User login
Permanent pacemaker in TAVR: Earlier implantation costs much less
PARIS – When a patient undergoing transcatheter aortic valve replacement needs a permanent pacemaker, the additional hospital costs are significantly less if the device is implanted within 24 hours post TAVR rather than later, Seth Clancy reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Not only the need for permanent pacemaker implantation but also the timing of the procedure as well as the management and monitoring of conduction disturbances have important resource use implications for TAVR,” observed Mr. Clancy of Edwards Lifesciences of Irvine, Calif.
He presented an economic analysis of all 12,148 TAVR hospitalizations included in the Medicare database for 2014. A key finding: The mean cost of TAVR hospitalizations with no permanent pacemaker implantation was $63,136, while for the 12% of TAVRs that did include permanent pacemaker implantation, the mean cost shot up to $80,441, for a difference of $17,305.
The additional cost of putting in a permanent pacemaker included nearly $8,000 for supplies, more than $2,600 for additional time in the operating room and/or catheterization laboratory, and in excess of $2,100 worth of extra ICU or cardiac care unit time.
Patients who received a permanent pacemaker during their TAVR hospitalization spent an average of 2.3 days longer in the hospital than the mean 6.6 days for patients who didn’t get a permanent pacemaker.
Drilling down further into the data, Mr. Clancy found that 41% of permanent pacemakers implanted during hospitalization for TAVR went in within 24 hours of the TAVR procedure. In a multivariate regression analysis adjusted for differences in patient demographics, comorbid conditions, and complications, those patients generated an average of $9,843 more in hospital costs than patients who didn’t get a permanent pacemaker during their TAVR hospitalization. However, patients who received a permanent pacemaker more than 24 hours after TAVR cost an average of $17,681 more and had a 2.72-day longer stay than patients who didn’t get a permanent pacemaker.
The need for a permanent pacemaker is a common complication following TAVR. This has been a sticking point for many cardiothoracic surgeons, who note that rates of permanent pacemaker implantation following surgical aortic valve replacement are far lower. Still, rates in TAVR patients have come down over time with advances in valve technology. Currently, permanent pacemaker implantation rates in TAVR patients are 5%-25%, depending upon the valve system, according to Mr. Clancy.
Advances in device design and techniques aimed at reducing the permanent pacemaker implantation rate substantially below the 12% figure seen in 2014 have the potential to generate substantial cost savings, he observed.
Session chair Mohammad Abdelghani, MD, of the Academic Medical Center at Amsterdam questioned whether the study results are relevant to European practice because of the large differences in health care costs.
Discussant Sonia Petronio, MD, expressed a more fundamental reservation.
“This is a very important subject – and a very dangerous one,” said Dr. Petronio of the University of Pisa (Italy). “It’s easier and less costly for a hospital to encourage increasing early permanent pacemaker implantation because the patient can go home earlier.”
“We don’t want to put in a pacemaker earlier to save money,” agreed Dr. Abdelghani. “This is not a cost-effectiveness analysis, it’s purely a cost analysis. Cost-effectiveness would take into account the long-term clinical outcomes and welfare of the patients. We would like to see that from you next year.”
Mr. Clancy is an employee of Edwards Lifesciences, which funded the study.
PARIS – When a patient undergoing transcatheter aortic valve replacement needs a permanent pacemaker, the additional hospital costs are significantly less if the device is implanted within 24 hours post TAVR rather than later, Seth Clancy reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Not only the need for permanent pacemaker implantation but also the timing of the procedure as well as the management and monitoring of conduction disturbances have important resource use implications for TAVR,” observed Mr. Clancy of Edwards Lifesciences of Irvine, Calif.
He presented an economic analysis of all 12,148 TAVR hospitalizations included in the Medicare database for 2014. A key finding: The mean cost of TAVR hospitalizations with no permanent pacemaker implantation was $63,136, while for the 12% of TAVRs that did include permanent pacemaker implantation, the mean cost shot up to $80,441, for a difference of $17,305.
The additional cost of putting in a permanent pacemaker included nearly $8,000 for supplies, more than $2,600 for additional time in the operating room and/or catheterization laboratory, and in excess of $2,100 worth of extra ICU or cardiac care unit time.
Patients who received a permanent pacemaker during their TAVR hospitalization spent an average of 2.3 days longer in the hospital than the mean 6.6 days for patients who didn’t get a permanent pacemaker.
Drilling down further into the data, Mr. Clancy found that 41% of permanent pacemakers implanted during hospitalization for TAVR went in within 24 hours of the TAVR procedure. In a multivariate regression analysis adjusted for differences in patient demographics, comorbid conditions, and complications, those patients generated an average of $9,843 more in hospital costs than patients who didn’t get a permanent pacemaker during their TAVR hospitalization. However, patients who received a permanent pacemaker more than 24 hours after TAVR cost an average of $17,681 more and had a 2.72-day longer stay than patients who didn’t get a permanent pacemaker.
The need for a permanent pacemaker is a common complication following TAVR. This has been a sticking point for many cardiothoracic surgeons, who note that rates of permanent pacemaker implantation following surgical aortic valve replacement are far lower. Still, rates in TAVR patients have come down over time with advances in valve technology. Currently, permanent pacemaker implantation rates in TAVR patients are 5%-25%, depending upon the valve system, according to Mr. Clancy.
Advances in device design and techniques aimed at reducing the permanent pacemaker implantation rate substantially below the 12% figure seen in 2014 have the potential to generate substantial cost savings, he observed.
Session chair Mohammad Abdelghani, MD, of the Academic Medical Center at Amsterdam questioned whether the study results are relevant to European practice because of the large differences in health care costs.
Discussant Sonia Petronio, MD, expressed a more fundamental reservation.
“This is a very important subject – and a very dangerous one,” said Dr. Petronio of the University of Pisa (Italy). “It’s easier and less costly for a hospital to encourage increasing early permanent pacemaker implantation because the patient can go home earlier.”
“We don’t want to put in a pacemaker earlier to save money,” agreed Dr. Abdelghani. “This is not a cost-effectiveness analysis, it’s purely a cost analysis. Cost-effectiveness would take into account the long-term clinical outcomes and welfare of the patients. We would like to see that from you next year.”
Mr. Clancy is an employee of Edwards Lifesciences, which funded the study.
PARIS – When a patient undergoing transcatheter aortic valve replacement needs a permanent pacemaker, the additional hospital costs are significantly less if the device is implanted within 24 hours post TAVR rather than later, Seth Clancy reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Not only the need for permanent pacemaker implantation but also the timing of the procedure as well as the management and monitoring of conduction disturbances have important resource use implications for TAVR,” observed Mr. Clancy of Edwards Lifesciences of Irvine, Calif.
He presented an economic analysis of all 12,148 TAVR hospitalizations included in the Medicare database for 2014. A key finding: The mean cost of TAVR hospitalizations with no permanent pacemaker implantation was $63,136, while for the 12% of TAVRs that did include permanent pacemaker implantation, the mean cost shot up to $80,441, for a difference of $17,305.
The additional cost of putting in a permanent pacemaker included nearly $8,000 for supplies, more than $2,600 for additional time in the operating room and/or catheterization laboratory, and in excess of $2,100 worth of extra ICU or cardiac care unit time.
Patients who received a permanent pacemaker during their TAVR hospitalization spent an average of 2.3 days longer in the hospital than the mean 6.6 days for patients who didn’t get a permanent pacemaker.
Drilling down further into the data, Mr. Clancy found that 41% of permanent pacemakers implanted during hospitalization for TAVR went in within 24 hours of the TAVR procedure. In a multivariate regression analysis adjusted for differences in patient demographics, comorbid conditions, and complications, those patients generated an average of $9,843 more in hospital costs than patients who didn’t get a permanent pacemaker during their TAVR hospitalization. However, patients who received a permanent pacemaker more than 24 hours after TAVR cost an average of $17,681 more and had a 2.72-day longer stay than patients who didn’t get a permanent pacemaker.
The need for a permanent pacemaker is a common complication following TAVR. This has been a sticking point for many cardiothoracic surgeons, who note that rates of permanent pacemaker implantation following surgical aortic valve replacement are far lower. Still, rates in TAVR patients have come down over time with advances in valve technology. Currently, permanent pacemaker implantation rates in TAVR patients are 5%-25%, depending upon the valve system, according to Mr. Clancy.
Advances in device design and techniques aimed at reducing the permanent pacemaker implantation rate substantially below the 12% figure seen in 2014 have the potential to generate substantial cost savings, he observed.
Session chair Mohammad Abdelghani, MD, of the Academic Medical Center at Amsterdam questioned whether the study results are relevant to European practice because of the large differences in health care costs.
Discussant Sonia Petronio, MD, expressed a more fundamental reservation.
“This is a very important subject – and a very dangerous one,” said Dr. Petronio of the University of Pisa (Italy). “It’s easier and less costly for a hospital to encourage increasing early permanent pacemaker implantation because the patient can go home earlier.”
“We don’t want to put in a pacemaker earlier to save money,” agreed Dr. Abdelghani. “This is not a cost-effectiveness analysis, it’s purely a cost analysis. Cost-effectiveness would take into account the long-term clinical outcomes and welfare of the patients. We would like to see that from you next year.”
Mr. Clancy is an employee of Edwards Lifesciences, which funded the study.
AT EUROPCR 2016
Key clinical point: The incremental cost of permanent pacemaker implantation more than 24 hours after transcatheter aortic valve replacement is almost twice as great as if the pacemaker goes in within 24 hours.
