User login
Official Newspaper of the American College of Surgeons
Hypoalbuminemia linked to increased surgical risks in obese patients
BALTIMORE – Hypoalbuminemia was identified as a significant risk factor for increased mortality and morbidity in obese patients undergoing elective general surgery, in a large study of patients from the ACS National Surgical Quality Improvement Program (NSQIP) database, Dr. Zachary C. Dietch reported at the annual meeting of the Surgical Infection Society.
The results suggest that surgeons may need to be more careful in evaluating protein deficiency in obese patients before surgery, said Dr. Dietch, a surgical resident at the University of Virginia, Charlottesville.
Protein-calorie deficiency is a well-known risk factor for complications, including infections and other surgical complications, but the risks of protein deficiency in different weight classes have not been well described. And while serum albumin is commonly used as an index for nutritional status and is known to correlate with adverse surgical outcomes, its use "as an index for nutrition status remains controversial," he noted.
But based on the results, "We feel that these risks likely reflect protein deficiency, and we feel that serum albumin appropriately reflects protein status in this population," he commented.
To evaluate the association of preoperative serum albumin and surgical complications by weight class, Dr. Dietch and his associates evaluated 240,000 general elective surgery patients, from the 2011 NSQIP database who had an elective procedure. After excluding certain groups of patients including those with systemic infections, cirrhosis, as well as those who were pregnant and those who had no preoperative albumin results available, they were left with about 86,000 patients.
Of these patients, 2,088 (about 2.4%) had a low serum albumin (below 3.0 g/dL); these patients tended to be older and tended to be in lower weight categories. Of those with hypoalbuminemia, 6.2% had a body mass index of 40 kg/m2 and greater and almost 22% had a BMI between 30-39 (a BMI of 30 and greater falls in the obese category), and they had higher rates of comorbidities.
After controlling for factors that included comorbidities, surgical wound classification, operation type and complexity, the interaction of hypoalbuminemia and BMI conferred a statistically significant increase in the risk of mortality among those with a BMI of 40 and above, with an odds ratio of 18.98; and among those with a BMI between 30 and 39, with an odds ratio of 3.14 – when compared with patients in lower weight categories, who had low serum albumin, Dr. Dietch said.
Among those with a BMI of 40 and greater who had hypoalbuminemia, the risk of all complications was significantly increased (OR, 3.13) and the risk of all infectious complications was significantly increased (2.59). The risk of all complications was not significantly increased among those with a BMI of 30-39.
"The impact of protein deficiency on outcomes among patients may not be appreciated by surgeons," he concluded. This was a hypothesis-generating study and future studies "should prospectively investigate preoperative nutritional interventions in at-risk patients regardless of BMI," he added, noting that the next step would be a pilot study.
The limitations of the study included the possibility that the NSQIP data did not capture confounding disease states, and no causal relationship between protein status and surgical complications could be established because of the observational nature of the study, he noted.
In response to an audience member’s comment that a low albumin can be a reflection of a proinflammatory state, Dr. Dietch said that he and his coinvestigators recognized this and attempted to eliminate patients with proinflammatory states, such as those with systemic infections and those with systemic inflammatory response syndrome.
The study was funded by a National Institutes of Health training grant. Dr. Dietch had no disclosures
BALTIMORE – Hypoalbuminemia was identified as a significant risk factor for increased mortality and morbidity in obese patients undergoing elective general surgery, in a large study of patients from the ACS National Surgical Quality Improvement Program (NSQIP) database, Dr. Zachary C. Dietch reported at the annual meeting of the Surgical Infection Society.
The results suggest that surgeons may need to be more careful in evaluating protein deficiency in obese patients before surgery, said Dr. Dietch, a surgical resident at the University of Virginia, Charlottesville.
Protein-calorie deficiency is a well-known risk factor for complications, including infections and other surgical complications, but the risks of protein deficiency in different weight classes have not been well described. And while serum albumin is commonly used as an index for nutritional status and is known to correlate with adverse surgical outcomes, its use "as an index for nutrition status remains controversial," he noted.
But based on the results, "We feel that these risks likely reflect protein deficiency, and we feel that serum albumin appropriately reflects protein status in this population," he commented.
To evaluate the association of preoperative serum albumin and surgical complications by weight class, Dr. Dietch and his associates evaluated 240,000 general elective surgery patients, from the 2011 NSQIP database who had an elective procedure. After excluding certain groups of patients including those with systemic infections, cirrhosis, as well as those who were pregnant and those who had no preoperative albumin results available, they were left with about 86,000 patients.
Of these patients, 2,088 (about 2.4%) had a low serum albumin (below 3.0 g/dL); these patients tended to be older and tended to be in lower weight categories. Of those with hypoalbuminemia, 6.2% had a body mass index of 40 kg/m2 and greater and almost 22% had a BMI between 30-39 (a BMI of 30 and greater falls in the obese category), and they had higher rates of comorbidities.
After controlling for factors that included comorbidities, surgical wound classification, operation type and complexity, the interaction of hypoalbuminemia and BMI conferred a statistically significant increase in the risk of mortality among those with a BMI of 40 and above, with an odds ratio of 18.98; and among those with a BMI between 30 and 39, with an odds ratio of 3.14 – when compared with patients in lower weight categories, who had low serum albumin, Dr. Dietch said.
Among those with a BMI of 40 and greater who had hypoalbuminemia, the risk of all complications was significantly increased (OR, 3.13) and the risk of all infectious complications was significantly increased (2.59). The risk of all complications was not significantly increased among those with a BMI of 30-39.
"The impact of protein deficiency on outcomes among patients may not be appreciated by surgeons," he concluded. This was a hypothesis-generating study and future studies "should prospectively investigate preoperative nutritional interventions in at-risk patients regardless of BMI," he added, noting that the next step would be a pilot study.
The limitations of the study included the possibility that the NSQIP data did not capture confounding disease states, and no causal relationship between protein status and surgical complications could be established because of the observational nature of the study, he noted.
In response to an audience member’s comment that a low albumin can be a reflection of a proinflammatory state, Dr. Dietch said that he and his coinvestigators recognized this and attempted to eliminate patients with proinflammatory states, such as those with systemic infections and those with systemic inflammatory response syndrome.
The study was funded by a National Institutes of Health training grant. Dr. Dietch had no disclosures
BALTIMORE – Hypoalbuminemia was identified as a significant risk factor for increased mortality and morbidity in obese patients undergoing elective general surgery, in a large study of patients from the ACS National Surgical Quality Improvement Program (NSQIP) database, Dr. Zachary C. Dietch reported at the annual meeting of the Surgical Infection Society.
The results suggest that surgeons may need to be more careful in evaluating protein deficiency in obese patients before surgery, said Dr. Dietch, a surgical resident at the University of Virginia, Charlottesville.
Protein-calorie deficiency is a well-known risk factor for complications, including infections and other surgical complications, but the risks of protein deficiency in different weight classes have not been well described. And while serum albumin is commonly used as an index for nutritional status and is known to correlate with adverse surgical outcomes, its use "as an index for nutrition status remains controversial," he noted.
But based on the results, "We feel that these risks likely reflect protein deficiency, and we feel that serum albumin appropriately reflects protein status in this population," he commented.
To evaluate the association of preoperative serum albumin and surgical complications by weight class, Dr. Dietch and his associates evaluated 240,000 general elective surgery patients, from the 2011 NSQIP database who had an elective procedure. After excluding certain groups of patients including those with systemic infections, cirrhosis, as well as those who were pregnant and those who had no preoperative albumin results available, they were left with about 86,000 patients.
Of these patients, 2,088 (about 2.4%) had a low serum albumin (below 3.0 g/dL); these patients tended to be older and tended to be in lower weight categories. Of those with hypoalbuminemia, 6.2% had a body mass index of 40 kg/m2 and greater and almost 22% had a BMI between 30-39 (a BMI of 30 and greater falls in the obese category), and they had higher rates of comorbidities.
After controlling for factors that included comorbidities, surgical wound classification, operation type and complexity, the interaction of hypoalbuminemia and BMI conferred a statistically significant increase in the risk of mortality among those with a BMI of 40 and above, with an odds ratio of 18.98; and among those with a BMI between 30 and 39, with an odds ratio of 3.14 – when compared with patients in lower weight categories, who had low serum albumin, Dr. Dietch said.
Among those with a BMI of 40 and greater who had hypoalbuminemia, the risk of all complications was significantly increased (OR, 3.13) and the risk of all infectious complications was significantly increased (2.59). The risk of all complications was not significantly increased among those with a BMI of 30-39.
"The impact of protein deficiency on outcomes among patients may not be appreciated by surgeons," he concluded. This was a hypothesis-generating study and future studies "should prospectively investigate preoperative nutritional interventions in at-risk patients regardless of BMI," he added, noting that the next step would be a pilot study.
The limitations of the study included the possibility that the NSQIP data did not capture confounding disease states, and no causal relationship between protein status and surgical complications could be established because of the observational nature of the study, he noted.
In response to an audience member’s comment that a low albumin can be a reflection of a proinflammatory state, Dr. Dietch said that he and his coinvestigators recognized this and attempted to eliminate patients with proinflammatory states, such as those with systemic infections and those with systemic inflammatory response syndrome.
The study was funded by a National Institutes of Health training grant. Dr. Dietch had no disclosures
AT THE SIS ANNUAL MEETING
Key clinical point: Carefully evaluate protein deficiency in obese patients before surgery.
Major finding: In hypoalbuminemic patients with a BMI of 40 and greater, the risks of complications or death after general elective surgery were increased (OR 3.13 and OR 18.98, respectively) vs. lower-weight patients
Data source: A study of approximately 86,000 general surgery patients enrolled in the American College of Surgeons NSQIP in 2011.
Disclosures: The study was funded by a National Institutes of Health training grant. Dr. Dietch had no disclosures.
Big Data and the art of medicine
Life is short, and the Art long to learn.
–Chaucer
If you are anything like us, you still hold firmly to the notion that medicine, at its core, is an art. Sure, medicine is informed by cutting-edge sciences, such as biochemistry and molecular biology. But one can’t capture the nuances of the patient interaction by studying the Krebs cycle, nor define the motivating forces driving physicians by looking through a microscope. On the contrary, physicians are artists, much like musicians, sculptors, or dancers. And, like any of these artists, it would seem that a physician’s craft should improve through "practice," not by studying data or using a computer. So how do we reconcile this in the era of "Big Data"? How can the "ones and zeros" living deep in the "guts" of our electronic health records (EHRs) promise to revolutionize an art that has relied solely on the judgment – or gut sense – of physicians for centuries? Here we will attempt to answer these questions and ponder whether or not we really can improve the art of medicine with the help of data.
It’s more than the ‘ones and zeros’
With the right information and the proper tools to analyze it, it is possible to conceive of an improvement in our ability to care for patients. Take, for example, the prevention of malignancies. Currently, early detection of cancer relies heavily on a physician’s knowledge of – and compliance with – current cancer screening guidelines. Success also depends on a patient’s willingness to come in for annual visits to receive the instruction. If the patient doesn’t show up for a physical, or if the provider neglects to mention the need for a colonoscopy when the patient does appear, the test may go unordered (much to the patient’s relief, perhaps!). But the right tools and analytics won’t let that happen. Instead, the technology will identify the highest-risk populations with ever-improving accuracy and notify both physician and patient of the need for action. With enough data, we may even be able to make observations in trends of cancer inheritance never before possible and predict cancer long before it might be detected by conventional screening protocols.
It pays to care about the data
Physicians may not realize it, but data can have a significant financial advantage, by improving reimbursement and decreasing the overall cost of care. This can be achieved in two ways. The first way is by using the data to paint a more accurate picture of patient complexity. Medicare assigns a risk-adjusted score to patient cohorts based on the severity of their diagnoses and reimburses Medicare Advantage plans based on that score: the higher the score, the better the reimbursement. Occasionally, those additional dollars are passed along to the treating physicians. But all too often physicians do not use ICD-9 codes properly on their claims, making their patients appear less complicated and thereby receiving lower reimbursement. Through emerging data collection tools, improper coding can be identified and corrected, and missed opportunities can be discovered early enough to capture additional funds.
The second way these tools can be used leads to direct benefit to the health care system in general, through improved medical cost management. By interfacing with insurers and analyzing claims, the software can identify patients who are high utilizers and can show trends in medical costs across a community or health system. This allows providers to target certain patients or disease states around which to build cost-containment strategies and create win-win scenarios that decrease hospital readmissions, limit cost, and improve patient quality of life.
We recently learned of a great example of this. Using a population management data tool, a community health system was able to identify a geographic area in their region with a large uninsured population. This group had a disproportionately high utilization of emergency medical services and very low care quality markers (such as diabetes control, vaccination rates, etc.). Through targeted outreach based on these data, the system was able to direct individuals into low-cost, high-quality primary care sites and reduce emergency service utilization to levels below the surrounding neighborhoods. Simultaneously, the health of the community improved through better disease management and care coordination. Finally, data analytics tools uncovered additional opportunities for savings by identifying expensive brand-name drug prescriptions that could be replaced with generic drug alternatives.
A reluctant revolution
As we have lamented on previous occasions, the adoption of health care information technology is often driven by artificial external forces, such as stimulus programs or regulatory requirements. The government has routinely used incentive payments and reimbursement adjustments in order to spur widespread acceptance of EHRs. Most infamously, the Meaningful Use Regulations program has become the poster child for government involvement in direct patient care. Through the use of annual payments over a 5-year period (combined with the threat of penalties for lack of compliance), Meaningful Use has almost single-handedly enabled the Big Data revolution in health care by requiring physicians to purchase electronic health records systems and use them for population management. While seemingly a good thing, most physicians would hardly regard these systems as "meaningful." In fact, many question if there is any value in having an electronic record at all.
