User login
Active psoriatic arthritis, ankylosing spondylitis linked to increase in adverse pregnancy outcomes
Women with psoriatic arthritis and ankylosing spondylitis generally have favorable pregnancy outcomes, but high disease activity during pregnancy could increase the risk of adverse labor and delivery outcomes, according to 2004-2018 data from the Organization of Teratology Information Specialists (OTIS) Autoimmune Disease Project.
Corticosteroid use further increased risk for preterm delivery among women with ankylosing spondylitis.
While more research is needed, these findings suggest that better obstetric outcomes might be achieved via better disease control and minimal use of corticosteroids, according to Chelsey J. F. Smith, MD, of the University of California, San Diego, and colleagues.
“Future studies are needed to confirm the novel findings seen in our study, as well as to continue to analyze the effect of different disease activity measures and medication use on pregnancy outcomes in these two chronic conditions,” Dr. Smith and coauthors said in a report on the study in Arthritis Care and Research.
Many women affected by psoriatic arthritis and ankylosing spondylitis are of child-bearing age and consider planning a family, according to the researchers. Data on pregnancy outcomes are lacking, they said, “often making it difficult for rheumatologists and obstetricians to counsel their patients effectively.”
The study from Dr. Smith and coinvestigators comprised 963 women who enrolled in the OTIS prospective cohort study within 20 weeks of gestation and delivered at least one live-born infant. Of that cohort, 129 had ankylosing spondylitis, 117 had psoriatic arthritis, and the remaining 717 served as a control group.
Psoriatic arthritis conferred an 81% increased risk for moderate preterm delivery at 32-36 weeks gestation, compared with healthier women, 13.7% and 7.7% respectively. Risk was increased among women with psoriatic arthritis for preterm labor, 16.2% and 8.4% (adjusted risk ratio, 2.05, 95% confidence interval, 1.21-3.48), caesarean delivery, 48.7% and 26.2% (aRR, 1.63, 95% CI, 1.26-2.12), and oligohydramnios, 25% and 11% (aRR, 3.79, 95% CI, 1.34-10.74). Women with psoriatic arthritis were 2 years older on average and their average body mass index was 27 kg/m2 vs. 24.5 kg/m2 in the control group.
In women with ankylosing spondylitis, risk of infant hospitalization in the neonatal intensive care unit was increased by 67%, 17.2% vs. 11.9% in the control group.
Active disease measured by the Health Assessment Questionnaire (HAQ) or Routine Assessment of Patient Index Data 3 (RAPID3) was linked to increased risk of adverse obstetric outcomes in some cases, the investigators said.
For example, risk of preterm delivery was increased in women with psoriatic arthritis who had active disease at 32 weeks as measured by HAQ (27 women) and RAPID3 (28 women) scores, while in ankylosing spondylitis, active disease measured at intake by RAPID3 (46 women) was associated with increased risk of caesarean delivery.
Medication use in women with psoriatic arthritis was not associated with increased preterm delivery risk. However, women with ankylosing spondylitis who used corticosteroids in the second trimester had an increased risk of preterm delivery.
The rate of corticosteroid use was “surprisingly high” at 38% among the women with ankylosing spondylitis, Dr. Smith and coinvestigators said.
“The 2016 American College of Rheumatology guidelines in fact recommend against the use of systemic corticosteroids for the treatment of ankylosing spondylitis, with the exception of short-term treatment with rapid tapering in circumstances such as flares during pregnancy, flares of concomitant inflammatory bowel disease, or flare of peripheral arthritis,” they said in their report.
Dr. Smith and coauthors reported no conflicts of interest. The OTIS Collaborative Research Group has received research funding from AbbVie, Amgen, Bristol-Myers Squibb, Janssen, Pfizer, and others.
SOURCE: Smith CJF et al. Arthritis Care Res. 2019 May 10. doi: 10.1002/acr.23924.
Women with psoriatic arthritis and ankylosing spondylitis generally have favorable pregnancy outcomes, but high disease activity during pregnancy could increase the risk of adverse labor and delivery outcomes, according to 2004-2018 data from the Organization of Teratology Information Specialists (OTIS) Autoimmune Disease Project.
Corticosteroid use further increased risk for preterm delivery among women with ankylosing spondylitis.
While more research is needed, these findings suggest that better obstetric outcomes might be achieved via better disease control and minimal use of corticosteroids, according to Chelsey J. F. Smith, MD, of the University of California, San Diego, and colleagues.
“Future studies are needed to confirm the novel findings seen in our study, as well as to continue to analyze the effect of different disease activity measures and medication use on pregnancy outcomes in these two chronic conditions,” Dr. Smith and coauthors said in a report on the study in Arthritis Care and Research.
Many women affected by psoriatic arthritis and ankylosing spondylitis are of child-bearing age and consider planning a family, according to the researchers. Data on pregnancy outcomes are lacking, they said, “often making it difficult for rheumatologists and obstetricians to counsel their patients effectively.”
The study from Dr. Smith and coinvestigators comprised 963 women who enrolled in the OTIS prospective cohort study within 20 weeks of gestation and delivered at least one live-born infant. Of that cohort, 129 had ankylosing spondylitis, 117 had psoriatic arthritis, and the remaining 717 served as a control group.
Psoriatic arthritis conferred an 81% increased risk for moderate preterm delivery at 32-36 weeks gestation, compared with healthier women, 13.7% and 7.7% respectively. Risk was increased among women with psoriatic arthritis for preterm labor, 16.2% and 8.4% (adjusted risk ratio, 2.05, 95% confidence interval, 1.21-3.48), caesarean delivery, 48.7% and 26.2% (aRR, 1.63, 95% CI, 1.26-2.12), and oligohydramnios, 25% and 11% (aRR, 3.79, 95% CI, 1.34-10.74). Women with psoriatic arthritis were 2 years older on average and their average body mass index was 27 kg/m2 vs. 24.5 kg/m2 in the control group.
In women with ankylosing spondylitis, risk of infant hospitalization in the neonatal intensive care unit was increased by 67%, 17.2% vs. 11.9% in the control group.
Active disease measured by the Health Assessment Questionnaire (HAQ) or Routine Assessment of Patient Index Data 3 (RAPID3) was linked to increased risk of adverse obstetric outcomes in some cases, the investigators said.
For example, risk of preterm delivery was increased in women with psoriatic arthritis who had active disease at 32 weeks as measured by HAQ (27 women) and RAPID3 (28 women) scores, while in ankylosing spondylitis, active disease measured at intake by RAPID3 (46 women) was associated with increased risk of caesarean delivery.
Medication use in women with psoriatic arthritis was not associated with increased preterm delivery risk. However, women with ankylosing spondylitis who used corticosteroids in the second trimester had an increased risk of preterm delivery.
The rate of corticosteroid use was “surprisingly high” at 38% among the women with ankylosing spondylitis, Dr. Smith and coinvestigators said.
“The 2016 American College of Rheumatology guidelines in fact recommend against the use of systemic corticosteroids for the treatment of ankylosing spondylitis, with the exception of short-term treatment with rapid tapering in circumstances such as flares during pregnancy, flares of concomitant inflammatory bowel disease, or flare of peripheral arthritis,” they said in their report.
Dr. Smith and coauthors reported no conflicts of interest. The OTIS Collaborative Research Group has received research funding from AbbVie, Amgen, Bristol-Myers Squibb, Janssen, Pfizer, and others.
SOURCE: Smith CJF et al. Arthritis Care Res. 2019 May 10. doi: 10.1002/acr.23924.
Women with psoriatic arthritis and ankylosing spondylitis generally have favorable pregnancy outcomes, but high disease activity during pregnancy could increase the risk of adverse labor and delivery outcomes, according to 2004-2018 data from the Organization of Teratology Information Specialists (OTIS) Autoimmune Disease Project.
Corticosteroid use further increased risk for preterm delivery among women with ankylosing spondylitis.
While more research is needed, these findings suggest that better obstetric outcomes might be achieved via better disease control and minimal use of corticosteroids, according to Chelsey J. F. Smith, MD, of the University of California, San Diego, and colleagues.
“Future studies are needed to confirm the novel findings seen in our study, as well as to continue to analyze the effect of different disease activity measures and medication use on pregnancy outcomes in these two chronic conditions,” Dr. Smith and coauthors said in a report on the study in Arthritis Care and Research.
Many women affected by psoriatic arthritis and ankylosing spondylitis are of child-bearing age and consider planning a family, according to the researchers. Data on pregnancy outcomes are lacking, they said, “often making it difficult for rheumatologists and obstetricians to counsel their patients effectively.”
The study from Dr. Smith and coinvestigators comprised 963 women who enrolled in the OTIS prospective cohort study within 20 weeks of gestation and delivered at least one live-born infant. Of that cohort, 129 had ankylosing spondylitis, 117 had psoriatic arthritis, and the remaining 717 served as a control group.
Psoriatic arthritis conferred an 81% increased risk for moderate preterm delivery at 32-36 weeks gestation, compared with healthier women, 13.7% and 7.7% respectively. Risk was increased among women with psoriatic arthritis for preterm labor, 16.2% and 8.4% (adjusted risk ratio, 2.05, 95% confidence interval, 1.21-3.48), caesarean delivery, 48.7% and 26.2% (aRR, 1.63, 95% CI, 1.26-2.12), and oligohydramnios, 25% and 11% (aRR, 3.79, 95% CI, 1.34-10.74). Women with psoriatic arthritis were 2 years older on average and their average body mass index was 27 kg/m2 vs. 24.5 kg/m2 in the control group.
In women with ankylosing spondylitis, risk of infant hospitalization in the neonatal intensive care unit was increased by 67%, 17.2% vs. 11.9% in the control group.
Active disease measured by the Health Assessment Questionnaire (HAQ) or Routine Assessment of Patient Index Data 3 (RAPID3) was linked to increased risk of adverse obstetric outcomes in some cases, the investigators said.
For example, risk of preterm delivery was increased in women with psoriatic arthritis who had active disease at 32 weeks as measured by HAQ (27 women) and RAPID3 (28 women) scores, while in ankylosing spondylitis, active disease measured at intake by RAPID3 (46 women) was associated with increased risk of caesarean delivery.
Medication use in women with psoriatic arthritis was not associated with increased preterm delivery risk. However, women with ankylosing spondylitis who used corticosteroids in the second trimester had an increased risk of preterm delivery.
The rate of corticosteroid use was “surprisingly high” at 38% among the women with ankylosing spondylitis, Dr. Smith and coinvestigators said.
“The 2016 American College of Rheumatology guidelines in fact recommend against the use of systemic corticosteroids for the treatment of ankylosing spondylitis, with the exception of short-term treatment with rapid tapering in circumstances such as flares during pregnancy, flares of concomitant inflammatory bowel disease, or flare of peripheral arthritis,” they said in their report.
Dr. Smith and coauthors reported no conflicts of interest. The OTIS Collaborative Research Group has received research funding from AbbVie, Amgen, Bristol-Myers Squibb, Janssen, Pfizer, and others.
SOURCE: Smith CJF et al. Arthritis Care Res. 2019 May 10. doi: 10.1002/acr.23924.
FROM ARTHRITIS CARE & RESEARCH
VA system lags in getting DMARDs to veterans with inflammatory arthritis
MADISON, WISC. – Only half of United States veterans with inflammatory arthritis received disease-modifying medication within 90 days of diagnosis if they received care within the Veterans Health Administration, according to a study presented at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
Over the study period, 58.2% of all inflammatory arthritis patients began a disease-modifying antirheumatic drug (DMARD) within 12 months of diagnosis. Rates of DMARD initiation were similar for patients with rheumatoid arthritis (RA, 57.7%) and psoriatic arthritis (PsA, 64.3%), said the first author of the poster presentation, Sogol S. Amjadi, DO, a resident physician at Bingham Memorial Hospital, Blackfoot, Idaho.
