User login
Immune agonist, checkpoint inhibitor combo shows good tolerability
CHICAGO – Combining two immunotherapies, one inhibiting immune suppression and the other stimulating immune activation, is well tolerated and shows activity for a variety of solid tumor types, according to a phase I trial presented at the annual meeting of the American Association of Clinical Oncology.
Investigators enrolled 51 patients with locally advanced or metastatic solid tumors of any type after progression on standard therapy to a phase Ib dose-escalation study using atezolizumab, a monoclonal antibody checkpoint inhibitor that targets PD-L1, in combination with MOXR0916 (MOXR), an agonist IgG1 monoclonal antibody targeting OX40, a costimulatory receptor. Atezolizumab received Food and Drug Administration approval in May 2016 for use in certain patients with urothelial carcinoma. There were 28 patients in a dose-escalation cohort of the study and 23 in a serial biopsy cohort. The dose of the drug combination was started at 12 mg and escalated to understand pharmacodynamic changes in the tumors.
“The pharmacokinetics of both MOXR0916 and atezolizumab were similar to their single-agent data, suggesting no interaction,” reported Dr. Jeffrey Infante of the Sarah Cannon Research Institute in Nashville, Tenn.
The drug combination was well tolerated through the entire escalation range of MOXR. There were no dose-limiting toxicities, and no maximal tolerated dose was reached. There were also no drug-related deaths or grade 4 toxicities or drug-related treatment discontinuations. One case of grade 3 pneumonitis, successfully managed with methylprednisolone and antibiotics, occurred at the MOXR 40-mg dose on cycle 4 of treatment in a patient with non–small-cell lung cancer, he said.
About half the patients (53%) experienced any form of adverse event on the drug combination, and only 8% were grade 2 or 3. There were very few adverse events of any one type, and they did not appear to cluster among patients on the higher MOXR doses. The most prevalent adverse events were nausea, fever, fatigue, and rash, and each was in the 8%-14% range and almost always grade 1.
Many patients showed efficacy of the regimens out to 6-7 cycles regardless of tumor type, and 8 of the 51 patients were still receiving the therapy past cycle 7 with partial responses.
The stimulatory molecule OX40 is not normally expressed on T cells, but it is expressed when antigen interacts with the T-cell receptor, and it can then interact with its ligand, OX40L. The result is production of inflammatory cytokines such as gamma-interferon, activation and survival of effector T cells, and production of memory T cells. At the same time, OX40 activity blocks the suppressive function of regulatory T cells.
“So a molecule that can be a cancer therapeutic such as an OX40 agonist has dual mechanisms of action,” Dr. Infante said. “It can costimulate effector T cells and at the same time inhibit regulatory T cells. Furthermore, there is a reduced risk of toxicity, potentially, as its activity is linked to antigen recognition.”
There is good rationale for using an OX40 agonist such as MOXR, either for its immune stimulatory function or to deactivate immune suppression by regulatory T cells, or both, said discussant Dr. Jedd Wolchok, chief, melanoma and immunotherapeutics service, Memorial Sloan-Kettering Cancer Center, New York. Dr. Infante’s dose-escalation study was “very nicely designed and showed quite good safety,” Dr. Wolchok said, though one thing he would have liked to have seen was a quantification of regulatory T cells in tumor biopsies.
“This [study] is very important considering that this is an agonist antibody, and the agonist agents need to be dosed very deliberatively, as was done here, to ensure safety of patients,” Dr. Wolchok said, adding that further research needs to target “optimal combinatorial partners” and explore other mechanistic biomarkers.
MOXR was given in this trial at escalating doses on a 3+3 design (0.8-1,200 mg) on the same day as atezolizumab 1,200 mg IV once every 3 weeks with a 21-day window for assessment of MOXR dose-limiting toxicities. MOXR doses of 300 mg maintained trough concentrations sufficient to saturate OX40 receptors. An expansion regimen using 300 mg MOXR with atezolizumab 1,200 mg every 3 weeks is underway and will assess efficacy in the treatment of melanoma, renal cell carcinoma, non–small-cell lung cancer, urothelial carcinoma, and triple-negative breast cancer.
The study was sponsored by Roche. Dr. Infante reported having no relevant financial disclosures. Dr. Wolchok owns stock in Potenza Therapeutics and Vesuvius Pharmaceuticals, has received travel expenses and/or has an advisory role with several other companies, and is a coinventor on an issued patent for DNA vaccines for the treatment of cancer in companion animals.
CHICAGO – Combining two immunotherapies, one inhibiting immune suppression and the other stimulating immune activation, is well tolerated and shows activity for a variety of solid tumor types, according to a phase I trial presented at the annual meeting of the American Association of Clinical Oncology.
Investigators enrolled 51 patients with locally advanced or metastatic solid tumors of any type after progression on standard therapy to a phase Ib dose-escalation study using atezolizumab, a monoclonal antibody checkpoint inhibitor that targets PD-L1, in combination with MOXR0916 (MOXR), an agonist IgG1 monoclonal antibody targeting OX40, a costimulatory receptor. Atezolizumab received Food and Drug Administration approval in May 2016 for use in certain patients with urothelial carcinoma. There were 28 patients in a dose-escalation cohort of the study and 23 in a serial biopsy cohort. The dose of the drug combination was started at 12 mg and escalated to understand pharmacodynamic changes in the tumors.
“The pharmacokinetics of both MOXR0916 and atezolizumab were similar to their single-agent data, suggesting no interaction,” reported Dr. Jeffrey Infante of the Sarah Cannon Research Institute in Nashville, Tenn.
The drug combination was well tolerated through the entire escalation range of MOXR. There were no dose-limiting toxicities, and no maximal tolerated dose was reached. There were also no drug-related deaths or grade 4 toxicities or drug-related treatment discontinuations. One case of grade 3 pneumonitis, successfully managed with methylprednisolone and antibiotics, occurred at the MOXR 40-mg dose on cycle 4 of treatment in a patient with non–small-cell lung cancer, he said.
About half the patients (53%) experienced any form of adverse event on the drug combination, and only 8% were grade 2 or 3. There were very few adverse events of any one type, and they did not appear to cluster among patients on the higher MOXR doses. The most prevalent adverse events were nausea, fever, fatigue, and rash, and each was in the 8%-14% range and almost always grade 1.
Many patients showed efficacy of the regimens out to 6-7 cycles regardless of tumor type, and 8 of the 51 patients were still receiving the therapy past cycle 7 with partial responses.
The stimulatory molecule OX40 is not normally expressed on T cells, but it is expressed when antigen interacts with the T-cell receptor, and it can then interact with its ligand, OX40L. The result is production of inflammatory cytokines such as gamma-interferon, activation and survival of effector T cells, and production of memory T cells. At the same time, OX40 activity blocks the suppressive function of regulatory T cells.
“So a molecule that can be a cancer therapeutic such as an OX40 agonist has dual mechanisms of action,” Dr. Infante said. “It can costimulate effector T cells and at the same time inhibit regulatory T cells. Furthermore, there is a reduced risk of toxicity, potentially, as its activity is linked to antigen recognition.”
