User login
Get Ready for CHEST 2018 in San Antonio
Have you been thinking about how great of a time you had at CHEST 2017? Or, perhaps you weren’t able to make it to CHEST 2017 and are looking forward to attending CHEST 2018? Well, we’d be happy to have you attend the annual meeting in sunny San Antonio, Texas, this fall. CHEST 2018 will occur earlier this year, from October 6-10, and we’ve got a few ways you can get involved leading up to the meeting.
CHEST 2018 Moderators
If you do not have original research to share, but believe you are qualified to moderate sessions, we have an opportunity for you! Moderating will take place on-site in San Antonio, and moderators will be recognized in the CHEST 2018 program and will receive a reduced registration rate to the meeting. See chestmeeting.chestnet.org.
CHEST Challenge 2018
Are you a US-based CHEST fellow-in-training? Compete with other programs across the country in CHEST Challenge 2018 for honor and prizes! The first round of the competition this year will consist of two parts; in addition to the traditional online quiz, there will be a number of social media challenges. The aggregate score for both of these components will be used to identify the top three-scoring teams. These top three teams will then be invited to send three fellows each to the CHEST Challenge Championship, a Jeopardy-style game show that takes place live during the CHEST Annual Meeting. http://www.chestnet.org/Hidden-Pages/CHEST-Challenge-US
CHEST Foundation Grants
We have had many talented and passionate people win our CHEST Foundation grants in research and community service. Each year, the CHEST Foundation offers grants to worthy research candidates, generous community service volunteers, and distinguished scholars in a field of expertise. Nearly 800 recipients worldwide have received more than $10 million in support and recognition of outstanding contributions to chest medicine.
How are you helping to champion lung health? The CHEST Foundation is accepting grant applications February 1 through April 9, 2018, in the following areas:
• CHEST Foundation Research Grant in Lung Cancer – $50,000 - $100,000 2-year grant*
• CHEST Foundation Research Grant in Asthma – $15,000 - $30,000 1-year grant*
• CHEST Foundation Research Grant in Pulmonary Arterial Hypertension – $25,000 - $50,000 1-year grant*
• CHEST Foundation and the Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency – $25,000 - $50,000 1-year grant*
• CHEST Foundation Research Grant in Pulmonary Fibrosis – $25,000 - $50,000 1-year grant*
• CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease – $30,000 1-year grant (multiple recipients selected)
• CHEST Foundation Research Grant in Venous Thromboembolism – $15,000 - $30,000 1-year grant*
• CHEST Foundation Research Grant in Nontuberculous Mycobacteria Disease – $25,000 - $50,000 1-year grant*
• CHEST Foundation Research Grant in Women’s Lung Health – $10,000 1-year grant
• CHEST Foundation Research Grant in Cystic Fibrosis – $30,000 1-year grant
• The Eli Lilly and Company Distinguished Scholar in Critical Care Medicine – $150,000 over 3 years
• CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP – $2,500- $15,000 1-year grant*
*Amount contingent on funding.
Learn more on how to apply now at chestfoundation.org/apply.
Things Happening in AprilDon’t forget to look out for CHEST 2018 registration, opening April 5. And, if you missed the first round of abstract submissions, submissions for late-breaking abstracts will open April 30. Stay updated on all things CHEST 2018 at chestmeeting.chestnet.org.
Have you been thinking about how great of a time you had at CHEST 2017? Or, perhaps you weren’t able to make it to CHEST 2017 and are looking forward to attending CHEST 2018? Well, we’d be happy to have you attend the annual meeting in sunny San Antonio, Texas, this fall. CHEST 2018 will occur earlier this year, from October 6-10, and we’ve got a few ways you can get involved leading up to the meeting.
CHEST 2018 Moderators
If you do not have original research to share, but believe you are qualified to moderate sessions, we have an opportunity for you! Moderating will take place on-site in San Antonio, and moderators will be recognized in the CHEST 2018 program and will receive a reduced registration rate to the meeting. See chestmeeting.chestnet.org.
CHEST Challenge 2018
Are you a US-based CHEST fellow-in-training? Compete with other programs across the country in CHEST Challenge 2018 for honor and prizes! The first round of the competition this year will consist of two parts; in addition to the traditional online quiz, there will be a number of social media challenges. The aggregate score for both of these components will be used to identify the top three-scoring teams. These top three teams will then be invited to send three fellows each to the CHEST Challenge Championship, a Jeopardy-style game show that takes place live during the CHEST Annual Meeting. http://www.chestnet.org/Hidden-Pages/CHEST-Challenge-US
CHEST Foundation Grants
We have had many talented and passionate people win our CHEST Foundation grants in research and community service. Each year, the CHEST Foundation offers grants to worthy research candidates, generous community service volunteers, and distinguished scholars in a field of expertise. Nearly 800 recipients worldwide have received more than $10 million in support and recognition of outstanding contributions to chest medicine.
How are you helping to champion lung health? The CHEST Foundation is accepting grant applications February 1 through April 9, 2018, in the following areas:
• CHEST Foundation Research Grant in Lung Cancer – $50,000 - $100,000 2-year grant*
• CHEST Foundation Research Grant in Asthma – $15,000 - $30,000 1-year grant*
• CHEST Foundation Research Grant in Pulmonary Arterial Hypertension – $25,000 - $50,000 1-year grant*
• CHEST Foundation and the Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency – $25,000 - $50,000 1-year grant*
• CHEST Foundation Research Grant in Pulmonary Fibrosis – $25,000 - $50,000 1-year grant*
• CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease – $30,000 1-year grant (multiple recipients selected)
• CHEST Foundation Research Grant in Venous Thromboembolism – $15,000 - $30,000 1-year grant*
• CHEST Foundation Research Grant in Nontuberculous Mycobacteria Disease – $25,000 - $50,000 1-year grant*
• CHEST Foundation Research Grant in Women’s Lung Health – $10,000 1-year grant
• CHEST Foundation Research Grant in Cystic Fibrosis – $30,000 1-year grant
• The Eli Lilly and Company Distinguished Scholar in Critical Care Medicine – $150,000 over 3 years
• CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP – $2,500- $15,000 1-year grant*
*Amount contingent on funding.
Learn more on how to apply now at chestfoundation.org/apply.
Things Happening in AprilDon’t forget to look out for CHEST 2018 registration, opening April 5. And, if you missed the first round of abstract submissions, submissions for late-breaking abstracts will open April 30. Stay updated on all things CHEST 2018 at chestmeeting.chestnet.org.
Have you been thinking about how great of a time you had at CHEST 2017? Or, perhaps you weren’t able to make it to CHEST 2017 and are looking forward to attending CHEST 2018? Well, we’d be happy to have you attend the annual meeting in sunny San Antonio, Texas, this fall. CHEST 2018 will occur earlier this year, from October 6-10, and we’ve got a few ways you can get involved leading up to the meeting.
CHEST 2018 Moderators
If you do not have original research to share, but believe you are qualified to moderate sessions, we have an opportunity for you! Moderating will take place on-site in San Antonio, and moderators will be recognized in the CHEST 2018 program and will receive a reduced registration rate to the meeting. See chestmeeting.chestnet.org.
CHEST Challenge 2018
Are you a US-based CHEST fellow-in-training? Compete with other programs across the country in CHEST Challenge 2018 for honor and prizes! The first round of the competition this year will consist of two parts; in addition to the traditional online quiz, there will be a number of social media challenges. The aggregate score for both of these components will be used to identify the top three-scoring teams. These top three teams will then be invited to send three fellows each to the CHEST Challenge Championship, a Jeopardy-style game show that takes place live during the CHEST Annual Meeting. http://www.chestnet.org/Hidden-Pages/CHEST-Challenge-US
CHEST Foundation Grants
We have had many talented and passionate people win our CHEST Foundation grants in research and community service. Each year, the CHEST Foundation offers grants to worthy research candidates, generous community service volunteers, and distinguished scholars in a field of expertise. Nearly 800 recipients worldwide have received more than $10 million in support and recognition of outstanding contributions to chest medicine.
How are you helping to champion lung health? The CHEST Foundation is accepting grant applications February 1 through April 9, 2018, in the following areas:
• CHEST Foundation Research Grant in Lung Cancer – $50,000 - $100,000 2-year grant*
• CHEST Foundation Research Grant in Asthma – $15,000 - $30,000 1-year grant*
• CHEST Foundation Research Grant in Pulmonary Arterial Hypertension – $25,000 - $50,000 1-year grant*
• CHEST Foundation and the Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency – $25,000 - $50,000 1-year grant*
• CHEST Foundation Research Grant in Pulmonary Fibrosis – $25,000 - $50,000 1-year grant*
• CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease – $30,000 1-year grant (multiple recipients selected)
• CHEST Foundation Research Grant in Venous Thromboembolism – $15,000 - $30,000 1-year grant*
• CHEST Foundation Research Grant in Nontuberculous Mycobacteria Disease – $25,000 - $50,000 1-year grant*
• CHEST Foundation Research Grant in Women’s Lung Health – $10,000 1-year grant
• CHEST Foundation Research Grant in Cystic Fibrosis – $30,000 1-year grant
• The Eli Lilly and Company Distinguished Scholar in Critical Care Medicine – $150,000 over 3 years
• CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP – $2,500- $15,000 1-year grant*
*Amount contingent on funding.
