User login
Megakaryocytes can control HSCs, team finds

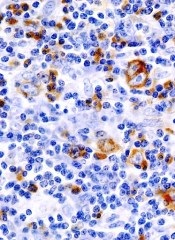
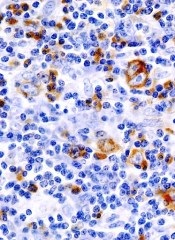
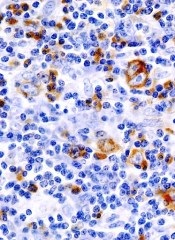
to a megakaryocyte (red)
Credit: Meng Zhao
For the first time, researchers have shown that hematopoietic stem cells (HSCs) can be directly controlled by their own progeny, megakaryocytes.
Preclinical experiments revealed that megakaryocytes maintain HSC quiescence during homeostasis and promote HSC regeneration after chemotherapeutic stress.
The discovery suggests megakaryocytes might be used to treat patients with low blood cell counts and to expand HSCs for transplant.
The researchers described these findings in Nature Medicine.
The team examined the relationship between megakaryocytes and HSCs in mouse bone marrow. And they discovered that, as a terminally differentiated progeny, megakaryocytes regulate HSCs by performing two previously unknown functions.
“Megakaryocytes can directly regulate the amount of hematopoietic stem cells by telling the cells when they need to keep in the quiescent stage and when they need to start proliferating to meet increased demand,” said study author Meng Zhao, PhD, of the Stowers Institute for Medical Research in Kansas City, Missouri.
The researchers found that the protein transforming growth factor B1 (TGF-B1), contained in megakaryocytes, signaled quiescence.
And, when under stress from chemotherapy, megakaryocytes signaled fibroblast growth factor 1 (FGF1), to stimulate HSC proliferation.
“Our findings suggest that megakaryocytes are required for the recovery of hematopoietic stem cells post-chemotherapy,” said Linheng Li, PhD, also of the Stowers Institute.
The discovery could provide insight for using megakaryocyte-derived factors, such as TGF-B1 and FGF1, clinically to facilitate the regeneration of HSCs, he added.
Engineering a megakaryocyte niche that supports the growth of HSCs in culture is the next step for the researchers. They are also investigating whether a megakaryocyte niche can be used to help expand human HSCs in vitro for transplant.
These findings are supported by similar research also reported in Nature Medicine. ![]()

to a megakaryocyte (red)
Credit: Meng Zhao
For the first time, researchers have shown that hematopoietic stem cells (HSCs) can be directly controlled by their own progeny, megakaryocytes.
Preclinical experiments revealed that megakaryocytes maintain HSC quiescence during homeostasis and promote HSC regeneration after chemotherapeutic stress.
The discovery suggests megakaryocytes might be used to treat patients with low blood cell counts and to expand HSCs for transplant.
The researchers described these findings in Nature Medicine.
The team examined the relationship between megakaryocytes and HSCs in mouse bone marrow. And they discovered that, as a terminally differentiated progeny, megakaryocytes regulate HSCs by performing two previously unknown functions.
“Megakaryocytes can directly regulate the amount of hematopoietic stem cells by telling the cells when they need to keep in the quiescent stage and when they need to start proliferating to meet increased demand,” said study author Meng Zhao, PhD, of the Stowers Institute for Medical Research in Kansas City, Missouri.
The researchers found that the protein transforming growth factor B1 (TGF-B1), contained in megakaryocytes, signaled quiescence.
And, when under stress from chemotherapy, megakaryocytes signaled fibroblast growth factor 1 (FGF1), to stimulate HSC proliferation.
“Our findings suggest that megakaryocytes are required for the recovery of hematopoietic stem cells post-chemotherapy,” said Linheng Li, PhD, also of the Stowers Institute.
The discovery could provide insight for using megakaryocyte-derived factors, such as TGF-B1 and FGF1, clinically to facilitate the regeneration of HSCs, he added.
Engineering a megakaryocyte niche that supports the growth of HSCs in culture is the next step for the researchers. They are also investigating whether a megakaryocyte niche can be used to help expand human HSCs in vitro for transplant.
These findings are supported by similar research also reported in Nature Medicine. ![]()

to a megakaryocyte (red)
Credit: Meng Zhao
For the first time, researchers have shown that hematopoietic stem cells (HSCs) can be directly controlled by their own progeny, megakaryocytes.
Preclinical experiments revealed that megakaryocytes maintain HSC quiescence during homeostasis and promote HSC regeneration after chemotherapeutic stress.
The discovery suggests megakaryocytes might be used to treat patients with low blood cell counts and to expand HSCs for transplant.
The researchers described these findings in Nature Medicine.
The team examined the relationship between megakaryocytes and HSCs in mouse bone marrow. And they discovered that, as a terminally differentiated progeny, megakaryocytes regulate HSCs by performing two previously unknown functions.
“Megakaryocytes can directly regulate the amount of hematopoietic stem cells by telling the cells when they need to keep in the quiescent stage and when they need to start proliferating to meet increased demand,” said study author Meng Zhao, PhD, of the Stowers Institute for Medical Research in Kansas City, Missouri.
The researchers found that the protein transforming growth factor B1 (TGF-B1), contained in megakaryocytes, signaled quiescence.
And, when under stress from chemotherapy, megakaryocytes signaled fibroblast growth factor 1 (FGF1), to stimulate HSC proliferation.
“Our findings suggest that megakaryocytes are required for the recovery of hematopoietic stem cells post-chemotherapy,” said Linheng Li, PhD, also of the Stowers Institute.
The discovery could provide insight for using megakaryocyte-derived factors, such as TGF-B1 and FGF1, clinically to facilitate the regeneration of HSCs, he added.
Engineering a megakaryocyte niche that supports the growth of HSCs in culture is the next step for the researchers. They are also investigating whether a megakaryocyte niche can be used to help expand human HSCs in vitro for transplant.
These findings are supported by similar research also reported in Nature Medicine. ![]()
CAR T cells can produce durable remissions

Credit: Penn Medicine
In a small study, 90% of children and adults with relapsed or refractory acute lymphoblastic leukemia (ALL) achieved remission after receiving CTL019, a chimeric antigen receptor (CAR) T-cell therapy.
Seven of these 27 patients ultimately relapsed, and 5 went on to receive additional therapy, including stem cell transplant.
Still, 15 of these heavily pretreated patients remained in remission at a median of 7 months of follow-up and did not require further treatment.
“[Patients] had relapsed as many as 4 times, including 60% whose cancers came back even after stem cell transplants,” said Stephan Grupp, MD, PhD, of the Children’s Hospital of Philadelphia in Pennsylvania.
“Their cancers were so aggressive they had no treatment options left. The durable responses we have observed with CTL019 therapy are unprecedented.”
Dr Grupp and his colleagues reported these results in NEJM. The new data build on preliminary findings presented at the 2013 ASH Annual Meeting and the 2012 ASH Annual Meeting.
CTL019 cells are a patient’s own T cells genetically engineered to express an anti-CD19 scFv coupled to CD3ζ signaling and 4-1BB co-stimulatory domains. The cells are activated and expanded ex vivo with anti-CD3 and anti-CD28 beads, then infused into patients.
In all, 30 patients received CTL019, including 25 children and young adults (ages 5 to 22) and 5 adults (ages 26 to 60). Three patients had primary refractory disease, 5 had relapsed once, and 22 patients had relapsed 2 or more times. Eighteen patients had received an allogeneic stem cell transplant.
Twenty-seven patients achieved a complete remission after an infusion of CTL019. Nineteen patients remain in remission, 15 of whom received CTL019 alone. Follow-up ranged from 1.4 months to 24 months.
Tests in patients who experienced complete remissions showed that their normal B cells had been eliminated along with their tumors. The researchers noted that persistent absence of normal B cells following CTL019 treatment indicates continued activity of the CAR T cells.
“Our results support that CTL019 can produce long-lasting remissions for certain heavily pretreated ALL patients without further therapy,” said Noelle Frey, MD, of the University of Pennsylvania in Philadelphia.
However, 5 patients did seek additional therapy, 3 of whom proceeded to allogeneic stem cell transplants while in remission.
Seven patients relapsed, between 6 weeks and 8.5 months after their infusions, including 3 whose cancers returned as CD19-negative leukemia that would not have been targeted by CTL019.
At 6 months, the overall survival rate was 78%, and the event-free survival rate was 67%.
All of the patients experienced cytokine release syndrome (CRS) within a few days of receiving CTL019, but they all fully recovered.
Twenty-two patients experienced mild to moderate CRS, which included varying degrees of flu-like symptoms, with high fevers, nausea, and muscle pain. Eight patients developed severe CRS, which required treatment for low blood pressure and breathing difficulties.
Nine patients were treated with tocilizumab, an immunosuppressant that inhibits the effects of the inflammatory cytokine IL-6, which have been found to spike during the most robust phase of the CAR T cells’ expansion in the body. Six patients also received short courses of steroids to combat CRS symptoms.
CTL019 was invented at The University of Pennsylvania but has been licensed to Novartis. In July, the US Food and Drug Administration granted CTL019 breakthrough therapy designation for the treatment of relapsed and refractory adult and pediatric ALL.
The first multicenter trial of CTL019 recently opened in the US, and additional multisite trials are expected to begin by the end of the year. ![]()

Credit: Penn Medicine
In a small study, 90% of children and adults with relapsed or refractory acute lymphoblastic leukemia (ALL) achieved remission after receiving CTL019, a chimeric antigen receptor (CAR) T-cell therapy.
Seven of these 27 patients ultimately relapsed, and 5 went on to receive additional therapy, including stem cell transplant.
Still, 15 of these heavily pretreated patients remained in remission at a median of 7 months of follow-up and did not require further treatment.
“[Patients] had relapsed as many as 4 times, including 60% whose cancers came back even after stem cell transplants,” said Stephan Grupp, MD, PhD, of the Children’s Hospital of Philadelphia in Pennsylvania.
“Their cancers were so aggressive they had no treatment options left. The durable responses we have observed with CTL019 therapy are unprecedented.”
Dr Grupp and his colleagues reported these results in NEJM. The new data build on preliminary findings presented at the 2013 ASH Annual Meeting and the 2012 ASH Annual Meeting.
CTL019 cells are a patient’s own T cells genetically engineered to express an anti-CD19 scFv coupled to CD3ζ signaling and 4-1BB co-stimulatory domains. The cells are activated and expanded ex vivo with anti-CD3 and anti-CD28 beads, then infused into patients.
In all, 30 patients received CTL019, including 25 children and young adults (ages 5 to 22) and 5 adults (ages 26 to 60). Three patients had primary refractory disease, 5 had relapsed once, and 22 patients had relapsed 2 or more times. Eighteen patients had received an allogeneic stem cell transplant.
Twenty-seven patients achieved a complete remission after an infusion of CTL019. Nineteen patients remain in remission, 15 of whom received CTL019 alone. Follow-up ranged from 1.4 months to 24 months.
Tests in patients who experienced complete remissions showed that their normal B cells had been eliminated along with their tumors. The researchers noted that persistent absence of normal B cells following CTL019 treatment indicates continued activity of the CAR T cells.
“Our results support that CTL019 can produce long-lasting remissions for certain heavily pretreated ALL patients without further therapy,” said Noelle Frey, MD, of the University of Pennsylvania in Philadelphia.
However, 5 patients did seek additional therapy, 3 of whom proceeded to allogeneic stem cell transplants while in remission.
Seven patients relapsed, between 6 weeks and 8.5 months after their infusions, including 3 whose cancers returned as CD19-negative leukemia that would not have been targeted by CTL019.
At 6 months, the overall survival rate was 78%, and the event-free survival rate was 67%.
All of the patients experienced cytokine release syndrome (CRS) within a few days of receiving CTL019, but they all fully recovered.
Twenty-two patients experienced mild to moderate CRS, which included varying degrees of flu-like symptoms, with high fevers, nausea, and muscle pain. Eight patients developed severe CRS, which required treatment for low blood pressure and breathing difficulties.
Nine patients were treated with tocilizumab, an immunosuppressant that inhibits the effects of the inflammatory cytokine IL-6, which have been found to spike during the most robust phase of the CAR T cells’ expansion in the body. Six patients also received short courses of steroids to combat CRS symptoms.
CTL019 was invented at The University of Pennsylvania but has been licensed to Novartis. In July, the US Food and Drug Administration granted CTL019 breakthrough therapy designation for the treatment of relapsed and refractory adult and pediatric ALL.
The first multicenter trial of CTL019 recently opened in the US, and additional multisite trials are expected to begin by the end of the year. ![]()

