User login
Everything We Say and Do: Hospitalists are leaders in designing inpatient experience
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively affect patients’ experience of care. This column highlights key takeaways from the SHM track of the upcoming 2017 Cleveland Clinic Patient Experience Empathy and Innovation Summit, May 22-24. Three hospitalist leaders describe their approach to leading the design of the inpatient experience.
What we say and do, and why
Like many forms of care improvement, we have found that health care providers and patients alike engage most proactively when they are directly involved in codesigning an approach or intervention for improving the experience of care. Here are some examples of how hospitalists can be effective leaders in cocreating the inpatient experience with patients and interdisciplinary colleagues.
Dr. Sliwka is medical director of patient and provider experience at University of California, San Francisco, Health; Dr. Kneeland is medical director for patient and provider experience at University of Colorado, Aurora, Hospital; Dr. Hoffman is medical director for patient relations at University of Wisconsin-Madison, Health.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively affect patients’ experience of care. This column highlights key takeaways from the SHM track of the upcoming 2017 Cleveland Clinic Patient Experience Empathy and Innovation Summit, May 22-24. Three hospitalist leaders describe their approach to leading the design of the inpatient experience.
What we say and do, and why
Like many forms of care improvement, we have found that health care providers and patients alike engage most proactively when they are directly involved in codesigning an approach or intervention for improving the experience of care. Here are some examples of how hospitalists can be effective leaders in cocreating the inpatient experience with patients and interdisciplinary colleagues.
Dr. Sliwka is medical director of patient and provider experience at University of California, San Francisco, Health; Dr. Kneeland is medical director for patient and provider experience at University of Colorado, Aurora, Hospital; Dr. Hoffman is medical director for patient relations at University of Wisconsin-Madison, Health.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively affect patients’ experience of care. This column highlights key takeaways from the SHM track of the upcoming 2017 Cleveland Clinic Patient Experience Empathy and Innovation Summit, May 22-24. Three hospitalist leaders describe their approach to leading the design of the inpatient experience.
What we say and do, and why
Like many forms of care improvement, we have found that health care providers and patients alike engage most proactively when they are directly involved in codesigning an approach or intervention for improving the experience of care. Here are some examples of how hospitalists can be effective leaders in cocreating the inpatient experience with patients and interdisciplinary colleagues.
Dr. Sliwka is medical director of patient and provider experience at University of California, San Francisco, Health; Dr. Kneeland is medical director for patient and provider experience at University of Colorado, Aurora, Hospital; Dr. Hoffman is medical director for patient relations at University of Wisconsin-Madison, Health.
SHM receives Eisenberg Award as part of I-PASS Study Group
The Society of Hospital Medicine is part of a patient safety research group that received the prestigious 2016 John M. Eisenberg Award for Innovation in Patient Safety and Quality presented annually by The Joint Commission and the National Quality Forum, two leading organizations that set standards in patient care as part of the I-PASS Study Group.
I-PASS comprises a suite of educational materials and interventions dedicated to improving patient safety by reducing miscommunication during patient handoffs that can lead to harmful medical errors. The team in SHM’s Center for Quality Improvement has been instrumental in supporting the I-PASS Study Group, which represents more than 50 hospitals from across North America.
“The Eisenberg Award for Innovation represents the highest patient safety and quality award in the country, and we are honored to be recognized for our role in this important program,” said Jenna Goldstein, director of SHM’s Center for Quality Improvement. “Our team’s participation in developing and sustaining the SHM I-PASS mentored implementation demonstrates our commitment to ensure safe and high-quality care for hospitalized patients.”
SHM previously won the 2011 Eisenberg Award at the national level for its mentored implementation program model. Through its mentored implementation framework and project management, SHM has supported the I-PASS program across the country at 32 hospitals of varying types, including pediatric and adult hospitals, academic medical centers, and community-based hospitals. SHM has offered both an I-PASS mentored implementation program, in which a physician mentor coaches hospital team members on evidence-based best practices in process improvement and culture change for safe patient handoffs, and an implementation guide, which contains strategies and tools needed to lead the quality improvement effort in the hospital.
In a large multicenter study published in the New England Journal of Medicine, implementation of I-PASS was associated with a 30% reduction in medical errors that harm patients. An estimated 80% of the most serious medical errors can be linked to communication failures, particularly during patient handoffs.
In addition to its work with I-PASS, SHM’s Center for Quality Improvement plays a prominent role in developing tools that empower clinicians to lead quality improvement efforts in their institutions.
Brett Radler is SHM’s communications specialist.
The Society of Hospital Medicine is part of a patient safety research group that received the prestigious 2016 John M. Eisenberg Award for Innovation in Patient Safety and Quality presented annually by The Joint Commission and the National Quality Forum, two leading organizations that set standards in patient care as part of the I-PASS Study Group.
I-PASS comprises a suite of educational materials and interventions dedicated to improving patient safety by reducing miscommunication during patient handoffs that can lead to harmful medical errors. The team in SHM’s Center for Quality Improvement has been instrumental in supporting the I-PASS Study Group, which represents more than 50 hospitals from across North America.
“The Eisenberg Award for Innovation represents the highest patient safety and quality award in the country, and we are honored to be recognized for our role in this important program,” said Jenna Goldstein, director of SHM’s Center for Quality Improvement. “Our team’s participation in developing and sustaining the SHM I-PASS mentored implementation demonstrates our commitment to ensure safe and high-quality care for hospitalized patients.”
SHM previously won the 2011 Eisenberg Award at the national level for its mentored implementation program model. Through its mentored implementation framework and project management, SHM has supported the I-PASS program across the country at 32 hospitals of varying types, including pediatric and adult hospitals, academic medical centers, and community-based hospitals. SHM has offered both an I-PASS mentored implementation program, in which a physician mentor coaches hospital team members on evidence-based best practices in process improvement and culture change for safe patient handoffs, and an implementation guide, which contains strategies and tools needed to lead the quality improvement effort in the hospital.
In a large multicenter study published in the New England Journal of Medicine, implementation of I-PASS was associated with a 30% reduction in medical errors that harm patients. An estimated 80% of the most serious medical errors can be linked to communication failures, particularly during patient handoffs.
In addition to its work with I-PASS, SHM’s Center for Quality Improvement plays a prominent role in developing tools that empower clinicians to lead quality improvement efforts in their institutions.
Brett Radler is SHM’s communications specialist.
The Society of Hospital Medicine is part of a patient safety research group that received the prestigious 2016 John M. Eisenberg Award for Innovation in Patient Safety and Quality presented annually by The Joint Commission and the National Quality Forum, two leading organizations that set standards in patient care as part of the I-PASS Study Group.
I-PASS comprises a suite of educational materials and interventions dedicated to improving patient safety by reducing miscommunication during patient handoffs that can lead to harmful medical errors. The team in SHM’s Center for Quality Improvement has been instrumental in supporting the I-PASS Study Group, which represents more than 50 hospitals from across North America.
“The Eisenberg Award for Innovation represents the highest patient safety and quality award in the country, and we are honored to be recognized for our role in this important program,” said Jenna Goldstein, director of SHM’s Center for Quality Improvement. “Our team’s participation in developing and sustaining the SHM I-PASS mentored implementation demonstrates our commitment to ensure safe and high-quality care for hospitalized patients.”
SHM previously won the 2011 Eisenberg Award at the national level for its mentored implementation program model. Through its mentored implementation framework and project management, SHM has supported the I-PASS program across the country at 32 hospitals of varying types, including pediatric and adult hospitals, academic medical centers, and community-based hospitals. SHM has offered both an I-PASS mentored implementation program, in which a physician mentor coaches hospital team members on evidence-based best practices in process improvement and culture change for safe patient handoffs, and an implementation guide, which contains strategies and tools needed to lead the quality improvement effort in the hospital.
In a large multicenter study published in the New England Journal of Medicine, implementation of I-PASS was associated with a 30% reduction in medical errors that harm patients. An estimated 80% of the most serious medical errors can be linked to communication failures, particularly during patient handoffs.
In addition to its work with I-PASS, SHM’s Center for Quality Improvement plays a prominent role in developing tools that empower clinicians to lead quality improvement efforts in their institutions.
Brett Radler is SHM’s communications specialist.
Tips from 'the father of modern networking'
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Evolution of a movement
One of the most enduring lessons I have learned during my time in hospital medicine is that hospitalists are always evolving, much like the specialty and healthcare system of which they are a part. And during my time as president of the Society of Hospital Medicine (SHM), I have come to realize how SHM provides its members with the resources to help us continue that evolution through our career journeys as a part of the hospital medicine movement.
Over a year ago, I ascended to president of SHM’s board of directors at HM16, the annual meeting in San Diego. Now, I am eagerly looking forward to HM17 next month, in Las Vegas, which we expect to be, yet again, the biggest, best, most innovative and most energetic gathering of hospitalists. As that meeting will mark the end of my tenure as president of the board, I’m also inclined to look back and survey what has happened over the last year, both personally and professionally.