Learn more on how to apply now at chestfoundation.org/apply.
Things Happening in AprilDon’t forget to look out for CHEST 2018 registration, opening April 5. And, if you missed the first round of abstract submissions, submissions for late-breaking abstracts will open April 30. Stay updated on all things CHEST 2018 at chestmeeting.chestnet.org.
NAMDRC Update Collaboration: Now More Than Ever
Ongoing hospital mergers, acquisitions, and closings demonstrate that reimbursement maximization and cost reduction are the twin sisters of health-care system reform. This focus is not going to change in the foreseeable future, as most experts now view “health system reform” as “health financing reform.”
Reports document that more than 50% of acute care hospitals in the United States experienced negative operating margins for the federal fiscal year ending September 30, 2017. Equally alarming is the increasing number of organizations either reducing or eliminating the roles of medical directors for clinical departments. Hospital and health system executives are increasingly engaging external consultants to find ways to decrease operating costs, with the caveat of maintaining or improving quality, safety, and patient satisfaction and engagement.
Given these cost reduction pressures, what can respiratory therapy medical directors and administrative directors do to ensure that quality and safety are ensured?
We believe that quality and safety can be maintained and improved in this bottom-line-focused environment if we collaborate with stakeholders and communicate the value of respiratory care services. Following are some examples of how to reinvigorate this collaboration. The list is far from complete, but we believe it is a good starting point for making a significant difference.
Science
We recognize that much of our practice is based on levels of evidence, and we must use this evidence as a basis for our services.
In talking and working with RT administrative directors across the country, we continue to see non-value-added “treatments” being provided, such as incentive spirometry and aerosolized acetylcysteine. Not only is this a waste of resources, but, because of it, our clinical RTs are not providing therapy.
One of the best opportunities to decrease cost is to eliminate waste. These services must be eliminated. For those patients who require secretion clearance/lung expansion, we can provide evidence-based services such as oscillating positive expiratory pressure.
Protocols
Respiratory care protocols have been around for decades, but surveys indicate that only half of all RT departments utilize them. Under the guidance of NAMDRC, the AARC has been educating RTs to transition from “treatments” to evidence-based protocols. Various barriers remain, and our challenge remains to implement proven care plans in every department.
Quality Assurance
The health-care industry made the transition from “Quality Control” to “Quality Assurance” several decades ago. However, many RT administrative directors lack the knowledge and/or resources necessary to create a comprehensive QA program, much less participate in clinical research. We suggest creating a standardized model to be adopted by RT departments across the country that would measure and communicate the value of respiratory care services.
Productivity/Staffing
An area where consultants and executives often focus their cost-saving efforts is staffing. Given that 50% to 60% of operating costs are personnel, this is to be expected.
Many organizations, however, are using the wrong metrics—such as procedures, CPT codes , and billables—to project staffing FTEs. Physicians and RTs understand that these metrics are not useful and must convince consultants and executives of this. The AARC Uniform Reporting Manual, which is currently being updated, is the best guide for determining appropriate staffing.
Education
Another common step in cost control has been the significant reduction or total elimination of education budgets.
During the past 5 years, RT leaders attending the AARC Summer Forum have been polled regarding whether they received financial assistance to attend the Management Section program. Sadly, the number attending on their own dime far surpasses those receiving financial assistance.
Additionally, the RT profession is witnessing more department-based education, which, in some cases, is not education at all, but marketing, cleverly packaged in the form of CEUs.
We fully understand these changes and recognize why they have occurred. However, we suggest the need to work together to differentiate marketing from education and ensure that clinical staff receive what is needed to ensure quality care.
It is vital for us to educate our physician leaders and pulmonary and critical care fellows on the science of respiratory care. There is a significant knowledge gap, and we have a great opportunity to improve the training of fellows. It is difficult to attract active medical directors if they don’t understand the science. We believe NAMDRC can play an important role by addressing these knowledge deficits.
Ongoing hospital mergers, acquisitions, and closings demonstrate that reimbursement maximization and cost reduction are the twin sisters of health-care system reform. This focus is not going to change in the foreseeable future, as most experts now view “health system reform” as “health financing reform.”
Reports document that more than 50% of acute care hospitals in the United States experienced negative operating margins for the federal fiscal year ending September 30, 2017. Equally alarming is the increasing number of organizations either reducing or eliminating the roles of medical directors for clinical departments. Hospital and health system executives are increasingly engaging external consultants to find ways to decrease operating costs, with the caveat of maintaining or improving quality, safety, and patient satisfaction and engagement.
Given these cost reduction pressures, what can respiratory therapy medical directors and administrative directors do to ensure that quality and safety are ensured?
We believe that quality and safety can be maintained and improved in this bottom-line-focused environment if we collaborate with stakeholders and communicate the value of respiratory care services. Following are some examples of how to reinvigorate this collaboration. The list is far from complete, but we believe it is a good starting point for making a significant difference.
Science
We recognize that much of our practice is based on levels of evidence, and we must use this evidence as a basis for our services.
In talking and working with RT administrative directors across the country, we continue to see non-value-added “treatments” being provided, such as incentive spirometry and aerosolized acetylcysteine. Not only is this a waste of resources, but, because of it, our clinical RTs are not providing therapy.
One of the best opportunities to decrease cost is to eliminate waste. These services must be eliminated. For those patients who require secretion clearance/lung expansion, we can provide evidence-based services such as oscillating positive expiratory pressure.
Protocols
Respiratory care protocols have been around for decades, but surveys indicate that only half of all RT departments utilize them. Under the guidance of NAMDRC, the AARC has been educating RTs to transition from “treatments” to evidence-based protocols. Various barriers remain, and our challenge remains to implement proven care plans in every department.
Quality Assurance
The health-care industry made the transition from “Quality Control” to “Quality Assurance” several decades ago. However, many RT administrative directors lack the knowledge and/or resources necessary to create a comprehensive QA program, much less participate in clinical research. We suggest creating a standardized model to be adopted by RT departments across the country that would measure and communicate the value of respiratory care services.
Productivity/Staffing
An area where consultants and executives often focus their cost-saving efforts is staffing. Given that 50% to 60% of operating costs are personnel, this is to be expected.
Many organizations, however, are using the wrong metrics—such as procedures, CPT codes , and billables—to project staffing FTEs. Physicians and RTs understand that these metrics are not useful and must convince consultants and executives of this. The AARC Uniform Reporting Manual, which is currently being updated, is the best guide for determining appropriate staffing.
Education
Another common step in cost control has been the significant reduction or total elimination of education budgets.
During the past 5 years, RT leaders attending the AARC Summer Forum have been polled regarding whether they received financial assistance to attend the Management Section program. Sadly, the number attending on their own dime far surpasses those receiving financial assistance.
Additionally, the RT profession is witnessing more department-based education, which, in some cases, is not education at all, but marketing, cleverly packaged in the form of CEUs.
We fully understand these changes and recognize why they have occurred. However, we suggest the need to work together to differentiate marketing from education and ensure that clinical staff receive what is needed to ensure quality care.
It is vital for us to educate our physician leaders and pulmonary and critical care fellows on the science of respiratory care. There is a significant knowledge gap, and we have a great opportunity to improve the training of fellows. It is difficult to attract active medical directors if they don’t understand the science. We believe NAMDRC can play an important role by addressing these knowledge deficits.
Ongoing hospital mergers, acquisitions, and closings demonstrate that reimbursement maximization and cost reduction are the twin sisters of health-care system reform. This focus is not going to change in the foreseeable future, as most experts now view “health system reform” as “health financing reform.”
Reports document that more than 50% of acute care hospitals in the United States experienced negative operating margins for the federal fiscal year ending September 30, 2017. Equally alarming is the increasing number of organizations either reducing or eliminating the roles of medical directors for clinical departments. Hospital and health system executives are increasingly engaging external consultants to find ways to decrease operating costs, with the caveat of maintaining or improving quality, safety, and patient satisfaction and engagement.
Given these cost reduction pressures, what can respiratory therapy medical directors and administrative directors do to ensure that quality and safety are ensured?
We believe that quality and safety can be maintained and improved in this bottom-line-focused environment if we collaborate with stakeholders and communicate the value of respiratory care services. Following are some examples of how to reinvigorate this collaboration. The list is far from complete, but we believe it is a good starting point for making a significant difference.
