User login
Official Newspaper of the American College of Surgeons
In Memoriam: Dr. George Sheldon, an icon in American surgery, passes away in June
George F. Sheldon, MD, FACS, an icon in American surgery and the American College of Surgeons (ACS), passed away Sunday, June 16. Dr. Sheldon was the Zack D. Owens Distinguished Professor of Surgery, University of North Carolina School of Medicine, Chapel Hill. His family was with him at the time of his passing.
Dr. Sheldon's contributions to American and international surgery, academic surgery, and the American College of Surgeons, as well as his accomplishments in general, are legendary. He continued to work with the College\'s leadership and staff until even this last week, offering his services in a number of areas. His dedication to the ACS has been recognized through his appointment and election to serve on the Board of Regents as an ACS President, as well as his receipt of the second ACS Lifetime Achievement Award last year.
A more complete reflection on the life and work of Dr. Sheldon will appear in the September issue of the Bulletin of the American College of Surgeons.
George F. Sheldon, MD, FACS, an icon in American surgery and the American College of Surgeons (ACS), passed away Sunday, June 16. Dr. Sheldon was the Zack D. Owens Distinguished Professor of Surgery, University of North Carolina School of Medicine, Chapel Hill. His family was with him at the time of his passing.
Dr. Sheldon's contributions to American and international surgery, academic surgery, and the American College of Surgeons, as well as his accomplishments in general, are legendary. He continued to work with the College\'s leadership and staff until even this last week, offering his services in a number of areas. His dedication to the ACS has been recognized through his appointment and election to serve on the Board of Regents as an ACS President, as well as his receipt of the second ACS Lifetime Achievement Award last year.
A more complete reflection on the life and work of Dr. Sheldon will appear in the September issue of the Bulletin of the American College of Surgeons.
George F. Sheldon, MD, FACS, an icon in American surgery and the American College of Surgeons (ACS), passed away Sunday, June 16. Dr. Sheldon was the Zack D. Owens Distinguished Professor of Surgery, University of North Carolina School of Medicine, Chapel Hill. His family was with him at the time of his passing.
Dr. Sheldon's contributions to American and international surgery, academic surgery, and the American College of Surgeons, as well as his accomplishments in general, are legendary. He continued to work with the College\'s leadership and staff until even this last week, offering his services in a number of areas. His dedication to the ACS has been recognized through his appointment and election to serve on the Board of Regents as an ACS President, as well as his receipt of the second ACS Lifetime Achievement Award last year.
A more complete reflection on the life and work of Dr. Sheldon will appear in the September issue of the Bulletin of the American College of Surgeons.
House committee unanimously passes SGR replacement
The demise of the Medicare Sustainable Growth Rate formula is a step closer to reality as the House Energy and Commerce Committee voted unanimously July 31 in favor of legislation that would remove the formula.
Both Democrats and Republicans on the committee supported the Medicare Patient Access and Quality Improvement Act of 2013 in a 51-0 vote. The legislation, H.R. 2810, was authored by Rep. Michael Burgess (R-Tex.), and developed with input from physician organizations.
If enacted, the legislation would replace the SGR with a 0.5% payment increase for physicians from 2014 through 2018. It would continue to support fee-for-service medicine, but also encourage the formation of new delivery models and reward reporting of quality data.
"In harnessing the ideas of the medical profession, and working as a team with Energy and Commerce Democrats as well as Ways and Means Republicans, we have crafted a policy that will not only get out of committee but has the merits to make it to the president’s desk," Rep. Fred Upton (R-Mich.), chairman of the Energy and Commerce Committee, said in a statement.
Rep. Henry Waxman (D-Calif.), the committee’s ranking minority member, said, "What is obvious today is that we have a bipartisan commitment to try to solve this problem. And that when we decide to work together, we can achieve positive results." He also noted that "in more than a decade of saying something needs to be done, I’m pleased that this committee is the first to act to bring this issue to the forefront."
The American College of Physicians said it was mostly pleased with the legislation and its progress. In addition to rewarding physician efficiency, "the bill promises to accelerate the growth of patient-centered medical homes, an innovative primary care delivery model that has been shown to improve outcomes and lower the costs of care for patients across the country," said Dr. Molly Cooke, ACP president, in a statement.
The college "looks forward to continuing to work with the House and Senate on a bipartisan basis to get legislation enacted this year that includes these and other key elements of the House Energy and Commerce Committee bill, plus additional improvements needed to accelerate the movement toward high-value, patient-centered health care."
The American Medical Association and the American Academy of Family Physicians also support the legislation. When the bill was approved by the Energy and Commerce Health Subcommittee, the AAFP said it was disappointed that the bill did not have higher payments for primary care.
During those deliberations, the AMA, AAFP, ACP, and some state medical societies also told the committee that a provision addressing misvalued codes could end up cutting physician pay. They’ve asked the committee to consider an amendment that would remove the misvalued code provisions from the bill; such an amendment was not considered by the committee.
The legislation still has a long path to passage. The House Ways and Means Committee and the Senate Finance Committee have also been working on legislation to replace the SGR. And so far, legislators in both houses have not addressed how to pay for an SGR fix.
Several Energy and Commerce Committee members acknowledged the looming financial reality during deliberations.
"One of the largest hurdles to overcome will be how to pay for the cost associated with fixing the SGR," said Rep. Eliot Engel (D-N.Y.). He urged his colleagues to continue the spirit of bipartisanship when figuring out the cost of replacement.
"We know that the work is not done," said Rep. Phil Gingrey (R-Ga.). "Any fiscally responsible bill in today’s budgetary environment must be paid for. I look forward to finding offsets that do not impact the practice of medicine but instead focus on good governance and combating waste," said the congressman, who is also an ob.gyn.
That work will likely come in September, when Congress returns from its summer recess.
[email protected] On Twitter @aliciaault
The demise of the Medicare Sustainable Growth Rate formula is a step closer to reality as the House Energy and Commerce Committee voted unanimously July 31 in favor of legislation that would remove the formula.
Both Democrats and Republicans on the committee supported the Medicare Patient Access and Quality Improvement Act of 2013 in a 51-0 vote. The legislation, H.R. 2810, was authored by Rep. Michael Burgess (R-Tex.), and developed with input from physician organizations.
If enacted, the legislation would replace the SGR with a 0.5% payment increase for physicians from 2014 through 2018. It would continue to support fee-for-service medicine, but also encourage the formation of new delivery models and reward reporting of quality data.
"In harnessing the ideas of the medical profession, and working as a team with Energy and Commerce Democrats as well as Ways and Means Republicans, we have crafted a policy that will not only get out of committee but has the merits to make it to the president’s desk," Rep. Fred Upton (R-Mich.), chairman of the Energy and Commerce Committee, said in a statement.
Rep. Henry Waxman (D-Calif.), the committee’s ranking minority member, said, "What is obvious today is that we have a bipartisan commitment to try to solve this problem. And that when we decide to work together, we can achieve positive results." He also noted that "in more than a decade of saying something needs to be done, I’m pleased that this committee is the first to act to bring this issue to the forefront."
The American College of Physicians said it was mostly pleased with the legislation and its progress. In addition to rewarding physician efficiency, "the bill promises to accelerate the growth of patient-centered medical homes, an innovative primary care delivery model that has been shown to improve outcomes and lower the costs of care for patients across the country," said Dr. Molly Cooke, ACP president, in a statement.
The college "looks forward to continuing to work with the House and Senate on a bipartisan basis to get legislation enacted this year that includes these and other key elements of the House Energy and Commerce Committee bill, plus additional improvements needed to accelerate the movement toward high-value, patient-centered health care."
The American Medical Association and the American Academy of Family Physicians also support the legislation. When the bill was approved by the Energy and Commerce Health Subcommittee, the AAFP said it was disappointed that the bill did not have higher payments for primary care.
During those deliberations, the AMA, AAFP, ACP, and some state medical societies also told the committee that a provision addressing misvalued codes could end up cutting physician pay. They’ve asked the committee to consider an amendment that would remove the misvalued code provisions from the bill; such an amendment was not considered by the committee.
The legislation still has a long path to passage. The House Ways and Means Committee and the Senate Finance Committee have also been working on legislation to replace the SGR. And so far, legislators in both houses have not addressed how to pay for an SGR fix.
Several Energy and Commerce Committee members acknowledged the looming financial reality during deliberations.
"One of the largest hurdles to overcome will be how to pay for the cost associated with fixing the SGR," said Rep. Eliot Engel (D-N.Y.). He urged his colleagues to continue the spirit of bipartisanship when figuring out the cost of replacement.
"We know that the work is not done," said Rep. Phil Gingrey (R-Ga.). "Any fiscally responsible bill in today’s budgetary environment must be paid for. I look forward to finding offsets that do not impact the practice of medicine but instead focus on good governance and combating waste," said the congressman, who is also an ob.gyn.
That work will likely come in September, when Congress returns from its summer recess.
[email protected] On Twitter @aliciaault
The demise of the Medicare Sustainable Growth Rate formula is a step closer to reality as the House Energy and Commerce Committee voted unanimously July 31 in favor of legislation that would remove the formula.
Both Democrats and Republicans on the committee supported the Medicare Patient Access and Quality Improvement Act of 2013 in a 51-0 vote. The legislation, H.R. 2810, was authored by Rep. Michael Burgess (R-Tex.), and developed with input from physician organizations.
If enacted, the legislation would replace the SGR with a 0.5% payment increase for physicians from 2014 through 2018. It would continue to support fee-for-service medicine, but also encourage the formation of new delivery models and reward reporting of quality data.
"In harnessing the ideas of the medical profession, and working as a team with Energy and Commerce Democrats as well as Ways and Means Republicans, we have crafted a policy that will not only get out of committee but has the merits to make it to the president’s desk," Rep. Fred Upton (R-Mich.), chairman of the Energy and Commerce Committee, said in a statement.
Rep. Henry Waxman (D-Calif.), the committee’s ranking minority member, said, "What is obvious today is that we have a bipartisan commitment to try to solve this problem. And that when we decide to work together, we can achieve positive results." He also noted that "in more than a decade of saying something needs to be done, I’m pleased that this committee is the first to act to bring this issue to the forefront."
The American College of Physicians said it was mostly pleased with the legislation and its progress. In addition to rewarding physician efficiency, "the bill promises to accelerate the growth of patient-centered medical homes, an innovative primary care delivery model that has been shown to improve outcomes and lower the costs of care for patients across the country," said Dr. Molly Cooke, ACP president, in a statement.
The college "looks forward to continuing to work with the House and Senate on a bipartisan basis to get legislation enacted this year that includes these and other key elements of the House Energy and Commerce Committee bill, plus additional improvements needed to accelerate the movement toward high-value, patient-centered health care."
The American Medical Association and the American Academy of Family Physicians also support the legislation. When the bill was approved by the Energy and Commerce Health Subcommittee, the AAFP said it was disappointed that the bill did not have higher payments for primary care.
During those deliberations, the AMA, AAFP, ACP, and some state medical societies also told the committee that a provision addressing misvalued codes could end up cutting physician pay. They’ve asked the committee to consider an amendment that would remove the misvalued code provisions from the bill; such an amendment was not considered by the committee.
