User login
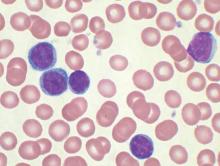
FDA approves venetoclax for CLL with 17p deletion
Venetoclax has been approved for the treatment of patients with chronic lymphocytic leukemia (CLL) who have a 17p deletion and who have been treated with a least one prior therapy, the Food and Drug Administration has announced.
The drug will be marketed as Venclexta, and is indicated for daily use after detection of a 17p deletion is confirmed through the use of the FDA-approved companion diagnostic test, the Vysis CLL FISH probe kit. A 17p deletion occurs in about 10% of patients with untreated CLL and in about 20% of patients with relapsed CLL. Venetoclax targets the B-cell lymphoma 2 (BCL-2) protein, according to the FDA press release.
“Up to half of people whose CLL progressed have 17p deletion,” Dr. Sandra Horning, chief medical officer and head of Global Product Development for Genentech, said in a press release issued by the company. Venclexta will be marketed by AbbVie and Genentech USA. The Vysis CLL FISH probe kit is manufactured by Abbott Molecular.
“For certain patients with CLL who have not had favorable outcomes with other therapies, Venclexta may provide a new option,” Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, said in a press release issued by the FDA.
The approval was based on a clinical trial of 106 patients who had CLL and 17p deletions and who had received at least one prior therapy. Trial participants took oral venetoclax daily, beginning with a 20 mg dose that was increased over a 5-week period to 400 mg. A complete or partial remission of CLL occurred in 80% of trial participants. Data on venetoclax also was presented at the annual meeting of the American Society of Hematology.
The most common side effects of venetoclax include neutropenia, diarrhea, nausea, anemia, upper respiratory tract infection, thrombocytopenia, and fatigue.
The FDA granted the Venclexta application breakthrough therapy designation, priority review status, and accelerated approval for this indication. Venclexta also received orphan drug designation.
On Twitter @maryjodales
Venetoclax has been approved for the treatment of patients with chronic lymphocytic leukemia (CLL) who have a 17p deletion and who have been treated with a least one prior therapy, the Food and Drug Administration has announced.
The drug will be marketed as Venclexta, and is indicated for daily use after detection of a 17p deletion is confirmed through the use of the FDA-approved companion diagnostic test, the Vysis CLL FISH probe kit. A 17p deletion occurs in about 10% of patients with untreated CLL and in about 20% of patients with relapsed CLL. Venetoclax targets the B-cell lymphoma 2 (BCL-2) protein, according to the FDA press release.
“Up to half of people whose CLL progressed have 17p deletion,” Dr. Sandra Horning, chief medical officer and head of Global Product Development for Genentech, said in a press release issued by the company. Venclexta will be marketed by AbbVie and Genentech USA. The Vysis CLL FISH probe kit is manufactured by Abbott Molecular.
“For certain patients with CLL who have not had favorable outcomes with other therapies, Venclexta may provide a new option,” Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, said in a press release issued by the FDA.
The approval was based on a clinical trial of 106 patients who had CLL and 17p deletions and who had received at least one prior therapy. Trial participants took oral venetoclax daily, beginning with a 20 mg dose that was increased over a 5-week period to 400 mg. A complete or partial remission of CLL occurred in 80% of trial participants. Data on venetoclax also was presented at the annual meeting of the American Society of Hematology.
The most common side effects of venetoclax include neutropenia, diarrhea, nausea, anemia, upper respiratory tract infection, thrombocytopenia, and fatigue.
The FDA granted the Venclexta application breakthrough therapy designation, priority review status, and accelerated approval for this indication. Venclexta also received orphan drug designation.
On Twitter @maryjodales
Venetoclax has been approved for the treatment of patients with chronic lymphocytic leukemia (CLL) who have a 17p deletion and who have been treated with a least one prior therapy, the Food and Drug Administration has announced.
The drug will be marketed as Venclexta, and is indicated for daily use after detection of a 17p deletion is confirmed through the use of the FDA-approved companion diagnostic test, the Vysis CLL FISH probe kit. A 17p deletion occurs in about 10% of patients with untreated CLL and in about 20% of patients with relapsed CLL. Venetoclax targets the B-cell lymphoma 2 (BCL-2) protein, according to the FDA press release.
“Up to half of people whose CLL progressed have 17p deletion,” Dr. Sandra Horning, chief medical officer and head of Global Product Development for Genentech, said in a press release issued by the company. Venclexta will be marketed by AbbVie and Genentech USA. The Vysis CLL FISH probe kit is manufactured by Abbott Molecular.
“For certain patients with CLL who have not had favorable outcomes with other therapies, Venclexta may provide a new option,” Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, said in a press release issued by the FDA.
The approval was based on a clinical trial of 106 patients who had CLL and 17p deletions and who had received at least one prior therapy. Trial participants took oral venetoclax daily, beginning with a 20 mg dose that was increased over a 5-week period to 400 mg. A complete or partial remission of CLL occurred in 80% of trial participants. Data on venetoclax also was presented at the annual meeting of the American Society of Hematology.
The most common side effects of venetoclax include neutropenia, diarrhea, nausea, anemia, upper respiratory tract infection, thrombocytopenia, and fatigue.
The FDA granted the Venclexta application breakthrough therapy designation, priority review status, and accelerated approval for this indication. Venclexta also received orphan drug designation.
On Twitter @maryjodales
Feds advance cancer moonshot with expert panel, outline of goals
Federal officials took the next step in their moonshot to end cancer by announcing on April 4 a blue ribbon panel to guide the effort.
A total of 28 leading researchers, clinicians, and patient advocates have been named to the panel charged with informing the scientific direction and goals of the National Cancer Moonshot Initiative, led by Vice President Joe Biden.
“This Blue Ribbon Panel will ensure that, as [the National Institutes of Health] allocates new resources through the Moonshot, decisions will be grounded in the best science,” Vice President Biden said in a statement. “I look forward to working with this panel and many others involved with the Moonshot to make unprecedented improvements in prevention, diagnosis, and treatment of cancer.”
The key goals of the initiative were set out simultaneously in a perspective from Dr. Francis S. Collins, NIH director, and Dr. Douglas R. Lowy, director of the National Cancer Institute. The editorial was published in the New England Journal of Medicine.
“Fueled by an additional $680 million in the proposed fiscal year 2017 budget for the NIH, plus additional resources for the Food and Drug Administration, the initiative will aim to accelerate progress toward the next generation of interventions that we hope will substantially reduce cancer incidence and dramatically improve patient outcomes,” Dr. Collins and Dr. Lowy wrote. “The NIH’s most compelling opportunities for progress will be set forth by late summer 2016 in a research plan informed by the deliberations of a blue-ribbon panel of experts, which will provide scientific input to the National Cancer Advisory Board. Some possible opportunities include vaccine development, early-detection technology, single-cell genomic analysis, immunotherapy, a focus on pediatric cancer, and enhanced data sharing.”
To read the full editorial, click here.
On Twitter @denisefulton
Federal officials took the next step in their moonshot to end cancer by announcing on April 4 a blue ribbon panel to guide the effort.
A total of 28 leading researchers, clinicians, and patient advocates have been named to the panel charged with informing the scientific direction and goals of the National Cancer Moonshot Initiative, led by Vice President Joe Biden.
“This Blue Ribbon Panel will ensure that, as [the National Institutes of Health] allocates new resources through the Moonshot, decisions will be grounded in the best science,” Vice President Biden said in a statement. “I look forward to working with this panel and many others involved with the Moonshot to make unprecedented improvements in prevention, diagnosis, and treatment of cancer.”
The key goals of the initiative were set out simultaneously in a perspective from Dr. Francis S. Collins, NIH director, and Dr. Douglas R. Lowy, director of the National Cancer Institute. The editorial was published in the New England Journal of Medicine.
