User login
ACS-COSECSA Women Scholars Program now accepting applications
To help address the severe shortage of surgeons in Sub-Saharan Africa, the American College of Surgeons (ACS) and the College of Surgeons of East, Central, and Southern Africa (COSECSA) have developed a scholarship program to support women in surgical residency, help them complete their training, and encourage other women in medicine to consider surgery as a profession.
The program is open to senior female surgical residents enrolled in the COSECSA region. Each $2,500 scholarship will go toward educational expenses, including accreditation, the fellowship examination, and five-years of membership dues to COSECSA and the ACS. Applicants should include a personal statement indicating future goals, a current curriculum vitae, and a letter of support from the surgical training program director. Completed applications should be sent via e-mail to [email protected] and will be reviewed in conjunction with the Operation Giving Back committee.
Applications are due no later than April 1. Contact [email protected] with any questions.
To help address the severe shortage of surgeons in Sub-Saharan Africa, the American College of Surgeons (ACS) and the College of Surgeons of East, Central, and Southern Africa (COSECSA) have developed a scholarship program to support women in surgical residency, help them complete their training, and encourage other women in medicine to consider surgery as a profession.
The program is open to senior female surgical residents enrolled in the COSECSA region. Each $2,500 scholarship will go toward educational expenses, including accreditation, the fellowship examination, and five-years of membership dues to COSECSA and the ACS. Applicants should include a personal statement indicating future goals, a current curriculum vitae, and a letter of support from the surgical training program director. Completed applications should be sent via e-mail to [email protected] and will be reviewed in conjunction with the Operation Giving Back committee.
Applications are due no later than April 1. Contact [email protected] with any questions.
To help address the severe shortage of surgeons in Sub-Saharan Africa, the American College of Surgeons (ACS) and the College of Surgeons of East, Central, and Southern Africa (COSECSA) have developed a scholarship program to support women in surgical residency, help them complete their training, and encourage other women in medicine to consider surgery as a profession.
The program is open to senior female surgical residents enrolled in the COSECSA region. Each $2,500 scholarship will go toward educational expenses, including accreditation, the fellowship examination, and five-years of membership dues to COSECSA and the ACS. Applicants should include a personal statement indicating future goals, a current curriculum vitae, and a letter of support from the surgical training program director. Completed applications should be sent via e-mail to [email protected] and will be reviewed in conjunction with the Operation Giving Back committee.
Applications are due no later than April 1. Contact [email protected] with any questions.
Get Pocket Versions of Practice Guidelines
SVS has partnered with Guidelines Central to create a Pocket Guide version of the new AAA guidelines. Also available are pocket guides on Management of Diabetic Foot, Peripheral Arterial Disease and Venous Leg Ulcers.
SVS members can access the digital versions for free; printed guidelines vary in price. The guidelines also are available as a bundled set. Slide sets of the guidelines, useful as educational tools, also are available online.
SVS has partnered with Guidelines Central to create a Pocket Guide version of the new AAA guidelines. Also available are pocket guides on Management of Diabetic Foot, Peripheral Arterial Disease and Venous Leg Ulcers.
SVS members can access the digital versions for free; printed guidelines vary in price. The guidelines also are available as a bundled set. Slide sets of the guidelines, useful as educational tools, also are available online.
SVS has partnered with Guidelines Central to create a Pocket Guide version of the new AAA guidelines. Also available are pocket guides on Management of Diabetic Foot, Peripheral Arterial Disease and Venous Leg Ulcers.
SVS members can access the digital versions for free; printed guidelines vary in price. The guidelines also are available as a bundled set. Slide sets of the guidelines, useful as educational tools, also are available online.
VAM Registration Now Open
Registration and housing for the 2018 Vascular Annual Meeting are now open. Register today for VAM, June 20 to 23 in Boston, including looking over housing options. Following a full day of postgraduate courses, VESS abstracts, workshops and international programming on Wednesday, June 20, abstract-based scientific sessions will open June 21 and continue to June 23. The Exhibit Hall will be open June 21 to 22.
Catch the highlights of this year's annual meeting here.
Registration and housing for the 2018 Vascular Annual Meeting are now open. Register today for VAM, June 20 to 23 in Boston, including looking over housing options. Following a full day of postgraduate courses, VESS abstracts, workshops and international programming on Wednesday, June 20, abstract-based scientific sessions will open June 21 and continue to June 23. The Exhibit Hall will be open June 21 to 22.
Catch the highlights of this year's annual meeting here.
Registration and housing for the 2018 Vascular Annual Meeting are now open. Register today for VAM, June 20 to 23 in Boston, including looking over housing options. Following a full day of postgraduate courses, VESS abstracts, workshops and international programming on Wednesday, June 20, abstract-based scientific sessions will open June 21 and continue to June 23. The Exhibit Hall will be open June 21 to 22.
Catch the highlights of this year's annual meeting here.
OSA Endotypes and Phenotypes: Toward Personalized OSA Care
Obstructive sleep apnea (OSA) contributes a major health burden to society due to its high prevalence and substantial neurocognitive and cardiovascular consequences. Estimates suggest that at least 10% of adults in North America are afflicted with OSA, making it probably the most common respiratory disease in the developed world (Peppard et al. Am J Epidemiol. 2013;177[9]:1006). Nasal CPAP is a highly efficacious therapy that has been shown to improve neurocognitive and cardiovascular outcomes. However, CPAP is not always well tolerated. Alternative therapies, such as oral appliances and upper airway surgery, have highly variable efficacy, and evidence of important clinical benefits are uncertain. Therefore, efforts are ongoing to determine optimal alternative strategies for therapy.
In order to treat any condition optimally, one needs to be able to predict who is at highest risk of developing the condition, then to assess the consequences if left untreated, and finally to be able to predict response to various treatment options. Currently, the OSA field is still in its early stages of our understanding. Clinically, we are often faced with patients who have varying presentations and manifestations, but, for reasons that are unclear. For instance, two individuals with the same body mass index may have very different clinical manifestations, one with severe OSA and one without any OSA. Similarly, two individuals with an apnea hypopnea index of 40 events per hour (ie, severe OSA) may have very different symptoms attributable to OSA, eg, one could be asymptomatic and the other could be debilitated from sleepiness. We and others have been making efforts to determine why these phenomenon occur. At present, the techniques to define mechanisms underlying OSA are labor-intensive, requiring one or two overnight experiments to gather meaningful data. Although we are gathering new insights based on these techniques, efforts are ongoing to simplify these approaches and to make assessment of pathophysiologic characteristics more accessible to the clinician (Orr et al. Am J Respir Crit Care Med. 2017 Nov 30. doi: 10.1164/rccm.201707-1357LE. [Epub ahead of print]).