The legislation still has a long path to passage. The House Ways and Means Committee and the Senate Finance Committee have also been working on legislation to replace the SGR. And so far, legislators in both houses have not addressed how to pay for an SGR fix.
Several Energy and Commerce Committee members acknowledged the looming financial reality during deliberations.
"One of the largest hurdles to overcome will be how to pay for the cost associated with fixing the SGR," said Rep. Eliot Engel (D-N.Y.). He urged his colleagues to continue the spirit of bipartisanship when figuring out the cost of replacement.
"We know that the work is not done," said Rep. Phil Gingrey (R-Ga.). "Any fiscally responsible bill in today’s budgetary environment must be paid for. I look forward to finding offsets that do not impact the practice of medicine but instead focus on good governance and combating waste," said the congressman, who is also an ob.gyn.
That work will likely come in September, when Congress returns from its summer recess.
[email protected] On Twitter @aliciaault
High BMI appears to cause gallstones
An elevated body mass index is not just associated with symptomatic gallstone disease, it appears to cause the disease, according to a report published in Hepatology (doi:10.1002/hep.26563).
Many epidemiologic and observational studies have noted a clear association between a high BMI and an increased risk for gallstones, but have not been able to pin down a causal effect. It was impossible to rule out confounding by some other factor, such as a high-fat diet, that simultaneously caused both the elevation in BMI and the elevation in risk for gallstones. Similarly, it was impossible to rule out reverse causation, such as the colicky pain of gallstone disease caused the physical inactivity that then led to a high BMI.
A new epidemiologic statistical approach known as Mendelian randomization is thought to avert both confounding and reverse causation by pinpointing the genetic variants that are linked to a high BMI (which are a constant throughout the lifespan) but that are not related to confounding factors, then determining whether they are also linked to gallstone disease. "If raised BMI truly is a causal factor in the development of gallstone disease, genetic variants that increase BMI would be expected to also increase risk of gallstone disease," said Dr. Stefan Stender of the department of clinical biochemistry, Rigshospitalet, University of Copenhagen, and his associates.
They studied 77,679 Danish adults from the general population who participated in two large prospective studies: the Copenhagen General Population Study (67,314 subjects) and the Copenhagen City Heart Study (10,365 subjects). All the participants had donated blood samples that could be used for DNA extraction and genotyping.
A total of 4,106 of these subjects developed symptomatic gallstone disease during follow-up of up to 34 years.
The researchers used genotyping to identify study subjects who carried any of the three polymorphisms that have the largest known effect sizes for association with BMI in European populations: FTO (rs9939609), MC4R (rs17782313), or TMEM18 (rs6548238). Each of these can be carried on two possible alleles, so any given subject could carry one to six affected alleles. The number of BMI-increasing alleles, from one to six, was determined for each study subject.
In an initial analysis of the data, the mean baseline BMI was 55% higher (11 kg/m2) in subjects carrying the most alleles compared with those carrying the fewest.
Increasing BMI was associated with a stepwise increase in the risk of developing symptomatic gallstone disease.
In the overall cohort, the risk of symptomatic gallstone disease was increased 7% for every 1-kg/m2 increase in BMI. In the Mendelian randomization cohort, the risk of gallstone disease increased 17% with every 1-kg/m2 increase in BMI. The concordance between these two estimates indicates that BMI itself is a causal risk factor for symptomatic gallstone disease, Dr. Stender and his associates said.
This study did not include data on gallstone composition and was not designed to examine the pathophysiologic mechanisms by which a high BMI causes gallstone formation. However, numerous other studies have proposed several possible mechanisms, they noted.
Obesity may raise cholesterol synthesis and hepatobiliary cholesterol efflux, "a key event in the development of cholesterol gallstones." High abdominal fat mass may induce gallbladder hypomotility and bile stasis, "another risk factor for gallstone formation."
In addition, substances secreted by or metabolized by adipocytes could influence gallstone formation. For example, estrogen is produced by adipocytes and may promote gallstone formation by raising the rate of hepatobiliary cholesterol efflux. And leptin, which is also secreted by adipocytes, may have lithogenic effects.
Adinopectin, another hormone secreted by adipocytes, has been linked to gallstones in both animal and human studies. And obesity-associated hyperinsulinemia may induce gallstone formation by causing the secretion of more lithogenic bile.
This study was limited in that it included only white people of Danish descent. "Because ethnic differences in gallstone prevalence are well known, the results reported here may not necessarily translate to other ethnicities," Dr. Stender and his colleagues said.
This study was supported by the Danish Medical Research Council, the Rigshospitalet at Copenhagen University, and the Odd Fellow Order. No financial conflicts of interest were reported.
An elevated body mass index is not just associated with symptomatic gallstone disease, it appears to cause the disease, according to a report published in Hepatology (doi:10.1002/hep.26563).
Many epidemiologic and observational studies have noted a clear association between a high BMI and an increased risk for gallstones, but have not been able to pin down a causal effect. It was impossible to rule out confounding by some other factor, such as a high-fat diet, that simultaneously caused both the elevation in BMI and the elevation in risk for gallstones. Similarly, it was impossible to rule out reverse causation, such as the colicky pain of gallstone disease caused the physical inactivity that then led to a high BMI.
A new epidemiologic statistical approach known as Mendelian randomization is thought to avert both confounding and reverse causation by pinpointing the genetic variants that are linked to a high BMI (which are a constant throughout the lifespan) but that are not related to confounding factors, then determining whether they are also linked to gallstone disease. "If raised BMI truly is a causal factor in the development of gallstone disease, genetic variants that increase BMI would be expected to also increase risk of gallstone disease," said Dr. Stefan Stender of the department of clinical biochemistry, Rigshospitalet, University of Copenhagen, and his associates.
They studied 77,679 Danish adults from the general population who participated in two large prospective studies: the Copenhagen General Population Study (67,314 subjects) and the Copenhagen City Heart Study (10,365 subjects). All the participants had donated blood samples that could be used for DNA extraction and genotyping.
A total of 4,106 of these subjects developed symptomatic gallstone disease during follow-up of up to 34 years.
The researchers used genotyping to identify study subjects who carried any of the three polymorphisms that have the largest known effect sizes for association with BMI in European populations: FTO (rs9939609), MC4R (rs17782313), or TMEM18 (rs6548238). Each of these can be carried on two possible alleles, so any given subject could carry one to six affected alleles. The number of BMI-increasing alleles, from one to six, was determined for each study subject.
In an initial analysis of the data, the mean baseline BMI was 55% higher (11 kg/m2) in subjects carrying the most alleles compared with those carrying the fewest.
Increasing BMI was associated with a stepwise increase in the risk of developing symptomatic gallstone disease.
In the overall cohort, the risk of symptomatic gallstone disease was increased 7% for every 1-kg/m2 increase in BMI. In the Mendelian randomization cohort, the risk of gallstone disease increased 17% with every 1-kg/m2 increase in BMI. The concordance between these two estimates indicates that BMI itself is a causal risk factor for symptomatic gallstone disease, Dr. Stender and his associates said.
This study did not include data on gallstone composition and was not designed to examine the pathophysiologic mechanisms by which a high BMI causes gallstone formation. However, numerous other studies have proposed several possible mechanisms, they noted.
Obesity may raise cholesterol synthesis and hepatobiliary cholesterol efflux, "a key event in the development of cholesterol gallstones." High abdominal fat mass may induce gallbladder hypomotility and bile stasis, "another risk factor for gallstone formation."
In addition, substances secreted by or metabolized by adipocytes could influence gallstone formation. For example, estrogen is produced by adipocytes and may promote gallstone formation by raising the rate of hepatobiliary cholesterol efflux. And leptin, which is also secreted by adipocytes, may have lithogenic effects.
Adinopectin, another hormone secreted by adipocytes, has been linked to gallstones in both animal and human studies. And obesity-associated hyperinsulinemia may induce gallstone formation by causing the secretion of more lithogenic bile.
This study was limited in that it included only white people of Danish descent. "Because ethnic differences in gallstone prevalence are well known, the results reported here may not necessarily translate to other ethnicities," Dr. Stender and his colleagues said.
This study was supported by the Danish Medical Research Council, the Rigshospitalet at Copenhagen University, and the Odd Fellow Order. No financial conflicts of interest were reported.
An elevated body mass index is not just associated with symptomatic gallstone disease, it appears to cause the disease, according to a report published in Hepatology (doi:10.1002/hep.26563).
Many epidemiologic and observational studies have noted a clear association between a high BMI and an increased risk for gallstones, but have not been able to pin down a causal effect. It was impossible to rule out confounding by some other factor, such as a high-fat diet, that simultaneously caused both the elevation in BMI and the elevation in risk for gallstones. Similarly, it was impossible to rule out reverse causation, such as the colicky pain of gallstone disease caused the physical inactivity that then led to a high BMI.
A new epidemiologic statistical approach known as Mendelian randomization is thought to avert both confounding and reverse causation by pinpointing the genetic variants that are linked to a high BMI (which are a constant throughout the lifespan) but that are not related to confounding factors, then determining whether they are also linked to gallstone disease. "If raised BMI truly is a causal factor in the development of gallstone disease, genetic variants that increase BMI would be expected to also increase risk of gallstone disease," said Dr. Stefan Stender of the department of clinical biochemistry, Rigshospitalet, University of Copenhagen, and his associates.
They studied 77,679 Danish adults from the general population who participated in two large prospective studies: the Copenhagen General Population Study (67,314 subjects) and the Copenhagen City Heart Study (10,365 subjects). All the participants had donated blood samples that could be used for DNA extraction and genotyping.
A total of 4,106 of these subjects developed symptomatic gallstone disease during follow-up of up to 34 years.
The researchers used genotyping to identify study subjects who carried any of the three polymorphisms that have the largest known effect sizes for association with BMI in European populations: FTO (rs9939609), MC4R (rs17782313), or TMEM18 (rs6548238). Each of these can be carried on two possible alleles, so any given subject could carry one to six affected alleles. The number of BMI-increasing alleles, from one to six, was determined for each study subject.
In an initial analysis of the data, the mean baseline BMI was 55% higher (11 kg/m2) in subjects carrying the most alleles compared with those carrying the fewest.
Increasing BMI was associated with a stepwise increase in the risk of developing symptomatic gallstone disease.
In the overall cohort, the risk of symptomatic gallstone disease was increased 7% for every 1-kg/m2 increase in BMI. In the Mendelian randomization cohort, the risk of gallstone disease increased 17% with every 1-kg/m2 increase in BMI. The concordance between these two estimates indicates that BMI itself is a causal risk factor for symptomatic gallstone disease, Dr. Stender and his associates said.
This study did not include data on gallstone composition and was not designed to examine the pathophysiologic mechanisms by which a high BMI causes gallstone formation. However, numerous other studies have proposed several possible mechanisms, they noted.
Obesity may raise cholesterol synthesis and hepatobiliary cholesterol efflux, "a key event in the development of cholesterol gallstones." High abdominal fat mass may induce gallbladder hypomotility and bile stasis, "another risk factor for gallstone formation."
