User login
Report card may foretell achalasia surgery outcomes
BALTIMORE – The Eckardt score has been established as a tool to evaluate outcomes of surgery for achalasia, but researchers have developed a report card that uses multiple variables that may provide a more accurate picture of surgical outcomes, according to results of study reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
“The use of an accurate score to assess outcomes after achalasia surgery shows outstanding results,” said Ealaf Shemmeri, MD, of Swedish Medical Center in Seattle. “Using patient-reported symptoms, objective measures, and rates of reinterventions organized into a report card provides a more comprehensive and informative view.”
The Eckardt score evaluates four symptoms to evaluate outcomes of surgery to treat achalasia: weight loss, retrosternal pain, regurgitation, and dysphagia. “However, it does not address the other changes that can occur after myotomy, including the quality of swallowing and the onset of reflux disease,” she said. “Thus, there is a need for a more comprehensive assessment of quality after achalasia treatment.”
So the Swedish investigators set out to devise a report card that provides “a comprehensive and informative assessment” of surgical myotomy outcomes, she said. This involved a retrospective, single-center chart review of 185 patients who had surgical myotomy for primary achalasia from 2005 to 2017.
To determine patient-reported outcomes, the report card defines success as an Eckardt score below 3, Dakkak dysphagia score above 40, and GERD-HRQL (health-related quality of life) score below 10. The objective measures consisted of DeMeester (pH) score below 14.72, no column at 5 minutes on timed barium swallow, normalized integrated relaxation pressure less than 15 on manometry, and absence of esophagitis on endoscopy. For the third pillar of the report card, no reintervention was recorded as a success, Dr. Shemmeri said.
Regarding the etiology of achalasia in the study population, 42 had type 1, 109 had type 2, and 34 had type 3. A total of 71 patients had per oral endoscopic myotomy and 114 had Heller myotomy, 92 with Dor fundoplication and 20 with Toupet. Major perioperative complications included four per oral endoscopic myotomy patients who developed a leak requiring intervention. Six patients required return to the operating room for persistent dysphagia, Dr. Shemmeri said.
After the procedures, 93% of study patients reported an Eckardt score less than 3. However, only 45% have a Dakkak dysphagia score greater than 40 and 71% had a GERD-HRQL score less than 10, Dr. Shemmeri said. The objective measures told a similar story: Integrated relaxation pressure normalized in 80%, barium clearance was achieved in 61%, normal esophageal mucosa was recorded in 71%, “but pH testing was normal only 50% of the time,” Dr. Shemmeri said.
“The final success of not needing intervention is 79%,” she said. At this point in the study, 139 patients were available for follow-up. Among the 29 who needed reintervention, 19 had dilation below 20 mm Hg, 3 underwent pneumatic dilation, and 2 had botulinum toxin. Two patients required a redo myotomy, two had antireflux surgery, and one had an esophagectomy.
“When you only focus on a singular outcome, you can miss the whole story that occurs after myotomy,” Dr. Shemmeri said. “Providing a comprehensive tool gives you the ability to identify areas for improvement in your achalasia practice. Its simplicity allows it to be applied in various settings.” In the academic setting, it can be a tool for evaluating technologies and approaches for postmyotomy management. In hospitals and surgeons’ practices, it can aid in quality improvement, comparative outcomes research, and in evaluating operative approaches to myotomy.
The outcomes highlight the high prevalence of GERD, thus stressing the importance of pH testing after myotomy, Dr. Shemmeri said. Her study team recommends pH testing at 6-month follow-up because patients may not always self-report the extent of esophagitis present. Coauthor Brian Louie, MD, also of Swedish Medical Center, added during the discussion that ongoing follow-up of achalasia patients is necessary to address issues patients encounter with their swallowing over time.
Dr. Shemmeri had no relevant financial relationships to disclose. Dr. Louie reported relationships with Boston Scientific, ERBE, and Olympus.
SOURCE: Shemmeri E et al. SAGES 2019, Presentation S085.
BALTIMORE – The Eckardt score has been established as a tool to evaluate outcomes of surgery for achalasia, but researchers have developed a report card that uses multiple variables that may provide a more accurate picture of surgical outcomes, according to results of study reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
“The use of an accurate score to assess outcomes after achalasia surgery shows outstanding results,” said Ealaf Shemmeri, MD, of Swedish Medical Center in Seattle. “Using patient-reported symptoms, objective measures, and rates of reinterventions organized into a report card provides a more comprehensive and informative view.”
The Eckardt score evaluates four symptoms to evaluate outcomes of surgery to treat achalasia: weight loss, retrosternal pain, regurgitation, and dysphagia. “However, it does not address the other changes that can occur after myotomy, including the quality of swallowing and the onset of reflux disease,” she said. “Thus, there is a need for a more comprehensive assessment of quality after achalasia treatment.”
So the Swedish investigators set out to devise a report card that provides “a comprehensive and informative assessment” of surgical myotomy outcomes, she said. This involved a retrospective, single-center chart review of 185 patients who had surgical myotomy for primary achalasia from 2005 to 2017.
To determine patient-reported outcomes, the report card defines success as an Eckardt score below 3, Dakkak dysphagia score above 40, and GERD-HRQL (health-related quality of life) score below 10. The objective measures consisted of DeMeester (pH) score below 14.72, no column at 5 minutes on timed barium swallow, normalized integrated relaxation pressure less than 15 on manometry, and absence of esophagitis on endoscopy. For the third pillar of the report card, no reintervention was recorded as a success, Dr. Shemmeri said.
Regarding the etiology of achalasia in the study population, 42 had type 1, 109 had type 2, and 34 had type 3. A total of 71 patients had per oral endoscopic myotomy and 114 had Heller myotomy, 92 with Dor fundoplication and 20 with Toupet. Major perioperative complications included four per oral endoscopic myotomy patients who developed a leak requiring intervention. Six patients required return to the operating room for persistent dysphagia, Dr. Shemmeri said.
After the procedures, 93% of study patients reported an Eckardt score less than 3. However, only 45% have a Dakkak dysphagia score greater than 40 and 71% had a GERD-HRQL score less than 10, Dr. Shemmeri said. The objective measures told a similar story: Integrated relaxation pressure normalized in 80%, barium clearance was achieved in 61%, normal esophageal mucosa was recorded in 71%, “but pH testing was normal only 50% of the time,” Dr. Shemmeri said.
“The final success of not needing intervention is 79%,” she said. At this point in the study, 139 patients were available for follow-up. Among the 29 who needed reintervention, 19 had dilation below 20 mm Hg, 3 underwent pneumatic dilation, and 2 had botulinum toxin. Two patients required a redo myotomy, two had antireflux surgery, and one had an esophagectomy.
“When you only focus on a singular outcome, you can miss the whole story that occurs after myotomy,” Dr. Shemmeri said. “Providing a comprehensive tool gives you the ability to identify areas for improvement in your achalasia practice. Its simplicity allows it to be applied in various settings.” In the academic setting, it can be a tool for evaluating technologies and approaches for postmyotomy management. In hospitals and surgeons’ practices, it can aid in quality improvement, comparative outcomes research, and in evaluating operative approaches to myotomy.
The outcomes highlight the high prevalence of GERD, thus stressing the importance of pH testing after myotomy, Dr. Shemmeri said. Her study team recommends pH testing at 6-month follow-up because patients may not always self-report the extent of esophagitis present. Coauthor Brian Louie, MD, also of Swedish Medical Center, added during the discussion that ongoing follow-up of achalasia patients is necessary to address issues patients encounter with their swallowing over time.
Dr. Shemmeri had no relevant financial relationships to disclose. Dr. Louie reported relationships with Boston Scientific, ERBE, and Olympus.
SOURCE: Shemmeri E et al. SAGES 2019, Presentation S085.
BALTIMORE – The Eckardt score has been established as a tool to evaluate outcomes of surgery for achalasia, but researchers have developed a report card that uses multiple variables that may provide a more accurate picture of surgical outcomes, according to results of study reported at the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.
“The use of an accurate score to assess outcomes after achalasia surgery shows outstanding results,” said Ealaf Shemmeri, MD, of Swedish Medical Center in Seattle. “Using patient-reported symptoms, objective measures, and rates of reinterventions organized into a report card provides a more comprehensive and informative view.”
The Eckardt score evaluates four symptoms to evaluate outcomes of surgery to treat achalasia: weight loss, retrosternal pain, regurgitation, and dysphagia. “However, it does not address the other changes that can occur after myotomy, including the quality of swallowing and the onset of reflux disease,” she said. “Thus, there is a need for a more comprehensive assessment of quality after achalasia treatment.”
So the Swedish investigators set out to devise a report card that provides “a comprehensive and informative assessment” of surgical myotomy outcomes, she said. This involved a retrospective, single-center chart review of 185 patients who had surgical myotomy for primary achalasia from 2005 to 2017.
To determine patient-reported outcomes, the report card defines success as an Eckardt score below 3, Dakkak dysphagia score above 40, and GERD-HRQL (health-related quality of life) score below 10. The objective measures consisted of DeMeester (pH) score below 14.72, no column at 5 minutes on timed barium swallow, normalized integrated relaxation pressure less than 15 on manometry, and absence of esophagitis on endoscopy. For the third pillar of the report card, no reintervention was recorded as a success, Dr. Shemmeri said.
Regarding the etiology of achalasia in the study population, 42 had type 1, 109 had type 2, and 34 had type 3. A total of 71 patients had per oral endoscopic myotomy and 114 had Heller myotomy, 92 with Dor fundoplication and 20 with Toupet. Major perioperative complications included four per oral endoscopic myotomy patients who developed a leak requiring intervention. Six patients required return to the operating room for persistent dysphagia, Dr. Shemmeri said.
After the procedures, 93% of study patients reported an Eckardt score less than 3. However, only 45% have a Dakkak dysphagia score greater than 40 and 71% had a GERD-HRQL score less than 10, Dr. Shemmeri said. The objective measures told a similar story: Integrated relaxation pressure normalized in 80%, barium clearance was achieved in 61%, normal esophageal mucosa was recorded in 71%, “but pH testing was normal only 50% of the time,” Dr. Shemmeri said.
“The final success of not needing intervention is 79%,” she said. At this point in the study, 139 patients were available for follow-up. Among the 29 who needed reintervention, 19 had dilation below 20 mm Hg, 3 underwent pneumatic dilation, and 2 had botulinum toxin. Two patients required a redo myotomy, two had antireflux surgery, and one had an esophagectomy.
“When you only focus on a singular outcome, you can miss the whole story that occurs after myotomy,” Dr. Shemmeri said. “Providing a comprehensive tool gives you the ability to identify areas for improvement in your achalasia practice. Its simplicity allows it to be applied in various settings.” In the academic setting, it can be a tool for evaluating technologies and approaches for postmyotomy management. In hospitals and surgeons’ practices, it can aid in quality improvement, comparative outcomes research, and in evaluating operative approaches to myotomy.
The outcomes highlight the high prevalence of GERD, thus stressing the importance of pH testing after myotomy, Dr. Shemmeri said. Her study team recommends pH testing at 6-month follow-up because patients may not always self-report the extent of esophagitis present. Coauthor Brian Louie, MD, also of Swedish Medical Center, added during the discussion that ongoing follow-up of achalasia patients is necessary to address issues patients encounter with their swallowing over time.
Dr. Shemmeri had no relevant financial relationships to disclose. Dr. Louie reported relationships with Boston Scientific, ERBE, and Olympus.
SOURCE: Shemmeri E et al. SAGES 2019, Presentation S085.
REPORTING FROM SAGES 2019
Look for functional esophageal disorders if GERD patients fail PPIs
In a small, first-in-kind study, functional heartburn or reflux hypersensitivity affected fully 75% of patients whose gastroesophageal reflux disease symptoms had not improved with once-daily proton pump inhibitor therapy.
At the same time, proton pump inhibitor (PPI) responders and nonresponders had similar impedance and pH parameters, reported Jason Abdallah, MD, of Case Western Reserve University, Cleveland, and his associates. The findings show “the important role of esophageal hypersensitivity in this patient population.” For these patients, the investigators suggested adding a neuromodulator and possibly psychotherapy, such as cognitive-behavioral therapy, hypnotherapy, relaxation techniques, mindfulness, and biofeedback.
Symptoms in up to 45% of patients with gastroesophageal reflux disease (GERD) persist despite once-daily PPI therapy, Dr. Abdallah and his associates wrote in Clinical Gastroenterology and Hepatology. For the study, they compared reflux characteristics and patterns between 13 patients whose GERD symptoms had fully resolved on standard once-daily PPIs and 16 patients who reported at least twice-weekly heartburn, regurgitation, or both for at least 3 months, despite treatment. Patients in both groups continued PPIs and underwent upper endoscopy and combined esophageal impedance–pH monitoring.
The average age of patients in this study was 54.5 years, with a standard deviation of 14.5 years. Demographic and clinical characteristics were similar between groups, and patients in both groups were receiving omeprazole, esomeprazole, or pantoprazole. Four (31%) PPI responders had abnormal pH test results, as did four (25%) nonresponders. Responders and nonresponders had similar numbers of reflux events; proportions of events that were acidic, weakly acidic, or alkaline; and mean total time with pH less than 4.0.
