User login
Early Career Pediatric Hospitalists
Pediatric hospital medicine (PHM) has established itself as a well‐defined field of pediatrics dedicated to improving the care of hospitalized children.[1] In 2010, the PHM core competencies were established to identify a specific knowledge base and skill set needed to provide the highest quality care for hospitalized children.[2] With these competencies, many are re‐evaluating training needs, particularly given the rapid advancement of the field.[1, 3] Previous workforce evaluations estimated that less than half of hospitalists surveyed had any specific hospitalist training.[4] In 2004 and 2008, studies of the current roles and training needs of pediatric hospitalists revealed advanced training needs in administration, research, quality improvement (QI), and education.[5, 6] Currently, there are 27 US PHM fellowship programs, but the majority of hospitalists are entering the field without PHM‐specific training. There is little evidence regarding our current residency and fellowship training models' abilities to help participants achieve proficiency in the PHM core competencies.
The objectives of this study were to compare the perceived PHM core competency achievements of fellowship and non‐fellowship‐trained early career pediatric hospitalists and identify perceived knowledge gaps in our current training models.
METHODS
Study Design
An anonymous Web‐based survey was conducted in November 2013. The survey was electronically distributed to the American Academy of Pediatrics (AAP) Section on Hospital Medicine (SOHM) Listserv, current PHM fellows present at the annual PHM Fellows Conference, as well as PHM division directors and fellowship directors to distribute to eligible hospitalists. The AAP SOHM Listserv functions as a convenience sample, representing the single largest listing of pediatric hospitalists, currently with over 2100 subscribers (email communication with Nicole Alexander, AAP Manager of the Division of Hospital and Surgical Services). An email announcing the survey was distributed to the aforementioned parties with 1 reminder email sent to the SOHM Listserv encouraging participation.
Inclusion criteria were current practicing hospitalists who had graduated from a US Accreditation Council for Graduate Medical Education‐approved residency program within the last 5 years. Recruiting individuals within 5 years of residency graduation was chosen in an effort to capture the experience of our current training models. Practicing hospitalists included current PHM fellows, PHM fellowship graduates (both defined as fellowship‐trained), and non‐fellowship‐trained individuals.
Survey Development
The survey obtained demographic data including type of residency training, chief residency, postresidency training, advanced degrees, practice environment, and professional positions. Competency was self‐assessed using an interactive sliding scale where participants could indicate their perceived competency by placing the cursor along a continuum with the anchors novice, competent, and expert. Each anchor was defined as follows: novice is the inability to perform the skill or require supervision/assistance to complete the activity; competent is the ability to perform unsupervised execution of a task, not requiring substantial mastery or advanced ability; and expert is demonstrating initiative and adaptability to special problem situations and can lead others in performing the skill.[7] Cursor position along the sliding scale was converted by the survey tool to a value from 0 to 100 for data analysis. Within each group, a mean score below 50 was considered an area respondents perceived themselves less than competent. Select PHM core competencies were chosen in consultation with the authors of the PHM core competencies to provide a representative sample from each of the 4 domains (Table 1) as well as restrict the survey to a reasonable length. The survey was pilot tested in small groups and revised for content and readability based on the feedback received.
| Clinical Diagnosis | Core Skills | Specialized Clinical Skills | Healthcare Systems |
|---|---|---|---|
| |||
| Abdominal pain | Bladder catheterization | Child abuse* | Advocacy* |
| ALTE | ECG interpretation | Hospice and palliative care | Business practice* |
| Asthma | Feeding tubes | Leading healthcare team* | Communication |
| Bone and joint infection | Fluid/electrolytes | Newborn care* | Quality improvement* |
| Bronchiolitis | IV access/ phlebotomy* | Technology‐dependent children* | Cost‐effective care* |
| CNS infections | Lumbar puncture* | Transport of the critically ill | Education* |
| Diabetes | Noninvasive monitoring | Evidence‐based medicine* | |
| Failure to thrive | Nutrition* | Health information systems | |
| Fever unknown origin | Oxygen delivery and airway management | Legal, risk management | |
| Gastroenteritis | Pain management* | Patient safety* | |
| Kawasaki disease | PALS | Research* | |
| Neonatal fever | Procedural sedation* | Transitions of care* | |
| Neonatal jaundice | Radiographic interpretation | ||
| Pneumonia | |||
| Respiratory failure | |||
| Seizures | |||
| Shock | |||
| Sickle cell disease | |||
| Skin and soft tissue infection | |||
| Upper airway infections | |||
| UTI | |||
| Single summative question included in the survey. | |||
Data Collection
Study data were collected and managed using the Research Electronic Data Capture (REDcap) tool hosted at Children's National Health System. REDcap is a secure, Web‐based application designed to support data capture for research studies.[8]
Data Analysis
Analysis was performed using SPSS version 22 (IBM, Armonk, NY). Demographic data comparing fellowship‐trained and non‐fellowship‐trained individuals were analyzed by [2] testing for categorical variables. Mean competency values between non‐fellows and those who have completed or are in the process of completing fellowship were analyzed using multiprobit regression. Values were adjusted for years since residency graduation (regardless of whether the individual was a current fellow, a fellowship graduate, or non‐fellowship‐trained), type of residency, and chief residency. P values were calculated based on the estimate and standard error of the slope term within the probit model. The effect of fellowship was qualitatively analyzed by comparing the values between the groups at different years since residency graduation. Incomplete data were excluded only for responses missing.
Institutional review board approval was obtained from Children's National Medical Center in Washington, DC.
RESULTS
One hundred ninety‐seven pediatric hospitalists responded to the survey. All were included in the analysis. One hundred forty‐seven respondents were non‐fellowship‐trained and 50 were PHM fellowship graduates or current PHM fellows. Demographic characteristics are listed in Table 2. Current and former PHM fellows were on average 2.1 years from residency graduation, whereas non‐fellowship‐trained hospitalists were 2.6 years from residency graduation (P=0.05). A significantly higher proportion of fellowship‐trained hospitalists reported working at a university‐affiliated free‐standing children's hospital, whereas a higher proportion of non‐fellowship‐trained hospitalists reported working at a non‐university‐affiliated community hospital. The majority of practice domains included hospitalists worked were similar between the 2 groups. A significantly higher proportion of fellowship‐trained hospitalists reported working in research and QI/safety. Surgical comanagement and newborn nursery were domains a significantly higher proportion of non‐fellowship‐trained hospitalists reported working.
| Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value | |
|---|---|---|---|
| |||
| Average years experience (since residency graduation) | 2.1 | 2.6 | 0.05 |
| Type of residency | 0.82 | ||
| Pediatric | 48 (96%) | 140 (95%) | |
| Medicine‐pediatric | 2 (4%) | 7 (5%) | |
| Family medicine | 0 | 0 | |
| Chief residency | 17 (34%) | 37 (25%) | 0.23 |
| Advanced degree obtained | 0.12 | ||
| Master's Public Health | 2 (4%) | 8 (5.5%) | |
| Master's of Education | 0 | 1 (0.7%) | |
| Master's Clinical and Translational Research | 1 (2%) | 0 | |
| Master's Business Administration | 1 (2%) | 0 | |
| PhD | 0 | 1 (0.7%) | |
| Other | 3 (6%) | 8 (5.5%) | |
| Currently pursuing | 14 (28%) | 6 (4.1%) | |
| Practice environment | |||
| University‐affiliated free‐standing children's hospital | 40 (80%) | 68 (46.3%) | <0.001 |
| University‐affiliated pediatric ward | 7 (14%) | 37 (25.2%) | 0.1 |
| University‐affiliated community hospital | 2 (4%) | 25 (17%) | 0.02 |
| Non‐university affiliated community hospital | 2 (4%) | 35 (23.8%) | 0.002 |
| Practice domain | |||
| General pediatrics inpatient unit | 49/49 (100%) | 139/143 (97.2%) | 0.24 |
| Subspecialty wards | 19/46 (41.3%) | 47/130 (36.1%) | 0.54 |
| Surgical comanagement | 36/46 (78.3%) | 119/133 (89.5%) | 0.05 |
| NICU | 8/47 (17.0%) | 36/128 (28.1%) | 0.13 |
| PICU | 11/47 (17.0%) | 16/126 (12.0%) | 0.08 |
| Intermediate care unit | 17/47 (36.2%) | 36/128 (28.1%) | 0.09 |
| ED | 16/47 (34.0%) | 55/128 (43.0%) | 0.42 |
| Newborn nursery | 11/45 (24.4%) | 68/132 (51.5%) | 0.002 |
| Sedation | 20/48 (41.7%) | 48/133 (36.1%) | 0.49 |
| Medical education | 47/48 (97.9%) | 123/137 (89.8%) | 0.08 |
| Hospital committee work | 42/48 (87.5%) | 109/138 (79.0%) | 0.3 |
| Research | 44/49 (90.0%) | 72/137 (52.6%) | <0.001 |
| Quality improvement/safety | 44/48 (91.7%) | 103/134 (76.9%) | 0.003 |
| Advocacy | 23/47 (47.9%) | 49/128 (38.2%) | 0.19 |
The adjusted mean perceived competency scores for fellowship and non‐fellowship‐trained hospitalists are shown in Table 3. Reported competency scores for management of common acute inpatient medical conditions in an otherwise healthy child were similar between the 2 groups. Both fellowship and non‐fellowship‐trained hospitalists reported feeling less than competent (scores <50) in sedation, understanding basic components of PHM business practice, and defining a relative value unit. Fellowship‐trained hospitalists indicated perceived competency (scores >50) in the remainder of the competencies surveyed. Non‐fellowship‐trained hospitalists additionally had average scores <50 with statistically significant lower reported competency scores than fellowship‐trained hospitalists in IV access/phlebotomy, managing emergencies in technology‐dependent children, performing Plan‐Do‐Study‐Act (PDSA) cycles to achieve QI, performing root‐cause analysis (RCA), defining basic statistical terms, and identifying resources required to conduct research. Non‐fellowship‐trained hospitalists reported statistically significant higher mean competency scores in pain management, newborn care, and transitions in care. In each of these competencies, though, mean scores for both groups were in the competent range.