Credit: Penn Medicine
In a small study, 90% of children and adults with relapsed or refractory acute lymphoblastic leukemia (ALL) achieved remission after receiving CTL019, a chimeric antigen receptor (CAR) T-cell therapy.
Seven of these 27 patients ultimately relapsed, and 5 went on to receive additional therapy, including stem cell transplant.
Still, 15 of these heavily pretreated patients remained in remission at a median of 7 months of follow-up and did not require further treatment.
“[Patients] had relapsed as many as 4 times, including 60% whose cancers came back even after stem cell transplants,” said Stephan Grupp, MD, PhD, of the Children’s Hospital of Philadelphia in Pennsylvania.
“Their cancers were so aggressive they had no treatment options left. The durable responses we have observed with CTL019 therapy are unprecedented.”
Dr Grupp and his colleagues reported these results in NEJM. The new data build on preliminary findings presented at the 2013 ASH Annual Meeting and the 2012 ASH Annual Meeting.
CTL019 cells are a patient’s own T cells genetically engineered to express an anti-CD19 scFv coupled to CD3ζ signaling and 4-1BB co-stimulatory domains. The cells are activated and expanded ex vivo with anti-CD3 and anti-CD28 beads, then infused into patients.
In all, 30 patients received CTL019, including 25 children and young adults (ages 5 to 22) and 5 adults (ages 26 to 60). Three patients had primary refractory disease, 5 had relapsed once, and 22 patients had relapsed 2 or more times. Eighteen patients had received an allogeneic stem cell transplant.
Twenty-seven patients achieved a complete remission after an infusion of CTL019. Nineteen patients remain in remission, 15 of whom received CTL019 alone. Follow-up ranged from 1.4 months to 24 months.
Tests in patients who experienced complete remissions showed that their normal B cells had been eliminated along with their tumors. The researchers noted that persistent absence of normal B cells following CTL019 treatment indicates continued activity of the CAR T cells.
“Our results support that CTL019 can produce long-lasting remissions for certain heavily pretreated ALL patients without further therapy,” said Noelle Frey, MD, of the University of Pennsylvania in Philadelphia.
However, 5 patients did seek additional therapy, 3 of whom proceeded to allogeneic stem cell transplants while in remission.
Seven patients relapsed, between 6 weeks and 8.5 months after their infusions, including 3 whose cancers returned as CD19-negative leukemia that would not have been targeted by CTL019.
At 6 months, the overall survival rate was 78%, and the event-free survival rate was 67%.
All of the patients experienced cytokine release syndrome (CRS) within a few days of receiving CTL019, but they all fully recovered.
Twenty-two patients experienced mild to moderate CRS, which included varying degrees of flu-like symptoms, with high fevers, nausea, and muscle pain. Eight patients developed severe CRS, which required treatment for low blood pressure and breathing difficulties.
Nine patients were treated with tocilizumab, an immunosuppressant that inhibits the effects of the inflammatory cytokine IL-6, which have been found to spike during the most robust phase of the CAR T cells’ expansion in the body. Six patients also received short courses of steroids to combat CRS symptoms.
CTL019 was invented at The University of Pennsylvania but has been licensed to Novartis. In July, the US Food and Drug Administration granted CTL019 breakthrough therapy designation for the treatment of relapsed and refractory adult and pediatric ALL.
The first multicenter trial of CTL019 recently opened in the US, and additional multisite trials are expected to begin by the end of the year. ![]()
CAR T cells serve as bridge to HSCT in ALL

Credit: Charles Haymond
An anti-CD19 chimeric antigen receptor (CAR) T-cell therapy can elicit complete responses (CRs) in heavily pretreated patients with acute lymphoblastic leukemia (ALL), results of a phase 1 trial suggest.
More than half of the 21 patients enrolled achieved a CR, and most of those patients went on to hematopoietic stem cell transplant (HSCT).
All 10 patients who underwent HSCT remain leukemia-free at a median follow-up of 10 months.
The CAR T cells did prompt some serious adverse effects, but all effects were fully reversible.
Crystal L. Mackall, MD, of the National Cancer Institute in Bethesda, Maryland, and her colleagues reported these results in The Lancet.
The phase 1 study enrolled patients ages 1 to 30 years who had relapsed or refractory ALL or non-Hodgkin lymphoma. Twenty patients had B-cell ALL, and 1 had diffuse large B-cell lymphoma (DLBCL). All of the patients had been heavily pretreated, and 8 had received a prior HSCT.
Patients received a conditioning regimen of cyclophosphamide and fludarabine, followed by a single infusion of CAR T cells: either 1×10⁶ CAR-transduced T cells per kg or 3×10⁶ CAR-transduced T cells per kg.
The CAR T cells were produced from each patient’s own peripheral blood mononuclear cells, modified using a gammaretroviral vector encoding the CAR, as well as a CD28 costimulatory moiety. After the dose-escalation phase, an expansion cohort was treated at the maximum-tolerated dose.
Twenty-one patients were enrolled and infused, but 2 of them did not receive the prescribed dose of CAR T cells, as the assigned dose could not be generated. The maximum-tolerated dose was 1×10⁶ CAR T cells per kg.
All toxicities were fully reversible. The most common non-hematologic grade 3 adverse events were fever (n=9), hypokalemia (n=9), fever and neutropenia (n=8), and cytokine release syndrome (n=3). Grade 4 cytokine release syndrome occurred in 3 patients.
At day 28, 12 patients had achieved a minimal residual disease (MRD)-negative CR. One patient had an MRD-positive CR, 1 had an MRD-positive CR with incomplete count recovery, and 3 patients had stable disease. Four patients, including the one with DLBCL, progressed.
Ten of the patients with an MRD-negative CR subsequently underwent HSCT, and all 10 remained disease-free with a median follow-up of 10 months.
“The results show that this treatment is feasible in many patients with ALL and can eradicate chemoresistant disease with an acceptable toxicity profile,” said Gary Schiller, MD, of the University of California, Los Angeles, who was not involved in this study.
“Further, the findings demonstrate substantially higher response rates than seen in the literature for the most recently approved agent for refractory ALL. CD19-CAR therapy represents a potentially important new tool to address the urgent need for new treatment modalities in these patients.”
Researchers previously reported positive results with this therapy in patients with chemotherapy-refractory DLBCL. ![]()

Credit: Charles Haymond
An anti-CD19 chimeric antigen receptor (CAR) T-cell therapy can elicit complete responses (CRs) in heavily pretreated patients with acute lymphoblastic leukemia (ALL), results of a phase 1 trial suggest.
More than half of the 21 patients enrolled achieved a CR, and most of those patients went on to hematopoietic stem cell transplant (HSCT).
All 10 patients who underwent HSCT remain leukemia-free at a median follow-up of 10 months.
The CAR T cells did prompt some serious adverse effects, but all effects were fully reversible.
Crystal L. Mackall, MD, of the National Cancer Institute in Bethesda, Maryland, and her colleagues reported these results in The Lancet.
The phase 1 study enrolled patients ages 1 to 30 years who had relapsed or refractory ALL or non-Hodgkin lymphoma. Twenty patients had B-cell ALL, and 1 had diffuse large B-cell lymphoma (DLBCL). All of the patients had been heavily pretreated, and 8 had received a prior HSCT.
Patients received a conditioning regimen of cyclophosphamide and fludarabine, followed by a single infusion of CAR T cells: either 1×10⁶ CAR-transduced T cells per kg or 3×10⁶ CAR-transduced T cells per kg.
The CAR T cells were produced from each patient’s own peripheral blood mononuclear cells, modified using a gammaretroviral vector encoding the CAR, as well as a CD28 costimulatory moiety. After the dose-escalation phase, an expansion cohort was treated at the maximum-tolerated dose.
Twenty-one patients were enrolled and infused, but 2 of them did not receive the prescribed dose of CAR T cells, as the assigned dose could not be generated. The maximum-tolerated dose was 1×10⁶ CAR T cells per kg.
All toxicities were fully reversible. The most common non-hematologic grade 3 adverse events were fever (n=9), hypokalemia (n=9), fever and neutropenia (n=8), and cytokine release syndrome (n=3). Grade 4 cytokine release syndrome occurred in 3 patients.
At day 28, 12 patients had achieved a minimal residual disease (MRD)-negative CR. One patient had an MRD-positive CR, 1 had an MRD-positive CR with incomplete count recovery, and 3 patients had stable disease. Four patients, including the one with DLBCL, progressed.
Ten of the patients with an MRD-negative CR subsequently underwent HSCT, and all 10 remained disease-free with a median follow-up of 10 months.
“The results show that this treatment is feasible in many patients with ALL and can eradicate chemoresistant disease with an acceptable toxicity profile,” said Gary Schiller, MD, of the University of California, Los Angeles, who was not involved in this study.
“Further, the findings demonstrate substantially higher response rates than seen in the literature for the most recently approved agent for refractory ALL. CD19-CAR therapy represents a potentially important new tool to address the urgent need for new treatment modalities in these patients.”
Researchers previously reported positive results with this therapy in patients with chemotherapy-refractory DLBCL. ![]()

Credit: Charles Haymond
An anti-CD19 chimeric antigen receptor (CAR) T-cell therapy can elicit complete responses (CRs) in heavily pretreated patients with acute lymphoblastic leukemia (ALL), results of a phase 1 trial suggest.
More than half of the 21 patients enrolled achieved a CR, and most of those patients went on to hematopoietic stem cell transplant (HSCT).
All 10 patients who underwent HSCT remain leukemia-free at a median follow-up of 10 months.
The CAR T cells did prompt some serious adverse effects, but all effects were fully reversible.
Crystal L. Mackall, MD, of the National Cancer Institute in Bethesda, Maryland, and her colleagues reported these results in The Lancet.
The phase 1 study enrolled patients ages 1 to 30 years who had relapsed or refractory ALL or non-Hodgkin lymphoma. Twenty patients had B-cell ALL, and 1 had diffuse large B-cell lymphoma (DLBCL). All of the patients had been heavily pretreated, and 8 had received a prior HSCT.
Patients received a conditioning regimen of cyclophosphamide and fludarabine, followed by a single infusion of CAR T cells: either 1×10⁶ CAR-transduced T cells per kg or 3×10⁶ CAR-transduced T cells per kg.
The CAR T cells were produced from each patient’s own peripheral blood mononuclear cells, modified using a gammaretroviral vector encoding the CAR, as well as a CD28 costimulatory moiety. After the dose-escalation phase, an expansion cohort was treated at the maximum-tolerated dose.
Twenty-one patients were enrolled and infused, but 2 of them did not receive the prescribed dose of CAR T cells, as the assigned dose could not be generated. The maximum-tolerated dose was 1×10⁶ CAR T cells per kg.
All toxicities were fully reversible. The most common non-hematologic grade 3 adverse events were fever (n=9), hypokalemia (n=9), fever and neutropenia (n=8), and cytokine release syndrome (n=3). Grade 4 cytokine release syndrome occurred in 3 patients.
At day 28, 12 patients had achieved a minimal residual disease (MRD)-negative CR. One patient had an MRD-positive CR, 1 had an MRD-positive CR with incomplete count recovery, and 3 patients had stable disease. Four patients, including the one with DLBCL, progressed.
Ten of the patients with an MRD-negative CR subsequently underwent HSCT, and all 10 remained disease-free with a median follow-up of 10 months.
“The results show that this treatment is feasible in many patients with ALL and can eradicate chemoresistant disease with an acceptable toxicity profile,” said Gary Schiller, MD, of the University of California, Los Angeles, who was not involved in this study.
“Further, the findings demonstrate substantially higher response rates than seen in the literature for the most recently approved agent for refractory ALL. CD19-CAR therapy represents a potentially important new tool to address the urgent need for new treatment modalities in these patients.”
Researchers previously reported positive results with this therapy in patients with chemotherapy-refractory DLBCL. ![]()
Shorter regimen can prevent GVHD