Additionally, most patients in both groups had normal endoscopic findings. One PPI responder had Los Angeles grade A erosive esophagitis, and two PPI responders had short-segment Barrett’s esophagus. Three PPI responders and two PPI nonresponders had nonobstructive Schatzki rings, and one PPI nonresponder had an esophageal stricture. Finally, five PPI responders (38%) and three nonresponders (19%) had hiatal hernias (P = .41).
In patients with GERD, “PPI failure” does not reflect a unique pattern of reflux events, acid exposure, or nonacidic reflux parameters, Dr. Abdallah and his associates concluded. The fact that most PPI nonresponders had a concurrent functional esophageal disorder – either reflux hypersensitivity or functional heartburn – “support[s] the hypothesis that PPI failure is primarily driven by esophageal hypersensitivity.”
This was a small study – recruitment “was hampered by the invasive nature of some of the procedures,” they wrote. “In addition, it is our experience that many patients who have responded to PPI [therapy] are reluctant to undergo invasive testing as part of a study protocol. Therefore, we believe that these types of prospective, invasive studies are rather difficult to perform but, at the same time, provide essential insight into the understanding of refractory GERD.”
No external funding sources were acknowledged. The senior author reported ties to Ironwood Pharmaceuticals, Mederi Therapeutics, Ethicon, AstraZeneca, and Takeda. The other researchers reported no conflicts of interest.
SOURCE: Abdallah J et al. Clin Gastroenterol Hepatol. 2018 Jun 15. doi: 10.1016/j.cgh.2018.09.006.
In a small, first-in-kind study, functional heartburn or reflux hypersensitivity affected fully 75% of patients whose gastroesophageal reflux disease symptoms had not improved with once-daily proton pump inhibitor therapy.
At the same time, proton pump inhibitor (PPI) responders and nonresponders had similar impedance and pH parameters, reported Jason Abdallah, MD, of Case Western Reserve University, Cleveland, and his associates. The findings show “the important role of esophageal hypersensitivity in this patient population.” For these patients, the investigators suggested adding a neuromodulator and possibly psychotherapy, such as cognitive-behavioral therapy, hypnotherapy, relaxation techniques, mindfulness, and biofeedback.
Symptoms in up to 45% of patients with gastroesophageal reflux disease (GERD) persist despite once-daily PPI therapy, Dr. Abdallah and his associates wrote in Clinical Gastroenterology and Hepatology. For the study, they compared reflux characteristics and patterns between 13 patients whose GERD symptoms had fully resolved on standard once-daily PPIs and 16 patients who reported at least twice-weekly heartburn, regurgitation, or both for at least 3 months, despite treatment. Patients in both groups continued PPIs and underwent upper endoscopy and combined esophageal impedance–pH monitoring.
The average age of patients in this study was 54.5 years, with a standard deviation of 14.5 years. Demographic and clinical characteristics were similar between groups, and patients in both groups were receiving omeprazole, esomeprazole, or pantoprazole. Four (31%) PPI responders had abnormal pH test results, as did four (25%) nonresponders. Responders and nonresponders had similar numbers of reflux events; proportions of events that were acidic, weakly acidic, or alkaline; and mean total time with pH less than 4.0.
Additionally, most patients in both groups had normal endoscopic findings. One PPI responder had Los Angeles grade A erosive esophagitis, and two PPI responders had short-segment Barrett’s esophagus. Three PPI responders and two PPI nonresponders had nonobstructive Schatzki rings, and one PPI nonresponder had an esophageal stricture. Finally, five PPI responders (38%) and three nonresponders (19%) had hiatal hernias (P = .41).
In patients with GERD, “PPI failure” does not reflect a unique pattern of reflux events, acid exposure, or nonacidic reflux parameters, Dr. Abdallah and his associates concluded. The fact that most PPI nonresponders had a concurrent functional esophageal disorder – either reflux hypersensitivity or functional heartburn – “support[s] the hypothesis that PPI failure is primarily driven by esophageal hypersensitivity.”
This was a small study – recruitment “was hampered by the invasive nature of some of the procedures,” they wrote. “In addition, it is our experience that many patients who have responded to PPI [therapy] are reluctant to undergo invasive testing as part of a study protocol. Therefore, we believe that these types of prospective, invasive studies are rather difficult to perform but, at the same time, provide essential insight into the understanding of refractory GERD.”
No external funding sources were acknowledged. The senior author reported ties to Ironwood Pharmaceuticals, Mederi Therapeutics, Ethicon, AstraZeneca, and Takeda. The other researchers reported no conflicts of interest.
SOURCE: Abdallah J et al. Clin Gastroenterol Hepatol. 2018 Jun 15. doi: 10.1016/j.cgh.2018.09.006.
In a small, first-in-kind study, functional heartburn or reflux hypersensitivity affected fully 75% of patients whose gastroesophageal reflux disease symptoms had not improved with once-daily proton pump inhibitor therapy.
At the same time, proton pump inhibitor (PPI) responders and nonresponders had similar impedance and pH parameters, reported Jason Abdallah, MD, of Case Western Reserve University, Cleveland, and his associates. The findings show “the important role of esophageal hypersensitivity in this patient population.” For these patients, the investigators suggested adding a neuromodulator and possibly psychotherapy, such as cognitive-behavioral therapy, hypnotherapy, relaxation techniques, mindfulness, and biofeedback.
Symptoms in up to 45% of patients with gastroesophageal reflux disease (GERD) persist despite once-daily PPI therapy, Dr. Abdallah and his associates wrote in Clinical Gastroenterology and Hepatology. For the study, they compared reflux characteristics and patterns between 13 patients whose GERD symptoms had fully resolved on standard once-daily PPIs and 16 patients who reported at least twice-weekly heartburn, regurgitation, or both for at least 3 months, despite treatment. Patients in both groups continued PPIs and underwent upper endoscopy and combined esophageal impedance–pH monitoring.
The average age of patients in this study was 54.5 years, with a standard deviation of 14.5 years. Demographic and clinical characteristics were similar between groups, and patients in both groups were receiving omeprazole, esomeprazole, or pantoprazole. Four (31%) PPI responders had abnormal pH test results, as did four (25%) nonresponders. Responders and nonresponders had similar numbers of reflux events; proportions of events that were acidic, weakly acidic, or alkaline; and mean total time with pH less than 4.0.
Additionally, most patients in both groups had normal endoscopic findings. One PPI responder had Los Angeles grade A erosive esophagitis, and two PPI responders had short-segment Barrett’s esophagus. Three PPI responders and two PPI nonresponders had nonobstructive Schatzki rings, and one PPI nonresponder had an esophageal stricture. Finally, five PPI responders (38%) and three nonresponders (19%) had hiatal hernias (P = .41).
In patients with GERD, “PPI failure” does not reflect a unique pattern of reflux events, acid exposure, or nonacidic reflux parameters, Dr. Abdallah and his associates concluded. The fact that most PPI nonresponders had a concurrent functional esophageal disorder – either reflux hypersensitivity or functional heartburn – “support[s] the hypothesis that PPI failure is primarily driven by esophageal hypersensitivity.”
This was a small study – recruitment “was hampered by the invasive nature of some of the procedures,” they wrote. “In addition, it is our experience that many patients who have responded to PPI [therapy] are reluctant to undergo invasive testing as part of a study protocol. Therefore, we believe that these types of prospective, invasive studies are rather difficult to perform but, at the same time, provide essential insight into the understanding of refractory GERD.”
No external funding sources were acknowledged. The senior author reported ties to Ironwood Pharmaceuticals, Mederi Therapeutics, Ethicon, AstraZeneca, and Takeda. The other researchers reported no conflicts of interest.
SOURCE: Abdallah J et al. Clin Gastroenterol Hepatol. 2018 Jun 15. doi: 10.1016/j.cgh.2018.09.006.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
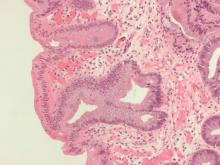
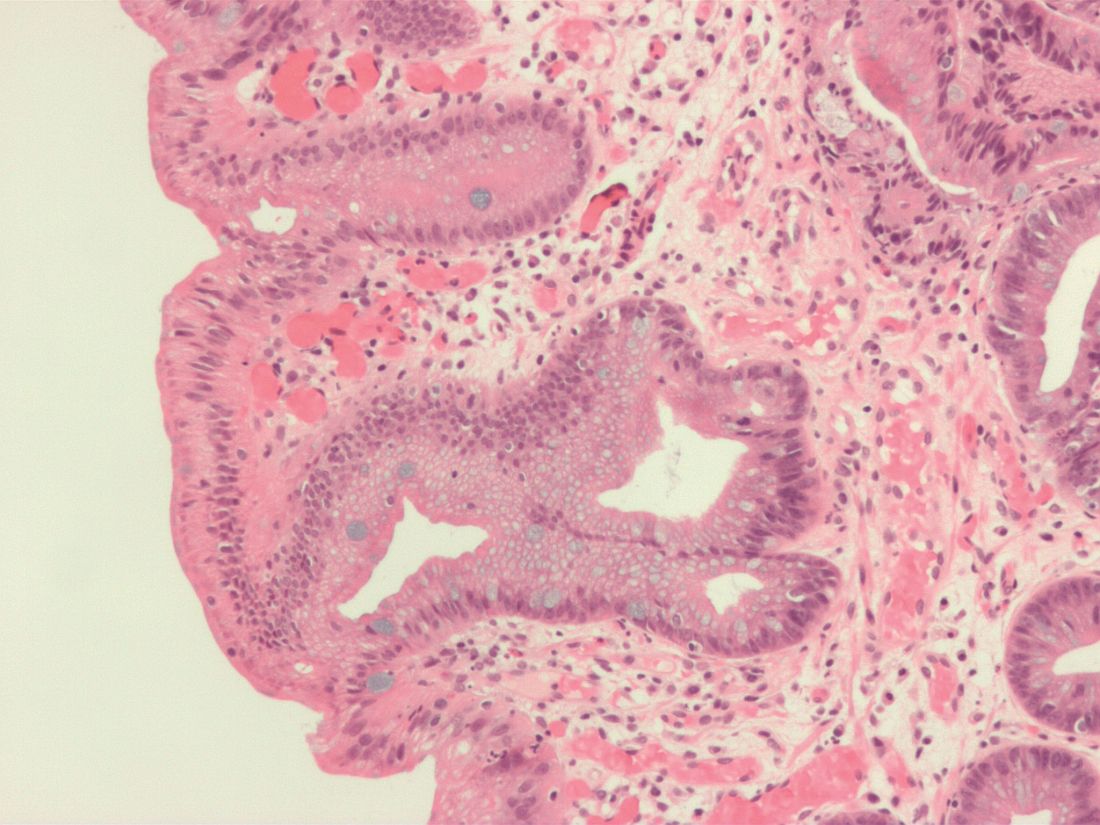
Mucosal impedance contour rapidly distinguished GERD, non-GERD, and eosinophilic esophagitis
.
Source: American Gastroenterological Association
Each group showed a significantly different (P less than .01) pattern of mucosal impedance (MI), or disruption of mucosal integrity, along the esophageal axis, wrote Dhyanesh A. Patel, MD, of Vanderbilt University Medical Center in Nashville, Tenn., and his associates. Patients without GERD had higher MI values along all esophageal segments, while GERD was characterized by below-normal values in the distal esophagus only, and eosinophilic esophagitis led to low values throughout the esophagus.
The findings were validated in a separate patient cohort, and the only reported adverse event was an episode of mild chest pain. “This contour heatmap could easily be employed to establish a diagnosis during endoscopy, independent of biopsy or pH monitoring,” the investigators wrote in Gastroenterology. They cautioned that the balloon catheter cannot be safely used in patients with severe fibrostenotic disease.
Current definitive diagnostics for GERD leave much to be desired. Transnasal probes are imprecise and uncomfortable, and they can be insensitive if discomfort causes patients to vary normal activity or skip meals. Wireless ambulatory pH monitoring is more tolerable but unreliable and measures only acidity of refluxed material at a single point along the esophagus. These tests also “fail to account for day-to-day variability of reflux, as they only provide a 24- to 48-hour snapshot of a disease process that is chronic in nature,” the researchers wrote. Eosinophilic esophagitis is becoming more common and usually requires proximal and distal biopsies for diagnosis.
Mucosal impedance contour pattern testing is based on the fact that both GERD and eosinophilic esophagitis involve increased distance between esophageal epithelial cells. The amount of intercellular dilatation correlates inversely with MI values. In proof-of-concept studies, individuals with GERD, non-GERD, eosinophilic esophagitis, and achalasia had distinct MI patterns. However, these studies tested a single-channel catheter system that took only point measurements and was subject to interoperator variability. To improve on this concept, Dr. Patel and his associates mounted radial and axial sensors on a balloon catheter to measure MI at 180-degree intervals along a 10-cm esophageal segment.
They tested the new device prospectively in 69 patients undergoing esophagogastroduodenoscopy with or without pH monitoring (which was used as the standard). In all, 24 patients had GERD, 21 had eosinophilic esophagitis, and 24 had normal findings. By using the intercept and slope of the balloon MI measurements, the researchers detected GERD with an area under the receiver operating characteristic curve (AUC) of 0.67, eosinophilic esophagitis with an AUC of 0.84, and non-GERD with an AUC of 0.83.