“Fueled by an additional $680 million in the proposed fiscal year 2017 budget for the NIH, plus additional resources for the Food and Drug Administration, the initiative will aim to accelerate progress toward the next generation of interventions that we hope will substantially reduce cancer incidence and dramatically improve patient outcomes,” Dr. Collins and Dr. Lowy wrote. “The NIH’s most compelling opportunities for progress will be set forth by late summer 2016 in a research plan informed by the deliberations of a blue-ribbon panel of experts, which will provide scientific input to the National Cancer Advisory Board. Some possible opportunities include vaccine development, early-detection technology, single-cell genomic analysis, immunotherapy, a focus on pediatric cancer, and enhanced data sharing.”
To read the full editorial, click here.
On Twitter @denisefulton
Federal officials took the next step in their moonshot to end cancer by announcing on April 4 a blue ribbon panel to guide the effort.
A total of 28 leading researchers, clinicians, and patient advocates have been named to the panel charged with informing the scientific direction and goals of the National Cancer Moonshot Initiative, led by Vice President Joe Biden.
“This Blue Ribbon Panel will ensure that, as [the National Institutes of Health] allocates new resources through the Moonshot, decisions will be grounded in the best science,” Vice President Biden said in a statement. “I look forward to working with this panel and many others involved with the Moonshot to make unprecedented improvements in prevention, diagnosis, and treatment of cancer.”
The key goals of the initiative were set out simultaneously in a perspective from Dr. Francis S. Collins, NIH director, and Dr. Douglas R. Lowy, director of the National Cancer Institute. The editorial was published in the New England Journal of Medicine.
“Fueled by an additional $680 million in the proposed fiscal year 2017 budget for the NIH, plus additional resources for the Food and Drug Administration, the initiative will aim to accelerate progress toward the next generation of interventions that we hope will substantially reduce cancer incidence and dramatically improve patient outcomes,” Dr. Collins and Dr. Lowy wrote. “The NIH’s most compelling opportunities for progress will be set forth by late summer 2016 in a research plan informed by the deliberations of a blue-ribbon panel of experts, which will provide scientific input to the National Cancer Advisory Board. Some possible opportunities include vaccine development, early-detection technology, single-cell genomic analysis, immunotherapy, a focus on pediatric cancer, and enhanced data sharing.”
To read the full editorial, click here.
On Twitter @denisefulton
FROM NEJM
RPS15 mutations prevalent in aggressive chronic lymphocytic leukemia
Mutations in the RPS15 gene occurred in 8 of 41 patients with relapsing chronic lymphocytic leukemia (CLL), and the mutations were present before treatment in 7 of the 8, a possible indication that the aberrations are early genetic events in aggressive CLL pathobiology.
RPS15 mutations may lead to defective p53 stability and increased degradation, representing a potential novel mechanism in CLL pathobiology. The findings suggest “RPS15-mutant cases should be treated with alternative regimens that act independently of the p53 pathway,” wrote Dr. Viktor Ljungström of the department of immunology, genetics, and pathology, Uppsala (Sweden) University, and colleagues (Blood 2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
In their study, the researchers performed whole exome sequencing of 110 samples collected before and after treatment from 41 patients with aggressive CLL that relapsed after a median of 2 years; 7 patients had mutations in RPS15 before treatment, and 8 had RPS15 mutations after treatment. The findings suggest that standard therapy with fludarabine, cyclophosphamide, and rituximab was not intrinsically mutagenic.
High frequencies of mutations were linked to poor outcome in both pretreated and relapse samples. These mutations included NOTCH1, TP53, ATM, SF3B1, MGA, and BIRC3. At least one mutation was seen before treatment in 26 of the 41 patients, and that rate rose to 33 of 41 patients at relapse. Two or more mutations were noted before treatment in 12 of 41 patients, and that rose to 15 of 41 at relapse.
In response to their findings, the researchers next performed targeted resequencing of the RPS15 hot spot (exon 4) in an extended series of 790 patients with CLL, intentionally enriched with 605 cases with adverse prognostic profiles. They found an additional 36 mutations in RPS15 (36/605, 6%). In contrast, none of the 185 patients with more favorable prognostic, IGHV-mutated CLL carried RPS15 mutations. RPS15-mutant patients without concomitant TP53 aberrations had an overall survival similar to other aggressive CLL subgroups, but none of the patients with both mutations survived at 10 years, compared with 59% of patients with wild-type RPS15 and wild-type TP53, “pointing to a dismal prognosis for RPS15-mutated CLL,” they wrote.
They also analyzed 30 cases with Richter syndrome (CLL transformed into diffuse large B-cell lymphoma), and only a single case was found to carry an RPS15 mutation, and the mutation was also observed in the preceding CLL phase. This finding indicates that RPS15 mutation probably does not underlie the transformation of CLL to Richter syndrome, according to the researchers.
Dr. Ljungström and coauthors reported having no relevant financial disclosures.
In support of the authors’ hypothesis that RPS15 mutations may be an early-acquired driver in high-risk disease, the variant allele frequency in eight serially analyzed cases remained static, with only one case gaining a mutation in RPS15, whereas the variable allele frequency increased at relapse for other well-characterized mutations in ATM, BIRC3, NFKBIE, and TP53.
Pilot experiments demonstrated specific interactions between TP53 and RPS15, and p53 stability was reduced in the presence of mutant RPS15.
The findings should prompt further investigation to determine if the consequences of RPS15 mutations depend on its interaction with TP53, or if the mutations found in other ribosomal proteins indicate a different mechanism related to the 40S subunit.
Given that RPS15 is not included in common academic or commercial sequencing panels, the presence of RPS15 mutations in other diseases may be underestimated as well.
More generally, are there other cancers with subgroups enriched for other benign-appearing genes?
Dr. James Blachly is with Wexner Medical Center, the Ohio State University, Columbus. These remarks were part of an editorial accompanying a report in Blood (2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
In support of the authors’ hypothesis that RPS15 mutations may be an early-acquired driver in high-risk disease, the variant allele frequency in eight serially analyzed cases remained static, with only one case gaining a mutation in RPS15, whereas the variable allele frequency increased at relapse for other well-characterized mutations in ATM, BIRC3, NFKBIE, and TP53.
Pilot experiments demonstrated specific interactions between TP53 and RPS15, and p53 stability was reduced in the presence of mutant RPS15.
The findings should prompt further investigation to determine if the consequences of RPS15 mutations depend on its interaction with TP53, or if the mutations found in other ribosomal proteins indicate a different mechanism related to the 40S subunit.
Given that RPS15 is not included in common academic or commercial sequencing panels, the presence of RPS15 mutations in other diseases may be underestimated as well.
More generally, are there other cancers with subgroups enriched for other benign-appearing genes?
Dr. James Blachly is with Wexner Medical Center, the Ohio State University, Columbus. These remarks were part of an editorial accompanying a report in Blood (2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
In support of the authors’ hypothesis that RPS15 mutations may be an early-acquired driver in high-risk disease, the variant allele frequency in eight serially analyzed cases remained static, with only one case gaining a mutation in RPS15, whereas the variable allele frequency increased at relapse for other well-characterized mutations in ATM, BIRC3, NFKBIE, and TP53.
Pilot experiments demonstrated specific interactions between TP53 and RPS15, and p53 stability was reduced in the presence of mutant RPS15.
The findings should prompt further investigation to determine if the consequences of RPS15 mutations depend on its interaction with TP53, or if the mutations found in other ribosomal proteins indicate a different mechanism related to the 40S subunit.
Given that RPS15 is not included in common academic or commercial sequencing panels, the presence of RPS15 mutations in other diseases may be underestimated as well.
More generally, are there other cancers with subgroups enriched for other benign-appearing genes?
Dr. James Blachly is with Wexner Medical Center, the Ohio State University, Columbus. These remarks were part of an editorial accompanying a report in Blood (2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
Mutations in the RPS15 gene occurred in 8 of 41 patients with relapsing chronic lymphocytic leukemia (CLL), and the mutations were present before treatment in 7 of the 8, a possible indication that the aberrations are early genetic events in aggressive CLL pathobiology.