Major finding: The mean cost of hospitalization for transcatheter aortic valve replacement without permanent pacemaker implication in Medicare patients in 2014 was $63,136, compared with $80,441 if they needed a pacemaker.
Data source: This was a retrospective study of the health care costs and lengths of stay for all 12,148 hospitalizations for transcatheter aortic valve replacement in the Medicare inpatient database for 2014.
Disclosures: The presenter is an employee of Edwards Lifesciences, which funded the study.
Wedge resection showed improved survival over SBRT for early-stage NSCLC
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
AT THE AATS ANNUAL MEETING
Key clinical point: Wedge resection outperformed SBRT in terms of mortality for early-stage NSCLC.
Major finding: In matched groups, SBRT was associated with significantly lower 5-year overall survival than was wedge resection (32% vs. 50%).
Data source: The study assessed more than 8.000 patients with early stage NSCLC who had either wedge resection or SBRT from the National Cancer Database from 2003 to 2011.
Disclosures: Dr. Yerokun had no relevant disclosures.
Challenging ‘dogma’ of allografts in infectious endocarditis
When a patient undergoes aortic valve replacement for infective endocarditis, conventional thinking holds that cardiac surgeons should use homografts because they have greater resistance to infection, but a recent study of more than 300 cases at two academic medical centers concluded that homografts may not necessarily offer such a benefit.
The study, published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1239-48), involved 304 consecutive adult patients on whom 30-40 different surgeons performed operations for active infective endocarditis (IE) in the aortic valve from 2002 to 2014.
“Our findings suggest that patient-specific factors, such as age and implant preference, as well as technical reconstructive considerations, should drive prosthetic choice, rather than surgical dogma,” said Joon Bum Kim, Ph.D., of Massachusetts General Hospital, Harvard Medical School, both in Boston, and Asan Medical Center in Seoul, Korea, and his colleagues.
The study found that cardiac surgeons favored homografts over conventional prostheses when the patient had prosthetic valve endocarditis (58.1% vs. 28.8%) and methicillin-resistant Staphylococcus aureus (25.6% vs. 12.1%), both significant differences.
“No significant benefit to the use of homografts was demonstrable with regard to resistance to reinfection in the setting of IE,” Dr. Kim and his colleagues said.
Because reinfection after valve replacement for IE is such a strong concern, the debate over which prosthesis is best has ensued for decades. The researchers pointed out that the evidence favoring autologous or allogeneic tissue over synthetic material in the infective field is weak, mostly built on single-armed observational studies without comparison to conventional prosthesis.
With that in mind, the researchers pooled data from two institutions to compare short- and long-term results for homograft vs. conventional prosthetic valves in patients with IE. In this study group, 86 (28.3%) had homografts, 139 (45.7%) had xenograft prostheses, and 79 (26%) mechanical prostheses. The homograft group had more than twice the rate of early death than did the conventional group – 19.8% vs. 9.2%, a significant difference (P = .019).
During follow-up, which ranged from 4.7 to 72.6 months, 60 patients (19.7%) of the total group died and 23 (7.7%) experienced reinfection, but rates did not vary between the homograft and conventional prosthesis groups, Dr. Kim and his colleagues reported.
Demographics were similar between the three groups with a few exceptions Those who received the mechanical prostheses were younger (mean age, 47.2 years vs. 55.6 and 59.8 for the homograft and xenograft groups, respectively), had lower rates of diabetes (5.1% vs. 10.5% and 12.2%) and had less-severe disease based on New York Heart Association functional class III or IV scores (34.2% vs. 54.7% and 53.2%). The types of IE pathogens also differed among the three groups; methicillin-resistant staphylococci was most common in the homograft group (25.6%), whereas the viridans group streptococci was the leading cause of IE in the mechanical (38% ) and xenograft groups (25.2% ).
The use of homografts involves a highly complex operation, typically requiring a complete aortic root replacement, which “may be the major drawback in recommending it to patients already at high risk of operative mortality,” the investigators wrote. The durability of homografts makes their use limited for younger patients, and such grafts are somewhat scarce and require cryopreservation. “Therefore, the notion that homografts are required may in practice present an obstacle to appropriate surgical management of patients who have IE,” Dr. Kim and his coauthors wrote. All patients but one in the homograft group received aortic arch replacement (98.8%) whereas 30 of the patients in the conventional group did so (13.8%).
The study findings are consistent with an earlier comparative study (Ann. Thorac. Surg. 2012;93:480-07), according to Dr. Kim and his colleagues. “These findings suggest that patient-specific factors, such as patient preferences and technical considerations, should be the principal drivers of choices of valve prostheses,” they said. “Furthermore, lack of access to homografts should not be considered an obstacle to surgical therapy for this serious condition.”
Coauthor Dr. Sundt disclosed that he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
The study by Dr. Kim and his colleagues joins a series of reports questioning conventional thinking on the use of homografts to prevent recurrent infective endocarditis (IE), but their propensity matching does not account for surgeon bias in selecting a prosthesis, Dr. James K. Kirklin of the University of Alabama at Birmingham said in his invited commentary (J Thorac. Cardiovasc Surg. 2016 May;151:1230-1).
For example, surgeon preference may account for the wide disparity in full root replacements, depending on the type of prosthesis, Dr. Kirklin said. “Some experienced homograft surgeons have preferred the intra-aortic cylinder technique or infracoronary implantation, which avoids the short-term and longer-term complexities of full root replacement and has demonstrated long-term structural durability equivalent to that of the full root replacement,” he said.
Also, experienced homograft surgeons may prefer the homograft for its resistance to infection and adaptability to severe root infection in individual patients, particularly in those with severe infection with an abscess. And he cautioned against the study’s implication that conventional prostheses are equivocal in the setting of IE.
“Of considerable importance, however, is the evidence-based conclusion that surgical referral of routine surgical aortic valve endocarditis to a center experienced with aortic homograft surgery is not necessary, and a justifiable expectation is that aortic valve endocarditis requiring operation can be safely and appropriately managed in centers with standard aortic valve surgery experience who do not have access to or experience with aortic valve homografts,” Dr. Kirklin concluded.
Dr. Kirklin had no financial relationships to disclose.

|
Dr. Christopher M. Feindel |
The series by Dr. Kim and his colleagues, one of the largest of acute infective endocarditis to date, provides further evidence that the type of prosthesis used in surgery for IE involving the aortic valve probably does not affect long-term outcomes or reinfection rates, Dr. Christopher M. Feindel of the University of Toronto said in his invited commentary (J Thorac Cardiovasc Surg. 2016 May;151:1249-50).
However, Dr. Feindel said, “numerous confounding factors” inherent in any observational study could raise questions about the conclusion.
“This article delivers an important message, although not all surgeons will agree with the statistical approach taken by Dr. Kim and his colleagues,” Dr. Feindel said. The propensity scoring method the study used lacked all baseline variables that affect treatment choice and outcomes, “a crucial assumption for effective use of the propensity score,” he said. However, given the multitude of variables in patients with acute and complex IE, he said most surgeons would be hard pressed to accept that’s even possible in the model the study used.
Dr. Feindel also said a close examination of the 115 patients who underwent root replacement would have been “very instructional,” and the lack of follow-up on valve-related complications in almost 25% of the patients is another limitation of the study.
Nonetheless, the conclusions of Dr. Kim and his colleagues are “reasonable,” Dr. Feindel said. “Clearly, this article contributes important additional information to the surgical management of IE that will help guide surgeons, especially when it comes to prosthesis of choice,” he concluded. “It is up to the reader to decide whether this report finally puts to rest the “dogma” that homografts should preferentially be used in the setting of IE.”
Dr. Feindel had no relationships to disclose.
The study by Dr. Kim and his colleagues joins a series of reports questioning conventional thinking on the use of homografts to prevent recurrent infective endocarditis (IE), but their propensity matching does not account for surgeon bias in selecting a prosthesis, Dr. James K. Kirklin of the University of Alabama at Birmingham said in his invited commentary (J Thorac. Cardiovasc Surg. 2016 May;151:1230-1).
For example, surgeon preference may account for the wide disparity in full root replacements, depending on the type of prosthesis, Dr. Kirklin said. “Some experienced homograft surgeons have preferred the intra-aortic cylinder technique or infracoronary implantation, which avoids the short-term and longer-term complexities of full root replacement and has demonstrated long-term structural durability equivalent to that of the full root replacement,” he said.
Also, experienced homograft surgeons may prefer the homograft for its resistance to infection and adaptability to severe root infection in individual patients, particularly in those with severe infection with an abscess. And he cautioned against the study’s implication that conventional prostheses are equivocal in the setting of IE.
“Of considerable importance, however, is the evidence-based conclusion that surgical referral of routine surgical aortic valve endocarditis to a center experienced with aortic homograft surgery is not necessary, and a justifiable expectation is that aortic valve endocarditis requiring operation can be safely and appropriately managed in centers with standard aortic valve surgery experience who do not have access to or experience with aortic valve homografts,” Dr. Kirklin concluded.
Dr. Kirklin had no financial relationships to disclose.

|
Dr. Christopher M. Feindel |
The series by Dr. Kim and his colleagues, one of the largest of acute infective endocarditis to date, provides further evidence that the type of prosthesis used in surgery for IE involving the aortic valve probably does not affect long-term outcomes or reinfection rates, Dr. Christopher M. Feindel of the University of Toronto said in his invited commentary (J Thorac Cardiovasc Surg. 2016 May;151:1249-50).