These findings held up in a separate validation cohort of 36 patients (28 with GERD and eight with eosinophilic esophagitis) from three tertiary care centers. The probability of eosinophilic esophagitis was highest in patients with low distal MI values (that is, a low intercept) and a low slope (showing that MI values remained low proximally). A low distal MI intercept with a steeper positive slope suggested GERD, while a higher distal MI intercept with a steep slope signified non-GERD.
The system “potentially obviates the need for 24- to 48-hour ambulatory wireless pH monitoring or esophageal biopsies for histopathology,” the researchers concluded. “This can help reduce diagnostic and treatment latency and might allow for monitoring disease activity over time.”
The National Institutes of Health funded the external validation analysis. Diversatek Healthcare, which patented the device together with Vanderbilt University, gave research funding to four coinvestigators, including the senior author. Dr. Patel and the other five coinvestigators reported having no conflicts of interest.
SOURCE: Patel DA et al. Gastroenterology. 2019 Jan 31. doi: 10.1053/j.gastro.2019.01.253.
Evaluating esophageal disorders such as GERD or eosinophilic esophagitis can be time consuming for patients in clinical practice and requires multiple visits to complete testing and obtain results. Other than visualizing complications of reflux such as erosive esophagitis or Barrett’s esophagus, there has been no immediate option to diagnose GERD in standard practice during routine endoscopy. Furthermore, the decision to pursue long-term medication or surgery for GERD relies on a brief pH assessment to be truly representative of a patient’s everyday symptoms. Follow-up of eosinophilic esophagitis requires repeated upper endoscopies with biopsies after every incremental change in medication or diet, which unsurprisingly, can reduce compliance with ongoing management for what is often a readily treatable condition.
Both GERD and eosinophilic esophagitis can be characterized by changes in esophageal mucosal impedance. Rather than directly measuring the pH or eosinophil counts, Dr. Patel and associates prospectively validated the diagnostic test performance of an add-on endoscopic mucosal impedance device that might enable the gastroenterologist to rule out GERD or rule in eosinophilic esophagitis during the index endoscopy with reasonable accuracy (AUC above 0.8 to rule out GERD or rule in eosinophilic esophagitis) while adding 2-3 minutes of procedure time. One patient was admitted for chest pain after use of the device but was discharged without complication, and the authors caution against use in severe fibrostenotic disease.
While work to refine a clinical prediction model with this technology is ongoing, the promise of diagnosing and following common esophageal conditions of GERD and eosinophilic esophagitis during endoscopy would have clear value in expediting care and enhancing compliance with treatment.
Eric D. Shah, MD, MBA, is assistant professor of medicine, director of gastrointestinal motility, esophageal, and swallowing disorders center, Geisel School of Medicine, Dartmouth College, Hanover, N.H. He has no disclosures.
Evaluating esophageal disorders such as GERD or eosinophilic esophagitis can be time consuming for patients in clinical practice and requires multiple visits to complete testing and obtain results. Other than visualizing complications of reflux such as erosive esophagitis or Barrett’s esophagus, there has been no immediate option to diagnose GERD in standard practice during routine endoscopy. Furthermore, the decision to pursue long-term medication or surgery for GERD relies on a brief pH assessment to be truly representative of a patient’s everyday symptoms. Follow-up of eosinophilic esophagitis requires repeated upper endoscopies with biopsies after every incremental change in medication or diet, which unsurprisingly, can reduce compliance with ongoing management for what is often a readily treatable condition.
Both GERD and eosinophilic esophagitis can be characterized by changes in esophageal mucosal impedance. Rather than directly measuring the pH or eosinophil counts, Dr. Patel and associates prospectively validated the diagnostic test performance of an add-on endoscopic mucosal impedance device that might enable the gastroenterologist to rule out GERD or rule in eosinophilic esophagitis during the index endoscopy with reasonable accuracy (AUC above 0.8 to rule out GERD or rule in eosinophilic esophagitis) while adding 2-3 minutes of procedure time. One patient was admitted for chest pain after use of the device but was discharged without complication, and the authors caution against use in severe fibrostenotic disease.
While work to refine a clinical prediction model with this technology is ongoing, the promise of diagnosing and following common esophageal conditions of GERD and eosinophilic esophagitis during endoscopy would have clear value in expediting care and enhancing compliance with treatment.
Eric D. Shah, MD, MBA, is assistant professor of medicine, director of gastrointestinal motility, esophageal, and swallowing disorders center, Geisel School of Medicine, Dartmouth College, Hanover, N.H. He has no disclosures.
Evaluating esophageal disorders such as GERD or eosinophilic esophagitis can be time consuming for patients in clinical practice and requires multiple visits to complete testing and obtain results. Other than visualizing complications of reflux such as erosive esophagitis or Barrett’s esophagus, there has been no immediate option to diagnose GERD in standard practice during routine endoscopy. Furthermore, the decision to pursue long-term medication or surgery for GERD relies on a brief pH assessment to be truly representative of a patient’s everyday symptoms. Follow-up of eosinophilic esophagitis requires repeated upper endoscopies with biopsies after every incremental change in medication or diet, which unsurprisingly, can reduce compliance with ongoing management for what is often a readily treatable condition.
Both GERD and eosinophilic esophagitis can be characterized by changes in esophageal mucosal impedance. Rather than directly measuring the pH or eosinophil counts, Dr. Patel and associates prospectively validated the diagnostic test performance of an add-on endoscopic mucosal impedance device that might enable the gastroenterologist to rule out GERD or rule in eosinophilic esophagitis during the index endoscopy with reasonable accuracy (AUC above 0.8 to rule out GERD or rule in eosinophilic esophagitis) while adding 2-3 minutes of procedure time. One patient was admitted for chest pain after use of the device but was discharged without complication, and the authors caution against use in severe fibrostenotic disease.
While work to refine a clinical prediction model with this technology is ongoing, the promise of diagnosing and following common esophageal conditions of GERD and eosinophilic esophagitis during endoscopy would have clear value in expediting care and enhancing compliance with treatment.
Eric D. Shah, MD, MBA, is assistant professor of medicine, director of gastrointestinal motility, esophageal, and swallowing disorders center, Geisel School of Medicine, Dartmouth College, Hanover, N.H. He has no disclosures.
.
Source: American Gastroenterological Association
Each group showed a significantly different (P less than .01) pattern of mucosal impedance (MI), or disruption of mucosal integrity, along the esophageal axis, wrote Dhyanesh A. Patel, MD, of Vanderbilt University Medical Center in Nashville, Tenn., and his associates. Patients without GERD had higher MI values along all esophageal segments, while GERD was characterized by below-normal values in the distal esophagus only, and eosinophilic esophagitis led to low values throughout the esophagus.
The findings were validated in a separate patient cohort, and the only reported adverse event was an episode of mild chest pain. “This contour heatmap could easily be employed to establish a diagnosis during endoscopy, independent of biopsy or pH monitoring,” the investigators wrote in Gastroenterology. They cautioned that the balloon catheter cannot be safely used in patients with severe fibrostenotic disease.
Current definitive diagnostics for GERD leave much to be desired. Transnasal probes are imprecise and uncomfortable, and they can be insensitive if discomfort causes patients to vary normal activity or skip meals. Wireless ambulatory pH monitoring is more tolerable but unreliable and measures only acidity of refluxed material at a single point along the esophagus. These tests also “fail to account for day-to-day variability of reflux, as they only provide a 24- to 48-hour snapshot of a disease process that is chronic in nature,” the researchers wrote. Eosinophilic esophagitis is becoming more common and usually requires proximal and distal biopsies for diagnosis.
Mucosal impedance contour pattern testing is based on the fact that both GERD and eosinophilic esophagitis involve increased distance between esophageal epithelial cells. The amount of intercellular dilatation correlates inversely with MI values. In proof-of-concept studies, individuals with GERD, non-GERD, eosinophilic esophagitis, and achalasia had distinct MI patterns. However, these studies tested a single-channel catheter system that took only point measurements and was subject to interoperator variability. To improve on this concept, Dr. Patel and his associates mounted radial and axial sensors on a balloon catheter to measure MI at 180-degree intervals along a 10-cm esophageal segment.
They tested the new device prospectively in 69 patients undergoing esophagogastroduodenoscopy with or without pH monitoring (which was used as the standard). In all, 24 patients had GERD, 21 had eosinophilic esophagitis, and 24 had normal findings. By using the intercept and slope of the balloon MI measurements, the researchers detected GERD with an area under the receiver operating characteristic curve (AUC) of 0.67, eosinophilic esophagitis with an AUC of 0.84, and non-GERD with an AUC of 0.83.
These findings held up in a separate validation cohort of 36 patients (28 with GERD and eight with eosinophilic esophagitis) from three tertiary care centers. The probability of eosinophilic esophagitis was highest in patients with low distal MI values (that is, a low intercept) and a low slope (showing that MI values remained low proximally). A low distal MI intercept with a steeper positive slope suggested GERD, while a higher distal MI intercept with a steep slope signified non-GERD.
The system “potentially obviates the need for 24- to 48-hour ambulatory wireless pH monitoring or esophageal biopsies for histopathology,” the researchers concluded. “This can help reduce diagnostic and treatment latency and might allow for monitoring disease activity over time.”
The National Institutes of Health funded the external validation analysis. Diversatek Healthcare, which patented the device together with Vanderbilt University, gave research funding to four coinvestigators, including the senior author. Dr. Patel and the other five coinvestigators reported having no conflicts of interest.
SOURCE: Patel DA et al. Gastroenterology. 2019 Jan 31. doi: 10.1053/j.gastro.2019.01.253.
.
Source: American Gastroenterological Association
Each group showed a significantly different (P less than .01) pattern of mucosal impedance (MI), or disruption of mucosal integrity, along the esophageal axis, wrote Dhyanesh A. Patel, MD, of Vanderbilt University Medical Center in Nashville, Tenn., and his associates. Patients without GERD had higher MI values along all esophageal segments, while GERD was characterized by below-normal values in the distal esophagus only, and eosinophilic esophagitis led to low values throughout the esophagus.
The findings were validated in a separate patient cohort, and the only reported adverse event was an episode of mild chest pain. “This contour heatmap could easily be employed to establish a diagnosis during endoscopy, independent of biopsy or pH monitoring,” the investigators wrote in Gastroenterology. They cautioned that the balloon catheter cannot be safely used in patients with severe fibrostenotic disease.
Current definitive diagnostics for GERD leave much to be desired. Transnasal probes are imprecise and uncomfortable, and they can be insensitive if discomfort causes patients to vary normal activity or skip meals. Wireless ambulatory pH monitoring is more tolerable but unreliable and measures only acidity of refluxed material at a single point along the esophagus. These tests also “fail to account for day-to-day variability of reflux, as they only provide a 24- to 48-hour snapshot of a disease process that is chronic in nature,” the researchers wrote. Eosinophilic esophagitis is becoming more common and usually requires proximal and distal biopsies for diagnosis.
Mucosal impedance contour pattern testing is based on the fact that both GERD and eosinophilic esophagitis involve increased distance between esophageal epithelial cells. The amount of intercellular dilatation correlates inversely with MI values. In proof-of-concept studies, individuals with GERD, non-GERD, eosinophilic esophagitis, and achalasia had distinct MI patterns. However, these studies tested a single-channel catheter system that took only point measurements and was subject to interoperator variability. To improve on this concept, Dr. Patel and his associates mounted radial and axial sensors on a balloon catheter to measure MI at 180-degree intervals along a 10-cm esophageal segment.
They tested the new device prospectively in 69 patients undergoing esophagogastroduodenoscopy with or without pH monitoring (which was used as the standard). In all, 24 patients had GERD, 21 had eosinophilic esophagitis, and 24 had normal findings. By using the intercept and slope of the balloon MI measurements, the researchers detected GERD with an area under the receiver operating characteristic curve (AUC) of 0.67, eosinophilic esophagitis with an AUC of 0.84, and non-GERD with an AUC of 0.83.
These findings held up in a separate validation cohort of 36 patients (28 with GERD and eight with eosinophilic esophagitis) from three tertiary care centers. The probability of eosinophilic esophagitis was highest in patients with low distal MI values (that is, a low intercept) and a low slope (showing that MI values remained low proximally). A low distal MI intercept with a steeper positive slope suggested GERD, while a higher distal MI intercept with a steep slope signified non-GERD.
The system “potentially obviates the need for 24- to 48-hour ambulatory wireless pH monitoring or esophageal biopsies for histopathology,” the researchers concluded. “This can help reduce diagnostic and treatment latency and might allow for monitoring disease activity over time.”
The National Institutes of Health funded the external validation analysis. Diversatek Healthcare, which patented the device together with Vanderbilt University, gave research funding to four coinvestigators, including the senior author. Dr. Patel and the other five coinvestigators reported having no conflicts of interest.
SOURCE: Patel DA et al. Gastroenterology. 2019 Jan 31. doi: 10.1053/j.gastro.2019.01.253.
