User login
Learn to Negotiate Physician Compensation Agreements
SVS and the SVS Community Practice Committee will hold an informative webinar for SVS members on April 30 on “Negotiating Physician Employment Agreements.” The 75-minute webinar will begin at 8 p.m. Eastern, 7 p.m. Central, 6 p.m. Mountain and 5 p.m. Pacific times. Topics will include current trends, regulatory overview and key contractual provisions. Register here.
SVS and the SVS Community Practice Committee will hold an informative webinar for SVS members on April 30 on “Negotiating Physician Employment Agreements.” The 75-minute webinar will begin at 8 p.m. Eastern, 7 p.m. Central, 6 p.m. Mountain and 5 p.m. Pacific times. Topics will include current trends, regulatory overview and key contractual provisions. Register here.
SVS and the SVS Community Practice Committee will hold an informative webinar for SVS members on April 30 on “Negotiating Physician Employment Agreements.” The 75-minute webinar will begin at 8 p.m. Eastern, 7 p.m. Central, 6 p.m. Mountain and 5 p.m. Pacific times. Topics will include current trends, regulatory overview and key contractual provisions. Register here.
SVS 2018 Vascular Annual Meeting to Host Vascular Teams
When: June 20-23
Where: Hynes Convention Center, Boston
Scientific Sessions: June 21-23
Exhibit Hall: June 21-22
Register: vsweb.org/VAM18
#VAM18
What’s happening this year at the Society for Vascular Surgery’s Vascular Annual Meeting?
- Enhanced online program planner that syncs with meeting app and makes it simple to plan your schedule. Follow this link to start now
- New opportunities for audience participation and discussion
- Programming aimed at physicians and the vascular team in all practice settings
- Cooperative scheduling with the Society for Vascular Nursing and physician assistants
- Great minds, stimulating discussions and events that include the entire vascular team
The 2018 VAM, sponsored by the SVS, will be at the Hynes Convention Center in Boston, Mass., June 20-23. The scientific sessions and exhibit hall open June 21. Registration numbers are already exceeding last year’s benchmarks, organizers said.
Abstracts for all the scientific sessions will be available in the June Journal of Vascular Surgery supplement.
Some of the highlights:
Inclusive. – This year’s meeting has a theme: The Vascular Team: Partners in Patient Care. Every member of the vascular team – surgeons, nurses, nurse practitioners, PAs – will find a reason to attend.
The meeting provides programming across all practice settings with an even stronger focus on practical, take-home information for all.
View Dr. Darling’s “wicked awesome” Welcome to VAM18 video
The Society for Vascular Nursing’s annual meeting will be in the same location June 20-21. Registration for the SVN meeting includes access to VAM.
This year, the newly established membership section for vascular PAs will present PA-focused education. Within just the past few months, more than 130 PAs joined SVS and many are expected to be at VAM.
An Intuitive Planner - VAM18 meeting will see a new online program planner that allows attendees to filter by session type, areas of interest, faculty, and more. Attendees can favorite a session to build their own meeting schedule. The online planner will sync with the new meeting mobile app, so that attendees can carry their schedule with them. The mobile app will be available through the SVS store in June.
Interactive sessions - Meeting organizers have added more opportunities for small group and audience interaction during and after sessions.
Industry’s best – This year’s Exhibit Hall will run for two days with longer hours each day than in previous years. It will feature the crowd-pleasing Vascular Live sessions each day, as well as exhibits showing off innovative devices and offering a chance to chat one-on-one with company representatives. To add to the festivities, a scavenger hunt will foster interaction.
Familiar favorites will be back – workshops, postgraduate courses, international sessions, posters, collaborative events with other societies and many, many chances to network and catch up with old friends. The essential VAM on Demand post-meeting slides, audio and video will help members revisit VAM anytime.
Learn more about the 2018 VAM here: All about VAM18
When: June 20-23
Where: Hynes Convention Center, Boston
Scientific Sessions: June 21-23
Exhibit Hall: June 21-22
Register: vsweb.org/VAM18
#VAM18
What’s happening this year at the Society for Vascular Surgery’s Vascular Annual Meeting?
- Enhanced online program planner that syncs with meeting app and makes it simple to plan your schedule. Follow this link to start now
- New opportunities for audience participation and discussion
- Programming aimed at physicians and the vascular team in all practice settings
- Cooperative scheduling with the Society for Vascular Nursing and physician assistants
- Great minds, stimulating discussions and events that include the entire vascular team
The 2018 VAM, sponsored by the SVS, will be at the Hynes Convention Center in Boston, Mass., June 20-23. The scientific sessions and exhibit hall open June 21. Registration numbers are already exceeding last year’s benchmarks, organizers said.
Abstracts for all the scientific sessions will be available in the June Journal of Vascular Surgery supplement.
Some of the highlights:
Inclusive. – This year’s meeting has a theme: The Vascular Team: Partners in Patient Care. Every member of the vascular team – surgeons, nurses, nurse practitioners, PAs – will find a reason to attend.
The meeting provides programming across all practice settings with an even stronger focus on practical, take-home information for all.
View Dr. Darling’s “wicked awesome” Welcome to VAM18 video
The Society for Vascular Nursing’s annual meeting will be in the same location June 20-21. Registration for the SVN meeting includes access to VAM.
This year, the newly established membership section for vascular PAs will present PA-focused education. Within just the past few months, more than 130 PAs joined SVS and many are expected to be at VAM.
An Intuitive Planner - VAM18 meeting will see a new online program planner that allows attendees to filter by session type, areas of interest, faculty, and more. Attendees can favorite a session to build their own meeting schedule. The online planner will sync with the new meeting mobile app, so that attendees can carry their schedule with them. The mobile app will be available through the SVS store in June.
Interactive sessions - Meeting organizers have added more opportunities for small group and audience interaction during and after sessions.
Industry’s best – This year’s Exhibit Hall will run for two days with longer hours each day than in previous years. It will feature the crowd-pleasing Vascular Live sessions each day, as well as exhibits showing off innovative devices and offering a chance to chat one-on-one with company representatives. To add to the festivities, a scavenger hunt will foster interaction.
Familiar favorites will be back – workshops, postgraduate courses, international sessions, posters, collaborative events with other societies and many, many chances to network and catch up with old friends. The essential VAM on Demand post-meeting slides, audio and video will help members revisit VAM anytime.
Learn more about the 2018 VAM here: All about VAM18
When: June 20-23
Where: Hynes Convention Center, Boston
Scientific Sessions: June 21-23
Exhibit Hall: June 21-22
Register: vsweb.org/VAM18
#VAM18
What’s happening this year at the Society for Vascular Surgery’s Vascular Annual Meeting?
- Enhanced online program planner that syncs with meeting app and makes it simple to plan your schedule. Follow this link to start now
- New opportunities for audience participation and discussion
- Programming aimed at physicians and the vascular team in all practice settings
- Cooperative scheduling with the Society for Vascular Nursing and physician assistants
- Great minds, stimulating discussions and events that include the entire vascular team
The 2018 VAM, sponsored by the SVS, will be at the Hynes Convention Center in Boston, Mass., June 20-23. The scientific sessions and exhibit hall open June 21. Registration numbers are already exceeding last year’s benchmarks, organizers said.
Abstracts for all the scientific sessions will be available in the June Journal of Vascular Surgery supplement.
Some of the highlights:
Inclusive. – This year’s meeting has a theme: The Vascular Team: Partners in Patient Care. Every member of the vascular team – surgeons, nurses, nurse practitioners, PAs – will find a reason to attend.
The meeting provides programming across all practice settings with an even stronger focus on practical, take-home information for all.
View Dr. Darling’s “wicked awesome” Welcome to VAM18 video
The Society for Vascular Nursing’s annual meeting will be in the same location June 20-21. Registration for the SVN meeting includes access to VAM.