In addition, substances secreted by or metabolized by adipocytes could influence gallstone formation. For example, estrogen is produced by adipocytes and may promote gallstone formation by raising the rate of hepatobiliary cholesterol efflux. And leptin, which is also secreted by adipocytes, may have lithogenic effects.
Adinopectin, another hormone secreted by adipocytes, has been linked to gallstones in both animal and human studies. And obesity-associated hyperinsulinemia may induce gallstone formation by causing the secretion of more lithogenic bile.
This study was limited in that it included only white people of Danish descent. "Because ethnic differences in gallstone prevalence are well known, the results reported here may not necessarily translate to other ethnicities," Dr. Stender and his colleagues said.
This study was supported by the Danish Medical Research Council, the Rigshospitalet at Copenhagen University, and the Odd Fellow Order. No financial conflicts of interest were reported.
FROM HEPATOLOGY
Major finding: In the overall cohort, the risk of symptomatic gallstone disease was increased 7% for every 1-kg/m2 increase in BMI, and in the Mendelian randomization cohort, the risk of gallstone disease increased 17% with every 1-kg/m2 increase in BMI.
Data source: A Mendelian randomization study involving 77,679 adults from the Danish general population who were genotyped to identify carriers of three BMI-increasing polymorphisms and who were followed for up to 34 years for the development of symptomatic gallstone disease.
Disclosures: This study was supported by the Danish Medical Research Council, the Rigshospitalet at Copenhagen University, and the Odd Fellow Order. No financial conflicts of interest were reported.
Early surgery for intracerebral bleeds may benefit a select few
LONDON – Approximately 2%-3% of patients with spontaneous intracerebral hemorrhage may benefit from early surgical removal of hematoma, according to the results of the second Surgical Trial in Lobar Intracerebral Hemorrhage.
As reported at the annual European Stroke Conference and published simultaneously in the Lancet, patients with superficial lesions and an unfavorable prognostic score appeared to benefit from early surgical intervention, compared with those given conservative medical treatment (odds ratio [OR] = 0.49, P =.02). Conversely, those with a good prognostic score did not seem to benefit (OR = 1.12, P = .57).
The primary analysis showed no significant benefit of early surgery overall, with 41.4% of 297 patients in the early surgery group and 37.7% of 286 patients in the conservative treatment group having a favorable outcome at 6 months, as determined by the 8-point extended Glasgow Outcome Scale (GOS-E) (P = .367).
"That’s a 3.7% absolute benefit, which is not enough to change surgical practice on its own," said Dr. A. David Mendelow, professor of neurosurgery at Newcastle University in Newcastle upon Tyne, England. "We were looking for a 12% benefit when we set out to do this trial," he added during a press conference.
A 6% decrease in mortality at 6 months was seen favoring surgery (18% vs. 24% for conservative therapy), but this was not statistically significant (P = .095).
"Intracerebral hemorrhage is not a homogenous condition," Dr. Mendelow said, adding that it can be a difficult decision to operate. Clinical manifestations can range from no apparent effects to severe disability and rapid death. "STICH [Surgical Trial in Lobar Intracerebral Hemorrhage] focused on patients that we are not quite sure about whether to operate or not," he said.
The hypothesis for the trial was based on the findings of the first STICH trial (Acta Neurochir. Suppl. 2006;96:65-8). The results of the trial were again neutral overall, but subgroup analyses showed that some groups of patients did worse with surgery, such as those with deep-seated bleeds, and some may fare better, such as those with superficial lobar hematomas.
STICH II therefore specifically recruited this latter group of patients to see if the effect was real or an artifact of the scientific analysis. In total, 601 conscious ICH patients with a median age of 65 years were recruited at 78 centers in 27 countries. Patients had to have a superficial lesion (1 cm or less from the cortical surface of the brain) that was between 10 mL and 100 mL in volume, and with no sign of intraventricular hemorrhage on CT scanning. Patients had to be recruited within 48 hours of the stroke and surgical intervention had to be performed within 12 hours (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)60986-1]). (A total of 6 patients were excluded or withdrew from the study before intervention, and after intervention another 12 withdrew, were lost to follow-up, or were alive but had an unknown status.)
The GOS-E was calculated from the answers to a questionnaire sent out to patients and their relatives 6 months following their stroke. A cutoff score of approximately 27 was used to categorize patients as having a good or bad prognosis. At baseline, about two-thirds of patients had a good prognosis, and the remainder had a poor prognosis.
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials,"
"One of the reasons, perhaps, for a lack of significance was the [number of] crossovers from initial conservative therapy to surgery," Dr. Mendelow said. Indeed, 21% of patients who were originally randomized to conservative treatment crossed over to the surgical arm. These patients had "clearly deteriorated" prior to having surgery, he said when presenting the findings. Furthermore, only 37% of these crossovers received surgery within the specified 12-hour time limit.
STICH provides the best, albeit insufficient, evidence to date on the role of surgery in ICH, Dr. Oliver Gautschi and Dr. Karl Schaller, both of the University of Geneva, commented in an editorial about the trial (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)61087-9]) .
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials," they wrote. "The overall result of this meta-analysis of patients with different types of intracerebral hemorrhage favors surgery."
The results of two other surgical studies, CLEAR III and MISTIE III, "are eagerly awaited," Dr. Gautschi and Dr. Schaller said, noting that, "decompressive hemicraniectomy might be a[nother] promising surgical procedure."
The U.K. Medical Research Council funded STICH II. Dr. Mendelow reported having no relevant financial disclosures.
LONDON – Approximately 2%-3% of patients with spontaneous intracerebral hemorrhage may benefit from early surgical removal of hematoma, according to the results of the second Surgical Trial in Lobar Intracerebral Hemorrhage.
As reported at the annual European Stroke Conference and published simultaneously in the Lancet, patients with superficial lesions and an unfavorable prognostic score appeared to benefit from early surgical intervention, compared with those given conservative medical treatment (odds ratio [OR] = 0.49, P =.02). Conversely, those with a good prognostic score did not seem to benefit (OR = 1.12, P = .57).
The primary analysis showed no significant benefit of early surgery overall, with 41.4% of 297 patients in the early surgery group and 37.7% of 286 patients in the conservative treatment group having a favorable outcome at 6 months, as determined by the 8-point extended Glasgow Outcome Scale (GOS-E) (P = .367).
"That’s a 3.7% absolute benefit, which is not enough to change surgical practice on its own," said Dr. A. David Mendelow, professor of neurosurgery at Newcastle University in Newcastle upon Tyne, England. "We were looking for a 12% benefit when we set out to do this trial," he added during a press conference.
A 6% decrease in mortality at 6 months was seen favoring surgery (18% vs. 24% for conservative therapy), but this was not statistically significant (P = .095).
"Intracerebral hemorrhage is not a homogenous condition," Dr. Mendelow said, adding that it can be a difficult decision to operate. Clinical manifestations can range from no apparent effects to severe disability and rapid death. "STICH [Surgical Trial in Lobar Intracerebral Hemorrhage] focused on patients that we are not quite sure about whether to operate or not," he said.
The hypothesis for the trial was based on the findings of the first STICH trial (Acta Neurochir. Suppl. 2006;96:65-8). The results of the trial were again neutral overall, but subgroup analyses showed that some groups of patients did worse with surgery, such as those with deep-seated bleeds, and some may fare better, such as those with superficial lobar hematomas.
STICH II therefore specifically recruited this latter group of patients to see if the effect was real or an artifact of the scientific analysis. In total, 601 conscious ICH patients with a median age of 65 years were recruited at 78 centers in 27 countries. Patients had to have a superficial lesion (1 cm or less from the cortical surface of the brain) that was between 10 mL and 100 mL in volume, and with no sign of intraventricular hemorrhage on CT scanning. Patients had to be recruited within 48 hours of the stroke and surgical intervention had to be performed within 12 hours (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)60986-1]). (A total of 6 patients were excluded or withdrew from the study before intervention, and after intervention another 12 withdrew, were lost to follow-up, or were alive but had an unknown status.)
The GOS-E was calculated from the answers to a questionnaire sent out to patients and their relatives 6 months following their stroke. A cutoff score of approximately 27 was used to categorize patients as having a good or bad prognosis. At baseline, about two-thirds of patients had a good prognosis, and the remainder had a poor prognosis.
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials,"
"One of the reasons, perhaps, for a lack of significance was the [number of] crossovers from initial conservative therapy to surgery," Dr. Mendelow said. Indeed, 21% of patients who were originally randomized to conservative treatment crossed over to the surgical arm. These patients had "clearly deteriorated" prior to having surgery, he said when presenting the findings. Furthermore, only 37% of these crossovers received surgery within the specified 12-hour time limit.
STICH provides the best, albeit insufficient, evidence to date on the role of surgery in ICH, Dr. Oliver Gautschi and Dr. Karl Schaller, both of the University of Geneva, commented in an editorial about the trial (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)61087-9]) .
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials," they wrote. "The overall result of this meta-analysis of patients with different types of intracerebral hemorrhage favors surgery."
The results of two other surgical studies, CLEAR III and MISTIE III, "are eagerly awaited," Dr. Gautschi and Dr. Schaller said, noting that, "decompressive hemicraniectomy might be a[nother] promising surgical procedure."
The U.K. Medical Research Council funded STICH II. Dr. Mendelow reported having no relevant financial disclosures.
LONDON – Approximately 2%-3% of patients with spontaneous intracerebral hemorrhage may benefit from early surgical removal of hematoma, according to the results of the second Surgical Trial in Lobar Intracerebral Hemorrhage.
As reported at the annual European Stroke Conference and published simultaneously in the Lancet, patients with superficial lesions and an unfavorable prognostic score appeared to benefit from early surgical intervention, compared with those given conservative medical treatment (odds ratio [OR] = 0.49, P =.02). Conversely, those with a good prognostic score did not seem to benefit (OR = 1.12, P = .57).
The primary analysis showed no significant benefit of early surgery overall, with 41.4% of 297 patients in the early surgery group and 37.7% of 286 patients in the conservative treatment group having a favorable outcome at 6 months, as determined by the 8-point extended Glasgow Outcome Scale (GOS-E) (P = .367).
"That’s a 3.7% absolute benefit, which is not enough to change surgical practice on its own," said Dr. A. David Mendelow, professor of neurosurgery at Newcastle University in Newcastle upon Tyne, England. "We were looking for a 12% benefit when we set out to do this trial," he added during a press conference.
A 6% decrease in mortality at 6 months was seen favoring surgery (18% vs. 24% for conservative therapy), but this was not statistically significant (P = .095).
"Intracerebral hemorrhage is not a homogenous condition," Dr. Mendelow said, adding that it can be a difficult decision to operate. Clinical manifestations can range from no apparent effects to severe disability and rapid death. "STICH [Surgical Trial in Lobar Intracerebral Hemorrhage] focused on patients that we are not quite sure about whether to operate or not," he said.
The hypothesis for the trial was based on the findings of the first STICH trial (Acta Neurochir. Suppl. 2006;96:65-8). The results of the trial were again neutral overall, but subgroup analyses showed that some groups of patients did worse with surgery, such as those with deep-seated bleeds, and some may fare better, such as those with superficial lobar hematomas.