Science
We recognize that much of our practice is based on levels of evidence, and we must use this evidence as a basis for our services.
In talking and working with RT administrative directors across the country, we continue to see non-value-added “treatments” being provided, such as incentive spirometry and aerosolized acetylcysteine. Not only is this a waste of resources, but, because of it, our clinical RTs are not providing therapy.
One of the best opportunities to decrease cost is to eliminate waste. These services must be eliminated. For those patients who require secretion clearance/lung expansion, we can provide evidence-based services such as oscillating positive expiratory pressure.
Protocols
Respiratory care protocols have been around for decades, but surveys indicate that only half of all RT departments utilize them. Under the guidance of NAMDRC, the AARC has been educating RTs to transition from “treatments” to evidence-based protocols. Various barriers remain, and our challenge remains to implement proven care plans in every department.
Quality Assurance
The health-care industry made the transition from “Quality Control” to “Quality Assurance” several decades ago. However, many RT administrative directors lack the knowledge and/or resources necessary to create a comprehensive QA program, much less participate in clinical research. We suggest creating a standardized model to be adopted by RT departments across the country that would measure and communicate the value of respiratory care services.
Productivity/Staffing
An area where consultants and executives often focus their cost-saving efforts is staffing. Given that 50% to 60% of operating costs are personnel, this is to be expected.
Many organizations, however, are using the wrong metrics—such as procedures, CPT codes , and billables—to project staffing FTEs. Physicians and RTs understand that these metrics are not useful and must convince consultants and executives of this. The AARC Uniform Reporting Manual, which is currently being updated, is the best guide for determining appropriate staffing.
Education
Another common step in cost control has been the significant reduction or total elimination of education budgets.
During the past 5 years, RT leaders attending the AARC Summer Forum have been polled regarding whether they received financial assistance to attend the Management Section program. Sadly, the number attending on their own dime far surpasses those receiving financial assistance.
Additionally, the RT profession is witnessing more department-based education, which, in some cases, is not education at all, but marketing, cleverly packaged in the form of CEUs.
We fully understand these changes and recognize why they have occurred. However, we suggest the need to work together to differentiate marketing from education and ensure that clinical staff receive what is needed to ensure quality care.
It is vital for us to educate our physician leaders and pulmonary and critical care fellows on the science of respiratory care. There is a significant knowledge gap, and we have a great opportunity to improve the training of fellows. It is difficult to attract active medical directors if they don’t understand the science. We believe NAMDRC can play an important role by addressing these knowledge deficits.
Turning Up the Heat on ICU Burnout
The work of critical care clinicians can create a perfect storm for emotional exhaustion, depersonalization, and reduced self-efficacy – widely known as burnout. Burnout is occurring in record numbers among physicians in general – more than twice as frequently as for non-health-care workers – and intensivists top the chart. Clinicians from all specialties in medicine today experience the frustrations of workplace chaos and loss of control, displacement of meaningful work with menial work, and ever increasing documentation requirements and electronic health record challenges – all contributing to burnout. Intensivists and other ICU professionals, such as advanced practice providers and nurses, however, experience the added challenge of working in a highly stressful environment characterized by fast-paced high-stakes decision making, long and irregular hours, and end-of-life scenarios often clouded by moral distress. These and other drivers contribute to high rates of burnout.
Being burned out takes its toll on health-care workers, contributing to psychological and physical manifestations, alcohol or substance abuse, posttraumatic stress disorder, and even suicidal ideation. Additionally, burnout carries important negative consequences for the organization and directly to the patient, including higher rates of employee turnover, lower quality of work, more medical errors, and reduced patient satisfaction. Unfortunately, burnout rates continue to rise with alarming speed.
Fortunately, there is increasing attention paid to the magnitude and potential impact of burnout, compelling important organizations to highlight the problem and assist clinicians in combating burnout and its consequences. For example, the National Academy of Medicine (NAM) has convened an Action Collaborative on Clinician Well-Being and Resilience and invited more than 100 organizations to publish their statement of commitment to improve clinician well-being and reduce clinician burnout (https://nam.edu/initiatives/clinician-resilience-and-well-being/). The American Medical Association (AMA) has developed modules and tools to assist clinicians and administrators in taking important steps to prevent burnout (https://www.stepsforward.org/modules/physician-burnout).
CHEST has been an active participant in addressing burnout in ICU professionals, including in an important partnership with the American Association of Critical-Care Nurses (AACN), the American Thoracic Society (ATS), and the Society of Critical Care Medicine (SCCM) - the Critical Care Societies Collaborative (CCSC). The CCSC, whose members include greater than 150,000 critical care professionals in the United States, has established a principle goal of mitigating ICU burnout (#StopICUBurnout). One of the first CCSC efforts was to publish a white paper simultaneously in all four journals of the CCSC professional societies that provides the rationale and direction for a “call for action” to tackle ICU burnout (Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. Burnout syndrome in critical care health care professionals: A call for action. Chest. 2016;150[1]:17). Recently, the CCSC sponsored a National Summit on the Prevention and Management of Burnout in the ICU (http://ccsconline.org/optimizing-the-workforce/burnout). Fifty-five invited participants brought wide ranging expertise and substantial enthusiasm to the task of deconstructing ICU burnout and identifying knowledge gaps and future directions. Areas of focused discussion included factors influencing burnout, identifying individuals with burnout, the value of organizational and individual interventions to prevent and manage burnout, and translation of these discussions into a research agenda. CHEST and the CCSC are committed to the goals of enhancing clinician well-being and eliminating burnout in the ICU.
The work of critical care clinicians can create a perfect storm for emotional exhaustion, depersonalization, and reduced self-efficacy – widely known as burnout. Burnout is occurring in record numbers among physicians in general – more than twice as frequently as for non-health-care workers – and intensivists top the chart. Clinicians from all specialties in medicine today experience the frustrations of workplace chaos and loss of control, displacement of meaningful work with menial work, and ever increasing documentation requirements and electronic health record challenges – all contributing to burnout. Intensivists and other ICU professionals, such as advanced practice providers and nurses, however, experience the added challenge of working in a highly stressful environment characterized by fast-paced high-stakes decision making, long and irregular hours, and end-of-life scenarios often clouded by moral distress. These and other drivers contribute to high rates of burnout.
Being burned out takes its toll on health-care workers, contributing to psychological and physical manifestations, alcohol or substance abuse, posttraumatic stress disorder, and even suicidal ideation. Additionally, burnout carries important negative consequences for the organization and directly to the patient, including higher rates of employee turnover, lower quality of work, more medical errors, and reduced patient satisfaction. Unfortunately, burnout rates continue to rise with alarming speed.
Fortunately, there is increasing attention paid to the magnitude and potential impact of burnout, compelling important organizations to highlight the problem and assist clinicians in combating burnout and its consequences. For example, the National Academy of Medicine (NAM) has convened an Action Collaborative on Clinician Well-Being and Resilience and invited more than 100 organizations to publish their statement of commitment to improve clinician well-being and reduce clinician burnout (https://nam.edu/initiatives/clinician-resilience-and-well-being/). The American Medical Association (AMA) has developed modules and tools to assist clinicians and administrators in taking important steps to prevent burnout (https://www.stepsforward.org/modules/physician-burnout).
CHEST has been an active participant in addressing burnout in ICU professionals, including in an important partnership with the American Association of Critical-Care Nurses (AACN), the American Thoracic Society (ATS), and the Society of Critical Care Medicine (SCCM) - the Critical Care Societies Collaborative (CCSC). The CCSC, whose members include greater than 150,000 critical care professionals in the United States, has established a principle goal of mitigating ICU burnout (#StopICUBurnout). One of the first CCSC efforts was to publish a white paper simultaneously in all four journals of the CCSC professional societies that provides the rationale and direction for a “call for action” to tackle ICU burnout (Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. Burnout syndrome in critical care health care professionals: A call for action. Chest. 2016;150[1]:17). Recently, the CCSC sponsored a National Summit on the Prevention and Management of Burnout in the ICU (http://ccsconline.org/optimizing-the-workforce/burnout). Fifty-five invited participants brought wide ranging expertise and substantial enthusiasm to the task of deconstructing ICU burnout and identifying knowledge gaps and future directions. Areas of focused discussion included factors influencing burnout, identifying individuals with burnout, the value of organizational and individual interventions to prevent and manage burnout, and translation of these discussions into a research agenda. CHEST and the CCSC are committed to the goals of enhancing clinician well-being and eliminating burnout in the ICU.
The work of critical care clinicians can create a perfect storm for emotional exhaustion, depersonalization, and reduced self-efficacy – widely known as burnout. Burnout is occurring in record numbers among physicians in general – more than twice as frequently as for non-health-care workers – and intensivists top the chart. Clinicians from all specialties in medicine today experience the frustrations of workplace chaos and loss of control, displacement of meaningful work with menial work, and ever increasing documentation requirements and electronic health record challenges – all contributing to burnout. Intensivists and other ICU professionals, such as advanced practice providers and nurses, however, experience the added challenge of working in a highly stressful environment characterized by fast-paced high-stakes decision making, long and irregular hours, and end-of-life scenarios often clouded by moral distress. These and other drivers contribute to high rates of burnout.
