User login
What is your diagnosis? - January 2019
Primary intestinal lymphangiectasia
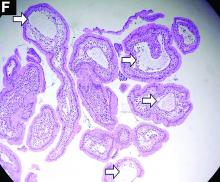
Histologic examination shows chronic inflammation of the ileum characterized by increased lymphoplasma cell infiltration of lamina propria without malignancy. Moreover, marked dilatation of lymphatic ducts that involved the mucosa was identified (Figure F, arrows; stain: hematoxylin and eosin; original magnification, ×100). On the basis of pathologic examinations, a diagnosis of primary intestinal lymphangiectasia (PIL) was made.
PIL is an extremely rare cause of protein-losing enteropathy characterized by the presence of dilated lymphatic channels in the mucosa, submucosa, or subserosa leading to protein-losing enteropathy.1 The true incidence and prevalence of this disease remains unclear. The disease affects males and females equally, and usually occurs in children and young adults. To date, less than 200 cases of PIL have been reported in the literature. The clinical manifestations of PIL may be asymptomatic or symptomatic such as abdominal pain, edema, diarrhea, and dyspnea. The diagnosis is based on the typical endoscopic findings of diffuse scattered mucosal white blebs with characteristic histologic findings of abnormal lymphatic dilatation. Double-balloon enteroscopy and capsule endoscopy are powerful modalities to evaluate the entire affected area of PIL.2 Although diet modification is a major treatment of PIL, several medicines have been reported to be useful such as corticosteroids, octreotide, and antiplasmin.3 Moreover, in patients with segmental lesions, surgery with local bowel resection is a useful treatment.3 In addition, PIL had a 5% risk of malignant transformation into lymphoma.3
References
1. Waldmann TA, Steinfeld JL, Dutcher TF, et al. The role of the gastrointestinal system in “idiopathic hypoproteinemia.” Gastroenterology. 1961;41:197-207.
2. Oh TG, Chung JW, Kim HM, et al. Primary intestinal lymphangiectasia diagnosed by capsule endoscopy and double balloon enteroscopy. World J Gastrointest Endosc. 2011;3:235-40.
3. Wen J, Tang Q, Wu, J. Primary intestinal lymphangiectasia: four case reports and a review of the literature. Dig Dis Sci. 2010;55:3466-72.
Primary intestinal lymphangiectasia
Histologic examination shows chronic inflammation of the ileum characterized by increased lymphoplasma cell infiltration of lamina propria without malignancy. Moreover, marked dilatation of lymphatic ducts that involved the mucosa was identified (Figure F, arrows; stain: hematoxylin and eosin; original magnification, ×100). On the basis of pathologic examinations, a diagnosis of primary intestinal lymphangiectasia (PIL) was made.
PIL is an extremely rare cause of protein-losing enteropathy characterized by the presence of dilated lymphatic channels in the mucosa, submucosa, or subserosa leading to protein-losing enteropathy.1 The true incidence and prevalence of this disease remains unclear. The disease affects males and females equally, and usually occurs in children and young adults. To date, less than 200 cases of PIL have been reported in the literature. The clinical manifestations of PIL may be asymptomatic or symptomatic such as abdominal pain, edema, diarrhea, and dyspnea. The diagnosis is based on the typical endoscopic findings of diffuse scattered mucosal white blebs with characteristic histologic findings of abnormal lymphatic dilatation. Double-balloon enteroscopy and capsule endoscopy are powerful modalities to evaluate the entire affected area of PIL.2 Although diet modification is a major treatment of PIL, several medicines have been reported to be useful such as corticosteroids, octreotide, and antiplasmin.3 Moreover, in patients with segmental lesions, surgery with local bowel resection is a useful treatment.3 In addition, PIL had a 5% risk of malignant transformation into lymphoma.3
References
1. Waldmann TA, Steinfeld JL, Dutcher TF, et al. The role of the gastrointestinal system in “idiopathic hypoproteinemia.” Gastroenterology. 1961;41:197-207.
2. Oh TG, Chung JW, Kim HM, et al. Primary intestinal lymphangiectasia diagnosed by capsule endoscopy and double balloon enteroscopy. World J Gastrointest Endosc. 2011;3:235-40.
3. Wen J, Tang Q, Wu, J. Primary intestinal lymphangiectasia: four case reports and a review of the literature. Dig Dis Sci. 2010;55:3466-72.
Primary intestinal lymphangiectasia
Histologic examination shows chronic inflammation of the ileum characterized by increased lymphoplasma cell infiltration of lamina propria without malignancy. Moreover, marked dilatation of lymphatic ducts that involved the mucosa was identified (Figure F, arrows; stain: hematoxylin and eosin; original magnification, ×100). On the basis of pathologic examinations, a diagnosis of primary intestinal lymphangiectasia (PIL) was made.
PIL is an extremely rare cause of protein-losing enteropathy characterized by the presence of dilated lymphatic channels in the mucosa, submucosa, or subserosa leading to protein-losing enteropathy.1 The true incidence and prevalence of this disease remains unclear. The disease affects males and females equally, and usually occurs in children and young adults. To date, less than 200 cases of PIL have been reported in the literature. The clinical manifestations of PIL may be asymptomatic or symptomatic such as abdominal pain, edema, diarrhea, and dyspnea. The diagnosis is based on the typical endoscopic findings of diffuse scattered mucosal white blebs with characteristic histologic findings of abnormal lymphatic dilatation. Double-balloon enteroscopy and capsule endoscopy are powerful modalities to evaluate the entire affected area of PIL.2 Although diet modification is a major treatment of PIL, several medicines have been reported to be useful such as corticosteroids, octreotide, and antiplasmin.3 Moreover, in patients with segmental lesions, surgery with local bowel resection is a useful treatment.3 In addition, PIL had a 5% risk of malignant transformation into lymphoma.3
References
1. Waldmann TA, Steinfeld JL, Dutcher TF, et al. The role of the gastrointestinal system in “idiopathic hypoproteinemia.” Gastroenterology. 1961;41:197-207.
2. Oh TG, Chung JW, Kim HM, et al. Primary intestinal lymphangiectasia diagnosed by capsule endoscopy and double balloon enteroscopy. World J Gastrointest Endosc. 2011;3:235-40.
3. Wen J, Tang Q, Wu, J. Primary intestinal lymphangiectasia: four case reports and a review of the literature. Dig Dis Sci. 2010;55:3466-72.
A 19-year-old boy presented to our hospital because of a 6-month history of progressive dyspnea and generalized edema. He developed cough, abdominal fullness, diarrhea, and leg edema 5 years ago.
Liver cirrhosis was suspected at that time. However, he seemed to have a poor response to medical treatment. Physical examination showed decreased breathing sounds and rales of the bilateral lower chest area, a distended abdomen with multiple purple striae, and edema of bilateral lower legs.
Laboratory tests showed a low serum total protein of 3.8 g/dL (normal range, 5.5–8), albumin of 2.0 g/dL (normal range, 3.8–5.4), total calcium of 7 mg/dL (normal range, 8.4–10.8), C-reactive protein of 11.02 mg/dL (normal, below 0.8). His hemogram showed a white blood cell count of 13,310 × 109/L (normal range, 3.5–11 × 109/L) with lymphocytopenia (9.8%).
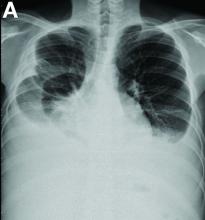
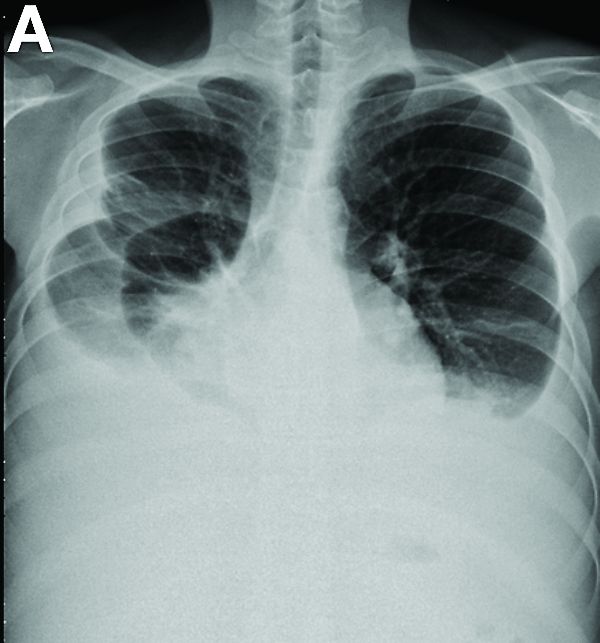
Other blood tests were within normal limits. The urinalysis and stool analysis were normal. Chest radiography showed bilateral pleural effusions (Figure A). Abdominal computed tomography demonstrated large ascites (Figure B). Paracentesis showed his serum ascites albumin gradient was 1.9 g/dL.
Subsequently, antegrade double-balloon enteroscopy (Fujinon EN-450T5; Fujinon, Saitama, Japan) demonstrated nodular mucosal lesions with a milk-like surface in the duodenum (Figure C).
Moreover, a snowflake appearance of mucosa was found in the jejunum and proximal ileum (Figure D). However, normal appearance of mucosa was identified in the middle ileum (Figure E). Biopsy specimens from these abnormal mucosal lesions were taken for pathology.
What is the diagnosis?
The SVS is working for you on burnout
Following a series of Vascular Specialist pieces highlighting the crisis of surgeon burnout and the unique challenges that face vascular surgeons, the SVS Wellness Task Force was formed in 2017. Recognizing that burnout may compromise recruitment and retention into our specialty, a particular threat at a time when our specialty faces projected increasing physician workforce needs, and that data suggests physician burnout compromises both patient quality of care and overall satisfaction, the task force was charged with proactively addressing vascular surgeon burnout. Our task force, comprising 21 engaged SVS members from across the country, has been working with strong support from leadership and administration to identify potential SVS targets for meaningful change.
The year 2018 was one of information gathering as we attempted clarify the severity of the problem and perceived member needs. We are grateful to our membership that have helped with this effort – for their time, for their insight, and for sharing their stories (some of which have been deeply personal). Two large-scale surveys were circulated to active SVS membership, both created with the assistance of the Mayo Clinic’s Division of Health Policy and Research.
The first survey was designed with a framework of validated wellness tools and well-described risk factors for burnout, then further “personalized” to incorporate unique challenges to the vascular surgeon. About 32% of our membership responded to this survey and alarmingly, when considering nonretired active SVS members, approximately one-third self-described depressive symptoms, 35% met criteria for burnout, and 8% self-reported suicidal thoughts in the last 12 months.
The second survey has only recently closed, focusing on the ergonomic challenges that we face across the spectrum of complex open and endovascular cases. Recognizing existing data that chronic pain and physical disability are associated with burnout, this data will be linked back to the original survey responses for association. Certainly there is more to come.
Concurrent with our survey initiatives, many of you participated in a Wellness Focus Group during VAM 2018. These focus groups intentionally considered the diversity of our membership across age, gender, practice setting, and region, revealing several important themes that threaten our wellness. It was no surprise that the EMR was identified as a clear threat to vascular surgery well-being and that this is not unique to our specialty. Importantly, our membership collectively feels “undervalued” at an institutional level. Specifically given the scope of comprehensive vascular care that we provide patients, a large part of our work includes both unpredictable acute vascular surgical care (such as intraoperative consultations for vascular trauma) and remedial salvage operations to manage vascular complications inflicted during care received from other physicians. This effort leaves us with little control over our time, often without perceived reciprocal clinical support, institutional support, or compensation.
Given this data, the Wellness Task Force is now strategizing efforts for change and supporting ongoing SVS initiatives. Our Task Force is currently:
- Collaborating with key EMR stakeholders with the goal of creating tools that can be shared across the specialty and addressing best practices for system-level support.
- Drafting a “public reply” to the Office of the National Coordinator for Health Information Technology’s “Strategy on Reducing Burden Relating to the Use of Health IT and EHRs” initiative.
- Collaborating with national experts to establish peer support tools and SVS networking opportunities that may help members cope with adverse outcomes and strategize the delivery of complex care.
- Identifying institutional best practices for surgeon wellness for broad dissemination.
- Supporting existing SVS initiatives that include the PAC/APM task force, branding initiatives through the PPO as we work to “own our space” and leverage our specialty and the community practice committee as the Society works proactively to optimize workload, fairness, and reward on a larger scale for membership.
We encourage everyone to stay tuned for periodic Vascular Specialist “Wellness Features” and to attend the Wellness Session at the 2019 VAM for interim progress that will feature the following discussions.
- (Re)Finding a meaningful career in vascular surgery.
- Ergonomic challenges to the vascular surgeon and strategies to mitigate the resulting threat of disability.
- EMR best practices to optimize efficiency.
- The role of peer support in vascular surgery, including the mitigation of second victim syndrome.
Surgeon burnout is a real threat to our workforce and the well-being of our colleagues and friends. Risk factors are multifactorial and will require broad, system-level change. The SVS remains fully committed to enhancing vascular surgeon wellness and this Task Force is grateful for your ongoing engagement and support.
Dr. Coleman is an associate professor of vascular surgery at the University of Michigan, Ann Arbor.
Following a series of Vascular Specialist pieces highlighting the crisis of surgeon burnout and the unique challenges that face vascular surgeons, the SVS Wellness Task Force was formed in 2017. Recognizing that burnout may compromise recruitment and retention into our specialty, a particular threat at a time when our specialty faces projected increasing physician workforce needs, and that data suggests physician burnout compromises both patient quality of care and overall satisfaction, the task force was charged with proactively addressing vascular surgeon burnout. Our task force, comprising 21 engaged SVS members from across the country, has been working with strong support from leadership and administration to identify potential SVS targets for meaningful change.
The year 2018 was one of information gathering as we attempted clarify the severity of the problem and perceived member needs. We are grateful to our membership that have helped with this effort – for their time, for their insight, and for sharing their stories (some of which have been deeply personal). Two large-scale surveys were circulated to active SVS membership, both created with the assistance of the Mayo Clinic’s Division of Health Policy and Research.
The first survey was designed with a framework of validated wellness tools and well-described risk factors for burnout, then further “personalized” to incorporate unique challenges to the vascular surgeon. About 32% of our membership responded to this survey and alarmingly, when considering nonretired active SVS members, approximately one-third self-described depressive symptoms, 35% met criteria for burnout, and 8% self-reported suicidal thoughts in the last 12 months.
The second survey has only recently closed, focusing on the ergonomic challenges that we face across the spectrum of complex open and endovascular cases. Recognizing existing data that chronic pain and physical disability are associated with burnout, this data will be linked back to the original survey responses for association. Certainly there is more to come.
Concurrent with our survey initiatives, many of you participated in a Wellness Focus Group during VAM 2018. These focus groups intentionally considered the diversity of our membership across age, gender, practice setting, and region, revealing several important themes that threaten our wellness. It was no surprise that the EMR was identified as a clear threat to vascular surgery well-being and that this is not unique to our specialty. Importantly, our membership collectively feels “undervalued” at an institutional level. Specifically given the scope of comprehensive vascular care that we provide patients, a large part of our work includes both unpredictable acute vascular surgical care (such as intraoperative consultations for vascular trauma) and remedial salvage operations to manage vascular complications inflicted during care received from other physicians. This effort leaves us with little control over our time, often without perceived reciprocal clinical support, institutional support, or compensation.
Given this data, the Wellness Task Force is now strategizing efforts for change and supporting ongoing SVS initiatives. Our Task Force is currently:
- Collaborating with key EMR stakeholders with the goal of creating tools that can be shared across the specialty and addressing best practices for system-level support.
- Drafting a “public reply” to the Office of the National Coordinator for Health Information Technology’s “Strategy on Reducing Burden Relating to the Use of Health IT and EHRs” initiative.
- Collaborating with national experts to establish peer support tools and SVS networking opportunities that may help members cope with adverse outcomes and strategize the delivery of complex care.
- Identifying institutional best practices for surgeon wellness for broad dissemination.
- Supporting existing SVS initiatives that include the PAC/APM task force, branding initiatives through the PPO as we work to “own our space” and leverage our specialty and the community practice committee as the Society works proactively to optimize workload, fairness, and reward on a larger scale for membership.
We encourage everyone to stay tuned for periodic Vascular Specialist “Wellness Features” and to attend the Wellness Session at the 2019 VAM for interim progress that will feature the following discussions.
- (Re)Finding a meaningful career in vascular surgery.
- Ergonomic challenges to the vascular surgeon and strategies to mitigate the resulting threat of disability.
- EMR best practices to optimize efficiency.
- The role of peer support in vascular surgery, including the mitigation of second victim syndrome.
Surgeon burnout is a real threat to our workforce and the well-being of our colleagues and friends. Risk factors are multifactorial and will require broad, system-level change. The SVS remains fully committed to enhancing vascular surgeon wellness and this Task Force is grateful for your ongoing engagement and support.
Dr. Coleman is an associate professor of vascular surgery at the University of Michigan, Ann Arbor.
Following a series of Vascular Specialist pieces highlighting the crisis of surgeon burnout and the unique challenges that face vascular surgeons, the SVS Wellness Task Force was formed in 2017. Recognizing that burnout may compromise recruitment and retention into our specialty, a particular threat at a time when our specialty faces projected increasing physician workforce needs, and that data suggests physician burnout compromises both patient quality of care and overall satisfaction, the task force was charged with proactively addressing vascular surgeon burnout. Our task force, comprising 21 engaged SVS members from across the country, has been working with strong support from leadership and administration to identify potential SVS targets for meaningful change.
The year 2018 was one of information gathering as we attempted clarify the severity of the problem and perceived member needs. We are grateful to our membership that have helped with this effort – for their time, for their insight, and for sharing their stories (some of which have been deeply personal). Two large-scale surveys were circulated to active SVS membership, both created with the assistance of the Mayo Clinic’s Division of Health Policy and Research.
The first survey was designed with a framework of validated wellness tools and well-described risk factors for burnout, then further “personalized” to incorporate unique challenges to the vascular surgeon. About 32% of our membership responded to this survey and alarmingly, when considering nonretired active SVS members, approximately one-third self-described depressive symptoms, 35% met criteria for burnout, and 8% self-reported suicidal thoughts in the last 12 months.
The second survey has only recently closed, focusing on the ergonomic challenges that we face across the spectrum of complex open and endovascular cases. Recognizing existing data that chronic pain and physical disability are associated with burnout, this data will be linked back to the original survey responses for association. Certainly there is more to come.
Concurrent with our survey initiatives, many of you participated in a Wellness Focus Group during VAM 2018. These focus groups intentionally considered the diversity of our membership across age, gender, practice setting, and region, revealing several important themes that threaten our wellness. It was no surprise that the EMR was identified as a clear threat to vascular surgery well-being and that this is not unique to our specialty. Importantly, our membership collectively feels “undervalued” at an institutional level. Specifically given the scope of comprehensive vascular care that we provide patients, a large part of our work includes both unpredictable acute vascular surgical care (such as intraoperative consultations for vascular trauma) and remedial salvage operations to manage vascular complications inflicted during care received from other physicians. This effort leaves us with little control over our time, often without perceived reciprocal clinical support, institutional support, or compensation.
Given this data, the Wellness Task Force is now strategizing efforts for change and supporting ongoing SVS initiatives. Our Task Force is currently:
- Collaborating with key EMR stakeholders with the goal of creating tools that can be shared across the specialty and addressing best practices for system-level support.
- Drafting a “public reply” to the Office of the National Coordinator for Health Information Technology’s “Strategy on Reducing Burden Relating to the Use of Health IT and EHRs” initiative.
- Collaborating with national experts to establish peer support tools and SVS networking opportunities that may help members cope with adverse outcomes and strategize the delivery of complex care.
- Identifying institutional best practices for surgeon wellness for broad dissemination.
- Supporting existing SVS initiatives that include the PAC/APM task force, branding initiatives through the PPO as we work to “own our space” and leverage our specialty and the community practice committee as the Society works proactively to optimize workload, fairness, and reward on a larger scale for membership.
We encourage everyone to stay tuned for periodic Vascular Specialist “Wellness Features” and to attend the Wellness Session at the 2019 VAM for interim progress that will feature the following discussions.
- (Re)Finding a meaningful career in vascular surgery.
- Ergonomic challenges to the vascular surgeon and strategies to mitigate the resulting threat of disability.
- EMR best practices to optimize efficiency.
- The role of peer support in vascular surgery, including the mitigation of second victim syndrome.
