User login
Drug shortages plague hematology, but preparedness helps
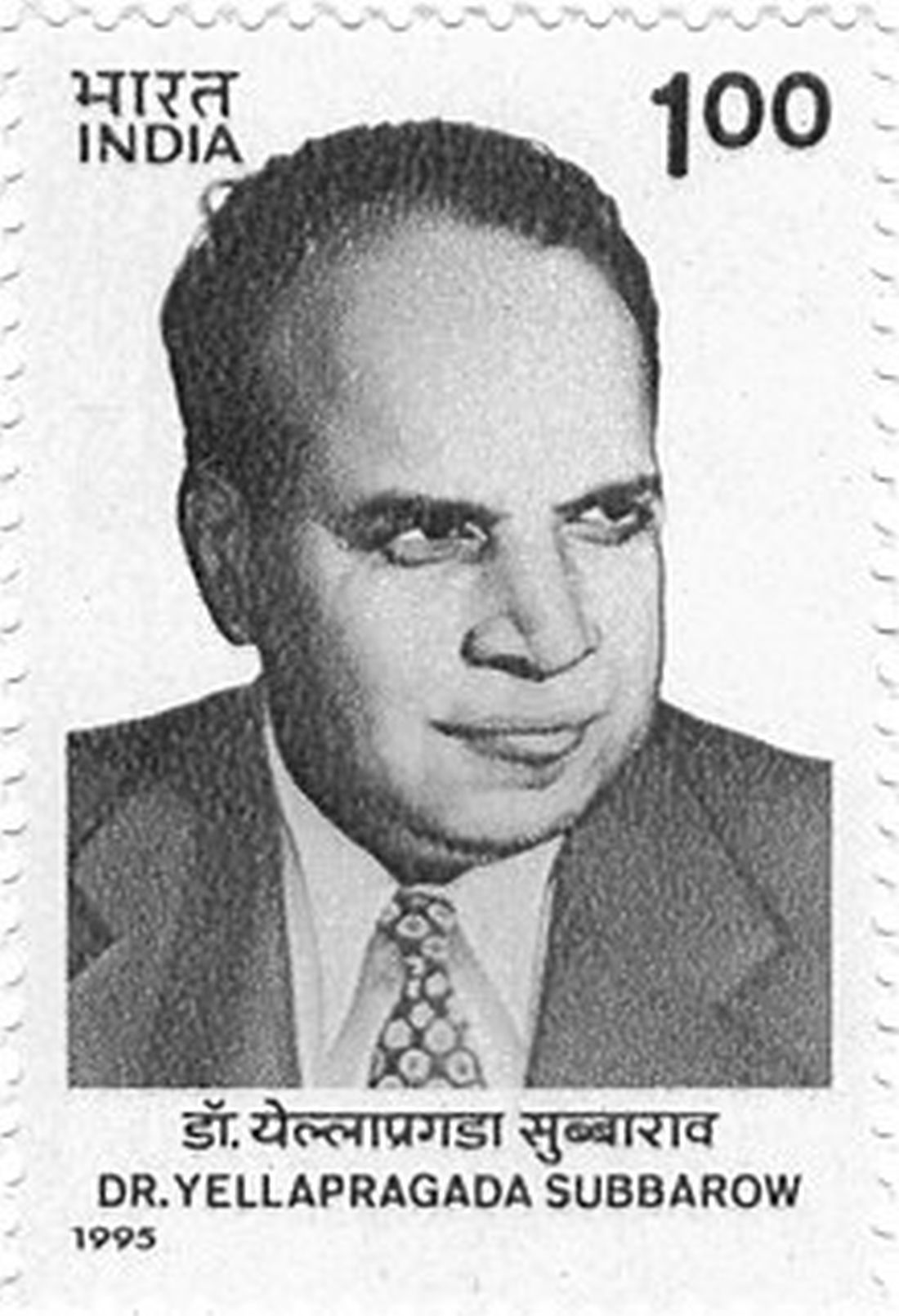
Just before he took a call from a reporter asking about the impact of drug shortages in hematology, Bill Greene, PharmD, chief pharmaceutical officer at St. Jude Children’s Research Hospital, had spent an hour on the phone overseeing his institution’s response to a hematology drug shortage. The chemotherapy drug fludarabine, used to treat chronic lymphocytic leukemia, was in short supply.
“There are 5 different manufacturers, but none of them have had drug available over the past 2 weeks,” Dr. Greene said. “We’re trying to chase some emergency supplies to be able to continue treatment for patients who’ve had their treatments initiated and planned.”
Over the past several years, this predicament has become common at hematology clinics across the country. In fact, management of scarce medication resources has become a significant part of Dr. Greene’s workload these days, as critical drugs fail to show up on time or manufacturer supplies run low at his hospital in Memphis.
This shortage of hematology drugs got a new dose of national attention, thanks to a recent episode of CBS News’ “60 Minutes.” Through interviews with physicians and parents of children who suddenly could not get vital medications, the report highlighted the recent shortage of another leukemia drug, vincristine.
“As a cancer mom, we shouldn’t be fighting for our children to get a drug that is needed,” Cyndi Valenta was quoted as saying. She recalled that when the shortage began in 2019, her 13-year-old son, a leukemia patient at Loma Linda (Calif.) University Hospital, felt frightened. Ms. Valenta said she felt a “gut-wrenching feeling of just fear and anger.” They were finally able to get doses of the drug after launching a social media campaign.
Such drug shortages are especially widespread in oncology and hematology, according to a survey of oncology pharmacists at 68 organizations nationwide. Published in the May 2022 issue of Oncology Practice, the study showed that 63% of institutions reported one or more drug shortages every month, with a 34% increase in 2019, compared with 2018. Treatment delays, reduced doses, or alternative regimens were reported by 75% of respondents, the authors wrote.
The pharmacists surveyed between May 2019 and July 2020 were asked about the three most hard-to-get chemotherapy and supportive care agents. Vincristine topped the list, followed by vinblastine, IVIG, leucovorin, and BCG, as well as difficult-to-obtain ropine, erwinia asparaginase, etoposide, and leuprolide. Several of these drugs are used to treat conditions such as lymphoma and leukemia.
Eighty-two percent of respondents reported shortages of decitabine (IV), often used as part of a cocktail with vinblastine and other drugs to treat Hodgkin lymphoma.
The reasons for drug shortages are varied. The CBS News report declared that “pharmaceutical companies have stopped producing many life-saving generic drugs because they make too little profit,” and it suggested that the federal government isn’t doing enough.
But government action actually might be making a difference. According to the FDA, the number of new drug shortages has fallen dramatically from 250 in 2011 to 41 in 2021, and the number of prevented drug shortages rose from nearly 200 to more than 300 over that same period. Still, the number of ongoing drug shortages has risen from around 40 in 2017 to about 80 in 2021.
Reasons for the paucity of certain drugs are often unclear. In a June 12, 2022 post, for example, the American Society of Health-System Pharmacists’ drug shortage database noted that the chemotherapy drug fludarabine was in short supply and provided details about when some of the 5 manufacturers expected to have it available. (This is the shortage that Dr. Greene was trying to manage.) But 4 of the 5 manufacturers “did not provide a reason,” and the fifth blamed manufacturing delays.
“There’s a lot of closely held trade secrets that hinder the ability to share good information,” said Dr. Greene. To make things more complicated, shipping times are often unreliable. “The product doesn’t show up today, we place another order. Sometimes it will show up tomorrow, sometimes it doesn’t,” he said. “If you’re not tracking it carefully, you deplete your own supply.”
Patients’ families have grown used to dealing with drug shortages, and “they’re less quick to blame personnel at our institution.”
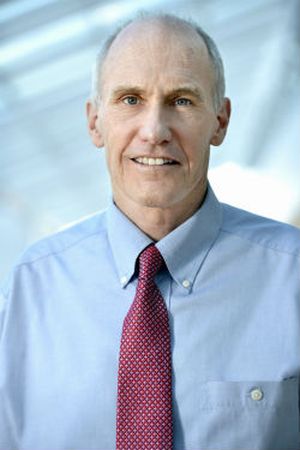
How can hematologists cope with this issue? “The best thing in the immediate term is to advocate for their hospital to have a pharmacist dedicated to shortage monitoring and taking proactive steps to obviate shortages,” hematologist/oncologist Andrew Hantel, MD, an instructor at Dana-Farber Cancer Institute, Harvard Medical School, Boston, said in an interview.
“We have ongoing communications with other large cancer centers and the FDA to recognize shortages early and develop plans to make sure we stay ahead of them,” Dr. Hantel said. “Most often this involves assessing supply, use rates, alternative manufacturers, and additional measures the Food and Drug Administration can take (for example, importation), and occasionally working with clinical teams to see if other medications are feasible alternatives.”
If a drug is unavailable, it can also be helpful to discuss alternative approaches. “We did not have any frank shortages of vincristine,” Dr. Hantel said, “but we did focus on conservation measures and considered different ethically appropriate ways to distribute vincristine if there was a point at which we did not have enough for everyone who needed it.”
If a drug is in short supply, options can include delaying treatment, giving an alternative, or providing the rest of the regimen without the scarce drug, he said. In a 2021 report in The Lancet Hematology, Dr. Hantel and his colleagues offered “model solutions for ethical allocation during cancer medicine shortages.”
The authors of the May 2022 drug-shortage report highlighted an alternative regimen in hematology. They noted that manufacturing delays have limited the supply of dacarbazine, used for Hodgkin lymphoma. Due to the current shortages, they wrote, clinicians are considering the use of escalated bleomycin, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone, replacing dacarbazine with procarbazine and using the doxorubicin, bleomycin, vinblastine, procarbazine, and prednisone regimen, or replacing dacarbazine with cyclophosphamide.
Dr. Greene emphasized the importance of tracking the news and the drug shortage websites run by the FDA and the American Society of Health-System Pharmacists.
It’s also crucial to have a good relationship with your wholesaler, he added, and to communicate about these problems within your facility. At his hospital, the pharmaceutical staff holds a multi-disciplinary meeting at least weekly to discuss the supply of medications. As he put it, “it’s a challenging environment.”
Dr. Greene and Dr. Hantel reported no relevant disclosures.
Just before he took a call from a reporter asking about the impact of drug shortages in hematology, Bill Greene, PharmD, chief pharmaceutical officer at St. Jude Children’s Research Hospital, had spent an hour on the phone overseeing his institution’s response to a hematology drug shortage. The chemotherapy drug fludarabine, used to treat chronic lymphocytic leukemia, was in short supply.
“There are 5 different manufacturers, but none of them have had drug available over the past 2 weeks,” Dr. Greene said. “We’re trying to chase some emergency supplies to be able to continue treatment for patients who’ve had their treatments initiated and planned.”
Over the past several years, this predicament has become common at hematology clinics across the country. In fact, management of scarce medication resources has become a significant part of Dr. Greene’s workload these days, as critical drugs fail to show up on time or manufacturer supplies run low at his hospital in Memphis.
This shortage of hematology drugs got a new dose of national attention, thanks to a recent episode of CBS News’ “60 Minutes.” Through interviews with physicians and parents of children who suddenly could not get vital medications, the report highlighted the recent shortage of another leukemia drug, vincristine.
“As a cancer mom, we shouldn’t be fighting for our children to get a drug that is needed,” Cyndi Valenta was quoted as saying. She recalled that when the shortage began in 2019, her 13-year-old son, a leukemia patient at Loma Linda (Calif.) University Hospital, felt frightened. Ms. Valenta said she felt a “gut-wrenching feeling of just fear and anger.” They were finally able to get doses of the drug after launching a social media campaign.
Such drug shortages are especially widespread in oncology and hematology, according to a survey of oncology pharmacists at 68 organizations nationwide. Published in the May 2022 issue of Oncology Practice, the study showed that 63% of institutions reported one or more drug shortages every month, with a 34% increase in 2019, compared with 2018. Treatment delays, reduced doses, or alternative regimens were reported by 75% of respondents, the authors wrote.
The pharmacists surveyed between May 2019 and July 2020 were asked about the three most hard-to-get chemotherapy and supportive care agents. Vincristine topped the list, followed by vinblastine, IVIG, leucovorin, and BCG, as well as difficult-to-obtain ropine, erwinia asparaginase, etoposide, and leuprolide. Several of these drugs are used to treat conditions such as lymphoma and leukemia.
Eighty-two percent of respondents reported shortages of decitabine (IV), often used as part of a cocktail with vinblastine and other drugs to treat Hodgkin lymphoma.
The reasons for drug shortages are varied. The CBS News report declared that “pharmaceutical companies have stopped producing many life-saving generic drugs because they make too little profit,” and it suggested that the federal government isn’t doing enough.
But government action actually might be making a difference. According to the FDA, the number of new drug shortages has fallen dramatically from 250 in 2011 to 41 in 2021, and the number of prevented drug shortages rose from nearly 200 to more than 300 over that same period. Still, the number of ongoing drug shortages has risen from around 40 in 2017 to about 80 in 2021.
Reasons for the paucity of certain drugs are often unclear. In a June 12, 2022 post, for example, the American Society of Health-System Pharmacists’ drug shortage database noted that the chemotherapy drug fludarabine was in short supply and provided details about when some of the 5 manufacturers expected to have it available. (This is the shortage that Dr. Greene was trying to manage.) But 4 of the 5 manufacturers “did not provide a reason,” and the fifth blamed manufacturing delays.
“There’s a lot of closely held trade secrets that hinder the ability to share good information,” said Dr. Greene. To make things more complicated, shipping times are often unreliable. “The product doesn’t show up today, we place another order. Sometimes it will show up tomorrow, sometimes it doesn’t,” he said. “If you’re not tracking it carefully, you deplete your own supply.”
Patients’ families have grown used to dealing with drug shortages, and “they’re less quick to blame personnel at our institution.”
How can hematologists cope with this issue? “The best thing in the immediate term is to advocate for their hospital to have a pharmacist dedicated to shortage monitoring and taking proactive steps to obviate shortages,” hematologist/oncologist Andrew Hantel, MD, an instructor at Dana-Farber Cancer Institute, Harvard Medical School, Boston, said in an interview.
“We have ongoing communications with other large cancer centers and the FDA to recognize shortages early and develop plans to make sure we stay ahead of them,” Dr. Hantel said. “Most often this involves assessing supply, use rates, alternative manufacturers, and additional measures the Food and Drug Administration can take (for example, importation), and occasionally working with clinical teams to see if other medications are feasible alternatives.”
If a drug is unavailable, it can also be helpful to discuss alternative approaches. “We did not have any frank shortages of vincristine,” Dr. Hantel said, “but we did focus on conservation measures and considered different ethically appropriate ways to distribute vincristine if there was a point at which we did not have enough for everyone who needed it.”
If a drug is in short supply, options can include delaying treatment, giving an alternative, or providing the rest of the regimen without the scarce drug, he said. In a 2021 report in The Lancet Hematology, Dr. Hantel and his colleagues offered “model solutions for ethical allocation during cancer medicine shortages.”
The authors of the May 2022 drug-shortage report highlighted an alternative regimen in hematology. They noted that manufacturing delays have limited the supply of dacarbazine, used for Hodgkin lymphoma. Due to the current shortages, they wrote, clinicians are considering the use of escalated bleomycin, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone, replacing dacarbazine with procarbazine and using the doxorubicin, bleomycin, vinblastine, procarbazine, and prednisone regimen, or replacing dacarbazine with cyclophosphamide.
Dr. Greene emphasized the importance of tracking the news and the drug shortage websites run by the FDA and the American Society of Health-System Pharmacists.
It’s also crucial to have a good relationship with your wholesaler, he added, and to communicate about these problems within your facility. At his hospital, the pharmaceutical staff holds a multi-disciplinary meeting at least weekly to discuss the supply of medications. As he put it, “it’s a challenging environment.”
Dr. Greene and Dr. Hantel reported no relevant disclosures.
Just before he took a call from a reporter asking about the impact of drug shortages in hematology, Bill Greene, PharmD, chief pharmaceutical officer at St. Jude Children’s Research Hospital, had spent an hour on the phone overseeing his institution’s response to a hematology drug shortage. The chemotherapy drug fludarabine, used to treat chronic lymphocytic leukemia, was in short supply.
“There are 5 different manufacturers, but none of them have had drug available over the past 2 weeks,” Dr. Greene said. “We’re trying to chase some emergency supplies to be able to continue treatment for patients who’ve had their treatments initiated and planned.”
Over the past several years, this predicament has become common at hematology clinics across the country. In fact, management of scarce medication resources has become a significant part of Dr. Greene’s workload these days, as critical drugs fail to show up on time or manufacturer supplies run low at his hospital in Memphis.
This shortage of hematology drugs got a new dose of national attention, thanks to a recent episode of CBS News’ “60 Minutes.” Through interviews with physicians and parents of children who suddenly could not get vital medications, the report highlighted the recent shortage of another leukemia drug, vincristine.
“As a cancer mom, we shouldn’t be fighting for our children to get a drug that is needed,” Cyndi Valenta was quoted as saying. She recalled that when the shortage began in 2019, her 13-year-old son, a leukemia patient at Loma Linda (Calif.) University Hospital, felt frightened. Ms. Valenta said she felt a “gut-wrenching feeling of just fear and anger.” They were finally able to get doses of the drug after launching a social media campaign.
Such drug shortages are especially widespread in oncology and hematology, according to a survey of oncology pharmacists at 68 organizations nationwide. Published in the May 2022 issue of Oncology Practice, the study showed that 63% of institutions reported one or more drug shortages every month, with a 34% increase in 2019, compared with 2018. Treatment delays, reduced doses, or alternative regimens were reported by 75% of respondents, the authors wrote.
The pharmacists surveyed between May 2019 and July 2020 were asked about the three most hard-to-get chemotherapy and supportive care agents. Vincristine topped the list, followed by vinblastine, IVIG, leucovorin, and BCG, as well as difficult-to-obtain ropine, erwinia asparaginase, etoposide, and leuprolide. Several of these drugs are used to treat conditions such as lymphoma and leukemia.
Eighty-two percent of respondents reported shortages of decitabine (IV), often used as part of a cocktail with vinblastine and other drugs to treat Hodgkin lymphoma.
The reasons for drug shortages are varied. The CBS News report declared that “pharmaceutical companies have stopped producing many life-saving generic drugs because they make too little profit,” and it suggested that the federal government isn’t doing enough.
But government action actually might be making a difference. According to the FDA, the number of new drug shortages has fallen dramatically from 250 in 2011 to 41 in 2021, and the number of prevented drug shortages rose from nearly 200 to more than 300 over that same period. Still, the number of ongoing drug shortages has risen from around 40 in 2017 to about 80 in 2021.
Reasons for the paucity of certain drugs are often unclear. In a June 12, 2022 post, for example, the American Society of Health-System Pharmacists’ drug shortage database noted that the chemotherapy drug fludarabine was in short supply and provided details about when some of the 5 manufacturers expected to have it available. (This is the shortage that Dr. Greene was trying to manage.) But 4 of the 5 manufacturers “did not provide a reason,” and the fifth blamed manufacturing delays.
“There’s a lot of closely held trade secrets that hinder the ability to share good information,” said Dr. Greene. To make things more complicated, shipping times are often unreliable. “The product doesn’t show up today, we place another order. Sometimes it will show up tomorrow, sometimes it doesn’t,” he said. “If you’re not tracking it carefully, you deplete your own supply.”
Patients’ families have grown used to dealing with drug shortages, and “they’re less quick to blame personnel at our institution.”
How can hematologists cope with this issue? “The best thing in the immediate term is to advocate for their hospital to have a pharmacist dedicated to shortage monitoring and taking proactive steps to obviate shortages,” hematologist/oncologist Andrew Hantel, MD, an instructor at Dana-Farber Cancer Institute, Harvard Medical School, Boston, said in an interview.
“We have ongoing communications with other large cancer centers and the FDA to recognize shortages early and develop plans to make sure we stay ahead of them,” Dr. Hantel said. “Most often this involves assessing supply, use rates, alternative manufacturers, and additional measures the Food and Drug Administration can take (for example, importation), and occasionally working with clinical teams to see if other medications are feasible alternatives.”
If a drug is unavailable, it can also be helpful to discuss alternative approaches. “We did not have any frank shortages of vincristine,” Dr. Hantel said, “but we did focus on conservation measures and considered different ethically appropriate ways to distribute vincristine if there was a point at which we did not have enough for everyone who needed it.”
If a drug is in short supply, options can include delaying treatment, giving an alternative, or providing the rest of the regimen without the scarce drug, he said. In a 2021 report in The Lancet Hematology, Dr. Hantel and his colleagues offered “model solutions for ethical allocation during cancer medicine shortages.”
The authors of the May 2022 drug-shortage report highlighted an alternative regimen in hematology. They noted that manufacturing delays have limited the supply of dacarbazine, used for Hodgkin lymphoma. Due to the current shortages, they wrote, clinicians are considering the use of escalated bleomycin, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone, replacing dacarbazine with procarbazine and using the doxorubicin, bleomycin, vinblastine, procarbazine, and prednisone regimen, or replacing dacarbazine with cyclophosphamide.
Dr. Greene emphasized the importance of tracking the news and the drug shortage websites run by the FDA and the American Society of Health-System Pharmacists.
It’s also crucial to have a good relationship with your wholesaler, he added, and to communicate about these problems within your facility. At his hospital, the pharmaceutical staff holds a multi-disciplinary meeting at least weekly to discuss the supply of medications. As he put it, “it’s a challenging environment.”
Dr. Greene and Dr. Hantel reported no relevant disclosures.
Third-generation Black woman physician makes cancer research history
When Jane Cooke Wright, MD, entered the medical profession in 1945, the notion that toxic drugs could target tumors struck many physicians and patients as outlandish. How could one poison be weaponized against another poison – a cancerous tumor – without creating more havoc? Let alone a combination of two or more chemicals?

Dr. Wright’s story would be extraordinary enough if she’d looked like most of her colleagues, but this surgeon and researcher stood apart. An African American woman at a time when medicine and science – like politics and law – were almost entirely the domain of White men, Dr. Wright had determination in her blood. Her father, once honored by a crowd of dignitaries that included a First Lady, persevered despite his horrific encounters with racism. She shared her father’s commitment to progress and added her own personal twists. She balanced elegance and beauty with scientific savvy, fierce ambition, and a refusal to be defined by anything other than her accomplishments.
“She didn’t focus on race, not at all,” her daughter Alison Jones, PhD, a psychologist in East Lansing, Mich., said in an interview. “Wherever she was, she wanted to be the best, not the best Black person. It was not about how she performed in a category, and she would get upset if someone said she was good as a Black physician.”
On the road to being the best, Dr. Jones said, her mother set a goal of curing cancer. National Cancer Research Month is a fitting opportunity to look back on a scientist dedicated to bringing humanity closer to that elusive achievement.
Medical legacy blazed in toil and trauma
A strong case could be made that Dr. Jane C. Wright and her father Louis Tompkins Wright, MD, are the most accomplished father-and-daughter team in all of medicine.
The elder Dr. Wright, son of a formerly enslaved man turned physician and a stepson of the first African American to graduate from Yale University, New Haven, Conn., himself graduated from Harvard Medical School in 1915. He earned a Purple Heart while serving in World War I, then went on to become the first Black surgeon to join the staff at Harlem Hospital.
Dr. Wright, who had witnessed mob violence and the aftermath of a lynching as a young man, became a supporter of the Harlem Renaissance and a prominent advocate for civil rights and integration. He served as chairman of the National Association for the Advancement of Colored People and was only the second Black member of the American College of Surgeons.
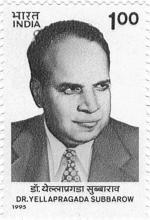
According to the 2009 book “Black Genius: Inspirational Portraits of African American Leaders,” he successfully treated the rare but devastating venereal disease lymphogranuloma venereum with a new antibiotic developed by his former colleague Yellapragada SubbaRow, MD. Dr. Wright even tried the drug himself, “as a lot of doctors in the olden days did,” according to another of his daughters, the late Barbara Wright Pierce, MD, who was quoted in “Black Genius.” She, too, was a physician.
