User login
Social Frailty Linked to Risk for Predementia Syndrome
TOPLINE:
Social frailty, the lack of resources to meet basic social needs, is associated with an increased risk for motoric cognitive risk syndrome (MCR), a predementia syndrome characterized by cognitive complaints and slow gait, results of a large, population-based study suggested.
METHODOLOGY:
- The study used 2011 (Round 1) to 2018 (Round 8) data on a discovery sample of 4657 individuals without MCR or dementia at baseline from the National Health and Aging Trends Study (NHATS), a longitudinal survey of older adult Medicare beneficiaries.
- Researchers also collected data on 3075 newly recruited individuals in Round 5 and followed to Round 8 as an independent validation sample to create a pooled sample of 7732 older adults, mean age 76.06, without MCR at baseline.
- Social frailty, assessed at baseline, included five social items: Going out less, not feeling confident, rarely visiting friends/family, not talking with others, and without live-in partner/spouse (researchers divided participants into normal [zero to one items] and social frailty [two to five items] groups).
- Individuals were considered to have MCR if they had both subjective cognitive complaints and slow gait speed (greater than 1 standard deviation below age-specific level) without dementia or mobility disability.
- Covariates included demographic and lifestyle data, presence of depression and/or anxiety symptoms, and number of chronic diseases.
TAKEAWAY:
- During a median follow-up period of 4 years, 10.35% individuals were diagnosed with MCR.
- After the researchers controlled for confounding factors, those with social frailty had an increased risk for MCR compared with the normal group (pooled sample: hazard ratio [HR], 1.57; 95% CI, 1.34-1.84; P < .001).
- Each additional unfavorable social item was associated with an increased risk for MCR (pooled sample: HR, 1.32; 95% CI, 1.22-1.43; P < .001).
- Results of stratified analyses across subgroups suggested individuals with social frailty had a significantly higher risk for incident MCR than that of those without social frailty, regardless of socioeconomic status, lifestyle factors, chronic diseases, and mental health.
IN PRACTICE:
The findings suggest assessing social frailty using simple questions “is an efficient tool for detecting older individuals with a high risk of MCR,” the authors wrote. They noted that the addition of such a tool in clinical practice may facilitate “timely implementation of prevention strategies.”
SOURCE:
The research was led by Hui Zhang, Human Phenome Institute, Zhangjiang Fudan International Innovation Centre, Fudan University, Shanghai, China. It was published online on January 29, 2024, in Alzheimer’s & Dementia.
LIMITATIONS:
The study was observational, so the association between social frailty and MCR is merely correlational. Due to the lack of genetic information in NHATS data, researchers didn’t evaluate the effect of genetic factors such as apolipoprotein E on the association between social frailty and MCR. Social frailty was assessed at a single time point. In addition, the researchers were unable examine the time sequence between social frailty and MCR and so could not determine the cause of this association.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China-Youth Science Fund, Shanghai Rising-Star Program, Shanghai Municipal Health Commission and Key Discipline Construction Project of Pudong Health, and Family Planning Commission of Shanghai. The authors reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Social frailty, the lack of resources to meet basic social needs, is associated with an increased risk for motoric cognitive risk syndrome (MCR), a predementia syndrome characterized by cognitive complaints and slow gait, results of a large, population-based study suggested.
METHODOLOGY:
- The study used 2011 (Round 1) to 2018 (Round 8) data on a discovery sample of 4657 individuals without MCR or dementia at baseline from the National Health and Aging Trends Study (NHATS), a longitudinal survey of older adult Medicare beneficiaries.
- Researchers also collected data on 3075 newly recruited individuals in Round 5 and followed to Round 8 as an independent validation sample to create a pooled sample of 7732 older adults, mean age 76.06, without MCR at baseline.
- Social frailty, assessed at baseline, included five social items: Going out less, not feeling confident, rarely visiting friends/family, not talking with others, and without live-in partner/spouse (researchers divided participants into normal [zero to one items] and social frailty [two to five items] groups).
- Individuals were considered to have MCR if they had both subjective cognitive complaints and slow gait speed (greater than 1 standard deviation below age-specific level) without dementia or mobility disability.
- Covariates included demographic and lifestyle data, presence of depression and/or anxiety symptoms, and number of chronic diseases.
TAKEAWAY:
- During a median follow-up period of 4 years, 10.35% individuals were diagnosed with MCR.
- After the researchers controlled for confounding factors, those with social frailty had an increased risk for MCR compared with the normal group (pooled sample: hazard ratio [HR], 1.57; 95% CI, 1.34-1.84; P < .001).
- Each additional unfavorable social item was associated with an increased risk for MCR (pooled sample: HR, 1.32; 95% CI, 1.22-1.43; P < .001).
- Results of stratified analyses across subgroups suggested individuals with social frailty had a significantly higher risk for incident MCR than that of those without social frailty, regardless of socioeconomic status, lifestyle factors, chronic diseases, and mental health.
IN PRACTICE:
The findings suggest assessing social frailty using simple questions “is an efficient tool for detecting older individuals with a high risk of MCR,” the authors wrote. They noted that the addition of such a tool in clinical practice may facilitate “timely implementation of prevention strategies.”
SOURCE:
The research was led by Hui Zhang, Human Phenome Institute, Zhangjiang Fudan International Innovation Centre, Fudan University, Shanghai, China. It was published online on January 29, 2024, in Alzheimer’s & Dementia.
LIMITATIONS:
The study was observational, so the association between social frailty and MCR is merely correlational. Due to the lack of genetic information in NHATS data, researchers didn’t evaluate the effect of genetic factors such as apolipoprotein E on the association between social frailty and MCR. Social frailty was assessed at a single time point. In addition, the researchers were unable examine the time sequence between social frailty and MCR and so could not determine the cause of this association.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China-Youth Science Fund, Shanghai Rising-Star Program, Shanghai Municipal Health Commission and Key Discipline Construction Project of Pudong Health, and Family Planning Commission of Shanghai. The authors reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Social frailty, the lack of resources to meet basic social needs, is associated with an increased risk for motoric cognitive risk syndrome (MCR), a predementia syndrome characterized by cognitive complaints and slow gait, results of a large, population-based study suggested.
METHODOLOGY:
- The study used 2011 (Round 1) to 2018 (Round 8) data on a discovery sample of 4657 individuals without MCR or dementia at baseline from the National Health and Aging Trends Study (NHATS), a longitudinal survey of older adult Medicare beneficiaries.
- Researchers also collected data on 3075 newly recruited individuals in Round 5 and followed to Round 8 as an independent validation sample to create a pooled sample of 7732 older adults, mean age 76.06, without MCR at baseline.
- Social frailty, assessed at baseline, included five social items: Going out less, not feeling confident, rarely visiting friends/family, not talking with others, and without live-in partner/spouse (researchers divided participants into normal [zero to one items] and social frailty [two to five items] groups).
- Individuals were considered to have MCR if they had both subjective cognitive complaints and slow gait speed (greater than 1 standard deviation below age-specific level) without dementia or mobility disability.
- Covariates included demographic and lifestyle data, presence of depression and/or anxiety symptoms, and number of chronic diseases.
TAKEAWAY:
- During a median follow-up period of 4 years, 10.35% individuals were diagnosed with MCR.
- After the researchers controlled for confounding factors, those with social frailty had an increased risk for MCR compared with the normal group (pooled sample: hazard ratio [HR], 1.57; 95% CI, 1.34-1.84; P < .001).
- Each additional unfavorable social item was associated with an increased risk for MCR (pooled sample: HR, 1.32; 95% CI, 1.22-1.43; P < .001).
- Results of stratified analyses across subgroups suggested individuals with social frailty had a significantly higher risk for incident MCR than that of those without social frailty, regardless of socioeconomic status, lifestyle factors, chronic diseases, and mental health.
IN PRACTICE:
The findings suggest assessing social frailty using simple questions “is an efficient tool for detecting older individuals with a high risk of MCR,” the authors wrote. They noted that the addition of such a tool in clinical practice may facilitate “timely implementation of prevention strategies.”
SOURCE:
The research was led by Hui Zhang, Human Phenome Institute, Zhangjiang Fudan International Innovation Centre, Fudan University, Shanghai, China. It was published online on January 29, 2024, in Alzheimer’s & Dementia.
LIMITATIONS:
The study was observational, so the association between social frailty and MCR is merely correlational. Due to the lack of genetic information in NHATS data, researchers didn’t evaluate the effect of genetic factors such as apolipoprotein E on the association between social frailty and MCR. Social frailty was assessed at a single time point. In addition, the researchers were unable examine the time sequence between social frailty and MCR and so could not determine the cause of this association.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China-Youth Science Fund, Shanghai Rising-Star Program, Shanghai Municipal Health Commission and Key Discipline Construction Project of Pudong Health, and Family Planning Commission of Shanghai. The authors reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
First Cases of Medically Acquired Alzheimer’s Disease Reported
Five people in the United Kingdom have been diagnosed with Alzheimer’s disease resulting from a medical treatment they received decades earlier, new research shows.
The individuals received treatment as children with human growth hormone extracted from pituitary glands of cadavers (c-hGH). Between 1958-1985, an estimated 30,000 people worldwide, mostly children, were treated with c-hGH for genetic disorders and growth hormone deficiencies.
The therapy was halted in 1985 after three patients in the US who received the treatment later died of Creutzfeldt-Jakob disease (CJD) transmitted through batches of c-hGH that were contaminated with disease-causing prions.
The new study builds on the investigators’ earlier work that showed the batches of c-hGH also contained amyloid-beta protein and that the protein could be transmitted decades later. These five cases were referred to or reviewed by researchers and clinicians at a prion clinic led by one of the lead researchers.
There are no reports of amyloid-beta transmission through any other medical or surgical procedures, researchers stress, and there is no evidence that amyloid-beta can be passed on during routine patient care or in daily activities.
“However, the recognition of transmission of amyloid-beta pathology in these rare situations should lead us to review measures to prevent accidental transmission via other medical or surgical procedures, in order to prevent such cases occurring in future,” lead author John Collinge, MD, director of the University of College London Institute of Prion Diseases, London, England, and leader of the UK’s National Prion Clinic, said in a press release.
“Importantly, our findings also suggest that Alzheimer’s and some other neurological conditions share similar disease processes to CJD, and this may have important implications for understanding and treating Alzheimer’s disease in the future,” Dr. Collinge continued.
The findings were published online January 29 in Nature Medicine.
Building on Earlier Work
The research builds on investigators’ previous 2015 work that found archived samples of c-hGH were also contaminated with amyloid-beta protein. In 2018, mouse studies showed that c-hGH samples stored for decades could still transmit amyloid-beta via injection.
Researchers said the findings suggested that individuals exposed to contaminated c-hGH who did not die from CJD might eventually develop AD.
Patients in the new study developed neurological symptoms consistent with AD between the ages of 38 and 55 years. The individual cases were either referred to or reviewed by experts in the National Prion Clinic in the UK between 2017 and 2022. The clinic coordinates the National Prion Monitoring Cohort, a longitudinal study of individuals with confirmed prion diseases.
Of the eight cases, three were diagnosed with AD before referral to the clinic; two others met criteria for an AD diagnosis; and three did not meet the criteria. Three of the patients — two of whom had AD — are now deceased.
All patients in the study received c-hGH prepared using a method called Wilhelmi or Hartree-modified Wilhelmi preparation (HWP).
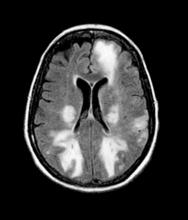
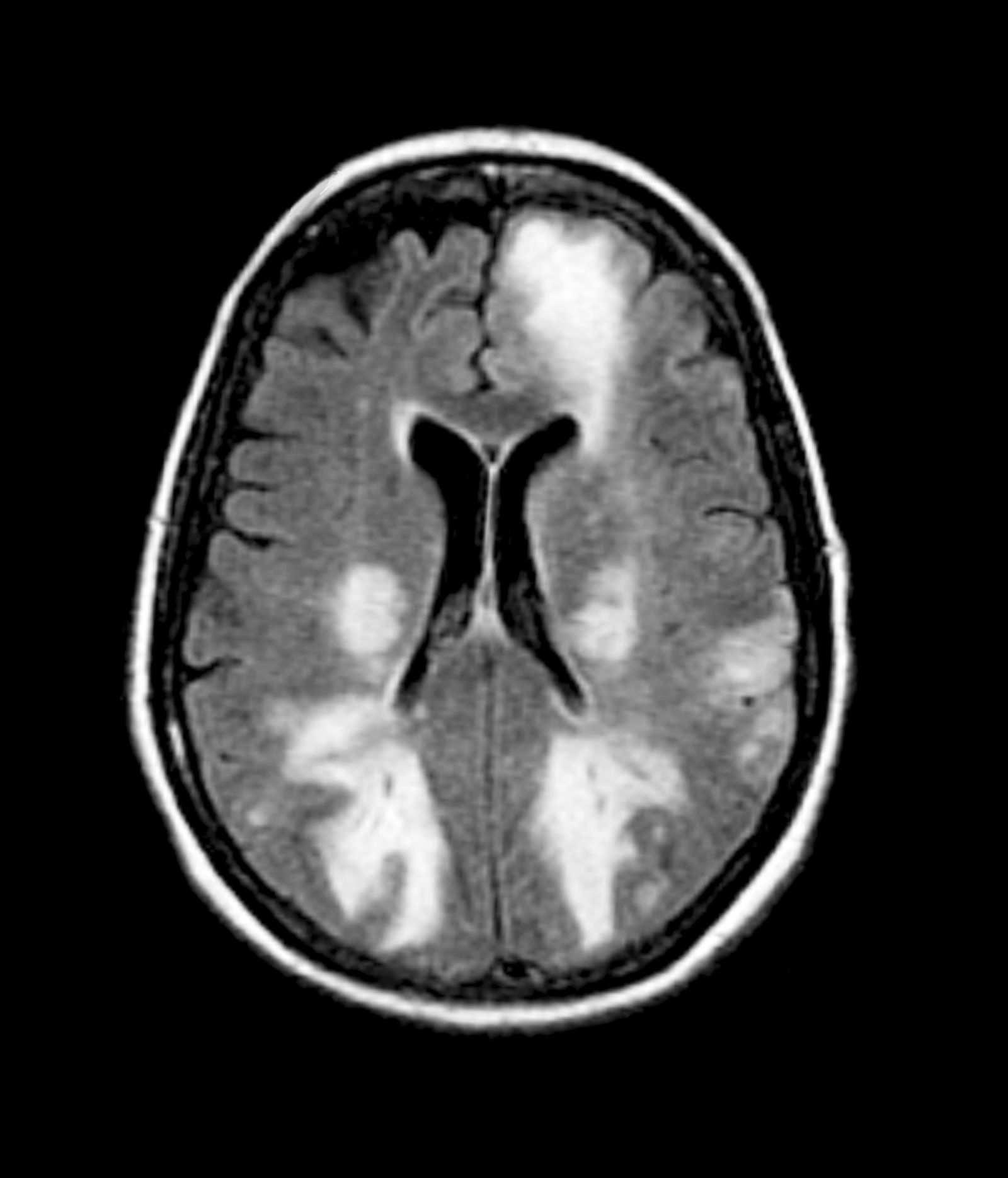
Biomarker analyses confirmed the AD diagnosis in two patients. Other cases showed either progressive brain volume loss on brain imaging or elevated cerebrospinal fluid total tau and phosphorylated tau, or evidence of amyloid-beta deposits on autopsy.
‘Potentially Transmissible’
The cases offered diverse presentations. Some were not symptomatic and some failed to meet current diagnostic criteria for sporadic Alzheimer’s disease. Treatment duration and frequency differed among those in the study, as did their age at treatment onset and completion. That and other factors could contribute to the diverse phenotype recorded in individuals, investigators note.
Investigators examined and ruled out other factors that might explain the individuals’ cognitive symptoms, including childhood intellectual disability, which has been linked to dementia risk, the underlying condition that prompted their treatment with c-hGH, growth hormone deficiency, and cranial radiotherapy, which four of the individuals had received. They also ruled out inherited disease in all five of the cases with samples available for testing.
“Taken together, the only factor common to all of the patients whom we describe is treatment with the HWP subtype of c-hGH,” the authors write. “Given the strong experimental evidence for A-beta transmission from relevant archived HWP c-hGH batches, we conclude that this is the most plausible explanation for the findings observed.”
Investigators say the findings show that, like other prion diseases, AD has three etiologies: sporadic, inherited, and rare acquired forms, or iatrogenic AD.
“The clinical syndrome developed by these individuals can, therefore, be termed iatrogenic Alzheimer’s disease, and Alzheimer’s disease should now be recognized as a potentially transmissible disorder,” the authors write.
“Our cases suggest that, similarly to what is observed in human prion diseases, iatrogenic forms of Alzheimer’s disease differ phenotypically from sporadic and inherited forms, with some individuals remaining asymptomatic despite exposure to A-beta seeds due to protective factors that, at present, are unknown,” they continue
‘Measure of Skepticism’
In an accompanying editorial, Mathias Jucker, PhD, of the Hertie Institute for Clinical Brain Research, University of Tübingen, Tübingen, Germany, and Lary C. Walker, PhD, in the Department of Neurology at Emory University, Atlanta, write that the findings should be considered “with a measure of skepticism.”
“The cases presented are diverse and complicated; the individuals had undergone a variety of medical interventions for various disorders earlier in life, and it is difficult to exclude a contribution of these circumstances to the complex disease phenotypes that appeared many years later,” they write.
However, they continue, “there is good reason to take the findings seriously.”
“From a practical standpoint, this report reinforces the potential of amyloid-beta seeds as targets for early prevention, and it underscores the importance of informed caution in the preparation of surgical instruments, handling of tissues, and implementation of therapeutic biologics, particularly those derived from human sources,” Dr. Jucker and Dr. Walker write.
Commenting on the findings for this news organization, Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association, says the idea that amyloid-beta is transmissible between individuals has been shown before.
“We’ve known for a long time that it is possible to create abnormal amyloid buildup — similar to that seen in Alzheimer’s – in the brain of an animal by injecting it with amyloid-beta. We also transfer human Alzheimer’s genes into animals to initiate abnormal, Alzheimer’s-like processes in their brains,” he said. “Thus, the idea that amyloid is transferable between individuals is not so novel as implied in the new paper.”
However, the study does highlight the importance of safety measures to prevent the accidental transmission of amyloid-beta, Weber added.
“It is a reasonable and actionable caution that the scientific and clinical communities must understand the possible risks and ensure that all methods of transmission are eliminated — for example, with complete and conscientious sterilization of surgical instruments,” he said. “Bottom line: We shouldn’t put amyloid-beta into people’s brains, either accidentally or on purpose, and appropriate measures should be in place to ensure that doesn’t happen.”