Whether or not their detractors admit it, EHRs do form the backbone of a new and very powerful information network – one which many believe has the power to revolutionize health care. While we certainly do not view the "data revolution" as the panacea others have claimed it to be, we do recognize that the right tools are emerging to enable physicians to learn from data and implement new, novel, and "disruptive" strategies to improve patient care.
Art is not static; the canvas, the paints, and the viewpoints change over time as experience evolves. Leonardo da Vinci furthered the world’s understanding of perspective. Pablo Picasso led a revolution in modern art. Each was different from his predecessors, and each expressed a human need to understand and portray the world in a manner consistent with his age. The same is true of our age and the art of medicine. The science has changed, as has the viewpoint and perspective from which we provide care. Our ability to record, retrieve, and understand health and disease will never be the same. But the attention to the patient is ever present. The necessity of interpreting the shifting world of health and disease to provide an empathic understanding of each patient’s individual and unique place in the world will never go away. Therein lies the Art.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference Inc., a software company that creates mobile apps.
Life is short, and the Art long to learn.
–Chaucer
If you are anything like us, you still hold firmly to the notion that medicine, at its core, is an art. Sure, medicine is informed by cutting-edge sciences, such as biochemistry and molecular biology. But one can’t capture the nuances of the patient interaction by studying the Krebs cycle, nor define the motivating forces driving physicians by looking through a microscope. On the contrary, physicians are artists, much like musicians, sculptors, or dancers. And, like any of these artists, it would seem that a physician’s craft should improve through "practice," not by studying data or using a computer. So how do we reconcile this in the era of "Big Data"? How can the "ones and zeros" living deep in the "guts" of our electronic health records (EHRs) promise to revolutionize an art that has relied solely on the judgment – or gut sense – of physicians for centuries? Here we will attempt to answer these questions and ponder whether or not we really can improve the art of medicine with the help of data.
It’s more than the ‘ones and zeros’
With the right information and the proper tools to analyze it, it is possible to conceive of an improvement in our ability to care for patients. Take, for example, the prevention of malignancies. Currently, early detection of cancer relies heavily on a physician’s knowledge of – and compliance with – current cancer screening guidelines. Success also depends on a patient’s willingness to come in for annual visits to receive the instruction. If the patient doesn’t show up for a physical, or if the provider neglects to mention the need for a colonoscopy when the patient does appear, the test may go unordered (much to the patient’s relief, perhaps!). But the right tools and analytics won’t let that happen. Instead, the technology will identify the highest-risk populations with ever-improving accuracy and notify both physician and patient of the need for action. With enough data, we may even be able to make observations in trends of cancer inheritance never before possible and predict cancer long before it might be detected by conventional screening protocols.
It pays to care about the data
Physicians may not realize it, but data can have a significant financial advantage, by improving reimbursement and decreasing the overall cost of care. This can be achieved in two ways. The first way is by using the data to paint a more accurate picture of patient complexity. Medicare assigns a risk-adjusted score to patient cohorts based on the severity of their diagnoses and reimburses Medicare Advantage plans based on that score: the higher the score, the better the reimbursement. Occasionally, those additional dollars are passed along to the treating physicians. But all too often physicians do not use ICD-9 codes properly on their claims, making their patients appear less complicated and thereby receiving lower reimbursement. Through emerging data collection tools, improper coding can be identified and corrected, and missed opportunities can be discovered early enough to capture additional funds.
The second way these tools can be used leads to direct benefit to the health care system in general, through improved medical cost management. By interfacing with insurers and analyzing claims, the software can identify patients who are high utilizers and can show trends in medical costs across a community or health system. This allows providers to target certain patients or disease states around which to build cost-containment strategies and create win-win scenarios that decrease hospital readmissions, limit cost, and improve patient quality of life.
We recently learned of a great example of this. Using a population management data tool, a community health system was able to identify a geographic area in their region with a large uninsured population. This group had a disproportionately high utilization of emergency medical services and very low care quality markers (such as diabetes control, vaccination rates, etc.). Through targeted outreach based on these data, the system was able to direct individuals into low-cost, high-quality primary care sites and reduce emergency service utilization to levels below the surrounding neighborhoods. Simultaneously, the health of the community improved through better disease management and care coordination. Finally, data analytics tools uncovered additional opportunities for savings by identifying expensive brand-name drug prescriptions that could be replaced with generic drug alternatives.
A reluctant revolution
As we have lamented on previous occasions, the adoption of health care information technology is often driven by artificial external forces, such as stimulus programs or regulatory requirements. The government has routinely used incentive payments and reimbursement adjustments in order to spur widespread acceptance of EHRs. Most infamously, the Meaningful Use Regulations program has become the poster child for government involvement in direct patient care. Through the use of annual payments over a 5-year period (combined with the threat of penalties for lack of compliance), Meaningful Use has almost single-handedly enabled the Big Data revolution in health care by requiring physicians to purchase electronic health records systems and use them for population management. While seemingly a good thing, most physicians would hardly regard these systems as "meaningful." In fact, many question if there is any value in having an electronic record at all.
Whether or not their detractors admit it, EHRs do form the backbone of a new and very powerful information network – one which many believe has the power to revolutionize health care. While we certainly do not view the "data revolution" as the panacea others have claimed it to be, we do recognize that the right tools are emerging to enable physicians to learn from data and implement new, novel, and "disruptive" strategies to improve patient care.
Art is not static; the canvas, the paints, and the viewpoints change over time as experience evolves. Leonardo da Vinci furthered the world’s understanding of perspective. Pablo Picasso led a revolution in modern art. Each was different from his predecessors, and each expressed a human need to understand and portray the world in a manner consistent with his age. The same is true of our age and the art of medicine. The science has changed, as has the viewpoint and perspective from which we provide care. Our ability to record, retrieve, and understand health and disease will never be the same. But the attention to the patient is ever present. The necessity of interpreting the shifting world of health and disease to provide an empathic understanding of each patient’s individual and unique place in the world will never go away. Therein lies the Art.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference Inc., a software company that creates mobile apps.
Life is short, and the Art long to learn.
–Chaucer
If you are anything like us, you still hold firmly to the notion that medicine, at its core, is an art. Sure, medicine is informed by cutting-edge sciences, such as biochemistry and molecular biology. But one can’t capture the nuances of the patient interaction by studying the Krebs cycle, nor define the motivating forces driving physicians by looking through a microscope. On the contrary, physicians are artists, much like musicians, sculptors, or dancers. And, like any of these artists, it would seem that a physician’s craft should improve through "practice," not by studying data or using a computer. So how do we reconcile this in the era of "Big Data"? How can the "ones and zeros" living deep in the "guts" of our electronic health records (EHRs) promise to revolutionize an art that has relied solely on the judgment – or gut sense – of physicians for centuries? Here we will attempt to answer these questions and ponder whether or not we really can improve the art of medicine with the help of data.
It’s more than the ‘ones and zeros’
With the right information and the proper tools to analyze it, it is possible to conceive of an improvement in our ability to care for patients. Take, for example, the prevention of malignancies. Currently, early detection of cancer relies heavily on a physician’s knowledge of – and compliance with – current cancer screening guidelines. Success also depends on a patient’s willingness to come in for annual visits to receive the instruction. If the patient doesn’t show up for a physical, or if the provider neglects to mention the need for a colonoscopy when the patient does appear, the test may go unordered (much to the patient’s relief, perhaps!). But the right tools and analytics won’t let that happen. Instead, the technology will identify the highest-risk populations with ever-improving accuracy and notify both physician and patient of the need for action. With enough data, we may even be able to make observations in trends of cancer inheritance never before possible and predict cancer long before it might be detected by conventional screening protocols.
It pays to care about the data
Physicians may not realize it, but data can have a significant financial advantage, by improving reimbursement and decreasing the overall cost of care. This can be achieved in two ways. The first way is by using the data to paint a more accurate picture of patient complexity. Medicare assigns a risk-adjusted score to patient cohorts based on the severity of their diagnoses and reimburses Medicare Advantage plans based on that score: the higher the score, the better the reimbursement. Occasionally, those additional dollars are passed along to the treating physicians. But all too often physicians do not use ICD-9 codes properly on their claims, making their patients appear less complicated and thereby receiving lower reimbursement. Through emerging data collection tools, improper coding can be identified and corrected, and missed opportunities can be discovered early enough to capture additional funds.
The second way these tools can be used leads to direct benefit to the health care system in general, through improved medical cost management. By interfacing with insurers and analyzing claims, the software can identify patients who are high utilizers and can show trends in medical costs across a community or health system. This allows providers to target certain patients or disease states around which to build cost-containment strategies and create win-win scenarios that decrease hospital readmissions, limit cost, and improve patient quality of life.
We recently learned of a great example of this. Using a population management data tool, a community health system was able to identify a geographic area in their region with a large uninsured population. This group had a disproportionately high utilization of emergency medical services and very low care quality markers (such as diabetes control, vaccination rates, etc.). Through targeted outreach based on these data, the system was able to direct individuals into low-cost, high-quality primary care sites and reduce emergency service utilization to levels below the surrounding neighborhoods. Simultaneously, the health of the community improved through better disease management and care coordination. Finally, data analytics tools uncovered additional opportunities for savings by identifying expensive brand-name drug prescriptions that could be replaced with generic drug alternatives.
A reluctant revolution
As we have lamented on previous occasions, the adoption of health care information technology is often driven by artificial external forces, such as stimulus programs or regulatory requirements. The government has routinely used incentive payments and reimbursement adjustments in order to spur widespread acceptance of EHRs. Most infamously, the Meaningful Use Regulations program has become the poster child for government involvement in direct patient care. Through the use of annual payments over a 5-year period (combined with the threat of penalties for lack of compliance), Meaningful Use has almost single-handedly enabled the Big Data revolution in health care by requiring physicians to purchase electronic health records systems and use them for population management. While seemingly a good thing, most physicians would hardly regard these systems as "meaningful." In fact, many question if there is any value in having an electronic record at all.
Whether or not their detractors admit it, EHRs do form the backbone of a new and very powerful information network – one which many believe has the power to revolutionize health care. While we certainly do not view the "data revolution" as the panacea others have claimed it to be, we do recognize that the right tools are emerging to enable physicians to learn from data and implement new, novel, and "disruptive" strategies to improve patient care.
Art is not static; the canvas, the paints, and the viewpoints change over time as experience evolves. Leonardo da Vinci furthered the world’s understanding of perspective. Pablo Picasso led a revolution in modern art. Each was different from his predecessors, and each expressed a human need to understand and portray the world in a manner consistent with his age. The same is true of our age and the art of medicine. The science has changed, as has the viewpoint and perspective from which we provide care. Our ability to record, retrieve, and understand health and disease will never be the same. But the attention to the patient is ever present. The necessity of interpreting the shifting world of health and disease to provide an empathic understanding of each patient’s individual and unique place in the world will never go away. Therein lies the Art.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. He is editor in chief of Redi-Reference Inc., a software company that creates mobile apps.
Data support suture vs. staple skin closure after cesarean delivery
CHICAGO – Suture closure of the skin incision after cesarean delivery was associated with significantly improved patient satisfaction, compared with staple closure, according to findings in a prospective, randomized, multicenter study of 746 women.
Suture closure also was associated with improved patient and physician assessments of cosmesis, compared with staple closure, Dr. Jonah Fleisher reported at the annual meeting of the American Congress of Obstetricians and Gynecologists.
The median interquartile range of overall "satisfaction with method of closure" scores on the validated Patient and Observer Scar Assessment Scale (POSAS) differed significantly for 299 suture patients and 307 staple patients for whom the data were available (scores of 10 vs. 9, respectively), as did median "satisfaction with appearance of skin incision" scores (also 10 vs. 9, respectively), said Dr. Fleisher of Geisinger Health System, Danville, Pa.
The cosmetic-specific question was included to help adjust for the multifactorial nature of the overall satisfaction score, which could be affected by the patient’s degree of pain, healing time, need for extra office visits, and frequency of complications, among other factors.
The two measures correlated positively, and both subjective and objective components of the POSAS favored suture closure, he noted.
Study participants were women undergoing cesarean delivery via low-transverse skin incisions at any of three participating centers. After fascia closure, the women were allocated to either the suture (type was surgeon’s choice) or metal staple closure group. Staples were removed between postoperative days 4 and 10.
About 1.3 million cesarean deliveries are performed each year in the United States, Dr. Fleisher said.
"Those scars that are formed as a result are very important to patients, both as far as cosmetic and general satisfaction ... and it turns out they are important to obstetricians, too," he added, noting that data to guide decision making are lacking.
In the current study, the differences between the suture and staple groups were significant, but patients in both groups had high rates of satisfaction.
"Given these considerations, I would suggest that we ought to incorporate wound complications rates into the decision of which method to use," he said.
An article that addresses the wound complication rates in this study is currently in press and scheduled for publication in the American Journal of Obstetrics & Gynecology in June. The data show a 57% lower complication rate with suture closure vs. staple closure, Dr. Fleisher said.
"The bottom line is, for all these reasons, we have moved to recommending suture closure in all transverse C-sections," he said.