In 1948, Dr. Jane C. Wright joined her father at Harlem Hospital’s Cancer Research Foundation. There the duo explored the cancer-fighting possibilities of a nitrogen mustard–like chemical agent that had been known since World War I to kill white blood cells. Ironically, Dr. Louis Wright himself suffered lifelong health problems because of an attack from the poisonous gas phosgene during his wartime service.
“Remissions were observed in patients with sarcoma, Hodgkin disease, and chronic myelogenous leukemia, mycosis fungoides, and lymphoma,” reported a 2013 obituary in the journal Oncology of the younger Dr. Wright. “They also performed early research into the clinical efficacy and toxicity of folic acid antagonists, documenting responses in 93 patients with various forms of incurable blood cancers and solid tumors.”
This research appears in a study that was authored by three Dr. Wrights – Dr. Louis T. Wright and his daughters Jane and Barbara.
“The elder Dr. Wright died in 1952, just months after 1,000 people – including Eleanor Roosevelt – honored him at a dinner to dedicate a Harlem Hospital library named after him. He was 61.
Scientific savvy mixed with modesty and elegance
After her father’s death, Dr. Janet C. Wright became director of the hospital’s cancer foundation. From the 1950s to the 1970s, she “worked out ways to use pieces of a patient’s own tumor, removed by surgery and grown in a nutrient culture medium in the laboratory, as a ‘guinea pig for testing drugs,’ ” according to the 1991 book “Black Scientists.” Previously, researchers had focused on mice as test subjects.
This approach also allowed Dr. Wright to determine if specific drugs such as methotrexate, a folic acid antagonist, would help specific patients. “She was looking for predictive activity for chemotherapeutic efficacy in vitro at a time when no one had good predictive tests,” wrote James F. Holland, MD, the late Mount Sinai School of Medicine oncologist, who was quoted in Dr. Wright’s 2013 Oncology obituary.
“Her strict attention to detail and concern for her patients helped determine effective dosing levels and establish treatment guidelines,” the Oncology obituary reported. “She treated patients that other physicians had given up on, and she was among the first small cadre of researchers to carefully test the effects of drugs against cancer in a clinical trial setting.”
Dr. Wright also focused on developing ways to administer chemotherapy, such using a catheter to reach difficult-to-access organs like the spleen without surgery, according to “Black Scientists.”
Along with her work, Dr. Wright’s appearance set her apart. According to “Black Genius,” a newspaper columnist dubbed her one of the 10 most beautiful Back woman in America, and Ebony Magazine in 1966 honored her as one of the best-dressed women in America. It featured a photograph of her in a stunning ivory and yellow brocade gown, noting that she was “in private life Mrs. David J. Jones.” (She’d married the Harvard University Law School graduate in 1946.)
Dr. Wright had a sense of modesty despite her accomplishments, according to her daughter Alison Jones. She even downplayed her own mental powers in a newspaper interview. “I know I’m a member of two minority groups,” she told The New York Post in 1967, “but I don’t think of myself that way. Sure, a woman has to try twice as hard. But – racial prejudice? I’ve met very little of it. It could be I met it – and wasn’t intelligent enough to recognize it.”
Sharp-eyed readers might have glimpsed her modesty nearly 2 decades later. In a 1984 article for the Journal of the National Medical Association, a society of African American physicians, she wrote about the past, present, and future of chemotherapy without noting her own prominent role in its development.
‘Global medical pioneer’ cofounds ASCO – and more
In the 1960s, Dr. Wright joined the influential President’s Commission on Heart Disease, Cancer, and Stroke and was named associate dean at New York Medical College, her alma mater, a first for a black woman at a prominent U.S. medical school. Even more importantly, Dr. Wright was the sole woman among seven physicians who founded the American Society of Clinical Oncology in Chicago in 1964. She served as ASCO’s first Secretary-Treasurer and was honored as its longest surviving founder when she passed away 9 years ago.
“Jane Wright had the vision to see that oncology was an important separate discipline within medicine with far-reaching implications for research and discovery,” Georgetown University Medical Center, Washington, oncologist Sandra M. Swain, MD, a former president of the ASCO and author of the 2013 Oncology obituary of Dr. Wright, said in an interview. “It is truly remarkable that, as a woman and an African American woman, she had a seat at the very small table for the formation of such an important group.”
As her friend and fellow oncologist Edith Mitchell, MD, said in a eulogy, “Dr. Wright led delegations of oncologists to China and the Soviet Union, and countries in Africa and Eastern Europe. She led medical teams providing medical and cancer care and education to other nurses and physicians in Ghana in 1957 and Kenya in 1961. From 1973 to 1984, she served as vice-president of the African Research and Medical foundation.”
Dr. Wright also raised two daughters. A 1968 Ebony article devoted to her career and family declared that neither of her teenagers was interested in medical careers. Their perspectives shifted, however – as had Dr. Wright’s. An undergraduate at Smith College, Dr. Wright majored in art, swam on the varsity team, and had a special affinity for German language studies before she switched to premed.
Like their mother, Dr. Wright’s daughters also changed paths, and they ultimately became the fourth generation of their family to enter the medical field. Dr. Alison Jones, the psychologist, currently works in a prison, while Jane Jones, MD, became a clinical psychiatrist. She’s now retired and lives in Guttenberg, N.J.
Both fondly remember their mother as a supportive force who insisted on excellence. “There couldn’t be any excuses for you not getting where you wanted to go,” Dr. Jane Jones recalled in an interview.
Nevertheless, Dr. Wright was still keenly aware of society’s limits. “She told me I had to be a doctor or lawyer,” Dr. Alison Jones said, “because that’s how you need to survive when you’re Black in America.”
Dr. Wright passed away in 2013 at age 93. “Dr. Jane C. Wright truly has made contributions that have changed the practice of medicine,” noted her friend Dr. Mitchell, an oncologist and a retired brigadier general with the U.S. Air Force who now teaches at Thomas Jefferson University, Philadelphia. “A true pioneer. A concerned mentor. A renowned researcher. A global teacher. A global medical pioneer. A talented researcher, beloved sister, wife, and mother, and a beautiful, kind, and loving human being.”
When Jane Cooke Wright, MD, entered the medical profession in 1945, the notion that toxic drugs could target tumors struck many physicians and patients as outlandish. How could one poison be weaponized against another poison – a cancerous tumor – without creating more havoc? Let alone a combination of two or more chemicals?

Dr. Wright’s story would be extraordinary enough if she’d looked like most of her colleagues, but this surgeon and researcher stood apart. An African American woman at a time when medicine and science – like politics and law – were almost entirely the domain of White men, Dr. Wright had determination in her blood. Her father, once honored by a crowd of dignitaries that included a First Lady, persevered despite his horrific encounters with racism. She shared her father’s commitment to progress and added her own personal twists. She balanced elegance and beauty with scientific savvy, fierce ambition, and a refusal to be defined by anything other than her accomplishments.
“She didn’t focus on race, not at all,” her daughter Alison Jones, PhD, a psychologist in East Lansing, Mich., said in an interview. “Wherever she was, she wanted to be the best, not the best Black person. It was not about how she performed in a category, and she would get upset if someone said she was good as a Black physician.”
On the road to being the best, Dr. Jones said, her mother set a goal of curing cancer. National Cancer Research Month is a fitting opportunity to look back on a scientist dedicated to bringing humanity closer to that elusive achievement.
Medical legacy blazed in toil and trauma
A strong case could be made that Dr. Jane C. Wright and her father Louis Tompkins Wright, MD, are the most accomplished father-and-daughter team in all of medicine.
The elder Dr. Wright, son of a formerly enslaved man turned physician and a stepson of the first African American to graduate from Yale University, New Haven, Conn., himself graduated from Harvard Medical School in 1915. He earned a Purple Heart while serving in World War I, then went on to become the first Black surgeon to join the staff at Harlem Hospital.
Dr. Wright, who had witnessed mob violence and the aftermath of a lynching as a young man, became a supporter of the Harlem Renaissance and a prominent advocate for civil rights and integration. He served as chairman of the National Association for the Advancement of Colored People and was only the second Black member of the American College of Surgeons.
According to the 2009 book “Black Genius: Inspirational Portraits of African American Leaders,” he successfully treated the rare but devastating venereal disease lymphogranuloma venereum with a new antibiotic developed by his former colleague Yellapragada SubbaRow, MD. Dr. Wright even tried the drug himself, “as a lot of doctors in the olden days did,” according to another of his daughters, the late Barbara Wright Pierce, MD, who was quoted in “Black Genius.” She, too, was a physician.
In 1948, Dr. Jane C. Wright joined her father at Harlem Hospital’s Cancer Research Foundation. There the duo explored the cancer-fighting possibilities of a nitrogen mustard–like chemical agent that had been known since World War I to kill white blood cells. Ironically, Dr. Louis Wright himself suffered lifelong health problems because of an attack from the poisonous gas phosgene during his wartime service.
“Remissions were observed in patients with sarcoma, Hodgkin disease, and chronic myelogenous leukemia, mycosis fungoides, and lymphoma,” reported a 2013 obituary in the journal Oncology of the younger Dr. Wright. “They also performed early research into the clinical efficacy and toxicity of folic acid antagonists, documenting responses in 93 patients with various forms of incurable blood cancers and solid tumors.”
This research appears in a study that was authored by three Dr. Wrights – Dr. Louis T. Wright and his daughters Jane and Barbara.
“The elder Dr. Wright died in 1952, just months after 1,000 people – including Eleanor Roosevelt – honored him at a dinner to dedicate a Harlem Hospital library named after him. He was 61.
Scientific savvy mixed with modesty and elegance
After her father’s death, Dr. Janet C. Wright became director of the hospital’s cancer foundation. From the 1950s to the 1970s, she “worked out ways to use pieces of a patient’s own tumor, removed by surgery and grown in a nutrient culture medium in the laboratory, as a ‘guinea pig for testing drugs,’ ” according to the 1991 book “Black Scientists.” Previously, researchers had focused on mice as test subjects.
This approach also allowed Dr. Wright to determine if specific drugs such as methotrexate, a folic acid antagonist, would help specific patients. “She was looking for predictive activity for chemotherapeutic efficacy in vitro at a time when no one had good predictive tests,” wrote James F. Holland, MD, the late Mount Sinai School of Medicine oncologist, who was quoted in Dr. Wright’s 2013 Oncology obituary.
“Her strict attention to detail and concern for her patients helped determine effective dosing levels and establish treatment guidelines,” the Oncology obituary reported. “She treated patients that other physicians had given up on, and she was among the first small cadre of researchers to carefully test the effects of drugs against cancer in a clinical trial setting.”
Dr. Wright also focused on developing ways to administer chemotherapy, such using a catheter to reach difficult-to-access organs like the spleen without surgery, according to “Black Scientists.”
Along with her work, Dr. Wright’s appearance set her apart. According to “Black Genius,” a newspaper columnist dubbed her one of the 10 most beautiful Back woman in America, and Ebony Magazine in 1966 honored her as one of the best-dressed women in America. It featured a photograph of her in a stunning ivory and yellow brocade gown, noting that she was “in private life Mrs. David J. Jones.” (She’d married the Harvard University Law School graduate in 1946.)
Dr. Wright had a sense of modesty despite her accomplishments, according to her daughter Alison Jones. She even downplayed her own mental powers in a newspaper interview. “I know I’m a member of two minority groups,” she told The New York Post in 1967, “but I don’t think of myself that way. Sure, a woman has to try twice as hard. But – racial prejudice? I’ve met very little of it. It could be I met it – and wasn’t intelligent enough to recognize it.”
Sharp-eyed readers might have glimpsed her modesty nearly 2 decades later. In a 1984 article for the Journal of the National Medical Association, a society of African American physicians, she wrote about the past, present, and future of chemotherapy without noting her own prominent role in its development.
‘Global medical pioneer’ cofounds ASCO – and more
In the 1960s, Dr. Wright joined the influential President’s Commission on Heart Disease, Cancer, and Stroke and was named associate dean at New York Medical College, her alma mater, a first for a black woman at a prominent U.S. medical school. Even more importantly, Dr. Wright was the sole woman among seven physicians who founded the American Society of Clinical Oncology in Chicago in 1964. She served as ASCO’s first Secretary-Treasurer and was honored as its longest surviving founder when she passed away 9 years ago.
“Jane Wright had the vision to see that oncology was an important separate discipline within medicine with far-reaching implications for research and discovery,” Georgetown University Medical Center, Washington, oncologist Sandra M. Swain, MD, a former president of the ASCO and author of the 2013 Oncology obituary of Dr. Wright, said in an interview. “It is truly remarkable that, as a woman and an African American woman, she had a seat at the very small table for the formation of such an important group.”
As her friend and fellow oncologist Edith Mitchell, MD, said in a eulogy, “Dr. Wright led delegations of oncologists to China and the Soviet Union, and countries in Africa and Eastern Europe. She led medical teams providing medical and cancer care and education to other nurses and physicians in Ghana in 1957 and Kenya in 1961. From 1973 to 1984, she served as vice-president of the African Research and Medical foundation.”
Dr. Wright also raised two daughters. A 1968 Ebony article devoted to her career and family declared that neither of her teenagers was interested in medical careers. Their perspectives shifted, however – as had Dr. Wright’s. An undergraduate at Smith College, Dr. Wright majored in art, swam on the varsity team, and had a special affinity for German language studies before she switched to premed.
Like their mother, Dr. Wright’s daughters also changed paths, and they ultimately became the fourth generation of their family to enter the medical field. Dr. Alison Jones, the psychologist, currently works in a prison, while Jane Jones, MD, became a clinical psychiatrist. She’s now retired and lives in Guttenberg, N.J.
Both fondly remember their mother as a supportive force who insisted on excellence. “There couldn’t be any excuses for you not getting where you wanted to go,” Dr. Jane Jones recalled in an interview.
Nevertheless, Dr. Wright was still keenly aware of society’s limits. “She told me I had to be a doctor or lawyer,” Dr. Alison Jones said, “because that’s how you need to survive when you’re Black in America.”
Dr. Wright passed away in 2013 at age 93. “Dr. Jane C. Wright truly has made contributions that have changed the practice of medicine,” noted her friend Dr. Mitchell, an oncologist and a retired brigadier general with the U.S. Air Force who now teaches at Thomas Jefferson University, Philadelphia. “A true pioneer. A concerned mentor. A renowned researcher. A global teacher. A global medical pioneer. A talented researcher, beloved sister, wife, and mother, and a beautiful, kind, and loving human being.”
When Jane Cooke Wright, MD, entered the medical profession in 1945, the notion that toxic drugs could target tumors struck many physicians and patients as outlandish. How could one poison be weaponized against another poison – a cancerous tumor – without creating more havoc? Let alone a combination of two or more chemicals?

Dr. Wright’s story would be extraordinary enough if she’d looked like most of her colleagues, but this surgeon and researcher stood apart. An African American woman at a time when medicine and science – like politics and law – were almost entirely the domain of White men, Dr. Wright had determination in her blood. Her father, once honored by a crowd of dignitaries that included a First Lady, persevered despite his horrific encounters with racism. She shared her father’s commitment to progress and added her own personal twists. She balanced elegance and beauty with scientific savvy, fierce ambition, and a refusal to be defined by anything other than her accomplishments.
“She didn’t focus on race, not at all,” her daughter Alison Jones, PhD, a psychologist in East Lansing, Mich., said in an interview. “Wherever she was, she wanted to be the best, not the best Black person. It was not about how she performed in a category, and she would get upset if someone said she was good as a Black physician.”
On the road to being the best, Dr. Jones said, her mother set a goal of curing cancer. National Cancer Research Month is a fitting opportunity to look back on a scientist dedicated to bringing humanity closer to that elusive achievement.
Medical legacy blazed in toil and trauma
A strong case could be made that Dr. Jane C. Wright and her father Louis Tompkins Wright, MD, are the most accomplished father-and-daughter team in all of medicine.
The elder Dr. Wright, son of a formerly enslaved man turned physician and a stepson of the first African American to graduate from Yale University, New Haven, Conn., himself graduated from Harvard Medical School in 1915. He earned a Purple Heart while serving in World War I, then went on to become the first Black surgeon to join the staff at Harlem Hospital.
Dr. Wright, who had witnessed mob violence and the aftermath of a lynching as a young man, became a supporter of the Harlem Renaissance and a prominent advocate for civil rights and integration. He served as chairman of the National Association for the Advancement of Colored People and was only the second Black member of the American College of Surgeons.
According to the 2009 book “Black Genius: Inspirational Portraits of African American Leaders,” he successfully treated the rare but devastating venereal disease lymphogranuloma venereum with a new antibiotic developed by his former colleague Yellapragada SubbaRow, MD. Dr. Wright even tried the drug himself, “as a lot of doctors in the olden days did,” according to another of his daughters, the late Barbara Wright Pierce, MD, who was quoted in “Black Genius.” She, too, was a physician.
In 1948, Dr. Jane C. Wright joined her father at Harlem Hospital’s Cancer Research Foundation. There the duo explored the cancer-fighting possibilities of a nitrogen mustard–like chemical agent that had been known since World War I to kill white blood cells. Ironically, Dr. Louis Wright himself suffered lifelong health problems because of an attack from the poisonous gas phosgene during his wartime service.
“Remissions were observed in patients with sarcoma, Hodgkin disease, and chronic myelogenous leukemia, mycosis fungoides, and lymphoma,” reported a 2013 obituary in the journal Oncology of the younger Dr. Wright. “They also performed early research into the clinical efficacy and toxicity of folic acid antagonists, documenting responses in 93 patients with various forms of incurable blood cancers and solid tumors.”
This research appears in a study that was authored by three Dr. Wrights – Dr. Louis T. Wright and his daughters Jane and Barbara.
“The elder Dr. Wright died in 1952, just months after 1,000 people – including Eleanor Roosevelt – honored him at a dinner to dedicate a Harlem Hospital library named after him. He was 61.
Scientific savvy mixed with modesty and elegance
After her father’s death, Dr. Janet C. Wright became director of the hospital’s cancer foundation. From the 1950s to the 1970s, she “worked out ways to use pieces of a patient’s own tumor, removed by surgery and grown in a nutrient culture medium in the laboratory, as a ‘guinea pig for testing drugs,’ ” according to the 1991 book “Black Scientists.” Previously, researchers had focused on mice as test subjects.
This approach also allowed Dr. Wright to determine if specific drugs such as methotrexate, a folic acid antagonist, would help specific patients. “She was looking for predictive activity for chemotherapeutic efficacy in vitro at a time when no one had good predictive tests,” wrote James F. Holland, MD, the late Mount Sinai School of Medicine oncologist, who was quoted in Dr. Wright’s 2013 Oncology obituary.
“Her strict attention to detail and concern for her patients helped determine effective dosing levels and establish treatment guidelines,” the Oncology obituary reported. “She treated patients that other physicians had given up on, and she was among the first small cadre of researchers to carefully test the effects of drugs against cancer in a clinical trial setting.”
Dr. Wright also focused on developing ways to administer chemotherapy, such using a catheter to reach difficult-to-access organs like the spleen without surgery, according to “Black Scientists.”
Along with her work, Dr. Wright’s appearance set her apart. According to “Black Genius,” a newspaper columnist dubbed her one of the 10 most beautiful Back woman in America, and Ebony Magazine in 1966 honored her as one of the best-dressed women in America. It featured a photograph of her in a stunning ivory and yellow brocade gown, noting that she was “in private life Mrs. David J. Jones.” (She’d married the Harvard University Law School graduate in 1946.)
Dr. Wright had a sense of modesty despite her accomplishments, according to her daughter Alison Jones. She even downplayed her own mental powers in a newspaper interview. “I know I’m a member of two minority groups,” she told The New York Post in 1967, “but I don’t think of myself that way. Sure, a woman has to try twice as hard. But – racial prejudice? I’ve met very little of it. It could be I met it – and wasn’t intelligent enough to recognize it.”
Sharp-eyed readers might have glimpsed her modesty nearly 2 decades later. In a 1984 article for the Journal of the National Medical Association, a society of African American physicians, she wrote about the past, present, and future of chemotherapy without noting her own prominent role in its development.
‘Global medical pioneer’ cofounds ASCO – and more
In the 1960s, Dr. Wright joined the influential President’s Commission on Heart Disease, Cancer, and Stroke and was named associate dean at New York Medical College, her alma mater, a first for a black woman at a prominent U.S. medical school. Even more importantly, Dr. Wright was the sole woman among seven physicians who founded the American Society of Clinical Oncology in Chicago in 1964. She served as ASCO’s first Secretary-Treasurer and was honored as its longest surviving founder when she passed away 9 years ago.
“Jane Wright had the vision to see that oncology was an important separate discipline within medicine with far-reaching implications for research and discovery,” Georgetown University Medical Center, Washington, oncologist Sandra M. Swain, MD, a former president of the ASCO and author of the 2013 Oncology obituary of Dr. Wright, said in an interview. “It is truly remarkable that, as a woman and an African American woman, she had a seat at the very small table for the formation of such an important group.”
As her friend and fellow oncologist Edith Mitchell, MD, said in a eulogy, “Dr. Wright led delegations of oncologists to China and the Soviet Union, and countries in Africa and Eastern Europe. She led medical teams providing medical and cancer care and education to other nurses and physicians in Ghana in 1957 and Kenya in 1961. From 1973 to 1984, she served as vice-president of the African Research and Medical foundation.”
Dr. Wright also raised two daughters. A 1968 Ebony article devoted to her career and family declared that neither of her teenagers was interested in medical careers. Their perspectives shifted, however – as had Dr. Wright’s. An undergraduate at Smith College, Dr. Wright majored in art, swam on the varsity team, and had a special affinity for German language studies before she switched to premed.
Like their mother, Dr. Wright’s daughters also changed paths, and they ultimately became the fourth generation of their family to enter the medical field. Dr. Alison Jones, the psychologist, currently works in a prison, while Jane Jones, MD, became a clinical psychiatrist. She’s now retired and lives in Guttenberg, N.J.
Both fondly remember their mother as a supportive force who insisted on excellence. “There couldn’t be any excuses for you not getting where you wanted to go,” Dr. Jane Jones recalled in an interview.
Nevertheless, Dr. Wright was still keenly aware of society’s limits. “She told me I had to be a doctor or lawyer,” Dr. Alison Jones said, “because that’s how you need to survive when you’re Black in America.”
Dr. Wright passed away in 2013 at age 93. “Dr. Jane C. Wright truly has made contributions that have changed the practice of medicine,” noted her friend Dr. Mitchell, an oncologist and a retired brigadier general with the U.S. Air Force who now teaches at Thomas Jefferson University, Philadelphia. “A true pioneer. A concerned mentor. A renowned researcher. A global teacher. A global medical pioneer. A talented researcher, beloved sister, wife, and mother, and a beautiful, kind, and loving human being.”
Young leukemia survivors still dying early, study shows
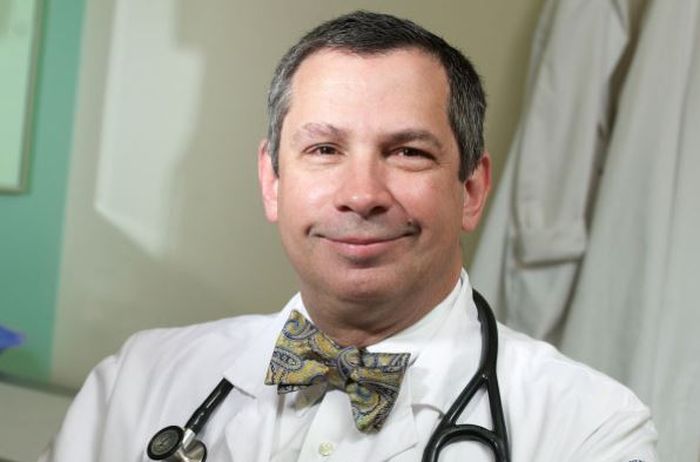
Although adolescents and young adults (AYAs) who survive leukemia are living much longer than ever before, their life spans are still shorter than those of the general population, a new study concludes.
