User login
Dermatological improvements translate to enhanced QoL in PsA
Key clinical point: Dermatological symptoms are substantially associated with the quality of life (QoL) in patients with active psoriatic arthritis (PsA) and improvements in dermatology measures could translate to clinically meaningful improvements in their QoL.
Major finding: Itch severity item (ISI) scores of 7-10, Physician’s Global Assessment of Psoriasis (PGA-PsO) scores of 4, and Patient’s Global Joint and Skin Assessment-Visual Analog Scale (PGJS-VAS) scores of 90-100 mm corresponded with Dermatology Life Quality Index (DLQI) scores categorized as having a very large effect on a patient’s life. An improvement of ≥3 points in ISI, ≥2 points in PGA-PsO, and ≥40 mm in PGJS-VAS translated to a clinically meaningful improvement in DLQI scores.
Study details: This post hoc analysis of two phase 3 studies, OPAL Broaden and OPAL Beyond, included 816 patients with active PsA and an inadequate response to previous therapies who received tofacitinib, adalimumab, or placebo.
Disclosures: This study was funded by Pfizer. Four authors reported being employees or stockholders of Pfizer. The other authors reported ties with several sources, including Pfizer.
Source: Taylor PC et al. Relationships of dermatologic symptoms and quality of life in patients with psoriatic arthritis: analysis of two tofacitinib phase III studies. J Dermatol Treat. 2022 (Apr 11). Doi: 10.1080/09546634.2022.2060924
Key clinical point: Dermatological symptoms are substantially associated with the quality of life (QoL) in patients with active psoriatic arthritis (PsA) and improvements in dermatology measures could translate to clinically meaningful improvements in their QoL.
Major finding: Itch severity item (ISI) scores of 7-10, Physician’s Global Assessment of Psoriasis (PGA-PsO) scores of 4, and Patient’s Global Joint and Skin Assessment-Visual Analog Scale (PGJS-VAS) scores of 90-100 mm corresponded with Dermatology Life Quality Index (DLQI) scores categorized as having a very large effect on a patient’s life. An improvement of ≥3 points in ISI, ≥2 points in PGA-PsO, and ≥40 mm in PGJS-VAS translated to a clinically meaningful improvement in DLQI scores.
Study details: This post hoc analysis of two phase 3 studies, OPAL Broaden and OPAL Beyond, included 816 patients with active PsA and an inadequate response to previous therapies who received tofacitinib, adalimumab, or placebo.
Disclosures: This study was funded by Pfizer. Four authors reported being employees or stockholders of Pfizer. The other authors reported ties with several sources, including Pfizer.
Source: Taylor PC et al. Relationships of dermatologic symptoms and quality of life in patients with psoriatic arthritis: analysis of two tofacitinib phase III studies. J Dermatol Treat. 2022 (Apr 11). Doi: 10.1080/09546634.2022.2060924
Key clinical point: Dermatological symptoms are substantially associated with the quality of life (QoL) in patients with active psoriatic arthritis (PsA) and improvements in dermatology measures could translate to clinically meaningful improvements in their QoL.
Major finding: Itch severity item (ISI) scores of 7-10, Physician’s Global Assessment of Psoriasis (PGA-PsO) scores of 4, and Patient’s Global Joint and Skin Assessment-Visual Analog Scale (PGJS-VAS) scores of 90-100 mm corresponded with Dermatology Life Quality Index (DLQI) scores categorized as having a very large effect on a patient’s life. An improvement of ≥3 points in ISI, ≥2 points in PGA-PsO, and ≥40 mm in PGJS-VAS translated to a clinically meaningful improvement in DLQI scores.
Study details: This post hoc analysis of two phase 3 studies, OPAL Broaden and OPAL Beyond, included 816 patients with active PsA and an inadequate response to previous therapies who received tofacitinib, adalimumab, or placebo.
Disclosures: This study was funded by Pfizer. Four authors reported being employees or stockholders of Pfizer. The other authors reported ties with several sources, including Pfizer.
Source: Taylor PC et al. Relationships of dermatologic symptoms and quality of life in patients with psoriatic arthritis: analysis of two tofacitinib phase III studies. J Dermatol Treat. 2022 (Apr 11). Doi: 10.1080/09546634.2022.2060924
PsA: Rapid and sustained improvement in pain with upadacitinib
Key clinical point: Upadacitinib led to early, clinically meaningful, and sustained improvements in pain in patients with psoriatic arthritis (PsA) and an inadequate response to prior biological or nonbiological disease-modifying antirheumatic drugs (b/nbDMARD).
Major finding: A significantly higher proportion of patients receiving 15 mg upadacitinib vs. placebo achieved ≥30%, ≥50%, and ≥70% reductions in pain as early as at 2 weeks (P < .05), with improvements sustained till week 56.
Study details: Findings are from an analysis of 2 phase 3 trials, SELECT-PsA 1 and SELECT-PsA 2 , including 1113 patients with active PsA and an inadequate response to ≥1 nb/bDMARD who were randomly assigned to receive 15 mg upadacitinib once daily, placebo, or adalimumab (only in the SELECT-PsA 1 study).
Disclosures: This study was sponsored by AbbVie. Eight authors declared serving as employees or owning stock/stock options in AbbVie and other authors reported ties with several sources, including AbbVie.
Source: McInnes IB et al. Effect of upadacitinib on reducing pain in patients with active psoriatic arthritis or ankylosing spondylitis: Post hoc analysis of three randomised clinical trials. RMD Open. 2022;8:e002049 (Mar 24). Doi: 10.1136/rmdopen-2021-002049
Key clinical point: Upadacitinib led to early, clinically meaningful, and sustained improvements in pain in patients with psoriatic arthritis (PsA) and an inadequate response to prior biological or nonbiological disease-modifying antirheumatic drugs (b/nbDMARD).
Major finding: A significantly higher proportion of patients receiving 15 mg upadacitinib vs. placebo achieved ≥30%, ≥50%, and ≥70% reductions in pain as early as at 2 weeks (P < .05), with improvements sustained till week 56.
Study details: Findings are from an analysis of 2 phase 3 trials, SELECT-PsA 1 and SELECT-PsA 2 , including 1113 patients with active PsA and an inadequate response to ≥1 nb/bDMARD who were randomly assigned to receive 15 mg upadacitinib once daily, placebo, or adalimumab (only in the SELECT-PsA 1 study).
Disclosures: This study was sponsored by AbbVie. Eight authors declared serving as employees or owning stock/stock options in AbbVie and other authors reported ties with several sources, including AbbVie.
