User login
CMV matching improves survival in HSCT recipients
Matching the cytomegalovirus (CMV) status of the donor and recipient of a hematopoietic stem cell transplant (HSCT) can significantly improve the recipient’s survival, according to a study published in Bone Marrow Transplantation.
In fact, researchers said they found evidence to suggest that CMV matching may abrogate the effect of a human leukocyte antigen (HLA) mismatch.
“This breakthrough will help us discover new and more effective ways to make sure patients in need of a transplant get the best possible match to cure blood cancer and blood disorders,” said study author Steven Marsh, PhD, of Anthony Nolan Research Institute, Royal Free Hospital in London, UK.
Dr Marsh and his colleagues studied 1271 patients who received T-cell-depleted grafts to treat a hematologic disorder, including acute or chronic leukemia, lymphoma, myeloma, myelodysplasia, and “other” disorders.
The 5-year overall survival in these patients was 40.6%.
The researchers found HSCT recipients with a 10/10 HLA-matched donor had significantly better overall survival (OS) and lower non-relapse mortality (NRM) than patients with a mismatched donor.
The 5-year OS was 43.1% for a 10/10 match, 35.6% for a 9/10 match, and 28.4% for a match less than 9/10 (P=0.001). NRM at 1 year was 20.3%, 26.0%, and 33.4%, respectively (P=0.007).
Similarly, HSCT recipients with a CMV-matched donor had significantly better OS and significantly lower NRM than recipients with a CMV-mismatched donor.
The 5-year OS was 44.1% for recipients with a CMV-matched donor and 32.2% for patients with a mismatched donor (P<0.001). NRM at 1 year was 19.1% and 30.4%, respectively (P<0.001)
Most of the associations between CMV/HLA matching and OS/NRM remained significant in multivariate analyses.
For recipients with more than 1 HLA mismatch, the relative risk (RR) of death was 1.43 (P=0.016), and the RR for NRM was 1.59 (P=0.028), when compared to patients who had received a 10/10 HLA-matched graft.
For recipients with a single mismatch, the RR for death was 1.21 (P=0.042), and the RR for NRM was 1.24 (P=0.14).
For recipients with a CMV mismatched donor, the RR for death was 1.40 (P<0.001), and the RR for NRM was 1.63 (P<0.001).
The researchers also assessed CMV and HLA status together. Compared to fully HLA-matched and CMV-matched recipients, the RRs for death were:
- 1.36 (P=0.003) for HLA matched/CMV mismatched
- 1.22 (P=0.062) for HLA mismatched/CMV matched
- 1.81 (P=0.001) for HLA and CMV mismatched.
The researchers said these results suggest it is possible to improve survival rates for patients with no HLA-matched donor by matching the CMV status of the donor and recipient.
As a result of the findings, experts at Anthony Nolan are exploring how to type donors for CMV when joining the stem cell donor register to allow CMV status to be taken into account when transplant centers are selecting potential donors for a patient.
“[B]y establishing that CMV matching has a significant impact on patient outcomes, we are making it easier for transplant centers to make informed choices about the donors they select for their patients,” Dr Marsh said. ![]()
Matching the cytomegalovirus (CMV) status of the donor and recipient of a hematopoietic stem cell transplant (HSCT) can significantly improve the recipient’s survival, according to a study published in Bone Marrow Transplantation.
In fact, researchers said they found evidence to suggest that CMV matching may abrogate the effect of a human leukocyte antigen (HLA) mismatch.
“This breakthrough will help us discover new and more effective ways to make sure patients in need of a transplant get the best possible match to cure blood cancer and blood disorders,” said study author Steven Marsh, PhD, of Anthony Nolan Research Institute, Royal Free Hospital in London, UK.
Dr Marsh and his colleagues studied 1271 patients who received T-cell-depleted grafts to treat a hematologic disorder, including acute or chronic leukemia, lymphoma, myeloma, myelodysplasia, and “other” disorders.
The 5-year overall survival in these patients was 40.6%.
The researchers found HSCT recipients with a 10/10 HLA-matched donor had significantly better overall survival (OS) and lower non-relapse mortality (NRM) than patients with a mismatched donor.
The 5-year OS was 43.1% for a 10/10 match, 35.6% for a 9/10 match, and 28.4% for a match less than 9/10 (P=0.001). NRM at 1 year was 20.3%, 26.0%, and 33.4%, respectively (P=0.007).
Similarly, HSCT recipients with a CMV-matched donor had significantly better OS and significantly lower NRM than recipients with a CMV-mismatched donor.
The 5-year OS was 44.1% for recipients with a CMV-matched donor and 32.2% for patients with a mismatched donor (P<0.001). NRM at 1 year was 19.1% and 30.4%, respectively (P<0.001)
Most of the associations between CMV/HLA matching and OS/NRM remained significant in multivariate analyses.
For recipients with more than 1 HLA mismatch, the relative risk (RR) of death was 1.43 (P=0.016), and the RR for NRM was 1.59 (P=0.028), when compared to patients who had received a 10/10 HLA-matched graft.
For recipients with a single mismatch, the RR for death was 1.21 (P=0.042), and the RR for NRM was 1.24 (P=0.14).
For recipients with a CMV mismatched donor, the RR for death was 1.40 (P<0.001), and the RR for NRM was 1.63 (P<0.001).
The researchers also assessed CMV and HLA status together. Compared to fully HLA-matched and CMV-matched recipients, the RRs for death were:
- 1.36 (P=0.003) for HLA matched/CMV mismatched
- 1.22 (P=0.062) for HLA mismatched/CMV matched
- 1.81 (P=0.001) for HLA and CMV mismatched.
The researchers said these results suggest it is possible to improve survival rates for patients with no HLA-matched donor by matching the CMV status of the donor and recipient.
As a result of the findings, experts at Anthony Nolan are exploring how to type donors for CMV when joining the stem cell donor register to allow CMV status to be taken into account when transplant centers are selecting potential donors for a patient.
“[B]y establishing that CMV matching has a significant impact on patient outcomes, we are making it easier for transplant centers to make informed choices about the donors they select for their patients,” Dr Marsh said. ![]()
Matching the cytomegalovirus (CMV) status of the donor and recipient of a hematopoietic stem cell transplant (HSCT) can significantly improve the recipient’s survival, according to a study published in Bone Marrow Transplantation.
In fact, researchers said they found evidence to suggest that CMV matching may abrogate the effect of a human leukocyte antigen (HLA) mismatch.
“This breakthrough will help us discover new and more effective ways to make sure patients in need of a transplant get the best possible match to cure blood cancer and blood disorders,” said study author Steven Marsh, PhD, of Anthony Nolan Research Institute, Royal Free Hospital in London, UK.
Dr Marsh and his colleagues studied 1271 patients who received T-cell-depleted grafts to treat a hematologic disorder, including acute or chronic leukemia, lymphoma, myeloma, myelodysplasia, and “other” disorders.
The 5-year overall survival in these patients was 40.6%.
The researchers found HSCT recipients with a 10/10 HLA-matched donor had significantly better overall survival (OS) and lower non-relapse mortality (NRM) than patients with a mismatched donor.
The 5-year OS was 43.1% for a 10/10 match, 35.6% for a 9/10 match, and 28.4% for a match less than 9/10 (P=0.001). NRM at 1 year was 20.3%, 26.0%, and 33.4%, respectively (P=0.007).
Similarly, HSCT recipients with a CMV-matched donor had significantly better OS and significantly lower NRM than recipients with a CMV-mismatched donor.
The 5-year OS was 44.1% for recipients with a CMV-matched donor and 32.2% for patients with a mismatched donor (P<0.001). NRM at 1 year was 19.1% and 30.4%, respectively (P<0.001)
Most of the associations between CMV/HLA matching and OS/NRM remained significant in multivariate analyses.
For recipients with more than 1 HLA mismatch, the relative risk (RR) of death was 1.43 (P=0.016), and the RR for NRM was 1.59 (P=0.028), when compared to patients who had received a 10/10 HLA-matched graft.
For recipients with a single mismatch, the RR for death was 1.21 (P=0.042), and the RR for NRM was 1.24 (P=0.14).
For recipients with a CMV mismatched donor, the RR for death was 1.40 (P<0.001), and the RR for NRM was 1.63 (P<0.001).
The researchers also assessed CMV and HLA status together. Compared to fully HLA-matched and CMV-matched recipients, the RRs for death were:
- 1.36 (P=0.003) for HLA matched/CMV mismatched
- 1.22 (P=0.062) for HLA mismatched/CMV matched
- 1.81 (P=0.001) for HLA and CMV mismatched.
The researchers said these results suggest it is possible to improve survival rates for patients with no HLA-matched donor by matching the CMV status of the donor and recipient.
As a result of the findings, experts at Anthony Nolan are exploring how to type donors for CMV when joining the stem cell donor register to allow CMV status to be taken into account when transplant centers are selecting potential donors for a patient.
“[B]y establishing that CMV matching has a significant impact on patient outcomes, we are making it easier for transplant centers to make informed choices about the donors they select for their patients,” Dr Marsh said. ![]()
Engineered bone marrow could make transplants safer
Engineers say they have developed biomimetic bone tissues that could one day provide new bone marrow for patients requiring transplants.
The team created bone tissues with functional bone marrow that can be filled with donor cells and implanted under the skin of mice.
The implant gives donor cells their own space to live and grow without competition, eliminating the need for a conditioning regimen to wipe out the host’s pre-existing cells prior to transplant.
“We’ve made an accessory bone that can separately accommodate donor cells,” explained Shyni Varghese, PhD, of the University of California, San Diego.
“This way, we can keep the host cells and bypass irradiation.”
In mice that received the engineered bone tissue, donor hematopoietic cells survived for at least 6 months and supplied the mice with new blood cells.
“In the future, our work could contribute to improved therapies for bone marrow disease,” said Yu-Ru Vernon Shih, PhD, a researcher in Dr Varghese’s lab.
The researchers noted that these implants would be limited to patients with non-malignant bone marrow diseases, such as aplastic anemia, where there aren’t any cancerous cells that need to be eliminated prior to transplant.
The team described their bone tissue implants in PNAS.
The implants mimic the structure of long bones in the body, consisting of an outer bone compartment and an inner marrow compartment.