The study found that the 10-year survival of AYA leukemia survivors was approximately 10% lower than that of the age-adjusted U.S. general population at large.
These differences persisted for up to 30 years of follow-up.
“We need to think about the long-term life span and the quality of life for our patients. Cure is not enough for our AYA cancer survivors,” said senior author Michael Roth, MD, associate professor of pediatric patient care and director of the Childhood Cancer Survivorship Clinic at the University of Texas MD Anderson Cancer Center, Houston.
“Once these patients reach the survivorship stage of their journey, they may encounter additional side effects as a result of intensive treatment, lack of access to quality health care, and other issues that may negatively impact their health and overall survival,” he said in a statement.
The study was published in Cancer Epidemiology, Biomarkers and Prevention.
Demographics play role in survival
AYAs were defined as those persons aged 15-39 years. For their study, Dr. Roth and colleagues used the Surveillance, Epidemiology, and End Results (SEER) registry to identify 1,938 AYA survivors of acute lymphoblastic leukemia (ALL) and 2,350 AYA survivors of acute myeloid leukemia (AML) who were diagnosed from 1980 to 2009. They were followed for a median of 12 years.
The median age at diagnosis was 23 years for ALL and 28 years for AML.
Among ALL survivors, 6% were Black, 7% were Asian or Pacific Islander, 29% were Hispanic, and 58% were White. Among AML survivors, 9% were Black, 10% were Asian or Pacific Islander, 22% were Hispanic, and 59% were White. Ten-year survival for ALL and AML survivors was 87% and 89%, respectively. For the general population, it was 99%.
For ALL survivors, the 10-year survival was 83% for those diagnosed in the 1980s; it was 88% for those diagnosed in the 1990s and in the 2000s. The pattern was similar for AML survivors: 82%, 90%, and 90%.
The most common cause of death during early survivorship was acute leukemia. Deaths plateaued approximately 10 years after the initial diagnosis.
“Some of these patients aren’t being fully cured of their initial cancer, so between 5 and 10 years post initial diagnosis, most of the deaths are due to disease progression or relapse, whereas after that, most of the deaths result from late side effects from treatment, including cardiovascular disease and secondary cancers,” Dr. Roth said. Mortality from other causes continued to rise during the survivorship period. Subsequent malignancies and cardiac disease were the most common causes of death for both ALL and AML survivors.
A recent study found that AYA cancer survivors face nearly a twofold higher risk of dying from a new primary cancer, compared with peers in the general population.
When looking at key demographics, the authors found that older age at diagnosis was significantly associated with differential long-term survival (P < .0001 for both ALL and AML). Each additional year older at diagnosis was associated with a 6% and 5% decrease in long-term survival for both types of leukemia.
The decade in which the diagnosis was made had a significant difference in long-term survival both for patients with ALL and those with AML. Long-term survival times for those diagnosed in the 1990s were more than twice those of patients diagnosed in the 1980s for ALL (unadjusted P = .008) and AML (unadjusted P = .0002). Survival times were also more than twice those of patients diagnosed in the 2000s versus the 1980s for ALL (unadjusted P = .009) and AML (unadjusted P = .0003).
No significant long-term survival differences were observed for those diagnosed in the 2000s, compared with the 1990s, for either leukemia.
“The data from the national registry used for this study gave us insights into some possible challenges AML and ALL patients may encounter throughout survivorship, but we need to more thoroughly survey their journey,” Dr. Roth said. “An examination of their socioeconomic status, comorbidities, access to quality health care, and other risk factors that may impact their survivorship is warranted.”
The research was supported by the National Cancer Institute at the National Institutes of Health, the Archer Charitable Foundation, and LyondellBasell. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although adolescents and young adults (AYAs) who survive leukemia are living much longer than ever before, their life spans are still shorter than those of the general population, a new study concludes.
The study found that the 10-year survival of AYA leukemia survivors was approximately 10% lower than that of the age-adjusted U.S. general population at large.
These differences persisted for up to 30 years of follow-up.
“We need to think about the long-term life span and the quality of life for our patients. Cure is not enough for our AYA cancer survivors,” said senior author Michael Roth, MD, associate professor of pediatric patient care and director of the Childhood Cancer Survivorship Clinic at the University of Texas MD Anderson Cancer Center, Houston.
“Once these patients reach the survivorship stage of their journey, they may encounter additional side effects as a result of intensive treatment, lack of access to quality health care, and other issues that may negatively impact their health and overall survival,” he said in a statement.
The study was published in Cancer Epidemiology, Biomarkers and Prevention.
Demographics play role in survival
AYAs were defined as those persons aged 15-39 years. For their study, Dr. Roth and colleagues used the Surveillance, Epidemiology, and End Results (SEER) registry to identify 1,938 AYA survivors of acute lymphoblastic leukemia (ALL) and 2,350 AYA survivors of acute myeloid leukemia (AML) who were diagnosed from 1980 to 2009. They were followed for a median of 12 years.
The median age at diagnosis was 23 years for ALL and 28 years for AML.
Among ALL survivors, 6% were Black, 7% were Asian or Pacific Islander, 29% were Hispanic, and 58% were White. Among AML survivors, 9% were Black, 10% were Asian or Pacific Islander, 22% were Hispanic, and 59% were White. Ten-year survival for ALL and AML survivors was 87% and 89%, respectively. For the general population, it was 99%.
For ALL survivors, the 10-year survival was 83% for those diagnosed in the 1980s; it was 88% for those diagnosed in the 1990s and in the 2000s. The pattern was similar for AML survivors: 82%, 90%, and 90%.
The most common cause of death during early survivorship was acute leukemia. Deaths plateaued approximately 10 years after the initial diagnosis.
“Some of these patients aren’t being fully cured of their initial cancer, so between 5 and 10 years post initial diagnosis, most of the deaths are due to disease progression or relapse, whereas after that, most of the deaths result from late side effects from treatment, including cardiovascular disease and secondary cancers,” Dr. Roth said. Mortality from other causes continued to rise during the survivorship period. Subsequent malignancies and cardiac disease were the most common causes of death for both ALL and AML survivors.
A recent study found that AYA cancer survivors face nearly a twofold higher risk of dying from a new primary cancer, compared with peers in the general population.
When looking at key demographics, the authors found that older age at diagnosis was significantly associated with differential long-term survival (P < .0001 for both ALL and AML). Each additional year older at diagnosis was associated with a 6% and 5% decrease in long-term survival for both types of leukemia.
The decade in which the diagnosis was made had a significant difference in long-term survival both for patients with ALL and those with AML. Long-term survival times for those diagnosed in the 1990s were more than twice those of patients diagnosed in the 1980s for ALL (unadjusted P = .008) and AML (unadjusted P = .0002). Survival times were also more than twice those of patients diagnosed in the 2000s versus the 1980s for ALL (unadjusted P = .009) and AML (unadjusted P = .0003).
No significant long-term survival differences were observed for those diagnosed in the 2000s, compared with the 1990s, for either leukemia.
“The data from the national registry used for this study gave us insights into some possible challenges AML and ALL patients may encounter throughout survivorship, but we need to more thoroughly survey their journey,” Dr. Roth said. “An examination of their socioeconomic status, comorbidities, access to quality health care, and other risk factors that may impact their survivorship is warranted.”
The research was supported by the National Cancer Institute at the National Institutes of Health, the Archer Charitable Foundation, and LyondellBasell. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although adolescents and young adults (AYAs) who survive leukemia are living much longer than ever before, their life spans are still shorter than those of the general population, a new study concludes.
The study found that the 10-year survival of AYA leukemia survivors was approximately 10% lower than that of the age-adjusted U.S. general population at large.
These differences persisted for up to 30 years of follow-up.
“We need to think about the long-term life span and the quality of life for our patients. Cure is not enough for our AYA cancer survivors,” said senior author Michael Roth, MD, associate professor of pediatric patient care and director of the Childhood Cancer Survivorship Clinic at the University of Texas MD Anderson Cancer Center, Houston.
“Once these patients reach the survivorship stage of their journey, they may encounter additional side effects as a result of intensive treatment, lack of access to quality health care, and other issues that may negatively impact their health and overall survival,” he said in a statement.
The study was published in Cancer Epidemiology, Biomarkers and Prevention.
Demographics play role in survival
AYAs were defined as those persons aged 15-39 years. For their study, Dr. Roth and colleagues used the Surveillance, Epidemiology, and End Results (SEER) registry to identify 1,938 AYA survivors of acute lymphoblastic leukemia (ALL) and 2,350 AYA survivors of acute myeloid leukemia (AML) who were diagnosed from 1980 to 2009. They were followed for a median of 12 years.
The median age at diagnosis was 23 years for ALL and 28 years for AML.
Among ALL survivors, 6% were Black, 7% were Asian or Pacific Islander, 29% were Hispanic, and 58% were White. Among AML survivors, 9% were Black, 10% were Asian or Pacific Islander, 22% were Hispanic, and 59% were White. Ten-year survival for ALL and AML survivors was 87% and 89%, respectively. For the general population, it was 99%.
For ALL survivors, the 10-year survival was 83% for those diagnosed in the 1980s; it was 88% for those diagnosed in the 1990s and in the 2000s. The pattern was similar for AML survivors: 82%, 90%, and 90%.
The most common cause of death during early survivorship was acute leukemia. Deaths plateaued approximately 10 years after the initial diagnosis.
“Some of these patients aren’t being fully cured of their initial cancer, so between 5 and 10 years post initial diagnosis, most of the deaths are due to disease progression or relapse, whereas after that, most of the deaths result from late side effects from treatment, including cardiovascular disease and secondary cancers,” Dr. Roth said. Mortality from other causes continued to rise during the survivorship period. Subsequent malignancies and cardiac disease were the most common causes of death for both ALL and AML survivors.
A recent study found that AYA cancer survivors face nearly a twofold higher risk of dying from a new primary cancer, compared with peers in the general population.
When looking at key demographics, the authors found that older age at diagnosis was significantly associated with differential long-term survival (P < .0001 for both ALL and AML). Each additional year older at diagnosis was associated with a 6% and 5% decrease in long-term survival for both types of leukemia.
The decade in which the diagnosis was made had a significant difference in long-term survival both for patients with ALL and those with AML. Long-term survival times for those diagnosed in the 1990s were more than twice those of patients diagnosed in the 1980s for ALL (unadjusted P = .008) and AML (unadjusted P = .0002). Survival times were also more than twice those of patients diagnosed in the 2000s versus the 1980s for ALL (unadjusted P = .009) and AML (unadjusted P = .0003).
No significant long-term survival differences were observed for those diagnosed in the 2000s, compared with the 1990s, for either leukemia.
“The data from the national registry used for this study gave us insights into some possible challenges AML and ALL patients may encounter throughout survivorship, but we need to more thoroughly survey their journey,” Dr. Roth said. “An examination of their socioeconomic status, comorbidities, access to quality health care, and other risk factors that may impact their survivorship is warranted.”
The research was supported by the National Cancer Institute at the National Institutes of Health, the Archer Charitable Foundation, and LyondellBasell. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANCER EPIDEMIOLOGY, BIOMARKERS AND PREVENTION
Ex–hospital porter a neglected giant of cancer research
We have a half-forgotten Indian immigrant to thank – a hospital night porter turned biochemist –for revolutionizing treatment of leukemia, the once deadly childhood scourge that is still the most common pediatric cancer.
Dr. Yellapragada SubbaRow has been called the “father of chemotherapy” for developing methotrexate, a powerful, inexpensive therapy for leukemia and other diseases, and he is celebrated for additional scientific achievements. Yet Dr. SubbaRow’s life was marked more by struggle than glory.
Born poor in southeastern India, he nearly succumbed to a tropical disease that killed two older brothers, and he didn’t focus on schoolwork until his father died. Later, prejudice dogged his years as an immigrant to the United States, and a blood clot took his life at the age of 53.
Scientifically, however, Dr. SubbaRow (pronounced sue-buh-rao) triumphed, despite mammoth challenges and a lack of recognition that persists to this day. National Cancer Research Month is a fitting time to look back on his extraordinary life and work and pay tribute to his accomplishments.
‘Yella,’ folic acid, and a paradigm shift
No one appreciates Dr. SubbaRow more than a cadre of Indian-born physicians who have kept his legacy alive in journal articles, presentations, and a Pulitzer Prize-winning book. Among them is author and oncologist Siddhartha Mukherjee, MD, who chronicled Dr. SubbaRow’s achievements in his New York Times No. 1 bestseller, “The Emperor of All Maladies: A Biography of Cancer.”
As Dr. Mukherjee wrote, Dr. SubbaRow was a “pioneer in many ways, a physician turned cellular physiologist, a chemist who had accidentally wandered into biology.” (Per Indian tradition, SubbaRow is the doctor’s first name, and Yellapragada is his surname, but medical literature uses SubbaRow as his cognomen, with some variations in spelling. Dr. Mukherjee wrote that his friends called him “Yella.”)
Dr. SubbaRow came to the United States in 1923, after enduring a difficult childhood and young adulthood. He’d survived bouts of religious fervor, childhood rebellion (including a bid to run away from home and become a banana trader), and a failed arranged marriage. His wife bore him a child who died in infancy. He left it all behind.
In Boston, medical officials rejected his degree. Broke, he worked for a time as a night porter at Brigham and Women’s Hospital in Boston, changing sheets and cleaning urinals. To a poor but proud high-caste Indian Brahmin, the culture shock of carrying out these tasks must have been especially jarring.
Dr. SubbaRow went on to earn a diploma from Harvard Medical School, also in Boston, and became a junior faculty member. As a foreigner, Dr. Mukherjee wrote, Dr. SubbaRow was a “reclusive, nocturnal, heavily accented vegetarian,” so different from his colleagues that advancement seemed impossible. Despite his pioneering biochemistry work, Harvard later declined to offer Dr. SubbaRow a tenured faculty position.
By the early 1940s, he took a job at an upstate New York pharmaceutical company called Lederle Labs (later purchased by Pfizer). At Lederle, Dr. SubbaRow strove to synthesize the vitamin known as folic acid. He ended up creating a kind of antivitamin, a lookalike that acted like folic acid but only succeeded in gumming up the works in receptors. But what good would it do to stop the body from absorbing folic acid? Plenty, it turned out.
Discoveries pile up, but credit and fame prove elusive
Dr. SubbaRow was no stranger to producing landmark biological work. He’d previously codiscovered phosphocreatine and ATP, which are crucial to muscular contractions. However, “in 1935, he had to disown the extent of his role in the discovery of the color test related to phosphorus, instead giving the credit to his co-author, who was being considered for promotion to a full professorship at Harvard,” wrote author Gerald Posner in his 2020 book, “Pharma: Greed, Lies and the Poisoning of America.”
Houston-area oncologist Kirtan Nautiyal, MD, who paid tribute to Dr. SubbaRow in a 2018 article, contended that “with his Indian instinct for self-effacement, he had irreparably sabotaged his own career.”
Dr. SubbaRow and his team also developed “the first effective treatment of filariasis, which causes elephantiasis of the lower limbs and genitals in millions of people, mainly in tropical countries,” Dr. Nautiyal wrote. “Later in the decade, his antibiotic program generated polymyxin, the first effective treatment against the class of bacteria called Gram negatives, and aureomycin, the first “broad-spectrum’ antibiotic.” (Aureomycin is also the first tetracycline antibiotic.)
Dr. SubbaRow’s discovery of a folic acid antagonist would again go largely unheralded. But first came the realization that folic acid made childhood leukemia worse, not better, and the prospect that this process could potentially be reversed.
Rise of methotrexate and fall of leukemia
In Boston, Sidney Farber, MD, a Boston pathologist, was desperate to help Robert Sandler, a 2-year-old leukemia patient. Dr. Farber contacted his ex-colleague Dr. SubbaRow to request a supply of aminopterin, an early version of methotrexate that Dr. SubbaRow and his team had developed. Dr. Farber injected Robert with the substance and within 3 days, the toddler’s white blood count started falling – fast. He stopped bleeding, resumed eating, and once again seemed almost identical to his twin brother, as Dr. Mukherjee wrote in his book.
Leukemia had never gone into remission before. Unfortunately, the treatment only worked temporarily. Robert, like other children treated with the drug, relapsed and died within months. But Dr. Farber “saw a door open” – a chemical, a kind of chemotherapy, that could turn back cancer. In the case of folic acid antagonists, they do so by stopping cancer cells from replicating.
Methotrexate, a related agent synthesized by Dr. SubbaRow, would become a mainstay of leukemia treatment and begin to produce long-term remission from acute lymphoblastic leukemia in 1970, when combination chemotherapy was developed.
Other cancers fell to methotrexate treatment. “Previous assumptions that cancer was nearly always fatal were revised, and the field of medical oncology (treatment of cancer with chemotherapy), which had not previously existed, was formally established in 1971,” according to the National Cancer Institute’s history of methotrexate. This account does not mention Dr. SubbaRow.
Death takes the doctor, but his legacy remains
In biographies, as well as his own words, Dr. SubbaRow comes across as a prickly, hard-driving workaholic who had little interest in intimate human connections. “It is not good to ask in every letter when I will be back,” he wrote to his wife back in India, before cutting off ties completely in the early 1930s. “I will come as early as possible. ... I do not want to write anything more.”
It seems, as his biographer S.P.K. Gupta noted, that “he was quite determined that the time allotted to him on Earth should be completely devoted to finding cures for ailments that plagued mankind.”
Still, Dr. SubbaRow’s research team was devoted to him, and he had plenty of reasons to be bitter, such as the prejudice and isolation he encountered in the United States and earlier, in British-run India. According to Mr. Posner’s book, even as a young medical student, Dr. SubbaRow heeded the call of Indian independence activist Mohandas Gandhi. He “refused the British surgical gown given him at school and instead donned a traditional and simple cotton Khadi. That act of defiance cost SubbaRow the college degree that was necessary for him to get into the State Medical College.”
During the last year of his life, Dr. SubbaRow faced yet another humiliation: In his landmark 1948 study about aminopterin as a treatment for leukemia, his colleague Dr. Farber failed to credit him, an “astonishing omission” as Yaddanapudi Ravindranath, MBBS, a pediatric hematologist/oncologist at Wayne State University, Detroit, put it. “From everything I know, Dr. Farber spent the rest of his career apologizing and trying to make amends for it,” Dr. Ravindranath said in an interview.
A career cut short, and a lasting legacy
In 1948, at the age of 53, Dr. SubbaRow suddenly died. “Many think Dr. SubbaRow would have won [the] Nobel Prize had he lived a few years longer,” said Dr. Ravindranath.
Like Dr. SubbaRow, Dr. Ravindranath was born in Andhra Pradesh state, near the city of Chennai formerly known as Madras. “Being a compatriot, in a way I continue his legacy, and I am obviously proud of him,” said Dr. Ravindranath, who has conducted his own landmark research regarding methotrexate and leukemia.
Nearly 75 years after Dr. SubbaRow’s death, Indian-born physicians like Dr. Ravindranath continue to honor him in print, trying to ensure that he’s not forgotten. Methotrexate remains a crucial treatment for leukemia, along with a long list of other ailments, including psoriasis.
Recognition for “Yella” may have come late and infrequently, but a Lederle Laboratories research library named after him offered Dr. SubbaRow a kind of immortality. A plaque there memorialized him in stone as a scientist, teacher, philosopher, and humanitarian, featuring the quote: “Science simply prolongs life. Religion deepens it.”
By all accounts, Dr. SubbaRow was a man of science and faith who had faith in science.
We have a half-forgotten Indian immigrant to thank – a hospital night porter turned biochemist –for revolutionizing treatment of leukemia, the once deadly childhood scourge that is still the most common pediatric cancer.
Dr. Yellapragada SubbaRow has been called the “father of chemotherapy” for developing methotrexate, a powerful, inexpensive therapy for leukemia and other diseases, and he is celebrated for additional scientific achievements. Yet Dr. SubbaRow’s life was marked more by struggle than glory.
Born poor in southeastern India, he nearly succumbed to a tropical disease that killed two older brothers, and he didn’t focus on schoolwork until his father died. Later, prejudice dogged his years as an immigrant to the United States, and a blood clot took his life at the age of 53.
Scientifically, however, Dr. SubbaRow (pronounced sue-buh-rao) triumphed, despite mammoth challenges and a lack of recognition that persists to this day. National Cancer Research Month is a fitting time to look back on his extraordinary life and work and pay tribute to his accomplishments.
‘Yella,’ folic acid, and a paradigm shift
No one appreciates Dr. SubbaRow more than a cadre of Indian-born physicians who have kept his legacy alive in journal articles, presentations, and a Pulitzer Prize-winning book. Among them is author and oncologist Siddhartha Mukherjee, MD, who chronicled Dr. SubbaRow’s achievements in his New York Times No. 1 bestseller, “The Emperor of All Maladies: A Biography of Cancer.”
As Dr. Mukherjee wrote, Dr. SubbaRow was a “pioneer in many ways, a physician turned cellular physiologist, a chemist who had accidentally wandered into biology.” (Per Indian tradition, SubbaRow is the doctor’s first name, and Yellapragada is his surname, but medical literature uses SubbaRow as his cognomen, with some variations in spelling. Dr. Mukherjee wrote that his friends called him “Yella.”)
Dr. SubbaRow came to the United States in 1923, after enduring a difficult childhood and young adulthood. He’d survived bouts of religious fervor, childhood rebellion (including a bid to run away from home and become a banana trader), and a failed arranged marriage. His wife bore him a child who died in infancy. He left it all behind.
In Boston, medical officials rejected his degree. Broke, he worked for a time as a night porter at Brigham and Women’s Hospital in Boston, changing sheets and cleaning urinals. To a poor but proud high-caste Indian Brahmin, the culture shock of carrying out these tasks must have been especially jarring.
Dr. SubbaRow went on to earn a diploma from Harvard Medical School, also in Boston, and became a junior faculty member. As a foreigner, Dr. Mukherjee wrote, Dr. SubbaRow was a “reclusive, nocturnal, heavily accented vegetarian,” so different from his colleagues that advancement seemed impossible. Despite his pioneering biochemistry work, Harvard later declined to offer Dr. SubbaRow a tenured faculty position.
By the early 1940s, he took a job at an upstate New York pharmaceutical company called Lederle Labs (later purchased by Pfizer). At Lederle, Dr. SubbaRow strove to synthesize the vitamin known as folic acid. He ended up creating a kind of antivitamin, a lookalike that acted like folic acid but only succeeded in gumming up the works in receptors. But what good would it do to stop the body from absorbing folic acid? Plenty, it turned out.
Discoveries pile up, but credit and fame prove elusive
Dr. SubbaRow was no stranger to producing landmark biological work. He’d previously codiscovered phosphocreatine and ATP, which are crucial to muscular contractions. However, “in 1935, he had to disown the extent of his role in the discovery of the color test related to phosphorus, instead giving the credit to his co-author, who was being considered for promotion to a full professorship at Harvard,” wrote author Gerald Posner in his 2020 book, “Pharma: Greed, Lies and the Poisoning of America.”
Houston-area oncologist Kirtan Nautiyal, MD, who paid tribute to Dr. SubbaRow in a 2018 article, contended that “with his Indian instinct for self-effacement, he had irreparably sabotaged his own career.”
Dr. SubbaRow and his team also developed “the first effective treatment of filariasis, which causes elephantiasis of the lower limbs and genitals in millions of people, mainly in tropical countries,” Dr. Nautiyal wrote. “Later in the decade, his antibiotic program generated polymyxin, the first effective treatment against the class of bacteria called Gram negatives, and aureomycin, the first “broad-spectrum’ antibiotic.” (Aureomycin is also the first tetracycline antibiotic.)