FROM GASTROENTEROLOGY
POEM outcomes ‘outstanding’ in achalasia with long-term follow-up
PHILADELPHIA – , Stavros N. Stavropoulos, MD, said at a meeting jointly provided by Rutgers and Global Academy for Medical Education.
“POEM represents a first-line treatment option for achalasia that has equivalent or superior efficacy to Heller [myotomy],” said Dr. Stavropoulos, MD, director of the program in advanced GI endoscopy at NYU Winthrop Hospital, Mineola, N.Y.
Although POEM is associated with more gastrointestinal reflux disease (GERD) than laparoscopic Heller myotomy, there is some evidence that the advantage of Heller in this respect may decrease over time, he told attendees.
“GERD after POEM is easily treatable with proton pump inhibitors (PPIs), with good patient satisfaction and no significant long-term GERD complications,” Dr. Stavropoulos said in a presentation on minimally invasive approaches to esophageal disorders.
NYU Winthrop Hospital was the site of the first human POEM outside of Japan, performed in 2009 by Dr. Stavropoulos, who along with colleagues recently published what he said is the largest single-operator POEM series in the Western hemisphere.
That report in Gastrointestinal Endoscopy (2018 Apr;87[4]:972-85) was based on 318 consecutive POEMs performed through October 2016. Dr. Stavropoulos and colleagues reported that over a median follow-up of 28 months they had a 95.7% clinical success rate, defined as a Eckardt score of 3 or more and no further treatment needed.
Those results suggested POEM should be a “treatment of choice” for challenging cases managed at centers who have a high level of experience with the procedure, the investigators said at the time.
Dr. Stavropoulos presented his center’s updated experience including 515 patients undergoing POEM, with a median follow-up of 37 months. About 50% of the patients were previously treated, including 73 (14% who underwent Heller myotomy).
Mean Eckardt scores were 7.7 preprocedure and 0.5 post procedure, while on timed barium swallow, emptying of 50% or greater at 5 minutes was seen in 96% of patients, and 100% emptying at 5 minutes was seen in 68%, according to data Dr. Stavropoulos presented.
Disease-free probability was 99% at 1 year and 90% at 5 years, he added.
There were no deaths, leaks, aborted procedures, or need for drains in this series, according to the investigator. Three percent of patients had a hospitalization exceeding 5 days, while 1% were readmitted because of minor adverse events related to POEM, such as dehydration, Dr. Stavropoulos reported.
In 2017, the American Gastroenterological Association published a clinical practice update “legitimizing” POEM as a first-line achalasia treatment, Dr. Stavropoulos said. That update said POEM should be performed in high-volume centers by experienced physicians.
Patients who experience GERD after POEM can be effectively treated with standard, once-daily PPI therapy, according to the expert.
“The absolute difference in GERD rates between laparoscopic Heller myotomy and POEM is 20%-25% at 1 year, but may decrease with time, and may be associated with inferior dysphagia relief in LHM patients,” Dr. Stavropoulos told attendees.
Dr. Stavropoulos disclosed that he is a consultant for Boston Scientific and ERBE.
Global Academy and this news organization are owned by the same company.
PHILADELPHIA – , Stavros N. Stavropoulos, MD, said at a meeting jointly provided by Rutgers and Global Academy for Medical Education.
“POEM represents a first-line treatment option for achalasia that has equivalent or superior efficacy to Heller [myotomy],” said Dr. Stavropoulos, MD, director of the program in advanced GI endoscopy at NYU Winthrop Hospital, Mineola, N.Y.
Although POEM is associated with more gastrointestinal reflux disease (GERD) than laparoscopic Heller myotomy, there is some evidence that the advantage of Heller in this respect may decrease over time, he told attendees.
“GERD after POEM is easily treatable with proton pump inhibitors (PPIs), with good patient satisfaction and no significant long-term GERD complications,” Dr. Stavropoulos said in a presentation on minimally invasive approaches to esophageal disorders.
NYU Winthrop Hospital was the site of the first human POEM outside of Japan, performed in 2009 by Dr. Stavropoulos, who along with colleagues recently published what he said is the largest single-operator POEM series in the Western hemisphere.
That report in Gastrointestinal Endoscopy (2018 Apr;87[4]:972-85) was based on 318 consecutive POEMs performed through October 2016. Dr. Stavropoulos and colleagues reported that over a median follow-up of 28 months they had a 95.7% clinical success rate, defined as a Eckardt score of 3 or more and no further treatment needed.
Those results suggested POEM should be a “treatment of choice” for challenging cases managed at centers who have a high level of experience with the procedure, the investigators said at the time.
Dr. Stavropoulos presented his center’s updated experience including 515 patients undergoing POEM, with a median follow-up of 37 months. About 50% of the patients were previously treated, including 73 (14% who underwent Heller myotomy).
Mean Eckardt scores were 7.7 preprocedure and 0.5 post procedure, while on timed barium swallow, emptying of 50% or greater at 5 minutes was seen in 96% of patients, and 100% emptying at 5 minutes was seen in 68%, according to data Dr. Stavropoulos presented.
Disease-free probability was 99% at 1 year and 90% at 5 years, he added.
There were no deaths, leaks, aborted procedures, or need for drains in this series, according to the investigator. Three percent of patients had a hospitalization exceeding 5 days, while 1% were readmitted because of minor adverse events related to POEM, such as dehydration, Dr. Stavropoulos reported.
In 2017, the American Gastroenterological Association published a clinical practice update “legitimizing” POEM as a first-line achalasia treatment, Dr. Stavropoulos said. That update said POEM should be performed in high-volume centers by experienced physicians.
Patients who experience GERD after POEM can be effectively treated with standard, once-daily PPI therapy, according to the expert.
“The absolute difference in GERD rates between laparoscopic Heller myotomy and POEM is 20%-25% at 1 year, but may decrease with time, and may be associated with inferior dysphagia relief in LHM patients,” Dr. Stavropoulos told attendees.
Dr. Stavropoulos disclosed that he is a consultant for Boston Scientific and ERBE.
Global Academy and this news organization are owned by the same company.
PHILADELPHIA – , Stavros N. Stavropoulos, MD, said at a meeting jointly provided by Rutgers and Global Academy for Medical Education.
“POEM represents a first-line treatment option for achalasia that has equivalent or superior efficacy to Heller [myotomy],” said Dr. Stavropoulos, MD, director of the program in advanced GI endoscopy at NYU Winthrop Hospital, Mineola, N.Y.
Although POEM is associated with more gastrointestinal reflux disease (GERD) than laparoscopic Heller myotomy, there is some evidence that the advantage of Heller in this respect may decrease over time, he told attendees.
“GERD after POEM is easily treatable with proton pump inhibitors (PPIs), with good patient satisfaction and no significant long-term GERD complications,” Dr. Stavropoulos said in a presentation on minimally invasive approaches to esophageal disorders.
NYU Winthrop Hospital was the site of the first human POEM outside of Japan, performed in 2009 by Dr. Stavropoulos, who along with colleagues recently published what he said is the largest single-operator POEM series in the Western hemisphere.
That report in Gastrointestinal Endoscopy (2018 Apr;87[4]:972-85) was based on 318 consecutive POEMs performed through October 2016. Dr. Stavropoulos and colleagues reported that over a median follow-up of 28 months they had a 95.7% clinical success rate, defined as a Eckardt score of 3 or more and no further treatment needed.
Those results suggested POEM should be a “treatment of choice” for challenging cases managed at centers who have a high level of experience with the procedure, the investigators said at the time.
Dr. Stavropoulos presented his center’s updated experience including 515 patients undergoing POEM, with a median follow-up of 37 months. About 50% of the patients were previously treated, including 73 (14% who underwent Heller myotomy).
Mean Eckardt scores were 7.7 preprocedure and 0.5 post procedure, while on timed barium swallow, emptying of 50% or greater at 5 minutes was seen in 96% of patients, and 100% emptying at 5 minutes was seen in 68%, according to data Dr. Stavropoulos presented.
Disease-free probability was 99% at 1 year and 90% at 5 years, he added.
There were no deaths, leaks, aborted procedures, or need for drains in this series, according to the investigator. Three percent of patients had a hospitalization exceeding 5 days, while 1% were readmitted because of minor adverse events related to POEM, such as dehydration, Dr. Stavropoulos reported.
In 2017, the American Gastroenterological Association published a clinical practice update “legitimizing” POEM as a first-line achalasia treatment, Dr. Stavropoulos said. That update said POEM should be performed in high-volume centers by experienced physicians.
Patients who experience GERD after POEM can be effectively treated with standard, once-daily PPI therapy, according to the expert.
“The absolute difference in GERD rates between laparoscopic Heller myotomy and POEM is 20%-25% at 1 year, but may decrease with time, and may be associated with inferior dysphagia relief in LHM patients,” Dr. Stavropoulos told attendees.
Dr. Stavropoulos disclosed that he is a consultant for Boston Scientific and ERBE.
Global Academy and this news organization are owned by the same company.
REPORTING FROM DIGESTIVE DISEASES: NEW ADVANCES
DDNA 2019 - Heartburn: Modern Diagnosis of GERD
AT DIGESTIVE DISEASES: NEW ADVANCES
Interactive online module improved detection of Barrett’s esophagus neoplasia
An online educational tool for endoscopists helped improve their detection of Barrett’s esophagus–related neoplasia (BORN), researchers reported in the April issue of Gastroenterology.
In tests administered before and after training, endoscopists increased their rates of BORN detection by a median of 30% (P less than .001), reported J.J. Bergman, MD, PhD, of the University of Amsterdam, together with his associates. “To our knowledge, this is the first validated online, interactive endoscopic training program in our field,” they wrote. “Widespread use of this tool might improve management of Barrett’s esophagus by general endoscopists.”
To develop the program, the investigators recorded high-definition videos of upper endoscopies of patients with either BORN or nondysplastic Barrett’s esophagus. They sent these videos to three experts, who used special tools to superimpose their delineations of lesions.
Next, 68 general endoscopists (fellows, early-career general gastroenterologists, and senior general gastroenterologists) watched four batches of 20 videos each. The researchers compared the assessors’ interpretations with the experts’ to identify the 25 videos with the most educational impact. These were then shown in four batches of five to 121 new assessors (five videos were reserved for pre- and post testing).
From the first to the fourth batch of training videos, assessors sequentially improved their scores for detection, delineation, agreement delineation, and relative delineation of BORN, the researchers said. Among the 121 assessors in the second phase of development, median rates of detection of BORN rose by 30% after training. Furthermore, from baseline to the end of the study, scores rose by 46% for detection, 129% for delineation, 105% for agreement delineation, and 106% for relative delineation (all P less than .001). These improvements did not depend on the country of origin of the assessors or their level of endoscopic experience.
This module requires the use of high-definition videos whose resolution is not lost during replay or when viewed on the web, the researchers emphasized. They noted that the module is active, not passive – learners select the video frame to position a biopsy mark and delineate the lesion, and the software then gives them tailored feedback on their choice. Learners also can add and remove the experts’ delineations as well as their own during feedback sessions at the end of each batch of videos. This enables them to “fully appreciate the subtle appearance of the lesion on the selected time frame,” the investigators wrote.
By completing the training module, “general endoscopists with a wide range of experience and from different countries of origin can substantially and conveniently increase their skills for detection and delineation of early BORN lesions,” they concluded. “Therefore, the module could provide training in an essential upper gastrointestinal endoscopic skill that is not otherwise readily available.”
The investigators disclosed no external funding sources. They reported having no conflicts of interest.
SOURCE: Bergman JJ et al. Gastroenterology. 2019 Jan 2. doi: 10.1053/j.gastro.2018.12.021.
Endoscopic mucosal resection and ablation strategies offer the potential for minimally invasive, curative treatment for patients with Barrett’s esophagus–associated intramucosal neoplasia. For the gastroenterologist interested in endoscopic prevention and management of esophageal cancer, however, achieving proficiency in performance of these endoscopic techniques represents only part of the requisite preparatory experience. Acquisition of cognitive skills in lesion recognition is a fundamental and underappreciated component to a successful endoscopic treatment paradigm.
General endoscopist assessors were grouped into three groups based on level of experience. Following completion of the training module, scores in lesion detection and delineation increased irrespective of level of endoscopist experience.
The module is free, CME-accredited, and available for online use. Any endoscopist who performs Barrett’s screening, surveillance, and therapy should be motivated and incentivized to engage with this important educational tool.
Patrick Yachimski, MD, MPH, AGAF, is associate professor of medicine, director of pancreatobiliary endoscopy, division of gastroenterology, hepatology & nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
Endoscopic mucosal resection and ablation strategies offer the potential for minimally invasive, curative treatment for patients with Barrett’s esophagus–associated intramucosal neoplasia. For the gastroenterologist interested in endoscopic prevention and management of esophageal cancer, however, achieving proficiency in performance of these endoscopic techniques represents only part of the requisite preparatory experience. Acquisition of cognitive skills in lesion recognition is a fundamental and underappreciated component to a successful endoscopic treatment paradigm.
General endoscopist assessors were grouped into three groups based on level of experience. Following completion of the training module, scores in lesion detection and delineation increased irrespective of level of endoscopist experience.