The implants are made of a porous hydrogel matrix. The outer matrix contains calcium phosphate minerals. Stem cells grown in this mineralized matrix differentiate into bone-building cells. The inner matrix houses donor stem cells that produce blood cells.
When implanted beneath the skin of mice, the structures matured into bone tissues that have a working blood vessel network and a bone marrow that supplies new blood cells.
After 4 weeks, the implanted marrow contained a mix of host and donor blood cells. This mix was still circulating in the bloodstream after 24 weeks.
The researchers said these findings suggest the implanted marrow is functional, donor cells can grow and survive for long time periods in the presence of host cells, and host and donor cells can travel between the implanted marrow and the host’s circulating blood via the blood vessel network formed in the implanted bone tissue.
In another set of experiments, the researchers took hematopoietic stem cells from the implanted marrow and transplanted them into a second group of mice that had their stem cells destroyed by radiation and drugs. The team found the transplanted cells had diffused into the bloodstream of these mice.
“We did these experiments to show that the bone marrow cells from the engineered bone tissues function similar to native bone,” Dr Shih said.
“We’re working on making this a platform to generate more bone marrow stem cells,” Dr Varghese added. “That would have useful applications for cell transplantations in the clinic.” ![]()
Engineers say they have developed biomimetic bone tissues that could one day provide new bone marrow for patients requiring transplants.
The team created bone tissues with functional bone marrow that can be filled with donor cells and implanted under the skin of mice.
The implant gives donor cells their own space to live and grow without competition, eliminating the need for a conditioning regimen to wipe out the host’s pre-existing cells prior to transplant.
“We’ve made an accessory bone that can separately accommodate donor cells,” explained Shyni Varghese, PhD, of the University of California, San Diego.
“This way, we can keep the host cells and bypass irradiation.”
In mice that received the engineered bone tissue, donor hematopoietic cells survived for at least 6 months and supplied the mice with new blood cells.
“In the future, our work could contribute to improved therapies for bone marrow disease,” said Yu-Ru Vernon Shih, PhD, a researcher in Dr Varghese’s lab.
The researchers noted that these implants would be limited to patients with non-malignant bone marrow diseases, such as aplastic anemia, where there aren’t any cancerous cells that need to be eliminated prior to transplant.
The team described their bone tissue implants in PNAS.
The implants mimic the structure of long bones in the body, consisting of an outer bone compartment and an inner marrow compartment.
The implants are made of a porous hydrogel matrix. The outer matrix contains calcium phosphate minerals. Stem cells grown in this mineralized matrix differentiate into bone-building cells. The inner matrix houses donor stem cells that produce blood cells.
When implanted beneath the skin of mice, the structures matured into bone tissues that have a working blood vessel network and a bone marrow that supplies new blood cells.
After 4 weeks, the implanted marrow contained a mix of host and donor blood cells. This mix was still circulating in the bloodstream after 24 weeks.
The researchers said these findings suggest the implanted marrow is functional, donor cells can grow and survive for long time periods in the presence of host cells, and host and donor cells can travel between the implanted marrow and the host’s circulating blood via the blood vessel network formed in the implanted bone tissue.
In another set of experiments, the researchers took hematopoietic stem cells from the implanted marrow and transplanted them into a second group of mice that had their stem cells destroyed by radiation and drugs. The team found the transplanted cells had diffused into the bloodstream of these mice.
“We did these experiments to show that the bone marrow cells from the engineered bone tissues function similar to native bone,” Dr Shih said.
“We’re working on making this a platform to generate more bone marrow stem cells,” Dr Varghese added. “That would have useful applications for cell transplantations in the clinic.” ![]()
Engineers say they have developed biomimetic bone tissues that could one day provide new bone marrow for patients requiring transplants.
The team created bone tissues with functional bone marrow that can be filled with donor cells and implanted under the skin of mice.
The implant gives donor cells their own space to live and grow without competition, eliminating the need for a conditioning regimen to wipe out the host’s pre-existing cells prior to transplant.
“We’ve made an accessory bone that can separately accommodate donor cells,” explained Shyni Varghese, PhD, of the University of California, San Diego.
“This way, we can keep the host cells and bypass irradiation.”
In mice that received the engineered bone tissue, donor hematopoietic cells survived for at least 6 months and supplied the mice with new blood cells.
“In the future, our work could contribute to improved therapies for bone marrow disease,” said Yu-Ru Vernon Shih, PhD, a researcher in Dr Varghese’s lab.
The researchers noted that these implants would be limited to patients with non-malignant bone marrow diseases, such as aplastic anemia, where there aren’t any cancerous cells that need to be eliminated prior to transplant.
The team described their bone tissue implants in PNAS.
The implants mimic the structure of long bones in the body, consisting of an outer bone compartment and an inner marrow compartment.
The implants are made of a porous hydrogel matrix. The outer matrix contains calcium phosphate minerals. Stem cells grown in this mineralized matrix differentiate into bone-building cells. The inner matrix houses donor stem cells that produce blood cells.
When implanted beneath the skin of mice, the structures matured into bone tissues that have a working blood vessel network and a bone marrow that supplies new blood cells.
After 4 weeks, the implanted marrow contained a mix of host and donor blood cells. This mix was still circulating in the bloodstream after 24 weeks.
The researchers said these findings suggest the implanted marrow is functional, donor cells can grow and survive for long time periods in the presence of host cells, and host and donor cells can travel between the implanted marrow and the host’s circulating blood via the blood vessel network formed in the implanted bone tissue.
In another set of experiments, the researchers took hematopoietic stem cells from the implanted marrow and transplanted them into a second group of mice that had their stem cells destroyed by radiation and drugs. The team found the transplanted cells had diffused into the bloodstream of these mice.
“We did these experiments to show that the bone marrow cells from the engineered bone tissues function similar to native bone,” Dr Shih said.
“We’re working on making this a platform to generate more bone marrow stem cells,” Dr Varghese added. “That would have useful applications for cell transplantations in the clinic.” ![]()
Study shows similar outcomes with RIC and MAC in MDS
Results of a phase 3 trial revealed similar outcomes in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) to treat myelodysplastic syndromes (MDS), regardless of the conditioning regimen they received.
Rates of engraftment, graft-vs-host disease (GVHD), relapse, and survival were similar between patients who received reduced-intensity conditioning (RIC) and those who received standard myeloablative conditioning (MAC) before HSCT.
Researchers reported these results in the Journal of Clinical Oncology.
“Our study shed new light on expected benefits of a reduced-intensity conditioning regimen that can be offered as a curative treatment approach, especially in older patients with MDS,” said study author Nicolaus Kröger, MD, of University Hospital Eppendorf in Hamburg, Germany.
Patient characteristics
The study, known as RICMAC, involved 129 patients who underwent HSCT between May 2004 and December 2012 at 18 transplant units in 7 countries.
Patients were randomized in a 1:1 ratio to RIC (n=65) or MAC (n=64) and were stratified according to donor type, age, and blast count.
The median age was 50 (range, 19-64) in the MAC arm and 51 (range, 22-63) in the RIC arm. The median blast percentage was 4% (range, 0-18) and 5% (range, 0-18), respectively.
According to IPSS, most patients in both arms had intermediate-I-risk disease (28 MAC, 25 RIC) or intermediate-II-risk disease (18 MAC, 24 RIC).
Similar numbers of patients in each arm had low cytogenetic risk (24 MAC, 28 RIC), intermediate cytogenetic risk (17 MAC, 13 RIC), and high cytogenetic risk (17 MAC, 18 RIC).
Thirty-three patients in the MAC arm and 32 in the RIC arm received ATG as GVHD prophylaxis.
Patients received grafts from matched related donors (17 MAC, 16 RIC), matched unrelated donors (36 MAC, 38 RIC), or mismatched related/unrelated donors (11 in both arms).
Most patients received peripheral blood stem cell grafts—61 in the MAC arm and 59 in the RIC arm.
Results
The researchers said engraftment was comparable between the arms. There were 4 graft failures in the MAC arm and 3 in the RIC arm (P=0.72). The median time to leukocyte engraftment was 15 days in both arms. The median time to platelet engraftment was 15 days in the RIC arm and 16 in the MAC arm (P=0.33).
There was no significant difference in the cumulative incidence of GVHD between the RIC and MAC arms:
- Grade 2-4 acute GVHD—32.3% and 37.5%, respectively
- Grade 3-4 acute GVHD—15% and 14%, respectively (P=0.35 for between-arm difference for all acute GVHD)
- Chronic GVHD—61.6% and 64.7%, respectively (P=0.76).
Though the occurrence of infection was similar between the MAC and RIC arms (48 and 44, respectively), the rate of infection was higher in the MAC arm than the RIC arm.
The rate of infection in the first 100 days was 6.9 per 100 person-years in the MAC arm and 4.3 in the RIC arm (P=0.002). The rate of infection during the total follow-up was 2.0 per 100 person-years in the MAC arm and 1.4 in the RIC arm (P=0.002).
There was no significant difference between the RIC and MAC arms with regard to the cumulative incidence of nonrelapse mortality after 1 year—16.9% and 25.3%, respectively (P=0.29).
And there was no significant difference in the cumulative incidence of relapse at 2 years—17% and 14.8%, respectively (P=0.6).
The 2-year relapse-free survival rate was similar in the MAC and RIC arms—58.3% and 62.4% (P=0.58)—as was the 2-year overall survival rate—63.2% and 76.3%, respectively (P=0.08). ![]()
Results of a phase 3 trial revealed similar outcomes in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) to treat myelodysplastic syndromes (MDS), regardless of the conditioning regimen they received.
Rates of engraftment, graft-vs-host disease (GVHD), relapse, and survival were similar between patients who received reduced-intensity conditioning (RIC) and those who received standard myeloablative conditioning (MAC) before HSCT.
Researchers reported these results in the Journal of Clinical Oncology.
“Our study shed new light on expected benefits of a reduced-intensity conditioning regimen that can be offered as a curative treatment approach, especially in older patients with MDS,” said study author Nicolaus Kröger, MD, of University Hospital Eppendorf in Hamburg, Germany.
Patient characteristics
The study, known as RICMAC, involved 129 patients who underwent HSCT between May 2004 and December 2012 at 18 transplant units in 7 countries.
Patients were randomized in a 1:1 ratio to RIC (n=65) or MAC (n=64) and were stratified according to donor type, age, and blast count.
