User login
Efficacy of KTE-C19 CAR T cells not compromised by prior blinatumomab
CHICAGO—Prior exposure to blinatumomab does not appear to affect the successful manufacture of KTE-C19 or its efficacy in patients with relapsed/refractory acute lymphoblastic leukemia (ALL), an investigator reported at the 2018 ASCO Annual Meeting.
The clinical benefit of KTE-C19, an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, was preserved regardless of whether patients were exposed to blinatumomab, said Bijal D. Shah, MD, of Moffitt Cancer Center in Tampa, Florida.
High rates of complete response and undetectable minimal residual disease (MRD) were independent of exposure to blinatumomab, a CD19/CD3 bispecific T-cell engager.
“We feel the results of these data support KTE-C19 as an effective option for adults with refractory leukemia, regardless of prior exposure to CD19-directed therapy,” Dr Shah reported at the meeting (abstract 7006*).
The current standard of care for adults with relapsed/refractory ALL includes blinatumomab, raising the question of whether prior exposure to this CD19-directed treatment could influence the manufacture or efficacy of KTE-C19.
Sara Cooley, MD, of Masonic Medical Center, University of Minnesota in Minneapolis, said results of this analysis suggest prior blinatumomab should not be a contraindication or concern in the context of KTE-C19.
“This remains to be shown with other CAR T-cell therapies,” she said in a presentation at ASCO on cellular therapy in leukemia.
The analysis by Dr Shah and co-investigators was based on ZUMA-3 (NCT02614066), a phase 1 study including adults with relapsed/refractory ALL who received KTE-C19 at doses of 0.5, 1, or 2 x 106 cells/kg.
They excluded patients in the highest dose cohort, who were required to be blinatumomab naïve, per protocol. That left 23 patients who received 0.5 or 1 x 106 cells/kg, of whom 11 had prior blinatumomab exposure and 12 did not.
Best overall response appeared to be independent of prior blinatumomab treatment, with a CR rate of 72% overall, and 63% and 80% for blinatumomab-exposed and blinatumomab-naïve patients, respectively.
The rate of undetectable MRD was likewise high at 88% in the prior blinatumomab group and 100% in the no-blinatumomab group.
Product characteristics did not vary according to blinatumomab exposure, though there was a trend toward a more differentiated phenotype in those patients who had received prior CD19-directed treatment, he said.
There were no significant differences between groups in the rate of grade 3 or greater cytokine release syndrome. Neurologic events were higher in the blinatumomab-naïve patients, though a higher percentage of those patients received the 1 x 106 cells/kg dose, Dr Shah reported.
Investigators also looked at CAR T levels by treatment.
“We cannot appreciate any significant differences between the blinatumomab-naïve and the blinatumomab-exposed groups,” Dr Shah told ASCO attendees.
The ZUMA-3 trial was sponsored by Kite, a Gilead Company.
*Data in the abstract differ from the presentation.
CHICAGO—Prior exposure to blinatumomab does not appear to affect the successful manufacture of KTE-C19 or its efficacy in patients with relapsed/refractory acute lymphoblastic leukemia (ALL), an investigator reported at the 2018 ASCO Annual Meeting.
The clinical benefit of KTE-C19, an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, was preserved regardless of whether patients were exposed to blinatumomab, said Bijal D. Shah, MD, of Moffitt Cancer Center in Tampa, Florida.
High rates of complete response and undetectable minimal residual disease (MRD) were independent of exposure to blinatumomab, a CD19/CD3 bispecific T-cell engager.
“We feel the results of these data support KTE-C19 as an effective option for adults with refractory leukemia, regardless of prior exposure to CD19-directed therapy,” Dr Shah reported at the meeting (abstract 7006*).
The current standard of care for adults with relapsed/refractory ALL includes blinatumomab, raising the question of whether prior exposure to this CD19-directed treatment could influence the manufacture or efficacy of KTE-C19.
Sara Cooley, MD, of Masonic Medical Center, University of Minnesota in Minneapolis, said results of this analysis suggest prior blinatumomab should not be a contraindication or concern in the context of KTE-C19.
“This remains to be shown with other CAR T-cell therapies,” she said in a presentation at ASCO on cellular therapy in leukemia.
The analysis by Dr Shah and co-investigators was based on ZUMA-3 (NCT02614066), a phase 1 study including adults with relapsed/refractory ALL who received KTE-C19 at doses of 0.5, 1, or 2 x 106 cells/kg.
They excluded patients in the highest dose cohort, who were required to be blinatumomab naïve, per protocol. That left 23 patients who received 0.5 or 1 x 106 cells/kg, of whom 11 had prior blinatumomab exposure and 12 did not.
Best overall response appeared to be independent of prior blinatumomab treatment, with a CR rate of 72% overall, and 63% and 80% for blinatumomab-exposed and blinatumomab-naïve patients, respectively.
The rate of undetectable MRD was likewise high at 88% in the prior blinatumomab group and 100% in the no-blinatumomab group.
Product characteristics did not vary according to blinatumomab exposure, though there was a trend toward a more differentiated phenotype in those patients who had received prior CD19-directed treatment, he said.
There were no significant differences between groups in the rate of grade 3 or greater cytokine release syndrome. Neurologic events were higher in the blinatumomab-naïve patients, though a higher percentage of those patients received the 1 x 106 cells/kg dose, Dr Shah reported.
Investigators also looked at CAR T levels by treatment.
“We cannot appreciate any significant differences between the blinatumomab-naïve and the blinatumomab-exposed groups,” Dr Shah told ASCO attendees.
The ZUMA-3 trial was sponsored by Kite, a Gilead Company.
*Data in the abstract differ from the presentation.
CHICAGO—Prior exposure to blinatumomab does not appear to affect the successful manufacture of KTE-C19 or its efficacy in patients with relapsed/refractory acute lymphoblastic leukemia (ALL), an investigator reported at the 2018 ASCO Annual Meeting.
The clinical benefit of KTE-C19, an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, was preserved regardless of whether patients were exposed to blinatumomab, said Bijal D. Shah, MD, of Moffitt Cancer Center in Tampa, Florida.
High rates of complete response and undetectable minimal residual disease (MRD) were independent of exposure to blinatumomab, a CD19/CD3 bispecific T-cell engager.
“We feel the results of these data support KTE-C19 as an effective option for adults with refractory leukemia, regardless of prior exposure to CD19-directed therapy,” Dr Shah reported at the meeting (abstract 7006*).
The current standard of care for adults with relapsed/refractory ALL includes blinatumomab, raising the question of whether prior exposure to this CD19-directed treatment could influence the manufacture or efficacy of KTE-C19.
Sara Cooley, MD, of Masonic Medical Center, University of Minnesota in Minneapolis, said results of this analysis suggest prior blinatumomab should not be a contraindication or concern in the context of KTE-C19.
“This remains to be shown with other CAR T-cell therapies,” she said in a presentation at ASCO on cellular therapy in leukemia.
The analysis by Dr Shah and co-investigators was based on ZUMA-3 (NCT02614066), a phase 1 study including adults with relapsed/refractory ALL who received KTE-C19 at doses of 0.5, 1, or 2 x 106 cells/kg.
They excluded patients in the highest dose cohort, who were required to be blinatumomab naïve, per protocol. That left 23 patients who received 0.5 or 1 x 106 cells/kg, of whom 11 had prior blinatumomab exposure and 12 did not.
Best overall response appeared to be independent of prior blinatumomab treatment, with a CR rate of 72% overall, and 63% and 80% for blinatumomab-exposed and blinatumomab-naïve patients, respectively.
The rate of undetectable MRD was likewise high at 88% in the prior blinatumomab group and 100% in the no-blinatumomab group.
Product characteristics did not vary according to blinatumomab exposure, though there was a trend toward a more differentiated phenotype in those patients who had received prior CD19-directed treatment, he said.
There were no significant differences between groups in the rate of grade 3 or greater cytokine release syndrome. Neurologic events were higher in the blinatumomab-naïve patients, though a higher percentage of those patients received the 1 x 106 cells/kg dose, Dr Shah reported.
Investigators also looked at CAR T levels by treatment.
“We cannot appreciate any significant differences between the blinatumomab-naïve and the blinatumomab-exposed groups,” Dr Shah told ASCO attendees.
The ZUMA-3 trial was sponsored by Kite, a Gilead Company.
*Data in the abstract differ from the presentation.
Dasatinib outcomes similar to imatinib in pediatric Ph+ ALL
Dasatinib used during induction and consolidation in the Children’s Oncology Group (COG) AALL0622 trial provided early response rates for children with Ph-positive (Ph+) acute lymphoblastic leukemia (ALL), according to investigators.
But the early response rates did not improve event-free survival (EFS) compared to the use of consolidation imatinib in the AALL0031 study.
Incidence of cranial relapse was more than doubled in AALL0622 compared to AALL0031.
The investigators believe the incidence of cranial relapse may explain the results of AALL0622.
“We cannot yet conclude that the current dasatinib plus chemotherapy combination is better than imatinib plus chemotherapy,” the authors stated.
AALL0622 was designed to be an improvement on AALL0031, which demonstrated that adding the tyrosine kinase inhibitor (TKI) imatinib to intensive chemotherapy in the consolidation phase significantly improved survival for children with Ph+ ALL.
In AALL0622 dasatinib was given early in induction (day 15) and then in consolidation with the hope that patients could achieve early remission.
Another departure from AALL0031 was that cranial irradiation was not provided for control of central nervous system (CNS) metastasis. Because dasatinib accumulates in the CNS, which is a ‘sanctuary site’ for leukemia, it was presumed that patients could benefit from a TKI yet be spared from cranial irradiation.
As expected, adding dasatinib mid-induction provided a complete remission rate of 98% at the end of induction (day 29), which was better than the 89% seen in AALL0031.
In addition, more patients in AALL0622 showed minimal residual disease (MRD) <0.01% at the end of induction: 59% vs 25% in AALL0031 (P <0.001). At the end of consolidation, corresponding rates were 89% vs 71% for AALL0031.
For the primary outcome, 3-year EFS was 84.6% for patients in AALL0622 in standard-risk patients. Five-year OS and EFS rates were 86% and 60%, respectively.
In patients with overt brain metastasis (CNS3 status), 5-year CNS relapse was 15% for patients in the AALL0622 study vs 6.6% for patients in the AALL031 study.
However, 5-year OS rates were similar in the two groups of patients: 86% for AALL0622 vs 81% for AALL0031.
HSCT
AALL0622 allowed the use of hematopoietic stem cell transplantation (HSCT) in high-risk patients as well as in standard-risk patients with a sibling donor.
Five-year OS and EFS for standard-risk patients (19% underwent HSCT at first remission) and high-risk patients (91% underwent HSCT in first remission) were similar.
Children who did not undergo HSCT had a similar 5-year OS of 88%, which suggested that children with Ph+ ALL should not undergo transplantation at first remission.
Samples from a subset of patients was analyzed for IKZF1 mutations and correlated with outcomes.
Five-year OS was 80% in those harboring the mutation versus 100% who had the wild-type gene (P=0.04); 4-year EFS was also significantly lower—10% vs 82% (P=0.04).
Screening for IKZF1 may be used to identify high-risk patients suitable for HSCT and/or alternate treatment, the authors note.
The investigators reported their findings in The Journal of Clinical Oncology.
Dasatinib used during induction and consolidation in the Children’s Oncology Group (COG) AALL0622 trial provided early response rates for children with Ph-positive (Ph+) acute lymphoblastic leukemia (ALL), according to investigators.
But the early response rates did not improve event-free survival (EFS) compared to the use of consolidation imatinib in the AALL0031 study.
Incidence of cranial relapse was more than doubled in AALL0622 compared to AALL0031.
The investigators believe the incidence of cranial relapse may explain the results of AALL0622.
“We cannot yet conclude that the current dasatinib plus chemotherapy combination is better than imatinib plus chemotherapy,” the authors stated.
AALL0622 was designed to be an improvement on AALL0031, which demonstrated that adding the tyrosine kinase inhibitor (TKI) imatinib to intensive chemotherapy in the consolidation phase significantly improved survival for children with Ph+ ALL.
In AALL0622 dasatinib was given early in induction (day 15) and then in consolidation with the hope that patients could achieve early remission.
Another departure from AALL0031 was that cranial irradiation was not provided for control of central nervous system (CNS) metastasis. Because dasatinib accumulates in the CNS, which is a ‘sanctuary site’ for leukemia, it was presumed that patients could benefit from a TKI yet be spared from cranial irradiation.
As expected, adding dasatinib mid-induction provided a complete remission rate of 98% at the end of induction (day 29), which was better than the 89% seen in AALL0031.
In addition, more patients in AALL0622 showed minimal residual disease (MRD) <0.01% at the end of induction: 59% vs 25% in AALL0031 (P <0.001). At the end of consolidation, corresponding rates were 89% vs 71% for AALL0031.
