User login
What are the best, worst states for physicians?
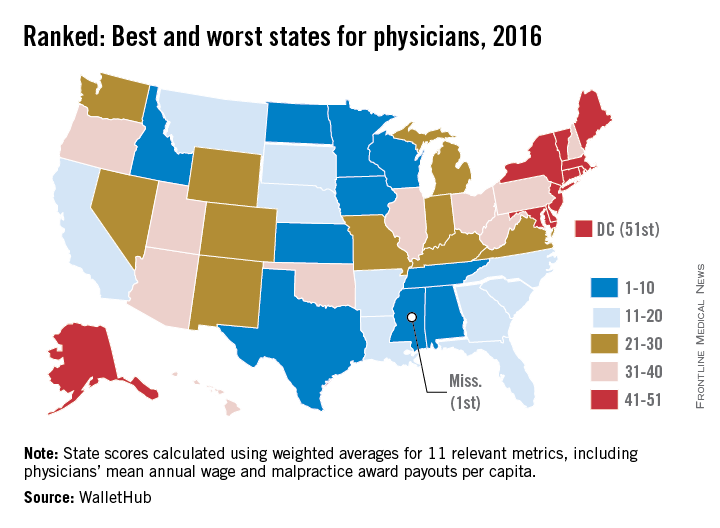
Should your future include a move to the South? A new report finds that Mississippi ranks as the best state to practice medicine, while the District of Columbia and New York are the least doctor-friendly areas in the United States.
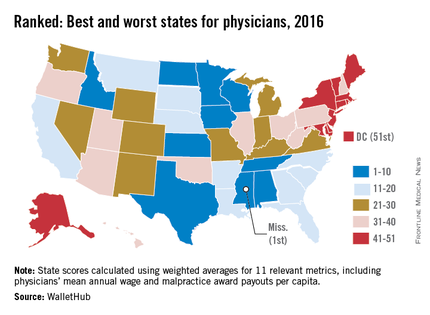
The survey, conducted by personal finance website WalletHub, compares all 50 states and D.C. across 11 metrics, including physician starting salary, medical malpractice climate, provider competition, and annual wages – adjusted for cost of living. Data was derived from the U.S. Census Bureau, the Bureau of Labor Statistics, the U.S. Department of Health and Human Services, and the Missouri Economic Research & Information Center, among other sources.
Researchers gave each metric a value between 0 and 100 and then calculated an overall score for each state using the weighted average across all metrics. Behind Mississippi, Iowa, Minnesota, and North Dakota ranked among the best states to practice medicine, according to the report. Rhode Island, Maryland, and Connecticut ranked among the worst, just slightly better than New York and D.C.
“There are an abundance of differences in terms of the working environments faced by doctors across the nation,” WalletHub analyst Jill Gonzalez said in an interview. “The results, while not too surprising, may certainly be eye opening for many new or soon-to-be doctors. Doctors should understand what they’re signing up for in terms of wages, malpractice rates, and job security when they move to another state to practice.”
View the entire WalletHub analysis here.
On Twitter @legal_med
Should your future include a move to the South? A new report finds that Mississippi ranks as the best state to practice medicine, while the District of Columbia and New York are the least doctor-friendly areas in the United States.
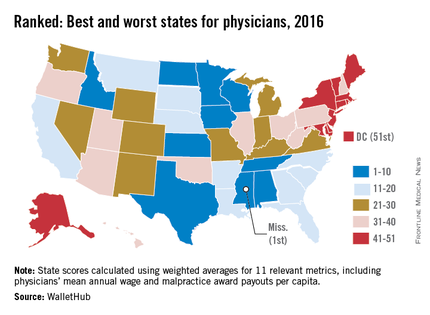
The survey, conducted by personal finance website WalletHub, compares all 50 states and D.C. across 11 metrics, including physician starting salary, medical malpractice climate, provider competition, and annual wages – adjusted for cost of living. Data was derived from the U.S. Census Bureau, the Bureau of Labor Statistics, the U.S. Department of Health and Human Services, and the Missouri Economic Research & Information Center, among other sources.
Researchers gave each metric a value between 0 and 100 and then calculated an overall score for each state using the weighted average across all metrics. Behind Mississippi, Iowa, Minnesota, and North Dakota ranked among the best states to practice medicine, according to the report. Rhode Island, Maryland, and Connecticut ranked among the worst, just slightly better than New York and D.C.
“There are an abundance of differences in terms of the working environments faced by doctors across the nation,” WalletHub analyst Jill Gonzalez said in an interview. “The results, while not too surprising, may certainly be eye opening for many new or soon-to-be doctors. Doctors should understand what they’re signing up for in terms of wages, malpractice rates, and job security when they move to another state to practice.”
View the entire WalletHub analysis here.
On Twitter @legal_med
Should your future include a move to the South? A new report finds that Mississippi ranks as the best state to practice medicine, while the District of Columbia and New York are the least doctor-friendly areas in the United States.
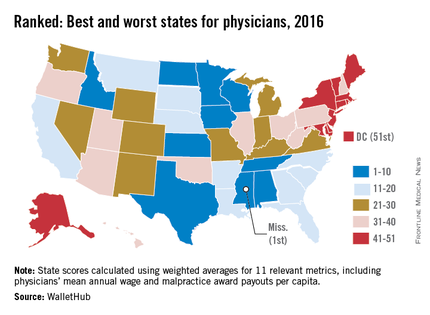
The survey, conducted by personal finance website WalletHub, compares all 50 states and D.C. across 11 metrics, including physician starting salary, medical malpractice climate, provider competition, and annual wages – adjusted for cost of living. Data was derived from the U.S. Census Bureau, the Bureau of Labor Statistics, the U.S. Department of Health and Human Services, and the Missouri Economic Research & Information Center, among other sources.
Researchers gave each metric a value between 0 and 100 and then calculated an overall score for each state using the weighted average across all metrics. Behind Mississippi, Iowa, Minnesota, and North Dakota ranked among the best states to practice medicine, according to the report. Rhode Island, Maryland, and Connecticut ranked among the worst, just slightly better than New York and D.C.
“There are an abundance of differences in terms of the working environments faced by doctors across the nation,” WalletHub analyst Jill Gonzalez said in an interview. “The results, while not too surprising, may certainly be eye opening for many new or soon-to-be doctors. Doctors should understand what they’re signing up for in terms of wages, malpractice rates, and job security when they move to another state to practice.”
View the entire WalletHub analysis here.
On Twitter @legal_med
Justices order new briefs in birth control mandate case
Less than a week after hearing oral arguments, Supreme Court justices have ordered both sides to provide new briefs in a religious freedom case that centers on the federal government’s contraception mandate.
In an unexpected move, the justices on March 29 directed attorneys to file supplemental briefs that propose alternatives to the government’s current accommodation under the mandate. The high court wants to know whether, and how, contraceptive coverage could be obtained by employees of religious nonprofits through the plaintiffs’ health plans in a way that does not require employer involvement.
The request is likely an attempt to avoid a 4-4 ruling in Zubik v. Burwell, while finding a way to spare religious nonprofits from participating in the process of providing birth control coverage, according to analysts.
“The court here is clearly looking to craft a win-win situation; a compromise where no one has to lose,” said Mark Goldfeder, a law professor at Emory University in Atlanta and director of the school’s law and religion student program. “The court is asking for the parties to help craft a process by which the affected employees can get their contraception easily covered, in a way that does not violate their employer’s religious beliefs.”
During oral arguments on March 23, the justices focused much attention on the process of the accommodation and how the arrangement unfolds between employers and the government, said Laurie Sobel, a senior policy analyst for the Henry J. Kaiser Family Foundation who attended the oral arguments.
“The fundamental issue in this case comes down to how the accommodation works,” Ms. Sobel said in an interview. “The petitioners believe the notification is the permission slip that triggers the coverage from the insurance companies. The government’s position is, ‘No, that’s just a notification, and the requirement to provide the coverage comes from the law.’ That came up a lot during arguments.”
The Supreme Court’s more conservative justices, including Justice Samuel A. Alito Jr. and Chief Justice John G. Roberts, were skeptical that the accommodation is the least restrictive means of advancing a compelling interest. The court’s four more liberal justices – particularly the three women on the court – appeared to support the accommodation, said Marci A. Hamilton, a law professor at Yeshiva University, New York, who also attended oral arguments.
Ms. Hamilton wrote a friend-of-the-court brief on behalf of Rep. Bobby Scott (D-Va.) in support of the government.
“[Plaintiffs’ attorney] Paul Clement was very quickly attacked by all three female Supreme Court justices,” Ms. Hamilton said in an interview. “It was really interesting that the female justices clearly took this to heart. They fundamentally identified with the contraceptive issue, and they really dominated the first part of the argument.”
Justice Ruth Bader Ginsburg countered the assertion that under the accommodation, notification by employers is treated by the government as an authorization for contraceptive coverage.
“It’s not an authorization,” Justice Ginsburg said during arguments. “The government, the law, the regulation requires it, but it doesn’t matter whether you say, yes or no. And you could say, ‘I fill out the form. I do not authorize. I do not permit.’ It won’t make any difference.”
The ACA’s accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities, such as churches. The plaintiffs – part of seven consolidated cases that include a Catholic bishop and an order of nuns – argue that the opt-out process put in place by the government makes them complicit in offering contraception coverage indirectly. Forcing them to cooperate with the accommodation violates their rights under the federal Religious Freedom Restoration Act, according to the plaintiffs.
The government contends that the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share their employers’ religious beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuit courts.
Chief Justice Roberts indicated agreement that the government is attempting to take control of the plaintiff’s health plans and provide coverage against the will of the nonprofit employers, said Mr. Goldfeder.
During arguments, Justice Roberts also made it clear that religious liberty versus reproductive rights is not at the center of the case, noted Mr. Goldfeder, who co-wrote a friend-of-the-court brief for the American Center for Law and Justice in support of the employers. Specifically, Justice Roberts stressed that the case is rooted in the employer’s objection to the government’s mechanism, not to employees receiving contraceptive care.
“The way this case has often been portrayed in the media, it has been about a clash between religious liberty and reproductive rights,” Mr. Goldfeder said in an interview. “As became clear in the arguments today, that is a false dichotomy, and a false narrative.”
Foreshadowing their latest move, justices and attorneys spent ample time arguing over whether an alternative paperwork process could satisfy both parties. Justice Alito asked whether it was possible that patients who do not get contraceptive coverage from their religious nonprofit employer could obtain a free contraceptive-only policy through the ACA insurance exchanges.
Solicitor General Donald B. Verrilli, Jr. dismissed that proposal.
“It’s not a less restrictive alternative because it has precisely the problem Congress was trying to overcome in the preventive services provision,” he said. “That [proposal] is not equally effective at achieving the government’s interest, because the whole point of this provision is that you get this care from your regular doctor as part of your regular health care without any barriers, including any copay barriers.”
The justices have several options in deciding the case, including choosing to rehear arguments at a later date. The Feb. 13 death of Justice Antonin Scalia could also mean a 4-4 split decision. If such a division occurs, the lower court rulings would stand.
