User login
‘Doomscrolling’ may be a significant driver of poor mental health
The past 2 years have been filled with worrisome global events, from the pandemic to the war in Ukraine, large-scale protests, mass shootings, and devastating wildfires. The 24-hour media coverage of these events can take a toll on “news addicts” who have an excessive urge to constantly check the news, researchers note.
Results from an online survey of more than 1,000 adults showed that nearly 17% showed signs of “severely problematic” news consumption.
These “doomscrollers” or “doomsurfers” scored high on all five problematic news consumption dimensions: being absorbed in news content, being consumed by thoughts about the news, attempting to alleviate feelings of threat by consuming more news, losing control over news consumption, and having news consumption interfere in daily life.
“We anticipated that a sizable portion of our sample would show signs of problematic news consumption. However, we were surprised to find that 17% of study participants suffer from the most severe level of problematic news consumption,” lead author Bryan McLaughlin, PhD, Texas Tech University, Lubbock, told this news organization. “This is certainly concerning and suggests the problem may be more widespread than we expected,” he said.
In addition, 74% of those with severe levels of problematic news consumption reported experiencing mental problems, and 61% reported physical problems.
“It’s important for health care providers to be aware that problematic news consumption may be a significant driver of mental and physical ill-being, especially because a lot of people might be unaware of the negative impact the news is having on their health,” Dr. McLaughlin said.
The findings were published online in Health Communication.
Emotionally invested
The researchers assessed data from an online survey of 1,100 adults (mean age, 40.5 years; 51% women) in the United States who were recruited in August 2021.
Among those surveyed, 27.3% reported “moderately problematic” news consumption, 27.5% reported minimally problematic news consumption, and 28.7% reported no problematic news consumption.
Perhaps not surprisingly, respondents with higher levels of problematic news consumption were significantly more likely to experience mental and physical ill-being than those with lower levels, even after accounting for demographics, personality traits, and overall news use, the researchers note.
Nearly three-quarters (74%) of those with severe levels of problematic news consumption reported experiencing mental ill-being “quite a bit” or “very much” – whereas frequent symptoms were only reported by 8% of all other study participants.
In addition, 61% of adults with severe problematic news consumption reported experiencing physical ill-being “quite a bit” or “very much,” compared with only 6.1% for all other study participants.
Dr. McLaughlin noted that one way to combat this problem is to help individuals develop a healthier relationship with the news – and mindfulness training may be one way to accomplish that.
“We have some preliminary evidence that individuals with high levels of mindfulness are much less susceptible to developing higher levels of problematic news consumption,” he said.
“Given this, mindfulness-based training could potentially help problematic news consumers follow the news without becoming so emotionally invested in it. We hope to examine the effectiveness of a mindfulness intervention in our future research,” he added.
Increased distress
Commenting on the study, Steven R. Thorp, PhD, ABPP, a professor at California School of Professional Psychology, Alliant International University, San Diego, said that he and his colleagues have noticed an increase in clients reporting distress about news consumption.
The survey by Dr. McLaughlin and colleagues “appears to be representative and has sufficient statistical power to address the issues,” said Dr. Thorp, who was not involved with the research.
“However, as the researchers note, it is a cross-sectional and correlational survey. So it’s possible that, as implied, people who ‘doomscroll’ are more likely to have physical and mental health problems that interfere with their functioning,” he added.
It is also possible that individuals with physical and mental health problems are more likely to be isolated and have restricted activities, thus leading to greater news consumption, Dr. Thorp noted. Alternatively, there could be an independent link between health and news consumption.
Most news is “sensational and not representative,” Dr. Thorp pointed out.
For example, “we are far more likely to hear about deaths from terrorist attacks or plane crashes than from heart attacks, though deaths from heart attacks are far more common,” he said.
“News also tends to be negative, rather than uplifting, and most news is not directly relevant to a person’s day-to-day functioning. Thus, for most people, the consumption of news may have more downsides than upsides,” Dr. Thorp added.
Still, many people want to stay informed about national and international events. So rather than following a “cold turkey” or abstinence model of stopping all news consumption, individuals could consider a “harm reduction” model of reducing time spent consuming news, Dr. Thorp noted.
Another thing to consider is the news source. “Some outlets and social media sites are designed to instill outrage, fear, or anger and to increase polarization, while others have been shown to provide balanced and less sensational coverage,” Dr. Thorp said.
“I also think it’s a good idea for providers to regularly ask about news consumption, along with learning about other daily activities that may enhance or diminish mental and physical health,” he added.
The research had no specific funding. Dr. McLaughlin and Dr. Thorp have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The past 2 years have been filled with worrisome global events, from the pandemic to the war in Ukraine, large-scale protests, mass shootings, and devastating wildfires. The 24-hour media coverage of these events can take a toll on “news addicts” who have an excessive urge to constantly check the news, researchers note.
Results from an online survey of more than 1,000 adults showed that nearly 17% showed signs of “severely problematic” news consumption.
These “doomscrollers” or “doomsurfers” scored high on all five problematic news consumption dimensions: being absorbed in news content, being consumed by thoughts about the news, attempting to alleviate feelings of threat by consuming more news, losing control over news consumption, and having news consumption interfere in daily life.
“We anticipated that a sizable portion of our sample would show signs of problematic news consumption. However, we were surprised to find that 17% of study participants suffer from the most severe level of problematic news consumption,” lead author Bryan McLaughlin, PhD, Texas Tech University, Lubbock, told this news organization. “This is certainly concerning and suggests the problem may be more widespread than we expected,” he said.
In addition, 74% of those with severe levels of problematic news consumption reported experiencing mental problems, and 61% reported physical problems.
“It’s important for health care providers to be aware that problematic news consumption may be a significant driver of mental and physical ill-being, especially because a lot of people might be unaware of the negative impact the news is having on their health,” Dr. McLaughlin said.
The findings were published online in Health Communication.
Emotionally invested
The researchers assessed data from an online survey of 1,100 adults (mean age, 40.5 years; 51% women) in the United States who were recruited in August 2021.
Among those surveyed, 27.3% reported “moderately problematic” news consumption, 27.5% reported minimally problematic news consumption, and 28.7% reported no problematic news consumption.
Perhaps not surprisingly, respondents with higher levels of problematic news consumption were significantly more likely to experience mental and physical ill-being than those with lower levels, even after accounting for demographics, personality traits, and overall news use, the researchers note.
Nearly three-quarters (74%) of those with severe levels of problematic news consumption reported experiencing mental ill-being “quite a bit” or “very much” – whereas frequent symptoms were only reported by 8% of all other study participants.
In addition, 61% of adults with severe problematic news consumption reported experiencing physical ill-being “quite a bit” or “very much,” compared with only 6.1% for all other study participants.
Dr. McLaughlin noted that one way to combat this problem is to help individuals develop a healthier relationship with the news – and mindfulness training may be one way to accomplish that.
“We have some preliminary evidence that individuals with high levels of mindfulness are much less susceptible to developing higher levels of problematic news consumption,” he said.
“Given this, mindfulness-based training could potentially help problematic news consumers follow the news without becoming so emotionally invested in it. We hope to examine the effectiveness of a mindfulness intervention in our future research,” he added.
Increased distress
Commenting on the study, Steven R. Thorp, PhD, ABPP, a professor at California School of Professional Psychology, Alliant International University, San Diego, said that he and his colleagues have noticed an increase in clients reporting distress about news consumption.
The survey by Dr. McLaughlin and colleagues “appears to be representative and has sufficient statistical power to address the issues,” said Dr. Thorp, who was not involved with the research.
“However, as the researchers note, it is a cross-sectional and correlational survey. So it’s possible that, as implied, people who ‘doomscroll’ are more likely to have physical and mental health problems that interfere with their functioning,” he added.
It is also possible that individuals with physical and mental health problems are more likely to be isolated and have restricted activities, thus leading to greater news consumption, Dr. Thorp noted. Alternatively, there could be an independent link between health and news consumption.
Most news is “sensational and not representative,” Dr. Thorp pointed out.
For example, “we are far more likely to hear about deaths from terrorist attacks or plane crashes than from heart attacks, though deaths from heart attacks are far more common,” he said.
“News also tends to be negative, rather than uplifting, and most news is not directly relevant to a person’s day-to-day functioning. Thus, for most people, the consumption of news may have more downsides than upsides,” Dr. Thorp added.
Still, many people want to stay informed about national and international events. So rather than following a “cold turkey” or abstinence model of stopping all news consumption, individuals could consider a “harm reduction” model of reducing time spent consuming news, Dr. Thorp noted.
Another thing to consider is the news source. “Some outlets and social media sites are designed to instill outrage, fear, or anger and to increase polarization, while others have been shown to provide balanced and less sensational coverage,” Dr. Thorp said.
“I also think it’s a good idea for providers to regularly ask about news consumption, along with learning about other daily activities that may enhance or diminish mental and physical health,” he added.
The research had no specific funding. Dr. McLaughlin and Dr. Thorp have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The past 2 years have been filled with worrisome global events, from the pandemic to the war in Ukraine, large-scale protests, mass shootings, and devastating wildfires. The 24-hour media coverage of these events can take a toll on “news addicts” who have an excessive urge to constantly check the news, researchers note.
Results from an online survey of more than 1,000 adults showed that nearly 17% showed signs of “severely problematic” news consumption.
These “doomscrollers” or “doomsurfers” scored high on all five problematic news consumption dimensions: being absorbed in news content, being consumed by thoughts about the news, attempting to alleviate feelings of threat by consuming more news, losing control over news consumption, and having news consumption interfere in daily life.
“We anticipated that a sizable portion of our sample would show signs of problematic news consumption. However, we were surprised to find that 17% of study participants suffer from the most severe level of problematic news consumption,” lead author Bryan McLaughlin, PhD, Texas Tech University, Lubbock, told this news organization. “This is certainly concerning and suggests the problem may be more widespread than we expected,” he said.
In addition, 74% of those with severe levels of problematic news consumption reported experiencing mental problems, and 61% reported physical problems.
“It’s important for health care providers to be aware that problematic news consumption may be a significant driver of mental and physical ill-being, especially because a lot of people might be unaware of the negative impact the news is having on their health,” Dr. McLaughlin said.
The findings were published online in Health Communication.
Emotionally invested
The researchers assessed data from an online survey of 1,100 adults (mean age, 40.5 years; 51% women) in the United States who were recruited in August 2021.
Among those surveyed, 27.3% reported “moderately problematic” news consumption, 27.5% reported minimally problematic news consumption, and 28.7% reported no problematic news consumption.
Perhaps not surprisingly, respondents with higher levels of problematic news consumption were significantly more likely to experience mental and physical ill-being than those with lower levels, even after accounting for demographics, personality traits, and overall news use, the researchers note.
Nearly three-quarters (74%) of those with severe levels of problematic news consumption reported experiencing mental ill-being “quite a bit” or “very much” – whereas frequent symptoms were only reported by 8% of all other study participants.
In addition, 61% of adults with severe problematic news consumption reported experiencing physical ill-being “quite a bit” or “very much,” compared with only 6.1% for all other study participants.
Dr. McLaughlin noted that one way to combat this problem is to help individuals develop a healthier relationship with the news – and mindfulness training may be one way to accomplish that.
“We have some preliminary evidence that individuals with high levels of mindfulness are much less susceptible to developing higher levels of problematic news consumption,” he said.
“Given this, mindfulness-based training could potentially help problematic news consumers follow the news without becoming so emotionally invested in it. We hope to examine the effectiveness of a mindfulness intervention in our future research,” he added.
Increased distress
Commenting on the study, Steven R. Thorp, PhD, ABPP, a professor at California School of Professional Psychology, Alliant International University, San Diego, said that he and his colleagues have noticed an increase in clients reporting distress about news consumption.
The survey by Dr. McLaughlin and colleagues “appears to be representative and has sufficient statistical power to address the issues,” said Dr. Thorp, who was not involved with the research.
“However, as the researchers note, it is a cross-sectional and correlational survey. So it’s possible that, as implied, people who ‘doomscroll’ are more likely to have physical and mental health problems that interfere with their functioning,” he added.
It is also possible that individuals with physical and mental health problems are more likely to be isolated and have restricted activities, thus leading to greater news consumption, Dr. Thorp noted. Alternatively, there could be an independent link between health and news consumption.
Most news is “sensational and not representative,” Dr. Thorp pointed out.
For example, “we are far more likely to hear about deaths from terrorist attacks or plane crashes than from heart attacks, though deaths from heart attacks are far more common,” he said.
“News also tends to be negative, rather than uplifting, and most news is not directly relevant to a person’s day-to-day functioning. Thus, for most people, the consumption of news may have more downsides than upsides,” Dr. Thorp added.
Still, many people want to stay informed about national and international events. So rather than following a “cold turkey” or abstinence model of stopping all news consumption, individuals could consider a “harm reduction” model of reducing time spent consuming news, Dr. Thorp noted.
Another thing to consider is the news source. “Some outlets and social media sites are designed to instill outrage, fear, or anger and to increase polarization, while others have been shown to provide balanced and less sensational coverage,” Dr. Thorp said.
“I also think it’s a good idea for providers to regularly ask about news consumption, along with learning about other daily activities that may enhance or diminish mental and physical health,” he added.
The research had no specific funding. Dr. McLaughlin and Dr. Thorp have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HEALTH COMMUNICATION
Distorted time perception during the pandemic tied to stress, poor mental health
ranging from difficulty keeping track of the days of the week to feeling that the hours either crawled by or sped up, new research suggests.
Results showed the sense of present focus, blurring weekdays and weekends together, and uncertainly about the future were reported by over 65% of the 5,661 survey respondents. And more than half reported the experience of feeling “time speeding up or slowing down,” report the investigators, led by E. Alison Holman, PhD, professor at the University of California, Irvine.
Significant predictors of these time distortions included being exposed to daily pandemic-related media and having a mental health diagnosis prior to the pandemic; secondary stress such as school closures and lockdown; financial stress; lifetime stress; and lifetime trauma exposure.
“Continuity between past experiences, present life, and future hopes is critical to one’s well-being, and disruption of that synergy presents mental health challenges,” Dr. Holman said in a news release.
“We were able to measure this in a nationally representative sample of Americans as they were experiencing a protracted collective trauma, which has never been done before, and this study is the first to document the prevalence and early predictors of these time distortions,” added Dr. Holman.
The findings were published online in Psychological Trauma: Theory, Research, Practice, and Policy.
Unique opportunity
During the pandemic, many people’s time perspective (TP), defined as “our view of time as it spans from our past into the future,” shifted as they “focused on the immediate, present danger of the COVID-19 pandemic and future plans became uncertain,” the investigators wrote.
Studies of convenience samples “suggested that many people experienced time slowing down, stopping, and/or speeding up as they coped with the challenges of the pandemic” – a phenomenon known as temporal disintegration (TD) in psychiatric literature.
Dr. Holman said in an interview that she researched TD after the Sept.11, 2001 World Trade Center attacks.
“We found that people who experienced that early sense of TD, the sense of ‘time falling apart,’ were more prone to getting stuck in the past and staying focused on the past event,” which led to feeling “more distress over time,” she said.
Research examining the prevalence of and psychosocial factors predicting TD are “quite rare” and studies examining TD “during an unfolding, protracted collective trauma are even rarer,” the researchers note. The COVID pandemic “presented a unique opportunity to conduct such a study,” the researchers wrote.
For their study, the investigators surveyed participants in the NORC AmeriSpeak online panel, a “probability-based panel” of 35,000 U.S. households selected at random from across the country.
The study was conducted in two waves: the first survey was administered March–April 2020, the second in September–October 2020.
Speeding up, slowing down
At wave 2, participants completed a 7-item index of TD symptoms experienced over the previous 6 months. To adjust for psychological processes that may have predisposed individuals to experience TD during the pandemic, the researchers included a Wave 1 measure of future uncertainty as a covariate.
Prepandemic health data had been collected prior to the current study.
Wave 1 participants completed a checklist reporting personal, work, and community-wide exposure to the COVID outbreak, including contracting the virus, sheltering in place, and experiencing secondary stressors. The extent and type of pandemic-related media exposure were also assessed.
At wave 2, they reported the extent of exposure to the coronavirus, financial exposures, and secondary stressors. They also completed a non–COVID-related stress/trauma exposure checklist and were asked to indicate whether the trauma, disaster, or bereavement took place prior to or during the pandemic.
The final sample consisted of 5,661 adults (52% female) who completed the wave 2 survey. Participants were divided into four age groups: 18-34, 35-49, 50-64, and 65 and older.
The most common experiences (reported by more than 65% of respondents) included being focused on the present moment, feeling that weekdays and weekends were the same, and feeling uncertain about the future.
Over half of respondents (50.4%) reported feeling as though time was speeding up, and 55.2% reported feeling as though time was slowing down. Some also reported feeling uncertain about the time of day (46.4%) and forgetting events they had just experienced (35.2%).
When the researchers controlled for feeling uncertain about the future, they found that women reported more TD than men (b = 0.11; 95% confidence interval, 0.07-0.14; P < .001).
At wave 1, associations were found between TD and COVID-related media exposure, prepandemic mental health diagnoses, and prepandemic non–COVID-related stress and trauma. At wave 2, associations were found between TD and COVID-related secondary and financial stressors (P < .001 for all).
In contrast, COVID-related work exposure at wave 1, being 45-59 years old, and living in the Midwest region were negatively associated with TD.
“The sense of the flow of the past into the present, and the present into the future is important for our mental health,” Dr. Holman said. “We need to remember who we have been, how that shaped who we are today, and where we want to go with our lives.”
Staying in the present moment is “good, when you’re doing it mindfully. But you still need to feel you can shape and work toward the future and have some sense of control,” she added.
Dr. Homan also recommended time-perspective therapy, which helps patients with PTSD to “build continuity across time – to understand and learn from the past, live in the present, and move toward the future.”
