User login
Prescription drug monitoring programs improve, but challenges remain
When Wisconsin introduced its first prescription drug monitoring program (PDMP) system in 2013, doctors found the system clunky and cumbersome to navigate, recalled Noel Deep, MD, an Antigo, Wis.–based internist and president of the Wisconsin Medical Society.
Physicians had to click through several screens and were then directed to log into another website to enter patient information and scan records.
The state’s PDMP is much improved today, Dr. Deep said. The Wisconsin Department of Safety and Professional Services launched an enhanced version of the PDMP in January, giving doctors time to learn the new system before its use became mandatory for prescribers in April. The system takes fewer clicks and communicates with practices’ electronic medical record.
“It is very easy, compared with what it was before,” Dr. Deep said in an interview. “I was one of those people who were skeptical, but I’ve been happy with the PDMP. It’s extremely quick. I know it’s a few more clicks, but it has also shown that, in Wisconsin, this has significantly decreased the use of prescription [opioid] medications.”
Across the country, physicians are experiencing similar ups and downs with state PDMPs as they work to manage the systems, juggle patient caseloads, and make the best prescribing decisions. Currently, 49 states, the District of Columbia, and Guam have operational PDMPs. Most databases generally require that Schedule II, III, and IV prescriptions be reported, explained Natalia Mazina, a San Francisco–based attorney who specializes in health and pharmacy law.
“Some states also require Schedule V, and some states even require certain noncontrolled substances to be reported,” she said in an interview. “That’s the biggest difference. There are also different agencies responsible for enforcement.”
States differ in the time allowed for prescribers and dispensers to report data, Ms. Mazina added. States such as New York and Utah, for instance, require real-time reporting, while Alabama and Louisiana require daily PDMP reporting. South Dakota requires reporting within 7 days of a prescription, while Alaska allows for monthly reporting. Training hours required for PDMP participation also vary by state.
More states are moving toward mandatory rather than voluntary PDMP systems. At least 34 states now specify circumstances in which prescribers, dispensers, or both must access a patient’s PDMP prescription history, according to a summary by the National Alliance for Model State Drug Laws. For doctors, the push toward mandated PDMPs has generated mixed feelings and led to legislative battles in some states.
“From a safety standpoint, [PDMPs are] a good thing,” Dr. Deep said. “From a physician standpoint, [some] people feel this is restricting the physician-patient relationship and dictating how much we can prescribe, when we can prescribe, and what we can do. That’s one of the downsides.”
Beneficial or burdensome?
When Georgia legislators proposed a law earlier this year that would tighten reporting requirements for their state’s PDMP, physician leaders fought back against what they viewed as excessive regulations.
An initial bill included reporting requirements not only for standard controlled substances but for stimulants such as Adderall, Vyvanse, Focalin, and Ritalin, and all other nonopioid controlled drugs. The early version of the bill also recommended civil and criminal penalties for physicians who violated the regulations.
The American College of Physicians Georgia Chapter and the Medical Association of Georgia successfully advocated for the two provisions to be removed from the bill’s final version, said W. Cody McClatchey, MD, chair of the ACP Georgia Chapter’s health and public policy committee.
“We are in the midst of an opioid epidemic,” Dr. McClatchey said in an interview. “It would have been unreasonable and costly for state government to mandate that prescribers check PDMP for controlled drugs not related to the opioid epidemic. [In addition], I felt strongly that prescribers should not be subject to criminal penalties for not checking the PDMP. We are already subject to civil and criminal penalties for intentionally or knowingly overprescribing controlled drugs. That is adequate protection for patients.”
Georgia’s law, signed in May, requires physicians and up to two certified staff to seek and review information from the PDMP every 90 days for any prescription outlined in the law that exceeds 3 days/26 pills for medical care, or 10 days/40 pills for surgical care. In addition, physicians must make a notation in the patient’s medical record stating the date and time upon which such inquiry was made, among other requirements.
The new requirements mean it will take longer to manage patients with chronic pain, anxiety, and depression who may need opioids and benzodiazepines because of the time necessary to access the PDMP, document that it was reviewed, and properly counsel the patient, Dr. McClatchey said. However, he noted that the additional time may allow physicians to charge a higher level of evaluation and management services. Doctors can minimize the impact of the rules by delegating many of the tasks to certified medical assistants and using “smartphrases” to document completion, he said.
“In my opinion, the final version of HB 249 strikes a fair balance between the needs of patients and the administrative burden on physicians,” he said. “Most physicians do not prescribe opioids and benzodiazepines on a continuing basis to many patients. Physicians who prescribe chronic opioids or benzodiazepines now have the ability to more accurately know when patients may be abusing opioids and benzodiazepines, which can be a matter of life or death.”
‘Well-designed regs keep patients safe’
In California, prescribers are encouraged but not yet required to check the Controlled Substance Utilization Review and Evaluation System (CURES) database before prescribing controlled substances. Under state law, checking the database will become mandatory 6 months after the California Department of Justice certifies that the CURES system is ready for statewide use and the department has adequate staff to handle the technical and administrative workload. When that will happen remains unclear.
It’s too early to know how well CURES will work once fully implemented, said Patricia Salber, MD, a Larkspur, Calif.–based internist and founder of the blog TheDoctorWeighsIn.com, but access to statewide data about patients’ medical and drug history is a positive for doctors.
“As a former emergency physician who has taken care of many drug-seeking patients, having access to statewide data about an individual’s drug use will be a valuable tool to help stem the tide of scheduled prescription drug abuse,” she said. “Given our mobile society, I would also like to eventually see a nationwide system.”
As new systems roll out, it’s important for physicians to give the databases a chance and advocate fixing the bugs, rather than condemning them because of logistics or initial glitches, Dr. Salber added.

“I think sometimes people blame rules and regulations for making their lives difficult, when in fact it is clunky design and implementation of the regulations that cause the problem,” she said. “Well-designed regulations can keep our patients safe, for example, by requiring adequate testing of the safety and efficacy of therapeutics. If regulations are found to be effective but burdensome, I believe the first response should not be to overturn the regulation, but rather to improve the way the regulation is carried out.”
For example, she noted that the California Medical Association successfully fought for state law language requiring the CURES process to be certified ready before requiring physicians to use the system.
Are PDMPs working?
Although PDMPs may be causing headaches for some, data show that they are having effective results against opioid abuse and overprescribing.
In Florida, opioid prescriptions decreased in 80% of counties from 2010 to 2015 after the state established a PDMP in combination with tighter regulation of pain clinics. In the first month after implementation of Florida’s PDMP, oxycodone deaths dropped by 25%, according to a 2015 study published in Drug and Alcohol Dependence (2015 May 1. doi: 10.1016/j.drugalcdep.2015.02.010).
Opioid prescriptions in Kentucky, New York, and Tennessee dropped after mandates that prescribers check their state PDMPs, according to a summary by the PDMP Center of Excellence at Brandeis University. In Kentucky, doses dispensed declined for hydrocodone (–10.3%), oxycodone (–11.6%), and oxymorphone (–35%), while in Tennessee the number of opioid prescriptions fell by 7%. In New York, total opioid prescriptions have dropped by more than 9% since the state’s PDMP went into effect.
In Wisconsin, an analysis after enactment of the state’s PDMP found a nearly 12% reduction in opioid prescriptions and a 13% reduction in opioid doses dispensed between the fourth quarter of 2015 and the fourth quarter of 2016, according to a report by the Wisconsin Department of Safety and Professional Services.
PDMPs also have altered physicians’ prescribing behaviors and changed patient care decisions, studies show. A review of medical providers in Ohio emergency departments found that 41% of those given PDMP data altered their prescribing for patients receiving multiple simultaneous narcotics prescriptions, according to the Brandeis University summary. Of those Ohio providers, 61% prescribed no narcotics or fewer narcotics than originally planned.
A survey of prescribers in Rhode Island and Connecticut found that those who used PDMP data were more likely than nonusers to take clinically appropriate action in response to suspected cases of prescription drug abuse or diversion by patients, such as conducting drug screens or referring them to substance abuse treatment.
Despite the positive impacts, however, challenges for PDMPs remain.
Dr. Deep noted that physicians in solo and small practices may have a harder time than employed physicians when it comes to checking databases, recording data, and delegating duties. In addition, differing PDMP regulations may not catch prescription drug abusers who go across state lines.
Most states with PDMPs share their PDMP data with other state PDMPs or share data with authorized users in other states. Florida can receive PDMP data from other jurisdictions and provide that data to authorized users in Florida, but it does not share its data with other states. Oregon allows only prescribers in California, Idaho, Nevada, and Washington state to access its database information.
PDMPs also are limited in what they tell physicians about patients, said Gregory A. Hood, MD, an internist in Lexington, Ky., and former governor of the American College of Physicians, Kentucky Chapter.
“PDMP is only helpful to a point,” he said in an interview. “Any PDMP has the inherent limitation that it only reports what is reported to it. This doesn’t tell us about whether the patient actually takes the medicine, gives or sells it away, or whether they use it appropriately or not. Patients can overuse for 3 of 4 weeks, buy a week on the street, or from someone they know, and we’re none the wiser, absent an informant.”
Kentucky’s database, called the Kentucky All Schedule Prescription Electronic Reporting System (KASPER), requires that prescribers and dispensers of controlled substances query the state’s electronic monitoring system before issuing new prescriptions or refills. To track illicit use of opiates, Kentucky also recently made gabapentin a Schedule V controlled substance, Dr. Hood said.
Whether PDMPs have a positive effect depends on what doctors do with the information they learn from the database, Dr. Hood said.
“Generally, PDMPs can help identify at least some who are seeking adverse gain,” he said. “Properly identifying someone with a medical issue and arranging proper care is a positive. Rote dropping of someone with a ‘dirty’ PDMP – as has been known to happen in some primary care and specialty offices – is difficult to view as a positive, particularly given shortages in both primary care and in pain management.”
[email protected] On Twitter @legal_med
When Wisconsin introduced its first prescription drug monitoring program (PDMP) system in 2013, doctors found the system clunky and cumbersome to navigate, recalled Noel Deep, MD, an Antigo, Wis.–based internist and president of the Wisconsin Medical Society.
Physicians had to click through several screens and were then directed to log into another website to enter patient information and scan records.
The state’s PDMP is much improved today, Dr. Deep said. The Wisconsin Department of Safety and Professional Services launched an enhanced version of the PDMP in January, giving doctors time to learn the new system before its use became mandatory for prescribers in April. The system takes fewer clicks and communicates with practices’ electronic medical record.
“It is very easy, compared with what it was before,” Dr. Deep said in an interview. “I was one of those people who were skeptical, but I’ve been happy with the PDMP. It’s extremely quick. I know it’s a few more clicks, but it has also shown that, in Wisconsin, this has significantly decreased the use of prescription [opioid] medications.”
Across the country, physicians are experiencing similar ups and downs with state PDMPs as they work to manage the systems, juggle patient caseloads, and make the best prescribing decisions. Currently, 49 states, the District of Columbia, and Guam have operational PDMPs. Most databases generally require that Schedule II, III, and IV prescriptions be reported, explained Natalia Mazina, a San Francisco–based attorney who specializes in health and pharmacy law.
“Some states also require Schedule V, and some states even require certain noncontrolled substances to be reported,” she said in an interview. “That’s the biggest difference. There are also different agencies responsible for enforcement.”
States differ in the time allowed for prescribers and dispensers to report data, Ms. Mazina added. States such as New York and Utah, for instance, require real-time reporting, while Alabama and Louisiana require daily PDMP reporting. South Dakota requires reporting within 7 days of a prescription, while Alaska allows for monthly reporting. Training hours required for PDMP participation also vary by state.
More states are moving toward mandatory rather than voluntary PDMP systems. At least 34 states now specify circumstances in which prescribers, dispensers, or both must access a patient’s PDMP prescription history, according to a summary by the National Alliance for Model State Drug Laws. For doctors, the push toward mandated PDMPs has generated mixed feelings and led to legislative battles in some states.
“From a safety standpoint, [PDMPs are] a good thing,” Dr. Deep said. “From a physician standpoint, [some] people feel this is restricting the physician-patient relationship and dictating how much we can prescribe, when we can prescribe, and what we can do. That’s one of the downsides.”
Beneficial or burdensome?
When Georgia legislators proposed a law earlier this year that would tighten reporting requirements for their state’s PDMP, physician leaders fought back against what they viewed as excessive regulations.
An initial bill included reporting requirements not only for standard controlled substances but for stimulants such as Adderall, Vyvanse, Focalin, and Ritalin, and all other nonopioid controlled drugs. The early version of the bill also recommended civil and criminal penalties for physicians who violated the regulations.
The American College of Physicians Georgia Chapter and the Medical Association of Georgia successfully advocated for the two provisions to be removed from the bill’s final version, said W. Cody McClatchey, MD, chair of the ACP Georgia Chapter’s health and public policy committee.
“We are in the midst of an opioid epidemic,” Dr. McClatchey said in an interview. “It would have been unreasonable and costly for state government to mandate that prescribers check PDMP for controlled drugs not related to the opioid epidemic. [In addition], I felt strongly that prescribers should not be subject to criminal penalties for not checking the PDMP. We are already subject to civil and criminal penalties for intentionally or knowingly overprescribing controlled drugs. That is adequate protection for patients.”
Georgia’s law, signed in May, requires physicians and up to two certified staff to seek and review information from the PDMP every 90 days for any prescription outlined in the law that exceeds 3 days/26 pills for medical care, or 10 days/40 pills for surgical care. In addition, physicians must make a notation in the patient’s medical record stating the date and time upon which such inquiry was made, among other requirements.
The new requirements mean it will take longer to manage patients with chronic pain, anxiety, and depression who may need opioids and benzodiazepines because of the time necessary to access the PDMP, document that it was reviewed, and properly counsel the patient, Dr. McClatchey said. However, he noted that the additional time may allow physicians to charge a higher level of evaluation and management services. Doctors can minimize the impact of the rules by delegating many of the tasks to certified medical assistants and using “smartphrases” to document completion, he said.
“In my opinion, the final version of HB 249 strikes a fair balance between the needs of patients and the administrative burden on physicians,” he said. “Most physicians do not prescribe opioids and benzodiazepines on a continuing basis to many patients. Physicians who prescribe chronic opioids or benzodiazepines now have the ability to more accurately know when patients may be abusing opioids and benzodiazepines, which can be a matter of life or death.”
‘Well-designed regs keep patients safe’
In California, prescribers are encouraged but not yet required to check the Controlled Substance Utilization Review and Evaluation System (CURES) database before prescribing controlled substances. Under state law, checking the database will become mandatory 6 months after the California Department of Justice certifies that the CURES system is ready for statewide use and the department has adequate staff to handle the technical and administrative workload. When that will happen remains unclear.
It’s too early to know how well CURES will work once fully implemented, said Patricia Salber, MD, a Larkspur, Calif.–based internist and founder of the blog TheDoctorWeighsIn.com, but access to statewide data about patients’ medical and drug history is a positive for doctors.
“As a former emergency physician who has taken care of many drug-seeking patients, having access to statewide data about an individual’s drug use will be a valuable tool to help stem the tide of scheduled prescription drug abuse,” she said. “Given our mobile society, I would also like to eventually see a nationwide system.”
As new systems roll out, it’s important for physicians to give the databases a chance and advocate fixing the bugs, rather than condemning them because of logistics or initial glitches, Dr. Salber added.

“I think sometimes people blame rules and regulations for making their lives difficult, when in fact it is clunky design and implementation of the regulations that cause the problem,” she said. “Well-designed regulations can keep our patients safe, for example, by requiring adequate testing of the safety and efficacy of therapeutics. If regulations are found to be effective but burdensome, I believe the first response should not be to overturn the regulation, but rather to improve the way the regulation is carried out.”
For example, she noted that the California Medical Association successfully fought for state law language requiring the CURES process to be certified ready before requiring physicians to use the system.
Are PDMPs working?
Although PDMPs may be causing headaches for some, data show that they are having effective results against opioid abuse and overprescribing.
In Florida, opioid prescriptions decreased in 80% of counties from 2010 to 2015 after the state established a PDMP in combination with tighter regulation of pain clinics. In the first month after implementation of Florida’s PDMP, oxycodone deaths dropped by 25%, according to a 2015 study published in Drug and Alcohol Dependence (2015 May 1. doi: 10.1016/j.drugalcdep.2015.02.010).
Opioid prescriptions in Kentucky, New York, and Tennessee dropped after mandates that prescribers check their state PDMPs, according to a summary by the PDMP Center of Excellence at Brandeis University. In Kentucky, doses dispensed declined for hydrocodone (–10.3%), oxycodone (–11.6%), and oxymorphone (–35%), while in Tennessee the number of opioid prescriptions fell by 7%. In New York, total opioid prescriptions have dropped by more than 9% since the state’s PDMP went into effect.
In Wisconsin, an analysis after enactment of the state’s PDMP found a nearly 12% reduction in opioid prescriptions and a 13% reduction in opioid doses dispensed between the fourth quarter of 2015 and the fourth quarter of 2016, according to a report by the Wisconsin Department of Safety and Professional Services.
PDMPs also have altered physicians’ prescribing behaviors and changed patient care decisions, studies show. A review of medical providers in Ohio emergency departments found that 41% of those given PDMP data altered their prescribing for patients receiving multiple simultaneous narcotics prescriptions, according to the Brandeis University summary. Of those Ohio providers, 61% prescribed no narcotics or fewer narcotics than originally planned.
A survey of prescribers in Rhode Island and Connecticut found that those who used PDMP data were more likely than nonusers to take clinically appropriate action in response to suspected cases of prescription drug abuse or diversion by patients, such as conducting drug screens or referring them to substance abuse treatment.
Despite the positive impacts, however, challenges for PDMPs remain.
Dr. Deep noted that physicians in solo and small practices may have a harder time than employed physicians when it comes to checking databases, recording data, and delegating duties. In addition, differing PDMP regulations may not catch prescription drug abusers who go across state lines.
