User login
Official Newspaper of the American College of Surgeons
New interventions improve symptoms of GERD
Patients with chronic gastroesophageal reflux disease (GERD) who have failed long-term proton pump inhibitor (PPI) therapy can benefit from surgical intervention with magnetic sphincter augmentation, according to a new study that has validated the long-term safety and efficacy of this procedure.
All 85 patients in the cohort had used PPIs at baseline, but this declined to 15.3% at 5 years. Moderate or severe regurgitation also decreased significantly. It was present in 57% of patients at baseline, but in 1.2% at the 5-year follow-up.
In a second related study, researchers found that compared with patients on esomeprazole therapy, GERD patients who underwent laparoscopic antireflux surgery (LARS), experienced significantly greater reductions in 24-hour esophageal acid exposure after 6 months and at 5 years. Both procedures were effective in achieving and maintaining a reduction in distal esophageal acid exposure down to a normal level, but LARS nearly abolished gastroesophageal acid reflux.
Both studies were published in the May issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.05.028; doi: 10.1016/j.cgh.2015.07.025).
Gastroesophageal reflux disease (GERD) is caused by excessive exposure of esophageal mucosa to gastric acid. Left unchecked, it can lead to chronic symptoms and complications, and is associated with a higher risk for Barrett’s esophagus and esophageal adenocarcinoma.
In the first study, Dr. Robert A. Ganz of Minnesota Gastroenterology PA, Plymouth, Minn., and colleagues, conducted a prospective international study that looked at the safety and efficacy of a magnetic device in adults with GERD.
The Food and Drug Administration approved this magnetic device in 2012, which augments lower esophageal sphincter function in patients with GERD, and the current paper now reports on the final results after 5 years of follow-up.
Quality of life, reflux control, use of PPIs, and side effects were evaluated, and the GERD health-related quality of life (GERD-HRQL) questionnaire was administered at baseline to patients on and off PPIs, and after placement of the device.
A partial response to PPIs was defined as a GERD-HRQL score of 10 or less on PPIs and a score of 15 or higher off PPIs, or a 6-point or more improvement when scores on vs. off PPI were compared.
During the follow-up period, there were no device erosions, migrations, or malfunctions. The median GERD-HRQL score was 27 in patients not taking PPIs and 11 in patients on PPIs at the start of the study. After 5 years with the device in place, this score decreased to 4.
All patients reported that they had the ability to belch and vomit if they needed to. The proportion of patients reporting bothersome swallowing was 5% at baseline and 6% at 5 years (P = .739), and bothersome gas-bloat was present in 52% at baseline but decreased to 8.3% at 5 years.
“Without a procedure to correct an incompetent lower esophageal sphincter, it is unlikely that continued medical therapy would have improved these reflux symptoms, and the severity and frequency of the symptoms may have worsened,” wrote the authors.
In the second study, Dr. Jan G. Hatlebakk of Haukeland University Hospital, Bergen, Norway, and his colleagues analyzed data from a prospective, randomized, open-label trial that compared the efficacy and safety of LARS with esomeprazole (20 or 40 mg/d) over a 5-year period in patients with chronic GERD.
Among patients in the LARS group (n = 116), the median 24-hour esophageal acid exposure was 8.6% at baseline and 0.7% after 6 months and 5 years (P less than .001 vs. baseline).
In the esomeprazole group (n = 151), the median 24-hour esophageal acid exposure was 8.8% at baseline, 2.1% after 6 months, and 1.9% after 5 years (P less than .001, therapy vs. baseline, and LARS vs. esomeprazole).
Gastric acidity was stable in both groups, and patients who needed a dose increase to 40 mg/d experienced more severe supine reflux at baseline, but less esophageal acid exposure (P less than .02) and gastric acidity after their dose was increased. Esophageal and intragastric pH parameters, both on and off therapy, did not seem to long-term symptom breakthrough.
“We found that neither intragastric nor intraesophageal pH parameters could predict the short- and long-term therapeutic outcome, which indicates that response to therapy in patients with GERD is individual and not related directly to normalization of acid reflux parameters alone,” wrote Dr. Hatlebakk and coauthors.
Patients with chronic gastroesophageal reflux disease (GERD) who have failed long-term proton pump inhibitor (PPI) therapy can benefit from surgical intervention with magnetic sphincter augmentation, according to a new study that has validated the long-term safety and efficacy of this procedure.
All 85 patients in the cohort had used PPIs at baseline, but this declined to 15.3% at 5 years. Moderate or severe regurgitation also decreased significantly. It was present in 57% of patients at baseline, but in 1.2% at the 5-year follow-up.
In a second related study, researchers found that compared with patients on esomeprazole therapy, GERD patients who underwent laparoscopic antireflux surgery (LARS), experienced significantly greater reductions in 24-hour esophageal acid exposure after 6 months and at 5 years. Both procedures were effective in achieving and maintaining a reduction in distal esophageal acid exposure down to a normal level, but LARS nearly abolished gastroesophageal acid reflux.
Both studies were published in the May issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.05.028; doi: 10.1016/j.cgh.2015.07.025).
Gastroesophageal reflux disease (GERD) is caused by excessive exposure of esophageal mucosa to gastric acid. Left unchecked, it can lead to chronic symptoms and complications, and is associated with a higher risk for Barrett’s esophagus and esophageal adenocarcinoma.
In the first study, Dr. Robert A. Ganz of Minnesota Gastroenterology PA, Plymouth, Minn., and colleagues, conducted a prospective international study that looked at the safety and efficacy of a magnetic device in adults with GERD.
The Food and Drug Administration approved this magnetic device in 2012, which augments lower esophageal sphincter function in patients with GERD, and the current paper now reports on the final results after 5 years of follow-up.
Quality of life, reflux control, use of PPIs, and side effects were evaluated, and the GERD health-related quality of life (GERD-HRQL) questionnaire was administered at baseline to patients on and off PPIs, and after placement of the device.
A partial response to PPIs was defined as a GERD-HRQL score of 10 or less on PPIs and a score of 15 or higher off PPIs, or a 6-point or more improvement when scores on vs. off PPI were compared.
During the follow-up period, there were no device erosions, migrations, or malfunctions. The median GERD-HRQL score was 27 in patients not taking PPIs and 11 in patients on PPIs at the start of the study. After 5 years with the device in place, this score decreased to 4.
All patients reported that they had the ability to belch and vomit if they needed to. The proportion of patients reporting bothersome swallowing was 5% at baseline and 6% at 5 years (P = .739), and bothersome gas-bloat was present in 52% at baseline but decreased to 8.3% at 5 years.
“Without a procedure to correct an incompetent lower esophageal sphincter, it is unlikely that continued medical therapy would have improved these reflux symptoms, and the severity and frequency of the symptoms may have worsened,” wrote the authors.
In the second study, Dr. Jan G. Hatlebakk of Haukeland University Hospital, Bergen, Norway, and his colleagues analyzed data from a prospective, randomized, open-label trial that compared the efficacy and safety of LARS with esomeprazole (20 or 40 mg/d) over a 5-year period in patients with chronic GERD.
Among patients in the LARS group (n = 116), the median 24-hour esophageal acid exposure was 8.6% at baseline and 0.7% after 6 months and 5 years (P less than .001 vs. baseline).
In the esomeprazole group (n = 151), the median 24-hour esophageal acid exposure was 8.8% at baseline, 2.1% after 6 months, and 1.9% after 5 years (P less than .001, therapy vs. baseline, and LARS vs. esomeprazole).
Gastric acidity was stable in both groups, and patients who needed a dose increase to 40 mg/d experienced more severe supine reflux at baseline, but less esophageal acid exposure (P less than .02) and gastric acidity after their dose was increased. Esophageal and intragastric pH parameters, both on and off therapy, did not seem to long-term symptom breakthrough.
“We found that neither intragastric nor intraesophageal pH parameters could predict the short- and long-term therapeutic outcome, which indicates that response to therapy in patients with GERD is individual and not related directly to normalization of acid reflux parameters alone,” wrote Dr. Hatlebakk and coauthors.
Patients with chronic gastroesophageal reflux disease (GERD) who have failed long-term proton pump inhibitor (PPI) therapy can benefit from surgical intervention with magnetic sphincter augmentation, according to a new study that has validated the long-term safety and efficacy of this procedure.
All 85 patients in the cohort had used PPIs at baseline, but this declined to 15.3% at 5 years. Moderate or severe regurgitation also decreased significantly. It was present in 57% of patients at baseline, but in 1.2% at the 5-year follow-up.
In a second related study, researchers found that compared with patients on esomeprazole therapy, GERD patients who underwent laparoscopic antireflux surgery (LARS), experienced significantly greater reductions in 24-hour esophageal acid exposure after 6 months and at 5 years. Both procedures were effective in achieving and maintaining a reduction in distal esophageal acid exposure down to a normal level, but LARS nearly abolished gastroesophageal acid reflux.
Both studies were published in the May issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.05.028; doi: 10.1016/j.cgh.2015.07.025).
Gastroesophageal reflux disease (GERD) is caused by excessive exposure of esophageal mucosa to gastric acid. Left unchecked, it can lead to chronic symptoms and complications, and is associated with a higher risk for Barrett’s esophagus and esophageal adenocarcinoma.
In the first study, Dr. Robert A. Ganz of Minnesota Gastroenterology PA, Plymouth, Minn., and colleagues, conducted a prospective international study that looked at the safety and efficacy of a magnetic device in adults with GERD.
The Food and Drug Administration approved this magnetic device in 2012, which augments lower esophageal sphincter function in patients with GERD, and the current paper now reports on the final results after 5 years of follow-up.
Quality of life, reflux control, use of PPIs, and side effects were evaluated, and the GERD health-related quality of life (GERD-HRQL) questionnaire was administered at baseline to patients on and off PPIs, and after placement of the device.
A partial response to PPIs was defined as a GERD-HRQL score of 10 or less on PPIs and a score of 15 or higher off PPIs, or a 6-point or more improvement when scores on vs. off PPI were compared.
During the follow-up period, there were no device erosions, migrations, or malfunctions. The median GERD-HRQL score was 27 in patients not taking PPIs and 11 in patients on PPIs at the start of the study. After 5 years with the device in place, this score decreased to 4.
All patients reported that they had the ability to belch and vomit if they needed to. The proportion of patients reporting bothersome swallowing was 5% at baseline and 6% at 5 years (P = .739), and bothersome gas-bloat was present in 52% at baseline but decreased to 8.3% at 5 years.
“Without a procedure to correct an incompetent lower esophageal sphincter, it is unlikely that continued medical therapy would have improved these reflux symptoms, and the severity and frequency of the symptoms may have worsened,” wrote the authors.
In the second study, Dr. Jan G. Hatlebakk of Haukeland University Hospital, Bergen, Norway, and his colleagues analyzed data from a prospective, randomized, open-label trial that compared the efficacy and safety of LARS with esomeprazole (20 or 40 mg/d) over a 5-year period in patients with chronic GERD.
Among patients in the LARS group (n = 116), the median 24-hour esophageal acid exposure was 8.6% at baseline and 0.7% after 6 months and 5 years (P less than .001 vs. baseline).
In the esomeprazole group (n = 151), the median 24-hour esophageal acid exposure was 8.8% at baseline, 2.1% after 6 months, and 1.9% after 5 years (P less than .001, therapy vs. baseline, and LARS vs. esomeprazole).
Gastric acidity was stable in both groups, and patients who needed a dose increase to 40 mg/d experienced more severe supine reflux at baseline, but less esophageal acid exposure (P less than .02) and gastric acidity after their dose was increased. Esophageal and intragastric pH parameters, both on and off therapy, did not seem to long-term symptom breakthrough.
“We found that neither intragastric nor intraesophageal pH parameters could predict the short- and long-term therapeutic outcome, which indicates that response to therapy in patients with GERD is individual and not related directly to normalization of acid reflux parameters alone,” wrote Dr. Hatlebakk and coauthors.
Infections kill many waiting for liver transplant, force others off list
AMSTERDAM – Infection is a major cause of death among patients waiting for a liver transplant, killing more than half of those who contracted one.
Infection also was the biggest reason that patients with end-stage liver disease withdrew from the transplant waiting list, a 9-year-long study has shown. Patients who developed an infection were six times more likely to withdraw than were those who did not, Dr. Loes Alferink wrote in a poster presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
“We need to focus on better prophylactic antibiotic strategies to save lives in patients with end-stage liver disease who are on the waiting list,” said Dr. Alferink of Erasmus Medical Center, Rotterdam, the Netherlands.
She and her colleagues examined the effect of infections on 312 patients who were waiting for a transplant at Erasmus Medical Center from the period of 2006-2013. During that time, a total of 317 infections developed in 144 patients. The infections were fatal in 58% of these patients.
These included spontaneous primary cholangitis (75); spontaneous bacterial peritonitis (61); urogenital (38), respiratory (30), and skin (25) infections; as well as primary bacteremia (22). Also, there were 18 cases of gastroenteritis and 12 cases of Candida esophagitis. The remainder were unspecified infections.