However, at 12 months after diagnosis, only 29.6% of ankylosing spondylitis (AS) patients had not been started on a DMARD. “The ankylosing spondylitis group really had the lowest DMARD initiation over time,” said Dr. Amjadi in an interview.
The study used diagnosis codes and natural language processing to look for incident cases of the three inflammatory arthritides (IAs) among patients receiving care within the Veterans Health Administration from 2007 through 2015.
In all, 12,118 patients with incident IA were identified. Of these, 9,711 had RA, 1,472 had PsA, and 935 had AS. Patients were mostly (91.3%) male, with a mean age of 63.7 years.
Over the study period, 41.2% of IA patients were dispensed a DMARD within 30 days of diagnosis, and 50% received a DMARD within 90 days of diagnosis. Patients with PsA or RA had similar rates of DMARD prescription within 30 days of diagnosis (about 42% and 43%, respectively).
The investigators discovered in their analysis that another factor in prompt treatment was access to specialty care.“Timely access to a rheumatology provider is likely important for early DMARD treatment,” wrote Dr. Amjadi and her coauthors in the poster accompanying the presentation. Of patients who did receive a DMARD, 82.7% had received rheumatology specialty care before nonbiologic DMARD dispensing, as had 90.0% of patients receiving biologic DMARDs. Over the entire study period, about 10% of all IA patients had biologic DMARD exposure.
There was a trend over time for increased DMARD dispensing, said the investigators. “The percentage of IA patients with DMARD exposure during the 12-month follow-up period increased from 48.8% in 2008 to 66.4% in 2015.”
For AS patients, early DMARD prescribing rates rose from about 20% in 2007 to nearly 30% in 2015. “DMARD treatment rates during the initial 12 months after diagnosis increased between 2007 and 2015, but nontreatment remained common, particularly in patients with AS,” wrote the investigators. “Delays in treatment for inflammatory arthritis are associated with unfavorable outcomes, including impaired quality of life, irreversible joint damage, and disability.”
The authors reported no conflicts of interest and no outside sources of funding.
MADISON, WISC. – Only half of United States veterans with inflammatory arthritis received disease-modifying medication within 90 days of diagnosis if they received care within the Veterans Health Administration, according to a study presented at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
Over the study period, 58.2% of all inflammatory arthritis patients began a disease-modifying antirheumatic drug (DMARD) within 12 months of diagnosis. Rates of DMARD initiation were similar for patients with rheumatoid arthritis (RA, 57.7%) and psoriatic arthritis (PsA, 64.3%), said the first author of the poster presentation, Sogol S. Amjadi, DO, a resident physician at Bingham Memorial Hospital, Blackfoot, Idaho.
However, at 12 months after diagnosis, only 29.6% of ankylosing spondylitis (AS) patients had not been started on a DMARD. “The ankylosing spondylitis group really had the lowest DMARD initiation over time,” said Dr. Amjadi in an interview.
The study used diagnosis codes and natural language processing to look for incident cases of the three inflammatory arthritides (IAs) among patients receiving care within the Veterans Health Administration from 2007 through 2015.
In all, 12,118 patients with incident IA were identified. Of these, 9,711 had RA, 1,472 had PsA, and 935 had AS. Patients were mostly (91.3%) male, with a mean age of 63.7 years.
Over the study period, 41.2% of IA patients were dispensed a DMARD within 30 days of diagnosis, and 50% received a DMARD within 90 days of diagnosis. Patients with PsA or RA had similar rates of DMARD prescription within 30 days of diagnosis (about 42% and 43%, respectively).
The investigators discovered in their analysis that another factor in prompt treatment was access to specialty care.“Timely access to a rheumatology provider is likely important for early DMARD treatment,” wrote Dr. Amjadi and her coauthors in the poster accompanying the presentation. Of patients who did receive a DMARD, 82.7% had received rheumatology specialty care before nonbiologic DMARD dispensing, as had 90.0% of patients receiving biologic DMARDs. Over the entire study period, about 10% of all IA patients had biologic DMARD exposure.
There was a trend over time for increased DMARD dispensing, said the investigators. “The percentage of IA patients with DMARD exposure during the 12-month follow-up period increased from 48.8% in 2008 to 66.4% in 2015.”
For AS patients, early DMARD prescribing rates rose from about 20% in 2007 to nearly 30% in 2015. “DMARD treatment rates during the initial 12 months after diagnosis increased between 2007 and 2015, but nontreatment remained common, particularly in patients with AS,” wrote the investigators. “Delays in treatment for inflammatory arthritis are associated with unfavorable outcomes, including impaired quality of life, irreversible joint damage, and disability.”
The authors reported no conflicts of interest and no outside sources of funding.
MADISON, WISC. – Only half of United States veterans with inflammatory arthritis received disease-modifying medication within 90 days of diagnosis if they received care within the Veterans Health Administration, according to a study presented at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN).
Over the study period, 58.2% of all inflammatory arthritis patients began a disease-modifying antirheumatic drug (DMARD) within 12 months of diagnosis. Rates of DMARD initiation were similar for patients with rheumatoid arthritis (RA, 57.7%) and psoriatic arthritis (PsA, 64.3%), said the first author of the poster presentation, Sogol S. Amjadi, DO, a resident physician at Bingham Memorial Hospital, Blackfoot, Idaho.
However, at 12 months after diagnosis, only 29.6% of ankylosing spondylitis (AS) patients had not been started on a DMARD. “The ankylosing spondylitis group really had the lowest DMARD initiation over time,” said Dr. Amjadi in an interview.
The study used diagnosis codes and natural language processing to look for incident cases of the three inflammatory arthritides (IAs) among patients receiving care within the Veterans Health Administration from 2007 through 2015.
In all, 12,118 patients with incident IA were identified. Of these, 9,711 had RA, 1,472 had PsA, and 935 had AS. Patients were mostly (91.3%) male, with a mean age of 63.7 years.
Over the study period, 41.2% of IA patients were dispensed a DMARD within 30 days of diagnosis, and 50% received a DMARD within 90 days of diagnosis. Patients with PsA or RA had similar rates of DMARD prescription within 30 days of diagnosis (about 42% and 43%, respectively).
The investigators discovered in their analysis that another factor in prompt treatment was access to specialty care.“Timely access to a rheumatology provider is likely important for early DMARD treatment,” wrote Dr. Amjadi and her coauthors in the poster accompanying the presentation. Of patients who did receive a DMARD, 82.7% had received rheumatology specialty care before nonbiologic DMARD dispensing, as had 90.0% of patients receiving biologic DMARDs. Over the entire study period, about 10% of all IA patients had biologic DMARD exposure.
There was a trend over time for increased DMARD dispensing, said the investigators. “The percentage of IA patients with DMARD exposure during the 12-month follow-up period increased from 48.8% in 2008 to 66.4% in 2015.”
For AS patients, early DMARD prescribing rates rose from about 20% in 2007 to nearly 30% in 2015. “DMARD treatment rates during the initial 12 months after diagnosis increased between 2007 and 2015, but nontreatment remained common, particularly in patients with AS,” wrote the investigators. “Delays in treatment for inflammatory arthritis are associated with unfavorable outcomes, including impaired quality of life, irreversible joint damage, and disability.”
The authors reported no conflicts of interest and no outside sources of funding.
REPORTING FROM SPARTAN 2019
Key clinical point:
Major finding: Overall, 58.2% of inflammatory arthritis patients received a DMARD within the first year of diagnosis.
Study details: Retrospective review of 12,118 incident cases of inflammatory arthritis in the Veterans Health Administration during the period from 2007 through 2015.
Disclosures: The authors reported no conflicts of interest and no outside sources of funding.
Source: Amjadi SS et al. SPARTAN 2019.
Ankylosing spondylitis patients taking COX-2 inhibitors may see fewer cardiovascular events
MADISON, WISC. – Patients with ankylosing spondylitis had a small but significant reduction in risk for cardiovascular events if they were taking cyclooxygenase-2 (COX-2) inhibitors, according to a new systematic review and meta-analysis.
The reduced risk observed in this analysis (risk ratio, 0.48; 95% confidence interval, 0.33-0.70) contrasts with the increased risk for cardiovascular events seen with COX-2 inhibitor use in the general population, said Paras Karmacharya, MBBS, speaking in an interview at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN). The overall effect was highly statistically significant (P = .0001), and the finding provides “reassuring” data for a population that’s known to have an elevated risk for cardiovascular events, he said.
“[W]e found in the subgroup analysis that COX-2 inhibitors were associated with a reduced risk of cardiovascular events as a whole,” an association also seen when looking just at ischemic stroke, Dr. Karmacharya said. “So that was sort of surprising; in the general population, there are some concerns about using COX-2 inhibitors.”
Looking at data for the nine studies that met criteria for inclusion in the meta-analysis, Dr. Karmacharya, a rheumatology fellow at the Mayo Clinic, Rochester, Minn., and his collaborators calculated risk ratios for a composite outcome of all cardiovascular events (CVE) for all individuals taking NSAIDs, compared with individuals with ankylosing spondylitis (AS) who were not taking NSAIDs. Here, they found a relative risk of 0.94 (95% CI, 0.50-1.75; P = .84).
Next, the investigators calculated a relative risk of 0.78 for the composite CVE outcome just for those taking nonselective NSAIDs (95% CI, 0.44-1.38; P = .40).
Along with NSAIDs, Dr. Karmacharya and his coauthors also looked at the relationship between tumor necrosis factor inhibitors (TNFIs) and cardiovascular events. They found a significantly increased risk for the composite endpoint among AS patients taking TNFIs (RR, 1.60; 95% CI, 1.05-2.41; P = .03), but the comparison was limited to only one study.
In their analysis, the investigators also broke out risk of acute coronary syndrome (ACS)/ischemic heart disease. “The only place where we found some increased risk was ACS and ischemic heart disease, and that was with nonselective NSAIDS,” Dr. Karmacharya said (RR, 1.21; 95% CI, 1.06-1.39; P = .005). No significant changes in relative risk for ACS and ischemic heart disease were seen for the total group of NSAID users, for the subgroups taking COX-2 inhibitors, or for those taking TNFIs.
Finally, the investigators found a relative risk of 0.58 for stroke among the full group of NSAID users and a relative risk of 0.59 for those taking COX-2 inhibitors, but no reduced risk for the subgroup taking nonselective NSAIDs (P = .02, .04, and .37, respectively).
“While NSAIDs are known to be associated with an increased risk of CVE in the general population, whether the anti-inflammatory effects of NSAIDs reduce or modify the CVE risk in AS is controversial,” Dr. Karmacharya and his collaborators wrote. In this context, the meta-analysis provides a useful perspective for rheumatologists who care for AS patients, Dr. Karmacharya said: “I think it’s important, because most of these patients are on NSAIDs long-term.”
However, all of the studies included in the meta-analysis were observational, with no randomized, controlled trials meeting inclusion criteria. Also, some analyses presented in the poster involved as few as two studies, so findings should be interpreted with caution, he added. “We don’t have a lot of studies included in the analysis. ... so we need more data for sure, but I think what data we have so far look reassuring.”
Dr. Karmacharya reported that he had no conflicts of interest, and reported no outside sources of funding.
MADISON, WISC. – Patients with ankylosing spondylitis had a small but significant reduction in risk for cardiovascular events if they were taking cyclooxygenase-2 (COX-2) inhibitors, according to a new systematic review and meta-analysis.
The reduced risk observed in this analysis (risk ratio, 0.48; 95% confidence interval, 0.33-0.70) contrasts with the increased risk for cardiovascular events seen with COX-2 inhibitor use in the general population, said Paras Karmacharya, MBBS, speaking in an interview at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN). The overall effect was highly statistically significant (P = .0001), and the finding provides “reassuring” data for a population that’s known to have an elevated risk for cardiovascular events, he said.