There is good rationale for using an OX40 agonist such as MOXR, either for its immune stimulatory function or to deactivate immune suppression by regulatory T cells, or both, said discussant Dr. Jedd Wolchok, chief, melanoma and immunotherapeutics service, Memorial Sloan-Kettering Cancer Center, New York. Dr. Infante’s dose-escalation study was “very nicely designed and showed quite good safety,” Dr. Wolchok said, though one thing he would have liked to have seen was a quantification of regulatory T cells in tumor biopsies.
“This [study] is very important considering that this is an agonist antibody, and the agonist agents need to be dosed very deliberatively, as was done here, to ensure safety of patients,” Dr. Wolchok said, adding that further research needs to target “optimal combinatorial partners” and explore other mechanistic biomarkers.
MOXR was given in this trial at escalating doses on a 3+3 design (0.8-1,200 mg) on the same day as atezolizumab 1,200 mg IV once every 3 weeks with a 21-day window for assessment of MOXR dose-limiting toxicities. MOXR doses of 300 mg maintained trough concentrations sufficient to saturate OX40 receptors. An expansion regimen using 300 mg MOXR with atezolizumab 1,200 mg every 3 weeks is underway and will assess efficacy in the treatment of melanoma, renal cell carcinoma, non–small-cell lung cancer, urothelial carcinoma, and triple-negative breast cancer.
The study was sponsored by Roche. Dr. Infante reported having no relevant financial disclosures. Dr. Wolchok owns stock in Potenza Therapeutics and Vesuvius Pharmaceuticals, has received travel expenses and/or has an advisory role with several other companies, and is a coinventor on an issued patent for DNA vaccines for the treatment of cancer in companion animals.
CHICAGO – Combining two immunotherapies, one inhibiting immune suppression and the other stimulating immune activation, is well tolerated and shows activity for a variety of solid tumor types, according to a phase I trial presented at the annual meeting of the American Association of Clinical Oncology.
Investigators enrolled 51 patients with locally advanced or metastatic solid tumors of any type after progression on standard therapy to a phase Ib dose-escalation study using atezolizumab, a monoclonal antibody checkpoint inhibitor that targets PD-L1, in combination with MOXR0916 (MOXR), an agonist IgG1 monoclonal antibody targeting OX40, a costimulatory receptor. Atezolizumab received Food and Drug Administration approval in May 2016 for use in certain patients with urothelial carcinoma. There were 28 patients in a dose-escalation cohort of the study and 23 in a serial biopsy cohort. The dose of the drug combination was started at 12 mg and escalated to understand pharmacodynamic changes in the tumors.
“The pharmacokinetics of both MOXR0916 and atezolizumab were similar to their single-agent data, suggesting no interaction,” reported Dr. Jeffrey Infante of the Sarah Cannon Research Institute in Nashville, Tenn.
The drug combination was well tolerated through the entire escalation range of MOXR. There were no dose-limiting toxicities, and no maximal tolerated dose was reached. There were also no drug-related deaths or grade 4 toxicities or drug-related treatment discontinuations. One case of grade 3 pneumonitis, successfully managed with methylprednisolone and antibiotics, occurred at the MOXR 40-mg dose on cycle 4 of treatment in a patient with non–small-cell lung cancer, he said.
About half the patients (53%) experienced any form of adverse event on the drug combination, and only 8% were grade 2 or 3. There were very few adverse events of any one type, and they did not appear to cluster among patients on the higher MOXR doses. The most prevalent adverse events were nausea, fever, fatigue, and rash, and each was in the 8%-14% range and almost always grade 1.
Many patients showed efficacy of the regimens out to 6-7 cycles regardless of tumor type, and 8 of the 51 patients were still receiving the therapy past cycle 7 with partial responses.
The stimulatory molecule OX40 is not normally expressed on T cells, but it is expressed when antigen interacts with the T-cell receptor, and it can then interact with its ligand, OX40L. The result is production of inflammatory cytokines such as gamma-interferon, activation and survival of effector T cells, and production of memory T cells. At the same time, OX40 activity blocks the suppressive function of regulatory T cells.
“So a molecule that can be a cancer therapeutic such as an OX40 agonist has dual mechanisms of action,” Dr. Infante said. “It can costimulate effector T cells and at the same time inhibit regulatory T cells. Furthermore, there is a reduced risk of toxicity, potentially, as its activity is linked to antigen recognition.”
There is good rationale for using an OX40 agonist such as MOXR, either for its immune stimulatory function or to deactivate immune suppression by regulatory T cells, or both, said discussant Dr. Jedd Wolchok, chief, melanoma and immunotherapeutics service, Memorial Sloan-Kettering Cancer Center, New York. Dr. Infante’s dose-escalation study was “very nicely designed and showed quite good safety,” Dr. Wolchok said, though one thing he would have liked to have seen was a quantification of regulatory T cells in tumor biopsies.
“This [study] is very important considering that this is an agonist antibody, and the agonist agents need to be dosed very deliberatively, as was done here, to ensure safety of patients,” Dr. Wolchok said, adding that further research needs to target “optimal combinatorial partners” and explore other mechanistic biomarkers.
MOXR was given in this trial at escalating doses on a 3+3 design (0.8-1,200 mg) on the same day as atezolizumab 1,200 mg IV once every 3 weeks with a 21-day window for assessment of MOXR dose-limiting toxicities. MOXR doses of 300 mg maintained trough concentrations sufficient to saturate OX40 receptors. An expansion regimen using 300 mg MOXR with atezolizumab 1,200 mg every 3 weeks is underway and will assess efficacy in the treatment of melanoma, renal cell carcinoma, non–small-cell lung cancer, urothelial carcinoma, and triple-negative breast cancer.
The study was sponsored by Roche. Dr. Infante reported having no relevant financial disclosures. Dr. Wolchok owns stock in Potenza Therapeutics and Vesuvius Pharmaceuticals, has received travel expenses and/or has an advisory role with several other companies, and is a coinventor on an issued patent for DNA vaccines for the treatment of cancer in companion animals.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Combining an immune agonist and a checkpoint inhibitor shows good tolerability.
Major finding: Eighty-five percent of adverse effects were grade 1; the rest were grade 2/3.
Data source: A phase Ib, open-label multicenter study of 51 patients.
Disclosures: The study was sponsored by Roche. Dr. Infante reported having no relevant financial disclosures. Dr. Wolchok owns stock in Potenza Therapeutics and Vesuvius Pharmaceuticals, has received travel expenses and/or has an advisory role with several other companies, and is a coinventor on an issued patent for DNA vaccines for the treatment of cancer in companion animals.
FDA grants accelerated approval to nivolumab for Hodgkin lymphoma
The Food and Drug Administration has granted accelerated approval to nivolumab for the treatment of patients with classical Hodgkin lymphoma (cHL) that has relapsed or progressed after autologous hematopoietic stem cell transplantation (HSCT) and posttransplantation brentuximab vedotin.
Approval was based on a 65% objective response rate in 95 patients treated with nivolumab following autologous HSCT and posttransplantation brentuximab vedotin. All patients in the single-arm, multicenter trial had relapsed or refractory cHL and were enrolled regardless of PD-L1 expression status. Patients received a median of 17 doses of nivolumab, the FDA said in a written statement.
The median time to response was 2.1 months (range, 0.7-5.7 months). The estimated median duration of response was 8.7 months.