However, Dr. Feindel said, “numerous confounding factors” inherent in any observational study could raise questions about the conclusion.
“This article delivers an important message, although not all surgeons will agree with the statistical approach taken by Dr. Kim and his colleagues,” Dr. Feindel said. The propensity scoring method the study used lacked all baseline variables that affect treatment choice and outcomes, “a crucial assumption for effective use of the propensity score,” he said. However, given the multitude of variables in patients with acute and complex IE, he said most surgeons would be hard pressed to accept that’s even possible in the model the study used.
Dr. Feindel also said a close examination of the 115 patients who underwent root replacement would have been “very instructional,” and the lack of follow-up on valve-related complications in almost 25% of the patients is another limitation of the study.
Nonetheless, the conclusions of Dr. Kim and his colleagues are “reasonable,” Dr. Feindel said. “Clearly, this article contributes important additional information to the surgical management of IE that will help guide surgeons, especially when it comes to prosthesis of choice,” he concluded. “It is up to the reader to decide whether this report finally puts to rest the “dogma” that homografts should preferentially be used in the setting of IE.”
Dr. Feindel had no relationships to disclose.
The study by Dr. Kim and his colleagues joins a series of reports questioning conventional thinking on the use of homografts to prevent recurrent infective endocarditis (IE), but their propensity matching does not account for surgeon bias in selecting a prosthesis, Dr. James K. Kirklin of the University of Alabama at Birmingham said in his invited commentary (J Thorac. Cardiovasc Surg. 2016 May;151:1230-1).
For example, surgeon preference may account for the wide disparity in full root replacements, depending on the type of prosthesis, Dr. Kirklin said. “Some experienced homograft surgeons have preferred the intra-aortic cylinder technique or infracoronary implantation, which avoids the short-term and longer-term complexities of full root replacement and has demonstrated long-term structural durability equivalent to that of the full root replacement,” he said.
Also, experienced homograft surgeons may prefer the homograft for its resistance to infection and adaptability to severe root infection in individual patients, particularly in those with severe infection with an abscess. And he cautioned against the study’s implication that conventional prostheses are equivocal in the setting of IE.
“Of considerable importance, however, is the evidence-based conclusion that surgical referral of routine surgical aortic valve endocarditis to a center experienced with aortic homograft surgery is not necessary, and a justifiable expectation is that aortic valve endocarditis requiring operation can be safely and appropriately managed in centers with standard aortic valve surgery experience who do not have access to or experience with aortic valve homografts,” Dr. Kirklin concluded.
Dr. Kirklin had no financial relationships to disclose.

|
Dr. Christopher M. Feindel |
The series by Dr. Kim and his colleagues, one of the largest of acute infective endocarditis to date, provides further evidence that the type of prosthesis used in surgery for IE involving the aortic valve probably does not affect long-term outcomes or reinfection rates, Dr. Christopher M. Feindel of the University of Toronto said in his invited commentary (J Thorac Cardiovasc Surg. 2016 May;151:1249-50).
However, Dr. Feindel said, “numerous confounding factors” inherent in any observational study could raise questions about the conclusion.
“This article delivers an important message, although not all surgeons will agree with the statistical approach taken by Dr. Kim and his colleagues,” Dr. Feindel said. The propensity scoring method the study used lacked all baseline variables that affect treatment choice and outcomes, “a crucial assumption for effective use of the propensity score,” he said. However, given the multitude of variables in patients with acute and complex IE, he said most surgeons would be hard pressed to accept that’s even possible in the model the study used.
Dr. Feindel also said a close examination of the 115 patients who underwent root replacement would have been “very instructional,” and the lack of follow-up on valve-related complications in almost 25% of the patients is another limitation of the study.
Nonetheless, the conclusions of Dr. Kim and his colleagues are “reasonable,” Dr. Feindel said. “Clearly, this article contributes important additional information to the surgical management of IE that will help guide surgeons, especially when it comes to prosthesis of choice,” he concluded. “It is up to the reader to decide whether this report finally puts to rest the “dogma” that homografts should preferentially be used in the setting of IE.”
Dr. Feindel had no relationships to disclose.
When a patient undergoes aortic valve replacement for infective endocarditis, conventional thinking holds that cardiac surgeons should use homografts because they have greater resistance to infection, but a recent study of more than 300 cases at two academic medical centers concluded that homografts may not necessarily offer such a benefit.
The study, published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1239-48), involved 304 consecutive adult patients on whom 30-40 different surgeons performed operations for active infective endocarditis (IE) in the aortic valve from 2002 to 2014.
“Our findings suggest that patient-specific factors, such as age and implant preference, as well as technical reconstructive considerations, should drive prosthetic choice, rather than surgical dogma,” said Joon Bum Kim, Ph.D., of Massachusetts General Hospital, Harvard Medical School, both in Boston, and Asan Medical Center in Seoul, Korea, and his colleagues.
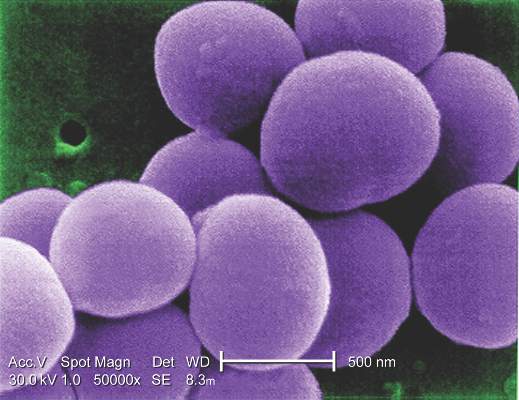
The study found that cardiac surgeons favored homografts over conventional prostheses when the patient had prosthetic valve endocarditis (58.1% vs. 28.8%) and methicillin-resistant Staphylococcus aureus (25.6% vs. 12.1%), both significant differences.
“No significant benefit to the use of homografts was demonstrable with regard to resistance to reinfection in the setting of IE,” Dr. Kim and his colleagues said.
Because reinfection after valve replacement for IE is such a strong concern, the debate over which prosthesis is best has ensued for decades. The researchers pointed out that the evidence favoring autologous or allogeneic tissue over synthetic material in the infective field is weak, mostly built on single-armed observational studies without comparison to conventional prosthesis.
With that in mind, the researchers pooled data from two institutions to compare short- and long-term results for homograft vs. conventional prosthetic valves in patients with IE. In this study group, 86 (28.3%) had homografts, 139 (45.7%) had xenograft prostheses, and 79 (26%) mechanical prostheses. The homograft group had more than twice the rate of early death than did the conventional group – 19.8% vs. 9.2%, a significant difference (P = .019).
During follow-up, which ranged from 4.7 to 72.6 months, 60 patients (19.7%) of the total group died and 23 (7.7%) experienced reinfection, but rates did not vary between the homograft and conventional prosthesis groups, Dr. Kim and his colleagues reported.
Demographics were similar between the three groups with a few exceptions Those who received the mechanical prostheses were younger (mean age, 47.2 years vs. 55.6 and 59.8 for the homograft and xenograft groups, respectively), had lower rates of diabetes (5.1% vs. 10.5% and 12.2%) and had less-severe disease based on New York Heart Association functional class III or IV scores (34.2% vs. 54.7% and 53.2%). The types of IE pathogens also differed among the three groups; methicillin-resistant staphylococci was most common in the homograft group (25.6%), whereas the viridans group streptococci was the leading cause of IE in the mechanical (38% ) and xenograft groups (25.2% ).
The use of homografts involves a highly complex operation, typically requiring a complete aortic root replacement, which “may be the major drawback in recommending it to patients already at high risk of operative mortality,” the investigators wrote. The durability of homografts makes their use limited for younger patients, and such grafts are somewhat scarce and require cryopreservation. “Therefore, the notion that homografts are required may in practice present an obstacle to appropriate surgical management of patients who have IE,” Dr. Kim and his coauthors wrote. All patients but one in the homograft group received aortic arch replacement (98.8%) whereas 30 of the patients in the conventional group did so (13.8%).
The study findings are consistent with an earlier comparative study (Ann. Thorac. Surg. 2012;93:480-07), according to Dr. Kim and his colleagues. “These findings suggest that patient-specific factors, such as patient preferences and technical considerations, should be the principal drivers of choices of valve prostheses,” they said. “Furthermore, lack of access to homografts should not be considered an obstacle to surgical therapy for this serious condition.”
Coauthor Dr. Sundt disclosed that he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
When a patient undergoes aortic valve replacement for infective endocarditis, conventional thinking holds that cardiac surgeons should use homografts because they have greater resistance to infection, but a recent study of more than 300 cases at two academic medical centers concluded that homografts may not necessarily offer such a benefit.
The study, published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1239-48), involved 304 consecutive adult patients on whom 30-40 different surgeons performed operations for active infective endocarditis (IE) in the aortic valve from 2002 to 2014.
“Our findings suggest that patient-specific factors, such as age and implant preference, as well as technical reconstructive considerations, should drive prosthetic choice, rather than surgical dogma,” said Joon Bum Kim, Ph.D., of Massachusetts General Hospital, Harvard Medical School, both in Boston, and Asan Medical Center in Seoul, Korea, and his colleagues.
The study found that cardiac surgeons favored homografts over conventional prostheses when the patient had prosthetic valve endocarditis (58.1% vs. 28.8%) and methicillin-resistant Staphylococcus aureus (25.6% vs. 12.1%), both significant differences.
