User login
Official Newspaper of the American College of Surgeons
Whither IPAB? Cost-cutting board is idle, but not gone
January came and went with nary a whisper from the once feared but now nearly forgotten Independent Payment Advisory Board.
Enacted as part of the Affordable Care Act and originally slated to have made its first cost-cutting recommendations by now, the IPAB has no members and has never met. For 2 years in a row, Congress and the President have stripped most of the board’s funding from the federal budget.
Under the ACA, the IPAB is charged with looking at 5-year Medicare spending trends and recommending cuts for the following year if per capita spending exceeds a set target.
The IPAB’s recommendations in any given year automatically take effect if Congress does not pass legislation to achieve the savings by Aug. 15. The board cannot recommend rationing care, increasing revenues, changing benefits, modifying eligibility, increasing cost-sharing, or changing the percentage of the premium that beneficiaries pay or the subsidies they receive under Medicare Part D.
Last year, the Medicare chief actuary determined spending would stay below the 2015 target, so the IPAB did not need to act. Further, the Congressional Budget Office has estimated that continuing slow growth in health care costs could mean that the board may not be called into play for another decade.
Physician organizations remain interested in either repealing the board or revising its scope and composition.
The American Medical Association objects to the IPAB on principle. In Feb. 2012, AMA Executive Vice President and CEO James L. Madara wrote to congressional leaders in support of a House bill to repeal the IPAB, noting that the IPAB "puts important health care payment and policy decisions in the hands of an independent body that has far too little accountability."
For the American Academy of Family Physicians, the IPAB "just isn’t a high priority right now," Dr. Reid Blackwelder, AAFP president, said in an interview.
The AAFP is more focused on replacing the Medicare Sustainable Growth Rate formula. Should the IPAB’s work get under way, the AAFP would go back to trying to get its recommendations reconsidered, Dr. Blackwelder said.
In fact, the AAFP isn’t completely opposed to the IPAB. "We like the concept, however, we really oppose the way the IPAB was set up," Dr. Blackwelder said.
The AAFP supports several changes to the IPAB, including:
• Addition of a primary care physician and a consumer representative to the board.
• A public comment period after IPAB recommendations are sent to Congress.
• Increased focus on quality improvement.
• Inclusion of all health care sectors – not just physician fees – in the board’s immediate mandate.
While the American College of Physicians supports the general concept of an independent panel to help evaluate Medicare fiscal soundness, it wants primary care representation and equal responsibility for meeting targets among all providers.
Bob Doherty, senior vice president of governmental affairs and public policy at the ACP, said that he does not expect any movement from the IPAB in the near future.
"The administration has made no effort to start the appointment process, which inevitably would run into Republican resistance to recommending appointees and Republican resistance in the Senate to their confirmation," he said. Mr. Doherty noted that many Democrats don’t support the IPAB, either.
That makes the IPAB "a fight that the administration and Democrats don’t need to take on now," Mr. Doherty said.
Paul N. Van de Water, a senior fellow at the Center on Budget and Policy Priorities in Washington, predicted that while action from the IPAB is unlikely in 2014, the board eventually will be called to action.
And, Mr. Van de Water said that he thought that physicians should take a more favorable view of the IPAB. "It allows for the application of expert human judgment about how a cost growth problem should be dealt with," he said.
"It’s not an SGR, an automatic formula that you are stuck with."
On Twitter @aliciaault
January came and went with nary a whisper from the once feared but now nearly forgotten Independent Payment Advisory Board.
Enacted as part of the Affordable Care Act and originally slated to have made its first cost-cutting recommendations by now, the IPAB has no members and has never met. For 2 years in a row, Congress and the President have stripped most of the board’s funding from the federal budget.
Under the ACA, the IPAB is charged with looking at 5-year Medicare spending trends and recommending cuts for the following year if per capita spending exceeds a set target.
The IPAB’s recommendations in any given year automatically take effect if Congress does not pass legislation to achieve the savings by Aug. 15. The board cannot recommend rationing care, increasing revenues, changing benefits, modifying eligibility, increasing cost-sharing, or changing the percentage of the premium that beneficiaries pay or the subsidies they receive under Medicare Part D.
Last year, the Medicare chief actuary determined spending would stay below the 2015 target, so the IPAB did not need to act. Further, the Congressional Budget Office has estimated that continuing slow growth in health care costs could mean that the board may not be called into play for another decade.
Physician organizations remain interested in either repealing the board or revising its scope and composition.
The American Medical Association objects to the IPAB on principle. In Feb. 2012, AMA Executive Vice President and CEO James L. Madara wrote to congressional leaders in support of a House bill to repeal the IPAB, noting that the IPAB "puts important health care payment and policy decisions in the hands of an independent body that has far too little accountability."
For the American Academy of Family Physicians, the IPAB "just isn’t a high priority right now," Dr. Reid Blackwelder, AAFP president, said in an interview.
The AAFP is more focused on replacing the Medicare Sustainable Growth Rate formula. Should the IPAB’s work get under way, the AAFP would go back to trying to get its recommendations reconsidered, Dr. Blackwelder said.
In fact, the AAFP isn’t completely opposed to the IPAB. "We like the concept, however, we really oppose the way the IPAB was set up," Dr. Blackwelder said.
The AAFP supports several changes to the IPAB, including:
• Addition of a primary care physician and a consumer representative to the board.
• A public comment period after IPAB recommendations are sent to Congress.
• Increased focus on quality improvement.
• Inclusion of all health care sectors – not just physician fees – in the board’s immediate mandate.
While the American College of Physicians supports the general concept of an independent panel to help evaluate Medicare fiscal soundness, it wants primary care representation and equal responsibility for meeting targets among all providers.
Bob Doherty, senior vice president of governmental affairs and public policy at the ACP, said that he does not expect any movement from the IPAB in the near future.
"The administration has made no effort to start the appointment process, which inevitably would run into Republican resistance to recommending appointees and Republican resistance in the Senate to their confirmation," he said. Mr. Doherty noted that many Democrats don’t support the IPAB, either.
That makes the IPAB "a fight that the administration and Democrats don’t need to take on now," Mr. Doherty said.
Paul N. Van de Water, a senior fellow at the Center on Budget and Policy Priorities in Washington, predicted that while action from the IPAB is unlikely in 2014, the board eventually will be called to action.
And, Mr. Van de Water said that he thought that physicians should take a more favorable view of the IPAB. "It allows for the application of expert human judgment about how a cost growth problem should be dealt with," he said.
"It’s not an SGR, an automatic formula that you are stuck with."
On Twitter @aliciaault
January came and went with nary a whisper from the once feared but now nearly forgotten Independent Payment Advisory Board.
Enacted as part of the Affordable Care Act and originally slated to have made its first cost-cutting recommendations by now, the IPAB has no members and has never met. For 2 years in a row, Congress and the President have stripped most of the board’s funding from the federal budget.
Under the ACA, the IPAB is charged with looking at 5-year Medicare spending trends and recommending cuts for the following year if per capita spending exceeds a set target.
The IPAB’s recommendations in any given year automatically take effect if Congress does not pass legislation to achieve the savings by Aug. 15. The board cannot recommend rationing care, increasing revenues, changing benefits, modifying eligibility, increasing cost-sharing, or changing the percentage of the premium that beneficiaries pay or the subsidies they receive under Medicare Part D.
Last year, the Medicare chief actuary determined spending would stay below the 2015 target, so the IPAB did not need to act. Further, the Congressional Budget Office has estimated that continuing slow growth in health care costs could mean that the board may not be called into play for another decade.
Physician organizations remain interested in either repealing the board or revising its scope and composition.
The American Medical Association objects to the IPAB on principle. In Feb. 2012, AMA Executive Vice President and CEO James L. Madara wrote to congressional leaders in support of a House bill to repeal the IPAB, noting that the IPAB "puts important health care payment and policy decisions in the hands of an independent body that has far too little accountability."
For the American Academy of Family Physicians, the IPAB "just isn’t a high priority right now," Dr. Reid Blackwelder, AAFP president, said in an interview.
The AAFP is more focused on replacing the Medicare Sustainable Growth Rate formula. Should the IPAB’s work get under way, the AAFP would go back to trying to get its recommendations reconsidered, Dr. Blackwelder said.
In fact, the AAFP isn’t completely opposed to the IPAB. "We like the concept, however, we really oppose the way the IPAB was set up," Dr. Blackwelder said.
The AAFP supports several changes to the IPAB, including:
• Addition of a primary care physician and a consumer representative to the board.
• A public comment period after IPAB recommendations are sent to Congress.
• Increased focus on quality improvement.
• Inclusion of all health care sectors – not just physician fees – in the board’s immediate mandate.
While the American College of Physicians supports the general concept of an independent panel to help evaluate Medicare fiscal soundness, it wants primary care representation and equal responsibility for meeting targets among all providers.
Bob Doherty, senior vice president of governmental affairs and public policy at the ACP, said that he does not expect any movement from the IPAB in the near future.
"The administration has made no effort to start the appointment process, which inevitably would run into Republican resistance to recommending appointees and Republican resistance in the Senate to their confirmation," he said. Mr. Doherty noted that many Democrats don’t support the IPAB, either.
That makes the IPAB "a fight that the administration and Democrats don’t need to take on now," Mr. Doherty said.
Paul N. Van de Water, a senior fellow at the Center on Budget and Policy Priorities in Washington, predicted that while action from the IPAB is unlikely in 2014, the board eventually will be called to action.
And, Mr. Van de Water said that he thought that physicians should take a more favorable view of the IPAB. "It allows for the application of expert human judgment about how a cost growth problem should be dealt with," he said.
"It’s not an SGR, an automatic formula that you are stuck with."
On Twitter @aliciaault
CT negative: Take the C-collars off already
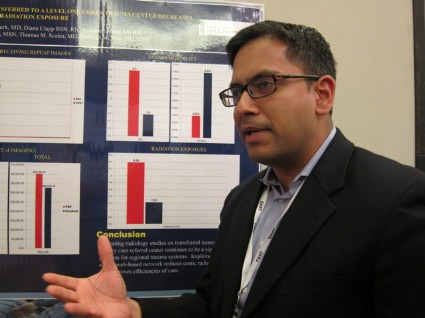
NAPLES, FLA. – Computed tomography of the cervical spine had 100% specificity and sensitivity in ruling out clinically significant fracture and ligamentous injuries after blunt trauma in a prospective cohort of 5,676 patients.
Patients with negative CT scans do not need further workup for possible ligamentous injury, as those were only identified in patients with a positive CT scan, Dr. Poornima Vanguri said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
"Patients with a normal CT do not need further imaging and collars should be cleared as soon as possible," the authors concluded.
The prospective study included all 5,676 blunt trauma alert patients seen at a Level 1 trauma center between January 2008 and December 2012. Their average age was 40.6 years, mean Glasgow Coma Scale (GCS) score 14.2, mean Injury Severity Score (ISS) 9.6, and mean length of stay 4.8 days.
Of these, 420 (7.2%) had any cervical spine injury and 2.6% died.
The incidence of fracture was 7.2% (409/5,676) and ligamentous injury 0.9% (52/5,676), said Dr. Vanguri, a general surgery resident at Virginia Commonwealth University in Richmond.
Patients with cervical spine injury versus those without were significantly older (46.3 years vs. 40.2 years), had significantly lower GCS scores (13.5 vs. 14.2), and had significantly higher ISS (18.9 vs. 8.9), average blood alcohol levels (666 mg/L vs. 538 mg/L), and average lactate levels (2.6 mmol/L vs. 2.4 mmol/L). Patients with cervical spine injuries also stayed significantly longer in the hospital (11.3 days vs. 4.3 days) and ICU (5.8 days vs. 1.4 days), and had more ventilator days (9.8 days vs. 4.1 days).
Of the 52 patients with ligamentous injury, 30 (57.7%) were suspected on CT, Dr. Vanguri noted. The remaining 22 without suspected ligamentous injury all had associated fractures identified by CT requiring further intervention. Thus, CT attained 100% sensitivity and specificity in ruling out cervical spine injuries, she said.
Notably, the incidence of ligamentous injury without fracture was 0.2% (10/5,676). Stepwise logistic regression identified only three independent predictors of ligamentous injury: cervical midline tenderness, abnormal alertness, and C-spine fracture on CT.
The poster presentation prompted a spirited debate at the meeting, with some attendees arguing that clearing collars in patients with a negative CT could leave practitioners and hospitals open to potential litigation if unstable fractures and/or ligamentous injuries are missed by not conducting further testing with magnetic resonance imaging (MRI).
The specter of litigation is always a possibility; however, the incidence of ligamentous injury without fracture was exceedingly low and prolonged C-collar use is not without consequences, argued senior author Dr. Therèse Duane, an ACS Fellow and trauma and critical care surgeon at the university.
"How many times do patients go home and 3 months later still have a collar on because they can’t get an MRI and now they have migraines, can’t work, and can’t drive? It’s huge," she said.
In the study, 77% of the 52 patients with ligamentous injury underwent MRI in addition to a CT scan, 48% had CT angiography of the neck, 40.4% had C-spine surgery, and 81% required prolonged collar use for treatment purposes of 6 weeks or longer.
Though current practice at the university is to clear collars in patients with a negative CT scan, research would be needed to determine whether this approach is feasible in the higher-risk patients with altered alertness, Dr. Duane observed.
Further studies are planned by the group looking at national databanks, as well as combining a decade worth of data at their institution, to define a C-spine clearance protocol.
Dr. Vanguri and her colleagues reported having no financial disclosures.
NAPLES, FLA. – Computed tomography of the cervical spine had 100% specificity and sensitivity in ruling out clinically significant fracture and ligamentous injuries after blunt trauma in a prospective cohort of 5,676 patients.
Patients with negative CT scans do not need further workup for possible ligamentous injury, as those were only identified in patients with a positive CT scan, Dr. Poornima Vanguri said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
"Patients with a normal CT do not need further imaging and collars should be cleared as soon as possible," the authors concluded.
The prospective study included all 5,676 blunt trauma alert patients seen at a Level 1 trauma center between January 2008 and December 2012. Their average age was 40.6 years, mean Glasgow Coma Scale (GCS) score 14.2, mean Injury Severity Score (ISS) 9.6, and mean length of stay 4.8 days.
Of these, 420 (7.2%) had any cervical spine injury and 2.6% died.
The incidence of fracture was 7.2% (409/5,676) and ligamentous injury 0.9% (52/5,676), said Dr. Vanguri, a general surgery resident at Virginia Commonwealth University in Richmond.
Patients with cervical spine injury versus those without were significantly older (46.3 years vs. 40.2 years), had significantly lower GCS scores (13.5 vs. 14.2), and had significantly higher ISS (18.9 vs. 8.9), average blood alcohol levels (666 mg/L vs. 538 mg/L), and average lactate levels (2.6 mmol/L vs. 2.4 mmol/L). Patients with cervical spine injuries also stayed significantly longer in the hospital (11.3 days vs. 4.3 days) and ICU (5.8 days vs. 1.4 days), and had more ventilator days (9.8 days vs. 4.1 days).
Of the 52 patients with ligamentous injury, 30 (57.7%) were suspected on CT, Dr. Vanguri noted. The remaining 22 without suspected ligamentous injury all had associated fractures identified by CT requiring further intervention. Thus, CT attained 100% sensitivity and specificity in ruling out cervical spine injuries, she said.
Notably, the incidence of ligamentous injury without fracture was 0.2% (10/5,676). Stepwise logistic regression identified only three independent predictors of ligamentous injury: cervical midline tenderness, abnormal alertness, and C-spine fracture on CT.
The poster presentation prompted a spirited debate at the meeting, with some attendees arguing that clearing collars in patients with a negative CT could leave practitioners and hospitals open to potential litigation if unstable fractures and/or ligamentous injuries are missed by not conducting further testing with magnetic resonance imaging (MRI).
The specter of litigation is always a possibility; however, the incidence of ligamentous injury without fracture was exceedingly low and prolonged C-collar use is not without consequences, argued senior author Dr. Therèse Duane, an ACS Fellow and trauma and critical care surgeon at the university.
"How many times do patients go home and 3 months later still have a collar on because they can’t get an MRI and now they have migraines, can’t work, and can’t drive? It’s huge," she said.
In the study, 77% of the 52 patients with ligamentous injury underwent MRI in addition to a CT scan, 48% had CT angiography of the neck, 40.4% had C-spine surgery, and 81% required prolonged collar use for treatment purposes of 6 weeks or longer.
Though current practice at the university is to clear collars in patients with a negative CT scan, research would be needed to determine whether this approach is feasible in the higher-risk patients with altered alertness, Dr. Duane observed.
Further studies are planned by the group looking at national databanks, as well as combining a decade worth of data at their institution, to define a C-spine clearance protocol.
Dr. Vanguri and her colleagues reported having no financial disclosures.
NAPLES, FLA. – Computed tomography of the cervical spine had 100% specificity and sensitivity in ruling out clinically significant fracture and ligamentous injuries after blunt trauma in a prospective cohort of 5,676 patients.
Patients with negative CT scans do not need further workup for possible ligamentous injury, as those were only identified in patients with a positive CT scan, Dr. Poornima Vanguri said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
"Patients with a normal CT do not need further imaging and collars should be cleared as soon as possible," the authors concluded.
The prospective study included all 5,676 blunt trauma alert patients seen at a Level 1 trauma center between January 2008 and December 2012. Their average age was 40.6 years, mean Glasgow Coma Scale (GCS) score 14.2, mean Injury Severity Score (ISS) 9.6, and mean length of stay 4.8 days.
Of these, 420 (7.2%) had any cervical spine injury and 2.6% died.
The incidence of fracture was 7.2% (409/5,676) and ligamentous injury 0.9% (52/5,676), said Dr. Vanguri, a general surgery resident at Virginia Commonwealth University in Richmond.
Patients with cervical spine injury versus those without were significantly older (46.3 years vs. 40.2 years), had significantly lower GCS scores (13.5 vs. 14.2), and had significantly higher ISS (18.9 vs. 8.9), average blood alcohol levels (666 mg/L vs. 538 mg/L), and average lactate levels (2.6 mmol/L vs. 2.4 mmol/L). Patients with cervical spine injuries also stayed significantly longer in the hospital (11.3 days vs. 4.3 days) and ICU (5.8 days vs. 1.4 days), and had more ventilator days (9.8 days vs. 4.1 days).
Of the 52 patients with ligamentous injury, 30 (57.7%) were suspected on CT, Dr. Vanguri noted. The remaining 22 without suspected ligamentous injury all had associated fractures identified by CT requiring further intervention. Thus, CT attained 100% sensitivity and specificity in ruling out cervical spine injuries, she said.
Notably, the incidence of ligamentous injury without fracture was 0.2% (10/5,676). Stepwise logistic regression identified only three independent predictors of ligamentous injury: cervical midline tenderness, abnormal alertness, and C-spine fracture on CT.
The poster presentation prompted a spirited debate at the meeting, with some attendees arguing that clearing collars in patients with a negative CT could leave practitioners and hospitals open to potential litigation if unstable fractures and/or ligamentous injuries are missed by not conducting further testing with magnetic resonance imaging (MRI).
The specter of litigation is always a possibility; however, the incidence of ligamentous injury without fracture was exceedingly low and prolonged C-collar use is not without consequences, argued senior author Dr. Therèse Duane, an ACS Fellow and trauma and critical care surgeon at the university.