“The impact will be that women employed by nonprofits in the 8th Circuit will be denied contraception coverage, but that women in all the other circuits will receive the coverage,” Ms. Hamilton said. “And we’ll be back to not having an answer from the Supreme Court. So all of the machinery that went into play for consideration of this case ... all of the entities that worked on it, will have to repeat itself. It will turn the whole exercise into something of a joke.”
In the two-page order issued March 29, the justices encouraged both parties to suggest ways in which the plaintiffs would have no legal obligation to provide contraceptive coverage, would not have to pay for such coverage, and would not be required to submit any separate notice to insurers, the government, or employees. New briefs are due by April 20.
On Twitter @legal_med
Less than a week after hearing oral arguments, Supreme Court justices have ordered both sides to provide new briefs in a religious freedom case that centers on the federal government’s contraception mandate.
In an unexpected move, the justices on March 29 directed attorneys to file supplemental briefs that propose alternatives to the government’s current accommodation under the mandate. The high court wants to know whether, and how, contraceptive coverage could be obtained by employees of religious nonprofits through the plaintiffs’ health plans in a way that does not require employer involvement.
The request is likely an attempt to avoid a 4-4 ruling in Zubik v. Burwell, while finding a way to spare religious nonprofits from participating in the process of providing birth control coverage, according to analysts.
“The court here is clearly looking to craft a win-win situation; a compromise where no one has to lose,” said Mark Goldfeder, a law professor at Emory University in Atlanta and director of the school’s law and religion student program. “The court is asking for the parties to help craft a process by which the affected employees can get their contraception easily covered, in a way that does not violate their employer’s religious beliefs.”
During oral arguments on March 23, the justices focused much attention on the process of the accommodation and how the arrangement unfolds between employers and the government, said Laurie Sobel, a senior policy analyst for the Henry J. Kaiser Family Foundation who attended the oral arguments.
“The fundamental issue in this case comes down to how the accommodation works,” Ms. Sobel said in an interview. “The petitioners believe the notification is the permission slip that triggers the coverage from the insurance companies. The government’s position is, ‘No, that’s just a notification, and the requirement to provide the coverage comes from the law.’ That came up a lot during arguments.”
The Supreme Court’s more conservative justices, including Justice Samuel A. Alito Jr. and Chief Justice John G. Roberts, were skeptical that the accommodation is the least restrictive means of advancing a compelling interest. The court’s four more liberal justices – particularly the three women on the court – appeared to support the accommodation, said Marci A. Hamilton, a law professor at Yeshiva University, New York, who also attended oral arguments.
Ms. Hamilton wrote a friend-of-the-court brief on behalf of Rep. Bobby Scott (D-Va.) in support of the government.
“[Plaintiffs’ attorney] Paul Clement was very quickly attacked by all three female Supreme Court justices,” Ms. Hamilton said in an interview. “It was really interesting that the female justices clearly took this to heart. They fundamentally identified with the contraceptive issue, and they really dominated the first part of the argument.”
Justice Ruth Bader Ginsburg countered the assertion that under the accommodation, notification by employers is treated by the government as an authorization for contraceptive coverage.
“It’s not an authorization,” Justice Ginsburg said during arguments. “The government, the law, the regulation requires it, but it doesn’t matter whether you say, yes or no. And you could say, ‘I fill out the form. I do not authorize. I do not permit.’ It won’t make any difference.”
The ACA’s accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities, such as churches. The plaintiffs – part of seven consolidated cases that include a Catholic bishop and an order of nuns – argue that the opt-out process put in place by the government makes them complicit in offering contraception coverage indirectly. Forcing them to cooperate with the accommodation violates their rights under the federal Religious Freedom Restoration Act, according to the plaintiffs.
The government contends that the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share their employers’ religious beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuit courts.
Chief Justice Roberts indicated agreement that the government is attempting to take control of the plaintiff’s health plans and provide coverage against the will of the nonprofit employers, said Mr. Goldfeder.
During arguments, Justice Roberts also made it clear that religious liberty versus reproductive rights is not at the center of the case, noted Mr. Goldfeder, who co-wrote a friend-of-the-court brief for the American Center for Law and Justice in support of the employers. Specifically, Justice Roberts stressed that the case is rooted in the employer’s objection to the government’s mechanism, not to employees receiving contraceptive care.
“The way this case has often been portrayed in the media, it has been about a clash between religious liberty and reproductive rights,” Mr. Goldfeder said in an interview. “As became clear in the arguments today, that is a false dichotomy, and a false narrative.”
Foreshadowing their latest move, justices and attorneys spent ample time arguing over whether an alternative paperwork process could satisfy both parties. Justice Alito asked whether it was possible that patients who do not get contraceptive coverage from their religious nonprofit employer could obtain a free contraceptive-only policy through the ACA insurance exchanges.
Solicitor General Donald B. Verrilli, Jr. dismissed that proposal.
“It’s not a less restrictive alternative because it has precisely the problem Congress was trying to overcome in the preventive services provision,” he said. “That [proposal] is not equally effective at achieving the government’s interest, because the whole point of this provision is that you get this care from your regular doctor as part of your regular health care without any barriers, including any copay barriers.”
The justices have several options in deciding the case, including choosing to rehear arguments at a later date. The Feb. 13 death of Justice Antonin Scalia could also mean a 4-4 split decision. If such a division occurs, the lower court rulings would stand.
“The impact will be that women employed by nonprofits in the 8th Circuit will be denied contraception coverage, but that women in all the other circuits will receive the coverage,” Ms. Hamilton said. “And we’ll be back to not having an answer from the Supreme Court. So all of the machinery that went into play for consideration of this case ... all of the entities that worked on it, will have to repeat itself. It will turn the whole exercise into something of a joke.”
In the two-page order issued March 29, the justices encouraged both parties to suggest ways in which the plaintiffs would have no legal obligation to provide contraceptive coverage, would not have to pay for such coverage, and would not be required to submit any separate notice to insurers, the government, or employees. New briefs are due by April 20.
On Twitter @legal_med
Less than a week after hearing oral arguments, Supreme Court justices have ordered both sides to provide new briefs in a religious freedom case that centers on the federal government’s contraception mandate.
In an unexpected move, the justices on March 29 directed attorneys to file supplemental briefs that propose alternatives to the government’s current accommodation under the mandate. The high court wants to know whether, and how, contraceptive coverage could be obtained by employees of religious nonprofits through the plaintiffs’ health plans in a way that does not require employer involvement.
The request is likely an attempt to avoid a 4-4 ruling in Zubik v. Burwell, while finding a way to spare religious nonprofits from participating in the process of providing birth control coverage, according to analysts.
“The court here is clearly looking to craft a win-win situation; a compromise where no one has to lose,” said Mark Goldfeder, a law professor at Emory University in Atlanta and director of the school’s law and religion student program. “The court is asking for the parties to help craft a process by which the affected employees can get their contraception easily covered, in a way that does not violate their employer’s religious beliefs.”
During oral arguments on March 23, the justices focused much attention on the process of the accommodation and how the arrangement unfolds between employers and the government, said Laurie Sobel, a senior policy analyst for the Henry J. Kaiser Family Foundation who attended the oral arguments.
“The fundamental issue in this case comes down to how the accommodation works,” Ms. Sobel said in an interview. “The petitioners believe the notification is the permission slip that triggers the coverage from the insurance companies. The government’s position is, ‘No, that’s just a notification, and the requirement to provide the coverage comes from the law.’ That came up a lot during arguments.”
The Supreme Court’s more conservative justices, including Justice Samuel A. Alito Jr. and Chief Justice John G. Roberts, were skeptical that the accommodation is the least restrictive means of advancing a compelling interest. The court’s four more liberal justices – particularly the three women on the court – appeared to support the accommodation, said Marci A. Hamilton, a law professor at Yeshiva University, New York, who also attended oral arguments.
Ms. Hamilton wrote a friend-of-the-court brief on behalf of Rep. Bobby Scott (D-Va.) in support of the government.
“[Plaintiffs’ attorney] Paul Clement was very quickly attacked by all three female Supreme Court justices,” Ms. Hamilton said in an interview. “It was really interesting that the female justices clearly took this to heart. They fundamentally identified with the contraceptive issue, and they really dominated the first part of the argument.”
Justice Ruth Bader Ginsburg countered the assertion that under the accommodation, notification by employers is treated by the government as an authorization for contraceptive coverage.
“It’s not an authorization,” Justice Ginsburg said during arguments. “The government, the law, the regulation requires it, but it doesn’t matter whether you say, yes or no. And you could say, ‘I fill out the form. I do not authorize. I do not permit.’ It won’t make any difference.”
The ACA’s accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities, such as churches. The plaintiffs – part of seven consolidated cases that include a Catholic bishop and an order of nuns – argue that the opt-out process put in place by the government makes them complicit in offering contraception coverage indirectly. Forcing them to cooperate with the accommodation violates their rights under the federal Religious Freedom Restoration Act, according to the plaintiffs.
The government contends that the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share their employers’ religious beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuit courts.
Chief Justice Roberts indicated agreement that the government is attempting to take control of the plaintiff’s health plans and provide coverage against the will of the nonprofit employers, said Mr. Goldfeder.
During arguments, Justice Roberts also made it clear that religious liberty versus reproductive rights is not at the center of the case, noted Mr. Goldfeder, who co-wrote a friend-of-the-court brief for the American Center for Law and Justice in support of the employers. Specifically, Justice Roberts stressed that the case is rooted in the employer’s objection to the government’s mechanism, not to employees receiving contraceptive care.
“The way this case has often been portrayed in the media, it has been about a clash between religious liberty and reproductive rights,” Mr. Goldfeder said in an interview. “As became clear in the arguments today, that is a false dichotomy, and a false narrative.”
Foreshadowing their latest move, justices and attorneys spent ample time arguing over whether an alternative paperwork process could satisfy both parties. Justice Alito asked whether it was possible that patients who do not get contraceptive coverage from their religious nonprofit employer could obtain a free contraceptive-only policy through the ACA insurance exchanges.
Solicitor General Donald B. Verrilli, Jr. dismissed that proposal.
“It’s not a less restrictive alternative because it has precisely the problem Congress was trying to overcome in the preventive services provision,” he said. “That [proposal] is not equally effective at achieving the government’s interest, because the whole point of this provision is that you get this care from your regular doctor as part of your regular health care without any barriers, including any copay barriers.”
The justices have several options in deciding the case, including choosing to rehear arguments at a later date. The Feb. 13 death of Justice Antonin Scalia could also mean a 4-4 split decision. If such a division occurs, the lower court rulings would stand.
“The impact will be that women employed by nonprofits in the 8th Circuit will be denied contraception coverage, but that women in all the other circuits will receive the coverage,” Ms. Hamilton said. “And we’ll be back to not having an answer from the Supreme Court. So all of the machinery that went into play for consideration of this case ... all of the entities that worked on it, will have to repeat itself. It will turn the whole exercise into something of a joke.”
In the two-page order issued March 29, the justices encouraged both parties to suggest ways in which the plaintiffs would have no legal obligation to provide contraceptive coverage, would not have to pay for such coverage, and would not be required to submit any separate notice to insurers, the government, or employees. New briefs are due by April 20.