The study was supported by the Medical Research Council, the National Institute for Health and Care Research (NIHR), the NIHR University College of London Hospital Biomedical Research Centre, Alzheimer’s Research UK, and the Stroke Association. Dr. Collinge is a shareholder and director of D-Gen, Ltd., an academic spin-out company working in the field of prion disease diagnosis, decontamination and therapeutics. Dr. Jucker and Dr. Walker report no conflicts of interest.
A version of this article appeared on Medscape.com.
Five people in the United Kingdom have been diagnosed with Alzheimer’s disease resulting from a medical treatment they received decades earlier, new research shows.
The individuals received treatment as children with human growth hormone extracted from pituitary glands of cadavers (c-hGH). Between 1958-1985, an estimated 30,000 people worldwide, mostly children, were treated with c-hGH for genetic disorders and growth hormone deficiencies.
The therapy was halted in 1985 after three patients in the US who received the treatment later died of Creutzfeldt-Jakob disease (CJD) transmitted through batches of c-hGH that were contaminated with disease-causing prions.
The new study builds on the investigators’ earlier work that showed the batches of c-hGH also contained amyloid-beta protein and that the protein could be transmitted decades later. These five cases were referred to or reviewed by researchers and clinicians at a prion clinic led by one of the lead researchers.
There are no reports of amyloid-beta transmission through any other medical or surgical procedures, researchers stress, and there is no evidence that amyloid-beta can be passed on during routine patient care or in daily activities.
“However, the recognition of transmission of amyloid-beta pathology in these rare situations should lead us to review measures to prevent accidental transmission via other medical or surgical procedures, in order to prevent such cases occurring in future,” lead author John Collinge, MD, director of the University of College London Institute of Prion Diseases, London, England, and leader of the UK’s National Prion Clinic, said in a press release.
“Importantly, our findings also suggest that Alzheimer’s and some other neurological conditions share similar disease processes to CJD, and this may have important implications for understanding and treating Alzheimer’s disease in the future,” Dr. Collinge continued.
The findings were published online January 29 in Nature Medicine.
Building on Earlier Work
The research builds on investigators’ previous 2015 work that found archived samples of c-hGH were also contaminated with amyloid-beta protein. In 2018, mouse studies showed that c-hGH samples stored for decades could still transmit amyloid-beta via injection.
Researchers said the findings suggested that individuals exposed to contaminated c-hGH who did not die from CJD might eventually develop AD.
Patients in the new study developed neurological symptoms consistent with AD between the ages of 38 and 55 years. The individual cases were either referred to or reviewed by experts in the National Prion Clinic in the UK between 2017 and 2022. The clinic coordinates the National Prion Monitoring Cohort, a longitudinal study of individuals with confirmed prion diseases.
Of the eight cases, three were diagnosed with AD before referral to the clinic; two others met criteria for an AD diagnosis; and three did not meet the criteria. Three of the patients — two of whom had AD — are now deceased.
All patients in the study received c-hGH prepared using a method called Wilhelmi or Hartree-modified Wilhelmi preparation (HWP).
Biomarker analyses confirmed the AD diagnosis in two patients. Other cases showed either progressive brain volume loss on brain imaging or elevated cerebrospinal fluid total tau and phosphorylated tau, or evidence of amyloid-beta deposits on autopsy.
‘Potentially Transmissible’
The cases offered diverse presentations. Some were not symptomatic and some failed to meet current diagnostic criteria for sporadic Alzheimer’s disease. Treatment duration and frequency differed among those in the study, as did their age at treatment onset and completion. That and other factors could contribute to the diverse phenotype recorded in individuals, investigators note.
Investigators examined and ruled out other factors that might explain the individuals’ cognitive symptoms, including childhood intellectual disability, which has been linked to dementia risk, the underlying condition that prompted their treatment with c-hGH, growth hormone deficiency, and cranial radiotherapy, which four of the individuals had received. They also ruled out inherited disease in all five of the cases with samples available for testing.
“Taken together, the only factor common to all of the patients whom we describe is treatment with the HWP subtype of c-hGH,” the authors write. “Given the strong experimental evidence for A-beta transmission from relevant archived HWP c-hGH batches, we conclude that this is the most plausible explanation for the findings observed.”
Investigators say the findings show that, like other prion diseases, AD has three etiologies: sporadic, inherited, and rare acquired forms, or iatrogenic AD.
“The clinical syndrome developed by these individuals can, therefore, be termed iatrogenic Alzheimer’s disease, and Alzheimer’s disease should now be recognized as a potentially transmissible disorder,” the authors write.
“Our cases suggest that, similarly to what is observed in human prion diseases, iatrogenic forms of Alzheimer’s disease differ phenotypically from sporadic and inherited forms, with some individuals remaining asymptomatic despite exposure to A-beta seeds due to protective factors that, at present, are unknown,” they continue
‘Measure of Skepticism’
In an accompanying editorial, Mathias Jucker, PhD, of the Hertie Institute for Clinical Brain Research, University of Tübingen, Tübingen, Germany, and Lary C. Walker, PhD, in the Department of Neurology at Emory University, Atlanta, write that the findings should be considered “with a measure of skepticism.”
“The cases presented are diverse and complicated; the individuals had undergone a variety of medical interventions for various disorders earlier in life, and it is difficult to exclude a contribution of these circumstances to the complex disease phenotypes that appeared many years later,” they write.
However, they continue, “there is good reason to take the findings seriously.”
“From a practical standpoint, this report reinforces the potential of amyloid-beta seeds as targets for early prevention, and it underscores the importance of informed caution in the preparation of surgical instruments, handling of tissues, and implementation of therapeutic biologics, particularly those derived from human sources,” Dr. Jucker and Dr. Walker write.
Commenting on the findings for this news organization, Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association, says the idea that amyloid-beta is transmissible between individuals has been shown before.
“We’ve known for a long time that it is possible to create abnormal amyloid buildup — similar to that seen in Alzheimer’s – in the brain of an animal by injecting it with amyloid-beta. We also transfer human Alzheimer’s genes into animals to initiate abnormal, Alzheimer’s-like processes in their brains,” he said. “Thus, the idea that amyloid is transferable between individuals is not so novel as implied in the new paper.”
However, the study does highlight the importance of safety measures to prevent the accidental transmission of amyloid-beta, Weber added.
“It is a reasonable and actionable caution that the scientific and clinical communities must understand the possible risks and ensure that all methods of transmission are eliminated — for example, with complete and conscientious sterilization of surgical instruments,” he said. “Bottom line: We shouldn’t put amyloid-beta into people’s brains, either accidentally or on purpose, and appropriate measures should be in place to ensure that doesn’t happen.”
The study was supported by the Medical Research Council, the National Institute for Health and Care Research (NIHR), the NIHR University College of London Hospital Biomedical Research Centre, Alzheimer’s Research UK, and the Stroke Association. Dr. Collinge is a shareholder and director of D-Gen, Ltd., an academic spin-out company working in the field of prion disease diagnosis, decontamination and therapeutics. Dr. Jucker and Dr. Walker report no conflicts of interest.
A version of this article appeared on Medscape.com.
Five people in the United Kingdom have been diagnosed with Alzheimer’s disease resulting from a medical treatment they received decades earlier, new research shows.
The individuals received treatment as children with human growth hormone extracted from pituitary glands of cadavers (c-hGH). Between 1958-1985, an estimated 30,000 people worldwide, mostly children, were treated with c-hGH for genetic disorders and growth hormone deficiencies.
The therapy was halted in 1985 after three patients in the US who received the treatment later died of Creutzfeldt-Jakob disease (CJD) transmitted through batches of c-hGH that were contaminated with disease-causing prions.
The new study builds on the investigators’ earlier work that showed the batches of c-hGH also contained amyloid-beta protein and that the protein could be transmitted decades later. These five cases were referred to or reviewed by researchers and clinicians at a prion clinic led by one of the lead researchers.
There are no reports of amyloid-beta transmission through any other medical or surgical procedures, researchers stress, and there is no evidence that amyloid-beta can be passed on during routine patient care or in daily activities.
“However, the recognition of transmission of amyloid-beta pathology in these rare situations should lead us to review measures to prevent accidental transmission via other medical or surgical procedures, in order to prevent such cases occurring in future,” lead author John Collinge, MD, director of the University of College London Institute of Prion Diseases, London, England, and leader of the UK’s National Prion Clinic, said in a press release.
“Importantly, our findings also suggest that Alzheimer’s and some other neurological conditions share similar disease processes to CJD, and this may have important implications for understanding and treating Alzheimer’s disease in the future,” Dr. Collinge continued.
The findings were published online January 29 in Nature Medicine.
Building on Earlier Work
The research builds on investigators’ previous 2015 work that found archived samples of c-hGH were also contaminated with amyloid-beta protein. In 2018, mouse studies showed that c-hGH samples stored for decades could still transmit amyloid-beta via injection.
Researchers said the findings suggested that individuals exposed to contaminated c-hGH who did not die from CJD might eventually develop AD.
Patients in the new study developed neurological symptoms consistent with AD between the ages of 38 and 55 years. The individual cases were either referred to or reviewed by experts in the National Prion Clinic in the UK between 2017 and 2022. The clinic coordinates the National Prion Monitoring Cohort, a longitudinal study of individuals with confirmed prion diseases.
Of the eight cases, three were diagnosed with AD before referral to the clinic; two others met criteria for an AD diagnosis; and three did not meet the criteria. Three of the patients — two of whom had AD — are now deceased.
All patients in the study received c-hGH prepared using a method called Wilhelmi or Hartree-modified Wilhelmi preparation (HWP).
Biomarker analyses confirmed the AD diagnosis in two patients. Other cases showed either progressive brain volume loss on brain imaging or elevated cerebrospinal fluid total tau and phosphorylated tau, or evidence of amyloid-beta deposits on autopsy.
‘Potentially Transmissible’
The cases offered diverse presentations. Some were not symptomatic and some failed to meet current diagnostic criteria for sporadic Alzheimer’s disease. Treatment duration and frequency differed among those in the study, as did their age at treatment onset and completion. That and other factors could contribute to the diverse phenotype recorded in individuals, investigators note.
Investigators examined and ruled out other factors that might explain the individuals’ cognitive symptoms, including childhood intellectual disability, which has been linked to dementia risk, the underlying condition that prompted their treatment with c-hGH, growth hormone deficiency, and cranial radiotherapy, which four of the individuals had received. They also ruled out inherited disease in all five of the cases with samples available for testing.
“Taken together, the only factor common to all of the patients whom we describe is treatment with the HWP subtype of c-hGH,” the authors write. “Given the strong experimental evidence for A-beta transmission from relevant archived HWP c-hGH batches, we conclude that this is the most plausible explanation for the findings observed.”
Investigators say the findings show that, like other prion diseases, AD has three etiologies: sporadic, inherited, and rare acquired forms, or iatrogenic AD.
“The clinical syndrome developed by these individuals can, therefore, be termed iatrogenic Alzheimer’s disease, and Alzheimer’s disease should now be recognized as a potentially transmissible disorder,” the authors write.
“Our cases suggest that, similarly to what is observed in human prion diseases, iatrogenic forms of Alzheimer’s disease differ phenotypically from sporadic and inherited forms, with some individuals remaining asymptomatic despite exposure to A-beta seeds due to protective factors that, at present, are unknown,” they continue
‘Measure of Skepticism’
In an accompanying editorial, Mathias Jucker, PhD, of the Hertie Institute for Clinical Brain Research, University of Tübingen, Tübingen, Germany, and Lary C. Walker, PhD, in the Department of Neurology at Emory University, Atlanta, write that the findings should be considered “with a measure of skepticism.”
“The cases presented are diverse and complicated; the individuals had undergone a variety of medical interventions for various disorders earlier in life, and it is difficult to exclude a contribution of these circumstances to the complex disease phenotypes that appeared many years later,” they write.
However, they continue, “there is good reason to take the findings seriously.”
“From a practical standpoint, this report reinforces the potential of amyloid-beta seeds as targets for early prevention, and it underscores the importance of informed caution in the preparation of surgical instruments, handling of tissues, and implementation of therapeutic biologics, particularly those derived from human sources,” Dr. Jucker and Dr. Walker write.
Commenting on the findings for this news organization, Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association, says the idea that amyloid-beta is transmissible between individuals has been shown before.
“We’ve known for a long time that it is possible to create abnormal amyloid buildup — similar to that seen in Alzheimer’s – in the brain of an animal by injecting it with amyloid-beta. We also transfer human Alzheimer’s genes into animals to initiate abnormal, Alzheimer’s-like processes in their brains,” he said. “Thus, the idea that amyloid is transferable between individuals is not so novel as implied in the new paper.”
However, the study does highlight the importance of safety measures to prevent the accidental transmission of amyloid-beta, Weber added.
“It is a reasonable and actionable caution that the scientific and clinical communities must understand the possible risks and ensure that all methods of transmission are eliminated — for example, with complete and conscientious sterilization of surgical instruments,” he said. “Bottom line: We shouldn’t put amyloid-beta into people’s brains, either accidentally or on purpose, and appropriate measures should be in place to ensure that doesn’t happen.”
The study was supported by the Medical Research Council, the National Institute for Health and Care Research (NIHR), the NIHR University College of London Hospital Biomedical Research Centre, Alzheimer’s Research UK, and the Stroke Association. Dr. Collinge is a shareholder and director of D-Gen, Ltd., an academic spin-out company working in the field of prion disease diagnosis, decontamination and therapeutics. Dr. Jucker and Dr. Walker report no conflicts of interest.
A version of this article appeared on Medscape.com.
FROM NATURE MEDICINE
Can Pet Ownership Ward Off Cognitive Decline?
TOPLINE:
, a new longitudinal cohort study showed. Investigators note the findings are important because previous research suggests older adults who live alone are at higher risk for dementia.
METHODOLOGY:
- Investigators analyzed data on 7945 participants aged 50 years and older (56% female; mean age, 66 years) from the English Longitudinal Study of Ageing (ELSA) and determined whether they lived alone or had a pet.
- Every couple of years for the next 8 years after baseline, participants were assessed for verbal cognition, verbal memory, and verbal fluency. Information about covariates including age, sex, employment status, educational level, and health was also collected.
- 35% of participants were pet owners, and 27% lived alone.
TAKEAWAY:
- Pet owners who lived alone had a slower rate of decline in verbal cognition (P = .009), verbal memory (P = .04), and verbal fluency (P = .03) compared with those without pets who lived alone.
- Stratified analysis showed that pet ownership was associated with slower rates of decline in composite verbal cognition, verbal memory, and verbal fluency but only among those who lived alone (all P < .001).
- There was no significant difference in rates of decline in composite verbal cognition, verbal memory, or verbal fluency between pet owners living alone and pet owners living with others.
IN PRACTICE:
“Pet ownership completely offset the associations of living alone with declining rates in verbal memory, verbal fluency, and composite verbal cognition. Our findings provide innovative insights for developing public health policies to slow cognitive decline in older adults living alone,” the authors wrote.
SOURCE:
Ciyong Lu, PhD, of Sun Yat-sen University in Guangzhou, China, led the study, which was published online on December 26, 2023, in JAMA Network Open.
LIMITATIONS:
Whereas cognitive function includes multiple components, the study only assessed verbal memory and verbal fluency. Also, the study did not gather information on the duration of pet ownership after baseline.
DISCLOSURES:
The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
, a new longitudinal cohort study showed. Investigators note the findings are important because previous research suggests older adults who live alone are at higher risk for dementia.
METHODOLOGY:
- Investigators analyzed data on 7945 participants aged 50 years and older (56% female; mean age, 66 years) from the English Longitudinal Study of Ageing (ELSA) and determined whether they lived alone or had a pet.
- Every couple of years for the next 8 years after baseline, participants were assessed for verbal cognition, verbal memory, and verbal fluency. Information about covariates including age, sex, employment status, educational level, and health was also collected.
- 35% of participants were pet owners, and 27% lived alone.
TAKEAWAY:
- Pet owners who lived alone had a slower rate of decline in verbal cognition (P = .009), verbal memory (P = .04), and verbal fluency (P = .03) compared with those without pets who lived alone.
- Stratified analysis showed that pet ownership was associated with slower rates of decline in composite verbal cognition, verbal memory, and verbal fluency but only among those who lived alone (all P < .001).
- There was no significant difference in rates of decline in composite verbal cognition, verbal memory, or verbal fluency between pet owners living alone and pet owners living with others.
IN PRACTICE:
“Pet ownership completely offset the associations of living alone with declining rates in verbal memory, verbal fluency, and composite verbal cognition. Our findings provide innovative insights for developing public health policies to slow cognitive decline in older adults living alone,” the authors wrote.
SOURCE:
Ciyong Lu, PhD, of Sun Yat-sen University in Guangzhou, China, led the study, which was published online on December 26, 2023, in JAMA Network Open.
LIMITATIONS:
Whereas cognitive function includes multiple components, the study only assessed verbal memory and verbal fluency. Also, the study did not gather information on the duration of pet ownership after baseline.
DISCLOSURES:
The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
, a new longitudinal cohort study showed. Investigators note the findings are important because previous research suggests older adults who live alone are at higher risk for dementia.
METHODOLOGY:
- Investigators analyzed data on 7945 participants aged 50 years and older (56% female; mean age, 66 years) from the English Longitudinal Study of Ageing (ELSA) and determined whether they lived alone or had a pet.
- Every couple of years for the next 8 years after baseline, participants were assessed for verbal cognition, verbal memory, and verbal fluency. Information about covariates including age, sex, employment status, educational level, and health was also collected.
- 35% of participants were pet owners, and 27% lived alone.
TAKEAWAY:
- Pet owners who lived alone had a slower rate of decline in verbal cognition (P = .009), verbal memory (P = .04), and verbal fluency (P = .03) compared with those without pets who lived alone.
- Stratified analysis showed that pet ownership was associated with slower rates of decline in composite verbal cognition, verbal memory, and verbal fluency but only among those who lived alone (all P < .001).
- There was no significant difference in rates of decline in composite verbal cognition, verbal memory, or verbal fluency between pet owners living alone and pet owners living with others.
IN PRACTICE:
“Pet ownership completely offset the associations of living alone with declining rates in verbal memory, verbal fluency, and composite verbal cognition. Our findings provide innovative insights for developing public health policies to slow cognitive decline in older adults living alone,” the authors wrote.
SOURCE:
Ciyong Lu, PhD, of Sun Yat-sen University in Guangzhou, China, led the study, which was published online on December 26, 2023, in JAMA Network Open.
LIMITATIONS:
Whereas cognitive function includes multiple components, the study only assessed verbal memory and verbal fluency. Also, the study did not gather information on the duration of pet ownership after baseline.
DISCLOSURES:
The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
A Healthy Dose of Superstition
Mr. Smith was once a nice guy.
These days, unfortunately, he’s anything but. The ravages of a neurodegenerative disease have left him demented, impulsive, and agitated.