The module is free, CME-accredited, and available for online use. Any endoscopist who performs Barrett’s screening, surveillance, and therapy should be motivated and incentivized to engage with this important educational tool.
Patrick Yachimski, MD, MPH, AGAF, is associate professor of medicine, director of pancreatobiliary endoscopy, division of gastroenterology, hepatology & nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
Endoscopic mucosal resection and ablation strategies offer the potential for minimally invasive, curative treatment for patients with Barrett’s esophagus–associated intramucosal neoplasia. For the gastroenterologist interested in endoscopic prevention and management of esophageal cancer, however, achieving proficiency in performance of these endoscopic techniques represents only part of the requisite preparatory experience. Acquisition of cognitive skills in lesion recognition is a fundamental and underappreciated component to a successful endoscopic treatment paradigm.
General endoscopist assessors were grouped into three groups based on level of experience. Following completion of the training module, scores in lesion detection and delineation increased irrespective of level of endoscopist experience.
The module is free, CME-accredited, and available for online use. Any endoscopist who performs Barrett’s screening, surveillance, and therapy should be motivated and incentivized to engage with this important educational tool.
Patrick Yachimski, MD, MPH, AGAF, is associate professor of medicine, director of pancreatobiliary endoscopy, division of gastroenterology, hepatology & nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
An online educational tool for endoscopists helped improve their detection of Barrett’s esophagus–related neoplasia (BORN), researchers reported in the April issue of Gastroenterology.
In tests administered before and after training, endoscopists increased their rates of BORN detection by a median of 30% (P less than .001), reported J.J. Bergman, MD, PhD, of the University of Amsterdam, together with his associates. “To our knowledge, this is the first validated online, interactive endoscopic training program in our field,” they wrote. “Widespread use of this tool might improve management of Barrett’s esophagus by general endoscopists.”
To develop the program, the investigators recorded high-definition videos of upper endoscopies of patients with either BORN or nondysplastic Barrett’s esophagus. They sent these videos to three experts, who used special tools to superimpose their delineations of lesions.
Next, 68 general endoscopists (fellows, early-career general gastroenterologists, and senior general gastroenterologists) watched four batches of 20 videos each. The researchers compared the assessors’ interpretations with the experts’ to identify the 25 videos with the most educational impact. These were then shown in four batches of five to 121 new assessors (five videos were reserved for pre- and post testing).
From the first to the fourth batch of training videos, assessors sequentially improved their scores for detection, delineation, agreement delineation, and relative delineation of BORN, the researchers said. Among the 121 assessors in the second phase of development, median rates of detection of BORN rose by 30% after training. Furthermore, from baseline to the end of the study, scores rose by 46% for detection, 129% for delineation, 105% for agreement delineation, and 106% for relative delineation (all P less than .001). These improvements did not depend on the country of origin of the assessors or their level of endoscopic experience.
This module requires the use of high-definition videos whose resolution is not lost during replay or when viewed on the web, the researchers emphasized. They noted that the module is active, not passive – learners select the video frame to position a biopsy mark and delineate the lesion, and the software then gives them tailored feedback on their choice. Learners also can add and remove the experts’ delineations as well as their own during feedback sessions at the end of each batch of videos. This enables them to “fully appreciate the subtle appearance of the lesion on the selected time frame,” the investigators wrote.
By completing the training module, “general endoscopists with a wide range of experience and from different countries of origin can substantially and conveniently increase their skills for detection and delineation of early BORN lesions,” they concluded. “Therefore, the module could provide training in an essential upper gastrointestinal endoscopic skill that is not otherwise readily available.”
The investigators disclosed no external funding sources. They reported having no conflicts of interest.
SOURCE: Bergman JJ et al. Gastroenterology. 2019 Jan 2. doi: 10.1053/j.gastro.2018.12.021.
An online educational tool for endoscopists helped improve their detection of Barrett’s esophagus–related neoplasia (BORN), researchers reported in the April issue of Gastroenterology.
In tests administered before and after training, endoscopists increased their rates of BORN detection by a median of 30% (P less than .001), reported J.J. Bergman, MD, PhD, of the University of Amsterdam, together with his associates. “To our knowledge, this is the first validated online, interactive endoscopic training program in our field,” they wrote. “Widespread use of this tool might improve management of Barrett’s esophagus by general endoscopists.”
To develop the program, the investigators recorded high-definition videos of upper endoscopies of patients with either BORN or nondysplastic Barrett’s esophagus. They sent these videos to three experts, who used special tools to superimpose their delineations of lesions.
Next, 68 general endoscopists (fellows, early-career general gastroenterologists, and senior general gastroenterologists) watched four batches of 20 videos each. The researchers compared the assessors’ interpretations with the experts’ to identify the 25 videos with the most educational impact. These were then shown in four batches of five to 121 new assessors (five videos were reserved for pre- and post testing).
From the first to the fourth batch of training videos, assessors sequentially improved their scores for detection, delineation, agreement delineation, and relative delineation of BORN, the researchers said. Among the 121 assessors in the second phase of development, median rates of detection of BORN rose by 30% after training. Furthermore, from baseline to the end of the study, scores rose by 46% for detection, 129% for delineation, 105% for agreement delineation, and 106% for relative delineation (all P less than .001). These improvements did not depend on the country of origin of the assessors or their level of endoscopic experience.
This module requires the use of high-definition videos whose resolution is not lost during replay or when viewed on the web, the researchers emphasized. They noted that the module is active, not passive – learners select the video frame to position a biopsy mark and delineate the lesion, and the software then gives them tailored feedback on their choice. Learners also can add and remove the experts’ delineations as well as their own during feedback sessions at the end of each batch of videos. This enables them to “fully appreciate the subtle appearance of the lesion on the selected time frame,” the investigators wrote.
By completing the training module, “general endoscopists with a wide range of experience and from different countries of origin can substantially and conveniently increase their skills for detection and delineation of early BORN lesions,” they concluded. “Therefore, the module could provide training in an essential upper gastrointestinal endoscopic skill that is not otherwise readily available.”
The investigators disclosed no external funding sources. They reported having no conflicts of interest.
SOURCE: Bergman JJ et al. Gastroenterology. 2019 Jan 2. doi: 10.1053/j.gastro.2018.12.021.
FROM GASTROENTEROLOGY
Barrett’s esophagus uncommon in patients with uncomplicated GERD
Uncomplicated gastroesophageal reflux disease (GERD) accounted for 13.5% of esophagogastroduodenoscopies, but 5.6% of these patients had suspected Barrett’s esophagus and only 1.4% had suspected long-segment Barrett’s esophagus, researchers reported. The study appears in the April issue of Clinical Gastroenterology and Hepatology.
“The prevalence of suspected Barrett’s esophagus is lower than in prior time periods. This raises questions about the utility of esophagogastroduodenoscopies to detect Barrett’s esophagus in patients with uncomplicated GERD,” wrote Emery C. Lin, MD, of Oregon Health and Science University, Portland, and his associates there and at Massachusetts General Hospital, Boston.
Symptoms of GERD affect more than one in four U.S. adults and are a risk factor for Barrett’s esophagus. However, the prevalence of Barrett’s esophagus is unclear in patients with dysphagia and in the era of proton pump inhibitors, the researchers said. The American Gastroenterological Association strongly discourages reflexively screening patients with GERD for Barrett’s esophagus, but “weakly recommends” screening GERD patients with multiple risk factors for Barrett’s esophagus, including chronic GERD, hiatal hernia, older age (50 years and up), white race, male sex, increased body mass index, and intra-abdominal adiposity.
To understand the prevalence and findings of esophagogastroduodenoscopy in patients with GERD without alarm symptoms (including weight loss, dysphagia, and bleeding), the investigators studied 543,103 of these procedures performed at 82 sites in the United States between 2003 and 2013. The data came from the National Endoscopic Database, which generates endoscopy reports using a structured computer form.
A total of 73,535 esophagogastroduodenoscopies (13.5%) were performed for GERD without alarm symptoms. Among these patients, 4,122 (5.6%) had suspected Barrett’s esophagus, of which 24.2% had suspected long-segment Barrett’s esophagus (3 cm or longer). Among patients with uncomplicated GERD, the prevalence of suspected Barrett’s esophagus was 5.6%, and the prevalence of long-segment disease was 1.4%.
Although male sex, older age, and white race were significant risk factors for suspected Barrett’s esophagus and suspected long-segment disease, 23.6% of esophagogastroduodenoscopies were performed in white men older than 50 years. “We find that low-risk populations with uncomplicated GERD make up a significant number of esophagogastroduodenoscopies done for uncomplicated GERD,” the investigators wrote. “If esophagogastroduodenoscopies were limited to patients that met the AGA criteria of being male, white, and age over 50, we would have detected 34 of 47 (72.3%) of esophageal tumors and found suspected Barrett’s esophagus in nearly 10%, while reducing the burden of endoscopy by more than 75%.”
Hiatal hernia was a significant correlate of suspected Barrett’s esophagus (odds ratio, 1.6), the researchers noted. Esophagitis was not associated with suspected Barrett’s esophagus overall but did correlate with long-segment disease. Esophagitis might mask underlying short-segment Barrett’s esophagus, and short-segment Barrett’s esophagus might be milder in nature and more responsive to antisecretory therapy, the researchers said. They noted that severe (grade C/D) esophagitis was strongly linked with both short-segment and long-segment Barrett’s esophagus.
The National Institute of Diabetes and Digestive and Kidney Diseases provided funding. The researchers reported having no conflicts of interest.
SOURCE: Lin EC et al. Clin Gastroenterol Hepatol. 2019 Apr. doi: 10.1016/j.cgh.2018.08.066.
The utility and cost-effectiveness of screening for Barrett’s esophagus with esophagogastroduodenoscopy (EGD) remain contentious issues. National GI societies currently recommend screening in only a limited high-risk population, mainly white men aged 50 or older with chronic GERD and one or more additional risk factors. It is unclear to what degree those guidelines are adhered to in clinical practice. This study by Lin et al. sheds further light on this issue. The investigators showed that a significant proportion (more than 10%) of EGDs were performed for uncomplicated GERD, with less than one-quarter of those patients meeting the minimal criteria for screening for Barrett’s esophagus. Among this group, the prevalence of Barrett’s esophagus was found to be lower than previously reported. The data offer compelling evidence that screening low-risk patients with uncomplicated GERD by using upper endoscopy is not cost effective, and is at best marginally cost effective if limited to the high-risk group identified by national GI societies. The question arises whether we should abandon screening for Barrett’s esophagus altogether.
The challenge, however, is that the incidence of esophageal adenocarcinoma continues to rise (albeit at a slower pace in recent years), and 5-year survival of patients diagnosed with esophageal adenocarcinoma remains extremely poor. Therefore, prevention remains the optimal strategy. The solution may lie in adopting a lower-cost screening modality that can replace endoscopy for this purpose, and while many such techniques are under investigation, further studies are required to find a widely applicable alternative to EGD.
Nabil M. Mansour, MD, is an assistant professor, department of medicine, section of gastroenterology and hepatology, Baylor College of Medicine, Houston. He has no conflicts of interest.
The utility and cost-effectiveness of screening for Barrett’s esophagus with esophagogastroduodenoscopy (EGD) remain contentious issues. National GI societies currently recommend screening in only a limited high-risk population, mainly white men aged 50 or older with chronic GERD and one or more additional risk factors. It is unclear to what degree those guidelines are adhered to in clinical practice. This study by Lin et al. sheds further light on this issue. The investigators showed that a significant proportion (more than 10%) of EGDs were performed for uncomplicated GERD, with less than one-quarter of those patients meeting the minimal criteria for screening for Barrett’s esophagus. Among this group, the prevalence of Barrett’s esophagus was found to be lower than previously reported. The data offer compelling evidence that screening low-risk patients with uncomplicated GERD by using upper endoscopy is not cost effective, and is at best marginally cost effective if limited to the high-risk group identified by national GI societies. The question arises whether we should abandon screening for Barrett’s esophagus altogether.
The challenge, however, is that the incidence of esophageal adenocarcinoma continues to rise (albeit at a slower pace in recent years), and 5-year survival of patients diagnosed with esophageal adenocarcinoma remains extremely poor. Therefore, prevention remains the optimal strategy. The solution may lie in adopting a lower-cost screening modality that can replace endoscopy for this purpose, and while many such techniques are under investigation, further studies are required to find a widely applicable alternative to EGD.
Nabil M. Mansour, MD, is an assistant professor, department of medicine, section of gastroenterology and hepatology, Baylor College of Medicine, Houston. He has no conflicts of interest.
The utility and cost-effectiveness of screening for Barrett’s esophagus with esophagogastroduodenoscopy (EGD) remain contentious issues. National GI societies currently recommend screening in only a limited high-risk population, mainly white men aged 50 or older with chronic GERD and one or more additional risk factors. It is unclear to what degree those guidelines are adhered to in clinical practice. This study by Lin et al. sheds further light on this issue. The investigators showed that a significant proportion (more than 10%) of EGDs were performed for uncomplicated GERD, with less than one-quarter of those patients meeting the minimal criteria for screening for Barrett’s esophagus. Among this group, the prevalence of Barrett’s esophagus was found to be lower than previously reported. The data offer compelling evidence that screening low-risk patients with uncomplicated GERD by using upper endoscopy is not cost effective, and is at best marginally cost effective if limited to the high-risk group identified by national GI societies. The question arises whether we should abandon screening for Barrett’s esophagus altogether.
