User login
Antibiotic use associated with triple-negative breast cancer mortality
SAN ANTONIO –
The study was recently presented at the San Antonio Breast Cancer Symposium by Julia D. Ransohoff, MD, of Stanford (Calif.) University.
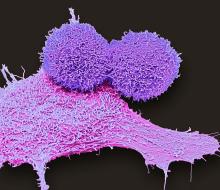
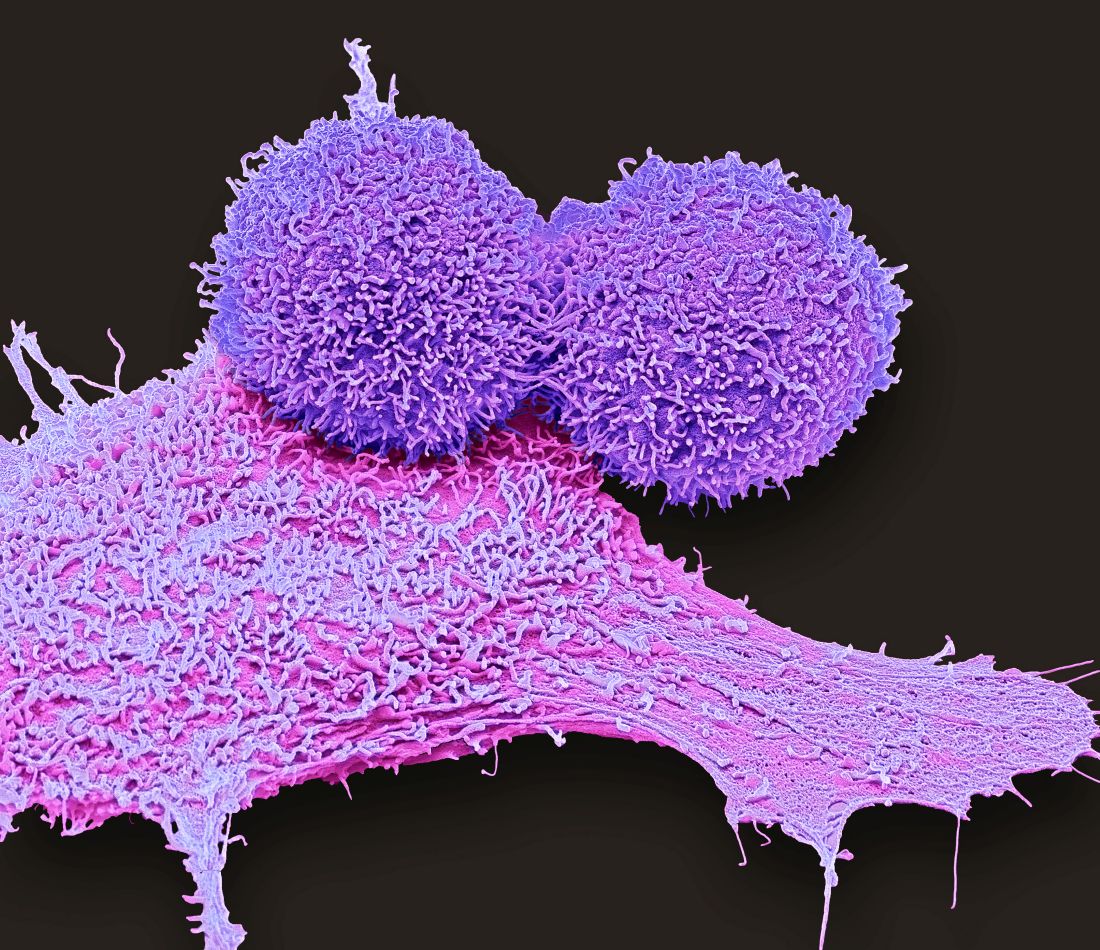
Gut-associated lymphoid tissues are the largest component of the immune system. They influence both local and systemic immune responses, but the use of antimicrobials can decrease circulating and tumor-infiltrating lymphocytes that effect the immune repertoire and in turn, the survival of women with triple-negative breast cancer.
Dr. Ransohoff and colleagues hypothesized that increasing antimicrobial exposure in the presence of time-varying absolute lymphocyte counts may lead to higher overall and breast cancer–specific mortality. Their analysis is based on data from the population-based Surveillance, Epidemiology, and End Results registry and electronic medical records from Stanford University and Sutter Health. It included 772 women who were treated for triple-negative breast cancer between 2000 and 2014. The women were followed for an average of 104 months.
In an earlier analysis of this same group, Dr. Ransohoff found that higher minimum absolute lymphocyte counts were associated with lower overall mortality (hazard ratio, 0.23; 95% confidence interval, 0.16-0.35) and breast cancer mortality (HR, 0.19; 95% CI, 0.11-0.34) The association between higher peripheral lymphocyte counts and tumor-infiltrating lymphocytes was significant.
In the analysis of relationships between antibiotic use and mortality, 85% of women (n = 654) were prescribed antibiotics after having been diagnosed with triple-negative breast cancer. The death rate among patients who were prescribed antibiotics was 23% (153/654), compared with 20% (24/118) among the patients who were not treated with antibiotics (which accounts for 15% of the entire group).
For total antibiotic exposure, the HR for overall mortality was 1.06 (95% CI, 1.03-1.09; P < .001) and 1.07 for breast cancer–specific mortality (95% CI, 1.04-1.10; P < .001). For unique antibiotic exposure (not counting repeat prescriptions of the same antibiotic), the HR for overall mortality was 1.17 (95% CI, 1.12-1.22; P < .001) and 1.18 for breast cancer–specific mortality (95% CI, 1.12-1.24; P < .001).
“These were all statistically significant associations derived from a statistical model that takes into account baseline patient characteristics, so the reported hazard ratios, to the best of our ability, represent the risk of death associated with antibiotic use adjusted for other baseline covariates. We’ve attempted to account for differences at baseline that may indicate patients are sicker, and so the reported risk represents mortality related with antibiotic exposure,” Dr. Ransohoff said.
Elucidating the role of the microbiome in mediating absolute lymphocyte counts and immune response may inform interventions to reduce triple-negative mortality, she said.
SAN ANTONIO –
The study was recently presented at the San Antonio Breast Cancer Symposium by Julia D. Ransohoff, MD, of Stanford (Calif.) University.
Gut-associated lymphoid tissues are the largest component of the immune system. They influence both local and systemic immune responses, but the use of antimicrobials can decrease circulating and tumor-infiltrating lymphocytes that effect the immune repertoire and in turn, the survival of women with triple-negative breast cancer.
Dr. Ransohoff and colleagues hypothesized that increasing antimicrobial exposure in the presence of time-varying absolute lymphocyte counts may lead to higher overall and breast cancer–specific mortality. Their analysis is based on data from the population-based Surveillance, Epidemiology, and End Results registry and electronic medical records from Stanford University and Sutter Health. It included 772 women who were treated for triple-negative breast cancer between 2000 and 2014. The women were followed for an average of 104 months.
In an earlier analysis of this same group, Dr. Ransohoff found that higher minimum absolute lymphocyte counts were associated with lower overall mortality (hazard ratio, 0.23; 95% confidence interval, 0.16-0.35) and breast cancer mortality (HR, 0.19; 95% CI, 0.11-0.34) The association between higher peripheral lymphocyte counts and tumor-infiltrating lymphocytes was significant.
In the analysis of relationships between antibiotic use and mortality, 85% of women (n = 654) were prescribed antibiotics after having been diagnosed with triple-negative breast cancer. The death rate among patients who were prescribed antibiotics was 23% (153/654), compared with 20% (24/118) among the patients who were not treated with antibiotics (which accounts for 15% of the entire group).
For total antibiotic exposure, the HR for overall mortality was 1.06 (95% CI, 1.03-1.09; P < .001) and 1.07 for breast cancer–specific mortality (95% CI, 1.04-1.10; P < .001). For unique antibiotic exposure (not counting repeat prescriptions of the same antibiotic), the HR for overall mortality was 1.17 (95% CI, 1.12-1.22; P < .001) and 1.18 for breast cancer–specific mortality (95% CI, 1.12-1.24; P < .001).
“These were all statistically significant associations derived from a statistical model that takes into account baseline patient characteristics, so the reported hazard ratios, to the best of our ability, represent the risk of death associated with antibiotic use adjusted for other baseline covariates. We’ve attempted to account for differences at baseline that may indicate patients are sicker, and so the reported risk represents mortality related with antibiotic exposure,” Dr. Ransohoff said.
Elucidating the role of the microbiome in mediating absolute lymphocyte counts and immune response may inform interventions to reduce triple-negative mortality, she said.
SAN ANTONIO –
The study was recently presented at the San Antonio Breast Cancer Symposium by Julia D. Ransohoff, MD, of Stanford (Calif.) University.
Gut-associated lymphoid tissues are the largest component of the immune system. They influence both local and systemic immune responses, but the use of antimicrobials can decrease circulating and tumor-infiltrating lymphocytes that effect the immune repertoire and in turn, the survival of women with triple-negative breast cancer.
Dr. Ransohoff and colleagues hypothesized that increasing antimicrobial exposure in the presence of time-varying absolute lymphocyte counts may lead to higher overall and breast cancer–specific mortality. Their analysis is based on data from the population-based Surveillance, Epidemiology, and End Results registry and electronic medical records from Stanford University and Sutter Health. It included 772 women who were treated for triple-negative breast cancer between 2000 and 2014. The women were followed for an average of 104 months.
In an earlier analysis of this same group, Dr. Ransohoff found that higher minimum absolute lymphocyte counts were associated with lower overall mortality (hazard ratio, 0.23; 95% confidence interval, 0.16-0.35) and breast cancer mortality (HR, 0.19; 95% CI, 0.11-0.34) The association between higher peripheral lymphocyte counts and tumor-infiltrating lymphocytes was significant.
In the analysis of relationships between antibiotic use and mortality, 85% of women (n = 654) were prescribed antibiotics after having been diagnosed with triple-negative breast cancer. The death rate among patients who were prescribed antibiotics was 23% (153/654), compared with 20% (24/118) among the patients who were not treated with antibiotics (which accounts for 15% of the entire group).
For total antibiotic exposure, the HR for overall mortality was 1.06 (95% CI, 1.03-1.09; P < .001) and 1.07 for breast cancer–specific mortality (95% CI, 1.04-1.10; P < .001). For unique antibiotic exposure (not counting repeat prescriptions of the same antibiotic), the HR for overall mortality was 1.17 (95% CI, 1.12-1.22; P < .001) and 1.18 for breast cancer–specific mortality (95% CI, 1.12-1.24; P < .001).
“These were all statistically significant associations derived from a statistical model that takes into account baseline patient characteristics, so the reported hazard ratios, to the best of our ability, represent the risk of death associated with antibiotic use adjusted for other baseline covariates. We’ve attempted to account for differences at baseline that may indicate patients are sicker, and so the reported risk represents mortality related with antibiotic exposure,” Dr. Ransohoff said.
Elucidating the role of the microbiome in mediating absolute lymphocyte counts and immune response may inform interventions to reduce triple-negative mortality, she said.
AT SABCS 2021
Omega-3 supplements may impact breast cancer risk
The study was presented by Katherine Cook, PhD, during a poster session at the San Antonio Breast Cancer Symposium. Dr. Cook is a researcher at Wake Forest University, Winston-Salem, N.C.
Obesity increases risk of breast cancer, but it also alters the composition of the gut microbiome. Obesity is associated with a greater frequency of Firmicute bacteria phyla, compared with Bacteroidetes phyla, while abnormally low ratios are associated with inflammatory bowel disease.
In mice, the researchers previously showed that diet can lead to changes in the microbiome of both the gut and the breast. They conducted fecal transplants between mice who were fed normal or high-fat diets (HFD), and then used a chemical carcinogenesis model to investigate the impact on tumor outcomes. They observed changes in the microbiota populations in both the gut and the mammary glands when mice fed a normal diet received fecal transplants from HFD mice. On the other hand, when HFD mice received fecal transplants from mice with normal diets, the transplants countered the increase in serum lipopolysaccharide levels associated with HFD. In vitro models showed that microbiota from HFD mice also altered the epithelial permeability of breast tissue, and infection of breast cancer cells with HFD microbiota led to greater proliferation.
The researchers also examined breast cancer tissue from women who received omega-3 PUFA supplements or placebo before undergoing primary tumor resection, and found that there were differences in the proportional abundance of specific microbes between tumor and adjacent normal tissue, with the former having excess of Lachnospiraceae and Ruminococcus. The finding suggests that these bacteria may grow better in a tumor microenvironment, and could play a role in breast cancer cell signaling. The supplements altered the microbiota of both normal and breast cancer tissue.
In the study presented at SABCS, the researchers analyzed fecal samples from 34 obese and overweight postmenopausal women involved in a weight-loss trial, who received 3.25 g/day of omega-3 PUFA supplements or placebo combined with calorie restriction and exercise. They performed metagenomic sequencing from the fecal samples at baseline and 6 months to determine microbiome populations.
Women who experienced weight loss, with or without omega-3 PUFA supplementation, had a decline in the abundance of Firmicutes phyla – a group linked to inflammation risk – as a percentage of overall bacterial phyla. The researchers found a similar trend among women who received omega-3 PUFA, regardless of how much weight they lost. At the species level, those who received supplements had higher proportional abundance of Phocaeicola massiliensis and reduced proportions of Faecalibacterium prausnitzii, R. lactaris, Blautia obeum, and Dorea formicigenerans (P < .05).
Weight loss combined with supplementation also seemed to affect gut microbiota, with subjects who lost more than 10% of their body weight and received omega-3 PUFA supplements having elevated Bacteriodetes and reduced Firmicutes, compared with all other groups (P < .05).
At 6 months, the researchers grouped women by mean body fat composition, and found both positive and negative correlations among different bacterial species. Finally, the researchers looked at serum levels of the inflammatory cytokines interleukin-6, monocyte chemoattractant protein-1 (MCP-1), and tumor necrosis factor–alpha at 6 months. Women with elevated levels of at least two cytokines had higher levels of two species of mucin-degrading bacteria. Levels of MCP-1 alone also correlated with greater proportions of mucin-degrading bacteria (P < .05).
The authors concluded that increasing omega-3 PUFA uptake to about 2% of total daily calorie intake could push the gut microbiome in a direction that improves intestinal permeability parameters and reduces chronic inflammation. These changes could lead to a reduction in the risk for postmenopausal breast cancer.
The study was funded by the Breast Cancer Research Foundation.
The study was presented by Katherine Cook, PhD, during a poster session at the San Antonio Breast Cancer Symposium. Dr. Cook is a researcher at Wake Forest University, Winston-Salem, N.C.
Obesity increases risk of breast cancer, but it also alters the composition of the gut microbiome. Obesity is associated with a greater frequency of Firmicute bacteria phyla, compared with Bacteroidetes phyla, while abnormally low ratios are associated with inflammatory bowel disease.
In mice, the researchers previously showed that diet can lead to changes in the microbiome of both the gut and the breast. They conducted fecal transplants between mice who were fed normal or high-fat diets (HFD), and then used a chemical carcinogenesis model to investigate the impact on tumor outcomes. They observed changes in the microbiota populations in both the gut and the mammary glands when mice fed a normal diet received fecal transplants from HFD mice. On the other hand, when HFD mice received fecal transplants from mice with normal diets, the transplants countered the increase in serum lipopolysaccharide levels associated with HFD. In vitro models showed that microbiota from HFD mice also altered the epithelial permeability of breast tissue, and infection of breast cancer cells with HFD microbiota led to greater proliferation.
The researchers also examined breast cancer tissue from women who received omega-3 PUFA supplements or placebo before undergoing primary tumor resection, and found that there were differences in the proportional abundance of specific microbes between tumor and adjacent normal tissue, with the former having excess of Lachnospiraceae and Ruminococcus. The finding suggests that these bacteria may grow better in a tumor microenvironment, and could play a role in breast cancer cell signaling. The supplements altered the microbiota of both normal and breast cancer tissue.
In the study presented at SABCS, the researchers analyzed fecal samples from 34 obese and overweight postmenopausal women involved in a weight-loss trial, who received 3.25 g/day of omega-3 PUFA supplements or placebo combined with calorie restriction and exercise. They performed metagenomic sequencing from the fecal samples at baseline and 6 months to determine microbiome populations.
Women who experienced weight loss, with or without omega-3 PUFA supplementation, had a decline in the abundance of Firmicutes phyla – a group linked to inflammation risk – as a percentage of overall bacterial phyla. The researchers found a similar trend among women who received omega-3 PUFA, regardless of how much weight they lost. At the species level, those who received supplements had higher proportional abundance of Phocaeicola massiliensis and reduced proportions of Faecalibacterium prausnitzii, R. lactaris, Blautia obeum, and Dorea formicigenerans (P < .05).