“[W]e found in the subgroup analysis that COX-2 inhibitors were associated with a reduced risk of cardiovascular events as a whole,” an association also seen when looking just at ischemic stroke, Dr. Karmacharya said. “So that was sort of surprising; in the general population, there are some concerns about using COX-2 inhibitors.”
Looking at data for the nine studies that met criteria for inclusion in the meta-analysis, Dr. Karmacharya, a rheumatology fellow at the Mayo Clinic, Rochester, Minn., and his collaborators calculated risk ratios for a composite outcome of all cardiovascular events (CVE) for all individuals taking NSAIDs, compared with individuals with ankylosing spondylitis (AS) who were not taking NSAIDs. Here, they found a relative risk of 0.94 (95% CI, 0.50-1.75; P = .84).
Next, the investigators calculated a relative risk of 0.78 for the composite CVE outcome just for those taking nonselective NSAIDs (95% CI, 0.44-1.38; P = .40).
Along with NSAIDs, Dr. Karmacharya and his coauthors also looked at the relationship between tumor necrosis factor inhibitors (TNFIs) and cardiovascular events. They found a significantly increased risk for the composite endpoint among AS patients taking TNFIs (RR, 1.60; 95% CI, 1.05-2.41; P = .03), but the comparison was limited to only one study.
In their analysis, the investigators also broke out risk of acute coronary syndrome (ACS)/ischemic heart disease. “The only place where we found some increased risk was ACS and ischemic heart disease, and that was with nonselective NSAIDS,” Dr. Karmacharya said (RR, 1.21; 95% CI, 1.06-1.39; P = .005). No significant changes in relative risk for ACS and ischemic heart disease were seen for the total group of NSAID users, for the subgroups taking COX-2 inhibitors, or for those taking TNFIs.
Finally, the investigators found a relative risk of 0.58 for stroke among the full group of NSAID users and a relative risk of 0.59 for those taking COX-2 inhibitors, but no reduced risk for the subgroup taking nonselective NSAIDs (P = .02, .04, and .37, respectively).
“While NSAIDs are known to be associated with an increased risk of CVE in the general population, whether the anti-inflammatory effects of NSAIDs reduce or modify the CVE risk in AS is controversial,” Dr. Karmacharya and his collaborators wrote. In this context, the meta-analysis provides a useful perspective for rheumatologists who care for AS patients, Dr. Karmacharya said: “I think it’s important, because most of these patients are on NSAIDs long-term.”
However, all of the studies included in the meta-analysis were observational, with no randomized, controlled trials meeting inclusion criteria. Also, some analyses presented in the poster involved as few as two studies, so findings should be interpreted with caution, he added. “We don’t have a lot of studies included in the analysis. ... so we need more data for sure, but I think what data we have so far look reassuring.”
Dr. Karmacharya reported that he had no conflicts of interest, and reported no outside sources of funding.
MADISON, WISC. – Patients with ankylosing spondylitis had a small but significant reduction in risk for cardiovascular events if they were taking cyclooxygenase-2 (COX-2) inhibitors, according to a new systematic review and meta-analysis.
The reduced risk observed in this analysis (risk ratio, 0.48; 95% confidence interval, 0.33-0.70) contrasts with the increased risk for cardiovascular events seen with COX-2 inhibitor use in the general population, said Paras Karmacharya, MBBS, speaking in an interview at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN). The overall effect was highly statistically significant (P = .0001), and the finding provides “reassuring” data for a population that’s known to have an elevated risk for cardiovascular events, he said.
“[W]e found in the subgroup analysis that COX-2 inhibitors were associated with a reduced risk of cardiovascular events as a whole,” an association also seen when looking just at ischemic stroke, Dr. Karmacharya said. “So that was sort of surprising; in the general population, there are some concerns about using COX-2 inhibitors.”
Looking at data for the nine studies that met criteria for inclusion in the meta-analysis, Dr. Karmacharya, a rheumatology fellow at the Mayo Clinic, Rochester, Minn., and his collaborators calculated risk ratios for a composite outcome of all cardiovascular events (CVE) for all individuals taking NSAIDs, compared with individuals with ankylosing spondylitis (AS) who were not taking NSAIDs. Here, they found a relative risk of 0.94 (95% CI, 0.50-1.75; P = .84).
Next, the investigators calculated a relative risk of 0.78 for the composite CVE outcome just for those taking nonselective NSAIDs (95% CI, 0.44-1.38; P = .40).
Along with NSAIDs, Dr. Karmacharya and his coauthors also looked at the relationship between tumor necrosis factor inhibitors (TNFIs) and cardiovascular events. They found a significantly increased risk for the composite endpoint among AS patients taking TNFIs (RR, 1.60; 95% CI, 1.05-2.41; P = .03), but the comparison was limited to only one study.
In their analysis, the investigators also broke out risk of acute coronary syndrome (ACS)/ischemic heart disease. “The only place where we found some increased risk was ACS and ischemic heart disease, and that was with nonselective NSAIDS,” Dr. Karmacharya said (RR, 1.21; 95% CI, 1.06-1.39; P = .005). No significant changes in relative risk for ACS and ischemic heart disease were seen for the total group of NSAID users, for the subgroups taking COX-2 inhibitors, or for those taking TNFIs.
Finally, the investigators found a relative risk of 0.58 for stroke among the full group of NSAID users and a relative risk of 0.59 for those taking COX-2 inhibitors, but no reduced risk for the subgroup taking nonselective NSAIDs (P = .02, .04, and .37, respectively).
“While NSAIDs are known to be associated with an increased risk of CVE in the general population, whether the anti-inflammatory effects of NSAIDs reduce or modify the CVE risk in AS is controversial,” Dr. Karmacharya and his collaborators wrote. In this context, the meta-analysis provides a useful perspective for rheumatologists who care for AS patients, Dr. Karmacharya said: “I think it’s important, because most of these patients are on NSAIDs long-term.”
However, all of the studies included in the meta-analysis were observational, with no randomized, controlled trials meeting inclusion criteria. Also, some analyses presented in the poster involved as few as two studies, so findings should be interpreted with caution, he added. “We don’t have a lot of studies included in the analysis. ... so we need more data for sure, but I think what data we have so far look reassuring.”
Dr. Karmacharya reported that he had no conflicts of interest, and reported no outside sources of funding.
REPORTING FROM SPARTAN 2019
Key clinical point: Individuals with ankylosing spondylitis (AS) who took cyclooxygenase 2 (COX-2) inhibitors had a reduced risk of cardiovascular events, compared with AS patients who were not using COX-2 inhibitors.
Major finding: Individuals with AS taking COX-2 inhibitors had a risk ratio of 0.48 for cardiovascular events (95% CI, 0.33-0.70; P = .001).
Study details: Systematic review and meta-analysis of nine observational studies that variably examined the association between NSAID use and tumor necrosis factor inhibitor use and cardiovascular events among individuals with AS.
Disclosures: The authors reported no conflicts of interest and no outside sources of funding.
Source: Karmacharya P. et al. SPARTAN 2019.
Experts agree on optimal use of MRI in axSpA
BIRMINGHAM, ENGLAND – An evidence-based approach coupled with expert consensus has been used to determine the best way to use MRI for the diagnosis of axial spondyloarthritis (axSpA).
Working under the auspices of the British Society for Spondyloarthritis (BRITSpA), a task force of nine rheumatologists and nine musculoskeletal radiologists with an interest in axSpA developed a set of seven recommendations that provide guidance on how to best to acquire and then interpret MRI images of the spine and sacroiliac joints.
The recommendations, which were published online (Rheumatology. 2019 May 2. doi: 10.1093/rheumatology/kez173), cover how to perform MRI when axSpA is suspected, such as by imaging both the sacroiliac joints and the spine, and provide guidance on the sequences and order of MRI planes to be used, and what features may increase the diagnostic confidence of axSpA.
The recommendations are as follows:
• When requesting an MRI for suspected axSpA, imaging of both the sacroiliac joints and the spine is recommended.
• T1-weighted and fat-suppressed, fluid-sensitive sequences are recommended for suspected axSpA.
• The minimum protocol when requesting an MRI for suspected axSpA should include sagittal images of the spine with extended lateral coverage and images of the sacroiliac joints that are in an oblique coronal plane to the joint.
• In the sacroiliac joints, the presence of bone marrow edema, fatty infiltration, or erosion is suggestive of the diagnosis of axSpA. The presence of more than one of these features increases the diagnostic confidence of axSpA.
• In the spine, the presence of multiple corner inflammatory lesions and/or multiple corner fatty lesions increases the diagnostic confidence of axSpA.
• In the sacroiliac joints and/or spine, the presence of characteristic new bone formation increases the diagnostic confidence of axSpA.
• The full range and combination of active and structural lesions of the sacroiliac joints and spine should be taken into account when deciding if the MRI scan is suggestive of axSpA or not.
The recommendations “are intended to standardize practice around the use of MRI,” said Alexis Jones, MBBS, MS (Rheumatology), a senior clinical research fellow at University College London Hospitals NHS Foundation Trust. She presented the recommendations on behalf of the expert task force at the annual conference of the British Society for Rheumatology.
“MRI has become an essential tool in axial spondyloarthritis. It facilitates earlier diagnoses and therefore has allowed for earlier initiation of treatment. It can be used to monitor the burden of inflammation and may predict response to therapy,” Dr. Jones said. Despite this, “there is significant inconsistency in the use of MRI” in clinical practice.
For instance, a survey performed in the United Kingdom (J Rheumatol. 2017;44[6]:780-5) highlighted the need for better collaboration between rheumatology and radiology departments to identify axSpA MRI lesions and develop appropriate protocols.
That survey showed that a quarter of radiologists were not aware of the term axSpA, and just 31% and 25%, respectively, were aware of Assessment of Spondyloarthritis international Society (ASAS) criteria for a positive MRI of the sacroiliac joints and spine. Furthermore, 18% of radiologists did not recognize bone marrow edema as a diagnostic feature of axSpA.
The heterogeneity in the performance of MRI in clinical practice could lead to a delay in diagnosis and potentially misdiagnosis, the task force’s lead author and consultant rheumatologist, Pedro Machado, MD, said in an interview.
“I think everyone has been focusing on demonstrating the value of MRI in the condition but then they forgot to look at the standardization aspect,” said Dr. Machado, who works at University College Hospital and the National Hospital for Neurology and Neurosurgery in London.
With that in mind, the BRITSpA-endorsed task force was set up and met to determine the scope of the recommendations. They looked at the evidence for the use of MRI in the diagnosis of axSpA and used two overarching principles to draft the recommendations: 1) the diagnosis of axSpA is based on clinical, laboratory, and imaging features; 2) Some patients with axSpA have isolated inflammation of the sacroiliac joints or spine.
“All of the recommendations were met with a high level of agreement, indicating a strong consensus” among rheumatologists and radiologists, Dr. Jones noted.
“These recommendations can be immediately applied to clinical practice,” said Dr. Machado, who noted that they should standardize practice and decrease heterogeneity around the use of MRI. “This will help ensure a more informed and consistent approach to the diagnosis of axSpA.”
One of the potential impacts of the recommendations, if followed, is that they may actually help to reduce health care costs, Dr. Machado suggested, because an optimized protocol would be used, making MRI more cost effective by not including sequences that do not add value in the condition.
The next task is to share the recommendations more widely and make sure they are applied in clinical practice.
A systematic literature review on which the recommendations were based was published simultaneously with the conference presentation (Rheumatology. 2019 May 2. doi: 10.1093/rheumatology/kez172).
The work was supported by BRITSpA. The authors had no relevant disclosures.
SOURCE: Bray TJP et al. Rheumatology 2019;58(suppl 3): Abstract 033. doi: 10.1093/rheumatology/kez105.032.
BIRMINGHAM, ENGLAND – An evidence-based approach coupled with expert consensus has been used to determine the best way to use MRI for the diagnosis of axial spondyloarthritis (axSpA).
