User login
Are You Delivering on the Promise of Higher Quality?
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
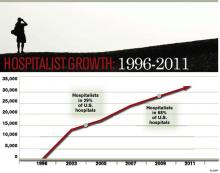
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
The Evidence
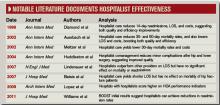
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
The Evidence
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
The Evidence
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
Discharge improvement
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.
HM=Improved Patient Care
GRAPEVINE, Texas—The most successful companies tend to have superior branding. Starbucks owns coffee. Disney owns family fun. And hospitalists own patient-safety and quality-improvement (QI) initiatives within their hospitals.
“We were pretty confident that if we embraced this, we would have a clear running field to ourselves,” says Robert Wachter, MD, MHM, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president, and author of the Wachter’s World blog. “No other physician field would do the same thing, and by owning the patient-safety field, we would distinguish ourselves.”
Now comes the really hard part, though.
Three keynote speakers at HM11—Dr. Wachter, AMA President Cecil Wilson, MD, and Robert Kocher, MD, a healthcare policy advisor to President Obama—pointed to hospitalists as the physician cohort that can help shepherd the conceptual reform passed last year by Congress into daily practice in America’s hospitals. And all three also point to HM’s role at the vanguard of patient safety as a primary reason why.
Hurdles will arise, Dr. Wilson says. A solo practitioner most of his career, he says hospitalists can play a key role in the coming years as more patients receive insurance, but looming doctor shortages could stymie the cause. While many caution that the flood of newly insured patients will overburden primary-care physicians (PCPs), the expected shortage of physicians will plague HM as well.
“Hospitalists are primary-care physicians; the vast majority of them are general internists,” Dr. Wilson says. “… So when we say that the number of people who are going into primary care, particularly general internal medicine, is reducing, that reduces not only the pool of physicians in the community, but also the hospitalist pool. We’re in that boat together.”
Dr. Kocher, director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., says hospitalists are in the best position to push for on-the-ground reform as they are the doctors who bridge all hospital departments, floors, and wards. He sees four broad areas where HM can take a particularly leading role:
- Increasing labor productivity. HM’s role as a link between specialties from cardiology to the pharmacy makes HM a natural conduit to push institutional values from a unique vantage point.
- Driving decision-making. Whether it’s recommending less costly drugs with similar outcomes, questioning whether expensive test batteries are truly necessary or being done for fear of missing something, or pausing to ask whether a “90-year-old hip replacement patient should receive orthopedic implants that will last far longer than their grandkids will be alive,” hospitalists can use their data to be a common-sense lynchpin of daily operations.
- Using technology to lower delivery costs. Many insurance companies are willing to enter into risk-based contracts with hospitals, but some hospital executives worry whether they will be able to perform well enough to justify the risk. “Hospitalists can help say, ‘We can do this. We can hit the thresholds.’ ”
- Shifting compensation models from “selling work RVUs to selling years of health.”
“The biggest thing [hospitalists] should begin doing,” Dr. Kocher adds, “is stop thinking about units of work, or RVUs, and start thinking about how much better patients can be by virtue of the care they’re delivering, how many readmissions are they avoiding, how many core measures/outcomes are they hitting, how much better is the patient experience, and how much smoother is the handoff.”
The push to improve quality and show better outcomes, of course, is intrinsically tied to payment reform. Bundled payments that reimburse a set fee for a case from pre-admission to a preset post-discharge deadline worry some hospitalists, who fear how the payments will be divvied up and who will be in charge of said payment decisions. Dr. Kocher says that even when the initial rules are set, the system is likely to evolve.
However, the hospitalist’s role as a driver of QI positions the field well, all three speakers noted. By quarterbacking patient handoffs and continuing to be seen by hospital executives as quality and safety leaders, HM groups can make the argument that they are worth the financial support they ask for in negotiations. Dr. Wachter adds that while quality research has become a staple of academics and residents, hospitalists should look to now tie value to the equation, effectively linking better patient outcomes to HM’s bottom line.
“There’s no question that physicians that can care for patients more efficiently, in a higher-quality way, in hospitals at lower costs, are going to do better no matter how the system evolves,” Dr. Kocher says. “I’m positive, as long as hospitalists are confident—and I think they should be—that they can deliver, more consistently, better care than those who aren’t hospitalists practicing in hospitals … and they’re going to do better economically.”
GRAPEVINE, Texas—The most successful companies tend to have superior branding. Starbucks owns coffee. Disney owns family fun. And hospitalists own patient-safety and quality-improvement (QI) initiatives within their hospitals.
“We were pretty confident that if we embraced this, we would have a clear running field to ourselves,” says Robert Wachter, MD, MHM, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president, and author of the Wachter’s World blog. “No other physician field would do the same thing, and by owning the patient-safety field, we would distinguish ourselves.”
Now comes the really hard part, though.
Three keynote speakers at HM11—Dr. Wachter, AMA President Cecil Wilson, MD, and Robert Kocher, MD, a healthcare policy advisor to President Obama—pointed to hospitalists as the physician cohort that can help shepherd the conceptual reform passed last year by Congress into daily practice in America’s hospitals. And all three also point to HM’s role at the vanguard of patient safety as a primary reason why.
Hurdles will arise, Dr. Wilson says. A solo practitioner most of his career, he says hospitalists can play a key role in the coming years as more patients receive insurance, but looming doctor shortages could stymie the cause. While many caution that the flood of newly insured patients will overburden primary-care physicians (PCPs), the expected shortage of physicians will plague HM as well.
“Hospitalists are primary-care physicians; the vast majority of them are general internists,” Dr. Wilson says. “… So when we say that the number of people who are going into primary care, particularly general internal medicine, is reducing, that reduces not only the pool of physicians in the community, but also the hospitalist pool. We’re in that boat together.”
Dr. Kocher, director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., says hospitalists are in the best position to push for on-the-ground reform as they are the doctors who bridge all hospital departments, floors, and wards. He sees four broad areas where HM can take a particularly leading role:
- Increasing labor productivity. HM’s role as a link between specialties from cardiology to the pharmacy makes HM a natural conduit to push institutional values from a unique vantage point.
- Driving decision-making. Whether it’s recommending less costly drugs with similar outcomes, questioning whether expensive test batteries are truly necessary or being done for fear of missing something, or pausing to ask whether a “90-year-old hip replacement patient should receive orthopedic implants that will last far longer than their grandkids will be alive,” hospitalists can use their data to be a common-sense lynchpin of daily operations.
- Using technology to lower delivery costs. Many insurance companies are willing to enter into risk-based contracts with hospitals, but some hospital executives worry whether they will be able to perform well enough to justify the risk. “Hospitalists can help say, ‘We can do this. We can hit the thresholds.’ ”
- Shifting compensation models from “selling work RVUs to selling years of health.”
“The biggest thing [hospitalists] should begin doing,” Dr. Kocher adds, “is stop thinking about units of work, or RVUs, and start thinking about how much better patients can be by virtue of the care they’re delivering, how many readmissions are they avoiding, how many core measures/outcomes are they hitting, how much better is the patient experience, and how much smoother is the handoff.”
The push to improve quality and show better outcomes, of course, is intrinsically tied to payment reform. Bundled payments that reimburse a set fee for a case from pre-admission to a preset post-discharge deadline worry some hospitalists, who fear how the payments will be divvied up and who will be in charge of said payment decisions. Dr. Kocher says that even when the initial rules are set, the system is likely to evolve.
However, the hospitalist’s role as a driver of QI positions the field well, all three speakers noted. By quarterbacking patient handoffs and continuing to be seen by hospital executives as quality and safety leaders, HM groups can make the argument that they are worth the financial support they ask for in negotiations. Dr. Wachter adds that while quality research has become a staple of academics and residents, hospitalists should look to now tie value to the equation, effectively linking better patient outcomes to HM’s bottom line.
“There’s no question that physicians that can care for patients more efficiently, in a higher-quality way, in hospitals at lower costs, are going to do better no matter how the system evolves,” Dr. Kocher says. “I’m positive, as long as hospitalists are confident—and I think they should be—that they can deliver, more consistently, better care than those who aren’t hospitalists practicing in hospitals … and they’re going to do better economically.”
GRAPEVINE, Texas—The most successful companies tend to have superior branding. Starbucks owns coffee. Disney owns family fun. And hospitalists own patient-safety and quality-improvement (QI) initiatives within their hospitals.
“We were pretty confident that if we embraced this, we would have a clear running field to ourselves,” says Robert Wachter, MD, MHM, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president, and author of the Wachter’s World blog. “No other physician field would do the same thing, and by owning the patient-safety field, we would distinguish ourselves.”
Now comes the really hard part, though.
Three keynote speakers at HM11—Dr. Wachter, AMA President Cecil Wilson, MD, and Robert Kocher, MD, a healthcare policy advisor to President Obama—pointed to hospitalists as the physician cohort that can help shepherd the conceptual reform passed last year by Congress into daily practice in America’s hospitals. And all three also point to HM’s role at the vanguard of patient safety as a primary reason why.
Hurdles will arise, Dr. Wilson says. A solo practitioner most of his career, he says hospitalists can play a key role in the coming years as more patients receive insurance, but looming doctor shortages could stymie the cause. While many caution that the flood of newly insured patients will overburden primary-care physicians (PCPs), the expected shortage of physicians will plague HM as well.
“Hospitalists are primary-care physicians; the vast majority of them are general internists,” Dr. Wilson says. “… So when we say that the number of people who are going into primary care, particularly general internal medicine, is reducing, that reduces not only the pool of physicians in the community, but also the hospitalist pool. We’re in that boat together.”
Dr. Kocher, director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., says hospitalists are in the best position to push for on-the-ground reform as they are the doctors who bridge all hospital departments, floors, and wards. He sees four broad areas where HM can take a particularly leading role:
- Increasing labor productivity. HM’s role as a link between specialties from cardiology to the pharmacy makes HM a natural conduit to push institutional values from a unique vantage point.
- Driving decision-making. Whether it’s recommending less costly drugs with similar outcomes, questioning whether expensive test batteries are truly necessary or being done for fear of missing something, or pausing to ask whether a “90-year-old hip replacement patient should receive orthopedic implants that will last far longer than their grandkids will be alive,” hospitalists can use their data to be a common-sense lynchpin of daily operations.
- Using technology to lower delivery costs. Many insurance companies are willing to enter into risk-based contracts with hospitals, but some hospital executives worry whether they will be able to perform well enough to justify the risk. “Hospitalists can help say, ‘We can do this. We can hit the thresholds.’ ”
- Shifting compensation models from “selling work RVUs to selling years of health.”
“The biggest thing [hospitalists] should begin doing,” Dr. Kocher adds, “is stop thinking about units of work, or RVUs, and start thinking about how much better patients can be by virtue of the care they’re delivering, how many readmissions are they avoiding, how many core measures/outcomes are they hitting, how much better is the patient experience, and how much smoother is the handoff.”
The push to improve quality and show better outcomes, of course, is intrinsically tied to payment reform. Bundled payments that reimburse a set fee for a case from pre-admission to a preset post-discharge deadline worry some hospitalists, who fear how the payments will be divvied up and who will be in charge of said payment decisions. Dr. Kocher says that even when the initial rules are set, the system is likely to evolve.
However, the hospitalist’s role as a driver of QI positions the field well, all three speakers noted. By quarterbacking patient handoffs and continuing to be seen by hospital executives as quality and safety leaders, HM groups can make the argument that they are worth the financial support they ask for in negotiations. Dr. Wachter adds that while quality research has become a staple of academics and residents, hospitalists should look to now tie value to the equation, effectively linking better patient outcomes to HM’s bottom line.
“There’s no question that physicians that can care for patients more efficiently, in a higher-quality way, in hospitals at lower costs, are going to do better no matter how the system evolves,” Dr. Kocher says. “I’m positive, as long as hospitalists are confident—and I think they should be—that they can deliver, more consistently, better care than those who aren’t hospitalists practicing in hospitals … and they’re going to do better economically.”
Under the Microscope: Medication Reconciliation

Boston hospitalist Jeffrey Schnipper, MD, MPH, FHM, is no stranger to quality initiatives aimed at medication reconciliation (MR). His research at Brigham and Women’s Hospital and Massachusetts General Hospital revealed a potential reduction of serious medical errors per patient to 0.3 from 1.4 in the past four years.
“I think those are achievable results,” he says. “This is all about doing those things better than we were always doing before.”
Now Dr. Schnipper will work to bring similar results to hospitals across America as principal investigator for SHM’s three-year, multicenter, MR quality-improvement study. The study, funded by a $1.5 million grant from the Agency for Healthcare Research and Quality (AHRQ), will develop a database to research the best practices in MR and provide a mentored implementation model for other hospitals to use.
The project also will include a package of materials and tools adaptable for any hospital, as well as an implementation guide with the mentored implementation model. “It really should be everything a site needs to improve its MR process,” says Dr. Schnipper, director of clinical research at the Brigham and Women’s Hospital Hospitalist Service and assistant professor at Harvard Medical School.