For the primary outcome, 3-year EFS was 84.6% for patients in AALL0622 in standard-risk patients. Five-year OS and EFS rates were 86% and 60%, respectively.
In patients with overt brain metastasis (CNS3 status), 5-year CNS relapse was 15% for patients in the AALL0622 study vs 6.6% for patients in the AALL031 study.
However, 5-year OS rates were similar in the two groups of patients: 86% for AALL0622 vs 81% for AALL0031.
HSCT
AALL0622 allowed the use of hematopoietic stem cell transplantation (HSCT) in high-risk patients as well as in standard-risk patients with a sibling donor.
Five-year OS and EFS for standard-risk patients (19% underwent HSCT at first remission) and high-risk patients (91% underwent HSCT in first remission) were similar.
Children who did not undergo HSCT had a similar 5-year OS of 88%, which suggested that children with Ph+ ALL should not undergo transplantation at first remission.
Samples from a subset of patients was analyzed for IKZF1 mutations and correlated with outcomes.
Five-year OS was 80% in those harboring the mutation versus 100% who had the wild-type gene (P=0.04); 4-year EFS was also significantly lower—10% vs 82% (P=0.04).
Screening for IKZF1 may be used to identify high-risk patients suitable for HSCT and/or alternate treatment, the authors note.
The investigators reported their findings in The Journal of Clinical Oncology.
Dasatinib used during induction and consolidation in the Children’s Oncology Group (COG) AALL0622 trial provided early response rates for children with Ph-positive (Ph+) acute lymphoblastic leukemia (ALL), according to investigators.
But the early response rates did not improve event-free survival (EFS) compared to the use of consolidation imatinib in the AALL0031 study.
Incidence of cranial relapse was more than doubled in AALL0622 compared to AALL0031.
The investigators believe the incidence of cranial relapse may explain the results of AALL0622.
“We cannot yet conclude that the current dasatinib plus chemotherapy combination is better than imatinib plus chemotherapy,” the authors stated.
AALL0622 was designed to be an improvement on AALL0031, which demonstrated that adding the tyrosine kinase inhibitor (TKI) imatinib to intensive chemotherapy in the consolidation phase significantly improved survival for children with Ph+ ALL.
In AALL0622 dasatinib was given early in induction (day 15) and then in consolidation with the hope that patients could achieve early remission.
Another departure from AALL0031 was that cranial irradiation was not provided for control of central nervous system (CNS) metastasis. Because dasatinib accumulates in the CNS, which is a ‘sanctuary site’ for leukemia, it was presumed that patients could benefit from a TKI yet be spared from cranial irradiation.
As expected, adding dasatinib mid-induction provided a complete remission rate of 98% at the end of induction (day 29), which was better than the 89% seen in AALL0031.
In addition, more patients in AALL0622 showed minimal residual disease (MRD) <0.01% at the end of induction: 59% vs 25% in AALL0031 (P <0.001). At the end of consolidation, corresponding rates were 89% vs 71% for AALL0031.
For the primary outcome, 3-year EFS was 84.6% for patients in AALL0622 in standard-risk patients. Five-year OS and EFS rates were 86% and 60%, respectively.
In patients with overt brain metastasis (CNS3 status), 5-year CNS relapse was 15% for patients in the AALL0622 study vs 6.6% for patients in the AALL031 study.
However, 5-year OS rates were similar in the two groups of patients: 86% for AALL0622 vs 81% for AALL0031.
HSCT
AALL0622 allowed the use of hematopoietic stem cell transplantation (HSCT) in high-risk patients as well as in standard-risk patients with a sibling donor.
Five-year OS and EFS for standard-risk patients (19% underwent HSCT at first remission) and high-risk patients (91% underwent HSCT in first remission) were similar.
Children who did not undergo HSCT had a similar 5-year OS of 88%, which suggested that children with Ph+ ALL should not undergo transplantation at first remission.
Samples from a subset of patients was analyzed for IKZF1 mutations and correlated with outcomes.
Five-year OS was 80% in those harboring the mutation versus 100% who had the wild-type gene (P=0.04); 4-year EFS was also significantly lower—10% vs 82% (P=0.04).
Screening for IKZF1 may be used to identify high-risk patients suitable for HSCT and/or alternate treatment, the authors note.
The investigators reported their findings in The Journal of Clinical Oncology.
MRD-negative status signals better outcomes in CAR T–treated ALL
CHICAGO – Minimal residual disease (MRD)–negative complete remission was strongly associated with improved survival outcomes in patients with B-cell acute lymphocytic leukemia (ALL) who received CD19 chimeric antigen receptor (CAR) T cells, results of a retrospective study showed.
Allogeneic hematopoietic stem cell transplant (HSCT) appeared to improve both disease-free and overall survival in those patients who had achieved MRD-negative complete remission, according to results of the study, which were presented at the annual meeting of the American Society of Clinical Oncology.
“Based upon our interaction testing, the potential benefit [of transplant] appears to exist in both good-risk and bad-risk patients as identified through multivariate modeling,” said study investigator Kevin Anthony Hay, MD, of Fred Hutchinson Cancer Research Center, Seattle.
In a comment on the results, Sarah Cooley, MD, noted that the benefits of allogeneic transplant were apparent regardless of whether the patients met criteria for the good-risk subgroup, which was defined by levels of lactate dehydrogenase (LDH) and platelets along with exposure to fludarabine as part of the conditioning regimen.
“I think this suggests that the goal at this point is to get patients to an MRD-negative state and to potentially curative transplant,” said Dr. Cooley, director of investigator-initiated research at Masonic Medical Center at the University of Minnesota, Minneapolis.
The retrospective analysis by Dr. Hay and his colleagues included 53 adults with relapsed or refractory ALL who had bone marrow or extramedullary disease at baseline and had received CD19 CAR T cells at or under the maximum tolerated dose at least 1 year prior to this analysis. Of that group, 45 (85%) achieved MRD-negative complete remission.
Those patients who did achieve MRD-negative complete remission had an improved median disease-free survival at 7.6 months versus 0.8 months (P less than .0001) and improved overall survival at 20.0 months versus 5.0 months (P = 0.014).
Most of the MRD-negative patients who relapsed did so within the first 6 months, an observation that led investigators to consider whether factors exist that could predict better outcomes.
In a multivariate analysis, they found three variables associated with disease free survival: higher LDH prior to lymphodepletion (hazard ratio, 1.39), along with higher platelet count prior to lymphodepletion and incorporation of fludarabine into the regimen, with hazard ratios of 0.65 and 0.34, respectively.
Using those three characteristics, investigators grouped patients as “good risk” if they had normal LDH, platelet count at or above 100 prior to lymphodepletion that included fludarabine. The 24-month disease-free survival for good-risk patients was 78%, and overall survival was 86%.
The role of allogeneic HSCT after ALL patients achieved MRD-negative complete remission with CAR T-cell therapy was one of the “major questions in the field,” Dr. Hay said.
In this analysis, Dr. Hay and colleagues found that patients who underwent transplant in MRD-negative complete remission had a 24-month disease free survival and overall survival of 61% and 72%, respectively, both of which were significantly higher than in patients with MRD-negative complete remission who had no transplant.
The disease-free survival benefit was not specific to the good-risk group, according to Dr. Hay, who said an interaction test demonstrated no significant interaction between risk group and allogeneic HSCT after CAR T-cell infusion (P = 0.53).
“This is a very important finding that should be further [studied] in an appropriately designed clinical trial,” Dr. Hay said during an oral presentation of the study results.
Dr. Hay and several coauthors reported financial disclosures related to Juno Therapeutics. Other disclosures reported by study coauthors included Cell Medica, Celgene, Eureka Therapeutics, Genentech/Roche, Gilead Sciences, Kite Pharma, Novartis, and others.
SOURCE: Hay KA. ASCO 2018, Abstract 7005.
CHICAGO – Minimal residual disease (MRD)–negative complete remission was strongly associated with improved survival outcomes in patients with B-cell acute lymphocytic leukemia (ALL) who received CD19 chimeric antigen receptor (CAR) T cells, results of a retrospective study showed.
Allogeneic hematopoietic stem cell transplant (HSCT) appeared to improve both disease-free and overall survival in those patients who had achieved MRD-negative complete remission, according to results of the study, which were presented at the annual meeting of the American Society of Clinical Oncology.
“Based upon our interaction testing, the potential benefit [of transplant] appears to exist in both good-risk and bad-risk patients as identified through multivariate modeling,” said study investigator Kevin Anthony Hay, MD, of Fred Hutchinson Cancer Research Center, Seattle.
In a comment on the results, Sarah Cooley, MD, noted that the benefits of allogeneic transplant were apparent regardless of whether the patients met criteria for the good-risk subgroup, which was defined by levels of lactate dehydrogenase (LDH) and platelets along with exposure to fludarabine as part of the conditioning regimen.
“I think this suggests that the goal at this point is to get patients to an MRD-negative state and to potentially curative transplant,” said Dr. Cooley, director of investigator-initiated research at Masonic Medical Center at the University of Minnesota, Minneapolis.
The retrospective analysis by Dr. Hay and his colleagues included 53 adults with relapsed or refractory ALL who had bone marrow or extramedullary disease at baseline and had received CD19 CAR T cells at or under the maximum tolerated dose at least 1 year prior to this analysis. Of that group, 45 (85%) achieved MRD-negative complete remission.
Those patients who did achieve MRD-negative complete remission had an improved median disease-free survival at 7.6 months versus 0.8 months (P less than .0001) and improved overall survival at 20.0 months versus 5.0 months (P = 0.014).
Most of the MRD-negative patients who relapsed did so within the first 6 months, an observation that led investigators to consider whether factors exist that could predict better outcomes.
In a multivariate analysis, they found three variables associated with disease free survival: higher LDH prior to lymphodepletion (hazard ratio, 1.39), along with higher platelet count prior to lymphodepletion and incorporation of fludarabine into the regimen, with hazard ratios of 0.65 and 0.34, respectively.
Using those three characteristics, investigators grouped patients as “good risk” if they had normal LDH, platelet count at or above 100 prior to lymphodepletion that included fludarabine. The 24-month disease-free survival for good-risk patients was 78%, and overall survival was 86%.
The role of allogeneic HSCT after ALL patients achieved MRD-negative complete remission with CAR T-cell therapy was one of the “major questions in the field,” Dr. Hay said.
In this analysis, Dr. Hay and colleagues found that patients who underwent transplant in MRD-negative complete remission had a 24-month disease free survival and overall survival of 61% and 72%, respectively, both of which were significantly higher than in patients with MRD-negative complete remission who had no transplant.
The disease-free survival benefit was not specific to the good-risk group, according to Dr. Hay, who said an interaction test demonstrated no significant interaction between risk group and allogeneic HSCT after CAR T-cell infusion (P = 0.53).
“This is a very important finding that should be further [studied] in an appropriately designed clinical trial,” Dr. Hay said during an oral presentation of the study results.
Dr. Hay and several coauthors reported financial disclosures related to Juno Therapeutics. Other disclosures reported by study coauthors included Cell Medica, Celgene, Eureka Therapeutics, Genentech/Roche, Gilead Sciences, Kite Pharma, Novartis, and others.
SOURCE: Hay KA. ASCO 2018, Abstract 7005.
CHICAGO – Minimal residual disease (MRD)–negative complete remission was strongly associated with improved survival outcomes in patients with B-cell acute lymphocytic leukemia (ALL) who received CD19 chimeric antigen receptor (CAR) T cells, results of a retrospective study showed.
Allogeneic hematopoietic stem cell transplant (HSCT) appeared to improve both disease-free and overall survival in those patients who had achieved MRD-negative complete remission, according to results of the study, which were presented at the annual meeting of the American Society of Clinical Oncology.
“Based upon our interaction testing, the potential benefit [of transplant] appears to exist in both good-risk and bad-risk patients as identified through multivariate modeling,” said study investigator Kevin Anthony Hay, MD, of Fred Hutchinson Cancer Research Center, Seattle.
In a comment on the results, Sarah Cooley, MD, noted that the benefits of allogeneic transplant were apparent regardless of whether the patients met criteria for the good-risk subgroup, which was defined by levels of lactate dehydrogenase (LDH) and platelets along with exposure to fludarabine as part of the conditioning regimen.
“I think this suggests that the goal at this point is to get patients to an MRD-negative state and to potentially curative transplant,” said Dr. Cooley, director of investigator-initiated research at Masonic Medical Center at the University of Minnesota, Minneapolis.
The retrospective analysis by Dr. Hay and his colleagues included 53 adults with relapsed or refractory ALL who had bone marrow or extramedullary disease at baseline and had received CD19 CAR T cells at or under the maximum tolerated dose at least 1 year prior to this analysis. Of that group, 45 (85%) achieved MRD-negative complete remission.
Those patients who did achieve MRD-negative complete remission had an improved median disease-free survival at 7.6 months versus 0.8 months (P less than .0001) and improved overall survival at 20.0 months versus 5.0 months (P = 0.014).