His family is trying to find placement for him, and in the meantime I’m doing my best to keep his behavior controlled. Like many things in medicine, this is as much art as science. A tablet of this, a capsule of that, increase this slightly, add something for PRN use ... a witch’s brew of modern medicine.
Because of his worsening, his wife was calling us several times a week with updates, not in an annoying way but in an “I need help” way. I began answering the phone myself if I saw her number come up, because it was easier and faster for me to deal with her directly, and I knew she wasn’t calling for fun.
A few months ago I stopped a medication that didn’t seem to be doing much and started a different one.
And then things went quiet. His wife’s calls went from 3-4 a week to none.
This worried me. I mean, maybe the new medicine was working. ... but the sudden silence was deafening.
One week went by, then two ... I did a Google search to make sure he and his wife hadn’t died or been in the news.
Of course, I could have picked up the phone and called his wife, but why tempt fate?
Three weeks ... I was sure my MA, who handles far more calls than I do, had probably noticed this, too.
It would have been easy to mention it, but even with 16 years of school and 5 years of medical training, not to mention 3,000-4,000 years of hard-earned science behind me, there was the old grade school notion of jinxing myself. To say something is to invite trouble.
Four weeks. Finally, his wife called in and reached my MA. The medication had been working, but now was wearing off and the dose needed to be adjusted. So we did that.
Afterward I mentioned the time lapse to my MA, that I’d been afraid of jinxing it by saying something to her, and she told me she’d been thinking the same thing.
Funny when you think about it. We’re both educated people, believers in science, and (I hope) intelligent. We’re living in a (by human standards) technologically advanced time.
Yet, the old superstitions are still there, the idea that we somehow have magical control over time, space, random chance, and the actions of others by not talking about a phone call (or the lack of one).
Surprisingly (or maybe not), this is pretty normal. When on call we never say “quiet,” for fear of enraging the mysterious Call Gods. If needed, we use “the Q word.”
We still try not to walk under ladders, avoid stepping on sidewalk cracks, carry good luck charms, cross fingers, and fight over wishbones.
Superstitions such as saying “bless you” or “gesundheit” when someone sneezes are so ingrained into us that they’re now part of good manners and polite society.
I’ve worked in quite a few hospitals over the years. Not one of them had a room on any floor that ended in 13, always jumping from 12 to 14.
Civilization is roughly 10,000-15,000 years old. We have the internet and can travel to (relatively nearby) space and back. We have probes exploring — and even leaving — our solar system.
But
I’m going to knock on wood now.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mr. Smith was once a nice guy.
These days, unfortunately, he’s anything but. The ravages of a neurodegenerative disease have left him demented, impulsive, and agitated.
His family is trying to find placement for him, and in the meantime I’m doing my best to keep his behavior controlled. Like many things in medicine, this is as much art as science. A tablet of this, a capsule of that, increase this slightly, add something for PRN use ... a witch’s brew of modern medicine.
Because of his worsening, his wife was calling us several times a week with updates, not in an annoying way but in an “I need help” way. I began answering the phone myself if I saw her number come up, because it was easier and faster for me to deal with her directly, and I knew she wasn’t calling for fun.
A few months ago I stopped a medication that didn’t seem to be doing much and started a different one.
And then things went quiet. His wife’s calls went from 3-4 a week to none.
This worried me. I mean, maybe the new medicine was working. ... but the sudden silence was deafening.
One week went by, then two ... I did a Google search to make sure he and his wife hadn’t died or been in the news.
Of course, I could have picked up the phone and called his wife, but why tempt fate?
Three weeks ... I was sure my MA, who handles far more calls than I do, had probably noticed this, too.
It would have been easy to mention it, but even with 16 years of school and 5 years of medical training, not to mention 3,000-4,000 years of hard-earned science behind me, there was the old grade school notion of jinxing myself. To say something is to invite trouble.
Four weeks. Finally, his wife called in and reached my MA. The medication had been working, but now was wearing off and the dose needed to be adjusted. So we did that.
Afterward I mentioned the time lapse to my MA, that I’d been afraid of jinxing it by saying something to her, and she told me she’d been thinking the same thing.
Funny when you think about it. We’re both educated people, believers in science, and (I hope) intelligent. We’re living in a (by human standards) technologically advanced time.
Yet, the old superstitions are still there, the idea that we somehow have magical control over time, space, random chance, and the actions of others by not talking about a phone call (or the lack of one).
Surprisingly (or maybe not), this is pretty normal. When on call we never say “quiet,” for fear of enraging the mysterious Call Gods. If needed, we use “the Q word.”
We still try not to walk under ladders, avoid stepping on sidewalk cracks, carry good luck charms, cross fingers, and fight over wishbones.
Superstitions such as saying “bless you” or “gesundheit” when someone sneezes are so ingrained into us that they’re now part of good manners and polite society.
I’ve worked in quite a few hospitals over the years. Not one of them had a room on any floor that ended in 13, always jumping from 12 to 14.
Civilization is roughly 10,000-15,000 years old. We have the internet and can travel to (relatively nearby) space and back. We have probes exploring — and even leaving — our solar system.
But
I’m going to knock on wood now.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mr. Smith was once a nice guy.
These days, unfortunately, he’s anything but. The ravages of a neurodegenerative disease have left him demented, impulsive, and agitated.
His family is trying to find placement for him, and in the meantime I’m doing my best to keep his behavior controlled. Like many things in medicine, this is as much art as science. A tablet of this, a capsule of that, increase this slightly, add something for PRN use ... a witch’s brew of modern medicine.
Because of his worsening, his wife was calling us several times a week with updates, not in an annoying way but in an “I need help” way. I began answering the phone myself if I saw her number come up, because it was easier and faster for me to deal with her directly, and I knew she wasn’t calling for fun.
A few months ago I stopped a medication that didn’t seem to be doing much and started a different one.
And then things went quiet. His wife’s calls went from 3-4 a week to none.
This worried me. I mean, maybe the new medicine was working. ... but the sudden silence was deafening.
One week went by, then two ... I did a Google search to make sure he and his wife hadn’t died or been in the news.
Of course, I could have picked up the phone and called his wife, but why tempt fate?
Three weeks ... I was sure my MA, who handles far more calls than I do, had probably noticed this, too.
It would have been easy to mention it, but even with 16 years of school and 5 years of medical training, not to mention 3,000-4,000 years of hard-earned science behind me, there was the old grade school notion of jinxing myself. To say something is to invite trouble.
Four weeks. Finally, his wife called in and reached my MA. The medication had been working, but now was wearing off and the dose needed to be adjusted. So we did that.
Afterward I mentioned the time lapse to my MA, that I’d been afraid of jinxing it by saying something to her, and she told me she’d been thinking the same thing.
Funny when you think about it. We’re both educated people, believers in science, and (I hope) intelligent. We’re living in a (by human standards) technologically advanced time.
Yet, the old superstitions are still there, the idea that we somehow have magical control over time, space, random chance, and the actions of others by not talking about a phone call (or the lack of one).
Surprisingly (or maybe not), this is pretty normal. When on call we never say “quiet,” for fear of enraging the mysterious Call Gods. If needed, we use “the Q word.”
We still try not to walk under ladders, avoid stepping on sidewalk cracks, carry good luck charms, cross fingers, and fight over wishbones.
Superstitions such as saying “bless you” or “gesundheit” when someone sneezes are so ingrained into us that they’re now part of good manners and polite society.
I’ve worked in quite a few hospitals over the years. Not one of them had a room on any floor that ended in 13, always jumping from 12 to 14.
Civilization is roughly 10,000-15,000 years old. We have the internet and can travel to (relatively nearby) space and back. We have probes exploring — and even leaving — our solar system.
But
I’m going to knock on wood now.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Multivitamins and Cognition: New Data From COSMOS
New data from the Cocoa Supplement and Multivitamin Outcomes Study (COSMOS) suggest that a daily multivitamin may help protect the aging brain. However, at least one expert has concerns about the study’s methodology and, as a result, the interpretation of its findings.
The meta-analysis of three separate cognition studies provides “strong and consistent evidence that taking a daily multivitamin, containing more than 20 essential micronutrients, can help prevent memory loss and slow down cognitive aging,” study investigator Chirag Vyas, MBBS, MPH, with Massachusetts General Hospital and Harvard Medical School, Boston, told this news organization.
“We are not now recommending multivitamin use, but the evidence is compelling that supports the promise of multivitamins to help prevent cognitive decline,” Dr. Vyas said.
The new data, from the cognitive substudies of COSMOS, were published online in the American Journal of Clinical Nutrition.
Clinically Meaningful Benefit?
To recap, COSMOS was a 2 x 2 factorial trial of coca extract (500 mg/d flavanols) and/or a daily commercial multivitamin-mineral (MVM) supplement for cardiovascular disease and cancer prevention among more than 21,000 US adults aged 60 years or older.
Neither the cocoa extract nor the MVM supplement had a significant impact on cancer or cardiovascular disease events.
COMOS-Mind was a substudy of 2262 participants aged 65 or older without dementia who completed telephone-based cognitive assessments at baseline and annually for 3 years.
As previously reported by this news organization in COSMOS-Mind, there was no cognitive benefit of daily cocoa extract, but daily MVM supplementation was associated with improved global cognition, episodic memory, and executive function. However, the difference in global cognitive function between MVM and placebo was small, with a mean 0.07-point improvement on the z-score at 3 years.
COSMOS-Web was a substudy of 3562 original participants who were evaluated annually for 3 years using an internet-based battery of neuropsychological tests.
In this analysis, those taking the MVM supplement performed better on a test for immediate memory recall (remembering a list of 20 words); they were able to remember an additional 0.71 word on average compared with 0.44 word in the placebo group. However, they did not improve on tests of memory retention, executive function, or novel object recognition.
The new data are from COSMOS-Clinic, an analysis of 573 participants who completed in-person cognitive assessments.
COSMOS-Clinic showed a modest benefit of MVM, compared with placebo, on global cognition over 2 years (mean difference, 0.06 SD units [SU]), with a significantly more favorable change in episodic memory (mean difference, 0.12 SU) but not in executive function/attention (mean difference, 0.04 SU), the researchers reported.
They also conducted a meta-analysis based on the three separate cognitive substudies, with 5200 nonoverlapping COSMOS participants.
The results showed “clear evidence” of MVM benefits on global cognition (mean difference, 0.07 SU; P = .0009) and episodic memory (mean difference, 0.06 SU; P =.0007), they reported, with the magnitude of effect on global cognition equivalent to reducing cognitive aging by 2 years.
In a statement, JoAnn Manson, MD, DrPH, chief of the Division of Preventive Medicine at Brigham and Women’s Hospital, who led the overall COSMOS trial, said that “the finding that a daily multivitamin improved memory and slowed cognitive aging in three separate placebo-controlled studies in COSMOS is exciting and further supports the promise of multivitamins as a safe, accessible, and affordable approach to protecting cognitive health in older adults.”
Not a Meta-analysis?
In an interview with this news organization, Christopher Labos, MD CM, MSc, a cardiologist and epidemiologist based in Montreal, Canada, who wasn’t involved in COSMOS, cautioned that the evidence to date on multivitamins for memory and brain health are “not all that impressive.”
Dr. Labos is a columnist for this news organization and previously has written about the COSMOS trial.
He said it is important to note that this “meta-analysis of COSMOS data, strictly speaking, is not a meta-analysis” because the patients were all from the original COSMOS study without including any additional patients, “so you don’t have any more data than what you started with.
“The fact that the results are consistent with the original trial is not surprising. In fact, it would be concerning if they were not consistent because they’re the same population. They were just assessed differently — by phone, online, or in person,” Dr. Labos explained.
“It is hard to tell what the benefit with multivitamins actually means in terms of hard clinical endpoints that matter to patients. Scoring a little bit better on a standardized test — I guess that’s a good thing, but does that mean you’re less likely to get dementia? I’m not sure we’re there yet,” he told this news organization.
The bottom line, said Dr. Labos, is that “at this point, the evidence does not support recommending multivitamins purely for brain health. There is also a cost and potential downside associated with their use.”
Also weighing in on the new analyses from COSMOS, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, said while there are now “positive, large-scale, long-term studies that show that multivitamin-mineral supplementation for older adults may slow cognitive aging, the Alzheimer’s Association is not ready to recommend widespread use of a multivitamin supplement to reduce risk of cognitive decline in older adults.
“Independent confirmatory studies are needed in larger, more diverse, and representative study populations. COSMOS-Clinic, for example, had less than 2% non-White in the multivitamin group and 5% non-White in the placebo group. It is critical that future treatments and preventions are effective in all populations,” Dr. Sexton told this news organization.
She noted that multivitamin supplements are “generally easy to find and relatively affordable. With confirmation, these promising findings have the potential to significantly impact public health — improving brain health, lowering healthcare costs, reducing caregiver burden — especially among older adults.”
The Alzheimer’s Association, Dr. Sexton said, “envisions a future where there are multiple treatments available that address the disease in multiple ways — like heart disease and cancer — and that can be combined into powerful combination therapies, in conjunction with brain-healthy guidelines for lifestyle, like diet and physical activity.”
The Alzheimer’s Association is leading a 2-year clinical trial known as US POINTER to evaluate whether lifestyle interventions that target multiple risk factors can protect cognition in older adults at increased risk for cognitive decline.
COSMOS-Clinic and the cognition studies in the meta-analysis were supported by investigator-initiated grants from Mars Edge, a segment of Mars Inc., and the National Institutes of Health. Multivitamin and placebo tablets and packaging were donated by Pfizer, Inc Consumer Healthcare (now Haleon). Disclosures for the COSMOS investigators are available with the original article. Dr. Labos and Dr. Sexton have no relevant disclosures.
A version of this article appeared on Medscape.com.
New data from the Cocoa Supplement and Multivitamin Outcomes Study (COSMOS) suggest that a daily multivitamin may help protect the aging brain. However, at least one expert has concerns about the study’s methodology and, as a result, the interpretation of its findings.
The meta-analysis of three separate cognition studies provides “strong and consistent evidence that taking a daily multivitamin, containing more than 20 essential micronutrients, can help prevent memory loss and slow down cognitive aging,” study investigator Chirag Vyas, MBBS, MPH, with Massachusetts General Hospital and Harvard Medical School, Boston, told this news organization.
“We are not now recommending multivitamin use, but the evidence is compelling that supports the promise of multivitamins to help prevent cognitive decline,” Dr. Vyas said.
The new data, from the cognitive substudies of COSMOS, were published online in the American Journal of Clinical Nutrition.
Clinically Meaningful Benefit?
To recap, COSMOS was a 2 x 2 factorial trial of coca extract (500 mg/d flavanols) and/or a daily commercial multivitamin-mineral (MVM) supplement for cardiovascular disease and cancer prevention among more than 21,000 US adults aged 60 years or older.
Neither the cocoa extract nor the MVM supplement had a significant impact on cancer or cardiovascular disease events.
COMOS-Mind was a substudy of 2262 participants aged 65 or older without dementia who completed telephone-based cognitive assessments at baseline and annually for 3 years.
As previously reported by this news organization in COSMOS-Mind, there was no cognitive benefit of daily cocoa extract, but daily MVM supplementation was associated with improved global cognition, episodic memory, and executive function. However, the difference in global cognitive function between MVM and placebo was small, with a mean 0.07-point improvement on the z-score at 3 years.
COSMOS-Web was a substudy of 3562 original participants who were evaluated annually for 3 years using an internet-based battery of neuropsychological tests.
In this analysis, those taking the MVM supplement performed better on a test for immediate memory recall (remembering a list of 20 words); they were able to remember an additional 0.71 word on average compared with 0.44 word in the placebo group. However, they did not improve on tests of memory retention, executive function, or novel object recognition.
The new data are from COSMOS-Clinic, an analysis of 573 participants who completed in-person cognitive assessments.
COSMOS-Clinic showed a modest benefit of MVM, compared with placebo, on global cognition over 2 years (mean difference, 0.06 SD units [SU]), with a significantly more favorable change in episodic memory (mean difference, 0.12 SU) but not in executive function/attention (mean difference, 0.04 SU), the researchers reported.
They also conducted a meta-analysis based on the three separate cognitive substudies, with 5200 nonoverlapping COSMOS participants.
The results showed “clear evidence” of MVM benefits on global cognition (mean difference, 0.07 SU; P = .0009) and episodic memory (mean difference, 0.06 SU; P =.0007), they reported, with the magnitude of effect on global cognition equivalent to reducing cognitive aging by 2 years.
In a statement, JoAnn Manson, MD, DrPH, chief of the Division of Preventive Medicine at Brigham and Women’s Hospital, who led the overall COSMOS trial, said that “the finding that a daily multivitamin improved memory and slowed cognitive aging in three separate placebo-controlled studies in COSMOS is exciting and further supports the promise of multivitamins as a safe, accessible, and affordable approach to protecting cognitive health in older adults.”
Not a Meta-analysis?
In an interview with this news organization, Christopher Labos, MD CM, MSc, a cardiologist and epidemiologist based in Montreal, Canada, who wasn’t involved in COSMOS, cautioned that the evidence to date on multivitamins for memory and brain health are “not all that impressive.”
Dr. Labos is a columnist for this news organization and previously has written about the COSMOS trial.
He said it is important to note that this “meta-analysis of COSMOS data, strictly speaking, is not a meta-analysis” because the patients were all from the original COSMOS study without including any additional patients, “so you don’t have any more data than what you started with.
“The fact that the results are consistent with the original trial is not surprising. In fact, it would be concerning if they were not consistent because they’re the same population. They were just assessed differently — by phone, online, or in person,” Dr. Labos explained.
“It is hard to tell what the benefit with multivitamins actually means in terms of hard clinical endpoints that matter to patients. Scoring a little bit better on a standardized test — I guess that’s a good thing, but does that mean you’re less likely to get dementia? I’m not sure we’re there yet,” he told this news organization.
The bottom line, said Dr. Labos, is that “at this point, the evidence does not support recommending multivitamins purely for brain health. There is also a cost and potential downside associated with their use.”
Also weighing in on the new analyses from COSMOS, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, said while there are now “positive, large-scale, long-term studies that show that multivitamin-mineral supplementation for older adults may slow cognitive aging, the Alzheimer’s Association is not ready to recommend widespread use of a multivitamin supplement to reduce risk of cognitive decline in older adults.
“Independent confirmatory studies are needed in larger, more diverse, and representative study populations. COSMOS-Clinic, for example, had less than 2% non-White in the multivitamin group and 5% non-White in the placebo group. It is critical that future treatments and preventions are effective in all populations,” Dr. Sexton told this news organization.
She noted that multivitamin supplements are “generally easy to find and relatively affordable. With confirmation, these promising findings have the potential to significantly impact public health — improving brain health, lowering healthcare costs, reducing caregiver burden — especially among older adults.”
The Alzheimer’s Association, Dr. Sexton said, “envisions a future where there are multiple treatments available that address the disease in multiple ways — like heart disease and cancer — and that can be combined into powerful combination therapies, in conjunction with brain-healthy guidelines for lifestyle, like diet and physical activity.”