This year, the newly established membership section for vascular PAs will present PA-focused education. Within just the past few months, more than 130 PAs joined SVS and many are expected to be at VAM.
An Intuitive Planner - VAM18 meeting will see a new online program planner that allows attendees to filter by session type, areas of interest, faculty, and more. Attendees can favorite a session to build their own meeting schedule. The online planner will sync with the new meeting mobile app, so that attendees can carry their schedule with them. The mobile app will be available through the SVS store in June.
Interactive sessions - Meeting organizers have added more opportunities for small group and audience interaction during and after sessions.
Industry’s best – This year’s Exhibit Hall will run for two days with longer hours each day than in previous years. It will feature the crowd-pleasing Vascular Live sessions each day, as well as exhibits showing off innovative devices and offering a chance to chat one-on-one with company representatives. To add to the festivities, a scavenger hunt will foster interaction.
Familiar favorites will be back – workshops, postgraduate courses, international sessions, posters, collaborative events with other societies and many, many chances to network and catch up with old friends. The essential VAM on Demand post-meeting slides, audio and video will help members revisit VAM anytime.
Learn more about the 2018 VAM here: All about VAM18
Five things to do around the convention center at CHEST 2018
Planning to attend CHEST 2018? We know you’re always on the go, so we’ve come up with a few quick things to do in San Antonio without having to go more than a few blocks outside of the convention center.
Whataburger
While some may be hardcore In-N-Out fans, there’s another well known burger joint in Texas with a location that happens to be next to the convention center on E Commerce St. Head on over to Whataburger and experience what the company calls a “bigger, better burger.”
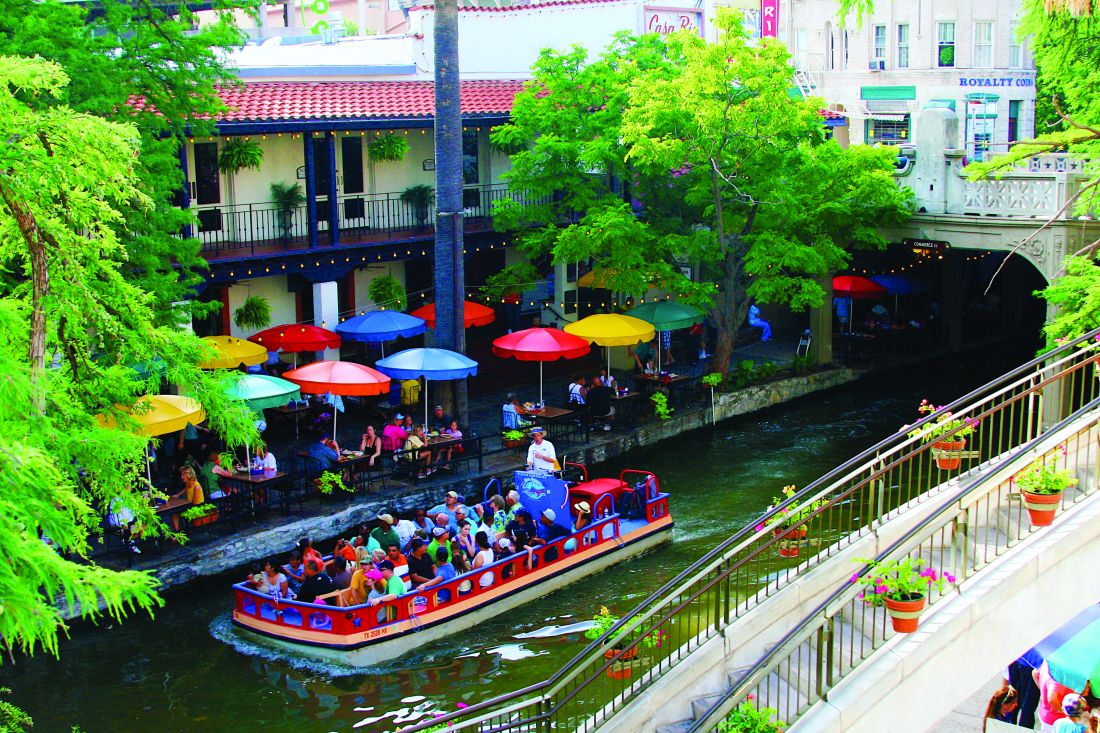
San Antonio Riverwalk
Want to experience the San Antonio, Texas atmosphere but don’t have time for a long excursion? The Henry B. Gonzalez Convention Center is a few steps away from the Riverwalk, which winds throughout the city. Off of the northwest corner of the convention center, take a stroll and experience the picturesque beauty of the San Antonio river, the restaurants, and the bright colorful surroundings.
La Villita Historic Arts Village
Interested in art? Interested in architecture? La Villita, located on the west side of the convention center on S Alamo St, is on the US government’s National Register of Historic Places as a Historic District. Take a look at different architectural styles, like adobe, early Victorian, and Texas vernacular limestone buildings. You’ll find markers throughout La Villita with information about each building’s history. You’ll also find local artists, custom art, and unique dining options.
Tower of the Americas
Exit the south end of the convention center to go to the Tower of the Americas for a spectacular view of the city. This 750-foot tall tower has an observation deck, revolving restaurant with panoramic views, a stationary bar, and a 4D theater adventure ride great for the whole family. This is a great stop for lunch, dinner, or a nice afternoon activity.
The Alamo
Lastly, if you have an hour to spare, take a tour of the Alamo that commemorates the 1836 siege and battle. There are free and ticketed activities, including audio or guided tours (ticketed) or history talks, visiting the Alamo Church, exhibitions, and more! Don’t forget to stop at the gift shop for a souvenir or two to take home.
Planning to attend CHEST 2018? We know you’re always on the go, so we’ve come up with a few quick things to do in San Antonio without having to go more than a few blocks outside of the convention center.
Whataburger
While some may be hardcore In-N-Out fans, there’s another well known burger joint in Texas with a location that happens to be next to the convention center on E Commerce St. Head on over to Whataburger and experience what the company calls a “bigger, better burger.”
San Antonio Riverwalk
Want to experience the San Antonio, Texas atmosphere but don’t have time for a long excursion? The Henry B. Gonzalez Convention Center is a few steps away from the Riverwalk, which winds throughout the city. Off of the northwest corner of the convention center, take a stroll and experience the picturesque beauty of the San Antonio river, the restaurants, and the bright colorful surroundings.
La Villita Historic Arts Village
Interested in art? Interested in architecture? La Villita, located on the west side of the convention center on S Alamo St, is on the US government’s National Register of Historic Places as a Historic District. Take a look at different architectural styles, like adobe, early Victorian, and Texas vernacular limestone buildings. You’ll find markers throughout La Villita with information about each building’s history. You’ll also find local artists, custom art, and unique dining options.
Tower of the Americas
Exit the south end of the convention center to go to the Tower of the Americas for a spectacular view of the city. This 750-foot tall tower has an observation deck, revolving restaurant with panoramic views, a stationary bar, and a 4D theater adventure ride great for the whole family. This is a great stop for lunch, dinner, or a nice afternoon activity.
The Alamo
Lastly, if you have an hour to spare, take a tour of the Alamo that commemorates the 1836 siege and battle. There are free and ticketed activities, including audio or guided tours (ticketed) or history talks, visiting the Alamo Church, exhibitions, and more! Don’t forget to stop at the gift shop for a souvenir or two to take home.
Planning to attend CHEST 2018? We know you’re always on the go, so we’ve come up with a few quick things to do in San Antonio without having to go more than a few blocks outside of the convention center.