Widespread distortion
In an interview, Ruth Ogden, PhD, a lecturer at Liverpool (England) John Moores University, said the findings “confirm those reported in Europe, South America, and the Middle East, that widespread distortion to time was common during the pandemic and that distortions to time were greatest amongst those most negatively affected by the pandemic.”
The results also support her own recent research in the United Kingdom “suggesting that distortions to time during the pandemic extend to our memory for the length of the pandemic, with most people believing that lockdowns lasted far longer than they actually did,” said Dr. Ogden, who was not involved with Dr. Holman and colleagues’ current study.
“This type of subjective lengthening of the pandemic may reinforce trauma by making the traumatic period seem longer, further damaging health and well-being,” she noted. “As the negative fallouts of the pandemic continue, it is important to establish the long-term effects of time distortions during the pandemic on mental health and well-being.”
The study was funded by U.S. National Science Foundation and the National Institute on Minority Health and Health Disparities. The investigators reported no relevant financial relationships. Dr. Ogden receives funding from the Wellcome Trust.
A version of this article first appeared on Medscape.com.
ranging from difficulty keeping track of the days of the week to feeling that the hours either crawled by or sped up, new research suggests.
Results showed the sense of present focus, blurring weekdays and weekends together, and uncertainly about the future were reported by over 65% of the 5,661 survey respondents. And more than half reported the experience of feeling “time speeding up or slowing down,” report the investigators, led by E. Alison Holman, PhD, professor at the University of California, Irvine.
Significant predictors of these time distortions included being exposed to daily pandemic-related media and having a mental health diagnosis prior to the pandemic; secondary stress such as school closures and lockdown; financial stress; lifetime stress; and lifetime trauma exposure.
“Continuity between past experiences, present life, and future hopes is critical to one’s well-being, and disruption of that synergy presents mental health challenges,” Dr. Holman said in a news release.
“We were able to measure this in a nationally representative sample of Americans as they were experiencing a protracted collective trauma, which has never been done before, and this study is the first to document the prevalence and early predictors of these time distortions,” added Dr. Holman.
The findings were published online in Psychological Trauma: Theory, Research, Practice, and Policy.
Unique opportunity
During the pandemic, many people’s time perspective (TP), defined as “our view of time as it spans from our past into the future,” shifted as they “focused on the immediate, present danger of the COVID-19 pandemic and future plans became uncertain,” the investigators wrote.
Studies of convenience samples “suggested that many people experienced time slowing down, stopping, and/or speeding up as they coped with the challenges of the pandemic” – a phenomenon known as temporal disintegration (TD) in psychiatric literature.
Dr. Holman said in an interview that she researched TD after the Sept.11, 2001 World Trade Center attacks.
“We found that people who experienced that early sense of TD, the sense of ‘time falling apart,’ were more prone to getting stuck in the past and staying focused on the past event,” which led to feeling “more distress over time,” she said.
Research examining the prevalence of and psychosocial factors predicting TD are “quite rare” and studies examining TD “during an unfolding, protracted collective trauma are even rarer,” the researchers note. The COVID pandemic “presented a unique opportunity to conduct such a study,” the researchers wrote.
For their study, the investigators surveyed participants in the NORC AmeriSpeak online panel, a “probability-based panel” of 35,000 U.S. households selected at random from across the country.
The study was conducted in two waves: the first survey was administered March–April 2020, the second in September–October 2020.
Speeding up, slowing down
At wave 2, participants completed a 7-item index of TD symptoms experienced over the previous 6 months. To adjust for psychological processes that may have predisposed individuals to experience TD during the pandemic, the researchers included a Wave 1 measure of future uncertainty as a covariate.
Prepandemic health data had been collected prior to the current study.
Wave 1 participants completed a checklist reporting personal, work, and community-wide exposure to the COVID outbreak, including contracting the virus, sheltering in place, and experiencing secondary stressors. The extent and type of pandemic-related media exposure were also assessed.
At wave 2, they reported the extent of exposure to the coronavirus, financial exposures, and secondary stressors. They also completed a non–COVID-related stress/trauma exposure checklist and were asked to indicate whether the trauma, disaster, or bereavement took place prior to or during the pandemic.
The final sample consisted of 5,661 adults (52% female) who completed the wave 2 survey. Participants were divided into four age groups: 18-34, 35-49, 50-64, and 65 and older.
The most common experiences (reported by more than 65% of respondents) included being focused on the present moment, feeling that weekdays and weekends were the same, and feeling uncertain about the future.
Over half of respondents (50.4%) reported feeling as though time was speeding up, and 55.2% reported feeling as though time was slowing down. Some also reported feeling uncertain about the time of day (46.4%) and forgetting events they had just experienced (35.2%).
When the researchers controlled for feeling uncertain about the future, they found that women reported more TD than men (b = 0.11; 95% confidence interval, 0.07-0.14; P < .001).
At wave 1, associations were found between TD and COVID-related media exposure, prepandemic mental health diagnoses, and prepandemic non–COVID-related stress and trauma. At wave 2, associations were found between TD and COVID-related secondary and financial stressors (P < .001 for all).
In contrast, COVID-related work exposure at wave 1, being 45-59 years old, and living in the Midwest region were negatively associated with TD.
“The sense of the flow of the past into the present, and the present into the future is important for our mental health,” Dr. Holman said. “We need to remember who we have been, how that shaped who we are today, and where we want to go with our lives.”
Staying in the present moment is “good, when you’re doing it mindfully. But you still need to feel you can shape and work toward the future and have some sense of control,” she added.
Dr. Homan also recommended time-perspective therapy, which helps patients with PTSD to “build continuity across time – to understand and learn from the past, live in the present, and move toward the future.”
Widespread distortion
In an interview, Ruth Ogden, PhD, a lecturer at Liverpool (England) John Moores University, said the findings “confirm those reported in Europe, South America, and the Middle East, that widespread distortion to time was common during the pandemic and that distortions to time were greatest amongst those most negatively affected by the pandemic.”
The results also support her own recent research in the United Kingdom “suggesting that distortions to time during the pandemic extend to our memory for the length of the pandemic, with most people believing that lockdowns lasted far longer than they actually did,” said Dr. Ogden, who was not involved with Dr. Holman and colleagues’ current study.
“This type of subjective lengthening of the pandemic may reinforce trauma by making the traumatic period seem longer, further damaging health and well-being,” she noted. “As the negative fallouts of the pandemic continue, it is important to establish the long-term effects of time distortions during the pandemic on mental health and well-being.”
The study was funded by U.S. National Science Foundation and the National Institute on Minority Health and Health Disparities. The investigators reported no relevant financial relationships. Dr. Ogden receives funding from the Wellcome Trust.
A version of this article first appeared on Medscape.com.
ranging from difficulty keeping track of the days of the week to feeling that the hours either crawled by or sped up, new research suggests.
Results showed the sense of present focus, blurring weekdays and weekends together, and uncertainly about the future were reported by over 65% of the 5,661 survey respondents. And more than half reported the experience of feeling “time speeding up or slowing down,” report the investigators, led by E. Alison Holman, PhD, professor at the University of California, Irvine.
Significant predictors of these time distortions included being exposed to daily pandemic-related media and having a mental health diagnosis prior to the pandemic; secondary stress such as school closures and lockdown; financial stress; lifetime stress; and lifetime trauma exposure.
“Continuity between past experiences, present life, and future hopes is critical to one’s well-being, and disruption of that synergy presents mental health challenges,” Dr. Holman said in a news release.
“We were able to measure this in a nationally representative sample of Americans as they were experiencing a protracted collective trauma, which has never been done before, and this study is the first to document the prevalence and early predictors of these time distortions,” added Dr. Holman.
The findings were published online in Psychological Trauma: Theory, Research, Practice, and Policy.
Unique opportunity
During the pandemic, many people’s time perspective (TP), defined as “our view of time as it spans from our past into the future,” shifted as they “focused on the immediate, present danger of the COVID-19 pandemic and future plans became uncertain,” the investigators wrote.
Studies of convenience samples “suggested that many people experienced time slowing down, stopping, and/or speeding up as they coped with the challenges of the pandemic” – a phenomenon known as temporal disintegration (TD) in psychiatric literature.
Dr. Holman said in an interview that she researched TD after the Sept.11, 2001 World Trade Center attacks.
“We found that people who experienced that early sense of TD, the sense of ‘time falling apart,’ were more prone to getting stuck in the past and staying focused on the past event,” which led to feeling “more distress over time,” she said.
Research examining the prevalence of and psychosocial factors predicting TD are “quite rare” and studies examining TD “during an unfolding, protracted collective trauma are even rarer,” the researchers note. The COVID pandemic “presented a unique opportunity to conduct such a study,” the researchers wrote.
For their study, the investigators surveyed participants in the NORC AmeriSpeak online panel, a “probability-based panel” of 35,000 U.S. households selected at random from across the country.
The study was conducted in two waves: the first survey was administered March–April 2020, the second in September–October 2020.
Speeding up, slowing down
At wave 2, participants completed a 7-item index of TD symptoms experienced over the previous 6 months. To adjust for psychological processes that may have predisposed individuals to experience TD during the pandemic, the researchers included a Wave 1 measure of future uncertainty as a covariate.
Prepandemic health data had been collected prior to the current study.
Wave 1 participants completed a checklist reporting personal, work, and community-wide exposure to the COVID outbreak, including contracting the virus, sheltering in place, and experiencing secondary stressors. The extent and type of pandemic-related media exposure were also assessed.
At wave 2, they reported the extent of exposure to the coronavirus, financial exposures, and secondary stressors. They also completed a non–COVID-related stress/trauma exposure checklist and were asked to indicate whether the trauma, disaster, or bereavement took place prior to or during the pandemic.
The final sample consisted of 5,661 adults (52% female) who completed the wave 2 survey. Participants were divided into four age groups: 18-34, 35-49, 50-64, and 65 and older.
The most common experiences (reported by more than 65% of respondents) included being focused on the present moment, feeling that weekdays and weekends were the same, and feeling uncertain about the future.
Over half of respondents (50.4%) reported feeling as though time was speeding up, and 55.2% reported feeling as though time was slowing down. Some also reported feeling uncertain about the time of day (46.4%) and forgetting events they had just experienced (35.2%).
When the researchers controlled for feeling uncertain about the future, they found that women reported more TD than men (b = 0.11; 95% confidence interval, 0.07-0.14; P < .001).
At wave 1, associations were found between TD and COVID-related media exposure, prepandemic mental health diagnoses, and prepandemic non–COVID-related stress and trauma. At wave 2, associations were found between TD and COVID-related secondary and financial stressors (P < .001 for all).
In contrast, COVID-related work exposure at wave 1, being 45-59 years old, and living in the Midwest region were negatively associated with TD.
“The sense of the flow of the past into the present, and the present into the future is important for our mental health,” Dr. Holman said. “We need to remember who we have been, how that shaped who we are today, and where we want to go with our lives.”
Staying in the present moment is “good, when you’re doing it mindfully. But you still need to feel you can shape and work toward the future and have some sense of control,” she added.
Dr. Homan also recommended time-perspective therapy, which helps patients with PTSD to “build continuity across time – to understand and learn from the past, live in the present, and move toward the future.”
Widespread distortion
In an interview, Ruth Ogden, PhD, a lecturer at Liverpool (England) John Moores University, said the findings “confirm those reported in Europe, South America, and the Middle East, that widespread distortion to time was common during the pandemic and that distortions to time were greatest amongst those most negatively affected by the pandemic.”
The results also support her own recent research in the United Kingdom “suggesting that distortions to time during the pandemic extend to our memory for the length of the pandemic, with most people believing that lockdowns lasted far longer than they actually did,” said Dr. Ogden, who was not involved with Dr. Holman and colleagues’ current study.
“This type of subjective lengthening of the pandemic may reinforce trauma by making the traumatic period seem longer, further damaging health and well-being,” she noted. “As the negative fallouts of the pandemic continue, it is important to establish the long-term effects of time distortions during the pandemic on mental health and well-being.”
The study was funded by U.S. National Science Foundation and the National Institute on Minority Health and Health Disparities. The investigators reported no relevant financial relationships. Dr. Ogden receives funding from the Wellcome Trust.
A version of this article first appeared on Medscape.com.
FROM PSYCHOLOGICAL TRAUMA: THEORY, RESEARCH, PRACTICE, AND POLICY
Stable, long-term opioid therapy safer than tapering?
Investigators analyzed data for almost 200,000 patients who did not have signs of opioid use disorder (OUD) and were receiving opioid treatment. The investigators compared three dosing strategies: abrupt withdrawal, gradual tapering, and continuation of the current stable dosage.
Results showed a higher adjusted cumulative incidence of opioid overdose or suicide events 11 months after baseline among participants for whom a tapered dosing strategy was utilized, compared with those who continued taking a stable dosage. The risk difference was 0.15% between taper and stable dosage and 0.33% between abrupt discontinuation and stable dosage.
“This study identified a small absolute increase in risk of harms associated with opioid tapering compared with a stable opioid dosage,” Marc LaRochelle, MD, MPH, assistant professor, Boston University, and colleagues write.
“These results do not suggest that policies of mandatory dosage tapering for individuals receiving a stable long-term opioid dosage without evidence of opioid misuse will reduce short-term harm via suicide and overdose,” they add.
The findings were published online in JAMA Network Open.
Benefits vs. harms
The investigators note that the Centers for Disease Control and Prevention, in its 2016 Guideline for Prescribing Opioids for Chronic Pain, “recommended tapering opioid dosages if benefits no longer outweigh harms.”
In response, “some health systems and U.S. states enacted stringent dose limits that were applied with few exceptions, regardless of individual patients’ risk of harms,” they write. By contrast, there have been “increasing reports of patients experiencing adverse effects from forced opioid tapers.”
Previous studies that identified harms associated with opioid tapering and discontinuation had several limitations, including a focus on discontinuation, which is “likely more destabilizing than gradual tapering,” the researchers write. There is also “a high potential for confounding” in these studies, they add.
The investigators sought to fill the research gap by drawing on 8-year data (Jan. 1, 2010, to Dec. 31, 2018) from a large database that includes adjudicated pharmacy, outpatient, and inpatient medical claims for individuals with commercial or Medicare Advantage insurance encompassing all 50 states, the District of Columbia, and Puerto Rico.
Notably, individuals who had received a diagnosis of substance use, abuse, or dependence or for whom there were indicators consistent with OUD were excluded.
The researchers compared the three treatment strategies during a 4-month treatment strategy assignment period (“grace period”) after baseline. Tapering was defined as “2 consecutive months with a mean MME [morphine milligram equivalent] reduction of 15% or more compared with the baseline month.”
All estimates were adjusted for potential confounders, including demographic and treatment characteristics, baseline year, region, insurance plan type, comorbid psychiatric and medical conditions, and the prescribing of other psychiatric medications, such as benzodiazepines, gabapentin, or pregabalin.
Patient-centered approaches
The final cohort that met inclusion criteria consisted of 199,836 individuals (45.1% men; mean age, 56.9 years). Of the total group, 57.6% were aged 45-64 years. There were 415,123 qualifying long-term opioid therapy episodes.
The largest percentage of the cohort (41.2%) were receiving a baseline mean MME of 50-89 mg/day, while 34% were receiving 90-199 mg/day and 23.5% were receiving at least 200 mg/day.
During the 6-month eligibility assessment period, 34.8% of the cohort were receiving benzodiazepine prescriptions, 18% had been diagnosed with comorbid anxiety, and 19.7% had been diagnosed with comorbid depression.
After the treatment assignment period, most treatment episodes (87.1%) were considered stable, 11.1% were considered a taper, and 1.8% were considered abrupt discontinuation.
Eleven months after baseline, the adjusted cumulative incidence of opioid overdose or suicide events was lowest for those who continued to receive a stable dose.
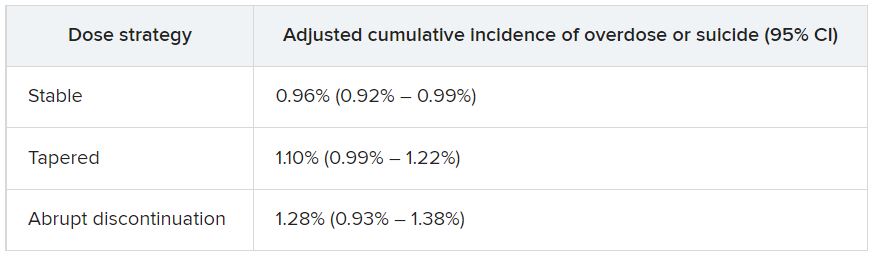
The risk differences between taper vs. stable dosage were 0.15% (95% confidence interval, 0.03%-0.26%), and the risk differences between abrupt discontinuation and stable dose were 0.33% (95% CI, −0.03%-0.74%). The risk ratios associated with taper vs. stable dosage and abrupt discontinuation vs. stable dosage were 1.15 (95% CI, 1.04-1.27) and 1.34 (95% CI, 0.97-1.79), respectively.
The adjusted cumulative incidence curves for overdose or suicide diverged at month 4 when comparing stable dosage and taper, with a higher incidence associated with the taper vs. stable dosage treatment strategies thereafter. However, when the researchers compared stable dosage with abrupt discontinuation, the event rates were similar.
A per protocol analysis, in which the researchers censored episodes involving lack of adherence to assigned treatment, yielded results similar to those of the main analysis.
“Policies establishing dosage thresholds or mandating tapers for all patients receiving long-term opioid therapy are not supported by existing data in terms of anticipated benefits even if, as we found, the rate of adverse outcomes is small,” the investigators write.
Instead, they encourage health care systems and clinicians to “continue to develop and implement patient-centered approaches to pain management for patients with established long-term opioid therapy.”
Protracted withdrawal?
Commenting on the study, A. Benjamin Srivastava, MD, assistant professor of clinical psychiatry, division on substance use disorders, Columbia University Medical Center, New York State Psychiatric Institute, New York, called the study “an important contribution to the literature” that “sheds further light on the risks associated with tapering.”