Weight loss combined with supplementation also seemed to affect gut microbiota, with subjects who lost more than 10% of their body weight and received omega-3 PUFA supplements having elevated Bacteriodetes and reduced Firmicutes, compared with all other groups (P < .05).
At 6 months, the researchers grouped women by mean body fat composition, and found both positive and negative correlations among different bacterial species. Finally, the researchers looked at serum levels of the inflammatory cytokines interleukin-6, monocyte chemoattractant protein-1 (MCP-1), and tumor necrosis factor–alpha at 6 months. Women with elevated levels of at least two cytokines had higher levels of two species of mucin-degrading bacteria. Levels of MCP-1 alone also correlated with greater proportions of mucin-degrading bacteria (P < .05).
The authors concluded that increasing omega-3 PUFA uptake to about 2% of total daily calorie intake could push the gut microbiome in a direction that improves intestinal permeability parameters and reduces chronic inflammation. These changes could lead to a reduction in the risk for postmenopausal breast cancer.
The study was funded by the Breast Cancer Research Foundation.
The study was presented by Katherine Cook, PhD, during a poster session at the San Antonio Breast Cancer Symposium. Dr. Cook is a researcher at Wake Forest University, Winston-Salem, N.C.
Obesity increases risk of breast cancer, but it also alters the composition of the gut microbiome. Obesity is associated with a greater frequency of Firmicute bacteria phyla, compared with Bacteroidetes phyla, while abnormally low ratios are associated with inflammatory bowel disease.
In mice, the researchers previously showed that diet can lead to changes in the microbiome of both the gut and the breast. They conducted fecal transplants between mice who were fed normal or high-fat diets (HFD), and then used a chemical carcinogenesis model to investigate the impact on tumor outcomes. They observed changes in the microbiota populations in both the gut and the mammary glands when mice fed a normal diet received fecal transplants from HFD mice. On the other hand, when HFD mice received fecal transplants from mice with normal diets, the transplants countered the increase in serum lipopolysaccharide levels associated with HFD. In vitro models showed that microbiota from HFD mice also altered the epithelial permeability of breast tissue, and infection of breast cancer cells with HFD microbiota led to greater proliferation.
The researchers also examined breast cancer tissue from women who received omega-3 PUFA supplements or placebo before undergoing primary tumor resection, and found that there were differences in the proportional abundance of specific microbes between tumor and adjacent normal tissue, with the former having excess of Lachnospiraceae and Ruminococcus. The finding suggests that these bacteria may grow better in a tumor microenvironment, and could play a role in breast cancer cell signaling. The supplements altered the microbiota of both normal and breast cancer tissue.
In the study presented at SABCS, the researchers analyzed fecal samples from 34 obese and overweight postmenopausal women involved in a weight-loss trial, who received 3.25 g/day of omega-3 PUFA supplements or placebo combined with calorie restriction and exercise. They performed metagenomic sequencing from the fecal samples at baseline and 6 months to determine microbiome populations.
Women who experienced weight loss, with or without omega-3 PUFA supplementation, had a decline in the abundance of Firmicutes phyla – a group linked to inflammation risk – as a percentage of overall bacterial phyla. The researchers found a similar trend among women who received omega-3 PUFA, regardless of how much weight they lost. At the species level, those who received supplements had higher proportional abundance of Phocaeicola massiliensis and reduced proportions of Faecalibacterium prausnitzii, R. lactaris, Blautia obeum, and Dorea formicigenerans (P < .05).
Weight loss combined with supplementation also seemed to affect gut microbiota, with subjects who lost more than 10% of their body weight and received omega-3 PUFA supplements having elevated Bacteriodetes and reduced Firmicutes, compared with all other groups (P < .05).
At 6 months, the researchers grouped women by mean body fat composition, and found both positive and negative correlations among different bacterial species. Finally, the researchers looked at serum levels of the inflammatory cytokines interleukin-6, monocyte chemoattractant protein-1 (MCP-1), and tumor necrosis factor–alpha at 6 months. Women with elevated levels of at least two cytokines had higher levels of two species of mucin-degrading bacteria. Levels of MCP-1 alone also correlated with greater proportions of mucin-degrading bacteria (P < .05).
The authors concluded that increasing omega-3 PUFA uptake to about 2% of total daily calorie intake could push the gut microbiome in a direction that improves intestinal permeability parameters and reduces chronic inflammation. These changes could lead to a reduction in the risk for postmenopausal breast cancer.
The study was funded by the Breast Cancer Research Foundation.
FROM SABCS 2021
Women struggle with benzodiazepine addiction post chemotherapy treatment
SAN ANTONIO – shows a new study.
While benzodiazepines and nonbenzodiazepine sedative-hypnotics are effective for these indications, misuse and increased health care utilization can ensue from their prolonged use, said Jacob C. Cogan, MD, a fellow in oncology/hematology at the Herbert Irving Comprehensive Cancer Center, Columbia University, New York. Dr. Cogan recently presented the results of the study at the San Antonio Breast Cancer Symposium.
The study included patients with breast cancer who received adjuvant chemotherapy between 2008 and 2017. Prescriptions for sedatives were divided into three periods: 365 days prior to chemotherapy to the start of chemotherapy (period one); start of chemotherapy to 90 days after the end of chemotherapy (period two); and 90-365 days after chemotherapy (period three). Patients who filled at least one benzodiazepine prescription in period two and patients who filled at least two benzodiazepine in period three were classified as new persistent benzodiazepine users. The same definitions were then used for nonbenzodiazepine sedative-hypnotics.
Among 17,532 benzodiazepine-naive patients (mean age, 57 years) and 21,863 nonbenzodiazepine sedative-hypnotic drug–naive patients (mean age, 56 years) who received adjuvant chemotherapy for breast cancer, lumpectomies were performed for a small majority (56.6% benzodiazepine naive, 55.1% nonbenzodiazepine sedative-hypnotics naive) versus mastectomy, and about half of patients received less than 4 months of chemotherapy (48.0% benzodiazepine naive, 48.6% nonbenzodiazepine sedative-hypnotics naive). Among benzodiazepine-naive patients, 4,447 (25.4%) filled at least one benzodiazepine prescription during chemotherapy, and 2,160 (9.9%) filled at least one nonbenzodiazepine sedative-hypnotic prescription during chemotherapy. The rate of new persistent benzodiazepine use after initial exposure during chemotherapy was 26.8% (n = 1,192). Similarly, 33.8% (n = 730) of nonbenzodiazepine sedative-hypnotics users became new persistent users. In addition, 115 patients became new persistent users of both types of sedative-hypnotics.
New persistent benzodiazepine use was associated with several characteristics: age 50-65 (odds ratio, 1.23; P = .01) and age greater than 65 (OR, 1.38, P = .005) relative to age less than 49; as well as Medicaid insurance, relative to commercial and Medicare insurance (OR, 1.68; P < .0001). Both new persistent benzodiazepine and nonbenzodiazepine sedative-hypnotics use was associated with chemotherapy duration of less than 4 months relative to 4 or more months of chemotherapy (OR, 1.17; P = .03 for benzodiazepines; OR, 1.58; P < .0001 for nonbenzodiazepine sedative-hypnotics).
It is not clear why shorter chemotherapy duration is associated with more new persistent use, Dr. Cogan said. “It may be that, paradoxically, a shorter duration of treatment could lead to more anxiety about recurrence. These patients may need closer monitoring of mental health symptoms and earlier referral for psychological services.”
Dr. Cogan said that providers should take steps to ensure that benzodiazepines and nonbenzodiazepine sedatives are used appropriately, which includes tapering dosages and, when appropriate, encouraging nonpharmacologic strategies.
There were no funding or other conflicts of interest associated with this study.
SAN ANTONIO – shows a new study.
While benzodiazepines and nonbenzodiazepine sedative-hypnotics are effective for these indications, misuse and increased health care utilization can ensue from their prolonged use, said Jacob C. Cogan, MD, a fellow in oncology/hematology at the Herbert Irving Comprehensive Cancer Center, Columbia University, New York. Dr. Cogan recently presented the results of the study at the San Antonio Breast Cancer Symposium.
The study included patients with breast cancer who received adjuvant chemotherapy between 2008 and 2017. Prescriptions for sedatives were divided into three periods: 365 days prior to chemotherapy to the start of chemotherapy (period one); start of chemotherapy to 90 days after the end of chemotherapy (period two); and 90-365 days after chemotherapy (period three). Patients who filled at least one benzodiazepine prescription in period two and patients who filled at least two benzodiazepine in period three were classified as new persistent benzodiazepine users. The same definitions were then used for nonbenzodiazepine sedative-hypnotics.
Among 17,532 benzodiazepine-naive patients (mean age, 57 years) and 21,863 nonbenzodiazepine sedative-hypnotic drug–naive patients (mean age, 56 years) who received adjuvant chemotherapy for breast cancer, lumpectomies were performed for a small majority (56.6% benzodiazepine naive, 55.1% nonbenzodiazepine sedative-hypnotics naive) versus mastectomy, and about half of patients received less than 4 months of chemotherapy (48.0% benzodiazepine naive, 48.6% nonbenzodiazepine sedative-hypnotics naive). Among benzodiazepine-naive patients, 4,447 (25.4%) filled at least one benzodiazepine prescription during chemotherapy, and 2,160 (9.9%) filled at least one nonbenzodiazepine sedative-hypnotic prescription during chemotherapy. The rate of new persistent benzodiazepine use after initial exposure during chemotherapy was 26.8% (n = 1,192). Similarly, 33.8% (n = 730) of nonbenzodiazepine sedative-hypnotics users became new persistent users. In addition, 115 patients became new persistent users of both types of sedative-hypnotics.
New persistent benzodiazepine use was associated with several characteristics: age 50-65 (odds ratio, 1.23; P = .01) and age greater than 65 (OR, 1.38, P = .005) relative to age less than 49; as well as Medicaid insurance, relative to commercial and Medicare insurance (OR, 1.68; P < .0001). Both new persistent benzodiazepine and nonbenzodiazepine sedative-hypnotics use was associated with chemotherapy duration of less than 4 months relative to 4 or more months of chemotherapy (OR, 1.17; P = .03 for benzodiazepines; OR, 1.58; P < .0001 for nonbenzodiazepine sedative-hypnotics).
It is not clear why shorter chemotherapy duration is associated with more new persistent use, Dr. Cogan said. “It may be that, paradoxically, a shorter duration of treatment could lead to more anxiety about recurrence. These patients may need closer monitoring of mental health symptoms and earlier referral for psychological services.”
Dr. Cogan said that providers should take steps to ensure that benzodiazepines and nonbenzodiazepine sedatives are used appropriately, which includes tapering dosages and, when appropriate, encouraging nonpharmacologic strategies.
There were no funding or other conflicts of interest associated with this study.
SAN ANTONIO – shows a new study.
While benzodiazepines and nonbenzodiazepine sedative-hypnotics are effective for these indications, misuse and increased health care utilization can ensue from their prolonged use, said Jacob C. Cogan, MD, a fellow in oncology/hematology at the Herbert Irving Comprehensive Cancer Center, Columbia University, New York. Dr. Cogan recently presented the results of the study at the San Antonio Breast Cancer Symposium.
The study included patients with breast cancer who received adjuvant chemotherapy between 2008 and 2017. Prescriptions for sedatives were divided into three periods: 365 days prior to chemotherapy to the start of chemotherapy (period one); start of chemotherapy to 90 days after the end of chemotherapy (period two); and 90-365 days after chemotherapy (period three). Patients who filled at least one benzodiazepine prescription in period two and patients who filled at least two benzodiazepine in period three were classified as new persistent benzodiazepine users. The same definitions were then used for nonbenzodiazepine sedative-hypnotics.
Among 17,532 benzodiazepine-naive patients (mean age, 57 years) and 21,863 nonbenzodiazepine sedative-hypnotic drug–naive patients (mean age, 56 years) who received adjuvant chemotherapy for breast cancer, lumpectomies were performed for a small majority (56.6% benzodiazepine naive, 55.1% nonbenzodiazepine sedative-hypnotics naive) versus mastectomy, and about half of patients received less than 4 months of chemotherapy (48.0% benzodiazepine naive, 48.6% nonbenzodiazepine sedative-hypnotics naive). Among benzodiazepine-naive patients, 4,447 (25.4%) filled at least one benzodiazepine prescription during chemotherapy, and 2,160 (9.9%) filled at least one nonbenzodiazepine sedative-hypnotic prescription during chemotherapy. The rate of new persistent benzodiazepine use after initial exposure during chemotherapy was 26.8% (n = 1,192). Similarly, 33.8% (n = 730) of nonbenzodiazepine sedative-hypnotics users became new persistent users. In addition, 115 patients became new persistent users of both types of sedative-hypnotics.
New persistent benzodiazepine use was associated with several characteristics: age 50-65 (odds ratio, 1.23; P = .01) and age greater than 65 (OR, 1.38, P = .005) relative to age less than 49; as well as Medicaid insurance, relative to commercial and Medicare insurance (OR, 1.68; P < .0001). Both new persistent benzodiazepine and nonbenzodiazepine sedative-hypnotics use was associated with chemotherapy duration of less than 4 months relative to 4 or more months of chemotherapy (OR, 1.17; P = .03 for benzodiazepines; OR, 1.58; P < .0001 for nonbenzodiazepine sedative-hypnotics).
It is not clear why shorter chemotherapy duration is associated with more new persistent use, Dr. Cogan said. “It may be that, paradoxically, a shorter duration of treatment could lead to more anxiety about recurrence. These patients may need closer monitoring of mental health symptoms and earlier referral for psychological services.”
Dr. Cogan said that providers should take steps to ensure that benzodiazepines and nonbenzodiazepine sedatives are used appropriately, which includes tapering dosages and, when appropriate, encouraging nonpharmacologic strategies.
There were no funding or other conflicts of interest associated with this study.
AT SABCS 2021
‘Surprising’ lack of benefit to adding palbociclib to endocrine therapy in early HR+/HER2– breast cancer
Two years of adjuvant palbociclib added to endocrine therapy failed to improve invasive disease-free survival or any other efficacy endpoint in patients with stage II-III HR-positive, HER2-negative breast cancer.
“These definitive findings from the PALLAS trial, already indicated by an interim analysis, are surprising given the established efficacy of palbociclib and other CDK4/6i [inhibitors] in advanced breast cancer,” according to lead author Michael Gnant, MD, professor in the department of surgery, Medical University of Vienna, and colleagues.
The results from the PALLAS trial were presented Dec. 7 at the San Antonio Breast Cancer Symposium and simultaneously published in the Journal of Clinical Oncology.
At a median follow-up of 31 months and at the final protocol-defined analysis, invasive disease-free survival events occurred in 253 (8.8%) of 2,884 patients who received the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor plus endocrine therapy and in 263 (9.1%) of 2,877 patients who received endocrine therapy alone. At 4 years, invasive disease-free survival rates were similar in the palbociclib group (84.2%) and standard treatment group (84.5%).
Caught by surprise
Studies have shown that combining CDK4/6 inhibitors and endocrine therapy prolongs progression-free survival (PFS) and overall survival in metastatic HR-positive, HER2-negative breast cancer, with good tolerability.
“CDK4/6 inhibitors have markedly changed outcomes in the metastatic setting and are now standard of care,” said Dr. Gnant, who presented the recent findings at SABCS. “It seem[ed] only logical to try to transfer these benefits to the curative setting of early breast cancer.”
But in 2020, palbociclib manufacturer Pfizer issued a press release noting that the PALLAS trial was unlikely to show a statistically significant improvement in the primary endpoint of invasive disease-free survival.
The results “caught many of us by surprise,” Kathy D. Miller, MD, codirector of the breast cancer program at the Melvin and Bren Simon Cancer Center at Indiana University, Indianapolis, wrote in response to this announcement.
The trial was based on strong science and incredibly positive results in the metastatic setting but did not meet its primary endpoint when incorporated into the adjuvant setting, Dr. Miller noted in a Medscape blog. “That is certainly not the result we had hoped for, and it’s not the result many of us were expecting.”
Dr. Miller emphasized that “more than anything else, this trial reminds us of the absolute necessity of putting our ideas to the test and doing appropriately powered, appropriately controlled, and well-conducted randomized trials.”
The PALLAS trial enrolled 5,796 patients from 406 centers in 21 countries worldwide over a 3-year period, with 5,761 included in the intention-to-treat population.
Participants were randomly assigned to receive 2 years of palbociclib (125 mg orally once daily, days 1-21 of a 28-day cycle) with adjuvant endocrine therapy or adjuvant endocrine therapy alone for at least 5 years.