The Alzheimer’s Association is leading a 2-year clinical trial known as US POINTER to evaluate whether lifestyle interventions that target multiple risk factors can protect cognition in older adults at increased risk for cognitive decline.
COSMOS-Clinic and the cognition studies in the meta-analysis were supported by investigator-initiated grants from Mars Edge, a segment of Mars Inc., and the National Institutes of Health. Multivitamin and placebo tablets and packaging were donated by Pfizer, Inc Consumer Healthcare (now Haleon). Disclosures for the COSMOS investigators are available with the original article. Dr. Labos and Dr. Sexton have no relevant disclosures.
A version of this article appeared on Medscape.com.
New data from the Cocoa Supplement and Multivitamin Outcomes Study (COSMOS) suggest that a daily multivitamin may help protect the aging brain. However, at least one expert has concerns about the study’s methodology and, as a result, the interpretation of its findings.
The meta-analysis of three separate cognition studies provides “strong and consistent evidence that taking a daily multivitamin, containing more than 20 essential micronutrients, can help prevent memory loss and slow down cognitive aging,” study investigator Chirag Vyas, MBBS, MPH, with Massachusetts General Hospital and Harvard Medical School, Boston, told this news organization.
“We are not now recommending multivitamin use, but the evidence is compelling that supports the promise of multivitamins to help prevent cognitive decline,” Dr. Vyas said.
The new data, from the cognitive substudies of COSMOS, were published online in the American Journal of Clinical Nutrition.
Clinically Meaningful Benefit?
To recap, COSMOS was a 2 x 2 factorial trial of coca extract (500 mg/d flavanols) and/or a daily commercial multivitamin-mineral (MVM) supplement for cardiovascular disease and cancer prevention among more than 21,000 US adults aged 60 years or older.
Neither the cocoa extract nor the MVM supplement had a significant impact on cancer or cardiovascular disease events.
COMOS-Mind was a substudy of 2262 participants aged 65 or older without dementia who completed telephone-based cognitive assessments at baseline and annually for 3 years.
As previously reported by this news organization in COSMOS-Mind, there was no cognitive benefit of daily cocoa extract, but daily MVM supplementation was associated with improved global cognition, episodic memory, and executive function. However, the difference in global cognitive function between MVM and placebo was small, with a mean 0.07-point improvement on the z-score at 3 years.
COSMOS-Web was a substudy of 3562 original participants who were evaluated annually for 3 years using an internet-based battery of neuropsychological tests.
In this analysis, those taking the MVM supplement performed better on a test for immediate memory recall (remembering a list of 20 words); they were able to remember an additional 0.71 word on average compared with 0.44 word in the placebo group. However, they did not improve on tests of memory retention, executive function, or novel object recognition.
The new data are from COSMOS-Clinic, an analysis of 573 participants who completed in-person cognitive assessments.
COSMOS-Clinic showed a modest benefit of MVM, compared with placebo, on global cognition over 2 years (mean difference, 0.06 SD units [SU]), with a significantly more favorable change in episodic memory (mean difference, 0.12 SU) but not in executive function/attention (mean difference, 0.04 SU), the researchers reported.
They also conducted a meta-analysis based on the three separate cognitive substudies, with 5200 nonoverlapping COSMOS participants.
The results showed “clear evidence” of MVM benefits on global cognition (mean difference, 0.07 SU; P = .0009) and episodic memory (mean difference, 0.06 SU; P =.0007), they reported, with the magnitude of effect on global cognition equivalent to reducing cognitive aging by 2 years.
In a statement, JoAnn Manson, MD, DrPH, chief of the Division of Preventive Medicine at Brigham and Women’s Hospital, who led the overall COSMOS trial, said that “the finding that a daily multivitamin improved memory and slowed cognitive aging in three separate placebo-controlled studies in COSMOS is exciting and further supports the promise of multivitamins as a safe, accessible, and affordable approach to protecting cognitive health in older adults.”
Not a Meta-analysis?
In an interview with this news organization, Christopher Labos, MD CM, MSc, a cardiologist and epidemiologist based in Montreal, Canada, who wasn’t involved in COSMOS, cautioned that the evidence to date on multivitamins for memory and brain health are “not all that impressive.”
Dr. Labos is a columnist for this news organization and previously has written about the COSMOS trial.
He said it is important to note that this “meta-analysis of COSMOS data, strictly speaking, is not a meta-analysis” because the patients were all from the original COSMOS study without including any additional patients, “so you don’t have any more data than what you started with.
“The fact that the results are consistent with the original trial is not surprising. In fact, it would be concerning if they were not consistent because they’re the same population. They were just assessed differently — by phone, online, or in person,” Dr. Labos explained.
“It is hard to tell what the benefit with multivitamins actually means in terms of hard clinical endpoints that matter to patients. Scoring a little bit better on a standardized test — I guess that’s a good thing, but does that mean you’re less likely to get dementia? I’m not sure we’re there yet,” he told this news organization.
The bottom line, said Dr. Labos, is that “at this point, the evidence does not support recommending multivitamins purely for brain health. There is also a cost and potential downside associated with their use.”
Also weighing in on the new analyses from COSMOS, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, said while there are now “positive, large-scale, long-term studies that show that multivitamin-mineral supplementation for older adults may slow cognitive aging, the Alzheimer’s Association is not ready to recommend widespread use of a multivitamin supplement to reduce risk of cognitive decline in older adults.
“Independent confirmatory studies are needed in larger, more diverse, and representative study populations. COSMOS-Clinic, for example, had less than 2% non-White in the multivitamin group and 5% non-White in the placebo group. It is critical that future treatments and preventions are effective in all populations,” Dr. Sexton told this news organization.
She noted that multivitamin supplements are “generally easy to find and relatively affordable. With confirmation, these promising findings have the potential to significantly impact public health — improving brain health, lowering healthcare costs, reducing caregiver burden — especially among older adults.”
The Alzheimer’s Association, Dr. Sexton said, “envisions a future where there are multiple treatments available that address the disease in multiple ways — like heart disease and cancer — and that can be combined into powerful combination therapies, in conjunction with brain-healthy guidelines for lifestyle, like diet and physical activity.”
The Alzheimer’s Association is leading a 2-year clinical trial known as US POINTER to evaluate whether lifestyle interventions that target multiple risk factors can protect cognition in older adults at increased risk for cognitive decline.
COSMOS-Clinic and the cognition studies in the meta-analysis were supported by investigator-initiated grants from Mars Edge, a segment of Mars Inc., and the National Institutes of Health. Multivitamin and placebo tablets and packaging were donated by Pfizer, Inc Consumer Healthcare (now Haleon). Disclosures for the COSMOS investigators are available with the original article. Dr. Labos and Dr. Sexton have no relevant disclosures.
A version of this article appeared on Medscape.com.
AMERICAN JOURNAL OF CLINICAL NUTRITION
Lipids and Dementia: A Complex and Evolving Story
The relationship between lipid levels and the development of dementia is an evolving but confusing landscape.
“This is an incredibly complex area, and there really isn’t a clear consensus on this subject because different lipid classes reflect different things,” according to Betsy Mills, PhD, assistant director of aging and Alzheimer’s prevention at the Alzheimer’s Drug Discovery Foundation.
Some studies suggest that excessive lipid levels may increase the risk of developing dementia and Alzheimer’s disease (AD). Others imply that elevated low-density lipoprotein (LDL) cholesterol or even triglycerides may offer some protection against subsequent dementia whereas higher levels of high-density lipoprotein (HDL) cholesterol, hitherto thought to be protective, may have a deleterious effect.
“It depends on what lipids you’re measuring, what you’re using to measure those lipids, what age the person is, and multiple other factors,” Dr. Mills told this news organization.
Teasing out the variables and potential mechanisms for the association between lipids and dementia risk necessitates understanding the role that lipids play in the healthy brain, the negative impact of brain lipid dysregulation, and the interplay between cholesterol in the central nervous system (CNS) and the cholesterol in the rest of the body.
Beyond Amyloid
The role of lipids in AD risk has historically been “overlooked,” says Scott Hansen, PhD, associate professor, Department of Molecular Medicine, Herbert Wertheim UF Scripps Institute for Biomedical Innovation and Technology, Florida.
“The common narrative is that amyloid is the culprit in AD and certainly that’s the case in familial AD,” he told this news organization. “It’s been assumed that because amyloid deposits are also found in the brains of people with late-onset AD — which is the vast majority of cases — amyloid is the cause, but that’s not clear at all.”
The “limited clinical success” of aducanumab, its “extremely small efficacy” — despite its obvious success in eradicating the amyloid plaques — suggests there’s “much more to the story than amyloid.”
He and a growing community of scientists recognize the role of inflammation and lipids. “The major finding of my lab is that cholesterol actually drives the synthesis of amyloid via inflammation. In other words, amyloid is downstream of cholesterol. Cholesterol drives the inflammation, and the inflammation drives amyloid,” he said.
‘Lipid Invasion Model’
Because the brain is an incredibly lipid-rich organ, Dr. Mills said that “any dysregulation in lipid homeostasis will impact the brain because cholesterol is needed for the myelin sheaths, cell membranes, and other functions.”
A healthy brain relies upon healthy lipid regulation, and “since the first description of AD over 100 years ago, the disease has been associated with altered lipids in the brain,” Dr. Hansen noted.
He cited the “ lipid invasion model” as a way of understanding brain lipid dysregulation. This hypothesis posits that AD is driven by external lipids that enter the brain as a result of damage to the blood-brain barrier (BBB).
“Cholesterol in the brain and cholesterol in the periphery — meaning, in the rest of the body, outside the brain — are separate,” Dr. Hansen explained. “The brain produces its own cholesterol and keeps tight control of it.”
Under normal circumstances, cholesterol from the diet doesn’t enter the brain. “Each pool of cholesterol — in the brain and in the periphery — has its own distinct regulatory mechanisms, target cells, and transport mechanisms.”
When the BBB has been compromised, it becomes permeable, allowing LDL cholesterol to enter the brain, said Dr. Hansen. Then the brain’s own lipoproteins transport the invading cholesterol, allowing it to be taken up by neurons. In turn, this causes neuronal amyloid levels to rise, ultimately leading to the creation of amyloid-b plaques. It also plays a role in tau phosphorylation. Both are key features of AD pathology.
Elevated levels of cholesterol and other lipids have been found in amyloid plaques, Dr. Hansen noted. Moreover, studies of brains of patients with AD have pointed to BBB damage.
And the risk factors for AD overlap with the risk factors for damage to the BBB (such as, aging, brain trauma, hypertension, stress, sleep deprivation, smoking, excess alcohol, obesity, diabetes, and APOE4 genotype), according to the lipid invasion model paper cited by Dr. Hansen.
‘Chicken and Egg’
“There is a strong link between the brain and the heart, and we know that cardiovascular risk factors have an overlap with dementia risk factors — especially vascular dementia,” said Dr. Mills.
She explained that an atherogenic lipid profile results in narrowing of the arteries, with less blood reaching the brain. “This can lead to stress in the brain, which drives inflammation and pathology.”
But cholesterol itself plays an important role in inflammation, Dr. Hansen said. In the periphery, it is “part of an integral response to tissue damage and infection.”
In the brain, once cholesterol is synthesized by the astrocytes, it is transported to neurons via the apolipoprotein E (APOE) protein, which plays a role in brain cholesterol homeostasis, Dr. Mills explained. Those with the ε4 allele of APOE (APOE4) tend to have faultier transport and storage of lipids in the brain, relative to the other APOE variants.
It’s known that individuals with APOE4 are particularly vulnerable to late-onset AD, Dr. Hansen observed. By contrast, APOE2 has a more protective effect. “Most people have APOE3, which is ‘in between,’ ” he said.
When there is neuronal uptake of “invading cholesterol,” not only is amyloid produced but also neuroinflammatory cytokines, further driving inflammation. A vicious cycle ensues: Cholesterol induces cytokine release; and cytokine release, in turn, induces cholesterol synthesis — which “suggests an autocatalytic function of cholesterol in the escalation of inflammation,” Dr. Hansen suggested. He noted that permeability of the BBB also allows inflammatory cytokines from elsewhere in the body to invade the brain, further driving inflammation.
Dr. Mills elaborated: “We know that generally, in dementia, there appear to be some changes in cholesterol metabolism in the brain, but it’s a chicken-and-egg question. We know that as the disease progresses, neurons are dying and getting remodeled. Do these changes have to do with the degenerative process, or are the changes in the cholesterol metabolism actually driving the degenerative disease process? It’s probably a combination, but it’s unclear at this point.”
Lipids in Plasma vs CSF
Dr. Mills explained that HDL particles in the brain differ from those in the periphery. “In the CNS, you have ‘HDL-like particles,’ which are similar in size and composition [to HDL in the periphery] but aren’t the same particles.” The brain itself generates HDL-like lipoproteins, which are produced by astrocytes and other glial cells and found in cerebrospinal fluid (CSF).
Dyslipidemia in the periphery can be a marker for cardiovascular pathology. In the brain, “it can be an indication that there is active damage going on, depending on which compartment you’re looking at.”
She noted that plasma lipid levels and brain CSF lipid levels are “very different.” Research suggests that HDL in the CSF exhibits similar heterogeneity to plasma HDL, but these CSF lipoproteins present at 100-fold lower concentrations, compared to plasma HDL and have unique combinations of protein subpopulations. Lipidomics analysis studies show that these compartments “get very different readings, in terms of the predominant lipid disease state, and they are regulated differently from the way lipids in the periphery are regulated.”
In the brain, the cholesterol “needs to get shuttled from glial cells to neurons,” so defects in the transport process can disrupt overall brain homeostasis, said Dr. Mills. But since the brain system is separate from the peripheral system, measuring plasma lipids is more likely to point to cardiovascular risks, while changes reflected in CSF lipids are “more indicative of alteration in lipid homeostasis in the brain.”
HDL and Triglycerides: A Complicated Story
Dr. Mills noted that HDL in the periphery is “very complicated,” and the idea that HDL, as a measure on its own, is “necessarily ‘good’ isn’t particularly informative.” Rather, HDL is “extremely heterogeneous, very diverse, has different lipid compositions, different classes, and different modifications.” For example, like oxidized LDL, oxidized HDL is also “bad,” preventing the HDL from having protective functions.
Similarly, the apolipoproteins associated with HDL can affect the function of the HDL. “Our understanding of the HDL-like particles in the CNS is limited, but we do understand the APOE4 link,” Dr. Mills said. “It seems that the HDL-like particles containing APOE2 or APOE3 are larger and are more effective at transferring the lipids and cholesterol linked to them relative to APOE4-containing particles.”
Because HDL is more complex than simply being “good,” measuring HDL doesn’t “give you the full story,” said Dr. Mills. She speculates that this may be why there are studies suggesting that high levels of HDL might not have protective benefits and might even be detrimental. This makes it difficult to look at population studies, where the different subclasses of HDL are not necessarily captured in depth.
Dr. Mills pointed to another confounding factor, which is that much of the risk for the development of AD appears to be related to the interaction of HDL, LDL, and triglycerides. “When you look at each of these individually, you get a lot of heterogeneity, and it’s unclear what’s driving what,” she said.
An advantage of observational studies is that they give information about which of these markers are associated with trends and disease risks in specific groups vs others.
“For example, higher levels of triglycerides are associated with cardiovascular risk more in women, relative to men,” she said. And the triglyceride-to-HDL ratio seems “particularly robust” as a measure of cardiovascular health and risk.
The interpretation of associations with triglycerides can be “tricky” and “confusing” because results differ so much between studies, she said. “There are differences between middle age and older age, which have to do with age-related changes in metabolism and lipid metabolism and not necessarily that the markers are indicating something different,” she said.
Some research has suggested that triglycerides may have a protective effect against dementia, noted Uma Naidoo, MD, director of nutritional and lifestyle psychiatry, Massachusetts General Hospital, and director of nutritional psychiatry at MGH Academy.
This may be because the brain “runs mostly on energy from burning triglycerides,” suggested Dr. Naidoo, author of the books Calm Your Mind With Food and This Is Your Brain on Food.
In addition, having higher levels of triglycerides may be linked with having overall healthier behaviors, Dr. Naidoo told this news organization.
Dr. Mills said that in middle-aged individuals, high levels of LDL-C and triglycerides are “often indicative of more atherogenic particles and risk to cardiovascular health, which is a generally negative trajectory. But in older individuals, things become more complicated because there are differences in terms of clearance of some of these particles, tissue clearance and distribution, and nutrient status. So for older individuals, it seems that fluctuations in either direction—either too high or too low—tend to be more informative that some overall dysregulation is going on the system.”
She emphasized that, in this “emerging area, looking at only one or two studies is confusing. But if you look at the spectrum of studies, you can see a pattern, which is that the regulation gets ‘off,’ as people age.”
The Potential Role of Statins
Dr. Mills speculated that there may be “neuroprotective benefits for some of the statins which appear to be related to cardiovascular benefits. But at this point, we don’t have any clear data whether statins actually directly impact brain cholesterol, since it’s a separate pool.”
They could help “by increasing blood flow and reducing narrowing of the arteries, but any direct impact on the brain is still under investigation.”
Dr. Hansen pointed to research suggesting statins taken at midlife appear to be cardioprotective and may be protective of brain health as well, whereas statins initiated in older age do not appear to have these benefits.
He speculated that one reason statins seem less helpful when initiated later in life is that the BBB has already been damaged by systemic inflammation in the periphery, and the neuroinflammatory process resulting in neuronal destruction is already underway. “I think statins aren’t going to fix that problem, so although lowering cholesterol can be helpful in some respects, it might be too late to affect cognition because the nerves have already died and won’t grow back.”
Can Dietary Approaches Help?
Dr. Naidoo said that when looking at neurologic and psychiatric disease, “it’s important to think about the ‘long game’ — how can we improve our blood and cardiovascular health earlier in life to help potentiate healthy aging?”
From a nutritional psychiatry standpoint, Dr. Naidoo focuses on nourishing the gut microbiome and decreasing inflammation. “A healthy and balanced microbiome supports cognition, while the composition of gut bacteria is actually drastically different in patients with neurological diseases, such as AD.”
She recommends a nutrient-dense, anti-inflammatory diet including probiotic-rich foods (such as kimchi, sauerkraut, plain yogurt, and miso). Moreover, “the quality and structure of our fatty acids may be relevant as well: Increasing our intake of polyunsaturated fatty acids and avoiding processed fats like trans fats and hydrogenated oils may benefit our overall brain health.”
Dr. Naidoo recommends extra-virgin olive oil as a source of healthy fat. Its consumption is linked to lower incidence of AD by way of encouraging autophagy, which she calls “our own process of “cellular cleanup.’”
Dr. Naidoo believes that clinicians’ guidance to patients should “focus on healthy nutrition and other lifestyle practices, such as exercise, outdoor time, good sleep, and stress reduction.”
