User login
Mentally ill and behind bars
The measure of a country’s greatness, Mahatma Gandhi said, should be based on how well it cares for its most vulnerable. Recently, I had the opportunity to work with members of a vulnerable population: men and women who have a mental illness and languish in jails and prisons around the country. My experience was eye-opening and heartbreaking.
Widespread incarceration of the mentally ill in a developed country such as the United States should be a national embarrassment. But this tragedy, which has reached an epidemic level, has been effectively shut out of the national conversation.
The problem has grown, and is enormous
By the estimate of the U.S. Department of Justice, more than one-half of people incarcerated in the United States are mentally ill and approximately 20% suffer from a serious mental illness.1,2 In fact, there are now 3 times as many mentally ill people in jail and prison as there are occupying psychiatric beds in hospitals.3 These numbers represent a considerable increase over the past 6 decades, and can be attributed to 2 major factors:
- A program of deinstitutionalization set in motion by the federal government in the 1950s called for shuttering of state psychiatric facilities around the country. This was a period of renewed national discourse on civil rights; for many people, the practice of institutionalization was considered a violation of civil rights. (Coincidentally, chlorpromazine was introduced about this time, and many experts believed that the drug would revolutionize outpatient management of psychiatric disorders.)
- More recently, heavy criminal penalties have been attached to convictions for possession and distribution of illegal substances—part of the government’s “war on drugs.”
As a consequence of these programs and policies, the United States has come full circle—routinely incarcerating the mentally ill as it did in the early 19th century, before reforms were initiated in response to the lobbying efforts of activist Dorothea Dix and her contemporaries.
My distressing, eye-opening experience
The time I spent with the incarcerated mentally ill was limited to a 6-month period at a county jail during residency. Yet the contrast between services provided to this population and those that are available to people in the community was immediately evident—and stark. The sheer number of adults in jails and prisons who require mental health care is such that the ratio of patients to psychiatrists, psychologists, and other mental health clinicians is shockingly skewed.
It does not take years of experience to figure out that a brief interview with an 18-year-old who is being jailed for the first time, has never seen a psychiatrist, and suffers panic attacks (or hallucinations, or suicidal thoughts) is a less-than-ideal clinical situation. Making that situation even more hazardous is that inmates have a high risk of suicide, particularly in the first 24 to 48 hours of incarceration.4
Other ethical issues arose during my stint in the correctional system: My patients frequently would be charged with prison-rule violations (there is evidence that mentally ill inmates are more likely to be charged with such violations2); on many such occasions, they would be placed in solitary confinement (“the hole”), a practice the United Nations has called “cruel, inhuman, and degrading: for the mentally ill5 and that, in turn, exacerbates the inmate’s psychiatric illness.6-11
Last, there are restrictions on the types of formulations of medications that can be prescribed, involuntary treatment, and other critical aspects of care that make the experience of providing care in this system frustrating for mental health providers.
Are there solutions?
One way to tackle this crisis might be to insert more psychiatrists and psychologists into the correctional system. A more sensible approach, however, would be to tackle the root cause and divert the mentally ill away from incarceration and into treatment—moving from a model of retribution and incapacitation to one of rehabilitation. For example:
- Several counties nationwide have adopted diversion programs that include so-called mental health courts and drug courts, with encouraging results12
- Police departments are establishing Crisis Intervention Teams
- Assisted outpatient treatment programs are growing in popularity.
Far more needs to be done, however. In the absence of a national debate on the problem of the incarcerated mentally ill, there is real risk that this population will continue to be ignored and that our mental health care infrastructure will remain inadequate for meeting their need for services.
1. American Psychiatric Association. Psychiatric services in jails and prisons: a task force report of the American Psychiatric Association. 2nd ed. Washington, DC: American Psychiatric Association; 2000:XIX.
2. U.S. Department of Justice. Bureau of Justice Statistics: special report. Mental health problems of prison and jail inmates. http://www.bjs.gov/content/pub/pdf/mhppji.pdf. Updated December 14, 2006. Accessed April 8, 2016.|
3. Torrey FE, Kennard AD, Eslinger D, et al. More mentally ill persons are in jails and prisons than hospitals: a survey of the states. http://www.treatmentadvocacycenter.org/storage/documents/final_jails_v_hospitals_study.pdf. Published May 2010. Accessed April 8, 2016.
4. U.S. Department of Justice. National study of jail suicide: 20 years later. http://static.nicic.gov/Library/024308.pdf. Published April 2010. Accessed April 8, 2016.
5. Méndez JE. Special Rapporteur on torture and other cruel, inhuman or degrading treatment or punishment. http://www.ohchr.org/EN/Issues/Torture/SRTorture/Pages/SRTortureIndex.aspx. Published 2011. Accessed April 8, 2016.
6. Daniel AE. Preventing suicide in prison: a collaborative responsibility of administrative, custodial, and clinical staff. J Am Acad Psychiatry Law. 2006;34(2):165-175.
7. White TW, Schimmel DJ, Frickey R. A comprehensive analysis of suicide in federal prisons: a fifteen-year review. J Correct Health Care. 2002;9(3):321-345.
8. Smith PS. The effects of solitary confinement on prison inmates: a brief history and review of the literature, crime and justice. Crime and Justice. 2006;34(1):441-528.
9. Grassian S. Psychopathological effects of solitary confinement. Am J Psychiatry. 1983;140(11):1450-1454.
10. Patterson RF, Hughes K. Review of completed suicides in the California Department of Corrections and Rehabilitation, 1999 to 2004. Psychiatr Serv. 2008;59(6):676-682.
11. Kaba F, Lewis A, Glowa-Kollisch S, et al. Solitary confinement and risk of self-harm among jail inmates. Am J Public Health. 2014;104(3):442-447.
12. McNiel DE, Binder RL. Effectiveness of a mental health court in reducing criminal recidivism and violence. Am J Psychiatry. 2007;164(9):1395-1403.
The measure of a country’s greatness, Mahatma Gandhi said, should be based on how well it cares for its most vulnerable. Recently, I had the opportunity to work with members of a vulnerable population: men and women who have a mental illness and languish in jails and prisons around the country. My experience was eye-opening and heartbreaking.
Widespread incarceration of the mentally ill in a developed country such as the United States should be a national embarrassment. But this tragedy, which has reached an epidemic level, has been effectively shut out of the national conversation.
The problem has grown, and is enormous
By the estimate of the U.S. Department of Justice, more than one-half of people incarcerated in the United States are mentally ill and approximately 20% suffer from a serious mental illness.1,2 In fact, there are now 3 times as many mentally ill people in jail and prison as there are occupying psychiatric beds in hospitals.3 These numbers represent a considerable increase over the past 6 decades, and can be attributed to 2 major factors:
- A program of deinstitutionalization set in motion by the federal government in the 1950s called for shuttering of state psychiatric facilities around the country. This was a period of renewed national discourse on civil rights; for many people, the practice of institutionalization was considered a violation of civil rights. (Coincidentally, chlorpromazine was introduced about this time, and many experts believed that the drug would revolutionize outpatient management of psychiatric disorders.)
- More recently, heavy criminal penalties have been attached to convictions for possession and distribution of illegal substances—part of the government’s “war on drugs.”
As a consequence of these programs and policies, the United States has come full circle—routinely incarcerating the mentally ill as it did in the early 19th century, before reforms were initiated in response to the lobbying efforts of activist Dorothea Dix and her contemporaries.
My distressing, eye-opening experience
The time I spent with the incarcerated mentally ill was limited to a 6-month period at a county jail during residency. Yet the contrast between services provided to this population and those that are available to people in the community was immediately evident—and stark. The sheer number of adults in jails and prisons who require mental health care is such that the ratio of patients to psychiatrists, psychologists, and other mental health clinicians is shockingly skewed.
It does not take years of experience to figure out that a brief interview with an 18-year-old who is being jailed for the first time, has never seen a psychiatrist, and suffers panic attacks (or hallucinations, or suicidal thoughts) is a less-than-ideal clinical situation. Making that situation even more hazardous is that inmates have a high risk of suicide, particularly in the first 24 to 48 hours of incarceration.4
Other ethical issues arose during my stint in the correctional system: My patients frequently would be charged with prison-rule violations (there is evidence that mentally ill inmates are more likely to be charged with such violations2); on many such occasions, they would be placed in solitary confinement (“the hole”), a practice the United Nations has called “cruel, inhuman, and degrading: for the mentally ill5 and that, in turn, exacerbates the inmate’s psychiatric illness.6-11
Last, there are restrictions on the types of formulations of medications that can be prescribed, involuntary treatment, and other critical aspects of care that make the experience of providing care in this system frustrating for mental health providers.
Are there solutions?
One way to tackle this crisis might be to insert more psychiatrists and psychologists into the correctional system. A more sensible approach, however, would be to tackle the root cause and divert the mentally ill away from incarceration and into treatment—moving from a model of retribution and incapacitation to one of rehabilitation. For example:
- Several counties nationwide have adopted diversion programs that include so-called mental health courts and drug courts, with encouraging results12
- Police departments are establishing Crisis Intervention Teams
- Assisted outpatient treatment programs are growing in popularity.
Far more needs to be done, however. In the absence of a national debate on the problem of the incarcerated mentally ill, there is real risk that this population will continue to be ignored and that our mental health care infrastructure will remain inadequate for meeting their need for services.
The measure of a country’s greatness, Mahatma Gandhi said, should be based on how well it cares for its most vulnerable. Recently, I had the opportunity to work with members of a vulnerable population: men and women who have a mental illness and languish in jails and prisons around the country. My experience was eye-opening and heartbreaking.
Widespread incarceration of the mentally ill in a developed country such as the United States should be a national embarrassment. But this tragedy, which has reached an epidemic level, has been effectively shut out of the national conversation.
The problem has grown, and is enormous
By the estimate of the U.S. Department of Justice, more than one-half of people incarcerated in the United States are mentally ill and approximately 20% suffer from a serious mental illness.1,2 In fact, there are now 3 times as many mentally ill people in jail and prison as there are occupying psychiatric beds in hospitals.3 These numbers represent a considerable increase over the past 6 decades, and can be attributed to 2 major factors:
- A program of deinstitutionalization set in motion by the federal government in the 1950s called for shuttering of state psychiatric facilities around the country. This was a period of renewed national discourse on civil rights; for many people, the practice of institutionalization was considered a violation of civil rights. (Coincidentally, chlorpromazine was introduced about this time, and many experts believed that the drug would revolutionize outpatient management of psychiatric disorders.)
- More recently, heavy criminal penalties have been attached to convictions for possession and distribution of illegal substances—part of the government’s “war on drugs.”
As a consequence of these programs and policies, the United States has come full circle—routinely incarcerating the mentally ill as it did in the early 19th century, before reforms were initiated in response to the lobbying efforts of activist Dorothea Dix and her contemporaries.
My distressing, eye-opening experience
The time I spent with the incarcerated mentally ill was limited to a 6-month period at a county jail during residency. Yet the contrast between services provided to this population and those that are available to people in the community was immediately evident—and stark. The sheer number of adults in jails and prisons who require mental health care is such that the ratio of patients to psychiatrists, psychologists, and other mental health clinicians is shockingly skewed.
It does not take years of experience to figure out that a brief interview with an 18-year-old who is being jailed for the first time, has never seen a psychiatrist, and suffers panic attacks (or hallucinations, or suicidal thoughts) is a less-than-ideal clinical situation. Making that situation even more hazardous is that inmates have a high risk of suicide, particularly in the first 24 to 48 hours of incarceration.4
Other ethical issues arose during my stint in the correctional system: My patients frequently would be charged with prison-rule violations (there is evidence that mentally ill inmates are more likely to be charged with such violations2); on many such occasions, they would be placed in solitary confinement (“the hole”), a practice the United Nations has called “cruel, inhuman, and degrading: for the mentally ill5 and that, in turn, exacerbates the inmate’s psychiatric illness.6-11
Last, there are restrictions on the types of formulations of medications that can be prescribed, involuntary treatment, and other critical aspects of care that make the experience of providing care in this system frustrating for mental health providers.
Are there solutions?
One way to tackle this crisis might be to insert more psychiatrists and psychologists into the correctional system. A more sensible approach, however, would be to tackle the root cause and divert the mentally ill away from incarceration and into treatment—moving from a model of retribution and incapacitation to one of rehabilitation. For example:
- Several counties nationwide have adopted diversion programs that include so-called mental health courts and drug courts, with encouraging results12
- Police departments are establishing Crisis Intervention Teams
- Assisted outpatient treatment programs are growing in popularity.
Far more needs to be done, however. In the absence of a national debate on the problem of the incarcerated mentally ill, there is real risk that this population will continue to be ignored and that our mental health care infrastructure will remain inadequate for meeting their need for services.
1. American Psychiatric Association. Psychiatric services in jails and prisons: a task force report of the American Psychiatric Association. 2nd ed. Washington, DC: American Psychiatric Association; 2000:XIX.
2. U.S. Department of Justice. Bureau of Justice Statistics: special report. Mental health problems of prison and jail inmates. http://www.bjs.gov/content/pub/pdf/mhppji.pdf. Updated December 14, 2006. Accessed April 8, 2016.|
3. Torrey FE, Kennard AD, Eslinger D, et al. More mentally ill persons are in jails and prisons than hospitals: a survey of the states. http://www.treatmentadvocacycenter.org/storage/documents/final_jails_v_hospitals_study.pdf. Published May 2010. Accessed April 8, 2016.
4. U.S. Department of Justice. National study of jail suicide: 20 years later. http://static.nicic.gov/Library/024308.pdf. Published April 2010. Accessed April 8, 2016.
5. Méndez JE. Special Rapporteur on torture and other cruel, inhuman or degrading treatment or punishment. http://www.ohchr.org/EN/Issues/Torture/SRTorture/Pages/SRTortureIndex.aspx. Published 2011. Accessed April 8, 2016.
6. Daniel AE. Preventing suicide in prison: a collaborative responsibility of administrative, custodial, and clinical staff. J Am Acad Psychiatry Law. 2006;34(2):165-175.
7. White TW, Schimmel DJ, Frickey R. A comprehensive analysis of suicide in federal prisons: a fifteen-year review. J Correct Health Care. 2002;9(3):321-345.
8. Smith PS. The effects of solitary confinement on prison inmates: a brief history and review of the literature, crime and justice. Crime and Justice. 2006;34(1):441-528.
9. Grassian S. Psychopathological effects of solitary confinement. Am J Psychiatry. 1983;140(11):1450-1454.
10. Patterson RF, Hughes K. Review of completed suicides in the California Department of Corrections and Rehabilitation, 1999 to 2004. Psychiatr Serv. 2008;59(6):676-682.
11. Kaba F, Lewis A, Glowa-Kollisch S, et al. Solitary confinement and risk of self-harm among jail inmates. Am J Public Health. 2014;104(3):442-447.
12. McNiel DE, Binder RL. Effectiveness of a mental health court in reducing criminal recidivism and violence. Am J Psychiatry. 2007;164(9):1395-1403.
1. American Psychiatric Association. Psychiatric services in jails and prisons: a task force report of the American Psychiatric Association. 2nd ed. Washington, DC: American Psychiatric Association; 2000:XIX.
2. U.S. Department of Justice. Bureau of Justice Statistics: special report. Mental health problems of prison and jail inmates. http://www.bjs.gov/content/pub/pdf/mhppji.pdf. Updated December 14, 2006. Accessed April 8, 2016.|
3. Torrey FE, Kennard AD, Eslinger D, et al. More mentally ill persons are in jails and prisons than hospitals: a survey of the states. http://www.treatmentadvocacycenter.org/storage/documents/final_jails_v_hospitals_study.pdf. Published May 2010. Accessed April 8, 2016.
4. U.S. Department of Justice. National study of jail suicide: 20 years later. http://static.nicic.gov/Library/024308.pdf. Published April 2010. Accessed April 8, 2016.
5. Méndez JE. Special Rapporteur on torture and other cruel, inhuman or degrading treatment or punishment. http://www.ohchr.org/EN/Issues/Torture/SRTorture/Pages/SRTortureIndex.aspx. Published 2011. Accessed April 8, 2016.
6. Daniel AE. Preventing suicide in prison: a collaborative responsibility of administrative, custodial, and clinical staff. J Am Acad Psychiatry Law. 2006;34(2):165-175.
7. White TW, Schimmel DJ, Frickey R. A comprehensive analysis of suicide in federal prisons: a fifteen-year review. J Correct Health Care. 2002;9(3):321-345.
8. Smith PS. The effects of solitary confinement on prison inmates: a brief history and review of the literature, crime and justice. Crime and Justice. 2006;34(1):441-528.
9. Grassian S. Psychopathological effects of solitary confinement. Am J Psychiatry. 1983;140(11):1450-1454.
10. Patterson RF, Hughes K. Review of completed suicides in the California Department of Corrections and Rehabilitation, 1999 to 2004. Psychiatr Serv. 2008;59(6):676-682.
11. Kaba F, Lewis A, Glowa-Kollisch S, et al. Solitary confinement and risk of self-harm among jail inmates. Am J Public Health. 2014;104(3):442-447.
12. McNiel DE, Binder RL. Effectiveness of a mental health court in reducing criminal recidivism and violence. Am J Psychiatry. 2007;164(9):1395-1403.
Don’t assume that psychiatric patients lack capacity to make decisions about care
Some practitioners of medicine—including psychiatrists—might equate “psychosis” with incapacity, but that isn’t necessarily true. Even patients who, by most measures, are deemed psychotic might be capable of making wise and thoughtful decisions about their life. The case I describe in this article demonstrates that fact.
While rotating on a busy consultation service, I was asked to evaluate the capacity of a woman who had a diagnosis of schizophrenia and was being seen for worsening auditory hallucinations and progressive weight loss. She had a complicated medical course that eventually led to multiple requests to the consult team for a capacity evaluation.
The question of capacity in this patient, and in the psychiatric population generally, motivated me to review the literature, because the assumption by many on the medical teams involved in this patient’s care was that psychiatric patients do not have the capacity to participate in their own care. My goal here is to clarify the misconceptions in regard to this situation.
CASE REPORT
Schizophrenia, weight loss, back pain
Ms. V, age 67, a resident of a group home for the past 6 years, was brought to the emergency department (ED) because of weight loss and auditory hallucinations that had developed during the past few months. She had a history of paranoid schizophrenia that included several psychiatric hospitalizations but no known medical history.
The patient appeared cachectic and dehydrated. When approached, she was pleasant and reported hearing voices of the “devil.”
“They are not scary,” she confided. “They talk to me about art and literature.”
Over the past 6 months, Ms. V had lost 60 lb; she was now bedridden because of back pain. Collateral information obtained from staff members at the group home indicated that she had refused to get out of bed, and only intermittently took her medications or ate meals during the past few months. In general, however, she had been relatively stable over the course of her psychiatric illness, was adherent to psychiatric treatment, and had had no psychiatric hospitalizations in the past 3 decades.
Ominous development. Although the ED staff was convinced that Ms. V needed psychiatric admission, we (the consult team) first requested a detailed medical workup, including imaging studies. A CT scan showed multiple metastatic foci throughout her spine. She was admitted to the medical service.
Respiratory distress developed; her condition deteriorated. Numerous capacity consults were requested because she refused a medical workup or to sign do-not-resuscitate and do-not-intubate orders. Each time an evaluation was performed, Ms. V was deemed by various clinicians on the consult service to have decision-making capacity.