As for whether the findings apply to other types of surgical operations, such as abdominal hysterectomy, Dr. Fleisher said there are many changes in pregnancy, including immunologic changes, that don’t necessarily apply to nonobstetric situations.
"There is some literature in the general surgery area about this, and some literature in gynecologic surgery, but given the immunologic changes – I think we’re seeing that even the adhesion data is not necessarily the same in those two contexts. ... I wouldn’t want to generalize from this to nonobstetric indications," he said.
This study was supported by Ethicon. Dr. Fleisher reported having no disclosures.
CHICAGO – Suture closure of the skin incision after cesarean delivery was associated with significantly improved patient satisfaction, compared with staple closure, according to findings in a prospective, randomized, multicenter study of 746 women.
Suture closure also was associated with improved patient and physician assessments of cosmesis, compared with staple closure, Dr. Jonah Fleisher reported at the annual meeting of the American Congress of Obstetricians and Gynecologists.
The median interquartile range of overall "satisfaction with method of closure" scores on the validated Patient and Observer Scar Assessment Scale (POSAS) differed significantly for 299 suture patients and 307 staple patients for whom the data were available (scores of 10 vs. 9, respectively), as did median "satisfaction with appearance of skin incision" scores (also 10 vs. 9, respectively), said Dr. Fleisher of Geisinger Health System, Danville, Pa.
The cosmetic-specific question was included to help adjust for the multifactorial nature of the overall satisfaction score, which could be affected by the patient’s degree of pain, healing time, need for extra office visits, and frequency of complications, among other factors.
The two measures correlated positively, and both subjective and objective components of the POSAS favored suture closure, he noted.
Study participants were women undergoing cesarean delivery via low-transverse skin incisions at any of three participating centers. After fascia closure, the women were allocated to either the suture (type was surgeon’s choice) or metal staple closure group. Staples were removed between postoperative days 4 and 10.
About 1.3 million cesarean deliveries are performed each year in the United States, Dr. Fleisher said.
"Those scars that are formed as a result are very important to patients, both as far as cosmetic and general satisfaction ... and it turns out they are important to obstetricians, too," he added, noting that data to guide decision making are lacking.
In the current study, the differences between the suture and staple groups were significant, but patients in both groups had high rates of satisfaction.
"Given these considerations, I would suggest that we ought to incorporate wound complications rates into the decision of which method to use," he said.
An article that addresses the wound complication rates in this study is currently in press and scheduled for publication in the American Journal of Obstetrics & Gynecology in June. The data show a 57% lower complication rate with suture closure vs. staple closure, Dr. Fleisher said.
"The bottom line is, for all these reasons, we have moved to recommending suture closure in all transverse C-sections," he said.
As for whether the findings apply to other types of surgical operations, such as abdominal hysterectomy, Dr. Fleisher said there are many changes in pregnancy, including immunologic changes, that don’t necessarily apply to nonobstetric situations.
"There is some literature in the general surgery area about this, and some literature in gynecologic surgery, but given the immunologic changes – I think we’re seeing that even the adhesion data is not necessarily the same in those two contexts. ... I wouldn’t want to generalize from this to nonobstetric indications," he said.
This study was supported by Ethicon. Dr. Fleisher reported having no disclosures.
CHICAGO – Suture closure of the skin incision after cesarean delivery was associated with significantly improved patient satisfaction, compared with staple closure, according to findings in a prospective, randomized, multicenter study of 746 women.
Suture closure also was associated with improved patient and physician assessments of cosmesis, compared with staple closure, Dr. Jonah Fleisher reported at the annual meeting of the American Congress of Obstetricians and Gynecologists.
The median interquartile range of overall "satisfaction with method of closure" scores on the validated Patient and Observer Scar Assessment Scale (POSAS) differed significantly for 299 suture patients and 307 staple patients for whom the data were available (scores of 10 vs. 9, respectively), as did median "satisfaction with appearance of skin incision" scores (also 10 vs. 9, respectively), said Dr. Fleisher of Geisinger Health System, Danville, Pa.
The cosmetic-specific question was included to help adjust for the multifactorial nature of the overall satisfaction score, which could be affected by the patient’s degree of pain, healing time, need for extra office visits, and frequency of complications, among other factors.
The two measures correlated positively, and both subjective and objective components of the POSAS favored suture closure, he noted.
Study participants were women undergoing cesarean delivery via low-transverse skin incisions at any of three participating centers. After fascia closure, the women were allocated to either the suture (type was surgeon’s choice) or metal staple closure group. Staples were removed between postoperative days 4 and 10.
About 1.3 million cesarean deliveries are performed each year in the United States, Dr. Fleisher said.
"Those scars that are formed as a result are very important to patients, both as far as cosmetic and general satisfaction ... and it turns out they are important to obstetricians, too," he added, noting that data to guide decision making are lacking.
In the current study, the differences between the suture and staple groups were significant, but patients in both groups had high rates of satisfaction.
"Given these considerations, I would suggest that we ought to incorporate wound complications rates into the decision of which method to use," he said.
An article that addresses the wound complication rates in this study is currently in press and scheduled for publication in the American Journal of Obstetrics & Gynecology in June. The data show a 57% lower complication rate with suture closure vs. staple closure, Dr. Fleisher said.
"The bottom line is, for all these reasons, we have moved to recommending suture closure in all transverse C-sections," he said.
As for whether the findings apply to other types of surgical operations, such as abdominal hysterectomy, Dr. Fleisher said there are many changes in pregnancy, including immunologic changes, that don’t necessarily apply to nonobstetric situations.
"There is some literature in the general surgery area about this, and some literature in gynecologic surgery, but given the immunologic changes – I think we’re seeing that even the adhesion data is not necessarily the same in those two contexts. ... I wouldn’t want to generalize from this to nonobstetric indications," he said.
This study was supported by Ethicon. Dr. Fleisher reported having no disclosures.
AT THE ACOG ANNUAL CLINICAL MEETING
Key clinical point: Patients and physicians preferred sutures over staples for skin closure after cesarean section.
Major finding: Satisfaction scores were 10 and 9 (interquartile range) for sutures vs. staples.
Data source: A prospective, multicenter, randomized trial involving 746 women.
Disclosures: This study was supported by Ethicon. Dr. Fleisher reported having no disclosures.
Answering subpoenas poses legal, privacy risks for doctors
Receiving a subpoena for information or testimony can make any physician feel nervous and apprehensive. The official-looking notices often arrive as certified mail, have a stamped deadline, and include an attorney’s signature.
But immediately fulfilling a subpoena without first accessing the request could land doctors in legal trouble.
"Understandably, many physicians don’t recognize that no judge has reviewed the propriety of a subpoena," said Michael J. Schoppmann, a New York–based health law attorney and managing partner for a health care litigation firm. "Most judges are not even aware of the subpoena. There’s an assumption by the physician that it has been vetted by the court and, in many cases, that is not true. With good intentions, we find physicians getting into trouble out of a desire to be compliant."
Before answering a subpoena, physicians should evaluate where the request originated, the status of the case, and who is involved, legal experts say. Frequently, a request for patient information or records is objected to by the patient’s attorney, said Michael J. Sacopulos, a medical liability defense attorney and founder of Medical Risk Institute (MRI) in Terre Haute, Ind. Physicians should ensure record requests are authorized by the patient or are bidden through a court order.
"Let’s say you’re not going to court, but they want information," Mr. Sacopulos said. "You have HIPAA issues at play. You still have an independent duty to safeguard patient information."
Mr. Schoppmann recommends that physicians contact the judge affiliated with the case and request guidance about how to proceed with a subpoena. The judge may deny the request because the records are inappropriate or allow the subpoena to proceed.
"It’s great protection because if we get an order from the court, that (shields the doctor) from the litigants later saying, ‘We did not want you to release those records.’" Mr. Schoppmann said.
In other instances, physicians may be subpoenaed to discuss a patient’s condition or treatment in a third-party case. For example, a patient who is suing an insurance carrier or third-party over a vehicle accident. Doctors have a responsibility to offer honest and unbiased testimony about their patient’s medical condition, said Steven Fitzer, a medical malpractice defense attorney in Tacoma, Wash. and former chair of the Washington State Bar Association Litigation Section. However, physicians should steer clear of providing opinions on medical matters unrelated to their expertise.
"A family practice doctor should offer thoughts and opinions and facts that are within his or her specialty," Mr. Fitzer said. "If (the doctor) regularly treats people who have whiplash and cervical strain, you can talk about that. But the family practice doctor shouldn’t be talking about neck surgery unless you do neck surgeries."
Physicians should also consider and address how their involvement with a case may affect their relationship with patients, Mr. Fitzer adds. Often, patients view their doctor as their supporter and expect their alliance during in a third-party lawsuit.
"Patients sometimes misunderstand that the role of the doctor in a deposition is to call it the way he or she sees it, not to be an advocate for the patient," he said. Doctors should "communicate that to the patient" beforehand.
Be wary of subpoenas for information or records that stem from a malpractice case in which the doctor is a named defendant, Mr. Sacopulos notes. In such instances, a plaintiff’s attorney may request details about a patient visit or ask about a doctor’s role in treating the patient within the continuum of care. But the attorney could really be fishing for more physicians to sue.
"They may have sued one or two physicians, but the statute of limitations has yet to run out," Mr. Sacopulos said. "They’ll sue one or two, then depose others to see if they can’t get some finger pointing and increase the litigation."
In addition, plaintiffs’ attorneys may hope that the subpoenaed physician makes statements to further enhance their case against another doctor, without hiring them as an expert witness.
"My advice would be if you are requested to offer testimony in a case that you are not a party to, you immediately contact your liability carrier," Mr. Sacopulos said. "Your medical malpractice carrier will most often provide an attorney for a deposition, even though you’re not a party."
Physicians should not let attorneys intimidate them with subpoenas or excessive demands for information. Some lawyers request thousands of pages of documents in a short timeframe and pressure the physician to comply, Mr. Schoppmann said. Other attorneys try to convince physicians to speak with them over the phone about the request and to provide patient information verbally.
Ensure that the scope, the timing, and the overall content of the request are appropriate before responding, Mr. Schoppmann stresses.
"The subpoena has to be reasonable," he said. "Step back and do not respond unduly aggressively. You could be subject to criticism later if you respond to an inappropriate subpoena. We want right, rather than quick."
Receiving a subpoena for information or testimony can make any physician feel nervous and apprehensive. The official-looking notices often arrive as certified mail, have a stamped deadline, and include an attorney’s signature.
But immediately fulfilling a subpoena without first accessing the request could land doctors in legal trouble.
"Understandably, many physicians don’t recognize that no judge has reviewed the propriety of a subpoena," said Michael J. Schoppmann, a New York–based health law attorney and managing partner for a health care litigation firm. "Most judges are not even aware of the subpoena. There’s an assumption by the physician that it has been vetted by the court and, in many cases, that is not true. With good intentions, we find physicians getting into trouble out of a desire to be compliant."
Before answering a subpoena, physicians should evaluate where the request originated, the status of the case, and who is involved, legal experts say. Frequently, a request for patient information or records is objected to by the patient’s attorney, said Michael J. Sacopulos, a medical liability defense attorney and founder of Medical Risk Institute (MRI) in Terre Haute, Ind. Physicians should ensure record requests are authorized by the patient or are bidden through a court order.
"Let’s say you’re not going to court, but they want information," Mr. Sacopulos said. "You have HIPAA issues at play. You still have an independent duty to safeguard patient information."
Mr. Schoppmann recommends that physicians contact the judge affiliated with the case and request guidance about how to proceed with a subpoena. The judge may deny the request because the records are inappropriate or allow the subpoena to proceed.
"It’s great protection because if we get an order from the court, that (shields the doctor) from the litigants later saying, ‘We did not want you to release those records.’" Mr. Schoppmann said.
In other instances, physicians may be subpoenaed to discuss a patient’s condition or treatment in a third-party case. For example, a patient who is suing an insurance carrier or third-party over a vehicle accident. Doctors have a responsibility to offer honest and unbiased testimony about their patient’s medical condition, said Steven Fitzer, a medical malpractice defense attorney in Tacoma, Wash. and former chair of the Washington State Bar Association Litigation Section. However, physicians should steer clear of providing opinions on medical matters unrelated to their expertise.
"A family practice doctor should offer thoughts and opinions and facts that are within his or her specialty," Mr. Fitzer said. "If (the doctor) regularly treats people who have whiplash and cervical strain, you can talk about that. But the family practice doctor shouldn’t be talking about neck surgery unless you do neck surgeries."
Physicians should also consider and address how their involvement with a case may affect their relationship with patients, Mr. Fitzer adds. Often, patients view their doctor as their supporter and expect their alliance during in a third-party lawsuit.
"Patients sometimes misunderstand that the role of the doctor in a deposition is to call it the way he or she sees it, not to be an advocate for the patient," he said. Doctors should "communicate that to the patient" beforehand.
Be wary of subpoenas for information or records that stem from a malpractice case in which the doctor is a named defendant, Mr. Sacopulos notes. In such instances, a plaintiff’s attorney may request details about a patient visit or ask about a doctor’s role in treating the patient within the continuum of care. But the attorney could really be fishing for more physicians to sue.
"They may have sued one or two physicians, but the statute of limitations has yet to run out," Mr. Sacopulos said. "They’ll sue one or two, then depose others to see if they can’t get some finger pointing and increase the litigation."
In addition, plaintiffs’ attorneys may hope that the subpoenaed physician makes statements to further enhance their case against another doctor, without hiring them as an expert witness.
