User login
Inpatient palliative care improves QOL for HSCT patients
ORLANDO, FL—New research shows that patients who received inpatient palliative care while undergoing hematopoietic stem cell transplant (HSCT) experienced significant improvements in quality of life (QOL), decreases in depression, and reductions in symptom burden compared to patients who received transplant care alone.
Areej R. El-Jawahri, MD, of Harvard Medical School in Boston, Massachusetts, presented these results at the 2017 BMT Tandem Meetings (abstract 49).
She noted that palliative care is rarely used for patients with hematologic malignancies, “in part, because of misperceptions equating palliative care with just end-of-life care.”
So Dr El-Jawahri and her colleagues decided to evaluate palliative care in patients with hematologic malignancies who were scheduled to undergo HSCT.
The researchers enrolled 160 patients on the trial. Eighty-one were randomized to receive inpatient palliative care integrated with transplant care (intervention arm), and 79 were randomized to transplant care alone (control).
The latter group could request palliative care consultations, but only 2 patients did so, Dr El-Jawahri pointed out.
Patients receiving the intervention had at least twice-weekly visits with a palliative care clinician throughout their hospitalization.
“Importantly, palliative care only followed patients during their transplant hospitalization,” Dr El-Jawahri noted. “This was purely an inpatient palliative care intervention.”
Palliative care focused primarily on managing patients’ symptoms, establishing rapport with patients and families, and helping them cope with their illness. The predominant symptoms addressed included pain, nausea, diarrhea, constipation, insomnia, fatigue, depression, and anxiety.
Researchers assessed QOL, symptom burden, and mood at baseline, during hospitalization (Week 2), and at 3 and 6 months using well-validated scales.
They assessed QOL using the Functional Assessment of Cancer Therapy-Bone Marrow Transplant (FACT-BMT) scale, mood using the Hospital Anxiety and Depression Scale (HADS) and Patient Health Questionnaire (PHQ-9), and symptom burden using the Edmonton Symptom Assessment Scale (ESAS).
They also measured post-traumatic stress (PTSD) at baseline as well as 3 and 6 months after HSCT using the PTSD checklist.
The primary endpoint of the study was patient-reported QOL at Week 2 of hospitalization. Researchers chose Week 2 because studies have shown the highest symptom burden and QOL deterioration during that period.
Demographics
Patients were a mean age of 57, and a little more than half were female. Most were white, had a college degree or higher, and were married.
Their diagnoses included, for the control and intervention arms, respectively: acute lymphoblastic leukemia (9%, 5%), acute myeloid leukemia/myelodysplastic syndromes (30%, 30%), myelofibrosis/chronic myeloid leukemia (9%, 10%), lymphoma (33%, 23%), and multiple myeloma (19%, 33%).
Results
At baseline, patients in each group had comparable QOL and mood scores.
However, at Week 2, after ANCOVA adjustment for baseline scores, patients in the intervention arm had a clinically and statistically significant effect of the intervention in all areas measured except for the PHQ-9 depression score.
In particular, the HADS depression and anxiety scores were significantly improved, at P=0.008 and P<0.001, respectively, compared to control.
At 3 months, the FACT-BMT (P=0.048), HADS-Depression (P=0.002), PHQ-9-Depression (P=0.002), and PTSD symptom (P=0.002) scores were significantly improved in the intervention group.
And at 6 months, the HADS-Depression assessment (P=0.024), the PHQ-9-Depression assessment (P=0.027), and the PTSD symptom assessment (P=0.013) remained significantly improved. However, there were no significant differences in anxiety between the 2 groups.
The researchers concluded that a relatively brief inpatient care intervention led to “remarkable sustained improvements” in depression and post-traumatic stress symptoms at 3 and 6 months after HSCT.
“This is the first study showing the benefits of palliative care for patients with hematologic malignancies undergoing stem cell transplant,” Dr El-Jawahri said.
“It’s also the first study showing the benefits of palliative care for patients with cancer pursuing curative therapy and extends the potential benefit of palliative care in a population of patients with serious illness. [T]he significant part of what palliative care does is helping patients and families cope with serious and potentially life-threatening illness.”
The researchers recommend future studies to evaluate the impact of early integration of palliative care for this patient population. ![]()
ORLANDO, FL—New research shows that patients who received inpatient palliative care while undergoing hematopoietic stem cell transplant (HSCT) experienced significant improvements in quality of life (QOL), decreases in depression, and reductions in symptom burden compared to patients who received transplant care alone.
Areej R. El-Jawahri, MD, of Harvard Medical School in Boston, Massachusetts, presented these results at the 2017 BMT Tandem Meetings (abstract 49).
She noted that palliative care is rarely used for patients with hematologic malignancies, “in part, because of misperceptions equating palliative care with just end-of-life care.”
So Dr El-Jawahri and her colleagues decided to evaluate palliative care in patients with hematologic malignancies who were scheduled to undergo HSCT.
The researchers enrolled 160 patients on the trial. Eighty-one were randomized to receive inpatient palliative care integrated with transplant care (intervention arm), and 79 were randomized to transplant care alone (control).
The latter group could request palliative care consultations, but only 2 patients did so, Dr El-Jawahri pointed out.
Patients receiving the intervention had at least twice-weekly visits with a palliative care clinician throughout their hospitalization.
“Importantly, palliative care only followed patients during their transplant hospitalization,” Dr El-Jawahri noted. “This was purely an inpatient palliative care intervention.”
Palliative care focused primarily on managing patients’ symptoms, establishing rapport with patients and families, and helping them cope with their illness. The predominant symptoms addressed included pain, nausea, diarrhea, constipation, insomnia, fatigue, depression, and anxiety.
Researchers assessed QOL, symptom burden, and mood at baseline, during hospitalization (Week 2), and at 3 and 6 months using well-validated scales.
They assessed QOL using the Functional Assessment of Cancer Therapy-Bone Marrow Transplant (FACT-BMT) scale, mood using the Hospital Anxiety and Depression Scale (HADS) and Patient Health Questionnaire (PHQ-9), and symptom burden using the Edmonton Symptom Assessment Scale (ESAS).
They also measured post-traumatic stress (PTSD) at baseline as well as 3 and 6 months after HSCT using the PTSD checklist.
The primary endpoint of the study was patient-reported QOL at Week 2 of hospitalization. Researchers chose Week 2 because studies have shown the highest symptom burden and QOL deterioration during that period.
Demographics
Patients were a mean age of 57, and a little more than half were female. Most were white, had a college degree or higher, and were married.
Their diagnoses included, for the control and intervention arms, respectively: acute lymphoblastic leukemia (9%, 5%), acute myeloid leukemia/myelodysplastic syndromes (30%, 30%), myelofibrosis/chronic myeloid leukemia (9%, 10%), lymphoma (33%, 23%), and multiple myeloma (19%, 33%).
Results
At baseline, patients in each group had comparable QOL and mood scores.
However, at Week 2, after ANCOVA adjustment for baseline scores, patients in the intervention arm had a clinically and statistically significant effect of the intervention in all areas measured except for the PHQ-9 depression score.
In particular, the HADS depression and anxiety scores were significantly improved, at P=0.008 and P<0.001, respectively, compared to control.
At 3 months, the FACT-BMT (P=0.048), HADS-Depression (P=0.002), PHQ-9-Depression (P=0.002), and PTSD symptom (P=0.002) scores were significantly improved in the intervention group.
And at 6 months, the HADS-Depression assessment (P=0.024), the PHQ-9-Depression assessment (P=0.027), and the PTSD symptom assessment (P=0.013) remained significantly improved. However, there were no significant differences in anxiety between the 2 groups.
The researchers concluded that a relatively brief inpatient care intervention led to “remarkable sustained improvements” in depression and post-traumatic stress symptoms at 3 and 6 months after HSCT.
“This is the first study showing the benefits of palliative care for patients with hematologic malignancies undergoing stem cell transplant,” Dr El-Jawahri said.
“It’s also the first study showing the benefits of palliative care for patients with cancer pursuing curative therapy and extends the potential benefit of palliative care in a population of patients with serious illness. [T]he significant part of what palliative care does is helping patients and families cope with serious and potentially life-threatening illness.”
The researchers recommend future studies to evaluate the impact of early integration of palliative care for this patient population. ![]()
ORLANDO, FL—New research shows that patients who received inpatient palliative care while undergoing hematopoietic stem cell transplant (HSCT) experienced significant improvements in quality of life (QOL), decreases in depression, and reductions in symptom burden compared to patients who received transplant care alone.
Areej R. El-Jawahri, MD, of Harvard Medical School in Boston, Massachusetts, presented these results at the 2017 BMT Tandem Meetings (abstract 49).
She noted that palliative care is rarely used for patients with hematologic malignancies, “in part, because of misperceptions equating palliative care with just end-of-life care.”
So Dr El-Jawahri and her colleagues decided to evaluate palliative care in patients with hematologic malignancies who were scheduled to undergo HSCT.
The researchers enrolled 160 patients on the trial. Eighty-one were randomized to receive inpatient palliative care integrated with transplant care (intervention arm), and 79 were randomized to transplant care alone (control).
The latter group could request palliative care consultations, but only 2 patients did so, Dr El-Jawahri pointed out.
Patients receiving the intervention had at least twice-weekly visits with a palliative care clinician throughout their hospitalization.
“Importantly, palliative care only followed patients during their transplant hospitalization,” Dr El-Jawahri noted. “This was purely an inpatient palliative care intervention.”
Palliative care focused primarily on managing patients’ symptoms, establishing rapport with patients and families, and helping them cope with their illness. The predominant symptoms addressed included pain, nausea, diarrhea, constipation, insomnia, fatigue, depression, and anxiety.
Researchers assessed QOL, symptom burden, and mood at baseline, during hospitalization (Week 2), and at 3 and 6 months using well-validated scales.
They assessed QOL using the Functional Assessment of Cancer Therapy-Bone Marrow Transplant (FACT-BMT) scale, mood using the Hospital Anxiety and Depression Scale (HADS) and Patient Health Questionnaire (PHQ-9), and symptom burden using the Edmonton Symptom Assessment Scale (ESAS).
They also measured post-traumatic stress (PTSD) at baseline as well as 3 and 6 months after HSCT using the PTSD checklist.
The primary endpoint of the study was patient-reported QOL at Week 2 of hospitalization. Researchers chose Week 2 because studies have shown the highest symptom burden and QOL deterioration during that period.
Demographics
Patients were a mean age of 57, and a little more than half were female. Most were white, had a college degree or higher, and were married.
Their diagnoses included, for the control and intervention arms, respectively: acute lymphoblastic leukemia (9%, 5%), acute myeloid leukemia/myelodysplastic syndromes (30%, 30%), myelofibrosis/chronic myeloid leukemia (9%, 10%), lymphoma (33%, 23%), and multiple myeloma (19%, 33%).
Results
At baseline, patients in each group had comparable QOL and mood scores.
However, at Week 2, after ANCOVA adjustment for baseline scores, patients in the intervention arm had a clinically and statistically significant effect of the intervention in all areas measured except for the PHQ-9 depression score.
In particular, the HADS depression and anxiety scores were significantly improved, at P=0.008 and P<0.001, respectively, compared to control.
At 3 months, the FACT-BMT (P=0.048), HADS-Depression (P=0.002), PHQ-9-Depression (P=0.002), and PTSD symptom (P=0.002) scores were significantly improved in the intervention group.
And at 6 months, the HADS-Depression assessment (P=0.024), the PHQ-9-Depression assessment (P=0.027), and the PTSD symptom assessment (P=0.013) remained significantly improved. However, there were no significant differences in anxiety between the 2 groups.
The researchers concluded that a relatively brief inpatient care intervention led to “remarkable sustained improvements” in depression and post-traumatic stress symptoms at 3 and 6 months after HSCT.
“This is the first study showing the benefits of palliative care for patients with hematologic malignancies undergoing stem cell transplant,” Dr El-Jawahri said.
“It’s also the first study showing the benefits of palliative care for patients with cancer pursuing curative therapy and extends the potential benefit of palliative care in a population of patients with serious illness. [T]he significant part of what palliative care does is helping patients and families cope with serious and potentially life-threatening illness.”
The researchers recommend future studies to evaluate the impact of early integration of palliative care for this patient population. ![]()
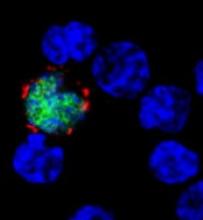
Immunotherapy receives fast track designation
The US Food and Drug Administration (FDA) has granted fast track designation to CMD-003 (baltaleucel-T) for patients with relapsed/refractory lymphoma and post-transplant lymphoproliferative disease associated with Epstein-Barr virus (EBV).
CMD-003 consists of patient-derived T cells that have been activated to kill malignant cells expressing antigens associated with EBV.
The T cells specifically target 4 EBV epitopes—LMP1, LMP2, EBNA, and BARF1.
CMD-003 is being developed by Cell Medica and the Baylor College of Medicine with funding provided, in part, by the Cancer Prevention and Research Institute of Texas.
About fast track designation
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the FDA’s fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
CMD-003-related research
CMD-003 is currently under investigation in the phase 2 CITADEL trial for patients with extranodal natural killer T-cell lymphoma and the phase 2 CIVIC trial for patients with EBV-associated diffuse large B-cell lymphoma, Hodgkin lymphoma, and post-transplant lymphoproliferative disease.
Researchers have not published results from any trials of CMD-003, but they have published results with EBV-specific T-cell products related to CMD-003.
In one study, published in the Journal of Clinical Oncology in 2014, researchers administered cytotoxic T lymphocytes (CTLs) in 50 patients with EBV-associated Hodgkin or non-Hodgkin lymphoma.
Twenty-nine of the patients were in remission when they received CTL infusions, but they were at a high risk of relapse. The remaining 21 patients had relapsed or refractory disease at the time of CTL infusion.
Twenty-seven of the patients who received CTLs as an adjuvant treatment remained in remission at 3.1 years after treatment.
Their 2-year event-free survival rate was 82%. None of the patients died of lymphoma, but 9 died from complications associated with the chemotherapy and radiation they had received.
Of the 21 patients with relapsed or refractory disease, 13 responded to CTL infusions, and 11 patients achieved a complete response. In this group, the 2-year event-free survival rate was about 50%.
The researchers said there were no toxicities that were definitively related to CTL infusion.
One patient had central nervous system deterioration 2 weeks after infusion. This was attributed to disease progression but could possibly have been treatment-related.
Another patient developed respiratory complications about 4 weeks after a second CTL infusion that may have been treatment-related. However, the researchers attributed it to an intercurrent infection, and the patient made a complete recovery.
The US Food and Drug Administration (FDA) has granted fast track designation to CMD-003 (baltaleucel-T) for patients with relapsed/refractory lymphoma and post-transplant lymphoproliferative disease associated with Epstein-Barr virus (EBV).
CMD-003 consists of patient-derived T cells that have been activated to kill malignant cells expressing antigens associated with EBV.
The T cells specifically target 4 EBV epitopes—LMP1, LMP2, EBNA, and BARF1.
CMD-003 is being developed by Cell Medica and the Baylor College of Medicine with funding provided, in part, by the Cancer Prevention and Research Institute of Texas.
About fast track designation
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the FDA’s fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
CMD-003-related research
CMD-003 is currently under investigation in the phase 2 CITADEL trial for patients with extranodal natural killer T-cell lymphoma and the phase 2 CIVIC trial for patients with EBV-associated diffuse large B-cell lymphoma, Hodgkin lymphoma, and post-transplant lymphoproliferative disease.
Researchers have not published results from any trials of CMD-003, but they have published results with EBV-specific T-cell products related to CMD-003.
In one study, published in the Journal of Clinical Oncology in 2014, researchers administered cytotoxic T lymphocytes (CTLs) in 50 patients with EBV-associated Hodgkin or non-Hodgkin lymphoma.
Twenty-nine of the patients were in remission when they received CTL infusions, but they were at a high risk of relapse. The remaining 21 patients had relapsed or refractory disease at the time of CTL infusion.
Twenty-seven of the patients who received CTLs as an adjuvant treatment remained in remission at 3.1 years after treatment.
Their 2-year event-free survival rate was 82%. None of the patients died of lymphoma, but 9 died from complications associated with the chemotherapy and radiation they had received.
Of the 21 patients with relapsed or refractory disease, 13 responded to CTL infusions, and 11 patients achieved a complete response. In this group, the 2-year event-free survival rate was about 50%.
The researchers said there were no toxicities that were definitively related to CTL infusion.
One patient had central nervous system deterioration 2 weeks after infusion. This was attributed to disease progression but could possibly have been treatment-related.
Another patient developed respiratory complications about 4 weeks after a second CTL infusion that may have been treatment-related. However, the researchers attributed it to an intercurrent infection, and the patient made a complete recovery.
The US Food and Drug Administration (FDA) has granted fast track designation to CMD-003 (baltaleucel-T) for patients with relapsed/refractory lymphoma and post-transplant lymphoproliferative disease associated with Epstein-Barr virus (EBV).
CMD-003 consists of patient-derived T cells that have been activated to kill malignant cells expressing antigens associated with EBV.
The T cells specifically target 4 EBV epitopes—LMP1, LMP2, EBNA, and BARF1.
CMD-003 is being developed by Cell Medica and the Baylor College of Medicine with funding provided, in part, by the Cancer Prevention and Research Institute of Texas.
About fast track designation
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the FDA’s fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the biologic license application or new drug application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
CMD-003-related research
CMD-003 is currently under investigation in the phase 2 CITADEL trial for patients with extranodal natural killer T-cell lymphoma and the phase 2 CIVIC trial for patients with EBV-associated diffuse large B-cell lymphoma, Hodgkin lymphoma, and post-transplant lymphoproliferative disease.
Researchers have not published results from any trials of CMD-003, but they have published results with EBV-specific T-cell products related to CMD-003.
In one study, published in the Journal of Clinical Oncology in 2014, researchers administered cytotoxic T lymphocytes (CTLs) in 50 patients with EBV-associated Hodgkin or non-Hodgkin lymphoma.
Twenty-nine of the patients were in remission when they received CTL infusions, but they were at a high risk of relapse. The remaining 21 patients had relapsed or refractory disease at the time of CTL infusion.
Twenty-seven of the patients who received CTLs as an adjuvant treatment remained in remission at 3.1 years after treatment.
Their 2-year event-free survival rate was 82%. None of the patients died of lymphoma, but 9 died from complications associated with the chemotherapy and radiation they had received.
Of the 21 patients with relapsed or refractory disease, 13 responded to CTL infusions, and 11 patients achieved a complete response. In this group, the 2-year event-free survival rate was about 50%.
The researchers said there were no toxicities that were definitively related to CTL infusion.
One patient had central nervous system deterioration 2 weeks after infusion. This was attributed to disease progression but could possibly have been treatment-related.
Another patient developed respiratory complications about 4 weeks after a second CTL infusion that may have been treatment-related. However, the researchers attributed it to an intercurrent infection, and the patient made a complete recovery.
Genetic profiling can guide HSCT in MDS, team says