We ultimately believe that a thorough analysis of a sleep recording combined with demographic data and other readily available clinical data (perhaps plasma biomarkers) may yield sufficient information for us to know why OSA is occurring and what interventions might be helpful for an individual patient. Currently, our use of the polysomnogram to derive only an apnea hypopnea index does not take full advantage of the available data. An apnea hypopnea index can be readily obtained from home sleep testing and does not truly provide much insight into why a given individual has OSA, what symptoms are attributable to OSA, and what interventions might be considered for the afflicted individual. By analogy, if the only useful data derived from an ECG were a heart rate, the test would rapidly become obsolete. Along these lines, if the only role for the sleep clinician was to prescribe CPAP to everyone with an AHI greater than 5/h, there would be little need or interest in specialized training. In contrast, we suggest that rich insights regarding pathophysiology and mechanisms should be gathered and may influence clinical management of patients afflicted with OSA. Thus, we encourage more thorough analyses of available data to maximize information gleaned and, ultimately, to optimize clinical outcomes.
Recent studies suggest that sleep apnea occurs for varying reasons, a concept that is now thought to be clinically important (Jordan et al. Lancet. 2014;383[9918]:736). We draw a crucial distinction between endotypes (mechanisms underlying disease) and phenotypes (clinical expression of disease). Important endotypes include compromised upper airway anatomy, dysfunction in pharyngeal dilator muscles, unstable ventilatory control (high loop gain), and low arousal threshold (wake up easily), among others. Important phenotypes of sleep apnea are emerging and still evolving to include minimally symptomatic OSA, OSA with daytime sleepiness, and OSA with major cardiometabolic risk, among others. Several important concepts have emerged regarding different OSA endotypes and phenotypes:
1 The mechanism underlying OSA may predict potential response to therapeutic interventions. For instance, the endotype of OSA with unstable ventilatory control (high loop gain) may respond to agents such as oxygen and acetazolamide, which serve to stabilize control of breathing. In patients with anatomical compromise at the level of the velopharynx, uvulopalatopharyngoplasty may be an effective intervention. For patients with multiple pathophysiologic abnormalities, combination therapy may be required to alleviate OSA (Edwards et al. Sleep. 2016;9[11]:1973).
2 Given that OSA has many underlying etiologies, efforts are underway to determine whether individuals with different risk factors for OSA develop their disease based on varying mechanisms. As an example, people with posttraumatic stress disorder (PTSD) may be at increased risk of OSA perhaps on the basis of a low threshold for arousal (Orr et al. JCSM. 2017, 13[1]: 57-63). Another example would be patients with neuromuscular disease who may be at risk of OSA primarily based on impaired pharyngeal dilator muscle function.
3 A new concept is emerging whereby endotypes of OSA may actually predict differing OSA phenotypes. In theory, loop gain-driven OSA may have different consequences from OSA driven by compromise of pharyngeal anatomy. To this point, data suggest that OSA in the elderly may not have as many consequences as OSA in younger people matched on severity of illness. OSA in the elderly has lower loop gain than OSA in younger people and is associated with less negative intrathoracic pressure at the time of arousal as compared with younger individuals with OSA (Kobayashi et al. Chest. 2010; 137[6]:1310). As such, the endotype of OSA in the elderly may explain why the clinical consequences are fewer than in the younger OSA counterparts.
4 The mechanism underlying OSA may be important in determining response to clinical interventions, such as nasal CPAP. Patients with a low arousal threshold may be prone to insomnia when placed on CPAP and could theoretically be poorly tolerant of therapy based on disrupted sleep architecture. Such patients may benefit from non-myorelaxant hypnotic therapy to consolidate sleep and improve CPAP adherence. In addition, patients with high loop gain (unstable ventilatory control) may be prone to develop central apneas when placed on CPAP therapy (Stanchina et al. Ann Am Thorac Soc. 2015;12[9]:1351). These patients may benefit from newer technologies, eg, auto or adaptive servo ventilation - ASV. High loop gain has also been shown to predict failure of upper airway surgery as a treatment for OSA by several groups (Li et al. JCSM. 2017;13[9]:1029). Such patients should, perhaps, undergo nonsurgical therapies for OSA.
We emphasize that some of the points being made are somewhat speculative and, thus, encourage further basic and clinical research to test our assumptions. Robust, multicenter clinical trials assessing hard outcomes will ultimately be required to change the current standard of care. Nonetheless, we believe that a more thorough understanding of OSA pathogenesis can help guide clinical care today and will be critical to the optimal treatment of afflicted individuals tomorrow.
Dr. Owens is Assistant Clinical Professor of Medicine; Dr. Deacon is a Post-Doctoral Research Scholar; and Dr. Malhotra is Kenneth M. Moser Professor of Medicine and Chief, Division of Pulmonary, Critical Care and Sleep Medicine, University of California San Diego.
Obstructive sleep apnea (OSA) contributes a major health burden to society due to its high prevalence and substantial neurocognitive and cardiovascular consequences. Estimates suggest that at least 10% of adults in North America are afflicted with OSA, making it probably the most common respiratory disease in the developed world (Peppard et al. Am J Epidemiol. 2013;177[9]:1006). Nasal CPAP is a highly efficacious therapy that has been shown to improve neurocognitive and cardiovascular outcomes. However, CPAP is not always well tolerated. Alternative therapies, such as oral appliances and upper airway surgery, have highly variable efficacy, and evidence of important clinical benefits are uncertain. Therefore, efforts are ongoing to determine optimal alternative strategies for therapy.