According to The Institute for Safe Medication Practices, MR is the process of comparing a patient’s medication orders with their previously prescribed medication regimen and communicating any necessary changes to patients and their next providers of care. More than 1.3 million medication errors occur annually in the U.S.; MR has been shown to eliminate as many as half of those errors and 20% of adverse medical events.
JoAnne Resnic, MBA, BSN, RN, senior project manager at SHM, says SHM will use the grant to fund research investigators, SHM’s project staff, and the development of a database for each of the study’s six sites to house their data collection and provide site-specific progress reports throughout the course of the study. SHM is working with consultants and physician co-investigators, a steering committee of nationally recognized thought leaders in medication reconciliation, a research pharmacist, and others to “help us take a pretty deep dive into the process and, hopefully, explain why some interventions work in some places and why they may not in others,” Resnic says.
According to Dr. Schnipper, SHM will conduct an interrupted time series at the sites, collecting baseline data for six months at each, then for 21 months after interventions begin. The study specifically will address 13 facets of medication reconciliation, scoring the facets based on their effectiveness (see Table 1, p. 6).
Each facet will be re-evaluated when different parts of the intervention are turned on, which should reveal “the most active ingredients that correspond to improved outcomes,” he says.
Dr. Schnipper emphasizes that there are two integral facets for improving MR: patient education and access to preadmission medication sources. Technology could be an answer to advancing these components, but it is not the sole link. “There may be ways to serve up the discharged medication list in a patient-friendly way using some IT or an image library of medications to help patients,” he says. “I do not foresee a medication reconciliation IT application, unfortunately.”
AHRQ selected SHM for the grant after a “peer review process [that] evaluates the merit of the applications against very rigorous criteria,” an AHRQ representative says. SHM was chosen “based upon its leadership and previous experience in medication reconciliation.” TH
Kevin Stevens is a staff writer based in New Jersey.

Boston hospitalist Jeffrey Schnipper, MD, MPH, FHM, is no stranger to quality initiatives aimed at medication reconciliation (MR). His research at Brigham and Women’s Hospital and Massachusetts General Hospital revealed a potential reduction of serious medical errors per patient to 0.3 from 1.4 in the past four years.
“I think those are achievable results,” he says. “This is all about doing those things better than we were always doing before.”
Now Dr. Schnipper will work to bring similar results to hospitals across America as principal investigator for SHM’s three-year, multicenter, MR quality-improvement study. The study, funded by a $1.5 million grant from the Agency for Healthcare Research and Quality (AHRQ), will develop a database to research the best practices in MR and provide a mentored implementation model for other hospitals to use.
The project also will include a package of materials and tools adaptable for any hospital, as well as an implementation guide with the mentored implementation model. “It really should be everything a site needs to improve its MR process,” says Dr. Schnipper, director of clinical research at the Brigham and Women’s Hospital Hospitalist Service and assistant professor at Harvard Medical School.
According to The Institute for Safe Medication Practices, MR is the process of comparing a patient’s medication orders with their previously prescribed medication regimen and communicating any necessary changes to patients and their next providers of care. More than 1.3 million medication errors occur annually in the U.S.; MR has been shown to eliminate as many as half of those errors and 20% of adverse medical events.
JoAnne Resnic, MBA, BSN, RN, senior project manager at SHM, says SHM will use the grant to fund research investigators, SHM’s project staff, and the development of a database for each of the study’s six sites to house their data collection and provide site-specific progress reports throughout the course of the study. SHM is working with consultants and physician co-investigators, a steering committee of nationally recognized thought leaders in medication reconciliation, a research pharmacist, and others to “help us take a pretty deep dive into the process and, hopefully, explain why some interventions work in some places and why they may not in others,” Resnic says.
According to Dr. Schnipper, SHM will conduct an interrupted time series at the sites, collecting baseline data for six months at each, then for 21 months after interventions begin. The study specifically will address 13 facets of medication reconciliation, scoring the facets based on their effectiveness (see Table 1, p. 6).
Each facet will be re-evaluated when different parts of the intervention are turned on, which should reveal “the most active ingredients that correspond to improved outcomes,” he says.
Dr. Schnipper emphasizes that there are two integral facets for improving MR: patient education and access to preadmission medication sources. Technology could be an answer to advancing these components, but it is not the sole link. “There may be ways to serve up the discharged medication list in a patient-friendly way using some IT or an image library of medications to help patients,” he says. “I do not foresee a medication reconciliation IT application, unfortunately.”
AHRQ selected SHM for the grant after a “peer review process [that] evaluates the merit of the applications against very rigorous criteria,” an AHRQ representative says. SHM was chosen “based upon its leadership and previous experience in medication reconciliation.” TH
Kevin Stevens is a staff writer based in New Jersey.

Boston hospitalist Jeffrey Schnipper, MD, MPH, FHM, is no stranger to quality initiatives aimed at medication reconciliation (MR). His research at Brigham and Women’s Hospital and Massachusetts General Hospital revealed a potential reduction of serious medical errors per patient to 0.3 from 1.4 in the past four years.
“I think those are achievable results,” he says. “This is all about doing those things better than we were always doing before.”
Now Dr. Schnipper will work to bring similar results to hospitals across America as principal investigator for SHM’s three-year, multicenter, MR quality-improvement study. The study, funded by a $1.5 million grant from the Agency for Healthcare Research and Quality (AHRQ), will develop a database to research the best practices in MR and provide a mentored implementation model for other hospitals to use.
The project also will include a package of materials and tools adaptable for any hospital, as well as an implementation guide with the mentored implementation model. “It really should be everything a site needs to improve its MR process,” says Dr. Schnipper, director of clinical research at the Brigham and Women’s Hospital Hospitalist Service and assistant professor at Harvard Medical School.
According to The Institute for Safe Medication Practices, MR is the process of comparing a patient’s medication orders with their previously prescribed medication regimen and communicating any necessary changes to patients and their next providers of care. More than 1.3 million medication errors occur annually in the U.S.; MR has been shown to eliminate as many as half of those errors and 20% of adverse medical events.
JoAnne Resnic, MBA, BSN, RN, senior project manager at SHM, says SHM will use the grant to fund research investigators, SHM’s project staff, and the development of a database for each of the study’s six sites to house their data collection and provide site-specific progress reports throughout the course of the study. SHM is working with consultants and physician co-investigators, a steering committee of nationally recognized thought leaders in medication reconciliation, a research pharmacist, and others to “help us take a pretty deep dive into the process and, hopefully, explain why some interventions work in some places and why they may not in others,” Resnic says.
According to Dr. Schnipper, SHM will conduct an interrupted time series at the sites, collecting baseline data for six months at each, then for 21 months after interventions begin. The study specifically will address 13 facets of medication reconciliation, scoring the facets based on their effectiveness (see Table 1, p. 6).
Each facet will be re-evaluated when different parts of the intervention are turned on, which should reveal “the most active ingredients that correspond to improved outcomes,” he says.
Dr. Schnipper emphasizes that there are two integral facets for improving MR: patient education and access to preadmission medication sources. Technology could be an answer to advancing these components, but it is not the sole link. “There may be ways to serve up the discharged medication list in a patient-friendly way using some IT or an image library of medications to help patients,” he says. “I do not foresee a medication reconciliation IT application, unfortunately.”
AHRQ selected SHM for the grant after a “peer review process [that] evaluates the merit of the applications against very rigorous criteria,” an AHRQ representative says. SHM was chosen “based upon its leadership and previous experience in medication reconciliation.” TH
Kevin Stevens is a staff writer based in New Jersey.
HM11 PREVIEW: Wachter’s Vision
When Robert Wachter, MD, MHM, delivers his keynote address to unofficially close HM11, he’ll toast the field he helped define. His remarks will coincide with the 15th anniversary of the article he and Lee Goldman, MD, coauthored in The New England Journal of Medicine that coined the term “hospitalist” and fostered an understanding that the HM movement was a true phenomenon.
The milestone presents the perfect opportunity to examine the specialty’s meteoric growth and celebrate the successes of its pioneers, says Dr. Wachter, a professor, chief of the Division of Hospital Medicine, and chief of the medical service at the University of California at San Francisco Medical Center. He also considers it an ideal time to examine the unforeseen developments of the past decade and a half, believing a critical analysis of a few key case studies can help lay the groundwork for an even brighter future.
“At 15, you’re in mid- to late adolescence,” Dr. Wachter says. “We can no longer say we’re this new kid on the block and, ‘Gee, whiz, isn’t this neat?’
“This is a good chance to reflect on things that went as we expected,” he adds. “It’s an even better chance to take a second look at things that were surprising but provide valuable lessons as we think about what the next 15 years are going to be like.”
Question: Fifteen years ago, did you envision HM would grow so quickly?
Answer: I had a sense this was a trend that was starting to emerge and could fill an important niche. At the same time, when Sergey (Brin) and Larry (Page) founded Google, I doubt they believed it would become a $200 billion company. In the beginning, I couldn’t have predicted what this would become.
Q: What surprised you most in the past 15 years?
A: I didn’t fully appreciate how quickly the push toward value would become a dominant theme. Once we discovered quality was important and there was a set of skills we needed to learn to improve it, we tackled it aggressively. It has been harder to tackle the cost part of the equation.
This goes beyond making sure patients don’t stay in the hospital longer than they need to. It means looking hard at the cost of care and the way we spend money, such as our patterns of ordering X-rays, consultants, and lab tests. I’m going to focus a fair amount on that.
Q: Why do you want to emphasize that point?
A: The cost of healthcare is going to bankrupt the country unless we get a handle on it. Our field needs to lead the way to show how a good, ethical physician not only focuses on improving quality of care, but also focuses on ridding the system of waste and of care that adds no real value to our patients. We’ve been a little sluggish in that area.
Q: What other surprises do you intend to discuss?
A: I didn’t anticipate the emergence of two different versions of the hospitalist field. One is the role of comanagement. The other is what I call the hyphenated hospitalist—these OB hospitalists and surgery hospitalists. This concept we came up with for general patients has been embraced by a variety of specialties. How do those people fit into our society and our field? Are they really part of us or are they fundamentally different? I think we need to think carefully about it.
Q: Why are the unexpected developments so important to consider?
A: Leaders in the field need to get really good at reading tea leaves. One of the ways you do that is to figure out, when you didn’t read them correctly the first time, why didn’t you? Could you have read them better if you were more clever or more thoughtful?
Q: What is the biggest challenge facing HM?
A: When we have been given new tasks and new opportunities, our members have stepped up to the plate and done what they’ve been asked to do as well, if not better, than expected. I’m a little fearful of the flip side. How we will meet the demand for our services? How do we ensure the job stays attractive and we don’t burn out? We have to demonstrate our value, but we have to make sure the jobs are truly sustainable and that we don’t shoot ourselves in the foot.
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
HM11’s visiting professor to serve as mentor, stimulate discussion
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
Q:What do you see as the solution?
A: I don’t think we’ll be able to meet all of the demand. There will be hospitals that can only partly staff the needs they have with hospitalists. I don’t want them to go too far down the quality curve. We need to be sure people entering the field are good and have the skills they need.
I think we’ll begin to ask important questions like, “Do I really need a hospitalist for this, or can I leverage fewer hospitalists with other nonphysician providers?” Or, “Can some of the work our hospitalists are doing be done as well and more cheaply by computers?” It opens a pathway to think more creatively about people and tasks and technologies.
Q: Despite the challenges associated with growth pressure, is HM better positioned for the future because of it?
A: Definitely. We will see a further extension of our reach into other areas of the hospital and healthcare system. We will continue to see our people begin as leaders in our world of hospital medicine but rapidly graduate to become hospital CEOs, chairs of departments of medicine, and major leaders in healthcare. There is a recognition that there’s no better training ground to be a leader in healthcare than to be a leader in our field. So I can’t help but be optimistic that our place in the world of healthcare is extraordinarily secure. HM11
Mark Leiser is a freelance writer based in New Jersey.
When Robert Wachter, MD, MHM, delivers his keynote address to unofficially close HM11, he’ll toast the field he helped define. His remarks will coincide with the 15th anniversary of the article he and Lee Goldman, MD, coauthored in The New England Journal of Medicine that coined the term “hospitalist” and fostered an understanding that the HM movement was a true phenomenon.
The milestone presents the perfect opportunity to examine the specialty’s meteoric growth and celebrate the successes of its pioneers, says Dr. Wachter, a professor, chief of the Division of Hospital Medicine, and chief of the medical service at the University of California at San Francisco Medical Center. He also considers it an ideal time to examine the unforeseen developments of the past decade and a half, believing a critical analysis of a few key case studies can help lay the groundwork for an even brighter future.
“At 15, you’re in mid- to late adolescence,” Dr. Wachter says. “We can no longer say we’re this new kid on the block and, ‘Gee, whiz, isn’t this neat?’
“This is a good chance to reflect on things that went as we expected,” he adds. “It’s an even better chance to take a second look at things that were surprising but provide valuable lessons as we think about what the next 15 years are going to be like.”