Dr. Srivastava, who was not involved with the research, noted that previous studies showing an increased prevalence of adverse events with tapering included participants with OUD or signs of opioid misuse, “potentially confounding findings.”
By contrast, the current study investigators specifically excluded patients with OUD/opioid misuse but still found a “slight increase in risk for opioid overdose and suicide, even when excluding for potential confounders,” he said.
Although causal implications require further investigation, “a source of these adverse outcomes may be unmanaged withdrawal that may be protracted,” Dr. Srivastava noted.
While abrupt discontinuation “may result in significant acute withdrawal symptoms, these should subside by 1-2 weeks at most,” he said.
Lowering the dose without discontinuation may lead to patients’ entering into “a dyshomeostatic state characterized by anxiety and dysphoria ... that may not be recognized by the prescribing clinician,” he added.
The brain “is still being primed by opioids [and] ‘wanting’ a higher dose. Thus, particular attention to withdrawal symptoms, both physical and psychiatric, is prudent when choosing to taper opioids vs. maintaining or discontinuing,” Dr. Srivastava said.
The study was funded by a grant from the CDC and a grant from the National Institute on Drug Abuse to one of the investigators. Dr. LaRochelle received grants from the CDC and NIDA during the conduct of the study and has received consulting fees for research paid to his institution from OptumLabs outside the submitted work. The other investigators’ disclosures are listed in the original article. Dr. Srivastava reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed data for almost 200,000 patients who did not have signs of opioid use disorder (OUD) and were receiving opioid treatment. The investigators compared three dosing strategies: abrupt withdrawal, gradual tapering, and continuation of the current stable dosage.
Results showed a higher adjusted cumulative incidence of opioid overdose or suicide events 11 months after baseline among participants for whom a tapered dosing strategy was utilized, compared with those who continued taking a stable dosage. The risk difference was 0.15% between taper and stable dosage and 0.33% between abrupt discontinuation and stable dosage.
“This study identified a small absolute increase in risk of harms associated with opioid tapering compared with a stable opioid dosage,” Marc LaRochelle, MD, MPH, assistant professor, Boston University, and colleagues write.
“These results do not suggest that policies of mandatory dosage tapering for individuals receiving a stable long-term opioid dosage without evidence of opioid misuse will reduce short-term harm via suicide and overdose,” they add.
The findings were published online in JAMA Network Open.
Benefits vs. harms
The investigators note that the Centers for Disease Control and Prevention, in its 2016 Guideline for Prescribing Opioids for Chronic Pain, “recommended tapering opioid dosages if benefits no longer outweigh harms.”
In response, “some health systems and U.S. states enacted stringent dose limits that were applied with few exceptions, regardless of individual patients’ risk of harms,” they write. By contrast, there have been “increasing reports of patients experiencing adverse effects from forced opioid tapers.”
Previous studies that identified harms associated with opioid tapering and discontinuation had several limitations, including a focus on discontinuation, which is “likely more destabilizing than gradual tapering,” the researchers write. There is also “a high potential for confounding” in these studies, they add.
The investigators sought to fill the research gap by drawing on 8-year data (Jan. 1, 2010, to Dec. 31, 2018) from a large database that includes adjudicated pharmacy, outpatient, and inpatient medical claims for individuals with commercial or Medicare Advantage insurance encompassing all 50 states, the District of Columbia, and Puerto Rico.
Notably, individuals who had received a diagnosis of substance use, abuse, or dependence or for whom there were indicators consistent with OUD were excluded.
The researchers compared the three treatment strategies during a 4-month treatment strategy assignment period (“grace period”) after baseline. Tapering was defined as “2 consecutive months with a mean MME [morphine milligram equivalent] reduction of 15% or more compared with the baseline month.”
All estimates were adjusted for potential confounders, including demographic and treatment characteristics, baseline year, region, insurance plan type, comorbid psychiatric and medical conditions, and the prescribing of other psychiatric medications, such as benzodiazepines, gabapentin, or pregabalin.
Patient-centered approaches
The final cohort that met inclusion criteria consisted of 199,836 individuals (45.1% men; mean age, 56.9 years). Of the total group, 57.6% were aged 45-64 years. There were 415,123 qualifying long-term opioid therapy episodes.
The largest percentage of the cohort (41.2%) were receiving a baseline mean MME of 50-89 mg/day, while 34% were receiving 90-199 mg/day and 23.5% were receiving at least 200 mg/day.
During the 6-month eligibility assessment period, 34.8% of the cohort were receiving benzodiazepine prescriptions, 18% had been diagnosed with comorbid anxiety, and 19.7% had been diagnosed with comorbid depression.
After the treatment assignment period, most treatment episodes (87.1%) were considered stable, 11.1% were considered a taper, and 1.8% were considered abrupt discontinuation.
Eleven months after baseline, the adjusted cumulative incidence of opioid overdose or suicide events was lowest for those who continued to receive a stable dose.
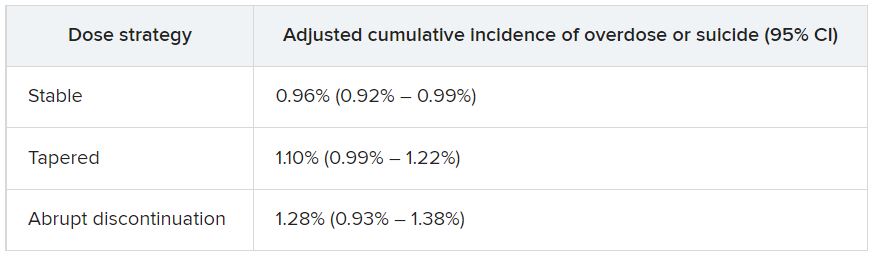
The risk differences between taper vs. stable dosage were 0.15% (95% confidence interval, 0.03%-0.26%), and the risk differences between abrupt discontinuation and stable dose were 0.33% (95% CI, −0.03%-0.74%). The risk ratios associated with taper vs. stable dosage and abrupt discontinuation vs. stable dosage were 1.15 (95% CI, 1.04-1.27) and 1.34 (95% CI, 0.97-1.79), respectively.
The adjusted cumulative incidence curves for overdose or suicide diverged at month 4 when comparing stable dosage and taper, with a higher incidence associated with the taper vs. stable dosage treatment strategies thereafter. However, when the researchers compared stable dosage with abrupt discontinuation, the event rates were similar.
A per protocol analysis, in which the researchers censored episodes involving lack of adherence to assigned treatment, yielded results similar to those of the main analysis.
“Policies establishing dosage thresholds or mandating tapers for all patients receiving long-term opioid therapy are not supported by existing data in terms of anticipated benefits even if, as we found, the rate of adverse outcomes is small,” the investigators write.
Instead, they encourage health care systems and clinicians to “continue to develop and implement patient-centered approaches to pain management for patients with established long-term opioid therapy.”
Protracted withdrawal?
Commenting on the study, A. Benjamin Srivastava, MD, assistant professor of clinical psychiatry, division on substance use disorders, Columbia University Medical Center, New York State Psychiatric Institute, New York, called the study “an important contribution to the literature” that “sheds further light on the risks associated with tapering.”
Dr. Srivastava, who was not involved with the research, noted that previous studies showing an increased prevalence of adverse events with tapering included participants with OUD or signs of opioid misuse, “potentially confounding findings.”
By contrast, the current study investigators specifically excluded patients with OUD/opioid misuse but still found a “slight increase in risk for opioid overdose and suicide, even when excluding for potential confounders,” he said.
Although causal implications require further investigation, “a source of these adverse outcomes may be unmanaged withdrawal that may be protracted,” Dr. Srivastava noted.
While abrupt discontinuation “may result in significant acute withdrawal symptoms, these should subside by 1-2 weeks at most,” he said.
Lowering the dose without discontinuation may lead to patients’ entering into “a dyshomeostatic state characterized by anxiety and dysphoria ... that may not be recognized by the prescribing clinician,” he added.
The brain “is still being primed by opioids [and] ‘wanting’ a higher dose. Thus, particular attention to withdrawal symptoms, both physical and psychiatric, is prudent when choosing to taper opioids vs. maintaining or discontinuing,” Dr. Srivastava said.
The study was funded by a grant from the CDC and a grant from the National Institute on Drug Abuse to one of the investigators. Dr. LaRochelle received grants from the CDC and NIDA during the conduct of the study and has received consulting fees for research paid to his institution from OptumLabs outside the submitted work. The other investigators’ disclosures are listed in the original article. Dr. Srivastava reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed data for almost 200,000 patients who did not have signs of opioid use disorder (OUD) and were receiving opioid treatment. The investigators compared three dosing strategies: abrupt withdrawal, gradual tapering, and continuation of the current stable dosage.
Results showed a higher adjusted cumulative incidence of opioid overdose or suicide events 11 months after baseline among participants for whom a tapered dosing strategy was utilized, compared with those who continued taking a stable dosage. The risk difference was 0.15% between taper and stable dosage and 0.33% between abrupt discontinuation and stable dosage.
“This study identified a small absolute increase in risk of harms associated with opioid tapering compared with a stable opioid dosage,” Marc LaRochelle, MD, MPH, assistant professor, Boston University, and colleagues write.
“These results do not suggest that policies of mandatory dosage tapering for individuals receiving a stable long-term opioid dosage without evidence of opioid misuse will reduce short-term harm via suicide and overdose,” they add.
The findings were published online in JAMA Network Open.
Benefits vs. harms
The investigators note that the Centers for Disease Control and Prevention, in its 2016 Guideline for Prescribing Opioids for Chronic Pain, “recommended tapering opioid dosages if benefits no longer outweigh harms.”
In response, “some health systems and U.S. states enacted stringent dose limits that were applied with few exceptions, regardless of individual patients’ risk of harms,” they write. By contrast, there have been “increasing reports of patients experiencing adverse effects from forced opioid tapers.”
Previous studies that identified harms associated with opioid tapering and discontinuation had several limitations, including a focus on discontinuation, which is “likely more destabilizing than gradual tapering,” the researchers write. There is also “a high potential for confounding” in these studies, they add.
The investigators sought to fill the research gap by drawing on 8-year data (Jan. 1, 2010, to Dec. 31, 2018) from a large database that includes adjudicated pharmacy, outpatient, and inpatient medical claims for individuals with commercial or Medicare Advantage insurance encompassing all 50 states, the District of Columbia, and Puerto Rico.
Notably, individuals who had received a diagnosis of substance use, abuse, or dependence or for whom there were indicators consistent with OUD were excluded.
The researchers compared the three treatment strategies during a 4-month treatment strategy assignment period (“grace period”) after baseline. Tapering was defined as “2 consecutive months with a mean MME [morphine milligram equivalent] reduction of 15% or more compared with the baseline month.”
All estimates were adjusted for potential confounders, including demographic and treatment characteristics, baseline year, region, insurance plan type, comorbid psychiatric and medical conditions, and the prescribing of other psychiatric medications, such as benzodiazepines, gabapentin, or pregabalin.
Patient-centered approaches
The final cohort that met inclusion criteria consisted of 199,836 individuals (45.1% men; mean age, 56.9 years). Of the total group, 57.6% were aged 45-64 years. There were 415,123 qualifying long-term opioid therapy episodes.
The largest percentage of the cohort (41.2%) were receiving a baseline mean MME of 50-89 mg/day, while 34% were receiving 90-199 mg/day and 23.5% were receiving at least 200 mg/day.
During the 6-month eligibility assessment period, 34.8% of the cohort were receiving benzodiazepine prescriptions, 18% had been diagnosed with comorbid anxiety, and 19.7% had been diagnosed with comorbid depression.
After the treatment assignment period, most treatment episodes (87.1%) were considered stable, 11.1% were considered a taper, and 1.8% were considered abrupt discontinuation.
Eleven months after baseline, the adjusted cumulative incidence of opioid overdose or suicide events was lowest for those who continued to receive a stable dose.
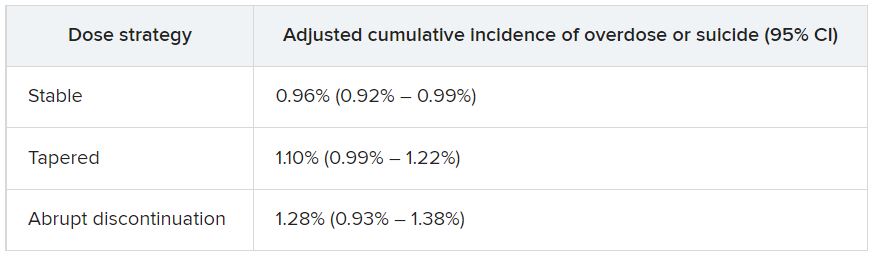
The risk differences between taper vs. stable dosage were 0.15% (95% confidence interval, 0.03%-0.26%), and the risk differences between abrupt discontinuation and stable dose were 0.33% (95% CI, −0.03%-0.74%). The risk ratios associated with taper vs. stable dosage and abrupt discontinuation vs. stable dosage were 1.15 (95% CI, 1.04-1.27) and 1.34 (95% CI, 0.97-1.79), respectively.
The adjusted cumulative incidence curves for overdose or suicide diverged at month 4 when comparing stable dosage and taper, with a higher incidence associated with the taper vs. stable dosage treatment strategies thereafter. However, when the researchers compared stable dosage with abrupt discontinuation, the event rates were similar.
A per protocol analysis, in which the researchers censored episodes involving lack of adherence to assigned treatment, yielded results similar to those of the main analysis.
“Policies establishing dosage thresholds or mandating tapers for all patients receiving long-term opioid therapy are not supported by existing data in terms of anticipated benefits even if, as we found, the rate of adverse outcomes is small,” the investigators write.
Instead, they encourage health care systems and clinicians to “continue to develop and implement patient-centered approaches to pain management for patients with established long-term opioid therapy.”
Protracted withdrawal?
Commenting on the study, A. Benjamin Srivastava, MD, assistant professor of clinical psychiatry, division on substance use disorders, Columbia University Medical Center, New York State Psychiatric Institute, New York, called the study “an important contribution to the literature” that “sheds further light on the risks associated with tapering.”
Dr. Srivastava, who was not involved with the research, noted that previous studies showing an increased prevalence of adverse events with tapering included participants with OUD or signs of opioid misuse, “potentially confounding findings.”
By contrast, the current study investigators specifically excluded patients with OUD/opioid misuse but still found a “slight increase in risk for opioid overdose and suicide, even when excluding for potential confounders,” he said.
Although causal implications require further investigation, “a source of these adverse outcomes may be unmanaged withdrawal that may be protracted,” Dr. Srivastava noted.
While abrupt discontinuation “may result in significant acute withdrawal symptoms, these should subside by 1-2 weeks at most,” he said.
Lowering the dose without discontinuation may lead to patients’ entering into “a dyshomeostatic state characterized by anxiety and dysphoria ... that may not be recognized by the prescribing clinician,” he added.
The brain “is still being primed by opioids [and] ‘wanting’ a higher dose. Thus, particular attention to withdrawal symptoms, both physical and psychiatric, is prudent when choosing to taper opioids vs. maintaining or discontinuing,” Dr. Srivastava said.
The study was funded by a grant from the CDC and a grant from the National Institute on Drug Abuse to one of the investigators. Dr. LaRochelle received grants from the CDC and NIDA during the conduct of the study and has received consulting fees for research paid to his institution from OptumLabs outside the submitted work. The other investigators’ disclosures are listed in the original article. Dr. Srivastava reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Psychedelic drug therapy a potential ‘breakthrough’ for alcohol dependence
Results from the first randomized, placebo-controlled trial of psilocybin for alcohol dependence showed that during the 8 months after first treatment dose, participants who received psilocybin had less than half as many heavy drinking days as their counterparts who received placebo.
In addition, 7 months after the last dose of medication, twice as many psilocybin-treated patients as placebo-treated patients were abstinent.
The effects observed with psilocybin were “considerably larger” than those of currently approved treatments for AUD, senior investigator Michael Bogenschutz, MD, psychiatrist and director of the NYU Langone Center for Psychedelic Medicine, New York, said during an Aug. 24 press briefing.
If the findings hold up in future trials, psilocybin will be a “real breakthrough” in the treatment of the condition, Dr. Bogenschutz said.
The findings were published online in JAMA Psychiatry.
83% reduction in drinking days
The study included 93 adults (mean age, 46 years) with alcohol dependence who consumed an average of seven drinks on the days they drank and had had at least four heavy drinking days during the month prior to treatment.
Of the participants, 48 were randomly assigned to receive two doses of psilocybin, and 45 were assigned to receive an antihistamine (diphenhydramine) placebo. Study medication was administered during 2 day-long sessions at week 4 and week 8.
The participants also received 12 psychotherapy sessions over a 12-week period. All were assessed at intervals from the beginning of the study until 32 weeks after the first medication session.
The primary outcome was percentage of days in which the patient drank heavily during the 32-week period following first medication dose. Heavy drinking was defined as having five or more drinks in a day for a man and four or more drinks in a day for a woman.
The percentage of heavy drinking days during the 32-week period was 9.7% for the psilocybin group and 23.6% for the placebo group, for a mean difference of 13.9% (P = .01).
“Compared to their baseline before the study, after receiving medication, the psilocybin group decreased their heavy drinking days by 83%, while the placebo group reduced their heavy drinking by 51%,” Dr. Bogenschutz reported.
During the last month of follow-up, which was 7 months after the final dose of study medication, 48% of the psilocybin group were entirely abstinent vs. 24% of the placebo group.
“It is remarkable that the effects of psilocybin treatment persisted for 7 months after people received the last dose of medication. This suggests that psilocybin is treating the underlying disorder of alcohol addiction rather than merely treating symptoms,” Dr. Bogenschutz noted.
Total alcohol consumption and problems related to alcohol use were also significantly less in the psilocybin group.
‘Encouraged and hopeful’
Adverse events related to psilocybin were mostly mild, self-limiting, and consistent with other recent trials that evaluated the drug’s effects in various conditions.