Genetic profiling can be used to determine which patients with myelodysplastic syndrome (MDS) are likely to benefit from allogeneic hematopoietic stem cell transplant (HSCT), according to research published in NEJM.
Targeted sequencing of 129 genes revealed mutations that, after adjustment for clinical variables, were associated with shorter survival and/or relapse after HSCT.
Patients with mutations in TP53, JAK2, and the RAS pathway tended to have worse outcomes after HSCT than patients without such mutations.
“Although donor stem cell transplantation is the only curative therapy for MDS, many patients die after transplantation, largely due to relapse of the disease or complications relating to the transplant itself,” said study author R. Coleman Lindsley, MD, PhD, of Dana-Farber Cancer Institute in Boston, Massachusetts.
“As physicians, one of our major challenges is to be able to predict which patients are most likely to benefit from a transplant. Improving our ability to identify patients who are most likely to have a relapse or to experience life-threatening complications from a transplant could lead to better pre-transplant therapies and strategies for preventing relapse.”
Researchers have long known that specific genetic mutations are closely related to the course MDS takes. With this study, Dr Lindsley and his colleagues sought to discover whether mutations can be used to predict how patients will fare following allogeneic HSCT.
The team analyzed blood samples from 1514 MDS patients, performing targeted sequencing of 129 genes. The genes were selected based on their known or suspected involvement in the pathogenesis of myeloid cancers or bone marrow failure syndromes.
Dr Lindsley and his colleagues then evaluated the association between mutations and HSCT outcomes, including overall survival, relapse, and death without relapse.
After adjusting for significant clinical variables, the researchers found that having mutated TP53 was significantly associated with shorter survival and shorter time to relapse after HSCT (P<0.001 for both comparisons). This was true whether patients received standard conditioning or reduced-intensity conditioning.
In patients age 40 and older who did not have TP53 mutations, mutations in RAS pathway genes (P=0.004) or JAK2 (P=0.001) were significantly associated with shorter survival.
The shorter survival in patients with mutated RAS pathway genes was due to a higher risk of relapse, while the shorter survival in patients with JAK2 mutations was due to a higher risk of death without relapse.
In contrast to TP53 mutations, the adverse effect of RAS mutations on survival and risk of relapse was evident only in patients who received reduced-intensity conditioning (P<0.001). This suggests these patients may benefit from higher intensity conditioning regimens, the researchers said.
This study also yielded insights about the biology of MDS in specific groups of patients.
For example, the researchers found that 4% of MDS patients between the ages of 18 and 40 had mutations associated with Shwachman-Diamond syndrome (in the SBDS gene), but most of them had not previously been diagnosed with the syndrome.
In each case, the patients had acquired a TP53 mutation, suggesting not only how MDS develops in patients with Schwachman-Diamond syndrome but also what underlies their poor prognosis after HSCT.
The researchers also analyzed patients with therapy-related MDS. The team found that TP53 mutations and mutations in PPM1D, a gene that regulates TP53 function, were far more common in these patients than in those with primary MDS (15% and 3%, respectively, P<0.001).
“In deciding whether a stem cell transplant is appropriate for a patient with MDS, it’s always necessary to balance the potential benefit with the risk of complications,” Dr Lindsley noted.
“Our findings offer physicians a guide—based on the genetic profile of the disease and certain clinical factors—to identifying patients for whom a transplant is appropriate, and the intensity of treatment most likely to be effective.” ![]()

Genetic profiling can be used to determine which patients with myelodysplastic syndrome (MDS) are likely to benefit from allogeneic hematopoietic stem cell transplant (HSCT), according to research published in NEJM.
Targeted sequencing of 129 genes revealed mutations that, after adjustment for clinical variables, were associated with shorter survival and/or relapse after HSCT.
Patients with mutations in TP53, JAK2, and the RAS pathway tended to have worse outcomes after HSCT than patients without such mutations.
“Although donor stem cell transplantation is the only curative therapy for MDS, many patients die after transplantation, largely due to relapse of the disease or complications relating to the transplant itself,” said study author R. Coleman Lindsley, MD, PhD, of Dana-Farber Cancer Institute in Boston, Massachusetts.
“As physicians, one of our major challenges is to be able to predict which patients are most likely to benefit from a transplant. Improving our ability to identify patients who are most likely to have a relapse or to experience life-threatening complications from a transplant could lead to better pre-transplant therapies and strategies for preventing relapse.”
Researchers have long known that specific genetic mutations are closely related to the course MDS takes. With this study, Dr Lindsley and his colleagues sought to discover whether mutations can be used to predict how patients will fare following allogeneic HSCT.
The team analyzed blood samples from 1514 MDS patients, performing targeted sequencing of 129 genes. The genes were selected based on their known or suspected involvement in the pathogenesis of myeloid cancers or bone marrow failure syndromes.
Dr Lindsley and his colleagues then evaluated the association between mutations and HSCT outcomes, including overall survival, relapse, and death without relapse.
After adjusting for significant clinical variables, the researchers found that having mutated TP53 was significantly associated with shorter survival and shorter time to relapse after HSCT (P<0.001 for both comparisons). This was true whether patients received standard conditioning or reduced-intensity conditioning.
In patients age 40 and older who did not have TP53 mutations, mutations in RAS pathway genes (P=0.004) or JAK2 (P=0.001) were significantly associated with shorter survival.
The shorter survival in patients with mutated RAS pathway genes was due to a higher risk of relapse, while the shorter survival in patients with JAK2 mutations was due to a higher risk of death without relapse.
In contrast to TP53 mutations, the adverse effect of RAS mutations on survival and risk of relapse was evident only in patients who received reduced-intensity conditioning (P<0.001). This suggests these patients may benefit from higher intensity conditioning regimens, the researchers said.
This study also yielded insights about the biology of MDS in specific groups of patients.
For example, the researchers found that 4% of MDS patients between the ages of 18 and 40 had mutations associated with Shwachman-Diamond syndrome (in the SBDS gene), but most of them had not previously been diagnosed with the syndrome.
In each case, the patients had acquired a TP53 mutation, suggesting not only how MDS develops in patients with Schwachman-Diamond syndrome but also what underlies their poor prognosis after HSCT.
The researchers also analyzed patients with therapy-related MDS. The team found that TP53 mutations and mutations in PPM1D, a gene that regulates TP53 function, were far more common in these patients than in those with primary MDS (15% and 3%, respectively, P<0.001).
“In deciding whether a stem cell transplant is appropriate for a patient with MDS, it’s always necessary to balance the potential benefit with the risk of complications,” Dr Lindsley noted.
“Our findings offer physicians a guide—based on the genetic profile of the disease and certain clinical factors—to identifying patients for whom a transplant is appropriate, and the intensity of treatment most likely to be effective.” ![]()

Genetic profiling can be used to determine which patients with myelodysplastic syndrome (MDS) are likely to benefit from allogeneic hematopoietic stem cell transplant (HSCT), according to research published in NEJM.
Targeted sequencing of 129 genes revealed mutations that, after adjustment for clinical variables, were associated with shorter survival and/or relapse after HSCT.
Patients with mutations in TP53, JAK2, and the RAS pathway tended to have worse outcomes after HSCT than patients without such mutations.
“Although donor stem cell transplantation is the only curative therapy for MDS, many patients die after transplantation, largely due to relapse of the disease or complications relating to the transplant itself,” said study author R. Coleman Lindsley, MD, PhD, of Dana-Farber Cancer Institute in Boston, Massachusetts.
“As physicians, one of our major challenges is to be able to predict which patients are most likely to benefit from a transplant. Improving our ability to identify patients who are most likely to have a relapse or to experience life-threatening complications from a transplant could lead to better pre-transplant therapies and strategies for preventing relapse.”
Researchers have long known that specific genetic mutations are closely related to the course MDS takes. With this study, Dr Lindsley and his colleagues sought to discover whether mutations can be used to predict how patients will fare following allogeneic HSCT.
The team analyzed blood samples from 1514 MDS patients, performing targeted sequencing of 129 genes. The genes were selected based on their known or suspected involvement in the pathogenesis of myeloid cancers or bone marrow failure syndromes.
Dr Lindsley and his colleagues then evaluated the association between mutations and HSCT outcomes, including overall survival, relapse, and death without relapse.
After adjusting for significant clinical variables, the researchers found that having mutated TP53 was significantly associated with shorter survival and shorter time to relapse after HSCT (P<0.001 for both comparisons). This was true whether patients received standard conditioning or reduced-intensity conditioning.
In patients age 40 and older who did not have TP53 mutations, mutations in RAS pathway genes (P=0.004) or JAK2 (P=0.001) were significantly associated with shorter survival.
The shorter survival in patients with mutated RAS pathway genes was due to a higher risk of relapse, while the shorter survival in patients with JAK2 mutations was due to a higher risk of death without relapse.
In contrast to TP53 mutations, the adverse effect of RAS mutations on survival and risk of relapse was evident only in patients who received reduced-intensity conditioning (P<0.001). This suggests these patients may benefit from higher intensity conditioning regimens, the researchers said.
This study also yielded insights about the biology of MDS in specific groups of patients.
For example, the researchers found that 4% of MDS patients between the ages of 18 and 40 had mutations associated with Shwachman-Diamond syndrome (in the SBDS gene), but most of them had not previously been diagnosed with the syndrome.
In each case, the patients had acquired a TP53 mutation, suggesting not only how MDS develops in patients with Schwachman-Diamond syndrome but also what underlies their poor prognosis after HSCT.
The researchers also analyzed patients with therapy-related MDS. The team found that TP53 mutations and mutations in PPM1D, a gene that regulates TP53 function, were far more common in these patients than in those with primary MDS (15% and 3%, respectively, P<0.001).
“In deciding whether a stem cell transplant is appropriate for a patient with MDS, it’s always necessary to balance the potential benefit with the risk of complications,” Dr Lindsley noted.
“Our findings offer physicians a guide—based on the genetic profile of the disease and certain clinical factors—to identifying patients for whom a transplant is appropriate, and the intensity of treatment most likely to be effective.” ![]()
Algorithm predicts NRM, GVHD after HSCT
A biomarker algorithm can identify patients with a high risk of graft-vs-host disease (GVHD) and non-relapse mortality (NRM) after hematopoietic stem cell transplant (HSCT), according to researchers.
The team found evidence to suggest that 2 proteins—ST2 and REG3α—present in blood drawn a week after HSCT can predict the likelihood of GVHD, including lethal GVHD, and NRM in patients with hematologic disorders.
James L.M. Ferrara, MD, of the Icahn School of Medicine at Mount Sinai in New York, New York, and his colleagues reported these findings in JCI Insight.
The researchers analyzed blood samples collected on day 7 after HSCT from 1287 patients. Of these, 620 samples were designated the training set.
The team measured the concentrations of 4 GVHD biomarkers—ST2, REG3α, TNFR1, and IL-2Rα—in the training set and used them to model 6-month NRM in an attempt to identify the best algorithm that defined 2 distinct risk groups.
The researchers applied the resulting algorithm to the test set of samples (n=309) and the validation set of samples (n=358).
The final algorithm used ST2 and REG3α concentrations to identify patients with a high and low risk of NRM at 6 months. Sixteen percent of patients in the training set belonged to the high-risk group, as did 17% of the test set and 20% of the validation set.
In the training set, the cumulative incidence of NRM at 6 months was 28% in the high-risk group and 7% in the low-risk group (P<0.001). The incidence was 33% and 7%, respectively (P<0.001), in the test set and 26% and 10%, respectively (P<0.001), in the validation set.
The high-risk patients were 3 times more likely to die from GVHD than low-risk patients in the overall cohort. The incidence of lethal GVHD was 19% and 6%, respectively (P<0.001).
GVHD-related mortality in the high-risk and low-risk groups, respectively, was 18% and 5% (P<0.001) in the training set, 24% and 4% (P<0.001) in the test set, and 14% and 5% (P<0.001) in the validation set.
The researchers said their algorithm can also be adapted to define 3 distinct risk groups at GVHD onset—Ann Arbor scores 1, 2, and 3.
The team dubbed their algorithm the “MAGIC algorithm,” after the Mount Sinai Acute GVHD International Consortium (MAGIC).
“The MAGIC algorithm gives doctors a roadmap to save many lives in the future,” Dr Ferrara said. “This simple blood test can determine which bone marrow transplant patients are at high risk for a lethal complication before it occurs. It will allow early intervention and potentially save many lives.”
Doctors at Mount Sinai are now designing clinical trials to determine whether immunotherapy drugs would benefit patients if the MAGIC algorithm determines they are at high risk for severe GVHD.
The researchers believe that if patients receive the drugs once the blood test is administered, which is well before symptoms develop, they would be spared the full force of GVHD, and fewer of them would die.
“This test will make bone marrow transplant safer and more effective for patients because it will guide adjustment of medications to protect against graft-vs-host disease,” said study author John Levine, MD, of the Icahn School of Medicine at Mount Sinai.
“If successful, the early use of the drugs would become a standard of care for bone marrow transplant patients.” ![]()
A biomarker algorithm can identify patients with a high risk of graft-vs-host disease (GVHD) and non-relapse mortality (NRM) after hematopoietic stem cell transplant (HSCT), according to researchers.
The team found evidence to suggest that 2 proteins—ST2 and REG3α—present in blood drawn a week after HSCT can predict the likelihood of GVHD, including lethal GVHD, and NRM in patients with hematologic disorders.
James L.M. Ferrara, MD, of the Icahn School of Medicine at Mount Sinai in New York, New York, and his colleagues reported these findings in JCI Insight.
The researchers analyzed blood samples collected on day 7 after HSCT from 1287 patients. Of these, 620 samples were designated the training set.
The team measured the concentrations of 4 GVHD biomarkers—ST2, REG3α, TNFR1, and IL-2Rα—in the training set and used them to model 6-month NRM in an attempt to identify the best algorithm that defined 2 distinct risk groups.
The researchers applied the resulting algorithm to the test set of samples (n=309) and the validation set of samples (n=358).
The final algorithm used ST2 and REG3α concentrations to identify patients with a high and low risk of NRM at 6 months. Sixteen percent of patients in the training set belonged to the high-risk group, as did 17% of the test set and 20% of the validation set.
In the training set, the cumulative incidence of NRM at 6 months was 28% in the high-risk group and 7% in the low-risk group (P<0.001). The incidence was 33% and 7%, respectively (P<0.001), in the test set and 26% and 10%, respectively (P<0.001), in the validation set.
The high-risk patients were 3 times more likely to die from GVHD than low-risk patients in the overall cohort. The incidence of lethal GVHD was 19% and 6%, respectively (P<0.001).
GVHD-related mortality in the high-risk and low-risk groups, respectively, was 18% and 5% (P<0.001) in the training set, 24% and 4% (P<0.001) in the test set, and 14% and 5% (P<0.001) in the validation set.
The researchers said their algorithm can also be adapted to define 3 distinct risk groups at GVHD onset—Ann Arbor scores 1, 2, and 3.
The team dubbed their algorithm the “MAGIC algorithm,” after the Mount Sinai Acute GVHD International Consortium (MAGIC).
“The MAGIC algorithm gives doctors a roadmap to save many lives in the future,” Dr Ferrara said. “This simple blood test can determine which bone marrow transplant patients are at high risk for a lethal complication before it occurs. It will allow early intervention and potentially save many lives.”
Doctors at Mount Sinai are now designing clinical trials to determine whether immunotherapy drugs would benefit patients if the MAGIC algorithm determines they are at high risk for severe GVHD.
The researchers believe that if patients receive the drugs once the blood test is administered, which is well before symptoms develop, they would be spared the full force of GVHD, and fewer of them would die.
“This test will make bone marrow transplant safer and more effective for patients because it will guide adjustment of medications to protect against graft-vs-host disease,” said study author John Levine, MD, of the Icahn School of Medicine at Mount Sinai.
“If successful, the early use of the drugs would become a standard of care for bone marrow transplant patients.” ![]()
A biomarker algorithm can identify patients with a high risk of graft-vs-host disease (GVHD) and non-relapse mortality (NRM) after hematopoietic stem cell transplant (HSCT), according to researchers.
The team found evidence to suggest that 2 proteins—ST2 and REG3α—present in blood drawn a week after HSCT can predict the likelihood of GVHD, including lethal GVHD, and NRM in patients with hematologic disorders.
James L.M. Ferrara, MD, of the Icahn School of Medicine at Mount Sinai in New York, New York, and his colleagues reported these findings in JCI Insight.
The researchers analyzed blood samples collected on day 7 after HSCT from 1287 patients. Of these, 620 samples were designated the training set.
The team measured the concentrations of 4 GVHD biomarkers—ST2, REG3α, TNFR1, and IL-2Rα—in the training set and used them to model 6-month NRM in an attempt to identify the best algorithm that defined 2 distinct risk groups.
The researchers applied the resulting algorithm to the test set of samples (n=309) and the validation set of samples (n=358).
The final algorithm used ST2 and REG3α concentrations to identify patients with a high and low risk of NRM at 6 months. Sixteen percent of patients in the training set belonged to the high-risk group, as did 17% of the test set and 20% of the validation set.
In the training set, the cumulative incidence of NRM at 6 months was 28% in the high-risk group and 7% in the low-risk group (P<0.001). The incidence was 33% and 7%, respectively (P<0.001), in the test set and 26% and 10%, respectively (P<0.001), in the validation set.
The high-risk patients were 3 times more likely to die from GVHD than low-risk patients in the overall cohort. The incidence of lethal GVHD was 19% and 6%, respectively (P<0.001).
GVHD-related mortality in the high-risk and low-risk groups, respectively, was 18% and 5% (P<0.001) in the training set, 24% and 4% (P<0.001) in the test set, and 14% and 5% (P<0.001) in the validation set.
The researchers said their algorithm can also be adapted to define 3 distinct risk groups at GVHD onset—Ann Arbor scores 1, 2, and 3.
The team dubbed their algorithm the “MAGIC algorithm,” after the Mount Sinai Acute GVHD International Consortium (MAGIC).
“The MAGIC algorithm gives doctors a roadmap to save many lives in the future,” Dr Ferrara said. “This simple blood test can determine which bone marrow transplant patients are at high risk for a lethal complication before it occurs. It will allow early intervention and potentially save many lives.”
Doctors at Mount Sinai are now designing clinical trials to determine whether immunotherapy drugs would benefit patients if the MAGIC algorithm determines they are at high risk for severe GVHD.
The researchers believe that if patients receive the drugs once the blood test is administered, which is well before symptoms develop, they would be spared the full force of GVHD, and fewer of them would die.
“This test will make bone marrow transplant safer and more effective for patients because it will guide adjustment of medications to protect against graft-vs-host disease,” said study author John Levine, MD, of the Icahn School of Medicine at Mount Sinai.
“If successful, the early use of the drugs would become a standard of care for bone marrow transplant patients.” ![]()
‘Alternative’ BMT deemed ‘promising’ for SAA