Credit: Chad McNeeley
Combining a couple of “promising” treatment approaches can prevent graft-vs-host disease (GVHD) as well as conventional therapy, researchers have reported in the Journal of Clinical Oncology.
They combined a 4-day myeloablative conditioning regimen of busulfan and fludarabine with 2 days of high-dose cyclophosphamide after transplant.
Typically, patients receive 6 months of immunosuppressive therapy to reduce their risk of GVHD.
The conditioning regimen and post-transplant cyclophosphamide have been tested separately in other studies and have good track records in controlling cancer and preventing severe GVHD.
Those successes led Leo Luznik, MD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues to combine the 2 therapies.
The team tested the combination in 92 patients with high-risk hematologic malignancies. Diagnoses included acute and chronic leukemias, multiple myeloma, non-Hodgkin lymphoma, and myelodysplastic syndromes. Patients had a median age of 49 (range, 21-65).
All patients received 40 mg/m2/day of intravenous (IV) fludarabine immediately before busulfan on all 4 days of conditioning. The busulfan dose of 130 mg/m2 IV daily was adjusted based on pharmacokinetics.
One or 2 days of rest were allowed before patients received a T-cell-replete bone marrow allograft. Forty-five patients had a matched, related donor, and 47 had a matched, unrelated donor.
Patients received 50 mg/kg/day of IV cyclophosphamide for 2 days, with the first dose starting 62 to 72 hours after the start of allograft infusion.
At 100 days after transplant, 51% of patients had developed grade 2-4 acute GVHD, and 15% had grade 3-4 acute GVHD. Fourteen percent of patients developed chronic GVHD.
The 2-year overall survival rate was 67%, and 2-year event-free survival was 62%.
Dr Luznik said he was encouraged by the low rate of chronic GVHD with the regimen. And he noted that percentages of acute GVHD are similar to those seen with the standard 6-month regimen of immunosuppressive drugs.
Reducing the post-transplant treatment to 2 days with cyclophosphamide, he said, “also allows for the earlier integration of other treatments.”
For example, immunotherapies used to eradicate any remaining cancer could be started much sooner with this regimen, said study author Christopher Kanakry, MD, of the Sidney Kimmel Cancer Center at Johns Hopkins.
“If you give patients immune cells to eradicate any remaining cancer cells that might be present,” he said, “those immune cells would not be prevented from doing their job by ongoing immune suppression drugs that are being used in patients treated with conventional transplant approaches.”
Dr Luznik said the researchers’ next step will be a phase 3 trial comparing this regimen to another experimental approach to prevent GVHD or to the more traditional 6-month immunosuppressive therapy.
Funding for this study was provided by Otsuka Pharmaceutical Co., Ltd. and the National Institutes of Health. ![]()

Credit: Chad McNeeley
Combining a couple of “promising” treatment approaches can prevent graft-vs-host disease (GVHD) as well as conventional therapy, researchers have reported in the Journal of Clinical Oncology.
They combined a 4-day myeloablative conditioning regimen of busulfan and fludarabine with 2 days of high-dose cyclophosphamide after transplant.
Typically, patients receive 6 months of immunosuppressive therapy to reduce their risk of GVHD.
The conditioning regimen and post-transplant cyclophosphamide have been tested separately in other studies and have good track records in controlling cancer and preventing severe GVHD.
Those successes led Leo Luznik, MD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues to combine the 2 therapies.
The team tested the combination in 92 patients with high-risk hematologic malignancies. Diagnoses included acute and chronic leukemias, multiple myeloma, non-Hodgkin lymphoma, and myelodysplastic syndromes. Patients had a median age of 49 (range, 21-65).
All patients received 40 mg/m2/day of intravenous (IV) fludarabine immediately before busulfan on all 4 days of conditioning. The busulfan dose of 130 mg/m2 IV daily was adjusted based on pharmacokinetics.
One or 2 days of rest were allowed before patients received a T-cell-replete bone marrow allograft. Forty-five patients had a matched, related donor, and 47 had a matched, unrelated donor.
Patients received 50 mg/kg/day of IV cyclophosphamide for 2 days, with the first dose starting 62 to 72 hours after the start of allograft infusion.
At 100 days after transplant, 51% of patients had developed grade 2-4 acute GVHD, and 15% had grade 3-4 acute GVHD. Fourteen percent of patients developed chronic GVHD.
The 2-year overall survival rate was 67%, and 2-year event-free survival was 62%.
Dr Luznik said he was encouraged by the low rate of chronic GVHD with the regimen. And he noted that percentages of acute GVHD are similar to those seen with the standard 6-month regimen of immunosuppressive drugs.
Reducing the post-transplant treatment to 2 days with cyclophosphamide, he said, “also allows for the earlier integration of other treatments.”
For example, immunotherapies used to eradicate any remaining cancer could be started much sooner with this regimen, said study author Christopher Kanakry, MD, of the Sidney Kimmel Cancer Center at Johns Hopkins.
“If you give patients immune cells to eradicate any remaining cancer cells that might be present,” he said, “those immune cells would not be prevented from doing their job by ongoing immune suppression drugs that are being used in patients treated with conventional transplant approaches.”
Dr Luznik said the researchers’ next step will be a phase 3 trial comparing this regimen to another experimental approach to prevent GVHD or to the more traditional 6-month immunosuppressive therapy.
Funding for this study was provided by Otsuka Pharmaceutical Co., Ltd. and the National Institutes of Health. ![]()

Credit: Chad McNeeley
Combining a couple of “promising” treatment approaches can prevent graft-vs-host disease (GVHD) as well as conventional therapy, researchers have reported in the Journal of Clinical Oncology.
They combined a 4-day myeloablative conditioning regimen of busulfan and fludarabine with 2 days of high-dose cyclophosphamide after transplant.
Typically, patients receive 6 months of immunosuppressive therapy to reduce their risk of GVHD.
The conditioning regimen and post-transplant cyclophosphamide have been tested separately in other studies and have good track records in controlling cancer and preventing severe GVHD.
Those successes led Leo Luznik, MD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues to combine the 2 therapies.
The team tested the combination in 92 patients with high-risk hematologic malignancies. Diagnoses included acute and chronic leukemias, multiple myeloma, non-Hodgkin lymphoma, and myelodysplastic syndromes. Patients had a median age of 49 (range, 21-65).
All patients received 40 mg/m2/day of intravenous (IV) fludarabine immediately before busulfan on all 4 days of conditioning. The busulfan dose of 130 mg/m2 IV daily was adjusted based on pharmacokinetics.
One or 2 days of rest were allowed before patients received a T-cell-replete bone marrow allograft. Forty-five patients had a matched, related donor, and 47 had a matched, unrelated donor.
Patients received 50 mg/kg/day of IV cyclophosphamide for 2 days, with the first dose starting 62 to 72 hours after the start of allograft infusion.
At 100 days after transplant, 51% of patients had developed grade 2-4 acute GVHD, and 15% had grade 3-4 acute GVHD. Fourteen percent of patients developed chronic GVHD.
The 2-year overall survival rate was 67%, and 2-year event-free survival was 62%.
Dr Luznik said he was encouraged by the low rate of chronic GVHD with the regimen. And he noted that percentages of acute GVHD are similar to those seen with the standard 6-month regimen of immunosuppressive drugs.
Reducing the post-transplant treatment to 2 days with cyclophosphamide, he said, “also allows for the earlier integration of other treatments.”
For example, immunotherapies used to eradicate any remaining cancer could be started much sooner with this regimen, said study author Christopher Kanakry, MD, of the Sidney Kimmel Cancer Center at Johns Hopkins.
“If you give patients immune cells to eradicate any remaining cancer cells that might be present,” he said, “those immune cells would not be prevented from doing their job by ongoing immune suppression drugs that are being used in patients treated with conventional transplant approaches.”
Dr Luznik said the researchers’ next step will be a phase 3 trial comparing this regimen to another experimental approach to prevent GVHD or to the more traditional 6-month immunosuppressive therapy.
Funding for this study was provided by Otsuka Pharmaceutical Co., Ltd. and the National Institutes of Health. ![]()
Ibrutinib fights chronic GVHD in mice

Preclinical research suggests the anticancer agent ibrutinib can ameliorate chronic graft-vs-host disease (GVHD).
Ibrutinib reduced the symptoms and progression of chronic GVHD in mouse models, and it decreased the activation of T and B cells isolated from patients with chronic GVHD.
These results indicate that T and B cells drive chronic GVHD and ibrutinib should be explored as a treatment option for human GVHD, according to investigators.
Bruce Blazar, MD, of the University of Minnesota in Minneapolis, and his colleagues described this work in The Journal of Clinical Investigation.
The team noted that CD4+ T cells and B cells mediate chronic GVHD, so it follows that targeting these populations might inhibit chronic GVHD pathogenesis.
As ibrutinib targets Th2 cells and B cells, the investigators decided to test whether the drug could reverse established chronic GVHD in 2 mouse models—a model of T cell–driven sclerodermatous chronic GVHD and an alloantibody-driven, multiorgan-system chronic GVHD model that induces bronchiolar obliterans.
Sclerodermatous chronic GVHD
The researchers first found that ibrutinib can reduce the clinical signs of sclerodermatous chronic GVHD. Fourteen days after treatment began, vehicle-treated mice and those that received cyclosporine exhibited sclerodermatous lesions, hair loss, hunched posture, and scabbing. But ibrutinib-treated mice did not.
Animals treated with ibrutinib had a significantly lower overall intensity of chronic GVHD—as measured by body weight, posture, mobility, hair loss, skin lesions, and vitality—than vehicle-treated mice (P=0.0184).
Ibrutinib also extended the median time to chronic GVHD progression by 14 days when compared to control. Thirty-three percent of ibrutinib-treated mice remained progression-free, compared to 12% of vehicle-treated mice (P<0.02).
Overall survival was 100% among ibrutinib-treated mice, 82% for cyclosporine-treated mice, and 88% for vehicle-treated mice.
The investigators also discovered that prolonged administration of ibrutinib is needed to reap the maximum therapeutic benefit in sclerodermatous chronic GVHD. Withdrawing treatment at day 60 enabled clinical breakthrough of chronic GVHD in a single mouse.
Alloantibody-driven chronic GVHD
In this model, ibrutinib inhibited the development of bronchiolar obliterans, as measured by pulmonary resistance (P=0.0090), elastance (P=0.0019), and compliance (P=0.0071).
In addition, there was less peribroncheolar collagen fibrosis among ibrutinib-treated animals and a significant reduction in pulmonary fibrosis (P<0.0001) compared to vehicle-treated controls.
However, continued therapy was necessary to see a long-term benefit with ibrutinib. Prophylactic ibrutinib given from day -2 to day 28 was not effective against chronic GVHD or bronchiolar obliterans.
Lastly, the investigators found that ibrutinib reduced the overall size, cellularity, and number of germinal center reactions (P<0.001), and the drug eliminated pulmonary immunoglobulin deposition (P<0.001).
Verifying the results
Additional experiments showed that mice lacking Bruton tyrosine kinase and IL-2 inducible T-cell kinase (both of which are inhibited by ibrutinib) did not develop chronic GVHD, which suggests these molecules are necessary for the condition to occur.
The investigators also discovered that ibrutinib reduced the activation of T and B cells from patients with active chronic GVHD.
CD4+ T cells pretreated with ibrutinib had lower surface expression of CD69 after ex vivo T-cell receptor stimulation using anti-CD3 (P=0.033). And purified B cells pretreated with ibrutinib showed lower levels of pBTK-Y223, pPLCγ2-Y1217, and pERK1/2.
Dr Blazar and his colleagues said these results indicate that B cells and T cells drive chronic GVHD and suggest that ibrutinib should be considered for testing in clinical trials of chronic GVHD. ![]()