The personal perspective is easy. I have a different position within my organization: president of Cleveland Clinic Akron General and the Southern Region, one which I would and could never have anticipated a year ago. It challenges, exhausts, exhilarates, and teaches me every day. I am also celebrating my 15th wedding anniversary and have three amazing children who seem to evolve in front of my eyes every day.
And, professionally, at HM16 (and on these pages a year ago), I framed what I felt were four critical directions for SHM and have a few thoughts on the work we have done over the last year.
1. Expand and engage SHM’s membership. SHM continues to be the envy of professional organizations, growing each year. More important than sole growth is our pursuit of connecting hospitalists to SHM’s resources and to each other; we have been incredibly active this past year. For instance, SHM is embarking on an engagement survey of HM groups, and is investing in new technologies to support membership. We are now a CME-accrediting organization and are moving the SHM Learning Portal to a new, enhanced platform. We launched a long-term communications strategy that is tied to engagement and a more nimble and mobile experience for our members. The SHM Leadership Academy sold out. HM17 is poised to be another success. And finally, we are increasingly appreciating that a strong SHM must have a vibrant chapter structure to ensure connections between our membership, staff, and board.
2. Focus on patient- and family-centered care. A look at the HM17 curriculum reinforces SHM’s awareness that patients and hospitalists must be more assertive in developing skills in communication and empathy. By doing so, they support a culture and environment wherein patients are active participants their care. Members of our Patient Experience Committee are presenting courses and workshops in Las Vegas, and last year’s annual meeting featured an entire pre-course on communication skills. Hospitalists play a signature role in the Cleveland Clinic’s national conference on improving the patient experience, and the committee has an advisory council of patients and advocates to guide their work.
3. Move assertively to define our role in an era of risk and reform. Last year’s national election will probably create policy upheavals that are difficult to either anticipate or plan for. However, the evolution of Medicare, Medicaid, and commercial payers toward passing risk (and reward) onto physicians, hospitals, and systems, likely is unstoppable. SHM held a board retreat with key hospital leaders (including Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at CMS and director of the Center for Medicare and Medicaid Innovation, and a keynote speaker at HM17) to outline a framework to engage and educate our membership by leveraging the work of our Public Policy, Education, and Practice Management committees.
4. Define our stance regarding specialty recognition: The complexities of this issue are political as well as logistical. SHM has continued to build out the infrastructure for Recognition of Focused Practice with the launch of SPARK ONE (our Focused Practice in Hospital Medicine exam preparation product), but the gaps between the curricula of internal medicine and family medicine residencies, and our daily clinical realities, will continue to exist for the foreseeable future. Pediatrics has established a board requirement for pediatric hospital medicine, but it is still unclear if this is the future of adult hospital medicine.
In sum
As I prepare to the pass to baton to Dr. Ron Greeno for 2017-18, I am reminded of one of the pearls of a former boss and mentor of mine who preached that career satisfaction comes from finding opportunities to achieve three goals: addressing meaningful challenges, working with compelling individuals, and learning something new every day. I would like to thank the board, SHM CEO Larry Wellikson, MD, MHM, and the society staff and volunteers, and, most of all, the many SHM members with whom I have met and spoken over the last year for providing me with exactly that opportunity.
I look forward to continuing to serve an active role in SHM, an organization that can provide you with those same opportunities and resources to help you grow, evolve and be an active participant in the hospital medicine movement.
One of the most enduring lessons I have learned during my time in hospital medicine is that hospitalists are always evolving, much like the specialty and healthcare system of which they are a part. And during my time as president of the Society of Hospital Medicine (SHM), I have come to realize how SHM provides its members with the resources to help us continue that evolution through our career journeys as a part of the hospital medicine movement.
Over a year ago, I ascended to president of SHM’s board of directors at HM16, the annual meeting in San Diego. Now, I am eagerly looking forward to HM17 next month, in Las Vegas, which we expect to be, yet again, the biggest, best, most innovative and most energetic gathering of hospitalists. As that meeting will mark the end of my tenure as president of the board, I’m also inclined to look back and survey what has happened over the last year, both personally and professionally.
The personal perspective is easy. I have a different position within my organization: president of Cleveland Clinic Akron General and the Southern Region, one which I would and could never have anticipated a year ago. It challenges, exhausts, exhilarates, and teaches me every day. I am also celebrating my 15th wedding anniversary and have three amazing children who seem to evolve in front of my eyes every day.
And, professionally, at HM16 (and on these pages a year ago), I framed what I felt were four critical directions for SHM and have a few thoughts on the work we have done over the last year.
1. Expand and engage SHM’s membership. SHM continues to be the envy of professional organizations, growing each year. More important than sole growth is our pursuit of connecting hospitalists to SHM’s resources and to each other; we have been incredibly active this past year. For instance, SHM is embarking on an engagement survey of HM groups, and is investing in new technologies to support membership. We are now a CME-accrediting organization and are moving the SHM Learning Portal to a new, enhanced platform. We launched a long-term communications strategy that is tied to engagement and a more nimble and mobile experience for our members. The SHM Leadership Academy sold out. HM17 is poised to be another success. And finally, we are increasingly appreciating that a strong SHM must have a vibrant chapter structure to ensure connections between our membership, staff, and board.
2. Focus on patient- and family-centered care. A look at the HM17 curriculum reinforces SHM’s awareness that patients and hospitalists must be more assertive in developing skills in communication and empathy. By doing so, they support a culture and environment wherein patients are active participants their care. Members of our Patient Experience Committee are presenting courses and workshops in Las Vegas, and last year’s annual meeting featured an entire pre-course on communication skills. Hospitalists play a signature role in the Cleveland Clinic’s national conference on improving the patient experience, and the committee has an advisory council of patients and advocates to guide their work.
3. Move assertively to define our role in an era of risk and reform. Last year’s national election will probably create policy upheavals that are difficult to either anticipate or plan for. However, the evolution of Medicare, Medicaid, and commercial payers toward passing risk (and reward) onto physicians, hospitals, and systems, likely is unstoppable. SHM held a board retreat with key hospital leaders (including Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at CMS and director of the Center for Medicare and Medicaid Innovation, and a keynote speaker at HM17) to outline a framework to engage and educate our membership by leveraging the work of our Public Policy, Education, and Practice Management committees.
4. Define our stance regarding specialty recognition: The complexities of this issue are political as well as logistical. SHM has continued to build out the infrastructure for Recognition of Focused Practice with the launch of SPARK ONE (our Focused Practice in Hospital Medicine exam preparation product), but the gaps between the curricula of internal medicine and family medicine residencies, and our daily clinical realities, will continue to exist for the foreseeable future. Pediatrics has established a board requirement for pediatric hospital medicine, but it is still unclear if this is the future of adult hospital medicine.
In sum
As I prepare to the pass to baton to Dr. Ron Greeno for 2017-18, I am reminded of one of the pearls of a former boss and mentor of mine who preached that career satisfaction comes from finding opportunities to achieve three goals: addressing meaningful challenges, working with compelling individuals, and learning something new every day. I would like to thank the board, SHM CEO Larry Wellikson, MD, MHM, and the society staff and volunteers, and, most of all, the many SHM members with whom I have met and spoken over the last year for providing me with exactly that opportunity.
I look forward to continuing to serve an active role in SHM, an organization that can provide you with those same opportunities and resources to help you grow, evolve and be an active participant in the hospital medicine movement.
One of the most enduring lessons I have learned during my time in hospital medicine is that hospitalists are always evolving, much like the specialty and healthcare system of which they are a part. And during my time as president of the Society of Hospital Medicine (SHM), I have come to realize how SHM provides its members with the resources to help us continue that evolution through our career journeys as a part of the hospital medicine movement.
Over a year ago, I ascended to president of SHM’s board of directors at HM16, the annual meeting in San Diego. Now, I am eagerly looking forward to HM17 next month, in Las Vegas, which we expect to be, yet again, the biggest, best, most innovative and most energetic gathering of hospitalists. As that meeting will mark the end of my tenure as president of the board, I’m also inclined to look back and survey what has happened over the last year, both personally and professionally.
The personal perspective is easy. I have a different position within my organization: president of Cleveland Clinic Akron General and the Southern Region, one which I would and could never have anticipated a year ago. It challenges, exhausts, exhilarates, and teaches me every day. I am also celebrating my 15th wedding anniversary and have three amazing children who seem to evolve in front of my eyes every day.
And, professionally, at HM16 (and on these pages a year ago), I framed what I felt were four critical directions for SHM and have a few thoughts on the work we have done over the last year.
1. Expand and engage SHM’s membership. SHM continues to be the envy of professional organizations, growing each year. More important than sole growth is our pursuit of connecting hospitalists to SHM’s resources and to each other; we have been incredibly active this past year. For instance, SHM is embarking on an engagement survey of HM groups, and is investing in new technologies to support membership. We are now a CME-accrediting organization and are moving the SHM Learning Portal to a new, enhanced platform. We launched a long-term communications strategy that is tied to engagement and a more nimble and mobile experience for our members. The SHM Leadership Academy sold out. HM17 is poised to be another success. And finally, we are increasingly appreciating that a strong SHM must have a vibrant chapter structure to ensure connections between our membership, staff, and board.
