User login
Certifications, training to increase addiction medicine specialists
Two new workforce developments aim to increase the number of addiction medicine specialists and provide new training opportunities in the subspecialty.
The American Board of Medical Specialties (ABMS) recently certified its first formal wave of addiction medicine physicians, adding 1,200 specialists to the field. Addiction medicine was first recognized as a subspecialty by ABMS in 2015, followed by the first certification exam in 2017.
The two developments “will change the landscape in substance use prevention, early intervention, and in addiction treatment and management,” said Lon R. Hays, MD, president of The Addiction Medicine Foundation, in Chevy Chase, Md., and director of the addiction medicine fellowship program at the University of Kentucky, Lexington.
“Many more trained physicians will be available to address the opioid crisis and other addictions,” Dr. Hays said in a statement. “They will also be able to help prevent and intervene early with unhealthy substance use in all its forms. For the first time, when aspiring physicians consider a career path, they will now have as an available choice an addiction medicine specialty that meets the highest standards of medicine.”
“When the American Board of Medical Specialties welcomed addiction medicine as its newest subspecialty, it in a lot of ways, legitimized our discipline,” Dr. Brennan said in an interview. “The American Board of Medical Specialties really represents the ‘House of Medicine.’ Being able to enter into that, it gives us a measure of credibility in the eyes of the public, and it basically codifies that these physicians who have passed this board exam have achieved a level of competency and knowledge that makes them trustworthy and safe to provide care to folks suffering from addiction.”
While the 1,200 additional addiction medicine specialists are an improvement, many more are needed, Dr. Brennan said, adding that he is optimistic that the new addiction medicine training opportunities provided by ACGME will help achieve higher numbers.
“For addiction medicine, we’ve had fellowships for about 10 years, but the funding for those fellowships was really challenging,” Dr. Brennan said. “Once you get ACGME-accredited, it gives you the ability to partake of [Centers for Medicare & Medicaid Services] funding that funds most of the graduate medical education residency fellowship spots in the United States. ACGME is the gold standard. I think that makes us much more potentially attractive for graduating physicians who are finishing their residencies.”
The certification of new addiction specialists is welcome news, particularly in the midst of the current epidemic, added Clif Knight, MD, senior vice president for education for the American Academy of Family Physicians.
“This is really good news [especially considering], the difficulty that the country is having with so much addiction – of course opioids are in the forefront – but there are so many different types of addiction,” he said in an interview. “This is good news that the certification is available and that physicians are pursuing obtaining additional expertise and recognition in their ability to treat addictions.”
Dr. Knight expressed appreciation that the ACGME training opportunities in addiction medicine are open to doctors of various specialties, he said.
“A lot of times subspecialty fellowships are only available to one specialty,” said Dr. Knight. “In this case, it looks like they’ve been very deliberate to make this available to multiple specialties. I think that really sends an important message that this is not just one specialty that is focused on [addiction medicine], but really should be something that all specialties are engaged and involved in.”
*This article was updated on 4/2/2018.
Two new workforce developments aim to increase the number of addiction medicine specialists and provide new training opportunities in the subspecialty.
The American Board of Medical Specialties (ABMS) recently certified its first formal wave of addiction medicine physicians, adding 1,200 specialists to the field. Addiction medicine was first recognized as a subspecialty by ABMS in 2015, followed by the first certification exam in 2017.
The two developments “will change the landscape in substance use prevention, early intervention, and in addiction treatment and management,” said Lon R. Hays, MD, president of The Addiction Medicine Foundation, in Chevy Chase, Md., and director of the addiction medicine fellowship program at the University of Kentucky, Lexington.
“Many more trained physicians will be available to address the opioid crisis and other addictions,” Dr. Hays said in a statement. “They will also be able to help prevent and intervene early with unhealthy substance use in all its forms. For the first time, when aspiring physicians consider a career path, they will now have as an available choice an addiction medicine specialty that meets the highest standards of medicine.”
“When the American Board of Medical Specialties welcomed addiction medicine as its newest subspecialty, it in a lot of ways, legitimized our discipline,” Dr. Brennan said in an interview. “The American Board of Medical Specialties really represents the ‘House of Medicine.’ Being able to enter into that, it gives us a measure of credibility in the eyes of the public, and it basically codifies that these physicians who have passed this board exam have achieved a level of competency and knowledge that makes them trustworthy and safe to provide care to folks suffering from addiction.”
While the 1,200 additional addiction medicine specialists are an improvement, many more are needed, Dr. Brennan said, adding that he is optimistic that the new addiction medicine training opportunities provided by ACGME will help achieve higher numbers.
“For addiction medicine, we’ve had fellowships for about 10 years, but the funding for those fellowships was really challenging,” Dr. Brennan said. “Once you get ACGME-accredited, it gives you the ability to partake of [Centers for Medicare & Medicaid Services] funding that funds most of the graduate medical education residency fellowship spots in the United States. ACGME is the gold standard. I think that makes us much more potentially attractive for graduating physicians who are finishing their residencies.”
The certification of new addiction specialists is welcome news, particularly in the midst of the current epidemic, added Clif Knight, MD, senior vice president for education for the American Academy of Family Physicians.
“This is really good news [especially considering], the difficulty that the country is having with so much addiction – of course opioids are in the forefront – but there are so many different types of addiction,” he said in an interview. “This is good news that the certification is available and that physicians are pursuing obtaining additional expertise and recognition in their ability to treat addictions.”
Dr. Knight expressed appreciation that the ACGME training opportunities in addiction medicine are open to doctors of various specialties, he said.
“A lot of times subspecialty fellowships are only available to one specialty,” said Dr. Knight. “In this case, it looks like they’ve been very deliberate to make this available to multiple specialties. I think that really sends an important message that this is not just one specialty that is focused on [addiction medicine], but really should be something that all specialties are engaged and involved in.”
*This article was updated on 4/2/2018.
Two new workforce developments aim to increase the number of addiction medicine specialists and provide new training opportunities in the subspecialty.
The American Board of Medical Specialties (ABMS) recently certified its first formal wave of addiction medicine physicians, adding 1,200 specialists to the field. Addiction medicine was first recognized as a subspecialty by ABMS in 2015, followed by the first certification exam in 2017.
The two developments “will change the landscape in substance use prevention, early intervention, and in addiction treatment and management,” said Lon R. Hays, MD, president of The Addiction Medicine Foundation, in Chevy Chase, Md., and director of the addiction medicine fellowship program at the University of Kentucky, Lexington.
“Many more trained physicians will be available to address the opioid crisis and other addictions,” Dr. Hays said in a statement. “They will also be able to help prevent and intervene early with unhealthy substance use in all its forms. For the first time, when aspiring physicians consider a career path, they will now have as an available choice an addiction medicine specialty that meets the highest standards of medicine.”
“When the American Board of Medical Specialties welcomed addiction medicine as its newest subspecialty, it in a lot of ways, legitimized our discipline,” Dr. Brennan said in an interview. “The American Board of Medical Specialties really represents the ‘House of Medicine.’ Being able to enter into that, it gives us a measure of credibility in the eyes of the public, and it basically codifies that these physicians who have passed this board exam have achieved a level of competency and knowledge that makes them trustworthy and safe to provide care to folks suffering from addiction.”
While the 1,200 additional addiction medicine specialists are an improvement, many more are needed, Dr. Brennan said, adding that he is optimistic that the new addiction medicine training opportunities provided by ACGME will help achieve higher numbers.
“For addiction medicine, we’ve had fellowships for about 10 years, but the funding for those fellowships was really challenging,” Dr. Brennan said. “Once you get ACGME-accredited, it gives you the ability to partake of [Centers for Medicare & Medicaid Services] funding that funds most of the graduate medical education residency fellowship spots in the United States. ACGME is the gold standard. I think that makes us much more potentially attractive for graduating physicians who are finishing their residencies.”
The certification of new addiction specialists is welcome news, particularly in the midst of the current epidemic, added Clif Knight, MD, senior vice president for education for the American Academy of Family Physicians.
“This is really good news [especially considering], the difficulty that the country is having with so much addiction – of course opioids are in the forefront – but there are so many different types of addiction,” he said in an interview. “This is good news that the certification is available and that physicians are pursuing obtaining additional expertise and recognition in their ability to treat addictions.”
Dr. Knight expressed appreciation that the ACGME training opportunities in addiction medicine are open to doctors of various specialties, he said.
“A lot of times subspecialty fellowships are only available to one specialty,” said Dr. Knight. “In this case, it looks like they’ve been very deliberate to make this available to multiple specialties. I think that really sends an important message that this is not just one specialty that is focused on [addiction medicine], but really should be something that all specialties are engaged and involved in.”
*This article was updated on 4/2/2018.
Could European data privacy rules cost you big?
U.S. health providers who treat foreign patients may want to take a closer look at their privacy policies to make sure they comply with new European Union data protection rules.
May 25 heralds the enforcement of the European Union’s General Data Protection Regulation (GDPR), a set of rules designed to strengthen and harmonize record protection for EU citizens and tighten how their data privacy is managed. The regulations protect various forms of electronic data including basic identity information, health and genetic data, and biometric information.
Treating a vacationing EU patient who needs unplanned treatment in the states is not likely to subject physicians to the GDPR, said Cynthia J. Larose, a privacy and data security attorney based in Boston.
“In general, the GDPR should not impact U.S. doctors who may incidentally treat an EU patient while that patient is here in the U.S.,” Ms. Larose said in an interview … If the EU patient presents at a U.S. health care provider for treatment, then the GDPR does not apply to her personal data in the possession of the U.S. health care provider – HIPAA applies. While the [GDPR] does have extraterritorial reach, you have to be doing something in the EU for the GDPR to apply.”
But other scenarios that could prove problematic, such as U.S. researchers studying patients in the EU, U.S. physicians providing telemedicine care to EU patients, and doctors who continue to monitor EU patients following treatment in the United States once patients return to their home country.
About 200,000 international visitors fly to the United States yearly for health treatment, of whom about 25% are from Europe, according to a 2015 report by the United States International Trade Commission.
Advertising medical services in the European Union is another way that U.S. physicians could be subject to the GDPR. For example, if a practice or hospital markets their specialty care on websites or other materials in the EU, this could fall under the GDPR umbrella, according to security experts.
“If you are advertising services to patients in the EU, and then they decide to obtain such services, that could trigger GDPR because the data subjects are in the EU and you are offering services to them,” said Elaine C. Zacharakis Loumbas, a health and security law attorney based in Chicago. “It becomes very fact specific.”
Like HIPAA, the GDPR requires that health providers disclose information to patients about where and how their data may be used. Mr. Barchie notes that in the United States, patient consent forms may generally include two or three potential uses for patient data such as marketing and medical research. The GDPR specifies that each potential usage of patient data requires its own separate consent form, he said.
“Let’s say you’re a clinic that specializes in diabetes [and] you’re used to taking data and sending it to a general database to [collect information] about diabetes,” Mr. Barchie said. “You can’t do that under GDPR. You would have to have a separate consent form for that. So one consent to provide your diabetes service, one consent form to maybe market to the [patient], and a separate consent form [regarding] the database.”
GDPR also requires the minimizing of personal data copies stored within multiple systems. In the United States, it’s not uncommon for there to be multiple copies of a person’s data in several places, which makes sense from an IT perspective, Mr. Barchie said. The GDPR however requires that data keepers limit the number of copies they maintain to only the most necessary information.
“[Under GDPR], you should send only the data that you need for that particular process,” he said. “For example, [in the case of] address, user name, and patient ID. If you only need the patient ID number, you should not send the patient name and address. You minimize the amount of data that you’re sending to be processed.”
Breach notification also is more stringent under the GDPR, compared with U.S. regulations. Under HIPAA, covered entities must notify the U.S. Department of Health & Human Services and affected patients of a data breach without unreasonable delay no later than 60 days following discovery of a breach. The GDPR requires that effected entities notify the supervisory authority “without undue delay and, where feasible, not later than 72 hours after having become aware of [the breach].” (The GDPR supervisory authority depends on the EU country affected.)
If determined that the personal data breach is “likely to result in a high risk to the rights and freedoms of individuals,” efforts must be made to communicate about the personal data breach with the affected data subjects “without undue delay,” according to the rules.
If unsure of whether your practices may fall under GDPR, experts advise discussing the question with a legal counselor, GDPR expert, or risk management team.
U.S. health providers who treat foreign patients may want to take a closer look at their privacy policies to make sure they comply with new European Union data protection rules.
May 25 heralds the enforcement of the European Union’s General Data Protection Regulation (GDPR), a set of rules designed to strengthen and harmonize record protection for EU citizens and tighten how their data privacy is managed. The regulations protect various forms of electronic data including basic identity information, health and genetic data, and biometric information.
Treating a vacationing EU patient who needs unplanned treatment in the states is not likely to subject physicians to the GDPR, said Cynthia J. Larose, a privacy and data security attorney based in Boston.
“In general, the GDPR should not impact U.S. doctors who may incidentally treat an EU patient while that patient is here in the U.S.,” Ms. Larose said in an interview … If the EU patient presents at a U.S. health care provider for treatment, then the GDPR does not apply to her personal data in the possession of the U.S. health care provider – HIPAA applies. While the [GDPR] does have extraterritorial reach, you have to be doing something in the EU for the GDPR to apply.”
But other scenarios that could prove problematic, such as U.S. researchers studying patients in the EU, U.S. physicians providing telemedicine care to EU patients, and doctors who continue to monitor EU patients following treatment in the United States once patients return to their home country.
About 200,000 international visitors fly to the United States yearly for health treatment, of whom about 25% are from Europe, according to a 2015 report by the United States International Trade Commission.
Advertising medical services in the European Union is another way that U.S. physicians could be subject to the GDPR. For example, if a practice or hospital markets their specialty care on websites or other materials in the EU, this could fall under the GDPR umbrella, according to security experts.
“If you are advertising services to patients in the EU, and then they decide to obtain such services, that could trigger GDPR because the data subjects are in the EU and you are offering services to them,” said Elaine C. Zacharakis Loumbas, a health and security law attorney based in Chicago. “It becomes very fact specific.”