Most of the MRD-negative patients who relapsed did so within the first 6 months, an observation that led investigators to consider whether factors exist that could predict better outcomes.
In a multivariate analysis, they found three variables associated with disease free survival: higher LDH prior to lymphodepletion (hazard ratio, 1.39), along with higher platelet count prior to lymphodepletion and incorporation of fludarabine into the regimen, with hazard ratios of 0.65 and 0.34, respectively.
Using those three characteristics, investigators grouped patients as “good risk” if they had normal LDH, platelet count at or above 100 prior to lymphodepletion that included fludarabine. The 24-month disease-free survival for good-risk patients was 78%, and overall survival was 86%.
The role of allogeneic HSCT after ALL patients achieved MRD-negative complete remission with CAR T-cell therapy was one of the “major questions in the field,” Dr. Hay said.
In this analysis, Dr. Hay and colleagues found that patients who underwent transplant in MRD-negative complete remission had a 24-month disease free survival and overall survival of 61% and 72%, respectively, both of which were significantly higher than in patients with MRD-negative complete remission who had no transplant.
The disease-free survival benefit was not specific to the good-risk group, according to Dr. Hay, who said an interaction test demonstrated no significant interaction between risk group and allogeneic HSCT after CAR T-cell infusion (P = 0.53).
“This is a very important finding that should be further [studied] in an appropriately designed clinical trial,” Dr. Hay said during an oral presentation of the study results.
Dr. Hay and several coauthors reported financial disclosures related to Juno Therapeutics. Other disclosures reported by study coauthors included Cell Medica, Celgene, Eureka Therapeutics, Genentech/Roche, Gilead Sciences, Kite Pharma, Novartis, and others.
SOURCE: Hay KA. ASCO 2018, Abstract 7005.
REPORTING FROM ASCO 2018
Key clinical point:
Major finding: Patients who achieved MRD-negative complete remission had an improved median disease-free survival at 7.6 months versus 0.8 months (P less than .0001)
Study details: A retrospective analysis including 53 patients with ALL who had bone marrow or extramedullary disease at baseline and had received CD19 CAR T cells at or under the maximum tolerated dose at least 1 year prior to this analysis.
Disclosures: Researchers reported financial ties to Juno Therapeutics, Cell Medica, Celgene, Eureka Therapeutics, Genentech/Roche, Gilead Sciences, Kite Pharma, Novartis, and others.
Source: Hay KA. ASCO 2018, Abstract 7005.
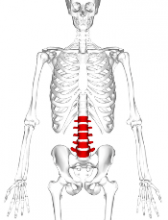
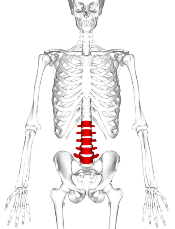
VF incidence increases significantly in kids after ALL treatment
A 6-year prospective study from the Canadian STOPP investigators revealed that following treatment for acute lymphoblastic leukemia (ALL), approximately 1 out of 3 children experiences vertebral fractures (VF) and 1 out of 5 children shows non-VF.
Glucocorticoid use and vertebral fractures at diagnosis emerged as significant predictive factors.
Investigators reported a cumulative incidence of 32.5% for vertebral fractures (VF) following treatment and 23.0% for non-VF after 6 years.
Thirty-nine percent of children with VF were asymptomatic.
“The osteotoxicity of leukemia and its treatment are underscored by the observation that the non-VF incidence was more than 2.5 times higher than the general pediatric population,” the study authors wrote, “whereas the VF incidence was increased more than 2000 times.”
The STOPP investigators—the Steroid-Associated Osteoporosis in the Pediatric Population Consortium—published their findings in the Journal of Bone and Mineral Research.
To document the incidence and predictors of fractures and profile who is at greatest risk, the STOPP investigators enrolled 186 children who were diagnosed and treated at 10 children’s hospitals across Canada between 2005 and 2007.
Median age at diagnosis was 5.3 years, median duration of follow-up was 6 years, and 38.1% were boys.
Approximately 4 out of 5 children were treated with Children’s Oncology Group protocols and 1 out of 5 was treated with the Dana-Farber protocols.
In girls, glucocorticoid exposure was 7.0 g/m2 and in boys it was 8.9 g/m2.
The entire cohort received 54.3% of the total cumulative glucocorticoid dose in the first year and 83.1% in the second year.
For VF, incidence at baseline was 15.1%. Skeletal fractures at any site were reported in 36% of the children over the 6-year period, 71% occurring during the first 2 years. No VF was reported in the sixth year.
Of 38 children with VF, 32 sustained at least 1 VF in the first 2 years and 77% occurred while on therapy or within 6 months of the last glucocorticoid dose. None of the children had disease relapse.
Non-VF were reported in 1.6% of children at baseline; incidence peaked at years 2 (5.4%) and 5 (4.8%) and none occurred in the sixth year.
Thirty-one non-VFs were reported in 26 children; 18 occurred in the first 2 years and 23 occurred on therapy or within 6 months of the last glucocorticoid dose.
The STOPP investigators showed that glucocorticoid exposure, VF, and low spine bone mineral density Z-scores at baseline were significant predictors for risk of VF.
“[This] observation suggests the importance of baseline spine phenotype (both VF and low lumbar spine bone mineral density) in signaling the potential for future bone morbidity,” the STOPP investigators note.
“In revealing that vertebral fractures are frequent in children with ALL on chemotherapy, and that older children and those with more severe collapse are at risk for residual vertebral deformities, strategies to prevent vertebral fractures in those at greatest risk for permanent sequelae now merit further study,” said lead author Leanne Ward, MD, of the University of Ottawa, Canada, in a statement.
The study was primarily supported by an operating grant from the Canadian Institutes for Health Research (CIHR) with additional funding from a CIHR New Investigator Award, a Canadian Child Health Clinician Scientist Career Enhancement Award, a University of Ottawa Research Chair Award, a Children’s Hospital of Eastern Ontario (CHEO) Research Institute Capacity Building Award, and the CHEO Departments of Pediatrics and Surgery. This work was also supported by the University of Alberta Women and Children’s Health Research Institute.
A 6-year prospective study from the Canadian STOPP investigators revealed that following treatment for acute lymphoblastic leukemia (ALL), approximately 1 out of 3 children experiences vertebral fractures (VF) and 1 out of 5 children shows non-VF.
Glucocorticoid use and vertebral fractures at diagnosis emerged as significant predictive factors.
Investigators reported a cumulative incidence of 32.5% for vertebral fractures (VF) following treatment and 23.0% for non-VF after 6 years.
Thirty-nine percent of children with VF were asymptomatic.
“The osteotoxicity of leukemia and its treatment are underscored by the observation that the non-VF incidence was more than 2.5 times higher than the general pediatric population,” the study authors wrote, “whereas the VF incidence was increased more than 2000 times.”
The STOPP investigators—the Steroid-Associated Osteoporosis in the Pediatric Population Consortium—published their findings in the Journal of Bone and Mineral Research.
To document the incidence and predictors of fractures and profile who is at greatest risk, the STOPP investigators enrolled 186 children who were diagnosed and treated at 10 children’s hospitals across Canada between 2005 and 2007.
Median age at diagnosis was 5.3 years, median duration of follow-up was 6 years, and 38.1% were boys.
Approximately 4 out of 5 children were treated with Children’s Oncology Group protocols and 1 out of 5 was treated with the Dana-Farber protocols.
In girls, glucocorticoid exposure was 7.0 g/m2 and in boys it was 8.9 g/m2.
The entire cohort received 54.3% of the total cumulative glucocorticoid dose in the first year and 83.1% in the second year.
For VF, incidence at baseline was 15.1%. Skeletal fractures at any site were reported in 36% of the children over the 6-year period, 71% occurring during the first 2 years. No VF was reported in the sixth year.
Of 38 children with VF, 32 sustained at least 1 VF in the first 2 years and 77% occurred while on therapy or within 6 months of the last glucocorticoid dose. None of the children had disease relapse.
Non-VF were reported in 1.6% of children at baseline; incidence peaked at years 2 (5.4%) and 5 (4.8%) and none occurred in the sixth year.
Thirty-one non-VFs were reported in 26 children; 18 occurred in the first 2 years and 23 occurred on therapy or within 6 months of the last glucocorticoid dose.
The STOPP investigators showed that glucocorticoid exposure, VF, and low spine bone mineral density Z-scores at baseline were significant predictors for risk of VF.
“[This] observation suggests the importance of baseline spine phenotype (both VF and low lumbar spine bone mineral density) in signaling the potential for future bone morbidity,” the STOPP investigators note.
“In revealing that vertebral fractures are frequent in children with ALL on chemotherapy, and that older children and those with more severe collapse are at risk for residual vertebral deformities, strategies to prevent vertebral fractures in those at greatest risk for permanent sequelae now merit further study,” said lead author Leanne Ward, MD, of the University of Ottawa, Canada, in a statement.
The study was primarily supported by an operating grant from the Canadian Institutes for Health Research (CIHR) with additional funding from a CIHR New Investigator Award, a Canadian Child Health Clinician Scientist Career Enhancement Award, a University of Ottawa Research Chair Award, a Children’s Hospital of Eastern Ontario (CHEO) Research Institute Capacity Building Award, and the CHEO Departments of Pediatrics and Surgery. This work was also supported by the University of Alberta Women and Children’s Health Research Institute.
A 6-year prospective study from the Canadian STOPP investigators revealed that following treatment for acute lymphoblastic leukemia (ALL), approximately 1 out of 3 children experiences vertebral fractures (VF) and 1 out of 5 children shows non-VF.
Glucocorticoid use and vertebral fractures at diagnosis emerged as significant predictive factors.
Investigators reported a cumulative incidence of 32.5% for vertebral fractures (VF) following treatment and 23.0% for non-VF after 6 years.
Thirty-nine percent of children with VF were asymptomatic.
“The osteotoxicity of leukemia and its treatment are underscored by the observation that the non-VF incidence was more than 2.5 times higher than the general pediatric population,” the study authors wrote, “whereas the VF incidence was increased more than 2000 times.”
The STOPP investigators—the Steroid-Associated Osteoporosis in the Pediatric Population Consortium—published their findings in the Journal of Bone and Mineral Research.
To document the incidence and predictors of fractures and profile who is at greatest risk, the STOPP investigators enrolled 186 children who were diagnosed and treated at 10 children’s hospitals across Canada between 2005 and 2007.
Median age at diagnosis was 5.3 years, median duration of follow-up was 6 years, and 38.1% were boys.
Approximately 4 out of 5 children were treated with Children’s Oncology Group protocols and 1 out of 5 was treated with the Dana-Farber protocols.
In girls, glucocorticoid exposure was 7.0 g/m2 and in boys it was 8.9 g/m2.
The entire cohort received 54.3% of the total cumulative glucocorticoid dose in the first year and 83.1% in the second year.
For VF, incidence at baseline was 15.1%. Skeletal fractures at any site were reported in 36% of the children over the 6-year period, 71% occurring during the first 2 years. No VF was reported in the sixth year.
Of 38 children with VF, 32 sustained at least 1 VF in the first 2 years and 77% occurred while on therapy or within 6 months of the last glucocorticoid dose. None of the children had disease relapse.
Non-VF were reported in 1.6% of children at baseline; incidence peaked at years 2 (5.4%) and 5 (4.8%) and none occurred in the sixth year.
Thirty-one non-VFs were reported in 26 children; 18 occurred in the first 2 years and 23 occurred on therapy or within 6 months of the last glucocorticoid dose.
The STOPP investigators showed that glucocorticoid exposure, VF, and low spine bone mineral density Z-scores at baseline were significant predictors for risk of VF.
“[This] observation suggests the importance of baseline spine phenotype (both VF and low lumbar spine bone mineral density) in signaling the potential for future bone morbidity,” the STOPP investigators note.
“In revealing that vertebral fractures are frequent in children with ALL on chemotherapy, and that older children and those with more severe collapse are at risk for residual vertebral deformities, strategies to prevent vertebral fractures in those at greatest risk for permanent sequelae now merit further study,” said lead author Leanne Ward, MD, of the University of Ottawa, Canada, in a statement.
The study was primarily supported by an operating grant from the Canadian Institutes for Health Research (CIHR) with additional funding from a CIHR New Investigator Award, a Canadian Child Health Clinician Scientist Career Enhancement Award, a University of Ottawa Research Chair Award, a Children’s Hospital of Eastern Ontario (CHEO) Research Institute Capacity Building Award, and the CHEO Departments of Pediatrics and Surgery. This work was also supported by the University of Alberta Women and Children’s Health Research Institute.
Early infection could prevent ALL, doc says
Childhood acute lymphoblastic leukemia (ALL) may be preventable, according to a researcher.
Mel Greaves, PhD, of The Institute of Cancer Research in London, UK, reviewed more than 30 years of research and concluded that ALL develops in 2 steps—genetic mutation before birth and further genetic change after birth triggered by infection.