Most states with PDMPs share their PDMP data with other state PDMPs or share data with authorized users in other states. Florida can receive PDMP data from other jurisdictions and provide that data to authorized users in Florida, but it does not share its data with other states. Oregon allows only prescribers in California, Idaho, Nevada, and Washington state to access its database information.
PDMPs also are limited in what they tell physicians about patients, said Gregory A. Hood, MD, an internist in Lexington, Ky., and former governor of the American College of Physicians, Kentucky Chapter.
“PDMP is only helpful to a point,” he said in an interview. “Any PDMP has the inherent limitation that it only reports what is reported to it. This doesn’t tell us about whether the patient actually takes the medicine, gives or sells it away, or whether they use it appropriately or not. Patients can overuse for 3 of 4 weeks, buy a week on the street, or from someone they know, and we’re none the wiser, absent an informant.”
Kentucky’s database, called the Kentucky All Schedule Prescription Electronic Reporting System (KASPER), requires that prescribers and dispensers of controlled substances query the state’s electronic monitoring system before issuing new prescriptions or refills. To track illicit use of opiates, Kentucky also recently made gabapentin a Schedule V controlled substance, Dr. Hood said.
Whether PDMPs have a positive effect depends on what doctors do with the information they learn from the database, Dr. Hood said.
“Generally, PDMPs can help identify at least some who are seeking adverse gain,” he said. “Properly identifying someone with a medical issue and arranging proper care is a positive. Rote dropping of someone with a ‘dirty’ PDMP – as has been known to happen in some primary care and specialty offices – is difficult to view as a positive, particularly given shortages in both primary care and in pain management.”
[email protected] On Twitter @legal_med
When Wisconsin introduced its first prescription drug monitoring program (PDMP) system in 2013, doctors found the system clunky and cumbersome to navigate, recalled Noel Deep, MD, an Antigo, Wis.–based internist and president of the Wisconsin Medical Society.
Physicians had to click through several screens and were then directed to log into another website to enter patient information and scan records.
The state’s PDMP is much improved today, Dr. Deep said. The Wisconsin Department of Safety and Professional Services launched an enhanced version of the PDMP in January, giving doctors time to learn the new system before its use became mandatory for prescribers in April. The system takes fewer clicks and communicates with practices’ electronic medical record.
“It is very easy, compared with what it was before,” Dr. Deep said in an interview. “I was one of those people who were skeptical, but I’ve been happy with the PDMP. It’s extremely quick. I know it’s a few more clicks, but it has also shown that, in Wisconsin, this has significantly decreased the use of prescription [opioid] medications.”
Across the country, physicians are experiencing similar ups and downs with state PDMPs as they work to manage the systems, juggle patient caseloads, and make the best prescribing decisions. Currently, 49 states, the District of Columbia, and Guam have operational PDMPs. Most databases generally require that Schedule II, III, and IV prescriptions be reported, explained Natalia Mazina, a San Francisco–based attorney who specializes in health and pharmacy law.
“Some states also require Schedule V, and some states even require certain noncontrolled substances to be reported,” she said in an interview. “That’s the biggest difference. There are also different agencies responsible for enforcement.”
States differ in the time allowed for prescribers and dispensers to report data, Ms. Mazina added. States such as New York and Utah, for instance, require real-time reporting, while Alabama and Louisiana require daily PDMP reporting. South Dakota requires reporting within 7 days of a prescription, while Alaska allows for monthly reporting. Training hours required for PDMP participation also vary by state.
More states are moving toward mandatory rather than voluntary PDMP systems. At least 34 states now specify circumstances in which prescribers, dispensers, or both must access a patient’s PDMP prescription history, according to a summary by the National Alliance for Model State Drug Laws. For doctors, the push toward mandated PDMPs has generated mixed feelings and led to legislative battles in some states.
“From a safety standpoint, [PDMPs are] a good thing,” Dr. Deep said. “From a physician standpoint, [some] people feel this is restricting the physician-patient relationship and dictating how much we can prescribe, when we can prescribe, and what we can do. That’s one of the downsides.”
Beneficial or burdensome?
When Georgia legislators proposed a law earlier this year that would tighten reporting requirements for their state’s PDMP, physician leaders fought back against what they viewed as excessive regulations.
An initial bill included reporting requirements not only for standard controlled substances but for stimulants such as Adderall, Vyvanse, Focalin, and Ritalin, and all other nonopioid controlled drugs. The early version of the bill also recommended civil and criminal penalties for physicians who violated the regulations.
The American College of Physicians Georgia Chapter and the Medical Association of Georgia successfully advocated for the two provisions to be removed from the bill’s final version, said W. Cody McClatchey, MD, chair of the ACP Georgia Chapter’s health and public policy committee.
“We are in the midst of an opioid epidemic,” Dr. McClatchey said in an interview. “It would have been unreasonable and costly for state government to mandate that prescribers check PDMP for controlled drugs not related to the opioid epidemic. [In addition], I felt strongly that prescribers should not be subject to criminal penalties for not checking the PDMP. We are already subject to civil and criminal penalties for intentionally or knowingly overprescribing controlled drugs. That is adequate protection for patients.”
Georgia’s law, signed in May, requires physicians and up to two certified staff to seek and review information from the PDMP every 90 days for any prescription outlined in the law that exceeds 3 days/26 pills for medical care, or 10 days/40 pills for surgical care. In addition, physicians must make a notation in the patient’s medical record stating the date and time upon which such inquiry was made, among other requirements.
The new requirements mean it will take longer to manage patients with chronic pain, anxiety, and depression who may need opioids and benzodiazepines because of the time necessary to access the PDMP, document that it was reviewed, and properly counsel the patient, Dr. McClatchey said. However, he noted that the additional time may allow physicians to charge a higher level of evaluation and management services. Doctors can minimize the impact of the rules by delegating many of the tasks to certified medical assistants and using “smartphrases” to document completion, he said.
“In my opinion, the final version of HB 249 strikes a fair balance between the needs of patients and the administrative burden on physicians,” he said. “Most physicians do not prescribe opioids and benzodiazepines on a continuing basis to many patients. Physicians who prescribe chronic opioids or benzodiazepines now have the ability to more accurately know when patients may be abusing opioids and benzodiazepines, which can be a matter of life or death.”
‘Well-designed regs keep patients safe’
In California, prescribers are encouraged but not yet required to check the Controlled Substance Utilization Review and Evaluation System (CURES) database before prescribing controlled substances. Under state law, checking the database will become mandatory 6 months after the California Department of Justice certifies that the CURES system is ready for statewide use and the department has adequate staff to handle the technical and administrative workload. When that will happen remains unclear.
It’s too early to know how well CURES will work once fully implemented, said Patricia Salber, MD, a Larkspur, Calif.–based internist and founder of the blog TheDoctorWeighsIn.com, but access to statewide data about patients’ medical and drug history is a positive for doctors.
“As a former emergency physician who has taken care of many drug-seeking patients, having access to statewide data about an individual’s drug use will be a valuable tool to help stem the tide of scheduled prescription drug abuse,” she said. “Given our mobile society, I would also like to eventually see a nationwide system.”
As new systems roll out, it’s important for physicians to give the databases a chance and advocate fixing the bugs, rather than condemning them because of logistics or initial glitches, Dr. Salber added.

“I think sometimes people blame rules and regulations for making their lives difficult, when in fact it is clunky design and implementation of the regulations that cause the problem,” she said. “Well-designed regulations can keep our patients safe, for example, by requiring adequate testing of the safety and efficacy of therapeutics. If regulations are found to be effective but burdensome, I believe the first response should not be to overturn the regulation, but rather to improve the way the regulation is carried out.”
For example, she noted that the California Medical Association successfully fought for state law language requiring the CURES process to be certified ready before requiring physicians to use the system.
Are PDMPs working?
Although PDMPs may be causing headaches for some, data show that they are having effective results against opioid abuse and overprescribing.
In Florida, opioid prescriptions decreased in 80% of counties from 2010 to 2015 after the state established a PDMP in combination with tighter regulation of pain clinics. In the first month after implementation of Florida’s PDMP, oxycodone deaths dropped by 25%, according to a 2015 study published in Drug and Alcohol Dependence (2015 May 1. doi: 10.1016/j.drugalcdep.2015.02.010).
Opioid prescriptions in Kentucky, New York, and Tennessee dropped after mandates that prescribers check their state PDMPs, according to a summary by the PDMP Center of Excellence at Brandeis University. In Kentucky, doses dispensed declined for hydrocodone (–10.3%), oxycodone (–11.6%), and oxymorphone (–35%), while in Tennessee the number of opioid prescriptions fell by 7%. In New York, total opioid prescriptions have dropped by more than 9% since the state’s PDMP went into effect.
In Wisconsin, an analysis after enactment of the state’s PDMP found a nearly 12% reduction in opioid prescriptions and a 13% reduction in opioid doses dispensed between the fourth quarter of 2015 and the fourth quarter of 2016, according to a report by the Wisconsin Department of Safety and Professional Services.
PDMPs also have altered physicians’ prescribing behaviors and changed patient care decisions, studies show. A review of medical providers in Ohio emergency departments found that 41% of those given PDMP data altered their prescribing for patients receiving multiple simultaneous narcotics prescriptions, according to the Brandeis University summary. Of those Ohio providers, 61% prescribed no narcotics or fewer narcotics than originally planned.
A survey of prescribers in Rhode Island and Connecticut found that those who used PDMP data were more likely than nonusers to take clinically appropriate action in response to suspected cases of prescription drug abuse or diversion by patients, such as conducting drug screens or referring them to substance abuse treatment.
Despite the positive impacts, however, challenges for PDMPs remain.
Dr. Deep noted that physicians in solo and small practices may have a harder time than employed physicians when it comes to checking databases, recording data, and delegating duties. In addition, differing PDMP regulations may not catch prescription drug abusers who go across state lines.
Most states with PDMPs share their PDMP data with other state PDMPs or share data with authorized users in other states. Florida can receive PDMP data from other jurisdictions and provide that data to authorized users in Florida, but it does not share its data with other states. Oregon allows only prescribers in California, Idaho, Nevada, and Washington state to access its database information.
PDMPs also are limited in what they tell physicians about patients, said Gregory A. Hood, MD, an internist in Lexington, Ky., and former governor of the American College of Physicians, Kentucky Chapter.
“PDMP is only helpful to a point,” he said in an interview. “Any PDMP has the inherent limitation that it only reports what is reported to it. This doesn’t tell us about whether the patient actually takes the medicine, gives or sells it away, or whether they use it appropriately or not. Patients can overuse for 3 of 4 weeks, buy a week on the street, or from someone they know, and we’re none the wiser, absent an informant.”
Kentucky’s database, called the Kentucky All Schedule Prescription Electronic Reporting System (KASPER), requires that prescribers and dispensers of controlled substances query the state’s electronic monitoring system before issuing new prescriptions or refills. To track illicit use of opiates, Kentucky also recently made gabapentin a Schedule V controlled substance, Dr. Hood said.
Whether PDMPs have a positive effect depends on what doctors do with the information they learn from the database, Dr. Hood said.
“Generally, PDMPs can help identify at least some who are seeking adverse gain,” he said. “Properly identifying someone with a medical issue and arranging proper care is a positive. Rote dropping of someone with a ‘dirty’ PDMP – as has been known to happen in some primary care and specialty offices – is difficult to view as a positive, particularly given shortages in both primary care and in pain management.”
[email protected] On Twitter @legal_med
Ruling: Apologies can’t be used against doctors in court
The Ohio Supreme Court has ruled that apologies by physicians that include an admission of fault cannot be used against them in court, upholding a lower court decision that spared a doctor’s comments from being heard at trial.
In a Sept. 12 decision, state Supreme Court justices concluded that Ohio’s apology statute protects both expressions of regret for an unanticipated outcome and acknowledgments that the patient’s treatment fell below the standard of care. The decision resolves a split among Ohio appeals courts over whether expressions of fault are admissible.
The decision declaring Ohio’s apology statute “unambiguous” is an important and clarifying ruling for physicians and settles the differing opinions of some lower courts, said Reginald Fields, director of external and professional relations for the Ohio State Medical Association.
“We applaud the high court’s decision,” Mr. Fields said in an interview. “Even the two dissenting justices agreed that the apology law is clear; they just questioned whether it applied in this particular case. This ruling likely means pending legislation thought to be needed to clarify the law is now unnecessary. The OSMA will now focus on other aspects of tort reform, such as ‘loss of chance’ claims and further elimination of frivolous lawsuits.”
The Ohio Association for Justice, the state’s plaintiffs’ bar did not respond to a request for comment.
The case of Stewart v. Vivian resulted from a lawsuit filed by Dennis Stewart against Cincinnati psychiatrist Rodney Vivian, MD, after the death of Mr. Stewart’s wife by suicide. Michelle Stewart was admitted to the emergency department of Mt. Orab MediCenter in February 2010 after attempting suicide and was later transferred to the psychiatric unit at Mercy Hospital Clermont in Batavia, Ohio. After consulting with nurses, Dr. Vivian ordered that a staff member of the psychiatric unit visually observe Ms. Stewart every 15 minutes, according to court documents. The next evening, Mr. Stewart arrived at the psychiatric unit to visit his wife and found her unconscious as a result of hanging.
Two days later, Dr. Vivian went to Ms. Stewart’s room in the intensive care unit to speak with family members. The content of the conversation between Dr. Vivian and family members is disputed. Family members allege that Dr. Vivian expressed that it was a “terrible situation” and that the patient had told Dr. Vivian that she “wanted to be dead” would “keep trying” to kill herself. Dr. Vivian testified that he told the family he was “sorry this has happened.” Ms. Stewart was later taken off life support and died.
In 2011, Mr. Stewart sued Dr. Vivian and Mercy Hospital Clermont for medical malpractice, loss of spousal consortium, and wrongful death. Dr. Vivian argued that his statements to family members in the ICU room were inadmissible under the state’s apology law because they were “intended to express commiseration, condolence, or sympathy.” Mr. Stewart countered that Dr. Vivian’s statements were admissible because they were not “pure expressions of apology, sympathy, commiseration, condolence, compassion, or a general sense of benevolence.” The trial court sided with Dr. Vivian and his statements were kept from trial testimony. The jury returned a verdict in favor of Dr. Vivian, concluding that he was not negligent in his assessment, care, or treatment.
The 12th District Court of Appeals ruled that Dr. Vivian’s statements were properly excluded, finding that the Ohio’s apology law is ambiguous because according to the term’s dictionary definition, “apology” may or may not include an admission of fault. But the decision conflicted with the case of Davis v. Wooster Orthopaedics & Sports Medicine, Inc. in which the Court of Appeals for the 9th District in Ohio determined Ohio’s apology statute protects from admission “pure expressions of apology, sympathy, commiseration, condolence, compassion, or a general sense of benevolence,” but not “admission of fault.”
Resolving the split, the Ohio Supreme Court concluded that the state law is unambiguous and that its legislative intent is to shield expressions of regret for unexpected outcomes that may include acknowledgments that the patient’s medical care fell below the standard of care.
Ohio Supreme Court Chief Justice Maureen O’Connor and Justice William M. O’Neill partially dissented. While they agreed with the majority’s holding regarding the intent of Ohio’s apology law, Justice O’Connor wrote that the Dr. Vivian’s statements fell outside the law’s protection.
“Dr. Vivian’s statements were not an apology nor did they express regret or a type of shared sadness associated with sympathy or commiseration,” she wrote in her dissent.
At least 36 states have apology laws that shield against certain statements, expressions, or other evidence related to disclosures being used against physicians in court.
[email protected]
On Twitter @legal_med
The Ohio Supreme Court has ruled that apologies by physicians that include an admission of fault cannot be used against them in court, upholding a lower court decision that spared a doctor’s comments from being heard at trial.
In a Sept. 12 decision, state Supreme Court justices concluded that Ohio’s apology statute protects both expressions of regret for an unanticipated outcome and acknowledgments that the patient’s treatment fell below the standard of care. The decision resolves a split among Ohio appeals courts over whether expressions of fault are admissible.
The decision declaring Ohio’s apology statute “unambiguous” is an important and clarifying ruling for physicians and settles the differing opinions of some lower courts, said Reginald Fields, director of external and professional relations for the Ohio State Medical Association.
“We applaud the high court’s decision,” Mr. Fields said in an interview. “Even the two dissenting justices agreed that the apology law is clear; they just questioned whether it applied in this particular case. This ruling likely means pending legislation thought to be needed to clarify the law is now unnecessary. The OSMA will now focus on other aspects of tort reform, such as ‘loss of chance’ claims and further elimination of frivolous lawsuits.”
The Ohio Association for Justice, the state’s plaintiffs’ bar did not respond to a request for comment.
The case of Stewart v. Vivian resulted from a lawsuit filed by Dennis Stewart against Cincinnati psychiatrist Rodney Vivian, MD, after the death of Mr. Stewart’s wife by suicide. Michelle Stewart was admitted to the emergency department of Mt. Orab MediCenter in February 2010 after attempting suicide and was later transferred to the psychiatric unit at Mercy Hospital Clermont in Batavia, Ohio. After consulting with nurses, Dr. Vivian ordered that a staff member of the psychiatric unit visually observe Ms. Stewart every 15 minutes, according to court documents. The next evening, Mr. Stewart arrived at the psychiatric unit to visit his wife and found her unconscious as a result of hanging.
Two days later, Dr. Vivian went to Ms. Stewart’s room in the intensive care unit to speak with family members. The content of the conversation between Dr. Vivian and family members is disputed. Family members allege that Dr. Vivian expressed that it was a “terrible situation” and that the patient had told Dr. Vivian that she “wanted to be dead” would “keep trying” to kill herself. Dr. Vivian testified that he told the family he was “sorry this has happened.” Ms. Stewart was later taken off life support and died.
In 2011, Mr. Stewart sued Dr. Vivian and Mercy Hospital Clermont for medical malpractice, loss of spousal consortium, and wrongful death. Dr. Vivian argued that his statements to family members in the ICU room were inadmissible under the state’s apology law because they were “intended to express commiseration, condolence, or sympathy.” Mr. Stewart countered that Dr. Vivian’s statements were admissible because they were not “pure expressions of apology, sympathy, commiseration, condolence, compassion, or a general sense of benevolence.” The trial court sided with Dr. Vivian and his statements were kept from trial testimony. The jury returned a verdict in favor of Dr. Vivian, concluding that he was not negligent in his assessment, care, or treatment.