Like HIPAA, the GDPR requires that health providers disclose information to patients about where and how their data may be used. Mr. Barchie notes that in the United States, patient consent forms may generally include two or three potential uses for patient data such as marketing and medical research. The GDPR specifies that each potential usage of patient data requires its own separate consent form, he said.
“Let’s say you’re a clinic that specializes in diabetes [and] you’re used to taking data and sending it to a general database to [collect information] about diabetes,” Mr. Barchie said. “You can’t do that under GDPR. You would have to have a separate consent form for that. So one consent to provide your diabetes service, one consent form to maybe market to the [patient], and a separate consent form [regarding] the database.”
GDPR also requires the minimizing of personal data copies stored within multiple systems. In the United States, it’s not uncommon for there to be multiple copies of a person’s data in several places, which makes sense from an IT perspective, Mr. Barchie said. The GDPR however requires that data keepers limit the number of copies they maintain to only the most necessary information.
“[Under GDPR], you should send only the data that you need for that particular process,” he said. “For example, [in the case of] address, user name, and patient ID. If you only need the patient ID number, you should not send the patient name and address. You minimize the amount of data that you’re sending to be processed.”
Breach notification also is more stringent under the GDPR, compared with U.S. regulations. Under HIPAA, covered entities must notify the U.S. Department of Health & Human Services and affected patients of a data breach without unreasonable delay no later than 60 days following discovery of a breach. The GDPR requires that effected entities notify the supervisory authority “without undue delay and, where feasible, not later than 72 hours after having become aware of [the breach].” (The GDPR supervisory authority depends on the EU country affected.)
If determined that the personal data breach is “likely to result in a high risk to the rights and freedoms of individuals,” efforts must be made to communicate about the personal data breach with the affected data subjects “without undue delay,” according to the rules.
If unsure of whether your practices may fall under GDPR, experts advise discussing the question with a legal counselor, GDPR expert, or risk management team.
U.S. health providers who treat foreign patients may want to take a closer look at their privacy policies to make sure they comply with new European Union data protection rules.
May 25 heralds the enforcement of the European Union’s General Data Protection Regulation (GDPR), a set of rules designed to strengthen and harmonize record protection for EU citizens and tighten how their data privacy is managed. The regulations protect various forms of electronic data including basic identity information, health and genetic data, and biometric information.
Treating a vacationing EU patient who needs unplanned treatment in the states is not likely to subject physicians to the GDPR, said Cynthia J. Larose, a privacy and data security attorney based in Boston.
“In general, the GDPR should not impact U.S. doctors who may incidentally treat an EU patient while that patient is here in the U.S.,” Ms. Larose said in an interview … If the EU patient presents at a U.S. health care provider for treatment, then the GDPR does not apply to her personal data in the possession of the U.S. health care provider – HIPAA applies. While the [GDPR] does have extraterritorial reach, you have to be doing something in the EU for the GDPR to apply.”
But other scenarios that could prove problematic, such as U.S. researchers studying patients in the EU, U.S. physicians providing telemedicine care to EU patients, and doctors who continue to monitor EU patients following treatment in the United States once patients return to their home country.
About 200,000 international visitors fly to the United States yearly for health treatment, of whom about 25% are from Europe, according to a 2015 report by the United States International Trade Commission.
Advertising medical services in the European Union is another way that U.S. physicians could be subject to the GDPR. For example, if a practice or hospital markets their specialty care on websites or other materials in the EU, this could fall under the GDPR umbrella, according to security experts.
“If you are advertising services to patients in the EU, and then they decide to obtain such services, that could trigger GDPR because the data subjects are in the EU and you are offering services to them,” said Elaine C. Zacharakis Loumbas, a health and security law attorney based in Chicago. “It becomes very fact specific.”
Like HIPAA, the GDPR requires that health providers disclose information to patients about where and how their data may be used. Mr. Barchie notes that in the United States, patient consent forms may generally include two or three potential uses for patient data such as marketing and medical research. The GDPR specifies that each potential usage of patient data requires its own separate consent form, he said.
“Let’s say you’re a clinic that specializes in diabetes [and] you’re used to taking data and sending it to a general database to [collect information] about diabetes,” Mr. Barchie said. “You can’t do that under GDPR. You would have to have a separate consent form for that. So one consent to provide your diabetes service, one consent form to maybe market to the [patient], and a separate consent form [regarding] the database.”
GDPR also requires the minimizing of personal data copies stored within multiple systems. In the United States, it’s not uncommon for there to be multiple copies of a person’s data in several places, which makes sense from an IT perspective, Mr. Barchie said. The GDPR however requires that data keepers limit the number of copies they maintain to only the most necessary information.
“[Under GDPR], you should send only the data that you need for that particular process,” he said. “For example, [in the case of] address, user name, and patient ID. If you only need the patient ID number, you should not send the patient name and address. You minimize the amount of data that you’re sending to be processed.”
Breach notification also is more stringent under the GDPR, compared with U.S. regulations. Under HIPAA, covered entities must notify the U.S. Department of Health & Human Services and affected patients of a data breach without unreasonable delay no later than 60 days following discovery of a breach. The GDPR requires that effected entities notify the supervisory authority “without undue delay and, where feasible, not later than 72 hours after having become aware of [the breach].” (The GDPR supervisory authority depends on the EU country affected.)
If determined that the personal data breach is “likely to result in a high risk to the rights and freedoms of individuals,” efforts must be made to communicate about the personal data breach with the affected data subjects “without undue delay,” according to the rules.
If unsure of whether your practices may fall under GDPR, experts advise discussing the question with a legal counselor, GDPR expert, or risk management team.
Justices appear skeptical of California’s abortion speech law
A California law that requires anti-abortion crisis pregnancy centers to provide women with information on abortion services was met with skepticism by U.S. Supreme Court justices during March 20 oral arguments.
The case revolves around California’s 2016 Reproductive Freedom, Accountability, Comprehensive Care, and Transparency (FACT) Act, which requires that pregnancy centers – many of which are anti-abortion – post notices about where patients can find free or low-cost abortion services. Another part of the law requires unlicensed pregnancy centers to disclose to women that they are not a licensed medical facility and have no medical professionals on staff.
The plaintiffs, led by the nonprofit National Institute of Family and Life Advocates (NIFLA), argue that the law violates the First Amendment by requiring speech and because the measure unfairly targets centers that discourage abortions. California officials contend that the law was needed to address concerns that nonprofit organizations, often religious, were misrepresenting themselves as full-service reproductive health clinics and misleading women about their options.
During oral arguments, justices peppered Joshua Klein, California deputy solicitor general, with questions about the law’s intent and why it appeared to single out certain pregnancy centers. Associate Justice Samuel Alito Jr., who is considered to be among the high court’s conservative members, asked why the law did not apply to for-profit centers.
“If you have a law that’s neutral on its face, but then it has a lot of crazy exemptions, and when you apply all the exemptions, what you’re left with is a very strange pattern and, gee, it turns out that just about the only clinics that are covered by this are pro-life clinics,” Justice Alito said during arguments. “Do you think it’s possible to infer intentional discrimination in that situation? Why does [the law] apply only for nonprofits and not for-profits? If the purpose is to get this information out to poor women, don’t you think there are examples of poor women who stumble into a for-profit facility?”
Mr. Klein responded that the law was designed to address scenarios in the state in which more transparency was needed.
“Your Honor, as a category, for-profit clinics do not seem to treat primarily women who need free and sliding-cost scale care in the same way,” Mr. Klein said. “Now I will say it’s always possible to imagine a new boundary for the law. But under intermediate scrutiny, a law does not need to be perfect and a legislature can concentrate its efforts at where the need for the law is most apparent.”
Associate Justice Elena Kagan, considered to be among the more liberal justices, raised a similar point when she expressed concern that the law had been “gerrymandered” to address some centers, but not others.
“There is a sense when you read this statute, Mr. Klein, there’s at least a question that arises as to whether this statute has been gerrymandered,” Justice Kagan said during arguments. “Because if it has been gerrymandered, that’s a serious issue. In other words, if, you know, it’s like, look, we have these general disclosure requirements, but we don’t really want to apply them generally, we just want to apply them to some speakers whose speech we don’t much like.”
Meanwhile, Associate Justice Sonia Sotomayor appeared to give credence to the California law, expressing doubt that the plaintiff’s activities were ethical and legitimate. She noted that she visited a website of one of the plaintiffs – Fallbrook Pregnancy Resource Center – and found photos of people in nurse uniforms standing next to an ultrasound machine as well as text that stated that staff will “educate clients about different abortion methods available and describe in medical terms different abortion procedures.”
“The website also says clients will be evaluated by nurses and that they follow all HIPAA regulations, which if they’re not a medical provider, they don’t have to follow,” Justice Sotomayor said. “If a reasonable person could look at this website and think that you’re giving medical advice, would the unlicensed notice be wrong?”
NIFLA attorney Michael Farris did not have a chance to respond to Justice Sotomayor’s question, but he argued throughout the session that California’s law takes an unjust aim at “pro-life pregnancy centers” by compelling licensed centers to point the way to an abortion and imposing onerous advertising rules on unlicensed centers.
In the end, both sides faced difficult questions from the justices about complex constitutional issues, said Heather Shumaker, an attorney for the National Women’s Law Center in Washington, who attended the oral arguments. The law center joined an amicus brief in the case in support of California.
However, Ms. Shumaker said her overall impression was that the arguments made clear the strong reasoning behind California’s law and its importance.
“I am confident that at least some members of the Supreme Court understood what was at stake here and understand that there is a layer of deception behind the actions of the anti-abortion centers,” she said in an interview.
Paul Sherman, a senior attorney for the Institute for Justice in Arlington, Va., said that based on the oral arguments, it appears likely California’s law will be struck down. Mr. Sherman coauthored the Institute for Justice’s amicus brief in support of NIFLA.
A number of physician associations have weighed in on NIFLA v. Becerra. The American Medical Association issued a court brief in support of California and the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics joined several other medical associations in a similar brief. The American Association of Pro-Life Obstetrician and Gynecologists joined the Christian Medical Association and others to submit a brief in support of NIFLA.
The Supreme Court is expected to rule on the case by this summer.
A California law that requires anti-abortion crisis pregnancy centers to provide women with information on abortion services was met with skepticism by U.S. Supreme Court justices during March 20 oral arguments.
The case revolves around California’s 2016 Reproductive Freedom, Accountability, Comprehensive Care, and Transparency (FACT) Act, which requires that pregnancy centers – many of which are anti-abortion – post notices about where patients can find free or low-cost abortion services. Another part of the law requires unlicensed pregnancy centers to disclose to women that they are not a licensed medical facility and have no medical professionals on staff.
The plaintiffs, led by the nonprofit National Institute of Family and Life Advocates (NIFLA), argue that the law violates the First Amendment by requiring speech and because the measure unfairly targets centers that discourage abortions. California officials contend that the law was needed to address concerns that nonprofit organizations, often religious, were misrepresenting themselves as full-service reproductive health clinics and misleading women about their options.
During oral arguments, justices peppered Joshua Klein, California deputy solicitor general, with questions about the law’s intent and why it appeared to single out certain pregnancy centers. Associate Justice Samuel Alito Jr., who is considered to be among the high court’s conservative members, asked why the law did not apply to for-profit centers.
“If you have a law that’s neutral on its face, but then it has a lot of crazy exemptions, and when you apply all the exemptions, what you’re left with is a very strange pattern and, gee, it turns out that just about the only clinics that are covered by this are pro-life clinics,” Justice Alito said during arguments. “Do you think it’s possible to infer intentional discrimination in that situation? Why does [the law] apply only for nonprofits and not for-profits? If the purpose is to get this information out to poor women, don’t you think there are examples of poor women who stumble into a for-profit facility?”
Mr. Klein responded that the law was designed to address scenarios in the state in which more transparency was needed.
“Your Honor, as a category, for-profit clinics do not seem to treat primarily women who need free and sliding-cost scale care in the same way,” Mr. Klein said. “Now I will say it’s always possible to imagine a new boundary for the law. But under intermediate scrutiny, a law does not need to be perfect and a legislature can concentrate its efforts at where the need for the law is most apparent.”
Associate Justice Elena Kagan, considered to be among the more liberal justices, raised a similar point when she expressed concern that the law had been “gerrymandered” to address some centers, but not others.
“There is a sense when you read this statute, Mr. Klein, there’s at least a question that arises as to whether this statute has been gerrymandered,” Justice Kagan said during arguments. “Because if it has been gerrymandered, that’s a serious issue. In other words, if, you know, it’s like, look, we have these general disclosure requirements, but we don’t really want to apply them generally, we just want to apply them to some speakers whose speech we don’t much like.”
Meanwhile, Associate Justice Sonia Sotomayor appeared to give credence to the California law, expressing doubt that the plaintiff’s activities were ethical and legitimate. She noted that she visited a website of one of the plaintiffs – Fallbrook Pregnancy Resource Center – and found photos of people in nurse uniforms standing next to an ultrasound machine as well as text that stated that staff will “educate clients about different abortion methods available and describe in medical terms different abortion procedures.”
“The website also says clients will be evaluated by nurses and that they follow all HIPAA regulations, which if they’re not a medical provider, they don’t have to follow,” Justice Sotomayor said. “If a reasonable person could look at this website and think that you’re giving medical advice, would the unlicensed notice be wrong?”
NIFLA attorney Michael Farris did not have a chance to respond to Justice Sotomayor’s question, but he argued throughout the session that California’s law takes an unjust aim at “pro-life pregnancy centers” by compelling licensed centers to point the way to an abortion and imposing onerous advertising rules on unlicensed centers.
In the end, both sides faced difficult questions from the justices about complex constitutional issues, said Heather Shumaker, an attorney for the National Women’s Law Center in Washington, who attended the oral arguments. The law center joined an amicus brief in the case in support of California.
However, Ms. Shumaker said her overall impression was that the arguments made clear the strong reasoning behind California’s law and its importance.
“I am confident that at least some members of the Supreme Court understood what was at stake here and understand that there is a layer of deception behind the actions of the anti-abortion centers,” she said in an interview.
Paul Sherman, a senior attorney for the Institute for Justice in Arlington, Va., said that based on the oral arguments, it appears likely California’s law will be struck down. Mr. Sherman coauthored the Institute for Justice’s amicus brief in support of NIFLA.