| Core Competency | Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value |
|---|---|---|---|
| |||
| Common diagnoses | 78.4 | 78.6 | 0.717 |
| Core skills | |||
| IV access/phlebotomy | 52.9 | 30.6 | 0.012 |
| Lumbar puncture | 76.2 | 77.0 | 0.245 |
| Sedation | 30.9 | 28.3 | 0.001 |
| Pain management | 70.7 | 72.6 | 0.014 |
| Nutrition | 68.0 | 66.1 | 0.026 |
| Specialized clinical skills | |||
| Leading a health care team | |||
| Team leadership | 74.9 | 72.0 | <0.001 |
| FCR | 75.3 | 72.6 | <0.001 |
| Technology‐dependent patient | |||
| General management | 71.4 | 65.9 | <0.001 |
| Emergencies | 53.2 | 49.4 | <0.001 |
| Newborn care | 56.6 | 61.6 | <0.001 |
| Child abuse | |||
| Diagnosing | 68.6 | 68.7 | 0.925 |
| Reporting | 68.9 | 68.5 | 0.630 |
| Healthcare systems | |||
| Transitions in care | 77.4 | 79.6 | 0.002 |
| Advocacy | 57.4 | 53.5 | <0.001 |
| Business practice | |||
| Basic components | 36.4 | 32.0 | <0.001 |
| Concept of RVU | 30.2 | 30.2 | 0.972 |
| Billing/coding | 61.4 | 63.9 | 0.004 |
| Quality Improvement | |||
| PDSA cycles | 63.7 | 42.8 | <0.001 |
| Best practice guidelines | 64.7 | 51.8 | <0.001 |
| Safety | |||
| Identify and address harm | 65.9 | 59.1 | <0.001 |
| Perform RCA | 56.7 | 36.0 | <0.001 |
| Cost‐effective care | 58.4 | 51.6 | <0.001 |
| Medical education | |||
| Needs assessment | 69.4 | 65.6 | <0.001 |
| Large group teaching | 67.6 | 60.6 | <0.001 |
| Small group teaching | 74.2 | 72.6 | 0.040 |
| Feedback | 73.8 | 68.9 | <0.001 |
| Evidence‐based medicine | |||
| Literature search | 75.9 | 69.0 | <0.001 |
| Literature appraisal | 63.4 | 57.2 | <0.001 |
| Apply study results | 70.2 | 64.8 | <0.001 |
| Research | |||
| Comparing study design | 62.6 | 54.1 | <0.001 |
| Basic statistics | 57.2 | 41.7 | <0.001 |
| Identifying resources | 56.0 | 36.1 | <0.001 |
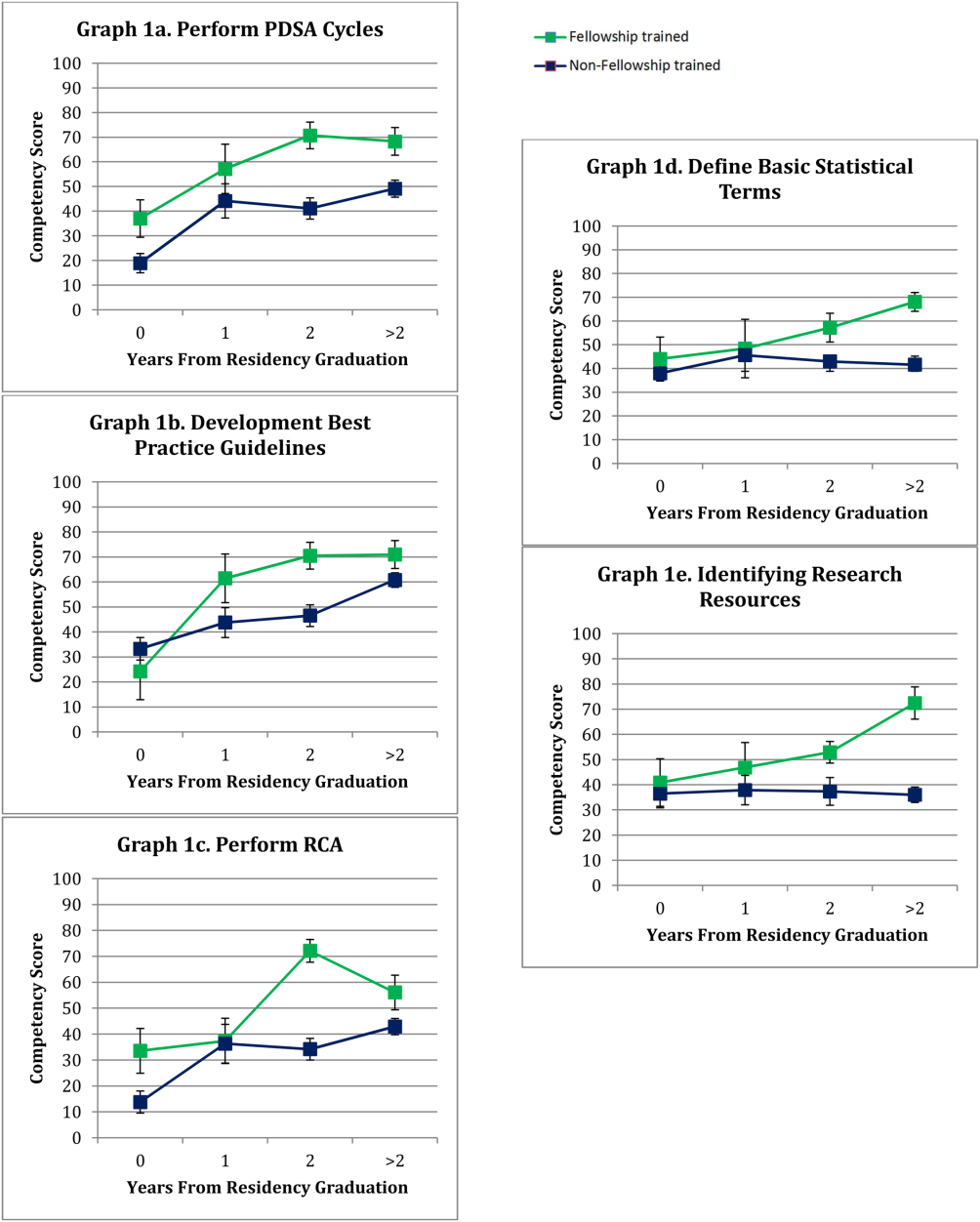
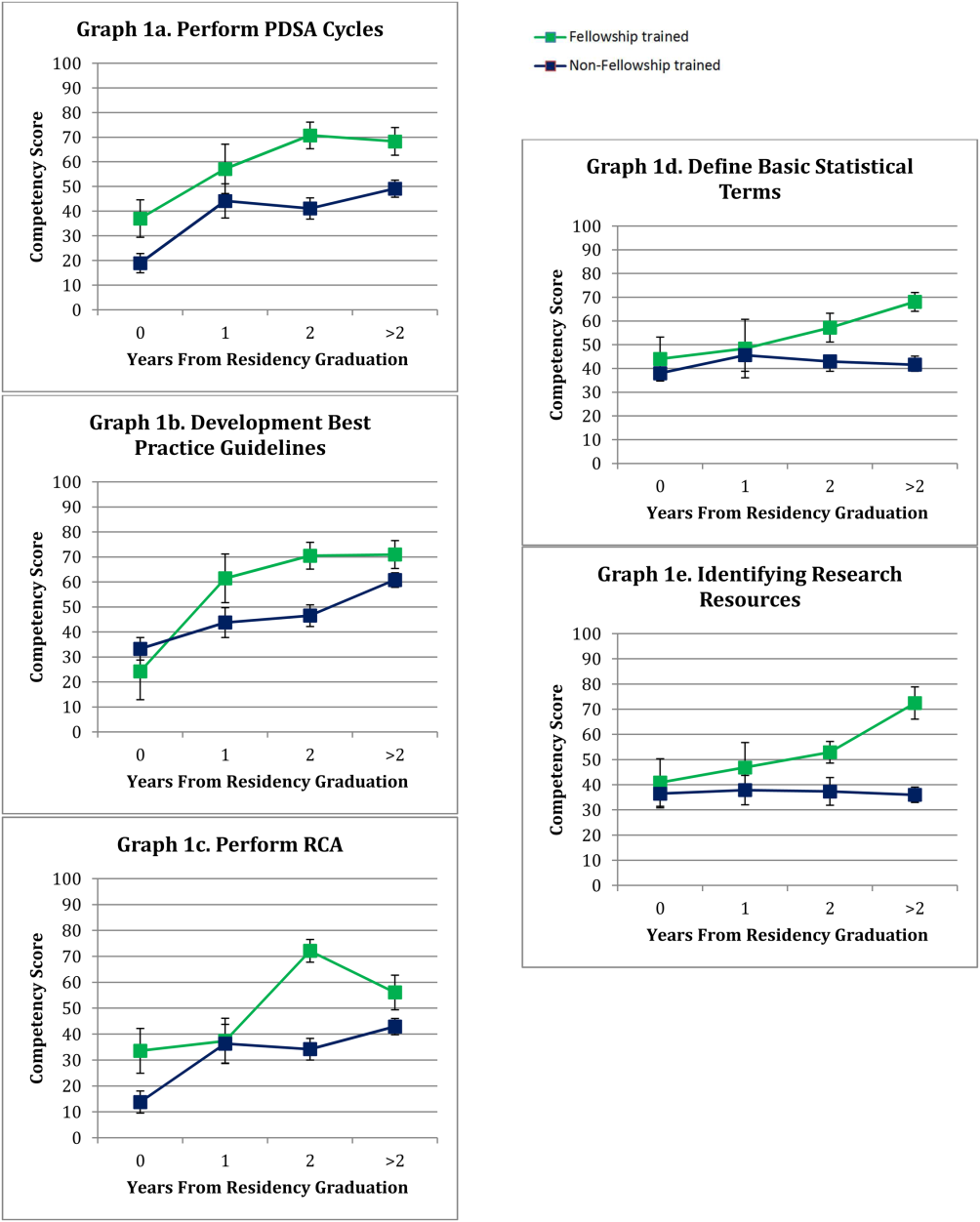
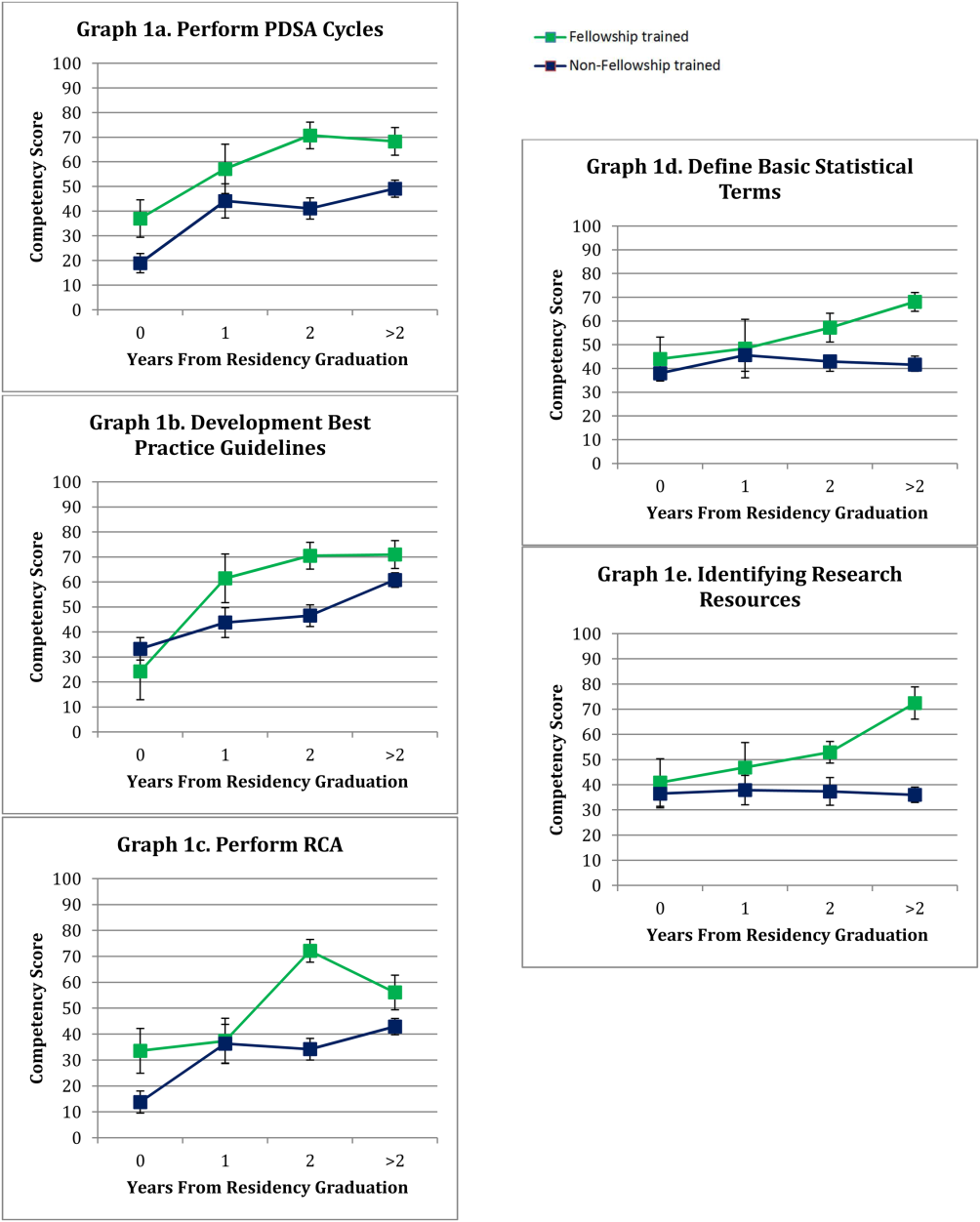
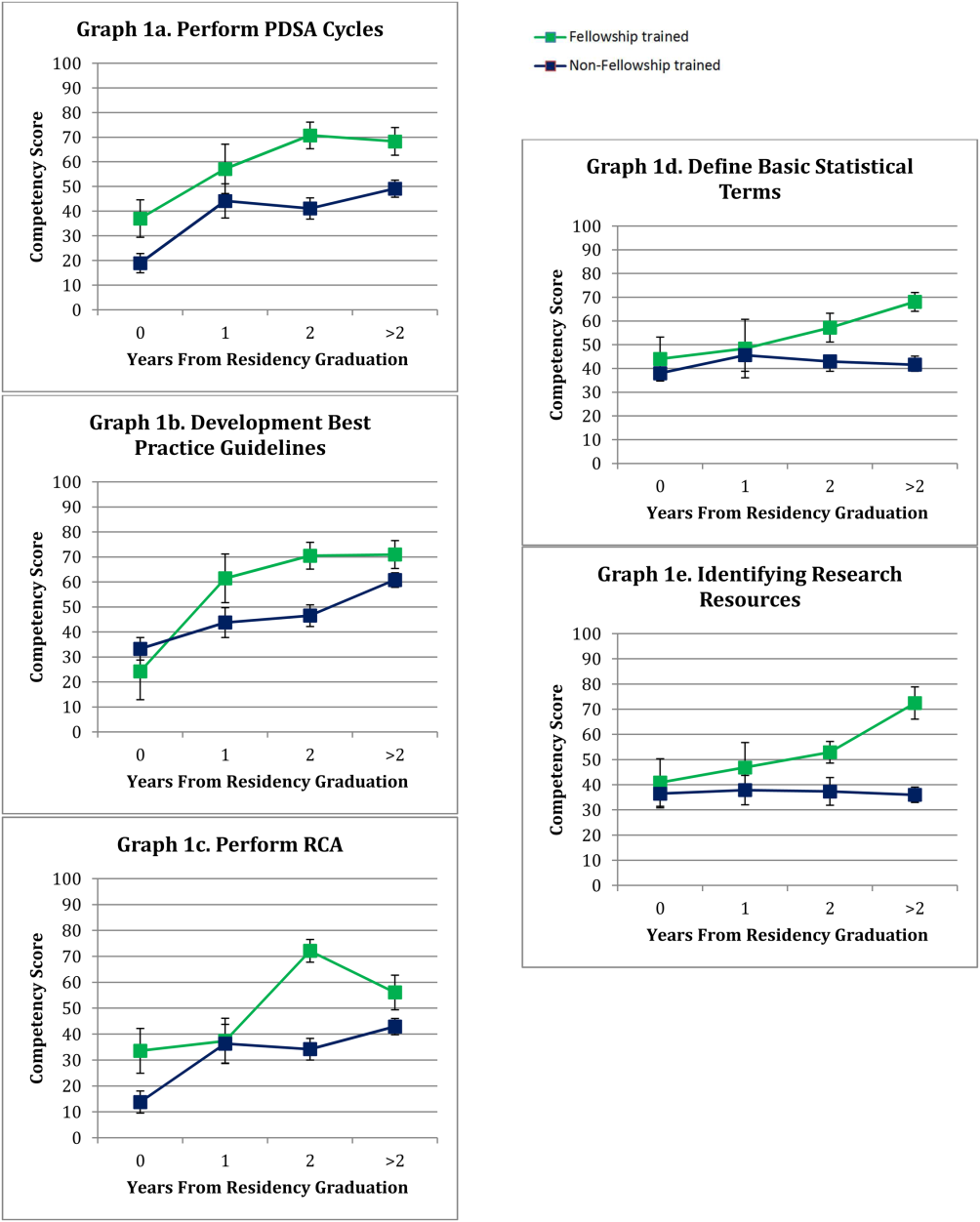
The mean adjusted competency scores in areas with some of the largest differences between the 2 groups were plotted by time since residency graduation and depicted in Figure 1. This does not represent a single cohort of hospitalists over time, rather individual hospitalists at different post‐graduate years from their residency graduation. In performing PDSA cycles, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean score indicating competency (57.3), whereas only non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation reported a mean score approaching competency (49.1) (Figure 1A). For development of best practice guidelines, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean competency score (61.8), similar to non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation (60.8) (Figure 1B). Competency in performing RCA was reported by fellowship‐trained hospitalists 2 years postresidency (72.1), whereas non‐fellowship‐trained hospitalists up to 5 years post‐residency report a mean score below competency (Figure 1C). Regarding research competencies, fellowship‐trained hospitalists reported increased perceived competency at each year postresidency graduation, whereas non‐fellowship‐trained hospitalists reported lower mean competency scores with each year post‐residency (Figure 1D,E).
DISCUSSION