The evidence suggests that infection early in life is beneficial to prime the immune system, but later infection without earlier priming can trigger ALL.
So priming the immune system in the first year of life could potentially prevent childhood ALL, according to Dr Greaves.
He outlined this theory in Nature Reviews Cancer.
Dr Greaves compiled more than 30 years of research into genetics, cell biology, immunology, epidemiology, and animal modelling of ALL.
The evidence led him to conclude that ALL begins with a genetic mutation that occurs before birth and predisposes a child to leukemia.
The disease is triggered later, in childhood, by exposure to one or more common infections. This primarily occurs in children who experienced “clean” childhoods in their first year of life, without much interaction with other infants or older children.
Dr Greaves challenged previous reports of possible environmental causes for ALL, such as ionizing radiation, electromagnetic waves, or man-made chemicals. He argued that none of these reports are supported by robust evidence.
Instead, he believes there is strong evidence suggesting that infection later in childhood, in the absence of earlier priming, can trigger ALL.
Dr Greaves’ studies of identical twins with ALL showed that 2 mutations were required for ALL development. The first arises in one twin in the womb but produces a population of pre-malignant cells that spread to the other twin via their shared blood supply. The second mutation arises after birth and is different in the twins.
Population studies and animal experiments suggest this second genetic hit can be triggered by infection, probably by a range of common viruses and bacteria. In one unique cluster of cases investigated by Dr Greaves and his colleagues, all cases were infected with flu virus.
In other work, researchers engineered mice with an active leukemia-initiating gene. When the team moved the mice from an ultra-clean, germ-free environment to one that had common microbes, the mice developed ALL.
Population studies have indicated that early exposure to infection in infancy, such as via day care attendance and breast feeding, can protect against ALL, probably by priming the immune system. This suggests childhood ALL may be preventable.
Dr Greaves is now investigating whether earlier exposure to harmless microbes could prevent leukemia in mice.
“I have spent more than 40 years researching childhood leukemia, and, over that time, there has been huge progress in our understanding of its biology and its treatment . . . ,” Dr Greaves said. “But it has always struck me that something big was missing, a gap in our knowledge [that failed to explain] why or how otherwise healthy children develop leukemia and whether this cancer is preventable.”
“This body of research is a culmination of decades of work and at last provides a credible explanation for how the major type of childhood leukemia develops. The research strongly suggests that ALL has a clear biological cause and is triggered by a variety of infections in predisposed children whose immune systems have not been properly primed. It also busts some persistent myths about the causes of leukemia, such as the damaging but unsubstantiated claims that the disease is commonly caused by exposure to electro-magnetic waves or pollution.”
“I hope this research will have a real impact on the lives of children. The most important implication is that most cases of childhood leukemia are likely to be preventable. It might be done in the same way that is currently under consideration for autoimmune disease or allergies, perhaps with simple and safe interventions to expose infants to a variety of common and harmless ‘bugs.’”
Childhood acute lymphoblastic leukemia (ALL) may be preventable, according to a researcher.
Mel Greaves, PhD, of The Institute of Cancer Research in London, UK, reviewed more than 30 years of research and concluded that ALL develops in 2 steps—genetic mutation before birth and further genetic change after birth triggered by infection.
The evidence suggests that infection early in life is beneficial to prime the immune system, but later infection without earlier priming can trigger ALL.
So priming the immune system in the first year of life could potentially prevent childhood ALL, according to Dr Greaves.
He outlined this theory in Nature Reviews Cancer.
Dr Greaves compiled more than 30 years of research into genetics, cell biology, immunology, epidemiology, and animal modelling of ALL.
The evidence led him to conclude that ALL begins with a genetic mutation that occurs before birth and predisposes a child to leukemia.
The disease is triggered later, in childhood, by exposure to one or more common infections. This primarily occurs in children who experienced “clean” childhoods in their first year of life, without much interaction with other infants or older children.
Dr Greaves challenged previous reports of possible environmental causes for ALL, such as ionizing radiation, electromagnetic waves, or man-made chemicals. He argued that none of these reports are supported by robust evidence.
Instead, he believes there is strong evidence suggesting that infection later in childhood, in the absence of earlier priming, can trigger ALL.
Dr Greaves’ studies of identical twins with ALL showed that 2 mutations were required for ALL development. The first arises in one twin in the womb but produces a population of pre-malignant cells that spread to the other twin via their shared blood supply. The second mutation arises after birth and is different in the twins.
Population studies and animal experiments suggest this second genetic hit can be triggered by infection, probably by a range of common viruses and bacteria. In one unique cluster of cases investigated by Dr Greaves and his colleagues, all cases were infected with flu virus.
In other work, researchers engineered mice with an active leukemia-initiating gene. When the team moved the mice from an ultra-clean, germ-free environment to one that had common microbes, the mice developed ALL.
Population studies have indicated that early exposure to infection in infancy, such as via day care attendance and breast feeding, can protect against ALL, probably by priming the immune system. This suggests childhood ALL may be preventable.
Dr Greaves is now investigating whether earlier exposure to harmless microbes could prevent leukemia in mice.
“I have spent more than 40 years researching childhood leukemia, and, over that time, there has been huge progress in our understanding of its biology and its treatment . . . ,” Dr Greaves said. “But it has always struck me that something big was missing, a gap in our knowledge [that failed to explain] why or how otherwise healthy children develop leukemia and whether this cancer is preventable.”
“This body of research is a culmination of decades of work and at last provides a credible explanation for how the major type of childhood leukemia develops. The research strongly suggests that ALL has a clear biological cause and is triggered by a variety of infections in predisposed children whose immune systems have not been properly primed. It also busts some persistent myths about the causes of leukemia, such as the damaging but unsubstantiated claims that the disease is commonly caused by exposure to electro-magnetic waves or pollution.”
“I hope this research will have a real impact on the lives of children. The most important implication is that most cases of childhood leukemia are likely to be preventable. It might be done in the same way that is currently under consideration for autoimmune disease or allergies, perhaps with simple and safe interventions to expose infants to a variety of common and harmless ‘bugs.’”
Childhood acute lymphoblastic leukemia (ALL) may be preventable, according to a researcher.
Mel Greaves, PhD, of The Institute of Cancer Research in London, UK, reviewed more than 30 years of research and concluded that ALL develops in 2 steps—genetic mutation before birth and further genetic change after birth triggered by infection.
The evidence suggests that infection early in life is beneficial to prime the immune system, but later infection without earlier priming can trigger ALL.
So priming the immune system in the first year of life could potentially prevent childhood ALL, according to Dr Greaves.
He outlined this theory in Nature Reviews Cancer.
Dr Greaves compiled more than 30 years of research into genetics, cell biology, immunology, epidemiology, and animal modelling of ALL.
The evidence led him to conclude that ALL begins with a genetic mutation that occurs before birth and predisposes a child to leukemia.
The disease is triggered later, in childhood, by exposure to one or more common infections. This primarily occurs in children who experienced “clean” childhoods in their first year of life, without much interaction with other infants or older children.
Dr Greaves challenged previous reports of possible environmental causes for ALL, such as ionizing radiation, electromagnetic waves, or man-made chemicals. He argued that none of these reports are supported by robust evidence.
Instead, he believes there is strong evidence suggesting that infection later in childhood, in the absence of earlier priming, can trigger ALL.
Dr Greaves’ studies of identical twins with ALL showed that 2 mutations were required for ALL development. The first arises in one twin in the womb but produces a population of pre-malignant cells that spread to the other twin via their shared blood supply. The second mutation arises after birth and is different in the twins.
Population studies and animal experiments suggest this second genetic hit can be triggered by infection, probably by a range of common viruses and bacteria. In one unique cluster of cases investigated by Dr Greaves and his colleagues, all cases were infected with flu virus.
In other work, researchers engineered mice with an active leukemia-initiating gene. When the team moved the mice from an ultra-clean, germ-free environment to one that had common microbes, the mice developed ALL.
Population studies have indicated that early exposure to infection in infancy, such as via day care attendance and breast feeding, can protect against ALL, probably by priming the immune system. This suggests childhood ALL may be preventable.
Dr Greaves is now investigating whether earlier exposure to harmless microbes could prevent leukemia in mice.
“I have spent more than 40 years researching childhood leukemia, and, over that time, there has been huge progress in our understanding of its biology and its treatment . . . ,” Dr Greaves said. “But it has always struck me that something big was missing, a gap in our knowledge [that failed to explain] why or how otherwise healthy children develop leukemia and whether this cancer is preventable.”
“This body of research is a culmination of decades of work and at last provides a credible explanation for how the major type of childhood leukemia develops. The research strongly suggests that ALL has a clear biological cause and is triggered by a variety of infections in predisposed children whose immune systems have not been properly primed. It also busts some persistent myths about the causes of leukemia, such as the damaging but unsubstantiated claims that the disease is commonly caused by exposure to electro-magnetic waves or pollution.”
“I hope this research will have a real impact on the lives of children. The most important implication is that most cases of childhood leukemia are likely to be preventable. It might be done in the same way that is currently under consideration for autoimmune disease or allergies, perhaps with simple and safe interventions to expose infants to a variety of common and harmless ‘bugs.’”
New regimens for youth with T-cell malignancies yield best outcomes yet
A set of novel chemotherapy regimens yield excellent outcomes—the best yet—among pediatric and young adult patients with T-cell malignancies, finds a phase 3 randomized controlled trial conducted by the Children’s Oncology Group (ALL0434).
“Despite very intense and complex chemotherapy, 20% of children and adolescents enrolled in Children’s Oncology Group T-cell leukemia trials between 2000 and 2005 did not survive. New drugs were needed to improve survival rates for T-cell malignancies,” lead study author Kimberly P. Dunsmore, MD, a professor at Virginia Tech, Roanoke, said in a press briefing leading up to the annual meeting of the American Society of Clinical Oncology.
The ALL0434 trial tested the addition of methotrexate (Trexall) and/or nelarabine (Arranon), a T cell–specific drug known to be efficacious in relapsed disease, to standard chemotherapy, with tailoring of the regimen to recurrence risk. Analyses were based on 1,545 patients with T-cell acute lymphoblastic leukemia (T-ALL) or T-cell lymphoblastic lymphoma (T-LL).
Results for all patients with T-ALL showed that, with addition of either or both drugs, more than 90% were alive at 4 years and more than 80% were leukemia free. Adding nelarabine to standard chemotherapy improved disease-free survival among the subset having intermediate- or high-risk disease, and the best outcomes were seen with addition of both nelarabine and an escalating dose of methotrexate.
Although patients with T-LL did not see benefit from addition of nelarabine, they still had an 85% rate of overall survival at 4 years.
“ALL0434 is the largest trial for children and young adults with T-cell malignancy ever conducted. It has the best-ever survival data,” Dr. Dunsmore commented.
“Our next steps will be to examine what implications and benefits may accrue when using nelarabine in protocols without cranial irradiation. This is to decrease long-term neurologic side effects, and we think it may be possible since nelarabine also reduces CNS relapses,” she said.
“This trial highlights how effective our pediatric and young adult oncologists are at accruing: This is a rare disease, and they were able to put more than 1,500 patients on trial with this rare disease over the course of time,” commented ASCO President Bruce E. Johnson, MD, FASCO.
The new combination regimens are noteworthy in that they improved survival by an absolute 10% without minimal increase in toxicity, he maintained.
“This is part of the paradigm where nelarabine had been approved [by the FDA] for relapsed or recurrent disease, and in this particular setting, it has been moved upfront, closer to the initial treatment, improving the outcomes for those patients,” elaborated Dr. Johnson, who is also a professor of medicine at the Dana-Farber Cancer Institute and a leader of the Dana-Farber/Harvard Cancer Center Lung Cancer Program, both in Boston.
Study details
The ALL0434 trial enrolled patients aged 1-30 years with newly diagnosed T-ALL or T-LL. After induction chemotherapy, all patients received standard chemotherapy, the Children’s Oncology Group augmented Berlin-Frankfurt-Munster regimen (N Engl J Med. 1998;338:1663-71), and depending on recurrence risk, cranial irradiation.
In addition to that regimen, they were randomly assigned to four arms, according to methotrexate dosing (high dose with leucovorin rescue in the inpatient setting vs. escalating dose in the outpatient setting) and nelarabine therapy (receipt vs. nonreceipt).
Among patients with T-ALL, those with low-risk disease were ineligible for nelarabine and did not receive cranial irradiation, whereas those with intermediate- and high-risk disease were randomized to all four arms, Dr. Dunsmore explained. In addition, those who did not achieve remission on induction chemotherapy were nonrandomly assigned to the high-dose methotrexate plus nelarabine arm.
Patients with T-LL were ineligible for high-dose methotrexate and were randomized to escalating-dose methotrexate with or without nelarabine.
Among all patients with T-ALL, the 4-year rate of overall survival was 90.2%, and the 4-year rate of disease-free survival was 84.1%, Dr. Dunsmore reported.