Working under the auspices of the British Society for Spondyloarthritis (BRITSpA), a task force of nine rheumatologists and nine musculoskeletal radiologists with an interest in axSpA developed a set of seven recommendations that provide guidance on how to best to acquire and then interpret MRI images of the spine and sacroiliac joints.
The recommendations, which were published online (Rheumatology. 2019 May 2. doi: 10.1093/rheumatology/kez173), cover how to perform MRI when axSpA is suspected, such as by imaging both the sacroiliac joints and the spine, and provide guidance on the sequences and order of MRI planes to be used, and what features may increase the diagnostic confidence of axSpA.
The recommendations are as follows:
• When requesting an MRI for suspected axSpA, imaging of both the sacroiliac joints and the spine is recommended.
• T1-weighted and fat-suppressed, fluid-sensitive sequences are recommended for suspected axSpA.
• The minimum protocol when requesting an MRI for suspected axSpA should include sagittal images of the spine with extended lateral coverage and images of the sacroiliac joints that are in an oblique coronal plane to the joint.
• In the sacroiliac joints, the presence of bone marrow edema, fatty infiltration, or erosion is suggestive of the diagnosis of axSpA. The presence of more than one of these features increases the diagnostic confidence of axSpA.
• In the spine, the presence of multiple corner inflammatory lesions and/or multiple corner fatty lesions increases the diagnostic confidence of axSpA.
• In the sacroiliac joints and/or spine, the presence of characteristic new bone formation increases the diagnostic confidence of axSpA.
• The full range and combination of active and structural lesions of the sacroiliac joints and spine should be taken into account when deciding if the MRI scan is suggestive of axSpA or not.
The recommendations “are intended to standardize practice around the use of MRI,” said Alexis Jones, MBBS, MS (Rheumatology), a senior clinical research fellow at University College London Hospitals NHS Foundation Trust. She presented the recommendations on behalf of the expert task force at the annual conference of the British Society for Rheumatology.
“MRI has become an essential tool in axial spondyloarthritis. It facilitates earlier diagnoses and therefore has allowed for earlier initiation of treatment. It can be used to monitor the burden of inflammation and may predict response to therapy,” Dr. Jones said. Despite this, “there is significant inconsistency in the use of MRI” in clinical practice.
For instance, a survey performed in the United Kingdom (J Rheumatol. 2017;44[6]:780-5) highlighted the need for better collaboration between rheumatology and radiology departments to identify axSpA MRI lesions and develop appropriate protocols.
That survey showed that a quarter of radiologists were not aware of the term axSpA, and just 31% and 25%, respectively, were aware of Assessment of Spondyloarthritis international Society (ASAS) criteria for a positive MRI of the sacroiliac joints and spine. Furthermore, 18% of radiologists did not recognize bone marrow edema as a diagnostic feature of axSpA.
The heterogeneity in the performance of MRI in clinical practice could lead to a delay in diagnosis and potentially misdiagnosis, the task force’s lead author and consultant rheumatologist, Pedro Machado, MD, said in an interview.
“I think everyone has been focusing on demonstrating the value of MRI in the condition but then they forgot to look at the standardization aspect,” said Dr. Machado, who works at University College Hospital and the National Hospital for Neurology and Neurosurgery in London.
With that in mind, the BRITSpA-endorsed task force was set up and met to determine the scope of the recommendations. They looked at the evidence for the use of MRI in the diagnosis of axSpA and used two overarching principles to draft the recommendations: 1) the diagnosis of axSpA is based on clinical, laboratory, and imaging features; 2) Some patients with axSpA have isolated inflammation of the sacroiliac joints or spine.
“All of the recommendations were met with a high level of agreement, indicating a strong consensus” among rheumatologists and radiologists, Dr. Jones noted.
“These recommendations can be immediately applied to clinical practice,” said Dr. Machado, who noted that they should standardize practice and decrease heterogeneity around the use of MRI. “This will help ensure a more informed and consistent approach to the diagnosis of axSpA.”
One of the potential impacts of the recommendations, if followed, is that they may actually help to reduce health care costs, Dr. Machado suggested, because an optimized protocol would be used, making MRI more cost effective by not including sequences that do not add value in the condition.
The next task is to share the recommendations more widely and make sure they are applied in clinical practice.
A systematic literature review on which the recommendations were based was published simultaneously with the conference presentation (Rheumatology. 2019 May 2. doi: 10.1093/rheumatology/kez172).
The work was supported by BRITSpA. The authors had no relevant disclosures.
SOURCE: Bray TJP et al. Rheumatology 2019;58(suppl 3): Abstract 033. doi: 10.1093/rheumatology/kez105.032.
BIRMINGHAM, ENGLAND – An evidence-based approach coupled with expert consensus has been used to determine the best way to use MRI for the diagnosis of axial spondyloarthritis (axSpA).
Working under the auspices of the British Society for Spondyloarthritis (BRITSpA), a task force of nine rheumatologists and nine musculoskeletal radiologists with an interest in axSpA developed a set of seven recommendations that provide guidance on how to best to acquire and then interpret MRI images of the spine and sacroiliac joints.
The recommendations, which were published online (Rheumatology. 2019 May 2. doi: 10.1093/rheumatology/kez173), cover how to perform MRI when axSpA is suspected, such as by imaging both the sacroiliac joints and the spine, and provide guidance on the sequences and order of MRI planes to be used, and what features may increase the diagnostic confidence of axSpA.
The recommendations are as follows:
• When requesting an MRI for suspected axSpA, imaging of both the sacroiliac joints and the spine is recommended.
• T1-weighted and fat-suppressed, fluid-sensitive sequences are recommended for suspected axSpA.
• The minimum protocol when requesting an MRI for suspected axSpA should include sagittal images of the spine with extended lateral coverage and images of the sacroiliac joints that are in an oblique coronal plane to the joint.
• In the sacroiliac joints, the presence of bone marrow edema, fatty infiltration, or erosion is suggestive of the diagnosis of axSpA. The presence of more than one of these features increases the diagnostic confidence of axSpA.
• In the spine, the presence of multiple corner inflammatory lesions and/or multiple corner fatty lesions increases the diagnostic confidence of axSpA.
• In the sacroiliac joints and/or spine, the presence of characteristic new bone formation increases the diagnostic confidence of axSpA.
• The full range and combination of active and structural lesions of the sacroiliac joints and spine should be taken into account when deciding if the MRI scan is suggestive of axSpA or not.
The recommendations “are intended to standardize practice around the use of MRI,” said Alexis Jones, MBBS, MS (Rheumatology), a senior clinical research fellow at University College London Hospitals NHS Foundation Trust. She presented the recommendations on behalf of the expert task force at the annual conference of the British Society for Rheumatology.
“MRI has become an essential tool in axial spondyloarthritis. It facilitates earlier diagnoses and therefore has allowed for earlier initiation of treatment. It can be used to monitor the burden of inflammation and may predict response to therapy,” Dr. Jones said. Despite this, “there is significant inconsistency in the use of MRI” in clinical practice.
For instance, a survey performed in the United Kingdom (J Rheumatol. 2017;44[6]:780-5) highlighted the need for better collaboration between rheumatology and radiology departments to identify axSpA MRI lesions and develop appropriate protocols.
That survey showed that a quarter of radiologists were not aware of the term axSpA, and just 31% and 25%, respectively, were aware of Assessment of Spondyloarthritis international Society (ASAS) criteria for a positive MRI of the sacroiliac joints and spine. Furthermore, 18% of radiologists did not recognize bone marrow edema as a diagnostic feature of axSpA.
The heterogeneity in the performance of MRI in clinical practice could lead to a delay in diagnosis and potentially misdiagnosis, the task force’s lead author and consultant rheumatologist, Pedro Machado, MD, said in an interview.
“I think everyone has been focusing on demonstrating the value of MRI in the condition but then they forgot to look at the standardization aspect,” said Dr. Machado, who works at University College Hospital and the National Hospital for Neurology and Neurosurgery in London.
With that in mind, the BRITSpA-endorsed task force was set up and met to determine the scope of the recommendations. They looked at the evidence for the use of MRI in the diagnosis of axSpA and used two overarching principles to draft the recommendations: 1) the diagnosis of axSpA is based on clinical, laboratory, and imaging features; 2) Some patients with axSpA have isolated inflammation of the sacroiliac joints or spine.
“All of the recommendations were met with a high level of agreement, indicating a strong consensus” among rheumatologists and radiologists, Dr. Jones noted.
“These recommendations can be immediately applied to clinical practice,” said Dr. Machado, who noted that they should standardize practice and decrease heterogeneity around the use of MRI. “This will help ensure a more informed and consistent approach to the diagnosis of axSpA.”
One of the potential impacts of the recommendations, if followed, is that they may actually help to reduce health care costs, Dr. Machado suggested, because an optimized protocol would be used, making MRI more cost effective by not including sequences that do not add value in the condition.
The next task is to share the recommendations more widely and make sure they are applied in clinical practice.
A systematic literature review on which the recommendations were based was published simultaneously with the conference presentation (Rheumatology. 2019 May 2. doi: 10.1093/rheumatology/kez172).
The work was supported by BRITSpA. The authors had no relevant disclosures.
SOURCE: Bray TJP et al. Rheumatology 2019;58(suppl 3): Abstract 033. doi: 10.1093/rheumatology/kez105.032.
REPORTING FROM BSR 2019
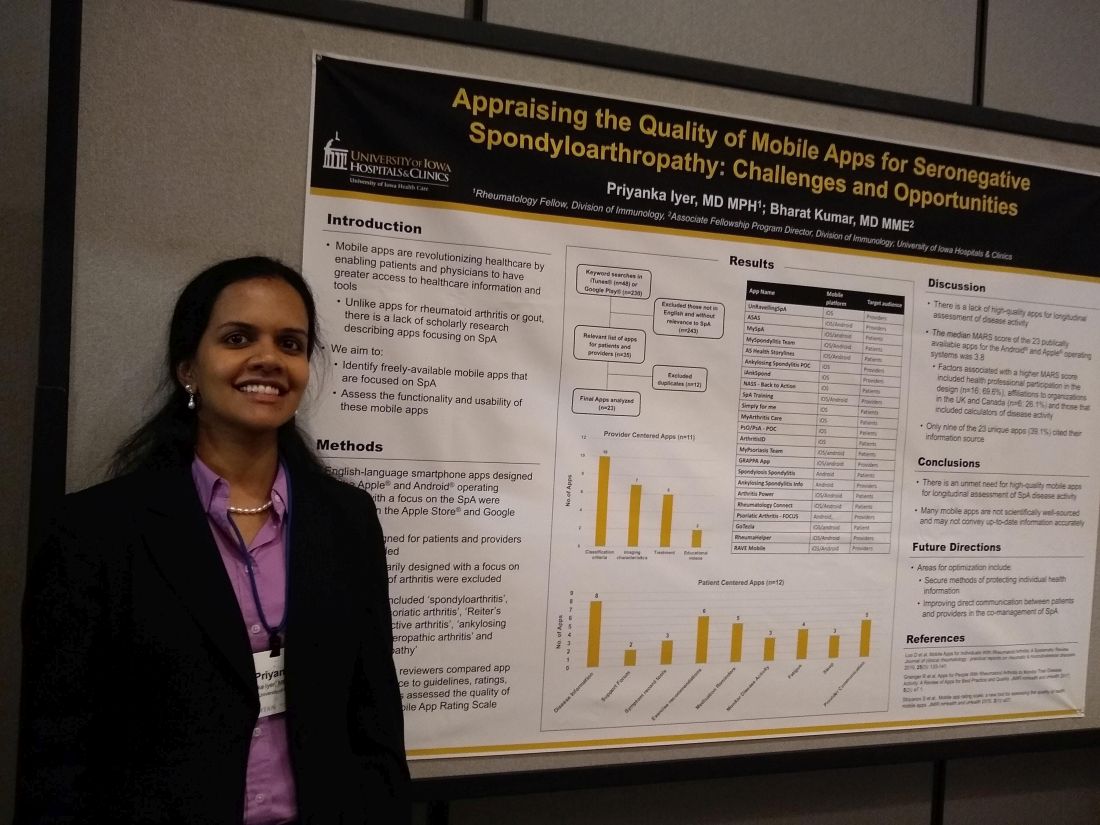
Mobile SpA apps abound, but there’s room for quality improvement
MADISON, WISC. – according to a recent review.
