User login
FDA considers regulating CBD products
The products can have drug-like effects on the body and contain CBD (cannabidiol) and THC (tetrahydrocannabinol). Both CBD and THC can be derived from hemp, which was legalized by Congress in 2018.
“Given what we know about the safety of CBD so far, it raises concerns for FDA about whether these existing regulatory pathways for food and dietary supplements are appropriate for this substance,” FDA Principal Deputy Commissioner Janet Woodcock, MD, told The Wall Street Journal.
A 2021 FDA report valued the CBD market at $4.6 billion and projected it to quadruple by 2026. The only FDA-approved CBD product is an oil called Epidiolex, which can be prescribed for the seizure-associated disease epilepsy. Research on CBD to treat other diseases is ongoing.
Food, beverage, and beauty products containing CBD are sold in stores and online in many forms, including oils, vaporized liquids, and oil-based capsules, but “research supporting the drug’s benefits is still limited,” the Mayo Clinic said.
Recently, investigations have found that many CBD products also contain THC, which can be derived from legal hemp in a form that is referred to as Delta 8 and produces a psychoactive high. The CDC warned in 2022 that people “mistook” THC products for CBD products, which are often sold at the same stores, and experienced “adverse events.”
The Centers for Disease Control and Prevention and FDA warn that much is unknown about CBD and delta-8 products. The CDC says known CBD risks include liver damage; interference with other drugs you are taking, which may lead to injury or serious side effects; drowsiness or sleepiness; diarrhea or changes in appetite; changes in mood, such as crankiness; potential negative effects on fetuses during pregnancy or on babies during breastfeeding; or unintentional poisoning of children when mistaking THC products for CBD products or due to containing other ingredients such as THC or pesticides.
“I don’t think that we can have the perfect be the enemy of the good when we’re looking at such a vast market that is so available and utilized,” Norman Birenbaum, a senior FDA adviser who is working on the regulatory issue, told the Journal. “You’ve got a widely unregulated market.”
A version of this article first appeared on WebMD.com.
The products can have drug-like effects on the body and contain CBD (cannabidiol) and THC (tetrahydrocannabinol). Both CBD and THC can be derived from hemp, which was legalized by Congress in 2018.
“Given what we know about the safety of CBD so far, it raises concerns for FDA about whether these existing regulatory pathways for food and dietary supplements are appropriate for this substance,” FDA Principal Deputy Commissioner Janet Woodcock, MD, told The Wall Street Journal.
A 2021 FDA report valued the CBD market at $4.6 billion and projected it to quadruple by 2026. The only FDA-approved CBD product is an oil called Epidiolex, which can be prescribed for the seizure-associated disease epilepsy. Research on CBD to treat other diseases is ongoing.
Food, beverage, and beauty products containing CBD are sold in stores and online in many forms, including oils, vaporized liquids, and oil-based capsules, but “research supporting the drug’s benefits is still limited,” the Mayo Clinic said.
Recently, investigations have found that many CBD products also contain THC, which can be derived from legal hemp in a form that is referred to as Delta 8 and produces a psychoactive high. The CDC warned in 2022 that people “mistook” THC products for CBD products, which are often sold at the same stores, and experienced “adverse events.”
The Centers for Disease Control and Prevention and FDA warn that much is unknown about CBD and delta-8 products. The CDC says known CBD risks include liver damage; interference with other drugs you are taking, which may lead to injury or serious side effects; drowsiness or sleepiness; diarrhea or changes in appetite; changes in mood, such as crankiness; potential negative effects on fetuses during pregnancy or on babies during breastfeeding; or unintentional poisoning of children when mistaking THC products for CBD products or due to containing other ingredients such as THC or pesticides.
“I don’t think that we can have the perfect be the enemy of the good when we’re looking at such a vast market that is so available and utilized,” Norman Birenbaum, a senior FDA adviser who is working on the regulatory issue, told the Journal. “You’ve got a widely unregulated market.”
A version of this article first appeared on WebMD.com.
The products can have drug-like effects on the body and contain CBD (cannabidiol) and THC (tetrahydrocannabinol). Both CBD and THC can be derived from hemp, which was legalized by Congress in 2018.
“Given what we know about the safety of CBD so far, it raises concerns for FDA about whether these existing regulatory pathways for food and dietary supplements are appropriate for this substance,” FDA Principal Deputy Commissioner Janet Woodcock, MD, told The Wall Street Journal.
A 2021 FDA report valued the CBD market at $4.6 billion and projected it to quadruple by 2026. The only FDA-approved CBD product is an oil called Epidiolex, which can be prescribed for the seizure-associated disease epilepsy. Research on CBD to treat other diseases is ongoing.
Food, beverage, and beauty products containing CBD are sold in stores and online in many forms, including oils, vaporized liquids, and oil-based capsules, but “research supporting the drug’s benefits is still limited,” the Mayo Clinic said.
Recently, investigations have found that many CBD products also contain THC, which can be derived from legal hemp in a form that is referred to as Delta 8 and produces a psychoactive high. The CDC warned in 2022 that people “mistook” THC products for CBD products, which are often sold at the same stores, and experienced “adverse events.”
The Centers for Disease Control and Prevention and FDA warn that much is unknown about CBD and delta-8 products. The CDC says known CBD risks include liver damage; interference with other drugs you are taking, which may lead to injury or serious side effects; drowsiness or sleepiness; diarrhea or changes in appetite; changes in mood, such as crankiness; potential negative effects on fetuses during pregnancy or on babies during breastfeeding; or unintentional poisoning of children when mistaking THC products for CBD products or due to containing other ingredients such as THC or pesticides.
“I don’t think that we can have the perfect be the enemy of the good when we’re looking at such a vast market that is so available and utilized,” Norman Birenbaum, a senior FDA adviser who is working on the regulatory issue, told the Journal. “You’ve got a widely unregulated market.”
A version of this article first appeared on WebMD.com.
Vegetarians suffer more depression than meat eaters
People who follow a vegetarian lifestyle have around twice as many depressive episodes as those who eat meat, according to the Brazilian Longitudinal Study of Adult Health.
What to know
, including the vegetarian social experience; depression itself may increase the likelihood of becoming vegetarian, or both vegetarianism and depression may be associated with guilt through factors involving the meat industry.
Adopting a vegetarian diet might affect one’s relationship with others and involvement in social activities and may sometimes be associated with teasing or other forms of social ostracism.
It is possible that being depressed and dwelling on negative thoughts cause people to be more likely to become vegetarian rather than the other way around.
Videos depicting violence and cruelty in the meat industry may affect depressed people, causing them to dwell on the images, feel guilty for their part in creating the demand for meat, and become vegetarian.
Survey data were collected in Brazil, a country famous for its meat-heavy diet, and while there has been a sharp increase in vegetarianism, vegetarians still account for less than 0.5%.
This is a summary of the article, “Association Between Meatless Diet and Depressive Episodes: A Cross-sectional Analysis of Baseline Data From the Longitudinal Study of Adult Health (ELSA-Brasil),” published in the Journal of Affective Disorders. The full article can be found at sciencedirect.com.
A version of this article first appeared on Medscape.com.
People who follow a vegetarian lifestyle have around twice as many depressive episodes as those who eat meat, according to the Brazilian Longitudinal Study of Adult Health.
What to know
, including the vegetarian social experience; depression itself may increase the likelihood of becoming vegetarian, or both vegetarianism and depression may be associated with guilt through factors involving the meat industry.
Adopting a vegetarian diet might affect one’s relationship with others and involvement in social activities and may sometimes be associated with teasing or other forms of social ostracism.
It is possible that being depressed and dwelling on negative thoughts cause people to be more likely to become vegetarian rather than the other way around.
Videos depicting violence and cruelty in the meat industry may affect depressed people, causing them to dwell on the images, feel guilty for their part in creating the demand for meat, and become vegetarian.
Survey data were collected in Brazil, a country famous for its meat-heavy diet, and while there has been a sharp increase in vegetarianism, vegetarians still account for less than 0.5%.
This is a summary of the article, “Association Between Meatless Diet and Depressive Episodes: A Cross-sectional Analysis of Baseline Data From the Longitudinal Study of Adult Health (ELSA-Brasil),” published in the Journal of Affective Disorders. The full article can be found at sciencedirect.com.
A version of this article first appeared on Medscape.com.
People who follow a vegetarian lifestyle have around twice as many depressive episodes as those who eat meat, according to the Brazilian Longitudinal Study of Adult Health.
What to know
, including the vegetarian social experience; depression itself may increase the likelihood of becoming vegetarian, or both vegetarianism and depression may be associated with guilt through factors involving the meat industry.
Adopting a vegetarian diet might affect one’s relationship with others and involvement in social activities and may sometimes be associated with teasing or other forms of social ostracism.
It is possible that being depressed and dwelling on negative thoughts cause people to be more likely to become vegetarian rather than the other way around.
Videos depicting violence and cruelty in the meat industry may affect depressed people, causing them to dwell on the images, feel guilty for their part in creating the demand for meat, and become vegetarian.
Survey data were collected in Brazil, a country famous for its meat-heavy diet, and while there has been a sharp increase in vegetarianism, vegetarians still account for less than 0.5%.
This is a summary of the article, “Association Between Meatless Diet and Depressive Episodes: A Cross-sectional Analysis of Baseline Data From the Longitudinal Study of Adult Health (ELSA-Brasil),” published in the Journal of Affective Disorders. The full article can be found at sciencedirect.com.
A version of this article first appeared on Medscape.com.
Depression: Think outside of the box for diagnosis, treatment
In the treatment of depression, clinicians are commonly dealing with a mix of comorbidities that are more complex than just depression, and as such, effective treatment options may likewise require thinking outside of the box – and beyond the definitions of the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision).
“The DSM-5 isn’t handed to us on tablets from Mount Sinai,” said Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral sciences at the Mulva Clinic for the Neurosciences at the University of Texas at Austin. He spoke at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Our patients don’t fall into these very convenient buckets,” Dr. Nemeroff said. “The problem with depression is patients have very high rates of morbidity and comorbidity.”
The array of potential psychiatric comorbidities that are common in depression is somewhat staggering: As many as 70% of patients also have social anxiety disorder; 67% of patients have obsessive-compulsive disorder (OCD); up to 65% of patients have panic disorder; 48% of patients have posttraumatic stress disorder (PTSD); and 42% have generalized anxiety disorder, Dr. Nemeroff said.
And while the DSM-5 may have all those bases covered, in real world clinical practice, cracking the code of each patient’s unique and often more complicated psychiatric profile – and how to best manage it – can be a challenge. But Dr. Nemeroff said important clues can guide the clinician’s path.
A key starting point is making sure to gauge the severity of the patient’s core depression with one of the validated depression scales – whether it’s the self-reported Beck Depression Inventory, the clinician-rated Hamilton Rating Scale for Depression, the clinician-rated Montgomery Asberg Depression Rating Scale, or the Inventory of Depressive Symptoms, clinicians should pick one and track the score with each visit, Dr. Nemeroff advised.
“It doesn’t matter which tool you prefer – most tend to like the Beck Depression Scale, but the bottom line is that you have to get a measure of severity at every visit,” he said.
Among the most important comorbidities to identify as soon as possible is bipolar disorder, due to the potential worsening of the condition that can occur among those patients if treated with antidepressants, Dr. Nemeroff said.
“The question of whether the patient is bipolar should always be in the back of your mind,” he cautioned. “And if patients have been started on antidepressants, the clues may become evident very quickly.”
The most important indicator that the patient has bipolar disorder “is if they tell you that they were prescribed an antidepressant and it resulted in an increase in what we know to be hypomania – they may describe it as agitation or an inability to sleep,” Dr. Nemeroff said.
Of note, the effect is much more common with SNRIs [serotonin norepinephrine reuptake inhibitors] than SSRIs [selective serotonin reuptake inhibitors], he said.
“The effect is particularly notable with venlafaxine,” he said. “But SNRIs all have the propensity to switch people with depression into hypomania, but only patients who have bipolar disorder.”
“If you give a patient 150 mg of venlafaxine and they switch to developing hypomania, you now have the diagnosis of bipolar disorder, and you can treat them appropriately.”
Other important clues of bipolarity in depressed patients include:
- Family history: Most cases are genetically driven.
- Earlier age of onset (younger than age 25): “If the patient tells you they were depressed prepuberty, you should be thinking about the possibility of bipolar disorder, as it often presents as depression in childhood.”
- Psychotic features: As many as 80% of patients with psychotic depression end up being bipolar, Dr. Nemeroff said.
- Atypical depression: For example, depression with hypersomnia, or having an increased appetite instead of decreased, or a high amount of anxiety.
Remission should be the goal of treatment, and Dr. Nemeroff said that in efforts to accomplish that with the help of medications, psychiatrists may need to think “outside of the box” – or beyond the label.
“Many practitioners become slaves to the PDR [Physicians’ Desk Reference],” he said. “It is only a guide to what the clinical trials show, and not a mandate in terms of dosing.”
“There’s often strong data in the literature that supports going to a higher dose, if necessary, and I have [plenty] of patients, for instance, on 450 or 600 mg of venlafaxine who had not responded to 150 or even 300 mg.”
Treatment resistance
When patients continue to fail to respond, regardless of dosing or medication adjustments, Dr. Nemeroff suggested that clinicians should consider the potential important reasons. For instance, in addition to comorbid psychiatric conditions, practitioners should determine if there are medical conditions that they are not aware of.
“Does the patient have an underlying medical condition, such as thyroid dysfunction, early Parkinson’s disease, or even something like cancer?” he said.
There is also the inevitable question of whether the patient is indeed taking the medication. “We know that 30% of our patients do not follow their prescriptions, so of course that’s an important question to ask,” Dr. Nemeroff said.
Finally, while some pharmacogenomic tests are emerging with the suggestion of identifying which patients may or may not respond to certain drugs, Dr. Nemeroff says he’s seen little convincing evidence of their benefits.
“We have a problem in this field in that we don’t have the kinds of markers that they do in oncology, so we’re left with having to generally play trial and error,” he said.
“But when it comes to these pharmacogenomic tests, there’s just no ‘there there’,” he asserted. “From what I’ve seen so far, it’s frankly neuro-mythology.”
Dr. Nemeroff disclosed that he receives grant/research support from the National Institutes of Health and serves as a consultant for and/or on the advisory boards of multiple pharmaceutical companies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
In the treatment of depression, clinicians are commonly dealing with a mix of comorbidities that are more complex than just depression, and as such, effective treatment options may likewise require thinking outside of the box – and beyond the definitions of the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision).
“The DSM-5 isn’t handed to us on tablets from Mount Sinai,” said Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral sciences at the Mulva Clinic for the Neurosciences at the University of Texas at Austin. He spoke at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Our patients don’t fall into these very convenient buckets,” Dr. Nemeroff said. “The problem with depression is patients have very high rates of morbidity and comorbidity.”
The array of potential psychiatric comorbidities that are common in depression is somewhat staggering: As many as 70% of patients also have social anxiety disorder; 67% of patients have obsessive-compulsive disorder (OCD); up to 65% of patients have panic disorder; 48% of patients have posttraumatic stress disorder (PTSD); and 42% have generalized anxiety disorder, Dr. Nemeroff said.
And while the DSM-5 may have all those bases covered, in real world clinical practice, cracking the code of each patient’s unique and often more complicated psychiatric profile – and how to best manage it – can be a challenge. But Dr. Nemeroff said important clues can guide the clinician’s path.
A key starting point is making sure to gauge the severity of the patient’s core depression with one of the validated depression scales – whether it’s the self-reported Beck Depression Inventory, the clinician-rated Hamilton Rating Scale for Depression, the clinician-rated Montgomery Asberg Depression Rating Scale, or the Inventory of Depressive Symptoms, clinicians should pick one and track the score with each visit, Dr. Nemeroff advised.