RPS15 mutations may lead to defective p53 stability and increased degradation, representing a potential novel mechanism in CLL pathobiology. The findings suggest “RPS15-mutant cases should be treated with alternative regimens that act independently of the p53 pathway,” wrote Dr. Viktor Ljungström of the department of immunology, genetics, and pathology, Uppsala (Sweden) University, and colleagues (Blood 2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
In their study, the researchers performed whole exome sequencing of 110 samples collected before and after treatment from 41 patients with aggressive CLL that relapsed after a median of 2 years; 7 patients had mutations in RPS15 before treatment, and 8 had RPS15 mutations after treatment. The findings suggest that standard therapy with fludarabine, cyclophosphamide, and rituximab was not intrinsically mutagenic.
High frequencies of mutations were linked to poor outcome in both pretreated and relapse samples. These mutations included NOTCH1, TP53, ATM, SF3B1, MGA, and BIRC3. At least one mutation was seen before treatment in 26 of the 41 patients, and that rate rose to 33 of 41 patients at relapse. Two or more mutations were noted before treatment in 12 of 41 patients, and that rose to 15 of 41 at relapse.
In response to their findings, the researchers next performed targeted resequencing of the RPS15 hot spot (exon 4) in an extended series of 790 patients with CLL, intentionally enriched with 605 cases with adverse prognostic profiles. They found an additional 36 mutations in RPS15 (36/605, 6%). In contrast, none of the 185 patients with more favorable prognostic, IGHV-mutated CLL carried RPS15 mutations. RPS15-mutant patients without concomitant TP53 aberrations had an overall survival similar to other aggressive CLL subgroups, but none of the patients with both mutations survived at 10 years, compared with 59% of patients with wild-type RPS15 and wild-type TP53, “pointing to a dismal prognosis for RPS15-mutated CLL,” they wrote.
They also analyzed 30 cases with Richter syndrome (CLL transformed into diffuse large B-cell lymphoma), and only a single case was found to carry an RPS15 mutation, and the mutation was also observed in the preceding CLL phase. This finding indicates that RPS15 mutation probably does not underlie the transformation of CLL to Richter syndrome, according to the researchers.
Dr. Ljungström and coauthors reported having no relevant financial disclosures.
Mutations in the RPS15 gene occurred in 8 of 41 patients with relapsing chronic lymphocytic leukemia (CLL), and the mutations were present before treatment in 7 of the 8, a possible indication that the aberrations are early genetic events in aggressive CLL pathobiology.
RPS15 mutations may lead to defective p53 stability and increased degradation, representing a potential novel mechanism in CLL pathobiology. The findings suggest “RPS15-mutant cases should be treated with alternative regimens that act independently of the p53 pathway,” wrote Dr. Viktor Ljungström of the department of immunology, genetics, and pathology, Uppsala (Sweden) University, and colleagues (Blood 2016 Feb 25. doi: 10.1182/blood-2015-10-674572).
In their study, the researchers performed whole exome sequencing of 110 samples collected before and after treatment from 41 patients with aggressive CLL that relapsed after a median of 2 years; 7 patients had mutations in RPS15 before treatment, and 8 had RPS15 mutations after treatment. The findings suggest that standard therapy with fludarabine, cyclophosphamide, and rituximab was not intrinsically mutagenic.
High frequencies of mutations were linked to poor outcome in both pretreated and relapse samples. These mutations included NOTCH1, TP53, ATM, SF3B1, MGA, and BIRC3. At least one mutation was seen before treatment in 26 of the 41 patients, and that rate rose to 33 of 41 patients at relapse. Two or more mutations were noted before treatment in 12 of 41 patients, and that rose to 15 of 41 at relapse.
In response to their findings, the researchers next performed targeted resequencing of the RPS15 hot spot (exon 4) in an extended series of 790 patients with CLL, intentionally enriched with 605 cases with adverse prognostic profiles. They found an additional 36 mutations in RPS15 (36/605, 6%). In contrast, none of the 185 patients with more favorable prognostic, IGHV-mutated CLL carried RPS15 mutations. RPS15-mutant patients without concomitant TP53 aberrations had an overall survival similar to other aggressive CLL subgroups, but none of the patients with both mutations survived at 10 years, compared with 59% of patients with wild-type RPS15 and wild-type TP53, “pointing to a dismal prognosis for RPS15-mutated CLL,” they wrote.
They also analyzed 30 cases with Richter syndrome (CLL transformed into diffuse large B-cell lymphoma), and only a single case was found to carry an RPS15 mutation, and the mutation was also observed in the preceding CLL phase. This finding indicates that RPS15 mutation probably does not underlie the transformation of CLL to Richter syndrome, according to the researchers.
Dr. Ljungström and coauthors reported having no relevant financial disclosures.
FROM BLOOD
Key clinical point: Aberrations in the RPS15 gene before therapy may be an indicator of aggressive pathobiology in chronic lymphocytic leukemia.
Major finding: Mutations in the RPS15 gene occurred in 8 of 41 patients with relapsing CLL, and the mutations were present before treatment in 7 of the 8.
Data sources: Whole exome sequencing of 110 samples collected before and after fludarabine, cyclophosphamide, and rituximab therapy from 41 patients with relapsed CLL.
Disclosures: Dr. Ljungström and coauthors reported having no relevant financial disclosures.
Idelalisib use halted in six combo therapy trials, FDA announces
An increased rate of adverse events, including deaths, have been reported in clinical trials with idelalisib (Zydelig) in combination with other cancer medicines, the U.S. Food and Drug Administration announced.
Gilead Sciences, Inc. has confirmed that they are stopping six clinical trials in patients with chronic lymphocytic leukemia, small lymphocytic lymphoma and indolent non-Hodgkin lymphomas. The FDA is reviewing the findings of the clinical trials and will communicate new information as necessary, according to the FDA press release.
Idelalisib is not approved for previously untreated chronic lymphocytic leukemia. It is approved by the FDA for the treatment of:
• Relapsed chronic lymphocytic leukemia, in combination with rituximab, in patients for whom rituximab alone would be considered appropriate therapy due to other co-morbidities.
• Relapsed follicular B-cell non-Hodgkin lymphoma in patients who have received at least two prior systemic therapies.
• Relapsed small lymphocytic lymphoma in patients who have received at least two prior systemic therapies.
Adverse events involving idelalisib should be reported to the FDA MedWatch program, the release advised.
On Twitter @maryjodales
An increased rate of adverse events, including deaths, have been reported in clinical trials with idelalisib (Zydelig) in combination with other cancer medicines, the U.S. Food and Drug Administration announced.
Gilead Sciences, Inc. has confirmed that they are stopping six clinical trials in patients with chronic lymphocytic leukemia, small lymphocytic lymphoma and indolent non-Hodgkin lymphomas. The FDA is reviewing the findings of the clinical trials and will communicate new information as necessary, according to the FDA press release.
Idelalisib is not approved for previously untreated chronic lymphocytic leukemia. It is approved by the FDA for the treatment of:
• Relapsed chronic lymphocytic leukemia, in combination with rituximab, in patients for whom rituximab alone would be considered appropriate therapy due to other co-morbidities.
• Relapsed follicular B-cell non-Hodgkin lymphoma in patients who have received at least two prior systemic therapies.
• Relapsed small lymphocytic lymphoma in patients who have received at least two prior systemic therapies.
Adverse events involving idelalisib should be reported to the FDA MedWatch program, the release advised.
On Twitter @maryjodales
An increased rate of adverse events, including deaths, have been reported in clinical trials with idelalisib (Zydelig) in combination with other cancer medicines, the U.S. Food and Drug Administration announced.
Gilead Sciences, Inc. has confirmed that they are stopping six clinical trials in patients with chronic lymphocytic leukemia, small lymphocytic lymphoma and indolent non-Hodgkin lymphomas. The FDA is reviewing the findings of the clinical trials and will communicate new information as necessary, according to the FDA press release.
Idelalisib is not approved for previously untreated chronic lymphocytic leukemia. It is approved by the FDA for the treatment of:
• Relapsed chronic lymphocytic leukemia, in combination with rituximab, in patients for whom rituximab alone would be considered appropriate therapy due to other co-morbidities.
