User login
Primary renal synovial sarcoma – a diagnostic dilemma
Soft tissue sarcomas are rare mesenchymal tumors that comprise 1% of all malignancies. Synovial sarcoma accounts for 5% to 10% of adult soft tissue sarcomas and usually occurs in close association with joint capsules, tendon sheaths, and bursa in the extremities of young and middle-aged adults.1 Synovial sarcomas have been reported in other unusual sites, including the head and neck, thoracic and abdominal wall, retroperitoneum, bone, pleura, and visceral organs such as the lung, prostate, or kidney.2 Primary renal synovial sarcoma is an extremely rare tumor accounting for <2% of all malignant renal tumors.3 To the best of our knowledge, fewer than 50 cases of primary renal synovial sarcoma have been described in the English literature.4 It presents as a diagnostic dilemma because of the dearth of specific clinical and imaging findings and is often confused with benign and malignant tumors. The differential diagnosis includes angiomyolipoma, renal cell carcinoma with sarcomatoid differentiation, metastatic sarcoma, hemangiopericytoma, malignant solitary fibrous tumor, Wilms tumor, and malignant peripheral nerve sheath tumor. Hence, a combination of histomorphologic, immunohistochemical, cytogenetic, and molecular studies that show a unique chromosomal translocation t(X;18) (p11;q11) is imperative in the diagnosis of primary renal synovial sarcoma.4 In the present report, we present the case of a 38-year-old man who was diagnosed with primary renal synovial sarcoma.
Case presentation and summary
A 38-year-old man with a medical history of gastroesophageal reflux disease and Barrett’s esophagus presented to our hospital for the first time with persistent and progressive right-sided flank and abdominal pain that was aggravated after a minor trauma to the back. There was no associated hematuria or dysuria.
Of note is that he had experienced intermittent flank pain for 2 years before this transfer. He had initially been diagnosed at his local hospital close to his home by ultrasound with an angiomyolipoma of 2 × 3 cm arising from the upper pole of his right kidney, which remained stable on repeat sonograms. About 22 months after his initial presentation at his local hospital, the flank pain increased, and a computed-tomographic (CT) scan revealed a perinephric hematoma that was thought to originate from a ruptured angiomyolipoma. He subsequently underwent embolization, but his symptoms recurred soon after. He presented again to his local hospital where CT imaging revealed a significant increase in the size of the retroperitoneal mass, and findings were suggestive of a hematoma. Subsequent angiogram did not reveal active extravasation, so a biopsy was performed.
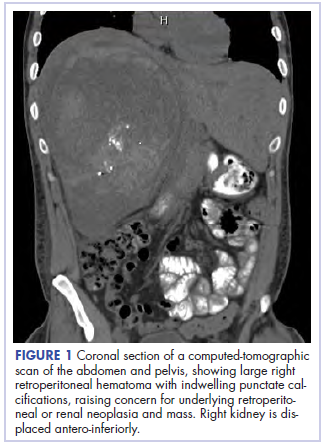
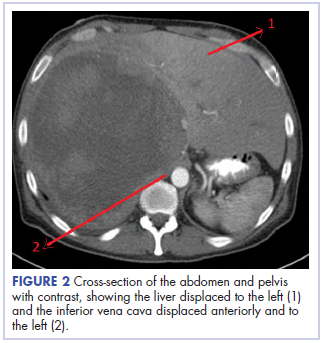
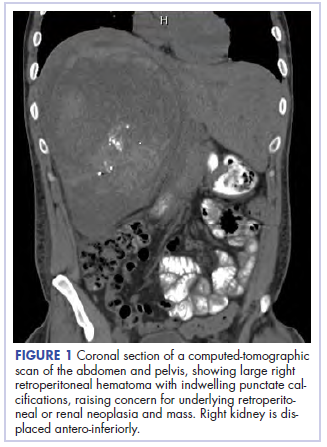
Before confirmatory pathologic evaluation could be completed, the patient presented to his local hospital again in excruciating pain. A CT scan of his abdomen and pelvis demonstrated a massive subacute on chronic hematoma in the right retroperitoneum measuring 22 × 19 × 18 cm, with calcifications originating from an upper pole right renal neoplasm. The right kidney was displaced antero-inferiorly, and the inferior vena cava was displaced anteriorly and to the left. The preliminary pathology returned with findings suggestive of sarcoma (Figures 1 and 2).
The patient was then transferred to our institution, where he was evaluated by medical and surgical oncology. A CT scan of the chest and magnetic-resonance imaging (MRI) of the brain did not reveal metastatic disease. He underwent exploratory laparotomy that involved the resection of a 22-cm retroperitoneal mass, right nephrectomy, right adrenalectomy, partial right hepatectomy, and a full thickness resection of the right postero-inferior diaphragm followed by mesh repair because of involvement by the tumor.
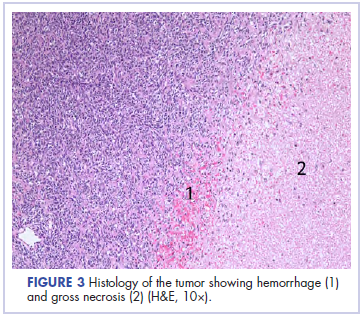
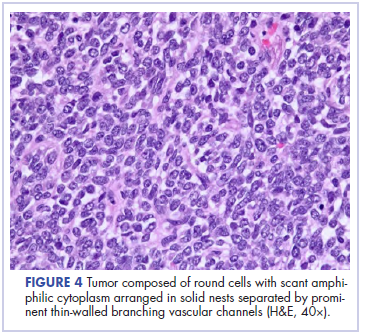
In its entirety, the specimen was a mass of 26 × 24 × 14 cm. It was sectioned to show extensively necrotic and hemorrhagic variegated white to tan-red parenchyma (Figure 3). Histology revealed a poorly differentiated malignant neoplasm composed of round cells with scant amphophilic cytoplasm arranged in solid, variably sized nests separated by prominent thin-walled branching vascular channels (Figure 4). The mitotic rate was high. It was determined to be a histologically ungraded sarcoma according to the French Federation of Comprehensive Cancer Centers system of grading soft tissue sarcomas; the margins were indeterminate. Immunohistochemistry was positive for EMA, TLE1, and negative for AE1/AE3, S100, STAT6, and Nkx2.2. Molecular pathology fluorescent in situ hybridization (FISH) analysis demonstrated positivity for SS18 gene rearrangement (SS18-SSX1 fusion).
After recovering from surgery, the patient received adjuvant chemotherapy with doxorubicin and ifosfamide. It has been almost 16 months since we first saw this patient. He was started on doxorubicin 20 mg/m2 on days 1 to 4, ifosfamide 2,500 mg on days 1 to 4, and mesna 800 mg on days 1 to 4, for a total of 6 cycles. He did well for the first 5 months, after which he developed disease recurrence in the postoperative nephrectomy bed (a biopsy showed it to be recurrent synovial sarcoma) as well as pulmonary nodules, for which he was started on trabectedin 1.5 mg/m2 every 3 weeks. Two months later, a CT scan showed an increase in the size of his retroperitoneal mass, and the treatment was changed to pazopanib 400 mg daily orally, on which he remained at the time of publication.
Discussion
Synovial sarcoma is the fourth most common type of soft tissue sarcoma, accounting for 2.5% to 10.5% of all primary soft tissue malignancies worldwide. It occurs most frequently in adolescents and young adults, with most patients presenting between the ages of 15 and 40 years. Median age of presentation is 36 years. Despite the nomenclature, synovial sarcoma does not arise in intra-articular locations but typically occurs in proximity to joints in the extremities. Synovial sarcomas are less commonly described in other sites, including the head and neck, mediastinum, intraperitoneum, retroperitoneum, lung, pleura, and kidney.4,5 Renal synovial sarcoma was first described in a published article by Argani and colleagues in 2000.5
Adult renal mesenchymal tumors are classified into benign and malignant tumors on the basis of the histologic features and clinicobiologic behavior.6,7 The benign esenchymal renal tumors include angiomyolipoma, leiomyoma, hemangioma, lymphangioma, juxtaglomerular cell tumor, renomedullary interstitial cell tumor (medullary fibroma), lipoma, solitary fibrous tumor, and schwannoma. Malignant renal tumors of mesenchymal origin include leiomyosarcoma, rhabdomyosarcoma, angiosarcoma, osteosarcoma, fibrosarcoma, malignant fibrous histiocytoma, solitary fibrous tumor, and synovial sarcoma.
Most of these tumor types cause the same nonspecific symptoms in patients – abdominal pain, flank pain, abdominal fullness, a palpable mass, and hematuria – although they can be clinically silent. The average duration of symptoms in synovial sarcoma is 2 to 4 years.8 The long duration of symptoms and initial slow growth of synovial sarcomas may give a false impression of a benign process.
A preoperative radiological diagnosis of primary renal synovial sarcoma may be suspected by analyzing the tumor’s growth patterns on CT scans.9 Renal synovial sarcomas often appear as large, well-defined soft tissue masses that can extend into the renal pelvis or into the perinephric region.9 A CT scan may identify soft tissue calcifications, especially subtle ones in areas where the tumor anatomy is complex. A CT scan may also reveal areas of hemorrhage, necrosis, or cyst formation within the tumor, and can easily confirm bone involvement. Intravenous contrast may help in differentiating the mass from adjacent muscle and neurovascular complex.9,10 On MRI, renal synovial sarcomas are often described as nonspecific heterogeneous masses, although they may also exhibit heterogeneous enhancement of hemorrhagic areas, calcifications, and air-fluid levels (known as “triple sign”) as well as septae. The triple sign may be identified as areas of low, intermediate, and high signal intensity, correlating with areas of hemorrhage, calcification, and air-fluid level.9,10 Signal intensity is about equal to that of skeletal muscle on T1-weighted MRI and higher than that of subcutaneous fat on T2-weighted MRI.
In the present case, the tumor was initially misdiagnosed as an angiomyolipoma, the most common benign tumor of the kidney. Angiomyolipomas are usually solid triphasic tumors arising from the renal cortex and are composed of 3 major elements: dysmorphic blood vessels, smooth muscle components, and adipose tissue. When angiomyolipomas are large enough, they are readily recognized by the identification of macroscopic fat within the tumor, either by CT scan or MRI.11 When they are small, they may be difficult to distinguish from a small cyst on CT because of volume averaging.
On pathology, synovial sarcoma has dual epithelial and mesenchymal differentiation. They are frequently multi-lobulated, and areas of necrosis, hemorrhage, and cyst formation are also common. There are 3 main histologic subtypes of synovial sarcoma: biphasic (20%-30%), monophasic (50%-60%), and poorly differentiated (15%-25%). Poorly differentiated synovial sarcomas are generally epithelioid in morphology, have high mitotic activity (usually 10-20 mitoses/10 high-power field; range is <5 for well differentiated, low-grade tumors), and can be confused with round cell tumors such as Ewing sarcoma. Poorly differentiated synovial sarcomas are high-grade tumors.
Immunohistochemical studies can confirm the pathological diagnosis. Synovial sarcomas usually stain positive for Bcl2, CD99/Mic2, CD56, Vim, and focally for EMA but negatively for desmin, actin, WT1, S-100, CD34, and CD31.5 Currently, the gold standard for diagnosis and hallmark for synovial sarcomas are the t (X;18) translocation and SYT-SSX gene fusion products (SYT-SSX1 in 67% and SYT-SSX2 in 33% of cases). These can be detected either by FISH or reverse-transcription polymerase chain reaction. This genetic alteration is identified in more than 90% of synovial sarcomas and is highly specific.
The role of SYT-SSX gene fusion in the pathogenesis of synovial sarcoma is an active area of investigation. The fusion of SYT with SSX translates into a fusion protein that binds to the transcription activator SMARCA4 that is involved in chromatin remodeling, thus displacing both the wildtype SYT and the tumor suppressor gene SMARCB1. The modified protein complex then binds at several super-enhancer loci, unlocking suppressed genes such as Sox2, which is known to be necessary for synovial sarcoma proliferation. Alterations in SMARCB1 are involved in several cancer types, implicating this event as a driver of these malignancies.12 This results in a global alteration in chromatin remodeling that needs to be better understood to design targeted therapies.
The clinical course of synovial sarcoma, regardless of the tissue of origin, is typically poor. Multiple clinical and pathologic factors, including tumor size, location, patient age, and presence of poorly differentiated areas, are thought to have prognostic significance. A tumor size of more than 5 cm at presentation has the greatest impact on prognosis, with studies showing 5-year survival rates of 64% for patients with tumors smaller than 5 cm and 26% for patients with masses greater than 5 cm.13,14 High-grade synovial sarcoma is favored in tumors that have cystic components, hemorrhage, and fluid levels and the triple sign.
Patients with tumors in the extremities have a more favorable prognosis than those with lesions in the head and neck area or axially, a feature that likely reflects better surgical control available for extremity lesions. Patient age of less than 15 to 20 years is also associated with a better long-term prognosis.15,16 Varela-Duran and Enzinger17 reported that the presence of extensive calcifications suggests improved long-term survival, with 5-year survival rates of 82% and decreased rates of local recurrence (32%) and metastatic disease (29%). The poorly differentiated subtype is associated with a worsened prognosis, with a 5-year survival rate of 20% through 30%.18,19 Other pathologic factors associated with worsened prognosis include presence of rhabdoid cells, extensive tumor necrosis, high nuclear grade, p53 mutations, and high mitotic rate (>10 mitoses/10 high-power field). More recently, the gene fusion type SYT-SSX2 (more common in monophasic lesions) has been associated with an improved prognosis, compared with that for SYT-SSX1, and an 89% metastasis-free survival.20
Although there are no guidelines for the treatment of primary renal synovial sarcoma because of the limited number of cases reported, surgery is considered the first choice. Adjuvant chemotherapy with an anthracycline (doxorubicin or epirubicin) combined with ifosfamide has been the most frequently used regimen in published cases, especially in those in which patients have poor prognostic factors as mentioned above.
Overall, the 5-year survival rate ranges from 36% to 76%.14 The clinical course of synovial sarcoma is characterized by a high rate of local recurrence (30%-50%) and metastatic disease (41%). Most metastases occur within the first 2 to 5 years after treatment cessation. Metastases are present in 16% to 25% of patients at their initial presentation, with the most frequent metastatic site being the lung, followed by the lymph nodes (4%-18%) and bone (8%-11%).
Conclusion
Primary renal synovial sarcoma is extremely rare, and preoperative diagnosis is difficult in the absence of specific clinical or imaging findings. A high index of suspicion combined with pathologic, immunohistochemical, cytogenetic, and molecular studies is essential for accurate diagnosis and subsequent treatment planning. The differential diagnosis of renal synovial sarcoma can be extensive, and our experience with this patient illustrates the diagnostic dilemma associated with renal synovial sarcoma.
1. Majumder A, Dey S, Khandakar B, Medda S, Chandra Paul P. Primary renal synovial sarcoma: a rare tumor with an atypical presentation. Arch Iran Med. 2014;17(10):726-728.
2. Fetsch JF, Meis JM. Synovial sarcoma of the abdominal wall. Cancer. 1993;72(2):469 477.
3. Wang Z, Zhong Z, Zhu L, et al. Primary synovial sarcoma of the kidney: a case report. Oncol Lett. 2015;10(6):3542-3544.
4. Abbas M, Dämmrich ME, Braubach P, et al. Synovial sarcoma of the kidney in a young patient with a review of the literature. Rare tumors. 2014;6(2):5393
5. Argani P, Faria PA, Epstein JI, et al. Primary renal synovial sarcoma: molecular and morphologic delineation of an entity previously included among embryonal sarcomas of the kidney. Am J Surg Pathol. 2000;24(8):1087-1096.
6. Eble JN, Sauter G, Epstein JI, Sesterhenn IA, eds. World Health Organization classification of tumours: pathology and genetics of tumours of the urinary system and male genital organs. Lyon, France: IARC; 2004.
7. Tamboli P, Ro JY, Amin MB, Ligato S, Ayala AG. Benign tumors and tumor-like lesions of the adult kidney. Part II: benign mesenchymal and mixed neoplasms, and tumor-like lesions. Adv Anat Pathol. 2000;7(1):47-66.
8. Weiss SW, Goldblum JR. Malignant soft tissue tumors of uncertain type. In: Weiss SW, Goldblum JR, eds. Enzinger and Weiss’s soft tissue tumors. 4th ed. St. Louis, MO: Mosby, 2001; 1483-1565.
9. Lacovelli R, Altavilla A, Ciardi A, et al. Clinical and pathological features of primary renal synovial sarcoma: analysis of 64 cases from 11 years of medical literature. BJU Int. 2012;110(10):1449-1454.
10. Alhazzani AR, El-Sharkawy MS, Hassan H. Primary retroperitoneal synovial sarcoma in CT and MRI. Urol Ann. 2010;2(1):39-41.
11. Katabathina VS, Vikram R, Nagar AM, Tamboli P, Menias CO, Prasad SR. Mesenchymal neoplasms of the kidney in adults: imaging spectrum with radiologic-pathologic correlation. Radiographics. 2010;30(6):1525-1540.