Being burned out takes its toll on health-care workers, contributing to psychological and physical manifestations, alcohol or substance abuse, posttraumatic stress disorder, and even suicidal ideation. Additionally, burnout carries important negative consequences for the organization and directly to the patient, including higher rates of employee turnover, lower quality of work, more medical errors, and reduced patient satisfaction. Unfortunately, burnout rates continue to rise with alarming speed.
Fortunately, there is increasing attention paid to the magnitude and potential impact of burnout, compelling important organizations to highlight the problem and assist clinicians in combating burnout and its consequences. For example, the National Academy of Medicine (NAM) has convened an Action Collaborative on Clinician Well-Being and Resilience and invited more than 100 organizations to publish their statement of commitment to improve clinician well-being and reduce clinician burnout (https://nam.edu/initiatives/clinician-resilience-and-well-being/). The American Medical Association (AMA) has developed modules and tools to assist clinicians and administrators in taking important steps to prevent burnout (https://www.stepsforward.org/modules/physician-burnout).
CHEST has been an active participant in addressing burnout in ICU professionals, including in an important partnership with the American Association of Critical-Care Nurses (AACN), the American Thoracic Society (ATS), and the Society of Critical Care Medicine (SCCM) - the Critical Care Societies Collaborative (CCSC). The CCSC, whose members include greater than 150,000 critical care professionals in the United States, has established a principle goal of mitigating ICU burnout (#StopICUBurnout). One of the first CCSC efforts was to publish a white paper simultaneously in all four journals of the CCSC professional societies that provides the rationale and direction for a “call for action” to tackle ICU burnout (Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. Burnout syndrome in critical care health care professionals: A call for action. Chest. 2016;150[1]:17). Recently, the CCSC sponsored a National Summit on the Prevention and Management of Burnout in the ICU (http://ccsconline.org/optimizing-the-workforce/burnout). Fifty-five invited participants brought wide ranging expertise and substantial enthusiasm to the task of deconstructing ICU burnout and identifying knowledge gaps and future directions. Areas of focused discussion included factors influencing burnout, identifying individuals with burnout, the value of organizational and individual interventions to prevent and manage burnout, and translation of these discussions into a research agenda. CHEST and the CCSC are committed to the goals of enhancing clinician well-being and eliminating burnout in the ICU.
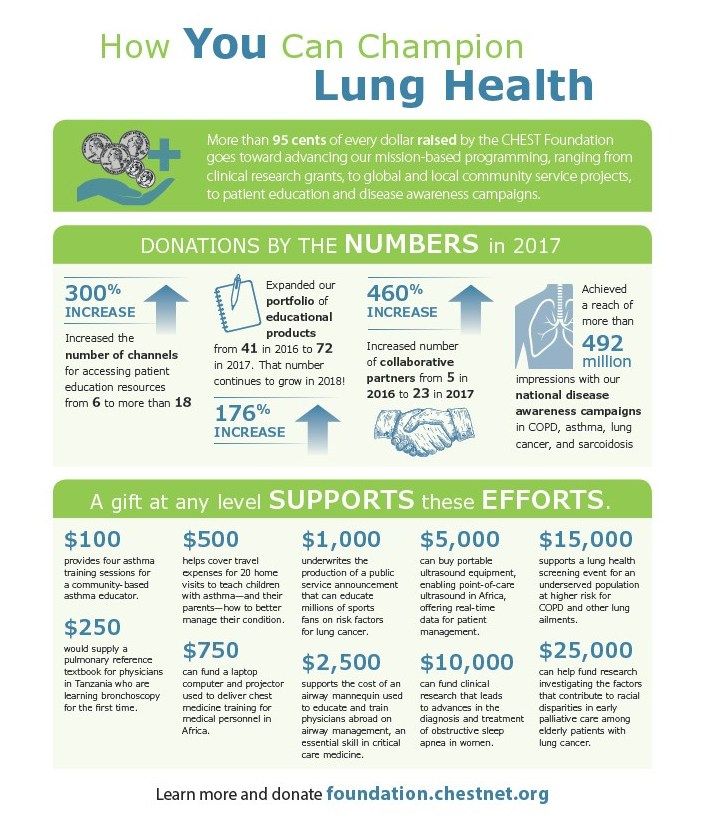
How You Can Champion Lung Health
More than 95 cents of every dollar raised by the CHEST Foundation goes toward advancing our mission-based programming, ranging from clinical research grants, to global and local community service projects, to patient education and disease awareness campaigns.
DONATIONS BY THE NUMBERS in 2017
300% INCREASE
176% INCREASE
Expanded our portfolio of educational products from 41 in 2016 to 72 in 2017. That number continues to grow in 2018!
460% INCREASE
Increased number of collaborative partners from 5 in 2016 to 23 in 2017.
Achieved a reach of more than 492 million impressions with our national disease awareness campaigns in COPD, asthma, lung cancer, and sarcoidosis
A gift at any level SUPPORTS these EFFORTS.
$100
provides four asthma training sessions for a community-based asthma educator.
$250
would supply a pulmonary referencer textbook for physicians in Tanzania who are learning bronchoscopy for the first time.
$500
helps cover travel expenses for 20 home visits to teach children with asthma—and their parents—how to better manage their condition.
$750
can fund a laptop computer and projector used to deliver chest medicine training for medical personnel in Africa.
$1,000
underwrites the production of a public service announcement that can educate millions of sports fans on risk factors for lung cancer.
$2,500
supports the cost of an airway mannequin used to educate and train physicians abroad on airway management, an essential skill in critical care medicine.
$5,000
can buy portable ultrasound equipment, enabling point-of-care ultrasound in Africa, offering real-time data for patient management.
$10,000
can fund clinical research that leads to advances in the diagnosis and treatment of obstructive sleep apnea in women.
$15,000
supports a lung health screening event for an underserved population at higher risk for COPD and other lung ailments.
$25,000
can help fund research investigating the factors that contribute to racial disparities in early palliative care among elderly patients with lung cancer.
Learn more and donate foundation.chestnet.org.
More than 95 cents of every dollar raised by the CHEST Foundation goes toward advancing our mission-based programming, ranging from clinical research grants, to global and local community service projects, to patient education and disease awareness campaigns.
DONATIONS BY THE NUMBERS in 2017
300% INCREASE
176% INCREASE
Expanded our portfolio of educational products from 41 in 2016 to 72 in 2017. That number continues to grow in 2018!
460% INCREASE
Increased number of collaborative partners from 5 in 2016 to 23 in 2017.
Achieved a reach of more than 492 million impressions with our national disease awareness campaigns in COPD, asthma, lung cancer, and sarcoidosis
A gift at any level SUPPORTS these EFFORTS.
$100
provides four asthma training sessions for a community-based asthma educator.
$250
would supply a pulmonary referencer textbook for physicians in Tanzania who are learning bronchoscopy for the first time.
$500
helps cover travel expenses for 20 home visits to teach children with asthma—and their parents—how to better manage their condition.
$750
can fund a laptop computer and projector used to deliver chest medicine training for medical personnel in Africa.
$1,000
underwrites the production of a public service announcement that can educate millions of sports fans on risk factors for lung cancer.
$2,500
supports the cost of an airway mannequin used to educate and train physicians abroad on airway management, an essential skill in critical care medicine.
$5,000
can buy portable ultrasound equipment, enabling point-of-care ultrasound in Africa, offering real-time data for patient management.
$10,000
can fund clinical research that leads to advances in the diagnosis and treatment of obstructive sleep apnea in women.
$15,000
supports a lung health screening event for an underserved population at higher risk for COPD and other lung ailments.
$25,000
can help fund research investigating the factors that contribute to racial disparities in early palliative care among elderly patients with lung cancer.
Learn more and donate foundation.chestnet.org.
More than 95 cents of every dollar raised by the CHEST Foundation goes toward advancing our mission-based programming, ranging from clinical research grants, to global and local community service projects, to patient education and disease awareness campaigns.
DONATIONS BY THE NUMBERS in 2017
300% INCREASE
176% INCREASE
Expanded our portfolio of educational products from 41 in 2016 to 72 in 2017. That number continues to grow in 2018!
460% INCREASE
Increased number of collaborative partners from 5 in 2016 to 23 in 2017.
Achieved a reach of more than 492 million impressions with our national disease awareness campaigns in COPD, asthma, lung cancer, and sarcoidosis
A gift at any level SUPPORTS these EFFORTS.
$100
provides four asthma training sessions for a community-based asthma educator.