The patient grew unhappy with the staff’s insistence that she undergo more tests regardless of her stated wishes. The palliative care service determined that further workup would not benefit her medically: Ms. V’s condition would be grave and her prognosis poor regardless of what treatment she received.
The medical team continued to believe that, because that this patient had a mental illness and was actively hallucinating, she did not have the capacity to refuse any proposed treatments and tests.
What is capacity?
Capacity is an assessment of a person’s ability to make rational decisions. This includes the ability to understand, appreciate, and manipulate information in reaching such decisions. Determining whether a patient has the capacity to accept or refuse treatment is a medical decision that any physician can make; however, consultation−liaison psychiatrists are the experts who often are involved in this activity, particularly in patients who have a psychiatric comorbidity.
Capacity is evaluated by assessing 4 standards; that is, whether a patient can:
- communicate choice about proposed treatment
- understand her (his) medical situation
- appreciate the situation and its consequences
- manipulate information to reach a rational decision.1-3
- manipulate information to reach a rational decision.
CASE REPORT continued
Although Ms. V’s health was deteriorating and her auditory hallucinations were becoming worse, she appeared insightful about her medical problems, understood her prognosis, and wanted comfort care. She understood that having multiple metastases meant a poor prognosis, and that a biopsy might yield a medical diagnosis. She stated, “If it were caught earlier and I was better able to tolerate treatment, it would make sense to know for sure, but now it doesn’t make sense. I just want to have no pain in my end.”
Misconceptions
In a study by Ganzini et al,4,5 395 consultation−liaison psychiatrists, geriatricians, and geriatric psychologists responded to a survey in which they rated types of misunderstandings by clinicians who refer patients for assessment of decision-making capacity. Seventy percent reported that it is common that, when a patient has a mental illness such as schizophrenia, practitioners think that the patient lacks capacity to make medical decisions. However, results of a meta-analysis by Jeste et al,6 in which the magnitude of impairment of decisional capacity in patients with schizophrenia was assessed in comparison to that of normal subjects, suggest that the presence of schizophrenia does not necessarily mean the patient has impaired capacity.
Voluntary participation in research. Many patients with schizophrenia volunteer to participate in clinical trials even when they are acutely psychotic and admitted to a psychiatric hospital. Given the importance placed on participants’ voluntary informed consent as a prerequisite for ethical conduct of research, the cognitive and emotional impairments associated with schizophrenia raise questions about patients’ capacity to consent.
As is true in other areas of functional capacity, the ability of patients with schizophrenia to make competent decisions relates more to their overall cognitive functioning than to the presence or absence of specific symptoms of the disorder.7 Documentation of longitudinal consent-related abilities among research participants with schizophrenia in the long-term Clinical Antipsychotic Trials of Intervention Effectiveness study indicated that most participants had stable or improved consent-related abilities. Although almost 25% of participants experienced substantial worsening, only 4% fell below the study’s capacity threshold for enrollment.8
What I learned from Ms. V
A diagnosis of schizophrenia does not automatically render a person unable to make decisions about medical care. Even patients who have severe mental illness might have significant intact areas of reality testing. Ethically, it is important to at least consider that the chronically mentally ill can understand treatment options and express consistent choices.
Healthcare providers might tend to exclude psychiatric patients from end-of-life decisions because they (1) are worried about the emotional fragility of such patients and (2) assume that patients lack capacity to participate in making such important decisions. The case presented here is an example of a patient with a severe psychiatric diagnosis being able to participate in her care despite her mental state.
1. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
2. Leo RJ. Competency and the capacity to make treatment decisions: a primer for primary care physicians. Prim Care Companion J Clin Psychiatry. 1999;1(5):131-141.
3. White MM, Lofwall MR. Challenges of the capacity evaluation for the consultation-liaison psychiatrist. J Psychiatr Pract. 2015;21(2):160-170.
4. Ganzini L, Volicer L, Nelson W, et al. Pitfalls in assessment of decision-making capacity. Psychosomatics. 2003;44(3):237-243.
5. Ganzini L, Volicer L, Nelson WA, et al. Ten myths about decision-making capacity. J Am Med Dir Assoc. 2005;6(3):S100-S104.
6. Jeste DV, Depp CA, Palmer BW. Magnitude of impairment in decisional capacity in people with schizophrenia compared to normal subjects: an overview. Schizophr Bull. 2005;32(1):121-128.
7. Appelbaum PS. Decisional capacity of patients with schizophrenia to consent to research: taking stock. Schizophr Bull. 2005;32(1):22-25.
8. Stroup TS, Appelbaum PS, Gu H, et al. Longitudinal consent-related abilities among research participants with schizophrenia: results from the CATIE study. Schizophr Res. 2011;130(1-3):47-52.
Some practitioners of medicine—including psychiatrists—might equate “psychosis” with incapacity, but that isn’t necessarily true. Even patients who, by most measures, are deemed psychotic might be capable of making wise and thoughtful decisions about their life. The case I describe in this article demonstrates that fact.
While rotating on a busy consultation service, I was asked to evaluate the capacity of a woman who had a diagnosis of schizophrenia and was being seen for worsening auditory hallucinations and progressive weight loss. She had a complicated medical course that eventually led to multiple requests to the consult team for a capacity evaluation.
The question of capacity in this patient, and in the psychiatric population generally, motivated me to review the literature, because the assumption by many on the medical teams involved in this patient’s care was that psychiatric patients do not have the capacity to participate in their own care. My goal here is to clarify the misconceptions in regard to this situation.
CASE REPORT
Schizophrenia, weight loss, back pain
Ms. V, age 67, a resident of a group home for the past 6 years, was brought to the emergency department (ED) because of weight loss and auditory hallucinations that had developed during the past few months. She had a history of paranoid schizophrenia that included several psychiatric hospitalizations but no known medical history.
The patient appeared cachectic and dehydrated. When approached, she was pleasant and reported hearing voices of the “devil.”
“They are not scary,” she confided. “They talk to me about art and literature.”
Over the past 6 months, Ms. V had lost 60 lb; she was now bedridden because of back pain. Collateral information obtained from staff members at the group home indicated that she had refused to get out of bed, and only intermittently took her medications or ate meals during the past few months. In general, however, she had been relatively stable over the course of her psychiatric illness, was adherent to psychiatric treatment, and had had no psychiatric hospitalizations in the past 3 decades.
Ominous development. Although the ED staff was convinced that Ms. V needed psychiatric admission, we (the consult team) first requested a detailed medical workup, including imaging studies. A CT scan showed multiple metastatic foci throughout her spine. She was admitted to the medical service.
Respiratory distress developed; her condition deteriorated. Numerous capacity consults were requested because she refused a medical workup or to sign do-not-resuscitate and do-not-intubate orders. Each time an evaluation was performed, Ms. V was deemed by various clinicians on the consult service to have decision-making capacity.
The patient grew unhappy with the staff’s insistence that she undergo more tests regardless of her stated wishes. The palliative care service determined that further workup would not benefit her medically: Ms. V’s condition would be grave and her prognosis poor regardless of what treatment she received.
The medical team continued to believe that, because that this patient had a mental illness and was actively hallucinating, she did not have the capacity to refuse any proposed treatments and tests.
What is capacity?
Capacity is an assessment of a person’s ability to make rational decisions. This includes the ability to understand, appreciate, and manipulate information in reaching such decisions. Determining whether a patient has the capacity to accept or refuse treatment is a medical decision that any physician can make; however, consultation−liaison psychiatrists are the experts who often are involved in this activity, particularly in patients who have a psychiatric comorbidity.
Capacity is evaluated by assessing 4 standards; that is, whether a patient can:
- communicate choice about proposed treatment
- understand her (his) medical situation
- appreciate the situation and its consequences
- manipulate information to reach a rational decision.1-3
- manipulate information to reach a rational decision.
CASE REPORT continued
Although Ms. V’s health was deteriorating and her auditory hallucinations were becoming worse, she appeared insightful about her medical problems, understood her prognosis, and wanted comfort care. She understood that having multiple metastases meant a poor prognosis, and that a biopsy might yield a medical diagnosis. She stated, “If it were caught earlier and I was better able to tolerate treatment, it would make sense to know for sure, but now it doesn’t make sense. I just want to have no pain in my end.”
Misconceptions
In a study by Ganzini et al,4,5 395 consultation−liaison psychiatrists, geriatricians, and geriatric psychologists responded to a survey in which they rated types of misunderstandings by clinicians who refer patients for assessment of decision-making capacity. Seventy percent reported that it is common that, when a patient has a mental illness such as schizophrenia, practitioners think that the patient lacks capacity to make medical decisions. However, results of a meta-analysis by Jeste et al,6 in which the magnitude of impairment of decisional capacity in patients with schizophrenia was assessed in comparison to that of normal subjects, suggest that the presence of schizophrenia does not necessarily mean the patient has impaired capacity.
Voluntary participation in research. Many patients with schizophrenia volunteer to participate in clinical trials even when they are acutely psychotic and admitted to a psychiatric hospital. Given the importance placed on participants’ voluntary informed consent as a prerequisite for ethical conduct of research, the cognitive and emotional impairments associated with schizophrenia raise questions about patients’ capacity to consent.
As is true in other areas of functional capacity, the ability of patients with schizophrenia to make competent decisions relates more to their overall cognitive functioning than to the presence or absence of specific symptoms of the disorder.7 Documentation of longitudinal consent-related abilities among research participants with schizophrenia in the long-term Clinical Antipsychotic Trials of Intervention Effectiveness study indicated that most participants had stable or improved consent-related abilities. Although almost 25% of participants experienced substantial worsening, only 4% fell below the study’s capacity threshold for enrollment.8
What I learned from Ms. V
A diagnosis of schizophrenia does not automatically render a person unable to make decisions about medical care. Even patients who have severe mental illness might have significant intact areas of reality testing. Ethically, it is important to at least consider that the chronically mentally ill can understand treatment options and express consistent choices.
Healthcare providers might tend to exclude psychiatric patients from end-of-life decisions because they (1) are worried about the emotional fragility of such patients and (2) assume that patients lack capacity to participate in making such important decisions. The case presented here is an example of a patient with a severe psychiatric diagnosis being able to participate in her care despite her mental state.
Some practitioners of medicine—including psychiatrists—might equate “psychosis” with incapacity, but that isn’t necessarily true. Even patients who, by most measures, are deemed psychotic might be capable of making wise and thoughtful decisions about their life. The case I describe in this article demonstrates that fact.
While rotating on a busy consultation service, I was asked to evaluate the capacity of a woman who had a diagnosis of schizophrenia and was being seen for worsening auditory hallucinations and progressive weight loss. She had a complicated medical course that eventually led to multiple requests to the consult team for a capacity evaluation.
The question of capacity in this patient, and in the psychiatric population generally, motivated me to review the literature, because the assumption by many on the medical teams involved in this patient’s care was that psychiatric patients do not have the capacity to participate in their own care. My goal here is to clarify the misconceptions in regard to this situation.
CASE REPORT
Schizophrenia, weight loss, back pain
Ms. V, age 67, a resident of a group home for the past 6 years, was brought to the emergency department (ED) because of weight loss and auditory hallucinations that had developed during the past few months. She had a history of paranoid schizophrenia that included several psychiatric hospitalizations but no known medical history.
The patient appeared cachectic and dehydrated. When approached, she was pleasant and reported hearing voices of the “devil.”
“They are not scary,” she confided. “They talk to me about art and literature.”
Over the past 6 months, Ms. V had lost 60 lb; she was now bedridden because of back pain. Collateral information obtained from staff members at the group home indicated that she had refused to get out of bed, and only intermittently took her medications or ate meals during the past few months. In general, however, she had been relatively stable over the course of her psychiatric illness, was adherent to psychiatric treatment, and had had no psychiatric hospitalizations in the past 3 decades.
Ominous development. Although the ED staff was convinced that Ms. V needed psychiatric admission, we (the consult team) first requested a detailed medical workup, including imaging studies. A CT scan showed multiple metastatic foci throughout her spine. She was admitted to the medical service.
Respiratory distress developed; her condition deteriorated. Numerous capacity consults were requested because she refused a medical workup or to sign do-not-resuscitate and do-not-intubate orders. Each time an evaluation was performed, Ms. V was deemed by various clinicians on the consult service to have decision-making capacity.
The patient grew unhappy with the staff’s insistence that she undergo more tests regardless of her stated wishes. The palliative care service determined that further workup would not benefit her medically: Ms. V’s condition would be grave and her prognosis poor regardless of what treatment she received.
The medical team continued to believe that, because that this patient had a mental illness and was actively hallucinating, she did not have the capacity to refuse any proposed treatments and tests.
What is capacity?
Capacity is an assessment of a person’s ability to make rational decisions. This includes the ability to understand, appreciate, and manipulate information in reaching such decisions. Determining whether a patient has the capacity to accept or refuse treatment is a medical decision that any physician can make; however, consultation−liaison psychiatrists are the experts who often are involved in this activity, particularly in patients who have a psychiatric comorbidity.
Capacity is evaluated by assessing 4 standards; that is, whether a patient can:
- communicate choice about proposed treatment
- understand her (his) medical situation
- appreciate the situation and its consequences
- manipulate information to reach a rational decision.1-3
- manipulate information to reach a rational decision.
CASE REPORT continued
Although Ms. V’s health was deteriorating and her auditory hallucinations were becoming worse, she appeared insightful about her medical problems, understood her prognosis, and wanted comfort care. She understood that having multiple metastases meant a poor prognosis, and that a biopsy might yield a medical diagnosis. She stated, “If it were caught earlier and I was better able to tolerate treatment, it would make sense to know for sure, but now it doesn’t make sense. I just want to have no pain in my end.”
Misconceptions
In a study by Ganzini et al,4,5 395 consultation−liaison psychiatrists, geriatricians, and geriatric psychologists responded to a survey in which they rated types of misunderstandings by clinicians who refer patients for assessment of decision-making capacity. Seventy percent reported that it is common that, when a patient has a mental illness such as schizophrenia, practitioners think that the patient lacks capacity to make medical decisions. However, results of a meta-analysis by Jeste et al,6 in which the magnitude of impairment of decisional capacity in patients with schizophrenia was assessed in comparison to that of normal subjects, suggest that the presence of schizophrenia does not necessarily mean the patient has impaired capacity.
Voluntary participation in research. Many patients with schizophrenia volunteer to participate in clinical trials even when they are acutely psychotic and admitted to a psychiatric hospital. Given the importance placed on participants’ voluntary informed consent as a prerequisite for ethical conduct of research, the cognitive and emotional impairments associated with schizophrenia raise questions about patients’ capacity to consent.
As is true in other areas of functional capacity, the ability of patients with schizophrenia to make competent decisions relates more to their overall cognitive functioning than to the presence or absence of specific symptoms of the disorder.7 Documentation of longitudinal consent-related abilities among research participants with schizophrenia in the long-term Clinical Antipsychotic Trials of Intervention Effectiveness study indicated that most participants had stable or improved consent-related abilities. Although almost 25% of participants experienced substantial worsening, only 4% fell below the study’s capacity threshold for enrollment.8
What I learned from Ms. V
A diagnosis of schizophrenia does not automatically render a person unable to make decisions about medical care. Even patients who have severe mental illness might have significant intact areas of reality testing. Ethically, it is important to at least consider that the chronically mentally ill can understand treatment options and express consistent choices.
Healthcare providers might tend to exclude psychiatric patients from end-of-life decisions because they (1) are worried about the emotional fragility of such patients and (2) assume that patients lack capacity to participate in making such important decisions. The case presented here is an example of a patient with a severe psychiatric diagnosis being able to participate in her care despite her mental state.
1. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
2. Leo RJ. Competency and the capacity to make treatment decisions: a primer for primary care physicians. Prim Care Companion J Clin Psychiatry. 1999;1(5):131-141.
3. White MM, Lofwall MR. Challenges of the capacity evaluation for the consultation-liaison psychiatrist. J Psychiatr Pract. 2015;21(2):160-170.
4. Ganzini L, Volicer L, Nelson W, et al. Pitfalls in assessment of decision-making capacity. Psychosomatics. 2003;44(3):237-243.
5. Ganzini L, Volicer L, Nelson WA, et al. Ten myths about decision-making capacity. J Am Med Dir Assoc. 2005;6(3):S100-S104.
6. Jeste DV, Depp CA, Palmer BW. Magnitude of impairment in decisional capacity in people with schizophrenia compared to normal subjects: an overview. Schizophr Bull. 2005;32(1):121-128.
7. Appelbaum PS. Decisional capacity of patients with schizophrenia to consent to research: taking stock. Schizophr Bull. 2005;32(1):22-25.
8. Stroup TS, Appelbaum PS, Gu H, et al. Longitudinal consent-related abilities among research participants with schizophrenia: results from the CATIE study. Schizophr Res. 2011;130(1-3):47-52.
1. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
2. Leo RJ. Competency and the capacity to make treatment decisions: a primer for primary care physicians. Prim Care Companion J Clin Psychiatry. 1999;1(5):131-141.
3. White MM, Lofwall MR. Challenges of the capacity evaluation for the consultation-liaison psychiatrist. J Psychiatr Pract. 2015;21(2):160-170.
4. Ganzini L, Volicer L, Nelson W, et al. Pitfalls in assessment of decision-making capacity. Psychosomatics. 2003;44(3):237-243.
5. Ganzini L, Volicer L, Nelson WA, et al. Ten myths about decision-making capacity. J Am Med Dir Assoc. 2005;6(3):S100-S104.
6. Jeste DV, Depp CA, Palmer BW. Magnitude of impairment in decisional capacity in people with schizophrenia compared to normal subjects: an overview. Schizophr Bull. 2005;32(1):121-128.
7. Appelbaum PS. Decisional capacity of patients with schizophrenia to consent to research: taking stock. Schizophr Bull. 2005;32(1):22-25.
8. Stroup TS, Appelbaum PS, Gu H, et al. Longitudinal consent-related abilities among research participants with schizophrenia: results from the CATIE study. Schizophr Res. 2011;130(1-3):47-52.
Intellectual disability impedes decision-making in organ transplantation
CASE REPORT Evaluation for renal transplant
Mr. B, age 21, who has a diagnosis of autism spectrum disorder and an IQ comparable to that of a 4-year-old, is referred for evaluation of his candidacy for renal transplant.
A few months earlier, Mr. B pulled out his temporary dialysis catheter. Now, he receives hemodialysis through an arteriovenous fistula in the arm, but requires constant supervision during dialysis.
At evaluation, Mr. B is accompanied by his parents and his older sister, who have been providing day-to-day care for him. They appear fully committed to his well-being.
Mr. B does not have a living donor.
Needed: Assessment of adaptive functioning
DSM-5 defines intellectual disability as a disorder with onset during the developmental period. It includes deficits of intellectual and adaptive functioning in conceptual, social, and practical domains.
Regrettably, many authors focus exclusively on intellectual functioning and IQ, classifying patients as having intellectual disability based on intelligence tests alone.1,2 Adaptive capabilities are insufficiently taken into consideration; there is an urgent need to supplement IQ testing with neuropsychological testing of a patient’s cognitive and adaptive functioning.
Landmark case
In 1995, Sandra Jensen, age 34, with trisomy 21 (Down syndrome) was denied a heart and lung transplant at 2 prominent academic institutions. The denial created a national debate; Jensen’s advocates persuaded one of the hospitals to reconsider.3,4
In 1996, Jensen received the transplant, but she died 18 months later from complications of immunosuppressive therapy. Her surgery was a landmark event; previously, no patient with trisomy 21 or intellectual disability had undergone organ transplantation.