Dr. Mills notes the importance of omega-3 fatty acids, such as docosahexaenoic acid (DHA) , for brain health. “DHA is a major lipid component of neuronal membranes,” she said. “Because of inefficiencies in metabolism with APOE4, people tend to metabolize more of the lipids on the membranes themselves, so they have higher lipid membrane turnover and a greater need to supplement. Supplementing particularly through diet, with foods such as fatty fish rich in omega-3, can help boost the levels to help keep neuronal membranes intact.”
What This Means for the Clinician
“At this point, we see all of these associations between lipids and dementia, but we haven’t worked out exactly what it means on the individual level for an individual patient,” said Dr. Mills. Certainly, the picture is complex, and the understanding is growing and shifting. “The clinical applications remain unclear.”
One potential clinical take-home is that clinicians might consider tracking lipid levels over time. “If you follow a patient and see an increase or decrease [in lipid levels], that can be informative.” Looking at ratios of lipids might be more useful than looking only at a change in a single measure. “If you see trends in a variety of measures that track with one another, it might be more of a sign that something is potentially wrong.”
Whether the patient should first try a lifestyle intervention or might need medication is a “personalized clinical decision, depending on the individual, their risk factors, and how their levels are going,” said Dr. Mills.
Dr. Mills, Dr. Hansen, and Dr. Naidoo declared no relevant financial relationships.
A version of this article appeared on Medscape.com.
The relationship between lipid levels and the development of dementia is an evolving but confusing landscape.
“This is an incredibly complex area, and there really isn’t a clear consensus on this subject because different lipid classes reflect different things,” according to Betsy Mills, PhD, assistant director of aging and Alzheimer’s prevention at the Alzheimer’s Drug Discovery Foundation.
Some studies suggest that excessive lipid levels may increase the risk of developing dementia and Alzheimer’s disease (AD). Others imply that elevated low-density lipoprotein (LDL) cholesterol or even triglycerides may offer some protection against subsequent dementia whereas higher levels of high-density lipoprotein (HDL) cholesterol, hitherto thought to be protective, may have a deleterious effect.
“It depends on what lipids you’re measuring, what you’re using to measure those lipids, what age the person is, and multiple other factors,” Dr. Mills told this news organization.
Teasing out the variables and potential mechanisms for the association between lipids and dementia risk necessitates understanding the role that lipids play in the healthy brain, the negative impact of brain lipid dysregulation, and the interplay between cholesterol in the central nervous system (CNS) and the cholesterol in the rest of the body.
Beyond Amyloid
The role of lipids in AD risk has historically been “overlooked,” says Scott Hansen, PhD, associate professor, Department of Molecular Medicine, Herbert Wertheim UF Scripps Institute for Biomedical Innovation and Technology, Florida.
“The common narrative is that amyloid is the culprit in AD and certainly that’s the case in familial AD,” he told this news organization. “It’s been assumed that because amyloid deposits are also found in the brains of people with late-onset AD — which is the vast majority of cases — amyloid is the cause, but that’s not clear at all.”
The “limited clinical success” of aducanumab, its “extremely small efficacy” — despite its obvious success in eradicating the amyloid plaques — suggests there’s “much more to the story than amyloid.”
He and a growing community of scientists recognize the role of inflammation and lipids. “The major finding of my lab is that cholesterol actually drives the synthesis of amyloid via inflammation. In other words, amyloid is downstream of cholesterol. Cholesterol drives the inflammation, and the inflammation drives amyloid,” he said.
‘Lipid Invasion Model’
Because the brain is an incredibly lipid-rich organ, Dr. Mills said that “any dysregulation in lipid homeostasis will impact the brain because cholesterol is needed for the myelin sheaths, cell membranes, and other functions.”
A healthy brain relies upon healthy lipid regulation, and “since the first description of AD over 100 years ago, the disease has been associated with altered lipids in the brain,” Dr. Hansen noted.
He cited the “ lipid invasion model” as a way of understanding brain lipid dysregulation. This hypothesis posits that AD is driven by external lipids that enter the brain as a result of damage to the blood-brain barrier (BBB).
“Cholesterol in the brain and cholesterol in the periphery — meaning, in the rest of the body, outside the brain — are separate,” Dr. Hansen explained. “The brain produces its own cholesterol and keeps tight control of it.”
Under normal circumstances, cholesterol from the diet doesn’t enter the brain. “Each pool of cholesterol — in the brain and in the periphery — has its own distinct regulatory mechanisms, target cells, and transport mechanisms.”
When the BBB has been compromised, it becomes permeable, allowing LDL cholesterol to enter the brain, said Dr. Hansen. Then the brain’s own lipoproteins transport the invading cholesterol, allowing it to be taken up by neurons. In turn, this causes neuronal amyloid levels to rise, ultimately leading to the creation of amyloid-b plaques. It also plays a role in tau phosphorylation. Both are key features of AD pathology.
Elevated levels of cholesterol and other lipids have been found in amyloid plaques, Dr. Hansen noted. Moreover, studies of brains of patients with AD have pointed to BBB damage.
And the risk factors for AD overlap with the risk factors for damage to the BBB (such as, aging, brain trauma, hypertension, stress, sleep deprivation, smoking, excess alcohol, obesity, diabetes, and APOE4 genotype), according to the lipid invasion model paper cited by Dr. Hansen.
‘Chicken and Egg’
“There is a strong link between the brain and the heart, and we know that cardiovascular risk factors have an overlap with dementia risk factors — especially vascular dementia,” said Dr. Mills.
She explained that an atherogenic lipid profile results in narrowing of the arteries, with less blood reaching the brain. “This can lead to stress in the brain, which drives inflammation and pathology.”
But cholesterol itself plays an important role in inflammation, Dr. Hansen said. In the periphery, it is “part of an integral response to tissue damage and infection.”
In the brain, once cholesterol is synthesized by the astrocytes, it is transported to neurons via the apolipoprotein E (APOE) protein, which plays a role in brain cholesterol homeostasis, Dr. Mills explained. Those with the ε4 allele of APOE (APOE4) tend to have faultier transport and storage of lipids in the brain, relative to the other APOE variants.
It’s known that individuals with APOE4 are particularly vulnerable to late-onset AD, Dr. Hansen observed. By contrast, APOE2 has a more protective effect. “Most people have APOE3, which is ‘in between,’ ” he said.
When there is neuronal uptake of “invading cholesterol,” not only is amyloid produced but also neuroinflammatory cytokines, further driving inflammation. A vicious cycle ensues: Cholesterol induces cytokine release; and cytokine release, in turn, induces cholesterol synthesis — which “suggests an autocatalytic function of cholesterol in the escalation of inflammation,” Dr. Hansen suggested. He noted that permeability of the BBB also allows inflammatory cytokines from elsewhere in the body to invade the brain, further driving inflammation.
Dr. Mills elaborated: “We know that generally, in dementia, there appear to be some changes in cholesterol metabolism in the brain, but it’s a chicken-and-egg question. We know that as the disease progresses, neurons are dying and getting remodeled. Do these changes have to do with the degenerative process, or are the changes in the cholesterol metabolism actually driving the degenerative disease process? It’s probably a combination, but it’s unclear at this point.”
Lipids in Plasma vs CSF
Dr. Mills explained that HDL particles in the brain differ from those in the periphery. “In the CNS, you have ‘HDL-like particles,’ which are similar in size and composition [to HDL in the periphery] but aren’t the same particles.” The brain itself generates HDL-like lipoproteins, which are produced by astrocytes and other glial cells and found in cerebrospinal fluid (CSF).
Dyslipidemia in the periphery can be a marker for cardiovascular pathology. In the brain, “it can be an indication that there is active damage going on, depending on which compartment you’re looking at.”
She noted that plasma lipid levels and brain CSF lipid levels are “very different.” Research suggests that HDL in the CSF exhibits similar heterogeneity to plasma HDL, but these CSF lipoproteins present at 100-fold lower concentrations, compared to plasma HDL and have unique combinations of protein subpopulations. Lipidomics analysis studies show that these compartments “get very different readings, in terms of the predominant lipid disease state, and they are regulated differently from the way lipids in the periphery are regulated.”
In the brain, the cholesterol “needs to get shuttled from glial cells to neurons,” so defects in the transport process can disrupt overall brain homeostasis, said Dr. Mills. But since the brain system is separate from the peripheral system, measuring plasma lipids is more likely to point to cardiovascular risks, while changes reflected in CSF lipids are “more indicative of alteration in lipid homeostasis in the brain.”
HDL and Triglycerides: A Complicated Story
Dr. Mills noted that HDL in the periphery is “very complicated,” and the idea that HDL, as a measure on its own, is “necessarily ‘good’ isn’t particularly informative.” Rather, HDL is “extremely heterogeneous, very diverse, has different lipid compositions, different classes, and different modifications.” For example, like oxidized LDL, oxidized HDL is also “bad,” preventing the HDL from having protective functions.
Similarly, the apolipoproteins associated with HDL can affect the function of the HDL. “Our understanding of the HDL-like particles in the CNS is limited, but we do understand the APOE4 link,” Dr. Mills said. “It seems that the HDL-like particles containing APOE2 or APOE3 are larger and are more effective at transferring the lipids and cholesterol linked to them relative to APOE4-containing particles.”
Because HDL is more complex than simply being “good,” measuring HDL doesn’t “give you the full story,” said Dr. Mills. She speculates that this may be why there are studies suggesting that high levels of HDL might not have protective benefits and might even be detrimental. This makes it difficult to look at population studies, where the different subclasses of HDL are not necessarily captured in depth.
Dr. Mills pointed to another confounding factor, which is that much of the risk for the development of AD appears to be related to the interaction of HDL, LDL, and triglycerides. “When you look at each of these individually, you get a lot of heterogeneity, and it’s unclear what’s driving what,” she said.
An advantage of observational studies is that they give information about which of these markers are associated with trends and disease risks in specific groups vs others.
“For example, higher levels of triglycerides are associated with cardiovascular risk more in women, relative to men,” she said. And the triglyceride-to-HDL ratio seems “particularly robust” as a measure of cardiovascular health and risk.
The interpretation of associations with triglycerides can be “tricky” and “confusing” because results differ so much between studies, she said. “There are differences between middle age and older age, which have to do with age-related changes in metabolism and lipid metabolism and not necessarily that the markers are indicating something different,” she said.
Some research has suggested that triglycerides may have a protective effect against dementia, noted Uma Naidoo, MD, director of nutritional and lifestyle psychiatry, Massachusetts General Hospital, and director of nutritional psychiatry at MGH Academy.
This may be because the brain “runs mostly on energy from burning triglycerides,” suggested Dr. Naidoo, author of the books Calm Your Mind With Food and This Is Your Brain on Food.
In addition, having higher levels of triglycerides may be linked with having overall healthier behaviors, Dr. Naidoo told this news organization.
Dr. Mills said that in middle-aged individuals, high levels of LDL-C and triglycerides are “often indicative of more atherogenic particles and risk to cardiovascular health, which is a generally negative trajectory. But in older individuals, things become more complicated because there are differences in terms of clearance of some of these particles, tissue clearance and distribution, and nutrient status. So for older individuals, it seems that fluctuations in either direction—either too high or too low—tend to be more informative that some overall dysregulation is going on the system.”
She emphasized that, in this “emerging area, looking at only one or two studies is confusing. But if you look at the spectrum of studies, you can see a pattern, which is that the regulation gets ‘off,’ as people age.”
The Potential Role of Statins
Dr. Mills speculated that there may be “neuroprotective benefits for some of the statins which appear to be related to cardiovascular benefits. But at this point, we don’t have any clear data whether statins actually directly impact brain cholesterol, since it’s a separate pool.”
They could help “by increasing blood flow and reducing narrowing of the arteries, but any direct impact on the brain is still under investigation.”
Dr. Hansen pointed to research suggesting statins taken at midlife appear to be cardioprotective and may be protective of brain health as well, whereas statins initiated in older age do not appear to have these benefits.
He speculated that one reason statins seem less helpful when initiated later in life is that the BBB has already been damaged by systemic inflammation in the periphery, and the neuroinflammatory process resulting in neuronal destruction is already underway. “I think statins aren’t going to fix that problem, so although lowering cholesterol can be helpful in some respects, it might be too late to affect cognition because the nerves have already died and won’t grow back.”
Can Dietary Approaches Help?
Dr. Naidoo said that when looking at neurologic and psychiatric disease, “it’s important to think about the ‘long game’ — how can we improve our blood and cardiovascular health earlier in life to help potentiate healthy aging?”
From a nutritional psychiatry standpoint, Dr. Naidoo focuses on nourishing the gut microbiome and decreasing inflammation. “A healthy and balanced microbiome supports cognition, while the composition of gut bacteria is actually drastically different in patients with neurological diseases, such as AD.”
She recommends a nutrient-dense, anti-inflammatory diet including probiotic-rich foods (such as kimchi, sauerkraut, plain yogurt, and miso). Moreover, “the quality and structure of our fatty acids may be relevant as well: Increasing our intake of polyunsaturated fatty acids and avoiding processed fats like trans fats and hydrogenated oils may benefit our overall brain health.”
Dr. Naidoo recommends extra-virgin olive oil as a source of healthy fat. Its consumption is linked to lower incidence of AD by way of encouraging autophagy, which she calls “our own process of “cellular cleanup.’”
Dr. Naidoo believes that clinicians’ guidance to patients should “focus on healthy nutrition and other lifestyle practices, such as exercise, outdoor time, good sleep, and stress reduction.”
Dr. Mills notes the importance of omega-3 fatty acids, such as docosahexaenoic acid (DHA) , for brain health. “DHA is a major lipid component of neuronal membranes,” she said. “Because of inefficiencies in metabolism with APOE4, people tend to metabolize more of the lipids on the membranes themselves, so they have higher lipid membrane turnover and a greater need to supplement. Supplementing particularly through diet, with foods such as fatty fish rich in omega-3, can help boost the levels to help keep neuronal membranes intact.”
What This Means for the Clinician
“At this point, we see all of these associations between lipids and dementia, but we haven’t worked out exactly what it means on the individual level for an individual patient,” said Dr. Mills. Certainly, the picture is complex, and the understanding is growing and shifting. “The clinical applications remain unclear.”
One potential clinical take-home is that clinicians might consider tracking lipid levels over time. “If you follow a patient and see an increase or decrease [in lipid levels], that can be informative.” Looking at ratios of lipids might be more useful than looking only at a change in a single measure. “If you see trends in a variety of measures that track with one another, it might be more of a sign that something is potentially wrong.”
Whether the patient should first try a lifestyle intervention or might need medication is a “personalized clinical decision, depending on the individual, their risk factors, and how their levels are going,” said Dr. Mills.
Dr. Mills, Dr. Hansen, and Dr. Naidoo declared no relevant financial relationships.
A version of this article appeared on Medscape.com.
The relationship between lipid levels and the development of dementia is an evolving but confusing landscape.
“This is an incredibly complex area, and there really isn’t a clear consensus on this subject because different lipid classes reflect different things,” according to Betsy Mills, PhD, assistant director of aging and Alzheimer’s prevention at the Alzheimer’s Drug Discovery Foundation.
Some studies suggest that excessive lipid levels may increase the risk of developing dementia and Alzheimer’s disease (AD). Others imply that elevated low-density lipoprotein (LDL) cholesterol or even triglycerides may offer some protection against subsequent dementia whereas higher levels of high-density lipoprotein (HDL) cholesterol, hitherto thought to be protective, may have a deleterious effect.
“It depends on what lipids you’re measuring, what you’re using to measure those lipids, what age the person is, and multiple other factors,” Dr. Mills told this news organization.
Teasing out the variables and potential mechanisms for the association between lipids and dementia risk necessitates understanding the role that lipids play in the healthy brain, the negative impact of brain lipid dysregulation, and the interplay between cholesterol in the central nervous system (CNS) and the cholesterol in the rest of the body.
Beyond Amyloid
The role of lipids in AD risk has historically been “overlooked,” says Scott Hansen, PhD, associate professor, Department of Molecular Medicine, Herbert Wertheim UF Scripps Institute for Biomedical Innovation and Technology, Florida.
“The common narrative is that amyloid is the culprit in AD and certainly that’s the case in familial AD,” he told this news organization. “It’s been assumed that because amyloid deposits are also found in the brains of people with late-onset AD — which is the vast majority of cases — amyloid is the cause, but that’s not clear at all.”
The “limited clinical success” of aducanumab, its “extremely small efficacy” — despite its obvious success in eradicating the amyloid plaques — suggests there’s “much more to the story than amyloid.”
He and a growing community of scientists recognize the role of inflammation and lipids. “The major finding of my lab is that cholesterol actually drives the synthesis of amyloid via inflammation. In other words, amyloid is downstream of cholesterol. Cholesterol drives the inflammation, and the inflammation drives amyloid,” he said.
‘Lipid Invasion Model’
Because the brain is an incredibly lipid-rich organ, Dr. Mills said that “any dysregulation in lipid homeostasis will impact the brain because cholesterol is needed for the myelin sheaths, cell membranes, and other functions.”
A healthy brain relies upon healthy lipid regulation, and “since the first description of AD over 100 years ago, the disease has been associated with altered lipids in the brain,” Dr. Hansen noted.
He cited the “ lipid invasion model” as a way of understanding brain lipid dysregulation. This hypothesis posits that AD is driven by external lipids that enter the brain as a result of damage to the blood-brain barrier (BBB).
“Cholesterol in the brain and cholesterol in the periphery — meaning, in the rest of the body, outside the brain — are separate,” Dr. Hansen explained. “The brain produces its own cholesterol and keeps tight control of it.”
Under normal circumstances, cholesterol from the diet doesn’t enter the brain. “Each pool of cholesterol — in the brain and in the periphery — has its own distinct regulatory mechanisms, target cells, and transport mechanisms.”
When the BBB has been compromised, it becomes permeable, allowing LDL cholesterol to enter the brain, said Dr. Hansen. Then the brain’s own lipoproteins transport the invading cholesterol, allowing it to be taken up by neurons. In turn, this causes neuronal amyloid levels to rise, ultimately leading to the creation of amyloid-b plaques. It also plays a role in tau phosphorylation. Both are key features of AD pathology.
Elevated levels of cholesterol and other lipids have been found in amyloid plaques, Dr. Hansen noted. Moreover, studies of brains of patients with AD have pointed to BBB damage.
And the risk factors for AD overlap with the risk factors for damage to the BBB (such as, aging, brain trauma, hypertension, stress, sleep deprivation, smoking, excess alcohol, obesity, diabetes, and APOE4 genotype), according to the lipid invasion model paper cited by Dr. Hansen.
‘Chicken and Egg’
“There is a strong link between the brain and the heart, and we know that cardiovascular risk factors have an overlap with dementia risk factors — especially vascular dementia,” said Dr. Mills.