$250
would supply a pulmonary referencer textbook for physicians in Tanzania who are learning bronchoscopy for the first time.
$500
helps cover travel expenses for 20 home visits to teach children with asthma—and their parents—how to better manage their condition.
$750
can fund a laptop computer and projector used to deliver chest medicine training for medical personnel in Africa.
$1,000
underwrites the production of a public service announcement that can educate millions of sports fans on risk factors for lung cancer.
$2,500
supports the cost of an airway mannequin used to educate and train physicians abroad on airway management, an essential skill in critical care medicine.
$5,000
can buy portable ultrasound equipment, enabling point-of-care ultrasound in Africa, offering real-time data for patient management.
$10,000
can fund clinical research that leads to advances in the diagnosis and treatment of obstructive sleep apnea in women.
$15,000
supports a lung health screening event for an underserved population at higher risk for COPD and other lung ailments.
$25,000
can help fund research investigating the factors that contribute to racial disparities in early palliative care among elderly patients with lung cancer.
Learn more and donate foundation.chestnet.org.
In Memoriam
W. Gerald Rainer, MD, FCCP, died November 14, 2017, one day after his 90th birthday Dr. Rainer was President of the American College of Chest Physicians in 1982-1983. He practiced thoracic and cardiovascular surgery for 50 years with St. Joseph Hospital in Denver as his professional home. He was a respected leader, researcher, and educator, helping and mentoring countless residents, fellows, and many other health-care professionals. Dr. Rainer was a distinguished clinical professor of surgery at the University of Colorado School of Medicine and served on many University boards and committees. He published prolifically in many respected surgical journals and was able to masterfully blend his private practice with strong academic involvement. As President of the American College of Chest Physicians and many other respected medical and surgical organizations, he was also actively involved in international professional societies. CHEST extends its condolences to Dr. Rainer’s wife of 67 years, Lois, and to his family and friends.
W. Gerald Rainer, MD, FCCP, died November 14, 2017, one day after his 90th birthday Dr. Rainer was President of the American College of Chest Physicians in 1982-1983. He practiced thoracic and cardiovascular surgery for 50 years with St. Joseph Hospital in Denver as his professional home. He was a respected leader, researcher, and educator, helping and mentoring countless residents, fellows, and many other health-care professionals. Dr. Rainer was a distinguished clinical professor of surgery at the University of Colorado School of Medicine and served on many University boards and committees. He published prolifically in many respected surgical journals and was able to masterfully blend his private practice with strong academic involvement. As President of the American College of Chest Physicians and many other respected medical and surgical organizations, he was also actively involved in international professional societies. CHEST extends its condolences to Dr. Rainer’s wife of 67 years, Lois, and to his family and friends.
W. Gerald Rainer, MD, FCCP, died November 14, 2017, one day after his 90th birthday Dr. Rainer was President of the American College of Chest Physicians in 1982-1983. He practiced thoracic and cardiovascular surgery for 50 years with St. Joseph Hospital in Denver as his professional home. He was a respected leader, researcher, and educator, helping and mentoring countless residents, fellows, and many other health-care professionals. Dr. Rainer was a distinguished clinical professor of surgery at the University of Colorado School of Medicine and served on many University boards and committees. He published prolifically in many respected surgical journals and was able to masterfully blend his private practice with strong academic involvement. As President of the American College of Chest Physicians and many other respected medical and surgical organizations, he was also actively involved in international professional societies. CHEST extends its condolences to Dr. Rainer’s wife of 67 years, Lois, and to his family and friends.
This Month in the Journal CHEST®
Original Research
Community-Acquired Pneumonia Visualized on CT Scans but Not Chest Radiographs: Pathogens, Severity, and Clinical Outcomes. By Dr. C. P. Upchurch, et al.
Commentary
CHEST: Home of the Clinician-Educator. By Dr. W. F. Kelly and Dr. A. S. Niven, on behalf of the CHEST Education Committee.
Original Research
Community-Acquired Pneumonia Visualized on CT Scans but Not Chest Radiographs: Pathogens, Severity, and Clinical Outcomes. By Dr. C. P. Upchurch, et al.
Commentary
CHEST: Home of the Clinician-Educator. By Dr. W. F. Kelly and Dr. A. S. Niven, on behalf of the CHEST Education Committee.
Original Research
Community-Acquired Pneumonia Visualized on CT Scans but Not Chest Radiographs: Pathogens, Severity, and Clinical Outcomes. By Dr. C. P. Upchurch, et al.
Commentary
CHEST: Home of the Clinician-Educator. By Dr. W. F. Kelly and Dr. A. S. Niven, on behalf of the CHEST Education Committee.
Eileen Metzger Bulger, MD, FACS, is new Chair of the ACS Committee on Trauma
Eileen Metzger Bulger, MD, FACS, chief of trauma and trauma medical director for adults and pediatrics, Harborview Medical Center, Seattle, WA, begins serving as the new Chair of the American College of Surgeons (ACS) Committee on Trauma (COT) this month. Dr. Bulger was appointed as the next COT Chair in October 2017 by the ACS Board of Regents. She is the 20th Chair of the COT, succeeding Ronald M. Stewart, MD, FACS, of San Antonio, TX.
“We look forward to Dr. Bulger’s exceptional vision and leadership as she directs the COT into its 96th year of working to improve the care of the injured patient. She is the perfect person to lead the COT into its next century of transforming care and reducing injuries across the globe,” Dr. Stewart said.
A diplomate of the American Board of Surgery, Dr. Bulger also is board certified in surgical critical care. She earned a medical doctorate at Cornell University Medical College, New York, NY (1992). She completed a residency in general surgery at the University of Washington (UW), Seattle (1992–1999), where she concurrently completed a two-year National Institutes of Health Trauma Research Fellowship during her years of residency training (1995–1997), and then went on to complete a surgical critical care fellowship at UW in 2000.
Recognized leadership
Throughout her career, Dr. Bulger has mentored many surgical residents in paper and scholarship competitions. For nearly two decades, she has served as the co-principal or principal investigator of a variety of innovative, grant-funded research projects related to trauma care, some of which focus on improving outcomes for crash injury victims, pediatric patients, and older adults.
Since her initial involvement with the COT in 2002, Dr. Bulger has contributed to many COT activities, often serving in a leadership role. She is a Course Instructor for the internationally recognized Advanced Traum
The COT is dedicated to all phases of injury care, from prevention to rehabilitation. The committee is supported by a network of 65 state and provincial committees, 11 international committees, and five military committees, and the majority of members are ACS Fellows.
Eileen Metzger Bulger, MD, FACS, chief of trauma and trauma medical director for adults and pediatrics, Harborview Medical Center, Seattle, WA, begins serving as the new Chair of the American College of Surgeons (ACS) Committee on Trauma (COT) this month. Dr. Bulger was appointed as the next COT Chair in October 2017 by the ACS Board of Regents. She is the 20th Chair of the COT, succeeding Ronald M. Stewart, MD, FACS, of San Antonio, TX.
“We look forward to Dr. Bulger’s exceptional vision and leadership as she directs the COT into its 96th year of working to improve the care of the injured patient. She is the perfect person to lead the COT into its next century of transforming care and reducing injuries across the globe,” Dr. Stewart said.
A diplomate of the American Board of Surgery, Dr. Bulger also is board certified in surgical critical care. She earned a medical doctorate at Cornell University Medical College, New York, NY (1992). She completed a residency in general surgery at the University of Washington (UW), Seattle (1992–1999), where she concurrently completed a two-year National Institutes of Health Trauma Research Fellowship during her years of residency training (1995–1997), and then went on to complete a surgical critical care fellowship at UW in 2000.
Recognized leadership
Throughout her career, Dr. Bulger has mentored many surgical residents in paper and scholarship competitions. For nearly two decades, she has served as the co-principal or principal investigator of a variety of innovative, grant-funded research projects related to trauma care, some of which focus on improving outcomes for crash injury victims, pediatric patients, and older adults.
Since her initial involvement with the COT in 2002, Dr. Bulger has contributed to many COT activities, often serving in a leadership role. She is a Course Instructor for the internationally recognized Advanced Traum
The COT is dedicated to all phases of injury care, from prevention to rehabilitation. The committee is supported by a network of 65 state and provincial committees, 11 international committees, and five military committees, and the majority of members are ACS Fellows.
Eileen Metzger Bulger, MD, FACS, chief of trauma and trauma medical director for adults and pediatrics, Harborview Medical Center, Seattle, WA, begins serving as the new Chair of the American College of Surgeons (ACS) Committee on Trauma (COT) this month. Dr. Bulger was appointed as the next COT Chair in October 2017 by the ACS Board of Regents. She is the 20th Chair of the COT, succeeding Ronald M. Stewart, MD, FACS, of San Antonio, TX.