The FDA also issued a warning for complications of allogeneic HSCT after nivolumab, reporting that transplant-related deaths have occurred. Health care professionals should follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease (GVHD), severe acute GVHD, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions, they said.
The most common adverse reactions in a second single-arm study used to evaluate safety (n = 263) were upper respiratory tract infection, cough, pyrexia, and diarrhea. Other immune-mediated adverse reactions, occurring in 1%-5% of patients, included rash, pneumonitis, hepatitis, hyperthyroidism, and colitis. The most common serious adverse reactions, which were reported in 1%-3% of patients, were pneumonia, pleural effusion, pneumonitis, pyrexia, infusion-related reaction, and rash.
Nivolumab is marketed as Opdivo by Bristol-Myers Squibb and has been previously approved to treat advanced renal cell carcinoma, lung cancer, and melanoma.
On Twitter @NikolaidesLaura
The Food and Drug Administration has granted accelerated approval to nivolumab for the treatment of patients with classical Hodgkin lymphoma (cHL) that has relapsed or progressed after autologous hematopoietic stem cell transplantation (HSCT) and posttransplantation brentuximab vedotin.
Approval was based on a 65% objective response rate in 95 patients treated with nivolumab following autologous HSCT and posttransplantation brentuximab vedotin. All patients in the single-arm, multicenter trial had relapsed or refractory cHL and were enrolled regardless of PD-L1 expression status. Patients received a median of 17 doses of nivolumab, the FDA said in a written statement.
The median time to response was 2.1 months (range, 0.7-5.7 months). The estimated median duration of response was 8.7 months.
The FDA also issued a warning for complications of allogeneic HSCT after nivolumab, reporting that transplant-related deaths have occurred. Health care professionals should follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease (GVHD), severe acute GVHD, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions, they said.
The most common adverse reactions in a second single-arm study used to evaluate safety (n = 263) were upper respiratory tract infection, cough, pyrexia, and diarrhea. Other immune-mediated adverse reactions, occurring in 1%-5% of patients, included rash, pneumonitis, hepatitis, hyperthyroidism, and colitis. The most common serious adverse reactions, which were reported in 1%-3% of patients, were pneumonia, pleural effusion, pneumonitis, pyrexia, infusion-related reaction, and rash.
Nivolumab is marketed as Opdivo by Bristol-Myers Squibb and has been previously approved to treat advanced renal cell carcinoma, lung cancer, and melanoma.
On Twitter @NikolaidesLaura
The Food and Drug Administration has granted accelerated approval to nivolumab for the treatment of patients with classical Hodgkin lymphoma (cHL) that has relapsed or progressed after autologous hematopoietic stem cell transplantation (HSCT) and posttransplantation brentuximab vedotin.
Approval was based on a 65% objective response rate in 95 patients treated with nivolumab following autologous HSCT and posttransplantation brentuximab vedotin. All patients in the single-arm, multicenter trial had relapsed or refractory cHL and were enrolled regardless of PD-L1 expression status. Patients received a median of 17 doses of nivolumab, the FDA said in a written statement.
The median time to response was 2.1 months (range, 0.7-5.7 months). The estimated median duration of response was 8.7 months.
The FDA also issued a warning for complications of allogeneic HSCT after nivolumab, reporting that transplant-related deaths have occurred. Health care professionals should follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease (GVHD), severe acute GVHD, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions, they said.
The most common adverse reactions in a second single-arm study used to evaluate safety (n = 263) were upper respiratory tract infection, cough, pyrexia, and diarrhea. Other immune-mediated adverse reactions, occurring in 1%-5% of patients, included rash, pneumonitis, hepatitis, hyperthyroidism, and colitis. The most common serious adverse reactions, which were reported in 1%-3% of patients, were pneumonia, pleural effusion, pneumonitis, pyrexia, infusion-related reaction, and rash.
Nivolumab is marketed as Opdivo by Bristol-Myers Squibb and has been previously approved to treat advanced renal cell carcinoma, lung cancer, and melanoma.
On Twitter @NikolaidesLaura
FDA approves lenvatinib for advanced renal cell carcinoma
The Food and Drug Administration has approved lenvatinib capsules, in combination with everolimus, for the treatment of patients with advanced renal cell carcinoma following one prior antiangiogenic therapy.
Approval was based on prolonged progression-free survival (PFS) in a randomized, phase II, open-label multicenter clinical trial of 153 patients, the FDA said in a written statement.
Patients who received lenvatinib plus everolimus (n = 51) had significantly prolonged PFS, compared with patients who received only everolimus (n = 50) (14.6 months vs. 5.5 months; HR, 0.40; 95% CI, 0.24-0.68; P = .0005) but not compared with patients who received lenvatinib alone (n = 52) (7.4 months; HR, 0.66; 95% CI, 0.30-1.10; P = .12). Of patients receiving the combination of drugs, 71% experienced adverse events, compared with 79% of patients receiving lenvatinib alone and 50% of patients receiving everolimus alone. The most common treatment-related adverse events reported included diarrhea, decreased appetite, and severe fatigue.
The FDA previously granted lenvatinib, marketed as Lenvima by Eisai, a breakthrough therapy designation and priority review.
“This is the only combination regimen to significantly prolong progression-free survival … when compared with a standard of care in patients with advanced renal cell carcinoma,” representatives from Eisai said in a written statement.
Lenvatinib was previously approved for the treatment of recurrent, progressive, radioactive iodine-refractory differentiated thyroid cancer in early 2015. However, in April 2016, the FDA released a safety warning about lenvatinib capsules for oral use.
“Serious tumor-related bleeds, including fatal hemorrhagic events in Lenvima-treated patients, have occurred in clinical trials and been reported in postmarketing experience,” reported the FDA in a written statement.
The recommended lenvatinib dosage for renal cell carcinoma patients is 18 mg/day, lower than the 24 mg/day that was recommended to thyroid cancer patients prior to the FDA’s warning.
On Twitter @JessCraig_OP
The Food and Drug Administration has approved lenvatinib capsules, in combination with everolimus, for the treatment of patients with advanced renal cell carcinoma following one prior antiangiogenic therapy.
Approval was based on prolonged progression-free survival (PFS) in a randomized, phase II, open-label multicenter clinical trial of 153 patients, the FDA said in a written statement.
Patients who received lenvatinib plus everolimus (n = 51) had significantly prolonged PFS, compared with patients who received only everolimus (n = 50) (14.6 months vs. 5.5 months; HR, 0.40; 95% CI, 0.24-0.68; P = .0005) but not compared with patients who received lenvatinib alone (n = 52) (7.4 months; HR, 0.66; 95% CI, 0.30-1.10; P = .12). Of patients receiving the combination of drugs, 71% experienced adverse events, compared with 79% of patients receiving lenvatinib alone and 50% of patients receiving everolimus alone. The most common treatment-related adverse events reported included diarrhea, decreased appetite, and severe fatigue.
The FDA previously granted lenvatinib, marketed as Lenvima by Eisai, a breakthrough therapy designation and priority review.
“This is the only combination regimen to significantly prolong progression-free survival … when compared with a standard of care in patients with advanced renal cell carcinoma,” representatives from Eisai said in a written statement.