Surgeon burnout is a real threat to our workforce and the well-being of our colleagues and friends. Risk factors are multifactorial and will require broad, system-level change. The SVS remains fully committed to enhancing vascular surgeon wellness and this Task Force is grateful for your ongoing engagement and support.
Dr. Coleman is an associate professor of vascular surgery at the University of Michigan, Ann Arbor.
Physician value thyself!
The Merriam-Webster dictionary defines value as “the regard that something is held to deserve; the importance, worth, or usefulness of something” and “relative worth, utility, or importance.” We usually assess our professional worth by how we are treated at work. In social valuing framework, we are given social status based on how others regard us for who we are, what we do, and what we are worth. This is described as “felt worth,” which encapsulates our feelings about how we are regarded by others, in contrast to self-esteem, which is more of an internally held belief.
Our power came from our relationship with our patients and our ability to communicate and influence our patients, peers and administrators. As owners of our practices and small businesses, our currency with hospitals and lawmakers was our ability to bring revenue to hospitals and patient concerns directly to legislators. Practicing in more than one hospital made us more valuable and hospitals battled with each other to provide us and our patients the latest tools and conveniences. In return, we gave our valuable time freely without compensation to hospitals as committee members, task force members, and sounding boards for the betterment of the community. If I were a conspiracy theorist, which I am not, and wanted to devalue physicians I would seek to weaken the physician-patient bond. The way to implement this would be for a single hospital employer to put us on a treadmill chasing work relative value units, give us hard-to-accomplish goals, and keep moving the goalpost. Like I said, I do not believe in conspiracies.
The tsunami of byzantine regulations, Stark laws, and complicated reimbursement formulas has sapped our energy to counter the devaluation. Some are glad to see physicians, particularly surgeons, get their comeuppance because we are perceived as having large egos. This may be true in some instances. Yet, it turns out that the top three job titles with the largest egos are: private household cooks, chief executives, and farm and ranch managers.1
Physicians are also reputed to be possessing dominant leadership styles and seen as bossy and disruptive. Hence, we are made to have frequent training in how to ameliorate our disruptive behavior tendencies. Again, this may be true in a few cases. However, while reports mention how many people witness such unacceptable behavior, there is no valid data about the incidence in practicing physicians. Research also does not support the view that physicians have dominant and aggressive personalities leading to such behavior.
One of the leading interpersonal skills model is Social Styles. We happen to teach this to our faculty at the Ohio State Medical Center’s Faculty Leadership Institute. Turns out that physicians and nurses are almost equally placed into the four quadrants of leadership styles: driving, expressive, amiable, and analytical. I found similar findings in our society members participating in a leadership session I moderated. Indeed, we rank very high on “versatility,” a measure that enables us to adapt our behaviors to fit with our patients and coworkers.
Reported burnout rates of 50% in physicians may or may not be accurate, but burnout is real and so is depression and so are physician suicides. I have witnessed six physician suicides in my career thus far. Teaching resilience, celebrating doctor’s day, and giving out a few awards are all interventions after the fact. Preventive measures like employers and hospitals prioritizing removing daily obstacles eliminating meaningless work, providing more resources to deal with EMRs, and making our lives easier at work, so we can get to our loved ones sooner would help.
Physicians have been largely excluded themselves from participating in the health care debate. We want to see empirical evidence before we sign on to every new proposed care model. Otherwise, we cling on to the status quo and therefore, decision makers tend to leave us out. More important, value-based payment models have not thus far led to reduction in the cost of health care. Despite poor engagement scores at major health systems, physicians are “managed” and sidelined, and mandates are “done to them, not with them.”
In my 40-year career, our devaluation has been a slow and painful process. It started with being called a “provider.” This devalues me. Call me by what I am and do. Physician. Doctor. That is what our patients call us. But, we have been pushed to acquiesce. So, why do physicians undervalue themselves and are unable to be confident of their value to employers and hospital executives?
Some have theorized that physicians have low self-esteem and that denial and rationalization are simply defense mechanisms. The low self-esteem is traced back to medical student days and considered “posttraumatic” disorder. In one study of 189 medical students, 50% reported a decrease in their self-esteem/confidence. The students blamed their residents and attendings for this reaction. Some degree of intimidation may continue into training and employment where it may be part of the culture. We need to change this cycle and treat our students, residents, and mentees with respect as future peers.
Another aspect is related to our own well-being. Most physicians value their patient’s health more than their own. That concept is drilled into us throughout our life. Our spouses complain that we care more about our patients than we do for our families. We often ignore warning signs of serious issues in our own health, always downplaying textbook symptoms of burnout, depression, and even MI. Being too busy is a badge of honor to indicate how successful and wanted we are. This also needs to change.
Sheryl Sandberg in her book “Lean in” discusses the “tiara syndrome,” mainly referring to women. I would suggest that this applies to a lot of physicians, both men and women. Physicians tend to keep their heads down, work hard, and expect someone to come compliment them and place a “tiara” over their head. We may be wary of being called “self-promoters.” Sometimes it is cultural baggage for immigrant physicians who are taught to not brag about their accomplishments. It may behoove us to judiciously make peers and leadership aware of our positive activities in and outside the health system.
Some see physicians not as “pillars of any community,” but as “technicians on an assembly line” or “pawns in a money-making game for hospital administrators.” This degree of pessimism among physicians in surveys is well known but there is good news.
In a 2016 survey based upon responses by 17,236 physicians, 63% were pessimistic or very pessimistic about the medical profession, down from 77% in 2012.2 In another poll, medical doctors were rated as having very high or high ratings of honesty and ethical standards by 65%, higher than all except nurses, military officers, and grade school teachers.3 When the health care debate was at its peak in 2009, a public poll on who they trusted to recommend the right thing for reforming the healthcare system placed physicians at the very top (73%)ahead of health care professors, researchers, hospitals, the President, and politicians. Gallup surveyed 7,000 physicians about engagement in four hierarchical levels: Confidence, Integrity, Pride and Passion. Physicians scored highly on the Pride items in the survey (feel proud to work and being treated with respect).4 In other words, if we are treated well, we feel proud to tell others where we work.
Finally, like many I may consider myself an expert in all sorts of things not relevant to practicing medicine. Yet, I respectfully suggest we stay away from political hot potatoes like nuclear disarmament, gun control, climate change, immigration, and other controversial issues because they distract us from our primary mission. I would hate to see us viewed like Hollywood.
References
1. www.chicagotribune.com/business/ct-payscale-ego-survey-0830-biz-20160829-story.html
2. www.medpagetoday.com/primarycare/generalprimarycare/60446
3. https://nurse.org/articles/gallup-ethical-standards-poll-nurses-rank-highest/
4.https://news.gallup.com/poll/120890/healthcare-americans-trust-physicians-politicians.aspx
Bhagwan Satiani, MD, MBA, is professor of clinical surgery in the division of vascular diseases and surgery at Ohio State University, Columbus. He blogs at www.savvy-medicine.com . Reach him on Twitter @savvycutter.
The Merriam-Webster dictionary defines value as “the regard that something is held to deserve; the importance, worth, or usefulness of something” and “relative worth, utility, or importance.” We usually assess our professional worth by how we are treated at work. In social valuing framework, we are given social status based on how others regard us for who we are, what we do, and what we are worth. This is described as “felt worth,” which encapsulates our feelings about how we are regarded by others, in contrast to self-esteem, which is more of an internally held belief.
Our power came from our relationship with our patients and our ability to communicate and influence our patients, peers and administrators. As owners of our practices and small businesses, our currency with hospitals and lawmakers was our ability to bring revenue to hospitals and patient concerns directly to legislators. Practicing in more than one hospital made us more valuable and hospitals battled with each other to provide us and our patients the latest tools and conveniences. In return, we gave our valuable time freely without compensation to hospitals as committee members, task force members, and sounding boards for the betterment of the community. If I were a conspiracy theorist, which I am not, and wanted to devalue physicians I would seek to weaken the physician-patient bond. The way to implement this would be for a single hospital employer to put us on a treadmill chasing work relative value units, give us hard-to-accomplish goals, and keep moving the goalpost. Like I said, I do not believe in conspiracies.
The tsunami of byzantine regulations, Stark laws, and complicated reimbursement formulas has sapped our energy to counter the devaluation. Some are glad to see physicians, particularly surgeons, get their comeuppance because we are perceived as having large egos. This may be true in some instances. Yet, it turns out that the top three job titles with the largest egos are: private household cooks, chief executives, and farm and ranch managers.1
Physicians are also reputed to be possessing dominant leadership styles and seen as bossy and disruptive. Hence, we are made to have frequent training in how to ameliorate our disruptive behavior tendencies. Again, this may be true in a few cases. However, while reports mention how many people witness such unacceptable behavior, there is no valid data about the incidence in practicing physicians. Research also does not support the view that physicians have dominant and aggressive personalities leading to such behavior.
One of the leading interpersonal skills model is Social Styles. We happen to teach this to our faculty at the Ohio State Medical Center’s Faculty Leadership Institute. Turns out that physicians and nurses are almost equally placed into the four quadrants of leadership styles: driving, expressive, amiable, and analytical. I found similar findings in our society members participating in a leadership session I moderated. Indeed, we rank very high on “versatility,” a measure that enables us to adapt our behaviors to fit with our patients and coworkers.
Reported burnout rates of 50% in physicians may or may not be accurate, but burnout is real and so is depression and so are physician suicides. I have witnessed six physician suicides in my career thus far. Teaching resilience, celebrating doctor’s day, and giving out a few awards are all interventions after the fact. Preventive measures like employers and hospitals prioritizing removing daily obstacles eliminating meaningless work, providing more resources to deal with EMRs, and making our lives easier at work, so we can get to our loved ones sooner would help.
Physicians have been largely excluded themselves from participating in the health care debate. We want to see empirical evidence before we sign on to every new proposed care model. Otherwise, we cling on to the status quo and therefore, decision makers tend to leave us out. More important, value-based payment models have not thus far led to reduction in the cost of health care. Despite poor engagement scores at major health systems, physicians are “managed” and sidelined, and mandates are “done to them, not with them.”
In my 40-year career, our devaluation has been a slow and painful process. It started with being called a “provider.” This devalues me. Call me by what I am and do. Physician. Doctor. That is what our patients call us. But, we have been pushed to acquiesce. So, why do physicians undervalue themselves and are unable to be confident of their value to employers and hospital executives?
Some have theorized that physicians have low self-esteem and that denial and rationalization are simply defense mechanisms. The low self-esteem is traced back to medical student days and considered “posttraumatic” disorder. In one study of 189 medical students, 50% reported a decrease in their self-esteem/confidence. The students blamed their residents and attendings for this reaction. Some degree of intimidation may continue into training and employment where it may be part of the culture. We need to change this cycle and treat our students, residents, and mentees with respect as future peers.
Another aspect is related to our own well-being. Most physicians value their patient’s health more than their own. That concept is drilled into us throughout our life. Our spouses complain that we care more about our patients than we do for our families. We often ignore warning signs of serious issues in our own health, always downplaying textbook symptoms of burnout, depression, and even MI. Being too busy is a badge of honor to indicate how successful and wanted we are. This also needs to change.
Sheryl Sandberg in her book “Lean in” discusses the “tiara syndrome,” mainly referring to women. I would suggest that this applies to a lot of physicians, both men and women. Physicians tend to keep their heads down, work hard, and expect someone to come compliment them and place a “tiara” over their head. We may be wary of being called “self-promoters.” Sometimes it is cultural baggage for immigrant physicians who are taught to not brag about their accomplishments. It may behoove us to judiciously make peers and leadership aware of our positive activities in and outside the health system.
Some see physicians not as “pillars of any community,” but as “technicians on an assembly line” or “pawns in a money-making game for hospital administrators.” This degree of pessimism among physicians in surveys is well known but there is good news.
In a 2016 survey based upon responses by 17,236 physicians, 63% were pessimistic or very pessimistic about the medical profession, down from 77% in 2012.2 In another poll, medical doctors were rated as having very high or high ratings of honesty and ethical standards by 65%, higher than all except nurses, military officers, and grade school teachers.3 When the health care debate was at its peak in 2009, a public poll on who they trusted to recommend the right thing for reforming the healthcare system placed physicians at the very top (73%)ahead of health care professors, researchers, hospitals, the President, and politicians. Gallup surveyed 7,000 physicians about engagement in four hierarchical levels: Confidence, Integrity, Pride and Passion. Physicians scored highly on the Pride items in the survey (feel proud to work and being treated with respect).4 In other words, if we are treated well, we feel proud to tell others where we work.
Finally, like many I may consider myself an expert in all sorts of things not relevant to practicing medicine. Yet, I respectfully suggest we stay away from political hot potatoes like nuclear disarmament, gun control, climate change, immigration, and other controversial issues because they distract us from our primary mission. I would hate to see us viewed like Hollywood.
References
1. www.chicagotribune.com/business/ct-payscale-ego-survey-0830-biz-20160829-story.html
2. www.medpagetoday.com/primarycare/generalprimarycare/60446
3. https://nurse.org/articles/gallup-ethical-standards-poll-nurses-rank-highest/
4.https://news.gallup.com/poll/120890/healthcare-americans-trust-physicians-politicians.aspx
Bhagwan Satiani, MD, MBA, is professor of clinical surgery in the division of vascular diseases and surgery at Ohio State University, Columbus. He blogs at www.savvy-medicine.com . Reach him on Twitter @savvycutter.
The Merriam-Webster dictionary defines value as “the regard that something is held to deserve; the importance, worth, or usefulness of something” and “relative worth, utility, or importance.” We usually assess our professional worth by how we are treated at work. In social valuing framework, we are given social status based on how others regard us for who we are, what we do, and what we are worth. This is described as “felt worth,” which encapsulates our feelings about how we are regarded by others, in contrast to self-esteem, which is more of an internally held belief.
Our power came from our relationship with our patients and our ability to communicate and influence our patients, peers and administrators. As owners of our practices and small businesses, our currency with hospitals and lawmakers was our ability to bring revenue to hospitals and patient concerns directly to legislators. Practicing in more than one hospital made us more valuable and hospitals battled with each other to provide us and our patients the latest tools and conveniences. In return, we gave our valuable time freely without compensation to hospitals as committee members, task force members, and sounding boards for the betterment of the community. If I were a conspiracy theorist, which I am not, and wanted to devalue physicians I would seek to weaken the physician-patient bond. The way to implement this would be for a single hospital employer to put us on a treadmill chasing work relative value units, give us hard-to-accomplish goals, and keep moving the goalpost. Like I said, I do not believe in conspiracies.
The tsunami of byzantine regulations, Stark laws, and complicated reimbursement formulas has sapped our energy to counter the devaluation. Some are glad to see physicians, particularly surgeons, get their comeuppance because we are perceived as having large egos. This may be true in some instances. Yet, it turns out that the top three job titles with the largest egos are: private household cooks, chief executives, and farm and ranch managers.1
Physicians are also reputed to be possessing dominant leadership styles and seen as bossy and disruptive. Hence, we are made to have frequent training in how to ameliorate our disruptive behavior tendencies. Again, this may be true in a few cases. However, while reports mention how many people witness such unacceptable behavior, there is no valid data about the incidence in practicing physicians. Research also does not support the view that physicians have dominant and aggressive personalities leading to such behavior.
One of the leading interpersonal skills model is Social Styles. We happen to teach this to our faculty at the Ohio State Medical Center’s Faculty Leadership Institute. Turns out that physicians and nurses are almost equally placed into the four quadrants of leadership styles: driving, expressive, amiable, and analytical. I found similar findings in our society members participating in a leadership session I moderated. Indeed, we rank very high on “versatility,” a measure that enables us to adapt our behaviors to fit with our patients and coworkers.
Reported burnout rates of 50% in physicians may or may not be accurate, but burnout is real and so is depression and so are physician suicides. I have witnessed six physician suicides in my career thus far. Teaching resilience, celebrating doctor’s day, and giving out a few awards are all interventions after the fact. Preventive measures like employers and hospitals prioritizing removing daily obstacles eliminating meaningless work, providing more resources to deal with EMRs, and making our lives easier at work, so we can get to our loved ones sooner would help.
Physicians have been largely excluded themselves from participating in the health care debate. We want to see empirical evidence before we sign on to every new proposed care model. Otherwise, we cling on to the status quo and therefore, decision makers tend to leave us out. More important, value-based payment models have not thus far led to reduction in the cost of health care. Despite poor engagement scores at major health systems, physicians are “managed” and sidelined, and mandates are “done to them, not with them.”
In my 40-year career, our devaluation has been a slow and painful process. It started with being called a “provider.” This devalues me. Call me by what I am and do. Physician. Doctor. That is what our patients call us. But, we have been pushed to acquiesce. So, why do physicians undervalue themselves and are unable to be confident of their value to employers and hospital executives?
Some have theorized that physicians have low self-esteem and that denial and rationalization are simply defense mechanisms. The low self-esteem is traced back to medical student days and considered “posttraumatic” disorder. In one study of 189 medical students, 50% reported a decrease in their self-esteem/confidence. The students blamed their residents and attendings for this reaction. Some degree of intimidation may continue into training and employment where it may be part of the culture. We need to change this cycle and treat our students, residents, and mentees with respect as future peers.
Another aspect is related to our own well-being. Most physicians value their patient’s health more than their own. That concept is drilled into us throughout our life. Our spouses complain that we care more about our patients than we do for our families. We often ignore warning signs of serious issues in our own health, always downplaying textbook symptoms of burnout, depression, and even MI. Being too busy is a badge of honor to indicate how successful and wanted we are. This also needs to change.
Sheryl Sandberg in her book “Lean in” discusses the “tiara syndrome,” mainly referring to women. I would suggest that this applies to a lot of physicians, both men and women. Physicians tend to keep their heads down, work hard, and expect someone to come compliment them and place a “tiara” over their head. We may be wary of being called “self-promoters.” Sometimes it is cultural baggage for immigrant physicians who are taught to not brag about their accomplishments. It may behoove us to judiciously make peers and leadership aware of our positive activities in and outside the health system.
Some see physicians not as “pillars of any community,” but as “technicians on an assembly line” or “pawns in a money-making game for hospital administrators.” This degree of pessimism among physicians in surveys is well known but there is good news.
In a 2016 survey based upon responses by 17,236 physicians, 63% were pessimistic or very pessimistic about the medical profession, down from 77% in 2012.2 In another poll, medical doctors were rated as having very high or high ratings of honesty and ethical standards by 65%, higher than all except nurses, military officers, and grade school teachers.3 When the health care debate was at its peak in 2009, a public poll on who they trusted to recommend the right thing for reforming the healthcare system placed physicians at the very top (73%)ahead of health care professors, researchers, hospitals, the President, and politicians. Gallup surveyed 7,000 physicians about engagement in four hierarchical levels: Confidence, Integrity, Pride and Passion. Physicians scored highly on the Pride items in the survey (feel proud to work and being treated with respect).4 In other words, if we are treated well, we feel proud to tell others where we work.
Finally, like many I may consider myself an expert in all sorts of things not relevant to practicing medicine. Yet, I respectfully suggest we stay away from political hot potatoes like nuclear disarmament, gun control, climate change, immigration, and other controversial issues because they distract us from our primary mission. I would hate to see us viewed like Hollywood.
References
1. www.chicagotribune.com/business/ct-payscale-ego-survey-0830-biz-20160829-story.html
2. www.medpagetoday.com/primarycare/generalprimarycare/60446
3. https://nurse.org/articles/gallup-ethical-standards-poll-nurses-rank-highest/
4.https://news.gallup.com/poll/120890/healthcare-americans-trust-physicians-politicians.aspx
Bhagwan Satiani, MD, MBA, is professor of clinical surgery in the division of vascular diseases and surgery at Ohio State University, Columbus. He blogs at www.savvy-medicine.com . Reach him on Twitter @savvycutter.
Knee and elbow rejuvenation
The cosmetic industry improves techniques for tightening faces, hands, necks, and decolletes; meanwhile, sagging elbows and knees, once ignored, also are a visible sign of aging. Modifying techniques commonly used for the face and neck can yield significant improvements in the elbows and knees. The elbows and knees naturally have looser skin to allow for joint movement; over time, the skin over these joints is exposed to sun damage, friction, and recurrent extension and flexion, which cause skin laxity and aging.
A combination approach addressing skin texture, collagen damage, rhytides, and fat deposition is the most effective method for knee and elbow rejuvenation.