“No significant benefit to the use of homografts was demonstrable with regard to resistance to reinfection in the setting of IE,” Dr. Kim and his colleagues said.
Because reinfection after valve replacement for IE is such a strong concern, the debate over which prosthesis is best has ensued for decades. The researchers pointed out that the evidence favoring autologous or allogeneic tissue over synthetic material in the infective field is weak, mostly built on single-armed observational studies without comparison to conventional prosthesis.
With that in mind, the researchers pooled data from two institutions to compare short- and long-term results for homograft vs. conventional prosthetic valves in patients with IE. In this study group, 86 (28.3%) had homografts, 139 (45.7%) had xenograft prostheses, and 79 (26%) mechanical prostheses. The homograft group had more than twice the rate of early death than did the conventional group – 19.8% vs. 9.2%, a significant difference (P = .019).
During follow-up, which ranged from 4.7 to 72.6 months, 60 patients (19.7%) of the total group died and 23 (7.7%) experienced reinfection, but rates did not vary between the homograft and conventional prosthesis groups, Dr. Kim and his colleagues reported.
Demographics were similar between the three groups with a few exceptions Those who received the mechanical prostheses were younger (mean age, 47.2 years vs. 55.6 and 59.8 for the homograft and xenograft groups, respectively), had lower rates of diabetes (5.1% vs. 10.5% and 12.2%) and had less-severe disease based on New York Heart Association functional class III or IV scores (34.2% vs. 54.7% and 53.2%). The types of IE pathogens also differed among the three groups; methicillin-resistant staphylococci was most common in the homograft group (25.6%), whereas the viridans group streptococci was the leading cause of IE in the mechanical (38% ) and xenograft groups (25.2% ).
The use of homografts involves a highly complex operation, typically requiring a complete aortic root replacement, which “may be the major drawback in recommending it to patients already at high risk of operative mortality,” the investigators wrote. The durability of homografts makes their use limited for younger patients, and such grafts are somewhat scarce and require cryopreservation. “Therefore, the notion that homografts are required may in practice present an obstacle to appropriate surgical management of patients who have IE,” Dr. Kim and his coauthors wrote. All patients but one in the homograft group received aortic arch replacement (98.8%) whereas 30 of the patients in the conventional group did so (13.8%).
The study findings are consistent with an earlier comparative study (Ann. Thorac. Surg. 2012;93:480-07), according to Dr. Kim and his colleagues. “These findings suggest that patient-specific factors, such as patient preferences and technical considerations, should be the principal drivers of choices of valve prostheses,” they said. “Furthermore, lack of access to homografts should not be considered an obstacle to surgical therapy for this serious condition.”
Coauthor Dr. Sundt disclosed that he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Use of homografts showed no significant benefit, compared with conventional prosthetic valves when the patient has infective endocarditis involving the aortic valve.
Major finding: The homograft group had more than twice the rate of early death than the conventional group, 19.8% vs. 9.2%, but in longer-term follow-up, the survival rates did not differ between groups.
Data source: 304 consecutive adult patients from the perspective database of two tertiary academic centers who had surgery for active infective endocarditis involving the aortic valve from 2002 to 2014.
Disclosures: Coauthor Dr. Sundt, disclosed he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
Additional antibiotics needed when implanting cryopreserved human aortic grafts
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The infection resistance of cryopreserved human allografts (CHAs) depends on antibiotic pretreatment during processing.
Major finding: Cardiac surgeons can recommend CHAs to patients either with active destructive infections or at high risk of reinfection, but they may want to apply additional antibiotic agents during implantation to enhance bacterial resistance.
Data source: Pieces of 10 CHAs were microbiologically tested in vitro and exposed to bacterial contamination and the number of attached bacteria quantified.
Disclosures: Dr. Steffen and her coauthors had no financial relationships to disclose.
VIDEO: Lobectomy quality requires linking outcomes to process change
BALTIMORE – An “introspective” analysis connecting patient outcomes with process changes may lead to significant surgical quality improvement, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
The case study detailed the University of Alabama at Birmingham School of Medicine’s attempt to identify the metrics used for the Society of Thoracic Surgeons lobectomy ranking, and show how the institution used root cause analysis with “lean” and process improvements to improve outcomes from Jan. 2006 until July 2014 in order to achieve a three star STS ranking.
UAB researchers found that their most common root cause analysis was failure to escalate care. The institution implemented process improvements such as increasing pulmonary rehabilitation prior to surgery, adding a respiratory therapist, eliminating (lean) non-valued steps, favoring stereotactic radiotherapy and segmentectomy instead of lobectomy for marginal patients, and using minimally invasive lobectomy. They ultimately achieved a three-star STS ranking.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Stephen D. Cassivi, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said in an interview that the research was important because it encourages surgeons to discuss and reevaluate quality improvement measures. He noted that early phases of surgical quality improvement was based on process measures, specifically around the idea that if surgeons were attentive to process measures, their outcome measures would improve. But over time, the emphasis on process measures has dissipated in favor of outcomes-focused analysis.
“Now that we have more robust [outcomes] data... we can examine our practices in a more thoughtful, data-driven, evidence-based way,” Dr. Cassivi said. He added that the shift from process measures to outcome measures is important in that surgeons can easily interpret and compare outcomes data across facilities. But he noted that there is a downside: If an institution’s outcome measures are not up to standard, it is sometimes difficult to determine why.
“The current way that the [outcomes] data are reported and processed is not easily interpretable into which processes we need to adapt,” Dr. Cassivi said. “There is still work that needs to be done, but [this paper] is a first step.”
Dr. Cassivi reported no relevant financial disclosures.
On Twitter @richpizzi
BALTIMORE – An “introspective” analysis connecting patient outcomes with process changes may lead to significant surgical quality improvement, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
The case study detailed the University of Alabama at Birmingham School of Medicine’s attempt to identify the metrics used for the Society of Thoracic Surgeons lobectomy ranking, and show how the institution used root cause analysis with “lean” and process improvements to improve outcomes from Jan. 2006 until July 2014 in order to achieve a three star STS ranking.
UAB researchers found that their most common root cause analysis was failure to escalate care. The institution implemented process improvements such as increasing pulmonary rehabilitation prior to surgery, adding a respiratory therapist, eliminating (lean) non-valued steps, favoring stereotactic radiotherapy and segmentectomy instead of lobectomy for marginal patients, and using minimally invasive lobectomy. They ultimately achieved a three-star STS ranking.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Stephen D. Cassivi, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said in an interview that the research was important because it encourages surgeons to discuss and reevaluate quality improvement measures. He noted that early phases of surgical quality improvement was based on process measures, specifically around the idea that if surgeons were attentive to process measures, their outcome measures would improve. But over time, the emphasis on process measures has dissipated in favor of outcomes-focused analysis.
“Now that we have more robust [outcomes] data... we can examine our practices in a more thoughtful, data-driven, evidence-based way,” Dr. Cassivi said. He added that the shift from process measures to outcome measures is important in that surgeons can easily interpret and compare outcomes data across facilities. But he noted that there is a downside: If an institution’s outcome measures are not up to standard, it is sometimes difficult to determine why.
“The current way that the [outcomes] data are reported and processed is not easily interpretable into which processes we need to adapt,” Dr. Cassivi said. “There is still work that needs to be done, but [this paper] is a first step.”
Dr. Cassivi reported no relevant financial disclosures.
On Twitter @richpizzi
BALTIMORE – An “introspective” analysis connecting patient outcomes with process changes may lead to significant surgical quality improvement, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
The case study detailed the University of Alabama at Birmingham School of Medicine’s attempt to identify the metrics used for the Society of Thoracic Surgeons lobectomy ranking, and show how the institution used root cause analysis with “lean” and process improvements to improve outcomes from Jan. 2006 until July 2014 in order to achieve a three star STS ranking.
UAB researchers found that their most common root cause analysis was failure to escalate care. The institution implemented process improvements such as increasing pulmonary rehabilitation prior to surgery, adding a respiratory therapist, eliminating (lean) non-valued steps, favoring stereotactic radiotherapy and segmentectomy instead of lobectomy for marginal patients, and using minimally invasive lobectomy. They ultimately achieved a three-star STS ranking.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Stephen D. Cassivi, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said in an interview that the research was important because it encourages surgeons to discuss and reevaluate quality improvement measures. He noted that early phases of surgical quality improvement was based on process measures, specifically around the idea that if surgeons were attentive to process measures, their outcome measures would improve. But over time, the emphasis on process measures has dissipated in favor of outcomes-focused analysis.
“Now that we have more robust [outcomes] data... we can examine our practices in a more thoughtful, data-driven, evidence-based way,” Dr. Cassivi said. He added that the shift from process measures to outcome measures is important in that surgeons can easily interpret and compare outcomes data across facilities. But he noted that there is a downside: If an institution’s outcome measures are not up to standard, it is sometimes difficult to determine why.
“The current way that the [outcomes] data are reported and processed is not easily interpretable into which processes we need to adapt,” Dr. Cassivi said. “There is still work that needs to be done, but [this paper] is a first step.”
Dr. Cassivi reported no relevant financial disclosures.
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
Transcatheter aortic valve implantation equivalent to surgical replacement
Transcatheter aortic valve implantation shows reductions in early and mid-term all-cause mortality similar to those with surgical aortic valve replacement, even in patients with low to intermediate surgical risk, a meta-analysis and systematic review has shown.