On Twitter @legal_med
VIDEO: Determining your practice’s fair market value in a quality-based world
AUSTIN, TEX. – The shift from fee-for-service to value-based health care raises important questions about determining a physician practice’s fair market value, according to financial analyst Albert “Chip” D. Hutzler.
How will the new systems impact valuation? What about commercial reasonableness of arrangements? In a video interview at an American Health Lawyers Association meeting, Mr. Hutzler of HealthCare Appraisers, Delray, Fla., discussed the intersection of fair market value and value-based care, and he offered guidance on how to prepare for the changes.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
AUSTIN, TEX. – The shift from fee-for-service to value-based health care raises important questions about determining a physician practice’s fair market value, according to financial analyst Albert “Chip” D. Hutzler.
How will the new systems impact valuation? What about commercial reasonableness of arrangements? In a video interview at an American Health Lawyers Association meeting, Mr. Hutzler of HealthCare Appraisers, Delray, Fla., discussed the intersection of fair market value and value-based care, and he offered guidance on how to prepare for the changes.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
AUSTIN, TEX. – The shift from fee-for-service to value-based health care raises important questions about determining a physician practice’s fair market value, according to financial analyst Albert “Chip” D. Hutzler.
How will the new systems impact valuation? What about commercial reasonableness of arrangements? In a video interview at an American Health Lawyers Association meeting, Mr. Hutzler of HealthCare Appraisers, Delray, Fla., discussed the intersection of fair market value and value-based care, and he offered guidance on how to prepare for the changes.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
AT THE PHYSICIANS AND HOSPITALS LAW INSTITUTE
Voluntary self-disclosure: Pros and cons of using the protocol
AUSTIN, TEX. – Using the federal government’s voluntary self-disclosure protocol to report potential program violations offers advantages and disadvantages.
On one hand, the protocol allows health providers to get in front of possible offenses and retain some control, according to Miami health law attorney Stephen H. Siegel. On the other hand, launching the process could draw increased government scrutiny to a practice.
However, it can pay to be safe, rather than sorry later, Mr. Siegel said at an American Health Lawyers Association meeting.
“You are far better [off] and in a much better position, being proactive than reactive,” Mr. Siegel said in an interview. “Being proactive is an indication that your intention is to do the right thing. Whereas reactive, certainly the government doesn’t view [your intention] that way.”
Several federal agencies offer voluntary disclosure protocols. The HHS Office of Inspector General (OIG) self-disclosure protocol was created in 1998 to enable the self-disclosure of potential health care fraud. The Centers for Medicare & Medicaid Services provides the voluntary self-disclosure protocol, which is limited to potential violations of the physician-self referral statute, also called the Stark Law. Self-disclosures can also be made to the Department of Justice, although the agency has no formal protocol.
Voluntary self-disclosure can limit the possibility of an external investigation and reduce criminal and civil liability, according to Mr. Siegel. In a self-disclosure case, doctors can typically expect to pay back 1.5 times the amount that was improperly paid by the government. Whereas, in a false claims act case, for example, physicians can wind up paying back treble damages, plus a fine of between $5,500 and $11,000. Other advantages to voluntary self-disclosure include an expedited resolution, better control over adverse publicity, and the neutralizing of whistle-blower threats and lawsuits.
Disadvantages include financial loss, potential reputation harm, no immunity from liability or prior commitments by government, and possible penalties for conduct that may have remained undiscovered and thus undisclosed.
“For the most part, doctors are not aware of [voluntary self-disclosure],” Mr. Siegel said in an interview. “They’re not using it. [However], I think voluntary disclosure is going to become more widely used as people realize the ability to control the risk associated with the process.”
A number of issues warrant voluntary self-disclosure in a practice setting: possible government overpayments, potential improper arrangements with service providers, demonstrable patient harm, falsification of medical records, medical directorship issues, inadequate staffing, or the practice of medicine without a license, among others.
Regardless of which agency handles the self-disclosure, the admission will likely make its way to other agencies.
“Be assured that the agencies are going to talk to each other,” Mr. Siegel said. “If you submit it to DOJ [Department of Justice], chances are, it’s going to go to OIG.”
After choosing which agency to direct the self-disclosure, submit a timely, complete, and transparent disclosure, he advised. Each disclosure protocol is specific. For example, the OIG requires the disclosing party to acknowledge that the conduct is a potential violation and explicitly identify the laws that were potentially violated. The disclosing party also must agree ensure that corrective actions are implemented and that potential misconduct has stopped by the time of disclosure or, for improper kickback arrangements, within 90 days of submission.
The process of voluntary self-disclosure can be slow, usually taking more than a year. The OIG and CMS also reserve the right to reject a voluntary disclosure, Mr. Siegel said. If the government has already initiated an investigation for instance, an agency may reject the self-disclosure.
The government considers a host of factors when choosing how to resolve a self-disclosure case including the effectiveness of preexisting compliance programs; the nature of the conduct and its financial impact; the doctor’s ability to repay; whether the discloser is a first‐time offender; whether the incident is isolated; efforts to correct the problem; the period of alleged conduct; how the matter was discovered; and the party’s level of cooperation.
Mr. Siegel stressed there are no guarantees about how a voluntary self-disclosure case may be settled and that the matter will depend on the circumstances.
“There is no one-size-fits-all approach to voluntary self‐disclosure,” he said. “These decisions should be made with the assistance of competent and experienced counsel.”
On Twitter @legal_med
AUSTIN, TEX. – Using the federal government’s voluntary self-disclosure protocol to report potential program violations offers advantages and disadvantages.
On one hand, the protocol allows health providers to get in front of possible offenses and retain some control, according to Miami health law attorney Stephen H. Siegel. On the other hand, launching the process could draw increased government scrutiny to a practice.
However, it can pay to be safe, rather than sorry later, Mr. Siegel said at an American Health Lawyers Association meeting.
“You are far better [off] and in a much better position, being proactive than reactive,” Mr. Siegel said in an interview. “Being proactive is an indication that your intention is to do the right thing. Whereas reactive, certainly the government doesn’t view [your intention] that way.”
Several federal agencies offer voluntary disclosure protocols. The HHS Office of Inspector General (OIG) self-disclosure protocol was created in 1998 to enable the self-disclosure of potential health care fraud. The Centers for Medicare & Medicaid Services provides the voluntary self-disclosure protocol, which is limited to potential violations of the physician-self referral statute, also called the Stark Law. Self-disclosures can also be made to the Department of Justice, although the agency has no formal protocol.
Voluntary self-disclosure can limit the possibility of an external investigation and reduce criminal and civil liability, according to Mr. Siegel. In a self-disclosure case, doctors can typically expect to pay back 1.5 times the amount that was improperly paid by the government. Whereas, in a false claims act case, for example, physicians can wind up paying back treble damages, plus a fine of between $5,500 and $11,000. Other advantages to voluntary self-disclosure include an expedited resolution, better control over adverse publicity, and the neutralizing of whistle-blower threats and lawsuits.
Disadvantages include financial loss, potential reputation harm, no immunity from liability or prior commitments by government, and possible penalties for conduct that may have remained undiscovered and thus undisclosed.
“For the most part, doctors are not aware of [voluntary self-disclosure],” Mr. Siegel said in an interview. “They’re not using it. [However], I think voluntary disclosure is going to become more widely used as people realize the ability to control the risk associated with the process.”
A number of issues warrant voluntary self-disclosure in a practice setting: possible government overpayments, potential improper arrangements with service providers, demonstrable patient harm, falsification of medical records, medical directorship issues, inadequate staffing, or the practice of medicine without a license, among others.
Regardless of which agency handles the self-disclosure, the admission will likely make its way to other agencies.
“Be assured that the agencies are going to talk to each other,” Mr. Siegel said. “If you submit it to DOJ [Department of Justice], chances are, it’s going to go to OIG.”
After choosing which agency to direct the self-disclosure, submit a timely, complete, and transparent disclosure, he advised. Each disclosure protocol is specific. For example, the OIG requires the disclosing party to acknowledge that the conduct is a potential violation and explicitly identify the laws that were potentially violated. The disclosing party also must agree ensure that corrective actions are implemented and that potential misconduct has stopped by the time of disclosure or, for improper kickback arrangements, within 90 days of submission.
The process of voluntary self-disclosure can be slow, usually taking more than a year. The OIG and CMS also reserve the right to reject a voluntary disclosure, Mr. Siegel said. If the government has already initiated an investigation for instance, an agency may reject the self-disclosure.
The government considers a host of factors when choosing how to resolve a self-disclosure case including the effectiveness of preexisting compliance programs; the nature of the conduct and its financial impact; the doctor’s ability to repay; whether the discloser is a first‐time offender; whether the incident is isolated; efforts to correct the problem; the period of alleged conduct; how the matter was discovered; and the party’s level of cooperation.
Mr. Siegel stressed there are no guarantees about how a voluntary self-disclosure case may be settled and that the matter will depend on the circumstances.
“There is no one-size-fits-all approach to voluntary self‐disclosure,” he said. “These decisions should be made with the assistance of competent and experienced counsel.”
On Twitter @legal_med
AUSTIN, TEX. – Using the federal government’s voluntary self-disclosure protocol to report potential program violations offers advantages and disadvantages.
On one hand, the protocol allows health providers to get in front of possible offenses and retain some control, according to Miami health law attorney Stephen H. Siegel. On the other hand, launching the process could draw increased government scrutiny to a practice.
However, it can pay to be safe, rather than sorry later, Mr. Siegel said at an American Health Lawyers Association meeting.
“You are far better [off] and in a much better position, being proactive than reactive,” Mr. Siegel said in an interview. “Being proactive is an indication that your intention is to do the right thing. Whereas reactive, certainly the government doesn’t view [your intention] that way.”
Several federal agencies offer voluntary disclosure protocols. The HHS Office of Inspector General (OIG) self-disclosure protocol was created in 1998 to enable the self-disclosure of potential health care fraud. The Centers for Medicare & Medicaid Services provides the voluntary self-disclosure protocol, which is limited to potential violations of the physician-self referral statute, also called the Stark Law. Self-disclosures can also be made to the Department of Justice, although the agency has no formal protocol.
Voluntary self-disclosure can limit the possibility of an external investigation and reduce criminal and civil liability, according to Mr. Siegel. In a self-disclosure case, doctors can typically expect to pay back 1.5 times the amount that was improperly paid by the government. Whereas, in a false claims act case, for example, physicians can wind up paying back treble damages, plus a fine of between $5,500 and $11,000. Other advantages to voluntary self-disclosure include an expedited resolution, better control over adverse publicity, and the neutralizing of whistle-blower threats and lawsuits.
Disadvantages include financial loss, potential reputation harm, no immunity from liability or prior commitments by government, and possible penalties for conduct that may have remained undiscovered and thus undisclosed.
“For the most part, doctors are not aware of [voluntary self-disclosure],” Mr. Siegel said in an interview. “They’re not using it. [However], I think voluntary disclosure is going to become more widely used as people realize the ability to control the risk associated with the process.”