Lenvatinib was previously approved for the treatment of recurrent, progressive, radioactive iodine-refractory differentiated thyroid cancer in early 2015. However, in April 2016, the FDA released a safety warning about lenvatinib capsules for oral use.
“Serious tumor-related bleeds, including fatal hemorrhagic events in Lenvima-treated patients, have occurred in clinical trials and been reported in postmarketing experience,” reported the FDA in a written statement.
The recommended lenvatinib dosage for renal cell carcinoma patients is 18 mg/day, lower than the 24 mg/day that was recommended to thyroid cancer patients prior to the FDA’s warning.
On Twitter @JessCraig_OP
The Food and Drug Administration has approved lenvatinib capsules, in combination with everolimus, for the treatment of patients with advanced renal cell carcinoma following one prior antiangiogenic therapy.
Approval was based on prolonged progression-free survival (PFS) in a randomized, phase II, open-label multicenter clinical trial of 153 patients, the FDA said in a written statement.
Patients who received lenvatinib plus everolimus (n = 51) had significantly prolonged PFS, compared with patients who received only everolimus (n = 50) (14.6 months vs. 5.5 months; HR, 0.40; 95% CI, 0.24-0.68; P = .0005) but not compared with patients who received lenvatinib alone (n = 52) (7.4 months; HR, 0.66; 95% CI, 0.30-1.10; P = .12). Of patients receiving the combination of drugs, 71% experienced adverse events, compared with 79% of patients receiving lenvatinib alone and 50% of patients receiving everolimus alone. The most common treatment-related adverse events reported included diarrhea, decreased appetite, and severe fatigue.
The FDA previously granted lenvatinib, marketed as Lenvima by Eisai, a breakthrough therapy designation and priority review.
“This is the only combination regimen to significantly prolong progression-free survival … when compared with a standard of care in patients with advanced renal cell carcinoma,” representatives from Eisai said in a written statement.
Lenvatinib was previously approved for the treatment of recurrent, progressive, radioactive iodine-refractory differentiated thyroid cancer in early 2015. However, in April 2016, the FDA released a safety warning about lenvatinib capsules for oral use.
“Serious tumor-related bleeds, including fatal hemorrhagic events in Lenvima-treated patients, have occurred in clinical trials and been reported in postmarketing experience,” reported the FDA in a written statement.
The recommended lenvatinib dosage for renal cell carcinoma patients is 18 mg/day, lower than the 24 mg/day that was recommended to thyroid cancer patients prior to the FDA’s warning.
On Twitter @JessCraig_OP
Immune checkpoint inhibitors have antitumor activity in gastric, esophageal cancers
SAN FRANCISCO – Two immune checkpoint inhibitors that help restore the antitumor response are active and well tolerated in patients with advanced, generally heavily pretreated gastric and esophageal cancers, according to a pair of early-phase trials reported at the Gastrointestinal Cancers Symposium.
Results from CheckMate-032 showed that nivolumab, an antibody that targets the cell surface receptor programmed death-1 (PD-1), yielded a response rate of 14% in patients with advanced gastric and related cancers. And updated results from KEYNOTE-028 showed that pembrolizumab, another antibody targeting PD-1, led to a response rate of 30% in patients with advanced esophageal and related cancers that expressed the ligand programmed death ligand 1 (PD-L1).
“Checkpoint inhibitors are clearly promising new agents ... All compounds are still in development, but we already have at least phase 1 data that they are effective,” commented invited discussant Dr. Markus H. Möhler of the University Medical Center Mainz (Germany). “Combination treatment strategies are clearly under investigation, and it is our task as a scientific community to look into interesting modern combinations, like combinations with antiangiogenic agents or maybe even with stem cell inhibition.”
He commended the KEYNOTE-028 investigators, in particular, for their development of a tumor gene signature that appeared to predict benefit from pembrolizumab.
“Molecular and immunological characterization of the patients is key, and we have seen now in the pembrolizumab study with the six-gene signature the first step in the right direction,” Dr. Möhler said, recommending that it be correlated with data from The Cancer Genome Atlas project, which has identified four distinct molecular subtypes of esophagogastric cancer.
“It is now clear that some of these subtypes express higher PD-L1 compared to the others, particularly inflamed subtypes,” he elaborated. “Therefore, it is clear that all the studies in the future really should try to look into the correlation with these four gene subgroups characterized.”
CheckMate-032 trial
Patients with a variety of solid tumors were eligible for CheckMate-032, a phase I/II trial. First author Dr. Dung T. Le reported results for 59 patients with locoregionally advanced or metastatic gastric cancer, esophageal, or gastroesophageal junction cancer who had received at least one prior therapy.
The patients were treated with nivolumab (Opdivo) every 2 weeks. (Nivolumab is currently FDA approved for the treatment of melanoma, non–small cell lung cancer, and renal cancer.)
With a median follow-up of 4.6 months, the response rate was 14%, reported Dr. Le of Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins, Baltimore, at the symposium, which was sponsored by ASCO, ASTRO, the American Gastroenterological Association, and the Society of Surgical Oncology.
However, “PD-L1 expression appears to be numerically associated with a higher objective response rate,” she noted. Specifically, the response rate was 27% among patients whose tumor cells showed 1% or greater PD-L1 staining, and an even higher 33% among those whose tumor cells showed 5% or greater PD-L1 staining.
Median overall survival was 5 months. The 6-month overall survival rate was 49%, and the 12-month rate was 36%.
“The adverse event profile was similar to that seen in patients with other tumor types,” Dr. Le commented.
In all, 17% of patients experienced grade 3 or 4 treatment-related adverse events, and 5% experienced grade 3 or 4 treatment-related serious adverse events. These events included elevation of liver enzymes, pneumonitis, fatigue, diarrhea, and vomiting. There were no treatment-related deaths.
KEYNOTE-028 trial
Patients with various types of advanced solid tumors were eligible for KEYNOTE-028, a phase Ib trial, if at least 1% of their tumor or inflammatory cells expressed PD-L1. First author Dr. Toshihiko Doi reported results for 23 patients with esophageal or gastroesophageal junction cancer who had experienced failure of standard therapy or were unable to tolerate it.
The patients were treated with pembrolizumab (Keytruda) every 2 weeks. (Pembrolizumab is currently FDA approved for the treatment of melanoma and non–small cell lung cancer.)
With a median follow-up of 7.1 months, the overall response rate was 30%, reported Dr. Doi of the National Cancer Center Hospital East in Chiba, Japan. By tumor histology, it was 29% for squamous cell carcinomas and 40% for adenocarcinomas.
He and his colleagues performed gene expression profiling of tumor tissue, identifying a six-gene interferon gamma signature that appeared predictive.
Specifically, patients with high signature scores, indicating more inflamed tumors, tended to have a better response rate than those with low scores (43% vs. 11%) as well as longer progression-free survival.
In all, 17% of patients experienced grade 3 treatment-related adverse events (reduced appetite, lymphopenia, liver disorder, and pruritic rash). There were no treatment-related deaths or discontinuations. With respect to adverse events of special interest because of their immune etiology, 9% of patients experienced hypothyroidism, 4% adrenal insufficiency, and 4% pruritic rash.