She explained that an atherogenic lipid profile results in narrowing of the arteries, with less blood reaching the brain. “This can lead to stress in the brain, which drives inflammation and pathology.”
But cholesterol itself plays an important role in inflammation, Dr. Hansen said. In the periphery, it is “part of an integral response to tissue damage and infection.”
In the brain, once cholesterol is synthesized by the astrocytes, it is transported to neurons via the apolipoprotein E (APOE) protein, which plays a role in brain cholesterol homeostasis, Dr. Mills explained. Those with the ε4 allele of APOE (APOE4) tend to have faultier transport and storage of lipids in the brain, relative to the other APOE variants.
It’s known that individuals with APOE4 are particularly vulnerable to late-onset AD, Dr. Hansen observed. By contrast, APOE2 has a more protective effect. “Most people have APOE3, which is ‘in between,’ ” he said.
When there is neuronal uptake of “invading cholesterol,” not only is amyloid produced but also neuroinflammatory cytokines, further driving inflammation. A vicious cycle ensues: Cholesterol induces cytokine release; and cytokine release, in turn, induces cholesterol synthesis — which “suggests an autocatalytic function of cholesterol in the escalation of inflammation,” Dr. Hansen suggested. He noted that permeability of the BBB also allows inflammatory cytokines from elsewhere in the body to invade the brain, further driving inflammation.
Dr. Mills elaborated: “We know that generally, in dementia, there appear to be some changes in cholesterol metabolism in the brain, but it’s a chicken-and-egg question. We know that as the disease progresses, neurons are dying and getting remodeled. Do these changes have to do with the degenerative process, or are the changes in the cholesterol metabolism actually driving the degenerative disease process? It’s probably a combination, but it’s unclear at this point.”
Lipids in Plasma vs CSF
Dr. Mills explained that HDL particles in the brain differ from those in the periphery. “In the CNS, you have ‘HDL-like particles,’ which are similar in size and composition [to HDL in the periphery] but aren’t the same particles.” The brain itself generates HDL-like lipoproteins, which are produced by astrocytes and other glial cells and found in cerebrospinal fluid (CSF).
Dyslipidemia in the periphery can be a marker for cardiovascular pathology. In the brain, “it can be an indication that there is active damage going on, depending on which compartment you’re looking at.”
She noted that plasma lipid levels and brain CSF lipid levels are “very different.” Research suggests that HDL in the CSF exhibits similar heterogeneity to plasma HDL, but these CSF lipoproteins present at 100-fold lower concentrations, compared to plasma HDL and have unique combinations of protein subpopulations. Lipidomics analysis studies show that these compartments “get very different readings, in terms of the predominant lipid disease state, and they are regulated differently from the way lipids in the periphery are regulated.”
In the brain, the cholesterol “needs to get shuttled from glial cells to neurons,” so defects in the transport process can disrupt overall brain homeostasis, said Dr. Mills. But since the brain system is separate from the peripheral system, measuring plasma lipids is more likely to point to cardiovascular risks, while changes reflected in CSF lipids are “more indicative of alteration in lipid homeostasis in the brain.”
HDL and Triglycerides: A Complicated Story
Dr. Mills noted that HDL in the periphery is “very complicated,” and the idea that HDL, as a measure on its own, is “necessarily ‘good’ isn’t particularly informative.” Rather, HDL is “extremely heterogeneous, very diverse, has different lipid compositions, different classes, and different modifications.” For example, like oxidized LDL, oxidized HDL is also “bad,” preventing the HDL from having protective functions.
Similarly, the apolipoproteins associated with HDL can affect the function of the HDL. “Our understanding of the HDL-like particles in the CNS is limited, but we do understand the APOE4 link,” Dr. Mills said. “It seems that the HDL-like particles containing APOE2 or APOE3 are larger and are more effective at transferring the lipids and cholesterol linked to them relative to APOE4-containing particles.”
Because HDL is more complex than simply being “good,” measuring HDL doesn’t “give you the full story,” said Dr. Mills. She speculates that this may be why there are studies suggesting that high levels of HDL might not have protective benefits and might even be detrimental. This makes it difficult to look at population studies, where the different subclasses of HDL are not necessarily captured in depth.
Dr. Mills pointed to another confounding factor, which is that much of the risk for the development of AD appears to be related to the interaction of HDL, LDL, and triglycerides. “When you look at each of these individually, you get a lot of heterogeneity, and it’s unclear what’s driving what,” she said.
An advantage of observational studies is that they give information about which of these markers are associated with trends and disease risks in specific groups vs others.
“For example, higher levels of triglycerides are associated with cardiovascular risk more in women, relative to men,” she said. And the triglyceride-to-HDL ratio seems “particularly robust” as a measure of cardiovascular health and risk.
The interpretation of associations with triglycerides can be “tricky” and “confusing” because results differ so much between studies, she said. “There are differences between middle age and older age, which have to do with age-related changes in metabolism and lipid metabolism and not necessarily that the markers are indicating something different,” she said.
Some research has suggested that triglycerides may have a protective effect against dementia, noted Uma Naidoo, MD, director of nutritional and lifestyle psychiatry, Massachusetts General Hospital, and director of nutritional psychiatry at MGH Academy.
This may be because the brain “runs mostly on energy from burning triglycerides,” suggested Dr. Naidoo, author of the books Calm Your Mind With Food and This Is Your Brain on Food.
In addition, having higher levels of triglycerides may be linked with having overall healthier behaviors, Dr. Naidoo told this news organization.
Dr. Mills said that in middle-aged individuals, high levels of LDL-C and triglycerides are “often indicative of more atherogenic particles and risk to cardiovascular health, which is a generally negative trajectory. But in older individuals, things become more complicated because there are differences in terms of clearance of some of these particles, tissue clearance and distribution, and nutrient status. So for older individuals, it seems that fluctuations in either direction—either too high or too low—tend to be more informative that some overall dysregulation is going on the system.”
She emphasized that, in this “emerging area, looking at only one or two studies is confusing. But if you look at the spectrum of studies, you can see a pattern, which is that the regulation gets ‘off,’ as people age.”
The Potential Role of Statins
Dr. Mills speculated that there may be “neuroprotective benefits for some of the statins which appear to be related to cardiovascular benefits. But at this point, we don’t have any clear data whether statins actually directly impact brain cholesterol, since it’s a separate pool.”
They could help “by increasing blood flow and reducing narrowing of the arteries, but any direct impact on the brain is still under investigation.”
Dr. Hansen pointed to research suggesting statins taken at midlife appear to be cardioprotective and may be protective of brain health as well, whereas statins initiated in older age do not appear to have these benefits.
He speculated that one reason statins seem less helpful when initiated later in life is that the BBB has already been damaged by systemic inflammation in the periphery, and the neuroinflammatory process resulting in neuronal destruction is already underway. “I think statins aren’t going to fix that problem, so although lowering cholesterol can be helpful in some respects, it might be too late to affect cognition because the nerves have already died and won’t grow back.”
Can Dietary Approaches Help?
Dr. Naidoo said that when looking at neurologic and psychiatric disease, “it’s important to think about the ‘long game’ — how can we improve our blood and cardiovascular health earlier in life to help potentiate healthy aging?”
From a nutritional psychiatry standpoint, Dr. Naidoo focuses on nourishing the gut microbiome and decreasing inflammation. “A healthy and balanced microbiome supports cognition, while the composition of gut bacteria is actually drastically different in patients with neurological diseases, such as AD.”
She recommends a nutrient-dense, anti-inflammatory diet including probiotic-rich foods (such as kimchi, sauerkraut, plain yogurt, and miso). Moreover, “the quality and structure of our fatty acids may be relevant as well: Increasing our intake of polyunsaturated fatty acids and avoiding processed fats like trans fats and hydrogenated oils may benefit our overall brain health.”
Dr. Naidoo recommends extra-virgin olive oil as a source of healthy fat. Its consumption is linked to lower incidence of AD by way of encouraging autophagy, which she calls “our own process of “cellular cleanup.’”
Dr. Naidoo believes that clinicians’ guidance to patients should “focus on healthy nutrition and other lifestyle practices, such as exercise, outdoor time, good sleep, and stress reduction.”
Dr. Mills notes the importance of omega-3 fatty acids, such as docosahexaenoic acid (DHA) , for brain health. “DHA is a major lipid component of neuronal membranes,” she said. “Because of inefficiencies in metabolism with APOE4, people tend to metabolize more of the lipids on the membranes themselves, so they have higher lipid membrane turnover and a greater need to supplement. Supplementing particularly through diet, with foods such as fatty fish rich in omega-3, can help boost the levels to help keep neuronal membranes intact.”
What This Means for the Clinician
“At this point, we see all of these associations between lipids and dementia, but we haven’t worked out exactly what it means on the individual level for an individual patient,” said Dr. Mills. Certainly, the picture is complex, and the understanding is growing and shifting. “The clinical applications remain unclear.”
One potential clinical take-home is that clinicians might consider tracking lipid levels over time. “If you follow a patient and see an increase or decrease [in lipid levels], that can be informative.” Looking at ratios of lipids might be more useful than looking only at a change in a single measure. “If you see trends in a variety of measures that track with one another, it might be more of a sign that something is potentially wrong.”
Whether the patient should first try a lifestyle intervention or might need medication is a “personalized clinical decision, depending on the individual, their risk factors, and how their levels are going,” said Dr. Mills.
Dr. Mills, Dr. Hansen, and Dr. Naidoo declared no relevant financial relationships.
A version of this article appeared on Medscape.com.
Appetite loss and unusual agitation
Given the patient's results on the genetic panel and MRI, as well as the noted cognitive decline and increased aggression, this patient is suspected of having limbic-predominant age-related TDP-43 encephalopathy (LATE) secondary to AD and is referred to the neurologist on her multidisciplinary care team for further consultation and testing.
AD is one of the most common forms of dementia. More than 6 million people in the United States have clinical AD or mild cognitive impairment because of AD. LATE is a new classification of dementia, identified in 2019, that mimics AD but is a unique disease entity driven by the misfolding of the protein TDP-43, which regulates gene expression in the brain. Misfolded TDP-43 protein is common among older adults aged ≥ 85 years, and about a quarter of this population has enough misfolded TDP-43 protein to affect their memory and cognition.
Diagnosing AD currently relies on a clinical approach. A complete physical examination, with a detailed neurologic examination and a mental status examination, is used to evaluate disease stage. Initial mental status testing evaluates attention and concentration, recent and remote memory, language, praxis, executive function, and visuospatial function. Because LATE is a newly discovered form of dementia, there are no set guidelines on diagnosing LATE and no robust biomarker for TDP-43. What is known about LATE has been gleaned mostly from retrospective clinicopathologic studies.
The LATE consensus working group reports that the clinical course of disease, as studied by autopsy-proven LATE neuropathologic change (LATE-NC), is described as an "amnestic cognitive syndrome that can evolve to incorporate multiple cognitive domains and ultimately to impair activities of daily living." Researchers are currently analyzing different clinical assessments and neuroimaging with MRI to characterize LATE. A group of international researchers recently published a set of clinical criteria for limbic-predominant amnestic neurodegenerative syndrome (LANS), which is associated with LATE-NC. Their criteria include "core, standard and advanced features that are measurable in vivo, including older age at evaluation, mild clinical syndrome, disproportionate hippocampal atrophy, impaired semantic memory, limbic hypometabolism, absence of neocortical degenerative patterns and low likelihood of neocortical tau, with degrees of certainty (highest, high, moderate, low)." Other neuroimaging studies of autopsy-confirmed LATE-NC have shown that atrophy is mostly focused in the medial temporal lobe with marked reduced hippocampal volume.
The group reports that LATE and AD probably share pathophysiologic mechanisms. One of the universally accepted hallmarks of AD is the formation of beta-amyloid plaques, which are dense, mostly insoluble deposits of beta-amyloid protein that develop around neurons in the hippocampus and other regions in the cerebral cortex used for decision-making. These plaques disrupt brain function and lead to brain atrophy. The LATE group also reports that this same pathology has been noted with LATE: "Many subjects with LATE-NC have comorbid brain pathologies, often including amyloid-beta plaques and tauopathy." That said, genetic studies have helped identify five genes with risk alleles for LATE (GRN, TMEM106B, ABCC9, KCNMB2, and APOE), suggesting disease-specific underlying mechanisms compared to AD.
Patient and caregiver education and guidance is vital with a dementia diagnosis. If LATE and/or AD are suspected, physicians should encourage the involvement of family and friends who agree to become more involved in the patient's care as the disease progresses. These individuals need to understand the patient's wishes around care, especially for the future when the patient is no longer able to make decisions. The patient may also consider establishing medical advance directives and durable power of attorney for medical and financial decision-making. Caregivers supporting the patient are encouraged to help balance the physical needs of the patient while maintaining respect for them as a competent adult to the extent allowed by the progression of their disease.
Because LATE is a new classification of dementia, there are no known effective treatments. One ongoing study is testing the use of autologous bone marrow–derived stem cells to help improve cognitive impairment among patients with LATE, AD, and other dementias. Current AD treatments are focused on symptomatic therapies that modulate neurotransmitters — either acetylcholine or glutamate. The standard medical treatment includes cholinesterase inhibitors and a partial N-methyl-D-aspartate antagonist. Two amyloid-directed antibodies (aducanumab, lecanemab) are currently available in the United States for individuals with AD exhibiting mild cognitive impairment or mild dementia. A third agent currently in clinical trials (donanemab) has shown significantly slowed clinical progression after 1.5 years among clinical trial participants with early symptomatic AD and amyloid and tau pathology.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Given the patient's results on the genetic panel and MRI, as well as the noted cognitive decline and increased aggression, this patient is suspected of having limbic-predominant age-related TDP-43 encephalopathy (LATE) secondary to AD and is referred to the neurologist on her multidisciplinary care team for further consultation and testing.
AD is one of the most common forms of dementia. More than 6 million people in the United States have clinical AD or mild cognitive impairment because of AD. LATE is a new classification of dementia, identified in 2019, that mimics AD but is a unique disease entity driven by the misfolding of the protein TDP-43, which regulates gene expression in the brain. Misfolded TDP-43 protein is common among older adults aged ≥ 85 years, and about a quarter of this population has enough misfolded TDP-43 protein to affect their memory and cognition.
Diagnosing AD currently relies on a clinical approach. A complete physical examination, with a detailed neurologic examination and a mental status examination, is used to evaluate disease stage. Initial mental status testing evaluates attention and concentration, recent and remote memory, language, praxis, executive function, and visuospatial function. Because LATE is a newly discovered form of dementia, there are no set guidelines on diagnosing LATE and no robust biomarker for TDP-43. What is known about LATE has been gleaned mostly from retrospective clinicopathologic studies.
The LATE consensus working group reports that the clinical course of disease, as studied by autopsy-proven LATE neuropathologic change (LATE-NC), is described as an "amnestic cognitive syndrome that can evolve to incorporate multiple cognitive domains and ultimately to impair activities of daily living." Researchers are currently analyzing different clinical assessments and neuroimaging with MRI to characterize LATE. A group of international researchers recently published a set of clinical criteria for limbic-predominant amnestic neurodegenerative syndrome (LANS), which is associated with LATE-NC. Their criteria include "core, standard and advanced features that are measurable in vivo, including older age at evaluation, mild clinical syndrome, disproportionate hippocampal atrophy, impaired semantic memory, limbic hypometabolism, absence of neocortical degenerative patterns and low likelihood of neocortical tau, with degrees of certainty (highest, high, moderate, low)." Other neuroimaging studies of autopsy-confirmed LATE-NC have shown that atrophy is mostly focused in the medial temporal lobe with marked reduced hippocampal volume.
The group reports that LATE and AD probably share pathophysiologic mechanisms. One of the universally accepted hallmarks of AD is the formation of beta-amyloid plaques, which are dense, mostly insoluble deposits of beta-amyloid protein that develop around neurons in the hippocampus and other regions in the cerebral cortex used for decision-making. These plaques disrupt brain function and lead to brain atrophy. The LATE group also reports that this same pathology has been noted with LATE: "Many subjects with LATE-NC have comorbid brain pathologies, often including amyloid-beta plaques and tauopathy." That said, genetic studies have helped identify five genes with risk alleles for LATE (GRN, TMEM106B, ABCC9, KCNMB2, and APOE), suggesting disease-specific underlying mechanisms compared to AD.
Patient and caregiver education and guidance is vital with a dementia diagnosis. If LATE and/or AD are suspected, physicians should encourage the involvement of family and friends who agree to become more involved in the patient's care as the disease progresses. These individuals need to understand the patient's wishes around care, especially for the future when the patient is no longer able to make decisions. The patient may also consider establishing medical advance directives and durable power of attorney for medical and financial decision-making. Caregivers supporting the patient are encouraged to help balance the physical needs of the patient while maintaining respect for them as a competent adult to the extent allowed by the progression of their disease.
Because LATE is a new classification of dementia, there are no known effective treatments. One ongoing study is testing the use of autologous bone marrow–derived stem cells to help improve cognitive impairment among patients with LATE, AD, and other dementias. Current AD treatments are focused on symptomatic therapies that modulate neurotransmitters — either acetylcholine or glutamate. The standard medical treatment includes cholinesterase inhibitors and a partial N-methyl-D-aspartate antagonist. Two amyloid-directed antibodies (aducanumab, lecanemab) are currently available in the United States for individuals with AD exhibiting mild cognitive impairment or mild dementia. A third agent currently in clinical trials (donanemab) has shown significantly slowed clinical progression after 1.5 years among clinical trial participants with early symptomatic AD and amyloid and tau pathology.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Given the patient's results on the genetic panel and MRI, as well as the noted cognitive decline and increased aggression, this patient is suspected of having limbic-predominant age-related TDP-43 encephalopathy (LATE) secondary to AD and is referred to the neurologist on her multidisciplinary care team for further consultation and testing.
AD is one of the most common forms of dementia. More than 6 million people in the United States have clinical AD or mild cognitive impairment because of AD. LATE is a new classification of dementia, identified in 2019, that mimics AD but is a unique disease entity driven by the misfolding of the protein TDP-43, which regulates gene expression in the brain. Misfolded TDP-43 protein is common among older adults aged ≥ 85 years, and about a quarter of this population has enough misfolded TDP-43 protein to affect their memory and cognition.
Diagnosing AD currently relies on a clinical approach. A complete physical examination, with a detailed neurologic examination and a mental status examination, is used to evaluate disease stage. Initial mental status testing evaluates attention and concentration, recent and remote memory, language, praxis, executive function, and visuospatial function. Because LATE is a newly discovered form of dementia, there are no set guidelines on diagnosing LATE and no robust biomarker for TDP-43. What is known about LATE has been gleaned mostly from retrospective clinicopathologic studies.