12. Sápi Z, Papp G, Szendrői M, et al. Epigenetic regulation of SMARCB1 by miR-206, -381 and -671- 5p is evident in a variety of SMARCB1 immunonegative soft tissue sarcomas, while miR-765 appears specific for epithelioid sarcoma. A miRNA study of 223 soft tissue sarcomas. Genes Chromosomes Cancer. 2016;55(10):786-802.
13. Ferrari A, Gronchi A, Casanova M, et al. Synovial sarcoma: a retrospective analysis of 271 patients of all ages treated at a single institution. Cancer. 2004;101(3):627-634.
14. Rangheard AS, Vanel D, Viala J, Schwaab G, Casiraghi O, Sigal R. Synovial sarcomas of the head and neck: CT and MR imaging findings of eight patients. Am J Neuroradiol. 2001;22(5):851-857.
15. Oda Y, Hashimoto H, Tsuneyoshi M, Takeshita S. Survival in synovial sarcoma: a multivariate study of prognostic factors with special emphasis on the comparison between early death and long-term survival. Am J Surg Pathol. 1993;17(1):35-44.
16. Raney RB. Synovial sarcoma in young people: background, prognostic factors and therapeutic questions. J Pediatr Hematol Oncol. 2005;27(4):207-211.
17. Varela-Duran J, Enzinger FM. Calcifying synovial sarcoma. Cancer. 1982;50(2):345-352.
18. Cagle LA, Mirra JM, Storm FK, Roe DJ, Eilber FR. Histologic features relating to prognosis in synovial sarcoma. Cancer. 1987;59(10):1810-1814.
19. Skytting B, Meis-Kindblom JM, Larsson O, et al. Synovial sarcoma – identification of favorable and unfavorable histologic types: a Scandinavian sarcoma group study of 104 cases. Acta Orthop Scand. 1999:70(6):543-554.
20. Murphey MD, Gibson MS, Jennings BT, Crespo-Rodríguez AM, Fanburg-Smith J, Gajewski DA. Imaging of synovial sarcoma with radiologic-pathologic correlation. Radiographics. 2006;26(5):1543-1565.
Soft tissue sarcomas are rare mesenchymal tumors that comprise 1% of all malignancies. Synovial sarcoma accounts for 5% to 10% of adult soft tissue sarcomas and usually occurs in close association with joint capsules, tendon sheaths, and bursa in the extremities of young and middle-aged adults.1 Synovial sarcomas have been reported in other unusual sites, including the head and neck, thoracic and abdominal wall, retroperitoneum, bone, pleura, and visceral organs such as the lung, prostate, or kidney.2 Primary renal synovial sarcoma is an extremely rare tumor accounting for <2% of all malignant renal tumors.3 To the best of our knowledge, fewer than 50 cases of primary renal synovial sarcoma have been described in the English literature.4 It presents as a diagnostic dilemma because of the dearth of specific clinical and imaging findings and is often confused with benign and malignant tumors. The differential diagnosis includes angiomyolipoma, renal cell carcinoma with sarcomatoid differentiation, metastatic sarcoma, hemangiopericytoma, malignant solitary fibrous tumor, Wilms tumor, and malignant peripheral nerve sheath tumor. Hence, a combination of histomorphologic, immunohistochemical, cytogenetic, and molecular studies that show a unique chromosomal translocation t(X;18) (p11;q11) is imperative in the diagnosis of primary renal synovial sarcoma.4 In the present report, we present the case of a 38-year-old man who was diagnosed with primary renal synovial sarcoma.
Case presentation and summary
A 38-year-old man with a medical history of gastroesophageal reflux disease and Barrett’s esophagus presented to our hospital for the first time with persistent and progressive right-sided flank and abdominal pain that was aggravated after a minor trauma to the back. There was no associated hematuria or dysuria.
Of note is that he had experienced intermittent flank pain for 2 years before this transfer. He had initially been diagnosed at his local hospital close to his home by ultrasound with an angiomyolipoma of 2 × 3 cm arising from the upper pole of his right kidney, which remained stable on repeat sonograms. About 22 months after his initial presentation at his local hospital, the flank pain increased, and a computed-tomographic (CT) scan revealed a perinephric hematoma that was thought to originate from a ruptured angiomyolipoma. He subsequently underwent embolization, but his symptoms recurred soon after. He presented again to his local hospital where CT imaging revealed a significant increase in the size of the retroperitoneal mass, and findings were suggestive of a hematoma. Subsequent angiogram did not reveal active extravasation, so a biopsy was performed.
Before confirmatory pathologic evaluation could be completed, the patient presented to his local hospital again in excruciating pain. A CT scan of his abdomen and pelvis demonstrated a massive subacute on chronic hematoma in the right retroperitoneum measuring 22 × 19 × 18 cm, with calcifications originating from an upper pole right renal neoplasm. The right kidney was displaced antero-inferiorly, and the inferior vena cava was displaced anteriorly and to the left. The preliminary pathology returned with findings suggestive of sarcoma (Figures 1 and 2).
The patient was then transferred to our institution, where he was evaluated by medical and surgical oncology. A CT scan of the chest and magnetic-resonance imaging (MRI) of the brain did not reveal metastatic disease. He underwent exploratory laparotomy that involved the resection of a 22-cm retroperitoneal mass, right nephrectomy, right adrenalectomy, partial right hepatectomy, and a full thickness resection of the right postero-inferior diaphragm followed by mesh repair because of involvement by the tumor.
In its entirety, the specimen was a mass of 26 × 24 × 14 cm. It was sectioned to show extensively necrotic and hemorrhagic variegated white to tan-red parenchyma (Figure 3). Histology revealed a poorly differentiated malignant neoplasm composed of round cells with scant amphophilic cytoplasm arranged in solid, variably sized nests separated by prominent thin-walled branching vascular channels (Figure 4). The mitotic rate was high. It was determined to be a histologically ungraded sarcoma according to the French Federation of Comprehensive Cancer Centers system of grading soft tissue sarcomas; the margins were indeterminate. Immunohistochemistry was positive for EMA, TLE1, and negative for AE1/AE3, S100, STAT6, and Nkx2.2. Molecular pathology fluorescent in situ hybridization (FISH) analysis demonstrated positivity for SS18 gene rearrangement (SS18-SSX1 fusion).
After recovering from surgery, the patient received adjuvant chemotherapy with doxorubicin and ifosfamide. It has been almost 16 months since we first saw this patient. He was started on doxorubicin 20 mg/m2 on days 1 to 4, ifosfamide 2,500 mg on days 1 to 4, and mesna 800 mg on days 1 to 4, for a total of 6 cycles. He did well for the first 5 months, after which he developed disease recurrence in the postoperative nephrectomy bed (a biopsy showed it to be recurrent synovial sarcoma) as well as pulmonary nodules, for which he was started on trabectedin 1.5 mg/m2 every 3 weeks. Two months later, a CT scan showed an increase in the size of his retroperitoneal mass, and the treatment was changed to pazopanib 400 mg daily orally, on which he remained at the time of publication.
Discussion
Synovial sarcoma is the fourth most common type of soft tissue sarcoma, accounting for 2.5% to 10.5% of all primary soft tissue malignancies worldwide. It occurs most frequently in adolescents and young adults, with most patients presenting between the ages of 15 and 40 years. Median age of presentation is 36 years. Despite the nomenclature, synovial sarcoma does not arise in intra-articular locations but typically occurs in proximity to joints in the extremities. Synovial sarcomas are less commonly described in other sites, including the head and neck, mediastinum, intraperitoneum, retroperitoneum, lung, pleura, and kidney.4,5 Renal synovial sarcoma was first described in a published article by Argani and colleagues in 2000.5
Adult renal mesenchymal tumors are classified into benign and malignant tumors on the basis of the histologic features and clinicobiologic behavior.6,7 The benign esenchymal renal tumors include angiomyolipoma, leiomyoma, hemangioma, lymphangioma, juxtaglomerular cell tumor, renomedullary interstitial cell tumor (medullary fibroma), lipoma, solitary fibrous tumor, and schwannoma. Malignant renal tumors of mesenchymal origin include leiomyosarcoma, rhabdomyosarcoma, angiosarcoma, osteosarcoma, fibrosarcoma, malignant fibrous histiocytoma, solitary fibrous tumor, and synovial sarcoma.
Most of these tumor types cause the same nonspecific symptoms in patients – abdominal pain, flank pain, abdominal fullness, a palpable mass, and hematuria – although they can be clinically silent. The average duration of symptoms in synovial sarcoma is 2 to 4 years.8 The long duration of symptoms and initial slow growth of synovial sarcomas may give a false impression of a benign process.
A preoperative radiological diagnosis of primary renal synovial sarcoma may be suspected by analyzing the tumor’s growth patterns on CT scans.9 Renal synovial sarcomas often appear as large, well-defined soft tissue masses that can extend into the renal pelvis or into the perinephric region.9 A CT scan may identify soft tissue calcifications, especially subtle ones in areas where the tumor anatomy is complex. A CT scan may also reveal areas of hemorrhage, necrosis, or cyst formation within the tumor, and can easily confirm bone involvement. Intravenous contrast may help in differentiating the mass from adjacent muscle and neurovascular complex.9,10 On MRI, renal synovial sarcomas are often described as nonspecific heterogeneous masses, although they may also exhibit heterogeneous enhancement of hemorrhagic areas, calcifications, and air-fluid levels (known as “triple sign”) as well as septae. The triple sign may be identified as areas of low, intermediate, and high signal intensity, correlating with areas of hemorrhage, calcification, and air-fluid level.9,10 Signal intensity is about equal to that of skeletal muscle on T1-weighted MRI and higher than that of subcutaneous fat on T2-weighted MRI.
In the present case, the tumor was initially misdiagnosed as an angiomyolipoma, the most common benign tumor of the kidney. Angiomyolipomas are usually solid triphasic tumors arising from the renal cortex and are composed of 3 major elements: dysmorphic blood vessels, smooth muscle components, and adipose tissue. When angiomyolipomas are large enough, they are readily recognized by the identification of macroscopic fat within the tumor, either by CT scan or MRI.11 When they are small, they may be difficult to distinguish from a small cyst on CT because of volume averaging.
On pathology, synovial sarcoma has dual epithelial and mesenchymal differentiation. They are frequently multi-lobulated, and areas of necrosis, hemorrhage, and cyst formation are also common. There are 3 main histologic subtypes of synovial sarcoma: biphasic (20%-30%), monophasic (50%-60%), and poorly differentiated (15%-25%). Poorly differentiated synovial sarcomas are generally epithelioid in morphology, have high mitotic activity (usually 10-20 mitoses/10 high-power field; range is <5 for well differentiated, low-grade tumors), and can be confused with round cell tumors such as Ewing sarcoma. Poorly differentiated synovial sarcomas are high-grade tumors.
Immunohistochemical studies can confirm the pathological diagnosis. Synovial sarcomas usually stain positive for Bcl2, CD99/Mic2, CD56, Vim, and focally for EMA but negatively for desmin, actin, WT1, S-100, CD34, and CD31.5 Currently, the gold standard for diagnosis and hallmark for synovial sarcomas are the t (X;18) translocation and SYT-SSX gene fusion products (SYT-SSX1 in 67% and SYT-SSX2 in 33% of cases). These can be detected either by FISH or reverse-transcription polymerase chain reaction. This genetic alteration is identified in more than 90% of synovial sarcomas and is highly specific.
The role of SYT-SSX gene fusion in the pathogenesis of synovial sarcoma is an active area of investigation. The fusion of SYT with SSX translates into a fusion protein that binds to the transcription activator SMARCA4 that is involved in chromatin remodeling, thus displacing both the wildtype SYT and the tumor suppressor gene SMARCB1. The modified protein complex then binds at several super-enhancer loci, unlocking suppressed genes such as Sox2, which is known to be necessary for synovial sarcoma proliferation. Alterations in SMARCB1 are involved in several cancer types, implicating this event as a driver of these malignancies.12 This results in a global alteration in chromatin remodeling that needs to be better understood to design targeted therapies.
The clinical course of synovial sarcoma, regardless of the tissue of origin, is typically poor. Multiple clinical and pathologic factors, including tumor size, location, patient age, and presence of poorly differentiated areas, are thought to have prognostic significance. A tumor size of more than 5 cm at presentation has the greatest impact on prognosis, with studies showing 5-year survival rates of 64% for patients with tumors smaller than 5 cm and 26% for patients with masses greater than 5 cm.13,14 High-grade synovial sarcoma is favored in tumors that have cystic components, hemorrhage, and fluid levels and the triple sign.
Patients with tumors in the extremities have a more favorable prognosis than those with lesions in the head and neck area or axially, a feature that likely reflects better surgical control available for extremity lesions. Patient age of less than 15 to 20 years is also associated with a better long-term prognosis.15,16 Varela-Duran and Enzinger17 reported that the presence of extensive calcifications suggests improved long-term survival, with 5-year survival rates of 82% and decreased rates of local recurrence (32%) and metastatic disease (29%). The poorly differentiated subtype is associated with a worsened prognosis, with a 5-year survival rate of 20% through 30%.18,19 Other pathologic factors associated with worsened prognosis include presence of rhabdoid cells, extensive tumor necrosis, high nuclear grade, p53 mutations, and high mitotic rate (>10 mitoses/10 high-power field). More recently, the gene fusion type SYT-SSX2 (more common in monophasic lesions) has been associated with an improved prognosis, compared with that for SYT-SSX1, and an 89% metastasis-free survival.20
Although there are no guidelines for the treatment of primary renal synovial sarcoma because of the limited number of cases reported, surgery is considered the first choice. Adjuvant chemotherapy with an anthracycline (doxorubicin or epirubicin) combined with ifosfamide has been the most frequently used regimen in published cases, especially in those in which patients have poor prognostic factors as mentioned above.
Overall, the 5-year survival rate ranges from 36% to 76%.14 The clinical course of synovial sarcoma is characterized by a high rate of local recurrence (30%-50%) and metastatic disease (41%). Most metastases occur within the first 2 to 5 years after treatment cessation. Metastases are present in 16% to 25% of patients at their initial presentation, with the most frequent metastatic site being the lung, followed by the lymph nodes (4%-18%) and bone (8%-11%).
Conclusion
Primary renal synovial sarcoma is extremely rare, and preoperative diagnosis is difficult in the absence of specific clinical or imaging findings. A high index of suspicion combined with pathologic, immunohistochemical, cytogenetic, and molecular studies is essential for accurate diagnosis and subsequent treatment planning. The differential diagnosis of renal synovial sarcoma can be extensive, and our experience with this patient illustrates the diagnostic dilemma associated with renal synovial sarcoma.
Soft tissue sarcomas are rare mesenchymal tumors that comprise 1% of all malignancies. Synovial sarcoma accounts for 5% to 10% of adult soft tissue sarcomas and usually occurs in close association with joint capsules, tendon sheaths, and bursa in the extremities of young and middle-aged adults.1 Synovial sarcomas have been reported in other unusual sites, including the head and neck, thoracic and abdominal wall, retroperitoneum, bone, pleura, and visceral organs such as the lung, prostate, or kidney.2 Primary renal synovial sarcoma is an extremely rare tumor accounting for <2% of all malignant renal tumors.3 To the best of our knowledge, fewer than 50 cases of primary renal synovial sarcoma have been described in the English literature.4 It presents as a diagnostic dilemma because of the dearth of specific clinical and imaging findings and is often confused with benign and malignant tumors. The differential diagnosis includes angiomyolipoma, renal cell carcinoma with sarcomatoid differentiation, metastatic sarcoma, hemangiopericytoma, malignant solitary fibrous tumor, Wilms tumor, and malignant peripheral nerve sheath tumor. Hence, a combination of histomorphologic, immunohistochemical, cytogenetic, and molecular studies that show a unique chromosomal translocation t(X;18) (p11;q11) is imperative in the diagnosis of primary renal synovial sarcoma.4 In the present report, we present the case of a 38-year-old man who was diagnosed with primary renal synovial sarcoma.
Case presentation and summary
A 38-year-old man with a medical history of gastroesophageal reflux disease and Barrett’s esophagus presented to our hospital for the first time with persistent and progressive right-sided flank and abdominal pain that was aggravated after a minor trauma to the back. There was no associated hematuria or dysuria.
Of note is that he had experienced intermittent flank pain for 2 years before this transfer. He had initially been diagnosed at his local hospital close to his home by ultrasound with an angiomyolipoma of 2 × 3 cm arising from the upper pole of his right kidney, which remained stable on repeat sonograms. About 22 months after his initial presentation at his local hospital, the flank pain increased, and a computed-tomographic (CT) scan revealed a perinephric hematoma that was thought to originate from a ruptured angiomyolipoma. He subsequently underwent embolization, but his symptoms recurred soon after. He presented again to his local hospital where CT imaging revealed a significant increase in the size of the retroperitoneal mass, and findings were suggestive of a hematoma. Subsequent angiogram did not reveal active extravasation, so a biopsy was performed.