A number of issues warrant voluntary self-disclosure in a practice setting: possible government overpayments, potential improper arrangements with service providers, demonstrable patient harm, falsification of medical records, medical directorship issues, inadequate staffing, or the practice of medicine without a license, among others.
Regardless of which agency handles the self-disclosure, the admission will likely make its way to other agencies.
“Be assured that the agencies are going to talk to each other,” Mr. Siegel said. “If you submit it to DOJ [Department of Justice], chances are, it’s going to go to OIG.”
After choosing which agency to direct the self-disclosure, submit a timely, complete, and transparent disclosure, he advised. Each disclosure protocol is specific. For example, the OIG requires the disclosing party to acknowledge that the conduct is a potential violation and explicitly identify the laws that were potentially violated. The disclosing party also must agree ensure that corrective actions are implemented and that potential misconduct has stopped by the time of disclosure or, for improper kickback arrangements, within 90 days of submission.
The process of voluntary self-disclosure can be slow, usually taking more than a year. The OIG and CMS also reserve the right to reject a voluntary disclosure, Mr. Siegel said. If the government has already initiated an investigation for instance, an agency may reject the self-disclosure.
The government considers a host of factors when choosing how to resolve a self-disclosure case including the effectiveness of preexisting compliance programs; the nature of the conduct and its financial impact; the doctor’s ability to repay; whether the discloser is a first‐time offender; whether the incident is isolated; efforts to correct the problem; the period of alleged conduct; how the matter was discovered; and the party’s level of cooperation.
Mr. Siegel stressed there are no guarantees about how a voluntary self-disclosure case may be settled and that the matter will depend on the circumstances.
“There is no one-size-fits-all approach to voluntary self‐disclosure,” he said. “These decisions should be made with the assistance of competent and experienced counsel.”
On Twitter @legal_med
EXPERT ANALYSIS FROM THE PHYSICIANS AND HOSPITALS LAW INSTITUTE
Feds launch phase 2 of HIPAA audits
The federal government has launched the second phase of its HIPAA Audit Program and will soon be identifying health providers it plans to target.
For the 2016 Phase 2 HIPAA Audit Program, auditors will review policies and procedures enacted by covered entities and their business associates to meet selected standards of the Privacy, Security, and Breach Notification Rules, according to a March 21 announcement by the Department of Health & Human Services Office for Civil Rights (OCR).
Physicians and other covered entities can expect an email at some point this year requesting that updated contact information be provided to the OCR. The office will then send health providers a pre-audit questionnaire to gather data about the practice’s size, type, and operations, according to the announcement. The government will use the data as well as other information to create audit subject pools. If an entity does not respond to the OCR’s contact request or the pre-audit questionnaire, the agency will use publicly available information about the practice.
Every covered entity and business associate is eligible for an audit, the OCR noted. For Phase 2, the government plans to identify health providers and business associates that represent a wide range of health care providers, health plans, health care clearinghouses and business associates to access HIPAA compliance across the industry. Sampling criteria for auditee selection will include size of the entity, affiliation with other health care organizations, whether an organization is public or private, geographic factors, and present enforcement activity with OCR. Entities with open complaints or that are currently undergoing investigations will not be chosen.
The first set of audits will be desk audits of covered entities followed by a second round of desk audits of business associates, OCR stated. OCR plans to complete all desk audits by December 2016. A third set of audits will be on site and will examine a broader scope of requirements under the HIPAA rules. Some desk auditees may be subject to a subsequent on-site audit, the government noted.
A list of frequently asked questions about the 2016 Phase 2 HIPAA Audit Program can be found on the OCR’s website.
Round 2 of the HIPAA audits follows a pilot program launched in 2011 and 2012 by OCR that assessed HIPAA controls and processes implemented by 115 covered entities. The second phase will draw on the results and experiences learned from the pilot program, according to OCR.
On Twitter @legal_med
The federal government has launched the second phase of its HIPAA Audit Program and will soon be identifying health providers it plans to target.
For the 2016 Phase 2 HIPAA Audit Program, auditors will review policies and procedures enacted by covered entities and their business associates to meet selected standards of the Privacy, Security, and Breach Notification Rules, according to a March 21 announcement by the Department of Health & Human Services Office for Civil Rights (OCR).
Physicians and other covered entities can expect an email at some point this year requesting that updated contact information be provided to the OCR. The office will then send health providers a pre-audit questionnaire to gather data about the practice’s size, type, and operations, according to the announcement. The government will use the data as well as other information to create audit subject pools. If an entity does not respond to the OCR’s contact request or the pre-audit questionnaire, the agency will use publicly available information about the practice.
Every covered entity and business associate is eligible for an audit, the OCR noted. For Phase 2, the government plans to identify health providers and business associates that represent a wide range of health care providers, health plans, health care clearinghouses and business associates to access HIPAA compliance across the industry. Sampling criteria for auditee selection will include size of the entity, affiliation with other health care organizations, whether an organization is public or private, geographic factors, and present enforcement activity with OCR. Entities with open complaints or that are currently undergoing investigations will not be chosen.
The first set of audits will be desk audits of covered entities followed by a second round of desk audits of business associates, OCR stated. OCR plans to complete all desk audits by December 2016. A third set of audits will be on site and will examine a broader scope of requirements under the HIPAA rules. Some desk auditees may be subject to a subsequent on-site audit, the government noted.
A list of frequently asked questions about the 2016 Phase 2 HIPAA Audit Program can be found on the OCR’s website.
Round 2 of the HIPAA audits follows a pilot program launched in 2011 and 2012 by OCR that assessed HIPAA controls and processes implemented by 115 covered entities. The second phase will draw on the results and experiences learned from the pilot program, according to OCR.
On Twitter @legal_med
The federal government has launched the second phase of its HIPAA Audit Program and will soon be identifying health providers it plans to target.
For the 2016 Phase 2 HIPAA Audit Program, auditors will review policies and procedures enacted by covered entities and their business associates to meet selected standards of the Privacy, Security, and Breach Notification Rules, according to a March 21 announcement by the Department of Health & Human Services Office for Civil Rights (OCR).
Physicians and other covered entities can expect an email at some point this year requesting that updated contact information be provided to the OCR. The office will then send health providers a pre-audit questionnaire to gather data about the practice’s size, type, and operations, according to the announcement. The government will use the data as well as other information to create audit subject pools. If an entity does not respond to the OCR’s contact request or the pre-audit questionnaire, the agency will use publicly available information about the practice.
Every covered entity and business associate is eligible for an audit, the OCR noted. For Phase 2, the government plans to identify health providers and business associates that represent a wide range of health care providers, health plans, health care clearinghouses and business associates to access HIPAA compliance across the industry. Sampling criteria for auditee selection will include size of the entity, affiliation with other health care organizations, whether an organization is public or private, geographic factors, and present enforcement activity with OCR. Entities with open complaints or that are currently undergoing investigations will not be chosen.
The first set of audits will be desk audits of covered entities followed by a second round of desk audits of business associates, OCR stated. OCR plans to complete all desk audits by December 2016. A third set of audits will be on site and will examine a broader scope of requirements under the HIPAA rules. Some desk auditees may be subject to a subsequent on-site audit, the government noted.
A list of frequently asked questions about the 2016 Phase 2 HIPAA Audit Program can be found on the OCR’s website.
Round 2 of the HIPAA audits follows a pilot program launched in 2011 and 2012 by OCR that assessed HIPAA controls and processes implemented by 115 covered entities. The second phase will draw on the results and experiences learned from the pilot program, according to OCR.
On Twitter @legal_med
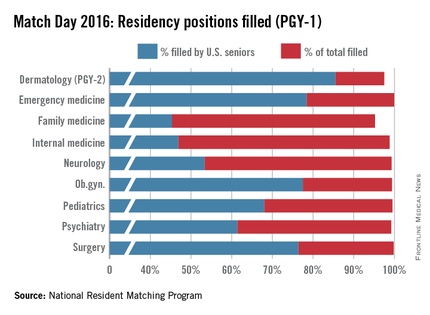
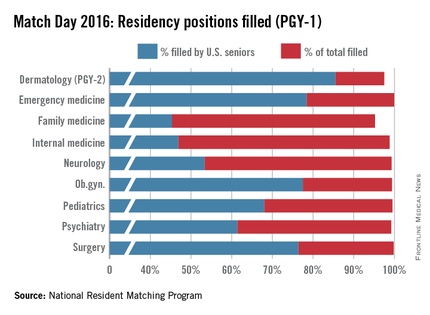
Match Day 2016: Residency spots rise, but growth still needed
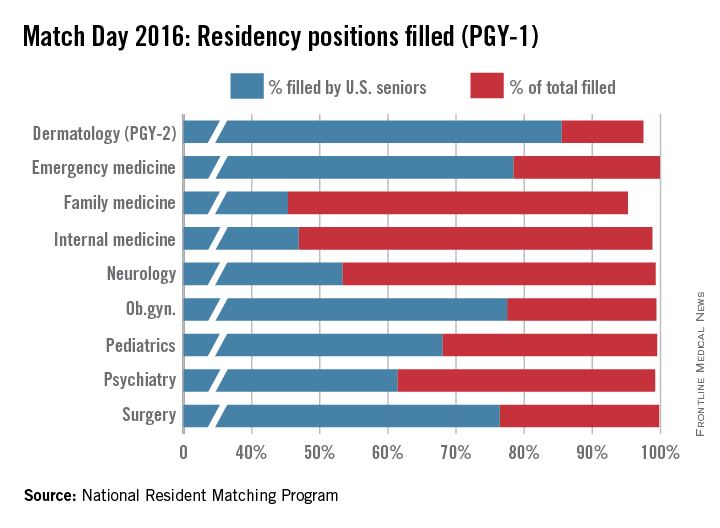
Medical school seniors scored a record number of available first-year slots in this year’s Main Residency Match, with both internal medicine and family medicine programs offering more spots to residents in 2016.
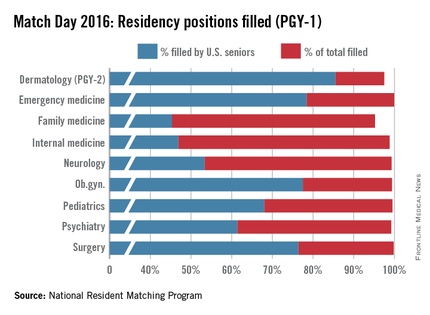
Continuing a 4-year growth trend, the number of available post-graduate year 1 (PGY-1) positions rose to 27,860 in 2016, 567 more spots than in 2015, and a record 18,668 U.S. allopathic medical school seniors registered for the match, 221 more than in 2015, according to data from the National Resident Matching Program (NRMP).
Family medicine residency programs offered 3,238 positions in 2016, up from 3,195 in the 2015 match. This year, greater than 95% of those positions were filled; 45% were filled by U.S. medical school graduates, the NRMP announced March 18.
Internal medicine experienced similar increases, with residency programs offering 7,024 positions this year, up from 6,770 positions in 2015. Just less than 99% of the positions were filled, with 47% filled by U.S. medical school graduates in this year’s Match.