Whataburger
While some may be hardcore In-N-Out fans, there’s another well known burger joint in Texas with a location that happens to be next to the convention center on E Commerce St. Head on over to Whataburger and experience what the company calls a “bigger, better burger.”
San Antonio Riverwalk
Want to experience the San Antonio, Texas atmosphere but don’t have time for a long excursion? The Henry B. Gonzalez Convention Center is a few steps away from the Riverwalk, which winds throughout the city. Off of the northwest corner of the convention center, take a stroll and experience the picturesque beauty of the San Antonio river, the restaurants, and the bright colorful surroundings.
La Villita Historic Arts Village
Interested in art? Interested in architecture? La Villita, located on the west side of the convention center on S Alamo St, is on the US government’s National Register of Historic Places as a Historic District. Take a look at different architectural styles, like adobe, early Victorian, and Texas vernacular limestone buildings. You’ll find markers throughout La Villita with information about each building’s history. You’ll also find local artists, custom art, and unique dining options.
Tower of the Americas
Exit the south end of the convention center to go to the Tower of the Americas for a spectacular view of the city. This 750-foot tall tower has an observation deck, revolving restaurant with panoramic views, a stationary bar, and a 4D theater adventure ride great for the whole family. This is a great stop for lunch, dinner, or a nice afternoon activity.
The Alamo
Lastly, if you have an hour to spare, take a tour of the Alamo that commemorates the 1836 siege and battle. There are free and ticketed activities, including audio or guided tours (ticketed) or history talks, visiting the Alamo Church, exhibitions, and more! Don’t forget to stop at the gift shop for a souvenir or two to take home.
New lung cancer screening guideline from CHEST
An update to CHEST’s lung cancer screening guideline, Screening for Lung Cancer: CHEST Guideline and Expert Panel Report, has just been published online in the journal CHEST®. This update was made possible by the hard work of my co-authors and the amazing support of the CHEST staff.
Our goal was to update the evidence base for the benefit, harms, and implementation of low-radiation dose chest CT screening, then use this evidence base to produce meaningful and usable recommendations. The process for developing the guideline followed the rigorous methodological standards of CHEST in which the evidence was gathered from a systematic literature review, and the overall quality of the body of evidence was assessed using the GRADE approach. Recommendations were developed and graded based on this assessment.
There are a few aspects of the new guidelines to highlight. First, we have updated some of the core recommendations; second, we have developed new recommendations related to the implementation of high-quality screening; and third, the CHEST approach to guideline development has evolved to allow us to provide recommendations in which the evidence allows and statements based on experience and expert consensus in which it does not. Through this process, we developed six graded recommendations and nine ungraded consensus-based statements.
In this update, a few changes to the core recommendations about who should be screened are worthy to note:
- We have recommended an increase to the upper age of the screen-eligible cohort from 74 to 77, in line with CMS coverage and reflecting the oldest age of participants in the National Lung Screening Trial at the end of the screening period.
- We have directly addressed the cohort of individuals who are at high risk for having/developing lung cancer based on clinical risk prediction calculators but do not meet the current eligibility criteria. We recommended that this cohort should not be routinely screened given the greater potential for this cohort to have comorbid conditions that would influence morbidity from the evaluation and treatment of screen-detected findings and death from any cause. We did, however, state that there will be individuals within the cohort deemed to be at high risk for lung cancer from a clinical risk prediction calculator who are healthy enough to benefit from lung cancer screening and that low-radiation dose CT screening could be considered in these individuals.
- We recommended against low-radiation dose CT screening in cohorts at low risk of developing lung cancer and in individuals with comorbidities that adversely influence their ability to tolerate the evaluation of screen-detected findings, tolerate treatment of an early stage screen-detected lung cancer, or that substantially limit their life expectancy.
- We also highlighted that screening is reserved for patients without symptoms that could be caused by the presence of lung cancer, stressing that all symptomatic patients should receive an appropriate diagnostic evaluation.
Our remaining recommendation and statements are focused on aspects of screening implementation that influence the balance of benefit and harms of screening and lend to an approach to screening that respects patient values. An extensive literature review, followed by a recommendation or statement, is provided to guide programs in the following areas:
- the choice of nodule size to define what constitutes a positive test;
- maximizing compliance with annual screening exams;
- developing a comprehensive approach to lung nodule management;
- minimizing overtreatment of potentially indolent lung cancers;
- the provision of evidence-based tobacco cessation treatment;
- providing effective counseling and shared decision-making visits prior to the low-radiation dose CT scan;
- how to perform the low-radiation dose CT scan;
- structured reporting of the exam results, management of non-nodule findings on the low radiation dose CT; and
- the development of data collection and reporting tools that are capable of assisting with quality improvement initiatives.
Throughout the recommendations and statements, we have tried to be sensitive to the variety of acceptable approaches to screening program organization, ranging from program structures that are entirely decentralized (test ordering, counseling, and management of the findings by the referring provider) to those that are entirely centralized (test ordering, counseling, and management of the findings by the screening program).
Though we have attempted to comprehensively evaluate the literature and balance available evidence with pragmatism and the needs of our patients, we recognize that well-intentioned and informed experts can have different opinions about aspects of our guidelines. This highlights the need for further research to guide the screening community. Most will agree that it is time to increase access to high- quality lung cancer screening programs across the country. We hope that the updated CHEST lung cancer screening guidelines can help catalyze this.
Coinciding with the publication of the guideline, CHEST has developed new e-learning modules on the benefits and harms of CT screening for lung cancer. The modules are based on the CHEST 2018 educational session on the Screening for Lung Cancer Guidelines. The modules are available at chestnet.org/lungcancerscreening.
An update to CHEST’s lung cancer screening guideline, Screening for Lung Cancer: CHEST Guideline and Expert Panel Report, has just been published online in the journal CHEST®. This update was made possible by the hard work of my co-authors and the amazing support of the CHEST staff.
Our goal was to update the evidence base for the benefit, harms, and implementation of low-radiation dose chest CT screening, then use this evidence base to produce meaningful and usable recommendations. The process for developing the guideline followed the rigorous methodological standards of CHEST in which the evidence was gathered from a systematic literature review, and the overall quality of the body of evidence was assessed using the GRADE approach. Recommendations were developed and graded based on this assessment.
There are a few aspects of the new guidelines to highlight. First, we have updated some of the core recommendations; second, we have developed new recommendations related to the implementation of high-quality screening; and third, the CHEST approach to guideline development has evolved to allow us to provide recommendations in which the evidence allows and statements based on experience and expert consensus in which it does not. Through this process, we developed six graded recommendations and nine ungraded consensus-based statements.
In this update, a few changes to the core recommendations about who should be screened are worthy to note:
- We have recommended an increase to the upper age of the screen-eligible cohort from 74 to 77, in line with CMS coverage and reflecting the oldest age of participants in the National Lung Screening Trial at the end of the screening period.
- We have directly addressed the cohort of individuals who are at high risk for having/developing lung cancer based on clinical risk prediction calculators but do not meet the current eligibility criteria. We recommended that this cohort should not be routinely screened given the greater potential for this cohort to have comorbid conditions that would influence morbidity from the evaluation and treatment of screen-detected findings and death from any cause. We did, however, state that there will be individuals within the cohort deemed to be at high risk for lung cancer from a clinical risk prediction calculator who are healthy enough to benefit from lung cancer screening and that low-radiation dose CT screening could be considered in these individuals.
- We recommended against low-radiation dose CT screening in cohorts at low risk of developing lung cancer and in individuals with comorbidities that adversely influence their ability to tolerate the evaluation of screen-detected findings, tolerate treatment of an early stage screen-detected lung cancer, or that substantially limit their life expectancy.
- We also highlighted that screening is reserved for patients without symptoms that could be caused by the presence of lung cancer, stressing that all symptomatic patients should receive an appropriate diagnostic evaluation.