“Further evaluation of pembrolizumab in esophageal cancer is ongoing,” Dr. Doi concluded, pointing to the KEYNOTE-180 trial, which is testing the agent as third-line therapy, and the KEYNOTE-181 trial, which is pitting it against treatment of physician’s choice as second-line therapy.
SAN FRANCISCO – Two immune checkpoint inhibitors that help restore the antitumor response are active and well tolerated in patients with advanced, generally heavily pretreated gastric and esophageal cancers, according to a pair of early-phase trials reported at the Gastrointestinal Cancers Symposium.
Results from CheckMate-032 showed that nivolumab, an antibody that targets the cell surface receptor programmed death-1 (PD-1), yielded a response rate of 14% in patients with advanced gastric and related cancers. And updated results from KEYNOTE-028 showed that pembrolizumab, another antibody targeting PD-1, led to a response rate of 30% in patients with advanced esophageal and related cancers that expressed the ligand programmed death ligand 1 (PD-L1).
“Checkpoint inhibitors are clearly promising new agents ... All compounds are still in development, but we already have at least phase 1 data that they are effective,” commented invited discussant Dr. Markus H. Möhler of the University Medical Center Mainz (Germany). “Combination treatment strategies are clearly under investigation, and it is our task as a scientific community to look into interesting modern combinations, like combinations with antiangiogenic agents or maybe even with stem cell inhibition.”
He commended the KEYNOTE-028 investigators, in particular, for their development of a tumor gene signature that appeared to predict benefit from pembrolizumab.
“Molecular and immunological characterization of the patients is key, and we have seen now in the pembrolizumab study with the six-gene signature the first step in the right direction,” Dr. Möhler said, recommending that it be correlated with data from The Cancer Genome Atlas project, which has identified four distinct molecular subtypes of esophagogastric cancer.
“It is now clear that some of these subtypes express higher PD-L1 compared to the others, particularly inflamed subtypes,” he elaborated. “Therefore, it is clear that all the studies in the future really should try to look into the correlation with these four gene subgroups characterized.”
CheckMate-032 trial
Patients with a variety of solid tumors were eligible for CheckMate-032, a phase I/II trial. First author Dr. Dung T. Le reported results for 59 patients with locoregionally advanced or metastatic gastric cancer, esophageal, or gastroesophageal junction cancer who had received at least one prior therapy.
The patients were treated with nivolumab (Opdivo) every 2 weeks. (Nivolumab is currently FDA approved for the treatment of melanoma, non–small cell lung cancer, and renal cancer.)
With a median follow-up of 4.6 months, the response rate was 14%, reported Dr. Le of Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins, Baltimore, at the symposium, which was sponsored by ASCO, ASTRO, the American Gastroenterological Association, and the Society of Surgical Oncology.
However, “PD-L1 expression appears to be numerically associated with a higher objective response rate,” she noted. Specifically, the response rate was 27% among patients whose tumor cells showed 1% or greater PD-L1 staining, and an even higher 33% among those whose tumor cells showed 5% or greater PD-L1 staining.
Median overall survival was 5 months. The 6-month overall survival rate was 49%, and the 12-month rate was 36%.
“The adverse event profile was similar to that seen in patients with other tumor types,” Dr. Le commented.
In all, 17% of patients experienced grade 3 or 4 treatment-related adverse events, and 5% experienced grade 3 or 4 treatment-related serious adverse events. These events included elevation of liver enzymes, pneumonitis, fatigue, diarrhea, and vomiting. There were no treatment-related deaths.
KEYNOTE-028 trial
Patients with various types of advanced solid tumors were eligible for KEYNOTE-028, a phase Ib trial, if at least 1% of their tumor or inflammatory cells expressed PD-L1. First author Dr. Toshihiko Doi reported results for 23 patients with esophageal or gastroesophageal junction cancer who had experienced failure of standard therapy or were unable to tolerate it.
The patients were treated with pembrolizumab (Keytruda) every 2 weeks. (Pembrolizumab is currently FDA approved for the treatment of melanoma and non–small cell lung cancer.)
With a median follow-up of 7.1 months, the overall response rate was 30%, reported Dr. Doi of the National Cancer Center Hospital East in Chiba, Japan. By tumor histology, it was 29% for squamous cell carcinomas and 40% for adenocarcinomas.
He and his colleagues performed gene expression profiling of tumor tissue, identifying a six-gene interferon gamma signature that appeared predictive.
Specifically, patients with high signature scores, indicating more inflamed tumors, tended to have a better response rate than those with low scores (43% vs. 11%) as well as longer progression-free survival.
In all, 17% of patients experienced grade 3 treatment-related adverse events (reduced appetite, lymphopenia, liver disorder, and pruritic rash). There were no treatment-related deaths or discontinuations. With respect to adverse events of special interest because of their immune etiology, 9% of patients experienced hypothyroidism, 4% adrenal insufficiency, and 4% pruritic rash.
“Further evaluation of pembrolizumab in esophageal cancer is ongoing,” Dr. Doi concluded, pointing to the KEYNOTE-180 trial, which is testing the agent as third-line therapy, and the KEYNOTE-181 trial, which is pitting it against treatment of physician’s choice as second-line therapy.
SAN FRANCISCO – Two immune checkpoint inhibitors that help restore the antitumor response are active and well tolerated in patients with advanced, generally heavily pretreated gastric and esophageal cancers, according to a pair of early-phase trials reported at the Gastrointestinal Cancers Symposium.
Results from CheckMate-032 showed that nivolumab, an antibody that targets the cell surface receptor programmed death-1 (PD-1), yielded a response rate of 14% in patients with advanced gastric and related cancers. And updated results from KEYNOTE-028 showed that pembrolizumab, another antibody targeting PD-1, led to a response rate of 30% in patients with advanced esophageal and related cancers that expressed the ligand programmed death ligand 1 (PD-L1).
“Checkpoint inhibitors are clearly promising new agents ... All compounds are still in development, but we already have at least phase 1 data that they are effective,” commented invited discussant Dr. Markus H. Möhler of the University Medical Center Mainz (Germany). “Combination treatment strategies are clearly under investigation, and it is our task as a scientific community to look into interesting modern combinations, like combinations with antiangiogenic agents or maybe even with stem cell inhibition.”
He commended the KEYNOTE-028 investigators, in particular, for their development of a tumor gene signature that appeared to predict benefit from pembrolizumab.
“Molecular and immunological characterization of the patients is key, and we have seen now in the pembrolizumab study with the six-gene signature the first step in the right direction,” Dr. Möhler said, recommending that it be correlated with data from The Cancer Genome Atlas project, which has identified four distinct molecular subtypes of esophagogastric cancer.
“It is now clear that some of these subtypes express higher PD-L1 compared to the others, particularly inflamed subtypes,” he elaborated. “Therefore, it is clear that all the studies in the future really should try to look into the correlation with these four gene subgroups characterized.”
CheckMate-032 trial
Patients with a variety of solid tumors were eligible for CheckMate-032, a phase I/II trial. First author Dr. Dung T. Le reported results for 59 patients with locoregionally advanced or metastatic gastric cancer, esophageal, or gastroesophageal junction cancer who had received at least one prior therapy.
The patients were treated with nivolumab (Opdivo) every 2 weeks. (Nivolumab is currently FDA approved for the treatment of melanoma, non–small cell lung cancer, and renal cancer.)