Question: Fifteen years ago, did you envision HM would grow so quickly?
Answer: I had a sense this was a trend that was starting to emerge and could fill an important niche. At the same time, when Sergey (Brin) and Larry (Page) founded Google, I doubt they believed it would become a $200 billion company. In the beginning, I couldn’t have predicted what this would become.
Q: What surprised you most in the past 15 years?
A: I didn’t fully appreciate how quickly the push toward value would become a dominant theme. Once we discovered quality was important and there was a set of skills we needed to learn to improve it, we tackled it aggressively. It has been harder to tackle the cost part of the equation.
This goes beyond making sure patients don’t stay in the hospital longer than they need to. It means looking hard at the cost of care and the way we spend money, such as our patterns of ordering X-rays, consultants, and lab tests. I’m going to focus a fair amount on that.
Q: Why do you want to emphasize that point?
A: The cost of healthcare is going to bankrupt the country unless we get a handle on it. Our field needs to lead the way to show how a good, ethical physician not only focuses on improving quality of care, but also focuses on ridding the system of waste and of care that adds no real value to our patients. We’ve been a little sluggish in that area.
Q: What other surprises do you intend to discuss?
A: I didn’t anticipate the emergence of two different versions of the hospitalist field. One is the role of comanagement. The other is what I call the hyphenated hospitalist—these OB hospitalists and surgery hospitalists. This concept we came up with for general patients has been embraced by a variety of specialties. How do those people fit into our society and our field? Are they really part of us or are they fundamentally different? I think we need to think carefully about it.
Q: Why are the unexpected developments so important to consider?
A: Leaders in the field need to get really good at reading tea leaves. One of the ways you do that is to figure out, when you didn’t read them correctly the first time, why didn’t you? Could you have read them better if you were more clever or more thoughtful?
Q: What is the biggest challenge facing HM?
A: When we have been given new tasks and new opportunities, our members have stepped up to the plate and done what they’ve been asked to do as well, if not better, than expected. I’m a little fearful of the flip side. How we will meet the demand for our services? How do we ensure the job stays attractive and we don’t burn out? We have to demonstrate our value, but we have to make sure the jobs are truly sustainable and that we don’t shoot ourselves in the foot.
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
HM11’s visiting professor to serve as mentor, stimulate discussion
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
Q:What do you see as the solution?
A: I don’t think we’ll be able to meet all of the demand. There will be hospitals that can only partly staff the needs they have with hospitalists. I don’t want them to go too far down the quality curve. We need to be sure people entering the field are good and have the skills they need.
I think we’ll begin to ask important questions like, “Do I really need a hospitalist for this, or can I leverage fewer hospitalists with other nonphysician providers?” Or, “Can some of the work our hospitalists are doing be done as well and more cheaply by computers?” It opens a pathway to think more creatively about people and tasks and technologies.
Q: Despite the challenges associated with growth pressure, is HM better positioned for the future because of it?
A: Definitely. We will see a further extension of our reach into other areas of the hospital and healthcare system. We will continue to see our people begin as leaders in our world of hospital medicine but rapidly graduate to become hospital CEOs, chairs of departments of medicine, and major leaders in healthcare. There is a recognition that there’s no better training ground to be a leader in healthcare than to be a leader in our field. So I can’t help but be optimistic that our place in the world of healthcare is extraordinarily secure. HM11
Mark Leiser is a freelance writer based in New Jersey.
When Robert Wachter, MD, MHM, delivers his keynote address to unofficially close HM11, he’ll toast the field he helped define. His remarks will coincide with the 15th anniversary of the article he and Lee Goldman, MD, coauthored in The New England Journal of Medicine that coined the term “hospitalist” and fostered an understanding that the HM movement was a true phenomenon.
The milestone presents the perfect opportunity to examine the specialty’s meteoric growth and celebrate the successes of its pioneers, says Dr. Wachter, a professor, chief of the Division of Hospital Medicine, and chief of the medical service at the University of California at San Francisco Medical Center. He also considers it an ideal time to examine the unforeseen developments of the past decade and a half, believing a critical analysis of a few key case studies can help lay the groundwork for an even brighter future.
“At 15, you’re in mid- to late adolescence,” Dr. Wachter says. “We can no longer say we’re this new kid on the block and, ‘Gee, whiz, isn’t this neat?’
“This is a good chance to reflect on things that went as we expected,” he adds. “It’s an even better chance to take a second look at things that were surprising but provide valuable lessons as we think about what the next 15 years are going to be like.”
Question: Fifteen years ago, did you envision HM would grow so quickly?
Answer: I had a sense this was a trend that was starting to emerge and could fill an important niche. At the same time, when Sergey (Brin) and Larry (Page) founded Google, I doubt they believed it would become a $200 billion company. In the beginning, I couldn’t have predicted what this would become.
Q: What surprised you most in the past 15 years?
A: I didn’t fully appreciate how quickly the push toward value would become a dominant theme. Once we discovered quality was important and there was a set of skills we needed to learn to improve it, we tackled it aggressively. It has been harder to tackle the cost part of the equation.
This goes beyond making sure patients don’t stay in the hospital longer than they need to. It means looking hard at the cost of care and the way we spend money, such as our patterns of ordering X-rays, consultants, and lab tests. I’m going to focus a fair amount on that.
Q: Why do you want to emphasize that point?
A: The cost of healthcare is going to bankrupt the country unless we get a handle on it. Our field needs to lead the way to show how a good, ethical physician not only focuses on improving quality of care, but also focuses on ridding the system of waste and of care that adds no real value to our patients. We’ve been a little sluggish in that area.
Q: What other surprises do you intend to discuss?
A: I didn’t anticipate the emergence of two different versions of the hospitalist field. One is the role of comanagement. The other is what I call the hyphenated hospitalist—these OB hospitalists and surgery hospitalists. This concept we came up with for general patients has been embraced by a variety of specialties. How do those people fit into our society and our field? Are they really part of us or are they fundamentally different? I think we need to think carefully about it.
Q: Why are the unexpected developments so important to consider?
A: Leaders in the field need to get really good at reading tea leaves. One of the ways you do that is to figure out, when you didn’t read them correctly the first time, why didn’t you? Could you have read them better if you were more clever or more thoughtful?
Q: What is the biggest challenge facing HM?
A: When we have been given new tasks and new opportunities, our members have stepped up to the plate and done what they’ve been asked to do as well, if not better, than expected. I’m a little fearful of the flip side. How we will meet the demand for our services? How do we ensure the job stays attractive and we don’t burn out? We have to demonstrate our value, but we have to make sure the jobs are truly sustainable and that we don’t shoot ourselves in the foot.
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
HM11’s visiting professor to serve as mentor, stimulate discussion
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
Q:What do you see as the solution?
A: I don’t think we’ll be able to meet all of the demand. There will be hospitals that can only partly staff the needs they have with hospitalists. I don’t want them to go too far down the quality curve. We need to be sure people entering the field are good and have the skills they need.
I think we’ll begin to ask important questions like, “Do I really need a hospitalist for this, or can I leverage fewer hospitalists with other nonphysician providers?” Or, “Can some of the work our hospitalists are doing be done as well and more cheaply by computers?” It opens a pathway to think more creatively about people and tasks and technologies.
Q: Despite the challenges associated with growth pressure, is HM better positioned for the future because of it?
A: Definitely. We will see a further extension of our reach into other areas of the hospital and healthcare system. We will continue to see our people begin as leaders in our world of hospital medicine but rapidly graduate to become hospital CEOs, chairs of departments of medicine, and major leaders in healthcare. There is a recognition that there’s no better training ground to be a leader in healthcare than to be a leader in our field. So I can’t help but be optimistic that our place in the world of healthcare is extraordinarily secure. HM11
Mark Leiser is a freelance writer based in New Jersey.
POLICY CORNER: Despite significant QI, disparities among poor Americans persist.
The Agency for Healthcare Research and Quality (AHRQ) recently released the annual National Healthcare Quality & Disparities Reports. The reports provide in-depth quality information on the overall population and divide this information along such subgroups as race, ethnicity, and education level. The report is more than 200 pages long, but it can be summarized in one sentence: If you are poor, the quality of your healthcare is likely to be poor.
Despite significant quality improvement (QI) in a number of areas, disparities among poor Americans persist. For example, the percentage of heart-attack patients who underwent procedures to unblock heart arteries within 90 minutes improved to 81% in 2008 from 42% in 2005. This is very positive news, but unfortunately, these and many other gains in quality only apply to higher-income populations.
A new section of the report focused on care coordination and transitions of care contains some statistics of particular interest to hospitalists. One statistic shows that the percentage of hospitalized adult patients with heart failure who were given complete written discharge instructions improved to 82.0% in 2008, up from 57.5% in 2005.
It is important to note that this number remains more or less constant across all racial/ethnic divisions. Could part of this improvement be attributed to the growth and success of the hospitalist movement?
Hospitalists know that despite the numbers, a successful transition does not simply include discharge instructions; it is the combination of those instructions, along with coordination with primary care, that prevents avoidable readmissions.
Unfortunately, 15% to 20% of low-income patients have no regular primary-care physician (PCP). If a condition begins to deteriorate, this group often has little choice but to return to the hospital.
In the absence of a PCP, it is the hospitalist who can provide patients with the tools they need to stay healthy after leaving the hospital.
Such assistance can range from ensuring that patients truly understand their discharge instructions to being a resource for future questions. Hospitalists are ahead of the game when it comes to quality and reducing disparities; it is just a matter of the other facets of healthcare catching up.
The National Healthcare Quality & Disparities reports are available at www.ahrq.gov/qual/qrdr10.htm. TH
The Agency for Healthcare Research and Quality (AHRQ) recently released the annual National Healthcare Quality & Disparities Reports. The reports provide in-depth quality information on the overall population and divide this information along such subgroups as race, ethnicity, and education level. The report is more than 200 pages long, but it can be summarized in one sentence: If you are poor, the quality of your healthcare is likely to be poor.
Despite significant quality improvement (QI) in a number of areas, disparities among poor Americans persist. For example, the percentage of heart-attack patients who underwent procedures to unblock heart arteries within 90 minutes improved to 81% in 2008 from 42% in 2005. This is very positive news, but unfortunately, these and many other gains in quality only apply to higher-income populations.
A new section of the report focused on care coordination and transitions of care contains some statistics of particular interest to hospitalists. One statistic shows that the percentage of hospitalized adult patients with heart failure who were given complete written discharge instructions improved to 82.0% in 2008, up from 57.5% in 2005.
It is important to note that this number remains more or less constant across all racial/ethnic divisions. Could part of this improvement be attributed to the growth and success of the hospitalist movement?
Hospitalists know that despite the numbers, a successful transition does not simply include discharge instructions; it is the combination of those instructions, along with coordination with primary care, that prevents avoidable readmissions.
Unfortunately, 15% to 20% of low-income patients have no regular primary-care physician (PCP). If a condition begins to deteriorate, this group often has little choice but to return to the hospital.
In the absence of a PCP, it is the hospitalist who can provide patients with the tools they need to stay healthy after leaving the hospital.
Such assistance can range from ensuring that patients truly understand their discharge instructions to being a resource for future questions. Hospitalists are ahead of the game when it comes to quality and reducing disparities; it is just a matter of the other facets of healthcare catching up.
The National Healthcare Quality & Disparities reports are available at www.ahrq.gov/qual/qrdr10.htm. TH
The Agency for Healthcare Research and Quality (AHRQ) recently released the annual National Healthcare Quality & Disparities Reports. The reports provide in-depth quality information on the overall population and divide this information along such subgroups as race, ethnicity, and education level. The report is more than 200 pages long, but it can be summarized in one sentence: If you are poor, the quality of your healthcare is likely to be poor.
Despite significant quality improvement (QI) in a number of areas, disparities among poor Americans persist. For example, the percentage of heart-attack patients who underwent procedures to unblock heart arteries within 90 minutes improved to 81% in 2008 from 42% in 2005. This is very positive news, but unfortunately, these and many other gains in quality only apply to higher-income populations.
A new section of the report focused on care coordination and transitions of care contains some statistics of particular interest to hospitalists. One statistic shows that the percentage of hospitalized adult patients with heart failure who were given complete written discharge instructions improved to 82.0% in 2008, up from 57.5% in 2005.
It is important to note that this number remains more or less constant across all racial/ethnic divisions. Could part of this improvement be attributed to the growth and success of the hospitalist movement?
Hospitalists know that despite the numbers, a successful transition does not simply include discharge instructions; it is the combination of those instructions, along with coordination with primary care, that prevents avoidable readmissions.
Unfortunately, 15% to 20% of low-income patients have no regular primary-care physician (PCP). If a condition begins to deteriorate, this group often has little choice but to return to the hospital.
In the absence of a PCP, it is the hospitalist who can provide patients with the tools they need to stay healthy after leaving the hospital.
Such assistance can range from ensuring that patients truly understand their discharge instructions to being a resource for future questions. Hospitalists are ahead of the game when it comes to quality and reducing disparities; it is just a matter of the other facets of healthcare catching up.