The death rate was highest in primary bacteremia, which killed about 40% of those who developed it. The rate was about 25% in respiratory infections, 20% in spontaneous primary bacteremia, 15% in esophagitis, 10% in gastroenteritis and urinary tract infections, and 10% in patients with multiple site infections.
The pathogens were gram negative (70) and gram positive (37) bacteria; Enterococcus faecium (15) and faecalis (3); yeasts (13); viruses (7); and mold (2). The remainder of the infections yielded a negative culture.
In 24 patients, multiple pathogens were identified. These patients had the highest rate of mortality, with almost half of them dying from their infection; one of the two patients with a mold infection also died. The death rate was 20% in patients with yeast infections, 18% in those with E. faecium, 15% in gram-positive infections, and 10% in gram-negative infections.
A multivariate analysis found several factors that increased the risk of dying from an infection. For every 10 years of increasing age, the risk of infection-related mortality doubled (odds ratio, 2); worse MELD (Model for End-Stage Liver Disease) scores increased the risk by 12%.
Patients with hepatic encephalopathy were 76% more likely to die from an infection, and those with refractory ascites faced a 2.5-fold increased risk. Mechanical ventilation was associated with more than a fivefold increased risk (OR, 5.72).
Patients who developed an infection were almost six times more likely to be withdrawn from the transplant waiting list (hazard ratio, 5.87). The regression analysis for withdrawal identified several factors that significantly increased the risk, including age, MELD score, and serum albumin. The biggest risk factor for withdrawal related to infection was refractory ascites, which more than doubled the risk (HR, 2.2).
Dr. Alferink had no financial disclosures.
On Twitter @Alz_Gal
AMSTERDAM – Infection is a major cause of death among patients waiting for a liver transplant, killing more than half of those who contracted one.
Infection also was the biggest reason that patients with end-stage liver disease withdrew from the transplant waiting list, a 9-year-long study has shown. Patients who developed an infection were six times more likely to withdraw than were those who did not, Dr. Loes Alferink wrote in a poster presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
“We need to focus on better prophylactic antibiotic strategies to save lives in patients with end-stage liver disease who are on the waiting list,” said Dr. Alferink of Erasmus Medical Center, Rotterdam, the Netherlands.
She and her colleagues examined the effect of infections on 312 patients who were waiting for a transplant at Erasmus Medical Center from the period of 2006-2013. During that time, a total of 317 infections developed in 144 patients. The infections were fatal in 58% of these patients.
These included spontaneous primary cholangitis (75); spontaneous bacterial peritonitis (61); urogenital (38), respiratory (30), and skin (25) infections; as well as primary bacteremia (22). Also, there were 18 cases of gastroenteritis and 12 cases of Candida esophagitis. The remainder were unspecified infections.
The death rate was highest in primary bacteremia, which killed about 40% of those who developed it. The rate was about 25% in respiratory infections, 20% in spontaneous primary bacteremia, 15% in esophagitis, 10% in gastroenteritis and urinary tract infections, and 10% in patients with multiple site infections.
The pathogens were gram negative (70) and gram positive (37) bacteria; Enterococcus faecium (15) and faecalis (3); yeasts (13); viruses (7); and mold (2). The remainder of the infections yielded a negative culture.
In 24 patients, multiple pathogens were identified. These patients had the highest rate of mortality, with almost half of them dying from their infection; one of the two patients with a mold infection also died. The death rate was 20% in patients with yeast infections, 18% in those with E. faecium, 15% in gram-positive infections, and 10% in gram-negative infections.
A multivariate analysis found several factors that increased the risk of dying from an infection. For every 10 years of increasing age, the risk of infection-related mortality doubled (odds ratio, 2); worse MELD (Model for End-Stage Liver Disease) scores increased the risk by 12%.
Patients with hepatic encephalopathy were 76% more likely to die from an infection, and those with refractory ascites faced a 2.5-fold increased risk. Mechanical ventilation was associated with more than a fivefold increased risk (OR, 5.72).
Patients who developed an infection were almost six times more likely to be withdrawn from the transplant waiting list (hazard ratio, 5.87). The regression analysis for withdrawal identified several factors that significantly increased the risk, including age, MELD score, and serum albumin. The biggest risk factor for withdrawal related to infection was refractory ascites, which more than doubled the risk (HR, 2.2).
Dr. Alferink had no financial disclosures.
On Twitter @Alz_Gal
AMSTERDAM – Infection is a major cause of death among patients waiting for a liver transplant, killing more than half of those who contracted one.
Infection also was the biggest reason that patients with end-stage liver disease withdrew from the transplant waiting list, a 9-year-long study has shown. Patients who developed an infection were six times more likely to withdraw than were those who did not, Dr. Loes Alferink wrote in a poster presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
“We need to focus on better prophylactic antibiotic strategies to save lives in patients with end-stage liver disease who are on the waiting list,” said Dr. Alferink of Erasmus Medical Center, Rotterdam, the Netherlands.
She and her colleagues examined the effect of infections on 312 patients who were waiting for a transplant at Erasmus Medical Center from the period of 2006-2013. During that time, a total of 317 infections developed in 144 patients. The infections were fatal in 58% of these patients.
These included spontaneous primary cholangitis (75); spontaneous bacterial peritonitis (61); urogenital (38), respiratory (30), and skin (25) infections; as well as primary bacteremia (22). Also, there were 18 cases of gastroenteritis and 12 cases of Candida esophagitis. The remainder were unspecified infections.
The death rate was highest in primary bacteremia, which killed about 40% of those who developed it. The rate was about 25% in respiratory infections, 20% in spontaneous primary bacteremia, 15% in esophagitis, 10% in gastroenteritis and urinary tract infections, and 10% in patients with multiple site infections.
The pathogens were gram negative (70) and gram positive (37) bacteria; Enterococcus faecium (15) and faecalis (3); yeasts (13); viruses (7); and mold (2). The remainder of the infections yielded a negative culture.
In 24 patients, multiple pathogens were identified. These patients had the highest rate of mortality, with almost half of them dying from their infection; one of the two patients with a mold infection also died. The death rate was 20% in patients with yeast infections, 18% in those with E. faecium, 15% in gram-positive infections, and 10% in gram-negative infections.
A multivariate analysis found several factors that increased the risk of dying from an infection. For every 10 years of increasing age, the risk of infection-related mortality doubled (odds ratio, 2); worse MELD (Model for End-Stage Liver Disease) scores increased the risk by 12%.
Patients with hepatic encephalopathy were 76% more likely to die from an infection, and those with refractory ascites faced a 2.5-fold increased risk. Mechanical ventilation was associated with more than a fivefold increased risk (OR, 5.72).
Patients who developed an infection were almost six times more likely to be withdrawn from the transplant waiting list (hazard ratio, 5.87). The regression analysis for withdrawal identified several factors that significantly increased the risk, including age, MELD score, and serum albumin. The biggest risk factor for withdrawal related to infection was refractory ascites, which more than doubled the risk (HR, 2.2).
Dr. Alferink had no financial disclosures.
On Twitter @Alz_Gal
AT ECCMID 2016
Key clinical point: Infections are a major cause of transplant wait-list withdrawal and death in patients with end-stage liver disease.
Major finding: Infections increased the risk of withdrawal by sixfold, and killed 58% of those who developed one.
Data source: A retrospective study of 144 patients who developed a total of 317 infections.
Disclosures: Dr. Alferink had no financial disclosures.
Search is on for cases of aggressive, ruxolitinib-associated skin cancers
ORLANDO – The hematologic cancer drug ruxolitinib seems to be associated with cases of aggressive nonmelanoma skin cancer.
After treating a very aggressive squamous cell carcinoma in a 55-year-old man treated with ruxolitinib for polycythemia vera, and hearing firsthand of three other similar cases, Dr. Fiona Zwald is collecting additional data on the association. She intends to publish these cases in a monograph as a warning to dermatologists, hematologists, oncologists, and other physicians who manage patients with hematologic malignancies, she said at the annual meeting of the American College of Mohs Surgery.
The prescribing information for ruxolitinib (Jakafi, Incyte Pharmaceuticals; Jakavi, Novartis) was updated in 2014 to warn that patients taking the drug face an increased risk of nonmelanoma skin cancers. The label also recommends that physicians inspect the skin regularly and urge patients to be alert for and report any new or changing lesions.
Despite the warnings and recommendations, cases are occurring – and some are quite serious, said Dr. Zwald, a Mohs surgeon in Atlanta.
“People should know this is actually happening. If you have experience with this medication, please let us know so we can compile this report. We are trying to assess the number of skin cancers before and after initiating this medication,” she said.
Ruxolitinib is an inhibitor of Janus kinase with a special affinity for the JAK1 and JAK2 subtypes. Like other cytokine-signaling molecules, their function depends on cell context; it may inhibit cell growth in one setting, and, in another, stimulate it. Ruxolitinib was initially approved in 2011 for the treatment of intermediate- and high-risk myelofibrosis, including primary myelofibrosis, post–polycythemia vera myelofibrosis, and post–essential thrombocythemia myelofibrosis.
In 2014, indications for ruxolitinib were expanded to include treatment of patients with polycythemia vera who have had an inadequate response to or are intolerant of hydroxyurea.
Dr. Zwald’s patient had a 10-year history of polycythemia vera. He was initially well controlled on the standard hydroxyurea treatment. In the meantime, he began working as a caddy at a major U.S. golf club. He developed many facial squamous cell carcinomas that were treated with excision and radiation. A year before he presented to Dr. Zwald, he stopped responding to hydroxyurea and was placed on ruxolitinib.
The patient presented with a 4-cm ulcerated lesion over part of his right temple and to the right helical crus; the lesion had developed over 3 months. Dr. Zwald consulted with the patient’s medical oncologist; treatment with ruxolitinib continued, albeit at a reduced dosage in light of recent events.
She performed Mohs surgery on the patient. It was a challenging case, she said, not the least because adequate anesthesia could not be achieved with local anesthetic. Preoperative staging showed no nodal spread.
“He did, unfortunately demonstrate a large, indurated mass located over one branch of the superficial temporal artery. At the helical crus there was an area of bound-down, fixed tumor. Knowing that I would not be able to fully resect this, I passed him on to the operating room,” Dr. Zwald said. “This tumor was found to extend down to the parotid capsule, but margins were clear.” The surgical defect was successfully repaired with a split-thickness skin graft.
The tumor recurred about 3 months later, and the patient underwent another surgery.
“This time we could not get clear surgical margins, and the tumor was approaching the external auditory meatus. Surgery was abandoned due to fears of complications to that area,” she said.
She presented the case at tumor board, during which she and her colleagues discussed adjuvant radiation. They initially abandoned this idea because he had already had so much radiation to his face. After the second surgery, they decide to proceed with radiation. “The next conversation we have will be whether to add another adjuvant therapy to treatment.”
She sent out the case and requests for feedback to the International Transplant Skin Cancer Collaborative, an 800-member consortium of dermatologists and Mohs surgeons who take care of transplant patients. She received information on three additional cases of aggressive squamous cell carcinoma (SCC) associated with ruxolitinib treatment:
• A patient with myelodysplastic syndrome with aggressive scalp SCC with cutaneous metastases.
• A patient with undifferentiated pleomorphic sarcoma of the scalp, several cutaneous SCCs.
• A patient with a myelodysplastic syndrome with in-transit metastases and explosive cutaneous SCCs. The patient has had the ruxolitinib dose reduced and may be switched to capecitabine.
Dr. Zwald noted that her patient was at risk for aggressive skin cancers for reasons in addition to ruxolitinib treatment.
“He was already immunosuppressed from his malignancy. He was on hydroxyurea, a drug that’s a cumulative phototoxin, and he’s out in the sun playing golf every day, and then was put on ruxolitinib. But the question we face now is how to try and stop this medication so we can get better treatment for him which will, of course, be very difficult.”
To contribute to Dr. Zwald’s case series, please email her at [email protected].
She had no relevant financial disclosures.
On Twitter @Alz_Gal
ORLANDO – The hematologic cancer drug ruxolitinib seems to be associated with cases of aggressive nonmelanoma skin cancer.
After treating a very aggressive squamous cell carcinoma in a 55-year-old man treated with ruxolitinib for polycythemia vera, and hearing firsthand of three other similar cases, Dr. Fiona Zwald is collecting additional data on the association. She intends to publish these cases in a monograph as a warning to dermatologists, hematologists, oncologists, and other physicians who manage patients with hematologic malignancies, she said at the annual meeting of the American College of Mohs Surgery.
The prescribing information for ruxolitinib (Jakafi, Incyte Pharmaceuticals; Jakavi, Novartis) was updated in 2014 to warn that patients taking the drug face an increased risk of nonmelanoma skin cancers. The label also recommends that physicians inspect the skin regularly and urge patients to be alert for and report any new or changing lesions.
Despite the warnings and recommendations, cases are occurring – and some are quite serious, said Dr. Zwald, a Mohs surgeon in Atlanta.
“People should know this is actually happening. If you have experience with this medication, please let us know so we can compile this report. We are trying to assess the number of skin cancers before and after initiating this medication,” she said.