Dr. Giuseppe Gargiulo of Federico II University in Naples, Italy, and coauthors analyzed data from five randomized trials and 31 observational matched studies comparing mortality outcomes in 16,638 patients undergoing transcatheter aortic valve implantation (TAVI) or surgical aortic valve replacement (SAVR).
Their analysis found no statistically significant difference between the two procedures in terms of early or midterm all-cause mortality, even among patients judged as being at low to intermediate surgical risk (Ann Intern Med. 2016 Jun 7. doi: 10.7326/M16-0060).
In terms of 2- to 5-year mortality, overall there was a statistically nonsignificant increase in the risk of all-cause mortality with TAVI (odds ratio, 1.28; 95% confidence interval, 0.97-1.69), although the long-term mortality outcomes in patients in the low to intermediate surgical risk subgroup were inconclusive.
However, the authors did note significantly reduced early all-cause mortality in individuals who underwent transfemoral TAVI compared to those who underwent SAVR (OR 0.68, 95%CI, 0.53 to 0.87).
The analysis also showed that individuals who underwent TAVI had a higher incidence of permanent pacemaker implantation, vascular complications, and moderate to severe paravalvular leak, while those who underwent SAVR had more frequent incidence of major bleeding, acute kidney injury, and new-onset atrial fibrillation.
“These findings, which apply to adults with severe aortic stenosis, consolidate the role of TAVI as an alternative to SAVR,” the authors wrote. “Indeed, TAVI techniques continue to improve, newer valves address the issue of paravalvular leak, the percentage of pacemakers is decreasing, and the rate of vascular complications is expected to be lowered as the result of smaller sheaths and improved procedural techniques.”
The researchers noted that elderly patients and those with coronary artery disease showed a greater benefit from TAVI than from SAVR, suggesting that this may be because these groups have a heightened risk that favors less invasive surgical approaches.
They also found greater reductions in early mortality with TAVI when a Sapien valve was implanted, compared to a CoreValve. They noted that this was due mostly to a single large study and the effect did not persist through to the midterm follow-up.
One author reported grants from the CardioPath PhD Program, Federico II University of Naples, and from the European Association of Percutaneous Coronary Interventions, outside the submitted work. Another author declared a consultancy for Edwards Lifesciences. There were no other conflicts of interest declared.
Transcatheter aortic valve implantation shows reductions in early and mid-term all-cause mortality similar to those with surgical aortic valve replacement, even in patients with low to intermediate surgical risk, a meta-analysis and systematic review has shown.
Dr. Giuseppe Gargiulo of Federico II University in Naples, Italy, and coauthors analyzed data from five randomized trials and 31 observational matched studies comparing mortality outcomes in 16,638 patients undergoing transcatheter aortic valve implantation (TAVI) or surgical aortic valve replacement (SAVR).
Their analysis found no statistically significant difference between the two procedures in terms of early or midterm all-cause mortality, even among patients judged as being at low to intermediate surgical risk (Ann Intern Med. 2016 Jun 7. doi: 10.7326/M16-0060).
In terms of 2- to 5-year mortality, overall there was a statistically nonsignificant increase in the risk of all-cause mortality with TAVI (odds ratio, 1.28; 95% confidence interval, 0.97-1.69), although the long-term mortality outcomes in patients in the low to intermediate surgical risk subgroup were inconclusive.
However, the authors did note significantly reduced early all-cause mortality in individuals who underwent transfemoral TAVI compared to those who underwent SAVR (OR 0.68, 95%CI, 0.53 to 0.87).
The analysis also showed that individuals who underwent TAVI had a higher incidence of permanent pacemaker implantation, vascular complications, and moderate to severe paravalvular leak, while those who underwent SAVR had more frequent incidence of major bleeding, acute kidney injury, and new-onset atrial fibrillation.
“These findings, which apply to adults with severe aortic stenosis, consolidate the role of TAVI as an alternative to SAVR,” the authors wrote. “Indeed, TAVI techniques continue to improve, newer valves address the issue of paravalvular leak, the percentage of pacemakers is decreasing, and the rate of vascular complications is expected to be lowered as the result of smaller sheaths and improved procedural techniques.”
The researchers noted that elderly patients and those with coronary artery disease showed a greater benefit from TAVI than from SAVR, suggesting that this may be because these groups have a heightened risk that favors less invasive surgical approaches.
They also found greater reductions in early mortality with TAVI when a Sapien valve was implanted, compared to a CoreValve. They noted that this was due mostly to a single large study and the effect did not persist through to the midterm follow-up.
One author reported grants from the CardioPath PhD Program, Federico II University of Naples, and from the European Association of Percutaneous Coronary Interventions, outside the submitted work. Another author declared a consultancy for Edwards Lifesciences. There were no other conflicts of interest declared.
Transcatheter aortic valve implantation shows reductions in early and mid-term all-cause mortality similar to those with surgical aortic valve replacement, even in patients with low to intermediate surgical risk, a meta-analysis and systematic review has shown.
Dr. Giuseppe Gargiulo of Federico II University in Naples, Italy, and coauthors analyzed data from five randomized trials and 31 observational matched studies comparing mortality outcomes in 16,638 patients undergoing transcatheter aortic valve implantation (TAVI) or surgical aortic valve replacement (SAVR).
Their analysis found no statistically significant difference between the two procedures in terms of early or midterm all-cause mortality, even among patients judged as being at low to intermediate surgical risk (Ann Intern Med. 2016 Jun 7. doi: 10.7326/M16-0060).
In terms of 2- to 5-year mortality, overall there was a statistically nonsignificant increase in the risk of all-cause mortality with TAVI (odds ratio, 1.28; 95% confidence interval, 0.97-1.69), although the long-term mortality outcomes in patients in the low to intermediate surgical risk subgroup were inconclusive.
However, the authors did note significantly reduced early all-cause mortality in individuals who underwent transfemoral TAVI compared to those who underwent SAVR (OR 0.68, 95%CI, 0.53 to 0.87).
The analysis also showed that individuals who underwent TAVI had a higher incidence of permanent pacemaker implantation, vascular complications, and moderate to severe paravalvular leak, while those who underwent SAVR had more frequent incidence of major bleeding, acute kidney injury, and new-onset atrial fibrillation.
“These findings, which apply to adults with severe aortic stenosis, consolidate the role of TAVI as an alternative to SAVR,” the authors wrote. “Indeed, TAVI techniques continue to improve, newer valves address the issue of paravalvular leak, the percentage of pacemakers is decreasing, and the rate of vascular complications is expected to be lowered as the result of smaller sheaths and improved procedural techniques.”
The researchers noted that elderly patients and those with coronary artery disease showed a greater benefit from TAVI than from SAVR, suggesting that this may be because these groups have a heightened risk that favors less invasive surgical approaches.
They also found greater reductions in early mortality with TAVI when a Sapien valve was implanted, compared to a CoreValve. They noted that this was due mostly to a single large study and the effect did not persist through to the midterm follow-up.
One author reported grants from the CardioPath PhD Program, Federico II University of Naples, and from the European Association of Percutaneous Coronary Interventions, outside the submitted work. Another author declared a consultancy for Edwards Lifesciences. There were no other conflicts of interest declared.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Transcatheter aortic valve implantation shows reductions in early and mid-term all-cause mortality similar to those of surgical aortic valve replacement.
Major finding: Transcatheter aortic valve implantation and surgical aortic valve replacement show similar reductions in mortality, even in patients at low to intermediate surgical risk.
Data source: Systematic review and meta-analysis.
Disclosures: One author reported grants from the CardioPath PhD Program, Federico II University of Naples, and from the European Association of Percutaneous Coronary Interventions, outside the submitted work. Another author declared a consultancy for Edwards Lifesciences. There were no other conflicts of interest declared.
Pulmonary function testing adds little to STS risk scores
Routine preoperative pulmonary function tests appear to have only limited utility in predicting outcomes in patients undergoing cardiothoracic surgery when the Society of Thoracic Surgeons risk score is available, according to the results of a retrospective study.
Dr. Alexander Ivanov of New York Methodist Hospital, Brooklyn, and his colleagues conducted a database analysis of 1,685 patients undergoing index cardiac surgery at New York Methodist Hospital between April 2004 and January 2014. They used the STS risk model version 2.73 to estimate postoperative risk of respiratory failure (defined as the need for mechanical ventilation greater than or equal to 72 hours, or reintubation), prolonged postoperative length of stay (defined as greater than 14 days), and 30-day all cause mortality in these patients, according to their report in The Journal of Thoracic and Cardiovascular Surgery (2016;151:1183-9).
They plotted the receiver operating characteristics curve for the STS score for each of these adverse events and compared the resulting area under the curve (AUC) with the AUC after adding pulmonary function testing parameters and COPD classifications.
A total of 1,412 patients had a calculated STS score, of which 751 underwent pulmonary function testing (53%). In general, patients who had pulmonary function testing were older and had higher rates of comorbidities and more complex cardiothoracic surgery compared with their counterparts, according to Dr. Ivanov. These patients also had significantly elevated STS risk for prolonged ventilation (12.4% vs. 10.3%), prolonged postoperative length of stay (8.9% vs. 7.2%), and 30-day mortality (2.7% vs. 2.2%).
The decision to perform pulmonary testing was left to the treating physician. Of those patients tested, 652 had bedside spirometry and 99 had formal laboratory testing. Forced expiratory volume in 1 second (FEV1) and forced volume vital capacity (FVC) values were determined by taking the best of three trials. COPD was diagnosed in cases of an FEV1/FVC ratio of less than 70%.