STICH II therefore specifically recruited this latter group of patients to see if the effect was real or an artifact of the scientific analysis. In total, 601 conscious ICH patients with a median age of 65 years were recruited at 78 centers in 27 countries. Patients had to have a superficial lesion (1 cm or less from the cortical surface of the brain) that was between 10 mL and 100 mL in volume, and with no sign of intraventricular hemorrhage on CT scanning. Patients had to be recruited within 48 hours of the stroke and surgical intervention had to be performed within 12 hours (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)60986-1]). (A total of 6 patients were excluded or withdrew from the study before intervention, and after intervention another 12 withdrew, were lost to follow-up, or were alive but had an unknown status.)
The GOS-E was calculated from the answers to a questionnaire sent out to patients and their relatives 6 months following their stroke. A cutoff score of approximately 27 was used to categorize patients as having a good or bad prognosis. At baseline, about two-thirds of patients had a good prognosis, and the remainder had a poor prognosis.
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials,"
"One of the reasons, perhaps, for a lack of significance was the [number of] crossovers from initial conservative therapy to surgery," Dr. Mendelow said. Indeed, 21% of patients who were originally randomized to conservative treatment crossed over to the surgical arm. These patients had "clearly deteriorated" prior to having surgery, he said when presenting the findings. Furthermore, only 37% of these crossovers received surgery within the specified 12-hour time limit.
STICH provides the best, albeit insufficient, evidence to date on the role of surgery in ICH, Dr. Oliver Gautschi and Dr. Karl Schaller, both of the University of Geneva, commented in an editorial about the trial (Lancet 2013 May 29 [doi:10.1016/S0140-6736(13)61087-9]) .
"The notion that early surgery might be beneficial in this subgroup of patients is supported by the results of the investigator’s updated meta-analysis of 15 trials," they wrote. "The overall result of this meta-analysis of patients with different types of intracerebral hemorrhage favors surgery."
The results of two other surgical studies, CLEAR III and MISTIE III, "are eagerly awaited," Dr. Gautschi and Dr. Schaller said, noting that, "decompressive hemicraniectomy might be a[nother] promising surgical procedure."
The U.K. Medical Research Council funded STICH II. Dr. Mendelow reported having no relevant financial disclosures.
AT THE EUROPEAN STROKE CONFERENCE
Major finding: A favorable outcome at 6 months was seen in 41% of the early surgery group and 38% of the conservative treatment group (P = .367).
Data source: STICH II, an international, multicenter prospective trial of 601 patients randomized to early surgery (within 12 hours) or medical treatment within 48 hours of a spontaneous superficial intracerebral hemorrhage.
Disclosures: The U.K. Medical Research Council funded STICH II. Dr. Mendelow reported having no relevant financial disclosures.
Low-dose perioperative steroids effective in IBD patients
Postoperative postural hypotension or adrenal insufficiency in patients with inflammatory bowel disease can be effectively prevented with low-dose rather than high-dose steroids, according to data published in the June 14 online issue of Annals of Surgery [doi: 10.1097/SLA.b013e318297adca].
"Corticosteroid-treated patients undergoing major colorectal surgery are commonly prescribed high-dose steroids to prevent perioperative adrenal insufficiency and cardiovascular collapse," wrote Dr. Karen Zaghiyan and her colleagues from Cedars-Sinai Medical Center, Los Angeles. "There is little evidence to support this practice."
A randomized, single-blinded noninferiority trial in 92 steroid-treated inflammatory bowel disease (IBD) patients undergoing major colorectal surgery showed that 96% of patients randomized to low-dose steroids and 95% of patients randomized to high-dose steroids did not exhibit postural hypotension on the first day after surgery (noninferiority 95% confidence interval, –0.08 to 0.09; P = .007).
"Because reports of postoperative adrenal insufficiency and hemodynamic collapse have implicated the first 24 hours after surgery as the most susceptible, and postural hypotension is likely to be a more reliable indicator of hemodynamic instability than supine hypotension, our primary endpoint was clinically meaningful," the researchers reported.
Patients were randomized to receive either 100 mg of IV hydrocortisone at the time of incision and three times daily for the first postoperative day, then tapered, or to low-dose IV hydrocortisone equivalent to presurgical oral dosing, followed by taper.
The primary outcome was the absence of postural hypotension on postoperative day 1, defined as a decrease in systolic blood pressure by 20 mm Hg after sitting from a supine position.
"We found no significant difference in perioperative factors, including operative time, intraoperative blood loss, volume of intravenous fluids administered, number of patients requiring intravenous fluid boluses, or blood transfusions between our two patient groups," the researchers reported.
The investigators also found no significant differences in other outcomes such as surgical or medical complications, length of postoperative stay, fatigue, nausea, and pain, although there was an insignificant trend toward more infectious complications in the high-dose steroid group.
The practice of administering high doses of corticosteroids perioperatively was sparked in the 1950s by two incidences of postoperative cardiovascular collapse and death in patients whose preoperative corticosteroids were discontinued before surgery, the authors said.
"However, high-dose corticosteroids are not without consequence and have been associated with various postoperative complications, including wound infection and anastomotic dehiscence," the authors reported.
Some studies had already suggested that steroid-treated patients undergoing surgery could remain on their baseline corticosteroid dose perioperatively; however, these studies were mostly focused on organ transplant recipients or included patients taking low maintenance doses of corticosteroids undergoing minor or moderate surgical procedures.
"Patients with IBD represent a unique study cohort because they are frequently taking high doses of steroids for a prolonged period of time, and surgery in these patients often involves major stress," the researchers reported.
"Although we recently published our retrospective data to suggest safety of low-dose steroids in steroid-treated IBD patients undergoing major colorectal surgery, this is the first prospective study to evaluate the role of stress-dose steroids in patients undergoing major abdominal and pelvic surgery," the investigators wrote.
There were no conflicts of interest declared.
Postoperative postural hypotension or adrenal insufficiency in patients with inflammatory bowel disease can be effectively prevented with low-dose rather than high-dose steroids, according to data published in the June 14 online issue of Annals of Surgery [doi: 10.1097/SLA.b013e318297adca].
"Corticosteroid-treated patients undergoing major colorectal surgery are commonly prescribed high-dose steroids to prevent perioperative adrenal insufficiency and cardiovascular collapse," wrote Dr. Karen Zaghiyan and her colleagues from Cedars-Sinai Medical Center, Los Angeles. "There is little evidence to support this practice."
A randomized, single-blinded noninferiority trial in 92 steroid-treated inflammatory bowel disease (IBD) patients undergoing major colorectal surgery showed that 96% of patients randomized to low-dose steroids and 95% of patients randomized to high-dose steroids did not exhibit postural hypotension on the first day after surgery (noninferiority 95% confidence interval, –0.08 to 0.09; P = .007).
"Because reports of postoperative adrenal insufficiency and hemodynamic collapse have implicated the first 24 hours after surgery as the most susceptible, and postural hypotension is likely to be a more reliable indicator of hemodynamic instability than supine hypotension, our primary endpoint was clinically meaningful," the researchers reported.
Patients were randomized to receive either 100 mg of IV hydrocortisone at the time of incision and three times daily for the first postoperative day, then tapered, or to low-dose IV hydrocortisone equivalent to presurgical oral dosing, followed by taper.
The primary outcome was the absence of postural hypotension on postoperative day 1, defined as a decrease in systolic blood pressure by 20 mm Hg after sitting from a supine position.
"We found no significant difference in perioperative factors, including operative time, intraoperative blood loss, volume of intravenous fluids administered, number of patients requiring intravenous fluid boluses, or blood transfusions between our two patient groups," the researchers reported.
The investigators also found no significant differences in other outcomes such as surgical or medical complications, length of postoperative stay, fatigue, nausea, and pain, although there was an insignificant trend toward more infectious complications in the high-dose steroid group.
The practice of administering high doses of corticosteroids perioperatively was sparked in the 1950s by two incidences of postoperative cardiovascular collapse and death in patients whose preoperative corticosteroids were discontinued before surgery, the authors said.
"However, high-dose corticosteroids are not without consequence and have been associated with various postoperative complications, including wound infection and anastomotic dehiscence," the authors reported.
Some studies had already suggested that steroid-treated patients undergoing surgery could remain on their baseline corticosteroid dose perioperatively; however, these studies were mostly focused on organ transplant recipients or included patients taking low maintenance doses of corticosteroids undergoing minor or moderate surgical procedures.
"Patients with IBD represent a unique study cohort because they are frequently taking high doses of steroids for a prolonged period of time, and surgery in these patients often involves major stress," the researchers reported.
"Although we recently published our retrospective data to suggest safety of low-dose steroids in steroid-treated IBD patients undergoing major colorectal surgery, this is the first prospective study to evaluate the role of stress-dose steroids in patients undergoing major abdominal and pelvic surgery," the investigators wrote.
There were no conflicts of interest declared.
Postoperative postural hypotension or adrenal insufficiency in patients with inflammatory bowel disease can be effectively prevented with low-dose rather than high-dose steroids, according to data published in the June 14 online issue of Annals of Surgery [doi: 10.1097/SLA.b013e318297adca].
"Corticosteroid-treated patients undergoing major colorectal surgery are commonly prescribed high-dose steroids to prevent perioperative adrenal insufficiency and cardiovascular collapse," wrote Dr. Karen Zaghiyan and her colleagues from Cedars-Sinai Medical Center, Los Angeles. "There is little evidence to support this practice."
A randomized, single-blinded noninferiority trial in 92 steroid-treated inflammatory bowel disease (IBD) patients undergoing major colorectal surgery showed that 96% of patients randomized to low-dose steroids and 95% of patients randomized to high-dose steroids did not exhibit postural hypotension on the first day after surgery (noninferiority 95% confidence interval, –0.08 to 0.09; P = .007).
"Because reports of postoperative adrenal insufficiency and hemodynamic collapse have implicated the first 24 hours after surgery as the most susceptible, and postural hypotension is likely to be a more reliable indicator of hemodynamic instability than supine hypotension, our primary endpoint was clinically meaningful," the researchers reported.
Patients were randomized to receive either 100 mg of IV hydrocortisone at the time of incision and three times daily for the first postoperative day, then tapered, or to low-dose IV hydrocortisone equivalent to presurgical oral dosing, followed by taper.
The primary outcome was the absence of postural hypotension on postoperative day 1, defined as a decrease in systolic blood pressure by 20 mm Hg after sitting from a supine position.
"We found no significant difference in perioperative factors, including operative time, intraoperative blood loss, volume of intravenous fluids administered, number of patients requiring intravenous fluid boluses, or blood transfusions between our two patient groups," the researchers reported.
The investigators also found no significant differences in other outcomes such as surgical or medical complications, length of postoperative stay, fatigue, nausea, and pain, although there was an insignificant trend toward more infectious complications in the high-dose steroid group.
The practice of administering high doses of corticosteroids perioperatively was sparked in the 1950s by two incidences of postoperative cardiovascular collapse and death in patients whose preoperative corticosteroids were discontinued before surgery, the authors said.
"However, high-dose corticosteroids are not without consequence and have been associated with various postoperative complications, including wound infection and anastomotic dehiscence," the authors reported.