A number of physician associations have weighed in on NIFLA v. Becerra. The American Medical Association issued a court brief in support of California and the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics joined several other medical associations in a similar brief. The American Association of Pro-Life Obstetrician and Gynecologists joined the Christian Medical Association and others to submit a brief in support of NIFLA.
The Supreme Court is expected to rule on the case by this summer.
A California law that requires anti-abortion crisis pregnancy centers to provide women with information on abortion services was met with skepticism by U.S. Supreme Court justices during March 20 oral arguments.
The case revolves around California’s 2016 Reproductive Freedom, Accountability, Comprehensive Care, and Transparency (FACT) Act, which requires that pregnancy centers – many of which are anti-abortion – post notices about where patients can find free or low-cost abortion services. Another part of the law requires unlicensed pregnancy centers to disclose to women that they are not a licensed medical facility and have no medical professionals on staff.
The plaintiffs, led by the nonprofit National Institute of Family and Life Advocates (NIFLA), argue that the law violates the First Amendment by requiring speech and because the measure unfairly targets centers that discourage abortions. California officials contend that the law was needed to address concerns that nonprofit organizations, often religious, were misrepresenting themselves as full-service reproductive health clinics and misleading women about their options.
During oral arguments, justices peppered Joshua Klein, California deputy solicitor general, with questions about the law’s intent and why it appeared to single out certain pregnancy centers. Associate Justice Samuel Alito Jr., who is considered to be among the high court’s conservative members, asked why the law did not apply to for-profit centers.
“If you have a law that’s neutral on its face, but then it has a lot of crazy exemptions, and when you apply all the exemptions, what you’re left with is a very strange pattern and, gee, it turns out that just about the only clinics that are covered by this are pro-life clinics,” Justice Alito said during arguments. “Do you think it’s possible to infer intentional discrimination in that situation? Why does [the law] apply only for nonprofits and not for-profits? If the purpose is to get this information out to poor women, don’t you think there are examples of poor women who stumble into a for-profit facility?”
Mr. Klein responded that the law was designed to address scenarios in the state in which more transparency was needed.
“Your Honor, as a category, for-profit clinics do not seem to treat primarily women who need free and sliding-cost scale care in the same way,” Mr. Klein said. “Now I will say it’s always possible to imagine a new boundary for the law. But under intermediate scrutiny, a law does not need to be perfect and a legislature can concentrate its efforts at where the need for the law is most apparent.”
Associate Justice Elena Kagan, considered to be among the more liberal justices, raised a similar point when she expressed concern that the law had been “gerrymandered” to address some centers, but not others.
“There is a sense when you read this statute, Mr. Klein, there’s at least a question that arises as to whether this statute has been gerrymandered,” Justice Kagan said during arguments. “Because if it has been gerrymandered, that’s a serious issue. In other words, if, you know, it’s like, look, we have these general disclosure requirements, but we don’t really want to apply them generally, we just want to apply them to some speakers whose speech we don’t much like.”
Meanwhile, Associate Justice Sonia Sotomayor appeared to give credence to the California law, expressing doubt that the plaintiff’s activities were ethical and legitimate. She noted that she visited a website of one of the plaintiffs – Fallbrook Pregnancy Resource Center – and found photos of people in nurse uniforms standing next to an ultrasound machine as well as text that stated that staff will “educate clients about different abortion methods available and describe in medical terms different abortion procedures.”
“The website also says clients will be evaluated by nurses and that they follow all HIPAA regulations, which if they’re not a medical provider, they don’t have to follow,” Justice Sotomayor said. “If a reasonable person could look at this website and think that you’re giving medical advice, would the unlicensed notice be wrong?”
NIFLA attorney Michael Farris did not have a chance to respond to Justice Sotomayor’s question, but he argued throughout the session that California’s law takes an unjust aim at “pro-life pregnancy centers” by compelling licensed centers to point the way to an abortion and imposing onerous advertising rules on unlicensed centers.
In the end, both sides faced difficult questions from the justices about complex constitutional issues, said Heather Shumaker, an attorney for the National Women’s Law Center in Washington, who attended the oral arguments. The law center joined an amicus brief in the case in support of California.
However, Ms. Shumaker said her overall impression was that the arguments made clear the strong reasoning behind California’s law and its importance.
“I am confident that at least some members of the Supreme Court understood what was at stake here and understand that there is a layer of deception behind the actions of the anti-abortion centers,” she said in an interview.
Paul Sherman, a senior attorney for the Institute for Justice in Arlington, Va., said that based on the oral arguments, it appears likely California’s law will be struck down. Mr. Sherman coauthored the Institute for Justice’s amicus brief in support of NIFLA.
A number of physician associations have weighed in on NIFLA v. Becerra. The American Medical Association issued a court brief in support of California and the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics joined several other medical associations in a similar brief. The American Association of Pro-Life Obstetrician and Gynecologists joined the Christian Medical Association and others to submit a brief in support of NIFLA.
The Supreme Court is expected to rule on the case by this summer.
Court: State cannot sue over religious exemption expansion
Massachusetts cannot sue the Trump administration for broadening exemptions to the Affordable Care Act’s contraceptive mandate, a district court has ruled.
In a March decision, the U.S. District Court for the District of Massachusetts concluded that the state lacks standing to sue the federal government and that it could not prove that its residents would be harmed by the expanded exemption.
Under two regulations, issued in October 2017 in the Federal Register, the Trump administration allowed that an expanded group of employers and insurers can object to paying for contraception coverage on religious or moral grounds. The new policy “better balances the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions,” according to the rule issued by the departments of Health & Human Services, Labor, and Treasury.
Several state attorneys general sued over the rules, including Massachusetts Attorney General Maura Healey (D). Ms. Healey argued that the rules violates women’s equal protection rights by restricting their ability to access contraception. The lawsuit also claimed the narrowing of the mandate allowed employers to unconstitutionally impose their religious and moral beliefs on employees.
“The [rules] jeopardize the health care of women in Massachusetts and nationwide, promote the religious freedom of corporations over the autonomy and health of women, and leave the states to bear additional health care costs both with regard to contraceptive and prenatal care as well as other services associated with unintended pregnancies and related negative health outcomes for both women and their children,” the lawsuit stated.
In his March 12 opinion however, U.S. District Judge Nathaniel M. Gorton dismissed the state’s claims, ruling that Massachusetts failed to prove its citizens will suffer future injury from the exemption expansion. The judge noted a 2017 law passed by Massachusetts called the ACCESS Act that requires certain employer-sponsored health plans to cover contraceptives without imposing out-of-pocket costs on employees. This law and other state regulations make Massachusetts less likely than women in other states to be affected negatively by the expanded exemption, said Judge Gorton, who was appointed to the bench by President George H.W. Bush.
In a statement, Ms. Healey said the state was disappointed in the decision, but remained steadfast in its commitment to “ensuring affordable and reliable reproductive health care for women.”
“Access to contraceptive coverage is a critical issue for the health, equality, and economic well-being of women and their families, and we will continue to fight for these protections.” Ms. Healey said.
The legal fight over the ACA’s contraceptive mandate exemption is far from over. The Massachusetts decision comes after federal judges in California and Pennsylvania halted the administration’s exemption rules. In December 2017, U.S. District Judge Haywood Gilliam Jr. temporarily blocked the exemption extension from going forward in favor of California and four other states that joined the lawsuit – New York, Delaware, Maryland, and Virginia. Earlier that month, U.S. District Judge Wendy Beetlestone ruled similarly in a decision for the U.S. District Court for the Eastern District of Pennsylvania. Both Mr. Gilliam and Ms. Beetlestone were appointed to the bench by President Obama.
The Trump administration has indicated that it plans to appeal the rulings. In a summary of the rules, the administration said the new policies will “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.”
Massachusetts cannot sue the Trump administration for broadening exemptions to the Affordable Care Act’s contraceptive mandate, a district court has ruled.
In a March decision, the U.S. District Court for the District of Massachusetts concluded that the state lacks standing to sue the federal government and that it could not prove that its residents would be harmed by the expanded exemption.
Under two regulations, issued in October 2017 in the Federal Register, the Trump administration allowed that an expanded group of employers and insurers can object to paying for contraception coverage on religious or moral grounds. The new policy “better balances the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions,” according to the rule issued by the departments of Health & Human Services, Labor, and Treasury.
Several state attorneys general sued over the rules, including Massachusetts Attorney General Maura Healey (D). Ms. Healey argued that the rules violates women’s equal protection rights by restricting their ability to access contraception. The lawsuit also claimed the narrowing of the mandate allowed employers to unconstitutionally impose their religious and moral beliefs on employees.
“The [rules] jeopardize the health care of women in Massachusetts and nationwide, promote the religious freedom of corporations over the autonomy and health of women, and leave the states to bear additional health care costs both with regard to contraceptive and prenatal care as well as other services associated with unintended pregnancies and related negative health outcomes for both women and their children,” the lawsuit stated.
In his March 12 opinion however, U.S. District Judge Nathaniel M. Gorton dismissed the state’s claims, ruling that Massachusetts failed to prove its citizens will suffer future injury from the exemption expansion. The judge noted a 2017 law passed by Massachusetts called the ACCESS Act that requires certain employer-sponsored health plans to cover contraceptives without imposing out-of-pocket costs on employees. This law and other state regulations make Massachusetts less likely than women in other states to be affected negatively by the expanded exemption, said Judge Gorton, who was appointed to the bench by President George H.W. Bush.
In a statement, Ms. Healey said the state was disappointed in the decision, but remained steadfast in its commitment to “ensuring affordable and reliable reproductive health care for women.”
“Access to contraceptive coverage is a critical issue for the health, equality, and economic well-being of women and their families, and we will continue to fight for these protections.” Ms. Healey said.
The legal fight over the ACA’s contraceptive mandate exemption is far from over. The Massachusetts decision comes after federal judges in California and Pennsylvania halted the administration’s exemption rules. In December 2017, U.S. District Judge Haywood Gilliam Jr. temporarily blocked the exemption extension from going forward in favor of California and four other states that joined the lawsuit – New York, Delaware, Maryland, and Virginia. Earlier that month, U.S. District Judge Wendy Beetlestone ruled similarly in a decision for the U.S. District Court for the Eastern District of Pennsylvania. Both Mr. Gilliam and Ms. Beetlestone were appointed to the bench by President Obama.
The Trump administration has indicated that it plans to appeal the rulings. In a summary of the rules, the administration said the new policies will “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.”
Massachusetts cannot sue the Trump administration for broadening exemptions to the Affordable Care Act’s contraceptive mandate, a district court has ruled.
In a March decision, the U.S. District Court for the District of Massachusetts concluded that the state lacks standing to sue the federal government and that it could not prove that its residents would be harmed by the expanded exemption.
Under two regulations, issued in October 2017 in the Federal Register, the Trump administration allowed that an expanded group of employers and insurers can object to paying for contraception coverage on religious or moral grounds. The new policy “better balances the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions,” according to the rule issued by the departments of Health & Human Services, Labor, and Treasury.
Several state attorneys general sued over the rules, including Massachusetts Attorney General Maura Healey (D). Ms. Healey argued that the rules violates women’s equal protection rights by restricting their ability to access contraception. The lawsuit also claimed the narrowing of the mandate allowed employers to unconstitutionally impose their religious and moral beliefs on employees.
“The [rules] jeopardize the health care of women in Massachusetts and nationwide, promote the religious freedom of corporations over the autonomy and health of women, and leave the states to bear additional health care costs both with regard to contraceptive and prenatal care as well as other services associated with unintended pregnancies and related negative health outcomes for both women and their children,” the lawsuit stated.
In his March 12 opinion however, U.S. District Judge Nathaniel M. Gorton dismissed the state’s claims, ruling that Massachusetts failed to prove its citizens will suffer future injury from the exemption expansion. The judge noted a 2017 law passed by Massachusetts called the ACCESS Act that requires certain employer-sponsored health plans to cover contraceptives without imposing out-of-pocket costs on employees. This law and other state regulations make Massachusetts less likely than women in other states to be affected negatively by the expanded exemption, said Judge Gorton, who was appointed to the bench by President George H.W. Bush.
In a statement, Ms. Healey said the state was disappointed in the decision, but remained steadfast in its commitment to “ensuring affordable and reliable reproductive health care for women.”
“Access to contraceptive coverage is a critical issue for the health, equality, and economic well-being of women and their families, and we will continue to fight for these protections.” Ms. Healey said.
The legal fight over the ACA’s contraceptive mandate exemption is far from over. The Massachusetts decision comes after federal judges in California and Pennsylvania halted the administration’s exemption rules. In December 2017, U.S. District Judge Haywood Gilliam Jr. temporarily blocked the exemption extension from going forward in favor of California and four other states that joined the lawsuit – New York, Delaware, Maryland, and Virginia. Earlier that month, U.S. District Judge Wendy Beetlestone ruled similarly in a decision for the U.S. District Court for the Eastern District of Pennsylvania. Both Mr. Gilliam and Ms. Beetlestone were appointed to the bench by President Obama.
The Trump administration has indicated that it plans to appeal the rulings. In a summary of the rules, the administration said the new policies will “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.”
ABS announces new certification exam
.
The new test, required every other year, consists of a 40-question, open-book assessment that surgeons can take on their own computers within the assessment time frame, according to a March 5 announcement. The previous 10-year exam consisted of nearly 250 questions and had to be completed at a highly secure testing center.
The assessment shift was made to address diplomates’ concerns that the prior exam was burdensome, stressful, and challenging to complete because of its rigid design and location requirements, ABS Chair Mary E. Klingensmith, MD, FACS, said in an interview.
“This new method, which allows a take-from-home or office format, is much less stressful, as both the setting, and the ability to choose the content area, give diplomates much more control,” Dr. Klingensmith said. “Additionally, the testing concepts and references will be provided in advance, should a diplomate desire to know these aspects.”
On March 11, the American College of Surgeons released a statement regarding the new assessment and suggested that, while the new approach is welcomed by the ACS, some details of the process are of concern to surgeons. “The American College of Surgeons (ACS) leadership has heard your concerns both through personal conversations with many of you and through your posts on ACS Communities. In fact, many in leadership share these concerns. We have been in discussions with ABS leadership and can tell you that they are also listening. They want to get this right.”
