User login
What’s new for CHEST 2019?
Head to New Orleans this October for CHEST Annual Meeting 2019 for the latest original research, postgraduate courses, interactive case-based discussions, simulation sessions, CHEST Games, and more! CHEST 2019 allows clinician members of the entire health-care team to stay up to date on pulmonary, critical care, and sleep medicine. There are many new and exciting things happening at CHEST 2019, and we are excited to give you a sneak peek.
The simulation sessions are better than ever and include a full day of cadaver-based courses and brand new hands-on sessions in bronchoscopy, advanced critical care echocardiography, and airway management, that will put your skills to the test. You don’t want to miss these simulation sessions that allow you to learn from our expert faculty to advance and develop valuable skills and apply your knowledge.
Visit CHEST in the exhibit hall to see the new additions we have added to amplify your experience. The new FISH Bowl innovation competition will allow you to learn about new solutions and ideas that were submitted in education and clinical disease for pulmonary, critical care, and sleep medicine. The finalists will be presenting live in Experience CHEST and competing for prizes in each category. CHEST games will be back again in a new space in the exhibit hall. Be sure to bring your team to play the popular Nodal Nemesis and the other games that test your skills in new and creative ways.
CHEST 2019 plans to make your life easier by providing you with the latest updates in patient care at the annual meeting, but we are also planning on making it easier in other ways. New this year, you can update your professional headshot in our new complimentary headshot booth. Plan on a visit to the new CHEST Wellness Zone. This area is designed to help you relax and recharge while at CHEST and includes meditation, posture consultants, aromatherapy, foot massage, and yoga. Attend CHEST 2019 with some peace of mind knowing that your children can be cared for at the Kiddie Corp childcare program for kids ages 6 months to 12 years.
According to William Kelly, MD, FCCP, CHEST 2019 Program Chair, “We are excited about these new opportunities that will help you improve your patient care. We’re taking concrete steps to make your learning, your practice, and your life a little easier.”
We look forward to seeing you at CHEST 2019 in New Orleans, Louisiana, October 19-23!
Head to New Orleans this October for CHEST Annual Meeting 2019 for the latest original research, postgraduate courses, interactive case-based discussions, simulation sessions, CHEST Games, and more! CHEST 2019 allows clinician members of the entire health-care team to stay up to date on pulmonary, critical care, and sleep medicine. There are many new and exciting things happening at CHEST 2019, and we are excited to give you a sneak peek.
The simulation sessions are better than ever and include a full day of cadaver-based courses and brand new hands-on sessions in bronchoscopy, advanced critical care echocardiography, and airway management, that will put your skills to the test. You don’t want to miss these simulation sessions that allow you to learn from our expert faculty to advance and develop valuable skills and apply your knowledge.
Visit CHEST in the exhibit hall to see the new additions we have added to amplify your experience. The new FISH Bowl innovation competition will allow you to learn about new solutions and ideas that were submitted in education and clinical disease for pulmonary, critical care, and sleep medicine. The finalists will be presenting live in Experience CHEST and competing for prizes in each category. CHEST games will be back again in a new space in the exhibit hall. Be sure to bring your team to play the popular Nodal Nemesis and the other games that test your skills in new and creative ways.
CHEST 2019 plans to make your life easier by providing you with the latest updates in patient care at the annual meeting, but we are also planning on making it easier in other ways. New this year, you can update your professional headshot in our new complimentary headshot booth. Plan on a visit to the new CHEST Wellness Zone. This area is designed to help you relax and recharge while at CHEST and includes meditation, posture consultants, aromatherapy, foot massage, and yoga. Attend CHEST 2019 with some peace of mind knowing that your children can be cared for at the Kiddie Corp childcare program for kids ages 6 months to 12 years.
According to William Kelly, MD, FCCP, CHEST 2019 Program Chair, “We are excited about these new opportunities that will help you improve your patient care. We’re taking concrete steps to make your learning, your practice, and your life a little easier.”
We look forward to seeing you at CHEST 2019 in New Orleans, Louisiana, October 19-23!
Head to New Orleans this October for CHEST Annual Meeting 2019 for the latest original research, postgraduate courses, interactive case-based discussions, simulation sessions, CHEST Games, and more! CHEST 2019 allows clinician members of the entire health-care team to stay up to date on pulmonary, critical care, and sleep medicine. There are many new and exciting things happening at CHEST 2019, and we are excited to give you a sneak peek.
The simulation sessions are better than ever and include a full day of cadaver-based courses and brand new hands-on sessions in bronchoscopy, advanced critical care echocardiography, and airway management, that will put your skills to the test. You don’t want to miss these simulation sessions that allow you to learn from our expert faculty to advance and develop valuable skills and apply your knowledge.
Visit CHEST in the exhibit hall to see the new additions we have added to amplify your experience. The new FISH Bowl innovation competition will allow you to learn about new solutions and ideas that were submitted in education and clinical disease for pulmonary, critical care, and sleep medicine. The finalists will be presenting live in Experience CHEST and competing for prizes in each category. CHEST games will be back again in a new space in the exhibit hall. Be sure to bring your team to play the popular Nodal Nemesis and the other games that test your skills in new and creative ways.
CHEST 2019 plans to make your life easier by providing you with the latest updates in patient care at the annual meeting, but we are also planning on making it easier in other ways. New this year, you can update your professional headshot in our new complimentary headshot booth. Plan on a visit to the new CHEST Wellness Zone. This area is designed to help you relax and recharge while at CHEST and includes meditation, posture consultants, aromatherapy, foot massage, and yoga. Attend CHEST 2019 with some peace of mind knowing that your children can be cared for at the Kiddie Corp childcare program for kids ages 6 months to 12 years.
According to William Kelly, MD, FCCP, CHEST 2019 Program Chair, “We are excited about these new opportunities that will help you improve your patient care. We’re taking concrete steps to make your learning, your practice, and your life a little easier.”
We look forward to seeing you at CHEST 2019 in New Orleans, Louisiana, October 19-23!
CHEST Foundation at Board Review
The CHEST Foundation is excited to be a part of this year’s CHEST Board Review in Phoenix, and we can’t wait to see you! We are hosting two receptions and invite you to attend and learn more about how the CHEST Foundation supports you, your colleagues, your patients, and the greater community while also taking the time to relax with your peers and board review faculty. The receptions are scheduled for Saturday, August 17 (for Sleep and Critical Care Board Review), and Wednesday, August 21 (for Pulmonary Board Review) immediately following your scheduled sessions. Please join us for hors d’oeuvres and beverages. This year, we are featuring surprise, guest speakers from CHEST leadership who will share why they are passionate about the Foundation’s mission and offer simple ways you can become further involved with the CHEST Foundation. You won’t want to miss this networking opportunity and the chance to learn more about what the Foundation has been doing!