“It doesn’t matter which tool you prefer – most tend to like the Beck Depression Scale, but the bottom line is that you have to get a measure of severity at every visit,” he said.
Among the most important comorbidities to identify as soon as possible is bipolar disorder, due to the potential worsening of the condition that can occur among those patients if treated with antidepressants, Dr. Nemeroff said.
“The question of whether the patient is bipolar should always be in the back of your mind,” he cautioned. “And if patients have been started on antidepressants, the clues may become evident very quickly.”
The most important indicator that the patient has bipolar disorder “is if they tell you that they were prescribed an antidepressant and it resulted in an increase in what we know to be hypomania – they may describe it as agitation or an inability to sleep,” Dr. Nemeroff said.
Of note, the effect is much more common with SNRIs [serotonin norepinephrine reuptake inhibitors] than SSRIs [selective serotonin reuptake inhibitors], he said.
“The effect is particularly notable with venlafaxine,” he said. “But SNRIs all have the propensity to switch people with depression into hypomania, but only patients who have bipolar disorder.”
“If you give a patient 150 mg of venlafaxine and they switch to developing hypomania, you now have the diagnosis of bipolar disorder, and you can treat them appropriately.”
Other important clues of bipolarity in depressed patients include:
- Family history: Most cases are genetically driven.
- Earlier age of onset (younger than age 25): “If the patient tells you they were depressed prepuberty, you should be thinking about the possibility of bipolar disorder, as it often presents as depression in childhood.”
- Psychotic features: As many as 80% of patients with psychotic depression end up being bipolar, Dr. Nemeroff said.
- Atypical depression: For example, depression with hypersomnia, or having an increased appetite instead of decreased, or a high amount of anxiety.
Remission should be the goal of treatment, and Dr. Nemeroff said that in efforts to accomplish that with the help of medications, psychiatrists may need to think “outside of the box” – or beyond the label.
“Many practitioners become slaves to the PDR [Physicians’ Desk Reference],” he said. “It is only a guide to what the clinical trials show, and not a mandate in terms of dosing.”
“There’s often strong data in the literature that supports going to a higher dose, if necessary, and I have [plenty] of patients, for instance, on 450 or 600 mg of venlafaxine who had not responded to 150 or even 300 mg.”
Treatment resistance
When patients continue to fail to respond, regardless of dosing or medication adjustments, Dr. Nemeroff suggested that clinicians should consider the potential important reasons. For instance, in addition to comorbid psychiatric conditions, practitioners should determine if there are medical conditions that they are not aware of.
“Does the patient have an underlying medical condition, such as thyroid dysfunction, early Parkinson’s disease, or even something like cancer?” he said.
There is also the inevitable question of whether the patient is indeed taking the medication. “We know that 30% of our patients do not follow their prescriptions, so of course that’s an important question to ask,” Dr. Nemeroff said.
Finally, while some pharmacogenomic tests are emerging with the suggestion of identifying which patients may or may not respond to certain drugs, Dr. Nemeroff says he’s seen little convincing evidence of their benefits.
“We have a problem in this field in that we don’t have the kinds of markers that they do in oncology, so we’re left with having to generally play trial and error,” he said.
“But when it comes to these pharmacogenomic tests, there’s just no ‘there there’,” he asserted. “From what I’ve seen so far, it’s frankly neuro-mythology.”
Dr. Nemeroff disclosed that he receives grant/research support from the National Institutes of Health and serves as a consultant for and/or on the advisory boards of multiple pharmaceutical companies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
In the treatment of depression, clinicians are commonly dealing with a mix of comorbidities that are more complex than just depression, and as such, effective treatment options may likewise require thinking outside of the box – and beyond the definitions of the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision).
“The DSM-5 isn’t handed to us on tablets from Mount Sinai,” said Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral sciences at the Mulva Clinic for the Neurosciences at the University of Texas at Austin. He spoke at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Our patients don’t fall into these very convenient buckets,” Dr. Nemeroff said. “The problem with depression is patients have very high rates of morbidity and comorbidity.”
The array of potential psychiatric comorbidities that are common in depression is somewhat staggering: As many as 70% of patients also have social anxiety disorder; 67% of patients have obsessive-compulsive disorder (OCD); up to 65% of patients have panic disorder; 48% of patients have posttraumatic stress disorder (PTSD); and 42% have generalized anxiety disorder, Dr. Nemeroff said.
And while the DSM-5 may have all those bases covered, in real world clinical practice, cracking the code of each patient’s unique and often more complicated psychiatric profile – and how to best manage it – can be a challenge. But Dr. Nemeroff said important clues can guide the clinician’s path.
A key starting point is making sure to gauge the severity of the patient’s core depression with one of the validated depression scales – whether it’s the self-reported Beck Depression Inventory, the clinician-rated Hamilton Rating Scale for Depression, the clinician-rated Montgomery Asberg Depression Rating Scale, or the Inventory of Depressive Symptoms, clinicians should pick one and track the score with each visit, Dr. Nemeroff advised.
“It doesn’t matter which tool you prefer – most tend to like the Beck Depression Scale, but the bottom line is that you have to get a measure of severity at every visit,” he said.
Among the most important comorbidities to identify as soon as possible is bipolar disorder, due to the potential worsening of the condition that can occur among those patients if treated with antidepressants, Dr. Nemeroff said.
“The question of whether the patient is bipolar should always be in the back of your mind,” he cautioned. “And if patients have been started on antidepressants, the clues may become evident very quickly.”
The most important indicator that the patient has bipolar disorder “is if they tell you that they were prescribed an antidepressant and it resulted in an increase in what we know to be hypomania – they may describe it as agitation or an inability to sleep,” Dr. Nemeroff said.
Of note, the effect is much more common with SNRIs [serotonin norepinephrine reuptake inhibitors] than SSRIs [selective serotonin reuptake inhibitors], he said.
“The effect is particularly notable with venlafaxine,” he said. “But SNRIs all have the propensity to switch people with depression into hypomania, but only patients who have bipolar disorder.”
“If you give a patient 150 mg of venlafaxine and they switch to developing hypomania, you now have the diagnosis of bipolar disorder, and you can treat them appropriately.”
Other important clues of bipolarity in depressed patients include:
- Family history: Most cases are genetically driven.
- Earlier age of onset (younger than age 25): “If the patient tells you they were depressed prepuberty, you should be thinking about the possibility of bipolar disorder, as it often presents as depression in childhood.”
- Psychotic features: As many as 80% of patients with psychotic depression end up being bipolar, Dr. Nemeroff said.
- Atypical depression: For example, depression with hypersomnia, or having an increased appetite instead of decreased, or a high amount of anxiety.
Remission should be the goal of treatment, and Dr. Nemeroff said that in efforts to accomplish that with the help of medications, psychiatrists may need to think “outside of the box” – or beyond the label.
“Many practitioners become slaves to the PDR [Physicians’ Desk Reference],” he said. “It is only a guide to what the clinical trials show, and not a mandate in terms of dosing.”
“There’s often strong data in the literature that supports going to a higher dose, if necessary, and I have [plenty] of patients, for instance, on 450 or 600 mg of venlafaxine who had not responded to 150 or even 300 mg.”
Treatment resistance
When patients continue to fail to respond, regardless of dosing or medication adjustments, Dr. Nemeroff suggested that clinicians should consider the potential important reasons. For instance, in addition to comorbid psychiatric conditions, practitioners should determine if there are medical conditions that they are not aware of.
“Does the patient have an underlying medical condition, such as thyroid dysfunction, early Parkinson’s disease, or even something like cancer?” he said.
There is also the inevitable question of whether the patient is indeed taking the medication. “We know that 30% of our patients do not follow their prescriptions, so of course that’s an important question to ask,” Dr. Nemeroff said.
Finally, while some pharmacogenomic tests are emerging with the suggestion of identifying which patients may or may not respond to certain drugs, Dr. Nemeroff says he’s seen little convincing evidence of their benefits.
“We have a problem in this field in that we don’t have the kinds of markers that they do in oncology, so we’re left with having to generally play trial and error,” he said.
“But when it comes to these pharmacogenomic tests, there’s just no ‘there there’,” he asserted. “From what I’ve seen so far, it’s frankly neuro-mythology.”
Dr. Nemeroff disclosed that he receives grant/research support from the National Institutes of Health and serves as a consultant for and/or on the advisory boards of multiple pharmaceutical companies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
FROM PSYCHOPHARMACOLOGY UPDATE
Alzheimer’s Association to CMS: Ditch restraints on amyloid drugs
In a letter addressed to CMS administrator Chiquita Brooks-LaSure, MPP, the association has asked the agency to remove the requirements for “coverage with evidence development” in its national coverage determination for FDA-approved anti-amyloid monoclonal antibodies.
The CMS coverage restrictions for anti-amyloid drugs were finalized in April on the basis of data available at the time.
Since then, new data from the CLARITY AD trial “clearly demonstrate a meaningful clinical benefit” from the investigational anti-amyloid agent lecanemab (Eisai/Biogen), Robert Egge, chief public policy officer for the Alzheimer’s Association, told this news organization.
The CLARITY AD results were published in the New England Journal of Medicine. Lecanemab is currently under accelerated review at the FDA.
The Alzheimer’s Association’s letter to the CMS includes a joint statement signed by more than 200 AD researchers and experts. All agree that the lecanemab results represent “significant new evidence” that necessitates reconsidering the restrictions on anti-amyloid agents.
“CMS has said it would look at new evidence, and now that evidence is here. We believe CMS recognizes this evidence for lecanemab is stronger than that for many treatments Medicare routinely covers,” Mr. Egge said.
‘No time to waste’
“With the timing of accelerated approvals for both lecanemab and donanemab in the next few months, the Alzheimer’s Association wants to ensure, if approved, that patients can access these treatments,” Mr. Egge noted.
“Because revisions to National Coverage Determinations can be a lengthy process, CMS needs to act quickly to minimize delays. People living with Alzheimer’s disease don’t have time to waste,” he added.
The Alzheimer’s Association estimates that every day, more than 2,000 individuals aged 65 or older may transition from mild dementia due to AD to a more advanced stage of the disease in which they may no longer be eligible for lecanemab and the other anti-amyloid agents currently being tested.
“Each day matters when it comes to slowing the progression of this disease,” Joanne Pike, DrPH, president and incoming chief executive officer for the Alzheimer’s Association, noted in a news release.
“The current CMS policy to severely limit access to these treatments eliminates people’s options, is resulting in continued irreversible disease progression, and contributes to greater health inequities. That’s not acceptable,” Dr. Pike said.
A version of this article first appeared on Medscape.com.
In a letter addressed to CMS administrator Chiquita Brooks-LaSure, MPP, the association has asked the agency to remove the requirements for “coverage with evidence development” in its national coverage determination for FDA-approved anti-amyloid monoclonal antibodies.
The CMS coverage restrictions for anti-amyloid drugs were finalized in April on the basis of data available at the time.
Since then, new data from the CLARITY AD trial “clearly demonstrate a meaningful clinical benefit” from the investigational anti-amyloid agent lecanemab (Eisai/Biogen), Robert Egge, chief public policy officer for the Alzheimer’s Association, told this news organization.
The CLARITY AD results were published in the New England Journal of Medicine. Lecanemab is currently under accelerated review at the FDA.
The Alzheimer’s Association’s letter to the CMS includes a joint statement signed by more than 200 AD researchers and experts. All agree that the lecanemab results represent “significant new evidence” that necessitates reconsidering the restrictions on anti-amyloid agents.
“CMS has said it would look at new evidence, and now that evidence is here. We believe CMS recognizes this evidence for lecanemab is stronger than that for many treatments Medicare routinely covers,” Mr. Egge said.
‘No time to waste’
“With the timing of accelerated approvals for both lecanemab and donanemab in the next few months, the Alzheimer’s Association wants to ensure, if approved, that patients can access these treatments,” Mr. Egge noted.
“Because revisions to National Coverage Determinations can be a lengthy process, CMS needs to act quickly to minimize delays. People living with Alzheimer’s disease don’t have time to waste,” he added.
The Alzheimer’s Association estimates that every day, more than 2,000 individuals aged 65 or older may transition from mild dementia due to AD to a more advanced stage of the disease in which they may no longer be eligible for lecanemab and the other anti-amyloid agents currently being tested.
“Each day matters when it comes to slowing the progression of this disease,” Joanne Pike, DrPH, president and incoming chief executive officer for the Alzheimer’s Association, noted in a news release.
“The current CMS policy to severely limit access to these treatments eliminates people’s options, is resulting in continued irreversible disease progression, and contributes to greater health inequities. That’s not acceptable,” Dr. Pike said.
A version of this article first appeared on Medscape.com.
In a letter addressed to CMS administrator Chiquita Brooks-LaSure, MPP, the association has asked the agency to remove the requirements for “coverage with evidence development” in its national coverage determination for FDA-approved anti-amyloid monoclonal antibodies.
The CMS coverage restrictions for anti-amyloid drugs were finalized in April on the basis of data available at the time.
Since then, new data from the CLARITY AD trial “clearly demonstrate a meaningful clinical benefit” from the investigational anti-amyloid agent lecanemab (Eisai/Biogen), Robert Egge, chief public policy officer for the Alzheimer’s Association, told this news organization.
The CLARITY AD results were published in the New England Journal of Medicine. Lecanemab is currently under accelerated review at the FDA.
The Alzheimer’s Association’s letter to the CMS includes a joint statement signed by more than 200 AD researchers and experts. All agree that the lecanemab results represent “significant new evidence” that necessitates reconsidering the restrictions on anti-amyloid agents.
“CMS has said it would look at new evidence, and now that evidence is here. We believe CMS recognizes this evidence for lecanemab is stronger than that for many treatments Medicare routinely covers,” Mr. Egge said.
‘No time to waste’
“With the timing of accelerated approvals for both lecanemab and donanemab in the next few months, the Alzheimer’s Association wants to ensure, if approved, that patients can access these treatments,” Mr. Egge noted.
“Because revisions to National Coverage Determinations can be a lengthy process, CMS needs to act quickly to minimize delays. People living with Alzheimer’s disease don’t have time to waste,” he added.
The Alzheimer’s Association estimates that every day, more than 2,000 individuals aged 65 or older may transition from mild dementia due to AD to a more advanced stage of the disease in which they may no longer be eligible for lecanemab and the other anti-amyloid agents currently being tested.
“Each day matters when it comes to slowing the progression of this disease,” Joanne Pike, DrPH, president and incoming chief executive officer for the Alzheimer’s Association, noted in a news release.
“The current CMS policy to severely limit access to these treatments eliminates people’s options, is resulting in continued irreversible disease progression, and contributes to greater health inequities. That’s not acceptable,” Dr. Pike said.
A version of this article first appeared on Medscape.com.
AAP offers new guidance on child exploitation and sex trafficking
In a new updated report, the American Academy of Pediatrics urges pediatricians to understand signs of exploitation and labor/sex trafficking and learn how to support children and adolescents who are targeted.
“It’s incredibly scary when you encounter someone you worry is a victim, and you don’t know how to help them, and they’re not saying what’s going on,” pediatrician and report coauthor Dana Kaplan, MD, of Staten Island (N.Y.) University Hospital, said in an interview. “Every case is so unique and different: There’s no algorithm of ‘If A, then B, then C.’ You have to approach each person as an individual, and it takes time to make sure you’re thinking things through about how to provide what’s needed.”
The AAP published the clinical report, which is intended to provide guidance to pediatricians, in the January 2023 issue of Pediatrics. The organization previously tackled this topic in a 2017 clinical report, and Dr. Kaplan said the new report includes updated recommendations.
As the new report notes, there aren’t reliable estimates of exploited children in the United States, although millions are thought to be trafficked and subjected to forced labor around the world. “By virtue of their young age, children and adolescents are vulnerable to manipulation and exploitation, because they have limited life experiences, a need for attachment and acceptance, an immature prefrontal cortex ... and limited options for action,” the report says.