2. Focus on patient- and family-centered care. A look at the HM17 curriculum reinforces SHM’s awareness that patients and hospitalists must be more assertive in developing skills in communication and empathy. By doing so, they support a culture and environment wherein patients are active participants their care. Members of our Patient Experience Committee are presenting courses and workshops in Las Vegas, and last year’s annual meeting featured an entire pre-course on communication skills. Hospitalists play a signature role in the Cleveland Clinic’s national conference on improving the patient experience, and the committee has an advisory council of patients and advocates to guide their work.
3. Move assertively to define our role in an era of risk and reform. Last year’s national election will probably create policy upheavals that are difficult to either anticipate or plan for. However, the evolution of Medicare, Medicaid, and commercial payers toward passing risk (and reward) onto physicians, hospitals, and systems, likely is unstoppable. SHM held a board retreat with key hospital leaders (including Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at CMS and director of the Center for Medicare and Medicaid Innovation, and a keynote speaker at HM17) to outline a framework to engage and educate our membership by leveraging the work of our Public Policy, Education, and Practice Management committees.
4. Define our stance regarding specialty recognition: The complexities of this issue are political as well as logistical. SHM has continued to build out the infrastructure for Recognition of Focused Practice with the launch of SPARK ONE (our Focused Practice in Hospital Medicine exam preparation product), but the gaps between the curricula of internal medicine and family medicine residencies, and our daily clinical realities, will continue to exist for the foreseeable future. Pediatrics has established a board requirement for pediatric hospital medicine, but it is still unclear if this is the future of adult hospital medicine.
In sum
As I prepare to the pass to baton to Dr. Ron Greeno for 2017-18, I am reminded of one of the pearls of a former boss and mentor of mine who preached that career satisfaction comes from finding opportunities to achieve three goals: addressing meaningful challenges, working with compelling individuals, and learning something new every day. I would like to thank the board, SHM CEO Larry Wellikson, MD, MHM, and the society staff and volunteers, and, most of all, the many SHM members with whom I have met and spoken over the last year for providing me with exactly that opportunity.
I look forward to continuing to serve an active role in SHM, an organization that can provide you with those same opportunities and resources to help you grow, evolve and be an active participant in the hospital medicine movement.
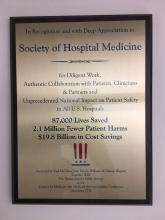
CMS recognizes Society of Hospital Medicine’s Center for Quality Improvement
PHILADELPHIA – The Society of Hospital Medicine (SHM)’s Center for Quality Improvement (QI) has been distinguished by the Centers for Medicare & Medicaid Services for maintaining an ongoing collaborative partnership with CMS to enhance patient safety.
The letter of recognition from Paul McGann, MD, Jean Moody-Williams, RN, MPP, and Dennis Wagner, MPA, of the CMS, to Jenna Goldstein, MA, director of SHM’s Center for QI, and Kevin Vuernick, MPA, senior project manager, noted: “Over the last several years, our team has been privileged to partner with you and the Society of Hospital Medicine on the work of quality improvement and patient safety. Without relationships like these, the results in the reduction of patient harm we have seen at a national scale, saving 87,000 lives and nearly $20 billion in cost savings, would never have been possible.”
In August 2016, CMS’ Hospital Improvement Innovation Networks contacted SHM to participate in their weekly Partnership for Patients (PfP) Pacing Event webinar to present strategies for reducing opioid use and preventing adverse drug events, including SHM’s Mentored Implementation pilot program on Reducing Adverse Drug Events Related to Opioids (RADEO). SHM’s contribution to this webinar was twofold: Thomas W. Frederickson, MD, the lead author of the RADEO guide and one of two program mentors, spoke about the development of the RADEO program and its importance in the acute care setting. Matthew Jared, MD, a hospitalist at St. Anthony Hospital in Oklahoma City, one of the five pilot RADEO sites, discussed his experience implementing specific RADEO interventions as well as the mentoring provided by Dr. Frederickson of the department of hospital medicine at CHI Health in Omaha, Neb.
As a result of this successful partnership, SHM was contacted in January to provide its perspective on best practices in managing inpatients receiving opioids and adverse drug event data collection. At that time, Mr. Vuernick discussed the lessons learned between RADEO’s pilot program and the second iteration of RADEO, which launched in November 2016.
For more information about SHM’s Center for QI, please visit www.hospitalmedicine.org/QI. For more information about SHM and hospital medicine, visit www.hospitalmedicine.org and follow SHM on Twitter at @SHMLive.
PHILADELPHIA – The Society of Hospital Medicine (SHM)’s Center for Quality Improvement (QI) has been distinguished by the Centers for Medicare & Medicaid Services for maintaining an ongoing collaborative partnership with CMS to enhance patient safety.
The letter of recognition from Paul McGann, MD, Jean Moody-Williams, RN, MPP, and Dennis Wagner, MPA, of the CMS, to Jenna Goldstein, MA, director of SHM’s Center for QI, and Kevin Vuernick, MPA, senior project manager, noted: “Over the last several years, our team has been privileged to partner with you and the Society of Hospital Medicine on the work of quality improvement and patient safety. Without relationships like these, the results in the reduction of patient harm we have seen at a national scale, saving 87,000 lives and nearly $20 billion in cost savings, would never have been possible.”
In August 2016, CMS’ Hospital Improvement Innovation Networks contacted SHM to participate in their weekly Partnership for Patients (PfP) Pacing Event webinar to present strategies for reducing opioid use and preventing adverse drug events, including SHM’s Mentored Implementation pilot program on Reducing Adverse Drug Events Related to Opioids (RADEO). SHM’s contribution to this webinar was twofold: Thomas W. Frederickson, MD, the lead author of the RADEO guide and one of two program mentors, spoke about the development of the RADEO program and its importance in the acute care setting. Matthew Jared, MD, a hospitalist at St. Anthony Hospital in Oklahoma City, one of the five pilot RADEO sites, discussed his experience implementing specific RADEO interventions as well as the mentoring provided by Dr. Frederickson of the department of hospital medicine at CHI Health in Omaha, Neb.
As a result of this successful partnership, SHM was contacted in January to provide its perspective on best practices in managing inpatients receiving opioids and adverse drug event data collection. At that time, Mr. Vuernick discussed the lessons learned between RADEO’s pilot program and the second iteration of RADEO, which launched in November 2016.
For more information about SHM’s Center for QI, please visit www.hospitalmedicine.org/QI. For more information about SHM and hospital medicine, visit www.hospitalmedicine.org and follow SHM on Twitter at @SHMLive.
PHILADELPHIA – The Society of Hospital Medicine (SHM)’s Center for Quality Improvement (QI) has been distinguished by the Centers for Medicare & Medicaid Services for maintaining an ongoing collaborative partnership with CMS to enhance patient safety.
The letter of recognition from Paul McGann, MD, Jean Moody-Williams, RN, MPP, and Dennis Wagner, MPA, of the CMS, to Jenna Goldstein, MA, director of SHM’s Center for QI, and Kevin Vuernick, MPA, senior project manager, noted: “Over the last several years, our team has been privileged to partner with you and the Society of Hospital Medicine on the work of quality improvement and patient safety. Without relationships like these, the results in the reduction of patient harm we have seen at a national scale, saving 87,000 lives and nearly $20 billion in cost savings, would never have been possible.”
In August 2016, CMS’ Hospital Improvement Innovation Networks contacted SHM to participate in their weekly Partnership for Patients (PfP) Pacing Event webinar to present strategies for reducing opioid use and preventing adverse drug events, including SHM’s Mentored Implementation pilot program on Reducing Adverse Drug Events Related to Opioids (RADEO). SHM’s contribution to this webinar was twofold: Thomas W. Frederickson, MD, the lead author of the RADEO guide and one of two program mentors, spoke about the development of the RADEO program and its importance in the acute care setting. Matthew Jared, MD, a hospitalist at St. Anthony Hospital in Oklahoma City, one of the five pilot RADEO sites, discussed his experience implementing specific RADEO interventions as well as the mentoring provided by Dr. Frederickson of the department of hospital medicine at CHI Health in Omaha, Neb.
As a result of this successful partnership, SHM was contacted in January to provide its perspective on best practices in managing inpatients receiving opioids and adverse drug event data collection. At that time, Mr. Vuernick discussed the lessons learned between RADEO’s pilot program and the second iteration of RADEO, which launched in November 2016.
For more information about SHM’s Center for QI, please visit www.hospitalmedicine.org/QI. For more information about SHM and hospital medicine, visit www.hospitalmedicine.org and follow SHM on Twitter at @SHMLive.
Here’s what’s trending at SHM
Hospitalist specialty code becomes official designation
On April 3, 2017, “hospitalist” becomes an official specialty designation under Medicare – the code itself is C6. Starting on that date, hospitalists can change their specialty designation on the Medicare enrollment application. Specialty codes are self-designated and describe the kind of medicine that health care providers practice. Appropriate use of specialty codes helps distinguish differences among providers and improves the quality of utilization data. SHM applied for a specialty code for hospitalists nearly 3 years ago, and the Centers for Medicare & Medicaid Services approved the application in February 2016.