“We’re very pleased with the way the numbers turned out,” said Dr. Philip A. Masters, clinical content development director for the American College of Physicians (ACP). “About 45% of new slots in this year’s Match were in internal medicine. So that coupled with a very high fill rate really suggests a continuing and an increased interest in the field.”
Dr. Wanda Filer, president of the American Academy of Family Physicians, said she was glad to see an increased number of medical school graduates matching to family medicine, but she stressed that the numbers are not enough.
“This nation needs far more family medicine physicians than the current numbers are achieving,” she said in an interview. “The growth in family medicine residency slots is not fast enough and our antiquated graduate medical education payment is misaligned with U.S. workforce needs. Additionally, poor accountability for federal dollars by some U.S. medical schools to deliver that workforce should be rapidly addressed.”
While ACP officials were satisfied with the overall internal medicine numbers, Dr. Masters said that the lack of medical students entering general internal medicine and primary care careers is concerning.
“The number of people in the regular categorical [internal medicine] training programs is a lot lower than it used to be,” Dr. Masters said in a interview. “A long time ago, upwards of half of people who went in categorical training pursued a career in general internal medicine. [Now], the overall trend tends to be away from primary care/general internal medicine. That is concerning because that’s what society really needs right now.”
Pediatric positions, meanwhile, rose slightly in 2016, growing to 2,689, with 21 more slots than last year. Just more than 99% were filled, and 68% were filled by U.S. seniors.
The NRMP data shows that of 18,668 U.S. allopathic seniors who registered for the Match this year, 18,187 submitted program choices and 17,057 matched to first-year positions. This is up from the 18,025 U.S. allopathic medical school seniors who submitted program preferences for the 2015 Match, of which 16,932 matched to first-year positions.
The larger scope of this year’s Match is likely attributed to growing enrollment among medical colleges, said NRMP President and CEO Mona Signer.
“Every year seems to be larger than the year before, at least, certainly recently,” Ms. Signer said in an interview. “It isn’t just a little bit larger. It’s a lot larger. Medical schools have been increasing enrollment and new medical schools have been [opened]. We certainly expect to see that trickle into the Match as those new schools begin to graduate their first classes and as those existing schools begin to graduate larger classes.”
But Ms. Signer agrees with others that larger Match numbers will not necessarily curb future physician shortages.
“The increasing enrollment in medical schools can’t help but at least address the physician-to-population ratio,” she said. “The issue is, are those new physicians gong to be in the specialties that we need? Obviously, we need more primary care physicians. It remains to be seen whether larger class sizes are going to result in a better physician-to-population ratio in primary care.”
On Twitter @legal_med
Medical school seniors scored a record number of available first-year slots in this year’s Main Residency Match, with both internal medicine and family medicine programs offering more spots to residents in 2016.
Continuing a 4-year growth trend, the number of available post-graduate year 1 (PGY-1) positions rose to 27,860 in 2016, 567 more spots than in 2015, and a record 18,668 U.S. allopathic medical school seniors registered for the match, 221 more than in 2015, according to data from the National Resident Matching Program (NRMP).
Family medicine residency programs offered 3,238 positions in 2016, up from 3,195 in the 2015 match. This year, greater than 95% of those positions were filled; 45% were filled by U.S. medical school graduates, the NRMP announced March 18.
Internal medicine experienced similar increases, with residency programs offering 7,024 positions this year, up from 6,770 positions in 2015. Just less than 99% of the positions were filled, with 47% filled by U.S. medical school graduates in this year’s Match.
“We’re very pleased with the way the numbers turned out,” said Dr. Philip A. Masters, clinical content development director for the American College of Physicians (ACP). “About 45% of new slots in this year’s Match were in internal medicine. So that coupled with a very high fill rate really suggests a continuing and an increased interest in the field.”
Dr. Wanda Filer, president of the American Academy of Family Physicians, said she was glad to see an increased number of medical school graduates matching to family medicine, but she stressed that the numbers are not enough.
“This nation needs far more family medicine physicians than the current numbers are achieving,” she said in an interview. “The growth in family medicine residency slots is not fast enough and our antiquated graduate medical education payment is misaligned with U.S. workforce needs. Additionally, poor accountability for federal dollars by some U.S. medical schools to deliver that workforce should be rapidly addressed.”
While ACP officials were satisfied with the overall internal medicine numbers, Dr. Masters said that the lack of medical students entering general internal medicine and primary care careers is concerning.
“The number of people in the regular categorical [internal medicine] training programs is a lot lower than it used to be,” Dr. Masters said in a interview. “A long time ago, upwards of half of people who went in categorical training pursued a career in general internal medicine. [Now], the overall trend tends to be away from primary care/general internal medicine. That is concerning because that’s what society really needs right now.”
Pediatric positions, meanwhile, rose slightly in 2016, growing to 2,689, with 21 more slots than last year. Just more than 99% were filled, and 68% were filled by U.S. seniors.
The NRMP data shows that of 18,668 U.S. allopathic seniors who registered for the Match this year, 18,187 submitted program choices and 17,057 matched to first-year positions. This is up from the 18,025 U.S. allopathic medical school seniors who submitted program preferences for the 2015 Match, of which 16,932 matched to first-year positions.
The larger scope of this year’s Match is likely attributed to growing enrollment among medical colleges, said NRMP President and CEO Mona Signer.
“Every year seems to be larger than the year before, at least, certainly recently,” Ms. Signer said in an interview. “It isn’t just a little bit larger. It’s a lot larger. Medical schools have been increasing enrollment and new medical schools have been [opened]. We certainly expect to see that trickle into the Match as those new schools begin to graduate their first classes and as those existing schools begin to graduate larger classes.”
But Ms. Signer agrees with others that larger Match numbers will not necessarily curb future physician shortages.
“The increasing enrollment in medical schools can’t help but at least address the physician-to-population ratio,” she said. “The issue is, are those new physicians gong to be in the specialties that we need? Obviously, we need more primary care physicians. It remains to be seen whether larger class sizes are going to result in a better physician-to-population ratio in primary care.”
On Twitter @legal_med
Medical school seniors scored a record number of available first-year slots in this year’s Main Residency Match, with both internal medicine and family medicine programs offering more spots to residents in 2016.
Continuing a 4-year growth trend, the number of available post-graduate year 1 (PGY-1) positions rose to 27,860 in 2016, 567 more spots than in 2015, and a record 18,668 U.S. allopathic medical school seniors registered for the match, 221 more than in 2015, according to data from the National Resident Matching Program (NRMP).
Family medicine residency programs offered 3,238 positions in 2016, up from 3,195 in the 2015 match. This year, greater than 95% of those positions were filled; 45% were filled by U.S. medical school graduates, the NRMP announced March 18.
Internal medicine experienced similar increases, with residency programs offering 7,024 positions this year, up from 6,770 positions in 2015. Just less than 99% of the positions were filled, with 47% filled by U.S. medical school graduates in this year’s Match.
“We’re very pleased with the way the numbers turned out,” said Dr. Philip A. Masters, clinical content development director for the American College of Physicians (ACP). “About 45% of new slots in this year’s Match were in internal medicine. So that coupled with a very high fill rate really suggests a continuing and an increased interest in the field.”
Dr. Wanda Filer, president of the American Academy of Family Physicians, said she was glad to see an increased number of medical school graduates matching to family medicine, but she stressed that the numbers are not enough.
“This nation needs far more family medicine physicians than the current numbers are achieving,” she said in an interview. “The growth in family medicine residency slots is not fast enough and our antiquated graduate medical education payment is misaligned with U.S. workforce needs. Additionally, poor accountability for federal dollars by some U.S. medical schools to deliver that workforce should be rapidly addressed.”
While ACP officials were satisfied with the overall internal medicine numbers, Dr. Masters said that the lack of medical students entering general internal medicine and primary care careers is concerning.
“The number of people in the regular categorical [internal medicine] training programs is a lot lower than it used to be,” Dr. Masters said in a interview. “A long time ago, upwards of half of people who went in categorical training pursued a career in general internal medicine. [Now], the overall trend tends to be away from primary care/general internal medicine. That is concerning because that’s what society really needs right now.”
Pediatric positions, meanwhile, rose slightly in 2016, growing to 2,689, with 21 more slots than last year. Just more than 99% were filled, and 68% were filled by U.S. seniors.
The NRMP data shows that of 18,668 U.S. allopathic seniors who registered for the Match this year, 18,187 submitted program choices and 17,057 matched to first-year positions. This is up from the 18,025 U.S. allopathic medical school seniors who submitted program preferences for the 2015 Match, of which 16,932 matched to first-year positions.
The larger scope of this year’s Match is likely attributed to growing enrollment among medical colleges, said NRMP President and CEO Mona Signer.
“Every year seems to be larger than the year before, at least, certainly recently,” Ms. Signer said in an interview. “It isn’t just a little bit larger. It’s a lot larger. Medical schools have been increasing enrollment and new medical schools have been [opened]. We certainly expect to see that trickle into the Match as those new schools begin to graduate their first classes and as those existing schools begin to graduate larger classes.”
But Ms. Signer agrees with others that larger Match numbers will not necessarily curb future physician shortages.
“The increasing enrollment in medical schools can’t help but at least address the physician-to-population ratio,” she said. “The issue is, are those new physicians gong to be in the specialties that we need? Obviously, we need more primary care physicians. It remains to be seen whether larger class sizes are going to result in a better physician-to-population ratio in primary care.”
On Twitter @legal_med
Supreme Court to hear debate over contraception coverage mandate
The U.S. Supreme Court will hear oral arguments March 23 in a case that pits the federal government against religious employers who oppose contraceptive use.
Zubik v. Burwell centers on whether an accommodation under the Affordable Care Act’s contraceptive mandate is enough to protect the religious freedoms of nonprofit employers with strongly held religious beliefs.
The ruling in Zubik will have broad implications for contraception care nationwide and the way in which the Religious Freedom Restoration Act (RFRA) is applied going forward, said Laurie Sobel, a senior policy analyst for the Henry J. Kaiser Family Foundation.
“Ultimately, if the court were to rule in favor of Zubik, it would mean the workers and dependents of nonprofits are at risk of losing some or all contraceptive coverage,” Ms. Sobel said during a March 16 Kaiser press briefing. “The burden on women to pay out of pocket has [been] shown to really limit their choices and possibly limit [all] contraceptives for them.”
The ACA’s accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities, such as churches. The plaintiffs – part of seven consolidated cases that include a Catholic bishop and an order of nuns – argue that the opt-out process put in place by the government makes them complicit in offering contraception coverage indirectly.
The government contends that the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share their employers’ religious beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuit courts.
The case comes down to whether the plaintiffs can prove the accommodation places a substantial burden on their religious conduct, and if so, whether the government can prove its provision is the least restrictive means of advancing a compelling interest, said Marci A. Hamilton, a law professor at the Benjamin N. Cardozo School of Law, Yeshiva University, New York.
“[If the court sides with Zubik], one possible precedent this could set is that religious objectors – the employers in these cases – will be able to limit independent third-party actions,” Ms. Hamilton said during the media conference. “It doesn’t matter the faith. You can have your decisions about birth control and the cost and reproductive care determined by the faith of your employer.”