The challenge, however, is that the incidence of esophageal adenocarcinoma continues to rise (albeit at a slower pace in recent years), and 5-year survival of patients diagnosed with esophageal adenocarcinoma remains extremely poor. Therefore, prevention remains the optimal strategy. The solution may lie in adopting a lower-cost screening modality that can replace endoscopy for this purpose, and while many such techniques are under investigation, further studies are required to find a widely applicable alternative to EGD.
Nabil M. Mansour, MD, is an assistant professor, department of medicine, section of gastroenterology and hepatology, Baylor College of Medicine, Houston. He has no conflicts of interest.
Uncomplicated gastroesophageal reflux disease (GERD) accounted for 13.5% of esophagogastroduodenoscopies, but 5.6% of these patients had suspected Barrett’s esophagus and only 1.4% had suspected long-segment Barrett’s esophagus, researchers reported. The study appears in the April issue of Clinical Gastroenterology and Hepatology.
“The prevalence of suspected Barrett’s esophagus is lower than in prior time periods. This raises questions about the utility of esophagogastroduodenoscopies to detect Barrett’s esophagus in patients with uncomplicated GERD,” wrote Emery C. Lin, MD, of Oregon Health and Science University, Portland, and his associates there and at Massachusetts General Hospital, Boston.
Symptoms of GERD affect more than one in four U.S. adults and are a risk factor for Barrett’s esophagus. However, the prevalence of Barrett’s esophagus is unclear in patients with dysphagia and in the era of proton pump inhibitors, the researchers said. The American Gastroenterological Association strongly discourages reflexively screening patients with GERD for Barrett’s esophagus, but “weakly recommends” screening GERD patients with multiple risk factors for Barrett’s esophagus, including chronic GERD, hiatal hernia, older age (50 years and up), white race, male sex, increased body mass index, and intra-abdominal adiposity.
To understand the prevalence and findings of esophagogastroduodenoscopy in patients with GERD without alarm symptoms (including weight loss, dysphagia, and bleeding), the investigators studied 543,103 of these procedures performed at 82 sites in the United States between 2003 and 2013. The data came from the National Endoscopic Database, which generates endoscopy reports using a structured computer form.
A total of 73,535 esophagogastroduodenoscopies (13.5%) were performed for GERD without alarm symptoms. Among these patients, 4,122 (5.6%) had suspected Barrett’s esophagus, of which 24.2% had suspected long-segment Barrett’s esophagus (3 cm or longer). Among patients with uncomplicated GERD, the prevalence of suspected Barrett’s esophagus was 5.6%, and the prevalence of long-segment disease was 1.4%.
Although male sex, older age, and white race were significant risk factors for suspected Barrett’s esophagus and suspected long-segment disease, 23.6% of esophagogastroduodenoscopies were performed in white men older than 50 years. “We find that low-risk populations with uncomplicated GERD make up a significant number of esophagogastroduodenoscopies done for uncomplicated GERD,” the investigators wrote. “If esophagogastroduodenoscopies were limited to patients that met the AGA criteria of being male, white, and age over 50, we would have detected 34 of 47 (72.3%) of esophageal tumors and found suspected Barrett’s esophagus in nearly 10%, while reducing the burden of endoscopy by more than 75%.”
Hiatal hernia was a significant correlate of suspected Barrett’s esophagus (odds ratio, 1.6), the researchers noted. Esophagitis was not associated with suspected Barrett’s esophagus overall but did correlate with long-segment disease. Esophagitis might mask underlying short-segment Barrett’s esophagus, and short-segment Barrett’s esophagus might be milder in nature and more responsive to antisecretory therapy, the researchers said. They noted that severe (grade C/D) esophagitis was strongly linked with both short-segment and long-segment Barrett’s esophagus.
The National Institute of Diabetes and Digestive and Kidney Diseases provided funding. The researchers reported having no conflicts of interest.
SOURCE: Lin EC et al. Clin Gastroenterol Hepatol. 2019 Apr. doi: 10.1016/j.cgh.2018.08.066.
Uncomplicated gastroesophageal reflux disease (GERD) accounted for 13.5% of esophagogastroduodenoscopies, but 5.6% of these patients had suspected Barrett’s esophagus and only 1.4% had suspected long-segment Barrett’s esophagus, researchers reported. The study appears in the April issue of Clinical Gastroenterology and Hepatology.
“The prevalence of suspected Barrett’s esophagus is lower than in prior time periods. This raises questions about the utility of esophagogastroduodenoscopies to detect Barrett’s esophagus in patients with uncomplicated GERD,” wrote Emery C. Lin, MD, of Oregon Health and Science University, Portland, and his associates there and at Massachusetts General Hospital, Boston.
Symptoms of GERD affect more than one in four U.S. adults and are a risk factor for Barrett’s esophagus. However, the prevalence of Barrett’s esophagus is unclear in patients with dysphagia and in the era of proton pump inhibitors, the researchers said. The American Gastroenterological Association strongly discourages reflexively screening patients with GERD for Barrett’s esophagus, but “weakly recommends” screening GERD patients with multiple risk factors for Barrett’s esophagus, including chronic GERD, hiatal hernia, older age (50 years and up), white race, male sex, increased body mass index, and intra-abdominal adiposity.
To understand the prevalence and findings of esophagogastroduodenoscopy in patients with GERD without alarm symptoms (including weight loss, dysphagia, and bleeding), the investigators studied 543,103 of these procedures performed at 82 sites in the United States between 2003 and 2013. The data came from the National Endoscopic Database, which generates endoscopy reports using a structured computer form.
A total of 73,535 esophagogastroduodenoscopies (13.5%) were performed for GERD without alarm symptoms. Among these patients, 4,122 (5.6%) had suspected Barrett’s esophagus, of which 24.2% had suspected long-segment Barrett’s esophagus (3 cm or longer). Among patients with uncomplicated GERD, the prevalence of suspected Barrett’s esophagus was 5.6%, and the prevalence of long-segment disease was 1.4%.
Although male sex, older age, and white race were significant risk factors for suspected Barrett’s esophagus and suspected long-segment disease, 23.6% of esophagogastroduodenoscopies were performed in white men older than 50 years. “We find that low-risk populations with uncomplicated GERD make up a significant number of esophagogastroduodenoscopies done for uncomplicated GERD,” the investigators wrote. “If esophagogastroduodenoscopies were limited to patients that met the AGA criteria of being male, white, and age over 50, we would have detected 34 of 47 (72.3%) of esophageal tumors and found suspected Barrett’s esophagus in nearly 10%, while reducing the burden of endoscopy by more than 75%.”
Hiatal hernia was a significant correlate of suspected Barrett’s esophagus (odds ratio, 1.6), the researchers noted. Esophagitis was not associated with suspected Barrett’s esophagus overall but did correlate with long-segment disease. Esophagitis might mask underlying short-segment Barrett’s esophagus, and short-segment Barrett’s esophagus might be milder in nature and more responsive to antisecretory therapy, the researchers said. They noted that severe (grade C/D) esophagitis was strongly linked with both short-segment and long-segment Barrett’s esophagus.
The National Institute of Diabetes and Digestive and Kidney Diseases provided funding. The researchers reported having no conflicts of interest.
SOURCE: Lin EC et al. Clin Gastroenterol Hepatol. 2019 Apr. doi: 10.1016/j.cgh.2018.08.066.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Long-term budesonide oral suspension well tolerated in EoE
Treatment with budesonide oral suspension (BOS) was generally well tolerated and maintained a histologic response in some patients with eosinophilic esophagitis (EoE), according to the results of the 24-week, open-label extension phase of a multicenter, randomized, placebo-controlled, industry-sponsored trial.
Rates of histologic response (up to 6 eosinophils per high-power field) were “modest” – 23% among patients who stayed on BOS throughout the study and 48.5% among patients who initiated BOS after 12 weeks on placebo, reported Evan S. Dellon, MD, MPH, of the University of North Carolina in Chapel Hill and his associates. However, these rates “need to be viewed in the context of a highly symptomatic and histologically severe population with eosinophilic esophagitis,” they contended. A total of 11% of budesonide initiators developed esophageal candidiasis, they reported in Clinical Gastroenterology and Hepatology.
Budesonide oral suspension is a mucoadherent formulation of topical corticosteroid that has recently been developed to treat EoE. Previously, during the randomized, double-blind component of this phase 2 trial, 93 patients aged 11-40 years with active EoE and dysphagia received either BOS (2 mg) or placebo twice daily (Gastroenterology. 2017 Mar;157[4]:776-86). After 12 weeks, rates of histologic response were 39% for BOS versus 3% for placebo, and BOS significantly improved patients’ mean peak eosinophil count and scores on the Dysphagia Symptom Questionnaire, compared with baseline and compared with the response in the placebo group. During the open-label extension phase, 45 BOS continuers and 37 BOS initiators received 2 mg once daily for 12 weeks and then had the option to increase the BOS dose to 1.5-2.0 mg twice daily.
The rate of drug-related adverse events was 19% among BOS initiators and 4% among BOS continuers. One patient in each group developed oral candidiasis, while four BOS initiators (11%) developed esophageal candidiasis. Three BOS continuers had subnormal morning cortisol levels; while these were subclinical cases, they merit attention since long-term corticosteroids for EoE have been linked with possible hypothalamic–pituitary–adrenal axis suppression, the researchers noted.
In addition, while BOS initiators tended to maintain their endoscopic response, only 42% of those with an initial histologic response maintained a histologic response after 36 weeks of treatment or when leaving the study. Post hoc analyses confirmed that prolonged BOS treatment does not increase the chances of histologic or endoscopic response. Prior studies have suggested that EoE can become steroid-refractory over time and that certain molecular and histologic markers might predict resistance, the investigators noted.
Meritage Pharma (now part of Shire) was involved in the study design and conduct, data collection and management, and manuscript review. Dr. Dellon disclosed research funding from Meritage and Shire and a consulting relationship with Shire, along with ties to several other pharmaceutical companies. All six coinvestigators also disclosed ties to Meritage, Shire, or both, and two are Shire employees and stockholders.
*This story was updated on Feb. 7, 2019.
SOURCE: Dellon ES et al. Clin Gastroenterol Hepatol. 2018 Jun 11. doi: 10.1016/j.cgh.2018.05.051.
Guidelines regarding the management of eosinophilic esophagitis (EoE) with topical steroids are still unclear with regard to dosing and duration. Here, Dellon et al. present evidence that long-term budesonide oral suspension (BOS) therapy is safe and efficacious. Both the BOS and placebo cohorts of the initial, 12-week trial demonstrated clinical and histologic improvement on BOS over this 24-week period, with few adverse events. Maintenance of histologic response was only seen in 42% in initial BOS responders, suggesting steroid tolerance or resistance may develop. Another important observation was that peak eosinphil count decreased steroid dosing.
Finally, these data support the notion that initial responders are unlikely to gain response with continued therapy and may be better served with early transition to alternatives. Further research is needed to clarify these issues and which patients may be predisposed to nonresponse or loss of response.
Reena V. Chokshi, MD , is assistant professor of medicine in the department of gastroenterology at Baylor College of Medicine, Houston.
Guidelines regarding the management of eosinophilic esophagitis (EoE) with topical steroids are still unclear with regard to dosing and duration. Here, Dellon et al. present evidence that long-term budesonide oral suspension (BOS) therapy is safe and efficacious. Both the BOS and placebo cohorts of the initial, 12-week trial demonstrated clinical and histologic improvement on BOS over this 24-week period, with few adverse events. Maintenance of histologic response was only seen in 42% in initial BOS responders, suggesting steroid tolerance or resistance may develop. Another important observation was that peak eosinphil count decreased steroid dosing.
Finally, these data support the notion that initial responders are unlikely to gain response with continued therapy and may be better served with early transition to alternatives. Further research is needed to clarify these issues and which patients may be predisposed to nonresponse or loss of response.
Reena V. Chokshi, MD , is assistant professor of medicine in the department of gastroenterology at Baylor College of Medicine, Houston.
Guidelines regarding the management of eosinophilic esophagitis (EoE) with topical steroids are still unclear with regard to dosing and duration. Here, Dellon et al. present evidence that long-term budesonide oral suspension (BOS) therapy is safe and efficacious. Both the BOS and placebo cohorts of the initial, 12-week trial demonstrated clinical and histologic improvement on BOS over this 24-week period, with few adverse events. Maintenance of histologic response was only seen in 42% in initial BOS responders, suggesting steroid tolerance or resistance may develop. Another important observation was that peak eosinphil count decreased steroid dosing.
Finally, these data support the notion that initial responders are unlikely to gain response with continued therapy and may be better served with early transition to alternatives. Further research is needed to clarify these issues and which patients may be predisposed to nonresponse or loss of response.
Reena V. Chokshi, MD , is assistant professor of medicine in the department of gastroenterology at Baylor College of Medicine, Houston.