"How many times do patients go home and 3 months later still have a collar on because they can’t get an MRI and now they have migraines, can’t work, and can’t drive? It’s huge," she said.
In the study, 77% of the 52 patients with ligamentous injury underwent MRI in addition to a CT scan, 48% had CT angiography of the neck, 40.4% had C-spine surgery, and 81% required prolonged collar use for treatment purposes of 6 weeks or longer.
Though current practice at the university is to clear collars in patients with a negative CT scan, research would be needed to determine whether this approach is feasible in the higher-risk patients with altered alertness, Dr. Duane observed.
Further studies are planned by the group looking at national databanks, as well as combining a decade worth of data at their institution, to define a C-spine clearance protocol.
Dr. Vanguri and her colleagues reported having no financial disclosures.
AT THE EAST SCIENTIFIC ASSEMBLY
Major finding: The incidence of fracture was 7.2% (409/5,676) and ligamentous injury 0.9% (52/5,676). CT cervical spine had 100% specificity and sensitivity in ruling out clinically significant fracture and ligamentous injuries.
Data source: A prospective study of 5,676 alert patients with blunt trauma.
Disclosures: Dr. Vanguri and her colleagues reported having no financial disclosures.
Recommended reading: top papers in the surgical literature
Members of the Surgery News Editorial Advisory Board and their colleagues contributed to the list below, which represents articles from the recent surgical literature that they found particularly interesting. We hope readers across surgical specialties will find this information useful.
Bariatric surgery
"Surgical skill and complication rates after bariatric surgery" (N. Engl. J. Med. 2013;369:1434-2).
The authors conducted a study involving 20 bariatric surgeons in Michigan who participated in a statewide collaborative improvement program. Each surgeon submitted a single representative videotape of himself or herself performing a laparoscopic gastric bypass, which was rated in various domains of technical skill on a scale of 1-5 (with higher scores indicating more advanced skill) by at least 10 peer surgeons who were unaware of the identity of the operating surgeon. The relationships between these skill ratings and risk-adjusted complication rates were assessed with data from a prospective, externally audited, clinical-outcomes registry involving 10,343 patients. The mean summary ratings of technical skill ranged from 2.6 to 4.8 across the 20 surgeons. The bottom quartile of surgical skill, compared with the top quartile, was associated with higher complication rates (14.5% vs. 5.2%; P less than .001) and higher mortality (0.26% vs. 0.05%; P = .01). The lowest quartile of skill also was significantly associated with longer operations and higher rates of reoperation and readmission. The findings suggest that peer rating of operative skill may be an effective strategy for assessing a surgeon’s proficiency, the authors wrote.
Dr. Caprice Greenberg is an ACS Fellow, associate professor of surgery, and director of the Wisconsin Surgical Outcomes Research Program, University of Wisconsin, Madison.
Dr. Henry A. Pitt is an ACS Fellow and chief quality officer, Temple University Health System, Philadelphia.
Bioinformatics
"The Randomized Registry Trial – The Next Disruptive Technology in Clinical Research?" (N. Engl. J. Med. 2013;369:1579-81).
This editorial discusses the emergence of randomized registry trials, scientific studies that leverage clinical information collected in observational registries to expedite the process the conducting of large-scale randomized controlled trials. Randomized registry trials are described as potentially "disruptive technologies," which may transform existing standards, procedures, and cost structures for comparative-effectiveness research.
"Telemedicine as a potential medium for teaching the advanced trauma life support (ATLS) course"(J. Surg. Educ. 2013;70:258-64).
This article describes a controlled trial that compared the performance of first-year family practice residents who were randomized to traditional in-person or telemedicine ATLS courses. There were no statistically significant differences between the groups in terms of post-ATLS multiple-choice question test performance, instructor evaluation of student skill station performance, and overall pass rate, nor were there significant differences in the participant evaluations of course components and overall course quality.
Dr. Grace Purcell Jackson is an ACS Fellow and assistant professor of surgery, pediatrics, and biomedical informatics, Vanderbilt University, Nashville, Tenn.
Endocrine surgery
"A prospective, assessor-blind evaluation of surgeon-performed transcutaneous laryngeal ultrasonography in vocal cord examination before and after thyroidectomy" (Surgery 2013;154:1158-65).
This year there has been increased debate about the role of pre and postoperative laryngoscopy for patients undergoing thyroidectomy. An alternative to laryngoscopy that is garnishing a great deal of attention and interest in the endocrine surgery community is the use of transcutaneous ultrasound to evaluate vocal cord function. In this study of a series of 204 patients, the surgeons were able to visualize the vocal cords in 95% of patients. In their hands, ultrasound had a sensitivity of 93.3% and a negative predictive value of 99.4%. As many surgeons already use ultrasound regularly in their practice, this technique offers great promise for helping to identify patients who may benefit most from a laryngoscopic examination.
"Association Between BRAF V600E Mutation and Mortality in Patients With Papillary Thyroid Cancer" (JAMA 2013;309:1493-1501).
BRAF V600E is an important oncogene in papillary thyroid cancer. While it has been shown to play a useful role in the diagnosis of thyroid cancer, its impact on tumor behavior and patient outcomes is a matter of great debate. While several studies have shown that BRAF V600E is associated with a higher rate of nodal disease and recurrence, it hadn’t been shown to impact survival. This study included 1,849 patients from more than 13 centers and 7 countries. The researchers in this large study that BRAF V600E was associated with an increased incidence of cancer-related death, adjusted HR 2.66 (95% CI, 1.4-4.55). However, when they controlled for other known prognostic factors such as lymph node metastases, extrathyroidal extension, and distant metastases, they found that significance was lost. While BRAF V600E may lead to a worse prognosis, it may not add additional information beyond the already known prognostic factors in papillary thyroid cancer.
Dr. Rebecca Sippel is an ACS Fellow and chief of endocrine surgery, University of Wisconsin-Madison
General surgery
"Complications of daytime elective laparoscopic cholecystectomies performed by surgeons who operated the night before" (JAMA 2013; 310:1837-41).
In total, 94,183 eligible elective laparoscopic cholecystectomies were performed between 2004 and 2011. Of these surgeries, there were 2,078 procedures in which 331 different surgeons across 102 community hospitals had operated between midnight and 7 a.m. the night before. Each "at-risk" surgery was randomly matched with four other elective laparoscopic cholecystectomies (n = 8,312) performed by the same surgeon, who had no evidence of having operated the night before. No significant association was found in conversion rates to open operations between surgeons when they operated the night before compared with when they did not operate the previous night. There was also no association between operating the night before vs. not operating the night before, and the risk of iatrogenic injuries.
This study showed that elective surgery on a day following a night operation did not suffer from increased technical complications. Work-hour restrictions have never been based on good science, and this good study goes a long way to support the community surgeon who performs emergency surgery at night, then works a regular schedule during the day. The authors used a clever approach, reasoning that conversion to open surgery, iatrogenic injury, or death were markers of technical complications, then compared patients who had their lap choles the day after their surgeons had operated the night before with matched controls, showing no increase in complications or deaths. For many surgeons in smaller communities, an acute care surgical service is not practical, and surgeons routinely have elective patients post call. Surgeons can use evidence like this to justify their practice decisions.
Dr. Mark Savarise is an ACS Fellow and clinical assistant professor of surgery, University of Utah, South Jordan Health Center, Salt Lake City.
Head and neck surgery
"Long-term results of RTOG 91-11: a comparison of three nonsurgical treatment strategies to preserve the larynx in patients with locally advanced larynx cancer" (J. Clin. Oncol. 2013;7:845-52).
The authors analyzed 520 patients with stage III or IV glottic or supraglottic squamous cell cancer who were randomly assigned to induction cisplatin/fluorouracil (PF) followed by radiation therapy (control arm), concomitant cisplatin/RT, or RT alone. The composite end point of laryngectomy-free survival (LFS) was the primary endpoint. Both chemotherapy regimens significantly improved laryngectomy-free survival (LFS) compared with RT alone. Overall survival did not differ significantly, although there was a possibility of worse outcome with concomitant relative to induction chemotherapy. Concomitant cisplatin/RT significantly improved the larynx preservation rate over induction PF followed by RT and over RT alone, whereas induction PF followed by RT was not better than treatment with RT alone. No difference in late effects was detected, but deaths not attributed to larynx cancer or treatment were higher with concomitant chemotherapy (30.8% vs. 20.8% with induction chemotherapy and 16.9% with RT alone).The authors concluded that these 10-year results show that induction PF followed by RT and concomitant cisplatin/RT show similar efficacy for the composite endpoint of LFS. Locoregional control and larynx preservation were significantly improved with concomitant cisplatin/RT compared with the induction arm or RT alone.
Dr. Mark Weissler is an ACS Fellow, the J.P. Riddle Distinguished Professor of Otolaryngology – Head and Neck Surgery at the University of North Carolina, Chapel Hill, and vice-chair of the Board of Regents of the ACS.
Infections
"Effect of daily chlorhexidine bathing on hospital-acquired infection" (N. Engl. J. Med. 2013;368:533-42).
The authors conducted a multicenter, cluster-randomized, nonblinded crossover trial of 7,727 patients to evaluate the effect of daily bathing with chlorhexidine-impregnated washcloths on the acquisition of multidrug-resistant organisms (MDROs) and the incidence of hospital-acquired bloodstream infections. Nine intensive care and bone marrow transplantation units in six hospitals were randomly assigned to bathe patients either with no-rinse 2% chlorhexidine–impregnated washcloths or with nonantimicrobial washcloths for a 6-month period, exchanged for the alternate product during the subsequent 6 months. The overall rate of MDRO acquisition was 5.10 cases per 1,000 patient-days with chlorhexidine bathing versus 6.60 cases per 1,000 patient-days with nonantimicrobial washcloths (P = .03), the equivalent of a 23% lower rate with chlorhexidine bathing. The overall rate of hospital-acquired bloodstream infections was 4.78 cases per 1,000 patient-days with chlorhexidine bathing versus 6.60 cases per 1,000 patient-days with nonantimicrobial washcloths (P = .007), a 28% lower rate with chlorhexidine-impregnated washcloths. No serious skin reactions were noted during either study period.
In a world of $2 million robots seeking better outcomes and cost-effectiveness, it is important to remember that simple maneuvers like using patient baths may do more to alleviate suffering and death than the latest Buck Rogers equipment. Every hospital large and small can do this and make a difference right away without a large capital expense or a steep learning curve.
Dr. Tyler G. Hughes is an ACS Fellow and is with the department of general surgery at McPherson (Kan.) Hospital, editor of the Rural Surgery Community website for the ACS, and chair of the ACS Advisory Council on Rural Surgery.
Lung cancer surgery
"Treatment of stage I and II non–small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines" (Chest 2013;143:e278S-313S).
Recommendations by the writing committee were based on an evidence-based review of the literature and in accordance with the approach described by the Guidelines Oversight Committee of the American College of Chest Physicians. Among their conclusions: Surgical resection remains the primary and preferred approach to the treatment of stage I and II NSCLC. Lobectomy or greater resection remains the preferred approach to T1b and larger tumors. Every patient should have systematic mediastinal lymph node sampling at the time of curative intent surgical resection, and mediastinal lymphadenectomy can be performed without increased morbidity. Perioperative morbidity and mortality are reduced and long-term survival is improved when surgical resection is performed by a board-certified thoracic surgeon. The use of adjuvant chemotherapy for stage II NSCLC is recommended and has shown benefit. The use of adjuvant radiation or chemotherapy for stage I NSCLC is of unproven benefit. There is growing evidence that SBRT provides greater local control than standard radiation therapy for high-risk and medically inoperable patients with NSCLC. The role of ablative therapies in the treatment of high-risk patients with stage I NSCLC is evolving.
This past year, the American College of Chest Physicians updated its guidelines on the management of lung cancer. These collective manuscripts have been vetted by its distinguished membership and represent the most up-to-date evidence-based guidelines for lung cancer treatment. An entire supplement of CHEST has been devoted to this third iteration of lung cancer guidelines and includes recommendations spanning the entire gamut of disease, from surgical resection to definitive chemoradiotherapy to palliative interventions. This represents the most significant literature contribution to the field in 2013.
Dr. Sudish Murthy is an ACS Fellow and surgical director of the Center for Major Airway Disease, Cleveland Clinic.
Pediatric surgery
"Multicenter Study of Pectus Excavatum, Final Report: Complications, Static/Exercise Pulmonary Function, and Anatomic Outcomes" (J. Am. Coll. Surg. 2013;217:1080-9).
Pectus excavatum, or funnel chest, has long been a frequently-performed operation by pediatric and thoracic surgeons. It represents a significant psychological and sometimes physical burden for patients with the deformity. However, the literature has not previously provided definitive evidence of improved physiologic function after repair of pectus excavatum, despite unquestionable cosmetic and psychological improvements that accompany correction. For this reason, health care payers have been resistant to approve surgery for pectus excavatum. This multicenter study – of more than 300 patients who underwent pectus repairs via the Nuss technique or some form of open correction – for the first time demonstrates a significant improvement in pulmonary function, VO2 max, and O2 pulse in patients with a CT index of greater than 3.2 (considered severe), with normal being less than 2.5. This data should provide ample physiological evidence to support the repair of severe pectus deformities.
"Risk-Adjusted Hospital Outcomes for Children’s Surgery" (Pediatrics 2013;132:e677-88).
The National Surgical Quality Improvement Program (NSQIP) has unequivocally been shown to provide adult hospitals with actionable quality data that can lead to improved surgical outcomes, and to discriminate between high and low performing hospitals. Similar data for pediatric hospitals have not been as compelling. In this study, more than 46,000 patients were entered into Pediatric NSQIP and analyzed. Not surprisingly, the overall mortality rate (0.3%), cumulative morbidity (5.8%), and surgical site infection rate (1.8%) were quite low. As has been shown in the trauma literature, mortality is not a discriminating factor for quality between pediatric institutions. However, the data from this study suggest that models can be developed wherein cumulative morbidity and surgical site infection rates can differentiate between institutions, and should lead to successful efforts to improve surgical outcomes in children.
Dr. Dennis Lund is an ACS Fellow and executive vice president, Phoenix Children’s Medical Group, surgeon-in-chief, Phoenix Children’s Hospital, and professor of child health and surgery, University of Arizona College of Medicine–Phoenix.
Trauma surgery
"Outcomes following ‘rescue’ superselective angioembolization for gastrointestinal hemorrhage in hemodynamically unstable patients" (J. Trauma Acute Care Surg. 2013;75:398-403).
The authors conducted a 10-year retrospective review of all hemodynamically unstable patients (systolic blood pressure less than 90 mm Hg and ongoing transfusion requirement) who underwent "rescue" SSAE for GIH after failed endoscopic management was performed. A total of 98 patients underwent SSAE for GIH; 47 were excluded because of lack of active contrast extravasation. Of the remaining 51 patients, 22 (43%) presented with a lower GIH and 29 (57%) with upper GIH. The majority (71%) underwent embolization with a permanent agent, while the remaining patients received a temporary agent (16%) or a combination (14%). The overall technical and clinical success rates were 98% and 71%, respectively. Of the 14 patients with technical success but clinical failure (rebleeding within 30 days) and the 1 patient with technical failure, 4 were managed successfully with reembolization, while 2 underwent successful endoscopic therapy, and 9 had surgical resections.
The authors concluded that SSAE, with reembolization if necessary, is an effective rescue treatment modality for hemodynamically unstable patients with active GIH. Of the patients, 20% will fail SSAE and require additional intervention. Ischemic complications were extremely rare.
"Platelets are dominant contributors to hypercoagulability after injury" (J. Trauma Acute Care Surg. 2013;74:756-65).
The authors randomized 50 surgical intensive care unit trauma patients to receive 5,000 IU of low-molecular-weight heparin (LMWH) daily (controls) or to thrombelastography (TEG)–guided prophylaxis, up to 5,000 IU twice daily with the addition of aspirin. Patients were followed up for 5 days. The control (n = 25) and TEG-guided prophylaxis (n = 25) groups were similar in age, body mass index, Injury Severity Score, and male sex. Fibrinogen levels and platelet counts did not differ, and increased LMWH did not affect clot strength between the control and study groups. The correlation of clot strength (G value) with fibrinogen was stronger on days 1 and 2 but was superseded by platelet count on days 3, 4, and 5. The authors concluded that increased LMWH seemed to increase platelet contribution to clot strength early in the study but failed to affect the overall rise clot strength. Over time, platelet count had the strongest correlation with clot strength, and in vitro studies demonstrated that increased platelet counts increase fibrin production and thrombus generation. These data suggest an important role for antiplatelet therapy in VTE prophylaxis following trauma, particularly after 48 hours, they stated.
Dr. Grace S. Rozycki is an ACS Fellow, Willis D. Gatch Professor of Surgery, executive vice chair of the department of surgery, and director of the Indiana Injury Institute, Indiana University, Indianapolis.
Members of the Surgery News Editorial Advisory Board and their colleagues contributed to the list below, which represents articles from the recent surgical literature that they found particularly interesting. We hope readers across surgical specialties will find this information useful.
Bariatric surgery
"Surgical skill and complication rates after bariatric surgery" (N. Engl. J. Med. 2013;369:1434-2).
The authors conducted a study involving 20 bariatric surgeons in Michigan who participated in a statewide collaborative improvement program. Each surgeon submitted a single representative videotape of himself or herself performing a laparoscopic gastric bypass, which was rated in various domains of technical skill on a scale of 1-5 (with higher scores indicating more advanced skill) by at least 10 peer surgeons who were unaware of the identity of the operating surgeon. The relationships between these skill ratings and risk-adjusted complication rates were assessed with data from a prospective, externally audited, clinical-outcomes registry involving 10,343 patients. The mean summary ratings of technical skill ranged from 2.6 to 4.8 across the 20 surgeons. The bottom quartile of surgical skill, compared with the top quartile, was associated with higher complication rates (14.5% vs. 5.2%; P less than .001) and higher mortality (0.26% vs. 0.05%; P = .01). The lowest quartile of skill also was significantly associated with longer operations and higher rates of reoperation and readmission. The findings suggest that peer rating of operative skill may be an effective strategy for assessing a surgeon’s proficiency, the authors wrote.
Dr. Caprice Greenberg is an ACS Fellow, associate professor of surgery, and director of the Wisconsin Surgical Outcomes Research Program, University of Wisconsin, Madison.
Dr. Henry A. Pitt is an ACS Fellow and chief quality officer, Temple University Health System, Philadelphia.
Bioinformatics
"The Randomized Registry Trial – The Next Disruptive Technology in Clinical Research?" (N. Engl. J. Med. 2013;369:1579-81).
This editorial discusses the emergence of randomized registry trials, scientific studies that leverage clinical information collected in observational registries to expedite the process the conducting of large-scale randomized controlled trials. Randomized registry trials are described as potentially "disruptive technologies," which may transform existing standards, procedures, and cost structures for comparative-effectiveness research.
"Telemedicine as a potential medium for teaching the advanced trauma life support (ATLS) course"(J. Surg. Educ. 2013;70:258-64).
This article describes a controlled trial that compared the performance of first-year family practice residents who were randomized to traditional in-person or telemedicine ATLS courses. There were no statistically significant differences between the groups in terms of post-ATLS multiple-choice question test performance, instructor evaluation of student skill station performance, and overall pass rate, nor were there significant differences in the participant evaluations of course components and overall course quality.