“We look forward to Dr. Bulger’s exceptional vision and leadership as she directs the COT into its 96th year of working to improve the care of the injured patient. She is the perfect person to lead the COT into its next century of transforming care and reducing injuries across the globe,” Dr. Stewart said.
A diplomate of the American Board of Surgery, Dr. Bulger also is board certified in surgical critical care. She earned a medical doctorate at Cornell University Medical College, New York, NY (1992). She completed a residency in general surgery at the University of Washington (UW), Seattle (1992–1999), where she concurrently completed a two-year National Institutes of Health Trauma Research Fellowship during her years of residency training (1995–1997), and then went on to complete a surgical critical care fellowship at UW in 2000.
Recognized leadership
Throughout her career, Dr. Bulger has mentored many surgical residents in paper and scholarship competitions. For nearly two decades, she has served as the co-principal or principal investigator of a variety of innovative, grant-funded research projects related to trauma care, some of which focus on improving outcomes for crash injury victims, pediatric patients, and older adults.
Since her initial involvement with the COT in 2002, Dr. Bulger has contributed to many COT activities, often serving in a leadership role. She is a Course Instructor for the internationally recognized Advanced Traum
The COT is dedicated to all phases of injury care, from prevention to rehabilitation. The committee is supported by a network of 65 state and provincial committees, 11 international committees, and five military committees, and the majority of members are ACS Fellows.
Bipartisan Budget Act of 2018 addresses ACS priorities
On February 9, Congress passed and President Trump signed into law the Bipartisan Budget Act of 2018. The law addresses many key physician and patient issues, including important technical corrections to the Merit-based Incentive Payment System (MIPS) that the American College of Surgeons (ACS) strongly favors.
The law addresses several other ACS priorities, including:
The addition of a long-term funding extension (10 years) for the Children’s Health Insurance Program (CHIP), ensuring that children continue to have access to surgical care
The inclusion of language that eases electronic health record system meaningful use requirements, alleviating some of the burdens imposed on physicians and their practices
Additional funding to address the opioid epidemic and to support the work of the National Institutes of Health Repeal of the Independent Payment Advisory Board
For more information, contact Mark Lukaszewski, ACS Congressional Lobbyist, at [email protected].
On February 9, Congress passed and President Trump signed into law the Bipartisan Budget Act of 2018. The law addresses many key physician and patient issues, including important technical corrections to the Merit-based Incentive Payment System (MIPS) that the American College of Surgeons (ACS) strongly favors.
The law addresses several other ACS priorities, including:
The addition of a long-term funding extension (10 years) for the Children’s Health Insurance Program (CHIP), ensuring that children continue to have access to surgical care
The inclusion of language that eases electronic health record system meaningful use requirements, alleviating some of the burdens imposed on physicians and their practices
Additional funding to address the opioid epidemic and to support the work of the National Institutes of Health Repeal of the Independent Payment Advisory Board
For more information, contact Mark Lukaszewski, ACS Congressional Lobbyist, at [email protected].
On February 9, Congress passed and President Trump signed into law the Bipartisan Budget Act of 2018. The law addresses many key physician and patient issues, including important technical corrections to the Merit-based Incentive Payment System (MIPS) that the American College of Surgeons (ACS) strongly favors.
The law addresses several other ACS priorities, including:
The addition of a long-term funding extension (10 years) for the Children’s Health Insurance Program (CHIP), ensuring that children continue to have access to surgical care
The inclusion of language that eases electronic health record system meaningful use requirements, alleviating some of the burdens imposed on physicians and their practices
Additional funding to address the opioid epidemic and to support the work of the National Institutes of Health Repeal of the Independent Payment Advisory Board
For more information, contact Mark Lukaszewski, ACS Congressional Lobbyist, at [email protected].
ACS delegation shapes policy at AMA HOD meeting
The American Medical Association (AMA) Interim Meeting of the House of Delegates (HOD) took place November 11–14, 2017, in Honolulu, HI. A total of 532 delegates were in attendance to debate the policy implications of 36 reports and 99 resolutions.
The American College of Surgeons (ACS) sent a six-member delegation to the meeting. The ACS also participates in AMA activities in other capacities, including in the AMA Young Physician Section Assembly, the AMA Resident and Fellow Section Assembly, and the AMA Council on Medical Education. These three groups met in conjunction with the HOD meeting. See the sidebar on page 74 for the list of ACS delegates and their other AMA roles.
ACS cosponsored issues
The AMA HOD brings together a variety of perspectives in medicine, and the job of the ACS delegation is to shape AMA policy consistent with College priorities. One way the ACS achieves this objective is by cosponsoring resolutions that have been submitted by other delegations and that are relevant to the College Fellowship. The ACS delegation cosponsored the following three resolutions at the November meeting—two on scope-of-practice issues and one on physician payment—all of which were adopted.
Resolution 214, Advanced Practice Registered Nurse (APRN) Compact, was initiated by the American Society of Anesthesiologists and strengthened with amendments. AMA policy opposes enactment of the Advanced APRN Multistate Compact because of its potential to supersede state laws that require APRNs to practice under physician supervision, as well as legislation that authorizes the independent practice of medicine by any individual who has not completed the state’s requirement for licensure to practice medicine. The AMA will convene an in-person meeting of relevant physician stakeholders to create a consistent national strategy to prevent fulfillment of the APRN Compact.
Resolution 230, Oppose Physician Assistant Independent Practice, with support from a spectrum of state medical and national specialty societies, continued the theme of opposition to legislation or regulation that allows physician extenders—in this case physician assistants—to practice independently. Another resolution addressed the emerging advanced physician assistant degree known as doctor of medical science. The AMA opposes holders of this degree from being recognized as a new category of health care practitioners licensed for the independent practice of medicine.
Resolution 808, Opposition to Reduced Payment for the 25-Modifier, was offered by the American Academy of Dermatology. The resolution was a response to private insurers discounting evaluation and management (E/M) codes by 50 percent when linked through the 25-modifier to a procedure on the same day. This resolution passed as simplified by amendment to have AMA aggressively and immediately advocate, through any legal means possible (such as direct payor negotiations, regulations, legislation, or litigation), for non-reduced allowable payment of appropriately reported 25-modifier E/M codes when linked with procedures.
Other HOD-adopted resolutions of interest
BOT (Board of Trustees) Report 5, Effective Peer Review, amended the AMA Physician and Medical Staff Member Bill of Rights to add “protection from any retaliatory actions” to the list of immunity rights when physicians participate in good faith peer-review activities. In testimony at the reference committee, the delegation highlighted the value of the new ACS “red book,” Optimal Resources for Surgical Quality and Safety, for establishing peer-review standards in surgical care.
Council on Science and Public Health Report 2, Targeted Education to Increase Organ Donation, amended the AMA policy, Methods to Increase the U.S. Organ Donor Pool. As a result, the AMA supports studies that evaluate the effectiveness of mandated choice and presumed consent models for increasing organ donation and urges development of effective methods to inform populations with historically low participation rates about donating.
Resolution 953, Fees for Taking Maintenance of Certification (MOC) Examination, amended AMA MOC policy to assert that the MOC process should reflect the cost of development and administration of the MOC components, ensure a fair fee structure, and not hinder patient care. The AMA will advocate that value in MOC includes cost-effectiveness with full financial transparency, respect for physicians’ time and patient care commitments, alignment of MOC requirements with other regulator and payor requirements, and adherence to an evidence basis for both MOC content and processes.
Not every item was viewed favorably at the AMA meeting. Council on Ethical and Judicial Affairs (CEJA) Report 1, Competence, Self-Assessment and Self-Awareness, sought to provide guidance for physicians in determining their own competence when practicing medicine. The council observed, “As an ethical responsibility, competence encompasses more than medical knowledge and skill. It requires physicians to understand that as a practical matter in the care of actual patients, competence is fluid and dependent on context.” Considerable testimony emphasized a lack of reliable tools and available resources to assist physicians in self-assessment. Thus, the report was referred back to CEJA for more work.
Surgical caucus
In addition to facilitating an agenda review and business meeting for surgeons, anesthesiologists, and emergency physicians, the caucus sponsored a popular education session, Hazards of the Deep: Trauma in Paradise. Michael Hayashi, MD, FACS, Chair of the Hawaii Committee on Trauma, discussed system challenges in caring for injured patients from geographically remote and less populated areas. Lieutenant Matthew Brown, MC, USN, an undersea/diving medical officer stationed at Pearl Harbor, HI, shared insights about injuries and medical conditions experienced by scuba divers, swimmers, surfers, and other beach enthusiasts.
Leadership transition
After extended service on the delegation, including eight years as Chair, Dr. Armstrong bid “aloha” to the HOD as a retiring delegate. Dr. Turner has accepted the role as Chair, maintaining continued College leadership in the HOD.