Some studies had already suggested that steroid-treated patients undergoing surgery could remain on their baseline corticosteroid dose perioperatively; however, these studies were mostly focused on organ transplant recipients or included patients taking low maintenance doses of corticosteroids undergoing minor or moderate surgical procedures.
"Patients with IBD represent a unique study cohort because they are frequently taking high doses of steroids for a prolonged period of time, and surgery in these patients often involves major stress," the researchers reported.
"Although we recently published our retrospective data to suggest safety of low-dose steroids in steroid-treated IBD patients undergoing major colorectal surgery, this is the first prospective study to evaluate the role of stress-dose steroids in patients undergoing major abdominal and pelvic surgery," the investigators wrote.
There were no conflicts of interest declared.
FROM ANNALS OF SURGERY
Major finding: Low-dose corticosteroids are as effective as high dose in preventing postoperative postural hypotension or adrenal insufficiency in patients with inflammatory bowel disease.
Data source: Randomized, single-blinded noninferiority trial in 92 patients.
Disclosures: No conflicts of interest were declared.
Tools help predict VTE after abdominal, thoracic surgery
Two simple-to-use calculation tools, which physicians can use to predict separately the 30-day risk of postoperative venous thromboembolism in hospital and after discharge, have been developed. Researchers based the two nomograms on the results of a retrospective analysis of more than 450,000 thoracic and abdominal surgical patients in the American College of Surgeons National Surgical Quality Improvement Program database.
"Substantial variation exists in the incidence of VTE [venous thromboembolism] and VTEDC [venous thromboembolism after hospital discharge] after abdominal or thoracic surgery, depending on patient and procedural factors," wrote Dr. Robert Canter, Dr. Dhruvil R. Shah, and colleagues at the University of California, Davis. They analyzed these factors to determine statistically significant risks in order to construct the predictive nomograms, according to their report published in the July issue of the Journal of Surgical Research. Dr. Canter is the senior author of the study and associate professor of surgery in the Division of Surgical Oncology at UC Davis.*
The authors used data obtained from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) to construct a nomogram by which physicians could use a ruler and draw lines from each separate risk factor on a no-yes gridline to a point score for that factor. By adding the point results for all factors, the total number of points could then be used to calculate the 30-day risk of developing a VTE. A separate nomogram using the same process was constructed for calculating the risk of a VTEDC.
The researchers assessed 471,867 patients who underwent inpatient abdominal or thoracic operations between 2005 and 2010. Patients who underwent primary vascular and spine operations were excluded. The overall unadjusted, 30-day incidence of postoperative VT) in these patients was 1.5% and that of VTEDC was 0.5%, and the annual incidence rates remained unchanged over the period studied. The median time to VTE was 9 days and the median time to VTEDC was 17 days, and these also did not change over the study period.
The majority of patients were white (75.5%) and men (59%), with a mean age of 54 years and a mean body mass index of 31 kg/m2; 93% of the patients were functionally independent.
Comorbidities included smoking (19%), history of preoperative infection or sepsis (16.5%), diabetes (15%), and a variety of cardiovascular conditions or procedures (9%). The vast majority of operations were abdominal (98%), with most performed on the gastrointestinal tract (51.5%). Thoracic operations accounted for 2.1%. Minimally invasive (excluding bariatric) surgery was performed in 37% of cases, with 20% of all operations performed for cancer. A total of 11% of patients experienced one or more major postoperative complications within 30 days of the operation, including post discharge.
Multivariate analysis showed that the significant predictors of both VTE and VTEDC were age, body mass index, presence of postoperative infection, operation for cancer, procedure type (primarily splenectomy), multivisceral resection, and nonbariatric laparoscopic surgery. Significant factors predicting VTE but not VTEDC were a history of chronic obstructive pulmonary disease, disseminated cancer, and emergent operation (J. Surg. Res. 2013;183:462-71).
In addition to the nomogram, the researchers used internally developed concordance indices to measure the probability of concordance between the predicted and measured outcomes and found that these were 0.77 for VTE and 0.67 for VTEDC. They acknowledge that the lower value for VTEDC is a probable indicator of unknown and uncaptured risk factors, possibly including socioeconomic status, a change in postoperative functional status,
Limitations of the study included those inherent to using the ACS-NSQUIP database, which meant that they could not identify patients who had a prior history of VTE or central line placement, both of which have been cited as VTE risk factors, according to the researchers. In addition, asymptomatic VTE events and events for which patients did not receive anticoagulation were not captured in the database.
"Although these nomograms require external validation to ensure reproducibility, these tools will aid clinicians, researchers, and administrators in determining which subset of patients undergoing abdominal or general thoracic general surgical operations are at highest risk for postoperative VTE and VTEDC. Our data may allow for more targeted quality improvement interventions to reduce VTE and VTEDC" in these patients, the researchers concluded.
The authors disclosed no conflicts that the editors of the journal determined should be reported in the article.
*UPDATED: This story was updated to include Dr. Canter's information and photo.
Two simple-to-use calculation tools, which physicians can use to predict separately the 30-day risk of postoperative venous thromboembolism in hospital and after discharge, have been developed. Researchers based the two nomograms on the results of a retrospective analysis of more than 450,000 thoracic and abdominal surgical patients in the American College of Surgeons National Surgical Quality Improvement Program database.
"Substantial variation exists in the incidence of VTE [venous thromboembolism] and VTEDC [venous thromboembolism after hospital discharge] after abdominal or thoracic surgery, depending on patient and procedural factors," wrote Dr. Robert Canter, Dr. Dhruvil R. Shah, and colleagues at the University of California, Davis. They analyzed these factors to determine statistically significant risks in order to construct the predictive nomograms, according to their report published in the July issue of the Journal of Surgical Research. Dr. Canter is the senior author of the study and associate professor of surgery in the Division of Surgical Oncology at UC Davis.*
The authors used data obtained from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) to construct a nomogram by which physicians could use a ruler and draw lines from each separate risk factor on a no-yes gridline to a point score for that factor. By adding the point results for all factors, the total number of points could then be used to calculate the 30-day risk of developing a VTE. A separate nomogram using the same process was constructed for calculating the risk of a VTEDC.
The researchers assessed 471,867 patients who underwent inpatient abdominal or thoracic operations between 2005 and 2010. Patients who underwent primary vascular and spine operations were excluded. The overall unadjusted, 30-day incidence of postoperative VT) in these patients was 1.5% and that of VTEDC was 0.5%, and the annual incidence rates remained unchanged over the period studied. The median time to VTE was 9 days and the median time to VTEDC was 17 days, and these also did not change over the study period.
The majority of patients were white (75.5%) and men (59%), with a mean age of 54 years and a mean body mass index of 31 kg/m2; 93% of the patients were functionally independent.
Comorbidities included smoking (19%), history of preoperative infection or sepsis (16.5%), diabetes (15%), and a variety of cardiovascular conditions or procedures (9%). The vast majority of operations were abdominal (98%), with most performed on the gastrointestinal tract (51.5%). Thoracic operations accounted for 2.1%. Minimally invasive (excluding bariatric) surgery was performed in 37% of cases, with 20% of all operations performed for cancer. A total of 11% of patients experienced one or more major postoperative complications within 30 days of the operation, including post discharge.
Multivariate analysis showed that the significant predictors of both VTE and VTEDC were age, body mass index, presence of postoperative infection, operation for cancer, procedure type (primarily splenectomy), multivisceral resection, and nonbariatric laparoscopic surgery. Significant factors predicting VTE but not VTEDC were a history of chronic obstructive pulmonary disease, disseminated cancer, and emergent operation (J. Surg. Res. 2013;183:462-71).
In addition to the nomogram, the researchers used internally developed concordance indices to measure the probability of concordance between the predicted and measured outcomes and found that these were 0.77 for VTE and 0.67 for VTEDC. They acknowledge that the lower value for VTEDC is a probable indicator of unknown and uncaptured risk factors, possibly including socioeconomic status, a change in postoperative functional status,
Limitations of the study included those inherent to using the ACS-NSQUIP database, which meant that they could not identify patients who had a prior history of VTE or central line placement, both of which have been cited as VTE risk factors, according to the researchers. In addition, asymptomatic VTE events and events for which patients did not receive anticoagulation were not captured in the database.
"Although these nomograms require external validation to ensure reproducibility, these tools will aid clinicians, researchers, and administrators in determining which subset of patients undergoing abdominal or general thoracic general surgical operations are at highest risk for postoperative VTE and VTEDC. Our data may allow for more targeted quality improvement interventions to reduce VTE and VTEDC" in these patients, the researchers concluded.
The authors disclosed no conflicts that the editors of the journal determined should be reported in the article.
*UPDATED: This story was updated to include Dr. Canter's information and photo.
Two simple-to-use calculation tools, which physicians can use to predict separately the 30-day risk of postoperative venous thromboembolism in hospital and after discharge, have been developed. Researchers based the two nomograms on the results of a retrospective analysis of more than 450,000 thoracic and abdominal surgical patients in the American College of Surgeons National Surgical Quality Improvement Program database.
"Substantial variation exists in the incidence of VTE [venous thromboembolism] and VTEDC [venous thromboembolism after hospital discharge] after abdominal or thoracic surgery, depending on patient and procedural factors," wrote Dr. Robert Canter, Dr. Dhruvil R. Shah, and colleagues at the University of California, Davis. They analyzed these factors to determine statistically significant risks in order to construct the predictive nomograms, according to their report published in the July issue of the Journal of Surgical Research. Dr. Canter is the senior author of the study and associate professor of surgery in the Division of Surgical Oncology at UC Davis.*
The authors used data obtained from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) to construct a nomogram by which physicians could use a ruler and draw lines from each separate risk factor on a no-yes gridline to a point score for that factor. By adding the point results for all factors, the total number of points could then be used to calculate the 30-day risk of developing a VTE. A separate nomogram using the same process was constructed for calculating the risk of a VTEDC.
The researchers assessed 471,867 patients who underwent inpatient abdominal or thoracic operations between 2005 and 2010. Patients who underwent primary vascular and spine operations were excluded. The overall unadjusted, 30-day incidence of postoperative VT) in these patients was 1.5% and that of VTEDC was 0.5%, and the annual incidence rates remained unchanged over the period studied. The median time to VTE was 9 days and the median time to VTEDC was 17 days, and these also did not change over the study period.
The majority of patients were white (75.5%) and men (59%), with a mean age of 54 years and a mean body mass index of 31 kg/m2; 93% of the patients were functionally independent.
Comorbidities included smoking (19%), history of preoperative infection or sepsis (16.5%), diabetes (15%), and a variety of cardiovascular conditions or procedures (9%). The vast majority of operations were abdominal (98%), with most performed on the gastrointestinal tract (51.5%). Thoracic operations accounted for 2.1%. Minimally invasive (excluding bariatric) surgery was performed in 37% of cases, with 20% of all operations performed for cancer. A total of 11% of patients experienced one or more major postoperative complications within 30 days of the operation, including post discharge.
Multivariate analysis showed that the significant predictors of both VTE and VTEDC were age, body mass index, presence of postoperative infection, operation for cancer, procedure type (primarily splenectomy), multivisceral resection, and nonbariatric laparoscopic surgery. Significant factors predicting VTE but not VTEDC were a history of chronic obstructive pulmonary disease, disseminated cancer, and emergent operation (J. Surg. Res. 2013;183:462-71).