For knees and elbows with loose skin and rhytides, in-office noninvasive and minimally invasive radio-frequency and light energy treatments are helpful in increasing collagen production and tissue tightening. Similarly, microfocused ultrasound has been shown to be a safe and effective skin tightening treatment for the knees. In comparison to the face, however, the skin around the elbows and knees can be thinner and has fewer sebaceous glands. Caution should be used particularly with minimally invasive radio-frequency techniques in order to protect the epidermal skin. Often, treatments have to be repeated to give optimal results, which are not apparent until 3-6 months after the initial procedure.
For knee skin with severe laxity, a comprehensive approach using polydioxanone (PDO) or poly-l-lactic acid (PLLA) threads in both the upper thighs and circumferentially around the knees provides collagen production and tightening of the loose skin. Treatment of the upper thighs is essential in providing a vector that lifts the skin of the knees. Treatments can be repeated, with results seen after 90 days. Thread lifts of the knees and thighs are highly effective, noninvasive procedures with little to no downtime and can be used for severe skin laxity, wrinkling, and thinning of the knee skin.
Loose, roughened knee and elbow skin can also be treated with nonablative factional resurfacing, radio-frequency microneedling, or a series of monthly treatments with PLLA and hyaluronic acid fillers injected in the superficial to mid-dermis. Both fractional resurfacing and dermal filler injections help stimulate collagen production and improve both fine rhytides and dermatoheliosis.
Adipose tissue around the knees can be treated with monthly deoxycholic acid injections (for a video of this procedure, go to https://drive.google.com/file/d/1rhw-nESy15AoDhKUrc25DDjKEun7RL4i/view). The volume of injection, however, is significantly higher than that recommended in the submental area. Two to four times the volume is needed per knee over a series of 3-6 treatments, depending on the amount of fat in the knees.
Cryolipolysis is also an effective option for fat pockets around the knees; however, in my experience, it can be difficult to fit the applicators onto the area of concern appropriately unless smaller applicators are applied.
With the increasing demand for body rejuvenation techniques, providers are adapting techniques used for the face and neck to lift, tighten, thin, and sculpt the knees and elbows. A combination approach using lasers, ultrasound, fillers, threads, and cryolipolysis can be effective for these areas. Results are obtainable when repeat treatments are performed; however, one must be patient because results are not seen for 6 months or more.
Dr. Lily Talakoub and Dr. Naissan Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Macedo O. et al. J Am Acad Dermatol. 2014;70(Suppl 1), Abstract P800, page AB193.
The cosmetic industry improves techniques for tightening faces, hands, necks, and decolletes; meanwhile, sagging elbows and knees, once ignored, also are a visible sign of aging. Modifying techniques commonly used for the face and neck can yield significant improvements in the elbows and knees. The elbows and knees naturally have looser skin to allow for joint movement; over time, the skin over these joints is exposed to sun damage, friction, and recurrent extension and flexion, which cause skin laxity and aging.
A combination approach addressing skin texture, collagen damage, rhytides, and fat deposition is the most effective method for knee and elbow rejuvenation.
For knees and elbows with loose skin and rhytides, in-office noninvasive and minimally invasive radio-frequency and light energy treatments are helpful in increasing collagen production and tissue tightening. Similarly, microfocused ultrasound has been shown to be a safe and effective skin tightening treatment for the knees. In comparison to the face, however, the skin around the elbows and knees can be thinner and has fewer sebaceous glands. Caution should be used particularly with minimally invasive radio-frequency techniques in order to protect the epidermal skin. Often, treatments have to be repeated to give optimal results, which are not apparent until 3-6 months after the initial procedure.
For knee skin with severe laxity, a comprehensive approach using polydioxanone (PDO) or poly-l-lactic acid (PLLA) threads in both the upper thighs and circumferentially around the knees provides collagen production and tightening of the loose skin. Treatment of the upper thighs is essential in providing a vector that lifts the skin of the knees. Treatments can be repeated, with results seen after 90 days. Thread lifts of the knees and thighs are highly effective, noninvasive procedures with little to no downtime and can be used for severe skin laxity, wrinkling, and thinning of the knee skin.
Loose, roughened knee and elbow skin can also be treated with nonablative factional resurfacing, radio-frequency microneedling, or a series of monthly treatments with PLLA and hyaluronic acid fillers injected in the superficial to mid-dermis. Both fractional resurfacing and dermal filler injections help stimulate collagen production and improve both fine rhytides and dermatoheliosis.
Adipose tissue around the knees can be treated with monthly deoxycholic acid injections (for a video of this procedure, go to https://drive.google.com/file/d/1rhw-nESy15AoDhKUrc25DDjKEun7RL4i/view). The volume of injection, however, is significantly higher than that recommended in the submental area. Two to four times the volume is needed per knee over a series of 3-6 treatments, depending on the amount of fat in the knees.
Cryolipolysis is also an effective option for fat pockets around the knees; however, in my experience, it can be difficult to fit the applicators onto the area of concern appropriately unless smaller applicators are applied.
With the increasing demand for body rejuvenation techniques, providers are adapting techniques used for the face and neck to lift, tighten, thin, and sculpt the knees and elbows. A combination approach using lasers, ultrasound, fillers, threads, and cryolipolysis can be effective for these areas. Results are obtainable when repeat treatments are performed; however, one must be patient because results are not seen for 6 months or more.
Dr. Lily Talakoub and Dr. Naissan Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Macedo O. et al. J Am Acad Dermatol. 2014;70(Suppl 1), Abstract P800, page AB193.
The cosmetic industry improves techniques for tightening faces, hands, necks, and decolletes; meanwhile, sagging elbows and knees, once ignored, also are a visible sign of aging. Modifying techniques commonly used for the face and neck can yield significant improvements in the elbows and knees. The elbows and knees naturally have looser skin to allow for joint movement; over time, the skin over these joints is exposed to sun damage, friction, and recurrent extension and flexion, which cause skin laxity and aging.
A combination approach addressing skin texture, collagen damage, rhytides, and fat deposition is the most effective method for knee and elbow rejuvenation.
For knees and elbows with loose skin and rhytides, in-office noninvasive and minimally invasive radio-frequency and light energy treatments are helpful in increasing collagen production and tissue tightening. Similarly, microfocused ultrasound has been shown to be a safe and effective skin tightening treatment for the knees. In comparison to the face, however, the skin around the elbows and knees can be thinner and has fewer sebaceous glands. Caution should be used particularly with minimally invasive radio-frequency techniques in order to protect the epidermal skin. Often, treatments have to be repeated to give optimal results, which are not apparent until 3-6 months after the initial procedure.
For knee skin with severe laxity, a comprehensive approach using polydioxanone (PDO) or poly-l-lactic acid (PLLA) threads in both the upper thighs and circumferentially around the knees provides collagen production and tightening of the loose skin. Treatment of the upper thighs is essential in providing a vector that lifts the skin of the knees. Treatments can be repeated, with results seen after 90 days. Thread lifts of the knees and thighs are highly effective, noninvasive procedures with little to no downtime and can be used for severe skin laxity, wrinkling, and thinning of the knee skin.
Loose, roughened knee and elbow skin can also be treated with nonablative factional resurfacing, radio-frequency microneedling, or a series of monthly treatments with PLLA and hyaluronic acid fillers injected in the superficial to mid-dermis. Both fractional resurfacing and dermal filler injections help stimulate collagen production and improve both fine rhytides and dermatoheliosis.
Adipose tissue around the knees can be treated with monthly deoxycholic acid injections (for a video of this procedure, go to https://drive.google.com/file/d/1rhw-nESy15AoDhKUrc25DDjKEun7RL4i/view). The volume of injection, however, is significantly higher than that recommended in the submental area. Two to four times the volume is needed per knee over a series of 3-6 treatments, depending on the amount of fat in the knees.
Cryolipolysis is also an effective option for fat pockets around the knees; however, in my experience, it can be difficult to fit the applicators onto the area of concern appropriately unless smaller applicators are applied.
With the increasing demand for body rejuvenation techniques, providers are adapting techniques used for the face and neck to lift, tighten, thin, and sculpt the knees and elbows. A combination approach using lasers, ultrasound, fillers, threads, and cryolipolysis can be effective for these areas. Results are obtainable when repeat treatments are performed; however, one must be patient because results are not seen for 6 months or more.
Dr. Lily Talakoub and Dr. Naissan Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
Macedo O. et al. J Am Acad Dermatol. 2014;70(Suppl 1), Abstract P800, page AB193.
Report criticizes VA’s suicide prevention efforts; author shares depression-fighting strategies
The suicide rate among veterans is almost double that of the general American population. It has been rising among those who served in the wars in Iraq and Afghanistan.
Rep. Tim Walz, the Minnesota Democrat who requested the investigation, reportedly said in a statement. “Unfortunately, VA failed to do that.”
Mr. Walz was referring to a failure in prevention efforts that was detailed in a Government Accountability Office report released recently and was the subject of an article in the New York Times. The report blames bureaucratic confusion and an absence of leadership – epitomized by several department vacancies.
“This is such an important issue; we need to be throwing everything we can at it,” said Caitin Thompson, PhD. She was director of the VA’s suicide prevention efforts but resigned in frustration in mid-2017. “It’s so ludicrous that money would be sitting on the table. Outreach is one of the first ways to engage with veterans and families about ways to get help. If we don’t have that, what do we have?”
Surviving the holidays with depression
The postcard image of the Christmas season is that of joyous celebration with family and friends. For many people, however, this image is false. Many complain about feelings of stress imposed by familial obligations, pressure to conform to those postcard myths, and the financial toll that all of that holiday largesse can exact.
Now add depression to this mix. How can those burdened by depression find some joy at this time of year? In a recent article in the Huffington Post, author Andrea Loewen advises staying away from social media and focusing on the positive.
“[Social media] is a double-edged sword: Either I see all the amazing things everyone else is doing and feel jealous/insignificant/left out, or I see that no one else is really posting and assume they must be too busy having incredible quality time with their families while I’m the unengaged loser scrolling Instagram,” Ms. Loewen wrote. “Either way, it’s bad news.”
One concrete practice that she engages in is taking a few minutes to think about and write down the positive things that happened each day.
“The list includes everything, big and small: from the thoughtful gift I wasn’t expecting to the simple observation that a friend seemed happy to see me,” Ms. Loewen wrote. “Depending on where I’m at in my depression, those seemingly tiny details can be vital reminders I hold a valuable place in the world.”
Artist perpetuates persistent myth
In some ways, Kanye West embraces his diagnosis of bipolar disorder. He calls the illness his “superpower,” and the art on his new album, “Ye,” includes the phrase: “I hate being Bi-Polar/it’s awesome.” But his decision to abandon his medications promotes a myth, Amanda Mull wrote in an opinion piece in the Atlantic.
“In apparently quitting his psychiatric medication for the sake of his creativity, Mr. West is promoting one of mental health’s most persistent and dangerous myths: that suffering is necessary for great art,” Ms. Mull wrote.
Philip R. Muskin, MD, who is affiliated with the department of psychiatry at Columbia University in New York, agreed that linking mental turmoil with creative genius is indeed problematic. “Creative people are not creative when they’re depressed, or so manic that no one can tolerate being with them and they start to merge into psychosis, or when they’re filled with numbing anxiety,” he said in the Atlantic article.
Esmé Weijun Wang concurred and offered a counterview to that of Mr. West. A novelist who has written about living with schizoaffective disorder, she said: “It may be true that mental illness has given me insights with which to work, creatively speaking, but it’s also made me too sick to use that creativity. The voice in my head that says, ‘Die, die, die’ is not a voice that encourages putting together a short story.”
For his part, Mr. West’s decision to stop taking his medicine threatens to undermine his own mental health. And his public musings could drive others away from treatment.
“Antiopioid backlash” causes pain
An article by Fox News has highlighted the daily toll that opioid addiction is exacting on Americans. Government efforts aimed at quelling the use of opioids by targeting availability have had the unintended consequence of the cut-off of prescriptions by many physicians. With that route turned off, many people are turning to other sources for pain relief – or are being left with no relief.
One person in the article related how his wife is unable to obtain pain relief for her neurologic and spinal diseases. “A welcome death has become a discussion,” he said.
Meanwhile, a 69-year-old veteran said the Department of Veterans Affairs ended his pain medication. “I now buy heroin on the street.”
Another person in the article, Herb Erne III, wrote: “As a nurse, I have seen addicts and the other end of opioid abuse. But there is another side to this crisis that people are not talking about, those that actually need pain medications but cannot get them because of the ‘fear factor’ of running afoul of the antiopioid – including legal ones taken safely under medical supervision – backlash.
“The chronically ill who do not abuse, who do not divert, have become the unintended victims of misguided and overzealous efforts by policy- and regulation-making bodies in the government,” he said.
Grandparents filling void
An article in the Detroit News reported on more carnage of the opioid crisis. In Michigan and elsewhere nationwide, increasing numbers of parents with opioid addiction are unable to safely care for their children or have died because of an overdose. Grandparents are stepping in to assume care.
Results of a national survey involving more than 1,000 grandparents found that 20% are the daily caregivers to their grandchildren. They can be on their own, without any financial aid from state or national programs. Other children without grandparents can be diverted to foster care.
It’s a role few grandparents anticipated. “Our system as a whole is messed up. It tears at my heart,” 47-year-old Christina Wasilewski said in the article. “Everyone keeps saying children are resilient, but only to a point.”
Ms. Wasilewski and her husband assumed care for their granddaughter when they discovered her in physical distress from lack of care.
In Michigan, the increase in the rate of opioid-related deaths slowed in 2017 but deaths still rose 9% from 2016 , according to the Michigan Department of Health & Human Services. The prior year the death rate was 35%. In Michigan, grandparents raising their grandchildren do not have legal parental rights for this care, including the right to seek medical care and to pursue educational options.
Ms. Wasilewski’s concern about these trends led her to launch the Caregiver Cafe, a support group for grandparents raising their grandchildren.
The suicide rate among veterans is almost double that of the general American population. It has been rising among those who served in the wars in Iraq and Afghanistan.
Rep. Tim Walz, the Minnesota Democrat who requested the investigation, reportedly said in a statement. “Unfortunately, VA failed to do that.”
Mr. Walz was referring to a failure in prevention efforts that was detailed in a Government Accountability Office report released recently and was the subject of an article in the New York Times. The report blames bureaucratic confusion and an absence of leadership – epitomized by several department vacancies.
“This is such an important issue; we need to be throwing everything we can at it,” said Caitin Thompson, PhD. She was director of the VA’s suicide prevention efforts but resigned in frustration in mid-2017. “It’s so ludicrous that money would be sitting on the table. Outreach is one of the first ways to engage with veterans and families about ways to get help. If we don’t have that, what do we have?”
Surviving the holidays with depression
The postcard image of the Christmas season is that of joyous celebration with family and friends. For many people, however, this image is false. Many complain about feelings of stress imposed by familial obligations, pressure to conform to those postcard myths, and the financial toll that all of that holiday largesse can exact.
Now add depression to this mix. How can those burdened by depression find some joy at this time of year? In a recent article in the Huffington Post, author Andrea Loewen advises staying away from social media and focusing on the positive.
“[Social media] is a double-edged sword: Either I see all the amazing things everyone else is doing and feel jealous/insignificant/left out, or I see that no one else is really posting and assume they must be too busy having incredible quality time with their families while I’m the unengaged loser scrolling Instagram,” Ms. Loewen wrote. “Either way, it’s bad news.”
One concrete practice that she engages in is taking a few minutes to think about and write down the positive things that happened each day.
“The list includes everything, big and small: from the thoughtful gift I wasn’t expecting to the simple observation that a friend seemed happy to see me,” Ms. Loewen wrote. “Depending on where I’m at in my depression, those seemingly tiny details can be vital reminders I hold a valuable place in the world.”
Artist perpetuates persistent myth
In some ways, Kanye West embraces his diagnosis of bipolar disorder. He calls the illness his “superpower,” and the art on his new album, “Ye,” includes the phrase: “I hate being Bi-Polar/it’s awesome.” But his decision to abandon his medications promotes a myth, Amanda Mull wrote in an opinion piece in the Atlantic.
“In apparently quitting his psychiatric medication for the sake of his creativity, Mr. West is promoting one of mental health’s most persistent and dangerous myths: that suffering is necessary for great art,” Ms. Mull wrote.
Philip R. Muskin, MD, who is affiliated with the department of psychiatry at Columbia University in New York, agreed that linking mental turmoil with creative genius is indeed problematic. “Creative people are not creative when they’re depressed, or so manic that no one can tolerate being with them and they start to merge into psychosis, or when they’re filled with numbing anxiety,” he said in the Atlantic article.
Esmé Weijun Wang concurred and offered a counterview to that of Mr. West. A novelist who has written about living with schizoaffective disorder, she said: “It may be true that mental illness has given me insights with which to work, creatively speaking, but it’s also made me too sick to use that creativity. The voice in my head that says, ‘Die, die, die’ is not a voice that encourages putting together a short story.”
For his part, Mr. West’s decision to stop taking his medicine threatens to undermine his own mental health. And his public musings could drive others away from treatment.
“Antiopioid backlash” causes pain
An article by Fox News has highlighted the daily toll that opioid addiction is exacting on Americans. Government efforts aimed at quelling the use of opioids by targeting availability have had the unintended consequence of the cut-off of prescriptions by many physicians. With that route turned off, many people are turning to other sources for pain relief – or are being left with no relief.
One person in the article related how his wife is unable to obtain pain relief for her neurologic and spinal diseases. “A welcome death has become a discussion,” he said.
Meanwhile, a 69-year-old veteran said the Department of Veterans Affairs ended his pain medication. “I now buy heroin on the street.”
Another person in the article, Herb Erne III, wrote: “As a nurse, I have seen addicts and the other end of opioid abuse. But there is another side to this crisis that people are not talking about, those that actually need pain medications but cannot get them because of the ‘fear factor’ of running afoul of the antiopioid – including legal ones taken safely under medical supervision – backlash.
“The chronically ill who do not abuse, who do not divert, have become the unintended victims of misguided and overzealous efforts by policy- and regulation-making bodies in the government,” he said.
Grandparents filling void
An article in the Detroit News reported on more carnage of the opioid crisis. In Michigan and elsewhere nationwide, increasing numbers of parents with opioid addiction are unable to safely care for their children or have died because of an overdose. Grandparents are stepping in to assume care.
Results of a national survey involving more than 1,000 grandparents found that 20% are the daily caregivers to their grandchildren. They can be on their own, without any financial aid from state or national programs. Other children without grandparents can be diverted to foster care.
It’s a role few grandparents anticipated. “Our system as a whole is messed up. It tears at my heart,” 47-year-old Christina Wasilewski said in the article. “Everyone keeps saying children are resilient, but only to a point.”
Ms. Wasilewski and her husband assumed care for their granddaughter when they discovered her in physical distress from lack of care.
In Michigan, the increase in the rate of opioid-related deaths slowed in 2017 but deaths still rose 9% from 2016 , according to the Michigan Department of Health & Human Services. The prior year the death rate was 35%. In Michigan, grandparents raising their grandchildren do not have legal parental rights for this care, including the right to seek medical care and to pursue educational options.
Ms. Wasilewski’s concern about these trends led her to launch the Caregiver Cafe, a support group for grandparents raising their grandchildren.
The suicide rate among veterans is almost double that of the general American population. It has been rising among those who served in the wars in Iraq and Afghanistan.
Rep. Tim Walz, the Minnesota Democrat who requested the investigation, reportedly said in a statement. “Unfortunately, VA failed to do that.”
Mr. Walz was referring to a failure in prevention efforts that was detailed in a Government Accountability Office report released recently and was the subject of an article in the New York Times. The report blames bureaucratic confusion and an absence of leadership – epitomized by several department vacancies.
“This is such an important issue; we need to be throwing everything we can at it,” said Caitin Thompson, PhD. She was director of the VA’s suicide prevention efforts but resigned in frustration in mid-2017. “It’s so ludicrous that money would be sitting on the table. Outreach is one of the first ways to engage with veterans and families about ways to get help. If we don’t have that, what do we have?”
Surviving the holidays with depression
The postcard image of the Christmas season is that of joyous celebration with family and friends. For many people, however, this image is false. Many complain about feelings of stress imposed by familial obligations, pressure to conform to those postcard myths, and the financial toll that all of that holiday largesse can exact.
Now add depression to this mix. How can those burdened by depression find some joy at this time of year? In a recent article in the Huffington Post, author Andrea Loewen advises staying away from social media and focusing on the positive.