In assessing the 23 publicly available apps aimed at patients or providers, the median score on a common assessment of smartphone apps was just 3.8 on a 5-point scale, said Priyanka Iyer, MBBS, MPH.
Speaking in an interview at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN), Dr. Iyer pointed out several ways that apps could be optimized. Foremost, she said, is providing secure ways to store and transmit protected health information. Also, apps still haven’t realized their potential to support true comanagement of spondyloarthritis (SpA) via secure, direct patient-provider communication.
“This is an area that we researched previously in rheumatoid arthritis and gout,” explained Dr. Iyer, a rheumatology fellow at the University of Iowa, Iowa City. “We found 23 apps that are available between the Android and iOS platforms; most of them are actually centered towards patients.” In their review, Dr. Iyer and coauthor, Bharat Kumar, MD, had excluded apps that primarily focused on other types of arthritis, using search terms that focused on SpA.
In looking at the 11 provider-centered apps and the 12 that were patient focused, Dr. Iyer and coauthor independently reviewed features of each app. Factors they considered included adherence to guidelines, amount of correct medical information provided, and specific features including capacity to store imaging and test results, and ability to host patient-provider communication.
Of the provider-centered apps, 10 contained appropriate classification criteria, and 7 also contained medical imaging characteristics of the target conditions. Six apps guided providers through treatment options, and two had educational videos.
Of the 12 patient-centered apps, 8 provided disease information, and 6 gave exercise recommendations. Five of the apps had prompts that reminded patients to take medication, and three had tools to help patients record and track symptoms. Similarly, three apps had features to help patients monitor disease activity. Two of the apps were primarily access points for a patient support forum.
Additionally, each app was evaluated by each reviewer using the Mobile App Rating Scale (MARS), said Dr. Iyer. “The overall rating was pretty low, at 3.8 [of a possible 5.0]. Factors that increased the MARS scores included affiliations to organizations in the United Kingdom and Canada; for patients who use these apps, their information is automatically transmitted to their providers, and they are able to also access imaging and most of their other health care information on the app.”
Another factor associated with a higher MARS score was design that included health professional participation, which was the case for 16 apps (69.6%). Apps that included calculators of disease activity were also more likely to achieve a higher MARS score, Dr. Iyer and coauthor wrote.
Notably, just 9 of 23 apps (39.1%) included citations referencing their source for medical information.
“I think future areas for improvement and for development of apps include securing individual health information to allow direct communication between patients and providers,” Dr. Iyer said. “I hope that some patients use these apps to learn, and to help their self-management improve.”
“There is an unmet need for high-quality mobile apps for longitudinal assessment of SpA disease activity,” Dr. Iyer and colleagues wrote in the poster accompanying the presentation. “Many mobile apps are not scientifically well sourced and may not convey up-to-date information accurately.”
The authors reported no conflicts of interest and no outside sources of funding.
SOURCE: Iyer P et al. SPARTAN 2019.
MADISON, WISC. – according to a recent review.
In assessing the 23 publicly available apps aimed at patients or providers, the median score on a common assessment of smartphone apps was just 3.8 on a 5-point scale, said Priyanka Iyer, MBBS, MPH.
Speaking in an interview at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN), Dr. Iyer pointed out several ways that apps could be optimized. Foremost, she said, is providing secure ways to store and transmit protected health information. Also, apps still haven’t realized their potential to support true comanagement of spondyloarthritis (SpA) via secure, direct patient-provider communication.
“This is an area that we researched previously in rheumatoid arthritis and gout,” explained Dr. Iyer, a rheumatology fellow at the University of Iowa, Iowa City. “We found 23 apps that are available between the Android and iOS platforms; most of them are actually centered towards patients.” In their review, Dr. Iyer and coauthor, Bharat Kumar, MD, had excluded apps that primarily focused on other types of arthritis, using search terms that focused on SpA.
In looking at the 11 provider-centered apps and the 12 that were patient focused, Dr. Iyer and coauthor independently reviewed features of each app. Factors they considered included adherence to guidelines, amount of correct medical information provided, and specific features including capacity to store imaging and test results, and ability to host patient-provider communication.
Of the provider-centered apps, 10 contained appropriate classification criteria, and 7 also contained medical imaging characteristics of the target conditions. Six apps guided providers through treatment options, and two had educational videos.
Of the 12 patient-centered apps, 8 provided disease information, and 6 gave exercise recommendations. Five of the apps had prompts that reminded patients to take medication, and three had tools to help patients record and track symptoms. Similarly, three apps had features to help patients monitor disease activity. Two of the apps were primarily access points for a patient support forum.
Additionally, each app was evaluated by each reviewer using the Mobile App Rating Scale (MARS), said Dr. Iyer. “The overall rating was pretty low, at 3.8 [of a possible 5.0]. Factors that increased the MARS scores included affiliations to organizations in the United Kingdom and Canada; for patients who use these apps, their information is automatically transmitted to their providers, and they are able to also access imaging and most of their other health care information on the app.”
Another factor associated with a higher MARS score was design that included health professional participation, which was the case for 16 apps (69.6%). Apps that included calculators of disease activity were also more likely to achieve a higher MARS score, Dr. Iyer and coauthor wrote.
Notably, just 9 of 23 apps (39.1%) included citations referencing their source for medical information.
“I think future areas for improvement and for development of apps include securing individual health information to allow direct communication between patients and providers,” Dr. Iyer said. “I hope that some patients use these apps to learn, and to help their self-management improve.”
“There is an unmet need for high-quality mobile apps for longitudinal assessment of SpA disease activity,” Dr. Iyer and colleagues wrote in the poster accompanying the presentation. “Many mobile apps are not scientifically well sourced and may not convey up-to-date information accurately.”
The authors reported no conflicts of interest and no outside sources of funding.
SOURCE: Iyer P et al. SPARTAN 2019.
MADISON, WISC. – according to a recent review.
In assessing the 23 publicly available apps aimed at patients or providers, the median score on a common assessment of smartphone apps was just 3.8 on a 5-point scale, said Priyanka Iyer, MBBS, MPH.
Speaking in an interview at the annual meeting of the Spondyloarthritis Research and Treatment Network (SPARTAN), Dr. Iyer pointed out several ways that apps could be optimized. Foremost, she said, is providing secure ways to store and transmit protected health information. Also, apps still haven’t realized their potential to support true comanagement of spondyloarthritis (SpA) via secure, direct patient-provider communication.
“This is an area that we researched previously in rheumatoid arthritis and gout,” explained Dr. Iyer, a rheumatology fellow at the University of Iowa, Iowa City. “We found 23 apps that are available between the Android and iOS platforms; most of them are actually centered towards patients.” In their review, Dr. Iyer and coauthor, Bharat Kumar, MD, had excluded apps that primarily focused on other types of arthritis, using search terms that focused on SpA.
In looking at the 11 provider-centered apps and the 12 that were patient focused, Dr. Iyer and coauthor independently reviewed features of each app. Factors they considered included adherence to guidelines, amount of correct medical information provided, and specific features including capacity to store imaging and test results, and ability to host patient-provider communication.
Of the provider-centered apps, 10 contained appropriate classification criteria, and 7 also contained medical imaging characteristics of the target conditions. Six apps guided providers through treatment options, and two had educational videos.
Of the 12 patient-centered apps, 8 provided disease information, and 6 gave exercise recommendations. Five of the apps had prompts that reminded patients to take medication, and three had tools to help patients record and track symptoms. Similarly, three apps had features to help patients monitor disease activity. Two of the apps were primarily access points for a patient support forum.
Additionally, each app was evaluated by each reviewer using the Mobile App Rating Scale (MARS), said Dr. Iyer. “The overall rating was pretty low, at 3.8 [of a possible 5.0]. Factors that increased the MARS scores included affiliations to organizations in the United Kingdom and Canada; for patients who use these apps, their information is automatically transmitted to their providers, and they are able to also access imaging and most of their other health care information on the app.”
Another factor associated with a higher MARS score was design that included health professional participation, which was the case for 16 apps (69.6%). Apps that included calculators of disease activity were also more likely to achieve a higher MARS score, Dr. Iyer and coauthor wrote.
Notably, just 9 of 23 apps (39.1%) included citations referencing their source for medical information.
“I think future areas for improvement and for development of apps include securing individual health information to allow direct communication between patients and providers,” Dr. Iyer said. “I hope that some patients use these apps to learn, and to help their self-management improve.”
“There is an unmet need for high-quality mobile apps for longitudinal assessment of SpA disease activity,” Dr. Iyer and colleagues wrote in the poster accompanying the presentation. “Many mobile apps are not scientifically well sourced and may not convey up-to-date information accurately.”
The authors reported no conflicts of interest and no outside sources of funding.
SOURCE: Iyer P et al. SPARTAN 2019.
REPORTING FROM SPARTAN 2019
Arthritis joint pain, inactivity vary greatly across U.S.
Almost 31% of the estimated 54 million adults in the United States with arthritis have severe joint pain, according to the Centers for Disease Control and Prevention.

Nationally, the prevalence of severe joint pain was 30.8% in adults with arthritis in 2017, but state-specific, age-standardized prevalences varied from a low of 20.8% in Colorado to 45.2% in Mississippi. Regionally, prevalences of both severe joint pain and physical inactivity in arthritis patients were highest in the Southeast, noted Dana Guglielmo, MPH, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion, Atlanta, and associates (MMWR 2019 May 3;68(17):381-7).
The prevalence of arthritis itself was lowest in the District of Columbia at 15.7% and highest in West Virginia at 34.6%. Alabama, at 30.4%, was the only other state above 30%. Colorado had the lowest physical inactivity rate (23.2%), while Kentucky had the highest (44.4%), the investigators said.
The differences among arthritis patients were demographic as well as geographic in 2017. The prevalence of severe joint pain was 33.0% among those aged 18-44 years and 35.6% in those 45-64 but only 25.1% in those aged 65 and older. Whites had a 27.4% prevalence of severe joint pain, compared with 42.0% for Hispanics and 50.9% for blacks. For arthritis patients with a college degree, the age-standardized prevalence of severe joint pain was 15.1%, compared with 35.5% for high school graduates and 54.1% for those with less than a high school degree, based on data from the Behavioral Risk Factor Surveillance System.
“Although persons with arthritis report that pain, or fear of causing or worsening it, is a substantial barrier to exercising, physical activity is an inexpensive intervention that can reduce pain, prevent or delay disability and limitations, and improve mental health, physical functioning, and quality of life with few adverse effects,” wrote Ms. Guglielmo and associates. Adults with severe joint pain “should engage in regular physical activity according to their abilities and avoid physical inactivity [since] even small amounts of physical activity can improve physical functioning in adults with joint conditions.”
SOURCE: Guglielmo D et al. MMWR 2019 May 3;68(17):381-7.
Almost 31% of the estimated 54 million adults in the United States with arthritis have severe joint pain, according to the Centers for Disease Control and Prevention.

Nationally, the prevalence of severe joint pain was 30.8% in adults with arthritis in 2017, but state-specific, age-standardized prevalences varied from a low of 20.8% in Colorado to 45.2% in Mississippi. Regionally, prevalences of both severe joint pain and physical inactivity in arthritis patients were highest in the Southeast, noted Dana Guglielmo, MPH, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion, Atlanta, and associates (MMWR 2019 May 3;68(17):381-7).