Before confirmatory pathologic evaluation could be completed, the patient presented to his local hospital again in excruciating pain. A CT scan of his abdomen and pelvis demonstrated a massive subacute on chronic hematoma in the right retroperitoneum measuring 22 × 19 × 18 cm, with calcifications originating from an upper pole right renal neoplasm. The right kidney was displaced antero-inferiorly, and the inferior vena cava was displaced anteriorly and to the left. The preliminary pathology returned with findings suggestive of sarcoma (Figures 1 and 2).
The patient was then transferred to our institution, where he was evaluated by medical and surgical oncology. A CT scan of the chest and magnetic-resonance imaging (MRI) of the brain did not reveal metastatic disease. He underwent exploratory laparotomy that involved the resection of a 22-cm retroperitoneal mass, right nephrectomy, right adrenalectomy, partial right hepatectomy, and a full thickness resection of the right postero-inferior diaphragm followed by mesh repair because of involvement by the tumor.
In its entirety, the specimen was a mass of 26 × 24 × 14 cm. It was sectioned to show extensively necrotic and hemorrhagic variegated white to tan-red parenchyma (Figure 3). Histology revealed a poorly differentiated malignant neoplasm composed of round cells with scant amphophilic cytoplasm arranged in solid, variably sized nests separated by prominent thin-walled branching vascular channels (Figure 4). The mitotic rate was high. It was determined to be a histologically ungraded sarcoma according to the French Federation of Comprehensive Cancer Centers system of grading soft tissue sarcomas; the margins were indeterminate. Immunohistochemistry was positive for EMA, TLE1, and negative for AE1/AE3, S100, STAT6, and Nkx2.2. Molecular pathology fluorescent in situ hybridization (FISH) analysis demonstrated positivity for SS18 gene rearrangement (SS18-SSX1 fusion).
After recovering from surgery, the patient received adjuvant chemotherapy with doxorubicin and ifosfamide. It has been almost 16 months since we first saw this patient. He was started on doxorubicin 20 mg/m2 on days 1 to 4, ifosfamide 2,500 mg on days 1 to 4, and mesna 800 mg on days 1 to 4, for a total of 6 cycles. He did well for the first 5 months, after which he developed disease recurrence in the postoperative nephrectomy bed (a biopsy showed it to be recurrent synovial sarcoma) as well as pulmonary nodules, for which he was started on trabectedin 1.5 mg/m2 every 3 weeks. Two months later, a CT scan showed an increase in the size of his retroperitoneal mass, and the treatment was changed to pazopanib 400 mg daily orally, on which he remained at the time of publication.
Discussion
Synovial sarcoma is the fourth most common type of soft tissue sarcoma, accounting for 2.5% to 10.5% of all primary soft tissue malignancies worldwide. It occurs most frequently in adolescents and young adults, with most patients presenting between the ages of 15 and 40 years. Median age of presentation is 36 years. Despite the nomenclature, synovial sarcoma does not arise in intra-articular locations but typically occurs in proximity to joints in the extremities. Synovial sarcomas are less commonly described in other sites, including the head and neck, mediastinum, intraperitoneum, retroperitoneum, lung, pleura, and kidney.4,5 Renal synovial sarcoma was first described in a published article by Argani and colleagues in 2000.5
Adult renal mesenchymal tumors are classified into benign and malignant tumors on the basis of the histologic features and clinicobiologic behavior.6,7 The benign esenchymal renal tumors include angiomyolipoma, leiomyoma, hemangioma, lymphangioma, juxtaglomerular cell tumor, renomedullary interstitial cell tumor (medullary fibroma), lipoma, solitary fibrous tumor, and schwannoma. Malignant renal tumors of mesenchymal origin include leiomyosarcoma, rhabdomyosarcoma, angiosarcoma, osteosarcoma, fibrosarcoma, malignant fibrous histiocytoma, solitary fibrous tumor, and synovial sarcoma.
Most of these tumor types cause the same nonspecific symptoms in patients – abdominal pain, flank pain, abdominal fullness, a palpable mass, and hematuria – although they can be clinically silent. The average duration of symptoms in synovial sarcoma is 2 to 4 years.8 The long duration of symptoms and initial slow growth of synovial sarcomas may give a false impression of a benign process.
A preoperative radiological diagnosis of primary renal synovial sarcoma may be suspected by analyzing the tumor’s growth patterns on CT scans.9 Renal synovial sarcomas often appear as large, well-defined soft tissue masses that can extend into the renal pelvis or into the perinephric region.9 A CT scan may identify soft tissue calcifications, especially subtle ones in areas where the tumor anatomy is complex. A CT scan may also reveal areas of hemorrhage, necrosis, or cyst formation within the tumor, and can easily confirm bone involvement. Intravenous contrast may help in differentiating the mass from adjacent muscle and neurovascular complex.9,10 On MRI, renal synovial sarcomas are often described as nonspecific heterogeneous masses, although they may also exhibit heterogeneous enhancement of hemorrhagic areas, calcifications, and air-fluid levels (known as “triple sign”) as well as septae. The triple sign may be identified as areas of low, intermediate, and high signal intensity, correlating with areas of hemorrhage, calcification, and air-fluid level.9,10 Signal intensity is about equal to that of skeletal muscle on T1-weighted MRI and higher than that of subcutaneous fat on T2-weighted MRI.
In the present case, the tumor was initially misdiagnosed as an angiomyolipoma, the most common benign tumor of the kidney. Angiomyolipomas are usually solid triphasic tumors arising from the renal cortex and are composed of 3 major elements: dysmorphic blood vessels, smooth muscle components, and adipose tissue. When angiomyolipomas are large enough, they are readily recognized by the identification of macroscopic fat within the tumor, either by CT scan or MRI.11 When they are small, they may be difficult to distinguish from a small cyst on CT because of volume averaging.
On pathology, synovial sarcoma has dual epithelial and mesenchymal differentiation. They are frequently multi-lobulated, and areas of necrosis, hemorrhage, and cyst formation are also common. There are 3 main histologic subtypes of synovial sarcoma: biphasic (20%-30%), monophasic (50%-60%), and poorly differentiated (15%-25%). Poorly differentiated synovial sarcomas are generally epithelioid in morphology, have high mitotic activity (usually 10-20 mitoses/10 high-power field; range is <5 for well differentiated, low-grade tumors), and can be confused with round cell tumors such as Ewing sarcoma. Poorly differentiated synovial sarcomas are high-grade tumors.
Immunohistochemical studies can confirm the pathological diagnosis. Synovial sarcomas usually stain positive for Bcl2, CD99/Mic2, CD56, Vim, and focally for EMA but negatively for desmin, actin, WT1, S-100, CD34, and CD31.5 Currently, the gold standard for diagnosis and hallmark for synovial sarcomas are the t (X;18) translocation and SYT-SSX gene fusion products (SYT-SSX1 in 67% and SYT-SSX2 in 33% of cases). These can be detected either by FISH or reverse-transcription polymerase chain reaction. This genetic alteration is identified in more than 90% of synovial sarcomas and is highly specific.
The role of SYT-SSX gene fusion in the pathogenesis of synovial sarcoma is an active area of investigation. The fusion of SYT with SSX translates into a fusion protein that binds to the transcription activator SMARCA4 that is involved in chromatin remodeling, thus displacing both the wildtype SYT and the tumor suppressor gene SMARCB1. The modified protein complex then binds at several super-enhancer loci, unlocking suppressed genes such as Sox2, which is known to be necessary for synovial sarcoma proliferation. Alterations in SMARCB1 are involved in several cancer types, implicating this event as a driver of these malignancies.12 This results in a global alteration in chromatin remodeling that needs to be better understood to design targeted therapies.
The clinical course of synovial sarcoma, regardless of the tissue of origin, is typically poor. Multiple clinical and pathologic factors, including tumor size, location, patient age, and presence of poorly differentiated areas, are thought to have prognostic significance. A tumor size of more than 5 cm at presentation has the greatest impact on prognosis, with studies showing 5-year survival rates of 64% for patients with tumors smaller than 5 cm and 26% for patients with masses greater than 5 cm.13,14 High-grade synovial sarcoma is favored in tumors that have cystic components, hemorrhage, and fluid levels and the triple sign.
Patients with tumors in the extremities have a more favorable prognosis than those with lesions in the head and neck area or axially, a feature that likely reflects better surgical control available for extremity lesions. Patient age of less than 15 to 20 years is also associated with a better long-term prognosis.15,16 Varela-Duran and Enzinger17 reported that the presence of extensive calcifications suggests improved long-term survival, with 5-year survival rates of 82% and decreased rates of local recurrence (32%) and metastatic disease (29%). The poorly differentiated subtype is associated with a worsened prognosis, with a 5-year survival rate of 20% through 30%.18,19 Other pathologic factors associated with worsened prognosis include presence of rhabdoid cells, extensive tumor necrosis, high nuclear grade, p53 mutations, and high mitotic rate (>10 mitoses/10 high-power field). More recently, the gene fusion type SYT-SSX2 (more common in monophasic lesions) has been associated with an improved prognosis, compared with that for SYT-SSX1, and an 89% metastasis-free survival.20
Although there are no guidelines for the treatment of primary renal synovial sarcoma because of the limited number of cases reported, surgery is considered the first choice. Adjuvant chemotherapy with an anthracycline (doxorubicin or epirubicin) combined with ifosfamide has been the most frequently used regimen in published cases, especially in those in which patients have poor prognostic factors as mentioned above.
Overall, the 5-year survival rate ranges from 36% to 76%.14 The clinical course of synovial sarcoma is characterized by a high rate of local recurrence (30%-50%) and metastatic disease (41%). Most metastases occur within the first 2 to 5 years after treatment cessation. Metastases are present in 16% to 25% of patients at their initial presentation, with the most frequent metastatic site being the lung, followed by the lymph nodes (4%-18%) and bone (8%-11%).
Conclusion
Primary renal synovial sarcoma is extremely rare, and preoperative diagnosis is difficult in the absence of specific clinical or imaging findings. A high index of suspicion combined with pathologic, immunohistochemical, cytogenetic, and molecular studies is essential for accurate diagnosis and subsequent treatment planning. The differential diagnosis of renal synovial sarcoma can be extensive, and our experience with this patient illustrates the diagnostic dilemma associated with renal synovial sarcoma.
1. Majumder A, Dey S, Khandakar B, Medda S, Chandra Paul P. Primary renal synovial sarcoma: a rare tumor with an atypical presentation. Arch Iran Med. 2014;17(10):726-728.
2. Fetsch JF, Meis JM. Synovial sarcoma of the abdominal wall. Cancer. 1993;72(2):469 477.
3. Wang Z, Zhong Z, Zhu L, et al. Primary synovial sarcoma of the kidney: a case report. Oncol Lett. 2015;10(6):3542-3544.
4. Abbas M, Dämmrich ME, Braubach P, et al. Synovial sarcoma of the kidney in a young patient with a review of the literature. Rare tumors. 2014;6(2):5393
5. Argani P, Faria PA, Epstein JI, et al. Primary renal synovial sarcoma: molecular and morphologic delineation of an entity previously included among embryonal sarcomas of the kidney. Am J Surg Pathol. 2000;24(8):1087-1096.
6. Eble JN, Sauter G, Epstein JI, Sesterhenn IA, eds. World Health Organization classification of tumours: pathology and genetics of tumours of the urinary system and male genital organs. Lyon, France: IARC; 2004.
7. Tamboli P, Ro JY, Amin MB, Ligato S, Ayala AG. Benign tumors and tumor-like lesions of the adult kidney. Part II: benign mesenchymal and mixed neoplasms, and tumor-like lesions. Adv Anat Pathol. 2000;7(1):47-66.
8. Weiss SW, Goldblum JR. Malignant soft tissue tumors of uncertain type. In: Weiss SW, Goldblum JR, eds. Enzinger and Weiss’s soft tissue tumors. 4th ed. St. Louis, MO: Mosby, 2001; 1483-1565.
9. Lacovelli R, Altavilla A, Ciardi A, et al. Clinical and pathological features of primary renal synovial sarcoma: analysis of 64 cases from 11 years of medical literature. BJU Int. 2012;110(10):1449-1454.
10. Alhazzani AR, El-Sharkawy MS, Hassan H. Primary retroperitoneal synovial sarcoma in CT and MRI. Urol Ann. 2010;2(1):39-41.
11. Katabathina VS, Vikram R, Nagar AM, Tamboli P, Menias CO, Prasad SR. Mesenchymal neoplasms of the kidney in adults: imaging spectrum with radiologic-pathologic correlation. Radiographics. 2010;30(6):1525-1540.
12. Sápi Z, Papp G, Szendrői M, et al. Epigenetic regulation of SMARCB1 by miR-206, -381 and -671- 5p is evident in a variety of SMARCB1 immunonegative soft tissue sarcomas, while miR-765 appears specific for epithelioid sarcoma. A miRNA study of 223 soft tissue sarcomas. Genes Chromosomes Cancer. 2016;55(10):786-802.
13. Ferrari A, Gronchi A, Casanova M, et al. Synovial sarcoma: a retrospective analysis of 271 patients of all ages treated at a single institution. Cancer. 2004;101(3):627-634.
14. Rangheard AS, Vanel D, Viala J, Schwaab G, Casiraghi O, Sigal R. Synovial sarcomas of the head and neck: CT and MR imaging findings of eight patients. Am J Neuroradiol. 2001;22(5):851-857.
15. Oda Y, Hashimoto H, Tsuneyoshi M, Takeshita S. Survival in synovial sarcoma: a multivariate study of prognostic factors with special emphasis on the comparison between early death and long-term survival. Am J Surg Pathol. 1993;17(1):35-44.
16. Raney RB. Synovial sarcoma in young people: background, prognostic factors and therapeutic questions. J Pediatr Hematol Oncol. 2005;27(4):207-211.
17. Varela-Duran J, Enzinger FM. Calcifying synovial sarcoma. Cancer. 1982;50(2):345-352.
18. Cagle LA, Mirra JM, Storm FK, Roe DJ, Eilber FR. Histologic features relating to prognosis in synovial sarcoma. Cancer. 1987;59(10):1810-1814.
19. Skytting B, Meis-Kindblom JM, Larsson O, et al. Synovial sarcoma – identification of favorable and unfavorable histologic types: a Scandinavian sarcoma group study of 104 cases. Acta Orthop Scand. 1999:70(6):543-554.
20. Murphey MD, Gibson MS, Jennings BT, Crespo-Rodríguez AM, Fanburg-Smith J, Gajewski DA. Imaging of synovial sarcoma with radiologic-pathologic correlation. Radiographics. 2006;26(5):1543-1565.
1. Majumder A, Dey S, Khandakar B, Medda S, Chandra Paul P. Primary renal synovial sarcoma: a rare tumor with an atypical presentation. Arch Iran Med. 2014;17(10):726-728.
2. Fetsch JF, Meis JM. Synovial sarcoma of the abdominal wall. Cancer. 1993;72(2):469 477.
3. Wang Z, Zhong Z, Zhu L, et al. Primary synovial sarcoma of the kidney: a case report. Oncol Lett. 2015;10(6):3542-3544.
4. Abbas M, Dämmrich ME, Braubach P, et al. Synovial sarcoma of the kidney in a young patient with a review of the literature. Rare tumors. 2014;6(2):5393
5. Argani P, Faria PA, Epstein JI, et al. Primary renal synovial sarcoma: molecular and morphologic delineation of an entity previously included among embryonal sarcomas of the kidney. Am J Surg Pathol. 2000;24(8):1087-1096.
6. Eble JN, Sauter G, Epstein JI, Sesterhenn IA, eds. World Health Organization classification of tumours: pathology and genetics of tumours of the urinary system and male genital organs. Lyon, France: IARC; 2004.
7. Tamboli P, Ro JY, Amin MB, Ligato S, Ayala AG. Benign tumors and tumor-like lesions of the adult kidney. Part II: benign mesenchymal and mixed neoplasms, and tumor-like lesions. Adv Anat Pathol. 2000;7(1):47-66.
8. Weiss SW, Goldblum JR. Malignant soft tissue tumors of uncertain type. In: Weiss SW, Goldblum JR, eds. Enzinger and Weiss’s soft tissue tumors. 4th ed. St. Louis, MO: Mosby, 2001; 1483-1565.
9. Lacovelli R, Altavilla A, Ciardi A, et al. Clinical and pathological features of primary renal synovial sarcoma: analysis of 64 cases from 11 years of medical literature. BJU Int. 2012;110(10):1449-1454.
10. Alhazzani AR, El-Sharkawy MS, Hassan H. Primary retroperitoneal synovial sarcoma in CT and MRI. Urol Ann. 2010;2(1):39-41.
11. Katabathina VS, Vikram R, Nagar AM, Tamboli P, Menias CO, Prasad SR. Mesenchymal neoplasms of the kidney in adults: imaging spectrum with radiologic-pathologic correlation. Radiographics. 2010;30(6):1525-1540.