Ruxolitinib is an inhibitor of Janus kinase with a special affinity for the JAK1 and JAK2 subtypes. Like other cytokine-signaling molecules, their function depends on cell context; it may inhibit cell growth in one setting, and, in another, stimulate it. Ruxolitinib was initially approved in 2011 for the treatment of intermediate- and high-risk myelofibrosis, including primary myelofibrosis, post–polycythemia vera myelofibrosis, and post–essential thrombocythemia myelofibrosis.
In 2014, indications for ruxolitinib were expanded to include treatment of patients with polycythemia vera who have had an inadequate response to or are intolerant of hydroxyurea.
Dr. Zwald’s patient had a 10-year history of polycythemia vera. He was initially well controlled on the standard hydroxyurea treatment. In the meantime, he began working as a caddy at a major U.S. golf club. He developed many facial squamous cell carcinomas that were treated with excision and radiation. A year before he presented to Dr. Zwald, he stopped responding to hydroxyurea and was placed on ruxolitinib.
The patient presented with a 4-cm ulcerated lesion over part of his right temple and to the right helical crus; the lesion had developed over 3 months. Dr. Zwald consulted with the patient’s medical oncologist; treatment with ruxolitinib continued, albeit at a reduced dosage in light of recent events.
She performed Mohs surgery on the patient. It was a challenging case, she said, not the least because adequate anesthesia could not be achieved with local anesthetic. Preoperative staging showed no nodal spread.
“He did, unfortunately demonstrate a large, indurated mass located over one branch of the superficial temporal artery. At the helical crus there was an area of bound-down, fixed tumor. Knowing that I would not be able to fully resect this, I passed him on to the operating room,” Dr. Zwald said. “This tumor was found to extend down to the parotid capsule, but margins were clear.” The surgical defect was successfully repaired with a split-thickness skin graft.
The tumor recurred about 3 months later, and the patient underwent another surgery.
“This time we could not get clear surgical margins, and the tumor was approaching the external auditory meatus. Surgery was abandoned due to fears of complications to that area,” she said.
She presented the case at tumor board, during which she and her colleagues discussed adjuvant radiation. They initially abandoned this idea because he had already had so much radiation to his face. After the second surgery, they decide to proceed with radiation. “The next conversation we have will be whether to add another adjuvant therapy to treatment.”
She sent out the case and requests for feedback to the International Transplant Skin Cancer Collaborative, an 800-member consortium of dermatologists and Mohs surgeons who take care of transplant patients. She received information on three additional cases of aggressive squamous cell carcinoma (SCC) associated with ruxolitinib treatment:
• A patient with myelodysplastic syndrome with aggressive scalp SCC with cutaneous metastases.
• A patient with undifferentiated pleomorphic sarcoma of the scalp, several cutaneous SCCs.
• A patient with a myelodysplastic syndrome with in-transit metastases and explosive cutaneous SCCs. The patient has had the ruxolitinib dose reduced and may be switched to capecitabine.
Dr. Zwald noted that her patient was at risk for aggressive skin cancers for reasons in addition to ruxolitinib treatment.
“He was already immunosuppressed from his malignancy. He was on hydroxyurea, a drug that’s a cumulative phototoxin, and he’s out in the sun playing golf every day, and then was put on ruxolitinib. But the question we face now is how to try and stop this medication so we can get better treatment for him which will, of course, be very difficult.”
To contribute to Dr. Zwald’s case series, please email her at [email protected].
She had no relevant financial disclosures.
On Twitter @Alz_Gal
ORLANDO – The hematologic cancer drug ruxolitinib seems to be associated with cases of aggressive nonmelanoma skin cancer.
After treating a very aggressive squamous cell carcinoma in a 55-year-old man treated with ruxolitinib for polycythemia vera, and hearing firsthand of three other similar cases, Dr. Fiona Zwald is collecting additional data on the association. She intends to publish these cases in a monograph as a warning to dermatologists, hematologists, oncologists, and other physicians who manage patients with hematologic malignancies, she said at the annual meeting of the American College of Mohs Surgery.
The prescribing information for ruxolitinib (Jakafi, Incyte Pharmaceuticals; Jakavi, Novartis) was updated in 2014 to warn that patients taking the drug face an increased risk of nonmelanoma skin cancers. The label also recommends that physicians inspect the skin regularly and urge patients to be alert for and report any new or changing lesions.
Despite the warnings and recommendations, cases are occurring – and some are quite serious, said Dr. Zwald, a Mohs surgeon in Atlanta.
“People should know this is actually happening. If you have experience with this medication, please let us know so we can compile this report. We are trying to assess the number of skin cancers before and after initiating this medication,” she said.
Ruxolitinib is an inhibitor of Janus kinase with a special affinity for the JAK1 and JAK2 subtypes. Like other cytokine-signaling molecules, their function depends on cell context; it may inhibit cell growth in one setting, and, in another, stimulate it. Ruxolitinib was initially approved in 2011 for the treatment of intermediate- and high-risk myelofibrosis, including primary myelofibrosis, post–polycythemia vera myelofibrosis, and post–essential thrombocythemia myelofibrosis.
In 2014, indications for ruxolitinib were expanded to include treatment of patients with polycythemia vera who have had an inadequate response to or are intolerant of hydroxyurea.
Dr. Zwald’s patient had a 10-year history of polycythemia vera. He was initially well controlled on the standard hydroxyurea treatment. In the meantime, he began working as a caddy at a major U.S. golf club. He developed many facial squamous cell carcinomas that were treated with excision and radiation. A year before he presented to Dr. Zwald, he stopped responding to hydroxyurea and was placed on ruxolitinib.
The patient presented with a 4-cm ulcerated lesion over part of his right temple and to the right helical crus; the lesion had developed over 3 months. Dr. Zwald consulted with the patient’s medical oncologist; treatment with ruxolitinib continued, albeit at a reduced dosage in light of recent events.
She performed Mohs surgery on the patient. It was a challenging case, she said, not the least because adequate anesthesia could not be achieved with local anesthetic. Preoperative staging showed no nodal spread.
“He did, unfortunately demonstrate a large, indurated mass located over one branch of the superficial temporal artery. At the helical crus there was an area of bound-down, fixed tumor. Knowing that I would not be able to fully resect this, I passed him on to the operating room,” Dr. Zwald said. “This tumor was found to extend down to the parotid capsule, but margins were clear.” The surgical defect was successfully repaired with a split-thickness skin graft.
The tumor recurred about 3 months later, and the patient underwent another surgery.
“This time we could not get clear surgical margins, and the tumor was approaching the external auditory meatus. Surgery was abandoned due to fears of complications to that area,” she said.
She presented the case at tumor board, during which she and her colleagues discussed adjuvant radiation. They initially abandoned this idea because he had already had so much radiation to his face. After the second surgery, they decide to proceed with radiation. “The next conversation we have will be whether to add another adjuvant therapy to treatment.”
She sent out the case and requests for feedback to the International Transplant Skin Cancer Collaborative, an 800-member consortium of dermatologists and Mohs surgeons who take care of transplant patients. She received information on three additional cases of aggressive squamous cell carcinoma (SCC) associated with ruxolitinib treatment:
• A patient with myelodysplastic syndrome with aggressive scalp SCC with cutaneous metastases.
• A patient with undifferentiated pleomorphic sarcoma of the scalp, several cutaneous SCCs.
• A patient with a myelodysplastic syndrome with in-transit metastases and explosive cutaneous SCCs. The patient has had the ruxolitinib dose reduced and may be switched to capecitabine.
Dr. Zwald noted that her patient was at risk for aggressive skin cancers for reasons in addition to ruxolitinib treatment.
“He was already immunosuppressed from his malignancy. He was on hydroxyurea, a drug that’s a cumulative phototoxin, and he’s out in the sun playing golf every day, and then was put on ruxolitinib. But the question we face now is how to try and stop this medication so we can get better treatment for him which will, of course, be very difficult.”
To contribute to Dr. Zwald’s case series, please email her at [email protected].
She had no relevant financial disclosures.
On Twitter @Alz_Gal
AT THE ACMS ANNUAL MEETING
Supreme Court case could expand false claims liability
A case before the U.S. Supreme Court could expand physicians’ liability under the False Claims Act (FCA).
The case of Escobar v. Universal Health Services centers on the theory of implied certification and how that legal test should be used to determine whether a claim for payment is fraudulent.
The case “is an opportunity for the Supreme Court to figure out how far the False Claims Act is going to stretch,” said Lawrence M. Kraus, a Boston health law attorney who attended the April 19 oral arguments. “On the practical level, it may have an impact as to whether [such] cases get dismissed at an early stage or whether they go into the discovery phase, which can be quite long, unpleasant, and expensive.”
The Escobar case arises from the death of a patient who was treated at a Lawrence, Mass., mental health clinic operated by Universal Health Services. The patient died from an alleged adverse reaction to medication prescribed for her by clinic staff, according to allegations by her family. The patient’s father, Julio Escobar, later learned counselors and psychologists involved in his daughter’s treatment were not licensed, were not properly supervised by a physician, and had lied about their medical credentials, according to court documents.
The Massachusetts Department of Public Health found the clinic had violated 14 distinct regulations, including those relating to staff licensure and supervision. As a result of the investigation, the clinic entered into a correction plan with the agency and paid a civil fine.
Mr. Escobar and his wife then filed suit under the FCA and the Massachusetts False Claims Act, claiming that Universal had presented false claims to Medicaid by seeking payments for services provided by unlicensed, unsupervised health care providers. Although the reimbursement claims submitted to the government accurately described the services provided and cited the correct charges, the plaintiffs alleged that because the clinic’s operations violated state requirements to participate in Medicaid, Universal had also violated the FCA. The federal government intervened in the case on behalf of the Escobars.
Universal countered that the FCA suit was invalid because a reimbursement claim cannot be false unless its details are untrue or inaccurate.
The plaintiffs, however, contend that a claim does not have to include explicit false statements to be fraudulent. Rather, their complaint relies on “implied certification,” a theory holding that any submission for government payment includes an implicit certification that the health provider has complied with all applicable contract requirements, laws, and regulations that could be a condition of payment. Universal falsely claimed entitlement when it submitted reimbursement requests that did not conform to applicable laws, the plaintiffs argued.
The 1st U.S. Circuit Court of Appeals ruled in favor of Escobar, and Universal appealed to the Supreme Court.
Circuit courts across the country have split on the issue, Mr. Kraus noted.
“There have been a number of different approaches from appeals courts in the country,” he said. “This is not a new issue, but one that the Supreme Court found important enough to decide.”
Why should doctors care about this case?
A ruling for the plaintiff could increase the chances that physicians are accused of an FCA violation after submitting a claim for payment, said William W. Horton, a Birmingham, Ala., health law attorney and chair of the American Bar Association Health Law Section.
“The problem that this raises for health care providers is: There is an enormous web of laws and regulations out there, many of which don’t have anything to do with whether a particular service was rendered or not,” Mr. Horton said in an interview “If you adopt the implied certification theory and take a broad view, than you significantly enhance the scope of claims that could be pursued under the False Claims Act.”
Mr. Horton provides this example: Take a physician group that has an in-office lab, and assume that for some technical reason, the group doesn’t satisfy the Stark Law exception for in-office ancillary services. If a physician in the group refers a Medicare patient to the lab and the group bills Medicare, that’s a Stark Law violation because the group didn’t meet the Stark exception, even if there’s no dispute over whether the patient needed the test or whether the test was done correctly, or whether the Medicare claim accurately reflected the charges, he said. By broadly applying the implied certification theory to this scenario, a case could be made that the practice violated the FCA in submitting the claim because the group was implicitly certifying that the claim did not result from a referral that violated the Stark Law.
“The group could be found liable for the enormous penalties available under the False Claims Act even though the services rendered were medically necessary and appropriate, and even though the group did not expressly certify, in so many words, that the claim did not result from a referral that violated the Stark Law,” Mr. Horton said.
Medical associations, including the American Medical Association and American Hospital Association have weighed in on the case in favor of Universal Health Services. In its brief, the AMA said there is a “sharp distinction” between statutory, regulatory, or contractual violations and false or fraudulent claims.
“Implied certification claims find no support in the statute and do not resemble claims Congress had in mind when enacting or amending the FCA,” according to the brief. “They deprive contractors of their constitutional rights to have notice that they are engaging in conduct subject to heightened sanctions.”
How might the Supreme Court rule?
During oral arguments on April 19, some justices appeared to indicate which way they are leaning, Mr. Kraus said.
Chief Justice John Roberts seemed concerned about the reach of the FCA under the implied certification theory. He raised questions about how people conducting business with the government would know about each and every regulation that could apply as a condition of payment.
Associate Justice Sonia Sotomayer and Associate Justice Elena Kagan appeared in favor of implied certification, while Associate Justice Samuel Alito Jr., Associate Justice Clarence Thomas, and Associate Justice Ruth Bader-Ginsberg did not display a strong opinion either way, Mr. Kraus said. Associate Justice Stephen Breyer appeared to be conflicted, asking for guidance from Roy T. Englert, an attorney for Universal Health Services.