Although attitudes and practices have changed in the past 2 decades, intellectual disability is still considered a relative contraindication to certain organ transplants.5
Why is intellectual disability still a contraindication?
Allocation of transplant organs is based primarily on the ethical principle of utilitarianism: ie, a morally good action is one that helps the greatest number of people. “Benefit” might take the form of the number of lives saved or the number of years added to a patient’s life.
There is little consensus on the definition of quality of life, with its debatable ideological standpoint that stands, at times, in contrast to distributive justice. Studies have shown that the long-term outcome for patients with intellectual disability who received a kidney transplant is comparable to the outcome after renal transplant for patients who are not intellectually disabled. In other studies, patients with intellectual disability and their caregivers report improvement in quality of life after transplant.
The goal of successful transplantation is improvement in quality of life and an increase in longevity. Compliance with all aspects of post-transplant treatment is essential—which is why intellectual disability remains a relative contraindication to heart transplantation in the guidelines of the International Society for Heart and Lung Transplantation. The society’s position is based on a theoretical rationale: ie, “concerns about compliance.”
Only 7 cases of successful long-term outcome after cardiac transplantation have been reported in patients with intellectual disability, and these were marked by the presence of the social and cognitive support necessary for post-transplant compliance with treatment.5 One of these 7 patients had a lengthy hospitalization 4 years after transplantation because of poor adherence to his medication regimen, following the functional decline of his primary caregiver.
Two-pronged evaluation is needed. Most patients undergoing organ transplantation receive a psychosocial assessment that varies from institution to institution. Intellectual disability can add complexity to the task of assessing candidacy for transplantation, however. In these patients, the availability and adequacy of caregivers is as important a part of decision-making as assessment of the patients themselves—yet studies of the assessment of caregivers are limited. The patient’s caregivers should be present during evaluation so that their knowledge, ability, and willingness to take on post-transplant responsibilities can be assessed. More research is needed on long-term outcomes of successful transplantation in patients with intellectual disability.
CASE CONTINUED Placement on hold
The transplant committee decides to postpone placing Mr. B on the transplant waiting list. Consensus is to revisit the question of placing him on the list at a later date.
What led to this decision?
The committee had several concerns about approving Mr. B for a transplant:
- His history of pulling out the catheter meant that he would require closer postoperative monitoring, because he would likely have drains and a urinary catheter inserted.
- Maintaining adequate oral hydration with a new kidney could be a challenge because Mr. B would not be able to comprehend how dehydration can destroy a new kidney.
- His parents believed that, after transplant, Mr. B would not be dependent on them; they failed to understand that he requires lifelong supervision to ensure compliance with immunosuppressive medications and return for follow-up.
The committee’s decision was aided by the rationale that dialysis is readily available and is a sustainable alternative to transplantation.
Mr. B’s case raises an ethical question
We speculate what the team’s decision about transplantation would have been if Mr. B (1) had a living donor or (2) was being considered for a heart, lung, or liver transplant—for which there is no analogous procedure to dialysis to sustain the patient.
1. Arciniegas DB, Filley CM. Implications of impaired cognition for organ transplant candidacy. Curr Opin Organ Transplant. 1999;4(2):168-172.
2. Dobbels F. Intellectual disability in pediatric transplantation: pitfalls and opportunities. Pediatr Transplant. 2014;18(7):658-660.
3. Martens MA, Jones L, Reiss S. Organ transplantation, organ donation and mental retardation. Pediatr Transplant. 2006;10(6):658-664.
4. Panocchia N, Bossola M, Vivanti G. Transplantation and mental retardation: what is the meaning of a discrimination? Am J Transplant. 2010;10(4):727-730.
5. Samelson-Jones E, Mancini D, Shapiro PA. Cardiac transplantation in adult patients with mental retardation: do outcomes support consensus guidelines? Psychosomatics. 2012;53(2):133-138.
CASE REPORT Evaluation for renal transplant
Mr. B, age 21, who has a diagnosis of autism spectrum disorder and an IQ comparable to that of a 4-year-old, is referred for evaluation of his candidacy for renal transplant.
A few months earlier, Mr. B pulled out his temporary dialysis catheter. Now, he receives hemodialysis through an arteriovenous fistula in the arm, but requires constant supervision during dialysis.
At evaluation, Mr. B is accompanied by his parents and his older sister, who have been providing day-to-day care for him. They appear fully committed to his well-being.
Mr. B does not have a living donor.
Needed: Assessment of adaptive functioning
DSM-5 defines intellectual disability as a disorder with onset during the developmental period. It includes deficits of intellectual and adaptive functioning in conceptual, social, and practical domains.
Regrettably, many authors focus exclusively on intellectual functioning and IQ, classifying patients as having intellectual disability based on intelligence tests alone.1,2 Adaptive capabilities are insufficiently taken into consideration; there is an urgent need to supplement IQ testing with neuropsychological testing of a patient’s cognitive and adaptive functioning.
Landmark case
In 1995, Sandra Jensen, age 34, with trisomy 21 (Down syndrome) was denied a heart and lung transplant at 2 prominent academic institutions. The denial created a national debate; Jensen’s advocates persuaded one of the hospitals to reconsider.3,4
In 1996, Jensen received the transplant, but she died 18 months later from complications of immunosuppressive therapy. Her surgery was a landmark event; previously, no patient with trisomy 21 or intellectual disability had undergone organ transplantation.
Although attitudes and practices have changed in the past 2 decades, intellectual disability is still considered a relative contraindication to certain organ transplants.5
Why is intellectual disability still a contraindication?
Allocation of transplant organs is based primarily on the ethical principle of utilitarianism: ie, a morally good action is one that helps the greatest number of people. “Benefit” might take the form of the number of lives saved or the number of years added to a patient’s life.
There is little consensus on the definition of quality of life, with its debatable ideological standpoint that stands, at times, in contrast to distributive justice. Studies have shown that the long-term outcome for patients with intellectual disability who received a kidney transplant is comparable to the outcome after renal transplant for patients who are not intellectually disabled. In other studies, patients with intellectual disability and their caregivers report improvement in quality of life after transplant.
The goal of successful transplantation is improvement in quality of life and an increase in longevity. Compliance with all aspects of post-transplant treatment is essential—which is why intellectual disability remains a relative contraindication to heart transplantation in the guidelines of the International Society for Heart and Lung Transplantation. The society’s position is based on a theoretical rationale: ie, “concerns about compliance.”
Only 7 cases of successful long-term outcome after cardiac transplantation have been reported in patients with intellectual disability, and these were marked by the presence of the social and cognitive support necessary for post-transplant compliance with treatment.5 One of these 7 patients had a lengthy hospitalization 4 years after transplantation because of poor adherence to his medication regimen, following the functional decline of his primary caregiver.
Two-pronged evaluation is needed. Most patients undergoing organ transplantation receive a psychosocial assessment that varies from institution to institution. Intellectual disability can add complexity to the task of assessing candidacy for transplantation, however. In these patients, the availability and adequacy of caregivers is as important a part of decision-making as assessment of the patients themselves—yet studies of the assessment of caregivers are limited. The patient’s caregivers should be present during evaluation so that their knowledge, ability, and willingness to take on post-transplant responsibilities can be assessed. More research is needed on long-term outcomes of successful transplantation in patients with intellectual disability.
CASE CONTINUED Placement on hold
The transplant committee decides to postpone placing Mr. B on the transplant waiting list. Consensus is to revisit the question of placing him on the list at a later date.
What led to this decision?
The committee had several concerns about approving Mr. B for a transplant:
- His history of pulling out the catheter meant that he would require closer postoperative monitoring, because he would likely have drains and a urinary catheter inserted.
- Maintaining adequate oral hydration with a new kidney could be a challenge because Mr. B would not be able to comprehend how dehydration can destroy a new kidney.
- His parents believed that, after transplant, Mr. B would not be dependent on them; they failed to understand that he requires lifelong supervision to ensure compliance with immunosuppressive medications and return for follow-up.
The committee’s decision was aided by the rationale that dialysis is readily available and is a sustainable alternative to transplantation.
Mr. B’s case raises an ethical question
We speculate what the team’s decision about transplantation would have been if Mr. B (1) had a living donor or (2) was being considered for a heart, lung, or liver transplant—for which there is no analogous procedure to dialysis to sustain the patient.
CASE REPORT Evaluation for renal transplant
Mr. B, age 21, who has a diagnosis of autism spectrum disorder and an IQ comparable to that of a 4-year-old, is referred for evaluation of his candidacy for renal transplant.
A few months earlier, Mr. B pulled out his temporary dialysis catheter. Now, he receives hemodialysis through an arteriovenous fistula in the arm, but requires constant supervision during dialysis.
At evaluation, Mr. B is accompanied by his parents and his older sister, who have been providing day-to-day care for him. They appear fully committed to his well-being.
Mr. B does not have a living donor.
Needed: Assessment of adaptive functioning
DSM-5 defines intellectual disability as a disorder with onset during the developmental period. It includes deficits of intellectual and adaptive functioning in conceptual, social, and practical domains.
Regrettably, many authors focus exclusively on intellectual functioning and IQ, classifying patients as having intellectual disability based on intelligence tests alone.1,2 Adaptive capabilities are insufficiently taken into consideration; there is an urgent need to supplement IQ testing with neuropsychological testing of a patient’s cognitive and adaptive functioning.
Landmark case
In 1995, Sandra Jensen, age 34, with trisomy 21 (Down syndrome) was denied a heart and lung transplant at 2 prominent academic institutions. The denial created a national debate; Jensen’s advocates persuaded one of the hospitals to reconsider.3,4
In 1996, Jensen received the transplant, but she died 18 months later from complications of immunosuppressive therapy. Her surgery was a landmark event; previously, no patient with trisomy 21 or intellectual disability had undergone organ transplantation.
Although attitudes and practices have changed in the past 2 decades, intellectual disability is still considered a relative contraindication to certain organ transplants.5
Why is intellectual disability still a contraindication?
Allocation of transplant organs is based primarily on the ethical principle of utilitarianism: ie, a morally good action is one that helps the greatest number of people. “Benefit” might take the form of the number of lives saved or the number of years added to a patient’s life.
There is little consensus on the definition of quality of life, with its debatable ideological standpoint that stands, at times, in contrast to distributive justice. Studies have shown that the long-term outcome for patients with intellectual disability who received a kidney transplant is comparable to the outcome after renal transplant for patients who are not intellectually disabled. In other studies, patients with intellectual disability and their caregivers report improvement in quality of life after transplant.
The goal of successful transplantation is improvement in quality of life and an increase in longevity. Compliance with all aspects of post-transplant treatment is essential—which is why intellectual disability remains a relative contraindication to heart transplantation in the guidelines of the International Society for Heart and Lung Transplantation. The society’s position is based on a theoretical rationale: ie, “concerns about compliance.”
Only 7 cases of successful long-term outcome after cardiac transplantation have been reported in patients with intellectual disability, and these were marked by the presence of the social and cognitive support necessary for post-transplant compliance with treatment.5 One of these 7 patients had a lengthy hospitalization 4 years after transplantation because of poor adherence to his medication regimen, following the functional decline of his primary caregiver.
Two-pronged evaluation is needed. Most patients undergoing organ transplantation receive a psychosocial assessment that varies from institution to institution. Intellectual disability can add complexity to the task of assessing candidacy for transplantation, however. In these patients, the availability and adequacy of caregivers is as important a part of decision-making as assessment of the patients themselves—yet studies of the assessment of caregivers are limited. The patient’s caregivers should be present during evaluation so that their knowledge, ability, and willingness to take on post-transplant responsibilities can be assessed. More research is needed on long-term outcomes of successful transplantation in patients with intellectual disability.
CASE CONTINUED Placement on hold
The transplant committee decides to postpone placing Mr. B on the transplant waiting list. Consensus is to revisit the question of placing him on the list at a later date.
What led to this decision?
The committee had several concerns about approving Mr. B for a transplant:
- His history of pulling out the catheter meant that he would require closer postoperative monitoring, because he would likely have drains and a urinary catheter inserted.
- Maintaining adequate oral hydration with a new kidney could be a challenge because Mr. B would not be able to comprehend how dehydration can destroy a new kidney.
- His parents believed that, after transplant, Mr. B would not be dependent on them; they failed to understand that he requires lifelong supervision to ensure compliance with immunosuppressive medications and return for follow-up.
The committee’s decision was aided by the rationale that dialysis is readily available and is a sustainable alternative to transplantation.
Mr. B’s case raises an ethical question
We speculate what the team’s decision about transplantation would have been if Mr. B (1) had a living donor or (2) was being considered for a heart, lung, or liver transplant—for which there is no analogous procedure to dialysis to sustain the patient.
1. Arciniegas DB, Filley CM. Implications of impaired cognition for organ transplant candidacy. Curr Opin Organ Transplant. 1999;4(2):168-172.
2. Dobbels F. Intellectual disability in pediatric transplantation: pitfalls and opportunities. Pediatr Transplant. 2014;18(7):658-660.
3. Martens MA, Jones L, Reiss S. Organ transplantation, organ donation and mental retardation. Pediatr Transplant. 2006;10(6):658-664.
4. Panocchia N, Bossola M, Vivanti G. Transplantation and mental retardation: what is the meaning of a discrimination? Am J Transplant. 2010;10(4):727-730.
5. Samelson-Jones E, Mancini D, Shapiro PA. Cardiac transplantation in adult patients with mental retardation: do outcomes support consensus guidelines? Psychosomatics. 2012;53(2):133-138.
1. Arciniegas DB, Filley CM. Implications of impaired cognition for organ transplant candidacy. Curr Opin Organ Transplant. 1999;4(2):168-172.
2. Dobbels F. Intellectual disability in pediatric transplantation: pitfalls and opportunities. Pediatr Transplant. 2014;18(7):658-660.
3. Martens MA, Jones L, Reiss S. Organ transplantation, organ donation and mental retardation. Pediatr Transplant. 2006;10(6):658-664.
4. Panocchia N, Bossola M, Vivanti G. Transplantation and mental retardation: what is the meaning of a discrimination? Am J Transplant. 2010;10(4):727-730.
5. Samelson-Jones E, Mancini D, Shapiro PA. Cardiac transplantation in adult patients with mental retardation: do outcomes support consensus guidelines? Psychosomatics. 2012;53(2):133-138.
The view from my office: How psychiatry residency programs have changed
As I approach my twentieth year as Residency Program Coordinator in the Department of Psychiatry at Saint Louis University School of Medicine, I’ve been reflecting on the many changes that have occurred: within our residency program; in the requirements that all residency programs must meet to continue as an Accreditation Council for Graduate Medical Education (ACGME)-accredited program; and in the overall scope of psychiatry residency training.
What has changed
During my time as Residency Program Coordinator, I have assisted 5 program directors and 3 associate program directors with day-to-day details of residency training. Our residency program has had couples, and a father and son; some residents even married each other while still in training.
The Electronic Residency Application System was not available until 2001; before that, applicants interested in being invited for an interview with a psychiatry residency program had to mail in their applications for review. This was a time-consuming, tedious process. In addition, residency programs today are required to use the American Board of Psychiatry and Neurology (ABPN) PreCERT credentialing program to verify training—instead of (as in the past) simply submitting a letter to ABPN that detailed the rotations and clinical skills examinations completed.
Residency programs have gone from evaluating residents by using the 6 competencies to the Milestones requirement from ACGME, which is the newest system of measuring residents’ competencies. Every month, the program faculty meets to discuss the progress of 1 of the classes of residents and the residents who are completing an individual self-assessment. Milestone scores for each resident are then reported to ACGME.
At one time, a resident’s files could be stored in a 2-inch binder; now, we need a 4-inch binder to accommodate required documentation! I am relieved—as, I am sure, many other residency program coordinators are—that residency programs are no longer required to prepare a Program Information Form but, instead, perform a self-study and, every 10 years, have a site visit. Last, every academic year, the Residency Program Coordinator is required to enter the incoming residents’ information into the graduate medical education track, ACGME, and PreCERT Web site systems.
Rewards of my position
As Residency Program Coordinator, I’ve had the rewarding experience of meeting physicians from all over the world without having to travel to other countries. Because I have a 3- or 4-year relationship with residents, I serve them in various roles: mentor, mother, confidante, motivator, and friend. As much as the job is rewarding, being the Residency Program Coordinator can, on some days, be overwhelming, particularly because I need to think “out of the box” to streamline decisions and thus avoid conflicts with program rotations and didactic schedules.
As I approach my twentieth year as Residency Program Coordinator in the Department of Psychiatry at Saint Louis University School of Medicine, I’ve been reflecting on the many changes that have occurred: within our residency program; in the requirements that all residency programs must meet to continue as an Accreditation Council for Graduate Medical Education (ACGME)-accredited program; and in the overall scope of psychiatry residency training.
What has changed
During my time as Residency Program Coordinator, I have assisted 5 program directors and 3 associate program directors with day-to-day details of residency training. Our residency program has had couples, and a father and son; some residents even married each other while still in training.
The Electronic Residency Application System was not available until 2001; before that, applicants interested in being invited for an interview with a psychiatry residency program had to mail in their applications for review. This was a time-consuming, tedious process. In addition, residency programs today are required to use the American Board of Psychiatry and Neurology (ABPN) PreCERT credentialing program to verify training—instead of (as in the past) simply submitting a letter to ABPN that detailed the rotations and clinical skills examinations completed.
Residency programs have gone from evaluating residents by using the 6 competencies to the Milestones requirement from ACGME, which is the newest system of measuring residents’ competencies. Every month, the program faculty meets to discuss the progress of 1 of the classes of residents and the residents who are completing an individual self-assessment. Milestone scores for each resident are then reported to ACGME.
At one time, a resident’s files could be stored in a 2-inch binder; now, we need a 4-inch binder to accommodate required documentation! I am relieved—as, I am sure, many other residency program coordinators are—that residency programs are no longer required to prepare a Program Information Form but, instead, perform a self-study and, every 10 years, have a site visit. Last, every academic year, the Residency Program Coordinator is required to enter the incoming residents’ information into the graduate medical education track, ACGME, and PreCERT Web site systems.
Rewards of my position
As Residency Program Coordinator, I’ve had the rewarding experience of meeting physicians from all over the world without having to travel to other countries. Because I have a 3- or 4-year relationship with residents, I serve them in various roles: mentor, mother, confidante, motivator, and friend. As much as the job is rewarding, being the Residency Program Coordinator can, on some days, be overwhelming, particularly because I need to think “out of the box” to streamline decisions and thus avoid conflicts with program rotations and didactic schedules.
As I approach my twentieth year as Residency Program Coordinator in the Department of Psychiatry at Saint Louis University School of Medicine, I’ve been reflecting on the many changes that have occurred: within our residency program; in the requirements that all residency programs must meet to continue as an Accreditation Council for Graduate Medical Education (ACGME)-accredited program; and in the overall scope of psychiatry residency training.
What has changed
During my time as Residency Program Coordinator, I have assisted 5 program directors and 3 associate program directors with day-to-day details of residency training. Our residency program has had couples, and a father and son; some residents even married each other while still in training.