Stand with your fellow hospitalists and make sure to declare “I’m a C6.”
Assess your knowledge in hospital medicine with SPARK ONE
SHM recently launched SPARK ONE, a comprehensive online self-assessment tool created specifically for hospital medicine professionals. The activity contains 450-plus vignette-style multiple-choice questions covering 100% of the American Board of Internal Medicine’s Focused Practice in Hospital Medicine (FPHM) exam blueprint. This online tool is your complete resource for successfully preparing for the FPHM exam, or assessing your general knowledge in hospital medicine.
White paper now available: Hospitalist Attitudes Toward Electronic Medical Records
SHM’s Health Information Technology Committee diligently analyzed survey results that captured hospitalists’ attitudes towards electronic medical records, resulting in a white paper now available. The purpose of this paper is to effect change on EHR systems by informing conversations with decision makers and to provide hospital medicine a definitive voice in the landscape of the tumultuous world of electronic medical record systems.
SHM believes hospitalists are especially qualified to evaluate these systems, and the survey results paint a grim picture of the effectiveness and usability of the systems that hospitalists spend the majority of their time interacting with. These results should serve as a call to action to accelerate the pace of advancement and innovation in health care technology.
By sharing these results, SHM hopes to raise awareness of the unacceptable performance of existing systems that contributes to slower-than-desired improvement in quality and safety as well as increasing provider frustration. SHM strongly believes that health care needs a renewed focus on initial goals of technology adoption. View the white paper at hospitalmedicine.org/EHR.
Join the Early-Career Academic Hospitalist Speed Mentoring Session at Hospital Medicine 2017
The SHM “speed mentoring” session, held on Tuesday, May 2 from noon to 1:00 p.m. at Hospital Medicine 2017, is designed to assist early-career hospitalists in specific areas of career development by providing a fresh perspective and rapid advice.
Early-career hospitalists will be matched with three senior advisors by area of interest. The “mentee” will spend 10-15 minutes with each advisor and will then rotate to the next advisor. After the session, there will be time for additional informal discussion and networking among advisors and peers.
Pre-registration by March 31, 2017 is required; it will not be possible to register for this activity on-site at HM17. There is no additional fee to register. Registration will be limited to the first 20 participants. Visit hospitalmedicine2017.org/academic today.
Now available: 4 new antimicrobial stewardship modules
SHM has developed four new antimicrobial stewardship modules to help you demonstrate an understanding of best practices to optimize and improve antimicrobial prescribing within your hospital:
1. Optimizing Antibiotic Use for Hospitalized Patients
2. Best Practices in Treatment of UTIs: “Low-Hanging Fruit”
3. Best Practices in Acute Bacterial Skin Infection
4. Antibiotic Use for Inpatient Respiratory Infections
View these resources at hospitalmedicine.org/abx.
Network with the largest gathering of pediatric hospital medicine professionals
Pediatric Hospital Medicine 2017 (PHM 2017) will be held July 20-23 at the Omni Nashville located in Nashville, Tenn. PHM 2017 offers an all-inclusive arrangement of educational and networking opportunities planned specifically for the pediatric hospital medicine professional. More than 100 concurrent sessions to choose from over the 4 days of the conference allow participants to get the best out of their PHM 2017 experience.
Earn free CME in the enhanced SHM Learning Portal
You asked, and we listened: Introducing the enhanced SHM Learning Portal! The SHM Learning Portal, the online learning home for hospitalists with all eLearning initiatives in one place, just launched a brand-new responsive design in March 2016.
Launching this summer, SHM’s new Learning Portal will offer a better way to access and track online CME, with member discounts to a growing library of content. For more information, visit www.shmlearningportal.org.
Bringing SHM to you with local chapter meetings
Attend a chapter meeting and experience SHM locally. Chapters provide focused educational topics through key speakers and presentations and the opportunity to network with other hospitalists in your area. Find a chapter meeting close to you at hospitalmedicine.org/chapters.
A new look for SHM’s Center for Hospital Innovation & Improvement
Just as hospital medicine is evolving, so is SHM’s group dedicated to developing quality improvement safety tools and programs to meet health care’s changing needs. SHM is proud to unveil a new look for its Center for Hospital Innovation & Improvement this month. Stay tuned for more, and visit hospitalmedicine.org/QI for the latest offerings in a variety of quality improvement topics and clinical areas.
Stand out as a leader with the Fellow in Hospital Medicine designation
Applications for SHM’s Fellow in Hospital Medicine designation open on April 17, 2017. You may be eligible if you have been a member of SHM for at least 3 years and have been involved in key quality improvement programs and leadership roles in hospital medicine. Learn more and apply at hospitalmedicine.org/fellows.
Mr. Radler is Communications Specialist at the Society of Hospital Medicine.
Hospitalist specialty code becomes official designation
On April 3, 2017, “hospitalist” becomes an official specialty designation under Medicare – the code itself is C6. Starting on that date, hospitalists can change their specialty designation on the Medicare enrollment application. Specialty codes are self-designated and describe the kind of medicine that health care providers practice. Appropriate use of specialty codes helps distinguish differences among providers and improves the quality of utilization data. SHM applied for a specialty code for hospitalists nearly 3 years ago, and the Centers for Medicare & Medicaid Services approved the application in February 2016.
Stand with your fellow hospitalists and make sure to declare “I’m a C6.”
Assess your knowledge in hospital medicine with SPARK ONE
SHM recently launched SPARK ONE, a comprehensive online self-assessment tool created specifically for hospital medicine professionals. The activity contains 450-plus vignette-style multiple-choice questions covering 100% of the American Board of Internal Medicine’s Focused Practice in Hospital Medicine (FPHM) exam blueprint. This online tool is your complete resource for successfully preparing for the FPHM exam, or assessing your general knowledge in hospital medicine.
White paper now available: Hospitalist Attitudes Toward Electronic Medical Records
SHM’s Health Information Technology Committee diligently analyzed survey results that captured hospitalists’ attitudes towards electronic medical records, resulting in a white paper now available. The purpose of this paper is to effect change on EHR systems by informing conversations with decision makers and to provide hospital medicine a definitive voice in the landscape of the tumultuous world of electronic medical record systems.
SHM believes hospitalists are especially qualified to evaluate these systems, and the survey results paint a grim picture of the effectiveness and usability of the systems that hospitalists spend the majority of their time interacting with. These results should serve as a call to action to accelerate the pace of advancement and innovation in health care technology.
By sharing these results, SHM hopes to raise awareness of the unacceptable performance of existing systems that contributes to slower-than-desired improvement in quality and safety as well as increasing provider frustration. SHM strongly believes that health care needs a renewed focus on initial goals of technology adoption. View the white paper at hospitalmedicine.org/EHR.
Join the Early-Career Academic Hospitalist Speed Mentoring Session at Hospital Medicine 2017
The SHM “speed mentoring” session, held on Tuesday, May 2 from noon to 1:00 p.m. at Hospital Medicine 2017, is designed to assist early-career hospitalists in specific areas of career development by providing a fresh perspective and rapid advice.
Early-career hospitalists will be matched with three senior advisors by area of interest. The “mentee” will spend 10-15 minutes with each advisor and will then rotate to the next advisor. After the session, there will be time for additional informal discussion and networking among advisors and peers.
Pre-registration by March 31, 2017 is required; it will not be possible to register for this activity on-site at HM17. There is no additional fee to register. Registration will be limited to the first 20 participants. Visit hospitalmedicine2017.org/academic today.
Now available: 4 new antimicrobial stewardship modules
SHM has developed four new antimicrobial stewardship modules to help you demonstrate an understanding of best practices to optimize and improve antimicrobial prescribing within your hospital:
1. Optimizing Antibiotic Use for Hospitalized Patients
2. Best Practices in Treatment of UTIs: “Low-Hanging Fruit”
3. Best Practices in Acute Bacterial Skin Infection
4. Antibiotic Use for Inpatient Respiratory Infections
View these resources at hospitalmedicine.org/abx.
Network with the largest gathering of pediatric hospital medicine professionals
Pediatric Hospital Medicine 2017 (PHM 2017) will be held July 20-23 at the Omni Nashville located in Nashville, Tenn. PHM 2017 offers an all-inclusive arrangement of educational and networking opportunities planned specifically for the pediatric hospital medicine professional. More than 100 concurrent sessions to choose from over the 4 days of the conference allow participants to get the best out of their PHM 2017 experience.
Earn free CME in the enhanced SHM Learning Portal
You asked, and we listened: Introducing the enhanced SHM Learning Portal! The SHM Learning Portal, the online learning home for hospitalists with all eLearning initiatives in one place, just launched a brand-new responsive design in March 2016.
Launching this summer, SHM’s new Learning Portal will offer a better way to access and track online CME, with member discounts to a growing library of content. For more information, visit www.shmlearningportal.org.
Bringing SHM to you with local chapter meetings
Attend a chapter meeting and experience SHM locally. Chapters provide focused educational topics through key speakers and presentations and the opportunity to network with other hospitalists in your area. Find a chapter meeting close to you at hospitalmedicine.org/chapters.