A ruling for Zubik would also throw a monkey wrench in the country’s long tradition of legislative accommodations, Ms. Hamilton said, noting that there are many laws that include accommodations for certain populations.
“That means the legislative weighing of harm and safety is going to be pushed aside and essentially, we’re going to be talking about, how can every single law including the accommodations be fine-tuned for one set of believers?”
The recent death of Associate Justice Antonin Scalia, who was the court’s most outspoken conservative, could significantly impact the case’s outcome, analysts said. Justice Scalia was among majority in the 5-4 decision in Burwell v. Hobby Lobby, a 2014 opinion that protected religiously devout owners of closely held, for-profit businesses from having to offer birth control under the mandate. His absence could mean a 4-4 split in the Zubik case, which would allow the lower court rulings to stand, said Lyle Denniston, a Supreme Court analyst who writes for SCOTUSblog.
“My own sense is that the court is going to try very hard to find a way to resolve this case without a 4-4 split,” Mr. Denniston said during the Kaiser media conference. “If the Supreme Court issues a 4-4 decision, that leaves division in the lower courts, and it will vary from region to region in the country as to what the rights for women under the ACA are.”
More than 70 briefs have been issued to the high court in support of or opposition to the plaintiffs, including pleas by religious organizations, women’s advocacy groups, law professors, medical associations, and attorneys.
The American College of Obstetricians and Gynecologists and the American Academy of Family Physicians wrote in a joint brief that contraception coverage under the ACA ensures that patients have access to medically appropriate contraception without regard to their ability to pay. At the same time, the law respects an employer’s sincerely held religious objections to contraception through the accommodation, the brief said.
However, the Council for Christian Colleges & Universities argues the government’s decision to exempt some religious employers from providing contraceptive coverage while requiring others to comply with the mandate “demonstrates that the government’s approach is not the least restrictive means necessary to advance its interests.”
“Civil rights should not vary based on whether that institution is or is not affiliated with a church or other house of worship,” the council wrote in its brief to the Supreme Court. “Religious exercise is not tied to one’s affiliation but rather the source and sincerity of one’s belief and the desire to exercise it. That truth appears to be one the government has been unable to grasp or comprehend as it decides who is sufficiently ‘religious’ to have religious beliefs worthy of protection.”
On Twitter @legal_med
The U.S. Supreme Court will hear oral arguments March 23 in a case that pits the federal government against religious employers who oppose contraceptive use.
Zubik v. Burwell centers on whether an accommodation under the Affordable Care Act’s contraceptive mandate is enough to protect the religious freedoms of nonprofit employers with strongly held religious beliefs.
The ruling in Zubik will have broad implications for contraception care nationwide and the way in which the Religious Freedom Restoration Act (RFRA) is applied going forward, said Laurie Sobel, a senior policy analyst for the Henry J. Kaiser Family Foundation.
“Ultimately, if the court were to rule in favor of Zubik, it would mean the workers and dependents of nonprofits are at risk of losing some or all contraceptive coverage,” Ms. Sobel said during a March 16 Kaiser press briefing. “The burden on women to pay out of pocket has [been] shown to really limit their choices and possibly limit [all] contraceptives for them.”
The ACA’s accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities, such as churches. The plaintiffs – part of seven consolidated cases that include a Catholic bishop and an order of nuns – argue that the opt-out process put in place by the government makes them complicit in offering contraception coverage indirectly.
The government contends that the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share their employers’ religious beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuit courts.
The case comes down to whether the plaintiffs can prove the accommodation places a substantial burden on their religious conduct, and if so, whether the government can prove its provision is the least restrictive means of advancing a compelling interest, said Marci A. Hamilton, a law professor at the Benjamin N. Cardozo School of Law, Yeshiva University, New York.
“[If the court sides with Zubik], one possible precedent this could set is that religious objectors – the employers in these cases – will be able to limit independent third-party actions,” Ms. Hamilton said during the media conference. “It doesn’t matter the faith. You can have your decisions about birth control and the cost and reproductive care determined by the faith of your employer.”
A ruling for Zubik would also throw a monkey wrench in the country’s long tradition of legislative accommodations, Ms. Hamilton said, noting that there are many laws that include accommodations for certain populations.
“That means the legislative weighing of harm and safety is going to be pushed aside and essentially, we’re going to be talking about, how can every single law including the accommodations be fine-tuned for one set of believers?”
The recent death of Associate Justice Antonin Scalia, who was the court’s most outspoken conservative, could significantly impact the case’s outcome, analysts said. Justice Scalia was among majority in the 5-4 decision in Burwell v. Hobby Lobby, a 2014 opinion that protected religiously devout owners of closely held, for-profit businesses from having to offer birth control under the mandate. His absence could mean a 4-4 split in the Zubik case, which would allow the lower court rulings to stand, said Lyle Denniston, a Supreme Court analyst who writes for SCOTUSblog.
“My own sense is that the court is going to try very hard to find a way to resolve this case without a 4-4 split,” Mr. Denniston said during the Kaiser media conference. “If the Supreme Court issues a 4-4 decision, that leaves division in the lower courts, and it will vary from region to region in the country as to what the rights for women under the ACA are.”
More than 70 briefs have been issued to the high court in support of or opposition to the plaintiffs, including pleas by religious organizations, women’s advocacy groups, law professors, medical associations, and attorneys.
The American College of Obstetricians and Gynecologists and the American Academy of Family Physicians wrote in a joint brief that contraception coverage under the ACA ensures that patients have access to medically appropriate contraception without regard to their ability to pay. At the same time, the law respects an employer’s sincerely held religious objections to contraception through the accommodation, the brief said.
However, the Council for Christian Colleges & Universities argues the government’s decision to exempt some religious employers from providing contraceptive coverage while requiring others to comply with the mandate “demonstrates that the government’s approach is not the least restrictive means necessary to advance its interests.”
“Civil rights should not vary based on whether that institution is or is not affiliated with a church or other house of worship,” the council wrote in its brief to the Supreme Court. “Religious exercise is not tied to one’s affiliation but rather the source and sincerity of one’s belief and the desire to exercise it. That truth appears to be one the government has been unable to grasp or comprehend as it decides who is sufficiently ‘religious’ to have religious beliefs worthy of protection.”
On Twitter @legal_med
The U.S. Supreme Court will hear oral arguments March 23 in a case that pits the federal government against religious employers who oppose contraceptive use.
Zubik v. Burwell centers on whether an accommodation under the Affordable Care Act’s contraceptive mandate is enough to protect the religious freedoms of nonprofit employers with strongly held religious beliefs.
The ruling in Zubik will have broad implications for contraception care nationwide and the way in which the Religious Freedom Restoration Act (RFRA) is applied going forward, said Laurie Sobel, a senior policy analyst for the Henry J. Kaiser Family Foundation.
“Ultimately, if the court were to rule in favor of Zubik, it would mean the workers and dependents of nonprofits are at risk of losing some or all contraceptive coverage,” Ms. Sobel said during a March 16 Kaiser press briefing. “The burden on women to pay out of pocket has [been] shown to really limit their choices and possibly limit [all] contraceptives for them.”
The ACA’s accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities, such as churches. The plaintiffs – part of seven consolidated cases that include a Catholic bishop and an order of nuns – argue that the opt-out process put in place by the government makes them complicit in offering contraception coverage indirectly.
The government contends that the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share their employers’ religious beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuit courts.
The case comes down to whether the plaintiffs can prove the accommodation places a substantial burden on their religious conduct, and if so, whether the government can prove its provision is the least restrictive means of advancing a compelling interest, said Marci A. Hamilton, a law professor at the Benjamin N. Cardozo School of Law, Yeshiva University, New York.
“[If the court sides with Zubik], one possible precedent this could set is that religious objectors – the employers in these cases – will be able to limit independent third-party actions,” Ms. Hamilton said during the media conference. “It doesn’t matter the faith. You can have your decisions about birth control and the cost and reproductive care determined by the faith of your employer.”
A ruling for Zubik would also throw a monkey wrench in the country’s long tradition of legislative accommodations, Ms. Hamilton said, noting that there are many laws that include accommodations for certain populations.
“That means the legislative weighing of harm and safety is going to be pushed aside and essentially, we’re going to be talking about, how can every single law including the accommodations be fine-tuned for one set of believers?”
The recent death of Associate Justice Antonin Scalia, who was the court’s most outspoken conservative, could significantly impact the case’s outcome, analysts said. Justice Scalia was among majority in the 5-4 decision in Burwell v. Hobby Lobby, a 2014 opinion that protected religiously devout owners of closely held, for-profit businesses from having to offer birth control under the mandate. His absence could mean a 4-4 split in the Zubik case, which would allow the lower court rulings to stand, said Lyle Denniston, a Supreme Court analyst who writes for SCOTUSblog.
“My own sense is that the court is going to try very hard to find a way to resolve this case without a 4-4 split,” Mr. Denniston said during the Kaiser media conference. “If the Supreme Court issues a 4-4 decision, that leaves division in the lower courts, and it will vary from region to region in the country as to what the rights for women under the ACA are.”
More than 70 briefs have been issued to the high court in support of or opposition to the plaintiffs, including pleas by religious organizations, women’s advocacy groups, law professors, medical associations, and attorneys.
The American College of Obstetricians and Gynecologists and the American Academy of Family Physicians wrote in a joint brief that contraception coverage under the ACA ensures that patients have access to medically appropriate contraception without regard to their ability to pay. At the same time, the law respects an employer’s sincerely held religious objections to contraception through the accommodation, the brief said.
However, the Council for Christian Colleges & Universities argues the government’s decision to exempt some religious employers from providing contraceptive coverage while requiring others to comply with the mandate “demonstrates that the government’s approach is not the least restrictive means necessary to advance its interests.”
“Civil rights should not vary based on whether that institution is or is not affiliated with a church or other house of worship,” the council wrote in its brief to the Supreme Court. “Religious exercise is not tied to one’s affiliation but rather the source and sincerity of one’s belief and the desire to exercise it. That truth appears to be one the government has been unable to grasp or comprehend as it decides who is sufficiently ‘religious’ to have religious beliefs worthy of protection.”
On Twitter @legal_med
VIDEO: How to navigate value-based care payer contracts
AUSTIN, TEX. – The shift from volume- to value-based care has become a regular hot topic among the medical community. But one rarely discussed question is how quality-based care will impact physician contracts with health plans, according to Bloomfield Hills, Mich., health law attorney Mark S. Kopson.
In a video interview at an American Health Lawyers Association meeting, Mr. Kopson discusses how to navigate payer contracts when operating within value-based care models. He addresses ideal terms to include in quality-based care contracts and how to mitigate legal risks with health plans.
“The contract language that works in volume-based contracts doesn’t work in value-based contracts,” Mr. Kopson explains. “We have to make a distinction between the two and recognize that there are risks and issues that have to be addressed in value-based arrangements.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
AUSTIN, TEX. – The shift from volume- to value-based care has become a regular hot topic among the medical community. But one rarely discussed question is how quality-based care will impact physician contracts with health plans, according to Bloomfield Hills, Mich., health law attorney Mark S. Kopson.