The Electronic Residency Application System was not available until 2001; before that, applicants interested in being invited for an interview with a psychiatry residency program had to mail in their applications for review. This was a time-consuming, tedious process. In addition, residency programs today are required to use the American Board of Psychiatry and Neurology (ABPN) PreCERT credentialing program to verify training—instead of (as in the past) simply submitting a letter to ABPN that detailed the rotations and clinical skills examinations completed.
Residency programs have gone from evaluating residents by using the 6 competencies to the Milestones requirement from ACGME, which is the newest system of measuring residents’ competencies. Every month, the program faculty meets to discuss the progress of 1 of the classes of residents and the residents who are completing an individual self-assessment. Milestone scores for each resident are then reported to ACGME.
At one time, a resident’s files could be stored in a 2-inch binder; now, we need a 4-inch binder to accommodate required documentation! I am relieved—as, I am sure, many other residency program coordinators are—that residency programs are no longer required to prepare a Program Information Form but, instead, perform a self-study and, every 10 years, have a site visit. Last, every academic year, the Residency Program Coordinator is required to enter the incoming residents’ information into the graduate medical education track, ACGME, and PreCERT Web site systems.
Rewards of my position
As Residency Program Coordinator, I’ve had the rewarding experience of meeting physicians from all over the world without having to travel to other countries. Because I have a 3- or 4-year relationship with residents, I serve them in various roles: mentor, mother, confidante, motivator, and friend. As much as the job is rewarding, being the Residency Program Coordinator can, on some days, be overwhelming, particularly because I need to think “out of the box” to streamline decisions and thus avoid conflicts with program rotations and didactic schedules.
Changing trends in diet pill use, from weight loss agent to recreational drug
The prevalence of obesity and obesity-related conditions in the United States is increasing. Many weight-loss products and dietary supplements are used in an attempt to combat this epidemic, but little evidence exists of their efficacy and safety.
We present a case report of a middle-age woman who developed severe psychotic symptoms while taking phentermine hydrochloride (HCl), a psychostimulant similar to amphetamine that is used as a weight-loss agent and for recreational purposes. Phentermine has been associated with mood and psychotic symptoms and has a tendency to cause psychological dependence and tolerance.
To investigate the risks and potential effects of using this drug, we searched OVID and PubMed databases using the search string “phentermine + psychosis.” We conclude that there is a need for awareness about early detection and treatment of reversible psychotic and mood symptoms caused by what might appear to be harmless weight-loss and energy pills.
Obesity epidemic, wide-ranging weight-loss effortsThere has been a dramatic increase in obesity in the United States in the past 20 years: More than one-third of adults and approximately 17% of children and adolescents are obese. Obesity-related conditions, such as heart disease, stroke, and type 2 diabetes mellitus, are leading causes of preventable death.1 Weight monitoring, a healthy lifestyle, surgical intervention, traditional herbs, and diet-pill supplements are some of the modalities used to address this epidemic.
Most so-called supplements for weight loss are exempt from FDA regulation. They do not undergo rigorous testing for safety. Furthermore, many contain controlled substances; some supplements are anti-seizure medications or other prescription drugs; and some are drugs not approved in the United States.2 Since the 1930s, such drugs as dinitrophenol, ephedrine, amphetamine, fenfluramine, and phentermine have flooded the market with the promise of quick weight loss.3,4
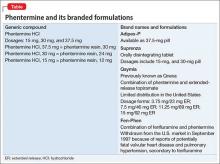
Phentermine, a contraction of “phenyltertiary-butylamine,” and its various types (Table) is a psychostimulant of the phenethylamine class, with a pharmacologic profile similar to that of amphetamine. It is known to yield false-positive immunoassay screening results for amphetamines.
CASE REPORT Acute psychotic break
Ms. B, age 37, with a history of postpartum depression, arrives at the emergency room reporting auditory hallucinations of her son and boyfriend; vivid visual hallucinations; and persecutory ideas toward her boyfriend, whom she believes had kidnapped her son. She also complains of insomnia and intermittent confusion for the past week.
Speech is pressured, fast, and difficult to comprehend at times; affect is labile and irritable. Ms. B denies suicidal ideation and is oriented to time, place, and person.
A urine drug screen is positive for amphetamine.
Pre-admission medications include alprazolam, 1 mg as needed, and zolpidem, 10 mg at bedtime, prescribed by Ms. B’s primary care physician for anxiety and insomnia. She discontinued these medications 3 weeks ago because of increased drowsiness at work. She denies other substance use and is unable to account for the positive urine drug screen.
Her medical history, physical examination, and a CT scan of the head are unremarkable. The components of a comprehensive metabolic panel and complete blood count are within normal limits.
After admission, in-depth assessment reveals that Ms. B has been taking phentermine, 37.5 mg (under the brand name Adipex-P), once daily since age 16 for weight loss. She recently discontinued the drug, abruptly, for 1 month, then resumed taking it at an unspecified higher dosage 1 week before she came to the emergency room, for what she said was recreational use and to meet the demands of her job, which required shift work and long hours.
Over the next few days in the hospital, Ms. B’s symptoms resolve as the drug is eliminated from her body. Speech becomes comprehensible and sleep improves. Affective distress diminishes considerably after admission; slight mood lability persists. She no longer reports perceptual disturbances or distress secondary to intrusive thoughts.
Ms. B is discharged 1 week after admission, with instructions to follow up at a dual-diagnosis outpatient program.
Pharmacologic profilePhentermine acts through sympathomimetic pathways by increasing brain noradrenaline and dopamine. The drug has no effect on serotonin.4,5 Phentermine can lead to elevated blood pressure and heart rate, palpitations, restlessness, and insomnia, and can suppress appetite. Increased sympathomimetic activity has been implicated in the ability of phentermine to induce psychotic symptoms.
The literature. Our PubMed search of “phentermine + psychosis” produced 13 results, including 6 case reports of phentermine use. Five citations were more than 4 decades old5-12; only 1 could be considered recent (2011).13
Patients in these reports developed psychotic or manic features after chronic or acute phentermine use, mainly for weight reduction. The most recent article13 mentioned 4 patients who were abusing diet pills recreationally (including “for lethargy”). As with Ms. B, in all 4 of those patients, phentermine precipitated the primary pathology (mania in bipolar disorder; depression in postpartum depression and substance abuse) or revealed underlying illness.
Changing landscape of use and abuseThere has been a trend observed in the pattern of diet pill use: Initially marketed as an appetite suppressant, these pills are now being abused across ethnic, racial, and socioeconomic groups, by males and females.14 There is also a scarcity of useful guidance for clinicians.
Not only are diet pills used by people with an eating disorder; their recreational use is an emerging problem. If reports12,13 continue to reveal that phentermine is a substance of abuse and has catastrophic effects on the user’s psyche, the need for stronger warnings and guidelines might be warranted to allow consumers to make an informed choice about using the drug.
Call for awarenessThe case we presented here exemplifies the importance of tighter regulation of both over-the-counter and prescription stimulant analogs. There is a need for awareness among practitioners about early detection and treatment of reversible psychotic and mood symptoms secondary to what might be promoted as, or appear to be, “harmless” weight loss and energy pills.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
This unfunded study was presented as a case report poster at the Annual Meeting of the Academy of Psychosomatic Medicine, November 2013, Tucson, Arizona, and at the Colloquium of Scholars of the Philadelphia Psychiatric Society, March 2014, Philadelphia, Pennsylvania.
Drug Brand Names
Alprazolam • Xanax
Fenfluramine • Pondimin
Phentermine HCl • Adipex-P, Fen-Phen, Qsymia, Suprenza
Topiramate • Topamax, Trokendi XR
Zolpidem • Ambien
1. Center for Disease Control. Division of nutrition, physical activity, and obesity. http://www.cdc.gov/obesity/data/adult. html. Updated September 14, 2015. Accessed October 27, 2015.
2. Retamero C, Rivera T, Murphy K. “Ephedra-free” diet pill-induced psychosis. Psychosomatics. 2011;52(6):579-582.
3. Cohen PA, Goday A, Swann JP. The return of rainbow diet pills. Am J Public Health. 2012;102(9):1676-1686.
4. Wellman PJ. Overview of adrenergic anorectic agents. Am J Clin Nutr. 1992;55(suppl 1):193S-198S.
5. Devan GS. Phentermine and psychosis. Br J Psychiatry. 1990;156:442-443.
6. Hoffman BF. Diet pill psychosis. Can Med Assoc J. 1977;116(4):351-355.
7. Hoffman BF. Diet pill psychosis: follow-up after 6 years. Can Med Assoc J. 1983;129(10):1077-1078.
8. Rubin RT. Acute psychotic reaction following ingestion of phentermine. Am J Psychiatry. 1964;120:1124-1125.
9. Schaffer CB, Pauli MW. Psychotic reaction caused by proprietary oral diet agent. Am J Psychiatry. 1980;137(10):1256-12567.
10. Lee SH, Liu CY, Yang YY. Schizophreniform-like psychotic disorder induced by phentermine: a case report. Zhonghua Yi Xue Za Zhi (Taipei). 1998;61(1):44-47.
11. Zimmer JE, Gregory RJ. Bipolar depression associated with fenfluramine and phentermine. J Clin Psychiatry. 1998;59(7):383-384.
12. Bagri S, Reddy G. Delirium with manic symptoms induced by diet pills. J Clin Psychiatry. 1998;59(2):83.
13. Alexander J, Cheng Y, Choudhary J, et al. Phentermine (Duromine) precipitated psychosis. Aust N Z J Psychiatry. 2011;45(8):684-685.
14. Pomeranz JL, Taylor LM, Austin SB. Over-the-counter and out-of-control: legal strategies to protect youths from abusing products for weight control. Am J Public Health. 2013;103(2):222-2253.
The prevalence of obesity and obesity-related conditions in the United States is increasing. Many weight-loss products and dietary supplements are used in an attempt to combat this epidemic, but little evidence exists of their efficacy and safety.
We present a case report of a middle-age woman who developed severe psychotic symptoms while taking phentermine hydrochloride (HCl), a psychostimulant similar to amphetamine that is used as a weight-loss agent and for recreational purposes. Phentermine has been associated with mood and psychotic symptoms and has a tendency to cause psychological dependence and tolerance.
To investigate the risks and potential effects of using this drug, we searched OVID and PubMed databases using the search string “phentermine + psychosis.” We conclude that there is a need for awareness about early detection and treatment of reversible psychotic and mood symptoms caused by what might appear to be harmless weight-loss and energy pills.
Obesity epidemic, wide-ranging weight-loss effortsThere has been a dramatic increase in obesity in the United States in the past 20 years: More than one-third of adults and approximately 17% of children and adolescents are obese. Obesity-related conditions, such as heart disease, stroke, and type 2 diabetes mellitus, are leading causes of preventable death.1 Weight monitoring, a healthy lifestyle, surgical intervention, traditional herbs, and diet-pill supplements are some of the modalities used to address this epidemic.
Most so-called supplements for weight loss are exempt from FDA regulation. They do not undergo rigorous testing for safety. Furthermore, many contain controlled substances; some supplements are anti-seizure medications or other prescription drugs; and some are drugs not approved in the United States.2 Since the 1930s, such drugs as dinitrophenol, ephedrine, amphetamine, fenfluramine, and phentermine have flooded the market with the promise of quick weight loss.3,4
Phentermine, a contraction of “phenyltertiary-butylamine,” and its various types (Table) is a psychostimulant of the phenethylamine class, with a pharmacologic profile similar to that of amphetamine. It is known to yield false-positive immunoassay screening results for amphetamines.
CASE REPORT Acute psychotic break
Ms. B, age 37, with a history of postpartum depression, arrives at the emergency room reporting auditory hallucinations of her son and boyfriend; vivid visual hallucinations; and persecutory ideas toward her boyfriend, whom she believes had kidnapped her son. She also complains of insomnia and intermittent confusion for the past week.
Speech is pressured, fast, and difficult to comprehend at times; affect is labile and irritable. Ms. B denies suicidal ideation and is oriented to time, place, and person.
A urine drug screen is positive for amphetamine.
Pre-admission medications include alprazolam, 1 mg as needed, and zolpidem, 10 mg at bedtime, prescribed by Ms. B’s primary care physician for anxiety and insomnia. She discontinued these medications 3 weeks ago because of increased drowsiness at work. She denies other substance use and is unable to account for the positive urine drug screen.
Her medical history, physical examination, and a CT scan of the head are unremarkable. The components of a comprehensive metabolic panel and complete blood count are within normal limits.
After admission, in-depth assessment reveals that Ms. B has been taking phentermine, 37.5 mg (under the brand name Adipex-P), once daily since age 16 for weight loss. She recently discontinued the drug, abruptly, for 1 month, then resumed taking it at an unspecified higher dosage 1 week before she came to the emergency room, for what she said was recreational use and to meet the demands of her job, which required shift work and long hours.
Over the next few days in the hospital, Ms. B’s symptoms resolve as the drug is eliminated from her body. Speech becomes comprehensible and sleep improves. Affective distress diminishes considerably after admission; slight mood lability persists. She no longer reports perceptual disturbances or distress secondary to intrusive thoughts.
Ms. B is discharged 1 week after admission, with instructions to follow up at a dual-diagnosis outpatient program.
Pharmacologic profilePhentermine acts through sympathomimetic pathways by increasing brain noradrenaline and dopamine. The drug has no effect on serotonin.4,5 Phentermine can lead to elevated blood pressure and heart rate, palpitations, restlessness, and insomnia, and can suppress appetite. Increased sympathomimetic activity has been implicated in the ability of phentermine to induce psychotic symptoms.
The literature. Our PubMed search of “phentermine + psychosis” produced 13 results, including 6 case reports of phentermine use. Five citations were more than 4 decades old5-12; only 1 could be considered recent (2011).13
Patients in these reports developed psychotic or manic features after chronic or acute phentermine use, mainly for weight reduction. The most recent article13 mentioned 4 patients who were abusing diet pills recreationally (including “for lethargy”). As with Ms. B, in all 4 of those patients, phentermine precipitated the primary pathology (mania in bipolar disorder; depression in postpartum depression and substance abuse) or revealed underlying illness.
Changing landscape of use and abuseThere has been a trend observed in the pattern of diet pill use: Initially marketed as an appetite suppressant, these pills are now being abused across ethnic, racial, and socioeconomic groups, by males and females.14 There is also a scarcity of useful guidance for clinicians.
Not only are diet pills used by people with an eating disorder; their recreational use is an emerging problem. If reports12,13 continue to reveal that phentermine is a substance of abuse and has catastrophic effects on the user’s psyche, the need for stronger warnings and guidelines might be warranted to allow consumers to make an informed choice about using the drug.
Call for awarenessThe case we presented here exemplifies the importance of tighter regulation of both over-the-counter and prescription stimulant analogs. There is a need for awareness among practitioners about early detection and treatment of reversible psychotic and mood symptoms secondary to what might be promoted as, or appear to be, “harmless” weight loss and energy pills.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
This unfunded study was presented as a case report poster at the Annual Meeting of the Academy of Psychosomatic Medicine, November 2013, Tucson, Arizona, and at the Colloquium of Scholars of the Philadelphia Psychiatric Society, March 2014, Philadelphia, Pennsylvania.
Drug Brand Names
Alprazolam • Xanax
Fenfluramine • Pondimin
Phentermine HCl • Adipex-P, Fen-Phen, Qsymia, Suprenza
Topiramate • Topamax, Trokendi XR
Zolpidem • Ambien
The prevalence of obesity and obesity-related conditions in the United States is increasing. Many weight-loss products and dietary supplements are used in an attempt to combat this epidemic, but little evidence exists of their efficacy and safety.
We present a case report of a middle-age woman who developed severe psychotic symptoms while taking phentermine hydrochloride (HCl), a psychostimulant similar to amphetamine that is used as a weight-loss agent and for recreational purposes. Phentermine has been associated with mood and psychotic symptoms and has a tendency to cause psychological dependence and tolerance.
To investigate the risks and potential effects of using this drug, we searched OVID and PubMed databases using the search string “phentermine + psychosis.” We conclude that there is a need for awareness about early detection and treatment of reversible psychotic and mood symptoms caused by what might appear to be harmless weight-loss and energy pills.
Obesity epidemic, wide-ranging weight-loss effortsThere has been a dramatic increase in obesity in the United States in the past 20 years: More than one-third of adults and approximately 17% of children and adolescents are obese. Obesity-related conditions, such as heart disease, stroke, and type 2 diabetes mellitus, are leading causes of preventable death.1 Weight monitoring, a healthy lifestyle, surgical intervention, traditional herbs, and diet-pill supplements are some of the modalities used to address this epidemic.
Most so-called supplements for weight loss are exempt from FDA regulation. They do not undergo rigorous testing for safety. Furthermore, many contain controlled substances; some supplements are anti-seizure medications or other prescription drugs; and some are drugs not approved in the United States.2 Since the 1930s, such drugs as dinitrophenol, ephedrine, amphetamine, fenfluramine, and phentermine have flooded the market with the promise of quick weight loss.3,4
Phentermine, a contraction of “phenyltertiary-butylamine,” and its various types (Table) is a psychostimulant of the phenethylamine class, with a pharmacologic profile similar to that of amphetamine. It is known to yield false-positive immunoassay screening results for amphetamines.
CASE REPORT Acute psychotic break
Ms. B, age 37, with a history of postpartum depression, arrives at the emergency room reporting auditory hallucinations of her son and boyfriend; vivid visual hallucinations; and persecutory ideas toward her boyfriend, whom she believes had kidnapped her son. She also complains of insomnia and intermittent confusion for the past week.
Speech is pressured, fast, and difficult to comprehend at times; affect is labile and irritable. Ms. B denies suicidal ideation and is oriented to time, place, and person.
A urine drug screen is positive for amphetamine.
Pre-admission medications include alprazolam, 1 mg as needed, and zolpidem, 10 mg at bedtime, prescribed by Ms. B’s primary care physician for anxiety and insomnia. She discontinued these medications 3 weeks ago because of increased drowsiness at work. She denies other substance use and is unable to account for the positive urine drug screen.
Her medical history, physical examination, and a CT scan of the head are unremarkable. The components of a comprehensive metabolic panel and complete blood count are within normal limits.
After admission, in-depth assessment reveals that Ms. B has been taking phentermine, 37.5 mg (under the brand name Adipex-P), once daily since age 16 for weight loss. She recently discontinued the drug, abruptly, for 1 month, then resumed taking it at an unspecified higher dosage 1 week before she came to the emergency room, for what she said was recreational use and to meet the demands of her job, which required shift work and long hours.
Over the next few days in the hospital, Ms. B’s symptoms resolve as the drug is eliminated from her body. Speech becomes comprehensible and sleep improves. Affective distress diminishes considerably after admission; slight mood lability persists. She no longer reports perceptual disturbances or distress secondary to intrusive thoughts.
Ms. B is discharged 1 week after admission, with instructions to follow up at a dual-diagnosis outpatient program.
Pharmacologic profilePhentermine acts through sympathomimetic pathways by increasing brain noradrenaline and dopamine. The drug has no effect on serotonin.4,5 Phentermine can lead to elevated blood pressure and heart rate, palpitations, restlessness, and insomnia, and can suppress appetite. Increased sympathomimetic activity has been implicated in the ability of phentermine to induce psychotic symptoms.