Our study results reveal significant differences in perceived competency between fellowship‐trained and non‐fellowship‐trained hospitalists, identifying several perceived knowledge gaps. Early career hospitalists, regardless of their training, perceive they have not achieved competency in sedation and aspects of PHM business practice. Early career hospitalists who did not pursue PHM fellowship training reported also feeling less than competent in intravenous access/phlebotomy, managing emergencies in technology‐dependent children, performing PDSA cycles to achieve QI, performing RCA, defining basic statistical terms, and identifying resources required to conduct research. Although both groups perceived themselves as competent in newborn care, pain management, and transitions in care, non‐fellowship‐trained hospitalists did report statistically significant higher competency scores compared to fellowship‐trained hospitalists in these skills.
Our findings support previous studies on the roles and training needs of pediatric hospitalists. In 2004, Ottolini et al. conducted a survey of pediatric hospitalists through Pediatric Research in Inpatient Settings, finding additional training needs in program/division management, practice guidelines, QI, safety, teaching, evidence‐based medicine (EBM), and research. The majority of hospitalists surveyed did not believe their pediatric residency training provided all of the skills necessary to practice as pediatric hospitalists.[5] Maniscalco et al. repeated the study in 2008 with similar findings.[6] In the field of adult internal medicine, Plauth et al. surveyed practicing hospitalists regarding the adequacy of their residency training, and found that systems issues (ie, QI, health economics, practice guidelines development) were reported as important to their current practice and not adequately emphasized in residency training.[9] Collectively, these findings highlight the need to critically evaluate our current training models' ability to prepare an individual for a career in hospital medicine. There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified,[1] but it is important to identify where the current knowledge gaps exist to optimize this process.
Not surprisingly, the majority of the hospitalists surveyed self‐reported competency in most of the clinical skills included. Residency training is heavily weighted toward acquisition of clinical skills, with a significant amount of time spent on inpatient clinical rotations.[10] The exception was sedation, which had some of the lowest mean perceived competency scores for all early career hospitalists surveyed. There is growing demand for safe and effective procedural sedation nationally, and pediatric hospitalists have been recognized as well poised to augment sedation services provided by anesthesiologists.[11, 12] This study demonstrates that current residency and PHM fellowship training may not adequately address this skill set to produce hospitalists prepared to take on this potential role.
Significant findings in the non‐clinical domains were the healthcare systems competencies. It is increasingly evident that a hospitalist's job description includes addressing communication, coordination of care, quality of care, and patient safety.[13] Yet, our findings indicate that non‐fellowship‐trained early career hospitalists do not feel competent in several of these aspects of hospital medicine practice. Our findings suggest that residency training alone may not provide adequate instruction for perceived competency, as no hospitalists with <1 year since residency graduation reported competency in PDSA cycles, best practice guidelines, and RCA. Interestingly, examining these competencies at different years following residency graduation, experience alone also does not ensure perceived competency early in one's career. Hospitalists are establishing themselves as a catalyst for change and the driving forces behind healthcare systems improvements within the hospital setting, often as our value added to an institution.[14, 15, 16, 17] Therefore, every pediatric hospitalist will need to acquire competency in these skills in a timely manner to effectively deliver high‐quality care to hospitalized children.