Treatment with budesonide oral suspension (BOS) was generally well tolerated and maintained a histologic response in some patients with eosinophilic esophagitis (EoE), according to the results of the 24-week, open-label extension phase of a multicenter, randomized, placebo-controlled, industry-sponsored trial.
Rates of histologic response (up to 6 eosinophils per high-power field) were “modest” – 23% among patients who stayed on BOS throughout the study and 48.5% among patients who initiated BOS after 12 weeks on placebo, reported Evan S. Dellon, MD, MPH, of the University of North Carolina in Chapel Hill and his associates. However, these rates “need to be viewed in the context of a highly symptomatic and histologically severe population with eosinophilic esophagitis,” they contended. A total of 11% of budesonide initiators developed esophageal candidiasis, they reported in Clinical Gastroenterology and Hepatology.
Budesonide oral suspension is a mucoadherent formulation of topical corticosteroid that has recently been developed to treat EoE. Previously, during the randomized, double-blind component of this phase 2 trial, 93 patients aged 11-40 years with active EoE and dysphagia received either BOS (2 mg) or placebo twice daily (Gastroenterology. 2017 Mar;157[4]:776-86). After 12 weeks, rates of histologic response were 39% for BOS versus 3% for placebo, and BOS significantly improved patients’ mean peak eosinophil count and scores on the Dysphagia Symptom Questionnaire, compared with baseline and compared with the response in the placebo group. During the open-label extension phase, 45 BOS continuers and 37 BOS initiators received 2 mg once daily for 12 weeks and then had the option to increase the BOS dose to 1.5-2.0 mg twice daily.
The rate of drug-related adverse events was 19% among BOS initiators and 4% among BOS continuers. One patient in each group developed oral candidiasis, while four BOS initiators (11%) developed esophageal candidiasis. Three BOS continuers had subnormal morning cortisol levels; while these were subclinical cases, they merit attention since long-term corticosteroids for EoE have been linked with possible hypothalamic–pituitary–adrenal axis suppression, the researchers noted.
In addition, while BOS initiators tended to maintain their endoscopic response, only 42% of those with an initial histologic response maintained a histologic response after 36 weeks of treatment or when leaving the study. Post hoc analyses confirmed that prolonged BOS treatment does not increase the chances of histologic or endoscopic response. Prior studies have suggested that EoE can become steroid-refractory over time and that certain molecular and histologic markers might predict resistance, the investigators noted.
Meritage Pharma (now part of Shire) was involved in the study design and conduct, data collection and management, and manuscript review. Dr. Dellon disclosed research funding from Meritage and Shire and a consulting relationship with Shire, along with ties to several other pharmaceutical companies. All six coinvestigators also disclosed ties to Meritage, Shire, or both, and two are Shire employees and stockholders.
*This story was updated on Feb. 7, 2019.
SOURCE: Dellon ES et al. Clin Gastroenterol Hepatol. 2018 Jun 11. doi: 10.1016/j.cgh.2018.05.051.
Treatment with budesonide oral suspension (BOS) was generally well tolerated and maintained a histologic response in some patients with eosinophilic esophagitis (EoE), according to the results of the 24-week, open-label extension phase of a multicenter, randomized, placebo-controlled, industry-sponsored trial.
Rates of histologic response (up to 6 eosinophils per high-power field) were “modest” – 23% among patients who stayed on BOS throughout the study and 48.5% among patients who initiated BOS after 12 weeks on placebo, reported Evan S. Dellon, MD, MPH, of the University of North Carolina in Chapel Hill and his associates. However, these rates “need to be viewed in the context of a highly symptomatic and histologically severe population with eosinophilic esophagitis,” they contended. A total of 11% of budesonide initiators developed esophageal candidiasis, they reported in Clinical Gastroenterology and Hepatology.
Budesonide oral suspension is a mucoadherent formulation of topical corticosteroid that has recently been developed to treat EoE. Previously, during the randomized, double-blind component of this phase 2 trial, 93 patients aged 11-40 years with active EoE and dysphagia received either BOS (2 mg) or placebo twice daily (Gastroenterology. 2017 Mar;157[4]:776-86). After 12 weeks, rates of histologic response were 39% for BOS versus 3% for placebo, and BOS significantly improved patients’ mean peak eosinophil count and scores on the Dysphagia Symptom Questionnaire, compared with baseline and compared with the response in the placebo group. During the open-label extension phase, 45 BOS continuers and 37 BOS initiators received 2 mg once daily for 12 weeks and then had the option to increase the BOS dose to 1.5-2.0 mg twice daily.
The rate of drug-related adverse events was 19% among BOS initiators and 4% among BOS continuers. One patient in each group developed oral candidiasis, while four BOS initiators (11%) developed esophageal candidiasis. Three BOS continuers had subnormal morning cortisol levels; while these were subclinical cases, they merit attention since long-term corticosteroids for EoE have been linked with possible hypothalamic–pituitary–adrenal axis suppression, the researchers noted.
In addition, while BOS initiators tended to maintain their endoscopic response, only 42% of those with an initial histologic response maintained a histologic response after 36 weeks of treatment or when leaving the study. Post hoc analyses confirmed that prolonged BOS treatment does not increase the chances of histologic or endoscopic response. Prior studies have suggested that EoE can become steroid-refractory over time and that certain molecular and histologic markers might predict resistance, the investigators noted.
Meritage Pharma (now part of Shire) was involved in the study design and conduct, data collection and management, and manuscript review. Dr. Dellon disclosed research funding from Meritage and Shire and a consulting relationship with Shire, along with ties to several other pharmaceutical companies. All six coinvestigators also disclosed ties to Meritage, Shire, or both, and two are Shire employees and stockholders.
*This story was updated on Feb. 7, 2019.
SOURCE: Dellon ES et al. Clin Gastroenterol Hepatol. 2018 Jun 11. doi: 10.1016/j.cgh.2018.05.051.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Budesonide oral suspension was well tolerated and maintained a histologic response in some patients with eosinophilic esophagitis.
Major finding: A total of 42% of initial histologic responders maintained a histologic response (less than 6 eosinophils per high-power field) after 24 weeks. Treatment was generally well tolerated, but 11% of initiators developed esophageal candidiasis.
Study details: Open-label extension study of a 12-week, multicenter, randomized, double-blind, placebo-controlled trial.
Disclosures: Meritage Pharma (now part of Shire) was involved in the study design and conduct, data collection and management, and manuscript review. Dr. Dellon disclosed research funding from Meritage and Shire and a consulting relationship with Shire, along with ties to several other pharmaceutical companies. All six coinvestigators also disclosed ties to Meritage, Shire, or both, and two are Shire employees and stockholders.
Source: Dellon ES et al. Clin Gastroenterol Hepatol. 2018 Jun 11. https://doi.org/10.1016/j.cgh.2018.05.051
Study supports swallowed topical steroids as maintenance for eosinophilic esophagitis
For adults with eosinophilic esophagitis, maintenance treatment with swallowed topical steroids was associated with significantly higher remission rates when compared with “steroid holidays” in a single-center retrospective observational study presented in the February issue of Clinical Gastroenterology and Hepatology.
At a median follow-up time of 5 years, the rate of complete (including clinical, endoscopic, and histologic) remission was 16.1% when patients were receiving swallowed topical steroids but only 1.3% when they were not on these or other maintenance therapies (that is, on “drug holidays”), reported Thomas Greuter, MD, of University Hospital Zürich and the Mayo Clinic in Rochester, Minn., and his associates. Swallowed topical steroids also were associated with significantly higher rates of each individual endpoint (P less than .001). Swallowed topical steroid therapy did not appear to cause dysplasia or mucosal atrophy, although esophageal candidiasis was confirmed in 2.7% of visits when patients were on treatment. “Given the good safety profile of low-dose swallowed topical steroid therapy, we advocate for prolonged treatment. Dose-finding trials are needed to achieve higher remission rates,” the investigators wrote in Clinical Gastroenterology and Hepatology.
Several studies have confirmed the efficacy of short-term swallowed topical steroids for treating eosinophilic esophagitis, but only one small randomized trial has evaluated longer-term treatment, and participants were followed for only 1 year. Dr. Greuter and his associates therefore analyzed retrospective data from 229 adults in Switzerland who received swallowed topical steroids for eosinophilic esophagitis between 2000 and 2014. Induction therapy consisted of 1 mg swallowed topical steroids twice daily, allowing 2-4 weeks for a clinical response. Patients then received infinite maintenance therapy with 0.25 mg swallowed topical steroids twice daily. Patients tended to be male and diagnosed in their late 30s. Endoscopy commonly showed corrugated rings, white exudates, edema, and furrows, and 35% of patients had strictures. Peak eosinophil count typically was 25 cells per high-power frame.
Among 819 follow-up visits, 336 (41%) occurred when patients were on maintenance swallowed topical steroid therapy. The median duration of maintenance therapy prior to a follow-up visit was 347 days (interquartile range, 90-750 days) or 677 doses (IQR, 280-1413 doses). The rate of clinical remission was 31% when patients were on maintenance treatment but only 4.5% when they were not (P less than .001). Respective rates of endoscopic and histologic remission were 48.8% versus 17.8% (P less than .001) and 44.8% versus 10.1% (P less than .001). After accounting for numerous demographic and clinical variables, the only significant predictors of clinical remission were treatment with swallowed topical steroids (odds ratio, 16.98; 95% confidence interval, 6.69-43.09) and a negative family history of esophageal eosinophilia (OR, 4.02; 95% CI, 1.41-11.47).
This study excluded patients whose eosinophilic esophagitis had responded to proton pump inhibitor therapy. Also, the maintenance dose of swallowed topical steroid dose (0.25 mg twice daily) probably was too low to achieve efficacious drug levels in the esophageal mucosa, which could explain the high proportion of treatment-refractory cases, according to the researchers. Evaluating a higher maintenance dose “would be of particular interest in the future,” they added.
The Swiss National Science Foundation provided partial funding. Dr. Greuter disclosed a travel grant from Falk Pharma GmbH and Vifor and an unrestricted research grant from Novartis.
SOURCE: Greuter T et al. Clin Gastroenterol Hepatol. 2018 Jun 11.
For adults with eosinophilic esophagitis, maintenance treatment with swallowed topical steroids was associated with significantly higher remission rates when compared with “steroid holidays” in a single-center retrospective observational study presented in the February issue of Clinical Gastroenterology and Hepatology.
At a median follow-up time of 5 years, the rate of complete (including clinical, endoscopic, and histologic) remission was 16.1% when patients were receiving swallowed topical steroids but only 1.3% when they were not on these or other maintenance therapies (that is, on “drug holidays”), reported Thomas Greuter, MD, of University Hospital Zürich and the Mayo Clinic in Rochester, Minn., and his associates. Swallowed topical steroids also were associated with significantly higher rates of each individual endpoint (P less than .001). Swallowed topical steroid therapy did not appear to cause dysplasia or mucosal atrophy, although esophageal candidiasis was confirmed in 2.7% of visits when patients were on treatment. “Given the good safety profile of low-dose swallowed topical steroid therapy, we advocate for prolonged treatment. Dose-finding trials are needed to achieve higher remission rates,” the investigators wrote in Clinical Gastroenterology and Hepatology.
Several studies have confirmed the efficacy of short-term swallowed topical steroids for treating eosinophilic esophagitis, but only one small randomized trial has evaluated longer-term treatment, and participants were followed for only 1 year. Dr. Greuter and his associates therefore analyzed retrospective data from 229 adults in Switzerland who received swallowed topical steroids for eosinophilic esophagitis between 2000 and 2014. Induction therapy consisted of 1 mg swallowed topical steroids twice daily, allowing 2-4 weeks for a clinical response. Patients then received infinite maintenance therapy with 0.25 mg swallowed topical steroids twice daily. Patients tended to be male and diagnosed in their late 30s. Endoscopy commonly showed corrugated rings, white exudates, edema, and furrows, and 35% of patients had strictures. Peak eosinophil count typically was 25 cells per high-power frame.
Among 819 follow-up visits, 336 (41%) occurred when patients were on maintenance swallowed topical steroid therapy. The median duration of maintenance therapy prior to a follow-up visit was 347 days (interquartile range, 90-750 days) or 677 doses (IQR, 280-1413 doses). The rate of clinical remission was 31% when patients were on maintenance treatment but only 4.5% when they were not (P less than .001). Respective rates of endoscopic and histologic remission were 48.8% versus 17.8% (P less than .001) and 44.8% versus 10.1% (P less than .001). After accounting for numerous demographic and clinical variables, the only significant predictors of clinical remission were treatment with swallowed topical steroids (odds ratio, 16.98; 95% confidence interval, 6.69-43.09) and a negative family history of esophageal eosinophilia (OR, 4.02; 95% CI, 1.41-11.47).
This study excluded patients whose eosinophilic esophagitis had responded to proton pump inhibitor therapy. Also, the maintenance dose of swallowed topical steroid dose (0.25 mg twice daily) probably was too low to achieve efficacious drug levels in the esophageal mucosa, which could explain the high proportion of treatment-refractory cases, according to the researchers. Evaluating a higher maintenance dose “would be of particular interest in the future,” they added.
The Swiss National Science Foundation provided partial funding. Dr. Greuter disclosed a travel grant from Falk Pharma GmbH and Vifor and an unrestricted research grant from Novartis.