“I’m asking for advice from you, from your point of view,” Justice Breyer said to Mr. Englert. “What the sentence in the opinion should say that describes the circumstances under which the person who submits a form saying, ‘I want a thousand dollars. I just supplied the guns or the medical care.’ ... When has that person committed fraud? – Or that’s what I want. What is the sentence you want me to write?”
Justices could rule a number of ways. They could uphold the appeals court decision, which would affirm a broad interpretation of implied certification theory. They could rule that the implied certification theory is valid, but it cannot be stretched as far as the appeals court expanded it. Justices could choose to reject the implied certification theory altogether and decide that the government must expressly identify every condition of payment in which a health provider is certifying compliance when they submit a claim, either on the claim form or by regulation. The high court could also split on the issue four to four, leaving intact the range of circuit court interpretations on implied certification across the country.
“There’s a very real question as to whether they’re going to be able to get a majority on any of those decisions because this is not an easy question,” Mr. Horton said. “The court has a pretty wide range of potential rulings available to it, but I don’t know what they’re going to be able to majority around, if they’re going to be able get a majority around any result at all.”
A decision in the case is expected by June.
On Twitter @legal_med
A case before the U.S. Supreme Court could expand physicians’ liability under the False Claims Act (FCA).
The case of Escobar v. Universal Health Services centers on the theory of implied certification and how that legal test should be used to determine whether a claim for payment is fraudulent.
The case “is an opportunity for the Supreme Court to figure out how far the False Claims Act is going to stretch,” said Lawrence M. Kraus, a Boston health law attorney who attended the April 19 oral arguments. “On the practical level, it may have an impact as to whether [such] cases get dismissed at an early stage or whether they go into the discovery phase, which can be quite long, unpleasant, and expensive.”
The Escobar case arises from the death of a patient who was treated at a Lawrence, Mass., mental health clinic operated by Universal Health Services. The patient died from an alleged adverse reaction to medication prescribed for her by clinic staff, according to allegations by her family. The patient’s father, Julio Escobar, later learned counselors and psychologists involved in his daughter’s treatment were not licensed, were not properly supervised by a physician, and had lied about their medical credentials, according to court documents.
The Massachusetts Department of Public Health found the clinic had violated 14 distinct regulations, including those relating to staff licensure and supervision. As a result of the investigation, the clinic entered into a correction plan with the agency and paid a civil fine.
Mr. Escobar and his wife then filed suit under the FCA and the Massachusetts False Claims Act, claiming that Universal had presented false claims to Medicaid by seeking payments for services provided by unlicensed, unsupervised health care providers. Although the reimbursement claims submitted to the government accurately described the services provided and cited the correct charges, the plaintiffs alleged that because the clinic’s operations violated state requirements to participate in Medicaid, Universal had also violated the FCA. The federal government intervened in the case on behalf of the Escobars.
Universal countered that the FCA suit was invalid because a reimbursement claim cannot be false unless its details are untrue or inaccurate.
The plaintiffs, however, contend that a claim does not have to include explicit false statements to be fraudulent. Rather, their complaint relies on “implied certification,” a theory holding that any submission for government payment includes an implicit certification that the health provider has complied with all applicable contract requirements, laws, and regulations that could be a condition of payment. Universal falsely claimed entitlement when it submitted reimbursement requests that did not conform to applicable laws, the plaintiffs argued.
The 1st U.S. Circuit Court of Appeals ruled in favor of Escobar, and Universal appealed to the Supreme Court.
Circuit courts across the country have split on the issue, Mr. Kraus noted.
“There have been a number of different approaches from appeals courts in the country,” he said. “This is not a new issue, but one that the Supreme Court found important enough to decide.”
Why should doctors care about this case?
A ruling for the plaintiff could increase the chances that physicians are accused of an FCA violation after submitting a claim for payment, said William W. Horton, a Birmingham, Ala., health law attorney and chair of the American Bar Association Health Law Section.
“The problem that this raises for health care providers is: There is an enormous web of laws and regulations out there, many of which don’t have anything to do with whether a particular service was rendered or not,” Mr. Horton said in an interview “If you adopt the implied certification theory and take a broad view, than you significantly enhance the scope of claims that could be pursued under the False Claims Act.”
Mr. Horton provides this example: Take a physician group that has an in-office lab, and assume that for some technical reason, the group doesn’t satisfy the Stark Law exception for in-office ancillary services. If a physician in the group refers a Medicare patient to the lab and the group bills Medicare, that’s a Stark Law violation because the group didn’t meet the Stark exception, even if there’s no dispute over whether the patient needed the test or whether the test was done correctly, or whether the Medicare claim accurately reflected the charges, he said. By broadly applying the implied certification theory to this scenario, a case could be made that the practice violated the FCA in submitting the claim because the group was implicitly certifying that the claim did not result from a referral that violated the Stark Law.
“The group could be found liable for the enormous penalties available under the False Claims Act even though the services rendered were medically necessary and appropriate, and even though the group did not expressly certify, in so many words, that the claim did not result from a referral that violated the Stark Law,” Mr. Horton said.
Medical associations, including the American Medical Association and American Hospital Association have weighed in on the case in favor of Universal Health Services. In its brief, the AMA said there is a “sharp distinction” between statutory, regulatory, or contractual violations and false or fraudulent claims.
“Implied certification claims find no support in the statute and do not resemble claims Congress had in mind when enacting or amending the FCA,” according to the brief. “They deprive contractors of their constitutional rights to have notice that they are engaging in conduct subject to heightened sanctions.”
How might the Supreme Court rule?
During oral arguments on April 19, some justices appeared to indicate which way they are leaning, Mr. Kraus said.
Chief Justice John Roberts seemed concerned about the reach of the FCA under the implied certification theory. He raised questions about how people conducting business with the government would know about each and every regulation that could apply as a condition of payment.
Associate Justice Sonia Sotomayer and Associate Justice Elena Kagan appeared in favor of implied certification, while Associate Justice Samuel Alito Jr., Associate Justice Clarence Thomas, and Associate Justice Ruth Bader-Ginsberg did not display a strong opinion either way, Mr. Kraus said. Associate Justice Stephen Breyer appeared to be conflicted, asking for guidance from Roy T. Englert, an attorney for Universal Health Services.
“I’m asking for advice from you, from your point of view,” Justice Breyer said to Mr. Englert. “What the sentence in the opinion should say that describes the circumstances under which the person who submits a form saying, ‘I want a thousand dollars. I just supplied the guns or the medical care.’ ... When has that person committed fraud? – Or that’s what I want. What is the sentence you want me to write?”
Justices could rule a number of ways. They could uphold the appeals court decision, which would affirm a broad interpretation of implied certification theory. They could rule that the implied certification theory is valid, but it cannot be stretched as far as the appeals court expanded it. Justices could choose to reject the implied certification theory altogether and decide that the government must expressly identify every condition of payment in which a health provider is certifying compliance when they submit a claim, either on the claim form or by regulation. The high court could also split on the issue four to four, leaving intact the range of circuit court interpretations on implied certification across the country.
“There’s a very real question as to whether they’re going to be able to get a majority on any of those decisions because this is not an easy question,” Mr. Horton said. “The court has a pretty wide range of potential rulings available to it, but I don’t know what they’re going to be able to majority around, if they’re going to be able get a majority around any result at all.”
A decision in the case is expected by June.
On Twitter @legal_med
A case before the U.S. Supreme Court could expand physicians’ liability under the False Claims Act (FCA).
The case of Escobar v. Universal Health Services centers on the theory of implied certification and how that legal test should be used to determine whether a claim for payment is fraudulent.
The case “is an opportunity for the Supreme Court to figure out how far the False Claims Act is going to stretch,” said Lawrence M. Kraus, a Boston health law attorney who attended the April 19 oral arguments. “On the practical level, it may have an impact as to whether [such] cases get dismissed at an early stage or whether they go into the discovery phase, which can be quite long, unpleasant, and expensive.”
The Escobar case arises from the death of a patient who was treated at a Lawrence, Mass., mental health clinic operated by Universal Health Services. The patient died from an alleged adverse reaction to medication prescribed for her by clinic staff, according to allegations by her family. The patient’s father, Julio Escobar, later learned counselors and psychologists involved in his daughter’s treatment were not licensed, were not properly supervised by a physician, and had lied about their medical credentials, according to court documents.
The Massachusetts Department of Public Health found the clinic had violated 14 distinct regulations, including those relating to staff licensure and supervision. As a result of the investigation, the clinic entered into a correction plan with the agency and paid a civil fine.
Mr. Escobar and his wife then filed suit under the FCA and the Massachusetts False Claims Act, claiming that Universal had presented false claims to Medicaid by seeking payments for services provided by unlicensed, unsupervised health care providers. Although the reimbursement claims submitted to the government accurately described the services provided and cited the correct charges, the plaintiffs alleged that because the clinic’s operations violated state requirements to participate in Medicaid, Universal had also violated the FCA. The federal government intervened in the case on behalf of the Escobars.
Universal countered that the FCA suit was invalid because a reimbursement claim cannot be false unless its details are untrue or inaccurate.
The plaintiffs, however, contend that a claim does not have to include explicit false statements to be fraudulent. Rather, their complaint relies on “implied certification,” a theory holding that any submission for government payment includes an implicit certification that the health provider has complied with all applicable contract requirements, laws, and regulations that could be a condition of payment. Universal falsely claimed entitlement when it submitted reimbursement requests that did not conform to applicable laws, the plaintiffs argued.
The 1st U.S. Circuit Court of Appeals ruled in favor of Escobar, and Universal appealed to the Supreme Court.
Circuit courts across the country have split on the issue, Mr. Kraus noted.
“There have been a number of different approaches from appeals courts in the country,” he said. “This is not a new issue, but one that the Supreme Court found important enough to decide.”
Why should doctors care about this case?
A ruling for the plaintiff could increase the chances that physicians are accused of an FCA violation after submitting a claim for payment, said William W. Horton, a Birmingham, Ala., health law attorney and chair of the American Bar Association Health Law Section.
“The problem that this raises for health care providers is: There is an enormous web of laws and regulations out there, many of which don’t have anything to do with whether a particular service was rendered or not,” Mr. Horton said in an interview “If you adopt the implied certification theory and take a broad view, than you significantly enhance the scope of claims that could be pursued under the False Claims Act.”
Mr. Horton provides this example: Take a physician group that has an in-office lab, and assume that for some technical reason, the group doesn’t satisfy the Stark Law exception for in-office ancillary services. If a physician in the group refers a Medicare patient to the lab and the group bills Medicare, that’s a Stark Law violation because the group didn’t meet the Stark exception, even if there’s no dispute over whether the patient needed the test or whether the test was done correctly, or whether the Medicare claim accurately reflected the charges, he said. By broadly applying the implied certification theory to this scenario, a case could be made that the practice violated the FCA in submitting the claim because the group was implicitly certifying that the claim did not result from a referral that violated the Stark Law.
“The group could be found liable for the enormous penalties available under the False Claims Act even though the services rendered were medically necessary and appropriate, and even though the group did not expressly certify, in so many words, that the claim did not result from a referral that violated the Stark Law,” Mr. Horton said.
Medical associations, including the American Medical Association and American Hospital Association have weighed in on the case in favor of Universal Health Services. In its brief, the AMA said there is a “sharp distinction” between statutory, regulatory, or contractual violations and false or fraudulent claims.
“Implied certification claims find no support in the statute and do not resemble claims Congress had in mind when enacting or amending the FCA,” according to the brief. “They deprive contractors of their constitutional rights to have notice that they are engaging in conduct subject to heightened sanctions.”
How might the Supreme Court rule?
During oral arguments on April 19, some justices appeared to indicate which way they are leaning, Mr. Kraus said.
Chief Justice John Roberts seemed concerned about the reach of the FCA under the implied certification theory. He raised questions about how people conducting business with the government would know about each and every regulation that could apply as a condition of payment.
Associate Justice Sonia Sotomayer and Associate Justice Elena Kagan appeared in favor of implied certification, while Associate Justice Samuel Alito Jr., Associate Justice Clarence Thomas, and Associate Justice Ruth Bader-Ginsberg did not display a strong opinion either way, Mr. Kraus said. Associate Justice Stephen Breyer appeared to be conflicted, asking for guidance from Roy T. Englert, an attorney for Universal Health Services.
“I’m asking for advice from you, from your point of view,” Justice Breyer said to Mr. Englert. “What the sentence in the opinion should say that describes the circumstances under which the person who submits a form saying, ‘I want a thousand dollars. I just supplied the guns or the medical care.’ ... When has that person committed fraud? – Or that’s what I want. What is the sentence you want me to write?”
Justices could rule a number of ways. They could uphold the appeals court decision, which would affirm a broad interpretation of implied certification theory. They could rule that the implied certification theory is valid, but it cannot be stretched as far as the appeals court expanded it. Justices could choose to reject the implied certification theory altogether and decide that the government must expressly identify every condition of payment in which a health provider is certifying compliance when they submit a claim, either on the claim form or by regulation. The high court could also split on the issue four to four, leaving intact the range of circuit court interpretations on implied certification across the country.
“There’s a very real question as to whether they’re going to be able to get a majority on any of those decisions because this is not an easy question,” Mr. Horton said. “The court has a pretty wide range of potential rulings available to it, but I don’t know what they’re going to be able to majority around, if they’re going to be able get a majority around any result at all.”