• Relapsed follicular B-cell non-Hodgkin lymphoma in patients who have received at least two prior systemic therapies.
• Relapsed small lymphocytic lymphoma in patients who have received at least two prior systemic therapies.
Adverse events involving idelalisib should be reported to the FDA MedWatch program, the release advised.
On Twitter @maryjodales
Ibrutinib approved as first-line therapy for all CLL patients
Ibrutinib (Imbruvica) has been approved as a first-line treatment for patients with chronic lymphocytic leukemia (CLL), irrespective of their treatment history, according to a statement issued by the manufacturer, AbbVie.
The approval is based on data from the randomized, multicenter, open-label phase III RESONATE-2 trial, which evaluated the use of ibrutinib versus chlorambucil in 269 treatment-naive patients with CLL or small lymphocytic lymphoma (SLL) aged 65 years or older. The RESONATE-2 data were presented at the 2015 annual meeting of the American Society of Hematology.
“The progression-free survival data seen in these previously untreated CLL patients are strong and encouraging,” Dr. Jan Burger of the University of Texas MD Anderson Cancer Center, Houston, and the lead investigator of RESONATE-2, said in the AbbVie statement. “This is especially important for first-line CLL patients, when considering the safety profile. This treatment represents another option for these patients.”
The National Comprehensive Cancer Network also recently published an update to its clinical practice guidelines for non-Hodgkin’s lymphomas, granting Imbruvica a category 1 recommendation for certain CLL patients, including as a first-line treatment option for frail CLL patients with significant comorbidities, as well as for CLL patients with or without del 17p or the genetic mutation TP53 who are 70 years or older, or younger patients with significant comorbidities, the AbbVie statement noted.
Imbruvica has been jointly developed and commercialized by Pharmacyclics LLC, an AbbVie company, and by Janssen Biotech.
Ibrutinib (Imbruvica) has been approved as a first-line treatment for patients with chronic lymphocytic leukemia (CLL), irrespective of their treatment history, according to a statement issued by the manufacturer, AbbVie.
The approval is based on data from the randomized, multicenter, open-label phase III RESONATE-2 trial, which evaluated the use of ibrutinib versus chlorambucil in 269 treatment-naive patients with CLL or small lymphocytic lymphoma (SLL) aged 65 years or older. The RESONATE-2 data were presented at the 2015 annual meeting of the American Society of Hematology.
“The progression-free survival data seen in these previously untreated CLL patients are strong and encouraging,” Dr. Jan Burger of the University of Texas MD Anderson Cancer Center, Houston, and the lead investigator of RESONATE-2, said in the AbbVie statement. “This is especially important for first-line CLL patients, when considering the safety profile. This treatment represents another option for these patients.”
The National Comprehensive Cancer Network also recently published an update to its clinical practice guidelines for non-Hodgkin’s lymphomas, granting Imbruvica a category 1 recommendation for certain CLL patients, including as a first-line treatment option for frail CLL patients with significant comorbidities, as well as for CLL patients with or without del 17p or the genetic mutation TP53 who are 70 years or older, or younger patients with significant comorbidities, the AbbVie statement noted.
Imbruvica has been jointly developed and commercialized by Pharmacyclics LLC, an AbbVie company, and by Janssen Biotech.
Ibrutinib (Imbruvica) has been approved as a first-line treatment for patients with chronic lymphocytic leukemia (CLL), irrespective of their treatment history, according to a statement issued by the manufacturer, AbbVie.
The approval is based on data from the randomized, multicenter, open-label phase III RESONATE-2 trial, which evaluated the use of ibrutinib versus chlorambucil in 269 treatment-naive patients with CLL or small lymphocytic lymphoma (SLL) aged 65 years or older. The RESONATE-2 data were presented at the 2015 annual meeting of the American Society of Hematology.
“The progression-free survival data seen in these previously untreated CLL patients are strong and encouraging,” Dr. Jan Burger of the University of Texas MD Anderson Cancer Center, Houston, and the lead investigator of RESONATE-2, said in the AbbVie statement. “This is especially important for first-line CLL patients, when considering the safety profile. This treatment represents another option for these patients.”
The National Comprehensive Cancer Network also recently published an update to its clinical practice guidelines for non-Hodgkin’s lymphomas, granting Imbruvica a category 1 recommendation for certain CLL patients, including as a first-line treatment option for frail CLL patients with significant comorbidities, as well as for CLL patients with or without del 17p or the genetic mutation TP53 who are 70 years or older, or younger patients with significant comorbidities, the AbbVie statement noted.
Imbruvica has been jointly developed and commercialized by Pharmacyclics LLC, an AbbVie company, and by Janssen Biotech.
Venetoclax shows promise for relapsed CLL, SLL
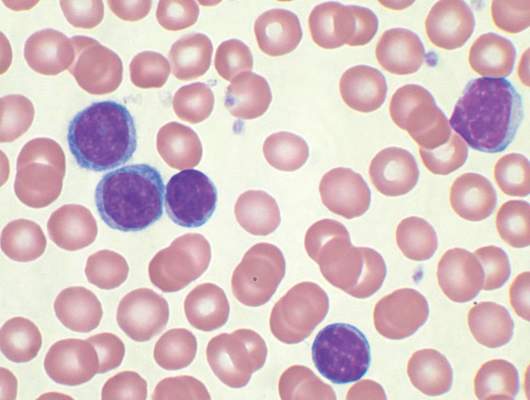
Daily oral treatment with venetoclax induced substantial responses with manageable adverse effects in patients with relapsed chronic lymphocytic leukemia or small lymphocytic lymphoma in a first-in-human phase I dose-escalation study.
The promising effects of the highly selective investigational inhibitor of BCL2 – a protein central to the survival of CLL cells – were noted even in patients with poor prognostic features, who comprised 89% of the cohort, reported Dr. Andrew W. Roberts of Royal Melbourne Hospital, Australia, and his colleagues. The study was published online Jan. 28 in The New England Journal of Medicine.
In the dose escalation phase of the study, 56 patients received active treatment at doses raging from 150 to 1,200 mg daily, and 60 additional patients received weekly stepwise ramp-up with doses beginning at 20 mg daily with weekly increases to 50 mg, 100 mg, and 200 mg daily up to the target dose of 400 mg daily. The patients had received a median of 3 previous therapies (range, 1-11).
Of 116 treated patients, 92 (79%) had a response, and 20% achieved complete remission, including 5% with no minimal residual disease on flow cytometry, the investigators said (N Engl J Med. 2016;374:311-22).
Venetoclax was active at all doses used in the study, and no maximum tolerated dose was identified.
Tumor lysis syndrome occurred in 10 patients, but clinically important sequelae occurred in only 3 of those patients, 2 of whom had severe sequelae. After adjustments were made to dosing schedule, no further cases occurred.
Other side effects included mild diarrhea, upper respiratory tract infection, nausea, and grade 3 or 4 neutropenia, which occurred in 41%-52% of patients. Serious adverse events included febrile neutropenia in 6% of patients, pneumonia in 4%, upper respiratory tract infection in 3%, and immune thrombocytopenia in 3%.
Among the patients with an adverse prognosis, treatment response rates ranged from 71% to 79%, depending on the subgroup. For example, the response rate was 79% in 70 patients with resistance to fludarabine, and 71% in 31 patients with chromosome 17p deletions.
New treatments, including ibrutinib monotherapy and idelalisib in combination with rituximab, have improved outcomes for patients with relapsed CLL, but despite these advances, complete remissions remain uncommon, the authors said.
“This first trial of venetoclax showed the potential of BCL2 antagonism as an additional therapeutic avenue for patients with relapsed CLL,” they wrote, adding that the 79% overall response rate in this study – including deep responses and complete responses without minimal residual disease in patients up to age 86 years and patients with poor prognostic factors – “provides support for further development of venetoclax as a treatment option for patients with heavily pretreated relapsed or refractory CLL or SLL.”