The National Healthcare Quality & Disparities reports are available at www.ahrq.gov/qual/qrdr10.htm. TH
POLICY CORNER: An inside look at the most pressing policy issues
On Feb. 16, the Agency for Healthcare Research and Quality (AHRQ) listed SHM as a patient safety organization (PSO). A PSO serves as an independent, external, expert organization that can collect, analyze, and aggregate information in order to develop insights into the underlying causes of patient-safety events. PSOs are designed to help clinicians, hospitals, and healthcare organizations improve patient safety and the quality of healthcare delivery.
PSO status allows SHM’s current quality-improvement (QI) activities to be conducted in a secure environment that is protected from legal discovery. AHRQ currently lists 78 PSOs, including the Society for Vascular Surgery PSO, the Emergency Medicine Patient Safety Foundation, and the Biomedical Research and Education Foundation. A full list is available at www.pso.ahrq.gov/listing/psolist.htm.
To achieve PSO status, SHM worked closely with AHRQ to meet specific guidelines and requirements. One of the requirements is that the mission and primary activity of a PSO must be to conduct activities that are designed to improve patient safety and the quality of healthcare delivery.
To comply, SHM formed a separate component within the Quality Initiatives Department strictly to pursue patient safety and quality activities.
The SHM PSO will be unique. While PSOs are required to collect patient-safety data and provide some form of feedback to contracted sites, few have their own QI initiatives, and even fewer are established by a national physician’s professional society.
These differences will help the SHM PSO stand out from the crowd and will present opportunities within the healthcare reform framework. The Affordable Care Act (ACA) requires significant QI among the nation’s hospitals.
Specifically pertaining to PSOs, Section 399KK, a rarely mentioned section of the ACA, requires the Health and Human Services to establish a program for hospitals with high readmission rates to improve their rates through the use of PSOs. The details of this program remain unclear, but based upon the little bit of information currently available, there could be positive overlap between SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) and the provision.
AHRQ’s recognition of the SHM PSO exemplifies SHM’s commitment to improving the quality of healthcare delivery. It also provides additional value to sites that implement SHM’s QI initiatives and will hopefully open new doors to SHM’s members. TH
On Feb. 16, the Agency for Healthcare Research and Quality (AHRQ) listed SHM as a patient safety organization (PSO). A PSO serves as an independent, external, expert organization that can collect, analyze, and aggregate information in order to develop insights into the underlying causes of patient-safety events. PSOs are designed to help clinicians, hospitals, and healthcare organizations improve patient safety and the quality of healthcare delivery.
PSO status allows SHM’s current quality-improvement (QI) activities to be conducted in a secure environment that is protected from legal discovery. AHRQ currently lists 78 PSOs, including the Society for Vascular Surgery PSO, the Emergency Medicine Patient Safety Foundation, and the Biomedical Research and Education Foundation. A full list is available at www.pso.ahrq.gov/listing/psolist.htm.
To achieve PSO status, SHM worked closely with AHRQ to meet specific guidelines and requirements. One of the requirements is that the mission and primary activity of a PSO must be to conduct activities that are designed to improve patient safety and the quality of healthcare delivery.
To comply, SHM formed a separate component within the Quality Initiatives Department strictly to pursue patient safety and quality activities.
The SHM PSO will be unique. While PSOs are required to collect patient-safety data and provide some form of feedback to contracted sites, few have their own QI initiatives, and even fewer are established by a national physician’s professional society.
These differences will help the SHM PSO stand out from the crowd and will present opportunities within the healthcare reform framework. The Affordable Care Act (ACA) requires significant QI among the nation’s hospitals.
Specifically pertaining to PSOs, Section 399KK, a rarely mentioned section of the ACA, requires the Health and Human Services to establish a program for hospitals with high readmission rates to improve their rates through the use of PSOs. The details of this program remain unclear, but based upon the little bit of information currently available, there could be positive overlap between SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) and the provision.
AHRQ’s recognition of the SHM PSO exemplifies SHM’s commitment to improving the quality of healthcare delivery. It also provides additional value to sites that implement SHM’s QI initiatives and will hopefully open new doors to SHM’s members. TH
On Feb. 16, the Agency for Healthcare Research and Quality (AHRQ) listed SHM as a patient safety organization (PSO). A PSO serves as an independent, external, expert organization that can collect, analyze, and aggregate information in order to develop insights into the underlying causes of patient-safety events. PSOs are designed to help clinicians, hospitals, and healthcare organizations improve patient safety and the quality of healthcare delivery.
PSO status allows SHM’s current quality-improvement (QI) activities to be conducted in a secure environment that is protected from legal discovery. AHRQ currently lists 78 PSOs, including the Society for Vascular Surgery PSO, the Emergency Medicine Patient Safety Foundation, and the Biomedical Research and Education Foundation. A full list is available at www.pso.ahrq.gov/listing/psolist.htm.
To achieve PSO status, SHM worked closely with AHRQ to meet specific guidelines and requirements. One of the requirements is that the mission and primary activity of a PSO must be to conduct activities that are designed to improve patient safety and the quality of healthcare delivery.
To comply, SHM formed a separate component within the Quality Initiatives Department strictly to pursue patient safety and quality activities.
The SHM PSO will be unique. While PSOs are required to collect patient-safety data and provide some form of feedback to contracted sites, few have their own QI initiatives, and even fewer are established by a national physician’s professional society.
These differences will help the SHM PSO stand out from the crowd and will present opportunities within the healthcare reform framework. The Affordable Care Act (ACA) requires significant QI among the nation’s hospitals.
Specifically pertaining to PSOs, Section 399KK, a rarely mentioned section of the ACA, requires the Health and Human Services to establish a program for hospitals with high readmission rates to improve their rates through the use of PSOs. The details of this program remain unclear, but based upon the little bit of information currently available, there could be positive overlap between SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) and the provision.
AHRQ’s recognition of the SHM PSO exemplifies SHM’s commitment to improving the quality of healthcare delivery. It also provides additional value to sites that implement SHM’s QI initiatives and will hopefully open new doors to SHM’s members. TH
Minivan, Major Lesson
I recently visited my parents in my ancestral home of Wisconsin. As parents of a certain age, they inexplicably are genetically predisposed to owning a minivan. Another quirk of their DNA is that they must own a new minivan. No sooner has the last wisp of new-car smell osmosed from the burled walnut interior than they are trading up to the newest, tricked-out minivan. Perhaps more puzzling is the manner of pride they display in their minivan.
Now, my dad, as if not readily apparent, is not cool. And to see him folded into the driver’s seat, his furry-ear-to-furry-ear grin signaling a self-satisfaction customarily reserved for his grandchildren, painstakingly recounting glory-day stories and 4:30 p.m. dinner buffets, further solidifies his place in the Annals of Uncool.
When I’m home, they tend to employ my chauffeur services (most likely in retribution for my peri-pubescent years), and on the first day back home, I stopped their newest ride near the back door of the house, foot idling on the brake while this exchange occurred: “That’s a fascinating story about how much more challenging the world was when you were my age, Dad. You are a true American hero. Would you like to get out here or in the garage?”
“Here,” he replied.
“OK, then get out,” I countered.
“I can’t,” he responded knowingly.
“Why not?” I queried, the patience seeping from my voice.
“Because the door’s not open,” he answered, seemingly mocking me.
“Then open it,” I replied, silently recounting the evidence for his institutionalization.
“I can’t,” he responded.
“Why not?” I replied again, this time calculating the likelihood that I was adopted.
“Because it’s locked,” came his retort.
“Then unlock it,” I answered, reconfirming my decision to move away for college.
“I can’t,” he replied, ostensibly encouraging parenticide.
“Why not?” I queried, strongly contemplating parenticide.
“Because you haven’t put the car in park,” he responded triumphantly.
A System So Safe
As a safety feature, the minivan needed to be in park before you could open the door to exit. I’ve never heard of anyone actually falling out of a moving car, but recollecting high school, I can fathom the right mix, type, and number of teenagers where possibility would meet inevitability. But, apparently, enough people are falling out of moving vehicles that car engineers have built a system that is so safe, this can’t happen. So no matter how hard someone tries, it just isn’t possible to fall out of a moving car (believe me, toward the end of a week of my father’s car stories, my mind had worked every possible angle).
Likewise, newer vehicles employ occupant-sensitive sensors that detect the weight, size, and position of the passenger to determine if the airbag should deploy. Rather than depending on the driver to turn the passenger-side airbag on or off, the car does it for you: heavy enough to trigger the sensor, and the airbag will deploy; too light, and the car assumes you are a child and doesn’t deploy. It’s a system that is so safe because it doesn’t depend on the operator to get it right.
Ditto motion sensors that detect objects behind the car while reversing (avoiding accidental back-overs), antilock brakes (to maintain control during panicked braking), traction control (improves stability during acceleration), electronic stability control (foils spinouts), tire-pressure-monitoring systems (avoids blowouts), daytime running lights (ensures others see you), rollover airbags (they stay inflated to keep you in the car), lane-departure warning (alerts you if you stray from your lane), and doors that automatically lock after the car starts (again, falling out of cars).
For all the negative press of late, car manufacturers understand safety.
A System Not So Safe
Contrast this to healthcare, in which 10% of patients will suffer a serious, preventable, adverse event during their hospital stay.1 Read that sentence again. That’s 10%; that’s preventable; that’s a number that has largely remained unchanged in the past decade. If 1 in 10 drivers suffered a serious adverse preventable auto accident, Congress would do nothing but hold automotive safety hearings.
In medicine, we still largely employ unsafe systems in which even the best doctors can, and do, hurt patients. Sure, we have made strides in this arena (oxygen tubing that only works if hooked up properly, smart pumps that avert IV dosing errors, CO2 monitors to detect proper endotracheal tube placement), but remarkably, in this era of patient safety, we still utilize systems that largely depend on the heroism of the individual.
As physicians, we are famously autonomous and value our professional independence, even to the degree that it might harm patients. We generally eschew standardization, believing that each patient is inherently different. In fact, the thrill of the improvisational theater that follows every patient’s chief compliant is one of the great satisfiers in medicine. We love that feeling that comes from sleuthing each case, deftly enacting a plan of action to shepherd the patient to health.
To suggest following protocols, guidelines, and checklists is derisively dismissed as “cookbook medicine.” To work in teams in which certain tasks are delegated to others is seen as weakness—we don’t need a system that utilizes a pharmacist; rather, we should know the doses of all medicines, their interactions, and the effect of renal and liver impairment on their clearance. To suggest otherwise is an insult to our Oslerian roots. To examine our errors, our system breakdowns, our patient harms is anathema to our practice, an admission of failure.
The result is that most of us continue to toil in systems that have become exponentially unsafe as healthcare has become more complex. Today, we still have a system that will more or less allow us to kill a patient by doing nothing more than forgetting the letter “g.” I can go to my hospital today and intend to write “4 grams of magnesium sulfate (MgSO4)” and inadvertently forget the “g” in “Mg.” This could result in an order for a lethal dose of morphine sulfate (MSO4). It’s that easy to hurt a patient. Now, you might say that would never happen, because the pharmacy would catch it. And this is likely. But is it guaranteed? Can you 100% ensure it wouldn’t happen? Consider that nearly 20% of medication doses administered in a hospital are done so incorrectly.2 Nearly 1 in 5. This is the type of system we are employing to stop this lethal overdose. Is this system, which depends on another human to prevent an error, foolproof, or just a snare waiting to prove you the fool?
This represents our opportunity. As hospitalists, the hospital is our tapestry, our system of care, our responsibility. Few others are as well-positioned to ensure that the systems that envelop our patients are highly functional, reliable, and safe. This will take work—work that will feel burdensome, underappreciated, undercompensated. And, fully recognizing that none of us went into medicine to become systems engineers, this will be hard.
However, if not us, who? Who will ensure that our fathers, our mothers, our children will be as safe in the hospital as they are on the drive to the hospital? TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Global health leaders join the World Health Organization to announce accelerated efforts to improve patient safety. World Health Organization website. Available at: www.who.int/mediacentre/news/releases/2004/pr74/en/. Accessed Feb. 14, 2011.
- Barker KN, Flynn EA, Pepper GA, Bates DW, Mikeal RL. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162(16):1897-1903.
I recently visited my parents in my ancestral home of Wisconsin. As parents of a certain age, they inexplicably are genetically predisposed to owning a minivan. Another quirk of their DNA is that they must own a new minivan. No sooner has the last wisp of new-car smell osmosed from the burled walnut interior than they are trading up to the newest, tricked-out minivan. Perhaps more puzzling is the manner of pride they display in their minivan.
Now, my dad, as if not readily apparent, is not cool. And to see him folded into the driver’s seat, his furry-ear-to-furry-ear grin signaling a self-satisfaction customarily reserved for his grandchildren, painstakingly recounting glory-day stories and 4:30 p.m. dinner buffets, further solidifies his place in the Annals of Uncool.