Source: McInnes IB et al. Effect of upadacitinib on reducing pain in patients with active psoriatic arthritis or ankylosing spondylitis: Post hoc analysis of three randomised clinical trials. RMD Open. 2022;8:e002049 (Mar 24). Doi: 10.1136/rmdopen-2021-002049
Key clinical point: Upadacitinib led to early, clinically meaningful, and sustained improvements in pain in patients with psoriatic arthritis (PsA) and an inadequate response to prior biological or nonbiological disease-modifying antirheumatic drugs (b/nbDMARD).
Major finding: A significantly higher proportion of patients receiving 15 mg upadacitinib vs. placebo achieved ≥30%, ≥50%, and ≥70% reductions in pain as early as at 2 weeks (P < .05), with improvements sustained till week 56.
Study details: Findings are from an analysis of 2 phase 3 trials, SELECT-PsA 1 and SELECT-PsA 2 , including 1113 patients with active PsA and an inadequate response to ≥1 nb/bDMARD who were randomly assigned to receive 15 mg upadacitinib once daily, placebo, or adalimumab (only in the SELECT-PsA 1 study).
Disclosures: This study was sponsored by AbbVie. Eight authors declared serving as employees or owning stock/stock options in AbbVie and other authors reported ties with several sources, including AbbVie.
Source: McInnes IB et al. Effect of upadacitinib on reducing pain in patients with active psoriatic arthritis or ankylosing spondylitis: Post hoc analysis of three randomised clinical trials. RMD Open. 2022;8:e002049 (Mar 24). Doi: 10.1136/rmdopen-2021-002049
Robust and sustained improvement with guselkumab in a diverse population of patients with PsA
Key clinical point: A dose of 100 mg guselkumab every 4 weeks (Q4W) or 8 weeks (Q8W) effectively improved the signs and symptoms of psoriatic arthritis (PsA) at week 24, with effects sustained till week 52, in subgroups of patients with diverse baseline characteristics.
Major finding: At week 24, a higher proportion of patients receiving guselkumab Q4W/Q8W (62%/60%) vs. placebo (29%) achieved ≥20% improvement in the American College of Rheumatology (ACR20) criteria, with guselkumab demonstrating superior efficacy over placebo regardless of baseline patient demographics, disease characteristics, or medication use, with effects sustained till week 52.
Study details: This post hoc analysis of two phase 3 trials, DISCOVER-1, and DISCOVER-2, and included 1120 patients with active PsA with an inadequate response to standard therapies who were randomly assigned to receive subcutaneous 100 mg guselkumab Q4W, 100 mg guselkumab Q8W, or placebo.
Disclosures: This study was funded by Janssen Research & Development, LLC. Six authors declared being employees of Janssen and owned stocks in Johnson & Johnson, the parent of Janssen. The other authors reported ties with several sources, including Janssen.
Source: Ritchlin CT et al. Sustained and improved guselkumab response in patients with active psoriatic arthritis regardless of baseline demographic and disease characteristics: Pooled results through week 52 of two phase III, randomised, placebo-controlled studies. RMD Open. 2022;8:e002195 (Mar 16). Doi: 10.1136/rmdopen-2022-002195
Key clinical point: A dose of 100 mg guselkumab every 4 weeks (Q4W) or 8 weeks (Q8W) effectively improved the signs and symptoms of psoriatic arthritis (PsA) at week 24, with effects sustained till week 52, in subgroups of patients with diverse baseline characteristics.
Major finding: At week 24, a higher proportion of patients receiving guselkumab Q4W/Q8W (62%/60%) vs. placebo (29%) achieved ≥20% improvement in the American College of Rheumatology (ACR20) criteria, with guselkumab demonstrating superior efficacy over placebo regardless of baseline patient demographics, disease characteristics, or medication use, with effects sustained till week 52.
Study details: This post hoc analysis of two phase 3 trials, DISCOVER-1, and DISCOVER-2, and included 1120 patients with active PsA with an inadequate response to standard therapies who were randomly assigned to receive subcutaneous 100 mg guselkumab Q4W, 100 mg guselkumab Q8W, or placebo.
Disclosures: This study was funded by Janssen Research & Development, LLC. Six authors declared being employees of Janssen and owned stocks in Johnson & Johnson, the parent of Janssen. The other authors reported ties with several sources, including Janssen.
Source: Ritchlin CT et al. Sustained and improved guselkumab response in patients with active psoriatic arthritis regardless of baseline demographic and disease characteristics: Pooled results through week 52 of two phase III, randomised, placebo-controlled studies. RMD Open. 2022;8:e002195 (Mar 16). Doi: 10.1136/rmdopen-2022-002195
Key clinical point: A dose of 100 mg guselkumab every 4 weeks (Q4W) or 8 weeks (Q8W) effectively improved the signs and symptoms of psoriatic arthritis (PsA) at week 24, with effects sustained till week 52, in subgroups of patients with diverse baseline characteristics.
Major finding: At week 24, a higher proportion of patients receiving guselkumab Q4W/Q8W (62%/60%) vs. placebo (29%) achieved ≥20% improvement in the American College of Rheumatology (ACR20) criteria, with guselkumab demonstrating superior efficacy over placebo regardless of baseline patient demographics, disease characteristics, or medication use, with effects sustained till week 52.
Study details: This post hoc analysis of two phase 3 trials, DISCOVER-1, and DISCOVER-2, and included 1120 patients with active PsA with an inadequate response to standard therapies who were randomly assigned to receive subcutaneous 100 mg guselkumab Q4W, 100 mg guselkumab Q8W, or placebo.
Disclosures: This study was funded by Janssen Research & Development, LLC. Six authors declared being employees of Janssen and owned stocks in Johnson & Johnson, the parent of Janssen. The other authors reported ties with several sources, including Janssen.
Source: Ritchlin CT et al. Sustained and improved guselkumab response in patients with active psoriatic arthritis regardless of baseline demographic and disease characteristics: Pooled results through week 52 of two phase III, randomised, placebo-controlled studies. RMD Open. 2022;8:e002195 (Mar 16). Doi: 10.1136/rmdopen-2022-002195
IL-17 inhibitors associated with higher treatment persistence in PsA
Key clinical point: Interleukin-17 (IL-17) inhibitors were associated with higher treatment persistence than tumor necrosis factor (TNF) inhibitors or IL-12/23 inhibitors in patients with psoriatic arthritis (PsA) who initiated treatment with biologics.
Major finding: Treatment persistence was higher with IL-17 inhibitors than TNF inhibitors (weighted hazard ratio [HR] 0.70; P < .001) or IL-12/23 inhibitor (weighted HR 0.69; P < .001); however, IL-12/23 and TNF inhibitors showed similar persistence (P = .70).
Study details: This nationwide cohort study included 16,892 adults with psoriasis and 6531 adults with PsA who initiated first-line treatment with TNF, IL-12/23, or IL-17 inhibitors.