Of note, the Food and Drug Administration on Jan. 28 – the date this study was released – granted venetoclax Breakthrough Therapy Designation for use in combination with hypomethylating agents for the treatment of acute myeloid leukemia patients who aren’t eligible for standard induction chemotherapy. The designation – the third for the agent – is supported by data from a single study of untreated patients aged 65 years or older with AML. Prior venetoclax Breakthrough Therapy Designations were granted in April 2015 for its use as monotherapy in patients with refractory CLL who have the 17p deletion genetic mutation, and in January for its use with rituximab for the treatment of relapsed/refractory CLL.
AbbVie and Genentech supported the study. Dr. Roberts reported receiving grant support and study drugs form AbbVie, serving as an investigator in trials sponsored by Genentech, AbbVie, Janssen, and Beigene, and receiving institutional research funding from Genentech for the development of venetoclax. His coauthors reported ties to various pharmaceutical companies.
Targeted therapies have fundamentally changed the management and outcomes of patients with CLL in recent years, and new findings for second-generation drugs offer even more promise, according to Dr. Wyndham H. Wilson.
Taken together with the recent finding that acalabrutinib has a high degree of Bruton’s tyrosine kinase (BTK) inhibition with lower toxicity than ibrutinib, the findings of Roberts et al. with respect to venetoclax suggest a possible new avenue for combination treatment, Dr. Wilson wrote in an editorial (N Engl J Med. 2016;374;4:386-8).
“The transformative characteristics of acalabrutinib and venetoclax arise from effective targeting of important survival pathways in CLL. Indeed, BTK inhibition produces durable responses, improves survival, and selects for mutations in the BTK-binding domain,” Dr. Wilson said, adding that BCL2 also plays an important role in CLL survival, as indicated by the activity of venetoclax.
While neither venetoclax nor acalabrutinib regularly induce complete remission, in vitro findings show that venetoclax and BTK inhibitors are synergistic, which suggests that combining the two might “further transform the targeted treatment of CLL,” he explained.
Dr. Wilson is with the National Cancer Institute, Bethesda, Md.
Targeted therapies have fundamentally changed the management and outcomes of patients with CLL in recent years, and new findings for second-generation drugs offer even more promise, according to Dr. Wyndham H. Wilson.
Taken together with the recent finding that acalabrutinib has a high degree of Bruton’s tyrosine kinase (BTK) inhibition with lower toxicity than ibrutinib, the findings of Roberts et al. with respect to venetoclax suggest a possible new avenue for combination treatment, Dr. Wilson wrote in an editorial (N Engl J Med. 2016;374;4:386-8).
“The transformative characteristics of acalabrutinib and venetoclax arise from effective targeting of important survival pathways in CLL. Indeed, BTK inhibition produces durable responses, improves survival, and selects for mutations in the BTK-binding domain,” Dr. Wilson said, adding that BCL2 also plays an important role in CLL survival, as indicated by the activity of venetoclax.
While neither venetoclax nor acalabrutinib regularly induce complete remission, in vitro findings show that venetoclax and BTK inhibitors are synergistic, which suggests that combining the two might “further transform the targeted treatment of CLL,” he explained.
Dr. Wilson is with the National Cancer Institute, Bethesda, Md.
Targeted therapies have fundamentally changed the management and outcomes of patients with CLL in recent years, and new findings for second-generation drugs offer even more promise, according to Dr. Wyndham H. Wilson.
Taken together with the recent finding that acalabrutinib has a high degree of Bruton’s tyrosine kinase (BTK) inhibition with lower toxicity than ibrutinib, the findings of Roberts et al. with respect to venetoclax suggest a possible new avenue for combination treatment, Dr. Wilson wrote in an editorial (N Engl J Med. 2016;374;4:386-8).
“The transformative characteristics of acalabrutinib and venetoclax arise from effective targeting of important survival pathways in CLL. Indeed, BTK inhibition produces durable responses, improves survival, and selects for mutations in the BTK-binding domain,” Dr. Wilson said, adding that BCL2 also plays an important role in CLL survival, as indicated by the activity of venetoclax.
While neither venetoclax nor acalabrutinib regularly induce complete remission, in vitro findings show that venetoclax and BTK inhibitors are synergistic, which suggests that combining the two might “further transform the targeted treatment of CLL,” he explained.
Dr. Wilson is with the National Cancer Institute, Bethesda, Md.
Daily oral treatment with venetoclax induced substantial responses with manageable adverse effects in patients with relapsed chronic lymphocytic leukemia or small lymphocytic lymphoma in a first-in-human phase I dose-escalation study.
The promising effects of the highly selective investigational inhibitor of BCL2 – a protein central to the survival of CLL cells – were noted even in patients with poor prognostic features, who comprised 89% of the cohort, reported Dr. Andrew W. Roberts of Royal Melbourne Hospital, Australia, and his colleagues. The study was published online Jan. 28 in The New England Journal of Medicine.
In the dose escalation phase of the study, 56 patients received active treatment at doses raging from 150 to 1,200 mg daily, and 60 additional patients received weekly stepwise ramp-up with doses beginning at 20 mg daily with weekly increases to 50 mg, 100 mg, and 200 mg daily up to the target dose of 400 mg daily. The patients had received a median of 3 previous therapies (range, 1-11).
Of 116 treated patients, 92 (79%) had a response, and 20% achieved complete remission, including 5% with no minimal residual disease on flow cytometry, the investigators said (N Engl J Med. 2016;374:311-22).
Venetoclax was active at all doses used in the study, and no maximum tolerated dose was identified.
Tumor lysis syndrome occurred in 10 patients, but clinically important sequelae occurred in only 3 of those patients, 2 of whom had severe sequelae. After adjustments were made to dosing schedule, no further cases occurred.
Other side effects included mild diarrhea, upper respiratory tract infection, nausea, and grade 3 or 4 neutropenia, which occurred in 41%-52% of patients. Serious adverse events included febrile neutropenia in 6% of patients, pneumonia in 4%, upper respiratory tract infection in 3%, and immune thrombocytopenia in 3%.
Among the patients with an adverse prognosis, treatment response rates ranged from 71% to 79%, depending on the subgroup. For example, the response rate was 79% in 70 patients with resistance to fludarabine, and 71% in 31 patients with chromosome 17p deletions.
New treatments, including ibrutinib monotherapy and idelalisib in combination with rituximab, have improved outcomes for patients with relapsed CLL, but despite these advances, complete remissions remain uncommon, the authors said.
“This first trial of venetoclax showed the potential of BCL2 antagonism as an additional therapeutic avenue for patients with relapsed CLL,” they wrote, adding that the 79% overall response rate in this study – including deep responses and complete responses without minimal residual disease in patients up to age 86 years and patients with poor prognostic factors – “provides support for further development of venetoclax as a treatment option for patients with heavily pretreated relapsed or refractory CLL or SLL.”
Of note, the Food and Drug Administration on Jan. 28 – the date this study was released – granted venetoclax Breakthrough Therapy Designation for use in combination with hypomethylating agents for the treatment of acute myeloid leukemia patients who aren’t eligible for standard induction chemotherapy. The designation – the third for the agent – is supported by data from a single study of untreated patients aged 65 years or older with AML. Prior venetoclax Breakthrough Therapy Designations were granted in April 2015 for its use as monotherapy in patients with refractory CLL who have the 17p deletion genetic mutation, and in January for its use with rituximab for the treatment of relapsed/refractory CLL.
AbbVie and Genentech supported the study. Dr. Roberts reported receiving grant support and study drugs form AbbVie, serving as an investigator in trials sponsored by Genentech, AbbVie, Janssen, and Beigene, and receiving institutional research funding from Genentech for the development of venetoclax. His coauthors reported ties to various pharmaceutical companies.
Daily oral treatment with venetoclax induced substantial responses with manageable adverse effects in patients with relapsed chronic lymphocytic leukemia or small lymphocytic lymphoma in a first-in-human phase I dose-escalation study.