Dr. SubbaRow’s discovery of a folic acid antagonist would again go largely unheralded. But first came the realization that folic acid made childhood leukemia worse, not better, and the prospect that this process could potentially be reversed.
Rise of methotrexate and fall of leukemia
In Boston, Sidney Farber, MD, a Boston pathologist, was desperate to help Robert Sandler, a 2-year-old leukemia patient. Dr. Farber contacted his ex-colleague Dr. SubbaRow to request a supply of aminopterin, an early version of methotrexate that Dr. SubbaRow and his team had developed. Dr. Farber injected Robert with the substance and within 3 days, the toddler’s white blood count started falling – fast. He stopped bleeding, resumed eating, and once again seemed almost identical to his twin brother, as Dr. Mukherjee wrote in his book.
Leukemia had never gone into remission before. Unfortunately, the treatment only worked temporarily. Robert, like other children treated with the drug, relapsed and died within months. But Dr. Farber “saw a door open” – a chemical, a kind of chemotherapy, that could turn back cancer. In the case of folic acid antagonists, they do so by stopping cancer cells from replicating.
Methotrexate, a related agent synthesized by Dr. SubbaRow, would become a mainstay of leukemia treatment and begin to produce long-term remission from acute lymphoblastic leukemia in 1970, when combination chemotherapy was developed.
Other cancers fell to methotrexate treatment. “Previous assumptions that cancer was nearly always fatal were revised, and the field of medical oncology (treatment of cancer with chemotherapy), which had not previously existed, was formally established in 1971,” according to the National Cancer Institute’s history of methotrexate. This account does not mention Dr. SubbaRow.
Death takes the doctor, but his legacy remains
In biographies, as well as his own words, Dr. SubbaRow comes across as a prickly, hard-driving workaholic who had little interest in intimate human connections. “It is not good to ask in every letter when I will be back,” he wrote to his wife back in India, before cutting off ties completely in the early 1930s. “I will come as early as possible. ... I do not want to write anything more.”
It seems, as his biographer S.P.K. Gupta noted, that “he was quite determined that the time allotted to him on Earth should be completely devoted to finding cures for ailments that plagued mankind.”
Still, Dr. SubbaRow’s research team was devoted to him, and he had plenty of reasons to be bitter, such as the prejudice and isolation he encountered in the United States and earlier, in British-run India. According to Mr. Posner’s book, even as a young medical student, Dr. SubbaRow heeded the call of Indian independence activist Mohandas Gandhi. He “refused the British surgical gown given him at school and instead donned a traditional and simple cotton Khadi. That act of defiance cost SubbaRow the college degree that was necessary for him to get into the State Medical College.”
During the last year of his life, Dr. SubbaRow faced yet another humiliation: In his landmark 1948 study about aminopterin as a treatment for leukemia, his colleague Dr. Farber failed to credit him, an “astonishing omission” as Yaddanapudi Ravindranath, MBBS, a pediatric hematologist/oncologist at Wayne State University, Detroit, put it. “From everything I know, Dr. Farber spent the rest of his career apologizing and trying to make amends for it,” Dr. Ravindranath said in an interview.
A career cut short, and a lasting legacy
In 1948, at the age of 53, Dr. SubbaRow suddenly died. “Many think Dr. SubbaRow would have won [the] Nobel Prize had he lived a few years longer,” said Dr. Ravindranath.
Like Dr. SubbaRow, Dr. Ravindranath was born in Andhra Pradesh state, near the city of Chennai formerly known as Madras. “Being a compatriot, in a way I continue his legacy, and I am obviously proud of him,” said Dr. Ravindranath, who has conducted his own landmark research regarding methotrexate and leukemia.
Nearly 75 years after Dr. SubbaRow’s death, Indian-born physicians like Dr. Ravindranath continue to honor him in print, trying to ensure that he’s not forgotten. Methotrexate remains a crucial treatment for leukemia, along with a long list of other ailments, including psoriasis.
Recognition for “Yella” may have come late and infrequently, but a Lederle Laboratories research library named after him offered Dr. SubbaRow a kind of immortality. A plaque there memorialized him in stone as a scientist, teacher, philosopher, and humanitarian, featuring the quote: “Science simply prolongs life. Religion deepens it.”
By all accounts, Dr. SubbaRow was a man of science and faith who had faith in science.
We have a half-forgotten Indian immigrant to thank – a hospital night porter turned biochemist –for revolutionizing treatment of leukemia, the once deadly childhood scourge that is still the most common pediatric cancer.
Dr. Yellapragada SubbaRow has been called the “father of chemotherapy” for developing methotrexate, a powerful, inexpensive therapy for leukemia and other diseases, and he is celebrated for additional scientific achievements. Yet Dr. SubbaRow’s life was marked more by struggle than glory.
Born poor in southeastern India, he nearly succumbed to a tropical disease that killed two older brothers, and he didn’t focus on schoolwork until his father died. Later, prejudice dogged his years as an immigrant to the United States, and a blood clot took his life at the age of 53.
Scientifically, however, Dr. SubbaRow (pronounced sue-buh-rao) triumphed, despite mammoth challenges and a lack of recognition that persists to this day. National Cancer Research Month is a fitting time to look back on his extraordinary life and work and pay tribute to his accomplishments.
‘Yella,’ folic acid, and a paradigm shift
No one appreciates Dr. SubbaRow more than a cadre of Indian-born physicians who have kept his legacy alive in journal articles, presentations, and a Pulitzer Prize-winning book. Among them is author and oncologist Siddhartha Mukherjee, MD, who chronicled Dr. SubbaRow’s achievements in his New York Times No. 1 bestseller, “The Emperor of All Maladies: A Biography of Cancer.”
As Dr. Mukherjee wrote, Dr. SubbaRow was a “pioneer in many ways, a physician turned cellular physiologist, a chemist who had accidentally wandered into biology.” (Per Indian tradition, SubbaRow is the doctor’s first name, and Yellapragada is his surname, but medical literature uses SubbaRow as his cognomen, with some variations in spelling. Dr. Mukherjee wrote that his friends called him “Yella.”)
Dr. SubbaRow came to the United States in 1923, after enduring a difficult childhood and young adulthood. He’d survived bouts of religious fervor, childhood rebellion (including a bid to run away from home and become a banana trader), and a failed arranged marriage. His wife bore him a child who died in infancy. He left it all behind.
In Boston, medical officials rejected his degree. Broke, he worked for a time as a night porter at Brigham and Women’s Hospital in Boston, changing sheets and cleaning urinals. To a poor but proud high-caste Indian Brahmin, the culture shock of carrying out these tasks must have been especially jarring.
Dr. SubbaRow went on to earn a diploma from Harvard Medical School, also in Boston, and became a junior faculty member. As a foreigner, Dr. Mukherjee wrote, Dr. SubbaRow was a “reclusive, nocturnal, heavily accented vegetarian,” so different from his colleagues that advancement seemed impossible. Despite his pioneering biochemistry work, Harvard later declined to offer Dr. SubbaRow a tenured faculty position.
By the early 1940s, he took a job at an upstate New York pharmaceutical company called Lederle Labs (later purchased by Pfizer). At Lederle, Dr. SubbaRow strove to synthesize the vitamin known as folic acid. He ended up creating a kind of antivitamin, a lookalike that acted like folic acid but only succeeded in gumming up the works in receptors. But what good would it do to stop the body from absorbing folic acid? Plenty, it turned out.
Discoveries pile up, but credit and fame prove elusive
Dr. SubbaRow was no stranger to producing landmark biological work. He’d previously codiscovered phosphocreatine and ATP, which are crucial to muscular contractions. However, “in 1935, he had to disown the extent of his role in the discovery of the color test related to phosphorus, instead giving the credit to his co-author, who was being considered for promotion to a full professorship at Harvard,” wrote author Gerald Posner in his 2020 book, “Pharma: Greed, Lies and the Poisoning of America.”
Houston-area oncologist Kirtan Nautiyal, MD, who paid tribute to Dr. SubbaRow in a 2018 article, contended that “with his Indian instinct for self-effacement, he had irreparably sabotaged his own career.”
Dr. SubbaRow and his team also developed “the first effective treatment of filariasis, which causes elephantiasis of the lower limbs and genitals in millions of people, mainly in tropical countries,” Dr. Nautiyal wrote. “Later in the decade, his antibiotic program generated polymyxin, the first effective treatment against the class of bacteria called Gram negatives, and aureomycin, the first “broad-spectrum’ antibiotic.” (Aureomycin is also the first tetracycline antibiotic.)
Dr. SubbaRow’s discovery of a folic acid antagonist would again go largely unheralded. But first came the realization that folic acid made childhood leukemia worse, not better, and the prospect that this process could potentially be reversed.
Rise of methotrexate and fall of leukemia
In Boston, Sidney Farber, MD, a Boston pathologist, was desperate to help Robert Sandler, a 2-year-old leukemia patient. Dr. Farber contacted his ex-colleague Dr. SubbaRow to request a supply of aminopterin, an early version of methotrexate that Dr. SubbaRow and his team had developed. Dr. Farber injected Robert with the substance and within 3 days, the toddler’s white blood count started falling – fast. He stopped bleeding, resumed eating, and once again seemed almost identical to his twin brother, as Dr. Mukherjee wrote in his book.
Leukemia had never gone into remission before. Unfortunately, the treatment only worked temporarily. Robert, like other children treated with the drug, relapsed and died within months. But Dr. Farber “saw a door open” – a chemical, a kind of chemotherapy, that could turn back cancer. In the case of folic acid antagonists, they do so by stopping cancer cells from replicating.
Methotrexate, a related agent synthesized by Dr. SubbaRow, would become a mainstay of leukemia treatment and begin to produce long-term remission from acute lymphoblastic leukemia in 1970, when combination chemotherapy was developed.
Other cancers fell to methotrexate treatment. “Previous assumptions that cancer was nearly always fatal were revised, and the field of medical oncology (treatment of cancer with chemotherapy), which had not previously existed, was formally established in 1971,” according to the National Cancer Institute’s history of methotrexate. This account does not mention Dr. SubbaRow.
Death takes the doctor, but his legacy remains
In biographies, as well as his own words, Dr. SubbaRow comes across as a prickly, hard-driving workaholic who had little interest in intimate human connections. “It is not good to ask in every letter when I will be back,” he wrote to his wife back in India, before cutting off ties completely in the early 1930s. “I will come as early as possible. ... I do not want to write anything more.”
It seems, as his biographer S.P.K. Gupta noted, that “he was quite determined that the time allotted to him on Earth should be completely devoted to finding cures for ailments that plagued mankind.”
Still, Dr. SubbaRow’s research team was devoted to him, and he had plenty of reasons to be bitter, such as the prejudice and isolation he encountered in the United States and earlier, in British-run India. According to Mr. Posner’s book, even as a young medical student, Dr. SubbaRow heeded the call of Indian independence activist Mohandas Gandhi. He “refused the British surgical gown given him at school and instead donned a traditional and simple cotton Khadi. That act of defiance cost SubbaRow the college degree that was necessary for him to get into the State Medical College.”
During the last year of his life, Dr. SubbaRow faced yet another humiliation: In his landmark 1948 study about aminopterin as a treatment for leukemia, his colleague Dr. Farber failed to credit him, an “astonishing omission” as Yaddanapudi Ravindranath, MBBS, a pediatric hematologist/oncologist at Wayne State University, Detroit, put it. “From everything I know, Dr. Farber spent the rest of his career apologizing and trying to make amends for it,” Dr. Ravindranath said in an interview.
A career cut short, and a lasting legacy
In 1948, at the age of 53, Dr. SubbaRow suddenly died. “Many think Dr. SubbaRow would have won [the] Nobel Prize had he lived a few years longer,” said Dr. Ravindranath.
Like Dr. SubbaRow, Dr. Ravindranath was born in Andhra Pradesh state, near the city of Chennai formerly known as Madras. “Being a compatriot, in a way I continue his legacy, and I am obviously proud of him,” said Dr. Ravindranath, who has conducted his own landmark research regarding methotrexate and leukemia.
Nearly 75 years after Dr. SubbaRow’s death, Indian-born physicians like Dr. Ravindranath continue to honor him in print, trying to ensure that he’s not forgotten. Methotrexate remains a crucial treatment for leukemia, along with a long list of other ailments, including psoriasis.
Recognition for “Yella” may have come late and infrequently, but a Lederle Laboratories research library named after him offered Dr. SubbaRow a kind of immortality. A plaque there memorialized him in stone as a scientist, teacher, philosopher, and humanitarian, featuring the quote: “Science simply prolongs life. Religion deepens it.”
By all accounts, Dr. SubbaRow was a man of science and faith who had faith in science.
Rare pediatric cancers persist 63 years after nuclear accident
Chernobyl. Fukushima. Three Mile Island.
The world knows these names all too well because of accidents there: complete or partial meltdowns of nuclear reactors that released massive amounts of cancer-causing radiation into the air, soil, and water.
The Santa Susana Field Lab is far less well-known, but no less infamous for what took place at this former rocket engine and nuclear energy test site just 28 miles northwest of downtown Los Angeles.
In July 1959, an accident involving one of 10 experimental nuclear reactors at the SSFL site released a cloud of harmful radiation and toxic chemicals over the surrounding area, including Simi Valley, San Gabriel Valley, Chatsworth, and Canoga Park. The small reactor had no containment vessel.
This accident resulted in a release of radioactive iodine estimated to be as much as 250 times that of the partial meltdown that would occur 2 decades later at Three Mile Island, a much larger commercial reactor that had a containment vessel.
Decades-long cover-up
In 1959, the public knew nothing about what happened at the site.
According to John Pace, then an employee at SSFL, the accident was covered up. Mr. Pace recounted the cover-up in the documentary “In the Dark of the Valley,” which first aired in November 2021 on MSNBC.
In fact, the accident at SSFL remained under wraps for 2 decades, according to Daniel Hirsch, former director of the Program on Environmental and Nuclear Policy at the University of California, Santa Cruz, and now president of Committee to Bridge the Gap, a nuclear policy nongovernmental organization.
“Students working with me while I was teaching at UCLA in 1979 uncovered these Atomic Energy Commission reports from Atomics International,” he said in an interview. “We had to order the documents from the annex to the UCLA Engineering Library. They were stored offsite, and it took a few days, and when we got them, we opened them up, and there were these fold-out photographs of the fuel [rods]. As we folded out the photographs further, we saw one photo with an arrow labeled ‘longitudinal cracks,’ and then other arrows showing other kinds of cracks, and then another arrow labeled ‘melted blob.’ ”
Mr. Hirsch and his students found that other accidents had occurred at SSFL, including a fuel fabrication system that leached plutonium, fires in a “hot” lab where irradiated nuclear fuel from around the United States was handled, and open-air burn pits where radioactive and toxic chemical wastes were illegally torched.
According to the Committee to Bridge the Gap, when the 2,800-acre SSFL site was being developed under the name Rocketdyne by aircraft maker North American Aviation, the area was sparsely populated, with nearly as many grazing animals as people in its hills and valleys.
North American Aviation later became part of Rockwell International, which in turn sold its aerospace and defense business units to the Boeing Company in 1996. Boeing, now in charge of the site and the cleanup efforts, is doing everything in its power to shirk or diminish its responsibility, Mr. Hirsch and other critics say.
Parents against SSFL
Today, more than 150,000 people live within 5 miles of SSFL, and more than half a million live within 10 miles.
Melissa Bumstead is one of those residents. She and her family live 3.7 miles from the Santa Susana site. When her toddler Grace was diagnosed with a rare form of leukemia in 2014, doctors told Ms. Bumstead there were no known links between her daughter’s cancer and environmental contamination.
But during Grace’s treatment at Children’s Hospital Los Angeles, her mother began meeting other parents who lived near her and had children facing equally rare cancers.
Lauren Hammersley, whose daughter Hazel was diagnosed with a rare brain tumor called neuroblastoma at age 2, lived about 10 miles from Ms. Bumstead on the other side of a mountain and just over 4 miles from SSFL.
On her street alone, Ms. Bumstead discovered three cases of pediatric cancer, including two children in adjacent homes who had the same rare brain tumor as Hazel Hammersley.
As Ms. Bumstead told Los Angeles National Public Radio station KCRW in 2021, “I started to panic because I knew that childhood cancer is extremely rare. There’s only 15,000 new cases every year out of 72 million children in America. So, the chance of knowing your neighbors, especially at an internationally renowned hospital like Children’s Hospital Los Angeles – we knew something wasn’t right.”
After a relapse of her tumor, Hazel died in 2018, a few months after her seventh birthday.
Cancer clusters
Hoping to understand why their kids were getting so sick, Ms. Bumstead and the other parents formed a Facebook group. They plotted their homes on Google Maps and found that they all lived within roughly 10 miles of one another. It would take another year for them to realize that the SSFL site was at the center of the circle.
Once they realized that being close to SSFL could be their common thread, Ms. Bumstead and parents in her group began to gradually piece together the story, linking unusual or unexplained illnesses in their families to potential radiation or toxic chemical exposures from the lab.
“What really convinced me that this was absolutely a problem was when I learned about the epidemiological study by Dr. Hal Morgenstern that found that residents living within 2 miles of the Santa Susana Field Lab actually had a 60% higher cancer incidence rate and that over 1,500 workers have been diagnosed with cancer just from the Santa Susana Field Lab,” she told KCRW.
In 2015, Ms. Bumstead and other parents formed Parents Against Santa Susana Field Lab to hold SSFL site owner Boeing accountable for radiologic and toxic contamination and to ensure that Boeing cleans the site and surrounding areas. The group “seeks to reduce, to the greatest extent possible, the number of local families who have to hear the words, ‘Your child has cancer.’ ”
No longer quite so rare
Dr. Morgenstern, now retired from the University of Michigan, declined to be interviewed for this article. But as he and colleagues reported to the Centers for Disease Control and Prevention’s Agency for Toxic Substances and Disease Registry in 2007, there were strong signs of a link between contamination of the site and cancer.
The researchers compared cancer rates of adults living within 2 miles and 2-5 miles from SSFL with those of adults living more than 5 miles away, in Ventura and Los Angeles counties. They found that from 1988 through 1995, residents living within 2 miles of SSFL had a 60% higher rate of cancers than the control group. These included cancers of the thyroid, oral and nasal cavities, pharynx, larynx, esophagus, and bladder, as well as blood cancers such as leukemia, lymphoma, and multiple myeloma.
In separate studies, the investigators found higher rates of certain cancers among workers at SSFL who were exposed to radiation and to hydrazine, a chemical in rocket fuel.
In an interview, Dr. Saro Armenian, a pediatric hematologist-oncologist who was not involved in the studies, said the 60% increase in cancer incidence, which translated into a 1.6-fold increase in risk, merits more investigation.
“In epidemiologic studies, a 1.6-fold risk is actually a pretty strong signal because typically, most signals that you get are somewhere around 1.1- to 1.2-fold increased risk,” noted Dr. Armenian, a specialist in pediatric cancer survivorship and outcomes at City of Hope National Medical Center in Duarte, Calif.
However, Dr. Thomas Mack, former director of the Los Angeles County Cancer Surveillance Program, contends that there is insufficient evidence to support a direct link between the 1959 reactor accident and recent incident cancers. Dr. Mack is currently a professor of preventive medicine and pathology at the University of Southern California in Los Angeles.
“I have evaluated concerns about local excesses of cancer at least 100 times, usually from county residents, but for a while I represented the CDC and the California cancer registry,” Dr. Mack said, in response to an emailed request for comment.
“So far I have seen no evidence of carcinogenic radionucleotides or chemical carcinogens from Santa Susana found in any meaningful amount in any nearby community, but if someone has such evidence that would constitute evidence, that needs a response,” Dr. Mack added.
Boeing and California
Boeing has said problems at SSFL were not responsible for the high cancer rates among children in the community.
In April 2007, in a statement opposing a bill before the California State Legislature that would compel Boeing to pay for SSFL site cleanup, the company said that “in contrast to the accusations made against The Boeing Company that falsely claim increased cancer rates in the communities surrounding SSFL, a recent study conducted by the University of Michigan School of Public Health just concluded the opposite.”
Yet as Dr. Morgenstern wrote in 2007 to California state Sen. Joe Simitian, then chair of the Committee on Environmental Quality: “For the period 1996 through 2002, we found that the incidence rate of thyroid cancer was more than 60% greater among residents living within 2 miles of SSFL than for residents living more than 5 miles from SSFL. The magnitude and consistency of the thyroid finding for both periods is especially provocative because of evidence from other studies linking thyroid cancer with environmental exposures originating at SSFL and found in the surrounding communities.”
Boeing chose to ignore the results and instead focused on the methods used in the study, where the authors acknowledged that they measured distance from the site rather than environmental exposures and thus could not conclusively link excess cancer rates to exposures arising from SSFL.
But Dr. Morgenstern emphasized the conclusion of the report: “Despite the methodologic limitations of this study, the findings suggest there may be elevated incidence rates of certain cancers near SSFL that have been linked in previous studies with hazardous substances used at Rocketdyne, some of which have been observed or projected to exist offsite.”
Failure to come clean
In 2008, a law that set standards for cleanup of the site was passed. But the law was overturned in 2014 after a legal challenge by Boeing.
That left in place a 2007 order of consent between Boeing, NASA, the U.S. Department of Energy, and the California Department of Toxic Substances Control (DTSC) that required cleanup of SSFL to a much less stringent standard.
As of last year, Boeing and DTSC had begun confidential, nonbinding agreements regarding the 2007 order of consent, according to Parents Against SSFL.
Among the contaminants lingering at the site are radioactive particles, chemical compounds, heavy metals, and polluted water.
“In fact, over 300 contaminants of concern have been found at the site, and they are refusing to clean it,” Mr. Hirsch said. “This company releases large amounts of carcinogens, and perhaps significant numbers of people get sick with cancer, and the company doesn’t go to prison. They get more federal contracts.”
A version of this article first appeared on WebMD.com.
April 20, 2022 – Editor’s note: This article has been updated to include an interview with Dr. Thomas Mack, former director of the Los Angeles County Cancer Surveillance Program, who contends that there is insufficient evidence to support a direct link between the 1959 reactor accident and recent incident cancers.
Chernobyl. Fukushima. Three Mile Island.
The world knows these names all too well because of accidents there: complete or partial meltdowns of nuclear reactors that released massive amounts of cancer-causing radiation into the air, soil, and water.
The Santa Susana Field Lab is far less well-known, but no less infamous for what took place at this former rocket engine and nuclear energy test site just 28 miles northwest of downtown Los Angeles.
In July 1959, an accident involving one of 10 experimental nuclear reactors at the SSFL site released a cloud of harmful radiation and toxic chemicals over the surrounding area, including Simi Valley, San Gabriel Valley, Chatsworth, and Canoga Park. The small reactor had no containment vessel.
This accident resulted in a release of radioactive iodine estimated to be as much as 250 times that of the partial meltdown that would occur 2 decades later at Three Mile Island, a much larger commercial reactor that had a containment vessel.
Decades-long cover-up
In 1959, the public knew nothing about what happened at the site.
According to John Pace, then an employee at SSFL, the accident was covered up. Mr. Pace recounted the cover-up in the documentary “In the Dark of the Valley,” which first aired in November 2021 on MSNBC.
In fact, the accident at SSFL remained under wraps for 2 decades, according to Daniel Hirsch, former director of the Program on Environmental and Nuclear Policy at the University of California, Santa Cruz, and now president of Committee to Bridge the Gap, a nuclear policy nongovernmental organization.
“Students working with me while I was teaching at UCLA in 1979 uncovered these Atomic Energy Commission reports from Atomics International,” he said in an interview. “We had to order the documents from the annex to the UCLA Engineering Library. They were stored offsite, and it took a few days, and when we got them, we opened them up, and there were these fold-out photographs of the fuel [rods]. As we folded out the photographs further, we saw one photo with an arrow labeled ‘longitudinal cracks,’ and then other arrows showing other kinds of cracks, and then another arrow labeled ‘melted blob.’ ”
Mr. Hirsch and his students found that other accidents had occurred at SSFL, including a fuel fabrication system that leached plutonium, fires in a “hot” lab where irradiated nuclear fuel from around the United States was handled, and open-air burn pits where radioactive and toxic chemical wastes were illegally torched.