Disclosures: The study did not report any source of funding. P Claudepierre reported receiving consulting fees and serving as an investigator for several pharmaceutical companies.
Source: Vegas LP et al. Long-term persistence of first-line biologics for patients with psoriasis and psoriatic arthritis in the french health insurance database. JAMA Dermatol. 2022 (Mar 23). Doi: 10.1001/jamadermatol.2022.0364
Key clinical point: Interleukin-17 (IL-17) inhibitors were associated with higher treatment persistence than tumor necrosis factor (TNF) inhibitors or IL-12/23 inhibitors in patients with psoriatic arthritis (PsA) who initiated treatment with biologics.
Major finding: Treatment persistence was higher with IL-17 inhibitors than TNF inhibitors (weighted hazard ratio [HR] 0.70; P < .001) or IL-12/23 inhibitor (weighted HR 0.69; P < .001); however, IL-12/23 and TNF inhibitors showed similar persistence (P = .70).
Study details: This nationwide cohort study included 16,892 adults with psoriasis and 6531 adults with PsA who initiated first-line treatment with TNF, IL-12/23, or IL-17 inhibitors.
Disclosures: The study did not report any source of funding. P Claudepierre reported receiving consulting fees and serving as an investigator for several pharmaceutical companies.
Source: Vegas LP et al. Long-term persistence of first-line biologics for patients with psoriasis and psoriatic arthritis in the french health insurance database. JAMA Dermatol. 2022 (Mar 23). Doi: 10.1001/jamadermatol.2022.0364
Key clinical point: Interleukin-17 (IL-17) inhibitors were associated with higher treatment persistence than tumor necrosis factor (TNF) inhibitors or IL-12/23 inhibitors in patients with psoriatic arthritis (PsA) who initiated treatment with biologics.
Major finding: Treatment persistence was higher with IL-17 inhibitors than TNF inhibitors (weighted hazard ratio [HR] 0.70; P < .001) or IL-12/23 inhibitor (weighted HR 0.69; P < .001); however, IL-12/23 and TNF inhibitors showed similar persistence (P = .70).
Study details: This nationwide cohort study included 16,892 adults with psoriasis and 6531 adults with PsA who initiated first-line treatment with TNF, IL-12/23, or IL-17 inhibitors.
Disclosures: The study did not report any source of funding. P Claudepierre reported receiving consulting fees and serving as an investigator for several pharmaceutical companies.
Source: Vegas LP et al. Long-term persistence of first-line biologics for patients with psoriasis and psoriatic arthritis in the french health insurance database. JAMA Dermatol. 2022 (Mar 23). Doi: 10.1001/jamadermatol.2022.0364
Clinical Edge Journal Scan Commentary: Type 2 DM May 2022
Heart failure with preserved ejection fraction (HFpEF) is common in elderly adults with type 2 diabetes (T2D), and these individuals are at high risk for frailty and cognitive impairment. Empagliflozin has been shown to reduce cardiovascular death or hospitalization for heart failure in individuals with HFpEF with or without diabetes, but little is known about the impact of empagliflozin on cognition in patients with diabetes and HFpEF. In a prospective observation study of 162 frail older adults with T2D and HFpEF, Mone and colleagues reported that after receiving empagliflozin for 1 month, there was a significant improvement in the Montreal Cognitive Assessment score, but no improvement was seen with metformin or insulin. Although the study was limited by its observational design, small sample size, and short follow-up, it indicates that improved cognition may be another unexpected benefit of empagliflozin in patients with HFpEF.
The Action to Control Cardiovascular Risk in Diabetes (ACCORD) study continues to provide valuable information for the management of T2D. ACCORD Lipid had previously shown that fenofibrate vs. placebo added to simvastatin did not reduce major atherosclerotic cardiovascular events in about 5500 patients with T2D who were at high risk for cardiovascular disease. Ferreira and colleagues have now reported that fenofibrate in ACCORD Lipid reduced hospitalization for heart failure or cardiovascular death by 18%, with the benefit predominantly in those treated with standard glucose-lowering therapy. This analysis was done post hoc and is hypothesis-generating for fenofibrate reducing HF-related events. The soon to be completed PROMINENT study of pemafibrate includes a secondary composite cardiovascular outcome with hospitalization for heart failure as a component, so more information regarding the impact of fibrates on heart failure will be available soon.
Diabetes is associated with a threefold greater risk for stroke and microvascular disease. In another analysis of ACCORD, Kaze and colleagues reported that a higher urine albumin‐to‐creatinine ratio and a lower estimated glomerular filtration rate were each independently associated with an increased risk for stroke. Although further adequately powered studies are required, this analysis suggests that prevention of kidney disease and its progression may help mitigate the risk for stroke in people with T2D.
People with severe mental illness (SMI), such as schizophrenia, bipolar disorder, or depression, are at increased risk for T2D, but it is unknown whether they are more likely to develop the complications of diabetes. Scheuer and colleagues published data from a large nationwide registry in Denmark. They found that, compared with people without SMI, people with SMI were more likely to develop nephropathy or cardiovascular disease, have an amputation, and that the nephropathy and cardiovascular disease occurred at younger ages in those with SMI. Although there are limitations with registry data, this study supports diabetes guidelines that recommend cardiorenal protection with sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide 1 (GLP-1) receptor agonists in patients with T2D who are at high risk for nephropathy progression and cardiovascular disease. Because this study suggests that SMI along with T2D confers greater risk for nephropathy and cardiovascular disease at younger ages, perhaps we should consider these cardiorenal protective agents early on in persons with T2D and SMI.
Heart failure with preserved ejection fraction (HFpEF) is common in elderly adults with type 2 diabetes (T2D), and these individuals are at high risk for frailty and cognitive impairment. Empagliflozin has been shown to reduce cardiovascular death or hospitalization for heart failure in individuals with HFpEF with or without diabetes, but little is known about the impact of empagliflozin on cognition in patients with diabetes and HFpEF. In a prospective observation study of 162 frail older adults with T2D and HFpEF, Mone and colleagues reported that after receiving empagliflozin for 1 month, there was a significant improvement in the Montreal Cognitive Assessment score, but no improvement was seen with metformin or insulin. Although the study was limited by its observational design, small sample size, and short follow-up, it indicates that improved cognition may be another unexpected benefit of empagliflozin in patients with HFpEF.
The Action to Control Cardiovascular Risk in Diabetes (ACCORD) study continues to provide valuable information for the management of T2D. ACCORD Lipid had previously shown that fenofibrate vs. placebo added to simvastatin did not reduce major atherosclerotic cardiovascular events in about 5500 patients with T2D who were at high risk for cardiovascular disease. Ferreira and colleagues have now reported that fenofibrate in ACCORD Lipid reduced hospitalization for heart failure or cardiovascular death by 18%, with the benefit predominantly in those treated with standard glucose-lowering therapy. This analysis was done post hoc and is hypothesis-generating for fenofibrate reducing HF-related events. The soon to be completed PROMINENT study of pemafibrate includes a secondary composite cardiovascular outcome with hospitalization for heart failure as a component, so more information regarding the impact of fibrates on heart failure will be available soon.