The promising effects of the highly selective investigational inhibitor of BCL2 – a protein central to the survival of CLL cells – were noted even in patients with poor prognostic features, who comprised 89% of the cohort, reported Dr. Andrew W. Roberts of Royal Melbourne Hospital, Australia, and his colleagues. The study was published online Jan. 28 in The New England Journal of Medicine.
In the dose escalation phase of the study, 56 patients received active treatment at doses raging from 150 to 1,200 mg daily, and 60 additional patients received weekly stepwise ramp-up with doses beginning at 20 mg daily with weekly increases to 50 mg, 100 mg, and 200 mg daily up to the target dose of 400 mg daily. The patients had received a median of 3 previous therapies (range, 1-11).
Of 116 treated patients, 92 (79%) had a response, and 20% achieved complete remission, including 5% with no minimal residual disease on flow cytometry, the investigators said (N Engl J Med. 2016;374:311-22).
Venetoclax was active at all doses used in the study, and no maximum tolerated dose was identified.
Tumor lysis syndrome occurred in 10 patients, but clinically important sequelae occurred in only 3 of those patients, 2 of whom had severe sequelae. After adjustments were made to dosing schedule, no further cases occurred.
Other side effects included mild diarrhea, upper respiratory tract infection, nausea, and grade 3 or 4 neutropenia, which occurred in 41%-52% of patients. Serious adverse events included febrile neutropenia in 6% of patients, pneumonia in 4%, upper respiratory tract infection in 3%, and immune thrombocytopenia in 3%.
Among the patients with an adverse prognosis, treatment response rates ranged from 71% to 79%, depending on the subgroup. For example, the response rate was 79% in 70 patients with resistance to fludarabine, and 71% in 31 patients with chromosome 17p deletions.
New treatments, including ibrutinib monotherapy and idelalisib in combination with rituximab, have improved outcomes for patients with relapsed CLL, but despite these advances, complete remissions remain uncommon, the authors said.
“This first trial of venetoclax showed the potential of BCL2 antagonism as an additional therapeutic avenue for patients with relapsed CLL,” they wrote, adding that the 79% overall response rate in this study – including deep responses and complete responses without minimal residual disease in patients up to age 86 years and patients with poor prognostic factors – “provides support for further development of venetoclax as a treatment option for patients with heavily pretreated relapsed or refractory CLL or SLL.”
Of note, the Food and Drug Administration on Jan. 28 – the date this study was released – granted venetoclax Breakthrough Therapy Designation for use in combination with hypomethylating agents for the treatment of acute myeloid leukemia patients who aren’t eligible for standard induction chemotherapy. The designation – the third for the agent – is supported by data from a single study of untreated patients aged 65 years or older with AML. Prior venetoclax Breakthrough Therapy Designations were granted in April 2015 for its use as monotherapy in patients with refractory CLL who have the 17p deletion genetic mutation, and in January for its use with rituximab for the treatment of relapsed/refractory CLL.
AbbVie and Genentech supported the study. Dr. Roberts reported receiving grant support and study drugs form AbbVie, serving as an investigator in trials sponsored by Genentech, AbbVie, Janssen, and Beigene, and receiving institutional research funding from Genentech for the development of venetoclax. His coauthors reported ties to various pharmaceutical companies.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Daily oral treatment with venetoclax induced substantial responses with manageable adverse effects in patients with relapsed chronic lymphocytic leukemia or small lymphocytic lymphoma in a first-in-human phase I dose-escalation study.
Major finding: Of 116 treated patients, 92 (79%) had a response, and 20% achieved complete remission, including 5% with no minimal residual disease on flow cytometry.
Data source: A phase I dose-escalation study involving 116 patients.
Disclosures: AbbVie and Genentech supported the study. Dr. Roberts reported receiving grant support and study drugs form AbbVie, serving as an investigator in trials sponsored by Genentech, AbbVie, Janssen, and Beigene, and receiving institutional research funding from Genentech for the development of venetoclax. His coauthors reported ties to various pharmaceutical companies.
Acalabrutinib yields 95% overall response in relapsed CLL
Acalabrutinib, an oral drug that is a more specific Bruton tyrosine kinase (BTK) inhibitor related to ibrutinib, produced a high response rate and durable remissions at a median 14 months of follow-up in an uncontrolled phase I/II trial of 61 adults with relapsed chronic lymphocytic leukemia, according to a report published online Jan. 28 in the New England Journal of Medicine.
The study patients had received a median of three previous therapies for CLL; 31% had chromosome 17p13.1 deletions, and 75% had unmutated immunoglobulin heavy-chain variable genes.
At the analysis, one patient had died from pneumonia at 13 months and CLL had progressed at 16 months in another patient. The overall response rate among the 60 evaluable patients was 95%, with a partial response in 85% and a partial response with lymphocytosis in 10%. The rate of stable disease was 5%. Adverse events were mostly mild and self-limiting; eight patients (13%) discontinued treatment, said Dr. John C. Byrd of the division of hematology, Ohio State University, Columbus, and his associates.
All 18 patients with chromosome 17p13.1 deletions responded to acalabrutinib, with a partial response in 89% and a partial response with lymphocytosis in 11%. One patient with a chromosome 17p13.1 deletion had disease progression, and this patient had a C481S (major clone) mutation in BTK and an L845F (minor clone) mutation in PLCγ2.
No cases of Richter’s transformation occurred.
Patients were treated at six sites in the United States and the United Kingdom. Four different doses of oral acalabrutinib were used in the first phase of the study; the drug’s low toxicity permitted a twice-daily 100-mg dose in phase II of the study. Twice-daily dosing promoted continuous levels of drug binding to BTK, according to the researchers. It is hoped that this approach will decrease drug resistance and will perhaps lower the rate of transformation into large-cell lymphoma.
Among patients who had cytopenia at entry into the study, platelet count improved in 62%, hemoglobin levels improved in 76%, and absolute neutrophil count improved in 80%. Among patients who had B symptoms (weight loss, night sweats, and fever) at study entry, those symptoms resolved in 88% by the third cycle of treatment and in 100% by the ninth cycle, Dr. Byrd and his associates said (N Engl J Med. 2016 Jan 28. doi: 10.1056/NEJMoa1509981). The most common adverse events were headache (43% of patients), diarrhea (39%), weight gain (26%), pyrexia (23%), and upper respiratory tract infection (23%). Fewer than 2% of patients developed severe diarrhea, rash, arthralgia, myalgia, bruising, or bleeding.
These findings offered strong justification to further investigate the efficacy and safety of acalabrutinib for relapsed CLL, and a phase III trial is now underway, the investigators added.
Acalabrutinib, an oral drug that is a more specific Bruton tyrosine kinase (BTK) inhibitor related to ibrutinib, produced a high response rate and durable remissions at a median 14 months of follow-up in an uncontrolled phase I/II trial of 61 adults with relapsed chronic lymphocytic leukemia, according to a report published online Jan. 28 in the New England Journal of Medicine.
The study patients had received a median of three previous therapies for CLL; 31% had chromosome 17p13.1 deletions, and 75% had unmutated immunoglobulin heavy-chain variable genes.
At the analysis, one patient had died from pneumonia at 13 months and CLL had progressed at 16 months in another patient. The overall response rate among the 60 evaluable patients was 95%, with a partial response in 85% and a partial response with lymphocytosis in 10%. The rate of stable disease was 5%. Adverse events were mostly mild and self-limiting; eight patients (13%) discontinued treatment, said Dr. John C. Byrd of the division of hematology, Ohio State University, Columbus, and his associates.
All 18 patients with chromosome 17p13.1 deletions responded to acalabrutinib, with a partial response in 89% and a partial response with lymphocytosis in 11%. One patient with a chromosome 17p13.1 deletion had disease progression, and this patient had a C481S (major clone) mutation in BTK and an L845F (minor clone) mutation in PLCγ2.
No cases of Richter’s transformation occurred.
Patients were treated at six sites in the United States and the United Kingdom. Four different doses of oral acalabrutinib were used in the first phase of the study; the drug’s low toxicity permitted a twice-daily 100-mg dose in phase II of the study. Twice-daily dosing promoted continuous levels of drug binding to BTK, according to the researchers. It is hoped that this approach will decrease drug resistance and will perhaps lower the rate of transformation into large-cell lymphoma.