Among these patients, 4.5% developed postoperative respiratory failure, and there was no statistically significant difference in the respiratory failure rate between patients with and without pulmonary function testing. In addition, there was no significant difference in 30-day mortality between these patients (1.9% vs. 2.1%). However, a total of 6.9% had a prolonged postoperative length of stay, with a significantly higher rate in the patients with pulmonary function testing than without (8.8% vs. 4.7%).
Dr. Ivanov and his colleagues found that the AUC of the STS score was 0.65 (95% confidence interval [CI], 0.55-0.74)for respiratory failure, 0.67 (95% CI, 0.6-0.74) for prolonged postoperative length of stay, and 0.74 (95% CI, 0.6-0.87) for 30-day mortality. Even though the STS score based upon clinical definitions of lung disease afforded only modest discriminatory ability for the three studied outcomes, they found that there was no significant added benefit to the predictive ability of these STS scores obtained by incorporating any of the pulmonary function testing parameters or COPD classifications studied.
“A possible physiological explanation for these findings may be that the examined pulmonary function testing variables do not depend solely on pulmonary parameters such as airway diameter, degree of obstruction, or lung elasticity, but rather on a patient’s effort and muscle “strength,” characteristics that are already well captured and accounted for in the current STS model,” the researchers stated.
“The STS score calculated with clinical information on lung disease status offers modest discriminatory ability for respiratory failure, prolonged postoperative length of stay, and 30-day mortality after CT surgery, which cannot be improved by adding PFT parameters or PFT-derived COPD categorization,” they wrote. “Therefore, routine preoperative PFTs may have only limited clinical utility in patients undergoing CT surgery when the STS score is readily available. Further prospective studies will be helpful in confirming these conclusions,” Dr. Ivanov and his colleagues noted.
The authors reported that they had nothing to disclose.
Chronic lung disease is one of the risk factors included in the STS model for mortality, renal failure, prolonged ventilation, sternal wound infection, reoperation, and length of hospital stay. Mild, moderate, and severe CLD increases the odds ratio for those complications. A total of 20% of almost 1 million patients used in developing the current STS risk model had CLD.

|
Dr. Juan A. Crestanello |
The authors found that none of the pulmonary function testing parameters added to the predictive ability of the STS risk model for operative mortality, prolonged ventilation, or prolonged length of hospital stay. Because CLD is 1 of 40 preoperative and operative variables used in the STS risk model, an improvement in discrimination of only 1 of 40 variables is very unlikely to improve the overall model.
One may be tempted to conclude that it is not worth performing pulmonary function testing before cardiac surgery. However, remember once again the importance of precise and accurate data to support risk stratification. In science, behind each word resides a precise definition; without a pulmonary function test, we cannot define chronic lung disease severity.
Dr. Juan A. Crestanello is in the division of cardiac surgery, Wexner Medical Center, Ohio State University, Columbus. His remarks are from an invited commentary (J Thorac Cardiovasc Surg. 2016;151:1189-90).
Chronic lung disease is one of the risk factors included in the STS model for mortality, renal failure, prolonged ventilation, sternal wound infection, reoperation, and length of hospital stay. Mild, moderate, and severe CLD increases the odds ratio for those complications. A total of 20% of almost 1 million patients used in developing the current STS risk model had CLD.

|
Dr. Juan A. Crestanello |
The authors found that none of the pulmonary function testing parameters added to the predictive ability of the STS risk model for operative mortality, prolonged ventilation, or prolonged length of hospital stay. Because CLD is 1 of 40 preoperative and operative variables used in the STS risk model, an improvement in discrimination of only 1 of 40 variables is very unlikely to improve the overall model.
One may be tempted to conclude that it is not worth performing pulmonary function testing before cardiac surgery. However, remember once again the importance of precise and accurate data to support risk stratification. In science, behind each word resides a precise definition; without a pulmonary function test, we cannot define chronic lung disease severity.
Dr. Juan A. Crestanello is in the division of cardiac surgery, Wexner Medical Center, Ohio State University, Columbus. His remarks are from an invited commentary (J Thorac Cardiovasc Surg. 2016;151:1189-90).
Chronic lung disease is one of the risk factors included in the STS model for mortality, renal failure, prolonged ventilation, sternal wound infection, reoperation, and length of hospital stay. Mild, moderate, and severe CLD increases the odds ratio for those complications. A total of 20% of almost 1 million patients used in developing the current STS risk model had CLD.

|
Dr. Juan A. Crestanello |
The authors found that none of the pulmonary function testing parameters added to the predictive ability of the STS risk model for operative mortality, prolonged ventilation, or prolonged length of hospital stay. Because CLD is 1 of 40 preoperative and operative variables used in the STS risk model, an improvement in discrimination of only 1 of 40 variables is very unlikely to improve the overall model.
One may be tempted to conclude that it is not worth performing pulmonary function testing before cardiac surgery. However, remember once again the importance of precise and accurate data to support risk stratification. In science, behind each word resides a precise definition; without a pulmonary function test, we cannot define chronic lung disease severity.
Dr. Juan A. Crestanello is in the division of cardiac surgery, Wexner Medical Center, Ohio State University, Columbus. His remarks are from an invited commentary (J Thorac Cardiovasc Surg. 2016;151:1189-90).
Routine preoperative pulmonary function tests appear to have only limited utility in predicting outcomes in patients undergoing cardiothoracic surgery when the Society of Thoracic Surgeons risk score is available, according to the results of a retrospective study.
Dr. Alexander Ivanov of New York Methodist Hospital, Brooklyn, and his colleagues conducted a database analysis of 1,685 patients undergoing index cardiac surgery at New York Methodist Hospital between April 2004 and January 2014. They used the STS risk model version 2.73 to estimate postoperative risk of respiratory failure (defined as the need for mechanical ventilation greater than or equal to 72 hours, or reintubation), prolonged postoperative length of stay (defined as greater than 14 days), and 30-day all cause mortality in these patients, according to their report in The Journal of Thoracic and Cardiovascular Surgery (2016;151:1183-9).
They plotted the receiver operating characteristics curve for the STS score for each of these adverse events and compared the resulting area under the curve (AUC) with the AUC after adding pulmonary function testing parameters and COPD classifications.
A total of 1,412 patients had a calculated STS score, of which 751 underwent pulmonary function testing (53%). In general, patients who had pulmonary function testing were older and had higher rates of comorbidities and more complex cardiothoracic surgery compared with their counterparts, according to Dr. Ivanov. These patients also had significantly elevated STS risk for prolonged ventilation (12.4% vs. 10.3%), prolonged postoperative length of stay (8.9% vs. 7.2%), and 30-day mortality (2.7% vs. 2.2%).
The decision to perform pulmonary testing was left to the treating physician. Of those patients tested, 652 had bedside spirometry and 99 had formal laboratory testing. Forced expiratory volume in 1 second (FEV1) and forced volume vital capacity (FVC) values were determined by taking the best of three trials. COPD was diagnosed in cases of an FEV1/FVC ratio of less than 70%.
Among these patients, 4.5% developed postoperative respiratory failure, and there was no statistically significant difference in the respiratory failure rate between patients with and without pulmonary function testing. In addition, there was no significant difference in 30-day mortality between these patients (1.9% vs. 2.1%). However, a total of 6.9% had a prolonged postoperative length of stay, with a significantly higher rate in the patients with pulmonary function testing than without (8.8% vs. 4.7%).
Dr. Ivanov and his colleagues found that the AUC of the STS score was 0.65 (95% confidence interval [CI], 0.55-0.74)for respiratory failure, 0.67 (95% CI, 0.6-0.74) for prolonged postoperative length of stay, and 0.74 (95% CI, 0.6-0.87) for 30-day mortality. Even though the STS score based upon clinical definitions of lung disease afforded only modest discriminatory ability for the three studied outcomes, they found that there was no significant added benefit to the predictive ability of these STS scores obtained by incorporating any of the pulmonary function testing parameters or COPD classifications studied.
“A possible physiological explanation for these findings may be that the examined pulmonary function testing variables do not depend solely on pulmonary parameters such as airway diameter, degree of obstruction, or lung elasticity, but rather on a patient’s effort and muscle “strength,” characteristics that are already well captured and accounted for in the current STS model,” the researchers stated.
“The STS score calculated with clinical information on lung disease status offers modest discriminatory ability for respiratory failure, prolonged postoperative length of stay, and 30-day mortality after CT surgery, which cannot be improved by adding PFT parameters or PFT-derived COPD categorization,” they wrote. “Therefore, routine preoperative PFTs may have only limited clinical utility in patients undergoing CT surgery when the STS score is readily available. Further prospective studies will be helpful in confirming these conclusions,” Dr. Ivanov and his colleagues noted.
The authors reported that they had nothing to disclose.
Routine preoperative pulmonary function tests appear to have only limited utility in predicting outcomes in patients undergoing cardiothoracic surgery when the Society of Thoracic Surgeons risk score is available, according to the results of a retrospective study.
Dr. Alexander Ivanov of New York Methodist Hospital, Brooklyn, and his colleagues conducted a database analysis of 1,685 patients undergoing index cardiac surgery at New York Methodist Hospital between April 2004 and January 2014. They used the STS risk model version 2.73 to estimate postoperative risk of respiratory failure (defined as the need for mechanical ventilation greater than or equal to 72 hours, or reintubation), prolonged postoperative length of stay (defined as greater than 14 days), and 30-day all cause mortality in these patients, according to their report in The Journal of Thoracic and Cardiovascular Surgery (2016;151:1183-9).