The median age was 50 (range, 19-64) in the MAC arm and 51 (range, 22-63) in the RIC arm. The median blast percentage was 4% (range, 0-18) and 5% (range, 0-18), respectively.
According to IPSS, most patients in both arms had intermediate-I-risk disease (28 MAC, 25 RIC) or intermediate-II-risk disease (18 MAC, 24 RIC).
Similar numbers of patients in each arm had low cytogenetic risk (24 MAC, 28 RIC), intermediate cytogenetic risk (17 MAC, 13 RIC), and high cytogenetic risk (17 MAC, 18 RIC).
Thirty-three patients in the MAC arm and 32 in the RIC arm received ATG as GVHD prophylaxis.
Patients received grafts from matched related donors (17 MAC, 16 RIC), matched unrelated donors (36 MAC, 38 RIC), or mismatched related/unrelated donors (11 in both arms).
Most patients received peripheral blood stem cell grafts—61 in the MAC arm and 59 in the RIC arm.
Results
The researchers said engraftment was comparable between the arms. There were 4 graft failures in the MAC arm and 3 in the RIC arm (P=0.72). The median time to leukocyte engraftment was 15 days in both arms. The median time to platelet engraftment was 15 days in the RIC arm and 16 in the MAC arm (P=0.33).
There was no significant difference in the cumulative incidence of GVHD between the RIC and MAC arms:
- Grade 2-4 acute GVHD—32.3% and 37.5%, respectively
- Grade 3-4 acute GVHD—15% and 14%, respectively (P=0.35 for between-arm difference for all acute GVHD)
- Chronic GVHD—61.6% and 64.7%, respectively (P=0.76).
Though the occurrence of infection was similar between the MAC and RIC arms (48 and 44, respectively), the rate of infection was higher in the MAC arm than the RIC arm.
The rate of infection in the first 100 days was 6.9 per 100 person-years in the MAC arm and 4.3 in the RIC arm (P=0.002). The rate of infection during the total follow-up was 2.0 per 100 person-years in the MAC arm and 1.4 in the RIC arm (P=0.002).
There was no significant difference between the RIC and MAC arms with regard to the cumulative incidence of nonrelapse mortality after 1 year—16.9% and 25.3%, respectively (P=0.29).
And there was no significant difference in the cumulative incidence of relapse at 2 years—17% and 14.8%, respectively (P=0.6).
The 2-year relapse-free survival rate was similar in the MAC and RIC arms—58.3% and 62.4% (P=0.58)—as was the 2-year overall survival rate—63.2% and 76.3%, respectively (P=0.08). ![]()
Results of a phase 3 trial revealed similar outcomes in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) to treat myelodysplastic syndromes (MDS), regardless of the conditioning regimen they received.
Rates of engraftment, graft-vs-host disease (GVHD), relapse, and survival were similar between patients who received reduced-intensity conditioning (RIC) and those who received standard myeloablative conditioning (MAC) before HSCT.
Researchers reported these results in the Journal of Clinical Oncology.
“Our study shed new light on expected benefits of a reduced-intensity conditioning regimen that can be offered as a curative treatment approach, especially in older patients with MDS,” said study author Nicolaus Kröger, MD, of University Hospital Eppendorf in Hamburg, Germany.
Patient characteristics
The study, known as RICMAC, involved 129 patients who underwent HSCT between May 2004 and December 2012 at 18 transplant units in 7 countries.
Patients were randomized in a 1:1 ratio to RIC (n=65) or MAC (n=64) and were stratified according to donor type, age, and blast count.
The median age was 50 (range, 19-64) in the MAC arm and 51 (range, 22-63) in the RIC arm. The median blast percentage was 4% (range, 0-18) and 5% (range, 0-18), respectively.
According to IPSS, most patients in both arms had intermediate-I-risk disease (28 MAC, 25 RIC) or intermediate-II-risk disease (18 MAC, 24 RIC).
Similar numbers of patients in each arm had low cytogenetic risk (24 MAC, 28 RIC), intermediate cytogenetic risk (17 MAC, 13 RIC), and high cytogenetic risk (17 MAC, 18 RIC).
Thirty-three patients in the MAC arm and 32 in the RIC arm received ATG as GVHD prophylaxis.
Patients received grafts from matched related donors (17 MAC, 16 RIC), matched unrelated donors (36 MAC, 38 RIC), or mismatched related/unrelated donors (11 in both arms).
Most patients received peripheral blood stem cell grafts—61 in the MAC arm and 59 in the RIC arm.
Results
The researchers said engraftment was comparable between the arms. There were 4 graft failures in the MAC arm and 3 in the RIC arm (P=0.72). The median time to leukocyte engraftment was 15 days in both arms. The median time to platelet engraftment was 15 days in the RIC arm and 16 in the MAC arm (P=0.33).
There was no significant difference in the cumulative incidence of GVHD between the RIC and MAC arms:
- Grade 2-4 acute GVHD—32.3% and 37.5%, respectively
- Grade 3-4 acute GVHD—15% and 14%, respectively (P=0.35 for between-arm difference for all acute GVHD)
- Chronic GVHD—61.6% and 64.7%, respectively (P=0.76).
Though the occurrence of infection was similar between the MAC and RIC arms (48 and 44, respectively), the rate of infection was higher in the MAC arm than the RIC arm.
The rate of infection in the first 100 days was 6.9 per 100 person-years in the MAC arm and 4.3 in the RIC arm (P=0.002). The rate of infection during the total follow-up was 2.0 per 100 person-years in the MAC arm and 1.4 in the RIC arm (P=0.002).
There was no significant difference between the RIC and MAC arms with regard to the cumulative incidence of nonrelapse mortality after 1 year—16.9% and 25.3%, respectively (P=0.29).
And there was no significant difference in the cumulative incidence of relapse at 2 years—17% and 14.8%, respectively (P=0.6).
The 2-year relapse-free survival rate was similar in the MAC and RIC arms—58.3% and 62.4% (P=0.58)—as was the 2-year overall survival rate—63.2% and 76.3%, respectively (P=0.08). ![]()
Cord blood product bests standard UCB transplant
The expanded umbilical cord blood (UCB) product NiCord can provide benefits over standard UCB transplant, according to research published in Biology of Blood and Marrow Transplantation.
NiCord is a stand-alone graft derived from a single UCB unit that has been expanded in culture and enriched with stem and progenitor cells.
The study showed that patients transplanted with NiCord had shorter time to engraftment, a lower risk of infection, and shorter hospital stays than patients who received standard UCB transplants.
On the other hand, there was no significant difference between the transplant groups when it came to grade 2-4 acute graft-versus-host disease (GVHD), relapse, or survival within 100 days of transplant.
“Our results indicate that rapid hematopoietic recovery from Gamida Cell’s NiCord transplantation approach is associated with clinical benefit,” said study author Mitchell Horwitz, MD, of Duke University School of Medicine in Durham, North Carolina.
Dr Horwitz receives research support from Gamida Cell Ltd., makers of NiCord.
Patient characteristics
The researchers compared 18 consecutive NiCord-transplanted patients and 86 consecutive patients who received standard UCB transplants. All of the patients received total body irradiation-based myeloablative conditioning.
In both arms, most patients received a double transplant. In the NiCord arm, 61.1% of patients (n=11) received NiCord along with a second unmanipulated UCB unit. In the standard UCB arm, 95.3% of patients (n=82) received a double UCB transplant.
Patients in the NiCord arm were older than patients in the standard UCB arm, with median ages of 45.5 (range, 42-57) and 37.5 (range, 28-51), respectively.
Most patients in both arms had acute leukemia or myelodysplastic syndromes (about 89%), although roughly 11% had lymphoid malignancies.
There were no significant differences between the arms when it came to patient sex, pre-transplant weight, cytomegalovirus serostatus, and Karnofsky Performance Status.
Results
The median time to neutrophil engraftment was 12.5 days (range, 10-18) in the NiCord arm and 27 days (range, 23-28) in the standard UCB arm (P<0.001).
All of the patients studied had at least 1 infection of any severity. However, patients in the NiCord arm had a significantly lower risk of infection than patients in the standard UCB arm.
In an analysis adjusted for age, disease stage, and grade 2-4 acute GVHD, the risk ratios (RRs) for NiCord versus standard UCB transplant were as follows:
- Total infection—RR=0.72, P=0.03
- Grade 2-3 infection—RR=0.38, P=0.001
- Bacterial infection—RR=0.42, P=0.008
- Grade 2-3 bacterial infection—RR=0.23, P=0.006.
Patients in the NiCord arm spent a mean of 72.4 days out of the hospital in the first 100 days after transplant, compared to 48.6 days for the standard UCB arm (P=0.001).
After the researchers adjusted for age and Karnofsky Performance Status, patients in the NiCord arm had a mean of 20.2 more days out of the hospital than their peers who received standard UCB (P=0.005).
The incidence of grade 2-4 acute GHVD was 55.6% in the NiCord arm and 41.9% in the standard UCB arm (P=0.31). The rate of second transplant was 5.6% and 11.6%, respectively (P=0.68).
The rate of relapse was 0% in the NiCord arm and 7% in the standard UCB arm (P=0.59). And the rate of death was 5.6% and 16.3%, respectively (P=0.46). ![]()
The expanded umbilical cord blood (UCB) product NiCord can provide benefits over standard UCB transplant, according to research published in Biology of Blood and Marrow Transplantation.
NiCord is a stand-alone graft derived from a single UCB unit that has been expanded in culture and enriched with stem and progenitor cells.
The study showed that patients transplanted with NiCord had shorter time to engraftment, a lower risk of infection, and shorter hospital stays than patients who received standard UCB transplants.
On the other hand, there was no significant difference between the transplant groups when it came to grade 2-4 acute graft-versus-host disease (GVHD), relapse, or survival within 100 days of transplant.
“Our results indicate that rapid hematopoietic recovery from Gamida Cell’s NiCord transplantation approach is associated with clinical benefit,” said study author Mitchell Horwitz, MD, of Duke University School of Medicine in Durham, North Carolina.
Dr Horwitz receives research support from Gamida Cell Ltd., makers of NiCord.
Patient characteristics
The researchers compared 18 consecutive NiCord-transplanted patients and 86 consecutive patients who received standard UCB transplants. All of the patients received total body irradiation-based myeloablative conditioning.