Diabetes is associated with a threefold greater risk for stroke and microvascular disease. In another analysis of ACCORD, Kaze and colleagues reported that a higher urine albumin‐to‐creatinine ratio and a lower estimated glomerular filtration rate were each independently associated with an increased risk for stroke. Although further adequately powered studies are required, this analysis suggests that prevention of kidney disease and its progression may help mitigate the risk for stroke in people with T2D.
People with severe mental illness (SMI), such as schizophrenia, bipolar disorder, or depression, are at increased risk for T2D, but it is unknown whether they are more likely to develop the complications of diabetes. Scheuer and colleagues published data from a large nationwide registry in Denmark. They found that, compared with people without SMI, people with SMI were more likely to develop nephropathy or cardiovascular disease, have an amputation, and that the nephropathy and cardiovascular disease occurred at younger ages in those with SMI. Although there are limitations with registry data, this study supports diabetes guidelines that recommend cardiorenal protection with sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide 1 (GLP-1) receptor agonists in patients with T2D who are at high risk for nephropathy progression and cardiovascular disease. Because this study suggests that SMI along with T2D confers greater risk for nephropathy and cardiovascular disease at younger ages, perhaps we should consider these cardiorenal protective agents early on in persons with T2D and SMI.
Heart failure with preserved ejection fraction (HFpEF) is common in elderly adults with type 2 diabetes (T2D), and these individuals are at high risk for frailty and cognitive impairment. Empagliflozin has been shown to reduce cardiovascular death or hospitalization for heart failure in individuals with HFpEF with or without diabetes, but little is known about the impact of empagliflozin on cognition in patients with diabetes and HFpEF. In a prospective observation study of 162 frail older adults with T2D and HFpEF, Mone and colleagues reported that after receiving empagliflozin for 1 month, there was a significant improvement in the Montreal Cognitive Assessment score, but no improvement was seen with metformin or insulin. Although the study was limited by its observational design, small sample size, and short follow-up, it indicates that improved cognition may be another unexpected benefit of empagliflozin in patients with HFpEF.
The Action to Control Cardiovascular Risk in Diabetes (ACCORD) study continues to provide valuable information for the management of T2D. ACCORD Lipid had previously shown that fenofibrate vs. placebo added to simvastatin did not reduce major atherosclerotic cardiovascular events in about 5500 patients with T2D who were at high risk for cardiovascular disease. Ferreira and colleagues have now reported that fenofibrate in ACCORD Lipid reduced hospitalization for heart failure or cardiovascular death by 18%, with the benefit predominantly in those treated with standard glucose-lowering therapy. This analysis was done post hoc and is hypothesis-generating for fenofibrate reducing HF-related events. The soon to be completed PROMINENT study of pemafibrate includes a secondary composite cardiovascular outcome with hospitalization for heart failure as a component, so more information regarding the impact of fibrates on heart failure will be available soon.
Diabetes is associated with a threefold greater risk for stroke and microvascular disease. In another analysis of ACCORD, Kaze and colleagues reported that a higher urine albumin‐to‐creatinine ratio and a lower estimated glomerular filtration rate were each independently associated with an increased risk for stroke. Although further adequately powered studies are required, this analysis suggests that prevention of kidney disease and its progression may help mitigate the risk for stroke in people with T2D.
People with severe mental illness (SMI), such as schizophrenia, bipolar disorder, or depression, are at increased risk for T2D, but it is unknown whether they are more likely to develop the complications of diabetes. Scheuer and colleagues published data from a large nationwide registry in Denmark. They found that, compared with people without SMI, people with SMI were more likely to develop nephropathy or cardiovascular disease, have an amputation, and that the nephropathy and cardiovascular disease occurred at younger ages in those with SMI. Although there are limitations with registry data, this study supports diabetes guidelines that recommend cardiorenal protection with sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide 1 (GLP-1) receptor agonists in patients with T2D who are at high risk for nephropathy progression and cardiovascular disease. Because this study suggests that SMI along with T2D confers greater risk for nephropathy and cardiovascular disease at younger ages, perhaps we should consider these cardiorenal protective agents early on in persons with T2D and SMI.
How are maternal and neonatal outcomes impacted by the contemporary practice of operative vaginal delivery?
Muraca GM, Boutin A, Razaz N, et al. Maternal and neonatal trauma following operative vaginal delivery. CMAJ. 2022;194:E1-E12. doi: 10.1503/cmaj.210841.
EXPERT COMMENTARY
Operative vaginal delivery is used to achieve and expedite safe vaginal birth while avoiding CD and its associated morbidities.1,2 Despite support from the American College of Obstetricians and Gynecologists (ACOG) for the use of OVD as an alternative to CD, OVD was used in only 3% of all US births in 2013, a shift from approximately 30% in 1987.1,3 Reported complications of OVD are biased by the level of experience of the operator, changes in practice, and by misinterpretation of the counterfactual.1
Outcomes of OVD should be compared with appropriate reference groups, namely, with second-stage CD births rather than with spontaneous vaginal births.4 With decreasing rates of OVD, evidence of contemporary data is needed on appropriately compared perinatal outcomes.4
Details of the study
Muraca and colleagues conducted an observational cohort study of births in Canada between 2013 and 2019 to assess the incidence of maternal and neonatal trauma following OVD. They used composites defined a priori— stratified by instrument, region, level of obstetric care, and institutional OVD volume.
Results. Among 1,326,191 live or stillbirths, 2.9% were attempted forceps deliveries and 8.4% were attempted vacuum deliveries. Following forceps delivery, the maternal trauma rate was 25.3% (95% confidence interval [CI], 24.8%–25.7%), and the neonatal trauma rate was 9.6 per 1,000 live births (95% CI, 8.6–10.6). Following vacuum delivery, maternal and neonatal trauma rates were 13.2% (95% CI, 13.0%–13.4%) and 9.6 per 1,000 live births (95% CI, 9.0–10.2), respectively. Maternal trauma was driven by higher order perineal lacerations. Some association was seen between increased forceps volume and decreased maternal trauma rates.
The authors concluded that in Canada, rates of maternal and neonatal trauma following OVD are higher than previously reported in consensus statements.
Study strengths and limitations
This large contemporary study uniquely stratified perinatal outcomes following OVD. The outcomes are well defined and meaningful, but some limitations affect the generalizability of the findings.