They plotted the receiver operating characteristics curve for the STS score for each of these adverse events and compared the resulting area under the curve (AUC) with the AUC after adding pulmonary function testing parameters and COPD classifications.
A total of 1,412 patients had a calculated STS score, of which 751 underwent pulmonary function testing (53%). In general, patients who had pulmonary function testing were older and had higher rates of comorbidities and more complex cardiothoracic surgery compared with their counterparts, according to Dr. Ivanov. These patients also had significantly elevated STS risk for prolonged ventilation (12.4% vs. 10.3%), prolonged postoperative length of stay (8.9% vs. 7.2%), and 30-day mortality (2.7% vs. 2.2%).
The decision to perform pulmonary testing was left to the treating physician. Of those patients tested, 652 had bedside spirometry and 99 had formal laboratory testing. Forced expiratory volume in 1 second (FEV1) and forced volume vital capacity (FVC) values were determined by taking the best of three trials. COPD was diagnosed in cases of an FEV1/FVC ratio of less than 70%.
Among these patients, 4.5% developed postoperative respiratory failure, and there was no statistically significant difference in the respiratory failure rate between patients with and without pulmonary function testing. In addition, there was no significant difference in 30-day mortality between these patients (1.9% vs. 2.1%). However, a total of 6.9% had a prolonged postoperative length of stay, with a significantly higher rate in the patients with pulmonary function testing than without (8.8% vs. 4.7%).
Dr. Ivanov and his colleagues found that the AUC of the STS score was 0.65 (95% confidence interval [CI], 0.55-0.74)for respiratory failure, 0.67 (95% CI, 0.6-0.74) for prolonged postoperative length of stay, and 0.74 (95% CI, 0.6-0.87) for 30-day mortality. Even though the STS score based upon clinical definitions of lung disease afforded only modest discriminatory ability for the three studied outcomes, they found that there was no significant added benefit to the predictive ability of these STS scores obtained by incorporating any of the pulmonary function testing parameters or COPD classifications studied.
“A possible physiological explanation for these findings may be that the examined pulmonary function testing variables do not depend solely on pulmonary parameters such as airway diameter, degree of obstruction, or lung elasticity, but rather on a patient’s effort and muscle “strength,” characteristics that are already well captured and accounted for in the current STS model,” the researchers stated.
“The STS score calculated with clinical information on lung disease status offers modest discriminatory ability for respiratory failure, prolonged postoperative length of stay, and 30-day mortality after CT surgery, which cannot be improved by adding PFT parameters or PFT-derived COPD categorization,” they wrote. “Therefore, routine preoperative PFTs may have only limited clinical utility in patients undergoing CT surgery when the STS score is readily available. Further prospective studies will be helpful in confirming these conclusions,” Dr. Ivanov and his colleagues noted.
The authors reported that they had nothing to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Additional pulmonary function testing adds little predictive value to STS risk scoring when available.
Major finding: There was no significant added benefit to the predictive ability of STS scores obtained by incorporating any of the pulmonary function testing parameters or COPD classifications studied, as determined by AUC analysis.
Data source: A retrospective, database analysis of 1,685 patients undergoing index cardiac surgery at a single center between April 2004 and January 2014.
Disclosures: The authors reported that they had no disclosures.
VIDEO: EVLP may extend lung preservation, quality for transplants
BALTIMORE – The use of ex vivo lung perfusion (EVLP) may allow for the safe transplantation of lungs preserved for more than 12 hours, according to a study presented at the annual meeting of the American Association for Thoracic Surgery.
A research team at the University of Toronto evaluated the outcomes of transplant patients who received a lung with a preservation time of over 12 hours between January 2006 and April 2015 and compared them to the general lung transplant population. Median hospital and ICU length of stay were similar between the two groups, and Kaplan-Meier survival curves between the two groups did not show any difference. Preservation time, donor PO2, and use of EVLP were not significant variables affecting survival.
Dr. Bartley P. Griffith, chief of cardiac surgery at the University of Maryland, Baltimore, and a discussant on the paper at the meeting, said that the findings of the study open up the possibility of a more “planned” approach to transplantation.
“Anything that not only extends preservation time, but perhaps even improves quality of preservation, would be a godsend,” Dr. Griffith said in a video interview. He cautioned that the “devil is in the details,” and that the data had to be examined closely. Nevertheless, Dr. Griffith said transplant surgeons should be grateful for the important work done by the University of Toronto team.
Dr. Griffith reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – The use of ex vivo lung perfusion (EVLP) may allow for the safe transplantation of lungs preserved for more than 12 hours, according to a study presented at the annual meeting of the American Association for Thoracic Surgery.
A research team at the University of Toronto evaluated the outcomes of transplant patients who received a lung with a preservation time of over 12 hours between January 2006 and April 2015 and compared them to the general lung transplant population. Median hospital and ICU length of stay were similar between the two groups, and Kaplan-Meier survival curves between the two groups did not show any difference. Preservation time, donor PO2, and use of EVLP were not significant variables affecting survival.
Dr. Bartley P. Griffith, chief of cardiac surgery at the University of Maryland, Baltimore, and a discussant on the paper at the meeting, said that the findings of the study open up the possibility of a more “planned” approach to transplantation.
“Anything that not only extends preservation time, but perhaps even improves quality of preservation, would be a godsend,” Dr. Griffith said in a video interview. He cautioned that the “devil is in the details,” and that the data had to be examined closely. Nevertheless, Dr. Griffith said transplant surgeons should be grateful for the important work done by the University of Toronto team.
Dr. Griffith reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – The use of ex vivo lung perfusion (EVLP) may allow for the safe transplantation of lungs preserved for more than 12 hours, according to a study presented at the annual meeting of the American Association for Thoracic Surgery.
A research team at the University of Toronto evaluated the outcomes of transplant patients who received a lung with a preservation time of over 12 hours between January 2006 and April 2015 and compared them to the general lung transplant population. Median hospital and ICU length of stay were similar between the two groups, and Kaplan-Meier survival curves between the two groups did not show any difference. Preservation time, donor PO2, and use of EVLP were not significant variables affecting survival.
Dr. Bartley P. Griffith, chief of cardiac surgery at the University of Maryland, Baltimore, and a discussant on the paper at the meeting, said that the findings of the study open up the possibility of a more “planned” approach to transplantation.
“Anything that not only extends preservation time, but perhaps even improves quality of preservation, would be a godsend,” Dr. Griffith said in a video interview. He cautioned that the “devil is in the details,” and that the data had to be examined closely. Nevertheless, Dr. Griffith said transplant surgeons should be grateful for the important work done by the University of Toronto team.
Dr. Griffith reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
VIDEO: Identifying patients who will benefit from pulmonary metastasectomy
BALTIMORE – New research from Memorial Sloan Kettering Cancer Center in New York could help surgeons better determine which patients with soft tissue sarcoma may benefit most from pulmonary metastasectomy.
The results of the research, presented at the annual meeting of the American Association for Thoracic Surgery, suggest that preoperative factors such as primary tumor histology and size, number of metastases, time from initial resection of the primary, absence of extrapulmonary disease, and thoracoscopic resection are associated with improved survival in STS patients.
Dr. Garrett L. Walsh, professor of surgery at the University of Texas MD Anderson Cancer Center, Houston, and a discussant on the paper at the meeting, said the study was important because it showed the power of a prospective surgical database, retrospectively viewed in this particular case. He said that the Sloan Kettering research was likely “as good as it’s going to get,” given that a randomized controlled trial is unlikely ever to occur with STS patients.
“Trying to select the patients we think are going to do well with surgery has always been one of the challenging aspects of thoracic surgery,” Dr. Walsh said in a video interview. “This paper may help with better selection of patients from that large cohort who are referred to us for pulmonary metastasectomy.”
Dr. Walsh reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – New research from Memorial Sloan Kettering Cancer Center in New York could help surgeons better determine which patients with soft tissue sarcoma may benefit most from pulmonary metastasectomy.
The results of the research, presented at the annual meeting of the American Association for Thoracic Surgery, suggest that preoperative factors such as primary tumor histology and size, number of metastases, time from initial resection of the primary, absence of extrapulmonary disease, and thoracoscopic resection are associated with improved survival in STS patients.
Dr. Garrett L. Walsh, professor of surgery at the University of Texas MD Anderson Cancer Center, Houston, and a discussant on the paper at the meeting, said the study was important because it showed the power of a prospective surgical database, retrospectively viewed in this particular case. He said that the Sloan Kettering research was likely “as good as it’s going to get,” given that a randomized controlled trial is unlikely ever to occur with STS patients.
“Trying to select the patients we think are going to do well with surgery has always been one of the challenging aspects of thoracic surgery,” Dr. Walsh said in a video interview. “This paper may help with better selection of patients from that large cohort who are referred to us for pulmonary metastasectomy.”
Dr. Walsh reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – New research from Memorial Sloan Kettering Cancer Center in New York could help surgeons better determine which patients with soft tissue sarcoma may benefit most from pulmonary metastasectomy.
The results of the research, presented at the annual meeting of the American Association for Thoracic Surgery, suggest that preoperative factors such as primary tumor histology and size, number of metastases, time from initial resection of the primary, absence of extrapulmonary disease, and thoracoscopic resection are associated with improved survival in STS patients.