Dr. Kaplan puts it this way: “By the nature of being a child, you’re vulnerable.”
Still, health care professionals often aren’t trained in regard to human trafficking, the report says, even though it’s clear that they “must remain alert for the possibility.”
Dr. Kaplan, who has special training in child abuse and often sees children at risk, cautioned that children usually don’t directly say that they need help. “That’s generally not the case. They don’t articulate what’s going on around them as unsafe, or concerning, or dangerous. If you go and see a doctor for 10 minutes, are you going to tell them everything?
Instead, clinicians must often rely on their own observations. The report lists multiple possible signs of exploitation.
- The patient is accompanied by a domineering adult who does not allow the child to answer questions or accompanied by an unrelated adult. Inconsistent information is provided by the patient or companion. There’s a delay in seeking medical care.
- The patient has multiple sexually transmitted infections, previous pregnancy or termination, and/or frequent visits for emergency contraception. There are signs of prior sexual abuse, assault, or other maltreatment.
- The patient is withdrawn, fearful, hostile, or has a suspicious demeanor. The patient is constantly checking his or her phone and appears anxious or afraid.
What should clinicians do if they suspect exploitation? The report recommends that health care organizations develop guidelines for workers to follow. For her part, Dr. Kaplan advises colleagues to let patients lead conversations and not dig too deeply into their lives.
“Don’t turn into an investigator. This is not [Law & Order] SVU,” she said. “Stay focused on what you’re trained to do – provide health care.”
That doesn’t mean clinicians should ignore signs of trouble. It’s crucial to develop trust with the patient over time, she said, and turn to a specialist in your community or institution if you have suspicions.
And be careful to not portray victims as perpetrators. The new report emphasizes that “it’s important for health care providers to emphasize to authorities that the patient is a victim of exploitation who needs services rather than a juvenile offender.”
The report also highlights the importance of creating an environment that supports clinicians themselves: “Self-care for the clinician is critical in preventing and addressing secondary traumatic stress. A work environment that fosters peer support, encourages open discussion of work-related stress, and implements reasonable work-life balance policies can help protect providers from secondary stress and its consequences.”
Resources for clinicians include the National Human Trafficking Hotline, the federal Office of Trafficking in Persons, and the Centers for Disease Control and Prevention’s domestic refugee screening guidelines.
The study has no external funding. The authors report no disclosures.
In a new updated report, the American Academy of Pediatrics urges pediatricians to understand signs of exploitation and labor/sex trafficking and learn how to support children and adolescents who are targeted.
“It’s incredibly scary when you encounter someone you worry is a victim, and you don’t know how to help them, and they’re not saying what’s going on,” pediatrician and report coauthor Dana Kaplan, MD, of Staten Island (N.Y.) University Hospital, said in an interview. “Every case is so unique and different: There’s no algorithm of ‘If A, then B, then C.’ You have to approach each person as an individual, and it takes time to make sure you’re thinking things through about how to provide what’s needed.”
The AAP published the clinical report, which is intended to provide guidance to pediatricians, in the January 2023 issue of Pediatrics. The organization previously tackled this topic in a 2017 clinical report, and Dr. Kaplan said the new report includes updated recommendations.
As the new report notes, there aren’t reliable estimates of exploited children in the United States, although millions are thought to be trafficked and subjected to forced labor around the world. “By virtue of their young age, children and adolescents are vulnerable to manipulation and exploitation, because they have limited life experiences, a need for attachment and acceptance, an immature prefrontal cortex ... and limited options for action,” the report says.
Dr. Kaplan puts it this way: “By the nature of being a child, you’re vulnerable.”
Still, health care professionals often aren’t trained in regard to human trafficking, the report says, even though it’s clear that they “must remain alert for the possibility.”
Dr. Kaplan, who has special training in child abuse and often sees children at risk, cautioned that children usually don’t directly say that they need help. “That’s generally not the case. They don’t articulate what’s going on around them as unsafe, or concerning, or dangerous. If you go and see a doctor for 10 minutes, are you going to tell them everything?
Instead, clinicians must often rely on their own observations. The report lists multiple possible signs of exploitation.
- The patient is accompanied by a domineering adult who does not allow the child to answer questions or accompanied by an unrelated adult. Inconsistent information is provided by the patient or companion. There’s a delay in seeking medical care.
- The patient has multiple sexually transmitted infections, previous pregnancy or termination, and/or frequent visits for emergency contraception. There are signs of prior sexual abuse, assault, or other maltreatment.
- The patient is withdrawn, fearful, hostile, or has a suspicious demeanor. The patient is constantly checking his or her phone and appears anxious or afraid.
What should clinicians do if they suspect exploitation? The report recommends that health care organizations develop guidelines for workers to follow. For her part, Dr. Kaplan advises colleagues to let patients lead conversations and not dig too deeply into their lives.
“Don’t turn into an investigator. This is not [Law & Order] SVU,” she said. “Stay focused on what you’re trained to do – provide health care.”
That doesn’t mean clinicians should ignore signs of trouble. It’s crucial to develop trust with the patient over time, she said, and turn to a specialist in your community or institution if you have suspicions.
And be careful to not portray victims as perpetrators. The new report emphasizes that “it’s important for health care providers to emphasize to authorities that the patient is a victim of exploitation who needs services rather than a juvenile offender.”
The report also highlights the importance of creating an environment that supports clinicians themselves: “Self-care for the clinician is critical in preventing and addressing secondary traumatic stress. A work environment that fosters peer support, encourages open discussion of work-related stress, and implements reasonable work-life balance policies can help protect providers from secondary stress and its consequences.”
Resources for clinicians include the National Human Trafficking Hotline, the federal Office of Trafficking in Persons, and the Centers for Disease Control and Prevention’s domestic refugee screening guidelines.
The study has no external funding. The authors report no disclosures.
In a new updated report, the American Academy of Pediatrics urges pediatricians to understand signs of exploitation and labor/sex trafficking and learn how to support children and adolescents who are targeted.
“It’s incredibly scary when you encounter someone you worry is a victim, and you don’t know how to help them, and they’re not saying what’s going on,” pediatrician and report coauthor Dana Kaplan, MD, of Staten Island (N.Y.) University Hospital, said in an interview. “Every case is so unique and different: There’s no algorithm of ‘If A, then B, then C.’ You have to approach each person as an individual, and it takes time to make sure you’re thinking things through about how to provide what’s needed.”
The AAP published the clinical report, which is intended to provide guidance to pediatricians, in the January 2023 issue of Pediatrics. The organization previously tackled this topic in a 2017 clinical report, and Dr. Kaplan said the new report includes updated recommendations.
As the new report notes, there aren’t reliable estimates of exploited children in the United States, although millions are thought to be trafficked and subjected to forced labor around the world. “By virtue of their young age, children and adolescents are vulnerable to manipulation and exploitation, because they have limited life experiences, a need for attachment and acceptance, an immature prefrontal cortex ... and limited options for action,” the report says.
Dr. Kaplan puts it this way: “By the nature of being a child, you’re vulnerable.”
Still, health care professionals often aren’t trained in regard to human trafficking, the report says, even though it’s clear that they “must remain alert for the possibility.”
Dr. Kaplan, who has special training in child abuse and often sees children at risk, cautioned that children usually don’t directly say that they need help. “That’s generally not the case. They don’t articulate what’s going on around them as unsafe, or concerning, or dangerous. If you go and see a doctor for 10 minutes, are you going to tell them everything?
Instead, clinicians must often rely on their own observations. The report lists multiple possible signs of exploitation.
- The patient is accompanied by a domineering adult who does not allow the child to answer questions or accompanied by an unrelated adult. Inconsistent information is provided by the patient or companion. There’s a delay in seeking medical care.
- The patient has multiple sexually transmitted infections, previous pregnancy or termination, and/or frequent visits for emergency contraception. There are signs of prior sexual abuse, assault, or other maltreatment.
- The patient is withdrawn, fearful, hostile, or has a suspicious demeanor. The patient is constantly checking his or her phone and appears anxious or afraid.
What should clinicians do if they suspect exploitation? The report recommends that health care organizations develop guidelines for workers to follow. For her part, Dr. Kaplan advises colleagues to let patients lead conversations and not dig too deeply into their lives.
“Don’t turn into an investigator. This is not [Law & Order] SVU,” she said. “Stay focused on what you’re trained to do – provide health care.”
That doesn’t mean clinicians should ignore signs of trouble. It’s crucial to develop trust with the patient over time, she said, and turn to a specialist in your community or institution if you have suspicions.
And be careful to not portray victims as perpetrators. The new report emphasizes that “it’s important for health care providers to emphasize to authorities that the patient is a victim of exploitation who needs services rather than a juvenile offender.”
The report also highlights the importance of creating an environment that supports clinicians themselves: “Self-care for the clinician is critical in preventing and addressing secondary traumatic stress. A work environment that fosters peer support, encourages open discussion of work-related stress, and implements reasonable work-life balance policies can help protect providers from secondary stress and its consequences.”
Resources for clinicians include the National Human Trafficking Hotline, the federal Office of Trafficking in Persons, and the Centers for Disease Control and Prevention’s domestic refugee screening guidelines.
The study has no external funding. The authors report no disclosures.
FROM PEDIATRICS
Greater handgrip strength tied to lower risk for depression
, new research suggests.
In a study of more than 115,000 adults, there was a significant association between stronger handgrip, up to 40 kg in men and 27 kg in women, and lower depression risk.
Investigators add that there was a “dose-response” association between physical strength and risk for depression.
“Being physically strong may serve as a preventive factor for depression in older adults, but this is limited to a maximum specific threshold for men and women,” Ruben Lopez-Bueno, PhD, of the department of physical medicine and nursing, University of Zaragoza, Spain, and colleagues write.
The findings were published online in the British Journal of Psychiatry.
Easy, fast, reliable
Depression is a major public health problem, and studies “aimed at examining preventive factors to tackle the increase in depression are required,” the investigators write.
They add that a “growing body of research” is examining the link between depression and muscle strength, with handgrip as an estimator, in healthy middle-aged and older adults.
Handgrip strength is an “easy-to-use, fast and reliable indicator of both sarcopenia (age-related loss of muscle mass) and dynapenia (age-related loss of muscle strength), both of which have been associated with depression,” the researchers note.
It is plausible that there is a “regulatory role of skeletal muscle on brain function affecting this condition,” they add.
They note that exercise seems to play a “key role” because it can improve muscle strength as well as muscle mass, downregulate systemic inflammation, and improve neuroplasticity, neuroendocrine, and oxidative stress responses.
Previous studies have relied either on cross-sectional or prospective cohort models and have focused mostly on a specific country, “not accounting for time-varying changes of both handgrip strength and relevant covariables.”
Moreover, previous evidence has been mixed regarding the “extent to which handgrip strength levels may associate with lower risk of depression, with study results ranging from weak to strong associations,” the investigators write.
So “higher-quality research with representative samples from different countries is required to better clarify the strength of such an association and to confirm directionality,” they add.
SHARE data
To fill this gap, the researchers turned to data from waves 1, 2, 4, 5, 6, and 7 of the Survey of Health, Ageing and Retirement in Europe (SHARE). This encompassed 115,601 individuals aged 50 years and older (mean age, 64.3 years; 54.3% women) residing in European countries and Israel (24 countries total).
Data from wave 3 were not used because handgrip measures were not used in that wave. In the other waves, a handheld dynamometer was used to measure handgrip strength.
The participants were divided into tertiles of handgrip strength, with the “first third” being the lowest tertile of strength and the “final third” representing the highest strength.
All participants were followed for a median of 7.3 years (792,459 person-years), during which 26.1% experienced a risk for depression, as reflected by scores on the EURO-D 12-item scale.
The investigators set the time scale as the months from study entry until either a first depression onset or the end of follow-up.
Covariates that the researchers accounted for included gender, age, education, country, body mass index, physical inactivity, smoking, alcohol consumption, whether living with a partner, wave of inclusion, chronic diseases, consumption of prescribed drugs, and fruit and vegetable consumption.
The researchers used two models: the first adjusted for gender and age at time of the interview, and the second adjusted for all confounders.
In the model that was adjusted only for gender and age, greater handgrip strength was associated with a significantly reduced risk for depression among participants in the second, third, and the final third in comparison with the first third (hazard ratio, 0.65; 95% confidence interval, 0.63-0.68; and HR, 0.50; 95% CI, 0.48-0.53, respectively).
The associations remained consistent in the fully adjusted model, although risk for depression was slightly attenuated in the second and final thirds compared with the first third (HR, 0.76; 95% CI, 0.71-0.81; and HR, 0.64; 95% CI, 0.59-0.69, respectively).
When the researchers conducted analyses using restricted cubic spline modeling, they found a significant association for each kilogram increase of handgrip strength and depression, up to 40 kg in men and 27 kg in women (HR, 1.39; 95% CI, 1.08-1.71; and HR, 1.28; 95% CI, 1.05-1.55, respectively).
There was no greater reduction in depression risk in those with handgrip strength above those values.
Potential depression screen
The investigators suggest several explanations for their findings. For example, handgrip strength has “been used as an overall indicator of health status, including sarcopenia,” they write.
Adults with sarcopenia have been found to be at greater risk for depression because of reduced muscle strength, since neurotrophins are produced by skeletal muscle, among other tissues, and are associated with improvement in mood.
From a psychological point of view, “being physically strong may lead to a sensation of psychological wellbeing,” the researchers write.
Moreover, being physically active “across the lifespan also promotes structural and functional changes in the brain, benefiting cognitive functioning and reducing the risk of neurodegeneration,” they write.
This can be important because aging adults with cognitive impairments can also experience neuromuscular impairments that “presumably will contribute to becoming weaker,” they note.
Overall, the findings “warrant strength training programmes aimed at older adults to reduce depression risk,” the investigators write. Clinicians “may consider using the observed handgrip strength thresholds to screen for potential depression risk in older adults,” they add.
Protective factor?
Commenting for this news organization, Julian Mutz, PhD, postdoctoral research associate at the Social, Genetic and Developmental Psychiatry Centre, King’s College, London, said the study “provides further evidence that physical strength may be a protective factor against depression in older adults.”
This confirms a “plethora of cross-sectional and longitudinal studies,” including one recently conducted by Dr. Mutz’s group.
The design of the current study “allowed the authors to address a number of key limitations of previous studies, for example, by including repeated measurements of grip strength and adjustment for potential confounding factors over time,” said Dr. Mutz, who was not involved with the research.
Additionally, “an important contribution of this study is that the authors show that higher grip strength is only associated with a lower risk of depression up to a specific threshold,” he noted.
“The clinical implication of this finding is that only individuals with grip strength below this threshold are at a higher risk of depression. These individuals especially may benefit from interventions aimed at increasing physical strength,” Dr. Mutz said.
The SHARE data collection has been funded by the European Commission and by DG Employment, Social Affairs and Inclusion. Additional funding was obtained from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, and the U.S. National Institute on Aging. Dr. Lopez-Bueno is supported by the European Union – Next Generation EU. The other investigators and Dr. Mutz have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
In a study of more than 115,000 adults, there was a significant association between stronger handgrip, up to 40 kg in men and 27 kg in women, and lower depression risk.
Investigators add that there was a “dose-response” association between physical strength and risk for depression.
“Being physically strong may serve as a preventive factor for depression in older adults, but this is limited to a maximum specific threshold for men and women,” Ruben Lopez-Bueno, PhD, of the department of physical medicine and nursing, University of Zaragoza, Spain, and colleagues write.
The findings were published online in the British Journal of Psychiatry.
Easy, fast, reliable
Depression is a major public health problem, and studies “aimed at examining preventive factors to tackle the increase in depression are required,” the investigators write.
They add that a “growing body of research” is examining the link between depression and muscle strength, with handgrip as an estimator, in healthy middle-aged and older adults.