"My advice would be if you are requested to offer testimony in a case that you are not a party to, you immediately contact your liability carrier," Mr. Sacopulos said. "Your medical malpractice carrier will most often provide an attorney for a deposition, even though you’re not a party."
Physicians should not let attorneys intimidate them with subpoenas or excessive demands for information. Some lawyers request thousands of pages of documents in a short timeframe and pressure the physician to comply, Mr. Schoppmann said. Other attorneys try to convince physicians to speak with them over the phone about the request and to provide patient information verbally.
Ensure that the scope, the timing, and the overall content of the request are appropriate before responding, Mr. Schoppmann stresses.
"The subpoena has to be reasonable," he said. "Step back and do not respond unduly aggressively. You could be subject to criticism later if you respond to an inappropriate subpoena. We want right, rather than quick."
Receiving a subpoena for information or testimony can make any physician feel nervous and apprehensive. The official-looking notices often arrive as certified mail, have a stamped deadline, and include an attorney’s signature.
But immediately fulfilling a subpoena without first accessing the request could land doctors in legal trouble.
"Understandably, many physicians don’t recognize that no judge has reviewed the propriety of a subpoena," said Michael J. Schoppmann, a New York–based health law attorney and managing partner for a health care litigation firm. "Most judges are not even aware of the subpoena. There’s an assumption by the physician that it has been vetted by the court and, in many cases, that is not true. With good intentions, we find physicians getting into trouble out of a desire to be compliant."
Before answering a subpoena, physicians should evaluate where the request originated, the status of the case, and who is involved, legal experts say. Frequently, a request for patient information or records is objected to by the patient’s attorney, said Michael J. Sacopulos, a medical liability defense attorney and founder of Medical Risk Institute (MRI) in Terre Haute, Ind. Physicians should ensure record requests are authorized by the patient or are bidden through a court order.
"Let’s say you’re not going to court, but they want information," Mr. Sacopulos said. "You have HIPAA issues at play. You still have an independent duty to safeguard patient information."
Mr. Schoppmann recommends that physicians contact the judge affiliated with the case and request guidance about how to proceed with a subpoena. The judge may deny the request because the records are inappropriate or allow the subpoena to proceed.
"It’s great protection because if we get an order from the court, that (shields the doctor) from the litigants later saying, ‘We did not want you to release those records.’" Mr. Schoppmann said.
In other instances, physicians may be subpoenaed to discuss a patient’s condition or treatment in a third-party case. For example, a patient who is suing an insurance carrier or third-party over a vehicle accident. Doctors have a responsibility to offer honest and unbiased testimony about their patient’s medical condition, said Steven Fitzer, a medical malpractice defense attorney in Tacoma, Wash. and former chair of the Washington State Bar Association Litigation Section. However, physicians should steer clear of providing opinions on medical matters unrelated to their expertise.
"A family practice doctor should offer thoughts and opinions and facts that are within his or her specialty," Mr. Fitzer said. "If (the doctor) regularly treats people who have whiplash and cervical strain, you can talk about that. But the family practice doctor shouldn’t be talking about neck surgery unless you do neck surgeries."
Physicians should also consider and address how their involvement with a case may affect their relationship with patients, Mr. Fitzer adds. Often, patients view their doctor as their supporter and expect their alliance during in a third-party lawsuit.
"Patients sometimes misunderstand that the role of the doctor in a deposition is to call it the way he or she sees it, not to be an advocate for the patient," he said. Doctors should "communicate that to the patient" beforehand.
Be wary of subpoenas for information or records that stem from a malpractice case in which the doctor is a named defendant, Mr. Sacopulos notes. In such instances, a plaintiff’s attorney may request details about a patient visit or ask about a doctor’s role in treating the patient within the continuum of care. But the attorney could really be fishing for more physicians to sue.
"They may have sued one or two physicians, but the statute of limitations has yet to run out," Mr. Sacopulos said. "They’ll sue one or two, then depose others to see if they can’t get some finger pointing and increase the litigation."
In addition, plaintiffs’ attorneys may hope that the subpoenaed physician makes statements to further enhance their case against another doctor, without hiring them as an expert witness.
"My advice would be if you are requested to offer testimony in a case that you are not a party to, you immediately contact your liability carrier," Mr. Sacopulos said. "Your medical malpractice carrier will most often provide an attorney for a deposition, even though you’re not a party."
Physicians should not let attorneys intimidate them with subpoenas or excessive demands for information. Some lawyers request thousands of pages of documents in a short timeframe and pressure the physician to comply, Mr. Schoppmann said. Other attorneys try to convince physicians to speak with them over the phone about the request and to provide patient information verbally.
Ensure that the scope, the timing, and the overall content of the request are appropriate before responding, Mr. Schoppmann stresses.
"The subpoena has to be reasonable," he said. "Step back and do not respond unduly aggressively. You could be subject to criticism later if you respond to an inappropriate subpoena. We want right, rather than quick."
Burwell gets a step closer to HHS helm
Sylvia Mathews Burwell, the nominee to become the next secretary of the Department of Health & Human Services, got a warm reception from senators in her first confirmation hearing.
Ms. Burwell, who is the current director of the Office of Management and Budget, was widely praised for her competence, compassion, and willingness to work with lawmakers of both parties. She was endorsed by Sen. John McCain (R-Ariz.), who favors replacing the Affordable Care Act. He said that regardless of how senators feel about the health law, they should confirm Ms. Burwell, because she is well qualified to lead HHS and will be more responsive than the current secretary, Kathleen Sebelius.
Sen. McCain added that he tried to discourage her from accepting the "thankless" job. "Who would recommend their friend take over as captain of the Titanic after it hit the iceberg?" he said.
During the 2-hour hearing, lawmakers on the Senate Committee on Health, Education, Labor & Pensions took advantage of their first chance to question Ms. Burwell, querying her on a range of issues from the shortage of primary care providers to the speed of drug approvals at the Food and Drug Administration.
When asked about her approach to employing the controversial Independent Payment Advisory Board, Ms. Burwell said she hopes that it will never be triggered, because the government will keep health care costs under control.
And when it comes to the past failures of HHS in managing the healthcare.gov rollout, Ms. Burwell said she learned that there needs to be a different approach to handling information technology procurement and delivery. She pledged to ensure there was "ownership and accountability" in the IT operations in the future.
She also promised GOP senators that she would share information with them. "I am here to serve the American people," she said.
Ms. Burwell is not expected to have a tough confirmation battle. New Senate rules allow her to be confirmed with only a majority vote, and she received a unanimous confirmation vote for her current post last April. She will face questioning next from the Senate Finance Committee.
Ms. Burwell, a Rhodes Scholar from Hinton, W.Va., previously served as president of the Walmart Foundation and as president of the global development program at the Bill & Melinda Gates Foundation. During the Clinton administration, she worked as deputy director of the Office of Management and Budget.
On Twitter @maryellenny
Sylvia Mathews Burwell, the nominee to become the next secretary of the Department of Health & Human Services, got a warm reception from senators in her first confirmation hearing.
Ms. Burwell, who is the current director of the Office of Management and Budget, was widely praised for her competence, compassion, and willingness to work with lawmakers of both parties. She was endorsed by Sen. John McCain (R-Ariz.), who favors replacing the Affordable Care Act. He said that regardless of how senators feel about the health law, they should confirm Ms. Burwell, because she is well qualified to lead HHS and will be more responsive than the current secretary, Kathleen Sebelius.
Sen. McCain added that he tried to discourage her from accepting the "thankless" job. "Who would recommend their friend take over as captain of the Titanic after it hit the iceberg?" he said.
During the 2-hour hearing, lawmakers on the Senate Committee on Health, Education, Labor & Pensions took advantage of their first chance to question Ms. Burwell, querying her on a range of issues from the shortage of primary care providers to the speed of drug approvals at the Food and Drug Administration.
When asked about her approach to employing the controversial Independent Payment Advisory Board, Ms. Burwell said she hopes that it will never be triggered, because the government will keep health care costs under control.
And when it comes to the past failures of HHS in managing the healthcare.gov rollout, Ms. Burwell said she learned that there needs to be a different approach to handling information technology procurement and delivery. She pledged to ensure there was "ownership and accountability" in the IT operations in the future.
She also promised GOP senators that she would share information with them. "I am here to serve the American people," she said.
Ms. Burwell is not expected to have a tough confirmation battle. New Senate rules allow her to be confirmed with only a majority vote, and she received a unanimous confirmation vote for her current post last April. She will face questioning next from the Senate Finance Committee.
Ms. Burwell, a Rhodes Scholar from Hinton, W.Va., previously served as president of the Walmart Foundation and as president of the global development program at the Bill & Melinda Gates Foundation. During the Clinton administration, she worked as deputy director of the Office of Management and Budget.
On Twitter @maryellenny
Sylvia Mathews Burwell, the nominee to become the next secretary of the Department of Health & Human Services, got a warm reception from senators in her first confirmation hearing.
Ms. Burwell, who is the current director of the Office of Management and Budget, was widely praised for her competence, compassion, and willingness to work with lawmakers of both parties. She was endorsed by Sen. John McCain (R-Ariz.), who favors replacing the Affordable Care Act. He said that regardless of how senators feel about the health law, they should confirm Ms. Burwell, because she is well qualified to lead HHS and will be more responsive than the current secretary, Kathleen Sebelius.
Sen. McCain added that he tried to discourage her from accepting the "thankless" job. "Who would recommend their friend take over as captain of the Titanic after it hit the iceberg?" he said.
During the 2-hour hearing, lawmakers on the Senate Committee on Health, Education, Labor & Pensions took advantage of their first chance to question Ms. Burwell, querying her on a range of issues from the shortage of primary care providers to the speed of drug approvals at the Food and Drug Administration.
When asked about her approach to employing the controversial Independent Payment Advisory Board, Ms. Burwell said she hopes that it will never be triggered, because the government will keep health care costs under control.
And when it comes to the past failures of HHS in managing the healthcare.gov rollout, Ms. Burwell said she learned that there needs to be a different approach to handling information technology procurement and delivery. She pledged to ensure there was "ownership and accountability" in the IT operations in the future.
She also promised GOP senators that she would share information with them. "I am here to serve the American people," she said.
Ms. Burwell is not expected to have a tough confirmation battle. New Senate rules allow her to be confirmed with only a majority vote, and she received a unanimous confirmation vote for her current post last April. She will face questioning next from the Senate Finance Committee.
Ms. Burwell, a Rhodes Scholar from Hinton, W.Va., previously served as president of the Walmart Foundation and as president of the global development program at the Bill & Melinda Gates Foundation. During the Clinton administration, she worked as deputy director of the Office of Management and Budget.
On Twitter @maryellenny
ABIM: Majority meeting Maintenance of Certification requirements
The American Board of Internal Medicine says that "a substantial majority" of the nation’s internists have met the new Maintenance of Certification requirements as of May 1, the deadline for doctors to be listed publicly on the ABIM’s website as having met those standards.
The ABIM reported that "despite vocal concerns" from physicians, some 150,000 have enrolled in the MOC program, 50,000 since the new requirements were instituted on Jan. 1.
As part of the new MOC, every 2 years, physicians who are certified by the ABIM must earn at least some points by completing some of the educational activities approved for MOC credit. At the 5-year mark, they must earn 100 points, as well as complete patient safety and patient survey activities, to be considered up to date. Previously, physicians were given 10 years to earn 100 points. They must also pass their board exam every 10 years.
"We are listening to the feedback we have received from the community about changes to our program, but at the same time the public is seeking a way to know that their doctor is ‘keeping up in their field,’" Dr. Richard Baron, ABIM president and chief executive officer, said in a statement.
A petition to overturn most of the MOC changes begun by Dr. Paul Teirstein, chief of cardiology and director of interventional cardiology for Scripps Clinic in La Jolla, Calif., has collected more than 14,000 signatures since it was posted in late March.
According to the ABIM, since Jan. 1, physicians have claimed more than 245,000 hours of Continuing Medical Education (CME) through their MOC involvement, and nearly 20,000 physicians have already met their MOC requirements through 2015.
"MOC has clearly sparked a national conversation focused on what regular assessments are appropriate for ongoing specialty certification," Dr. Baron said. "We must look at how the MOC process meets the needs of physicians, patients, and others who rely on it as an indicator of a provider’s expertise."
The ABIM continues to say that MOC is needed because it is desired by patients and payers. "Those who choose to meet ABIM’s MOC requirements are differentiating themselves from some of their colleagues. They are saying, ‘I’m a cardiologist or oncologist, or whatever specialty they are certified in, who is meeting a standard set by my peers.’ That is a powerful statement to make to their patients, and to themselves," Dr. Clarence H. Braddock III, chair-elect of the ABIM Board of Directors, said in the ABIM statement.
The Board also said it is responding to criticism by making changes to the MOC program, including giving "credit" for activities physicians already are doing to maintain their knowledge base and improve their practices. It said it recognizes more than 270 programs created by medical societies, health systems, and others and that 32,000 ABIM diplomates already have fulfilled some requirements of MOC using those pathways.
"We recognize that the MOC program is not perfect, and we are committed to constant assessment of it," said Dr. Baron.
That may not be enough for some physicians.
Another group, Change Board Recertification, was started in 2010 with the aim of completely overhauling the MOC process.
On Twitter @aliciaault
The new MOC requirements that became effective on Jan. 1, 2014, have met with significant criticism from practicing physicians. Nevertheless, the majority of physicians with time-limited board certifications have enrolled in the program, as hospital privileges and insurance reimbursements are often linked to active certification.