Finally, research was another area in which non‐fellowship‐trained hospitalists had low self‐perceived competency. When evaluating competency at different years postresidency graduation, non‐fellowship‐trained individuals appeared to lose a sense of competency each year, whereas fellowship‐trained hospitalists reported escalating competency with each year post‐residency. This finding may be due to the fellowship training itself, mentorship established in fellowship, or resources available in their chosen practice environment following fellowship. In 2011, Bekmezian et al. found that the majority of pediatric hospitalists wanted to conduct research but cited lack of dedicated time and mentorship as barriers to their productivity.[18] High‐quality studies including clinical, QI, and comparative effectiveness research are necessary to allow practicing hospitalists to make better decisions regarding patient care and to advance the field. This need transcends practice environment evidenced by the latest movement to transition away from the more traditional academic and non‐academic nomenclature. Even if one is not planning to conduct research, a basic foundation of research knowledge is required to critically appraise literature and apply EBM principles to clinical practice. This study suggests these skills are not being adequately obtained in residency for perceived competency or acquired with experience alone early in one's career.
There are several limitations of this study that should be considered. Most notably, the competency scores are based on self‐perceived assessments and therefore are not validated with objective measures of an individual's knowledge and skill, risking bias based on an individual's level of personal insight. We also did not quantify differences in training experience based on specific institutions, residency size, patient volume, and exposure to a hospitalist service, which could influence perceived competency and generalizability. Similarly, there is wide variation in current PHM fellowship curriculums, which is not accounted for in this study. Professional competency is challenging to define as well as measure.[19] Although this study is based on subjective measures, one can postulate that self‐perceived competency may impact an individual's approach to clinical practice, projects pursued, and career aspirations.
A second significant limitation was our inability to accurately determine a response rate. Other pediatric hospitalist surveys have faced similar limitations utilizing the AAP SOHM Listserv, because there is no centralized database of practicing hospitalists.[18, 20, 21] Attempts to collect workforce data from the American Board of Pediatrics (ABP) regarding estimates of the number of hospitalists within 5 years of their residency graduation revealed that they changed their data collection methods during our study period, therefore direct comparisons could not be made before and after 2012 (email communication with Cathy Koenig, Psychometric Data Analyst, ABP). Additionally, the AAP SOHM Listserv does not collect demographic data on subscribers, therefore we were unable to determine how many of the 2100 subscribers are within 5 years of their residency graduation. Nevertheless, it is the largest listserv of pediatric hospitalists and enabled us to attempt to collect data from the most representative population. PHM fellowship programs have also rapidly expanded, and only recently has there been a more centralized, comprehensive database of programs and fellows. With the available information, we could not accurately estimate a response rate. Despite the potential for response bias and small sample size, we feel the information collected is a valuable first look at important and timely data that can inform future studies.
Overall, this study provides important information regarding the perceived competency of early career pediatric hospitalists. Although different practice environments may afford different experiences and influence competency over time, we believe the majority of the PHM core competencies transcend practice environment and are ones all early career hospitalists should strive to achieve. To ensure the ongoing advancement of our field, we must guarantee that hospitalists are provided the resources and training to attain these competencies. This may include developing hospital medicine residency tracks, continuing medical education offerings, and/or PHM fellowships whose objectives are aligned with the established core competencies. Although this study was not designed to determine which of these options are optimal, the results can help identify the existing gaps to inform curriculum development in the future. As our field continues to evolve and advance, it will be important to continuously re‐evaluate our training programs' abilities to produce pediatric hospitalists with clinical, quality, scholarly, and leadership skills that meet our field's core competency standards.
CONCLUSIONS
Early career pediatric hospitalists report deficits in several of the PHM core competencies, which should be considered when designing PHM‐specific training in the future. PHM fellowship‐trained hospitalists report higher levels of self‐perceived competency in many core areas.
Disclosure: Nothing to report.
- , , , et al. Pediatric hospital medicine: a strategic planning roundtable to chart the future. J Hosp Med. 2012;7(4):329–334.
- , , , et al. The Pediatric Hospital Medicine Core Competencies Supplement: a Framework for Curriculum Development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(suppl 2):i–xv, 1–114.
- , . Pediatric hospital medicine and education: why we can't stand still. JAMA Pediatr. 2013;167(5):412–413.
- , , Research Advisory Committee of the American Board of Pediatrics. Pediatric hospitalists: training, current practice, and career goals. J Hosp Med. 2009;4(3):179–186.
- , , , . PRIS Survey: pediatric hospitalist roles and training needs. Pediatr Res. 2004;55:360A.
- , , , , . Current roles and training needs of pediatric hospitalists: a study from the Pediatric Research in Inpatient Settings (PRIS) Network. Paper presented at: Pediatric Academic Societies; 2008; Honolulu, HI.
- , , , . From the educational bench to the clinical bedside: translating the Dreyfus developmental model to the learning of clinical skills. Acad Med. 2008;83(8):761–767.
- , , , , , . Research Electronic Data Capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- , , , . Hospitalists' perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111(3):247–254.
- Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Pediatrics. 2012. Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/320_pediatrics_07012013.pdf. Accessed August 14, 2014.
- , . Pediatric sedation. Pediatr Clin North Am. 2014;61(4):703–717.
- , , , , . Development of a pediatric hospitalist sedation service: training and implementation. J Hosp Med. 2012;7(4):335–339.
- , , , et al. Guiding principles for pediatric hospital medicine programs. Pediatrics. 2013;132(4):782–786.
- , , , . Pediatric hospitalists: a systematic review of the literature. Pediatrics. 2006;117(5):1736–1744.
- , . Pediatric hospitalist systems versus traditional models of care: effect on quality and cost outcomes. J Hosp Med. 2012;7(4):350–357.
- . Pediatric hospital medicine: historical perspectives, inspired future. Curr Probl Pediatr Adolesc Health Care. 2012;42(5):107–112.
- . Pediatric hospitalists working in community hospitals. Pediatr Clin North Am. 2014;61(4):681–691.
- , , . Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38–44.
- , . Defining and assessing professional competence. JAMA. 2002;287(2):226–235.
- , , . Transition of care: what Is the pediatric hospitalist's role? An exploratory survey of current attitudes. J Hosp Med. 2012;7(4):277–281.
- , , . Association between practice setting and pediatric hospitalist career satisfaction. Hosp Pediatr. 2013;3(3):285–291.
Pediatric hospital medicine (PHM) has established itself as a well‐defined field of pediatrics dedicated to improving the care of hospitalized children.[1] In 2010, the PHM core competencies were established to identify a specific knowledge base and skill set needed to provide the highest quality care for hospitalized children.[2] With these competencies, many are re‐evaluating training needs, particularly given the rapid advancement of the field.[1, 3] Previous workforce evaluations estimated that less than half of hospitalists surveyed had any specific hospitalist training.[4] In 2004 and 2008, studies of the current roles and training needs of pediatric hospitalists revealed advanced training needs in administration, research, quality improvement (QI), and education.[5, 6] Currently, there are 27 US PHM fellowship programs, but the majority of hospitalists are entering the field without PHM‐specific training. There is little evidence regarding our current residency and fellowship training models' abilities to help participants achieve proficiency in the PHM core competencies.
The objectives of this study were to compare the perceived PHM core competency achievements of fellowship and non‐fellowship‐trained early career pediatric hospitalists and identify perceived knowledge gaps in our current training models.
METHODS
Study Design
An anonymous Web‐based survey was conducted in November 2013. The survey was electronically distributed to the American Academy of Pediatrics (AAP) Section on Hospital Medicine (SOHM) Listserv, current PHM fellows present at the annual PHM Fellows Conference, as well as PHM division directors and fellowship directors to distribute to eligible hospitalists. The AAP SOHM Listserv functions as a convenience sample, representing the single largest listing of pediatric hospitalists, currently with over 2100 subscribers (email communication with Nicole Alexander, AAP Manager of the Division of Hospital and Surgical Services). An email announcing the survey was distributed to the aforementioned parties with 1 reminder email sent to the SOHM Listserv encouraging participation.
Inclusion criteria were current practicing hospitalists who had graduated from a US Accreditation Council for Graduate Medical Education‐approved residency program within the last 5 years. Recruiting individuals within 5 years of residency graduation was chosen in an effort to capture the experience of our current training models. Practicing hospitalists included current PHM fellows, PHM fellowship graduates (both defined as fellowship‐trained), and non‐fellowship‐trained individuals.
Survey Development
The survey obtained demographic data including type of residency training, chief residency, postresidency training, advanced degrees, practice environment, and professional positions. Competency was self‐assessed using an interactive sliding scale where participants could indicate their perceived competency by placing the cursor along a continuum with the anchors novice, competent, and expert. Each anchor was defined as follows: novice is the inability to perform the skill or require supervision/assistance to complete the activity; competent is the ability to perform unsupervised execution of a task, not requiring substantial mastery or advanced ability; and expert is demonstrating initiative and adaptability to special problem situations and can lead others in performing the skill.[7] Cursor position along the sliding scale was converted by the survey tool to a value from 0 to 100 for data analysis. Within each group, a mean score below 50 was considered an area respondents perceived themselves less than competent. Select PHM core competencies were chosen in consultation with the authors of the PHM core competencies to provide a representative sample from each of the 4 domains (Table 1) as well as restrict the survey to a reasonable length. The survey was pilot tested in small groups and revised for content and readability based on the feedback received.
| Clinical Diagnosis | Core Skills | Specialized Clinical Skills | Healthcare Systems |
|---|---|---|---|
| |||
| Abdominal pain | Bladder catheterization | Child abuse* | Advocacy* |
| ALTE | ECG interpretation | Hospice and palliative care | Business practice* |
| Asthma | Feeding tubes | Leading healthcare team* | Communication |
| Bone and joint infection | Fluid/electrolytes | Newborn care* | Quality improvement* |
| Bronchiolitis | IV access/ phlebotomy* | Technology‐dependent children* | Cost‐effective care* |
| CNS infections | Lumbar puncture* | Transport of the critically ill | Education* |
| Diabetes | Noninvasive monitoring | Evidence‐based medicine* | |
| Failure to thrive | Nutrition* | Health information systems | |
| Fever unknown origin | Oxygen delivery and airway management | Legal, risk management | |
| Gastroenteritis | Pain management* | Patient safety* | |
| Kawasaki disease | PALS | Research* | |
| Neonatal fever | Procedural sedation* | Transitions of care* | |
| Neonatal jaundice | Radiographic interpretation | ||
| Pneumonia | |||
| Respiratory failure | |||
| Seizures | |||
| Shock | |||
| Sickle cell disease | |||
| Skin and soft tissue infection | |||
| Upper airway infections | |||
| UTI | |||
| Single summative question included in the survey. | |||
Data Collection
Study data were collected and managed using the Research Electronic Data Capture (REDcap) tool hosted at Children's National Health System. REDcap is a secure, Web‐based application designed to support data capture for research studies.[8]
Data Analysis
Analysis was performed using SPSS version 22 (IBM, Armonk, NY). Demographic data comparing fellowship‐trained and non‐fellowship‐trained individuals were analyzed by [2] testing for categorical variables. Mean competency values between non‐fellows and those who have completed or are in the process of completing fellowship were analyzed using multiprobit regression. Values were adjusted for years since residency graduation (regardless of whether the individual was a current fellow, a fellowship graduate, or non‐fellowship‐trained), type of residency, and chief residency. P values were calculated based on the estimate and standard error of the slope term within the probit model. The effect of fellowship was qualitatively analyzed by comparing the values between the groups at different years since residency graduation. Incomplete data were excluded only for responses missing.