According to the Committee to Bridge the Gap, when the 2,800-acre SSFL site was being developed under the name Rocketdyne by aircraft maker North American Aviation, the area was sparsely populated, with nearly as many grazing animals as people in its hills and valleys.
North American Aviation later became part of Rockwell International, which in turn sold its aerospace and defense business units to the Boeing Company in 1996. Boeing, now in charge of the site and the cleanup efforts, is doing everything in its power to shirk or diminish its responsibility, Mr. Hirsch and other critics say.
Parents against SSFL
Today, more than 150,000 people live within 5 miles of SSFL, and more than half a million live within 10 miles.
Melissa Bumstead is one of those residents. She and her family live 3.7 miles from the Santa Susana site. When her toddler Grace was diagnosed with a rare form of leukemia in 2014, doctors told Ms. Bumstead there were no known links between her daughter’s cancer and environmental contamination.
But during Grace’s treatment at Children’s Hospital Los Angeles, her mother began meeting other parents who lived near her and had children facing equally rare cancers.
Lauren Hammersley, whose daughter Hazel was diagnosed with a rare brain tumor called neuroblastoma at age 2, lived about 10 miles from Ms. Bumstead on the other side of a mountain and just over 4 miles from SSFL.
On her street alone, Ms. Bumstead discovered three cases of pediatric cancer, including two children in adjacent homes who had the same rare brain tumor as Hazel Hammersley.
As Ms. Bumstead told Los Angeles National Public Radio station KCRW in 2021, “I started to panic because I knew that childhood cancer is extremely rare. There’s only 15,000 new cases every year out of 72 million children in America. So, the chance of knowing your neighbors, especially at an internationally renowned hospital like Children’s Hospital Los Angeles – we knew something wasn’t right.”
After a relapse of her tumor, Hazel died in 2018, a few months after her seventh birthday.
Cancer clusters
Hoping to understand why their kids were getting so sick, Ms. Bumstead and the other parents formed a Facebook group. They plotted their homes on Google Maps and found that they all lived within roughly 10 miles of one another. It would take another year for them to realize that the SSFL site was at the center of the circle.
Once they realized that being close to SSFL could be their common thread, Ms. Bumstead and parents in her group began to gradually piece together the story, linking unusual or unexplained illnesses in their families to potential radiation or toxic chemical exposures from the lab.
“What really convinced me that this was absolutely a problem was when I learned about the epidemiological study by Dr. Hal Morgenstern that found that residents living within 2 miles of the Santa Susana Field Lab actually had a 60% higher cancer incidence rate and that over 1,500 workers have been diagnosed with cancer just from the Santa Susana Field Lab,” she told KCRW.
In 2015, Ms. Bumstead and other parents formed Parents Against Santa Susana Field Lab to hold SSFL site owner Boeing accountable for radiologic and toxic contamination and to ensure that Boeing cleans the site and surrounding areas. The group “seeks to reduce, to the greatest extent possible, the number of local families who have to hear the words, ‘Your child has cancer.’ ”
No longer quite so rare
Dr. Morgenstern, now retired from the University of Michigan, declined to be interviewed for this article. But as he and colleagues reported to the Centers for Disease Control and Prevention’s Agency for Toxic Substances and Disease Registry in 2007, there were strong signs of a link between contamination of the site and cancer.
The researchers compared cancer rates of adults living within 2 miles and 2-5 miles from SSFL with those of adults living more than 5 miles away, in Ventura and Los Angeles counties. They found that from 1988 through 1995, residents living within 2 miles of SSFL had a 60% higher rate of cancers than the control group. These included cancers of the thyroid, oral and nasal cavities, pharynx, larynx, esophagus, and bladder, as well as blood cancers such as leukemia, lymphoma, and multiple myeloma.
In separate studies, the investigators found higher rates of certain cancers among workers at SSFL who were exposed to radiation and to hydrazine, a chemical in rocket fuel.
In an interview, Dr. Saro Armenian, a pediatric hematologist-oncologist who was not involved in the studies, said the 60% increase in cancer incidence, which translated into a 1.6-fold increase in risk, merits more investigation.
“In epidemiologic studies, a 1.6-fold risk is actually a pretty strong signal because typically, most signals that you get are somewhere around 1.1- to 1.2-fold increased risk,” noted Dr. Armenian, a specialist in pediatric cancer survivorship and outcomes at City of Hope National Medical Center in Duarte, Calif.
However, Dr. Thomas Mack, former director of the Los Angeles County Cancer Surveillance Program, contends that there is insufficient evidence to support a direct link between the 1959 reactor accident and recent incident cancers. Dr. Mack is currently a professor of preventive medicine and pathology at the University of Southern California in Los Angeles.
“I have evaluated concerns about local excesses of cancer at least 100 times, usually from county residents, but for a while I represented the CDC and the California cancer registry,” Dr. Mack said, in response to an emailed request for comment.
“So far I have seen no evidence of carcinogenic radionucleotides or chemical carcinogens from Santa Susana found in any meaningful amount in any nearby community, but if someone has such evidence that would constitute evidence, that needs a response,” Dr. Mack added.
Boeing and California
Boeing has said problems at SSFL were not responsible for the high cancer rates among children in the community.
In April 2007, in a statement opposing a bill before the California State Legislature that would compel Boeing to pay for SSFL site cleanup, the company said that “in contrast to the accusations made against The Boeing Company that falsely claim increased cancer rates in the communities surrounding SSFL, a recent study conducted by the University of Michigan School of Public Health just concluded the opposite.”
Yet as Dr. Morgenstern wrote in 2007 to California state Sen. Joe Simitian, then chair of the Committee on Environmental Quality: “For the period 1996 through 2002, we found that the incidence rate of thyroid cancer was more than 60% greater among residents living within 2 miles of SSFL than for residents living more than 5 miles from SSFL. The magnitude and consistency of the thyroid finding for both periods is especially provocative because of evidence from other studies linking thyroid cancer with environmental exposures originating at SSFL and found in the surrounding communities.”
Boeing chose to ignore the results and instead focused on the methods used in the study, where the authors acknowledged that they measured distance from the site rather than environmental exposures and thus could not conclusively link excess cancer rates to exposures arising from SSFL.
But Dr. Morgenstern emphasized the conclusion of the report: “Despite the methodologic limitations of this study, the findings suggest there may be elevated incidence rates of certain cancers near SSFL that have been linked in previous studies with hazardous substances used at Rocketdyne, some of which have been observed or projected to exist offsite.”
Failure to come clean
In 2008, a law that set standards for cleanup of the site was passed. But the law was overturned in 2014 after a legal challenge by Boeing.
That left in place a 2007 order of consent between Boeing, NASA, the U.S. Department of Energy, and the California Department of Toxic Substances Control (DTSC) that required cleanup of SSFL to a much less stringent standard.
As of last year, Boeing and DTSC had begun confidential, nonbinding agreements regarding the 2007 order of consent, according to Parents Against SSFL.
Among the contaminants lingering at the site are radioactive particles, chemical compounds, heavy metals, and polluted water.
“In fact, over 300 contaminants of concern have been found at the site, and they are refusing to clean it,” Mr. Hirsch said. “This company releases large amounts of carcinogens, and perhaps significant numbers of people get sick with cancer, and the company doesn’t go to prison. They get more federal contracts.”
A version of this article first appeared on WebMD.com.
April 20, 2022 – Editor’s note: This article has been updated to include an interview with Dr. Thomas Mack, former director of the Los Angeles County Cancer Surveillance Program, who contends that there is insufficient evidence to support a direct link between the 1959 reactor accident and recent incident cancers.
Chernobyl. Fukushima. Three Mile Island.
The world knows these names all too well because of accidents there: complete or partial meltdowns of nuclear reactors that released massive amounts of cancer-causing radiation into the air, soil, and water.
The Santa Susana Field Lab is far less well-known, but no less infamous for what took place at this former rocket engine and nuclear energy test site just 28 miles northwest of downtown Los Angeles.
In July 1959, an accident involving one of 10 experimental nuclear reactors at the SSFL site released a cloud of harmful radiation and toxic chemicals over the surrounding area, including Simi Valley, San Gabriel Valley, Chatsworth, and Canoga Park. The small reactor had no containment vessel.
This accident resulted in a release of radioactive iodine estimated to be as much as 250 times that of the partial meltdown that would occur 2 decades later at Three Mile Island, a much larger commercial reactor that had a containment vessel.
Decades-long cover-up
In 1959, the public knew nothing about what happened at the site.
According to John Pace, then an employee at SSFL, the accident was covered up. Mr. Pace recounted the cover-up in the documentary “In the Dark of the Valley,” which first aired in November 2021 on MSNBC.
In fact, the accident at SSFL remained under wraps for 2 decades, according to Daniel Hirsch, former director of the Program on Environmental and Nuclear Policy at the University of California, Santa Cruz, and now president of Committee to Bridge the Gap, a nuclear policy nongovernmental organization.
“Students working with me while I was teaching at UCLA in 1979 uncovered these Atomic Energy Commission reports from Atomics International,” he said in an interview. “We had to order the documents from the annex to the UCLA Engineering Library. They were stored offsite, and it took a few days, and when we got them, we opened them up, and there were these fold-out photographs of the fuel [rods]. As we folded out the photographs further, we saw one photo with an arrow labeled ‘longitudinal cracks,’ and then other arrows showing other kinds of cracks, and then another arrow labeled ‘melted blob.’ ”
Mr. Hirsch and his students found that other accidents had occurred at SSFL, including a fuel fabrication system that leached plutonium, fires in a “hot” lab where irradiated nuclear fuel from around the United States was handled, and open-air burn pits where radioactive and toxic chemical wastes were illegally torched.
According to the Committee to Bridge the Gap, when the 2,800-acre SSFL site was being developed under the name Rocketdyne by aircraft maker North American Aviation, the area was sparsely populated, with nearly as many grazing animals as people in its hills and valleys.
North American Aviation later became part of Rockwell International, which in turn sold its aerospace and defense business units to the Boeing Company in 1996. Boeing, now in charge of the site and the cleanup efforts, is doing everything in its power to shirk or diminish its responsibility, Mr. Hirsch and other critics say.
Parents against SSFL
Today, more than 150,000 people live within 5 miles of SSFL, and more than half a million live within 10 miles.
Melissa Bumstead is one of those residents. She and her family live 3.7 miles from the Santa Susana site. When her toddler Grace was diagnosed with a rare form of leukemia in 2014, doctors told Ms. Bumstead there were no known links between her daughter’s cancer and environmental contamination.
But during Grace’s treatment at Children’s Hospital Los Angeles, her mother began meeting other parents who lived near her and had children facing equally rare cancers.
Lauren Hammersley, whose daughter Hazel was diagnosed with a rare brain tumor called neuroblastoma at age 2, lived about 10 miles from Ms. Bumstead on the other side of a mountain and just over 4 miles from SSFL.
On her street alone, Ms. Bumstead discovered three cases of pediatric cancer, including two children in adjacent homes who had the same rare brain tumor as Hazel Hammersley.
As Ms. Bumstead told Los Angeles National Public Radio station KCRW in 2021, “I started to panic because I knew that childhood cancer is extremely rare. There’s only 15,000 new cases every year out of 72 million children in America. So, the chance of knowing your neighbors, especially at an internationally renowned hospital like Children’s Hospital Los Angeles – we knew something wasn’t right.”
After a relapse of her tumor, Hazel died in 2018, a few months after her seventh birthday.
Cancer clusters
Hoping to understand why their kids were getting so sick, Ms. Bumstead and the other parents formed a Facebook group. They plotted their homes on Google Maps and found that they all lived within roughly 10 miles of one another. It would take another year for them to realize that the SSFL site was at the center of the circle.
Once they realized that being close to SSFL could be their common thread, Ms. Bumstead and parents in her group began to gradually piece together the story, linking unusual or unexplained illnesses in their families to potential radiation or toxic chemical exposures from the lab.
“What really convinced me that this was absolutely a problem was when I learned about the epidemiological study by Dr. Hal Morgenstern that found that residents living within 2 miles of the Santa Susana Field Lab actually had a 60% higher cancer incidence rate and that over 1,500 workers have been diagnosed with cancer just from the Santa Susana Field Lab,” she told KCRW.
In 2015, Ms. Bumstead and other parents formed Parents Against Santa Susana Field Lab to hold SSFL site owner Boeing accountable for radiologic and toxic contamination and to ensure that Boeing cleans the site and surrounding areas. The group “seeks to reduce, to the greatest extent possible, the number of local families who have to hear the words, ‘Your child has cancer.’ ”
No longer quite so rare
Dr. Morgenstern, now retired from the University of Michigan, declined to be interviewed for this article. But as he and colleagues reported to the Centers for Disease Control and Prevention’s Agency for Toxic Substances and Disease Registry in 2007, there were strong signs of a link between contamination of the site and cancer.
The researchers compared cancer rates of adults living within 2 miles and 2-5 miles from SSFL with those of adults living more than 5 miles away, in Ventura and Los Angeles counties. They found that from 1988 through 1995, residents living within 2 miles of SSFL had a 60% higher rate of cancers than the control group. These included cancers of the thyroid, oral and nasal cavities, pharynx, larynx, esophagus, and bladder, as well as blood cancers such as leukemia, lymphoma, and multiple myeloma.
In separate studies, the investigators found higher rates of certain cancers among workers at SSFL who were exposed to radiation and to hydrazine, a chemical in rocket fuel.
In an interview, Dr. Saro Armenian, a pediatric hematologist-oncologist who was not involved in the studies, said the 60% increase in cancer incidence, which translated into a 1.6-fold increase in risk, merits more investigation.
“In epidemiologic studies, a 1.6-fold risk is actually a pretty strong signal because typically, most signals that you get are somewhere around 1.1- to 1.2-fold increased risk,” noted Dr. Armenian, a specialist in pediatric cancer survivorship and outcomes at City of Hope National Medical Center in Duarte, Calif.
However, Dr. Thomas Mack, former director of the Los Angeles County Cancer Surveillance Program, contends that there is insufficient evidence to support a direct link between the 1959 reactor accident and recent incident cancers. Dr. Mack is currently a professor of preventive medicine and pathology at the University of Southern California in Los Angeles.
“I have evaluated concerns about local excesses of cancer at least 100 times, usually from county residents, but for a while I represented the CDC and the California cancer registry,” Dr. Mack said, in response to an emailed request for comment.
“So far I have seen no evidence of carcinogenic radionucleotides or chemical carcinogens from Santa Susana found in any meaningful amount in any nearby community, but if someone has such evidence that would constitute evidence, that needs a response,” Dr. Mack added.
Boeing and California
Boeing has said problems at SSFL were not responsible for the high cancer rates among children in the community.
In April 2007, in a statement opposing a bill before the California State Legislature that would compel Boeing to pay for SSFL site cleanup, the company said that “in contrast to the accusations made against The Boeing Company that falsely claim increased cancer rates in the communities surrounding SSFL, a recent study conducted by the University of Michigan School of Public Health just concluded the opposite.”
Yet as Dr. Morgenstern wrote in 2007 to California state Sen. Joe Simitian, then chair of the Committee on Environmental Quality: “For the period 1996 through 2002, we found that the incidence rate of thyroid cancer was more than 60% greater among residents living within 2 miles of SSFL than for residents living more than 5 miles from SSFL. The magnitude and consistency of the thyroid finding for both periods is especially provocative because of evidence from other studies linking thyroid cancer with environmental exposures originating at SSFL and found in the surrounding communities.”
Boeing chose to ignore the results and instead focused on the methods used in the study, where the authors acknowledged that they measured distance from the site rather than environmental exposures and thus could not conclusively link excess cancer rates to exposures arising from SSFL.
But Dr. Morgenstern emphasized the conclusion of the report: “Despite the methodologic limitations of this study, the findings suggest there may be elevated incidence rates of certain cancers near SSFL that have been linked in previous studies with hazardous substances used at Rocketdyne, some of which have been observed or projected to exist offsite.”
Failure to come clean
In 2008, a law that set standards for cleanup of the site was passed. But the law was overturned in 2014 after a legal challenge by Boeing.
That left in place a 2007 order of consent between Boeing, NASA, the U.S. Department of Energy, and the California Department of Toxic Substances Control (DTSC) that required cleanup of SSFL to a much less stringent standard.
As of last year, Boeing and DTSC had begun confidential, nonbinding agreements regarding the 2007 order of consent, according to Parents Against SSFL.
Among the contaminants lingering at the site are radioactive particles, chemical compounds, heavy metals, and polluted water.
“In fact, over 300 contaminants of concern have been found at the site, and they are refusing to clean it,” Mr. Hirsch said. “This company releases large amounts of carcinogens, and perhaps significant numbers of people get sick with cancer, and the company doesn’t go to prison. They get more federal contracts.”
A version of this article first appeared on WebMD.com.
April 20, 2022 – Editor’s note: This article has been updated to include an interview with Dr. Thomas Mack, former director of the Los Angeles County Cancer Surveillance Program, who contends that there is insufficient evidence to support a direct link between the 1959 reactor accident and recent incident cancers.
CLL patients ‘cured’: 10 years post infusion, CAR T cells persist
“We can now conclude that CAR T cells can actually cure patients with leukemia based on these results,” said senior author Carl H. June, MD, in a press briefing on the study published in Nature.
“The major finding from this paper is that, 10 years down the road, you can find these [CAR T] cells,” Dr. June, director of the Center for Cellular Immunotherapies, University of Pennsylvania, Philadelphia, added. “The cells have evolved, and that was a big surprise ... but they are still able to kill leukemia cells 10 years after infusion.”
CAR T-cell therapy, in which patients’ own T cells are removed, reprogrammed in a lab to recognize and attack cancer cells, and then infused back into the patients, has transformed treatment of various blood cancers and shows often-remarkable results in achieving remissions.
While the treatment has become a routine therapy for certain leukemias, long-term results on the fate and function of the cells over time has been highly anticipated.
In the first published observations of a 10-year follow-up of patients treated with CAR T cells, Dr. June and colleagues described the findings for two patients, both with CLL, who back in 2010 were among the first to be treated with this groundbreaking therapy at the University of Pennsylvania.
A decade later, the CAR T cells are found to have remained detectable in both patients, who achieved complete remission in their first year of treatment, and both have sustained that remission.
Notably, the cells have evolved over the years – from initially being dominated by killer T cells to being dominated primarily by proliferative CD4-positive CAR T cells – with one of the patients exclusively having CD4-positive cells at year 9.3.
“The killer T cells did the initial heavy lifting of eliminating the tumor, “ first author J. Joseph Melenhorst, PhD, said in an interview.
“Once their job was done, those cells went down to very low levels, but the CD4-positive population persisted,” said Dr. Melenhorst, who established the lab at the University of Pennsylvania to follow patients treated with CAR T-cell therapy. “[This] delayed phase of immune response against cancer is a novel insight, and we were surprised to see it.”
Dr. Melenhorst noted that the clonal makeup of the CD4-positive cells importantly stabilized and became dominated by a small number of clones, suggesting further sustainability.
When one of the two patients, Doug Olson, who participated in the press conference, donated his cells back to the center after 9.3 years, the researchers found that his cells were still capable of destroying leukemia cells in the lab.
“Ten years [post infusion], we can’t find any of the leukemia cells and we still have the CAR T cells that are on patrol and on surveillance for residual leukemia,” Dr. June said.
One challenge of the otherwise desirable elimination of leukemia cells is that some aspects of sustaining CAR T-cell activity become problematic.
“The aspect of how the remission is maintained [is] very hard to study in a patient when there is no leukemia at all,” Dr. June explained. “It could be the last cell was gone within 3 weeks [of treatment], or it could be that the [cancer cells] are coming up like whack-a-moles, and they are killed because these CAR T cells are on patrol.”
Sadly, the other CLL patient, Bill Ludwig, who was first to receive the CAR T-cell treatment, died in 2021 from COVID-19.
Effects in other blood diseases similar?
CAR T-cell therapy is currently approved in the United States for several blood cancers, and whether similar long-term patterns of the cells may be observed in other patient and cancer types remains to be seen, Dr. Melenhorst said.
“I think in CLL we will see something similar, but in other diseases, we have yet to learn,” he said. “It may depend on issues including which domain has been engineered into the CAR.”
While the prospect of some patients being “cured” is exciting, responses to the therapy have generally been mixed. In CLL, for instance, full remissions have been observed to be maintained in about a quarter of patients, with higher rates observed in some lymphomas and pediatric ALL patients, Dr. Melenhorst explained.
The effects of CAR T-cell therapy in solid cancers have so far been more disappointing, with no research centers reproducing the kinds of results that have been seen with blood cancers.
“There appear to be a number of reasons, including that the [solid] tumor is more complex, and these solid cancers have ways to evade the immune system that need to be overcome,” Dr. June explained.
And despite the more encouraging findings in blood cancers, even with those, “the biggest disappointment is that CAR T-cell therapy doesn’t work all the time. It doesn’t work in every patient,” coauthor David Porter, MD, the University of Pennsylvania oncologist who treated the two patients, said in the press briefing.
“I think the importance of the Nature study is that we are starting to learn the mechanisms of why and how this works, so that we can start to get at how to make it work for more people,” Dr. Porter added. “But what we do see is that, when it works, it really is beyond what we expected 10 or 11 years ago.”
Speaking in the press briefing, Mr. Olson described how several weeks after his treatment in 2010, he became very ill with what has become known as the common, short-term side effect of cytokine release syndrome.
However, after Mr. Olson recovered a few days later, Dr. Porter gave him the remarkable news that “we cannot find a single cancer cell. You appear completely free of CLL.”
Mr. Olson reported that he has since lived a “full life,” kept working, and has even run some half-marathons.
Dr. June confided that the current 10-year results far exceed the team’s early expectations for CAR T-cell therapy. “After Doug [initially] signed his informed consent document for this, we thought that the cells would all be gone within a month or 2. The fact that they have survived for 10 years was a major surprise – and a happy one at that.”
Dr. June, Dr. Melenhorst, and Dr. Porter reported holding patents related to CAR T-cell manufacturing and biomarker discovery.
“We can now conclude that CAR T cells can actually cure patients with leukemia based on these results,” said senior author Carl H. June, MD, in a press briefing on the study published in Nature.
“The major finding from this paper is that, 10 years down the road, you can find these [CAR T] cells,” Dr. June, director of the Center for Cellular Immunotherapies, University of Pennsylvania, Philadelphia, added. “The cells have evolved, and that was a big surprise ... but they are still able to kill leukemia cells 10 years after infusion.”
CAR T-cell therapy, in which patients’ own T cells are removed, reprogrammed in a lab to recognize and attack cancer cells, and then infused back into the patients, has transformed treatment of various blood cancers and shows often-remarkable results in achieving remissions.
While the treatment has become a routine therapy for certain leukemias, long-term results on the fate and function of the cells over time has been highly anticipated.
In the first published observations of a 10-year follow-up of patients treated with CAR T cells, Dr. June and colleagues described the findings for two patients, both with CLL, who back in 2010 were among the first to be treated with this groundbreaking therapy at the University of Pennsylvania.
A decade later, the CAR T cells are found to have remained detectable in both patients, who achieved complete remission in their first year of treatment, and both have sustained that remission.
Notably, the cells have evolved over the years – from initially being dominated by killer T cells to being dominated primarily by proliferative CD4-positive CAR T cells – with one of the patients exclusively having CD4-positive cells at year 9.3.
“The killer T cells did the initial heavy lifting of eliminating the tumor, “ first author J. Joseph Melenhorst, PhD, said in an interview.