Dr. Grace Purcell Jackson is an ACS Fellow and assistant professor of surgery, pediatrics, and biomedical informatics, Vanderbilt University, Nashville, Tenn.
Endocrine surgery
"A prospective, assessor-blind evaluation of surgeon-performed transcutaneous laryngeal ultrasonography in vocal cord examination before and after thyroidectomy" (Surgery 2013;154:1158-65).
This year there has been increased debate about the role of pre and postoperative laryngoscopy for patients undergoing thyroidectomy. An alternative to laryngoscopy that is garnishing a great deal of attention and interest in the endocrine surgery community is the use of transcutaneous ultrasound to evaluate vocal cord function. In this study of a series of 204 patients, the surgeons were able to visualize the vocal cords in 95% of patients. In their hands, ultrasound had a sensitivity of 93.3% and a negative predictive value of 99.4%. As many surgeons already use ultrasound regularly in their practice, this technique offers great promise for helping to identify patients who may benefit most from a laryngoscopic examination.
"Association Between BRAF V600E Mutation and Mortality in Patients With Papillary Thyroid Cancer" (JAMA 2013;309:1493-1501).
BRAF V600E is an important oncogene in papillary thyroid cancer. While it has been shown to play a useful role in the diagnosis of thyroid cancer, its impact on tumor behavior and patient outcomes is a matter of great debate. While several studies have shown that BRAF V600E is associated with a higher rate of nodal disease and recurrence, it hadn’t been shown to impact survival. This study included 1,849 patients from more than 13 centers and 7 countries. The researchers in this large study that BRAF V600E was associated with an increased incidence of cancer-related death, adjusted HR 2.66 (95% CI, 1.4-4.55). However, when they controlled for other known prognostic factors such as lymph node metastases, extrathyroidal extension, and distant metastases, they found that significance was lost. While BRAF V600E may lead to a worse prognosis, it may not add additional information beyond the already known prognostic factors in papillary thyroid cancer.
Dr. Rebecca Sippel is an ACS Fellow and chief of endocrine surgery, University of Wisconsin-Madison
General surgery
"Complications of daytime elective laparoscopic cholecystectomies performed by surgeons who operated the night before" (JAMA 2013; 310:1837-41).
In total, 94,183 eligible elective laparoscopic cholecystectomies were performed between 2004 and 2011. Of these surgeries, there were 2,078 procedures in which 331 different surgeons across 102 community hospitals had operated between midnight and 7 a.m. the night before. Each "at-risk" surgery was randomly matched with four other elective laparoscopic cholecystectomies (n = 8,312) performed by the same surgeon, who had no evidence of having operated the night before. No significant association was found in conversion rates to open operations between surgeons when they operated the night before compared with when they did not operate the previous night. There was also no association between operating the night before vs. not operating the night before, and the risk of iatrogenic injuries.
This study showed that elective surgery on a day following a night operation did not suffer from increased technical complications. Work-hour restrictions have never been based on good science, and this good study goes a long way to support the community surgeon who performs emergency surgery at night, then works a regular schedule during the day. The authors used a clever approach, reasoning that conversion to open surgery, iatrogenic injury, or death were markers of technical complications, then compared patients who had their lap choles the day after their surgeons had operated the night before with matched controls, showing no increase in complications or deaths. For many surgeons in smaller communities, an acute care surgical service is not practical, and surgeons routinely have elective patients post call. Surgeons can use evidence like this to justify their practice decisions.
Dr. Mark Savarise is an ACS Fellow and clinical assistant professor of surgery, University of Utah, South Jordan Health Center, Salt Lake City.
Head and neck surgery
"Long-term results of RTOG 91-11: a comparison of three nonsurgical treatment strategies to preserve the larynx in patients with locally advanced larynx cancer" (J. Clin. Oncol. 2013;7:845-52).
The authors analyzed 520 patients with stage III or IV glottic or supraglottic squamous cell cancer who were randomly assigned to induction cisplatin/fluorouracil (PF) followed by radiation therapy (control arm), concomitant cisplatin/RT, or RT alone. The composite end point of laryngectomy-free survival (LFS) was the primary endpoint. Both chemotherapy regimens significantly improved laryngectomy-free survival (LFS) compared with RT alone. Overall survival did not differ significantly, although there was a possibility of worse outcome with concomitant relative to induction chemotherapy. Concomitant cisplatin/RT significantly improved the larynx preservation rate over induction PF followed by RT and over RT alone, whereas induction PF followed by RT was not better than treatment with RT alone. No difference in late effects was detected, but deaths not attributed to larynx cancer or treatment were higher with concomitant chemotherapy (30.8% vs. 20.8% with induction chemotherapy and 16.9% with RT alone).The authors concluded that these 10-year results show that induction PF followed by RT and concomitant cisplatin/RT show similar efficacy for the composite endpoint of LFS. Locoregional control and larynx preservation were significantly improved with concomitant cisplatin/RT compared with the induction arm or RT alone.
Dr. Mark Weissler is an ACS Fellow, the J.P. Riddle Distinguished Professor of Otolaryngology – Head and Neck Surgery at the University of North Carolina, Chapel Hill, and vice-chair of the Board of Regents of the ACS.
Infections
"Effect of daily chlorhexidine bathing on hospital-acquired infection" (N. Engl. J. Med. 2013;368:533-42).
The authors conducted a multicenter, cluster-randomized, nonblinded crossover trial of 7,727 patients to evaluate the effect of daily bathing with chlorhexidine-impregnated washcloths on the acquisition of multidrug-resistant organisms (MDROs) and the incidence of hospital-acquired bloodstream infections. Nine intensive care and bone marrow transplantation units in six hospitals were randomly assigned to bathe patients either with no-rinse 2% chlorhexidine–impregnated washcloths or with nonantimicrobial washcloths for a 6-month period, exchanged for the alternate product during the subsequent 6 months. The overall rate of MDRO acquisition was 5.10 cases per 1,000 patient-days with chlorhexidine bathing versus 6.60 cases per 1,000 patient-days with nonantimicrobial washcloths (P = .03), the equivalent of a 23% lower rate with chlorhexidine bathing. The overall rate of hospital-acquired bloodstream infections was 4.78 cases per 1,000 patient-days with chlorhexidine bathing versus 6.60 cases per 1,000 patient-days with nonantimicrobial washcloths (P = .007), a 28% lower rate with chlorhexidine-impregnated washcloths. No serious skin reactions were noted during either study period.
In a world of $2 million robots seeking better outcomes and cost-effectiveness, it is important to remember that simple maneuvers like using patient baths may do more to alleviate suffering and death than the latest Buck Rogers equipment. Every hospital large and small can do this and make a difference right away without a large capital expense or a steep learning curve.
Dr. Tyler G. Hughes is an ACS Fellow and is with the department of general surgery at McPherson (Kan.) Hospital, editor of the Rural Surgery Community website for the ACS, and chair of the ACS Advisory Council on Rural Surgery.
Lung cancer surgery
"Treatment of stage I and II non–small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines" (Chest 2013;143:e278S-313S).
Recommendations by the writing committee were based on an evidence-based review of the literature and in accordance with the approach described by the Guidelines Oversight Committee of the American College of Chest Physicians. Among their conclusions: Surgical resection remains the primary and preferred approach to the treatment of stage I and II NSCLC. Lobectomy or greater resection remains the preferred approach to T1b and larger tumors. Every patient should have systematic mediastinal lymph node sampling at the time of curative intent surgical resection, and mediastinal lymphadenectomy can be performed without increased morbidity. Perioperative morbidity and mortality are reduced and long-term survival is improved when surgical resection is performed by a board-certified thoracic surgeon. The use of adjuvant chemotherapy for stage II NSCLC is recommended and has shown benefit. The use of adjuvant radiation or chemotherapy for stage I NSCLC is of unproven benefit. There is growing evidence that SBRT provides greater local control than standard radiation therapy for high-risk and medically inoperable patients with NSCLC. The role of ablative therapies in the treatment of high-risk patients with stage I NSCLC is evolving.
This past year, the American College of Chest Physicians updated its guidelines on the management of lung cancer. These collective manuscripts have been vetted by its distinguished membership and represent the most up-to-date evidence-based guidelines for lung cancer treatment. An entire supplement of CHEST has been devoted to this third iteration of lung cancer guidelines and includes recommendations spanning the entire gamut of disease, from surgical resection to definitive chemoradiotherapy to palliative interventions. This represents the most significant literature contribution to the field in 2013.
Dr. Sudish Murthy is an ACS Fellow and surgical director of the Center for Major Airway Disease, Cleveland Clinic.
Pediatric surgery
"Multicenter Study of Pectus Excavatum, Final Report: Complications, Static/Exercise Pulmonary Function, and Anatomic Outcomes" (J. Am. Coll. Surg. 2013;217:1080-9).
Pectus excavatum, or funnel chest, has long been a frequently-performed operation by pediatric and thoracic surgeons. It represents a significant psychological and sometimes physical burden for patients with the deformity. However, the literature has not previously provided definitive evidence of improved physiologic function after repair of pectus excavatum, despite unquestionable cosmetic and psychological improvements that accompany correction. For this reason, health care payers have been resistant to approve surgery for pectus excavatum. This multicenter study – of more than 300 patients who underwent pectus repairs via the Nuss technique or some form of open correction – for the first time demonstrates a significant improvement in pulmonary function, VO2 max, and O2 pulse in patients with a CT index of greater than 3.2 (considered severe), with normal being less than 2.5. This data should provide ample physiological evidence to support the repair of severe pectus deformities.
"Risk-Adjusted Hospital Outcomes for Children’s Surgery" (Pediatrics 2013;132:e677-88).
The National Surgical Quality Improvement Program (NSQIP) has unequivocally been shown to provide adult hospitals with actionable quality data that can lead to improved surgical outcomes, and to discriminate between high and low performing hospitals. Similar data for pediatric hospitals have not been as compelling. In this study, more than 46,000 patients were entered into Pediatric NSQIP and analyzed. Not surprisingly, the overall mortality rate (0.3%), cumulative morbidity (5.8%), and surgical site infection rate (1.8%) were quite low. As has been shown in the trauma literature, mortality is not a discriminating factor for quality between pediatric institutions. However, the data from this study suggest that models can be developed wherein cumulative morbidity and surgical site infection rates can differentiate between institutions, and should lead to successful efforts to improve surgical outcomes in children.
Dr. Dennis Lund is an ACS Fellow and executive vice president, Phoenix Children’s Medical Group, surgeon-in-chief, Phoenix Children’s Hospital, and professor of child health and surgery, University of Arizona College of Medicine–Phoenix.
Trauma surgery
"Outcomes following ‘rescue’ superselective angioembolization for gastrointestinal hemorrhage in hemodynamically unstable patients" (J. Trauma Acute Care Surg. 2013;75:398-403).
The authors conducted a 10-year retrospective review of all hemodynamically unstable patients (systolic blood pressure less than 90 mm Hg and ongoing transfusion requirement) who underwent "rescue" SSAE for GIH after failed endoscopic management was performed. A total of 98 patients underwent SSAE for GIH; 47 were excluded because of lack of active contrast extravasation. Of the remaining 51 patients, 22 (43%) presented with a lower GIH and 29 (57%) with upper GIH. The majority (71%) underwent embolization with a permanent agent, while the remaining patients received a temporary agent (16%) or a combination (14%). The overall technical and clinical success rates were 98% and 71%, respectively. Of the 14 patients with technical success but clinical failure (rebleeding within 30 days) and the 1 patient with technical failure, 4 were managed successfully with reembolization, while 2 underwent successful endoscopic therapy, and 9 had surgical resections.
The authors concluded that SSAE, with reembolization if necessary, is an effective rescue treatment modality for hemodynamically unstable patients with active GIH. Of the patients, 20% will fail SSAE and require additional intervention. Ischemic complications were extremely rare.
"Platelets are dominant contributors to hypercoagulability after injury" (J. Trauma Acute Care Surg. 2013;74:756-65).
The authors randomized 50 surgical intensive care unit trauma patients to receive 5,000 IU of low-molecular-weight heparin (LMWH) daily (controls) or to thrombelastography (TEG)–guided prophylaxis, up to 5,000 IU twice daily with the addition of aspirin. Patients were followed up for 5 days. The control (n = 25) and TEG-guided prophylaxis (n = 25) groups were similar in age, body mass index, Injury Severity Score, and male sex. Fibrinogen levels and platelet counts did not differ, and increased LMWH did not affect clot strength between the control and study groups. The correlation of clot strength (G value) with fibrinogen was stronger on days 1 and 2 but was superseded by platelet count on days 3, 4, and 5. The authors concluded that increased LMWH seemed to increase platelet contribution to clot strength early in the study but failed to affect the overall rise clot strength. Over time, platelet count had the strongest correlation with clot strength, and in vitro studies demonstrated that increased platelet counts increase fibrin production and thrombus generation. These data suggest an important role for antiplatelet therapy in VTE prophylaxis following trauma, particularly after 48 hours, they stated.
Dr. Grace S. Rozycki is an ACS Fellow, Willis D. Gatch Professor of Surgery, executive vice chair of the department of surgery, and director of the Indiana Injury Institute, Indiana University, Indianapolis.
Members of the Surgery News Editorial Advisory Board and their colleagues contributed to the list below, which represents articles from the recent surgical literature that they found particularly interesting. We hope readers across surgical specialties will find this information useful.
Bariatric surgery
"Surgical skill and complication rates after bariatric surgery" (N. Engl. J. Med. 2013;369:1434-2).
The authors conducted a study involving 20 bariatric surgeons in Michigan who participated in a statewide collaborative improvement program. Each surgeon submitted a single representative videotape of himself or herself performing a laparoscopic gastric bypass, which was rated in various domains of technical skill on a scale of 1-5 (with higher scores indicating more advanced skill) by at least 10 peer surgeons who were unaware of the identity of the operating surgeon. The relationships between these skill ratings and risk-adjusted complication rates were assessed with data from a prospective, externally audited, clinical-outcomes registry involving 10,343 patients. The mean summary ratings of technical skill ranged from 2.6 to 4.8 across the 20 surgeons. The bottom quartile of surgical skill, compared with the top quartile, was associated with higher complication rates (14.5% vs. 5.2%; P less than .001) and higher mortality (0.26% vs. 0.05%; P = .01). The lowest quartile of skill also was significantly associated with longer operations and higher rates of reoperation and readmission. The findings suggest that peer rating of operative skill may be an effective strategy for assessing a surgeon’s proficiency, the authors wrote.
Dr. Caprice Greenberg is an ACS Fellow, associate professor of surgery, and director of the Wisconsin Surgical Outcomes Research Program, University of Wisconsin, Madison.
Dr. Henry A. Pitt is an ACS Fellow and chief quality officer, Temple University Health System, Philadelphia.
Bioinformatics
"The Randomized Registry Trial – The Next Disruptive Technology in Clinical Research?" (N. Engl. J. Med. 2013;369:1579-81).
This editorial discusses the emergence of randomized registry trials, scientific studies that leverage clinical information collected in observational registries to expedite the process the conducting of large-scale randomized controlled trials. Randomized registry trials are described as potentially "disruptive technologies," which may transform existing standards, procedures, and cost structures for comparative-effectiveness research.
"Telemedicine as a potential medium for teaching the advanced trauma life support (ATLS) course"(J. Surg. Educ. 2013;70:258-64).
This article describes a controlled trial that compared the performance of first-year family practice residents who were randomized to traditional in-person or telemedicine ATLS courses. There were no statistically significant differences between the groups in terms of post-ATLS multiple-choice question test performance, instructor evaluation of student skill station performance, and overall pass rate, nor were there significant differences in the participant evaluations of course components and overall course quality.
Dr. Grace Purcell Jackson is an ACS Fellow and assistant professor of surgery, pediatrics, and biomedical informatics, Vanderbilt University, Nashville, Tenn.
Endocrine surgery
"A prospective, assessor-blind evaluation of surgeon-performed transcutaneous laryngeal ultrasonography in vocal cord examination before and after thyroidectomy" (Surgery 2013;154:1158-65).
This year there has been increased debate about the role of pre and postoperative laryngoscopy for patients undergoing thyroidectomy. An alternative to laryngoscopy that is garnishing a great deal of attention and interest in the endocrine surgery community is the use of transcutaneous ultrasound to evaluate vocal cord function. In this study of a series of 204 patients, the surgeons were able to visualize the vocal cords in 95% of patients. In their hands, ultrasound had a sensitivity of 93.3% and a negative predictive value of 99.4%. As many surgeons already use ultrasound regularly in their practice, this technique offers great promise for helping to identify patients who may benefit most from a laryngoscopic examination.
"Association Between BRAF V600E Mutation and Mortality in Patients With Papillary Thyroid Cancer" (JAMA 2013;309:1493-1501).
BRAF V600E is an important oncogene in papillary thyroid cancer. While it has been shown to play a useful role in the diagnosis of thyroid cancer, its impact on tumor behavior and patient outcomes is a matter of great debate. While several studies have shown that BRAF V600E is associated with a higher rate of nodal disease and recurrence, it hadn’t been shown to impact survival. This study included 1,849 patients from more than 13 centers and 7 countries. The researchers in this large study that BRAF V600E was associated with an increased incidence of cancer-related death, adjusted HR 2.66 (95% CI, 1.4-4.55). However, when they controlled for other known prognostic factors such as lymph node metastases, extrathyroidal extension, and distant metastases, they found that significance was lost. While BRAF V600E may lead to a worse prognosis, it may not add additional information beyond the already known prognostic factors in papillary thyroid cancer.
Dr. Rebecca Sippel is an ACS Fellow and chief of endocrine surgery, University of Wisconsin-Madison
General surgery
"Complications of daytime elective laparoscopic cholecystectomies performed by surgeons who operated the night before" (JAMA 2013; 310:1837-41).
In total, 94,183 eligible elective laparoscopic cholecystectomies were performed between 2004 and 2011. Of these surgeries, there were 2,078 procedures in which 331 different surgeons across 102 community hospitals had operated between midnight and 7 a.m. the night before. Each "at-risk" surgery was randomly matched with four other elective laparoscopic cholecystectomies (n = 8,312) performed by the same surgeon, who had no evidence of having operated the night before. No significant association was found in conversion rates to open operations between surgeons when they operated the night before compared with when they did not operate the previous night. There was also no association between operating the night before vs. not operating the night before, and the risk of iatrogenic injuries.
This study showed that elective surgery on a day following a night operation did not suffer from increased technical complications. Work-hour restrictions have never been based on good science, and this good study goes a long way to support the community surgeon who performs emergency surgery at night, then works a regular schedule during the day. The authors used a clever approach, reasoning that conversion to open surgery, iatrogenic injury, or death were markers of technical complications, then compared patients who had their lap choles the day after their surgeons had operated the night before with matched controls, showing no increase in complications or deaths. For many surgeons in smaller communities, an acute care surgical service is not practical, and surgeons routinely have elective patients post call. Surgeons can use evidence like this to justify their practice decisions.
Dr. Mark Savarise is an ACS Fellow and clinical assistant professor of surgery, University of Utah, South Jordan Health Center, Salt Lake City.
Head and neck surgery
"Long-term results of RTOG 91-11: a comparison of three nonsurgical treatment strategies to preserve the larynx in patients with locally advanced larynx cancer" (J. Clin. Oncol. 2013;7:845-52).