Institutional review board approval was obtained from Children's National Medical Center in Washington, DC.
RESULTS
One hundred ninety‐seven pediatric hospitalists responded to the survey. All were included in the analysis. One hundred forty‐seven respondents were non‐fellowship‐trained and 50 were PHM fellowship graduates or current PHM fellows. Demographic characteristics are listed in Table 2. Current and former PHM fellows were on average 2.1 years from residency graduation, whereas non‐fellowship‐trained hospitalists were 2.6 years from residency graduation (P=0.05). A significantly higher proportion of fellowship‐trained hospitalists reported working at a university‐affiliated free‐standing children's hospital, whereas a higher proportion of non‐fellowship‐trained hospitalists reported working at a non‐university‐affiliated community hospital. The majority of practice domains included hospitalists worked were similar between the 2 groups. A significantly higher proportion of fellowship‐trained hospitalists reported working in research and QI/safety. Surgical comanagement and newborn nursery were domains a significantly higher proportion of non‐fellowship‐trained hospitalists reported working.
| Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value | |
|---|---|---|---|
| |||
| Average years experience (since residency graduation) | 2.1 | 2.6 | 0.05 |
| Type of residency | 0.82 | ||
| Pediatric | 48 (96%) | 140 (95%) | |
| Medicine‐pediatric | 2 (4%) | 7 (5%) | |
| Family medicine | 0 | 0 | |
| Chief residency | 17 (34%) | 37 (25%) | 0.23 |
| Advanced degree obtained | 0.12 | ||
| Master's Public Health | 2 (4%) | 8 (5.5%) | |
| Master's of Education | 0 | 1 (0.7%) | |
| Master's Clinical and Translational Research | 1 (2%) | 0 | |
| Master's Business Administration | 1 (2%) | 0 | |
| PhD | 0 | 1 (0.7%) | |
| Other | 3 (6%) | 8 (5.5%) | |
| Currently pursuing | 14 (28%) | 6 (4.1%) | |
| Practice environment | |||
| University‐affiliated free‐standing children's hospital | 40 (80%) | 68 (46.3%) | <0.001 |
| University‐affiliated pediatric ward | 7 (14%) | 37 (25.2%) | 0.1 |
| University‐affiliated community hospital | 2 (4%) | 25 (17%) | 0.02 |
| Non‐university affiliated community hospital | 2 (4%) | 35 (23.8%) | 0.002 |
| Practice domain | |||
| General pediatrics inpatient unit | 49/49 (100%) | 139/143 (97.2%) | 0.24 |
| Subspecialty wards | 19/46 (41.3%) | 47/130 (36.1%) | 0.54 |
| Surgical comanagement | 36/46 (78.3%) | 119/133 (89.5%) | 0.05 |
| NICU | 8/47 (17.0%) | 36/128 (28.1%) | 0.13 |
| PICU | 11/47 (17.0%) | 16/126 (12.0%) | 0.08 |
| Intermediate care unit | 17/47 (36.2%) | 36/128 (28.1%) | 0.09 |
| ED | 16/47 (34.0%) | 55/128 (43.0%) | 0.42 |
| Newborn nursery | 11/45 (24.4%) | 68/132 (51.5%) | 0.002 |
| Sedation | 20/48 (41.7%) | 48/133 (36.1%) | 0.49 |
| Medical education | 47/48 (97.9%) | 123/137 (89.8%) | 0.08 |
| Hospital committee work | 42/48 (87.5%) | 109/138 (79.0%) | 0.3 |
| Research | 44/49 (90.0%) | 72/137 (52.6%) | <0.001 |
| Quality improvement/safety | 44/48 (91.7%) | 103/134 (76.9%) | 0.003 |
| Advocacy | 23/47 (47.9%) | 49/128 (38.2%) | 0.19 |
The adjusted mean perceived competency scores for fellowship and non‐fellowship‐trained hospitalists are shown in Table 3. Reported competency scores for management of common acute inpatient medical conditions in an otherwise healthy child were similar between the 2 groups. Both fellowship and non‐fellowship‐trained hospitalists reported feeling less than competent (scores <50) in sedation, understanding basic components of PHM business practice, and defining a relative value unit. Fellowship‐trained hospitalists indicated perceived competency (scores >50) in the remainder of the competencies surveyed. Non‐fellowship‐trained hospitalists additionally had average scores <50 with statistically significant lower reported competency scores than fellowship‐trained hospitalists in IV access/phlebotomy, managing emergencies in technology‐dependent children, performing Plan‐Do‐Study‐Act (PDSA) cycles to achieve QI, performing root‐cause analysis (RCA), defining basic statistical terms, and identifying resources required to conduct research. Non‐fellowship‐trained hospitalists reported statistically significant higher mean competency scores in pain management, newborn care, and transitions in care. In each of these competencies, though, mean scores for both groups were in the competent range.
| Core Competency | Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value |
|---|---|---|---|
| |||
| Common diagnoses | 78.4 | 78.6 | 0.717 |
| Core skills | |||
| IV access/phlebotomy | 52.9 | 30.6 | 0.012 |
| Lumbar puncture | 76.2 | 77.0 | 0.245 |
| Sedation | 30.9 | 28.3 | 0.001 |
| Pain management | 70.7 | 72.6 | 0.014 |
| Nutrition | 68.0 | 66.1 | 0.026 |
| Specialized clinical skills | |||
| Leading a health care team | |||
| Team leadership | 74.9 | 72.0 | <0.001 |
| FCR | 75.3 | 72.6 | <0.001 |
| Technology‐dependent patient | |||
| General management | 71.4 | 65.9 | <0.001 |
| Emergencies | 53.2 | 49.4 | <0.001 |
| Newborn care | 56.6 | 61.6 | <0.001 |
| Child abuse | |||
| Diagnosing | 68.6 | 68.7 | 0.925 |
| Reporting | 68.9 | 68.5 | 0.630 |
| Healthcare systems | |||
| Transitions in care | 77.4 | 79.6 | 0.002 |
| Advocacy | 57.4 | 53.5 | <0.001 |
| Business practice | |||
| Basic components | 36.4 | 32.0 | <0.001 |
| Concept of RVU | 30.2 | 30.2 | 0.972 |
| Billing/coding | 61.4 | 63.9 | 0.004 |
| Quality Improvement | |||
| PDSA cycles | 63.7 | 42.8 | <0.001 |
| Best practice guidelines | 64.7 | 51.8 | <0.001 |
| Safety | |||
| Identify and address harm | 65.9 | 59.1 | <0.001 |
| Perform RCA | 56.7 | 36.0 | <0.001 |
| Cost‐effective care | 58.4 | 51.6 | <0.001 |
| Medical education | |||
| Needs assessment | 69.4 | 65.6 | <0.001 |
| Large group teaching | 67.6 | 60.6 | <0.001 |
| Small group teaching | 74.2 | 72.6 | 0.040 |
| Feedback | 73.8 | 68.9 | <0.001 |
| Evidence‐based medicine | |||
| Literature search | 75.9 | 69.0 | <0.001 |
| Literature appraisal | 63.4 | 57.2 | <0.001 |
| Apply study results | 70.2 | 64.8 | <0.001 |
| Research | |||
| Comparing study design | 62.6 | 54.1 | <0.001 |
| Basic statistics | 57.2 | 41.7 | <0.001 |
| Identifying resources | 56.0 | 36.1 | <0.001 |
The mean adjusted competency scores in areas with some of the largest differences between the 2 groups were plotted by time since residency graduation and depicted in Figure 1. This does not represent a single cohort of hospitalists over time, rather individual hospitalists at different post‐graduate years from their residency graduation. In performing PDSA cycles, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean score indicating competency (57.3), whereas only non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation reported a mean score approaching competency (49.1) (Figure 1A). For development of best practice guidelines, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean competency score (61.8), similar to non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation (60.8) (Figure 1B). Competency in performing RCA was reported by fellowship‐trained hospitalists 2 years postresidency (72.1), whereas non‐fellowship‐trained hospitalists up to 5 years post‐residency report a mean score below competency (Figure 1C). Regarding research competencies, fellowship‐trained hospitalists reported increased perceived competency at each year postresidency graduation, whereas non‐fellowship‐trained hospitalists reported lower mean competency scores with each year post‐residency (Figure 1D,E).
DISCUSSION
Our study results reveal significant differences in perceived competency between fellowship‐trained and non‐fellowship‐trained hospitalists, identifying several perceived knowledge gaps. Early career hospitalists, regardless of their training, perceive they have not achieved competency in sedation and aspects of PHM business practice. Early career hospitalists who did not pursue PHM fellowship training reported also feeling less than competent in intravenous access/phlebotomy, managing emergencies in technology‐dependent children, performing PDSA cycles to achieve QI, performing RCA, defining basic statistical terms, and identifying resources required to conduct research. Although both groups perceived themselves as competent in newborn care, pain management, and transitions in care, non‐fellowship‐trained hospitalists did report statistically significant higher competency scores compared to fellowship‐trained hospitalists in these skills.