First, stillbirths were included for the maternal composite outcome, yet the incidence of this within the study population is not reported. Operative vaginal deliveries that involve stillbirths can be complex; a subgroup analysis excluding these would aid in interpretation.
Second, complicated OVDs, including sequential use of forceps and vacuum and OVDs from midpelvic station, were included; ACOG recommends against both these practices in routine circumstances due to known increases in maternal and neonatal morbidity.1 As such, the inclusion of these OVDs may bias results away from the null.
Finally, despite discussing the role of episiotomy, the episiotomy rate in this cohort is not reported.
Despite these limitations, the study by Muraca and colleagues is a positive step forward toward understanding the role of OVD in contemporary obstetric practice, and it uniquely ascertains the impact of OVD volume outcomes that previously had been an elusive exposure ●
While it is important to understand perinatal outcomes following OVD in a contemporary cohort, utilizing the correct cohort and reference group is critical.4 Risks for maternal and neonatal trauma follow OVD; however, outcomes vary based on appropriate selection of OVD candidates and adherence to recommended national guidelines.1,4 The infrequency of OVD raises concerns regarding adequate training for obstetricians, which should be prioritized so that they can offer OVD as a safe alternative to CD birth.3
HAYLEY E. MILLER, MD, AND DANIELLE M. PANELLI, MD
- American College of Obstetricians and Gynecologists. Operative vaginal birth: ACOG practice bulletin, number 219. Obstet Gynecol. 2020;135:e149-e159.
- Spong CY, Berghella V, Wenstrom KD, et al. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists workshop. Obstet Gynecol. 2012;120:1181-1193.
- Zahniser SC, Kendrick JS, Franks AL, et al. Trends in obstetric operative procedures, 1980 to 1987. Am J Public Health. 1992;82:1340-1344.
- Panelli DM, Leonard SA, Joudi N, et al. Severe maternal and neonatal morbidity after attempted operative vaginal delivery. Am J Obstet Gynecol MFM. 2021;3: 100339.
Muraca GM, Boutin A, Razaz N, et al. Maternal and neonatal trauma following operative vaginal delivery. CMAJ. 2022;194:E1-E12. doi: 10.1503/cmaj.210841.
EXPERT COMMENTARY
Operative vaginal delivery is used to achieve and expedite safe vaginal birth while avoiding CD and its associated morbidities.1,2 Despite support from the American College of Obstetricians and Gynecologists (ACOG) for the use of OVD as an alternative to CD, OVD was used in only 3% of all US births in 2013, a shift from approximately 30% in 1987.1,3 Reported complications of OVD are biased by the level of experience of the operator, changes in practice, and by misinterpretation of the counterfactual.1
Outcomes of OVD should be compared with appropriate reference groups, namely, with second-stage CD births rather than with spontaneous vaginal births.4 With decreasing rates of OVD, evidence of contemporary data is needed on appropriately compared perinatal outcomes.4
Details of the study
Muraca and colleagues conducted an observational cohort study of births in Canada between 2013 and 2019 to assess the incidence of maternal and neonatal trauma following OVD. They used composites defined a priori— stratified by instrument, region, level of obstetric care, and institutional OVD volume.
Results. Among 1,326,191 live or stillbirths, 2.9% were attempted forceps deliveries and 8.4% were attempted vacuum deliveries. Following forceps delivery, the maternal trauma rate was 25.3% (95% confidence interval [CI], 24.8%–25.7%), and the neonatal trauma rate was 9.6 per 1,000 live births (95% CI, 8.6–10.6). Following vacuum delivery, maternal and neonatal trauma rates were 13.2% (95% CI, 13.0%–13.4%) and 9.6 per 1,000 live births (95% CI, 9.0–10.2), respectively. Maternal trauma was driven by higher order perineal lacerations. Some association was seen between increased forceps volume and decreased maternal trauma rates.
The authors concluded that in Canada, rates of maternal and neonatal trauma following OVD are higher than previously reported in consensus statements.
Study strengths and limitations
This large contemporary study uniquely stratified perinatal outcomes following OVD. The outcomes are well defined and meaningful, but some limitations affect the generalizability of the findings.
First, stillbirths were included for the maternal composite outcome, yet the incidence of this within the study population is not reported. Operative vaginal deliveries that involve stillbirths can be complex; a subgroup analysis excluding these would aid in interpretation.
Second, complicated OVDs, including sequential use of forceps and vacuum and OVDs from midpelvic station, were included; ACOG recommends against both these practices in routine circumstances due to known increases in maternal and neonatal morbidity.1 As such, the inclusion of these OVDs may bias results away from the null.
Finally, despite discussing the role of episiotomy, the episiotomy rate in this cohort is not reported.
Despite these limitations, the study by Muraca and colleagues is a positive step forward toward understanding the role of OVD in contemporary obstetric practice, and it uniquely ascertains the impact of OVD volume outcomes that previously had been an elusive exposure ●
While it is important to understand perinatal outcomes following OVD in a contemporary cohort, utilizing the correct cohort and reference group is critical.4 Risks for maternal and neonatal trauma follow OVD; however, outcomes vary based on appropriate selection of OVD candidates and adherence to recommended national guidelines.1,4 The infrequency of OVD raises concerns regarding adequate training for obstetricians, which should be prioritized so that they can offer OVD as a safe alternative to CD birth.3
HAYLEY E. MILLER, MD, AND DANIELLE M. PANELLI, MD
Muraca GM, Boutin A, Razaz N, et al. Maternal and neonatal trauma following operative vaginal delivery. CMAJ. 2022;194:E1-E12. doi: 10.1503/cmaj.210841.
EXPERT COMMENTARY
Operative vaginal delivery is used to achieve and expedite safe vaginal birth while avoiding CD and its associated morbidities.1,2 Despite support from the American College of Obstetricians and Gynecologists (ACOG) for the use of OVD as an alternative to CD, OVD was used in only 3% of all US births in 2013, a shift from approximately 30% in 1987.1,3 Reported complications of OVD are biased by the level of experience of the operator, changes in practice, and by misinterpretation of the counterfactual.1
Outcomes of OVD should be compared with appropriate reference groups, namely, with second-stage CD births rather than with spontaneous vaginal births.4 With decreasing rates of OVD, evidence of contemporary data is needed on appropriately compared perinatal outcomes.4
Details of the study
Muraca and colleagues conducted an observational cohort study of births in Canada between 2013 and 2019 to assess the incidence of maternal and neonatal trauma following OVD. They used composites defined a priori— stratified by instrument, region, level of obstetric care, and institutional OVD volume.