“[Social media] is a double-edged sword: Either I see all the amazing things everyone else is doing and feel jealous/insignificant/left out, or I see that no one else is really posting and assume they must be too busy having incredible quality time with their families while I’m the unengaged loser scrolling Instagram,” Ms. Loewen wrote. “Either way, it’s bad news.”
One concrete practice that she engages in is taking a few minutes to think about and write down the positive things that happened each day.
“The list includes everything, big and small: from the thoughtful gift I wasn’t expecting to the simple observation that a friend seemed happy to see me,” Ms. Loewen wrote. “Depending on where I’m at in my depression, those seemingly tiny details can be vital reminders I hold a valuable place in the world.”
Artist perpetuates persistent myth
In some ways, Kanye West embraces his diagnosis of bipolar disorder. He calls the illness his “superpower,” and the art on his new album, “Ye,” includes the phrase: “I hate being Bi-Polar/it’s awesome.” But his decision to abandon his medications promotes a myth, Amanda Mull wrote in an opinion piece in the Atlantic.
“In apparently quitting his psychiatric medication for the sake of his creativity, Mr. West is promoting one of mental health’s most persistent and dangerous myths: that suffering is necessary for great art,” Ms. Mull wrote.
Philip R. Muskin, MD, who is affiliated with the department of psychiatry at Columbia University in New York, agreed that linking mental turmoil with creative genius is indeed problematic. “Creative people are not creative when they’re depressed, or so manic that no one can tolerate being with them and they start to merge into psychosis, or when they’re filled with numbing anxiety,” he said in the Atlantic article.
Esmé Weijun Wang concurred and offered a counterview to that of Mr. West. A novelist who has written about living with schizoaffective disorder, she said: “It may be true that mental illness has given me insights with which to work, creatively speaking, but it’s also made me too sick to use that creativity. The voice in my head that says, ‘Die, die, die’ is not a voice that encourages putting together a short story.”
For his part, Mr. West’s decision to stop taking his medicine threatens to undermine his own mental health. And his public musings could drive others away from treatment.
“Antiopioid backlash” causes pain
An article by Fox News has highlighted the daily toll that opioid addiction is exacting on Americans. Government efforts aimed at quelling the use of opioids by targeting availability have had the unintended consequence of the cut-off of prescriptions by many physicians. With that route turned off, many people are turning to other sources for pain relief – or are being left with no relief.
One person in the article related how his wife is unable to obtain pain relief for her neurologic and spinal diseases. “A welcome death has become a discussion,” he said.
Meanwhile, a 69-year-old veteran said the Department of Veterans Affairs ended his pain medication. “I now buy heroin on the street.”
Another person in the article, Herb Erne III, wrote: “As a nurse, I have seen addicts and the other end of opioid abuse. But there is another side to this crisis that people are not talking about, those that actually need pain medications but cannot get them because of the ‘fear factor’ of running afoul of the antiopioid – including legal ones taken safely under medical supervision – backlash.
“The chronically ill who do not abuse, who do not divert, have become the unintended victims of misguided and overzealous efforts by policy- and regulation-making bodies in the government,” he said.
Grandparents filling void
An article in the Detroit News reported on more carnage of the opioid crisis. In Michigan and elsewhere nationwide, increasing numbers of parents with opioid addiction are unable to safely care for their children or have died because of an overdose. Grandparents are stepping in to assume care.
Results of a national survey involving more than 1,000 grandparents found that 20% are the daily caregivers to their grandchildren. They can be on their own, without any financial aid from state or national programs. Other children without grandparents can be diverted to foster care.
It’s a role few grandparents anticipated. “Our system as a whole is messed up. It tears at my heart,” 47-year-old Christina Wasilewski said in the article. “Everyone keeps saying children are resilient, but only to a point.”
Ms. Wasilewski and her husband assumed care for their granddaughter when they discovered her in physical distress from lack of care.
In Michigan, the increase in the rate of opioid-related deaths slowed in 2017 but deaths still rose 9% from 2016 , according to the Michigan Department of Health & Human Services. The prior year the death rate was 35%. In Michigan, grandparents raising their grandchildren do not have legal parental rights for this care, including the right to seek medical care and to pursue educational options.
Ms. Wasilewski’s concern about these trends led her to launch the Caregiver Cafe, a support group for grandparents raising their grandchildren.
Michigan police receive training to recognize mental illness
Responding to a police call can prove dangerous. In those kinds of high-pressure situations, agitation or other manifestations of mental illness might be mistaken for violent intent – with disastrous results.
In Kalamazoo, Mich., crime response training now includes subduing suspects without using violent force. “Through training and education, and scenarios that we use in the training, [the officers] start to detect the different cues or indicators where they start to see that this is really a crisis event. And we treat it as a medical issue and get that person the help that they need,” said Rafael Diaz, executive lieutenant with the Kalamazoo Department of Public Safety in an interview on Michigan NPR.
In the training, called the Crisis Intervention Team model, the goal is to slow down the pace of the interaction and keep some distance between themselves and the suspect after officers recognize signs of mental illness. Both responses can lower the chances of a lash-out response.
“The number of injuries to officers goes down, the number of injuries to the person in crisis goes down, and there is a huge benefit to society there if you don’t have to use physical force,” Mr. Diaz said.
Animal neglect and mental health
Images of neglected and abused livestock on farms can inspire thoughts of how someone could mistreat the animals in their care. “Frankly, if you can’t understand that, it’s probably a good thing. It means you haven’t been in the depths of low, low mental health, depression, and anxiety,” Andria Jones-Bitton, DVM, PhD, said in an interview with the Western Producer.
Dr. Jones-Bitton is a veterinarian and epidemiologist at the Ontario Veterinary College in Guelph. She is studying the mental health and mental resilience of farmers and veterinarians.
“If farmers are struggling with their own well-being and motivation, they’re likely going to find it difficult to invest in improving animal welfare. When we’re mentally unwell, it’s hard to care for ourselves, let alone to care for others, even when those others are really important to us,” she said.
A national survey of Canadian farmers by Dr. Jones-Bitton showed high levels of stress and diminished ability to cope with the pressures that come with running a livestock farm. “What makes me the most upset is I have everything I’ve ever dreamed of – love, family, and a farm, and all I feel is overwhelmed out of control and sad,” one respondent said.
The problems are not unique to Canada. Studies from Ireland, for example, documented an association between animal neglect cases and the mental health, drug/alcohol addiction, and social problems of farmers.
“Even if you didn’t care about the humans that were struggling and you only cared about the animal welfare, you’d be wise to address the issue of farmer stress,” Dr. Jones-Britton said.
Depression and rural America
A recent “Farming in Tough Times” workshop that convened in Minnesota focused on the mental health of farmers. Making a living is challenging for many reasons. One is that prices for commodities are set by others.
“I realized that I can’t change the situation that we’re in. I can’t change milk prices. I can’t stop farms from going bankrupt. But I can change how we are. And we are together, and that really does matter,” said dairy farmer Brenda Rudolph during the workshop, according to a report from the St. Cloud Times, which is part of the USA Today network.
“There is a conversation you people have to have in America, rural America, that says, depression is part of your life. It is not a sign of weakness. It’s a sign of reality,” said Dennis Hoiberg, a farming consultant based in Australia who spoke at the workshop. He added that, from his perspective, the United States still tends to be more repressed about mental health issues than elsewhere in the world – with the focus on stress and not on resiliency.
“Most of you folk are proud folk, and most you folk are very proud of what you do,” Mr. Hoiberg said. “You’re also psychologically exposed because you are a true believer [in what you do].”
Advice offered to lessen the tough times included noticing the beauty in the world, breaking down problems into small chunks that are more easily dealt with and then moving on to the next, sleep, and a good diet.
People with mental illness languishing
Public defenders in Colorado are seeking to have dozens of people diagnosed with mental illness who are in jail awaiting trial set free until their court date. The usual scenario in Colorado for someone charged with a crime and jailed who is deemed mentally incompetent is treatment within 28 days. However, this system is broken and wait times are far longer – in one instance 270 days.
“Many of them are there for very, very low level offenses and they’re holding in jail for way longer than a person who did not suffer from mental illness would be in custody,” said Maureen Cain, policy liaison for the public defender’s office in an interview with the Denver Post. “They are being incarcerated for their mental illness, not really because of the crime they committed.” Responses from judges have ranged from immediate release to finding the incarcerated person guilty of contempt and sending them back to jail.
The Colorado Department of Human Services is in charge of people who have been jailed but have been found to be incompetent to stand trial. Officials there have say they do not have enough bed space or capacity to get people moved out of jail within 28 days.
“We are in a situation where [the human services department] is in breach, and I need to know what efforts are being made to bring it back into compliance,” said federal Judge Nina Y. Wang. “These individuals are not being served, and frankly, the state is not being served.”
“Cruel” practice confined youth
A federal class action lawsuit filed against the Departmental of Children and Family Services (DCFS) in the Chicago area alleges that, from 2015 to 2017, more than 800 youth were being confined to psychiatric hospitals even when they were cleared for discharge. The problem goes back decades and is getting worse, the lawsuit contends.
“I spent Thanksgiving, Christmas, New Year’s, Easter, and my 16th birthday in the hospital,” said Skylar, who’s now 19 years old. “I only got to go outside one time. I felt like a prisoner; I felt very depressed.”
As reported on Chicago’s WGN9 News, the delay between clearance for discharge and actual freedom is a month or more in many of the cases. Acting Cook County Public Guardian Charles Golbert said the practice is “cruel, unusual, and illegal. It’s a violation of the children’s civil and most basic human rights.”
Many of the youth had been incarcerated for setting fires and self-harm and had been rejected by foster parents and other providers, in some cases their own families, who were concerned with the possible behavior of the youth after their release.
“Blame the children is the wrong response from DCFS,” said attorney Russell Ainsworth. “DCFS should be apologizing for not addressing this issue and for violating the Constitution.”
Responding to a police call can prove dangerous. In those kinds of high-pressure situations, agitation or other manifestations of mental illness might be mistaken for violent intent – with disastrous results.
In Kalamazoo, Mich., crime response training now includes subduing suspects without using violent force. “Through training and education, and scenarios that we use in the training, [the officers] start to detect the different cues or indicators where they start to see that this is really a crisis event. And we treat it as a medical issue and get that person the help that they need,” said Rafael Diaz, executive lieutenant with the Kalamazoo Department of Public Safety in an interview on Michigan NPR.
In the training, called the Crisis Intervention Team model, the goal is to slow down the pace of the interaction and keep some distance between themselves and the suspect after officers recognize signs of mental illness. Both responses can lower the chances of a lash-out response.
“The number of injuries to officers goes down, the number of injuries to the person in crisis goes down, and there is a huge benefit to society there if you don’t have to use physical force,” Mr. Diaz said.
Animal neglect and mental health
Images of neglected and abused livestock on farms can inspire thoughts of how someone could mistreat the animals in their care. “Frankly, if you can’t understand that, it’s probably a good thing. It means you haven’t been in the depths of low, low mental health, depression, and anxiety,” Andria Jones-Bitton, DVM, PhD, said in an interview with the Western Producer.
Dr. Jones-Bitton is a veterinarian and epidemiologist at the Ontario Veterinary College in Guelph. She is studying the mental health and mental resilience of farmers and veterinarians.
“If farmers are struggling with their own well-being and motivation, they’re likely going to find it difficult to invest in improving animal welfare. When we’re mentally unwell, it’s hard to care for ourselves, let alone to care for others, even when those others are really important to us,” she said.
A national survey of Canadian farmers by Dr. Jones-Bitton showed high levels of stress and diminished ability to cope with the pressures that come with running a livestock farm. “What makes me the most upset is I have everything I’ve ever dreamed of – love, family, and a farm, and all I feel is overwhelmed out of control and sad,” one respondent said.
The problems are not unique to Canada. Studies from Ireland, for example, documented an association between animal neglect cases and the mental health, drug/alcohol addiction, and social problems of farmers.
“Even if you didn’t care about the humans that were struggling and you only cared about the animal welfare, you’d be wise to address the issue of farmer stress,” Dr. Jones-Britton said.
Depression and rural America
A recent “Farming in Tough Times” workshop that convened in Minnesota focused on the mental health of farmers. Making a living is challenging for many reasons. One is that prices for commodities are set by others.
“I realized that I can’t change the situation that we’re in. I can’t change milk prices. I can’t stop farms from going bankrupt. But I can change how we are. And we are together, and that really does matter,” said dairy farmer Brenda Rudolph during the workshop, according to a report from the St. Cloud Times, which is part of the USA Today network.
“There is a conversation you people have to have in America, rural America, that says, depression is part of your life. It is not a sign of weakness. It’s a sign of reality,” said Dennis Hoiberg, a farming consultant based in Australia who spoke at the workshop. He added that, from his perspective, the United States still tends to be more repressed about mental health issues than elsewhere in the world – with the focus on stress and not on resiliency.
“Most of you folk are proud folk, and most you folk are very proud of what you do,” Mr. Hoiberg said. “You’re also psychologically exposed because you are a true believer [in what you do].”
Advice offered to lessen the tough times included noticing the beauty in the world, breaking down problems into small chunks that are more easily dealt with and then moving on to the next, sleep, and a good diet.
People with mental illness languishing
Public defenders in Colorado are seeking to have dozens of people diagnosed with mental illness who are in jail awaiting trial set free until their court date. The usual scenario in Colorado for someone charged with a crime and jailed who is deemed mentally incompetent is treatment within 28 days. However, this system is broken and wait times are far longer – in one instance 270 days.
“Many of them are there for very, very low level offenses and they’re holding in jail for way longer than a person who did not suffer from mental illness would be in custody,” said Maureen Cain, policy liaison for the public defender’s office in an interview with the Denver Post. “They are being incarcerated for their mental illness, not really because of the crime they committed.” Responses from judges have ranged from immediate release to finding the incarcerated person guilty of contempt and sending them back to jail.
The Colorado Department of Human Services is in charge of people who have been jailed but have been found to be incompetent to stand trial. Officials there have say they do not have enough bed space or capacity to get people moved out of jail within 28 days.
“We are in a situation where [the human services department] is in breach, and I need to know what efforts are being made to bring it back into compliance,” said federal Judge Nina Y. Wang. “These individuals are not being served, and frankly, the state is not being served.”
“Cruel” practice confined youth
A federal class action lawsuit filed against the Departmental of Children and Family Services (DCFS) in the Chicago area alleges that, from 2015 to 2017, more than 800 youth were being confined to psychiatric hospitals even when they were cleared for discharge. The problem goes back decades and is getting worse, the lawsuit contends.
“I spent Thanksgiving, Christmas, New Year’s, Easter, and my 16th birthday in the hospital,” said Skylar, who’s now 19 years old. “I only got to go outside one time. I felt like a prisoner; I felt very depressed.”
As reported on Chicago’s WGN9 News, the delay between clearance for discharge and actual freedom is a month or more in many of the cases. Acting Cook County Public Guardian Charles Golbert said the practice is “cruel, unusual, and illegal. It’s a violation of the children’s civil and most basic human rights.”
Many of the youth had been incarcerated for setting fires and self-harm and had been rejected by foster parents and other providers, in some cases their own families, who were concerned with the possible behavior of the youth after their release.
“Blame the children is the wrong response from DCFS,” said attorney Russell Ainsworth. “DCFS should be apologizing for not addressing this issue and for violating the Constitution.”
Responding to a police call can prove dangerous. In those kinds of high-pressure situations, agitation or other manifestations of mental illness might be mistaken for violent intent – with disastrous results.
In Kalamazoo, Mich., crime response training now includes subduing suspects without using violent force. “Through training and education, and scenarios that we use in the training, [the officers] start to detect the different cues or indicators where they start to see that this is really a crisis event. And we treat it as a medical issue and get that person the help that they need,” said Rafael Diaz, executive lieutenant with the Kalamazoo Department of Public Safety in an interview on Michigan NPR.
In the training, called the Crisis Intervention Team model, the goal is to slow down the pace of the interaction and keep some distance between themselves and the suspect after officers recognize signs of mental illness. Both responses can lower the chances of a lash-out response.
“The number of injuries to officers goes down, the number of injuries to the person in crisis goes down, and there is a huge benefit to society there if you don’t have to use physical force,” Mr. Diaz said.
Animal neglect and mental health
Images of neglected and abused livestock on farms can inspire thoughts of how someone could mistreat the animals in their care. “Frankly, if you can’t understand that, it’s probably a good thing. It means you haven’t been in the depths of low, low mental health, depression, and anxiety,” Andria Jones-Bitton, DVM, PhD, said in an interview with the Western Producer.
Dr. Jones-Bitton is a veterinarian and epidemiologist at the Ontario Veterinary College in Guelph. She is studying the mental health and mental resilience of farmers and veterinarians.
“If farmers are struggling with their own well-being and motivation, they’re likely going to find it difficult to invest in improving animal welfare. When we’re mentally unwell, it’s hard to care for ourselves, let alone to care for others, even when those others are really important to us,” she said.
A national survey of Canadian farmers by Dr. Jones-Bitton showed high levels of stress and diminished ability to cope with the pressures that come with running a livestock farm. “What makes me the most upset is I have everything I’ve ever dreamed of – love, family, and a farm, and all I feel is overwhelmed out of control and sad,” one respondent said.
The problems are not unique to Canada. Studies from Ireland, for example, documented an association between animal neglect cases and the mental health, drug/alcohol addiction, and social problems of farmers.
“Even if you didn’t care about the humans that were struggling and you only cared about the animal welfare, you’d be wise to address the issue of farmer stress,” Dr. Jones-Britton said.
Depression and rural America
A recent “Farming in Tough Times” workshop that convened in Minnesota focused on the mental health of farmers. Making a living is challenging for many reasons. One is that prices for commodities are set by others.
“I realized that I can’t change the situation that we’re in. I can’t change milk prices. I can’t stop farms from going bankrupt. But I can change how we are. And we are together, and that really does matter,” said dairy farmer Brenda Rudolph during the workshop, according to a report from the St. Cloud Times, which is part of the USA Today network.
“There is a conversation you people have to have in America, rural America, that says, depression is part of your life. It is not a sign of weakness. It’s a sign of reality,” said Dennis Hoiberg, a farming consultant based in Australia who spoke at the workshop. He added that, from his perspective, the United States still tends to be more repressed about mental health issues than elsewhere in the world – with the focus on stress and not on resiliency.
“Most of you folk are proud folk, and most you folk are very proud of what you do,” Mr. Hoiberg said. “You’re also psychologically exposed because you are a true believer [in what you do].”
Advice offered to lessen the tough times included noticing the beauty in the world, breaking down problems into small chunks that are more easily dealt with and then moving on to the next, sleep, and a good diet.
People with mental illness languishing
Public defenders in Colorado are seeking to have dozens of people diagnosed with mental illness who are in jail awaiting trial set free until their court date. The usual scenario in Colorado for someone charged with a crime and jailed who is deemed mentally incompetent is treatment within 28 days. However, this system is broken and wait times are far longer – in one instance 270 days.
“Many of them are there for very, very low level offenses and they’re holding in jail for way longer than a person who did not suffer from mental illness would be in custody,” said Maureen Cain, policy liaison for the public defender’s office in an interview with the Denver Post. “They are being incarcerated for their mental illness, not really because of the crime they committed.” Responses from judges have ranged from immediate release to finding the incarcerated person guilty of contempt and sending them back to jail.
The Colorado Department of Human Services is in charge of people who have been jailed but have been found to be incompetent to stand trial. Officials there have say they do not have enough bed space or capacity to get people moved out of jail within 28 days.
“We are in a situation where [the human services department] is in breach, and I need to know what efforts are being made to bring it back into compliance,” said federal Judge Nina Y. Wang. “These individuals are not being served, and frankly, the state is not being served.”
“Cruel” practice confined youth
A federal class action lawsuit filed against the Departmental of Children and Family Services (DCFS) in the Chicago area alleges that, from 2015 to 2017, more than 800 youth were being confined to psychiatric hospitals even when they were cleared for discharge. The problem goes back decades and is getting worse, the lawsuit contends.
“I spent Thanksgiving, Christmas, New Year’s, Easter, and my 16th birthday in the hospital,” said Skylar, who’s now 19 years old. “I only got to go outside one time. I felt like a prisoner; I felt very depressed.”
As reported on Chicago’s WGN9 News, the delay between clearance for discharge and actual freedom is a month or more in many of the cases. Acting Cook County Public Guardian Charles Golbert said the practice is “cruel, unusual, and illegal. It’s a violation of the children’s civil and most basic human rights.”