Handgrip strength is an “easy-to-use, fast and reliable indicator of both sarcopenia (age-related loss of muscle mass) and dynapenia (age-related loss of muscle strength), both of which have been associated with depression,” the researchers note.
It is plausible that there is a “regulatory role of skeletal muscle on brain function affecting this condition,” they add.
They note that exercise seems to play a “key role” because it can improve muscle strength as well as muscle mass, downregulate systemic inflammation, and improve neuroplasticity, neuroendocrine, and oxidative stress responses.
Previous studies have relied either on cross-sectional or prospective cohort models and have focused mostly on a specific country, “not accounting for time-varying changes of both handgrip strength and relevant covariables.”
Moreover, previous evidence has been mixed regarding the “extent to which handgrip strength levels may associate with lower risk of depression, with study results ranging from weak to strong associations,” the investigators write.
So “higher-quality research with representative samples from different countries is required to better clarify the strength of such an association and to confirm directionality,” they add.
SHARE data
To fill this gap, the researchers turned to data from waves 1, 2, 4, 5, 6, and 7 of the Survey of Health, Ageing and Retirement in Europe (SHARE). This encompassed 115,601 individuals aged 50 years and older (mean age, 64.3 years; 54.3% women) residing in European countries and Israel (24 countries total).
Data from wave 3 were not used because handgrip measures were not used in that wave. In the other waves, a handheld dynamometer was used to measure handgrip strength.
The participants were divided into tertiles of handgrip strength, with the “first third” being the lowest tertile of strength and the “final third” representing the highest strength.
All participants were followed for a median of 7.3 years (792,459 person-years), during which 26.1% experienced a risk for depression, as reflected by scores on the EURO-D 12-item scale.
The investigators set the time scale as the months from study entry until either a first depression onset or the end of follow-up.
Covariates that the researchers accounted for included gender, age, education, country, body mass index, physical inactivity, smoking, alcohol consumption, whether living with a partner, wave of inclusion, chronic diseases, consumption of prescribed drugs, and fruit and vegetable consumption.
The researchers used two models: the first adjusted for gender and age at time of the interview, and the second adjusted for all confounders.
In the model that was adjusted only for gender and age, greater handgrip strength was associated with a significantly reduced risk for depression among participants in the second, third, and the final third in comparison with the first third (hazard ratio, 0.65; 95% confidence interval, 0.63-0.68; and HR, 0.50; 95% CI, 0.48-0.53, respectively).
The associations remained consistent in the fully adjusted model, although risk for depression was slightly attenuated in the second and final thirds compared with the first third (HR, 0.76; 95% CI, 0.71-0.81; and HR, 0.64; 95% CI, 0.59-0.69, respectively).
When the researchers conducted analyses using restricted cubic spline modeling, they found a significant association for each kilogram increase of handgrip strength and depression, up to 40 kg in men and 27 kg in women (HR, 1.39; 95% CI, 1.08-1.71; and HR, 1.28; 95% CI, 1.05-1.55, respectively).
There was no greater reduction in depression risk in those with handgrip strength above those values.
Potential depression screen
The investigators suggest several explanations for their findings. For example, handgrip strength has “been used as an overall indicator of health status, including sarcopenia,” they write.
Adults with sarcopenia have been found to be at greater risk for depression because of reduced muscle strength, since neurotrophins are produced by skeletal muscle, among other tissues, and are associated with improvement in mood.
From a psychological point of view, “being physically strong may lead to a sensation of psychological wellbeing,” the researchers write.
Moreover, being physically active “across the lifespan also promotes structural and functional changes in the brain, benefiting cognitive functioning and reducing the risk of neurodegeneration,” they write.
This can be important because aging adults with cognitive impairments can also experience neuromuscular impairments that “presumably will contribute to becoming weaker,” they note.
Overall, the findings “warrant strength training programmes aimed at older adults to reduce depression risk,” the investigators write. Clinicians “may consider using the observed handgrip strength thresholds to screen for potential depression risk in older adults,” they add.
Protective factor?
Commenting for this news organization, Julian Mutz, PhD, postdoctoral research associate at the Social, Genetic and Developmental Psychiatry Centre, King’s College, London, said the study “provides further evidence that physical strength may be a protective factor against depression in older adults.”
This confirms a “plethora of cross-sectional and longitudinal studies,” including one recently conducted by Dr. Mutz’s group.
The design of the current study “allowed the authors to address a number of key limitations of previous studies, for example, by including repeated measurements of grip strength and adjustment for potential confounding factors over time,” said Dr. Mutz, who was not involved with the research.
Additionally, “an important contribution of this study is that the authors show that higher grip strength is only associated with a lower risk of depression up to a specific threshold,” he noted.
“The clinical implication of this finding is that only individuals with grip strength below this threshold are at a higher risk of depression. These individuals especially may benefit from interventions aimed at increasing physical strength,” Dr. Mutz said.
The SHARE data collection has been funded by the European Commission and by DG Employment, Social Affairs and Inclusion. Additional funding was obtained from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, and the U.S. National Institute on Aging. Dr. Lopez-Bueno is supported by the European Union – Next Generation EU. The other investigators and Dr. Mutz have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
In a study of more than 115,000 adults, there was a significant association between stronger handgrip, up to 40 kg in men and 27 kg in women, and lower depression risk.
Investigators add that there was a “dose-response” association between physical strength and risk for depression.
“Being physically strong may serve as a preventive factor for depression in older adults, but this is limited to a maximum specific threshold for men and women,” Ruben Lopez-Bueno, PhD, of the department of physical medicine and nursing, University of Zaragoza, Spain, and colleagues write.
The findings were published online in the British Journal of Psychiatry.
Easy, fast, reliable
Depression is a major public health problem, and studies “aimed at examining preventive factors to tackle the increase in depression are required,” the investigators write.
They add that a “growing body of research” is examining the link between depression and muscle strength, with handgrip as an estimator, in healthy middle-aged and older adults.
Handgrip strength is an “easy-to-use, fast and reliable indicator of both sarcopenia (age-related loss of muscle mass) and dynapenia (age-related loss of muscle strength), both of which have been associated with depression,” the researchers note.
It is plausible that there is a “regulatory role of skeletal muscle on brain function affecting this condition,” they add.
They note that exercise seems to play a “key role” because it can improve muscle strength as well as muscle mass, downregulate systemic inflammation, and improve neuroplasticity, neuroendocrine, and oxidative stress responses.
Previous studies have relied either on cross-sectional or prospective cohort models and have focused mostly on a specific country, “not accounting for time-varying changes of both handgrip strength and relevant covariables.”
Moreover, previous evidence has been mixed regarding the “extent to which handgrip strength levels may associate with lower risk of depression, with study results ranging from weak to strong associations,” the investigators write.
So “higher-quality research with representative samples from different countries is required to better clarify the strength of such an association and to confirm directionality,” they add.
SHARE data
To fill this gap, the researchers turned to data from waves 1, 2, 4, 5, 6, and 7 of the Survey of Health, Ageing and Retirement in Europe (SHARE). This encompassed 115,601 individuals aged 50 years and older (mean age, 64.3 years; 54.3% women) residing in European countries and Israel (24 countries total).
Data from wave 3 were not used because handgrip measures were not used in that wave. In the other waves, a handheld dynamometer was used to measure handgrip strength.
The participants were divided into tertiles of handgrip strength, with the “first third” being the lowest tertile of strength and the “final third” representing the highest strength.
All participants were followed for a median of 7.3 years (792,459 person-years), during which 26.1% experienced a risk for depression, as reflected by scores on the EURO-D 12-item scale.
The investigators set the time scale as the months from study entry until either a first depression onset or the end of follow-up.
Covariates that the researchers accounted for included gender, age, education, country, body mass index, physical inactivity, smoking, alcohol consumption, whether living with a partner, wave of inclusion, chronic diseases, consumption of prescribed drugs, and fruit and vegetable consumption.
The researchers used two models: the first adjusted for gender and age at time of the interview, and the second adjusted for all confounders.
In the model that was adjusted only for gender and age, greater handgrip strength was associated with a significantly reduced risk for depression among participants in the second, third, and the final third in comparison with the first third (hazard ratio, 0.65; 95% confidence interval, 0.63-0.68; and HR, 0.50; 95% CI, 0.48-0.53, respectively).
The associations remained consistent in the fully adjusted model, although risk for depression was slightly attenuated in the second and final thirds compared with the first third (HR, 0.76; 95% CI, 0.71-0.81; and HR, 0.64; 95% CI, 0.59-0.69, respectively).
When the researchers conducted analyses using restricted cubic spline modeling, they found a significant association for each kilogram increase of handgrip strength and depression, up to 40 kg in men and 27 kg in women (HR, 1.39; 95% CI, 1.08-1.71; and HR, 1.28; 95% CI, 1.05-1.55, respectively).
There was no greater reduction in depression risk in those with handgrip strength above those values.
Potential depression screen
The investigators suggest several explanations for their findings. For example, handgrip strength has “been used as an overall indicator of health status, including sarcopenia,” they write.
Adults with sarcopenia have been found to be at greater risk for depression because of reduced muscle strength, since neurotrophins are produced by skeletal muscle, among other tissues, and are associated with improvement in mood.
From a psychological point of view, “being physically strong may lead to a sensation of psychological wellbeing,” the researchers write.
Moreover, being physically active “across the lifespan also promotes structural and functional changes in the brain, benefiting cognitive functioning and reducing the risk of neurodegeneration,” they write.
This can be important because aging adults with cognitive impairments can also experience neuromuscular impairments that “presumably will contribute to becoming weaker,” they note.
Overall, the findings “warrant strength training programmes aimed at older adults to reduce depression risk,” the investigators write. Clinicians “may consider using the observed handgrip strength thresholds to screen for potential depression risk in older adults,” they add.
Protective factor?
Commenting for this news organization, Julian Mutz, PhD, postdoctoral research associate at the Social, Genetic and Developmental Psychiatry Centre, King’s College, London, said the study “provides further evidence that physical strength may be a protective factor against depression in older adults.”
This confirms a “plethora of cross-sectional and longitudinal studies,” including one recently conducted by Dr. Mutz’s group.
The design of the current study “allowed the authors to address a number of key limitations of previous studies, for example, by including repeated measurements of grip strength and adjustment for potential confounding factors over time,” said Dr. Mutz, who was not involved with the research.
Additionally, “an important contribution of this study is that the authors show that higher grip strength is only associated with a lower risk of depression up to a specific threshold,” he noted.
“The clinical implication of this finding is that only individuals with grip strength below this threshold are at a higher risk of depression. These individuals especially may benefit from interventions aimed at increasing physical strength,” Dr. Mutz said.
The SHARE data collection has been funded by the European Commission and by DG Employment, Social Affairs and Inclusion. Additional funding was obtained from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, and the U.S. National Institute on Aging. Dr. Lopez-Bueno is supported by the European Union – Next Generation EU. The other investigators and Dr. Mutz have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF PSYCHIATRY
Can a common artificial sweetener fuel anxiety?
In a new preclinical study, investigators observed that mice that drank water containing aspartame exhibited pronounced anxiety-like behaviors in a variety of maze tests.
This behavior occurred at aspartame doses equivalent to less than 15% of the maximum daily human intake recommended by the U.S. Food and Drug Administration.
“It was such a robust anxiety-like trait that I don’t think any of us were anticipating we would see. It was completely unexpected. Usually you see subtle changes,” lead author Sara Jones, doctoral candidate at Florida State University, Tallahassee, said in a news release.
The findings were published online in Proceedings of the National Academy of Sciences.
Transgenerational transmission
When consumed, aspartame becomes aspartic acid, phenylalanine, and methanol – all of which can have potent effects on the central nervous system, the researchers point out.
Exposing the mice to aspartame also produced changes in the expression of genes regulating excitation-inhibition balance in the amygdala, a brain region that regulates anxiety and fear.
Giving the mice diazepam, which is used to treat generalized anxiety disorder, alleviated the anxiety behavior in the animals.
“The anxiety, its response to diazepam, and the changes in amygdala gene expression are not limited to the aspartame-exposed individuals but also appear in up to two generations descending from the aspartame-exposed males,” the researchers report.
“Extrapolation of the findings to humans suggests that aspartame consumption at doses below the FDA recommended maximum daily intake may produce neurobehavioral changes in aspartame-consuming individuals and their descendants,” they write.
“Thus, human population at risk of aspartame’s potential mental health effects may be larger than current expectations, which only include aspartame-consuming individuals,” they add.
Far from harmless?
The investigators plan to publish additional data from the study that focus on how aspartame affected memory in the mice.
In future research, they hope to identify molecular mechanisms that influence the transmission of aspartame’s effect across generations.
The Florida State University study joins several others that discount the long-held notion that aspartame and other nonnutritive sweeteners have no effect on the body.
As reported by this news organization, in a recent study researchers found that these sugar substitutes are not metabolically inert and can alter the gut microbiome in a way that can influence blood glucose levels.
Artificial sweeteners have also been linked to an increased risk for heart disease and stroke and for cancer.
The study was funded by the Jim and Betty Ann Rodgers Chair Fund at Florida State University and by the Bryan Robinson Foundation. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a new preclinical study, investigators observed that mice that drank water containing aspartame exhibited pronounced anxiety-like behaviors in a variety of maze tests.
This behavior occurred at aspartame doses equivalent to less than 15% of the maximum daily human intake recommended by the U.S. Food and Drug Administration.
“It was such a robust anxiety-like trait that I don’t think any of us were anticipating we would see. It was completely unexpected. Usually you see subtle changes,” lead author Sara Jones, doctoral candidate at Florida State University, Tallahassee, said in a news release.
The findings were published online in Proceedings of the National Academy of Sciences.
Transgenerational transmission
When consumed, aspartame becomes aspartic acid, phenylalanine, and methanol – all of which can have potent effects on the central nervous system, the researchers point out.
Exposing the mice to aspartame also produced changes in the expression of genes regulating excitation-inhibition balance in the amygdala, a brain region that regulates anxiety and fear.
Giving the mice diazepam, which is used to treat generalized anxiety disorder, alleviated the anxiety behavior in the animals.
“The anxiety, its response to diazepam, and the changes in amygdala gene expression are not limited to the aspartame-exposed individuals but also appear in up to two generations descending from the aspartame-exposed males,” the researchers report.
“Extrapolation of the findings to humans suggests that aspartame consumption at doses below the FDA recommended maximum daily intake may produce neurobehavioral changes in aspartame-consuming individuals and their descendants,” they write.
“Thus, human population at risk of aspartame’s potential mental health effects may be larger than current expectations, which only include aspartame-consuming individuals,” they add.
Far from harmless?
The investigators plan to publish additional data from the study that focus on how aspartame affected memory in the mice.
In future research, they hope to identify molecular mechanisms that influence the transmission of aspartame’s effect across generations.
The Florida State University study joins several others that discount the long-held notion that aspartame and other nonnutritive sweeteners have no effect on the body.
As reported by this news organization, in a recent study researchers found that these sugar substitutes are not metabolically inert and can alter the gut microbiome in a way that can influence blood glucose levels.
Artificial sweeteners have also been linked to an increased risk for heart disease and stroke and for cancer.
The study was funded by the Jim and Betty Ann Rodgers Chair Fund at Florida State University and by the Bryan Robinson Foundation. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a new preclinical study, investigators observed that mice that drank water containing aspartame exhibited pronounced anxiety-like behaviors in a variety of maze tests.
This behavior occurred at aspartame doses equivalent to less than 15% of the maximum daily human intake recommended by the U.S. Food and Drug Administration.
“It was such a robust anxiety-like trait that I don’t think any of us were anticipating we would see. It was completely unexpected. Usually you see subtle changes,” lead author Sara Jones, doctoral candidate at Florida State University, Tallahassee, said in a news release.