12. Sápi Z, Papp G, Szendrői M, et al. Epigenetic regulation of SMARCB1 by miR-206, -381 and -671- 5p is evident in a variety of SMARCB1 immunonegative soft tissue sarcomas, while miR-765 appears specific for epithelioid sarcoma. A miRNA study of 223 soft tissue sarcomas. Genes Chromosomes Cancer. 2016;55(10):786-802.
13. Ferrari A, Gronchi A, Casanova M, et al. Synovial sarcoma: a retrospective analysis of 271 patients of all ages treated at a single institution. Cancer. 2004;101(3):627-634.
14. Rangheard AS, Vanel D, Viala J, Schwaab G, Casiraghi O, Sigal R. Synovial sarcomas of the head and neck: CT and MR imaging findings of eight patients. Am J Neuroradiol. 2001;22(5):851-857.
15. Oda Y, Hashimoto H, Tsuneyoshi M, Takeshita S. Survival in synovial sarcoma: a multivariate study of prognostic factors with special emphasis on the comparison between early death and long-term survival. Am J Surg Pathol. 1993;17(1):35-44.
16. Raney RB. Synovial sarcoma in young people: background, prognostic factors and therapeutic questions. J Pediatr Hematol Oncol. 2005;27(4):207-211.
17. Varela-Duran J, Enzinger FM. Calcifying synovial sarcoma. Cancer. 1982;50(2):345-352.
18. Cagle LA, Mirra JM, Storm FK, Roe DJ, Eilber FR. Histologic features relating to prognosis in synovial sarcoma. Cancer. 1987;59(10):1810-1814.
19. Skytting B, Meis-Kindblom JM, Larsson O, et al. Synovial sarcoma – identification of favorable and unfavorable histologic types: a Scandinavian sarcoma group study of 104 cases. Acta Orthop Scand. 1999:70(6):543-554.
20. Murphey MD, Gibson MS, Jennings BT, Crespo-Rodríguez AM, Fanburg-Smith J, Gajewski DA. Imaging of synovial sarcoma with radiologic-pathologic correlation. Radiographics. 2006;26(5):1543-1565.
TKIs and immunotherapy hold promise for alveolar soft part sarcoma
Alveolar soft part sarcoma (ASPS) has often proven to be resistant to conventional doxorubicin-based chemotherapy, but tyrosine kinase inhibitors (TKIs) and immune checkpoint inhibitors (ICIs) may provide new treatment strategies for this rare type of sarcoma, according to a literature review.
A rare, translocation-driven sarcoma of the soft tissues, ASPS often affects young adults and is characterized by indolent behavior and early metastasis. Despite its resistance to chemotherapy, studies indicate that survival is often prolonged in patients with metastatic disease. The literature has shown 5-year survival rates at about 60%, and this percentage has remained fairly consistent for the past 3 decades.
Luca Paoluzzi, MD, of New York University, and Robert G. Maki, MD, PhD, of Hofstra University, Hempstead, N.Y., reviewed the literature from 1952 to March 2018, in order to gain a better understanding of ASPS and the opportunities “for the translation of such knowledge into clinical practice,” they wrote in JAMA.
From a therapeutic standpoint, ASPS is characterized by sensitivity to vascular endothelial growth factor receptor–predominant TKIs, compared with other soft tissue sarcomas (STS), and recent data have emphasized that it is responsive to new immunotherapy regimens including ICIs. Pazopanib is currently the only agent that has received regulatory approval for use in STS refractory to other treatments and it appears to have consistent activity in metastatic ASPS. Management of ASPS generally also involves surgical resection and/or systemic treatment for metastatic disease. Conventional agents such as anthracycline-based chemotherapy have demonstrated a poor response rate lower than 10%, and while a complete resection may be curative, metastases are common and can occur years after resection of the primary tumor.
Conversely, ICIs “represent a promising area of drug development in ASPS; the data to date are limited but encouraging,” wrote Dr. Paoluzzi and Dr. Maki.
They pointed to one study that included 50 patients with sarcoma with 14 different subtypes of STS who were enrolled in immunotherapy trials conducted at the University of Texas MD Anderson Cancer Center, Houston. There were two pretreated patients with ASPS (two to four prior lines) in the cohort who received antiprogrammed death-ligand 1–based therapy, and achieved a partial response bordering on a complete response that lasted 8 and 12 months. An additional two patients achieved stable disease.
Another paper, presented at the 2017 Connective Tissue Oncology Society annual meeting, presented preliminary data from a phase 2 study that showed four of nine evaluable patients with ASPS treated with the TKI axitinib, combined with pembrolizumab, achieved a partial response. Three others had stable disease.
“Pathway-driven basket trials facilitate the enrollment of patients with such uncommon cancers and should provide valuable information regarding a second type of immune responsiveness to ICIs, one that is not a function of high tumor mutational burden,” the authors concluded.
No outside funding sources were reported. Dr. Maki reported receiving consultant fees from numerous sources and research support to New York University from Immune Design, Immunocore, Eli Lilly, Presage Biosciences, TRACON Pharmaceuticals, SARC, Regeneron, and Genentech. No other conflicts were reported.
SOURCE: doi: 10.1001/jamaoncol.2018.4490.
Alveolar soft part sarcoma (ASPS) has often proven to be resistant to conventional doxorubicin-based chemotherapy, but tyrosine kinase inhibitors (TKIs) and immune checkpoint inhibitors (ICIs) may provide new treatment strategies for this rare type of sarcoma, according to a literature review.
A rare, translocation-driven sarcoma of the soft tissues, ASPS often affects young adults and is characterized by indolent behavior and early metastasis. Despite its resistance to chemotherapy, studies indicate that survival is often prolonged in patients with metastatic disease. The literature has shown 5-year survival rates at about 60%, and this percentage has remained fairly consistent for the past 3 decades.
Luca Paoluzzi, MD, of New York University, and Robert G. Maki, MD, PhD, of Hofstra University, Hempstead, N.Y., reviewed the literature from 1952 to March 2018, in order to gain a better understanding of ASPS and the opportunities “for the translation of such knowledge into clinical practice,” they wrote in JAMA.
From a therapeutic standpoint, ASPS is characterized by sensitivity to vascular endothelial growth factor receptor–predominant TKIs, compared with other soft tissue sarcomas (STS), and recent data have emphasized that it is responsive to new immunotherapy regimens including ICIs. Pazopanib is currently the only agent that has received regulatory approval for use in STS refractory to other treatments and it appears to have consistent activity in metastatic ASPS. Management of ASPS generally also involves surgical resection and/or systemic treatment for metastatic disease. Conventional agents such as anthracycline-based chemotherapy have demonstrated a poor response rate lower than 10%, and while a complete resection may be curative, metastases are common and can occur years after resection of the primary tumor.
Conversely, ICIs “represent a promising area of drug development in ASPS; the data to date are limited but encouraging,” wrote Dr. Paoluzzi and Dr. Maki.
They pointed to one study that included 50 patients with sarcoma with 14 different subtypes of STS who were enrolled in immunotherapy trials conducted at the University of Texas MD Anderson Cancer Center, Houston. There were two pretreated patients with ASPS (two to four prior lines) in the cohort who received antiprogrammed death-ligand 1–based therapy, and achieved a partial response bordering on a complete response that lasted 8 and 12 months. An additional two patients achieved stable disease.
Another paper, presented at the 2017 Connective Tissue Oncology Society annual meeting, presented preliminary data from a phase 2 study that showed four of nine evaluable patients with ASPS treated with the TKI axitinib, combined with pembrolizumab, achieved a partial response. Three others had stable disease.
“Pathway-driven basket trials facilitate the enrollment of patients with such uncommon cancers and should provide valuable information regarding a second type of immune responsiveness to ICIs, one that is not a function of high tumor mutational burden,” the authors concluded.
No outside funding sources were reported. Dr. Maki reported receiving consultant fees from numerous sources and research support to New York University from Immune Design, Immunocore, Eli Lilly, Presage Biosciences, TRACON Pharmaceuticals, SARC, Regeneron, and Genentech. No other conflicts were reported.
SOURCE: doi: 10.1001/jamaoncol.2018.4490.
Alveolar soft part sarcoma (ASPS) has often proven to be resistant to conventional doxorubicin-based chemotherapy, but tyrosine kinase inhibitors (TKIs) and immune checkpoint inhibitors (ICIs) may provide new treatment strategies for this rare type of sarcoma, according to a literature review.
A rare, translocation-driven sarcoma of the soft tissues, ASPS often affects young adults and is characterized by indolent behavior and early metastasis. Despite its resistance to chemotherapy, studies indicate that survival is often prolonged in patients with metastatic disease. The literature has shown 5-year survival rates at about 60%, and this percentage has remained fairly consistent for the past 3 decades.
Luca Paoluzzi, MD, of New York University, and Robert G. Maki, MD, PhD, of Hofstra University, Hempstead, N.Y., reviewed the literature from 1952 to March 2018, in order to gain a better understanding of ASPS and the opportunities “for the translation of such knowledge into clinical practice,” they wrote in JAMA.
From a therapeutic standpoint, ASPS is characterized by sensitivity to vascular endothelial growth factor receptor–predominant TKIs, compared with other soft tissue sarcomas (STS), and recent data have emphasized that it is responsive to new immunotherapy regimens including ICIs. Pazopanib is currently the only agent that has received regulatory approval for use in STS refractory to other treatments and it appears to have consistent activity in metastatic ASPS. Management of ASPS generally also involves surgical resection and/or systemic treatment for metastatic disease. Conventional agents such as anthracycline-based chemotherapy have demonstrated a poor response rate lower than 10%, and while a complete resection may be curative, metastases are common and can occur years after resection of the primary tumor.
Conversely, ICIs “represent a promising area of drug development in ASPS; the data to date are limited but encouraging,” wrote Dr. Paoluzzi and Dr. Maki.
They pointed to one study that included 50 patients with sarcoma with 14 different subtypes of STS who were enrolled in immunotherapy trials conducted at the University of Texas MD Anderson Cancer Center, Houston. There were two pretreated patients with ASPS (two to four prior lines) in the cohort who received antiprogrammed death-ligand 1–based therapy, and achieved a partial response bordering on a complete response that lasted 8 and 12 months. An additional two patients achieved stable disease.
Another paper, presented at the 2017 Connective Tissue Oncology Society annual meeting, presented preliminary data from a phase 2 study that showed four of nine evaluable patients with ASPS treated with the TKI axitinib, combined with pembrolizumab, achieved a partial response. Three others had stable disease.
“Pathway-driven basket trials facilitate the enrollment of patients with such uncommon cancers and should provide valuable information regarding a second type of immune responsiveness to ICIs, one that is not a function of high tumor mutational burden,” the authors concluded.
No outside funding sources were reported. Dr. Maki reported receiving consultant fees from numerous sources and research support to New York University from Immune Design, Immunocore, Eli Lilly, Presage Biosciences, TRACON Pharmaceuticals, SARC, Regeneron, and Genentech. No other conflicts were reported.
SOURCE: doi: 10.1001/jamaoncol.2018.4490.
FROM JAMA
Key clinical point: Alveolar soft part sarcoma has often proven to be resistant to conventional doxorubicin-based chemotherapy, tyrosine kinase inhibitors and immune checkpoint inhibitors may provide new treatment strategies.
Major finding: In one study of sarcoma patients enrolled in immunotherapy trials, two pretreated patients with alveolar soft part sarcoma (two to four prior lines) who received antiprogrammed death-ligand 1–based therapy achieved partial responses, bordering on a complete response, that lasted 8 and 12 months.
Study details: A review of literature concerning treatment for alveolar soft part sarcoma.
Disclosures: No outside funding sources were reported. Dr. Maki reported receiving consultant fees from numerous sources and research support to New York University from Immune Design, Immunocore, Eli Lilly, Presage Biosciences, TRACON Pharmaceuticals, SARC, Regeneron, and Genentech. No other conflicts were reported.
Source:
Predicting treatment response in leiomyosarcoma, liposarcoma
Aberrations in oncogenic pathways and immune modulation influence treatment response in patients with metastatic leiomyosarcoma or liposarcoma, based on an analysis of whole-exome sequencing of tumor samples from patients in a completed phase 3 randomized trial comparing trabectedin and dacarbazine.
In that trial, trabectedin benefit was mostly seen in patients with leiomyosarcoma, as well as in patients with myxoid/round cell sarcomas, and less so in those with dedifferentiated and pleomorphic liposarcomas.
Gurpreet Kapoor, PhD, of LabConnect, Seattle, and colleagues examined aberrations in oncogenic pathways (DNA damage response, PI3K, MDM2-p53) and in immune modulation and then correlated the genomic aberrations with prospective data on clinical outcomes in the trial.
For the study, presented at the annual meeting of the American Society of Clinical Oncology in Chicago, archival tumor samples were collected from 456 of the 518 patients; 180 had uterine leiomyosarcomas, 149 had nonuterine leiomyosarcomas, 66 had dedifferentiated liposarcomas, 46 had myxoid liposarcomas, and 15 had pleomorphic liposarcomas.
Peripheral blood samples from a subset of 346 patients were also analyzed as matched normal to filter noise from nonpathogenic variants in the whole-exome sequencing.
Consistent with sarcoma data from The Cancer Genome Atlas, frequent homozygous gene deletions with relatively low mutational load were noted in these leiomyosarcoma and liposarcoma samples. TP53 and RB1 alterations were more frequent in leiomyosarcomas than in liposarcomas and were not associated with clinical outcomes. Analyses of 103 DNA damage-response genes found somatic alterations exceeded 20% across subtypes and correlated with improved progression-free survival in only uterine leiomyosarcomas (hazard ratio, 0.63; P = .03).
Genomic alterations in PI3K pathway genes were noted in 30% of myxoid liposarcomas and were associated with a worse rate of progression-free survival (HR, 3.0; P = .045).
A trend towards better overall survival was noted in dedifferentiated liposarcoma patients with MDM2 amplification as compared with normal MDM2 copy number.
Certain subtype-specific genomic aberrations in immune modulation pathways were associated with worse clinical outcomes in patients with uterine leiomyosarcoma or dedifferentiated liposarcoma. Alterations in immune suppressors were associated with improved clinical outcomes in nonuterine leiomyosarcomas and alterations in lipid metabolism were associated with improved clinical outcomes in dedifferentiated liposarcomas.
The invited discussant for the study, Mark Andrew Dickson, MD, of Memorial Sloan Kettering Cancer Center, New York, noted that “the real take-home here is that the TMBs (tumor mutation burdens) are relatively low across all of the L-type sarcomas.
“The pattern and prevalence of genomic aberrations that we’re seeing in this cohort of patients prospectively analyzed on a clinical trial are consistent with prior reports. ... including CDK4 and MDM2 in dedifferentiated liposarcoma, PI3-kinase in some myxoid/round cells, p53 in leiomyosarcoma and liposarcoma, and so on.”
Generally, tumor mutation burden is low in L-type sarcomas, and there are some intriguing associations with benefit to therapies, such as PI3-kinase pathway and potential resistance to trabectedin and high tumor mutation burden and potential sensitivity to trabectedin, that need to be explored and validated in another larger cohort, he said.
“I also am increasingly coming to terms with the fact that the tumors like leiomyosarcoma, which have low tumor mutation burden, and which so far have proven fairly immune to immunotherapy, based on all of the negative PD-1 data that we’ve seen, and that also have recurrent, relatively unactionable mutations, like p53 and Rb, remain very difficult to treat,” Dr. Dickson concluded.
SOURCE: Kapoor G et al. ASCO 2018, Abstract 11513.
Aberrations in oncogenic pathways and immune modulation influence treatment response in patients with metastatic leiomyosarcoma or liposarcoma, based on an analysis of whole-exome sequencing of tumor samples from patients in a completed phase 3 randomized trial comparing trabectedin and dacarbazine.
In that trial, trabectedin benefit was mostly seen in patients with leiomyosarcoma, as well as in patients with myxoid/round cell sarcomas, and less so in those with dedifferentiated and pleomorphic liposarcomas.
Gurpreet Kapoor, PhD, of LabConnect, Seattle, and colleagues examined aberrations in oncogenic pathways (DNA damage response, PI3K, MDM2-p53) and in immune modulation and then correlated the genomic aberrations with prospective data on clinical outcomes in the trial.
For the study, presented at the annual meeting of the American Society of Clinical Oncology in Chicago, archival tumor samples were collected from 456 of the 518 patients; 180 had uterine leiomyosarcomas, 149 had nonuterine leiomyosarcomas, 66 had dedifferentiated liposarcomas, 46 had myxoid liposarcomas, and 15 had pleomorphic liposarcomas.
Peripheral blood samples from a subset of 346 patients were also analyzed as matched normal to filter noise from nonpathogenic variants in the whole-exome sequencing.
Consistent with sarcoma data from The Cancer Genome Atlas, frequent homozygous gene deletions with relatively low mutational load were noted in these leiomyosarcoma and liposarcoma samples. TP53 and RB1 alterations were more frequent in leiomyosarcomas than in liposarcomas and were not associated with clinical outcomes. Analyses of 103 DNA damage-response genes found somatic alterations exceeded 20% across subtypes and correlated with improved progression-free survival in only uterine leiomyosarcomas (hazard ratio, 0.63; P = .03).