Our remaining recommendation and statements are focused on aspects of screening implementation that influence the balance of benefit and harms of screening and lend to an approach to screening that respects patient values. An extensive literature review, followed by a recommendation or statement, is provided to guide programs in the following areas:
- the choice of nodule size to define what constitutes a positive test;
- maximizing compliance with annual screening exams;
- developing a comprehensive approach to lung nodule management;
- minimizing overtreatment of potentially indolent lung cancers;
- the provision of evidence-based tobacco cessation treatment;
- providing effective counseling and shared decision-making visits prior to the low-radiation dose CT scan;
- how to perform the low-radiation dose CT scan;
- structured reporting of the exam results, management of non-nodule findings on the low radiation dose CT; and
- the development of data collection and reporting tools that are capable of assisting with quality improvement initiatives.
Throughout the recommendations and statements, we have tried to be sensitive to the variety of acceptable approaches to screening program organization, ranging from program structures that are entirely decentralized (test ordering, counseling, and management of the findings by the referring provider) to those that are entirely centralized (test ordering, counseling, and management of the findings by the screening program).
Though we have attempted to comprehensively evaluate the literature and balance available evidence with pragmatism and the needs of our patients, we recognize that well-intentioned and informed experts can have different opinions about aspects of our guidelines. This highlights the need for further research to guide the screening community. Most will agree that it is time to increase access to high- quality lung cancer screening programs across the country. We hope that the updated CHEST lung cancer screening guidelines can help catalyze this.
Coinciding with the publication of the guideline, CHEST has developed new e-learning modules on the benefits and harms of CT screening for lung cancer. The modules are based on the CHEST 2018 educational session on the Screening for Lung Cancer Guidelines. The modules are available at chestnet.org/lungcancerscreening.
An update to CHEST’s lung cancer screening guideline, Screening for Lung Cancer: CHEST Guideline and Expert Panel Report, has just been published online in the journal CHEST®. This update was made possible by the hard work of my co-authors and the amazing support of the CHEST staff.
Our goal was to update the evidence base for the benefit, harms, and implementation of low-radiation dose chest CT screening, then use this evidence base to produce meaningful and usable recommendations. The process for developing the guideline followed the rigorous methodological standards of CHEST in which the evidence was gathered from a systematic literature review, and the overall quality of the body of evidence was assessed using the GRADE approach. Recommendations were developed and graded based on this assessment.
There are a few aspects of the new guidelines to highlight. First, we have updated some of the core recommendations; second, we have developed new recommendations related to the implementation of high-quality screening; and third, the CHEST approach to guideline development has evolved to allow us to provide recommendations in which the evidence allows and statements based on experience and expert consensus in which it does not. Through this process, we developed six graded recommendations and nine ungraded consensus-based statements.
In this update, a few changes to the core recommendations about who should be screened are worthy to note:
- We have recommended an increase to the upper age of the screen-eligible cohort from 74 to 77, in line with CMS coverage and reflecting the oldest age of participants in the National Lung Screening Trial at the end of the screening period.
- We have directly addressed the cohort of individuals who are at high risk for having/developing lung cancer based on clinical risk prediction calculators but do not meet the current eligibility criteria. We recommended that this cohort should not be routinely screened given the greater potential for this cohort to have comorbid conditions that would influence morbidity from the evaluation and treatment of screen-detected findings and death from any cause. We did, however, state that there will be individuals within the cohort deemed to be at high risk for lung cancer from a clinical risk prediction calculator who are healthy enough to benefit from lung cancer screening and that low-radiation dose CT screening could be considered in these individuals.
- We recommended against low-radiation dose CT screening in cohorts at low risk of developing lung cancer and in individuals with comorbidities that adversely influence their ability to tolerate the evaluation of screen-detected findings, tolerate treatment of an early stage screen-detected lung cancer, or that substantially limit their life expectancy.
- We also highlighted that screening is reserved for patients without symptoms that could be caused by the presence of lung cancer, stressing that all symptomatic patients should receive an appropriate diagnostic evaluation.
Our remaining recommendation and statements are focused on aspects of screening implementation that influence the balance of benefit and harms of screening and lend to an approach to screening that respects patient values. An extensive literature review, followed by a recommendation or statement, is provided to guide programs in the following areas:
- the choice of nodule size to define what constitutes a positive test;
- maximizing compliance with annual screening exams;
- developing a comprehensive approach to lung nodule management;
- minimizing overtreatment of potentially indolent lung cancers;
- the provision of evidence-based tobacco cessation treatment;
- providing effective counseling and shared decision-making visits prior to the low-radiation dose CT scan;
- how to perform the low-radiation dose CT scan;
- structured reporting of the exam results, management of non-nodule findings on the low radiation dose CT; and
- the development of data collection and reporting tools that are capable of assisting with quality improvement initiatives.
Throughout the recommendations and statements, we have tried to be sensitive to the variety of acceptable approaches to screening program organization, ranging from program structures that are entirely decentralized (test ordering, counseling, and management of the findings by the referring provider) to those that are entirely centralized (test ordering, counseling, and management of the findings by the screening program).
Though we have attempted to comprehensively evaluate the literature and balance available evidence with pragmatism and the needs of our patients, we recognize that well-intentioned and informed experts can have different opinions about aspects of our guidelines. This highlights the need for further research to guide the screening community. Most will agree that it is time to increase access to high- quality lung cancer screening programs across the country. We hope that the updated CHEST lung cancer screening guidelines can help catalyze this.
Coinciding with the publication of the guideline, CHEST has developed new e-learning modules on the benefits and harms of CT screening for lung cancer. The modules are based on the CHEST 2018 educational session on the Screening for Lung Cancer Guidelines. The modules are available at chestnet.org/lungcancerscreening.
Bringing respiratory care to asthma clinics in Guyana
How it all started
The study abroad project was truly a goal and vision that came about after returning to Guyana after approximately 46 years. I was born in Guyana but left as a child and returned later and joined a mission group. In 2015, I began a personal journey of missionary service with the team of Bridge Global Medical Missions (BGMM) in Georgetown, Guyana. I was the first respiratory therapist to join the team.
I remember during the first few days in the hospitals I was told that there was “a lot of wheezing” in the EDs. Treating patients consisted of just administrating short-acting nebulizer treatments, but I remember being very impressed with the ICU at the main public hospital, Georgetown Public Hospital Corporation (GPHC), because they had the ventilators I could use. However, physicians only managed the patients while the nurses were left to monitor the ventilators and equipment, which they did not understand.
At the Linden Hospital in Guyana, the ED was constantly full of the “wheezers,” and the ICU only had ventilators that were basically nonfunctioning due to language barriers or a lack of biomed professionals. One of my fondest memories was fixing two ventilators from China. I could get the ventilators to work and explain the basic modes because in my mind, it was just a ventilator, and they could see the modes. The problem was the language was all in Chinese! So, we all got together: a Cuban doctor, a Cuban biomed, and a nurse with a translation program and, finally, changed the language to English. It was an interesting day!
When we were on our study abroad trip this past January, I was able to place an intubated patient on that same ventilator. After my first visit to Linden Hospital, I addressed a few of my observations with the medical director, and I will never forget his comment. He said, “I thought respiratory would just come do some nebulizer treatments and show us oxygen.”
Study abroad and respiratory care
Then the vision of my project began, because I needed to show him the scope of the practice of a respiratory therapist. I asked Dr. Heyliger-Thomas of BGMM if she could assist me in promoting a study abroad program in Guyana with the Ministry of Health. It was very important for me to bring my students to Guyana for many reasons, the most important being the profession was needed there, and our students would be excellent representatives.