The 12th District Court of Appeals ruled that Dr. Vivian’s statements were properly excluded, finding that the Ohio’s apology law is ambiguous because according to the term’s dictionary definition, “apology” may or may not include an admission of fault. But the decision conflicted with the case of Davis v. Wooster Orthopaedics & Sports Medicine, Inc. in which the Court of Appeals for the 9th District in Ohio determined Ohio’s apology statute protects from admission “pure expressions of apology, sympathy, commiseration, condolence, compassion, or a general sense of benevolence,” but not “admission of fault.”
Resolving the split, the Ohio Supreme Court concluded that the state law is unambiguous and that its legislative intent is to shield expressions of regret for unexpected outcomes that may include acknowledgments that the patient’s medical care fell below the standard of care.
Ohio Supreme Court Chief Justice Maureen O’Connor and Justice William M. O’Neill partially dissented. While they agreed with the majority’s holding regarding the intent of Ohio’s apology law, Justice O’Connor wrote that the Dr. Vivian’s statements fell outside the law’s protection.
“Dr. Vivian’s statements were not an apology nor did they express regret or a type of shared sadness associated with sympathy or commiseration,” she wrote in her dissent.
At least 36 states have apology laws that shield against certain statements, expressions, or other evidence related to disclosures being used against physicians in court.
[email protected]
On Twitter @legal_med
The Ohio Supreme Court has ruled that apologies by physicians that include an admission of fault cannot be used against them in court, upholding a lower court decision that spared a doctor’s comments from being heard at trial.
In a Sept. 12 decision, state Supreme Court justices concluded that Ohio’s apology statute protects both expressions of regret for an unanticipated outcome and acknowledgments that the patient’s treatment fell below the standard of care. The decision resolves a split among Ohio appeals courts over whether expressions of fault are admissible.
The decision declaring Ohio’s apology statute “unambiguous” is an important and clarifying ruling for physicians and settles the differing opinions of some lower courts, said Reginald Fields, director of external and professional relations for the Ohio State Medical Association.
“We applaud the high court’s decision,” Mr. Fields said in an interview. “Even the two dissenting justices agreed that the apology law is clear; they just questioned whether it applied in this particular case. This ruling likely means pending legislation thought to be needed to clarify the law is now unnecessary. The OSMA will now focus on other aspects of tort reform, such as ‘loss of chance’ claims and further elimination of frivolous lawsuits.”
The Ohio Association for Justice, the state’s plaintiffs’ bar did not respond to a request for comment.
The case of Stewart v. Vivian resulted from a lawsuit filed by Dennis Stewart against Cincinnati psychiatrist Rodney Vivian, MD, after the death of Mr. Stewart’s wife by suicide. Michelle Stewart was admitted to the emergency department of Mt. Orab MediCenter in February 2010 after attempting suicide and was later transferred to the psychiatric unit at Mercy Hospital Clermont in Batavia, Ohio. After consulting with nurses, Dr. Vivian ordered that a staff member of the psychiatric unit visually observe Ms. Stewart every 15 minutes, according to court documents. The next evening, Mr. Stewart arrived at the psychiatric unit to visit his wife and found her unconscious as a result of hanging.
Two days later, Dr. Vivian went to Ms. Stewart’s room in the intensive care unit to speak with family members. The content of the conversation between Dr. Vivian and family members is disputed. Family members allege that Dr. Vivian expressed that it was a “terrible situation” and that the patient had told Dr. Vivian that she “wanted to be dead” would “keep trying” to kill herself. Dr. Vivian testified that he told the family he was “sorry this has happened.” Ms. Stewart was later taken off life support and died.
In 2011, Mr. Stewart sued Dr. Vivian and Mercy Hospital Clermont for medical malpractice, loss of spousal consortium, and wrongful death. Dr. Vivian argued that his statements to family members in the ICU room were inadmissible under the state’s apology law because they were “intended to express commiseration, condolence, or sympathy.” Mr. Stewart countered that Dr. Vivian’s statements were admissible because they were not “pure expressions of apology, sympathy, commiseration, condolence, compassion, or a general sense of benevolence.” The trial court sided with Dr. Vivian and his statements were kept from trial testimony. The jury returned a verdict in favor of Dr. Vivian, concluding that he was not negligent in his assessment, care, or treatment.
The 12th District Court of Appeals ruled that Dr. Vivian’s statements were properly excluded, finding that the Ohio’s apology law is ambiguous because according to the term’s dictionary definition, “apology” may or may not include an admission of fault. But the decision conflicted with the case of Davis v. Wooster Orthopaedics & Sports Medicine, Inc. in which the Court of Appeals for the 9th District in Ohio determined Ohio’s apology statute protects from admission “pure expressions of apology, sympathy, commiseration, condolence, compassion, or a general sense of benevolence,” but not “admission of fault.”
Resolving the split, the Ohio Supreme Court concluded that the state law is unambiguous and that its legislative intent is to shield expressions of regret for unexpected outcomes that may include acknowledgments that the patient’s medical care fell below the standard of care.
Ohio Supreme Court Chief Justice Maureen O’Connor and Justice William M. O’Neill partially dissented. While they agreed with the majority’s holding regarding the intent of Ohio’s apology law, Justice O’Connor wrote that the Dr. Vivian’s statements fell outside the law’s protection.
“Dr. Vivian’s statements were not an apology nor did they express regret or a type of shared sadness associated with sympathy or commiseration,” she wrote in her dissent.
At least 36 states have apology laws that shield against certain statements, expressions, or other evidence related to disclosures being used against physicians in court.
[email protected]
On Twitter @legal_med
HHS Secretary resigns amid flight criticism
U.S. Department of Health & Human Services Secretary Tom Price, MD, has resigned from his post following furor over his use of private planes for government business paid for by taxpayers.
In a Sept. 29 press statement, White House press secretary Sarah Huckabee Sanders said Dr. Price offered his resignation early Sept. 29 and that President Trump accepted. Don J. Wright, deputy assistant secretary for health and director of the office of disease prevention and health promotion, will serve as Acting Secretary effective Sept. 30, according to the statement.
Dr. Price’s resignation comes after widespread criticism over his alleged repeated use of taxpayer-funded charter flights. Politico first broke the story, reporting that he has taken at least 24 flights on private charter planes at taxpayers’ expense since early May, costing an estimated $400,000-$500,000. After the reports, Dr. Price announced that he planned to write a personal check to the government for $60,000 to cover the cost of the flights.
During a press briefing on Sept. 29, President Trump said he was “disappointed” with Dr. Price’s actions, and that the White House was looking into the accusations.
“I felt very badly because Secretary Price is a good man, but we are looking into it, and we’re looking into it very strongly,” President Trump said at the briefing.
In his resignation letter, posted on Twitter, Dr. Price expressed remorse for having created a distraction for the administration and said he was grateful for the opportunity to have served as HHS Secretary.
“I have spent 40 years both as a doctor and public servant putting people first,” Dr. Price said in his resignation letter. “I regret that the recent events have created a distraction from these important objectives. Success on these issues is more important than any one person. In order for you to move forward without further disruption, I am officially tendering my resignation.”
[email protected]
On Twitter @legal_med
U.S. Department of Health & Human Services Secretary Tom Price, MD, has resigned from his post following furor over his use of private planes for government business paid for by taxpayers.
In a Sept. 29 press statement, White House press secretary Sarah Huckabee Sanders said Dr. Price offered his resignation early Sept. 29 and that President Trump accepted. Don J. Wright, deputy assistant secretary for health and director of the office of disease prevention and health promotion, will serve as Acting Secretary effective Sept. 30, according to the statement.
Dr. Price’s resignation comes after widespread criticism over his alleged repeated use of taxpayer-funded charter flights. Politico first broke the story, reporting that he has taken at least 24 flights on private charter planes at taxpayers’ expense since early May, costing an estimated $400,000-$500,000. After the reports, Dr. Price announced that he planned to write a personal check to the government for $60,000 to cover the cost of the flights.
During a press briefing on Sept. 29, President Trump said he was “disappointed” with Dr. Price’s actions, and that the White House was looking into the accusations.
“I felt very badly because Secretary Price is a good man, but we are looking into it, and we’re looking into it very strongly,” President Trump said at the briefing.
In his resignation letter, posted on Twitter, Dr. Price expressed remorse for having created a distraction for the administration and said he was grateful for the opportunity to have served as HHS Secretary.
“I have spent 40 years both as a doctor and public servant putting people first,” Dr. Price said in his resignation letter. “I regret that the recent events have created a distraction from these important objectives. Success on these issues is more important than any one person. In order for you to move forward without further disruption, I am officially tendering my resignation.”
[email protected]
On Twitter @legal_med
U.S. Department of Health & Human Services Secretary Tom Price, MD, has resigned from his post following furor over his use of private planes for government business paid for by taxpayers.
In a Sept. 29 press statement, White House press secretary Sarah Huckabee Sanders said Dr. Price offered his resignation early Sept. 29 and that President Trump accepted. Don J. Wright, deputy assistant secretary for health and director of the office of disease prevention and health promotion, will serve as Acting Secretary effective Sept. 30, according to the statement.
Dr. Price’s resignation comes after widespread criticism over his alleged repeated use of taxpayer-funded charter flights. Politico first broke the story, reporting that he has taken at least 24 flights on private charter planes at taxpayers’ expense since early May, costing an estimated $400,000-$500,000. After the reports, Dr. Price announced that he planned to write a personal check to the government for $60,000 to cover the cost of the flights.
During a press briefing on Sept. 29, President Trump said he was “disappointed” with Dr. Price’s actions, and that the White House was looking into the accusations.
“I felt very badly because Secretary Price is a good man, but we are looking into it, and we’re looking into it very strongly,” President Trump said at the briefing.
In his resignation letter, posted on Twitter, Dr. Price expressed remorse for having created a distraction for the administration and said he was grateful for the opportunity to have served as HHS Secretary.
“I have spent 40 years both as a doctor and public servant putting people first,” Dr. Price said in his resignation letter. “I regret that the recent events have created a distraction from these important objectives. Success on these issues is more important than any one person. In order for you to move forward without further disruption, I am officially tendering my resignation.”
[email protected]
On Twitter @legal_med
ECHO rheumatology programs increase access, improve care
As in many places throughout the country, rheumatologists are in short supply in southern Arizona. Patients frequently wait up to 6 months to visit a rheumatologist at Banner University Medical Center (BUMC) in Tucson, and many drive between 3 and 4 hours for the appointment, said Dominick G. Sudano, MD, a rheumatologist at BUMC, which is affiliated with the University of Arizona.
[polldaddy:9823712]
The high demand for rheumatologists and lack of timely access led the University of Arizona to develop a program that will train primary care providers at remote sites to treat rheumatic diseases. The program, a partnership between the university’s Arizona Telemedicine Program and the University of Arizona Center for Rural Health, will use the popular ECHO (Extension for Community Healthcare Outcomes) model, founded by the University of New Mexico in Albuquerque, which aims to increase workforce capacity by sharing medical knowledge.
A unique model of care
As part of the program, set to launch this month, Dr. Sudano will hold rheumatology training sessions via telemedicine for primary care physicians and other nonphysicians at four remote sites around Arizona. Participating sites include Canyonlands Healthcare, North County Healthcare, and Northern Arizona Healthcare – all located in the northern part of the state – and Copper Queen Community Hospital in southern Arizona.
The virtual sessions will include both educational topics and the opportunity for local doctors and health professionals to present patient cases to Dr. Sudano for guidance. The local doctors and health professionals will eventually treat rheumatic cases in their communities, while cases identified as severe will still be referred to rheumatologists.
The university’s Arizona Telemedicine Program was fortunate to receive a $17,700 grant from Lilly to launch the 1-year rheumatology ECHO pilot program, Dr. Sudano noted. The grant will enable the program to get off the ground, while administrators search for additional funding sources to become sustainable, he said.
Dr. Sudano credits the assistance and support of the University of New Mexico and its ECHO leaders for helping the University of Arizona build its ECHO rheumatology program and helping administrators address the details of setting up the program.
“[The University of New Mexico] was immensely helpful,” he said. “They have immersion sessions about once a month and you spend [time] working with their team. They work with you to get the logistics ironed out.”
A spreading movement
The University of New Mexico (UNM) has good reason to assist other health and academic medical centers in launching their own ECHO programs. UNM’s mission is to continue building the ECHO movement and accomplish its goal of “touching 1 billion lives” by 2025, said Sanjeev Arora, MD, a gastroenterologist at UNM and founder/director of the university’s Project ECHO.
“There was a great shortage of specialists to treat hepatitis C so I came up with this idea of ECHO to bring access to care to everyone in New Mexico who needed care,” he said. “The second part of the idea was, if we could do that for hepatitis C, we could do that for a lot of other problems like rheumatoid arthritis, like addiction, like diabetes.”
Project ECHO has now spread to medical centers and hospitals across the country, with programs that center on asthma, HIV infection, cardiac risk reduction, chronic pain management, geriatrics, palliative care, substance abuse, and obesity, among others. The model is now in 139 academic hubs in 24 countries with more than 65 health conditions targeted, according to Dr. Arora. Replication sites focus on four key principles of ECHO: technology used to leverage scarce health care expertise and resources; best practices shared to standardize care across disparate health care delivery systems; case-based learning used as the primary modality to build knowledge, confidence, and expertise; and evaluations conducted to monitor outcomes.
Data show the care patients receive via the ECHO model is equal to that of care provided by university-based specialists. A 2011 report published in the New England Journal of Medicine, for example, found that a sustained viral response to treatment for hepatitis C was achieved in 58% of patients managed at the university and by 58% of patients managed by primary care physicians at rural and prison sites who participated in Project ECHO (N Engl J Med. 2011;364:2199-2207). Response rates to different subtypes of hepatitis C also did not differ significantly between the two groups.
The ECHO model has also greatly improved access and outcomes for hepatitis C patients in Northern Arizona, said Colleen Hopkins, telehealth coordinator at North Country Healthcare in Flagstaff. North Country Healthcare has participated in a hepatitis C ECHO program since 2012, linking its chain of 14 community health centers with a hepatologist-educator at St. Joseph’s Hospital and Medical Center in Phoenix, 140 miles to the south.
“In 2011, more than 950 patients in the health system’s network had a hepatitis C diagnosis, but the majority did not have access to care,” Ms. Hopkins said in an interview.
“To date, over 500 patients have received care for their liver disease in rural Northern Arizona,” she said. “These numbers continue to climb as our awareness has caused an increase in screening and various outreach efforts ... Overall, our providers and patients are empowered by having access to specialty care; they are living longer healthier lives as well as keeping money in our communities.”
Rheumatology and the ECHO model
The volume of rheumatic conditions encountered by primary care physicians and the shortage of specialists make rheumatology a logical fit for the ECHO model, Dr. Arora said. Rheumatoid arthritis, osteoarthritis, osteoporosis, fibromyalgia, and joint pain account for as many as one in five visits to primary care doctors, he noted.
“Osteoporosis and rheumatoid arthritis produce massive disability in the world,” he said. “Treatment exists, but it’s not getting to patients. ECHO can fundamentally transform the field of rheumatology if it’s adopted widely.”
However, compared with other specialty ECHO models, there are not many rheumatology ECHO programs in operation. Dr. Arora is hopeful that as word spreads about how well rheumatology fits into the ECHO structure, more programs will develop, he said.
“We have found over the years that with our training these providers – both physicians and nonphysician – are able to function as well as a specially trained [rheumatologist],” Dr. Bankhurst said. “We help them as needed by our weekly teleconference where they present cases to us and those cases which appear to be most difficult, we see immediately in our clinics.”
The program has led to decreased referrals to the university from outlying areas and more care access for patients in rural areas, Dr. Bankhurst said. A university study is underway to analyze clinical outcomes for rheumatoid arthritis as conducted by distant provider sites compared with treatment at the university clinic.
“It’s my perspective, based on 12 years of experience, that they’ll be identical,” he said.
Setting up such ECHO programs is not without challenges. Financial support for telecommunication equipment in all needed areas can be difficult, Dr. Bankhurst said. Recruiting individuals who are well motivated to participate in the program can also be a challenge.
“It needs a commitment by the administration,” he said. “It does take time from other activities. It requires dedicated time away from a busy clinic.”
[email protected]
On Twitter @legal_med
As in many places throughout the country, rheumatologists are in short supply in southern Arizona. Patients frequently wait up to 6 months to visit a rheumatologist at Banner University Medical Center (BUMC) in Tucson, and many drive between 3 and 4 hours for the appointment, said Dominick G. Sudano, MD, a rheumatologist at BUMC, which is affiliated with the University of Arizona.
[polldaddy:9823712]
The high demand for rheumatologists and lack of timely access led the University of Arizona to develop a program that will train primary care providers at remote sites to treat rheumatic diseases. The program, a partnership between the university’s Arizona Telemedicine Program and the University of Arizona Center for Rural Health, will use the popular ECHO (Extension for Community Healthcare Outcomes) model, founded by the University of New Mexico in Albuquerque, which aims to increase workforce capacity by sharing medical knowledge.
A unique model of care
As part of the program, set to launch this month, Dr. Sudano will hold rheumatology training sessions via telemedicine for primary care physicians and other nonphysicians at four remote sites around Arizona. Participating sites include Canyonlands Healthcare, North County Healthcare, and Northern Arizona Healthcare – all located in the northern part of the state – and Copper Queen Community Hospital in southern Arizona.
The virtual sessions will include both educational topics and the opportunity for local doctors and health professionals to present patient cases to Dr. Sudano for guidance. The local doctors and health professionals will eventually treat rheumatic cases in their communities, while cases identified as severe will still be referred to rheumatologists.
The university’s Arizona Telemedicine Program was fortunate to receive a $17,700 grant from Lilly to launch the 1-year rheumatology ECHO pilot program, Dr. Sudano noted. The grant will enable the program to get off the ground, while administrators search for additional funding sources to become sustainable, he said.