In both arms, most patients received a double transplant. In the NiCord arm, 61.1% of patients (n=11) received NiCord along with a second unmanipulated UCB unit. In the standard UCB arm, 95.3% of patients (n=82) received a double UCB transplant.
Patients in the NiCord arm were older than patients in the standard UCB arm, with median ages of 45.5 (range, 42-57) and 37.5 (range, 28-51), respectively.
Most patients in both arms had acute leukemia or myelodysplastic syndromes (about 89%), although roughly 11% had lymphoid malignancies.
There were no significant differences between the arms when it came to patient sex, pre-transplant weight, cytomegalovirus serostatus, and Karnofsky Performance Status.
Results
The median time to neutrophil engraftment was 12.5 days (range, 10-18) in the NiCord arm and 27 days (range, 23-28) in the standard UCB arm (P<0.001).
All of the patients studied had at least 1 infection of any severity. However, patients in the NiCord arm had a significantly lower risk of infection than patients in the standard UCB arm.
In an analysis adjusted for age, disease stage, and grade 2-4 acute GVHD, the risk ratios (RRs) for NiCord versus standard UCB transplant were as follows:
- Total infection—RR=0.72, P=0.03
- Grade 2-3 infection—RR=0.38, P=0.001
- Bacterial infection—RR=0.42, P=0.008
- Grade 2-3 bacterial infection—RR=0.23, P=0.006.
Patients in the NiCord arm spent a mean of 72.4 days out of the hospital in the first 100 days after transplant, compared to 48.6 days for the standard UCB arm (P=0.001).
After the researchers adjusted for age and Karnofsky Performance Status, patients in the NiCord arm had a mean of 20.2 more days out of the hospital than their peers who received standard UCB (P=0.005).
The incidence of grade 2-4 acute GHVD was 55.6% in the NiCord arm and 41.9% in the standard UCB arm (P=0.31). The rate of second transplant was 5.6% and 11.6%, respectively (P=0.68).
The rate of relapse was 0% in the NiCord arm and 7% in the standard UCB arm (P=0.59). And the rate of death was 5.6% and 16.3%, respectively (P=0.46). ![]()
The expanded umbilical cord blood (UCB) product NiCord can provide benefits over standard UCB transplant, according to research published in Biology of Blood and Marrow Transplantation.
NiCord is a stand-alone graft derived from a single UCB unit that has been expanded in culture and enriched with stem and progenitor cells.
The study showed that patients transplanted with NiCord had shorter time to engraftment, a lower risk of infection, and shorter hospital stays than patients who received standard UCB transplants.
On the other hand, there was no significant difference between the transplant groups when it came to grade 2-4 acute graft-versus-host disease (GVHD), relapse, or survival within 100 days of transplant.
“Our results indicate that rapid hematopoietic recovery from Gamida Cell’s NiCord transplantation approach is associated with clinical benefit,” said study author Mitchell Horwitz, MD, of Duke University School of Medicine in Durham, North Carolina.
Dr Horwitz receives research support from Gamida Cell Ltd., makers of NiCord.
Patient characteristics
The researchers compared 18 consecutive NiCord-transplanted patients and 86 consecutive patients who received standard UCB transplants. All of the patients received total body irradiation-based myeloablative conditioning.
In both arms, most patients received a double transplant. In the NiCord arm, 61.1% of patients (n=11) received NiCord along with a second unmanipulated UCB unit. In the standard UCB arm, 95.3% of patients (n=82) received a double UCB transplant.
Patients in the NiCord arm were older than patients in the standard UCB arm, with median ages of 45.5 (range, 42-57) and 37.5 (range, 28-51), respectively.
Most patients in both arms had acute leukemia or myelodysplastic syndromes (about 89%), although roughly 11% had lymphoid malignancies.
There were no significant differences between the arms when it came to patient sex, pre-transplant weight, cytomegalovirus serostatus, and Karnofsky Performance Status.
Results
The median time to neutrophil engraftment was 12.5 days (range, 10-18) in the NiCord arm and 27 days (range, 23-28) in the standard UCB arm (P<0.001).
All of the patients studied had at least 1 infection of any severity. However, patients in the NiCord arm had a significantly lower risk of infection than patients in the standard UCB arm.
In an analysis adjusted for age, disease stage, and grade 2-4 acute GVHD, the risk ratios (RRs) for NiCord versus standard UCB transplant were as follows:
- Total infection—RR=0.72, P=0.03
- Grade 2-3 infection—RR=0.38, P=0.001
- Bacterial infection—RR=0.42, P=0.008
- Grade 2-3 bacterial infection—RR=0.23, P=0.006.
Patients in the NiCord arm spent a mean of 72.4 days out of the hospital in the first 100 days after transplant, compared to 48.6 days for the standard UCB arm (P=0.001).
After the researchers adjusted for age and Karnofsky Performance Status, patients in the NiCord arm had a mean of 20.2 more days out of the hospital than their peers who received standard UCB (P=0.005).
The incidence of grade 2-4 acute GHVD was 55.6% in the NiCord arm and 41.9% in the standard UCB arm (P=0.31). The rate of second transplant was 5.6% and 11.6%, respectively (P=0.68).
The rate of relapse was 0% in the NiCord arm and 7% in the standard UCB arm (P=0.59). And the rate of death was 5.6% and 16.3%, respectively (P=0.46). ![]()
Method could prevent GVHD while preserving GVL effect
Researchers believe they have found a way to prevent graft-versus-host disease (GVHD) after hematopoietic stem cell transplant (HSCT) while preserving a strong graft-versus-leukemia (GVL) effect.
In experiments with mice, the team found that temporary in vivo depletion of CD4+ T cells soon after HSCT prevented GVHD without inhibiting GVL effects.
The depletion of CD4+ cells essentially caused CD8+ cells to become exhausted in their quest to destroy normal tissue but strengthened in their fight against leukemia, which meant the CD8+ cells could eliminate leukemic cells without causing GVHD.
Defu Zeng, MD, of City of Hope in Duarte, California, and his colleagues recounted these findings in the Journal of Clinical Investigation.
The researchers were able to achieve temporary in vivo depletion of CD4+ T cells by injecting mice with an anti-CD4 monoclonal antibody (mAb).
The team found that a single injection of the mAb given immediately after HSCT prevented acute but not chronic GVHD. Three injections of the mAb—given on days 0, 14, and 28—prevented both types of GVHD.
The researchers said their results suggest GVHD is more effectively prevented by temporary in vivo depletion of donor CD4+ T cells early after HSCT than by ex vivo depletion of donor CD4+ T cells.
This is because treatment with an anti-CD4 mAb temporarily depletes both the injected mature CD4+ T cells and the CD4+ T cells generated de novo from the marrow progenitors early after HSCT.
In explaining the mechanism behind their observations, the researchers noted that the interaction between PD-L1 and CD80 has been shown to exacerbate GVHD, but costimulation of CD80 and PD-1 ameliorates GVHD.
In their experiments, the team found that depleting CD4+ T cells increased serum IFN-γ and reduced IL-2 concentrations. And this led to upregulation of PD-L1 expression by recipient tissues and donor CD8+ T cells.
The researchers said that, in GVHD target tissues, the interactions of PD-L1 and PD-1 on donor CD8+ T cells caused anergy, exhaustion, and apoptosis. These effects prevented the development of GVHD.
On the other hand, in lymphoid tissues, the interactions of PD-L1 and CD80 augmented CD8+ T-cell expansion without increasing anergy, exhaustion, or apoptosis. This allowed for the preservation of GVL effects.
“If successfully translated into clinical application, this [CD4+ T-cell-depleting] regimen may represent one of the novel approaches that allow strong GVL effects without causing GVHD,” Dr Zeng said.
“This kind of regimen has the potential to promote widespread application of allogenic [HSCT] as a curative therapy for hematological malignancies.” ![]()
Researchers believe they have found a way to prevent graft-versus-host disease (GVHD) after hematopoietic stem cell transplant (HSCT) while preserving a strong graft-versus-leukemia (GVL) effect.
In experiments with mice, the team found that temporary in vivo depletion of CD4+ T cells soon after HSCT prevented GVHD without inhibiting GVL effects.
The depletion of CD4+ cells essentially caused CD8+ cells to become exhausted in their quest to destroy normal tissue but strengthened in their fight against leukemia, which meant the CD8+ cells could eliminate leukemic cells without causing GVHD.
Defu Zeng, MD, of City of Hope in Duarte, California, and his colleagues recounted these findings in the Journal of Clinical Investigation.
The researchers were able to achieve temporary in vivo depletion of CD4+ T cells by injecting mice with an anti-CD4 monoclonal antibody (mAb).
The team found that a single injection of the mAb given immediately after HSCT prevented acute but not chronic GVHD. Three injections of the mAb—given on days 0, 14, and 28—prevented both types of GVHD.
The researchers said their results suggest GVHD is more effectively prevented by temporary in vivo depletion of donor CD4+ T cells early after HSCT than by ex vivo depletion of donor CD4+ T cells.
This is because treatment with an anti-CD4 mAb temporarily depletes both the injected mature CD4+ T cells and the CD4+ T cells generated de novo from the marrow progenitors early after HSCT.
In explaining the mechanism behind their observations, the researchers noted that the interaction between PD-L1 and CD80 has been shown to exacerbate GVHD, but costimulation of CD80 and PD-1 ameliorates GVHD.
In their experiments, the team found that depleting CD4+ T cells increased serum IFN-γ and reduced IL-2 concentrations. And this led to upregulation of PD-L1 expression by recipient tissues and donor CD8+ T cells.
The researchers said that, in GVHD target tissues, the interactions of PD-L1 and PD-1 on donor CD8+ T cells caused anergy, exhaustion, and apoptosis. These effects prevented the development of GVHD.
On the other hand, in lymphoid tissues, the interactions of PD-L1 and CD80 augmented CD8+ T-cell expansion without increasing anergy, exhaustion, or apoptosis. This allowed for the preservation of GVL effects.
“If successfully translated into clinical application, this [CD4+ T-cell-depleting] regimen may represent one of the novel approaches that allow strong GVL effects without causing GVHD,” Dr Zeng said.