However, the current investigators note that they implemented measures to ensure safety, including careful medical and psychiatric screening, therapy, and monitoring that was provided by well-trained therapists, including a licensed psychiatrist. In addition, medications were available to treat acute psychiatric reactions.
A cited limitation of the study was that blinding was not maintained because the average intensity of experience with psilocybin was high, whereas it was low with diphenhydramine.
This difference undermined the masking of treatment such that more than 90% of participants and therapists correctly guessed the treatment assignment.
Another limitation was that objective measures to validate self-reported drinking outcomes were available for only 54% of study participants.
Despite these limitations, the study builds on earlier work by the NYU team that showed that two doses of psilocybin taken over a period of 8 weeks significantly reduced alcohol use and cravings in patients with AUD.
“We’re very encouraged by these findings and hopeful about where they could lead. Personally, it’s been very meaningful and rewarding for me to do this work and inspiring to witness the remarkable recoveries that some of our participants have experienced,” Dr. Bogenschutz told briefing attendees.
Urgent need
The authors of an accompanying editorial note that novel medications for alcohol dependence are “sorely needed. Recent renewed interest in the potential of hallucinogens for treating psychiatric disorders, including AUD, represents a potential move in that direction.”
Henry Kranzler, MD, and Emily Hartwell, PhD, both with the Center for Studies of Addiction, University of Pennsylvania, Philadelphia, write that the new findings “underscore the potential of developing psilocybin as an addition to the alcohol treatment pharmacopeia.”
They question, however, the feasibility of using hallucinogens in routine clinical practice because intensive psychotherapy, such as that provided in this study, requires a significant investment of time and labor.
“Such concomitant therapy, if necessary to realize the therapeutic benefits of psilocybin for treating AUD, could limit its uptake by clinicians,” Dr. Kranzler and Dr. Hartwell write.
The study was funded by the Heffter Research Institute and by individual donations from Carey and Claudia Turnbull, Dr. Efrem Nulman, Rodrigo Niño, and Cody Swift. Dr. Bogenschutz reports having received research funds from and serving as a consultant to Mind Medicine, the Multidisciplinary Association for Psychedelic Studies, B. More, AJNA Labs, Beckley Psytech, Journey Colab, and Bright Minds Biosciences. Dr. Kranzler and Dr. Hartwell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from the first randomized, placebo-controlled trial of psilocybin for alcohol dependence showed that during the 8 months after first treatment dose, participants who received psilocybin had less than half as many heavy drinking days as their counterparts who received placebo.
In addition, 7 months after the last dose of medication, twice as many psilocybin-treated patients as placebo-treated patients were abstinent.
The effects observed with psilocybin were “considerably larger” than those of currently approved treatments for AUD, senior investigator Michael Bogenschutz, MD, psychiatrist and director of the NYU Langone Center for Psychedelic Medicine, New York, said during an Aug. 24 press briefing.
If the findings hold up in future trials, psilocybin will be a “real breakthrough” in the treatment of the condition, Dr. Bogenschutz said.
The findings were published online in JAMA Psychiatry.
83% reduction in drinking days
The study included 93 adults (mean age, 46 years) with alcohol dependence who consumed an average of seven drinks on the days they drank and had had at least four heavy drinking days during the month prior to treatment.
Of the participants, 48 were randomly assigned to receive two doses of psilocybin, and 45 were assigned to receive an antihistamine (diphenhydramine) placebo. Study medication was administered during 2 day-long sessions at week 4 and week 8.
The participants also received 12 psychotherapy sessions over a 12-week period. All were assessed at intervals from the beginning of the study until 32 weeks after the first medication session.
The primary outcome was percentage of days in which the patient drank heavily during the 32-week period following first medication dose. Heavy drinking was defined as having five or more drinks in a day for a man and four or more drinks in a day for a woman.
The percentage of heavy drinking days during the 32-week period was 9.7% for the psilocybin group and 23.6% for the placebo group, for a mean difference of 13.9% (P = .01).
“Compared to their baseline before the study, after receiving medication, the psilocybin group decreased their heavy drinking days by 83%, while the placebo group reduced their heavy drinking by 51%,” Dr. Bogenschutz reported.
During the last month of follow-up, which was 7 months after the final dose of study medication, 48% of the psilocybin group were entirely abstinent vs. 24% of the placebo group.
“It is remarkable that the effects of psilocybin treatment persisted for 7 months after people received the last dose of medication. This suggests that psilocybin is treating the underlying disorder of alcohol addiction rather than merely treating symptoms,” Dr. Bogenschutz noted.
Total alcohol consumption and problems related to alcohol use were also significantly less in the psilocybin group.
‘Encouraged and hopeful’
Adverse events related to psilocybin were mostly mild, self-limiting, and consistent with other recent trials that evaluated the drug’s effects in various conditions.
However, the current investigators note that they implemented measures to ensure safety, including careful medical and psychiatric screening, therapy, and monitoring that was provided by well-trained therapists, including a licensed psychiatrist. In addition, medications were available to treat acute psychiatric reactions.
A cited limitation of the study was that blinding was not maintained because the average intensity of experience with psilocybin was high, whereas it was low with diphenhydramine.
This difference undermined the masking of treatment such that more than 90% of participants and therapists correctly guessed the treatment assignment.
Another limitation was that objective measures to validate self-reported drinking outcomes were available for only 54% of study participants.
Despite these limitations, the study builds on earlier work by the NYU team that showed that two doses of psilocybin taken over a period of 8 weeks significantly reduced alcohol use and cravings in patients with AUD.
“We’re very encouraged by these findings and hopeful about where they could lead. Personally, it’s been very meaningful and rewarding for me to do this work and inspiring to witness the remarkable recoveries that some of our participants have experienced,” Dr. Bogenschutz told briefing attendees.
Urgent need
The authors of an accompanying editorial note that novel medications for alcohol dependence are “sorely needed. Recent renewed interest in the potential of hallucinogens for treating psychiatric disorders, including AUD, represents a potential move in that direction.”
Henry Kranzler, MD, and Emily Hartwell, PhD, both with the Center for Studies of Addiction, University of Pennsylvania, Philadelphia, write that the new findings “underscore the potential of developing psilocybin as an addition to the alcohol treatment pharmacopeia.”
They question, however, the feasibility of using hallucinogens in routine clinical practice because intensive psychotherapy, such as that provided in this study, requires a significant investment of time and labor.
“Such concomitant therapy, if necessary to realize the therapeutic benefits of psilocybin for treating AUD, could limit its uptake by clinicians,” Dr. Kranzler and Dr. Hartwell write.
The study was funded by the Heffter Research Institute and by individual donations from Carey and Claudia Turnbull, Dr. Efrem Nulman, Rodrigo Niño, and Cody Swift. Dr. Bogenschutz reports having received research funds from and serving as a consultant to Mind Medicine, the Multidisciplinary Association for Psychedelic Studies, B. More, AJNA Labs, Beckley Psytech, Journey Colab, and Bright Minds Biosciences. Dr. Kranzler and Dr. Hartwell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from the first randomized, placebo-controlled trial of psilocybin for alcohol dependence showed that during the 8 months after first treatment dose, participants who received psilocybin had less than half as many heavy drinking days as their counterparts who received placebo.
In addition, 7 months after the last dose of medication, twice as many psilocybin-treated patients as placebo-treated patients were abstinent.
The effects observed with psilocybin were “considerably larger” than those of currently approved treatments for AUD, senior investigator Michael Bogenschutz, MD, psychiatrist and director of the NYU Langone Center for Psychedelic Medicine, New York, said during an Aug. 24 press briefing.
If the findings hold up in future trials, psilocybin will be a “real breakthrough” in the treatment of the condition, Dr. Bogenschutz said.
The findings were published online in JAMA Psychiatry.
83% reduction in drinking days
The study included 93 adults (mean age, 46 years) with alcohol dependence who consumed an average of seven drinks on the days they drank and had had at least four heavy drinking days during the month prior to treatment.
Of the participants, 48 were randomly assigned to receive two doses of psilocybin, and 45 were assigned to receive an antihistamine (diphenhydramine) placebo. Study medication was administered during 2 day-long sessions at week 4 and week 8.
The participants also received 12 psychotherapy sessions over a 12-week period. All were assessed at intervals from the beginning of the study until 32 weeks after the first medication session.
The primary outcome was percentage of days in which the patient drank heavily during the 32-week period following first medication dose. Heavy drinking was defined as having five or more drinks in a day for a man and four or more drinks in a day for a woman.
The percentage of heavy drinking days during the 32-week period was 9.7% for the psilocybin group and 23.6% for the placebo group, for a mean difference of 13.9% (P = .01).
“Compared to their baseline before the study, after receiving medication, the psilocybin group decreased their heavy drinking days by 83%, while the placebo group reduced their heavy drinking by 51%,” Dr. Bogenschutz reported.
During the last month of follow-up, which was 7 months after the final dose of study medication, 48% of the psilocybin group were entirely abstinent vs. 24% of the placebo group.
“It is remarkable that the effects of psilocybin treatment persisted for 7 months after people received the last dose of medication. This suggests that psilocybin is treating the underlying disorder of alcohol addiction rather than merely treating symptoms,” Dr. Bogenschutz noted.
Total alcohol consumption and problems related to alcohol use were also significantly less in the psilocybin group.
‘Encouraged and hopeful’
Adverse events related to psilocybin were mostly mild, self-limiting, and consistent with other recent trials that evaluated the drug’s effects in various conditions.
However, the current investigators note that they implemented measures to ensure safety, including careful medical and psychiatric screening, therapy, and monitoring that was provided by well-trained therapists, including a licensed psychiatrist. In addition, medications were available to treat acute psychiatric reactions.
A cited limitation of the study was that blinding was not maintained because the average intensity of experience with psilocybin was high, whereas it was low with diphenhydramine.
This difference undermined the masking of treatment such that more than 90% of participants and therapists correctly guessed the treatment assignment.
Another limitation was that objective measures to validate self-reported drinking outcomes were available for only 54% of study participants.
Despite these limitations, the study builds on earlier work by the NYU team that showed that two doses of psilocybin taken over a period of 8 weeks significantly reduced alcohol use and cravings in patients with AUD.
“We’re very encouraged by these findings and hopeful about where they could lead. Personally, it’s been very meaningful and rewarding for me to do this work and inspiring to witness the remarkable recoveries that some of our participants have experienced,” Dr. Bogenschutz told briefing attendees.
Urgent need
The authors of an accompanying editorial note that novel medications for alcohol dependence are “sorely needed. Recent renewed interest in the potential of hallucinogens for treating psychiatric disorders, including AUD, represents a potential move in that direction.”
Henry Kranzler, MD, and Emily Hartwell, PhD, both with the Center for Studies of Addiction, University of Pennsylvania, Philadelphia, write that the new findings “underscore the potential of developing psilocybin as an addition to the alcohol treatment pharmacopeia.”
They question, however, the feasibility of using hallucinogens in routine clinical practice because intensive psychotherapy, such as that provided in this study, requires a significant investment of time and labor.
“Such concomitant therapy, if necessary to realize the therapeutic benefits of psilocybin for treating AUD, could limit its uptake by clinicians,” Dr. Kranzler and Dr. Hartwell write.
The study was funded by the Heffter Research Institute and by individual donations from Carey and Claudia Turnbull, Dr. Efrem Nulman, Rodrigo Niño, and Cody Swift. Dr. Bogenschutz reports having received research funds from and serving as a consultant to Mind Medicine, the Multidisciplinary Association for Psychedelic Studies, B. More, AJNA Labs, Beckley Psytech, Journey Colab, and Bright Minds Biosciences. Dr. Kranzler and Dr. Hartwell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Adult ADHD improved by home-based, noninvasive brain stimulation
Results from the sham-controlled trial also showed that the tDCS treatment was both safe and well tolerated.
Overall, the findings suggest that the device could be a nondrug alternative for treating this patient population, Douglas Teixeira Leffa, MD, PhD, department of psychiatry, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil, and colleagues note.
“This is particularly relevant since a vast body of literature describes low long-term adherence rates and persistence to pharmacological treatment in patients with ADHD,” they write.
The findings were published online in JAMA Psychiatry.
Avoiding office visits
A noninvasive technique that is easy to use and relatively inexpensive, tDCS involves applying a low-intensity current over the scalp to modulate cortical excitability and induce neuroplasticity. Home-use tDCS devices, which avoid the need for daily office visits for stimulation sessions, have been validated in previous clinical samples.
The current study included 64 adults with ADHD who are not taking stimulants. They had moderate or severe symptoms of inattention, with an inattention score of 21 or higher on the clinician-administered Adult ADHD Self-Report Scale version 1.1 (CASRS).
The CASRS includes nine questions related to inattention symptoms (CASRS-I) and nine related to hyperactivity-impulsivity symptoms (CASRS-HI). The score can vary from 0 to 36 for each domain, with higher scores indicating increased symptoms.
Researchers randomly assigned participants to receive either active or sham stimulation.
The tDCS device used in the study delivered a current with 35-cm2 electrodes (7 cm by 5 cm). The anodal and cathodal electrodes were positioned corresponding to the right and left dorsolateral prefrontal cortex (DLPFC), respectively.
The investigators note that decreased activation in the right DLPFC has been reported before in patients with ADHD during tasks that require attention.
After learning to use the device, participants underwent 30-minute daily sessions of tDCS (2-mA direct constant current) for 4 weeks for a total of 28 sessions.
Devices programmed for sham treatment delivered a 30-second ramp-up (0-2 mA) stimulation followed by a 30-second ramp-down (2-0 mA) at the beginning, middle, and end of the application. This mimicked the tactile sensations reported with tDCS and has been shown to be a reliable sham protocol.
Participants were encouraged to perform the stimulation sessions at the same time of day. To improve adherence, they received daily text message reminders.
Nine patients discontinued treatment, two in the sham group and seven in the active group. However, patients who finished the trial completed a mean 25 of 28 sessions.
Window of opportunity?
The mean inattention score on CASRS-I at week 4, the primary outcome, was 18.88 in the active tDCS group vs. 23.63 in the sham tDCS group. There was a statistically significant treatment by time interaction for CASRS-I (beta interaction, –3.18; 95% confidence interval, –4.60 to –1.75; P < .001), showing decreased inattention symptoms in the active vs. sham groups.
The estimated Cohen’s d was 1.23 (95% CI, .67-1.78), indicating at least a moderate effect. This effect was similar to that reported with trigeminal nerve stimulation (TNS), the first approved device-based therapy for ADHD, and to that of atomoxetine, the second-line treatment for ADHD, the researchers note.
About one-third of patients (34.3%) in the active tDCS group achieved a 30% reduction in CASRS-I score, compared with 6.2% in the sham tDCS group.
There was no statistically significant difference in the secondary outcome of hyperactivity-impulsivity symptoms evaluated with the CASRS-HI. This may be because hyperactivity-impulsivity in ADHD is associated with a hypoactivation in the right inferior frontal cortex rather than the right DLPFC, the investigators write.
There were also no significant group differences in other secondary outcomes, including depression, anxiety, and executive function.
Adverse events (AE) were mostly mild and included skin redness and scalp burn. There were no severe or serious AEs.
Using a home-based tDCS device allows for considerably more sessions, with 28 being the highest number so far applied to patients with ADHD. This, the researchers note, is important because evidence suggests increased efficacy of tDCS with extended periods of treatment.
The home-based device “opens a new window of opportunity, especially for participants who live in geographically remote areas or have physical or cognitive disabilities that may hinder access to clinical centers,” they write.
Although a study limitation was the relatively high dropout rate in the active group, which might bias interpretation of the findings, only two of seven dropouts in the active group left because of an AE, the investigators note.
Patients received training in using the device, but there was no remote monitoring of sessions. In addition, the study population, which was relatively homogeneous with participants having no moderate to severe symptoms of depression or anxiety, differed from the usual patients with ADHD who are treated in clinical centers, the researchers point out.
As well, the study included only patients not taking pharmacologic treatment for ADHD – so the findings might not be generalizable to other patients, they add.
‘Just a first step’
Commenting on the study, Mark George, MD, distinguished professor of psychiatry, radiology, and neurology, Medical University of South Carolina, Charleston, noted that although this was a single-center study with a relatively small sample size, it is still important.
Showing it is possible to do high-quality tDCS studies at home “is a huge advance,” said Dr. George, who was not involved with the research.
“Home treatment is cheaper and easier for patients and allows many people to get treatment who would not be able to make it to the clinic daily for treatment,” he added.
He noted the study showed “a clear improvement in ADHD,” which is important because better treatments are needed.
However, he cautioned that this is “just a first step” and more studies are needed. For example, he said, it is not clear whether improvements persist and if patients need to self-treat forever, as they would with a medication.
Dr. George also noted that although the study used “a pioneering research device” with several safety features, many home-based tDCS devices on the market do not have those.
“I don’t advise patients to do this now. Further studies are needed for FDA approval and general public use,” he said.
The study was funded by the National Council for Scientific and Technological Development, the Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul, the Brain & Behavior Research Foundation, Fundação de Amparo à Pesquisa do Estado de São Paulo, and the Brazilian Innovation Agency. Dr. Leffa reported having received grants from the Brain & Behavior Research Foundation, the National Council for Scientific and Technological Development, and Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul during the conduction of the study. Dr. George reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from the sham-controlled trial also showed that the tDCS treatment was both safe and well tolerated.
Overall, the findings suggest that the device could be a nondrug alternative for treating this patient population, Douglas Teixeira Leffa, MD, PhD, department of psychiatry, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil, and colleagues note.
“This is particularly relevant since a vast body of literature describes low long-term adherence rates and persistence to pharmacological treatment in patients with ADHD,” they write.
The findings were published online in JAMA Psychiatry.