A decision in the case is expected by June.
On Twitter @legal_med
Admission to surgical service appears optimal for adhesive small-bowel obstruction
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
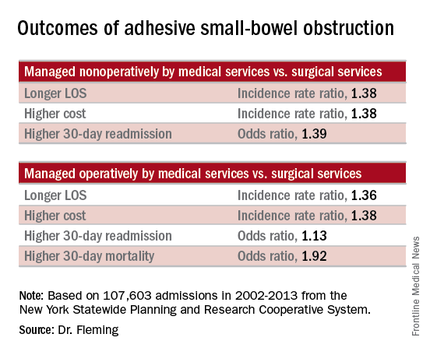
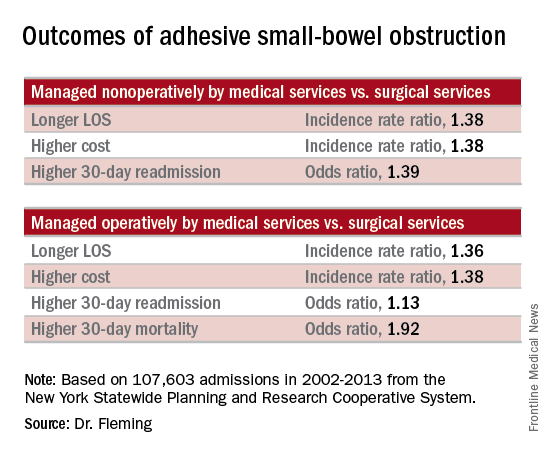
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
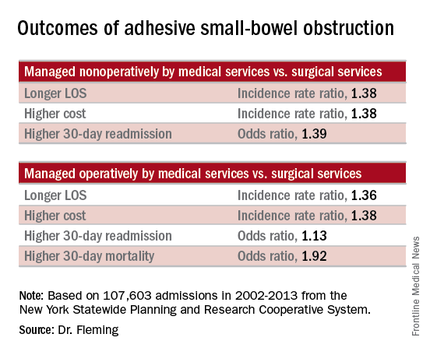
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
CHICAGO – Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggested.
Admission of patients with adhesive small-bowel obstruction (SBO) to medical teams is associated with higher health care costs and worse outcomes; thus, policies favoring primary admission to surgical services could substantially reduce costs and improve outcomes, Dr. Fergal J. Fleming of the University of Rochester (N.Y.) Medical Center reported at the annual meeting of the American Surgical Association.
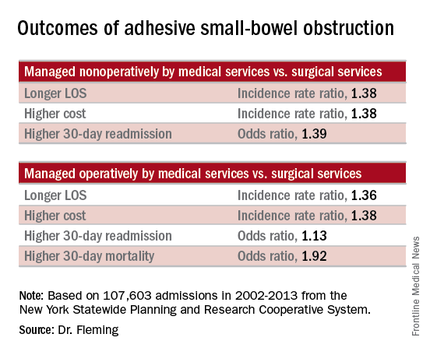
Of 107,603 admissions among patients in the data set, including 78% who were nonoperative and 22% who were operative, 43% were admitted to medical services, and 57% were admitted to surgical services. After several variables, including patient, physician, and hospital-level factors, were controlled for, patients managed nonoperatively primarily by medical services (vs. surgical services) had a longer length of stay (incidence rate ratio, 1.38), higher total cost (incidence rate ratio, 1.38), and higher 30-day readmission rate (odds ratio, 1.39). In addition, those managed operatively primarily by medical services (vs. surgical services) had a greater delay in time to surgical intervention (incidence rate ratio, 1.84), a longer length of stay (incidence rate ratio, 1.36), greater inpatient costs (incidence rate ratio, 1.38), and higher 30-day mortality and 30-day readmission rates (odds ratios, 1.92 and 1.13, respectively), Dr. Fleming said.
Based on these findings and on adjusted population-attributable risk estimates, management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion. In addition, 2,500 deaths and 30,000 readmissions could be avoided annually in the United States, he noted.
Patients with adhesive small-bowel obstruction are known to have high health care utilization. Many patients are admitted to hospitalists – perhaps because most patients are managed nonoperatively, but outcome comparisons between primary medical and surgical services have been limited to single-institution studies, Dr. Fleming said.
Historically, patients with adhesive SBO were managed by surgical services, but with current management strategies, the vast majority are successfully managed without surgery, and a shift over time has resulted in more patients receiving primary management by medical services, he explained.
The current study evaluated the impact of admission to primary medical vs. surgical services on health care utilization and outcomes for adhesive SBO using a population-based data set: the New York Statewide Planning and Research Cooperative System. The system was queried for unscheduled adhesive small bowl obstruction admissions from 2002 to 2013.
Even after adjustment for the older age and increased medical comorbidities of those managed by medical vs. surgical services, the findings demonstrated that outcomes are better with primary management by surgical services, he said, adding that “experience undoubtedly plays a role,” as surgical attendings admit a higher volume of adhesive SBO patients per year.
“We feel this data strongly supports the notion that small-bowel obstruction is a surgical disease and issue, and is best managed by surgeons. … Patients with adhesive small-bowel obstruction should be admitted to surgical service,” he said.
Further, while health care delivery is continually evolving and changing, changes in models of care like that seen over time in the surgical vs. medical service management of adhesive small-bowel obstruction should be studied prospectively before widespread adoption, he said.
Dr. Fleming reported having no relevant financial disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point: Patients with adhesive small-bowel obstruction should be managed by a primary surgical team rather than a medical team, findings from a population-based study suggest.
Major finding: Management by a primary surgical team could result in 1.3 million fewer inpatient days and savings of $2.2 billion.
Data source: A population-based study of more than 107,600 hospital admissions
Disclosures: Dr. Fleming reported having no relevant financial disclosures.
Opioid reform legislation passes House committee
The House Energy & Commerce Committee has passed a comprehensive package of bills designed to curb the nation’s opioid epidemic.
Eleven opioid-related bills passed the full committee by voice vote on April 27 and April 28. Key provisions of the legislation would:
• Create an interagency task force to review best practices for pain management and prescribing.
• Require annual updates of federal opioid-prescribing guidelines.
• Authorize grants to test coprescribing opioids with buprenorphine or naloxone.
• Limit the number of pills prescribed.
• Increase the number of patients that a qualified addiction treatment specialist could see annually.
• Require an FDA advisory committee to review any new opioid proposed without abuse-deterrent properties.
• Require a detailed assessment of currently available inpatient and outpatient treatment beds.
• Prohibit the sale dextromethorphan-containing products to minors.
The full Senate also has a package of opioid-related bills to consider. On March 17, the Senate Committee on Health, Education, Labor and Pensions moved similar legislation to the Senate floor, including bills that would increase addiction patient panels, require coprescribing, and mandate insurance coverage of addiction treatment as required by current mental health parity laws.
Earlier this year, in a near unanimous vote, the Senate passed the Comprehensive Addiction and Recovery Act, which calls for the creation of a federal pain management best practices interagency task force. No funding was attached to the legislation, however, and companion legislation remains in committee in the House.
Although the opioid bills had bipartisan support in the Energy & Commerce Committee, rancor may yet surface. During mark-up, three amendments were defeated mostly along party lines. The amendments would have increased the number of patients each qualified provider can treat with buprenorphine to a variety of levels – one amendment called for a maximum of 250 patients while others called for as many as 300 or 500. Supporters of the amendments said higher numbers would ensure treatment for many more patients while opponents expressed concern about sacrificing quality of care for quantity.
Another defeated amendment called for a $1 billion appropriation for increased opioid treatment, echoing President Obama’s call earlier this year. Opponents painted the proposal as “fiscally irresponsible.”
At press time, the House had not scheduled consideration on the opioid bills.
On Twitter @whitneymcknight
The House Energy & Commerce Committee has passed a comprehensive package of bills designed to curb the nation’s opioid epidemic.
Eleven opioid-related bills passed the full committee by voice vote on April 27 and April 28. Key provisions of the legislation would:
• Create an interagency task force to review best practices for pain management and prescribing.
• Require annual updates of federal opioid-prescribing guidelines.
• Authorize grants to test coprescribing opioids with buprenorphine or naloxone.
• Limit the number of pills prescribed.
• Increase the number of patients that a qualified addiction treatment specialist could see annually.
• Require an FDA advisory committee to review any new opioid proposed without abuse-deterrent properties.
• Require a detailed assessment of currently available inpatient and outpatient treatment beds.
• Prohibit the sale dextromethorphan-containing products to minors.
The full Senate also has a package of opioid-related bills to consider. On March 17, the Senate Committee on Health, Education, Labor and Pensions moved similar legislation to the Senate floor, including bills that would increase addiction patient panels, require coprescribing, and mandate insurance coverage of addiction treatment as required by current mental health parity laws.
Earlier this year, in a near unanimous vote, the Senate passed the Comprehensive Addiction and Recovery Act, which calls for the creation of a federal pain management best practices interagency task force. No funding was attached to the legislation, however, and companion legislation remains in committee in the House.
Although the opioid bills had bipartisan support in the Energy & Commerce Committee, rancor may yet surface. During mark-up, three amendments were defeated mostly along party lines. The amendments would have increased the number of patients each qualified provider can treat with buprenorphine to a variety of levels – one amendment called for a maximum of 250 patients while others called for as many as 300 or 500. Supporters of the amendments said higher numbers would ensure treatment for many more patients while opponents expressed concern about sacrificing quality of care for quantity.
Another defeated amendment called for a $1 billion appropriation for increased opioid treatment, echoing President Obama’s call earlier this year. Opponents painted the proposal as “fiscally irresponsible.”
At press time, the House had not scheduled consideration on the opioid bills.
On Twitter @whitneymcknight
The House Energy & Commerce Committee has passed a comprehensive package of bills designed to curb the nation’s opioid epidemic.
Eleven opioid-related bills passed the full committee by voice vote on April 27 and April 28. Key provisions of the legislation would:
• Create an interagency task force to review best practices for pain management and prescribing.
• Require annual updates of federal opioid-prescribing guidelines.
• Authorize grants to test coprescribing opioids with buprenorphine or naloxone.
• Limit the number of pills prescribed.
• Increase the number of patients that a qualified addiction treatment specialist could see annually.
• Require an FDA advisory committee to review any new opioid proposed without abuse-deterrent properties.
• Require a detailed assessment of currently available inpatient and outpatient treatment beds.
• Prohibit the sale dextromethorphan-containing products to minors.
The full Senate also has a package of opioid-related bills to consider. On March 17, the Senate Committee on Health, Education, Labor and Pensions moved similar legislation to the Senate floor, including bills that would increase addiction patient panels, require coprescribing, and mandate insurance coverage of addiction treatment as required by current mental health parity laws.
Earlier this year, in a near unanimous vote, the Senate passed the Comprehensive Addiction and Recovery Act, which calls for the creation of a federal pain management best practices interagency task force. No funding was attached to the legislation, however, and companion legislation remains in committee in the House.
Although the opioid bills had bipartisan support in the Energy & Commerce Committee, rancor may yet surface. During mark-up, three amendments were defeated mostly along party lines. The amendments would have increased the number of patients each qualified provider can treat with buprenorphine to a variety of levels – one amendment called for a maximum of 250 patients while others called for as many as 300 or 500. Supporters of the amendments said higher numbers would ensure treatment for many more patients while opponents expressed concern about sacrificing quality of care for quantity.
Another defeated amendment called for a $1 billion appropriation for increased opioid treatment, echoing President Obama’s call earlier this year. Opponents painted the proposal as “fiscally irresponsible.”
At press time, the House had not scheduled consideration on the opioid bills.
On Twitter @whitneymcknight
FROM A HOUSE ENERGY & COMMERCE COMMITTEE HEARING
Training impacted performance of surgical quality measures
INDIAN WELLS, CALIF. – Surgeons with fellowship training in female pelvic medicine and reconstructive surgery were significantly more likely to perform proposed quality measures at the time of hysterectomy for pelvic organ prolapse, compared with those who lack such training, a single-center study showed.
“The Physician Quality Reporting System was instituted as part of recent health care reform, with the aim of improving the reporting of quality measures, with the overall goal of improving the quality of care provided to patients throughout all areas of medicine,” Dr. Emily Adams-Piper said at the annual scientific meeting of the Society of Gynecologic Surgeons. “While there are many types of quality measures, including outcome measures and patient satisfaction measures, process measures may be the most directly applicable for the practicing clinician, because they provide recommended actions during specific patient encounters that can guide practice.”
Dr. Adams-Piper, a resident physician in the division of urogynecology at the University of California, Irvine, and her associates set out to investigate the use of proposed quality measures at the time of hysterectomy for pelvic organ prolapse (POP) among women receiving care from Southern California Permanente Medical Group, a large HMO.
They wanted to know if training background affected the rate of performance of four different quality measures related to hysterectomy for POP: offering conservative treatment prior to the surgical treatment of POP, quantitative assessment of POP with either a Baden-Walker or a POP-Q exam, apical support procedure performed at the time of hysterectomy for prolapse, and performance of intraoperative cystoscopy.