Of the 40 questions on the new exam, 20 questions will cover core surgical principles, while the other 20 will cover a practice-related area of the diplomate’s choosing. For 2018, diplomates can select from four practice-related areas: general surgery, abdomen, alimentary tract, or breast. More areas are planned based on future feedback from diplomates and surgical societies. Other aspects of the new exam include:
- Topics and references for the various areas will be published in advance on the ABS website.
- Diplomates will be provided with immediate feedback, and will have two opportunities to answer a question correctly.
- A final score of 80% correct will be required to pass.
- Once the assessment is started, diplomates will have 2 weeks to complete the test, with the ability to save and continue when convenient.
The purpose of the new assessment is to provide practicing surgeons with a timely, relevant, and accessible method to stay current with surgical practice knowledge,” Dr. Klingensmith said.
“By selecting a practice-specific area of their own choosing, surgeons will no longer have to study for and be tested upon the entire breadth of general surgery; instead they can focus on those areas that most reflect their practice,” she said. “By submitting to a learning exercise every 2 years, which is focused in the areas of an individual surgeon’s practice, I expect important aspects of knowledge will be transmitted and integrated into a surgeon’s practice. This new program will provide practicing surgeons with an accessible method for keeping up with the constantly changing landscape of surgical practice.”
The new exam is part of an ongoing effort by ABS to revamp its maintenance of certification requirements after widespread criticism that its past provisions were burdensome and irrelevant. In July, ABS announced that it was extending its continuing medical education reporting cycle from 3 to 5 years and reducing the number of required self-assessment by a third. Surgeons now have to report 150 credits over 5 years, 50 from self-assessment CMEs. Under the old system, it was 90 credits over 3 years, 60 of which had to include self-assessment.
After the July announcement, ABS sent surveys to all diplomates to gather feedback about alternatives to the 10-year exam. Nearly 10,000 surgeons responded, according to an ABS summary. The majority of respondents said they wanted more frequent, lower-stakes, open-book assessments that would be required no frequently than every 2 years. Most surgeons were also in favor of being tested on both surgery concepts and practice-specific content.
For 2019 and beyond, the ABS’ Component Boards – Vascular, Pediatric Surgery, Surgical, and Critical Care – will develop their continuous certification processes, Dr. Klingensmith said. Additional areas for the surgery exam also will be developed in collaboration with specialty societies.
In the meantime, registration for the new general surgery assessment opens Aug. 1. The assessment will be available from Sept. 7 to Nov. 5, during which time diplomates can take the assessment at their convenience.
For more information, go to the continuous certification section on the ABS website.
.
The new test, required every other year, consists of a 40-question, open-book assessment that surgeons can take on their own computers within the assessment time frame, according to a March 5 announcement. The previous 10-year exam consisted of nearly 250 questions and had to be completed at a highly secure testing center.
The assessment shift was made to address diplomates’ concerns that the prior exam was burdensome, stressful, and challenging to complete because of its rigid design and location requirements, ABS Chair Mary E. Klingensmith, MD, FACS, said in an interview.
“This new method, which allows a take-from-home or office format, is much less stressful, as both the setting, and the ability to choose the content area, give diplomates much more control,” Dr. Klingensmith said. “Additionally, the testing concepts and references will be provided in advance, should a diplomate desire to know these aspects.”
On March 11, the American College of Surgeons released a statement regarding the new assessment and suggested that, while the new approach is welcomed by the ACS, some details of the process are of concern to surgeons. “The American College of Surgeons (ACS) leadership has heard your concerns both through personal conversations with many of you and through your posts on ACS Communities. In fact, many in leadership share these concerns. We have been in discussions with ABS leadership and can tell you that they are also listening. They want to get this right.”
Of the 40 questions on the new exam, 20 questions will cover core surgical principles, while the other 20 will cover a practice-related area of the diplomate’s choosing. For 2018, diplomates can select from four practice-related areas: general surgery, abdomen, alimentary tract, or breast. More areas are planned based on future feedback from diplomates and surgical societies. Other aspects of the new exam include:
- Topics and references for the various areas will be published in advance on the ABS website.
- Diplomates will be provided with immediate feedback, and will have two opportunities to answer a question correctly.
- A final score of 80% correct will be required to pass.
- Once the assessment is started, diplomates will have 2 weeks to complete the test, with the ability to save and continue when convenient.
The purpose of the new assessment is to provide practicing surgeons with a timely, relevant, and accessible method to stay current with surgical practice knowledge,” Dr. Klingensmith said.
“By selecting a practice-specific area of their own choosing, surgeons will no longer have to study for and be tested upon the entire breadth of general surgery; instead they can focus on those areas that most reflect their practice,” she said. “By submitting to a learning exercise every 2 years, which is focused in the areas of an individual surgeon’s practice, I expect important aspects of knowledge will be transmitted and integrated into a surgeon’s practice. This new program will provide practicing surgeons with an accessible method for keeping up with the constantly changing landscape of surgical practice.”
The new exam is part of an ongoing effort by ABS to revamp its maintenance of certification requirements after widespread criticism that its past provisions were burdensome and irrelevant. In July, ABS announced that it was extending its continuing medical education reporting cycle from 3 to 5 years and reducing the number of required self-assessment by a third. Surgeons now have to report 150 credits over 5 years, 50 from self-assessment CMEs. Under the old system, it was 90 credits over 3 years, 60 of which had to include self-assessment.
After the July announcement, ABS sent surveys to all diplomates to gather feedback about alternatives to the 10-year exam. Nearly 10,000 surgeons responded, according to an ABS summary. The majority of respondents said they wanted more frequent, lower-stakes, open-book assessments that would be required no frequently than every 2 years. Most surgeons were also in favor of being tested on both surgery concepts and practice-specific content.
For 2019 and beyond, the ABS’ Component Boards – Vascular, Pediatric Surgery, Surgical, and Critical Care – will develop their continuous certification processes, Dr. Klingensmith said. Additional areas for the surgery exam also will be developed in collaboration with specialty societies.
In the meantime, registration for the new general surgery assessment opens Aug. 1. The assessment will be available from Sept. 7 to Nov. 5, during which time diplomates can take the assessment at their convenience.
For more information, go to the continuous certification section on the ABS website.
.
The new test, required every other year, consists of a 40-question, open-book assessment that surgeons can take on their own computers within the assessment time frame, according to a March 5 announcement. The previous 10-year exam consisted of nearly 250 questions and had to be completed at a highly secure testing center.
The assessment shift was made to address diplomates’ concerns that the prior exam was burdensome, stressful, and challenging to complete because of its rigid design and location requirements, ABS Chair Mary E. Klingensmith, MD, FACS, said in an interview.
“This new method, which allows a take-from-home or office format, is much less stressful, as both the setting, and the ability to choose the content area, give diplomates much more control,” Dr. Klingensmith said. “Additionally, the testing concepts and references will be provided in advance, should a diplomate desire to know these aspects.”
On March 11, the American College of Surgeons released a statement regarding the new assessment and suggested that, while the new approach is welcomed by the ACS, some details of the process are of concern to surgeons. “The American College of Surgeons (ACS) leadership has heard your concerns both through personal conversations with many of you and through your posts on ACS Communities. In fact, many in leadership share these concerns. We have been in discussions with ABS leadership and can tell you that they are also listening. They want to get this right.”
Of the 40 questions on the new exam, 20 questions will cover core surgical principles, while the other 20 will cover a practice-related area of the diplomate’s choosing. For 2018, diplomates can select from four practice-related areas: general surgery, abdomen, alimentary tract, or breast. More areas are planned based on future feedback from diplomates and surgical societies. Other aspects of the new exam include:
- Topics and references for the various areas will be published in advance on the ABS website.
- Diplomates will be provided with immediate feedback, and will have two opportunities to answer a question correctly.
- A final score of 80% correct will be required to pass.
- Once the assessment is started, diplomates will have 2 weeks to complete the test, with the ability to save and continue when convenient.
The purpose of the new assessment is to provide practicing surgeons with a timely, relevant, and accessible method to stay current with surgical practice knowledge,” Dr. Klingensmith said.
“By selecting a practice-specific area of their own choosing, surgeons will no longer have to study for and be tested upon the entire breadth of general surgery; instead they can focus on those areas that most reflect their practice,” she said. “By submitting to a learning exercise every 2 years, which is focused in the areas of an individual surgeon’s practice, I expect important aspects of knowledge will be transmitted and integrated into a surgeon’s practice. This new program will provide practicing surgeons with an accessible method for keeping up with the constantly changing landscape of surgical practice.”
The new exam is part of an ongoing effort by ABS to revamp its maintenance of certification requirements after widespread criticism that its past provisions were burdensome and irrelevant. In July, ABS announced that it was extending its continuing medical education reporting cycle from 3 to 5 years and reducing the number of required self-assessment by a third. Surgeons now have to report 150 credits over 5 years, 50 from self-assessment CMEs. Under the old system, it was 90 credits over 3 years, 60 of which had to include self-assessment.
After the July announcement, ABS sent surveys to all diplomates to gather feedback about alternatives to the 10-year exam. Nearly 10,000 surgeons responded, according to an ABS summary. The majority of respondents said they wanted more frequent, lower-stakes, open-book assessments that would be required no frequently than every 2 years. Most surgeons were also in favor of being tested on both surgery concepts and practice-specific content.
For 2019 and beyond, the ABS’ Component Boards – Vascular, Pediatric Surgery, Surgical, and Critical Care – will develop their continuous certification processes, Dr. Klingensmith said. Additional areas for the surgery exam also will be developed in collaboration with specialty societies.
In the meantime, registration for the new general surgery assessment opens Aug. 1. The assessment will be available from Sept. 7 to Nov. 5, during which time diplomates can take the assessment at their convenience.
For more information, go to the continuous certification section on the ABS website.
Supreme Court declines to hear DACA case
The U.S. Supreme Court has declined to decide for now whether the Deferred Action for Childhood Arrivals (DACA) program should continue, turning down a request by the Trump administration to hear the case early. The Feb. 26 decision allows the DACA program to remain in effect under a district court ruling and sends the case back to the appeals court.
The Trump administration has called DACA, an Obama administration policy that protected from deportation immigrants who were brought to the United States illegally as children and authorized them to work in the United States, an “unconstitutional overreach of executive branch power” by the former administration that deliberately sought to undermine the legislative branch.
President Trump announced in September 2016 that he would phase out the DACA program and gave Congress 6 months to pass legislation that would replace DACA or preserve some of its provisions or he would terminate it. They have made little progress toward agreeing on replacement legislation for DACA since then.
A number of plaintiffs sued the Trump administration over the program’s rescission, including the University of California, several states, and a group of individuals who remain in the United States because of DACA. The plaintiffs alleged the rescission violated the Administrative Procedure Act because it was an abuse of discretion and deprived those affected by DACA of “constitutionally protected property and liberty interests without due process of law.”
In a Jan. 9 opinion, the United States District Court for the Northern District of California sided with the plaintiffs, ruling that they were likely to succeed on their claims that the rescission “was arbitrary, capricious, an abuse of discretion, or not otherwise in accordance with law.” The court ordered the government to continue accepting DACA renewal applications while the challenges continued through the court system. Rather than pursuing an appeal, the U.S. Department of Justice requested that the Supreme Court take up the case.
In its Feb. 26 order, the high court declined to hear the case, writing, “it is assumed the court of appeals will act expeditiously to decide this case.”
Jirayut New Latthivongskorn, a co-plaintiff in the case and a medical student with DACA status at the University of California, San Francisco, said the Supreme Court made the right decision. Mr. Latthivongskorn, who came to the United States from Thailand when he was 9 years old, is cofounder of Pre-Health Dreamers, a network of undocumented students who plan to pursue medical careers. He is in his third year at UCSF and is slated to graduate in 2019 after completing the university’s Program in Medical Education for the Urban Underserved.
The Department of Justice expressed disappointment at the Supreme Court’s decision not to take up the case and said it will continue to strongly defend the case.
“While we were hopeful for a different outcome, the Supreme Court very rarely grants certiorari before judgment, though in our view it was warranted for the extraordinary injunction requiring the Department of Homeland Security to maintain DACA,” DOJ spokesman Devin O’Malley said in a statement. “We will continue to defend DHS’ lawful authority to wind down DACA in an orderly manner.”
The U.S. Supreme Court has declined to decide for now whether the Deferred Action for Childhood Arrivals (DACA) program should continue, turning down a request by the Trump administration to hear the case early. The Feb. 26 decision allows the DACA program to remain in effect under a district court ruling and sends the case back to the appeals court.
The Trump administration has called DACA, an Obama administration policy that protected from deportation immigrants who were brought to the United States illegally as children and authorized them to work in the United States, an “unconstitutional overreach of executive branch power” by the former administration that deliberately sought to undermine the legislative branch.
President Trump announced in September 2016 that he would phase out the DACA program and gave Congress 6 months to pass legislation that would replace DACA or preserve some of its provisions or he would terminate it. They have made little progress toward agreeing on replacement legislation for DACA since then.
A number of plaintiffs sued the Trump administration over the program’s rescission, including the University of California, several states, and a group of individuals who remain in the United States because of DACA. The plaintiffs alleged the rescission violated the Administrative Procedure Act because it was an abuse of discretion and deprived those affected by DACA of “constitutionally protected property and liberty interests without due process of law.”
In a Jan. 9 opinion, the United States District Court for the Northern District of California sided with the plaintiffs, ruling that they were likely to succeed on their claims that the rescission “was arbitrary, capricious, an abuse of discretion, or not otherwise in accordance with law.” The court ordered the government to continue accepting DACA renewal applications while the challenges continued through the court system. Rather than pursuing an appeal, the U.S. Department of Justice requested that the Supreme Court take up the case.
In its Feb. 26 order, the high court declined to hear the case, writing, “it is assumed the court of appeals will act expeditiously to decide this case.”
Jirayut New Latthivongskorn, a co-plaintiff in the case and a medical student with DACA status at the University of California, San Francisco, said the Supreme Court made the right decision. Mr. Latthivongskorn, who came to the United States from Thailand when he was 9 years old, is cofounder of Pre-Health Dreamers, a network of undocumented students who plan to pursue medical careers. He is in his third year at UCSF and is slated to graduate in 2019 after completing the university’s Program in Medical Education for the Urban Underserved.