Photo by Chad McNeeley
Researchers have reported a “promising” treatment approach for
refractory, severe aplastic anemia (SAA).
The
regimen consists of nonmyeloablative conditioning, bone marrow
transplants (BMTs) from “alternative” donors, and graft-vs-host disease
(GVHD) prophylaxis.
All 16 SAA patients who received this treatment
achieved engraftment and were completely cleared of disease.
There were 2 cases of acute and chronic GVHD, but they resolved.
All patients were ultimately able to stop immunosuppressive therapy.
Robert Brodsky, MD, of Sidney Kimmel Cancer Center in Baltimore, Maryland, and his colleagues reported these findings in Biology of Blood and Marrow Transplantation.
“Our findings have the potential to greatly widen treatment options for the vast majority of severe aplastic anemia patients,” Dr Brodsky said.
He and his colleagues tested their approach in 16 SAA patients between 11 and 69 years of age. Each of the patients had failed to respond to immunosuppressive therapy and other treatments.
The patients received conditioning with antithymocyte globulin, fludarabine, low-dose cyclophosphamide, and total body irradiation.
They then received BMTs. Thirteen of the donors were haploidentical related, 2 were fully matched unrelated, and 1 was mismatched unrelated.
Three and 4 days after BMT, the patients received cyclophosphamide at 50 mg/kg/day as GVHD prophylaxis. They then received mycophenolate mofetil on days 5 through 35 and tacrolimus from day 5 through 1 year.
The median time to neutrophil recovery (over 1000 × 103/mm3 for 3 consecutive days) was 19 days (range, 16 to 27). The median time to red cell engraftment was 25 days (range, 2 to 58). And the median time to the last platelet transfusion (to keep platelet counts over 50 × 103/mm3) was 27.5 days (range, 22 to 108).
At a median follow-up of 21 months (range, 3 to 64), all 16 patients were still alive, disease-free, and no longer required transfusions.
Two patients did develop grade 1/2 acute skin GVHD. They also had mild chronic GVHD of the skin/mouth, which required systemic steroids.
One of these patients was able to come off all immunosuppressive therapy by 15 months, and the other was able to do so by 17 months. All of the other patients stopped immunosuppressive therapy at 1 year.
Ending all therapy related to their disease has been life-changing for these patients, said study author Amy DeZern, MD, also of the Sidney Kimmel Cancer Center.
“It’s like night and day,” she said. “They go from not knowing if they have a future to hoping for what they’d hoped for before they got sick. It’s that transformative.”
Successful BMTs using partially matched donors open up the transplant option to nearly all patients with SAA, especially minority patients, added Dr Brodsky.
“Now, a therapy that used to be available to 25% to 30% of patients with severe aplastic anemia is potentially available to more than 95%,” he said. ![]()

Photo by Chad McNeeley
Researchers have reported a “promising” treatment approach for
refractory, severe aplastic anemia (SAA).
The
regimen consists of nonmyeloablative conditioning, bone marrow
transplants (BMTs) from “alternative” donors, and graft-vs-host disease
(GVHD) prophylaxis.
All 16 SAA patients who received this treatment
achieved engraftment and were completely cleared of disease.
There were 2 cases of acute and chronic GVHD, but they resolved.
All patients were ultimately able to stop immunosuppressive therapy.
Robert Brodsky, MD, of Sidney Kimmel Cancer Center in Baltimore, Maryland, and his colleagues reported these findings in Biology of Blood and Marrow Transplantation.
“Our findings have the potential to greatly widen treatment options for the vast majority of severe aplastic anemia patients,” Dr Brodsky said.
He and his colleagues tested their approach in 16 SAA patients between 11 and 69 years of age. Each of the patients had failed to respond to immunosuppressive therapy and other treatments.
The patients received conditioning with antithymocyte globulin, fludarabine, low-dose cyclophosphamide, and total body irradiation.
They then received BMTs. Thirteen of the donors were haploidentical related, 2 were fully matched unrelated, and 1 was mismatched unrelated.
Three and 4 days after BMT, the patients received cyclophosphamide at 50 mg/kg/day as GVHD prophylaxis. They then received mycophenolate mofetil on days 5 through 35 and tacrolimus from day 5 through 1 year.
The median time to neutrophil recovery (over 1000 × 103/mm3 for 3 consecutive days) was 19 days (range, 16 to 27). The median time to red cell engraftment was 25 days (range, 2 to 58). And the median time to the last platelet transfusion (to keep platelet counts over 50 × 103/mm3) was 27.5 days (range, 22 to 108).
At a median follow-up of 21 months (range, 3 to 64), all 16 patients were still alive, disease-free, and no longer required transfusions.
Two patients did develop grade 1/2 acute skin GVHD. They also had mild chronic GVHD of the skin/mouth, which required systemic steroids.
One of these patients was able to come off all immunosuppressive therapy by 15 months, and the other was able to do so by 17 months. All of the other patients stopped immunosuppressive therapy at 1 year.
Ending all therapy related to their disease has been life-changing for these patients, said study author Amy DeZern, MD, also of the Sidney Kimmel Cancer Center.
“It’s like night and day,” she said. “They go from not knowing if they have a future to hoping for what they’d hoped for before they got sick. It’s that transformative.”
Successful BMTs using partially matched donors open up the transplant option to nearly all patients with SAA, especially minority patients, added Dr Brodsky.
“Now, a therapy that used to be available to 25% to 30% of patients with severe aplastic anemia is potentially available to more than 95%,” he said. ![]()

Photo by Chad McNeeley
Researchers have reported a “promising” treatment approach for
refractory, severe aplastic anemia (SAA).
The
regimen consists of nonmyeloablative conditioning, bone marrow
transplants (BMTs) from “alternative” donors, and graft-vs-host disease
(GVHD) prophylaxis.
All 16 SAA patients who received this treatment
achieved engraftment and were completely cleared of disease.
There were 2 cases of acute and chronic GVHD, but they resolved.
All patients were ultimately able to stop immunosuppressive therapy.
Robert Brodsky, MD, of Sidney Kimmel Cancer Center in Baltimore, Maryland, and his colleagues reported these findings in Biology of Blood and Marrow Transplantation.
“Our findings have the potential to greatly widen treatment options for the vast majority of severe aplastic anemia patients,” Dr Brodsky said.
He and his colleagues tested their approach in 16 SAA patients between 11 and 69 years of age. Each of the patients had failed to respond to immunosuppressive therapy and other treatments.
The patients received conditioning with antithymocyte globulin, fludarabine, low-dose cyclophosphamide, and total body irradiation.
They then received BMTs. Thirteen of the donors were haploidentical related, 2 were fully matched unrelated, and 1 was mismatched unrelated.
Three and 4 days after BMT, the patients received cyclophosphamide at 50 mg/kg/day as GVHD prophylaxis. They then received mycophenolate mofetil on days 5 through 35 and tacrolimus from day 5 through 1 year.
The median time to neutrophil recovery (over 1000 × 103/mm3 for 3 consecutive days) was 19 days (range, 16 to 27). The median time to red cell engraftment was 25 days (range, 2 to 58). And the median time to the last platelet transfusion (to keep platelet counts over 50 × 103/mm3) was 27.5 days (range, 22 to 108).
At a median follow-up of 21 months (range, 3 to 64), all 16 patients were still alive, disease-free, and no longer required transfusions.
Two patients did develop grade 1/2 acute skin GVHD. They also had mild chronic GVHD of the skin/mouth, which required systemic steroids.
One of these patients was able to come off all immunosuppressive therapy by 15 months, and the other was able to do so by 17 months. All of the other patients stopped immunosuppressive therapy at 1 year.
Ending all therapy related to their disease has been life-changing for these patients, said study author Amy DeZern, MD, also of the Sidney Kimmel Cancer Center.
“It’s like night and day,” she said. “They go from not knowing if they have a future to hoping for what they’d hoped for before they got sick. It’s that transformative.”
Successful BMTs using partially matched donors open up the transplant option to nearly all patients with SAA, especially minority patients, added Dr Brodsky.
“Now, a therapy that used to be available to 25% to 30% of patients with severe aplastic anemia is potentially available to more than 95%,” he said. ![]()
Approach may provide better treatment of GVHD, team says

Photo by Aaron Logan
Preclinical research suggests that targeting 2 kinases may provide an approach to treating graft-vs-host-disease (GVHD) that does not compromise the tumor-fighting capabilities of the immune system.
Researchers said that dual inhibition of Aurora kinase A and JAK2, attenuating CD28 costimulation and IL-6-mediated signal transduction, respectively, can fight GVHD without destroying potential antitumor cytotoxic T lymphocyte (CTL) responses.
The team detailed these findings in Science Translational Medicine.
“It is known that Aurora kinase A and JAK2 pathway activation contributes to GVHD,” said study author Brian C. Betts, MD, of H. Lee Moffitt Cancer Center & Research Institute in Tampa, Florida.
“However, drugs that inhibit either protein alone do not completely prevent GVHD. We hypothesized that co-treatment with drugs that target both Aurora kinase A and JAK2 could prevent GVHD better than either drug alone.”
In fact, Dr Betts and his colleagues engineered and tested 2 compounds that inhibit both Aurora kinase A and JAK2—AJI-100 and AJI-214.
The team then compared the AJI analogs to the Aurora kinase A inhibitor alisertib, the JAK2 inhibitor TG101348, the combination of alisertib and TG101348, and dimethyl sulfoxide (DMSO) control.
The researchers first found that AJI-214 and AJI-100 “exerted significant suppression of T cells” in vitro, suppressing alloreactive T-cell proliferation with a potency that was similar to that of alisertib and TG101348 in combination.
The team noted that inhibition of Aurora kinase A and JAK2—with either AJI analog or alisertib and TG101348 in combination—significantly reduced alloreactive conventional T cells (Tconv) and helper T cells (TH1 and TH17) but permitted the differentiation of inducible regulatory T cells (iTregs).
In fact, the researchers said that dual inhibition of Aurora kinase A and JAK2 supports potent CD39+ iTregs. They observed higher CD39 cell surface density among AJI-214–treated iTregs, which resulted in improved scavenging of extracellular adenosine triphosphate, when compared to DMSO-treated iTregs.
The team then tested AJI-100 in mouse models of GVHD, as this drug has better bioavailability than AJI-214.
AJI-100 significantly improved the overall survival of the mice and reduced the severity of GVHD, compared to vehicle control (P=0.003).
In comparison, alisertib and TG101348 in combination significantly delayed the onset and severity of GVHD when compared to vehicle or TG101348 alone (P<0.0001 and P=0.0001). But the combination did not significantly improve survival in the mice.
Next, the researchers tested the effects of AJI-100 on CTLs by generating human antitumor CTLs in xenotransplanted mice. The mice received AJI-100 or vehicle control, as well as irradiated U937 cells. Unvaccinated, xenotransplanted mice served as negative controls.
The team said AJI-100 did not inhibit CTL generation because CD8+ CTLs from AJI-100–treated and vehicle-treated mice demonstrated similarly enhanced killing capacity against U937 targets in vitro, when compared to unvaccinated controls.
Additional experiments in mice showed that AJI-100 significantly increases the ratio of Tregs to activated Tconv while eliminating TH17 and TH1 cells.
The researchers therefore concluded that inhibiting CD28 and IL-6 signal transduction pathways in donor T cells may increase the Treg/Tconv ratio, prevent GVHD, and preserve antitumor CTLs.
“This novel prevention strategy warrants further investigation because of its potential to reduce the risk of GVHD and possibly be more effective and selective than commonly used GVHD treatments currently available today,” Dr Betts said. ![]()