Patients who underwent hysterectomy for POP in 2008 were eligible for the study. The researchers reviewed electronic medical records for clinical and demographic data and categorized surgeons by their level of training.
“They were considered fellowship trained if they had pursued additional formal subspecialty training in female pelvic medicine and reconstructive surgery,” Dr. Adams-Piper explained. “Surgeons were considered grandfathered if they subsequently took the FPMRS [Female Pelvic Medicine and Reconstructive Surgery] boards when they became available in 2013. Surgeons were considered generalist if they fit into neither of these two categories and completed a residency in ob.gyn.”
Chi-squared tests were used to compare demographics and performance of the proposed quality measures. Of the 662 hysterectomies performed in 2008, 328 were included in the final analysis. The mean patient age was 60 years, the mean parity was 2.9, and the mean body mass index was 27.9 kg/m2.
Overall performance of the four proposed quality measures was high, ranging from 82%-87%. More than half of quality assessments (58%) were performed with the POP-Q exam, while the majority of apical support procedures were uterosacral ligament vault suspensions (67%), followed by sacrocolpopexy (18%), McCall culdoplasty (12%), and sacrospinous ligament fixation (3%).
When categorized by training, fellowship-trained surgeons performed 133 hysterectomies, “grandfathered” surgeons performed 55, and generalist gynecologic surgeons performed 140. Fellowship-trained surgeons performed each of the four proposed quality measures more often than did grandfathered surgeons, who performed them more often than generalist gynecologic surgeons did.
Specifically, conservative treatment was offered by 94% of fellowship-trained surgeons, 87% of grandfathered surgeons, and 76% of generalist gynecologic surgeons (P = .0002). Qualitative preoperative assessment of POP was performed by 99% of fellowship-trained surgeons, 93% of grandfathered surgeons, and 73% of generalist gynecologic surgeons (three-way comparison reached statistical significance, with a P less than .0001).
Apical repair was performed by 96% of fellowship-trained surgeons, 82% of grandfathered surgeons, and 69% of generalist gynecologic surgeons (P less than .0001). Finally, cystoscopy was performed by 98% of fellowship-trained surgeons, 91% of grandfathered surgeons, and 72% of generalist gynecologic surgeons (P less than .0001).
When the researchers evaluated the cumulative performance of all measures in the same patient, fellowship-trained surgeons had the highest rates (89%, compared with 62% of grandfathered surgeons, and 39% of generalist gynecologic surgeons; P less than .0001).
“When we looked at the patient characteristics and their distribution across the surgeon training backgrounds, we found no significant differences in the age, BMI, gravidity, or parity of the subjects that underwent surgeries with the three groups,” Dr. Adams-Piper said.
She acknowledged certain limitations of the study, including the fact that it reflects clinical practice in a single health care delivery system, it relied on prior documentation, and it evaluated data from 2008.
“From this study we can conclude that perioperative practice patterns differ by surgeon training background,” she said. “However, in order for the proposed quality measures to be clinically meaningful, they must be correlated with patient-centered outcomes.”
Dr. Adams-Piper reported having no financial disclosures. The meeting was jointly sponsored by the American College of Surgeons.
INDIAN WELLS, CALIF. – Surgeons with fellowship training in female pelvic medicine and reconstructive surgery were significantly more likely to perform proposed quality measures at the time of hysterectomy for pelvic organ prolapse, compared with those who lack such training, a single-center study showed.
“The Physician Quality Reporting System was instituted as part of recent health care reform, with the aim of improving the reporting of quality measures, with the overall goal of improving the quality of care provided to patients throughout all areas of medicine,” Dr. Emily Adams-Piper said at the annual scientific meeting of the Society of Gynecologic Surgeons. “While there are many types of quality measures, including outcome measures and patient satisfaction measures, process measures may be the most directly applicable for the practicing clinician, because they provide recommended actions during specific patient encounters that can guide practice.”
Dr. Adams-Piper, a resident physician in the division of urogynecology at the University of California, Irvine, and her associates set out to investigate the use of proposed quality measures at the time of hysterectomy for pelvic organ prolapse (POP) among women receiving care from Southern California Permanente Medical Group, a large HMO.
They wanted to know if training background affected the rate of performance of four different quality measures related to hysterectomy for POP: offering conservative treatment prior to the surgical treatment of POP, quantitative assessment of POP with either a Baden-Walker or a POP-Q exam, apical support procedure performed at the time of hysterectomy for prolapse, and performance of intraoperative cystoscopy.
Patients who underwent hysterectomy for POP in 2008 were eligible for the study. The researchers reviewed electronic medical records for clinical and demographic data and categorized surgeons by their level of training.
“They were considered fellowship trained if they had pursued additional formal subspecialty training in female pelvic medicine and reconstructive surgery,” Dr. Adams-Piper explained. “Surgeons were considered grandfathered if they subsequently took the FPMRS [Female Pelvic Medicine and Reconstructive Surgery] boards when they became available in 2013. Surgeons were considered generalist if they fit into neither of these two categories and completed a residency in ob.gyn.”
Chi-squared tests were used to compare demographics and performance of the proposed quality measures. Of the 662 hysterectomies performed in 2008, 328 were included in the final analysis. The mean patient age was 60 years, the mean parity was 2.9, and the mean body mass index was 27.9 kg/m2.
Overall performance of the four proposed quality measures was high, ranging from 82%-87%. More than half of quality assessments (58%) were performed with the POP-Q exam, while the majority of apical support procedures were uterosacral ligament vault suspensions (67%), followed by sacrocolpopexy (18%), McCall culdoplasty (12%), and sacrospinous ligament fixation (3%).
When categorized by training, fellowship-trained surgeons performed 133 hysterectomies, “grandfathered” surgeons performed 55, and generalist gynecologic surgeons performed 140. Fellowship-trained surgeons performed each of the four proposed quality measures more often than did grandfathered surgeons, who performed them more often than generalist gynecologic surgeons did.
Specifically, conservative treatment was offered by 94% of fellowship-trained surgeons, 87% of grandfathered surgeons, and 76% of generalist gynecologic surgeons (P = .0002). Qualitative preoperative assessment of POP was performed by 99% of fellowship-trained surgeons, 93% of grandfathered surgeons, and 73% of generalist gynecologic surgeons (three-way comparison reached statistical significance, with a P less than .0001).
Apical repair was performed by 96% of fellowship-trained surgeons, 82% of grandfathered surgeons, and 69% of generalist gynecologic surgeons (P less than .0001). Finally, cystoscopy was performed by 98% of fellowship-trained surgeons, 91% of grandfathered surgeons, and 72% of generalist gynecologic surgeons (P less than .0001).
When the researchers evaluated the cumulative performance of all measures in the same patient, fellowship-trained surgeons had the highest rates (89%, compared with 62% of grandfathered surgeons, and 39% of generalist gynecologic surgeons; P less than .0001).
“When we looked at the patient characteristics and their distribution across the surgeon training backgrounds, we found no significant differences in the age, BMI, gravidity, or parity of the subjects that underwent surgeries with the three groups,” Dr. Adams-Piper said.
She acknowledged certain limitations of the study, including the fact that it reflects clinical practice in a single health care delivery system, it relied on prior documentation, and it evaluated data from 2008.
“From this study we can conclude that perioperative practice patterns differ by surgeon training background,” she said. “However, in order for the proposed quality measures to be clinically meaningful, they must be correlated with patient-centered outcomes.”
Dr. Adams-Piper reported having no financial disclosures. The meeting was jointly sponsored by the American College of Surgeons.
INDIAN WELLS, CALIF. – Surgeons with fellowship training in female pelvic medicine and reconstructive surgery were significantly more likely to perform proposed quality measures at the time of hysterectomy for pelvic organ prolapse, compared with those who lack such training, a single-center study showed.
“The Physician Quality Reporting System was instituted as part of recent health care reform, with the aim of improving the reporting of quality measures, with the overall goal of improving the quality of care provided to patients throughout all areas of medicine,” Dr. Emily Adams-Piper said at the annual scientific meeting of the Society of Gynecologic Surgeons. “While there are many types of quality measures, including outcome measures and patient satisfaction measures, process measures may be the most directly applicable for the practicing clinician, because they provide recommended actions during specific patient encounters that can guide practice.”
Dr. Adams-Piper, a resident physician in the division of urogynecology at the University of California, Irvine, and her associates set out to investigate the use of proposed quality measures at the time of hysterectomy for pelvic organ prolapse (POP) among women receiving care from Southern California Permanente Medical Group, a large HMO.
They wanted to know if training background affected the rate of performance of four different quality measures related to hysterectomy for POP: offering conservative treatment prior to the surgical treatment of POP, quantitative assessment of POP with either a Baden-Walker or a POP-Q exam, apical support procedure performed at the time of hysterectomy for prolapse, and performance of intraoperative cystoscopy.
Patients who underwent hysterectomy for POP in 2008 were eligible for the study. The researchers reviewed electronic medical records for clinical and demographic data and categorized surgeons by their level of training.
“They were considered fellowship trained if they had pursued additional formal subspecialty training in female pelvic medicine and reconstructive surgery,” Dr. Adams-Piper explained. “Surgeons were considered grandfathered if they subsequently took the FPMRS [Female Pelvic Medicine and Reconstructive Surgery] boards when they became available in 2013. Surgeons were considered generalist if they fit into neither of these two categories and completed a residency in ob.gyn.”
Chi-squared tests were used to compare demographics and performance of the proposed quality measures. Of the 662 hysterectomies performed in 2008, 328 were included in the final analysis. The mean patient age was 60 years, the mean parity was 2.9, and the mean body mass index was 27.9 kg/m2.
Overall performance of the four proposed quality measures was high, ranging from 82%-87%. More than half of quality assessments (58%) were performed with the POP-Q exam, while the majority of apical support procedures were uterosacral ligament vault suspensions (67%), followed by sacrocolpopexy (18%), McCall culdoplasty (12%), and sacrospinous ligament fixation (3%).
When categorized by training, fellowship-trained surgeons performed 133 hysterectomies, “grandfathered” surgeons performed 55, and generalist gynecologic surgeons performed 140. Fellowship-trained surgeons performed each of the four proposed quality measures more often than did grandfathered surgeons, who performed them more often than generalist gynecologic surgeons did.
Specifically, conservative treatment was offered by 94% of fellowship-trained surgeons, 87% of grandfathered surgeons, and 76% of generalist gynecologic surgeons (P = .0002). Qualitative preoperative assessment of POP was performed by 99% of fellowship-trained surgeons, 93% of grandfathered surgeons, and 73% of generalist gynecologic surgeons (three-way comparison reached statistical significance, with a P less than .0001).
Apical repair was performed by 96% of fellowship-trained surgeons, 82% of grandfathered surgeons, and 69% of generalist gynecologic surgeons (P less than .0001). Finally, cystoscopy was performed by 98% of fellowship-trained surgeons, 91% of grandfathered surgeons, and 72% of generalist gynecologic surgeons (P less than .0001).
When the researchers evaluated the cumulative performance of all measures in the same patient, fellowship-trained surgeons had the highest rates (89%, compared with 62% of grandfathered surgeons, and 39% of generalist gynecologic surgeons; P less than .0001).
“When we looked at the patient characteristics and their distribution across the surgeon training backgrounds, we found no significant differences in the age, BMI, gravidity, or parity of the subjects that underwent surgeries with the three groups,” Dr. Adams-Piper said.
She acknowledged certain limitations of the study, including the fact that it reflects clinical practice in a single health care delivery system, it relied on prior documentation, and it evaluated data from 2008.
“From this study we can conclude that perioperative practice patterns differ by surgeon training background,” she said. “However, in order for the proposed quality measures to be clinically meaningful, they must be correlated with patient-centered outcomes.”
Dr. Adams-Piper reported having no financial disclosures. The meeting was jointly sponsored by the American College of Surgeons.
AT SGS 2016
Key clinical point: The level of surgical training impacted performance of proposed quality measures at the time of hysterectomy for pelvic organ prolapse.
Major finding: Fellowship-trained surgeons in female pelvic medicine and reconstructive surgery were significantly more likely to perform proposed quality measures relating to hysterectomy for pelvic organ prolapse at 89%, compared with 39% of generalist gynecologic surgeons.
Data source: A review 328 hysterectomies performed in 2008 by surgeons in a Southern California HMO.
Disclosures: Dr. Adams-Piper reported having no financial disclosures.
Surgery, pessary are both good options for treating prolapse
INDIAN WELLS, CALIF. – Both surgery and pessary are effective at helping women with pelvic organ prolapse attain pre-treatment goals, improvements in quality of life, and improvements in patient-reported outcome scores, results from a prospective cohort study demonstrated.
“Women seeking care for pelvic organ prolapse have a wide range of severity in symptoms and they often have highly individual goals for treatment,” Dr. Kyle J. Wohlrab said at the annual scientific meeting of the Society of Gynecologic Surgeons. “We know that when we attain those goals, we help their quality of life.”