“This kind of regimen has the potential to promote widespread application of allogenic [HSCT] as a curative therapy for hematological malignancies.” ![]()
Researchers believe they have found a way to prevent graft-versus-host disease (GVHD) after hematopoietic stem cell transplant (HSCT) while preserving a strong graft-versus-leukemia (GVL) effect.
In experiments with mice, the team found that temporary in vivo depletion of CD4+ T cells soon after HSCT prevented GVHD without inhibiting GVL effects.
The depletion of CD4+ cells essentially caused CD8+ cells to become exhausted in their quest to destroy normal tissue but strengthened in their fight against leukemia, which meant the CD8+ cells could eliminate leukemic cells without causing GVHD.
Defu Zeng, MD, of City of Hope in Duarte, California, and his colleagues recounted these findings in the Journal of Clinical Investigation.
The researchers were able to achieve temporary in vivo depletion of CD4+ T cells by injecting mice with an anti-CD4 monoclonal antibody (mAb).
The team found that a single injection of the mAb given immediately after HSCT prevented acute but not chronic GVHD. Three injections of the mAb—given on days 0, 14, and 28—prevented both types of GVHD.
The researchers said their results suggest GVHD is more effectively prevented by temporary in vivo depletion of donor CD4+ T cells early after HSCT than by ex vivo depletion of donor CD4+ T cells.
This is because treatment with an anti-CD4 mAb temporarily depletes both the injected mature CD4+ T cells and the CD4+ T cells generated de novo from the marrow progenitors early after HSCT.
In explaining the mechanism behind their observations, the researchers noted that the interaction between PD-L1 and CD80 has been shown to exacerbate GVHD, but costimulation of CD80 and PD-1 ameliorates GVHD.
In their experiments, the team found that depleting CD4+ T cells increased serum IFN-γ and reduced IL-2 concentrations. And this led to upregulation of PD-L1 expression by recipient tissues and donor CD8+ T cells.
The researchers said that, in GVHD target tissues, the interactions of PD-L1 and PD-1 on donor CD8+ T cells caused anergy, exhaustion, and apoptosis. These effects prevented the development of GVHD.
On the other hand, in lymphoid tissues, the interactions of PD-L1 and CD80 augmented CD8+ T-cell expansion without increasing anergy, exhaustion, or apoptosis. This allowed for the preservation of GVL effects.
“If successfully translated into clinical application, this [CD4+ T-cell-depleting] regimen may represent one of the novel approaches that allow strong GVL effects without causing GVHD,” Dr Zeng said.
“This kind of regimen has the potential to promote widespread application of allogenic [HSCT] as a curative therapy for hematological malignancies.” ![]()
Cells are key to specification of HSCs, team says
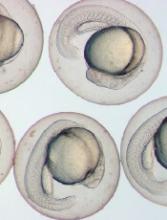
Experiments in zebrafish embryos have suggested that trunk neural crest cells play a key role in the specification of hematopoietic stem cells (HSCs).
Researchers believe this finding could be used to aid the creation of HSCs in the lab and ultimately help improve access to HSC transplant.
“The research will likely open new avenues of investigation in stem cell biology and blood development and provide insight to aid efforts to make transplantable hematopoietic stem cells in the lab,” said Wilson Clements, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Clements and Erich W. Damm, PhD, also of St. Jude, described this research in Nature Cell Biology.
The researchers noted that scientists have yet to achieve in vitro specification of normal HSCs with a high level of engraftment and normal multilineage potential. And this suggests key specification signals remain unknown.
The pair pointed out that, in all vertebrates, HSCs arise from hemogenic endothelium in the ventral floor of the dorsal aorta. And stromal cells residing in stem cell microenvironments often act as a niche to contribute cues that regulate behavior.
“Researchers have speculated that the endothelial cells that give rise to blood-forming stem cells are surrounded by a support niche of other cells whose identity and origins were unknown,” Dr Damm said. “Our results support the existence of a niche and identify trunk neural crest cells as an occupant.”
Trunk neural crest cells are made in the developing spinal cord and migrate throughout the embryo. The cells eventually give rise to a variety of adult cells, including neurons and glial cells in the sympathetic and parasympathetic nervous system.
Using time-lapse video, Drs Clements and Damm tracked the migration of neural crest cells in the transparent embryos of zebrafish. (Zebrafish and humans share nearly identical blood systems.)
After about 20 hours, the neural crest cells had reached the developing aorta. After hour 24, the migrating cells had cozied up to the endothelial cells in the aorta, which then turned on genes, such as runx1, indicating their conversion to HSCs.
Additional experiments revealed that migration of neural crest cells to the dorsal aorta is dependent on platelet-derived growth factor signaling, and this signaling is required for HSC specification.
Likewise, the physical association of neural crest cells with the pre-hematopoietic dorsal aorta is required for initiation of the hematopoietic program and HSC specification.
Drs Clements and Damm said these results suggest neural crest cells are key cellular components of the HSC specification niche that can be profiled to identify unknown HSC specification signals. ![]()
Experiments in zebrafish embryos have suggested that trunk neural crest cells play a key role in the specification of hematopoietic stem cells (HSCs).
Researchers believe this finding could be used to aid the creation of HSCs in the lab and ultimately help improve access to HSC transplant.
“The research will likely open new avenues of investigation in stem cell biology and blood development and provide insight to aid efforts to make transplantable hematopoietic stem cells in the lab,” said Wilson Clements, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Clements and Erich W. Damm, PhD, also of St. Jude, described this research in Nature Cell Biology.
The researchers noted that scientists have yet to achieve in vitro specification of normal HSCs with a high level of engraftment and normal multilineage potential. And this suggests key specification signals remain unknown.
The pair pointed out that, in all vertebrates, HSCs arise from hemogenic endothelium in the ventral floor of the dorsal aorta. And stromal cells residing in stem cell microenvironments often act as a niche to contribute cues that regulate behavior.
“Researchers have speculated that the endothelial cells that give rise to blood-forming stem cells are surrounded by a support niche of other cells whose identity and origins were unknown,” Dr Damm said. “Our results support the existence of a niche and identify trunk neural crest cells as an occupant.”
Trunk neural crest cells are made in the developing spinal cord and migrate throughout the embryo. The cells eventually give rise to a variety of adult cells, including neurons and glial cells in the sympathetic and parasympathetic nervous system.
Using time-lapse video, Drs Clements and Damm tracked the migration of neural crest cells in the transparent embryos of zebrafish. (Zebrafish and humans share nearly identical blood systems.)
After about 20 hours, the neural crest cells had reached the developing aorta. After hour 24, the migrating cells had cozied up to the endothelial cells in the aorta, which then turned on genes, such as runx1, indicating their conversion to HSCs.
Additional experiments revealed that migration of neural crest cells to the dorsal aorta is dependent on platelet-derived growth factor signaling, and this signaling is required for HSC specification.
Likewise, the physical association of neural crest cells with the pre-hematopoietic dorsal aorta is required for initiation of the hematopoietic program and HSC specification.
Drs Clements and Damm said these results suggest neural crest cells are key cellular components of the HSC specification niche that can be profiled to identify unknown HSC specification signals. ![]()
Experiments in zebrafish embryos have suggested that trunk neural crest cells play a key role in the specification of hematopoietic stem cells (HSCs).
Researchers believe this finding could be used to aid the creation of HSCs in the lab and ultimately help improve access to HSC transplant.
“The research will likely open new avenues of investigation in stem cell biology and blood development and provide insight to aid efforts to make transplantable hematopoietic stem cells in the lab,” said Wilson Clements, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Clements and Erich W. Damm, PhD, also of St. Jude, described this research in Nature Cell Biology.
The researchers noted that scientists have yet to achieve in vitro specification of normal HSCs with a high level of engraftment and normal multilineage potential. And this suggests key specification signals remain unknown.
The pair pointed out that, in all vertebrates, HSCs arise from hemogenic endothelium in the ventral floor of the dorsal aorta. And stromal cells residing in stem cell microenvironments often act as a niche to contribute cues that regulate behavior.
“Researchers have speculated that the endothelial cells that give rise to blood-forming stem cells are surrounded by a support niche of other cells whose identity and origins were unknown,” Dr Damm said. “Our results support the existence of a niche and identify trunk neural crest cells as an occupant.”
Trunk neural crest cells are made in the developing spinal cord and migrate throughout the embryo. The cells eventually give rise to a variety of adult cells, including neurons and glial cells in the sympathetic and parasympathetic nervous system.
Using time-lapse video, Drs Clements and Damm tracked the migration of neural crest cells in the transparent embryos of zebrafish. (Zebrafish and humans share nearly identical blood systems.)
After about 20 hours, the neural crest cells had reached the developing aorta. After hour 24, the migrating cells had cozied up to the endothelial cells in the aorta, which then turned on genes, such as runx1, indicating their conversion to HSCs.
Additional experiments revealed that migration of neural crest cells to the dorsal aorta is dependent on platelet-derived growth factor signaling, and this signaling is required for HSC specification.
Likewise, the physical association of neural crest cells with the pre-hematopoietic dorsal aorta is required for initiation of the hematopoietic program and HSC specification.
Drs Clements and Damm said these results suggest neural crest cells are key cellular components of the HSC specification niche that can be profiled to identify unknown HSC specification signals. ![]()
Weighing risks, benefits of autologous HSCT in MM
The use of autologous transplant after a 3-drug induction regimen for multiple myeloma (MM) prolongs progression-free survival (PFS) but not overall survival (OS), according to new research.
In a phase 3 trial, newly diagnosed MM patients who received lenalidomide, bortezomib, and dexamethasone (RVD) followed by an autologous hematopoietic stem cell transplant (HSCT) had significantly better PFS but similar OS when compared to patients who only received RVD.
In addition, HSCT recipients had significantly higher rates of high-grade blood and lymphatic system disorders, gastrointestinal events, and infections.
The study also showed that OS outcomes were similar for patients who received HSCT after completing treatment with RVD and patients who were in the RVD-only treatment arm but underwent HSCT later, as salvage therapy.
Researchers believe this suggests MM patients can potentially choose when to undergo a transplant.
The team reported their findings in NEJM. The study was supported by grants from Celgene and Janssen and by funds from the French Ministry of Health Programme Hospitalier de Recherche Clinique and from the French National Research Agency.