Our findings support previous studies on the roles and training needs of pediatric hospitalists. In 2004, Ottolini et al. conducted a survey of pediatric hospitalists through Pediatric Research in Inpatient Settings, finding additional training needs in program/division management, practice guidelines, QI, safety, teaching, evidence‐based medicine (EBM), and research. The majority of hospitalists surveyed did not believe their pediatric residency training provided all of the skills necessary to practice as pediatric hospitalists.[5] Maniscalco et al. repeated the study in 2008 with similar findings.[6] In the field of adult internal medicine, Plauth et al. surveyed practicing hospitalists regarding the adequacy of their residency training, and found that systems issues (ie, QI, health economics, practice guidelines development) were reported as important to their current practice and not adequately emphasized in residency training.[9] Collectively, these findings highlight the need to critically evaluate our current training models' ability to prepare an individual for a career in hospital medicine. There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified,[1] but it is important to identify where the current knowledge gaps exist to optimize this process.
Not surprisingly, the majority of the hospitalists surveyed self‐reported competency in most of the clinical skills included. Residency training is heavily weighted toward acquisition of clinical skills, with a significant amount of time spent on inpatient clinical rotations.[10] The exception was sedation, which had some of the lowest mean perceived competency scores for all early career hospitalists surveyed. There is growing demand for safe and effective procedural sedation nationally, and pediatric hospitalists have been recognized as well poised to augment sedation services provided by anesthesiologists.[11, 12] This study demonstrates that current residency and PHM fellowship training may not adequately address this skill set to produce hospitalists prepared to take on this potential role.
Significant findings in the non‐clinical domains were the healthcare systems competencies. It is increasingly evident that a hospitalist's job description includes addressing communication, coordination of care, quality of care, and patient safety.[13] Yet, our findings indicate that non‐fellowship‐trained early career hospitalists do not feel competent in several of these aspects of hospital medicine practice. Our findings suggest that residency training alone may not provide adequate instruction for perceived competency, as no hospitalists with <1 year since residency graduation reported competency in PDSA cycles, best practice guidelines, and RCA. Interestingly, examining these competencies at different years following residency graduation, experience alone also does not ensure perceived competency early in one's career. Hospitalists are establishing themselves as a catalyst for change and the driving forces behind healthcare systems improvements within the hospital setting, often as our value added to an institution.[14, 15, 16, 17] Therefore, every pediatric hospitalist will need to acquire competency in these skills in a timely manner to effectively deliver high‐quality care to hospitalized children.
Finally, research was another area in which non‐fellowship‐trained hospitalists had low self‐perceived competency. When evaluating competency at different years postresidency graduation, non‐fellowship‐trained individuals appeared to lose a sense of competency each year, whereas fellowship‐trained hospitalists reported escalating competency with each year post‐residency. This finding may be due to the fellowship training itself, mentorship established in fellowship, or resources available in their chosen practice environment following fellowship. In 2011, Bekmezian et al. found that the majority of pediatric hospitalists wanted to conduct research but cited lack of dedicated time and mentorship as barriers to their productivity.[18] High‐quality studies including clinical, QI, and comparative effectiveness research are necessary to allow practicing hospitalists to make better decisions regarding patient care and to advance the field. This need transcends practice environment evidenced by the latest movement to transition away from the more traditional academic and non‐academic nomenclature. Even if one is not planning to conduct research, a basic foundation of research knowledge is required to critically appraise literature and apply EBM principles to clinical practice. This study suggests these skills are not being adequately obtained in residency for perceived competency or acquired with experience alone early in one's career.
There are several limitations of this study that should be considered. Most notably, the competency scores are based on self‐perceived assessments and therefore are not validated with objective measures of an individual's knowledge and skill, risking bias based on an individual's level of personal insight. We also did not quantify differences in training experience based on specific institutions, residency size, patient volume, and exposure to a hospitalist service, which could influence perceived competency and generalizability. Similarly, there is wide variation in current PHM fellowship curriculums, which is not accounted for in this study. Professional competency is challenging to define as well as measure.[19] Although this study is based on subjective measures, one can postulate that self‐perceived competency may impact an individual's approach to clinical practice, projects pursued, and career aspirations.
A second significant limitation was our inability to accurately determine a response rate. Other pediatric hospitalist surveys have faced similar limitations utilizing the AAP SOHM Listserv, because there is no centralized database of practicing hospitalists.[18, 20, 21] Attempts to collect workforce data from the American Board of Pediatrics (ABP) regarding estimates of the number of hospitalists within 5 years of their residency graduation revealed that they changed their data collection methods during our study period, therefore direct comparisons could not be made before and after 2012 (email communication with Cathy Koenig, Psychometric Data Analyst, ABP). Additionally, the AAP SOHM Listserv does not collect demographic data on subscribers, therefore we were unable to determine how many of the 2100 subscribers are within 5 years of their residency graduation. Nevertheless, it is the largest listserv of pediatric hospitalists and enabled us to attempt to collect data from the most representative population. PHM fellowship programs have also rapidly expanded, and only recently has there been a more centralized, comprehensive database of programs and fellows. With the available information, we could not accurately estimate a response rate. Despite the potential for response bias and small sample size, we feel the information collected is a valuable first look at important and timely data that can inform future studies.
Overall, this study provides important information regarding the perceived competency of early career pediatric hospitalists. Although different practice environments may afford different experiences and influence competency over time, we believe the majority of the PHM core competencies transcend practice environment and are ones all early career hospitalists should strive to achieve. To ensure the ongoing advancement of our field, we must guarantee that hospitalists are provided the resources and training to attain these competencies. This may include developing hospital medicine residency tracks, continuing medical education offerings, and/or PHM fellowships whose objectives are aligned with the established core competencies. Although this study was not designed to determine which of these options are optimal, the results can help identify the existing gaps to inform curriculum development in the future. As our field continues to evolve and advance, it will be important to continuously re‐evaluate our training programs' abilities to produce pediatric hospitalists with clinical, quality, scholarly, and leadership skills that meet our field's core competency standards.
CONCLUSIONS
Early career pediatric hospitalists report deficits in several of the PHM core competencies, which should be considered when designing PHM‐specific training in the future. PHM fellowship‐trained hospitalists report higher levels of self‐perceived competency in many core areas.
Disclosure: Nothing to report.
Pediatric hospital medicine (PHM) has established itself as a well‐defined field of pediatrics dedicated to improving the care of hospitalized children.[1] In 2010, the PHM core competencies were established to identify a specific knowledge base and skill set needed to provide the highest quality care for hospitalized children.[2] With these competencies, many are re‐evaluating training needs, particularly given the rapid advancement of the field.[1, 3] Previous workforce evaluations estimated that less than half of hospitalists surveyed had any specific hospitalist training.[4] In 2004 and 2008, studies of the current roles and training needs of pediatric hospitalists revealed advanced training needs in administration, research, quality improvement (QI), and education.[5, 6] Currently, there are 27 US PHM fellowship programs, but the majority of hospitalists are entering the field without PHM‐specific training. There is little evidence regarding our current residency and fellowship training models' abilities to help participants achieve proficiency in the PHM core competencies.
The objectives of this study were to compare the perceived PHM core competency achievements of fellowship and non‐fellowship‐trained early career pediatric hospitalists and identify perceived knowledge gaps in our current training models.
METHODS
Study Design
An anonymous Web‐based survey was conducted in November 2013. The survey was electronically distributed to the American Academy of Pediatrics (AAP) Section on Hospital Medicine (SOHM) Listserv, current PHM fellows present at the annual PHM Fellows Conference, as well as PHM division directors and fellowship directors to distribute to eligible hospitalists. The AAP SOHM Listserv functions as a convenience sample, representing the single largest listing of pediatric hospitalists, currently with over 2100 subscribers (email communication with Nicole Alexander, AAP Manager of the Division of Hospital and Surgical Services). An email announcing the survey was distributed to the aforementioned parties with 1 reminder email sent to the SOHM Listserv encouraging participation.
Inclusion criteria were current practicing hospitalists who had graduated from a US Accreditation Council for Graduate Medical Education‐approved residency program within the last 5 years. Recruiting individuals within 5 years of residency graduation was chosen in an effort to capture the experience of our current training models. Practicing hospitalists included current PHM fellows, PHM fellowship graduates (both defined as fellowship‐trained), and non‐fellowship‐trained individuals.
Survey Development
The survey obtained demographic data including type of residency training, chief residency, postresidency training, advanced degrees, practice environment, and professional positions. Competency was self‐assessed using an interactive sliding scale where participants could indicate their perceived competency by placing the cursor along a continuum with the anchors novice, competent, and expert. Each anchor was defined as follows: novice is the inability to perform the skill or require supervision/assistance to complete the activity; competent is the ability to perform unsupervised execution of a task, not requiring substantial mastery or advanced ability; and expert is demonstrating initiative and adaptability to special problem situations and can lead others in performing the skill.[7] Cursor position along the sliding scale was converted by the survey tool to a value from 0 to 100 for data analysis. Within each group, a mean score below 50 was considered an area respondents perceived themselves less than competent. Select PHM core competencies were chosen in consultation with the authors of the PHM core competencies to provide a representative sample from each of the 4 domains (Table 1) as well as restrict the survey to a reasonable length. The survey was pilot tested in small groups and revised for content and readability based on the feedback received.
| Clinical Diagnosis | Core Skills | Specialized Clinical Skills | Healthcare Systems |
|---|---|---|---|
| |||
| Abdominal pain | Bladder catheterization | Child abuse* | Advocacy* |
| ALTE | ECG interpretation | Hospice and palliative care | Business practice* |
| Asthma | Feeding tubes | Leading healthcare team* | Communication |
| Bone and joint infection | Fluid/electrolytes | Newborn care* | Quality improvement* |
| Bronchiolitis | IV access/ phlebotomy* | Technology‐dependent children* | Cost‐effective care* |
| CNS infections | Lumbar puncture* | Transport of the critically ill | Education* |
| Diabetes | Noninvasive monitoring | Evidence‐based medicine* | |
| Failure to thrive | Nutrition* | Health information systems | |
| Fever unknown origin | Oxygen delivery and airway management | Legal, risk management | |
| Gastroenteritis | Pain management* | Patient safety* | |
| Kawasaki disease | PALS | Research* | |
| Neonatal fever | Procedural sedation* | Transitions of care* | |
| Neonatal jaundice | Radiographic interpretation | ||
| Pneumonia | |||
| Respiratory failure | |||
| Seizures | |||
| Shock | |||
| Sickle cell disease | |||
| Skin and soft tissue infection | |||
| Upper airway infections | |||
| UTI | |||
| Single summative question included in the survey. | |||
Data Collection
Study data were collected and managed using the Research Electronic Data Capture (REDcap) tool hosted at Children's National Health System. REDcap is a secure, Web‐based application designed to support data capture for research studies.[8]
Data Analysis
Analysis was performed using SPSS version 22 (IBM, Armonk, NY). Demographic data comparing fellowship‐trained and non‐fellowship‐trained individuals were analyzed by [2] testing for categorical variables. Mean competency values between non‐fellows and those who have completed or are in the process of completing fellowship were analyzed using multiprobit regression. Values were adjusted for years since residency graduation (regardless of whether the individual was a current fellow, a fellowship graduate, or non‐fellowship‐trained), type of residency, and chief residency. P values were calculated based on the estimate and standard error of the slope term within the probit model. The effect of fellowship was qualitatively analyzed by comparing the values between the groups at different years since residency graduation. Incomplete data were excluded only for responses missing.