Preclinical research suggests the anticancer agent ibrutinib can ameliorate chronic graft-vs-host disease (GVHD).
Ibrutinib reduced the symptoms and progression of chronic GVHD in mouse models, and it decreased the activation of T and B cells isolated from patients with chronic GVHD.
These results indicate that T and B cells drive chronic GVHD and ibrutinib should be explored as a treatment option for human GVHD, according to investigators.
Bruce Blazar, MD, of the University of Minnesota in Minneapolis, and his colleagues described this work in The Journal of Clinical Investigation.
The team noted that CD4+ T cells and B cells mediate chronic GVHD, so it follows that targeting these populations might inhibit chronic GVHD pathogenesis.
As ibrutinib targets Th2 cells and B cells, the investigators decided to test whether the drug could reverse established chronic GVHD in 2 mouse models—a model of T cell–driven sclerodermatous chronic GVHD and an alloantibody-driven, multiorgan-system chronic GVHD model that induces bronchiolar obliterans.
Sclerodermatous chronic GVHD
The researchers first found that ibrutinib can reduce the clinical signs of sclerodermatous chronic GVHD. Fourteen days after treatment began, vehicle-treated mice and those that received cyclosporine exhibited sclerodermatous lesions, hair loss, hunched posture, and scabbing. But ibrutinib-treated mice did not.
Animals treated with ibrutinib had a significantly lower overall intensity of chronic GVHD—as measured by body weight, posture, mobility, hair loss, skin lesions, and vitality—than vehicle-treated mice (P=0.0184).
Ibrutinib also extended the median time to chronic GVHD progression by 14 days when compared to control. Thirty-three percent of ibrutinib-treated mice remained progression-free, compared to 12% of vehicle-treated mice (P<0.02).
Overall survival was 100% among ibrutinib-treated mice, 82% for cyclosporine-treated mice, and 88% for vehicle-treated mice.
The investigators also discovered that prolonged administration of ibrutinib is needed to reap the maximum therapeutic benefit in sclerodermatous chronic GVHD. Withdrawing treatment at day 60 enabled clinical breakthrough of chronic GVHD in a single mouse.
Alloantibody-driven chronic GVHD
In this model, ibrutinib inhibited the development of bronchiolar obliterans, as measured by pulmonary resistance (P=0.0090), elastance (P=0.0019), and compliance (P=0.0071).
In addition, there was less peribroncheolar collagen fibrosis among ibrutinib-treated animals and a significant reduction in pulmonary fibrosis (P<0.0001) compared to vehicle-treated controls.
However, continued therapy was necessary to see a long-term benefit with ibrutinib. Prophylactic ibrutinib given from day -2 to day 28 was not effective against chronic GVHD or bronchiolar obliterans.
Lastly, the investigators found that ibrutinib reduced the overall size, cellularity, and number of germinal center reactions (P<0.001), and the drug eliminated pulmonary immunoglobulin deposition (P<0.001).
Verifying the results
Additional experiments showed that mice lacking Bruton tyrosine kinase and IL-2 inducible T-cell kinase (both of which are inhibited by ibrutinib) did not develop chronic GVHD, which suggests these molecules are necessary for the condition to occur.
The investigators also discovered that ibrutinib reduced the activation of T and B cells from patients with active chronic GVHD.
CD4+ T cells pretreated with ibrutinib had lower surface expression of CD69 after ex vivo T-cell receptor stimulation using anti-CD3 (P=0.033). And purified B cells pretreated with ibrutinib showed lower levels of pBTK-Y223, pPLCγ2-Y1217, and pERK1/2.
Dr Blazar and his colleagues said these results indicate that B cells and T cells drive chronic GVHD and suggest that ibrutinib should be considered for testing in clinical trials of chronic GVHD. ![]()

Preclinical research suggests the anticancer agent ibrutinib can ameliorate chronic graft-vs-host disease (GVHD).
Ibrutinib reduced the symptoms and progression of chronic GVHD in mouse models, and it decreased the activation of T and B cells isolated from patients with chronic GVHD.
These results indicate that T and B cells drive chronic GVHD and ibrutinib should be explored as a treatment option for human GVHD, according to investigators.
Bruce Blazar, MD, of the University of Minnesota in Minneapolis, and his colleagues described this work in The Journal of Clinical Investigation.
The team noted that CD4+ T cells and B cells mediate chronic GVHD, so it follows that targeting these populations might inhibit chronic GVHD pathogenesis.
As ibrutinib targets Th2 cells and B cells, the investigators decided to test whether the drug could reverse established chronic GVHD in 2 mouse models—a model of T cell–driven sclerodermatous chronic GVHD and an alloantibody-driven, multiorgan-system chronic GVHD model that induces bronchiolar obliterans.
Sclerodermatous chronic GVHD
The researchers first found that ibrutinib can reduce the clinical signs of sclerodermatous chronic GVHD. Fourteen days after treatment began, vehicle-treated mice and those that received cyclosporine exhibited sclerodermatous lesions, hair loss, hunched posture, and scabbing. But ibrutinib-treated mice did not.
Animals treated with ibrutinib had a significantly lower overall intensity of chronic GVHD—as measured by body weight, posture, mobility, hair loss, skin lesions, and vitality—than vehicle-treated mice (P=0.0184).
Ibrutinib also extended the median time to chronic GVHD progression by 14 days when compared to control. Thirty-three percent of ibrutinib-treated mice remained progression-free, compared to 12% of vehicle-treated mice (P<0.02).
Overall survival was 100% among ibrutinib-treated mice, 82% for cyclosporine-treated mice, and 88% for vehicle-treated mice.
The investigators also discovered that prolonged administration of ibrutinib is needed to reap the maximum therapeutic benefit in sclerodermatous chronic GVHD. Withdrawing treatment at day 60 enabled clinical breakthrough of chronic GVHD in a single mouse.
Alloantibody-driven chronic GVHD
In this model, ibrutinib inhibited the development of bronchiolar obliterans, as measured by pulmonary resistance (P=0.0090), elastance (P=0.0019), and compliance (P=0.0071).
In addition, there was less peribroncheolar collagen fibrosis among ibrutinib-treated animals and a significant reduction in pulmonary fibrosis (P<0.0001) compared to vehicle-treated controls.
However, continued therapy was necessary to see a long-term benefit with ibrutinib. Prophylactic ibrutinib given from day -2 to day 28 was not effective against chronic GVHD or bronchiolar obliterans.
Lastly, the investigators found that ibrutinib reduced the overall size, cellularity, and number of germinal center reactions (P<0.001), and the drug eliminated pulmonary immunoglobulin deposition (P<0.001).
Verifying the results
Additional experiments showed that mice lacking Bruton tyrosine kinase and IL-2 inducible T-cell kinase (both of which are inhibited by ibrutinib) did not develop chronic GVHD, which suggests these molecules are necessary for the condition to occur.
The investigators also discovered that ibrutinib reduced the activation of T and B cells from patients with active chronic GVHD.
CD4+ T cells pretreated with ibrutinib had lower surface expression of CD69 after ex vivo T-cell receptor stimulation using anti-CD3 (P=0.033). And purified B cells pretreated with ibrutinib showed lower levels of pBTK-Y223, pPLCγ2-Y1217, and pERK1/2.
Dr Blazar and his colleagues said these results indicate that B cells and T cells drive chronic GVHD and suggest that ibrutinib should be considered for testing in clinical trials of chronic GVHD. ![]()
Consolidation can improve PFS in HL
Consolidation therapy with brentuximab vedotin can improve progression-free survival (PFS) for Hodgkin lymphoma (HL) patients who have undergone a transplant, according to a phase 3 study.
The trial, known as AETHERA, is a comparison of single-agent brentuximab vedotin to placebo in patients with HL who were at risk of relapse following autologous stem cell transplant (ASCT).
Brentuximab vedotin conferred a 75% improvement in PFS over placebo.
However, there was no significant difference in overall survival between the 2 treatment arms.
These results were recently announced by Seattle Genetics Inc. and Takeda Pharmaceutical Company Limited, the companies developing brentuximab vedotin (Adcetris).
The companies said more complete results from AETHERA will be presented at the 2014 ASH Annual Meeting in December.
AETHERA is a randomized, double-blind, placebo-controlled study designed to evaluate the potential of brentuximab vedotin to extend PFS post-ASCT in patients with HL who have at least one risk factor for progression. In addition to the primary endpoint of PFS, secondary endpoints included overall survival, safety, and tolerability.
Patients were eligible if they had risk factors for residual HL, defined as a history of refractory HL, those who relapse or progress within a year of receiving frontline chemotherapy, and/or those who have disease outside of the lymph nodes at the time of pre-ASCT relapse.
The study included 329 patients who received brentuximab vedotin or placebo every 3 weeks for up to a year.
The researchers assessed PFS a minimum of 2 years after the initiation of treatment for all patients. There was a significant improvement in PFS with brentuximab vedotin compared to placebo (hazard ratio=0.57; P=0.001).
However, a prespecified interim analysis of overall survival showed no significant difference between the treatment arms.
Patients in both arms who experienced progression received a variety of subsequent therapies. Most patients on the placebo arm received brentuximab vedotin after progression.
A further analysis of overall survival is planned in 2016. The safety profile of brentuximab vedotin in the AETHERA trial was generally consistent with the existing prescribing information.
“We anticipate reporting more complete AETHERA data at the ASH Annual Meeting in December and intend to submit a supplemental Biologics License Application to the FDA in 2015 for approval in this setting,” said Clay B. Siegall, PhD, President and Chief Executive Officer of Seattle Genetics.
The FDA has already granted brentuximab vedotin accelerated approval to treat HL patients after ASCT failure or after the failure of at least 2 prior multiagent chemotherapy regimens in patients who are not ASCT candidates. The FDA also granted the drug accelerated approval to treat systemic anaplastic large cell lymphoma after the failure of at least 1 prior multiagent chemotherapy regimen.
The European Commission granted brentuximab vedotin conditional marketing authorization for the same indications. In both cases, the drug can gain full, traditional approval once studies have shown it confers a clinical benefit.
Brentuximab vedotin has a boxed warning detailing the risk of progressive multifocal leukoencephalopathy associated with use of the drug. The drug has also been shown to pose a risk of pulmonary toxicity when combined with bleomycin. ![]()
Consolidation therapy with brentuximab vedotin can improve progression-free survival (PFS) for Hodgkin lymphoma (HL) patients who have undergone a transplant, according to a phase 3 study.
The trial, known as AETHERA, is a comparison of single-agent brentuximab vedotin to placebo in patients with HL who were at risk of relapse following autologous stem cell transplant (ASCT).
Brentuximab vedotin conferred a 75% improvement in PFS over placebo.
However, there was no significant difference in overall survival between the 2 treatment arms.
These results were recently announced by Seattle Genetics Inc. and Takeda Pharmaceutical Company Limited, the companies developing brentuximab vedotin (Adcetris).
The companies said more complete results from AETHERA will be presented at the 2014 ASH Annual Meeting in December.
AETHERA is a randomized, double-blind, placebo-controlled study designed to evaluate the potential of brentuximab vedotin to extend PFS post-ASCT in patients with HL who have at least one risk factor for progression. In addition to the primary endpoint of PFS, secondary endpoints included overall survival, safety, and tolerability.
Patients were eligible if they had risk factors for residual HL, defined as a history of refractory HL, those who relapse or progress within a year of receiving frontline chemotherapy, and/or those who have disease outside of the lymph nodes at the time of pre-ASCT relapse.
The study included 329 patients who received brentuximab vedotin or placebo every 3 weeks for up to a year.
The researchers assessed PFS a minimum of 2 years after the initiation of treatment for all patients. There was a significant improvement in PFS with brentuximab vedotin compared to placebo (hazard ratio=0.57; P=0.001).
However, a prespecified interim analysis of overall survival showed no significant difference between the treatment arms.
Patients in both arms who experienced progression received a variety of subsequent therapies. Most patients on the placebo arm received brentuximab vedotin after progression.
A further analysis of overall survival is planned in 2016. The safety profile of brentuximab vedotin in the AETHERA trial was generally consistent with the existing prescribing information.
“We anticipate reporting more complete AETHERA data at the ASH Annual Meeting in December and intend to submit a supplemental Biologics License Application to the FDA in 2015 for approval in this setting,” said Clay B. Siegall, PhD, President and Chief Executive Officer of Seattle Genetics.
The FDA has already granted brentuximab vedotin accelerated approval to treat HL patients after ASCT failure or after the failure of at least 2 prior multiagent chemotherapy regimens in patients who are not ASCT candidates. The FDA also granted the drug accelerated approval to treat systemic anaplastic large cell lymphoma after the failure of at least 1 prior multiagent chemotherapy regimen.
The European Commission granted brentuximab vedotin conditional marketing authorization for the same indications. In both cases, the drug can gain full, traditional approval once studies have shown it confers a clinical benefit.
Brentuximab vedotin has a boxed warning detailing the risk of progressive multifocal leukoencephalopathy associated with use of the drug. The drug has also been shown to pose a risk of pulmonary toxicity when combined with bleomycin. ![]()
Consolidation therapy with brentuximab vedotin can improve progression-free survival (PFS) for Hodgkin lymphoma (HL) patients who have undergone a transplant, according to a phase 3 study.
The trial, known as AETHERA, is a comparison of single-agent brentuximab vedotin to placebo in patients with HL who were at risk of relapse following autologous stem cell transplant (ASCT).
Brentuximab vedotin conferred a 75% improvement in PFS over placebo.
However, there was no significant difference in overall survival between the 2 treatment arms.
These results were recently announced by Seattle Genetics Inc. and Takeda Pharmaceutical Company Limited, the companies developing brentuximab vedotin (Adcetris).
The companies said more complete results from AETHERA will be presented at the 2014 ASH Annual Meeting in December.
AETHERA is a randomized, double-blind, placebo-controlled study designed to evaluate the potential of brentuximab vedotin to extend PFS post-ASCT in patients with HL who have at least one risk factor for progression. In addition to the primary endpoint of PFS, secondary endpoints included overall survival, safety, and tolerability.
Patients were eligible if they had risk factors for residual HL, defined as a history of refractory HL, those who relapse or progress within a year of receiving frontline chemotherapy, and/or those who have disease outside of the lymph nodes at the time of pre-ASCT relapse.
The study included 329 patients who received brentuximab vedotin or placebo every 3 weeks for up to a year.
The researchers assessed PFS a minimum of 2 years after the initiation of treatment for all patients. There was a significant improvement in PFS with brentuximab vedotin compared to placebo (hazard ratio=0.57; P=0.001).
However, a prespecified interim analysis of overall survival showed no significant difference between the treatment arms.
Patients in both arms who experienced progression received a variety of subsequent therapies. Most patients on the placebo arm received brentuximab vedotin after progression.
A further analysis of overall survival is planned in 2016. The safety profile of brentuximab vedotin in the AETHERA trial was generally consistent with the existing prescribing information.
“We anticipate reporting more complete AETHERA data at the ASH Annual Meeting in December and intend to submit a supplemental Biologics License Application to the FDA in 2015 for approval in this setting,” said Clay B. Siegall, PhD, President and Chief Executive Officer of Seattle Genetics.
The FDA has already granted brentuximab vedotin accelerated approval to treat HL patients after ASCT failure or after the failure of at least 2 prior multiagent chemotherapy regimens in patients who are not ASCT candidates. The FDA also granted the drug accelerated approval to treat systemic anaplastic large cell lymphoma after the failure of at least 1 prior multiagent chemotherapy regimen.
The European Commission granted brentuximab vedotin conditional marketing authorization for the same indications. In both cases, the drug can gain full, traditional approval once studies have shown it confers a clinical benefit.
Brentuximab vedotin has a boxed warning detailing the risk of progressive multifocal leukoencephalopathy associated with use of the drug. The drug has also been shown to pose a risk of pulmonary toxicity when combined with bleomycin. ![]()
Preventing cancer-related infection