This summer, we are focused on supporting young and early-career clinicians and are raising money at this year’s at Board Review to support travel grants to CHEST 2019. These travel grants provide early-career clinicians the funds needed to attend CHEST 2019. This program further develops the future leaders of CHEST and allows clinicians to take full advantage of career-development and networking opportunities that the annual meeting offers. If you’re interested in how you can make a difference in someone’s life, visit our website (foundation.chestnet.org), or find us at Board Review! We would love to share more with you about all the great work the Foundation is doing.
We can’t wait to see you in Phoenix to celebrate all your hard work!
The CHEST Foundation is excited to be a part of this year’s CHEST Board Review in Phoenix, and we can’t wait to see you! We are hosting two receptions and invite you to attend and learn more about how the CHEST Foundation supports you, your colleagues, your patients, and the greater community while also taking the time to relax with your peers and board review faculty. The receptions are scheduled for Saturday, August 17 (for Sleep and Critical Care Board Review), and Wednesday, August 21 (for Pulmonary Board Review) immediately following your scheduled sessions. Please join us for hors d’oeuvres and beverages. This year, we are featuring surprise, guest speakers from CHEST leadership who will share why they are passionate about the Foundation’s mission and offer simple ways you can become further involved with the CHEST Foundation. You won’t want to miss this networking opportunity and the chance to learn more about what the Foundation has been doing!
This summer, we are focused on supporting young and early-career clinicians and are raising money at this year’s at Board Review to support travel grants to CHEST 2019. These travel grants provide early-career clinicians the funds needed to attend CHEST 2019. This program further develops the future leaders of CHEST and allows clinicians to take full advantage of career-development and networking opportunities that the annual meeting offers. If you’re interested in how you can make a difference in someone’s life, visit our website (foundation.chestnet.org), or find us at Board Review! We would love to share more with you about all the great work the Foundation is doing.
We can’t wait to see you in Phoenix to celebrate all your hard work!
The CHEST Foundation is excited to be a part of this year’s CHEST Board Review in Phoenix, and we can’t wait to see you! We are hosting two receptions and invite you to attend and learn more about how the CHEST Foundation supports you, your colleagues, your patients, and the greater community while also taking the time to relax with your peers and board review faculty. The receptions are scheduled for Saturday, August 17 (for Sleep and Critical Care Board Review), and Wednesday, August 21 (for Pulmonary Board Review) immediately following your scheduled sessions. Please join us for hors d’oeuvres and beverages. This year, we are featuring surprise, guest speakers from CHEST leadership who will share why they are passionate about the Foundation’s mission and offer simple ways you can become further involved with the CHEST Foundation. You won’t want to miss this networking opportunity and the chance to learn more about what the Foundation has been doing!
This summer, we are focused on supporting young and early-career clinicians and are raising money at this year’s at Board Review to support travel grants to CHEST 2019. These travel grants provide early-career clinicians the funds needed to attend CHEST 2019. This program further develops the future leaders of CHEST and allows clinicians to take full advantage of career-development and networking opportunities that the annual meeting offers. If you’re interested in how you can make a difference in someone’s life, visit our website (foundation.chestnet.org), or find us at Board Review! We would love to share more with you about all the great work the Foundation is doing.
We can’t wait to see you in Phoenix to celebrate all your hard work!
In Memoriam: Mark J. Rosen, MD, Master FCCP
Past President (2006-2007) of the American College of Chest Physicians, leader, educator, mentor, and friend, Dr. Mark Rosen, Master FCCP, died on July 3, 2019. Dr. Rosen’s distinguished career in pulmonary and critical care medicine spanned more than 4 decades, marked by his deep commitments to medical education and patient care. His research and administrative accomplishments at New York City and Long Island hospitals were many, but clinical medicine and teaching were always at the top of his list. Mark’s unmistakable way of incorporating both clarity and humor into his roles of clinician, teacher, colleague, and friend provided us all with respect and adoration for this unforgettable individual.
Mark’s distinguished leadership involvement with CHEST began well before his term as President. Two years after completing his fellowships in pulmonary and critical care medicine, he became an FCCP in 1982, and his engagement with the American College of Chest Physicians began. During the 1990s and into the 2000s, Mark provided CHEST with his teaching expertise serving as faculty and director for the Pulmonary Board Review Courses. In 1998, he was Chair of the CHEST Annual Meeting, and from 1999 to 2005, he served on the ACCP-SEEK Editorial Boards for Pulmonary Disease and Critical Care Medicine. Mark served on the CHEST Board of Regents for many years, on the CHEST Foundation Board of Trustees, and as a Chair or member on numerous CHEST committees, some of which included Education, Nominations, Membership, Marketing, and Finance. He was the CHEST Governor for the City of New York and Chair of the Council of Governors. His leadership in all of these capacities was exemplary, as was his guidance as CHEST President from 2006 to 2007. Most recently, Mark served as CHEST Director of Global Education and Strategic Development (2011-2014) followed by CHEST Medical Director (2014-2016). Mark strived to uphold and strengthen the quality of the education that CHEST provided to all health-care professionals. His imprint on the educational and clinical foundations of CHEST, along with the many friendships he made along the way, will be remembered always.
CHEST extends heartfelt condolences to Mark’s wife of 37 years, Ilene, and the Rosen family and many friends and colleagues.
Past President (2006-2007) of the American College of Chest Physicians, leader, educator, mentor, and friend, Dr. Mark Rosen, Master FCCP, died on July 3, 2019. Dr. Rosen’s distinguished career in pulmonary and critical care medicine spanned more than 4 decades, marked by his deep commitments to medical education and patient care. His research and administrative accomplishments at New York City and Long Island hospitals were many, but clinical medicine and teaching were always at the top of his list. Mark’s unmistakable way of incorporating both clarity and humor into his roles of clinician, teacher, colleague, and friend provided us all with respect and adoration for this unforgettable individual.