In addition to the nomogram, the researchers used internally developed concordance indices to measure the probability of concordance between the predicted and measured outcomes and found that these were 0.77 for VTE and 0.67 for VTEDC. They acknowledge that the lower value for VTEDC is a probable indicator of unknown and uncaptured risk factors, possibly including socioeconomic status, a change in postoperative functional status,
Limitations of the study included those inherent to using the ACS-NSQUIP database, which meant that they could not identify patients who had a prior history of VTE or central line placement, both of which have been cited as VTE risk factors, according to the researchers. In addition, asymptomatic VTE events and events for which patients did not receive anticoagulation were not captured in the database.
"Although these nomograms require external validation to ensure reproducibility, these tools will aid clinicians, researchers, and administrators in determining which subset of patients undergoing abdominal or general thoracic general surgical operations are at highest risk for postoperative VTE and VTEDC. Our data may allow for more targeted quality improvement interventions to reduce VTE and VTEDC" in these patients, the researchers concluded.
The authors disclosed no conflicts that the editors of the journal determined should be reported in the article.
*UPDATED: This story was updated to include Dr. Canter's information and photo.
FROM THE JOURNAL OF SURGICAL RESEARCH
More hospitals providing palliative care
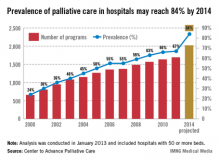
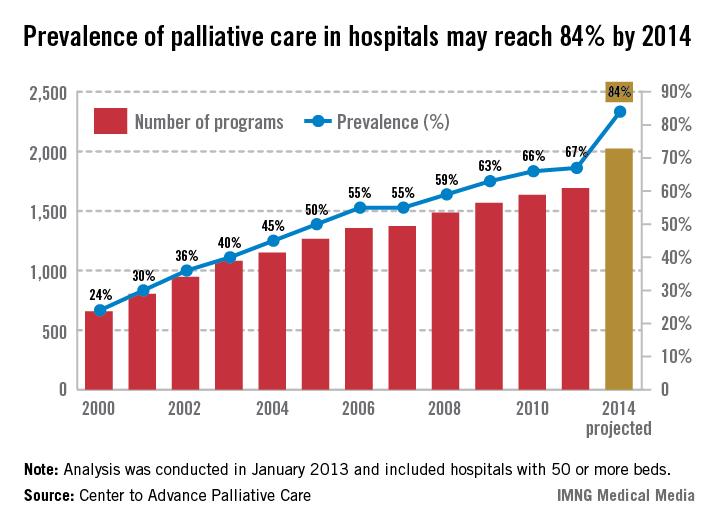
The prevalence of palliative care programs in U.S. hospitals is expected to reach 84% by 2014, according to an analysis from the Center to Advance Palliative Care.
From 2000 to 2011, the number of hospitals with 50 or more beds that had a palliative care program went from 658 to 1,692, an increase of 157%. If that trend continues, there should be 2,023 hospitals – approximately 84% – providing palliative care in the United States by 2014, the CAPC reported.
The CAPC analysis, conducted in January 2013, involved data from the American Hospital Association and the center’s own National Palliative Care Registry.
The prevalence of palliative care programs in U.S. hospitals is expected to reach 84% by 2014, according to an analysis from the Center to Advance Palliative Care.
From 2000 to 2011, the number of hospitals with 50 or more beds that had a palliative care program went from 658 to 1,692, an increase of 157%. If that trend continues, there should be 2,023 hospitals – approximately 84% – providing palliative care in the United States by 2014, the CAPC reported.
The CAPC analysis, conducted in January 2013, involved data from the American Hospital Association and the center’s own National Palliative Care Registry.
The prevalence of palliative care programs in U.S. hospitals is expected to reach 84% by 2014, according to an analysis from the Center to Advance Palliative Care.
From 2000 to 2011, the number of hospitals with 50 or more beds that had a palliative care program went from 658 to 1,692, an increase of 157%. If that trend continues, there should be 2,023 hospitals – approximately 84% – providing palliative care in the United States by 2014, the CAPC reported.
The CAPC analysis, conducted in January 2013, involved data from the American Hospital Association and the center’s own National Palliative Care Registry.
Postop pneumonia risk strong for subset of thoracic surgery patients
SAN DIEGO – For thoracic surgery patients, being on neoadjuvant chemotherapy, having chronic obstructive pulmonary disease, and a weight loss of greater than 10% were all associated with the development of postoperative pneumonia, results from a single-center study showed.
At the national conference of the American College of Surgeons/National Surgical Quality Improvement Program, Dr. Elisabeth Dexter noted that after the first ACS/NSQIP data harvest at the Roswell Park Cancer Institute in Buffalo, N.Y., the risk of postoperative pneumonia was found to be 4.4%, compared with a rate of 1.1% in all other NSQIP hospitals.
"Of particular note, the thoracic surgery service had a high incidence of 13.2%," said Dr. Dexter, an attending surgeon in the department of thoracic surgery at the Institute. "The high incidence of our postoperative pneumonia was likely [affected] by our thoracic surgery service because our thoracic surgery service had an increased percentage of the abstracted NSQIP data in our cohort, from 12% to 14%, compared with other NSQIP hospitals of similar academic size abstracting 2%. When we found this high postoperative pneumonia rate, we decided to query our NSQIP data and our tumor registry between July 1, 2011, and Oct. 8, 2012, to ask the question: Is there an increased incidence of postoperative pneumonia in thoracic surgery patients who received neoadjuvant chemotherapy compared with those who did not?"
Dr. Dexter and her associates cross-referenced ACS/NSQIP data on 1,723 patients at the cancer center with the tumor registry. Of the 1,723 patients, 1,645 had no postoperative pneumonia while 78 did. Compared with the non-pneumonia patients, those who had pneumonia tended to be older (a mean of 67 vs. 60 years, respectively; odds ratio, 1.05; P less than .001), more likely to be male (59% vs. 37%; OR, 2.48; P less than .001), have chronic obstructive pulmonary disease (35% vs. 9%; OR, 5.08; P less than .001), be a smoker (36% vs. 24%; OR, 1.75; P = .021), and had lost more than 10% of body weight (10% vs. 2.5%; OR, 4.47; P less than .001).
On univariate analysis, postoperative pneumonia was associated with being on neoadjuvant chemotherapy (4.2% vs. 14%; OR, 3.75; P less than .001).
In addition, certain surgical subspecialties at the Institute had a high incidence of postoperative pneumonia, including thoracic surgery (46%), GI surgery (21%), and gynecology (12%).
When the researchers included the entire cohort of patients, those who were on neoadjuvant therapy had an increased incidence of postoperative pneumonia, compared with those who were not on neoadjuvant chemotherapy (P = .001). When thoracic surgery patients were excluded from the analysis, non-thoracic surgery patients who were on neoadjuvant chemotherapy had no increased incidence of postoperative pneumonia, compared with the patients who were not on neoadjuvant chemotherapy (P = .681). On multivariate analysis, significant variables associated with postoperative pneumonia were being on neoadjuvant chemotherapy (P= .001), having chronic obstructive pulmonary disease (P less than .0001), and having weight loss of greater than 10% (P = .004).
"Institutions with disproportionately busy complex thoracic surgery programs may have rates of postoperative pneumonia skewed higher than predicted by NSQIP models," Dr. Dexter concluded. "Optimization of nutritional status and COPD treatment in neoadjuvant chemotherapy patients may reduce postoperative pneumonia risk and incidence. Balance of oncologic benefit of neoadjuvant chemotherapy versus risk and morbidity of postoperative chemotherapy warrants future study in thoracic surgery patients."
Dr. Dexter said that she had no relevant financial conflicts to make.
SAN DIEGO – For thoracic surgery patients, being on neoadjuvant chemotherapy, having chronic obstructive pulmonary disease, and a weight loss of greater than 10% were all associated with the development of postoperative pneumonia, results from a single-center study showed.
At the national conference of the American College of Surgeons/National Surgical Quality Improvement Program, Dr. Elisabeth Dexter noted that after the first ACS/NSQIP data harvest at the Roswell Park Cancer Institute in Buffalo, N.Y., the risk of postoperative pneumonia was found to be 4.4%, compared with a rate of 1.1% in all other NSQIP hospitals.
"Of particular note, the thoracic surgery service had a high incidence of 13.2%," said Dr. Dexter, an attending surgeon in the department of thoracic surgery at the Institute. "The high incidence of our postoperative pneumonia was likely [affected] by our thoracic surgery service because our thoracic surgery service had an increased percentage of the abstracted NSQIP data in our cohort, from 12% to 14%, compared with other NSQIP hospitals of similar academic size abstracting 2%. When we found this high postoperative pneumonia rate, we decided to query our NSQIP data and our tumor registry between July 1, 2011, and Oct. 8, 2012, to ask the question: Is there an increased incidence of postoperative pneumonia in thoracic surgery patients who received neoadjuvant chemotherapy compared with those who did not?"
Dr. Dexter and her associates cross-referenced ACS/NSQIP data on 1,723 patients at the cancer center with the tumor registry. Of the 1,723 patients, 1,645 had no postoperative pneumonia while 78 did. Compared with the non-pneumonia patients, those who had pneumonia tended to be older (a mean of 67 vs. 60 years, respectively; odds ratio, 1.05; P less than .001), more likely to be male (59% vs. 37%; OR, 2.48; P less than .001), have chronic obstructive pulmonary disease (35% vs. 9%; OR, 5.08; P less than .001), be a smoker (36% vs. 24%; OR, 1.75; P = .021), and had lost more than 10% of body weight (10% vs. 2.5%; OR, 4.47; P less than .001).
On univariate analysis, postoperative pneumonia was associated with being on neoadjuvant chemotherapy (4.2% vs. 14%; OR, 3.75; P less than .001).
In addition, certain surgical subspecialties at the Institute had a high incidence of postoperative pneumonia, including thoracic surgery (46%), GI surgery (21%), and gynecology (12%).
When the researchers included the entire cohort of patients, those who were on neoadjuvant therapy had an increased incidence of postoperative pneumonia, compared with those who were not on neoadjuvant chemotherapy (P = .001). When thoracic surgery patients were excluded from the analysis, non-thoracic surgery patients who were on neoadjuvant chemotherapy had no increased incidence of postoperative pneumonia, compared with the patients who were not on neoadjuvant chemotherapy (P = .681). On multivariate analysis, significant variables associated with postoperative pneumonia were being on neoadjuvant chemotherapy (P= .001), having chronic obstructive pulmonary disease (P less than .0001), and having weight loss of greater than 10% (P = .004).
"Institutions with disproportionately busy complex thoracic surgery programs may have rates of postoperative pneumonia skewed higher than predicted by NSQIP models," Dr. Dexter concluded. "Optimization of nutritional status and COPD treatment in neoadjuvant chemotherapy patients may reduce postoperative pneumonia risk and incidence. Balance of oncologic benefit of neoadjuvant chemotherapy versus risk and morbidity of postoperative chemotherapy warrants future study in thoracic surgery patients."
Dr. Dexter said that she had no relevant financial conflicts to make.