The findings were published online in Proceedings of the National Academy of Sciences.
Transgenerational transmission
When consumed, aspartame becomes aspartic acid, phenylalanine, and methanol – all of which can have potent effects on the central nervous system, the researchers point out.
Exposing the mice to aspartame also produced changes in the expression of genes regulating excitation-inhibition balance in the amygdala, a brain region that regulates anxiety and fear.
Giving the mice diazepam, which is used to treat generalized anxiety disorder, alleviated the anxiety behavior in the animals.
“The anxiety, its response to diazepam, and the changes in amygdala gene expression are not limited to the aspartame-exposed individuals but also appear in up to two generations descending from the aspartame-exposed males,” the researchers report.
“Extrapolation of the findings to humans suggests that aspartame consumption at doses below the FDA recommended maximum daily intake may produce neurobehavioral changes in aspartame-consuming individuals and their descendants,” they write.
“Thus, human population at risk of aspartame’s potential mental health effects may be larger than current expectations, which only include aspartame-consuming individuals,” they add.
Far from harmless?
The investigators plan to publish additional data from the study that focus on how aspartame affected memory in the mice.
In future research, they hope to identify molecular mechanisms that influence the transmission of aspartame’s effect across generations.
The Florida State University study joins several others that discount the long-held notion that aspartame and other nonnutritive sweeteners have no effect on the body.
As reported by this news organization, in a recent study researchers found that these sugar substitutes are not metabolically inert and can alter the gut microbiome in a way that can influence blood glucose levels.
Artificial sweeteners have also been linked to an increased risk for heart disease and stroke and for cancer.
The study was funded by the Jim and Betty Ann Rodgers Chair Fund at Florida State University and by the Bryan Robinson Foundation. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
Whom to screen for anxiety and depression: Updated USPSTF recommendations
In September 2022, the US Preventive Services Task Force (USPSTF) released 2 sets of draft recommendations on screening for 3 mental health conditions in adults: anxiety, depression, and suicide risk.1,2 These draft recommendations are summarized in TABLE 11-4 along with finalized recommendations on the same topics for children and adolescents, published in October 2022.3,4
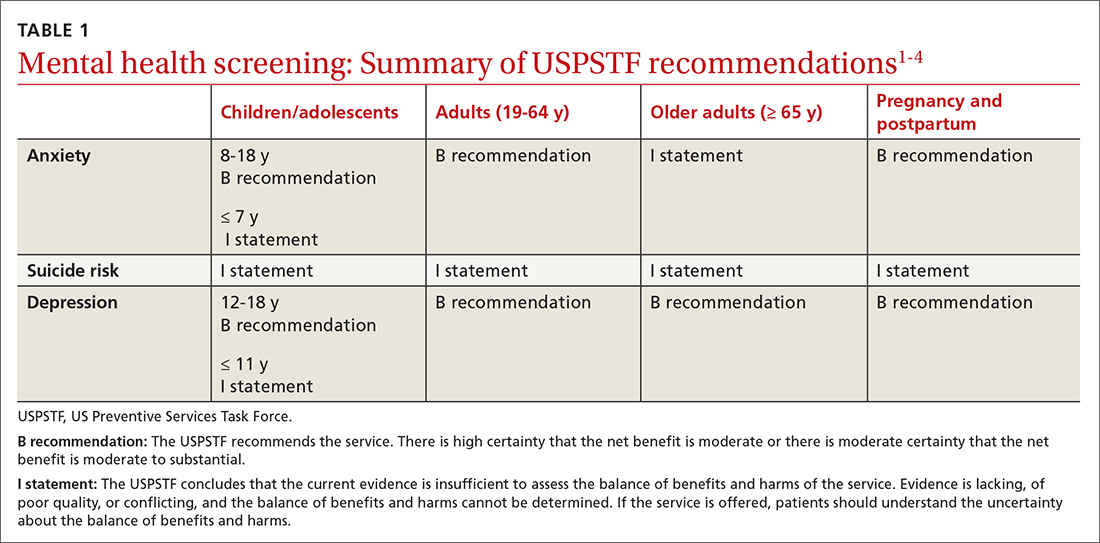
The recommendations on depression and suicide risk screening in adults are updates of previous recommendations (2016 for depression and 2014 for suicide risk) with no major changes. Screening for anxiety is a topic addressed for the first time this year for adults and for children and adolescents.1,3
The recommendations are fairly consistent between age groups. A “B” recommendation supports screening for major depression in all patients starting at age 12 years, including during pregnancy and the postpartum period. (See TABLE 1 for grade definitions.) For all age groups, evidence was insufficient to recommend screening for suicide risk. A “B” recommendation was also assigned to screening for anxiety in those ages 8 to 64 years. The USPSTF believes the evidence is insufficient to make a recommendation on screening for anxiety among adults ≥ 65 years of age.
The anxiety disorders common to both children and adults included in the USPSTF recommendations are generalized anxiety disorder, social anxiety disorder, panic disorder, separation anxiety disorder, phobias, selective mutism, and anxiety type not specified. For adults, the USPSTF also includes substance/medication-induced anxiety and anxiety due to other medical conditions.
Adults with anxiety often present with generalized complaints such as sleep disturbance, pain, and other somatic disorders that can remain undiagnosed for years. The USPSTF cites a lifetime prevalence of anxiety disorders of 26.4% for men and 40.4% for women, although the data used are 10 years old.5 The cited rate of generalized anxiety in pregnancy is 8.5% to 10.5%, and in the postpartum period, 4.4% to 10.8%.6
The data on direct benefits and harms of screening for anxiety in adults through age 64 are sparse. Nevertheless, the USPSTF deemed that screening tests for anxiety have adequate accuracy and that psychological interventions for anxiety result in moderate reduction of anxiety symptoms. Pharmacologic interventions produce a small benefit, although there is a lack of evidence for pharmacotherapy in pregnant and postpartum women. There is even less evidence of benefit for treatment in adults ≥ 65 years of age.1
How anxiety screening tests compare
Screening tests for anxiety in adults reviewed by the USPSTF included the Generalized Anxiety Disorder (GAD) scale and the Edinburgh Postnatal Depression Scale (EPDS) anxiety subscale.1 The most studied tools are the GAD-2 and GAD-7.
Continue to: The sensitivity and specificity...
The sensitivity and specificity of each test depends on the cutoff used. With the GAD-2, a cutoff of 2 or more resulted in a sensitivity of 94% and a specificity of 68% for detecting generalized anxiety.7 A cutoff of 3 or more resulted in a sensitivity of 81% and a specificity of 86%.7 The GAD-7, using 10 as a cutoff, achieves a sensitivity of 79% and a specificity of 89%.7 Given the similar performance of the 2 options, the GAD-2 (TABLE 28,9) is probably preferable for use in primary care because of its ease of administration.
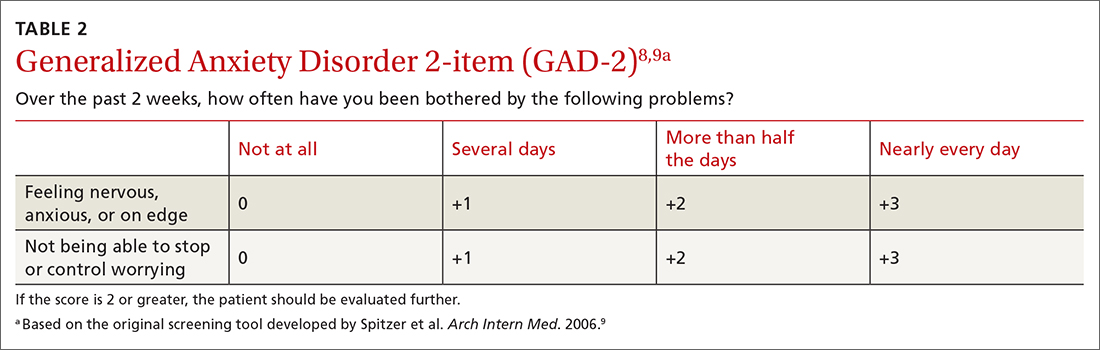
The tests evaluated by the USPSTF for anxiety screening in children and adolescents ≥ 8 years of age included the Screen for Child Anxiety Related Disorders (SCARED) and the Patient Health Questionnaire–Adolescent (PHQ-A).3 These tools ask more questions than the adult screening tools do: 41 for the SCARED and 13 for the PHQ-A. The sensitivity of SCARED for generalized anxiety disorder was 64% and the specificity was 63%.10 The sensitivity of the PHQ-A was 50% and the specificity was 98%.10
Various versions of all of these screening tools can be easily located on the internet. Search for them using the acronyms.
Screening for major depression
The depression screening tests the USPSTF examined were various versions of the Patient Health Questionnaire (PHQ), the Center for Epidemiologic Studies Depression Scale (CES-D), the Geriatric Depression Scale (GDS) in older adults, and the EPDS in postpartum and pregnant persons.7
A 2-question version of the PHQ was found to have a sensitivity of 91% with a specificity of 67%. The 9-question PHQ was found to have a similar sensitivity (88%) but better specificity (85%).7 TABLE 311 lists the 2 questions in the PHQ-2 and explains how to score the results.
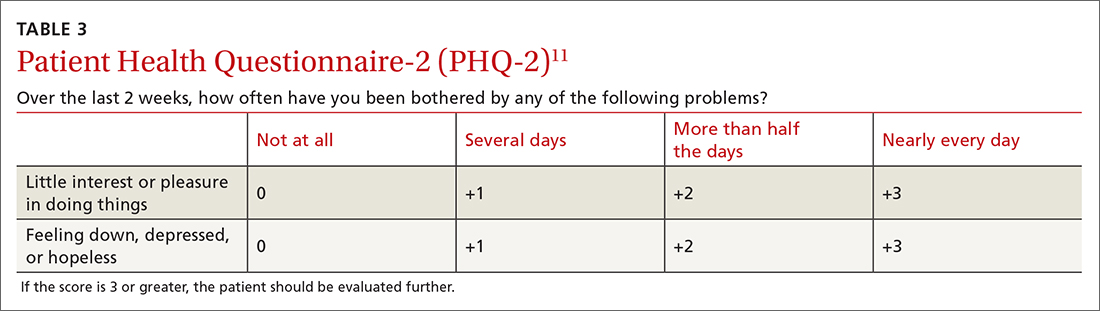
Continue to: The most commonly...
The most commonly studied screening tool for adolescents is the PHQ-A. Its sensitivity is 73% and specificity is 94%.12
The GAD-2 and PHQ-2 have the same possible answers and scores and can be combined into a 4-question screening tool to assess for anxiety and depression. If an initial screen for anxiety or depression (or both) is positive, further diagnostic testing and follow-up are needed.
Frequency of screening
The USPSTF recognized that limited information on the frequency of screening for both anxiety and depression does not support any recommendation on this matter. It suggested screening everyone once and then basing the need for subsequent screening tests on clinical judgment after considering risk factors and life events, with periodic rescreening of those at high risk. Finally, USPSTF recognized the many challenges to implementing screening tests for mental health conditions in primary care practice, but offered little practical advice on how to do this.
Suicide risk screening
As for the evidence on benefits and harms of screening for suicide risk in all age groups, the USPSTF still regards it as insufficient to make a recommendation. The lack of evidence applies to all aspects of screening, including the accuracy of the various screening tools and the potential benefits and harms of preventive interventions.2,7
Next steps
The recommendations on screening for depression, suicide risk, and anxiety in adults have been published as a draft, and the public comment period will be over by the time of this publication. The USPSTF generally takes 6 to 9 months to consider all the public comments and to publish final recommendations. The final recommendations on these topics for children and adolescents have been published since drafts were made available last April. There were no major changes between the draft and final versions.
1. USPSTF. Screening for anxiety in adults. Draft recommendation statement. Published September 20, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/draft-recommendation/anxiety-adults-screening
2. USPSTF. Screening for depression and suicide risk in adults. Updated September 14, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/draft-update-summary/screening-depression-suicide-risk-adults
3. USPSTF. Anxiety in children and adolescents: screening. Published October 11, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/recommendation/screening-anxiety-children-adolescents
4. USPSTF. Depression and suicide risk in children and adolescents: screening. Final recommendation statement. Published October 11, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/recommendation/screening-depression-suicide-risk-children-adolescents
5. Kessler RC, Petukhova M, Sampson NA, et al. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012;21:169-184. doi: 10.1002/mpr.1359
6. Misri S, Abizadeh J, Sanders S, et al. Perinatal generalized anxiety disorder: assessment and treatment. J Womens Health (Larchmt). 2015;24:762-770. doi: 10.1089/jwh.2014.5150
7. O’Connor E, Henninger M, Perdue LA, et al. Screening for depression, anxiety, and suicide risk in adults: a systematic evidence review for the US Preventive Services Task Force. Accessed November 22, 2022. www.uspreventiveservicestaskforce.org/home/getfilebytoken/dpG5pjV5yCew8fXvctFJNK
8. Sapra A, Bhandari P, Sharma S, et al. Using Generalized Anxiety Disorder-2 (GAD-2) and GAD-7 in a primary care setting. Cureus. 2020;12:e8224. doi: 10.7759/cureus.8224
9. Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-1097. doi: 10.1001/archinte.166.10.1092
10. Viswanathan M, Wallace IF, Middleton JC, et al. Screening for anxiety in children and adolescents: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2022;328:1445-1455. doi: 10.1001/jama.2022.16303
11. Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire‐2: validity of a two‐item depression screener. Med Care. 2003;41:1284‐1292. doi: 10.1097/01.MLR.0000093487.78664.3C
12. Viswanathan M, Wallace IF, Middleton JC, et al. Screening for depression and suicide risk in children and adolescents: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2022;328:1543-1556. doi:10.1001/jama.2022.16310
In September 2022, the US Preventive Services Task Force (USPSTF) released 2 sets of draft recommendations on screening for 3 mental health conditions in adults: anxiety, depression, and suicide risk.1,2 These draft recommendations are summarized in TABLE 11-4 along with finalized recommendations on the same topics for children and adolescents, published in October 2022.3,4
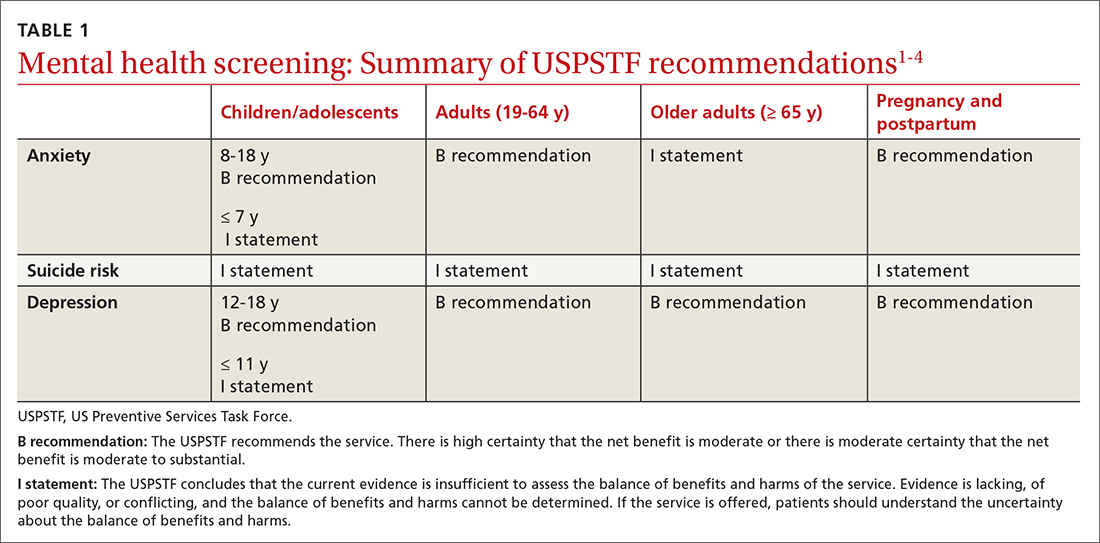
The recommendations on depression and suicide risk screening in adults are updates of previous recommendations (2016 for depression and 2014 for suicide risk) with no major changes. Screening for anxiety is a topic addressed for the first time this year for adults and for children and adolescents.1,3
The recommendations are fairly consistent between age groups. A “B” recommendation supports screening for major depression in all patients starting at age 12 years, including during pregnancy and the postpartum period. (See TABLE 1 for grade definitions.) For all age groups, evidence was insufficient to recommend screening for suicide risk. A “B” recommendation was also assigned to screening for anxiety in those ages 8 to 64 years. The USPSTF believes the evidence is insufficient to make a recommendation on screening for anxiety among adults ≥ 65 years of age.