Whereas it is largely agreed that some measure of ongoing knowledge and competence is vital to setting standards for the profession and protecting the interests of patients, many physicians raise significant concerns regarding the current process. These include overly burdensome costs and time commitments as well as relevance to actual practice.
Finally, there is a paucity of data demonstrating that the MOC recertification process actually translates to improved physician performance in the clinical setting. A number of recommendations have been suggested to improve the recertification process. These include decreasing the costs of recertification by the ABIM; customizing the process to dovetail with an individual physician's actual practice; testing not only rote knowledge, but also physician ability to accesses and utilize information; and further research to demonstrate efficacy in achieving and demonstrating physician competence.
The new MOC requirements that became effective on Jan. 1, 2014, have met with significant criticism from practicing physicians. Nevertheless, the majority of physicians with time-limited board certifications have enrolled in the program, as hospital privileges and insurance reimbursements are often linked to active certification.
Whereas it is largely agreed that some measure of ongoing knowledge and competence is vital to setting standards for the profession and protecting the interests of patients, many physicians raise significant concerns regarding the current process. These include overly burdensome costs and time commitments as well as relevance to actual practice.
Finally, there is a paucity of data demonstrating that the MOC recertification process actually translates to improved physician performance in the clinical setting. A number of recommendations have been suggested to improve the recertification process. These include decreasing the costs of recertification by the ABIM; customizing the process to dovetail with an individual physician's actual practice; testing not only rote knowledge, but also physician ability to accesses and utilize information; and further research to demonstrate efficacy in achieving and demonstrating physician competence.
The new MOC requirements that became effective on Jan. 1, 2014, have met with significant criticism from practicing physicians. Nevertheless, the majority of physicians with time-limited board certifications have enrolled in the program, as hospital privileges and insurance reimbursements are often linked to active certification.
Whereas it is largely agreed that some measure of ongoing knowledge and competence is vital to setting standards for the profession and protecting the interests of patients, many physicians raise significant concerns regarding the current process. These include overly burdensome costs and time commitments as well as relevance to actual practice.
Finally, there is a paucity of data demonstrating that the MOC recertification process actually translates to improved physician performance in the clinical setting. A number of recommendations have been suggested to improve the recertification process. These include decreasing the costs of recertification by the ABIM; customizing the process to dovetail with an individual physician's actual practice; testing not only rote knowledge, but also physician ability to accesses and utilize information; and further research to demonstrate efficacy in achieving and demonstrating physician competence.
The American Board of Internal Medicine says that "a substantial majority" of the nation’s internists have met the new Maintenance of Certification requirements as of May 1, the deadline for doctors to be listed publicly on the ABIM’s website as having met those standards.
The ABIM reported that "despite vocal concerns" from physicians, some 150,000 have enrolled in the MOC program, 50,000 since the new requirements were instituted on Jan. 1.
As part of the new MOC, every 2 years, physicians who are certified by the ABIM must earn at least some points by completing some of the educational activities approved for MOC credit. At the 5-year mark, they must earn 100 points, as well as complete patient safety and patient survey activities, to be considered up to date. Previously, physicians were given 10 years to earn 100 points. They must also pass their board exam every 10 years.
"We are listening to the feedback we have received from the community about changes to our program, but at the same time the public is seeking a way to know that their doctor is ‘keeping up in their field,’" Dr. Richard Baron, ABIM president and chief executive officer, said in a statement.
A petition to overturn most of the MOC changes begun by Dr. Paul Teirstein, chief of cardiology and director of interventional cardiology for Scripps Clinic in La Jolla, Calif., has collected more than 14,000 signatures since it was posted in late March.
According to the ABIM, since Jan. 1, physicians have claimed more than 245,000 hours of Continuing Medical Education (CME) through their MOC involvement, and nearly 20,000 physicians have already met their MOC requirements through 2015.
"MOC has clearly sparked a national conversation focused on what regular assessments are appropriate for ongoing specialty certification," Dr. Baron said. "We must look at how the MOC process meets the needs of physicians, patients, and others who rely on it as an indicator of a provider’s expertise."
The ABIM continues to say that MOC is needed because it is desired by patients and payers. "Those who choose to meet ABIM’s MOC requirements are differentiating themselves from some of their colleagues. They are saying, ‘I’m a cardiologist or oncologist, or whatever specialty they are certified in, who is meeting a standard set by my peers.’ That is a powerful statement to make to their patients, and to themselves," Dr. Clarence H. Braddock III, chair-elect of the ABIM Board of Directors, said in the ABIM statement.
The Board also said it is responding to criticism by making changes to the MOC program, including giving "credit" for activities physicians already are doing to maintain their knowledge base and improve their practices. It said it recognizes more than 270 programs created by medical societies, health systems, and others and that 32,000 ABIM diplomates already have fulfilled some requirements of MOC using those pathways.
"We recognize that the MOC program is not perfect, and we are committed to constant assessment of it," said Dr. Baron.
That may not be enough for some physicians.
Another group, Change Board Recertification, was started in 2010 with the aim of completely overhauling the MOC process.
On Twitter @aliciaault
The American Board of Internal Medicine says that "a substantial majority" of the nation’s internists have met the new Maintenance of Certification requirements as of May 1, the deadline for doctors to be listed publicly on the ABIM’s website as having met those standards.
The ABIM reported that "despite vocal concerns" from physicians, some 150,000 have enrolled in the MOC program, 50,000 since the new requirements were instituted on Jan. 1.
As part of the new MOC, every 2 years, physicians who are certified by the ABIM must earn at least some points by completing some of the educational activities approved for MOC credit. At the 5-year mark, they must earn 100 points, as well as complete patient safety and patient survey activities, to be considered up to date. Previously, physicians were given 10 years to earn 100 points. They must also pass their board exam every 10 years.
"We are listening to the feedback we have received from the community about changes to our program, but at the same time the public is seeking a way to know that their doctor is ‘keeping up in their field,’" Dr. Richard Baron, ABIM president and chief executive officer, said in a statement.
A petition to overturn most of the MOC changes begun by Dr. Paul Teirstein, chief of cardiology and director of interventional cardiology for Scripps Clinic in La Jolla, Calif., has collected more than 14,000 signatures since it was posted in late March.
According to the ABIM, since Jan. 1, physicians have claimed more than 245,000 hours of Continuing Medical Education (CME) through their MOC involvement, and nearly 20,000 physicians have already met their MOC requirements through 2015.
"MOC has clearly sparked a national conversation focused on what regular assessments are appropriate for ongoing specialty certification," Dr. Baron said. "We must look at how the MOC process meets the needs of physicians, patients, and others who rely on it as an indicator of a provider’s expertise."
The ABIM continues to say that MOC is needed because it is desired by patients and payers. "Those who choose to meet ABIM’s MOC requirements are differentiating themselves from some of their colleagues. They are saying, ‘I’m a cardiologist or oncologist, or whatever specialty they are certified in, who is meeting a standard set by my peers.’ That is a powerful statement to make to their patients, and to themselves," Dr. Clarence H. Braddock III, chair-elect of the ABIM Board of Directors, said in the ABIM statement.
The Board also said it is responding to criticism by making changes to the MOC program, including giving "credit" for activities physicians already are doing to maintain their knowledge base and improve their practices. It said it recognizes more than 270 programs created by medical societies, health systems, and others and that 32,000 ABIM diplomates already have fulfilled some requirements of MOC using those pathways.
"We recognize that the MOC program is not perfect, and we are committed to constant assessment of it," said Dr. Baron.
That may not be enough for some physicians.
Another group, Change Board Recertification, was started in 2010 with the aim of completely overhauling the MOC process.
On Twitter @aliciaault
Doctors’ first steps after lawsuit filing are vital, warn attorneys
Receiving notice that a patient is suing can spark a range of emotions in physicians, including fear, anger, hurt, and helplessness. But litigation experts stress that after a filing, physicians must rein in their feelings and focus on immediate next steps – crucial actions that can significantly impact the suit and its outcome.
"Doctors have two reactions to getting sued – either they’re very sad or they’re very angry," said Steven Fitzer, a medical liability defense attorney at Fitzer, Leighton & Fitzer, P.S., in Tacoma, Wash., and former chair of the Washington State Bar Association Litigation Section. "Relaxing and composing yourself are important because a lawsuit is a marathon – not a sprint."
American Medical Association data show 60% of physicians will be sued by the time they reach 55 years of age. The average span of a medical malpractice claim from start to close is generally about 2.5 years, although many suits progress longer. While most medical liability claims do not end in trial, defense attorneys say knowing how to respond to a lawsuit can raise doctors’ chances of a quicker, more ideal resolution.
First and foremost, physicians should notify their malpractice insurance carrier as soon as possible after lawsuit papers are served, said Matt Mitcham, senior vice president of claims for MagMutual Insurance Company, a medical liability insurer that operates in the Southeast. Employed physicians should immediately alert their risk management department.
"All suits have a limited time for providing a response, and there are severe consequences for not meeting these deadlines," Mr. Mitcham said. "In addition, physicians need to provide their defense team with as much time as possible to prepare a response."
Doctors should resist the desire to contact patients or their families in an attempt to work out the situation themselves, adds Mr. Fitzer, who recently shared lawsuit preparation tips in two video playlists for The Doctors Company, a national medical malpractice insurer.
"Particularly with family practice physicians, they tend to have a long and strong bond with their patients and their patients’ families, and they think, ‘If I just call and ask what’s going on, we can just fix this all right here,’ " he said. "That never works. The patient or their lawyer will take whatever you say in or out of context and use it against you."
Another action to avoid after a lawsuit filing is making additions or changes to patient records, said Mr. Mitcham.
"The original records should never be altered under any circumstance," he said. "Today’s forensic specialists are experts in identifying changes, and by altering records, a physician can potentially turn a defensible case into one that is indefensible."
Securing an attorney that doctors trust and with whom they can aptly communicate is also essential, said Michael F. Ball, a medical liability defense attorney and partner at McCormick Barstow, LLP, in Fresno, Calif. Most doctors may not realize they can typically choose from a panel of attorneys used by their insurer, he said. Physicians can also ask to view the attorney panel and conduct their own research before requesting a specific lawyer.
Mr. Ball counsels his clients to focus only on the task at hand during each stage of a lawsuit, rather than worry about future phases or a possible trial. For example, during the deposition stage, physicians should prepare by understanding the deposition’s purpose, reading through the record, and being clear on what questions may be asked. A deposition is a witness’s sworn, out-of-court testimony used to gather information as part of the discovery process.
"Some [physicians] don’t review the record as closely as they should," he said. "There’s no substitute for real preparation."
Additionally, depositions are a stage in which a physician’s emotions may come bubbling to the surface, notes Angela Dodge, Ph.D., founding partner of Dodge Consulting & Publications, LLP, a litigation consulting firm in the Seattle-Tacoma area.
"A doctor may go into a deposition feeling very angry and resentful because a patient they believe they gave good care to is now suing," said Ms. Dodge, author of the book "When Good Doctors Get Sued: A Practical Guide for Physicians Involved in Malpractice Lawsuits, and Winning at Jury Selection." "We counsel them on the importance of setting that aside because it could interfere with" their success.
Negative emotions by doctors may be interpreted by plaintiffs’ attorneys as guilt or defensiveness and used to fuel their claims, she said. Doctors should also focus only on the questions being asked during a deposition and not offer up any further or additional information. For instance, in a recent case, a doctor was asked about a specific part of his education. In response, the physician provided unnecessary information about his entire medical education, including his experience operating on pigs, how pig anatomy is relevant to human medicine, and other needless details, Ms. Dodge said.
"He was so anxious to explain how he gained his expertise; he forgot that the question was [only] where and when he gained his expertise," she said.
Litigation counselors point to strong cooperation among physicians, insurers, and defense attorneys as one of the most vital components to the successful handling of a lawsuit.
"The legal system can be a very daunting place for physicians, but when the malpractice carrier and defense attorney work together as a team, they can help the physician navigate the process and hopefully win the case," Mr. Mitcham said.
A 2011 study in the New England Journal of Medicine estimated that 75% of physicians in "low-risk" specialties and virtually 100% of physicians in "high-risk" specialties could expect to face a malpractice claim sometime in their career (N. Engl. J. Med. 2011;365:629-36). However, 60% of liability claims against doctors are dropped, withdrawn, or dismissed without payment, and physicians are found not negligent in over 90% of cases that do go to trial.
While there are no readily available national statistics on the actual number of claims filed, there is data, compiled by the federal government’s National Practitioner Data Bank (NPDB), suggesting that the number of cases filed has been dropping in the last decade.

|
|
The NPDB issues an annual report that includes the number of medical malpractice payments made each year for the preceding 10 years. For nearly every year in the past decade, the number of medical malpractice payments made on behalf of all practitioners reported to the NPDB has decreased. Between 2002 and 2011, the number of medical malpractice payments decreased nearly 40%, declining steadily from 18,696 to 11,424.
Also, in the past 10 years, the number of medical malpractice payments reported to the NPDB, attributed to physicians and dentists, has decreased steadily from 17,155 to 10,038. Between 2003 and 2011, the total amount paid out fell from $4.5 billion to less than $3.2 billion, a 29% drop. State tort-reform laws limiting noneconomic damages, growth in risk management responses to adverse events, and the growing use of apology and disclosure likely have contributed to this trend.
Dr. James A.L. Mathers, Jr., is a past president of the American College of Chest Physicians, and is recently retired with 30 years of private practice experience in pulmonary, critical care, and sleep medicine.