Photo by Aaron Logan
Preclinical research suggests that targeting 2 kinases may provide an approach to treating graft-vs-host-disease (GVHD) that does not compromise the tumor-fighting capabilities of the immune system.
Researchers said that dual inhibition of Aurora kinase A and JAK2, attenuating CD28 costimulation and IL-6-mediated signal transduction, respectively, can fight GVHD without destroying potential antitumor cytotoxic T lymphocyte (CTL) responses.
The team detailed these findings in Science Translational Medicine.
“It is known that Aurora kinase A and JAK2 pathway activation contributes to GVHD,” said study author Brian C. Betts, MD, of H. Lee Moffitt Cancer Center & Research Institute in Tampa, Florida.
“However, drugs that inhibit either protein alone do not completely prevent GVHD. We hypothesized that co-treatment with drugs that target both Aurora kinase A and JAK2 could prevent GVHD better than either drug alone.”
In fact, Dr Betts and his colleagues engineered and tested 2 compounds that inhibit both Aurora kinase A and JAK2—AJI-100 and AJI-214.
The team then compared the AJI analogs to the Aurora kinase A inhibitor alisertib, the JAK2 inhibitor TG101348, the combination of alisertib and TG101348, and dimethyl sulfoxide (DMSO) control.
The researchers first found that AJI-214 and AJI-100 “exerted significant suppression of T cells” in vitro, suppressing alloreactive T-cell proliferation with a potency that was similar to that of alisertib and TG101348 in combination.
The team noted that inhibition of Aurora kinase A and JAK2—with either AJI analog or alisertib and TG101348 in combination—significantly reduced alloreactive conventional T cells (Tconv) and helper T cells (TH1 and TH17) but permitted the differentiation of inducible regulatory T cells (iTregs).
In fact, the researchers said that dual inhibition of Aurora kinase A and JAK2 supports potent CD39+ iTregs. They observed higher CD39 cell surface density among AJI-214–treated iTregs, which resulted in improved scavenging of extracellular adenosine triphosphate, when compared to DMSO-treated iTregs.
The team then tested AJI-100 in mouse models of GVHD, as this drug has better bioavailability than AJI-214.
AJI-100 significantly improved the overall survival of the mice and reduced the severity of GVHD, compared to vehicle control (P=0.003).
In comparison, alisertib and TG101348 in combination significantly delayed the onset and severity of GVHD when compared to vehicle or TG101348 alone (P<0.0001 and P=0.0001). But the combination did not significantly improve survival in the mice.
Next, the researchers tested the effects of AJI-100 on CTLs by generating human antitumor CTLs in xenotransplanted mice. The mice received AJI-100 or vehicle control, as well as irradiated U937 cells. Unvaccinated, xenotransplanted mice served as negative controls.
The team said AJI-100 did not inhibit CTL generation because CD8+ CTLs from AJI-100–treated and vehicle-treated mice demonstrated similarly enhanced killing capacity against U937 targets in vitro, when compared to unvaccinated controls.
Additional experiments in mice showed that AJI-100 significantly increases the ratio of Tregs to activated Tconv while eliminating TH17 and TH1 cells.
The researchers therefore concluded that inhibiting CD28 and IL-6 signal transduction pathways in donor T cells may increase the Treg/Tconv ratio, prevent GVHD, and preserve antitumor CTLs.
“This novel prevention strategy warrants further investigation because of its potential to reduce the risk of GVHD and possibly be more effective and selective than commonly used GVHD treatments currently available today,” Dr Betts said. ![]()

Photo by Aaron Logan
Preclinical research suggests that targeting 2 kinases may provide an approach to treating graft-vs-host-disease (GVHD) that does not compromise the tumor-fighting capabilities of the immune system.
Researchers said that dual inhibition of Aurora kinase A and JAK2, attenuating CD28 costimulation and IL-6-mediated signal transduction, respectively, can fight GVHD without destroying potential antitumor cytotoxic T lymphocyte (CTL) responses.
The team detailed these findings in Science Translational Medicine.
“It is known that Aurora kinase A and JAK2 pathway activation contributes to GVHD,” said study author Brian C. Betts, MD, of H. Lee Moffitt Cancer Center & Research Institute in Tampa, Florida.
“However, drugs that inhibit either protein alone do not completely prevent GVHD. We hypothesized that co-treatment with drugs that target both Aurora kinase A and JAK2 could prevent GVHD better than either drug alone.”
In fact, Dr Betts and his colleagues engineered and tested 2 compounds that inhibit both Aurora kinase A and JAK2—AJI-100 and AJI-214.
The team then compared the AJI analogs to the Aurora kinase A inhibitor alisertib, the JAK2 inhibitor TG101348, the combination of alisertib and TG101348, and dimethyl sulfoxide (DMSO) control.
The researchers first found that AJI-214 and AJI-100 “exerted significant suppression of T cells” in vitro, suppressing alloreactive T-cell proliferation with a potency that was similar to that of alisertib and TG101348 in combination.
The team noted that inhibition of Aurora kinase A and JAK2—with either AJI analog or alisertib and TG101348 in combination—significantly reduced alloreactive conventional T cells (Tconv) and helper T cells (TH1 and TH17) but permitted the differentiation of inducible regulatory T cells (iTregs).
In fact, the researchers said that dual inhibition of Aurora kinase A and JAK2 supports potent CD39+ iTregs. They observed higher CD39 cell surface density among AJI-214–treated iTregs, which resulted in improved scavenging of extracellular adenosine triphosphate, when compared to DMSO-treated iTregs.
The team then tested AJI-100 in mouse models of GVHD, as this drug has better bioavailability than AJI-214.
AJI-100 significantly improved the overall survival of the mice and reduced the severity of GVHD, compared to vehicle control (P=0.003).
In comparison, alisertib and TG101348 in combination significantly delayed the onset and severity of GVHD when compared to vehicle or TG101348 alone (P<0.0001 and P=0.0001). But the combination did not significantly improve survival in the mice.
Next, the researchers tested the effects of AJI-100 on CTLs by generating human antitumor CTLs in xenotransplanted mice. The mice received AJI-100 or vehicle control, as well as irradiated U937 cells. Unvaccinated, xenotransplanted mice served as negative controls.
The team said AJI-100 did not inhibit CTL generation because CD8+ CTLs from AJI-100–treated and vehicle-treated mice demonstrated similarly enhanced killing capacity against U937 targets in vitro, when compared to unvaccinated controls.
Additional experiments in mice showed that AJI-100 significantly increases the ratio of Tregs to activated Tconv while eliminating TH17 and TH1 cells.
The researchers therefore concluded that inhibiting CD28 and IL-6 signal transduction pathways in donor T cells may increase the Treg/Tconv ratio, prevent GVHD, and preserve antitumor CTLs.
“This novel prevention strategy warrants further investigation because of its potential to reduce the risk of GVHD and possibly be more effective and selective than commonly used GVHD treatments currently available today,” Dr Betts said. ![]()
Study reveals CML patients likely to benefit from HSCT long-term

Photo by Chad McNeeley
SAN DIEGO—Researchers believe they have identified patients with chronic myeloid leukemia (CML) who are likely to derive long-term benefit from allogeneic hematopoietic stem cell transplant (allo-HSCT).
The researchers found that CML patients have a low risk of long-term morbidity if they undergo HSCT before the age of 45, are conditioned with busulfan and cyclophosphamide (Bu/Cy), and receive a graft from a matched, related donor (MRD).
Jessica Wu, of the University of Alabama at Birmingham, presented these findings at the 2016 ASH Annual Meeting (abstract 823*).
Wu noted that allogeneic HSCT is potentially curative for CML, but this method of treatment has been on the decline since the introduction of tyrosine kinase inhibitors (TKIs). And today, few CML patients undergo allo-HSCT.
She said that although TKIs can induce remission in CML patients, the drugs also fail to eradicate leukemia, can produce side effects that impact patients’ quality of life, and come with a significant financial burden (estimated at $92,000 to $138,000 per patient per year).
With this in mind, Wu and her colleagues set out to determine if certain CML patients might benefit from allo-HSCT long-term. The team also wanted to quantify overall and cause-specific late mortality after allo-HSCT and the long-term burden of severe/life-threatening chronic health conditions after allo-HSCT.
Patient population
The researchers studied 637 CML patients treated with allo-HSCT between 1981 and 2010 at City of Hope in Duarte, California, or the University of Minnesota in Minneapolis/Saint Paul. The patients had to have survived at least 2 years post-transplant.
About 60% of patients were male, and 67% were non-Hispanic white. Their median age at HSCT was 36.4 years, and 65% received an MRD graft. Nineteen percent of patients were transplanted in 1980-1989, 52% were transplanted in 1990-1999, and 29% were transplanted in 2000-2010.
Fifty-eight percent of patients received Cy/total body irradiation (TBI), 18% received Bu/Cy, and 3% received reduced-intensity conditioning (RIC).
Sixty-one percent of patients had chronic graft-vs-host disease (cGVHD), and 32% had high-risk disease at the time of HSCT.
Survival
The patients were followed for a median of 16.7 years. Thirty percent (n=192) died after surviving at least 2 years post-HSCT.
The median time to death was 8.3 years (range, 2-29.5), and the median age at death was 49.2 (range, 7.8-69.8). At 20 years from HSCT, the overall survival was 68.6%.
HSCT recipients had a 4.4-fold increased risk of death compared with the age-, sex-, and race-matched general population.
“Non-relapse mortality was the major contributor to late mortality, with infection, second malignancies, and cGVHD being the most common causes of death,” Wu said.
Non-relapse mortality was 20%, and relapse-related mortality was 4%. Eight percent of patients died of infection, 6.3% died of cGVHD, and 3.7% died of second malignancies.
Health outcomes
Patients who were still alive at the time of the study were asked to complete the BMTSS-2 health questionnaire, which was used to examine the risk of grade 3/4 chronic health conditions.
A total of 288 patients completed the questionnaire, as did a sibling comparison group of 404 individuals.
Among the patients, the median age at allo-HSCT was 37.5 (range, 3.6-71.4), and the median duration of follow-up was 13.9 years (range, 2-34.6).
Sixty-two percent of patients received an MRD graft, and 38% had a matched, unrelated donor. Eighty-three percent of patients had TBI-based conditioning, 16% received Bu/Cy, and 2.7% received RIC.
The prevalence of grade 3/4 chronic health conditions was significantly higher among patients than among siblings—38% and 24%, respectively (P<0.0001).
The odds ratio (OR)—adjusted for age, sex, race, and socioeconomic status—was 2.7 (P<0.0001).
The cumulative incidence of any grade 3/4 condition at 20 years after HSCT was 47.2% among patients. Common conditions were diabetes (14.9%), second malignancies (12.6%), and coronary artery disease (10%).
The researchers found the risk of grade 3/4 morbidity was significantly higher for the following patient groups:
- Those age 45 and older (hazard ratio [HR]=3.3, P<0.0001)
- Patients with a matched, unrelated donor (HR=3.0, P<0.0001)
- Those who received peripheral blood or cord blood grafts as opposed to bone marrow (HR=2.7, P=0.006).
(This analysis was adjusted for race/ethnicity, sex, education, household income, insurance, cGVHD, and conditioning regimen).
Lower risk
To identify subpopulations with a reduced risk of long-term morbidity, the researchers calculated the risk in various CML patient groups compared to siblings.
The overall OR for CML patients compared with siblings was 2.7 (P<0.0001).
The OR for patients in first chronic phase who underwent HSCT before the age of 45 and had an MRD was 1.5 (P=0.1).
The OR for CML patients in first chronic phase who underwent HSCT before the age of 45, had an MRD, and received Bu/Cy conditioning was 0.8 (P=0.7).
“[W]e found that patients who received a matched, related donor transplant under the age of 45, with busulfan/cyclophosphamide, carried the same burden of morbidity as the sibling cohort,” Wu said. “These findings could help inform decisions regarding therapeutic options for the management of CML.”
Wu noted that the limited sample size in this study prevented the researchers from examining outcomes with RIC. And a lack of data at analysis prevented them from examining pre-HSCT and post-HSCT management of CML, the interval between diagnosis and HSCT, and the life-long economic burden of allo-HSCT.
However, she said data collection is ongoing, and the researchers hope to address some of these limitations.![]()
*Information presented at the meeting differs from the abstract.