The authors analyzed 520 patients with stage III or IV glottic or supraglottic squamous cell cancer who were randomly assigned to induction cisplatin/fluorouracil (PF) followed by radiation therapy (control arm), concomitant cisplatin/RT, or RT alone. The composite end point of laryngectomy-free survival (LFS) was the primary endpoint. Both chemotherapy regimens significantly improved laryngectomy-free survival (LFS) compared with RT alone. Overall survival did not differ significantly, although there was a possibility of worse outcome with concomitant relative to induction chemotherapy. Concomitant cisplatin/RT significantly improved the larynx preservation rate over induction PF followed by RT and over RT alone, whereas induction PF followed by RT was not better than treatment with RT alone. No difference in late effects was detected, but deaths not attributed to larynx cancer or treatment were higher with concomitant chemotherapy (30.8% vs. 20.8% with induction chemotherapy and 16.9% with RT alone).The authors concluded that these 10-year results show that induction PF followed by RT and concomitant cisplatin/RT show similar efficacy for the composite endpoint of LFS. Locoregional control and larynx preservation were significantly improved with concomitant cisplatin/RT compared with the induction arm or RT alone.
Dr. Mark Weissler is an ACS Fellow, the J.P. Riddle Distinguished Professor of Otolaryngology – Head and Neck Surgery at the University of North Carolina, Chapel Hill, and vice-chair of the Board of Regents of the ACS.
Infections
"Effect of daily chlorhexidine bathing on hospital-acquired infection" (N. Engl. J. Med. 2013;368:533-42).
The authors conducted a multicenter, cluster-randomized, nonblinded crossover trial of 7,727 patients to evaluate the effect of daily bathing with chlorhexidine-impregnated washcloths on the acquisition of multidrug-resistant organisms (MDROs) and the incidence of hospital-acquired bloodstream infections. Nine intensive care and bone marrow transplantation units in six hospitals were randomly assigned to bathe patients either with no-rinse 2% chlorhexidine–impregnated washcloths or with nonantimicrobial washcloths for a 6-month period, exchanged for the alternate product during the subsequent 6 months. The overall rate of MDRO acquisition was 5.10 cases per 1,000 patient-days with chlorhexidine bathing versus 6.60 cases per 1,000 patient-days with nonantimicrobial washcloths (P = .03), the equivalent of a 23% lower rate with chlorhexidine bathing. The overall rate of hospital-acquired bloodstream infections was 4.78 cases per 1,000 patient-days with chlorhexidine bathing versus 6.60 cases per 1,000 patient-days with nonantimicrobial washcloths (P = .007), a 28% lower rate with chlorhexidine-impregnated washcloths. No serious skin reactions were noted during either study period.
In a world of $2 million robots seeking better outcomes and cost-effectiveness, it is important to remember that simple maneuvers like using patient baths may do more to alleviate suffering and death than the latest Buck Rogers equipment. Every hospital large and small can do this and make a difference right away without a large capital expense or a steep learning curve.
Dr. Tyler G. Hughes is an ACS Fellow and is with the department of general surgery at McPherson (Kan.) Hospital, editor of the Rural Surgery Community website for the ACS, and chair of the ACS Advisory Council on Rural Surgery.
Lung cancer surgery
"Treatment of stage I and II non–small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines" (Chest 2013;143:e278S-313S).
Recommendations by the writing committee were based on an evidence-based review of the literature and in accordance with the approach described by the Guidelines Oversight Committee of the American College of Chest Physicians. Among their conclusions: Surgical resection remains the primary and preferred approach to the treatment of stage I and II NSCLC. Lobectomy or greater resection remains the preferred approach to T1b and larger tumors. Every patient should have systematic mediastinal lymph node sampling at the time of curative intent surgical resection, and mediastinal lymphadenectomy can be performed without increased morbidity. Perioperative morbidity and mortality are reduced and long-term survival is improved when surgical resection is performed by a board-certified thoracic surgeon. The use of adjuvant chemotherapy for stage II NSCLC is recommended and has shown benefit. The use of adjuvant radiation or chemotherapy for stage I NSCLC is of unproven benefit. There is growing evidence that SBRT provides greater local control than standard radiation therapy for high-risk and medically inoperable patients with NSCLC. The role of ablative therapies in the treatment of high-risk patients with stage I NSCLC is evolving.
This past year, the American College of Chest Physicians updated its guidelines on the management of lung cancer. These collective manuscripts have been vetted by its distinguished membership and represent the most up-to-date evidence-based guidelines for lung cancer treatment. An entire supplement of CHEST has been devoted to this third iteration of lung cancer guidelines and includes recommendations spanning the entire gamut of disease, from surgical resection to definitive chemoradiotherapy to palliative interventions. This represents the most significant literature contribution to the field in 2013.
Dr. Sudish Murthy is an ACS Fellow and surgical director of the Center for Major Airway Disease, Cleveland Clinic.
Pediatric surgery
"Multicenter Study of Pectus Excavatum, Final Report: Complications, Static/Exercise Pulmonary Function, and Anatomic Outcomes" (J. Am. Coll. Surg. 2013;217:1080-9).
Pectus excavatum, or funnel chest, has long been a frequently-performed operation by pediatric and thoracic surgeons. It represents a significant psychological and sometimes physical burden for patients with the deformity. However, the literature has not previously provided definitive evidence of improved physiologic function after repair of pectus excavatum, despite unquestionable cosmetic and psychological improvements that accompany correction. For this reason, health care payers have been resistant to approve surgery for pectus excavatum. This multicenter study – of more than 300 patients who underwent pectus repairs via the Nuss technique or some form of open correction – for the first time demonstrates a significant improvement in pulmonary function, VO2 max, and O2 pulse in patients with a CT index of greater than 3.2 (considered severe), with normal being less than 2.5. This data should provide ample physiological evidence to support the repair of severe pectus deformities.
"Risk-Adjusted Hospital Outcomes for Children’s Surgery" (Pediatrics 2013;132:e677-88).
The National Surgical Quality Improvement Program (NSQIP) has unequivocally been shown to provide adult hospitals with actionable quality data that can lead to improved surgical outcomes, and to discriminate between high and low performing hospitals. Similar data for pediatric hospitals have not been as compelling. In this study, more than 46,000 patients were entered into Pediatric NSQIP and analyzed. Not surprisingly, the overall mortality rate (0.3%), cumulative morbidity (5.8%), and surgical site infection rate (1.8%) were quite low. As has been shown in the trauma literature, mortality is not a discriminating factor for quality between pediatric institutions. However, the data from this study suggest that models can be developed wherein cumulative morbidity and surgical site infection rates can differentiate between institutions, and should lead to successful efforts to improve surgical outcomes in children.
Dr. Dennis Lund is an ACS Fellow and executive vice president, Phoenix Children’s Medical Group, surgeon-in-chief, Phoenix Children’s Hospital, and professor of child health and surgery, University of Arizona College of Medicine–Phoenix.
Trauma surgery
"Outcomes following ‘rescue’ superselective angioembolization for gastrointestinal hemorrhage in hemodynamically unstable patients" (J. Trauma Acute Care Surg. 2013;75:398-403).
The authors conducted a 10-year retrospective review of all hemodynamically unstable patients (systolic blood pressure less than 90 mm Hg and ongoing transfusion requirement) who underwent "rescue" SSAE for GIH after failed endoscopic management was performed. A total of 98 patients underwent SSAE for GIH; 47 were excluded because of lack of active contrast extravasation. Of the remaining 51 patients, 22 (43%) presented with a lower GIH and 29 (57%) with upper GIH. The majority (71%) underwent embolization with a permanent agent, while the remaining patients received a temporary agent (16%) or a combination (14%). The overall technical and clinical success rates were 98% and 71%, respectively. Of the 14 patients with technical success but clinical failure (rebleeding within 30 days) and the 1 patient with technical failure, 4 were managed successfully with reembolization, while 2 underwent successful endoscopic therapy, and 9 had surgical resections.
The authors concluded that SSAE, with reembolization if necessary, is an effective rescue treatment modality for hemodynamically unstable patients with active GIH. Of the patients, 20% will fail SSAE and require additional intervention. Ischemic complications were extremely rare.
"Platelets are dominant contributors to hypercoagulability after injury" (J. Trauma Acute Care Surg. 2013;74:756-65).
The authors randomized 50 surgical intensive care unit trauma patients to receive 5,000 IU of low-molecular-weight heparin (LMWH) daily (controls) or to thrombelastography (TEG)–guided prophylaxis, up to 5,000 IU twice daily with the addition of aspirin. Patients were followed up for 5 days. The control (n = 25) and TEG-guided prophylaxis (n = 25) groups were similar in age, body mass index, Injury Severity Score, and male sex. Fibrinogen levels and platelet counts did not differ, and increased LMWH did not affect clot strength between the control and study groups. The correlation of clot strength (G value) with fibrinogen was stronger on days 1 and 2 but was superseded by platelet count on days 3, 4, and 5. The authors concluded that increased LMWH seemed to increase platelet contribution to clot strength early in the study but failed to affect the overall rise clot strength. Over time, platelet count had the strongest correlation with clot strength, and in vitro studies demonstrated that increased platelet counts increase fibrin production and thrombus generation. These data suggest an important role for antiplatelet therapy in VTE prophylaxis following trauma, particularly after 48 hours, they stated.
Dr. Grace S. Rozycki is an ACS Fellow, Willis D. Gatch Professor of Surgery, executive vice chair of the department of surgery, and director of the Indiana Injury Institute, Indiana University, Indianapolis.
Poor accrual halts one in five cancer clinical trials
Almost one-fifth of adult cancer clinical trials fail to reach completion for reasons unrelated to efficacy or adverse effects, according to data being reported at the 2014 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology. Poor accrual is the leading cause.
Trials were more likely to fail completion if they were phase II, single center, funded by industry, or conducted solely in the United States. Trials among patients with genitourinary cancers were no more or less likely to fail than trials among patients with other cancers.
"These findings really underscore the clinical trial accrual problem that we have in the United States. Not only does poor accrual lead to more expensive trials and trials that generate answers much more slowly, but it also prevents many trials from generating answers at all," senior author Dr. Matthew D. Galsky, director of the genitourinary medical oncology program, Icahn School of Medicine at Mount Sinai, New York, said in a press briefing at the 2014 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology.
The study is not meant to indict any specific stakeholders, Dr. Galsky stressed. "Rather, what we wanted to do was hold up a mirror to our activities as a cancer clinical trials community and really ask whether the system is optimized to bring better treatments to our patients as efficiently as possible. And clearly there is some work to do.
"Based on this analysis and others, it’s apparent that we need better collaboration and communication within the system and to use novel approaches to increase accrual to cancer clinical trials, which has really been quite steady at 3% to 5% of the adult cancer population for decades."
"This is a really interesting presentation which casts some light on one of the major frustrations that I think ... our whole community shares in designing and implementing clinical trials," said press briefing moderator Dr. Charles J. Ryan, leader of the genitourinary medical oncology program at the University of California, San Francisco. "Hopefully, this may be the beginning of a broader discussion that helps improve some of the efficiencies here."
Dr. Galsky speculated that the explanation for poor accrual is multifactorial. "Clearly, we need to engage patients more in the design of trials. We need to design trials that are more pragmatic; eligibility for trials is often so restrictive that only the patients who are the fittest and represent kind of an extreme of cancer patients can actually enroll," he said.
Other issues likely include financial barriers (such as whether insurers reimburse the costs of care for patients in trials); geographic accessibility; and the time and regulatory burdens of participating, especially as they affect community oncology practices. "Addressing the cancer clinical trials enterprise at large requires making the burden of participation lower because that does address accrual, that does address generalizability, that does address accessibility. It’s a problem that needs to be part of this conversation," Dr. Galsky maintained.
Dr. Ryan, the moderator, cited rapid treatment advances as yet another possible reason for poor accrual. "Some trials may take 2 or 3 years to accrue. During the first year, the standards of care may be one thing, and during the third year, the standards of care may have changed. We are really seeing very rapid evolution in our standards of care, so that could be one issue," he elaborated.
Introducing the study, Dr. Galsky noted that trials that fail to complete (that is, close without enrolling the intended number of patients) represent a major inefficiency of the cancer clinical trials enterprise. "Such trials contribute little knowledge, waste finite resources, and potentially divert patients from participating in other trials," he said.
The Institute of Medicine previously issued a report suggesting that about 40% of trials sponsored by the National Cancer Institute fail to achieve completion. But such trials account for only about 15% of all cancer trials.
The researchers analyzed 7,776 phase II or III interventional adult cancer clinical trials registered on ClinicalTrials.gov that had start dates between 2005 and 2011. They searched for those that had failed to reach completion, meaning that the trial had been stopped and had a "terminated" or "withdrawn" status.
The trials had a total of about 48,000 patients. Overall, 10% were trials in prostate, kidney, bladder, or testicular cancer.
The cumulative incidence of failure to reach completion for reasons unrelated to the efficacy or safety of the intervention was about 20%, according to Dr. Galsky.
Among all noncompleted trials, the largest share, 39%, failed to achieve completion because of poor accrual, topping other reasons such as logistics and efficacy/safety.
Trials were more likely to fail completion if they were funded by industry as compared with the federal government (hazard ratio, 1.97), were phase II as compared with phase III (HR, 1.29), or were single center as compared with multicenter (HR, 1.93).
On the other hand, trials were less likely to fail completion if they were conducted solely outside the United States (HR, 0.65) or both in and outside the United States (HR, 0.67), as compared with solely in the United States.
Dr. Galsky disclosed no relevant conflicts of interest.
Almost one-fifth of adult cancer clinical trials fail to reach completion for reasons unrelated to efficacy or adverse effects, according to data being reported at the 2014 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology. Poor accrual is the leading cause.
Trials were more likely to fail completion if they were phase II, single center, funded by industry, or conducted solely in the United States. Trials among patients with genitourinary cancers were no more or less likely to fail than trials among patients with other cancers.
"These findings really underscore the clinical trial accrual problem that we have in the United States. Not only does poor accrual lead to more expensive trials and trials that generate answers much more slowly, but it also prevents many trials from generating answers at all," senior author Dr. Matthew D. Galsky, director of the genitourinary medical oncology program, Icahn School of Medicine at Mount Sinai, New York, said in a press briefing at the 2014 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology.
The study is not meant to indict any specific stakeholders, Dr. Galsky stressed. "Rather, what we wanted to do was hold up a mirror to our activities as a cancer clinical trials community and really ask whether the system is optimized to bring better treatments to our patients as efficiently as possible. And clearly there is some work to do.
"Based on this analysis and others, it’s apparent that we need better collaboration and communication within the system and to use novel approaches to increase accrual to cancer clinical trials, which has really been quite steady at 3% to 5% of the adult cancer population for decades."
"This is a really interesting presentation which casts some light on one of the major frustrations that I think ... our whole community shares in designing and implementing clinical trials," said press briefing moderator Dr. Charles J. Ryan, leader of the genitourinary medical oncology program at the University of California, San Francisco. "Hopefully, this may be the beginning of a broader discussion that helps improve some of the efficiencies here."
Dr. Galsky speculated that the explanation for poor accrual is multifactorial. "Clearly, we need to engage patients more in the design of trials. We need to design trials that are more pragmatic; eligibility for trials is often so restrictive that only the patients who are the fittest and represent kind of an extreme of cancer patients can actually enroll," he said.
Other issues likely include financial barriers (such as whether insurers reimburse the costs of care for patients in trials); geographic accessibility; and the time and regulatory burdens of participating, especially as they affect community oncology practices. "Addressing the cancer clinical trials enterprise at large requires making the burden of participation lower because that does address accrual, that does address generalizability, that does address accessibility. It’s a problem that needs to be part of this conversation," Dr. Galsky maintained.
Dr. Ryan, the moderator, cited rapid treatment advances as yet another possible reason for poor accrual. "Some trials may take 2 or 3 years to accrue. During the first year, the standards of care may be one thing, and during the third year, the standards of care may have changed. We are really seeing very rapid evolution in our standards of care, so that could be one issue," he elaborated.
Introducing the study, Dr. Galsky noted that trials that fail to complete (that is, close without enrolling the intended number of patients) represent a major inefficiency of the cancer clinical trials enterprise. "Such trials contribute little knowledge, waste finite resources, and potentially divert patients from participating in other trials," he said.
The Institute of Medicine previously issued a report suggesting that about 40% of trials sponsored by the National Cancer Institute fail to achieve completion. But such trials account for only about 15% of all cancer trials.
The researchers analyzed 7,776 phase II or III interventional adult cancer clinical trials registered on ClinicalTrials.gov that had start dates between 2005 and 2011. They searched for those that had failed to reach completion, meaning that the trial had been stopped and had a "terminated" or "withdrawn" status.
The trials had a total of about 48,000 patients. Overall, 10% were trials in prostate, kidney, bladder, or testicular cancer.
The cumulative incidence of failure to reach completion for reasons unrelated to the efficacy or safety of the intervention was about 20%, according to Dr. Galsky.
Among all noncompleted trials, the largest share, 39%, failed to achieve completion because of poor accrual, topping other reasons such as logistics and efficacy/safety.
Trials were more likely to fail completion if they were funded by industry as compared with the federal government (hazard ratio, 1.97), were phase II as compared with phase III (HR, 1.29), or were single center as compared with multicenter (HR, 1.93).
On the other hand, trials were less likely to fail completion if they were conducted solely outside the United States (HR, 0.65) or both in and outside the United States (HR, 0.67), as compared with solely in the United States.
Dr. Galsky disclosed no relevant conflicts of interest.
Almost one-fifth of adult cancer clinical trials fail to reach completion for reasons unrelated to efficacy or adverse effects, according to data being reported at the 2014 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology. Poor accrual is the leading cause.
Trials were more likely to fail completion if they were phase II, single center, funded by industry, or conducted solely in the United States. Trials among patients with genitourinary cancers were no more or less likely to fail than trials among patients with other cancers.
"These findings really underscore the clinical trial accrual problem that we have in the United States. Not only does poor accrual lead to more expensive trials and trials that generate answers much more slowly, but it also prevents many trials from generating answers at all," senior author Dr. Matthew D. Galsky, director of the genitourinary medical oncology program, Icahn School of Medicine at Mount Sinai, New York, said in a press briefing at the 2014 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology.
The study is not meant to indict any specific stakeholders, Dr. Galsky stressed. "Rather, what we wanted to do was hold up a mirror to our activities as a cancer clinical trials community and really ask whether the system is optimized to bring better treatments to our patients as efficiently as possible. And clearly there is some work to do.
"Based on this analysis and others, it’s apparent that we need better collaboration and communication within the system and to use novel approaches to increase accrual to cancer clinical trials, which has really been quite steady at 3% to 5% of the adult cancer population for decades."
"This is a really interesting presentation which casts some light on one of the major frustrations that I think ... our whole community shares in designing and implementing clinical trials," said press briefing moderator Dr. Charles J. Ryan, leader of the genitourinary medical oncology program at the University of California, San Francisco. "Hopefully, this may be the beginning of a broader discussion that helps improve some of the efficiencies here."
Dr. Galsky speculated that the explanation for poor accrual is multifactorial. "Clearly, we need to engage patients more in the design of trials. We need to design trials that are more pragmatic; eligibility for trials is often so restrictive that only the patients who are the fittest and represent kind of an extreme of cancer patients can actually enroll," he said.