“Once their job was done, those cells went down to very low levels, but the CD4-positive population persisted,” said Dr. Melenhorst, who established the lab at the University of Pennsylvania to follow patients treated with CAR T-cell therapy. “[This] delayed phase of immune response against cancer is a novel insight, and we were surprised to see it.”
Dr. Melenhorst noted that the clonal makeup of the CD4-positive cells importantly stabilized and became dominated by a small number of clones, suggesting further sustainability.
When one of the two patients, Doug Olson, who participated in the press conference, donated his cells back to the center after 9.3 years, the researchers found that his cells were still capable of destroying leukemia cells in the lab.
“Ten years [post infusion], we can’t find any of the leukemia cells and we still have the CAR T cells that are on patrol and on surveillance for residual leukemia,” Dr. June said.
One challenge of the otherwise desirable elimination of leukemia cells is that some aspects of sustaining CAR T-cell activity become problematic.
“The aspect of how the remission is maintained [is] very hard to study in a patient when there is no leukemia at all,” Dr. June explained. “It could be the last cell was gone within 3 weeks [of treatment], or it could be that the [cancer cells] are coming up like whack-a-moles, and they are killed because these CAR T cells are on patrol.”
Sadly, the other CLL patient, Bill Ludwig, who was first to receive the CAR T-cell treatment, died in 2021 from COVID-19.
Effects in other blood diseases similar?
CAR T-cell therapy is currently approved in the United States for several blood cancers, and whether similar long-term patterns of the cells may be observed in other patient and cancer types remains to be seen, Dr. Melenhorst said.
“I think in CLL we will see something similar, but in other diseases, we have yet to learn,” he said. “It may depend on issues including which domain has been engineered into the CAR.”
While the prospect of some patients being “cured” is exciting, responses to the therapy have generally been mixed. In CLL, for instance, full remissions have been observed to be maintained in about a quarter of patients, with higher rates observed in some lymphomas and pediatric ALL patients, Dr. Melenhorst explained.
The effects of CAR T-cell therapy in solid cancers have so far been more disappointing, with no research centers reproducing the kinds of results that have been seen with blood cancers.
“There appear to be a number of reasons, including that the [solid] tumor is more complex, and these solid cancers have ways to evade the immune system that need to be overcome,” Dr. June explained.
And despite the more encouraging findings in blood cancers, even with those, “the biggest disappointment is that CAR T-cell therapy doesn’t work all the time. It doesn’t work in every patient,” coauthor David Porter, MD, the University of Pennsylvania oncologist who treated the two patients, said in the press briefing.
“I think the importance of the Nature study is that we are starting to learn the mechanisms of why and how this works, so that we can start to get at how to make it work for more people,” Dr. Porter added. “But what we do see is that, when it works, it really is beyond what we expected 10 or 11 years ago.”
Speaking in the press briefing, Mr. Olson described how several weeks after his treatment in 2010, he became very ill with what has become known as the common, short-term side effect of cytokine release syndrome.
However, after Mr. Olson recovered a few days later, Dr. Porter gave him the remarkable news that “we cannot find a single cancer cell. You appear completely free of CLL.”
Mr. Olson reported that he has since lived a “full life,” kept working, and has even run some half-marathons.
Dr. June confided that the current 10-year results far exceed the team’s early expectations for CAR T-cell therapy. “After Doug [initially] signed his informed consent document for this, we thought that the cells would all be gone within a month or 2. The fact that they have survived for 10 years was a major surprise – and a happy one at that.”
Dr. June, Dr. Melenhorst, and Dr. Porter reported holding patents related to CAR T-cell manufacturing and biomarker discovery.
“We can now conclude that CAR T cells can actually cure patients with leukemia based on these results,” said senior author Carl H. June, MD, in a press briefing on the study published in Nature.
“The major finding from this paper is that, 10 years down the road, you can find these [CAR T] cells,” Dr. June, director of the Center for Cellular Immunotherapies, University of Pennsylvania, Philadelphia, added. “The cells have evolved, and that was a big surprise ... but they are still able to kill leukemia cells 10 years after infusion.”
CAR T-cell therapy, in which patients’ own T cells are removed, reprogrammed in a lab to recognize and attack cancer cells, and then infused back into the patients, has transformed treatment of various blood cancers and shows often-remarkable results in achieving remissions.
While the treatment has become a routine therapy for certain leukemias, long-term results on the fate and function of the cells over time has been highly anticipated.
In the first published observations of a 10-year follow-up of patients treated with CAR T cells, Dr. June and colleagues described the findings for two patients, both with CLL, who back in 2010 were among the first to be treated with this groundbreaking therapy at the University of Pennsylvania.
A decade later, the CAR T cells are found to have remained detectable in both patients, who achieved complete remission in their first year of treatment, and both have sustained that remission.
Notably, the cells have evolved over the years – from initially being dominated by killer T cells to being dominated primarily by proliferative CD4-positive CAR T cells – with one of the patients exclusively having CD4-positive cells at year 9.3.
“The killer T cells did the initial heavy lifting of eliminating the tumor, “ first author J. Joseph Melenhorst, PhD, said in an interview.
“Once their job was done, those cells went down to very low levels, but the CD4-positive population persisted,” said Dr. Melenhorst, who established the lab at the University of Pennsylvania to follow patients treated with CAR T-cell therapy. “[This] delayed phase of immune response against cancer is a novel insight, and we were surprised to see it.”
Dr. Melenhorst noted that the clonal makeup of the CD4-positive cells importantly stabilized and became dominated by a small number of clones, suggesting further sustainability.
When one of the two patients, Doug Olson, who participated in the press conference, donated his cells back to the center after 9.3 years, the researchers found that his cells were still capable of destroying leukemia cells in the lab.
“Ten years [post infusion], we can’t find any of the leukemia cells and we still have the CAR T cells that are on patrol and on surveillance for residual leukemia,” Dr. June said.
One challenge of the otherwise desirable elimination of leukemia cells is that some aspects of sustaining CAR T-cell activity become problematic.
“The aspect of how the remission is maintained [is] very hard to study in a patient when there is no leukemia at all,” Dr. June explained. “It could be the last cell was gone within 3 weeks [of treatment], or it could be that the [cancer cells] are coming up like whack-a-moles, and they are killed because these CAR T cells are on patrol.”
Sadly, the other CLL patient, Bill Ludwig, who was first to receive the CAR T-cell treatment, died in 2021 from COVID-19.
Effects in other blood diseases similar?
CAR T-cell therapy is currently approved in the United States for several blood cancers, and whether similar long-term patterns of the cells may be observed in other patient and cancer types remains to be seen, Dr. Melenhorst said.
“I think in CLL we will see something similar, but in other diseases, we have yet to learn,” he said. “It may depend on issues including which domain has been engineered into the CAR.”
While the prospect of some patients being “cured” is exciting, responses to the therapy have generally been mixed. In CLL, for instance, full remissions have been observed to be maintained in about a quarter of patients, with higher rates observed in some lymphomas and pediatric ALL patients, Dr. Melenhorst explained.
The effects of CAR T-cell therapy in solid cancers have so far been more disappointing, with no research centers reproducing the kinds of results that have been seen with blood cancers.
“There appear to be a number of reasons, including that the [solid] tumor is more complex, and these solid cancers have ways to evade the immune system that need to be overcome,” Dr. June explained.
And despite the more encouraging findings in blood cancers, even with those, “the biggest disappointment is that CAR T-cell therapy doesn’t work all the time. It doesn’t work in every patient,” coauthor David Porter, MD, the University of Pennsylvania oncologist who treated the two patients, said in the press briefing.
“I think the importance of the Nature study is that we are starting to learn the mechanisms of why and how this works, so that we can start to get at how to make it work for more people,” Dr. Porter added. “But what we do see is that, when it works, it really is beyond what we expected 10 or 11 years ago.”
Speaking in the press briefing, Mr. Olson described how several weeks after his treatment in 2010, he became very ill with what has become known as the common, short-term side effect of cytokine release syndrome.
However, after Mr. Olson recovered a few days later, Dr. Porter gave him the remarkable news that “we cannot find a single cancer cell. You appear completely free of CLL.”
Mr. Olson reported that he has since lived a “full life,” kept working, and has even run some half-marathons.
Dr. June confided that the current 10-year results far exceed the team’s early expectations for CAR T-cell therapy. “After Doug [initially] signed his informed consent document for this, we thought that the cells would all be gone within a month or 2. The fact that they have survived for 10 years was a major surprise – and a happy one at that.”
Dr. June, Dr. Melenhorst, and Dr. Porter reported holding patents related to CAR T-cell manufacturing and biomarker discovery.
FROM NATURE
100 coauthored papers, 10 years: Cancer transplant pioneers model 'team science'
On July 29, 2021, Sergio Giralt, MD, deputy division head of the division of hematologic malignancies and Miguel-Angel Perales, MD, chief of the adult bone marrow transplant service at MSKCC, published their 100th peer-reviewed paper as coauthors. Listing hundreds of such articles on a CV is standard for top-tier physicians, but the pair had gone one better: 100 publications written together in 10 years.
Their centenary article hit scientific newsstands almost exactly a decade after their first joint paper, which appeared in September 2011, not long after they met.
Born in Cuba, Dr. Giralt grew up in Venezuela. From the age of 14, he knew that medicine was his path, and in 1984 he earned a medical degree from the Universidad Central de Venezuela, Caracas. Next came a research position at Harvard Medical School, a residency at the Good Samaritan Hospital, Cincinnati, and a fellowship at the University of Texas MD Anderson Cancer Center, Houston. Dr. Giralt arrived at MSKCC in 2010 as the new chief of the adult bone marrow transplant service. There he was introduced to a new colleague, Dr. Perales. They soon learned that in addition to expertise in hematology, they had second language in common: Spanish.
Dr. Giralt said: “We both have a Spanish background and in a certain sense, there was an affinity there. ... We both have shared experiences.”
Dr. Perales was brought up in Belgium, a European nation with three official languages: French, Dutch, and German. He speaks five tongues in all and learned Spanish from his father, who came from Spain.
Fluency in Spanish enables both physicians to take care of the many New Yorkers who are more comfortable in that language – especially when navigating cancer treatment. However, both Dr. Giralt and Dr. Perales said that a second language is more than a professional tool. They described the enjoyable change of persona that happens when they switch to Spanish.
“People who are multilingual have different roles [as much as] different languages,” said Dr. Perales. “When I’m in Spanish, part of my brain is [thinking back to] summer vacations and hanging out with my cousins.”
When it comes to clinical science, however, English is the language of choice.
Global leaders in HSCT
Dr. Giralt and Dr. Perales are known worldwide in the field of allogeneic HSCT, a potentially curative treatment for an elongating list of both malignant and nonmalignant diseases.
In 1973, MSKCC conducted the first bone-marrow transplant from an unrelated donor. Fifty years on, medical oncologists in the United States conduct approximately 8,500 allogeneic transplants each year, 72% to treat acute leukemias or myelodysplastic syndrome (MDS).
However, stripping the immune system with intensive chemotherapy ‘conditioning,’ then rebuilding it with non-diseased donor hematopoietic cells is a hazardous undertaking. Older patients are less likely to survive the intensive conditioning, so historically have missed out. Also, even with a good human leukocyte antigen (HLA) match, the recipient needs often brutal immunosuppression.
Since Dr. Giralt and Dr. Perales began their partnership in 2010, the goals of their work have not changed: to develop safer, lower-intensity transplantation suitable for older, more vulnerable patients and reduce fearsome posttransplant sequelae such as graft-versus-host disease (GVHD).
Dr. Giralt’s publication list spans more than 600 peer-reviewed papers, articles and book chapters, almost exclusively on HSCT. Dr. Perales has more than 300 publication credits on the topic.
The two paired up on their first paper just months after Dr. Giralt arrived at MSKCC. That article, published in Biology of Blood and Marrow Transplantation, compared umbilical cord blood for HSCT with donor blood in 367 people with a variety of hematologic malignancies, including acute and chronic leukemias, MDS, and lymphoma.
The MSKCC team found that transplant-related mortality in the first 180 days was higher for the cord blood (21%), but thereafter mortality and relapse were much lower than for donated blood, with the result that 2-year progression-free survival of 55% was similar. Dr. Perales, Dr. Giralt and their coauthors concluded that the data provided “strong support” for further work on cord blood as an alternative stem-cell source.
During their first decade of collaboration, Dr. Giralt and Dr. Perales worked on any promising avenue that could improve outcomes and the experience of HSCT recipients, including reduced-intensity conditioning regimens to allow older adults to benefit from curative HSCT and donor T-cell depletion by CD34 selection, to reduce graft-versus-host disease (GVHD).
The CD34 protein is typically found on the surface of early stage and highly active stem cell types. Selecting these cell types using a range of techniques can eliminate many other potentially interfering or inactive cells. This enriches the transplant population with the most effective cells and can lower the risk of GVHD.
The 100th paper on which Dr. Giralt and Dr. Perales were coauthors was published in Blood Advances on July 27, 2021. The retrospective study examined the fate of 58 MSKCC patients with a rare form of chronic lymphocytic leukemia, CLL with Richter’s transformation (CLL-RT). It was the largest such study to date of this rare disease.
M.D. Anderson Cancer Center had shown in 2006 that, despite chemotherapy, overall survival in patients with CLL-RT was approximately 8 months. HSCT improved survival dramatically (75% at 3 years; n = 7). However, with the advent of novel targeted drugs for CLL such as ibrutinib (Imbruvica), venetoclax (Venclexta), or idelalisib (Zydelig), the MSKCC team asked themselves: What was the role of reduced-intensive conditioning HSCT? Was it even safe? Among other findings, Dr. Giralt and Dr. Perales’ 100th paper showed that reduced-intensity HSCT remained a viable alternative after a CLL-RT patient progressed on a novel agent.
Impact of the pandemic
When COVID-19 hit, the team lost many research staff and developed a huge backlog, said Dr. Giralt. He and Dr. Perales realized that they needed to be “thoughtful and careful” about which studies to continue. “For example, the CD-34 selection trials we did not close because these are our workhorse trials,” Dr. Giralt said. “We have people we need to treat, and some of the patients that we need to treat can only be treated on trial.”
The team was also able to pivot some of their work into COVID 19 itself, and they collected crucial information on HSCT in recovered COVID-19 patients, as an example.
“We were living through a critical time, but that doesn’t mean we [aren’t] obligated to continue our mission, our research mission,” said Dr. Giralt. “It really is team science. The way we look at it ... there’s a common thread: We both like to do allogeneic transplant, and we both believe in trying to make CD-34 selection better. So we’re both very much [working on] how can we improve what we call ‘the Memorial way’ of doing transplants. Where we separate is, Miguel does primarily lymphoma. He doesn’t do myeloma [like me]. So in those two areas, we’re helping develop the junior faculty in a different way.”
Something more in common
Right from the start, Dr. Perales and Dr. Giralt also shared a commitment to mentoring. Since 2010, Dr. Perales has mentored 22 up-and-coming junior faculty, including 10 from Europe (8 from Spain) and 2 from Latin America.
“[It makes] the research enterprise much more productive but [these young scientists] really increase the visibility of the program,” said Dr. Giralt.
He cited Dr. Perales’ track record of mentoring as one of the reasons for his promotion to chief of the adult bone marrow transplant service. In March 2020, Dr. Perales seamlessly stepped into Dr. Giralt’s shoes, while Dr. Giralt moved on to his present role as deputy division head of the division of hematologic malignancies.
Dr. Perales said: “The key aspect [of these promotions] is the fantastic working relationship that we’ve had over the years. ... I consider Sergio my mentor, but also a good friend and colleague. And so I think it’s this ability that we’ve had to work together and that relationship of trust, which has been key.”
“Sergio is somebody who lifts people up,” Dr. Perales added. “Many people will tell you that Sergio has helped them in their career. ... And I think that’s a lesson I’ve learned from him: training the next generation. And [that’s] not just in the U.S., but outside. I think that’s a key role that we have. And our responsibility.”
Asked to comment on their 100th-paper milestone, Dr. Perales firmly turned the spotlight from himself and Dr. Giralt to the junior investigators who have passed through the doors of the bone-marrow transplant program: “This body of work represents not just our collaboration but also the many contributions of our team at MSK ... and beyond MSK.”
This article was updated 1/26/22.
On July 29, 2021, Sergio Giralt, MD, deputy division head of the division of hematologic malignancies and Miguel-Angel Perales, MD, chief of the adult bone marrow transplant service at MSKCC, published their 100th peer-reviewed paper as coauthors. Listing hundreds of such articles on a CV is standard for top-tier physicians, but the pair had gone one better: 100 publications written together in 10 years.
Their centenary article hit scientific newsstands almost exactly a decade after their first joint paper, which appeared in September 2011, not long after they met.
Born in Cuba, Dr. Giralt grew up in Venezuela. From the age of 14, he knew that medicine was his path, and in 1984 he earned a medical degree from the Universidad Central de Venezuela, Caracas. Next came a research position at Harvard Medical School, a residency at the Good Samaritan Hospital, Cincinnati, and a fellowship at the University of Texas MD Anderson Cancer Center, Houston. Dr. Giralt arrived at MSKCC in 2010 as the new chief of the adult bone marrow transplant service. There he was introduced to a new colleague, Dr. Perales. They soon learned that in addition to expertise in hematology, they had second language in common: Spanish.
Dr. Giralt said: “We both have a Spanish background and in a certain sense, there was an affinity there. ... We both have shared experiences.”
Dr. Perales was brought up in Belgium, a European nation with three official languages: French, Dutch, and German. He speaks five tongues in all and learned Spanish from his father, who came from Spain.
Fluency in Spanish enables both physicians to take care of the many New Yorkers who are more comfortable in that language – especially when navigating cancer treatment. However, both Dr. Giralt and Dr. Perales said that a second language is more than a professional tool. They described the enjoyable change of persona that happens when they switch to Spanish.
“People who are multilingual have different roles [as much as] different languages,” said Dr. Perales. “When I’m in Spanish, part of my brain is [thinking back to] summer vacations and hanging out with my cousins.”
When it comes to clinical science, however, English is the language of choice.
Global leaders in HSCT
Dr. Giralt and Dr. Perales are known worldwide in the field of allogeneic HSCT, a potentially curative treatment for an elongating list of both malignant and nonmalignant diseases.
In 1973, MSKCC conducted the first bone-marrow transplant from an unrelated donor. Fifty years on, medical oncologists in the United States conduct approximately 8,500 allogeneic transplants each year, 72% to treat acute leukemias or myelodysplastic syndrome (MDS).
However, stripping the immune system with intensive chemotherapy ‘conditioning,’ then rebuilding it with non-diseased donor hematopoietic cells is a hazardous undertaking. Older patients are less likely to survive the intensive conditioning, so historically have missed out. Also, even with a good human leukocyte antigen (HLA) match, the recipient needs often brutal immunosuppression.
Since Dr. Giralt and Dr. Perales began their partnership in 2010, the goals of their work have not changed: to develop safer, lower-intensity transplantation suitable for older, more vulnerable patients and reduce fearsome posttransplant sequelae such as graft-versus-host disease (GVHD).
Dr. Giralt’s publication list spans more than 600 peer-reviewed papers, articles and book chapters, almost exclusively on HSCT. Dr. Perales has more than 300 publication credits on the topic.
The two paired up on their first paper just months after Dr. Giralt arrived at MSKCC. That article, published in Biology of Blood and Marrow Transplantation, compared umbilical cord blood for HSCT with donor blood in 367 people with a variety of hematologic malignancies, including acute and chronic leukemias, MDS, and lymphoma.
The MSKCC team found that transplant-related mortality in the first 180 days was higher for the cord blood (21%), but thereafter mortality and relapse were much lower than for donated blood, with the result that 2-year progression-free survival of 55% was similar. Dr. Perales, Dr. Giralt and their coauthors concluded that the data provided “strong support” for further work on cord blood as an alternative stem-cell source.
During their first decade of collaboration, Dr. Giralt and Dr. Perales worked on any promising avenue that could improve outcomes and the experience of HSCT recipients, including reduced-intensity conditioning regimens to allow older adults to benefit from curative HSCT and donor T-cell depletion by CD34 selection, to reduce graft-versus-host disease (GVHD).
The CD34 protein is typically found on the surface of early stage and highly active stem cell types. Selecting these cell types using a range of techniques can eliminate many other potentially interfering or inactive cells. This enriches the transplant population with the most effective cells and can lower the risk of GVHD.
The 100th paper on which Dr. Giralt and Dr. Perales were coauthors was published in Blood Advances on July 27, 2021. The retrospective study examined the fate of 58 MSKCC patients with a rare form of chronic lymphocytic leukemia, CLL with Richter’s transformation (CLL-RT). It was the largest such study to date of this rare disease.
M.D. Anderson Cancer Center had shown in 2006 that, despite chemotherapy, overall survival in patients with CLL-RT was approximately 8 months. HSCT improved survival dramatically (75% at 3 years; n = 7). However, with the advent of novel targeted drugs for CLL such as ibrutinib (Imbruvica), venetoclax (Venclexta), or idelalisib (Zydelig), the MSKCC team asked themselves: What was the role of reduced-intensive conditioning HSCT? Was it even safe? Among other findings, Dr. Giralt and Dr. Perales’ 100th paper showed that reduced-intensity HSCT remained a viable alternative after a CLL-RT patient progressed on a novel agent.
Impact of the pandemic
When COVID-19 hit, the team lost many research staff and developed a huge backlog, said Dr. Giralt. He and Dr. Perales realized that they needed to be “thoughtful and careful” about which studies to continue. “For example, the CD-34 selection trials we did not close because these are our workhorse trials,” Dr. Giralt said. “We have people we need to treat, and some of the patients that we need to treat can only be treated on trial.”
The team was also able to pivot some of their work into COVID 19 itself, and they collected crucial information on HSCT in recovered COVID-19 patients, as an example.
“We were living through a critical time, but that doesn’t mean we [aren’t] obligated to continue our mission, our research mission,” said Dr. Giralt. “It really is team science. The way we look at it ... there’s a common thread: We both like to do allogeneic transplant, and we both believe in trying to make CD-34 selection better. So we’re both very much [working on] how can we improve what we call ‘the Memorial way’ of doing transplants. Where we separate is, Miguel does primarily lymphoma. He doesn’t do myeloma [like me]. So in those two areas, we’re helping develop the junior faculty in a different way.”
Something more in common
Right from the start, Dr. Perales and Dr. Giralt also shared a commitment to mentoring. Since 2010, Dr. Perales has mentored 22 up-and-coming junior faculty, including 10 from Europe (8 from Spain) and 2 from Latin America.
“[It makes] the research enterprise much more productive but [these young scientists] really increase the visibility of the program,” said Dr. Giralt.
He cited Dr. Perales’ track record of mentoring as one of the reasons for his promotion to chief of the adult bone marrow transplant service. In March 2020, Dr. Perales seamlessly stepped into Dr. Giralt’s shoes, while Dr. Giralt moved on to his present role as deputy division head of the division of hematologic malignancies.
Dr. Perales said: “The key aspect [of these promotions] is the fantastic working relationship that we’ve had over the years. ... I consider Sergio my mentor, but also a good friend and colleague. And so I think it’s this ability that we’ve had to work together and that relationship of trust, which has been key.”
“Sergio is somebody who lifts people up,” Dr. Perales added. “Many people will tell you that Sergio has helped them in their career. ... And I think that’s a lesson I’ve learned from him: training the next generation. And [that’s] not just in the U.S., but outside. I think that’s a key role that we have. And our responsibility.”
Asked to comment on their 100th-paper milestone, Dr. Perales firmly turned the spotlight from himself and Dr. Giralt to the junior investigators who have passed through the doors of the bone-marrow transplant program: “This body of work represents not just our collaboration but also the many contributions of our team at MSK ... and beyond MSK.”
This article was updated 1/26/22.