Dr. Gnant and colleagues found that the primary endpoint – invasive disease-free survival – did not differ significantly different between the two treatment groups (hazard ratio, 0.96; P = .65). Secondary endpoints in the palbociclib versus no-palbociclib groups were also similar: 4-year survival rates for invasive breast cancer-free survival were 85.4% versus 86%, distant recurrence-free survival was 86.2% versus 87.8%, locoregional recurrence-free survival was 96.8% versus 95.4%, and overall survival was 93.8% versus 95.2%.
The main side effect of palbociclib was neutropenia, but there were no new safety signals, Dr. Gnant explained. He noted, however, that the rates of palbociclib discontinuation were monitored closely and were substantial. At 1 year, 30% of patients discontinued palbociclib and by 24 months, 45% had stopped.
Not the final word?
An interim analysis of the phase 3 monarchE trial did not align with the PALLAS trial.
The monarchE trial found that adding the CDK4/6 inhibitor abemaciclib (Verzenio) to endocrine therapy for 2 years significantly reduced the risk of early recurrence, compared with endocrine therapy alone in the same patient populations – those with early HR-positive, HER2-negative breast cancer. The researchers reported the combination was associated with a 25% relative risk reduction of invasive disease-free survival (HR, 0.75; P =.0096).
The research was presented at the ESMO Virtual Congress 2020 and simultaneously published in the Journal of Clinical Oncology.
Dr. Miller speculated how about how these two drugs that look so similar in the metastatic setting have given such different results in the adjuvant setting. One potential reason is pure chance.
“Any study, no matter how many zeros in the P value, could be simply the play of chance,” she said in an interview. “And that is true for negative and positive studies.”
The fault could also lie in the study design. “Remember, these are agents that we think of as reversing endocrine resistance and extending the benefit of hormone therapy,” she pointed out. “And yet we looked at very early results. Perhaps the study design was just wrong for palbociclib.”
Yet another possibility: The relative potency of those two CDK4/6 inhibitors could differ. “In a metastatic setting, that did not seem to affect effectiveness, but it clearly affected the toxicity profile. Perhaps in the adjuvant setting, those differences really do drive differences in efficacy,” she said.
Dr. Gnant also speculated that differences in the treatment schedules for the two drugs, as abemaciclib is taken continuously without a break, could potentially explain the different efficacies in the early breast cancer setting.
He called for long-term follow up, saying it’s essential for comprehensively examining outcomes in HR-positive luminal breast cancers.
“Ongoing analyses in the Trans-PALLAS translational and clinical science program, with almost 6,000 tumor blocks and tens of thousands of blood samples, will improve understanding of CD4/6 inhibition as well as contemporary management of HR-positive, HER2-negative breast cancer,” Dr. Gnant said.
The trial was funded by Pfizer, who provided study drug and financial support. In addition, the academic organizations ABCSG and AFT supported the trial by providing human resources. Dr. Gnant reported employment at Sandoz; receiving honoraria from Amgen, Novartis, AstraZeneca, Lilly; and consulting or advisory roles at Daiichi Sankyo, Veracyte, Tolmar¸ LifeBrain, and Lilly.
A version of this article first appeared on Medscape.com.
Two years of adjuvant palbociclib added to endocrine therapy failed to improve invasive disease-free survival or any other efficacy endpoint in patients with stage II-III HR-positive, HER2-negative breast cancer.
“These definitive findings from the PALLAS trial, already indicated by an interim analysis, are surprising given the established efficacy of palbociclib and other CDK4/6i [inhibitors] in advanced breast cancer,” according to lead author Michael Gnant, MD, professor in the department of surgery, Medical University of Vienna, and colleagues.
The results from the PALLAS trial were presented Dec. 7 at the San Antonio Breast Cancer Symposium and simultaneously published in the Journal of Clinical Oncology.
At a median follow-up of 31 months and at the final protocol-defined analysis, invasive disease-free survival events occurred in 253 (8.8%) of 2,884 patients who received the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor plus endocrine therapy and in 263 (9.1%) of 2,877 patients who received endocrine therapy alone. At 4 years, invasive disease-free survival rates were similar in the palbociclib group (84.2%) and standard treatment group (84.5%).
Caught by surprise
Studies have shown that combining CDK4/6 inhibitors and endocrine therapy prolongs progression-free survival (PFS) and overall survival in metastatic HR-positive, HER2-negative breast cancer, with good tolerability.
“CDK4/6 inhibitors have markedly changed outcomes in the metastatic setting and are now standard of care,” said Dr. Gnant, who presented the recent findings at SABCS. “It seem[ed] only logical to try to transfer these benefits to the curative setting of early breast cancer.”
But in 2020, palbociclib manufacturer Pfizer issued a press release noting that the PALLAS trial was unlikely to show a statistically significant improvement in the primary endpoint of invasive disease-free survival.
The results “caught many of us by surprise,” Kathy D. Miller, MD, codirector of the breast cancer program at the Melvin and Bren Simon Cancer Center at Indiana University, Indianapolis, wrote in response to this announcement.
The trial was based on strong science and incredibly positive results in the metastatic setting but did not meet its primary endpoint when incorporated into the adjuvant setting, Dr. Miller noted in a Medscape blog. “That is certainly not the result we had hoped for, and it’s not the result many of us were expecting.”
Dr. Miller emphasized that “more than anything else, this trial reminds us of the absolute necessity of putting our ideas to the test and doing appropriately powered, appropriately controlled, and well-conducted randomized trials.”
The PALLAS trial enrolled 5,796 patients from 406 centers in 21 countries worldwide over a 3-year period, with 5,761 included in the intention-to-treat population.
Participants were randomly assigned to receive 2 years of palbociclib (125 mg orally once daily, days 1-21 of a 28-day cycle) with adjuvant endocrine therapy or adjuvant endocrine therapy alone for at least 5 years.
Dr. Gnant and colleagues found that the primary endpoint – invasive disease-free survival – did not differ significantly different between the two treatment groups (hazard ratio, 0.96; P = .65). Secondary endpoints in the palbociclib versus no-palbociclib groups were also similar: 4-year survival rates for invasive breast cancer-free survival were 85.4% versus 86%, distant recurrence-free survival was 86.2% versus 87.8%, locoregional recurrence-free survival was 96.8% versus 95.4%, and overall survival was 93.8% versus 95.2%.
The main side effect of palbociclib was neutropenia, but there were no new safety signals, Dr. Gnant explained. He noted, however, that the rates of palbociclib discontinuation were monitored closely and were substantial. At 1 year, 30% of patients discontinued palbociclib and by 24 months, 45% had stopped.
Not the final word?
An interim analysis of the phase 3 monarchE trial did not align with the PALLAS trial.
The monarchE trial found that adding the CDK4/6 inhibitor abemaciclib (Verzenio) to endocrine therapy for 2 years significantly reduced the risk of early recurrence, compared with endocrine therapy alone in the same patient populations – those with early HR-positive, HER2-negative breast cancer. The researchers reported the combination was associated with a 25% relative risk reduction of invasive disease-free survival (HR, 0.75; P =.0096).
The research was presented at the ESMO Virtual Congress 2020 and simultaneously published in the Journal of Clinical Oncology.
Dr. Miller speculated how about how these two drugs that look so similar in the metastatic setting have given such different results in the adjuvant setting. One potential reason is pure chance.
“Any study, no matter how many zeros in the P value, could be simply the play of chance,” she said in an interview. “And that is true for negative and positive studies.”
The fault could also lie in the study design. “Remember, these are agents that we think of as reversing endocrine resistance and extending the benefit of hormone therapy,” she pointed out. “And yet we looked at very early results. Perhaps the study design was just wrong for palbociclib.”
Yet another possibility: The relative potency of those two CDK4/6 inhibitors could differ. “In a metastatic setting, that did not seem to affect effectiveness, but it clearly affected the toxicity profile. Perhaps in the adjuvant setting, those differences really do drive differences in efficacy,” she said.
Dr. Gnant also speculated that differences in the treatment schedules for the two drugs, as abemaciclib is taken continuously without a break, could potentially explain the different efficacies in the early breast cancer setting.
He called for long-term follow up, saying it’s essential for comprehensively examining outcomes in HR-positive luminal breast cancers.
“Ongoing analyses in the Trans-PALLAS translational and clinical science program, with almost 6,000 tumor blocks and tens of thousands of blood samples, will improve understanding of CD4/6 inhibition as well as contemporary management of HR-positive, HER2-negative breast cancer,” Dr. Gnant said.
The trial was funded by Pfizer, who provided study drug and financial support. In addition, the academic organizations ABCSG and AFT supported the trial by providing human resources. Dr. Gnant reported employment at Sandoz; receiving honoraria from Amgen, Novartis, AstraZeneca, Lilly; and consulting or advisory roles at Daiichi Sankyo, Veracyte, Tolmar¸ LifeBrain, and Lilly.
A version of this article first appeared on Medscape.com.
Two years of adjuvant palbociclib added to endocrine therapy failed to improve invasive disease-free survival or any other efficacy endpoint in patients with stage II-III HR-positive, HER2-negative breast cancer.
“These definitive findings from the PALLAS trial, already indicated by an interim analysis, are surprising given the established efficacy of palbociclib and other CDK4/6i [inhibitors] in advanced breast cancer,” according to lead author Michael Gnant, MD, professor in the department of surgery, Medical University of Vienna, and colleagues.
The results from the PALLAS trial were presented Dec. 7 at the San Antonio Breast Cancer Symposium and simultaneously published in the Journal of Clinical Oncology.
At a median follow-up of 31 months and at the final protocol-defined analysis, invasive disease-free survival events occurred in 253 (8.8%) of 2,884 patients who received the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor plus endocrine therapy and in 263 (9.1%) of 2,877 patients who received endocrine therapy alone. At 4 years, invasive disease-free survival rates were similar in the palbociclib group (84.2%) and standard treatment group (84.5%).
Caught by surprise
Studies have shown that combining CDK4/6 inhibitors and endocrine therapy prolongs progression-free survival (PFS) and overall survival in metastatic HR-positive, HER2-negative breast cancer, with good tolerability.
“CDK4/6 inhibitors have markedly changed outcomes in the metastatic setting and are now standard of care,” said Dr. Gnant, who presented the recent findings at SABCS. “It seem[ed] only logical to try to transfer these benefits to the curative setting of early breast cancer.”
But in 2020, palbociclib manufacturer Pfizer issued a press release noting that the PALLAS trial was unlikely to show a statistically significant improvement in the primary endpoint of invasive disease-free survival.
The results “caught many of us by surprise,” Kathy D. Miller, MD, codirector of the breast cancer program at the Melvin and Bren Simon Cancer Center at Indiana University, Indianapolis, wrote in response to this announcement.
The trial was based on strong science and incredibly positive results in the metastatic setting but did not meet its primary endpoint when incorporated into the adjuvant setting, Dr. Miller noted in a Medscape blog. “That is certainly not the result we had hoped for, and it’s not the result many of us were expecting.”
Dr. Miller emphasized that “more than anything else, this trial reminds us of the absolute necessity of putting our ideas to the test and doing appropriately powered, appropriately controlled, and well-conducted randomized trials.”
The PALLAS trial enrolled 5,796 patients from 406 centers in 21 countries worldwide over a 3-year period, with 5,761 included in the intention-to-treat population.
Participants were randomly assigned to receive 2 years of palbociclib (125 mg orally once daily, days 1-21 of a 28-day cycle) with adjuvant endocrine therapy or adjuvant endocrine therapy alone for at least 5 years.
Dr. Gnant and colleagues found that the primary endpoint – invasive disease-free survival – did not differ significantly different between the two treatment groups (hazard ratio, 0.96; P = .65). Secondary endpoints in the palbociclib versus no-palbociclib groups were also similar: 4-year survival rates for invasive breast cancer-free survival were 85.4% versus 86%, distant recurrence-free survival was 86.2% versus 87.8%, locoregional recurrence-free survival was 96.8% versus 95.4%, and overall survival was 93.8% versus 95.2%.
The main side effect of palbociclib was neutropenia, but there were no new safety signals, Dr. Gnant explained. He noted, however, that the rates of palbociclib discontinuation were monitored closely and were substantial. At 1 year, 30% of patients discontinued palbociclib and by 24 months, 45% had stopped.
Not the final word?
An interim analysis of the phase 3 monarchE trial did not align with the PALLAS trial.
The monarchE trial found that adding the CDK4/6 inhibitor abemaciclib (Verzenio) to endocrine therapy for 2 years significantly reduced the risk of early recurrence, compared with endocrine therapy alone in the same patient populations – those with early HR-positive, HER2-negative breast cancer. The researchers reported the combination was associated with a 25% relative risk reduction of invasive disease-free survival (HR, 0.75; P =.0096).
The research was presented at the ESMO Virtual Congress 2020 and simultaneously published in the Journal of Clinical Oncology.
Dr. Miller speculated how about how these two drugs that look so similar in the metastatic setting have given such different results in the adjuvant setting. One potential reason is pure chance.
“Any study, no matter how many zeros in the P value, could be simply the play of chance,” she said in an interview. “And that is true for negative and positive studies.”
The fault could also lie in the study design. “Remember, these are agents that we think of as reversing endocrine resistance and extending the benefit of hormone therapy,” she pointed out. “And yet we looked at very early results. Perhaps the study design was just wrong for palbociclib.”
Yet another possibility: The relative potency of those two CDK4/6 inhibitors could differ. “In a metastatic setting, that did not seem to affect effectiveness, but it clearly affected the toxicity profile. Perhaps in the adjuvant setting, those differences really do drive differences in efficacy,” she said.
Dr. Gnant also speculated that differences in the treatment schedules for the two drugs, as abemaciclib is taken continuously without a break, could potentially explain the different efficacies in the early breast cancer setting.
He called for long-term follow up, saying it’s essential for comprehensively examining outcomes in HR-positive luminal breast cancers.
“Ongoing analyses in the Trans-PALLAS translational and clinical science program, with almost 6,000 tumor blocks and tens of thousands of blood samples, will improve understanding of CD4/6 inhibition as well as contemporary management of HR-positive, HER2-negative breast cancer,” Dr. Gnant said.
The trial was funded by Pfizer, who provided study drug and financial support. In addition, the academic organizations ABCSG and AFT supported the trial by providing human resources. Dr. Gnant reported employment at Sandoz; receiving honoraria from Amgen, Novartis, AstraZeneca, Lilly; and consulting or advisory roles at Daiichi Sankyo, Veracyte, Tolmar¸ LifeBrain, and Lilly.
A version of this article first appeared on Medscape.com.
FROM SABCS 2021
The evolving HER2+ metastatic breast cancer landscape: Novel agents and promising combination therapies
Recent therapeutic advances in HER2-positive metastatic breast cancer (MBC) have begun to reshape the treatment landscape for patients. Since late 2019, the U.S. Food and Drug Administration (FDA) has approved a handful of novel agents for HER2-positive MBC — most notably, the antibody-drug conjugate (ADC) trastuzumab deruxtecan in December 2019 and the tyrosine kinase inhibitors (TKIs) tucatinib and neratinib in 2020. According to the National Cancer Institute›s Surveillance, Epidemiology, and End Results (SEER) program, the 5-year survival rate for patients with advanced disease was already on the rise between 2004 and 2018, and
“I’ve been involved in the HER2 space for a long time and have watched the field evolve,” said Adam Brufsky, MD, PhD, associate chief in the division of hematology/oncology and co-director of the Comprehensive Breast Cancer Center at the University of Pittsburgh School of Medicine. “The fact that we’re now talking about fourth- and fifth-line therapies for HER2-positive MBC represents a major advance in the management of these patients.”
Oncologists are still building on this progress, focusing on designing more targeted therapies as well as studying different combinations of available agents. The main goal of treatment, experts say, is to prolong patients’ systemic response and prevent recurrences, especially in the brain. This news organization spoke to Dr. Brufksy and others about promising agents and therapeutic strategies on the horizon to treat HER2-positive MBC.
Inside emerging ADCs
Because many patients develop resistance to trastuzumab emtansine (T-DM1) — the first FDA-approved ADC in breast cancer — researchers have focused on developing the next generation of ADCs with more potent payloads, different linkers, and distinct mechanisms of action, according to Sayeh Lavasani, MD, MS, a medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County.
The second-generation ADC trastuzumab deruxtecan showed “really dramatic” results in HER2-positive MBC, demonstrating progression-free survival of 16 months, remarked Kevin Kalinsky, MD, acting associate professor in the department of hematology and medical oncology at Emory University School of Medicine in Atlanta and director of the Glenn Family Breast Center at the Winship Cancer Institute of Emory University. “These outcomes further changed how we treat patients with metastatic disease and prompted considerable excitement over the potential to develop novel ADCs to treat HER2-positive MBC.”