Next meeting
The next meeting of the AMA HOD is scheduled for June 9–13 in Chicago, IL. In addition to debate on numerous issues, elections for AMA officers, trustees, and councils will be held at the meeting. Surgeons with suggestions for potential resolutions or questions about ACS activities at the AMA HOD should e-mail [email protected]
ACS Delegation at the AMA HOD
John H. Armstrong, MD, FACS (Delegation Chair), acute care surgery, Tampa, FL
Brian J. Gavitt, MD, MPH (also Young Physicians Section delegate), general surgery, Cincinnati, OH
Jacob Moalem, MD, FACS, general surgery, Rochester, NY
Leigh A. Neumayer, MD, FACS, general surgery, Tucson, AZ; Chair, ACS Board of Regents
Naveen F. Sangji, MD (also Resident and Fellow Section delegate), general surgery resident, Boston, MA
Patricia L. Turner, MD, FACS, general surgery, Chicago, IL; Director, ACS Division of Member Services; member and immediate past-chair, AMA Council on Medical EducationDr. Armstrong is affiliate associate professor of surgery, University of South Florida Morsani College of Medicine, Tampa, and former Florida Surgeon General and Secretary of Health (2012–2016). He is a member, ACS Health Policy and Advocacy Group, and Past-Chair, ACS Professional Association political action committee (ACSPA-SurgeonsPAC).
Mr. Sutton is Manager, State Affairs, ACS Division of Advocacy and Health Policy.
The American Medical Association (AMA) Interim Meeting of the House of Delegates (HOD) took place November 11–14, 2017, in Honolulu, HI. A total of 532 delegates were in attendance to debate the policy implications of 36 reports and 99 resolutions.
The American College of Surgeons (ACS) sent a six-member delegation to the meeting. The ACS also participates in AMA activities in other capacities, including in the AMA Young Physician Section Assembly, the AMA Resident and Fellow Section Assembly, and the AMA Council on Medical Education. These three groups met in conjunction with the HOD meeting. See the sidebar on page 74 for the list of ACS delegates and their other AMA roles.
ACS cosponsored issues
The AMA HOD brings together a variety of perspectives in medicine, and the job of the ACS delegation is to shape AMA policy consistent with College priorities. One way the ACS achieves this objective is by cosponsoring resolutions that have been submitted by other delegations and that are relevant to the College Fellowship. The ACS delegation cosponsored the following three resolutions at the November meeting—two on scope-of-practice issues and one on physician payment—all of which were adopted.
Resolution 214, Advanced Practice Registered Nurse (APRN) Compact, was initiated by the American Society of Anesthesiologists and strengthened with amendments. AMA policy opposes enactment of the Advanced APRN Multistate Compact because of its potential to supersede state laws that require APRNs to practice under physician supervision, as well as legislation that authorizes the independent practice of medicine by any individual who has not completed the state’s requirement for licensure to practice medicine. The AMA will convene an in-person meeting of relevant physician stakeholders to create a consistent national strategy to prevent fulfillment of the APRN Compact.
Resolution 230, Oppose Physician Assistant Independent Practice, with support from a spectrum of state medical and national specialty societies, continued the theme of opposition to legislation or regulation that allows physician extenders—in this case physician assistants—to practice independently. Another resolution addressed the emerging advanced physician assistant degree known as doctor of medical science. The AMA opposes holders of this degree from being recognized as a new category of health care practitioners licensed for the independent practice of medicine.
Resolution 808, Opposition to Reduced Payment for the 25-Modifier, was offered by the American Academy of Dermatology. The resolution was a response to private insurers discounting evaluation and management (E/M) codes by 50 percent when linked through the 25-modifier to a procedure on the same day. This resolution passed as simplified by amendment to have AMA aggressively and immediately advocate, through any legal means possible (such as direct payor negotiations, regulations, legislation, or litigation), for non-reduced allowable payment of appropriately reported 25-modifier E/M codes when linked with procedures.
Other HOD-adopted resolutions of interest
BOT (Board of Trustees) Report 5, Effective Peer Review, amended the AMA Physician and Medical Staff Member Bill of Rights to add “protection from any retaliatory actions” to the list of immunity rights when physicians participate in good faith peer-review activities. In testimony at the reference committee, the delegation highlighted the value of the new ACS “red book,” Optimal Resources for Surgical Quality and Safety, for establishing peer-review standards in surgical care.
Council on Science and Public Health Report 2, Targeted Education to Increase Organ Donation, amended the AMA policy, Methods to Increase the U.S. Organ Donor Pool. As a result, the AMA supports studies that evaluate the effectiveness of mandated choice and presumed consent models for increasing organ donation and urges development of effective methods to inform populations with historically low participation rates about donating.
Resolution 953, Fees for Taking Maintenance of Certification (MOC) Examination, amended AMA MOC policy to assert that the MOC process should reflect the cost of development and administration of the MOC components, ensure a fair fee structure, and not hinder patient care. The AMA will advocate that value in MOC includes cost-effectiveness with full financial transparency, respect for physicians’ time and patient care commitments, alignment of MOC requirements with other regulator and payor requirements, and adherence to an evidence basis for both MOC content and processes.
Not every item was viewed favorably at the AMA meeting. Council on Ethical and Judicial Affairs (CEJA) Report 1, Competence, Self-Assessment and Self-Awareness, sought to provide guidance for physicians in determining their own competence when practicing medicine. The council observed, “As an ethical responsibility, competence encompasses more than medical knowledge and skill. It requires physicians to understand that as a practical matter in the care of actual patients, competence is fluid and dependent on context.” Considerable testimony emphasized a lack of reliable tools and available resources to assist physicians in self-assessment. Thus, the report was referred back to CEJA for more work.
Surgical caucus
In addition to facilitating an agenda review and business meeting for surgeons, anesthesiologists, and emergency physicians, the caucus sponsored a popular education session, Hazards of the Deep: Trauma in Paradise. Michael Hayashi, MD, FACS, Chair of the Hawaii Committee on Trauma, discussed system challenges in caring for injured patients from geographically remote and less populated areas. Lieutenant Matthew Brown, MC, USN, an undersea/diving medical officer stationed at Pearl Harbor, HI, shared insights about injuries and medical conditions experienced by scuba divers, swimmers, surfers, and other beach enthusiasts.
Leadership transition
After extended service on the delegation, including eight years as Chair, Dr. Armstrong bid “aloha” to the HOD as a retiring delegate. Dr. Turner has accepted the role as Chair, maintaining continued College leadership in the HOD.
Next meeting
The next meeting of the AMA HOD is scheduled for June 9–13 in Chicago, IL. In addition to debate on numerous issues, elections for AMA officers, trustees, and councils will be held at the meeting. Surgeons with suggestions for potential resolutions or questions about ACS activities at the AMA HOD should e-mail [email protected]
ACS Delegation at the AMA HOD
John H. Armstrong, MD, FACS (Delegation Chair), acute care surgery, Tampa, FL
Brian J. Gavitt, MD, MPH (also Young Physicians Section delegate), general surgery, Cincinnati, OH
Jacob Moalem, MD, FACS, general surgery, Rochester, NY
Leigh A. Neumayer, MD, FACS, general surgery, Tucson, AZ; Chair, ACS Board of Regents
Naveen F. Sangji, MD (also Resident and Fellow Section delegate), general surgery resident, Boston, MA
Patricia L. Turner, MD, FACS, general surgery, Chicago, IL; Director, ACS Division of Member Services; member and immediate past-chair, AMA Council on Medical EducationDr. Armstrong is affiliate associate professor of surgery, University of South Florida Morsani College of Medicine, Tampa, and former Florida Surgeon General and Secretary of Health (2012–2016). He is a member, ACS Health Policy and Advocacy Group, and Past-Chair, ACS Professional Association political action committee (ACSPA-SurgeonsPAC).
Mr. Sutton is Manager, State Affairs, ACS Division of Advocacy and Health Policy.
The American Medical Association (AMA) Interim Meeting of the House of Delegates (HOD) took place November 11–14, 2017, in Honolulu, HI. A total of 532 delegates were in attendance to debate the policy implications of 36 reports and 99 resolutions.
The American College of Surgeons (ACS) sent a six-member delegation to the meeting. The ACS also participates in AMA activities in other capacities, including in the AMA Young Physician Section Assembly, the AMA Resident and Fellow Section Assembly, and the AMA Council on Medical Education. These three groups met in conjunction with the HOD meeting. See the sidebar on page 74 for the list of ACS delegates and their other AMA roles.
ACS cosponsored issues
The AMA HOD brings together a variety of perspectives in medicine, and the job of the ACS delegation is to shape AMA policy consistent with College priorities. One way the ACS achieves this objective is by cosponsoring resolutions that have been submitted by other delegations and that are relevant to the College Fellowship. The ACS delegation cosponsored the following three resolutions at the November meeting—two on scope-of-practice issues and one on physician payment—all of which were adopted.