Among patients who had cytopenia at entry into the study, platelet count improved in 62%, hemoglobin levels improved in 76%, and absolute neutrophil count improved in 80%. Among patients who had B symptoms (weight loss, night sweats, and fever) at study entry, those symptoms resolved in 88% by the third cycle of treatment and in 100% by the ninth cycle, Dr. Byrd and his associates said (N Engl J Med. 2016 Jan 28. doi: 10.1056/NEJMoa1509981). The most common adverse events were headache (43% of patients), diarrhea (39%), weight gain (26%), pyrexia (23%), and upper respiratory tract infection (23%). Fewer than 2% of patients developed severe diarrhea, rash, arthralgia, myalgia, bruising, or bleeding.
These findings offered strong justification to further investigate the efficacy and safety of acalabrutinib for relapsed CLL, and a phase III trial is now underway, the investigators added.
Acalabrutinib, an oral drug that is a more specific Bruton tyrosine kinase (BTK) inhibitor related to ibrutinib, produced a high response rate and durable remissions at a median 14 months of follow-up in an uncontrolled phase I/II trial of 61 adults with relapsed chronic lymphocytic leukemia, according to a report published online Jan. 28 in the New England Journal of Medicine.
The study patients had received a median of three previous therapies for CLL; 31% had chromosome 17p13.1 deletions, and 75% had unmutated immunoglobulin heavy-chain variable genes.
At the analysis, one patient had died from pneumonia at 13 months and CLL had progressed at 16 months in another patient. The overall response rate among the 60 evaluable patients was 95%, with a partial response in 85% and a partial response with lymphocytosis in 10%. The rate of stable disease was 5%. Adverse events were mostly mild and self-limiting; eight patients (13%) discontinued treatment, said Dr. John C. Byrd of the division of hematology, Ohio State University, Columbus, and his associates.
All 18 patients with chromosome 17p13.1 deletions responded to acalabrutinib, with a partial response in 89% and a partial response with lymphocytosis in 11%. One patient with a chromosome 17p13.1 deletion had disease progression, and this patient had a C481S (major clone) mutation in BTK and an L845F (minor clone) mutation in PLCγ2.
No cases of Richter’s transformation occurred.
Patients were treated at six sites in the United States and the United Kingdom. Four different doses of oral acalabrutinib were used in the first phase of the study; the drug’s low toxicity permitted a twice-daily 100-mg dose in phase II of the study. Twice-daily dosing promoted continuous levels of drug binding to BTK, according to the researchers. It is hoped that this approach will decrease drug resistance and will perhaps lower the rate of transformation into large-cell lymphoma.
Among patients who had cytopenia at entry into the study, platelet count improved in 62%, hemoglobin levels improved in 76%, and absolute neutrophil count improved in 80%. Among patients who had B symptoms (weight loss, night sweats, and fever) at study entry, those symptoms resolved in 88% by the third cycle of treatment and in 100% by the ninth cycle, Dr. Byrd and his associates said (N Engl J Med. 2016 Jan 28. doi: 10.1056/NEJMoa1509981). The most common adverse events were headache (43% of patients), diarrhea (39%), weight gain (26%), pyrexia (23%), and upper respiratory tract infection (23%). Fewer than 2% of patients developed severe diarrhea, rash, arthralgia, myalgia, bruising, or bleeding.
These findings offered strong justification to further investigate the efficacy and safety of acalabrutinib for relapsed CLL, and a phase III trial is now underway, the investigators added.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Acalabrutinib, a more selective and therefore less-toxic relative of ibrutinib, produced a high response rate and durable remission in relapsed CLL.
Major finding: Acalabrutinib showed robust clinical activity, with an overall response rate of 95%, only one patient death, and only one case of CLL progression.
Data source: A multicenter phase I/II industry-sponsored clinical trial involving 61 patients followed for 14 months.
Disclosures: This trial was supported by Acerta Pharma, which was involved in study design and data analysis; it was also supported by the National Cancer Institute, the Leukemia and Lymphoma Society, the Four Winds Foundation, the Sullivan Chronic Lymphocytic Leukemia Research Fund, Mr. and Mrs. Michael Thomas, Al and Midge Lipkin, and the D. Warren Brown Foundation. Dr. Byrd reported receiving research grants from Acerta and serving as an unpaid consultant for Acerta, AbbVie, Genentech, Janssen, and Pharmacyclics; his associates reported ties to numerous industry sources.
Ofatumumab approved for extended treatment of CLL patients in complete or partial response
Ofatumumab has been approved for extended treatment of patients who are in complete or partial response after at least two lines of therapy for recurrent or progressive chronic lymphocytic leukemia (CLL), the U.S. Food and Drug Administration announced on Jan. 19.
Ofatumumab (Arzerra Injection, Novartis Pharmaceuticals) was previously approved for treatment-naive patients with CLL for whom fludarabine-based therapy was considered inappropriate and for patients with CLL refractory to fludarabine and alemtuzumab.
Approval of the new indication was based on the results of a randomized, open-label trial that found improved progression-free survival with ofatumumab as compared with observation in patients whose disease had a complete or partial response after at least two lines of prior therapy, the FDA said in a press release.
In the study, 238 patients were randomized to ofatumumab and 236 to observation. Patients in the ofatumumab arm had received a range of two to five prior therapies. The median progression-free survival was significantly longer with ofatumumab at 29.4 months (95% confidence interval, 26.2-34.2) than with observation at 15.2 months (95% CI, 11.8-18.8).
Of patients treated with ofatumumab, 33% reported serious adverse reactions. The most common were pneumonia, pyrexia, and neutropenia (including febrile neutropenia).
The recommended dose and schedule for ofatumumab therapy is 300 mg by intravenous infusion on day 1 followed by 1,000 mg on day 8, and then 7 weeks later, and then every 8 weeks thereafter for up to a maximum of 2 years.
Full prescribing information is available at http://www.accessdata.fda.gov/drugsatfda_docs/label/2016/125326s062lbl.pdf.
Ofatumumab has been approved for extended treatment of patients who are in complete or partial response after at least two lines of therapy for recurrent or progressive chronic lymphocytic leukemia (CLL), the U.S. Food and Drug Administration announced on Jan. 19.
Ofatumumab (Arzerra Injection, Novartis Pharmaceuticals) was previously approved for treatment-naive patients with CLL for whom fludarabine-based therapy was considered inappropriate and for patients with CLL refractory to fludarabine and alemtuzumab.
Approval of the new indication was based on the results of a randomized, open-label trial that found improved progression-free survival with ofatumumab as compared with observation in patients whose disease had a complete or partial response after at least two lines of prior therapy, the FDA said in a press release.
In the study, 238 patients were randomized to ofatumumab and 236 to observation. Patients in the ofatumumab arm had received a range of two to five prior therapies. The median progression-free survival was significantly longer with ofatumumab at 29.4 months (95% confidence interval, 26.2-34.2) than with observation at 15.2 months (95% CI, 11.8-18.8).
Of patients treated with ofatumumab, 33% reported serious adverse reactions. The most common were pneumonia, pyrexia, and neutropenia (including febrile neutropenia).
The recommended dose and schedule for ofatumumab therapy is 300 mg by intravenous infusion on day 1 followed by 1,000 mg on day 8, and then 7 weeks later, and then every 8 weeks thereafter for up to a maximum of 2 years.
Full prescribing information is available at http://www.accessdata.fda.gov/drugsatfda_docs/label/2016/125326s062lbl.pdf.
Ofatumumab has been approved for extended treatment of patients who are in complete or partial response after at least two lines of therapy for recurrent or progressive chronic lymphocytic leukemia (CLL), the U.S. Food and Drug Administration announced on Jan. 19.
Ofatumumab (Arzerra Injection, Novartis Pharmaceuticals) was previously approved for treatment-naive patients with CLL for whom fludarabine-based therapy was considered inappropriate and for patients with CLL refractory to fludarabine and alemtuzumab.