A new look for SHM’s Center for Hospital Innovation & Improvement
Just as hospital medicine is evolving, so is SHM’s group dedicated to developing quality improvement safety tools and programs to meet health care’s changing needs. SHM is proud to unveil a new look for its Center for Hospital Innovation & Improvement this month. Stay tuned for more, and visit hospitalmedicine.org/QI for the latest offerings in a variety of quality improvement topics and clinical areas.
Stand out as a leader with the Fellow in Hospital Medicine designation
Applications for SHM’s Fellow in Hospital Medicine designation open on April 17, 2017. You may be eligible if you have been a member of SHM for at least 3 years and have been involved in key quality improvement programs and leadership roles in hospital medicine. Learn more and apply at hospitalmedicine.org/fellows.
Mr. Radler is Communications Specialist at the Society of Hospital Medicine.
Hospitalist specialty code becomes official designation
On April 3, 2017, “hospitalist” becomes an official specialty designation under Medicare – the code itself is C6. Starting on that date, hospitalists can change their specialty designation on the Medicare enrollment application. Specialty codes are self-designated and describe the kind of medicine that health care providers practice. Appropriate use of specialty codes helps distinguish differences among providers and improves the quality of utilization data. SHM applied for a specialty code for hospitalists nearly 3 years ago, and the Centers for Medicare & Medicaid Services approved the application in February 2016.
Stand with your fellow hospitalists and make sure to declare “I’m a C6.”
Assess your knowledge in hospital medicine with SPARK ONE
SHM recently launched SPARK ONE, a comprehensive online self-assessment tool created specifically for hospital medicine professionals. The activity contains 450-plus vignette-style multiple-choice questions covering 100% of the American Board of Internal Medicine’s Focused Practice in Hospital Medicine (FPHM) exam blueprint. This online tool is your complete resource for successfully preparing for the FPHM exam, or assessing your general knowledge in hospital medicine.
White paper now available: Hospitalist Attitudes Toward Electronic Medical Records
SHM’s Health Information Technology Committee diligently analyzed survey results that captured hospitalists’ attitudes towards electronic medical records, resulting in a white paper now available. The purpose of this paper is to effect change on EHR systems by informing conversations with decision makers and to provide hospital medicine a definitive voice in the landscape of the tumultuous world of electronic medical record systems.
SHM believes hospitalists are especially qualified to evaluate these systems, and the survey results paint a grim picture of the effectiveness and usability of the systems that hospitalists spend the majority of their time interacting with. These results should serve as a call to action to accelerate the pace of advancement and innovation in health care technology.
By sharing these results, SHM hopes to raise awareness of the unacceptable performance of existing systems that contributes to slower-than-desired improvement in quality and safety as well as increasing provider frustration. SHM strongly believes that health care needs a renewed focus on initial goals of technology adoption. View the white paper at hospitalmedicine.org/EHR.
Join the Early-Career Academic Hospitalist Speed Mentoring Session at Hospital Medicine 2017
The SHM “speed mentoring” session, held on Tuesday, May 2 from noon to 1:00 p.m. at Hospital Medicine 2017, is designed to assist early-career hospitalists in specific areas of career development by providing a fresh perspective and rapid advice.
Early-career hospitalists will be matched with three senior advisors by area of interest. The “mentee” will spend 10-15 minutes with each advisor and will then rotate to the next advisor. After the session, there will be time for additional informal discussion and networking among advisors and peers.
Pre-registration by March 31, 2017 is required; it will not be possible to register for this activity on-site at HM17. There is no additional fee to register. Registration will be limited to the first 20 participants. Visit hospitalmedicine2017.org/academic today.
Now available: 4 new antimicrobial stewardship modules
SHM has developed four new antimicrobial stewardship modules to help you demonstrate an understanding of best practices to optimize and improve antimicrobial prescribing within your hospital:
1. Optimizing Antibiotic Use for Hospitalized Patients
2. Best Practices in Treatment of UTIs: “Low-Hanging Fruit”
3. Best Practices in Acute Bacterial Skin Infection
4. Antibiotic Use for Inpatient Respiratory Infections
View these resources at hospitalmedicine.org/abx.
Network with the largest gathering of pediatric hospital medicine professionals
Pediatric Hospital Medicine 2017 (PHM 2017) will be held July 20-23 at the Omni Nashville located in Nashville, Tenn. PHM 2017 offers an all-inclusive arrangement of educational and networking opportunities planned specifically for the pediatric hospital medicine professional. More than 100 concurrent sessions to choose from over the 4 days of the conference allow participants to get the best out of their PHM 2017 experience.
Earn free CME in the enhanced SHM Learning Portal
You asked, and we listened: Introducing the enhanced SHM Learning Portal! The SHM Learning Portal, the online learning home for hospitalists with all eLearning initiatives in one place, just launched a brand-new responsive design in March 2016.
Launching this summer, SHM’s new Learning Portal will offer a better way to access and track online CME, with member discounts to a growing library of content. For more information, visit www.shmlearningportal.org.
Bringing SHM to you with local chapter meetings
Attend a chapter meeting and experience SHM locally. Chapters provide focused educational topics through key speakers and presentations and the opportunity to network with other hospitalists in your area. Find a chapter meeting close to you at hospitalmedicine.org/chapters.
A new look for SHM’s Center for Hospital Innovation & Improvement
Just as hospital medicine is evolving, so is SHM’s group dedicated to developing quality improvement safety tools and programs to meet health care’s changing needs. SHM is proud to unveil a new look for its Center for Hospital Innovation & Improvement this month. Stay tuned for more, and visit hospitalmedicine.org/QI for the latest offerings in a variety of quality improvement topics and clinical areas.
Stand out as a leader with the Fellow in Hospital Medicine designation
Applications for SHM’s Fellow in Hospital Medicine designation open on April 17, 2017. You may be eligible if you have been a member of SHM for at least 3 years and have been involved in key quality improvement programs and leadership roles in hospital medicine. Learn more and apply at hospitalmedicine.org/fellows.
Mr. Radler is Communications Specialist at the Society of Hospital Medicine.
What’s new at HM17
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”
Everything We Say and Do: Discussing advance care planning
Editor’s note: “Everything We Say and Do” is an informational series developed by the Society of Hospital Medicine’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experiences of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I empower all of my patients by giving them the opportunity to consider advance care planning.
Why I do it
Everyone deserves advance care planning, and every health care encounter, including a hospitalization, is an opportunity to better identify and document patients’ wishes for care should they become unable to express them. If we wait for patients to develop serious advanced illness before having advance care planning conversations, we risk depriving them of the care they would want in these situations. Additionally, we place a huge burden on family members who may struggle with excruciatingly difficult decisions in the absence of guidance about their loved one’s wishes.
How I do it
I start by identifying which components of advance care planning each patient needs, using a simple algorithm (see figure). All of my patients are queried about code status, and I give them the opportunity to better understand the value of having a healthcare proxy and advance directives, if they are not already in place.
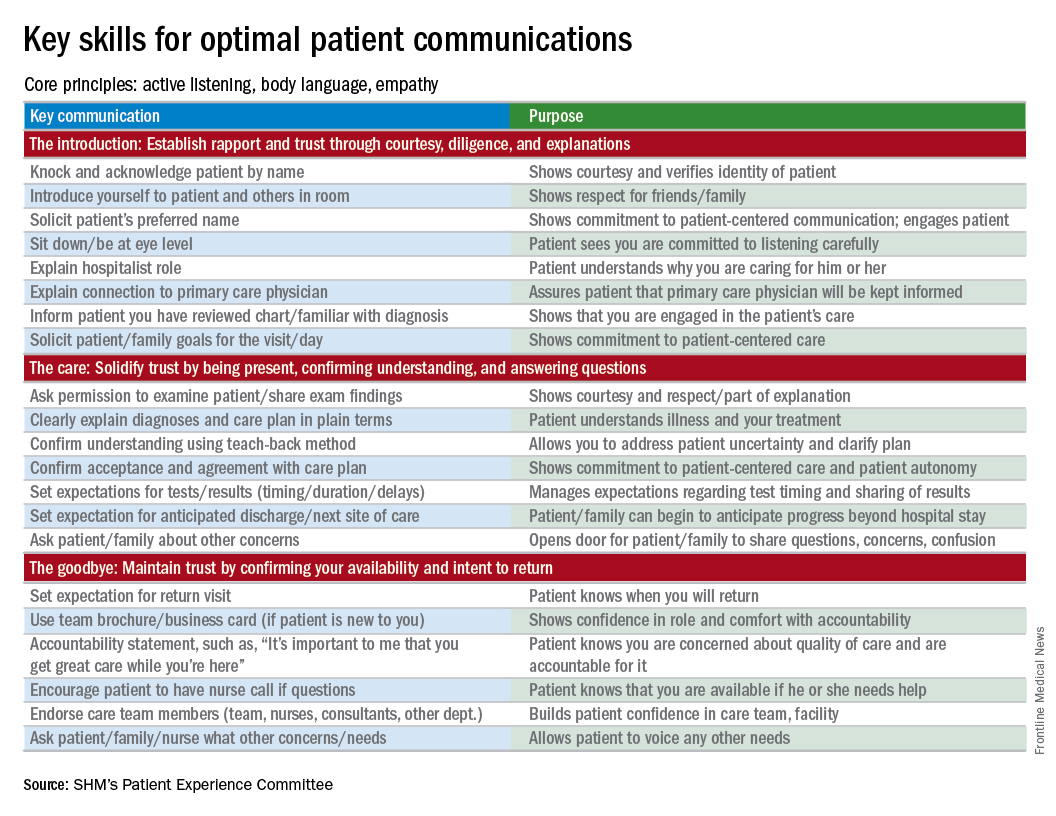
For the remainder of this column, I’m going to focus on patients who have an acute and/or chronic treatable illness – those who require simpler advance-care-planning conversations.