Most recently, two investigational ADCs — trastuzumab duocarmazine (SYD985) and ARX788 — have stood out. The FDA granted fast-track designations to trastuzumab duocarmazine in January 2018 and ARX788 in January 2021. Trastuzumab duocarmazine, the furthest along the pipeline, has shown promising results so far. In June 2021, Netherlands-based biopharmaceutical company Byondis reported preliminary phase 3 data from the TULIP trial. The open-label, randomized phase 3 study enrolled 436 patients with HER2-positive locally advanced or metastatic disease that had progressed on previous anti-HER2 regimens. The company shared early results that trastuzumab duocarmazine achieved its progression-free survival primary endpoint, marking a significant improvement over physician’s choice of chemotherapy, and promised more detailed results to come later this year.
Although only in early-phase trials, ARX788 has also shown robust anti-HER2 activity as well as low toxicity in HER2-positive tumors, according to recent data. The findings from two phase 1 studies, presented at the June 2021 virtual American Society for Clinical Oncology meeting (abstract 1038), revealed an overall response rate of 74% in the breast cancer cohort, but the investigators acknowledged it was too early to report median progression-free survival outcomes. Preclinical data also showed activity in HER2-low and T-DM1–resistant tumors.
Despite the encouraging initial findings, Dr. Kalinsky remains cautiously optimistic about long-term outcomes for both ADCs. “These data are hot off the press, but it’s too soon to know how these two ADCs and others in the pipeline will measure up to approved therapies,” he commented. As experts learn more about the efficacy of these novel ADCs, Dr. Brufsky would also like to better understand resistance mechanisms and how to integrate these agents into current treatment strategies. “The cellular biology of HER2-positive MBC is complicated, and many factors in these tumor cells affect where ADCs are released, how resistance develops, and whether or not resistance to one ADC applies to others,” Dr. Brufsky remarked. “As we gather more data, we’ll understand resistance mechanisms better and begin to figure out where to go with treatment sequencing.”
TKIs and beyond
In addition to ADCs, TKIs continue to make their mark in the targeted HER2 therapeutic space. The approvals of tucatinib and neratinib last year represented an important advance in treating HER2-positive MBC, particularly for patients with brain metastases. The HER2CLIMB trial, for instance, found that tucatinib combined with trastuzumab and capecitabine had a 4.5-month overall survival advantage compared with placebo (21.9 vs 17.4) and a median progression-free survival advantage of 5.4 months in patients with active brain metastases (9.5 vs 4.1) and 8.3 months in patients with stable metastases (13.9 vs 5.6).
Given this progress, experts are looking to add new TKIs to the armamentarium. In particular, pyrotinib — already approved in China for treating HER2-positive MBC — has demonstrated significantly longer progression-free survival compared with a standard TKI, lapatinib. The phase 3 PHOEBE trial results, published in The Lancet in early 2021, found a median progression-free survival of 12.5 months in patients randomly assigned to receive pyrotinib plus capecitabine compared with 6.8 months in those receiving lapatinib plus capecitabine. The investigators also reported “manageable toxicity”; diarrhea was the most common grade 3 adverse event, occurring in 31% of the pyrotinib group vs. 8% of the lapatinib group, and overall serious adverse events occurred in 10% of patients receiving pyrotinib vs. 8% of those receiving lapatinib.
More recent data on pyrotinib come from the phase 2 PERMEATE trial, which focused on the safety and efficacy of the agent in patients with advanced disease and brain metastases. The investigators, who presented their findings at the 2021 virtual ASCO meeting (abstract 1037), reported that radiation therapy–naive patients receiving pyrotinib plus capecitabine had an overall response rate of 74.6% in the central nervous system. Patients experiencing progression after whole-brain or stereotactic radiation therapy, however, had a comparatively lower overall response rate of 42.1%.
Similarly, median progression-free survival was much higher in the radiation therapy–naive patients (12.1 vs 5.6 months in the radiation therapy cohort). Similar to the PHOEBE trial, the most common grade 3 adverse event was diarrhea (23.1%), followed by decreased neutrophil and white blood cell counts (12.8% for both), anemia (9%), and hand-foot syndrome (7.7%). The main question for Dr. Kalinsky is how well pyrotinib will ultimately stack up to tucatinib and neratinib. “Pyrotinib — like neratinib — was shown to be superior to lapatinib plus capecitabine , but its role may be limited by its gastrointestinal toxicity,” he said. In addition to research focused on expanding the selection of novel ADCs and TKIs, researchers are also exploring new combinations of approved treatments and whether these combinations can be used earlier in treatment sequencing.
Take the CompassHER2 trials. The ongoing phase 3 trial in patients with high-risk HER2-positive breast cancer and residual disease will explore whether tucatinib plus T-DM1 compared with T-DM1 alone improves overall survival and recurrence-free survival and prevents brain metastases. Another possibility currently under investigation is pairing tucatinib and trastuzumab deruxtecan, instead of T-DM1. “Overall, it’s exciting that we are increasing the number of therapeutic options and combinations,” commented Debu Tripathy, MD, professor and chairman in the department of breast medical oncology at the University of Texas MD Anderson Cancer Center in Houston. “Having more choices allows us to tailor therapies to manage resistance and prolong patients’ responses.”
Curbing brain metastasis, according to Dr. Brufksy, is particularly important, and experts need to explore the extent to which ADCs can penetrate the blood-brain barrier. Already, a subgroup analysis of the DESTINY-Breast01 trial found that trastuzumab deruxtecan appeared to be active in patients with brain metastases. Investigators reported an overall response rate of 58.3% and a median progression-free survival of 18.1 months — results in line with those in the general study cohort — but the study population did not include patients with untreated or progressive brain metastases. A phase 2 study currently under way will examine whether patients with HER2-positive and HER2-low breast cancer who have untreated or progressive brain metastases respond to trastuzumab deruxtecan as well. Ultimately, Dr. Brufksy hopes the recent successes with preventing brain metastases in pediatric acute lymphoblastic leukemia (ALL) foreshadow what›s to come in HER2-positive MBC.
“When we figured out how to treat brain metastases prophylactically in childhood ALL, we saw a huge improvement in the cure rate, which is ultimately my vision for HER2-positive disease,” Dr. Brufsky remarked. “Are there cures for HER2-positive MBC on the horizon? We don’t know yet, but the field has really exploded in recent years.”
A version of this article first appeared on Medscape.com.
Recent therapeutic advances in HER2-positive metastatic breast cancer (MBC) have begun to reshape the treatment landscape for patients. Since late 2019, the U.S. Food and Drug Administration (FDA) has approved a handful of novel agents for HER2-positive MBC — most notably, the antibody-drug conjugate (ADC) trastuzumab deruxtecan in December 2019 and the tyrosine kinase inhibitors (TKIs) tucatinib and neratinib in 2020. According to the National Cancer Institute›s Surveillance, Epidemiology, and End Results (SEER) program, the 5-year survival rate for patients with advanced disease was already on the rise between 2004 and 2018, and
“I’ve been involved in the HER2 space for a long time and have watched the field evolve,” said Adam Brufsky, MD, PhD, associate chief in the division of hematology/oncology and co-director of the Comprehensive Breast Cancer Center at the University of Pittsburgh School of Medicine. “The fact that we’re now talking about fourth- and fifth-line therapies for HER2-positive MBC represents a major advance in the management of these patients.”
Oncologists are still building on this progress, focusing on designing more targeted therapies as well as studying different combinations of available agents. The main goal of treatment, experts say, is to prolong patients’ systemic response and prevent recurrences, especially in the brain. This news organization spoke to Dr. Brufksy and others about promising agents and therapeutic strategies on the horizon to treat HER2-positive MBC.
Inside emerging ADCs
Because many patients develop resistance to trastuzumab emtansine (T-DM1) — the first FDA-approved ADC in breast cancer — researchers have focused on developing the next generation of ADCs with more potent payloads, different linkers, and distinct mechanisms of action, according to Sayeh Lavasani, MD, MS, a medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County.
The second-generation ADC trastuzumab deruxtecan showed “really dramatic” results in HER2-positive MBC, demonstrating progression-free survival of 16 months, remarked Kevin Kalinsky, MD, acting associate professor in the department of hematology and medical oncology at Emory University School of Medicine in Atlanta and director of the Glenn Family Breast Center at the Winship Cancer Institute of Emory University. “These outcomes further changed how we treat patients with metastatic disease and prompted considerable excitement over the potential to develop novel ADCs to treat HER2-positive MBC.”
Most recently, two investigational ADCs — trastuzumab duocarmazine (SYD985) and ARX788 — have stood out. The FDA granted fast-track designations to trastuzumab duocarmazine in January 2018 and ARX788 in January 2021. Trastuzumab duocarmazine, the furthest along the pipeline, has shown promising results so far. In June 2021, Netherlands-based biopharmaceutical company Byondis reported preliminary phase 3 data from the TULIP trial. The open-label, randomized phase 3 study enrolled 436 patients with HER2-positive locally advanced or metastatic disease that had progressed on previous anti-HER2 regimens. The company shared early results that trastuzumab duocarmazine achieved its progression-free survival primary endpoint, marking a significant improvement over physician’s choice of chemotherapy, and promised more detailed results to come later this year.
Although only in early-phase trials, ARX788 has also shown robust anti-HER2 activity as well as low toxicity in HER2-positive tumors, according to recent data. The findings from two phase 1 studies, presented at the June 2021 virtual American Society for Clinical Oncology meeting (abstract 1038), revealed an overall response rate of 74% in the breast cancer cohort, but the investigators acknowledged it was too early to report median progression-free survival outcomes. Preclinical data also showed activity in HER2-low and T-DM1–resistant tumors.
Despite the encouraging initial findings, Dr. Kalinsky remains cautiously optimistic about long-term outcomes for both ADCs. “These data are hot off the press, but it’s too soon to know how these two ADCs and others in the pipeline will measure up to approved therapies,” he commented. As experts learn more about the efficacy of these novel ADCs, Dr. Brufsky would also like to better understand resistance mechanisms and how to integrate these agents into current treatment strategies. “The cellular biology of HER2-positive MBC is complicated, and many factors in these tumor cells affect where ADCs are released, how resistance develops, and whether or not resistance to one ADC applies to others,” Dr. Brufsky remarked. “As we gather more data, we’ll understand resistance mechanisms better and begin to figure out where to go with treatment sequencing.”
TKIs and beyond
In addition to ADCs, TKIs continue to make their mark in the targeted HER2 therapeutic space. The approvals of tucatinib and neratinib last year represented an important advance in treating HER2-positive MBC, particularly for patients with brain metastases. The HER2CLIMB trial, for instance, found that tucatinib combined with trastuzumab and capecitabine had a 4.5-month overall survival advantage compared with placebo (21.9 vs 17.4) and a median progression-free survival advantage of 5.4 months in patients with active brain metastases (9.5 vs 4.1) and 8.3 months in patients with stable metastases (13.9 vs 5.6).
Given this progress, experts are looking to add new TKIs to the armamentarium. In particular, pyrotinib — already approved in China for treating HER2-positive MBC — has demonstrated significantly longer progression-free survival compared with a standard TKI, lapatinib. The phase 3 PHOEBE trial results, published in The Lancet in early 2021, found a median progression-free survival of 12.5 months in patients randomly assigned to receive pyrotinib plus capecitabine compared with 6.8 months in those receiving lapatinib plus capecitabine. The investigators also reported “manageable toxicity”; diarrhea was the most common grade 3 adverse event, occurring in 31% of the pyrotinib group vs. 8% of the lapatinib group, and overall serious adverse events occurred in 10% of patients receiving pyrotinib vs. 8% of those receiving lapatinib.
More recent data on pyrotinib come from the phase 2 PERMEATE trial, which focused on the safety and efficacy of the agent in patients with advanced disease and brain metastases. The investigators, who presented their findings at the 2021 virtual ASCO meeting (abstract 1037), reported that radiation therapy–naive patients receiving pyrotinib plus capecitabine had an overall response rate of 74.6% in the central nervous system. Patients experiencing progression after whole-brain or stereotactic radiation therapy, however, had a comparatively lower overall response rate of 42.1%.
Similarly, median progression-free survival was much higher in the radiation therapy–naive patients (12.1 vs 5.6 months in the radiation therapy cohort). Similar to the PHOEBE trial, the most common grade 3 adverse event was diarrhea (23.1%), followed by decreased neutrophil and white blood cell counts (12.8% for both), anemia (9%), and hand-foot syndrome (7.7%). The main question for Dr. Kalinsky is how well pyrotinib will ultimately stack up to tucatinib and neratinib. “Pyrotinib — like neratinib — was shown to be superior to lapatinib plus capecitabine , but its role may be limited by its gastrointestinal toxicity,” he said. In addition to research focused on expanding the selection of novel ADCs and TKIs, researchers are also exploring new combinations of approved treatments and whether these combinations can be used earlier in treatment sequencing.
Take the CompassHER2 trials. The ongoing phase 3 trial in patients with high-risk HER2-positive breast cancer and residual disease will explore whether tucatinib plus T-DM1 compared with T-DM1 alone improves overall survival and recurrence-free survival and prevents brain metastases. Another possibility currently under investigation is pairing tucatinib and trastuzumab deruxtecan, instead of T-DM1. “Overall, it’s exciting that we are increasing the number of therapeutic options and combinations,” commented Debu Tripathy, MD, professor and chairman in the department of breast medical oncology at the University of Texas MD Anderson Cancer Center in Houston. “Having more choices allows us to tailor therapies to manage resistance and prolong patients’ responses.”
Curbing brain metastasis, according to Dr. Brufksy, is particularly important, and experts need to explore the extent to which ADCs can penetrate the blood-brain barrier. Already, a subgroup analysis of the DESTINY-Breast01 trial found that trastuzumab deruxtecan appeared to be active in patients with brain metastases. Investigators reported an overall response rate of 58.3% and a median progression-free survival of 18.1 months — results in line with those in the general study cohort — but the study population did not include patients with untreated or progressive brain metastases. A phase 2 study currently under way will examine whether patients with HER2-positive and HER2-low breast cancer who have untreated or progressive brain metastases respond to trastuzumab deruxtecan as well. Ultimately, Dr. Brufksy hopes the recent successes with preventing brain metastases in pediatric acute lymphoblastic leukemia (ALL) foreshadow what›s to come in HER2-positive MBC.
“When we figured out how to treat brain metastases prophylactically in childhood ALL, we saw a huge improvement in the cure rate, which is ultimately my vision for HER2-positive disease,” Dr. Brufsky remarked. “Are there cures for HER2-positive MBC on the horizon? We don’t know yet, but the field has really exploded in recent years.”
A version of this article first appeared on Medscape.com.
Recent therapeutic advances in HER2-positive metastatic breast cancer (MBC) have begun to reshape the treatment landscape for patients. Since late 2019, the U.S. Food and Drug Administration (FDA) has approved a handful of novel agents for HER2-positive MBC — most notably, the antibody-drug conjugate (ADC) trastuzumab deruxtecan in December 2019 and the tyrosine kinase inhibitors (TKIs) tucatinib and neratinib in 2020. According to the National Cancer Institute›s Surveillance, Epidemiology, and End Results (SEER) program, the 5-year survival rate for patients with advanced disease was already on the rise between 2004 and 2018, and
“I’ve been involved in the HER2 space for a long time and have watched the field evolve,” said Adam Brufsky, MD, PhD, associate chief in the division of hematology/oncology and co-director of the Comprehensive Breast Cancer Center at the University of Pittsburgh School of Medicine. “The fact that we’re now talking about fourth- and fifth-line therapies for HER2-positive MBC represents a major advance in the management of these patients.”
Oncologists are still building on this progress, focusing on designing more targeted therapies as well as studying different combinations of available agents. The main goal of treatment, experts say, is to prolong patients’ systemic response and prevent recurrences, especially in the brain. This news organization spoke to Dr. Brufksy and others about promising agents and therapeutic strategies on the horizon to treat HER2-positive MBC.
Inside emerging ADCs
Because many patients develop resistance to trastuzumab emtansine (T-DM1) — the first FDA-approved ADC in breast cancer — researchers have focused on developing the next generation of ADCs with more potent payloads, different linkers, and distinct mechanisms of action, according to Sayeh Lavasani, MD, MS, a medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County.
The second-generation ADC trastuzumab deruxtecan showed “really dramatic” results in HER2-positive MBC, demonstrating progression-free survival of 16 months, remarked Kevin Kalinsky, MD, acting associate professor in the department of hematology and medical oncology at Emory University School of Medicine in Atlanta and director of the Glenn Family Breast Center at the Winship Cancer Institute of Emory University. “These outcomes further changed how we treat patients with metastatic disease and prompted considerable excitement over the potential to develop novel ADCs to treat HER2-positive MBC.”