Dr. Wohlrab, of the Division of Female Pelvic Medicine and Reconstructive Surgery at Women and Infants Hospital, Providence, R.I., and his associates set out to compare goal attainment between women who chose surgery versus pessary for treatment of their pelvic organ prolapse. Their secondary aim was to evaluate the association between improvements in symptoms and quality of life scores with goal attainment.
Women were eligible if they had symptomatic bulge symptoms and stage 2 or greater pelvic organ prolapse. They were enrolled when they chose either surgery or pessary for treatment and had a successful pessary fitting. The study participants were asked what their 10 most important goals for treatment were, and the researchers categorized them as functional goals (physical, social, emotional, and sexual) or symptom goals (prolapse, urinary, bowel, and pain/discomfort).
The secondary study outcomes were patient-reported outcomes based on the Pelvic Floor Distress Inventory-20 (PFDI-20), the Pelvic Floor Impact Questionnaire-short form 7 (PFIQ-7), the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12), and the Body Image Scale (BIS), which were administered at baseline, 6 months, and 12 months.
A total of 160 women were studied, 80 in each treatment group. Compared with those in the pessary group, women in the surgical group were younger at baseline (a mean of 59 years vs. 64 years), and had less severe prolapse (Pelvic Organ Prolapse Quantification System stage 2 vs. 3), but they had worse PFDI-20 scores (a mean of 126 vs. 104) and BIS scores (a mean of 32 vs. 22).
Dr. Wohlrab and his associates found that 75% of patients in the surgery group achieved all of their functional goals, compared with 58% of those in the pessary group, a difference that did not reach statistical significance except in the category of physical function, which favored patients in the surgery group (87% of goals attained, vs. 62% of those in the pessary group; P = .03).
At the same time, 74% of patients in the surgery group achieved all of their symptom goals, compared with 70% of those in the pessary group, a difference that did not reach statistical significance (P = .7).
Both surgery and pessary groups had significant improvements in the PFDI-20, PFIQ-7, and the BIS scores from baseline (P less than .05 for all). Mean scores on the PISQ-12 also improved from baseline in the surgery group (P less than .05), but not in the pessary group.
Dr. Wohlrab reported having no financial disclosures. The meeting was jointly sponsored by the American College of Surgeons.
INDIAN WELLS, CALIF. – Both surgery and pessary are effective at helping women with pelvic organ prolapse attain pre-treatment goals, improvements in quality of life, and improvements in patient-reported outcome scores, results from a prospective cohort study demonstrated.
“Women seeking care for pelvic organ prolapse have a wide range of severity in symptoms and they often have highly individual goals for treatment,” Dr. Kyle J. Wohlrab said at the annual scientific meeting of the Society of Gynecologic Surgeons. “We know that when we attain those goals, we help their quality of life.”
Dr. Wohlrab, of the Division of Female Pelvic Medicine and Reconstructive Surgery at Women and Infants Hospital, Providence, R.I., and his associates set out to compare goal attainment between women who chose surgery versus pessary for treatment of their pelvic organ prolapse. Their secondary aim was to evaluate the association between improvements in symptoms and quality of life scores with goal attainment.
Women were eligible if they had symptomatic bulge symptoms and stage 2 or greater pelvic organ prolapse. They were enrolled when they chose either surgery or pessary for treatment and had a successful pessary fitting. The study participants were asked what their 10 most important goals for treatment were, and the researchers categorized them as functional goals (physical, social, emotional, and sexual) or symptom goals (prolapse, urinary, bowel, and pain/discomfort).
The secondary study outcomes were patient-reported outcomes based on the Pelvic Floor Distress Inventory-20 (PFDI-20), the Pelvic Floor Impact Questionnaire-short form 7 (PFIQ-7), the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12), and the Body Image Scale (BIS), which were administered at baseline, 6 months, and 12 months.
A total of 160 women were studied, 80 in each treatment group. Compared with those in the pessary group, women in the surgical group were younger at baseline (a mean of 59 years vs. 64 years), and had less severe prolapse (Pelvic Organ Prolapse Quantification System stage 2 vs. 3), but they had worse PFDI-20 scores (a mean of 126 vs. 104) and BIS scores (a mean of 32 vs. 22).
Dr. Wohlrab and his associates found that 75% of patients in the surgery group achieved all of their functional goals, compared with 58% of those in the pessary group, a difference that did not reach statistical significance except in the category of physical function, which favored patients in the surgery group (87% of goals attained, vs. 62% of those in the pessary group; P = .03).
At the same time, 74% of patients in the surgery group achieved all of their symptom goals, compared with 70% of those in the pessary group, a difference that did not reach statistical significance (P = .7).
Both surgery and pessary groups had significant improvements in the PFDI-20, PFIQ-7, and the BIS scores from baseline (P less than .05 for all). Mean scores on the PISQ-12 also improved from baseline in the surgery group (P less than .05), but not in the pessary group.
Dr. Wohlrab reported having no financial disclosures. The meeting was jointly sponsored by the American College of Surgeons.
INDIAN WELLS, CALIF. – Both surgery and pessary are effective at helping women with pelvic organ prolapse attain pre-treatment goals, improvements in quality of life, and improvements in patient-reported outcome scores, results from a prospective cohort study demonstrated.
“Women seeking care for pelvic organ prolapse have a wide range of severity in symptoms and they often have highly individual goals for treatment,” Dr. Kyle J. Wohlrab said at the annual scientific meeting of the Society of Gynecologic Surgeons. “We know that when we attain those goals, we help their quality of life.”
Dr. Wohlrab, of the Division of Female Pelvic Medicine and Reconstructive Surgery at Women and Infants Hospital, Providence, R.I., and his associates set out to compare goal attainment between women who chose surgery versus pessary for treatment of their pelvic organ prolapse. Their secondary aim was to evaluate the association between improvements in symptoms and quality of life scores with goal attainment.
Women were eligible if they had symptomatic bulge symptoms and stage 2 or greater pelvic organ prolapse. They were enrolled when they chose either surgery or pessary for treatment and had a successful pessary fitting. The study participants were asked what their 10 most important goals for treatment were, and the researchers categorized them as functional goals (physical, social, emotional, and sexual) or symptom goals (prolapse, urinary, bowel, and pain/discomfort).
The secondary study outcomes were patient-reported outcomes based on the Pelvic Floor Distress Inventory-20 (PFDI-20), the Pelvic Floor Impact Questionnaire-short form 7 (PFIQ-7), the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12), and the Body Image Scale (BIS), which were administered at baseline, 6 months, and 12 months.
A total of 160 women were studied, 80 in each treatment group. Compared with those in the pessary group, women in the surgical group were younger at baseline (a mean of 59 years vs. 64 years), and had less severe prolapse (Pelvic Organ Prolapse Quantification System stage 2 vs. 3), but they had worse PFDI-20 scores (a mean of 126 vs. 104) and BIS scores (a mean of 32 vs. 22).
Dr. Wohlrab and his associates found that 75% of patients in the surgery group achieved all of their functional goals, compared with 58% of those in the pessary group, a difference that did not reach statistical significance except in the category of physical function, which favored patients in the surgery group (87% of goals attained, vs. 62% of those in the pessary group; P = .03).
At the same time, 74% of patients in the surgery group achieved all of their symptom goals, compared with 70% of those in the pessary group, a difference that did not reach statistical significance (P = .7).
Both surgery and pessary groups had significant improvements in the PFDI-20, PFIQ-7, and the BIS scores from baseline (P less than .05 for all). Mean scores on the PISQ-12 also improved from baseline in the surgery group (P less than .05), but not in the pessary group.
Dr. Wohlrab reported having no financial disclosures. The meeting was jointly sponsored by the American College of Surgeons.
AT SGS 2016
Key clinical point: Both surgery and pessary were effective in helping women with pelvic organ prolapse reach pre-treatment functional and symptom goals.
Major finding: Seventy-five percent of patients in the surgery group achieved all of their pre-treatment functional goals, compared with 58% of those in the pessary group, a difference that did not reach statistical significance.
Data source: A prospective cohort study of 180 women who chose either surgery or pessary for treatment of pelvic organ prolapse.
Disclosures: Dr. Wohlrab reported having no financial disclosures.
CMS promises streamlined, flexible program to replace meaningful use
Meaningful use would get a new name and an emphasis on flexibility under a proposal from the Centers for Medicare & Medicaid Services.
“We’re proposing today to replace meaningful use in the physician office with a new effort that moves the emphasis away from the use of information technology to one that supports patient care, supported by better and more connected technology,” CMS Acting Administrator Andy Slavitt said during an April 27 press teleconference to introduce the changes.
“The program, Advancing Care Information, is designed to be far simpler, less burdensome, and more flexible,” Mr. Slavitt said. “If this proposal is finalized, it will replace the current meaningful use program for physician offices and will be effective January 1, 2017, along with the other components of the MACRA implementations.”
Mr. Slavitt and Dr. Karen DeSalvo, National Coordinator for Health Information Technology, noted in a blog postthat the improvements “should increase providers’ ability to use technology in ways that are more relevant to their needs and the needs of their patients.”
The changes come as part of a larger proposed regulation to implement the Medicare Access and CHIP Reauthorization Act, released online April 27 and scheduled for publication in the Federal Register on May 9.
MACRA will create two systems under which doctors will be paid for the quality of care they provide. The changes to the meaningful use program will affect physicians who choose to participate in the Merit-based Incentive Payment System (MIPS). Under the proposed rule, efforts under the new Advancing Care Information program would account for 25% of the score used to determine pay for office-based physicians under Medicare.
The key difference between the proposed program and meaningful use is that physicians will no longer be faced with an all-or-nothing requirement for meeting criteria to qualify for extra payments under the MIPS program.
Advancing Care Information has been divided into two parts. The first is reporting measures and has been streamlined to 11 measures, down from 18. Reporting on computerized physician order entry and clinical decision support measures have been eliminated.
The second part is based on performance measures, with multiple pathways to achieve those targets, which allow physicians to select the measures that best align with their needs.
There also is an opportunity to earn an extra point if a physician is reporting to more than one public health registry.
“We’ve also taken this opportunity to really focus more on aligning quality, on seeing that we are streamlining workflow and creating opportunities for electronic health record and health IT developers to create products that really meet the needs and expectations of clinicians and providers on the front lines,” Dr. DeSalvo said during the April 27 call.
The proposal also emphasizes interoperability, information exchange, and security measures and requires that patients be able to access their health care information easily through the use of apps and other consumer-friendly technology, according to the blog post.
The proposed rule also emphasizes open data sharing and interoperability, something that has been a continual drag on the current meaningful use program.
Comments on the proposed rule can be made at www.regulations.gov and are due June 26.
Meaningful use would get a new name and an emphasis on flexibility under a proposal from the Centers for Medicare & Medicaid Services.
“We’re proposing today to replace meaningful use in the physician office with a new effort that moves the emphasis away from the use of information technology to one that supports patient care, supported by better and more connected technology,” CMS Acting Administrator Andy Slavitt said during an April 27 press teleconference to introduce the changes.
“The program, Advancing Care Information, is designed to be far simpler, less burdensome, and more flexible,” Mr. Slavitt said. “If this proposal is finalized, it will replace the current meaningful use program for physician offices and will be effective January 1, 2017, along with the other components of the MACRA implementations.”
Mr. Slavitt and Dr. Karen DeSalvo, National Coordinator for Health Information Technology, noted in a blog postthat the improvements “should increase providers’ ability to use technology in ways that are more relevant to their needs and the needs of their patients.”
The changes come as part of a larger proposed regulation to implement the Medicare Access and CHIP Reauthorization Act, released online April 27 and scheduled for publication in the Federal Register on May 9.
MACRA will create two systems under which doctors will be paid for the quality of care they provide. The changes to the meaningful use program will affect physicians who choose to participate in the Merit-based Incentive Payment System (MIPS). Under the proposed rule, efforts under the new Advancing Care Information program would account for 25% of the score used to determine pay for office-based physicians under Medicare.
The key difference between the proposed program and meaningful use is that physicians will no longer be faced with an all-or-nothing requirement for meeting criteria to qualify for extra payments under the MIPS program.
Advancing Care Information has been divided into two parts. The first is reporting measures and has been streamlined to 11 measures, down from 18. Reporting on computerized physician order entry and clinical decision support measures have been eliminated.
The second part is based on performance measures, with multiple pathways to achieve those targets, which allow physicians to select the measures that best align with their needs.
There also is an opportunity to earn an extra point if a physician is reporting to more than one public health registry.
“We’ve also taken this opportunity to really focus more on aligning quality, on seeing that we are streamlining workflow and creating opportunities for electronic health record and health IT developers to create products that really meet the needs and expectations of clinicians and providers on the front lines,” Dr. DeSalvo said during the April 27 call.
The proposal also emphasizes interoperability, information exchange, and security measures and requires that patients be able to access their health care information easily through the use of apps and other consumer-friendly technology, according to the blog post.
The proposed rule also emphasizes open data sharing and interoperability, something that has been a continual drag on the current meaningful use program.
Comments on the proposed rule can be made at www.regulations.gov and are due June 26.
Meaningful use would get a new name and an emphasis on flexibility under a proposal from the Centers for Medicare & Medicaid Services.