Dr. Sudano credits the assistance and support of the University of New Mexico and its ECHO leaders for helping the University of Arizona build its ECHO rheumatology program and helping administrators address the details of setting up the program.
“[The University of New Mexico] was immensely helpful,” he said. “They have immersion sessions about once a month and you spend [time] working with their team. They work with you to get the logistics ironed out.”
A spreading movement
The University of New Mexico (UNM) has good reason to assist other health and academic medical centers in launching their own ECHO programs. UNM’s mission is to continue building the ECHO movement and accomplish its goal of “touching 1 billion lives” by 2025, said Sanjeev Arora, MD, a gastroenterologist at UNM and founder/director of the university’s Project ECHO.
“There was a great shortage of specialists to treat hepatitis C so I came up with this idea of ECHO to bring access to care to everyone in New Mexico who needed care,” he said. “The second part of the idea was, if we could do that for hepatitis C, we could do that for a lot of other problems like rheumatoid arthritis, like addiction, like diabetes.”
Project ECHO has now spread to medical centers and hospitals across the country, with programs that center on asthma, HIV infection, cardiac risk reduction, chronic pain management, geriatrics, palliative care, substance abuse, and obesity, among others. The model is now in 139 academic hubs in 24 countries with more than 65 health conditions targeted, according to Dr. Arora. Replication sites focus on four key principles of ECHO: technology used to leverage scarce health care expertise and resources; best practices shared to standardize care across disparate health care delivery systems; case-based learning used as the primary modality to build knowledge, confidence, and expertise; and evaluations conducted to monitor outcomes.
Data show the care patients receive via the ECHO model is equal to that of care provided by university-based specialists. A 2011 report published in the New England Journal of Medicine, for example, found that a sustained viral response to treatment for hepatitis C was achieved in 58% of patients managed at the university and by 58% of patients managed by primary care physicians at rural and prison sites who participated in Project ECHO (N Engl J Med. 2011;364:2199-2207). Response rates to different subtypes of hepatitis C also did not differ significantly between the two groups.
The ECHO model has also greatly improved access and outcomes for hepatitis C patients in Northern Arizona, said Colleen Hopkins, telehealth coordinator at North Country Healthcare in Flagstaff. North Country Healthcare has participated in a hepatitis C ECHO program since 2012, linking its chain of 14 community health centers with a hepatologist-educator at St. Joseph’s Hospital and Medical Center in Phoenix, 140 miles to the south.
“In 2011, more than 950 patients in the health system’s network had a hepatitis C diagnosis, but the majority did not have access to care,” Ms. Hopkins said in an interview.
“To date, over 500 patients have received care for their liver disease in rural Northern Arizona,” she said. “These numbers continue to climb as our awareness has caused an increase in screening and various outreach efforts ... Overall, our providers and patients are empowered by having access to specialty care; they are living longer healthier lives as well as keeping money in our communities.”
Rheumatology and the ECHO model
The volume of rheumatic conditions encountered by primary care physicians and the shortage of specialists make rheumatology a logical fit for the ECHO model, Dr. Arora said. Rheumatoid arthritis, osteoarthritis, osteoporosis, fibromyalgia, and joint pain account for as many as one in five visits to primary care doctors, he noted.
“Osteoporosis and rheumatoid arthritis produce massive disability in the world,” he said. “Treatment exists, but it’s not getting to patients. ECHO can fundamentally transform the field of rheumatology if it’s adopted widely.”
However, compared with other specialty ECHO models, there are not many rheumatology ECHO programs in operation. Dr. Arora is hopeful that as word spreads about how well rheumatology fits into the ECHO structure, more programs will develop, he said.
“We have found over the years that with our training these providers – both physicians and nonphysician – are able to function as well as a specially trained [rheumatologist],” Dr. Bankhurst said. “We help them as needed by our weekly teleconference where they present cases to us and those cases which appear to be most difficult, we see immediately in our clinics.”
The program has led to decreased referrals to the university from outlying areas and more care access for patients in rural areas, Dr. Bankhurst said. A university study is underway to analyze clinical outcomes for rheumatoid arthritis as conducted by distant provider sites compared with treatment at the university clinic.
“It’s my perspective, based on 12 years of experience, that they’ll be identical,” he said.
Setting up such ECHO programs is not without challenges. Financial support for telecommunication equipment in all needed areas can be difficult, Dr. Bankhurst said. Recruiting individuals who are well motivated to participate in the program can also be a challenge.
“It needs a commitment by the administration,” he said. “It does take time from other activities. It requires dedicated time away from a busy clinic.”
[email protected]
On Twitter @legal_med
As in many places throughout the country, rheumatologists are in short supply in southern Arizona. Patients frequently wait up to 6 months to visit a rheumatologist at Banner University Medical Center (BUMC) in Tucson, and many drive between 3 and 4 hours for the appointment, said Dominick G. Sudano, MD, a rheumatologist at BUMC, which is affiliated with the University of Arizona.
[polldaddy:9823712]
The high demand for rheumatologists and lack of timely access led the University of Arizona to develop a program that will train primary care providers at remote sites to treat rheumatic diseases. The program, a partnership between the university’s Arizona Telemedicine Program and the University of Arizona Center for Rural Health, will use the popular ECHO (Extension for Community Healthcare Outcomes) model, founded by the University of New Mexico in Albuquerque, which aims to increase workforce capacity by sharing medical knowledge.
A unique model of care
As part of the program, set to launch this month, Dr. Sudano will hold rheumatology training sessions via telemedicine for primary care physicians and other nonphysicians at four remote sites around Arizona. Participating sites include Canyonlands Healthcare, North County Healthcare, and Northern Arizona Healthcare – all located in the northern part of the state – and Copper Queen Community Hospital in southern Arizona.
The virtual sessions will include both educational topics and the opportunity for local doctors and health professionals to present patient cases to Dr. Sudano for guidance. The local doctors and health professionals will eventually treat rheumatic cases in their communities, while cases identified as severe will still be referred to rheumatologists.
The university’s Arizona Telemedicine Program was fortunate to receive a $17,700 grant from Lilly to launch the 1-year rheumatology ECHO pilot program, Dr. Sudano noted. The grant will enable the program to get off the ground, while administrators search for additional funding sources to become sustainable, he said.
Dr. Sudano credits the assistance and support of the University of New Mexico and its ECHO leaders for helping the University of Arizona build its ECHO rheumatology program and helping administrators address the details of setting up the program.
“[The University of New Mexico] was immensely helpful,” he said. “They have immersion sessions about once a month and you spend [time] working with their team. They work with you to get the logistics ironed out.”
A spreading movement
The University of New Mexico (UNM) has good reason to assist other health and academic medical centers in launching their own ECHO programs. UNM’s mission is to continue building the ECHO movement and accomplish its goal of “touching 1 billion lives” by 2025, said Sanjeev Arora, MD, a gastroenterologist at UNM and founder/director of the university’s Project ECHO.
“There was a great shortage of specialists to treat hepatitis C so I came up with this idea of ECHO to bring access to care to everyone in New Mexico who needed care,” he said. “The second part of the idea was, if we could do that for hepatitis C, we could do that for a lot of other problems like rheumatoid arthritis, like addiction, like diabetes.”
Project ECHO has now spread to medical centers and hospitals across the country, with programs that center on asthma, HIV infection, cardiac risk reduction, chronic pain management, geriatrics, palliative care, substance abuse, and obesity, among others. The model is now in 139 academic hubs in 24 countries with more than 65 health conditions targeted, according to Dr. Arora. Replication sites focus on four key principles of ECHO: technology used to leverage scarce health care expertise and resources; best practices shared to standardize care across disparate health care delivery systems; case-based learning used as the primary modality to build knowledge, confidence, and expertise; and evaluations conducted to monitor outcomes.
Data show the care patients receive via the ECHO model is equal to that of care provided by university-based specialists. A 2011 report published in the New England Journal of Medicine, for example, found that a sustained viral response to treatment for hepatitis C was achieved in 58% of patients managed at the university and by 58% of patients managed by primary care physicians at rural and prison sites who participated in Project ECHO (N Engl J Med. 2011;364:2199-2207). Response rates to different subtypes of hepatitis C also did not differ significantly between the two groups.
The ECHO model has also greatly improved access and outcomes for hepatitis C patients in Northern Arizona, said Colleen Hopkins, telehealth coordinator at North Country Healthcare in Flagstaff. North Country Healthcare has participated in a hepatitis C ECHO program since 2012, linking its chain of 14 community health centers with a hepatologist-educator at St. Joseph’s Hospital and Medical Center in Phoenix, 140 miles to the south.
“In 2011, more than 950 patients in the health system’s network had a hepatitis C diagnosis, but the majority did not have access to care,” Ms. Hopkins said in an interview.
“To date, over 500 patients have received care for their liver disease in rural Northern Arizona,” she said. “These numbers continue to climb as our awareness has caused an increase in screening and various outreach efforts ... Overall, our providers and patients are empowered by having access to specialty care; they are living longer healthier lives as well as keeping money in our communities.”
Rheumatology and the ECHO model
The volume of rheumatic conditions encountered by primary care physicians and the shortage of specialists make rheumatology a logical fit for the ECHO model, Dr. Arora said. Rheumatoid arthritis, osteoarthritis, osteoporosis, fibromyalgia, and joint pain account for as many as one in five visits to primary care doctors, he noted.
“Osteoporosis and rheumatoid arthritis produce massive disability in the world,” he said. “Treatment exists, but it’s not getting to patients. ECHO can fundamentally transform the field of rheumatology if it’s adopted widely.”
However, compared with other specialty ECHO models, there are not many rheumatology ECHO programs in operation. Dr. Arora is hopeful that as word spreads about how well rheumatology fits into the ECHO structure, more programs will develop, he said.
“We have found over the years that with our training these providers – both physicians and nonphysician – are able to function as well as a specially trained [rheumatologist],” Dr. Bankhurst said. “We help them as needed by our weekly teleconference where they present cases to us and those cases which appear to be most difficult, we see immediately in our clinics.”
The program has led to decreased referrals to the university from outlying areas and more care access for patients in rural areas, Dr. Bankhurst said. A university study is underway to analyze clinical outcomes for rheumatoid arthritis as conducted by distant provider sites compared with treatment at the university clinic.
“It’s my perspective, based on 12 years of experience, that they’ll be identical,” he said.
Setting up such ECHO programs is not without challenges. Financial support for telecommunication equipment in all needed areas can be difficult, Dr. Bankhurst said. Recruiting individuals who are well motivated to participate in the program can also be a challenge.
“It needs a commitment by the administration,” he said. “It does take time from other activities. It requires dedicated time away from a busy clinic.”
[email protected]
On Twitter @legal_med
After newest travel restrictions, Supreme Court defers hearing on old policy
The U.S. Supreme Court will not hear oral arguments over President Trump’s controversial travel ban in light of new travel restrictions issued by the Trump administration that may render the case moot.
President Trump released new regulations Sept. 24 that prohibit travel to the United States from seven countries, most of which were covered in his original travel ban. Those include citizens of Iran, Libya, Syria, Yemen, Somalia, Chad, and North Korea. In addition, citizens of Iraq and certain citizens of Venezuela will face restrictions or heightened scrutiny when traveling to the United States.
Meanwhile, the Supreme Court Sept. 25 canceled oral arguments in the case of Trump v. Hawaii et al., which had challenged the second iteration of the president’s travel ban issued in March. Justices asked that each party file briefs by Oct. 5, addressing whether the legal challenge is now moot.
Unlike his two previous bans, President Trump’s new travel restrictions give each country its own set of travel restrictions. Most of the regulations prohibit immigration to the United States permanently and ban such nationals from working, studying, or visiting the United States.
Iran, however, will still be able to send its residents on student exchanges to the United States, although they will be subject to enhanced screening and vetting requirements. Certain Venezuelan government officials and their families are barred from coming to the United States under the new rules, and Somalian citizens will no longer be able to immigrate to America, but they can visit with heightened vetting.
The new order takes effect Oct. 18.
[email protected]
On Twitter @legal_med
The U.S. Supreme Court will not hear oral arguments over President Trump’s controversial travel ban in light of new travel restrictions issued by the Trump administration that may render the case moot.
President Trump released new regulations Sept. 24 that prohibit travel to the United States from seven countries, most of which were covered in his original travel ban. Those include citizens of Iran, Libya, Syria, Yemen, Somalia, Chad, and North Korea. In addition, citizens of Iraq and certain citizens of Venezuela will face restrictions or heightened scrutiny when traveling to the United States.
Meanwhile, the Supreme Court Sept. 25 canceled oral arguments in the case of Trump v. Hawaii et al., which had challenged the second iteration of the president’s travel ban issued in March. Justices asked that each party file briefs by Oct. 5, addressing whether the legal challenge is now moot.
Unlike his two previous bans, President Trump’s new travel restrictions give each country its own set of travel restrictions. Most of the regulations prohibit immigration to the United States permanently and ban such nationals from working, studying, or visiting the United States.
Iran, however, will still be able to send its residents on student exchanges to the United States, although they will be subject to enhanced screening and vetting requirements. Certain Venezuelan government officials and their families are barred from coming to the United States under the new rules, and Somalian citizens will no longer be able to immigrate to America, but they can visit with heightened vetting.
The new order takes effect Oct. 18.
[email protected]
On Twitter @legal_med
The U.S. Supreme Court will not hear oral arguments over President Trump’s controversial travel ban in light of new travel restrictions issued by the Trump administration that may render the case moot.
President Trump released new regulations Sept. 24 that prohibit travel to the United States from seven countries, most of which were covered in his original travel ban. Those include citizens of Iran, Libya, Syria, Yemen, Somalia, Chad, and North Korea. In addition, citizens of Iraq and certain citizens of Venezuela will face restrictions or heightened scrutiny when traveling to the United States.
Meanwhile, the Supreme Court Sept. 25 canceled oral arguments in the case of Trump v. Hawaii et al., which had challenged the second iteration of the president’s travel ban issued in March. Justices asked that each party file briefs by Oct. 5, addressing whether the legal challenge is now moot.
Unlike his two previous bans, President Trump’s new travel restrictions give each country its own set of travel restrictions. Most of the regulations prohibit immigration to the United States permanently and ban such nationals from working, studying, or visiting the United States.
Iran, however, will still be able to send its residents on student exchanges to the United States, although they will be subject to enhanced screening and vetting requirements. Certain Venezuelan government officials and their families are barred from coming to the United States under the new rules, and Somalian citizens will no longer be able to immigrate to America, but they can visit with heightened vetting.
The new order takes effect Oct. 18.
[email protected]
On Twitter @legal_med
Readmission rates linked to hospital quality measures
Poorer-performing hospitals have higher readmission rates than better-performing hospitals for patients with similar diagnoses, a study shows.
Lead author Harlan M. Krumholz, MD, of Yale University, New Haven, Conn., and his colleagues analyzed Centers for Medicare and Medicaid Services hospital-wide readmission data and divided data from July 2014 through June 2015 into two random samples. Researchers used the first sample to calculate the risk-standardized readmission rate within 30 days for each hospital and classified hospitals into performance quartiles, with a lower readmission rate indicating better performance. The second study sample included patients who had two admissions for similar diagnoses at different hospitals that occurred more than 1 month and less than 1 year apart. Researchers compared the observed readmission rates among patients who had been admitted to hospitals in different performance quartiles. The analysis included all discharges occurring from July 1, 2014, through June 30, 2015, from short-term acute care or critical access hospitals in the United States involving Medicare patients who were aged 65 years or older.
Results found that among the patients hospitalized more than once for similar diagnoses at different hospitals, the readmission rate was significantly higher among patients admitted to the worst-performing quartile of hospitals than among those admitted to the best-performing quartile (absolute difference in readmission rate, 2.0 percentage points; 95% confidence interval, 0.4-3.5; P = .001) (N Engl J Med. 2017. doi: 10.1056/NEJMsa1702321). The differences in the comparisons of the other quartiles were smaller and not significant, according to the study. 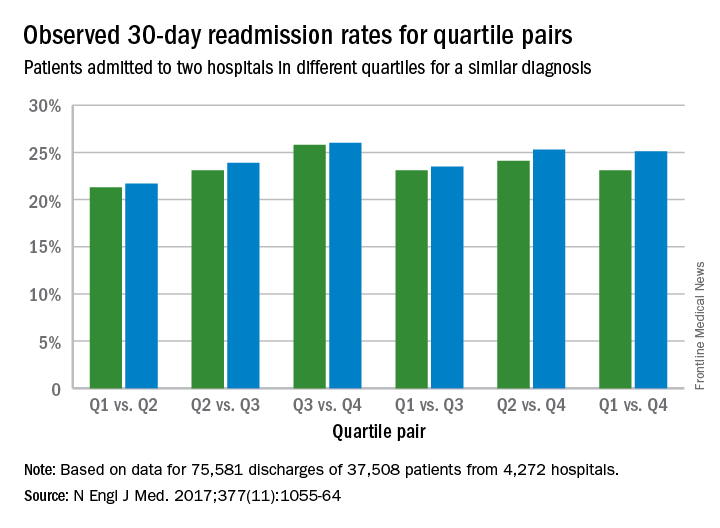
The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors, study authors concluded.
“This study addresses a persistent concern that national readmission measures may reflect differences in unmeasured factors rather than in hospital performance,” study authors noted in the study. “The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors. By studying patients who were admitted twice within 1 year with similar diagnoses to different hospitals, this study design was able to isolate hospital signals of performance while minimizing differences among the patients. In these cases, because the same patients had similar admissions at two hospitals, the characteristics of the patients, including their level of social disadvantage, level of education, or degree of underlying illness, were broadly the same. The alignment of the differences that we observed with the results of the CMS hospital-wide readmission measure also adds to evidence that the readmission measure classifies true differences in performance.”
Dr. Krumholz and seven coauthors reported receiving support from contracts with the Center for Medicare and Medicaid Services to develop and reevaluate performance measures that are used for public reporting.
[email protected]
On Twitter @legal_med
Poorer-performing hospitals have higher readmission rates than better-performing hospitals for patients with similar diagnoses, a study shows.