Genomic alterations in PI3K pathway genes were noted in 30% of myxoid liposarcomas and were associated with a worse rate of progression-free survival (HR, 3.0; P = .045).
A trend towards better overall survival was noted in dedifferentiated liposarcoma patients with MDM2 amplification as compared with normal MDM2 copy number.
Certain subtype-specific genomic aberrations in immune modulation pathways were associated with worse clinical outcomes in patients with uterine leiomyosarcoma or dedifferentiated liposarcoma. Alterations in immune suppressors were associated with improved clinical outcomes in nonuterine leiomyosarcomas and alterations in lipid metabolism were associated with improved clinical outcomes in dedifferentiated liposarcomas.
The invited discussant for the study, Mark Andrew Dickson, MD, of Memorial Sloan Kettering Cancer Center, New York, noted that “the real take-home here is that the TMBs (tumor mutation burdens) are relatively low across all of the L-type sarcomas.
“The pattern and prevalence of genomic aberrations that we’re seeing in this cohort of patients prospectively analyzed on a clinical trial are consistent with prior reports. ... including CDK4 and MDM2 in dedifferentiated liposarcoma, PI3-kinase in some myxoid/round cells, p53 in leiomyosarcoma and liposarcoma, and so on.”
Generally, tumor mutation burden is low in L-type sarcomas, and there are some intriguing associations with benefit to therapies, such as PI3-kinase pathway and potential resistance to trabectedin and high tumor mutation burden and potential sensitivity to trabectedin, that need to be explored and validated in another larger cohort, he said.
“I also am increasingly coming to terms with the fact that the tumors like leiomyosarcoma, which have low tumor mutation burden, and which so far have proven fairly immune to immunotherapy, based on all of the negative PD-1 data that we’ve seen, and that also have recurrent, relatively unactionable mutations, like p53 and Rb, remain very difficult to treat,” Dr. Dickson concluded.
SOURCE: Kapoor G et al. ASCO 2018, Abstract 11513.
Aberrations in oncogenic pathways and immune modulation influence treatment response in patients with metastatic leiomyosarcoma or liposarcoma, based on an analysis of whole-exome sequencing of tumor samples from patients in a completed phase 3 randomized trial comparing trabectedin and dacarbazine.
In that trial, trabectedin benefit was mostly seen in patients with leiomyosarcoma, as well as in patients with myxoid/round cell sarcomas, and less so in those with dedifferentiated and pleomorphic liposarcomas.
Gurpreet Kapoor, PhD, of LabConnect, Seattle, and colleagues examined aberrations in oncogenic pathways (DNA damage response, PI3K, MDM2-p53) and in immune modulation and then correlated the genomic aberrations with prospective data on clinical outcomes in the trial.
For the study, presented at the annual meeting of the American Society of Clinical Oncology in Chicago, archival tumor samples were collected from 456 of the 518 patients; 180 had uterine leiomyosarcomas, 149 had nonuterine leiomyosarcomas, 66 had dedifferentiated liposarcomas, 46 had myxoid liposarcomas, and 15 had pleomorphic liposarcomas.
Peripheral blood samples from a subset of 346 patients were also analyzed as matched normal to filter noise from nonpathogenic variants in the whole-exome sequencing.
Consistent with sarcoma data from The Cancer Genome Atlas, frequent homozygous gene deletions with relatively low mutational load were noted in these leiomyosarcoma and liposarcoma samples. TP53 and RB1 alterations were more frequent in leiomyosarcomas than in liposarcomas and were not associated with clinical outcomes. Analyses of 103 DNA damage-response genes found somatic alterations exceeded 20% across subtypes and correlated with improved progression-free survival in only uterine leiomyosarcomas (hazard ratio, 0.63; P = .03).
Genomic alterations in PI3K pathway genes were noted in 30% of myxoid liposarcomas and were associated with a worse rate of progression-free survival (HR, 3.0; P = .045).
A trend towards better overall survival was noted in dedifferentiated liposarcoma patients with MDM2 amplification as compared with normal MDM2 copy number.
Certain subtype-specific genomic aberrations in immune modulation pathways were associated with worse clinical outcomes in patients with uterine leiomyosarcoma or dedifferentiated liposarcoma. Alterations in immune suppressors were associated with improved clinical outcomes in nonuterine leiomyosarcomas and alterations in lipid metabolism were associated with improved clinical outcomes in dedifferentiated liposarcomas.
The invited discussant for the study, Mark Andrew Dickson, MD, of Memorial Sloan Kettering Cancer Center, New York, noted that “the real take-home here is that the TMBs (tumor mutation burdens) are relatively low across all of the L-type sarcomas.
“The pattern and prevalence of genomic aberrations that we’re seeing in this cohort of patients prospectively analyzed on a clinical trial are consistent with prior reports. ... including CDK4 and MDM2 in dedifferentiated liposarcoma, PI3-kinase in some myxoid/round cells, p53 in leiomyosarcoma and liposarcoma, and so on.”
Generally, tumor mutation burden is low in L-type sarcomas, and there are some intriguing associations with benefit to therapies, such as PI3-kinase pathway and potential resistance to trabectedin and high tumor mutation burden and potential sensitivity to trabectedin, that need to be explored and validated in another larger cohort, he said.
“I also am increasingly coming to terms with the fact that the tumors like leiomyosarcoma, which have low tumor mutation burden, and which so far have proven fairly immune to immunotherapy, based on all of the negative PD-1 data that we’ve seen, and that also have recurrent, relatively unactionable mutations, like p53 and Rb, remain very difficult to treat,” Dr. Dickson concluded.
SOURCE: Kapoor G et al. ASCO 2018, Abstract 11513.
REPORTING FROM ASCO 2018
Key clinical point: Aberrations in oncogenic pathways and immune modulation influence treatment response in patients with metastatic leiomyosarcoma or liposarcoma.
Major finding: Genomic alterations in PI3K pathway genes were noted in 30% of myxoid liposarcomas and were associated with a worse rate of progression-free survival (HR, 3.0; P = .045).
Study details: Archival tumor samples were collected from 456 of the 518 patients; 180 had uterine leiomyosarcomas, 149 had nonuterine leiomyosarcomas, 66 had dedifferentiated liposarcomas, 46 had myxoid liposarcomas, and 15 had pleomorphic liposarcomas in the completed phase 3 randomized trial comparing trabectedin and dacarbazine.
Disclosures: Dr. Kapoor is employed by LabConnect, Seattle. Research funding was supplied by Janssen Research & Development.
Source: Kapoor G et al. ASCO 2018, Abstract 11513.
FDA lifts partial hold on tazemetostat trials
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
Improved survival in liposarcoma
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PARP inhibitor plus trabectedin shows promise for sarcoma
A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma, the recent TOMAS trial found.
High PARP1 expression was associated with treatment response, reported Giovanni Grignani, MD, of the Medical Oncology_Sarcoma Unit at Istituto di Ricovero e Cura a Carattere Scientifico in Candiolo, Italy, and his colleagues.
PARP inhibitors prevent repair of DNA damage, suggesting potential synergisms with DNA-damaging anticancer agents. Preclinical models support this strategy; however, clinical trials have found that toxicities restrict doses below antitumor activity levels.
“In view of these findings, trabectedin could be an ideal drug to use in combination with PARP1/2 inhibitors for two reasons: its favourable haemopoietic toxicity profile and its unique mechanisms of action,” the authors wrote in The Lancet Oncology. Trabectedin bends the minor groove of DNA toward the major groove, which activates PARP1 in an attempt to repair the damage. Preclinical trials showed that a PARP inhibitor such as olaparib would block this PARP1 activation, ultimately resulting in a more robust response than with either drug alone.
The phase 1b, open-label TOMAS trial involved 50 patients with sarcoma who had experienced disease progression after standard therapy. The study was divided into two cohorts: dose-escalation and dose-expansion. Patients received a median of four cycles of therapy with a median follow-up of 10 months (some patients are still undergoing treatment). The primary endpoint was maximum tolerated dose. The investigators also evaluated pharmacokinetics, pharmacodynamics, and various response measures.
Although adverse events occurred, these were manageable, and the authors concluded that the combination is safe for further investigation. The most common grade 3 or higher adverse events were lymphopenia (64%), neutropenia (62%), thrombocytopenia (28%), anemia (26%), hypophosphatemia (40%), and alanine aminotransferase elevation (18%). The maximum tolerated dose (recommended phase 2 dose) was olaparib 150 mg twice daily and trabectedin 1.1 mg/m2 every 3 weeks.
“These doses allowed us to minimize the need for dose reductions and continue treatment for as long as tumour control was maintained,” the authors wrote. Previous treatments impacted tolerability. The researchers noted that “patients who had received more than two lines of therapy had a higher risk of developing dose-limiting toxicities than those patients who had been treated with only one line of therapy.”
Overall, 14% of patients responded to therapy. Six-month progression-free survival was more common in patients with soft tissue sarcoma (38%) than other tumor types. More patients with high PARP1 expression achieved 6-month PFS compared with patients who had low PARP1 expression (59% vs. 8%; P = .01).
“The combination of olaparib and trabectedin exploits the potential of two different first-in-class drugs and shows tolerability and activity in homologous repair-proficient tumors,” the authors concluded.
They are planning two phase 2 studies in the future; one “comparing trabectedin alone versus the combination of trabectedin and olaparib, stratifying patients according to PARP1 expression,” and an “after-platinum-failure study of patients with ovarian cancer regardless of patients’ BRCA1/2 and BRCAness status.”
The TOMAS trial was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
SOURCE: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
The phase 1b TOMAS trial by Grignani et al. showed that PARP inhibitor combination therapy may be a safe and effective option for patients with sarcoma, and a phase 2 study is warranted, according to Benjamin A. Nacev, MD, and William D. Tap, MD.
PARP inhibitors mitigate DNA damage repair, suggesting potential for synergistic combinations with DNA-damaging anticancer agents. Unfortunately, previous combinations have revealed toxicity issues.
“The first clinical example of this approach was the combination of the alkylating drug temozolomide and the PARP inhibitor rucaparib, which was hampered by dose-limiting myelosuppression,” Dr. Nacev and Dr. Tap wrote in an editorial in The Lancet Oncology.
In the TOMAS trial, Grignani et al. assessed a combination of trabectedin and the PARP inhibitor olaparib. Preclinical data showed synergistic activity in sarcoma cell lines, and the authors predicted tolerable myelosuppression with trabectedin.
Their predictions yielded promising results: Approximately one-third of patients with soft-tissue sarcoma were progression free at 6 months. Although myelosuppression did occur, the adverse event profile was tolerable.
As drug synergisms are biologically complex, “a key success of the TOMAS trial is the effective use of exploratory pharmacodynamic endpoints including PARP1 expression, PARylation, and mutational status of the DNA damage repair pathway.”
“For example, efficacy in the TOMAS trial correlated with PARP1 expression, with greater 6-month progression-free survival in the high PARP1 expression group than the low expression group.”
“The TOMAS investigators should be commended for doing the important bench-to-bedside approach of rationally designing and testing a drug combination to leverage available active drugs. We agree with the authors’ call for further investigation of trabectedin and olaparib in a randomised phase 2 trial in soft tissue sarcoma.”
William D. Tap, MD is chief of the Sarcoma Medical Oncology Service and Benjamin A. Nacev, MD is a third-year medical oncology/hematology fellow at Memorial Sloan Kettering Cancer Center in New York. Dr. Tap reported personal fees from Eli Lilly, Novartis, Eisai, and others. These comments are adapted from their accompanying editorial .
The phase 1b TOMAS trial by Grignani et al. showed that PARP inhibitor combination therapy may be a safe and effective option for patients with sarcoma, and a phase 2 study is warranted, according to Benjamin A. Nacev, MD, and William D. Tap, MD.
PARP inhibitors mitigate DNA damage repair, suggesting potential for synergistic combinations with DNA-damaging anticancer agents. Unfortunately, previous combinations have revealed toxicity issues.
“The first clinical example of this approach was the combination of the alkylating drug temozolomide and the PARP inhibitor rucaparib, which was hampered by dose-limiting myelosuppression,” Dr. Nacev and Dr. Tap wrote in an editorial in The Lancet Oncology.
In the TOMAS trial, Grignani et al. assessed a combination of trabectedin and the PARP inhibitor olaparib. Preclinical data showed synergistic activity in sarcoma cell lines, and the authors predicted tolerable myelosuppression with trabectedin.
Their predictions yielded promising results: Approximately one-third of patients with soft-tissue sarcoma were progression free at 6 months. Although myelosuppression did occur, the adverse event profile was tolerable.
As drug synergisms are biologically complex, “a key success of the TOMAS trial is the effective use of exploratory pharmacodynamic endpoints including PARP1 expression, PARylation, and mutational status of the DNA damage repair pathway.”
“For example, efficacy in the TOMAS trial correlated with PARP1 expression, with greater 6-month progression-free survival in the high PARP1 expression group than the low expression group.”
“The TOMAS investigators should be commended for doing the important bench-to-bedside approach of rationally designing and testing a drug combination to leverage available active drugs. We agree with the authors’ call for further investigation of trabectedin and olaparib in a randomised phase 2 trial in soft tissue sarcoma.”
William D. Tap, MD is chief of the Sarcoma Medical Oncology Service and Benjamin A. Nacev, MD is a third-year medical oncology/hematology fellow at Memorial Sloan Kettering Cancer Center in New York. Dr. Tap reported personal fees from Eli Lilly, Novartis, Eisai, and others. These comments are adapted from their accompanying editorial .
The phase 1b TOMAS trial by Grignani et al. showed that PARP inhibitor combination therapy may be a safe and effective option for patients with sarcoma, and a phase 2 study is warranted, according to Benjamin A. Nacev, MD, and William D. Tap, MD.
PARP inhibitors mitigate DNA damage repair, suggesting potential for synergistic combinations with DNA-damaging anticancer agents. Unfortunately, previous combinations have revealed toxicity issues.
“The first clinical example of this approach was the combination of the alkylating drug temozolomide and the PARP inhibitor rucaparib, which was hampered by dose-limiting myelosuppression,” Dr. Nacev and Dr. Tap wrote in an editorial in The Lancet Oncology.
In the TOMAS trial, Grignani et al. assessed a combination of trabectedin and the PARP inhibitor olaparib. Preclinical data showed synergistic activity in sarcoma cell lines, and the authors predicted tolerable myelosuppression with trabectedin.
Their predictions yielded promising results: Approximately one-third of patients with soft-tissue sarcoma were progression free at 6 months. Although myelosuppression did occur, the adverse event profile was tolerable.
As drug synergisms are biologically complex, “a key success of the TOMAS trial is the effective use of exploratory pharmacodynamic endpoints including PARP1 expression, PARylation, and mutational status of the DNA damage repair pathway.”
“For example, efficacy in the TOMAS trial correlated with PARP1 expression, with greater 6-month progression-free survival in the high PARP1 expression group than the low expression group.”
“The TOMAS investigators should be commended for doing the important bench-to-bedside approach of rationally designing and testing a drug combination to leverage available active drugs. We agree with the authors’ call for further investigation of trabectedin and olaparib in a randomised phase 2 trial in soft tissue sarcoma.”
William D. Tap, MD is chief of the Sarcoma Medical Oncology Service and Benjamin A. Nacev, MD is a third-year medical oncology/hematology fellow at Memorial Sloan Kettering Cancer Center in New York. Dr. Tap reported personal fees from Eli Lilly, Novartis, Eisai, and others. These comments are adapted from their accompanying editorial .
A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma, the recent TOMAS trial found.
High PARP1 expression was associated with treatment response, reported Giovanni Grignani, MD, of the Medical Oncology_Sarcoma Unit at Istituto di Ricovero e Cura a Carattere Scientifico in Candiolo, Italy, and his colleagues.
PARP inhibitors prevent repair of DNA damage, suggesting potential synergisms with DNA-damaging anticancer agents. Preclinical models support this strategy; however, clinical trials have found that toxicities restrict doses below antitumor activity levels.
“In view of these findings, trabectedin could be an ideal drug to use in combination with PARP1/2 inhibitors for two reasons: its favourable haemopoietic toxicity profile and its unique mechanisms of action,” the authors wrote in The Lancet Oncology. Trabectedin bends the minor groove of DNA toward the major groove, which activates PARP1 in an attempt to repair the damage. Preclinical trials showed that a PARP inhibitor such as olaparib would block this PARP1 activation, ultimately resulting in a more robust response than with either drug alone.
The phase 1b, open-label TOMAS trial involved 50 patients with sarcoma who had experienced disease progression after standard therapy. The study was divided into two cohorts: dose-escalation and dose-expansion. Patients received a median of four cycles of therapy with a median follow-up of 10 months (some patients are still undergoing treatment). The primary endpoint was maximum tolerated dose. The investigators also evaluated pharmacokinetics, pharmacodynamics, and various response measures.