Resolution 214, Advanced Practice Registered Nurse (APRN) Compact, was initiated by the American Society of Anesthesiologists and strengthened with amendments. AMA policy opposes enactment of the Advanced APRN Multistate Compact because of its potential to supersede state laws that require APRNs to practice under physician supervision, as well as legislation that authorizes the independent practice of medicine by any individual who has not completed the state’s requirement for licensure to practice medicine. The AMA will convene an in-person meeting of relevant physician stakeholders to create a consistent national strategy to prevent fulfillment of the APRN Compact.
Resolution 230, Oppose Physician Assistant Independent Practice, with support from a spectrum of state medical and national specialty societies, continued the theme of opposition to legislation or regulation that allows physician extenders—in this case physician assistants—to practice independently. Another resolution addressed the emerging advanced physician assistant degree known as doctor of medical science. The AMA opposes holders of this degree from being recognized as a new category of health care practitioners licensed for the independent practice of medicine.
Resolution 808, Opposition to Reduced Payment for the 25-Modifier, was offered by the American Academy of Dermatology. The resolution was a response to private insurers discounting evaluation and management (E/M) codes by 50 percent when linked through the 25-modifier to a procedure on the same day. This resolution passed as simplified by amendment to have AMA aggressively and immediately advocate, through any legal means possible (such as direct payor negotiations, regulations, legislation, or litigation), for non-reduced allowable payment of appropriately reported 25-modifier E/M codes when linked with procedures.
Other HOD-adopted resolutions of interest
BOT (Board of Trustees) Report 5, Effective Peer Review, amended the AMA Physician and Medical Staff Member Bill of Rights to add “protection from any retaliatory actions” to the list of immunity rights when physicians participate in good faith peer-review activities. In testimony at the reference committee, the delegation highlighted the value of the new ACS “red book,” Optimal Resources for Surgical Quality and Safety, for establishing peer-review standards in surgical care.
Council on Science and Public Health Report 2, Targeted Education to Increase Organ Donation, amended the AMA policy, Methods to Increase the U.S. Organ Donor Pool. As a result, the AMA supports studies that evaluate the effectiveness of mandated choice and presumed consent models for increasing organ donation and urges development of effective methods to inform populations with historically low participation rates about donating.
Resolution 953, Fees for Taking Maintenance of Certification (MOC) Examination, amended AMA MOC policy to assert that the MOC process should reflect the cost of development and administration of the MOC components, ensure a fair fee structure, and not hinder patient care. The AMA will advocate that value in MOC includes cost-effectiveness with full financial transparency, respect for physicians’ time and patient care commitments, alignment of MOC requirements with other regulator and payor requirements, and adherence to an evidence basis for both MOC content and processes.
Not every item was viewed favorably at the AMA meeting. Council on Ethical and Judicial Affairs (CEJA) Report 1, Competence, Self-Assessment and Self-Awareness, sought to provide guidance for physicians in determining their own competence when practicing medicine. The council observed, “As an ethical responsibility, competence encompasses more than medical knowledge and skill. It requires physicians to understand that as a practical matter in the care of actual patients, competence is fluid and dependent on context.” Considerable testimony emphasized a lack of reliable tools and available resources to assist physicians in self-assessment. Thus, the report was referred back to CEJA for more work.
Surgical caucus
In addition to facilitating an agenda review and business meeting for surgeons, anesthesiologists, and emergency physicians, the caucus sponsored a popular education session, Hazards of the Deep: Trauma in Paradise. Michael Hayashi, MD, FACS, Chair of the Hawaii Committee on Trauma, discussed system challenges in caring for injured patients from geographically remote and less populated areas. Lieutenant Matthew Brown, MC, USN, an undersea/diving medical officer stationed at Pearl Harbor, HI, shared insights about injuries and medical conditions experienced by scuba divers, swimmers, surfers, and other beach enthusiasts.
Leadership transition
After extended service on the delegation, including eight years as Chair, Dr. Armstrong bid “aloha” to the HOD as a retiring delegate. Dr. Turner has accepted the role as Chair, maintaining continued College leadership in the HOD.
Next meeting
The next meeting of the AMA HOD is scheduled for June 9–13 in Chicago, IL. In addition to debate on numerous issues, elections for AMA officers, trustees, and councils will be held at the meeting. Surgeons with suggestions for potential resolutions or questions about ACS activities at the AMA HOD should e-mail [email protected]
ACS Delegation at the AMA HOD
John H. Armstrong, MD, FACS (Delegation Chair), acute care surgery, Tampa, FL
Brian J. Gavitt, MD, MPH (also Young Physicians Section delegate), general surgery, Cincinnati, OH
Jacob Moalem, MD, FACS, general surgery, Rochester, NY
Leigh A. Neumayer, MD, FACS, general surgery, Tucson, AZ; Chair, ACS Board of Regents
Naveen F. Sangji, MD (also Resident and Fellow Section delegate), general surgery resident, Boston, MA
Patricia L. Turner, MD, FACS, general surgery, Chicago, IL; Director, ACS Division of Member Services; member and immediate past-chair, AMA Council on Medical EducationDr. Armstrong is affiliate associate professor of surgery, University of South Florida Morsani College of Medicine, Tampa, and former Florida Surgeon General and Secretary of Health (2012–2016). He is a member, ACS Health Policy and Advocacy Group, and Past-Chair, ACS Professional Association political action committee (ACSPA-SurgeonsPAC).
Mr. Sutton is Manager, State Affairs, ACS Division of Advocacy and Health Policy.
Register for an upcoming 2018 ACS General Surgery Coding Workshop
Registration is open to attend an American College of Surgeons (ACS) 2018 General Surgery Coding Workshop. With Medicare and third-party payor policy and coding changes taking effect this year, it is imperative that surgeons have accurate and up-to-date information to protect their reimbursements and optimize efficiency.
During the coding workshop, you will learn how to report surgical procedures and medical services and will have access to the tools necessary to succeed, including a coding workbook to keep for future reference with checklists, resource guides, templates, and examples. Physicians receive up to 6.5 AMA PRA Category 1 Credits™ for each day of participation. In addition, each day of the workshop meets AAPC guidelines for 6.5 continuing education units.
The ACS will offer the following five remaining coding workshops in 2018:
Chicago, IL, April 12–13
New York, NY, May 17–19
Nashville, TN, August 9–10
Chicago, IL, November 1–3
The ACS also will offer a three-day course, including a day devoted to trauma and critical care coding at the New York City and (November) Chicago workshops.
Register for a course at www.karenzupko.com/workshops2/gensurg-workshops/. For more information about the 2018 ACS coding workshops, visit the ACS website www.facs.org/advocacy/practmanagement/workshops or e-mail
Registration is open to attend an American College of Surgeons (ACS) 2018 General Surgery Coding Workshop. With Medicare and third-party payor policy and coding changes taking effect this year, it is imperative that surgeons have accurate and up-to-date information to protect their reimbursements and optimize efficiency.
During the coding workshop, you will learn how to report surgical procedures and medical services and will have access to the tools necessary to succeed, including a coding workbook to keep for future reference with checklists, resource guides, templates, and examples. Physicians receive up to 6.5 AMA PRA Category 1 Credits™ for each day of participation. In addition, each day of the workshop meets AAPC guidelines for 6.5 continuing education units.
The ACS will offer the following five remaining coding workshops in 2018:
Chicago, IL, April 12–13
New York, NY, May 17–19
Nashville, TN, August 9–10
Chicago, IL, November 1–3
The ACS also will offer a three-day course, including a day devoted to trauma and critical care coding at the New York City and (November) Chicago workshops.
Register for a course at www.karenzupko.com/workshops2/gensurg-workshops/. For more information about the 2018 ACS coding workshops, visit the ACS website www.facs.org/advocacy/practmanagement/workshops or e-mail
Registration is open to attend an American College of Surgeons (ACS) 2018 General Surgery Coding Workshop. With Medicare and third-party payor policy and coding changes taking effect this year, it is imperative that surgeons have accurate and up-to-date information to protect their reimbursements and optimize efficiency.
During the coding workshop, you will learn how to report surgical procedures and medical services and will have access to the tools necessary to succeed, including a coding workbook to keep for future reference with checklists, resource guides, templates, and examples. Physicians receive up to 6.5 AMA PRA Category 1 Credits™ for each day of participation. In addition, each day of the workshop meets AAPC guidelines for 6.5 continuing education units.
The ACS will offer the following five remaining coding workshops in 2018:
Chicago, IL, April 12–13
New York, NY, May 17–19
Nashville, TN, August 9–10
Chicago, IL, November 1–3
The ACS also will offer a three-day course, including a day devoted to trauma and critical care coding at the New York City and (November) Chicago workshops.
Register for a course at www.karenzupko.com/workshops2/gensurg-workshops/. For more information about the 2018 ACS coding workshops, visit the ACS website www.facs.org/advocacy/practmanagement/workshops or e-mail