Approval of the new indication was based on the results of a randomized, open-label trial that found improved progression-free survival with ofatumumab as compared with observation in patients whose disease had a complete or partial response after at least two lines of prior therapy, the FDA said in a press release.
In the study, 238 patients were randomized to ofatumumab and 236 to observation. Patients in the ofatumumab arm had received a range of two to five prior therapies. The median progression-free survival was significantly longer with ofatumumab at 29.4 months (95% confidence interval, 26.2-34.2) than with observation at 15.2 months (95% CI, 11.8-18.8).
Of patients treated with ofatumumab, 33% reported serious adverse reactions. The most common were pneumonia, pyrexia, and neutropenia (including febrile neutropenia).
The recommended dose and schedule for ofatumumab therapy is 300 mg by intravenous infusion on day 1 followed by 1,000 mg on day 8, and then 7 weeks later, and then every 8 weeks thereafter for up to a maximum of 2 years.
Full prescribing information is available at http://www.accessdata.fda.gov/drugsatfda_docs/label/2016/125326s062lbl.pdf.
Venetoclax gets 79% overall response rate in high-risk CLL
ORLANDO – Venetoclax monotherapy achieved an overall response rate of 79% in a high-risk population of 107 patients with relapsed or refractory del(17p) chronic lymphocytic leukemia, Dr. Stephan Stilgenbauer reported in a late-breaking abstract at the annual meeting of the American Society of Hematology.
Of the 85 responders, the response was maintained at 1 year in 85%. Of the 45 patients assessed for minimal residual disease in the blood, 18 achieved MRD negativity. Ten of these 18 patients also had bone marrow assessments and six were MRD negative.
Dr. Stilgenbauer of the University of Ulm (Germany), discussed the implications of the phase II study findings in our exclusive interview at ASH, as well as phase III study plans and the use of venetoclax in combination therapies.
He receives honoraria or research funding from a wide range of companies, including AbbVie and Genentech, the companies collaborating on the development of venetoclax.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @maryjodales
ORLANDO – Venetoclax monotherapy achieved an overall response rate of 79% in a high-risk population of 107 patients with relapsed or refractory del(17p) chronic lymphocytic leukemia, Dr. Stephan Stilgenbauer reported in a late-breaking abstract at the annual meeting of the American Society of Hematology.
Of the 85 responders, the response was maintained at 1 year in 85%. Of the 45 patients assessed for minimal residual disease in the blood, 18 achieved MRD negativity. Ten of these 18 patients also had bone marrow assessments and six were MRD negative.
Dr. Stilgenbauer of the University of Ulm (Germany), discussed the implications of the phase II study findings in our exclusive interview at ASH, as well as phase III study plans and the use of venetoclax in combination therapies.
He receives honoraria or research funding from a wide range of companies, including AbbVie and Genentech, the companies collaborating on the development of venetoclax.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @maryjodales
ORLANDO – Venetoclax monotherapy achieved an overall response rate of 79% in a high-risk population of 107 patients with relapsed or refractory del(17p) chronic lymphocytic leukemia, Dr. Stephan Stilgenbauer reported in a late-breaking abstract at the annual meeting of the American Society of Hematology.
Of the 85 responders, the response was maintained at 1 year in 85%. Of the 45 patients assessed for minimal residual disease in the blood, 18 achieved MRD negativity. Ten of these 18 patients also had bone marrow assessments and six were MRD negative.
Dr. Stilgenbauer of the University of Ulm (Germany), discussed the implications of the phase II study findings in our exclusive interview at ASH, as well as phase III study plans and the use of venetoclax in combination therapies.
He receives honoraria or research funding from a wide range of companies, including AbbVie and Genentech, the companies collaborating on the development of venetoclax.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @maryjodales
AT ASH 2015
Ibrutinib response durable at 1 year in CLL patients who relapsed after allogeneic stem cell transplants
Ibrutinib may prove useful for patients whose chronic lymphocytic leukemia (CLL) relapses after allogeneic stem cell transplantation, Dr. C. S. Link and colleagues reported.
Ibrutinib has shown efficacy in patients with high-risk CLL, but there are few data from patients who relapsed after allogeneic stem cell transplantation, wrote Dr. Link of the Medizinische Klinik und Poliklinik I, Universitätsklinikum Carl Gustav Carus and the DFG Research Center for Regenerative Therapies, both at the Technische Universität Dresden (Germany).
The researchers performed analyses on cytokine levels and direct measuring of CD4 Th1 and CD4 Th2 cells in a study of five CLL patients treated with ibrutinib for relapse after allogeneic transplants. All patients had partial responses to ibrutinib and one had a minimal residual disease–negative remission.
At 1 year, none of the patients had relapsed; however, one patient died of pneumonia while on ibrutinib treatment. No other unexpected adverse events were observed, the researchers reported in the study, which was published online on Jan. 11.
No substantial changes in T-cell distribution in favor of a CD4 Th1 T-cell shift were noted based on flow cytometry and analyses of T cell–mediated cytokine levels. No acute exacerbations of graft-versus-host disease occurred.
Click here to read the study (Bone Marrow Transplant. 2016 Jan 11. doi: 10.1038/bmt.2015.339).
On Twitter @maryjodales
Ibrutinib may prove useful for patients whose chronic lymphocytic leukemia (CLL) relapses after allogeneic stem cell transplantation, Dr. C. S. Link and colleagues reported.
Ibrutinib has shown efficacy in patients with high-risk CLL, but there are few data from patients who relapsed after allogeneic stem cell transplantation, wrote Dr. Link of the Medizinische Klinik und Poliklinik I, Universitätsklinikum Carl Gustav Carus and the DFG Research Center for Regenerative Therapies, both at the Technische Universität Dresden (Germany).
The researchers performed analyses on cytokine levels and direct measuring of CD4 Th1 and CD4 Th2 cells in a study of five CLL patients treated with ibrutinib for relapse after allogeneic transplants. All patients had partial responses to ibrutinib and one had a minimal residual disease–negative remission.
At 1 year, none of the patients had relapsed; however, one patient died of pneumonia while on ibrutinib treatment. No other unexpected adverse events were observed, the researchers reported in the study, which was published online on Jan. 11.
No substantial changes in T-cell distribution in favor of a CD4 Th1 T-cell shift were noted based on flow cytometry and analyses of T cell–mediated cytokine levels. No acute exacerbations of graft-versus-host disease occurred.
Click here to read the study (Bone Marrow Transplant. 2016 Jan 11. doi: 10.1038/bmt.2015.339).
On Twitter @maryjodales
Ibrutinib may prove useful for patients whose chronic lymphocytic leukemia (CLL) relapses after allogeneic stem cell transplantation, Dr. C. S. Link and colleagues reported.
Ibrutinib has shown efficacy in patients with high-risk CLL, but there are few data from patients who relapsed after allogeneic stem cell transplantation, wrote Dr. Link of the Medizinische Klinik und Poliklinik I, Universitätsklinikum Carl Gustav Carus and the DFG Research Center for Regenerative Therapies, both at the Technische Universität Dresden (Germany).
The researchers performed analyses on cytokine levels and direct measuring of CD4 Th1 and CD4 Th2 cells in a study of five CLL patients treated with ibrutinib for relapse after allogeneic transplants. All patients had partial responses to ibrutinib and one had a minimal residual disease–negative remission.
At 1 year, none of the patients had relapsed; however, one patient died of pneumonia while on ibrutinib treatment. No other unexpected adverse events were observed, the researchers reported in the study, which was published online on Jan. 11.
No substantial changes in T-cell distribution in favor of a CD4 Th1 T-cell shift were noted based on flow cytometry and analyses of T cell–mediated cytokine levels. No acute exacerbations of graft-versus-host disease occurred.
Click here to read the study (Bone Marrow Transplant. 2016 Jan 11. doi: 10.1038/bmt.2015.339).
On Twitter @maryjodales
FROM BONE MARROW TRANSPLANTATION