“Over the past decade, drugs that modulate the immune system and agents known as proteasome inhibitors have shown a great deal of promise in patients with multiple myeloma, when used in combination with chemotherapy,” said study author Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“This led us to propose that these combinations could be used selectively with established modalities such as transplant for patients with newly diagnosed myeloma, and this, in turn, raised questions about where and how transplant should be fit into the therapeutic paradigm. Our trial sought to comprehensively address these issues in a prospective fashion, and provide a foundation for future studies as the next generation of agents, such as monoclonal antibodies, impact the field.”
The study enrolled 700 adult patients under the age of 65 who were newly diagnosed with MM. They were treated at 69 centers in France, Belgium, and Switzerland.
The patients were randomized to 2 treatment arms. Both groups received 3 initial cycles of RVD.
One group then received 5 more cycles of RVD. The other received high-dose chemotherapy (melphalan) followed by an autologous HSCT and 2 additional cycles of RVD.
Patients in both groups then received lenalidomide as maintenance therapy for 1 year or until they progressed, experienced unacceptable adverse events (AEs), or withdrew consent.
Response and survival
The complete response rate was significantly higher in the HSCT arm than the RVD-alone arm—59% and 48%, respectively (P=0.03).
And there was a significantly higher percentage of patients who were negative for minimal residual disease in the HSCT arm than in the RVD arm—79% and 65%, respectively (P<0.001).
The median PFS was significantly longer in the HSCT arm than the RVD arm—50 months and 36 months, respectively (P<0.001). The researchers said this benefit was observed across all patient subgroups, including those stratified according to International Staging System stage and cytogenetic risk.
There was no significant between-group difference in the rate of OS at 4 years, which was 81% in the HSCT arm and 82% in the RVD arm.
Subsequent therapy
In the RVD arm, 207 patients progressed, and 172 received second-line therapy, which was followed by salvage HSCT in 136 patients (79%).
In the HSCT arm, 149 patients progressed, and 123 received second-line therapy, which was followed by a second HSCT in 21 patients (17%).
Safety
Nine percent of patients in the RVD arm and 11% in the HSCT arm discontinued treatment due to AEs. There were 2 treatment-related deaths in the RVD arm and 6 in the HSCT arm.
Grade 3/4 AEs with a significantly higher incidence in the HSCT arm than the RVD arm were blood and lymphatic system disorders (95% and 64%, respectively, P<0.001), gastrointestinal disorders (28% and 7%, respectively, P<0.001), and infections (20% and 9%, respectively, P<0.001).
Thirteen patients in the RVD arm and 17 in the HSCT arm had at least 1 invasive second primary malignancy (P=0.36). Acute myeloid leukemia occurred in 1 patient in the RVD arm and 4 in the HSCT arm (P=0.21).
The researchers said these results suggest the benefits of HSCT plus RVD must be weighed against the increased risk of toxicity associated with high-dose chemotherapy plus HSCT, particularly since HSCT after progression might be as effective as early HSCT for ensuring long-term OS. ![]()
The use of autologous transplant after a 3-drug induction regimen for multiple myeloma (MM) prolongs progression-free survival (PFS) but not overall survival (OS), according to new research.
In a phase 3 trial, newly diagnosed MM patients who received lenalidomide, bortezomib, and dexamethasone (RVD) followed by an autologous hematopoietic stem cell transplant (HSCT) had significantly better PFS but similar OS when compared to patients who only received RVD.
In addition, HSCT recipients had significantly higher rates of high-grade blood and lymphatic system disorders, gastrointestinal events, and infections.
The study also showed that OS outcomes were similar for patients who received HSCT after completing treatment with RVD and patients who were in the RVD-only treatment arm but underwent HSCT later, as salvage therapy.
Researchers believe this suggests MM patients can potentially choose when to undergo a transplant.
The team reported their findings in NEJM. The study was supported by grants from Celgene and Janssen and by funds from the French Ministry of Health Programme Hospitalier de Recherche Clinique and from the French National Research Agency.
“Over the past decade, drugs that modulate the immune system and agents known as proteasome inhibitors have shown a great deal of promise in patients with multiple myeloma, when used in combination with chemotherapy,” said study author Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“This led us to propose that these combinations could be used selectively with established modalities such as transplant for patients with newly diagnosed myeloma, and this, in turn, raised questions about where and how transplant should be fit into the therapeutic paradigm. Our trial sought to comprehensively address these issues in a prospective fashion, and provide a foundation for future studies as the next generation of agents, such as monoclonal antibodies, impact the field.”
The study enrolled 700 adult patients under the age of 65 who were newly diagnosed with MM. They were treated at 69 centers in France, Belgium, and Switzerland.
The patients were randomized to 2 treatment arms. Both groups received 3 initial cycles of RVD.
One group then received 5 more cycles of RVD. The other received high-dose chemotherapy (melphalan) followed by an autologous HSCT and 2 additional cycles of RVD.
Patients in both groups then received lenalidomide as maintenance therapy for 1 year or until they progressed, experienced unacceptable adverse events (AEs), or withdrew consent.
Response and survival
The complete response rate was significantly higher in the HSCT arm than the RVD-alone arm—59% and 48%, respectively (P=0.03).
And there was a significantly higher percentage of patients who were negative for minimal residual disease in the HSCT arm than in the RVD arm—79% and 65%, respectively (P<0.001).
The median PFS was significantly longer in the HSCT arm than the RVD arm—50 months and 36 months, respectively (P<0.001). The researchers said this benefit was observed across all patient subgroups, including those stratified according to International Staging System stage and cytogenetic risk.
There was no significant between-group difference in the rate of OS at 4 years, which was 81% in the HSCT arm and 82% in the RVD arm.
Subsequent therapy
In the RVD arm, 207 patients progressed, and 172 received second-line therapy, which was followed by salvage HSCT in 136 patients (79%).
In the HSCT arm, 149 patients progressed, and 123 received second-line therapy, which was followed by a second HSCT in 21 patients (17%).
Safety
Nine percent of patients in the RVD arm and 11% in the HSCT arm discontinued treatment due to AEs. There were 2 treatment-related deaths in the RVD arm and 6 in the HSCT arm.
Grade 3/4 AEs with a significantly higher incidence in the HSCT arm than the RVD arm were blood and lymphatic system disorders (95% and 64%, respectively, P<0.001), gastrointestinal disorders (28% and 7%, respectively, P<0.001), and infections (20% and 9%, respectively, P<0.001).
Thirteen patients in the RVD arm and 17 in the HSCT arm had at least 1 invasive second primary malignancy (P=0.36). Acute myeloid leukemia occurred in 1 patient in the RVD arm and 4 in the HSCT arm (P=0.21).
The researchers said these results suggest the benefits of HSCT plus RVD must be weighed against the increased risk of toxicity associated with high-dose chemotherapy plus HSCT, particularly since HSCT after progression might be as effective as early HSCT for ensuring long-term OS. ![]()
The use of autologous transplant after a 3-drug induction regimen for multiple myeloma (MM) prolongs progression-free survival (PFS) but not overall survival (OS), according to new research.
In a phase 3 trial, newly diagnosed MM patients who received lenalidomide, bortezomib, and dexamethasone (RVD) followed by an autologous hematopoietic stem cell transplant (HSCT) had significantly better PFS but similar OS when compared to patients who only received RVD.
In addition, HSCT recipients had significantly higher rates of high-grade blood and lymphatic system disorders, gastrointestinal events, and infections.
The study also showed that OS outcomes were similar for patients who received HSCT after completing treatment with RVD and patients who were in the RVD-only treatment arm but underwent HSCT later, as salvage therapy.
Researchers believe this suggests MM patients can potentially choose when to undergo a transplant.
The team reported their findings in NEJM. The study was supported by grants from Celgene and Janssen and by funds from the French Ministry of Health Programme Hospitalier de Recherche Clinique and from the French National Research Agency.
“Over the past decade, drugs that modulate the immune system and agents known as proteasome inhibitors have shown a great deal of promise in patients with multiple myeloma, when used in combination with chemotherapy,” said study author Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“This led us to propose that these combinations could be used selectively with established modalities such as transplant for patients with newly diagnosed myeloma, and this, in turn, raised questions about where and how transplant should be fit into the therapeutic paradigm. Our trial sought to comprehensively address these issues in a prospective fashion, and provide a foundation for future studies as the next generation of agents, such as monoclonal antibodies, impact the field.”
The study enrolled 700 adult patients under the age of 65 who were newly diagnosed with MM. They were treated at 69 centers in France, Belgium, and Switzerland.
The patients were randomized to 2 treatment arms. Both groups received 3 initial cycles of RVD.
One group then received 5 more cycles of RVD. The other received high-dose chemotherapy (melphalan) followed by an autologous HSCT and 2 additional cycles of RVD.
Patients in both groups then received lenalidomide as maintenance therapy for 1 year or until they progressed, experienced unacceptable adverse events (AEs), or withdrew consent.
Response and survival
The complete response rate was significantly higher in the HSCT arm than the RVD-alone arm—59% and 48%, respectively (P=0.03).
And there was a significantly higher percentage of patients who were negative for minimal residual disease in the HSCT arm than in the RVD arm—79% and 65%, respectively (P<0.001).
The median PFS was significantly longer in the HSCT arm than the RVD arm—50 months and 36 months, respectively (P<0.001). The researchers said this benefit was observed across all patient subgroups, including those stratified according to International Staging System stage and cytogenetic risk.
There was no significant between-group difference in the rate of OS at 4 years, which was 81% in the HSCT arm and 82% in the RVD arm.
Subsequent therapy
In the RVD arm, 207 patients progressed, and 172 received second-line therapy, which was followed by salvage HSCT in 136 patients (79%).
In the HSCT arm, 149 patients progressed, and 123 received second-line therapy, which was followed by a second HSCT in 21 patients (17%).
Safety
Nine percent of patients in the RVD arm and 11% in the HSCT arm discontinued treatment due to AEs. There were 2 treatment-related deaths in the RVD arm and 6 in the HSCT arm.
Grade 3/4 AEs with a significantly higher incidence in the HSCT arm than the RVD arm were blood and lymphatic system disorders (95% and 64%, respectively, P<0.001), gastrointestinal disorders (28% and 7%, respectively, P<0.001), and infections (20% and 9%, respectively, P<0.001).