In order to treat any condition optimally, one needs to be able to predict who is at highest risk of developing the condition, then to assess the consequences if left untreated, and finally to be able to predict response to various treatment options. Currently, the OSA field is still in its early stages of our understanding. Clinically, we are often faced with patients who have varying presentations and manifestations, but, for reasons that are unclear. For instance, two individuals with the same body mass index may have very different clinical manifestations, one with severe OSA and one without any OSA. Similarly, two individuals with an apnea hypopnea index of 40 events per hour (ie, severe OSA) may have very different symptoms attributable to OSA, eg, one could be asymptomatic and the other could be debilitated from sleepiness. We and others have been making efforts to determine why these phenomenon occur. At present, the techniques to define mechanisms underlying OSA are labor-intensive, requiring one or two overnight experiments to gather meaningful data. Although we are gathering new insights based on these techniques, efforts are ongoing to simplify these approaches and to make assessment of pathophysiologic characteristics more accessible to the clinician (Orr et al. Am J Respir Crit Care Med. 2017 Nov 30. doi: 10.1164/rccm.201707-1357LE. [Epub ahead of print]).
We ultimately believe that a thorough analysis of a sleep recording combined with demographic data and other readily available clinical data (perhaps plasma biomarkers) may yield sufficient information for us to know why OSA is occurring and what interventions might be helpful for an individual patient. Currently, our use of the polysomnogram to derive only an apnea hypopnea index does not take full advantage of the available data. An apnea hypopnea index can be readily obtained from home sleep testing and does not truly provide much insight into why a given individual has OSA, what symptoms are attributable to OSA, and what interventions might be considered for the afflicted individual. By analogy, if the only useful data derived from an ECG were a heart rate, the test would rapidly become obsolete. Along these lines, if the only role for the sleep clinician was to prescribe CPAP to everyone with an AHI greater than 5/h, there would be little need or interest in specialized training. In contrast, we suggest that rich insights regarding pathophysiology and mechanisms should be gathered and may influence clinical management of patients afflicted with OSA. Thus, we encourage more thorough analyses of available data to maximize information gleaned and, ultimately, to optimize clinical outcomes.
Recent studies suggest that sleep apnea occurs for varying reasons, a concept that is now thought to be clinically important (Jordan et al. Lancet. 2014;383[9918]:736). We draw a crucial distinction between endotypes (mechanisms underlying disease) and phenotypes (clinical expression of disease). Important endotypes include compromised upper airway anatomy, dysfunction in pharyngeal dilator muscles, unstable ventilatory control (high loop gain), and low arousal threshold (wake up easily), among others. Important phenotypes of sleep apnea are emerging and still evolving to include minimally symptomatic OSA, OSA with daytime sleepiness, and OSA with major cardiometabolic risk, among others. Several important concepts have emerged regarding different OSA endotypes and phenotypes:
1 The mechanism underlying OSA may predict potential response to therapeutic interventions. For instance, the endotype of OSA with unstable ventilatory control (high loop gain) may respond to agents such as oxygen and acetazolamide, which serve to stabilize control of breathing. In patients with anatomical compromise at the level of the velopharynx, uvulopalatopharyngoplasty may be an effective intervention. For patients with multiple pathophysiologic abnormalities, combination therapy may be required to alleviate OSA (Edwards et al. Sleep. 2016;9[11]:1973).
2 Given that OSA has many underlying etiologies, efforts are underway to determine whether individuals with different risk factors for OSA develop their disease based on varying mechanisms. As an example, people with posttraumatic stress disorder (PTSD) may be at increased risk of OSA perhaps on the basis of a low threshold for arousal (Orr et al. JCSM. 2017, 13[1]: 57-63). Another example would be patients with neuromuscular disease who may be at risk of OSA primarily based on impaired pharyngeal dilator muscle function.
3 A new concept is emerging whereby endotypes of OSA may actually predict differing OSA phenotypes. In theory, loop gain-driven OSA may have different consequences from OSA driven by compromise of pharyngeal anatomy. To this point, data suggest that OSA in the elderly may not have as many consequences as OSA in younger people matched on severity of illness. OSA in the elderly has lower loop gain than OSA in younger people and is associated with less negative intrathoracic pressure at the time of arousal as compared with younger individuals with OSA (Kobayashi et al. Chest. 2010; 137[6]:1310). As such, the endotype of OSA in the elderly may explain why the clinical consequences are fewer than in the younger OSA counterparts.
4 The mechanism underlying OSA may be important in determining response to clinical interventions, such as nasal CPAP. Patients with a low arousal threshold may be prone to insomnia when placed on CPAP and could theoretically be poorly tolerant of therapy based on disrupted sleep architecture. Such patients may benefit from non-myorelaxant hypnotic therapy to consolidate sleep and improve CPAP adherence. In addition, patients with high loop gain (unstable ventilatory control) may be prone to develop central apneas when placed on CPAP therapy (Stanchina et al. Ann Am Thorac Soc. 2015;12[9]:1351). These patients may benefit from newer technologies, eg, auto or adaptive servo ventilation - ASV. High loop gain has also been shown to predict failure of upper airway surgery as a treatment for OSA by several groups (Li et al. JCSM. 2017;13[9]:1029). Such patients should, perhaps, undergo nonsurgical therapies for OSA.
We emphasize that some of the points being made are somewhat speculative and, thus, encourage further basic and clinical research to test our assumptions. Robust, multicenter clinical trials assessing hard outcomes will ultimately be required to change the current standard of care. Nonetheless, we believe that a more thorough understanding of OSA pathogenesis can help guide clinical care today and will be critical to the optimal treatment of afflicted individuals tomorrow.
Dr. Owens is Assistant Clinical Professor of Medicine; Dr. Deacon is a Post-Doctoral Research Scholar; and Dr. Malhotra is Kenneth M. Moser Professor of Medicine and Chief, Division of Pulmonary, Critical Care and Sleep Medicine, University of California San Diego.
Obstructive sleep apnea (OSA) contributes a major health burden to society due to its high prevalence and substantial neurocognitive and cardiovascular consequences. Estimates suggest that at least 10% of adults in North America are afflicted with OSA, making it probably the most common respiratory disease in the developed world (Peppard et al. Am J Epidemiol. 2013;177[9]:1006). Nasal CPAP is a highly efficacious therapy that has been shown to improve neurocognitive and cardiovascular outcomes. However, CPAP is not always well tolerated. Alternative therapies, such as oral appliances and upper airway surgery, have highly variable efficacy, and evidence of important clinical benefits are uncertain. Therefore, efforts are ongoing to determine optimal alternative strategies for therapy.