The anxiety disorders common to both children and adults included in the USPSTF recommendations are generalized anxiety disorder, social anxiety disorder, panic disorder, separation anxiety disorder, phobias, selective mutism, and anxiety type not specified. For adults, the USPSTF also includes substance/medication-induced anxiety and anxiety due to other medical conditions.
Adults with anxiety often present with generalized complaints such as sleep disturbance, pain, and other somatic disorders that can remain undiagnosed for years. The USPSTF cites a lifetime prevalence of anxiety disorders of 26.4% for men and 40.4% for women, although the data used are 10 years old.5 The cited rate of generalized anxiety in pregnancy is 8.5% to 10.5%, and in the postpartum period, 4.4% to 10.8%.6
The data on direct benefits and harms of screening for anxiety in adults through age 64 are sparse. Nevertheless, the USPSTF deemed that screening tests for anxiety have adequate accuracy and that psychological interventions for anxiety result in moderate reduction of anxiety symptoms. Pharmacologic interventions produce a small benefit, although there is a lack of evidence for pharmacotherapy in pregnant and postpartum women. There is even less evidence of benefit for treatment in adults ≥ 65 years of age.1
How anxiety screening tests compare
Screening tests for anxiety in adults reviewed by the USPSTF included the Generalized Anxiety Disorder (GAD) scale and the Edinburgh Postnatal Depression Scale (EPDS) anxiety subscale.1 The most studied tools are the GAD-2 and GAD-7.
Continue to: The sensitivity and specificity...
The sensitivity and specificity of each test depends on the cutoff used. With the GAD-2, a cutoff of 2 or more resulted in a sensitivity of 94% and a specificity of 68% for detecting generalized anxiety.7 A cutoff of 3 or more resulted in a sensitivity of 81% and a specificity of 86%.7 The GAD-7, using 10 as a cutoff, achieves a sensitivity of 79% and a specificity of 89%.7 Given the similar performance of the 2 options, the GAD-2 (TABLE 28,9) is probably preferable for use in primary care because of its ease of administration.
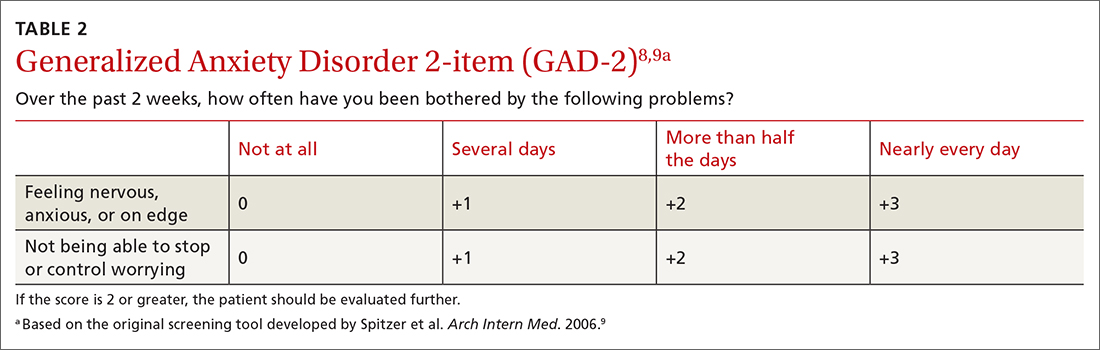
The tests evaluated by the USPSTF for anxiety screening in children and adolescents ≥ 8 years of age included the Screen for Child Anxiety Related Disorders (SCARED) and the Patient Health Questionnaire–Adolescent (PHQ-A).3 These tools ask more questions than the adult screening tools do: 41 for the SCARED and 13 for the PHQ-A. The sensitivity of SCARED for generalized anxiety disorder was 64% and the specificity was 63%.10 The sensitivity of the PHQ-A was 50% and the specificity was 98%.10
Various versions of all of these screening tools can be easily located on the internet. Search for them using the acronyms.
Screening for major depression
The depression screening tests the USPSTF examined were various versions of the Patient Health Questionnaire (PHQ), the Center for Epidemiologic Studies Depression Scale (CES-D), the Geriatric Depression Scale (GDS) in older adults, and the EPDS in postpartum and pregnant persons.7
A 2-question version of the PHQ was found to have a sensitivity of 91% with a specificity of 67%. The 9-question PHQ was found to have a similar sensitivity (88%) but better specificity (85%).7 TABLE 311 lists the 2 questions in the PHQ-2 and explains how to score the results.
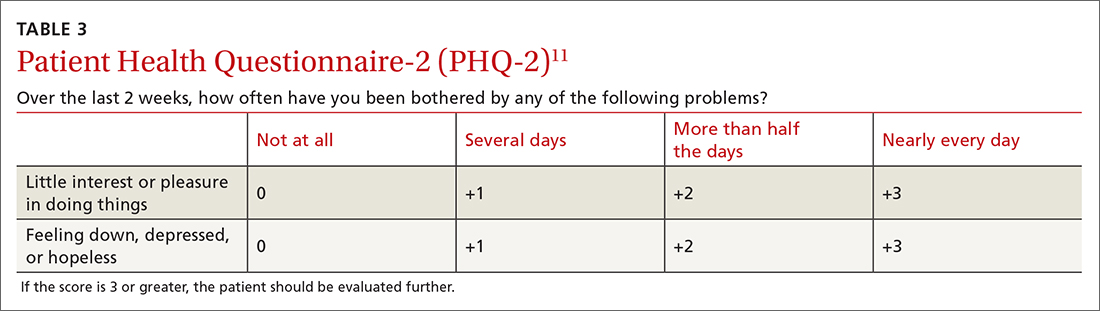
Continue to: The most commonly...
The most commonly studied screening tool for adolescents is the PHQ-A. Its sensitivity is 73% and specificity is 94%.12
The GAD-2 and PHQ-2 have the same possible answers and scores and can be combined into a 4-question screening tool to assess for anxiety and depression. If an initial screen for anxiety or depression (or both) is positive, further diagnostic testing and follow-up are needed.
Frequency of screening
The USPSTF recognized that limited information on the frequency of screening for both anxiety and depression does not support any recommendation on this matter. It suggested screening everyone once and then basing the need for subsequent screening tests on clinical judgment after considering risk factors and life events, with periodic rescreening of those at high risk. Finally, USPSTF recognized the many challenges to implementing screening tests for mental health conditions in primary care practice, but offered little practical advice on how to do this.
Suicide risk screening
As for the evidence on benefits and harms of screening for suicide risk in all age groups, the USPSTF still regards it as insufficient to make a recommendation. The lack of evidence applies to all aspects of screening, including the accuracy of the various screening tools and the potential benefits and harms of preventive interventions.2,7
Next steps
The recommendations on screening for depression, suicide risk, and anxiety in adults have been published as a draft, and the public comment period will be over by the time of this publication. The USPSTF generally takes 6 to 9 months to consider all the public comments and to publish final recommendations. The final recommendations on these topics for children and adolescents have been published since drafts were made available last April. There were no major changes between the draft and final versions.
In September 2022, the US Preventive Services Task Force (USPSTF) released 2 sets of draft recommendations on screening for 3 mental health conditions in adults: anxiety, depression, and suicide risk.1,2 These draft recommendations are summarized in TABLE 11-4 along with finalized recommendations on the same topics for children and adolescents, published in October 2022.3,4
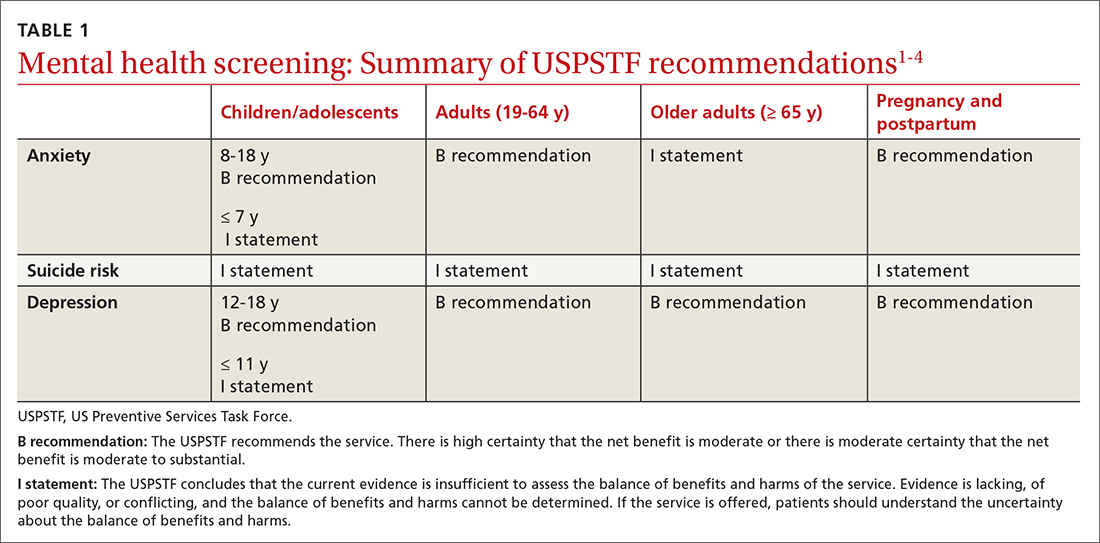
The recommendations on depression and suicide risk screening in adults are updates of previous recommendations (2016 for depression and 2014 for suicide risk) with no major changes. Screening for anxiety is a topic addressed for the first time this year for adults and for children and adolescents.1,3
The recommendations are fairly consistent between age groups. A “B” recommendation supports screening for major depression in all patients starting at age 12 years, including during pregnancy and the postpartum period. (See TABLE 1 for grade definitions.) For all age groups, evidence was insufficient to recommend screening for suicide risk. A “B” recommendation was also assigned to screening for anxiety in those ages 8 to 64 years. The USPSTF believes the evidence is insufficient to make a recommendation on screening for anxiety among adults ≥ 65 years of age.
The anxiety disorders common to both children and adults included in the USPSTF recommendations are generalized anxiety disorder, social anxiety disorder, panic disorder, separation anxiety disorder, phobias, selective mutism, and anxiety type not specified. For adults, the USPSTF also includes substance/medication-induced anxiety and anxiety due to other medical conditions.
Adults with anxiety often present with generalized complaints such as sleep disturbance, pain, and other somatic disorders that can remain undiagnosed for years. The USPSTF cites a lifetime prevalence of anxiety disorders of 26.4% for men and 40.4% for women, although the data used are 10 years old.5 The cited rate of generalized anxiety in pregnancy is 8.5% to 10.5%, and in the postpartum period, 4.4% to 10.8%.6
The data on direct benefits and harms of screening for anxiety in adults through age 64 are sparse. Nevertheless, the USPSTF deemed that screening tests for anxiety have adequate accuracy and that psychological interventions for anxiety result in moderate reduction of anxiety symptoms. Pharmacologic interventions produce a small benefit, although there is a lack of evidence for pharmacotherapy in pregnant and postpartum women. There is even less evidence of benefit for treatment in adults ≥ 65 years of age.1
How anxiety screening tests compare
Screening tests for anxiety in adults reviewed by the USPSTF included the Generalized Anxiety Disorder (GAD) scale and the Edinburgh Postnatal Depression Scale (EPDS) anxiety subscale.1 The most studied tools are the GAD-2 and GAD-7.
Continue to: The sensitivity and specificity...
The sensitivity and specificity of each test depends on the cutoff used. With the GAD-2, a cutoff of 2 or more resulted in a sensitivity of 94% and a specificity of 68% for detecting generalized anxiety.7 A cutoff of 3 or more resulted in a sensitivity of 81% and a specificity of 86%.7 The GAD-7, using 10 as a cutoff, achieves a sensitivity of 79% and a specificity of 89%.7 Given the similar performance of the 2 options, the GAD-2 (TABLE 28,9) is probably preferable for use in primary care because of its ease of administration.
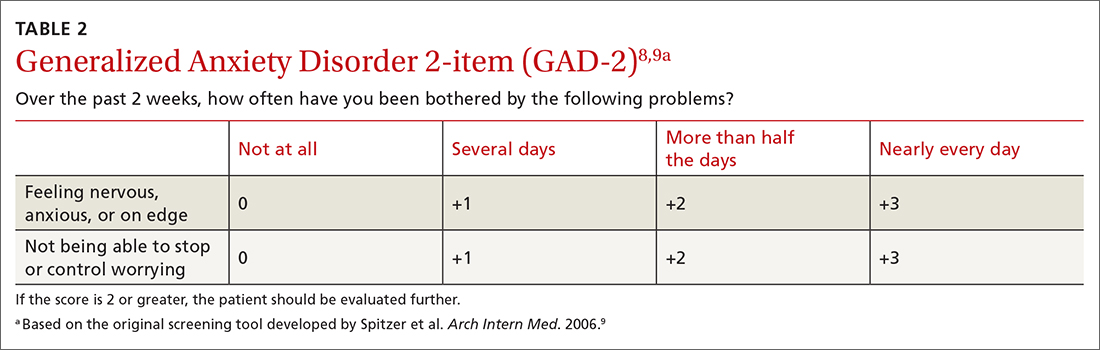
The tests evaluated by the USPSTF for anxiety screening in children and adolescents ≥ 8 years of age included the Screen for Child Anxiety Related Disorders (SCARED) and the Patient Health Questionnaire–Adolescent (PHQ-A).3 These tools ask more questions than the adult screening tools do: 41 for the SCARED and 13 for the PHQ-A. The sensitivity of SCARED for generalized anxiety disorder was 64% and the specificity was 63%.10 The sensitivity of the PHQ-A was 50% and the specificity was 98%.10
Various versions of all of these screening tools can be easily located on the internet. Search for them using the acronyms.
Screening for major depression
The depression screening tests the USPSTF examined were various versions of the Patient Health Questionnaire (PHQ), the Center for Epidemiologic Studies Depression Scale (CES-D), the Geriatric Depression Scale (GDS) in older adults, and the EPDS in postpartum and pregnant persons.7
A 2-question version of the PHQ was found to have a sensitivity of 91% with a specificity of 67%. The 9-question PHQ was found to have a similar sensitivity (88%) but better specificity (85%).7 TABLE 311 lists the 2 questions in the PHQ-2 and explains how to score the results.
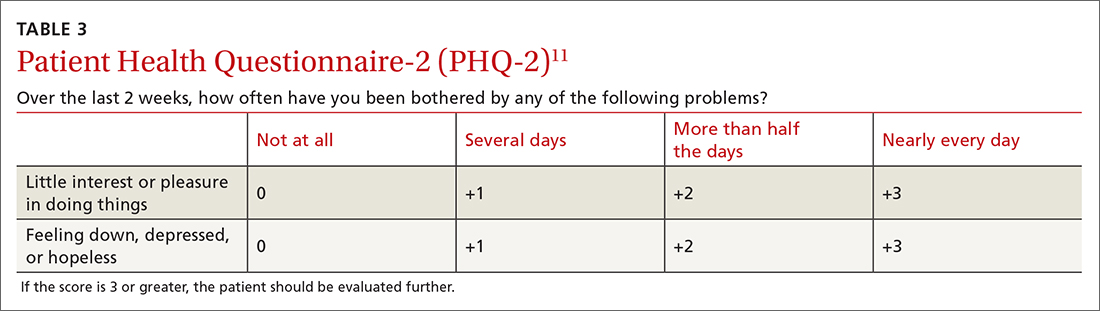
Continue to: The most commonly...