Many of the youth had been incarcerated for setting fires and self-harm and had been rejected by foster parents and other providers, in some cases their own families, who were concerned with the possible behavior of the youth after their release.
“Blame the children is the wrong response from DCFS,” said attorney Russell Ainsworth. “DCFS should be apologizing for not addressing this issue and for violating the Constitution.”
Hospital medicine fellowships
Is it the right choice for me?
As Dr. Melanie Schaffer neared the end of her family medicine residency in the spring of 2015, she found herself considering a hospital medicine fellowship. Unsure if she could get a hospitalist job in an urban market given the outpatient focus of her training, Dr. Schaffer began searching for fellowships on the Society of Hospital Medicine website.1
Likewise, in 2014 Dr. Micah Prochaska was seriously contemplating a hospital medicine fellowship. He was about to graduate from internal medicine residency at the University of Chicago and was eager to gain skills and experience in clinical research.
In 2006, there were a total of 16 HM fellowship programs in the United States, catering to graduates of internal medicine, family medicine, and pediatric residencies.2 Since that time, the number of hospital medicine fellowships has grown considerably, paralleling the explosive growth of hospital medicine as a specialty. For example, at one point in the summer of 2018, the SHM website listed 13 clinical family practice fellowships, 29 internal medicine fellowships, and 26 pediatric fellowships. Each fellowship emphasized different aspects of hospital medicine including clinical practice, research, quality improvement, and leadership.
Now more than ever, residents interested in hospital medicine may get overwhelmed by the multitude of options for fellowship training. And the question remains: why pursue fellowship training in the first place?
“I learned that as a family physician it is harder to get a job as a hospitalist outside of smaller communities, and I wanted to have extra training and credentials,” Dr. Schaffer said. “I pursued a fellowship in hospital medicine to hone my inpatient skills, obtain more ICU exposure, and work on procedures.”
Dr. Schaffer’s online search eventually led her to the Advanced Hospital Medicine Fellowship at Swedish Medical Center in Seattle. This 1-year hospital medicine fellowship started in 2008 with an intentional clinical focus, aiming to provide additional training opportunities in hospital medicine primarily to family medicine residency graduates.
“The goal of our program is to bridge the gap between the training of family medicine and internal medicine so our trainees can refine and develop their inpatient skills,” said Dr. David Wilson, program director of the Swedish Hospitalist Fellowship.
During her fellowship year, Dr. Schaffer was caring for hospitalized adult patients on a general medical ward, with supervision from a dedicated group of teaching hospitalists. She also completed rotations in the ICU, on subspecialty services, and received advanced training in point-of-care ultrasound.
Now in her second year of practice as a full time adult hospitalist at Swedish Medical Center, Dr. Schaffer believes her year of hospital medicine fellowship prepared her well for her current position.
“I am constantly using the tools and knowledge I acquired during my fellowship year,” she said. “I would encourage anyone who has an interest in working on procedural skills and gaining more ICU exposure to pursue a similar fellowship.”
In contrast to Dr. Schaffer, Dr. Prochaska was satisfied with his clinical training but chose to pursue a hospital medicine fellowship to develop research skills. Prior to starting the 2-year Hospitalist Scholars Training Program at the University of Chicago in 2014, Dr. Prochaska had a clear vision of becoming a hospital medicine health outcomes investigator, and believed this career would not be possible without the additional training offered by a research-focused fellowship program.
The Hospitalist Scholars Program at the University of Chicago, one of the first programs of its kind, offers a built-in master’s degree to all participants. At the conclusion of his fellowship training in 2016, Dr. Prochaska completed his Master’s in Health Sciences, which gives considerable attention to biostatistics and epidemiology. According to Dr. Prochaska, the key to becoming a successful academic researcher lies in one’s ability to write grants and receive funding, a skill he honed during this fellowship.
Now on faculty at the University of Chicago in the Section of Hospital Medicine, Dr. Prochaska devotes approximately 75% of his time to research and 25% to patient care.
Beyond the research training and experience he gained during his hospital medicine fellowship, Dr. Prochaska said he values the mentorship afforded to him. He noted that one of the most meaningful experiences during his 2 years of fellowship was having the opportunity to sit down with his program directors, Dr. Vineet Arora and Dr. David Meltzer, to discuss the trajectory of his career in academic medicine.
“It is hard to find senior mentors in hospital medicine,” Dr. Prochaska said. “You could get a master’s degree on your own, but with the fellowship program, your mentors can help you think about the next steps in your career.”
For Dr. Schaffer and Dr. Prochaska, fellowship provided training and experience well-matched to their individual goals and helped foster their careers in hospital medicine. For some, however, a fellowship may not be a necessary step on the path to becoming a hospitalist. Many leaders in the field of hospital medicine have advanced in their careers without further training. In addition, receiving little more than a resident’s salary for an additional year or more during fellowship may not be financially tenable for some. Given the ongoing demand for hospitalists across the country, the lack of a fellowship on your resume may not significantly diminish your chances of securing a position, especially in the community setting.
In the end, the decision of whether to pursue a hospital medicine fellowship is a personal one, and the programs available are as varied as the individuals completing them. “Any hospitalist interested in more than simply patient care – potentially QI, medical education, policy, or administration – should consider a fellowship,” Dr. Prochaska said. “Hospitalists have a unique opportunity to be involved in all these areas, but there are absolutely critical skills you need to develop beyond your clinical skills to succeed.” Fellowships are one way to enhance these nonclinical skills.
The best advice to those considering a hospital medicine fellowship? Dedicate some time to engage in self-assessment and goal setting, before jumping to SHM’s online list of programs.
Ask yourself: “Where do I see myself in 10 years? What do I wish to accomplish in my career as a hospitalist? What additional training (clinical, research, quality improvement, leadership) might I need to achieve these goals? Will completion of a hospital medicine fellowship help me make this vision a reality?”
For Dr. Schaffer, a clinical practice–focused hospital medicine fellowship served as a necessary bridge between her family medicine residency and her current position as an adult hospitalist. While for Dr. Prochaska, a research-intensive hospital medicine fellowship was a key step in launching his academic career.
Of course, for many trainees at the end of residency, your self-assessment may lead you in the opposite direction. In that case it is time to find your first “real job” as an attending physician. But if you feel you need more training to meet your personal goals you should rest assured – whether now or in the future, there is almost certainly a hospital medicine fellowship that is right for you.
Dr. Schouten is a hospitalist at Mayo Clinic in Rochester, Minn., and serves on the Society of Hospital Medicine Physicians in Training Committee. Dr. Sundar is a hospitalist at Emory Saint Joseph’s Hospital in Sandy Springs, Ga., and serves as the Site Assistant Director for Education.
References
1. www.hospitalmedicine.org/membership/hospitalist-fellowships/
2. Ranji et al. “Hospital medicine fellowships: Works in progress.” American J Med. 2006 Jan;119(1):72.e1-7. doi: 10.1016/j.amjmed.2005.07.061.
Is it the right choice for me?
Is it the right choice for me?
As Dr. Melanie Schaffer neared the end of her family medicine residency in the spring of 2015, she found herself considering a hospital medicine fellowship. Unsure if she could get a hospitalist job in an urban market given the outpatient focus of her training, Dr. Schaffer began searching for fellowships on the Society of Hospital Medicine website.1
Likewise, in 2014 Dr. Micah Prochaska was seriously contemplating a hospital medicine fellowship. He was about to graduate from internal medicine residency at the University of Chicago and was eager to gain skills and experience in clinical research.
In 2006, there were a total of 16 HM fellowship programs in the United States, catering to graduates of internal medicine, family medicine, and pediatric residencies.2 Since that time, the number of hospital medicine fellowships has grown considerably, paralleling the explosive growth of hospital medicine as a specialty. For example, at one point in the summer of 2018, the SHM website listed 13 clinical family practice fellowships, 29 internal medicine fellowships, and 26 pediatric fellowships. Each fellowship emphasized different aspects of hospital medicine including clinical practice, research, quality improvement, and leadership.
Now more than ever, residents interested in hospital medicine may get overwhelmed by the multitude of options for fellowship training. And the question remains: why pursue fellowship training in the first place?
“I learned that as a family physician it is harder to get a job as a hospitalist outside of smaller communities, and I wanted to have extra training and credentials,” Dr. Schaffer said. “I pursued a fellowship in hospital medicine to hone my inpatient skills, obtain more ICU exposure, and work on procedures.”
Dr. Schaffer’s online search eventually led her to the Advanced Hospital Medicine Fellowship at Swedish Medical Center in Seattle. This 1-year hospital medicine fellowship started in 2008 with an intentional clinical focus, aiming to provide additional training opportunities in hospital medicine primarily to family medicine residency graduates.
“The goal of our program is to bridge the gap between the training of family medicine and internal medicine so our trainees can refine and develop their inpatient skills,” said Dr. David Wilson, program director of the Swedish Hospitalist Fellowship.
During her fellowship year, Dr. Schaffer was caring for hospitalized adult patients on a general medical ward, with supervision from a dedicated group of teaching hospitalists. She also completed rotations in the ICU, on subspecialty services, and received advanced training in point-of-care ultrasound.
Now in her second year of practice as a full time adult hospitalist at Swedish Medical Center, Dr. Schaffer believes her year of hospital medicine fellowship prepared her well for her current position.
“I am constantly using the tools and knowledge I acquired during my fellowship year,” she said. “I would encourage anyone who has an interest in working on procedural skills and gaining more ICU exposure to pursue a similar fellowship.”
In contrast to Dr. Schaffer, Dr. Prochaska was satisfied with his clinical training but chose to pursue a hospital medicine fellowship to develop research skills. Prior to starting the 2-year Hospitalist Scholars Training Program at the University of Chicago in 2014, Dr. Prochaska had a clear vision of becoming a hospital medicine health outcomes investigator, and believed this career would not be possible without the additional training offered by a research-focused fellowship program.
The Hospitalist Scholars Program at the University of Chicago, one of the first programs of its kind, offers a built-in master’s degree to all participants. At the conclusion of his fellowship training in 2016, Dr. Prochaska completed his Master’s in Health Sciences, which gives considerable attention to biostatistics and epidemiology. According to Dr. Prochaska, the key to becoming a successful academic researcher lies in one’s ability to write grants and receive funding, a skill he honed during this fellowship.
Now on faculty at the University of Chicago in the Section of Hospital Medicine, Dr. Prochaska devotes approximately 75% of his time to research and 25% to patient care.
Beyond the research training and experience he gained during his hospital medicine fellowship, Dr. Prochaska said he values the mentorship afforded to him. He noted that one of the most meaningful experiences during his 2 years of fellowship was having the opportunity to sit down with his program directors, Dr. Vineet Arora and Dr. David Meltzer, to discuss the trajectory of his career in academic medicine.
“It is hard to find senior mentors in hospital medicine,” Dr. Prochaska said. “You could get a master’s degree on your own, but with the fellowship program, your mentors can help you think about the next steps in your career.”
For Dr. Schaffer and Dr. Prochaska, fellowship provided training and experience well-matched to their individual goals and helped foster their careers in hospital medicine. For some, however, a fellowship may not be a necessary step on the path to becoming a hospitalist. Many leaders in the field of hospital medicine have advanced in their careers without further training. In addition, receiving little more than a resident’s salary for an additional year or more during fellowship may not be financially tenable for some. Given the ongoing demand for hospitalists across the country, the lack of a fellowship on your resume may not significantly diminish your chances of securing a position, especially in the community setting.
In the end, the decision of whether to pursue a hospital medicine fellowship is a personal one, and the programs available are as varied as the individuals completing them. “Any hospitalist interested in more than simply patient care – potentially QI, medical education, policy, or administration – should consider a fellowship,” Dr. Prochaska said. “Hospitalists have a unique opportunity to be involved in all these areas, but there are absolutely critical skills you need to develop beyond your clinical skills to succeed.” Fellowships are one way to enhance these nonclinical skills.
The best advice to those considering a hospital medicine fellowship? Dedicate some time to engage in self-assessment and goal setting, before jumping to SHM’s online list of programs.
Ask yourself: “Where do I see myself in 10 years? What do I wish to accomplish in my career as a hospitalist? What additional training (clinical, research, quality improvement, leadership) might I need to achieve these goals? Will completion of a hospital medicine fellowship help me make this vision a reality?”
For Dr. Schaffer, a clinical practice–focused hospital medicine fellowship served as a necessary bridge between her family medicine residency and her current position as an adult hospitalist. While for Dr. Prochaska, a research-intensive hospital medicine fellowship was a key step in launching his academic career.
Of course, for many trainees at the end of residency, your self-assessment may lead you in the opposite direction. In that case it is time to find your first “real job” as an attending physician. But if you feel you need more training to meet your personal goals you should rest assured – whether now or in the future, there is almost certainly a hospital medicine fellowship that is right for you.
Dr. Schouten is a hospitalist at Mayo Clinic in Rochester, Minn., and serves on the Society of Hospital Medicine Physicians in Training Committee. Dr. Sundar is a hospitalist at Emory Saint Joseph’s Hospital in Sandy Springs, Ga., and serves as the Site Assistant Director for Education.
References
1. www.hospitalmedicine.org/membership/hospitalist-fellowships/
2. Ranji et al. “Hospital medicine fellowships: Works in progress.” American J Med. 2006 Jan;119(1):72.e1-7. doi: 10.1016/j.amjmed.2005.07.061.
As Dr. Melanie Schaffer neared the end of her family medicine residency in the spring of 2015, she found herself considering a hospital medicine fellowship. Unsure if she could get a hospitalist job in an urban market given the outpatient focus of her training, Dr. Schaffer began searching for fellowships on the Society of Hospital Medicine website.1
Likewise, in 2014 Dr. Micah Prochaska was seriously contemplating a hospital medicine fellowship. He was about to graduate from internal medicine residency at the University of Chicago and was eager to gain skills and experience in clinical research.
In 2006, there were a total of 16 HM fellowship programs in the United States, catering to graduates of internal medicine, family medicine, and pediatric residencies.2 Since that time, the number of hospital medicine fellowships has grown considerably, paralleling the explosive growth of hospital medicine as a specialty. For example, at one point in the summer of 2018, the SHM website listed 13 clinical family practice fellowships, 29 internal medicine fellowships, and 26 pediatric fellowships. Each fellowship emphasized different aspects of hospital medicine including clinical practice, research, quality improvement, and leadership.
Now more than ever, residents interested in hospital medicine may get overwhelmed by the multitude of options for fellowship training. And the question remains: why pursue fellowship training in the first place?
“I learned that as a family physician it is harder to get a job as a hospitalist outside of smaller communities, and I wanted to have extra training and credentials,” Dr. Schaffer said. “I pursued a fellowship in hospital medicine to hone my inpatient skills, obtain more ICU exposure, and work on procedures.”
Dr. Schaffer’s online search eventually led her to the Advanced Hospital Medicine Fellowship at Swedish Medical Center in Seattle. This 1-year hospital medicine fellowship started in 2008 with an intentional clinical focus, aiming to provide additional training opportunities in hospital medicine primarily to family medicine residency graduates.
“The goal of our program is to bridge the gap between the training of family medicine and internal medicine so our trainees can refine and develop their inpatient skills,” said Dr. David Wilson, program director of the Swedish Hospitalist Fellowship.
During her fellowship year, Dr. Schaffer was caring for hospitalized adult patients on a general medical ward, with supervision from a dedicated group of teaching hospitalists. She also completed rotations in the ICU, on subspecialty services, and received advanced training in point-of-care ultrasound.
Now in her second year of practice as a full time adult hospitalist at Swedish Medical Center, Dr. Schaffer believes her year of hospital medicine fellowship prepared her well for her current position.
“I am constantly using the tools and knowledge I acquired during my fellowship year,” she said. “I would encourage anyone who has an interest in working on procedural skills and gaining more ICU exposure to pursue a similar fellowship.”
In contrast to Dr. Schaffer, Dr. Prochaska was satisfied with his clinical training but chose to pursue a hospital medicine fellowship to develop research skills. Prior to starting the 2-year Hospitalist Scholars Training Program at the University of Chicago in 2014, Dr. Prochaska had a clear vision of becoming a hospital medicine health outcomes investigator, and believed this career would not be possible without the additional training offered by a research-focused fellowship program.
The Hospitalist Scholars Program at the University of Chicago, one of the first programs of its kind, offers a built-in master’s degree to all participants. At the conclusion of his fellowship training in 2016, Dr. Prochaska completed his Master’s in Health Sciences, which gives considerable attention to biostatistics and epidemiology. According to Dr. Prochaska, the key to becoming a successful academic researcher lies in one’s ability to write grants and receive funding, a skill he honed during this fellowship.
Now on faculty at the University of Chicago in the Section of Hospital Medicine, Dr. Prochaska devotes approximately 75% of his time to research and 25% to patient care.
Beyond the research training and experience he gained during his hospital medicine fellowship, Dr. Prochaska said he values the mentorship afforded to him. He noted that one of the most meaningful experiences during his 2 years of fellowship was having the opportunity to sit down with his program directors, Dr. Vineet Arora and Dr. David Meltzer, to discuss the trajectory of his career in academic medicine.
“It is hard to find senior mentors in hospital medicine,” Dr. Prochaska said. “You could get a master’s degree on your own, but with the fellowship program, your mentors can help you think about the next steps in your career.”
For Dr. Schaffer and Dr. Prochaska, fellowship provided training and experience well-matched to their individual goals and helped foster their careers in hospital medicine. For some, however, a fellowship may not be a necessary step on the path to becoming a hospitalist. Many leaders in the field of hospital medicine have advanced in their careers without further training. In addition, receiving little more than a resident’s salary for an additional year or more during fellowship may not be financially tenable for some. Given the ongoing demand for hospitalists across the country, the lack of a fellowship on your resume may not significantly diminish your chances of securing a position, especially in the community setting.
In the end, the decision of whether to pursue a hospital medicine fellowship is a personal one, and the programs available are as varied as the individuals completing them. “Any hospitalist interested in more than simply patient care – potentially QI, medical education, policy, or administration – should consider a fellowship,” Dr. Prochaska said. “Hospitalists have a unique opportunity to be involved in all these areas, but there are absolutely critical skills you need to develop beyond your clinical skills to succeed.” Fellowships are one way to enhance these nonclinical skills.
The best advice to those considering a hospital medicine fellowship? Dedicate some time to engage in self-assessment and goal setting, before jumping to SHM’s online list of programs.
Ask yourself: “Where do I see myself in 10 years? What do I wish to accomplish in my career as a hospitalist? What additional training (clinical, research, quality improvement, leadership) might I need to achieve these goals? Will completion of a hospital medicine fellowship help me make this vision a reality?”
For Dr. Schaffer, a clinical practice–focused hospital medicine fellowship served as a necessary bridge between her family medicine residency and her current position as an adult hospitalist. While for Dr. Prochaska, a research-intensive hospital medicine fellowship was a key step in launching his academic career.
Of course, for many trainees at the end of residency, your self-assessment may lead you in the opposite direction. In that case it is time to find your first “real job” as an attending physician. But if you feel you need more training to meet your personal goals you should rest assured – whether now or in the future, there is almost certainly a hospital medicine fellowship that is right for you.
Dr. Schouten is a hospitalist at Mayo Clinic in Rochester, Minn., and serves on the Society of Hospital Medicine Physicians in Training Committee. Dr. Sundar is a hospitalist at Emory Saint Joseph’s Hospital in Sandy Springs, Ga., and serves as the Site Assistant Director for Education.
References
1. www.hospitalmedicine.org/membership/hospitalist-fellowships/
2. Ranji et al. “Hospital medicine fellowships: Works in progress.” American J Med. 2006 Jan;119(1):72.e1-7. doi: 10.1016/j.amjmed.2005.07.061.
Medical marijuana for autism facing good prospects in Colorado
Five years after the legalization of marijuana in Colorado, anticipated legislation in 2019 could see home delivery of cannabis and cannabis-related products, and expanded medical availability.
Governor-elect Jared Polis, who takes office in the new year, probably will take a different approach from outgoing Gov. John Hickenlooper, according to a recent article in the Denver Post. Mr. Hickenlooper vetoed previous legislation intended to increase drug’s accessibility.
“ says Albert Gutierrez, CEO of MedPharm Holdings, a cannabis research and cultivation company.
“You’re going to probably have more variety from these companies, whether they’re offering drinks or chocolate bars. But these companies are going to be the household names that people are going to come to know over the next 30, 50, 100 years,” he says.