In 2015, the study “Introduction of spirometry into clinical practice in Georgetown, Guyana: quality and diagnostic outcomes” highlighted increased physician referral to the country’s only COPD/asthma clinic. I wanted to promote the importance of study abroad and international mission work, especially when promoting the care of asthma and the pulmonary patient, which I believe we did. The main project during study abroad was to test the school-aged children in Linden, thereby showing that there was undiagnosed asthma.
The 2 days that we were in Linden brought the largest sign-up for their clinic. When we did our screening at Mackenzie High School, we were able to utilize the portable spirometers and printer purchased by the CHEST Foundation community service grant. We are still collecting data, but the one thing that was revealed was the difficulty in obtaining medication for the treatment of asthma and COPD in some areas.
This project was also a learning experience for our students in many ways: in how they performed their interviews, how the culture affected the way their patients answered their questionnaires, and even how they performed on the tests. The value to the student and the individual of working within a different culture, far away from the norms of North America, allows them to appreciate their patients, the work they do, and their interprofessional team in a whole new light.
I want this experience to have an impact on each student’s life. You are a teacher, an instructor, a mentor, professor, and much more when traveling with 10 students. The most satisfying moment is the transformation you see in them. They are no longer timid and unsure of themselves; they have greater confidence in their abilities and a deeper understanding of the needs of a patient. They finally understand the importance of culture as it pertains to health care.
The effect of the CHEST Foundation grant
Applying for the CHEST Foundation community service grant was the largest grant I had ever attempted. Having a support system behind you is the most important piece of advice I can give to future grant applicants. I could not have completed my grant without our grant team at Texas State University. They truly had my back; and close to the deadline when it seemed insurmountable, they helped push me through it. The other piece of advice is to have a true vision and stick to that vision. The most difficult part of my project was the budget, prioritizing the things or people that I needed. Honestly, I needed help here, because for me, I needed everything. I had to make choices and leave some things out. I focused on what the actual need was for the many.
My ultimate goal for Guyana is to promote and show the need for respiratory care professionals to have that education offered at the University of Guyana as part of its allied health program and assist those in the application to the International Fellowship Program of the American Association of Respiratory Care—there has never been a fellow from Guyana. I believe that Guyana will have the resources, and with assistance, could achieve the goal. My vision and goal started in 2016, and I want to achieve it in the next 10 years.
I would like to thank all the CHEST Foundation donors from the bottom of my heart. This project was real and, as a CHEST member myself, it encourages me to be a better donor. Thank you—for it was and is much appreciated. Finally, I would like to express my thanks to my Co-Assistant Program Director, Holly Wise (Mass Communications) and Amber Hazelett, RRT (RC assistant), and the BGMM team for their entire support throughout the study abroad journey.
(This article was previous published in CHEST Thought Leaders.)
This grant is supported in full by the CHEST Foundation. Donors like you make grants like this possible. Thank you for your generosity and passion for community service and moving the needle forward on improving patient outcomes. To support community service initiatives, and the next generation of lung health champions, please go to foundation.chestnet.org/donate
How it all started
The study abroad project was truly a goal and vision that came about after returning to Guyana after approximately 46 years. I was born in Guyana but left as a child and returned later and joined a mission group. In 2015, I began a personal journey of missionary service with the team of Bridge Global Medical Missions (BGMM) in Georgetown, Guyana. I was the first respiratory therapist to join the team.
I remember during the first few days in the hospitals I was told that there was “a lot of wheezing” in the EDs. Treating patients consisted of just administrating short-acting nebulizer treatments, but I remember being very impressed with the ICU at the main public hospital, Georgetown Public Hospital Corporation (GPHC), because they had the ventilators I could use. However, physicians only managed the patients while the nurses were left to monitor the ventilators and equipment, which they did not understand.
At the Linden Hospital in Guyana, the ED was constantly full of the “wheezers,” and the ICU only had ventilators that were basically nonfunctioning due to language barriers or a lack of biomed professionals. One of my fondest memories was fixing two ventilators from China. I could get the ventilators to work and explain the basic modes because in my mind, it was just a ventilator, and they could see the modes. The problem was the language was all in Chinese! So, we all got together: a Cuban doctor, a Cuban biomed, and a nurse with a translation program and, finally, changed the language to English. It was an interesting day!
When we were on our study abroad trip this past January, I was able to place an intubated patient on that same ventilator. After my first visit to Linden Hospital, I addressed a few of my observations with the medical director, and I will never forget his comment. He said, “I thought respiratory would just come do some nebulizer treatments and show us oxygen.”
Study abroad and respiratory care
Then the vision of my project began, because I needed to show him the scope of the practice of a respiratory therapist. I asked Dr. Heyliger-Thomas of BGMM if she could assist me in promoting a study abroad program in Guyana with the Ministry of Health. It was very important for me to bring my students to Guyana for many reasons, the most important being the profession was needed there, and our students would be excellent representatives.
In 2015, the study “Introduction of spirometry into clinical practice in Georgetown, Guyana: quality and diagnostic outcomes” highlighted increased physician referral to the country’s only COPD/asthma clinic. I wanted to promote the importance of study abroad and international mission work, especially when promoting the care of asthma and the pulmonary patient, which I believe we did. The main project during study abroad was to test the school-aged children in Linden, thereby showing that there was undiagnosed asthma.
The 2 days that we were in Linden brought the largest sign-up for their clinic. When we did our screening at Mackenzie High School, we were able to utilize the portable spirometers and printer purchased by the CHEST Foundation community service grant. We are still collecting data, but the one thing that was revealed was the difficulty in obtaining medication for the treatment of asthma and COPD in some areas.
This project was also a learning experience for our students in many ways: in how they performed their interviews, how the culture affected the way their patients answered their questionnaires, and even how they performed on the tests. The value to the student and the individual of working within a different culture, far away from the norms of North America, allows them to appreciate their patients, the work they do, and their interprofessional team in a whole new light.
I want this experience to have an impact on each student’s life. You are a teacher, an instructor, a mentor, professor, and much more when traveling with 10 students. The most satisfying moment is the transformation you see in them. They are no longer timid and unsure of themselves; they have greater confidence in their abilities and a deeper understanding of the needs of a patient. They finally understand the importance of culture as it pertains to health care.
The effect of the CHEST Foundation grant
Applying for the CHEST Foundation community service grant was the largest grant I had ever attempted. Having a support system behind you is the most important piece of advice I can give to future grant applicants. I could not have completed my grant without our grant team at Texas State University. They truly had my back; and close to the deadline when it seemed insurmountable, they helped push me through it. The other piece of advice is to have a true vision and stick to that vision. The most difficult part of my project was the budget, prioritizing the things or people that I needed. Honestly, I needed help here, because for me, I needed everything. I had to make choices and leave some things out. I focused on what the actual need was for the many.
My ultimate goal for Guyana is to promote and show the need for respiratory care professionals to have that education offered at the University of Guyana as part of its allied health program and assist those in the application to the International Fellowship Program of the American Association of Respiratory Care—there has never been a fellow from Guyana. I believe that Guyana will have the resources, and with assistance, could achieve the goal. My vision and goal started in 2016, and I want to achieve it in the next 10 years.
I would like to thank all the CHEST Foundation donors from the bottom of my heart. This project was real and, as a CHEST member myself, it encourages me to be a better donor. Thank you—for it was and is much appreciated. Finally, I would like to express my thanks to my Co-Assistant Program Director, Holly Wise (Mass Communications) and Amber Hazelett, RRT (RC assistant), and the BGMM team for their entire support throughout the study abroad journey.
(This article was previous published in CHEST Thought Leaders.)