Lead author Harlan M. Krumholz, MD, of Yale University, New Haven, Conn., and his colleagues analyzed Centers for Medicare and Medicaid Services hospital-wide readmission data and divided data from July 2014 through June 2015 into two random samples. Researchers used the first sample to calculate the risk-standardized readmission rate within 30 days for each hospital and classified hospitals into performance quartiles, with a lower readmission rate indicating better performance. The second study sample included patients who had two admissions for similar diagnoses at different hospitals that occurred more than 1 month and less than 1 year apart. Researchers compared the observed readmission rates among patients who had been admitted to hospitals in different performance quartiles. The analysis included all discharges occurring from July 1, 2014, through June 30, 2015, from short-term acute care or critical access hospitals in the United States involving Medicare patients who were aged 65 years or older.
Results found that among the patients hospitalized more than once for similar diagnoses at different hospitals, the readmission rate was significantly higher among patients admitted to the worst-performing quartile of hospitals than among those admitted to the best-performing quartile (absolute difference in readmission rate, 2.0 percentage points; 95% confidence interval, 0.4-3.5; P = .001) (N Engl J Med. 2017. doi: 10.1056/NEJMsa1702321). The differences in the comparisons of the other quartiles were smaller and not significant, according to the study. 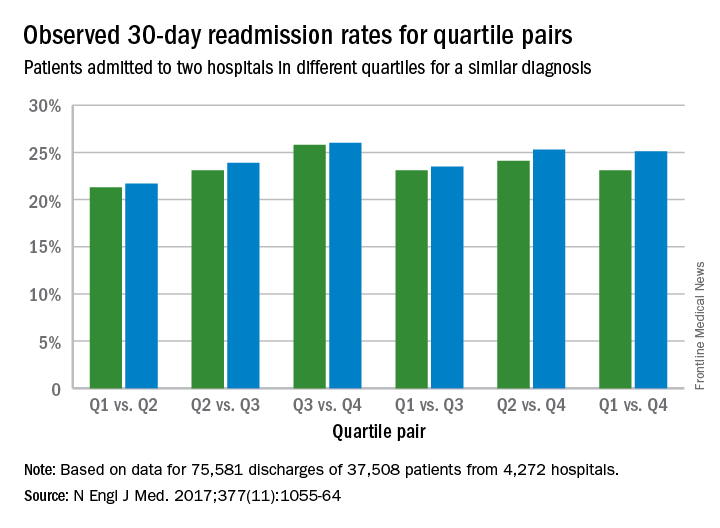
The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors, study authors concluded.
“This study addresses a persistent concern that national readmission measures may reflect differences in unmeasured factors rather than in hospital performance,” study authors noted in the study. “The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors. By studying patients who were admitted twice within 1 year with similar diagnoses to different hospitals, this study design was able to isolate hospital signals of performance while minimizing differences among the patients. In these cases, because the same patients had similar admissions at two hospitals, the characteristics of the patients, including their level of social disadvantage, level of education, or degree of underlying illness, were broadly the same. The alignment of the differences that we observed with the results of the CMS hospital-wide readmission measure also adds to evidence that the readmission measure classifies true differences in performance.”
Dr. Krumholz and seven coauthors reported receiving support from contracts with the Center for Medicare and Medicaid Services to develop and reevaluate performance measures that are used for public reporting.
[email protected]
On Twitter @legal_med
Poorer-performing hospitals have higher readmission rates than better-performing hospitals for patients with similar diagnoses, a study shows.
Lead author Harlan M. Krumholz, MD, of Yale University, New Haven, Conn., and his colleagues analyzed Centers for Medicare and Medicaid Services hospital-wide readmission data and divided data from July 2014 through June 2015 into two random samples. Researchers used the first sample to calculate the risk-standardized readmission rate within 30 days for each hospital and classified hospitals into performance quartiles, with a lower readmission rate indicating better performance. The second study sample included patients who had two admissions for similar diagnoses at different hospitals that occurred more than 1 month and less than 1 year apart. Researchers compared the observed readmission rates among patients who had been admitted to hospitals in different performance quartiles. The analysis included all discharges occurring from July 1, 2014, through June 30, 2015, from short-term acute care or critical access hospitals in the United States involving Medicare patients who were aged 65 years or older.
Results found that among the patients hospitalized more than once for similar diagnoses at different hospitals, the readmission rate was significantly higher among patients admitted to the worst-performing quartile of hospitals than among those admitted to the best-performing quartile (absolute difference in readmission rate, 2.0 percentage points; 95% confidence interval, 0.4-3.5; P = .001) (N Engl J Med. 2017. doi: 10.1056/NEJMsa1702321). The differences in the comparisons of the other quartiles were smaller and not significant, according to the study. 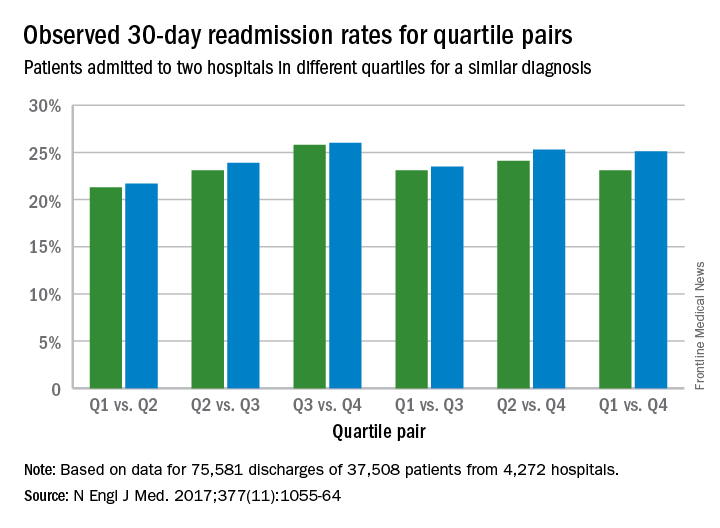
The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors, study authors concluded.
“This study addresses a persistent concern that national readmission measures may reflect differences in unmeasured factors rather than in hospital performance,” study authors noted in the study. “The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors. By studying patients who were admitted twice within 1 year with similar diagnoses to different hospitals, this study design was able to isolate hospital signals of performance while minimizing differences among the patients. In these cases, because the same patients had similar admissions at two hospitals, the characteristics of the patients, including their level of social disadvantage, level of education, or degree of underlying illness, were broadly the same. The alignment of the differences that we observed with the results of the CMS hospital-wide readmission measure also adds to evidence that the readmission measure classifies true differences in performance.”
Dr. Krumholz and seven coauthors reported receiving support from contracts with the Center for Medicare and Medicaid Services to develop and reevaluate performance measures that are used for public reporting.
[email protected]
On Twitter @legal_med
FROM NEJM
Key clinical point:
Major finding: The readmission rate was significantly higher among patients admitted to the worst-performing quartile of hospitals than among those admitted to the best-performing quartile (absolute difference in readmission rate, 2.0 percentage points).
Data source: Analysis of Centers for Medicare and Medicaid Services hospital-wide readmission data from July 2014 through June 2015.
Disclosures: Dr. Krumholz and seven coauthors reported receiving support from contracts with the Center for Medicare and Medicaid Services to develop and reevaluate performance measures that are used for public reporting.
DACA program in limbo after White House attitude changes
The fate of the Deferred Action for Childhood Arrivals (DACA) program remains uncertain after an unexpected change of tune by President Donald J. Trump to support of protecting young undocumented immigrants from deportation.
Earlier this month, President Trump announced he would phase out the Obama administration’s DACA program, a policy that protected immigrants who came to the United States as children from deportation and authorized them to work in the United States. In a Sept. 5 statement, President Trump said winding down the DACA program was in the nation’s best interest, and that there can be no principled immigration reform if the executive branch is able to “rewrite or nullify federal laws at will.” The Trump administration allowed Congress 6 months to pass legislation that would replace DACA or preserve some of its provisions before the program terminated in March 2018.
In a series of tweets on Sept. 14, President Trump expressed support for those currently protected under DACA, stating an agreement to address the program was in the works.
“Does anybody really want to throw out good, educated, and accomplished young people who have jobs, some serving in the military?” President Trump tweeted. “They have been in our country for many years through no fault of their own – brought in by parents at young age. Plus BIG border security. ... No deal was made last night on DACA. Massive border security would have to be agreed to in exchange for consent. Would be subject to vote.”
“As Congress debates the best ways to address illegal immigration through strong border security and interior enforcement, DACA should be part of those discussions,” Sen. McConnell said in a statement. “We look forward to receiving the Trump administration’s legislative proposal as we continue our work on these issues.”
DACA demise could strand medical students
The DACA program was created by the Obama administration in 2012 as a way of protecting young, undocumented immigrants from deportation after Congress repeatedly blocked legislation that would develop such a safe haven. The policy allowed about 800,000 young adults brought to the United States illegally as children to work legally in the United States and remain in the country without fear of deportation.
If the Trump administration moves forward with termination, the program’s end will affect the growing number of medical students with DACA status and likely jeopardize the funding invested in their training. Sixty-two medical schools accept applications from DACA applicants, according to the Association of American Medical Colleges. For the 2016-2017 school year, 113 students with DACA status applied to U.S. medical schools, and there were 65 medical students enrolled who had DACA status. AAMC does not collect data on medical students with DACA status; the National Resident Matching Program, likewise, does not collect data on residents with DACA status.
“It’s a tragic decision,” Dr. Kuczewski said of the President’s Sept. 5 announcement to end DACA. “It once again puts a cloud over these young people who DACA has given the first real opportunity to come out of the shadows, be educated, and serve the community. Now they’re returned back to the situation of uncertainty.”
If DACA ends, current DACA medical students may not be able to finish their training, and those close to completion may not be able to use their degrees in the workforce, Dr. Kuczewski said. Since they are not citizens, DACA students do not qualify for federal student loans, so medical schools must find ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Loyola’s Stritch School of Medicine, Dr. Kuczewski said. However, such loan programs require DACA status. Without DACA or another path to citizenship, medical students in the middle of training will not be able to obtain financial aid to finish their training, he said. The work authorization that DACA provided will also be eliminated.
Dr. Kuczewski said his university plans to advocate strongly for Congress to pass legislation to protect DACA youth, such as the Development, Relief, and Education for Alien Minors (DREAM) Act. The legislation, which dates back to 2001 with a renewed bill in 2017, would shield young immigrants from deportation and offer a path to citizenship.
“We are going to advocate strongly because we believe this is common sense,” he said. “You don’t just throw away the talents of these young people and the investments they’ve made in their education and the investments we’ve made in them. DACA has given many people the chance to see these young people as students, as employees, as colleagues, and we hope that helps people to mobilize.”
Medical groups push for DREAM Act passage
Dozens of physician and medical associations are also pushing Congress to pass the DREAM Act. On Sept. 14, more than 50 medical and health care groups, including the American Medical Association, the American Academy of Family Physicians, the American College of Physicians, the American Academy of Dermatology Association, and the American Academy of Pediatrics sent a letter to congressional leaders urging them to pass the bill.
“On behalf of the undersigned health professions organizations, we urge you to ensure that all members of the health care workforce with Deferred Action for Childhood Arrivals (DACA) status are able to continue their employment, education, training, and research, with passage of a permanent legislative remedy, such as the bipartisan, bicameral Dream Act of 2017,” the letter stated. “By providing a legal pathway to permanent residency for undocumented Americans brought to the U.S. as children, Congress can help our country produce a diverse and culturally responsive health care workforce to meet the needs of underserved populations, improve cultural awareness, and promote health equity.”
The Immigration Reform Law Institute praised President Trump’s Sept. 5 decision to rescind the DACA program, calling the policy an affront to Congress and a violation of the U.S. Constitution.
“Contrary to former President Obama’s claims, not only is DACA not authorized by federal statute, but prior to the unlawful program, deferred action has only ever been applied to small numbers of illegal aliens on a case-by-case basis,” Dale Wilcox, executive director, said in a statement. “Applying it to approximately 15% of the illegal alien population was never a proper exercise of the president’s discretion under the Constitution and is inconsistent with the president’s duty to take care that the laws be faithfully executed. By rescinding DACA, President Trump has put an end to the previous administration’s flagrant violation of our immigration laws and its abuse of hard-working American taxpayers.”
[email protected]
On Twitter @legal_med
The fate of the Deferred Action for Childhood Arrivals (DACA) program remains uncertain after an unexpected change of tune by President Donald J. Trump to support of protecting young undocumented immigrants from deportation.
Earlier this month, President Trump announced he would phase out the Obama administration’s DACA program, a policy that protected immigrants who came to the United States as children from deportation and authorized them to work in the United States. In a Sept. 5 statement, President Trump said winding down the DACA program was in the nation’s best interest, and that there can be no principled immigration reform if the executive branch is able to “rewrite or nullify federal laws at will.” The Trump administration allowed Congress 6 months to pass legislation that would replace DACA or preserve some of its provisions before the program terminated in March 2018.
In a series of tweets on Sept. 14, President Trump expressed support for those currently protected under DACA, stating an agreement to address the program was in the works.
“Does anybody really want to throw out good, educated, and accomplished young people who have jobs, some serving in the military?” President Trump tweeted. “They have been in our country for many years through no fault of their own – brought in by parents at young age. Plus BIG border security. ... No deal was made last night on DACA. Massive border security would have to be agreed to in exchange for consent. Would be subject to vote.”
“As Congress debates the best ways to address illegal immigration through strong border security and interior enforcement, DACA should be part of those discussions,” Sen. McConnell said in a statement. “We look forward to receiving the Trump administration’s legislative proposal as we continue our work on these issues.”
DACA demise could strand medical students
The DACA program was created by the Obama administration in 2012 as a way of protecting young, undocumented immigrants from deportation after Congress repeatedly blocked legislation that would develop such a safe haven. The policy allowed about 800,000 young adults brought to the United States illegally as children to work legally in the United States and remain in the country without fear of deportation.
If the Trump administration moves forward with termination, the program’s end will affect the growing number of medical students with DACA status and likely jeopardize the funding invested in their training. Sixty-two medical schools accept applications from DACA applicants, according to the Association of American Medical Colleges. For the 2016-2017 school year, 113 students with DACA status applied to U.S. medical schools, and there were 65 medical students enrolled who had DACA status. AAMC does not collect data on medical students with DACA status; the National Resident Matching Program, likewise, does not collect data on residents with DACA status.
“It’s a tragic decision,” Dr. Kuczewski said of the President’s Sept. 5 announcement to end DACA. “It once again puts a cloud over these young people who DACA has given the first real opportunity to come out of the shadows, be educated, and serve the community. Now they’re returned back to the situation of uncertainty.”
If DACA ends, current DACA medical students may not be able to finish their training, and those close to completion may not be able to use their degrees in the workforce, Dr. Kuczewski said. Since they are not citizens, DACA students do not qualify for federal student loans, so medical schools must find ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Loyola’s Stritch School of Medicine, Dr. Kuczewski said. However, such loan programs require DACA status. Without DACA or another path to citizenship, medical students in the middle of training will not be able to obtain financial aid to finish their training, he said. The work authorization that DACA provided will also be eliminated.
Dr. Kuczewski said his university plans to advocate strongly for Congress to pass legislation to protect DACA youth, such as the Development, Relief, and Education for Alien Minors (DREAM) Act. The legislation, which dates back to 2001 with a renewed bill in 2017, would shield young immigrants from deportation and offer a path to citizenship.
“We are going to advocate strongly because we believe this is common sense,” he said. “You don’t just throw away the talents of these young people and the investments they’ve made in their education and the investments we’ve made in them. DACA has given many people the chance to see these young people as students, as employees, as colleagues, and we hope that helps people to mobilize.”
Medical groups push for DREAM Act passage
Dozens of physician and medical associations are also pushing Congress to pass the DREAM Act. On Sept. 14, more than 50 medical and health care groups, including the American Medical Association, the American Academy of Family Physicians, the American College of Physicians, the American Academy of Dermatology Association, and the American Academy of Pediatrics sent a letter to congressional leaders urging them to pass the bill.
“On behalf of the undersigned health professions organizations, we urge you to ensure that all members of the health care workforce with Deferred Action for Childhood Arrivals (DACA) status are able to continue their employment, education, training, and research, with passage of a permanent legislative remedy, such as the bipartisan, bicameral Dream Act of 2017,” the letter stated. “By providing a legal pathway to permanent residency for undocumented Americans brought to the U.S. as children, Congress can help our country produce a diverse and culturally responsive health care workforce to meet the needs of underserved populations, improve cultural awareness, and promote health equity.”
The Immigration Reform Law Institute praised President Trump’s Sept. 5 decision to rescind the DACA program, calling the policy an affront to Congress and a violation of the U.S. Constitution.
“Contrary to former President Obama’s claims, not only is DACA not authorized by federal statute, but prior to the unlawful program, deferred action has only ever been applied to small numbers of illegal aliens on a case-by-case basis,” Dale Wilcox, executive director, said in a statement. “Applying it to approximately 15% of the illegal alien population was never a proper exercise of the president’s discretion under the Constitution and is inconsistent with the president’s duty to take care that the laws be faithfully executed. By rescinding DACA, President Trump has put an end to the previous administration’s flagrant violation of our immigration laws and its abuse of hard-working American taxpayers.”
[email protected]
On Twitter @legal_med
The fate of the Deferred Action for Childhood Arrivals (DACA) program remains uncertain after an unexpected change of tune by President Donald J. Trump to support of protecting young undocumented immigrants from deportation.
Earlier this month, President Trump announced he would phase out the Obama administration’s DACA program, a policy that protected immigrants who came to the United States as children from deportation and authorized them to work in the United States. In a Sept. 5 statement, President Trump said winding down the DACA program was in the nation’s best interest, and that there can be no principled immigration reform if the executive branch is able to “rewrite or nullify federal laws at will.” The Trump administration allowed Congress 6 months to pass legislation that would replace DACA or preserve some of its provisions before the program terminated in March 2018.
In a series of tweets on Sept. 14, President Trump expressed support for those currently protected under DACA, stating an agreement to address the program was in the works.