Most recently, two investigational ADCs — trastuzumab duocarmazine (SYD985) and ARX788 — have stood out. The FDA granted fast-track designations to trastuzumab duocarmazine in January 2018 and ARX788 in January 2021. Trastuzumab duocarmazine, the furthest along the pipeline, has shown promising results so far. In June 2021, Netherlands-based biopharmaceutical company Byondis reported preliminary phase 3 data from the TULIP trial. The open-label, randomized phase 3 study enrolled 436 patients with HER2-positive locally advanced or metastatic disease that had progressed on previous anti-HER2 regimens. The company shared early results that trastuzumab duocarmazine achieved its progression-free survival primary endpoint, marking a significant improvement over physician’s choice of chemotherapy, and promised more detailed results to come later this year.
Although only in early-phase trials, ARX788 has also shown robust anti-HER2 activity as well as low toxicity in HER2-positive tumors, according to recent data. The findings from two phase 1 studies, presented at the June 2021 virtual American Society for Clinical Oncology meeting (abstract 1038), revealed an overall response rate of 74% in the breast cancer cohort, but the investigators acknowledged it was too early to report median progression-free survival outcomes. Preclinical data also showed activity in HER2-low and T-DM1–resistant tumors.
Despite the encouraging initial findings, Dr. Kalinsky remains cautiously optimistic about long-term outcomes for both ADCs. “These data are hot off the press, but it’s too soon to know how these two ADCs and others in the pipeline will measure up to approved therapies,” he commented. As experts learn more about the efficacy of these novel ADCs, Dr. Brufsky would also like to better understand resistance mechanisms and how to integrate these agents into current treatment strategies. “The cellular biology of HER2-positive MBC is complicated, and many factors in these tumor cells affect where ADCs are released, how resistance develops, and whether or not resistance to one ADC applies to others,” Dr. Brufsky remarked. “As we gather more data, we’ll understand resistance mechanisms better and begin to figure out where to go with treatment sequencing.”
TKIs and beyond
In addition to ADCs, TKIs continue to make their mark in the targeted HER2 therapeutic space. The approvals of tucatinib and neratinib last year represented an important advance in treating HER2-positive MBC, particularly for patients with brain metastases. The HER2CLIMB trial, for instance, found that tucatinib combined with trastuzumab and capecitabine had a 4.5-month overall survival advantage compared with placebo (21.9 vs 17.4) and a median progression-free survival advantage of 5.4 months in patients with active brain metastases (9.5 vs 4.1) and 8.3 months in patients with stable metastases (13.9 vs 5.6).
Given this progress, experts are looking to add new TKIs to the armamentarium. In particular, pyrotinib — already approved in China for treating HER2-positive MBC — has demonstrated significantly longer progression-free survival compared with a standard TKI, lapatinib. The phase 3 PHOEBE trial results, published in The Lancet in early 2021, found a median progression-free survival of 12.5 months in patients randomly assigned to receive pyrotinib plus capecitabine compared with 6.8 months in those receiving lapatinib plus capecitabine. The investigators also reported “manageable toxicity”; diarrhea was the most common grade 3 adverse event, occurring in 31% of the pyrotinib group vs. 8% of the lapatinib group, and overall serious adverse events occurred in 10% of patients receiving pyrotinib vs. 8% of those receiving lapatinib.
More recent data on pyrotinib come from the phase 2 PERMEATE trial, which focused on the safety and efficacy of the agent in patients with advanced disease and brain metastases. The investigators, who presented their findings at the 2021 virtual ASCO meeting (abstract 1037), reported that radiation therapy–naive patients receiving pyrotinib plus capecitabine had an overall response rate of 74.6% in the central nervous system. Patients experiencing progression after whole-brain or stereotactic radiation therapy, however, had a comparatively lower overall response rate of 42.1%.
Similarly, median progression-free survival was much higher in the radiation therapy–naive patients (12.1 vs 5.6 months in the radiation therapy cohort). Similar to the PHOEBE trial, the most common grade 3 adverse event was diarrhea (23.1%), followed by decreased neutrophil and white blood cell counts (12.8% for both), anemia (9%), and hand-foot syndrome (7.7%). The main question for Dr. Kalinsky is how well pyrotinib will ultimately stack up to tucatinib and neratinib. “Pyrotinib — like neratinib — was shown to be superior to lapatinib plus capecitabine , but its role may be limited by its gastrointestinal toxicity,” he said. In addition to research focused on expanding the selection of novel ADCs and TKIs, researchers are also exploring new combinations of approved treatments and whether these combinations can be used earlier in treatment sequencing.
Take the CompassHER2 trials. The ongoing phase 3 trial in patients with high-risk HER2-positive breast cancer and residual disease will explore whether tucatinib plus T-DM1 compared with T-DM1 alone improves overall survival and recurrence-free survival and prevents brain metastases. Another possibility currently under investigation is pairing tucatinib and trastuzumab deruxtecan, instead of T-DM1. “Overall, it’s exciting that we are increasing the number of therapeutic options and combinations,” commented Debu Tripathy, MD, professor and chairman in the department of breast medical oncology at the University of Texas MD Anderson Cancer Center in Houston. “Having more choices allows us to tailor therapies to manage resistance and prolong patients’ responses.”
Curbing brain metastasis, according to Dr. Brufksy, is particularly important, and experts need to explore the extent to which ADCs can penetrate the blood-brain barrier. Already, a subgroup analysis of the DESTINY-Breast01 trial found that trastuzumab deruxtecan appeared to be active in patients with brain metastases. Investigators reported an overall response rate of 58.3% and a median progression-free survival of 18.1 months — results in line with those in the general study cohort — but the study population did not include patients with untreated or progressive brain metastases. A phase 2 study currently under way will examine whether patients with HER2-positive and HER2-low breast cancer who have untreated or progressive brain metastases respond to trastuzumab deruxtecan as well. Ultimately, Dr. Brufksy hopes the recent successes with preventing brain metastases in pediatric acute lymphoblastic leukemia (ALL) foreshadow what›s to come in HER2-positive MBC.
“When we figured out how to treat brain metastases prophylactically in childhood ALL, we saw a huge improvement in the cure rate, which is ultimately my vision for HER2-positive disease,” Dr. Brufsky remarked. “Are there cures for HER2-positive MBC on the horizon? We don’t know yet, but the field has really exploded in recent years.”
A version of this article first appeared on Medscape.com.
Genomic instability varies between breast cancer subtypes
More than 1,000 patients with TNBC, ER+ breast cancer, or ovarian cancer from five cohorts were examined for genomic instability scores (GIS) and the presence of BRCA deficiency, which showed that, while GIS was similar in BRCA-deficient TNBC and ovarian cancer, it was significantly different in ER+ breast cancer.
The analysis, presented at the San Antonio Breast Cancer Symposium, showed that the genomic instability scores threshold, which could be used to dictate a patient’s treatment, should be lower for ER+ breast cancer than for TNBC.
“This indicates that different GIS thresholds are appropriate for breast cancer subtypes, and that the GIS threshold developed for ovarian caner is not appropriate for ER+ breast cancer,” said lead author Kirsten Timms, PhD, from Myriad Genetics.
This, she noted, is “consistent with the fact that ovarian cancer and TNBC are known to have similar molecular signatures.”
The researchers suggest that the “more inclusive” thresholds assessed in the study should be examined in further studies “to determine whether these cutoffs are associated with a benefit from treatment with DNA-targeting agents,” such as poly (ADP-ribose) polymerase (PARP) inhibitors.
Thomas P. Slavin, MD, chief medical officer at Myriad Genetics, said in an interview that there is “not a one size fits all” for GIS thresholds.
“When you look at ER+ breast cancer you see we need a different cutoff because it’s probably not as driven by homologous recombination deficiency [HRD], as least as a whole, compared to the other two,” he said. “There’s a little less genomic instability.”
He continued that their results suggest around half of TNBC patients have a GIS score that indicates the presence of significant HRD, which is “spot on for what we see with ovarian cancer” and “those people should respond pretty well to PARP-inhibitor therapies,” which is currently being investigated in clinical trials.
“But even in the ER+ group, when we look at the thresholds we used in this research, still about a third have what looks like a substantial amount of HRD, so that’s a huge biomarker,” Dr. Slavin said.
He explained that the importance of their score is that, rather than looking for the causes of HRD, they are looking for the consequences.
“We don’t know all the causes of why, all of a sudden, a tumor cell looks like it can’t replicate through homologous combination [but] what this test does is it says: ‘We don’t really care what the cause is ... we can just look at the genomic scarring and the consequences.’ ”
Elena Provenzano, MD, CRUK Therapeutic Discovery Laboratories, Cambridge (England) University Hospitals NHS Foundation Trust, who was not involved in the study, said in an interview it is “interesting work.”
“We have a personalized breast cancer program here in Cambridge and we’re running trials where we use PARP inhibitors and platinum-based therapy, and what we’re using to make these sorts of decisions is COSMIC mutational signatures associated with genetic instability. And I guess we also look at the total mutational burden,” Dr. Provenzano said.
She continued that the GIS is one of several ways of measuring HRD. “So the question is how it compares with the other measures that are being used to assess whether or not patients are suitable for PARP inhibitor and platinum-based therapy.”
Dr. Provenzano underlined that it has been known since the “early 2000s” that breast cancer is a group of different diseases. “Even within those categories there’s quite a lot of tumor types,” so it “makes sense you need to adjust the threshold slightly for it to become relevant to types of breast cancer.”
She added that the “holy grail in oncology is this concept of personalized medicine, so all these tests help us make sure that the right patient is getting the right treatment.
“At the moment TNBC is often getting treated in a similar way, although we know that there are different biological subtypes, so while there’s a significant group that falls into this BRCA-deficient group that are going to respond to PARPs there are other types that don’t.
“So these sorts of tests help us decide which subset are going to help us the most, and for the others ones we potentially need to identify other treatments as being optimal,” Dr. Provenzano said.
Previous studies have shown that HR-deficient tumors may benefit from treatment with DNA-damaging agents, and that tools such as the three-biomarker GIS can be used to identify HR deficiency.
The Food and Drug Administration has already approved a GIS threshold for identifying HR deficiency in ovarian cancer of 42, which was set as the 5th percentile for BRCA-deficient tumors. However, a recent published in Molecular Cancer Research, and a second published on MDPI Open Access Journals, indicated that a lower, first percentile, cutoff of at least 33 was associated with improved outcomes after platinum-based treatment.
As TNBC is known to have a similar molecular profile to ovarian cancer, the researchers investigated whether it has a different GIS threshold to that in ER+ breast cancer, gathering data on patients newly diagnosed with ovarian cancer, TNBC, or ER+ breast cancer from across five cohorts.
They included 127 ovarian cancer patients from Nature, 434 ovarian cancer, 44 TNBC, and 213 ER+ breast cancer patients from The Cancer Genome Atlas, 55 TNBC and 112 ER+ breast cancer patients from Breast Cancer Research, 19 TNBC and 25 ER+ breast cancer patients from TBCRC 008, and 56 ER+ breast cancer patients from OlympiAD.
GIS was defined as a combination of loss of heterozygosity, telomeric-allellic imbalance, and large-scale state transitions, identified through next-generation sequencing, and GIS distributions were compared between cancer types and subtypes.
The team also determined the presence of BRCA deficiency, finding that, among BRCA deficient tumors, the GIS distribution among patients with ER+ breast cancer was significantly different from that seen in both ovarian cancer (P = 9.6 x 10–5) and TNBC (P = 2.1 x 10–4).
The first percentile of a normal distribution of BRCA-deficient ER+ breast cancers indicated a GIS threshold of 24, with 45.1% of all ER+ tumors at or above this threshold found to be GIS positive. This translated into 98.7% of BRCA-deficient tumors and 32.7% that were BRCA intact.
The results also showed, however, that the GIS distribution for TNBC was not significantly different from that seen in ovarian cancer (P = .72), with the threshold of at least 33 Identifying 64.4% of TNBC tumors as GIS positive. This equated to 100% of BRCA-deficient tumors and 41.7% that were BRCA intact.
Dr. Timms and Dr. Slavin are employed by Myriad Genetics, who funded the study.
More than 1,000 patients with TNBC, ER+ breast cancer, or ovarian cancer from five cohorts were examined for genomic instability scores (GIS) and the presence of BRCA deficiency, which showed that, while GIS was similar in BRCA-deficient TNBC and ovarian cancer, it was significantly different in ER+ breast cancer.
The analysis, presented at the San Antonio Breast Cancer Symposium, showed that the genomic instability scores threshold, which could be used to dictate a patient’s treatment, should be lower for ER+ breast cancer than for TNBC.
“This indicates that different GIS thresholds are appropriate for breast cancer subtypes, and that the GIS threshold developed for ovarian caner is not appropriate for ER+ breast cancer,” said lead author Kirsten Timms, PhD, from Myriad Genetics.
This, she noted, is “consistent with the fact that ovarian cancer and TNBC are known to have similar molecular signatures.”
The researchers suggest that the “more inclusive” thresholds assessed in the study should be examined in further studies “to determine whether these cutoffs are associated with a benefit from treatment with DNA-targeting agents,” such as poly (ADP-ribose) polymerase (PARP) inhibitors.
Thomas P. Slavin, MD, chief medical officer at Myriad Genetics, said in an interview that there is “not a one size fits all” for GIS thresholds.
“When you look at ER+ breast cancer you see we need a different cutoff because it’s probably not as driven by homologous recombination deficiency [HRD], as least as a whole, compared to the other two,” he said. “There’s a little less genomic instability.”
He continued that their results suggest around half of TNBC patients have a GIS score that indicates the presence of significant HRD, which is “spot on for what we see with ovarian cancer” and “those people should respond pretty well to PARP-inhibitor therapies,” which is currently being investigated in clinical trials.
“But even in the ER+ group, when we look at the thresholds we used in this research, still about a third have what looks like a substantial amount of HRD, so that’s a huge biomarker,” Dr. Slavin said.
He explained that the importance of their score is that, rather than looking for the causes of HRD, they are looking for the consequences.
“We don’t know all the causes of why, all of a sudden, a tumor cell looks like it can’t replicate through homologous combination [but] what this test does is it says: ‘We don’t really care what the cause is ... we can just look at the genomic scarring and the consequences.’ ”
Elena Provenzano, MD, CRUK Therapeutic Discovery Laboratories, Cambridge (England) University Hospitals NHS Foundation Trust, who was not involved in the study, said in an interview it is “interesting work.”
“We have a personalized breast cancer program here in Cambridge and we’re running trials where we use PARP inhibitors and platinum-based therapy, and what we’re using to make these sorts of decisions is COSMIC mutational signatures associated with genetic instability. And I guess we also look at the total mutational burden,” Dr. Provenzano said.
She continued that the GIS is one of several ways of measuring HRD. “So the question is how it compares with the other measures that are being used to assess whether or not patients are suitable for PARP inhibitor and platinum-based therapy.”
Dr. Provenzano underlined that it has been known since the “early 2000s” that breast cancer is a group of different diseases. “Even within those categories there’s quite a lot of tumor types,” so it “makes sense you need to adjust the threshold slightly for it to become relevant to types of breast cancer.”
She added that the “holy grail in oncology is this concept of personalized medicine, so all these tests help us make sure that the right patient is getting the right treatment.
“At the moment TNBC is often getting treated in a similar way, although we know that there are different biological subtypes, so while there’s a significant group that falls into this BRCA-deficient group that are going to respond to PARPs there are other types that don’t.
“So these sorts of tests help us decide which subset are going to help us the most, and for the others ones we potentially need to identify other treatments as being optimal,” Dr. Provenzano said.
Previous studies have shown that HR-deficient tumors may benefit from treatment with DNA-damaging agents, and that tools such as the three-biomarker GIS can be used to identify HR deficiency.
The Food and Drug Administration has already approved a GIS threshold for identifying HR deficiency in ovarian cancer of 42, which was set as the 5th percentile for BRCA-deficient tumors. However, a recent published in Molecular Cancer Research, and a second published on MDPI Open Access Journals, indicated that a lower, first percentile, cutoff of at least 33 was associated with improved outcomes after platinum-based treatment.
As TNBC is known to have a similar molecular profile to ovarian cancer, the researchers investigated whether it has a different GIS threshold to that in ER+ breast cancer, gathering data on patients newly diagnosed with ovarian cancer, TNBC, or ER+ breast cancer from across five cohorts.
They included 127 ovarian cancer patients from Nature, 434 ovarian cancer, 44 TNBC, and 213 ER+ breast cancer patients from The Cancer Genome Atlas, 55 TNBC and 112 ER+ breast cancer patients from Breast Cancer Research, 19 TNBC and 25 ER+ breast cancer patients from TBCRC 008, and 56 ER+ breast cancer patients from OlympiAD.
GIS was defined as a combination of loss of heterozygosity, telomeric-allellic imbalance, and large-scale state transitions, identified through next-generation sequencing, and GIS distributions were compared between cancer types and subtypes.
The team also determined the presence of BRCA deficiency, finding that, among BRCA deficient tumors, the GIS distribution among patients with ER+ breast cancer was significantly different from that seen in both ovarian cancer (P = 9.6 x 10–5) and TNBC (P = 2.1 x 10–4).