A 2011 study in the New England Journal of Medicine estimated that 75% of physicians in "low-risk" specialties and virtually 100% of physicians in "high-risk" specialties could expect to face a malpractice claim sometime in their career (N. Engl. J. Med. 2011;365:629-36). However, 60% of liability claims against doctors are dropped, withdrawn, or dismissed without payment, and physicians are found not negligent in over 90% of cases that do go to trial.
While there are no readily available national statistics on the actual number of claims filed, there is data, compiled by the federal government’s National Practitioner Data Bank (NPDB), suggesting that the number of cases filed has been dropping in the last decade.

|
|
The NPDB issues an annual report that includes the number of medical malpractice payments made each year for the preceding 10 years. For nearly every year in the past decade, the number of medical malpractice payments made on behalf of all practitioners reported to the NPDB has decreased. Between 2002 and 2011, the number of medical malpractice payments decreased nearly 40%, declining steadily from 18,696 to 11,424.
Also, in the past 10 years, the number of medical malpractice payments reported to the NPDB, attributed to physicians and dentists, has decreased steadily from 17,155 to 10,038. Between 2003 and 2011, the total amount paid out fell from $4.5 billion to less than $3.2 billion, a 29% drop. State tort-reform laws limiting noneconomic damages, growth in risk management responses to adverse events, and the growing use of apology and disclosure likely have contributed to this trend.
Dr. James A.L. Mathers, Jr., is a past president of the American College of Chest Physicians, and is recently retired with 30 years of private practice experience in pulmonary, critical care, and sleep medicine.
A 2011 study in the New England Journal of Medicine estimated that 75% of physicians in "low-risk" specialties and virtually 100% of physicians in "high-risk" specialties could expect to face a malpractice claim sometime in their career (N. Engl. J. Med. 2011;365:629-36). However, 60% of liability claims against doctors are dropped, withdrawn, or dismissed without payment, and physicians are found not negligent in over 90% of cases that do go to trial.
While there are no readily available national statistics on the actual number of claims filed, there is data, compiled by the federal government’s National Practitioner Data Bank (NPDB), suggesting that the number of cases filed has been dropping in the last decade.

|
|
The NPDB issues an annual report that includes the number of medical malpractice payments made each year for the preceding 10 years. For nearly every year in the past decade, the number of medical malpractice payments made on behalf of all practitioners reported to the NPDB has decreased. Between 2002 and 2011, the number of medical malpractice payments decreased nearly 40%, declining steadily from 18,696 to 11,424.
Also, in the past 10 years, the number of medical malpractice payments reported to the NPDB, attributed to physicians and dentists, has decreased steadily from 17,155 to 10,038. Between 2003 and 2011, the total amount paid out fell from $4.5 billion to less than $3.2 billion, a 29% drop. State tort-reform laws limiting noneconomic damages, growth in risk management responses to adverse events, and the growing use of apology and disclosure likely have contributed to this trend.
Dr. James A.L. Mathers, Jr., is a past president of the American College of Chest Physicians, and is recently retired with 30 years of private practice experience in pulmonary, critical care, and sleep medicine.
Receiving notice that a patient is suing can spark a range of emotions in physicians, including fear, anger, hurt, and helplessness. But litigation experts stress that after a filing, physicians must rein in their feelings and focus on immediate next steps – crucial actions that can significantly impact the suit and its outcome.
"Doctors have two reactions to getting sued – either they’re very sad or they’re very angry," said Steven Fitzer, a medical liability defense attorney at Fitzer, Leighton & Fitzer, P.S., in Tacoma, Wash., and former chair of the Washington State Bar Association Litigation Section. "Relaxing and composing yourself are important because a lawsuit is a marathon – not a sprint."
American Medical Association data show 60% of physicians will be sued by the time they reach 55 years of age. The average span of a medical malpractice claim from start to close is generally about 2.5 years, although many suits progress longer. While most medical liability claims do not end in trial, defense attorneys say knowing how to respond to a lawsuit can raise doctors’ chances of a quicker, more ideal resolution.
First and foremost, physicians should notify their malpractice insurance carrier as soon as possible after lawsuit papers are served, said Matt Mitcham, senior vice president of claims for MagMutual Insurance Company, a medical liability insurer that operates in the Southeast. Employed physicians should immediately alert their risk management department.
"All suits have a limited time for providing a response, and there are severe consequences for not meeting these deadlines," Mr. Mitcham said. "In addition, physicians need to provide their defense team with as much time as possible to prepare a response."
Doctors should resist the desire to contact patients or their families in an attempt to work out the situation themselves, adds Mr. Fitzer, who recently shared lawsuit preparation tips in two video playlists for The Doctors Company, a national medical malpractice insurer.
"Particularly with family practice physicians, they tend to have a long and strong bond with their patients and their patients’ families, and they think, ‘If I just call and ask what’s going on, we can just fix this all right here,’ " he said. "That never works. The patient or their lawyer will take whatever you say in or out of context and use it against you."
Another action to avoid after a lawsuit filing is making additions or changes to patient records, said Mr. Mitcham.
"The original records should never be altered under any circumstance," he said. "Today’s forensic specialists are experts in identifying changes, and by altering records, a physician can potentially turn a defensible case into one that is indefensible."
Securing an attorney that doctors trust and with whom they can aptly communicate is also essential, said Michael F. Ball, a medical liability defense attorney and partner at McCormick Barstow, LLP, in Fresno, Calif. Most doctors may not realize they can typically choose from a panel of attorneys used by their insurer, he said. Physicians can also ask to view the attorney panel and conduct their own research before requesting a specific lawyer.
Mr. Ball counsels his clients to focus only on the task at hand during each stage of a lawsuit, rather than worry about future phases or a possible trial. For example, during the deposition stage, physicians should prepare by understanding the deposition’s purpose, reading through the record, and being clear on what questions may be asked. A deposition is a witness’s sworn, out-of-court testimony used to gather information as part of the discovery process.
"Some [physicians] don’t review the record as closely as they should," he said. "There’s no substitute for real preparation."
Additionally, depositions are a stage in which a physician’s emotions may come bubbling to the surface, notes Angela Dodge, Ph.D., founding partner of Dodge Consulting & Publications, LLP, a litigation consulting firm in the Seattle-Tacoma area.
"A doctor may go into a deposition feeling very angry and resentful because a patient they believe they gave good care to is now suing," said Ms. Dodge, author of the book "When Good Doctors Get Sued: A Practical Guide for Physicians Involved in Malpractice Lawsuits, and Winning at Jury Selection." "We counsel them on the importance of setting that aside because it could interfere with" their success.
Negative emotions by doctors may be interpreted by plaintiffs’ attorneys as guilt or defensiveness and used to fuel their claims, she said. Doctors should also focus only on the questions being asked during a deposition and not offer up any further or additional information. For instance, in a recent case, a doctor was asked about a specific part of his education. In response, the physician provided unnecessary information about his entire medical education, including his experience operating on pigs, how pig anatomy is relevant to human medicine, and other needless details, Ms. Dodge said.
"He was so anxious to explain how he gained his expertise; he forgot that the question was [only] where and when he gained his expertise," she said.
Litigation counselors point to strong cooperation among physicians, insurers, and defense attorneys as one of the most vital components to the successful handling of a lawsuit.
"The legal system can be a very daunting place for physicians, but when the malpractice carrier and defense attorney work together as a team, they can help the physician navigate the process and hopefully win the case," Mr. Mitcham said.
Receiving notice that a patient is suing can spark a range of emotions in physicians, including fear, anger, hurt, and helplessness. But litigation experts stress that after a filing, physicians must rein in their feelings and focus on immediate next steps – crucial actions that can significantly impact the suit and its outcome.
"Doctors have two reactions to getting sued – either they’re very sad or they’re very angry," said Steven Fitzer, a medical liability defense attorney at Fitzer, Leighton & Fitzer, P.S., in Tacoma, Wash., and former chair of the Washington State Bar Association Litigation Section. "Relaxing and composing yourself are important because a lawsuit is a marathon – not a sprint."
American Medical Association data show 60% of physicians will be sued by the time they reach 55 years of age. The average span of a medical malpractice claim from start to close is generally about 2.5 years, although many suits progress longer. While most medical liability claims do not end in trial, defense attorneys say knowing how to respond to a lawsuit can raise doctors’ chances of a quicker, more ideal resolution.
First and foremost, physicians should notify their malpractice insurance carrier as soon as possible after lawsuit papers are served, said Matt Mitcham, senior vice president of claims for MagMutual Insurance Company, a medical liability insurer that operates in the Southeast. Employed physicians should immediately alert their risk management department.
"All suits have a limited time for providing a response, and there are severe consequences for not meeting these deadlines," Mr. Mitcham said. "In addition, physicians need to provide their defense team with as much time as possible to prepare a response."
Doctors should resist the desire to contact patients or their families in an attempt to work out the situation themselves, adds Mr. Fitzer, who recently shared lawsuit preparation tips in two video playlists for The Doctors Company, a national medical malpractice insurer.
"Particularly with family practice physicians, they tend to have a long and strong bond with their patients and their patients’ families, and they think, ‘If I just call and ask what’s going on, we can just fix this all right here,’ " he said. "That never works. The patient or their lawyer will take whatever you say in or out of context and use it against you."
Another action to avoid after a lawsuit filing is making additions or changes to patient records, said Mr. Mitcham.
"The original records should never be altered under any circumstance," he said. "Today’s forensic specialists are experts in identifying changes, and by altering records, a physician can potentially turn a defensible case into one that is indefensible."
Securing an attorney that doctors trust and with whom they can aptly communicate is also essential, said Michael F. Ball, a medical liability defense attorney and partner at McCormick Barstow, LLP, in Fresno, Calif. Most doctors may not realize they can typically choose from a panel of attorneys used by their insurer, he said. Physicians can also ask to view the attorney panel and conduct their own research before requesting a specific lawyer.
Mr. Ball counsels his clients to focus only on the task at hand during each stage of a lawsuit, rather than worry about future phases or a possible trial. For example, during the deposition stage, physicians should prepare by understanding the deposition’s purpose, reading through the record, and being clear on what questions may be asked. A deposition is a witness’s sworn, out-of-court testimony used to gather information as part of the discovery process.
"Some [physicians] don’t review the record as closely as they should," he said. "There’s no substitute for real preparation."
Additionally, depositions are a stage in which a physician’s emotions may come bubbling to the surface, notes Angela Dodge, Ph.D., founding partner of Dodge Consulting & Publications, LLP, a litigation consulting firm in the Seattle-Tacoma area.
"A doctor may go into a deposition feeling very angry and resentful because a patient they believe they gave good care to is now suing," said Ms. Dodge, author of the book "When Good Doctors Get Sued: A Practical Guide for Physicians Involved in Malpractice Lawsuits, and Winning at Jury Selection." "We counsel them on the importance of setting that aside because it could interfere with" their success.
Negative emotions by doctors may be interpreted by plaintiffs’ attorneys as guilt or defensiveness and used to fuel their claims, she said. Doctors should also focus only on the questions being asked during a deposition and not offer up any further or additional information. For instance, in a recent case, a doctor was asked about a specific part of his education. In response, the physician provided unnecessary information about his entire medical education, including his experience operating on pigs, how pig anatomy is relevant to human medicine, and other needless details, Ms. Dodge said.
"He was so anxious to explain how he gained his expertise; he forgot that the question was [only] where and when he gained his expertise," she said.
Litigation counselors point to strong cooperation among physicians, insurers, and defense attorneys as one of the most vital components to the successful handling of a lawsuit.
"The legal system can be a very daunting place for physicians, but when the malpractice carrier and defense attorney work together as a team, they can help the physician navigate the process and hopefully win the case," Mr. Mitcham said.
Physician offices provided $10.5 billion in uncompensated care in 2013
Office-based physicians provided an estimated $10.5 billion worth of in-kind services and charity care to the uninsured in 2013, according to an analysis of uncompensated care in the United States.
Total expenditures for care to the uninsured were projected by using two methods: One used data from the federal Medical Expenditure Panel Survey (MEPS), and the other "used published secondary data from health care providers and government sources," said Teresa A. Coughlin and her associates at the Urban Institute in Washington.
The MEPS data yielded a total uncompensated expenditure of $84.9 billion for 2013, while the second analysis projected a total cost of $74.9 billion. The difference reflects the exclusion of information from some sources in the second analysis, such as drugs provided at no charge by some pharmaceutical companies, and conservative assumptions made about uncompensated care provided by publicly funded sources such as the U.S. Department of Veterans Affairs and the Indian Health Service, they said (Health Aff. 2014;33:807-14).
The $10.5 billion in care provided by office-based physicians represents 14% of the $74.9 billion from the second analysis. The largest share (59.5%, or $44.6 billion) was provided by hospitals, with the other $19.8 billion (26.4%) coming from community sources funded by the VA, IHS, local and state health departments, and automobile and home-owners insurance, Ms. Coughlin and her associates reported.
The MEPS data could not be used to see how costs of uncompensated care were divided among providers and which funding sources paid for such care, so only the second analysis estimated physicians’ share, the investigators noted.
The study was part of a project for the Kaiser Commission on Medicaid and the Uninsured.