Other issues likely include financial barriers (such as whether insurers reimburse the costs of care for patients in trials); geographic accessibility; and the time and regulatory burdens of participating, especially as they affect community oncology practices. "Addressing the cancer clinical trials enterprise at large requires making the burden of participation lower because that does address accrual, that does address generalizability, that does address accessibility. It’s a problem that needs to be part of this conversation," Dr. Galsky maintained.
Dr. Ryan, the moderator, cited rapid treatment advances as yet another possible reason for poor accrual. "Some trials may take 2 or 3 years to accrue. During the first year, the standards of care may be one thing, and during the third year, the standards of care may have changed. We are really seeing very rapid evolution in our standards of care, so that could be one issue," he elaborated.
Introducing the study, Dr. Galsky noted that trials that fail to complete (that is, close without enrolling the intended number of patients) represent a major inefficiency of the cancer clinical trials enterprise. "Such trials contribute little knowledge, waste finite resources, and potentially divert patients from participating in other trials," he said.
The Institute of Medicine previously issued a report suggesting that about 40% of trials sponsored by the National Cancer Institute fail to achieve completion. But such trials account for only about 15% of all cancer trials.
The researchers analyzed 7,776 phase II or III interventional adult cancer clinical trials registered on ClinicalTrials.gov that had start dates between 2005 and 2011. They searched for those that had failed to reach completion, meaning that the trial had been stopped and had a "terminated" or "withdrawn" status.
The trials had a total of about 48,000 patients. Overall, 10% were trials in prostate, kidney, bladder, or testicular cancer.
The cumulative incidence of failure to reach completion for reasons unrelated to the efficacy or safety of the intervention was about 20%, according to Dr. Galsky.
Among all noncompleted trials, the largest share, 39%, failed to achieve completion because of poor accrual, topping other reasons such as logistics and efficacy/safety.
Trials were more likely to fail completion if they were funded by industry as compared with the federal government (hazard ratio, 1.97), were phase II as compared with phase III (HR, 1.29), or were single center as compared with multicenter (HR, 1.93).
On the other hand, trials were less likely to fail completion if they were conducted solely outside the United States (HR, 0.65) or both in and outside the United States (HR, 0.67), as compared with solely in the United States.
Dr. Galsky disclosed no relevant conflicts of interest.
AT THE GENITOURINARY CANCERS SYMPOSIUM
Major finding: About 20% of cancer clinical trials fail to reach completion for reasons unrelated to efficacy or toxicity, and the most common reason is poor accrual.
Data source: An analysis of 7,776 phase II and III interventional clinical trials involving adults with cancer.
Disclosures: Dr. Galsky disclosed no relevant conflicts of interest.
Striking trends emerge in SLE joint replacement
SNOWMASS, COLO. – Total knee replacement surgery rates in patients with systemic lupus erythematosus jumped sixfold nationally during a recent 15-year span – and buried within this statistic is some very good news.
The sharp rise in total knee replacement (TKR) among systemic lupus erythematosus (SLE) patients has been driven by a hefty increase in operations performed for osteoarthritis, while TKR for active SLE in the knee has declined. These trends reflect the increased longevity of patients with SLE resulting from improved medical management. For the first time, large numbers of SLE patients are surviving to an age when they, like other Americans, are more vulnerable to osteoarthritis, Dr. Susan M. Goodman explained at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
"Lupus is no longer the highly mortal disease that it was," she observed. "Clearly, patients are surviving and – I don’t know how else to put it – they’ve become middle-aged women who are having knee replacements, which is kind of a success."
She presented highlights of a soon-to-be-published study involving analysis of 10 state databases including nearly 2.8 million arthroplasties performed during 1991-2005. The rate of TKR in SLE patients climbed sixfold from 0.03 per 100,000 population in 1991 to 0.18 per 100,000 in 2005. Meanwhile, total hip replacement (THR) in SLE patients showed a modest but statistically significant increase from 0.11 to 0.18 cases per 100,000.
The proportion of lupus patients undergoing arthroplasty for avascular necrosis fell from 53% in 1991 to 24% in 2005, while the proportion undergoing arthroplasty because they developed osteoarthritis went from 23% to 61%.
Virtually all of the increase in total arthroplasties among SLE patients occurred in women aged 45 years and older. Their rate more than tripled during the study years, going from 0.076 to 0.271 cases per 100,000. Rates in female SLE patients aged 44 years and younger actually took a significant drop from 0.073 to 0.067 per 100,000. Rates in males aged 44 and younger remained flat over time, while men aged 45 and up showed a modest increase from a low baseline rate of 0.009 cases per 100,000 in 1991 to 0.034 per 100,000 in 2005, according to Dr. Goodman, a rheumatologist at the Hospital for Special Surgery and Cornell University, New York.
The proportion of TKRs among all arthroplasties performed in SLE patients increased from 16% in 1991 to 48% in 2005. Meanwhile, THRs decreased from 66% of all arthroplasties to 40%. Other joint replacements didn’t change much over time.
A particularly striking finding in the study was that the mean age at the time of arthroplasty in SLE patients increased by nearly a decade – 47.3 years in 1991 to 56.8 years in 2005. In contrast, the mean age at arthroplasty for osteoarthritis patients without SLE decreased from 71.5 to 69.0 years.
Dr. Goodman turned to additional studies by her research group and other investigators to provide a picture of arthroplasty outcomes in SLE patients.
In-hospital postoperative mortality was found to be increased in SLE patients, compared with rheumatoid arthritis patients or controls undergoing TKR or THR in a study of more than 1.5 million TKRs and THRs included in the Nationwide Inpatient Sample for 1993-2006. The Nationwide Inpatient Sample is the largest all-payer inpatient health care database in the United States.
In a multivariate logistic regression analysis adjusted for comorbidities, hospital type, and other potential confounders, investigators at Stanford (Calif.) University found that SLE patients undergoing THR had a 3.5-fold increased risk of death, compared with controls. This was driven by a 4.9-fold increased death risk in SLE patients undergoing nonelective THR or TKR, typically because of a fracture. In contrast, the rate of in-hospital death following TKR or THR in rheumatoid arthritis patients wasn’t significantly different from controls. The one comorbidity present on admission that was associated with markedly increased postoperative mortality was renal disease in SLE patients (J. Rheumatol. 2010;37:1467-72).
"Baseline renal dysfunction really seems to be a marker in lupus patients for bad perioperative outcome," Dr. Goodman observed, adding that there is a need for "increased vigilance" regarding this comorbidity.
A study of 57 SLE patients and 107 age-matched osteoarthritis patients who underwent THR at the Hospital for Special Surgery demonstrated that the lupus patients had more baseline comorbidities as reflected in their mean Charlson Comorbidity Index of 1.9, compared with 0.3 in the osteoarthritis group. Seventy-nine percent of the SLE patients, but none of the osteoarthritis patients, were on immunosuppressant therapy. The lupus patients had a 19% incidence of postoperative major adverse events, including deep vein thrombosis, arrhythmia, acute renal insufficiency, or additional surgery, compared with a 6% rate in the osteoarthritis group. The 6-day mean length of stay in the SLE group was a full day longer than that of the osteoarthritis patients, according to Dr. Goodman.
Another Hospital for Special Surgery study included 56 SLE patients undergoing THR and 45 with TKR, as well as 108 age-matched controls undergoing THR and 89 with TKR. The SLE patients had significantly worse baseline Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and function scores than did the osteoarthritis patients. At 2 years of follow-up, however, all four groups ended up with very good pain and function outcomes, with WOMAC scores in the 80-92 range.
Yet despite these excellent outcomes, the SLE patients still felt more limited by their chronic disease. This was reflected in their lower health-related quality of life on the SF-36 physical component summary score at 2 years of follow-up: 39 in the SLE THR patients, compared with 50.1 in the osteoarthritis THR group, and 38 in the SLE TKR patients, compared with 48.4 in the osteoarthritis controls.
This and other studies paint a picture of contemporary SLE patients undergoing TKR as more closely resembling osteoarthritis patients with TKR than SLE patients undergoing THR. The average age of the SLE TKR patients, at 62.4 years, was 8 years older than the SLE THR group. The SLE TKR group’s mean body mass index of 31.5 kg/m2 was 5 kg/m2 greater than in the SLE THR group. And none of the SLE TKR patients had avascular necrosis, compared with one-third of those undergoing THR.
Dr. Goodman reported having no relevant financial relationships.
SNOWMASS, COLO. – Total knee replacement surgery rates in patients with systemic lupus erythematosus jumped sixfold nationally during a recent 15-year span – and buried within this statistic is some very good news.
The sharp rise in total knee replacement (TKR) among systemic lupus erythematosus (SLE) patients has been driven by a hefty increase in operations performed for osteoarthritis, while TKR for active SLE in the knee has declined. These trends reflect the increased longevity of patients with SLE resulting from improved medical management. For the first time, large numbers of SLE patients are surviving to an age when they, like other Americans, are more vulnerable to osteoarthritis, Dr. Susan M. Goodman explained at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
"Lupus is no longer the highly mortal disease that it was," she observed. "Clearly, patients are surviving and – I don’t know how else to put it – they’ve become middle-aged women who are having knee replacements, which is kind of a success."
She presented highlights of a soon-to-be-published study involving analysis of 10 state databases including nearly 2.8 million arthroplasties performed during 1991-2005. The rate of TKR in SLE patients climbed sixfold from 0.03 per 100,000 population in 1991 to 0.18 per 100,000 in 2005. Meanwhile, total hip replacement (THR) in SLE patients showed a modest but statistically significant increase from 0.11 to 0.18 cases per 100,000.
The proportion of lupus patients undergoing arthroplasty for avascular necrosis fell from 53% in 1991 to 24% in 2005, while the proportion undergoing arthroplasty because they developed osteoarthritis went from 23% to 61%.
Virtually all of the increase in total arthroplasties among SLE patients occurred in women aged 45 years and older. Their rate more than tripled during the study years, going from 0.076 to 0.271 cases per 100,000. Rates in female SLE patients aged 44 years and younger actually took a significant drop from 0.073 to 0.067 per 100,000. Rates in males aged 44 and younger remained flat over time, while men aged 45 and up showed a modest increase from a low baseline rate of 0.009 cases per 100,000 in 1991 to 0.034 per 100,000 in 2005, according to Dr. Goodman, a rheumatologist at the Hospital for Special Surgery and Cornell University, New York.
The proportion of TKRs among all arthroplasties performed in SLE patients increased from 16% in 1991 to 48% in 2005. Meanwhile, THRs decreased from 66% of all arthroplasties to 40%. Other joint replacements didn’t change much over time.
A particularly striking finding in the study was that the mean age at the time of arthroplasty in SLE patients increased by nearly a decade – 47.3 years in 1991 to 56.8 years in 2005. In contrast, the mean age at arthroplasty for osteoarthritis patients without SLE decreased from 71.5 to 69.0 years.
Dr. Goodman turned to additional studies by her research group and other investigators to provide a picture of arthroplasty outcomes in SLE patients.
In-hospital postoperative mortality was found to be increased in SLE patients, compared with rheumatoid arthritis patients or controls undergoing TKR or THR in a study of more than 1.5 million TKRs and THRs included in the Nationwide Inpatient Sample for 1993-2006. The Nationwide Inpatient Sample is the largest all-payer inpatient health care database in the United States.
In a multivariate logistic regression analysis adjusted for comorbidities, hospital type, and other potential confounders, investigators at Stanford (Calif.) University found that SLE patients undergoing THR had a 3.5-fold increased risk of death, compared with controls. This was driven by a 4.9-fold increased death risk in SLE patients undergoing nonelective THR or TKR, typically because of a fracture. In contrast, the rate of in-hospital death following TKR or THR in rheumatoid arthritis patients wasn’t significantly different from controls. The one comorbidity present on admission that was associated with markedly increased postoperative mortality was renal disease in SLE patients (J. Rheumatol. 2010;37:1467-72).
"Baseline renal dysfunction really seems to be a marker in lupus patients for bad perioperative outcome," Dr. Goodman observed, adding that there is a need for "increased vigilance" regarding this comorbidity.
A study of 57 SLE patients and 107 age-matched osteoarthritis patients who underwent THR at the Hospital for Special Surgery demonstrated that the lupus patients had more baseline comorbidities as reflected in their mean Charlson Comorbidity Index of 1.9, compared with 0.3 in the osteoarthritis group. Seventy-nine percent of the SLE patients, but none of the osteoarthritis patients, were on immunosuppressant therapy. The lupus patients had a 19% incidence of postoperative major adverse events, including deep vein thrombosis, arrhythmia, acute renal insufficiency, or additional surgery, compared with a 6% rate in the osteoarthritis group. The 6-day mean length of stay in the SLE group was a full day longer than that of the osteoarthritis patients, according to Dr. Goodman.
Another Hospital for Special Surgery study included 56 SLE patients undergoing THR and 45 with TKR, as well as 108 age-matched controls undergoing THR and 89 with TKR. The SLE patients had significantly worse baseline Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and function scores than did the osteoarthritis patients. At 2 years of follow-up, however, all four groups ended up with very good pain and function outcomes, with WOMAC scores in the 80-92 range.
Yet despite these excellent outcomes, the SLE patients still felt more limited by their chronic disease. This was reflected in their lower health-related quality of life on the SF-36 physical component summary score at 2 years of follow-up: 39 in the SLE THR patients, compared with 50.1 in the osteoarthritis THR group, and 38 in the SLE TKR patients, compared with 48.4 in the osteoarthritis controls.
This and other studies paint a picture of contemporary SLE patients undergoing TKR as more closely resembling osteoarthritis patients with TKR than SLE patients undergoing THR. The average age of the SLE TKR patients, at 62.4 years, was 8 years older than the SLE THR group. The SLE TKR group’s mean body mass index of 31.5 kg/m2 was 5 kg/m2 greater than in the SLE THR group. And none of the SLE TKR patients had avascular necrosis, compared with one-third of those undergoing THR.
Dr. Goodman reported having no relevant financial relationships.
SNOWMASS, COLO. – Total knee replacement surgery rates in patients with systemic lupus erythematosus jumped sixfold nationally during a recent 15-year span – and buried within this statistic is some very good news.
The sharp rise in total knee replacement (TKR) among systemic lupus erythematosus (SLE) patients has been driven by a hefty increase in operations performed for osteoarthritis, while TKR for active SLE in the knee has declined. These trends reflect the increased longevity of patients with SLE resulting from improved medical management. For the first time, large numbers of SLE patients are surviving to an age when they, like other Americans, are more vulnerable to osteoarthritis, Dr. Susan M. Goodman explained at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
"Lupus is no longer the highly mortal disease that it was," she observed. "Clearly, patients are surviving and – I don’t know how else to put it – they’ve become middle-aged women who are having knee replacements, which is kind of a success."
She presented highlights of a soon-to-be-published study involving analysis of 10 state databases including nearly 2.8 million arthroplasties performed during 1991-2005. The rate of TKR in SLE patients climbed sixfold from 0.03 per 100,000 population in 1991 to 0.18 per 100,000 in 2005. Meanwhile, total hip replacement (THR) in SLE patients showed a modest but statistically significant increase from 0.11 to 0.18 cases per 100,000.
The proportion of lupus patients undergoing arthroplasty for avascular necrosis fell from 53% in 1991 to 24% in 2005, while the proportion undergoing arthroplasty because they developed osteoarthritis went from 23% to 61%.
Virtually all of the increase in total arthroplasties among SLE patients occurred in women aged 45 years and older. Their rate more than tripled during the study years, going from 0.076 to 0.271 cases per 100,000. Rates in female SLE patients aged 44 years and younger actually took a significant drop from 0.073 to 0.067 per 100,000. Rates in males aged 44 and younger remained flat over time, while men aged 45 and up showed a modest increase from a low baseline rate of 0.009 cases per 100,000 in 1991 to 0.034 per 100,000 in 2005, according to Dr. Goodman, a rheumatologist at the Hospital for Special Surgery and Cornell University, New York.
The proportion of TKRs among all arthroplasties performed in SLE patients increased from 16% in 1991 to 48% in 2005. Meanwhile, THRs decreased from 66% of all arthroplasties to 40%. Other joint replacements didn’t change much over time.
A particularly striking finding in the study was that the mean age at the time of arthroplasty in SLE patients increased by nearly a decade – 47.3 years in 1991 to 56.8 years in 2005. In contrast, the mean age at arthroplasty for osteoarthritis patients without SLE decreased from 71.5 to 69.0 years.
Dr. Goodman turned to additional studies by her research group and other investigators to provide a picture of arthroplasty outcomes in SLE patients.
In-hospital postoperative mortality was found to be increased in SLE patients, compared with rheumatoid arthritis patients or controls undergoing TKR or THR in a study of more than 1.5 million TKRs and THRs included in the Nationwide Inpatient Sample for 1993-2006. The Nationwide Inpatient Sample is the largest all-payer inpatient health care database in the United States.
In a multivariate logistic regression analysis adjusted for comorbidities, hospital type, and other potential confounders, investigators at Stanford (Calif.) University found that SLE patients undergoing THR had a 3.5-fold increased risk of death, compared with controls. This was driven by a 4.9-fold increased death risk in SLE patients undergoing nonelective THR or TKR, typically because of a fracture. In contrast, the rate of in-hospital death following TKR or THR in rheumatoid arthritis patients wasn’t significantly different from controls. The one comorbidity present on admission that was associated with markedly increased postoperative mortality was renal disease in SLE patients (J. Rheumatol. 2010;37:1467-72).
"Baseline renal dysfunction really seems to be a marker in lupus patients for bad perioperative outcome," Dr. Goodman observed, adding that there is a need for "increased vigilance" regarding this comorbidity.
A study of 57 SLE patients and 107 age-matched osteoarthritis patients who underwent THR at the Hospital for Special Surgery demonstrated that the lupus patients had more baseline comorbidities as reflected in their mean Charlson Comorbidity Index of 1.9, compared with 0.3 in the osteoarthritis group. Seventy-nine percent of the SLE patients, but none of the osteoarthritis patients, were on immunosuppressant therapy. The lupus patients had a 19% incidence of postoperative major adverse events, including deep vein thrombosis, arrhythmia, acute renal insufficiency, or additional surgery, compared with a 6% rate in the osteoarthritis group. The 6-day mean length of stay in the SLE group was a full day longer than that of the osteoarthritis patients, according to Dr. Goodman.
Another Hospital for Special Surgery study included 56 SLE patients undergoing THR and 45 with TKR, as well as 108 age-matched controls undergoing THR and 89 with TKR. The SLE patients had significantly worse baseline Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and function scores than did the osteoarthritis patients. At 2 years of follow-up, however, all four groups ended up with very good pain and function outcomes, with WOMAC scores in the 80-92 range.
Yet despite these excellent outcomes, the SLE patients still felt more limited by their chronic disease. This was reflected in their lower health-related quality of life on the SF-36 physical component summary score at 2 years of follow-up: 39 in the SLE THR patients, compared with 50.1 in the osteoarthritis THR group, and 38 in the SLE TKR patients, compared with 48.4 in the osteoarthritis controls.
This and other studies paint a picture of contemporary SLE patients undergoing TKR as more closely resembling osteoarthritis patients with TKR than SLE patients undergoing THR. The average age of the SLE TKR patients, at 62.4 years, was 8 years older than the SLE THR group. The SLE TKR group’s mean body mass index of 31.5 kg/m2 was 5 kg/m2 greater than in the SLE THR group. And none of the SLE TKR patients had avascular necrosis, compared with one-third of those undergoing THR.