Photo by Chad McNeeley
SAN DIEGO—Researchers believe they have identified patients with chronic myeloid leukemia (CML) who are likely to derive long-term benefit from allogeneic hematopoietic stem cell transplant (allo-HSCT).
The researchers found that CML patients have a low risk of long-term morbidity if they undergo HSCT before the age of 45, are conditioned with busulfan and cyclophosphamide (Bu/Cy), and receive a graft from a matched, related donor (MRD).
Jessica Wu, of the University of Alabama at Birmingham, presented these findings at the 2016 ASH Annual Meeting (abstract 823*).
Wu noted that allogeneic HSCT is potentially curative for CML, but this method of treatment has been on the decline since the introduction of tyrosine kinase inhibitors (TKIs). And today, few CML patients undergo allo-HSCT.
She said that although TKIs can induce remission in CML patients, the drugs also fail to eradicate leukemia, can produce side effects that impact patients’ quality of life, and come with a significant financial burden (estimated at $92,000 to $138,000 per patient per year).
With this in mind, Wu and her colleagues set out to determine if certain CML patients might benefit from allo-HSCT long-term. The team also wanted to quantify overall and cause-specific late mortality after allo-HSCT and the long-term burden of severe/life-threatening chronic health conditions after allo-HSCT.
Patient population
The researchers studied 637 CML patients treated with allo-HSCT between 1981 and 2010 at City of Hope in Duarte, California, or the University of Minnesota in Minneapolis/Saint Paul. The patients had to have survived at least 2 years post-transplant.
About 60% of patients were male, and 67% were non-Hispanic white. Their median age at HSCT was 36.4 years, and 65% received an MRD graft. Nineteen percent of patients were transplanted in 1980-1989, 52% were transplanted in 1990-1999, and 29% were transplanted in 2000-2010.
Fifty-eight percent of patients received Cy/total body irradiation (TBI), 18% received Bu/Cy, and 3% received reduced-intensity conditioning (RIC).
Sixty-one percent of patients had chronic graft-vs-host disease (cGVHD), and 32% had high-risk disease at the time of HSCT.
Survival
The patients were followed for a median of 16.7 years. Thirty percent (n=192) died after surviving at least 2 years post-HSCT.
The median time to death was 8.3 years (range, 2-29.5), and the median age at death was 49.2 (range, 7.8-69.8). At 20 years from HSCT, the overall survival was 68.6%.
HSCT recipients had a 4.4-fold increased risk of death compared with the age-, sex-, and race-matched general population.
“Non-relapse mortality was the major contributor to late mortality, with infection, second malignancies, and cGVHD being the most common causes of death,” Wu said.
Non-relapse mortality was 20%, and relapse-related mortality was 4%. Eight percent of patients died of infection, 6.3% died of cGVHD, and 3.7% died of second malignancies.
Health outcomes
Patients who were still alive at the time of the study were asked to complete the BMTSS-2 health questionnaire, which was used to examine the risk of grade 3/4 chronic health conditions.
A total of 288 patients completed the questionnaire, as did a sibling comparison group of 404 individuals.
Among the patients, the median age at allo-HSCT was 37.5 (range, 3.6-71.4), and the median duration of follow-up was 13.9 years (range, 2-34.6).
Sixty-two percent of patients received an MRD graft, and 38% had a matched, unrelated donor. Eighty-three percent of patients had TBI-based conditioning, 16% received Bu/Cy, and 2.7% received RIC.
The prevalence of grade 3/4 chronic health conditions was significantly higher among patients than among siblings—38% and 24%, respectively (P<0.0001).
The odds ratio (OR)—adjusted for age, sex, race, and socioeconomic status—was 2.7 (P<0.0001).
The cumulative incidence of any grade 3/4 condition at 20 years after HSCT was 47.2% among patients. Common conditions were diabetes (14.9%), second malignancies (12.6%), and coronary artery disease (10%).
The researchers found the risk of grade 3/4 morbidity was significantly higher for the following patient groups:
- Those age 45 and older (hazard ratio [HR]=3.3, P<0.0001)
- Patients with a matched, unrelated donor (HR=3.0, P<0.0001)
- Those who received peripheral blood or cord blood grafts as opposed to bone marrow (HR=2.7, P=0.006).
(This analysis was adjusted for race/ethnicity, sex, education, household income, insurance, cGVHD, and conditioning regimen).
Lower risk
To identify subpopulations with a reduced risk of long-term morbidity, the researchers calculated the risk in various CML patient groups compared to siblings.
The overall OR for CML patients compared with siblings was 2.7 (P<0.0001).
The OR for patients in first chronic phase who underwent HSCT before the age of 45 and had an MRD was 1.5 (P=0.1).
The OR for CML patients in first chronic phase who underwent HSCT before the age of 45, had an MRD, and received Bu/Cy conditioning was 0.8 (P=0.7).
“[W]e found that patients who received a matched, related donor transplant under the age of 45, with busulfan/cyclophosphamide, carried the same burden of morbidity as the sibling cohort,” Wu said. “These findings could help inform decisions regarding therapeutic options for the management of CML.”
Wu noted that the limited sample size in this study prevented the researchers from examining outcomes with RIC. And a lack of data at analysis prevented them from examining pre-HSCT and post-HSCT management of CML, the interval between diagnosis and HSCT, and the life-long economic burden of allo-HSCT.
However, she said data collection is ongoing, and the researchers hope to address some of these limitations.![]()
*Information presented at the meeting differs from the abstract.

Photo by Chad McNeeley
SAN DIEGO—Researchers believe they have identified patients with chronic myeloid leukemia (CML) who are likely to derive long-term benefit from allogeneic hematopoietic stem cell transplant (allo-HSCT).
The researchers found that CML patients have a low risk of long-term morbidity if they undergo HSCT before the age of 45, are conditioned with busulfan and cyclophosphamide (Bu/Cy), and receive a graft from a matched, related donor (MRD).
Jessica Wu, of the University of Alabama at Birmingham, presented these findings at the 2016 ASH Annual Meeting (abstract 823*).
Wu noted that allogeneic HSCT is potentially curative for CML, but this method of treatment has been on the decline since the introduction of tyrosine kinase inhibitors (TKIs). And today, few CML patients undergo allo-HSCT.
She said that although TKIs can induce remission in CML patients, the drugs also fail to eradicate leukemia, can produce side effects that impact patients’ quality of life, and come with a significant financial burden (estimated at $92,000 to $138,000 per patient per year).
With this in mind, Wu and her colleagues set out to determine if certain CML patients might benefit from allo-HSCT long-term. The team also wanted to quantify overall and cause-specific late mortality after allo-HSCT and the long-term burden of severe/life-threatening chronic health conditions after allo-HSCT.
Patient population
The researchers studied 637 CML patients treated with allo-HSCT between 1981 and 2010 at City of Hope in Duarte, California, or the University of Minnesota in Minneapolis/Saint Paul. The patients had to have survived at least 2 years post-transplant.
About 60% of patients were male, and 67% were non-Hispanic white. Their median age at HSCT was 36.4 years, and 65% received an MRD graft. Nineteen percent of patients were transplanted in 1980-1989, 52% were transplanted in 1990-1999, and 29% were transplanted in 2000-2010.
Fifty-eight percent of patients received Cy/total body irradiation (TBI), 18% received Bu/Cy, and 3% received reduced-intensity conditioning (RIC).
Sixty-one percent of patients had chronic graft-vs-host disease (cGVHD), and 32% had high-risk disease at the time of HSCT.
Survival
The patients were followed for a median of 16.7 years. Thirty percent (n=192) died after surviving at least 2 years post-HSCT.
The median time to death was 8.3 years (range, 2-29.5), and the median age at death was 49.2 (range, 7.8-69.8). At 20 years from HSCT, the overall survival was 68.6%.
HSCT recipients had a 4.4-fold increased risk of death compared with the age-, sex-, and race-matched general population.
“Non-relapse mortality was the major contributor to late mortality, with infection, second malignancies, and cGVHD being the most common causes of death,” Wu said.
Non-relapse mortality was 20%, and relapse-related mortality was 4%. Eight percent of patients died of infection, 6.3% died of cGVHD, and 3.7% died of second malignancies.
Health outcomes
Patients who were still alive at the time of the study were asked to complete the BMTSS-2 health questionnaire, which was used to examine the risk of grade 3/4 chronic health conditions.
A total of 288 patients completed the questionnaire, as did a sibling comparison group of 404 individuals.
Among the patients, the median age at allo-HSCT was 37.5 (range, 3.6-71.4), and the median duration of follow-up was 13.9 years (range, 2-34.6).
Sixty-two percent of patients received an MRD graft, and 38% had a matched, unrelated donor. Eighty-three percent of patients had TBI-based conditioning, 16% received Bu/Cy, and 2.7% received RIC.
The prevalence of grade 3/4 chronic health conditions was significantly higher among patients than among siblings—38% and 24%, respectively (P<0.0001).
The odds ratio (OR)—adjusted for age, sex, race, and socioeconomic status—was 2.7 (P<0.0001).
The cumulative incidence of any grade 3/4 condition at 20 years after HSCT was 47.2% among patients. Common conditions were diabetes (14.9%), second malignancies (12.6%), and coronary artery disease (10%).
The researchers found the risk of grade 3/4 morbidity was significantly higher for the following patient groups:
- Those age 45 and older (hazard ratio [HR]=3.3, P<0.0001)
- Patients with a matched, unrelated donor (HR=3.0, P<0.0001)
- Those who received peripheral blood or cord blood grafts as opposed to bone marrow (HR=2.7, P=0.006).
(This analysis was adjusted for race/ethnicity, sex, education, household income, insurance, cGVHD, and conditioning regimen).
Lower risk
To identify subpopulations with a reduced risk of long-term morbidity, the researchers calculated the risk in various CML patient groups compared to siblings.
The overall OR for CML patients compared with siblings was 2.7 (P<0.0001).
The OR for patients in first chronic phase who underwent HSCT before the age of 45 and had an MRD was 1.5 (P=0.1).
The OR for CML patients in first chronic phase who underwent HSCT before the age of 45, had an MRD, and received Bu/Cy conditioning was 0.8 (P=0.7).
“[W]e found that patients who received a matched, related donor transplant under the age of 45, with busulfan/cyclophosphamide, carried the same burden of morbidity as the sibling cohort,” Wu said. “These findings could help inform decisions regarding therapeutic options for the management of CML.”
Wu noted that the limited sample size in this study prevented the researchers from examining outcomes with RIC. And a lack of data at analysis prevented them from examining pre-HSCT and post-HSCT management of CML, the interval between diagnosis and HSCT, and the life-long economic burden of allo-HSCT.
However, she said data collection is ongoing, and the researchers hope to address some of these limitations.![]()
*Information presented at the meeting differs from the abstract.
Restrictive transfusion strategy should be standard after HSCT, doc says

Photo from UAB Hospital
SAN DIEGO—Results of the phase 3 TRIST study support the use of a restrictive red blood cell (RBC) transfusion strategy in patients undergoing hematopoietic stem cell transplant (HSCT) to treat hematologic disorders.
The study suggests a restrictive strategy—in which patients receive 2 RBC units if their hemoglobin level is below 70 g/L—is non-inferior to a liberal strategy—in which patients receive 2 units if their hemoglobin level is below 90 g/L.
Clinical outcomes and health-related quality of life (HRQOL) were similar with both strategies.
Therefore, a restrictive strategy should be considered the standard of care in patients undergoing HSCT, according to study investigator Jason Tay, MD, of the University of Calgary/Tom Baker Cancer Center in Alberta, Canada.
Dr Tay presented results of the TRIST study at the 2016 ASH Annual Meeting (abstract 1032*).
He noted that recent AABB guidelines recommend using a restrictive RBC transfusion strategy in most circumstances. However, these recommendations do not apply to patients treated for hematologic or oncologic diseases who are at risk of bleeding, as there is a lack of randomized trials in such patients.
So Dr Tay and his colleagues decided to conduct a randomized, controlled trial comparing 2 RBC transfusion strategies in patients undergoing HSCT to treat hematologic disorders.
The study enrolled 300 patients who underwent HSCT between March 28, 2011, and February 3, 2016, at 4 Canadian centers.
The patients were randomized to 1 of 2 transfusion strategies from day 0 to day 100 post-HSCT:
- Restrictive strategy (n=149)—patients received 2 RBC units if their hemoglobin levels were below 70 g/L, to target a hemoglobin level of 70-90 g/L
- Liberal strategy (n=150)—patients received 2 RBC units if their hemoglobin levels were below 90 g/L, to target a hemoglobin level of 90-110 g/L.
The median age was 57.47 (range, 48.94-62.66) in the restrictive group and 56.04 (range, 48.27-62.24) in the liberal group. Most patients were male—65.10% and 62.67%, respectively.
Patients had acute leukemia (25.50% and 24.00%, respectively), chronic leukemia (6.71% and 6.00%), myeloproliferative disorders (2.68% and 2.00%), lymphoma (30.87% and 33.33%), myeloma (24.16% and 28.00%), and other disorders (10.07% and 6.67%, respectively).
About half of patients in each transfusion group received an autologous HSCT (49.66% and 50.00%, respectively), and about half received an allogeneic HSCT (50.34% and 50.00%, respectively).
Transfusion use
The total number of RBC units transfused was 407 in the restrictive group and 753 in the liberal group. The median number of RBC units transfused per patient was 2 (range, 0-2) and 4 (range, 2-6), respectively. The mean number was 2.73 and 5.02, respectively (P=0.0004).
The total number of RBC transfusion episodes was 234 in the restrictive group and 407 in the liberal group. The median number per patient was 1 (range, 0-2) and 2 (range, 1-3), respectively, and the mean was 1.57 and 2.70, respectively (P=0.002).
The median storage duration of the RBC units transfused was 17 days (range, 13-23) in the restrictive group and 20 days (range, 15-25) in the liberal group. The mean was 18.46 and 19.95, respectively (P=0.0003).
The between-group difference in the overall mean pre-transfusion hemoglobin per patient over the study period was 13.71 g/L.
The median number of platelet units transfused was 2 (range, 1-3) in the
restrictive group and 3 (range, 1-4) in the liberal group. The mean was 3.84 and 3.61, respectively (P=0.6930).
The median number of platelet transfusion episodes was 2 for both groups (range, 1-3 and
1-4, respectively). The mean was 3.84 in the restrictive group and 3.61 in the liberal group (P=0.77).
Adherence
In both groups, there were cases of non-adherence to the trigger hemoglobin value.
There were 49 non-adherent patients (32.89%) in the restrictive group—35 in whom an RBC transfusion occurred above the assigned trigger and 14 in whom a transfusion did not occur when the assigned trigger was reached.
There were 83 non-adherent patients (55.3%) in the liberal group—11 in whom an RBC transfusion occurred above the assigned trigger and 72 in whom a transfusion did not occur when the assigned trigger was reached.
Sixty-nine patients (46.31%) in the restrictive group and 21 (14%) in the liberal group never received an RBC transfusion.
Outcomes
The study’s primary endpoint was HRQOL, as measured by the FACT-BMT scale.
The total FACT-BMT score at day 100 was 116.3 (range, 98-129.2) in the restrictive group and 109.2 (range, 92.1-125.2) in the liberal group (P<0.0001 for non-inferiority).
Non-inferiority in HRQOL was shown for all other time points assessed as well—day 7 (P<0.001), day 14 (P<0.0001), day 28 (P<0.0001), and day 60 (P<0.0001). Total FACT-BMT scores at all time points were higher for patients in the restrictive group than the liberal one.
The study’s secondary endpoints included clinical outcomes and FACT-Anemia scores at several time points.
There was no significant difference in clinical outcomes between the restrictive and liberal transfusion groups.
There were 2 cases of transplant-related mortality in the restrictive group and 4 in the liberal group (P=0.42). And there were 4 cases of sinusoidal obstruction syndrome in both groups (P=0.98).
The median Bearman toxicity score at day 28 was 2 in both groups (range, 1-3 and 1-4, respectively). The mean was 2.5 in the restrictive group and 2.8 in the liberal group (P=0.33).
There was no significant between-group difference in WHO bleeding score at day 14 (P=0.13), day 28 (P=0.81), or day 100 (P=0.28).
There was no significant difference between the transfusion groups in the length of hospital stay for patients who received autologous HSCT (P=0.95) or allogeneic HSCT (P=0.23) or in the number of hospital readmissions for patients who received autologous HSCT (P=0.29) or allogeneic HSCT (P=0.81).
The total FACT-Anemia score was significantly higher in the restrictive transfusion group at day 7 (P=0.03) and day 60 (P=0.03) post-HSCT.
However, there was no significant between-group difference in FACT-Anemia score at 14 days (P=0.07), 28 days (P=0.51), or 100 days (P=0.14).
Dr Tay said these results suggest a restrictive RBC transfusion strategy is non-inferior to a liberal one in patients undergoing HSCT to treat a hematologic disorder.
“Moreover, a restrictive strategy is safe and results in less blood transfusions,” he said. “We’d like to suggest that a strategy of 70 g/L can be considered the standard of care in patients undergoing a stem cell transplantation.” ![]()
*Information presented at the meeting differs from the abstract.