Credit: CDC/Kimberly Smith
and Christine Ford
NEW YORK—Hand washing is still the single most effective method to prevent the transmission of infection, but additional measures can reduce the risk of cancer-related infections, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
In her presentation, Laura Zitella, RN, of the Stanford Cancer Institute in California, discussed current recommendations for pharmacologic and non-pharmacologic infection prophylaxis.
She noted that NCCN Guidelines on the Prevention and Treatment of Cancer-Related Infections state that the highest risk of infection is in patients undergoing allogeneic hematopoietic stem cell transplant (HSCT), acute leukemia patients undergoing induction or consolidation therapy, patients receiving alemtuzumab therapy, patients with graft-vs-host disease (GVHD) treated with high-dose steroids, and patients with neutropenia anticipated to last greater than 10 days.
Antibiotic prophylaxis
Prior to 2005, Zitella said, no survival benefit was observed for antibiotic prophylaxis. All of this changed with the results of a meta-analysis. The analysis included 95 randomized, controlled trials and 9283 patients, the majority having acute leukemia or undergoing HSCT.
For the first time, antibiotic prophylaxis was shown to confer a survival benefit. In neutropenic patients, prophylaxis reduced overall mortality by 33% and infection-related mortality by 42%, compared with placebo or no treatment.
Prophylaxis is not recommended for low-risk neutropenic patients, Zitella said, because it is not proven to decrease morality.
And the drugs of choice are levofloxacin (500-750 mg PO daily) or ciprofloxacin (500-750 mg PO twice daily).
Colony-stimulating factors
Consensus guidelines for the use of colony-stimulating factors (CSFs) are a compilation of ASCO, EORTC, ESMO, and NCCN guidelines.
CSFs may be used prophylactically to prevent chemotherapy-induced neutropenia, febrile neutropenia, and infection. They reduce the duration of hospitalization, the duration of parenteral antibiotics, and have shown a survival benefit.
CSFs are recommended if the risk of febrile neutropenia is 20% or greater. CSFs are not routinely recommended for patients undergoing radiation treatment, acute myeloid leukemia induction, or patients with Hodgkin lymphoma.
Antifungal prophylaxis
Zitella noted that fluconazole is the best-studied antifungal prophylaxis and is recommended as the primary prophylaxis for HSCT patients.
In double-blind, placebo-controlled trials, fluconazole reduced mucosal candidiasis and invasive Candida infections in patients undergoing HSCT. And it improved survival at day 110 after transplant.
Posaconazole prophylaxis has proven effective in patients with acute myeloid leukemia or myelodysplastic syndromes undergoing intensive chemotherapy. The drug reduced invasive fungal infections, including aspergillosis, and improved survival.
For patients with GVHD on immunosuppressive therapy, posaconazole and fluconazole prophylaxis were equivalent in preventing invasive fungal infections. However, posaconazole reduced the incidence of invasive aspergillosis and fungal-related mortality.
The NCCN guidelines, Zitella said, spell out which antifungal agents should be used for each disease or therapeutic intervention.
Antiviral prophylaxis
HSV and VZV
Patients requiring antiviral prophylaxis for herpes simplex virus (HSV) and varicella zoster virus (VZV) should be seropositive and have acute leukemia, GVHD treated with steroids, prior HSV reactivation under treatment, or have undergone HSCT.
Zitella pointed out that patients treated with proteasome inhibitors, such as bortezomib, alemtuzumab, or purine analaogs, such as fludarabine, are more at risk and should also receive antiviral prophylaxis.
Recommended drugs include valacyclovir, acyclovir, or famciclovir.
CMV
Cytomegalovirus-positive (CMV+) patients at high risk include those who have received an allogeneic HSCT or treatment with alemtuzumab.
Zitella explained that for these patients, prophylaxis is uncommon, and a pre-emptive strategy should be used, including testing 3 to 6 months after transplant or in the setting of GVHD and 2 months after alemtuzumab therapy.
CMV viremia should be treated with valganciclovir, ganciclovir, foscarnet, or cidofovir.
HBV
Zitella noted that 30% of the world population has been infected with hepatitis B virus (HBV), and reactivation during cancer treatment can lead to fulminant hepatitis and death.
NCCN recommends that patients undergoing immunosuppressive therapy, allogeneic HSCT candidates, patients receiving anti-CD20 monoclonal antibodies, those treated with alemtuzumab, and patients receiving systemic therapy who have an obvious risk factor for HBV infection should be tested.
Entecavir, tenofovir, adefovir, telbivudine, or lamivudine may be used to prevent HBV reactivation.
Pneumocystis pneumonia prophylaxis
Patients undergoing allogeneic HSCT, patients with acute lymphoblastic leukemia, those treated with alemtuzumab, and those with a CD4 count below 200 cells/mcL should receive pneumocystis pneumonia prophylaxis.
Trimethorpim/sulfamethoxazole is the drug of choice. Atovaquone, dapsone, and inhaled or IV pentamidine are alternatives.
Vaccines
Zitella pointed out that recommended vaccines include influenza, pneumococcal, and tetanus, diphtheria, and acellular pertussis.
She cautioned that live attenuated vaccines should not be given to cancer patients. Other vaccines to avoid include smallpox; measles, mumps, and rubella; varicella zoster; rotavirus; yellow fever; oral typhoid; BCG; and oral polio vaccine.
Neutropenic precautions
Low microbial diets are a hot topic among patients undergoing cancer treatment, Zitella said. Fresh fruits and vegetables used to be restricted, but no studies show that dietary restrictions decrease the risk of infection.
Zitella stressed, however, that standard food safety recommendations of the USDA/FDA should be followed.
She also noted that HEPA filtration is protective against molds in high-risk patients, antiseptic bathing has contradictory evidence, the benefit of laminar airflow is unclear, and protective isolation has not been proven to reduce the risk of infection. ![]()

Credit: CDC/Kimberly Smith
and Christine Ford
NEW YORK—Hand washing is still the single most effective method to prevent the transmission of infection, but additional measures can reduce the risk of cancer-related infections, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
In her presentation, Laura Zitella, RN, of the Stanford Cancer Institute in California, discussed current recommendations for pharmacologic and non-pharmacologic infection prophylaxis.
She noted that NCCN Guidelines on the Prevention and Treatment of Cancer-Related Infections state that the highest risk of infection is in patients undergoing allogeneic hematopoietic stem cell transplant (HSCT), acute leukemia patients undergoing induction or consolidation therapy, patients receiving alemtuzumab therapy, patients with graft-vs-host disease (GVHD) treated with high-dose steroids, and patients with neutropenia anticipated to last greater than 10 days.
Antibiotic prophylaxis
Prior to 2005, Zitella said, no survival benefit was observed for antibiotic prophylaxis. All of this changed with the results of a meta-analysis. The analysis included 95 randomized, controlled trials and 9283 patients, the majority having acute leukemia or undergoing HSCT.
For the first time, antibiotic prophylaxis was shown to confer a survival benefit. In neutropenic patients, prophylaxis reduced overall mortality by 33% and infection-related mortality by 42%, compared with placebo or no treatment.
Prophylaxis is not recommended for low-risk neutropenic patients, Zitella said, because it is not proven to decrease morality.
And the drugs of choice are levofloxacin (500-750 mg PO daily) or ciprofloxacin (500-750 mg PO twice daily).
Colony-stimulating factors
Consensus guidelines for the use of colony-stimulating factors (CSFs) are a compilation of ASCO, EORTC, ESMO, and NCCN guidelines.
CSFs may be used prophylactically to prevent chemotherapy-induced neutropenia, febrile neutropenia, and infection. They reduce the duration of hospitalization, the duration of parenteral antibiotics, and have shown a survival benefit.
CSFs are recommended if the risk of febrile neutropenia is 20% or greater. CSFs are not routinely recommended for patients undergoing radiation treatment, acute myeloid leukemia induction, or patients with Hodgkin lymphoma.
Antifungal prophylaxis
Zitella noted that fluconazole is the best-studied antifungal prophylaxis and is recommended as the primary prophylaxis for HSCT patients.
In double-blind, placebo-controlled trials, fluconazole reduced mucosal candidiasis and invasive Candida infections in patients undergoing HSCT. And it improved survival at day 110 after transplant.
Posaconazole prophylaxis has proven effective in patients with acute myeloid leukemia or myelodysplastic syndromes undergoing intensive chemotherapy. The drug reduced invasive fungal infections, including aspergillosis, and improved survival.
For patients with GVHD on immunosuppressive therapy, posaconazole and fluconazole prophylaxis were equivalent in preventing invasive fungal infections. However, posaconazole reduced the incidence of invasive aspergillosis and fungal-related mortality.
The NCCN guidelines, Zitella said, spell out which antifungal agents should be used for each disease or therapeutic intervention.
Antiviral prophylaxis
HSV and VZV
Patients requiring antiviral prophylaxis for herpes simplex virus (HSV) and varicella zoster virus (VZV) should be seropositive and have acute leukemia, GVHD treated with steroids, prior HSV reactivation under treatment, or have undergone HSCT.
Zitella pointed out that patients treated with proteasome inhibitors, such as bortezomib, alemtuzumab, or purine analaogs, such as fludarabine, are more at risk and should also receive antiviral prophylaxis.
Recommended drugs include valacyclovir, acyclovir, or famciclovir.
CMV
Cytomegalovirus-positive (CMV+) patients at high risk include those who have received an allogeneic HSCT or treatment with alemtuzumab.
Zitella explained that for these patients, prophylaxis is uncommon, and a pre-emptive strategy should be used, including testing 3 to 6 months after transplant or in the setting of GVHD and 2 months after alemtuzumab therapy.
CMV viremia should be treated with valganciclovir, ganciclovir, foscarnet, or cidofovir.
HBV
Zitella noted that 30% of the world population has been infected with hepatitis B virus (HBV), and reactivation during cancer treatment can lead to fulminant hepatitis and death.
NCCN recommends that patients undergoing immunosuppressive therapy, allogeneic HSCT candidates, patients receiving anti-CD20 monoclonal antibodies, those treated with alemtuzumab, and patients receiving systemic therapy who have an obvious risk factor for HBV infection should be tested.
Entecavir, tenofovir, adefovir, telbivudine, or lamivudine may be used to prevent HBV reactivation.
Pneumocystis pneumonia prophylaxis
Patients undergoing allogeneic HSCT, patients with acute lymphoblastic leukemia, those treated with alemtuzumab, and those with a CD4 count below 200 cells/mcL should receive pneumocystis pneumonia prophylaxis.
Trimethorpim/sulfamethoxazole is the drug of choice. Atovaquone, dapsone, and inhaled or IV pentamidine are alternatives.
Vaccines
Zitella pointed out that recommended vaccines include influenza, pneumococcal, and tetanus, diphtheria, and acellular pertussis.
She cautioned that live attenuated vaccines should not be given to cancer patients. Other vaccines to avoid include smallpox; measles, mumps, and rubella; varicella zoster; rotavirus; yellow fever; oral typhoid; BCG; and oral polio vaccine.
Neutropenic precautions
Low microbial diets are a hot topic among patients undergoing cancer treatment, Zitella said. Fresh fruits and vegetables used to be restricted, but no studies show that dietary restrictions decrease the risk of infection.
Zitella stressed, however, that standard food safety recommendations of the USDA/FDA should be followed.
She also noted that HEPA filtration is protective against molds in high-risk patients, antiseptic bathing has contradictory evidence, the benefit of laminar airflow is unclear, and protective isolation has not been proven to reduce the risk of infection. ![]()