The prevalence of arthritis itself was lowest in the District of Columbia at 15.7% and highest in West Virginia at 34.6%. Alabama, at 30.4%, was the only other state above 30%. Colorado had the lowest physical inactivity rate (23.2%), while Kentucky had the highest (44.4%), the investigators said.
The differences among arthritis patients were demographic as well as geographic in 2017. The prevalence of severe joint pain was 33.0% among those aged 18-44 years and 35.6% in those 45-64 but only 25.1% in those aged 65 and older. Whites had a 27.4% prevalence of severe joint pain, compared with 42.0% for Hispanics and 50.9% for blacks. For arthritis patients with a college degree, the age-standardized prevalence of severe joint pain was 15.1%, compared with 35.5% for high school graduates and 54.1% for those with less than a high school degree, based on data from the Behavioral Risk Factor Surveillance System.
“Although persons with arthritis report that pain, or fear of causing or worsening it, is a substantial barrier to exercising, physical activity is an inexpensive intervention that can reduce pain, prevent or delay disability and limitations, and improve mental health, physical functioning, and quality of life with few adverse effects,” wrote Ms. Guglielmo and associates. Adults with severe joint pain “should engage in regular physical activity according to their abilities and avoid physical inactivity [since] even small amounts of physical activity can improve physical functioning in adults with joint conditions.”
SOURCE: Guglielmo D et al. MMWR 2019 May 3;68(17):381-7.
Almost 31% of the estimated 54 million adults in the United States with arthritis have severe joint pain, according to the Centers for Disease Control and Prevention.

Nationally, the prevalence of severe joint pain was 30.8% in adults with arthritis in 2017, but state-specific, age-standardized prevalences varied from a low of 20.8% in Colorado to 45.2% in Mississippi. Regionally, prevalences of both severe joint pain and physical inactivity in arthritis patients were highest in the Southeast, noted Dana Guglielmo, MPH, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion, Atlanta, and associates (MMWR 2019 May 3;68(17):381-7).
The prevalence of arthritis itself was lowest in the District of Columbia at 15.7% and highest in West Virginia at 34.6%. Alabama, at 30.4%, was the only other state above 30%. Colorado had the lowest physical inactivity rate (23.2%), while Kentucky had the highest (44.4%), the investigators said.
The differences among arthritis patients were demographic as well as geographic in 2017. The prevalence of severe joint pain was 33.0% among those aged 18-44 years and 35.6% in those 45-64 but only 25.1% in those aged 65 and older. Whites had a 27.4% prevalence of severe joint pain, compared with 42.0% for Hispanics and 50.9% for blacks. For arthritis patients with a college degree, the age-standardized prevalence of severe joint pain was 15.1%, compared with 35.5% for high school graduates and 54.1% for those with less than a high school degree, based on data from the Behavioral Risk Factor Surveillance System.
“Although persons with arthritis report that pain, or fear of causing or worsening it, is a substantial barrier to exercising, physical activity is an inexpensive intervention that can reduce pain, prevent or delay disability and limitations, and improve mental health, physical functioning, and quality of life with few adverse effects,” wrote Ms. Guglielmo and associates. Adults with severe joint pain “should engage in regular physical activity according to their abilities and avoid physical inactivity [since] even small amounts of physical activity can improve physical functioning in adults with joint conditions.”
SOURCE: Guglielmo D et al. MMWR 2019 May 3;68(17):381-7.
FROM MMWR
FDA approves new etanercept biosimilar, Eticovo
The Food and Drug Administration has approved Eticovo (etanercept-ykro), a biosimilar of Enbrel (etanercept), for the treatment of several different rheumatologic and dermatologic conditions.
FDA approval was based in part on the results of a phase 3 trial in which 596 patients with moderate to severe rheumatoid arthritis uncontrolled by methotrexate received either Eticovo or Enbrel. The American College of Rheumatology 20% response rate after 24 weeks was 78.1% for Eticovo and 80.3% for Enbrel; the two drugs were statistically equivalent. Both groups had statistically equivalent rates of treatment-emergent adverse events (55.2% vs. 58.2%).
According to the label, Eticovo is a tumor necrosis factor blocker approved for the treatment of rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, and plaque psoriasis in patients aged 4 years or older. The most common adverse events associated with the drug include infections and injection site reactions.
Eticovo is the second etanercept biosimilar approved by the FDA. The first FDA-approved etanercept biosimilar, etanercept-szzs (Erelzi), is currently facing a legal challenge from Amgen, the manufacturer of Enbrel.
The Food and Drug Administration has approved Eticovo (etanercept-ykro), a biosimilar of Enbrel (etanercept), for the treatment of several different rheumatologic and dermatologic conditions.
FDA approval was based in part on the results of a phase 3 trial in which 596 patients with moderate to severe rheumatoid arthritis uncontrolled by methotrexate received either Eticovo or Enbrel. The American College of Rheumatology 20% response rate after 24 weeks was 78.1% for Eticovo and 80.3% for Enbrel; the two drugs were statistically equivalent. Both groups had statistically equivalent rates of treatment-emergent adverse events (55.2% vs. 58.2%).
According to the label, Eticovo is a tumor necrosis factor blocker approved for the treatment of rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, and plaque psoriasis in patients aged 4 years or older. The most common adverse events associated with the drug include infections and injection site reactions.
Eticovo is the second etanercept biosimilar approved by the FDA. The first FDA-approved etanercept biosimilar, etanercept-szzs (Erelzi), is currently facing a legal challenge from Amgen, the manufacturer of Enbrel.
The Food and Drug Administration has approved Eticovo (etanercept-ykro), a biosimilar of Enbrel (etanercept), for the treatment of several different rheumatologic and dermatologic conditions.
FDA approval was based in part on the results of a phase 3 trial in which 596 patients with moderate to severe rheumatoid arthritis uncontrolled by methotrexate received either Eticovo or Enbrel. The American College of Rheumatology 20% response rate after 24 weeks was 78.1% for Eticovo and 80.3% for Enbrel; the two drugs were statistically equivalent. Both groups had statistically equivalent rates of treatment-emergent adverse events (55.2% vs. 58.2%).
According to the label, Eticovo is a tumor necrosis factor blocker approved for the treatment of rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, and plaque psoriasis in patients aged 4 years or older. The most common adverse events associated with the drug include infections and injection site reactions.
Eticovo is the second etanercept biosimilar approved by the FDA. The first FDA-approved etanercept biosimilar, etanercept-szzs (Erelzi), is currently facing a legal challenge from Amgen, the manufacturer of Enbrel.
Ixekizumab posts positive results in phase 3 nr-axSpA trial
Eli Lilly has announced positive results from COAST-X, a 52-week, placebo-controlled, phase 3 trial evaluating ixekizumab (Taltz) in biologic disease-modifying antirheumatic drug–naive patients with nonradiographic axial spondyloarthritis (nr-axSpA).
Ixekizumab met the primary endpoint of statistically significant improvement in nr-axSpA symptoms as measured by Assessment of Spondyloarthritis International Society 40 response at both week 16 and week 52, compared with patients who received placebo. The drug also met all secondary endpoints, including significant improvement in Ankylosing Spondylitis Disease Activity Score, significant improvement in Bath Ankylosing Spondylitis Disease Activity, proportion of patients achieving low disease activity, significant improvement in sacroiliac joint inflammation as assessed by MRI, and significant improvement in 36-Item Short Form Health Survey Physical Component Summary score.
The safety profile of ixekizumab was broadly similar to what has been seen in previous phase 3 trials; the most common adverse events include injection site reactions, upper respiratory tract infections, nausea, and tinea infections, the company said.
“Nonradiographic axSpA is a challenging diagnosis that is not only missed in clinics, but also has limited treatment options for physicians to offer patients. The COAST-X results offer compelling evidence that Taltz could provide a much-needed new alternative if approved for this patient population,” Atul A. Deodhar, MD, professor of medicine at Oregon Health & Science University, Portland, and clinical investigator for the COAST program, said in the press release.
Find the full press release on the Eli Lilly website.
Eli Lilly has announced positive results from COAST-X, a 52-week, placebo-controlled, phase 3 trial evaluating ixekizumab (Taltz) in biologic disease-modifying antirheumatic drug–naive patients with nonradiographic axial spondyloarthritis (nr-axSpA).
Ixekizumab met the primary endpoint of statistically significant improvement in nr-axSpA symptoms as measured by Assessment of Spondyloarthritis International Society 40 response at both week 16 and week 52, compared with patients who received placebo. The drug also met all secondary endpoints, including significant improvement in Ankylosing Spondylitis Disease Activity Score, significant improvement in Bath Ankylosing Spondylitis Disease Activity, proportion of patients achieving low disease activity, significant improvement in sacroiliac joint inflammation as assessed by MRI, and significant improvement in 36-Item Short Form Health Survey Physical Component Summary score.
The safety profile of ixekizumab was broadly similar to what has been seen in previous phase 3 trials; the most common adverse events include injection site reactions, upper respiratory tract infections, nausea, and tinea infections, the company said.
“Nonradiographic axSpA is a challenging diagnosis that is not only missed in clinics, but also has limited treatment options for physicians to offer patients. The COAST-X results offer compelling evidence that Taltz could provide a much-needed new alternative if approved for this patient population,” Atul A. Deodhar, MD, professor of medicine at Oregon Health & Science University, Portland, and clinical investigator for the COAST program, said in the press release.
Find the full press release on the Eli Lilly website.
Eli Lilly has announced positive results from COAST-X, a 52-week, placebo-controlled, phase 3 trial evaluating ixekizumab (Taltz) in biologic disease-modifying antirheumatic drug–naive patients with nonradiographic axial spondyloarthritis (nr-axSpA).
Ixekizumab met the primary endpoint of statistically significant improvement in nr-axSpA symptoms as measured by Assessment of Spondyloarthritis International Society 40 response at both week 16 and week 52, compared with patients who received placebo. The drug also met all secondary endpoints, including significant improvement in Ankylosing Spondylitis Disease Activity Score, significant improvement in Bath Ankylosing Spondylitis Disease Activity, proportion of patients achieving low disease activity, significant improvement in sacroiliac joint inflammation as assessed by MRI, and significant improvement in 36-Item Short Form Health Survey Physical Component Summary score.
The safety profile of ixekizumab was broadly similar to what has been seen in previous phase 3 trials; the most common adverse events include injection site reactions, upper respiratory tract infections, nausea, and tinea infections, the company said.
“Nonradiographic axSpA is a challenging diagnosis that is not only missed in clinics, but also has limited treatment options for physicians to offer patients. The COAST-X results offer compelling evidence that Taltz could provide a much-needed new alternative if approved for this patient population,” Atul A. Deodhar, MD, professor of medicine at Oregon Health & Science University, Portland, and clinical investigator for the COAST program, said in the press release.
Find the full press release on the Eli Lilly website.
Referral system aims to slash axial spondyloarthritis diagnostic delay
Low back pain. A bane of human existence.
Almost everyone – 90% of us in fact – will have at least one bout of it. Snow shoveling, too much weight on the barbell, a strange twist while carrying in the groceries. A quick visit to a primary care doc, a prescription NSAID, a few days or weeks of rest, and a gradual resolution of symptoms is the usual course.
But in Toronto, a small group of clinicians aims to change this clinical picture. They’ve developed a secondary screening program to identify back pain patients at risk of axSpA, potentially bypassing the diagnostic merry-go-round, years of pain, and disease progression. Success relies on the alertness of primary care and the expertise of advanced practice physical therapists to make sure the right patients arrive in the rheumatologist’s office.
“We know the delay is on average 8-10 years, and often by the time a patient does show up in a rheumatology office, much damage has occurred,” Laura Passalent, a clinician researcher at University Health Network, Toronto, said in an interview. “But spondyloarthritis gets lost in the background noise of mechanical and musculoskeletal back pain, so it’s hard for primary care to accurately diagnose, and patients often bounce around the health care system for years before someone finally suspects. We are trying to change that paradigm, reduce the time to diagnosis, and identify patients earlier. If we can, we can treat earlier, and the evidence suggests that, like early treatment in RA, we can prevent disease progression.”