To comfortably initiate the conversation about advance care planning, I always start by asking permission. I commonly say, “There are a couple of important items I discuss with all of my patients to make sure they get the care they want. Would it be okay for us to talk about those now?” This respectfully puts the patient in control. I then initiate a discussion of code status by saying, “It’s important that all of us on your care team know what you would like us to do if you got so sick that we couldn’t communicate with you. I’m not expecting this to happen, but I ask all my patients this question so that we have your instructions.” From there, the conversation evolves depending on whether the patient has any familiarity with this question and its implications.
To introduce the concept of a health care proxy and advance directives, I ask, “Have you ever thought about who you might choose to make medical decisions on your behalf if you became too sick to make those decisions yourself?” Then, finally, I share the following information, usually referring to the blank advance directives document they received in their admission packet: “There is a valuable way to put your wishes about specific care options in writing so others will know your wishes if you’re unable to communicate with them. Would you like to talk about that right now?” Again, this gives the patient control of the situation and an opportunity to decline the conversation if they are not interested or comfortable at that time.
It’s important to document the nature and outcome of these conversations. Keep in mind, advance care planning discussions need not occur at the time of admission. In fact, admission may be the worst time for some patients, further underscoring the importance of documentation so that subsequent providers can see whether advance care planning has been addressed during the hospital stay.
Note: For useful educational resources that address goals-of-care conversations in patients toward the end of life, the Center to Advance Palliative Care (www.capc.org) has a number of educational courses that address these important communication skills.
Dr. Rudolph is vice president of physician development and patient experience for Sound Physicians, Tacoma, Wash. and chair of the SHM Patient Experience Committee .
Reference
1. Moss, A.H., Ganjoo, J, Sharma S, et al. Utility of the “Surprise” Question to Identify Dialysis Patients with High Mortality. Clinical Journal of the American Society of Nephrology: CJASN. 2008;3(5):1379-84. doi:10.2215/CJN.00940208.
Editor’s note: “Everything We Say and Do” is an informational series developed by the Society of Hospital Medicine’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experiences of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I empower all of my patients by giving them the opportunity to consider advance care planning.
Why I do it
Everyone deserves advance care planning, and every health care encounter, including a hospitalization, is an opportunity to better identify and document patients’ wishes for care should they become unable to express them. If we wait for patients to develop serious advanced illness before having advance care planning conversations, we risk depriving them of the care they would want in these situations. Additionally, we place a huge burden on family members who may struggle with excruciatingly difficult decisions in the absence of guidance about their loved one’s wishes.
How I do it
I start by identifying which components of advance care planning each patient needs, using a simple algorithm (see figure). All of my patients are queried about code status, and I give them the opportunity to better understand the value of having a healthcare proxy and advance directives, if they are not already in place.
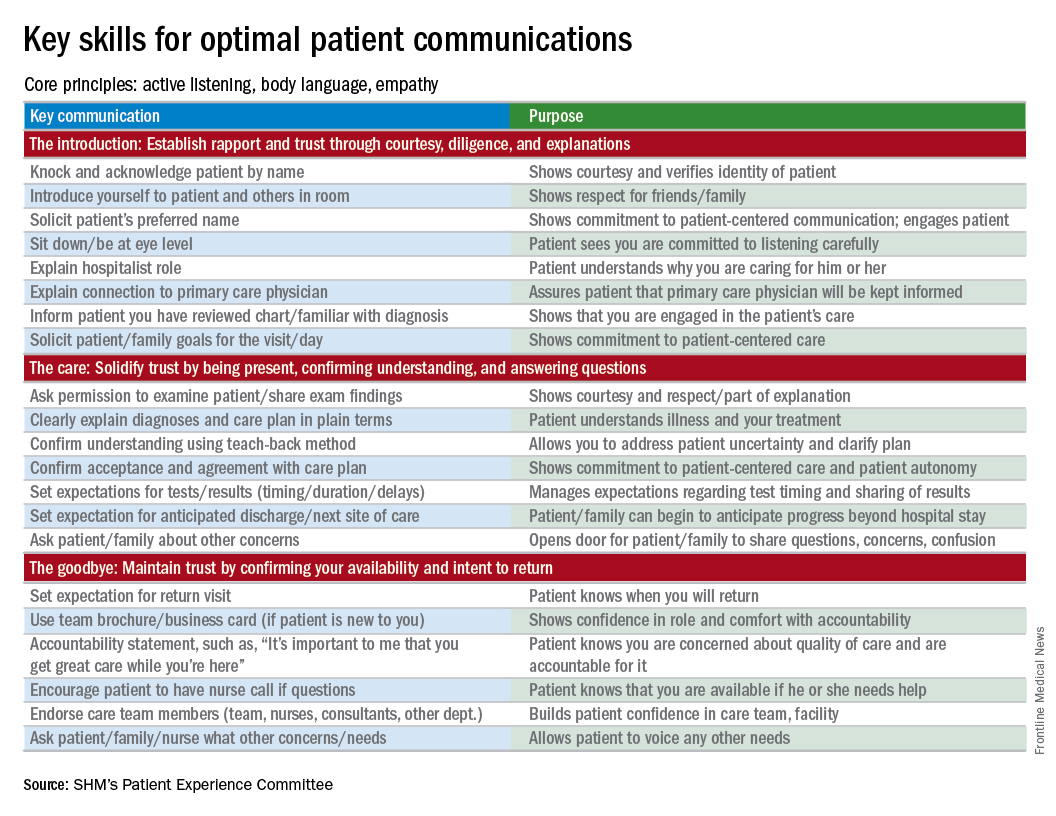
For the remainder of this column, I’m going to focus on patients who have an acute and/or chronic treatable illness – those who require simpler advance-care-planning conversations.
To comfortably initiate the conversation about advance care planning, I always start by asking permission. I commonly say, “There are a couple of important items I discuss with all of my patients to make sure they get the care they want. Would it be okay for us to talk about those now?” This respectfully puts the patient in control. I then initiate a discussion of code status by saying, “It’s important that all of us on your care team know what you would like us to do if you got so sick that we couldn’t communicate with you. I’m not expecting this to happen, but I ask all my patients this question so that we have your instructions.” From there, the conversation evolves depending on whether the patient has any familiarity with this question and its implications.
To introduce the concept of a health care proxy and advance directives, I ask, “Have you ever thought about who you might choose to make medical decisions on your behalf if you became too sick to make those decisions yourself?” Then, finally, I share the following information, usually referring to the blank advance directives document they received in their admission packet: “There is a valuable way to put your wishes about specific care options in writing so others will know your wishes if you’re unable to communicate with them. Would you like to talk about that right now?” Again, this gives the patient control of the situation and an opportunity to decline the conversation if they are not interested or comfortable at that time.
It’s important to document the nature and outcome of these conversations. Keep in mind, advance care planning discussions need not occur at the time of admission. In fact, admission may be the worst time for some patients, further underscoring the importance of documentation so that subsequent providers can see whether advance care planning has been addressed during the hospital stay.
Note: For useful educational resources that address goals-of-care conversations in patients toward the end of life, the Center to Advance Palliative Care (www.capc.org) has a number of educational courses that address these important communication skills.
Dr. Rudolph is vice president of physician development and patient experience for Sound Physicians, Tacoma, Wash. and chair of the SHM Patient Experience Committee .
Reference
1. Moss, A.H., Ganjoo, J, Sharma S, et al. Utility of the “Surprise” Question to Identify Dialysis Patients with High Mortality. Clinical Journal of the American Society of Nephrology: CJASN. 2008;3(5):1379-84. doi:10.2215/CJN.00940208.
Editor’s note: “Everything We Say and Do” is an informational series developed by the Society of Hospital Medicine’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experiences of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I empower all of my patients by giving them the opportunity to consider advance care planning.
Why I do it
Everyone deserves advance care planning, and every health care encounter, including a hospitalization, is an opportunity to better identify and document patients’ wishes for care should they become unable to express them. If we wait for patients to develop serious advanced illness before having advance care planning conversations, we risk depriving them of the care they would want in these situations. Additionally, we place a huge burden on family members who may struggle with excruciatingly difficult decisions in the absence of guidance about their loved one’s wishes.
How I do it
I start by identifying which components of advance care planning each patient needs, using a simple algorithm (see figure). All of my patients are queried about code status, and I give them the opportunity to better understand the value of having a healthcare proxy and advance directives, if they are not already in place.