Mark’s distinguished leadership involvement with CHEST began well before his term as President. Two years after completing his fellowships in pulmonary and critical care medicine, he became an FCCP in 1982, and his engagement with the American College of Chest Physicians began. During the 1990s and into the 2000s, Mark provided CHEST with his teaching expertise serving as faculty and director for the Pulmonary Board Review Courses. In 1998, he was Chair of the CHEST Annual Meeting, and from 1999 to 2005, he served on the ACCP-SEEK Editorial Boards for Pulmonary Disease and Critical Care Medicine. Mark served on the CHEST Board of Regents for many years, on the CHEST Foundation Board of Trustees, and as a Chair or member on numerous CHEST committees, some of which included Education, Nominations, Membership, Marketing, and Finance. He was the CHEST Governor for the City of New York and Chair of the Council of Governors. His leadership in all of these capacities was exemplary, as was his guidance as CHEST President from 2006 to 2007. Most recently, Mark served as CHEST Director of Global Education and Strategic Development (2011-2014) followed by CHEST Medical Director (2014-2016). Mark strived to uphold and strengthen the quality of the education that CHEST provided to all health-care professionals. His imprint on the educational and clinical foundations of CHEST, along with the many friendships he made along the way, will be remembered always.
CHEST extends heartfelt condolences to Mark’s wife of 37 years, Ilene, and the Rosen family and many friends and colleagues.
Past President (2006-2007) of the American College of Chest Physicians, leader, educator, mentor, and friend, Dr. Mark Rosen, Master FCCP, died on July 3, 2019. Dr. Rosen’s distinguished career in pulmonary and critical care medicine spanned more than 4 decades, marked by his deep commitments to medical education and patient care. His research and administrative accomplishments at New York City and Long Island hospitals were many, but clinical medicine and teaching were always at the top of his list. Mark’s unmistakable way of incorporating both clarity and humor into his roles of clinician, teacher, colleague, and friend provided us all with respect and adoration for this unforgettable individual.
Mark’s distinguished leadership involvement with CHEST began well before his term as President. Two years after completing his fellowships in pulmonary and critical care medicine, he became an FCCP in 1982, and his engagement with the American College of Chest Physicians began. During the 1990s and into the 2000s, Mark provided CHEST with his teaching expertise serving as faculty and director for the Pulmonary Board Review Courses. In 1998, he was Chair of the CHEST Annual Meeting, and from 1999 to 2005, he served on the ACCP-SEEK Editorial Boards for Pulmonary Disease and Critical Care Medicine. Mark served on the CHEST Board of Regents for many years, on the CHEST Foundation Board of Trustees, and as a Chair or member on numerous CHEST committees, some of which included Education, Nominations, Membership, Marketing, and Finance. He was the CHEST Governor for the City of New York and Chair of the Council of Governors. His leadership in all of these capacities was exemplary, as was his guidance as CHEST President from 2006 to 2007. Most recently, Mark served as CHEST Director of Global Education and Strategic Development (2011-2014) followed by CHEST Medical Director (2014-2016). Mark strived to uphold and strengthen the quality of the education that CHEST provided to all health-care professionals. His imprint on the educational and clinical foundations of CHEST, along with the many friendships he made along the way, will be remembered always.
CHEST extends heartfelt condolences to Mark’s wife of 37 years, Ilene, and the Rosen family and many friends and colleagues.
New Editor in Chief takes the reins
CHEST welcomed Peter J. Mazzone, MD, MPH, FCCP, in July, as the new Editor in Chief of the journal CHEST®. Dr. Mazzone is the Director of the Lung Cancer Program and Lung Cancer Screening Program for the Respiratory Institute at the Cleveland Clinic in Ohio.
His clinical interests include nodule management and the prevention, screening, diagnosis, staging, and characterization of lung cancer; his research has focused on the development of molecular biomarkers for lung cancer detection. Dr. Mazzone has been a member of CHEST since 1999 and an FCCP since 2004. He has served in several CHEST leadership positions, including member of the CHEST Lung Cancer Living Guidelines Steering Committee and program chair for the CHEST 2017 annual meeting, among others. Dr. Mazzone has provided some insights into the structure and strategies of the journal going forward, so don’t miss his editorial in the July issue of CHEST®.
CHEST welcomed Peter J. Mazzone, MD, MPH, FCCP, in July, as the new Editor in Chief of the journal CHEST®. Dr. Mazzone is the Director of the Lung Cancer Program and Lung Cancer Screening Program for the Respiratory Institute at the Cleveland Clinic in Ohio.
His clinical interests include nodule management and the prevention, screening, diagnosis, staging, and characterization of lung cancer; his research has focused on the development of molecular biomarkers for lung cancer detection. Dr. Mazzone has been a member of CHEST since 1999 and an FCCP since 2004. He has served in several CHEST leadership positions, including member of the CHEST Lung Cancer Living Guidelines Steering Committee and program chair for the CHEST 2017 annual meeting, among others. Dr. Mazzone has provided some insights into the structure and strategies of the journal going forward, so don’t miss his editorial in the July issue of CHEST®.
CHEST welcomed Peter J. Mazzone, MD, MPH, FCCP, in July, as the new Editor in Chief of the journal CHEST®. Dr. Mazzone is the Director of the Lung Cancer Program and Lung Cancer Screening Program for the Respiratory Institute at the Cleveland Clinic in Ohio.
His clinical interests include nodule management and the prevention, screening, diagnosis, staging, and characterization of lung cancer; his research has focused on the development of molecular biomarkers for lung cancer detection. Dr. Mazzone has been a member of CHEST since 1999 and an FCCP since 2004. He has served in several CHEST leadership positions, including member of the CHEST Lung Cancer Living Guidelines Steering Committee and program chair for the CHEST 2017 annual meeting, among others. Dr. Mazzone has provided some insights into the structure and strategies of the journal going forward, so don’t miss his editorial in the July issue of CHEST®.
Environmental Scan: Economy and workforce
The health care workforce is being transformed by profound demographic changes and the steady growth of the U.S. health sector. In addition, the movement of physicians out of private practice to employment by medical centers has accelerated. And a new generation of health care professionals is demanding a sustainable work/life balance. These trends will combine to change the work environment of chest physicians.
Spending
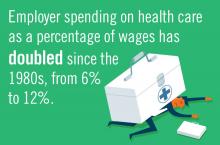
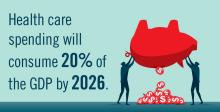
The United States spends about twice as much on health care as any other industrialized nation and this fact is driving an increasingly urgent public discussion about options and means of reducing costs.1 Medicare and Medicaid already account for about a quarter of federal government spending and those numbers are expected to rise as baby boomers age.1 Employer spending on health care as a percentage of wages has doubled since the 1980s.2
Workforce supply
An expanding health care sector means a growing demand for health care labor. Health care occupations are projected to grow 18% from 2016 to 2026, faster than the average for all occupations and adding 2.4 million new jobs to the economy.3 Expert testimony before the U.S. Senate Committee on Health, Education, Labor, and Pensions in May 2018 projected shortages of physicians in the coming years. According to estimates of the Health Resources and Services Administration (HRSA), there is a need for 13,800 additional primary care physicians in areas – especially rural – that are designated as health professional shortage areas. Signs of a worsening situation include projected shortages of 20,000 primary care physicians by 2025, according to HRSA, and 42,600-121,300 physicians by 2030, according to the Association of American Medical Colleges. The demand for physicians will exceed supply by 46,000-90,000 by 2025. An update to that research increased the projected shortage range to 61,700-94,700 by 2025.4 These shortages will result in recruiting challenges for many medical centers, especially those in rural areas.