The literature. Our PubMed search of “phentermine + psychosis” produced 13 results, including 6 case reports of phentermine use. Five citations were more than 4 decades old5-12; only 1 could be considered recent (2011).13
Patients in these reports developed psychotic or manic features after chronic or acute phentermine use, mainly for weight reduction. The most recent article13 mentioned 4 patients who were abusing diet pills recreationally (including “for lethargy”). As with Ms. B, in all 4 of those patients, phentermine precipitated the primary pathology (mania in bipolar disorder; depression in postpartum depression and substance abuse) or revealed underlying illness.
Changing landscape of use and abuseThere has been a trend observed in the pattern of diet pill use: Initially marketed as an appetite suppressant, these pills are now being abused across ethnic, racial, and socioeconomic groups, by males and females.14 There is also a scarcity of useful guidance for clinicians.
Not only are diet pills used by people with an eating disorder; their recreational use is an emerging problem. If reports12,13 continue to reveal that phentermine is a substance of abuse and has catastrophic effects on the user’s psyche, the need for stronger warnings and guidelines might be warranted to allow consumers to make an informed choice about using the drug.
Call for awarenessThe case we presented here exemplifies the importance of tighter regulation of both over-the-counter and prescription stimulant analogs. There is a need for awareness among practitioners about early detection and treatment of reversible psychotic and mood symptoms secondary to what might be promoted as, or appear to be, “harmless” weight loss and energy pills.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
This unfunded study was presented as a case report poster at the Annual Meeting of the Academy of Psychosomatic Medicine, November 2013, Tucson, Arizona, and at the Colloquium of Scholars of the Philadelphia Psychiatric Society, March 2014, Philadelphia, Pennsylvania.
Drug Brand Names
Alprazolam • Xanax
Fenfluramine • Pondimin
Phentermine HCl • Adipex-P, Fen-Phen, Qsymia, Suprenza
Topiramate • Topamax, Trokendi XR
Zolpidem • Ambien
1. Center for Disease Control. Division of nutrition, physical activity, and obesity. http://www.cdc.gov/obesity/data/adult. html. Updated September 14, 2015. Accessed October 27, 2015.
2. Retamero C, Rivera T, Murphy K. “Ephedra-free” diet pill-induced psychosis. Psychosomatics. 2011;52(6):579-582.
3. Cohen PA, Goday A, Swann JP. The return of rainbow diet pills. Am J Public Health. 2012;102(9):1676-1686.
4. Wellman PJ. Overview of adrenergic anorectic agents. Am J Clin Nutr. 1992;55(suppl 1):193S-198S.
5. Devan GS. Phentermine and psychosis. Br J Psychiatry. 1990;156:442-443.
6. Hoffman BF. Diet pill psychosis. Can Med Assoc J. 1977;116(4):351-355.
7. Hoffman BF. Diet pill psychosis: follow-up after 6 years. Can Med Assoc J. 1983;129(10):1077-1078.
8. Rubin RT. Acute psychotic reaction following ingestion of phentermine. Am J Psychiatry. 1964;120:1124-1125.
9. Schaffer CB, Pauli MW. Psychotic reaction caused by proprietary oral diet agent. Am J Psychiatry. 1980;137(10):1256-12567.
10. Lee SH, Liu CY, Yang YY. Schizophreniform-like psychotic disorder induced by phentermine: a case report. Zhonghua Yi Xue Za Zhi (Taipei). 1998;61(1):44-47.
11. Zimmer JE, Gregory RJ. Bipolar depression associated with fenfluramine and phentermine. J Clin Psychiatry. 1998;59(7):383-384.
12. Bagri S, Reddy G. Delirium with manic symptoms induced by diet pills. J Clin Psychiatry. 1998;59(2):83.
13. Alexander J, Cheng Y, Choudhary J, et al. Phentermine (Duromine) precipitated psychosis. Aust N Z J Psychiatry. 2011;45(8):684-685.
14. Pomeranz JL, Taylor LM, Austin SB. Over-the-counter and out-of-control: legal strategies to protect youths from abusing products for weight control. Am J Public Health. 2013;103(2):222-2253.
1. Center for Disease Control. Division of nutrition, physical activity, and obesity. http://www.cdc.gov/obesity/data/adult. html. Updated September 14, 2015. Accessed October 27, 2015.
2. Retamero C, Rivera T, Murphy K. “Ephedra-free” diet pill-induced psychosis. Psychosomatics. 2011;52(6):579-582.
3. Cohen PA, Goday A, Swann JP. The return of rainbow diet pills. Am J Public Health. 2012;102(9):1676-1686.
4. Wellman PJ. Overview of adrenergic anorectic agents. Am J Clin Nutr. 1992;55(suppl 1):193S-198S.
5. Devan GS. Phentermine and psychosis. Br J Psychiatry. 1990;156:442-443.
6. Hoffman BF. Diet pill psychosis. Can Med Assoc J. 1977;116(4):351-355.
7. Hoffman BF. Diet pill psychosis: follow-up after 6 years. Can Med Assoc J. 1983;129(10):1077-1078.
8. Rubin RT. Acute psychotic reaction following ingestion of phentermine. Am J Psychiatry. 1964;120:1124-1125.
9. Schaffer CB, Pauli MW. Psychotic reaction caused by proprietary oral diet agent. Am J Psychiatry. 1980;137(10):1256-12567.
10. Lee SH, Liu CY, Yang YY. Schizophreniform-like psychotic disorder induced by phentermine: a case report. Zhonghua Yi Xue Za Zhi (Taipei). 1998;61(1):44-47.
11. Zimmer JE, Gregory RJ. Bipolar depression associated with fenfluramine and phentermine. J Clin Psychiatry. 1998;59(7):383-384.
12. Bagri S, Reddy G. Delirium with manic symptoms induced by diet pills. J Clin Psychiatry. 1998;59(2):83.
13. Alexander J, Cheng Y, Choudhary J, et al. Phentermine (Duromine) precipitated psychosis. Aust N Z J Psychiatry. 2011;45(8):684-685.
14. Pomeranz JL, Taylor LM, Austin SB. Over-the-counter and out-of-control: legal strategies to protect youths from abusing products for weight control. Am J Public Health. 2013;103(2):222-2253.
The value and veracity of psychiatric themes depicted in modern cinema
Perhaps more than any other medical specialty, psychiatry enjoys a longstanding and, at times, complicated relationship with cinema. Recent award-winning films, such as Still Alice, Silver Linings Playbook, and Birdman: Or (The Unexpected Virtue of Ignorance) continue traditions rooted in One Flew Over the Cuckoo’s Nest, Martha Marcy May Marlene, Spellbound, and dozens of other films. Through these films, psychiatry is afforded exposure unavailable to most medical specialties. This exposure has proven to be a double-edged sword, however.
Exposure vs accurate portrayal
Relative benefits and disadvantages of psychiatry’s position in film and popular media are difficult to calculate. A film such as Still Alice can provide a vivid, concrete personal narrative of a patient with Alzheimer’s disease, equipping millions of viewers with knowledge that might otherwise remain esoteric and inaccessible. Martha Marcy May Marlene offers a similar stage for posttraumatic stress disorder (PTSD), as does Spellbound for dissociative amnesia.
Such exposure comes at a cost, inevitably, because information about psychiatry is incorporated into a dramatic storyline assembled by filmmakers who are not medical professionals and who are bound by conflicting pressures. At times, those pressures outweigh the desire to accurately portray psychiatric illness.
‘Magical realism’
Two of last year’s celebrated films, Birdman and Still Alice, have continued the longstanding tradition of portraying mental illness in film. Medicine often is touted as art and science; film likewise sits at this intersection. However, filmmakers are artists, primarily, and the nature of storytelling is to emphasize art over scientific accuracy.
The main character in Birdman, for example, manifests psychosis, but many of his presenting signs and symptoms are incongruent with any diagnosable form of psychosis. To tell its story, the film employs magical realism, a celebrated literary and film technique. Although magical realism might detract from the accuracy of the condition portrayed, it adds cinematic appeal to the film, likely creates more entertainment value, and, in turn, garners appreciation from a broader audience.
Expansion of medical information, accurate and otherwise
As in the 1970’s, we are, today, in the midst of rapidly evolving societal norms. One of the most rapid changes is in how the public acquires information. We are in the midst of the “Googlification” of medical knowledge and the expansion of online medical resources. These resources can, simultaneously, inform and mislead the public.
Popular films behave in much the same way. There is no motion picture-guild requirement that mentally ill characters in films such as Birdman meet any set of psychiatric criteria, from DSM-5 or elsewhere. Similarly, the fact that psychiatrists do not control the information in films that portray mental illness comes as no surprise.
‘One flew East, one flew West…’
The tension between engaging storytelling and medical accuracy certainly is not a new phenomenon, extending not only to representations of disease but to representations of treatment. Consider director Miloš Forman’s seminal 1975 film, One Flew Over the Cuckoo’s Nest, whose chief importance for psychiatry rests not in its individualized representations of patients but in a portrayal of the environment in which they are treated. Louise Fletcher’s Academy Award-winning portrayal of cruel Nurse Ratched has lingered in the public consciousness, remaining a prominent image for many Americans when they think of a psychiatric institution.
When Cuckoo’s Nest was released, it was considered by critics to be an “exploration of society’s enforcement of conformism” that “almost willfully overlooked the realities of mental illness”1 so that it could vivify its protagonist’s struggle against tyrannical Nurse Ratched. The film’s primary intent might not have been to make a statement about the injustices of the time, but it has certainly had a lasting effect on the public’s perception of psychiatric illness and treatment.
Films offer an opportunity for discussion
Films on the theme of psychiatry and mental illness have long held a distinctive position in the canon of Western cinema. In this vein, films from the past year have made timely contributions to the genre. Although Still Alice and Birdman might prove to be ground-breaking in changing societal views over time, we must not expect them to do so.
Nevertheless, psychiatry ought to take advantage of popular films’ wide exposure and ability to destigmatize mental illness—rather than lament medical inaccuracies in these films.
Cinema is, first and foremost, an art. Although patients and the public might pick up misconceptions about psychosis, Alzheimer’s disease, or PTSD because popular films take artistic liberty about mental illness, psychiatrists are available to set the record straight. After all, psychiatry has long been about managing perceptions, and patient education is at the core of our specialty.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Reference
1. Ebert R. “One Flew Over The Cuckoo’s Nest (review). http://www.rogerebert.com/reviews/great-movie-one-flew-overthe-cuckoos-nest-1975. February 2, 2003. Accessed September 9, 2015.
Perhaps more than any other medical specialty, psychiatry enjoys a longstanding and, at times, complicated relationship with cinema. Recent award-winning films, such as Still Alice, Silver Linings Playbook, and Birdman: Or (The Unexpected Virtue of Ignorance) continue traditions rooted in One Flew Over the Cuckoo’s Nest, Martha Marcy May Marlene, Spellbound, and dozens of other films. Through these films, psychiatry is afforded exposure unavailable to most medical specialties. This exposure has proven to be a double-edged sword, however.
Exposure vs accurate portrayal
Relative benefits and disadvantages of psychiatry’s position in film and popular media are difficult to calculate. A film such as Still Alice can provide a vivid, concrete personal narrative of a patient with Alzheimer’s disease, equipping millions of viewers with knowledge that might otherwise remain esoteric and inaccessible. Martha Marcy May Marlene offers a similar stage for posttraumatic stress disorder (PTSD), as does Spellbound for dissociative amnesia.
Such exposure comes at a cost, inevitably, because information about psychiatry is incorporated into a dramatic storyline assembled by filmmakers who are not medical professionals and who are bound by conflicting pressures. At times, those pressures outweigh the desire to accurately portray psychiatric illness.
‘Magical realism’
Two of last year’s celebrated films, Birdman and Still Alice, have continued the longstanding tradition of portraying mental illness in film. Medicine often is touted as art and science; film likewise sits at this intersection. However, filmmakers are artists, primarily, and the nature of storytelling is to emphasize art over scientific accuracy.
The main character in Birdman, for example, manifests psychosis, but many of his presenting signs and symptoms are incongruent with any diagnosable form of psychosis. To tell its story, the film employs magical realism, a celebrated literary and film technique. Although magical realism might detract from the accuracy of the condition portrayed, it adds cinematic appeal to the film, likely creates more entertainment value, and, in turn, garners appreciation from a broader audience.
Expansion of medical information, accurate and otherwise
As in the 1970’s, we are, today, in the midst of rapidly evolving societal norms. One of the most rapid changes is in how the public acquires information. We are in the midst of the “Googlification” of medical knowledge and the expansion of online medical resources. These resources can, simultaneously, inform and mislead the public.
Popular films behave in much the same way. There is no motion picture-guild requirement that mentally ill characters in films such as Birdman meet any set of psychiatric criteria, from DSM-5 or elsewhere. Similarly, the fact that psychiatrists do not control the information in films that portray mental illness comes as no surprise.
‘One flew East, one flew West…’
The tension between engaging storytelling and medical accuracy certainly is not a new phenomenon, extending not only to representations of disease but to representations of treatment. Consider director Miloš Forman’s seminal 1975 film, One Flew Over the Cuckoo’s Nest, whose chief importance for psychiatry rests not in its individualized representations of patients but in a portrayal of the environment in which they are treated. Louise Fletcher’s Academy Award-winning portrayal of cruel Nurse Ratched has lingered in the public consciousness, remaining a prominent image for many Americans when they think of a psychiatric institution.
When Cuckoo’s Nest was released, it was considered by critics to be an “exploration of society’s enforcement of conformism” that “almost willfully overlooked the realities of mental illness”1 so that it could vivify its protagonist’s struggle against tyrannical Nurse Ratched. The film’s primary intent might not have been to make a statement about the injustices of the time, but it has certainly had a lasting effect on the public’s perception of psychiatric illness and treatment.
Films offer an opportunity for discussion
Films on the theme of psychiatry and mental illness have long held a distinctive position in the canon of Western cinema. In this vein, films from the past year have made timely contributions to the genre. Although Still Alice and Birdman might prove to be ground-breaking in changing societal views over time, we must not expect them to do so.
Nevertheless, psychiatry ought to take advantage of popular films’ wide exposure and ability to destigmatize mental illness—rather than lament medical inaccuracies in these films.
Cinema is, first and foremost, an art. Although patients and the public might pick up misconceptions about psychosis, Alzheimer’s disease, or PTSD because popular films take artistic liberty about mental illness, psychiatrists are available to set the record straight. After all, psychiatry has long been about managing perceptions, and patient education is at the core of our specialty.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Perhaps more than any other medical specialty, psychiatry enjoys a longstanding and, at times, complicated relationship with cinema. Recent award-winning films, such as Still Alice, Silver Linings Playbook, and Birdman: Or (The Unexpected Virtue of Ignorance) continue traditions rooted in One Flew Over the Cuckoo’s Nest, Martha Marcy May Marlene, Spellbound, and dozens of other films. Through these films, psychiatry is afforded exposure unavailable to most medical specialties. This exposure has proven to be a double-edged sword, however.
Exposure vs accurate portrayal
Relative benefits and disadvantages of psychiatry’s position in film and popular media are difficult to calculate. A film such as Still Alice can provide a vivid, concrete personal narrative of a patient with Alzheimer’s disease, equipping millions of viewers with knowledge that might otherwise remain esoteric and inaccessible. Martha Marcy May Marlene offers a similar stage for posttraumatic stress disorder (PTSD), as does Spellbound for dissociative amnesia.
Such exposure comes at a cost, inevitably, because information about psychiatry is incorporated into a dramatic storyline assembled by filmmakers who are not medical professionals and who are bound by conflicting pressures. At times, those pressures outweigh the desire to accurately portray psychiatric illness.
‘Magical realism’
Two of last year’s celebrated films, Birdman and Still Alice, have continued the longstanding tradition of portraying mental illness in film. Medicine often is touted as art and science; film likewise sits at this intersection. However, filmmakers are artists, primarily, and the nature of storytelling is to emphasize art over scientific accuracy.
The main character in Birdman, for example, manifests psychosis, but many of his presenting signs and symptoms are incongruent with any diagnosable form of psychosis. To tell its story, the film employs magical realism, a celebrated literary and film technique. Although magical realism might detract from the accuracy of the condition portrayed, it adds cinematic appeal to the film, likely creates more entertainment value, and, in turn, garners appreciation from a broader audience.
Expansion of medical information, accurate and otherwise
As in the 1970’s, we are, today, in the midst of rapidly evolving societal norms. One of the most rapid changes is in how the public acquires information. We are in the midst of the “Googlification” of medical knowledge and the expansion of online medical resources. These resources can, simultaneously, inform and mislead the public.
Popular films behave in much the same way. There is no motion picture-guild requirement that mentally ill characters in films such as Birdman meet any set of psychiatric criteria, from DSM-5 or elsewhere. Similarly, the fact that psychiatrists do not control the information in films that portray mental illness comes as no surprise.
‘One flew East, one flew West…’
The tension between engaging storytelling and medical accuracy certainly is not a new phenomenon, extending not only to representations of disease but to representations of treatment. Consider director Miloš Forman’s seminal 1975 film, One Flew Over the Cuckoo’s Nest, whose chief importance for psychiatry rests not in its individualized representations of patients but in a portrayal of the environment in which they are treated. Louise Fletcher’s Academy Award-winning portrayal of cruel Nurse Ratched has lingered in the public consciousness, remaining a prominent image for many Americans when they think of a psychiatric institution.
When Cuckoo’s Nest was released, it was considered by critics to be an “exploration of society’s enforcement of conformism” that “almost willfully overlooked the realities of mental illness”1 so that it could vivify its protagonist’s struggle against tyrannical Nurse Ratched. The film’s primary intent might not have been to make a statement about the injustices of the time, but it has certainly had a lasting effect on the public’s perception of psychiatric illness and treatment.
Films offer an opportunity for discussion
Films on the theme of psychiatry and mental illness have long held a distinctive position in the canon of Western cinema. In this vein, films from the past year have made timely contributions to the genre. Although Still Alice and Birdman might prove to be ground-breaking in changing societal views over time, we must not expect them to do so.
Nevertheless, psychiatry ought to take advantage of popular films’ wide exposure and ability to destigmatize mental illness—rather than lament medical inaccuracies in these films.
Cinema is, first and foremost, an art. Although patients and the public might pick up misconceptions about psychosis, Alzheimer’s disease, or PTSD because popular films take artistic liberty about mental illness, psychiatrists are available to set the record straight. After all, psychiatry has long been about managing perceptions, and patient education is at the core of our specialty.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Reference
1. Ebert R. “One Flew Over The Cuckoo’s Nest (review). http://www.rogerebert.com/reviews/great-movie-one-flew-overthe-cuckoos-nest-1975. February 2, 2003. Accessed September 9, 2015.
Reference
1. Ebert R. “One Flew Over The Cuckoo’s Nest (review). http://www.rogerebert.com/reviews/great-movie-one-flew-overthe-cuckoos-nest-1975. February 2, 2003. Accessed September 9, 2015.
For residents, technology can put professionalism and reputation at risk
As mobile devices permeate our professional lives, resident disengagement, social media, and communications with patients all present a risk of breaches in professionalism for unwary trainees.