In a video interview at an American Health Lawyers Association meeting, Mr. Kopson discusses how to navigate payer contracts when operating within value-based care models. He addresses ideal terms to include in quality-based care contracts and how to mitigate legal risks with health plans.
“The contract language that works in volume-based contracts doesn’t work in value-based contracts,” Mr. Kopson explains. “We have to make a distinction between the two and recognize that there are risks and issues that have to be addressed in value-based arrangements.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
AUSTIN, TEX. – The shift from volume- to value-based care has become a regular hot topic among the medical community. But one rarely discussed question is how quality-based care will impact physician contracts with health plans, according to Bloomfield Hills, Mich., health law attorney Mark S. Kopson.
In a video interview at an American Health Lawyers Association meeting, Mr. Kopson discusses how to navigate payer contracts when operating within value-based care models. He addresses ideal terms to include in quality-based care contracts and how to mitigate legal risks with health plans.
“The contract language that works in volume-based contracts doesn’t work in value-based contracts,” Mr. Kopson explains. “We have to make a distinction between the two and recognize that there are risks and issues that have to be addressed in value-based arrangements.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
EXPERT ANALYSIS FROM THE PHYSICIANS AND HOSPITALS LAW INSTITUTE
VIDEO: How proposed patient substance use privacy rule impacts physicians
Health providers have until April 11 to offer perspective on a proposed rule that would loosen restrictions over the redisclosure of patient records involving substance abuse.
The U.S. Department of Health and Human Services in early February announced suggested revisions to the Confidentiality of Alcohol and Drug Abuse Patient Records regulations, known as 42 CFR Part 2. The changes, published Feb. 9 in the Federal Register, aim to facilitate the transfer of health information within new care models while protecting patient privacy.
The proposed rule seeks to broaden the consent process for re-releasing substance use records to make it easier for health information exchanges to obtain health data, Chicago health law attorney Gerald “Jud” DeLoss said at an American Health Lawyers Association (AHLA) meeting.
In this video interview at the AHLA conference, Mr. DeLoss breaks down the proposed modifications and discusses how the rule, if made final, would affect physician practices. He also addresses how the rule would impact the intersection of behavioral health and primary care treatment.
“I think the proposed rule goes a long way in terms of advancing the goals of integrated care between behavioral health and primary care,” Mr. DeLoss said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
Health providers have until April 11 to offer perspective on a proposed rule that would loosen restrictions over the redisclosure of patient records involving substance abuse.
The U.S. Department of Health and Human Services in early February announced suggested revisions to the Confidentiality of Alcohol and Drug Abuse Patient Records regulations, known as 42 CFR Part 2. The changes, published Feb. 9 in the Federal Register, aim to facilitate the transfer of health information within new care models while protecting patient privacy.
The proposed rule seeks to broaden the consent process for re-releasing substance use records to make it easier for health information exchanges to obtain health data, Chicago health law attorney Gerald “Jud” DeLoss said at an American Health Lawyers Association (AHLA) meeting.
In this video interview at the AHLA conference, Mr. DeLoss breaks down the proposed modifications and discusses how the rule, if made final, would affect physician practices. He also addresses how the rule would impact the intersection of behavioral health and primary care treatment.
“I think the proposed rule goes a long way in terms of advancing the goals of integrated care between behavioral health and primary care,” Mr. DeLoss said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
Health providers have until April 11 to offer perspective on a proposed rule that would loosen restrictions over the redisclosure of patient records involving substance abuse.
The U.S. Department of Health and Human Services in early February announced suggested revisions to the Confidentiality of Alcohol and Drug Abuse Patient Records regulations, known as 42 CFR Part 2. The changes, published Feb. 9 in the Federal Register, aim to facilitate the transfer of health information within new care models while protecting patient privacy.
The proposed rule seeks to broaden the consent process for re-releasing substance use records to make it easier for health information exchanges to obtain health data, Chicago health law attorney Gerald “Jud” DeLoss said at an American Health Lawyers Association (AHLA) meeting.
In this video interview at the AHLA conference, Mr. DeLoss breaks down the proposed modifications and discusses how the rule, if made final, would affect physician practices. He also addresses how the rule would impact the intersection of behavioral health and primary care treatment.
“I think the proposed rule goes a long way in terms of advancing the goals of integrated care between behavioral health and primary care,” Mr. DeLoss said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
Justices appear split over Texas abortion regulations
The Supreme Court justices appear split along ideological lines over whether two Texas abortion regulations unconstitutionally restrict women’s access to the procedure.
During oral arguments March 2 in Whole Woman’s Health v. Hellerstedt, justices expressed differing viewpoints on a Texas law that requires abortion providers to have admitting privileges at a hospital within 30 miles and another rule that requires abortion clinics to meet the same standards as those of ambulatory surgical centers (ASCs). Justices also seemed to disagree about whether enough evidence exists to prove the closure of more than 20 abortion clinics in the state is directly related to the Texas legislation, HB2.
“I think it was pretty clear the four [more liberal] justices would vote to strike down this law,” said Gretchen Borchelt, an attorney for the National Women’s Law Center (NWLC) who attended oral arguments. “They made it pretty clear that they don’t think there’s any evidence that the law is necessary. It’s less clear where the other justices line up. With abortion cases, it’s often a [split] decision and [Associate Justice Anthony] Kennedy has been the swing vote in the past.”
From Justice Kennedy’s line of questioning during the debate, it was difficult to tell which direction he was leaning, said Ms. Borchelt, who is NWLC vice president for health and reproductive rights. The NWLC issued a brief in the case in support of the plaintiff.
Whole Woman’s Health v. Hellerstedt centers on whether Texas HB2 imposes an undue burden on a patient’s right to get an abortion. The plaintiffs, who are clinics and doctors, argue that both restrictions are unnecessary and limit access to abortion services. The Texas Department of State Health Services argues that the restrictions are reasonable and effective measures that raise the standard of care for abortion patients and ensure health and safety.
The 5th U.S. Circuit Court of Appeals sided with the state, a decision that will stand should the high court split 4-4. Antonin Scalia, Supreme Court Associate Justice and the ninth member of the high court, died Feb. 13.
Justices display preferences
During oral arguments, Justice Samuel A. Alito Jr. and Chief Justice John G. Roberts expressed skepticism that abortion clinic closures in Texas were related to the regulations. They questioned why Whole Woman’s Health had not included more evidence in the record linking the events.
“There is very little specific evidence in the record in this case with respect to why any particular clinic closed,” Justice Alito said during arguments. “I mean, I could give you examples: Planned Parenthood Center for Choice, Bryan, Texas ... The Huffington Post reported that this was closed as a result of the 2011 Texas Women’s Program bill which cut funding for family planning services. It’s not the law that we’re talking about here.”
Meanwhile, Associate Justice Sonia Sotomayor and Associate Justice Ruth Bader Ginsburg grilled Texas Solicitor General Scott A. Keller about the health benefits derived from the state’s regulations, asking why women undergoing nonsurgical abortions were required to take medications at an ambulatory surgical facility.
For his part, Mr. Keller defended the state’s regulations, saying the legislation improves continuity of care, increases clinical competence, and prevents miscommunication and patient abandonment. Requiring patients to take abortion-inducing medication in an ASC aids in the event of a complication, he said.
But Stephanie Toti, lead attorney for Whole Woman’s Health, and Donald B. Verrilli, Jr., the Solicitor General of the United States, argued the state’s regulations are unnecessary and create substantial obstacles to abortion access.
“This law closes most abortion facilities in the state, puts extreme stress on the few facilities that remain open, and exponentially increases the obstacles confronting women who seek abortions in the state,” Verrilli said during arguments. “And it does all of that on the basis of a medical justification that cannot withstand any meaningful scrutiny, that the American Medical Association has told you is groundless and that the district court found will actually operate in practice to increase health risks to women and not decrease [risks].”
Ruling could hinge on Justice Kennedy
Legal analysts said it was significant that the justices focused so much time on the link between clinic closures and the Texas law.
If the justices believe there is a lack of evidence in this regard, they may remand the case to the 5th Circuit for further development, said Ilya Shapiro, a senior fellow at the Cato Institute, a conservative public policy research organization. The high court may choose this route to avoid making a decision with only eight justices, Mr. Shapiro said.
“It would be kicking the can down the street,” he said. “A 4-4 ruling, the court doesn’t like to issue those if they can avoid them. If it can achieve agreement on narrower ways of resolving cases, I think it’s going to try to do that.”
If the justices move forward with deciding the core of the case, the vote will likely come down to Justice Kennedy, said Ruthann Robson, a law professor at the City University of New York School of Law and co-editor of the Constitutional Law Professor’s Blog.
While Justice Alito seemed to favor the state’s side, Justice Thomas was predictably silent, and Justice Roberts appeared to lean toward the state’s side, on the condition it could prove a rational basis for enacting HB2, she said. But Justice Kennedy is the mystery vote, she noted, adding that he was in the majority of the 1992 decision in Planned Parenthood of Southeastern Pennsylvania v. Casey, which upheld Roe v. Wade.
“He seems to be in the middle on this issue,” Ms. Robson said. “Justice Kennedy did seem to be troubled during arguments about the idea that nonsurgical abortions being curtailed could cause women to have more surgical abortions. He specifically asked the Texas [solicitor general] about this.”
Given Justice Kennedy’s strong opposition to the so-called “partial birth” abortion procedure, expressed in the 2007 Gonzales v. Carhart case, it would seem he would be especially concerned with late-term abortions, she said.
Ms. Robson said she was surprised with the depth to which the justices compared abortion with other medical procedures during the debate and questioned the differences in safety. Justice Ginsburg, for instance, noted the statistical dangers of childbirth, colonoscopies, and dental procedures and inquired why Texas had not placed similar restrictions on those practices.
“That’s really at the heart of the case,” Ms. Robson said. “If abortion is not more dangerous than other procedures, the question is, why isn’t the state protecting women’s health in colonoscopies and dental procedures and other kinds of things? At the heart of the case is the problem of legislators seemingly acting to decrease abortion in the guise of protecting women’s health.”
A split vote, which would uphold the appeals decision, or a remand of the case could come as early as March 7, Mr. Shapiro said. If justices decide to issue an opinion, the ruling would likely come at the end of the court’s term in June.
On Twitter @legal_med
The Supreme Court justices appear split along ideological lines over whether two Texas abortion regulations unconstitutionally restrict women’s access to the procedure.
During oral arguments March 2 in Whole Woman’s Health v. Hellerstedt, justices expressed differing viewpoints on a Texas law that requires abortion providers to have admitting privileges at a hospital within 30 miles and another rule that requires abortion clinics to meet the same standards as those of ambulatory surgical centers (ASCs). Justices also seemed to disagree about whether enough evidence exists to prove the closure of more than 20 abortion clinics in the state is directly related to the Texas legislation, HB2.
“I think it was pretty clear the four [more liberal] justices would vote to strike down this law,” said Gretchen Borchelt, an attorney for the National Women’s Law Center (NWLC) who attended oral arguments. “They made it pretty clear that they don’t think there’s any evidence that the law is necessary. It’s less clear where the other justices line up. With abortion cases, it’s often a [split] decision and [Associate Justice Anthony] Kennedy has been the swing vote in the past.”