Employment
Private practice is becoming the less common structure of employment for physicians. According to American Medical Association data, physician ownership of practices dropped below 50% for the first time in 2016.5 The trend toward employed versus private practice physicians is expected to continue. The size of practices is growing, with about one-third of physicians working in a hospital-owned practice or employed directly by a hospital and around 40% in practices of 10 physicians or more.5 Of every 10 physician practices, 3 were hospital owned in 2016.6 Physicians are being called upon to do more data entry and administrative work; 21% of physicians’ time is now spent on nonclinical paperwork.7 The ripple-out effects of what amounts to a seismic shift in the work structure and work environment for physicians are only beginning to be studied in terms of overall personal satisfaction and impact on patient care.
Stephanie M. Levine, MD, FCCP, the designate president of the American College of Chest Physicians and professor of medicine in the division of pulmonary diseases and critical care medicine at the University of Texas, San Antonio, recognizes the significance of the move from private practice to employment and suggests that advantages could be offset by some potential negatives practicing chest physicians. She noted, “Pros include potentially more job security, more predictable work hours, perhaps a reduction in some of the traditional administrative ‘hassles’ with running a private practice, and possibly a better and healthier work/life balance. Some think that physician input and leadership in the employed model may have more influence on a health care system than in an individual private practice. Nonclinical work may be decreased, but it is not clear that this is true.
“The negatives include a loss of autonomy, a potential loss of personal ownership of our patients’ health, and the loss of a unique personal culture of private practice. Physicians may be subject to metrics imposed by the employer. In addition, we may see more job turnover since physicians could be less invested emotionally and financially; fewer patients seen since the structure is often salary based and not based on productivity; and increased shift work, set work hours, and schedules. Thus, the employer-based model may actually contribute to the ongoing physician shortage.”
Dr. Levine stressed the role of training programs to prepare physicians for what may lie ahead. “Training programs must prepare physicians for what to expect as employees.”
Changing expectations
An evolution of expectations about a healthy work/life balance has occurred in many professions, including the health care profession. While younger practitioners may be more likely to embrace the changes occurring within health care, they are often more vocal about their desire for a healthy work/life balance and may be less likely to spend time away from family and friends rather than completing administrative tasks. Parenting is increasingly regarded by women and men as compatible with a full and rewarding career as a physician. So these changing expectations about work/life balances mean health care institutions will have to adjust their own expectations in order to recruit and maintain top-quality staff.
Stress and burnout
Workforce shortages, overwhelming administrative tasks, and a variety of forces that come with employment in a large medical system are causing stress and burnout in many physicians. In a 2018 Medscape study of more than 15,000 physicians, 42% reported burnout, and 15% admitted to experiencing either clinical or colloquial forms of depression.8 Dr. Levine acknowledges that many chest physicians are at risk for burnout. “In our field of medicine, particularly with those that practice in an intensive care setting, we are faced with the high stress and emotional experiences we encounter in the life and death nature of our jobs. We care for the sickest patient population, and are often facing life and death clinical needs as well as end-of-life discussions and care. Burnout is a potential threat to both patient safety and the quality of healthcare that we practice.”
Dr. Levine strongly urges colleagues to remain vigilant to this potentially devastating condition in their fellow physicians and in themselves. She said, “If you suspect you are feeling the symptoms of burnout, or have been told so by a colleague, then talk to a peer or colleague, take personal time to do something you enjoy, and/or join a support group. But better than that, try to preempt burnout by developing a strong emotional peer support group in or out of work, practicing mindfulness training, and paying attention to wellness and self-care.”
Burnout is finally being recognized by medical institutions as a significant factor in physician health and performance, and in the recruitment and attrition of staff. Dr. Levine sees progress in how health care institutions deal with burnout, wellness, and work/life balance among staff and trainees. In a hopeful note, Dr. Levine suggested that institutional responses to burnout and the workplace factors that fuel burnout may improve work conditions for physicians in the future.
These trends in the U.S. economy and workforce will mean a steady growth of the health care sector for the foreseeable future, continued political and social pressure to control costs, fewer physicians in private practice, and a potential move away from unhealthy work/life ratios currently so common among physicians.
Dr. Levine concluded that it is up to training programs to prepare trainees for these sea changes to the practice of medicine.
References
1. https://www.healthleadersmedia.com/finance/healthcare-spending-20-gdp-thats-economy-wide-problem
2. PwC Health Research Institute
3. https://www.bls.gov/ooh/healthcare/home.htm
4. https://www.hfma.org/Content.aspx?id=60811
5. https://www.ama-assn.org/about-ama/research/physician-practice-benchmark-survey
6. http://www.physiciansadvocacyinstitute.org/
7. https://omahamedical.com/wp-content/uploads/2016/12/2016-Survey-of-Americas-Physicians-Practice-Patterns-and-Perspectives.pdf
8. https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235
The health care workforce is being transformed by profound demographic changes and the steady growth of the U.S. health sector. In addition, the movement of physicians out of private practice to employment by medical centers has accelerated. And a new generation of health care professionals is demanding a sustainable work/life balance. These trends will combine to change the work environment of chest physicians.
Spending
The United States spends about twice as much on health care as any other industrialized nation and this fact is driving an increasingly urgent public discussion about options and means of reducing costs.1 Medicare and Medicaid already account for about a quarter of federal government spending and those numbers are expected to rise as baby boomers age.1 Employer spending on health care as a percentage of wages has doubled since the 1980s.2
Workforce supply
An expanding health care sector means a growing demand for health care labor. Health care occupations are projected to grow 18% from 2016 to 2026, faster than the average for all occupations and adding 2.4 million new jobs to the economy.3 Expert testimony before the U.S. Senate Committee on Health, Education, Labor, and Pensions in May 2018 projected shortages of physicians in the coming years. According to estimates of the Health Resources and Services Administration (HRSA), there is a need for 13,800 additional primary care physicians in areas – especially rural – that are designated as health professional shortage areas. Signs of a worsening situation include projected shortages of 20,000 primary care physicians by 2025, according to HRSA, and 42,600-121,300 physicians by 2030, according to the Association of American Medical Colleges. The demand for physicians will exceed supply by 46,000-90,000 by 2025. An update to that research increased the projected shortage range to 61,700-94,700 by 2025.4 These shortages will result in recruiting challenges for many medical centers, especially those in rural areas.