In order to treat any condition optimally, one needs to be able to predict who is at highest risk of developing the condition, then to assess the consequences if left untreated, and finally to be able to predict response to various treatment options. Currently, the OSA field is still in its early stages of our understanding. Clinically, we are often faced with patients who have varying presentations and manifestations, but, for reasons that are unclear. For instance, two individuals with the same body mass index may have very different clinical manifestations, one with severe OSA and one without any OSA. Similarly, two individuals with an apnea hypopnea index of 40 events per hour (ie, severe OSA) may have very different symptoms attributable to OSA, eg, one could be asymptomatic and the other could be debilitated from sleepiness. We and others have been making efforts to determine why these phenomenon occur. At present, the techniques to define mechanisms underlying OSA are labor-intensive, requiring one or two overnight experiments to gather meaningful data. Although we are gathering new insights based on these techniques, efforts are ongoing to simplify these approaches and to make assessment of pathophysiologic characteristics more accessible to the clinician (Orr et al. Am J Respir Crit Care Med. 2017 Nov 30. doi: 10.1164/rccm.201707-1357LE. [Epub ahead of print]).
We ultimately believe that a thorough analysis of a sleep recording combined with demographic data and other readily available clinical data (perhaps plasma biomarkers) may yield sufficient information for us to know why OSA is occurring and what interventions might be helpful for an individual patient. Currently, our use of the polysomnogram to derive only an apnea hypopnea index does not take full advantage of the available data. An apnea hypopnea index can be readily obtained from home sleep testing and does not truly provide much insight into why a given individual has OSA, what symptoms are attributable to OSA, and what interventions might be considered for the afflicted individual. By analogy, if the only useful data derived from an ECG were a heart rate, the test would rapidly become obsolete. Along these lines, if the only role for the sleep clinician was to prescribe CPAP to everyone with an AHI greater than 5/h, there would be little need or interest in specialized training. In contrast, we suggest that rich insights regarding pathophysiology and mechanisms should be gathered and may influence clinical management of patients afflicted with OSA. Thus, we encourage more thorough analyses of available data to maximize information gleaned and, ultimately, to optimize clinical outcomes.
Recent studies suggest that sleep apnea occurs for varying reasons, a concept that is now thought to be clinically important (Jordan et al. Lancet. 2014;383[9918]:736). We draw a crucial distinction between endotypes (mechanisms underlying disease) and phenotypes (clinical expression of disease). Important endotypes include compromised upper airway anatomy, dysfunction in pharyngeal dilator muscles, unstable ventilatory control (high loop gain), and low arousal threshold (wake up easily), among others. Important phenotypes of sleep apnea are emerging and still evolving to include minimally symptomatic OSA, OSA with daytime sleepiness, and OSA with major cardiometabolic risk, among others. Several important concepts have emerged regarding different OSA endotypes and phenotypes:
1 The mechanism underlying OSA may predict potential response to therapeutic interventions. For instance, the endotype of OSA with unstable ventilatory control (high loop gain) may respond to agents such as oxygen and acetazolamide, which serve to stabilize control of breathing. In patients with anatomical compromise at the level of the velopharynx, uvulopalatopharyngoplasty may be an effective intervention. For patients with multiple pathophysiologic abnormalities, combination therapy may be required to alleviate OSA (Edwards et al. Sleep. 2016;9[11]:1973).
2 Given that OSA has many underlying etiologies, efforts are underway to determine whether individuals with different risk factors for OSA develop their disease based on varying mechanisms. As an example, people with posttraumatic stress disorder (PTSD) may be at increased risk of OSA perhaps on the basis of a low threshold for arousal (Orr et al. JCSM. 2017, 13[1]: 57-63). Another example would be patients with neuromuscular disease who may be at risk of OSA primarily based on impaired pharyngeal dilator muscle function.
3 A new concept is emerging whereby endotypes of OSA may actually predict differing OSA phenotypes. In theory, loop gain-driven OSA may have different consequences from OSA driven by compromise of pharyngeal anatomy. To this point, data suggest that OSA in the elderly may not have as many consequences as OSA in younger people matched on severity of illness. OSA in the elderly has lower loop gain than OSA in younger people and is associated with less negative intrathoracic pressure at the time of arousal as compared with younger individuals with OSA (Kobayashi et al. Chest. 2010; 137[6]:1310). As such, the endotype of OSA in the elderly may explain why the clinical consequences are fewer than in the younger OSA counterparts.
4 The mechanism underlying OSA may be important in determining response to clinical interventions, such as nasal CPAP. Patients with a low arousal threshold may be prone to insomnia when placed on CPAP and could theoretically be poorly tolerant of therapy based on disrupted sleep architecture. Such patients may benefit from non-myorelaxant hypnotic therapy to consolidate sleep and improve CPAP adherence. In addition, patients with high loop gain (unstable ventilatory control) may be prone to develop central apneas when placed on CPAP therapy (Stanchina et al. Ann Am Thorac Soc. 2015;12[9]:1351). These patients may benefit from newer technologies, eg, auto or adaptive servo ventilation - ASV. High loop gain has also been shown to predict failure of upper airway surgery as a treatment for OSA by several groups (Li et al. JCSM. 2017;13[9]:1029). Such patients should, perhaps, undergo nonsurgical therapies for OSA.
We emphasize that some of the points being made are somewhat speculative and, thus, encourage further basic and clinical research to test our assumptions. Robust, multicenter clinical trials assessing hard outcomes will ultimately be required to change the current standard of care. Nonetheless, we believe that a more thorough understanding of OSA pathogenesis can help guide clinical care today and will be critical to the optimal treatment of afflicted individuals tomorrow.
Dr. Owens is Assistant Clinical Professor of Medicine; Dr. Deacon is a Post-Doctoral Research Scholar; and Dr. Malhotra is Kenneth M. Moser Professor of Medicine and Chief, Division of Pulmonary, Critical Care and Sleep Medicine, University of California San Diego.
Women, Apply for Leadership Training Grant
Through the Leadership Development and Diversity Committee, the SVS continues its strong commitment to leadership development in women. The Women's Leadership Training Grant seeks to identify female surgeons who want to sharpen their leadership skills. A $5,000 award will defray costs for travel, hotel accommodations and registration expenses to attend relevant courses and/or other leadership training opportunities and activities. Application deadline is March 14.