Institutional review board approval was obtained from Children's National Medical Center in Washington, DC.
RESULTS
One hundred ninety‐seven pediatric hospitalists responded to the survey. All were included in the analysis. One hundred forty‐seven respondents were non‐fellowship‐trained and 50 were PHM fellowship graduates or current PHM fellows. Demographic characteristics are listed in Table 2. Current and former PHM fellows were on average 2.1 years from residency graduation, whereas non‐fellowship‐trained hospitalists were 2.6 years from residency graduation (P=0.05). A significantly higher proportion of fellowship‐trained hospitalists reported working at a university‐affiliated free‐standing children's hospital, whereas a higher proportion of non‐fellowship‐trained hospitalists reported working at a non‐university‐affiliated community hospital. The majority of practice domains included hospitalists worked were similar between the 2 groups. A significantly higher proportion of fellowship‐trained hospitalists reported working in research and QI/safety. Surgical comanagement and newborn nursery were domains a significantly higher proportion of non‐fellowship‐trained hospitalists reported working.
| Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value | |
|---|---|---|---|
| |||
| Average years experience (since residency graduation) | 2.1 | 2.6 | 0.05 |
| Type of residency | 0.82 | ||
| Pediatric | 48 (96%) | 140 (95%) | |
| Medicine‐pediatric | 2 (4%) | 7 (5%) | |
| Family medicine | 0 | 0 | |
| Chief residency | 17 (34%) | 37 (25%) | 0.23 |
| Advanced degree obtained | 0.12 | ||
| Master's Public Health | 2 (4%) | 8 (5.5%) | |
| Master's of Education | 0 | 1 (0.7%) | |
| Master's Clinical and Translational Research | 1 (2%) | 0 | |
| Master's Business Administration | 1 (2%) | 0 | |
| PhD | 0 | 1 (0.7%) | |
| Other | 3 (6%) | 8 (5.5%) | |
| Currently pursuing | 14 (28%) | 6 (4.1%) | |
| Practice environment | |||
| University‐affiliated free‐standing children's hospital | 40 (80%) | 68 (46.3%) | <0.001 |
| University‐affiliated pediatric ward | 7 (14%) | 37 (25.2%) | 0.1 |
| University‐affiliated community hospital | 2 (4%) | 25 (17%) | 0.02 |
| Non‐university affiliated community hospital | 2 (4%) | 35 (23.8%) | 0.002 |
| Practice domain | |||
| General pediatrics inpatient unit | 49/49 (100%) | 139/143 (97.2%) | 0.24 |
| Subspecialty wards | 19/46 (41.3%) | 47/130 (36.1%) | 0.54 |
| Surgical comanagement | 36/46 (78.3%) | 119/133 (89.5%) | 0.05 |
| NICU | 8/47 (17.0%) | 36/128 (28.1%) | 0.13 |
| PICU | 11/47 (17.0%) | 16/126 (12.0%) | 0.08 |
| Intermediate care unit | 17/47 (36.2%) | 36/128 (28.1%) | 0.09 |
| ED | 16/47 (34.0%) | 55/128 (43.0%) | 0.42 |
| Newborn nursery | 11/45 (24.4%) | 68/132 (51.5%) | 0.002 |
| Sedation | 20/48 (41.7%) | 48/133 (36.1%) | 0.49 |
| Medical education | 47/48 (97.9%) | 123/137 (89.8%) | 0.08 |
| Hospital committee work | 42/48 (87.5%) | 109/138 (79.0%) | 0.3 |
| Research | 44/49 (90.0%) | 72/137 (52.6%) | <0.001 |
| Quality improvement/safety | 44/48 (91.7%) | 103/134 (76.9%) | 0.003 |
| Advocacy | 23/47 (47.9%) | 49/128 (38.2%) | 0.19 |
The adjusted mean perceived competency scores for fellowship and non‐fellowship‐trained hospitalists are shown in Table 3. Reported competency scores for management of common acute inpatient medical conditions in an otherwise healthy child were similar between the 2 groups. Both fellowship and non‐fellowship‐trained hospitalists reported feeling less than competent (scores <50) in sedation, understanding basic components of PHM business practice, and defining a relative value unit. Fellowship‐trained hospitalists indicated perceived competency (scores >50) in the remainder of the competencies surveyed. Non‐fellowship‐trained hospitalists additionally had average scores <50 with statistically significant lower reported competency scores than fellowship‐trained hospitalists in IV access/phlebotomy, managing emergencies in technology‐dependent children, performing Plan‐Do‐Study‐Act (PDSA) cycles to achieve QI, performing root‐cause analysis (RCA), defining basic statistical terms, and identifying resources required to conduct research. Non‐fellowship‐trained hospitalists reported statistically significant higher mean competency scores in pain management, newborn care, and transitions in care. In each of these competencies, though, mean scores for both groups were in the competent range.
| Core Competency | Fellowship Trained, n=50 | Non‐Fellowship‐Trained, n=147 | P Value |
|---|---|---|---|
| |||
| Common diagnoses | 78.4 | 78.6 | 0.717 |
| Core skills | |||
| IV access/phlebotomy | 52.9 | 30.6 | 0.012 |
| Lumbar puncture | 76.2 | 77.0 | 0.245 |
| Sedation | 30.9 | 28.3 | 0.001 |
| Pain management | 70.7 | 72.6 | 0.014 |
| Nutrition | 68.0 | 66.1 | 0.026 |
| Specialized clinical skills | |||
| Leading a health care team | |||
| Team leadership | 74.9 | 72.0 | <0.001 |
| FCR | 75.3 | 72.6 | <0.001 |
| Technology‐dependent patient | |||
| General management | 71.4 | 65.9 | <0.001 |
| Emergencies | 53.2 | 49.4 | <0.001 |
| Newborn care | 56.6 | 61.6 | <0.001 |
| Child abuse | |||
| Diagnosing | 68.6 | 68.7 | 0.925 |
| Reporting | 68.9 | 68.5 | 0.630 |
| Healthcare systems | |||
| Transitions in care | 77.4 | 79.6 | 0.002 |
| Advocacy | 57.4 | 53.5 | <0.001 |
| Business practice | |||
| Basic components | 36.4 | 32.0 | <0.001 |
| Concept of RVU | 30.2 | 30.2 | 0.972 |
| Billing/coding | 61.4 | 63.9 | 0.004 |
| Quality Improvement | |||
| PDSA cycles | 63.7 | 42.8 | <0.001 |
| Best practice guidelines | 64.7 | 51.8 | <0.001 |
| Safety | |||
| Identify and address harm | 65.9 | 59.1 | <0.001 |
| Perform RCA | 56.7 | 36.0 | <0.001 |
| Cost‐effective care | 58.4 | 51.6 | <0.001 |
| Medical education | |||
| Needs assessment | 69.4 | 65.6 | <0.001 |
| Large group teaching | 67.6 | 60.6 | <0.001 |
| Small group teaching | 74.2 | 72.6 | 0.040 |
| Feedback | 73.8 | 68.9 | <0.001 |
| Evidence‐based medicine | |||
| Literature search | 75.9 | 69.0 | <0.001 |
| Literature appraisal | 63.4 | 57.2 | <0.001 |
| Apply study results | 70.2 | 64.8 | <0.001 |
| Research | |||
| Comparing study design | 62.6 | 54.1 | <0.001 |
| Basic statistics | 57.2 | 41.7 | <0.001 |
| Identifying resources | 56.0 | 36.1 | <0.001 |
The mean adjusted competency scores in areas with some of the largest differences between the 2 groups were plotted by time since residency graduation and depicted in Figure 1. This does not represent a single cohort of hospitalists over time, rather individual hospitalists at different post‐graduate years from their residency graduation. In performing PDSA cycles, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean score indicating competency (57.3), whereas only non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation reported a mean score approaching competency (49.1) (Figure 1A). For development of best practice guidelines, fellowship‐trained hospitalists 1 year postresidency graduation reported a mean competency score (61.8), similar to non‐fellowship‐trained hospitalists 3 to 5 years postresidency graduation (60.8) (Figure 1B). Competency in performing RCA was reported by fellowship‐trained hospitalists 2 years postresidency (72.1), whereas non‐fellowship‐trained hospitalists up to 5 years post‐residency report a mean score below competency (Figure 1C). Regarding research competencies, fellowship‐trained hospitalists reported increased perceived competency at each year postresidency graduation, whereas non‐fellowship‐trained hospitalists reported lower mean competency scores with each year post‐residency (Figure 1D,E).
DISCUSSION
Our study results reveal significant differences in perceived competency between fellowship‐trained and non‐fellowship‐trained hospitalists, identifying several perceived knowledge gaps. Early career hospitalists, regardless of their training, perceive they have not achieved competency in sedation and aspects of PHM business practice. Early career hospitalists who did not pursue PHM fellowship training reported also feeling less than competent in intravenous access/phlebotomy, managing emergencies in technology‐dependent children, performing PDSA cycles to achieve QI, performing RCA, defining basic statistical terms, and identifying resources required to conduct research. Although both groups perceived themselves as competent in newborn care, pain management, and transitions in care, non‐fellowship‐trained hospitalists did report statistically significant higher competency scores compared to fellowship‐trained hospitalists in these skills.
Our findings support previous studies on the roles and training needs of pediatric hospitalists. In 2004, Ottolini et al. conducted a survey of pediatric hospitalists through Pediatric Research in Inpatient Settings, finding additional training needs in program/division management, practice guidelines, QI, safety, teaching, evidence‐based medicine (EBM), and research. The majority of hospitalists surveyed did not believe their pediatric residency training provided all of the skills necessary to practice as pediatric hospitalists.[5] Maniscalco et al. repeated the study in 2008 with similar findings.[6] In the field of adult internal medicine, Plauth et al. surveyed practicing hospitalists regarding the adequacy of their residency training, and found that systems issues (ie, QI, health economics, practice guidelines development) were reported as important to their current practice and not adequately emphasized in residency training.[9] Collectively, these findings highlight the need to critically evaluate our current training models' ability to prepare an individual for a career in hospital medicine. There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified,[1] but it is important to identify where the current knowledge gaps exist to optimize this process.