The first percentile of a normal distribution of BRCA-deficient ER+ breast cancers indicated a GIS threshold of 24, with 45.1% of all ER+ tumors at or above this threshold found to be GIS positive. This translated into 98.7% of BRCA-deficient tumors and 32.7% that were BRCA intact.
The results also showed, however, that the GIS distribution for TNBC was not significantly different from that seen in ovarian cancer (P = .72), with the threshold of at least 33 Identifying 64.4% of TNBC tumors as GIS positive. This equated to 100% of BRCA-deficient tumors and 41.7% that were BRCA intact.
Dr. Timms and Dr. Slavin are employed by Myriad Genetics, who funded the study.
More than 1,000 patients with TNBC, ER+ breast cancer, or ovarian cancer from five cohorts were examined for genomic instability scores (GIS) and the presence of BRCA deficiency, which showed that, while GIS was similar in BRCA-deficient TNBC and ovarian cancer, it was significantly different in ER+ breast cancer.
The analysis, presented at the San Antonio Breast Cancer Symposium, showed that the genomic instability scores threshold, which could be used to dictate a patient’s treatment, should be lower for ER+ breast cancer than for TNBC.
“This indicates that different GIS thresholds are appropriate for breast cancer subtypes, and that the GIS threshold developed for ovarian caner is not appropriate for ER+ breast cancer,” said lead author Kirsten Timms, PhD, from Myriad Genetics.
This, she noted, is “consistent with the fact that ovarian cancer and TNBC are known to have similar molecular signatures.”
The researchers suggest that the “more inclusive” thresholds assessed in the study should be examined in further studies “to determine whether these cutoffs are associated with a benefit from treatment with DNA-targeting agents,” such as poly (ADP-ribose) polymerase (PARP) inhibitors.
Thomas P. Slavin, MD, chief medical officer at Myriad Genetics, said in an interview that there is “not a one size fits all” for GIS thresholds.
“When you look at ER+ breast cancer you see we need a different cutoff because it’s probably not as driven by homologous recombination deficiency [HRD], as least as a whole, compared to the other two,” he said. “There’s a little less genomic instability.”
He continued that their results suggest around half of TNBC patients have a GIS score that indicates the presence of significant HRD, which is “spot on for what we see with ovarian cancer” and “those people should respond pretty well to PARP-inhibitor therapies,” which is currently being investigated in clinical trials.
“But even in the ER+ group, when we look at the thresholds we used in this research, still about a third have what looks like a substantial amount of HRD, so that’s a huge biomarker,” Dr. Slavin said.
He explained that the importance of their score is that, rather than looking for the causes of HRD, they are looking for the consequences.
“We don’t know all the causes of why, all of a sudden, a tumor cell looks like it can’t replicate through homologous combination [but] what this test does is it says: ‘We don’t really care what the cause is ... we can just look at the genomic scarring and the consequences.’ ”
Elena Provenzano, MD, CRUK Therapeutic Discovery Laboratories, Cambridge (England) University Hospitals NHS Foundation Trust, who was not involved in the study, said in an interview it is “interesting work.”
“We have a personalized breast cancer program here in Cambridge and we’re running trials where we use PARP inhibitors and platinum-based therapy, and what we’re using to make these sorts of decisions is COSMIC mutational signatures associated with genetic instability. And I guess we also look at the total mutational burden,” Dr. Provenzano said.
She continued that the GIS is one of several ways of measuring HRD. “So the question is how it compares with the other measures that are being used to assess whether or not patients are suitable for PARP inhibitor and platinum-based therapy.”
Dr. Provenzano underlined that it has been known since the “early 2000s” that breast cancer is a group of different diseases. “Even within those categories there’s quite a lot of tumor types,” so it “makes sense you need to adjust the threshold slightly for it to become relevant to types of breast cancer.”
She added that the “holy grail in oncology is this concept of personalized medicine, so all these tests help us make sure that the right patient is getting the right treatment.
“At the moment TNBC is often getting treated in a similar way, although we know that there are different biological subtypes, so while there’s a significant group that falls into this BRCA-deficient group that are going to respond to PARPs there are other types that don’t.
“So these sorts of tests help us decide which subset are going to help us the most, and for the others ones we potentially need to identify other treatments as being optimal,” Dr. Provenzano said.
Previous studies have shown that HR-deficient tumors may benefit from treatment with DNA-damaging agents, and that tools such as the three-biomarker GIS can be used to identify HR deficiency.
The Food and Drug Administration has already approved a GIS threshold for identifying HR deficiency in ovarian cancer of 42, which was set as the 5th percentile for BRCA-deficient tumors. However, a recent published in Molecular Cancer Research, and a second published on MDPI Open Access Journals, indicated that a lower, first percentile, cutoff of at least 33 was associated with improved outcomes after platinum-based treatment.
As TNBC is known to have a similar molecular profile to ovarian cancer, the researchers investigated whether it has a different GIS threshold to that in ER+ breast cancer, gathering data on patients newly diagnosed with ovarian cancer, TNBC, or ER+ breast cancer from across five cohorts.
They included 127 ovarian cancer patients from Nature, 434 ovarian cancer, 44 TNBC, and 213 ER+ breast cancer patients from The Cancer Genome Atlas, 55 TNBC and 112 ER+ breast cancer patients from Breast Cancer Research, 19 TNBC and 25 ER+ breast cancer patients from TBCRC 008, and 56 ER+ breast cancer patients from OlympiAD.
GIS was defined as a combination of loss of heterozygosity, telomeric-allellic imbalance, and large-scale state transitions, identified through next-generation sequencing, and GIS distributions were compared between cancer types and subtypes.
The team also determined the presence of BRCA deficiency, finding that, among BRCA deficient tumors, the GIS distribution among patients with ER+ breast cancer was significantly different from that seen in both ovarian cancer (P = 9.6 x 10–5) and TNBC (P = 2.1 x 10–4).
The first percentile of a normal distribution of BRCA-deficient ER+ breast cancers indicated a GIS threshold of 24, with 45.1% of all ER+ tumors at or above this threshold found to be GIS positive. This translated into 98.7% of BRCA-deficient tumors and 32.7% that were BRCA intact.
The results also showed, however, that the GIS distribution for TNBC was not significantly different from that seen in ovarian cancer (P = .72), with the threshold of at least 33 Identifying 64.4% of TNBC tumors as GIS positive. This equated to 100% of BRCA-deficient tumors and 41.7% that were BRCA intact.
Dr. Timms and Dr. Slavin are employed by Myriad Genetics, who funded the study.
FROM SABCS 2021
Ongoing HER2 breast cancer therapy may cost an additional $68,000 per patient
The current funding policy in British Columbia restricts patients to two lines of HER2-directed therapy for metastatic breast cancer, but accessing continued HER2 suppression has become more complex as novel agents have emerged, Emily Jackson, MD, and colleagues explained (in poster PD8-09) at the San Antonio Breast Cancer Symposium.
Continuing HER2 suppression has improved progression free survival (PFS) and overall survival (OS), but the financial implications of adapting funding policies to “reflect increasing lines of proven HER2 treatment” are unclear, they noted.
Drug funding is provided through the provincial government, but it can take months – and sometimes years – from when a drug is approved by Health Canada and when provincial protocols are approved and funding is made available, Dr. Jackson, co-chief resident (PGY5) at BC Cancer, Vancouver, said in an interview.
During that “lag time,” the province is negotiating drug prices with pharmaceutical companies and determining “which patients are eligible and under which circumstances,” she said.
To assess the potential costs, the investigators analyzed data from the BC Cancer outcomes unit, which collects clinical and outcome information on 85% of all patients diagnosed with breast cancer in the province. Information on therapy use was obtained from the BC Cancer pharmacy database.
Of 230 patients who received any HER2 treatment for metastatic breast cancer dispensed by BC Cancer between 2013 and 2018, 112 (49%) were eligible to continue beyond their second line of therapy.
“Of these, 86 patients accessed continued HER2-directed therapy, while 26 were eligible but unable to access continued HER2Rx,” they reported, noting that “the remaining 51% (n = 118) were not eligible for consideration of further HER2Rx due to either stable disease (n = 61) or deterioration precluding treatment (n = 57).”
At median follow-up of 42.2 months, the median number of lines of therapy in the entire study population was three. The median number of cycles in those who received HER2-directed therapy beyond second-line therapy was 33.
The median overall survival was 37.5 months for those who were eligible but did not continue HER2, compared with 57.9 months for those who did continue, they found.
The overall survival difference was not statistically significant (P = .13), but this was likely due to the small number of patients included in the initial analysis, Dr. Jackson said, noting that the finding is “hypothesis generating,” and should be further assessed.
Notably, most patients who continued HER2 therapy did so through pharmaceutical company compassionate access programs or clinical trials, she said.
The “conservative estimated cost per cycle of HER2Rx” was based on currently available trastuzumab biosimilars, and the potential financial implications were calculated based on the current cost of commonly used third-line therapies.
The findings demonstrate that most patients access continued treatment despite prohibitive funding policies, and suggest that significant increases in cost per patient can be expected if funding policies don’t evolve to meet treatment needs, they concluded, noting that “if these trends in survival continue we would expect an additional cost of $68,000 per patient over current costs.
“As the cost of novel therapies are likely to be higher than currently available biosimilars, there will be significant implications for both private payer and public payer healthcare systems,” they added.
A larger, more comprehensive analysis of the data is planned, said Dr. Jackson, who did not disclose any funding or other conflicts of interest associated with this study.
The current funding policy in British Columbia restricts patients to two lines of HER2-directed therapy for metastatic breast cancer, but accessing continued HER2 suppression has become more complex as novel agents have emerged, Emily Jackson, MD, and colleagues explained (in poster PD8-09) at the San Antonio Breast Cancer Symposium.
Continuing HER2 suppression has improved progression free survival (PFS) and overall survival (OS), but the financial implications of adapting funding policies to “reflect increasing lines of proven HER2 treatment” are unclear, they noted.
Drug funding is provided through the provincial government, but it can take months – and sometimes years – from when a drug is approved by Health Canada and when provincial protocols are approved and funding is made available, Dr. Jackson, co-chief resident (PGY5) at BC Cancer, Vancouver, said in an interview.
During that “lag time,” the province is negotiating drug prices with pharmaceutical companies and determining “which patients are eligible and under which circumstances,” she said.
To assess the potential costs, the investigators analyzed data from the BC Cancer outcomes unit, which collects clinical and outcome information on 85% of all patients diagnosed with breast cancer in the province. Information on therapy use was obtained from the BC Cancer pharmacy database.
Of 230 patients who received any HER2 treatment for metastatic breast cancer dispensed by BC Cancer between 2013 and 2018, 112 (49%) were eligible to continue beyond their second line of therapy.
“Of these, 86 patients accessed continued HER2-directed therapy, while 26 were eligible but unable to access continued HER2Rx,” they reported, noting that “the remaining 51% (n = 118) were not eligible for consideration of further HER2Rx due to either stable disease (n = 61) or deterioration precluding treatment (n = 57).”
At median follow-up of 42.2 months, the median number of lines of therapy in the entire study population was three. The median number of cycles in those who received HER2-directed therapy beyond second-line therapy was 33.
The median overall survival was 37.5 months for those who were eligible but did not continue HER2, compared with 57.9 months for those who did continue, they found.
The overall survival difference was not statistically significant (P = .13), but this was likely due to the small number of patients included in the initial analysis, Dr. Jackson said, noting that the finding is “hypothesis generating,” and should be further assessed.
Notably, most patients who continued HER2 therapy did so through pharmaceutical company compassionate access programs or clinical trials, she said.
The “conservative estimated cost per cycle of HER2Rx” was based on currently available trastuzumab biosimilars, and the potential financial implications were calculated based on the current cost of commonly used third-line therapies.
The findings demonstrate that most patients access continued treatment despite prohibitive funding policies, and suggest that significant increases in cost per patient can be expected if funding policies don’t evolve to meet treatment needs, they concluded, noting that “if these trends in survival continue we would expect an additional cost of $68,000 per patient over current costs.
“As the cost of novel therapies are likely to be higher than currently available biosimilars, there will be significant implications for both private payer and public payer healthcare systems,” they added.
A larger, more comprehensive analysis of the data is planned, said Dr. Jackson, who did not disclose any funding or other conflicts of interest associated with this study.
The current funding policy in British Columbia restricts patients to two lines of HER2-directed therapy for metastatic breast cancer, but accessing continued HER2 suppression has become more complex as novel agents have emerged, Emily Jackson, MD, and colleagues explained (in poster PD8-09) at the San Antonio Breast Cancer Symposium.
Continuing HER2 suppression has improved progression free survival (PFS) and overall survival (OS), but the financial implications of adapting funding policies to “reflect increasing lines of proven HER2 treatment” are unclear, they noted.
Drug funding is provided through the provincial government, but it can take months – and sometimes years – from when a drug is approved by Health Canada and when provincial protocols are approved and funding is made available, Dr. Jackson, co-chief resident (PGY5) at BC Cancer, Vancouver, said in an interview.
During that “lag time,” the province is negotiating drug prices with pharmaceutical companies and determining “which patients are eligible and under which circumstances,” she said.
To assess the potential costs, the investigators analyzed data from the BC Cancer outcomes unit, which collects clinical and outcome information on 85% of all patients diagnosed with breast cancer in the province. Information on therapy use was obtained from the BC Cancer pharmacy database.
Of 230 patients who received any HER2 treatment for metastatic breast cancer dispensed by BC Cancer between 2013 and 2018, 112 (49%) were eligible to continue beyond their second line of therapy.
“Of these, 86 patients accessed continued HER2-directed therapy, while 26 were eligible but unable to access continued HER2Rx,” they reported, noting that “the remaining 51% (n = 118) were not eligible for consideration of further HER2Rx due to either stable disease (n = 61) or deterioration precluding treatment (n = 57).”
At median follow-up of 42.2 months, the median number of lines of therapy in the entire study population was three. The median number of cycles in those who received HER2-directed therapy beyond second-line therapy was 33.
The median overall survival was 37.5 months for those who were eligible but did not continue HER2, compared with 57.9 months for those who did continue, they found.
The overall survival difference was not statistically significant (P = .13), but this was likely due to the small number of patients included in the initial analysis, Dr. Jackson said, noting that the finding is “hypothesis generating,” and should be further assessed.
Notably, most patients who continued HER2 therapy did so through pharmaceutical company compassionate access programs or clinical trials, she said.
The “conservative estimated cost per cycle of HER2Rx” was based on currently available trastuzumab biosimilars, and the potential financial implications were calculated based on the current cost of commonly used third-line therapies.
The findings demonstrate that most patients access continued treatment despite prohibitive funding policies, and suggest that significant increases in cost per patient can be expected if funding policies don’t evolve to meet treatment needs, they concluded, noting that “if these trends in survival continue we would expect an additional cost of $68,000 per patient over current costs.
“As the cost of novel therapies are likely to be higher than currently available biosimilars, there will be significant implications for both private payer and public payer healthcare systems,” they added.
A larger, more comprehensive analysis of the data is planned, said Dr. Jackson, who did not disclose any funding or other conflicts of interest associated with this study.
FROM SABCS 2021
1 in 7 breast cancers are overdiagnosed
A new model based on data from the Breast Cancer Surveillance Consortium (BCSC) suggests that overdiagnosis of screen-detected breast cancer is less frequent than estimates from excess-incidence studies, but the model also takes into account indolent tumors and produced a higher estimate than previous models that didn’t consider this factor.
“There is a pronounced lack of consensus of the true rate of overdiagnosis in the contemporary U.S. mammography practice. This uncertainty about the extent of overdiagnosis is a problem for the development of guidelines and policies. By overcoming shortcomings of previous studies, we produced a defensible estimate of overdiagnosis in contemporary U.S. mammography practice. About one in seven screen-detected cancers in women (between 50 and 74 years) undergoing biennial screening will be overdiagnosed, and about one in three overdiagnosed cancers are attributed to the detection of nonprogressive cancers,” said Marc D. Ryser, PhD, in an interview. Dr. Ryser is an expert in mathematical and statistical modeling in population health science at Duke University, Durham, N.C. He presented the results of the model at the 2021 San Antonio Breast Cancer Symposium.
Previous models have come up with estimates ranging from 0% to 54%, but the heterogeneity makes them difficult to compare. “They differ in study populations, estimation methods and their definitions of overdiagnosis,” Dr. Ryser said.
There are two general ways to estimate overdiagnosis. One is a model-based approach that works out the tumor latency using models of disease natural history and clinical data, and then uses that to predict overdiagnosis. But these models may not account or indolent tumors, or tumors that would not likely cause death during the patient’s lifetime, and the assumptions behind the models can be opaque. On the other hand, the excess-incidence strategy compares incidence in screened versus unscreened populations and assumes that excess cancers in the screened group is caused by overdiagnosis, but this can be affected by bias.