Through the Leadership Development and Diversity Committee, the SVS continues its strong commitment to leadership development in women. The Women's Leadership Training Grant seeks to identify female surgeons who want to sharpen their leadership skills. A $5,000 award will defray costs for travel, hotel accommodations and registration expenses to attend relevant courses and/or other leadership training opportunities and activities. Application deadline is March 14.
Through the Leadership Development and Diversity Committee, the SVS continues its strong commitment to leadership development in women. The Women's Leadership Training Grant seeks to identify female surgeons who want to sharpen their leadership skills. A $5,000 award will defray costs for travel, hotel accommodations and registration expenses to attend relevant courses and/or other leadership training opportunities and activities. Application deadline is March 14.
Apply for Disaster Relief Funds by March 16
The SVS Foundation will accept applications through March 16 for funds from its Disaster Relief Fund. The fund can be used for recovery efforts in areas that have experienced catastrophes.
Monies support programs, initiated by SVS members, that provide short-term emergency assistance and longer-term aid for vascular surgery practices and vascular patients in disaster-devastated communities.
The SVS Foundation will accept applications through March 16 for funds from its Disaster Relief Fund. The fund can be used for recovery efforts in areas that have experienced catastrophes.
Monies support programs, initiated by SVS members, that provide short-term emergency assistance and longer-term aid for vascular surgery practices and vascular patients in disaster-devastated communities.
The SVS Foundation will accept applications through March 16 for funds from its Disaster Relief Fund. The fund can be used for recovery efforts in areas that have experienced catastrophes.
Monies support programs, initiated by SVS members, that provide short-term emergency assistance and longer-term aid for vascular surgery practices and vascular patients in disaster-devastated communities.
VAM Registration Opens This Week
It's nearly here! The 2018 Vascular Annual Meeting takes a big step forward this week with the opening of housing and registration. Prepare to sign up for VAM, June 20 to 23 in Boston.
Following a full day of postgraduate courses, VESS abstracts, workshops and international programming, abstract-based scientific sessions will open June 21 and continue to June 23. The Exhibit Hall will be open June 21 to 22.
Catch the highlights of this year's annual meeting here.
It's nearly here! The 2018 Vascular Annual Meeting takes a big step forward this week with the opening of housing and registration. Prepare to sign up for VAM, June 20 to 23 in Boston.
Following a full day of postgraduate courses, VESS abstracts, workshops and international programming, abstract-based scientific sessions will open June 21 and continue to June 23. The Exhibit Hall will be open June 21 to 22.
Catch the highlights of this year's annual meeting here.
It's nearly here! The 2018 Vascular Annual Meeting takes a big step forward this week with the opening of housing and registration. Prepare to sign up for VAM, June 20 to 23 in Boston.
Following a full day of postgraduate courses, VESS abstracts, workshops and international programming, abstract-based scientific sessions will open June 21 and continue to June 23. The Exhibit Hall will be open June 21 to 22.
Catch the highlights of this year's annual meeting here.
Know the danger signs of CVI and VTE in pregnant patients
A new review of the literature on chronic venous insufficiency in pregnant women reveals considerable guidance for their treatment. CVI occurs in up to 80% of pregnant women, while around 7 of every 1,000 pregnant mothers face venous thromboembolism and pulmonary embolism.
As reported in the March edition of the Journal of Vascular Surgery: Venous and Lymphatic Disorders, clinicians from Johns Hopkins Hospital and the Greater Baltimore Medical Center led by vascular surgeon Dr. Jennifer Heller, analyzed 80 studies related to pregnancy, VTE and CVI.
Pregnancy causes significant hemodynamic changes within the circulatory system. While these are considered essential for the health of the developing fetus, the changes place considerable stress on the expectant mother’s heart and lower extremity veins.
Chronic venous insufficiency (CVI), marked by varicose veins, pain, edema, itching, skin discoloration, night cramps and heaviness are all common, particularly during the third trimester. Venous thromboembolism (VTE) and pulmonary embolism (PE) affects pregnant women nearly five times more than non-pregnant women. In fact, VTE is the number one cause of maternal death in developing countries.
With regards to the hemodynamic and physiologic changes, the review reveals pregnancy:
- Decreases systemic vascular resistance
- Increases heart rate
- Increases cardiac output
- Decreases deep venous blood flow
- Increases deep vein diameters, and
- Induces a hypercoagulable state
Treatment strategies for primary CVI in pregnancy, which occurs in up to 80% of women, were reviewed and include indications for non-pharmacologic therapies (compression, reflexology, water emersion), and pharmacologic treatments (non-steroidal anti-inflammatory drugs, fondaparinux, and low-molecular-weight heparin).
With an incidence up to 7 per 1,000 pregnancies, acute VTE remains an important issue in pregnancy. The authors provided a thorough review of VTE prevention during pregnancy, and VTE treatment during pregnancy (including indications for caval filters and management of iliofemoral thrombosis).
“It is important for physicians to comprehend the full extent of the hemodynamic factors that contribute to the increased risk of lower extremity venous disease as well as the most appropriate and effective evidence-based management options,” stated Dr. Heller. “While prophylaxis and treatment of VTE has been extensively studied in pregnancy, further research is required to look at the potential effectiveness and long-term safety profiles of new oral anticoagulants in the mother and fetus.”
She also hopes that future randomized trials will evaluate treatment strategies to relieve symptoms associated with chronic venous insufficiency during pregnancy.
Complete understanding of these issues helps physicians prepare their patients for these eventualities during pregnancy and treat venous complications effectively.
To download the complete article, open access through April 30, click here.
A new review of the literature on chronic venous insufficiency in pregnant women reveals considerable guidance for their treatment. CVI occurs in up to 80% of pregnant women, while around 7 of every 1,000 pregnant mothers face venous thromboembolism and pulmonary embolism.
As reported in the March edition of the Journal of Vascular Surgery: Venous and Lymphatic Disorders, clinicians from Johns Hopkins Hospital and the Greater Baltimore Medical Center led by vascular surgeon Dr. Jennifer Heller, analyzed 80 studies related to pregnancy, VTE and CVI.