Disease-free survival was better with escalating-dose methotrexate than with high-dose methotrexate (89.8% vs. 78%).
Addition of nelarabine for patients with T-ALL having intermediate- or high-risk disease improved disease-free survival, from 83% without the drug to 88% with the drug (P = .0450), and reduced the rate of CNS relapse. Disease-free survival was highest, at 91%, among those who received both escalating-dose methotrexate and nelarabine.
Among the patients who did not achieve remission from induction chemotherapy, the 4-year rate of overall survival was 54%. “This is important because it’s more than double the past survival rates,” Dr. Dunsmore noted.
Patients with T-LL fared similarly well whether they received nelarabine or not; fully 85% overall were still alive at 4 years.
In terms of adverse effects of nelarabine therapy, the rate of peripheral neuropathy (motor or sensory), one of the more problematic adverse effects of the drug, was 8% in the trial population overall and did not exceed 9% in any treatment arm, she reported.
Dr. Dunsmore disclosed that an immediate family member is an employee of and has a leadership role with TypeZero Technologies; that she receives travel, accommodations, and/or expenses from Novo Nordisk; and that an immediate family member receives travel, accommodations, and/or expenses from Tandem Diabetes Care. The study received funding from the Cancer Therapy Evaluation Program within the National Cancer Institute/National Institutes of Health and received support from the St. Baldrick’s Foundation.
SOURCE: Dunsmore KP et al. ASCO 2018, Abstract 10500.
A set of novel chemotherapy regimens yield excellent outcomes—the best yet—among pediatric and young adult patients with T-cell malignancies, finds a phase 3 randomized controlled trial conducted by the Children’s Oncology Group (ALL0434).
“Despite very intense and complex chemotherapy, 20% of children and adolescents enrolled in Children’s Oncology Group T-cell leukemia trials between 2000 and 2005 did not survive. New drugs were needed to improve survival rates for T-cell malignancies,” lead study author Kimberly P. Dunsmore, MD, a professor at Virginia Tech, Roanoke, said in a press briefing leading up to the annual meeting of the American Society of Clinical Oncology.
The ALL0434 trial tested the addition of methotrexate (Trexall) and/or nelarabine (Arranon), a T cell–specific drug known to be efficacious in relapsed disease, to standard chemotherapy, with tailoring of the regimen to recurrence risk. Analyses were based on 1,545 patients with T-cell acute lymphoblastic leukemia (T-ALL) or T-cell lymphoblastic lymphoma (T-LL).
Results for all patients with T-ALL showed that, with addition of either or both drugs, more than 90% were alive at 4 years and more than 80% were leukemia free. Adding nelarabine to standard chemotherapy improved disease-free survival among the subset having intermediate- or high-risk disease, and the best outcomes were seen with addition of both nelarabine and an escalating dose of methotrexate.
Although patients with T-LL did not see benefit from addition of nelarabine, they still had an 85% rate of overall survival at 4 years.
“ALL0434 is the largest trial for children and young adults with T-cell malignancy ever conducted. It has the best-ever survival data,” Dr. Dunsmore commented.
“Our next steps will be to examine what implications and benefits may accrue when using nelarabine in protocols without cranial irradiation. This is to decrease long-term neurologic side effects, and we think it may be possible since nelarabine also reduces CNS relapses,” she said.
“This trial highlights how effective our pediatric and young adult oncologists are at accruing: This is a rare disease, and they were able to put more than 1,500 patients on trial with this rare disease over the course of time,” commented ASCO President Bruce E. Johnson, MD, FASCO.
The new combination regimens are noteworthy in that they improved survival by an absolute 10% without minimal increase in toxicity, he maintained.
“This is part of the paradigm where nelarabine had been approved [by the FDA] for relapsed or recurrent disease, and in this particular setting, it has been moved upfront, closer to the initial treatment, improving the outcomes for those patients,” elaborated Dr. Johnson, who is also a professor of medicine at the Dana-Farber Cancer Institute and a leader of the Dana-Farber/Harvard Cancer Center Lung Cancer Program, both in Boston.
Study details
The ALL0434 trial enrolled patients aged 1-30 years with newly diagnosed T-ALL or T-LL. After induction chemotherapy, all patients received standard chemotherapy, the Children’s Oncology Group augmented Berlin-Frankfurt-Munster regimen (N Engl J Med. 1998;338:1663-71), and depending on recurrence risk, cranial irradiation.
In addition to that regimen, they were randomly assigned to four arms, according to methotrexate dosing (high dose with leucovorin rescue in the inpatient setting vs. escalating dose in the outpatient setting) and nelarabine therapy (receipt vs. nonreceipt).
Among patients with T-ALL, those with low-risk disease were ineligible for nelarabine and did not receive cranial irradiation, whereas those with intermediate- and high-risk disease were randomized to all four arms, Dr. Dunsmore explained. In addition, those who did not achieve remission on induction chemotherapy were nonrandomly assigned to the high-dose methotrexate plus nelarabine arm.
Patients with T-LL were ineligible for high-dose methotrexate and were randomized to escalating-dose methotrexate with or without nelarabine.
Among all patients with T-ALL, the 4-year rate of overall survival was 90.2%, and the 4-year rate of disease-free survival was 84.1%, Dr. Dunsmore reported.
Disease-free survival was better with escalating-dose methotrexate than with high-dose methotrexate (89.8% vs. 78%).
Addition of nelarabine for patients with T-ALL having intermediate- or high-risk disease improved disease-free survival, from 83% without the drug to 88% with the drug (P = .0450), and reduced the rate of CNS relapse. Disease-free survival was highest, at 91%, among those who received both escalating-dose methotrexate and nelarabine.
Among the patients who did not achieve remission from induction chemotherapy, the 4-year rate of overall survival was 54%. “This is important because it’s more than double the past survival rates,” Dr. Dunsmore noted.
Patients with T-LL fared similarly well whether they received nelarabine or not; fully 85% overall were still alive at 4 years.
In terms of adverse effects of nelarabine therapy, the rate of peripheral neuropathy (motor or sensory), one of the more problematic adverse effects of the drug, was 8% in the trial population overall and did not exceed 9% in any treatment arm, she reported.
Dr. Dunsmore disclosed that an immediate family member is an employee of and has a leadership role with TypeZero Technologies; that she receives travel, accommodations, and/or expenses from Novo Nordisk; and that an immediate family member receives travel, accommodations, and/or expenses from Tandem Diabetes Care. The study received funding from the Cancer Therapy Evaluation Program within the National Cancer Institute/National Institutes of Health and received support from the St. Baldrick’s Foundation.
SOURCE: Dunsmore KP et al. ASCO 2018, Abstract 10500.
A set of novel chemotherapy regimens yield excellent outcomes—the best yet—among pediatric and young adult patients with T-cell malignancies, finds a phase 3 randomized controlled trial conducted by the Children’s Oncology Group (ALL0434).
“Despite very intense and complex chemotherapy, 20% of children and adolescents enrolled in Children’s Oncology Group T-cell leukemia trials between 2000 and 2005 did not survive. New drugs were needed to improve survival rates for T-cell malignancies,” lead study author Kimberly P. Dunsmore, MD, a professor at Virginia Tech, Roanoke, said in a press briefing leading up to the annual meeting of the American Society of Clinical Oncology.
The ALL0434 trial tested the addition of methotrexate (Trexall) and/or nelarabine (Arranon), a T cell–specific drug known to be efficacious in relapsed disease, to standard chemotherapy, with tailoring of the regimen to recurrence risk. Analyses were based on 1,545 patients with T-cell acute lymphoblastic leukemia (T-ALL) or T-cell lymphoblastic lymphoma (T-LL).
Results for all patients with T-ALL showed that, with addition of either or both drugs, more than 90% were alive at 4 years and more than 80% were leukemia free. Adding nelarabine to standard chemotherapy improved disease-free survival among the subset having intermediate- or high-risk disease, and the best outcomes were seen with addition of both nelarabine and an escalating dose of methotrexate.
Although patients with T-LL did not see benefit from addition of nelarabine, they still had an 85% rate of overall survival at 4 years.
“ALL0434 is the largest trial for children and young adults with T-cell malignancy ever conducted. It has the best-ever survival data,” Dr. Dunsmore commented.
“Our next steps will be to examine what implications and benefits may accrue when using nelarabine in protocols without cranial irradiation. This is to decrease long-term neurologic side effects, and we think it may be possible since nelarabine also reduces CNS relapses,” she said.
“This trial highlights how effective our pediatric and young adult oncologists are at accruing: This is a rare disease, and they were able to put more than 1,500 patients on trial with this rare disease over the course of time,” commented ASCO President Bruce E. Johnson, MD, FASCO.
The new combination regimens are noteworthy in that they improved survival by an absolute 10% without minimal increase in toxicity, he maintained.
“This is part of the paradigm where nelarabine had been approved [by the FDA] for relapsed or recurrent disease, and in this particular setting, it has been moved upfront, closer to the initial treatment, improving the outcomes for those patients,” elaborated Dr. Johnson, who is also a professor of medicine at the Dana-Farber Cancer Institute and a leader of the Dana-Farber/Harvard Cancer Center Lung Cancer Program, both in Boston.
Study details
The ALL0434 trial enrolled patients aged 1-30 years with newly diagnosed T-ALL or T-LL. After induction chemotherapy, all patients received standard chemotherapy, the Children’s Oncology Group augmented Berlin-Frankfurt-Munster regimen (N Engl J Med. 1998;338:1663-71), and depending on recurrence risk, cranial irradiation.
In addition to that regimen, they were randomly assigned to four arms, according to methotrexate dosing (high dose with leucovorin rescue in the inpatient setting vs. escalating dose in the outpatient setting) and nelarabine therapy (receipt vs. nonreceipt).
Among patients with T-ALL, those with low-risk disease were ineligible for nelarabine and did not receive cranial irradiation, whereas those with intermediate- and high-risk disease were randomized to all four arms, Dr. Dunsmore explained. In addition, those who did not achieve remission on induction chemotherapy were nonrandomly assigned to the high-dose methotrexate plus nelarabine arm.
Patients with T-LL were ineligible for high-dose methotrexate and were randomized to escalating-dose methotrexate with or without nelarabine.
Among all patients with T-ALL, the 4-year rate of overall survival was 90.2%, and the 4-year rate of disease-free survival was 84.1%, Dr. Dunsmore reported.
Disease-free survival was better with escalating-dose methotrexate than with high-dose methotrexate (89.8% vs. 78%).
Addition of nelarabine for patients with T-ALL having intermediate- or high-risk disease improved disease-free survival, from 83% without the drug to 88% with the drug (P = .0450), and reduced the rate of CNS relapse. Disease-free survival was highest, at 91%, among those who received both escalating-dose methotrexate and nelarabine.
Among the patients who did not achieve remission from induction chemotherapy, the 4-year rate of overall survival was 54%. “This is important because it’s more than double the past survival rates,” Dr. Dunsmore noted.
Patients with T-LL fared similarly well whether they received nelarabine or not; fully 85% overall were still alive at 4 years.
In terms of adverse effects of nelarabine therapy, the rate of peripheral neuropathy (motor or sensory), one of the more problematic adverse effects of the drug, was 8% in the trial population overall and did not exceed 9% in any treatment arm, she reported.
Dr. Dunsmore disclosed that an immediate family member is an employee of and has a leadership role with TypeZero Technologies; that she receives travel, accommodations, and/or expenses from Novo Nordisk; and that an immediate family member receives travel, accommodations, and/or expenses from Tandem Diabetes Care. The study received funding from the Cancer Therapy Evaluation Program within the National Cancer Institute/National Institutes of Health and received support from the St. Baldrick’s Foundation.
SOURCE: Dunsmore KP et al. ASCO 2018, Abstract 10500.
REPORTING FROM ASCO 2018
Key clinical point:
Major finding: Patients with T-ALL had a 4-year rate of overall survival of 90.2% and disease-free survival of 84.1%; patients with T-LL had a 4-year rate of overall survival of 85%.
Study details: Phase 3 randomized controlled trial among 1,545 youth with T-ALL or T-LL testing various regimens of methotrexate and/or nelarabine with standard chemotherapy (ALL0434).
Disclosures: Dr. Dunsmore disclosed that an immediate family member is an employee of and has a leadership role with TypeZero; that she receives travel, accommodations, and/or expenses from Novo Nordisk; and that an immediate family member receives travel, accommodations, and/or expenses from Tandem Diabetes Care. The study received funding from the Cancer Therapy Evaluation Program within the National Cancer Institute/National Institutes of Health and received support from the St. Baldrick’s Foundation.
Source: Dunsmore KP et al. ASCO 2018, Abstract 10500.
Pediatric cancers are on the rise
PITTSBURGH – The incidence of many pediatric cancers are on the rise, and the increase is occurring in nearly all demographic groups studied, according to the latest data from the U.S. Centers for Disease Control and Prevention.