Encroaching technology and resident disengagement
It is pointless to be some kind of Luddite and reject the transformative tide of technology—mobile devices in particular—in psychiatry.1 Yet commentators have remarked on the potential that technology has to damage the professionalism of physicians.2
We are dismayed to observe that, nationally, residents seem at times more absorbed with their social media accounts, e-mail, text messages, and Web browsers than by Grand Rounds and didactic lectures provided by faculty. We believe that this electronic preoccupation shows a level of disrespect; indeed, self-control does matter, and is an inherent facet of professionalism.3
We are under no illusion that, when we give small-group didactic presentations to medical students, they will stop surfing the Internet, e-mailing, and texting: Frankly, we aren’t that riveting. We certainly appreciate, however, students’ discretion by generally using their mobile devices out of our view.
Last, we find it interesting that, despite the greater formality of national medical meetings, we see more blatant use of mobile devices by residents when greater respect is, arguably, warranted. Perhaps the anonymity of a larger audience is to blame for that phenomenon.
Social media
The rise of social media presents particular concerns for the professionalism of residents. In a recent study of applicants to residency, 46% of all applicants maintained a Facebook profile; 16% of those who maintained a profile have posted unprofessional content there.4 (In our experience, the percentage of residents who have a social media or other online presence is considerably greater than 46%.)
Using social media presents risks: for example, if a resident were to post to her (his) social media profile that she (he) was “tired” or had been out “partying with friends.” Like it or not, we, as residents, speak not just as individuals but as representatives of our training program and institution. Should a resident’s patient suffer an adverse outcome the day after the physician posts a 3 AM image of herself out drinking, she might be exposing herself, her institution, or both, to liability.
Correspondence with patients
E-mail and texting correspondence with patients present their own professionalism dilemmas, with regard to legal liability, confidentiality, boundary violations, and “netiquette” issues.5-7 In our experience, the rapid-fire nature of texting can lead a resident to write without appropriate deliberation or to respond outside of business hours. In doing so, the boundary between what is professional and what is purely personal can be blurred. Furthermore, unless our patients have signed a consent form that articulates the acceptable uses of e-mail and text communication,7 we risk exposing ourselves to liability if a patient notifies us of an urgent matter by e-mail at a time when we are inaccessible.
Our residency class is fairly divided on texting patients. However, we (the authors) sometimes feel comfortable exchanging text messages about scheduling with our psychotherapy patients.
Admittedly, texting with a patient can easily become a slippery slope when a patient texts about a scheduling matter well outside of business hours. The path of least resistance would be to reply at the moment, but we have learned that the wiser course is to wait and reply during business hours (even though that adds another item to the to-do list).
Even more challenging is when a psychotherapy patient pushes boundaries further, for example, by texting about a non-emergent psychotherapy concern that should be addressed in a therapy session. Although non-emergent texts about a psychotherapy matter clearly represent a pressing concern to the patient, boundaries can be blurred if a resident, reluctant to risk offending a patient, addresses the matter directly. The benefit of having these experiences during residency is that a psychotherapy supervisor is available to provide guidance.
Better understanding of these risks is needed
Resident disengagement, social media, and correspondence with patients can present pitfalls for unwary residents. They have the potential to create a breach in professionalism and, as a result, increase our exposure to liability. The solution? We believe it isn’t to restrict use of technology, but to continue to study these slippery slopes and how we should address them. Ultimately, by continuing to embrace professionalism, we enhance the reputation of psychiatry and of medicine broadly.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. DeJong SM. Networking, professionalism and the internet: what practicing psychiatrists need to know about Facebook, LinkedIn,and beyond. Psychiatric Times. http://www.psychiatrictimes.com/career/networking-professionalism-and-internet.Published December 7, 2012. Accessed June 22, 2015.
2. Blumenthal D. Doctors in a wired world: can professionalism survive connectivity? Milbank Q. 2002;80(3):525-546, iv.
3. Hershberger PJ, Zryd TW, Rodes MB, et al. Professionalism: self-control matters. Med Teach. 2010;32(1):e36-e41.
4. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
5. DeJong SM, Benjamin S, Anzia JM, et al. Professionalism and the internet in psychiatry: what to teach and how to teach it. Acad Psychiatry. 2012;36(5):356-362.
6. DeJong SM, Gorrindo T. To text or not to text: applying clinical and professionalism principles to decisions about text messaging with patients. J Am Acad Child Adolesc Psychiatry.2014;53(7):713-715.
7. Reynolds A, Mossman D. Before you hit ‘send’: will an e-mail to your patient put you at legal risk? Current Psychiatry. 2015;14(6):33,38,39,42.
As mobile devices permeate our professional lives, resident disengagement, social media, and communications with patients all present a risk of breaches in professionalism for unwary trainees.
Encroaching technology and resident disengagement
It is pointless to be some kind of Luddite and reject the transformative tide of technology—mobile devices in particular—in psychiatry.1 Yet commentators have remarked on the potential that technology has to damage the professionalism of physicians.2
We are dismayed to observe that, nationally, residents seem at times more absorbed with their social media accounts, e-mail, text messages, and Web browsers than by Grand Rounds and didactic lectures provided by faculty. We believe that this electronic preoccupation shows a level of disrespect; indeed, self-control does matter, and is an inherent facet of professionalism.3
We are under no illusion that, when we give small-group didactic presentations to medical students, they will stop surfing the Internet, e-mailing, and texting: Frankly, we aren’t that riveting. We certainly appreciate, however, students’ discretion by generally using their mobile devices out of our view.
Last, we find it interesting that, despite the greater formality of national medical meetings, we see more blatant use of mobile devices by residents when greater respect is, arguably, warranted. Perhaps the anonymity of a larger audience is to blame for that phenomenon.
Social media
The rise of social media presents particular concerns for the professionalism of residents. In a recent study of applicants to residency, 46% of all applicants maintained a Facebook profile; 16% of those who maintained a profile have posted unprofessional content there.4 (In our experience, the percentage of residents who have a social media or other online presence is considerably greater than 46%.)
Using social media presents risks: for example, if a resident were to post to her (his) social media profile that she (he) was “tired” or had been out “partying with friends.” Like it or not, we, as residents, speak not just as individuals but as representatives of our training program and institution. Should a resident’s patient suffer an adverse outcome the day after the physician posts a 3 AM image of herself out drinking, she might be exposing herself, her institution, or both, to liability.
Correspondence with patients
E-mail and texting correspondence with patients present their own professionalism dilemmas, with regard to legal liability, confidentiality, boundary violations, and “netiquette” issues.5-7 In our experience, the rapid-fire nature of texting can lead a resident to write without appropriate deliberation or to respond outside of business hours. In doing so, the boundary between what is professional and what is purely personal can be blurred. Furthermore, unless our patients have signed a consent form that articulates the acceptable uses of e-mail and text communication,7 we risk exposing ourselves to liability if a patient notifies us of an urgent matter by e-mail at a time when we are inaccessible.
Our residency class is fairly divided on texting patients. However, we (the authors) sometimes feel comfortable exchanging text messages about scheduling with our psychotherapy patients.
Admittedly, texting with a patient can easily become a slippery slope when a patient texts about a scheduling matter well outside of business hours. The path of least resistance would be to reply at the moment, but we have learned that the wiser course is to wait and reply during business hours (even though that adds another item to the to-do list).
Even more challenging is when a psychotherapy patient pushes boundaries further, for example, by texting about a non-emergent psychotherapy concern that should be addressed in a therapy session. Although non-emergent texts about a psychotherapy matter clearly represent a pressing concern to the patient, boundaries can be blurred if a resident, reluctant to risk offending a patient, addresses the matter directly. The benefit of having these experiences during residency is that a psychotherapy supervisor is available to provide guidance.
Better understanding of these risks is needed
Resident disengagement, social media, and correspondence with patients can present pitfalls for unwary residents. They have the potential to create a breach in professionalism and, as a result, increase our exposure to liability. The solution? We believe it isn’t to restrict use of technology, but to continue to study these slippery slopes and how we should address them. Ultimately, by continuing to embrace professionalism, we enhance the reputation of psychiatry and of medicine broadly.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
As mobile devices permeate our professional lives, resident disengagement, social media, and communications with patients all present a risk of breaches in professionalism for unwary trainees.
Encroaching technology and resident disengagement
It is pointless to be some kind of Luddite and reject the transformative tide of technology—mobile devices in particular—in psychiatry.1 Yet commentators have remarked on the potential that technology has to damage the professionalism of physicians.2
We are dismayed to observe that, nationally, residents seem at times more absorbed with their social media accounts, e-mail, text messages, and Web browsers than by Grand Rounds and didactic lectures provided by faculty. We believe that this electronic preoccupation shows a level of disrespect; indeed, self-control does matter, and is an inherent facet of professionalism.3
We are under no illusion that, when we give small-group didactic presentations to medical students, they will stop surfing the Internet, e-mailing, and texting: Frankly, we aren’t that riveting. We certainly appreciate, however, students’ discretion by generally using their mobile devices out of our view.
Last, we find it interesting that, despite the greater formality of national medical meetings, we see more blatant use of mobile devices by residents when greater respect is, arguably, warranted. Perhaps the anonymity of a larger audience is to blame for that phenomenon.
Social media
The rise of social media presents particular concerns for the professionalism of residents. In a recent study of applicants to residency, 46% of all applicants maintained a Facebook profile; 16% of those who maintained a profile have posted unprofessional content there.4 (In our experience, the percentage of residents who have a social media or other online presence is considerably greater than 46%.)
Using social media presents risks: for example, if a resident were to post to her (his) social media profile that she (he) was “tired” or had been out “partying with friends.” Like it or not, we, as residents, speak not just as individuals but as representatives of our training program and institution. Should a resident’s patient suffer an adverse outcome the day after the physician posts a 3 AM image of herself out drinking, she might be exposing herself, her institution, or both, to liability.
Correspondence with patients
E-mail and texting correspondence with patients present their own professionalism dilemmas, with regard to legal liability, confidentiality, boundary violations, and “netiquette” issues.5-7 In our experience, the rapid-fire nature of texting can lead a resident to write without appropriate deliberation or to respond outside of business hours. In doing so, the boundary between what is professional and what is purely personal can be blurred. Furthermore, unless our patients have signed a consent form that articulates the acceptable uses of e-mail and text communication,7 we risk exposing ourselves to liability if a patient notifies us of an urgent matter by e-mail at a time when we are inaccessible.
Our residency class is fairly divided on texting patients. However, we (the authors) sometimes feel comfortable exchanging text messages about scheduling with our psychotherapy patients.
Admittedly, texting with a patient can easily become a slippery slope when a patient texts about a scheduling matter well outside of business hours. The path of least resistance would be to reply at the moment, but we have learned that the wiser course is to wait and reply during business hours (even though that adds another item to the to-do list).
Even more challenging is when a psychotherapy patient pushes boundaries further, for example, by texting about a non-emergent psychotherapy concern that should be addressed in a therapy session. Although non-emergent texts about a psychotherapy matter clearly represent a pressing concern to the patient, boundaries can be blurred if a resident, reluctant to risk offending a patient, addresses the matter directly. The benefit of having these experiences during residency is that a psychotherapy supervisor is available to provide guidance.
Better understanding of these risks is needed
Resident disengagement, social media, and correspondence with patients can present pitfalls for unwary residents. They have the potential to create a breach in professionalism and, as a result, increase our exposure to liability. The solution? We believe it isn’t to restrict use of technology, but to continue to study these slippery slopes and how we should address them. Ultimately, by continuing to embrace professionalism, we enhance the reputation of psychiatry and of medicine broadly.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. DeJong SM. Networking, professionalism and the internet: what practicing psychiatrists need to know about Facebook, LinkedIn,and beyond. Psychiatric Times. http://www.psychiatrictimes.com/career/networking-professionalism-and-internet.Published December 7, 2012. Accessed June 22, 2015.
2. Blumenthal D. Doctors in a wired world: can professionalism survive connectivity? Milbank Q. 2002;80(3):525-546, iv.
3. Hershberger PJ, Zryd TW, Rodes MB, et al. Professionalism: self-control matters. Med Teach. 2010;32(1):e36-e41.
4. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
5. DeJong SM, Benjamin S, Anzia JM, et al. Professionalism and the internet in psychiatry: what to teach and how to teach it. Acad Psychiatry. 2012;36(5):356-362.
6. DeJong SM, Gorrindo T. To text or not to text: applying clinical and professionalism principles to decisions about text messaging with patients. J Am Acad Child Adolesc Psychiatry.2014;53(7):713-715.
7. Reynolds A, Mossman D. Before you hit ‘send’: will an e-mail to your patient put you at legal risk? Current Psychiatry. 2015;14(6):33,38,39,42.
1. DeJong SM. Networking, professionalism and the internet: what practicing psychiatrists need to know about Facebook, LinkedIn,and beyond. Psychiatric Times. http://www.psychiatrictimes.com/career/networking-professionalism-and-internet.Published December 7, 2012. Accessed June 22, 2015.
2. Blumenthal D. Doctors in a wired world: can professionalism survive connectivity? Milbank Q. 2002;80(3):525-546, iv.
3. Hershberger PJ, Zryd TW, Rodes MB, et al. Professionalism: self-control matters. Med Teach. 2010;32(1):e36-e41.
4. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
5. DeJong SM, Benjamin S, Anzia JM, et al. Professionalism and the internet in psychiatry: what to teach and how to teach it. Acad Psychiatry. 2012;36(5):356-362.
6. DeJong SM, Gorrindo T. To text or not to text: applying clinical and professionalism principles to decisions about text messaging with patients. J Am Acad Child Adolesc Psychiatry.2014;53(7):713-715.
7. Reynolds A, Mossman D. Before you hit ‘send’: will an e-mail to your patient put you at legal risk? Current Psychiatry. 2015;14(6):33,38,39,42.
Reducing the likelihood that a patient will be readmitted: A resident's perspective
Over the past year, as a part of a treatment team, I encountered many discharged patients who did not heed their physician’s instructions—be it rehabilitation advice, follow-up appointments, or adherence to a drug regimen. Consequently, these patients found themselves back in the inpatient unit a few days later. A cycle of admission−discharge−readmission began for them.
I have witnessed conflicting emotions on the part of the staff (nurses and residents) toward these patients. Some staff are empathetic to their needs; others see the recurrent admissions as a ruse to find food and shelter and get attention.
In this article, I explore several aspects of this behavioral pattern and possible reasons for it, and describe the staff’s reaction to a returning patient in one case.
CASE REPORT Depressed and heavily intoxicated
Mr. R, age 35, with a history of major depressive disorder and nonadherence to treatment, is brought to the emergency room (ER) by emergency medical services because he is heavily intoxicated (blood alcohol level, >200 mg/dL). Mr. R has had 4 admissions to the inpatient psychiatry unit in the past 6 months, including 2 in the past 30 days.
After a few hours’ stay in the ER, Mr. R’s blood alcohol level drops to <100 mg/dL. He is being prepared for discharge to follow-up with outpatient psychiatric services when he begins complaining of chest pain. A cardiac workup is negative; he is again prepared for discharge when he begins reporting suicidal ideation, with a plan to jump in front of traffic.
Mr. R is admitted to the inpatient psychiatry unit.
During Mr. R’s hospitalization, he admits that he lied about being suicidal because he recently lost his job and is homeless and in dire need of food and shelter. He stays in the inpatient unit for 6 days.
An unexpected ‘adverse reaction’
During the hospital stay, staff members, who initially were concerned about Mr. R’s condition, underwent a striking transformation in their attitude toward the patient once his suicidal ideation was exposed as a hoax: They became less receptive to his needs.
The staff’s experience with Mr. R also altered their approach to other patients, who were put under unnecessary scrutiny in response to heightened suspicion of feigned illness—a classic case of “once bitten, twice shy.” The staff felt betrayed by Mr. R’s false claim of being suicidal.
Furthermore, I noticed self-doubt creeping into the minds of the residents who had admitted Mr. R. Consequently, they advocated that he should be discharged patients of an acute care bed.
The attending physicians and other members of the staff remained compassionate toward the patient, however; instead of condemning him, they tried to understand the root cause of why he sought admission: Was it nonadherence with his medication regimen? Substance abuse? Social issues? These staff members were opposed to discharging Mr. R because they believed that forced discharge would encourage him to further manipulate the system—and he would be back in the ER.
CASE CONCLUDED
The medical team concludes that it is prudent to prepare a well-thought-out discharge plan for Mr. R. He is allowed to remain as an inpatient until his social issues are addressed; he is plugged into the rehabilitation program for his alcohol addiction, with a plan for close outpatient psychiatry follow-up.
One year later, Mr. R has not been admitted again.
How to tackle shortcomings of the system
Because of changing hospital policies, an acute shortage of psychiatry inpatient beds, and the reluctance of insurance companies to reimburse for an extended stay, these beds are often hurriedly evacuated and patients are discharged prematurely to make room for acutely ill patients.1 Such policies can lead to failure to reach a therapeutic medication dosage or establish an appropriate disposition plan. Patients might relapse and find their way back to the inpatient unit.
Even though this is a system—not a personal—shortcoming, these patients are viewed negatively and are unwelcome when they return to the hospital. Notably, longer hospital stays do not necessarily lead to better care or fewer readmissions. Patients who have a longer length of stay are, in fact, sicker and have inadequate community and social support.1,2
After a year’s experience as a psychiatry resident, I came to understand that, before discharging a patient from the inpatient unit, a resident should pose a few questions to himself (herself), including:
• What is the likelihood that the patient will adhere to his (her) medication regimen?
• Where is the patient going to get his medications? Will he (she) be able to pay for them?
• Does he have a substance use disorder?
• Have the patient’s personal circumstances changed since he was admitted? If so, how?
Finding answers to these questions and working on solutions can help minimize the readmission rate.
The post-discharge component of care has a significant role, too, including psycho-education of the patient and the family regarding:
• ongoing psychiatric disease
• potential side effects of medications
• post-discharge telephone calls
• timely follow-up (within 2 or 3 weeks)
• good communication with the outpatient provider, through telephone calls or a faxed discharge summary.2,3
I’ve learned that it isn’t uncommon for health care providers to give in to negative emotions and become frustrated. For residents and other members of the team alike, it is important to talk to one’s supervisor and colleagues about that frustration. It is the duty of every member of the treatment team to support each another and maintain a therapeutic posture on the unit.
At the end of every day, of course, what matters is the well-being of our patients.
Disclosure
Dr. Sharma reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Botha UA, Koen L, Joska JA, et al. The revolving door phenomenon in psychiatry: comparing low-frequency and high-frequency users in psychiatry inpatient services in a developing country. Soc Psychiatry Psychiatr Epidemiol. 2010;45(4):461-468.
2. Clary C, Dever A, Schweizer E. Psychiatric inpatient’s knowledge of medication at hospital discharge. Hosp Community Psychiatry. 1992;43(2):140-144.
3. Boyer CA, McAlpine DD, Pottick KJ, et al. Identifying risk factors and key strategies in linkage to outpatient psychiatric care. Am J Psychiatry. 2000;157(10):1592-1598.
Over the past year, as a part of a treatment team, I encountered many discharged patients who did not heed their physician’s instructions—be it rehabilitation advice, follow-up appointments, or adherence to a drug regimen. Consequently, these patients found themselves back in the inpatient unit a few days later. A cycle of admission−discharge−readmission began for them.
I have witnessed conflicting emotions on the part of the staff (nurses and residents) toward these patients. Some staff are empathetic to their needs; others see the recurrent admissions as a ruse to find food and shelter and get attention.
In this article, I explore several aspects of this behavioral pattern and possible reasons for it, and describe the staff’s reaction to a returning patient in one case.