Credit: CDC/Kimberly Smith
and Christine Ford
NEW YORK—Hand washing is still the single most effective method to prevent the transmission of infection, but additional measures can reduce the risk of cancer-related infections, according to a speaker at the NCCN 9th Annual Congress: Hematologic Malignancies.
In her presentation, Laura Zitella, RN, of the Stanford Cancer Institute in California, discussed current recommendations for pharmacologic and non-pharmacologic infection prophylaxis.
She noted that NCCN Guidelines on the Prevention and Treatment of Cancer-Related Infections state that the highest risk of infection is in patients undergoing allogeneic hematopoietic stem cell transplant (HSCT), acute leukemia patients undergoing induction or consolidation therapy, patients receiving alemtuzumab therapy, patients with graft-vs-host disease (GVHD) treated with high-dose steroids, and patients with neutropenia anticipated to last greater than 10 days.
Antibiotic prophylaxis
Prior to 2005, Zitella said, no survival benefit was observed for antibiotic prophylaxis. All of this changed with the results of a meta-analysis. The analysis included 95 randomized, controlled trials and 9283 patients, the majority having acute leukemia or undergoing HSCT.
For the first time, antibiotic prophylaxis was shown to confer a survival benefit. In neutropenic patients, prophylaxis reduced overall mortality by 33% and infection-related mortality by 42%, compared with placebo or no treatment.
Prophylaxis is not recommended for low-risk neutropenic patients, Zitella said, because it is not proven to decrease morality.
And the drugs of choice are levofloxacin (500-750 mg PO daily) or ciprofloxacin (500-750 mg PO twice daily).
Colony-stimulating factors
Consensus guidelines for the use of colony-stimulating factors (CSFs) are a compilation of ASCO, EORTC, ESMO, and NCCN guidelines.
CSFs may be used prophylactically to prevent chemotherapy-induced neutropenia, febrile neutropenia, and infection. They reduce the duration of hospitalization, the duration of parenteral antibiotics, and have shown a survival benefit.
CSFs are recommended if the risk of febrile neutropenia is 20% or greater. CSFs are not routinely recommended for patients undergoing radiation treatment, acute myeloid leukemia induction, or patients with Hodgkin lymphoma.
Antifungal prophylaxis
Zitella noted that fluconazole is the best-studied antifungal prophylaxis and is recommended as the primary prophylaxis for HSCT patients.
In double-blind, placebo-controlled trials, fluconazole reduced mucosal candidiasis and invasive Candida infections in patients undergoing HSCT. And it improved survival at day 110 after transplant.
Posaconazole prophylaxis has proven effective in patients with acute myeloid leukemia or myelodysplastic syndromes undergoing intensive chemotherapy. The drug reduced invasive fungal infections, including aspergillosis, and improved survival.
For patients with GVHD on immunosuppressive therapy, posaconazole and fluconazole prophylaxis were equivalent in preventing invasive fungal infections. However, posaconazole reduced the incidence of invasive aspergillosis and fungal-related mortality.
The NCCN guidelines, Zitella said, spell out which antifungal agents should be used for each disease or therapeutic intervention.
Antiviral prophylaxis
HSV and VZV
Patients requiring antiviral prophylaxis for herpes simplex virus (HSV) and varicella zoster virus (VZV) should be seropositive and have acute leukemia, GVHD treated with steroids, prior HSV reactivation under treatment, or have undergone HSCT.
Zitella pointed out that patients treated with proteasome inhibitors, such as bortezomib, alemtuzumab, or purine analaogs, such as fludarabine, are more at risk and should also receive antiviral prophylaxis.
Recommended drugs include valacyclovir, acyclovir, or famciclovir.
CMV
Cytomegalovirus-positive (CMV+) patients at high risk include those who have received an allogeneic HSCT or treatment with alemtuzumab.
Zitella explained that for these patients, prophylaxis is uncommon, and a pre-emptive strategy should be used, including testing 3 to 6 months after transplant or in the setting of GVHD and 2 months after alemtuzumab therapy.
CMV viremia should be treated with valganciclovir, ganciclovir, foscarnet, or cidofovir.
HBV
Zitella noted that 30% of the world population has been infected with hepatitis B virus (HBV), and reactivation during cancer treatment can lead to fulminant hepatitis and death.
NCCN recommends that patients undergoing immunosuppressive therapy, allogeneic HSCT candidates, patients receiving anti-CD20 monoclonal antibodies, those treated with alemtuzumab, and patients receiving systemic therapy who have an obvious risk factor for HBV infection should be tested.
Entecavir, tenofovir, adefovir, telbivudine, or lamivudine may be used to prevent HBV reactivation.
Pneumocystis pneumonia prophylaxis
Patients undergoing allogeneic HSCT, patients with acute lymphoblastic leukemia, those treated with alemtuzumab, and those with a CD4 count below 200 cells/mcL should receive pneumocystis pneumonia prophylaxis.
Trimethorpim/sulfamethoxazole is the drug of choice. Atovaquone, dapsone, and inhaled or IV pentamidine are alternatives.
Vaccines
Zitella pointed out that recommended vaccines include influenza, pneumococcal, and tetanus, diphtheria, and acellular pertussis.
She cautioned that live attenuated vaccines should not be given to cancer patients. Other vaccines to avoid include smallpox; measles, mumps, and rubella; varicella zoster; rotavirus; yellow fever; oral typhoid; BCG; and oral polio vaccine.
Neutropenic precautions
Low microbial diets are a hot topic among patients undergoing cancer treatment, Zitella said. Fresh fruits and vegetables used to be restricted, but no studies show that dietary restrictions decrease the risk of infection.
Zitella stressed, however, that standard food safety recommendations of the USDA/FDA should be followed.
She also noted that HEPA filtration is protective against molds in high-risk patients, antiseptic bathing has contradictory evidence, the benefit of laminar airflow is unclear, and protective isolation has not been proven to reduce the risk of infection.
Split decision on role of upfront transplant in MM

Credit: Chad McNeeley
NEW YORK—A debate on the pros and cons of upfront transplant in symptomatic multiple myeloma (MM) yielded a split decision from the audience during the NCCN 9th Annual Congress: Hematologic Malignancies.
Sergio Giralt, MD, of Memorial Sloan Kettering Cancer Center in New York, argued for upfront transplant, pointing out that long-term MM survivors have transplant as upfront therapy.
Kenneth Anderson, MD, of Dana Farber/Brigham and Women’s Cancer Center in Boston, took the stance that, in the past 10 years, there has been a
revolution in novel therapies that has significantly improved survival in MM.
For upfront transplant
Dr Giralt cited the 36-month follow-up of the E4A03 landmark analysis of patients who went off therapy after 4 cycles of lenalidomide/dexamethasone to pursue early stem cell transplant and those who continued treatment until disease progression.
Regardless of whether the patients were younger than 65 years or between 65 and 70, the patients who had an early transplant had superior progression-free survival (PFS) and overall survival (OS) compared to those who did not.
Dr Giralt added that bortezomib should be a component of induction therapy prior to autologous stem cell transplant (ASCT). Even though there is no survival benefit with bortezomib-based regimens, he said, there is significant improvement in PFS, as shown in a meta-analysis of phase 3 European studies.
The E4A03 landmark study also determined that the more intense the treatment, the better the outcome. So patients with double ASCT had a significantly longer PFS than patients who only had a single transplant.
This held true for OS as well, and included patients with 17p deletion and/or t(4;14) who failed to achieve complete remission after bortezomib-based induction regimens.
An analysis of 27,987 MM patients with a median age of 68 years (range, 19 to 90) revealed that of the patients who survived 10 years or more, 16.5% had ASCT as part of their initial therapy.
Dr Giralt concluded that the preponderance of evidence supports high-dose melphalan and ASCT as upfront consolidation therapy for MM. And until results of randomized trials investigating combination therapies are reported, melphalan consolidation should be considered the standard of care for all eligible patients with MM.
Against upfront transplant
Dr Anderson countered with data showing limited or no improvement in survival with ASCT, including evidence from studies by Attal, Fermand, Blade, Child, and Barlogie.
ASCT confers only modest PFS advantage, he said, showing results of the Barlogie study in which patients undergoing ASCT had a 25-month PFS, compared with a 21-month PFS with VBMCP (vincristine, carmustine, melphalan, cyclophosphamide, and prednisone).
“In the last 10 to 15 years, there has been a revolution in myeloma,” Dr Anderson said. “We have a lot of novel agents here today, and we have even more coming. It’s a hugely exciting time.”
Dr Anderson pointed out that since the introduction of novel agents, survival has improved between 2006 and 2010, compared to the period between 2001 and 2005, and particularly in patients older than 65 years (P=0.001).
Transplant has also changed, he said. Novel therapies have been integrated into the transplant paradigm, either before, as induction and consolidation therapy, or after, as maintenance. He indicated that this begs the question as to whether we really need the transplant component.
There has also been unprecedented use of triplets in combination therapy, Dr Anderson said, resulting in overall response rates upwards of 90%. For example, carfilzomib in combination with lenalidomide and dexamethasone prompted an overall response rate of 94%, with a stringent complete response (CR), CR, and near CR of 53%.
“It’s a new day in myeloma,” he said. “It’s taken us a long time, but we’re worrying about minimal residual disease (MRD) now. We’re worried about getting to the endpoint of 1 myeloma cell in 1 million normal cells.”
The point is, he added, that with novel therapies, such as carfilzomib, lenalidomide, and dexamethasone, patients who achieve a complete response can become MRD negative, suggesting an unprecedented extent of response without transplant.
MRD negativity may also be accomplished with oral agents, such as ixazomib. The depth of response with ixazomib increases over the course of treatment, with 27% achieving stringent CR or CR with a median duration of response of 13.8 months, and 82% of patients attaining MRD-negative status.
“In the absence of transplant,” Dr Anderson said, “this is an unprecedented response.”
Dr Anderson also pointed out that in the era of novel agents, there is no difference in outcome between early or delayed transplant. The 4-year OS in transplant-eligible patients who received initial therapy with lenalidomide was 80%, regardless of the timing of ASCT.
And in one trial, patients who received a delayed transplant fared better in OS than those transplanted early.
Dr Anderson said there is a parallel, international phase 3 study underway (IFM/DFCI2009) that will provide an answer to the debate on upfront transplant in the not-too-distant future.