The Department of Justice expressed disappointment at the Supreme Court’s decision not to take up the case and said it will continue to strongly defend the case.
“While we were hopeful for a different outcome, the Supreme Court very rarely grants certiorari before judgment, though in our view it was warranted for the extraordinary injunction requiring the Department of Homeland Security to maintain DACA,” DOJ spokesman Devin O’Malley said in a statement. “We will continue to defend DHS’ lawful authority to wind down DACA in an orderly manner.”
The U.S. Supreme Court has declined to decide for now whether the Deferred Action for Childhood Arrivals (DACA) program should continue, turning down a request by the Trump administration to hear the case early. The Feb. 26 decision allows the DACA program to remain in effect under a district court ruling and sends the case back to the appeals court.
The Trump administration has called DACA, an Obama administration policy that protected from deportation immigrants who were brought to the United States illegally as children and authorized them to work in the United States, an “unconstitutional overreach of executive branch power” by the former administration that deliberately sought to undermine the legislative branch.
President Trump announced in September 2016 that he would phase out the DACA program and gave Congress 6 months to pass legislation that would replace DACA or preserve some of its provisions or he would terminate it. They have made little progress toward agreeing on replacement legislation for DACA since then.
A number of plaintiffs sued the Trump administration over the program’s rescission, including the University of California, several states, and a group of individuals who remain in the United States because of DACA. The plaintiffs alleged the rescission violated the Administrative Procedure Act because it was an abuse of discretion and deprived those affected by DACA of “constitutionally protected property and liberty interests without due process of law.”
In a Jan. 9 opinion, the United States District Court for the Northern District of California sided with the plaintiffs, ruling that they were likely to succeed on their claims that the rescission “was arbitrary, capricious, an abuse of discretion, or not otherwise in accordance with law.” The court ordered the government to continue accepting DACA renewal applications while the challenges continued through the court system. Rather than pursuing an appeal, the U.S. Department of Justice requested that the Supreme Court take up the case.
In its Feb. 26 order, the high court declined to hear the case, writing, “it is assumed the court of appeals will act expeditiously to decide this case.”
Jirayut New Latthivongskorn, a co-plaintiff in the case and a medical student with DACA status at the University of California, San Francisco, said the Supreme Court made the right decision. Mr. Latthivongskorn, who came to the United States from Thailand when he was 9 years old, is cofounder of Pre-Health Dreamers, a network of undocumented students who plan to pursue medical careers. He is in his third year at UCSF and is slated to graduate in 2019 after completing the university’s Program in Medical Education for the Urban Underserved.
The Department of Justice expressed disappointment at the Supreme Court’s decision not to take up the case and said it will continue to strongly defend the case.
“While we were hopeful for a different outcome, the Supreme Court very rarely grants certiorari before judgment, though in our view it was warranted for the extraordinary injunction requiring the Department of Homeland Security to maintain DACA,” DOJ spokesman Devin O’Malley said in a statement. “We will continue to defend DHS’ lawful authority to wind down DACA in an orderly manner.”
Will Indiana Medicaid work requirements pass legal muster?
The recent federal waiver allowing work requirements for Indiana’s Medicaid program has sparked controversy from all sides and led to a debate that analysts say is likely to end in court.
Indiana’s waiver, green-lighted by the U.S. Department of Health & Human Services in February, requires certain Medicaid recipients to work an average of 20 hours a week, be enrolled in school, or participate in a job search/training program in order to qualify for assistance. Proponents say the requirements are a practical approach to improving self-sufficiency for able-bodied Medicaid patients by incentivizing work and community engagement. Critics argue the requirements are burdensome for the state’s most vulnerable populations and jeopardize medical care for some 30,000 recipients. But will the requirements pass legal muster in a court of law?
Typically, when arguments arise over state Medicaid program provisions, they center on whether the requirements help or hinder the program, Mr. Salo said in an interview.
“There isn’t really a clear-cut, black-and-white definition of the purposes of Medicaid written down in the statute,” he said. “Practically speaking, it’s a fairly subjective term. Clearly, the Obama administration said, ‘We don’t think [work requirement] policies further the objectives of the Medicaid program.’ I don’t think there’s anything that would preclude a new administration from saying, ‘We have a slightly different opinion of what the purposes of the Medicaid program are.’ ”
However, Leonardo Cuello, director of health policy for the National Health Law Program, says Indiana’s new requirements are illegal and clearly run contrary to the purpose of the Medicaid program. While the program’s work requirements are taking the spotlight, he notes that the new provisions also include lockout periods if paperwork is late and removes transportation assistance for medical care.
The National Health Law Program is a coplaintiff in a lawsuit challenging similar Medicaid requirements in Kentucky. Like Indiana’s waiver, Kentucky’s approved plan includes lockout provisions for failing to pay premiums on time and has work requirements for able-bodied adult enrollees. Mr. Cuello said his organization is looking closely at taking legal action against Indiana’s waiver as well.
In a statement, HHS Secretary Alex Azar said the approval of Indiana’s expanded Medicaid program is in line with a Trump administration policy to support state efforts to “improve Medicaid enrollee health outcomes and promote independence by incentivizing community engagement among able-bodied, working-age Medicaid beneficiaries.” The policy responds to numerous state requests to test programs through Medicaid demonstration projects under which work and other types of community engagement would be a condition of Medicaid coverage, according to the announcement.
“We look forward to collaborating with Indiana on this next evolution of [the Healthy Indiana Plan], which serves as another example of the Trump administration’s support of state-led efforts and innovative reforms to make our HHS programs really work for Americans,” Mr. Azar said in the statement.
Another legal question that may arise against Indiana’s work requirements for Medicaid is whether the provisions are part of a true “experiment.”
“These waivers are at the broad discretion of the government,” Mr. Blumstein said in an interview. “I think [Indiana’s plan] is compatible with an overall welfare strategy that’s designed to cut costs, to get folks jobs, and then ultimately, into private sector health insurance. In principal, these things are good to try.”
Mr. Blumstein said that he believes HHS has a strong legal position in defending Indiana’s waiver program, but that doesn’t mean a judge will agree, he said.
“Will a court somewhere find against the government? Against Indiana? I can’t say,” he said. “There’s a lot of hostility to change, and some judges share that hostility to change. But based on my TennCare experience, courts should bend over backward to give flexibility to the states to experiment in this way, if they’re approved by the federal government.”
Mr. Cuello of the National Health Law Program said the Indiana and Kentucky waivers both fail to demonstrate any experimental value. Studies show that when such requirements are enforced, patients drop out of Medicaid or forgo medical care.
“These waivers fail a legality test because they’re not part of any experiment,” he said. “An experiment would be: Here’s an innovative way we have for how to provide health care. These are not experiments.”
At press time, eight states had pending waiver requests at the Centers for Medicare & Medicaid Services that would require work as a condition of eligibility for expansion adults and/or traditional populations.
The recent federal waiver allowing work requirements for Indiana’s Medicaid program has sparked controversy from all sides and led to a debate that analysts say is likely to end in court.
Indiana’s waiver, green-lighted by the U.S. Department of Health & Human Services in February, requires certain Medicaid recipients to work an average of 20 hours a week, be enrolled in school, or participate in a job search/training program in order to qualify for assistance. Proponents say the requirements are a practical approach to improving self-sufficiency for able-bodied Medicaid patients by incentivizing work and community engagement. Critics argue the requirements are burdensome for the state’s most vulnerable populations and jeopardize medical care for some 30,000 recipients. But will the requirements pass legal muster in a court of law?
Typically, when arguments arise over state Medicaid program provisions, they center on whether the requirements help or hinder the program, Mr. Salo said in an interview.
“There isn’t really a clear-cut, black-and-white definition of the purposes of Medicaid written down in the statute,” he said. “Practically speaking, it’s a fairly subjective term. Clearly, the Obama administration said, ‘We don’t think [work requirement] policies further the objectives of the Medicaid program.’ I don’t think there’s anything that would preclude a new administration from saying, ‘We have a slightly different opinion of what the purposes of the Medicaid program are.’ ”
However, Leonardo Cuello, director of health policy for the National Health Law Program, says Indiana’s new requirements are illegal and clearly run contrary to the purpose of the Medicaid program. While the program’s work requirements are taking the spotlight, he notes that the new provisions also include lockout periods if paperwork is late and removes transportation assistance for medical care.
The National Health Law Program is a coplaintiff in a lawsuit challenging similar Medicaid requirements in Kentucky. Like Indiana’s waiver, Kentucky’s approved plan includes lockout provisions for failing to pay premiums on time and has work requirements for able-bodied adult enrollees. Mr. Cuello said his organization is looking closely at taking legal action against Indiana’s waiver as well.
In a statement, HHS Secretary Alex Azar said the approval of Indiana’s expanded Medicaid program is in line with a Trump administration policy to support state efforts to “improve Medicaid enrollee health outcomes and promote independence by incentivizing community engagement among able-bodied, working-age Medicaid beneficiaries.” The policy responds to numerous state requests to test programs through Medicaid demonstration projects under which work and other types of community engagement would be a condition of Medicaid coverage, according to the announcement.
“We look forward to collaborating with Indiana on this next evolution of [the Healthy Indiana Plan], which serves as another example of the Trump administration’s support of state-led efforts and innovative reforms to make our HHS programs really work for Americans,” Mr. Azar said in the statement.
Another legal question that may arise against Indiana’s work requirements for Medicaid is whether the provisions are part of a true “experiment.”
“These waivers are at the broad discretion of the government,” Mr. Blumstein said in an interview. “I think [Indiana’s plan] is compatible with an overall welfare strategy that’s designed to cut costs, to get folks jobs, and then ultimately, into private sector health insurance. In principal, these things are good to try.”
Mr. Blumstein said that he believes HHS has a strong legal position in defending Indiana’s waiver program, but that doesn’t mean a judge will agree, he said.
“Will a court somewhere find against the government? Against Indiana? I can’t say,” he said. “There’s a lot of hostility to change, and some judges share that hostility to change. But based on my TennCare experience, courts should bend over backward to give flexibility to the states to experiment in this way, if they’re approved by the federal government.”
Mr. Cuello of the National Health Law Program said the Indiana and Kentucky waivers both fail to demonstrate any experimental value. Studies show that when such requirements are enforced, patients drop out of Medicaid or forgo medical care.
“These waivers fail a legality test because they’re not part of any experiment,” he said. “An experiment would be: Here’s an innovative way we have for how to provide health care. These are not experiments.”
At press time, eight states had pending waiver requests at the Centers for Medicare & Medicaid Services that would require work as a condition of eligibility for expansion adults and/or traditional populations.
The recent federal waiver allowing work requirements for Indiana’s Medicaid program has sparked controversy from all sides and led to a debate that analysts say is likely to end in court.
Indiana’s waiver, green-lighted by the U.S. Department of Health & Human Services in February, requires certain Medicaid recipients to work an average of 20 hours a week, be enrolled in school, or participate in a job search/training program in order to qualify for assistance. Proponents say the requirements are a practical approach to improving self-sufficiency for able-bodied Medicaid patients by incentivizing work and community engagement. Critics argue the requirements are burdensome for the state’s most vulnerable populations and jeopardize medical care for some 30,000 recipients. But will the requirements pass legal muster in a court of law?
Typically, when arguments arise over state Medicaid program provisions, they center on whether the requirements help or hinder the program, Mr. Salo said in an interview.
“There isn’t really a clear-cut, black-and-white definition of the purposes of Medicaid written down in the statute,” he said. “Practically speaking, it’s a fairly subjective term. Clearly, the Obama administration said, ‘We don’t think [work requirement] policies further the objectives of the Medicaid program.’ I don’t think there’s anything that would preclude a new administration from saying, ‘We have a slightly different opinion of what the purposes of the Medicaid program are.’ ”
However, Leonardo Cuello, director of health policy for the National Health Law Program, says Indiana’s new requirements are illegal and clearly run contrary to the purpose of the Medicaid program. While the program’s work requirements are taking the spotlight, he notes that the new provisions also include lockout periods if paperwork is late and removes transportation assistance for medical care.
The National Health Law Program is a coplaintiff in a lawsuit challenging similar Medicaid requirements in Kentucky. Like Indiana’s waiver, Kentucky’s approved plan includes lockout provisions for failing to pay premiums on time and has work requirements for able-bodied adult enrollees. Mr. Cuello said his organization is looking closely at taking legal action against Indiana’s waiver as well.
In a statement, HHS Secretary Alex Azar said the approval of Indiana’s expanded Medicaid program is in line with a Trump administration policy to support state efforts to “improve Medicaid enrollee health outcomes and promote independence by incentivizing community engagement among able-bodied, working-age Medicaid beneficiaries.” The policy responds to numerous state requests to test programs through Medicaid demonstration projects under which work and other types of community engagement would be a condition of Medicaid coverage, according to the announcement.
“We look forward to collaborating with Indiana on this next evolution of [the Healthy Indiana Plan], which serves as another example of the Trump administration’s support of state-led efforts and innovative reforms to make our HHS programs really work for Americans,” Mr. Azar said in the statement.
Another legal question that may arise against Indiana’s work requirements for Medicaid is whether the provisions are part of a true “experiment.”
“These waivers are at the broad discretion of the government,” Mr. Blumstein said in an interview. “I think [Indiana’s plan] is compatible with an overall welfare strategy that’s designed to cut costs, to get folks jobs, and then ultimately, into private sector health insurance. In principal, these things are good to try.”
Mr. Blumstein said that he believes HHS has a strong legal position in defending Indiana’s waiver program, but that doesn’t mean a judge will agree, he said.
“Will a court somewhere find against the government? Against Indiana? I can’t say,” he said. “There’s a lot of hostility to change, and some judges share that hostility to change. But based on my TennCare experience, courts should bend over backward to give flexibility to the states to experiment in this way, if they’re approved by the federal government.”
Mr. Cuello of the National Health Law Program said the Indiana and Kentucky waivers both fail to demonstrate any experimental value. Studies show that when such requirements are enforced, patients drop out of Medicaid or forgo medical care.
“These waivers fail a legality test because they’re not part of any experiment,” he said. “An experiment would be: Here’s an innovative way we have for how to provide health care. These are not experiments.”