“We’re proposing today to replace meaningful use in the physician office with a new effort that moves the emphasis away from the use of information technology to one that supports patient care, supported by better and more connected technology,” CMS Acting Administrator Andy Slavitt said during an April 27 press teleconference to introduce the changes.
“The program, Advancing Care Information, is designed to be far simpler, less burdensome, and more flexible,” Mr. Slavitt said. “If this proposal is finalized, it will replace the current meaningful use program for physician offices and will be effective January 1, 2017, along with the other components of the MACRA implementations.”
Mr. Slavitt and Dr. Karen DeSalvo, National Coordinator for Health Information Technology, noted in a blog postthat the improvements “should increase providers’ ability to use technology in ways that are more relevant to their needs and the needs of their patients.”
The changes come as part of a larger proposed regulation to implement the Medicare Access and CHIP Reauthorization Act, released online April 27 and scheduled for publication in the Federal Register on May 9.
MACRA will create two systems under which doctors will be paid for the quality of care they provide. The changes to the meaningful use program will affect physicians who choose to participate in the Merit-based Incentive Payment System (MIPS). Under the proposed rule, efforts under the new Advancing Care Information program would account for 25% of the score used to determine pay for office-based physicians under Medicare.
The key difference between the proposed program and meaningful use is that physicians will no longer be faced with an all-or-nothing requirement for meeting criteria to qualify for extra payments under the MIPS program.
Advancing Care Information has been divided into two parts. The first is reporting measures and has been streamlined to 11 measures, down from 18. Reporting on computerized physician order entry and clinical decision support measures have been eliminated.
The second part is based on performance measures, with multiple pathways to achieve those targets, which allow physicians to select the measures that best align with their needs.
There also is an opportunity to earn an extra point if a physician is reporting to more than one public health registry.
“We’ve also taken this opportunity to really focus more on aligning quality, on seeing that we are streamlining workflow and creating opportunities for electronic health record and health IT developers to create products that really meet the needs and expectations of clinicians and providers on the front lines,” Dr. DeSalvo said during the April 27 call.
The proposal also emphasizes interoperability, information exchange, and security measures and requires that patients be able to access their health care information easily through the use of apps and other consumer-friendly technology, according to the blog post.
The proposed rule also emphasizes open data sharing and interoperability, something that has been a continual drag on the current meaningful use program.
Comments on the proposed rule can be made at www.regulations.gov and are due June 26.
Premenopausal age linked to lower sexual function after gynecologic cancer surgery
INDIAN WELLS, CALIF. – Premenopausal age was associated with a greater temporary decline in sexual desire 1 month after undergoing surgery for suspected gynecologic malignancies, results from an ancillary analysis showed.
“Sexual health is an important dimension of quality of life for women with gynecologic cancer,” Dr. C. Emi Bretschneider, lead study author, said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Limited data exists on the impact of surgery for treatment of gynecologic cancer on patient-reported sexual desire and interest.”
In an effort to evaluate the impact on sexual function in women undergoing surgery for presumed or known gynecologic malignancies, the researchers performed an ancillary analysis of a cohort study analyzing quality-of-life and operative outcomes in 185 women who underwent gynecologic oncology procedures at the University of North Carolina, Chapel Hill, between October 2013 and October 2014.
Study participants completed the Patient-Reported Outcomes Measurement Information System Sexual Function and Satisfaction Questionnaire (PROMIS-SFQ) at baseline and at 1, 3, and 6 months postoperatively. The questionnaire evaluates four subdomains of sexual function: global satisfaction with sex life, interest in sexual activity, lubrication, and vaginal discomfort. The researchers used student t-test and linear regression to compare mean score changes between cancer types, surgical route, menopausal status, and postoperative complications, said Dr. Bretschneider of the university’s department of obstetrics and gynecology.
Of the 281 patients initially enrolled, 185 (66%) completed the PROMIS-SFQ at baseline and at 1 month postoperatively, forming the primary cohort from which the researchers performed the analysis. Of these 185 patients, 170 (92%) completed the PROMIS-SFQ at 3 months and 174 (94%) completed the survey at 6 months postoperatively.
The average age of patients at baseline was 56 years: most (77%) were white, mean body mass index was 32.9 kg/m2, 62% were partnered, and 63% underwent minimally invasive procedures. Following surgery, 131 of the patients (71%) were diagnosed with a malignancy, most commonly uterine cancer (84%), followed by ovarian (23%), cervical (17%), and vulvar cancer (3%).
Dr. Bretschneider reported that the mean baseline sexual interest score among all study participants was 44.8. At 1 month postoperatively, the mean scores decreased a mean of 3.8 points from baseline to 41. By 3 and 6 months postoperatively, the mean sexual interest scores increased from baseline by 1.9 and 2.7 points, respectively, to 46.7 and 47.5.
Women younger than age 55 years had a greater decrease in sexual interest between baseline and 1 month postoperatively, compared with their counterparts aged 55 and older (a mean of –5.5 vs. –2.3 points, respectively; P = .02).
On multivariate analysis adjusted for cancer diagnosis, minimally invasive surgery, and cancer site, women younger than age 55 continued to have a greater decrease in sexual interest between baseline and 1 month postoperatively, compared with their counterparts aged 55 and older (a mean of –4.59 points). Additionally, women who had cancer had a greater drop in sexual desire, compared with those with benign disease (a mean of –5.6 points).
“This study offers new information on the impact of surgery on sexual function for women with gynecologic cancer,” Dr. Bretschneider said at the meeting, which was jointly sponsored by the American College of Surgeons. “The study was further strengthened by its prospective design and well-characterized, large cohort of women.” Weaknesses, she continued, include its generalizability, “which may be limited, as the study cohort was recruited from a single academic institution. Also, the small sample size for some cancer sites reduced our ability to sense cancer site as a causal agent for sexual dysfunction.”
Dr. Bretschneider reported having no financial disclosures.
INDIAN WELLS, CALIF. – Premenopausal age was associated with a greater temporary decline in sexual desire 1 month after undergoing surgery for suspected gynecologic malignancies, results from an ancillary analysis showed.
“Sexual health is an important dimension of quality of life for women with gynecologic cancer,” Dr. C. Emi Bretschneider, lead study author, said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Limited data exists on the impact of surgery for treatment of gynecologic cancer on patient-reported sexual desire and interest.”
In an effort to evaluate the impact on sexual function in women undergoing surgery for presumed or known gynecologic malignancies, the researchers performed an ancillary analysis of a cohort study analyzing quality-of-life and operative outcomes in 185 women who underwent gynecologic oncology procedures at the University of North Carolina, Chapel Hill, between October 2013 and October 2014.
Study participants completed the Patient-Reported Outcomes Measurement Information System Sexual Function and Satisfaction Questionnaire (PROMIS-SFQ) at baseline and at 1, 3, and 6 months postoperatively. The questionnaire evaluates four subdomains of sexual function: global satisfaction with sex life, interest in sexual activity, lubrication, and vaginal discomfort. The researchers used student t-test and linear regression to compare mean score changes between cancer types, surgical route, menopausal status, and postoperative complications, said Dr. Bretschneider of the university’s department of obstetrics and gynecology.
Of the 281 patients initially enrolled, 185 (66%) completed the PROMIS-SFQ at baseline and at 1 month postoperatively, forming the primary cohort from which the researchers performed the analysis. Of these 185 patients, 170 (92%) completed the PROMIS-SFQ at 3 months and 174 (94%) completed the survey at 6 months postoperatively.
The average age of patients at baseline was 56 years: most (77%) were white, mean body mass index was 32.9 kg/m2, 62% were partnered, and 63% underwent minimally invasive procedures. Following surgery, 131 of the patients (71%) were diagnosed with a malignancy, most commonly uterine cancer (84%), followed by ovarian (23%), cervical (17%), and vulvar cancer (3%).
Dr. Bretschneider reported that the mean baseline sexual interest score among all study participants was 44.8. At 1 month postoperatively, the mean scores decreased a mean of 3.8 points from baseline to 41. By 3 and 6 months postoperatively, the mean sexual interest scores increased from baseline by 1.9 and 2.7 points, respectively, to 46.7 and 47.5.
Women younger than age 55 years had a greater decrease in sexual interest between baseline and 1 month postoperatively, compared with their counterparts aged 55 and older (a mean of –5.5 vs. –2.3 points, respectively; P = .02).
On multivariate analysis adjusted for cancer diagnosis, minimally invasive surgery, and cancer site, women younger than age 55 continued to have a greater decrease in sexual interest between baseline and 1 month postoperatively, compared with their counterparts aged 55 and older (a mean of –4.59 points). Additionally, women who had cancer had a greater drop in sexual desire, compared with those with benign disease (a mean of –5.6 points).
“This study offers new information on the impact of surgery on sexual function for women with gynecologic cancer,” Dr. Bretschneider said at the meeting, which was jointly sponsored by the American College of Surgeons. “The study was further strengthened by its prospective design and well-characterized, large cohort of women.” Weaknesses, she continued, include its generalizability, “which may be limited, as the study cohort was recruited from a single academic institution. Also, the small sample size for some cancer sites reduced our ability to sense cancer site as a causal agent for sexual dysfunction.”
Dr. Bretschneider reported having no financial disclosures.
INDIAN WELLS, CALIF. – Premenopausal age was associated with a greater temporary decline in sexual desire 1 month after undergoing surgery for suspected gynecologic malignancies, results from an ancillary analysis showed.
“Sexual health is an important dimension of quality of life for women with gynecologic cancer,” Dr. C. Emi Bretschneider, lead study author, said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Limited data exists on the impact of surgery for treatment of gynecologic cancer on patient-reported sexual desire and interest.”
In an effort to evaluate the impact on sexual function in women undergoing surgery for presumed or known gynecologic malignancies, the researchers performed an ancillary analysis of a cohort study analyzing quality-of-life and operative outcomes in 185 women who underwent gynecologic oncology procedures at the University of North Carolina, Chapel Hill, between October 2013 and October 2014.
Study participants completed the Patient-Reported Outcomes Measurement Information System Sexual Function and Satisfaction Questionnaire (PROMIS-SFQ) at baseline and at 1, 3, and 6 months postoperatively. The questionnaire evaluates four subdomains of sexual function: global satisfaction with sex life, interest in sexual activity, lubrication, and vaginal discomfort. The researchers used student t-test and linear regression to compare mean score changes between cancer types, surgical route, menopausal status, and postoperative complications, said Dr. Bretschneider of the university’s department of obstetrics and gynecology.
Of the 281 patients initially enrolled, 185 (66%) completed the PROMIS-SFQ at baseline and at 1 month postoperatively, forming the primary cohort from which the researchers performed the analysis. Of these 185 patients, 170 (92%) completed the PROMIS-SFQ at 3 months and 174 (94%) completed the survey at 6 months postoperatively.
The average age of patients at baseline was 56 years: most (77%) were white, mean body mass index was 32.9 kg/m2, 62% were partnered, and 63% underwent minimally invasive procedures. Following surgery, 131 of the patients (71%) were diagnosed with a malignancy, most commonly uterine cancer (84%), followed by ovarian (23%), cervical (17%), and vulvar cancer (3%).
Dr. Bretschneider reported that the mean baseline sexual interest score among all study participants was 44.8. At 1 month postoperatively, the mean scores decreased a mean of 3.8 points from baseline to 41. By 3 and 6 months postoperatively, the mean sexual interest scores increased from baseline by 1.9 and 2.7 points, respectively, to 46.7 and 47.5.
Women younger than age 55 years had a greater decrease in sexual interest between baseline and 1 month postoperatively, compared with their counterparts aged 55 and older (a mean of –5.5 vs. –2.3 points, respectively; P = .02).
On multivariate analysis adjusted for cancer diagnosis, minimally invasive surgery, and cancer site, women younger than age 55 continued to have a greater decrease in sexual interest between baseline and 1 month postoperatively, compared with their counterparts aged 55 and older (a mean of –4.59 points). Additionally, women who had cancer had a greater drop in sexual desire, compared with those with benign disease (a mean of –5.6 points).
“This study offers new information on the impact of surgery on sexual function for women with gynecologic cancer,” Dr. Bretschneider said at the meeting, which was jointly sponsored by the American College of Surgeons. “The study was further strengthened by its prospective design and well-characterized, large cohort of women.” Weaknesses, she continued, include its generalizability, “which may be limited, as the study cohort was recruited from a single academic institution. Also, the small sample size for some cancer sites reduced our ability to sense cancer site as a causal agent for sexual dysfunction.”
Dr. Bretschneider reported having no financial disclosures.
AT SGS 2016
Key clinical point: Premenopausal age was associated with a greater temporary decline in sexual function following gynecologic oncology procedures.
Major finding: Women younger than age 55 years had a greater decrease in sexual interest between baseline and 1 month postoperatively, compared with their counterparts aged 55 and older (a mean of –5.5 vs. –2.3 points on the PROMIS-SFQ, respectively; P = .02).
Data source: An ancillary analysis of a cohort study analyzing quality-of-life and operative outcomes in 185 women who underwent gynecologic oncology procedures between October 2013 and October 2014.
Disclosures: Dr. Bretschneider reported having no financial disclosures.