To get around these limitations, Dr. Ryser’s group used a model-based approach, but also allowed for indolent tumors. They ensured transparency of the underlying assumptions of the model, and took advantage of a contemporary, high-quality data source in the BCSC.
They used individual mammography screening and breast cancer diagnosis records from 35,986 women aged 50-74 years, who were first screened between 2000 and 2018. To estimate overdiagnosis caused by indolent tumors, they used the risk of non–breast cancer mortality from age cohort–adjusted annual mortality risks. There were a total 82,677 screens and 718 cases of breast cancer diagnosed. 3.6% of detected tumor were indolent (95% credible interval, 0.2%-13.8%). The predicted overdiagnosis rate for a biennial screening program was 15.3% (95% prediction interval, 9.7%-25.2%). 6.0% of overdiagnosis was projected to be caused by indolent tumors (95% PI, 0.2%-19.0%) that don’t progress at all, and 9.3% to tumors that would progress, but not fast enough to cause mortality during the individual’s lifetime. An annual screening program had a predicted overdiagnosis rate of 14.6% (95% PI, 9.4%-23.9%).
Dr. Ryser identified some specific studies that used the same definition of overdiagnosis as his group used, and compared them with the 15.3% incidence that his group determined. Excess-incidence studies produced higher estimates, while modeling studies produced lower estimates.
The model did not distinguish between ductal carcinoma in situ and invasive cancers, and it did not account for patient race and breast density.
The study was funded by the National Institutes of Health. Dr. Ryser has no relevant financial disclosures.
A new model based on data from the Breast Cancer Surveillance Consortium (BCSC) suggests that overdiagnosis of screen-detected breast cancer is less frequent than estimates from excess-incidence studies, but the model also takes into account indolent tumors and produced a higher estimate than previous models that didn’t consider this factor.
“There is a pronounced lack of consensus of the true rate of overdiagnosis in the contemporary U.S. mammography practice. This uncertainty about the extent of overdiagnosis is a problem for the development of guidelines and policies. By overcoming shortcomings of previous studies, we produced a defensible estimate of overdiagnosis in contemporary U.S. mammography practice. About one in seven screen-detected cancers in women (between 50 and 74 years) undergoing biennial screening will be overdiagnosed, and about one in three overdiagnosed cancers are attributed to the detection of nonprogressive cancers,” said Marc D. Ryser, PhD, in an interview. Dr. Ryser is an expert in mathematical and statistical modeling in population health science at Duke University, Durham, N.C. He presented the results of the model at the 2021 San Antonio Breast Cancer Symposium.
Previous models have come up with estimates ranging from 0% to 54%, but the heterogeneity makes them difficult to compare. “They differ in study populations, estimation methods and their definitions of overdiagnosis,” Dr. Ryser said.
There are two general ways to estimate overdiagnosis. One is a model-based approach that works out the tumor latency using models of disease natural history and clinical data, and then uses that to predict overdiagnosis. But these models may not account or indolent tumors, or tumors that would not likely cause death during the patient’s lifetime, and the assumptions behind the models can be opaque. On the other hand, the excess-incidence strategy compares incidence in screened versus unscreened populations and assumes that excess cancers in the screened group is caused by overdiagnosis, but this can be affected by bias.
To get around these limitations, Dr. Ryser’s group used a model-based approach, but also allowed for indolent tumors. They ensured transparency of the underlying assumptions of the model, and took advantage of a contemporary, high-quality data source in the BCSC.
They used individual mammography screening and breast cancer diagnosis records from 35,986 women aged 50-74 years, who were first screened between 2000 and 2018. To estimate overdiagnosis caused by indolent tumors, they used the risk of non–breast cancer mortality from age cohort–adjusted annual mortality risks. There were a total 82,677 screens and 718 cases of breast cancer diagnosed. 3.6% of detected tumor were indolent (95% credible interval, 0.2%-13.8%). The predicted overdiagnosis rate for a biennial screening program was 15.3% (95% prediction interval, 9.7%-25.2%). 6.0% of overdiagnosis was projected to be caused by indolent tumors (95% PI, 0.2%-19.0%) that don’t progress at all, and 9.3% to tumors that would progress, but not fast enough to cause mortality during the individual’s lifetime. An annual screening program had a predicted overdiagnosis rate of 14.6% (95% PI, 9.4%-23.9%).
Dr. Ryser identified some specific studies that used the same definition of overdiagnosis as his group used, and compared them with the 15.3% incidence that his group determined. Excess-incidence studies produced higher estimates, while modeling studies produced lower estimates.
The model did not distinguish between ductal carcinoma in situ and invasive cancers, and it did not account for patient race and breast density.
The study was funded by the National Institutes of Health. Dr. Ryser has no relevant financial disclosures.
A new model based on data from the Breast Cancer Surveillance Consortium (BCSC) suggests that overdiagnosis of screen-detected breast cancer is less frequent than estimates from excess-incidence studies, but the model also takes into account indolent tumors and produced a higher estimate than previous models that didn’t consider this factor.
“There is a pronounced lack of consensus of the true rate of overdiagnosis in the contemporary U.S. mammography practice. This uncertainty about the extent of overdiagnosis is a problem for the development of guidelines and policies. By overcoming shortcomings of previous studies, we produced a defensible estimate of overdiagnosis in contemporary U.S. mammography practice. About one in seven screen-detected cancers in women (between 50 and 74 years) undergoing biennial screening will be overdiagnosed, and about one in three overdiagnosed cancers are attributed to the detection of nonprogressive cancers,” said Marc D. Ryser, PhD, in an interview. Dr. Ryser is an expert in mathematical and statistical modeling in population health science at Duke University, Durham, N.C. He presented the results of the model at the 2021 San Antonio Breast Cancer Symposium.
Previous models have come up with estimates ranging from 0% to 54%, but the heterogeneity makes them difficult to compare. “They differ in study populations, estimation methods and their definitions of overdiagnosis,” Dr. Ryser said.
There are two general ways to estimate overdiagnosis. One is a model-based approach that works out the tumor latency using models of disease natural history and clinical data, and then uses that to predict overdiagnosis. But these models may not account or indolent tumors, or tumors that would not likely cause death during the patient’s lifetime, and the assumptions behind the models can be opaque. On the other hand, the excess-incidence strategy compares incidence in screened versus unscreened populations and assumes that excess cancers in the screened group is caused by overdiagnosis, but this can be affected by bias.
To get around these limitations, Dr. Ryser’s group used a model-based approach, but also allowed for indolent tumors. They ensured transparency of the underlying assumptions of the model, and took advantage of a contemporary, high-quality data source in the BCSC.
They used individual mammography screening and breast cancer diagnosis records from 35,986 women aged 50-74 years, who were first screened between 2000 and 2018. To estimate overdiagnosis caused by indolent tumors, they used the risk of non–breast cancer mortality from age cohort–adjusted annual mortality risks. There were a total 82,677 screens and 718 cases of breast cancer diagnosed. 3.6% of detected tumor were indolent (95% credible interval, 0.2%-13.8%). The predicted overdiagnosis rate for a biennial screening program was 15.3% (95% prediction interval, 9.7%-25.2%). 6.0% of overdiagnosis was projected to be caused by indolent tumors (95% PI, 0.2%-19.0%) that don’t progress at all, and 9.3% to tumors that would progress, but not fast enough to cause mortality during the individual’s lifetime. An annual screening program had a predicted overdiagnosis rate of 14.6% (95% PI, 9.4%-23.9%).
Dr. Ryser identified some specific studies that used the same definition of overdiagnosis as his group used, and compared them with the 15.3% incidence that his group determined. Excess-incidence studies produced higher estimates, while modeling studies produced lower estimates.
The model did not distinguish between ductal carcinoma in situ and invasive cancers, and it did not account for patient race and breast density.
The study was funded by the National Institutes of Health. Dr. Ryser has no relevant financial disclosures.
FROM SABCS 2021
Vitamin D counters bone density loss with aromatase inhibitors
Among women with breast cancer being treated with aromatase inhibitors (AI), supplementation with vitamin D and calcium protected against bone loss after 5 years, according to results from a prospective cohort study in Brazil. The study found no difference in bone mineral density outcomes at 5 years between women with hormone receptor–positive cancers treated with aromatase inhibitors (AIG) and triple negative or HER-2 positive patients who were treated with another therapy (CG).
About two-thirds of women with breast cancer have tumors that are positive for hormone receptors, and so are often treated with endocrine therapy such as selective estrogen receptor modulators or AI. However, there are concerns that AI treatment may lead to a loss of bone mineral density and impacts on quality of life. This loss is influenced by a range of factors, including body weight, physical activity, smoking, alcohol consumption, corticosteroid use, calcium in the diet, and circulating levels of vitamin D.
Vitamin D helps to regulate absorption of calcium and phosphorus, ensuring that their plasma concentrations are high enough for adequate bone health. But vitamin D deficiency is a common problem, even in tropical areas such as Brazil. “It is high in the general population and especially in postmenopausal breast cancer patients. Thus, vitamin D and calcium supplementation has an impact on these women’s lives,” said lead author Marcelo Antonini, MD, who presented the study (abstract P1-13-04) at the San Antonio Breast Cancer Symposium. He is a researcher at Hospital Servidor Publico Estadual in São Paulo, Brazil.
Although the findings are encouraging, more work needs to be done before it leads to a change in practice. “Larger studies must be carried out to prove this theory; however, in noncancer patients we have already well established the benefits of vitamin D and calcium supplementation,” Dr. Antonini said in an interview
The researchers examined women before the start of treatment, at 6 months, and at 5 years. Those with vitamin D levels below 30 ng/mL received 7,000 IU/day for 8 weeks, followed by a 1,000 IU/day maintenance dose. Subjects with osteopenia received a calcium supplement (500 mg calcium carbonate), and those with osteoporosis received 4 mg zoledronic acid (Zometa, Novartis).
There were 140 patients in both the AIG and CG groups. The average age was 65 years. Sixty-four percent of the AIG group and 71% of the CG group were vitamin D deficient at baseline. At 5 years, the frequencies were 17% and 16%, respectively. Both groups showed significant declines in bone mineral density in the femoral neck and femur at both 6 months and 5 years, but there was no significant difference between them. There was no significant difference between the two groups with respect to bone density loss in the spine.
The study is limited by the fact that it was conducted at a single center and had a small population size.
Another prospective observational study, published earlier this year, looked at vitamin D supplementation in 741 patients (mean age 61.9 years) being treated with aromatase inhibitors, whose baseline vitamin D levels were less 30 ng/mL. They received 16,000 IU dose of oral calcifediol every 2 weeks. At 3 months, individuals who achieved vitamin D levels of 40 ng/mL or higher were less likely to have joint pain (P < .05). At 12 months, data from 473 patients showed that for every 10-ng/mL increase in serum vitamin D at 3 months, there was a reduction in loss of bone marrow density in the lumbar spine (adjusted beta = +0.177%, P < .05), though there were no associations between vitamin D levels and BMD of the femur or total hip.
“Our results suggest that optimal levels of vitamin D are associated with a reduced risk of joint pain related to AI treatment. A target threshold (of vitamin D) levels was set at 40 ng/mL to significantly reduce the increase in joint pain. The authors noted that this threshold is well above the goal of 20 ng/mL recommended by the 2010 Institute of Medicine report.
The study did not receive external funding. Dr. Antonini has no relevant financial disclosures.
Among women with breast cancer being treated with aromatase inhibitors (AI), supplementation with vitamin D and calcium protected against bone loss after 5 years, according to results from a prospective cohort study in Brazil. The study found no difference in bone mineral density outcomes at 5 years between women with hormone receptor–positive cancers treated with aromatase inhibitors (AIG) and triple negative or HER-2 positive patients who were treated with another therapy (CG).
About two-thirds of women with breast cancer have tumors that are positive for hormone receptors, and so are often treated with endocrine therapy such as selective estrogen receptor modulators or AI. However, there are concerns that AI treatment may lead to a loss of bone mineral density and impacts on quality of life. This loss is influenced by a range of factors, including body weight, physical activity, smoking, alcohol consumption, corticosteroid use, calcium in the diet, and circulating levels of vitamin D.
Vitamin D helps to regulate absorption of calcium and phosphorus, ensuring that their plasma concentrations are high enough for adequate bone health. But vitamin D deficiency is a common problem, even in tropical areas such as Brazil. “It is high in the general population and especially in postmenopausal breast cancer patients. Thus, vitamin D and calcium supplementation has an impact on these women’s lives,” said lead author Marcelo Antonini, MD, who presented the study (abstract P1-13-04) at the San Antonio Breast Cancer Symposium. He is a researcher at Hospital Servidor Publico Estadual in São Paulo, Brazil.
Although the findings are encouraging, more work needs to be done before it leads to a change in practice. “Larger studies must be carried out to prove this theory; however, in noncancer patients we have already well established the benefits of vitamin D and calcium supplementation,” Dr. Antonini said in an interview
The researchers examined women before the start of treatment, at 6 months, and at 5 years. Those with vitamin D levels below 30 ng/mL received 7,000 IU/day for 8 weeks, followed by a 1,000 IU/day maintenance dose. Subjects with osteopenia received a calcium supplement (500 mg calcium carbonate), and those with osteoporosis received 4 mg zoledronic acid (Zometa, Novartis).
There were 140 patients in both the AIG and CG groups. The average age was 65 years. Sixty-four percent of the AIG group and 71% of the CG group were vitamin D deficient at baseline. At 5 years, the frequencies were 17% and 16%, respectively. Both groups showed significant declines in bone mineral density in the femoral neck and femur at both 6 months and 5 years, but there was no significant difference between them. There was no significant difference between the two groups with respect to bone density loss in the spine.
The study is limited by the fact that it was conducted at a single center and had a small population size.
Another prospective observational study, published earlier this year, looked at vitamin D supplementation in 741 patients (mean age 61.9 years) being treated with aromatase inhibitors, whose baseline vitamin D levels were less 30 ng/mL. They received 16,000 IU dose of oral calcifediol every 2 weeks. At 3 months, individuals who achieved vitamin D levels of 40 ng/mL or higher were less likely to have joint pain (P < .05). At 12 months, data from 473 patients showed that for every 10-ng/mL increase in serum vitamin D at 3 months, there was a reduction in loss of bone marrow density in the lumbar spine (adjusted beta = +0.177%, P < .05), though there were no associations between vitamin D levels and BMD of the femur or total hip.
“Our results suggest that optimal levels of vitamin D are associated with a reduced risk of joint pain related to AI treatment. A target threshold (of vitamin D) levels was set at 40 ng/mL to significantly reduce the increase in joint pain. The authors noted that this threshold is well above the goal of 20 ng/mL recommended by the 2010 Institute of Medicine report.
The study did not receive external funding. Dr. Antonini has no relevant financial disclosures.
Among women with breast cancer being treated with aromatase inhibitors (AI), supplementation with vitamin D and calcium protected against bone loss after 5 years, according to results from a prospective cohort study in Brazil. The study found no difference in bone mineral density outcomes at 5 years between women with hormone receptor–positive cancers treated with aromatase inhibitors (AIG) and triple negative or HER-2 positive patients who were treated with another therapy (CG).
About two-thirds of women with breast cancer have tumors that are positive for hormone receptors, and so are often treated with endocrine therapy such as selective estrogen receptor modulators or AI. However, there are concerns that AI treatment may lead to a loss of bone mineral density and impacts on quality of life. This loss is influenced by a range of factors, including body weight, physical activity, smoking, alcohol consumption, corticosteroid use, calcium in the diet, and circulating levels of vitamin D.
Vitamin D helps to regulate absorption of calcium and phosphorus, ensuring that their plasma concentrations are high enough for adequate bone health. But vitamin D deficiency is a common problem, even in tropical areas such as Brazil. “It is high in the general population and especially in postmenopausal breast cancer patients. Thus, vitamin D and calcium supplementation has an impact on these women’s lives,” said lead author Marcelo Antonini, MD, who presented the study (abstract P1-13-04) at the San Antonio Breast Cancer Symposium. He is a researcher at Hospital Servidor Publico Estadual in São Paulo, Brazil.
Although the findings are encouraging, more work needs to be done before it leads to a change in practice. “Larger studies must be carried out to prove this theory; however, in noncancer patients we have already well established the benefits of vitamin D and calcium supplementation,” Dr. Antonini said in an interview
The researchers examined women before the start of treatment, at 6 months, and at 5 years. Those with vitamin D levels below 30 ng/mL received 7,000 IU/day for 8 weeks, followed by a 1,000 IU/day maintenance dose. Subjects with osteopenia received a calcium supplement (500 mg calcium carbonate), and those with osteoporosis received 4 mg zoledronic acid (Zometa, Novartis).