At press time, eight states had pending waiver requests at the Centers for Medicare & Medicaid Services that would require work as a condition of eligibility for expansion adults and/or traditional populations.
Cyberliability insurance: Should you purchase a policy?
As hackers become more sophisticated, these .
In 2017, there were at least 477 publicly reported health data breaches in the United States, affecting some 5.6 million patients, up from 450 health care breaches in 2016, according to Protenus, a health care cybersecurity vendor that tracks data breaches reported to the U.S. Department of Health & Human Services.
“A breach is very expensive,” said Mr. Cohen, chair for the New York City Bar Association Committee on Medical Malpractice. “You have the fine to the Office for Civil Rights, which can be in the millions of dollars, and you’re going to have to ameliorate the breach, which can be hundreds of dollars per person, let alone deal with lawsuits from the patients.”
Cyberliability: What’s the risk?
Cyberliability refers to legal dangers arising from data breaches, privacy law violations, and ransomware/cyberextortion threats, as well as data loss and business interruption from computer system failures.
Of the 477 breaches in 2017 analyzed by Protenus, 37% were from hacking, 37% resulted from insider incidents, and 16% stemmed from data loss or theft. About 10% of cases resulted from unknown reasons, according to the report.
Data breaches caused by hackers and malware attacks are rising in the health care sector, said Katherine Keefe, global head of breach response services for Beazley, a national cyberliability insurer and risk management company. Beazley handled 2,615 data breaches in 2017, more than half of which were health care–related, Ms. Keefe said in an interview. The top three causes of health care breaches reported to Beazley in 2017 were accidental disclosure, hack or malware, and insider incidents, according to a recent report from that company
“We see an awful lot of that,” Ms. Keefe said. “There’s been a real surge in successful phishing emails and social engineering that enables criminals to identify medical practice leaders. It’s not hard to dress up an email to look like it’s coming from a specific individual. There are all kinds of increasingly sophisticated tactics to trick people into letting criminals into their systems or tricking people into forwarding money or valuable information.”
Hackers frequently use phishing emails to get employees to download a payload, the portion of malware that performs malicious actions, Mr. Cohen added. Once downloaded, payloads can do significant damage to a medical practice.
“Once you get hit with these payloads, not only can they start pulling information out of the computer system, they can also start doing things, such as turning on laptop cameras, reading emails, listening in on computer microphones,” he said. “All they need is one employee to click.”
Considering cybercoverage
To protect themselves from potential breach expenses, more medical practices are purchasing cyberliability insurance policies. A 2017 survey of 270 insurance brokers and 125 underwriters found that health care has more first-time buyers of stand-alone cyberliability insurance than does any other industry.
However, Mr. Cohen advises that practices should do their research before buying and be aware of the different types of policies, coverage limits, and insurance options.
“Be careful about what it covers,” he said. “Are they going to pay for all the amelioration for all the patients affected? Some policies will cover ‘repairing and disinfecting the system,’ but they will not likely cover all the [Office for Civil Rights] fines.”
The Doctors Company, a national medical liability insurer, provides $50,000 in cybersecurity coverage to all its insured physician members and the option to increase coverage by $1 million in additional protection, according to Crystal Brown, senior vice president of underwriting for the Doctors Company. The coverage protects against regulatory and liability claims arising from theft, loss, or accidental transmission of patient or financial information as well as the cost of data recovery. Another policy offered protects against claims arising from administrative actions pertaining to utilization, licensing, credentialing, and misconduct.
Meanwhile, national medical liability insurer ProAssurance offers health providers a basic cyberliability coverage endorsement in most states on its medical professional liability policy. The insurer also has a branded cyberprogram that allows clients to buy additional and broader coverage at a discounted premium.
“In today’s electronic environment, we are hearing about breaches occurring at both small and large health care practices,” said Melanie Tullos, vice president for ProAssurance. “Small physician practices are just as vulnerable, if not more so, to a cyberbreach and should take the necessary steps to protect patient data against an attack at all measures, including, but not limited to, purchasing cyberliability coverage.
The price of cyberliability insurance varies by risk and other factors, Ms. Tullos said. Generally, the cost of a $1 million cyberliability policy for a single physician practice is less than $1,000, whereas a group of 10 physicians can pay up to $8,000-$9,000, she said in an interview.
Beazley offers policies that cover the expenses and services associated with investigating whether a data breach has occurred, responding to breaches, and liability that may arise from the breach, said Ms. Keefe, of Beazley, which works with companies such as the Doctors Company to provide coverage and also works with state-run malpractice programs to offer a cyberliability component for a small, additional premium, she said.
Ms. Keefe stressed that cyberliability coverage can ensure that physician practices don’t run up a hefty bill in the event of a data breach by paying for separate specialists and damage control.
“One of the reasons doctors should have cyberliability coverage are the costs associated with figuring out what to do if patient records are lost or stolen,” she said. “The cost of hiring a lawyer, hiring a forensics investigator to assess the situation, the cost of notifying the patients, and taking all the steps required by HIPAA can really add up. Most practices don’t have those costs built into their annual budgets. A cyberpolicy acts as a buffer against those expenses.”
Manage risk before a breach
Of course, there is plenty that practices can do to prevent – and protect themselves from – a health data breach before it happens. Providing employee awareness training is an important step, said Craig Musgrave, chief information officer of the Doctors Company. Institute a training program for staff at all levels and go over the basics, such as refraining from opening emails from senders they don’t know, Mr. Musgrave wrote in a recent column. Updating all software regularly and backing up data is also essential. And Mr. Musgrave emphasizes the importance of “whitelisting.”
“Health care systems are fragmented in their management of systems and data,” Mr. Musgrave wrote in his column. “Their ability to patch legacy systems and employ cybersecurity staff varies enormously. Therefore, application whitelisting is essential. Rather than blacklisting known malicious software, an application whitelist prevents the launching of any executable program (known or unknown) that does not have explicit authorization. This, in combination with strong firewalls and network segmentation tools like micro-segmentation, provides stronger security.”
In addition, consider implementing data security policies and incident response protocols as well as employee training on securing patient data, ProAssurance’s Ms. Tullos said.
“A breach can also occur within a third-party vendors system and infiltrate the physician’s records, so it is important to discuss cybersecurity with those vendors and all parties should purchase cyberliability insurance,” she said.
Michael E. Nelson, MD, FCCP, comments: Being old enough to remember a paper chart and scheduling book, I can't help but marvel at the how the electronic health record (EHR) has fallen short of its expectations and added to the cost of medical care. Well, let's add cybersecurity insurance to the cost of doing business. While I love the ability to look at a chest x-ray or CT without a viewbox, I can't think of many other things that the EHR has done to make me a more efficient physician. It has, however, spawned many cottage industries that provide "must have" services with their attendant fees. The ever-increasing regulatory and administrative burdens and costs placed on physicians' practices is making it impossible for smaller practices to remain financially viable, leaving smaller communities without medical services. I don't think this was the intent when we decided to "modernize" medicine. It makes me want to go back to those Halcyon days of the paper chart - try phishing one of those, you hackers.
Michael E. Nelson, MD, FCCP, comments: Being old enough to remember a paper chart and scheduling book, I can't help but marvel at the how the electronic health record (EHR) has fallen short of its expectations and added to the cost of medical care. Well, let's add cybersecurity insurance to the cost of doing business. While I love the ability to look at a chest x-ray or CT without a viewbox, I can't think of many other things that the EHR has done to make me a more efficient physician. It has, however, spawned many cottage industries that provide "must have" services with their attendant fees. The ever-increasing regulatory and administrative burdens and costs placed on physicians' practices is making it impossible for smaller practices to remain financially viable, leaving smaller communities without medical services. I don't think this was the intent when we decided to "modernize" medicine. It makes me want to go back to those Halcyon days of the paper chart - try phishing one of those, you hackers.
Michael E. Nelson, MD, FCCP, comments: Being old enough to remember a paper chart and scheduling book, I can't help but marvel at the how the electronic health record (EHR) has fallen short of its expectations and added to the cost of medical care. Well, let's add cybersecurity insurance to the cost of doing business. While I love the ability to look at a chest x-ray or CT without a viewbox, I can't think of many other things that the EHR has done to make me a more efficient physician. It has, however, spawned many cottage industries that provide "must have" services with their attendant fees. The ever-increasing regulatory and administrative burdens and costs placed on physicians' practices is making it impossible for smaller practices to remain financially viable, leaving smaller communities without medical services. I don't think this was the intent when we decided to "modernize" medicine. It makes me want to go back to those Halcyon days of the paper chart - try phishing one of those, you hackers.
As hackers become more sophisticated, these .
In 2017, there were at least 477 publicly reported health data breaches in the United States, affecting some 5.6 million patients, up from 450 health care breaches in 2016, according to Protenus, a health care cybersecurity vendor that tracks data breaches reported to the U.S. Department of Health & Human Services.
“A breach is very expensive,” said Mr. Cohen, chair for the New York City Bar Association Committee on Medical Malpractice. “You have the fine to the Office for Civil Rights, which can be in the millions of dollars, and you’re going to have to ameliorate the breach, which can be hundreds of dollars per person, let alone deal with lawsuits from the patients.”
Cyberliability: What’s the risk?
Cyberliability refers to legal dangers arising from data breaches, privacy law violations, and ransomware/cyberextortion threats, as well as data loss and business interruption from computer system failures.
Of the 477 breaches in 2017 analyzed by Protenus, 37% were from hacking, 37% resulted from insider incidents, and 16% stemmed from data loss or theft. About 10% of cases resulted from unknown reasons, according to the report.
Data breaches caused by hackers and malware attacks are rising in the health care sector, said Katherine Keefe, global head of breach response services for Beazley, a national cyberliability insurer and risk management company. Beazley handled 2,615 data breaches in 2017, more than half of which were health care–related, Ms. Keefe said in an interview. The top three causes of health care breaches reported to Beazley in 2017 were accidental disclosure, hack or malware, and insider incidents, according to a recent report from that company
“We see an awful lot of that,” Ms. Keefe said. “There’s been a real surge in successful phishing emails and social engineering that enables criminals to identify medical practice leaders. It’s not hard to dress up an email to look like it’s coming from a specific individual. There are all kinds of increasingly sophisticated tactics to trick people into letting criminals into their systems or tricking people into forwarding money or valuable information.”
Hackers frequently use phishing emails to get employees to download a payload, the portion of malware that performs malicious actions, Mr. Cohen added. Once downloaded, payloads can do significant damage to a medical practice.
“Once you get hit with these payloads, not only can they start pulling information out of the computer system, they can also start doing things, such as turning on laptop cameras, reading emails, listening in on computer microphones,” he said. “All they need is one employee to click.”
Considering cybercoverage
To protect themselves from potential breach expenses, more medical practices are purchasing cyberliability insurance policies. A 2017 survey of 270 insurance brokers and 125 underwriters found that health care has more first-time buyers of stand-alone cyberliability insurance than does any other industry.
However, Mr. Cohen advises that practices should do their research before buying and be aware of the different types of policies, coverage limits, and insurance options.
“Be careful about what it covers,” he said. “Are they going to pay for all the amelioration for all the patients affected? Some policies will cover ‘repairing and disinfecting the system,’ but they will not likely cover all the [Office for Civil Rights] fines.”
The Doctors Company, a national medical liability insurer, provides $50,000 in cybersecurity coverage to all its insured physician members and the option to increase coverage by $1 million in additional protection, according to Crystal Brown, senior vice president of underwriting for the Doctors Company. The coverage protects against regulatory and liability claims arising from theft, loss, or accidental transmission of patient or financial information as well as the cost of data recovery. Another policy offered protects against claims arising from administrative actions pertaining to utilization, licensing, credentialing, and misconduct.
Meanwhile, national medical liability insurer ProAssurance offers health providers a basic cyberliability coverage endorsement in most states on its medical professional liability policy. The insurer also has a branded cyberprogram that allows clients to buy additional and broader coverage at a discounted premium.
“In today’s electronic environment, we are hearing about breaches occurring at both small and large health care practices,” said Melanie Tullos, vice president for ProAssurance. “Small physician practices are just as vulnerable, if not more so, to a cyberbreach and should take the necessary steps to protect patient data against an attack at all measures, including, but not limited to, purchasing cyberliability coverage.
The price of cyberliability insurance varies by risk and other factors, Ms. Tullos said. Generally, the cost of a $1 million cyberliability policy for a single physician practice is less than $1,000, whereas a group of 10 physicians can pay up to $8,000-$9,000, she said in an interview.
Beazley offers policies that cover the expenses and services associated with investigating whether a data breach has occurred, responding to breaches, and liability that may arise from the breach, said Ms. Keefe, of Beazley, which works with companies such as the Doctors Company to provide coverage and also works with state-run malpractice programs to offer a cyberliability component for a small, additional premium, she said.
Ms. Keefe stressed that cyberliability coverage can ensure that physician practices don’t run up a hefty bill in the event of a data breach by paying for separate specialists and damage control.
“One of the reasons doctors should have cyberliability coverage are the costs associated with figuring out what to do if patient records are lost or stolen,” she said. “The cost of hiring a lawyer, hiring a forensics investigator to assess the situation, the cost of notifying the patients, and taking all the steps required by HIPAA can really add up. Most practices don’t have those costs built into their annual budgets. A cyberpolicy acts as a buffer against those expenses.”
Manage risk before a breach
Of course, there is plenty that practices can do to prevent – and protect themselves from – a health data breach before it happens. Providing employee awareness training is an important step, said Craig Musgrave, chief information officer of the Doctors Company. Institute a training program for staff at all levels and go over the basics, such as refraining from opening emails from senders they don’t know, Mr. Musgrave wrote in a recent column. Updating all software regularly and backing up data is also essential. And Mr. Musgrave emphasizes the importance of “whitelisting.”
“Health care systems are fragmented in their management of systems and data,” Mr. Musgrave wrote in his column. “Their ability to patch legacy systems and employ cybersecurity staff varies enormously. Therefore, application whitelisting is essential. Rather than blacklisting known malicious software, an application whitelist prevents the launching of any executable program (known or unknown) that does not have explicit authorization. This, in combination with strong firewalls and network segmentation tools like micro-segmentation, provides stronger security.”
In addition, consider implementing data security policies and incident response protocols as well as employee training on securing patient data, ProAssurance’s Ms. Tullos said.