With a median follow-up of 4.6 months, the response rate was 14%, reported Dr. Le of Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins, Baltimore, at the symposium, which was sponsored by ASCO, ASTRO, the American Gastroenterological Association, and the Society of Surgical Oncology.
However, “PD-L1 expression appears to be numerically associated with a higher objective response rate,” she noted. Specifically, the response rate was 27% among patients whose tumor cells showed 1% or greater PD-L1 staining, and an even higher 33% among those whose tumor cells showed 5% or greater PD-L1 staining.
Median overall survival was 5 months. The 6-month overall survival rate was 49%, and the 12-month rate was 36%.
“The adverse event profile was similar to that seen in patients with other tumor types,” Dr. Le commented.
In all, 17% of patients experienced grade 3 or 4 treatment-related adverse events, and 5% experienced grade 3 or 4 treatment-related serious adverse events. These events included elevation of liver enzymes, pneumonitis, fatigue, diarrhea, and vomiting. There were no treatment-related deaths.
KEYNOTE-028 trial
Patients with various types of advanced solid tumors were eligible for KEYNOTE-028, a phase Ib trial, if at least 1% of their tumor or inflammatory cells expressed PD-L1. First author Dr. Toshihiko Doi reported results for 23 patients with esophageal or gastroesophageal junction cancer who had experienced failure of standard therapy or were unable to tolerate it.
The patients were treated with pembrolizumab (Keytruda) every 2 weeks. (Pembrolizumab is currently FDA approved for the treatment of melanoma and non–small cell lung cancer.)
With a median follow-up of 7.1 months, the overall response rate was 30%, reported Dr. Doi of the National Cancer Center Hospital East in Chiba, Japan. By tumor histology, it was 29% for squamous cell carcinomas and 40% for adenocarcinomas.
He and his colleagues performed gene expression profiling of tumor tissue, identifying a six-gene interferon gamma signature that appeared predictive.
Specifically, patients with high signature scores, indicating more inflamed tumors, tended to have a better response rate than those with low scores (43% vs. 11%) as well as longer progression-free survival.
In all, 17% of patients experienced grade 3 treatment-related adverse events (reduced appetite, lymphopenia, liver disorder, and pruritic rash). There were no treatment-related deaths or discontinuations. With respect to adverse events of special interest because of their immune etiology, 9% of patients experienced hypothyroidism, 4% adrenal insufficiency, and 4% pruritic rash.
“Further evaluation of pembrolizumab in esophageal cancer is ongoing,” Dr. Doi concluded, pointing to the KEYNOTE-180 trial, which is testing the agent as third-line therapy, and the KEYNOTE-181 trial, which is pitting it against treatment of physician’s choice as second-line therapy.
AT THE GASTROINTESTINAL CANCERS SYMPOSIUM
Key clinical point: Nivolumab and pembrolizumab appear active and well tolerated in patients with previously treated esophagogastric cancers.
Major finding: The overall response rate was 14% with nivolumab in gastric and related cancers, and 30% with pembrolizumab in PD-L1–positive esophageal and related cancers.
Data source: An analysis of 59 patients with advanced gastric and related cancers treated on a phase I/II trial (CheckMate-032 trial), and 23 patients with advanced PD-L1–positive esophageal and related cancers treated on a phase Ib trial (KEYNOTE-028).
Disclosures: Dr. Le disclosed that she receives research funding from Aduro Biotech, Bristol-Myers Squibb, and Merck. CheckMate-032 was sponsored by Bristol-Myers Squibb. Dr. Doi disclosed that he receives honoraria from Chugai Pharma and Novartis; has consulting roles and receives research funding from several pharmaceutical companies. KEYNOTE-028 was sponsored by Merck Sharp & Dohme Corp. Dr. Möhler disclosed honoraria and travel expenses from and advisory roles with several pharmaceutical companies.
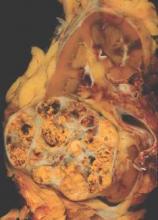
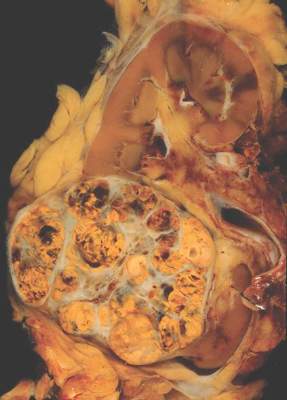
Individualized approach improves surveillance after renal cell carcinoma resection
A novel approach to oncologic surveillance after surgical resection for renal cell carcinoma (RCC) that incorporates patient age, Charlson comorbidity index, pathologic tumor stage, and relapse location–specific data, may provide better recommendations for surveillance duration than current guidelines, researchers reported.
“By providing more individualized recommendations and by eliminating oversimplified time thresholds for surveillance, this strategy, we believe, represents an improvement over current guidelines,” wrote Dr. Suzanne Stewart-Merrill of the department of urology, Mayo Clinic, Rochester, Minn., and colleagues (J Clin Oncol. 2015 Sep 7. doi: 10.1200/JCO.2015.61.8009).
Guidelines suggest surveillance durations based on cumulative incidence of recurrences, but do not account for individual patient risk factors. Adherence to the guidelines could miss up to one-third of all recurrences, the authors noted. The longest surveillance duration advocated by the National Comprehensive Cancer Network or the American Urological Association is 5 years.
Researchers used Weibull models for risk of recurrence, stratified by stage and relapse location, combined with risk estimates for non-RCC death, to estimate the optimum surveillance duration. For example, for patients aged 50-59 years with pT1Nx-0 disease and a Charlson comorbidity index of less than or equal to 1, risk of non-RCC death exceeded the risk of abdominal recurrence at 7 years, marking the recommended surveillance duration for that subgroup. The recommended surveillance duration for patients with similar characteristics aged 60-69 years is 2.5 years, and for patients aged 70-79 years it is 1.5 years.
When taking into account individual risk factors, the method produced a wide range of surveillance durations. For patients under 50 years old with pT1Nx-0 disease and a Charlson comorbidity index less than or equal to 1, the risk of non-RCC death did not exceed the risk of abdominal recurrence for more than 20 years. By contrast, patients with pT1Nx-0 disease and Charlson comorbidity index greater than or equal to 2, had a higher risk of non-RCC death than risk of abdominal recurrence at 30 days after surgery.
The retrospective study of 2,511 patients who underwent surgical resection for M0 sporadic RCC between 1990 and 2008 had a median follow up of 9.0 years (interquartile range 6.4-12.7 years).
The researchers noted that recurrences beyond 5 years are fairly common, with up to 15% of patients, by one study’s estimate, experiencing recurrence during the decade following surgery. Cumulative incidence of recurrence does not capture how a patient’s risk of recurrence changes with time or how comorbid conditions influence risk.
The proposed surveillance method results in shorter surveillance durations for some patients and longer surveillance durations than currently recommended for others. This diversity in stopping points “better reflects the range of disease courses appreciated in patients with RCC on the basis of the interplay that occurs between the risk of recurrence and other competing health factors,” Dr. Stewart-Merrill and associates explained.
Dr. Stewart-Merrill reported having no disclosures.