“Does anybody really want to throw out good, educated, and accomplished young people who have jobs, some serving in the military?” President Trump tweeted. “They have been in our country for many years through no fault of their own – brought in by parents at young age. Plus BIG border security. ... No deal was made last night on DACA. Massive border security would have to be agreed to in exchange for consent. Would be subject to vote.”
“As Congress debates the best ways to address illegal immigration through strong border security and interior enforcement, DACA should be part of those discussions,” Sen. McConnell said in a statement. “We look forward to receiving the Trump administration’s legislative proposal as we continue our work on these issues.”
DACA demise could strand medical students
The DACA program was created by the Obama administration in 2012 as a way of protecting young, undocumented immigrants from deportation after Congress repeatedly blocked legislation that would develop such a safe haven. The policy allowed about 800,000 young adults brought to the United States illegally as children to work legally in the United States and remain in the country without fear of deportation.
If the Trump administration moves forward with termination, the program’s end will affect the growing number of medical students with DACA status and likely jeopardize the funding invested in their training. Sixty-two medical schools accept applications from DACA applicants, according to the Association of American Medical Colleges. For the 2016-2017 school year, 113 students with DACA status applied to U.S. medical schools, and there were 65 medical students enrolled who had DACA status. AAMC does not collect data on medical students with DACA status; the National Resident Matching Program, likewise, does not collect data on residents with DACA status.
“It’s a tragic decision,” Dr. Kuczewski said of the President’s Sept. 5 announcement to end DACA. “It once again puts a cloud over these young people who DACA has given the first real opportunity to come out of the shadows, be educated, and serve the community. Now they’re returned back to the situation of uncertainty.”
If DACA ends, current DACA medical students may not be able to finish their training, and those close to completion may not be able to use their degrees in the workforce, Dr. Kuczewski said. Since they are not citizens, DACA students do not qualify for federal student loans, so medical schools must find ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Loyola’s Stritch School of Medicine, Dr. Kuczewski said. However, such loan programs require DACA status. Without DACA or another path to citizenship, medical students in the middle of training will not be able to obtain financial aid to finish their training, he said. The work authorization that DACA provided will also be eliminated.
Dr. Kuczewski said his university plans to advocate strongly for Congress to pass legislation to protect DACA youth, such as the Development, Relief, and Education for Alien Minors (DREAM) Act. The legislation, which dates back to 2001 with a renewed bill in 2017, would shield young immigrants from deportation and offer a path to citizenship.
“We are going to advocate strongly because we believe this is common sense,” he said. “You don’t just throw away the talents of these young people and the investments they’ve made in their education and the investments we’ve made in them. DACA has given many people the chance to see these young people as students, as employees, as colleagues, and we hope that helps people to mobilize.”
Medical groups push for DREAM Act passage
Dozens of physician and medical associations are also pushing Congress to pass the DREAM Act. On Sept. 14, more than 50 medical and health care groups, including the American Medical Association, the American Academy of Family Physicians, the American College of Physicians, the American Academy of Dermatology Association, and the American Academy of Pediatrics sent a letter to congressional leaders urging them to pass the bill.
“On behalf of the undersigned health professions organizations, we urge you to ensure that all members of the health care workforce with Deferred Action for Childhood Arrivals (DACA) status are able to continue their employment, education, training, and research, with passage of a permanent legislative remedy, such as the bipartisan, bicameral Dream Act of 2017,” the letter stated. “By providing a legal pathway to permanent residency for undocumented Americans brought to the U.S. as children, Congress can help our country produce a diverse and culturally responsive health care workforce to meet the needs of underserved populations, improve cultural awareness, and promote health equity.”
The Immigration Reform Law Institute praised President Trump’s Sept. 5 decision to rescind the DACA program, calling the policy an affront to Congress and a violation of the U.S. Constitution.
“Contrary to former President Obama’s claims, not only is DACA not authorized by federal statute, but prior to the unlawful program, deferred action has only ever been applied to small numbers of illegal aliens on a case-by-case basis,” Dale Wilcox, executive director, said in a statement. “Applying it to approximately 15% of the illegal alien population was never a proper exercise of the president’s discretion under the Constitution and is inconsistent with the president’s duty to take care that the laws be faithfully executed. By rescinding DACA, President Trump has put an end to the previous administration’s flagrant violation of our immigration laws and its abuse of hard-working American taxpayers.”
[email protected]
On Twitter @legal_med
Regional differences in surgical outcomes could unfairly skew bundled payments
Risk-adjusted adverse outcomes for elective colorectal surgery vary significantly across regions in the United States, and, therefore, regionally based Medicare payments could disadvantage some hospitals.
The findings, presented at the annual Central Surgical Association meeting, suggest that alternative payment models (APMs) should consider regional benchmarks as a variable when evaluating quality and pricing of episodes of care to level the playing field among hospitals, the study authors said.
All hospitals with a minimum of 20 evaluable colorectal resection cases from the master data set regardless of coding quality were identified for comparative outcomes. For hospital analysis, the total number of patients with one or more adverse outcomes (AOs) was tabulated. The total predicted AOs were then set equal to the number of observed events for each hospital by multiplication of the hospital-specific predicted value by the ratio of observed-to-predicted events for the entire final hospital population of patients.
Hospitals were then sorted by the nine Census Bureau regions: region 1 (New England), region 2 (Middle Atlantic), region 3 (South Atlantic), region 4 (East South Central), region 5 (West South Central), region 6 (East North Central), region 7 (West North Central), region 8 (Mountain), and region 9 (Pacific).
Within each region, total patients, total observed AOs, and total predicted AOs were derived from the prediction models. Region-specific standard deviations (SDs) were computed and overall region z scores and risk-adjusted AO rates were calculated for comparison.
A total of 1,497 hospitals had 86,624 patients for the comparative analysis of hospitals with 20 or more qualifying cases. Hospitals averaged 57.9 cases with a median of 43 for the study period. Among the AOs, there were 947 IpD (1.1%), 7,268 prLOS (8.4%), 762 PD90 (0.9%), and 14,552 RA90 (16.8%) patients. An additional 1,130 patients died during or following readmission within the 90-day postdischarge period for total postoperative deaths including inpatient and 90 days following discharge of 2,839 (3.3%). Total patients with one or more AOs were 21,064 (24.3%).
Among the hospitals, 49 (3.3%) had z scores of –2.0 or less. These best-performing hospitals had a median z score of –2.24 and a median risk-adjusted AO rate of 10.8%. A total of 159 hospitals (10.6%) had z scores that were greater than –2.0 but less than or equal to –1.0. These hospitals had a median risk-adjusted AO rate of 15.1%. There were 66 hospitals (4.4%) with z scores greater than +2.0. These suboptimal-performing hospitals had a z score of +2.39 and a median risk-adjusted AO rate of 38.8%. A total of 209 hospitals (14.0%) had z scores greater than or equal to +1.0 but less than +2.0. They had a median risk-adjusted AO rate of 32.5%.
Findings showed a nearly 5-SD difference between the Pacific region and the New England region. In addition, the results showed a 2.5% absolute risk–adjusted adverse outcome rate difference between the top- and the lowest-performing regions.
What findings could mean for bundled payments
The findings raise concerns about a lopsided playing field for hospitals when it comes to bundled payments, according to the study authors.
“What that means is if you have more readmissions and more complications and your historical profile is being used to pay for care going forward, regions of the country with poorer outcomes would get higher prices than those areas with better outcomes,” Dr. Fry, executive vice president, clinical outcomes management, MPA Healthcare Solutions, Chicago, said in an interview.
The Centers for Medicare & Medicaid Services has used performance of the Census Bureau region as a major factor in defining target price at the beginning of the Comprehensive Care for Joint Replacement bundled payment program. Regional performance will become the exclusive basis for the target price as the program matures into successive years, the study authors noted. A colorectal surgery bundle has not yet been proposed by Medicare, but because it’s a common operation with relatively high adverse outcomes rates, it is expected to be included in a future bundled payment strategy, according to the investigators.
Dr. Fry and his coauthors concluded that hospitals and surgeons may find meeting the target price of a bundled payment to improve margins or avoid losses more difficult for any inpatient operation if they are in a best-performing region.
A 2.5% adverse outcome rate difference between regions may not seem like much, but the variance could mean a wide disparity in payments, Dr. Fry said.
“We have done previous research with colon operations and identified that a readmission after an elective colon operation costs about an additional $30,000,” he said. “If cases being done in poorer-performing areas of the country have two or three more readmissions per 100 patients, then it means those areas are going to be paid on average $1,000 more per case than would be the circumstance for those areas where outcomes are better.”
By these parameters, the CMS would basically be rewarding care that is suboptimal in the regions with high adverse outcome rates, he said.
“APMs are going to evolve in health care,” Dr. Fry said. “I feel that regional and local outcomes, as illustrated in this article, are different, and that a national standard for expected outcomes needs to be the benchmark. The national benchmark becomes a method to stimulate hospitals and surgeons to know what the results of their care really are and how they compare nationally.”
Perspectives on the study
However, it remains unclear whether adjustment for quality measures should be based on regions, and, if so, how those regions should be broken down, said Dr. Whitcomb, who is cofounder and past president of the Society of Hospital Medicine. Another question is whether adjustments should take into consideration the characteristics of hospitals, he said, for example, the general demographics of patients who visit academic medical centers, compared with the demographics of community hospitals. Dr. Whitcomb also noted that programs such as the Hospital Readmissions Reduction Program has faced criticism for not factoring in the disproportionately high share of low socioeconomic status patients at some hospitals.
“The paper raises the important issue of comparing apples to apples when quality measures are used to determine payment under alternative payment models,” Dr. Whitcomb said in an interview. “But a number of questions remain about how risk should be adjusted and how benchmarking should occur between hospitals.”
“The overall average adverse outcome in the study was 24.3%, but 16.8% of that 24% is due to readmissions,” he said in an interview. “Length of stay and readmissions are correlated – people who tend to have long lengths of stay tend to be readmitted. If you add those two rates together in the study, almost all of the outcome rate is the length of stay and readmissions. You could argue [that] mortality [should] be more heavily weighted than length of stay and readmissions.”
In regard to adjusting risk by region, there is good research that utilization of procedures varies dramatically by region and that some of this variation may have more to do with overutilization of procedures, Dr. Pitt added.
“I would think that risk adjusting for type of operation, diagnosis, and socioeconomic status –across the country – would be more appropriate than risk adjusting by region where there may be major differences in patient selection and indication for operation,” he said.
For example, there is currently an international debate about the management of diverticulitis, including whether and when to operate as well as what procedure(s) to perform.
“It may be in one region, there’s a very low threshold to operate, whereas in another region, there’s a high threshold to operate,” he said. “And the operations that are done may be very different in one region than another.”
Dr. Fry and his colleagues are planning future research in this area, and he said he hopes their studies will impact how the CMS rolls out its bundled payment programs in the future.
“What we’re trying to stimulate is for payment models to be nationally indexed and not regionally indexed,” he said. “CMS is doing that now with [Medicare Severity–Diagnosis Related Groups]. They are paying a price for a total joint replacement, a price for a colon resection, a price for a heart operation – and they do make adjustments based on the local wage and price index, but the core payment is linked to a national payment model, and that’s what we would like to see happen with the bundled payment initiative.”
[email protected]
On Twitter @legal_med
Risk-adjusted adverse outcomes for elective colorectal surgery vary significantly across regions in the United States, and, therefore, regionally based Medicare payments could disadvantage some hospitals.
The findings, presented at the annual Central Surgical Association meeting, suggest that alternative payment models (APMs) should consider regional benchmarks as a variable when evaluating quality and pricing of episodes of care to level the playing field among hospitals, the study authors said.
All hospitals with a minimum of 20 evaluable colorectal resection cases from the master data set regardless of coding quality were identified for comparative outcomes. For hospital analysis, the total number of patients with one or more adverse outcomes (AOs) was tabulated. The total predicted AOs were then set equal to the number of observed events for each hospital by multiplication of the hospital-specific predicted value by the ratio of observed-to-predicted events for the entire final hospital population of patients.
Hospitals were then sorted by the nine Census Bureau regions: region 1 (New England), region 2 (Middle Atlantic), region 3 (South Atlantic), region 4 (East South Central), region 5 (West South Central), region 6 (East North Central), region 7 (West North Central), region 8 (Mountain), and region 9 (Pacific).
Within each region, total patients, total observed AOs, and total predicted AOs were derived from the prediction models. Region-specific standard deviations (SDs) were computed and overall region z scores and risk-adjusted AO rates were calculated for comparison.
A total of 1,497 hospitals had 86,624 patients for the comparative analysis of hospitals with 20 or more qualifying cases. Hospitals averaged 57.9 cases with a median of 43 for the study period. Among the AOs, there were 947 IpD (1.1%), 7,268 prLOS (8.4%), 762 PD90 (0.9%), and 14,552 RA90 (16.8%) patients. An additional 1,130 patients died during or following readmission within the 90-day postdischarge period for total postoperative deaths including inpatient and 90 days following discharge of 2,839 (3.3%). Total patients with one or more AOs were 21,064 (24.3%).
Among the hospitals, 49 (3.3%) had z scores of –2.0 or less. These best-performing hospitals had a median z score of –2.24 and a median risk-adjusted AO rate of 10.8%. A total of 159 hospitals (10.6%) had z scores that were greater than –2.0 but less than or equal to –1.0. These hospitals had a median risk-adjusted AO rate of 15.1%. There were 66 hospitals (4.4%) with z scores greater than +2.0. These suboptimal-performing hospitals had a z score of +2.39 and a median risk-adjusted AO rate of 38.8%. A total of 209 hospitals (14.0%) had z scores greater than or equal to +1.0 but less than +2.0. They had a median risk-adjusted AO rate of 32.5%.
Findings showed a nearly 5-SD difference between the Pacific region and the New England region. In addition, the results showed a 2.5% absolute risk–adjusted adverse outcome rate difference between the top- and the lowest-performing regions.
What findings could mean for bundled payments
The findings raise concerns about a lopsided playing field for hospitals when it comes to bundled payments, according to the study authors.
“What that means is if you have more readmissions and more complications and your historical profile is being used to pay for care going forward, regions of the country with poorer outcomes would get higher prices than those areas with better outcomes,” Dr. Fry, executive vice president, clinical outcomes management, MPA Healthcare Solutions, Chicago, said in an interview.
The Centers for Medicare & Medicaid Services has used performance of the Census Bureau region as a major factor in defining target price at the beginning of the Comprehensive Care for Joint Replacement bundled payment program. Regional performance will become the exclusive basis for the target price as the program matures into successive years, the study authors noted. A colorectal surgery bundle has not yet been proposed by Medicare, but because it’s a common operation with relatively high adverse outcomes rates, it is expected to be included in a future bundled payment strategy, according to the investigators.
Dr. Fry and his coauthors concluded that hospitals and surgeons may find meeting the target price of a bundled payment to improve margins or avoid losses more difficult for any inpatient operation if they are in a best-performing region.
A 2.5% adverse outcome rate difference between regions may not seem like much, but the variance could mean a wide disparity in payments, Dr. Fry said.
“We have done previous research with colon operations and identified that a readmission after an elective colon operation costs about an additional $30,000,” he said. “If cases being done in poorer-performing areas of the country have two or three more readmissions per 100 patients, then it means those areas are going to be paid on average $1,000 more per case than would be the circumstance for those areas where outcomes are better.”
By these parameters, the CMS would basically be rewarding care that is suboptimal in the regions with high adverse outcome rates, he said.
“APMs are going to evolve in health care,” Dr. Fry said. “I feel that regional and local outcomes, as illustrated in this article, are different, and that a national standard for expected outcomes needs to be the benchmark. The national benchmark becomes a method to stimulate hospitals and surgeons to know what the results of their care really are and how they compare nationally.”
Perspectives on the study
However, it remains unclear whether adjustment for quality measures should be based on regions, and, if so, how those regions should be broken down, said Dr. Whitcomb, who is cofounder and past president of the Society of Hospital Medicine. Another question is whether adjustments should take into consideration the characteristics of hospitals, he said, for example, the general demographics of patients who visit academic medical centers, compared with the demographics of community hospitals. Dr. Whitcomb also noted that programs such as the Hospital Readmissions Reduction Program has faced criticism for not factoring in the disproportionately high share of low socioeconomic status patients at some hospitals.
“The paper raises the important issue of comparing apples to apples when quality measures are used to determine payment under alternative payment models,” Dr. Whitcomb said in an interview. “But a number of questions remain about how risk should be adjusted and how benchmarking should occur between hospitals.”
“The overall average adverse outcome in the study was 24.3%, but 16.8% of that 24% is due to readmissions,” he said in an interview. “Length of stay and readmissions are correlated – people who tend to have long lengths of stay tend to be readmitted. If you add those two rates together in the study, almost all of the outcome rate is the length of stay and readmissions. You could argue [that] mortality [should] be more heavily weighted than length of stay and readmissions.”
In regard to adjusting risk by region, there is good research that utilization of procedures varies dramatically by region and that some of this variation may have more to do with overutilization of procedures, Dr. Pitt added.
“I would think that risk adjusting for type of operation, diagnosis, and socioeconomic status –across the country – would be more appropriate than risk adjusting by region where there may be major differences in patient selection and indication for operation,” he said.
For example, there is currently an international debate about the management of diverticulitis, including whether and when to operate as well as what procedure(s) to perform.
“It may be in one region, there’s a very low threshold to operate, whereas in another region, there’s a high threshold to operate,” he said. “And the operations that are done may be very different in one region than another.”
Dr. Fry and his colleagues are planning future research in this area, and he said he hopes their studies will impact how the CMS rolls out its bundled payment programs in the future.
“What we’re trying to stimulate is for payment models to be nationally indexed and not regionally indexed,” he said. “CMS is doing that now with [Medicare Severity–Diagnosis Related Groups]. They are paying a price for a total joint replacement, a price for a colon resection, a price for a heart operation – and they do make adjustments based on the local wage and price index, but the core payment is linked to a national payment model, and that’s what we would like to see happen with the bundled payment initiative.”