Pediatric cancers that increased significantly in incidence from 2001 through 2014, compared with previous time periods, include thyroid carcinoma, hepatic tumors, lymphomas, renal tumors, and brain tumors. Other cancer types remained unchanged, except malignant melanoma, which saw a significant decline in incidence over the same period, reported David A. Siegel, MD, of the Epidemic Intelligence Service at the CDC in Atlanta.
Recent studies of trends in pediatric cancer have either used data from before 2010 or covered less than a third of the U.S. population, the investigators noted.
To get a more accurate estimate of current trends, the investigators relied on the United States Cancer Statistics, which combines data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Program of Cancer Registries. Together, the combined databases cover 100% of the U.S. population.
Dr. Siegel and his colleagues looked at cancer incidence rates and trends among individuals younger than 20 years of age from across 48 states from 2001 to 2014 – Mississippi, Nevada, and the District of Columbia were not included.
They used a joinpoint regression method to calculate average annual percent change (AAPC) in rates, then stratified rates and trends by sex, age, and race/ethnicity; location; economic status; and cancer type.
During the 14-year period of the study, there were a total of 196,200 incident cases of pediatric cancer, for an overall cancer incidence rate of 173 per million. The pediatric cancer with the highest incident rate was leukemia of any type (45.6 per million), brain tumors (30.8), and lymphomas (26.0).
Incidence rates were highest among males, patients from infancy through age 4, non-Hispanic whites, children who live in the Northeast region, those who live in the wealthiest counties, and those who live in urban/metropolitan counties. The overall pediatric cancer incidence rate increased, with an AAPC of 0.7 (95% confidence interval, 0.5-0.8).
“Rates increased in each stratum of sex, age, and race/ethnicity (except non-Hispanic American Indian/Alaska Native), region, economic status, and rural/urban classification,” the investigators wrote.
Cancers with significantly increased AAPC included thyroid carcinomas (AAPC, 4.8), hepatic tumors (2.5), lymphomas (1.7), renal tumors (0.6), and brain tumors (all types, 0.4).
There were no significant changes in the incidence of either germ cell cancer, retinoblastoma, leukemia, neuroblastoma, soft-tissue sarcomas, or bone tumors.
The only significant decrease over the study period was in the incidence of melanoma in children (–2.6).
“Possible causes of increasing rates might include changes in diagnostic, coding, and reporting standards, increased detection, population-based changes (such as increasing obesity), and environmental exposures,” they wrote.
Public health campaigns about the dangers of UV exposure and promoting the use of sunscreens may account for the decline in the incidence of malignant melanoma, they suggested.
The study was supported by the CDC. Dr. Siegel and coauthors are CDC employees. They reported having no conflicts of interest.
SOURCE: Siegel DA et al. ASPHO 2018, Abstract 605.
PITTSBURGH – The incidence of many pediatric cancers are on the rise, and the increase is occurring in nearly all demographic groups studied, according to the latest data from the U.S. Centers for Disease Control and Prevention.
Pediatric cancers that increased significantly in incidence from 2001 through 2014, compared with previous time periods, include thyroid carcinoma, hepatic tumors, lymphomas, renal tumors, and brain tumors. Other cancer types remained unchanged, except malignant melanoma, which saw a significant decline in incidence over the same period, reported David A. Siegel, MD, of the Epidemic Intelligence Service at the CDC in Atlanta.
Recent studies of trends in pediatric cancer have either used data from before 2010 or covered less than a third of the U.S. population, the investigators noted.
To get a more accurate estimate of current trends, the investigators relied on the United States Cancer Statistics, which combines data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Program of Cancer Registries. Together, the combined databases cover 100% of the U.S. population.
Dr. Siegel and his colleagues looked at cancer incidence rates and trends among individuals younger than 20 years of age from across 48 states from 2001 to 2014 – Mississippi, Nevada, and the District of Columbia were not included.
They used a joinpoint regression method to calculate average annual percent change (AAPC) in rates, then stratified rates and trends by sex, age, and race/ethnicity; location; economic status; and cancer type.
During the 14-year period of the study, there were a total of 196,200 incident cases of pediatric cancer, for an overall cancer incidence rate of 173 per million. The pediatric cancer with the highest incident rate was leukemia of any type (45.6 per million), brain tumors (30.8), and lymphomas (26.0).
Incidence rates were highest among males, patients from infancy through age 4, non-Hispanic whites, children who live in the Northeast region, those who live in the wealthiest counties, and those who live in urban/metropolitan counties. The overall pediatric cancer incidence rate increased, with an AAPC of 0.7 (95% confidence interval, 0.5-0.8).
“Rates increased in each stratum of sex, age, and race/ethnicity (except non-Hispanic American Indian/Alaska Native), region, economic status, and rural/urban classification,” the investigators wrote.
Cancers with significantly increased AAPC included thyroid carcinomas (AAPC, 4.8), hepatic tumors (2.5), lymphomas (1.7), renal tumors (0.6), and brain tumors (all types, 0.4).
There were no significant changes in the incidence of either germ cell cancer, retinoblastoma, leukemia, neuroblastoma, soft-tissue sarcomas, or bone tumors.
The only significant decrease over the study period was in the incidence of melanoma in children (–2.6).
“Possible causes of increasing rates might include changes in diagnostic, coding, and reporting standards, increased detection, population-based changes (such as increasing obesity), and environmental exposures,” they wrote.
Public health campaigns about the dangers of UV exposure and promoting the use of sunscreens may account for the decline in the incidence of malignant melanoma, they suggested.
The study was supported by the CDC. Dr. Siegel and coauthors are CDC employees. They reported having no conflicts of interest.
SOURCE: Siegel DA et al. ASPHO 2018, Abstract 605.
PITTSBURGH – The incidence of many pediatric cancers are on the rise, and the increase is occurring in nearly all demographic groups studied, according to the latest data from the U.S. Centers for Disease Control and Prevention.
Pediatric cancers that increased significantly in incidence from 2001 through 2014, compared with previous time periods, include thyroid carcinoma, hepatic tumors, lymphomas, renal tumors, and brain tumors. Other cancer types remained unchanged, except malignant melanoma, which saw a significant decline in incidence over the same period, reported David A. Siegel, MD, of the Epidemic Intelligence Service at the CDC in Atlanta.
Recent studies of trends in pediatric cancer have either used data from before 2010 or covered less than a third of the U.S. population, the investigators noted.
To get a more accurate estimate of current trends, the investigators relied on the United States Cancer Statistics, which combines data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Program of Cancer Registries. Together, the combined databases cover 100% of the U.S. population.
Dr. Siegel and his colleagues looked at cancer incidence rates and trends among individuals younger than 20 years of age from across 48 states from 2001 to 2014 – Mississippi, Nevada, and the District of Columbia were not included.
They used a joinpoint regression method to calculate average annual percent change (AAPC) in rates, then stratified rates and trends by sex, age, and race/ethnicity; location; economic status; and cancer type.
During the 14-year period of the study, there were a total of 196,200 incident cases of pediatric cancer, for an overall cancer incidence rate of 173 per million. The pediatric cancer with the highest incident rate was leukemia of any type (45.6 per million), brain tumors (30.8), and lymphomas (26.0).
Incidence rates were highest among males, patients from infancy through age 4, non-Hispanic whites, children who live in the Northeast region, those who live in the wealthiest counties, and those who live in urban/metropolitan counties. The overall pediatric cancer incidence rate increased, with an AAPC of 0.7 (95% confidence interval, 0.5-0.8).
“Rates increased in each stratum of sex, age, and race/ethnicity (except non-Hispanic American Indian/Alaska Native), region, economic status, and rural/urban classification,” the investigators wrote.
Cancers with significantly increased AAPC included thyroid carcinomas (AAPC, 4.8), hepatic tumors (2.5), lymphomas (1.7), renal tumors (0.6), and brain tumors (all types, 0.4).
There were no significant changes in the incidence of either germ cell cancer, retinoblastoma, leukemia, neuroblastoma, soft-tissue sarcomas, or bone tumors.
The only significant decrease over the study period was in the incidence of melanoma in children (–2.6).
“Possible causes of increasing rates might include changes in diagnostic, coding, and reporting standards, increased detection, population-based changes (such as increasing obesity), and environmental exposures,” they wrote.
Public health campaigns about the dangers of UV exposure and promoting the use of sunscreens may account for the decline in the incidence of malignant melanoma, they suggested.
The study was supported by the CDC. Dr. Siegel and coauthors are CDC employees. They reported having no conflicts of interest.
SOURCE: Siegel DA et al. ASPHO 2018, Abstract 605.
REPORTING FROM ASPHO 2018
Key clinical point: Major finding: From 2001 to 2014, there were 196,200 incident cases of pediatric cancer for an overall cancer incidence rate of 173 per 1 million.
Study details: A review of data from the United States Cancer Statistics for children under age 20.
Disclosures: The CDC supported the study. Dr. Siegel and his coauthors are CDC employees. They reported having no conflicts of interest.
Source: Siegel DA et al. ASPHO 2018, Abstract 605.
Regimen can improve DFS in newly diagnosed T-ALL
The addition of nelarabine can improve treatment outcomes for certain patients with T-cell acute lymphoblastic leukemia (T-ALL), according to a phase 3 trial.
Patients with newly diagnosed, intermediate- or high-risk T-ALL had a significant improvement in 4-year disease-free survival (DFS) if they received nelarabine in addition to chemotherapy and cranial irradiation.
The DFS benefit with nelarabine was significant for patients who received high-dose methotrexate but not for those who received escalating-dose methotrexate.
This study also included patients with T-cell lymphoblastic lymphoma (T-LL), and they did not experience an improvement in DFS with the addition of nelarabine.
Kimberly Dunsmore, MD, of Virginia Tech Carilion School of Medicine in Roanoke, presented these results in a press briefing in advance of the 2018 ASCO Annual Meeting. Additional results are scheduled to be presented at the meeting as abstract 10500.
This research was supported by the National Cancer Institute/National Institutes of Health and St. Baldrick’s Foundation. The researchers’ disclosures are listed with the abstract.
Patients and treatment
The trial enrolled 1895 patients, ages 1 to 30, who were newly diagnosed with T-ALL (94%) or T-LL (6%).
Patients received standard 4-drug induction chemotherapy, and 1307 of these patients were then randomized to 1 of 4 treatment arms.
Regardless of which arm they were randomized to, patients received an 11-drug chemotherapy regimen—the augmented Berlin-Frankfurt-Munster regimen. Intermediate- and high-risk patients in all 4 arms also received cranial irradiation.
In the first treatment arm, T-LL (n=58) and T-ALL (n=372) patients received escalating-dose methotrexate without leucovorin rescue and pegaspargase (C-MTX).
In the second treatment arm, patients with intermediate- and high-risk T-ALL (n=147) and T-LL (n=60) received C-MTX plus nelarabine (six 5-day courses at 650 mg/m2/day).
In the third arm, T-ALL patients (n=451) received high-dose methotrexate with leucovorin rescue (HD-MTX). T-LL patients were not eligible for this arm or the fourth treatment arm.
In the fourth arm, intermediate- and high-risk T-ALL patients (n=219) received HD-MTX and nelarabine (same schedule as above). This included 43 T-ALL patients who had induction failure and were assigned to this arm non-randomly.
Results
For T-ALL patients, the 4-year disease-free survival (DFS) rate was 84%, and the 4-year overall survival rate was 90%.
There was a significant improvement in DFS for T-ALL patients who received nelarabine compared to those who did not—89% and 83%, respectively (P=0.0332).
“Historically, about 80% of people [with T-ALL] live at least 4 years after being treated for their disease, but we felt we could and must do better,” Dr Dunsmore said. “Our trial shows that we could further increase survival rates by about 10%, which is very encouraging.”
Dr Dunsmore also noted that patients who received nelarabine had fewer central nervous system relapses.
Among T-ALL patients who received C-MTX, there was no significant difference in DFS for those who received nelarabine and those who did not—92% and 90%, respectively (P=0.3825).
However, for patients who received HD-MTX, the difference in DFS was significant. The DFS rate was 86% in patients who received nelarabine and 78% in those who did not (P=0.024).
For the T-ALL patients who failed induction and were assigned to HD-MTX and nelarabine, the 4-year DFS rate was 55%.
Patients with T-LL did not benefit from the addition of nelarabine. The 4-year DFS rate was 85% in the nelarabine recipients and 89% in non-recipients (P=0.2788).
There were no significant differences in overall toxicity or peripheral neurotoxicity between the treatment arms.
Dr Dunsmore said the next step with this research will be to examine the implications and potential benefits of using nelarabine in treatment protocols that do not include cranial radiation.
The addition of nelarabine can improve treatment outcomes for certain patients with T-cell acute lymphoblastic leukemia (T-ALL), according to a phase 3 trial.
Patients with newly diagnosed, intermediate- or high-risk T-ALL had a significant improvement in 4-year disease-free survival (DFS) if they received nelarabine in addition to chemotherapy and cranial irradiation.