The most commonly studied screening tool for adolescents is the PHQ-A. Its sensitivity is 73% and specificity is 94%.12
The GAD-2 and PHQ-2 have the same possible answers and scores and can be combined into a 4-question screening tool to assess for anxiety and depression. If an initial screen for anxiety or depression (or both) is positive, further diagnostic testing and follow-up are needed.
Frequency of screening
The USPSTF recognized that limited information on the frequency of screening for both anxiety and depression does not support any recommendation on this matter. It suggested screening everyone once and then basing the need for subsequent screening tests on clinical judgment after considering risk factors and life events, with periodic rescreening of those at high risk. Finally, USPSTF recognized the many challenges to implementing screening tests for mental health conditions in primary care practice, but offered little practical advice on how to do this.
Suicide risk screening
As for the evidence on benefits and harms of screening for suicide risk in all age groups, the USPSTF still regards it as insufficient to make a recommendation. The lack of evidence applies to all aspects of screening, including the accuracy of the various screening tools and the potential benefits and harms of preventive interventions.2,7
Next steps
The recommendations on screening for depression, suicide risk, and anxiety in adults have been published as a draft, and the public comment period will be over by the time of this publication. The USPSTF generally takes 6 to 9 months to consider all the public comments and to publish final recommendations. The final recommendations on these topics for children and adolescents have been published since drafts were made available last April. There were no major changes between the draft and final versions.
1. USPSTF. Screening for anxiety in adults. Draft recommendation statement. Published September 20, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/draft-recommendation/anxiety-adults-screening
2. USPSTF. Screening for depression and suicide risk in adults. Updated September 14, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/draft-update-summary/screening-depression-suicide-risk-adults
3. USPSTF. Anxiety in children and adolescents: screening. Published October 11, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/recommendation/screening-anxiety-children-adolescents
4. USPSTF. Depression and suicide risk in children and adolescents: screening. Final recommendation statement. Published October 11, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/recommendation/screening-depression-suicide-risk-children-adolescents
5. Kessler RC, Petukhova M, Sampson NA, et al. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012;21:169-184. doi: 10.1002/mpr.1359
6. Misri S, Abizadeh J, Sanders S, et al. Perinatal generalized anxiety disorder: assessment and treatment. J Womens Health (Larchmt). 2015;24:762-770. doi: 10.1089/jwh.2014.5150
7. O’Connor E, Henninger M, Perdue LA, et al. Screening for depression, anxiety, and suicide risk in adults: a systematic evidence review for the US Preventive Services Task Force. Accessed November 22, 2022. www.uspreventiveservicestaskforce.org/home/getfilebytoken/dpG5pjV5yCew8fXvctFJNK
8. Sapra A, Bhandari P, Sharma S, et al. Using Generalized Anxiety Disorder-2 (GAD-2) and GAD-7 in a primary care setting. Cureus. 2020;12:e8224. doi: 10.7759/cureus.8224
9. Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-1097. doi: 10.1001/archinte.166.10.1092
10. Viswanathan M, Wallace IF, Middleton JC, et al. Screening for anxiety in children and adolescents: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2022;328:1445-1455. doi: 10.1001/jama.2022.16303
11. Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire‐2: validity of a two‐item depression screener. Med Care. 2003;41:1284‐1292. doi: 10.1097/01.MLR.0000093487.78664.3C
12. Viswanathan M, Wallace IF, Middleton JC, et al. Screening for depression and suicide risk in children and adolescents: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2022;328:1543-1556. doi:10.1001/jama.2022.16310
1. USPSTF. Screening for anxiety in adults. Draft recommendation statement. Published September 20, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/draft-recommendation/anxiety-adults-screening
2. USPSTF. Screening for depression and suicide risk in adults. Updated September 14, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/draft-update-summary/screening-depression-suicide-risk-adults
3. USPSTF. Anxiety in children and adolescents: screening. Published October 11, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/recommendation/screening-anxiety-children-adolescents
4. USPSTF. Depression and suicide risk in children and adolescents: screening. Final recommendation statement. Published October 11, 2022. Accessed November 22, 2022. https://uspreventiveservicestaskforce.org/uspstf/recommendation/screening-depression-suicide-risk-children-adolescents
5. Kessler RC, Petukhova M, Sampson NA, et al. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012;21:169-184. doi: 10.1002/mpr.1359
6. Misri S, Abizadeh J, Sanders S, et al. Perinatal generalized anxiety disorder: assessment and treatment. J Womens Health (Larchmt). 2015;24:762-770. doi: 10.1089/jwh.2014.5150
7. O’Connor E, Henninger M, Perdue LA, et al. Screening for depression, anxiety, and suicide risk in adults: a systematic evidence review for the US Preventive Services Task Force. Accessed November 22, 2022. www.uspreventiveservicestaskforce.org/home/getfilebytoken/dpG5pjV5yCew8fXvctFJNK
8. Sapra A, Bhandari P, Sharma S, et al. Using Generalized Anxiety Disorder-2 (GAD-2) and GAD-7 in a primary care setting. Cureus. 2020;12:e8224. doi: 10.7759/cureus.8224
9. Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-1097. doi: 10.1001/archinte.166.10.1092
10. Viswanathan M, Wallace IF, Middleton JC, et al. Screening for anxiety in children and adolescents: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2022;328:1445-1455. doi: 10.1001/jama.2022.16303
11. Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire‐2: validity of a two‐item depression screener. Med Care. 2003;41:1284‐1292. doi: 10.1097/01.MLR.0000093487.78664.3C
12. Viswanathan M, Wallace IF, Middleton JC, et al. Screening for depression and suicide risk in children and adolescents: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2022;328:1543-1556. doi:10.1001/jama.2022.16310
Behavioral treatment tied to lower medical, pharmacy costs
Results of a large retrospective study showed that patients newly diagnosed with a BHC who receive OPBHT following diagnosis incur lower medical and pharmacy costs over roughly the next 1 to 2 years, compared with peers who don’t receive OPBHT.
“Our findings suggest that promoting OPBHT as part of a population health strategy is associated with improved overall medical spending, particularly among adults,” the investigators write.
The study was published online in JAMA Network Open.
Common, undertreated
Nearly a quarter of adults in the United States have a BHC, and they incur greater medical costs than those without a BHC. However, diagnosis of a BHC is often delayed, and most affected individuals receive little to no treatment.
In their cost analysis, Johanna Bellon, PhD, and colleagues with Evernorth Health, St. Louis, analyzed commercial insurance claims data for 203,401 U.S. individuals newly diagnosed with one or more BHCs between 2017 and 2018.
About half of participants had depression and/or anxiety, 11% had substance use or alcohol use disorder, and 6% had a higher-acuity diagnosis, such as bipolar disorder, severe depression, eating disorder, psychotic disorder, or autism spectrum disorder.
About 1 in 5 (22%) had at least one chronic medical condition along with their BHC.
The researchers found that having at least one OPBHT visit was associated with lower medical and pharmacy costs during 15- and 27-month follow-up periods.
Over 15 months, the adjusted mean per member per month (PMPM) medical/pharmacy cost was $686 with no OPBHT visit, compared with $571 with one or more OPBHT visits.
Over 27 months, the adjusted mean PMPM was $464 with no OPBHT, versus $391 with one or more OPBHT visits.
Dose-response effect
In addition, there was a “dose-response” relationship between OPBHT and medical/pharmacy costs, such that estimated cost savings were significantly lower in the treated versus the untreated groups at almost every level of treatment.
“Our findings were also largely age independent, especially over 15 months, suggesting that OPBHT has favorable effects among children, young adults, and adults,” the researchers report.
“This is promising given that disease etiology and progression, treatment paradigms, presence of comorbid medical conditions, and overall medical and pharmacy costs differ among the three groups,” they say.
Notably, the dataset largely encompassed in-person OPBHT, because the study period preceded the transition into virtual care that occurred in 2020.
However, overall use of OPBHT was low – older adults, adults with lower income, individuals with comorbid medical conditions, and persons of racial and ethnic minorities were less likely to receive OPBHT, they found.
“These findings support the cost-effectiveness of practitioner- and insurance-based interventions to increase OPBHT utilization, which is a critical resource as new BHC diagnoses continue to increase,” the researchers say.
“Future research should validate these findings in other populations, including government-insured individuals, and explore data by chronic disease category, over longer time horizons, by type and quality of OPBHT, by type of medical spending, within subpopulations with BHCs, and including virtual and digital behavioral health services,” they suggest.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large retrospective study showed that patients newly diagnosed with a BHC who receive OPBHT following diagnosis incur lower medical and pharmacy costs over roughly the next 1 to 2 years, compared with peers who don’t receive OPBHT.
“Our findings suggest that promoting OPBHT as part of a population health strategy is associated with improved overall medical spending, particularly among adults,” the investigators write.
The study was published online in JAMA Network Open.
Common, undertreated
Nearly a quarter of adults in the United States have a BHC, and they incur greater medical costs than those without a BHC. However, diagnosis of a BHC is often delayed, and most affected individuals receive little to no treatment.
In their cost analysis, Johanna Bellon, PhD, and colleagues with Evernorth Health, St. Louis, analyzed commercial insurance claims data for 203,401 U.S. individuals newly diagnosed with one or more BHCs between 2017 and 2018.
About half of participants had depression and/or anxiety, 11% had substance use or alcohol use disorder, and 6% had a higher-acuity diagnosis, such as bipolar disorder, severe depression, eating disorder, psychotic disorder, or autism spectrum disorder.
About 1 in 5 (22%) had at least one chronic medical condition along with their BHC.
The researchers found that having at least one OPBHT visit was associated with lower medical and pharmacy costs during 15- and 27-month follow-up periods.
Over 15 months, the adjusted mean per member per month (PMPM) medical/pharmacy cost was $686 with no OPBHT visit, compared with $571 with one or more OPBHT visits.
Over 27 months, the adjusted mean PMPM was $464 with no OPBHT, versus $391 with one or more OPBHT visits.
Dose-response effect
In addition, there was a “dose-response” relationship between OPBHT and medical/pharmacy costs, such that estimated cost savings were significantly lower in the treated versus the untreated groups at almost every level of treatment.
“Our findings were also largely age independent, especially over 15 months, suggesting that OPBHT has favorable effects among children, young adults, and adults,” the researchers report.
“This is promising given that disease etiology and progression, treatment paradigms, presence of comorbid medical conditions, and overall medical and pharmacy costs differ among the three groups,” they say.
Notably, the dataset largely encompassed in-person OPBHT, because the study period preceded the transition into virtual care that occurred in 2020.
However, overall use of OPBHT was low – older adults, adults with lower income, individuals with comorbid medical conditions, and persons of racial and ethnic minorities were less likely to receive OPBHT, they found.
“These findings support the cost-effectiveness of practitioner- and insurance-based interventions to increase OPBHT utilization, which is a critical resource as new BHC diagnoses continue to increase,” the researchers say.
“Future research should validate these findings in other populations, including government-insured individuals, and explore data by chronic disease category, over longer time horizons, by type and quality of OPBHT, by type of medical spending, within subpopulations with BHCs, and including virtual and digital behavioral health services,” they suggest.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large retrospective study showed that patients newly diagnosed with a BHC who receive OPBHT following diagnosis incur lower medical and pharmacy costs over roughly the next 1 to 2 years, compared with peers who don’t receive OPBHT.
“Our findings suggest that promoting OPBHT as part of a population health strategy is associated with improved overall medical spending, particularly among adults,” the investigators write.
The study was published online in JAMA Network Open.
Common, undertreated
Nearly a quarter of adults in the United States have a BHC, and they incur greater medical costs than those without a BHC. However, diagnosis of a BHC is often delayed, and most affected individuals receive little to no treatment.
In their cost analysis, Johanna Bellon, PhD, and colleagues with Evernorth Health, St. Louis, analyzed commercial insurance claims data for 203,401 U.S. individuals newly diagnosed with one or more BHCs between 2017 and 2018.
About half of participants had depression and/or anxiety, 11% had substance use or alcohol use disorder, and 6% had a higher-acuity diagnosis, such as bipolar disorder, severe depression, eating disorder, psychotic disorder, or autism spectrum disorder.
About 1 in 5 (22%) had at least one chronic medical condition along with their BHC.
The researchers found that having at least one OPBHT visit was associated with lower medical and pharmacy costs during 15- and 27-month follow-up periods.
Over 15 months, the adjusted mean per member per month (PMPM) medical/pharmacy cost was $686 with no OPBHT visit, compared with $571 with one or more OPBHT visits.
Over 27 months, the adjusted mean PMPM was $464 with no OPBHT, versus $391 with one or more OPBHT visits.
Dose-response effect
In addition, there was a “dose-response” relationship between OPBHT and medical/pharmacy costs, such that estimated cost savings were significantly lower in the treated versus the untreated groups at almost every level of treatment.
“Our findings were also largely age independent, especially over 15 months, suggesting that OPBHT has favorable effects among children, young adults, and adults,” the researchers report.
“This is promising given that disease etiology and progression, treatment paradigms, presence of comorbid medical conditions, and overall medical and pharmacy costs differ among the three groups,” they say.
Notably, the dataset largely encompassed in-person OPBHT, because the study period preceded the transition into virtual care that occurred in 2020.
However, overall use of OPBHT was low – older adults, adults with lower income, individuals with comorbid medical conditions, and persons of racial and ethnic minorities were less likely to receive OPBHT, they found.
“These findings support the cost-effectiveness of practitioner- and insurance-based interventions to increase OPBHT utilization, which is a critical resource as new BHC diagnoses continue to increase,” the researchers say.
“Future research should validate these findings in other populations, including government-insured individuals, and explore data by chronic disease category, over longer time horizons, by type and quality of OPBHT, by type of medical spending, within subpopulations with BHCs, and including virtual and digital behavioral health services,” they suggest.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Aerobic exercise augments PTSD therapy
Investigators randomly assigned individuals with PTSD to receive either exposure therapy with aerobic exercise or exposure therapy with passive stretching for 9 weeks. At 6 months post intervention, participants in the aerobic exercise group showed greater reductions in PTSD severity, compared with those in the stretching group.
“There is a critical need to improve outcomes for treating people with PTSD, and this finding points to one potentially cheap and ready-to-use strategy that all clinicians could employ with most patients,” lead author Richard Bryant, MPsych, PhD, DSc, director of the Traumatic Stress Clinic and Scientia Professor of Psychology at the University of New South Wales, Sydney, told this news organization.
The study was published online in The Lancet Psychiatry.
Promoting BDNF
“Trauma-focused psychotherapy is the recommended treatment for PTSD, but up to half of patients do not respond to this treatment,” Dr. Bryant said.
“We know that brain-derived neurotrophic factors [BDNF] are critical for synaptic plasticity, which underpins the learning that occurs in therapy so that reminders of trauma are no longer fear-provoking,” he continued. “Preclinical animal and human research inform us that brief aerobic exercise can promote BDNF and new learning that inhibits fear responses.”
The researchers “hypothesized that brief exercise after exposure therapy to trauma memories – which is the key ingredient of trauma-focused psychotherapy – would lead to greater reductions in PTSD, relative to standard trauma-focused therapy,” he said.
To investigate the question, the researchers randomly assigned 130 adults with PTSD (mean age, 39 years; 61% female; 76% White) to receive nine 90-minute sessions of exposure therapy with either aerobic exercise or passive stretching (n = 65 in each group).