A novel approach to oncologic surveillance after surgical resection for renal cell carcinoma (RCC) that incorporates patient age, Charlson comorbidity index, pathologic tumor stage, and relapse location–specific data, may provide better recommendations for surveillance duration than current guidelines, researchers reported.
“By providing more individualized recommendations and by eliminating oversimplified time thresholds for surveillance, this strategy, we believe, represents an improvement over current guidelines,” wrote Dr. Suzanne Stewart-Merrill of the department of urology, Mayo Clinic, Rochester, Minn., and colleagues (J Clin Oncol. 2015 Sep 7. doi: 10.1200/JCO.2015.61.8009).
Guidelines suggest surveillance durations based on cumulative incidence of recurrences, but do not account for individual patient risk factors. Adherence to the guidelines could miss up to one-third of all recurrences, the authors noted. The longest surveillance duration advocated by the National Comprehensive Cancer Network or the American Urological Association is 5 years.
Researchers used Weibull models for risk of recurrence, stratified by stage and relapse location, combined with risk estimates for non-RCC death, to estimate the optimum surveillance duration. For example, for patients aged 50-59 years with pT1Nx-0 disease and a Charlson comorbidity index of less than or equal to 1, risk of non-RCC death exceeded the risk of abdominal recurrence at 7 years, marking the recommended surveillance duration for that subgroup. The recommended surveillance duration for patients with similar characteristics aged 60-69 years is 2.5 years, and for patients aged 70-79 years it is 1.5 years.
When taking into account individual risk factors, the method produced a wide range of surveillance durations. For patients under 50 years old with pT1Nx-0 disease and a Charlson comorbidity index less than or equal to 1, the risk of non-RCC death did not exceed the risk of abdominal recurrence for more than 20 years. By contrast, patients with pT1Nx-0 disease and Charlson comorbidity index greater than or equal to 2, had a higher risk of non-RCC death than risk of abdominal recurrence at 30 days after surgery.
The retrospective study of 2,511 patients who underwent surgical resection for M0 sporadic RCC between 1990 and 2008 had a median follow up of 9.0 years (interquartile range 6.4-12.7 years).
The researchers noted that recurrences beyond 5 years are fairly common, with up to 15% of patients, by one study’s estimate, experiencing recurrence during the decade following surgery. Cumulative incidence of recurrence does not capture how a patient’s risk of recurrence changes with time or how comorbid conditions influence risk.
The proposed surveillance method results in shorter surveillance durations for some patients and longer surveillance durations than currently recommended for others. This diversity in stopping points “better reflects the range of disease courses appreciated in patients with RCC on the basis of the interplay that occurs between the risk of recurrence and other competing health factors,” Dr. Stewart-Merrill and associates explained.
Dr. Stewart-Merrill reported having no disclosures.
A novel approach to oncologic surveillance after surgical resection for renal cell carcinoma (RCC) that incorporates patient age, Charlson comorbidity index, pathologic tumor stage, and relapse location–specific data, may provide better recommendations for surveillance duration than current guidelines, researchers reported.
“By providing more individualized recommendations and by eliminating oversimplified time thresholds for surveillance, this strategy, we believe, represents an improvement over current guidelines,” wrote Dr. Suzanne Stewart-Merrill of the department of urology, Mayo Clinic, Rochester, Minn., and colleagues (J Clin Oncol. 2015 Sep 7. doi: 10.1200/JCO.2015.61.8009).
Guidelines suggest surveillance durations based on cumulative incidence of recurrences, but do not account for individual patient risk factors. Adherence to the guidelines could miss up to one-third of all recurrences, the authors noted. The longest surveillance duration advocated by the National Comprehensive Cancer Network or the American Urological Association is 5 years.
Researchers used Weibull models for risk of recurrence, stratified by stage and relapse location, combined with risk estimates for non-RCC death, to estimate the optimum surveillance duration. For example, for patients aged 50-59 years with pT1Nx-0 disease and a Charlson comorbidity index of less than or equal to 1, risk of non-RCC death exceeded the risk of abdominal recurrence at 7 years, marking the recommended surveillance duration for that subgroup. The recommended surveillance duration for patients with similar characteristics aged 60-69 years is 2.5 years, and for patients aged 70-79 years it is 1.5 years.
When taking into account individual risk factors, the method produced a wide range of surveillance durations. For patients under 50 years old with pT1Nx-0 disease and a Charlson comorbidity index less than or equal to 1, the risk of non-RCC death did not exceed the risk of abdominal recurrence for more than 20 years. By contrast, patients with pT1Nx-0 disease and Charlson comorbidity index greater than or equal to 2, had a higher risk of non-RCC death than risk of abdominal recurrence at 30 days after surgery.
The retrospective study of 2,511 patients who underwent surgical resection for M0 sporadic RCC between 1990 and 2008 had a median follow up of 9.0 years (interquartile range 6.4-12.7 years).
The researchers noted that recurrences beyond 5 years are fairly common, with up to 15% of patients, by one study’s estimate, experiencing recurrence during the decade following surgery. Cumulative incidence of recurrence does not capture how a patient’s risk of recurrence changes with time or how comorbid conditions influence risk.
The proposed surveillance method results in shorter surveillance durations for some patients and longer surveillance durations than currently recommended for others. This diversity in stopping points “better reflects the range of disease courses appreciated in patients with RCC on the basis of the interplay that occurs between the risk of recurrence and other competing health factors,” Dr. Stewart-Merrill and associates explained.
Dr. Stewart-Merrill reported having no disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: An individualized approach to surveillance after surgical resection in patients with renal cell carcinoma may provide better patient benefit and resource allocation.
Major finding: Weibull models for risk of recurrence, stratified by stage and relapse location, combined with risk estimates for non-RCC death, provided the basis for recommendations on surveillance duration.
Data source: Retrospective study of 2,511 patients who underwent surgical resection for M0 sporadic RCC between 1990 and 2008, with a median follow up of 9.0 years (interquartile range 6.4-12.7 years).
Disclosures: Dr. Stewart-Merrill reported having no disclosures.
Nivolumab benefits patients with previously treated renal cell carcinoma
After a median follow-up of 45 months, the anti–PD-1 antibody nivolumab showed benefit in a majority of patients who had previously received one to five treatments for renal cell carcinoma, according to a report published online March 23 in the Journal of Clinical Oncology.
The previously treated cohort included 71% who had received two prior systemic treatments and 44% who had received three or more prior treatments for renal cell carcinoma (RCC). Out of the total 34 patients, 10 (29%) had objective responses, nine (27%) had stable disease for at least 24 weeks, 2 (6%) had stable disease for at least 48 weeks, and 3 patients (9%) had unconventional immune-related responses, which can include reduction in target lesions in the presence of new lesions or regression after initial progression (J. Clin. Oncol. 2015 Mar. 23 [doi:10.1200/JCO.2014.58.1041]).
“The results of our study suggest that nivolumab can be administered safely in an outpatient setting to pretreated patients with RCC and demonstrate durable clinical activity. Blockade of the PD-1 pathway may represent an important new target for RCC therapy,” wrote Dr. David F. McDermott of Harvard Medical School and Beth Israel Deaconess Medical Center, Boston, and his colleagues.