Pregnancy causes significant hemodynamic changes within the circulatory system. While these are considered essential for the health of the developing fetus, the changes place considerable stress on the expectant mother’s heart and lower extremity veins.
Chronic venous insufficiency (CVI), marked by varicose veins, pain, edema, itching, skin discoloration, night cramps and heaviness are all common, particularly during the third trimester. Venous thromboembolism (VTE) and pulmonary embolism (PE) affects pregnant women nearly five times more than non-pregnant women. In fact, VTE is the number one cause of maternal death in developing countries.
With regards to the hemodynamic and physiologic changes, the review reveals pregnancy:
- Decreases systemic vascular resistance
- Increases heart rate
- Increases cardiac output
- Decreases deep venous blood flow
- Increases deep vein diameters, and
- Induces a hypercoagulable state
Treatment strategies for primary CVI in pregnancy, which occurs in up to 80% of women, were reviewed and include indications for non-pharmacologic therapies (compression, reflexology, water emersion), and pharmacologic treatments (non-steroidal anti-inflammatory drugs, fondaparinux, and low-molecular-weight heparin).
With an incidence up to 7 per 1,000 pregnancies, acute VTE remains an important issue in pregnancy. The authors provided a thorough review of VTE prevention during pregnancy, and VTE treatment during pregnancy (including indications for caval filters and management of iliofemoral thrombosis).
“It is important for physicians to comprehend the full extent of the hemodynamic factors that contribute to the increased risk of lower extremity venous disease as well as the most appropriate and effective evidence-based management options,” stated Dr. Heller. “While prophylaxis and treatment of VTE has been extensively studied in pregnancy, further research is required to look at the potential effectiveness and long-term safety profiles of new oral anticoagulants in the mother and fetus.”
She also hopes that future randomized trials will evaluate treatment strategies to relieve symptoms associated with chronic venous insufficiency during pregnancy.
Complete understanding of these issues helps physicians prepare their patients for these eventualities during pregnancy and treat venous complications effectively.
To download the complete article, open access through April 30, click here.
A new review of the literature on chronic venous insufficiency in pregnant women reveals considerable guidance for their treatment. CVI occurs in up to 80% of pregnant women, while around 7 of every 1,000 pregnant mothers face venous thromboembolism and pulmonary embolism.
As reported in the March edition of the Journal of Vascular Surgery: Venous and Lymphatic Disorders, clinicians from Johns Hopkins Hospital and the Greater Baltimore Medical Center led by vascular surgeon Dr. Jennifer Heller, analyzed 80 studies related to pregnancy, VTE and CVI.
Pregnancy causes significant hemodynamic changes within the circulatory system. While these are considered essential for the health of the developing fetus, the changes place considerable stress on the expectant mother’s heart and lower extremity veins.
Chronic venous insufficiency (CVI), marked by varicose veins, pain, edema, itching, skin discoloration, night cramps and heaviness are all common, particularly during the third trimester. Venous thromboembolism (VTE) and pulmonary embolism (PE) affects pregnant women nearly five times more than non-pregnant women. In fact, VTE is the number one cause of maternal death in developing countries.
With regards to the hemodynamic and physiologic changes, the review reveals pregnancy:
- Decreases systemic vascular resistance
- Increases heart rate
- Increases cardiac output
- Decreases deep venous blood flow
- Increases deep vein diameters, and
- Induces a hypercoagulable state
Treatment strategies for primary CVI in pregnancy, which occurs in up to 80% of women, were reviewed and include indications for non-pharmacologic therapies (compression, reflexology, water emersion), and pharmacologic treatments (non-steroidal anti-inflammatory drugs, fondaparinux, and low-molecular-weight heparin).
With an incidence up to 7 per 1,000 pregnancies, acute VTE remains an important issue in pregnancy. The authors provided a thorough review of VTE prevention during pregnancy, and VTE treatment during pregnancy (including indications for caval filters and management of iliofemoral thrombosis).
“It is important for physicians to comprehend the full extent of the hemodynamic factors that contribute to the increased risk of lower extremity venous disease as well as the most appropriate and effective evidence-based management options,” stated Dr. Heller. “While prophylaxis and treatment of VTE has been extensively studied in pregnancy, further research is required to look at the potential effectiveness and long-term safety profiles of new oral anticoagulants in the mother and fetus.”
She also hopes that future randomized trials will evaluate treatment strategies to relieve symptoms associated with chronic venous insufficiency during pregnancy.
Complete understanding of these issues helps physicians prepare their patients for these eventualities during pregnancy and treat venous complications effectively.
To download the complete article, open access through April 30, click here.
RAS Inhibitors Show Promise for CLTI Patients After Interventions
Physicians should consider prescribing high-dose angiotensin inhibitors for patients with chronic limb-threatening ischemia (CLTI), a recent study from Harvard University suggests.
The report was published in the March edition of the Journal of Vascular Surgery by researchers from the Division of Vascular and Endovascular Surgery from the Beth Israel Deaconess Medical Center led by vascular surgeon Dr. Marc Schermerhorn.
The team conducted a retrospective review of 1,161 patients between 2005 and 2014 and evaluated the effect of renin-angiotensin system (RAS) inhibition on mortality in patients undergoing revascularization (both endovascular and surgical bypass) for CLTI.
In this population, RAS inhibition resulted in:
• Reduced mortality (67% versus 54% survival at three years)
• Lower 30-day myocardial infarction (1.6% versus 4.3%)
• No difference in major adverse limb events, amputation, or reinterventions
“These benefits were restricted to those prescribed high-dose RAS inhibition, and not realized in those on lower doses,” noted first author Dr. Thomas Bodewes. As such, the authors recommend that, “physicians should strive to maintain patients on high-dose RAS inhibition, provided that such doses are tolerated in terms of blood pressure.”
Patients with CLTI are heavily burdened with atherosclerosis, which affects nearly all important vascular beds, including the cerebral, coronary, peripheral, renal and mesenteric circulatory systems.
A growing body of evidence suggests that renin-angiotensin system (RAS) inhibition has multiple cardiovascular benefits including:
• Blood pressure control
• Decrease in preload and afterload
• Stabilization of plaque
• Inhibition of smooth muscle proliferation
• Improved vascular endothelial function
• Reduced ventricular hypertrophy
• Enhanced fibrinolysis
Despite this evidence, questions remain. The authors note that this was a retrospective single institution review and despite adjustment for multiple variables, the association between RAS inhibitor use and long-term outcomes may be confounded by other factors including some that were unmeasured.