This grant is supported in full by the CHEST Foundation. Donors like you make grants like this possible. Thank you for your generosity and passion for community service and moving the needle forward on improving patient outcomes. To support community service initiatives, and the next generation of lung health champions, please go to foundation.chestnet.org/donate
How it all started
The study abroad project was truly a goal and vision that came about after returning to Guyana after approximately 46 years. I was born in Guyana but left as a child and returned later and joined a mission group. In 2015, I began a personal journey of missionary service with the team of Bridge Global Medical Missions (BGMM) in Georgetown, Guyana. I was the first respiratory therapist to join the team.
I remember during the first few days in the hospitals I was told that there was “a lot of wheezing” in the EDs. Treating patients consisted of just administrating short-acting nebulizer treatments, but I remember being very impressed with the ICU at the main public hospital, Georgetown Public Hospital Corporation (GPHC), because they had the ventilators I could use. However, physicians only managed the patients while the nurses were left to monitor the ventilators and equipment, which they did not understand.
At the Linden Hospital in Guyana, the ED was constantly full of the “wheezers,” and the ICU only had ventilators that were basically nonfunctioning due to language barriers or a lack of biomed professionals. One of my fondest memories was fixing two ventilators from China. I could get the ventilators to work and explain the basic modes because in my mind, it was just a ventilator, and they could see the modes. The problem was the language was all in Chinese! So, we all got together: a Cuban doctor, a Cuban biomed, and a nurse with a translation program and, finally, changed the language to English. It was an interesting day!
When we were on our study abroad trip this past January, I was able to place an intubated patient on that same ventilator. After my first visit to Linden Hospital, I addressed a few of my observations with the medical director, and I will never forget his comment. He said, “I thought respiratory would just come do some nebulizer treatments and show us oxygen.”
Study abroad and respiratory care
Then the vision of my project began, because I needed to show him the scope of the practice of a respiratory therapist. I asked Dr. Heyliger-Thomas of BGMM if she could assist me in promoting a study abroad program in Guyana with the Ministry of Health. It was very important for me to bring my students to Guyana for many reasons, the most important being the profession was needed there, and our students would be excellent representatives.
In 2015, the study “Introduction of spirometry into clinical practice in Georgetown, Guyana: quality and diagnostic outcomes” highlighted increased physician referral to the country’s only COPD/asthma clinic. I wanted to promote the importance of study abroad and international mission work, especially when promoting the care of asthma and the pulmonary patient, which I believe we did. The main project during study abroad was to test the school-aged children in Linden, thereby showing that there was undiagnosed asthma.
The 2 days that we were in Linden brought the largest sign-up for their clinic. When we did our screening at Mackenzie High School, we were able to utilize the portable spirometers and printer purchased by the CHEST Foundation community service grant. We are still collecting data, but the one thing that was revealed was the difficulty in obtaining medication for the treatment of asthma and COPD in some areas.
This project was also a learning experience for our students in many ways: in how they performed their interviews, how the culture affected the way their patients answered their questionnaires, and even how they performed on the tests. The value to the student and the individual of working within a different culture, far away from the norms of North America, allows them to appreciate their patients, the work they do, and their interprofessional team in a whole new light.
I want this experience to have an impact on each student’s life. You are a teacher, an instructor, a mentor, professor, and much more when traveling with 10 students. The most satisfying moment is the transformation you see in them. They are no longer timid and unsure of themselves; they have greater confidence in their abilities and a deeper understanding of the needs of a patient. They finally understand the importance of culture as it pertains to health care.
The effect of the CHEST Foundation grant
Applying for the CHEST Foundation community service grant was the largest grant I had ever attempted. Having a support system behind you is the most important piece of advice I can give to future grant applicants. I could not have completed my grant without our grant team at Texas State University. They truly had my back; and close to the deadline when it seemed insurmountable, they helped push me through it. The other piece of advice is to have a true vision and stick to that vision. The most difficult part of my project was the budget, prioritizing the things or people that I needed. Honestly, I needed help here, because for me, I needed everything. I had to make choices and leave some things out. I focused on what the actual need was for the many.
My ultimate goal for Guyana is to promote and show the need for respiratory care professionals to have that education offered at the University of Guyana as part of its allied health program and assist those in the application to the International Fellowship Program of the American Association of Respiratory Care—there has never been a fellow from Guyana. I believe that Guyana will have the resources, and with assistance, could achieve the goal. My vision and goal started in 2016, and I want to achieve it in the next 10 years.
I would like to thank all the CHEST Foundation donors from the bottom of my heart. This project was real and, as a CHEST member myself, it encourages me to be a better donor. Thank you—for it was and is much appreciated. Finally, I would like to express my thanks to my Co-Assistant Program Director, Holly Wise (Mass Communications) and Amber Hazelett, RRT (RC assistant), and the BGMM team for their entire support throughout the study abroad journey.
(This article was previous published in CHEST Thought Leaders.)
This grant is supported in full by the CHEST Foundation. Donors like you make grants like this possible. Thank you for your generosity and passion for community service and moving the needle forward on improving patient outcomes. To support community service initiatives, and the next generation of lung health champions, please go to foundation.chestnet.org/donate
FDA to host meeting about sleep apnea devices
You are invited to attend this open meeting on April 16, held at the FDA White Oak Campus in Silver Spring, Md. (https://www.fda.gov/MedicalDevices/NewsEvents/WorkshopsConferences/ucm596147.htm). The FDA is soliciting ideas or opinions about criteria or processes for FDA review of medical devices to diagnose or treat sleep apnea. CHEST is represented by Dr. Neil Freedman ([email protected]) and Dr. Barbara Phillips ([email protected]) who also welcome your input by email prior to the meeting. Home testing, “apps,” and the criteria to diagnose sleep apnea and/or its resolution are among the topics to be discussed.
You are invited to attend this open meeting on April 16, held at the FDA White Oak Campus in Silver Spring, Md. (https://www.fda.gov/MedicalDevices/NewsEvents/WorkshopsConferences/ucm596147.htm). The FDA is soliciting ideas or opinions about criteria or processes for FDA review of medical devices to diagnose or treat sleep apnea. CHEST is represented by Dr. Neil Freedman ([email protected]) and Dr. Barbara Phillips ([email protected]) who also welcome your input by email prior to the meeting. Home testing, “apps,” and the criteria to diagnose sleep apnea and/or its resolution are among the topics to be discussed.
You are invited to attend this open meeting on April 16, held at the FDA White Oak Campus in Silver Spring, Md. (https://www.fda.gov/MedicalDevices/NewsEvents/WorkshopsConferences/ucm596147.htm). The FDA is soliciting ideas or opinions about criteria or processes for FDA review of medical devices to diagnose or treat sleep apnea. CHEST is represented by Dr. Neil Freedman ([email protected]) and Dr. Barbara Phillips ([email protected]) who also welcome your input by email prior to the meeting. Home testing, “apps,” and the criteria to diagnose sleep apnea and/or its resolution are among the topics to be discussed.
“No consequence” Knowledge Check-In expands
In 2018, ABIM is introducing the new Knowledge Check-In assessment option, an every-2-year assessment option serving as an alternative to the 10-year assessment model. Initially, for 2018, this option will be piloted for both Internal Medicine and Nephrology. In 2019, the Knowledge Check-In will expand to several additional specialties, including Pulmonary Disease. The remaining specialties, including Critical Care Medicine, will become available in 2020.
Previously, ABIM announced that physicians taking the Knowledge Check-In in 2018—the initial year it is offered in Internal Medicine or Nephrology—would have another chance to take it again 2 years later if they were unsuccessful, even if they were due to pass the exam that year. Based on feedback ABIM received from the physician community, this feature is now being extended to include all other Internal Medicine subspecialties in the future. Therefore, if a physician opts to take the Knowledge Check-In the first year it is offered in their subspecialty and is unsuccessful, they will get at least one additional opportunity to take it 2 years later.