The DFS benefit with nelarabine was significant for patients who received high-dose methotrexate but not for those who received escalating-dose methotrexate.
This study also included patients with T-cell lymphoblastic lymphoma (T-LL), and they did not experience an improvement in DFS with the addition of nelarabine.
Kimberly Dunsmore, MD, of Virginia Tech Carilion School of Medicine in Roanoke, presented these results in a press briefing in advance of the 2018 ASCO Annual Meeting. Additional results are scheduled to be presented at the meeting as abstract 10500.
This research was supported by the National Cancer Institute/National Institutes of Health and St. Baldrick’s Foundation. The researchers’ disclosures are listed with the abstract.
Patients and treatment
The trial enrolled 1895 patients, ages 1 to 30, who were newly diagnosed with T-ALL (94%) or T-LL (6%).
Patients received standard 4-drug induction chemotherapy, and 1307 of these patients were then randomized to 1 of 4 treatment arms.
Regardless of which arm they were randomized to, patients received an 11-drug chemotherapy regimen—the augmented Berlin-Frankfurt-Munster regimen. Intermediate- and high-risk patients in all 4 arms also received cranial irradiation.
In the first treatment arm, T-LL (n=58) and T-ALL (n=372) patients received escalating-dose methotrexate without leucovorin rescue and pegaspargase (C-MTX).
In the second treatment arm, patients with intermediate- and high-risk T-ALL (n=147) and T-LL (n=60) received C-MTX plus nelarabine (six 5-day courses at 650 mg/m2/day).
In the third arm, T-ALL patients (n=451) received high-dose methotrexate with leucovorin rescue (HD-MTX). T-LL patients were not eligible for this arm or the fourth treatment arm.
In the fourth arm, intermediate- and high-risk T-ALL patients (n=219) received HD-MTX and nelarabine (same schedule as above). This included 43 T-ALL patients who had induction failure and were assigned to this arm non-randomly.
Results
For T-ALL patients, the 4-year disease-free survival (DFS) rate was 84%, and the 4-year overall survival rate was 90%.
There was a significant improvement in DFS for T-ALL patients who received nelarabine compared to those who did not—89% and 83%, respectively (P=0.0332).
“Historically, about 80% of people [with T-ALL] live at least 4 years after being treated for their disease, but we felt we could and must do better,” Dr Dunsmore said. “Our trial shows that we could further increase survival rates by about 10%, which is very encouraging.”
Dr Dunsmore also noted that patients who received nelarabine had fewer central nervous system relapses.
Among T-ALL patients who received C-MTX, there was no significant difference in DFS for those who received nelarabine and those who did not—92% and 90%, respectively (P=0.3825).
However, for patients who received HD-MTX, the difference in DFS was significant. The DFS rate was 86% in patients who received nelarabine and 78% in those who did not (P=0.024).
For the T-ALL patients who failed induction and were assigned to HD-MTX and nelarabine, the 4-year DFS rate was 55%.
Patients with T-LL did not benefit from the addition of nelarabine. The 4-year DFS rate was 85% in the nelarabine recipients and 89% in non-recipients (P=0.2788).
There were no significant differences in overall toxicity or peripheral neurotoxicity between the treatment arms.
Dr Dunsmore said the next step with this research will be to examine the implications and potential benefits of using nelarabine in treatment protocols that do not include cranial radiation.
The addition of nelarabine can improve treatment outcomes for certain patients with T-cell acute lymphoblastic leukemia (T-ALL), according to a phase 3 trial.
Patients with newly diagnosed, intermediate- or high-risk T-ALL had a significant improvement in 4-year disease-free survival (DFS) if they received nelarabine in addition to chemotherapy and cranial irradiation.
The DFS benefit with nelarabine was significant for patients who received high-dose methotrexate but not for those who received escalating-dose methotrexate.
This study also included patients with T-cell lymphoblastic lymphoma (T-LL), and they did not experience an improvement in DFS with the addition of nelarabine.
Kimberly Dunsmore, MD, of Virginia Tech Carilion School of Medicine in Roanoke, presented these results in a press briefing in advance of the 2018 ASCO Annual Meeting. Additional results are scheduled to be presented at the meeting as abstract 10500.
This research was supported by the National Cancer Institute/National Institutes of Health and St. Baldrick’s Foundation. The researchers’ disclosures are listed with the abstract.
Patients and treatment
The trial enrolled 1895 patients, ages 1 to 30, who were newly diagnosed with T-ALL (94%) or T-LL (6%).
Patients received standard 4-drug induction chemotherapy, and 1307 of these patients were then randomized to 1 of 4 treatment arms.
Regardless of which arm they were randomized to, patients received an 11-drug chemotherapy regimen—the augmented Berlin-Frankfurt-Munster regimen. Intermediate- and high-risk patients in all 4 arms also received cranial irradiation.
In the first treatment arm, T-LL (n=58) and T-ALL (n=372) patients received escalating-dose methotrexate without leucovorin rescue and pegaspargase (C-MTX).
In the second treatment arm, patients with intermediate- and high-risk T-ALL (n=147) and T-LL (n=60) received C-MTX plus nelarabine (six 5-day courses at 650 mg/m2/day).
In the third arm, T-ALL patients (n=451) received high-dose methotrexate with leucovorin rescue (HD-MTX). T-LL patients were not eligible for this arm or the fourth treatment arm.
In the fourth arm, intermediate- and high-risk T-ALL patients (n=219) received HD-MTX and nelarabine (same schedule as above). This included 43 T-ALL patients who had induction failure and were assigned to this arm non-randomly.
Results
For T-ALL patients, the 4-year disease-free survival (DFS) rate was 84%, and the 4-year overall survival rate was 90%.
There was a significant improvement in DFS for T-ALL patients who received nelarabine compared to those who did not—89% and 83%, respectively (P=0.0332).
“Historically, about 80% of people [with T-ALL] live at least 4 years after being treated for their disease, but we felt we could and must do better,” Dr Dunsmore said. “Our trial shows that we could further increase survival rates by about 10%, which is very encouraging.”
Dr Dunsmore also noted that patients who received nelarabine had fewer central nervous system relapses.
Among T-ALL patients who received C-MTX, there was no significant difference in DFS for those who received nelarabine and those who did not—92% and 90%, respectively (P=0.3825).
However, for patients who received HD-MTX, the difference in DFS was significant. The DFS rate was 86% in patients who received nelarabine and 78% in those who did not (P=0.024).
For the T-ALL patients who failed induction and were assigned to HD-MTX and nelarabine, the 4-year DFS rate was 55%.
Patients with T-LL did not benefit from the addition of nelarabine. The 4-year DFS rate was 85% in the nelarabine recipients and 89% in non-recipients (P=0.2788).
There were no significant differences in overall toxicity or peripheral neurotoxicity between the treatment arms.
Dr Dunsmore said the next step with this research will be to examine the implications and potential benefits of using nelarabine in treatment protocols that do not include cranial radiation.
Children with Down syndrome and ALL have good outcomes today
PITTSBURGH – In the current era, children with Down syndrome who have standard risk B-cell precursor acute lymphoblastic leukemia have event-free and overall survival rates nearly as good as those of other children with standard-risk B–ALL, results of a Children’s Oncology Group study show.
Among 5,311 children enrolled in the COG AALL0331 trial, a study of combination chemotherapy for young patients with newly diagnosed ALL, the 5-year event-free survival (EFS) rate for children with Down syndrome was 86%, compared with 89% for children without Down syndrome (P = .025).
Although the differences in EFS and OS were significant, ”overall in this study, Down syndrome ALL had an excellent outcome that was similar to those patients without Down syndrome,” she said at the annual meeting of the American Society of Pediatric Hematology/Oncology.
The trial confirmed her group’s previous finding that there is a low rate of favorable cytogenetic features in patients with Down syndrome ALL; nonetheless, in the current study, 5-year continuous complete remission rates for standard-risk average, low, and high in patients with Down syndrome were similar to those for patients without Down syndrome, she said.
In the trial, patients were treated with a three-drug induction regimen, and following induction were assigned to standard-risk low, average, or high groups based on leukemia genetics and initial response to therapy.
Of the 5,311 children enrolled, 141 (2.7%) had Down syndrome, and these patients received risk-stratified therapy with additional supportive care guidelines, including leucovorin rescue after intrathecal methotrexate until maintenance. The care team strongly encouraged hospitalizations during high-risk blocks for this subgroup of patients until they experienced neutrophil recovery.
At the end of induction, patients who were judged to be standard-risk average were then randomized in a 2x2 design to either standard or intensified consolidation, and to standard interim maintenance with delayed intensification, or to intensified interim maintenance with delayed intensification.
The intensified interim maintenance with delayed intensification randomization was closed in 2008 because of superior results with escalating intravenous methotrexate during interim maintenance for standard-risk ALL patients treated in the CCG 1991 trial. Subsequently, all patients enrolled in AALL0331 received escalating intravenous methotrexate during interim maintenance.
Also in AALL0331, patients with Down syndrome who had standard-high ALL were given intensified consolidation and a single vs. double intensified interim maintenance with delayed intensification; patients without Down syndrome and standard risk high received the double intensified interim maintenance regimen.
Standard-risk low Down syndrome patients and non–Down syndrome patients participated in a randomization to additional pegaspargase doses during consolidation and interim maintenance.
There were no significant differences between patients with or without Down syndrome in the proportion of either rapid or slow early responses. Significantly fewer patients with Down syndrome had standard-risk low disease, and significantly more had average or high-risk disease.
Patients with Down syndrome initially had 11.5% excess risk for death during induction, but following additional treatment modifications, the excess risk decreased to 1.7%.
Among patients with Down syndrome, one died during intensive consolidation, and two died during delayed intensification. All three deaths were due to infections. No patients with Down syndrome died during maintenance.
Patients with Down syndrome also had a significantly increased risk for infection during induction (P less than .0001).
For patients with standard-risk low disease, 5-year EFS was 100% for those with Down syndrome, compared with 95.35% for patients without. Respective rates for standard risk average and high disease were 88.07% vs. 89.63%. and 82.35% vs. 86.18%.
Down syndrome was not an independent risk factor for survival in multivariate analyses accounting for risk group, Dr. Maloney said.
COG AALL0331 was supported by the National Cancer Institute. Dr. Maloney reported having no financial disclosures.
SOURCE: Maloney K et al. ASPHO 2018, Abstract PP 2001.
PITTSBURGH – In the current era, children with Down syndrome who have standard risk B-cell precursor acute lymphoblastic leukemia have event-free and overall survival rates nearly as good as those of other children with standard-risk B–ALL, results of a Children’s Oncology Group study show.
Among 5,311 children enrolled in the COG AALL0331 trial, a study of combination chemotherapy for young patients with newly diagnosed ALL, the 5-year event-free survival (EFS) rate for children with Down syndrome was 86%, compared with 89% for children without Down syndrome (P = .025).
Although the differences in EFS and OS were significant, ”overall in this study, Down syndrome ALL had an excellent outcome that was similar to those patients without Down syndrome,” she said at the annual meeting of the American Society of Pediatric Hematology/Oncology.
The trial confirmed her group’s previous finding that there is a low rate of favorable cytogenetic features in patients with Down syndrome ALL; nonetheless, in the current study, 5-year continuous complete remission rates for standard-risk average, low, and high in patients with Down syndrome were similar to those for patients without Down syndrome, she said.
In the trial, patients were treated with a three-drug induction regimen, and following induction were assigned to standard-risk low, average, or high groups based on leukemia genetics and initial response to therapy.
Of the 5,311 children enrolled, 141 (2.7%) had Down syndrome, and these patients received risk-stratified therapy with additional supportive care guidelines, including leucovorin rescue after intrathecal methotrexate until maintenance. The care team strongly encouraged hospitalizations during high-risk blocks for this subgroup of patients until they experienced neutrophil recovery.
At the end of induction, patients who were judged to be standard-risk average were then randomized in a 2x2 design to either standard or intensified consolidation, and to standard interim maintenance with delayed intensification, or to intensified interim maintenance with delayed intensification.
The intensified interim maintenance with delayed intensification randomization was closed in 2008 because of superior results with escalating intravenous methotrexate during interim maintenance for standard-risk ALL patients treated in the CCG 1991 trial. Subsequently, all patients enrolled in AALL0331 received escalating intravenous methotrexate during interim maintenance.
Also in AALL0331, patients with Down syndrome who had standard-high ALL were given intensified consolidation and a single vs. double intensified interim maintenance with delayed intensification; patients without Down syndrome and standard risk high received the double intensified interim maintenance regimen.
Standard-risk low Down syndrome patients and non–Down syndrome patients participated in a randomization to additional pegaspargase doses during consolidation and interim maintenance.
There were no significant differences between patients with or without Down syndrome in the proportion of either rapid or slow early responses. Significantly fewer patients with Down syndrome had standard-risk low disease, and significantly more had average or high-risk disease.