Not everyone is on board. “We should all be able to agree that Colorado’s increasingly potent marijuana products are harmful to youth and that we have a collective responsibility to protect Colorado kids,” writes Henny Lasley, the cofounder of Smart Colorado, which was formed in opposition to the legalization of marijuana in the state.
The availability of medical marijuana for people diagnosed with autism spectrum disorders is among the vetoed initiatives that are likely to reemerge in 2019. That bill reportedly was opposed by the Colorado Child and Adolescent Psychiatric Society, the Colorado Psychiatric Society, and by Larry Wolk, MD, who recently stepped down as chief medical officer of the state’s department of public health and environment.
Adjusting to life after fires
The latest wildfires have been vanquished in California. For those affected recently and in the past several years has come the reality that the draw of living on the edge of nature means living surrounded by tinder-dry terrain. It’s a great location – until it ignites.
A year ago, the Thomas Fire devastated Ventura and Santa Barbara counties, burning more than 440 square miles. Few people died, but more than 1,000 buildings were destroyed – and hundreds of people were left homeless. A year later, in the Clearpoint neighborhood of Ventura, residential lots sit empty, their owners having abandoned the effort to rebuild. Others, like Sandra and Ed Fuller, are choosing to begin again. The beauty of the area that pulled them there years ago remains strong.
They have come to terms with losing their home to the fire. “I think it was a sort of a breaking point where there was just a flood of peace that kind of went through. It’s like there is nothing we can do about this. We know what we have to do now. We’ll just get on with it,” Ed Fuller says in an interview with NPR.
Having the Christmas season looming has been a boost to their spirits and planning. “My wife is absolutely obsessed that she’s ready for Christmas. Last Christmas we sort of lost.”
The invisibility of asexuality
It can be hard for some to fathom that sex just isn’t important for some. “They are the friends and family members who don’t express any desire to pursue sexual intimacy, who don’t often or ever seem interested in conventional dating, and who get pushed to the sidelines in any conversation about sexual health,” Kate Sloan writes in a recent article in the Walrus.
“Much like same-sex attraction decades ago, this nonattraction was initially (and is sometimes still) conflated with a sexual-desire disorder, worthy of pathologization and medical treatment with pharmaceuticals or therapy. But scientists have confirmed asexuality isn’t a medical issue; it is a sexual orientation on the same plane as heterosexuality, homosexuality, and bisexuality,” Ms. Sloan writes.
“If someone is gay, as an example, it’s pretty easy to say, ‘Okay, well, I experience the same type of attraction that everyone else does, it’s just pointed at a different gender,’ ” says Brian Langevin, executive director of the nonprofit organization Asexual Outreach. “For asexual people ... they might not even know that sexual attraction exists, and to them, the whole world could seem very confusing.”
Meanwhile, a 2013 study in British Columbia showed that asexual individuals are more likely to be socially isolated, depressed, and anxious.
“True emotional intimacy is created, according to psychology, by honesty, empathy, and listening,” Ms. Sloan writes. “When we oversimplify relationships by insisting, on a sociocultural level, that sex is the ultimate key to and only sign of a profound connection, we deprive ourselves of the more holistic affinities available to us if we look for more.”
Fundamental churches face allegations
Joy Evans Ryder was 15 when she reportedly was raped by Dave Hyles, youth director at her Baptist church in Hammond, Ind. She was not the youth director’s only alleged victim. He never faced charges; in a scenario strikingly similar to that of hundreds of Roman Catholic priests, he escaped local prosecution by being moved on to other assignments.
An investigation by the Fort Worth (Tex.) Star-Telegram has unearthed a decades-old cover-up of more than 400 cases of sexual abuse at independent fundamental Baptist churches across the United States.
Former members of congregations point to the cultlike power of many independent fundamental Baptist churches and the constant pressure to never question pastors or leave the church.
“We didn’t have a compound ... but it may as well have been. Our mind was the compound,” says a former member. Some of the abused believed that if they disobeyed the pastor or left the church, God would kill them or their family.
Some independent fundamental Baptist churches preach separation from the world, nonbelievers, and Christians with other religious views. A natural outcome, according to Josh Elliott, a former member of Vineyard’s Oklahoma City church, is that for any issues, “even legal issues, you go to the pastor first, not the police. ... You don’t report to police because the pastor is the ultimate authority, not the government.”
“I see a culture where pastoral authority is taken to a level that’s beyond what the Scripture teaches,” says Tim Heck, who was a deacon at Faith Baptist Church in Wildomar, Calif., and whose daughter said she had been abused by the youth pastor there. “I think the independent fundamental Baptists have lost their way.”
Adam Lanza’s ‘separateness’ exposed
Written musings and other documents by Adam Lanza – who slaughtered 20 first-graders and six teachers at Sandy Hook Elementary School in Newtown, Conn., on Dec. 14, 2012 – have been reported by the Hartford Courant.
Adam Lanza was challenged by speech and sensory issues as a child but had a keen intellect. That potential was eclipsed in his teenage years by paranoia, disdain for relationships, and contempt for others, the documents show. Family, teachers, and counselors were aware of his isolation. And, with time, his obsessions and mental/physical deterioration grew. But the documents make clear that no one really had a full grasp of the person he was becoming.
“As a teenager, his sensory condition made him exceedingly sensitive to textures, sound, light, and movement. He shunned his classmates, bothered by their choice of clothes and the noises they made. He cultivated a set of ground rules that fed his separateness,” write reporters Josh Kovner and Dave Altimari. The critical addition to this toxic brew was an absence of empathy and social compassion, according to Harold I. Schwartz, MD, a psychiatrist and former member of the Sandy Hook Advisory Commission, which studied the shootings.
“In this mental state, known as solipsism, only the solipsist is real. Everyone else in the world is a cardboard cutout, placed there for your benefit and otherwise devoid of meaning or value. It is the most extreme end of one form of malignant narcissism. If the victims have no value, then there is nothing to constrain you from shooting them,” Dr. Schwartz says.
In a note accompanying the article, the editors write: “Understanding what a mass killer was thinking not only paints a clearer picture of the individual, it helps us identify and understand red flags that could be part of a prevention formula for future mass shootings.”
Five years after the legalization of marijuana in Colorado, anticipated legislation in 2019 could see home delivery of cannabis and cannabis-related products, and expanded medical availability.
Governor-elect Jared Polis, who takes office in the new year, probably will take a different approach from outgoing Gov. John Hickenlooper, according to a recent article in the Denver Post. Mr. Hickenlooper vetoed previous legislation intended to increase drug’s accessibility.
“ says Albert Gutierrez, CEO of MedPharm Holdings, a cannabis research and cultivation company.
“You’re going to probably have more variety from these companies, whether they’re offering drinks or chocolate bars. But these companies are going to be the household names that people are going to come to know over the next 30, 50, 100 years,” he says.
Not everyone is on board. “We should all be able to agree that Colorado’s increasingly potent marijuana products are harmful to youth and that we have a collective responsibility to protect Colorado kids,” writes Henny Lasley, the cofounder of Smart Colorado, which was formed in opposition to the legalization of marijuana in the state.
The availability of medical marijuana for people diagnosed with autism spectrum disorders is among the vetoed initiatives that are likely to reemerge in 2019. That bill reportedly was opposed by the Colorado Child and Adolescent Psychiatric Society, the Colorado Psychiatric Society, and by Larry Wolk, MD, who recently stepped down as chief medical officer of the state’s department of public health and environment.
Adjusting to life after fires
The latest wildfires have been vanquished in California. For those affected recently and in the past several years has come the reality that the draw of living on the edge of nature means living surrounded by tinder-dry terrain. It’s a great location – until it ignites.
A year ago, the Thomas Fire devastated Ventura and Santa Barbara counties, burning more than 440 square miles. Few people died, but more than 1,000 buildings were destroyed – and hundreds of people were left homeless. A year later, in the Clearpoint neighborhood of Ventura, residential lots sit empty, their owners having abandoned the effort to rebuild. Others, like Sandra and Ed Fuller, are choosing to begin again. The beauty of the area that pulled them there years ago remains strong.
They have come to terms with losing their home to the fire. “I think it was a sort of a breaking point where there was just a flood of peace that kind of went through. It’s like there is nothing we can do about this. We know what we have to do now. We’ll just get on with it,” Ed Fuller says in an interview with NPR.
Having the Christmas season looming has been a boost to their spirits and planning. “My wife is absolutely obsessed that she’s ready for Christmas. Last Christmas we sort of lost.”
The invisibility of asexuality
It can be hard for some to fathom that sex just isn’t important for some. “They are the friends and family members who don’t express any desire to pursue sexual intimacy, who don’t often or ever seem interested in conventional dating, and who get pushed to the sidelines in any conversation about sexual health,” Kate Sloan writes in a recent article in the Walrus.
“Much like same-sex attraction decades ago, this nonattraction was initially (and is sometimes still) conflated with a sexual-desire disorder, worthy of pathologization and medical treatment with pharmaceuticals or therapy. But scientists have confirmed asexuality isn’t a medical issue; it is a sexual orientation on the same plane as heterosexuality, homosexuality, and bisexuality,” Ms. Sloan writes.
“If someone is gay, as an example, it’s pretty easy to say, ‘Okay, well, I experience the same type of attraction that everyone else does, it’s just pointed at a different gender,’ ” says Brian Langevin, executive director of the nonprofit organization Asexual Outreach. “For asexual people ... they might not even know that sexual attraction exists, and to them, the whole world could seem very confusing.”
Meanwhile, a 2013 study in British Columbia showed that asexual individuals are more likely to be socially isolated, depressed, and anxious.
“True emotional intimacy is created, according to psychology, by honesty, empathy, and listening,” Ms. Sloan writes. “When we oversimplify relationships by insisting, on a sociocultural level, that sex is the ultimate key to and only sign of a profound connection, we deprive ourselves of the more holistic affinities available to us if we look for more.”
Fundamental churches face allegations
Joy Evans Ryder was 15 when she reportedly was raped by Dave Hyles, youth director at her Baptist church in Hammond, Ind. She was not the youth director’s only alleged victim. He never faced charges; in a scenario strikingly similar to that of hundreds of Roman Catholic priests, he escaped local prosecution by being moved on to other assignments.
An investigation by the Fort Worth (Tex.) Star-Telegram has unearthed a decades-old cover-up of more than 400 cases of sexual abuse at independent fundamental Baptist churches across the United States.
Former members of congregations point to the cultlike power of many independent fundamental Baptist churches and the constant pressure to never question pastors or leave the church.
“We didn’t have a compound ... but it may as well have been. Our mind was the compound,” says a former member. Some of the abused believed that if they disobeyed the pastor or left the church, God would kill them or their family.
Some independent fundamental Baptist churches preach separation from the world, nonbelievers, and Christians with other religious views. A natural outcome, according to Josh Elliott, a former member of Vineyard’s Oklahoma City church, is that for any issues, “even legal issues, you go to the pastor first, not the police. ... You don’t report to police because the pastor is the ultimate authority, not the government.”
“I see a culture where pastoral authority is taken to a level that’s beyond what the Scripture teaches,” says Tim Heck, who was a deacon at Faith Baptist Church in Wildomar, Calif., and whose daughter said she had been abused by the youth pastor there. “I think the independent fundamental Baptists have lost their way.”
Adam Lanza’s ‘separateness’ exposed
Written musings and other documents by Adam Lanza – who slaughtered 20 first-graders and six teachers at Sandy Hook Elementary School in Newtown, Conn., on Dec. 14, 2012 – have been reported by the Hartford Courant.
Adam Lanza was challenged by speech and sensory issues as a child but had a keen intellect. That potential was eclipsed in his teenage years by paranoia, disdain for relationships, and contempt for others, the documents show. Family, teachers, and counselors were aware of his isolation. And, with time, his obsessions and mental/physical deterioration grew. But the documents make clear that no one really had a full grasp of the person he was becoming.
“As a teenager, his sensory condition made him exceedingly sensitive to textures, sound, light, and movement. He shunned his classmates, bothered by their choice of clothes and the noises they made. He cultivated a set of ground rules that fed his separateness,” write reporters Josh Kovner and Dave Altimari. The critical addition to this toxic brew was an absence of empathy and social compassion, according to Harold I. Schwartz, MD, a psychiatrist and former member of the Sandy Hook Advisory Commission, which studied the shootings.
“In this mental state, known as solipsism, only the solipsist is real. Everyone else in the world is a cardboard cutout, placed there for your benefit and otherwise devoid of meaning or value. It is the most extreme end of one form of malignant narcissism. If the victims have no value, then there is nothing to constrain you from shooting them,” Dr. Schwartz says.
In a note accompanying the article, the editors write: “Understanding what a mass killer was thinking not only paints a clearer picture of the individual, it helps us identify and understand red flags that could be part of a prevention formula for future mass shootings.”
Five years after the legalization of marijuana in Colorado, anticipated legislation in 2019 could see home delivery of cannabis and cannabis-related products, and expanded medical availability.
Governor-elect Jared Polis, who takes office in the new year, probably will take a different approach from outgoing Gov. John Hickenlooper, according to a recent article in the Denver Post. Mr. Hickenlooper vetoed previous legislation intended to increase drug’s accessibility.
“ says Albert Gutierrez, CEO of MedPharm Holdings, a cannabis research and cultivation company.
“You’re going to probably have more variety from these companies, whether they’re offering drinks or chocolate bars. But these companies are going to be the household names that people are going to come to know over the next 30, 50, 100 years,” he says.
Not everyone is on board. “We should all be able to agree that Colorado’s increasingly potent marijuana products are harmful to youth and that we have a collective responsibility to protect Colorado kids,” writes Henny Lasley, the cofounder of Smart Colorado, which was formed in opposition to the legalization of marijuana in the state.
The availability of medical marijuana for people diagnosed with autism spectrum disorders is among the vetoed initiatives that are likely to reemerge in 2019. That bill reportedly was opposed by the Colorado Child and Adolescent Psychiatric Society, the Colorado Psychiatric Society, and by Larry Wolk, MD, who recently stepped down as chief medical officer of the state’s department of public health and environment.
Adjusting to life after fires
The latest wildfires have been vanquished in California. For those affected recently and in the past several years has come the reality that the draw of living on the edge of nature means living surrounded by tinder-dry terrain. It’s a great location – until it ignites.
A year ago, the Thomas Fire devastated Ventura and Santa Barbara counties, burning more than 440 square miles. Few people died, but more than 1,000 buildings were destroyed – and hundreds of people were left homeless. A year later, in the Clearpoint neighborhood of Ventura, residential lots sit empty, their owners having abandoned the effort to rebuild. Others, like Sandra and Ed Fuller, are choosing to begin again. The beauty of the area that pulled them there years ago remains strong.
They have come to terms with losing their home to the fire. “I think it was a sort of a breaking point where there was just a flood of peace that kind of went through. It’s like there is nothing we can do about this. We know what we have to do now. We’ll just get on with it,” Ed Fuller says in an interview with NPR.
Having the Christmas season looming has been a boost to their spirits and planning. “My wife is absolutely obsessed that she’s ready for Christmas. Last Christmas we sort of lost.”
The invisibility of asexuality
It can be hard for some to fathom that sex just isn’t important for some. “They are the friends and family members who don’t express any desire to pursue sexual intimacy, who don’t often or ever seem interested in conventional dating, and who get pushed to the sidelines in any conversation about sexual health,” Kate Sloan writes in a recent article in the Walrus.
“Much like same-sex attraction decades ago, this nonattraction was initially (and is sometimes still) conflated with a sexual-desire disorder, worthy of pathologization and medical treatment with pharmaceuticals or therapy. But scientists have confirmed asexuality isn’t a medical issue; it is a sexual orientation on the same plane as heterosexuality, homosexuality, and bisexuality,” Ms. Sloan writes.
“If someone is gay, as an example, it’s pretty easy to say, ‘Okay, well, I experience the same type of attraction that everyone else does, it’s just pointed at a different gender,’ ” says Brian Langevin, executive director of the nonprofit organization Asexual Outreach. “For asexual people ... they might not even know that sexual attraction exists, and to them, the whole world could seem very confusing.”
Meanwhile, a 2013 study in British Columbia showed that asexual individuals are more likely to be socially isolated, depressed, and anxious.
“True emotional intimacy is created, according to psychology, by honesty, empathy, and listening,” Ms. Sloan writes. “When we oversimplify relationships by insisting, on a sociocultural level, that sex is the ultimate key to and only sign of a profound connection, we deprive ourselves of the more holistic affinities available to us if we look for more.”
Fundamental churches face allegations
Joy Evans Ryder was 15 when she reportedly was raped by Dave Hyles, youth director at her Baptist church in Hammond, Ind. She was not the youth director’s only alleged victim. He never faced charges; in a scenario strikingly similar to that of hundreds of Roman Catholic priests, he escaped local prosecution by being moved on to other assignments.
An investigation by the Fort Worth (Tex.) Star-Telegram has unearthed a decades-old cover-up of more than 400 cases of sexual abuse at independent fundamental Baptist churches across the United States.
Former members of congregations point to the cultlike power of many independent fundamental Baptist churches and the constant pressure to never question pastors or leave the church.
“We didn’t have a compound ... but it may as well have been. Our mind was the compound,” says a former member. Some of the abused believed that if they disobeyed the pastor or left the church, God would kill them or their family.
Some independent fundamental Baptist churches preach separation from the world, nonbelievers, and Christians with other religious views. A natural outcome, according to Josh Elliott, a former member of Vineyard’s Oklahoma City church, is that for any issues, “even legal issues, you go to the pastor first, not the police. ... You don’t report to police because the pastor is the ultimate authority, not the government.”
“I see a culture where pastoral authority is taken to a level that’s beyond what the Scripture teaches,” says Tim Heck, who was a deacon at Faith Baptist Church in Wildomar, Calif., and whose daughter said she had been abused by the youth pastor there. “I think the independent fundamental Baptists have lost their way.”
Adam Lanza’s ‘separateness’ exposed
Written musings and other documents by Adam Lanza – who slaughtered 20 first-graders and six teachers at Sandy Hook Elementary School in Newtown, Conn., on Dec. 14, 2012 – have been reported by the Hartford Courant.
Adam Lanza was challenged by speech and sensory issues as a child but had a keen intellect. That potential was eclipsed in his teenage years by paranoia, disdain for relationships, and contempt for others, the documents show. Family, teachers, and counselors were aware of his isolation. And, with time, his obsessions and mental/physical deterioration grew. But the documents make clear that no one really had a full grasp of the person he was becoming.
“As a teenager, his sensory condition made him exceedingly sensitive to textures, sound, light, and movement. He shunned his classmates, bothered by their choice of clothes and the noises they made. He cultivated a set of ground rules that fed his separateness,” write reporters Josh Kovner and Dave Altimari. The critical addition to this toxic brew was an absence of empathy and social compassion, according to Harold I. Schwartz, MD, a psychiatrist and former member of the Sandy Hook Advisory Commission, which studied the shootings.
“In this mental state, known as solipsism, only the solipsist is real. Everyone else in the world is a cardboard cutout, placed there for your benefit and otherwise devoid of meaning or value. It is the most extreme end of one form of malignant narcissism. If the victims have no value, then there is nothing to constrain you from shooting them,” Dr. Schwartz says.
In a note accompanying the article, the editors write: “Understanding what a mass killer was thinking not only paints a clearer picture of the individual, it helps us identify and understand red flags that could be part of a prevention formula for future mass shootings.”
Uptick in adult syphilis means congenital syphilis may be lurking
While many pediatric clinicians have not frequently managed newborns of mothers with reactive syphilis serology, increased adult syphilis may change that.1
Diagnosing/managing congenital syphilis is not always clear cut. A positive rapid plasma reagin (RPR) titer in a newborn may not indicate congenital infection but merely may reflect transplacental, passively acquired maternal IgG from the mother’s current or previous infection rather than antibodies produced by the newborn. Because currently no IgM assay for syphilis is recommended by the Centers for Disease Control and Prevention for newborn testing, we must deal with IgG test results.
Often initial management decisions are needed while the infant’s status is evolving. The questions to answer to make final decisions include the following2:
- Was the mother actively infected with Treponema pallidum during pregnancy?
- If so, was the mother appropriately treated and when?
- Does the infant have any clinical, laboratory, or radiographic evidence of syphilis?
- How do the mother’s and infant’s nontreponemal serologic titers (NTT) compare at delivery using the same test?