Dr. Garrett L. Walsh, professor of surgery at the University of Texas MD Anderson Cancer Center, Houston, and a discussant on the paper at the meeting, said the study was important because it showed the power of a prospective surgical database, retrospectively viewed in this particular case. He said that the Sloan Kettering research was likely “as good as it’s going to get,” given that a randomized controlled trial is unlikely ever to occur with STS patients.
“Trying to select the patients we think are going to do well with surgery has always been one of the challenging aspects of thoracic surgery,” Dr. Walsh said in a video interview. “This paper may help with better selection of patients from that large cohort who are referred to us for pulmonary metastasectomy.”
Dr. Walsh reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
Rotor ablation for atrial fibrillation strikes out in first randomized trial
SAN FRANCISCO – Focal impulse and rotor modulation-guided ablation for persistent atrial fibrillation – either alone or in conjunction with other procedures – increased procedural times without improving outcomes, according to the first randomized trial to assess its utility.
In fact, enrollment in the rotor ablation-only (RA) arm was halted early for futility. “There was 100% recurrence” of atrial fibrillation (AF), said senior investigator Dr. Andrea Natale, executive medical director of the Texas Cardiac Arrhythmia Institute, Austin.
“I’m surprised it took this long for a randomized study, because this system has been around for 5 or 6 years,” noted Dr. Natale. “Our community should demand these sorts of studies earlier, because it’s not fair for patients to go on with a procedure for years that has not been proven to be effective.
“For us, unless there is a new version of rotor mapping that I feel is significantly different, this will be the end of rotor ablation in my lab with this system [the Topera Physiologic Rotor Mapping Solution],” Dr. Natale said at the annual scientific sessions of the Heart Rhythm Society.
In the study, his team randomized 29 patients to RA only, 42 to RA plus pulmonary vein antral isolation (PVAI), and 42 to PVAI plus posterior wall and nonpulmonary vein trigger ablation.
At about 1 year, four RA-only patients (14%), 22 RA plus PVAI patients (52%), and 32 patients in the PVAI plus trigger group (76%) were free of AF and atrial tachycardias without antiarrhythmic drugs (P < .0001).
Meanwhile, RA alone and RA plus PVAI cases took about 230 minutes, while the more effective PVAI plus trigger approach took about 130 minutes (P < .001).
There was “a very poor outcome with rotor-only ablation,” Dr. Natale said. “There isn’t a benefit either alone or as an add-on strategy, at least with this mapping software.”
Perhaps “people who think rotors don’t exist are right,” he added. On the other hand, maybe the basket mapping catheter doesn’t touch enough of the left atrium, or the software that makes sense of what the catheter detects needs to be improved, Dr. Natale noted.
All the patients were undergoing their first ablation. They were in their early 60s, on average, and most were men. The mean left atrium diameter was about 47 mm, and mean left ventricle ejection fraction about 55%. There were no statistically significant differences between the study arms, and no significant differences in outcomes between the 70% of patients with persistent AF and the 30% with long-standing persistent AF.
There was no industry funding for the work. Dr. Natale disclosed relationships with Biosense Webster, Boston Scientific, Janssen, Medtronic, and St. Jude Medical.
My gut sense is that there’s something to rotor mapping, but we are not there yet. There are a lot of investment dollars and a lot of bright people working on this. It really is the Holy Grail to find the source of AF.
Dr. John Day is the director of Intermountain Heart Rhythm Specialists in Murray, Utah, and the current president of the Hearth Rhythm Society. He had no disclosures.
My gut sense is that there’s something to rotor mapping, but we are not there yet. There are a lot of investment dollars and a lot of bright people working on this. It really is the Holy Grail to find the source of AF.
Dr. John Day is the director of Intermountain Heart Rhythm Specialists in Murray, Utah, and the current president of the Hearth Rhythm Society. He had no disclosures.
My gut sense is that there’s something to rotor mapping, but we are not there yet. There are a lot of investment dollars and a lot of bright people working on this. It really is the Holy Grail to find the source of AF.
Dr. John Day is the director of Intermountain Heart Rhythm Specialists in Murray, Utah, and the current president of the Hearth Rhythm Society. He had no disclosures.
SAN FRANCISCO – Focal impulse and rotor modulation-guided ablation for persistent atrial fibrillation – either alone or in conjunction with other procedures – increased procedural times without improving outcomes, according to the first randomized trial to assess its utility.
In fact, enrollment in the rotor ablation-only (RA) arm was halted early for futility. “There was 100% recurrence” of atrial fibrillation (AF), said senior investigator Dr. Andrea Natale, executive medical director of the Texas Cardiac Arrhythmia Institute, Austin.
“I’m surprised it took this long for a randomized study, because this system has been around for 5 or 6 years,” noted Dr. Natale. “Our community should demand these sorts of studies earlier, because it’s not fair for patients to go on with a procedure for years that has not been proven to be effective.
“For us, unless there is a new version of rotor mapping that I feel is significantly different, this will be the end of rotor ablation in my lab with this system [the Topera Physiologic Rotor Mapping Solution],” Dr. Natale said at the annual scientific sessions of the Heart Rhythm Society.
In the study, his team randomized 29 patients to RA only, 42 to RA plus pulmonary vein antral isolation (PVAI), and 42 to PVAI plus posterior wall and nonpulmonary vein trigger ablation.
At about 1 year, four RA-only patients (14%), 22 RA plus PVAI patients (52%), and 32 patients in the PVAI plus trigger group (76%) were free of AF and atrial tachycardias without antiarrhythmic drugs (P < .0001).
Meanwhile, RA alone and RA plus PVAI cases took about 230 minutes, while the more effective PVAI plus trigger approach took about 130 minutes (P < .001).
There was “a very poor outcome with rotor-only ablation,” Dr. Natale said. “There isn’t a benefit either alone or as an add-on strategy, at least with this mapping software.”
Perhaps “people who think rotors don’t exist are right,” he added. On the other hand, maybe the basket mapping catheter doesn’t touch enough of the left atrium, or the software that makes sense of what the catheter detects needs to be improved, Dr. Natale noted.
All the patients were undergoing their first ablation. They were in their early 60s, on average, and most were men. The mean left atrium diameter was about 47 mm, and mean left ventricle ejection fraction about 55%. There were no statistically significant differences between the study arms, and no significant differences in outcomes between the 70% of patients with persistent AF and the 30% with long-standing persistent AF.
There was no industry funding for the work. Dr. Natale disclosed relationships with Biosense Webster, Boston Scientific, Janssen, Medtronic, and St. Jude Medical.
SAN FRANCISCO – Focal impulse and rotor modulation-guided ablation for persistent atrial fibrillation – either alone or in conjunction with other procedures – increased procedural times without improving outcomes, according to the first randomized trial to assess its utility.
In fact, enrollment in the rotor ablation-only (RA) arm was halted early for futility. “There was 100% recurrence” of atrial fibrillation (AF), said senior investigator Dr. Andrea Natale, executive medical director of the Texas Cardiac Arrhythmia Institute, Austin.
“I’m surprised it took this long for a randomized study, because this system has been around for 5 or 6 years,” noted Dr. Natale. “Our community should demand these sorts of studies earlier, because it’s not fair for patients to go on with a procedure for years that has not been proven to be effective.
“For us, unless there is a new version of rotor mapping that I feel is significantly different, this will be the end of rotor ablation in my lab with this system [the Topera Physiologic Rotor Mapping Solution],” Dr. Natale said at the annual scientific sessions of the Heart Rhythm Society.
In the study, his team randomized 29 patients to RA only, 42 to RA plus pulmonary vein antral isolation (PVAI), and 42 to PVAI plus posterior wall and nonpulmonary vein trigger ablation.
At about 1 year, four RA-only patients (14%), 22 RA plus PVAI patients (52%), and 32 patients in the PVAI plus trigger group (76%) were free of AF and atrial tachycardias without antiarrhythmic drugs (P < .0001).
Meanwhile, RA alone and RA plus PVAI cases took about 230 minutes, while the more effective PVAI plus trigger approach took about 130 minutes (P < .001).
There was “a very poor outcome with rotor-only ablation,” Dr. Natale said. “There isn’t a benefit either alone or as an add-on strategy, at least with this mapping software.”
Perhaps “people who think rotors don’t exist are right,” he added. On the other hand, maybe the basket mapping catheter doesn’t touch enough of the left atrium, or the software that makes sense of what the catheter detects needs to be improved, Dr. Natale noted.
All the patients were undergoing their first ablation. They were in their early 60s, on average, and most were men. The mean left atrium diameter was about 47 mm, and mean left ventricle ejection fraction about 55%. There were no statistically significant differences between the study arms, and no significant differences in outcomes between the 70% of patients with persistent AF and the 30% with long-standing persistent AF.
There was no industry funding for the work. Dr. Natale disclosed relationships with Biosense Webster, Boston Scientific, Janssen, Medtronic, and St. Jude Medical.
AT HEART RHYTHM 2016
Key clinical point: Focal impulse and rotor modulation-guided ablation for persistent atrial fibrillation – either alone or in conjunction with other procedures – increased procedural times without improving outcomes.
Major finding: At about 1 year, four rotor ablation-only patients (14%), 22 RA plus pulmonary vein antral isolation patients (52.4%), and 32 patients in the PVAI plus trigger group (76%) were free of atrial fibrillation and atrial tachycardias without antiarrhythmic drugs (P < .0001).
Data source: A randomized trial in 113 persistent AF patients.
Disclosures: There was no industry funding for the work. The senior investigator disclosed relationships with Biosense Webster, Boston Scientific, Janssen, Medtronic, and St. Jude Medical.