Credit: Chad McNeeley
NEW YORK—A debate on the pros and cons of upfront transplant in symptomatic multiple myeloma (MM) yielded a split decision from the audience during the NCCN 9th Annual Congress: Hematologic Malignancies.
Sergio Giralt, MD, of Memorial Sloan Kettering Cancer Center in New York, argued for upfront transplant, pointing out that long-term MM survivors have transplant as upfront therapy.
Kenneth Anderson, MD, of Dana Farber/Brigham and Women’s Cancer Center in Boston, took the stance that, in the past 10 years, there has been a
revolution in novel therapies that has significantly improved survival in MM.
For upfront transplant
Dr Giralt cited the 36-month follow-up of the E4A03 landmark analysis of patients who went off therapy after 4 cycles of lenalidomide/dexamethasone to pursue early stem cell transplant and those who continued treatment until disease progression.
Regardless of whether the patients were younger than 65 years or between 65 and 70, the patients who had an early transplant had superior progression-free survival (PFS) and overall survival (OS) compared to those who did not.
Dr Giralt added that bortezomib should be a component of induction therapy prior to autologous stem cell transplant (ASCT). Even though there is no survival benefit with bortezomib-based regimens, he said, there is significant improvement in PFS, as shown in a meta-analysis of phase 3 European studies.
The E4A03 landmark study also determined that the more intense the treatment, the better the outcome. So patients with double ASCT had a significantly longer PFS than patients who only had a single transplant.
This held true for OS as well, and included patients with 17p deletion and/or t(4;14) who failed to achieve complete remission after bortezomib-based induction regimens.
An analysis of 27,987 MM patients with a median age of 68 years (range, 19 to 90) revealed that of the patients who survived 10 years or more, 16.5% had ASCT as part of their initial therapy.
Dr Giralt concluded that the preponderance of evidence supports high-dose melphalan and ASCT as upfront consolidation therapy for MM. And until results of randomized trials investigating combination therapies are reported, melphalan consolidation should be considered the standard of care for all eligible patients with MM.
Against upfront transplant
Dr Anderson countered with data showing limited or no improvement in survival with ASCT, including evidence from studies by Attal, Fermand, Blade, Child, and Barlogie.
ASCT confers only modest PFS advantage, he said, showing results of the Barlogie study in which patients undergoing ASCT had a 25-month PFS, compared with a 21-month PFS with VBMCP (vincristine, carmustine, melphalan, cyclophosphamide, and prednisone).
“In the last 10 to 15 years, there has been a revolution in myeloma,” Dr Anderson said. “We have a lot of novel agents here today, and we have even more coming. It’s a hugely exciting time.”
Dr Anderson pointed out that since the introduction of novel agents, survival has improved between 2006 and 2010, compared to the period between 2001 and 2005, and particularly in patients older than 65 years (P=0.001).
Transplant has also changed, he said. Novel therapies have been integrated into the transplant paradigm, either before, as induction and consolidation therapy, or after, as maintenance. He indicated that this begs the question as to whether we really need the transplant component.
There has also been unprecedented use of triplets in combination therapy, Dr Anderson said, resulting in overall response rates upwards of 90%. For example, carfilzomib in combination with lenalidomide and dexamethasone prompted an overall response rate of 94%, with a stringent complete response (CR), CR, and near CR of 53%.
“It’s a new day in myeloma,” he said. “It’s taken us a long time, but we’re worrying about minimal residual disease (MRD) now. We’re worried about getting to the endpoint of 1 myeloma cell in 1 million normal cells.”
The point is, he added, that with novel therapies, such as carfilzomib, lenalidomide, and dexamethasone, patients who achieve a complete response can become MRD negative, suggesting an unprecedented extent of response without transplant.
MRD negativity may also be accomplished with oral agents, such as ixazomib. The depth of response with ixazomib increases over the course of treatment, with 27% achieving stringent CR or CR with a median duration of response of 13.8 months, and 82% of patients attaining MRD-negative status.
“In the absence of transplant,” Dr Anderson said, “this is an unprecedented response.”
Dr Anderson also pointed out that in the era of novel agents, there is no difference in outcome between early or delayed transplant. The 4-year OS in transplant-eligible patients who received initial therapy with lenalidomide was 80%, regardless of the timing of ASCT.
And in one trial, patients who received a delayed transplant fared better in OS than those transplanted early.
Dr Anderson said there is a parallel, international phase 3 study underway (IFM/DFCI2009) that will provide an answer to the debate on upfront transplant in the not-too-distant future.

Credit: Chad McNeeley
NEW YORK—A debate on the pros and cons of upfront transplant in symptomatic multiple myeloma (MM) yielded a split decision from the audience during the NCCN 9th Annual Congress: Hematologic Malignancies.
Sergio Giralt, MD, of Memorial Sloan Kettering Cancer Center in New York, argued for upfront transplant, pointing out that long-term MM survivors have transplant as upfront therapy.
Kenneth Anderson, MD, of Dana Farber/Brigham and Women’s Cancer Center in Boston, took the stance that, in the past 10 years, there has been a
revolution in novel therapies that has significantly improved survival in MM.
For upfront transplant
Dr Giralt cited the 36-month follow-up of the E4A03 landmark analysis of patients who went off therapy after 4 cycles of lenalidomide/dexamethasone to pursue early stem cell transplant and those who continued treatment until disease progression.
Regardless of whether the patients were younger than 65 years or between 65 and 70, the patients who had an early transplant had superior progression-free survival (PFS) and overall survival (OS) compared to those who did not.
Dr Giralt added that bortezomib should be a component of induction therapy prior to autologous stem cell transplant (ASCT). Even though there is no survival benefit with bortezomib-based regimens, he said, there is significant improvement in PFS, as shown in a meta-analysis of phase 3 European studies.
The E4A03 landmark study also determined that the more intense the treatment, the better the outcome. So patients with double ASCT had a significantly longer PFS than patients who only had a single transplant.
This held true for OS as well, and included patients with 17p deletion and/or t(4;14) who failed to achieve complete remission after bortezomib-based induction regimens.
An analysis of 27,987 MM patients with a median age of 68 years (range, 19 to 90) revealed that of the patients who survived 10 years or more, 16.5% had ASCT as part of their initial therapy.
Dr Giralt concluded that the preponderance of evidence supports high-dose melphalan and ASCT as upfront consolidation therapy for MM. And until results of randomized trials investigating combination therapies are reported, melphalan consolidation should be considered the standard of care for all eligible patients with MM.
Against upfront transplant
Dr Anderson countered with data showing limited or no improvement in survival with ASCT, including evidence from studies by Attal, Fermand, Blade, Child, and Barlogie.
ASCT confers only modest PFS advantage, he said, showing results of the Barlogie study in which patients undergoing ASCT had a 25-month PFS, compared with a 21-month PFS with VBMCP (vincristine, carmustine, melphalan, cyclophosphamide, and prednisone).
“In the last 10 to 15 years, there has been a revolution in myeloma,” Dr Anderson said. “We have a lot of novel agents here today, and we have even more coming. It’s a hugely exciting time.”
Dr Anderson pointed out that since the introduction of novel agents, survival has improved between 2006 and 2010, compared to the period between 2001 and 2005, and particularly in patients older than 65 years (P=0.001).
Transplant has also changed, he said. Novel therapies have been integrated into the transplant paradigm, either before, as induction and consolidation therapy, or after, as maintenance. He indicated that this begs the question as to whether we really need the transplant component.
There has also been unprecedented use of triplets in combination therapy, Dr Anderson said, resulting in overall response rates upwards of 90%. For example, carfilzomib in combination with lenalidomide and dexamethasone prompted an overall response rate of 94%, with a stringent complete response (CR), CR, and near CR of 53%.
“It’s a new day in myeloma,” he said. “It’s taken us a long time, but we’re worrying about minimal residual disease (MRD) now. We’re worried about getting to the endpoint of 1 myeloma cell in 1 million normal cells.”
The point is, he added, that with novel therapies, such as carfilzomib, lenalidomide, and dexamethasone, patients who achieve a complete response can become MRD negative, suggesting an unprecedented extent of response without transplant.
MRD negativity may also be accomplished with oral agents, such as ixazomib. The depth of response with ixazomib increases over the course of treatment, with 27% achieving stringent CR or CR with a median duration of response of 13.8 months, and 82% of patients attaining MRD-negative status.
“In the absence of transplant,” Dr Anderson said, “this is an unprecedented response.”
Dr Anderson also pointed out that in the era of novel agents, there is no difference in outcome between early or delayed transplant. The 4-year OS in transplant-eligible patients who received initial therapy with lenalidomide was 80%, regardless of the timing of ASCT.
And in one trial, patients who received a delayed transplant fared better in OS than those transplanted early.
Dr Anderson said there is a parallel, international phase 3 study underway (IFM/DFCI2009) that will provide an answer to the debate on upfront transplant in the not-too-distant future.
Molecule enables ‘robust’ expansion of cord blood cells

Credit: NHS
Investigators say they have identified a molecule that allows for robust ex vivo expansion of human cord blood (CB) cells.
CB cells expanded with this molecule, known as UM171, were capable of human hematopoietic reconstitution in NSG mice, an effect that lasted more than 6 months.
The researchers believe UM171 acts by enhancing the long-term-hematopoietic stem cell (LT-HSC) self-renewal machinery independently of AhR suppression.
Guy Sauvageau, MD, PhD, of the University of Montreal in Quebec, Canada, and his colleagues identified UM171 and described the discovery in Science.
The team first screened a library of 5280 low-molecular-weight compounds looking for those with the ability to expand human CD34+CD45RA- mobilized peripheral blood cells, which are enriched in LT-HSCs.
They got 7 hits, and only 2 of these—UM729 and UM118428—did not suppress the AhR pathway. The researchers selected UM729 for further characterization and optimization because it demonstrated superior activity in expanding CD34+CD45RA- cells.
The investigators analyzed more than 300 newly synthesized analogs of UM729 and identified one that was 10 to 20 times more potent than UM729. That compound was UM171.
UM171 could expand CD34+CD45RA- cells at concentrations of 17 nM to 19 nM. The highest expansion of multipotent progenitors and long-term culture-initiating cells occurred on day 12.
The effect of UM171 required its constant presence in the media, and the compound lacked direct mitogenic activity. UM171 did not affect the division rate of phenotypically primitive cell populations.
The researchers compared UM171 to SR1 (a compound known to promote self-renewal of HSCs) in fed-batch culture. They found that frequencies of CD34+ CB cells were similar in cultures containing SR1 and those containing UM171. But CD34+CD45RA- cells were more abundant with UM171 (P<0.005).
The team then evaluated LT-HSC populations. Twenty weeks after CD34+ CB cells were transplanted into mice, LT-HSC frequencies were similar in mice that received control and SR1-expanded cells. But LT-HSC frequencies were 13-fold higher in the mice that received UM171-expanded cells.
Next, the investigators assessed human hematopoietic reconstitution in NSG mice transplanted with fresh or expanded cells. They observed 2 patterns of reconstitution. One was from predominantly lymphomyeloid LT-HSCs that occurred with high cell doses in most conditions.
And the other was from LT-HSCs that display a lymphoid-deficient differentiation phenotype mostly observed with UM171 treatment, with or without SR1. However, UM171 did not negatively affect B lymphopoiesis or the frequency or number of lymphomyeloid LT-HSCs.
The impact of UM171 on LT-HSCs was preserved at 30 weeks post-transplant. And myeloid cell output was slightly augmented, a phenomenon that has been observed with normal, unexpanded cells.
The researchers also transplanted UM171-treated LT-HSC populations into secondary recipients. And they found the cells were still competent, but they had no advantage over unmanipulated CD34+ cells.
A clinical study of UM171 and a new type of bioreactor developed for stem cell culture is set to begin this December. The cells will be expanded at Maisonneuve-Rosemont Hospital, and grafts will be distributed to patients in Montreal, Quebec City, and Vancouver. The investigators expect tangible results will be available in December 2015.

Credit: NHS
Investigators say they have identified a molecule that allows for robust ex vivo expansion of human cord blood (CB) cells.
CB cells expanded with this molecule, known as UM171, were capable of human hematopoietic reconstitution in NSG mice, an effect that lasted more than 6 months.
The researchers believe UM171 acts by enhancing the long-term-hematopoietic stem cell (LT-HSC) self-renewal machinery independently of AhR suppression.
Guy Sauvageau, MD, PhD, of the University of Montreal in Quebec, Canada, and his colleagues identified UM171 and described the discovery in Science.
The team first screened a library of 5280 low-molecular-weight compounds looking for those with the ability to expand human CD34+CD45RA- mobilized peripheral blood cells, which are enriched in LT-HSCs.
They got 7 hits, and only 2 of these—UM729 and UM118428—did not suppress the AhR pathway. The researchers selected UM729 for further characterization and optimization because it demonstrated superior activity in expanding CD34+CD45RA- cells.
The investigators analyzed more than 300 newly synthesized analogs of UM729 and identified one that was 10 to 20 times more potent than UM729. That compound was UM171.
UM171 could expand CD34+CD45RA- cells at concentrations of 17 nM to 19 nM. The highest expansion of multipotent progenitors and long-term culture-initiating cells occurred on day 12.
The effect of UM171 required its constant presence in the media, and the compound lacked direct mitogenic activity. UM171 did not affect the division rate of phenotypically primitive cell populations.
The researchers compared UM171 to SR1 (a compound known to promote self-renewal of HSCs) in fed-batch culture. They found that frequencies of CD34+ CB cells were similar in cultures containing SR1 and those containing UM171. But CD34+CD45RA- cells were more abundant with UM171 (P<0.005).
The team then evaluated LT-HSC populations. Twenty weeks after CD34+ CB cells were transplanted into mice, LT-HSC frequencies were similar in mice that received control and SR1-expanded cells. But LT-HSC frequencies were 13-fold higher in the mice that received UM171-expanded cells.
Next, the investigators assessed human hematopoietic reconstitution in NSG mice transplanted with fresh or expanded cells. They observed 2 patterns of reconstitution. One was from predominantly lymphomyeloid LT-HSCs that occurred with high cell doses in most conditions.
And the other was from LT-HSCs that display a lymphoid-deficient differentiation phenotype mostly observed with UM171 treatment, with or without SR1. However, UM171 did not negatively affect B lymphopoiesis or the frequency or number of lymphomyeloid LT-HSCs.
The impact of UM171 on LT-HSCs was preserved at 30 weeks post-transplant. And myeloid cell output was slightly augmented, a phenomenon that has been observed with normal, unexpanded cells.
The researchers also transplanted UM171-treated LT-HSC populations into secondary recipients. And they found the cells were still competent, but they had no advantage over unmanipulated CD34+ cells.
A clinical study of UM171 and a new type of bioreactor developed for stem cell culture is set to begin this December. The cells will be expanded at Maisonneuve-Rosemont Hospital, and grafts will be distributed to patients in Montreal, Quebec City, and Vancouver. The investigators expect tangible results will be available in December 2015.