Note: All infants assessed for congenital syphilis need a full evaluation for HIV.
Managing the infant of a mother with positive tests3,4
All such neonates need an examination for evidence of congenital syphilis. The clinical signs of congenital syphilis in neonates include nonimmune hydrops, jaundice, hepatosplenomegaly, rhinitis, skin rash, and pseudoparalysis of extremity. Also, consider dark-field examination or polymerase chain reaction (PCR) of lesions (such as bullae) or secretions (nasal). If available, have the placenta examined histologically (silver stain) or by PCR (Clinical Laboratory Improvement Amendments–validated test). Skeletal radiographic surveys are more useful for stillborn than live born infants. (The complete algorithm can be found in Figure 3.10 of reference 4.)
Order a quantitative NTT, using the Venereal Disease Research Laboratory (VDRL) test or RPR test on neonatal serum. Umbilical cord blood is not appropriate because of potential maternal blood contamination, which could give a false-positive result, or Wharton’s jelly, which could give a false-negative result. Use of treponemal-specific tests that are used for maternal diagnosis – such as T. pallidum particle agglutination (TP-PA), T. pallidum enzyme-linked immunosorbent assay (TP-EIA), fluorescent treponemal antibody absorption (FTA-ABS) test, or T. pallidum chemiluminescence immunoassay (TP-CIA) – on neonatal serum is not recommended because of difficulties in interpretation.
Diagnostic results allow designation of an infant into one of four CDC categories: proven/highly probable syphilis; possible syphilis; syphilis less likely; and syphilis unlikely. Treatment recommendations are based on these categories.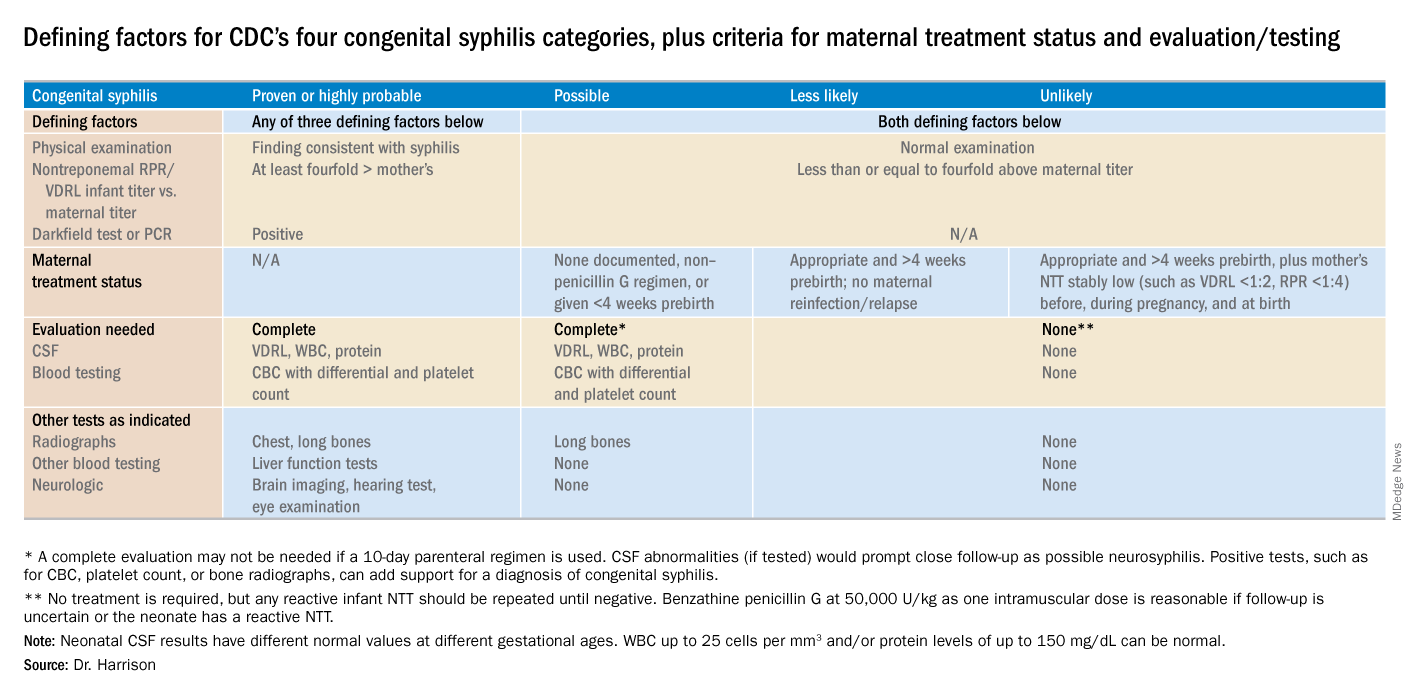
Proven or highly probable syphilis
There are two alternative recommended 10-day treatment regimens.
A. Aqueous crystalline penicillin G 100,000-150,000 U/kg per day by IV at 50,000 U/kg per dose, given every 12 hours through 7 days of age or every 8 hours if greater than 7 days old.
B. Procaine penicillin G at 50,000 U/kg per dose intramuscularly in one dose each day.
More than 1 day of missed therapy requires restarting a new 10-day course. Use of other antimicrobial agents (such as ampicillin) is not validated, so any empiric ampicillin initially given for possible sepsis does not count toward the 10-day penicillin regimen. If nonpenicillin drugs must be used, close serologic follow-up must occur to ensure adequacy of response to therapy.
Possible syphilis
There are three alternative regimens, the same two as in proven/highly probable syphilis (above) plus a single-dose option
A. Aqueous crystalline penicillin G, as described above.
B. Procaine penicillin G, as described above.
C. Benzathine penicillin G at 50,000 U/kg per dose intramuscularly in a single dose.
Note: To be eligible for regimen C, an infant must have a complete evaluation that is normal (cerebrospinal fluid [CSF] examination, long-bone radiographs, and complete blood count with platelet count) and follow-up must be assured. Exception: Neonates born to mothers with untreated early syphilis at the time of delivery are at increased risk for congenital syphilis, and the 10-day course of penicillin G may be considered even if the complete evaluation is normal and follow-up is certain.
Less likely syphilis
One antibiotic regimen is available, but no treatment also may be an option.
A. Benzathine penicillin G as described above.
B. If mother’s NTT has decreased at least fourfold after appropriate early syphilis therapy or remained stably low, which indicates latent syphilis (VDRL less than 1:2; RPR less than 1:4), no treatment is an option but requires repeat serology every 2-3 months until infant is 6 months old.
Unlikely syphilis
No treatment is recommended unless follow-up is uncertain, in which case it is appropriate to give the infant benzathine penicillin G as described above.
Infant with positive NTT at birth
All neonates with reactive NTT need careful follow-up examinations and repeat NTT every 2-3 months until nonreactive. NTT in infants who are not treated because of less likely or unlikely syphilis status should drop by 3 months and be nonreactive by 6 months; this indicates NTT was passively transferred maternal IgG. If NTT remains reactive at 6 months, the infant is likely infected and needs treatment. Persistent NTT at 6-12 months in treated neonates should trigger repeat CSF examination and infectious diseases consultation about a possible repeat of the 10-day penicillin G regimen. If the mother was seroreactive, but the newborn’s NTT was negative at birth, testing of the infant’s NTT needs repeating at 3 months to exclude the possibility that the congenital syphilis was incubating when prior testing occurred at birth. Note: Treponemal-specific tests are not useful in assessing treatment because detectable maternal IgG treponemal antibody can persist at least 15 months.
Neonates with abnormal CSF at birth
Repeat cerebrospinal fluid evaluation every 6 months until results normalize. Persistently reactive CSF VDRL or abnormal CSF indexes not caused by another known cause requires retreatment for possible neurosyphilis, as well as consultation with an expert.
Summary
NTT are the essential test for newborns and some degree of laboratory or imaging work up often are needed. Consider consulting an expert in infectious diseases and/or perinatology if the gray areas do not readily become clear. Treatment of the correct patients with the right drug for the right duration remains the goal, as usual.
Dr. Harrison is a professor of pediatrics at University of Missouri-Kansas City and Director of Research Affairs in the pediatric infectious diseases division at Children’s Mercy Hospital – Kansas City. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. MMWR. 2015 Nov 13;64(44);1241-5.
2. “Congenital Syphilis,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
3. “Syphilis During Pregnancy,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
4. Syphilis – Section 3: Summaries of Infectious Diseases. Red Book Online. 2018.
While many pediatric clinicians have not frequently managed newborns of mothers with reactive syphilis serology, increased adult syphilis may change that.1
Diagnosing/managing congenital syphilis is not always clear cut. A positive rapid plasma reagin (RPR) titer in a newborn may not indicate congenital infection but merely may reflect transplacental, passively acquired maternal IgG from the mother’s current or previous infection rather than antibodies produced by the newborn. Because currently no IgM assay for syphilis is recommended by the Centers for Disease Control and Prevention for newborn testing, we must deal with IgG test results.
Often initial management decisions are needed while the infant’s status is evolving. The questions to answer to make final decisions include the following2:
- Was the mother actively infected with Treponema pallidum during pregnancy?
- If so, was the mother appropriately treated and when?
- Does the infant have any clinical, laboratory, or radiographic evidence of syphilis?
- How do the mother’s and infant’s nontreponemal serologic titers (NTT) compare at delivery using the same test?
Note: All infants assessed for congenital syphilis need a full evaluation for HIV.
Managing the infant of a mother with positive tests3,4
All such neonates need an examination for evidence of congenital syphilis. The clinical signs of congenital syphilis in neonates include nonimmune hydrops, jaundice, hepatosplenomegaly, rhinitis, skin rash, and pseudoparalysis of extremity. Also, consider dark-field examination or polymerase chain reaction (PCR) of lesions (such as bullae) or secretions (nasal). If available, have the placenta examined histologically (silver stain) or by PCR (Clinical Laboratory Improvement Amendments–validated test). Skeletal radiographic surveys are more useful for stillborn than live born infants. (The complete algorithm can be found in Figure 3.10 of reference 4.)
Order a quantitative NTT, using the Venereal Disease Research Laboratory (VDRL) test or RPR test on neonatal serum. Umbilical cord blood is not appropriate because of potential maternal blood contamination, which could give a false-positive result, or Wharton’s jelly, which could give a false-negative result. Use of treponemal-specific tests that are used for maternal diagnosis – such as T. pallidum particle agglutination (TP-PA), T. pallidum enzyme-linked immunosorbent assay (TP-EIA), fluorescent treponemal antibody absorption (FTA-ABS) test, or T. pallidum chemiluminescence immunoassay (TP-CIA) – on neonatal serum is not recommended because of difficulties in interpretation.
Diagnostic results allow designation of an infant into one of four CDC categories: proven/highly probable syphilis; possible syphilis; syphilis less likely; and syphilis unlikely. Treatment recommendations are based on these categories.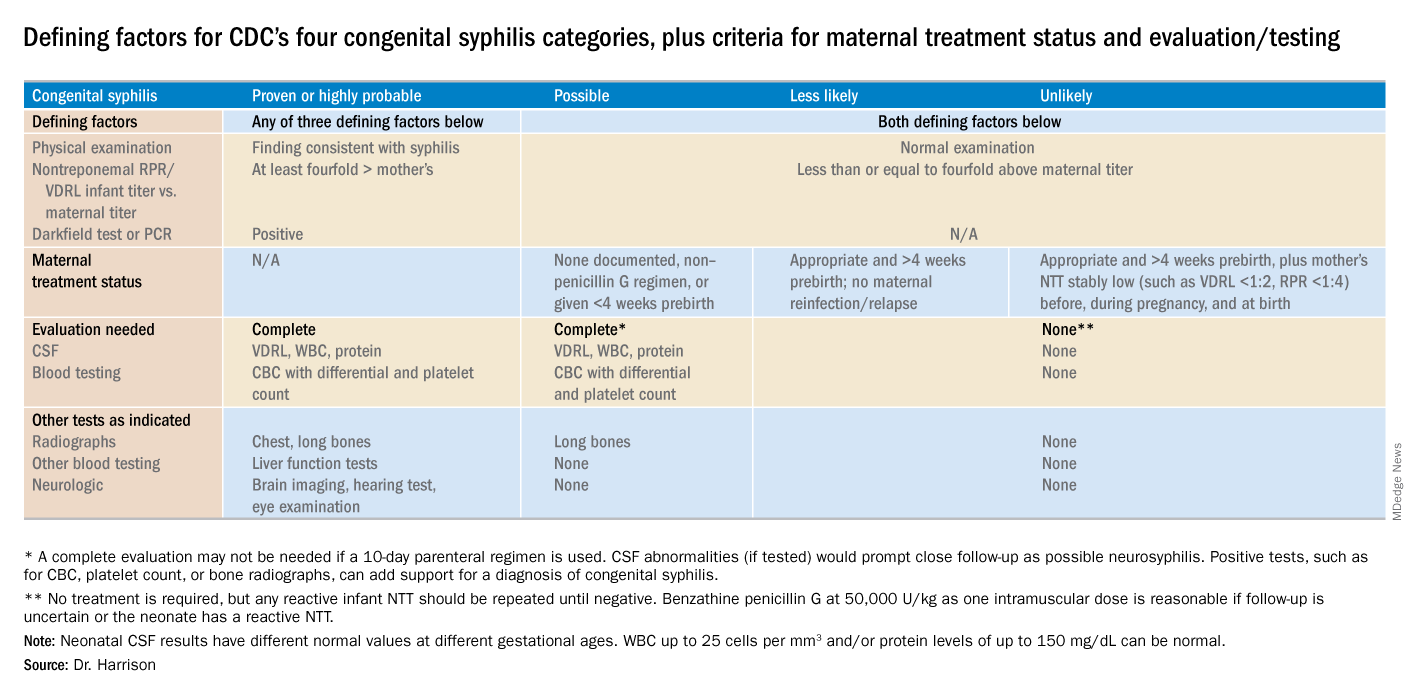
Proven or highly probable syphilis
There are two alternative recommended 10-day treatment regimens.
A. Aqueous crystalline penicillin G 100,000-150,000 U/kg per day by IV at 50,000 U/kg per dose, given every 12 hours through 7 days of age or every 8 hours if greater than 7 days old.
B. Procaine penicillin G at 50,000 U/kg per dose intramuscularly in one dose each day.
More than 1 day of missed therapy requires restarting a new 10-day course. Use of other antimicrobial agents (such as ampicillin) is not validated, so any empiric ampicillin initially given for possible sepsis does not count toward the 10-day penicillin regimen. If nonpenicillin drugs must be used, close serologic follow-up must occur to ensure adequacy of response to therapy.
Possible syphilis
There are three alternative regimens, the same two as in proven/highly probable syphilis (above) plus a single-dose option
A. Aqueous crystalline penicillin G, as described above.
B. Procaine penicillin G, as described above.
C. Benzathine penicillin G at 50,000 U/kg per dose intramuscularly in a single dose.
Note: To be eligible for regimen C, an infant must have a complete evaluation that is normal (cerebrospinal fluid [CSF] examination, long-bone radiographs, and complete blood count with platelet count) and follow-up must be assured. Exception: Neonates born to mothers with untreated early syphilis at the time of delivery are at increased risk for congenital syphilis, and the 10-day course of penicillin G may be considered even if the complete evaluation is normal and follow-up is certain.
Less likely syphilis
One antibiotic regimen is available, but no treatment also may be an option.
A. Benzathine penicillin G as described above.
B. If mother’s NTT has decreased at least fourfold after appropriate early syphilis therapy or remained stably low, which indicates latent syphilis (VDRL less than 1:2; RPR less than 1:4), no treatment is an option but requires repeat serology every 2-3 months until infant is 6 months old.
Unlikely syphilis
No treatment is recommended unless follow-up is uncertain, in which case it is appropriate to give the infant benzathine penicillin G as described above.
Infant with positive NTT at birth
All neonates with reactive NTT need careful follow-up examinations and repeat NTT every 2-3 months until nonreactive. NTT in infants who are not treated because of less likely or unlikely syphilis status should drop by 3 months and be nonreactive by 6 months; this indicates NTT was passively transferred maternal IgG. If NTT remains reactive at 6 months, the infant is likely infected and needs treatment. Persistent NTT at 6-12 months in treated neonates should trigger repeat CSF examination and infectious diseases consultation about a possible repeat of the 10-day penicillin G regimen. If the mother was seroreactive, but the newborn’s NTT was negative at birth, testing of the infant’s NTT needs repeating at 3 months to exclude the possibility that the congenital syphilis was incubating when prior testing occurred at birth. Note: Treponemal-specific tests are not useful in assessing treatment because detectable maternal IgG treponemal antibody can persist at least 15 months.
Neonates with abnormal CSF at birth
Repeat cerebrospinal fluid evaluation every 6 months until results normalize. Persistently reactive CSF VDRL or abnormal CSF indexes not caused by another known cause requires retreatment for possible neurosyphilis, as well as consultation with an expert.
Summary
NTT are the essential test for newborns and some degree of laboratory or imaging work up often are needed. Consider consulting an expert in infectious diseases and/or perinatology if the gray areas do not readily become clear. Treatment of the correct patients with the right drug for the right duration remains the goal, as usual.
Dr. Harrison is a professor of pediatrics at University of Missouri-Kansas City and Director of Research Affairs in the pediatric infectious diseases division at Children’s Mercy Hospital – Kansas City. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. MMWR. 2015 Nov 13;64(44);1241-5.
2. “Congenital Syphilis,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
3. “Syphilis During Pregnancy,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
4. Syphilis – Section 3: Summaries of Infectious Diseases. Red Book Online. 2018.
While many pediatric clinicians have not frequently managed newborns of mothers with reactive syphilis serology, increased adult syphilis may change that.1
Diagnosing/managing congenital syphilis is not always clear cut. A positive rapid plasma reagin (RPR) titer in a newborn may not indicate congenital infection but merely may reflect transplacental, passively acquired maternal IgG from the mother’s current or previous infection rather than antibodies produced by the newborn. Because currently no IgM assay for syphilis is recommended by the Centers for Disease Control and Prevention for newborn testing, we must deal with IgG test results.
Often initial management decisions are needed while the infant’s status is evolving. The questions to answer to make final decisions include the following2:
- Was the mother actively infected with Treponema pallidum during pregnancy?
- If so, was the mother appropriately treated and when?
- Does the infant have any clinical, laboratory, or radiographic evidence of syphilis?
- How do the mother’s and infant’s nontreponemal serologic titers (NTT) compare at delivery using the same test?
Note: All infants assessed for congenital syphilis need a full evaluation for HIV.
Managing the infant of a mother with positive tests3,4
All such neonates need an examination for evidence of congenital syphilis. The clinical signs of congenital syphilis in neonates include nonimmune hydrops, jaundice, hepatosplenomegaly, rhinitis, skin rash, and pseudoparalysis of extremity. Also, consider dark-field examination or polymerase chain reaction (PCR) of lesions (such as bullae) or secretions (nasal). If available, have the placenta examined histologically (silver stain) or by PCR (Clinical Laboratory Improvement Amendments–validated test). Skeletal radiographic surveys are more useful for stillborn than live born infants. (The complete algorithm can be found in Figure 3.10 of reference 4.)
Order a quantitative NTT, using the Venereal Disease Research Laboratory (VDRL) test or RPR test on neonatal serum. Umbilical cord blood is not appropriate because of potential maternal blood contamination, which could give a false-positive result, or Wharton’s jelly, which could give a false-negative result. Use of treponemal-specific tests that are used for maternal diagnosis – such as T. pallidum particle agglutination (TP-PA), T. pallidum enzyme-linked immunosorbent assay (TP-EIA), fluorescent treponemal antibody absorption (FTA-ABS) test, or T. pallidum chemiluminescence immunoassay (TP-CIA) – on neonatal serum is not recommended because of difficulties in interpretation.