The LATE consensus working group reports that the clinical course of disease, as studied by autopsy-proven LATE neuropathologic change (LATE-NC), is described as an "amnestic cognitive syndrome that can evolve to incorporate multiple cognitive domains and ultimately to impair activities of daily living." Researchers are currently analyzing different clinical assessments and neuroimaging with MRI to characterize LATE. A group of international researchers recently published a set of clinical criteria for limbic-predominant amnestic neurodegenerative syndrome (LANS), which is associated with LATE-NC. Their criteria include "core, standard and advanced features that are measurable in vivo, including older age at evaluation, mild clinical syndrome, disproportionate hippocampal atrophy, impaired semantic memory, limbic hypometabolism, absence of neocortical degenerative patterns and low likelihood of neocortical tau, with degrees of certainty (highest, high, moderate, low)." Other neuroimaging studies of autopsy-confirmed LATE-NC have shown that atrophy is mostly focused in the medial temporal lobe with marked reduced hippocampal volume.
The group reports that LATE and AD probably share pathophysiologic mechanisms. One of the universally accepted hallmarks of AD is the formation of beta-amyloid plaques, which are dense, mostly insoluble deposits of beta-amyloid protein that develop around neurons in the hippocampus and other regions in the cerebral cortex used for decision-making. These plaques disrupt brain function and lead to brain atrophy. The LATE group also reports that this same pathology has been noted with LATE: "Many subjects with LATE-NC have comorbid brain pathologies, often including amyloid-beta plaques and tauopathy." That said, genetic studies have helped identify five genes with risk alleles for LATE (GRN, TMEM106B, ABCC9, KCNMB2, and APOE), suggesting disease-specific underlying mechanisms compared to AD.
Patient and caregiver education and guidance is vital with a dementia diagnosis. If LATE and/or AD are suspected, physicians should encourage the involvement of family and friends who agree to become more involved in the patient's care as the disease progresses. These individuals need to understand the patient's wishes around care, especially for the future when the patient is no longer able to make decisions. The patient may also consider establishing medical advance directives and durable power of attorney for medical and financial decision-making. Caregivers supporting the patient are encouraged to help balance the physical needs of the patient while maintaining respect for them as a competent adult to the extent allowed by the progression of their disease.
Because LATE is a new classification of dementia, there are no known effective treatments. One ongoing study is testing the use of autologous bone marrow–derived stem cells to help improve cognitive impairment among patients with LATE, AD, and other dementias. Current AD treatments are focused on symptomatic therapies that modulate neurotransmitters — either acetylcholine or glutamate. The standard medical treatment includes cholinesterase inhibitors and a partial N-methyl-D-aspartate antagonist. Two amyloid-directed antibodies (aducanumab, lecanemab) are currently available in the United States for individuals with AD exhibiting mild cognitive impairment or mild dementia. A third agent currently in clinical trials (donanemab) has shown significantly slowed clinical progression after 1.5 years among clinical trial participants with early symptomatic AD and amyloid and tau pathology.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
An 85-year-old woman presents to her geriatrician with her daughter, who is her primary caregiver. Seven years ago, the patient was diagnosed with mild Alzheimer's disease (AD). Her symptoms at diagnosis were irritability, forgetfulness, and panic attacks. Cognitive, behavioral, and functional assessments showed levels of decline; neurologic examination revealed mild hyposmia. The patient has been living with her daughter ever since her AD diagnosis.
At today's visit, the daughter reports that her mother has been experiencing loss of appetite and wide mood fluctuations with moments of unusual agitation. In addition, she tells the geriatrician that her mother has had trouble maintaining her balance and seems to have lost her sense of time. The patient has difficulty remembering what month and day it is, and how long it's been since her brother came to visit — which has been every Sunday like clockwork since the patient moved in with her daughter. The daughter also notes that her mother loses track of the story line when she is watching movie and TV shows lately.
The physician orders a brain MRI and genetic panel. MRI reveals atrophy in the frontal cortex as well as the medial temporal lobe, with hippocampal sclerosis. The genetic panel shows APOE and TMEM106 mutations.
Modifiable Risk Factors for Young-Onset Dementia Flagged
TOPLINE:
In addition to better known risk factors such as diabetes, stroke, heart disease, and depression, findings of a large study suggested vitamin D deficiency, elevated C-reactive protein (CRP) levels, and social isolation increase the risk for young-onset dementia (YOD).
METHODOLOGY:
- The study included 356,052 participants younger than 65 years (mean baseline age, 54.6 years) without dementia from the UK Biobank, an ongoing prospective cohort study.
- Participants underwent a comprehensive baseline assessment, provided biological samples, completed touch screen questionnaires, and underwent a physical examination.
- Researchers identified incident all-cause YOD cases from hospital inpatient registers or death register linkage.
- The researchers detected 39 potential risk factors and grouped them into domains of sociodemographic, genetic, lifestyle, environmental, vitamin D and CRP levels, cardiometabolic, psychiatric, and other factors.
- Researchers analyzed incidence rates of YOD for 5-year age bands starting at age 40 years and separately for men and women.
TAKEAWAY:
- During a mean follow-up of 8.12 years, there were 485 incident YOD cases (incidence rate of 16.8 per 100,000 person-years; 95% CI 15.4-18.3).
- The final analysis identified 15 risk factors associated with significantly higher incidence of YOD, including traditional factors like stroke (hazard ratio [HR], 2.07), heart disease (HR, 1.61), diabetes (HR, 1.65), and depression (HR, 3.25) but also less-recognized risk factors like vitamin D deficiency (< 10 ng/mL; HR, 1.59), high CRP levels (> 1 mg/dL; HR, 1.54), and social isolation (infrequent visits to friends or family; HR, 1.53), with lower socioeconomic status (HR, 1.82), having two apolipoprotein E epsilon-4 alleles (HR, 1.87), orthostatic hypotension, which the authors said may be an early sign of Parkinson dementia or Lewy body dementia (HR, 4.20), and hearing impairment (HR, 1.56) also increasing risk.
- Interestingly, some alcohol use seemed to be protective (moderate or heavy alcohol use had a lower association with YOD than alcohol abstinence, possibly due to the “healthy drinker effect” where people who drink are healthier than abstainers who may have illnesses preventing them from drinking, said the authors), as was higher education level and higher than normative handgrip strength (less strength is a proxy for physical frailty).
- Men with diabetes had higher YOD risk than those without diabetes, while there was no association with diabetes in women; on the other hand, women with high CRP levels had greater YOD risk than those with low levels, while there was no association with CRP in men.
IN PRACTICE:
“While further exploration of these risk factors is necessary to identify potential underlying mechanisms, addressing these modifiable factors may prove effective in mitigating the risk of developing YOD and can be readily integrated in current dementia prevention initiatives,” the investigators wrote.
SOURCE:
The study was led by Stevie Hendriks, PhD, Department of Psychiatry and Neuropsychology, Maastricht University, Maastricht, the Netherlands. It was published online in JAMA Neurology.
LIMITATIONS:
The study was observational and so can’t infer causality. Several factors were based on self-reported data, which might be a source of response bias. Factors not considered in the study, for example, family history of dementia and drug (other than alcohol) use disorder, may have confounded associations. Some factors including orthostatic hypotension had few exposed cases, leading to decreased power to detect associations. Hospital and death records may not have captured all YOD cases. The UK Biobank is overrepresented by healthy and White participants, so results may not be generalizable to other racial and ethnic groups. The analyses only focused on all-cause dementia.
DISCLOSURES:
The study was supported by Alzheimer Netherlands. Hendriks has no relevant conflicts of interest; see paper for disclosures of other authors.
A version of this article appeared on Medscape.com.
TOPLINE:
In addition to better known risk factors such as diabetes, stroke, heart disease, and depression, findings of a large study suggested vitamin D deficiency, elevated C-reactive protein (CRP) levels, and social isolation increase the risk for young-onset dementia (YOD).
METHODOLOGY:
- The study included 356,052 participants younger than 65 years (mean baseline age, 54.6 years) without dementia from the UK Biobank, an ongoing prospective cohort study.
- Participants underwent a comprehensive baseline assessment, provided biological samples, completed touch screen questionnaires, and underwent a physical examination.
- Researchers identified incident all-cause YOD cases from hospital inpatient registers or death register linkage.
- The researchers detected 39 potential risk factors and grouped them into domains of sociodemographic, genetic, lifestyle, environmental, vitamin D and CRP levels, cardiometabolic, psychiatric, and other factors.
- Researchers analyzed incidence rates of YOD for 5-year age bands starting at age 40 years and separately for men and women.
TAKEAWAY:
- During a mean follow-up of 8.12 years, there were 485 incident YOD cases (incidence rate of 16.8 per 100,000 person-years; 95% CI 15.4-18.3).
- The final analysis identified 15 risk factors associated with significantly higher incidence of YOD, including traditional factors like stroke (hazard ratio [HR], 2.07), heart disease (HR, 1.61), diabetes (HR, 1.65), and depression (HR, 3.25) but also less-recognized risk factors like vitamin D deficiency (< 10 ng/mL; HR, 1.59), high CRP levels (> 1 mg/dL; HR, 1.54), and social isolation (infrequent visits to friends or family; HR, 1.53), with lower socioeconomic status (HR, 1.82), having two apolipoprotein E epsilon-4 alleles (HR, 1.87), orthostatic hypotension, which the authors said may be an early sign of Parkinson dementia or Lewy body dementia (HR, 4.20), and hearing impairment (HR, 1.56) also increasing risk.
- Interestingly, some alcohol use seemed to be protective (moderate or heavy alcohol use had a lower association with YOD than alcohol abstinence, possibly due to the “healthy drinker effect” where people who drink are healthier than abstainers who may have illnesses preventing them from drinking, said the authors), as was higher education level and higher than normative handgrip strength (less strength is a proxy for physical frailty).
- Men with diabetes had higher YOD risk than those without diabetes, while there was no association with diabetes in women; on the other hand, women with high CRP levels had greater YOD risk than those with low levels, while there was no association with CRP in men.
IN PRACTICE:
“While further exploration of these risk factors is necessary to identify potential underlying mechanisms, addressing these modifiable factors may prove effective in mitigating the risk of developing YOD and can be readily integrated in current dementia prevention initiatives,” the investigators wrote.
SOURCE:
The study was led by Stevie Hendriks, PhD, Department of Psychiatry and Neuropsychology, Maastricht University, Maastricht, the Netherlands. It was published online in JAMA Neurology.
LIMITATIONS:
The study was observational and so can’t infer causality. Several factors were based on self-reported data, which might be a source of response bias. Factors not considered in the study, for example, family history of dementia and drug (other than alcohol) use disorder, may have confounded associations. Some factors including orthostatic hypotension had few exposed cases, leading to decreased power to detect associations. Hospital and death records may not have captured all YOD cases. The UK Biobank is overrepresented by healthy and White participants, so results may not be generalizable to other racial and ethnic groups. The analyses only focused on all-cause dementia.
DISCLOSURES:
The study was supported by Alzheimer Netherlands. Hendriks has no relevant conflicts of interest; see paper for disclosures of other authors.
A version of this article appeared on Medscape.com.
TOPLINE:
In addition to better known risk factors such as diabetes, stroke, heart disease, and depression, findings of a large study suggested vitamin D deficiency, elevated C-reactive protein (CRP) levels, and social isolation increase the risk for young-onset dementia (YOD).
METHODOLOGY:
- The study included 356,052 participants younger than 65 years (mean baseline age, 54.6 years) without dementia from the UK Biobank, an ongoing prospective cohort study.
- Participants underwent a comprehensive baseline assessment, provided biological samples, completed touch screen questionnaires, and underwent a physical examination.
- Researchers identified incident all-cause YOD cases from hospital inpatient registers or death register linkage.
- The researchers detected 39 potential risk factors and grouped them into domains of sociodemographic, genetic, lifestyle, environmental, vitamin D and CRP levels, cardiometabolic, psychiatric, and other factors.
- Researchers analyzed incidence rates of YOD for 5-year age bands starting at age 40 years and separately for men and women.
TAKEAWAY:
- During a mean follow-up of 8.12 years, there were 485 incident YOD cases (incidence rate of 16.8 per 100,000 person-years; 95% CI 15.4-18.3).
- The final analysis identified 15 risk factors associated with significantly higher incidence of YOD, including traditional factors like stroke (hazard ratio [HR], 2.07), heart disease (HR, 1.61), diabetes (HR, 1.65), and depression (HR, 3.25) but also less-recognized risk factors like vitamin D deficiency (< 10 ng/mL; HR, 1.59), high CRP levels (> 1 mg/dL; HR, 1.54), and social isolation (infrequent visits to friends or family; HR, 1.53), with lower socioeconomic status (HR, 1.82), having two apolipoprotein E epsilon-4 alleles (HR, 1.87), orthostatic hypotension, which the authors said may be an early sign of Parkinson dementia or Lewy body dementia (HR, 4.20), and hearing impairment (HR, 1.56) also increasing risk.
- Interestingly, some alcohol use seemed to be protective (moderate or heavy alcohol use had a lower association with YOD than alcohol abstinence, possibly due to the “healthy drinker effect” where people who drink are healthier than abstainers who may have illnesses preventing them from drinking, said the authors), as was higher education level and higher than normative handgrip strength (less strength is a proxy for physical frailty).
- Men with diabetes had higher YOD risk than those without diabetes, while there was no association with diabetes in women; on the other hand, women with high CRP levels had greater YOD risk than those with low levels, while there was no association with CRP in men.
IN PRACTICE:
“While further exploration of these risk factors is necessary to identify potential underlying mechanisms, addressing these modifiable factors may prove effective in mitigating the risk of developing YOD and can be readily integrated in current dementia prevention initiatives,” the investigators wrote.
SOURCE:
The study was led by Stevie Hendriks, PhD, Department of Psychiatry and Neuropsychology, Maastricht University, Maastricht, the Netherlands. It was published online in JAMA Neurology.
LIMITATIONS:
The study was observational and so can’t infer causality. Several factors were based on self-reported data, which might be a source of response bias. Factors not considered in the study, for example, family history of dementia and drug (other than alcohol) use disorder, may have confounded associations. Some factors including orthostatic hypotension had few exposed cases, leading to decreased power to detect associations. Hospital and death records may not have captured all YOD cases. The UK Biobank is overrepresented by healthy and White participants, so results may not be generalizable to other racial and ethnic groups. The analyses only focused on all-cause dementia.
DISCLOSURES:
The study was supported by Alzheimer Netherlands. Hendriks has no relevant conflicts of interest; see paper for disclosures of other authors.
A version of this article appeared on Medscape.com.
Poor Oral Health Tied to Worse Brain Health
In a large observational study of middle-aged adults without stroke or dementia, poor oral health was strongly associated with multiple neuroimaging markers of white matter injury.
“Because the neuroimaging markers evaluated in this study precede and are established risk factors of stroke and dementia, our results suggest that oral health, an easily modifiable process, may be a promising target for very early interventions focused on improving brain health,” wrote the authors, led by Cyprien A. Rivier, MD, MS, with the Department of Neurology, Yale University School of Medicine, New Haven, Connecticut.
The study was published online on December 20, 2023, in Neurology.
Research data came from 40,175 adults (mean age, 55 years; 53% women) with no history of stroke or dementia who enrolled in the UK Biobank from 2006 to 2010 and had brain MRI between 2014 and 2016.
Altogether, 5470 (14%) participants had poor oral health, defined as the presence of dentures or loose teeth. Those with poor (vs optimal) oral health were older, more likely to be male, and had higher prevalence of hypertension, hypercholesterolemia, diabetes, overweight/obesity, and current or past smoking history.
In a multivariable model, poor oral health was associated with a 9% increase in white matter hyperintensity (WMH) volume (P < .001), a well-established marker of clinically silent cerebrovascular disease.
Poor oral health was also associated with a 10% change in aggregate fractional anisotropy (FA) score (P < .001) and a 5% change in aggregate mean diffusivity (MD) score (P < .001), two diffusion tensor imaging metrics that accurately represent white matter disintegrity.
Genetic analyses using Mendelian randomization confirmed these associations. Individuals who were genetically prone to poor oral health had a 30% increase in WMH volume (P < .001), 43% change in aggregate FA score (P < .001), and 10% change in aggregate MD score (P < .01), the researchers reported.
These findings, they noted, add to prior epidemiologic evidence for an association between poor oral health and a higher risk for clinical outcomes related to brain health, including cognitive decline.
‘Huge Dividends’
The authors of an accompanying editorial praised the authors for looking at the consequences of poor oral health in a “new and powerful way by using as their outcome MRI-defined white matter injury, which is associated with, but antedates by many years, cognitive decline and stroke.”
“The fact that these imaging changes are seen in asymptomatic persons offers the hope that if the association is causal, interventions to improve oral health could pay huge dividends in subsequent brain health,” wrote Steven J. Kittner, MD, MPH, and Breana L. Taylor, MD, with the Department of Neurology, University of Maryland School of Medicine in Baltimore.
“The mechanisms mediating the relationship between the oral health genetic risk score and white matter injury are likely to be complex, but the authors have taken an important step forward in addressing a hypothesis of immense public health importance,” they added.
Data from the World Health Organization suggested that oral diseases, which are largely preventable, affect nearly 3.5 billion people globally, with three out of four people affected in middle-income countries.
Funding for the study was provided in part by grants from the National Institutes of Health, the American Heart Association, and the Neurocritical Care Society Research Fellowship. The authors and editorialists disclosed no relevant conflicts of interest.
Megan Brooks has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
In a large observational study of middle-aged adults without stroke or dementia, poor oral health was strongly associated with multiple neuroimaging markers of white matter injury.
“Because the neuroimaging markers evaluated in this study precede and are established risk factors of stroke and dementia, our results suggest that oral health, an easily modifiable process, may be a promising target for very early interventions focused on improving brain health,” wrote the authors, led by Cyprien A. Rivier, MD, MS, with the Department of Neurology, Yale University School of Medicine, New Haven, Connecticut.
The study was published online on December 20, 2023, in Neurology.
Research data came from 40,175 adults (mean age, 55 years; 53% women) with no history of stroke or dementia who enrolled in the UK Biobank from 2006 to 2010 and had brain MRI between 2014 and 2016.
Altogether, 5470 (14%) participants had poor oral health, defined as the presence of dentures or loose teeth. Those with poor (vs optimal) oral health were older, more likely to be male, and had higher prevalence of hypertension, hypercholesterolemia, diabetes, overweight/obesity, and current or past smoking history.
In a multivariable model, poor oral health was associated with a 9% increase in white matter hyperintensity (WMH) volume (P < .001), a well-established marker of clinically silent cerebrovascular disease.
Poor oral health was also associated with a 10% change in aggregate fractional anisotropy (FA) score (P < .001) and a 5% change in aggregate mean diffusivity (MD) score (P < .001), two diffusion tensor imaging metrics that accurately represent white matter disintegrity.
Genetic analyses using Mendelian randomization confirmed these associations. Individuals who were genetically prone to poor oral health had a 30% increase in WMH volume (P < .001), 43% change in aggregate FA score (P < .001), and 10% change in aggregate MD score (P < .01), the researchers reported.