Employment
Private practice is becoming the less common structure of employment for physicians. According to American Medical Association data, physician ownership of practices dropped below 50% for the first time in 2016.5 The trend toward employed versus private practice physicians is expected to continue. The size of practices is growing, with about one-third of physicians working in a hospital-owned practice or employed directly by a hospital and around 40% in practices of 10 physicians or more.5 Of every 10 physician practices, 3 were hospital owned in 2016.6 Physicians are being called upon to do more data entry and administrative work; 21% of physicians’ time is now spent on nonclinical paperwork.7 The ripple-out effects of what amounts to a seismic shift in the work structure and work environment for physicians are only beginning to be studied in terms of overall personal satisfaction and impact on patient care.
Stephanie M. Levine, MD, FCCP, the designate president of the American College of Chest Physicians and professor of medicine in the division of pulmonary diseases and critical care medicine at the University of Texas, San Antonio, recognizes the significance of the move from private practice to employment and suggests that advantages could be offset by some potential negatives practicing chest physicians. She noted, “Pros include potentially more job security, more predictable work hours, perhaps a reduction in some of the traditional administrative ‘hassles’ with running a private practice, and possibly a better and healthier work/life balance. Some think that physician input and leadership in the employed model may have more influence on a health care system than in an individual private practice. Nonclinical work may be decreased, but it is not clear that this is true.
“The negatives include a loss of autonomy, a potential loss of personal ownership of our patients’ health, and the loss of a unique personal culture of private practice. Physicians may be subject to metrics imposed by the employer. In addition, we may see more job turnover since physicians could be less invested emotionally and financially; fewer patients seen since the structure is often salary based and not based on productivity; and increased shift work, set work hours, and schedules. Thus, the employer-based model may actually contribute to the ongoing physician shortage.”
Dr. Levine stressed the role of training programs to prepare physicians for what may lie ahead. “Training programs must prepare physicians for what to expect as employees.”
Changing expectations
An evolution of expectations about a healthy work/life balance has occurred in many professions, including the health care profession. While younger practitioners may be more likely to embrace the changes occurring within health care, they are often more vocal about their desire for a healthy work/life balance and may be less likely to spend time away from family and friends rather than completing administrative tasks. Parenting is increasingly regarded by women and men as compatible with a full and rewarding career as a physician. So these changing expectations about work/life balances mean health care institutions will have to adjust their own expectations in order to recruit and maintain top-quality staff.
Stress and burnout
Workforce shortages, overwhelming administrative tasks, and a variety of forces that come with employment in a large medical system are causing stress and burnout in many physicians. In a 2018 Medscape study of more than 15,000 physicians, 42% reported burnout, and 15% admitted to experiencing either clinical or colloquial forms of depression.8 Dr. Levine acknowledges that many chest physicians are at risk for burnout. “In our field of medicine, particularly with those that practice in an intensive care setting, we are faced with the high stress and emotional experiences we encounter in the life and death nature of our jobs. We care for the sickest patient population, and are often facing life and death clinical needs as well as end-of-life discussions and care. Burnout is a potential threat to both patient safety and the quality of healthcare that we practice.”
Dr. Levine strongly urges colleagues to remain vigilant to this potentially devastating condition in their fellow physicians and in themselves. She said, “If you suspect you are feeling the symptoms of burnout, or have been told so by a colleague, then talk to a peer or colleague, take personal time to do something you enjoy, and/or join a support group. But better than that, try to preempt burnout by developing a strong emotional peer support group in or out of work, practicing mindfulness training, and paying attention to wellness and self-care.”
Burnout is finally being recognized by medical institutions as a significant factor in physician health and performance, and in the recruitment and attrition of staff. Dr. Levine sees progress in how health care institutions deal with burnout, wellness, and work/life balance among staff and trainees. In a hopeful note, Dr. Levine suggested that institutional responses to burnout and the workplace factors that fuel burnout may improve work conditions for physicians in the future.
These trends in the U.S. economy and workforce will mean a steady growth of the health care sector for the foreseeable future, continued political and social pressure to control costs, fewer physicians in private practice, and a potential move away from unhealthy work/life ratios currently so common among physicians.
Dr. Levine concluded that it is up to training programs to prepare trainees for these sea changes to the practice of medicine.
References
1. https://www.healthleadersmedia.com/finance/healthcare-spending-20-gdp-thats-economy-wide-problem
2. PwC Health Research Institute
3. https://www.bls.gov/ooh/healthcare/home.htm
4. https://www.hfma.org/Content.aspx?id=60811
5. https://www.ama-assn.org/about-ama/research/physician-practice-benchmark-survey
6. http://www.physiciansadvocacyinstitute.org/
7. https://omahamedical.com/wp-content/uploads/2016/12/2016-Survey-of-Americas-Physicians-Practice-Patterns-and-Perspectives.pdf
8. https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235
The health care workforce is being transformed by profound demographic changes and the steady growth of the U.S. health sector. In addition, the movement of physicians out of private practice to employment by medical centers has accelerated. And a new generation of health care professionals is demanding a sustainable work/life balance. These trends will combine to change the work environment of chest physicians.
Spending
The United States spends about twice as much on health care as any other industrialized nation and this fact is driving an increasingly urgent public discussion about options and means of reducing costs.1 Medicare and Medicaid already account for about a quarter of federal government spending and those numbers are expected to rise as baby boomers age.1 Employer spending on health care as a percentage of wages has doubled since the 1980s.2
Workforce supply
An expanding health care sector means a growing demand for health care labor. Health care occupations are projected to grow 18% from 2016 to 2026, faster than the average for all occupations and adding 2.4 million new jobs to the economy.3 Expert testimony before the U.S. Senate Committee on Health, Education, Labor, and Pensions in May 2018 projected shortages of physicians in the coming years. According to estimates of the Health Resources and Services Administration (HRSA), there is a need for 13,800 additional primary care physicians in areas – especially rural – that are designated as health professional shortage areas. Signs of a worsening situation include projected shortages of 20,000 primary care physicians by 2025, according to HRSA, and 42,600-121,300 physicians by 2030, according to the Association of American Medical Colleges. The demand for physicians will exceed supply by 46,000-90,000 by 2025. An update to that research increased the projected shortage range to 61,700-94,700 by 2025.4 These shortages will result in recruiting challenges for many medical centers, especially those in rural areas.