SAN DIEGO – For thoracic surgery patients, being on neoadjuvant chemotherapy, having chronic obstructive pulmonary disease, and a weight loss of greater than 10% were all associated with the development of postoperative pneumonia, results from a single-center study showed.
At the national conference of the American College of Surgeons/National Surgical Quality Improvement Program, Dr. Elisabeth Dexter noted that after the first ACS/NSQIP data harvest at the Roswell Park Cancer Institute in Buffalo, N.Y., the risk of postoperative pneumonia was found to be 4.4%, compared with a rate of 1.1% in all other NSQIP hospitals.
"Of particular note, the thoracic surgery service had a high incidence of 13.2%," said Dr. Dexter, an attending surgeon in the department of thoracic surgery at the Institute. "The high incidence of our postoperative pneumonia was likely [affected] by our thoracic surgery service because our thoracic surgery service had an increased percentage of the abstracted NSQIP data in our cohort, from 12% to 14%, compared with other NSQIP hospitals of similar academic size abstracting 2%. When we found this high postoperative pneumonia rate, we decided to query our NSQIP data and our tumor registry between July 1, 2011, and Oct. 8, 2012, to ask the question: Is there an increased incidence of postoperative pneumonia in thoracic surgery patients who received neoadjuvant chemotherapy compared with those who did not?"
Dr. Dexter and her associates cross-referenced ACS/NSQIP data on 1,723 patients at the cancer center with the tumor registry. Of the 1,723 patients, 1,645 had no postoperative pneumonia while 78 did. Compared with the non-pneumonia patients, those who had pneumonia tended to be older (a mean of 67 vs. 60 years, respectively; odds ratio, 1.05; P less than .001), more likely to be male (59% vs. 37%; OR, 2.48; P less than .001), have chronic obstructive pulmonary disease (35% vs. 9%; OR, 5.08; P less than .001), be a smoker (36% vs. 24%; OR, 1.75; P = .021), and had lost more than 10% of body weight (10% vs. 2.5%; OR, 4.47; P less than .001).
On univariate analysis, postoperative pneumonia was associated with being on neoadjuvant chemotherapy (4.2% vs. 14%; OR, 3.75; P less than .001).
In addition, certain surgical subspecialties at the Institute had a high incidence of postoperative pneumonia, including thoracic surgery (46%), GI surgery (21%), and gynecology (12%).
When the researchers included the entire cohort of patients, those who were on neoadjuvant therapy had an increased incidence of postoperative pneumonia, compared with those who were not on neoadjuvant chemotherapy (P = .001). When thoracic surgery patients were excluded from the analysis, non-thoracic surgery patients who were on neoadjuvant chemotherapy had no increased incidence of postoperative pneumonia, compared with the patients who were not on neoadjuvant chemotherapy (P = .681). On multivariate analysis, significant variables associated with postoperative pneumonia were being on neoadjuvant chemotherapy (P= .001), having chronic obstructive pulmonary disease (P less than .0001), and having weight loss of greater than 10% (P = .004).
"Institutions with disproportionately busy complex thoracic surgery programs may have rates of postoperative pneumonia skewed higher than predicted by NSQIP models," Dr. Dexter concluded. "Optimization of nutritional status and COPD treatment in neoadjuvant chemotherapy patients may reduce postoperative pneumonia risk and incidence. Balance of oncologic benefit of neoadjuvant chemotherapy versus risk and morbidity of postoperative chemotherapy warrants future study in thoracic surgery patients."
Dr. Dexter said that she had no relevant financial conflicts to make.
AT THE ACS NSQIP NATIONAL CONFERENCE
Major finding: On multivariate analysis, significant variables associated with postoperative pneumonia were being on neoadjuvant chemotherapy (P = .001), having COPD (P less than .0001), and having weight loss of greater than 10% (P = .004).
Data source: A study of 1,723 patients who underwent surgery at Roswell Park Cancer Institute in Buffalo, N.Y. Of the postoperative pneumonia cases that developed, 46% were from the thoracic surgery service.
Disclosures: Dr. Dexter said that she had no relevant financial disclosures to make.
Preoperative screening program helped reduce 30-day mortality
SAN DIEGO – The implementation of an intensive preoperative screening and intervention process led to a significant decrease in 30-day mortality for general surgery and vascular procedures, results from a single-center study demonstrated.
In 2007, Carilion Roanoke (Va.) Memorial Hospital became a member of the American College of Surgeons/National Surgical Quality Improvement Program (ACS/NSQIP). "After receiving our first report, it became evident that surgical mortality at our institution was significantly higher than expected and significantly higher than the national average," Dr. Agathoklis Konstantinidis said at the ACS/NSQIP National Conference. "After further evaluation of this data, it became obvious that we were operating on people with several undiagnosed, untreated medical diseases such as diabetes, obstructive sleep apnea, hypertension, lung disease, and renal disease that all constituted significant preoperative risk factors."
In an effort to improve surgical mortality at the hospital, Dr. Konstantinidis and his associates implemented a strict preoperative screening and intervention program that began in January 2010. Since that time, every patient scheduled for surgery is required to undergo a preoperative screening appointment with a registered nurse who performs an extensive computer-based checklist of risk factors for heart disease, renal disease, abnormal EKG, sleep apnea, and pulmonary disease.
"If a problem is identified, the surgery is postponed until the issue is addressed, either by the primary care physician or by the surgeon who is directly involved in the care of the patient, and in close communication with other specialists, such as those in internal medicine, family practice, and endocrinology," explained Dr. Konstantinidis, who is a surgeon at the hospital.
Between July 2007 and December 2009 – prior to initiation of the preoperative screening and intervention program – the odds ratios for 30-day mortality in all cases were 1.40, 1.43, 1.58, and 1.56 in successive reporting periods. Beginning with the first report after implementation of the preoperative screening and intervention program, 30-day mortality in all cases progressively decreased in successive reporting periods (OR, 1.26, 1.19, 1.14, and 0.86, respectively), with similar reductions in both general surgery (OR, 0.92) and vascular surgery (OR, 0.92) for the last year.
"After the implementation of our new preoperative screening and intervention process, overall 30-day surgical mortality at our institution decreased from 3.5% to 1.9%, which is clinically and also statistically significant based on the P value (P = .007)," Dr. Konstantinidis said.
He went on to report that out of 5,866 patients who underwent screening in 2012 alone, 3,691 had undiagnosed obstructive sleep apnea, 2,361 had an abnormal preoperative EKG, 437 had undiagnosed diabetes, 192 had undiagnosed hypertension, and 167 had undiagnosed shortness of breath. "As a result of the screening intervention, surgery was canceled in 218 patients, and 147 were referred to cardiology specialists for further evaluation," he said.
Dr. Konstantinidis said that he had no relevant financial conflicts to disclose.
Carilion Roanoke (Va.) Memorial Hospital, American College of Surgeons/National Surgical Quality Improvement Program (ACS/NSQIP), Dr. Agathoklis Konstantinidis, ACS/NSQIP National Conference, diabetes, obstructive sleep apnea, hypertension, lung disease, renal disease, preoperative risk factors, improve surgical mortality,
SAN DIEGO – The implementation of an intensive preoperative screening and intervention process led to a significant decrease in 30-day mortality for general surgery and vascular procedures, results from a single-center study demonstrated.
In 2007, Carilion Roanoke (Va.) Memorial Hospital became a member of the American College of Surgeons/National Surgical Quality Improvement Program (ACS/NSQIP). "After receiving our first report, it became evident that surgical mortality at our institution was significantly higher than expected and significantly higher than the national average," Dr. Agathoklis Konstantinidis said at the ACS/NSQIP National Conference. "After further evaluation of this data, it became obvious that we were operating on people with several undiagnosed, untreated medical diseases such as diabetes, obstructive sleep apnea, hypertension, lung disease, and renal disease that all constituted significant preoperative risk factors."
In an effort to improve surgical mortality at the hospital, Dr. Konstantinidis and his associates implemented a strict preoperative screening and intervention program that began in January 2010. Since that time, every patient scheduled for surgery is required to undergo a preoperative screening appointment with a registered nurse who performs an extensive computer-based checklist of risk factors for heart disease, renal disease, abnormal EKG, sleep apnea, and pulmonary disease.
"If a problem is identified, the surgery is postponed until the issue is addressed, either by the primary care physician or by the surgeon who is directly involved in the care of the patient, and in close communication with other specialists, such as those in internal medicine, family practice, and endocrinology," explained Dr. Konstantinidis, who is a surgeon at the hospital.
Between July 2007 and December 2009 – prior to initiation of the preoperative screening and intervention program – the odds ratios for 30-day mortality in all cases were 1.40, 1.43, 1.58, and 1.56 in successive reporting periods. Beginning with the first report after implementation of the preoperative screening and intervention program, 30-day mortality in all cases progressively decreased in successive reporting periods (OR, 1.26, 1.19, 1.14, and 0.86, respectively), with similar reductions in both general surgery (OR, 0.92) and vascular surgery (OR, 0.92) for the last year.
"After the implementation of our new preoperative screening and intervention process, overall 30-day surgical mortality at our institution decreased from 3.5% to 1.9%, which is clinically and also statistically significant based on the P value (P = .007)," Dr. Konstantinidis said.
He went on to report that out of 5,866 patients who underwent screening in 2012 alone, 3,691 had undiagnosed obstructive sleep apnea, 2,361 had an abnormal preoperative EKG, 437 had undiagnosed diabetes, 192 had undiagnosed hypertension, and 167 had undiagnosed shortness of breath. "As a result of the screening intervention, surgery was canceled in 218 patients, and 147 were referred to cardiology specialists for further evaluation," he said.
Dr. Konstantinidis said that he had no relevant financial conflicts to disclose.
SAN DIEGO – The implementation of an intensive preoperative screening and intervention process led to a significant decrease in 30-day mortality for general surgery and vascular procedures, results from a single-center study demonstrated.
In 2007, Carilion Roanoke (Va.) Memorial Hospital became a member of the American College of Surgeons/National Surgical Quality Improvement Program (ACS/NSQIP). "After receiving our first report, it became evident that surgical mortality at our institution was significantly higher than expected and significantly higher than the national average," Dr. Agathoklis Konstantinidis said at the ACS/NSQIP National Conference. "After further evaluation of this data, it became obvious that we were operating on people with several undiagnosed, untreated medical diseases such as diabetes, obstructive sleep apnea, hypertension, lung disease, and renal disease that all constituted significant preoperative risk factors."
In an effort to improve surgical mortality at the hospital, Dr. Konstantinidis and his associates implemented a strict preoperative screening and intervention program that began in January 2010. Since that time, every patient scheduled for surgery is required to undergo a preoperative screening appointment with a registered nurse who performs an extensive computer-based checklist of risk factors for heart disease, renal disease, abnormal EKG, sleep apnea, and pulmonary disease.
"If a problem is identified, the surgery is postponed until the issue is addressed, either by the primary care physician or by the surgeon who is directly involved in the care of the patient, and in close communication with other specialists, such as those in internal medicine, family practice, and endocrinology," explained Dr. Konstantinidis, who is a surgeon at the hospital.