Although adverse events occurred, these were manageable, and the authors concluded that the combination is safe for further investigation. The most common grade 3 or higher adverse events were lymphopenia (64%), neutropenia (62%), thrombocytopenia (28%), anemia (26%), hypophosphatemia (40%), and alanine aminotransferase elevation (18%). The maximum tolerated dose (recommended phase 2 dose) was olaparib 150 mg twice daily and trabectedin 1.1 mg/m2 every 3 weeks.
“These doses allowed us to minimize the need for dose reductions and continue treatment for as long as tumour control was maintained,” the authors wrote. Previous treatments impacted tolerability. The researchers noted that “patients who had received more than two lines of therapy had a higher risk of developing dose-limiting toxicities than those patients who had been treated with only one line of therapy.”
Overall, 14% of patients responded to therapy. Six-month progression-free survival was more common in patients with soft tissue sarcoma (38%) than other tumor types. More patients with high PARP1 expression achieved 6-month PFS compared with patients who had low PARP1 expression (59% vs. 8%; P = .01).
“The combination of olaparib and trabectedin exploits the potential of two different first-in-class drugs and shows tolerability and activity in homologous repair-proficient tumors,” the authors concluded.
They are planning two phase 2 studies in the future; one “comparing trabectedin alone versus the combination of trabectedin and olaparib, stratifying patients according to PARP1 expression,” and an “after-platinum-failure study of patients with ovarian cancer regardless of patients’ BRCA1/2 and BRCAness status.”
The TOMAS trial was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
SOURCE: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma, the recent TOMAS trial found.
High PARP1 expression was associated with treatment response, reported Giovanni Grignani, MD, of the Medical Oncology_Sarcoma Unit at Istituto di Ricovero e Cura a Carattere Scientifico in Candiolo, Italy, and his colleagues.
PARP inhibitors prevent repair of DNA damage, suggesting potential synergisms with DNA-damaging anticancer agents. Preclinical models support this strategy; however, clinical trials have found that toxicities restrict doses below antitumor activity levels.
“In view of these findings, trabectedin could be an ideal drug to use in combination with PARP1/2 inhibitors for two reasons: its favourable haemopoietic toxicity profile and its unique mechanisms of action,” the authors wrote in The Lancet Oncology. Trabectedin bends the minor groove of DNA toward the major groove, which activates PARP1 in an attempt to repair the damage. Preclinical trials showed that a PARP inhibitor such as olaparib would block this PARP1 activation, ultimately resulting in a more robust response than with either drug alone.
The phase 1b, open-label TOMAS trial involved 50 patients with sarcoma who had experienced disease progression after standard therapy. The study was divided into two cohorts: dose-escalation and dose-expansion. Patients received a median of four cycles of therapy with a median follow-up of 10 months (some patients are still undergoing treatment). The primary endpoint was maximum tolerated dose. The investigators also evaluated pharmacokinetics, pharmacodynamics, and various response measures.
Although adverse events occurred, these were manageable, and the authors concluded that the combination is safe for further investigation. The most common grade 3 or higher adverse events were lymphopenia (64%), neutropenia (62%), thrombocytopenia (28%), anemia (26%), hypophosphatemia (40%), and alanine aminotransferase elevation (18%). The maximum tolerated dose (recommended phase 2 dose) was olaparib 150 mg twice daily and trabectedin 1.1 mg/m2 every 3 weeks.
“These doses allowed us to minimize the need for dose reductions and continue treatment for as long as tumour control was maintained,” the authors wrote. Previous treatments impacted tolerability. The researchers noted that “patients who had received more than two lines of therapy had a higher risk of developing dose-limiting toxicities than those patients who had been treated with only one line of therapy.”
Overall, 14% of patients responded to therapy. Six-month progression-free survival was more common in patients with soft tissue sarcoma (38%) than other tumor types. More patients with high PARP1 expression achieved 6-month PFS compared with patients who had low PARP1 expression (59% vs. 8%; P = .01).
“The combination of olaparib and trabectedin exploits the potential of two different first-in-class drugs and shows tolerability and activity in homologous repair-proficient tumors,” the authors concluded.
They are planning two phase 2 studies in the future; one “comparing trabectedin alone versus the combination of trabectedin and olaparib, stratifying patients according to PARP1 expression,” and an “after-platinum-failure study of patients with ovarian cancer regardless of patients’ BRCA1/2 and BRCAness status.”
The TOMAS trial was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
SOURCE: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
FROM THE LANCET ONCOLOGY
Key clinical point: A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma.
Major finding: Of those with high PARP1 expression, 59% were progression free 6 months after treatment.
Study details: TOMAS was an open-label phase 1b trial involving 50 patients with sarcoma who had disease progression after standard therapy.
Disclosures: The study was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
Source: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
HIV-associated Kaposi sarcoma responds to checkpoint inhibitors
Checkpoint inhibitor therapy is effective for patients with HIV-associated Kaposi sarcoma (KS), a recent study has found.
Partial or complete remission was achieved by a majority of patients; others currently have stable disease lasting longer than 6 months, reported Natalie Galanina, MD, of Rebecca and John Moores Cancer Center at the University of California, San Diego, and her colleagues. Earlier this year, investigators reported similar responses to checkpoint inhibitors in two patients with KS that wasn’t associated with HIV.
“An association has been demonstrated between chronic viral infection, malignancy, and up-regulation of programmed death receptor 1 (PD-1) on CD8+ cytotoxic T-lymphocytes,” the authors wrote in Cancer Immunology Research. In particular, “HIV-specific CD8+ T cells have increased PD-1 expression, which … promotes a cellular milieu conducive to oncogenesis.” These factors, together with the results from the previous study, have suggested that checkpoint inhibitors may be effective for patients with HIV-associated KS.
The retrospective study involved 320 patients treated with immunotherapy at Moores Cancer Center from August 2013 through December 2017. From this group, nine cases of HIV-associated KS were found. Median CD4 count was 256 cells/mcL and median viral load was 20 copies/mL. Eight patients were treated with nivolumab and one was treated with pembrolizumab. Median age was 44 years. All patients were male and receiving antiretroviral therapy.
Six patients (67%) achieved remission, with five attaining partial remission and one attaining complete remission (gastrointestinal disease). Of the remaining three patients, two currently have stable disease lasting longer than 6 months, and one has stable disease lasting longer than 3 months.
Muscle aches, pruritus, and low-grade fever were the most common adverse events. No grade 3 or higher drug-related adverse events occurred.
“Most of our patients received one to four prior lines of therapy but still responded to checkpoint blockade,” the authors wrote. “Our observations suggest that patients with HIV-associated KS have high [response rates] to PD-1 checkpoint blockade, without significant toxicity, even in the presence of low [tumor mutational burden] and/or lack of PD-L1 expression.”
Authors reported compensation from Incyte, Genentech, Merck, Pfizer, and others.
SOURCE: Galanina et al. Cancer Immunol Res. doi: 10.1158/2326-6066.CIR-18-0121.
Checkpoint inhibitor therapy is effective for patients with HIV-associated Kaposi sarcoma (KS), a recent study has found.
Partial or complete remission was achieved by a majority of patients; others currently have stable disease lasting longer than 6 months, reported Natalie Galanina, MD, of Rebecca and John Moores Cancer Center at the University of California, San Diego, and her colleagues. Earlier this year, investigators reported similar responses to checkpoint inhibitors in two patients with KS that wasn’t associated with HIV.
“An association has been demonstrated between chronic viral infection, malignancy, and up-regulation of programmed death receptor 1 (PD-1) on CD8+ cytotoxic T-lymphocytes,” the authors wrote in Cancer Immunology Research. In particular, “HIV-specific CD8+ T cells have increased PD-1 expression, which … promotes a cellular milieu conducive to oncogenesis.” These factors, together with the results from the previous study, have suggested that checkpoint inhibitors may be effective for patients with HIV-associated KS.
The retrospective study involved 320 patients treated with immunotherapy at Moores Cancer Center from August 2013 through December 2017. From this group, nine cases of HIV-associated KS were found. Median CD4 count was 256 cells/mcL and median viral load was 20 copies/mL. Eight patients were treated with nivolumab and one was treated with pembrolizumab. Median age was 44 years. All patients were male and receiving antiretroviral therapy.
Six patients (67%) achieved remission, with five attaining partial remission and one attaining complete remission (gastrointestinal disease). Of the remaining three patients, two currently have stable disease lasting longer than 6 months, and one has stable disease lasting longer than 3 months.
Muscle aches, pruritus, and low-grade fever were the most common adverse events. No grade 3 or higher drug-related adverse events occurred.
“Most of our patients received one to four prior lines of therapy but still responded to checkpoint blockade,” the authors wrote. “Our observations suggest that patients with HIV-associated KS have high [response rates] to PD-1 checkpoint blockade, without significant toxicity, even in the presence of low [tumor mutational burden] and/or lack of PD-L1 expression.”
Authors reported compensation from Incyte, Genentech, Merck, Pfizer, and others.
SOURCE: Galanina et al. Cancer Immunol Res. doi: 10.1158/2326-6066.CIR-18-0121.
Checkpoint inhibitor therapy is effective for patients with HIV-associated Kaposi sarcoma (KS), a recent study has found.
Partial or complete remission was achieved by a majority of patients; others currently have stable disease lasting longer than 6 months, reported Natalie Galanina, MD, of Rebecca and John Moores Cancer Center at the University of California, San Diego, and her colleagues. Earlier this year, investigators reported similar responses to checkpoint inhibitors in two patients with KS that wasn’t associated with HIV.
“An association has been demonstrated between chronic viral infection, malignancy, and up-regulation of programmed death receptor 1 (PD-1) on CD8+ cytotoxic T-lymphocytes,” the authors wrote in Cancer Immunology Research. In particular, “HIV-specific CD8+ T cells have increased PD-1 expression, which … promotes a cellular milieu conducive to oncogenesis.” These factors, together with the results from the previous study, have suggested that checkpoint inhibitors may be effective for patients with HIV-associated KS.
The retrospective study involved 320 patients treated with immunotherapy at Moores Cancer Center from August 2013 through December 2017. From this group, nine cases of HIV-associated KS were found. Median CD4 count was 256 cells/mcL and median viral load was 20 copies/mL. Eight patients were treated with nivolumab and one was treated with pembrolizumab. Median age was 44 years. All patients were male and receiving antiretroviral therapy.
Six patients (67%) achieved remission, with five attaining partial remission and one attaining complete remission (gastrointestinal disease). Of the remaining three patients, two currently have stable disease lasting longer than 6 months, and one has stable disease lasting longer than 3 months.
Muscle aches, pruritus, and low-grade fever were the most common adverse events. No grade 3 or higher drug-related adverse events occurred.
“Most of our patients received one to four prior lines of therapy but still responded to checkpoint blockade,” the authors wrote. “Our observations suggest that patients with HIV-associated KS have high [response rates] to PD-1 checkpoint blockade, without significant toxicity, even in the presence of low [tumor mutational burden] and/or lack of PD-L1 expression.”
Authors reported compensation from Incyte, Genentech, Merck, Pfizer, and others.
SOURCE: Galanina et al. Cancer Immunol Res. doi: 10.1158/2326-6066.CIR-18-0121.
FROM CANCER IMMUNOLOGY RESEARCH
Key clinical point: Checkpoint inhibitor therapy is effective for patients with HIV-associated Kaposi sarcoma.
Major finding: Two-thirds of patients (67%) with HIV-associated Kaposi sarcoma achieved partial or complete remission when treated with immune checkpoint blockade.
Study details: A retrospective study involving nine patients with Kaposi sarcoma treated with either nivolumab or pembrolizumab at the Rebecca and John Moores Cancer Center at the University of California, San Diego, (UCSD) from August 2013 through December 2017.
Disclosures: Authors reported compensation from Incyte, Genentech, Merck, Pfizer, and others.
Source: Galanina et al. Cancer Immunol Res. 2018 Sept 7. doi: 10.1158/2326-6066.CIR-18-0121.
Novel molecular assay: Promising results in bone and soft tissue tumor evaluation
, according to researchers.
The technique of anchored multiplex polymerase chain reaction (AMP)–based targeted next-generation sequencing (NGS) had a failure rate of 14% but, nonetheless, worked favorably when compared with conventional techniques, which were associated with several false positives in this study, the researchers reported in the Journal of Molecular Diagnostics.
Two new fusion partners for the USP6 gene were found using AMP-based targeted NGS in this study, which thus contributed to the “further unraveling of the molecular landscape” for these tumors, added corresponding author Judith V.M.G. Bovée, MD, PhD, of the department of pathology at Leiden (the Netherlands) University Medical Center and her colleagues.
While the genetics of bone and soft tissue tumors have diagnostic value in clinical practice, standard fluorescence in situ hybridization (FISH) and reverse transcriptase PCR are associated with several drawbacks, such as a high false negative rate in the case of FISH, Dr. Bovée and her coauthors wrote.
Accordingly, the researchers evaluated the applicability of a targeted sequencing assay (Archer FusionPlex Sarcoma kit, which was developed by ArcherDX) aimed at 26 genes relevant to bone and soft tissue tumor diagnostics.
Besides allowing for assessment of multiple target genes in a single assay, this technique circumvents the need to know both fusion partners for translocation detection, which opens up the possibility of identifying novel or rare fusion partners, investigators noted.
AMP-based targeted NGS was used to evaluate 81 bone and soft tissue tumor samples, and of those, 48 cases showed a fusion. For the remaining 33 cases in which no fusion was detected, 22 were considered truly negative because samples met all criteria for good quality, while the remaining 11 (14%) were considered not reliable because of insufficient quality, investigators reported.
The samples were also evaluated through use of FISH, reverse transcriptase PCR, or both in 58 cases and use of immunohistochemistry in 16 cases; for the remaining seven cases, no assay or immunohistochemistry could be applied because of a lack of availability, according to investigators.
Among the 48 entities that were fusion-positive according to AMP-based targeted NGS, 29 were validated using standard molecular assays, and of those, 25 had concordant results. Further analysis of the four discordant cases with a third independent technique confirmed the AMP-based targeted NGS findings, according to the published report.
Among the 22 fusion-negative high-quality samples, 19 were validated using FISH, and one case was found to be discordant; however, despite use of a third independent technique, this discrepancy could not be resolved, investigators said.
The AMP-based targeted NGS technique identified COL1A1 and SEC31A as novel fusion partners for USP6 in two cases of nodular fasciitis. Those fusion partners had been previously described in aneurysmal bone cysts, according to investigators.
Despite the promising results for the novel assay, conventional methods were sufficient in this study to confirm translocations in straightforward cases and ordinary rearrangements, according to the investigators.
“Both reverse transcription PCR and FISH are not only quick and easy to conduct but are also of low cost and high analytical validity and accuracy, which make them attractive methods,” they wrote.
The work by Dr. Bovée and her colleagues was supported by Leiden University Medical Center. The department of pathology and the department of cell and chemical biology at the medical center receive royalty payments from Kreatech/Leica, which provided a COL1A1/PDGFB fusion probe used in the research.
SOURCE: Lam SW et al. J Mol Diagn. 2018 Aug 20;20(5):653-63.
, according to researchers.
The technique of anchored multiplex polymerase chain reaction (AMP)–based targeted next-generation sequencing (NGS) had a failure rate of 14% but, nonetheless, worked favorably when compared with conventional techniques, which were associated with several false positives in this study, the researchers reported in the Journal of Molecular Diagnostics.
Two new fusion partners for the USP6 gene were found using AMP-based targeted NGS in this study, which thus contributed to the “further unraveling of the molecular landscape” for these tumors, added corresponding author Judith V.M.G. Bovée, MD, PhD, of the department of pathology at Leiden (the Netherlands) University Medical Center and her colleagues.
While the genetics of bone and soft tissue tumors have diagnostic value in clinical practice, standard fluorescence in situ hybridization (FISH) and reverse transcriptase PCR are associated with several drawbacks, such as a high false negative rate in the case of FISH, Dr. Bovée and her coauthors wrote.
Accordingly, the researchers evaluated the applicability of a targeted sequencing assay (Archer FusionPlex Sarcoma kit, which was developed by ArcherDX) aimed at 26 genes relevant to bone and soft tissue tumor diagnostics.
Besides allowing for assessment of multiple target genes in a single assay, this technique circumvents the need to know both fusion partners for translocation detection, which opens up the possibility of identifying novel or rare fusion partners, investigators noted.
AMP-based targeted NGS was used to evaluate 81 bone and soft tissue tumor samples, and of those, 48 cases showed a fusion. For the remaining 33 cases in which no fusion was detected, 22 were considered truly negative because samples met all criteria for good quality, while the remaining 11 (14%) were considered not reliable because of insufficient quality, investigators reported.
The samples were also evaluated through use of FISH, reverse transcriptase PCR, or both in 58 cases and use of immunohistochemistry in 16 cases; for the remaining seven cases, no assay or immunohistochemistry could be applied because of a lack of availability, according to investigators.