Employment
Private practice is becoming the less common structure of employment for physicians. According to American Medical Association data, physician ownership of practices dropped below 50% for the first time in 2016.5 The trend toward employed versus private practice physicians is expected to continue. The size of practices is growing, with about one-third of physicians working in a hospital-owned practice or employed directly by a hospital and around 40% in practices of 10 physicians or more.5 Of every 10 physician practices, 3 were hospital owned in 2016.6 Physicians are being called upon to do more data entry and administrative work; 21% of physicians’ time is now spent on nonclinical paperwork.7 The ripple-out effects of what amounts to a seismic shift in the work structure and work environment for physicians are only beginning to be studied in terms of overall personal satisfaction and impact on patient care.
Stephanie M. Levine, MD, FCCP, the designate president of the American College of Chest Physicians and professor of medicine in the division of pulmonary diseases and critical care medicine at the University of Texas, San Antonio, recognizes the significance of the move from private practice to employment and suggests that advantages could be offset by some potential negatives practicing chest physicians. She noted, “Pros include potentially more job security, more predictable work hours, perhaps a reduction in some of the traditional administrative ‘hassles’ with running a private practice, and possibly a better and healthier work/life balance. Some think that physician input and leadership in the employed model may have more influence on a health care system than in an individual private practice. Nonclinical work may be decreased, but it is not clear that this is true.
“The negatives include a loss of autonomy, a potential loss of personal ownership of our patients’ health, and the loss of a unique personal culture of private practice. Physicians may be subject to metrics imposed by the employer. In addition, we may see more job turnover since physicians could be less invested emotionally and financially; fewer patients seen since the structure is often salary based and not based on productivity; and increased shift work, set work hours, and schedules. Thus, the employer-based model may actually contribute to the ongoing physician shortage.”
Dr. Levine stressed the role of training programs to prepare physicians for what may lie ahead. “Training programs must prepare physicians for what to expect as employees.”
Changing expectations
An evolution of expectations about a healthy work/life balance has occurred in many professions, including the health care profession. While younger practitioners may be more likely to embrace the changes occurring within health care, they are often more vocal about their desire for a healthy work/life balance and may be less likely to spend time away from family and friends rather than completing administrative tasks. Parenting is increasingly regarded by women and men as compatible with a full and rewarding career as a physician. So these changing expectations about work/life balances mean health care institutions will have to adjust their own expectations in order to recruit and maintain top-quality staff.
Stress and burnout
Workforce shortages, overwhelming administrative tasks, and a variety of forces that come with employment in a large medical system are causing stress and burnout in many physicians. In a 2018 Medscape study of more than 15,000 physicians, 42% reported burnout, and 15% admitted to experiencing either clinical or colloquial forms of depression.8 Dr. Levine acknowledges that many chest physicians are at risk for burnout. “In our field of medicine, particularly with those that practice in an intensive care setting, we are faced with the high stress and emotional experiences we encounter in the life and death nature of our jobs. We care for the sickest patient population, and are often facing life and death clinical needs as well as end-of-life discussions and care. Burnout is a potential threat to both patient safety and the quality of healthcare that we practice.”
Dr. Levine strongly urges colleagues to remain vigilant to this potentially devastating condition in their fellow physicians and in themselves. She said, “If you suspect you are feeling the symptoms of burnout, or have been told so by a colleague, then talk to a peer or colleague, take personal time to do something you enjoy, and/or join a support group. But better than that, try to preempt burnout by developing a strong emotional peer support group in or out of work, practicing mindfulness training, and paying attention to wellness and self-care.”
Burnout is finally being recognized by medical institutions as a significant factor in physician health and performance, and in the recruitment and attrition of staff. Dr. Levine sees progress in how health care institutions deal with burnout, wellness, and work/life balance among staff and trainees. In a hopeful note, Dr. Levine suggested that institutional responses to burnout and the workplace factors that fuel burnout may improve work conditions for physicians in the future.
These trends in the U.S. economy and workforce will mean a steady growth of the health care sector for the foreseeable future, continued political and social pressure to control costs, fewer physicians in private practice, and a potential move away from unhealthy work/life ratios currently so common among physicians.
Dr. Levine concluded that it is up to training programs to prepare trainees for these sea changes to the practice of medicine.
References
1. https://www.healthleadersmedia.com/finance/healthcare-spending-20-gdp-thats-economy-wide-problem
2. PwC Health Research Institute
3. https://www.bls.gov/ooh/healthcare/home.htm
4. https://www.hfma.org/Content.aspx?id=60811
5. https://www.ama-assn.org/about-ama/research/physician-practice-benchmark-survey
6. http://www.physiciansadvocacyinstitute.org/
7. https://omahamedical.com/wp-content/uploads/2016/12/2016-Survey-of-Americas-Physicians-Practice-Patterns-and-Perspectives.pdf
8. https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235
Propose Ideas for Sessions for VAM 2020
The Society for Vascular Surgery seeks proposals for invited sessions for the 2020 Vascular Annual Meeting, to be held June 17 to 20 in Toronto, Ontario, Canada. Scientific sessions will be June 18 to 20 and exhibits will be open June 18 to 19. Proposals should include the session's educational benefit, a short outline of the program topic, session goals and target audience, among other information. Obtain the information/submission form here. Email completed forms to [email protected].
The Society for Vascular Surgery seeks proposals for invited sessions for the 2020 Vascular Annual Meeting, to be held June 17 to 20 in Toronto, Ontario, Canada. Scientific sessions will be June 18 to 20 and exhibits will be open June 18 to 19. Proposals should include the session's educational benefit, a short outline of the program topic, session goals and target audience, among other information. Obtain the information/submission form here. Email completed forms to [email protected].
The Society for Vascular Surgery seeks proposals for invited sessions for the 2020 Vascular Annual Meeting, to be held June 17 to 20 in Toronto, Ontario, Canada. Scientific sessions will be June 18 to 20 and exhibits will be open June 18 to 19. Proposals should include the session's educational benefit, a short outline of the program topic, session goals and target audience, among other information. Obtain the information/submission form here. Email completed forms to [email protected].
VAM on Demand Now Available
All who attended the 2019 Vascular Annual Meeting can now review sessions they attended, as well as “attend” those that they missed. Those who weren’t at VAM can now experience all they missed. Slides and audio presentations of nearly every session are included in the now available VAM on Demand. The cost for one year of access is $199 for VAM attendees and $499 for non-attendees. Those who purchased VAM on Demand before the meeting ended can visit this site to gain access by logging in with their SVS credentials.