Between July 2007 and December 2009 – prior to initiation of the preoperative screening and intervention program – the odds ratios for 30-day mortality in all cases were 1.40, 1.43, 1.58, and 1.56 in successive reporting periods. Beginning with the first report after implementation of the preoperative screening and intervention program, 30-day mortality in all cases progressively decreased in successive reporting periods (OR, 1.26, 1.19, 1.14, and 0.86, respectively), with similar reductions in both general surgery (OR, 0.92) and vascular surgery (OR, 0.92) for the last year.
"After the implementation of our new preoperative screening and intervention process, overall 30-day surgical mortality at our institution decreased from 3.5% to 1.9%, which is clinically and also statistically significant based on the P value (P = .007)," Dr. Konstantinidis said.
He went on to report that out of 5,866 patients who underwent screening in 2012 alone, 3,691 had undiagnosed obstructive sleep apnea, 2,361 had an abnormal preoperative EKG, 437 had undiagnosed diabetes, 192 had undiagnosed hypertension, and 167 had undiagnosed shortness of breath. "As a result of the screening intervention, surgery was canceled in 218 patients, and 147 were referred to cardiology specialists for further evaluation," he said.
Dr. Konstantinidis said that he had no relevant financial conflicts to disclose.
Carilion Roanoke (Va.) Memorial Hospital, American College of Surgeons/National Surgical Quality Improvement Program (ACS/NSQIP), Dr. Agathoklis Konstantinidis, ACS/NSQIP National Conference, diabetes, obstructive sleep apnea, hypertension, lung disease, renal disease, preoperative risk factors, improve surgical mortality,
Carilion Roanoke (Va.) Memorial Hospital, American College of Surgeons/National Surgical Quality Improvement Program (ACS/NSQIP), Dr. Agathoklis Konstantinidis, ACS/NSQIP National Conference, diabetes, obstructive sleep apnea, hypertension, lung disease, renal disease, preoperative risk factors, improve surgical mortality,
AT THE ACS NSQIP NATIONAL CONFERENCE
Major finding: After implementation of a new preoperative screening and intervention process, overall 30-day surgical mortality decreased from 3.5% to 1.9%, which reached clinical and statistical significance (P = .007).
Data source: A single-center study of patients who underwent general surgery and vascular surgery procedures between 2007 and 2011 at Carilion Roanoke (Va.) Memorial Hospital.
Disclosures: Dr. Konstantinidis said that he had no relevant financial conflicts to disclose.
TVS useful for diagnosis of adenomyosis and leiomyoma
SAN DIEGO – Transvaginal ultrasound is accurate, sensitive, and specific in the diagnosis of leiomyoma and coexisting adenomyosis and leiomyoma, results from a single-center study showed.
"Menorrhagia is a very common condition which female patients are suffering from many days of the month," Dr. Magdi Hanafi, FACS, said in an interview after the American College of Surgeons/National Surgical Quality Improvement Program National Conference, where the study was presented at a poster session.
"It interferes with their normal day-to-day life and work, and causes anemia and its subsequent complications. Two of the common causes of menorrhagia are adenomyosis and leiomyoma. These two conditions are frequently missed by some gynecologists – especially adenomyosis – clinically and on some occasions by pelvic ultrasound."
Dr. Hanafi, medical director of Gyn. and Fertility Specialists at Saint Joseph’s Hospital of Atlanta, retrospectively evaluated 163 women with a preoperative transvaginal ultrasound (TVS) diagnosis of adenomyosis, leiomyoma, and adenomyosis with coexisting leiomyoma. Of the 163 patients, 130 underwent hysterectomy and 33 symptomatic patients underwent myomectomy with excision of the surrounding myometrium, which presumably contained adenomyosis. Following surgery, hospital pathologists performed a histological examination and recorded the diagnosis.
The mean age of the patients was 44 years. Dr. Hanafi reported that 123 of the patients were positively diagnosed with adenomyosis via TVS. Among these, histopathologic confirmation of TVS diagnosis of adenomyosis was positive in 93 patients (76%) and negative in 30 (24%). The sensitivity, specificity, and accuracy of TVS in the diagnosis of adenomyosis were 85% (P less than .0001), 43% (P = .41), and 71%, respectively. "This demonstrates that TVS diagnosis of adenomyosis is sensitive, but not specific," he said.
Histopathologic data on leiomyoma was complete in 134 of the patients. Among these, histopathologic confirmation of TVS diagnosis of leiomyoma was positive in 133 patients (99%) and negative in 1 (1%). The sensitivity, specificity, and accuracy of TVS in the diagnosis of leiomyoma were 96% (P less than .0001), 96% (P less than .0001), and 96%, respectively.
"In other published studies in the diagnosis of adenomyosis, combined adenomyosis and leiomyoma was not mentioned," Dr. Hanafi commented. "This combination is more common than we ever thought before, and all gynecologists should think of this combined condition in menorrhagic patients in their differential diagnosis."
He concluded that office TVS "is a very valuable procedure in the diagnosis of adenomyosis, leiomyoma, or combined [adenomyosis and leiomyoma]. It is sensitive and accurate in the diagnosis of leiomyoma, adenomyosis, or [the combination], but not specific in the diagnosis of adenomyosis alone."
Dr. Hanafi said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Transvaginal ultrasound is accurate, sensitive, and specific in the diagnosis of leiomyoma and coexisting adenomyosis and leiomyoma, results from a single-center study showed.
"Menorrhagia is a very common condition which female patients are suffering from many days of the month," Dr. Magdi Hanafi, FACS, said in an interview after the American College of Surgeons/National Surgical Quality Improvement Program National Conference, where the study was presented at a poster session.
"It interferes with their normal day-to-day life and work, and causes anemia and its subsequent complications. Two of the common causes of menorrhagia are adenomyosis and leiomyoma. These two conditions are frequently missed by some gynecologists – especially adenomyosis – clinically and on some occasions by pelvic ultrasound."
Dr. Hanafi, medical director of Gyn. and Fertility Specialists at Saint Joseph’s Hospital of Atlanta, retrospectively evaluated 163 women with a preoperative transvaginal ultrasound (TVS) diagnosis of adenomyosis, leiomyoma, and adenomyosis with coexisting leiomyoma. Of the 163 patients, 130 underwent hysterectomy and 33 symptomatic patients underwent myomectomy with excision of the surrounding myometrium, which presumably contained adenomyosis. Following surgery, hospital pathologists performed a histological examination and recorded the diagnosis.
The mean age of the patients was 44 years. Dr. Hanafi reported that 123 of the patients were positively diagnosed with adenomyosis via TVS. Among these, histopathologic confirmation of TVS diagnosis of adenomyosis was positive in 93 patients (76%) and negative in 30 (24%). The sensitivity, specificity, and accuracy of TVS in the diagnosis of adenomyosis were 85% (P less than .0001), 43% (P = .41), and 71%, respectively. "This demonstrates that TVS diagnosis of adenomyosis is sensitive, but not specific," he said.
Histopathologic data on leiomyoma was complete in 134 of the patients. Among these, histopathologic confirmation of TVS diagnosis of leiomyoma was positive in 133 patients (99%) and negative in 1 (1%). The sensitivity, specificity, and accuracy of TVS in the diagnosis of leiomyoma were 96% (P less than .0001), 96% (P less than .0001), and 96%, respectively.
"In other published studies in the diagnosis of adenomyosis, combined adenomyosis and leiomyoma was not mentioned," Dr. Hanafi commented. "This combination is more common than we ever thought before, and all gynecologists should think of this combined condition in menorrhagic patients in their differential diagnosis."
He concluded that office TVS "is a very valuable procedure in the diagnosis of adenomyosis, leiomyoma, or combined [adenomyosis and leiomyoma]. It is sensitive and accurate in the diagnosis of leiomyoma, adenomyosis, or [the combination], but not specific in the diagnosis of adenomyosis alone."
Dr. Hanafi said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Transvaginal ultrasound is accurate, sensitive, and specific in the diagnosis of leiomyoma and coexisting adenomyosis and leiomyoma, results from a single-center study showed.
"Menorrhagia is a very common condition which female patients are suffering from many days of the month," Dr. Magdi Hanafi, FACS, said in an interview after the American College of Surgeons/National Surgical Quality Improvement Program National Conference, where the study was presented at a poster session.
"It interferes with their normal day-to-day life and work, and causes anemia and its subsequent complications. Two of the common causes of menorrhagia are adenomyosis and leiomyoma. These two conditions are frequently missed by some gynecologists – especially adenomyosis – clinically and on some occasions by pelvic ultrasound."
Dr. Hanafi, medical director of Gyn. and Fertility Specialists at Saint Joseph’s Hospital of Atlanta, retrospectively evaluated 163 women with a preoperative transvaginal ultrasound (TVS) diagnosis of adenomyosis, leiomyoma, and adenomyosis with coexisting leiomyoma. Of the 163 patients, 130 underwent hysterectomy and 33 symptomatic patients underwent myomectomy with excision of the surrounding myometrium, which presumably contained adenomyosis. Following surgery, hospital pathologists performed a histological examination and recorded the diagnosis.
The mean age of the patients was 44 years. Dr. Hanafi reported that 123 of the patients were positively diagnosed with adenomyosis via TVS. Among these, histopathologic confirmation of TVS diagnosis of adenomyosis was positive in 93 patients (76%) and negative in 30 (24%). The sensitivity, specificity, and accuracy of TVS in the diagnosis of adenomyosis were 85% (P less than .0001), 43% (P = .41), and 71%, respectively. "This demonstrates that TVS diagnosis of adenomyosis is sensitive, but not specific," he said.
Histopathologic data on leiomyoma was complete in 134 of the patients. Among these, histopathologic confirmation of TVS diagnosis of leiomyoma was positive in 133 patients (99%) and negative in 1 (1%). The sensitivity, specificity, and accuracy of TVS in the diagnosis of leiomyoma were 96% (P less than .0001), 96% (P less than .0001), and 96%, respectively.
"In other published studies in the diagnosis of adenomyosis, combined adenomyosis and leiomyoma was not mentioned," Dr. Hanafi commented. "This combination is more common than we ever thought before, and all gynecologists should think of this combined condition in menorrhagic patients in their differential diagnosis."
He concluded that office TVS "is a very valuable procedure in the diagnosis of adenomyosis, leiomyoma, or combined [adenomyosis and leiomyoma]. It is sensitive and accurate in the diagnosis of leiomyoma, adenomyosis, or [the combination], but not specific in the diagnosis of adenomyosis alone."
Dr. Hanafi said that he had no relevant financial conflicts to disclose.
AT THE ACS NSQIP NATIONAL CONFERENCE
Major finding: The sensitivity, specificity, and accuracy of transvaginal ultrasound in the diagnosis of adenomyosis were 85% (P less than .0001), 43% (P = .41), and 71%, respectively. At the same time, the sensitivity, specificity, and accuracy of TVS in the diagnosis of adenomyosis were 96% (P less than .0001), 96% (P less than .0001), and 96%, respectively.
Data source: A retrospective study of 163 female patients with a preoperative TVS diagnosis of adenomyosis, leiomyoma, and adenomyosis with coexisting leiomyoma.
Disclosures: Dr. Hanafi said that he had no relevant financial conflicts to disclose.