Among the 48 entities that were fusion-positive according to AMP-based targeted NGS, 29 were validated using standard molecular assays, and of those, 25 had concordant results. Further analysis of the four discordant cases with a third independent technique confirmed the AMP-based targeted NGS findings, according to the published report.
Among the 22 fusion-negative high-quality samples, 19 were validated using FISH, and one case was found to be discordant; however, despite use of a third independent technique, this discrepancy could not be resolved, investigators said.
The AMP-based targeted NGS technique identified COL1A1 and SEC31A as novel fusion partners for USP6 in two cases of nodular fasciitis. Those fusion partners had been previously described in aneurysmal bone cysts, according to investigators.
Despite the promising results for the novel assay, conventional methods were sufficient in this study to confirm translocations in straightforward cases and ordinary rearrangements, according to the investigators.
“Both reverse transcription PCR and FISH are not only quick and easy to conduct but are also of low cost and high analytical validity and accuracy, which make them attractive methods,” they wrote.
The work by Dr. Bovée and her colleagues was supported by Leiden University Medical Center. The department of pathology and the department of cell and chemical biology at the medical center receive royalty payments from Kreatech/Leica, which provided a COL1A1/PDGFB fusion probe used in the research.
SOURCE: Lam SW et al. J Mol Diagn. 2018 Aug 20;20(5):653-63.
, according to researchers.
The technique of anchored multiplex polymerase chain reaction (AMP)–based targeted next-generation sequencing (NGS) had a failure rate of 14% but, nonetheless, worked favorably when compared with conventional techniques, which were associated with several false positives in this study, the researchers reported in the Journal of Molecular Diagnostics.
Two new fusion partners for the USP6 gene were found using AMP-based targeted NGS in this study, which thus contributed to the “further unraveling of the molecular landscape” for these tumors, added corresponding author Judith V.M.G. Bovée, MD, PhD, of the department of pathology at Leiden (the Netherlands) University Medical Center and her colleagues.
While the genetics of bone and soft tissue tumors have diagnostic value in clinical practice, standard fluorescence in situ hybridization (FISH) and reverse transcriptase PCR are associated with several drawbacks, such as a high false negative rate in the case of FISH, Dr. Bovée and her coauthors wrote.
Accordingly, the researchers evaluated the applicability of a targeted sequencing assay (Archer FusionPlex Sarcoma kit, which was developed by ArcherDX) aimed at 26 genes relevant to bone and soft tissue tumor diagnostics.
Besides allowing for assessment of multiple target genes in a single assay, this technique circumvents the need to know both fusion partners for translocation detection, which opens up the possibility of identifying novel or rare fusion partners, investigators noted.
AMP-based targeted NGS was used to evaluate 81 bone and soft tissue tumor samples, and of those, 48 cases showed a fusion. For the remaining 33 cases in which no fusion was detected, 22 were considered truly negative because samples met all criteria for good quality, while the remaining 11 (14%) were considered not reliable because of insufficient quality, investigators reported.
The samples were also evaluated through use of FISH, reverse transcriptase PCR, or both in 58 cases and use of immunohistochemistry in 16 cases; for the remaining seven cases, no assay or immunohistochemistry could be applied because of a lack of availability, according to investigators.
Among the 48 entities that were fusion-positive according to AMP-based targeted NGS, 29 were validated using standard molecular assays, and of those, 25 had concordant results. Further analysis of the four discordant cases with a third independent technique confirmed the AMP-based targeted NGS findings, according to the published report.
Among the 22 fusion-negative high-quality samples, 19 were validated using FISH, and one case was found to be discordant; however, despite use of a third independent technique, this discrepancy could not be resolved, investigators said.
The AMP-based targeted NGS technique identified COL1A1 and SEC31A as novel fusion partners for USP6 in two cases of nodular fasciitis. Those fusion partners had been previously described in aneurysmal bone cysts, according to investigators.
Despite the promising results for the novel assay, conventional methods were sufficient in this study to confirm translocations in straightforward cases and ordinary rearrangements, according to the investigators.
“Both reverse transcription PCR and FISH are not only quick and easy to conduct but are also of low cost and high analytical validity and accuracy, which make them attractive methods,” they wrote.
The work by Dr. Bovée and her colleagues was supported by Leiden University Medical Center. The department of pathology and the department of cell and chemical biology at the medical center receive royalty payments from Kreatech/Leica, which provided a COL1A1/PDGFB fusion probe used in the research.
SOURCE: Lam SW et al. J Mol Diagn. 2018 Aug 20;20(5):653-63.
FROM THE JOURNAL OF MOLECULAR DIAGNOSTICS
Key clinical point: Anchored multiplex PCR (AMP)-based targeted next-generation sequencing (NGS) may be superior to conventional molecular assays in the evaluation of bone and soft tissue tumor samples.
Major finding: Standard techniques yielded 4 false negatives out of 29 samples that were fusion-positive by AMP-based targeted NGS.
Study details: Analysis of 81 bone and soft tissue tumor samples evaluated by AMP-based targeted NGS and conventional techniques.
Disclosures: The research was supported by Leiden (the Netherlands) University Medical Center, which receives royalty payments from Kreatech/Leica.
Source: Lam SW et al. J Mol Diagn. 2018 Aug 20;20(5):653-63.
SEAL: Selinexor extends PFS in advanced dedifferentiated liposarcoma
The investigational drug selinexor appears to be improving progression-free survival in patients with advanced dedifferentiated liposarcoma, based on phase 2 results from the randomized, placebo-controlled SEAL study.
But the statistical significance of the improvements varied depending on whether progression-free survival (PFS) was assessed by the World Health Organization criteria, which looks at two-dimensional measurements of these irregular three-dimensional objects, or RECIST v1.1 criteria, which only looks at a unidimensional measure, reported Mrinal M. Gounder, MD, of Memorial Sloan Kettering Cancer Center, New York, at the annual meeting of the American Society of Clinical Oncology. When tumor response was based on WHO criteria, there was no difference in median PFS for the 24 patients on active therapy (1.4 months) and the 27 patients on placebo (1.8 months). By RECIST v1.1 criteria, however, median PFS was 5.6 months with selinexor.
Dedifferentiated liposarcoma is incurable, and palliative therapies are associated with an overall survival of 11-20 months in these patients. Selinexor is an oral selective inhibitor of exportin-1 which exports proteins from the nucleus into the cytoplasm. The drug appears to prevent p53 from leaving the nucleus, thereby protecting it from overexpressed MDM2, which is a negative regulator of p53, but the drug might have other potential mechanisms of action.
The double-blind study included 56 evaluable patients who had progressive dedifferentiated liposarcoma and had received at least one prior systemic therapy. Patients’ median age was 61 years and they had received a median of two prior therapies. Patients were randomized to get either 60 mg of selinexor (26 patients) or placebo (30 patients) twice weekly until their disease progressed or they were no longer able to tolerate therapy. Patients whose disease progressed on placebo (24 patients) were allowed to cross over to open-label selinexor therapy.
Treatments were unblinded for 51 of the patients, 24 on selinexor and 27 on placebo. Disease progression as confirmed by Independent Central Radiological Review using WHO criteria was the main reason for ending blinded treatment.
Grade 1/2 adverse events for selinexor versus placebo, respectively, were nausea (85% vs. 31%), anorexia (62% vs. 14%), and fatigue (58% vs. 45%). The comparable rates of grade 3/4 adverse events were hyponatremia (15% vs. 0%), anemia (15% vs. 7%), and thrombocytopenia (12% vs. 0%). Selinexor dose was reduced because of adverse events in 12 patients.
In a discussion of the study’s implications, Mark Andrew Dickson, MD, also of Memorial Sloan Kettering Cancer Center, called the adverse events profile “mostly manageable but predictable grade 1/2 adverse events ... and median progression-free survival of 5 and a half months is quite encouraging.
“Changing response assessment method midtrial in a study with progression-free survival as the primary endpoint is obviously problematic, but it also highlights how difficult it is to measure three-dimensional tumors like complex retroperitoneal liposarcomas, which move and change and grow and shrink over time,” he said. “And I would conclude that RECIST is probably the worst method of tumor assessment for sarcoma, except for all the other methods of tumor assessment.”
To illustrate the difficulty of measuring tumor response, Dr. Dickson presented examples of different tumor shapes and scenarios where one method would indicate tumor progression and the other would indicate stable disease.
“There can be differences between the two methods in how progression responds and is determined. And you can do this experiment with a number of different shapes and find scenarios where one method would call it progression at a different time than the other. So this is really critically important when we look at the results of the clinical trial, because it was designed to look at WHO PFS. And you can see that, based on that, there was no significant difference between the selinexor and placebo arm,” he said.
Additionally, he reviewed cases from the study where “either way you measure this, you can see that [the] tumor is getting smaller over time,” as well as cases where the tumor grew in patients on placebo first, but decreased in size after switching to the active therapy.
“The improvement in progression-free survival is promising and ... selinexor probably does have activity in dediff lipo compared to historical data,” said Dr. Dickson, adding that he looks forward to selinexor progressing to a randomized, phase 3 trial and “seeing those data perhaps next year.”
Dr. Gounder disclosed financial relationships with multiple drug companies including Karyopharm Therapeutics, the maker of selinexor. Dr. Dickson disclosed a consult or adviser role with Celgene and research funding from Eli Lilly.
SOURCE: Gounder M et al. ASCO 2018, Abstract 11512.
The investigational drug selinexor appears to be improving progression-free survival in patients with advanced dedifferentiated liposarcoma, based on phase 2 results from the randomized, placebo-controlled SEAL study.
But the statistical significance of the improvements varied depending on whether progression-free survival (PFS) was assessed by the World Health Organization criteria, which looks at two-dimensional measurements of these irregular three-dimensional objects, or RECIST v1.1 criteria, which only looks at a unidimensional measure, reported Mrinal M. Gounder, MD, of Memorial Sloan Kettering Cancer Center, New York, at the annual meeting of the American Society of Clinical Oncology. When tumor response was based on WHO criteria, there was no difference in median PFS for the 24 patients on active therapy (1.4 months) and the 27 patients on placebo (1.8 months). By RECIST v1.1 criteria, however, median PFS was 5.6 months with selinexor.
Dedifferentiated liposarcoma is incurable, and palliative therapies are associated with an overall survival of 11-20 months in these patients. Selinexor is an oral selective inhibitor of exportin-1 which exports proteins from the nucleus into the cytoplasm. The drug appears to prevent p53 from leaving the nucleus, thereby protecting it from overexpressed MDM2, which is a negative regulator of p53, but the drug might have other potential mechanisms of action.
The double-blind study included 56 evaluable patients who had progressive dedifferentiated liposarcoma and had received at least one prior systemic therapy. Patients’ median age was 61 years and they had received a median of two prior therapies. Patients were randomized to get either 60 mg of selinexor (26 patients) or placebo (30 patients) twice weekly until their disease progressed or they were no longer able to tolerate therapy. Patients whose disease progressed on placebo (24 patients) were allowed to cross over to open-label selinexor therapy.
Treatments were unblinded for 51 of the patients, 24 on selinexor and 27 on placebo. Disease progression as confirmed by Independent Central Radiological Review using WHO criteria was the main reason for ending blinded treatment.
Grade 1/2 adverse events for selinexor versus placebo, respectively, were nausea (85% vs. 31%), anorexia (62% vs. 14%), and fatigue (58% vs. 45%). The comparable rates of grade 3/4 adverse events were hyponatremia (15% vs. 0%), anemia (15% vs. 7%), and thrombocytopenia (12% vs. 0%). Selinexor dose was reduced because of adverse events in 12 patients.
In a discussion of the study’s implications, Mark Andrew Dickson, MD, also of Memorial Sloan Kettering Cancer Center, called the adverse events profile “mostly manageable but predictable grade 1/2 adverse events ... and median progression-free survival of 5 and a half months is quite encouraging.
“Changing response assessment method midtrial in a study with progression-free survival as the primary endpoint is obviously problematic, but it also highlights how difficult it is to measure three-dimensional tumors like complex retroperitoneal liposarcomas, which move and change and grow and shrink over time,” he said. “And I would conclude that RECIST is probably the worst method of tumor assessment for sarcoma, except for all the other methods of tumor assessment.”
To illustrate the difficulty of measuring tumor response, Dr. Dickson presented examples of different tumor shapes and scenarios where one method would indicate tumor progression and the other would indicate stable disease.
“There can be differences between the two methods in how progression responds and is determined. And you can do this experiment with a number of different shapes and find scenarios where one method would call it progression at a different time than the other. So this is really critically important when we look at the results of the clinical trial, because it was designed to look at WHO PFS. And you can see that, based on that, there was no significant difference between the selinexor and placebo arm,” he said.
Additionally, he reviewed cases from the study where “either way you measure this, you can see that [the] tumor is getting smaller over time,” as well as cases where the tumor grew in patients on placebo first, but decreased in size after switching to the active therapy.
“The improvement in progression-free survival is promising and ... selinexor probably does have activity in dediff lipo compared to historical data,” said Dr. Dickson, adding that he looks forward to selinexor progressing to a randomized, phase 3 trial and “seeing those data perhaps next year.”
Dr. Gounder disclosed financial relationships with multiple drug companies including Karyopharm Therapeutics, the maker of selinexor. Dr. Dickson disclosed a consult or adviser role with Celgene and research funding from Eli Lilly.
SOURCE: Gounder M et al. ASCO 2018, Abstract 11512.
The investigational drug selinexor appears to be improving progression-free survival in patients with advanced dedifferentiated liposarcoma, based on phase 2 results from the randomized, placebo-controlled SEAL study.
But the statistical significance of the improvements varied depending on whether progression-free survival (PFS) was assessed by the World Health Organization criteria, which looks at two-dimensional measurements of these irregular three-dimensional objects, or RECIST v1.1 criteria, which only looks at a unidimensional measure, reported Mrinal M. Gounder, MD, of Memorial Sloan Kettering Cancer Center, New York, at the annual meeting of the American Society of Clinical Oncology. When tumor response was based on WHO criteria, there was no difference in median PFS for the 24 patients on active therapy (1.4 months) and the 27 patients on placebo (1.8 months). By RECIST v1.1 criteria, however, median PFS was 5.6 months with selinexor.
Dedifferentiated liposarcoma is incurable, and palliative therapies are associated with an overall survival of 11-20 months in these patients. Selinexor is an oral selective inhibitor of exportin-1 which exports proteins from the nucleus into the cytoplasm. The drug appears to prevent p53 from leaving the nucleus, thereby protecting it from overexpressed MDM2, which is a negative regulator of p53, but the drug might have other potential mechanisms of action.
The double-blind study included 56 evaluable patients who had progressive dedifferentiated liposarcoma and had received at least one prior systemic therapy. Patients’ median age was 61 years and they had received a median of two prior therapies. Patients were randomized to get either 60 mg of selinexor (26 patients) or placebo (30 patients) twice weekly until their disease progressed or they were no longer able to tolerate therapy. Patients whose disease progressed on placebo (24 patients) were allowed to cross over to open-label selinexor therapy.
Treatments were unblinded for 51 of the patients, 24 on selinexor and 27 on placebo. Disease progression as confirmed by Independent Central Radiological Review using WHO criteria was the main reason for ending blinded treatment.
Grade 1/2 adverse events for selinexor versus placebo, respectively, were nausea (85% vs. 31%), anorexia (62% vs. 14%), and fatigue (58% vs. 45%). The comparable rates of grade 3/4 adverse events were hyponatremia (15% vs. 0%), anemia (15% vs. 7%), and thrombocytopenia (12% vs. 0%). Selinexor dose was reduced because of adverse events in 12 patients.
In a discussion of the study’s implications, Mark Andrew Dickson, MD, also of Memorial Sloan Kettering Cancer Center, called the adverse events profile “mostly manageable but predictable grade 1/2 adverse events ... and median progression-free survival of 5 and a half months is quite encouraging.
“Changing response assessment method midtrial in a study with progression-free survival as the primary endpoint is obviously problematic, but it also highlights how difficult it is to measure three-dimensional tumors like complex retroperitoneal liposarcomas, which move and change and grow and shrink over time,” he said. “And I would conclude that RECIST is probably the worst method of tumor assessment for sarcoma, except for all the other methods of tumor assessment.”
To illustrate the difficulty of measuring tumor response, Dr. Dickson presented examples of different tumor shapes and scenarios where one method would indicate tumor progression and the other would indicate stable disease.
“There can be differences between the two methods in how progression responds and is determined. And you can do this experiment with a number of different shapes and find scenarios where one method would call it progression at a different time than the other. So this is really critically important when we look at the results of the clinical trial, because it was designed to look at WHO PFS. And you can see that, based on that, there was no significant difference between the selinexor and placebo arm,” he said.
Additionally, he reviewed cases from the study where “either way you measure this, you can see that [the] tumor is getting smaller over time,” as well as cases where the tumor grew in patients on placebo first, but decreased in size after switching to the active therapy.
“The improvement in progression-free survival is promising and ... selinexor probably does have activity in dediff lipo compared to historical data,” said Dr. Dickson, adding that he looks forward to selinexor progressing to a randomized, phase 3 trial and “seeing those data perhaps next year.”