All who attended the 2019 Vascular Annual Meeting can now review sessions they attended, as well as “attend” those that they missed. Those who weren’t at VAM can now experience all they missed. Slides and audio presentations of nearly every session are included in the now available VAM on Demand. The cost for one year of access is $199 for VAM attendees and $499 for non-attendees. Those who purchased VAM on Demand before the meeting ended can visit this site to gain access by logging in with their SVS credentials.
All who attended the 2019 Vascular Annual Meeting can now review sessions they attended, as well as “attend” those that they missed. Those who weren’t at VAM can now experience all they missed. Slides and audio presentations of nearly every session are included in the now available VAM on Demand. The cost for one year of access is $199 for VAM attendees and $499 for non-attendees. Those who purchased VAM on Demand before the meeting ended can visit this site to gain access by logging in with their SVS credentials.
AGA remembers Dr. Henry T. Lynch
Henry T. Lynch, MD, came from a humble background, growing up in a rough neighborhood in New York City. He enlisted in the Navy and served in the South Pacific during World War II. Afterward, Dr. Lynch focused his efforts on completing his education, which eventually lead him to the medical field.
After obtaining his high-school equivalency, and completing his undergraduate degree at the University of Oklahoma and his master’s degree in clinical psychology at the University of Denver, his path turned toward the field in which he would make his thrilling and unprecedented discoveries. He studied for a PhD in human genetics at the University of Texas at Austin and received his medical degree from the University of Texas Medical Branch in Galveston. He completed his internship at St. Mary’s Hospital in Evansville, Indiana, and his residency in internal medicine at the University of Nebraska College of Medicine. His first faculty appointment was at The University of Texas MD Anderson Cancer Center.
In 1967, he accepted a position at Creighton, in Omaha, Neb., where he would spend the rest of his storied career. Dr. Lynch was a professor at Creighton University School of Medicine, and the founder and director of the Hereditary Cancer Center at Creighton, established in 1984. He served as chair of the institution’s Department of Preventive Medicine and Public Health, and was named the inaugural holder of the Charles F. and Mary C. Heider Endowed Chair in Cancer Research at Creighton.
A patient he encountered in 1962 – an alcoholic that drank because he believed he would die of colon cancer since everyone in his family had – was the catalyst for his groundbreaking work into the possibility of a hereditary component to some forms of cancer. During this time, it was understood that carcinogenic chemicals and viruses were the primary cause of cancer.
Dr. Lynch provided the first complete description of hereditary nonpolyposis colorectal cancer, a form of colon cancer eventually renamed Lynch syndrome. He continued his research, eventually identifying a hereditary form of breast and ovarian cancers, melanoma, and prostate and pancreatic cancers. His efforts also resulted in one of the world’s largest databases of family cancer histories.
Dr. Lynch passed away on June 2, 2019, at the age of 91. AGA members are sharing their stories and the impact Dr. Lynch had on their work in the AGA Community.
Lucas Franki contributed to this report.
Henry T. Lynch, MD, came from a humble background, growing up in a rough neighborhood in New York City. He enlisted in the Navy and served in the South Pacific during World War II. Afterward, Dr. Lynch focused his efforts on completing his education, which eventually lead him to the medical field.
After obtaining his high-school equivalency, and completing his undergraduate degree at the University of Oklahoma and his master’s degree in clinical psychology at the University of Denver, his path turned toward the field in which he would make his thrilling and unprecedented discoveries. He studied for a PhD in human genetics at the University of Texas at Austin and received his medical degree from the University of Texas Medical Branch in Galveston. He completed his internship at St. Mary’s Hospital in Evansville, Indiana, and his residency in internal medicine at the University of Nebraska College of Medicine. His first faculty appointment was at The University of Texas MD Anderson Cancer Center.
In 1967, he accepted a position at Creighton, in Omaha, Neb., where he would spend the rest of his storied career. Dr. Lynch was a professor at Creighton University School of Medicine, and the founder and director of the Hereditary Cancer Center at Creighton, established in 1984. He served as chair of the institution’s Department of Preventive Medicine and Public Health, and was named the inaugural holder of the Charles F. and Mary C. Heider Endowed Chair in Cancer Research at Creighton.
A patient he encountered in 1962 – an alcoholic that drank because he believed he would die of colon cancer since everyone in his family had – was the catalyst for his groundbreaking work into the possibility of a hereditary component to some forms of cancer. During this time, it was understood that carcinogenic chemicals and viruses were the primary cause of cancer.
Dr. Lynch provided the first complete description of hereditary nonpolyposis colorectal cancer, a form of colon cancer eventually renamed Lynch syndrome. He continued his research, eventually identifying a hereditary form of breast and ovarian cancers, melanoma, and prostate and pancreatic cancers. His efforts also resulted in one of the world’s largest databases of family cancer histories.
Dr. Lynch passed away on June 2, 2019, at the age of 91. AGA members are sharing their stories and the impact Dr. Lynch had on their work in the AGA Community.
Lucas Franki contributed to this report.
Henry T. Lynch, MD, came from a humble background, growing up in a rough neighborhood in New York City. He enlisted in the Navy and served in the South Pacific during World War II. Afterward, Dr. Lynch focused his efforts on completing his education, which eventually lead him to the medical field.
After obtaining his high-school equivalency, and completing his undergraduate degree at the University of Oklahoma and his master’s degree in clinical psychology at the University of Denver, his path turned toward the field in which he would make his thrilling and unprecedented discoveries. He studied for a PhD in human genetics at the University of Texas at Austin and received his medical degree from the University of Texas Medical Branch in Galveston. He completed his internship at St. Mary’s Hospital in Evansville, Indiana, and his residency in internal medicine at the University of Nebraska College of Medicine. His first faculty appointment was at The University of Texas MD Anderson Cancer Center.
In 1967, he accepted a position at Creighton, in Omaha, Neb., where he would spend the rest of his storied career. Dr. Lynch was a professor at Creighton University School of Medicine, and the founder and director of the Hereditary Cancer Center at Creighton, established in 1984. He served as chair of the institution’s Department of Preventive Medicine and Public Health, and was named the inaugural holder of the Charles F. and Mary C. Heider Endowed Chair in Cancer Research at Creighton.
A patient he encountered in 1962 – an alcoholic that drank because he believed he would die of colon cancer since everyone in his family had – was the catalyst for his groundbreaking work into the possibility of a hereditary component to some forms of cancer. During this time, it was understood that carcinogenic chemicals and viruses were the primary cause of cancer.