CASE REPORT Depressed and heavily intoxicated
Mr. R, age 35, with a history of major depressive disorder and nonadherence to treatment, is brought to the emergency room (ER) by emergency medical services because he is heavily intoxicated (blood alcohol level, >200 mg/dL). Mr. R has had 4 admissions to the inpatient psychiatry unit in the past 6 months, including 2 in the past 30 days.
After a few hours’ stay in the ER, Mr. R’s blood alcohol level drops to <100 mg/dL. He is being prepared for discharge to follow-up with outpatient psychiatric services when he begins complaining of chest pain. A cardiac workup is negative; he is again prepared for discharge when he begins reporting suicidal ideation, with a plan to jump in front of traffic.
Mr. R is admitted to the inpatient psychiatry unit.
During Mr. R’s hospitalization, he admits that he lied about being suicidal because he recently lost his job and is homeless and in dire need of food and shelter. He stays in the inpatient unit for 6 days.
An unexpected ‘adverse reaction’
During the hospital stay, staff members, who initially were concerned about Mr. R’s condition, underwent a striking transformation in their attitude toward the patient once his suicidal ideation was exposed as a hoax: They became less receptive to his needs.
The staff’s experience with Mr. R also altered their approach to other patients, who were put under unnecessary scrutiny in response to heightened suspicion of feigned illness—a classic case of “once bitten, twice shy.” The staff felt betrayed by Mr. R’s false claim of being suicidal.
Furthermore, I noticed self-doubt creeping into the minds of the residents who had admitted Mr. R. Consequently, they advocated that he should be discharged patients of an acute care bed.
The attending physicians and other members of the staff remained compassionate toward the patient, however; instead of condemning him, they tried to understand the root cause of why he sought admission: Was it nonadherence with his medication regimen? Substance abuse? Social issues? These staff members were opposed to discharging Mr. R because they believed that forced discharge would encourage him to further manipulate the system—and he would be back in the ER.
CASE CONCLUDED
The medical team concludes that it is prudent to prepare a well-thought-out discharge plan for Mr. R. He is allowed to remain as an inpatient until his social issues are addressed; he is plugged into the rehabilitation program for his alcohol addiction, with a plan for close outpatient psychiatry follow-up.
One year later, Mr. R has not been admitted again.
How to tackle shortcomings of the system
Because of changing hospital policies, an acute shortage of psychiatry inpatient beds, and the reluctance of insurance companies to reimburse for an extended stay, these beds are often hurriedly evacuated and patients are discharged prematurely to make room for acutely ill patients.1 Such policies can lead to failure to reach a therapeutic medication dosage or establish an appropriate disposition plan. Patients might relapse and find their way back to the inpatient unit.
Even though this is a system—not a personal—shortcoming, these patients are viewed negatively and are unwelcome when they return to the hospital. Notably, longer hospital stays do not necessarily lead to better care or fewer readmissions. Patients who have a longer length of stay are, in fact, sicker and have inadequate community and social support.1,2
After a year’s experience as a psychiatry resident, I came to understand that, before discharging a patient from the inpatient unit, a resident should pose a few questions to himself (herself), including:
• What is the likelihood that the patient will adhere to his (her) medication regimen?
• Where is the patient going to get his medications? Will he (she) be able to pay for them?
• Does he have a substance use disorder?
• Have the patient’s personal circumstances changed since he was admitted? If so, how?
Finding answers to these questions and working on solutions can help minimize the readmission rate.
The post-discharge component of care has a significant role, too, including psycho-education of the patient and the family regarding:
• ongoing psychiatric disease
• potential side effects of medications
• post-discharge telephone calls
• timely follow-up (within 2 or 3 weeks)
• good communication with the outpatient provider, through telephone calls or a faxed discharge summary.2,3
I’ve learned that it isn’t uncommon for health care providers to give in to negative emotions and become frustrated. For residents and other members of the team alike, it is important to talk to one’s supervisor and colleagues about that frustration. It is the duty of every member of the treatment team to support each another and maintain a therapeutic posture on the unit.
At the end of every day, of course, what matters is the well-being of our patients.
Disclosure
Dr. Sharma reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Over the past year, as a part of a treatment team, I encountered many discharged patients who did not heed their physician’s instructions—be it rehabilitation advice, follow-up appointments, or adherence to a drug regimen. Consequently, these patients found themselves back in the inpatient unit a few days later. A cycle of admission−discharge−readmission began for them.
I have witnessed conflicting emotions on the part of the staff (nurses and residents) toward these patients. Some staff are empathetic to their needs; others see the recurrent admissions as a ruse to find food and shelter and get attention.
In this article, I explore several aspects of this behavioral pattern and possible reasons for it, and describe the staff’s reaction to a returning patient in one case.
CASE REPORT Depressed and heavily intoxicated
Mr. R, age 35, with a history of major depressive disorder and nonadherence to treatment, is brought to the emergency room (ER) by emergency medical services because he is heavily intoxicated (blood alcohol level, >200 mg/dL). Mr. R has had 4 admissions to the inpatient psychiatry unit in the past 6 months, including 2 in the past 30 days.
After a few hours’ stay in the ER, Mr. R’s blood alcohol level drops to <100 mg/dL. He is being prepared for discharge to follow-up with outpatient psychiatric services when he begins complaining of chest pain. A cardiac workup is negative; he is again prepared for discharge when he begins reporting suicidal ideation, with a plan to jump in front of traffic.
Mr. R is admitted to the inpatient psychiatry unit.
During Mr. R’s hospitalization, he admits that he lied about being suicidal because he recently lost his job and is homeless and in dire need of food and shelter. He stays in the inpatient unit for 6 days.
An unexpected ‘adverse reaction’
During the hospital stay, staff members, who initially were concerned about Mr. R’s condition, underwent a striking transformation in their attitude toward the patient once his suicidal ideation was exposed as a hoax: They became less receptive to his needs.
The staff’s experience with Mr. R also altered their approach to other patients, who were put under unnecessary scrutiny in response to heightened suspicion of feigned illness—a classic case of “once bitten, twice shy.” The staff felt betrayed by Mr. R’s false claim of being suicidal.
Furthermore, I noticed self-doubt creeping into the minds of the residents who had admitted Mr. R. Consequently, they advocated that he should be discharged patients of an acute care bed.
The attending physicians and other members of the staff remained compassionate toward the patient, however; instead of condemning him, they tried to understand the root cause of why he sought admission: Was it nonadherence with his medication regimen? Substance abuse? Social issues? These staff members were opposed to discharging Mr. R because they believed that forced discharge would encourage him to further manipulate the system—and he would be back in the ER.
CASE CONCLUDED
The medical team concludes that it is prudent to prepare a well-thought-out discharge plan for Mr. R. He is allowed to remain as an inpatient until his social issues are addressed; he is plugged into the rehabilitation program for his alcohol addiction, with a plan for close outpatient psychiatry follow-up.
One year later, Mr. R has not been admitted again.
How to tackle shortcomings of the system
Because of changing hospital policies, an acute shortage of psychiatry inpatient beds, and the reluctance of insurance companies to reimburse for an extended stay, these beds are often hurriedly evacuated and patients are discharged prematurely to make room for acutely ill patients.1 Such policies can lead to failure to reach a therapeutic medication dosage or establish an appropriate disposition plan. Patients might relapse and find their way back to the inpatient unit.
Even though this is a system—not a personal—shortcoming, these patients are viewed negatively and are unwelcome when they return to the hospital. Notably, longer hospital stays do not necessarily lead to better care or fewer readmissions. Patients who have a longer length of stay are, in fact, sicker and have inadequate community and social support.1,2
After a year’s experience as a psychiatry resident, I came to understand that, before discharging a patient from the inpatient unit, a resident should pose a few questions to himself (herself), including:
• What is the likelihood that the patient will adhere to his (her) medication regimen?
• Where is the patient going to get his medications? Will he (she) be able to pay for them?
• Does he have a substance use disorder?
• Have the patient’s personal circumstances changed since he was admitted? If so, how?
Finding answers to these questions and working on solutions can help minimize the readmission rate.
The post-discharge component of care has a significant role, too, including psycho-education of the patient and the family regarding:
• ongoing psychiatric disease
• potential side effects of medications
• post-discharge telephone calls
• timely follow-up (within 2 or 3 weeks)
• good communication with the outpatient provider, through telephone calls or a faxed discharge summary.2,3
I’ve learned that it isn’t uncommon for health care providers to give in to negative emotions and become frustrated. For residents and other members of the team alike, it is important to talk to one’s supervisor and colleagues about that frustration. It is the duty of every member of the treatment team to support each another and maintain a therapeutic posture on the unit.
At the end of every day, of course, what matters is the well-being of our patients.
Disclosure
Dr. Sharma reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Botha UA, Koen L, Joska JA, et al. The revolving door phenomenon in psychiatry: comparing low-frequency and high-frequency users in psychiatry inpatient services in a developing country. Soc Psychiatry Psychiatr Epidemiol. 2010;45(4):461-468.
2. Clary C, Dever A, Schweizer E. Psychiatric inpatient’s knowledge of medication at hospital discharge. Hosp Community Psychiatry. 1992;43(2):140-144.
3. Boyer CA, McAlpine DD, Pottick KJ, et al. Identifying risk factors and key strategies in linkage to outpatient psychiatric care. Am J Psychiatry. 2000;157(10):1592-1598.
1. Botha UA, Koen L, Joska JA, et al. The revolving door phenomenon in psychiatry: comparing low-frequency and high-frequency users in psychiatry inpatient services in a developing country. Soc Psychiatry Psychiatr Epidemiol. 2010;45(4):461-468.
2. Clary C, Dever A, Schweizer E. Psychiatric inpatient’s knowledge of medication at hospital discharge. Hosp Community Psychiatry. 1992;43(2):140-144.
3. Boyer CA, McAlpine DD, Pottick KJ, et al. Identifying risk factors and key strategies in linkage to outpatient psychiatric care. Am J Psychiatry. 2000;157(10):1592-1598.
Good medical care for psychiatric patients is imperative
The first year of residency came faster than I had expected and concluded just as quickly. At times, it felt like medical school, with different rotations, adjusting to newly formed teams, dealing with the pressures of getting the right diagnosis and treatment, managing the unrelenting speed of rounds, and trying to make a difference for the better. I must be honest – there were times when I was counting down the days for the rotation to end so that I could begin focusing and working directly in the mental health field.
Now, in my second year, the pace has improved, and the rotations resemble the work and patient population that I chose during the match process. Nonetheless, I am thankful for the time spent and the knowledge gained during my intern year, because it is only now that I understand the true value of my first-year experiences and the need to continue getting a well-rounded medical education for the benefit of my patients.
During my second year of residency, I have come across multiple instances of health disparities for people with mental illness. While working in several inpatient units, I have witnessed delayed time of visit from medical/surgical or ob.gyn. consults, shorter evaluation times from visiting consulting personnel, and postponed follow-up appointments for general medical conditions. I remember one occasion when a patient with urinary incontinence waited 3 days until internal medicine completed its consult. These experiences remind me of the conversations I had in medical school. Some of my colleagues would say, “Psychiatric patients are difficult.” Others were honest in admitting that they were scared to even enter a psychiatric inpatient unit.
Medical comorbidities common
During one 24-hour shift, I was paged to the inpatient unit. A new admission from that afternoon was complaining of “toe pain.”
The patient had been admitted for suicidal ideation and alcohol withdrawal. He reported tripping over a concrete step 2 weeks prior to admission. Under examination, he had an open laceration with purulent, foul-smelling discharge, erythema, and edema around the wound. The patient had signs of cellulitis, had a possible fracture of the phalanx, and was at risk for osteomyelitis.
He had been medically cleared at another facility prior to his admission, where he also had complained of toe pain. At that time, however, he was told, “You are not here for that,” and the extremity was not examined during the medical clearance. I ordered a referral, imaging was completed, and antibiotic treatment was started for his infection. Unfortunately, this is not an incidental or isolated case; situations similar to this one have become more frequent than we would like for those with mental illness.
Often, psychiatric patients are overlooked and undertreated. We frequently are the only physicians who evaluate the patient and help improve their quality of life. After reviewing the literature, I found countless studies concluding that patients who have a psychiatric diagnosis often have increased medical comorbidity and even increased mortality. A review and meta-analysis published earlier this year suggested that “people with mental disorders often do not receive preventive services, such as immunizations, cancer screenings, and tobacco counseling, and often receive a lower quality of care for medical conditions” (JAMA Psychiatry 2015;72:334-41). The researchers also found that “mortality was significantly higher among people with mental disorders than among the comparison population.”
Focusing on mind, body
I knew I wanted to be a psychiatrist since my early years in training. Initially, I was drawn toward psychology, in which I completed a bachelor’s degree, but my world turned around after a conversation with the father of a high school classmate. He told me: “I commend you on your decision to want to help people; however, I would like to give you food for thought. If your goal is to be of service to your patients and provide care, it would be to their benefit to address not only the mind but also the body” (which, coincidentally, is the theme of this year’s American Psychiatric Association meeting in Toronto.)
At that time, I was weighing becoming a clinician versus a physician; after all, both have instrumental roles in treatment. Yet, those words resonate now in my life for a new reason, namely, that my duty as an advocate for mental health is not only to treat psychiatric disorders but also to work toward treating general medical conditions.
I have been fortunate to cross paths with mentors who helped strengthen my commitment to well-rounded care and a multidisciplinary approach for the mentally ill. I am thankful to have worked with Dr. Jill Williams, who stressed the need to treat tobacco dependence, and Dr. Anthony Tobia, who emphasized the need to rule out substance- and medication-induced disorders prior to treatment. I have had the pleasure of working with many other attending psychiatrists who not only focused on psychiatric symptoms and diagnosis but stressed the need to address the medical care of our patients.
If I can understand my patients by learning about human behavior, conditioning, defense mechanisms, and interpersonal relationships and also focus on pathophysiology, comorbid conditions, differential diagnosis, and exacerbating medical conditions, I will be able to give them the best medical care possible.
Dr. Poulsen, a second-year psychiatry resident at the Robert Wood Johnson Medical School, Piscataway, N.J., is interested in cultural psychiatry and advocacy, and in pursuing a fellowship in child and adolescent psychiatry. After obtaining a bachelor of science degree at the University of Florida, Gainesville, he earned a medical degree at the University of Puerto Rico. He is currently serving in multiple leadership positions, including vice president of the New Jersey Psychiatric Association (NJPA) Residents Chapter and NJPA chapter advocacy coordinator. In addition, he has been selected as resident-fellow representative of the APA’s Area 3.
The first year of residency came faster than I had expected and concluded just as quickly. At times, it felt like medical school, with different rotations, adjusting to newly formed teams, dealing with the pressures of getting the right diagnosis and treatment, managing the unrelenting speed of rounds, and trying to make a difference for the better. I must be honest – there were times when I was counting down the days for the rotation to end so that I could begin focusing and working directly in the mental health field.
Now, in my second year, the pace has improved, and the rotations resemble the work and patient population that I chose during the match process. Nonetheless, I am thankful for the time spent and the knowledge gained during my intern year, because it is only now that I understand the true value of my first-year experiences and the need to continue getting a well-rounded medical education for the benefit of my patients.
During my second year of residency, I have come across multiple instances of health disparities for people with mental illness. While working in several inpatient units, I have witnessed delayed time of visit from medical/surgical or ob.gyn. consults, shorter evaluation times from visiting consulting personnel, and postponed follow-up appointments for general medical conditions. I remember one occasion when a patient with urinary incontinence waited 3 days until internal medicine completed its consult. These experiences remind me of the conversations I had in medical school. Some of my colleagues would say, “Psychiatric patients are difficult.” Others were honest in admitting that they were scared to even enter a psychiatric inpatient unit.
Medical comorbidities common
During one 24-hour shift, I was paged to the inpatient unit. A new admission from that afternoon was complaining of “toe pain.”
The patient had been admitted for suicidal ideation and alcohol withdrawal. He reported tripping over a concrete step 2 weeks prior to admission. Under examination, he had an open laceration with purulent, foul-smelling discharge, erythema, and edema around the wound. The patient had signs of cellulitis, had a possible fracture of the phalanx, and was at risk for osteomyelitis.
He had been medically cleared at another facility prior to his admission, where he also had complained of toe pain. At that time, however, he was told, “You are not here for that,” and the extremity was not examined during the medical clearance. I ordered a referral, imaging was completed, and antibiotic treatment was started for his infection. Unfortunately, this is not an incidental or isolated case; situations similar to this one have become more frequent than we would like for those with mental illness.
Often, psychiatric patients are overlooked and undertreated. We frequently are the only physicians who evaluate the patient and help improve their quality of life. After reviewing the literature, I found countless studies concluding that patients who have a psychiatric diagnosis often have increased medical comorbidity and even increased mortality. A review and meta-analysis published earlier this year suggested that “people with mental disorders often do not receive preventive services, such as immunizations, cancer screenings, and tobacco counseling, and often receive a lower quality of care for medical conditions” (JAMA Psychiatry 2015;72:334-41). The researchers also found that “mortality was significantly higher among people with mental disorders than among the comparison population.”
Focusing on mind, body
I knew I wanted to be a psychiatrist since my early years in training. Initially, I was drawn toward psychology, in which I completed a bachelor’s degree, but my world turned around after a conversation with the father of a high school classmate. He told me: “I commend you on your decision to want to help people; however, I would like to give you food for thought. If your goal is to be of service to your patients and provide care, it would be to their benefit to address not only the mind but also the body” (which, coincidentally, is the theme of this year’s American Psychiatric Association meeting in Toronto.)
At that time, I was weighing becoming a clinician versus a physician; after all, both have instrumental roles in treatment. Yet, those words resonate now in my life for a new reason, namely, that my duty as an advocate for mental health is not only to treat psychiatric disorders but also to work toward treating general medical conditions.
I have been fortunate to cross paths with mentors who helped strengthen my commitment to well-rounded care and a multidisciplinary approach for the mentally ill. I am thankful to have worked with Dr. Jill Williams, who stressed the need to treat tobacco dependence, and Dr. Anthony Tobia, who emphasized the need to rule out substance- and medication-induced disorders prior to treatment. I have had the pleasure of working with many other attending psychiatrists who not only focused on psychiatric symptoms and diagnosis but stressed the need to address the medical care of our patients.
If I can understand my patients by learning about human behavior, conditioning, defense mechanisms, and interpersonal relationships and also focus on pathophysiology, comorbid conditions, differential diagnosis, and exacerbating medical conditions, I will be able to give them the best medical care possible.
Dr. Poulsen, a second-year psychiatry resident at the Robert Wood Johnson Medical School, Piscataway, N.J., is interested in cultural psychiatry and advocacy, and in pursuing a fellowship in child and adolescent psychiatry. After obtaining a bachelor of science degree at the University of Florida, Gainesville, he earned a medical degree at the University of Puerto Rico. He is currently serving in multiple leadership positions, including vice president of the New Jersey Psychiatric Association (NJPA) Residents Chapter and NJPA chapter advocacy coordinator. In addition, he has been selected as resident-fellow representative of the APA’s Area 3.
The first year of residency came faster than I had expected and concluded just as quickly. At times, it felt like medical school, with different rotations, adjusting to newly formed teams, dealing with the pressures of getting the right diagnosis and treatment, managing the unrelenting speed of rounds, and trying to make a difference for the better. I must be honest – there were times when I was counting down the days for the rotation to end so that I could begin focusing and working directly in the mental health field.