Photo from UAB Hospital
SAN DIEGO—Results of the phase 3 TRIST study support the use of a restrictive red blood cell (RBC) transfusion strategy in patients undergoing hematopoietic stem cell transplant (HSCT) to treat hematologic disorders.
The study suggests a restrictive strategy—in which patients receive 2 RBC units if their hemoglobin level is below 70 g/L—is non-inferior to a liberal strategy—in which patients receive 2 units if their hemoglobin level is below 90 g/L.
Clinical outcomes and health-related quality of life (HRQOL) were similar with both strategies.
Therefore, a restrictive strategy should be considered the standard of care in patients undergoing HSCT, according to study investigator Jason Tay, MD, of the University of Calgary/Tom Baker Cancer Center in Alberta, Canada.
Dr Tay presented results of the TRIST study at the 2016 ASH Annual Meeting (abstract 1032*).
He noted that recent AABB guidelines recommend using a restrictive RBC transfusion strategy in most circumstances. However, these recommendations do not apply to patients treated for hematologic or oncologic diseases who are at risk of bleeding, as there is a lack of randomized trials in such patients.
So Dr Tay and his colleagues decided to conduct a randomized, controlled trial comparing 2 RBC transfusion strategies in patients undergoing HSCT to treat hematologic disorders.
The study enrolled 300 patients who underwent HSCT between March 28, 2011, and February 3, 2016, at 4 Canadian centers.
The patients were randomized to 1 of 2 transfusion strategies from day 0 to day 100 post-HSCT:
- Restrictive strategy (n=149)—patients received 2 RBC units if their hemoglobin levels were below 70 g/L, to target a hemoglobin level of 70-90 g/L
- Liberal strategy (n=150)—patients received 2 RBC units if their hemoglobin levels were below 90 g/L, to target a hemoglobin level of 90-110 g/L.
The median age was 57.47 (range, 48.94-62.66) in the restrictive group and 56.04 (range, 48.27-62.24) in the liberal group. Most patients were male—65.10% and 62.67%, respectively.
Patients had acute leukemia (25.50% and 24.00%, respectively), chronic leukemia (6.71% and 6.00%), myeloproliferative disorders (2.68% and 2.00%), lymphoma (30.87% and 33.33%), myeloma (24.16% and 28.00%), and other disorders (10.07% and 6.67%, respectively).
About half of patients in each transfusion group received an autologous HSCT (49.66% and 50.00%, respectively), and about half received an allogeneic HSCT (50.34% and 50.00%, respectively).
Transfusion use
The total number of RBC units transfused was 407 in the restrictive group and 753 in the liberal group. The median number of RBC units transfused per patient was 2 (range, 0-2) and 4 (range, 2-6), respectively. The mean number was 2.73 and 5.02, respectively (P=0.0004).
The total number of RBC transfusion episodes was 234 in the restrictive group and 407 in the liberal group. The median number per patient was 1 (range, 0-2) and 2 (range, 1-3), respectively, and the mean was 1.57 and 2.70, respectively (P=0.002).
The median storage duration of the RBC units transfused was 17 days (range, 13-23) in the restrictive group and 20 days (range, 15-25) in the liberal group. The mean was 18.46 and 19.95, respectively (P=0.0003).
The between-group difference in the overall mean pre-transfusion hemoglobin per patient over the study period was 13.71 g/L.
The median number of platelet units transfused was 2 (range, 1-3) in the
restrictive group and 3 (range, 1-4) in the liberal group. The mean was 3.84 and 3.61, respectively (P=0.6930).
The median number of platelet transfusion episodes was 2 for both groups (range, 1-3 and
1-4, respectively). The mean was 3.84 in the restrictive group and 3.61 in the liberal group (P=0.77).
Adherence
In both groups, there were cases of non-adherence to the trigger hemoglobin value.
There were 49 non-adherent patients (32.89%) in the restrictive group—35 in whom an RBC transfusion occurred above the assigned trigger and 14 in whom a transfusion did not occur when the assigned trigger was reached.
There were 83 non-adherent patients (55.3%) in the liberal group—11 in whom an RBC transfusion occurred above the assigned trigger and 72 in whom a transfusion did not occur when the assigned trigger was reached.
Sixty-nine patients (46.31%) in the restrictive group and 21 (14%) in the liberal group never received an RBC transfusion.
Outcomes
The study’s primary endpoint was HRQOL, as measured by the FACT-BMT scale.
The total FACT-BMT score at day 100 was 116.3 (range, 98-129.2) in the restrictive group and 109.2 (range, 92.1-125.2) in the liberal group (P<0.0001 for non-inferiority).
Non-inferiority in HRQOL was shown for all other time points assessed as well—day 7 (P<0.001), day 14 (P<0.0001), day 28 (P<0.0001), and day 60 (P<0.0001). Total FACT-BMT scores at all time points were higher for patients in the restrictive group than the liberal one.
The study’s secondary endpoints included clinical outcomes and FACT-Anemia scores at several time points.
There was no significant difference in clinical outcomes between the restrictive and liberal transfusion groups.
There were 2 cases of transplant-related mortality in the restrictive group and 4 in the liberal group (P=0.42). And there were 4 cases of sinusoidal obstruction syndrome in both groups (P=0.98).
The median Bearman toxicity score at day 28 was 2 in both groups (range, 1-3 and 1-4, respectively). The mean was 2.5 in the restrictive group and 2.8 in the liberal group (P=0.33).
There was no significant between-group difference in WHO bleeding score at day 14 (P=0.13), day 28 (P=0.81), or day 100 (P=0.28).
There was no significant difference between the transfusion groups in the length of hospital stay for patients who received autologous HSCT (P=0.95) or allogeneic HSCT (P=0.23) or in the number of hospital readmissions for patients who received autologous HSCT (P=0.29) or allogeneic HSCT (P=0.81).
The total FACT-Anemia score was significantly higher in the restrictive transfusion group at day 7 (P=0.03) and day 60 (P=0.03) post-HSCT.
However, there was no significant between-group difference in FACT-Anemia score at 14 days (P=0.07), 28 days (P=0.51), or 100 days (P=0.14).
Dr Tay said these results suggest a restrictive RBC transfusion strategy is non-inferior to a liberal one in patients undergoing HSCT to treat a hematologic disorder.
“Moreover, a restrictive strategy is safe and results in less blood transfusions,” he said. “We’d like to suggest that a strategy of 70 g/L can be considered the standard of care in patients undergoing a stem cell transplantation.” ![]()
*Information presented at the meeting differs from the abstract.

Photo from UAB Hospital
SAN DIEGO—Results of the phase 3 TRIST study support the use of a restrictive red blood cell (RBC) transfusion strategy in patients undergoing hematopoietic stem cell transplant (HSCT) to treat hematologic disorders.
The study suggests a restrictive strategy—in which patients receive 2 RBC units if their hemoglobin level is below 70 g/L—is non-inferior to a liberal strategy—in which patients receive 2 units if their hemoglobin level is below 90 g/L.
Clinical outcomes and health-related quality of life (HRQOL) were similar with both strategies.
Therefore, a restrictive strategy should be considered the standard of care in patients undergoing HSCT, according to study investigator Jason Tay, MD, of the University of Calgary/Tom Baker Cancer Center in Alberta, Canada.
Dr Tay presented results of the TRIST study at the 2016 ASH Annual Meeting (abstract 1032*).
He noted that recent AABB guidelines recommend using a restrictive RBC transfusion strategy in most circumstances. However, these recommendations do not apply to patients treated for hematologic or oncologic diseases who are at risk of bleeding, as there is a lack of randomized trials in such patients.
So Dr Tay and his colleagues decided to conduct a randomized, controlled trial comparing 2 RBC transfusion strategies in patients undergoing HSCT to treat hematologic disorders.
The study enrolled 300 patients who underwent HSCT between March 28, 2011, and February 3, 2016, at 4 Canadian centers.
The patients were randomized to 1 of 2 transfusion strategies from day 0 to day 100 post-HSCT:
- Restrictive strategy (n=149)—patients received 2 RBC units if their hemoglobin levels were below 70 g/L, to target a hemoglobin level of 70-90 g/L
- Liberal strategy (n=150)—patients received 2 RBC units if their hemoglobin levels were below 90 g/L, to target a hemoglobin level of 90-110 g/L.
The median age was 57.47 (range, 48.94-62.66) in the restrictive group and 56.04 (range, 48.27-62.24) in the liberal group. Most patients were male—65.10% and 62.67%, respectively.
Patients had acute leukemia (25.50% and 24.00%, respectively), chronic leukemia (6.71% and 6.00%), myeloproliferative disorders (2.68% and 2.00%), lymphoma (30.87% and 33.33%), myeloma (24.16% and 28.00%), and other disorders (10.07% and 6.67%, respectively).
About half of patients in each transfusion group received an autologous HSCT (49.66% and 50.00%, respectively), and about half received an allogeneic HSCT (50.34% and 50.00%, respectively).
Transfusion use
The total number of RBC units transfused was 407 in the restrictive group and 753 in the liberal group. The median number of RBC units transfused per patient was 2 (range, 0-2) and 4 (range, 2-6), respectively. The mean number was 2.73 and 5.02, respectively (P=0.0004).
The total number of RBC transfusion episodes was 234 in the restrictive group and 407 in the liberal group. The median number per patient was 1 (range, 0-2) and 2 (range, 1-3), respectively, and the mean was 1.57 and 2.70, respectively (P=0.002).
The median storage duration of the RBC units transfused was 17 days (range, 13-23) in the restrictive group and 20 days (range, 15-25) in the liberal group. The mean was 18.46 and 19.95, respectively (P=0.0003).
The between-group difference in the overall mean pre-transfusion hemoglobin per patient over the study period was 13.71 g/L.
The median number of platelet units transfused was 2 (range, 1-3) in the
restrictive group and 3 (range, 1-4) in the liberal group. The mean was 3.84 and 3.61, respectively (P=0.6930).
The median number of platelet transfusion episodes was 2 for both groups (range, 1-3 and
1-4, respectively). The mean was 3.84 in the restrictive group and 3.61 in the liberal group (P=0.77).
Adherence
In both groups, there were cases of non-adherence to the trigger hemoglobin value.
There were 49 non-adherent patients (32.89%) in the restrictive group—35 in whom an RBC transfusion occurred above the assigned trigger and 14 in whom a transfusion did not occur when the assigned trigger was reached.
There were 83 non-adherent patients (55.3%) in the liberal group—11 in whom an RBC transfusion occurred above the assigned trigger and 72 in whom a transfusion did not occur when the assigned trigger was reached.
Sixty-nine patients (46.31%) in the restrictive group and 21 (14%) in the liberal group never received an RBC transfusion.
Outcomes
The study’s primary endpoint was HRQOL, as measured by the FACT-BMT scale.
The total FACT-BMT score at day 100 was 116.3 (range, 98-129.2) in the restrictive group and 109.2 (range, 92.1-125.2) in the liberal group (P<0.0001 for non-inferiority).
Non-inferiority in HRQOL was shown for all other time points assessed as well—day 7 (P<0.001), day 14 (P<0.0001), day 28 (P<0.0001), and day 60 (P<0.0001). Total FACT-BMT scores at all time points were higher for patients in the restrictive group than the liberal one.
The study’s secondary endpoints included clinical outcomes and FACT-Anemia scores at several time points.
There was no significant difference in clinical outcomes between the restrictive and liberal transfusion groups.
There were 2 cases of transplant-related mortality in the restrictive group and 4 in the liberal group (P=0.42). And there were 4 cases of sinusoidal obstruction syndrome in both groups (P=0.98).
The median Bearman toxicity score at day 28 was 2 in both groups (range, 1-3 and 1-4, respectively). The mean was 2.5 in the restrictive group and 2.8 in the liberal group (P=0.33).
There was no significant between-group difference in WHO bleeding score at day 14 (P=0.13), day 28 (P=0.81), or day 100 (P=0.28).
There was no significant difference between the transfusion groups in the length of hospital stay for patients who received autologous HSCT (P=0.95) or allogeneic HSCT (P=0.23) or in the number of hospital readmissions for patients who received autologous HSCT (P=0.29) or allogeneic HSCT (P=0.81).
The total FACT-Anemia score was significantly higher in the restrictive transfusion group at day 7 (P=0.03) and day 60 (P=0.03) post-HSCT.
However, there was no significant between-group difference in FACT-Anemia score at 14 days (P=0.07), 28 days (P=0.51), or 100 days (P=0.14).
Dr Tay said these results suggest a restrictive RBC transfusion strategy is non-inferior to a liberal one in patients undergoing HSCT to treat a hematologic disorder.
“Moreover, a restrictive strategy is safe and results in less blood transfusions,” he said. “We’d like to suggest that a strategy of 70 g/L can be considered the standard of care in patients undergoing a stem cell transplantation.”
*Information presented at the meeting differs from the abstract.
Potential treatment for cGVHD after steroid failure

2016 ASH Annual Meeting
SAN DIEGO—Ibrutinib, a Bruton’s tyrosine kinase inhibitor approved to treat chronic lymphocytic leukemia and other hematologic diseases, appears to provide relief for patients suffering from chronic graft-versus-host disease (cGVHD) after failing corticosteroid therapy.
At present, no approved therapy exists for these patients. Ibrutinib reduced the severity of cGVHD in preclinical models and has been used successfully in the post-allogeneic transplant setting.
The US Food and Drug Administration granted ibrutinib breakthrough therapy and orphan drug designations as a potential treatment for cGVHD.
David Miklos, MD, of Stanford University in California, explained at the 2016 ASH Annual Meeting that, in cGVHD, healthy B cells have been corrupted to produce self-reactive antibody complexes, and the T cells are killing healthy tissues and cells.
This destructive process involves the Bruton’s tyrosine kinase molecule, which can be inhibited and thereby block some of the downstream cGVHD pathogenesis.
“And to this aim, we went about testing the benefits of ibrutinib in the treatment of steroid-refractory chronic graft-versus-host disease,” Dr Miklos said.
In phase 1 of the study, investigators tested the 420 mg oral once-daily dose. They found no dose-limiting toxicities.
“So this dose was carried forward into the phase 2 study,” Dr Miklos said.
He presented results of the phase 2 study at the meeting as a late-breaking abstract (LBA-3).
Study design
Patients were eligible for the study if they had steroid-dependent or -refractory cGVHD. They had to have 3 or fewer prior treatments, and they could continue other systemic immunosuppression if they were using it.
They had to have erythematous rash on more than 25% of their body surface or a total mouth score of more than 4 as defined by National Institutes of Health (NIH) criteria.
Patients with cGVHD had to have failed frontline therapy.
They were treated with the phase 1 dose until progression of cGVHD or unacceptable toxicity.
The primary endpoint was cGVHD response per NIH 2005 response criteria.
Secondary endpoints included rate of sustained response, change in Lee cGVHD symptom scale, changes in corticosteroid requirement over time, and safety endpoints.
Investigators enrolled 42 patients, the first of whom was dosed in July 2014.
Patient demographics
Patients were a median age of 56 (range, 19–74), and 52% were male.
The median time from allogeneic transplant to the diagnosis of cGVHD was 7.6 months (range, 1.5–76.0), and the median time from initial cGVHD diagnosis to start of ibrutinib therapy was 13.7 months (range, 1.1–63.2).
Most patients had mouth (86%), skin (81%), or gastrointestinal (33%) cGVHD involvement.
And most patients had received matched (88%), unrelated (60%), nonmyeloablative (57%) peripheral blood stem cell (88%) transplants.
“This was a heavily treated patient population,” Dr Miklos said.
They had received a median of 2 (range, 1–3) prior regimens, with a median prednisone dose at enrollment of 0.3 mg/kg/day.
Prior cGVHD therapies included corticosteroids (100%), tacrolimus (50%), extracorporeal photopheresis (33%), rituximab (26%), mycophenolate mofetil (24%), cyclosporine (19%), sirolimus (17%), and other immunosuppressants (5%).
Results
The overall response rate was 67%, including 9 complete responses and 19 partial responses. Seventy-nine percent responded by the first assessment, and 71% of the 28 responders had a sustained cGVHD response of at least 5 months.
Investigators observed responses across multiple organs. Eighty percent (20/25) of patients with at least 2 involved organs at baseline responded in at least 2 organs, and 56% (5/9) of patients with 3 or more involved organs at baseline responded in at least 3 organs.
“These responses seen across all organs and in multiple organs suggest that the ibrutinib is actually targeting the underlying process of chronic GVHD and not simply masking the symptoms of chronic GVHD,” Dr Miklos noted.
Median corticosteroid use decreased throughout the ibrutinib treatment period. Twenty-six patients (62%) reduced steroid doses to less than 0.15/mg/kg/day while on ibrutinib.
Five responders discontinued all corticosteroid treatment.
Dr Miklos pointed out that baseline steroid dose did not vary between those patients who had responses and those who did not.
And ibrutinib produced clinically meaning improvement in the Lee symptom scale score among patients who responded.
Discontinuation and toxicity
At a median follow-up of 14 months, 12 patients were still on ibrutinib therapy.
“Only 5 patients discontinued for the progression of chronic GVHD,” Dr Miklos noted.
Other reasons for discontinuation included adverse events (AEs, n=14), patient decision (n=6), investigator decision (n=2), recurrence or progression of original malignancy (n=2), and noncompliance with study drug (n=1).
“The AE profile largely reflects what has been seen with ibrutinib use in the patients being treated for malignancies,” Dr Miklos said. “They also reflect adverse events that we see in patients receiving corticosteroids for the treatment of chronic GVHD.”
Treatment-emergent AEs occurring in more than 15% of patients included fatigue, diarrhea, muscle spasms, nausea, bruising, upper respiratory tract infection, pneumonia, pyrexia, headache, and fall.
Serious AEs occurred in 22 patients (52%), including pneumonia (n=6), septic shock (n=2), and pyrexia (n=2).
Two patients died while on study due to multilobular pneumonia and bronchopulmonary aspergillosis.
Exploratory endpoints
Investigators measured plasma levels of various factors following ibrutinib therapy through the first 90 days. Proinflammatory, chemotactic, and fibrotic factors decreased significantly while patients were on ibrutinib.
“This indicates that the cellular inflammation, the immune recruitment, and the fibrosis at the root of chronic GVHD was improving,” Dr Mikos said.
These factors included IFNγ, TNFα, IP-10, and CXCL9—biomarkers associated with cGVHD.
“We believe the efficacy of ibrutinib in this population supports further study in frontline treatment of chronic GVHD in a randomized, double-blinded study,” Dr Miklos concluded.
The current study was sponsored by Pharmacyclics, Inc.