Thirteen patients in the RVD arm and 17 in the HSCT arm had at least 1 invasive second primary malignancy (P=0.36). Acute myeloid leukemia occurred in 1 patient in the RVD arm and 4 in the HSCT arm (P=0.21).
The researchers said these results suggest the benefits of HSCT plus RVD must be weighed against the increased risk of toxicity associated with high-dose chemotherapy plus HSCT, particularly since HSCT after progression might be as effective as early HSCT for ensuring long-term OS.
Drug induces remission in patient with severe TA-TMA
MARSEILLE—An investigational drug has successfully treated a severe case of transplant-associated thrombotic microangiopathy (TA-TMA), according to a presentation at the 43rd Annual Meeting of the European Society for Blood and Marrow Transplantation.
The drug is OMS721, a monoclonal antibody targeting mannan-binding lectin-associated serine protease-2 (MASP-2), the effector enzyme of the lectin pathway of the complement system.
The patient received OMS721, which is being developed by Omeros Corporation, under a compassionate-use protocol.
Marco Zecca, MD, of the Fondazione IRCCS Policlinico San Matteo in Italy, and his colleagues provided details on this patient in a poster presented at the meeting (Physician Poster Abstracts-Day 1, abstract A437).
The female patient had undergone a hematopoietic stem cell transplant to treat Diamond‐Blackfan anemia. At age 14, she received a transplant from an HLA-compatible, unrelated donor.
Seven months later, she was diagnosed with TA-TMA. The patient was initially treated with eculizumab but had to stop taking the drug after she developed acute pulmonary edema.
She was then treated with plasma exchange but experienced a TA-TMA relapse at 11 months. The patient was again treated with eculizumab and again had to discontinue the drug after developing acute pulmonary edema.
The patient’s condition continued to worsen, and she soon required hemodialysis 3 times a week as well as daily platelet transfusions.
Dr Zecca requested OMS721 as compassionate-use treatment for the patient, and Omeros complied.
Two months after starting OMS721, the patient was able to discontinue hemodialysis and decrease her platelet transfusion requirements. She did not experience any adverse events related to OMS721.
Recently, the patient’s dose was tapered, but she developed a viral infection that reactivated her TA-TMA.
A return to the original dose of OMS721 was successful. Now, the patient no longer requires dialysis or transfusions.
“This patient had severe TMA that I believe would have caused her death,” Dr Zecca said. “Her positive response to OMS721 treatment, both initially and following her virus-induced relapse during tapering, was impressive.”
“The results of OMS721 treatment in this challenge-rechallenge scenario underscore the important effects of the drug. Since the poster was produced, her TMA has remained in remission, and we have been able to discontinue her platelet transfusions. Her rapid response has been heartening, and we all are grateful for this remarkable outcome.”
MARSEILLE—An investigational drug has successfully treated a severe case of transplant-associated thrombotic microangiopathy (TA-TMA), according to a presentation at the 43rd Annual Meeting of the European Society for Blood and Marrow Transplantation.
The drug is OMS721, a monoclonal antibody targeting mannan-binding lectin-associated serine protease-2 (MASP-2), the effector enzyme of the lectin pathway of the complement system.
The patient received OMS721, which is being developed by Omeros Corporation, under a compassionate-use protocol.
Marco Zecca, MD, of the Fondazione IRCCS Policlinico San Matteo in Italy, and his colleagues provided details on this patient in a poster presented at the meeting (Physician Poster Abstracts-Day 1, abstract A437).
The female patient had undergone a hematopoietic stem cell transplant to treat Diamond‐Blackfan anemia. At age 14, she received a transplant from an HLA-compatible, unrelated donor.
Seven months later, she was diagnosed with TA-TMA. The patient was initially treated with eculizumab but had to stop taking the drug after she developed acute pulmonary edema.
She was then treated with plasma exchange but experienced a TA-TMA relapse at 11 months. The patient was again treated with eculizumab and again had to discontinue the drug after developing acute pulmonary edema.
The patient’s condition continued to worsen, and she soon required hemodialysis 3 times a week as well as daily platelet transfusions.
Dr Zecca requested OMS721 as compassionate-use treatment for the patient, and Omeros complied.
Two months after starting OMS721, the patient was able to discontinue hemodialysis and decrease her platelet transfusion requirements. She did not experience any adverse events related to OMS721.
Recently, the patient’s dose was tapered, but she developed a viral infection that reactivated her TA-TMA.
A return to the original dose of OMS721 was successful. Now, the patient no longer requires dialysis or transfusions.
“This patient had severe TMA that I believe would have caused her death,” Dr Zecca said. “Her positive response to OMS721 treatment, both initially and following her virus-induced relapse during tapering, was impressive.”
“The results of OMS721 treatment in this challenge-rechallenge scenario underscore the important effects of the drug. Since the poster was produced, her TMA has remained in remission, and we have been able to discontinue her platelet transfusions. Her rapid response has been heartening, and we all are grateful for this remarkable outcome.”
MARSEILLE—An investigational drug has successfully treated a severe case of transplant-associated thrombotic microangiopathy (TA-TMA), according to a presentation at the 43rd Annual Meeting of the European Society for Blood and Marrow Transplantation.
The drug is OMS721, a monoclonal antibody targeting mannan-binding lectin-associated serine protease-2 (MASP-2), the effector enzyme of the lectin pathway of the complement system.
The patient received OMS721, which is being developed by Omeros Corporation, under a compassionate-use protocol.
Marco Zecca, MD, of the Fondazione IRCCS Policlinico San Matteo in Italy, and his colleagues provided details on this patient in a poster presented at the meeting (Physician Poster Abstracts-Day 1, abstract A437).
The female patient had undergone a hematopoietic stem cell transplant to treat Diamond‐Blackfan anemia. At age 14, she received a transplant from an HLA-compatible, unrelated donor.
Seven months later, she was diagnosed with TA-TMA. The patient was initially treated with eculizumab but had to stop taking the drug after she developed acute pulmonary edema.
She was then treated with plasma exchange but experienced a TA-TMA relapse at 11 months. The patient was again treated with eculizumab and again had to discontinue the drug after developing acute pulmonary edema.
The patient’s condition continued to worsen, and she soon required hemodialysis 3 times a week as well as daily platelet transfusions.
Dr Zecca requested OMS721 as compassionate-use treatment for the patient, and Omeros complied.
Two months after starting OMS721, the patient was able to discontinue hemodialysis and decrease her platelet transfusion requirements. She did not experience any adverse events related to OMS721.
Recently, the patient’s dose was tapered, but she developed a viral infection that reactivated her TA-TMA.
A return to the original dose of OMS721 was successful. Now, the patient no longer requires dialysis or transfusions.
“This patient had severe TMA that I believe would have caused her death,” Dr Zecca said. “Her positive response to OMS721 treatment, both initially and following her virus-induced relapse during tapering, was impressive.”
“The results of OMS721 treatment in this challenge-rechallenge scenario underscore the important effects of the drug. Since the poster was produced, her TMA has remained in remission, and we have been able to discontinue her platelet transfusions. Her rapid response has been heartening, and we all are grateful for this remarkable outcome.”
EMA recommends orphan designation for cord blood product
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has recommended that NiCord® receive orphan designation as a treatment for patients who require a hematopoietic stem cell transplant.
NiCord is a stand-alone graft derived from a single umbilical cord blood unit that has been expanded in culture and enriched with stem and progenitor cells.
NiCord already has orphan designation in the European Union as a treatment for patients with acute myeloid leukemia.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval. The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The European Commission typically makes a decision within 30 days.
NiCord also has orphan designation and breakthrough designation from the US Food and Drug Administration for the treatment of hematologic malignancies.
NiCord research
Data from the pilot study of NiCord suggested the therapy can provide a clinically meaningful improvement in time to neutrophil engraftment over traditional cord blood transplant.
And research presented at EBMT 2016 showed that patients who received NiCord had fewer infections, shorter hospital stays, quicker platelet engraftment, and improved non-relapse mortality when compared to patients who received a traditional cord blood transplant.
NiCord is currently being studied in a phase 3 registration study as a graft for patients with hematologic malignancies who do not have a rapidly available, fully matched donor.
Gamida Cell, the company developing NiCord, announced last month that the first patient in the study had been transplanted.
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has recommended that NiCord® receive orphan designation as a treatment for patients who require a hematopoietic stem cell transplant.
NiCord is a stand-alone graft derived from a single umbilical cord blood unit that has been expanded in culture and enriched with stem and progenitor cells.
NiCord already has orphan designation in the European Union as a treatment for patients with acute myeloid leukemia.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval. The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The European Commission typically makes a decision within 30 days.
NiCord also has orphan designation and breakthrough designation from the US Food and Drug Administration for the treatment of hematologic malignancies.
NiCord research
Data from the pilot study of NiCord suggested the therapy can provide a clinically meaningful improvement in time to neutrophil engraftment over traditional cord blood transplant.
And research presented at EBMT 2016 showed that patients who received NiCord had fewer infections, shorter hospital stays, quicker platelet engraftment, and improved non-relapse mortality when compared to patients who received a traditional cord blood transplant.
NiCord is currently being studied in a phase 3 registration study as a graft for patients with hematologic malignancies who do not have a rapidly available, fully matched donor.
Gamida Cell, the company developing NiCord, announced last month that the first patient in the study had been transplanted.
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has recommended that NiCord® receive orphan designation as a treatment for patients who require a hematopoietic stem cell transplant.
NiCord is a stand-alone graft derived from a single umbilical cord blood unit that has been expanded in culture and enriched with stem and progenitor cells.
NiCord already has orphan designation in the European Union as a treatment for patients with acute myeloid leukemia.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval. The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The European Commission typically makes a decision within 30 days.
NiCord also has orphan designation and breakthrough designation from the US Food and Drug Administration for the treatment of hematologic malignancies.
NiCord research
Data from the pilot study of NiCord suggested the therapy can provide a clinically meaningful improvement in time to neutrophil engraftment over traditional cord blood transplant.
And research presented at EBMT 2016 showed that patients who received NiCord had fewer infections, shorter hospital stays, quicker platelet engraftment, and improved non-relapse mortality when compared to patients who received a traditional cord blood transplant.
NiCord is currently being studied in a phase 3 registration study as a graft for patients with hematologic malignancies who do not have a rapidly available, fully matched donor.
Gamida Cell, the company developing NiCord, announced last month that the first patient in the study had been transplanted.