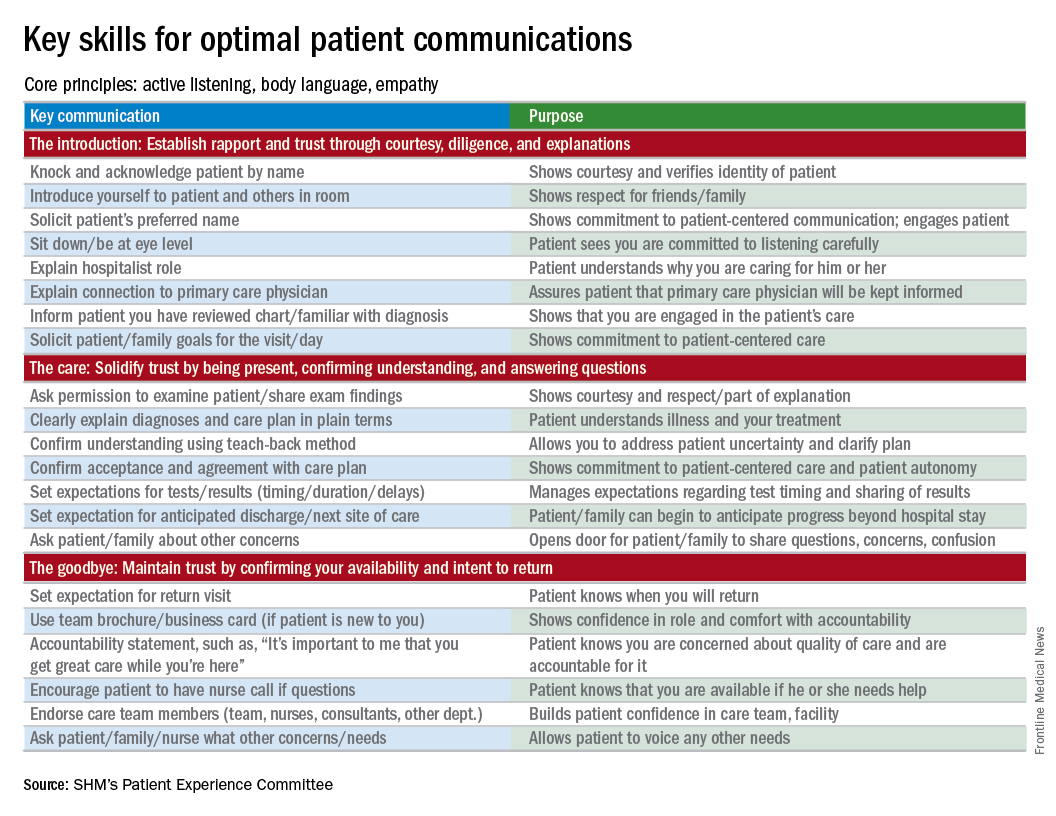
For the remainder of this column, I’m going to focus on patients who have an acute and/or chronic treatable illness – those who require simpler advance-care-planning conversations.
To comfortably initiate the conversation about advance care planning, I always start by asking permission. I commonly say, “There are a couple of important items I discuss with all of my patients to make sure they get the care they want. Would it be okay for us to talk about those now?” This respectfully puts the patient in control. I then initiate a discussion of code status by saying, “It’s important that all of us on your care team know what you would like us to do if you got so sick that we couldn’t communicate with you. I’m not expecting this to happen, but I ask all my patients this question so that we have your instructions.” From there, the conversation evolves depending on whether the patient has any familiarity with this question and its implications.
To introduce the concept of a health care proxy and advance directives, I ask, “Have you ever thought about who you might choose to make medical decisions on your behalf if you became too sick to make those decisions yourself?” Then, finally, I share the following information, usually referring to the blank advance directives document they received in their admission packet: “There is a valuable way to put your wishes about specific care options in writing so others will know your wishes if you’re unable to communicate with them. Would you like to talk about that right now?” Again, this gives the patient control of the situation and an opportunity to decline the conversation if they are not interested or comfortable at that time.
It’s important to document the nature and outcome of these conversations. Keep in mind, advance care planning discussions need not occur at the time of admission. In fact, admission may be the worst time for some patients, further underscoring the importance of documentation so that subsequent providers can see whether advance care planning has been addressed during the hospital stay.
Note: For useful educational resources that address goals-of-care conversations in patients toward the end of life, the Center to Advance Palliative Care (www.capc.org) has a number of educational courses that address these important communication skills.
Dr. Rudolph is vice president of physician development and patient experience for Sound Physicians, Tacoma, Wash. and chair of the SHM Patient Experience Committee .
Reference
1. Moss, A.H., Ganjoo, J, Sharma S, et al. Utility of the “Surprise” Question to Identify Dialysis Patients with High Mortality. Clinical Journal of the American Society of Nephrology: CJASN. 2008;3(5):1379-84. doi:10.2215/CJN.00940208.
Fellow in Hospital Medicine designation symbolizes physician commitment to hospital medicine
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Umesh Sharma, MD, MBA, FHM, chair of the division of community hospital medicine at Mayo Clinic. Umesh became a Fellow in Hospital Medicine in 2016 and has found great value in attending the annual meeting each year.
What inspired you to join SHM, and what prompted you to apply for the Fellow in Hospital Medicine designation?
How did you use SHM resources to help you in your pathway to Fellowship in Hospital Medicine?
There are specific eligibility requirements for the Fellow in Hospital Medicine designation, including a minimum of 5 years as a practicing hospitalist and 3 years as an SHM member, endorsements from two active members, regular meeting attendance and more. SHM provides a checklist for Fellow applicants online and an FAQ page to make the application process as user-friendly as possible. A friend of mine, Dr. Deepak Pahuja, is a Fellow, and he mentored me throughout the process.
How else has SHM contributed to your professional growth and provided you with tools you need to lead hospitalists at Mayo Clinic?
There are many resources that SHM provides to help with professional growth both online and at in-person meetings. I referenced the Key Principles and Characteristics of an Effective Hospital Medicine Group, an online assessment guide, in my role as department chair in La Crosse, Wisc., to resurrect a hospital medicine group, secure resources, hire career hospitalists, and create a well-functioning, well-managed, efficient, effective group with zero turnover during a span of 4 years.
By focusing on the leadership track at annual meetings, I have been able to gain knowledge on proven leadership strategies and enhance my skills, which I have applied on many occasions in my practice. Being able to talk to multisite hospital medicine group colleagues in person helped me to learn best practices in how to successfully manage the integration of 14 hospital medicine community hospital sites across Mayo Midwest. I was able to get ideas on effectively understanding and managing challenges, like recruitment retention, staffing to workloads, and scope of practice, among others. SHM promotes peer-to-peer learning and has helped me share and learn best practices as it relates to the clinical and nonclinical aspect of the practice of hospital medicine.
What one piece of advice would you give fellow hospitalists during this transformational time in health care?
This is an exciting time in health care, especially for hospital medicine professionals, who are at the forefront of providing value-based care. Every change is an opportunity to improve and innovate; the best way to handle change is to embrace and lead it.
Ms. Steele is SHM’s communications coordinator.
To apply for the Fellow in Hospital Medicine designation, visit www.hospitalmedicine.org/fellows.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Umesh Sharma, MD, MBA, FHM, chair of the division of community hospital medicine at Mayo Clinic. Umesh became a Fellow in Hospital Medicine in 2016 and has found great value in attending the annual meeting each year.
What inspired you to join SHM, and what prompted you to apply for the Fellow in Hospital Medicine designation?
How did you use SHM resources to help you in your pathway to Fellowship in Hospital Medicine?
There are specific eligibility requirements for the Fellow in Hospital Medicine designation, including a minimum of 5 years as a practicing hospitalist and 3 years as an SHM member, endorsements from two active members, regular meeting attendance and more. SHM provides a checklist for Fellow applicants online and an FAQ page to make the application process as user-friendly as possible. A friend of mine, Dr. Deepak Pahuja, is a Fellow, and he mentored me throughout the process.
How else has SHM contributed to your professional growth and provided you with tools you need to lead hospitalists at Mayo Clinic?
There are many resources that SHM provides to help with professional growth both online and at in-person meetings. I referenced the Key Principles and Characteristics of an Effective Hospital Medicine Group, an online assessment guide, in my role as department chair in La Crosse, Wisc., to resurrect a hospital medicine group, secure resources, hire career hospitalists, and create a well-functioning, well-managed, efficient, effective group with zero turnover during a span of 4 years.
By focusing on the leadership track at annual meetings, I have been able to gain knowledge on proven leadership strategies and enhance my skills, which I have applied on many occasions in my practice. Being able to talk to multisite hospital medicine group colleagues in person helped me to learn best practices in how to successfully manage the integration of 14 hospital medicine community hospital sites across Mayo Midwest. I was able to get ideas on effectively understanding and managing challenges, like recruitment retention, staffing to workloads, and scope of practice, among others. SHM promotes peer-to-peer learning and has helped me share and learn best practices as it relates to the clinical and nonclinical aspect of the practice of hospital medicine.