Diagnostic results allow designation of an infant into one of four CDC categories: proven/highly probable syphilis; possible syphilis; syphilis less likely; and syphilis unlikely. Treatment recommendations are based on these categories.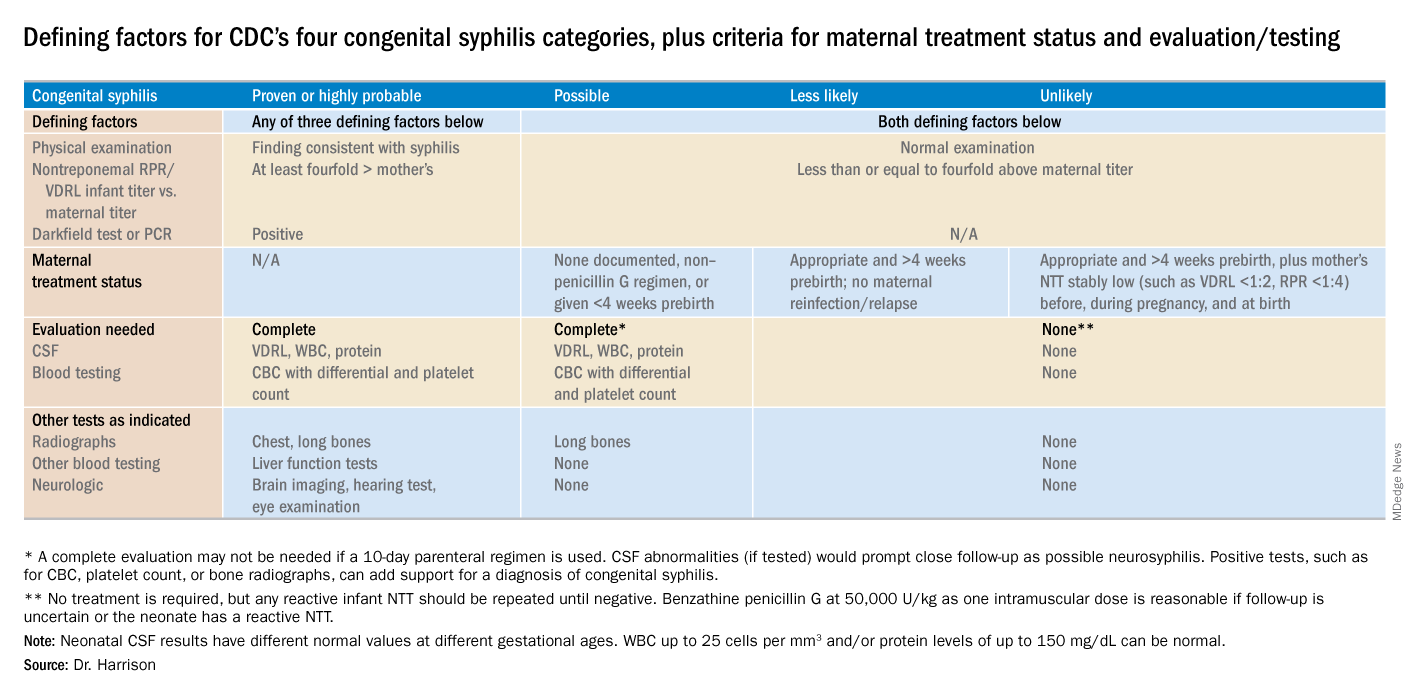
Proven or highly probable syphilis
There are two alternative recommended 10-day treatment regimens.
A. Aqueous crystalline penicillin G 100,000-150,000 U/kg per day by IV at 50,000 U/kg per dose, given every 12 hours through 7 days of age or every 8 hours if greater than 7 days old.
B. Procaine penicillin G at 50,000 U/kg per dose intramuscularly in one dose each day.
More than 1 day of missed therapy requires restarting a new 10-day course. Use of other antimicrobial agents (such as ampicillin) is not validated, so any empiric ampicillin initially given for possible sepsis does not count toward the 10-day penicillin regimen. If nonpenicillin drugs must be used, close serologic follow-up must occur to ensure adequacy of response to therapy.
Possible syphilis
There are three alternative regimens, the same two as in proven/highly probable syphilis (above) plus a single-dose option
A. Aqueous crystalline penicillin G, as described above.
B. Procaine penicillin G, as described above.
C. Benzathine penicillin G at 50,000 U/kg per dose intramuscularly in a single dose.
Note: To be eligible for regimen C, an infant must have a complete evaluation that is normal (cerebrospinal fluid [CSF] examination, long-bone radiographs, and complete blood count with platelet count) and follow-up must be assured. Exception: Neonates born to mothers with untreated early syphilis at the time of delivery are at increased risk for congenital syphilis, and the 10-day course of penicillin G may be considered even if the complete evaluation is normal and follow-up is certain.
Less likely syphilis
One antibiotic regimen is available, but no treatment also may be an option.
A. Benzathine penicillin G as described above.
B. If mother’s NTT has decreased at least fourfold after appropriate early syphilis therapy or remained stably low, which indicates latent syphilis (VDRL less than 1:2; RPR less than 1:4), no treatment is an option but requires repeat serology every 2-3 months until infant is 6 months old.
Unlikely syphilis
No treatment is recommended unless follow-up is uncertain, in which case it is appropriate to give the infant benzathine penicillin G as described above.
Infant with positive NTT at birth
All neonates with reactive NTT need careful follow-up examinations and repeat NTT every 2-3 months until nonreactive. NTT in infants who are not treated because of less likely or unlikely syphilis status should drop by 3 months and be nonreactive by 6 months; this indicates NTT was passively transferred maternal IgG. If NTT remains reactive at 6 months, the infant is likely infected and needs treatment. Persistent NTT at 6-12 months in treated neonates should trigger repeat CSF examination and infectious diseases consultation about a possible repeat of the 10-day penicillin G regimen. If the mother was seroreactive, but the newborn’s NTT was negative at birth, testing of the infant’s NTT needs repeating at 3 months to exclude the possibility that the congenital syphilis was incubating when prior testing occurred at birth. Note: Treponemal-specific tests are not useful in assessing treatment because detectable maternal IgG treponemal antibody can persist at least 15 months.
Neonates with abnormal CSF at birth
Repeat cerebrospinal fluid evaluation every 6 months until results normalize. Persistently reactive CSF VDRL or abnormal CSF indexes not caused by another known cause requires retreatment for possible neurosyphilis, as well as consultation with an expert.
Summary
NTT are the essential test for newborns and some degree of laboratory or imaging work up often are needed. Consider consulting an expert in infectious diseases and/or perinatology if the gray areas do not readily become clear. Treatment of the correct patients with the right drug for the right duration remains the goal, as usual.
Dr. Harrison is a professor of pediatrics at University of Missouri-Kansas City and Director of Research Affairs in the pediatric infectious diseases division at Children’s Mercy Hospital – Kansas City. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. MMWR. 2015 Nov 13;64(44);1241-5.
2. “Congenital Syphilis,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
3. “Syphilis During Pregnancy,” 2015 Sexually Transmitted Diseases Treatment Guidelines.
4. Syphilis – Section 3: Summaries of Infectious Diseases. Red Book Online. 2018.
Letter to the Editor: Strengthening the relationships between transferring and accepting surgeons
“Nobody is happy when a patient needs to be transferred.” As the general surgery group who receives requests for transfer of patients to our tertiary care hospital, we understand and sympathize with many of the issues raised in Dr. Puls’ article (“Rural Surgery – A view from the front lines” ‘I need to transfer this patient,” ACS Surgery News, September 2018, p. 7).
There is no doubt that sometimes patients benefit from support only available at a tertiary care center. The need can be for subspeciality surgical expertise, but many times it is driven by other available hospital-level support (critical care, interventional radiology, etc.).
Transfers are time consuming for physicians on both ends – while referring physicians have the responsibility of reaching out, accepting physicians have the responsibility of timely response to a request, regardless of other demands on their time and attention. We agree wholeheartedly with Dr. Puls’s argument that the phone call process “should not be delegated to the hospitalist or anyone else.” The benefit of speaking directly to the surgeon who has personally evaluated the patient cannot be overemphasized. When referrals for surgical care are initiated by the hospitalist or emergency department physician caring for a patient, there is almost always a lack of clarity around the surgical history, reason for transfer, and ongoing needs of the patient. It is our practice to request to speak to the surgeon who has evaluated and cared for the patient so we can fully understand the clinical course. It is the rare, typically life-threatening, situation in which we transfer patients without this crucial conversation.
Another crucial conversation, one in which the receiving physicians have room for improvement, is that of closing the loop after transfer. Dr. Puls recommended that there be periodic communication between the referring physician and the accepting physician, as well as closing the loop at the time the patient is discharged. There is a lack of “best practice” and infrastructure to support this work in many institutions, including ours, in part complicated by the variable EHRs utilized by individual hospitals. We believe the burden of this communication is shared by both parties and critical to optimal patient outcomes. At our hospital, we are currently working on standardizing this process and hope it will continue to strengthen the relationships we are building with our community surgeons.
At the end of the day, referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients, by optimally matching patient needs with appropriate resources. or this reason, we disagree with Dr. Puls’ statement that “accepting physicians at larger hospitals should be treated like gold.” The work of “networking” should not be placed solely on the shoulders of rural surgeons. We believe it is best practice for the tertiary care hospital team to visit their community hospitals to better understand their resources, rather than the other way around. The Atrium Health National Surgical Quality Improvement Program Collaborative has been a valuable platform for making these connections for hospitals within our system and provides infrastructure for ongoing collaboration. Surgeons at tertiary care centers should also make themselves available for phone consultation for the complicated patient for whom a surgeon may simply need a second opinion. Not all “transfer calls” result in a transfer, and if both parties agree that the patient can continue to receive the same care at the local hospital that is often in his or her best interest.
Strengthening relationships with our community surgeons will allow surgeons at tertiary care centers to partner with them to optimally match patient needs to available resources. We truly appreciate our referring surgeons and thank them for the incredible work they do in serving our communities. Without their care on the front lines, we would not be able to provide the complex care and support to patients who need it most.
I very much appreciate the comments made by Drs. Reinke, Matthews, Paton, and Schiffern of the Carolinas Medical Center, Atrium Health, regarding my commentary on a rural surgeon’s take on transferring patients. They have provided the important perspective of the surgeon at a tertiary care center accepting a transferred patient. They also point out some of the important responsibilities that accepting surgeons have regarding the patient transfer process. If all tertiary facilities had the philosophy described by Drs. Reinke, Matthews, Paton, and Schiffern regarding patient transfers, many more patients would benefit
I agree that more easily arranged phone consultations between a rural surgeon and a tertiary surgeon regarding the need for a potential patient transfer would be helpful. Sometimes the simple reassurance from a tertiary care surgeon that the rural surgeon is doing the right thing, and the comfort the patient and his/her family derives from knowing that their surgeon has spoken with a surgeon at a tertiary care center, can be enough to prevent the need for an immediate transfer.
I also agree that “closing the loop” after a transfer is an important responsibility of both the transferring surgeon and the accepting surgeon. This is difficult partly because everyone is busy, but also because of factors such as the incompatibility of EHRs. Perhaps if part of the transfer process involved the transferring surgeon and accepting surgeon exchanging cell phone numbers and email addresses, then a quick phone call, text, or email every couple of days could help to “close the loop.
I accept their mild criticism of my statement that “accepting physicians at larger hospitals should be treated like gold” since they really are saying that there is a shared responsibility between tertiary care surgeons and rural surgeons to develop relationships that allow for the optimal care of transferred patients. I couldn’t agree more with their statement that “referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients.” When we do this, we are treating the patient like gold, which is our ultimate objective.
Mark Puls, MD, FACS, is a general surgeon in Alpena, Mich. He serves as vice chair of the ACS Advisory Council for Rural Surgery. octor’s Name and Bio
I very much appreciate the comments made by Drs. Reinke, Matthews, Paton, and Schiffern of the Carolinas Medical Center, Atrium Health, regarding my commentary on a rural surgeon’s take on transferring patients. They have provided the important perspective of the surgeon at a tertiary care center accepting a transferred patient. They also point out some of the important responsibilities that accepting surgeons have regarding the patient transfer process. If all tertiary facilities had the philosophy described by Drs. Reinke, Matthews, Paton, and Schiffern regarding patient transfers, many more patients would benefit
I agree that more easily arranged phone consultations between a rural surgeon and a tertiary surgeon regarding the need for a potential patient transfer would be helpful. Sometimes the simple reassurance from a tertiary care surgeon that the rural surgeon is doing the right thing, and the comfort the patient and his/her family derives from knowing that their surgeon has spoken with a surgeon at a tertiary care center, can be enough to prevent the need for an immediate transfer.
I also agree that “closing the loop” after a transfer is an important responsibility of both the transferring surgeon and the accepting surgeon. This is difficult partly because everyone is busy, but also because of factors such as the incompatibility of EHRs. Perhaps if part of the transfer process involved the transferring surgeon and accepting surgeon exchanging cell phone numbers and email addresses, then a quick phone call, text, or email every couple of days could help to “close the loop.
I accept their mild criticism of my statement that “accepting physicians at larger hospitals should be treated like gold” since they really are saying that there is a shared responsibility between tertiary care surgeons and rural surgeons to develop relationships that allow for the optimal care of transferred patients. I couldn’t agree more with their statement that “referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients.” When we do this, we are treating the patient like gold, which is our ultimate objective.
Mark Puls, MD, FACS, is a general surgeon in Alpena, Mich. He serves as vice chair of the ACS Advisory Council for Rural Surgery. octor’s Name and Bio
I very much appreciate the comments made by Drs. Reinke, Matthews, Paton, and Schiffern of the Carolinas Medical Center, Atrium Health, regarding my commentary on a rural surgeon’s take on transferring patients. They have provided the important perspective of the surgeon at a tertiary care center accepting a transferred patient. They also point out some of the important responsibilities that accepting surgeons have regarding the patient transfer process. If all tertiary facilities had the philosophy described by Drs. Reinke, Matthews, Paton, and Schiffern regarding patient transfers, many more patients would benefit
I agree that more easily arranged phone consultations between a rural surgeon and a tertiary surgeon regarding the need for a potential patient transfer would be helpful. Sometimes the simple reassurance from a tertiary care surgeon that the rural surgeon is doing the right thing, and the comfort the patient and his/her family derives from knowing that their surgeon has spoken with a surgeon at a tertiary care center, can be enough to prevent the need for an immediate transfer.
I also agree that “closing the loop” after a transfer is an important responsibility of both the transferring surgeon and the accepting surgeon. This is difficult partly because everyone is busy, but also because of factors such as the incompatibility of EHRs. Perhaps if part of the transfer process involved the transferring surgeon and accepting surgeon exchanging cell phone numbers and email addresses, then a quick phone call, text, or email every couple of days could help to “close the loop.
I accept their mild criticism of my statement that “accepting physicians at larger hospitals should be treated like gold” since they really are saying that there is a shared responsibility between tertiary care surgeons and rural surgeons to develop relationships that allow for the optimal care of transferred patients. I couldn’t agree more with their statement that “referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients.” When we do this, we are treating the patient like gold, which is our ultimate objective.
Mark Puls, MD, FACS, is a general surgeon in Alpena, Mich. He serves as vice chair of the ACS Advisory Council for Rural Surgery. octor’s Name and Bio
“Nobody is happy when a patient needs to be transferred.” As the general surgery group who receives requests for transfer of patients to our tertiary care hospital, we understand and sympathize with many of the issues raised in Dr. Puls’ article (“Rural Surgery – A view from the front lines” ‘I need to transfer this patient,” ACS Surgery News, September 2018, p. 7).
There is no doubt that sometimes patients benefit from support only available at a tertiary care center. The need can be for subspeciality surgical expertise, but many times it is driven by other available hospital-level support (critical care, interventional radiology, etc.).
Transfers are time consuming for physicians on both ends – while referring physicians have the responsibility of reaching out, accepting physicians have the responsibility of timely response to a request, regardless of other demands on their time and attention. We agree wholeheartedly with Dr. Puls’s argument that the phone call process “should not be delegated to the hospitalist or anyone else.” The benefit of speaking directly to the surgeon who has personally evaluated the patient cannot be overemphasized. When referrals for surgical care are initiated by the hospitalist or emergency department physician caring for a patient, there is almost always a lack of clarity around the surgical history, reason for transfer, and ongoing needs of the patient. It is our practice to request to speak to the surgeon who has evaluated and cared for the patient so we can fully understand the clinical course. It is the rare, typically life-threatening, situation in which we transfer patients without this crucial conversation.
Another crucial conversation, one in which the receiving physicians have room for improvement, is that of closing the loop after transfer. Dr. Puls recommended that there be periodic communication between the referring physician and the accepting physician, as well as closing the loop at the time the patient is discharged. There is a lack of “best practice” and infrastructure to support this work in many institutions, including ours, in part complicated by the variable EHRs utilized by individual hospitals. We believe the burden of this communication is shared by both parties and critical to optimal patient outcomes. At our hospital, we are currently working on standardizing this process and hope it will continue to strengthen the relationships we are building with our community surgeons.
At the end of the day, referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients, by optimally matching patient needs with appropriate resources. or this reason, we disagree with Dr. Puls’ statement that “accepting physicians at larger hospitals should be treated like gold.” The work of “networking” should not be placed solely on the shoulders of rural surgeons. We believe it is best practice for the tertiary care hospital team to visit their community hospitals to better understand their resources, rather than the other way around. The Atrium Health National Surgical Quality Improvement Program Collaborative has been a valuable platform for making these connections for hospitals within our system and provides infrastructure for ongoing collaboration. Surgeons at tertiary care centers should also make themselves available for phone consultation for the complicated patient for whom a surgeon may simply need a second opinion. Not all “transfer calls” result in a transfer, and if both parties agree that the patient can continue to receive the same care at the local hospital that is often in his or her best interest.
Strengthening relationships with our community surgeons will allow surgeons at tertiary care centers to partner with them to optimally match patient needs to available resources. We truly appreciate our referring surgeons and thank them for the incredible work they do in serving our communities. Without their care on the front lines, we would not be able to provide the complex care and support to patients who need it most.
“Nobody is happy when a patient needs to be transferred.” As the general surgery group who receives requests for transfer of patients to our tertiary care hospital, we understand and sympathize with many of the issues raised in Dr. Puls’ article (“Rural Surgery – A view from the front lines” ‘I need to transfer this patient,” ACS Surgery News, September 2018, p. 7).
There is no doubt that sometimes patients benefit from support only available at a tertiary care center. The need can be for subspeciality surgical expertise, but many times it is driven by other available hospital-level support (critical care, interventional radiology, etc.).
Transfers are time consuming for physicians on both ends – while referring physicians have the responsibility of reaching out, accepting physicians have the responsibility of timely response to a request, regardless of other demands on their time and attention. We agree wholeheartedly with Dr. Puls’s argument that the phone call process “should not be delegated to the hospitalist or anyone else.” The benefit of speaking directly to the surgeon who has personally evaluated the patient cannot be overemphasized. When referrals for surgical care are initiated by the hospitalist or emergency department physician caring for a patient, there is almost always a lack of clarity around the surgical history, reason for transfer, and ongoing needs of the patient. It is our practice to request to speak to the surgeon who has evaluated and cared for the patient so we can fully understand the clinical course. It is the rare, typically life-threatening, situation in which we transfer patients without this crucial conversation.
Another crucial conversation, one in which the receiving physicians have room for improvement, is that of closing the loop after transfer. Dr. Puls recommended that there be periodic communication between the referring physician and the accepting physician, as well as closing the loop at the time the patient is discharged. There is a lack of “best practice” and infrastructure to support this work in many institutions, including ours, in part complicated by the variable EHRs utilized by individual hospitals. We believe the burden of this communication is shared by both parties and critical to optimal patient outcomes. At our hospital, we are currently working on standardizing this process and hope it will continue to strengthen the relationships we are building with our community surgeons.
At the end of the day, referring physicians and accepting physicians should function as team members with a shared goal – to always provide excellent surgical care to patients, by optimally matching patient needs with appropriate resources. or this reason, we disagree with Dr. Puls’ statement that “accepting physicians at larger hospitals should be treated like gold.” The work of “networking” should not be placed solely on the shoulders of rural surgeons. We believe it is best practice for the tertiary care hospital team to visit their community hospitals to better understand their resources, rather than the other way around. The Atrium Health National Surgical Quality Improvement Program Collaborative has been a valuable platform for making these connections for hospitals within our system and provides infrastructure for ongoing collaboration. Surgeons at tertiary care centers should also make themselves available for phone consultation for the complicated patient for whom a surgeon may simply need a second opinion. Not all “transfer calls” result in a transfer, and if both parties agree that the patient can continue to receive the same care at the local hospital that is often in his or her best interest.
Strengthening relationships with our community surgeons will allow surgeons at tertiary care centers to partner with them to optimally match patient needs to available resources. We truly appreciate our referring surgeons and thank them for the incredible work they do in serving our communities. Without their care on the front lines, we would not be able to provide the complex care and support to patients who need it most.