There are relatively modest number of non-white patients, and actual use of the medications beyond hospital discharge among the study patients is unknown. There are potential side effects to the use of RAS inhibitors that providers must consider in the dosing of these medications. Larger confirmatory studies are needed to confirm these findings and strengthen the evidence.
ClIck here to read the full-article, which is free to non-subscribers until April 30.
Physicians should consider prescribing high-dose angiotensin inhibitors for patients with chronic limb-threatening ischemia (CLTI), a recent study from Harvard University suggests.
The report was published in the March edition of the Journal of Vascular Surgery by researchers from the Division of Vascular and Endovascular Surgery from the Beth Israel Deaconess Medical Center led by vascular surgeon Dr. Marc Schermerhorn.
The team conducted a retrospective review of 1,161 patients between 2005 and 2014 and evaluated the effect of renin-angiotensin system (RAS) inhibition on mortality in patients undergoing revascularization (both endovascular and surgical bypass) for CLTI.
In this population, RAS inhibition resulted in:
• Reduced mortality (67% versus 54% survival at three years)
• Lower 30-day myocardial infarction (1.6% versus 4.3%)
• No difference in major adverse limb events, amputation, or reinterventions
“These benefits were restricted to those prescribed high-dose RAS inhibition, and not realized in those on lower doses,” noted first author Dr. Thomas Bodewes. As such, the authors recommend that, “physicians should strive to maintain patients on high-dose RAS inhibition, provided that such doses are tolerated in terms of blood pressure.”
Patients with CLTI are heavily burdened with atherosclerosis, which affects nearly all important vascular beds, including the cerebral, coronary, peripheral, renal and mesenteric circulatory systems.
A growing body of evidence suggests that renin-angiotensin system (RAS) inhibition has multiple cardiovascular benefits including:
• Blood pressure control
• Decrease in preload and afterload
• Stabilization of plaque
• Inhibition of smooth muscle proliferation
• Improved vascular endothelial function
• Reduced ventricular hypertrophy
• Enhanced fibrinolysis
Despite this evidence, questions remain. The authors note that this was a retrospective single institution review and despite adjustment for multiple variables, the association between RAS inhibitor use and long-term outcomes may be confounded by other factors including some that were unmeasured.
There are relatively modest number of non-white patients, and actual use of the medications beyond hospital discharge among the study patients is unknown. There are potential side effects to the use of RAS inhibitors that providers must consider in the dosing of these medications. Larger confirmatory studies are needed to confirm these findings and strengthen the evidence.
ClIck here to read the full-article, which is free to non-subscribers until April 30.
Physicians should consider prescribing high-dose angiotensin inhibitors for patients with chronic limb-threatening ischemia (CLTI), a recent study from Harvard University suggests.
The report was published in the March edition of the Journal of Vascular Surgery by researchers from the Division of Vascular and Endovascular Surgery from the Beth Israel Deaconess Medical Center led by vascular surgeon Dr. Marc Schermerhorn.
The team conducted a retrospective review of 1,161 patients between 2005 and 2014 and evaluated the effect of renin-angiotensin system (RAS) inhibition on mortality in patients undergoing revascularization (both endovascular and surgical bypass) for CLTI.
In this population, RAS inhibition resulted in:
• Reduced mortality (67% versus 54% survival at three years)
• Lower 30-day myocardial infarction (1.6% versus 4.3%)
• No difference in major adverse limb events, amputation, or reinterventions
“These benefits were restricted to those prescribed high-dose RAS inhibition, and not realized in those on lower doses,” noted first author Dr. Thomas Bodewes. As such, the authors recommend that, “physicians should strive to maintain patients on high-dose RAS inhibition, provided that such doses are tolerated in terms of blood pressure.”
Patients with CLTI are heavily burdened with atherosclerosis, which affects nearly all important vascular beds, including the cerebral, coronary, peripheral, renal and mesenteric circulatory systems.
A growing body of evidence suggests that renin-angiotensin system (RAS) inhibition has multiple cardiovascular benefits including:
• Blood pressure control
• Decrease in preload and afterload
• Stabilization of plaque
• Inhibition of smooth muscle proliferation
• Improved vascular endothelial function
• Reduced ventricular hypertrophy
• Enhanced fibrinolysis
Despite this evidence, questions remain. The authors note that this was a retrospective single institution review and despite adjustment for multiple variables, the association between RAS inhibitor use and long-term outcomes may be confounded by other factors including some that were unmeasured.
There are relatively modest number of non-white patients, and actual use of the medications beyond hospital discharge among the study patients is unknown. There are potential side effects to the use of RAS inhibitors that providers must consider in the dosing of these medications. Larger confirmatory studies are needed to confirm these findings and strengthen the evidence.
ClIck here to read the full-article, which is free to non-subscribers until April 30.
Legacy Society members sustain research
AGA Legacy Society members share a desire to guarantee long-term support for digestive disease research. Through their foresight and generosity, they help ensure the continued momentum of discovery and patient education that has characterized GI medicine in recent decades. Legacy Society member donations directly support young GI investigators as they establish independent research careers.
Legacy Society members are the most generous individual donors to the AGA Research Foundation. Members of the AGA Legacy Society provide tax-deductible gifts to the AGA Research Foundation of $5,000 or more per year for 5 years ($25,000 total) or $50,000 or more in a planned gift, such as a bequest. All Legacy Society contributions go directly to support research awards.
AGA members support young researchers at a critical decision point in their lives – when many consider giving up their research careers due to a lack of funding. “I am honored to be a recipient of the Research Scholar Award. I would like to thank the foundation for their generous contribution that will fund a crucial transition in my career,” said Jose Saenz, MD, PhD, Washington University School of Medicine and 2017 AGA – Gastric Cancer Foundation Research Scholar Award recipient.
The AGA Research Foundation’s mission is to raise funds to support young researchers in gastroenterology and hepatology. Gifts to the foundation support researchers working towards developing new treatments and diagnostics for patients with GI conditions.