Dr. Lynch provided the first complete description of hereditary nonpolyposis colorectal cancer, a form of colon cancer eventually renamed Lynch syndrome. He continued his research, eventually identifying a hereditary form of breast and ovarian cancers, melanoma, and prostate and pancreatic cancers. His efforts also resulted in one of the world’s largest databases of family cancer histories.
Dr. Lynch passed away on June 2, 2019, at the age of 91. AGA members are sharing their stories and the impact Dr. Lynch had on their work in the AGA Community.
Lucas Franki contributed to this report.
Top AGA Community patient cases
Physicians with difficult patient scenarios bring their questions to the AGA Community (https://community.gastro.org) to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. In case you missed it, here are the most popular clinical discussions shared in the forum recently:
1. Crohn’s disease, Infliximab and liver abscess
(http://ow.ly/MehK30p2UZr)
2. Positive Cologuard testing in patient on blood thinners
(http://ow.ly/lJXF30p2V12)
3. Recombinant zoster vaccine in IBD patients on biologics
(http://ow.ly/FWGA30p2V1F)
4. Hair loss and Crohn’s disease
(http://ow.ly/C6Sa30p2V2h)
Access these clinical cases and more discussions at https://community.gastro.org/discussions.
Physicians with difficult patient scenarios bring their questions to the AGA Community (https://community.gastro.org) to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. In case you missed it, here are the most popular clinical discussions shared in the forum recently:
1. Crohn’s disease, Infliximab and liver abscess
(http://ow.ly/MehK30p2UZr)
2. Positive Cologuard testing in patient on blood thinners
(http://ow.ly/lJXF30p2V12)
3. Recombinant zoster vaccine in IBD patients on biologics
(http://ow.ly/FWGA30p2V1F)
4. Hair loss and Crohn’s disease
(http://ow.ly/C6Sa30p2V2h)
Access these clinical cases and more discussions at https://community.gastro.org/discussions.
Physicians with difficult patient scenarios bring their questions to the AGA Community (https://community.gastro.org) to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. In case you missed it, here are the most popular clinical discussions shared in the forum recently:
1. Crohn’s disease, Infliximab and liver abscess
(http://ow.ly/MehK30p2UZr)
2. Positive Cologuard testing in patient on blood thinners
(http://ow.ly/lJXF30p2V12)
3. Recombinant zoster vaccine in IBD patients on biologics
(http://ow.ly/FWGA30p2V1F)
4. Hair loss and Crohn’s disease
(http://ow.ly/C6Sa30p2V2h)
Access these clinical cases and more discussions at https://community.gastro.org/discussions.
Remember the AGA Research Foundation in your will or living trust
What if all you had to do to ensure that the AGA Research Foundation can have an impact for years to come is to write a simple sentence? Sound impossible?
The AGA Research Foundation provides a key source of funding at a critical juncture in young investigators’ career. Securing the future of the talented investigators we serve really is as simple as one sentence. By including a gift to the AGA Research Foundation in your will, you can support our mission tomorrow without giving away any of your assets today.
Including the AGA Research Foundation in your will is a popular gift to give because it is:
- Affordable. The actual giving of your gift occurs after your lifetime, so your current income is not affected.
- Flexible. Until your will goes into effect, you are free to alter your plans or change your mind.
- Versatile. You can give a specific item, a set amount of money or a percentage of your estate. You can also make your gift contingent upon certain events.
We hope you’ll consider including a gift to the AGA Research Foundation in your will or living trust. It’s simple – just a few sentences in your will or trust are all that is needed. The official bequest language for the AGA Research Foundation is: “I, [name], of [city, state, ZIP], give, devise and bequeath to the AGA Research Foundation [written amount or percentage of the estate or description of property] for its unrestricted use and purpose.”
Join others in donating to the AGA Research Foundation and help fill the funding gap and protect the next generation of investigators.
Please contact us for more information at [email protected] or visit http://gastro.planmylegacy.org/.
What if all you had to do to ensure that the AGA Research Foundation can have an impact for years to come is to write a simple sentence? Sound impossible?
The AGA Research Foundation provides a key source of funding at a critical juncture in young investigators’ career. Securing the future of the talented investigators we serve really is as simple as one sentence. By including a gift to the AGA Research Foundation in your will, you can support our mission tomorrow without giving away any of your assets today.
Including the AGA Research Foundation in your will is a popular gift to give because it is:
- Affordable. The actual giving of your gift occurs after your lifetime, so your current income is not affected.
- Flexible. Until your will goes into effect, you are free to alter your plans or change your mind.
- Versatile. You can give a specific item, a set amount of money or a percentage of your estate. You can also make your gift contingent upon certain events.
We hope you’ll consider including a gift to the AGA Research Foundation in your will or living trust. It’s simple – just a few sentences in your will or trust are all that is needed. The official bequest language for the AGA Research Foundation is: “I, [name], of [city, state, ZIP], give, devise and bequeath to the AGA Research Foundation [written amount or percentage of the estate or description of property] for its unrestricted use and purpose.”
Join others in donating to the AGA Research Foundation and help fill the funding gap and protect the next generation of investigators.
Please contact us for more information at [email protected] or visit http://gastro.planmylegacy.org/.
What if all you had to do to ensure that the AGA Research Foundation can have an impact for years to come is to write a simple sentence? Sound impossible?
The AGA Research Foundation provides a key source of funding at a critical juncture in young investigators’ career. Securing the future of the talented investigators we serve really is as simple as one sentence. By including a gift to the AGA Research Foundation in your will, you can support our mission tomorrow without giving away any of your assets today.
Including the AGA Research Foundation in your will is a popular gift to give because it is:
- Affordable. The actual giving of your gift occurs after your lifetime, so your current income is not affected.
- Flexible. Until your will goes into effect, you are free to alter your plans or change your mind.
- Versatile. You can give a specific item, a set amount of money or a percentage of your estate. You can also make your gift contingent upon certain events.
We hope you’ll consider including a gift to the AGA Research Foundation in your will or living trust. It’s simple – just a few sentences in your will or trust are all that is needed. The official bequest language for the AGA Research Foundation is: “I, [name], of [city, state, ZIP], give, devise and bequeath to the AGA Research Foundation [written amount or percentage of the estate or description of property] for its unrestricted use and purpose.”
Join others in donating to the AGA Research Foundation and help fill the funding gap and protect the next generation of investigators.
Please contact us for more information at [email protected] or visit http://gastro.planmylegacy.org/.