SOURCE: Greuter T et al. Clin Gastroenterol Hepatol. 2018 Jun 11.
For adults with eosinophilic esophagitis, maintenance treatment with swallowed topical steroids was associated with significantly higher remission rates when compared with “steroid holidays” in a single-center retrospective observational study presented in the February issue of Clinical Gastroenterology and Hepatology.
At a median follow-up time of 5 years, the rate of complete (including clinical, endoscopic, and histologic) remission was 16.1% when patients were receiving swallowed topical steroids but only 1.3% when they were not on these or other maintenance therapies (that is, on “drug holidays”), reported Thomas Greuter, MD, of University Hospital Zürich and the Mayo Clinic in Rochester, Minn., and his associates. Swallowed topical steroids also were associated with significantly higher rates of each individual endpoint (P less than .001). Swallowed topical steroid therapy did not appear to cause dysplasia or mucosal atrophy, although esophageal candidiasis was confirmed in 2.7% of visits when patients were on treatment. “Given the good safety profile of low-dose swallowed topical steroid therapy, we advocate for prolonged treatment. Dose-finding trials are needed to achieve higher remission rates,” the investigators wrote in Clinical Gastroenterology and Hepatology.
Several studies have confirmed the efficacy of short-term swallowed topical steroids for treating eosinophilic esophagitis, but only one small randomized trial has evaluated longer-term treatment, and participants were followed for only 1 year. Dr. Greuter and his associates therefore analyzed retrospective data from 229 adults in Switzerland who received swallowed topical steroids for eosinophilic esophagitis between 2000 and 2014. Induction therapy consisted of 1 mg swallowed topical steroids twice daily, allowing 2-4 weeks for a clinical response. Patients then received infinite maintenance therapy with 0.25 mg swallowed topical steroids twice daily. Patients tended to be male and diagnosed in their late 30s. Endoscopy commonly showed corrugated rings, white exudates, edema, and furrows, and 35% of patients had strictures. Peak eosinophil count typically was 25 cells per high-power frame.
Among 819 follow-up visits, 336 (41%) occurred when patients were on maintenance swallowed topical steroid therapy. The median duration of maintenance therapy prior to a follow-up visit was 347 days (interquartile range, 90-750 days) or 677 doses (IQR, 280-1413 doses). The rate of clinical remission was 31% when patients were on maintenance treatment but only 4.5% when they were not (P less than .001). Respective rates of endoscopic and histologic remission were 48.8% versus 17.8% (P less than .001) and 44.8% versus 10.1% (P less than .001). After accounting for numerous demographic and clinical variables, the only significant predictors of clinical remission were treatment with swallowed topical steroids (odds ratio, 16.98; 95% confidence interval, 6.69-43.09) and a negative family history of esophageal eosinophilia (OR, 4.02; 95% CI, 1.41-11.47).
This study excluded patients whose eosinophilic esophagitis had responded to proton pump inhibitor therapy. Also, the maintenance dose of swallowed topical steroid dose (0.25 mg twice daily) probably was too low to achieve efficacious drug levels in the esophageal mucosa, which could explain the high proportion of treatment-refractory cases, according to the researchers. Evaluating a higher maintenance dose “would be of particular interest in the future,” they added.
The Swiss National Science Foundation provided partial funding. Dr. Greuter disclosed a travel grant from Falk Pharma GmbH and Vifor and an unrestricted research grant from Novartis.
SOURCE: Greuter T et al. Clin Gastroenterol Hepatol. 2018 Jun 11.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Swallowed topical steroids appear to increase remission rates among adults with eosinophilic esophagitis.
Major finding: After a median of 5 years of follow-up, rates of clinical remission were 16.1% and 1.3%, respectively (P less than .001).
Study details: Retrospective cohort study of 229 adults with eosinophilic esophagitis.
Disclosures: The Swiss National Science Foundation provided partial funding. Dr. Greuter disclosed a travel grant from Falk Pharma GmbH and Vifor and an unrestricted research grant from Novartis.
Source: Greuter T et al. Clin Gastroenterol Hepatol. 2018 Jun 11.
No difference between PPI prophylaxis, placebo for GI bleeding
There was no significant difference in mortality between critically ill patients who received pantoprazole prophylaxis for gastrointestinal bleeding, and those who received placebo, new findings suggest.
In a multicenter, randomized trial of 3,298 adult patients at risk for gastrointestinal bleeding, 510 patients (31.1%) in the pantoprazole group and 499 (30.4%) in the placebo group had died at 90 days (relative risk, 1.02; 95% confidence interval, 0.91-1.13; P = .76). The results were published in the New England Journal of Medicine.
Patients were aged 18 years or older; had been admitted to the ICU for an acute condition in one of six international centers; and had at least one risk factor for gastrointestinal bleeding including shock, use of anticoagulant agents, renal replacement therapy, mechanical ventilation (expected to last more than 24 hours), any history of liver disease, or any history of or ongoing coagulopathy. A total of 1,645 patients were randomly assigned to receive 40 mg of intravenous pantoprazole once daily and 1,653 received placebo, reported Mette Krag, MD, of the department of intensive care at Rigshospitalet in Copenhagen, and her coauthors.
The primary outcome was 90-day mortality. Secondary outcomes were clinically important events in the ICU, clinically important gastrointestinal bleeding in the ICU, infectious adverse events in the ICU, and days alive without the use of life support within the 90-day period.
One or more clinically important events occurred in 21.9% of patients in the pantoprazole group and in 22.6% in the placebo group (RR, 0.96; 95% CI, 0.83-1.11). In the pantoprazole group, 2.5% of patients had clinically important gastrointestinal bleeding, compared with 4.2% in the placebo group, Dr. Krag and her coauthors wrote.
The findings are similar to other recently published results, which showed “no significant differences ... in the rates of death or infectious complications between patients receiving placebo or no prophylaxis and those receiving proton pump inhibitors,” the authors wrote.
Dr. Krag reported financial support from Innovation Fund Denmark, Ehrenreich’s Foundation, and several other organizations.
SOURCE: Krag M et al. N Engl J Med. 2018 Dec 6. doi: 10.1056/NEJMoa1714919.
This article was updated 12/6/18.
“The take-home message from this trial is that, given the low incidence of clinically important upper gastrointestinal bleeding in the ICU, prophylaxis with a PPI [proton pump inhibitor], if initiated, should be reserved for seriously ill patients who are at high risk for this complication,” wrote Alan Barkun, MD, CM, of McGill University, Montreal, and Marc Bardou, MD, PhD, of the Centre Hospitalier Universitaire Dijon–Bourgogne (France), in an editorial published with the study.
Though 90-day mortality was similar between groups in this trial, “the between-group difference in the rate of important upper gastrointestinal bleeding may still support the recommendation of using a prophylactic PPI” given the absence of a difference in the rate of adverse events between the two groups, they added.
Dr. Barkun reported no disclosures; Dr. Bardou reported support from the French Medicines Agency.
“The take-home message from this trial is that, given the low incidence of clinically important upper gastrointestinal bleeding in the ICU, prophylaxis with a PPI [proton pump inhibitor], if initiated, should be reserved for seriously ill patients who are at high risk for this complication,” wrote Alan Barkun, MD, CM, of McGill University, Montreal, and Marc Bardou, MD, PhD, of the Centre Hospitalier Universitaire Dijon–Bourgogne (France), in an editorial published with the study.
Though 90-day mortality was similar between groups in this trial, “the between-group difference in the rate of important upper gastrointestinal bleeding may still support the recommendation of using a prophylactic PPI” given the absence of a difference in the rate of adverse events between the two groups, they added.
Dr. Barkun reported no disclosures; Dr. Bardou reported support from the French Medicines Agency.
“The take-home message from this trial is that, given the low incidence of clinically important upper gastrointestinal bleeding in the ICU, prophylaxis with a PPI [proton pump inhibitor], if initiated, should be reserved for seriously ill patients who are at high risk for this complication,” wrote Alan Barkun, MD, CM, of McGill University, Montreal, and Marc Bardou, MD, PhD, of the Centre Hospitalier Universitaire Dijon–Bourgogne (France), in an editorial published with the study.
Though 90-day mortality was similar between groups in this trial, “the between-group difference in the rate of important upper gastrointestinal bleeding may still support the recommendation of using a prophylactic PPI” given the absence of a difference in the rate of adverse events between the two groups, they added.
Dr. Barkun reported no disclosures; Dr. Bardou reported support from the French Medicines Agency.
There was no significant difference in mortality between critically ill patients who received pantoprazole prophylaxis for gastrointestinal bleeding, and those who received placebo, new findings suggest.
In a multicenter, randomized trial of 3,298 adult patients at risk for gastrointestinal bleeding, 510 patients (31.1%) in the pantoprazole group and 499 (30.4%) in the placebo group had died at 90 days (relative risk, 1.02; 95% confidence interval, 0.91-1.13; P = .76). The results were published in the New England Journal of Medicine.
Patients were aged 18 years or older; had been admitted to the ICU for an acute condition in one of six international centers; and had at least one risk factor for gastrointestinal bleeding including shock, use of anticoagulant agents, renal replacement therapy, mechanical ventilation (expected to last more than 24 hours), any history of liver disease, or any history of or ongoing coagulopathy. A total of 1,645 patients were randomly assigned to receive 40 mg of intravenous pantoprazole once daily and 1,653 received placebo, reported Mette Krag, MD, of the department of intensive care at Rigshospitalet in Copenhagen, and her coauthors.
The primary outcome was 90-day mortality. Secondary outcomes were clinically important events in the ICU, clinically important gastrointestinal bleeding in the ICU, infectious adverse events in the ICU, and days alive without the use of life support within the 90-day period.
One or more clinically important events occurred in 21.9% of patients in the pantoprazole group and in 22.6% in the placebo group (RR, 0.96; 95% CI, 0.83-1.11). In the pantoprazole group, 2.5% of patients had clinically important gastrointestinal bleeding, compared with 4.2% in the placebo group, Dr. Krag and her coauthors wrote.
The findings are similar to other recently published results, which showed “no significant differences ... in the rates of death or infectious complications between patients receiving placebo or no prophylaxis and those receiving proton pump inhibitors,” the authors wrote.
Dr. Krag reported financial support from Innovation Fund Denmark, Ehrenreich’s Foundation, and several other organizations.
SOURCE: Krag M et al. N Engl J Med. 2018 Dec 6. doi: 10.1056/NEJMoa1714919.
This article was updated 12/6/18.
There was no significant difference in mortality between critically ill patients who received pantoprazole prophylaxis for gastrointestinal bleeding, and those who received placebo, new findings suggest.
In a multicenter, randomized trial of 3,298 adult patients at risk for gastrointestinal bleeding, 510 patients (31.1%) in the pantoprazole group and 499 (30.4%) in the placebo group had died at 90 days (relative risk, 1.02; 95% confidence interval, 0.91-1.13; P = .76). The results were published in the New England Journal of Medicine.
Patients were aged 18 years or older; had been admitted to the ICU for an acute condition in one of six international centers; and had at least one risk factor for gastrointestinal bleeding including shock, use of anticoagulant agents, renal replacement therapy, mechanical ventilation (expected to last more than 24 hours), any history of liver disease, or any history of or ongoing coagulopathy. A total of 1,645 patients were randomly assigned to receive 40 mg of intravenous pantoprazole once daily and 1,653 received placebo, reported Mette Krag, MD, of the department of intensive care at Rigshospitalet in Copenhagen, and her coauthors.
The primary outcome was 90-day mortality. Secondary outcomes were clinically important events in the ICU, clinically important gastrointestinal bleeding in the ICU, infectious adverse events in the ICU, and days alive without the use of life support within the 90-day period.
One or more clinically important events occurred in 21.9% of patients in the pantoprazole group and in 22.6% in the placebo group (RR, 0.96; 95% CI, 0.83-1.11). In the pantoprazole group, 2.5% of patients had clinically important gastrointestinal bleeding, compared with 4.2% in the placebo group, Dr. Krag and her coauthors wrote.
The findings are similar to other recently published results, which showed “no significant differences ... in the rates of death or infectious complications between patients receiving placebo or no prophylaxis and those receiving proton pump inhibitors,” the authors wrote.
Dr. Krag reported financial support from Innovation Fund Denmark, Ehrenreich’s Foundation, and several other organizations.
SOURCE: Krag M et al. N Engl J Med. 2018 Dec 6. doi: 10.1056/NEJMoa1714919.
This article was updated 12/6/18.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: There was no significant difference in mortality between patients who received pantoprazole prophylaxis for gastrointestinal bleeding, and those who received placebo.
Major finding: Just over 31% of patients in the pantoprazole group and 30.4% in the placebo group had died at 90 days (relative risk, 1.02; 95% confidence interval, 0.91-1.13; P = .76).
Study details: A multicenter, randomized trial of 3,298 adult ICU patients at risk for gastrointestinal bleeding.
Disclosures: Dr. Krag reported financial support from Innovation Fund Denmark, Ehrenreich’s Foundation, and several other organizations.
Source: Krag M et al. N Engl J Med. 2018 Dec 6. doi: 10.1056/NEJMoa1714919.