Dr. Goodman reported having no relevant financial relationships.
EXPERT ANALYSIS FROM THE WINTER RHEUMATOLOGY SYMPOSIUM
Cloud-based network reduces repeat trauma imaging
NAPLES, FLA. – Implementing a cloud-based network for sharing radiological images reduced radiation exposure and costs at a Level 1 tertiary care trauma center.
The number of trauma patients who underwent the exact same imaging study decreased significantly from 62% to 47% in the 6 months after the network was available (P less than .01).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This resulted in a significant 19.2% decline in radiation exposure (mean 8.39 mSv vs. 7.23 mSv; P less than .01), Dr. Mayur Narayan reported at the annual meeting of the Eastern Association for the Surgery of Trauma.
"I think it’s a potential game changer," he said. "... The concept is important. The way we’re doing business currently is not sustainable."
Patients transferred within a regional trauma system to a tertiary care referral center frequently have prior radiology studies, but often undergo repeat imaging because of poor image quality, incompatible imaging software, or misplaced imaging discs. This can delay patient management, bring unwelcome radiation, and raise health care costs, explained Dr. Narayan, with the R Adams Cowley Shock Trauma Center at the University of Maryland Medical Center in Baltimore.
To reverse this trend, the center set up a secure, electronic (lifeIMAGE) network that uses a single platform for all medical image exchanges. Physicians can retrieve outside exams via the cloud or merge any or all picture archiving and communication system (PACS) data into their own PACS.
Ten hospitals are now on board and prospective data have been analyzed for 1,950 patients transferred to the trauma center between Jan. 1 and June 30, 2011, (pre-network) and between Jan. 1 and June 30, 2012, (post-network). About 8,500 patients are transferred to the trauma center annually from across the state. Patients in both time periods had similar demographics and Injury Severity Scores (mean 12).
In the 6 months after the network was implemented, the cost of imaging per patient dropped 18.7% ($413 vs. $333; P less than .01), while total imaging costs declined from $401,765 to $326,756 during the same period, Dr. Narayan said.
The most common repeat study in the analysis was an abdominal pelvic CT scan.
Inexplicably, hospital length of stay also declined from 4.4 days to 3.8 days (P = .07), he said. In-hospital mortality was unchanged (3.8% vs. 4.4%; P = .52).
The network cost Cowley Shock Trauma about $30,000 to set up, but other hospital groups are working to provide similar software for free, Dr. Narayan noted.
"The upfront costs should go away," he said.
During a discussion of the poster, one attendee said they set up a similar cloud-based system for their region, but no one used it. "I think it’s because small hospitals don’t see a lot of trauma. They have one or two patients maybe a month that would require transfer and with different people at the CT scanner every night, there’s no uniformity on how to do it," he said.
Others, however, noted that image sharing between hospitals has been fully integrated into their transfer algorithm, prompting calls between hospital radiology units, so that PAC files and patient record numbers have already been merged before the patient ever arrives in the trauma bay.
The Radiological Society of North America has also harnessed cloud-based computing to allow consumers to share their images and interpretations with any provider, regardless of institutional affiliation. According to 20-month follow-up data reported in late 2013, four out of five patients and 9 out of 10 physicians were satisfied with the RSNA Image Share network. A full 90% of patients were comfortable with the amount of privacy provided by the network, though some criticized the site for being "clunky" to navigate.
Dr. Narayan reported having no financial disclosures.
NAPLES, FLA. – Implementing a cloud-based network for sharing radiological images reduced radiation exposure and costs at a Level 1 tertiary care trauma center.
The number of trauma patients who underwent the exact same imaging study decreased significantly from 62% to 47% in the 6 months after the network was available (P less than .01).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This resulted in a significant 19.2% decline in radiation exposure (mean 8.39 mSv vs. 7.23 mSv; P less than .01), Dr. Mayur Narayan reported at the annual meeting of the Eastern Association for the Surgery of Trauma.
"I think it’s a potential game changer," he said. "... The concept is important. The way we’re doing business currently is not sustainable."
Patients transferred within a regional trauma system to a tertiary care referral center frequently have prior radiology studies, but often undergo repeat imaging because of poor image quality, incompatible imaging software, or misplaced imaging discs. This can delay patient management, bring unwelcome radiation, and raise health care costs, explained Dr. Narayan, with the R Adams Cowley Shock Trauma Center at the University of Maryland Medical Center in Baltimore.
To reverse this trend, the center set up a secure, electronic (lifeIMAGE) network that uses a single platform for all medical image exchanges. Physicians can retrieve outside exams via the cloud or merge any or all picture archiving and communication system (PACS) data into their own PACS.
Ten hospitals are now on board and prospective data have been analyzed for 1,950 patients transferred to the trauma center between Jan. 1 and June 30, 2011, (pre-network) and between Jan. 1 and June 30, 2012, (post-network). About 8,500 patients are transferred to the trauma center annually from across the state. Patients in both time periods had similar demographics and Injury Severity Scores (mean 12).
In the 6 months after the network was implemented, the cost of imaging per patient dropped 18.7% ($413 vs. $333; P less than .01), while total imaging costs declined from $401,765 to $326,756 during the same period, Dr. Narayan said.
The most common repeat study in the analysis was an abdominal pelvic CT scan.
Inexplicably, hospital length of stay also declined from 4.4 days to 3.8 days (P = .07), he said. In-hospital mortality was unchanged (3.8% vs. 4.4%; P = .52).
The network cost Cowley Shock Trauma about $30,000 to set up, but other hospital groups are working to provide similar software for free, Dr. Narayan noted.
"The upfront costs should go away," he said.
During a discussion of the poster, one attendee said they set up a similar cloud-based system for their region, but no one used it. "I think it’s because small hospitals don’t see a lot of trauma. They have one or two patients maybe a month that would require transfer and with different people at the CT scanner every night, there’s no uniformity on how to do it," he said.
Others, however, noted that image sharing between hospitals has been fully integrated into their transfer algorithm, prompting calls between hospital radiology units, so that PAC files and patient record numbers have already been merged before the patient ever arrives in the trauma bay.
The Radiological Society of North America has also harnessed cloud-based computing to allow consumers to share their images and interpretations with any provider, regardless of institutional affiliation. According to 20-month follow-up data reported in late 2013, four out of five patients and 9 out of 10 physicians were satisfied with the RSNA Image Share network. A full 90% of patients were comfortable with the amount of privacy provided by the network, though some criticized the site for being "clunky" to navigate.
Dr. Narayan reported having no financial disclosures.
NAPLES, FLA. – Implementing a cloud-based network for sharing radiological images reduced radiation exposure and costs at a Level 1 tertiary care trauma center.
The number of trauma patients who underwent the exact same imaging study decreased significantly from 62% to 47% in the 6 months after the network was available (P less than .01).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This resulted in a significant 19.2% decline in radiation exposure (mean 8.39 mSv vs. 7.23 mSv; P less than .01), Dr. Mayur Narayan reported at the annual meeting of the Eastern Association for the Surgery of Trauma.
"I think it’s a potential game changer," he said. "... The concept is important. The way we’re doing business currently is not sustainable."
Patients transferred within a regional trauma system to a tertiary care referral center frequently have prior radiology studies, but often undergo repeat imaging because of poor image quality, incompatible imaging software, or misplaced imaging discs. This can delay patient management, bring unwelcome radiation, and raise health care costs, explained Dr. Narayan, with the R Adams Cowley Shock Trauma Center at the University of Maryland Medical Center in Baltimore.
To reverse this trend, the center set up a secure, electronic (lifeIMAGE) network that uses a single platform for all medical image exchanges. Physicians can retrieve outside exams via the cloud or merge any or all picture archiving and communication system (PACS) data into their own PACS.
Ten hospitals are now on board and prospective data have been analyzed for 1,950 patients transferred to the trauma center between Jan. 1 and June 30, 2011, (pre-network) and between Jan. 1 and June 30, 2012, (post-network). About 8,500 patients are transferred to the trauma center annually from across the state. Patients in both time periods had similar demographics and Injury Severity Scores (mean 12).
In the 6 months after the network was implemented, the cost of imaging per patient dropped 18.7% ($413 vs. $333; P less than .01), while total imaging costs declined from $401,765 to $326,756 during the same period, Dr. Narayan said.
The most common repeat study in the analysis was an abdominal pelvic CT scan.
Inexplicably, hospital length of stay also declined from 4.4 days to 3.8 days (P = .07), he said. In-hospital mortality was unchanged (3.8% vs. 4.4%; P = .52).
The network cost Cowley Shock Trauma about $30,000 to set up, but other hospital groups are working to provide similar software for free, Dr. Narayan noted.
"The upfront costs should go away," he said.
During a discussion of the poster, one attendee said they set up a similar cloud-based system for their region, but no one used it. "I think it’s because small hospitals don’t see a lot of trauma. They have one or two patients maybe a month that would require transfer and with different people at the CT scanner every night, there’s no uniformity on how to do it," he said.
Others, however, noted that image sharing between hospitals has been fully integrated into their transfer algorithm, prompting calls between hospital radiology units, so that PAC files and patient record numbers have already been merged before the patient ever arrives in the trauma bay.
The Radiological Society of North America has also harnessed cloud-based computing to allow consumers to share their images and interpretations with any provider, regardless of institutional affiliation. According to 20-month follow-up data reported in late 2013, four out of five patients and 9 out of 10 physicians were satisfied with the RSNA Image Share network. A full 90% of patients were comfortable with the amount of privacy provided by the network, though some criticized the site for being "clunky" to navigate.
Dr. Narayan reported having no financial disclosures.
AT EAST 2014
Major finding: The number of patients who underwent repeat imaging declined from 62% to 47% in the 6 months after the network was implemented (P less than .01).
Data source: Prospective data review of 1,950 trauma patients.
Disclosures: Dr. Narayan reported having no financial disclosures.
Military’s top doc: Medical lessons from Iraq saved lives in Boston bombings
Dr. Jonathan Woodson fielded e-mails in his Pentagon office last April from nervous colleagues in Boston.
His fellow vascular surgeons there wanted to know if more attacks were coming in the Marathon bombings. "When you work at the Pentagon, everyone thinks you have total situational awareness," said Dr. Woodson, assistant secretary of defense for health affairs.
His former colleagues, however, also wanted tips on how to care for bombing victims, and knew that military surgeons like Dr. Woodson had answers. Before President Obama tapped him in 2010 to become the military’s top doctor and oversee the Pentagon’s $50 billion-plus medical budget, he’d scrubbed in on battlefield cases in Kosovo, Iraq, and Afghanistan, in addition to performing his vascular surgery and administrative duties at Boston University and Boston Medical Center.
"We’ve been dealing with [improvised explosive device] injuries for over a decade," said Dr. Woodson, a brigadier general in the U.S. Army Reserve.
"The good news is, I had trained some of the folks who worked" on the bombing victims, and "they knew what my techniques were." Still, there were discussions about particular fixes; hypertrophic bone growths, infections, and other wound complications; and ways to help young people recover from devastating injuries. Many of the lessons came from Dr. Woodson’s military service.
The back-and-forth about the Boston attacks highlights how important it is for military and civilian physicians to cross-pollinate. In the past, "there’s always been a cadre of usually academic surgeons and physicians who maintain contact with the military. I think [it] is very important to formalize these connections. One of my strategic imperatives is to make sure we invest in partnerships [with] academic medical centers and key professional organizations" so that war innovations make it into civilian practice, and, in turn, are remembered for future conflicts.
"There’s the potential for this expertise to be lost," said Dr. Woodson, who was finishing a paper with two colleagues on the history of military medical innovations (Semin. Vasc. Surg. 2010;23:235-42) when he was nominated to serve as the secretary of defense’s principal adviser on health issues.
There’ve been many innovations in recent years, including the recognition that extensive fasciotomies can save badly damaged limbs.
At the start of Operation Iraqi Freedom in 2003, Dr. Woodson was in northern Kuwait running a makeshift U.S. military hospital out of a commandeered Kuwaiti facility. "As the troops went over the berm, we were taking the first wave of casualties," performing surgery in full chemical-attack gear. "Luckily," the incoming Scud missiles weren’t very accurate. It was a humbling experience," he said.
A young soldier was helicoptered in with a crushed leg after a hit to his armored vehicle. "We did an interposition graft to repair the popliteal artery," and, because of severe swelling, extensive fasciotomies to prevent compartment syndrome; the soldier still had his leg when he was airlifted out. Although not standard practice at the time, that case and others like it quickly demonstrated "the benefit of doing four-compartment fasciotomies early on to preserve limbs. Fasciotomies are now [used routinely] to address these injuries," Dr. Woodson said.
Tourniquets – which "prior to this conflict had a very bad reputation" – have proved their worth in recent battles as well, a lesson that helped save lives in Boston. Likewise, the military has learned the value of temporary vascular shunts, narrow tubing – most often Argyle carotid artery shunts – to bypass tears or reconnect severed vessels when there’s no time for a definitive repair. "We [also] came to understand very early on the need for aggressive blood replacement. Previously, protocols called for lactated Ringer’s or saline infusions, but we realized they just lead to massive soft tissue edema, increased lung water," and other problems, he said.
Currently, Dr. Woodson and his military colleagues are helping coach the rehabilitation of the Boston bombing victims. Rehab has seen "major advances in the military that are now finding their way into civilian practice," including improved prosthetics; better understanding of rehabilitation psychology; and recognition of subtle traumatic brain, eye, ear, and other injuries that can derail recovery efforts, he said.
"Because soldiers were athletes before [their injury], they often have aggressive goals in mind. Some want to return to swimming, surfing, or skiing. We try to meet those goals ... to get them fully reincorporated into the lives they want to lead"; adaptive sports programs help, among other things. It’s a very appropriate strategy for the Boston bombing survivors, since many were athletes, he said.
Dr. Jonathan Woodson fielded e-mails in his Pentagon office last April from nervous colleagues in Boston.
His fellow vascular surgeons there wanted to know if more attacks were coming in the Marathon bombings. "When you work at the Pentagon, everyone thinks you have total situational awareness," said Dr. Woodson, assistant secretary of defense for health affairs.
His former colleagues, however, also wanted tips on how to care for bombing victims, and knew that military surgeons like Dr. Woodson had answers. Before President Obama tapped him in 2010 to become the military’s top doctor and oversee the Pentagon’s $50 billion-plus medical budget, he’d scrubbed in on battlefield cases in Kosovo, Iraq, and Afghanistan, in addition to performing his vascular surgery and administrative duties at Boston University and Boston Medical Center.
"We’ve been dealing with [improvised explosive device] injuries for over a decade," said Dr. Woodson, a brigadier general in the U.S. Army Reserve.
"The good news is, I had trained some of the folks who worked" on the bombing victims, and "they knew what my techniques were." Still, there were discussions about particular fixes; hypertrophic bone growths, infections, and other wound complications; and ways to help young people recover from devastating injuries. Many of the lessons came from Dr. Woodson’s military service.
The back-and-forth about the Boston attacks highlights how important it is for military and civilian physicians to cross-pollinate. In the past, "there’s always been a cadre of usually academic surgeons and physicians who maintain contact with the military. I think [it] is very important to formalize these connections. One of my strategic imperatives is to make sure we invest in partnerships [with] academic medical centers and key professional organizations" so that war innovations make it into civilian practice, and, in turn, are remembered for future conflicts.
"There’s the potential for this expertise to be lost," said Dr. Woodson, who was finishing a paper with two colleagues on the history of military medical innovations (Semin. Vasc. Surg. 2010;23:235-42) when he was nominated to serve as the secretary of defense’s principal adviser on health issues.
There’ve been many innovations in recent years, including the recognition that extensive fasciotomies can save badly damaged limbs.
At the start of Operation Iraqi Freedom in 2003, Dr. Woodson was in northern Kuwait running a makeshift U.S. military hospital out of a commandeered Kuwaiti facility. "As the troops went over the berm, we were taking the first wave of casualties," performing surgery in full chemical-attack gear. "Luckily," the incoming Scud missiles weren’t very accurate. It was a humbling experience," he said.
A young soldier was helicoptered in with a crushed leg after a hit to his armored vehicle. "We did an interposition graft to repair the popliteal artery," and, because of severe swelling, extensive fasciotomies to prevent compartment syndrome; the soldier still had his leg when he was airlifted out. Although not standard practice at the time, that case and others like it quickly demonstrated "the benefit of doing four-compartment fasciotomies early on to preserve limbs. Fasciotomies are now [used routinely] to address these injuries," Dr. Woodson said.
Tourniquets – which "prior to this conflict had a very bad reputation" – have proved their worth in recent battles as well, a lesson that helped save lives in Boston. Likewise, the military has learned the value of temporary vascular shunts, narrow tubing – most often Argyle carotid artery shunts – to bypass tears or reconnect severed vessels when there’s no time for a definitive repair. "We [also] came to understand very early on the need for aggressive blood replacement. Previously, protocols called for lactated Ringer’s or saline infusions, but we realized they just lead to massive soft tissue edema, increased lung water," and other problems, he said.
Currently, Dr. Woodson and his military colleagues are helping coach the rehabilitation of the Boston bombing victims. Rehab has seen "major advances in the military that are now finding their way into civilian practice," including improved prosthetics; better understanding of rehabilitation psychology; and recognition of subtle traumatic brain, eye, ear, and other injuries that can derail recovery efforts, he said.
"Because soldiers were athletes before [their injury], they often have aggressive goals in mind. Some want to return to swimming, surfing, or skiing. We try to meet those goals ... to get them fully reincorporated into the lives they want to lead"; adaptive sports programs help, among other things. It’s a very appropriate strategy for the Boston bombing survivors, since many were athletes, he said.
Dr. Jonathan Woodson fielded e-mails in his Pentagon office last April from nervous colleagues in Boston.
His fellow vascular surgeons there wanted to know if more attacks were coming in the Marathon bombings. "When you work at the Pentagon, everyone thinks you have total situational awareness," said Dr. Woodson, assistant secretary of defense for health affairs.
His former colleagues, however, also wanted tips on how to care for bombing victims, and knew that military surgeons like Dr. Woodson had answers. Before President Obama tapped him in 2010 to become the military’s top doctor and oversee the Pentagon’s $50 billion-plus medical budget, he’d scrubbed in on battlefield cases in Kosovo, Iraq, and Afghanistan, in addition to performing his vascular surgery and administrative duties at Boston University and Boston Medical Center.
"We’ve been dealing with [improvised explosive device] injuries for over a decade," said Dr. Woodson, a brigadier general in the U.S. Army Reserve.
"The good news is, I had trained some of the folks who worked" on the bombing victims, and "they knew what my techniques were." Still, there were discussions about particular fixes; hypertrophic bone growths, infections, and other wound complications; and ways to help young people recover from devastating injuries. Many of the lessons came from Dr. Woodson’s military service.
The back-and-forth about the Boston attacks highlights how important it is for military and civilian physicians to cross-pollinate. In the past, "there’s always been a cadre of usually academic surgeons and physicians who maintain contact with the military. I think [it] is very important to formalize these connections. One of my strategic imperatives is to make sure we invest in partnerships [with] academic medical centers and key professional organizations" so that war innovations make it into civilian practice, and, in turn, are remembered for future conflicts.