Credit: NHS
Investigators say they have identified a molecule that allows for robust ex vivo expansion of human cord blood (CB) cells.
CB cells expanded with this molecule, known as UM171, were capable of human hematopoietic reconstitution in NSG mice, an effect that lasted more than 6 months.
The researchers believe UM171 acts by enhancing the long-term-hematopoietic stem cell (LT-HSC) self-renewal machinery independently of AhR suppression.
Guy Sauvageau, MD, PhD, of the University of Montreal in Quebec, Canada, and his colleagues identified UM171 and described the discovery in Science.
The team first screened a library of 5280 low-molecular-weight compounds looking for those with the ability to expand human CD34+CD45RA- mobilized peripheral blood cells, which are enriched in LT-HSCs.
They got 7 hits, and only 2 of these—UM729 and UM118428—did not suppress the AhR pathway. The researchers selected UM729 for further characterization and optimization because it demonstrated superior activity in expanding CD34+CD45RA- cells.
The investigators analyzed more than 300 newly synthesized analogs of UM729 and identified one that was 10 to 20 times more potent than UM729. That compound was UM171.
UM171 could expand CD34+CD45RA- cells at concentrations of 17 nM to 19 nM. The highest expansion of multipotent progenitors and long-term culture-initiating cells occurred on day 12.
The effect of UM171 required its constant presence in the media, and the compound lacked direct mitogenic activity. UM171 did not affect the division rate of phenotypically primitive cell populations.
The researchers compared UM171 to SR1 (a compound known to promote self-renewal of HSCs) in fed-batch culture. They found that frequencies of CD34+ CB cells were similar in cultures containing SR1 and those containing UM171. But CD34+CD45RA- cells were more abundant with UM171 (P<0.005).
The team then evaluated LT-HSC populations. Twenty weeks after CD34+ CB cells were transplanted into mice, LT-HSC frequencies were similar in mice that received control and SR1-expanded cells. But LT-HSC frequencies were 13-fold higher in the mice that received UM171-expanded cells.
Next, the investigators assessed human hematopoietic reconstitution in NSG mice transplanted with fresh or expanded cells. They observed 2 patterns of reconstitution. One was from predominantly lymphomyeloid LT-HSCs that occurred with high cell doses in most conditions.
And the other was from LT-HSCs that display a lymphoid-deficient differentiation phenotype mostly observed with UM171 treatment, with or without SR1. However, UM171 did not negatively affect B lymphopoiesis or the frequency or number of lymphomyeloid LT-HSCs.
The impact of UM171 on LT-HSCs was preserved at 30 weeks post-transplant. And myeloid cell output was slightly augmented, a phenomenon that has been observed with normal, unexpanded cells.
The researchers also transplanted UM171-treated LT-HSC populations into secondary recipients. And they found the cells were still competent, but they had no advantage over unmanipulated CD34+ cells.
A clinical study of UM171 and a new type of bioreactor developed for stem cell culture is set to begin this December. The cells will be expanded at Maisonneuve-Rosemont Hospital, and grafts will be distributed to patients in Montreal, Quebec City, and Vancouver. The investigators expect tangible results will be available in December 2015.
New assay could prove useful in HSCT

Credit: Chad McNeeley
Researchers say they’ve developed an assay that allows for ultrasensitive DNA detection.
This haplotype-based assay could be used to detect relapse in patients who have undergone hematopoietic stem cell transplant (HSCT).
In fact, the researchers believe it would enable relapse detection earlier than existing microsatellite-based assays.
The new assay could also be used to detect microchimerism in solid organ transplants, in forensics, and for patient identification.
James Eshleman, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues described this assay in The Journal of Molecular Diagnostics.
The team noted that most bone marrow engraftment testing currently uses microsatellites or short tandem repeats that are resolved by capillary electrophoresis.
“Repeat testing will only detect DNA that makes up at least 1% of a DNA sample, so it’s not great for situations in which results depend on small amounts of material within a larger sample,” Dr Eshleman said.
In these situations, evaluating single-nucleotide polymorphisms (SNPs) might seem like a better choice, but this method has a high error rate. Dr Eshleman and his colleagues found they could circumvent this problem by analyzing blocks of closely spaced SNPs, or haplotypes.
To test their method, the researchers chose the HLA-A locus. They aligned common HLA-A alleles and identified a region containing 18 closely spaced SNPs. The team then tested a series of primers surrounding this region and selected the best pair on the basis of amplification efficiency and specificity.
They found it easy to differentiate some combinations of HLA-A alleles but not others. For instance, they discovered that 11 SNPs differentiate allele A*01 from A*02. But A*02 and HLA-A* 68:01:01:01 have a single SNP difference.
To test the possible cross talk between molecules that vary by 11 SNPs, the researchers sequenced 2 samples—one homozygous for A*01 and another homozygous for A*02—and analyzed each for the other allele. They found that, when there are enough discriminating SNPs between 2 individuals’ alleles, the haplotype assay is highly specific.
To evaluate the assay’s accuracy and limit of detection, the researchers generated various dilutions of 2 cell lines with known HLA-A genotypes. They made dilutions with cell mixes varying from 1 in 1 million (0.0001%) to 1 in 100 (1%), using 10 million cells for each dilution.
The team isolated DNA and performed PCR using 600 ng of DNA. And they sequenced each sample at least twice.
The assay proved highly precise at the 0.1% cell mix but less precise at the 0.01% cell mix.
“[Nevertheless,] we could detect cells when they made up just 0.01% of the mixture, which is a big improvement over the current method, which can only detect DNA that makes up 1% to 5% of a sample,” Dr Eshleman said.
The researchers also used their assay to test samples from 18 HSCT patients whose donor-patient HLA genotypes varied by at least 4 SNPs. All but 1 sample tested positive for some level of patient DNA, and the positives ranged from 0.001% to 1.47% patient DNA.
Finally, the team analyzed the human genome using the 1000 Genomes database and identified many additional loci that could be used with their assay.

Credit: Chad McNeeley
Researchers say they’ve developed an assay that allows for ultrasensitive DNA detection.
This haplotype-based assay could be used to detect relapse in patients who have undergone hematopoietic stem cell transplant (HSCT).
In fact, the researchers believe it would enable relapse detection earlier than existing microsatellite-based assays.
The new assay could also be used to detect microchimerism in solid organ transplants, in forensics, and for patient identification.
James Eshleman, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues described this assay in The Journal of Molecular Diagnostics.
The team noted that most bone marrow engraftment testing currently uses microsatellites or short tandem repeats that are resolved by capillary electrophoresis.
“Repeat testing will only detect DNA that makes up at least 1% of a DNA sample, so it’s not great for situations in which results depend on small amounts of material within a larger sample,” Dr Eshleman said.
In these situations, evaluating single-nucleotide polymorphisms (SNPs) might seem like a better choice, but this method has a high error rate. Dr Eshleman and his colleagues found they could circumvent this problem by analyzing blocks of closely spaced SNPs, or haplotypes.
To test their method, the researchers chose the HLA-A locus. They aligned common HLA-A alleles and identified a region containing 18 closely spaced SNPs. The team then tested a series of primers surrounding this region and selected the best pair on the basis of amplification efficiency and specificity.
They found it easy to differentiate some combinations of HLA-A alleles but not others. For instance, they discovered that 11 SNPs differentiate allele A*01 from A*02. But A*02 and HLA-A* 68:01:01:01 have a single SNP difference.
To test the possible cross talk between molecules that vary by 11 SNPs, the researchers sequenced 2 samples—one homozygous for A*01 and another homozygous for A*02—and analyzed each for the other allele. They found that, when there are enough discriminating SNPs between 2 individuals’ alleles, the haplotype assay is highly specific.
To evaluate the assay’s accuracy and limit of detection, the researchers generated various dilutions of 2 cell lines with known HLA-A genotypes. They made dilutions with cell mixes varying from 1 in 1 million (0.0001%) to 1 in 100 (1%), using 10 million cells for each dilution.
The team isolated DNA and performed PCR using 600 ng of DNA. And they sequenced each sample at least twice.
The assay proved highly precise at the 0.1% cell mix but less precise at the 0.01% cell mix.
“[Nevertheless,] we could detect cells when they made up just 0.01% of the mixture, which is a big improvement over the current method, which can only detect DNA that makes up 1% to 5% of a sample,” Dr Eshleman said.
The researchers also used their assay to test samples from 18 HSCT patients whose donor-patient HLA genotypes varied by at least 4 SNPs. All but 1 sample tested positive for some level of patient DNA, and the positives ranged from 0.001% to 1.47% patient DNA.
Finally, the team analyzed the human genome using the 1000 Genomes database and identified many additional loci that could be used with their assay.

Credit: Chad McNeeley
Researchers say they’ve developed an assay that allows for ultrasensitive DNA detection.
This haplotype-based assay could be used to detect relapse in patients who have undergone hematopoietic stem cell transplant (HSCT).
In fact, the researchers believe it would enable relapse detection earlier than existing microsatellite-based assays.
The new assay could also be used to detect microchimerism in solid organ transplants, in forensics, and for patient identification.
James Eshleman, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues described this assay in The Journal of Molecular Diagnostics.
The team noted that most bone marrow engraftment testing currently uses microsatellites or short tandem repeats that are resolved by capillary electrophoresis.
“Repeat testing will only detect DNA that makes up at least 1% of a DNA sample, so it’s not great for situations in which results depend on small amounts of material within a larger sample,” Dr Eshleman said.
In these situations, evaluating single-nucleotide polymorphisms (SNPs) might seem like a better choice, but this method has a high error rate. Dr Eshleman and his colleagues found they could circumvent this problem by analyzing blocks of closely spaced SNPs, or haplotypes.
To test their method, the researchers chose the HLA-A locus. They aligned common HLA-A alleles and identified a region containing 18 closely spaced SNPs. The team then tested a series of primers surrounding this region and selected the best pair on the basis of amplification efficiency and specificity.
They found it easy to differentiate some combinations of HLA-A alleles but not others. For instance, they discovered that 11 SNPs differentiate allele A*01 from A*02. But A*02 and HLA-A* 68:01:01:01 have a single SNP difference.
To test the possible cross talk between molecules that vary by 11 SNPs, the researchers sequenced 2 samples—one homozygous for A*01 and another homozygous for A*02—and analyzed each for the other allele. They found that, when there are enough discriminating SNPs between 2 individuals’ alleles, the haplotype assay is highly specific.
To evaluate the assay’s accuracy and limit of detection, the researchers generated various dilutions of 2 cell lines with known HLA-A genotypes. They made dilutions with cell mixes varying from 1 in 1 million (0.0001%) to 1 in 100 (1%), using 10 million cells for each dilution.
The team isolated DNA and performed PCR using 600 ng of DNA. And they sequenced each sample at least twice.
The assay proved highly precise at the 0.1% cell mix but less precise at the 0.01% cell mix.
“[Nevertheless,] we could detect cells when they made up just 0.01% of the mixture, which is a big improvement over the current method, which can only detect DNA that makes up 1% to 5% of a sample,” Dr Eshleman said.
The researchers also used their assay to test samples from 18 HSCT patients whose donor-patient HLA genotypes varied by at least 4 SNPs. All but 1 sample tested positive for some level of patient DNA, and the positives ranged from 0.001% to 1.47% patient DNA.
Finally, the team analyzed the human genome using the 1000 Genomes database and identified many additional loci that could be used with their assay.