“A breach can also occur within a third-party vendors system and infiltrate the physician’s records, so it is important to discuss cybersecurity with those vendors and all parties should purchase cyberliability insurance,” she said.
As hackers become more sophisticated, these .
In 2017, there were at least 477 publicly reported health data breaches in the United States, affecting some 5.6 million patients, up from 450 health care breaches in 2016, according to Protenus, a health care cybersecurity vendor that tracks data breaches reported to the U.S. Department of Health & Human Services.
“A breach is very expensive,” said Mr. Cohen, chair for the New York City Bar Association Committee on Medical Malpractice. “You have the fine to the Office for Civil Rights, which can be in the millions of dollars, and you’re going to have to ameliorate the breach, which can be hundreds of dollars per person, let alone deal with lawsuits from the patients.”
Cyberliability: What’s the risk?
Cyberliability refers to legal dangers arising from data breaches, privacy law violations, and ransomware/cyberextortion threats, as well as data loss and business interruption from computer system failures.
Of the 477 breaches in 2017 analyzed by Protenus, 37% were from hacking, 37% resulted from insider incidents, and 16% stemmed from data loss or theft. About 10% of cases resulted from unknown reasons, according to the report.
Data breaches caused by hackers and malware attacks are rising in the health care sector, said Katherine Keefe, global head of breach response services for Beazley, a national cyberliability insurer and risk management company. Beazley handled 2,615 data breaches in 2017, more than half of which were health care–related, Ms. Keefe said in an interview. The top three causes of health care breaches reported to Beazley in 2017 were accidental disclosure, hack or malware, and insider incidents, according to a recent report from that company
“We see an awful lot of that,” Ms. Keefe said. “There’s been a real surge in successful phishing emails and social engineering that enables criminals to identify medical practice leaders. It’s not hard to dress up an email to look like it’s coming from a specific individual. There are all kinds of increasingly sophisticated tactics to trick people into letting criminals into their systems or tricking people into forwarding money or valuable information.”
Hackers frequently use phishing emails to get employees to download a payload, the portion of malware that performs malicious actions, Mr. Cohen added. Once downloaded, payloads can do significant damage to a medical practice.
“Once you get hit with these payloads, not only can they start pulling information out of the computer system, they can also start doing things, such as turning on laptop cameras, reading emails, listening in on computer microphones,” he said. “All they need is one employee to click.”
Considering cybercoverage
To protect themselves from potential breach expenses, more medical practices are purchasing cyberliability insurance policies. A 2017 survey of 270 insurance brokers and 125 underwriters found that health care has more first-time buyers of stand-alone cyberliability insurance than does any other industry.
However, Mr. Cohen advises that practices should do their research before buying and be aware of the different types of policies, coverage limits, and insurance options.
“Be careful about what it covers,” he said. “Are they going to pay for all the amelioration for all the patients affected? Some policies will cover ‘repairing and disinfecting the system,’ but they will not likely cover all the [Office for Civil Rights] fines.”
The Doctors Company, a national medical liability insurer, provides $50,000 in cybersecurity coverage to all its insured physician members and the option to increase coverage by $1 million in additional protection, according to Crystal Brown, senior vice president of underwriting for the Doctors Company. The coverage protects against regulatory and liability claims arising from theft, loss, or accidental transmission of patient or financial information as well as the cost of data recovery. Another policy offered protects against claims arising from administrative actions pertaining to utilization, licensing, credentialing, and misconduct.
Meanwhile, national medical liability insurer ProAssurance offers health providers a basic cyberliability coverage endorsement in most states on its medical professional liability policy. The insurer also has a branded cyberprogram that allows clients to buy additional and broader coverage at a discounted premium.
“In today’s electronic environment, we are hearing about breaches occurring at both small and large health care practices,” said Melanie Tullos, vice president for ProAssurance. “Small physician practices are just as vulnerable, if not more so, to a cyberbreach and should take the necessary steps to protect patient data against an attack at all measures, including, but not limited to, purchasing cyberliability coverage.
The price of cyberliability insurance varies by risk and other factors, Ms. Tullos said. Generally, the cost of a $1 million cyberliability policy for a single physician practice is less than $1,000, whereas a group of 10 physicians can pay up to $8,000-$9,000, she said in an interview.
Beazley offers policies that cover the expenses and services associated with investigating whether a data breach has occurred, responding to breaches, and liability that may arise from the breach, said Ms. Keefe, of Beazley, which works with companies such as the Doctors Company to provide coverage and also works with state-run malpractice programs to offer a cyberliability component for a small, additional premium, she said.
Ms. Keefe stressed that cyberliability coverage can ensure that physician practices don’t run up a hefty bill in the event of a data breach by paying for separate specialists and damage control.
“One of the reasons doctors should have cyberliability coverage are the costs associated with figuring out what to do if patient records are lost or stolen,” she said. “The cost of hiring a lawyer, hiring a forensics investigator to assess the situation, the cost of notifying the patients, and taking all the steps required by HIPAA can really add up. Most practices don’t have those costs built into their annual budgets. A cyberpolicy acts as a buffer against those expenses.”
Manage risk before a breach
Of course, there is plenty that practices can do to prevent – and protect themselves from – a health data breach before it happens. Providing employee awareness training is an important step, said Craig Musgrave, chief information officer of the Doctors Company. Institute a training program for staff at all levels and go over the basics, such as refraining from opening emails from senders they don’t know, Mr. Musgrave wrote in a recent column. Updating all software regularly and backing up data is also essential. And Mr. Musgrave emphasizes the importance of “whitelisting.”
“Health care systems are fragmented in their management of systems and data,” Mr. Musgrave wrote in his column. “Their ability to patch legacy systems and employ cybersecurity staff varies enormously. Therefore, application whitelisting is essential. Rather than blacklisting known malicious software, an application whitelist prevents the launching of any executable program (known or unknown) that does not have explicit authorization. This, in combination with strong firewalls and network segmentation tools like micro-segmentation, provides stronger security.”
In addition, consider implementing data security policies and incident response protocols as well as employee training on securing patient data, ProAssurance’s Ms. Tullos said.
“A breach can also occur within a third-party vendors system and infiltrate the physician’s records, so it is important to discuss cybersecurity with those vendors and all parties should purchase cyberliability insurance,” she said.
Transparency lacking in oncology clinical pathways
The use of oncology clinical pathways (OCPs) is rapidly rising as more data suggest that they can reduce cost and improve quality. But amid the advantages to pathways, there are growing concerns about hidden conflicts of interest.
“There is a lot of promise from these pathways in delivering the right care to the right patient at the right time,” said Bobby Daly, MD, an oncologist and health services researcher at Memorial Sloan Kettering Cancer Center in New York. “But oncologists and patients really want to understand how these pathways are being developed. The issue of transparency is one that patients and providers feel strongly about.”
While collaboration with industry is the key to innovation, Dr. Daly wrote that “to ensure patient and clinician trust and maintain their momentum in the value space, pathway developers will need to be transparent about [financial conflicts of interest] and how those interests are managed.”
Pathways: What’s the problem?
But as pathways have become more prevalent, concerns have emerged among physicians about who is making pathway treatment decisions and, specifically, about instances in which medications are being selected without disclosure of investments or financial relationships that could influence those decisions, said Robin Zon, MD, chair of the ASCO Task Force on Clinical Pathways.
“In addition, there have been concerns about the methodology of how treatments decisions are made with regard to efficacy, toxicity, and cost, as well as the weighting of these factors in making decisions for the pathway program,” Dr. Zon said in an interview.
Taken together, the mounting questions led to an analysis and by the ASCO task force.
“What the task force found was that standards defining high-quality pathways did not exist, so we became concerned that there could be a risk for wide variations with regards to the quality, utility, functionality, and impact of pathway programs,” Dr. Zon said.
The findings were the catalyst behind a March 2016 ASCO policy statement aimed at ensuring that clinical pathways in oncology promote – not hinder – cancer care. The task force called on pathway developers to adopt a process that was consistent and transparent to all stakeholders and to disclose potential conflicts of interest by the companies and individuals involved in pathway development.
“The criteria were developed to address the multiple issues brought to our attention by ASCO members and to be used as possible standards for pathway development, implementation, and evolution,” Dr. Zon said.
Meanwhile, the Cleveland Clinic has been utilizing pathways for more than 5 years and has published nearly 50 clinical pathways related to cancer care, Dr. Kalaycio said.
“Our care paths were designed to help physicians make clinical decisions that are in the best interest of their patients and the Cleveland Clinic,” he said in an interview. “These care paths are here for clinical reasons, not for financial reasons – we might ultimately use them to make financial decisions, but that’s not why they were developed. In contrast, the [JAMA Oncology study] is referring to pathways that are being developed by for-profit companies to control cost – big, big difference.”
The problem is that some insurers want to hide the identity of their advisors and how much they are being paid, which creates uncertainty about the validity of their pathways, he said. Dr. Kalaycio noted that the individuals selected for pathway panels and committees are often those who conducted the studies that the pathways are based upon and that those studies are frequently supported by the pharmaceutical industry.
“There is always going to be some degree of conflict of interest and as long as that’s disclosed, that’s fine,” he said. “It’s when you try to hide who’s getting paid for what that you get into trouble because you can’t say with certainty that someone’s not getting paid off.”
To address the transparency void, the California legislature in 2017 introduced the Oncology Clinical Pathways Act. The bill would have required health plans that develop and implement OCPs to provide the names, qualifications, affiliations, and conflicts of anyone involved in the research or analysis for an oncology clinical pathway if it were requested by a physician or surgeon. The bill died in committee.
Health plans push back
America’s Health Insurance Plans (AHIP) spokeswoman Cathryn Donaldson said health plans are being unfairly targeted in the drive toward more transparency. The recent efforts are an attempt to single out clinical care pathways developed by health plans as needing additional oversight standards while ignoring pathways that are developed by drug distributors, hospital systems, academic institutions, and others, Ms. Donaldson said in an interview.
ASCO’s Dr. Zon stressed that the criteria her task force created for pathways is aimed at all types of developers.
“In other words, we felt that the criteria should apply across all the pathway program developers whether they were provider or payer facing,” Dr. Zon said. “We also did not differentiate between not-for-profit and for-profit entities. Standards for high-quality criteria should apply to any pathway program being developed regardless of the source.”
Dr. Daly added that every entity that develops a pathway should have some policy around conflict of interest and how to address any transparency issues that may arise. Despite the recent debate over transparency, Dr. Daly said he believes the future of pathways is bright.
“I think the future is that pathways hold a lot of promise,” he said. “But I think we really need to ensure that the pathways that are being employed are of high quality because they influence how patients are treated.”
Dr. Daly serves as a director of Quadrant Holdings Corporation and receives compensation from this entity. This news organization is a subsidiary of Quadrant Holdings Corporation.
The use of oncology clinical pathways (OCPs) is rapidly rising as more data suggest that they can reduce cost and improve quality. But amid the advantages to pathways, there are growing concerns about hidden conflicts of interest.
“There is a lot of promise from these pathways in delivering the right care to the right patient at the right time,” said Bobby Daly, MD, an oncologist and health services researcher at Memorial Sloan Kettering Cancer Center in New York. “But oncologists and patients really want to understand how these pathways are being developed. The issue of transparency is one that patients and providers feel strongly about.”
While collaboration with industry is the key to innovation, Dr. Daly wrote that “to ensure patient and clinician trust and maintain their momentum in the value space, pathway developers will need to be transparent about [financial conflicts of interest] and how those interests are managed.”
Pathways: What’s the problem?
But as pathways have become more prevalent, concerns have emerged among physicians about who is making pathway treatment decisions and, specifically, about instances in which medications are being selected without disclosure of investments or financial relationships that could influence those decisions, said Robin Zon, MD, chair of the ASCO Task Force on Clinical Pathways.
“In addition, there have been concerns about the methodology of how treatments decisions are made with regard to efficacy, toxicity, and cost, as well as the weighting of these factors in making decisions for the pathway program,” Dr. Zon said in an interview.
Taken together, the mounting questions led to an analysis and by the ASCO task force.
“What the task force found was that standards defining high-quality pathways did not exist, so we became concerned that there could be a risk for wide variations with regards to the quality, utility, functionality, and impact of pathway programs,” Dr. Zon said.
The findings were the catalyst behind a March 2016 ASCO policy statement aimed at ensuring that clinical pathways in oncology promote – not hinder – cancer care. The task force called on pathway developers to adopt a process that was consistent and transparent to all stakeholders and to disclose potential conflicts of interest by the companies and individuals involved in pathway development.
“The criteria were developed to address the multiple issues brought to our attention by ASCO members and to be used as possible standards for pathway development, implementation, and evolution,” Dr. Zon said.
Meanwhile, the Cleveland Clinic has been utilizing pathways for more than 5 years and has published nearly 50 clinical pathways related to cancer care, Dr. Kalaycio said.
“Our care paths were designed to help physicians make clinical decisions that are in the best interest of their patients and the Cleveland Clinic,” he said in an interview. “These care paths are here for clinical reasons, not for financial reasons – we might ultimately use them to make financial decisions, but that’s not why they were developed. In contrast, the [JAMA Oncology study] is referring to pathways that are being developed by for-profit companies to control cost – big, big difference.”
The problem is that some insurers want to hide the identity of their advisors and how much they are being paid, which creates uncertainty about the validity of their pathways, he said. Dr. Kalaycio noted that the individuals selected for pathway panels and committees are often those who conducted the studies that the pathways are based upon and that those studies are frequently supported by the pharmaceutical industry.
“There is always going to be some degree of conflict of interest and as long as that’s disclosed, that’s fine,” he said. “It’s when you try to hide who’s getting paid for what that you get into trouble because you can’t say with certainty that someone’s not getting paid off.”
To address the transparency void, the California legislature in 2017 introduced the Oncology Clinical Pathways Act. The bill would have required health plans that develop and implement OCPs to provide the names, qualifications, affiliations, and conflicts of anyone involved in the research or analysis for an oncology clinical pathway if it were requested by a physician or surgeon. The bill died in committee.