Results. Among 1,326,191 live or stillbirths, 2.9% were attempted forceps deliveries and 8.4% were attempted vacuum deliveries. Following forceps delivery, the maternal trauma rate was 25.3% (95% confidence interval [CI], 24.8%–25.7%), and the neonatal trauma rate was 9.6 per 1,000 live births (95% CI, 8.6–10.6). Following vacuum delivery, maternal and neonatal trauma rates were 13.2% (95% CI, 13.0%–13.4%) and 9.6 per 1,000 live births (95% CI, 9.0–10.2), respectively. Maternal trauma was driven by higher order perineal lacerations. Some association was seen between increased forceps volume and decreased maternal trauma rates.
The authors concluded that in Canada, rates of maternal and neonatal trauma following OVD are higher than previously reported in consensus statements.
Study strengths and limitations
This large contemporary study uniquely stratified perinatal outcomes following OVD. The outcomes are well defined and meaningful, but some limitations affect the generalizability of the findings.
First, stillbirths were included for the maternal composite outcome, yet the incidence of this within the study population is not reported. Operative vaginal deliveries that involve stillbirths can be complex; a subgroup analysis excluding these would aid in interpretation.
Second, complicated OVDs, including sequential use of forceps and vacuum and OVDs from midpelvic station, were included; ACOG recommends against both these practices in routine circumstances due to known increases in maternal and neonatal morbidity.1 As such, the inclusion of these OVDs may bias results away from the null.
Finally, despite discussing the role of episiotomy, the episiotomy rate in this cohort is not reported.
Despite these limitations, the study by Muraca and colleagues is a positive step forward toward understanding the role of OVD in contemporary obstetric practice, and it uniquely ascertains the impact of OVD volume outcomes that previously had been an elusive exposure ●
While it is important to understand perinatal outcomes following OVD in a contemporary cohort, utilizing the correct cohort and reference group is critical.4 Risks for maternal and neonatal trauma follow OVD; however, outcomes vary based on appropriate selection of OVD candidates and adherence to recommended national guidelines.1,4 The infrequency of OVD raises concerns regarding adequate training for obstetricians, which should be prioritized so that they can offer OVD as a safe alternative to CD birth.3
HAYLEY E. MILLER, MD, AND DANIELLE M. PANELLI, MD
- American College of Obstetricians and Gynecologists. Operative vaginal birth: ACOG practice bulletin, number 219. Obstet Gynecol. 2020;135:e149-e159.
- Spong CY, Berghella V, Wenstrom KD, et al. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists workshop. Obstet Gynecol. 2012;120:1181-1193.
- Zahniser SC, Kendrick JS, Franks AL, et al. Trends in obstetric operative procedures, 1980 to 1987. Am J Public Health. 1992;82:1340-1344.
- Panelli DM, Leonard SA, Joudi N, et al. Severe maternal and neonatal morbidity after attempted operative vaginal delivery. Am J Obstet Gynecol MFM. 2021;3: 100339.
- American College of Obstetricians and Gynecologists. Operative vaginal birth: ACOG practice bulletin, number 219. Obstet Gynecol. 2020;135:e149-e159.
- Spong CY, Berghella V, Wenstrom KD, et al. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists workshop. Obstet Gynecol. 2012;120:1181-1193.
- Zahniser SC, Kendrick JS, Franks AL, et al. Trends in obstetric operative procedures, 1980 to 1987. Am J Public Health. 1992;82:1340-1344.
- Panelli DM, Leonard SA, Joudi N, et al. Severe maternal and neonatal morbidity after attempted operative vaginal delivery. Am J Obstet Gynecol MFM. 2021;3: 100339.
Infectious disease pop quiz: Clinical challenge #24 for the ObGyn
What are the 2 most likely causes for persistent fever in a patient who is being treated with antibiotics for postcesarean endometritis?
Continue to the answer...
The 2 most likely causes of a poor response to treatment for postcesarean endometritis are a resistant microorganism and wound infection. Less common causes of persistent postoperative fever include septic pelvic vein thrombophlebitis, pelvic abscess, retained products of conception, reactivation of a connective tissue disorder, and drug fever.
- Duff P. Maternal and perinatal infections: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al. Gabbe’s Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021:1124-1146.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TJ, et al. Creasy & Resnik’s Maternal-Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:862-919.
What are the 2 most likely causes for persistent fever in a patient who is being treated with antibiotics for postcesarean endometritis?
Continue to the answer...
The 2 most likely causes of a poor response to treatment for postcesarean endometritis are a resistant microorganism and wound infection. Less common causes of persistent postoperative fever include septic pelvic vein thrombophlebitis, pelvic abscess, retained products of conception, reactivation of a connective tissue disorder, and drug fever.
What are the 2 most likely causes for persistent fever in a patient who is being treated with antibiotics for postcesarean endometritis?
Continue to the answer...
The 2 most likely causes of a poor response to treatment for postcesarean endometritis are a resistant microorganism and wound infection. Less common causes of persistent postoperative fever include septic pelvic vein thrombophlebitis, pelvic abscess, retained products of conception, reactivation of a connective tissue disorder, and drug fever.
- Duff P. Maternal and perinatal infections: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al. Gabbe’s Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021:1124-1146.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TJ, et al. Creasy & Resnik’s Maternal-Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:862-919.
- Duff P. Maternal and perinatal infections: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al. Gabbe’s Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021:1124-1146.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TJ, et al. Creasy & Resnik’s Maternal-Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:862-919.
Optimizing the Suboptimal: Hepatocellular Carcinoma Surveillance Guide for Primary Care Practitioners
The goal of this activity is to update primary care practitioners (PCPs) on risk factors and trends in hepatocellular carcinoma (HCC) development, as well as guideline recommendations and best practices for collaborating with specialists in HCC surveillance.
Click here to access this content now
The goal of this activity is to update primary care practitioners (PCPs) on risk factors and trends in hepatocellular carcinoma (HCC) development, as well as guideline recommendations and best practices for collaborating with specialists in HCC surveillance.
Click here to access this content now
The goal of this activity is to update primary care practitioners (PCPs) on risk factors and trends in hepatocellular carcinoma (HCC) development, as well as guideline recommendations and best practices for collaborating with specialists in HCC surveillance.
Click here to access this content now
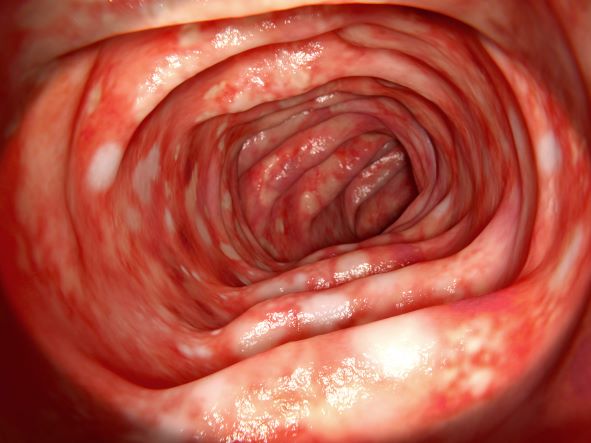
Abdominal cramping and diarrhea
On the basis of the patient's history and presentation, the likely diagnosis is extensive UC. Extensive colitis is defined by the presence of disease activity proximal to the splenic flexure. Because disease activity in UC is dynamic, up to half of patients who present with proctitis and 70% of those who present with left-sided colitis go on to develop extensive colitis on follow-up.