From Justice Kennedy’s line of questioning during the debate, it was difficult to tell which direction he was leaning, said Ms. Borchelt, who is NWLC vice president for health and reproductive rights. The NWLC issued a brief in the case in support of the plaintiff.
Whole Woman’s Health v. Hellerstedt centers on whether Texas HB2 imposes an undue burden on a patient’s right to get an abortion. The plaintiffs, who are clinics and doctors, argue that both restrictions are unnecessary and limit access to abortion services. The Texas Department of State Health Services argues that the restrictions are reasonable and effective measures that raise the standard of care for abortion patients and ensure health and safety.
The 5th U.S. Circuit Court of Appeals sided with the state, a decision that will stand should the high court split 4-4. Antonin Scalia, Supreme Court Associate Justice and the ninth member of the high court, died Feb. 13.
Justices display preferences
During oral arguments, Justice Samuel A. Alito Jr. and Chief Justice John G. Roberts expressed skepticism that abortion clinic closures in Texas were related to the regulations. They questioned why Whole Woman’s Health had not included more evidence in the record linking the events.
“There is very little specific evidence in the record in this case with respect to why any particular clinic closed,” Justice Alito said during arguments. “I mean, I could give you examples: Planned Parenthood Center for Choice, Bryan, Texas ... The Huffington Post reported that this was closed as a result of the 2011 Texas Women’s Program bill which cut funding for family planning services. It’s not the law that we’re talking about here.”
Meanwhile, Associate Justice Sonia Sotomayor and Associate Justice Ruth Bader Ginsburg grilled Texas Solicitor General Scott A. Keller about the health benefits derived from the state’s regulations, asking why women undergoing nonsurgical abortions were required to take medications at an ambulatory surgical facility.
For his part, Mr. Keller defended the state’s regulations, saying the legislation improves continuity of care, increases clinical competence, and prevents miscommunication and patient abandonment. Requiring patients to take abortion-inducing medication in an ASC aids in the event of a complication, he said.
But Stephanie Toti, lead attorney for Whole Woman’s Health, and Donald B. Verrilli, Jr., the Solicitor General of the United States, argued the state’s regulations are unnecessary and create substantial obstacles to abortion access.
“This law closes most abortion facilities in the state, puts extreme stress on the few facilities that remain open, and exponentially increases the obstacles confronting women who seek abortions in the state,” Verrilli said during arguments. “And it does all of that on the basis of a medical justification that cannot withstand any meaningful scrutiny, that the American Medical Association has told you is groundless and that the district court found will actually operate in practice to increase health risks to women and not decrease [risks].”
Ruling could hinge on Justice Kennedy
Legal analysts said it was significant that the justices focused so much time on the link between clinic closures and the Texas law.
If the justices believe there is a lack of evidence in this regard, they may remand the case to the 5th Circuit for further development, said Ilya Shapiro, a senior fellow at the Cato Institute, a conservative public policy research organization. The high court may choose this route to avoid making a decision with only eight justices, Mr. Shapiro said.
“It would be kicking the can down the street,” he said. “A 4-4 ruling, the court doesn’t like to issue those if they can avoid them. If it can achieve agreement on narrower ways of resolving cases, I think it’s going to try to do that.”
If the justices move forward with deciding the core of the case, the vote will likely come down to Justice Kennedy, said Ruthann Robson, a law professor at the City University of New York School of Law and co-editor of the Constitutional Law Professor’s Blog.
While Justice Alito seemed to favor the state’s side, Justice Thomas was predictably silent, and Justice Roberts appeared to lean toward the state’s side, on the condition it could prove a rational basis for enacting HB2, she said. But Justice Kennedy is the mystery vote, she noted, adding that he was in the majority of the 1992 decision in Planned Parenthood of Southeastern Pennsylvania v. Casey, which upheld Roe v. Wade.
“He seems to be in the middle on this issue,” Ms. Robson said. “Justice Kennedy did seem to be troubled during arguments about the idea that nonsurgical abortions being curtailed could cause women to have more surgical abortions. He specifically asked the Texas [solicitor general] about this.”
Given Justice Kennedy’s strong opposition to the so-called “partial birth” abortion procedure, expressed in the 2007 Gonzales v. Carhart case, it would seem he would be especially concerned with late-term abortions, she said.
Ms. Robson said she was surprised with the depth to which the justices compared abortion with other medical procedures during the debate and questioned the differences in safety. Justice Ginsburg, for instance, noted the statistical dangers of childbirth, colonoscopies, and dental procedures and inquired why Texas had not placed similar restrictions on those practices.
“That’s really at the heart of the case,” Ms. Robson said. “If abortion is not more dangerous than other procedures, the question is, why isn’t the state protecting women’s health in colonoscopies and dental procedures and other kinds of things? At the heart of the case is the problem of legislators seemingly acting to decrease abortion in the guise of protecting women’s health.”
A split vote, which would uphold the appeals decision, or a remand of the case could come as early as March 7, Mr. Shapiro said. If justices decide to issue an opinion, the ruling would likely come at the end of the court’s term in June.
On Twitter @legal_med
The Supreme Court justices appear split along ideological lines over whether two Texas abortion regulations unconstitutionally restrict women’s access to the procedure.
During oral arguments March 2 in Whole Woman’s Health v. Hellerstedt, justices expressed differing viewpoints on a Texas law that requires abortion providers to have admitting privileges at a hospital within 30 miles and another rule that requires abortion clinics to meet the same standards as those of ambulatory surgical centers (ASCs). Justices also seemed to disagree about whether enough evidence exists to prove the closure of more than 20 abortion clinics in the state is directly related to the Texas legislation, HB2.
“I think it was pretty clear the four [more liberal] justices would vote to strike down this law,” said Gretchen Borchelt, an attorney for the National Women’s Law Center (NWLC) who attended oral arguments. “They made it pretty clear that they don’t think there’s any evidence that the law is necessary. It’s less clear where the other justices line up. With abortion cases, it’s often a [split] decision and [Associate Justice Anthony] Kennedy has been the swing vote in the past.”
From Justice Kennedy’s line of questioning during the debate, it was difficult to tell which direction he was leaning, said Ms. Borchelt, who is NWLC vice president for health and reproductive rights. The NWLC issued a brief in the case in support of the plaintiff.
Whole Woman’s Health v. Hellerstedt centers on whether Texas HB2 imposes an undue burden on a patient’s right to get an abortion. The plaintiffs, who are clinics and doctors, argue that both restrictions are unnecessary and limit access to abortion services. The Texas Department of State Health Services argues that the restrictions are reasonable and effective measures that raise the standard of care for abortion patients and ensure health and safety.
The 5th U.S. Circuit Court of Appeals sided with the state, a decision that will stand should the high court split 4-4. Antonin Scalia, Supreme Court Associate Justice and the ninth member of the high court, died Feb. 13.
Justices display preferences
During oral arguments, Justice Samuel A. Alito Jr. and Chief Justice John G. Roberts expressed skepticism that abortion clinic closures in Texas were related to the regulations. They questioned why Whole Woman’s Health had not included more evidence in the record linking the events.
“There is very little specific evidence in the record in this case with respect to why any particular clinic closed,” Justice Alito said during arguments. “I mean, I could give you examples: Planned Parenthood Center for Choice, Bryan, Texas ... The Huffington Post reported that this was closed as a result of the 2011 Texas Women’s Program bill which cut funding for family planning services. It’s not the law that we’re talking about here.”
Meanwhile, Associate Justice Sonia Sotomayor and Associate Justice Ruth Bader Ginsburg grilled Texas Solicitor General Scott A. Keller about the health benefits derived from the state’s regulations, asking why women undergoing nonsurgical abortions were required to take medications at an ambulatory surgical facility.
For his part, Mr. Keller defended the state’s regulations, saying the legislation improves continuity of care, increases clinical competence, and prevents miscommunication and patient abandonment. Requiring patients to take abortion-inducing medication in an ASC aids in the event of a complication, he said.
But Stephanie Toti, lead attorney for Whole Woman’s Health, and Donald B. Verrilli, Jr., the Solicitor General of the United States, argued the state’s regulations are unnecessary and create substantial obstacles to abortion access.
“This law closes most abortion facilities in the state, puts extreme stress on the few facilities that remain open, and exponentially increases the obstacles confronting women who seek abortions in the state,” Verrilli said during arguments. “And it does all of that on the basis of a medical justification that cannot withstand any meaningful scrutiny, that the American Medical Association has told you is groundless and that the district court found will actually operate in practice to increase health risks to women and not decrease [risks].”
Ruling could hinge on Justice Kennedy
Legal analysts said it was significant that the justices focused so much time on the link between clinic closures and the Texas law.
If the justices believe there is a lack of evidence in this regard, they may remand the case to the 5th Circuit for further development, said Ilya Shapiro, a senior fellow at the Cato Institute, a conservative public policy research organization. The high court may choose this route to avoid making a decision with only eight justices, Mr. Shapiro said.
“It would be kicking the can down the street,” he said. “A 4-4 ruling, the court doesn’t like to issue those if they can avoid them. If it can achieve agreement on narrower ways of resolving cases, I think it’s going to try to do that.”
If the justices move forward with deciding the core of the case, the vote will likely come down to Justice Kennedy, said Ruthann Robson, a law professor at the City University of New York School of Law and co-editor of the Constitutional Law Professor’s Blog.
While Justice Alito seemed to favor the state’s side, Justice Thomas was predictably silent, and Justice Roberts appeared to lean toward the state’s side, on the condition it could prove a rational basis for enacting HB2, she said. But Justice Kennedy is the mystery vote, she noted, adding that he was in the majority of the 1992 decision in Planned Parenthood of Southeastern Pennsylvania v. Casey, which upheld Roe v. Wade.
“He seems to be in the middle on this issue,” Ms. Robson said. “Justice Kennedy did seem to be troubled during arguments about the idea that nonsurgical abortions being curtailed could cause women to have more surgical abortions. He specifically asked the Texas [solicitor general] about this.”
Given Justice Kennedy’s strong opposition to the so-called “partial birth” abortion procedure, expressed in the 2007 Gonzales v. Carhart case, it would seem he would be especially concerned with late-term abortions, she said.
Ms. Robson said she was surprised with the depth to which the justices compared abortion with other medical procedures during the debate and questioned the differences in safety. Justice Ginsburg, for instance, noted the statistical dangers of childbirth, colonoscopies, and dental procedures and inquired why Texas had not placed similar restrictions on those practices.
“That’s really at the heart of the case,” Ms. Robson said. “If abortion is not more dangerous than other procedures, the question is, why isn’t the state protecting women’s health in colonoscopies and dental procedures and other kinds of things? At the heart of the case is the problem of legislators seemingly acting to decrease abortion in the guise of protecting women’s health.”
A split vote, which would uphold the appeals decision, or a remand of the case could come as early as March 7, Mr. Shapiro said. If justices decide to issue an opinion, the ruling would likely come at the end of the court’s term in June.
On Twitter @legal_med