2016 ASH Annual Meeting
SAN DIEGO—Ibrutinib, a Bruton’s tyrosine kinase inhibitor approved to treat chronic lymphocytic leukemia and other hematologic diseases, appears to provide relief for patients suffering from chronic graft-versus-host disease (cGVHD) after failing corticosteroid therapy.
At present, no approved therapy exists for these patients. Ibrutinib reduced the severity of cGVHD in preclinical models and has been used successfully in the post-allogeneic transplant setting.
The US Food and Drug Administration granted ibrutinib breakthrough therapy and orphan drug designations as a potential treatment for cGVHD.
David Miklos, MD, of Stanford University in California, explained at the 2016 ASH Annual Meeting that, in cGVHD, healthy B cells have been corrupted to produce self-reactive antibody complexes, and the T cells are killing healthy tissues and cells.
This destructive process involves the Bruton’s tyrosine kinase molecule, which can be inhibited and thereby block some of the downstream cGVHD pathogenesis.
“And to this aim, we went about testing the benefits of ibrutinib in the treatment of steroid-refractory chronic graft-versus-host disease,” Dr Miklos said.
In phase 1 of the study, investigators tested the 420 mg oral once-daily dose. They found no dose-limiting toxicities.
“So this dose was carried forward into the phase 2 study,” Dr Miklos said.
He presented results of the phase 2 study at the meeting as a late-breaking abstract (LBA-3).
Study design
Patients were eligible for the study if they had steroid-dependent or -refractory cGVHD. They had to have 3 or fewer prior treatments, and they could continue other systemic immunosuppression if they were using it.
They had to have erythematous rash on more than 25% of their body surface or a total mouth score of more than 4 as defined by National Institutes of Health (NIH) criteria.
Patients with cGVHD had to have failed frontline therapy.
They were treated with the phase 1 dose until progression of cGVHD or unacceptable toxicity.
The primary endpoint was cGVHD response per NIH 2005 response criteria.
Secondary endpoints included rate of sustained response, change in Lee cGVHD symptom scale, changes in corticosteroid requirement over time, and safety endpoints.
Investigators enrolled 42 patients, the first of whom was dosed in July 2014.
Patient demographics
Patients were a median age of 56 (range, 19–74), and 52% were male.
The median time from allogeneic transplant to the diagnosis of cGVHD was 7.6 months (range, 1.5–76.0), and the median time from initial cGVHD diagnosis to start of ibrutinib therapy was 13.7 months (range, 1.1–63.2).
Most patients had mouth (86%), skin (81%), or gastrointestinal (33%) cGVHD involvement.
And most patients had received matched (88%), unrelated (60%), nonmyeloablative (57%) peripheral blood stem cell (88%) transplants.
“This was a heavily treated patient population,” Dr Miklos said.
They had received a median of 2 (range, 1–3) prior regimens, with a median prednisone dose at enrollment of 0.3 mg/kg/day.
Prior cGVHD therapies included corticosteroids (100%), tacrolimus (50%), extracorporeal photopheresis (33%), rituximab (26%), mycophenolate mofetil (24%), cyclosporine (19%), sirolimus (17%), and other immunosuppressants (5%).
Results
The overall response rate was 67%, including 9 complete responses and 19 partial responses. Seventy-nine percent responded by the first assessment, and 71% of the 28 responders had a sustained cGVHD response of at least 5 months.
Investigators observed responses across multiple organs. Eighty percent (20/25) of patients with at least 2 involved organs at baseline responded in at least 2 organs, and 56% (5/9) of patients with 3 or more involved organs at baseline responded in at least 3 organs.
“These responses seen across all organs and in multiple organs suggest that the ibrutinib is actually targeting the underlying process of chronic GVHD and not simply masking the symptoms of chronic GVHD,” Dr Miklos noted.
Median corticosteroid use decreased throughout the ibrutinib treatment period. Twenty-six patients (62%) reduced steroid doses to less than 0.15/mg/kg/day while on ibrutinib.
Five responders discontinued all corticosteroid treatment.
Dr Miklos pointed out that baseline steroid dose did not vary between those patients who had responses and those who did not.
And ibrutinib produced clinically meaning improvement in the Lee symptom scale score among patients who responded.
Discontinuation and toxicity
At a median follow-up of 14 months, 12 patients were still on ibrutinib therapy.
“Only 5 patients discontinued for the progression of chronic GVHD,” Dr Miklos noted.
Other reasons for discontinuation included adverse events (AEs, n=14), patient decision (n=6), investigator decision (n=2), recurrence or progression of original malignancy (n=2), and noncompliance with study drug (n=1).
“The AE profile largely reflects what has been seen with ibrutinib use in the patients being treated for malignancies,” Dr Miklos said. “They also reflect adverse events that we see in patients receiving corticosteroids for the treatment of chronic GVHD.”
Treatment-emergent AEs occurring in more than 15% of patients included fatigue, diarrhea, muscle spasms, nausea, bruising, upper respiratory tract infection, pneumonia, pyrexia, headache, and fall.
Serious AEs occurred in 22 patients (52%), including pneumonia (n=6), septic shock (n=2), and pyrexia (n=2).
Two patients died while on study due to multilobular pneumonia and bronchopulmonary aspergillosis.
Exploratory endpoints
Investigators measured plasma levels of various factors following ibrutinib therapy through the first 90 days. Proinflammatory, chemotactic, and fibrotic factors decreased significantly while patients were on ibrutinib.
“This indicates that the cellular inflammation, the immune recruitment, and the fibrosis at the root of chronic GVHD was improving,” Dr Mikos said.
These factors included IFNγ, TNFα, IP-10, and CXCL9—biomarkers associated with cGVHD.
“We believe the efficacy of ibrutinib in this population supports further study in frontline treatment of chronic GVHD in a randomized, double-blinded study,” Dr Miklos concluded.
The current study was sponsored by Pharmacyclics, Inc.

2016 ASH Annual Meeting
SAN DIEGO—Ibrutinib, a Bruton’s tyrosine kinase inhibitor approved to treat chronic lymphocytic leukemia and other hematologic diseases, appears to provide relief for patients suffering from chronic graft-versus-host disease (cGVHD) after failing corticosteroid therapy.
At present, no approved therapy exists for these patients. Ibrutinib reduced the severity of cGVHD in preclinical models and has been used successfully in the post-allogeneic transplant setting.
The US Food and Drug Administration granted ibrutinib breakthrough therapy and orphan drug designations as a potential treatment for cGVHD.
David Miklos, MD, of Stanford University in California, explained at the 2016 ASH Annual Meeting that, in cGVHD, healthy B cells have been corrupted to produce self-reactive antibody complexes, and the T cells are killing healthy tissues and cells.
This destructive process involves the Bruton’s tyrosine kinase molecule, which can be inhibited and thereby block some of the downstream cGVHD pathogenesis.
“And to this aim, we went about testing the benefits of ibrutinib in the treatment of steroid-refractory chronic graft-versus-host disease,” Dr Miklos said.
In phase 1 of the study, investigators tested the 420 mg oral once-daily dose. They found no dose-limiting toxicities.
“So this dose was carried forward into the phase 2 study,” Dr Miklos said.
He presented results of the phase 2 study at the meeting as a late-breaking abstract (LBA-3).
Study design
Patients were eligible for the study if they had steroid-dependent or -refractory cGVHD. They had to have 3 or fewer prior treatments, and they could continue other systemic immunosuppression if they were using it.
They had to have erythematous rash on more than 25% of their body surface or a total mouth score of more than 4 as defined by National Institutes of Health (NIH) criteria.
Patients with cGVHD had to have failed frontline therapy.
They were treated with the phase 1 dose until progression of cGVHD or unacceptable toxicity.
The primary endpoint was cGVHD response per NIH 2005 response criteria.
Secondary endpoints included rate of sustained response, change in Lee cGVHD symptom scale, changes in corticosteroid requirement over time, and safety endpoints.
Investigators enrolled 42 patients, the first of whom was dosed in July 2014.
Patient demographics
Patients were a median age of 56 (range, 19–74), and 52% were male.
The median time from allogeneic transplant to the diagnosis of cGVHD was 7.6 months (range, 1.5–76.0), and the median time from initial cGVHD diagnosis to start of ibrutinib therapy was 13.7 months (range, 1.1–63.2).
Most patients had mouth (86%), skin (81%), or gastrointestinal (33%) cGVHD involvement.
And most patients had received matched (88%), unrelated (60%), nonmyeloablative (57%) peripheral blood stem cell (88%) transplants.
“This was a heavily treated patient population,” Dr Miklos said.
They had received a median of 2 (range, 1–3) prior regimens, with a median prednisone dose at enrollment of 0.3 mg/kg/day.
Prior cGVHD therapies included corticosteroids (100%), tacrolimus (50%), extracorporeal photopheresis (33%), rituximab (26%), mycophenolate mofetil (24%), cyclosporine (19%), sirolimus (17%), and other immunosuppressants (5%).
Results
The overall response rate was 67%, including 9 complete responses and 19 partial responses. Seventy-nine percent responded by the first assessment, and 71% of the 28 responders had a sustained cGVHD response of at least 5 months.
Investigators observed responses across multiple organs. Eighty percent (20/25) of patients with at least 2 involved organs at baseline responded in at least 2 organs, and 56% (5/9) of patients with 3 or more involved organs at baseline responded in at least 3 organs.
“These responses seen across all organs and in multiple organs suggest that the ibrutinib is actually targeting the underlying process of chronic GVHD and not simply masking the symptoms of chronic GVHD,” Dr Miklos noted.
Median corticosteroid use decreased throughout the ibrutinib treatment period. Twenty-six patients (62%) reduced steroid doses to less than 0.15/mg/kg/day while on ibrutinib.
Five responders discontinued all corticosteroid treatment.
Dr Miklos pointed out that baseline steroid dose did not vary between those patients who had responses and those who did not.
And ibrutinib produced clinically meaning improvement in the Lee symptom scale score among patients who responded.
Discontinuation and toxicity
At a median follow-up of 14 months, 12 patients were still on ibrutinib therapy.
“Only 5 patients discontinued for the progression of chronic GVHD,” Dr Miklos noted.
Other reasons for discontinuation included adverse events (AEs, n=14), patient decision (n=6), investigator decision (n=2), recurrence or progression of original malignancy (n=2), and noncompliance with study drug (n=1).
“The AE profile largely reflects what has been seen with ibrutinib use in the patients being treated for malignancies,” Dr Miklos said. “They also reflect adverse events that we see in patients receiving corticosteroids for the treatment of chronic GVHD.”
Treatment-emergent AEs occurring in more than 15% of patients included fatigue, diarrhea, muscle spasms, nausea, bruising, upper respiratory tract infection, pneumonia, pyrexia, headache, and fall.
Serious AEs occurred in 22 patients (52%), including pneumonia (n=6), septic shock (n=2), and pyrexia (n=2).
Two patients died while on study due to multilobular pneumonia and bronchopulmonary aspergillosis.
Exploratory endpoints
Investigators measured plasma levels of various factors following ibrutinib therapy through the first 90 days. Proinflammatory, chemotactic, and fibrotic factors decreased significantly while patients were on ibrutinib.
“This indicates that the cellular inflammation, the immune recruitment, and the fibrosis at the root of chronic GVHD was improving,” Dr Mikos said.
These factors included IFNγ, TNFα, IP-10, and CXCL9—biomarkers associated with cGVHD.
“We believe the efficacy of ibrutinib in this population supports further study in frontline treatment of chronic GVHD in a randomized, double-blinded study,” Dr Miklos concluded.
The current study was sponsored by Pharmacyclics, Inc.
Rinse could provide short-term treatment of oral cGVHD