For more information visit www.abim.org/checkin.
In 2018, ABIM is introducing the new Knowledge Check-In assessment option, an every-2-year assessment option serving as an alternative to the 10-year assessment model. Initially, for 2018, this option will be piloted for both Internal Medicine and Nephrology. In 2019, the Knowledge Check-In will expand to several additional specialties, including Pulmonary Disease. The remaining specialties, including Critical Care Medicine, will become available in 2020.
Previously, ABIM announced that physicians taking the Knowledge Check-In in 2018—the initial year it is offered in Internal Medicine or Nephrology—would have another chance to take it again 2 years later if they were unsuccessful, even if they were due to pass the exam that year. Based on feedback ABIM received from the physician community, this feature is now being extended to include all other Internal Medicine subspecialties in the future. Therefore, if a physician opts to take the Knowledge Check-In the first year it is offered in their subspecialty and is unsuccessful, they will get at least one additional opportunity to take it 2 years later.
For more information visit www.abim.org/checkin.
In 2018, ABIM is introducing the new Knowledge Check-In assessment option, an every-2-year assessment option serving as an alternative to the 10-year assessment model. Initially, for 2018, this option will be piloted for both Internal Medicine and Nephrology. In 2019, the Knowledge Check-In will expand to several additional specialties, including Pulmonary Disease. The remaining specialties, including Critical Care Medicine, will become available in 2020.
Previously, ABIM announced that physicians taking the Knowledge Check-In in 2018—the initial year it is offered in Internal Medicine or Nephrology—would have another chance to take it again 2 years later if they were unsuccessful, even if they were due to pass the exam that year. Based on feedback ABIM received from the physician community, this feature is now being extended to include all other Internal Medicine subspecialties in the future. Therefore, if a physician opts to take the Knowledge Check-In the first year it is offered in their subspecialty and is unsuccessful, they will get at least one additional opportunity to take it 2 years later.
For more information visit www.abim.org/checkin.
New strategic plan for CHEST
We are pleased to announce the completion of a new, multiyear strategic plan for CHEST. Over the past few years, key stakeholders have provided essential input, resulting in a plan that identifies a very focused set of priorities we’ll pursue to help achieve our overarching strategy. Having selected these priorities, which leverage our strengths and strategic advantages, we are committed to dedicating sufficient resources toward their accomplishment over the next several years.
Each year, the plan will be reviewed and modified to reflect changes to CHEST priorities.
A strategic plan is an important tool for our organization because it truly does focus and direct our efforts and resources. Guided by our 2013-2017 strategic plan, we were able to accomplish the following:
- Developed events, products, and services that produced meaningful education for the CHEST community and generated positive financial margins;
- Optimized our membership model to increase engagement of all clinicians on the health-care team;
- Enhanced our global presence through guideline development and increased educational offerings;
- Launched a new Association Management System (AMS) and made strides to becoming a data-driven organization;
- Built and moved into a new building that enhanced our ability to develop and host courses in the CHEST Innovation, Simulation, and Training Center;
- Increased our visibility through our rebrand as “CHEST”;
- Fostered relationships and collaborated with other organizations to promote lung health through the CHEST Foundation; and
- Met our budget goals and financial covenants with our bank, and increased the CHEST Foundation’s corpus for grants and awards.
This new strategic plan can be found on chestnet.org under the “About” section. As members of CHEST, we invite you to review what’s outlined and become familiar with what the plan encompasses. This plan provides details to help you understand the future direction of CHEST, and we know you’ll support us in these important endeavors.
We are pleased to announce the completion of a new, multiyear strategic plan for CHEST. Over the past few years, key stakeholders have provided essential input, resulting in a plan that identifies a very focused set of priorities we’ll pursue to help achieve our overarching strategy. Having selected these priorities, which leverage our strengths and strategic advantages, we are committed to dedicating sufficient resources toward their accomplishment over the next several years.
Each year, the plan will be reviewed and modified to reflect changes to CHEST priorities.
A strategic plan is an important tool for our organization because it truly does focus and direct our efforts and resources. Guided by our 2013-2017 strategic plan, we were able to accomplish the following:
- Developed events, products, and services that produced meaningful education for the CHEST community and generated positive financial margins;
- Optimized our membership model to increase engagement of all clinicians on the health-care team;
- Enhanced our global presence through guideline development and increased educational offerings;
- Launched a new Association Management System (AMS) and made strides to becoming a data-driven organization;
- Built and moved into a new building that enhanced our ability to develop and host courses in the CHEST Innovation, Simulation, and Training Center;
- Increased our visibility through our rebrand as “CHEST”;
- Fostered relationships and collaborated with other organizations to promote lung health through the CHEST Foundation; and
- Met our budget goals and financial covenants with our bank, and increased the CHEST Foundation’s corpus for grants and awards.
This new strategic plan can be found on chestnet.org under the “About” section. As members of CHEST, we invite you to review what’s outlined and become familiar with what the plan encompasses. This plan provides details to help you understand the future direction of CHEST, and we know you’ll support us in these important endeavors.
We are pleased to announce the completion of a new, multiyear strategic plan for CHEST. Over the past few years, key stakeholders have provided essential input, resulting in a plan that identifies a very focused set of priorities we’ll pursue to help achieve our overarching strategy. Having selected these priorities, which leverage our strengths and strategic advantages, we are committed to dedicating sufficient resources toward their accomplishment over the next several years.
Each year, the plan will be reviewed and modified to reflect changes to CHEST priorities.
A strategic plan is an important tool for our organization because it truly does focus and direct our efforts and resources. Guided by our 2013-2017 strategic plan, we were able to accomplish the following:
- Developed events, products, and services that produced meaningful education for the CHEST community and generated positive financial margins;
- Optimized our membership model to increase engagement of all clinicians on the health-care team;
- Enhanced our global presence through guideline development and increased educational offerings;
- Launched a new Association Management System (AMS) and made strides to becoming a data-driven organization;
- Built and moved into a new building that enhanced our ability to develop and host courses in the CHEST Innovation, Simulation, and Training Center;
- Increased our visibility through our rebrand as “CHEST”;
- Fostered relationships and collaborated with other organizations to promote lung health through the CHEST Foundation; and
- Met our budget goals and financial covenants with our bank, and increased the CHEST Foundation’s corpus for grants and awards.
This new strategic plan can be found on chestnet.org under the “About” section. As members of CHEST, we invite you to review what’s outlined and become familiar with what the plan encompasses. This plan provides details to help you understand the future direction of CHEST, and we know you’ll support us in these important endeavors.
This month in the journal CHEST®
Giants In Chest Medicine
Professor Emeritus Elizabeth F. Juniper, MCSP, MSc
By Dr. P. M. O’Byrne
Original Research
A Population-Based Cohort Study on the Drug-Specific Effect of Statins on Sepsis Outcome.
A Multicenter Randomized Trial of a Checklist for Endotracheal Intubation of Critically Ill Adults.
By Dr. D. R. Janz, et al.
Determinants of Unintentional Leaks During CPAP Treatment in OSA.
By Dr. M. Lebret, et al.
Evidence-Based Medicine
Screening for Lung Cancer: CHEST Guideline and Expert Panel Report.
By Dr. P. J. Mazzone, et al.
Treating Cough Due to Non-CF and CF Bronchiectasis With Nonpharmacological Airway Clearance: CHEST Expert Panel Report.
By Dr. A. T. Hill, et al.
Giants In Chest Medicine
Professor Emeritus Elizabeth F. Juniper, MCSP, MSc
By Dr. P. M. O’Byrne
Original Research
A Population-Based Cohort Study on the Drug-Specific Effect of Statins on Sepsis Outcome.