Not surprisingly, the majority of the hospitalists surveyed self‐reported competency in most of the clinical skills included. Residency training is heavily weighted toward acquisition of clinical skills, with a significant amount of time spent on inpatient clinical rotations.[10] The exception was sedation, which had some of the lowest mean perceived competency scores for all early career hospitalists surveyed. There is growing demand for safe and effective procedural sedation nationally, and pediatric hospitalists have been recognized as well poised to augment sedation services provided by anesthesiologists.[11, 12] This study demonstrates that current residency and PHM fellowship training may not adequately address this skill set to produce hospitalists prepared to take on this potential role.
Significant findings in the non‐clinical domains were the healthcare systems competencies. It is increasingly evident that a hospitalist's job description includes addressing communication, coordination of care, quality of care, and patient safety.[13] Yet, our findings indicate that non‐fellowship‐trained early career hospitalists do not feel competent in several of these aspects of hospital medicine practice. Our findings suggest that residency training alone may not provide adequate instruction for perceived competency, as no hospitalists with <1 year since residency graduation reported competency in PDSA cycles, best practice guidelines, and RCA. Interestingly, examining these competencies at different years following residency graduation, experience alone also does not ensure perceived competency early in one's career. Hospitalists are establishing themselves as a catalyst for change and the driving forces behind healthcare systems improvements within the hospital setting, often as our value added to an institution.[14, 15, 16, 17] Therefore, every pediatric hospitalist will need to acquire competency in these skills in a timely manner to effectively deliver high‐quality care to hospitalized children.
Finally, research was another area in which non‐fellowship‐trained hospitalists had low self‐perceived competency. When evaluating competency at different years postresidency graduation, non‐fellowship‐trained individuals appeared to lose a sense of competency each year, whereas fellowship‐trained hospitalists reported escalating competency with each year post‐residency. This finding may be due to the fellowship training itself, mentorship established in fellowship, or resources available in their chosen practice environment following fellowship. In 2011, Bekmezian et al. found that the majority of pediatric hospitalists wanted to conduct research but cited lack of dedicated time and mentorship as barriers to their productivity.[18] High‐quality studies including clinical, QI, and comparative effectiveness research are necessary to allow practicing hospitalists to make better decisions regarding patient care and to advance the field. This need transcends practice environment evidenced by the latest movement to transition away from the more traditional academic and non‐academic nomenclature. Even if one is not planning to conduct research, a basic foundation of research knowledge is required to critically appraise literature and apply EBM principles to clinical practice. This study suggests these skills are not being adequately obtained in residency for perceived competency or acquired with experience alone early in one's career.
There are several limitations of this study that should be considered. Most notably, the competency scores are based on self‐perceived assessments and therefore are not validated with objective measures of an individual's knowledge and skill, risking bias based on an individual's level of personal insight. We also did not quantify differences in training experience based on specific institutions, residency size, patient volume, and exposure to a hospitalist service, which could influence perceived competency and generalizability. Similarly, there is wide variation in current PHM fellowship curriculums, which is not accounted for in this study. Professional competency is challenging to define as well as measure.[19] Although this study is based on subjective measures, one can postulate that self‐perceived competency may impact an individual's approach to clinical practice, projects pursued, and career aspirations.
A second significant limitation was our inability to accurately determine a response rate. Other pediatric hospitalist surveys have faced similar limitations utilizing the AAP SOHM Listserv, because there is no centralized database of practicing hospitalists.[18, 20, 21] Attempts to collect workforce data from the American Board of Pediatrics (ABP) regarding estimates of the number of hospitalists within 5 years of their residency graduation revealed that they changed their data collection methods during our study period, therefore direct comparisons could not be made before and after 2012 (email communication with Cathy Koenig, Psychometric Data Analyst, ABP). Additionally, the AAP SOHM Listserv does not collect demographic data on subscribers, therefore we were unable to determine how many of the 2100 subscribers are within 5 years of their residency graduation. Nevertheless, it is the largest listserv of pediatric hospitalists and enabled us to attempt to collect data from the most representative population. PHM fellowship programs have also rapidly expanded, and only recently has there been a more centralized, comprehensive database of programs and fellows. With the available information, we could not accurately estimate a response rate. Despite the potential for response bias and small sample size, we feel the information collected is a valuable first look at important and timely data that can inform future studies.
Overall, this study provides important information regarding the perceived competency of early career pediatric hospitalists. Although different practice environments may afford different experiences and influence competency over time, we believe the majority of the PHM core competencies transcend practice environment and are ones all early career hospitalists should strive to achieve. To ensure the ongoing advancement of our field, we must guarantee that hospitalists are provided the resources and training to attain these competencies. This may include developing hospital medicine residency tracks, continuing medical education offerings, and/or PHM fellowships whose objectives are aligned with the established core competencies. Although this study was not designed to determine which of these options are optimal, the results can help identify the existing gaps to inform curriculum development in the future. As our field continues to evolve and advance, it will be important to continuously re‐evaluate our training programs' abilities to produce pediatric hospitalists with clinical, quality, scholarly, and leadership skills that meet our field's core competency standards.
CONCLUSIONS
Early career pediatric hospitalists report deficits in several of the PHM core competencies, which should be considered when designing PHM‐specific training in the future. PHM fellowship‐trained hospitalists report higher levels of self‐perceived competency in many core areas.
Disclosure: Nothing to report.
- , , , et al. Pediatric hospital medicine: a strategic planning roundtable to chart the future. J Hosp Med. 2012;7(4):329–334.
- , , , et al. The Pediatric Hospital Medicine Core Competencies Supplement: a Framework for Curriculum Development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(suppl 2):i–xv, 1–114.
- , . Pediatric hospital medicine and education: why we can't stand still. JAMA Pediatr. 2013;167(5):412–413.
- , , Research Advisory Committee of the American Board of Pediatrics. Pediatric hospitalists: training, current practice, and career goals. J Hosp Med. 2009;4(3):179–186.
- , , , . PRIS Survey: pediatric hospitalist roles and training needs. Pediatr Res. 2004;55:360A.
- , , , , . Current roles and training needs of pediatric hospitalists: a study from the Pediatric Research in Inpatient Settings (PRIS) Network. Paper presented at: Pediatric Academic Societies; 2008; Honolulu, HI.
- , , , . From the educational bench to the clinical bedside: translating the Dreyfus developmental model to the learning of clinical skills. Acad Med. 2008;83(8):761–767.
- , , , , , . Research Electronic Data Capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- , , , . Hospitalists' perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111(3):247–254.
- Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Pediatrics. 2012. Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/320_pediatrics_07012013.pdf. Accessed August 14, 2014.
- , . Pediatric sedation. Pediatr Clin North Am. 2014;61(4):703–717.
- , , , , . Development of a pediatric hospitalist sedation service: training and implementation. J Hosp Med. 2012;7(4):335–339.
- , , , et al. Guiding principles for pediatric hospital medicine programs. Pediatrics. 2013;132(4):782–786.
- , , , . Pediatric hospitalists: a systematic review of the literature. Pediatrics. 2006;117(5):1736–1744.
- , . Pediatric hospitalist systems versus traditional models of care: effect on quality and cost outcomes. J Hosp Med. 2012;7(4):350–357.
- . Pediatric hospital medicine: historical perspectives, inspired future. Curr Probl Pediatr Adolesc Health Care. 2012;42(5):107–112.
- . Pediatric hospitalists working in community hospitals. Pediatr Clin North Am. 2014;61(4):681–691.
- , , . Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38–44.
- , . Defining and assessing professional competence. JAMA. 2002;287(2):226–235.
- , , . Transition of care: what Is the pediatric hospitalist's role? An exploratory survey of current attitudes. J Hosp Med. 2012;7(4):277–281.
- , , . Association between practice setting and pediatric hospitalist career satisfaction. Hosp Pediatr. 2013;3(3):285–291.
- , , , et al. Pediatric hospital medicine: a strategic planning roundtable to chart the future. J Hosp Med. 2012;7(4):329–334.
- , , , et al. The Pediatric Hospital Medicine Core Competencies Supplement: a Framework for Curriculum Development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(suppl 2):i–xv, 1–114.
- , . Pediatric hospital medicine and education: why we can't stand still. JAMA Pediatr. 2013;167(5):412–413.
- , , Research Advisory Committee of the American Board of Pediatrics. Pediatric hospitalists: training, current practice, and career goals. J Hosp Med. 2009;4(3):179–186.
- , , , . PRIS Survey: pediatric hospitalist roles and training needs. Pediatr Res. 2004;55:360A.
- , , , , . Current roles and training needs of pediatric hospitalists: a study from the Pediatric Research in Inpatient Settings (PRIS) Network. Paper presented at: Pediatric Academic Societies; 2008; Honolulu, HI.
- , , , . From the educational bench to the clinical bedside: translating the Dreyfus developmental model to the learning of clinical skills. Acad Med. 2008;83(8):761–767.
- , , , , , . Research Electronic Data Capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- , , , . Hospitalists' perceptions of their residency training needs: results of a national survey. Am J Med. 2001;111(3):247–254.
- Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Pediatrics. 2012. Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/320_pediatrics_07012013.pdf. Accessed August 14, 2014.
- , . Pediatric sedation. Pediatr Clin North Am. 2014;61(4):703–717.
- , , , , . Development of a pediatric hospitalist sedation service: training and implementation. J Hosp Med. 2012;7(4):335–339.
- , , , et al. Guiding principles for pediatric hospital medicine programs. Pediatrics. 2013;132(4):782–786.
- , , , . Pediatric hospitalists: a systematic review of the literature. Pediatrics. 2006;117(5):1736–1744.
- , . Pediatric hospitalist systems versus traditional models of care: effect on quality and cost outcomes. J Hosp Med. 2012;7(4):350–357.
- . Pediatric hospital medicine: historical perspectives, inspired future. Curr Probl Pediatr Adolesc Health Care. 2012;42(5):107–112.
- . Pediatric hospitalists working in community hospitals. Pediatr Clin North Am. 2014;61(4):681–691.
- , , . Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38–44.
- , . Defining and assessing professional competence. JAMA. 2002;287(2):226–235.
- , , . Transition of care: what Is the pediatric hospitalist's role? An exploratory survey of current attitudes. J Hosp Med. 2012;7(4):277–281.
- , , . Association between practice setting and pediatric hospitalist career satisfaction. Hosp Pediatr. 2013;3(3):285–291.
© 2015 Society of Hospital Medicine