On the basis of the workup, it appears that this patient's UC has transitioned from left-sided to extensive disease, given the loss of treatment response. Endoscopic evaluation of patients with loss of treatment response may reveal patchiness of the histologic activity, as seen in this case.
Extensive colitis is a poor prognostic factor in UC, as is systemic steroid requirement, young age at diagnosis, and an elevated C-reactive protein level or erythrocyte sedimentation rate, all of which are associated with higher rates of colectomy. Over time, patients living with extensive ulcerative colitis develop an increased risk for colorectal cancer. Routine colonoscopic screening and surveillance are recommended for these high-risk patients.
UC most often presents as a continuously inflamed segment involving the distal rectum and extending proximally. Endoscopic features of inflammation include loss of vascular markings; granularity and friability of the mucosa; erosions; and, in the setting of severe inflammation, ulcerations and spontaneous bleeding. The diagnosis of UC involves both a lower gastrointestinal endoscopic examination and histologic confirmation. In general, a complete colonoscopy including examination of the terminal ileum should be performed, allowing clinicians to assess the full extent of the disease while ruling out distal ileal involvement, which is characteristic of Crohn's disease.
Evaluation of UC during relapses should include assessment of symptom severity and potential triggers, including enteric infections, use of nonsteroidal anti-inflammatory drugs, and recent smoking cessation. Nonadherence to therapy is common in patients with UC and may lead to relapse.
To treat a patient like the one represented here, the American College of Gastroenterology guidelines recommend oral 5-ASA at a dose of at least 2 g/d to induce remission. However, because this patient lost response to this treatment, the next step in the guidelines are appropriate oral systemic corticosteroids.
Bhupinder S. Anand, MD, Professor, Department of Medicine, Baylor College of Medicine, Houston, TX
Bhupinder S. Anand, MD, has disclosed no relevant financial relationships
On the basis of the patient's history and presentation, the likely diagnosis is extensive UC. Extensive colitis is defined by the presence of disease activity proximal to the splenic flexure. Because disease activity in UC is dynamic, up to half of patients who present with proctitis and 70% of those who present with left-sided colitis go on to develop extensive colitis on follow-up.
On the basis of the workup, it appears that this patient's UC has transitioned from left-sided to extensive disease, given the loss of treatment response. Endoscopic evaluation of patients with loss of treatment response may reveal patchiness of the histologic activity, as seen in this case.
Extensive colitis is a poor prognostic factor in UC, as is systemic steroid requirement, young age at diagnosis, and an elevated C-reactive protein level or erythrocyte sedimentation rate, all of which are associated with higher rates of colectomy. Over time, patients living with extensive ulcerative colitis develop an increased risk for colorectal cancer. Routine colonoscopic screening and surveillance are recommended for these high-risk patients.
UC most often presents as a continuously inflamed segment involving the distal rectum and extending proximally. Endoscopic features of inflammation include loss of vascular markings; granularity and friability of the mucosa; erosions; and, in the setting of severe inflammation, ulcerations and spontaneous bleeding. The diagnosis of UC involves both a lower gastrointestinal endoscopic examination and histologic confirmation. In general, a complete colonoscopy including examination of the terminal ileum should be performed, allowing clinicians to assess the full extent of the disease while ruling out distal ileal involvement, which is characteristic of Crohn's disease.
Evaluation of UC during relapses should include assessment of symptom severity and potential triggers, including enteric infections, use of nonsteroidal anti-inflammatory drugs, and recent smoking cessation. Nonadherence to therapy is common in patients with UC and may lead to relapse.
To treat a patient like the one represented here, the American College of Gastroenterology guidelines recommend oral 5-ASA at a dose of at least 2 g/d to induce remission. However, because this patient lost response to this treatment, the next step in the guidelines are appropriate oral systemic corticosteroids.
Bhupinder S. Anand, MD, Professor, Department of Medicine, Baylor College of Medicine, Houston, TX
Bhupinder S. Anand, MD, has disclosed no relevant financial relationships
On the basis of the patient's history and presentation, the likely diagnosis is extensive UC. Extensive colitis is defined by the presence of disease activity proximal to the splenic flexure. Because disease activity in UC is dynamic, up to half of patients who present with proctitis and 70% of those who present with left-sided colitis go on to develop extensive colitis on follow-up.
On the basis of the workup, it appears that this patient's UC has transitioned from left-sided to extensive disease, given the loss of treatment response. Endoscopic evaluation of patients with loss of treatment response may reveal patchiness of the histologic activity, as seen in this case.
Extensive colitis is a poor prognostic factor in UC, as is systemic steroid requirement, young age at diagnosis, and an elevated C-reactive protein level or erythrocyte sedimentation rate, all of which are associated with higher rates of colectomy. Over time, patients living with extensive ulcerative colitis develop an increased risk for colorectal cancer. Routine colonoscopic screening and surveillance are recommended for these high-risk patients.
UC most often presents as a continuously inflamed segment involving the distal rectum and extending proximally. Endoscopic features of inflammation include loss of vascular markings; granularity and friability of the mucosa; erosions; and, in the setting of severe inflammation, ulcerations and spontaneous bleeding. The diagnosis of UC involves both a lower gastrointestinal endoscopic examination and histologic confirmation. In general, a complete colonoscopy including examination of the terminal ileum should be performed, allowing clinicians to assess the full extent of the disease while ruling out distal ileal involvement, which is characteristic of Crohn's disease.
Evaluation of UC during relapses should include assessment of symptom severity and potential triggers, including enteric infections, use of nonsteroidal anti-inflammatory drugs, and recent smoking cessation. Nonadherence to therapy is common in patients with UC and may lead to relapse.
To treat a patient like the one represented here, the American College of Gastroenterology guidelines recommend oral 5-ASA at a dose of at least 2 g/d to induce remission. However, because this patient lost response to this treatment, the next step in the guidelines are appropriate oral systemic corticosteroids.