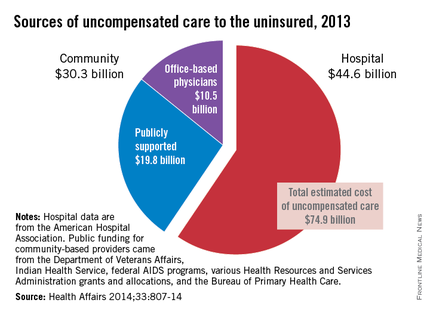
Office-based physicians provided an estimated $10.5 billion worth of in-kind services and charity care to the uninsured in 2013, according to an analysis of uncompensated care in the United States.
Total expenditures for care to the uninsured were projected by using two methods: One used data from the federal Medical Expenditure Panel Survey (MEPS), and the other "used published secondary data from health care providers and government sources," said Teresa A. Coughlin and her associates at the Urban Institute in Washington.
The MEPS data yielded a total uncompensated expenditure of $84.9 billion for 2013, while the second analysis projected a total cost of $74.9 billion. The difference reflects the exclusion of information from some sources in the second analysis, such as drugs provided at no charge by some pharmaceutical companies, and conservative assumptions made about uncompensated care provided by publicly funded sources such as the U.S. Department of Veterans Affairs and the Indian Health Service, they said (Health Aff. 2014;33:807-14).
The $10.5 billion in care provided by office-based physicians represents 14% of the $74.9 billion from the second analysis. The largest share (59.5%, or $44.6 billion) was provided by hospitals, with the other $19.8 billion (26.4%) coming from community sources funded by the VA, IHS, local and state health departments, and automobile and home-owners insurance, Ms. Coughlin and her associates reported.
The MEPS data could not be used to see how costs of uncompensated care were divided among providers and which funding sources paid for such care, so only the second analysis estimated physicians’ share, the investigators noted.
The study was part of a project for the Kaiser Commission on Medicaid and the Uninsured.
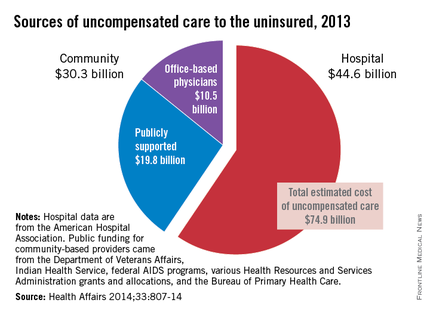
Office-based physicians provided an estimated $10.5 billion worth of in-kind services and charity care to the uninsured in 2013, according to an analysis of uncompensated care in the United States.
Total expenditures for care to the uninsured were projected by using two methods: One used data from the federal Medical Expenditure Panel Survey (MEPS), and the other "used published secondary data from health care providers and government sources," said Teresa A. Coughlin and her associates at the Urban Institute in Washington.
The MEPS data yielded a total uncompensated expenditure of $84.9 billion for 2013, while the second analysis projected a total cost of $74.9 billion. The difference reflects the exclusion of information from some sources in the second analysis, such as drugs provided at no charge by some pharmaceutical companies, and conservative assumptions made about uncompensated care provided by publicly funded sources such as the U.S. Department of Veterans Affairs and the Indian Health Service, they said (Health Aff. 2014;33:807-14).
The $10.5 billion in care provided by office-based physicians represents 14% of the $74.9 billion from the second analysis. The largest share (59.5%, or $44.6 billion) was provided by hospitals, with the other $19.8 billion (26.4%) coming from community sources funded by the VA, IHS, local and state health departments, and automobile and home-owners insurance, Ms. Coughlin and her associates reported.
The MEPS data could not be used to see how costs of uncompensated care were divided among providers and which funding sources paid for such care, so only the second analysis estimated physicians’ share, the investigators noted.
The study was part of a project for the Kaiser Commission on Medicaid and the Uninsured.
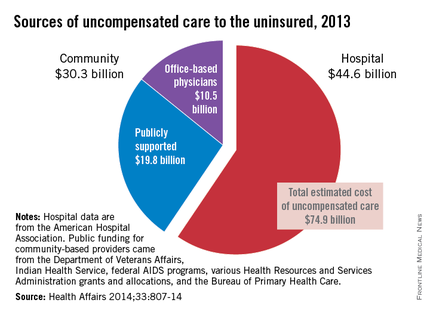
FROM HEALTH AFFAIRS
Federal legislation would provide doctors litigation safe harbor
Physician leaders are voicing support for a proposed federal law that aims to reduce litigation against doctors, lower health care costs, and establish more fairness in the analyzing of malpractice claims. The Saving Lives, Saving Costs Act, introduced in March by Rep. Dr. Ami Bera, (D-CA), would provide safe harbor protection to doctors who are sued if they followed evidence-based clinical guidelines.
"The Bera/Barr bill would accomplish two very important things," said Dr. John C. Jennings, president of the American Congress of Obstetricians and Gynecologists and professor of obstetrics and gynecology at Texas Tech University Health Sciences Center at the Permian Basin. "First, it would provide an incentive for every physician to follow the best clinical guidelines developed by his or her specialty, reducing care variations and potentially increasing patient safety and quality of care. Second, it would provide an affirmative defense for physicians who have followed their specialties’ guidelines and find themselves in the middle of a malpractice suit."
Under the bill, clinical guidelines developed by professional medical organizations would be used to determine whether a plaintiff’s lawsuit could continue against a physician defendant. If a doctor adhered to the approved guidelines during the time of the alleged malpractice event, the case would be removed from court proceedings, while a medical review panel investigated the claim. The bill would also allow for relevant cases to be moved from state to federal court if they involved federal dollars such as Medicare.The bill was referred to the Subcommittee on the Constitution and Civil Justice on March 20 for review.
Dr. Bera declined to comment for this article. In a statement, he said the measure is a practical way to decrease the skyrocketing cost of health care and to ensure the malpractice system works better for patients and physicians.
"As a doctor, I know that physicians want to do what’s best for their patients, and promoting evidence-based medicine will help us do that," he said.
The proposed safe harbor measure is a beneficial initiative that would potentially have a positive impact on multiple aspects of the health care system, adds Dr. David A. Fleming, president-elect of the American College of Physicians and chair of the department of medicine for the University of Missouri–Columbia.
"I think anything that standardized a patient-centered and evidence-based approach to care will serve only to improve clinical outcomes and decrease health care costs, as well as decrease liability costs at every level," Dr. Fleming said in an interview. "Encouraging the use of generally accepted and evidence-based clinical guidelines, as promoted by the Saving Lives, Saving Costs federal bill, is a good way to reach that."
Dr. Fleming noted an ACP position paper published in April that discusses the medical liability crisis physicians continue to face and outlines innovative solutions for a better malpractice environment. "Medical Liability Reform – Innovative Solutions for New Health Care System," also provides an update on state-based medical liability activities and summarizes traditional and newer tort reform proposals.
The paper highlights the positive effect of such state reforms as caps on noneconomic damages, injury funds, stronger expert witness rules, and alternative dispute resolution initiatives such as apology, disclosure, and compensation programs. The report provides nine approaches that should be incorporated into a multifaceted medical malpractice reform initiative, including passage of a comprehensive tort reform package, oversight of medical liability insurers, and development of effective safe harbor protections that improve quality of care, increase efficiency, and reduce costs.
As for federal reform, Dr. Fleming said legislation at the congressional level often faces successful challenges by trial attorneys and advocacy groups that argue plaintiffs’ rights would be violated. The politicization of the issue is also a problem, he said. However, federal tort reform is still possible and physicians should keep advocating significant changes by Congress, he said.
"The litigious environment in which we live continues to contribute to a sense of fear and consternation by practicing physicians that affects how they relate to patients and undoubtedly adds to health care costs," Dr. Fleming said.
Along with the Saving Lives, Saving Costs bills, doctors are closely watching several other federal malpractice reform measures under review. For instance, the Health Care Safety Net Enhancement Act would help ensure that physicians furnishing medical services, pursuant to the Emergency Medical Treatment & Active Labor Act (EMTALA), receive the same liability coverage currently extended to health professionals who provide Medicaid services at free clinics. The bill has been referred to the Subcommittee on Health.
Meanwhile, the Standard of Care Protection Act of 2013 would ensure that provisions of the Affordable Care Act and other federal laws cannot be used to create new standards of care for medical liability lawsuits. The proposed law was included in the recent Medicare Sustainable Growth Rate Formula bill, which passed out of the Energy and Commerce Committee.
"With so many changes occurring in the health care system, physicians are rightly concerned that federal rules and regulations could result in new, unwarranted, liability exposures," Dr. Jennings said. "This legislation helps safeguard physicians."
Physician leaders are voicing support for a proposed federal law that aims to reduce litigation against doctors, lower health care costs, and establish more fairness in the analyzing of malpractice claims. The Saving Lives, Saving Costs Act, introduced in March by Rep. Dr. Ami Bera, (D-CA), would provide safe harbor protection to doctors who are sued if they followed evidence-based clinical guidelines.
"The Bera/Barr bill would accomplish two very important things," said Dr. John C. Jennings, president of the American Congress of Obstetricians and Gynecologists and professor of obstetrics and gynecology at Texas Tech University Health Sciences Center at the Permian Basin. "First, it would provide an incentive for every physician to follow the best clinical guidelines developed by his or her specialty, reducing care variations and potentially increasing patient safety and quality of care. Second, it would provide an affirmative defense for physicians who have followed their specialties’ guidelines and find themselves in the middle of a malpractice suit."
Under the bill, clinical guidelines developed by professional medical organizations would be used to determine whether a plaintiff’s lawsuit could continue against a physician defendant. If a doctor adhered to the approved guidelines during the time of the alleged malpractice event, the case would be removed from court proceedings, while a medical review panel investigated the claim. The bill would also allow for relevant cases to be moved from state to federal court if they involved federal dollars such as Medicare.The bill was referred to the Subcommittee on the Constitution and Civil Justice on March 20 for review.
Dr. Bera declined to comment for this article. In a statement, he said the measure is a practical way to decrease the skyrocketing cost of health care and to ensure the malpractice system works better for patients and physicians.
"As a doctor, I know that physicians want to do what’s best for their patients, and promoting evidence-based medicine will help us do that," he said.
The proposed safe harbor measure is a beneficial initiative that would potentially have a positive impact on multiple aspects of the health care system, adds Dr. David A. Fleming, president-elect of the American College of Physicians and chair of the department of medicine for the University of Missouri–Columbia.
"I think anything that standardized a patient-centered and evidence-based approach to care will serve only to improve clinical outcomes and decrease health care costs, as well as decrease liability costs at every level," Dr. Fleming said in an interview. "Encouraging the use of generally accepted and evidence-based clinical guidelines, as promoted by the Saving Lives, Saving Costs federal bill, is a good way to reach that."
Dr. Fleming noted an ACP position paper published in April that discusses the medical liability crisis physicians continue to face and outlines innovative solutions for a better malpractice environment. "Medical Liability Reform – Innovative Solutions for New Health Care System," also provides an update on state-based medical liability activities and summarizes traditional and newer tort reform proposals.
The paper highlights the positive effect of such state reforms as caps on noneconomic damages, injury funds, stronger expert witness rules, and alternative dispute resolution initiatives such as apology, disclosure, and compensation programs. The report provides nine approaches that should be incorporated into a multifaceted medical malpractice reform initiative, including passage of a comprehensive tort reform package, oversight of medical liability insurers, and development of effective safe harbor protections that improve quality of care, increase efficiency, and reduce costs.
As for federal reform, Dr. Fleming said legislation at the congressional level often faces successful challenges by trial attorneys and advocacy groups that argue plaintiffs’ rights would be violated. The politicization of the issue is also a problem, he said. However, federal tort reform is still possible and physicians should keep advocating significant changes by Congress, he said.
"The litigious environment in which we live continues to contribute to a sense of fear and consternation by practicing physicians that affects how they relate to patients and undoubtedly adds to health care costs," Dr. Fleming said.
Along with the Saving Lives, Saving Costs bills, doctors are closely watching several other federal malpractice reform measures under review. For instance, the Health Care Safety Net Enhancement Act would help ensure that physicians furnishing medical services, pursuant to the Emergency Medical Treatment & Active Labor Act (EMTALA), receive the same liability coverage currently extended to health professionals who provide Medicaid services at free clinics. The bill has been referred to the Subcommittee on Health.
Meanwhile, the Standard of Care Protection Act of 2013 would ensure that provisions of the Affordable Care Act and other federal laws cannot be used to create new standards of care for medical liability lawsuits. The proposed law was included in the recent Medicare Sustainable Growth Rate Formula bill, which passed out of the Energy and Commerce Committee.
"With so many changes occurring in the health care system, physicians are rightly concerned that federal rules and regulations could result in new, unwarranted, liability exposures," Dr. Jennings said. "This legislation helps safeguard physicians."
Physician leaders are voicing support for a proposed federal law that aims to reduce litigation against doctors, lower health care costs, and establish more fairness in the analyzing of malpractice claims. The Saving Lives, Saving Costs Act, introduced in March by Rep. Dr. Ami Bera, (D-CA), would provide safe harbor protection to doctors who are sued if they followed evidence-based clinical guidelines.
"The Bera/Barr bill would accomplish two very important things," said Dr. John C. Jennings, president of the American Congress of Obstetricians and Gynecologists and professor of obstetrics and gynecology at Texas Tech University Health Sciences Center at the Permian Basin. "First, it would provide an incentive for every physician to follow the best clinical guidelines developed by his or her specialty, reducing care variations and potentially increasing patient safety and quality of care. Second, it would provide an affirmative defense for physicians who have followed their specialties’ guidelines and find themselves in the middle of a malpractice suit."