Dr. Gounder disclosed financial relationships with multiple drug companies including Karyopharm Therapeutics, the maker of selinexor. Dr. Dickson disclosed a consult or adviser role with Celgene and research funding from Eli Lilly.
SOURCE: Gounder M et al. ASCO 2018, Abstract 11512.
FROM ASCO 2018
Key clinical point: The investigational drug selinexor appears to be improving progression-free survival (PFS) in patients with advanced dedifferentiated liposarcoma.
Major finding: When tumor response was based on World Health Organization criteria, there was no difference in median PFS for the 24 patients on active therapy (1.4 months) and the 27 patients on placebo (1.8 months). By RECIST v1.1 criteria, however, median PFS was 5.6 months with selinexor.
Study details: Phase 2 results from 56 patients with dedifferentiated liposarcoma in the randomized, placebo-controlled SEAL study.
Disclosures: Dr. Gounder reported financial relationships with multiple drug companies including Karyopharm Therapeutics, the maker of selinexor. Dr. Dickson reported a consultant or adviser role with Celgene and research funding from Eli Lilly.
Source: Gounder M et al. ASCO 2018, Abstract 11512.
Chromoplexy linked to aggressive Ewing sarcomas
Chromoplexy, a sudden burst of complex, loop-like gene rearrangements that gives rise to a fusion gene, appears to be associated with aggressive Ewing sarcomas, based on a study of 124 tumors reported in Science.
Ewing sarcomas with complex karyotypes are associated with a poorer prognosis compared with those with simpler karyotypes. The new findings show that these complex karyotypes are the product of chromoplexy, and that chromoplexy-generated fusions arise early, giving rise to both primary and relapse Ewing sarcoma tumors, which can continue to evolve in parallel.
Analysis of the sequence context surrounding chromoplexy breaks may provide clues and potentially point to a therapeutic vulnerability that could be used to treat Ewing sarcomas. Further, given the preference of chromoplexy events for transcriptionally active regions, Ewing sarcomas arising from chromoplexy may be responsive to immune checkpoint inhibition.
In a study of the whole genomes of 124 Ewing sarcomas, chromoplexy rather than simple reciprocal translocations defined the gene fusions seen in 52 tumors (42%). Ewing sarcoma involves fusions between EWSR1, a gene encoding an RNA binding protein, and E26 transformation-specific (ETS) transcription factors.
“Our analyses reveal rearrangement bursts (chromoplectic loops) as a source of gene fusion in human bone and soft tissue tumors. Ewing sarcomas with complex karyotypes are associated with a poorer prognosis than those with simpler karyotypes, and here we show chromoplexy as the mechanism in 42% of tumors. It is possible that the chromoplectic tumor’s additional gene disruptions and fusions contribute to the difference in patient survival,” wrote Nathaniel D. Anderson of the Hospital for Sick Children, Toronto, and the University of Toronto, and his colleagues.
Standard reciprocal translocations involve DNA breaks in two fusion partners. Chromoplexy involves three or more breakpoints in the genome. A loop pattern emerges as these three or more broken chromosome ends are forced to find a new partner. The result is the formation of functional EWSR1-FLI1 or EWSR1-ERG fusions that, upon expression, provide a selective growth or survival advantage
The researchers found that the loop rearrangements always contained the disease-defining fusion at the center, but they disrupted multiple additional genes. The loops occurred preferentially in early replicating and transcriptionally active genomic regions.
They found similar loops forming canonical fusions in three other sarcoma types.
“Our whole-genome sequence data support a model in which there is an early clone of (Ewing sarcoma), containing EWSR1-ETS and chromoplexy, arising at least 1 year before diagnosis, which gives rise to both the primary and metastatic or relapse tumors. Whether the bursts ... are chance events or driven by specific mutational processes, akin to the RAG machinery operative in leukemia, remains to be established. As an increasing and diverse number of tumor genome sequences become available, we may be able to define further rearrangement processes that underlie fusion genes and thus unravel the causes of fusion-driven human cancers,” the researchers wrote.
The clinical features and demographics of the study patients were typical of Ewing sarcoma patients. Average patient age at diagnosis was 14.8 years (2.8 to 36.6 years); the male to female ratio was 1.38:1; and 14 patients had relapsed, with 13 having died from their disease.
About half of fusions between the EWS RNA binding protein 1 (EWSR1) gene on chromosome 22 and an E26 transformation-specific (ETS) family transcription factor gene, either FLI1 at 11q24 or ERG at 21q11 arose via chromoplexy.
SOURCE: Anderson et al. Science 2018 Aug 31. doi: 10.1126/science.aam8419.
The contribution of genetic analysis to the current standard of care for Ewing sarcoma is limited to confirmation of the diagnostic EWSR1-FLI1 or EWSR1-ERG fusions. The discovery of genomic patterns associated with subsets of Ewing sarcomas raises the question of whether additional molecular diagnostic modalities are warranted. If chromoplexy events are important clinical biomarkers for disease aggressiveness in this tumor, as the authors suggest, their findings may support a new indication for clinical whole genome sequencing.
Analysis of additional patient samples will be needed, however, to confirm that the presence of chromoplexy is an independent prognostic predictor in Ewing sarcoma. This is because the researchers find that chromoplexy-driven Ewing sarcoma more likely contains tumor protein 53 (TP53) mutations. Because TP53 and stromal antigen 2 (STAG2) mutations and genomic complexity have each been associated with more aggressive Ewing sarcoma, dissecting the contribution of these factors to poor clinical outcomes in chromoplexy-derived Ewing sarcoma will be an important area of future work.
More generally, the study has important clinical implications for the genomic diagnosis of these and other cancers, as well as the expanding biological role of complex rearrangements in cancer evolution.
Could chromoplexy events in Ewing sarcoma be linked, for example, to the activity of an aberrantly expressed endogenous transposase such as PiggyBac transposase 5 (PGBD5), which was recently implicated in the genesis of the pathogenic gene rearrangements in childhood malignant rhabdoid tumors? An alternative possibility is a constitutional or acquired DNA repair defect (Science 2018 Aug 31. doi: 10.1126/science.aau8231).
Marcin Imielinski is with the Meyer Cancer Center, Cornell University, and the New York Genome Center, New York. Marc Ladanyi is with Memorial Sloan Kettering Cancer Center, New York. They made their remarks in an editorial in Science that accompanied the study.
The contribution of genetic analysis to the current standard of care for Ewing sarcoma is limited to confirmation of the diagnostic EWSR1-FLI1 or EWSR1-ERG fusions. The discovery of genomic patterns associated with subsets of Ewing sarcomas raises the question of whether additional molecular diagnostic modalities are warranted. If chromoplexy events are important clinical biomarkers for disease aggressiveness in this tumor, as the authors suggest, their findings may support a new indication for clinical whole genome sequencing.
Analysis of additional patient samples will be needed, however, to confirm that the presence of chromoplexy is an independent prognostic predictor in Ewing sarcoma. This is because the researchers find that chromoplexy-driven Ewing sarcoma more likely contains tumor protein 53 (TP53) mutations. Because TP53 and stromal antigen 2 (STAG2) mutations and genomic complexity have each been associated with more aggressive Ewing sarcoma, dissecting the contribution of these factors to poor clinical outcomes in chromoplexy-derived Ewing sarcoma will be an important area of future work.
More generally, the study has important clinical implications for the genomic diagnosis of these and other cancers, as well as the expanding biological role of complex rearrangements in cancer evolution.
Could chromoplexy events in Ewing sarcoma be linked, for example, to the activity of an aberrantly expressed endogenous transposase such as PiggyBac transposase 5 (PGBD5), which was recently implicated in the genesis of the pathogenic gene rearrangements in childhood malignant rhabdoid tumors? An alternative possibility is a constitutional or acquired DNA repair defect (Science 2018 Aug 31. doi: 10.1126/science.aau8231).
Marcin Imielinski is with the Meyer Cancer Center, Cornell University, and the New York Genome Center, New York. Marc Ladanyi is with Memorial Sloan Kettering Cancer Center, New York. They made their remarks in an editorial in Science that accompanied the study.
The contribution of genetic analysis to the current standard of care for Ewing sarcoma is limited to confirmation of the diagnostic EWSR1-FLI1 or EWSR1-ERG fusions. The discovery of genomic patterns associated with subsets of Ewing sarcomas raises the question of whether additional molecular diagnostic modalities are warranted. If chromoplexy events are important clinical biomarkers for disease aggressiveness in this tumor, as the authors suggest, their findings may support a new indication for clinical whole genome sequencing.
Analysis of additional patient samples will be needed, however, to confirm that the presence of chromoplexy is an independent prognostic predictor in Ewing sarcoma. This is because the researchers find that chromoplexy-driven Ewing sarcoma more likely contains tumor protein 53 (TP53) mutations. Because TP53 and stromal antigen 2 (STAG2) mutations and genomic complexity have each been associated with more aggressive Ewing sarcoma, dissecting the contribution of these factors to poor clinical outcomes in chromoplexy-derived Ewing sarcoma will be an important area of future work.
More generally, the study has important clinical implications for the genomic diagnosis of these and other cancers, as well as the expanding biological role of complex rearrangements in cancer evolution.
Could chromoplexy events in Ewing sarcoma be linked, for example, to the activity of an aberrantly expressed endogenous transposase such as PiggyBac transposase 5 (PGBD5), which was recently implicated in the genesis of the pathogenic gene rearrangements in childhood malignant rhabdoid tumors? An alternative possibility is a constitutional or acquired DNA repair defect (Science 2018 Aug 31. doi: 10.1126/science.aau8231).
Marcin Imielinski is with the Meyer Cancer Center, Cornell University, and the New York Genome Center, New York. Marc Ladanyi is with Memorial Sloan Kettering Cancer Center, New York. They made their remarks in an editorial in Science that accompanied the study.
Chromoplexy, a sudden burst of complex, loop-like gene rearrangements that gives rise to a fusion gene, appears to be associated with aggressive Ewing sarcomas, based on a study of 124 tumors reported in Science.
Ewing sarcomas with complex karyotypes are associated with a poorer prognosis compared with those with simpler karyotypes. The new findings show that these complex karyotypes are the product of chromoplexy, and that chromoplexy-generated fusions arise early, giving rise to both primary and relapse Ewing sarcoma tumors, which can continue to evolve in parallel.
Analysis of the sequence context surrounding chromoplexy breaks may provide clues and potentially point to a therapeutic vulnerability that could be used to treat Ewing sarcomas. Further, given the preference of chromoplexy events for transcriptionally active regions, Ewing sarcomas arising from chromoplexy may be responsive to immune checkpoint inhibition.
In a study of the whole genomes of 124 Ewing sarcomas, chromoplexy rather than simple reciprocal translocations defined the gene fusions seen in 52 tumors (42%). Ewing sarcoma involves fusions between EWSR1, a gene encoding an RNA binding protein, and E26 transformation-specific (ETS) transcription factors.
“Our analyses reveal rearrangement bursts (chromoplectic loops) as a source of gene fusion in human bone and soft tissue tumors. Ewing sarcomas with complex karyotypes are associated with a poorer prognosis than those with simpler karyotypes, and here we show chromoplexy as the mechanism in 42% of tumors. It is possible that the chromoplectic tumor’s additional gene disruptions and fusions contribute to the difference in patient survival,” wrote Nathaniel D. Anderson of the Hospital for Sick Children, Toronto, and the University of Toronto, and his colleagues.
Standard reciprocal translocations involve DNA breaks in two fusion partners. Chromoplexy involves three or more breakpoints in the genome. A loop pattern emerges as these three or more broken chromosome ends are forced to find a new partner. The result is the formation of functional EWSR1-FLI1 or EWSR1-ERG fusions that, upon expression, provide a selective growth or survival advantage
The researchers found that the loop rearrangements always contained the disease-defining fusion at the center, but they disrupted multiple additional genes. The loops occurred preferentially in early replicating and transcriptionally active genomic regions.
They found similar loops forming canonical fusions in three other sarcoma types.
“Our whole-genome sequence data support a model in which there is an early clone of (Ewing sarcoma), containing EWSR1-ETS and chromoplexy, arising at least 1 year before diagnosis, which gives rise to both the primary and metastatic or relapse tumors. Whether the bursts ... are chance events or driven by specific mutational processes, akin to the RAG machinery operative in leukemia, remains to be established. As an increasing and diverse number of tumor genome sequences become available, we may be able to define further rearrangement processes that underlie fusion genes and thus unravel the causes of fusion-driven human cancers,” the researchers wrote.
The clinical features and demographics of the study patients were typical of Ewing sarcoma patients. Average patient age at diagnosis was 14.8 years (2.8 to 36.6 years); the male to female ratio was 1.38:1; and 14 patients had relapsed, with 13 having died from their disease.
About half of fusions between the EWS RNA binding protein 1 (EWSR1) gene on chromosome 22 and an E26 transformation-specific (ETS) family transcription factor gene, either FLI1 at 11q24 or ERG at 21q11 arose via chromoplexy.
SOURCE: Anderson et al. Science 2018 Aug 31. doi: 10.1126/science.aam8419.
Chromoplexy, a sudden burst of complex, loop-like gene rearrangements that gives rise to a fusion gene, appears to be associated with aggressive Ewing sarcomas, based on a study of 124 tumors reported in Science.
Ewing sarcomas with complex karyotypes are associated with a poorer prognosis compared with those with simpler karyotypes. The new findings show that these complex karyotypes are the product of chromoplexy, and that chromoplexy-generated fusions arise early, giving rise to both primary and relapse Ewing sarcoma tumors, which can continue to evolve in parallel.
Analysis of the sequence context surrounding chromoplexy breaks may provide clues and potentially point to a therapeutic vulnerability that could be used to treat Ewing sarcomas. Further, given the preference of chromoplexy events for transcriptionally active regions, Ewing sarcomas arising from chromoplexy may be responsive to immune checkpoint inhibition.
In a study of the whole genomes of 124 Ewing sarcomas, chromoplexy rather than simple reciprocal translocations defined the gene fusions seen in 52 tumors (42%). Ewing sarcoma involves fusions between EWSR1, a gene encoding an RNA binding protein, and E26 transformation-specific (ETS) transcription factors.
“Our analyses reveal rearrangement bursts (chromoplectic loops) as a source of gene fusion in human bone and soft tissue tumors. Ewing sarcomas with complex karyotypes are associated with a poorer prognosis than those with simpler karyotypes, and here we show chromoplexy as the mechanism in 42% of tumors. It is possible that the chromoplectic tumor’s additional gene disruptions and fusions contribute to the difference in patient survival,” wrote Nathaniel D. Anderson of the Hospital for Sick Children, Toronto, and the University of Toronto, and his colleagues.
Standard reciprocal translocations involve DNA breaks in two fusion partners. Chromoplexy involves three or more breakpoints in the genome. A loop pattern emerges as these three or more broken chromosome ends are forced to find a new partner. The result is the formation of functional EWSR1-FLI1 or EWSR1-ERG fusions that, upon expression, provide a selective growth or survival advantage
The researchers found that the loop rearrangements always contained the disease-defining fusion at the center, but they disrupted multiple additional genes. The loops occurred preferentially in early replicating and transcriptionally active genomic regions.
They found similar loops forming canonical fusions in three other sarcoma types.
“Our whole-genome sequence data support a model in which there is an early clone of (Ewing sarcoma), containing EWSR1-ETS and chromoplexy, arising at least 1 year before diagnosis, which gives rise to both the primary and metastatic or relapse tumors. Whether the bursts ... are chance events or driven by specific mutational processes, akin to the RAG machinery operative in leukemia, remains to be established. As an increasing and diverse number of tumor genome sequences become available, we may be able to define further rearrangement processes that underlie fusion genes and thus unravel the causes of fusion-driven human cancers,” the researchers wrote.
The clinical features and demographics of the study patients were typical of Ewing sarcoma patients. Average patient age at diagnosis was 14.8 years (2.8 to 36.6 years); the male to female ratio was 1.38:1; and 14 patients had relapsed, with 13 having died from their disease.
About half of fusions between the EWS RNA binding protein 1 (EWSR1) gene on chromosome 22 and an E26 transformation-specific (ETS) family transcription factor gene, either FLI1 at 11q24 or ERG at 21q11 arose via chromoplexy.
SOURCE: Anderson et al. Science 2018 Aug 31. doi: 10.1126/science.aam8419.
FROM SCIENCE
Key clinical point: Chromoplexy, a sudden burst of complex, loop-like gene rearrangements that gives rise to a fusion gene, appears to be associated with aggressive Ewing sarcomas.
Major finding: Chromoplexy rather than simple reciprocal translocations defined the gene fusions seen in 42% of Ewing sarcoma tumors.
Study details: A study of the whole genomes of 124 Ewing sarcomas.
Disclosures: This research project was conducted with support from C17 and partially funded by Ewings Cancer Foundation of Canada and Childhood Cancer Canada Foundation. The authors declared no competing interests.
Source: Anderson et al. Science 2018 Aug 31. doi: 10.1126/science.aam8419.