Bhupinder S. Anand, MD, Professor, Department of Medicine, Baylor College of Medicine, Houston, TX
Bhupinder S. Anand, MD, has disclosed no relevant financial relationships
A 46-year-old man presents with abdominal cramping and diarrhea and reports about five bowel movements per day for the past 2 weeks. Height is 5 ft 9 in and weight is 157 lb (BMI, 23.2). History is significant for ulcerative colitis (UC), diagnosed about 20 years ago with proctitis and having progressed about 8 years ago to left-sided disease. He smoked "lightly" through his 20s. Until about a month ago, the patient had been able to maintain remission with oral 5-aminosalicylic acid (ASA) therapy (2 g/d). Endoscopy shows granularity and friability of the mucosa with the inflamed segment extending proximal to the splenic flexure, though there is patchiness of the histologic activity. Colonoscopy rules out distal ileal involvement. Stool culture is negative.
Recent unintended weight loss
PCOS is most often defined according to the Rotterdam criteria, which stipulate that at least two of the following be present: irregular ovulation, biochemical/clinical hyperandrogenism, and polycystic ovaries (seen in the MRI scan above). Insulin resistance is part of the pathogenesis of PCOS, and insulin resistance is associated with T2D in PCOS.
In fact, PCOS is an independent risk factor for T2D, even after adjustment for BMI and obesity. Even normal-weight women with PCOS have an increased risk for T2D. More than half of women with PCOS develop T2D by age 40.
Even though family history and obesity are major contributors in the development of diabetes in patients with PCOS, diabetes can still occur in lean patients with PCOS who have no family history, mainly secondary to insulin resistance.
The Endocrine Society recommends that all individuals with PCOS undergo an oral glucose tolerance test every 3-5 years, with more frequent screening for those who develop symptoms of T2D, significant weight gain, or central adiposity. In guidelines published in 2015 by the American Association of Clinical Endocrinologists, the American College of Endocrinology, and the Androgen Excess and PCOS Society, an annual oral glucose tolerance test is recommended for patients with PCOS and impaired glucose tolerance, whereas those with a family history of T2D or a BMI above 30 should be screened every 1-2 years.
Management of T2D with PCOS is similar to that of T2D without PCOS. Accordingly, metformin and lifestyle changes are the treatments of choice; any antidiabetic agent may be added in patients who do not achieve glycemic targets despite treatment with metformin.
Romesh K. Khardori, MD, PhD, Professor, Department of Internal Medicine, Division of Diabetes, Endocrine, and Metabolic Disorders, Eastern Virginia Medical School; EVMS Medical Group, Norfolk, Virginia
Romesh K. Khardori, MD, PhD, has disclosed no relevant financial relationships
PCOS is most often defined according to the Rotterdam criteria, which stipulate that at least two of the following be present: irregular ovulation, biochemical/clinical hyperandrogenism, and polycystic ovaries (seen in the MRI scan above). Insulin resistance is part of the pathogenesis of PCOS, and insulin resistance is associated with T2D in PCOS.
In fact, PCOS is an independent risk factor for T2D, even after adjustment for BMI and obesity. Even normal-weight women with PCOS have an increased risk for T2D. More than half of women with PCOS develop T2D by age 40.
Even though family history and obesity are major contributors in the development of diabetes in patients with PCOS, diabetes can still occur in lean patients with PCOS who have no family history, mainly secondary to insulin resistance.
The Endocrine Society recommends that all individuals with PCOS undergo an oral glucose tolerance test every 3-5 years, with more frequent screening for those who develop symptoms of T2D, significant weight gain, or central adiposity. In guidelines published in 2015 by the American Association of Clinical Endocrinologists, the American College of Endocrinology, and the Androgen Excess and PCOS Society, an annual oral glucose tolerance test is recommended for patients with PCOS and impaired glucose tolerance, whereas those with a family history of T2D or a BMI above 30 should be screened every 1-2 years.
Management of T2D with PCOS is similar to that of T2D without PCOS. Accordingly, metformin and lifestyle changes are the treatments of choice; any antidiabetic agent may be added in patients who do not achieve glycemic targets despite treatment with metformin.
Romesh K. Khardori, MD, PhD, Professor, Department of Internal Medicine, Division of Diabetes, Endocrine, and Metabolic Disorders, Eastern Virginia Medical School; EVMS Medical Group, Norfolk, Virginia
Romesh K. Khardori, MD, PhD, has disclosed no relevant financial relationships
PCOS is most often defined according to the Rotterdam criteria, which stipulate that at least two of the following be present: irregular ovulation, biochemical/clinical hyperandrogenism, and polycystic ovaries (seen in the MRI scan above). Insulin resistance is part of the pathogenesis of PCOS, and insulin resistance is associated with T2D in PCOS.
In fact, PCOS is an independent risk factor for T2D, even after adjustment for BMI and obesity. Even normal-weight women with PCOS have an increased risk for T2D. More than half of women with PCOS develop T2D by age 40.
Even though family history and obesity are major contributors in the development of diabetes in patients with PCOS, diabetes can still occur in lean patients with PCOS who have no family history, mainly secondary to insulin resistance.
The Endocrine Society recommends that all individuals with PCOS undergo an oral glucose tolerance test every 3-5 years, with more frequent screening for those who develop symptoms of T2D, significant weight gain, or central adiposity. In guidelines published in 2015 by the American Association of Clinical Endocrinologists, the American College of Endocrinology, and the Androgen Excess and PCOS Society, an annual oral glucose tolerance test is recommended for patients with PCOS and impaired glucose tolerance, whereas those with a family history of T2D or a BMI above 30 should be screened every 1-2 years.
Management of T2D with PCOS is similar to that of T2D without PCOS. Accordingly, metformin and lifestyle changes are the treatments of choice; any antidiabetic agent may be added in patients who do not achieve glycemic targets despite treatment with metformin.
Romesh K. Khardori, MD, PhD, Professor, Department of Internal Medicine, Division of Diabetes, Endocrine, and Metabolic Disorders, Eastern Virginia Medical School; EVMS Medical Group, Norfolk, Virginia
Romesh K. Khardori, MD, PhD, has disclosed no relevant financial relationships
A 36-year-old woman presents with recent unintended weight loss of 12 lb in 2 months. Currently, she weighs 153 lb (BMI 24.7). She complains of increased thirst, increased urination, lack of energy, and fatigue.
Metabolic workup reveals that A1c is 7.1%, fasting blood glucose level is 131 mg/dL, oral glucose tolerance test level is 210 mg/dL, and random blood glucose level is 215 mg/dL, all of which are diagnostic for type 2 diabetes (T2D). She has no family history of diabetes.
A lipid panel shows a low-density lipoprotein cholesterol of 140 mg/dL, high-density lipoprotein cholesterol 38 mg/dL, and triglycerides 210 mg/dL. Blood pressure is 150/95 mm Hg.
The patient had been diagnosed with polycystic ovary syndrome (PCOS) at age 33, during a workup for infertility. At the time of her PCOS diagnosis, she weighed 190 lb (BMI, 30.7). She gave birth to an 8-lb son 14 months ago.