Patients with Down syndrome initially had 11.5% excess risk for death during induction, but following additional treatment modifications, the excess risk decreased to 1.7%.
Among patients with Down syndrome, one died during intensive consolidation, and two died during delayed intensification. All three deaths were due to infections. No patients with Down syndrome died during maintenance.
Patients with Down syndrome also had a significantly increased risk for infection during induction (P less than .0001).
For patients with standard-risk low disease, 5-year EFS was 100% for those with Down syndrome, compared with 95.35% for patients without. Respective rates for standard risk average and high disease were 88.07% vs. 89.63%. and 82.35% vs. 86.18%.
Down syndrome was not an independent risk factor for survival in multivariate analyses accounting for risk group, Dr. Maloney said.
COG AALL0331 was supported by the National Cancer Institute. Dr. Maloney reported having no financial disclosures.
SOURCE: Maloney K et al. ASPHO 2018, Abstract PP 2001.
PITTSBURGH – In the current era, children with Down syndrome who have standard risk B-cell precursor acute lymphoblastic leukemia have event-free and overall survival rates nearly as good as those of other children with standard-risk B–ALL, results of a Children’s Oncology Group study show.
Among 5,311 children enrolled in the COG AALL0331 trial, a study of combination chemotherapy for young patients with newly diagnosed ALL, the 5-year event-free survival (EFS) rate for children with Down syndrome was 86%, compared with 89% for children without Down syndrome (P = .025).
Although the differences in EFS and OS were significant, ”overall in this study, Down syndrome ALL had an excellent outcome that was similar to those patients without Down syndrome,” she said at the annual meeting of the American Society of Pediatric Hematology/Oncology.
The trial confirmed her group’s previous finding that there is a low rate of favorable cytogenetic features in patients with Down syndrome ALL; nonetheless, in the current study, 5-year continuous complete remission rates for standard-risk average, low, and high in patients with Down syndrome were similar to those for patients without Down syndrome, she said.
In the trial, patients were treated with a three-drug induction regimen, and following induction were assigned to standard-risk low, average, or high groups based on leukemia genetics and initial response to therapy.
Of the 5,311 children enrolled, 141 (2.7%) had Down syndrome, and these patients received risk-stratified therapy with additional supportive care guidelines, including leucovorin rescue after intrathecal methotrexate until maintenance. The care team strongly encouraged hospitalizations during high-risk blocks for this subgroup of patients until they experienced neutrophil recovery.
At the end of induction, patients who were judged to be standard-risk average were then randomized in a 2x2 design to either standard or intensified consolidation, and to standard interim maintenance with delayed intensification, or to intensified interim maintenance with delayed intensification.
The intensified interim maintenance with delayed intensification randomization was closed in 2008 because of superior results with escalating intravenous methotrexate during interim maintenance for standard-risk ALL patients treated in the CCG 1991 trial. Subsequently, all patients enrolled in AALL0331 received escalating intravenous methotrexate during interim maintenance.
Also in AALL0331, patients with Down syndrome who had standard-high ALL were given intensified consolidation and a single vs. double intensified interim maintenance with delayed intensification; patients without Down syndrome and standard risk high received the double intensified interim maintenance regimen.
Standard-risk low Down syndrome patients and non–Down syndrome patients participated in a randomization to additional pegaspargase doses during consolidation and interim maintenance.
There were no significant differences between patients with or without Down syndrome in the proportion of either rapid or slow early responses. Significantly fewer patients with Down syndrome had standard-risk low disease, and significantly more had average or high-risk disease.
Patients with Down syndrome initially had 11.5% excess risk for death during induction, but following additional treatment modifications, the excess risk decreased to 1.7%.
Among patients with Down syndrome, one died during intensive consolidation, and two died during delayed intensification. All three deaths were due to infections. No patients with Down syndrome died during maintenance.
Patients with Down syndrome also had a significantly increased risk for infection during induction (P less than .0001).
For patients with standard-risk low disease, 5-year EFS was 100% for those with Down syndrome, compared with 95.35% for patients without. Respective rates for standard risk average and high disease were 88.07% vs. 89.63%. and 82.35% vs. 86.18%.
Down syndrome was not an independent risk factor for survival in multivariate analyses accounting for risk group, Dr. Maloney said.
COG AALL0331 was supported by the National Cancer Institute. Dr. Maloney reported having no financial disclosures.
SOURCE: Maloney K et al. ASPHO 2018, Abstract PP 2001.
REPORTING FROM ASPHO 2018
Key clinical point:
Major finding: The 5-year event-free survival rate for children with Down syndrome was 86% vs. 89% for children without Down syndrome (P = .025).
Study details: Follow-up of 5,311 children with newly diagnosed ALL in the COG AALL0331 trial.
Disclosures: COG AALL0331 was supported by the National Cancer Institute. Dr. Maloney reported having no financial disclosures.
Source: Maloney K et al. ASPHO 2018, Abstract PP 2001.
Cooperation can drive T-ALL, study shows
Overexpression of HOXA9 and activated JAK/STAT signaling cooperate to drive the development of T-cell acute lymphoblastic leukemia (ALL), according to researchers.
The team found that JAK3 mutations are significantly associated with elevated HOXA9 expression in T-ALL, and co-expression of HOXA9 and JAK3 mutations prompt “rapid” leukemia development in mice.
In addition, STAT5 and HOXA9 occupy similar genetic loci, which results in increased JAK-STAT signaling in leukemia cells.
These discoveries, and results of subsequent experiments, suggested that PIM1 and JAK1 are potential therapeutic targets for T-ALL.
Jan Cools, PhD, of VIB-KU Leuven Center for Cancer Biology in Leuven, Belgium, and his colleagues described this research in Cancer Discovery.
“JAK3/STAT5 mutations are important in ALL since they stimulate the growth of the cells,” Dr Cools said. “[W]e found that JAK3/STAT5 mutations frequently occur together with HOXA9 mutations.”
In analyzing data from 2 cohorts of T-ALL patients, the researchers found that IL7R/JAK/STAT5 mutations were more frequent in HOXA+ cases, and HOXA9 was “the most important upregulated gene of the HOXA cluster.” (HOXA9 expression levels were significantly higher than HOXA10 or HOXA11 levels.)
“We examined the cooperation between JAK3/STAT5 mutation and HOXA9, [and] we observed that HOXA9 boosts the effects of other genes, leading to tumor development,” said study author Charles de Bock, PhD, of VIB-KU Leuven.
“As a result, when JAK3/STAT5 mutations and HOXA9 are both present, leukemia develops more rapidly and aggressively.”
The researchers found that co-expression of HOXA9 and the JAK3 M511I mutation led to rapid leukemia development in mice. Animals with co-expression of HOXA9 and JAK3 (M511I) developed leukemia that was characterized by an increase in peripheral white blood cell counts that exceeded 10,000 cells/mm3 within 30 days.
In addition, these mice had a significant decrease in disease-free survival compared to mice with JAK3 (M511I) alone. The median disease-free survival was 25 days and 126.5 days, respectively (P<0.0001).
Further analysis revealed co-localization of HOXA9 and STAT5. The researchers also found that HOXA9 enhances transcriptional activity of STAT5 in leukemia cells.
The team said this reconfirms STAT5 as “a major central player” in T-ALL, and it suggests that STAT5 target genes such as PIM1 could be therapeutic targets for T-ALL.
To test this theory, the researchers inhibited both PIM1 and JAK1 in JAK/STAT mutant T-ALL. The PIM1 inhibitor AZD1208 and the JAK1/2 inhibitor ruxolitinib demonstrated synergy and significantly reduced leukemia burden in vivo.
Overexpression of HOXA9 and activated JAK/STAT signaling cooperate to drive the development of T-cell acute lymphoblastic leukemia (ALL), according to researchers.
The team found that JAK3 mutations are significantly associated with elevated HOXA9 expression in T-ALL, and co-expression of HOXA9 and JAK3 mutations prompt “rapid” leukemia development in mice.
In addition, STAT5 and HOXA9 occupy similar genetic loci, which results in increased JAK-STAT signaling in leukemia cells.
These discoveries, and results of subsequent experiments, suggested that PIM1 and JAK1 are potential therapeutic targets for T-ALL.
Jan Cools, PhD, of VIB-KU Leuven Center for Cancer Biology in Leuven, Belgium, and his colleagues described this research in Cancer Discovery.
“JAK3/STAT5 mutations are important in ALL since they stimulate the growth of the cells,” Dr Cools said. “[W]e found that JAK3/STAT5 mutations frequently occur together with HOXA9 mutations.”
In analyzing data from 2 cohorts of T-ALL patients, the researchers found that IL7R/JAK/STAT5 mutations were more frequent in HOXA+ cases, and HOXA9 was “the most important upregulated gene of the HOXA cluster.” (HOXA9 expression levels were significantly higher than HOXA10 or HOXA11 levels.)
“We examined the cooperation between JAK3/STAT5 mutation and HOXA9, [and] we observed that HOXA9 boosts the effects of other genes, leading to tumor development,” said study author Charles de Bock, PhD, of VIB-KU Leuven.
“As a result, when JAK3/STAT5 mutations and HOXA9 are both present, leukemia develops more rapidly and aggressively.”
The researchers found that co-expression of HOXA9 and the JAK3 M511I mutation led to rapid leukemia development in mice. Animals with co-expression of HOXA9 and JAK3 (M511I) developed leukemia that was characterized by an increase in peripheral white blood cell counts that exceeded 10,000 cells/mm3 within 30 days.
In addition, these mice had a significant decrease in disease-free survival compared to mice with JAK3 (M511I) alone. The median disease-free survival was 25 days and 126.5 days, respectively (P<0.0001).
Further analysis revealed co-localization of HOXA9 and STAT5. The researchers also found that HOXA9 enhances transcriptional activity of STAT5 in leukemia cells.
The team said this reconfirms STAT5 as “a major central player” in T-ALL, and it suggests that STAT5 target genes such as PIM1 could be therapeutic targets for T-ALL.
To test this theory, the researchers inhibited both PIM1 and JAK1 in JAK/STAT mutant T-ALL. The PIM1 inhibitor AZD1208 and the JAK1/2 inhibitor ruxolitinib demonstrated synergy and significantly reduced leukemia burden in vivo.
Overexpression of HOXA9 and activated JAK/STAT signaling cooperate to drive the development of T-cell acute lymphoblastic leukemia (ALL), according to researchers.
The team found that JAK3 mutations are significantly associated with elevated HOXA9 expression in T-ALL, and co-expression of HOXA9 and JAK3 mutations prompt “rapid” leukemia development in mice.
In addition, STAT5 and HOXA9 occupy similar genetic loci, which results in increased JAK-STAT signaling in leukemia cells.
These discoveries, and results of subsequent experiments, suggested that PIM1 and JAK1 are potential therapeutic targets for T-ALL.
Jan Cools, PhD, of VIB-KU Leuven Center for Cancer Biology in Leuven, Belgium, and his colleagues described this research in Cancer Discovery.
“JAK3/STAT5 mutations are important in ALL since they stimulate the growth of the cells,” Dr Cools said. “[W]e found that JAK3/STAT5 mutations frequently occur together with HOXA9 mutations.”
In analyzing data from 2 cohorts of T-ALL patients, the researchers found that IL7R/JAK/STAT5 mutations were more frequent in HOXA+ cases, and HOXA9 was “the most important upregulated gene of the HOXA cluster.” (HOXA9 expression levels were significantly higher than HOXA10 or HOXA11 levels.)
“We examined the cooperation between JAK3/STAT5 mutation and HOXA9, [and] we observed that HOXA9 boosts the effects of other genes, leading to tumor development,” said study author Charles de Bock, PhD, of VIB-KU Leuven.
“As a result, when JAK3/STAT5 mutations and HOXA9 are both present, leukemia develops more rapidly and aggressively.”
The researchers found that co-expression of HOXA9 and the JAK3 M511I mutation led to rapid leukemia development in mice. Animals with co-expression of HOXA9 and JAK3 (M511I) developed leukemia that was characterized by an increase in peripheral white blood cell counts that exceeded 10,000 cells/mm3 within 30 days.
In addition, these mice had a significant decrease in disease-free survival compared to mice with JAK3 (M511I) alone. The median disease-free survival was 25 days and 126.5 days, respectively (P<0.0001).
Further analysis revealed co-localization of HOXA9 and STAT5. The researchers also found that HOXA9 enhances transcriptional activity of STAT5 in leukemia cells.
The team said this reconfirms STAT5 as “a major central player” in T-ALL, and it suggests that STAT5 target genes such as PIM1 could be therapeutic targets for T-ALL.
To test this theory, the researchers inhibited both PIM1 and JAK1 in JAK/STAT mutant T-ALL. The PIM1 inhibitor AZD1208 and the JAK1/2 inhibitor ruxolitinib demonstrated synergy and significantly reduced leukemia burden in vivo.