[email protected]
On Twitter @legal_med
Risk-adjusted adverse outcomes for elective colorectal surgery vary significantly across regions in the United States, and, therefore, regionally based Medicare payments could disadvantage some hospitals.
The findings, presented at the annual Central Surgical Association meeting, suggest that alternative payment models (APMs) should consider regional benchmarks as a variable when evaluating quality and pricing of episodes of care to level the playing field among hospitals, the study authors said.
All hospitals with a minimum of 20 evaluable colorectal resection cases from the master data set regardless of coding quality were identified for comparative outcomes. For hospital analysis, the total number of patients with one or more adverse outcomes (AOs) was tabulated. The total predicted AOs were then set equal to the number of observed events for each hospital by multiplication of the hospital-specific predicted value by the ratio of observed-to-predicted events for the entire final hospital population of patients.
Hospitals were then sorted by the nine Census Bureau regions: region 1 (New England), region 2 (Middle Atlantic), region 3 (South Atlantic), region 4 (East South Central), region 5 (West South Central), region 6 (East North Central), region 7 (West North Central), region 8 (Mountain), and region 9 (Pacific).
Within each region, total patients, total observed AOs, and total predicted AOs were derived from the prediction models. Region-specific standard deviations (SDs) were computed and overall region z scores and risk-adjusted AO rates were calculated for comparison.
A total of 1,497 hospitals had 86,624 patients for the comparative analysis of hospitals with 20 or more qualifying cases. Hospitals averaged 57.9 cases with a median of 43 for the study period. Among the AOs, there were 947 IpD (1.1%), 7,268 prLOS (8.4%), 762 PD90 (0.9%), and 14,552 RA90 (16.8%) patients. An additional 1,130 patients died during or following readmission within the 90-day postdischarge period for total postoperative deaths including inpatient and 90 days following discharge of 2,839 (3.3%). Total patients with one or more AOs were 21,064 (24.3%).
Among the hospitals, 49 (3.3%) had z scores of –2.0 or less. These best-performing hospitals had a median z score of –2.24 and a median risk-adjusted AO rate of 10.8%. A total of 159 hospitals (10.6%) had z scores that were greater than –2.0 but less than or equal to –1.0. These hospitals had a median risk-adjusted AO rate of 15.1%. There were 66 hospitals (4.4%) with z scores greater than +2.0. These suboptimal-performing hospitals had a z score of +2.39 and a median risk-adjusted AO rate of 38.8%. A total of 209 hospitals (14.0%) had z scores greater than or equal to +1.0 but less than +2.0. They had a median risk-adjusted AO rate of 32.5%.
Findings showed a nearly 5-SD difference between the Pacific region and the New England region. In addition, the results showed a 2.5% absolute risk–adjusted adverse outcome rate difference between the top- and the lowest-performing regions.
What findings could mean for bundled payments
The findings raise concerns about a lopsided playing field for hospitals when it comes to bundled payments, according to the study authors.
“What that means is if you have more readmissions and more complications and your historical profile is being used to pay for care going forward, regions of the country with poorer outcomes would get higher prices than those areas with better outcomes,” Dr. Fry, executive vice president, clinical outcomes management, MPA Healthcare Solutions, Chicago, said in an interview.
The Centers for Medicare & Medicaid Services has used performance of the Census Bureau region as a major factor in defining target price at the beginning of the Comprehensive Care for Joint Replacement bundled payment program. Regional performance will become the exclusive basis for the target price as the program matures into successive years, the study authors noted. A colorectal surgery bundle has not yet been proposed by Medicare, but because it’s a common operation with relatively high adverse outcomes rates, it is expected to be included in a future bundled payment strategy, according to the investigators.
Dr. Fry and his coauthors concluded that hospitals and surgeons may find meeting the target price of a bundled payment to improve margins or avoid losses more difficult for any inpatient operation if they are in a best-performing region.
A 2.5% adverse outcome rate difference between regions may not seem like much, but the variance could mean a wide disparity in payments, Dr. Fry said.
“We have done previous research with colon operations and identified that a readmission after an elective colon operation costs about an additional $30,000,” he said. “If cases being done in poorer-performing areas of the country have two or three more readmissions per 100 patients, then it means those areas are going to be paid on average $1,000 more per case than would be the circumstance for those areas where outcomes are better.”
By these parameters, the CMS would basically be rewarding care that is suboptimal in the regions with high adverse outcome rates, he said.
“APMs are going to evolve in health care,” Dr. Fry said. “I feel that regional and local outcomes, as illustrated in this article, are different, and that a national standard for expected outcomes needs to be the benchmark. The national benchmark becomes a method to stimulate hospitals and surgeons to know what the results of their care really are and how they compare nationally.”
Perspectives on the study
However, it remains unclear whether adjustment for quality measures should be based on regions, and, if so, how those regions should be broken down, said Dr. Whitcomb, who is cofounder and past president of the Society of Hospital Medicine. Another question is whether adjustments should take into consideration the characteristics of hospitals, he said, for example, the general demographics of patients who visit academic medical centers, compared with the demographics of community hospitals. Dr. Whitcomb also noted that programs such as the Hospital Readmissions Reduction Program has faced criticism for not factoring in the disproportionately high share of low socioeconomic status patients at some hospitals.
“The paper raises the important issue of comparing apples to apples when quality measures are used to determine payment under alternative payment models,” Dr. Whitcomb said in an interview. “But a number of questions remain about how risk should be adjusted and how benchmarking should occur between hospitals.”
“The overall average adverse outcome in the study was 24.3%, but 16.8% of that 24% is due to readmissions,” he said in an interview. “Length of stay and readmissions are correlated – people who tend to have long lengths of stay tend to be readmitted. If you add those two rates together in the study, almost all of the outcome rate is the length of stay and readmissions. You could argue [that] mortality [should] be more heavily weighted than length of stay and readmissions.”
In regard to adjusting risk by region, there is good research that utilization of procedures varies dramatically by region and that some of this variation may have more to do with overutilization of procedures, Dr. Pitt added.
“I would think that risk adjusting for type of operation, diagnosis, and socioeconomic status –across the country – would be more appropriate than risk adjusting by region where there may be major differences in patient selection and indication for operation,” he said.
For example, there is currently an international debate about the management of diverticulitis, including whether and when to operate as well as what procedure(s) to perform.
“It may be in one region, there’s a very low threshold to operate, whereas in another region, there’s a high threshold to operate,” he said. “And the operations that are done may be very different in one region than another.”
Dr. Fry and his colleagues are planning future research in this area, and he said he hopes their studies will impact how the CMS rolls out its bundled payment programs in the future.
“What we’re trying to stimulate is for payment models to be nationally indexed and not regionally indexed,” he said. “CMS is doing that now with [Medicare Severity–Diagnosis Related Groups]. They are paying a price for a total joint replacement, a price for a colon resection, a price for a heart operation – and they do make adjustments based on the local wage and price index, but the core payment is linked to a national payment model, and that’s what we would like to see happen with the bundled payment initiative.”
[email protected]
On Twitter @legal_med
Analysis: Actual cancer drug R&D costs are far less than widely publicized sum
Research and development costs for cancer drugs are far lower than previous estimates, according to a new analysis, casting doubt on the common justifications by drug companies for the high prices of such medications.
The median cost to develop a cancer drug was $648 million, compared with the widely publicized figure of $2.7 billion, the study’s researchers said.
Lead investigator Vinay Prasad, MD, of Oregon Health and Science University in Portland, and Sham Mailankody, MBBS, of Memorial Sloan Kettering Cancer Center in New York, studied U.S. Securities and Exchange Commission filings for drug companies with no drugs on the market that received Food and Drug Administration approval for a cancer drug from Jan. 1, 2006, through Dec. 31, 2015. Researchers estimated cumulative research and development spending from initiation of drug development activity to date of approval. Earnings were identified from the time of approval to the present. Ten drugs and companies were included in the analysis.
Investigators found that the median time to develop a drug was 7.3 years. Five companies (50%) developed drugs that received accelerated approval from the FDA, and five drugs (50%) received regular approval. Five of the 10 drugs (50%) act on a novel target (ibrutinib, brentuximab vedotin, ruxolitinib, cabozantinib, and eculizumab), whereas the other five drugs (50%) are next-in-class drugs with a mechanism of action similar to that of a previously approved drug.
Results showed the median cost of developing a single drug in 2017 U.S. dollars was $648 million (range, $157.3 million to $1.95 billion), and the mean development cost was $719.8 million (JAMA Intern Med. 2017 Sep 11 doi: 10.1001/jamainternmed.2017.3601).
Drugs that received accelerated approval cost less to develop than did those that received regular approval, although that finding was not statistically significant, according to the study. From the time of approval to December 2016 – or until the company sold or licensed the compound to another company – the total revenue of the 10 drugs was $67 billion. The median revenue for these companies was $1.66 billion (range, $204.1 million to $22.3 billion), and the average revenue was $6.7 billion. Nine of the 10 drugs had revenues greater than their research and development spending. Revenue from sales of four drugs (ponatinib, ibrutinib, enzalutamide, and eculizumab) was more than 10-fold higher than research and development spending.
The analysis offers a transparent estimate of research and development spending on cancer drugs, the study authors said, and has implications for the current debate on drug pricing. They noted that prior estimates for the cost to develop one new drug range from $320 million to $2.7 billion, markedly lower than the study’s $648 million finding.
“In a short period, development cost is more than recouped, and some companies boast more than a 10-fold higher revenue than [research and development] spending – a sum not seen in other sectors of the economy,” the researchers explained. “Future work regarding the cost of cancer drugs may be facilitated by more, not less, transparency in the biopharmaceutical industry.”
Regarding their work, the authors noted that the data set is small, the filings studied are subject to strict guidelines and regulation, the analysis pertains only to cancer drugs, and potential tax breaks applied to research and development costs for drug companies are not accounted for.
Dr. Mailankody reported serving as a principal investigator for clinical trials with research funding from Juno Therapeutics and Takeda Oncology. He also reported receiving personal fees for speaking at the Wedbush Pacgrow Healthcare Conference 2016. No other disclosures were reported.
[email protected]
On Twitter @legal_med
To counter increasing public alarm over high drug prices, industry leaders regularly assert that the substantial investment in researching and developing new products, and the riskiness of that enterprise, justify charging Americans the highest prices in the world for medicines.
To support the assertion, the industry’s trade group relies on an industry-funded study first produced in 1979 by the Tufts University Center for the Study of Drug Development. The most recent iteration of the study, updated in 2014, claims it takes more than 10 years and nearly $2.7 billion in capital to develop a single drug. In inflation-adjusted dollars, the study’s estimate for developing a new drug has more than doubled in the past decade and is more than 10 times the original 1979 figure.
In this issue of JAMA Internal Medicine, study authors Vinay Prasad, MD, MPH, and Sham Mailankody, MBBS, report that the actual cost of developing a new drug is approximately one-fourth the Tufts study estimate. The implications of the present study seem clear. Current pharmaceutical industry pricing policies are unrelated to the cost of research and development. Policymakers can safely take steps to rein in drug prices without fear of jeopardizing innovation.
Merrill Goozner is editor emeritus for Modern Healthcare in Chicago. He is also author of “The $800 Million Pill: The Truth Behind the Cost of New Drugs.” He made these remarks in an invited commentary accompanying the study (JAMA Intern Med. 2017 Sep 11 doi: 10.1001/jamainternmed.2017.4997).
To counter increasing public alarm over high drug prices, industry leaders regularly assert that the substantial investment in researching and developing new products, and the riskiness of that enterprise, justify charging Americans the highest prices in the world for medicines.
To support the assertion, the industry’s trade group relies on an industry-funded study first produced in 1979 by the Tufts University Center for the Study of Drug Development. The most recent iteration of the study, updated in 2014, claims it takes more than 10 years and nearly $2.7 billion in capital to develop a single drug. In inflation-adjusted dollars, the study’s estimate for developing a new drug has more than doubled in the past decade and is more than 10 times the original 1979 figure.
In this issue of JAMA Internal Medicine, study authors Vinay Prasad, MD, MPH, and Sham Mailankody, MBBS, report that the actual cost of developing a new drug is approximately one-fourth the Tufts study estimate. The implications of the present study seem clear. Current pharmaceutical industry pricing policies are unrelated to the cost of research and development. Policymakers can safely take steps to rein in drug prices without fear of jeopardizing innovation.
Merrill Goozner is editor emeritus for Modern Healthcare in Chicago. He is also author of “The $800 Million Pill: The Truth Behind the Cost of New Drugs.” He made these remarks in an invited commentary accompanying the study (JAMA Intern Med. 2017 Sep 11 doi: 10.1001/jamainternmed.2017.4997).
To counter increasing public alarm over high drug prices, industry leaders regularly assert that the substantial investment in researching and developing new products, and the riskiness of that enterprise, justify charging Americans the highest prices in the world for medicines.
To support the assertion, the industry’s trade group relies on an industry-funded study first produced in 1979 by the Tufts University Center for the Study of Drug Development. The most recent iteration of the study, updated in 2014, claims it takes more than 10 years and nearly $2.7 billion in capital to develop a single drug. In inflation-adjusted dollars, the study’s estimate for developing a new drug has more than doubled in the past decade and is more than 10 times the original 1979 figure.
In this issue of JAMA Internal Medicine, study authors Vinay Prasad, MD, MPH, and Sham Mailankody, MBBS, report that the actual cost of developing a new drug is approximately one-fourth the Tufts study estimate. The implications of the present study seem clear. Current pharmaceutical industry pricing policies are unrelated to the cost of research and development. Policymakers can safely take steps to rein in drug prices without fear of jeopardizing innovation.
Merrill Goozner is editor emeritus for Modern Healthcare in Chicago. He is also author of “The $800 Million Pill: The Truth Behind the Cost of New Drugs.” He made these remarks in an invited commentary accompanying the study (JAMA Intern Med. 2017 Sep 11 doi: 10.1001/jamainternmed.2017.4997).
Research and development costs for cancer drugs are far lower than previous estimates, according to a new analysis, casting doubt on the common justifications by drug companies for the high prices of such medications.
The median cost to develop a cancer drug was $648 million, compared with the widely publicized figure of $2.7 billion, the study’s researchers said.
Lead investigator Vinay Prasad, MD, of Oregon Health and Science University in Portland, and Sham Mailankody, MBBS, of Memorial Sloan Kettering Cancer Center in New York, studied U.S. Securities and Exchange Commission filings for drug companies with no drugs on the market that received Food and Drug Administration approval for a cancer drug from Jan. 1, 2006, through Dec. 31, 2015. Researchers estimated cumulative research and development spending from initiation of drug development activity to date of approval. Earnings were identified from the time of approval to the present. Ten drugs and companies were included in the analysis.
Investigators found that the median time to develop a drug was 7.3 years. Five companies (50%) developed drugs that received accelerated approval from the FDA, and five drugs (50%) received regular approval. Five of the 10 drugs (50%) act on a novel target (ibrutinib, brentuximab vedotin, ruxolitinib, cabozantinib, and eculizumab), whereas the other five drugs (50%) are next-in-class drugs with a mechanism of action similar to that of a previously approved drug.
Results showed the median cost of developing a single drug in 2017 U.S. dollars was $648 million (range, $157.3 million to $1.95 billion), and the mean development cost was $719.8 million (JAMA Intern Med. 2017 Sep 11 doi: 10.1001/jamainternmed.2017.3601).
Drugs that received accelerated approval cost less to develop than did those that received regular approval, although that finding was not statistically significant, according to the study. From the time of approval to December 2016 – or until the company sold or licensed the compound to another company – the total revenue of the 10 drugs was $67 billion. The median revenue for these companies was $1.66 billion (range, $204.1 million to $22.3 billion), and the average revenue was $6.7 billion. Nine of the 10 drugs had revenues greater than their research and development spending. Revenue from sales of four drugs (ponatinib, ibrutinib, enzalutamide, and eculizumab) was more than 10-fold higher than research and development spending.
The analysis offers a transparent estimate of research and development spending on cancer drugs, the study authors said, and has implications for the current debate on drug pricing. They noted that prior estimates for the cost to develop one new drug range from $320 million to $2.7 billion, markedly lower than the study’s $648 million finding.
“In a short period, development cost is more than recouped, and some companies boast more than a 10-fold higher revenue than [research and development] spending – a sum not seen in other sectors of the economy,” the researchers explained. “Future work regarding the cost of cancer drugs may be facilitated by more, not less, transparency in the biopharmaceutical industry.”
Regarding their work, the authors noted that the data set is small, the filings studied are subject to strict guidelines and regulation, the analysis pertains only to cancer drugs, and potential tax breaks applied to research and development costs for drug companies are not accounted for.
Dr. Mailankody reported serving as a principal investigator for clinical trials with research funding from Juno Therapeutics and Takeda Oncology. He also reported receiving personal fees for speaking at the Wedbush Pacgrow Healthcare Conference 2016. No other disclosures were reported.
[email protected]
On Twitter @legal_med
Research and development costs for cancer drugs are far lower than previous estimates, according to a new analysis, casting doubt on the common justifications by drug companies for the high prices of such medications.
The median cost to develop a cancer drug was $648 million, compared with the widely publicized figure of $2.7 billion, the study’s researchers said.
Lead investigator Vinay Prasad, MD, of Oregon Health and Science University in Portland, and Sham Mailankody, MBBS, of Memorial Sloan Kettering Cancer Center in New York, studied U.S. Securities and Exchange Commission filings for drug companies with no drugs on the market that received Food and Drug Administration approval for a cancer drug from Jan. 1, 2006, through Dec. 31, 2015. Researchers estimated cumulative research and development spending from initiation of drug development activity to date of approval. Earnings were identified from the time of approval to the present. Ten drugs and companies were included in the analysis.
Investigators found that the median time to develop a drug was 7.3 years. Five companies (50%) developed drugs that received accelerated approval from the FDA, and five drugs (50%) received regular approval. Five of the 10 drugs (50%) act on a novel target (ibrutinib, brentuximab vedotin, ruxolitinib, cabozantinib, and eculizumab), whereas the other five drugs (50%) are next-in-class drugs with a mechanism of action similar to that of a previously approved drug.