As in rheumatoid arthritis, getting patients on biologics sooner rather than later improves radiologic outcomes, daily function, and quality of life. Studies bear that out, including one by Ms. Passalent’s rheumatologist colleagues, Robert Inman, MD, and Nigel Haroon, MD, PhD, also with UHN. Their study of 334 patients with ankylosing spondylitis found that early treatment with a tumor necrosis factor (TNF) inhibitor reduced the odds of disease progression by up to 50% and was especially effective in those who got early treatment (Arthritis Rheum. 2013 Oct;65[10]:2645-54). Those who started at least 10 years after symptom onset were twice as likely to progress. Those who were on biologics for more than 50% of their disease duration were three times less likely to progress.
“It’s known that biologics improve the signs and symptoms of SpA, and the great majority of patients feel better on them,” Dr. Inman said in an interview. “But the really important outcomes are preventing structural damage, a finding already well established in RA. This study changed our thoughts on altering the natural history of this disease.”
Diagnostic delays worsen long-term outcomes in axSpA, just as in RA, but unlike RA, axSpA has no stepwise diagnostic algorithm, Dr. Inman said. “We had a real problem identifying a simple, reliable pathway for referrals. One of the strategies we investigated was this screening clinic model to facilitate appropriate and early referrals that are no longer dependent on primary care physicians.”
Community back pain clinics
Raja Rampersaud, MD, a spine surgeon at UHN, developed the first model – a community clinic that triages and treats people with low back pain. Primary care providers refer into the clinics, and advanced practice clinicians work with patients to create care plans. These might include low-level medical therapy, exercise, and other self-management techniques.
Ms. Passalent and her team partnered with these clinics in a pilot project to identify axSpA patients. The team provided clinician education and referral criteria for patients. These include back pain of more than 3 months’ duration in patients younger than 50 years who have other signs of inflammatory back pain. Primary care providers can refer such patients to a secondary screening program, run by an advanced care clinician, that further refines the diagnosis.
The clinic work-up includes the following:
- History, involving a description of back pain, peripheral joint involvement, and extra-articular manifestations.
- Physical exam looking at spinal mobility and vital signs, as well as tender/swollen joints, enthesitis, and dactylitis.
- Investigations that include pelvis and lateral lumbar and cervical spine radiographs, HLA-B27 testing, and measurements of C-reactive protein and erythrocyte sedimentation rate.
For those who don’t tick the axSpA boxes, the practitioner provides education on self-management, basic nonpharmacologic interventions, exercise guidance, and referrals back into primary care for their therapy.
But those who screen positive receive a direct rheumatology referral. This is an especially important component of the program because, like the United States, Canada has a chronic shortage of rheumatologists. However, in Canada there can be even greater distances than in the United States between a patient’s town and the closest rheumatology office. The back pain screening clinic reduced waiting time from up to 2 years to around 3 weeks – a notable accomplishment in a country with only about 500 rheumatologists – less than 1 per 75,000 residents.
First data
Ms. Passalent and the team presented their initial data from this model at recent annual meetings of the Canadian Rheumatology Association and the American College of Rheumatology (Arthritis Rheumatol. 2018;70[suppl 10]:Abstract 661).
During the first 3 years of the project, 410 patients were seen. Time from primary care referral to the secondary clinic appointment was roughly 22 days. These patients were young, with a mean age of about 37 years, and had experienced back pain for an average of 7 years. About 14% were positive for HLA-B27, but that characteristic signal actually performed poorly as an independent axSpA screen. It was highly specific (94%) but not very sensitive (28%), with a 71% positive and negative predictive value.
Assessment by the advanced care provider, on the other hand, had 90% specificity and 68% sensitivity. The negative and positive predictive values were 80% and 84%, respectively.
Among those who had a rheumatology consult, 18% received an axSpA diagnosis.
“We were very pleased to be able to decrease the time to diagnosis, from 9 years to 6 or 7,” Ms. Passalent said. “It’s still a long time, but you have to keep in mind this program is just getting started.”
Other benefits
It’s proven that early treatment prevents bone damage and improves spine-related function and quality of life for these patients. But if biologics help bone inflammation, could they also benefit the extra-articular manifestations that often accompany axSpA?
“The main comorbidities are anterior uveitis, inflammatory bowel diseases, and psoriasis,” Dr. Inman said. “In our cohort, 35% have uveitis, 12% have IBD, and 10% have psoriasis. Those are significant numbers, and the damage accrues over time. They are all inflammatory and maybe autoimmune.”
These extra-articular manifestations influence individual treatment plans, he said. “The presence of skin, eye, or joint inflammation does inform our selection. Generally, though, blocking TNF-alpha with a monoclonal antibody should also effectively treat these other issues in addition to SpA.”
A 2018 review touched on the uveitis/SpA treatment connection (Perm J. 2018;22:17-041. doi: 10.7812/TPP/17-041). Biologics – especially TNF blockers – are excellent choices for refractory uveitis and may confer a double benefit in patients with both diseases. Biologic choices for IBD and psoriasis also typically overlap those used in axSpA.
The literature is still evolving on this concept of cotreatment, Dr. Inman said, but it could represent an exciting option to prevent damage in multiple systems with one approach.
The future
Ms. Passalent, Dr. Inman, and Dr. Haroon see good things ahead for everyone involved in axSpA if the secondary screening clinic protocol expands throughout Canada.
“The thing that impresses me as a frontline worker, you can be an agent of change. If you’re surrounded by the right people and a supportive organization, you really can help to influence transformative change. It doesn’t happen overnight, but if you stick to it and work with the right champions, it’s amazing what influence on patient care you can have,” Ms. Passalent said.
Dr. Inman, Dr. Haroon, and Ms. Passalent have been consultants and received research funds from several pharmaceutical companies.
Low back pain. A bane of human existence.
Almost everyone – 90% of us in fact – will have at least one bout of it. Snow shoveling, too much weight on the barbell, a strange twist while carrying in the groceries. A quick visit to a primary care doc, a prescription NSAID, a few days or weeks of rest, and a gradual resolution of symptoms is the usual course.
But in Toronto, a small group of clinicians aims to change this clinical picture. They’ve developed a secondary screening program to identify back pain patients at risk of axSpA, potentially bypassing the diagnostic merry-go-round, years of pain, and disease progression. Success relies on the alertness of primary care and the expertise of advanced practice physical therapists to make sure the right patients arrive in the rheumatologist’s office.
“We know the delay is on average 8-10 years, and often by the time a patient does show up in a rheumatology office, much damage has occurred,” Laura Passalent, a clinician researcher at University Health Network, Toronto, said in an interview. “But spondyloarthritis gets lost in the background noise of mechanical and musculoskeletal back pain, so it’s hard for primary care to accurately diagnose, and patients often bounce around the health care system for years before someone finally suspects. We are trying to change that paradigm, reduce the time to diagnosis, and identify patients earlier. If we can, we can treat earlier, and the evidence suggests that, like early treatment in RA, we can prevent disease progression.”
As in rheumatoid arthritis, getting patients on biologics sooner rather than later improves radiologic outcomes, daily function, and quality of life. Studies bear that out, including one by Ms. Passalent’s rheumatologist colleagues, Robert Inman, MD, and Nigel Haroon, MD, PhD, also with UHN. Their study of 334 patients with ankylosing spondylitis found that early treatment with a tumor necrosis factor (TNF) inhibitor reduced the odds of disease progression by up to 50% and was especially effective in those who got early treatment (Arthritis Rheum. 2013 Oct;65[10]:2645-54). Those who started at least 10 years after symptom onset were twice as likely to progress. Those who were on biologics for more than 50% of their disease duration were three times less likely to progress.
“It’s known that biologics improve the signs and symptoms of SpA, and the great majority of patients feel better on them,” Dr. Inman said in an interview. “But the really important outcomes are preventing structural damage, a finding already well established in RA. This study changed our thoughts on altering the natural history of this disease.”
Diagnostic delays worsen long-term outcomes in axSpA, just as in RA, but unlike RA, axSpA has no stepwise diagnostic algorithm, Dr. Inman said. “We had a real problem identifying a simple, reliable pathway for referrals. One of the strategies we investigated was this screening clinic model to facilitate appropriate and early referrals that are no longer dependent on primary care physicians.”
Community back pain clinics
Raja Rampersaud, MD, a spine surgeon at UHN, developed the first model – a community clinic that triages and treats people with low back pain. Primary care providers refer into the clinics, and advanced practice clinicians work with patients to create care plans. These might include low-level medical therapy, exercise, and other self-management techniques.
Ms. Passalent and her team partnered with these clinics in a pilot project to identify axSpA patients. The team provided clinician education and referral criteria for patients. These include back pain of more than 3 months’ duration in patients younger than 50 years who have other signs of inflammatory back pain. Primary care providers can refer such patients to a secondary screening program, run by an advanced care clinician, that further refines the diagnosis.
The clinic work-up includes the following:
- History, involving a description of back pain, peripheral joint involvement, and extra-articular manifestations.
- Physical exam looking at spinal mobility and vital signs, as well as tender/swollen joints, enthesitis, and dactylitis.
- Investigations that include pelvis and lateral lumbar and cervical spine radiographs, HLA-B27 testing, and measurements of C-reactive protein and erythrocyte sedimentation rate.
For those who don’t tick the axSpA boxes, the practitioner provides education on self-management, basic nonpharmacologic interventions, exercise guidance, and referrals back into primary care for their therapy.
But those who screen positive receive a direct rheumatology referral. This is an especially important component of the program because, like the United States, Canada has a chronic shortage of rheumatologists. However, in Canada there can be even greater distances than in the United States between a patient’s town and the closest rheumatology office. The back pain screening clinic reduced waiting time from up to 2 years to around 3 weeks – a notable accomplishment in a country with only about 500 rheumatologists – less than 1 per 75,000 residents.
First data
Ms. Passalent and the team presented their initial data from this model at recent annual meetings of the Canadian Rheumatology Association and the American College of Rheumatology (Arthritis Rheumatol. 2018;70[suppl 10]:Abstract 661).
During the first 3 years of the project, 410 patients were seen. Time from primary care referral to the secondary clinic appointment was roughly 22 days. These patients were young, with a mean age of about 37 years, and had experienced back pain for an average of 7 years. About 14% were positive for HLA-B27, but that characteristic signal actually performed poorly as an independent axSpA screen. It was highly specific (94%) but not very sensitive (28%), with a 71% positive and negative predictive value.
Assessment by the advanced care provider, on the other hand, had 90% specificity and 68% sensitivity. The negative and positive predictive values were 80% and 84%, respectively.
Among those who had a rheumatology consult, 18% received an axSpA diagnosis.
“We were very pleased to be able to decrease the time to diagnosis, from 9 years to 6 or 7,” Ms. Passalent said. “It’s still a long time, but you have to keep in mind this program is just getting started.”
Other benefits
It’s proven that early treatment prevents bone damage and improves spine-related function and quality of life for these patients. But if biologics help bone inflammation, could they also benefit the extra-articular manifestations that often accompany axSpA?
“The main comorbidities are anterior uveitis, inflammatory bowel diseases, and psoriasis,” Dr. Inman said. “In our cohort, 35% have uveitis, 12% have IBD, and 10% have psoriasis. Those are significant numbers, and the damage accrues over time. They are all inflammatory and maybe autoimmune.”
These extra-articular manifestations influence individual treatment plans, he said. “The presence of skin, eye, or joint inflammation does inform our selection. Generally, though, blocking TNF-alpha with a monoclonal antibody should also effectively treat these other issues in addition to SpA.”