Avoiding office visits
A noninvasive technique that is easy to use and relatively inexpensive, tDCS involves applying a low-intensity current over the scalp to modulate cortical excitability and induce neuroplasticity. Home-use tDCS devices, which avoid the need for daily office visits for stimulation sessions, have been validated in previous clinical samples.
The current study included 64 adults with ADHD who are not taking stimulants. They had moderate or severe symptoms of inattention, with an inattention score of 21 or higher on the clinician-administered Adult ADHD Self-Report Scale version 1.1 (CASRS).
The CASRS includes nine questions related to inattention symptoms (CASRS-I) and nine related to hyperactivity-impulsivity symptoms (CASRS-HI). The score can vary from 0 to 36 for each domain, with higher scores indicating increased symptoms.
Researchers randomly assigned participants to receive either active or sham stimulation.
The tDCS device used in the study delivered a current with 35-cm2 electrodes (7 cm by 5 cm). The anodal and cathodal electrodes were positioned corresponding to the right and left dorsolateral prefrontal cortex (DLPFC), respectively.
The investigators note that decreased activation in the right DLPFC has been reported before in patients with ADHD during tasks that require attention.
After learning to use the device, participants underwent 30-minute daily sessions of tDCS (2-mA direct constant current) for 4 weeks for a total of 28 sessions.
Devices programmed for sham treatment delivered a 30-second ramp-up (0-2 mA) stimulation followed by a 30-second ramp-down (2-0 mA) at the beginning, middle, and end of the application. This mimicked the tactile sensations reported with tDCS and has been shown to be a reliable sham protocol.
Participants were encouraged to perform the stimulation sessions at the same time of day. To improve adherence, they received daily text message reminders.
Nine patients discontinued treatment, two in the sham group and seven in the active group. However, patients who finished the trial completed a mean 25 of 28 sessions.
Window of opportunity?
The mean inattention score on CASRS-I at week 4, the primary outcome, was 18.88 in the active tDCS group vs. 23.63 in the sham tDCS group. There was a statistically significant treatment by time interaction for CASRS-I (beta interaction, –3.18; 95% confidence interval, –4.60 to –1.75; P < .001), showing decreased inattention symptoms in the active vs. sham groups.
The estimated Cohen’s d was 1.23 (95% CI, .67-1.78), indicating at least a moderate effect. This effect was similar to that reported with trigeminal nerve stimulation (TNS), the first approved device-based therapy for ADHD, and to that of atomoxetine, the second-line treatment for ADHD, the researchers note.
About one-third of patients (34.3%) in the active tDCS group achieved a 30% reduction in CASRS-I score, compared with 6.2% in the sham tDCS group.
There was no statistically significant difference in the secondary outcome of hyperactivity-impulsivity symptoms evaluated with the CASRS-HI. This may be because hyperactivity-impulsivity in ADHD is associated with a hypoactivation in the right inferior frontal cortex rather than the right DLPFC, the investigators write.
There were also no significant group differences in other secondary outcomes, including depression, anxiety, and executive function.
Adverse events (AE) were mostly mild and included skin redness and scalp burn. There were no severe or serious AEs.
Using a home-based tDCS device allows for considerably more sessions, with 28 being the highest number so far applied to patients with ADHD. This, the researchers note, is important because evidence suggests increased efficacy of tDCS with extended periods of treatment.
The home-based device “opens a new window of opportunity, especially for participants who live in geographically remote areas or have physical or cognitive disabilities that may hinder access to clinical centers,” they write.
Although a study limitation was the relatively high dropout rate in the active group, which might bias interpretation of the findings, only two of seven dropouts in the active group left because of an AE, the investigators note.
Patients received training in using the device, but there was no remote monitoring of sessions. In addition, the study population, which was relatively homogeneous with participants having no moderate to severe symptoms of depression or anxiety, differed from the usual patients with ADHD who are treated in clinical centers, the researchers point out.
As well, the study included only patients not taking pharmacologic treatment for ADHD – so the findings might not be generalizable to other patients, they add.
‘Just a first step’
Commenting on the study, Mark George, MD, distinguished professor of psychiatry, radiology, and neurology, Medical University of South Carolina, Charleston, noted that although this was a single-center study with a relatively small sample size, it is still important.
Showing it is possible to do high-quality tDCS studies at home “is a huge advance,” said Dr. George, who was not involved with the research.
“Home treatment is cheaper and easier for patients and allows many people to get treatment who would not be able to make it to the clinic daily for treatment,” he added.
He noted the study showed “a clear improvement in ADHD,” which is important because better treatments are needed.
However, he cautioned that this is “just a first step” and more studies are needed. For example, he said, it is not clear whether improvements persist and if patients need to self-treat forever, as they would with a medication.
Dr. George also noted that although the study used “a pioneering research device” with several safety features, many home-based tDCS devices on the market do not have those.
“I don’t advise patients to do this now. Further studies are needed for FDA approval and general public use,” he said.
The study was funded by the National Council for Scientific and Technological Development, the Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul, the Brain & Behavior Research Foundation, Fundação de Amparo à Pesquisa do Estado de São Paulo, and the Brazilian Innovation Agency. Dr. Leffa reported having received grants from the Brain & Behavior Research Foundation, the National Council for Scientific and Technological Development, and Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul during the conduction of the study. Dr. George reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from the sham-controlled trial also showed that the tDCS treatment was both safe and well tolerated.
Overall, the findings suggest that the device could be a nondrug alternative for treating this patient population, Douglas Teixeira Leffa, MD, PhD, department of psychiatry, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil, and colleagues note.
“This is particularly relevant since a vast body of literature describes low long-term adherence rates and persistence to pharmacological treatment in patients with ADHD,” they write.
The findings were published online in JAMA Psychiatry.
Avoiding office visits
A noninvasive technique that is easy to use and relatively inexpensive, tDCS involves applying a low-intensity current over the scalp to modulate cortical excitability and induce neuroplasticity. Home-use tDCS devices, which avoid the need for daily office visits for stimulation sessions, have been validated in previous clinical samples.
The current study included 64 adults with ADHD who are not taking stimulants. They had moderate or severe symptoms of inattention, with an inattention score of 21 or higher on the clinician-administered Adult ADHD Self-Report Scale version 1.1 (CASRS).
The CASRS includes nine questions related to inattention symptoms (CASRS-I) and nine related to hyperactivity-impulsivity symptoms (CASRS-HI). The score can vary from 0 to 36 for each domain, with higher scores indicating increased symptoms.
Researchers randomly assigned participants to receive either active or sham stimulation.
The tDCS device used in the study delivered a current with 35-cm2 electrodes (7 cm by 5 cm). The anodal and cathodal electrodes were positioned corresponding to the right and left dorsolateral prefrontal cortex (DLPFC), respectively.
The investigators note that decreased activation in the right DLPFC has been reported before in patients with ADHD during tasks that require attention.
After learning to use the device, participants underwent 30-minute daily sessions of tDCS (2-mA direct constant current) for 4 weeks for a total of 28 sessions.
Devices programmed for sham treatment delivered a 30-second ramp-up (0-2 mA) stimulation followed by a 30-second ramp-down (2-0 mA) at the beginning, middle, and end of the application. This mimicked the tactile sensations reported with tDCS and has been shown to be a reliable sham protocol.
Participants were encouraged to perform the stimulation sessions at the same time of day. To improve adherence, they received daily text message reminders.
Nine patients discontinued treatment, two in the sham group and seven in the active group. However, patients who finished the trial completed a mean 25 of 28 sessions.
Window of opportunity?
The mean inattention score on CASRS-I at week 4, the primary outcome, was 18.88 in the active tDCS group vs. 23.63 in the sham tDCS group. There was a statistically significant treatment by time interaction for CASRS-I (beta interaction, –3.18; 95% confidence interval, –4.60 to –1.75; P < .001), showing decreased inattention symptoms in the active vs. sham groups.
The estimated Cohen’s d was 1.23 (95% CI, .67-1.78), indicating at least a moderate effect. This effect was similar to that reported with trigeminal nerve stimulation (TNS), the first approved device-based therapy for ADHD, and to that of atomoxetine, the second-line treatment for ADHD, the researchers note.
About one-third of patients (34.3%) in the active tDCS group achieved a 30% reduction in CASRS-I score, compared with 6.2% in the sham tDCS group.
There was no statistically significant difference in the secondary outcome of hyperactivity-impulsivity symptoms evaluated with the CASRS-HI. This may be because hyperactivity-impulsivity in ADHD is associated with a hypoactivation in the right inferior frontal cortex rather than the right DLPFC, the investigators write.
There were also no significant group differences in other secondary outcomes, including depression, anxiety, and executive function.
Adverse events (AE) were mostly mild and included skin redness and scalp burn. There were no severe or serious AEs.
Using a home-based tDCS device allows for considerably more sessions, with 28 being the highest number so far applied to patients with ADHD. This, the researchers note, is important because evidence suggests increased efficacy of tDCS with extended periods of treatment.
The home-based device “opens a new window of opportunity, especially for participants who live in geographically remote areas or have physical or cognitive disabilities that may hinder access to clinical centers,” they write.
Although a study limitation was the relatively high dropout rate in the active group, which might bias interpretation of the findings, only two of seven dropouts in the active group left because of an AE, the investigators note.
Patients received training in using the device, but there was no remote monitoring of sessions. In addition, the study population, which was relatively homogeneous with participants having no moderate to severe symptoms of depression or anxiety, differed from the usual patients with ADHD who are treated in clinical centers, the researchers point out.
As well, the study included only patients not taking pharmacologic treatment for ADHD – so the findings might not be generalizable to other patients, they add.
‘Just a first step’
Commenting on the study, Mark George, MD, distinguished professor of psychiatry, radiology, and neurology, Medical University of South Carolina, Charleston, noted that although this was a single-center study with a relatively small sample size, it is still important.
Showing it is possible to do high-quality tDCS studies at home “is a huge advance,” said Dr. George, who was not involved with the research.
“Home treatment is cheaper and easier for patients and allows many people to get treatment who would not be able to make it to the clinic daily for treatment,” he added.
He noted the study showed “a clear improvement in ADHD,” which is important because better treatments are needed.
However, he cautioned that this is “just a first step” and more studies are needed. For example, he said, it is not clear whether improvements persist and if patients need to self-treat forever, as they would with a medication.
Dr. George also noted that although the study used “a pioneering research device” with several safety features, many home-based tDCS devices on the market do not have those.
“I don’t advise patients to do this now. Further studies are needed for FDA approval and general public use,” he said.
The study was funded by the National Council for Scientific and Technological Development, the Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul, the Brain & Behavior Research Foundation, Fundação de Amparo à Pesquisa do Estado de São Paulo, and the Brazilian Innovation Agency. Dr. Leffa reported having received grants from the Brain & Behavior Research Foundation, the National Council for Scientific and Technological Development, and Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul during the conduction of the study. Dr. George reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
‘I missed it’: Coping with medical error
Thursday night
It was 9 o’clock at night when my phone rang. I didn’t recognize the number but decided to answer it anyway. It was my doctor.
“Chase, I got your labs back and you have a critically low level. I spoke with someone at the hospital, I think I know what is happening, but I need you to go to the pharmacy right now and get a medicine.” She explained further and as I listened electric currents ran through my thighs until I could barely feel my legs.
“I’m so sorry, Chase. I missed it. It was low the last time we did your labs 9 months ago, and I missed it.”
In disbelief, I continued to listen as she instructed me about the next steps I was to take and prepared me for what was to come the next day.
“If you notice any changes overnight, go straight to the ED.”
My chest tingled and I could barely breathe. My mind struggled to comprehend what was happening. I looked at my husband sitting close by on the couch. He looked concerned. I tuned back in and heard her say: “Is your husband there? Can I talk to him?”
“Yes,” is all I could manage, and I handed him the phone. I sat while he listened and asked his questions. My breathing came back under my control, my legs felt wiry, and restlessness set in. “I have to get out of here,” I thought. “I have to go and pick up this medicine.”
Monday afternoon
I am sitting across from a PGY3 resident I have been treating since his intern year, as part of his treatment plan for managing a chronic mental illness that began in medical school. Earlier in the day, I received an urgent message from him requesting an emergency appointment.
Within a few minutes of sitting down, the story from his weekend call shift tumbled out of him. His speech became pressured, and his eyes welled with tears as he recounted in detail the steps he had taken to care for a very sick patient overnight.
“I missed it.” The dam broke and he sat sobbing in front of me, his body trembling.
I sat silently across from him. Willing him to breathe.
In time, his breathing came back under his control, and he slowly regained his composure. He continued: “I got the imaging, and I missed a bleed.”
Failure and shame
I can recall memorable moments from my training when I came to understand that what I initially perceived to be a mistake was instead part of the work. An example from our practice involves a patient whom I was comanaging with her primary care provider (PCP). She was not doing well following a critical work event. When I met with her after the event, she admitted having thoughts of suicide, refused a voluntary inpatient admission, and would not have met criteria for an involuntary admission. My hands were tied.
Together we created a plan to keep her safe, which included paging her PCP after hours if needed. I told her PCP before leaving that night that he might hear from her and that if she reached out, she would require hospitalization.
I arrived at work the following day, and her PCP shared with me that our patient had overdosed on medication, paged him, and was admitted to the unit.
He seemed forlorn.
I was both relieved by the news and confused by his reaction. I had hoped that she would choose a higher level of care than what we could provide her as an outpatient. I said: “This is good. She followed the plan.”
Her overdose was, of course, not part of the plan. She was struggling with several internal conflicts, including having mixed feelings about coming into the hospital; but, when the critical moment happened and she was faced with a decision to call for help or possibly die, she chose to call her PCP and have him paged as we had talked about.
I looked at her PCP. “You helped get her to where she needed to be.”
In the years of working side by side with medically trained colleagues, I have time and again needed to reframe for them that what they perceive to be a “failure” or a “crisis” is often a catalyst for change. The patient I comanaged with the PCP was a highly skilled caregiver and, as such, had been having a hard time asking for help. The hospitalization that her PCP facilitated allowed her to receive the care she needed and created an opportunity for family and friends to show up for her. Their support fed her, and she only made gains from that point on.
My training had taught me that respecting a patient’s autonomy was of the utmost importance. This instills confidence in patients as the authority in their lives. For a clinician to do this, a certain amount of helplessness must be tolerated. As I became better at identifying these moments of helplessness, feelings of failure and shame transformed.
Medical error
Sitting across from the PGY3 resident who I had met with weekly for the past 3 years, I thought about his error.
I thought about my phone call 4 nights earlier. My doctor was called at home by a lab technician, who never met their patients but was simply following protocol and alerted my doctor to the worsening number that she should have been aware of 9 months earlier.
Just like my doctor’s lapse of attention, my patient’s error was not a moment of helplessness to be tolerated. These were mistakes, and there was no way around it.
“People make mistakes.” I said simply.
We sat silently for a time.
I don’t remember who broke the silence. The conversation that followed was centered on our humanity and our capability for both compassion and fallibility. Afterward, I wondered who my doctor confided in and hoped she had a similar conversation.
Dr. Levesque is a clinical psychologist and clinical assistant professor of psychiatry at the Geisel School of Medicine at Dartmouth, Hanover, N.H., where she also serves on the Committee for a Respectful Learning Environment.
A version of this article first appeared on Medscape.com.
Thursday night
It was 9 o’clock at night when my phone rang. I didn’t recognize the number but decided to answer it anyway. It was my doctor.
“Chase, I got your labs back and you have a critically low level. I spoke with someone at the hospital, I think I know what is happening, but I need you to go to the pharmacy right now and get a medicine.” She explained further and as I listened electric currents ran through my thighs until I could barely feel my legs.
“I’m so sorry, Chase. I missed it. It was low the last time we did your labs 9 months ago, and I missed it.”
In disbelief, I continued to listen as she instructed me about the next steps I was to take and prepared me for what was to come the next day.
“If you notice any changes overnight, go straight to the ED.”
My chest tingled and I could barely breathe. My mind struggled to comprehend what was happening. I looked at my husband sitting close by on the couch. He looked concerned. I tuned back in and heard her say: “Is your husband there? Can I talk to him?”
“Yes,” is all I could manage, and I handed him the phone. I sat while he listened and asked his questions. My breathing came back under my control, my legs felt wiry, and restlessness set in. “I have to get out of here,” I thought. “I have to go and pick up this medicine.”
Monday afternoon
I am sitting across from a PGY3 resident I have been treating since his intern year, as part of his treatment plan for managing a chronic mental illness that began in medical school. Earlier in the day, I received an urgent message from him requesting an emergency appointment.
Within a few minutes of sitting down, the story from his weekend call shift tumbled out of him. His speech became pressured, and his eyes welled with tears as he recounted in detail the steps he had taken to care for a very sick patient overnight.
“I missed it.” The dam broke and he sat sobbing in front of me, his body trembling.
I sat silently across from him. Willing him to breathe.
In time, his breathing came back under his control, and he slowly regained his composure. He continued: “I got the imaging, and I missed a bleed.”
Failure and shame
I can recall memorable moments from my training when I came to understand that what I initially perceived to be a mistake was instead part of the work. An example from our practice involves a patient whom I was comanaging with her primary care provider (PCP). She was not doing well following a critical work event. When I met with her after the event, she admitted having thoughts of suicide, refused a voluntary inpatient admission, and would not have met criteria for an involuntary admission. My hands were tied.
Together we created a plan to keep her safe, which included paging her PCP after hours if needed. I told her PCP before leaving that night that he might hear from her and that if she reached out, she would require hospitalization.
I arrived at work the following day, and her PCP shared with me that our patient had overdosed on medication, paged him, and was admitted to the unit.
He seemed forlorn.
I was both relieved by the news and confused by his reaction. I had hoped that she would choose a higher level of care than what we could provide her as an outpatient. I said: “This is good. She followed the plan.”
Her overdose was, of course, not part of the plan. She was struggling with several internal conflicts, including having mixed feelings about coming into the hospital; but, when the critical moment happened and she was faced with a decision to call for help or possibly die, she chose to call her PCP and have him paged as we had talked about.