Under the bill, clinical guidelines developed by professional medical organizations would be used to determine whether a plaintiff’s lawsuit could continue against a physician defendant. If a doctor adhered to the approved guidelines during the time of the alleged malpractice event, the case would be removed from court proceedings, while a medical review panel investigated the claim. The bill would also allow for relevant cases to be moved from state to federal court if they involved federal dollars such as Medicare.The bill was referred to the Subcommittee on the Constitution and Civil Justice on March 20 for review.
Dr. Bera declined to comment for this article. In a statement, he said the measure is a practical way to decrease the skyrocketing cost of health care and to ensure the malpractice system works better for patients and physicians.
"As a doctor, I know that physicians want to do what’s best for their patients, and promoting evidence-based medicine will help us do that," he said.
The proposed safe harbor measure is a beneficial initiative that would potentially have a positive impact on multiple aspects of the health care system, adds Dr. David A. Fleming, president-elect of the American College of Physicians and chair of the department of medicine for the University of Missouri–Columbia.
"I think anything that standardized a patient-centered and evidence-based approach to care will serve only to improve clinical outcomes and decrease health care costs, as well as decrease liability costs at every level," Dr. Fleming said in an interview. "Encouraging the use of generally accepted and evidence-based clinical guidelines, as promoted by the Saving Lives, Saving Costs federal bill, is a good way to reach that."
Dr. Fleming noted an ACP position paper published in April that discusses the medical liability crisis physicians continue to face and outlines innovative solutions for a better malpractice environment. "Medical Liability Reform – Innovative Solutions for New Health Care System," also provides an update on state-based medical liability activities and summarizes traditional and newer tort reform proposals.
The paper highlights the positive effect of such state reforms as caps on noneconomic damages, injury funds, stronger expert witness rules, and alternative dispute resolution initiatives such as apology, disclosure, and compensation programs. The report provides nine approaches that should be incorporated into a multifaceted medical malpractice reform initiative, including passage of a comprehensive tort reform package, oversight of medical liability insurers, and development of effective safe harbor protections that improve quality of care, increase efficiency, and reduce costs.
As for federal reform, Dr. Fleming said legislation at the congressional level often faces successful challenges by trial attorneys and advocacy groups that argue plaintiffs’ rights would be violated. The politicization of the issue is also a problem, he said. However, federal tort reform is still possible and physicians should keep advocating significant changes by Congress, he said.
"The litigious environment in which we live continues to contribute to a sense of fear and consternation by practicing physicians that affects how they relate to patients and undoubtedly adds to health care costs," Dr. Fleming said.
Along with the Saving Lives, Saving Costs bills, doctors are closely watching several other federal malpractice reform measures under review. For instance, the Health Care Safety Net Enhancement Act would help ensure that physicians furnishing medical services, pursuant to the Emergency Medical Treatment & Active Labor Act (EMTALA), receive the same liability coverage currently extended to health professionals who provide Medicaid services at free clinics. The bill has been referred to the Subcommittee on Health.
Meanwhile, the Standard of Care Protection Act of 2013 would ensure that provisions of the Affordable Care Act and other federal laws cannot be used to create new standards of care for medical liability lawsuits. The proposed law was included in the recent Medicare Sustainable Growth Rate Formula bill, which passed out of the Energy and Commerce Committee.
"With so many changes occurring in the health care system, physicians are rightly concerned that federal rules and regulations could result in new, unwarranted, liability exposures," Dr. Jennings said. "This legislation helps safeguard physicians."
Insurers address ACA 90-day grace period issue
Representatives of major insurance companies assured lawmakers that they have systems in place by which physicians can check whether patients newly insured through the state and federal health exchanges were up to date on payments for their premiums and thus eligible for coverage.
The insurers – Aetna, Cigna, Health Care Service Corporation, and Wellpoint – appeared May 7 before the House Energy and Commerce Oversight and Investigations Subcommittee to answer questions about how many enrollees under the Affordable Care Act’s state and federal health insurance exchanges have paid their premiums.
Rep. Michael Burgess (R-Tex.), a physician and a subcommittee member, said that he was especially concerned about the 90-day grace period that could create a situation in which care delivered by doctors is not covered by insurance companies.
The grace period was built into the Affordable Care Act.
According to the law, patients must pay their first month’s premium to be considered enrolled and verified as insured. After that, however, they have 90 days to pay the next premium. If the patient doesn’t pay for the second month, the insurer can hold or "pend" all claims. By the third month, if the patient still has not paid, the insurer can terminate the policy. The physician is left to collect from the patient whatever is owed for all outstanding claims.
The insurance company officials who testified at the hearing said that they had systems in place that gave physicians the ability to determine if a patient was current on payments and thus eligible for coverage. They did not give much detail beyond that.
Paul Wingle, executive director of individual business and public exchange operations and strategy at Aetna, said that doctors can call Aetna for updates on a patient’s payment status.
Brian Evanko, president of the individual segment at Cigna, said that physicians and hospitals can call or check online for a patient’s current insurance eligibility. J. Darren Rodgers, a senior vice president and marketing officer at Health Care Service Corporation, and Dennis Matheis, president of exchange strategy for Wellpoint, also said that their companies offered similar services for physicians to verify eligibility.
Rep. Burgess said that he still had concerns that physicians could end up delivering uncompensated care.
The insurers also said that, so far, it appears that a majority of exchange plan enrollees are paying their premiums.
Aetna enrolled 600,000 individuals by the third week in April. Of those, 500,000 have paid, said Mr. Wingle, noting that, since many enrollees have not reached the payment due date for coverage, the figure is "dynamic."
Cigna’s Mr. Evanko did not give enrollment or payment data.
Health Care Service Corporation had 830,000 applications for coverage – 600,000 on the exchanges and 230,000 from outside the exchanges, said Mr. Rodgers. In January, February, and March, 85%-88% of exchange plan enrollees had paid.
The payment rate dropped to 83% on April 1; May figures were incomplete, he said.
Mr. Matheis of Wellpoint testified that "we are seeing strong membership growth and large percentages of our newly enrolled customers are successfully paying their premiums by the due date."
He said that, overall, 70% of premiums have been paid, but that figure includes enrollees whose payments were not yet due. For those whose premium deadline has passed, the payment rate is up to 90%, said Mr. Matheis.
Rep. Tim Murphy (R-Pa.), chairman of the oversight and investigations subcommittee, said that the data submitted to the panel by insurers in late April "paints an uneven picture about the status of enrollment and payment through April 15."
A report issued by the Energy and Commerce Committee on April 30 claimed that data from insurers showed that 67% of the enrollees in the federal exchanges had paid their first month’s premium. Rep. Murphy said that the report showed a wild variation in payment rates by state, and that more information was needed.
"We recognize that many individuals still have time to pay their first month’s premium, which is why we have asked the insurers to update this information on May 20," he said.
On Twitter @aliciaault
Representatives of major insurance companies assured lawmakers that they have systems in place by which physicians can check whether patients newly insured through the state and federal health exchanges were up to date on payments for their premiums and thus eligible for coverage.
The insurers – Aetna, Cigna, Health Care Service Corporation, and Wellpoint – appeared May 7 before the House Energy and Commerce Oversight and Investigations Subcommittee to answer questions about how many enrollees under the Affordable Care Act’s state and federal health insurance exchanges have paid their premiums.
Rep. Michael Burgess (R-Tex.), a physician and a subcommittee member, said that he was especially concerned about the 90-day grace period that could create a situation in which care delivered by doctors is not covered by insurance companies.
The grace period was built into the Affordable Care Act.
According to the law, patients must pay their first month’s premium to be considered enrolled and verified as insured. After that, however, they have 90 days to pay the next premium. If the patient doesn’t pay for the second month, the insurer can hold or "pend" all claims. By the third month, if the patient still has not paid, the insurer can terminate the policy. The physician is left to collect from the patient whatever is owed for all outstanding claims.
The insurance company officials who testified at the hearing said that they had systems in place that gave physicians the ability to determine if a patient was current on payments and thus eligible for coverage. They did not give much detail beyond that.
Paul Wingle, executive director of individual business and public exchange operations and strategy at Aetna, said that doctors can call Aetna for updates on a patient’s payment status.
Brian Evanko, president of the individual segment at Cigna, said that physicians and hospitals can call or check online for a patient’s current insurance eligibility. J. Darren Rodgers, a senior vice president and marketing officer at Health Care Service Corporation, and Dennis Matheis, president of exchange strategy for Wellpoint, also said that their companies offered similar services for physicians to verify eligibility.
Rep. Burgess said that he still had concerns that physicians could end up delivering uncompensated care.
The insurers also said that, so far, it appears that a majority of exchange plan enrollees are paying their premiums.
Aetna enrolled 600,000 individuals by the third week in April. Of those, 500,000 have paid, said Mr. Wingle, noting that, since many enrollees have not reached the payment due date for coverage, the figure is "dynamic."
Cigna’s Mr. Evanko did not give enrollment or payment data.
Health Care Service Corporation had 830,000 applications for coverage – 600,000 on the exchanges and 230,000 from outside the exchanges, said Mr. Rodgers. In January, February, and March, 85%-88% of exchange plan enrollees had paid.
The payment rate dropped to 83% on April 1; May figures were incomplete, he said.
Mr. Matheis of Wellpoint testified that "we are seeing strong membership growth and large percentages of our newly enrolled customers are successfully paying their premiums by the due date."
He said that, overall, 70% of premiums have been paid, but that figure includes enrollees whose payments were not yet due. For those whose premium deadline has passed, the payment rate is up to 90%, said Mr. Matheis.
Rep. Tim Murphy (R-Pa.), chairman of the oversight and investigations subcommittee, said that the data submitted to the panel by insurers in late April "paints an uneven picture about the status of enrollment and payment through April 15."
A report issued by the Energy and Commerce Committee on April 30 claimed that data from insurers showed that 67% of the enrollees in the federal exchanges had paid their first month’s premium. Rep. Murphy said that the report showed a wild variation in payment rates by state, and that more information was needed.
"We recognize that many individuals still have time to pay their first month’s premium, which is why we have asked the insurers to update this information on May 20," he said.
On Twitter @aliciaault
Representatives of major insurance companies assured lawmakers that they have systems in place by which physicians can check whether patients newly insured through the state and federal health exchanges were up to date on payments for their premiums and thus eligible for coverage.
The insurers – Aetna, Cigna, Health Care Service Corporation, and Wellpoint – appeared May 7 before the House Energy and Commerce Oversight and Investigations Subcommittee to answer questions about how many enrollees under the Affordable Care Act’s state and federal health insurance exchanges have paid their premiums.
Rep. Michael Burgess (R-Tex.), a physician and a subcommittee member, said that he was especially concerned about the 90-day grace period that could create a situation in which care delivered by doctors is not covered by insurance companies.
The grace period was built into the Affordable Care Act.
According to the law, patients must pay their first month’s premium to be considered enrolled and verified as insured. After that, however, they have 90 days to pay the next premium. If the patient doesn’t pay for the second month, the insurer can hold or "pend" all claims. By the third month, if the patient still has not paid, the insurer can terminate the policy. The physician is left to collect from the patient whatever is owed for all outstanding claims.
The insurance company officials who testified at the hearing said that they had systems in place that gave physicians the ability to determine if a patient was current on payments and thus eligible for coverage. They did not give much detail beyond that.
Paul Wingle, executive director of individual business and public exchange operations and strategy at Aetna, said that doctors can call Aetna for updates on a patient’s payment status.
Brian Evanko, president of the individual segment at Cigna, said that physicians and hospitals can call or check online for a patient’s current insurance eligibility. J. Darren Rodgers, a senior vice president and marketing officer at Health Care Service Corporation, and Dennis Matheis, president of exchange strategy for Wellpoint, also said that their companies offered similar services for physicians to verify eligibility.
Rep. Burgess said that he still had concerns that physicians could end up delivering uncompensated care.
The insurers also said that, so far, it appears that a majority of exchange plan enrollees are paying their premiums.
Aetna enrolled 600,000 individuals by the third week in April. Of those, 500,000 have paid, said Mr. Wingle, noting that, since many enrollees have not reached the payment due date for coverage, the figure is "dynamic."
Cigna’s Mr. Evanko did not give enrollment or payment data.
Health Care Service Corporation had 830,000 applications for coverage – 600,000 on the exchanges and 230,000 from outside the exchanges, said Mr. Rodgers. In January, February, and March, 85%-88% of exchange plan enrollees had paid.
The payment rate dropped to 83% on April 1; May figures were incomplete, he said.
Mr. Matheis of Wellpoint testified that "we are seeing strong membership growth and large percentages of our newly enrolled customers are successfully paying their premiums by the due date."
He said that, overall, 70% of premiums have been paid, but that figure includes enrollees whose payments were not yet due. For those whose premium deadline has passed, the payment rate is up to 90%, said Mr. Matheis.
Rep. Tim Murphy (R-Pa.), chairman of the oversight and investigations subcommittee, said that the data submitted to the panel by insurers in late April "paints an uneven picture about the status of enrollment and payment through April 15."
A report issued by the Energy and Commerce Committee on April 30 claimed that data from insurers showed that 67% of the enrollees in the federal exchanges had paid their first month’s premium. Rep. Murphy said that the report showed a wild variation in payment rates by state, and that more information was needed.
"We recognize that many individuals still have time to pay their first month’s premium, which is why we have asked the insurers to update this information on May 20," he said.
On Twitter @aliciaault