When I’m home, they tend to employ my chauffeur services (most likely in retribution for my peri-pubescent years), and on the first day back home, I stopped their newest ride near the back door of the house, foot idling on the brake while this exchange occurred: “That’s a fascinating story about how much more challenging the world was when you were my age, Dad. You are a true American hero. Would you like to get out here or in the garage?”
“Here,” he replied.
“OK, then get out,” I countered.
“I can’t,” he responded knowingly.
“Why not?” I queried, the patience seeping from my voice.
“Because the door’s not open,” he answered, seemingly mocking me.
“Then open it,” I replied, silently recounting the evidence for his institutionalization.
“I can’t,” he responded.
“Why not?” I replied again, this time calculating the likelihood that I was adopted.
“Because it’s locked,” came his retort.
“Then unlock it,” I answered, reconfirming my decision to move away for college.
“I can’t,” he replied, ostensibly encouraging parenticide.
“Why not?” I queried, strongly contemplating parenticide.
“Because you haven’t put the car in park,” he responded triumphantly.
A System So Safe
As a safety feature, the minivan needed to be in park before you could open the door to exit. I’ve never heard of anyone actually falling out of a moving car, but recollecting high school, I can fathom the right mix, type, and number of teenagers where possibility would meet inevitability. But, apparently, enough people are falling out of moving vehicles that car engineers have built a system that is so safe, this can’t happen. So no matter how hard someone tries, it just isn’t possible to fall out of a moving car (believe me, toward the end of a week of my father’s car stories, my mind had worked every possible angle).
Likewise, newer vehicles employ occupant-sensitive sensors that detect the weight, size, and position of the passenger to determine if the airbag should deploy. Rather than depending on the driver to turn the passenger-side airbag on or off, the car does it for you: heavy enough to trigger the sensor, and the airbag will deploy; too light, and the car assumes you are a child and doesn’t deploy. It’s a system that is so safe because it doesn’t depend on the operator to get it right.
Ditto motion sensors that detect objects behind the car while reversing (avoiding accidental back-overs), antilock brakes (to maintain control during panicked braking), traction control (improves stability during acceleration), electronic stability control (foils spinouts), tire-pressure-monitoring systems (avoids blowouts), daytime running lights (ensures others see you), rollover airbags (they stay inflated to keep you in the car), lane-departure warning (alerts you if you stray from your lane), and doors that automatically lock after the car starts (again, falling out of cars).
For all the negative press of late, car manufacturers understand safety.
A System Not So Safe
Contrast this to healthcare, in which 10% of patients will suffer a serious, preventable, adverse event during their hospital stay.1 Read that sentence again. That’s 10%; that’s preventable; that’s a number that has largely remained unchanged in the past decade. If 1 in 10 drivers suffered a serious adverse preventable auto accident, Congress would do nothing but hold automotive safety hearings.
In medicine, we still largely employ unsafe systems in which even the best doctors can, and do, hurt patients. Sure, we have made strides in this arena (oxygen tubing that only works if hooked up properly, smart pumps that avert IV dosing errors, CO2 monitors to detect proper endotracheal tube placement), but remarkably, in this era of patient safety, we still utilize systems that largely depend on the heroism of the individual.
As physicians, we are famously autonomous and value our professional independence, even to the degree that it might harm patients. We generally eschew standardization, believing that each patient is inherently different. In fact, the thrill of the improvisational theater that follows every patient’s chief compliant is one of the great satisfiers in medicine. We love that feeling that comes from sleuthing each case, deftly enacting a plan of action to shepherd the patient to health.
To suggest following protocols, guidelines, and checklists is derisively dismissed as “cookbook medicine.” To work in teams in which certain tasks are delegated to others is seen as weakness—we don’t need a system that utilizes a pharmacist; rather, we should know the doses of all medicines, their interactions, and the effect of renal and liver impairment on their clearance. To suggest otherwise is an insult to our Oslerian roots. To examine our errors, our system breakdowns, our patient harms is anathema to our practice, an admission of failure.
The result is that most of us continue to toil in systems that have become exponentially unsafe as healthcare has become more complex. Today, we still have a system that will more or less allow us to kill a patient by doing nothing more than forgetting the letter “g.” I can go to my hospital today and intend to write “4 grams of magnesium sulfate (MgSO4)” and inadvertently forget the “g” in “Mg.” This could result in an order for a lethal dose of morphine sulfate (MSO4). It’s that easy to hurt a patient. Now, you might say that would never happen, because the pharmacy would catch it. And this is likely. But is it guaranteed? Can you 100% ensure it wouldn’t happen? Consider that nearly 20% of medication doses administered in a hospital are done so incorrectly.2 Nearly 1 in 5. This is the type of system we are employing to stop this lethal overdose. Is this system, which depends on another human to prevent an error, foolproof, or just a snare waiting to prove you the fool?
This represents our opportunity. As hospitalists, the hospital is our tapestry, our system of care, our responsibility. Few others are as well-positioned to ensure that the systems that envelop our patients are highly functional, reliable, and safe. This will take work—work that will feel burdensome, underappreciated, undercompensated. And, fully recognizing that none of us went into medicine to become systems engineers, this will be hard.
However, if not us, who? Who will ensure that our fathers, our mothers, our children will be as safe in the hospital as they are on the drive to the hospital? TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Global health leaders join the World Health Organization to announce accelerated efforts to improve patient safety. World Health Organization website. Available at: www.who.int/mediacentre/news/releases/2004/pr74/en/. Accessed Feb. 14, 2011.
- Barker KN, Flynn EA, Pepper GA, Bates DW, Mikeal RL. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162(16):1897-1903.
I recently visited my parents in my ancestral home of Wisconsin. As parents of a certain age, they inexplicably are genetically predisposed to owning a minivan. Another quirk of their DNA is that they must own a new minivan. No sooner has the last wisp of new-car smell osmosed from the burled walnut interior than they are trading up to the newest, tricked-out minivan. Perhaps more puzzling is the manner of pride they display in their minivan.
Now, my dad, as if not readily apparent, is not cool. And to see him folded into the driver’s seat, his furry-ear-to-furry-ear grin signaling a self-satisfaction customarily reserved for his grandchildren, painstakingly recounting glory-day stories and 4:30 p.m. dinner buffets, further solidifies his place in the Annals of Uncool.
When I’m home, they tend to employ my chauffeur services (most likely in retribution for my peri-pubescent years), and on the first day back home, I stopped their newest ride near the back door of the house, foot idling on the brake while this exchange occurred: “That’s a fascinating story about how much more challenging the world was when you were my age, Dad. You are a true American hero. Would you like to get out here or in the garage?”
“Here,” he replied.
“OK, then get out,” I countered.
“I can’t,” he responded knowingly.
“Why not?” I queried, the patience seeping from my voice.
“Because the door’s not open,” he answered, seemingly mocking me.
“Then open it,” I replied, silently recounting the evidence for his institutionalization.
“I can’t,” he responded.
“Why not?” I replied again, this time calculating the likelihood that I was adopted.
“Because it’s locked,” came his retort.
“Then unlock it,” I answered, reconfirming my decision to move away for college.
“I can’t,” he replied, ostensibly encouraging parenticide.
“Why not?” I queried, strongly contemplating parenticide.
“Because you haven’t put the car in park,” he responded triumphantly.
A System So Safe
As a safety feature, the minivan needed to be in park before you could open the door to exit. I’ve never heard of anyone actually falling out of a moving car, but recollecting high school, I can fathom the right mix, type, and number of teenagers where possibility would meet inevitability. But, apparently, enough people are falling out of moving vehicles that car engineers have built a system that is so safe, this can’t happen. So no matter how hard someone tries, it just isn’t possible to fall out of a moving car (believe me, toward the end of a week of my father’s car stories, my mind had worked every possible angle).
Likewise, newer vehicles employ occupant-sensitive sensors that detect the weight, size, and position of the passenger to determine if the airbag should deploy. Rather than depending on the driver to turn the passenger-side airbag on or off, the car does it for you: heavy enough to trigger the sensor, and the airbag will deploy; too light, and the car assumes you are a child and doesn’t deploy. It’s a system that is so safe because it doesn’t depend on the operator to get it right.
Ditto motion sensors that detect objects behind the car while reversing (avoiding accidental back-overs), antilock brakes (to maintain control during panicked braking), traction control (improves stability during acceleration), electronic stability control (foils spinouts), tire-pressure-monitoring systems (avoids blowouts), daytime running lights (ensures others see you), rollover airbags (they stay inflated to keep you in the car), lane-departure warning (alerts you if you stray from your lane), and doors that automatically lock after the car starts (again, falling out of cars).
For all the negative press of late, car manufacturers understand safety.
A System Not So Safe
Contrast this to healthcare, in which 10% of patients will suffer a serious, preventable, adverse event during their hospital stay.1 Read that sentence again. That’s 10%; that’s preventable; that’s a number that has largely remained unchanged in the past decade. If 1 in 10 drivers suffered a serious adverse preventable auto accident, Congress would do nothing but hold automotive safety hearings.
In medicine, we still largely employ unsafe systems in which even the best doctors can, and do, hurt patients. Sure, we have made strides in this arena (oxygen tubing that only works if hooked up properly, smart pumps that avert IV dosing errors, CO2 monitors to detect proper endotracheal tube placement), but remarkably, in this era of patient safety, we still utilize systems that largely depend on the heroism of the individual.
As physicians, we are famously autonomous and value our professional independence, even to the degree that it might harm patients. We generally eschew standardization, believing that each patient is inherently different. In fact, the thrill of the improvisational theater that follows every patient’s chief compliant is one of the great satisfiers in medicine. We love that feeling that comes from sleuthing each case, deftly enacting a plan of action to shepherd the patient to health.
To suggest following protocols, guidelines, and checklists is derisively dismissed as “cookbook medicine.” To work in teams in which certain tasks are delegated to others is seen as weakness—we don’t need a system that utilizes a pharmacist; rather, we should know the doses of all medicines, their interactions, and the effect of renal and liver impairment on their clearance. To suggest otherwise is an insult to our Oslerian roots. To examine our errors, our system breakdowns, our patient harms is anathema to our practice, an admission of failure.
The result is that most of us continue to toil in systems that have become exponentially unsafe as healthcare has become more complex. Today, we still have a system that will more or less allow us to kill a patient by doing nothing more than forgetting the letter “g.” I can go to my hospital today and intend to write “4 grams of magnesium sulfate (MgSO4)” and inadvertently forget the “g” in “Mg.” This could result in an order for a lethal dose of morphine sulfate (MSO4). It’s that easy to hurt a patient. Now, you might say that would never happen, because the pharmacy would catch it. And this is likely. But is it guaranteed? Can you 100% ensure it wouldn’t happen? Consider that nearly 20% of medication doses administered in a hospital are done so incorrectly.2 Nearly 1 in 5. This is the type of system we are employing to stop this lethal overdose. Is this system, which depends on another human to prevent an error, foolproof, or just a snare waiting to prove you the fool?
This represents our opportunity. As hospitalists, the hospital is our tapestry, our system of care, our responsibility. Few others are as well-positioned to ensure that the systems that envelop our patients are highly functional, reliable, and safe. This will take work—work that will feel burdensome, underappreciated, undercompensated. And, fully recognizing that none of us went into medicine to become systems engineers, this will be hard.
However, if not us, who? Who will ensure that our fathers, our mothers, our children will be as safe in the hospital as they are on the drive to the hospital? TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Global health leaders join the World Health Organization to announce accelerated efforts to improve patient safety. World Health Organization website. Available at: www.who.int/mediacentre/news/releases/2004/pr74/en/. Accessed Feb. 14, 2011.
- Barker KN, Flynn EA, Pepper GA, Bates DW, Mikeal RL. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162(16):1897-1903.
The Story of Us
From the outset, HM has been about efficiency. And there was nothing wrong with that, for value is quality divided by cost. But in our story, we found that mere efficiency was not enough: The lowering of the denominator (cost) had to be met with an escalation of the numerator (quality) to ensure value.
And see us as being born in the right place at the right time. For with the national focus turning to the need for quality and patient safety, hospital medicine was in the right place and the right time to heed the call to action: appropriately stepping up to enact efforts to make the slope of the line (on a chart of quality vs. cost) “STEEEPER” … finding systems innovations to make care Safe, Timely, Efficient, Effective, Equitable, and Patient-centered.
Of course, the story continued with the Affordable Care Act and healthcare reform, greatly accelerating our evolution as change agents. And now we find ourselves fully invested in a “change the system” mentality, perfectly positioned to meaningfully change healthcare for millions of people. But threats loom—specifically, the “R” in the STEEEPER mnemonic: the risks to quality in the face of healthcare reform.
So in the next chapter of our story, I present to you our challenge: how to overcome the threats to quality in the context of healthcare reform. The first three are presented here; in subsequent articles, I will address the remainder. Overcoming all threats will hinge on mastering the four truisms of cultural change:
- Systems drive function;
- Every system is perfectly designed to produce the outcomes that it does;
- This is not an issue of people needing to try harder; and
- The “no blame” culture begins with a paradigm shift from the “person at fault” to the “system at fault.”