I looked at her PCP. “You helped get her to where she needed to be.”
In the years of working side by side with medically trained colleagues, I have time and again needed to reframe for them that what they perceive to be a “failure” or a “crisis” is often a catalyst for change. The patient I comanaged with the PCP was a highly skilled caregiver and, as such, had been having a hard time asking for help. The hospitalization that her PCP facilitated allowed her to receive the care she needed and created an opportunity for family and friends to show up for her. Their support fed her, and she only made gains from that point on.
My training had taught me that respecting a patient’s autonomy was of the utmost importance. This instills confidence in patients as the authority in their lives. For a clinician to do this, a certain amount of helplessness must be tolerated. As I became better at identifying these moments of helplessness, feelings of failure and shame transformed.
Medical error
Sitting across from the PGY3 resident who I had met with weekly for the past 3 years, I thought about his error.
I thought about my phone call 4 nights earlier. My doctor was called at home by a lab technician, who never met their patients but was simply following protocol and alerted my doctor to the worsening number that she should have been aware of 9 months earlier.
Just like my doctor’s lapse of attention, my patient’s error was not a moment of helplessness to be tolerated. These were mistakes, and there was no way around it.
“People make mistakes.” I said simply.
We sat silently for a time.
I don’t remember who broke the silence. The conversation that followed was centered on our humanity and our capability for both compassion and fallibility. Afterward, I wondered who my doctor confided in and hoped she had a similar conversation.
Dr. Levesque is a clinical psychologist and clinical assistant professor of psychiatry at the Geisel School of Medicine at Dartmouth, Hanover, N.H., where she also serves on the Committee for a Respectful Learning Environment.
A version of this article first appeared on Medscape.com.
Thursday night
It was 9 o’clock at night when my phone rang. I didn’t recognize the number but decided to answer it anyway. It was my doctor.
“Chase, I got your labs back and you have a critically low level. I spoke with someone at the hospital, I think I know what is happening, but I need you to go to the pharmacy right now and get a medicine.” She explained further and as I listened electric currents ran through my thighs until I could barely feel my legs.
“I’m so sorry, Chase. I missed it. It was low the last time we did your labs 9 months ago, and I missed it.”
In disbelief, I continued to listen as she instructed me about the next steps I was to take and prepared me for what was to come the next day.
“If you notice any changes overnight, go straight to the ED.”
My chest tingled and I could barely breathe. My mind struggled to comprehend what was happening. I looked at my husband sitting close by on the couch. He looked concerned. I tuned back in and heard her say: “Is your husband there? Can I talk to him?”
“Yes,” is all I could manage, and I handed him the phone. I sat while he listened and asked his questions. My breathing came back under my control, my legs felt wiry, and restlessness set in. “I have to get out of here,” I thought. “I have to go and pick up this medicine.”
Monday afternoon
I am sitting across from a PGY3 resident I have been treating since his intern year, as part of his treatment plan for managing a chronic mental illness that began in medical school. Earlier in the day, I received an urgent message from him requesting an emergency appointment.
Within a few minutes of sitting down, the story from his weekend call shift tumbled out of him. His speech became pressured, and his eyes welled with tears as he recounted in detail the steps he had taken to care for a very sick patient overnight.
“I missed it.” The dam broke and he sat sobbing in front of me, his body trembling.
I sat silently across from him. Willing him to breathe.
In time, his breathing came back under his control, and he slowly regained his composure. He continued: “I got the imaging, and I missed a bleed.”
Failure and shame
I can recall memorable moments from my training when I came to understand that what I initially perceived to be a mistake was instead part of the work. An example from our practice involves a patient whom I was comanaging with her primary care provider (PCP). She was not doing well following a critical work event. When I met with her after the event, she admitted having thoughts of suicide, refused a voluntary inpatient admission, and would not have met criteria for an involuntary admission. My hands were tied.
Together we created a plan to keep her safe, which included paging her PCP after hours if needed. I told her PCP before leaving that night that he might hear from her and that if she reached out, she would require hospitalization.
I arrived at work the following day, and her PCP shared with me that our patient had overdosed on medication, paged him, and was admitted to the unit.
He seemed forlorn.
I was both relieved by the news and confused by his reaction. I had hoped that she would choose a higher level of care than what we could provide her as an outpatient. I said: “This is good. She followed the plan.”
Her overdose was, of course, not part of the plan. She was struggling with several internal conflicts, including having mixed feelings about coming into the hospital; but, when the critical moment happened and she was faced with a decision to call for help or possibly die, she chose to call her PCP and have him paged as we had talked about.
I looked at her PCP. “You helped get her to where she needed to be.”
In the years of working side by side with medically trained colleagues, I have time and again needed to reframe for them that what they perceive to be a “failure” or a “crisis” is often a catalyst for change. The patient I comanaged with the PCP was a highly skilled caregiver and, as such, had been having a hard time asking for help. The hospitalization that her PCP facilitated allowed her to receive the care she needed and created an opportunity for family and friends to show up for her. Their support fed her, and she only made gains from that point on.
My training had taught me that respecting a patient’s autonomy was of the utmost importance. This instills confidence in patients as the authority in their lives. For a clinician to do this, a certain amount of helplessness must be tolerated. As I became better at identifying these moments of helplessness, feelings of failure and shame transformed.
Medical error
Sitting across from the PGY3 resident who I had met with weekly for the past 3 years, I thought about his error.
I thought about my phone call 4 nights earlier. My doctor was called at home by a lab technician, who never met their patients but was simply following protocol and alerted my doctor to the worsening number that she should have been aware of 9 months earlier.
Just like my doctor’s lapse of attention, my patient’s error was not a moment of helplessness to be tolerated. These were mistakes, and there was no way around it.
“People make mistakes.” I said simply.
We sat silently for a time.
I don’t remember who broke the silence. The conversation that followed was centered on our humanity and our capability for both compassion and fallibility. Afterward, I wondered who my doctor confided in and hoped she had a similar conversation.
Dr. Levesque is a clinical psychologist and clinical assistant professor of psychiatry at the Geisel School of Medicine at Dartmouth, Hanover, N.H., where she also serves on the Committee for a Respectful Learning Environment.
A version of this article first appeared on Medscape.com.
FDA approves ‘rapid-acting’ oral drug for major depression
The U.S. Food and Drug Administration has approved the first oral N-methyl D-aspartate (NMDA) receptor antagonist for the treatment of major depressive disorder (MDD) in adults, its manufacturer has announced.
Auvelity (Axsome Therapeutics) is a proprietary extended-release oral tablet containing dextromethorphan (45 mg) and bupropion (105 mg).
,” the company said in a news release.
“The approval of Auvelity represents a milestone in depression treatment based on its novel oral NMDA antagonist mechanism, its rapid antidepressant efficacy demonstrated in controlled trials, and a relatively favorable safety profile,” Maurizio Fava, MD, psychiatrist-in-chief, Massachusetts General Hospital, Boston, added in the release.
‘Milestone’ in depression treatment?
Dr. Fava noted that nearly two-thirds of patients treated with currently available antidepressants fail to respond adequately, and those who do may not achieve clinically meaningful responses for up to 6-8 weeks.
“Given the debilitating nature of depression, the efficacy of Auvelity observed at 1 week and sustained thereafter may have a significant impact on the current treatment paradigm for this condition,” he said.
The company noted the drug was studied in a comprehensive clinical program that included more than 1,100 patients with MDD.
The efficacy of the drug was demonstrated in the GEMINI placebo-controlled study – with confirmatory evidence provided by the ASCEND study, which compared it with bupropion sustained-release tablets.
Axsome said it expects to launch the new oral medication in the fourth quarter of this year. It is not approved for use in children.
The full prescribing information and medication guide are available online.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved the first oral N-methyl D-aspartate (NMDA) receptor antagonist for the treatment of major depressive disorder (MDD) in adults, its manufacturer has announced.
Auvelity (Axsome Therapeutics) is a proprietary extended-release oral tablet containing dextromethorphan (45 mg) and bupropion (105 mg).
,” the company said in a news release.
“The approval of Auvelity represents a milestone in depression treatment based on its novel oral NMDA antagonist mechanism, its rapid antidepressant efficacy demonstrated in controlled trials, and a relatively favorable safety profile,” Maurizio Fava, MD, psychiatrist-in-chief, Massachusetts General Hospital, Boston, added in the release.
‘Milestone’ in depression treatment?
Dr. Fava noted that nearly two-thirds of patients treated with currently available antidepressants fail to respond adequately, and those who do may not achieve clinically meaningful responses for up to 6-8 weeks.
“Given the debilitating nature of depression, the efficacy of Auvelity observed at 1 week and sustained thereafter may have a significant impact on the current treatment paradigm for this condition,” he said.
The company noted the drug was studied in a comprehensive clinical program that included more than 1,100 patients with MDD.
The efficacy of the drug was demonstrated in the GEMINI placebo-controlled study – with confirmatory evidence provided by the ASCEND study, which compared it with bupropion sustained-release tablets.
Axsome said it expects to launch the new oral medication in the fourth quarter of this year. It is not approved for use in children.
The full prescribing information and medication guide are available online.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved the first oral N-methyl D-aspartate (NMDA) receptor antagonist for the treatment of major depressive disorder (MDD) in adults, its manufacturer has announced.
Auvelity (Axsome Therapeutics) is a proprietary extended-release oral tablet containing dextromethorphan (45 mg) and bupropion (105 mg).
,” the company said in a news release.
“The approval of Auvelity represents a milestone in depression treatment based on its novel oral NMDA antagonist mechanism, its rapid antidepressant efficacy demonstrated in controlled trials, and a relatively favorable safety profile,” Maurizio Fava, MD, psychiatrist-in-chief, Massachusetts General Hospital, Boston, added in the release.
‘Milestone’ in depression treatment?
Dr. Fava noted that nearly two-thirds of patients treated with currently available antidepressants fail to respond adequately, and those who do may not achieve clinically meaningful responses for up to 6-8 weeks.
“Given the debilitating nature of depression, the efficacy of Auvelity observed at 1 week and sustained thereafter may have a significant impact on the current treatment paradigm for this condition,” he said.
The company noted the drug was studied in a comprehensive clinical program that included more than 1,100 patients with MDD.
The efficacy of the drug was demonstrated in the GEMINI placebo-controlled study – with confirmatory evidence provided by the ASCEND study, which compared it with bupropion sustained-release tablets.
Axsome said it expects to launch the new oral medication in the fourth quarter of this year. It is not approved for use in children.
The full prescribing information and medication guide are available online.
A version of this article first appeared on Medscape.com.
Watching TV, using computer have opposite ties to dementia risk
The relationship to dementia with these activities remained strong no matter how much physical activity a person did, the authors wrote in Proceedings of the National Academy of Sciences.
Both watching TV and using a computer have been linked to increased risk of chronic disease and mortality, while exercise and physical activity (PA) have shown benefit in reducing cognitive decline, structural brain atrophy, and dementia risk in older adults, the authors wrote.
The authors said they wanted to try to understand the effects of watching TV and using computers on dementia risk, because people in the United States and Europe have been engaging in both of these activities more often.
They concluded that it’s not the sitting part of sedentary behavior (SB) that potentially has the effect on dementia but what people are doing while sitting.
Some of the results were surprising, lead author David Raichlen, PhD, professor of Human and Evolutionary Biology at University of Southern California, Los Angeles, said in an interview.
Previous literature on sedentary behaviors have documented their negative effects on a wide range of health outcomes, rather than finding positive associations, he explained.
More than 140,000 included in study
The researchers conducted their prospective cohort study using data from the United Kingdom Biobank. After excluding people younger than 60, those with prevalent dementia at the start of follow-up, and those without complete data, 146,651 participants were included.
The participants were followed from their baseline visit until they received a dementia diagnosis, died, were lost to follow-up, or were last admitted to the hospital.
TV-watching time was linked with an increased risk of incident dementia (HR [95% confidence interval] = 1.31 [1.23-1.40]), and computer use was linked with a reduced risk of incident dementia HR [95% CI] = 0.80 [0.76-0.85]).
TV’s link with higher dementia risk increased in those who had the highest use, compared with those who had the lowest use (HR [95% CI] = 1.28 [1.18-1.39].
Similarly, the link with risk reduction for dementia with computer use increased with more use.
Both medium and high computer time were associated with reduced risk of incident dementia (HR [95% CI] = 0.70 [0.64-0.76] and HR [95% CI] = 0.76 [0.70-0.83] respectively).
Dr. Raichlen pointed out that the high use of TV in this study was 4 or more hours a day and computer use – which included leisure use, not work use – had benefits on dementia risk after just half an hour.
These results remained significant after researchers adjusted for demographic, health, and lifestyle variables, including time spent on physical activity, sleeping, obesity, alcohol consumption, smoking status, diet scores, education level, body mass index, and employment type.
Physical is still better than sedentary activity
One potential reason for the different effects on dementia risk in the two activities studied, the authors write, is that sitting down to watch TV is associated with “uniquely low levels of muscle activity and energy expenditure, compared with sitting to use a computer.”
Andrew Budson, MD, chief of Cognitive & Behavioral Neurology and Associate Chief of Staff for Education for the VA Boston Healthcare System, Mass., who was not part of the study, said he thinks a more likely explanation for the study findings lies in the active versus passive tasks required in the two kinds of viewing that the authors reference.
“When we’re doing cognitive activity involving using the computer, we’re using large parts of our cortex to carry out that activity, whereas when we’re watching TV, there are probably relatively small amounts of our brain that are actually active,” Dr. Budson, author of Seven Steps to Managing Your Memory, explained in an interview.
“This is one of the first times I’ve been convinced that even when the computer activity isn’t completely new and novel, it may be beneficial,” Dr. Budson said.
It would be much better to do physical activity, but if the choice is sedentary activity, active cognitive activities, such as computer use, are better than TV watching, he continued.
The results of the current study are consistent with previous work showing that the type of sedentary behavior matters, according to the authors.
“Several studies have shown that TV time is associated with mortality and poor cardiometabolic biomarkers, whereas computer time is not,” they wrote.
A limitation of the study is that sedentary behaviors were self-reported via questionnaires, and there may be errors in recall.
“The use of objective methods for measuring both SB and PA are needed in future studies,” they write.
The authors receive support from the National Institutes of Health, the State of Arizona, the Arizona Department of Health Services, and the McKnight Brain Research Foundation. Neither the authors nor Dr. Budson declared relevant financial relationships.
The relationship to dementia with these activities remained strong no matter how much physical activity a person did, the authors wrote in Proceedings of the National Academy of Sciences.
Both watching TV and using a computer have been linked to increased risk of chronic disease and mortality, while exercise and physical activity (PA) have shown benefit in reducing cognitive decline, structural brain atrophy, and dementia risk in older adults, the authors wrote.
The authors said they wanted to try to understand the effects of watching TV and using computers on dementia risk, because people in the United States and Europe have been engaging in both of these activities more often.
They concluded that it’s not the sitting part of sedentary behavior (SB) that potentially has the effect on dementia but what people are doing while sitting.
Some of the results were surprising, lead author David Raichlen, PhD, professor of Human and Evolutionary Biology at University of Southern California, Los Angeles, said in an interview.
Previous literature on sedentary behaviors have documented their negative effects on a wide range of health outcomes, rather than finding positive associations, he explained.
More than 140,000 included in study
The researchers conducted their prospective cohort study using data from the United Kingdom Biobank. After excluding people younger than 60, those with prevalent dementia at the start of follow-up, and those without complete data, 146,651 participants were included.
The participants were followed from their baseline visit until they received a dementia diagnosis, died, were lost to follow-up, or were last admitted to the hospital.
TV-watching time was linked with an increased risk of incident dementia (HR [95% confidence interval] = 1.31 [1.23-1.40]), and computer use was linked with a reduced risk of incident dementia HR [95% CI] = 0.80 [0.76-0.85]).
TV’s link with higher dementia risk increased in those who had the highest use, compared with those who had the lowest use (HR [95% CI] = 1.28 [1.18-1.39].
Similarly, the link with risk reduction for dementia with computer use increased with more use.
Both medium and high computer time were associated with reduced risk of incident dementia (HR [95% CI] = 0.70 [0.64-0.76] and HR [95% CI] = 0.76 [0.70-0.83] respectively).
Dr. Raichlen pointed out that the high use of TV in this study was 4 or more hours a day and computer use – which included leisure use, not work use – had benefits on dementia risk after just half an hour.
These results remained significant after researchers adjusted for demographic, health, and lifestyle variables, including time spent on physical activity, sleeping, obesity, alcohol consumption, smoking status, diet scores, education level, body mass index, and employment type.
Physical is still better than sedentary activity
One potential reason for the different effects on dementia risk in the two activities studied, the authors write, is that sitting down to watch TV is associated with “uniquely low levels of muscle activity and energy expenditure, compared with sitting to use a computer.”
Andrew Budson, MD, chief of Cognitive & Behavioral Neurology and Associate Chief of Staff for Education for the VA Boston Healthcare System, Mass., who was not part of the study, said he thinks a more likely explanation for the study findings lies in the active versus passive tasks required in the two kinds of viewing that the authors reference.
“When we’re doing cognitive activity involving using the computer, we’re using large parts of our cortex to carry out that activity, whereas when we’re watching TV, there are probably relatively small amounts of our brain that are actually active,” Dr. Budson, author of Seven Steps to Managing Your Memory, explained in an interview.
“This is one of the first times I’ve been convinced that even when the computer activity isn’t completely new and novel, it may be beneficial,” Dr. Budson said.
It would be much better to do physical activity, but if the choice is sedentary activity, active cognitive activities, such as computer use, are better than TV watching, he continued.
The results of the current study are consistent with previous work showing that the type of sedentary behavior matters, according to the authors.
“Several studies have shown that TV time is associated with mortality and poor cardiometabolic biomarkers, whereas computer time is not,” they wrote.