On July 29, 2021, Sergio Giralt, MD, deputy division head of the division of hematologic malignancies and Miguel-Angel Perales, MD, chief of the adult bone marrow transplant service at MSKCC, published their 100th peer-reviewed paper as coauthors. Listing hundreds of such articles on a CV is standard for top-tier physicians, but the pair had gone one better: 100 publications written together in 10 years.
Their centenary article hit scientific newsstands almost exactly a decade after their first joint paper, which appeared in September 2011, not long after they met.
Born in Cuba, Dr. Giralt grew up in Venezuela. From the age of 14, he knew that medicine was his path, and in 1984 he earned a medical degree from the Universidad Central de Venezuela, Caracas. Next came a research position at Harvard Medical School, a residency at the Good Samaritan Hospital, Cincinnati, and a fellowship at the University of Texas MD Anderson Cancer Center, Houston. Dr. Giralt arrived at MSKCC in 2010 as the new chief of the adult bone marrow transplant service. There he was introduced to a new colleague, Dr. Perales. They soon learned that in addition to expertise in hematology, they had second language in common: Spanish.
Dr. Giralt said: “We both have a Spanish background and in a certain sense, there was an affinity there. ... We both have shared experiences.”
Dr. Perales was brought up in Belgium, a European nation with three official languages: French, Dutch, and German. He speaks five tongues in all and learned Spanish from his father, who came from Spain.
Fluency in Spanish enables both physicians to take care of the many New Yorkers who are more comfortable in that language – especially when navigating cancer treatment. However, both Dr. Giralt and Dr. Perales said that a second language is more than a professional tool. They described the enjoyable change of persona that happens when they switch to Spanish.
“People who are multilingual have different roles [as much as] different languages,” said Dr. Perales. “When I’m in Spanish, part of my brain is [thinking back to] summer vacations and hanging out with my cousins.”
When it comes to clinical science, however, English is the language of choice.
Global leaders in HSCT
Dr. Giralt and Dr. Perales are known worldwide in the field of allogeneic HSCT, a potentially curative treatment for an elongating list of both malignant and nonmalignant diseases.
In 1973, MSKCC conducted the first bone-marrow transplant from an unrelated donor. Fifty years on, medical oncologists in the United States conduct approximately 8,500 allogeneic transplants each year, 72% to treat acute leukemias or myelodysplastic syndrome (MDS).
However, stripping the immune system with intensive chemotherapy ‘conditioning,’ then rebuilding it with non-diseased donor hematopoietic cells is a hazardous undertaking. Older patients are less likely to survive the intensive conditioning, so historically have missed out. Also, even with a good human leukocyte antigen (HLA) match, the recipient needs often brutal immunosuppression.
Since Dr. Giralt and Dr. Perales began their partnership in 2010, the goals of their work have not changed: to develop safer, lower-intensity transplantation suitable for older, more vulnerable patients and reduce fearsome posttransplant sequelae such as graft-versus-host disease (GVHD).
Dr. Giralt’s publication list spans more than 600 peer-reviewed papers, articles and book chapters, almost exclusively on HSCT. Dr. Perales has more than 300 publication credits on the topic.
The two paired up on their first paper just months after Dr. Giralt arrived at MSKCC. That article, published in Biology of Blood and Marrow Transplantation, compared umbilical cord blood for HSCT with donor blood in 367 people with a variety of hematologic malignancies, including acute and chronic leukemias, MDS, and lymphoma.
The MSKCC team found that transplant-related mortality in the first 180 days was higher for the cord blood (21%), but thereafter mortality and relapse were much lower than for donated blood, with the result that 2-year progression-free survival of 55% was similar. Dr. Perales, Dr. Giralt and their coauthors concluded that the data provided “strong support” for further work on cord blood as an alternative stem-cell source.
During their first decade of collaboration, Dr. Giralt and Dr. Perales worked on any promising avenue that could improve outcomes and the experience of HSCT recipients, including reduced-intensity conditioning regimens to allow older adults to benefit from curative HSCT and donor T-cell depletion by CD34 selection, to reduce graft-versus-host disease (GVHD).
The CD34 protein is typically found on the surface of early stage and highly active stem cell types. Selecting these cell types using a range of techniques can eliminate many other potentially interfering or inactive cells. This enriches the transplant population with the most effective cells and can lower the risk of GVHD.
The 100th paper on which Dr. Giralt and Dr. Perales were coauthors was published in Blood Advances on July 27, 2021. The retrospective study examined the fate of 58 MSKCC patients with a rare form of chronic lymphocytic leukemia, CLL with Richter’s transformation (CLL-RT). It was the largest such study to date of this rare disease.
M.D. Anderson Cancer Center had shown in 2006 that, despite chemotherapy, overall survival in patients with CLL-RT was approximately 8 months. HSCT improved survival dramatically (75% at 3 years; n = 7). However, with the advent of novel targeted drugs for CLL such as ibrutinib (Imbruvica), venetoclax (Venclexta), or idelalisib (Zydelig), the MSKCC team asked themselves: What was the role of reduced-intensive conditioning HSCT? Was it even safe? Among other findings, Dr. Giralt and Dr. Perales’ 100th paper showed that reduced-intensity HSCT remained a viable alternative after a CLL-RT patient progressed on a novel agent.
Impact of the pandemic
When COVID-19 hit, the team lost many research staff and developed a huge backlog, said Dr. Giralt. He and Dr. Perales realized that they needed to be “thoughtful and careful” about which studies to continue. “For example, the CD-34 selection trials we did not close because these are our workhorse trials,” Dr. Giralt said. “We have people we need to treat, and some of the patients that we need to treat can only be treated on trial.”
The team was also able to pivot some of their work into COVID 19 itself, and they collected crucial information on HSCT in recovered COVID-19 patients, as an example.
“We were living through a critical time, but that doesn’t mean we [aren’t] obligated to continue our mission, our research mission,” said Dr. Giralt. “It really is team science. The way we look at it ... there’s a common thread: We both like to do allogeneic transplant, and we both believe in trying to make CD-34 selection better. So we’re both very much [working on] how can we improve what we call ‘the Memorial way’ of doing transplants. Where we separate is, Miguel does primarily lymphoma. He doesn’t do myeloma [like me]. So in those two areas, we’re helping develop the junior faculty in a different way.”
Something more in common
Right from the start, Dr. Perales and Dr. Giralt also shared a commitment to mentoring. Since 2010, Dr. Perales has mentored 22 up-and-coming junior faculty, including 10 from Europe (8 from Spain) and 2 from Latin America.
“[It makes] the research enterprise much more productive but [these young scientists] really increase the visibility of the program,” said Dr. Giralt.
He cited Dr. Perales’ track record of mentoring as one of the reasons for his promotion to chief of the adult bone marrow transplant service. In March 2020, Dr. Perales seamlessly stepped into Dr. Giralt’s shoes, while Dr. Giralt moved on to his present role as deputy division head of the division of hematologic malignancies.
Dr. Perales said: “The key aspect [of these promotions] is the fantastic working relationship that we’ve had over the years. ... I consider Sergio my mentor, but also a good friend and colleague. And so I think it’s this ability that we’ve had to work together and that relationship of trust, which has been key.”
“Sergio is somebody who lifts people up,” Dr. Perales added. “Many people will tell you that Sergio has helped them in their career. ... And I think that’s a lesson I’ve learned from him: training the next generation. And [that’s] not just in the U.S., but outside. I think that’s a key role that we have. And our responsibility.”
Asked to comment on their 100th-paper milestone, Dr. Perales firmly turned the spotlight from himself and Dr. Giralt to the junior investigators who have passed through the doors of the bone-marrow transplant program: “This body of work represents not just our collaboration but also the many contributions of our team at MSK ... and beyond MSK.”
This article was updated 1/26/22.
DKMS: Small nonprofit to world’s largest stem cell donor registry
When Mechtild Harf was diagnosed with acute leukemia in 1990, physicians told her and her husband Peter that a bone marrow transplant was her best hope for survival. Back then, her native Germany had only 3,000 registered donors, and none was a match.
“My dad just went crazy, you know, to save his wife,” recalled Katharina Harf, who was a young teen at the time of her mother’s diagnosis.
In the course of 1 year, the Harfs recruited more than 68,000 potential bone marrow donors, but their heroic efforts couldn’t save Mechtild.
“She unfortunately didn’t make it. She died because of leukemia,” Katharina said.
Although Mechtild Harf did not survive, her legacy lives on in the bone marrow and stem cell donor recruitment organization DKMS (Deutsche Knochenmarkspenderdatei, or German Bone Marrow Donor Center).
In May of 1991, Peter Harf and Gerhard Ehninger, MD, the hematologist who treated Mechtild, founded DKMS with the mission, as its website states, “to provide as many blood cancer patients as possible with a second chance at life.”
From its German roots, the nonprofit organization has extended its mission to the United States (where it was initially known as Delete Blood Cancer DKMS), Poland, the United Kingdom, Chile, and in 2021, to South Africa.
Three decades after her mother’s death, Katharina Harf serves as Executive Chairwoman of DKMS U.S., based in New York.
World’s largest registry
“DKMS has the largest number of unrelated donors of any organization in the world,” noted Richard E. Champlin, MD, chair of the department of stem cell transplantation and cellular therapy at the University of Texas MD Anderson Cancer Center in Houston.
“In a large fraction of our donor searches, we find matches that are in the DKMS registry,” he said in an interview,
Alexander Schmidt, MD, PhD, global chief medical officer for DKMS, said that approximately 25% of all registered donors worldwide were recruited by his organization, and 39% of all unrelated donor transplants are made with peripheral blood stem cell or bone marrow products, donated by volunteers who are recruited by DKMS.
Since its founding, DKMS has registered 7.1 million potential donors in Germany, who made a total of 80,000 stem cell donations. DKMS U.S., which began operations in 2004, has registered 1.1 million donors and enabled 4,700 donations.
Global partners
DKMS partners with donor centers and recruitment organizations in each country where it operates. In the United States, DKMS works with the National Marrow Donor Program (NMDP) and its “Be The Match” donor registry.
“DKMS donors, both those from DKMS in Germany and those from DKMS in the United States are also listed in the NMDP registry, to make it easier for US search coordinators to accept these donors,” Dr. Schmidt explained in an interview.
The international cooperation and coordination makes it possible for a donor in the UK, for example, to save a life of a patient in Germany, the U.S., Chile, India, or many other parts of the world – anywhere that can be reached in time for a patient in need to receive a stem cell donation.
Pandemic affects donations
But, as with just about every aspect of life, the COVID-19 pandemic has created enormous challenges for recruiters, donor centers, and stem cell transplant centers.
Dr. Schmidt said that decline in donations during the pandemic was less severe than initially feared, with a decrease of just 3.5% in 2020, compared with the prepandemic year of 2019. In contrast, though, the average annual growth rate for donations prior to the pandemic was about 4%.
“Nevertheless, at the beginning of the pandemic in March 2020, for a few days things looked quite terrible, because all the borders were closed and flights were canceled, and about 50% of all stem cell products go abroad, and between 20% and 25% go intercontinental,” Dr. Schmidt said.
However, close cooperation and coordination between donor centers and national health authorities soon resolved the problem and helped insure that the flow of life-saving donations could continue with minimal disruption, he noted.
“I don’t think we had any product that could not be delivered at the end of the day, due to the pandemic,” he told this news organization.
Workforce and clinical problems
Although the flow of donations within and between nations has continued, the COVID-19 pandemic has had profound negative effects on transplant centers, particularly during the wave of infections caused by the Omicron variant, according to a transplant expert.
“With this most recent strain and how transmissible it is, what we’re dealing with is mass workforce shortages,” said Yi-Bin Chen, MD, director of the bone marrow transplant program at Massachusetts General Hospital in Boston.
“On top of a short-staffed hospital, you then take a very transmissible variant and deplete it even more due to the need to quarantine,” he said in an interview.
Both Dr. Champlin and Dr. Chen said that on-again, off-again pandemic travel bans and donor illnesses have necessitated first obtaining products and cryopreserving them before starting the recipient on a conditioning regimen for the transplant.
“The problem is that, while you can preserve peripheral blood stem cells pretty reliably, cryopreserving bone marrow is a bit more difficult,” Dr. Chen said.
In addition, evidence from recent studies comparing stem cell sources suggest that outcomes are less good with cryopreserved products than with fresh products, and with peripheral blood stem cells compared with bone marrow.
“But you’ve got to make do. A transplant with a cryopreserved product is better than no transplant,” Dr. Chen said.
To make things even more frustrating, as the pandemic waxed and waned throughout 2020 and 2021, the recommendations from donor centers seesawed between using fresh or cryopreserved product, making it difficult to plan a transplant for an individual patient.
The Omicron wave has also resulted in a much higher rate of donor dropout than anticipated, making it that much harder to schedule a transplant, Dr. Chen noted.
‘Every patient saved’
The pandemic will eventually subside, however, while the need for stem cell transplantation to treat hematologic malignancies will continue.
DKMS recently launched special aid programs to improve access to stem cell transplants in developing nations by offering financial support, free HLA typing, and other services.
In addition to its core mission of recruiting donors, DKMS is dedicated to improving the quality and efficiency of stem cell transplants. For example, in 2017 scientists in DKMS’ Life Science Lab created an antibody test for donor cytomegalovirus (CMV) infection, using a simple buccal swab rather than a more invasive blood sample. CMV infections can compromise the integrity of stem cell grafts and could be fatal to immunocompromised transplant recipients.
The last word goes to Mechtild Harf’s daughter Katharina.
“My big dream is that every patient will be saved from blood cancer,” she said in a video posted on the DKMS website. “When they get sick, we have a solution for them, whether it’s because they need a donor, with research, building hospitals, providing them with the best medical care we can. I will just keep fighting and keep spreading the word, recruiting donors, raising money – all the things that it takes for us to delete blood cancer.”
“I have to believe that this dream will come true because otherwise, why dream, right?” she said.
Dr. Champlin was the recipient of a Mechtild Harf Science Award and is a member of the board of DKMS U.S. Dr. Schmidt is employed by DKMS. Dr. Chen reported having no relevant disclosures.
When Mechtild Harf was diagnosed with acute leukemia in 1990, physicians told her and her husband Peter that a bone marrow transplant was her best hope for survival. Back then, her native Germany had only 3,000 registered donors, and none was a match.
“My dad just went crazy, you know, to save his wife,” recalled Katharina Harf, who was a young teen at the time of her mother’s diagnosis.
In the course of 1 year, the Harfs recruited more than 68,000 potential bone marrow donors, but their heroic efforts couldn’t save Mechtild.
“She unfortunately didn’t make it. She died because of leukemia,” Katharina said.
Although Mechtild Harf did not survive, her legacy lives on in the bone marrow and stem cell donor recruitment organization DKMS (Deutsche Knochenmarkspenderdatei, or German Bone Marrow Donor Center).
In May of 1991, Peter Harf and Gerhard Ehninger, MD, the hematologist who treated Mechtild, founded DKMS with the mission, as its website states, “to provide as many blood cancer patients as possible with a second chance at life.”
From its German roots, the nonprofit organization has extended its mission to the United States (where it was initially known as Delete Blood Cancer DKMS), Poland, the United Kingdom, Chile, and in 2021, to South Africa.
Three decades after her mother’s death, Katharina Harf serves as Executive Chairwoman of DKMS U.S., based in New York.
World’s largest registry
“DKMS has the largest number of unrelated donors of any organization in the world,” noted Richard E. Champlin, MD, chair of the department of stem cell transplantation and cellular therapy at the University of Texas MD Anderson Cancer Center in Houston.
“In a large fraction of our donor searches, we find matches that are in the DKMS registry,” he said in an interview,
Alexander Schmidt, MD, PhD, global chief medical officer for DKMS, said that approximately 25% of all registered donors worldwide were recruited by his organization, and 39% of all unrelated donor transplants are made with peripheral blood stem cell or bone marrow products, donated by volunteers who are recruited by DKMS.
Since its founding, DKMS has registered 7.1 million potential donors in Germany, who made a total of 80,000 stem cell donations. DKMS U.S., which began operations in 2004, has registered 1.1 million donors and enabled 4,700 donations.
Global partners
DKMS partners with donor centers and recruitment organizations in each country where it operates. In the United States, DKMS works with the National Marrow Donor Program (NMDP) and its “Be The Match” donor registry.
“DKMS donors, both those from DKMS in Germany and those from DKMS in the United States are also listed in the NMDP registry, to make it easier for US search coordinators to accept these donors,” Dr. Schmidt explained in an interview.
The international cooperation and coordination makes it possible for a donor in the UK, for example, to save a life of a patient in Germany, the U.S., Chile, India, or many other parts of the world – anywhere that can be reached in time for a patient in need to receive a stem cell donation.
Pandemic affects donations
But, as with just about every aspect of life, the COVID-19 pandemic has created enormous challenges for recruiters, donor centers, and stem cell transplant centers.
Dr. Schmidt said that decline in donations during the pandemic was less severe than initially feared, with a decrease of just 3.5% in 2020, compared with the prepandemic year of 2019. In contrast, though, the average annual growth rate for donations prior to the pandemic was about 4%.
“Nevertheless, at the beginning of the pandemic in March 2020, for a few days things looked quite terrible, because all the borders were closed and flights were canceled, and about 50% of all stem cell products go abroad, and between 20% and 25% go intercontinental,” Dr. Schmidt said.
However, close cooperation and coordination between donor centers and national health authorities soon resolved the problem and helped insure that the flow of life-saving donations could continue with minimal disruption, he noted.
“I don’t think we had any product that could not be delivered at the end of the day, due to the pandemic,” he told this news organization.
Workforce and clinical problems
Although the flow of donations within and between nations has continued, the COVID-19 pandemic has had profound negative effects on transplant centers, particularly during the wave of infections caused by the Omicron variant, according to a transplant expert.
“With this most recent strain and how transmissible it is, what we’re dealing with is mass workforce shortages,” said Yi-Bin Chen, MD, director of the bone marrow transplant program at Massachusetts General Hospital in Boston.
“On top of a short-staffed hospital, you then take a very transmissible variant and deplete it even more due to the need to quarantine,” he said in an interview.
Both Dr. Champlin and Dr. Chen said that on-again, off-again pandemic travel bans and donor illnesses have necessitated first obtaining products and cryopreserving them before starting the recipient on a conditioning regimen for the transplant.
“The problem is that, while you can preserve peripheral blood stem cells pretty reliably, cryopreserving bone marrow is a bit more difficult,” Dr. Chen said.
In addition, evidence from recent studies comparing stem cell sources suggest that outcomes are less good with cryopreserved products than with fresh products, and with peripheral blood stem cells compared with bone marrow.
“But you’ve got to make do. A transplant with a cryopreserved product is better than no transplant,” Dr. Chen said.
To make things even more frustrating, as the pandemic waxed and waned throughout 2020 and 2021, the recommendations from donor centers seesawed between using fresh or cryopreserved product, making it difficult to plan a transplant for an individual patient.
The Omicron wave has also resulted in a much higher rate of donor dropout than anticipated, making it that much harder to schedule a transplant, Dr. Chen noted.
‘Every patient saved’
The pandemic will eventually subside, however, while the need for stem cell transplantation to treat hematologic malignancies will continue.
DKMS recently launched special aid programs to improve access to stem cell transplants in developing nations by offering financial support, free HLA typing, and other services.
In addition to its core mission of recruiting donors, DKMS is dedicated to improving the quality and efficiency of stem cell transplants. For example, in 2017 scientists in DKMS’ Life Science Lab created an antibody test for donor cytomegalovirus (CMV) infection, using a simple buccal swab rather than a more invasive blood sample. CMV infections can compromise the integrity of stem cell grafts and could be fatal to immunocompromised transplant recipients.
The last word goes to Mechtild Harf’s daughter Katharina.
“My big dream is that every patient will be saved from blood cancer,” she said in a video posted on the DKMS website. “When they get sick, we have a solution for them, whether it’s because they need a donor, with research, building hospitals, providing them with the best medical care we can. I will just keep fighting and keep spreading the word, recruiting donors, raising money – all the things that it takes for us to delete blood cancer.”
“I have to believe that this dream will come true because otherwise, why dream, right?” she said.
Dr. Champlin was the recipient of a Mechtild Harf Science Award and is a member of the board of DKMS U.S. Dr. Schmidt is employed by DKMS. Dr. Chen reported having no relevant disclosures.
When Mechtild Harf was diagnosed with acute leukemia in 1990, physicians told her and her husband Peter that a bone marrow transplant was her best hope for survival. Back then, her native Germany had only 3,000 registered donors, and none was a match.
“My dad just went crazy, you know, to save his wife,” recalled Katharina Harf, who was a young teen at the time of her mother’s diagnosis.
In the course of 1 year, the Harfs recruited more than 68,000 potential bone marrow donors, but their heroic efforts couldn’t save Mechtild.
“She unfortunately didn’t make it. She died because of leukemia,” Katharina said.
Although Mechtild Harf did not survive, her legacy lives on in the bone marrow and stem cell donor recruitment organization DKMS (Deutsche Knochenmarkspenderdatei, or German Bone Marrow Donor Center).
In May of 1991, Peter Harf and Gerhard Ehninger, MD, the hematologist who treated Mechtild, founded DKMS with the mission, as its website states, “to provide as many blood cancer patients as possible with a second chance at life.”
From its German roots, the nonprofit organization has extended its mission to the United States (where it was initially known as Delete Blood Cancer DKMS), Poland, the United Kingdom, Chile, and in 2021, to South Africa.
Three decades after her mother’s death, Katharina Harf serves as Executive Chairwoman of DKMS U.S., based in New York.
World’s largest registry
“DKMS has the largest number of unrelated donors of any organization in the world,” noted Richard E. Champlin, MD, chair of the department of stem cell transplantation and cellular therapy at the University of Texas MD Anderson Cancer Center in Houston.
“In a large fraction of our donor searches, we find matches that are in the DKMS registry,” he said in an interview,
Alexander Schmidt, MD, PhD, global chief medical officer for DKMS, said that approximately 25% of all registered donors worldwide were recruited by his organization, and 39% of all unrelated donor transplants are made with peripheral blood stem cell or bone marrow products, donated by volunteers who are recruited by DKMS.
Since its founding, DKMS has registered 7.1 million potential donors in Germany, who made a total of 80,000 stem cell donations. DKMS U.S., which began operations in 2004, has registered 1.1 million donors and enabled 4,700 donations.
Global partners
DKMS partners with donor centers and recruitment organizations in each country where it operates. In the United States, DKMS works with the National Marrow Donor Program (NMDP) and its “Be The Match” donor registry.
“DKMS donors, both those from DKMS in Germany and those from DKMS in the United States are also listed in the NMDP registry, to make it easier for US search coordinators to accept these donors,” Dr. Schmidt explained in an interview.
The international cooperation and coordination makes it possible for a donor in the UK, for example, to save a life of a patient in Germany, the U.S., Chile, India, or many other parts of the world – anywhere that can be reached in time for a patient in need to receive a stem cell donation.
Pandemic affects donations
But, as with just about every aspect of life, the COVID-19 pandemic has created enormous challenges for recruiters, donor centers, and stem cell transplant centers.
Dr. Schmidt said that decline in donations during the pandemic was less severe than initially feared, with a decrease of just 3.5% in 2020, compared with the prepandemic year of 2019. In contrast, though, the average annual growth rate for donations prior to the pandemic was about 4%.
“Nevertheless, at the beginning of the pandemic in March 2020, for a few days things looked quite terrible, because all the borders were closed and flights were canceled, and about 50% of all stem cell products go abroad, and between 20% and 25% go intercontinental,” Dr. Schmidt said.
However, close cooperation and coordination between donor centers and national health authorities soon resolved the problem and helped insure that the flow of life-saving donations could continue with minimal disruption, he noted.
“I don’t think we had any product that could not be delivered at the end of the day, due to the pandemic,” he told this news organization.
Workforce and clinical problems
Although the flow of donations within and between nations has continued, the COVID-19 pandemic has had profound negative effects on transplant centers, particularly during the wave of infections caused by the Omicron variant, according to a transplant expert.