Threat 1: Failure to Fund Quality
SHM elected to merge its annual State of Hospital Medicine survey with the MGMA. Though not without risk, this has resulted in the anticipated benefits. The MGMA collaboration brings greater leverage in working with the C-suite, which is pre-programmed to react to MGMA surveys. From the most recent MGMA survey comes good news: The financial compensation for hospitalists has increased. A sobering insight, however, is that this increase in compensation has been met with a corresponding increase in work intensity—RVUs. Further, the link between RVUs and compensation appears to be tightening, quantifying what has long been of concern: The time devoted to the nonclinical “value added” duties of the hospitalist is shrinking.
The threat to the culture of quality is captured in the single question: How many RVUs is a quality-improvement (QI) project worth? I’m not sure we have that answer. But without an answer, it is difficult to believe that meaningful QI can be expected without time to do so. And again, as the gap between compensation and RVUs narrows, one is left wondering if there will soon be a day where there is no value-added time remaining to perform QI at all.
Fortunately, the Affordable Care Act might provide some movement in the right direction via value-based purchasing. Linking quality outcomes to financial reimbursement is a big step forward in the hospitalist’s quest to leverage the C-suite in trading RVUs for devoted QI time. Although we still are left asking the question of how many RVUs a QI project is worth, value-based purchasing at least sets the stage for the conversation. But in the interim, it is still upon hospitalists to design these QI projects, and to learn the skills necessary to see the design to its fruition.
Threat 2: Quality Stops at Core Measures
It is hard to argue that fulfilling “core measures” is a bad thing. Nonetheless, the core measures were not meant to be quality; instead, they were meant as surrogate measures of quality. The presumption of the core-measures initiative is that the system would exist without direct attention to the core measures, operating as it ordinarily would with generic attention to meeting all standards of quality for all diseases. And at some point in time, the core measures would be assessed to give an overall assessment of the system’s quality.
What has evolved, however, is a concerted attention to meeting the core measures, with little regard to the overall culture of quality.
Let’s say you were tasked with improving the public school system in your state. As a measure of the improvement, you choose five of the 1,000 schools as “core measure” schools. The state board of education is told that the performance of these five sample schools will be assessed at the end of the year, and financial support for the system as a whole will hinge on their performance. The intended result is that attention would be paid to improving the performance of every school in the system, and this improvement would be reflected in the performance of the five sample schools. The board of education could take the route of improving all schools, but the more pragmatic route would be to funnel all resources into these five schools, to the detriment of resources for the other 995 schools. The performance of the core measure schools would dramatically improve, and funding would be secured. But ask yourself: Did the performance of the school system as a whole actually improve?
Such is the risk of the core measures in healthcare. The original intent of the core measures was to instill a culture of QI for all points of care. And this has been a valuable contribution to changing the consciousness of the healthcare system. The presumption was that the core measures would be “seeds,” and that by emphasizing these select measures, the QI culture eventually would spread to all aspects of patient care. But this plan hinged on the presumption that that there is an unlimited amount of mental energy and resources to be devoted to all tasks within healthcare. The reality is that there is a fixed amount of intellectual energy and resources to be devoted to the various aspects of healthcare. One wonders if the overemphasis on meeting the core measures might actually have taken the wind out of the sails for QI in other non-core-measure patient care.
The implications are twofold. By definition, a core measure has to be applicable to all healthcare systems, and with a fixed amount of mental energy and resources, there is a real risk that what portion is reserved for QI finds its way only to the core indicators, especially if they are overemphasized in the system. The second implication is captured in our experience with time to antibiotics. With meeting the core indicator as the priority, many systems instituted the “work-around”: Give antibiotics to every patient presenting to the ED, and you will be sure to have met the four-hour window in the core indicator. The result was an exponential increase in inappropriate antibiotic administration and radiographic tests, all because meeting the indicator became more important than the overall goal.
As stewards of the hospital system, it is upon us to ensure that the original intent of core measures remains secure: The core measures seed a culture of quality, but do not become ends in and of themselves. QI apart from the core measures must remain an equal priority, and it is the hospitalist who will be central in ensuring this comes to fruition.
Threat 3: Misplaced Incentives
There is an interesting anecdote in Steven Levitt and Stephen Dubner’s book Freakonomics.1 The story begins with a daycare center struggling with a problem: Some parents are showing up late to pick up their children at the end of the day, and this is costing the center in the way of overtime charges for the staff. To solve the problem, the center elects to institute a financial disincentive: Those showing up late to pick up their children will pay a modest financial penalty.
Fast-forward to months after the policy was put in place. The result? An exponential increase in the number of parents showing up late to pick up their children.
How do you explain worsening performance in spite of a financial disincentive? The answer resides in understanding human behavior. According to the authors, there are three primary motivations in life: financial, social, and moral. As ugly as it sounds, the decisions people make in life are driven by one of these three motivations. There is nothing wrong with providing incentives for behavior; incentives work.
But the danger arises when incentives are mismatched to behaviors. For example, if a financial outcome is the goal, then financial incentives make sense. If a social outcome (people should play better as a team) is the goal, the social incentives make sense (public recognition). But when the incentives get misaligned with their respective goals, trouble results.
What went wrong with the daycare’s plan is simple—most of the parents were motivated to pick up their children on time out of moral (“I gave my word”) or social (“I don’t want to be talked about by other parents”) incentives. But once a financial incentive was offered, the daycare center had essentially given the parents a way out in absolving their social and moral obligations. The parents had essentially cost-adjusted their behavior.
If you think this couldn’t happen to the healthcare system, let me ask you this. As a hospitalist, I see all of my patients early in the morning, because I see it as part of my obligation to the hospital team to discharge patients by 11 a.m. (social motivation).
But what if the CEO released this directive: “You will see all of your patients early in the morning, or you will take a $1,000 a year pay cut.” Is it possible that I might cost-adjust the $1,000 in exchange for sleeping in a little later and not having to deal with the morning traffic? I don’t know.
When it comes to financial incentives, there is a valley in the U-shaped curve. When the financial incentive is trivial, it is disregarded and the social/moral motivations of behavior persist (the kids are picked up on time; I persist in seeing patients early in the morning). When the financial incentive is huge, the financial incentive trumps all social/moral motivations, ensuring compliance with the goal behavior (every kid is picked up on time to avoid a penalty; I see all patients early in the day to avoid a larger penalty).
But in between is the risk zone: When the person feels they are paying an appropriate penance for not complying with the goal behavior, the financial disincentive absolves any social/moral guilt.
Healthcare reform is about incentives—and there is nothing wrong with that. But as the stewards of the inpatient healthcare system, it is upon us as hospitalists to ensure that the incentives remain matched to their intended goals, and that the untoward consequences of the incentives do not adversely affect the quality and safety of a patient’s care.
It is safe to say that the Affordable Care Act of 2010 moves us closer to a true environment of quality and patient safety. But it is equally safe to say that meaningful change will require more than what the law can provide. As stewards of the inpatient system, we have a responsibility to ensure that the healthcare system, particularly in how it responds to incentives, evolves to remain patient-centered, effective, and safe.
The next chapter in our story—the hospitalists’ story—will be one of accountability and responsibility. While there are things the government can do, the majority of what needs to be done will come directly from us. TH
Dr. Wiese is president of SHM.
Reference
- Levitt SD, Dubner SJ. Freakonomics: A Rogue Economist Explores the Hidden Side of Everything. New York City: William Morrow; 2005.
From the outset, HM has been about efficiency. And there was nothing wrong with that, for value is quality divided by cost. But in our story, we found that mere efficiency was not enough: The lowering of the denominator (cost) had to be met with an escalation of the numerator (quality) to ensure value.
And see us as being born in the right place at the right time. For with the national focus turning to the need for quality and patient safety, hospital medicine was in the right place and the right time to heed the call to action: appropriately stepping up to enact efforts to make the slope of the line (on a chart of quality vs. cost) “STEEEPER” … finding systems innovations to make care Safe, Timely, Efficient, Effective, Equitable, and Patient-centered.
Of course, the story continued with the Affordable Care Act and healthcare reform, greatly accelerating our evolution as change agents. And now we find ourselves fully invested in a “change the system” mentality, perfectly positioned to meaningfully change healthcare for millions of people. But threats loom—specifically, the “R” in the STEEEPER mnemonic: the risks to quality in the face of healthcare reform.
So in the next chapter of our story, I present to you our challenge: how to overcome the threats to quality in the context of healthcare reform. The first three are presented here; in subsequent articles, I will address the remainder. Overcoming all threats will hinge on mastering the four truisms of cultural change:
- Systems drive function;
- Every system is perfectly designed to produce the outcomes that it does;
- This is not an issue of people needing to try harder; and
- The “no blame” culture begins with a paradigm shift from the “person at fault” to the “system at fault.”
Threat 1: Failure to Fund Quality
SHM elected to merge its annual State of Hospital Medicine survey with the MGMA. Though not without risk, this has resulted in the anticipated benefits. The MGMA collaboration brings greater leverage in working with the C-suite, which is pre-programmed to react to MGMA surveys. From the most recent MGMA survey comes good news: The financial compensation for hospitalists has increased. A sobering insight, however, is that this increase in compensation has been met with a corresponding increase in work intensity—RVUs. Further, the link between RVUs and compensation appears to be tightening, quantifying what has long been of concern: The time devoted to the nonclinical “value added” duties of the hospitalist is shrinking.
The threat to the culture of quality is captured in the single question: How many RVUs is a quality-improvement (QI) project worth? I’m not sure we have that answer. But without an answer, it is difficult to believe that meaningful QI can be expected without time to do so. And again, as the gap between compensation and RVUs narrows, one is left wondering if there will soon be a day where there is no value-added time remaining to perform QI at all.
Fortunately, the Affordable Care Act might provide some movement in the right direction via value-based purchasing. Linking quality outcomes to financial reimbursement is a big step forward in the hospitalist’s quest to leverage the C-suite in trading RVUs for devoted QI time. Although we still are left asking the question of how many RVUs a QI project is worth, value-based purchasing at least sets the stage for the conversation. But in the interim, it is still upon hospitalists to design these QI projects, and to learn the skills necessary to see the design to its fruition.
Threat 2: Quality Stops at Core Measures
It is hard to argue that fulfilling “core measures” is a bad thing. Nonetheless, the core measures were not meant to be quality; instead, they were meant as surrogate measures of quality. The presumption of the core-measures initiative is that the system would exist without direct attention to the core measures, operating as it ordinarily would with generic attention to meeting all standards of quality for all diseases. And at some point in time, the core measures would be assessed to give an overall assessment of the system’s quality.
What has evolved, however, is a concerted attention to meeting the core measures, with little regard to the overall culture of quality.
Let’s say you were tasked with improving the public school system in your state. As a measure of the improvement, you choose five of the 1,000 schools as “core measure” schools. The state board of education is told that the performance of these five sample schools will be assessed at the end of the year, and financial support for the system as a whole will hinge on their performance. The intended result is that attention would be paid to improving the performance of every school in the system, and this improvement would be reflected in the performance of the five sample schools. The board of education could take the route of improving all schools, but the more pragmatic route would be to funnel all resources into these five schools, to the detriment of resources for the other 995 schools. The performance of the core measure schools would dramatically improve, and funding would be secured. But ask yourself: Did the performance of the school system as a whole actually improve?
Such is the risk of the core measures in healthcare. The original intent of the core measures was to instill a culture of QI for all points of care. And this has been a valuable contribution to changing the consciousness of the healthcare system. The presumption was that the core measures would be “seeds,” and that by emphasizing these select measures, the QI culture eventually would spread to all aspects of patient care. But this plan hinged on the presumption that that there is an unlimited amount of mental energy and resources to be devoted to all tasks within healthcare. The reality is that there is a fixed amount of intellectual energy and resources to be devoted to the various aspects of healthcare. One wonders if the overemphasis on meeting the core measures might actually have taken the wind out of the sails for QI in other non-core-measure patient care.
The implications are twofold. By definition, a core measure has to be applicable to all healthcare systems, and with a fixed amount of mental energy and resources, there is a real risk that what portion is reserved for QI finds its way only to the core indicators, especially if they are overemphasized in the system. The second implication is captured in our experience with time to antibiotics. With meeting the core indicator as the priority, many systems instituted the “work-around”: Give antibiotics to every patient presenting to the ED, and you will be sure to have met the four-hour window in the core indicator. The result was an exponential increase in inappropriate antibiotic administration and radiographic tests, all because meeting the indicator became more important than the overall goal.
As stewards of the hospital system, it is upon us to ensure that the original intent of core measures remains secure: The core measures seed a culture of quality, but do not become ends in and of themselves. QI apart from the core measures must remain an equal priority, and it is the hospitalist who will be central in ensuring this comes to fruition.