Allo-HSCT cures adult with congenital dyserythropoietic anemia
Physicians have reported what they believe is the first case of an allogeneic hematopoietic stem cell transplant (allo-HSCT) curing an adult with congenital dyserythropoietic anemia (CDA).
The patient, David Levy, was previously transfusion-dependent and suffered from iron overload, severe pain, and other adverse effects of his illness.
Levy was denied a transplant for years, but, in 2014, he received a non-myeloablative allo-HSCT from a matched, unrelated donor.
Now, Levy no longer requires transfusions, iron chelation, or immunosuppression, and says he is able to live a normal life.
Damiano Rondelli, MD, of the University of Illinois at Chicago, and his colleagues described Levy’s case in a letter to Bone Marrow Transplantation.
Levy was diagnosed with CDA at 4 months of age and was treated with regular blood transfusions for most of his life. He was 24 when the pain from his illness became so severe that he had to withdraw from graduate school.
“I spent the following years doing nothing—no work, no school, no social contact—because all I could focus on was managing my pain and getting my health back on track,” Levy said.
By age 32, Levy required transfusions every 2 to 3 weeks, had undergone a splenectomy, had an enlarged liver, and was suffering from fatigue, heart palpitations, and iron overload.
“It was bad,” Levy said. “I had been through enough pain. I was angry and depressed, and I wanted a cure. That’s why I started emailing Dr Rondelli.”
Dr Rondelli said that because of Levy’s range of illnesses and inability to tolerate chemotherapy and radiation, several institutions had denied him the possibility of a transplant.
However, Dr Rondelli and his colleagues had reported success with chemotherapy-free allo-HSCT in patients with sickle cell disease. So Dr Rondelli performed Levy’s transplant in 2014.
Levy received a peripheral blood stem cell transplant from an unrelated donor who was a 10/10 HLA match but ABO incompatible. He received conditioning with rabbit anti-thymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
Levy also received graft-vs-host disease (GVHD) prophylaxis consisting of high-dose cyclophosphamide, mycophenolate mofetil, and sirolimus. And he received standard antibacterial, antifungal, antiviral, and anti-Pneumocystis jiroveci prophylaxis.
Levy experienced platelet engraftment on day 20 and neutrophil engraftment on day 21. Whole-blood donor-cell chimerism was 98.7% on day 30 and 100% on day 60 and beyond.
Levy did develop transient hemolytic anemia due to the ABO incompatibility. He was given a total of 10 units of packed red blood cells until day 78.
Levy was tapered off all immunosuppression at 12 months and has shown no signs of acute or chronic GVHD.
At 24 months after HSCT, Levy’s hemoglobin was 13.7 g/dL, and his ferritin was 376 ng/mL. He has had no iron chelation since the transplant.
“The transplant was hard, and I had some complications, but I am back to normal now,” said Levy, who is now 35.
“I still have some pain and some lingering issues from the years my condition was not properly managed, but I can be independent now. That is the most important thing to me.”
Levy is finishing his doctorate in psychology and running group therapy sessions at a behavioral health hospital.
Dr Rondelli said the potential of this treatment approach is promising.
“The use of this transplant protocol may represent a safe therapeutic strategy to treat adult patients with many types of congenital anemias—perhaps the only possible cure,” he said.
“For many adult patients with a blood disorder, treatment options have been limited because they are often not sick enough to qualify for a risky procedure, or they are too sick to tolerate the toxic drugs used alongside a standard transplant. This procedure gives some adults the option of a stem cell transplant, which was not previously available.”
Physicians have reported what they believe is the first case of an allogeneic hematopoietic stem cell transplant (allo-HSCT) curing an adult with congenital dyserythropoietic anemia (CDA).
The patient, David Levy, was previously transfusion-dependent and suffered from iron overload, severe pain, and other adverse effects of his illness.
Levy was denied a transplant for years, but, in 2014, he received a non-myeloablative allo-HSCT from a matched, unrelated donor.
Now, Levy no longer requires transfusions, iron chelation, or immunosuppression, and says he is able to live a normal life.
Damiano Rondelli, MD, of the University of Illinois at Chicago, and his colleagues described Levy’s case in a letter to Bone Marrow Transplantation.
Levy was diagnosed with CDA at 4 months of age and was treated with regular blood transfusions for most of his life. He was 24 when the pain from his illness became so severe that he had to withdraw from graduate school.
“I spent the following years doing nothing—no work, no school, no social contact—because all I could focus on was managing my pain and getting my health back on track,” Levy said.
By age 32, Levy required transfusions every 2 to 3 weeks, had undergone a splenectomy, had an enlarged liver, and was suffering from fatigue, heart palpitations, and iron overload.
“It was bad,” Levy said. “I had been through enough pain. I was angry and depressed, and I wanted a cure. That’s why I started emailing Dr Rondelli.”
Dr Rondelli said that because of Levy’s range of illnesses and inability to tolerate chemotherapy and radiation, several institutions had denied him the possibility of a transplant.
However, Dr Rondelli and his colleagues had reported success with chemotherapy-free allo-HSCT in patients with sickle cell disease. So Dr Rondelli performed Levy’s transplant in 2014.
Levy received a peripheral blood stem cell transplant from an unrelated donor who was a 10/10 HLA match but ABO incompatible. He received conditioning with rabbit anti-thymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
Levy also received graft-vs-host disease (GVHD) prophylaxis consisting of high-dose cyclophosphamide, mycophenolate mofetil, and sirolimus. And he received standard antibacterial, antifungal, antiviral, and anti-Pneumocystis jiroveci prophylaxis.
Levy experienced platelet engraftment on day 20 and neutrophil engraftment on day 21. Whole-blood donor-cell chimerism was 98.7% on day 30 and 100% on day 60 and beyond.
Levy did develop transient hemolytic anemia due to the ABO incompatibility. He was given a total of 10 units of packed red blood cells until day 78.
Levy was tapered off all immunosuppression at 12 months and has shown no signs of acute or chronic GVHD.
At 24 months after HSCT, Levy’s hemoglobin was 13.7 g/dL, and his ferritin was 376 ng/mL. He has had no iron chelation since the transplant.
“The transplant was hard, and I had some complications, but I am back to normal now,” said Levy, who is now 35.
“I still have some pain and some lingering issues from the years my condition was not properly managed, but I can be independent now. That is the most important thing to me.”
Levy is finishing his doctorate in psychology and running group therapy sessions at a behavioral health hospital.
Dr Rondelli said the potential of this treatment approach is promising.
“The use of this transplant protocol may represent a safe therapeutic strategy to treat adult patients with many types of congenital anemias—perhaps the only possible cure,” he said.
“For many adult patients with a blood disorder, treatment options have been limited because they are often not sick enough to qualify for a risky procedure, or they are too sick to tolerate the toxic drugs used alongside a standard transplant. This procedure gives some adults the option of a stem cell transplant, which was not previously available.”
Physicians have reported what they believe is the first case of an allogeneic hematopoietic stem cell transplant (allo-HSCT) curing an adult with congenital dyserythropoietic anemia (CDA).
The patient, David Levy, was previously transfusion-dependent and suffered from iron overload, severe pain, and other adverse effects of his illness.
Levy was denied a transplant for years, but, in 2014, he received a non-myeloablative allo-HSCT from a matched, unrelated donor.
Now, Levy no longer requires transfusions, iron chelation, or immunosuppression, and says he is able to live a normal life.
Damiano Rondelli, MD, of the University of Illinois at Chicago, and his colleagues described Levy’s case in a letter to Bone Marrow Transplantation.
Levy was diagnosed with CDA at 4 months of age and was treated with regular blood transfusions for most of his life. He was 24 when the pain from his illness became so severe that he had to withdraw from graduate school.
“I spent the following years doing nothing—no work, no school, no social contact—because all I could focus on was managing my pain and getting my health back on track,” Levy said.
By age 32, Levy required transfusions every 2 to 3 weeks, had undergone a splenectomy, had an enlarged liver, and was suffering from fatigue, heart palpitations, and iron overload.
“It was bad,” Levy said. “I had been through enough pain. I was angry and depressed, and I wanted a cure. That’s why I started emailing Dr Rondelli.”
Dr Rondelli said that because of Levy’s range of illnesses and inability to tolerate chemotherapy and radiation, several institutions had denied him the possibility of a transplant.
However, Dr Rondelli and his colleagues had reported success with chemotherapy-free allo-HSCT in patients with sickle cell disease. So Dr Rondelli performed Levy’s transplant in 2014.
Levy received a peripheral blood stem cell transplant from an unrelated donor who was a 10/10 HLA match but ABO incompatible. He received conditioning with rabbit anti-thymocyte globulin, fludarabine, cyclophosphamide, and total body irradiation.
Levy also received graft-vs-host disease (GVHD) prophylaxis consisting of high-dose cyclophosphamide, mycophenolate mofetil, and sirolimus. And he received standard antibacterial, antifungal, antiviral, and anti-Pneumocystis jiroveci prophylaxis.
Levy experienced platelet engraftment on day 20 and neutrophil engraftment on day 21. Whole-blood donor-cell chimerism was 98.7% on day 30 and 100% on day 60 and beyond.
Levy did develop transient hemolytic anemia due to the ABO incompatibility. He was given a total of 10 units of packed red blood cells until day 78.
Levy was tapered off all immunosuppression at 12 months and has shown no signs of acute or chronic GVHD.
At 24 months after HSCT, Levy’s hemoglobin was 13.7 g/dL, and his ferritin was 376 ng/mL. He has had no iron chelation since the transplant.
“The transplant was hard, and I had some complications, but I am back to normal now,” said Levy, who is now 35.
“I still have some pain and some lingering issues from the years my condition was not properly managed, but I can be independent now. That is the most important thing to me.”
Levy is finishing his doctorate in psychology and running group therapy sessions at a behavioral health hospital.
Dr Rondelli said the potential of this treatment approach is promising.
“The use of this transplant protocol may represent a safe therapeutic strategy to treat adult patients with many types of congenital anemias—perhaps the only possible cure,” he said.
“For many adult patients with a blood disorder, treatment options have been limited because they are often not sick enough to qualify for a risky procedure, or they are too sick to tolerate the toxic drugs used alongside a standard transplant. This procedure gives some adults the option of a stem cell transplant, which was not previously available.”