“With this most recent strain and how transmissible it is, what we’re dealing with is mass workforce shortages,” said Yi-Bin Chen, MD, director of the bone marrow transplant program at Massachusetts General Hospital in Boston.
“On top of a short-staffed hospital, you then take a very transmissible variant and deplete it even more due to the need to quarantine,” he said in an interview.
Both Dr. Champlin and Dr. Chen said that on-again, off-again pandemic travel bans and donor illnesses have necessitated first obtaining products and cryopreserving them before starting the recipient on a conditioning regimen for the transplant.
“The problem is that, while you can preserve peripheral blood stem cells pretty reliably, cryopreserving bone marrow is a bit more difficult,” Dr. Chen said.
In addition, evidence from recent studies comparing stem cell sources suggest that outcomes are less good with cryopreserved products than with fresh products, and with peripheral blood stem cells compared with bone marrow.
“But you’ve got to make do. A transplant with a cryopreserved product is better than no transplant,” Dr. Chen said.
To make things even more frustrating, as the pandemic waxed and waned throughout 2020 and 2021, the recommendations from donor centers seesawed between using fresh or cryopreserved product, making it difficult to plan a transplant for an individual patient.
The Omicron wave has also resulted in a much higher rate of donor dropout than anticipated, making it that much harder to schedule a transplant, Dr. Chen noted.
‘Every patient saved’
The pandemic will eventually subside, however, while the need for stem cell transplantation to treat hematologic malignancies will continue.
DKMS recently launched special aid programs to improve access to stem cell transplants in developing nations by offering financial support, free HLA typing, and other services.
In addition to its core mission of recruiting donors, DKMS is dedicated to improving the quality and efficiency of stem cell transplants. For example, in 2017 scientists in DKMS’ Life Science Lab created an antibody test for donor cytomegalovirus (CMV) infection, using a simple buccal swab rather than a more invasive blood sample. CMV infections can compromise the integrity of stem cell grafts and could be fatal to immunocompromised transplant recipients.
The last word goes to Mechtild Harf’s daughter Katharina.
“My big dream is that every patient will be saved from blood cancer,” she said in a video posted on the DKMS website. “When they get sick, we have a solution for them, whether it’s because they need a donor, with research, building hospitals, providing them with the best medical care we can. I will just keep fighting and keep spreading the word, recruiting donors, raising money – all the things that it takes for us to delete blood cancer.”
“I have to believe that this dream will come true because otherwise, why dream, right?” she said.
Dr. Champlin was the recipient of a Mechtild Harf Science Award and is a member of the board of DKMS U.S. Dr. Schmidt is employed by DKMS. Dr. Chen reported having no relevant disclosures.
ASH studies look at racial disparities in ALL care, outcomes
Among almost 25,000 children and young adults up to 31 years old, all of whom participated in Children’s Oncology Group studies since 2004, 5-year event free survival (EFS) was 87.4% for White patients, 82.8% for Hispanic patients, and 81.9% for Black patients.
When socioeconomics and disease characteristics such as CNS involvement, white blood cell lineage, and induction status were taken into account, the risk of having a survival event fell from 37% to 11% higher for Hispanic patients versus White patients but from 45% to 32% for Black patients versus White patients.
However, there was no explicit adjustment in the study for acuity at presentation, body mass index, adherence to protocols, or Philadelphia chromosome (PH)-like disease, which is more common among Hispanic patients.
Even so, lead investigator Sumit Gupta, MD, a pediatric blood cancer specialist at the University of Toronto, said that even with the potential confounders, lingering differences in outcomes raise questions about equal access to care and other matters, and suggest that there are still “uncomfortable things to consider, things like ... structural racism” and a system that delivers “systemically different care to patients across racial” groups.
Another report presented at the meeting with 295 patients 18-40 years old found that Hispanic patients had 3-year overall survival comparable to that of White patients despite a higher prevalence of PH-like disease, perhaps because Hispanic patients had higher treatment adherence than did White patients at 76% versus 56%, said lead investigator Lori Muffly, MD, a bone and marrow transplant specialist at Stanford (Calif.) University.
However, Hispanic ALL patients were underrepresented in the study because the investigators didn’t recruit in Texas and Florida, states with higher percentages of young Hispanic ALL patients, and recruitment in California fell short of the prevalence of young Hispanic patients in that state. The work was a substudy of CALGB 10403, a trial of pediatric regimens in adolescents and young adults.
“It’s a relatively easy maneuver, going to where the patients are. When groups are thinking about multicenter trials, it has to be part of the dialogue from the beginning,” Dr. Muffly said.
Black patients in the review had fewer days in treatment and a higher prevalence of T-cell disease, and didn’t do as well as other groups.
Together, the studies “offer insight into the magnitude of racial and ethnic disparities in care among young people with” ALL, said Mikkael Sekeres, MD, chief of the division of hematology at the University of Miami, who moderated the presentations.
Dr. Gupta and his team found outcome differences only in relapsed B-cell ALL, not T-cell disease. B-cell disease has a more rigorous maintenance schedule, so it could be that there’s a difference in sticking to follow-up between various groups or less rigorous monitoring by pediatric oncologists in some groups, he said.
Dr. Gupta’s study was funded by the National Cancer Institute and others. Dr. Muffly didn’t report a funding source, but reported ties to Pfizer, Amgen, and other companies. Dr. Gupta is involved with Jazz Pharmaceuticals.
Among almost 25,000 children and young adults up to 31 years old, all of whom participated in Children’s Oncology Group studies since 2004, 5-year event free survival (EFS) was 87.4% for White patients, 82.8% for Hispanic patients, and 81.9% for Black patients.
When socioeconomics and disease characteristics such as CNS involvement, white blood cell lineage, and induction status were taken into account, the risk of having a survival event fell from 37% to 11% higher for Hispanic patients versus White patients but from 45% to 32% for Black patients versus White patients.
However, there was no explicit adjustment in the study for acuity at presentation, body mass index, adherence to protocols, or Philadelphia chromosome (PH)-like disease, which is more common among Hispanic patients.
Even so, lead investigator Sumit Gupta, MD, a pediatric blood cancer specialist at the University of Toronto, said that even with the potential confounders, lingering differences in outcomes raise questions about equal access to care and other matters, and suggest that there are still “uncomfortable things to consider, things like ... structural racism” and a system that delivers “systemically different care to patients across racial” groups.
Another report presented at the meeting with 295 patients 18-40 years old found that Hispanic patients had 3-year overall survival comparable to that of White patients despite a higher prevalence of PH-like disease, perhaps because Hispanic patients had higher treatment adherence than did White patients at 76% versus 56%, said lead investigator Lori Muffly, MD, a bone and marrow transplant specialist at Stanford (Calif.) University.
However, Hispanic ALL patients were underrepresented in the study because the investigators didn’t recruit in Texas and Florida, states with higher percentages of young Hispanic ALL patients, and recruitment in California fell short of the prevalence of young Hispanic patients in that state. The work was a substudy of CALGB 10403, a trial of pediatric regimens in adolescents and young adults.
“It’s a relatively easy maneuver, going to where the patients are. When groups are thinking about multicenter trials, it has to be part of the dialogue from the beginning,” Dr. Muffly said.
Black patients in the review had fewer days in treatment and a higher prevalence of T-cell disease, and didn’t do as well as other groups.
Together, the studies “offer insight into the magnitude of racial and ethnic disparities in care among young people with” ALL, said Mikkael Sekeres, MD, chief of the division of hematology at the University of Miami, who moderated the presentations.
Dr. Gupta and his team found outcome differences only in relapsed B-cell ALL, not T-cell disease. B-cell disease has a more rigorous maintenance schedule, so it could be that there’s a difference in sticking to follow-up between various groups or less rigorous monitoring by pediatric oncologists in some groups, he said.
Dr. Gupta’s study was funded by the National Cancer Institute and others. Dr. Muffly didn’t report a funding source, but reported ties to Pfizer, Amgen, and other companies. Dr. Gupta is involved with Jazz Pharmaceuticals.
Among almost 25,000 children and young adults up to 31 years old, all of whom participated in Children’s Oncology Group studies since 2004, 5-year event free survival (EFS) was 87.4% for White patients, 82.8% for Hispanic patients, and 81.9% for Black patients.
When socioeconomics and disease characteristics such as CNS involvement, white blood cell lineage, and induction status were taken into account, the risk of having a survival event fell from 37% to 11% higher for Hispanic patients versus White patients but from 45% to 32% for Black patients versus White patients.
However, there was no explicit adjustment in the study for acuity at presentation, body mass index, adherence to protocols, or Philadelphia chromosome (PH)-like disease, which is more common among Hispanic patients.
Even so, lead investigator Sumit Gupta, MD, a pediatric blood cancer specialist at the University of Toronto, said that even with the potential confounders, lingering differences in outcomes raise questions about equal access to care and other matters, and suggest that there are still “uncomfortable things to consider, things like ... structural racism” and a system that delivers “systemically different care to patients across racial” groups.
Another report presented at the meeting with 295 patients 18-40 years old found that Hispanic patients had 3-year overall survival comparable to that of White patients despite a higher prevalence of PH-like disease, perhaps because Hispanic patients had higher treatment adherence than did White patients at 76% versus 56%, said lead investigator Lori Muffly, MD, a bone and marrow transplant specialist at Stanford (Calif.) University.
However, Hispanic ALL patients were underrepresented in the study because the investigators didn’t recruit in Texas and Florida, states with higher percentages of young Hispanic ALL patients, and recruitment in California fell short of the prevalence of young Hispanic patients in that state. The work was a substudy of CALGB 10403, a trial of pediatric regimens in adolescents and young adults.
“It’s a relatively easy maneuver, going to where the patients are. When groups are thinking about multicenter trials, it has to be part of the dialogue from the beginning,” Dr. Muffly said.
Black patients in the review had fewer days in treatment and a higher prevalence of T-cell disease, and didn’t do as well as other groups.
Together, the studies “offer insight into the magnitude of racial and ethnic disparities in care among young people with” ALL, said Mikkael Sekeres, MD, chief of the division of hematology at the University of Miami, who moderated the presentations.
Dr. Gupta and his team found outcome differences only in relapsed B-cell ALL, not T-cell disease. B-cell disease has a more rigorous maintenance schedule, so it could be that there’s a difference in sticking to follow-up between various groups or less rigorous monitoring by pediatric oncologists in some groups, he said.
Dr. Gupta’s study was funded by the National Cancer Institute and others. Dr. Muffly didn’t report a funding source, but reported ties to Pfizer, Amgen, and other companies. Dr. Gupta is involved with Jazz Pharmaceuticals.
FROM ASH 2021
TKI/BiTE combo extends survival of older patients with Ph+ALL
ATLANTA – Older patients with acute lymphoblastic leukemia positive for the Philadelphia chromosome (Ph+ALL) are often not fit enough to withstand intensive chemotherapy and stem cell transplants, but remissions with alternative therapies are usually short lived.
Now, results from an ongoing study suggest that the combination of the
The new results were reported by investigators in the SWOG Cancer Research Network and come from a cohort of 25 patients with a median age of 73 years with newly diagnosed Ph+ALL or ALL with dasatinib-sensitive fusions of mutations (Ph-like ALL).
Nearly all (23 of 25 patients, 92%) had complete remissions, and 5 of 16 patients for whom minimal residual disease (MRD) data were available were MRD negative at day 28, said Anjali Advani, MD, from the Cleveland Clinic.
At a median follow-up of 1.7 years, the estimated 3-year disease-free survival rate was 80%, and the estimated overall survival rate was 85%, the investigators reported in a poster presentation at the annual meeting of the American Society of Hematology.
“I think the biggest question will be longer-term follow-up. We clearly see high remission rates in this population, but the issue is whether in these elderly patients who are not candidates for chemo we can prolong remission by the addition of other treatments, such as blinatumomab,” she said in an interview with this news organization.
“The follow-up is reasonable at this point, and as we get longer follow-up, if the current 3-year survival estimates hold up, that would be very encouraging,” she said.
Early promise
A leukemia specialist who was not involved in the study told this news organization that the results are promising, but added that it’s too early to make definitive judgments about the efficacy of the combination.
“People have used just a tyrosine kinase inhibitor and prednisone in these patients and gotten remissions, but they just don’t last,” said Peter Emanuel, MD, from CHI St. Vincent Infirmary in Little Rock, Ark.
“The promise with this approach is that you’re getting a longer-lasting remission – maybe not a cure, but a longer-lasting remission – without having to use intensive chemotherapy,” he said.
“It’s still a pretty small study, so I think this is going to require a bigger trial, looking at more patients, but it’s certainly very encouraging and very promising,” he added.
Hanno Hock, MD, PhD, a leukemia researcher at the Mass General Cancer Center in Boston, said in an interview that “the whole idea here is to add this newer agent, blinatumomab, to make those good initial responses more durable, and it looks like it is able to do that with very impressive initial data,” he said.
“The caveat is that this is still early, and one needs to wait and see how it all pans out, but it’s very well tolerated, and definitely the next logical step in trying to offer something to people who cannot tolerate more aggressive therapy such as transplant,” Dr. Hock added.
Study results
The new results come from a feasibility cohort of patients enrolled in the SWOG S1318 trial, which studied blinatumomab plus chemotherapy and prednisone in older patients with Ph-ALL, as well as blinatumomab, dasatinib, and prednisone in older adults with Ph+ ALL.
Patients 65 and older with newly diagnosed or relapsed/refractory Ph+ALL or Ph-like ALL and no central nervous system disease were eligible for the arm of the trial described here. All patients with data reported in this analysis had newly diagnosed ALL.
Patients first received a single induction cycle of dasatinib and prednisone and were then evaluated for response. Patients with a complete remission (CR) or CR with incomplete recovery of blood counts (CRi) would then undergo prednisone tapering while continuing dasatinib until day 84. Patients without a CR or CRi at day 28 who had remissions by day 56 then also continued dasatinib until day 84.
Those patients still in remission at day 84 went on to three cycles of blinatumomab and dasatinib, followed by dasatinib and prednisone maintenance until unacceptable toxicity or disease progression. Patients may remain on maintenance for up to 10 years after registration.
Patients who do not have a CR or CRi by day 84 can receive reinduction with up to two total cycles of blinatumomab, with those who get a remission moving on to the blinatumomab/ dasatinib combination and those who do not going off protocol.
Of the 25 patients, 23 had a CR following dasatinib/prednisone induction. As noted, 5 of 16 patients evaluable for MRD were MRD negative.
Four patients did not receive postremission therapy, two because of adverse events, one who went on to transplant, and one because of insurance issues.
In a safety review early in the study, 4 of 12 evaluable patients were found to have dose-limiting toxicities, including one case each of grade 3 dyspnea and gastrointestinal pain (in a single patient), hypertension, dyspnea, and hyperglycemia.
These adverse events were deemed acceptable by both U.S. Food and Drug Administration and National Cancer Institute reviewers, and this arm of the study was allowed to continue, Dr. Advani noted.
The study was funded by grants from the National Institutes of Health. Dr. Advani disclosed financial relationships with several companies. Dr. Emanuel and Dr. Hock have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ATLANTA – Older patients with acute lymphoblastic leukemia positive for the Philadelphia chromosome (Ph+ALL) are often not fit enough to withstand intensive chemotherapy and stem cell transplants, but remissions with alternative therapies are usually short lived.
Now, results from an ongoing study suggest that the combination of the
The new results were reported by investigators in the SWOG Cancer Research Network and come from a cohort of 25 patients with a median age of 73 years with newly diagnosed Ph+ALL or ALL with dasatinib-sensitive fusions of mutations (Ph-like ALL).
Nearly all (23 of 25 patients, 92%) had complete remissions, and 5 of 16 patients for whom minimal residual disease (MRD) data were available were MRD negative at day 28, said Anjali Advani, MD, from the Cleveland Clinic.
At a median follow-up of 1.7 years, the estimated 3-year disease-free survival rate was 80%, and the estimated overall survival rate was 85%, the investigators reported in a poster presentation at the annual meeting of the American Society of Hematology.
“I think the biggest question will be longer-term follow-up. We clearly see high remission rates in this population, but the issue is whether in these elderly patients who are not candidates for chemo we can prolong remission by the addition of other treatments, such as blinatumomab,” she said in an interview with this news organization.
“The follow-up is reasonable at this point, and as we get longer follow-up, if the current 3-year survival estimates hold up, that would be very encouraging,” she said.
Early promise
A leukemia specialist who was not involved in the study told this news organization that the results are promising, but added that it’s too early to make definitive judgments about the efficacy of the combination.
“People have used just a tyrosine kinase inhibitor and prednisone in these patients and gotten remissions, but they just don’t last,” said Peter Emanuel, MD, from CHI St. Vincent Infirmary in Little Rock, Ark.
“The promise with this approach is that you’re getting a longer-lasting remission – maybe not a cure, but a longer-lasting remission – without having to use intensive chemotherapy,” he said.
“It’s still a pretty small study, so I think this is going to require a bigger trial, looking at more patients, but it’s certainly very encouraging and very promising,” he added.
Hanno Hock, MD, PhD, a leukemia researcher at the Mass General Cancer Center in Boston, said in an interview that “the whole idea here is to add this newer agent, blinatumomab, to make those good initial responses more durable, and it looks like it is able to do that with very impressive initial data,” he said.
“The caveat is that this is still early, and one needs to wait and see how it all pans out, but it’s very well tolerated, and definitely the next logical step in trying to offer something to people who cannot tolerate more aggressive therapy such as transplant,” Dr. Hock added.
Study results
The new results come from a feasibility cohort of patients enrolled in the SWOG S1318 trial, which studied blinatumomab plus chemotherapy and prednisone in older patients with Ph-ALL, as well as blinatumomab, dasatinib, and prednisone in older adults with Ph+ ALL.
Patients 65 and older with newly diagnosed or relapsed/refractory Ph+ALL or Ph-like ALL and no central nervous system disease were eligible for the arm of the trial described here. All patients with data reported in this analysis had newly diagnosed ALL.
Patients first received a single induction cycle of dasatinib and prednisone and were then evaluated for response. Patients with a complete remission (CR) or CR with incomplete recovery of blood counts (CRi) would then undergo prednisone tapering while continuing dasatinib until day 84. Patients without a CR or CRi at day 28 who had remissions by day 56 then also continued dasatinib until day 84.
Those patients still in remission at day 84 went on to three cycles of blinatumomab and dasatinib, followed by dasatinib and prednisone maintenance until unacceptable toxicity or disease progression. Patients may remain on maintenance for up to 10 years after registration.
Patients who do not have a CR or CRi by day 84 can receive reinduction with up to two total cycles of blinatumomab, with those who get a remission moving on to the blinatumomab/ dasatinib combination and those who do not going off protocol.
Of the 25 patients, 23 had a CR following dasatinib/prednisone induction. As noted, 5 of 16 patients evaluable for MRD were MRD negative.
Four patients did not receive postremission therapy, two because of adverse events, one who went on to transplant, and one because of insurance issues.
In a safety review early in the study, 4 of 12 evaluable patients were found to have dose-limiting toxicities, including one case each of grade 3 dyspnea and gastrointestinal pain (in a single patient), hypertension, dyspnea, and hyperglycemia.
These adverse events were deemed acceptable by both U.S. Food and Drug Administration and National Cancer Institute reviewers, and this arm of the study was allowed to continue, Dr. Advani noted.
The study was funded by grants from the National Institutes of Health. Dr. Advani disclosed financial relationships with several companies. Dr. Emanuel and Dr. Hock have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ATLANTA – Older patients with acute lymphoblastic leukemia positive for the Philadelphia chromosome (Ph+ALL) are often not fit enough to withstand intensive chemotherapy and stem cell transplants, but remissions with alternative therapies are usually short lived.
Now, results from an ongoing study suggest that the combination of the
The new results were reported by investigators in the SWOG Cancer Research Network and come from a cohort of 25 patients with a median age of 73 years with newly diagnosed Ph+ALL or ALL with dasatinib-sensitive fusions of mutations (Ph-like ALL).
Nearly all (23 of 25 patients, 92%) had complete remissions, and 5 of 16 patients for whom minimal residual disease (MRD) data were available were MRD negative at day 28, said Anjali Advani, MD, from the Cleveland Clinic.
At a median follow-up of 1.7 years, the estimated 3-year disease-free survival rate was 80%, and the estimated overall survival rate was 85%, the investigators reported in a poster presentation at the annual meeting of the American Society of Hematology.
“I think the biggest question will be longer-term follow-up. We clearly see high remission rates in this population, but the issue is whether in these elderly patients who are not candidates for chemo we can prolong remission by the addition of other treatments, such as blinatumomab,” she said in an interview with this news organization.
“The follow-up is reasonable at this point, and as we get longer follow-up, if the current 3-year survival estimates hold up, that would be very encouraging,” she said.
Early promise
A leukemia specialist who was not involved in the study told this news organization that the results are promising, but added that it’s too early to make definitive judgments about the efficacy of the combination.
“People have used just a tyrosine kinase inhibitor and prednisone in these patients and gotten remissions, but they just don’t last,” said Peter Emanuel, MD, from CHI St. Vincent Infirmary in Little Rock, Ark.
“The promise with this approach is that you’re getting a longer-lasting remission – maybe not a cure, but a longer-lasting remission – without having to use intensive chemotherapy,” he said.
“It’s still a pretty small study, so I think this is going to require a bigger trial, looking at more patients, but it’s certainly very encouraging and very promising,” he added.
Hanno Hock, MD, PhD, a leukemia researcher at the Mass General Cancer Center in Boston, said in an interview that “the whole idea here is to add this newer agent, blinatumomab, to make those good initial responses more durable, and it looks like it is able to do that with very impressive initial data,” he said.
“The caveat is that this is still early, and one needs to wait and see how it all pans out, but it’s very well tolerated, and definitely the next logical step in trying to offer something to people who cannot tolerate more aggressive therapy such as transplant,” Dr. Hock added.
Study results
The new results come from a feasibility cohort of patients enrolled in the SWOG S1318 trial, which studied blinatumomab plus chemotherapy and prednisone in older patients with Ph-ALL, as well as blinatumomab, dasatinib, and prednisone in older adults with Ph+ ALL.
Patients 65 and older with newly diagnosed or relapsed/refractory Ph+ALL or Ph-like ALL and no central nervous system disease were eligible for the arm of the trial described here. All patients with data reported in this analysis had newly diagnosed ALL.
Patients first received a single induction cycle of dasatinib and prednisone and were then evaluated for response. Patients with a complete remission (CR) or CR with incomplete recovery of blood counts (CRi) would then undergo prednisone tapering while continuing dasatinib until day 84. Patients without a CR or CRi at day 28 who had remissions by day 56 then also continued dasatinib until day 84.
Those patients still in remission at day 84 went on to three cycles of blinatumomab and dasatinib, followed by dasatinib and prednisone maintenance until unacceptable toxicity or disease progression. Patients may remain on maintenance for up to 10 years after registration.
Patients who do not have a CR or CRi by day 84 can receive reinduction with up to two total cycles of blinatumomab, with those who get a remission moving on to the blinatumomab/ dasatinib combination and those who do not going off protocol.
Of the 25 patients, 23 had a CR following dasatinib/prednisone induction. As noted, 5 of 16 patients evaluable for MRD were MRD negative.
Four patients did not receive postremission therapy, two because of adverse events, one who went on to transplant, and one because of insurance issues.
In a safety review early in the study, 4 of 12 evaluable patients were found to have dose-limiting toxicities, including one case each of grade 3 dyspnea and gastrointestinal pain (in a single patient), hypertension, dyspnea, and hyperglycemia.
These adverse events were deemed acceptable by both U.S. Food and Drug Administration and National Cancer Institute reviewers, and this arm of the study was allowed to continue, Dr. Advani noted.
The study was funded by grants from the National Institutes of Health. Dr. Advani disclosed financial relationships with several companies. Dr. Emanuel and Dr. Hock have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ASH 2021