Threat 3: Misplaced Incentives
There is an interesting anecdote in Steven Levitt and Stephen Dubner’s book Freakonomics.1 The story begins with a daycare center struggling with a problem: Some parents are showing up late to pick up their children at the end of the day, and this is costing the center in the way of overtime charges for the staff. To solve the problem, the center elects to institute a financial disincentive: Those showing up late to pick up their children will pay a modest financial penalty.
Fast-forward to months after the policy was put in place. The result? An exponential increase in the number of parents showing up late to pick up their children.
How do you explain worsening performance in spite of a financial disincentive? The answer resides in understanding human behavior. According to the authors, there are three primary motivations in life: financial, social, and moral. As ugly as it sounds, the decisions people make in life are driven by one of these three motivations. There is nothing wrong with providing incentives for behavior; incentives work.
But the danger arises when incentives are mismatched to behaviors. For example, if a financial outcome is the goal, then financial incentives make sense. If a social outcome (people should play better as a team) is the goal, the social incentives make sense (public recognition). But when the incentives get misaligned with their respective goals, trouble results.
What went wrong with the daycare’s plan is simple—most of the parents were motivated to pick up their children on time out of moral (“I gave my word”) or social (“I don’t want to be talked about by other parents”) incentives. But once a financial incentive was offered, the daycare center had essentially given the parents a way out in absolving their social and moral obligations. The parents had essentially cost-adjusted their behavior.
If you think this couldn’t happen to the healthcare system, let me ask you this. As a hospitalist, I see all of my patients early in the morning, because I see it as part of my obligation to the hospital team to discharge patients by 11 a.m. (social motivation).
But what if the CEO released this directive: “You will see all of your patients early in the morning, or you will take a $1,000 a year pay cut.” Is it possible that I might cost-adjust the $1,000 in exchange for sleeping in a little later and not having to deal with the morning traffic? I don’t know.
When it comes to financial incentives, there is a valley in the U-shaped curve. When the financial incentive is trivial, it is disregarded and the social/moral motivations of behavior persist (the kids are picked up on time; I persist in seeing patients early in the morning). When the financial incentive is huge, the financial incentive trumps all social/moral motivations, ensuring compliance with the goal behavior (every kid is picked up on time to avoid a penalty; I see all patients early in the day to avoid a larger penalty).
But in between is the risk zone: When the person feels they are paying an appropriate penance for not complying with the goal behavior, the financial disincentive absolves any social/moral guilt.
Healthcare reform is about incentives—and there is nothing wrong with that. But as the stewards of the inpatient healthcare system, it is upon us as hospitalists to ensure that the incentives remain matched to their intended goals, and that the untoward consequences of the incentives do not adversely affect the quality and safety of a patient’s care.
It is safe to say that the Affordable Care Act of 2010 moves us closer to a true environment of quality and patient safety. But it is equally safe to say that meaningful change will require more than what the law can provide. As stewards of the inpatient system, we have a responsibility to ensure that the healthcare system, particularly in how it responds to incentives, evolves to remain patient-centered, effective, and safe.
The next chapter in our story—the hospitalists’ story—will be one of accountability and responsibility. While there are things the government can do, the majority of what needs to be done will come directly from us. TH
Dr. Wiese is president of SHM.
Reference
- Levitt SD, Dubner SJ. Freakonomics: A Rogue Economist Explores the Hidden Side of Everything. New York City: William Morrow; 2005.
From the outset, HM has been about efficiency. And there was nothing wrong with that, for value is quality divided by cost. But in our story, we found that mere efficiency was not enough: The lowering of the denominator (cost) had to be met with an escalation of the numerator (quality) to ensure value.
And see us as being born in the right place at the right time. For with the national focus turning to the need for quality and patient safety, hospital medicine was in the right place and the right time to heed the call to action: appropriately stepping up to enact efforts to make the slope of the line (on a chart of quality vs. cost) “STEEEPER” … finding systems innovations to make care Safe, Timely, Efficient, Effective, Equitable, and Patient-centered.
Of course, the story continued with the Affordable Care Act and healthcare reform, greatly accelerating our evolution as change agents. And now we find ourselves fully invested in a “change the system” mentality, perfectly positioned to meaningfully change healthcare for millions of people. But threats loom—specifically, the “R” in the STEEEPER mnemonic: the risks to quality in the face of healthcare reform.
So in the next chapter of our story, I present to you our challenge: how to overcome the threats to quality in the context of healthcare reform. The first three are presented here; in subsequent articles, I will address the remainder. Overcoming all threats will hinge on mastering the four truisms of cultural change:
- Systems drive function;
- Every system is perfectly designed to produce the outcomes that it does;
- This is not an issue of people needing to try harder; and
- The “no blame” culture begins with a paradigm shift from the “person at fault” to the “system at fault.”
Threat 1: Failure to Fund Quality
SHM elected to merge its annual State of Hospital Medicine survey with the MGMA. Though not without risk, this has resulted in the anticipated benefits. The MGMA collaboration brings greater leverage in working with the C-suite, which is pre-programmed to react to MGMA surveys. From the most recent MGMA survey comes good news: The financial compensation for hospitalists has increased. A sobering insight, however, is that this increase in compensation has been met with a corresponding increase in work intensity—RVUs. Further, the link between RVUs and compensation appears to be tightening, quantifying what has long been of concern: The time devoted to the nonclinical “value added” duties of the hospitalist is shrinking.
The threat to the culture of quality is captured in the single question: How many RVUs is a quality-improvement (QI) project worth? I’m not sure we have that answer. But without an answer, it is difficult to believe that meaningful QI can be expected without time to do so. And again, as the gap between compensation and RVUs narrows, one is left wondering if there will soon be a day where there is no value-added time remaining to perform QI at all.
Fortunately, the Affordable Care Act might provide some movement in the right direction via value-based purchasing. Linking quality outcomes to financial reimbursement is a big step forward in the hospitalist’s quest to leverage the C-suite in trading RVUs for devoted QI time. Although we still are left asking the question of how many RVUs a QI project is worth, value-based purchasing at least sets the stage for the conversation. But in the interim, it is still upon hospitalists to design these QI projects, and to learn the skills necessary to see the design to its fruition.
Threat 2: Quality Stops at Core Measures
It is hard to argue that fulfilling “core measures” is a bad thing. Nonetheless, the core measures were not meant to be quality; instead, they were meant as surrogate measures of quality. The presumption of the core-measures initiative is that the system would exist without direct attention to the core measures, operating as it ordinarily would with generic attention to meeting all standards of quality for all diseases. And at some point in time, the core measures would be assessed to give an overall assessment of the system’s quality.
What has evolved, however, is a concerted attention to meeting the core measures, with little regard to the overall culture of quality.
Let’s say you were tasked with improving the public school system in your state. As a measure of the improvement, you choose five of the 1,000 schools as “core measure” schools. The state board of education is told that the performance of these five sample schools will be assessed at the end of the year, and financial support for the system as a whole will hinge on their performance. The intended result is that attention would be paid to improving the performance of every school in the system, and this improvement would be reflected in the performance of the five sample schools. The board of education could take the route of improving all schools, but the more pragmatic route would be to funnel all resources into these five schools, to the detriment of resources for the other 995 schools. The performance of the core measure schools would dramatically improve, and funding would be secured. But ask yourself: Did the performance of the school system as a whole actually improve?
Such is the risk of the core measures in healthcare. The original intent of the core measures was to instill a culture of QI for all points of care. And this has been a valuable contribution to changing the consciousness of the healthcare system. The presumption was that the core measures would be “seeds,” and that by emphasizing these select measures, the QI culture eventually would spread to all aspects of patient care. But this plan hinged on the presumption that that there is an unlimited amount of mental energy and resources to be devoted to all tasks within healthcare. The reality is that there is a fixed amount of intellectual energy and resources to be devoted to the various aspects of healthcare. One wonders if the overemphasis on meeting the core measures might actually have taken the wind out of the sails for QI in other non-core-measure patient care.
The implications are twofold. By definition, a core measure has to be applicable to all healthcare systems, and with a fixed amount of mental energy and resources, there is a real risk that what portion is reserved for QI finds its way only to the core indicators, especially if they are overemphasized in the system. The second implication is captured in our experience with time to antibiotics. With meeting the core indicator as the priority, many systems instituted the “work-around”: Give antibiotics to every patient presenting to the ED, and you will be sure to have met the four-hour window in the core indicator. The result was an exponential increase in inappropriate antibiotic administration and radiographic tests, all because meeting the indicator became more important than the overall goal.
As stewards of the hospital system, it is upon us to ensure that the original intent of core measures remains secure: The core measures seed a culture of quality, but do not become ends in and of themselves. QI apart from the core measures must remain an equal priority, and it is the hospitalist who will be central in ensuring this comes to fruition.
Threat 3: Misplaced Incentives
There is an interesting anecdote in Steven Levitt and Stephen Dubner’s book Freakonomics.1 The story begins with a daycare center struggling with a problem: Some parents are showing up late to pick up their children at the end of the day, and this is costing the center in the way of overtime charges for the staff. To solve the problem, the center elects to institute a financial disincentive: Those showing up late to pick up their children will pay a modest financial penalty.
Fast-forward to months after the policy was put in place. The result? An exponential increase in the number of parents showing up late to pick up their children.
How do you explain worsening performance in spite of a financial disincentive? The answer resides in understanding human behavior. According to the authors, there are three primary motivations in life: financial, social, and moral. As ugly as it sounds, the decisions people make in life are driven by one of these three motivations. There is nothing wrong with providing incentives for behavior; incentives work.
But the danger arises when incentives are mismatched to behaviors. For example, if a financial outcome is the goal, then financial incentives make sense. If a social outcome (people should play better as a team) is the goal, the social incentives make sense (public recognition). But when the incentives get misaligned with their respective goals, trouble results.
What went wrong with the daycare’s plan is simple—most of the parents were motivated to pick up their children on time out of moral (“I gave my word”) or social (“I don’t want to be talked about by other parents”) incentives. But once a financial incentive was offered, the daycare center had essentially given the parents a way out in absolving their social and moral obligations. The parents had essentially cost-adjusted their behavior.
If you think this couldn’t happen to the healthcare system, let me ask you this. As a hospitalist, I see all of my patients early in the morning, because I see it as part of my obligation to the hospital team to discharge patients by 11 a.m. (social motivation).
But what if the CEO released this directive: “You will see all of your patients early in the morning, or you will take a $1,000 a year pay cut.” Is it possible that I might cost-adjust the $1,000 in exchange for sleeping in a little later and not having to deal with the morning traffic? I don’t know.
When it comes to financial incentives, there is a valley in the U-shaped curve. When the financial incentive is trivial, it is disregarded and the social/moral motivations of behavior persist (the kids are picked up on time; I persist in seeing patients early in the morning). When the financial incentive is huge, the financial incentive trumps all social/moral motivations, ensuring compliance with the goal behavior (every kid is picked up on time to avoid a penalty; I see all patients early in the day to avoid a larger penalty).
But in between is the risk zone: When the person feels they are paying an appropriate penance for not complying with the goal behavior, the financial disincentive absolves any social/moral guilt.
Healthcare reform is about incentives—and there is nothing wrong with that. But as the stewards of the inpatient healthcare system, it is upon us as hospitalists to ensure that the incentives remain matched to their intended goals, and that the untoward consequences of the incentives do not adversely affect the quality and safety of a patient’s care.
It is safe to say that the Affordable Care Act of 2010 moves us closer to a true environment of quality and patient safety. But it is equally safe to say that meaningful change will require more than what the law can provide. As stewards of the inpatient system, we have a responsibility to ensure that the healthcare system, particularly in how it responds to incentives, evolves to remain patient-centered, effective, and safe.
The next chapter in our story—the hospitalists’ story—will be one of accountability and responsibility. While there are things the government can do, the majority of what needs to be done will come directly from us. TH
Dr. Wiese is president of SHM.
Reference
- Levitt SD, Dubner SJ. Freakonomics: A Rogue Economist Explores the Hidden Side of Everything. New York City: William Morrow; 2005.
Gettin’ Dirty
Several months ago, my toilet broke. You should also know that I’m not particularly handy. So when I first realized that the toilet bowl seemed to fill constantly, I got a little stressed out.
How much was it going cost to call in a plumber on the weekend?
What kind of a water bill was I going to have?
Was this a serious problem?
I took a quick peek in the tank, but that just made me more confused. I was paralyzed by a lack of know-how.
Normally, I would have just Googled a local plumber. But that day, I decided to do something different. Maybe it was because it was the fantasy football offseason. Maybe it was because my wife had started to ask my father-in-law to change light bulbs around the house. Or, maybe, I wanted to learn to actually fix the problem. A few hours later, after an Internet lesson in toilet physiology, a $4.12 trip to Home Depot, and a wet pair of hands, I had replaced my first toilet flapper.
This wasn’t the rebuilding of a car engine, but it was a clear DIY step toward self-improvement. Easily the most memorable moment here was my sense of accomplishment.
I felt empowered.