A limitation of the study is that sedentary behaviors were self-reported via questionnaires, and there may be errors in recall.
“The use of objective methods for measuring both SB and PA are needed in future studies,” they write.
The authors receive support from the National Institutes of Health, the State of Arizona, the Arizona Department of Health Services, and the McKnight Brain Research Foundation. Neither the authors nor Dr. Budson declared relevant financial relationships.
The relationship to dementia with these activities remained strong no matter how much physical activity a person did, the authors wrote in Proceedings of the National Academy of Sciences.
Both watching TV and using a computer have been linked to increased risk of chronic disease and mortality, while exercise and physical activity (PA) have shown benefit in reducing cognitive decline, structural brain atrophy, and dementia risk in older adults, the authors wrote.
The authors said they wanted to try to understand the effects of watching TV and using computers on dementia risk, because people in the United States and Europe have been engaging in both of these activities more often.
They concluded that it’s not the sitting part of sedentary behavior (SB) that potentially has the effect on dementia but what people are doing while sitting.
Some of the results were surprising, lead author David Raichlen, PhD, professor of Human and Evolutionary Biology at University of Southern California, Los Angeles, said in an interview.
Previous literature on sedentary behaviors have documented their negative effects on a wide range of health outcomes, rather than finding positive associations, he explained.
More than 140,000 included in study
The researchers conducted their prospective cohort study using data from the United Kingdom Biobank. After excluding people younger than 60, those with prevalent dementia at the start of follow-up, and those without complete data, 146,651 participants were included.
The participants were followed from their baseline visit until they received a dementia diagnosis, died, were lost to follow-up, or were last admitted to the hospital.
TV-watching time was linked with an increased risk of incident dementia (HR [95% confidence interval] = 1.31 [1.23-1.40]), and computer use was linked with a reduced risk of incident dementia HR [95% CI] = 0.80 [0.76-0.85]).
TV’s link with higher dementia risk increased in those who had the highest use, compared with those who had the lowest use (HR [95% CI] = 1.28 [1.18-1.39].
Similarly, the link with risk reduction for dementia with computer use increased with more use.
Both medium and high computer time were associated with reduced risk of incident dementia (HR [95% CI] = 0.70 [0.64-0.76] and HR [95% CI] = 0.76 [0.70-0.83] respectively).
Dr. Raichlen pointed out that the high use of TV in this study was 4 or more hours a day and computer use – which included leisure use, not work use – had benefits on dementia risk after just half an hour.
These results remained significant after researchers adjusted for demographic, health, and lifestyle variables, including time spent on physical activity, sleeping, obesity, alcohol consumption, smoking status, diet scores, education level, body mass index, and employment type.
Physical is still better than sedentary activity
One potential reason for the different effects on dementia risk in the two activities studied, the authors write, is that sitting down to watch TV is associated with “uniquely low levels of muscle activity and energy expenditure, compared with sitting to use a computer.”
Andrew Budson, MD, chief of Cognitive & Behavioral Neurology and Associate Chief of Staff for Education for the VA Boston Healthcare System, Mass., who was not part of the study, said he thinks a more likely explanation for the study findings lies in the active versus passive tasks required in the two kinds of viewing that the authors reference.
“When we’re doing cognitive activity involving using the computer, we’re using large parts of our cortex to carry out that activity, whereas when we’re watching TV, there are probably relatively small amounts of our brain that are actually active,” Dr. Budson, author of Seven Steps to Managing Your Memory, explained in an interview.
“This is one of the first times I’ve been convinced that even when the computer activity isn’t completely new and novel, it may be beneficial,” Dr. Budson said.
It would be much better to do physical activity, but if the choice is sedentary activity, active cognitive activities, such as computer use, are better than TV watching, he continued.
The results of the current study are consistent with previous work showing that the type of sedentary behavior matters, according to the authors.
“Several studies have shown that TV time is associated with mortality and poor cardiometabolic biomarkers, whereas computer time is not,” they wrote.
A limitation of the study is that sedentary behaviors were self-reported via questionnaires, and there may be errors in recall.
“The use of objective methods for measuring both SB and PA are needed in future studies,” they write.
The authors receive support from the National Institutes of Health, the State of Arizona, the Arizona Department of Health Services, and the McKnight Brain Research Foundation. Neither the authors nor Dr. Budson declared relevant financial relationships.
FROM PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
New panic disorder model flags risk for recurrence, persistence
Investigators based in France and the United States analyzed data for almost 800 patients with DSM-IV–diagnosed PD.
Results showed that having a “general psychopathology factor,” defined as the shared effects of all comorbid conditions, or PD liability, significantly and independently predicted 3-year recurrence or persistence of PD symptoms.
Having a lower physical health-related quality of life (QOL), a greater number of stressful life events, and not seeking treatment at baseline were also significant and independent predictors.
“This integrative model could help clinicians to identify individuals at high risk of recurrence or persistence of panic disorder and provide content for future research,” Valentin Scheer, MD, MPH, a resident in psychiatry at AP-HP, Assistance Publique, Hôpitaux de Paris, and colleagues wrote.
The findings were published online in the Journal of Clinical Psychiatry.
Integration needed
PD is a disabling disorder with a “chronic course” – and a recurrence rate ranging from 25% to 50%, the investigators noted.
“Because of the heterogeneous course of PD, there is a need to develop a comprehensive predictive model of recurrence or persistence,” they wrote. This could “help practitioners adapt therapeutic strategies and develop prevention strategies in high-risk individuals.”
Most previous studies that have investigated risk factors for PD recurrence and persistence have relied on clinical samples, often with limited sample sizes.
Moreover, each risk factor, when considered individually, accounts for only a “small proportion” of the variance in risk, the researchers noted. The co-occurrence of these risk factors “suggests the need to combine them into a broad multivariable model.”
However, currently proposed integrative models do not identify independent predictors or mitigate the influence of confounding variables. To fill this gap, the investigators conducted a study using structural equation modeling “to take into account multiple correlations across predictors.”
They drew on data from 775 participants (mean age, 40 years) in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). For the current analysis, they examined two waves of NESARC (2001-2002 and 2004-2005) to “build a comprehensive model” of the 3-year recurrence or persistence of PD.
The researchers used a “latent variable approach” that simultaneously examined the effect of the following five groups of potential predictors of recurrence or persistence: PD severity, severity of comorbidity, family history of psychiatric disorders, sociodemographic characteristics, and treatment-seeking behavior.
They also distinguished between risk factors responsible for recurrence and those responsible for persistence.
Psychiatric diagnoses were determined on the basis of the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV. Participants also completed Version 2 of the Short Form 12-Item Health Survey, which assesses both mental and physical QOL over the previous 4 weeks.
Early treatment needed
Among participants with a 12-month diagnosis of PD at wave 1, 13% had persistent PD and 27.6% had recurrent PD during the 3-year period. The mean duration of illness was 9.5 years.
A greater number of lifetime panic attacks, the presence of any Axis I or II comorbid disorder, and any Axis I disorder, especially social anxiety disorder, were significantly associated with 3-year risk for recurrence and for persistence.
Sweating, choking, paresthesias, the comorbid disorders of mania/hypomania and general anxiety disorder, nicotine dependence, lower mental and physical QOL scores, and exposure to a greater number of stressful life events in the previous year were all significantly associated with 3-year risk for recurrence.
Only variables shown with a P value were statistically significant, “with the a priori fixed at .05,” the researchers noted.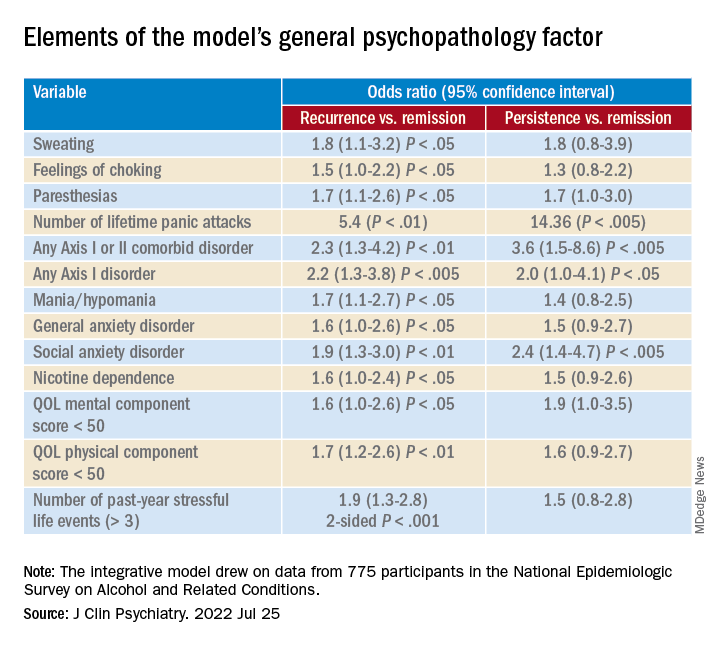
A combination of psychopathology factors, such as the shared effect of all comorbid psychiatric conditions, PD liability, lower physical health-related QOL, more life stressors during the past year, and not seeking treatment at baseline “significantly and independently” predicted recurrence or persistence of symptoms between the two waves (all Ps < .05), the investigators reported.
One study limitation cited was that several psychiatric disorders known to be associated with PD recurrence or persistence, such as borderline personality disorder, were not examined. Additionally, the study used a 3-year follow-up period – and the results might have differed for other follow-up time frames, the researchers noted.
Nevertheless, the findings constitute a “comprehensive model” to predict recurrence and persistence of PD, they wrote. Moreover, early treatment-seeking behavior “should be promoted, as it may reduce the risk of recurrence.”
Not much new?
Commenting on the study, Peter Roy-Byrne, MD, professor of psychiatry, University of Washington, Seattle, noted, “there is not much that is new here.”
Dr. Roy-Byrne, who was not involved with the study, said that a “general theme for years has been that more severe illness, whether you measure it by greater number of other Axis I disorders or symptom severity or a general psychopathology factor, usually predicts worse outcome – here codified as persistence and recurrence.”
Greater stress and reluctance to seek treatment may also predict worse outcomes, he noted.
In addition, the study “did not examine another very important factor: the degree of social connection/social support that someone has,” Dr. Roy-Byrne said. However, “perhaps some of this was contained in specific life events.”
A version of this article first appeared on Medscape.com.
Investigators based in France and the United States analyzed data for almost 800 patients with DSM-IV–diagnosed PD.
Results showed that having a “general psychopathology factor,” defined as the shared effects of all comorbid conditions, or PD liability, significantly and independently predicted 3-year recurrence or persistence of PD symptoms.
Having a lower physical health-related quality of life (QOL), a greater number of stressful life events, and not seeking treatment at baseline were also significant and independent predictors.
“This integrative model could help clinicians to identify individuals at high risk of recurrence or persistence of panic disorder and provide content for future research,” Valentin Scheer, MD, MPH, a resident in psychiatry at AP-HP, Assistance Publique, Hôpitaux de Paris, and colleagues wrote.
The findings were published online in the Journal of Clinical Psychiatry.
Integration needed
PD is a disabling disorder with a “chronic course” – and a recurrence rate ranging from 25% to 50%, the investigators noted.
“Because of the heterogeneous course of PD, there is a need to develop a comprehensive predictive model of recurrence or persistence,” they wrote. This could “help practitioners adapt therapeutic strategies and develop prevention strategies in high-risk individuals.”
Most previous studies that have investigated risk factors for PD recurrence and persistence have relied on clinical samples, often with limited sample sizes.
Moreover, each risk factor, when considered individually, accounts for only a “small proportion” of the variance in risk, the researchers noted. The co-occurrence of these risk factors “suggests the need to combine them into a broad multivariable model.”
However, currently proposed integrative models do not identify independent predictors or mitigate the influence of confounding variables. To fill this gap, the investigators conducted a study using structural equation modeling “to take into account multiple correlations across predictors.”
They drew on data from 775 participants (mean age, 40 years) in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). For the current analysis, they examined two waves of NESARC (2001-2002 and 2004-2005) to “build a comprehensive model” of the 3-year recurrence or persistence of PD.
The researchers used a “latent variable approach” that simultaneously examined the effect of the following five groups of potential predictors of recurrence or persistence: PD severity, severity of comorbidity, family history of psychiatric disorders, sociodemographic characteristics, and treatment-seeking behavior.
They also distinguished between risk factors responsible for recurrence and those responsible for persistence.
Psychiatric diagnoses were determined on the basis of the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV. Participants also completed Version 2 of the Short Form 12-Item Health Survey, which assesses both mental and physical QOL over the previous 4 weeks.
Early treatment needed
Among participants with a 12-month diagnosis of PD at wave 1, 13% had persistent PD and 27.6% had recurrent PD during the 3-year period. The mean duration of illness was 9.5 years.
A greater number of lifetime panic attacks, the presence of any Axis I or II comorbid disorder, and any Axis I disorder, especially social anxiety disorder, were significantly associated with 3-year risk for recurrence and for persistence.
Sweating, choking, paresthesias, the comorbid disorders of mania/hypomania and general anxiety disorder, nicotine dependence, lower mental and physical QOL scores, and exposure to a greater number of stressful life events in the previous year were all significantly associated with 3-year risk for recurrence.
Only variables shown with a P value were statistically significant, “with the a priori fixed at .05,” the researchers noted.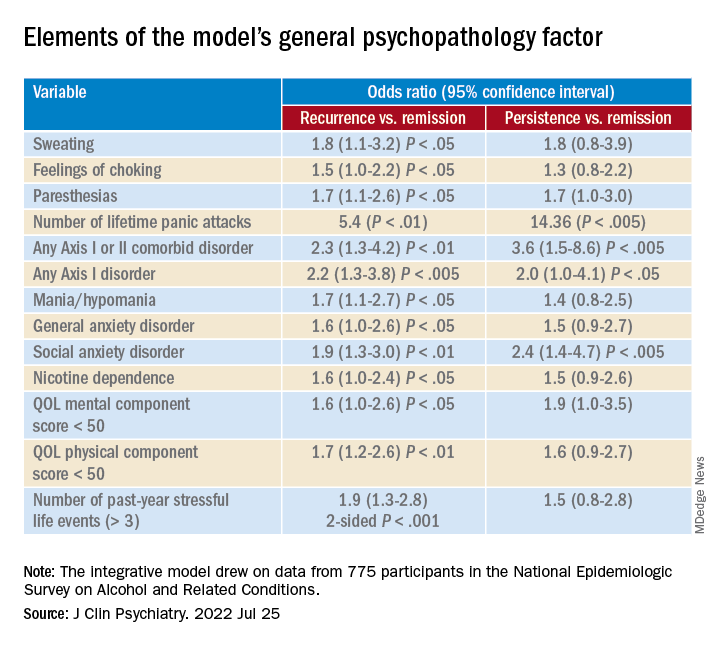
A combination of psychopathology factors, such as the shared effect of all comorbid psychiatric conditions, PD liability, lower physical health-related QOL, more life stressors during the past year, and not seeking treatment at baseline “significantly and independently” predicted recurrence or persistence of symptoms between the two waves (all Ps < .05), the investigators reported.
One study limitation cited was that several psychiatric disorders known to be associated with PD recurrence or persistence, such as borderline personality disorder, were not examined. Additionally, the study used a 3-year follow-up period – and the results might have differed for other follow-up time frames, the researchers noted.
Nevertheless, the findings constitute a “comprehensive model” to predict recurrence and persistence of PD, they wrote. Moreover, early treatment-seeking behavior “should be promoted, as it may reduce the risk of recurrence.”
Not much new?
Commenting on the study, Peter Roy-Byrne, MD, professor of psychiatry, University of Washington, Seattle, noted, “there is not much that is new here.”
Dr. Roy-Byrne, who was not involved with the study, said that a “general theme for years has been that more severe illness, whether you measure it by greater number of other Axis I disorders or symptom severity or a general psychopathology factor, usually predicts worse outcome – here codified as persistence and recurrence.”
Greater stress and reluctance to seek treatment may also predict worse outcomes, he noted.
In addition, the study “did not examine another very important factor: the degree of social connection/social support that someone has,” Dr. Roy-Byrne said. However, “perhaps some of this was contained in specific life events.”
A version of this article first appeared on Medscape.com.
Investigators based in France and the United States analyzed data for almost 800 patients with DSM-IV–diagnosed PD.
Results showed that having a “general psychopathology factor,” defined as the shared effects of all comorbid conditions, or PD liability, significantly and independently predicted 3-year recurrence or persistence of PD symptoms.
Having a lower physical health-related quality of life (QOL), a greater number of stressful life events, and not seeking treatment at baseline were also significant and independent predictors.
“This integrative model could help clinicians to identify individuals at high risk of recurrence or persistence of panic disorder and provide content for future research,” Valentin Scheer, MD, MPH, a resident in psychiatry at AP-HP, Assistance Publique, Hôpitaux de Paris, and colleagues wrote.
The findings were published online in the Journal of Clinical Psychiatry.
Integration needed
PD is a disabling disorder with a “chronic course” – and a recurrence rate ranging from 25% to 50%, the investigators noted.
“Because of the heterogeneous course of PD, there is a need to develop a comprehensive predictive model of recurrence or persistence,” they wrote. This could “help practitioners adapt therapeutic strategies and develop prevention strategies in high-risk individuals.”
Most previous studies that have investigated risk factors for PD recurrence and persistence have relied on clinical samples, often with limited sample sizes.
Moreover, each risk factor, when considered individually, accounts for only a “small proportion” of the variance in risk, the researchers noted. The co-occurrence of these risk factors “suggests the need to combine them into a broad multivariable model.”
However, currently proposed integrative models do not identify independent predictors or mitigate the influence of confounding variables. To fill this gap, the investigators conducted a study using structural equation modeling “to take into account multiple correlations across predictors.”
They drew on data from 775 participants (mean age, 40 years) in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). For the current analysis, they examined two waves of NESARC (2001-2002 and 2004-2005) to “build a comprehensive model” of the 3-year recurrence or persistence of PD.