"There’s the potential for this expertise to be lost," said Dr. Woodson, who was finishing a paper with two colleagues on the history of military medical innovations (Semin. Vasc. Surg. 2010;23:235-42) when he was nominated to serve as the secretary of defense’s principal adviser on health issues.
There’ve been many innovations in recent years, including the recognition that extensive fasciotomies can save badly damaged limbs.
At the start of Operation Iraqi Freedom in 2003, Dr. Woodson was in northern Kuwait running a makeshift U.S. military hospital out of a commandeered Kuwaiti facility. "As the troops went over the berm, we were taking the first wave of casualties," performing surgery in full chemical-attack gear. "Luckily," the incoming Scud missiles weren’t very accurate. It was a humbling experience," he said.
A young soldier was helicoptered in with a crushed leg after a hit to his armored vehicle. "We did an interposition graft to repair the popliteal artery," and, because of severe swelling, extensive fasciotomies to prevent compartment syndrome; the soldier still had his leg when he was airlifted out. Although not standard practice at the time, that case and others like it quickly demonstrated "the benefit of doing four-compartment fasciotomies early on to preserve limbs. Fasciotomies are now [used routinely] to address these injuries," Dr. Woodson said.
Tourniquets – which "prior to this conflict had a very bad reputation" – have proved their worth in recent battles as well, a lesson that helped save lives in Boston. Likewise, the military has learned the value of temporary vascular shunts, narrow tubing – most often Argyle carotid artery shunts – to bypass tears or reconnect severed vessels when there’s no time for a definitive repair. "We [also] came to understand very early on the need for aggressive blood replacement. Previously, protocols called for lactated Ringer’s or saline infusions, but we realized they just lead to massive soft tissue edema, increased lung water," and other problems, he said.
Currently, Dr. Woodson and his military colleagues are helping coach the rehabilitation of the Boston bombing victims. Rehab has seen "major advances in the military that are now finding their way into civilian practice," including improved prosthetics; better understanding of rehabilitation psychology; and recognition of subtle traumatic brain, eye, ear, and other injuries that can derail recovery efforts, he said.
"Because soldiers were athletes before [their injury], they often have aggressive goals in mind. Some want to return to swimming, surfing, or skiing. We try to meet those goals ... to get them fully reincorporated into the lives they want to lead"; adaptive sports programs help, among other things. It’s a very appropriate strategy for the Boston bombing survivors, since many were athletes, he said.
Complications after gastric cancer resection portend poor outcomes
SAN FRANCISCO – Postoperative complications are prognostic for poor outcomes in patients undergoing resection of gastric cancer, researchers reported at the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
The team retrospectively analyzed data collected in the U.S. Gastric Cancer Collaborative, a joint effort of seven moderate- to high-volume academic institutions across the United States. Analyses were based on 850 patients who underwent curative resection of gastric or gastroesophageal junction adenocarcinoma by abdominal approach from 2000 to 2012.
Complications occurred within a month of surgery in 40% of the patients, reported coauthor Dr. Ryan C. Fields of Washington University in St. Louis. These patients were 20% less likely to receive adjuvant therapy than were their peers with an uncomplicated postoperative course. And during a median follow-up of almost 3 years, those with postop complications were 60% more likely to die after potential confounding factors were taken into account.
"The particular strength of this data set is the cross-section of real-world treatments and outcomes that it represents," Dr. Fields noted.
Patients who had complications were older, had higher levels of comorbidity and complexity, underwent more extensive surgery, and had more advanced disease. "We could potentially identify preoperatively [these patients] in an attempt to reduce the chance of complications," he said.
Not included in this analysis was "the finding of muscular sarcopenia as measured from the psoas muscle on a preoperative CT scan. There are ongoing studies using this measure to identify patients who may benefit from a short course of intensive physical therapy and nutritional supplementation prior to surgery in an attempt to reduce complications," he added.
The study was limited by its retrospective and nonrandomized design, and factors such as selection bias and missing data may have affected outcomes, Dr. Fields acknowledged. The researchers are therefore conducting further analyses using propensity matching and imputation.
The data set "may not be representative of (patients in) other countries or importantly of the nearly 40% of patients with gastric cancer that are treated at non-university, community-based hospitals in the United States," he added. "I would argue, however, that if we accept the relationship between volume and outcomes that has been shown to be significant in gastrectomy, the effect of complications on outcomes would be expected to be even more significant in these settings."
Groups stratified by Clavien-Dindo score were too small to draw definitive conclusions, but there were trends whereby worse complications had a greater negative impact on outcome, Dr. Fields said.
"One of the problems that we have – as an oncologic community –is there is no real consistent definition of complications in a lot of this literature," he added, which may be generating some of the disparate findings. For example, the severity of a wound infection can range widely, with more severe infections affecting decisions about whether to delay or even withhold adjuvant therapy.
In the study, there were a total of 699 complications in 342 patients, "highlighting the ... observation that often complications can beget further complications," according to Dr. Fields.
More than one-third of the complications (37%) were of Clavien-Dindo grade III or IV, requiring care more invasive than simple treatment at the bedside or with intravenous medications.
The most common were anemia/bleeding (12%), wound infections (8%), pneumonia (6%), and respiratory failure requiring reintubation (6%).
Relative to counterparts without complications, patients who had complications were on average significantly older and had significantly higher American Society of Anesthesiologists scores (reflecting greater preoperative comorbidity and complexity), more extensive and complex surgery, and more advanced cancer.
"Importantly, we did not find neoadjuvant therapy to be associated with an increase in postoperative complications, and this is consistent with literature in other solid tumor types, such as pancreatic cancer and rectal cancer," noted Dr. Fields, who disclosed no conflicts of interest related to the study. Also, the extent of lymphadenectomy was not associated with this outcome.
A minority of patients had a laparoscopic surgery, and the number was too small to say whether this factor influenced complication rate, he said.
"What we can surmise, one, from the literature, and two, is that the specific complications that are oftentimes reduced with laparoscopy and minimally invasive surgery certainly relate to wound infection and wound problems for sure," Dr. Fields commented. "So I think if we can do anything to achieve the same oncologic goals and reduce the morbidity of an operation, and improve the ability of patients to get on adjuvant therapy, that’s going to be critical. And laparoscopy may be a way to do that in gastric cancer. It may be more challenging in some of the bulkier, more advanced tumors to apply it globally, but I think it certainly holds promise for that exact point."
Overall, 60% of patients without complications received adjuvant therapy, compared with 48% of patients with complications (P = .001).
In multivariate analyses conducted after a median follow-up of 35 months, patients who experienced postoperative complications still had shorter median survival (25 vs. 45 months) and were more likely to die (hazard ratio, 1.6; P = .004).
Other significant risk factors were receipt of neoadjuvant therapy, perineural invasion, and stage III or IV disease.
Dr. Fields disclosed no relevant conflicts of interest.
SAN FRANCISCO – Postoperative complications are prognostic for poor outcomes in patients undergoing resection of gastric cancer, researchers reported at the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
The team retrospectively analyzed data collected in the U.S. Gastric Cancer Collaborative, a joint effort of seven moderate- to high-volume academic institutions across the United States. Analyses were based on 850 patients who underwent curative resection of gastric or gastroesophageal junction adenocarcinoma by abdominal approach from 2000 to 2012.
Complications occurred within a month of surgery in 40% of the patients, reported coauthor Dr. Ryan C. Fields of Washington University in St. Louis. These patients were 20% less likely to receive adjuvant therapy than were their peers with an uncomplicated postoperative course. And during a median follow-up of almost 3 years, those with postop complications were 60% more likely to die after potential confounding factors were taken into account.
"The particular strength of this data set is the cross-section of real-world treatments and outcomes that it represents," Dr. Fields noted.
Patients who had complications were older, had higher levels of comorbidity and complexity, underwent more extensive surgery, and had more advanced disease. "We could potentially identify preoperatively [these patients] in an attempt to reduce the chance of complications," he said.
Not included in this analysis was "the finding of muscular sarcopenia as measured from the psoas muscle on a preoperative CT scan. There are ongoing studies using this measure to identify patients who may benefit from a short course of intensive physical therapy and nutritional supplementation prior to surgery in an attempt to reduce complications," he added.
The study was limited by its retrospective and nonrandomized design, and factors such as selection bias and missing data may have affected outcomes, Dr. Fields acknowledged. The researchers are therefore conducting further analyses using propensity matching and imputation.
The data set "may not be representative of (patients in) other countries or importantly of the nearly 40% of patients with gastric cancer that are treated at non-university, community-based hospitals in the United States," he added. "I would argue, however, that if we accept the relationship between volume and outcomes that has been shown to be significant in gastrectomy, the effect of complications on outcomes would be expected to be even more significant in these settings."
Groups stratified by Clavien-Dindo score were too small to draw definitive conclusions, but there were trends whereby worse complications had a greater negative impact on outcome, Dr. Fields said.
"One of the problems that we have – as an oncologic community –is there is no real consistent definition of complications in a lot of this literature," he added, which may be generating some of the disparate findings. For example, the severity of a wound infection can range widely, with more severe infections affecting decisions about whether to delay or even withhold adjuvant therapy.
In the study, there were a total of 699 complications in 342 patients, "highlighting the ... observation that often complications can beget further complications," according to Dr. Fields.
More than one-third of the complications (37%) were of Clavien-Dindo grade III or IV, requiring care more invasive than simple treatment at the bedside or with intravenous medications.
The most common were anemia/bleeding (12%), wound infections (8%), pneumonia (6%), and respiratory failure requiring reintubation (6%).
Relative to counterparts without complications, patients who had complications were on average significantly older and had significantly higher American Society of Anesthesiologists scores (reflecting greater preoperative comorbidity and complexity), more extensive and complex surgery, and more advanced cancer.
"Importantly, we did not find neoadjuvant therapy to be associated with an increase in postoperative complications, and this is consistent with literature in other solid tumor types, such as pancreatic cancer and rectal cancer," noted Dr. Fields, who disclosed no conflicts of interest related to the study. Also, the extent of lymphadenectomy was not associated with this outcome.
A minority of patients had a laparoscopic surgery, and the number was too small to say whether this factor influenced complication rate, he said.
"What we can surmise, one, from the literature, and two, is that the specific complications that are oftentimes reduced with laparoscopy and minimally invasive surgery certainly relate to wound infection and wound problems for sure," Dr. Fields commented. "So I think if we can do anything to achieve the same oncologic goals and reduce the morbidity of an operation, and improve the ability of patients to get on adjuvant therapy, that’s going to be critical. And laparoscopy may be a way to do that in gastric cancer. It may be more challenging in some of the bulkier, more advanced tumors to apply it globally, but I think it certainly holds promise for that exact point."
Overall, 60% of patients without complications received adjuvant therapy, compared with 48% of patients with complications (P = .001).
In multivariate analyses conducted after a median follow-up of 35 months, patients who experienced postoperative complications still had shorter median survival (25 vs. 45 months) and were more likely to die (hazard ratio, 1.6; P = .004).
Other significant risk factors were receipt of neoadjuvant therapy, perineural invasion, and stage III or IV disease.
Dr. Fields disclosed no relevant conflicts of interest.
SAN FRANCISCO – Postoperative complications are prognostic for poor outcomes in patients undergoing resection of gastric cancer, researchers reported at the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
The team retrospectively analyzed data collected in the U.S. Gastric Cancer Collaborative, a joint effort of seven moderate- to high-volume academic institutions across the United States. Analyses were based on 850 patients who underwent curative resection of gastric or gastroesophageal junction adenocarcinoma by abdominal approach from 2000 to 2012.
Complications occurred within a month of surgery in 40% of the patients, reported coauthor Dr. Ryan C. Fields of Washington University in St. Louis. These patients were 20% less likely to receive adjuvant therapy than were their peers with an uncomplicated postoperative course. And during a median follow-up of almost 3 years, those with postop complications were 60% more likely to die after potential confounding factors were taken into account.
"The particular strength of this data set is the cross-section of real-world treatments and outcomes that it represents," Dr. Fields noted.
Patients who had complications were older, had higher levels of comorbidity and complexity, underwent more extensive surgery, and had more advanced disease. "We could potentially identify preoperatively [these patients] in an attempt to reduce the chance of complications," he said.
Not included in this analysis was "the finding of muscular sarcopenia as measured from the psoas muscle on a preoperative CT scan. There are ongoing studies using this measure to identify patients who may benefit from a short course of intensive physical therapy and nutritional supplementation prior to surgery in an attempt to reduce complications," he added.
The study was limited by its retrospective and nonrandomized design, and factors such as selection bias and missing data may have affected outcomes, Dr. Fields acknowledged. The researchers are therefore conducting further analyses using propensity matching and imputation.
The data set "may not be representative of (patients in) other countries or importantly of the nearly 40% of patients with gastric cancer that are treated at non-university, community-based hospitals in the United States," he added. "I would argue, however, that if we accept the relationship between volume and outcomes that has been shown to be significant in gastrectomy, the effect of complications on outcomes would be expected to be even more significant in these settings."
Groups stratified by Clavien-Dindo score were too small to draw definitive conclusions, but there were trends whereby worse complications had a greater negative impact on outcome, Dr. Fields said.
"One of the problems that we have – as an oncologic community –is there is no real consistent definition of complications in a lot of this literature," he added, which may be generating some of the disparate findings. For example, the severity of a wound infection can range widely, with more severe infections affecting decisions about whether to delay or even withhold adjuvant therapy.
In the study, there were a total of 699 complications in 342 patients, "highlighting the ... observation that often complications can beget further complications," according to Dr. Fields.
More than one-third of the complications (37%) were of Clavien-Dindo grade III or IV, requiring care more invasive than simple treatment at the bedside or with intravenous medications.
The most common were anemia/bleeding (12%), wound infections (8%), pneumonia (6%), and respiratory failure requiring reintubation (6%).
Relative to counterparts without complications, patients who had complications were on average significantly older and had significantly higher American Society of Anesthesiologists scores (reflecting greater preoperative comorbidity and complexity), more extensive and complex surgery, and more advanced cancer.
"Importantly, we did not find neoadjuvant therapy to be associated with an increase in postoperative complications, and this is consistent with literature in other solid tumor types, such as pancreatic cancer and rectal cancer," noted Dr. Fields, who disclosed no conflicts of interest related to the study. Also, the extent of lymphadenectomy was not associated with this outcome.
A minority of patients had a laparoscopic surgery, and the number was too small to say whether this factor influenced complication rate, he said.
"What we can surmise, one, from the literature, and two, is that the specific complications that are oftentimes reduced with laparoscopy and minimally invasive surgery certainly relate to wound infection and wound problems for sure," Dr. Fields commented. "So I think if we can do anything to achieve the same oncologic goals and reduce the morbidity of an operation, and improve the ability of patients to get on adjuvant therapy, that’s going to be critical. And laparoscopy may be a way to do that in gastric cancer. It may be more challenging in some of the bulkier, more advanced tumors to apply it globally, but I think it certainly holds promise for that exact point."
Overall, 60% of patients without complications received adjuvant therapy, compared with 48% of patients with complications (P = .001).
In multivariate analyses conducted after a median follow-up of 35 months, patients who experienced postoperative complications still had shorter median survival (25 vs. 45 months) and were more likely to die (hazard ratio, 1.6; P = .004).
Other significant risk factors were receipt of neoadjuvant therapy, perineural invasion, and stage III or IV disease.
Dr. Fields disclosed no relevant conflicts of interest.
AT THE GASTROINTESTINAL CANCERS SYMPOSIUM
Major finding: Patients experiencing postoperative complications were more likely to die (HR, 1.6) and less likely to receive adjuvant therapy (48% vs. 60%).
Data source: A retrospective cohort study of 850 patients who underwent curative resection of gastric or gastroesophageal junction adenocarcinoma by abdominal approach
Disclosures: Dr. Fields disclosed no relevant conflicts of interest.
Testing now is critical to ICD-10 readiness
Still not prepared for the switch over to ICD-10? Experts say there’s still time to catch up before the Oct. 1 compliance date.
In an ideal world, physicians, their coders, and office staff would have already fully assessed the cost of transitioning to ICD-10, would have undergone training about how to improve clinical documentation and appropriate use of the new diagnosis codes, and would have internally tested their upgraded software. That would leave more than half a year to complete external testing with health plans to ensure that they get paid in October.
The reality? Few are on track to meet those milestones on time.
"Everybody is behind, not just practices," said Robert Tennant, senior policy adviser at the Medical Group Management Association (MGMA). For a practice to be ready for ICD-10, the "key trading partners have to be ready and our surveys are indicating that they are not," he said.
Those partners include practice management software vendors, electronic health record (EHR) vendors, clearinghouses, and private and public payers.
So does that mean another ICD-10 delay is likely? The Centers for Medicare and Medicaid Services says no.
Part of the reason may be that health plans, which are investing money in upgrading their own systems, are pushing the agency to move forward on time. They are signaling to the government that they don’t want another delay, Mr. Tennant said.
The MGMA is advising its members to prepare for an Oct. 1 launch of ICD-10. But Mr. Tennant said he’s not entirely convinced that the CMS will stick to the date if much of the health care industry is unprepared to make the switch.
"Claims have to be paid," he said. "The system cannot grind to a halt because practices that aren’t paid can’t see patients."
Start with training
Assuming that most physician offices have assessed which parts of their practice management and EHR systems need to be upgraded, and have determined the cost for upgrades and training, it’s time to get familiar with the new diagnosis coding system.
Coders and billers will need the most training on the new coding methodology, but doctors still need to get familiar with the level of documentation that’s need for their most frequently used codes. In general, the new system calls for great specificity, though it’s not an absolute rule.
For instance, the classification for asthma has changed from ICD-9 to ICD-10. Physicians will need to provide more specific documentation about the severity level (moderately persistent, severely persistent, etc.) for their coders to select the appropriate ICD-10 code, according to Kathryn DeVault, a coding expert at the American Health Information Management Association (AHIMA).
"The good news is that as different as ICD-10 and ICD-9 are, they are similar," Ms. DeVault said. "If there’s a familiarity or comfort level working with ICD-9, it’s a natural transition to ICD-10."
While there are some significant changes, especially related to orthopedic codes, for many subspecialties the differences will be minimal, she said.
Ms. DeVault recommended having the practice manager or lead coder identify the top 20 diagnosis codes for every physician in the practice and build some education around those frequently used codes.
She cautioned doctors not to skimp on the time and money needed to thoroughly train themselves and their staffs. "The key here is to do it right and do it right the first time," she said.
Check the books
Physicians and their staff also need to evaluate their current cash flow and revenue cycle, including the age of account balances, billing lag time, and other issues that may result in delayed or denied claims, said Asia Blunt, practice management strategist at the American Academy of Family Physicians. Correct those problems now, she said, then reevaluate between April and August.
Experts at the AAFP are recommending that physicians put aside a cash reserve, if possible, to cover expenses during the first 3 months of the transition in case large numbers of claims are denied. (See below for more tips on planning for the worst.)
Testing with vendors, payers
Internal and external testing is also key. Before Oct. 1, practices should have completed end-to-end testing of their upgraded systems, ensuring that everything works smoothly from the time they code a claim to when they receive payment from the health insurer.
Practices can begin internal testing as soon as they have upgraded their software. But external testing will depend on when clearinghouses and health plans are ready.
The CMS will provide the first testing opportunity March 3-7. The agency will hold a national ICD-10 testing week allowing practices and clearinghouses to submit claims using the new coding system. Practices will receive an acknowledgement that the claims were either accepted or rejected by the system. Practices must register in advance through their local Medicare Administrative Contractor (MAC) website to test. Find your local MAC here.