There were no differences at baseline in sociodemographic characteristics or psychopathology measures, although the mean age of the stretching group was slightly older than that of the aerobic group (40 years vs. 37 years, respectively), and there was a slightly higher proportion of women in the stretching group (68% vs. 54%).
Participants did not differ on weekly exercise either at baseline, immediately post treatment, or at 6-week follow-up.
PTSD severity (the primary outcome) was measured using the clinician-administered PTSD scale CAPS-2, with assessments conducted at baseline, 1 week post treatment, and 6 months post treatment.
The aerobic exercise regimen was tailored to each participant, based on an assessment of his/her aerobic target zone.
The exposure therapy sessions were identical for both groups. Following the exposure sessions, participants engaged in their respective exercises: Those in the passive stretching group engaged in 20 minutes of exercise, while those in the aerobic group participated in a total of 20 minutes of exercise, with 10 conducted at their personal aerobic target heart rate.
“This level of exercise was chosen because BDNF concentration in the serum is increased by two 3-minute bouts of aerobic exercise, and 10 minutes of aerobic exercise can facilitate extinction learning,” the authors explained.
The aerobic activity consisted of running on a stepper exercise platform while having cardiac activity recorded. A small portion (10%) of the therapy sessions were recorded and rated for treatment fidelity.
Change in PTSD was the primary outcome, with secondary outcomes consisting of changes in depression, anxiety, alcohol use disorder, and posttraumatic cognitions.
Few barriers
The researchers found no significant differences in PTSD severity, as measured by CAPS-2 score, between treatment groups at 10 weeks – that is, immediately post treatment (mean difference, 7.0; 95% confidence interval, –2.3 to 16.4; P = .14).
However, significantly greater reductions in PTSD severity were found in the aerobic versus the stretching group at 6-month follow-up (mean difference, 12.1;95% CI, 2.4-21.8; P = .023), pointing to a “moderate effect size” (d = 0.6; 95% CI, 0.1-1.1]).
Although there were no differences found at 6-month assessment between rates of PTSD diagnosis (25% of the aerobic vs 27% of the stretching group), more participants in the aerobic group reached a “minimal clinically important difference,” compared to those in the stretching group (96% vs. 84%, respectively, x2 = 4.4; P = .036).
There were also superior benefits found in the aerobic versus the stretching group on depression severity at 6 months (a secondary outcome), with a mean difference in Beck Depression Inventory-2 score of 5.7 (95% CI, 0.5-10.9; P = .022), yielding a “moderate effect size” (d = 0.5; 95% CI, 0.1-1.0]).
There were no adverse events associated with the intervention, and almost all the sessions (88%) complied with the treatment protocol.
The researchers noted several limitations. For example, they did not obtain plasma to measure BDNF concentrations, so they could not “infer whether the mechanism of change involved BDNF.”
In addition, they did not perform sex-specific analyses. “Future studies could increase the sample size to investigate sex differences because females display less BDNF change following exercise than do males,” they wrote.
Nevertheless, the study “provides initial evidence of a simple and accessible strategy that clinicians could readily apply in combination with exposure therapy,” they stated. “Whereas many pharmacologic interventions pose barriers, including cost, requirement for prescriptions, and patient resistance to drugs, exercise offers clinicians a strategy that can be implemented with few barriers.”
Dr. Bryant emphasized that one study “does not represent a body of evidence, and so it is essential that this finding be replicated in other trials before it can be recommended for clinical use.” He noted that other trials are “currently underway.”
Easy augmentation
In a comment, Barbara Rothbaum, PhD, professor in psychiatry and director of the Trauma and Anxiety Recovery Program at Emory University, Atlanta, called it a “well-controlled trial augmenting exposure therapy for PTSD with brief aerobic exercise and finding some benefits of the augmented condition at 6 months posttreatment but not immediately posttreatment.”
The study’s methodology – that is, using independent standard assessment of PTSD and rating audio recordings of therapy sessions for treatment fidelity and quality – can lead us to “be confident in their [the researchers’] conclusions,” she said.
Dr. Rothbaum, who was not associated with this study, described research into methods to augment exposure therapy for PTSD as “timely and clinically relevant.”
Exercise “would be an easy augmentation for many clinicians if it is helpful,” she noted.
The study was funded by the Australian National Health and Medical Research Council. The authors and Dr. Rothbaum reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators randomly assigned individuals with PTSD to receive either exposure therapy with aerobic exercise or exposure therapy with passive stretching for 9 weeks. At 6 months post intervention, participants in the aerobic exercise group showed greater reductions in PTSD severity, compared with those in the stretching group.
“There is a critical need to improve outcomes for treating people with PTSD, and this finding points to one potentially cheap and ready-to-use strategy that all clinicians could employ with most patients,” lead author Richard Bryant, MPsych, PhD, DSc, director of the Traumatic Stress Clinic and Scientia Professor of Psychology at the University of New South Wales, Sydney, told this news organization.
The study was published online in The Lancet Psychiatry.
Promoting BDNF
“Trauma-focused psychotherapy is the recommended treatment for PTSD, but up to half of patients do not respond to this treatment,” Dr. Bryant said.
“We know that brain-derived neurotrophic factors [BDNF] are critical for synaptic plasticity, which underpins the learning that occurs in therapy so that reminders of trauma are no longer fear-provoking,” he continued. “Preclinical animal and human research inform us that brief aerobic exercise can promote BDNF and new learning that inhibits fear responses.”
The researchers “hypothesized that brief exercise after exposure therapy to trauma memories – which is the key ingredient of trauma-focused psychotherapy – would lead to greater reductions in PTSD, relative to standard trauma-focused therapy,” he said.
To investigate the question, the researchers randomly assigned 130 adults with PTSD (mean age, 39 years; 61% female; 76% White) to receive nine 90-minute sessions of exposure therapy with either aerobic exercise or passive stretching (n = 65 in each group).
There were no differences at baseline in sociodemographic characteristics or psychopathology measures, although the mean age of the stretching group was slightly older than that of the aerobic group (40 years vs. 37 years, respectively), and there was a slightly higher proportion of women in the stretching group (68% vs. 54%).
Participants did not differ on weekly exercise either at baseline, immediately post treatment, or at 6-week follow-up.
PTSD severity (the primary outcome) was measured using the clinician-administered PTSD scale CAPS-2, with assessments conducted at baseline, 1 week post treatment, and 6 months post treatment.
The aerobic exercise regimen was tailored to each participant, based on an assessment of his/her aerobic target zone.
The exposure therapy sessions were identical for both groups. Following the exposure sessions, participants engaged in their respective exercises: Those in the passive stretching group engaged in 20 minutes of exercise, while those in the aerobic group participated in a total of 20 minutes of exercise, with 10 conducted at their personal aerobic target heart rate.
“This level of exercise was chosen because BDNF concentration in the serum is increased by two 3-minute bouts of aerobic exercise, and 10 minutes of aerobic exercise can facilitate extinction learning,” the authors explained.
The aerobic activity consisted of running on a stepper exercise platform while having cardiac activity recorded. A small portion (10%) of the therapy sessions were recorded and rated for treatment fidelity.
Change in PTSD was the primary outcome, with secondary outcomes consisting of changes in depression, anxiety, alcohol use disorder, and posttraumatic cognitions.
Few barriers
The researchers found no significant differences in PTSD severity, as measured by CAPS-2 score, between treatment groups at 10 weeks – that is, immediately post treatment (mean difference, 7.0; 95% confidence interval, –2.3 to 16.4; P = .14).
However, significantly greater reductions in PTSD severity were found in the aerobic versus the stretching group at 6-month follow-up (mean difference, 12.1;95% CI, 2.4-21.8; P = .023), pointing to a “moderate effect size” (d = 0.6; 95% CI, 0.1-1.1]).
Although there were no differences found at 6-month assessment between rates of PTSD diagnosis (25% of the aerobic vs 27% of the stretching group), more participants in the aerobic group reached a “minimal clinically important difference,” compared to those in the stretching group (96% vs. 84%, respectively, x2 = 4.4; P = .036).
There were also superior benefits found in the aerobic versus the stretching group on depression severity at 6 months (a secondary outcome), with a mean difference in Beck Depression Inventory-2 score of 5.7 (95% CI, 0.5-10.9; P = .022), yielding a “moderate effect size” (d = 0.5; 95% CI, 0.1-1.0]).
There were no adverse events associated with the intervention, and almost all the sessions (88%) complied with the treatment protocol.
The researchers noted several limitations. For example, they did not obtain plasma to measure BDNF concentrations, so they could not “infer whether the mechanism of change involved BDNF.”
In addition, they did not perform sex-specific analyses. “Future studies could increase the sample size to investigate sex differences because females display less BDNF change following exercise than do males,” they wrote.
Nevertheless, the study “provides initial evidence of a simple and accessible strategy that clinicians could readily apply in combination with exposure therapy,” they stated. “Whereas many pharmacologic interventions pose barriers, including cost, requirement for prescriptions, and patient resistance to drugs, exercise offers clinicians a strategy that can be implemented with few barriers.”
Dr. Bryant emphasized that one study “does not represent a body of evidence, and so it is essential that this finding be replicated in other trials before it can be recommended for clinical use.” He noted that other trials are “currently underway.”
Easy augmentation
In a comment, Barbara Rothbaum, PhD, professor in psychiatry and director of the Trauma and Anxiety Recovery Program at Emory University, Atlanta, called it a “well-controlled trial augmenting exposure therapy for PTSD with brief aerobic exercise and finding some benefits of the augmented condition at 6 months posttreatment but not immediately posttreatment.”
The study’s methodology – that is, using independent standard assessment of PTSD and rating audio recordings of therapy sessions for treatment fidelity and quality – can lead us to “be confident in their [the researchers’] conclusions,” she said.
Dr. Rothbaum, who was not associated with this study, described research into methods to augment exposure therapy for PTSD as “timely and clinically relevant.”
Exercise “would be an easy augmentation for many clinicians if it is helpful,” she noted.
The study was funded by the Australian National Health and Medical Research Council. The authors and Dr. Rothbaum reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators randomly assigned individuals with PTSD to receive either exposure therapy with aerobic exercise or exposure therapy with passive stretching for 9 weeks. At 6 months post intervention, participants in the aerobic exercise group showed greater reductions in PTSD severity, compared with those in the stretching group.
“There is a critical need to improve outcomes for treating people with PTSD, and this finding points to one potentially cheap and ready-to-use strategy that all clinicians could employ with most patients,” lead author Richard Bryant, MPsych, PhD, DSc, director of the Traumatic Stress Clinic and Scientia Professor of Psychology at the University of New South Wales, Sydney, told this news organization.
The study was published online in The Lancet Psychiatry.
Promoting BDNF
“Trauma-focused psychotherapy is the recommended treatment for PTSD, but up to half of patients do not respond to this treatment,” Dr. Bryant said.
“We know that brain-derived neurotrophic factors [BDNF] are critical for synaptic plasticity, which underpins the learning that occurs in therapy so that reminders of trauma are no longer fear-provoking,” he continued. “Preclinical animal and human research inform us that brief aerobic exercise can promote BDNF and new learning that inhibits fear responses.”
The researchers “hypothesized that brief exercise after exposure therapy to trauma memories – which is the key ingredient of trauma-focused psychotherapy – would lead to greater reductions in PTSD, relative to standard trauma-focused therapy,” he said.
To investigate the question, the researchers randomly assigned 130 adults with PTSD (mean age, 39 years; 61% female; 76% White) to receive nine 90-minute sessions of exposure therapy with either aerobic exercise or passive stretching (n = 65 in each group).
There were no differences at baseline in sociodemographic characteristics or psychopathology measures, although the mean age of the stretching group was slightly older than that of the aerobic group (40 years vs. 37 years, respectively), and there was a slightly higher proportion of women in the stretching group (68% vs. 54%).
Participants did not differ on weekly exercise either at baseline, immediately post treatment, or at 6-week follow-up.
PTSD severity (the primary outcome) was measured using the clinician-administered PTSD scale CAPS-2, with assessments conducted at baseline, 1 week post treatment, and 6 months post treatment.
The aerobic exercise regimen was tailored to each participant, based on an assessment of his/her aerobic target zone.
The exposure therapy sessions were identical for both groups. Following the exposure sessions, participants engaged in their respective exercises: Those in the passive stretching group engaged in 20 minutes of exercise, while those in the aerobic group participated in a total of 20 minutes of exercise, with 10 conducted at their personal aerobic target heart rate.
“This level of exercise was chosen because BDNF concentration in the serum is increased by two 3-minute bouts of aerobic exercise, and 10 minutes of aerobic exercise can facilitate extinction learning,” the authors explained.
The aerobic activity consisted of running on a stepper exercise platform while having cardiac activity recorded. A small portion (10%) of the therapy sessions were recorded and rated for treatment fidelity.
Change in PTSD was the primary outcome, with secondary outcomes consisting of changes in depression, anxiety, alcohol use disorder, and posttraumatic cognitions.
Few barriers
The researchers found no significant differences in PTSD severity, as measured by CAPS-2 score, between treatment groups at 10 weeks – that is, immediately post treatment (mean difference, 7.0; 95% confidence interval, –2.3 to 16.4; P = .14).
However, significantly greater reductions in PTSD severity were found in the aerobic versus the stretching group at 6-month follow-up (mean difference, 12.1;95% CI, 2.4-21.8; P = .023), pointing to a “moderate effect size” (d = 0.6; 95% CI, 0.1-1.1]).
Although there were no differences found at 6-month assessment between rates of PTSD diagnosis (25% of the aerobic vs 27% of the stretching group), more participants in the aerobic group reached a “minimal clinically important difference,” compared to those in the stretching group (96% vs. 84%, respectively, x2 = 4.4; P = .036).
There were also superior benefits found in the aerobic versus the stretching group on depression severity at 6 months (a secondary outcome), with a mean difference in Beck Depression Inventory-2 score of 5.7 (95% CI, 0.5-10.9; P = .022), yielding a “moderate effect size” (d = 0.5; 95% CI, 0.1-1.0]).
There were no adverse events associated with the intervention, and almost all the sessions (88%) complied with the treatment protocol.
The researchers noted several limitations. For example, they did not obtain plasma to measure BDNF concentrations, so they could not “infer whether the mechanism of change involved BDNF.”
In addition, they did not perform sex-specific analyses. “Future studies could increase the sample size to investigate sex differences because females display less BDNF change following exercise than do males,” they wrote.
Nevertheless, the study “provides initial evidence of a simple and accessible strategy that clinicians could readily apply in combination with exposure therapy,” they stated. “Whereas many pharmacologic interventions pose barriers, including cost, requirement for prescriptions, and patient resistance to drugs, exercise offers clinicians a strategy that can be implemented with few barriers.”
Dr. Bryant emphasized that one study “does not represent a body of evidence, and so it is essential that this finding be replicated in other trials before it can be recommended for clinical use.” He noted that other trials are “currently underway.”
Easy augmentation
In a comment, Barbara Rothbaum, PhD, professor in psychiatry and director of the Trauma and Anxiety Recovery Program at Emory University, Atlanta, called it a “well-controlled trial augmenting exposure therapy for PTSD with brief aerobic exercise and finding some benefits of the augmented condition at 6 months posttreatment but not immediately posttreatment.”
The study’s methodology – that is, using independent standard assessment of PTSD and rating audio recordings of therapy sessions for treatment fidelity and quality – can lead us to “be confident in their [the researchers’] conclusions,” she said.
Dr. Rothbaum, who was not associated with this study, described research into methods to augment exposure therapy for PTSD as “timely and clinically relevant.”
Exercise “would be an easy augmentation for many clinicians if it is helpful,” she noted.
The study was funded by the Australian National Health and Medical Research Council. The authors and Dr. Rothbaum reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET PSYCHIATRY