The researchers used a “latent variable approach” that simultaneously examined the effect of the following five groups of potential predictors of recurrence or persistence: PD severity, severity of comorbidity, family history of psychiatric disorders, sociodemographic characteristics, and treatment-seeking behavior.
They also distinguished between risk factors responsible for recurrence and those responsible for persistence.
Psychiatric diagnoses were determined on the basis of the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV. Participants also completed Version 2 of the Short Form 12-Item Health Survey, which assesses both mental and physical QOL over the previous 4 weeks.
Early treatment needed
Among participants with a 12-month diagnosis of PD at wave 1, 13% had persistent PD and 27.6% had recurrent PD during the 3-year period. The mean duration of illness was 9.5 years.
A greater number of lifetime panic attacks, the presence of any Axis I or II comorbid disorder, and any Axis I disorder, especially social anxiety disorder, were significantly associated with 3-year risk for recurrence and for persistence.
Sweating, choking, paresthesias, the comorbid disorders of mania/hypomania and general anxiety disorder, nicotine dependence, lower mental and physical QOL scores, and exposure to a greater number of stressful life events in the previous year were all significantly associated with 3-year risk for recurrence.
Only variables shown with a P value were statistically significant, “with the a priori fixed at .05,” the researchers noted.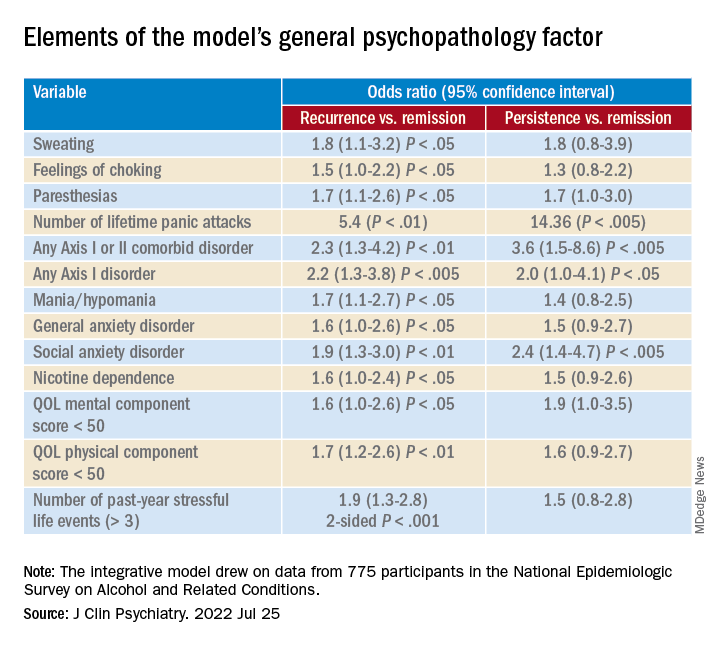
A combination of psychopathology factors, such as the shared effect of all comorbid psychiatric conditions, PD liability, lower physical health-related QOL, more life stressors during the past year, and not seeking treatment at baseline “significantly and independently” predicted recurrence or persistence of symptoms between the two waves (all Ps < .05), the investigators reported.
One study limitation cited was that several psychiatric disorders known to be associated with PD recurrence or persistence, such as borderline personality disorder, were not examined. Additionally, the study used a 3-year follow-up period – and the results might have differed for other follow-up time frames, the researchers noted.
Nevertheless, the findings constitute a “comprehensive model” to predict recurrence and persistence of PD, they wrote. Moreover, early treatment-seeking behavior “should be promoted, as it may reduce the risk of recurrence.”
Not much new?
Commenting on the study, Peter Roy-Byrne, MD, professor of psychiatry, University of Washington, Seattle, noted, “there is not much that is new here.”
Dr. Roy-Byrne, who was not involved with the study, said that a “general theme for years has been that more severe illness, whether you measure it by greater number of other Axis I disorders or symptom severity or a general psychopathology factor, usually predicts worse outcome – here codified as persistence and recurrence.”
Greater stress and reluctance to seek treatment may also predict worse outcomes, he noted.
In addition, the study “did not examine another very important factor: the degree of social connection/social support that someone has,” Dr. Roy-Byrne said. However, “perhaps some of this was contained in specific life events.”
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
Siblings of children with chronic health conditions may have increased mental health risks
Siblings of children with chronic health conditions could be at an increased risk for depression, according to a new report.
In a systematic review of 34 studies, siblings of children with chronic health conditions had significantly higher scores on depressive rating scales than individuals without a sibling with a chronic health condition (standardized mean difference = 0.53; P < .001). Findings related to other clinical health outcomes, such as physical health conditions or mortality, were inconsistent.
“We’ve known for a long time that siblings of kids with chronic conditions undergo stress, and there have been conflicting data on how that stress is manifested in terms of their own health,” senior study author Eyal Cohen, MD, program head for child health evaluative sciences at the Hospital for Sick Children, Toronto, told this news organization.
“For some siblings, having the experience of being raised with a child with a chronic condition may be an asset and build resiliency, while other siblings may feel strong negative emotions, such as sadness, anger, and fear,” he said. “Although we know that this experience is stressful for many siblings, it is important to know whether it changes their health outcomes, so that appropriate support can be put in place for those who need it.”
The study was published online in the Journal of Pediatrics.
Risk for psychological challenges
About a quarter of children in the United States have a mental, emotional, developmental, or behavioral condition, and more than a third have at least one current or lifelong health condition, the study authors write. A childhood chronic health condition can affect family members through worse mental health outcomes, increased stress, and poorer health-related quality of life.
Dr. Cohen and colleagues conducted a systematic review and meta-analysis to assess the clinical mental and physical health outcomes of siblings of children with chronic health conditions in comparison with siblings of healthy children or normative data.
The research team included English-language studies that reported on clinically diagnosable mental or physical health outcomes among siblings of persons younger than 18 years who had a chronic health condition. They included a comparison group and used an experimental or observational design for their study. The researchers analyzed 34 studies, including 28 that reported on mental health, 3 that reported on physical health, and 3 that reported on mortality.
Overall, siblings of children with chronic health conditions had significantly higher scores on depression rating scales than their comparison groups. Siblings’ anxiety scores weren’t substantially higher, however (standard mean difference = 0.21; P = .07).
The effects for confirmed psychiatric diagnoses, physical health outcomes, and mortality could not be included in the meta-analysis, owing to the limited number of studies and the high level of heterogeneity among the studies.
Dr. Cohen noted that although the researchers weren’t surprised that siblings may be at increased risk of mental health challenges, they were surprised by the limited data regarding physical health.
“At a minimum, our findings support the importance of asking open-ended questions about how a family is doing during clinical encounters,” he said. “These siblings may also benefit from programs such as support groups or summer camps, which have been shown to improve mental health and behavioral outcomes in siblings of children with chronic health conditions, such as cancer and neurodevelopmental disabilities.”
Future studies should assess the specific risk factors for mental health problems in siblings of children with chronic health conditions, Dr. Cohen said. Additional research could also investigate the design and effectiveness of interventions that address these concerns.
Message of inclusiveness
“The message that resonates with me is about the interventions and resources needed to support siblings,” Linda Nguyen, a doctoral student in rehabilitation science and researcher with the CanChild Center for Childhood Disability Research at McMaster University in Hamilton, Ont., told this news organization.
Ms. Nguyen, who wasn’t involved with this study, has researched the resources available to siblings in Canada and has found a lack of support options, particularly when it comes to specific health care management roles.
“Consistently throughout my research, I’ve seen the need for resources that go beyond a focus on siblings’ well-being and instead support them in their different roles,” she said. “Some want to be friends, mentors, supporters, and caregivers for their siblings in the future.”
Siblings often adopt different roles as they form their own identity, Ms. Nguyen noted, which becomes a larger part of the health care conversation as children with chronic conditions make the transition from pediatric to adult health care. Siblings want to be asked how they’d like to be involved, she said. Some would like to be involved with health care appointments, the chronic condition community, research, and policy making.
“At the societal level and public level, there’s also a message of inclusiveness and making sure that we’re welcoming youth with disabilities and chronic conditions,” Jan Willem Gorter, MD, PhD, a professor of pediatrics and scientist for CanChild at McMaster University, told this news organization.
Dr. Gorter, who also was not involved with this study, noted that children with chronic conditions often feel left behind, which can influence the involvement of their siblings as well.
“There are a lot of places in the world where children with disabilities go to special schools, and they spend a lot of time in a different world, with different experiences than their siblings,” he said. “At the public health level, we want to advocate for an inclusive society and support the whole family, which benefits everybody.”
The study was funded by the Canadian Institutes of Health Research and the CHILD-BRIGHT Network summer studentship, which is supported by the Canadian Institute for Health Research Strategy for Patient-Oriented Research. Dr. Cohen, Ms. Nguyen, and Dr. Gorter have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Siblings of children with chronic health conditions could be at an increased risk for depression, according to a new report.
In a systematic review of 34 studies, siblings of children with chronic health conditions had significantly higher scores on depressive rating scales than individuals without a sibling with a chronic health condition (standardized mean difference = 0.53; P < .001). Findings related to other clinical health outcomes, such as physical health conditions or mortality, were inconsistent.
“We’ve known for a long time that siblings of kids with chronic conditions undergo stress, and there have been conflicting data on how that stress is manifested in terms of their own health,” senior study author Eyal Cohen, MD, program head for child health evaluative sciences at the Hospital for Sick Children, Toronto, told this news organization.
“For some siblings, having the experience of being raised with a child with a chronic condition may be an asset and build resiliency, while other siblings may feel strong negative emotions, such as sadness, anger, and fear,” he said. “Although we know that this experience is stressful for many siblings, it is important to know whether it changes their health outcomes, so that appropriate support can be put in place for those who need it.”
The study was published online in the Journal of Pediatrics.
Risk for psychological challenges
About a quarter of children in the United States have a mental, emotional, developmental, or behavioral condition, and more than a third have at least one current or lifelong health condition, the study authors write. A childhood chronic health condition can affect family members through worse mental health outcomes, increased stress, and poorer health-related quality of life.
Dr. Cohen and colleagues conducted a systematic review and meta-analysis to assess the clinical mental and physical health outcomes of siblings of children with chronic health conditions in comparison with siblings of healthy children or normative data.
The research team included English-language studies that reported on clinically diagnosable mental or physical health outcomes among siblings of persons younger than 18 years who had a chronic health condition. They included a comparison group and used an experimental or observational design for their study. The researchers analyzed 34 studies, including 28 that reported on mental health, 3 that reported on physical health, and 3 that reported on mortality.
Overall, siblings of children with chronic health conditions had significantly higher scores on depression rating scales than their comparison groups. Siblings’ anxiety scores weren’t substantially higher, however (standard mean difference = 0.21; P = .07).
The effects for confirmed psychiatric diagnoses, physical health outcomes, and mortality could not be included in the meta-analysis, owing to the limited number of studies and the high level of heterogeneity among the studies.
Dr. Cohen noted that although the researchers weren’t surprised that siblings may be at increased risk of mental health challenges, they were surprised by the limited data regarding physical health.
“At a minimum, our findings support the importance of asking open-ended questions about how a family is doing during clinical encounters,” he said. “These siblings may also benefit from programs such as support groups or summer camps, which have been shown to improve mental health and behavioral outcomes in siblings of children with chronic health conditions, such as cancer and neurodevelopmental disabilities.”
Future studies should assess the specific risk factors for mental health problems in siblings of children with chronic health conditions, Dr. Cohen said. Additional research could also investigate the design and effectiveness of interventions that address these concerns.
Message of inclusiveness
“The message that resonates with me is about the interventions and resources needed to support siblings,” Linda Nguyen, a doctoral student in rehabilitation science and researcher with the CanChild Center for Childhood Disability Research at McMaster University in Hamilton, Ont., told this news organization.
Ms. Nguyen, who wasn’t involved with this study, has researched the resources available to siblings in Canada and has found a lack of support options, particularly when it comes to specific health care management roles.
“Consistently throughout my research, I’ve seen the need for resources that go beyond a focus on siblings’ well-being and instead support them in their different roles,” she said. “Some want to be friends, mentors, supporters, and caregivers for their siblings in the future.”
Siblings often adopt different roles as they form their own identity, Ms. Nguyen noted, which becomes a larger part of the health care conversation as children with chronic conditions make the transition from pediatric to adult health care. Siblings want to be asked how they’d like to be involved, she said. Some would like to be involved with health care appointments, the chronic condition community, research, and policy making.
“At the societal level and public level, there’s also a message of inclusiveness and making sure that we’re welcoming youth with disabilities and chronic conditions,” Jan Willem Gorter, MD, PhD, a professor of pediatrics and scientist for CanChild at McMaster University, told this news organization.
Dr. Gorter, who also was not involved with this study, noted that children with chronic conditions often feel left behind, which can influence the involvement of their siblings as well.
“There are a lot of places in the world where children with disabilities go to special schools, and they spend a lot of time in a different world, with different experiences than their siblings,” he said. “At the public health level, we want to advocate for an inclusive society and support the whole family, which benefits everybody.”
The study was funded by the Canadian Institutes of Health Research and the CHILD-BRIGHT Network summer studentship, which is supported by the Canadian Institute for Health Research Strategy for Patient-Oriented Research. Dr. Cohen, Ms. Nguyen, and Dr. Gorter have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Siblings of children with chronic health conditions could be at an increased risk for depression, according to a new report.
In a systematic review of 34 studies, siblings of children with chronic health conditions had significantly higher scores on depressive rating scales than individuals without a sibling with a chronic health condition (standardized mean difference = 0.53; P < .001). Findings related to other clinical health outcomes, such as physical health conditions or mortality, were inconsistent.
“We’ve known for a long time that siblings of kids with chronic conditions undergo stress, and there have been conflicting data on how that stress is manifested in terms of their own health,” senior study author Eyal Cohen, MD, program head for child health evaluative sciences at the Hospital for Sick Children, Toronto, told this news organization.
“For some siblings, having the experience of being raised with a child with a chronic condition may be an asset and build resiliency, while other siblings may feel strong negative emotions, such as sadness, anger, and fear,” he said. “Although we know that this experience is stressful for many siblings, it is important to know whether it changes their health outcomes, so that appropriate support can be put in place for those who need it.”
The study was published online in the Journal of Pediatrics.
Risk for psychological challenges
About a quarter of children in the United States have a mental, emotional, developmental, or behavioral condition, and more than a third have at least one current or lifelong health condition, the study authors write. A childhood chronic health condition can affect family members through worse mental health outcomes, increased stress, and poorer health-related quality of life.
Dr. Cohen and colleagues conducted a systematic review and meta-analysis to assess the clinical mental and physical health outcomes of siblings of children with chronic health conditions in comparison with siblings of healthy children or normative data.
The research team included English-language studies that reported on clinically diagnosable mental or physical health outcomes among siblings of persons younger than 18 years who had a chronic health condition. They included a comparison group and used an experimental or observational design for their study. The researchers analyzed 34 studies, including 28 that reported on mental health, 3 that reported on physical health, and 3 that reported on mortality.
Overall, siblings of children with chronic health conditions had significantly higher scores on depression rating scales than their comparison groups. Siblings’ anxiety scores weren’t substantially higher, however (standard mean difference = 0.21; P = .07).
The effects for confirmed psychiatric diagnoses, physical health outcomes, and mortality could not be included in the meta-analysis, owing to the limited number of studies and the high level of heterogeneity among the studies.
Dr. Cohen noted that although the researchers weren’t surprised that siblings may be at increased risk of mental health challenges, they were surprised by the limited data regarding physical health.
“At a minimum, our findings support the importance of asking open-ended questions about how a family is doing during clinical encounters,” he said. “These siblings may also benefit from programs such as support groups or summer camps, which have been shown to improve mental health and behavioral outcomes in siblings of children with chronic health conditions, such as cancer and neurodevelopmental disabilities.”
Future studies should assess the specific risk factors for mental health problems in siblings of children with chronic health conditions, Dr. Cohen said. Additional research could also investigate the design and effectiveness of interventions that address these concerns.
Message of inclusiveness
“The message that resonates with me is about the interventions and resources needed to support siblings,” Linda Nguyen, a doctoral student in rehabilitation science and researcher with the CanChild Center for Childhood Disability Research at McMaster University in Hamilton, Ont., told this news organization.
Ms. Nguyen, who wasn’t involved with this study, has researched the resources available to siblings in Canada and has found a lack of support options, particularly when it comes to specific health care management roles.
“Consistently throughout my research, I’ve seen the need for resources that go beyond a focus on siblings’ well-being and instead support them in their different roles,” she said. “Some want to be friends, mentors, supporters, and caregivers for their siblings in the future.”
Siblings often adopt different roles as they form their own identity, Ms. Nguyen noted, which becomes a larger part of the health care conversation as children with chronic conditions make the transition from pediatric to adult health care. Siblings want to be asked how they’d like to be involved, she said. Some would like to be involved with health care appointments, the chronic condition community, research, and policy making.
“At the societal level and public level, there’s also a message of inclusiveness and making sure that we’re welcoming youth with disabilities and chronic conditions,” Jan Willem Gorter, MD, PhD, a professor of pediatrics and scientist for CanChild at McMaster University, told this news organization.
Dr. Gorter, who also was not involved with this study, noted that children with chronic conditions often feel left behind, which can influence the involvement of their siblings as well.
“There are a lot of places in the world where children with disabilities go to special schools, and they spend a lot of time in a different world, with different experiences than their siblings,” he said. “At the public health level, we want to advocate for an inclusive society and support the whole family, which benefits everybody.”
The study was funded by the Canadian Institutes of Health Research and the CHILD-BRIGHT Network summer studentship, which is supported by the Canadian Institute for Health Research Strategy for Patient-Oriented Research. Dr. Cohen, Ms. Nguyen, and Dr. Gorter have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF PEDIATRICS