One Part Science, One Part Art
It’s taken me a while to realize this, but I’ve begun to take advantage of improvement opportunities at work as well. No, I haven’t been moonlighting as a plumber for my hospital. I’ve just been fortunate to be part of a trifecta of rewarding quality-improvement (QI) projects over the past year. Before I’d gotten my hands dirty with these, my understanding of QI was fairly naive. I’d heard about Plan-Do-Study-Act many times. I had listened to a talk at a national conference. And I had kept up with the general medical literature on the subject.
But none of those activities had truly prepared me for experience of actually doing the work on my own.
By taking on a project, an ambitious attempt to reduce continuous pulse oximetry use, I experienced a crash course in both the science and the art of process improvement. I was forced to overcome my “I don’t know how” inertia. And with expert guidance in the form of a clinical safety and effectiveness class, I learned the importance of run charts (science) and a well-crafted multidisciplinary team (art) in changing established but inefficient behavior.
Our rates of continuous pulse oximetry usage dropped by 50%, and cost savings were $12,000 per year on one unit. These results made my prior attempts at change—years of complaining about ingrained nursing culture—look infantile. (OK, maybe it was ineffective, but who hasn’t complained about the overuse of continuous monitoring?)
I haven’t met a pediatric hospitalist who wouldn’t understand the symbolic importance of this success. But I know of many hospitalists who have not yet participated in meaningful QI project. Imagine calling a plumber who grasped the flush and fill mechanism of a toilet but had never touched real porcelain. Here’s an even better analogy: What if doctors could get licensed without having touched real patients?
If pediatric hospitalists are to transform the care delivery of hospitalized children, and quality learning only comes through hands-on training, then we need some more hands in the pot.
Discharge Improvement
On the heels of my first project, I was fortunate enough to augment my education through another effort—this time with a cohort of fellow pediatric hospitalists. This was a national collaborative to improve discharge handoffs, and I will admit that, at the outset, I was as puzzled as the first time I pulled the lid off the tank of the toilet. There were just too many permutations on PCP communication at the participating institutions, and some felt our aim of timely discharge handoffs was unattainable.
What carried me through, however, was the collective and infectious DIY—no, QIY (Quality Improve-it-Yourself) attitude of the group. We were all learning, and regular participation in the collaborative essentially guaranteed improvement. We achieved our aim of 90% communication with PCPs within two days of discharge. The secret was simple: The more you do, the more you learn.
Pediatric hospitalists can transform care delivery through a focus on safe and quality care, but the tools to accomplish this must come through post-residency, on-the-job learning. This QI know-how must efficiently spread among our ranks through practical and project-based educational efforts. It’s “see one, do one, teach one,” but we’re not talking about lumbar punctures anymore.
This is a journey in which we all take on the responsibility of rolling up our sleeves and simply learn by doing. And here is where the third leg of my as-yet-unfinished QI course unfolds.
Through my involvement with the Value in Inpatient Pediatrics (VIP) Network, I’ve gained a newfound vision for what the future might hold. VIP has evolved from a benchmarking project focused on bronchiolitis to an improvement network that will incorporate projects similar to the discharge handoff collaborative above.
In the process, a model for how to rapidly spread QI learning has emerged. The capacity lies in the network’s rapidly growing connectivity. The power comes from the individuals: motivated, card-carrying pediatric hospitalists from a wide array of sites. Collaborative learning harbors the potential to exponentially increase the pace at which we improve.
The future of our quality care is bright. I see an open network of improvement doers and learners. I see collaboration on quality and safety initiatives in all manner of hospitals and communities. I see that this will all be built upon a foundation of hard work and a QIY attitude.
You, too, will play a role.
Just don’t be afraid to get your hands a little dirty. TH
Dr. Shen is medical director of hospital medicine at Dell Children’s Medical Center in Austin, Texas. He is pediatric editor of The Hospitalist.
Several months ago, my toilet broke. You should also know that I’m not particularly handy. So when I first realized that the toilet bowl seemed to fill constantly, I got a little stressed out.
How much was it going cost to call in a plumber on the weekend?
What kind of a water bill was I going to have?
Was this a serious problem?
I took a quick peek in the tank, but that just made me more confused. I was paralyzed by a lack of know-how.
Normally, I would have just Googled a local plumber. But that day, I decided to do something different. Maybe it was because it was the fantasy football offseason. Maybe it was because my wife had started to ask my father-in-law to change light bulbs around the house. Or, maybe, I wanted to learn to actually fix the problem. A few hours later, after an Internet lesson in toilet physiology, a $4.12 trip to Home Depot, and a wet pair of hands, I had replaced my first toilet flapper.
This wasn’t the rebuilding of a car engine, but it was a clear DIY step toward self-improvement. Easily the most memorable moment here was my sense of accomplishment.
I felt empowered.
One Part Science, One Part Art
It’s taken me a while to realize this, but I’ve begun to take advantage of improvement opportunities at work as well. No, I haven’t been moonlighting as a plumber for my hospital. I’ve just been fortunate to be part of a trifecta of rewarding quality-improvement (QI) projects over the past year. Before I’d gotten my hands dirty with these, my understanding of QI was fairly naive. I’d heard about Plan-Do-Study-Act many times. I had listened to a talk at a national conference. And I had kept up with the general medical literature on the subject.
But none of those activities had truly prepared me for experience of actually doing the work on my own.
By taking on a project, an ambitious attempt to reduce continuous pulse oximetry use, I experienced a crash course in both the science and the art of process improvement. I was forced to overcome my “I don’t know how” inertia. And with expert guidance in the form of a clinical safety and effectiveness class, I learned the importance of run charts (science) and a well-crafted multidisciplinary team (art) in changing established but inefficient behavior.
Our rates of continuous pulse oximetry usage dropped by 50%, and cost savings were $12,000 per year on one unit. These results made my prior attempts at change—years of complaining about ingrained nursing culture—look infantile. (OK, maybe it was ineffective, but who hasn’t complained about the overuse of continuous monitoring?)
I haven’t met a pediatric hospitalist who wouldn’t understand the symbolic importance of this success. But I know of many hospitalists who have not yet participated in meaningful QI project. Imagine calling a plumber who grasped the flush and fill mechanism of a toilet but had never touched real porcelain. Here’s an even better analogy: What if doctors could get licensed without having touched real patients?
If pediatric hospitalists are to transform the care delivery of hospitalized children, and quality learning only comes through hands-on training, then we need some more hands in the pot.
Discharge Improvement
On the heels of my first project, I was fortunate enough to augment my education through another effort—this time with a cohort of fellow pediatric hospitalists. This was a national collaborative to improve discharge handoffs, and I will admit that, at the outset, I was as puzzled as the first time I pulled the lid off the tank of the toilet. There were just too many permutations on PCP communication at the participating institutions, and some felt our aim of timely discharge handoffs was unattainable.
What carried me through, however, was the collective and infectious DIY—no, QIY (Quality Improve-it-Yourself) attitude of the group. We were all learning, and regular participation in the collaborative essentially guaranteed improvement. We achieved our aim of 90% communication with PCPs within two days of discharge. The secret was simple: The more you do, the more you learn.
Pediatric hospitalists can transform care delivery through a focus on safe and quality care, but the tools to accomplish this must come through post-residency, on-the-job learning. This QI know-how must efficiently spread among our ranks through practical and project-based educational efforts. It’s “see one, do one, teach one,” but we’re not talking about lumbar punctures anymore.
This is a journey in which we all take on the responsibility of rolling up our sleeves and simply learn by doing. And here is where the third leg of my as-yet-unfinished QI course unfolds.
Through my involvement with the Value in Inpatient Pediatrics (VIP) Network, I’ve gained a newfound vision for what the future might hold. VIP has evolved from a benchmarking project focused on bronchiolitis to an improvement network that will incorporate projects similar to the discharge handoff collaborative above.
In the process, a model for how to rapidly spread QI learning has emerged. The capacity lies in the network’s rapidly growing connectivity. The power comes from the individuals: motivated, card-carrying pediatric hospitalists from a wide array of sites. Collaborative learning harbors the potential to exponentially increase the pace at which we improve.
The future of our quality care is bright. I see an open network of improvement doers and learners. I see collaboration on quality and safety initiatives in all manner of hospitals and communities. I see that this will all be built upon a foundation of hard work and a QIY attitude.
You, too, will play a role.
Just don’t be afraid to get your hands a little dirty. TH
Dr. Shen is medical director of hospital medicine at Dell Children’s Medical Center in Austin, Texas. He is pediatric editor of The Hospitalist.
Several months ago, my toilet broke. You should also know that I’m not particularly handy. So when I first realized that the toilet bowl seemed to fill constantly, I got a little stressed out.
How much was it going cost to call in a plumber on the weekend?
What kind of a water bill was I going to have?
Was this a serious problem?
I took a quick peek in the tank, but that just made me more confused. I was paralyzed by a lack of know-how.
Normally, I would have just Googled a local plumber. But that day, I decided to do something different. Maybe it was because it was the fantasy football offseason. Maybe it was because my wife had started to ask my father-in-law to change light bulbs around the house. Or, maybe, I wanted to learn to actually fix the problem. A few hours later, after an Internet lesson in toilet physiology, a $4.12 trip to Home Depot, and a wet pair of hands, I had replaced my first toilet flapper.
This wasn’t the rebuilding of a car engine, but it was a clear DIY step toward self-improvement. Easily the most memorable moment here was my sense of accomplishment.
I felt empowered.
One Part Science, One Part Art
It’s taken me a while to realize this, but I’ve begun to take advantage of improvement opportunities at work as well. No, I haven’t been moonlighting as a plumber for my hospital. I’ve just been fortunate to be part of a trifecta of rewarding quality-improvement (QI) projects over the past year. Before I’d gotten my hands dirty with these, my understanding of QI was fairly naive. I’d heard about Plan-Do-Study-Act many times. I had listened to a talk at a national conference. And I had kept up with the general medical literature on the subject.
But none of those activities had truly prepared me for experience of actually doing the work on my own.
By taking on a project, an ambitious attempt to reduce continuous pulse oximetry use, I experienced a crash course in both the science and the art of process improvement. I was forced to overcome my “I don’t know how” inertia. And with expert guidance in the form of a clinical safety and effectiveness class, I learned the importance of run charts (science) and a well-crafted multidisciplinary team (art) in changing established but inefficient behavior.
Our rates of continuous pulse oximetry usage dropped by 50%, and cost savings were $12,000 per year on one unit. These results made my prior attempts at change—years of complaining about ingrained nursing culture—look infantile. (OK, maybe it was ineffective, but who hasn’t complained about the overuse of continuous monitoring?)
I haven’t met a pediatric hospitalist who wouldn’t understand the symbolic importance of this success. But I know of many hospitalists who have not yet participated in meaningful QI project. Imagine calling a plumber who grasped the flush and fill mechanism of a toilet but had never touched real porcelain. Here’s an even better analogy: What if doctors could get licensed without having touched real patients?
If pediatric hospitalists are to transform the care delivery of hospitalized children, and quality learning only comes through hands-on training, then we need some more hands in the pot.
Discharge Improvement
On the heels of my first project, I was fortunate enough to augment my education through another effort—this time with a cohort of fellow pediatric hospitalists. This was a national collaborative to improve discharge handoffs, and I will admit that, at the outset, I was as puzzled as the first time I pulled the lid off the tank of the toilet. There were just too many permutations on PCP communication at the participating institutions, and some felt our aim of timely discharge handoffs was unattainable.
What carried me through, however, was the collective and infectious DIY—no, QIY (Quality Improve-it-Yourself) attitude of the group. We were all learning, and regular participation in the collaborative essentially guaranteed improvement. We achieved our aim of 90% communication with PCPs within two days of discharge. The secret was simple: The more you do, the more you learn.
Pediatric hospitalists can transform care delivery through a focus on safe and quality care, but the tools to accomplish this must come through post-residency, on-the-job learning. This QI know-how must efficiently spread among our ranks through practical and project-based educational efforts. It’s “see one, do one, teach one,” but we’re not talking about lumbar punctures anymore.
This is a journey in which we all take on the responsibility of rolling up our sleeves and simply learn by doing. And here is where the third leg of my as-yet-unfinished QI course unfolds.
Through my involvement with the Value in Inpatient Pediatrics (VIP) Network, I’ve gained a newfound vision for what the future might hold. VIP has evolved from a benchmarking project focused on bronchiolitis to an improvement network that will incorporate projects similar to the discharge handoff collaborative above.
In the process, a model for how to rapidly spread QI learning has emerged. The capacity lies in the network’s rapidly growing connectivity. The power comes from the individuals: motivated, card-carrying pediatric hospitalists from a wide array of sites. Collaborative learning harbors the potential to exponentially increase the pace at which we improve.
The future of our quality care is bright. I see an open network of improvement doers and learners. I see collaboration on quality and safety initiatives in all manner of hospitals and communities. I see that this will all be built upon a foundation of hard work and a QIY attitude.
You, too, will play a role.
Just don’t be afraid to get your hands a little dirty. TH
Dr. Shen is medical director of hospital medicine at Dell Children’s Medical Center in Austin, Texas. He is pediatric editor of The Hospitalist.