A Multicenter Randomized Trial of a Checklist for Endotracheal Intubation of Critically Ill Adults.
By Dr. D. R. Janz, et al.
Determinants of Unintentional Leaks During CPAP Treatment in OSA.
By Dr. M. Lebret, et al.
Evidence-Based Medicine
Screening for Lung Cancer: CHEST Guideline and Expert Panel Report.
By Dr. P. J. Mazzone, et al.
Treating Cough Due to Non-CF and CF Bronchiectasis With Nonpharmacological Airway Clearance: CHEST Expert Panel Report.
By Dr. A. T. Hill, et al.
Giants In Chest Medicine
Professor Emeritus Elizabeth F. Juniper, MCSP, MSc
By Dr. P. M. O’Byrne
Original Research
A Population-Based Cohort Study on the Drug-Specific Effect of Statins on Sepsis Outcome.
A Multicenter Randomized Trial of a Checklist for Endotracheal Intubation of Critically Ill Adults.
By Dr. D. R. Janz, et al.
Determinants of Unintentional Leaks During CPAP Treatment in OSA.
By Dr. M. Lebret, et al.
Evidence-Based Medicine
Screening for Lung Cancer: CHEST Guideline and Expert Panel Report.
By Dr. P. J. Mazzone, et al.
Treating Cough Due to Non-CF and CF Bronchiectasis With Nonpharmacological Airway Clearance: CHEST Expert Panel Report.
By Dr. A. T. Hill, et al.
SAVE LIVES: Clean your hands
The World Health Organization (WHO) has announced its annual SAVE LIVES: Clean Your Hands 2018 campaign (Saito, et al. J Hosp Infect. 2018;98[4]:321), designating May 5, 2018, as world hand hygiene day.
Health-care-associated infections are a major patient safety problem. Unfortunately, their spread is common in hospitals and ICUs around the globe. The vehicle for these infections, including multidrug-resistant organisms, is frequently the contaminated hands of health-care workers. Health-care-acquired infections, as any other infection, can lead to sepsis and death. Infections acquired in the ICU are especially deadly, with mortalities that can be as high as 80%. Proper hand hygiene, despite being simple and inexpensive, is the single most important means of reducing the prevalence of hospital-acquired infections and the spread of antimicrobial resistance.
We have known about the significance of hand washing since the early 19th century. More recent data show that hand washing can reduce the overall prevalence of hospital-acquired infections and the cross-transmission of multidrug-resistant organisms. It is estimated that we can prevent 15% to 30% of these infections with adequate hand washing alone.
Despite the clear benefit and the understanding of the importance of hand washing, compliance with this simple intervention is only about 50%. Health-care workers tend to overestimate these rates, self-reporting a compliance of 75%. Even the latter number represents a lot of missed opportunities, and we must do something about it.
A multifaceted approach that combines education with written material, reminders, and continued feedback on performance can have an important effect on hand washing compliance and rates of hospital-acquired infections.
Sepsis is the single most important cause of death in hospitals in the United States. The campaign (http://www.who.int/infection-prevention/campaigns/clean-hands/en/), sponsored by the World Health Organization, should serve as a reminder to all health-care workers about the importance of adequate hand washing and as an opportunity to improve our compliance moving forward.
Despite the progress made, there is still a lot of room for improvement. We can have an impact on the number of deaths from sepsis by preventing them to occur in the first place. Wash your hands and do it well, it does not cost us anything.
Remember: It is in our hands – prevent sepsis and save lives!
Shruti Gadre, MD
Steering Committee Member, Critical Care NetWork
Angel Coz, MD, FCCP
Chair, Critical Care NetWork
The World Health Organization (WHO) has announced its annual SAVE LIVES: Clean Your Hands 2018 campaign (Saito, et al. J Hosp Infect. 2018;98[4]:321), designating May 5, 2018, as world hand hygiene day.
Health-care-associated infections are a major patient safety problem. Unfortunately, their spread is common in hospitals and ICUs around the globe. The vehicle for these infections, including multidrug-resistant organisms, is frequently the contaminated hands of health-care workers. Health-care-acquired infections, as any other infection, can lead to sepsis and death. Infections acquired in the ICU are especially deadly, with mortalities that can be as high as 80%. Proper hand hygiene, despite being simple and inexpensive, is the single most important means of reducing the prevalence of hospital-acquired infections and the spread of antimicrobial resistance.
We have known about the significance of hand washing since the early 19th century. More recent data show that hand washing can reduce the overall prevalence of hospital-acquired infections and the cross-transmission of multidrug-resistant organisms. It is estimated that we can prevent 15% to 30% of these infections with adequate hand washing alone.
Despite the clear benefit and the understanding of the importance of hand washing, compliance with this simple intervention is only about 50%. Health-care workers tend to overestimate these rates, self-reporting a compliance of 75%. Even the latter number represents a lot of missed opportunities, and we must do something about it.
A multifaceted approach that combines education with written material, reminders, and continued feedback on performance can have an important effect on hand washing compliance and rates of hospital-acquired infections.
Sepsis is the single most important cause of death in hospitals in the United States. The campaign (http://www.who.int/infection-prevention/campaigns/clean-hands/en/), sponsored by the World Health Organization, should serve as a reminder to all health-care workers about the importance of adequate hand washing and as an opportunity to improve our compliance moving forward.
Despite the progress made, there is still a lot of room for improvement. We can have an impact on the number of deaths from sepsis by preventing them to occur in the first place. Wash your hands and do it well, it does not cost us anything.
Remember: It is in our hands – prevent sepsis and save lives!
Shruti Gadre, MD
Steering Committee Member, Critical Care NetWork
Angel Coz, MD, FCCP
Chair, Critical Care NetWork
The World Health Organization (WHO) has announced its annual SAVE LIVES: Clean Your Hands 2018 campaign (Saito, et al. J Hosp Infect. 2018;98[4]:321), designating May 5, 2018, as world hand hygiene day.
Health-care-associated infections are a major patient safety problem. Unfortunately, their spread is common in hospitals and ICUs around the globe. The vehicle for these infections, including multidrug-resistant organisms, is frequently the contaminated hands of health-care workers. Health-care-acquired infections, as any other infection, can lead to sepsis and death. Infections acquired in the ICU are especially deadly, with mortalities that can be as high as 80%. Proper hand hygiene, despite being simple and inexpensive, is the single most important means of reducing the prevalence of hospital-acquired infections and the spread of antimicrobial resistance.
We have known about the significance of hand washing since the early 19th century. More recent data show that hand washing can reduce the overall prevalence of hospital-acquired infections and the cross-transmission of multidrug-resistant organisms. It is estimated that we can prevent 15% to 30% of these infections with adequate hand washing alone.
Despite the clear benefit and the understanding of the importance of hand washing, compliance with this simple intervention is only about 50%. Health-care workers tend to overestimate these rates, self-reporting a compliance of 75%. Even the latter number represents a lot of missed opportunities, and we must do something about it.
A multifaceted approach that combines education with written material, reminders, and continued feedback on performance can have an important effect on hand washing compliance and rates of hospital-acquired infections.
Sepsis is the single most important cause of death in hospitals in the United States. The campaign (http://www.who.int/infection-prevention/campaigns/clean-hands/en/), sponsored by the World Health Organization, should serve as a reminder to all health-care workers about the importance of adequate hand washing and as an opportunity to improve our compliance moving forward.
Despite the progress made, there is still a lot of room for improvement. We can have an impact on the number of deaths from sepsis by preventing them to occur in the first place. Wash your hands and do it well, it does not cost us anything.
Remember: It is in our hands – prevent sepsis and save lives!
Shruti Gadre, MD
Steering Committee Member, Critical Care NetWork
Angel Coz, MD, FCCP
Chair, Critical Care NetWork