There were 140 patients in both the AIG and CG groups. The average age was 65 years. Sixty-four percent of the AIG group and 71% of the CG group were vitamin D deficient at baseline. At 5 years, the frequencies were 17% and 16%, respectively. Both groups showed significant declines in bone mineral density in the femoral neck and femur at both 6 months and 5 years, but there was no significant difference between them. There was no significant difference between the two groups with respect to bone density loss in the spine.
The study is limited by the fact that it was conducted at a single center and had a small population size.
Another prospective observational study, published earlier this year, looked at vitamin D supplementation in 741 patients (mean age 61.9 years) being treated with aromatase inhibitors, whose baseline vitamin D levels were less 30 ng/mL. They received 16,000 IU dose of oral calcifediol every 2 weeks. At 3 months, individuals who achieved vitamin D levels of 40 ng/mL or higher were less likely to have joint pain (P < .05). At 12 months, data from 473 patients showed that for every 10-ng/mL increase in serum vitamin D at 3 months, there was a reduction in loss of bone marrow density in the lumbar spine (adjusted beta = +0.177%, P < .05), though there were no associations between vitamin D levels and BMD of the femur or total hip.
“Our results suggest that optimal levels of vitamin D are associated with a reduced risk of joint pain related to AI treatment. A target threshold (of vitamin D) levels was set at 40 ng/mL to significantly reduce the increase in joint pain. The authors noted that this threshold is well above the goal of 20 ng/mL recommended by the 2010 Institute of Medicine report.
The study did not receive external funding. Dr. Antonini has no relevant financial disclosures.
FROM SABCS 2021
Metformin does not improve outcomes in early breast cancer
In the primary analysis, the addition of metformin to standard therapy in moderate/high-risk hormone receptor positive or negative breast cancer did not improve invasive disease–free survival (IDFS), overall survival, or other breast outcomes, explained lead author Pamela J. Goodwin, MD, FRCPC, professor of medicine at the University of Toronto. “Metformin should not be used as breast cancer treatment in this population.”
However, an exploratory analysis suggested that metformin may have a beneficial effect in women with HER2-positive breast cancer, Dr. Goodwin noted.
In this subset, IDFS was improved in patients who received metformin (hazard ratio, 0.64; P = .03), as was overall survival (HR, 0.53; P = .04).
The findings were presented at the San Antonio Breast Cancer Symposium.
“This trial arose from the observation that obesity is associated with poor breast cancer outcomes, and insulin levels are higher in obesity and may be more strongly associated with breast cancer outcomes than obesity,” said Dr. Goodwin.
Metformin was used because of its ability to promote modest weight loss and lower insulin by about 15%-20% in nondiabetic breast cancer survivors. It has also shown anticancer effects in preclinical studies. “In some window of opportunity neoadjuvant studies, it has been shown to reduce Ki67 in breast cancer cells,” she said. “And in preclinical in vitro and in vivo research, it slows growth of breast cancer.”
In addition, emerging evidence from observational studies suggests that the use of metformin to treat diabetes in breast cancer patients may be associated with better outcomes, strengthening the rationale for the study.
The negative results in breast cancer follow recent reports of negative findings in lung cancer, when metformin was found to be ineffective when used alongside chemotherapy in locally advanced lung cancer, as reported by this news organization.
No benefit seen
Metformin was compared to placebo in the phase 3 CCTG MA.32 trial, conducted in 3,649 patients aged 18-74 years with T1-3 N0-3 M0 breast cancer. All patients were treated with standard therapy and were randomized to receive metformin 850 mg twice daily for 5 years or placebo.
In 2016, “futility was declared in ER/PR-negative patients” after a second interim analysis conducted at 29.6 months’ median follow-up, Dr. Goodwin noted. The intervention was stopped in that group, although blinding and follow-up continued.
After that, the study’s primary analysis focused on the 2,533 ER/PR-positive patients (mean age, 52.7 years; mean body mass index, 28.8; approx. 60% postmenopausal).
Just over half of these patients had T2 tumor stage, and most disease was grade 2 or 3.
In addition, 16.5% (of metformin) and 17.4% (of placebo) patients had HER2-positive disease, with the majority (97%) of all HER2 patients receiving trastuzumab.
There was no difference between the two groups in IDFS events, occurring in 18.5% of patients receiving metformin and 18.3% who received placebo, with most (75.6%) events due to breast cancer (HR, 1.01; P = .92).
There were 131 deaths in the metformin arm and 119 in the placebo arm, with most (75.8%) of the deaths related to breast cancer (HR, 1.10; P = .47).
Other breast cancer outcomes had similar results, including distant disease-free survival (HR, 0.99; P = .94) and breast cancer–free interval (HR, 0.98; P = .87), both of which showed no advantage for metformin.
Possible HER2 advantage
However, the exploratory analysis suggested there may be an advantage for patients with HER2-positive disease, but primarily those who had at least one C allele of a prespecified ATM associated rs11212617 SNP. These patients achieved a higher pathologic complete response rate with metformin than that of those without the allele.
There were 620 patients with HER2-positive disease analyzed, with 99.4% receiving chemotherapy and 96.5% receiving trastuzumab. There were 99 IDFS events, and 47 OS events.
In the entire HER2-positive cohort, patients who received metformin had fewer IDFS events (HR, 0.64; P = .026) compared with the placebo arm. Mortality was lower with metformin (HR for overall survival, 0.53; P = .038).
“Subjects with HER2-positive breast cancer, notably those with at least one C allele of the ATM-associated rs11212617 SNP, experienced improved IDFS and overall survival with metformin,” Dr. Goodwin concluded. “However, no P-value ‘spend’ was allocated to this comparison. As a result, it requires replication in a prospective trial focusing on the HER2-positive population.”
More research?
Stephanie Bernik, MD, chief of breast surgery, Mount Sinai West, and associate professor of breast surgery, Icahn School of Medicine at Mount Sinai, New York, was approached by this news organization for an independent comment.
“It has long been known that obesity, which often correlates with diabetes, increases a woman’s risk of breast cancer,” she said.
“This study tried to show that using a medication that helps control insulin levels, even in those without diabetes, might decrease one’s risk of breast cancer,” she said. “Unfortunately, using metformin had no effect on outcomes in this study, even though it has shown promise in other studies. Perhaps more research needs to be carried out to try to pinpoint which mechanisms of action, if any, might be helpful to combat cancer in those with and without diabetes.”
The study was funded by the Canadian Cancer Trials Group, Cancer Therapy Evaluation Program, Breast Cancer Researcher Foundation, Susan G. Komen for the Cure, Canadian Cancer Society, Apotex, Swiss Cancer Research, and the Canadian Breast Cancer Foundation. Dr. Goodwin has no disclosures.
A version of this article first appeared on Medscape.com.
In the primary analysis, the addition of metformin to standard therapy in moderate/high-risk hormone receptor positive or negative breast cancer did not improve invasive disease–free survival (IDFS), overall survival, or other breast outcomes, explained lead author Pamela J. Goodwin, MD, FRCPC, professor of medicine at the University of Toronto. “Metformin should not be used as breast cancer treatment in this population.”
However, an exploratory analysis suggested that metformin may have a beneficial effect in women with HER2-positive breast cancer, Dr. Goodwin noted.
In this subset, IDFS was improved in patients who received metformin (hazard ratio, 0.64; P = .03), as was overall survival (HR, 0.53; P = .04).
The findings were presented at the San Antonio Breast Cancer Symposium.
“This trial arose from the observation that obesity is associated with poor breast cancer outcomes, and insulin levels are higher in obesity and may be more strongly associated with breast cancer outcomes than obesity,” said Dr. Goodwin.
Metformin was used because of its ability to promote modest weight loss and lower insulin by about 15%-20% in nondiabetic breast cancer survivors. It has also shown anticancer effects in preclinical studies. “In some window of opportunity neoadjuvant studies, it has been shown to reduce Ki67 in breast cancer cells,” she said. “And in preclinical in vitro and in vivo research, it slows growth of breast cancer.”
In addition, emerging evidence from observational studies suggests that the use of metformin to treat diabetes in breast cancer patients may be associated with better outcomes, strengthening the rationale for the study.
The negative results in breast cancer follow recent reports of negative findings in lung cancer, when metformin was found to be ineffective when used alongside chemotherapy in locally advanced lung cancer, as reported by this news organization.
No benefit seen
Metformin was compared to placebo in the phase 3 CCTG MA.32 trial, conducted in 3,649 patients aged 18-74 years with T1-3 N0-3 M0 breast cancer. All patients were treated with standard therapy and were randomized to receive metformin 850 mg twice daily for 5 years or placebo.
In 2016, “futility was declared in ER/PR-negative patients” after a second interim analysis conducted at 29.6 months’ median follow-up, Dr. Goodwin noted. The intervention was stopped in that group, although blinding and follow-up continued.
After that, the study’s primary analysis focused on the 2,533 ER/PR-positive patients (mean age, 52.7 years; mean body mass index, 28.8; approx. 60% postmenopausal).
Just over half of these patients had T2 tumor stage, and most disease was grade 2 or 3.
In addition, 16.5% (of metformin) and 17.4% (of placebo) patients had HER2-positive disease, with the majority (97%) of all HER2 patients receiving trastuzumab.
There was no difference between the two groups in IDFS events, occurring in 18.5% of patients receiving metformin and 18.3% who received placebo, with most (75.6%) events due to breast cancer (HR, 1.01; P = .92).
There were 131 deaths in the metformin arm and 119 in the placebo arm, with most (75.8%) of the deaths related to breast cancer (HR, 1.10; P = .47).
Other breast cancer outcomes had similar results, including distant disease-free survival (HR, 0.99; P = .94) and breast cancer–free interval (HR, 0.98; P = .87), both of which showed no advantage for metformin.
Possible HER2 advantage
However, the exploratory analysis suggested there may be an advantage for patients with HER2-positive disease, but primarily those who had at least one C allele of a prespecified ATM associated rs11212617 SNP. These patients achieved a higher pathologic complete response rate with metformin than that of those without the allele.
There were 620 patients with HER2-positive disease analyzed, with 99.4% receiving chemotherapy and 96.5% receiving trastuzumab. There were 99 IDFS events, and 47 OS events.
In the entire HER2-positive cohort, patients who received metformin had fewer IDFS events (HR, 0.64; P = .026) compared with the placebo arm. Mortality was lower with metformin (HR for overall survival, 0.53; P = .038).
“Subjects with HER2-positive breast cancer, notably those with at least one C allele of the ATM-associated rs11212617 SNP, experienced improved IDFS and overall survival with metformin,” Dr. Goodwin concluded. “However, no P-value ‘spend’ was allocated to this comparison. As a result, it requires replication in a prospective trial focusing on the HER2-positive population.”
More research?
Stephanie Bernik, MD, chief of breast surgery, Mount Sinai West, and associate professor of breast surgery, Icahn School of Medicine at Mount Sinai, New York, was approached by this news organization for an independent comment.
“It has long been known that obesity, which often correlates with diabetes, increases a woman’s risk of breast cancer,” she said.
“This study tried to show that using a medication that helps control insulin levels, even in those without diabetes, might decrease one’s risk of breast cancer,” she said. “Unfortunately, using metformin had no effect on outcomes in this study, even though it has shown promise in other studies. Perhaps more research needs to be carried out to try to pinpoint which mechanisms of action, if any, might be helpful to combat cancer in those with and without diabetes.”
The study was funded by the Canadian Cancer Trials Group, Cancer Therapy Evaluation Program, Breast Cancer Researcher Foundation, Susan G. Komen for the Cure, Canadian Cancer Society, Apotex, Swiss Cancer Research, and the Canadian Breast Cancer Foundation. Dr. Goodwin has no disclosures.
A version of this article first appeared on Medscape.com.
In the primary analysis, the addition of metformin to standard therapy in moderate/high-risk hormone receptor positive or negative breast cancer did not improve invasive disease–free survival (IDFS), overall survival, or other breast outcomes, explained lead author Pamela J. Goodwin, MD, FRCPC, professor of medicine at the University of Toronto. “Metformin should not be used as breast cancer treatment in this population.”
However, an exploratory analysis suggested that metformin may have a beneficial effect in women with HER2-positive breast cancer, Dr. Goodwin noted.
In this subset, IDFS was improved in patients who received metformin (hazard ratio, 0.64; P = .03), as was overall survival (HR, 0.53; P = .04).
The findings were presented at the San Antonio Breast Cancer Symposium.
“This trial arose from the observation that obesity is associated with poor breast cancer outcomes, and insulin levels are higher in obesity and may be more strongly associated with breast cancer outcomes than obesity,” said Dr. Goodwin.
Metformin was used because of its ability to promote modest weight loss and lower insulin by about 15%-20% in nondiabetic breast cancer survivors. It has also shown anticancer effects in preclinical studies. “In some window of opportunity neoadjuvant studies, it has been shown to reduce Ki67 in breast cancer cells,” she said. “And in preclinical in vitro and in vivo research, it slows growth of breast cancer.”
In addition, emerging evidence from observational studies suggests that the use of metformin to treat diabetes in breast cancer patients may be associated with better outcomes, strengthening the rationale for the study.
The negative results in breast cancer follow recent reports of negative findings in lung cancer, when metformin was found to be ineffective when used alongside chemotherapy in locally advanced lung cancer, as reported by this news organization.
No benefit seen
Metformin was compared to placebo in the phase 3 CCTG MA.32 trial, conducted in 3,649 patients aged 18-74 years with T1-3 N0-3 M0 breast cancer. All patients were treated with standard therapy and were randomized to receive metformin 850 mg twice daily for 5 years or placebo.
In 2016, “futility was declared in ER/PR-negative patients” after a second interim analysis conducted at 29.6 months’ median follow-up, Dr. Goodwin noted. The intervention was stopped in that group, although blinding and follow-up continued.
After that, the study’s primary analysis focused on the 2,533 ER/PR-positive patients (mean age, 52.7 years; mean body mass index, 28.8; approx. 60% postmenopausal).
Just over half of these patients had T2 tumor stage, and most disease was grade 2 or 3.
In addition, 16.5% (of metformin) and 17.4% (of placebo) patients had HER2-positive disease, with the majority (97%) of all HER2 patients receiving trastuzumab.
There was no difference between the two groups in IDFS events, occurring in 18.5% of patients receiving metformin and 18.3% who received placebo, with most (75.6%) events due to breast cancer (HR, 1.01; P = .92).
There were 131 deaths in the metformin arm and 119 in the placebo arm, with most (75.8%) of the deaths related to breast cancer (HR, 1.10; P = .47).
Other breast cancer outcomes had similar results, including distant disease-free survival (HR, 0.99; P = .94) and breast cancer–free interval (HR, 0.98; P = .87), both of which showed no advantage for metformin.
Possible HER2 advantage
However, the exploratory analysis suggested there may be an advantage for patients with HER2-positive disease, but primarily those who had at least one C allele of a prespecified ATM associated rs11212617 SNP. These patients achieved a higher pathologic complete response rate with metformin than that of those without the allele.
There were 620 patients with HER2-positive disease analyzed, with 99.4% receiving chemotherapy and 96.5% receiving trastuzumab. There were 99 IDFS events, and 47 OS events.
In the entire HER2-positive cohort, patients who received metformin had fewer IDFS events (HR, 0.64; P = .026) compared with the placebo arm. Mortality was lower with metformin (HR for overall survival, 0.53; P = .038).
“Subjects with HER2-positive breast cancer, notably those with at least one C allele of the ATM-associated rs11212617 SNP, experienced improved IDFS and overall survival with metformin,” Dr. Goodwin concluded. “However, no P-value ‘spend’ was allocated to this comparison. As a result, it requires replication in a prospective trial focusing on the HER2-positive population.”
More research?
Stephanie Bernik, MD, chief of breast surgery, Mount Sinai West, and associate professor of breast surgery, Icahn School of Medicine at Mount Sinai, New York, was approached by this news organization for an independent comment.
“It has long been known that obesity, which often correlates with diabetes, increases a woman’s risk of breast cancer,” she said.
“This study tried to show that using a medication that helps control insulin levels, even in those without diabetes, might decrease one’s risk of breast cancer,” she said. “Unfortunately, using metformin had no effect on outcomes in this study, even though it has shown promise in other studies. Perhaps more research needs to be carried out to try to pinpoint which mechanisms of action, if any, might be helpful to combat cancer in those with and without diabetes.”
The study was funded by the Canadian Cancer Trials Group, Cancer Therapy Evaluation Program, Breast Cancer Researcher Foundation, Susan G. Komen for the Cure, Canadian Cancer Society, Apotex, Swiss Cancer Research, and the Canadian Breast Cancer Foundation. Dr. Goodwin has no disclosures.
A version of this article first appeared on Medscape.com.
FROM SABCS 2021