Adverse events of any grade were experienced by 29 (85%) patients, and 6 patients had grade 3-4 events. The toxicities, the most frequent of which were fatigue (14), rash (9), diarrhea (6), and pruritus (6), were consistent with immune-related mechanisms. The investigators noted that the favorable safety profile may permit the antibody to be used in combination and adjuvant regimens.
Patients received intravenous nivolumab 1 mg/kg (18 patients) or 10 mg/kg (16 patients) in an outpatient setting twice per week for up to 96 weeks. Some degree of tumor shrinkage occurred in 20 of 34 patients. Among the 10 patients with objective responses, the median duration was 12.9 months (range, 8.4-29.1+ months, with four responses ongoing at the time of analysis). Overall survival rates at 1, 2, and 3 years were 71%, 48%, and 44%, respectively, and the median overall survival was 22.4 months.
While the results are encouraging, the authors added that more research to understand the mechanism of action is needed to optimize the use of anti–PD-1 antibodies. Studies have shown that tumor expression of PD-L1 increases the likelihood of benefit from anti–PD-1, but not in all cases.
“A more comprehensive understanding of why some patients with PD-L1–negative tumors respond to PD-1 pathway blockade, while many with PD-L1–positive tumors fail to do so, will be critical to improving patient selection and developing anti–PD-1–based combination strategies for RCC,” they wrote.
Dr. McDermott reported having consulting or advisory roles with Bristol-Myers Squibb, Merck, Genentech/Roche, and Pfizer. Many of his coauthors reported ties to several industry sources.
After a median follow-up of 45 months, the anti–PD-1 antibody nivolumab showed benefit in a majority of patients who had previously received one to five treatments for renal cell carcinoma, according to a report published online March 23 in the Journal of Clinical Oncology.
The previously treated cohort included 71% who had received two prior systemic treatments and 44% who had received three or more prior treatments for renal cell carcinoma (RCC). Out of the total 34 patients, 10 (29%) had objective responses, nine (27%) had stable disease for at least 24 weeks, 2 (6%) had stable disease for at least 48 weeks, and 3 patients (9%) had unconventional immune-related responses, which can include reduction in target lesions in the presence of new lesions or regression after initial progression (J. Clin. Oncol. 2015 Mar. 23 [doi:10.1200/JCO.2014.58.1041]).
“The results of our study suggest that nivolumab can be administered safely in an outpatient setting to pretreated patients with RCC and demonstrate durable clinical activity. Blockade of the PD-1 pathway may represent an important new target for RCC therapy,” wrote Dr. David F. McDermott of Harvard Medical School and Beth Israel Deaconess Medical Center, Boston, and his colleagues.
Adverse events of any grade were experienced by 29 (85%) patients, and 6 patients had grade 3-4 events. The toxicities, the most frequent of which were fatigue (14), rash (9), diarrhea (6), and pruritus (6), were consistent with immune-related mechanisms. The investigators noted that the favorable safety profile may permit the antibody to be used in combination and adjuvant regimens.
Patients received intravenous nivolumab 1 mg/kg (18 patients) or 10 mg/kg (16 patients) in an outpatient setting twice per week for up to 96 weeks. Some degree of tumor shrinkage occurred in 20 of 34 patients. Among the 10 patients with objective responses, the median duration was 12.9 months (range, 8.4-29.1+ months, with four responses ongoing at the time of analysis). Overall survival rates at 1, 2, and 3 years were 71%, 48%, and 44%, respectively, and the median overall survival was 22.4 months.
While the results are encouraging, the authors added that more research to understand the mechanism of action is needed to optimize the use of anti–PD-1 antibodies. Studies have shown that tumor expression of PD-L1 increases the likelihood of benefit from anti–PD-1, but not in all cases.
“A more comprehensive understanding of why some patients with PD-L1–negative tumors respond to PD-1 pathway blockade, while many with PD-L1–positive tumors fail to do so, will be critical to improving patient selection and developing anti–PD-1–based combination strategies for RCC,” they wrote.
Dr. McDermott reported having consulting or advisory roles with Bristol-Myers Squibb, Merck, Genentech/Roche, and Pfizer. Many of his coauthors reported ties to several industry sources.
After a median follow-up of 45 months, the anti–PD-1 antibody nivolumab showed benefit in a majority of patients who had previously received one to five treatments for renal cell carcinoma, according to a report published online March 23 in the Journal of Clinical Oncology.
The previously treated cohort included 71% who had received two prior systemic treatments and 44% who had received three or more prior treatments for renal cell carcinoma (RCC). Out of the total 34 patients, 10 (29%) had objective responses, nine (27%) had stable disease for at least 24 weeks, 2 (6%) had stable disease for at least 48 weeks, and 3 patients (9%) had unconventional immune-related responses, which can include reduction in target lesions in the presence of new lesions or regression after initial progression (J. Clin. Oncol. 2015 Mar. 23 [doi:10.1200/JCO.2014.58.1041]).
“The results of our study suggest that nivolumab can be administered safely in an outpatient setting to pretreated patients with RCC and demonstrate durable clinical activity. Blockade of the PD-1 pathway may represent an important new target for RCC therapy,” wrote Dr. David F. McDermott of Harvard Medical School and Beth Israel Deaconess Medical Center, Boston, and his colleagues.
Adverse events of any grade were experienced by 29 (85%) patients, and 6 patients had grade 3-4 events. The toxicities, the most frequent of which were fatigue (14), rash (9), diarrhea (6), and pruritus (6), were consistent with immune-related mechanisms. The investigators noted that the favorable safety profile may permit the antibody to be used in combination and adjuvant regimens.
Patients received intravenous nivolumab 1 mg/kg (18 patients) or 10 mg/kg (16 patients) in an outpatient setting twice per week for up to 96 weeks. Some degree of tumor shrinkage occurred in 20 of 34 patients. Among the 10 patients with objective responses, the median duration was 12.9 months (range, 8.4-29.1+ months, with four responses ongoing at the time of analysis). Overall survival rates at 1, 2, and 3 years were 71%, 48%, and 44%, respectively, and the median overall survival was 22.4 months.
While the results are encouraging, the authors added that more research to understand the mechanism of action is needed to optimize the use of anti–PD-1 antibodies. Studies have shown that tumor expression of PD-L1 increases the likelihood of benefit from anti–PD-1, but not in all cases.
“A more comprehensive understanding of why some patients with PD-L1–negative tumors respond to PD-1 pathway blockade, while many with PD-L1–positive tumors fail to do so, will be critical to improving patient selection and developing anti–PD-1–based combination strategies for RCC,” they wrote.
Dr. McDermott reported having consulting or advisory roles with Bristol-Myers Squibb, Merck, Genentech/Roche, and Pfizer. Many of his coauthors reported ties to several industry sources.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: A majority of previously treated patients with renal cell carcinoma benefited from nivolumab.
Major finding: At a median 45-month follow-up, 29% of patients had objective responses, 27% had stable disease, and 9% had developed unconventional immune-related responses.
Data source: From 2008 to 2012, 34 patients received intravenous nivolumab, 1 or 10 mg/kg, twice per week for up to 96 weeks.
Disclosures: Dr. McDermott reported having consulting or advisory roles with Bristol-Myers Squibb, Merck, Genentech/Roche, and Pfizer. Many of his coauthors reported ties to several industry sources.