Results showed the median cost of developing a single drug in 2017 U.S. dollars was $648 million (range, $157.3 million to $1.95 billion), and the mean development cost was $719.8 million (JAMA Intern Med. 2017 Sep 11 doi: 10.1001/jamainternmed.2017.3601).
Drugs that received accelerated approval cost less to develop than did those that received regular approval, although that finding was not statistically significant, according to the study. From the time of approval to December 2016 – or until the company sold or licensed the compound to another company – the total revenue of the 10 drugs was $67 billion. The median revenue for these companies was $1.66 billion (range, $204.1 million to $22.3 billion), and the average revenue was $6.7 billion. Nine of the 10 drugs had revenues greater than their research and development spending. Revenue from sales of four drugs (ponatinib, ibrutinib, enzalutamide, and eculizumab) was more than 10-fold higher than research and development spending.
The analysis offers a transparent estimate of research and development spending on cancer drugs, the study authors said, and has implications for the current debate on drug pricing. They noted that prior estimates for the cost to develop one new drug range from $320 million to $2.7 billion, markedly lower than the study’s $648 million finding.
“In a short period, development cost is more than recouped, and some companies boast more than a 10-fold higher revenue than [research and development] spending – a sum not seen in other sectors of the economy,” the researchers explained. “Future work regarding the cost of cancer drugs may be facilitated by more, not less, transparency in the biopharmaceutical industry.”
Regarding their work, the authors noted that the data set is small, the filings studied are subject to strict guidelines and regulation, the analysis pertains only to cancer drugs, and potential tax breaks applied to research and development costs for drug companies are not accounted for.
Dr. Mailankody reported serving as a principal investigator for clinical trials with research funding from Juno Therapeutics and Takeda Oncology. He also reported receiving personal fees for speaking at the Wedbush Pacgrow Healthcare Conference 2016. No other disclosures were reported.
[email protected]
On Twitter @legal_med
FROM JAMA INTERNAL MEDICINE
Key clinical point:
Major finding: The median cost to develop a cancer drug was $648 million, compared with the widely publicized figure of $2.7 billion.
Data source: A case study of U.S. Securities and Exchange Commission filings for drug companies that received approval by the Food and Drug Administration for a cancer drug from Jan. 1, 2006, through Dec. 31, 2015.
Disclosures: Dr. Mailankody reported serving as principal investigator for clinical trials with research funding from Juno Therapeutics and Takeda Oncology. He also reported receiving personal fees for speaking at the Wedbush PacGrow Healthcare Conference 2016. No other disclosures were reported.
Trump administration ends DACA program, stranding medical students
President Trump has ended the Obama administration’s Deferred Action for Childhood Arrivals (DACA) program, a policy that protected immigrants who came to the United States as children from deportation and authorized them to work in the United States.
In a Sept. 5 press conference, Attorney General Jeff Sessions called the DACA program an unconstitutional overreach of executive branch power by the former administration that deliberately sought to undermine the legislative branch. Rollback of the DACA program will begin immediately, Mr. Sessions said, with the program expiring completely on March 5, 2018.
“The effect of this unilateral executive amnesty, among other things, contributed to a surge of minors at the southern border that yielded terrible humanitarian consequences,” Mr. Sessions said during the press conference. “[DACA has] also denied jobs to hundreds of thousands of Americans by allowing those same illegal aliens to take those jobs. To have a lawful system of immigration that serves the national interest, we cannot admit everyone. Therefore the nation must set and enforce a limit on how many immigrants we admit and that means all cannot be accepted.”
In a statement issued shortly after the press conference, President Trump said winding down the DACA program is in the nation’s best interest, and that there can be no principled immigration reform if the executive branch is able to “rewrite or nullify federal laws at will.
“As President, my highest duty is to defend the American people and the Constitution of the United States of America,” President Trump said in the statement. “At the same time, I do not favor punishing children, most of whom are now adults, for the actions of their parents. But we must also recognize that we are nation of opportunity because we are a nation of laws.”
The DACA program was created by the Obama administration in 2012 as a way of protecting young, undocumented immigrants from deportation after Congress repeatedly blocked legislation that would develop such a safe haven. The policy allowed about 800,000 young adults brought to the United States illegally as children to work legally in the U.S. and remain in the country without the fear of deportation.
The program’s end will affect the growing number of medical students with DACA status and likely jeopardize the funding invested in their training. Sixty-two medical schools accept applications from DACA applicants, according to the Association of American Medical Colleges (AAMC). For the 2016 -2017 school year, 113 students with DACA status applied to US medical schools, and there were 65 medical students enrolled who had DACA status. AAMC does not collect data on medical students with DACA status; the National Resident Matching Program, likewise, does not collect data on residents with DACA status.
Loyola University in Chicago is one institute that could be significantly impacted by recension of DACA. The university has accepted more students with DACA status than any other U.S. medical school, and currently has 32 DACA students attending, said Mark Kuczewski, Ph.D., chair of medical education at Loyola University.
“It’s a tragic decision,” he said in an interview. “It once again puts a cloud over these young people who DACA has given the first real opportunity to come out of the shadows, be educated, and serve the community. Now they’re returned back to the situation of uncertainty.”
The decision to end DACA means that current DACA medical students may not be able to finish their training and that those close to completion may not be able to use their degrees in the workforce, Dr. Kuczewski said. Since they are not citizens, DACA students do not qualify for federal student loans, so medical schools must find ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Loyola’s Stritch School of Medicine, Dr. Kuczewski said. However, such loan programs require DACA status. Without DACA or another path to citizenship, medical students in the middle of training will not be able to obtain financial aid to finish their training, he said. The work authorization that DACA provided will also be eliminated.
Dr. Kuczewski said his university plans to advocate strongly for Congress to pass legislation to protect DACA youth, such as the Dream Act of 2017.
“We are going to advocate strongly because we believe this is common sense,” he said. “You don’t just throw away the talents of these young people and the investments they’ve made in their education and the investments we’ve made in them. DACA has given many people the chance to see these young people as students, as employees, as colleagues, and we hope that helps people to mobilize.”
In a statement, Jack Ende, MD, president of the American College of Physicians, said President Trump’s decision to end the DACA program threatens to deny the country the talents of more than half a million individuals making enormous contributions and will also undermine public health and medical education.
“Today’s executive order has the potential to gravely impact public health,” Dr. Ende said in the statement. “We know that noncitizens and undocumented immigrants are more likely to lack health insurance coverage. If the nearly 800,000 people who are currently benefiting from DACA have their protections removed, many will avoid seeking health care in order to reduce the risk of detection and deportation. … Those who seek to serve in the health care professions will be denied that opportunity.”
The Immigration Reform Law Institute praised President Trump’s decision to rescind the DACA program, calling the policy an affront to Congress and a violation of the U.S. Constitution.
“Contrary to former President Obama’s claims, not only is DACA not authorized by federal statute, but prior to the unlawful program, deferred action has only ever been applied to small numbers of illegal aliens on a case-by-case basis,” Dale Wilcox, executive director, said in a statement. “Applying it to approximately 15% of the illegal alien population was never a proper exercise of the president’s discretion under the Constitution and is inconsistent with the president’s duty to take care that the laws be faithfully executed. By rescinding DACA, President Trump has put an end to the previous administration’s flagrant violation of our immigration laws and its abuse of hard-working American taxpayers.”
In a memorandum issued Sept. 5, the Department of Homeland Security said it will begin winding down the DACA program, while providing a limited window in which it will adjudicate certain requests for DACA and associated applications. DHS will adjudicate, on an individual, case-by-case basis, properly filed pending DACA initial requests and associated applications for employment authorization documents that have been accepted by the department as of Sept.5, 2017, according to the memorandum. All DACA initial requests and associated applications filed after this date will be rejected.
[email protected]
On Twitter @legal_med
President Trump has ended the Obama administration’s Deferred Action for Childhood Arrivals (DACA) program, a policy that protected immigrants who came to the United States as children from deportation and authorized them to work in the United States.
In a Sept. 5 press conference, Attorney General Jeff Sessions called the DACA program an unconstitutional overreach of executive branch power by the former administration that deliberately sought to undermine the legislative branch. Rollback of the DACA program will begin immediately, Mr. Sessions said, with the program expiring completely on March 5, 2018.
“The effect of this unilateral executive amnesty, among other things, contributed to a surge of minors at the southern border that yielded terrible humanitarian consequences,” Mr. Sessions said during the press conference. “[DACA has] also denied jobs to hundreds of thousands of Americans by allowing those same illegal aliens to take those jobs. To have a lawful system of immigration that serves the national interest, we cannot admit everyone. Therefore the nation must set and enforce a limit on how many immigrants we admit and that means all cannot be accepted.”
In a statement issued shortly after the press conference, President Trump said winding down the DACA program is in the nation’s best interest, and that there can be no principled immigration reform if the executive branch is able to “rewrite or nullify federal laws at will.
“As President, my highest duty is to defend the American people and the Constitution of the United States of America,” President Trump said in the statement. “At the same time, I do not favor punishing children, most of whom are now adults, for the actions of their parents. But we must also recognize that we are nation of opportunity because we are a nation of laws.”
The DACA program was created by the Obama administration in 2012 as a way of protecting young, undocumented immigrants from deportation after Congress repeatedly blocked legislation that would develop such a safe haven. The policy allowed about 800,000 young adults brought to the United States illegally as children to work legally in the U.S. and remain in the country without the fear of deportation.
The program’s end will affect the growing number of medical students with DACA status and likely jeopardize the funding invested in their training. Sixty-two medical schools accept applications from DACA applicants, according to the Association of American Medical Colleges (AAMC). For the 2016 -2017 school year, 113 students with DACA status applied to US medical schools, and there were 65 medical students enrolled who had DACA status. AAMC does not collect data on medical students with DACA status; the National Resident Matching Program, likewise, does not collect data on residents with DACA status.
Loyola University in Chicago is one institute that could be significantly impacted by recension of DACA. The university has accepted more students with DACA status than any other U.S. medical school, and currently has 32 DACA students attending, said Mark Kuczewski, Ph.D., chair of medical education at Loyola University.
“It’s a tragic decision,” he said in an interview. “It once again puts a cloud over these young people who DACA has given the first real opportunity to come out of the shadows, be educated, and serve the community. Now they’re returned back to the situation of uncertainty.”
The decision to end DACA means that current DACA medical students may not be able to finish their training and that those close to completion may not be able to use their degrees in the workforce, Dr. Kuczewski said. Since they are not citizens, DACA students do not qualify for federal student loans, so medical schools must find ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Loyola’s Stritch School of Medicine, Dr. Kuczewski said. However, such loan programs require DACA status. Without DACA or another path to citizenship, medical students in the middle of training will not be able to obtain financial aid to finish their training, he said. The work authorization that DACA provided will also be eliminated.
Dr. Kuczewski said his university plans to advocate strongly for Congress to pass legislation to protect DACA youth, such as the Dream Act of 2017.
“We are going to advocate strongly because we believe this is common sense,” he said. “You don’t just throw away the talents of these young people and the investments they’ve made in their education and the investments we’ve made in them. DACA has given many people the chance to see these young people as students, as employees, as colleagues, and we hope that helps people to mobilize.”
In a statement, Jack Ende, MD, president of the American College of Physicians, said President Trump’s decision to end the DACA program threatens to deny the country the talents of more than half a million individuals making enormous contributions and will also undermine public health and medical education.
“Today’s executive order has the potential to gravely impact public health,” Dr. Ende said in the statement. “We know that noncitizens and undocumented immigrants are more likely to lack health insurance coverage. If the nearly 800,000 people who are currently benefiting from DACA have their protections removed, many will avoid seeking health care in order to reduce the risk of detection and deportation. … Those who seek to serve in the health care professions will be denied that opportunity.”
The Immigration Reform Law Institute praised President Trump’s decision to rescind the DACA program, calling the policy an affront to Congress and a violation of the U.S. Constitution.
“Contrary to former President Obama’s claims, not only is DACA not authorized by federal statute, but prior to the unlawful program, deferred action has only ever been applied to small numbers of illegal aliens on a case-by-case basis,” Dale Wilcox, executive director, said in a statement. “Applying it to approximately 15% of the illegal alien population was never a proper exercise of the president’s discretion under the Constitution and is inconsistent with the president’s duty to take care that the laws be faithfully executed. By rescinding DACA, President Trump has put an end to the previous administration’s flagrant violation of our immigration laws and its abuse of hard-working American taxpayers.”
In a memorandum issued Sept. 5, the Department of Homeland Security said it will begin winding down the DACA program, while providing a limited window in which it will adjudicate certain requests for DACA and associated applications. DHS will adjudicate, on an individual, case-by-case basis, properly filed pending DACA initial requests and associated applications for employment authorization documents that have been accepted by the department as of Sept.5, 2017, according to the memorandum. All DACA initial requests and associated applications filed after this date will be rejected.
[email protected]
On Twitter @legal_med
President Trump has ended the Obama administration’s Deferred Action for Childhood Arrivals (DACA) program, a policy that protected immigrants who came to the United States as children from deportation and authorized them to work in the United States.
In a Sept. 5 press conference, Attorney General Jeff Sessions called the DACA program an unconstitutional overreach of executive branch power by the former administration that deliberately sought to undermine the legislative branch. Rollback of the DACA program will begin immediately, Mr. Sessions said, with the program expiring completely on March 5, 2018.
“The effect of this unilateral executive amnesty, among other things, contributed to a surge of minors at the southern border that yielded terrible humanitarian consequences,” Mr. Sessions said during the press conference. “[DACA has] also denied jobs to hundreds of thousands of Americans by allowing those same illegal aliens to take those jobs. To have a lawful system of immigration that serves the national interest, we cannot admit everyone. Therefore the nation must set and enforce a limit on how many immigrants we admit and that means all cannot be accepted.”
In a statement issued shortly after the press conference, President Trump said winding down the DACA program is in the nation’s best interest, and that there can be no principled immigration reform if the executive branch is able to “rewrite or nullify federal laws at will.
“As President, my highest duty is to defend the American people and the Constitution of the United States of America,” President Trump said in the statement. “At the same time, I do not favor punishing children, most of whom are now adults, for the actions of their parents. But we must also recognize that we are nation of opportunity because we are a nation of laws.”
The DACA program was created by the Obama administration in 2012 as a way of protecting young, undocumented immigrants from deportation after Congress repeatedly blocked legislation that would develop such a safe haven. The policy allowed about 800,000 young adults brought to the United States illegally as children to work legally in the U.S. and remain in the country without the fear of deportation.
The program’s end will affect the growing number of medical students with DACA status and likely jeopardize the funding invested in their training. Sixty-two medical schools accept applications from DACA applicants, according to the Association of American Medical Colleges (AAMC). For the 2016 -2017 school year, 113 students with DACA status applied to US medical schools, and there were 65 medical students enrolled who had DACA status. AAMC does not collect data on medical students with DACA status; the National Resident Matching Program, likewise, does not collect data on residents with DACA status.
Loyola University in Chicago is one institute that could be significantly impacted by recension of DACA. The university has accepted more students with DACA status than any other U.S. medical school, and currently has 32 DACA students attending, said Mark Kuczewski, Ph.D., chair of medical education at Loyola University.
“It’s a tragic decision,” he said in an interview. “It once again puts a cloud over these young people who DACA has given the first real opportunity to come out of the shadows, be educated, and serve the community. Now they’re returned back to the situation of uncertainty.”
The decision to end DACA means that current DACA medical students may not be able to finish their training and that those close to completion may not be able to use their degrees in the workforce, Dr. Kuczewski said. Since they are not citizens, DACA students do not qualify for federal student loans, so medical schools must find ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Loyola’s Stritch School of Medicine, Dr. Kuczewski said. However, such loan programs require DACA status. Without DACA or another path to citizenship, medical students in the middle of training will not be able to obtain financial aid to finish their training, he said. The work authorization that DACA provided will also be eliminated.
Dr. Kuczewski said his university plans to advocate strongly for Congress to pass legislation to protect DACA youth, such as the Dream Act of 2017.
“We are going to advocate strongly because we believe this is common sense,” he said. “You don’t just throw away the talents of these young people and the investments they’ve made in their education and the investments we’ve made in them. DACA has given many people the chance to see these young people as students, as employees, as colleagues, and we hope that helps people to mobilize.”
In a statement, Jack Ende, MD, president of the American College of Physicians, said President Trump’s decision to end the DACA program threatens to deny the country the talents of more than half a million individuals making enormous contributions and will also undermine public health and medical education.
“Today’s executive order has the potential to gravely impact public health,” Dr. Ende said in the statement. “We know that noncitizens and undocumented immigrants are more likely to lack health insurance coverage. If the nearly 800,000 people who are currently benefiting from DACA have their protections removed, many will avoid seeking health care in order to reduce the risk of detection and deportation. … Those who seek to serve in the health care professions will be denied that opportunity.”
The Immigration Reform Law Institute praised President Trump’s decision to rescind the DACA program, calling the policy an affront to Congress and a violation of the U.S. Constitution.
“Contrary to former President Obama’s claims, not only is DACA not authorized by federal statute, but prior to the unlawful program, deferred action has only ever been applied to small numbers of illegal aliens on a case-by-case basis,” Dale Wilcox, executive director, said in a statement. “Applying it to approximately 15% of the illegal alien population was never a proper exercise of the president’s discretion under the Constitution and is inconsistent with the president’s duty to take care that the laws be faithfully executed. By rescinding DACA, President Trump has put an end to the previous administration’s flagrant violation of our immigration laws and its abuse of hard-working American taxpayers.”
In a memorandum issued Sept. 5, the Department of Homeland Security said it will begin winding down the DACA program, while providing a limited window in which it will adjudicate certain requests for DACA and associated applications. DHS will adjudicate, on an individual, case-by-case basis, properly filed pending DACA initial requests and associated applications for employment authorization documents that have been accepted by the department as of Sept.5, 2017, according to the memorandum. All DACA initial requests and associated applications filed after this date will be rejected.
[email protected]
On Twitter @legal_med