These findings, they noted, add to prior epidemiologic evidence for an association between poor oral health and a higher risk for clinical outcomes related to brain health, including cognitive decline.
‘Huge Dividends’
The authors of an accompanying editorial praised the authors for looking at the consequences of poor oral health in a “new and powerful way by using as their outcome MRI-defined white matter injury, which is associated with, but antedates by many years, cognitive decline and stroke.”
“The fact that these imaging changes are seen in asymptomatic persons offers the hope that if the association is causal, interventions to improve oral health could pay huge dividends in subsequent brain health,” wrote Steven J. Kittner, MD, MPH, and Breana L. Taylor, MD, with the Department of Neurology, University of Maryland School of Medicine in Baltimore.
“The mechanisms mediating the relationship between the oral health genetic risk score and white matter injury are likely to be complex, but the authors have taken an important step forward in addressing a hypothesis of immense public health importance,” they added.
Data from the World Health Organization suggested that oral diseases, which are largely preventable, affect nearly 3.5 billion people globally, with three out of four people affected in middle-income countries.
Funding for the study was provided in part by grants from the National Institutes of Health, the American Heart Association, and the Neurocritical Care Society Research Fellowship. The authors and editorialists disclosed no relevant conflicts of interest.
Megan Brooks has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
In a large observational study of middle-aged adults without stroke or dementia, poor oral health was strongly associated with multiple neuroimaging markers of white matter injury.
“Because the neuroimaging markers evaluated in this study precede and are established risk factors of stroke and dementia, our results suggest that oral health, an easily modifiable process, may be a promising target for very early interventions focused on improving brain health,” wrote the authors, led by Cyprien A. Rivier, MD, MS, with the Department of Neurology, Yale University School of Medicine, New Haven, Connecticut.
The study was published online on December 20, 2023, in Neurology.
Research data came from 40,175 adults (mean age, 55 years; 53% women) with no history of stroke or dementia who enrolled in the UK Biobank from 2006 to 2010 and had brain MRI between 2014 and 2016.
Altogether, 5470 (14%) participants had poor oral health, defined as the presence of dentures or loose teeth. Those with poor (vs optimal) oral health were older, more likely to be male, and had higher prevalence of hypertension, hypercholesterolemia, diabetes, overweight/obesity, and current or past smoking history.
In a multivariable model, poor oral health was associated with a 9% increase in white matter hyperintensity (WMH) volume (P < .001), a well-established marker of clinically silent cerebrovascular disease.
Poor oral health was also associated with a 10% change in aggregate fractional anisotropy (FA) score (P < .001) and a 5% change in aggregate mean diffusivity (MD) score (P < .001), two diffusion tensor imaging metrics that accurately represent white matter disintegrity.
Genetic analyses using Mendelian randomization confirmed these associations. Individuals who were genetically prone to poor oral health had a 30% increase in WMH volume (P < .001), 43% change in aggregate FA score (P < .001), and 10% change in aggregate MD score (P < .01), the researchers reported.
These findings, they noted, add to prior epidemiologic evidence for an association between poor oral health and a higher risk for clinical outcomes related to brain health, including cognitive decline.
‘Huge Dividends’
The authors of an accompanying editorial praised the authors for looking at the consequences of poor oral health in a “new and powerful way by using as their outcome MRI-defined white matter injury, which is associated with, but antedates by many years, cognitive decline and stroke.”
“The fact that these imaging changes are seen in asymptomatic persons offers the hope that if the association is causal, interventions to improve oral health could pay huge dividends in subsequent brain health,” wrote Steven J. Kittner, MD, MPH, and Breana L. Taylor, MD, with the Department of Neurology, University of Maryland School of Medicine in Baltimore.
“The mechanisms mediating the relationship between the oral health genetic risk score and white matter injury are likely to be complex, but the authors have taken an important step forward in addressing a hypothesis of immense public health importance,” they added.
Data from the World Health Organization suggested that oral diseases, which are largely preventable, affect nearly 3.5 billion people globally, with three out of four people affected in middle-income countries.
Funding for the study was provided in part by grants from the National Institutes of Health, the American Heart Association, and the Neurocritical Care Society Research Fellowship. The authors and editorialists disclosed no relevant conflicts of interest.
Megan Brooks has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Epilepsy Linked to Earlier, More Rapid, Cognitive Decline
ORLANDO — People with epilepsy are more likely to decline cognitively compared with those without epilepsy, new research suggests.
Results of the large, longitudinal study show that seizures predicted earlier conversion time from normal cognition to mild cognitive impairment (MCI) but were not associated with conversion from MCI to dementia.
“Modifiable cardiovascular risk factors such as hypertension and diabetes need to be treated more aggressively because they can impact cognition, but epilepsy is another risk factor that needs to be treated in a timely fashion because it appears to be also associated with cognitive impairment,” said study investigator Ifrah Zawar MD, assistant professor, Department of Neurology, University of Virginia in Charlottesville.
The study (abstract #2.172) was presented on December 2 at the American Epilepsy Society annual meeting.
An Understudied Issue
Comorbid seizures occur in up to 64% of those with dementia, and patients with dementia and epilepsy have a more aggressive disease course, faster cognitive decline, and more severe neuronal loss, Dr. Zawar told Medscape Medical News.
But the impact of seizures on the conversion of cognitively healthy to MCI and from MCI to dementia, after accounting for cardiovascular risk factors, has not been well studied.
Researchers analyzed longitudinal data of 13,726 patients, mean age about 70 years, who were cognitively healthy or had mild cognitive impairment (MCI). Participants were recruited from 39 Alzheimer’s Disease (AD) centers in the United States from 2005 to 2021.
Investigators categorized participants into three groups: active (having had seizures in the past year and/or requiring active treatment; N = 118), resolved (not on any treatment for the past year and not having seizures; N = 226), and no seizures (never having had seizures; N = 13,382).
The primary outcome was conversion from cognitively healthy to MCI/dementia and from MCI to dementia in those with and without active epilepsy and resolved epilepsy.
Factors associated with conversion from cognitively healthy to MCI among those with current or active epilepsy included older age (P <.001 for ages 60-80 years and P =.002 for age 80 years or older vs younger than 60 years), male sex (P <.001), lower education (P <.001), hypertension (P <.001), and diabetes (P <.001).
The hazard ratio (HR) for earlier conversion from healthy to worse cognition among those with active epilepsy was 1.76 (95% CI, 1.38-2.24; P <.001), even after accounting for risk factors.
Kaplan-Meier curves showed that the median time to convert from healthy cognition to MCI among people with active epilepsy was about 5 years compared with about 9 years for those with resolved epilepsy and 10.5 years for those without epilepsy.
The story was similar for faster conversion from MCI to dementia. Compared with having no epilepsy, the HR for faster conversion for active epilepsy was 1.44 (95% CI, 1.20-1.73; P <.001).
In addition, the median time to conversion from MCI to dementia was about 3 years for those with active epilepsy compared with about 5 years for those with resolved epilepsy and about 5 years for those without epilepsy.
“It’s important for physicians to understand that uncontrolled epilepsy or active epilepsy is going to impact patients’ cognition adversely, which in itself is associated with increased comorbidity and mortality,” said Dr. Zawar.
The mechanism driving the acceleration to worse cognition in people with epilepsy is “complicated and involves a multitude of factors,” she said.
The researchers did not specifically investigate how use of antiseizure medications correlated with cognitive outcomes, but Dr. Zawar believes that “epilepsy in itself impacts cognition.”
The researchers also didn’t have EEG data for study participants who were recruited from Alzheimer’s disease centers where EEGs aren’t routinely carried out, so such data for many patients may not necessarily exist, said Dr. Zawar.
Important Research
Commenting for this news organization, Bruce Hermann, PhD, professor emeritus, Department of Neurology, University of Wisconsin School of Medicine and Public Health, said that the study is important because of the, “tremendous interest and concern about aging with epilepsy.”
“We want to know how people with chronic epilepsy age cognitively and what’s the cognitive course of those who have late onset epilepsy, particularly those with unknown etiology,” he added.
Dr. Hermann noted that much of the research in this area has been relatively small and single-center investigations.
“These larger-scale investigations from outside the epilepsy community are so important because they have data on large numbers of subjects, they have cognitive data, and follow-ups over long periods of time, and they’re providing some really novel information,” Dr. Hermann said.
He added that terms used in the dementia world such as MCI and frank dementia are somewhat foreign to epileptologists. In addition, interventions to delay, treat, or prevent cognitive decline such as exercise, diet, social activity, and mental stimulation that are regularly discussed by dementia experts are underrepresented in the epilepsy world.
“The things they talk about in memory clinics in the aging world almost routinely have not penetrated to the epilepsy clinics for aging individuals and for the epilepsy community in general.”
The study used the Montreal Cognitive Assessment to identify cognitive decline. “It would be nice to see how these people look with traditional neuropsychological tests,” said Dr. Hermann.
He added that information on the impact of epilepsy on different MCI phenotypes, for example, pure memory impairment subtype; pure nonmemory subtype; and multiple domain subtype, would also be useful.
The study was supported by the AES and the Alzheimer’s Association.
Dr. Zawar and Dr. Hermann report no relevant disclosures.
A version of this article appeared on Medscape.com.
ORLANDO — People with epilepsy are more likely to decline cognitively compared with those without epilepsy, new research suggests.
Results of the large, longitudinal study show that seizures predicted earlier conversion time from normal cognition to mild cognitive impairment (MCI) but were not associated with conversion from MCI to dementia.
“Modifiable cardiovascular risk factors such as hypertension and diabetes need to be treated more aggressively because they can impact cognition, but epilepsy is another risk factor that needs to be treated in a timely fashion because it appears to be also associated with cognitive impairment,” said study investigator Ifrah Zawar MD, assistant professor, Department of Neurology, University of Virginia in Charlottesville.
The study (abstract #2.172) was presented on December 2 at the American Epilepsy Society annual meeting.
An Understudied Issue
Comorbid seizures occur in up to 64% of those with dementia, and patients with dementia and epilepsy have a more aggressive disease course, faster cognitive decline, and more severe neuronal loss, Dr. Zawar told Medscape Medical News.
But the impact of seizures on the conversion of cognitively healthy to MCI and from MCI to dementia, after accounting for cardiovascular risk factors, has not been well studied.
Researchers analyzed longitudinal data of 13,726 patients, mean age about 70 years, who were cognitively healthy or had mild cognitive impairment (MCI). Participants were recruited from 39 Alzheimer’s Disease (AD) centers in the United States from 2005 to 2021.
Investigators categorized participants into three groups: active (having had seizures in the past year and/or requiring active treatment; N = 118), resolved (not on any treatment for the past year and not having seizures; N = 226), and no seizures (never having had seizures; N = 13,382).
The primary outcome was conversion from cognitively healthy to MCI/dementia and from MCI to dementia in those with and without active epilepsy and resolved epilepsy.
Factors associated with conversion from cognitively healthy to MCI among those with current or active epilepsy included older age (P <.001 for ages 60-80 years and P =.002 for age 80 years or older vs younger than 60 years), male sex (P <.001), lower education (P <.001), hypertension (P <.001), and diabetes (P <.001).
The hazard ratio (HR) for earlier conversion from healthy to worse cognition among those with active epilepsy was 1.76 (95% CI, 1.38-2.24; P <.001), even after accounting for risk factors.
Kaplan-Meier curves showed that the median time to convert from healthy cognition to MCI among people with active epilepsy was about 5 years compared with about 9 years for those with resolved epilepsy and 10.5 years for those without epilepsy.
The story was similar for faster conversion from MCI to dementia. Compared with having no epilepsy, the HR for faster conversion for active epilepsy was 1.44 (95% CI, 1.20-1.73; P <.001).
In addition, the median time to conversion from MCI to dementia was about 3 years for those with active epilepsy compared with about 5 years for those with resolved epilepsy and about 5 years for those without epilepsy.
“It’s important for physicians to understand that uncontrolled epilepsy or active epilepsy is going to impact patients’ cognition adversely, which in itself is associated with increased comorbidity and mortality,” said Dr. Zawar.
The mechanism driving the acceleration to worse cognition in people with epilepsy is “complicated and involves a multitude of factors,” she said.
The researchers did not specifically investigate how use of antiseizure medications correlated with cognitive outcomes, but Dr. Zawar believes that “epilepsy in itself impacts cognition.”
The researchers also didn’t have EEG data for study participants who were recruited from Alzheimer’s disease centers where EEGs aren’t routinely carried out, so such data for many patients may not necessarily exist, said Dr. Zawar.
Important Research
Commenting for this news organization, Bruce Hermann, PhD, professor emeritus, Department of Neurology, University of Wisconsin School of Medicine and Public Health, said that the study is important because of the, “tremendous interest and concern about aging with epilepsy.”
“We want to know how people with chronic epilepsy age cognitively and what’s the cognitive course of those who have late onset epilepsy, particularly those with unknown etiology,” he added.
Dr. Hermann noted that much of the research in this area has been relatively small and single-center investigations.
“These larger-scale investigations from outside the epilepsy community are so important because they have data on large numbers of subjects, they have cognitive data, and follow-ups over long periods of time, and they’re providing some really novel information,” Dr. Hermann said.
He added that terms used in the dementia world such as MCI and frank dementia are somewhat foreign to epileptologists. In addition, interventions to delay, treat, or prevent cognitive decline such as exercise, diet, social activity, and mental stimulation that are regularly discussed by dementia experts are underrepresented in the epilepsy world.
“The things they talk about in memory clinics in the aging world almost routinely have not penetrated to the epilepsy clinics for aging individuals and for the epilepsy community in general.”
The study used the Montreal Cognitive Assessment to identify cognitive decline. “It would be nice to see how these people look with traditional neuropsychological tests,” said Dr. Hermann.
He added that information on the impact of epilepsy on different MCI phenotypes, for example, pure memory impairment subtype; pure nonmemory subtype; and multiple domain subtype, would also be useful.
The study was supported by the AES and the Alzheimer’s Association.
Dr. Zawar and Dr. Hermann report no relevant disclosures.
A version of this article appeared on Medscape.com.
ORLANDO — People with epilepsy are more likely to decline cognitively compared with those without epilepsy, new research suggests.
Results of the large, longitudinal study show that seizures predicted earlier conversion time from normal cognition to mild cognitive impairment (MCI) but were not associated with conversion from MCI to dementia.
“Modifiable cardiovascular risk factors such as hypertension and diabetes need to be treated more aggressively because they can impact cognition, but epilepsy is another risk factor that needs to be treated in a timely fashion because it appears to be also associated with cognitive impairment,” said study investigator Ifrah Zawar MD, assistant professor, Department of Neurology, University of Virginia in Charlottesville.
The study (abstract #2.172) was presented on December 2 at the American Epilepsy Society annual meeting.
An Understudied Issue
Comorbid seizures occur in up to 64% of those with dementia, and patients with dementia and epilepsy have a more aggressive disease course, faster cognitive decline, and more severe neuronal loss, Dr. Zawar told Medscape Medical News.
But the impact of seizures on the conversion of cognitively healthy to MCI and from MCI to dementia, after accounting for cardiovascular risk factors, has not been well studied.
Researchers analyzed longitudinal data of 13,726 patients, mean age about 70 years, who were cognitively healthy or had mild cognitive impairment (MCI). Participants were recruited from 39 Alzheimer’s Disease (AD) centers in the United States from 2005 to 2021.
Investigators categorized participants into three groups: active (having had seizures in the past year and/or requiring active treatment; N = 118), resolved (not on any treatment for the past year and not having seizures; N = 226), and no seizures (never having had seizures; N = 13,382).
The primary outcome was conversion from cognitively healthy to MCI/dementia and from MCI to dementia in those with and without active epilepsy and resolved epilepsy.
Factors associated with conversion from cognitively healthy to MCI among those with current or active epilepsy included older age (P <.001 for ages 60-80 years and P =.002 for age 80 years or older vs younger than 60 years), male sex (P <.001), lower education (P <.001), hypertension (P <.001), and diabetes (P <.001).
The hazard ratio (HR) for earlier conversion from healthy to worse cognition among those with active epilepsy was 1.76 (95% CI, 1.38-2.24; P <.001), even after accounting for risk factors.
Kaplan-Meier curves showed that the median time to convert from healthy cognition to MCI among people with active epilepsy was about 5 years compared with about 9 years for those with resolved epilepsy and 10.5 years for those without epilepsy.
The story was similar for faster conversion from MCI to dementia. Compared with having no epilepsy, the HR for faster conversion for active epilepsy was 1.44 (95% CI, 1.20-1.73; P <.001).
In addition, the median time to conversion from MCI to dementia was about 3 years for those with active epilepsy compared with about 5 years for those with resolved epilepsy and about 5 years for those without epilepsy.
“It’s important for physicians to understand that uncontrolled epilepsy or active epilepsy is going to impact patients’ cognition adversely, which in itself is associated with increased comorbidity and mortality,” said Dr. Zawar.
The mechanism driving the acceleration to worse cognition in people with epilepsy is “complicated and involves a multitude of factors,” she said.
The researchers did not specifically investigate how use of antiseizure medications correlated with cognitive outcomes, but Dr. Zawar believes that “epilepsy in itself impacts cognition.”
The researchers also didn’t have EEG data for study participants who were recruited from Alzheimer’s disease centers where EEGs aren’t routinely carried out, so such data for many patients may not necessarily exist, said Dr. Zawar.
Important Research
Commenting for this news organization, Bruce Hermann, PhD, professor emeritus, Department of Neurology, University of Wisconsin School of Medicine and Public Health, said that the study is important because of the, “tremendous interest and concern about aging with epilepsy.”
“We want to know how people with chronic epilepsy age cognitively and what’s the cognitive course of those who have late onset epilepsy, particularly those with unknown etiology,” he added.
Dr. Hermann noted that much of the research in this area has been relatively small and single-center investigations.
“These larger-scale investigations from outside the epilepsy community are so important because they have data on large numbers of subjects, they have cognitive data, and follow-ups over long periods of time, and they’re providing some really novel information,” Dr. Hermann said.
He added that terms used in the dementia world such as MCI and frank dementia are somewhat foreign to epileptologists. In addition, interventions to delay, treat, or prevent cognitive decline such as exercise, diet, social activity, and mental stimulation that are regularly discussed by dementia experts are underrepresented in the epilepsy world.
“The things they talk about in memory clinics in the aging world almost routinely have not penetrated to the epilepsy clinics for aging individuals and for the epilepsy community in general.”
The study used the Montreal Cognitive Assessment to identify cognitive decline. “It would be nice to see how these people look with traditional neuropsychological tests,” said Dr. Hermann.
He added that information on the impact of epilepsy on different MCI phenotypes, for example, pure memory impairment subtype; pure nonmemory subtype; and multiple domain subtype, would also be useful.
The study was supported by the AES and the Alzheimer’s Association.
Dr. Zawar and Dr. Hermann report no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM AES 2023