Photo courtesy of NIH
SAN DIEGO—Results of a phase 2 study suggest an oral mouth rinse formulation of the steroid clobetasol could provide short-term treatment of oral chronic graft-vs-host disease (cGVHD).
A majority of patients had a greater than 25% improvement in their cGVHD after using the clobetasol rinse, and patients reported improvements in oral health-related quality of life.
The rinse even proved effective in patients who had failed prior treatment with clobetasol ointment.
However, researchers found evidence to suggest the clobetasol rinse is not suitable for unmonitored, long-term use, as some patients experienced adrenal suppression.
Jacqueline W. Mays, DDS, PhD, of the National Institutes of Health (NIH) in Bethesda, Maryland, presented these findings at the 2016 ASH Annual Meeting (abstract 826).
Dr Mays noted that topical therapy for oral cGVHD is intended to spare patients from exposure to systemic immunosuppressive agents.
According to NIH consensus criteria, dexamethasone is recommended as the first-line topical therapy for these patients. However, clinical trial data suggest only 29% to 58% of patients respond to this therapy.
Second-line treatment is not well-established, but it typically consists of topical steroids in a gel or ointment formulation. Unfortunately, patient compliance is an issue with this type of treatment.
“If you can imagine trying to apply something in a petrolatum base to the inside of your very wet wall cavity, you can imagine that’s a challenge for a healthy individual, much less for a chronic graft-vs-host disease patient who often will have joint mobility and fine motor issues,” Dr Mays said.
“So this leads to frequent treatment failures of topical regimens, not only due to the drug agents but also due to patient compliance.”
Dr Mays noted that clobetasol is a superpotent synthetic glucocorticoid that has been used off-label in ointment form to treat refractory oral GVHD.
In an attempt to overcome the application challenges with this ointment and improve patient adherence to oral cGVHD treatment, Dr Mays and her colleagues decided to investigate a clobetasol 0.05% solution formulated as an oral rinse in an aqueous base.
The team tested the rinse in a phase 2 trial with an initial 2-week randomized, double-blind, placebo-controlled period.
Patient population
The trial enrolled and randomized 36 patients with oral cGVHD. The patients had an Oral Mucositis Rating Scale (OMRS) score of ≥20 with moderate erythema and/or ulceration. They also had stable or tapering systemic therapy during the 2 weeks prior to starting the study and for the duration of the blinded period.
The patients’ median age was 42 (range, 18-68), and 20 were male. Thirty-five patients received ablative conditioning, 18 received a related-donor transplant, 34 received a matched-donor transplant, and 30 received a peripheral blood stem cell graft.
The median time from cGVHD diagnosis to trial enrollment was 257 days (range, 15-3013). Thirty-six patients had mouth cGVHD, 21 had skin cGVHD, 26 had eye cGVHD, 14 had gastrointestinal cGVHD, 16 had liver cGVHD, 11 had lung cGVHD, and 10 had cGVHD of the joints and fascia.
Six patients had not received any prior oral topical therapy. The other 30 patients had a median of 2 prior oral topical therapies. Eleven patients had received prior clobetasol ointment.
Treatment
The patients were randomized to receive clobetasol or placebo rinse for 2 weeks (blinded period). After that, all patients received clobetasol rinse until they completed 28 days of treatment.
The patients were required to perform a 2-minute swish with 10 ml of clobetasol rinse 3 times daily and a once-daily swish with nystatin (100,000 u/ml) rinse for antifungal prophylaxis. The patients continued on systemic pneumocystis, antiviral, and antifungal prophylaxis, per NIH cGVHD guidelines.
Thirty-two of the patients completed treatment, using the clobetasol rinse for the full 28 days.
Four patients went off study before completing 28 days of treatment. One of these patients could not tolerate the rinse. This patient had gastrointestinal issues that were attributed (by the patient and the physician) to use of the study drug.
Two patients went off study because they could not make it to the NIH for follow-up visits, and 1 patient died. The death was unrelated to the study drug.
Safety
Dr Mays noted that small amounts of clobetasol were detectable in the bloodstream, but she and her colleagues found this was not directly correlated to patient serum cortisol levels.
However, the researchers did observe a significant drop in serum cortisol levels from baseline to day 28, suggesting the rinse has an adrenal impact.
On the other hand, the peripheral lymphocyte profile was unchanged by the use of clobetasol rinse, which suggests there were no significant systemic immunosuppressive effects.
Adverse events considered possibly or probably related to clobetasol rinse included herpes simplex virus reactivation (n=3, grade 2-3), oral candidiasis (n=3, grade 2), other oral viral infection (n=1, grade 2), facial edema (n=3, grade 1), and adrenal suppression (6 grade 1 and 1 grade 2).
Dr Mays noted that many of the patients came on the study with adrenal suppression, but the clobetasol rinse had an additional impact.
Efficacy
The study’s primary endpoint was change in oral cGVHD severity scale at day 28 compared to baseline. Complete response was defined as a score of 0 on the erythema and ulceration components. Partial response was defined as a 25% decrease in score.
Progression was defined as a 25% increase in initial score. Stable disease was defined as a status that does not meet the criteria for progression or response.
Ninety-one percent of patients had a greater than 25% improvement in oral cGVHD severity scale. Nineteen percent of patients had a complete response, 72% of patients had a partial response, and 9% had stable disease. None of the patients progressed.
Dr Mays noted that patients who failed treatment with prior clobetasol ointment responded similarly to the clobetasol rinse when compared with the full study cohort.
Among the 11 patients with prior clobetasol ointment, 18% had a complete response, 73% had a partial response, 9% had stable disease, and none progressed.
Clobetasol rinse significantly decreased the clinical OMRS score (P<0.0001) and improved cGVHD pathology diagnosis (P=0.0001).
Patients reported a significant improvement in oral health-based quality of life (P=0.0008) after completing treatment, as well as significant improvements in oral pain (P=0.017) and oral sensitivity (P=0.0081).
Though saliva production did not change significantly from baseline to day 28, patients reported a significant improvement in oral dryness (P=0.014).
The blinded period of the study showed that placebo treatment was not effective. There was a significant difference between the placebo and clobetasol groups with regard to improvement in OMRS score from baseline to day 14 (P=0.0031).
“We found clobetasol oral rinse to be both effective and safe for short-term treatment of oral mucosal cGVHD and hope that it will improve sparing of systemic immunosuppressants in this patient population,” Dr Mays said. “Its risk profile is generally not suitable for unmonitored, long-term use.”

Photo courtesy of NIH
SAN DIEGO—Results of a phase 2 study suggest an oral mouth rinse formulation of the steroid clobetasol could provide short-term treatment of oral chronic graft-vs-host disease (cGVHD).
A majority of patients had a greater than 25% improvement in their cGVHD after using the clobetasol rinse, and patients reported improvements in oral health-related quality of life.
The rinse even proved effective in patients who had failed prior treatment with clobetasol ointment.
However, researchers found evidence to suggest the clobetasol rinse is not suitable for unmonitored, long-term use, as some patients experienced adrenal suppression.
Jacqueline W. Mays, DDS, PhD, of the National Institutes of Health (NIH) in Bethesda, Maryland, presented these findings at the 2016 ASH Annual Meeting (abstract 826).
Dr Mays noted that topical therapy for oral cGVHD is intended to spare patients from exposure to systemic immunosuppressive agents.
According to NIH consensus criteria, dexamethasone is recommended as the first-line topical therapy for these patients. However, clinical trial data suggest only 29% to 58% of patients respond to this therapy.
Second-line treatment is not well-established, but it typically consists of topical steroids in a gel or ointment formulation. Unfortunately, patient compliance is an issue with this type of treatment.
“If you can imagine trying to apply something in a petrolatum base to the inside of your very wet wall cavity, you can imagine that’s a challenge for a healthy individual, much less for a chronic graft-vs-host disease patient who often will have joint mobility and fine motor issues,” Dr Mays said.
“So this leads to frequent treatment failures of topical regimens, not only due to the drug agents but also due to patient compliance.”
Dr Mays noted that clobetasol is a superpotent synthetic glucocorticoid that has been used off-label in ointment form to treat refractory oral GVHD.
In an attempt to overcome the application challenges with this ointment and improve patient adherence to oral cGVHD treatment, Dr Mays and her colleagues decided to investigate a clobetasol 0.05% solution formulated as an oral rinse in an aqueous base.
The team tested the rinse in a phase 2 trial with an initial 2-week randomized, double-blind, placebo-controlled period.
Patient population
The trial enrolled and randomized 36 patients with oral cGVHD. The patients had an Oral Mucositis Rating Scale (OMRS) score of ≥20 with moderate erythema and/or ulceration. They also had stable or tapering systemic therapy during the 2 weeks prior to starting the study and for the duration of the blinded period.
The patients’ median age was 42 (range, 18-68), and 20 were male. Thirty-five patients received ablative conditioning, 18 received a related-donor transplant, 34 received a matched-donor transplant, and 30 received a peripheral blood stem cell graft.
The median time from cGVHD diagnosis to trial enrollment was 257 days (range, 15-3013). Thirty-six patients had mouth cGVHD, 21 had skin cGVHD, 26 had eye cGVHD, 14 had gastrointestinal cGVHD, 16 had liver cGVHD, 11 had lung cGVHD, and 10 had cGVHD of the joints and fascia.
Six patients had not received any prior oral topical therapy. The other 30 patients had a median of 2 prior oral topical therapies. Eleven patients had received prior clobetasol ointment.
Treatment
The patients were randomized to receive clobetasol or placebo rinse for 2 weeks (blinded period). After that, all patients received clobetasol rinse until they completed 28 days of treatment.
The patients were required to perform a 2-minute swish with 10 ml of clobetasol rinse 3 times daily and a once-daily swish with nystatin (100,000 u/ml) rinse for antifungal prophylaxis. The patients continued on systemic pneumocystis, antiviral, and antifungal prophylaxis, per NIH cGVHD guidelines.
Thirty-two of the patients completed treatment, using the clobetasol rinse for the full 28 days.
Four patients went off study before completing 28 days of treatment. One of these patients could not tolerate the rinse. This patient had gastrointestinal issues that were attributed (by the patient and the physician) to use of the study drug.
Two patients went off study because they could not make it to the NIH for follow-up visits, and 1 patient died. The death was unrelated to the study drug.
Safety
Dr Mays noted that small amounts of clobetasol were detectable in the bloodstream, but she and her colleagues found this was not directly correlated to patient serum cortisol levels.
However, the researchers did observe a significant drop in serum cortisol levels from baseline to day 28, suggesting the rinse has an adrenal impact.
On the other hand, the peripheral lymphocyte profile was unchanged by the use of clobetasol rinse, which suggests there were no significant systemic immunosuppressive effects.
Adverse events considered possibly or probably related to clobetasol rinse included herpes simplex virus reactivation (n=3, grade 2-3), oral candidiasis (n=3, grade 2), other oral viral infection (n=1, grade 2), facial edema (n=3, grade 1), and adrenal suppression (6 grade 1 and 1 grade 2).
Dr Mays noted that many of the patients came on the study with adrenal suppression, but the clobetasol rinse had an additional impact.
Efficacy
The study’s primary endpoint was change in oral cGVHD severity scale at day 28 compared to baseline. Complete response was defined as a score of 0 on the erythema and ulceration components. Partial response was defined as a 25% decrease in score.
Progression was defined as a 25% increase in initial score. Stable disease was defined as a status that does not meet the criteria for progression or response.
Ninety-one percent of patients had a greater than 25% improvement in oral cGVHD severity scale. Nineteen percent of patients had a complete response, 72% of patients had a partial response, and 9% had stable disease. None of the patients progressed.
Dr Mays noted that patients who failed treatment with prior clobetasol ointment responded similarly to the clobetasol rinse when compared with the full study cohort.
Among the 11 patients with prior clobetasol ointment, 18% had a complete response, 73% had a partial response, 9% had stable disease, and none progressed.
Clobetasol rinse significantly decreased the clinical OMRS score (P<0.0001) and improved cGVHD pathology diagnosis (P=0.0001).
Patients reported a significant improvement in oral health-based quality of life (P=0.0008) after completing treatment, as well as significant improvements in oral pain (P=0.017) and oral sensitivity (P=0.0081).
Though saliva production did not change significantly from baseline to day 28, patients reported a significant improvement in oral dryness (P=0.014).
The blinded period of the study showed that placebo treatment was not effective. There was a significant difference between the placebo and clobetasol groups with regard to improvement in OMRS score from baseline to day 14 (P=0.0031).
“We found clobetasol oral rinse to be both effective and safe for short-term treatment of oral mucosal cGVHD and hope that it will improve sparing of systemic immunosuppressants in this patient population,” Dr Mays said. “Its risk profile is generally not suitable for unmonitored, long-term use.”

Photo courtesy of NIH
SAN DIEGO—Results of a phase 2 study suggest an oral mouth rinse formulation of the steroid clobetasol could provide short-term treatment of oral chronic graft-vs-host disease (cGVHD).
A majority of patients had a greater than 25% improvement in their cGVHD after using the clobetasol rinse, and patients reported improvements in oral health-related quality of life.
The rinse even proved effective in patients who had failed prior treatment with clobetasol ointment.
However, researchers found evidence to suggest the clobetasol rinse is not suitable for unmonitored, long-term use, as some patients experienced adrenal suppression.
Jacqueline W. Mays, DDS, PhD, of the National Institutes of Health (NIH) in Bethesda, Maryland, presented these findings at the 2016 ASH Annual Meeting (abstract 826).
Dr Mays noted that topical therapy for oral cGVHD is intended to spare patients from exposure to systemic immunosuppressive agents.
According to NIH consensus criteria, dexamethasone is recommended as the first-line topical therapy for these patients. However, clinical trial data suggest only 29% to 58% of patients respond to this therapy.
Second-line treatment is not well-established, but it typically consists of topical steroids in a gel or ointment formulation. Unfortunately, patient compliance is an issue with this type of treatment.
“If you can imagine trying to apply something in a petrolatum base to the inside of your very wet wall cavity, you can imagine that’s a challenge for a healthy individual, much less for a chronic graft-vs-host disease patient who often will have joint mobility and fine motor issues,” Dr Mays said.
“So this leads to frequent treatment failures of topical regimens, not only due to the drug agents but also due to patient compliance.”
Dr Mays noted that clobetasol is a superpotent synthetic glucocorticoid that has been used off-label in ointment form to treat refractory oral GVHD.
In an attempt to overcome the application challenges with this ointment and improve patient adherence to oral cGVHD treatment, Dr Mays and her colleagues decided to investigate a clobetasol 0.05% solution formulated as an oral rinse in an aqueous base.
The team tested the rinse in a phase 2 trial with an initial 2-week randomized, double-blind, placebo-controlled period.
Patient population
The trial enrolled and randomized 36 patients with oral cGVHD. The patients had an Oral Mucositis Rating Scale (OMRS) score of ≥20 with moderate erythema and/or ulceration. They also had stable or tapering systemic therapy during the 2 weeks prior to starting the study and for the duration of the blinded period.
The patients’ median age was 42 (range, 18-68), and 20 were male. Thirty-five patients received ablative conditioning, 18 received a related-donor transplant, 34 received a matched-donor transplant, and 30 received a peripheral blood stem cell graft.
The median time from cGVHD diagnosis to trial enrollment was 257 days (range, 15-3013). Thirty-six patients had mouth cGVHD, 21 had skin cGVHD, 26 had eye cGVHD, 14 had gastrointestinal cGVHD, 16 had liver cGVHD, 11 had lung cGVHD, and 10 had cGVHD of the joints and fascia.
Six patients had not received any prior oral topical therapy. The other 30 patients had a median of 2 prior oral topical therapies. Eleven patients had received prior clobetasol ointment.
Treatment
The patients were randomized to receive clobetasol or placebo rinse for 2 weeks (blinded period). After that, all patients received clobetasol rinse until they completed 28 days of treatment.
The patients were required to perform a 2-minute swish with 10 ml of clobetasol rinse 3 times daily and a once-daily swish with nystatin (100,000 u/ml) rinse for antifungal prophylaxis. The patients continued on systemic pneumocystis, antiviral, and antifungal prophylaxis, per NIH cGVHD guidelines.
Thirty-two of the patients completed treatment, using the clobetasol rinse for the full 28 days.
Four patients went off study before completing 28 days of treatment. One of these patients could not tolerate the rinse. This patient had gastrointestinal issues that were attributed (by the patient and the physician) to use of the study drug.
Two patients went off study because they could not make it to the NIH for follow-up visits, and 1 patient died. The death was unrelated to the study drug.
Safety
Dr Mays noted that small amounts of clobetasol were detectable in the bloodstream, but she and her colleagues found this was not directly correlated to patient serum cortisol levels.
However, the researchers did observe a significant drop in serum cortisol levels from baseline to day 28, suggesting the rinse has an adrenal impact.
On the other hand, the peripheral lymphocyte profile was unchanged by the use of clobetasol rinse, which suggests there were no significant systemic immunosuppressive effects.
Adverse events considered possibly or probably related to clobetasol rinse included herpes simplex virus reactivation (n=3, grade 2-3), oral candidiasis (n=3, grade 2), other oral viral infection (n=1, grade 2), facial edema (n=3, grade 1), and adrenal suppression (6 grade 1 and 1 grade 2).
Dr Mays noted that many of the patients came on the study with adrenal suppression, but the clobetasol rinse had an additional impact.
Efficacy
The study’s primary endpoint was change in oral cGVHD severity scale at day 28 compared to baseline. Complete response was defined as a score of 0 on the erythema and ulceration components. Partial response was defined as a 25% decrease in score.
Progression was defined as a 25% increase in initial score. Stable disease was defined as a status that does not meet the criteria for progression or response.
Ninety-one percent of patients had a greater than 25% improvement in oral cGVHD severity scale. Nineteen percent of patients had a complete response, 72% of patients had a partial response, and 9% had stable disease. None of the patients progressed.
Dr Mays noted that patients who failed treatment with prior clobetasol ointment responded similarly to the clobetasol rinse when compared with the full study cohort.
Among the 11 patients with prior clobetasol ointment, 18% had a complete response, 73% had a partial response, 9% had stable disease, and none progressed.
Clobetasol rinse significantly decreased the clinical OMRS score (P<0.0001) and improved cGVHD pathology diagnosis (P=0.0001).
Patients reported a significant improvement in oral health-based quality of life (P=0.0008) after completing treatment, as well as significant improvements in oral pain (P=0.017) and oral sensitivity (P=0.0081).
Though saliva production did not change significantly from baseline to day 28, patients reported a significant improvement in oral dryness (P=0.014).
The blinded period of the study showed that placebo treatment was not effective. There was a significant difference between the placebo and clobetasol groups with regard to improvement in OMRS score from baseline to day 14 (P=0.0031).
“We found clobetasol oral rinse to be both effective and safe for short-term treatment of oral mucosal cGVHD and hope that it will improve sparing of systemic immunosuppressants in this patient population,” Dr Mays said. “Its risk profile is generally not suitable for unmonitored, long-term use.”