Health plans push back
America’s Health Insurance Plans (AHIP) spokeswoman Cathryn Donaldson said health plans are being unfairly targeted in the drive toward more transparency. The recent efforts are an attempt to single out clinical care pathways developed by health plans as needing additional oversight standards while ignoring pathways that are developed by drug distributors, hospital systems, academic institutions, and others, Ms. Donaldson said in an interview.
ASCO’s Dr. Zon stressed that the criteria her task force created for pathways is aimed at all types of developers.
“In other words, we felt that the criteria should apply across all the pathway program developers whether they were provider or payer facing,” Dr. Zon said. “We also did not differentiate between not-for-profit and for-profit entities. Standards for high-quality criteria should apply to any pathway program being developed regardless of the source.”
Dr. Daly added that every entity that develops a pathway should have some policy around conflict of interest and how to address any transparency issues that may arise. Despite the recent debate over transparency, Dr. Daly said he believes the future of pathways is bright.
“I think the future is that pathways hold a lot of promise,” he said. “But I think we really need to ensure that the pathways that are being employed are of high quality because they influence how patients are treated.”
Dr. Daly serves as a director of Quadrant Holdings Corporation and receives compensation from this entity. This news organization is a subsidiary of Quadrant Holdings Corporation.
The use of oncology clinical pathways (OCPs) is rapidly rising as more data suggest that they can reduce cost and improve quality. But amid the advantages to pathways, there are growing concerns about hidden conflicts of interest.
“There is a lot of promise from these pathways in delivering the right care to the right patient at the right time,” said Bobby Daly, MD, an oncologist and health services researcher at Memorial Sloan Kettering Cancer Center in New York. “But oncologists and patients really want to understand how these pathways are being developed. The issue of transparency is one that patients and providers feel strongly about.”
While collaboration with industry is the key to innovation, Dr. Daly wrote that “to ensure patient and clinician trust and maintain their momentum in the value space, pathway developers will need to be transparent about [financial conflicts of interest] and how those interests are managed.”
Pathways: What’s the problem?
But as pathways have become more prevalent, concerns have emerged among physicians about who is making pathway treatment decisions and, specifically, about instances in which medications are being selected without disclosure of investments or financial relationships that could influence those decisions, said Robin Zon, MD, chair of the ASCO Task Force on Clinical Pathways.
“In addition, there have been concerns about the methodology of how treatments decisions are made with regard to efficacy, toxicity, and cost, as well as the weighting of these factors in making decisions for the pathway program,” Dr. Zon said in an interview.
Taken together, the mounting questions led to an analysis and by the ASCO task force.
“What the task force found was that standards defining high-quality pathways did not exist, so we became concerned that there could be a risk for wide variations with regards to the quality, utility, functionality, and impact of pathway programs,” Dr. Zon said.
The findings were the catalyst behind a March 2016 ASCO policy statement aimed at ensuring that clinical pathways in oncology promote – not hinder – cancer care. The task force called on pathway developers to adopt a process that was consistent and transparent to all stakeholders and to disclose potential conflicts of interest by the companies and individuals involved in pathway development.
“The criteria were developed to address the multiple issues brought to our attention by ASCO members and to be used as possible standards for pathway development, implementation, and evolution,” Dr. Zon said.
Meanwhile, the Cleveland Clinic has been utilizing pathways for more than 5 years and has published nearly 50 clinical pathways related to cancer care, Dr. Kalaycio said.
“Our care paths were designed to help physicians make clinical decisions that are in the best interest of their patients and the Cleveland Clinic,” he said in an interview. “These care paths are here for clinical reasons, not for financial reasons – we might ultimately use them to make financial decisions, but that’s not why they were developed. In contrast, the [JAMA Oncology study] is referring to pathways that are being developed by for-profit companies to control cost – big, big difference.”
The problem is that some insurers want to hide the identity of their advisors and how much they are being paid, which creates uncertainty about the validity of their pathways, he said. Dr. Kalaycio noted that the individuals selected for pathway panels and committees are often those who conducted the studies that the pathways are based upon and that those studies are frequently supported by the pharmaceutical industry.
“There is always going to be some degree of conflict of interest and as long as that’s disclosed, that’s fine,” he said. “It’s when you try to hide who’s getting paid for what that you get into trouble because you can’t say with certainty that someone’s not getting paid off.”
To address the transparency void, the California legislature in 2017 introduced the Oncology Clinical Pathways Act. The bill would have required health plans that develop and implement OCPs to provide the names, qualifications, affiliations, and conflicts of anyone involved in the research or analysis for an oncology clinical pathway if it were requested by a physician or surgeon. The bill died in committee.
Health plans push back
America’s Health Insurance Plans (AHIP) spokeswoman Cathryn Donaldson said health plans are being unfairly targeted in the drive toward more transparency. The recent efforts are an attempt to single out clinical care pathways developed by health plans as needing additional oversight standards while ignoring pathways that are developed by drug distributors, hospital systems, academic institutions, and others, Ms. Donaldson said in an interview.
ASCO’s Dr. Zon stressed that the criteria her task force created for pathways is aimed at all types of developers.
“In other words, we felt that the criteria should apply across all the pathway program developers whether they were provider or payer facing,” Dr. Zon said. “We also did not differentiate between not-for-profit and for-profit entities. Standards for high-quality criteria should apply to any pathway program being developed regardless of the source.”
Dr. Daly added that every entity that develops a pathway should have some policy around conflict of interest and how to address any transparency issues that may arise. Despite the recent debate over transparency, Dr. Daly said he believes the future of pathways is bright.
“I think the future is that pathways hold a lot of promise,” he said. “But I think we really need to ensure that the pathways that are being employed are of high quality because they influence how patients are treated.”
Dr. Daly serves as a director of Quadrant Holdings Corporation and receives compensation from this entity. This news organization is a subsidiary of Quadrant Holdings Corporation.
Study: Half of doctors sued by age 55
By age 55, nearly half of physicians have been sued for malpractice, with general surgeons and obstetricians-gynecologists facing the highest lawsuit risks, according to data from the America Medical Association.
Investigators with the AMA surveyed 3,500 postresidency physicians who were not employed by the federal government. Findings show that the probability of getting sued increases with age, and that male doctors are more likely to be sued than female physicians. For example, only 8% of doctors under 40 have been sued, compared to nearly half of physicians over age 54, the study found. In addition, nearly 40% of male physicians have been sued over the course of their careers, compared with 23% of female doctors.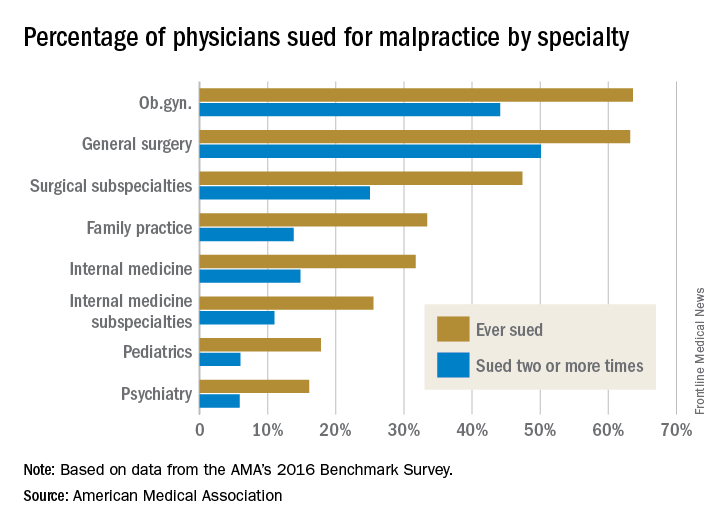
Employed physicians were no more or less likely than were physician-owners to have been sued. In addition, while solo practitioners had more claims filed against them than did doctors in single-specialty groups, the estimate was not statistically significant.
In a second report, an analysis showed the average expense incurred during a medical liability claim is $54,165 – a 65% increase since 2006. For the study, the AMA analyzed data from PIAA, a trade association for the medical professional liability insurance industry, and evaluated payments, expenses, and claim disposition within a sample of 90,473 medical liability claims that closed between 2006 and 2015.
Only 7% of claims were decided by a trial verdict with the vast majority (88%) won by the defendant health care provider. In about 25% of claims, a payment was paid to the plaintiff. The average indemnity payment to a plaintiff was $365,503 and the median payment was $200,000.
The new research paints a bleak picture of physicians’ experiences with medical liability claims and the associated cost burdens on the health system, AMA President David O. Barbe, MD, said in a statement.
“Even though the vast majority of claims are dropped, dismissed, or withdrawn, the heavy cost associated with a litigious climate takes a significant financial toll on our health care system when the nation is working to reduce unnecessary health care costs,” Dr. Barbe said.
By age 55, nearly half of physicians have been sued for malpractice, with general surgeons and obstetricians-gynecologists facing the highest lawsuit risks, according to data from the America Medical Association.
Investigators with the AMA surveyed 3,500 postresidency physicians who were not employed by the federal government. Findings show that the probability of getting sued increases with age, and that male doctors are more likely to be sued than female physicians. For example, only 8% of doctors under 40 have been sued, compared to nearly half of physicians over age 54, the study found. In addition, nearly 40% of male physicians have been sued over the course of their careers, compared with 23% of female doctors.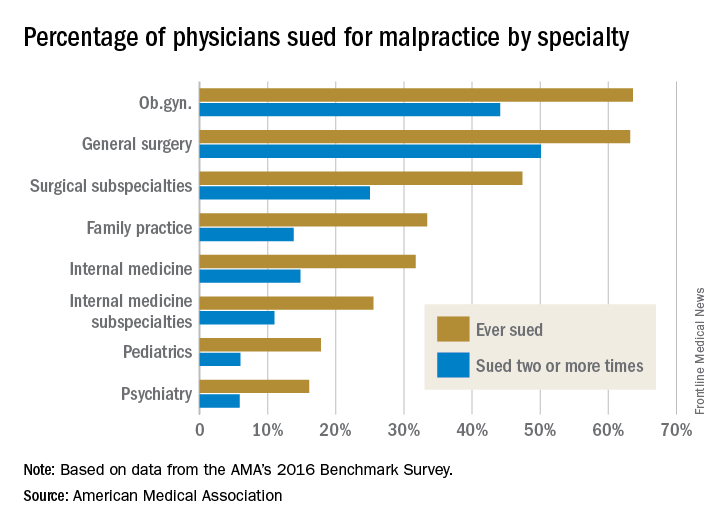
Employed physicians were no more or less likely than were physician-owners to have been sued. In addition, while solo practitioners had more claims filed against them than did doctors in single-specialty groups, the estimate was not statistically significant.
In a second report, an analysis showed the average expense incurred during a medical liability claim is $54,165 – a 65% increase since 2006. For the study, the AMA analyzed data from PIAA, a trade association for the medical professional liability insurance industry, and evaluated payments, expenses, and claim disposition within a sample of 90,473 medical liability claims that closed between 2006 and 2015.
Only 7% of claims were decided by a trial verdict with the vast majority (88%) won by the defendant health care provider. In about 25% of claims, a payment was paid to the plaintiff. The average indemnity payment to a plaintiff was $365,503 and the median payment was $200,000.
The new research paints a bleak picture of physicians’ experiences with medical liability claims and the associated cost burdens on the health system, AMA President David O. Barbe, MD, said in a statement.
“Even though the vast majority of claims are dropped, dismissed, or withdrawn, the heavy cost associated with a litigious climate takes a significant financial toll on our health care system when the nation is working to reduce unnecessary health care costs,” Dr. Barbe said.
By age 55, nearly half of physicians have been sued for malpractice, with general surgeons and obstetricians-gynecologists facing the highest lawsuit risks, according to data from the America Medical Association.
Investigators with the AMA surveyed 3,500 postresidency physicians who were not employed by the federal government. Findings show that the probability of getting sued increases with age, and that male doctors are more likely to be sued than female physicians. For example, only 8% of doctors under 40 have been sued, compared to nearly half of physicians over age 54, the study found. In addition, nearly 40% of male physicians have been sued over the course of their careers, compared with 23% of female doctors.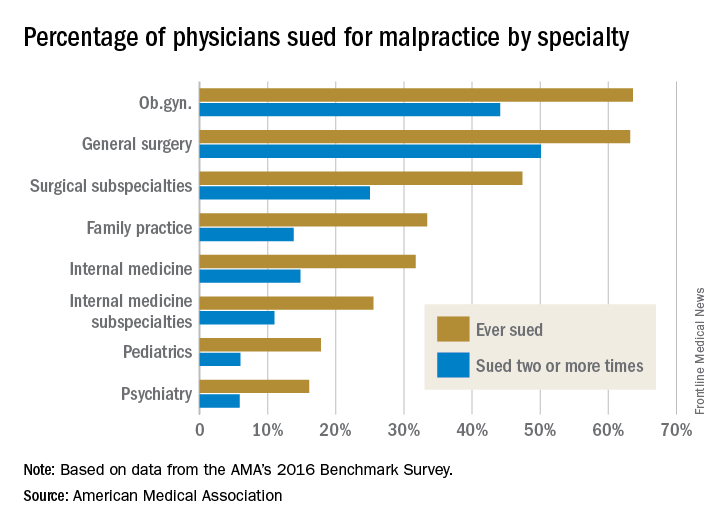
Employed physicians were no more or less likely than were physician-owners to have been sued. In addition, while solo practitioners had more claims filed against them than did doctors in single-specialty groups, the estimate was not statistically significant.
In a second report, an analysis showed the average expense incurred during a medical liability claim is $54,165 – a 65% increase since 2006. For the study, the AMA analyzed data from PIAA, a trade association for the medical professional liability insurance industry, and evaluated payments, expenses, and claim disposition within a sample of 90,473 medical liability claims that closed between 2006 and 2015.
Only 7% of claims were decided by a trial verdict with the vast majority (88%) won by the defendant health care provider. In about 25% of claims, a payment was paid to the plaintiff. The average indemnity payment to a plaintiff was $365,503 and the median payment was $200,000.
The new research paints a bleak picture of physicians’ experiences with medical liability claims and the associated cost burdens on the health system, AMA President David O. Barbe, MD, said in a statement.
“Even though the vast majority of claims are dropped, dismissed, or withdrawn, the heavy cost associated with a litigious climate takes a significant financial toll on our health care system when the nation is working to reduce unnecessary health care costs,” Dr. Barbe said.