What one piece of advice would you give fellow hospitalists during this transformational time in health care?
This is an exciting time in health care, especially for hospital medicine professionals, who are at the forefront of providing value-based care. Every change is an opportunity to improve and innovate; the best way to handle change is to embrace and lead it.
Ms. Steele is SHM’s communications coordinator.
To apply for the Fellow in Hospital Medicine designation, visit www.hospitalmedicine.org/fellows.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Umesh Sharma, MD, MBA, FHM, chair of the division of community hospital medicine at Mayo Clinic. Umesh became a Fellow in Hospital Medicine in 2016 and has found great value in attending the annual meeting each year.
What inspired you to join SHM, and what prompted you to apply for the Fellow in Hospital Medicine designation?
How did you use SHM resources to help you in your pathway to Fellowship in Hospital Medicine?
There are specific eligibility requirements for the Fellow in Hospital Medicine designation, including a minimum of 5 years as a practicing hospitalist and 3 years as an SHM member, endorsements from two active members, regular meeting attendance and more. SHM provides a checklist for Fellow applicants online and an FAQ page to make the application process as user-friendly as possible. A friend of mine, Dr. Deepak Pahuja, is a Fellow, and he mentored me throughout the process.
How else has SHM contributed to your professional growth and provided you with tools you need to lead hospitalists at Mayo Clinic?
There are many resources that SHM provides to help with professional growth both online and at in-person meetings. I referenced the Key Principles and Characteristics of an Effective Hospital Medicine Group, an online assessment guide, in my role as department chair in La Crosse, Wisc., to resurrect a hospital medicine group, secure resources, hire career hospitalists, and create a well-functioning, well-managed, efficient, effective group with zero turnover during a span of 4 years.
By focusing on the leadership track at annual meetings, I have been able to gain knowledge on proven leadership strategies and enhance my skills, which I have applied on many occasions in my practice. Being able to talk to multisite hospital medicine group colleagues in person helped me to learn best practices in how to successfully manage the integration of 14 hospital medicine community hospital sites across Mayo Midwest. I was able to get ideas on effectively understanding and managing challenges, like recruitment retention, staffing to workloads, and scope of practice, among others. SHM promotes peer-to-peer learning and has helped me share and learn best practices as it relates to the clinical and nonclinical aspect of the practice of hospital medicine.
What one piece of advice would you give fellow hospitalists during this transformational time in health care?
This is an exciting time in health care, especially for hospital medicine professionals, who are at the forefront of providing value-based care. Every change is an opportunity to improve and innovate; the best way to handle change is to embrace and lead it.
Ms. Steele is SHM’s communications coordinator.
To apply for the Fellow in Hospital Medicine designation, visit www.hospitalmedicine.org/fellows.
HM17: Plenaries – Conway and DeSalvo
The first two plenary addresses at HM17 are focused on policy at a time when the dynamically evolving U.S. health care delivery system may seem daunting, opaque, and labyrinthine.
Some might view the health care landscape as hopelessly confusing. Yet both of the keynote speakers use the same word for what they hope to leave their listeners with: optimism.
“Though it feels uncertain in the headlines, the reality is that the health care world feels pretty united in that we need to continue the progress we’ve made on moving away from the fee-for-service model and to let people practice medicine the way they want – to work better as teams and focus on patients and outcomes,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) and former national coordinator for health information technology.
“I would view it as an opportunity as well,” said Dr. Conway, who still moonlights as a pediatric academic hospitalist on weekends in greater Washington, D.C. “I think the pieces are coming together. Everything from data, to new payment models, to the MACRA Medicare Physician payment legislation, really suggests a time of positive change.”
Dr. DeSalvo, a former political appointee, joined HHS as the national coordinator for health information technology in 2014 and soon thereafter assumed the acting assistant secretary role. Dr. Conway has attained one of the country’s highest-ranking public health care jobs since joining CMS in 2011. He retained the top post at CMS while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited a confirmation hearing before the U.S. Senate. Dr. Conway’s prior title was principal deputy administrator and CMS chief medical officer.
“I don’t want people to lose sight of the fact that there’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes,” she said. “Hospitalists, quite frankly, have been leading that for their entire existence. They really understand in great granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has established a path that must be followed. The public sector move away from fee-for-service has combined with emerging technology platforms to create a new age where physicians and insurers can judge, in real time, how well care is working.
“We’re now in a feedback loop where we can say – ‘When we’ve built a care system like this or when we pay this way, we are actually seeing improved outcomes’ – and change doesn’t take as long,” Dr. DeSalvo said.
Dr. Conway, whose working title for his speech is “Health care System Transformation,” said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable care organizations (ACOs), value-based purchasing (VBP), alternative payment models (APM), and the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. He noted that, as innovations lead to better and more coordinated patient care, hospitalists, patients, and hospitals would all benefit.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged with these new payment models, help lead them, and provide better patient care as a part of them.”
The first two plenary addresses at HM17 are focused on policy at a time when the dynamically evolving U.S. health care delivery system may seem daunting, opaque, and labyrinthine.
Some might view the health care landscape as hopelessly confusing. Yet both of the keynote speakers use the same word for what they hope to leave their listeners with: optimism.
“Though it feels uncertain in the headlines, the reality is that the health care world feels pretty united in that we need to continue the progress we’ve made on moving away from the fee-for-service model and to let people practice medicine the way they want – to work better as teams and focus on patients and outcomes,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) and former national coordinator for health information technology.
“I would view it as an opportunity as well,” said Dr. Conway, who still moonlights as a pediatric academic hospitalist on weekends in greater Washington, D.C. “I think the pieces are coming together. Everything from data, to new payment models, to the MACRA Medicare Physician payment legislation, really suggests a time of positive change.”
Dr. DeSalvo, a former political appointee, joined HHS as the national coordinator for health information technology in 2014 and soon thereafter assumed the acting assistant secretary role. Dr. Conway has attained one of the country’s highest-ranking public health care jobs since joining CMS in 2011. He retained the top post at CMS while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited a confirmation hearing before the U.S. Senate. Dr. Conway’s prior title was principal deputy administrator and CMS chief medical officer.
“I don’t want people to lose sight of the fact that there’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes,” she said. “Hospitalists, quite frankly, have been leading that for their entire existence. They really understand in great granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has established a path that must be followed. The public sector move away from fee-for-service has combined with emerging technology platforms to create a new age where physicians and insurers can judge, in real time, how well care is working.
“We’re now in a feedback loop where we can say – ‘When we’ve built a care system like this or when we pay this way, we are actually seeing improved outcomes’ – and change doesn’t take as long,” Dr. DeSalvo said.
Dr. Conway, whose working title for his speech is “Health care System Transformation,” said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable care organizations (ACOs), value-based purchasing (VBP), alternative payment models (APM), and the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. He noted that, as innovations lead to better and more coordinated patient care, hospitalists, patients, and hospitals would all benefit.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged with these new payment models, help lead them, and provide better patient care as a part of them.”
The first two plenary addresses at HM17 are focused on policy at a time when the dynamically evolving U.S. health care delivery system may seem daunting, opaque, and labyrinthine.
Some might view the health care landscape as hopelessly confusing. Yet both of the keynote speakers use the same word for what they hope to leave their listeners with: optimism.
“Though it feels uncertain in the headlines, the reality is that the health care world feels pretty united in that we need to continue the progress we’ve made on moving away from the fee-for-service model and to let people practice medicine the way they want – to work better as teams and focus on patients and outcomes,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) and former national coordinator for health information technology.
“I would view it as an opportunity as well,” said Dr. Conway, who still moonlights as a pediatric academic hospitalist on weekends in greater Washington, D.C. “I think the pieces are coming together. Everything from data, to new payment models, to the MACRA Medicare Physician payment legislation, really suggests a time of positive change.”
Dr. DeSalvo, a former political appointee, joined HHS as the national coordinator for health information technology in 2014 and soon thereafter assumed the acting assistant secretary role. Dr. Conway has attained one of the country’s highest-ranking public health care jobs since joining CMS in 2011. He retained the top post at CMS while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited a confirmation hearing before the U.S. Senate. Dr. Conway’s prior title was principal deputy administrator and CMS chief medical officer.
“I don’t want people to lose sight of the fact that there’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes,” she said. “Hospitalists, quite frankly, have been leading that for their entire existence. They really understand in great granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has established a path that must be followed. The public sector move away from fee-for-service has combined with emerging technology platforms to create a new age where physicians and insurers can judge, in real time, how well care is working.
“We’re now in a feedback loop where we can say – ‘When we’ve built a care system like this or when we pay this way, we are actually seeing improved outcomes’ – and change doesn’t take as long,” Dr. DeSalvo said.
Dr. Conway, whose working title for his speech is “Health care System Transformation,” said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable care organizations (ACOs), value-based purchasing (VBP), alternative payment models (APM), and the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. He noted that, as innovations lead to better and more coordinated patient care, hospitalists, patients, and hospitals would all benefit.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged with these new payment models, help lead them, and provide better patient care as a part of them.”