But this type of front-end testing is only a first step, Mr. Tennant said. Front-end testing determines whether the claim contains an ICD-10 code and if it is in the right place and the right format. But practices will need to conduct further testing with payers to determine if the code they used is appropriate and whether they will get paid.
For instance, when submitting a claim for a sprained ankle under ICD-10, the coder might specify right or left ankle, or leave it as unspecified. Depending on the health insurer’s policy around the code, the insurer could pay the claim, reject it, or hold or "pend" it while seeking additional information. The complicating factor, Mr. Tennant said, is that each health insurer has different coding policies and those policies have yet to be released for ICD-10.
"It’s very frustrating for everybody," Mr. Tennant said.
To minimize the impact, Mr. Tennant recommended identifying the payers responsible for the majority of your claims. Keep in contact with them about the release of their payment policies and testing schedules, he said.
"Be aggressive in your outreach to those plans," he said.
Contingency plans
Just in case a worst-case scenario develops, Mr. Tennant offered the advice on ICD-10 contingency plans:
• Research back-up options for practice management systems and clearinghouses. If the vendors aren’t providing a clear answer on when they will be ready to offer upgrades and testing, start researching alternatives. Ask colleagues if they have vendors that are prepared for the transition.
• Don’t rely on one coder. Train more than one staff member on how to use the new coding system. That way, if the chief coder leaves 3 weeks before the compliance date, someone else can step in.
• Limit vacations around the Oct. 1 compliance date. This is not a time to operate short staffed.
• Don’t wait around for health plans to start ICD-10 testing. Start with context testing. Take a subset of high-dollar, high-volume ICD-9 claims that have already been paid by the health plan and practice coding them in ICD-10. Similarly, begin to code claims in parallel in both ICD-9 and ICD-10 and move them through your internal workflow. In both of these testing approaches, check if the documentation provided is sufficient to identify the best ICD-10 code. If not, it’s time for more training.
• Ensure you have enough cash to operate in case claims are rejected or delayed. Setting aside cash reserves is a good move. Consider postponing major capital investments for a few months before and after Oct. 1. Obtaining a line of credit to cover a few months of operating expenses is another option.
• Submit as many of claims as possible with ICD-9 codes before Oct. 1.
Free ICD-10 resources
• ICD-10 guide with checklists and timelines (CMS).
• Sample letter to gauge vendors’ ICD-10 readiness (AHIMA).
• Cost calculator and ICD-10 timeline (AAFP).
• Twelve step transition plan, white papers, and practice tool (AMA)
On Twitter @maryellenny
Still not prepared for the switch over to ICD-10? Experts say there’s still time to catch up before the Oct. 1 compliance date.
In an ideal world, physicians, their coders, and office staff would have already fully assessed the cost of transitioning to ICD-10, would have undergone training about how to improve clinical documentation and appropriate use of the new diagnosis codes, and would have internally tested their upgraded software. That would leave more than half a year to complete external testing with health plans to ensure that they get paid in October.
The reality? Few are on track to meet those milestones on time.
"Everybody is behind, not just practices," said Robert Tennant, senior policy adviser at the Medical Group Management Association (MGMA). For a practice to be ready for ICD-10, the "key trading partners have to be ready and our surveys are indicating that they are not," he said.
Those partners include practice management software vendors, electronic health record (EHR) vendors, clearinghouses, and private and public payers.
So does that mean another ICD-10 delay is likely? The Centers for Medicare and Medicaid Services says no.
Part of the reason may be that health plans, which are investing money in upgrading their own systems, are pushing the agency to move forward on time. They are signaling to the government that they don’t want another delay, Mr. Tennant said.
The MGMA is advising its members to prepare for an Oct. 1 launch of ICD-10. But Mr. Tennant said he’s not entirely convinced that the CMS will stick to the date if much of the health care industry is unprepared to make the switch.
"Claims have to be paid," he said. "The system cannot grind to a halt because practices that aren’t paid can’t see patients."
Start with training
Assuming that most physician offices have assessed which parts of their practice management and EHR systems need to be upgraded, and have determined the cost for upgrades and training, it’s time to get familiar with the new diagnosis coding system.
Coders and billers will need the most training on the new coding methodology, but doctors still need to get familiar with the level of documentation that’s need for their most frequently used codes. In general, the new system calls for great specificity, though it’s not an absolute rule.
For instance, the classification for asthma has changed from ICD-9 to ICD-10. Physicians will need to provide more specific documentation about the severity level (moderately persistent, severely persistent, etc.) for their coders to select the appropriate ICD-10 code, according to Kathryn DeVault, a coding expert at the American Health Information Management Association (AHIMA).
"The good news is that as different as ICD-10 and ICD-9 are, they are similar," Ms. DeVault said. "If there’s a familiarity or comfort level working with ICD-9, it’s a natural transition to ICD-10."
While there are some significant changes, especially related to orthopedic codes, for many subspecialties the differences will be minimal, she said.
Ms. DeVault recommended having the practice manager or lead coder identify the top 20 diagnosis codes for every physician in the practice and build some education around those frequently used codes.
She cautioned doctors not to skimp on the time and money needed to thoroughly train themselves and their staffs. "The key here is to do it right and do it right the first time," she said.
Check the books
Physicians and their staff also need to evaluate their current cash flow and revenue cycle, including the age of account balances, billing lag time, and other issues that may result in delayed or denied claims, said Asia Blunt, practice management strategist at the American Academy of Family Physicians. Correct those problems now, she said, then reevaluate between April and August.
Experts at the AAFP are recommending that physicians put aside a cash reserve, if possible, to cover expenses during the first 3 months of the transition in case large numbers of claims are denied. (See below for more tips on planning for the worst.)
Testing with vendors, payers
Internal and external testing is also key. Before Oct. 1, practices should have completed end-to-end testing of their upgraded systems, ensuring that everything works smoothly from the time they code a claim to when they receive payment from the health insurer.
Practices can begin internal testing as soon as they have upgraded their software. But external testing will depend on when clearinghouses and health plans are ready.
The CMS will provide the first testing opportunity March 3-7. The agency will hold a national ICD-10 testing week allowing practices and clearinghouses to submit claims using the new coding system. Practices will receive an acknowledgement that the claims were either accepted or rejected by the system. Practices must register in advance through their local Medicare Administrative Contractor (MAC) website to test. Find your local MAC here.
But this type of front-end testing is only a first step, Mr. Tennant said. Front-end testing determines whether the claim contains an ICD-10 code and if it is in the right place and the right format. But practices will need to conduct further testing with payers to determine if the code they used is appropriate and whether they will get paid.
For instance, when submitting a claim for a sprained ankle under ICD-10, the coder might specify right or left ankle, or leave it as unspecified. Depending on the health insurer’s policy around the code, the insurer could pay the claim, reject it, or hold or "pend" it while seeking additional information. The complicating factor, Mr. Tennant said, is that each health insurer has different coding policies and those policies have yet to be released for ICD-10.
"It’s very frustrating for everybody," Mr. Tennant said.
To minimize the impact, Mr. Tennant recommended identifying the payers responsible for the majority of your claims. Keep in contact with them about the release of their payment policies and testing schedules, he said.
"Be aggressive in your outreach to those plans," he said.
Contingency plans
Just in case a worst-case scenario develops, Mr. Tennant offered the advice on ICD-10 contingency plans:
• Research back-up options for practice management systems and clearinghouses. If the vendors aren’t providing a clear answer on when they will be ready to offer upgrades and testing, start researching alternatives. Ask colleagues if they have vendors that are prepared for the transition.
• Don’t rely on one coder. Train more than one staff member on how to use the new coding system. That way, if the chief coder leaves 3 weeks before the compliance date, someone else can step in.
• Limit vacations around the Oct. 1 compliance date. This is not a time to operate short staffed.
• Don’t wait around for health plans to start ICD-10 testing. Start with context testing. Take a subset of high-dollar, high-volume ICD-9 claims that have already been paid by the health plan and practice coding them in ICD-10. Similarly, begin to code claims in parallel in both ICD-9 and ICD-10 and move them through your internal workflow. In both of these testing approaches, check if the documentation provided is sufficient to identify the best ICD-10 code. If not, it’s time for more training.
• Ensure you have enough cash to operate in case claims are rejected or delayed. Setting aside cash reserves is a good move. Consider postponing major capital investments for a few months before and after Oct. 1. Obtaining a line of credit to cover a few months of operating expenses is another option.
• Submit as many of claims as possible with ICD-9 codes before Oct. 1.
Free ICD-10 resources
• ICD-10 guide with checklists and timelines (CMS).
• Sample letter to gauge vendors’ ICD-10 readiness (AHIMA).
• Cost calculator and ICD-10 timeline (AAFP).
• Twelve step transition plan, white papers, and practice tool (AMA)
On Twitter @maryellenny
Still not prepared for the switch over to ICD-10? Experts say there’s still time to catch up before the Oct. 1 compliance date.
In an ideal world, physicians, their coders, and office staff would have already fully assessed the cost of transitioning to ICD-10, would have undergone training about how to improve clinical documentation and appropriate use of the new diagnosis codes, and would have internally tested their upgraded software. That would leave more than half a year to complete external testing with health plans to ensure that they get paid in October.
The reality? Few are on track to meet those milestones on time.
"Everybody is behind, not just practices," said Robert Tennant, senior policy adviser at the Medical Group Management Association (MGMA). For a practice to be ready for ICD-10, the "key trading partners have to be ready and our surveys are indicating that they are not," he said.
Those partners include practice management software vendors, electronic health record (EHR) vendors, clearinghouses, and private and public payers.
So does that mean another ICD-10 delay is likely? The Centers for Medicare and Medicaid Services says no.
Part of the reason may be that health plans, which are investing money in upgrading their own systems, are pushing the agency to move forward on time. They are signaling to the government that they don’t want another delay, Mr. Tennant said.
The MGMA is advising its members to prepare for an Oct. 1 launch of ICD-10. But Mr. Tennant said he’s not entirely convinced that the CMS will stick to the date if much of the health care industry is unprepared to make the switch.
"Claims have to be paid," he said. "The system cannot grind to a halt because practices that aren’t paid can’t see patients."
Start with training
Assuming that most physician offices have assessed which parts of their practice management and EHR systems need to be upgraded, and have determined the cost for upgrades and training, it’s time to get familiar with the new diagnosis coding system.
Coders and billers will need the most training on the new coding methodology, but doctors still need to get familiar with the level of documentation that’s need for their most frequently used codes. In general, the new system calls for great specificity, though it’s not an absolute rule.
For instance, the classification for asthma has changed from ICD-9 to ICD-10. Physicians will need to provide more specific documentation about the severity level (moderately persistent, severely persistent, etc.) for their coders to select the appropriate ICD-10 code, according to Kathryn DeVault, a coding expert at the American Health Information Management Association (AHIMA).
"The good news is that as different as ICD-10 and ICD-9 are, they are similar," Ms. DeVault said. "If there’s a familiarity or comfort level working with ICD-9, it’s a natural transition to ICD-10."
While there are some significant changes, especially related to orthopedic codes, for many subspecialties the differences will be minimal, she said.
Ms. DeVault recommended having the practice manager or lead coder identify the top 20 diagnosis codes for every physician in the practice and build some education around those frequently used codes.
She cautioned doctors not to skimp on the time and money needed to thoroughly train themselves and their staffs. "The key here is to do it right and do it right the first time," she said.
Check the books
Physicians and their staff also need to evaluate their current cash flow and revenue cycle, including the age of account balances, billing lag time, and other issues that may result in delayed or denied claims, said Asia Blunt, practice management strategist at the American Academy of Family Physicians. Correct those problems now, she said, then reevaluate between April and August.
Experts at the AAFP are recommending that physicians put aside a cash reserve, if possible, to cover expenses during the first 3 months of the transition in case large numbers of claims are denied. (See below for more tips on planning for the worst.)
Testing with vendors, payers
Internal and external testing is also key. Before Oct. 1, practices should have completed end-to-end testing of their upgraded systems, ensuring that everything works smoothly from the time they code a claim to when they receive payment from the health insurer.
Practices can begin internal testing as soon as they have upgraded their software. But external testing will depend on when clearinghouses and health plans are ready.
The CMS will provide the first testing opportunity March 3-7. The agency will hold a national ICD-10 testing week allowing practices and clearinghouses to submit claims using the new coding system. Practices will receive an acknowledgement that the claims were either accepted or rejected by the system. Practices must register in advance through their local Medicare Administrative Contractor (MAC) website to test. Find your local MAC here.
But this type of front-end testing is only a first step, Mr. Tennant said. Front-end testing determines whether the claim contains an ICD-10 code and if it is in the right place and the right format. But practices will need to conduct further testing with payers to determine if the code they used is appropriate and whether they will get paid.
For instance, when submitting a claim for a sprained ankle under ICD-10, the coder might specify right or left ankle, or leave it as unspecified. Depending on the health insurer’s policy around the code, the insurer could pay the claim, reject it, or hold or "pend" it while seeking additional information. The complicating factor, Mr. Tennant said, is that each health insurer has different coding policies and those policies have yet to be released for ICD-10.
"It’s very frustrating for everybody," Mr. Tennant said.
To minimize the impact, Mr. Tennant recommended identifying the payers responsible for the majority of your claims. Keep in contact with them about the release of their payment policies and testing schedules, he said.
"Be aggressive in your outreach to those plans," he said.
Contingency plans
Just in case a worst-case scenario develops, Mr. Tennant offered the advice on ICD-10 contingency plans:
• Research back-up options for practice management systems and clearinghouses. If the vendors aren’t providing a clear answer on when they will be ready to offer upgrades and testing, start researching alternatives. Ask colleagues if they have vendors that are prepared for the transition.
• Don’t rely on one coder. Train more than one staff member on how to use the new coding system. That way, if the chief coder leaves 3 weeks before the compliance date, someone else can step in.
• Limit vacations around the Oct. 1 compliance date. This is not a time to operate short staffed.
• Don’t wait around for health plans to start ICD-10 testing. Start with context testing. Take a subset of high-dollar, high-volume ICD-9 claims that have already been paid by the health plan and practice coding them in ICD-10. Similarly, begin to code claims in parallel in both ICD-9 and ICD-10 and move them through your internal workflow. In both of these testing approaches, check if the documentation provided is sufficient to identify the best ICD-10 code. If not, it’s time for more training.
• Ensure you have enough cash to operate in case claims are rejected or delayed. Setting aside cash reserves is a good move. Consider postponing major capital investments for a few months before and after Oct. 1. Obtaining a line of credit to cover a few months of operating expenses is another option.
• Submit as many of claims as possible with ICD-9 codes before Oct. 1.
Free ICD-10 resources
• ICD-10 guide with checklists and timelines (CMS).
• Sample letter to gauge vendors’ ICD-10 readiness (AHIMA).
• Cost calculator and ICD-10 timeline (AAFP).
• Twelve step transition plan, white papers, and practice tool (AMA)
On Twitter @maryellenny
SGR fix could cost as much as $150 billion
Current proposals to repeal the Medicare Sustainable Growth Rate formula and replace it with a new payment system could cost anywhere from $121 billion to $150 billion over the next decade, according to new estimates from the Congressional Budget Office.
Legislation (H.R. 2810) approved by the House Ways and Means Committee in December is the least expensive option. It would cost about $121 billion over 10 years, according to the CBO projection. That bill includes 2 years of 0.5% pay updates for physicians and begins to partially tie payment to performance.
A more expensive option (S. 1871), approved by the Senate Finance Committee in December, would cost $150.4 billion through 2023, the CBO estimated. The Senate version would freeze physician payments for the next decade, but would allow physicians to earn more by participating in alternative payment models or another incentive program that measures quality of care and resource use.
The additional cost for this bill comes from extending some Medicare and Medicaid programs; the physician payment portion alone would cost about $111.5 billion over 10 years, CBO predicted.
The price tag will have a big impact on whether Congress can pass an SGR repeal bill this year. The Medicare fee cut for 2014 – which was to kick in Jan. 1 – was replaced by a 0.5% physician pay increase through March 31. But the cut will take effect on April 1 if Congress does not enact either another temporary SGR fix or a permanent repeal of the formula.
While there has been widespread bipartisan support for SGR repeal, there has yet to be any serious discussion of how lawmakers would pay for the fix. Physician groups, which have been deeply involved in the policy discussions surrounding SGR repeal, have also remained silent on how to pay for it.
On Twitter @maryellenny
Current proposals to repeal the Medicare Sustainable Growth Rate formula and replace it with a new payment system could cost anywhere from $121 billion to $150 billion over the next decade, according to new estimates from the Congressional Budget Office.
Legislation (H.R. 2810) approved by the House Ways and Means Committee in December is the least expensive option. It would cost about $121 billion over 10 years, according to the CBO projection. That bill includes 2 years of 0.5% pay updates for physicians and begins to partially tie payment to performance.
A more expensive option (S. 1871), approved by the Senate Finance Committee in December, would cost $150.4 billion through 2023, the CBO estimated. The Senate version would freeze physician payments for the next decade, but would allow physicians to earn more by participating in alternative payment models or another incentive program that measures quality of care and resource use.
The additional cost for this bill comes from extending some Medicare and Medicaid programs; the physician payment portion alone would cost about $111.5 billion over 10 years, CBO predicted.
The price tag will have a big impact on whether Congress can pass an SGR repeal bill this year. The Medicare fee cut for 2014 – which was to kick in Jan. 1 – was replaced by a 0.5% physician pay increase through March 31. But the cut will take effect on April 1 if Congress does not enact either another temporary SGR fix or a permanent repeal of the formula.
While there has been widespread bipartisan support for SGR repeal, there has yet to be any serious discussion of how lawmakers would pay for the fix. Physician groups, which have been deeply involved in the policy discussions surrounding SGR repeal, have also remained silent on how to pay for it.
On Twitter @maryellenny
Current proposals to repeal the Medicare Sustainable Growth Rate formula and replace it with a new payment system could cost anywhere from $121 billion to $150 billion over the next decade, according to new estimates from the Congressional Budget Office.
Legislation (H.R. 2810) approved by the House Ways and Means Committee in December is the least expensive option. It would cost about $121 billion over 10 years, according to the CBO projection. That bill includes 2 years of 0.5% pay updates for physicians and begins to partially tie payment to performance.
A more expensive option (S. 1871), approved by the Senate Finance Committee in December, would cost $150.4 billion through 2023, the CBO estimated. The Senate version would freeze physician payments for the next decade, but would allow physicians to earn more by participating in alternative payment models or another incentive program that measures quality of care and resource use.
The additional cost for this bill comes from extending some Medicare and Medicaid programs; the physician payment portion alone would cost about $111.5 billion over 10 years, CBO predicted.
The price tag will have a big impact on whether Congress can pass an SGR repeal bill this year. The Medicare fee cut for 2014 – which was to kick in Jan. 1 – was replaced by a 0.5% physician pay increase through March 31. But the cut will take effect on April 1 if Congress does not enact either another temporary SGR fix or a permanent repeal of the formula.
While there has been widespread bipartisan support for SGR repeal, there has yet to be any serious discussion of how lawmakers would pay for the fix. Physician groups, which have been deeply involved in the policy discussions surrounding SGR repeal, have also remained silent on how to pay for it.
On Twitter @maryellenny