“I am extremely grateful to be selected for this award. I would like to thank the foundation donors for their generous support. This award will me build a research program to better understand mechanisms that promote growth of cholangiocarcinoma,” remarks Silvia Affe, PhD, Columbia University, 2017 AGA Research Scholar recipient.
Donors who make gifts at the Legacy Society level before DDW will receive an invitation to the annual Benefactors’ Dinner at the Folger Shakespeare Library in Washington, DC. Individuals interested in learning more about Legacy Society membership may contact Stacey Hinton Tuneski, Senior Director of Development at [email protected] or via phone (301) 222-4005. More information on the AGA Legacy Society including the current roster and acceptance form is available on the foundation’s website at www.gastro.org/legacysociety.
The makings of a grand celebration
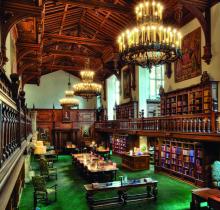
Beginning with a memorable gathering at the United States Library of Congress in 2007, the AGA Benefactors’ Dinner has welcomed members of the AGA Legacy Society and other AGA dignitaries to special locations nationwide. The Folger Shakespeare Library will be the location of the 2018 AGA Research Foundation Benefactors Dinner during DDW in Washington, DC. Just steps from the Capitol, the Great Hall and Pastor Reading room are a spectacular setting for an enjoyable evening with friends. Members of the AGA Legacy Society will be among the distinguished honorees at the annual event.
AGA Legacy Society members share a desire to guarantee long-term support for digestive disease research. Through their foresight and generosity, they help ensure the continued momentum of discovery and patient education that has characterized GI medicine in recent decades. Legacy Society member donations directly support young GI investigators as they establish independent research careers.
Legacy Society members are the most generous individual donors to the AGA Research Foundation. Members of the AGA Legacy Society provide tax-deductible gifts to the AGA Research Foundation of $5,000 or more per year for 5 years ($25,000 total) or $50,000 or more in a planned gift, such as a bequest. All Legacy Society contributions go directly to support research awards.
AGA members support young researchers at a critical decision point in their lives – when many consider giving up their research careers due to a lack of funding. “I am honored to be a recipient of the Research Scholar Award. I would like to thank the foundation for their generous contribution that will fund a crucial transition in my career,” said Jose Saenz, MD, PhD, Washington University School of Medicine and 2017 AGA – Gastric Cancer Foundation Research Scholar Award recipient.
The AGA Research Foundation’s mission is to raise funds to support young researchers in gastroenterology and hepatology. Gifts to the foundation support researchers working towards developing new treatments and diagnostics for patients with GI conditions.
“I am extremely grateful to be selected for this award. I would like to thank the foundation donors for their generous support. This award will me build a research program to better understand mechanisms that promote growth of cholangiocarcinoma,” remarks Silvia Affe, PhD, Columbia University, 2017 AGA Research Scholar recipient.
Donors who make gifts at the Legacy Society level before DDW will receive an invitation to the annual Benefactors’ Dinner at the Folger Shakespeare Library in Washington, DC. Individuals interested in learning more about Legacy Society membership may contact Stacey Hinton Tuneski, Senior Director of Development at [email protected] or via phone (301) 222-4005. More information on the AGA Legacy Society including the current roster and acceptance form is available on the foundation’s website at www.gastro.org/legacysociety.
The makings of a grand celebration
Beginning with a memorable gathering at the United States Library of Congress in 2007, the AGA Benefactors’ Dinner has welcomed members of the AGA Legacy Society and other AGA dignitaries to special locations nationwide. The Folger Shakespeare Library will be the location of the 2018 AGA Research Foundation Benefactors Dinner during DDW in Washington, DC. Just steps from the Capitol, the Great Hall and Pastor Reading room are a spectacular setting for an enjoyable evening with friends. Members of the AGA Legacy Society will be among the distinguished honorees at the annual event.
AGA Legacy Society members share a desire to guarantee long-term support for digestive disease research. Through their foresight and generosity, they help ensure the continued momentum of discovery and patient education that has characterized GI medicine in recent decades. Legacy Society member donations directly support young GI investigators as they establish independent research careers.
Legacy Society members are the most generous individual donors to the AGA Research Foundation. Members of the AGA Legacy Society provide tax-deductible gifts to the AGA Research Foundation of $5,000 or more per year for 5 years ($25,000 total) or $50,000 or more in a planned gift, such as a bequest. All Legacy Society contributions go directly to support research awards.
AGA members support young researchers at a critical decision point in their lives – when many consider giving up their research careers due to a lack of funding. “I am honored to be a recipient of the Research Scholar Award. I would like to thank the foundation for their generous contribution that will fund a crucial transition in my career,” said Jose Saenz, MD, PhD, Washington University School of Medicine and 2017 AGA – Gastric Cancer Foundation Research Scholar Award recipient.
The AGA Research Foundation’s mission is to raise funds to support young researchers in gastroenterology and hepatology. Gifts to the foundation support researchers working towards developing new treatments and diagnostics for patients with GI conditions.
“I am extremely grateful to be selected for this award. I would like to thank the foundation donors for their generous support. This award will me build a research program to better understand mechanisms that promote growth of cholangiocarcinoma,” remarks Silvia Affe, PhD, Columbia University, 2017 AGA Research Scholar recipient.
Donors who make gifts at the Legacy Society level before DDW will receive an invitation to the annual Benefactors’ Dinner at the Folger Shakespeare Library in Washington, DC. Individuals interested in learning more about Legacy Society membership may contact Stacey Hinton Tuneski, Senior Director of Development at [email protected] or via phone (301) 222-4005. More information on the AGA Legacy Society including the current roster and acceptance form is available on the foundation’s website at www.gastro.org/legacysociety.
The makings of a grand celebration
Beginning with a memorable gathering at the United States Library of Congress in 2007, the AGA Benefactors’ Dinner has welcomed members of the AGA Legacy Society and other AGA dignitaries to special locations nationwide. The Folger Shakespeare Library will be the location of the 2018 AGA Research Foundation Benefactors Dinner during DDW in Washington, DC. Just steps from the Capitol, the Great Hall and Pastor Reading room are a spectacular setting for an enjoyable evening with friends. Members of the AGA Legacy Society will be among the distinguished honorees at the annual event.