A 2018 review touched on the uveitis/SpA treatment connection (Perm J. 2018;22:17-041. doi: 10.7812/TPP/17-041). Biologics – especially TNF blockers – are excellent choices for refractory uveitis and may confer a double benefit in patients with both diseases. Biologic choices for IBD and psoriasis also typically overlap those used in axSpA.
The literature is still evolving on this concept of cotreatment, Dr. Inman said, but it could represent an exciting option to prevent damage in multiple systems with one approach.
The future
Ms. Passalent, Dr. Inman, and Dr. Haroon see good things ahead for everyone involved in axSpA if the secondary screening clinic protocol expands throughout Canada.
“The thing that impresses me as a frontline worker, you can be an agent of change. If you’re surrounded by the right people and a supportive organization, you really can help to influence transformative change. It doesn’t happen overnight, but if you stick to it and work with the right champions, it’s amazing what influence on patient care you can have,” Ms. Passalent said.
Dr. Inman, Dr. Haroon, and Ms. Passalent have been consultants and received research funds from several pharmaceutical companies.
Low back pain. A bane of human existence.
Almost everyone – 90% of us in fact – will have at least one bout of it. Snow shoveling, too much weight on the barbell, a strange twist while carrying in the groceries. A quick visit to a primary care doc, a prescription NSAID, a few days or weeks of rest, and a gradual resolution of symptoms is the usual course.
But in Toronto, a small group of clinicians aims to change this clinical picture. They’ve developed a secondary screening program to identify back pain patients at risk of axSpA, potentially bypassing the diagnostic merry-go-round, years of pain, and disease progression. Success relies on the alertness of primary care and the expertise of advanced practice physical therapists to make sure the right patients arrive in the rheumatologist’s office.
“We know the delay is on average 8-10 years, and often by the time a patient does show up in a rheumatology office, much damage has occurred,” Laura Passalent, a clinician researcher at University Health Network, Toronto, said in an interview. “But spondyloarthritis gets lost in the background noise of mechanical and musculoskeletal back pain, so it’s hard for primary care to accurately diagnose, and patients often bounce around the health care system for years before someone finally suspects. We are trying to change that paradigm, reduce the time to diagnosis, and identify patients earlier. If we can, we can treat earlier, and the evidence suggests that, like early treatment in RA, we can prevent disease progression.”
As in rheumatoid arthritis, getting patients on biologics sooner rather than later improves radiologic outcomes, daily function, and quality of life. Studies bear that out, including one by Ms. Passalent’s rheumatologist colleagues, Robert Inman, MD, and Nigel Haroon, MD, PhD, also with UHN. Their study of 334 patients with ankylosing spondylitis found that early treatment with a tumor necrosis factor (TNF) inhibitor reduced the odds of disease progression by up to 50% and was especially effective in those who got early treatment (Arthritis Rheum. 2013 Oct;65[10]:2645-54). Those who started at least 10 years after symptom onset were twice as likely to progress. Those who were on biologics for more than 50% of their disease duration were three times less likely to progress.
“It’s known that biologics improve the signs and symptoms of SpA, and the great majority of patients feel better on them,” Dr. Inman said in an interview. “But the really important outcomes are preventing structural damage, a finding already well established in RA. This study changed our thoughts on altering the natural history of this disease.”
Diagnostic delays worsen long-term outcomes in axSpA, just as in RA, but unlike RA, axSpA has no stepwise diagnostic algorithm, Dr. Inman said. “We had a real problem identifying a simple, reliable pathway for referrals. One of the strategies we investigated was this screening clinic model to facilitate appropriate and early referrals that are no longer dependent on primary care physicians.”
Community back pain clinics
Raja Rampersaud, MD, a spine surgeon at UHN, developed the first model – a community clinic that triages and treats people with low back pain. Primary care providers refer into the clinics, and advanced practice clinicians work with patients to create care plans. These might include low-level medical therapy, exercise, and other self-management techniques.
Ms. Passalent and her team partnered with these clinics in a pilot project to identify axSpA patients. The team provided clinician education and referral criteria for patients. These include back pain of more than 3 months’ duration in patients younger than 50 years who have other signs of inflammatory back pain. Primary care providers can refer such patients to a secondary screening program, run by an advanced care clinician, that further refines the diagnosis.
The clinic work-up includes the following:
- History, involving a description of back pain, peripheral joint involvement, and extra-articular manifestations.
- Physical exam looking at spinal mobility and vital signs, as well as tender/swollen joints, enthesitis, and dactylitis.
- Investigations that include pelvis and lateral lumbar and cervical spine radiographs, HLA-B27 testing, and measurements of C-reactive protein and erythrocyte sedimentation rate.
For those who don’t tick the axSpA boxes, the practitioner provides education on self-management, basic nonpharmacologic interventions, exercise guidance, and referrals back into primary care for their therapy.
But those who screen positive receive a direct rheumatology referral. This is an especially important component of the program because, like the United States, Canada has a chronic shortage of rheumatologists. However, in Canada there can be even greater distances than in the United States between a patient’s town and the closest rheumatology office. The back pain screening clinic reduced waiting time from up to 2 years to around 3 weeks – a notable accomplishment in a country with only about 500 rheumatologists – less than 1 per 75,000 residents.
First data
Ms. Passalent and the team presented their initial data from this model at recent annual meetings of the Canadian Rheumatology Association and the American College of Rheumatology (Arthritis Rheumatol. 2018;70[suppl 10]:Abstract 661).
During the first 3 years of the project, 410 patients were seen. Time from primary care referral to the secondary clinic appointment was roughly 22 days. These patients were young, with a mean age of about 37 years, and had experienced back pain for an average of 7 years. About 14% were positive for HLA-B27, but that characteristic signal actually performed poorly as an independent axSpA screen. It was highly specific (94%) but not very sensitive (28%), with a 71% positive and negative predictive value.
Assessment by the advanced care provider, on the other hand, had 90% specificity and 68% sensitivity. The negative and positive predictive values were 80% and 84%, respectively.
Among those who had a rheumatology consult, 18% received an axSpA diagnosis.
“We were very pleased to be able to decrease the time to diagnosis, from 9 years to 6 or 7,” Ms. Passalent said. “It’s still a long time, but you have to keep in mind this program is just getting started.”
Other benefits
It’s proven that early treatment prevents bone damage and improves spine-related function and quality of life for these patients. But if biologics help bone inflammation, could they also benefit the extra-articular manifestations that often accompany axSpA?
“The main comorbidities are anterior uveitis, inflammatory bowel diseases, and psoriasis,” Dr. Inman said. “In our cohort, 35% have uveitis, 12% have IBD, and 10% have psoriasis. Those are significant numbers, and the damage accrues over time. They are all inflammatory and maybe autoimmune.”
These extra-articular manifestations influence individual treatment plans, he said. “The presence of skin, eye, or joint inflammation does inform our selection. Generally, though, blocking TNF-alpha with a monoclonal antibody should also effectively treat these other issues in addition to SpA.”
A 2018 review touched on the uveitis/SpA treatment connection (Perm J. 2018;22:17-041. doi: 10.7812/TPP/17-041). Biologics – especially TNF blockers – are excellent choices for refractory uveitis and may confer a double benefit in patients with both diseases. Biologic choices for IBD and psoriasis also typically overlap those used in axSpA.
The literature is still evolving on this concept of cotreatment, Dr. Inman said, but it could represent an exciting option to prevent damage in multiple systems with one approach.
The future
Ms. Passalent, Dr. Inman, and Dr. Haroon see good things ahead for everyone involved in axSpA if the secondary screening clinic protocol expands throughout Canada.
“The thing that impresses me as a frontline worker, you can be an agent of change. If you’re surrounded by the right people and a supportive organization, you really can help to influence transformative change. It doesn’t happen overnight, but if you stick to it and work with the right champions, it’s amazing what influence on patient care you can have,” Ms. Passalent said.
Dr. Inman, Dr. Haroon, and Ms. Passalent have been consultants and received research funds from several pharmaceutical companies.
Cimzia becomes first FDA-approved treatment for nonradiographic axial spondyloarthritis
, with objective evidence of inflammation, making it the first treatment approved by the agency for the condition.
The FDA approved the tumor necrosis factor inhibitor based on results from a randomized clinical trial in 317 adult patients with nonradiographic axial spondyloarthritis (nr-axSpA) who had elevated C-reactive protein levels and/or sacroiliitis (inflammation of the sacroiliac joints) on MRI.
The trial entailed 52 weeks of double-blind therapy with certolizumab at a starting dose of 400 mg on weeks 0, 2, and 4 followed by 200 mg every 2 weeks, or placebo. The Ankylosing Spondylitis Disease Activity Score Major Improvement rate, defined as at least a 2-point improvement from baseline, was 47% in the active treatment arm, compared with 7% on placebo. The Assessment in Ankylosing Spondylitis International Society 40% response rate, a more patient-reported outcome measure, was 57% in the certolizumab group and 16% in controls (Arthritis Rheumatol. 2019 March 8. doi: 10.1002/art.40866).
The overall safety profile observed in the Cimzia treatment group was consistent with the known safety profile of certolizumab.
Cimzia was first approved in 2008 and has FDA-approved indications for adult patients with Crohn’s disease, moderate to severe rheumatoid arthritis, active ankylosing spondylitis and moderate to severe plaque psoriasis who are candidates for systemic therapy or phototherapy.
, with objective evidence of inflammation, making it the first treatment approved by the agency for the condition.
The FDA approved the tumor necrosis factor inhibitor based on results from a randomized clinical trial in 317 adult patients with nonradiographic axial spondyloarthritis (nr-axSpA) who had elevated C-reactive protein levels and/or sacroiliitis (inflammation of the sacroiliac joints) on MRI.
The trial entailed 52 weeks of double-blind therapy with certolizumab at a starting dose of 400 mg on weeks 0, 2, and 4 followed by 200 mg every 2 weeks, or placebo. The Ankylosing Spondylitis Disease Activity Score Major Improvement rate, defined as at least a 2-point improvement from baseline, was 47% in the active treatment arm, compared with 7% on placebo. The Assessment in Ankylosing Spondylitis International Society 40% response rate, a more patient-reported outcome measure, was 57% in the certolizumab group and 16% in controls (Arthritis Rheumatol. 2019 March 8. doi: 10.1002/art.40866).
The overall safety profile observed in the Cimzia treatment group was consistent with the known safety profile of certolizumab.
Cimzia was first approved in 2008 and has FDA-approved indications for adult patients with Crohn’s disease, moderate to severe rheumatoid arthritis, active ankylosing spondylitis and moderate to severe plaque psoriasis who are candidates for systemic therapy or phototherapy.
, with objective evidence of inflammation, making it the first treatment approved by the agency for the condition.
The FDA approved the tumor necrosis factor inhibitor based on results from a randomized clinical trial in 317 adult patients with nonradiographic axial spondyloarthritis (nr-axSpA) who had elevated C-reactive protein levels and/or sacroiliitis (inflammation of the sacroiliac joints) on MRI.
The trial entailed 52 weeks of double-blind therapy with certolizumab at a starting dose of 400 mg on weeks 0, 2, and 4 followed by 200 mg every 2 weeks, or placebo. The Ankylosing Spondylitis Disease Activity Score Major Improvement rate, defined as at least a 2-point improvement from baseline, was 47% in the active treatment arm, compared with 7% on placebo. The Assessment in Ankylosing Spondylitis International Society 40% response rate, a more patient-reported outcome measure, was 57% in the certolizumab group and 16% in controls (Arthritis Rheumatol. 2019 March 8. doi: 10.1002/art.40866).
The overall safety profile observed in the Cimzia treatment group was consistent with the known safety profile of certolizumab.
Cimzia was first approved in 2008 and has FDA-approved indications for adult patients with Crohn’s disease, moderate to severe rheumatoid arthritis, active ankylosing spondylitis and moderate to severe plaque psoriasis who are candidates for systemic therapy or phototherapy.