Now, in my second year, the pace has improved, and the rotations resemble the work and patient population that I chose during the match process. Nonetheless, I am thankful for the time spent and the knowledge gained during my intern year, because it is only now that I understand the true value of my first-year experiences and the need to continue getting a well-rounded medical education for the benefit of my patients.
During my second year of residency, I have come across multiple instances of health disparities for people with mental illness. While working in several inpatient units, I have witnessed delayed time of visit from medical/surgical or ob.gyn. consults, shorter evaluation times from visiting consulting personnel, and postponed follow-up appointments for general medical conditions. I remember one occasion when a patient with urinary incontinence waited 3 days until internal medicine completed its consult. These experiences remind me of the conversations I had in medical school. Some of my colleagues would say, “Psychiatric patients are difficult.” Others were honest in admitting that they were scared to even enter a psychiatric inpatient unit.
Medical comorbidities common
During one 24-hour shift, I was paged to the inpatient unit. A new admission from that afternoon was complaining of “toe pain.”
The patient had been admitted for suicidal ideation and alcohol withdrawal. He reported tripping over a concrete step 2 weeks prior to admission. Under examination, he had an open laceration with purulent, foul-smelling discharge, erythema, and edema around the wound. The patient had signs of cellulitis, had a possible fracture of the phalanx, and was at risk for osteomyelitis.
He had been medically cleared at another facility prior to his admission, where he also had complained of toe pain. At that time, however, he was told, “You are not here for that,” and the extremity was not examined during the medical clearance. I ordered a referral, imaging was completed, and antibiotic treatment was started for his infection. Unfortunately, this is not an incidental or isolated case; situations similar to this one have become more frequent than we would like for those with mental illness.
Often, psychiatric patients are overlooked and undertreated. We frequently are the only physicians who evaluate the patient and help improve their quality of life. After reviewing the literature, I found countless studies concluding that patients who have a psychiatric diagnosis often have increased medical comorbidity and even increased mortality. A review and meta-analysis published earlier this year suggested that “people with mental disorders often do not receive preventive services, such as immunizations, cancer screenings, and tobacco counseling, and often receive a lower quality of care for medical conditions” (JAMA Psychiatry 2015;72:334-41). The researchers also found that “mortality was significantly higher among people with mental disorders than among the comparison population.”
Focusing on mind, body
I knew I wanted to be a psychiatrist since my early years in training. Initially, I was drawn toward psychology, in which I completed a bachelor’s degree, but my world turned around after a conversation with the father of a high school classmate. He told me: “I commend you on your decision to want to help people; however, I would like to give you food for thought. If your goal is to be of service to your patients and provide care, it would be to their benefit to address not only the mind but also the body” (which, coincidentally, is the theme of this year’s American Psychiatric Association meeting in Toronto.)
At that time, I was weighing becoming a clinician versus a physician; after all, both have instrumental roles in treatment. Yet, those words resonate now in my life for a new reason, namely, that my duty as an advocate for mental health is not only to treat psychiatric disorders but also to work toward treating general medical conditions.
I have been fortunate to cross paths with mentors who helped strengthen my commitment to well-rounded care and a multidisciplinary approach for the mentally ill. I am thankful to have worked with Dr. Jill Williams, who stressed the need to treat tobacco dependence, and Dr. Anthony Tobia, who emphasized the need to rule out substance- and medication-induced disorders prior to treatment. I have had the pleasure of working with many other attending psychiatrists who not only focused on psychiatric symptoms and diagnosis but stressed the need to address the medical care of our patients.
If I can understand my patients by learning about human behavior, conditioning, defense mechanisms, and interpersonal relationships and also focus on pathophysiology, comorbid conditions, differential diagnosis, and exacerbating medical conditions, I will be able to give them the best medical care possible.
Dr. Poulsen, a second-year psychiatry resident at the Robert Wood Johnson Medical School, Piscataway, N.J., is interested in cultural psychiatry and advocacy, and in pursuing a fellowship in child and adolescent psychiatry. After obtaining a bachelor of science degree at the University of Florida, Gainesville, he earned a medical degree at the University of Puerto Rico. He is currently serving in multiple leadership positions, including vice president of the New Jersey Psychiatric Association (NJPA) Residents Chapter and NJPA chapter advocacy coordinator. In addition, he has been selected as resident-fellow representative of the APA’s Area 3.
‘Screen-time transferential interference’ in encounters with patients
I cannot recall the last time that I had a good look at the cashier who was scanning my grocery purchases. I could not tell you what color eyes he (or she?) had or how he styled his hair. This isn’t for lack of an effort to recall, or a manifestation of poor memory or absentmindedness. Rather, I think that the situation reflects a larger cultural shift that has gained momentum since the beginning of the new century: that is, the effect of a preponderance of so-called screen time in our lives.
In that mundane scene in the grocery store, screen time encompasses the impersonal and mechanical act of swiping my debit card, entering my PIN, and impatiently waiting for the receipt to print. All the while, I stand awkwardly, eyes downcast and fixed on the display of the card reader, ignoring the human being directly across from me.
Obsession with screens
Our engagement with screen time has grown to pandemic proportions, and television is no longer the main culprit. According to a Nielsen global consumer report,1 in 2010 in the United States, people spent an average of 5 hours a day in front of the “boob tube.” Even if we take that statistic with a grain of salt, it still represents only the most visible tip of the media iceberg. Smartphones, laptop and desktop monitors, portable gaming consoles, electronic tablets, PIN pad displays, video billboards, and any number of other LED and LCD screen surfaces have infiltrated the landscape.
Whereas most recent epidemiologic studies have addressed the deleterious effects of so-called sit time (sedentary activities with or without a screen) on physical health, I would like to address the deleterious effect of screen time on mental health and relational connectedness and the relevance of that screen time to psychiatric practice.
The ‘techno-bubble of private space’
Almond,2 in a humorous social commentary, “Connection Error,” conducted an impromptu experiment in which he attempted to connect spontaneously with strangers, especially those who had a smartphone, in Boston. His narrative navigates the gamut of human interaction, from tedious and boorish to comedic and absurd, noting that, conspicuously, “smartphone users have created a techno-bubble of private space” in which they are physically present but emotionally unavailable.
A chance encounter with a young professional led Almond to this conclusion:
It’s precisely the intrusive alienation of the “techno-bubble” that blunders into the modern patient-physician interaction in my clinical psychiatric practice in a busy outpatient clinic at a university medical center. Specifically, the ever-glowing, ever-distracting computer monitor sitting between me and my patient, with its promise of digital information at my fingertips, serves more to distance me from my patient than to connect us in a meaningful, human way. Just as I can’t recall the countenance of the grocery-store cashier, I miss the delicate, information-laden, minute-to-minute social interaction with the patient because it competes with the electronic intruder.
What’s at risk when a computer screen is in the room?
Transference in the psychotherapeutic encounter is an established tenet of psychoanalytic theory. In “Basic theory of psychoanalysis,”3 Waelder defines transference as “not simply the attribution to new objects of characteristics of old ones but the attempt to re-establish and relive, with whatever object will permit it, an infantile situation much longed for because it was once either greatly enjoyed or greatly missed.” This definition applies to the positive pole of transferential phenomena—and it is this position that is desired in a successful patient−physician encounter.
A patient’s warm and genial regard toward a provider secures trust, cooperation, and faith in the healing process. Establishment of positive transference toward the physician is essential to enhance the clinical encounter, regardless of what early object (caring mother, omnipotent father) is being projected onto the physician.
Attunement. Research into infant observation has revealed the critical role of caretaker responsiveness in the development of early infantile emotional regulation. Tronick et al4 demonstrated the importance of interactional reciprocity in the mother−child dyad.
In a series of experiments using the so-called still-face paradigm, Tronick et al4 saw that infants quickly fall into a state of despair and related negative affects when the mother assumes an unresponsive and detached still face. These episodes intentionally produce infant-mother emotional misattunement, which, although instantly damaging, can be successfully repaired through re-attunement by the mother. It is the primary caretaker’s ability to reconnect and repair that is paramount to the infant’s healthy psychological development.
This sentiment is echoed in Winnicott’s concept of the “good-enough” mother (or parent), formulated years earlier, in which failures in infant−caretaker attunement are inevitable and to be expected—as long as repair outcompetes deficiency.5
Divided attention: Patient or screen? Or both?
What we can understand by applying the ideas of transference and optimal attunement to the clinical encounter is how important uninterrupted face-to-face time with the patient is. Indeed, nonverbal communication from the patient, expressed though body language and facial articulation, is particularly salient to the practice of psychiatry. Information technology— especially the electronic health record—now encroaches on the time-honored central dyad of the patient-physician interaction by introducing a third entity into the traditional encounter.
Clinical misattunement, as understood through the still-face paradigm, increases in proportion to a provider’s need to divide his (her) attention between the patient and the computer screen. And, as the degree of misattunement increases, positive transference is more difficult to establish and maintain. The quality of the clinical encounter then deteriorates, undermining the care of the patient and reducing physician satisfaction.
Acknowledgment
Philip LeFevre, MD, Department of Neurology & Psychiatry, Saint Louis University, St. Louis, Missouri, provided inspiration and encouragement in the development of the manuscript.
Disclosure
Dr. Afanasevich reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. The Nielsen Company. How people watch: a global Nielsen consumer report. http://www.nielsen.com/content/dam/ corporate/mx/reports/2011/Lo-que-la-gente-ve.pdf. Published August 2010. Accessed March 17, 2015.
2. Almond S. Connection error. Spirit Magazine. April 2014:76-86.
3. Waelder R. Basic theory of psychoanalysis. New York, NY: International Universities Press; 1960.
4. Tronick E, Als H, Adamson L, et al. The infant’s response to entrapment between contradictory messages in face-to-face interaction. J Am Acad Child Psychiatry. 1978;17(1):1-13.
5. Winnicott DW. The child, the family, and the outside world. London, United Kingdom: Penguin Books; 1964.
I cannot recall the last time that I had a good look at the cashier who was scanning my grocery purchases. I could not tell you what color eyes he (or she?) had or how he styled his hair. This isn’t for lack of an effort to recall, or a manifestation of poor memory or absentmindedness. Rather, I think that the situation reflects a larger cultural shift that has gained momentum since the beginning of the new century: that is, the effect of a preponderance of so-called screen time in our lives.
In that mundane scene in the grocery store, screen time encompasses the impersonal and mechanical act of swiping my debit card, entering my PIN, and impatiently waiting for the receipt to print. All the while, I stand awkwardly, eyes downcast and fixed on the display of the card reader, ignoring the human being directly across from me.
Obsession with screens
Our engagement with screen time has grown to pandemic proportions, and television is no longer the main culprit. According to a Nielsen global consumer report,1 in 2010 in the United States, people spent an average of 5 hours a day in front of the “boob tube.” Even if we take that statistic with a grain of salt, it still represents only the most visible tip of the media iceberg. Smartphones, laptop and desktop monitors, portable gaming consoles, electronic tablets, PIN pad displays, video billboards, and any number of other LED and LCD screen surfaces have infiltrated the landscape.
Whereas most recent epidemiologic studies have addressed the deleterious effects of so-called sit time (sedentary activities with or without a screen) on physical health, I would like to address the deleterious effect of screen time on mental health and relational connectedness and the relevance of that screen time to psychiatric practice.
The ‘techno-bubble of private space’
Almond,2 in a humorous social commentary, “Connection Error,” conducted an impromptu experiment in which he attempted to connect spontaneously with strangers, especially those who had a smartphone, in Boston. His narrative navigates the gamut of human interaction, from tedious and boorish to comedic and absurd, noting that, conspicuously, “smartphone users have created a techno-bubble of private space” in which they are physically present but emotionally unavailable.
A chance encounter with a young professional led Almond to this conclusion:
It’s precisely the intrusive alienation of the “techno-bubble” that blunders into the modern patient-physician interaction in my clinical psychiatric practice in a busy outpatient clinic at a university medical center. Specifically, the ever-glowing, ever-distracting computer monitor sitting between me and my patient, with its promise of digital information at my fingertips, serves more to distance me from my patient than to connect us in a meaningful, human way. Just as I can’t recall the countenance of the grocery-store cashier, I miss the delicate, information-laden, minute-to-minute social interaction with the patient because it competes with the electronic intruder.
What’s at risk when a computer screen is in the room?
Transference in the psychotherapeutic encounter is an established tenet of psychoanalytic theory. In “Basic theory of psychoanalysis,”3 Waelder defines transference as “not simply the attribution to new objects of characteristics of old ones but the attempt to re-establish and relive, with whatever object will permit it, an infantile situation much longed for because it was once either greatly enjoyed or greatly missed.” This definition applies to the positive pole of transferential phenomena—and it is this position that is desired in a successful patient−physician encounter.
A patient’s warm and genial regard toward a provider secures trust, cooperation, and faith in the healing process. Establishment of positive transference toward the physician is essential to enhance the clinical encounter, regardless of what early object (caring mother, omnipotent father) is being projected onto the physician.
Attunement. Research into infant observation has revealed the critical role of caretaker responsiveness in the development of early infantile emotional regulation. Tronick et al4 demonstrated the importance of interactional reciprocity in the mother−child dyad.
In a series of experiments using the so-called still-face paradigm, Tronick et al4 saw that infants quickly fall into a state of despair and related negative affects when the mother assumes an unresponsive and detached still face. These episodes intentionally produce infant-mother emotional misattunement, which, although instantly damaging, can be successfully repaired through re-attunement by the mother. It is the primary caretaker’s ability to reconnect and repair that is paramount to the infant’s healthy psychological development.
This sentiment is echoed in Winnicott’s concept of the “good-enough” mother (or parent), formulated years earlier, in which failures in infant−caretaker attunement are inevitable and to be expected—as long as repair outcompetes deficiency.5
Divided attention: Patient or screen? Or both?
What we can understand by applying the ideas of transference and optimal attunement to the clinical encounter is how important uninterrupted face-to-face time with the patient is. Indeed, nonverbal communication from the patient, expressed though body language and facial articulation, is particularly salient to the practice of psychiatry. Information technology— especially the electronic health record—now encroaches on the time-honored central dyad of the patient-physician interaction by introducing a third entity into the traditional encounter.
Clinical misattunement, as understood through the still-face paradigm, increases in proportion to a provider’s need to divide his (her) attention between the patient and the computer screen. And, as the degree of misattunement increases, positive transference is more difficult to establish and maintain. The quality of the clinical encounter then deteriorates, undermining the care of the patient and reducing physician satisfaction.
Acknowledgment
Philip LeFevre, MD, Department of Neurology & Psychiatry, Saint Louis University, St. Louis, Missouri, provided inspiration and encouragement in the development of the manuscript.
Disclosure
Dr. Afanasevich reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
I cannot recall the last time that I had a good look at the cashier who was scanning my grocery purchases. I could not tell you what color eyes he (or she?) had or how he styled his hair. This isn’t for lack of an effort to recall, or a manifestation of poor memory or absentmindedness. Rather, I think that the situation reflects a larger cultural shift that has gained momentum since the beginning of the new century: that is, the effect of a preponderance of so-called screen time in our lives.
In that mundane scene in the grocery store, screen time encompasses the impersonal and mechanical act of swiping my debit card, entering my PIN, and impatiently waiting for the receipt to print. All the while, I stand awkwardly, eyes downcast and fixed on the display of the card reader, ignoring the human being directly across from me.
Obsession with screens
Our engagement with screen time has grown to pandemic proportions, and television is no longer the main culprit. According to a Nielsen global consumer report,1 in 2010 in the United States, people spent an average of 5 hours a day in front of the “boob tube.” Even if we take that statistic with a grain of salt, it still represents only the most visible tip of the media iceberg. Smartphones, laptop and desktop monitors, portable gaming consoles, electronic tablets, PIN pad displays, video billboards, and any number of other LED and LCD screen surfaces have infiltrated the landscape.
Whereas most recent epidemiologic studies have addressed the deleterious effects of so-called sit time (sedentary activities with or without a screen) on physical health, I would like to address the deleterious effect of screen time on mental health and relational connectedness and the relevance of that screen time to psychiatric practice.
The ‘techno-bubble of private space’
Almond,2 in a humorous social commentary, “Connection Error,” conducted an impromptu experiment in which he attempted to connect spontaneously with strangers, especially those who had a smartphone, in Boston. His narrative navigates the gamut of human interaction, from tedious and boorish to comedic and absurd, noting that, conspicuously, “smartphone users have created a techno-bubble of private space” in which they are physically present but emotionally unavailable.
A chance encounter with a young professional led Almond to this conclusion:
It’s precisely the intrusive alienation of the “techno-bubble” that blunders into the modern patient-physician interaction in my clinical psychiatric practice in a busy outpatient clinic at a university medical center. Specifically, the ever-glowing, ever-distracting computer monitor sitting between me and my patient, with its promise of digital information at my fingertips, serves more to distance me from my patient than to connect us in a meaningful, human way. Just as I can’t recall the countenance of the grocery-store cashier, I miss the delicate, information-laden, minute-to-minute social interaction with the patient because it competes with the electronic intruder.
What’s at risk when a computer screen is in the room?
Transference in the psychotherapeutic encounter is an established tenet of psychoanalytic theory. In “Basic theory of psychoanalysis,”3 Waelder defines transference as “not simply the attribution to new objects of characteristics of old ones but the attempt to re-establish and relive, with whatever object will permit it, an infantile situation much longed for because it was once either greatly enjoyed or greatly missed.” This definition applies to the positive pole of transferential phenomena—and it is this position that is desired in a successful patient−physician encounter.
A patient’s warm and genial regard toward a provider secures trust, cooperation, and faith in the healing process. Establishment of positive transference toward the physician is essential to enhance the clinical encounter, regardless of what early object (caring mother, omnipotent father) is being projected onto the physician.
Attunement. Research into infant observation has revealed the critical role of caretaker responsiveness in the development of early infantile emotional regulation. Tronick et al4 demonstrated the importance of interactional reciprocity in the mother−child dyad.
In a series of experiments using the so-called still-face paradigm, Tronick et al4 saw that infants quickly fall into a state of despair and related negative affects when the mother assumes an unresponsive and detached still face. These episodes intentionally produce infant-mother emotional misattunement, which, although instantly damaging, can be successfully repaired through re-attunement by the mother. It is the primary caretaker’s ability to reconnect and repair that is paramount to the infant’s healthy psychological development.
This sentiment is echoed in Winnicott’s concept of the “good-enough” mother (or parent), formulated years earlier, in which failures in infant−caretaker attunement are inevitable and to be expected—as long as repair outcompetes deficiency.5
Divided attention: Patient or screen? Or both?
What we can understand by applying the ideas of transference and optimal attunement to the clinical encounter is how important uninterrupted face-to-face time with the patient is. Indeed, nonverbal communication from the patient, expressed though body language and facial articulation, is particularly salient to the practice of psychiatry. Information technology— especially the electronic health record—now encroaches on the time-honored central dyad of the patient-physician interaction by introducing a third entity into the traditional encounter.
Clinical misattunement, as understood through the still-face paradigm, increases in proportion to a provider’s need to divide his (her) attention between the patient and the computer screen. And, as the degree of misattunement increases, positive transference is more difficult to establish and maintain. The quality of the clinical encounter then deteriorates, undermining the care of the patient and reducing physician satisfaction.
Acknowledgment
Philip LeFevre, MD, Department of Neurology & Psychiatry, Saint Louis University, St. Louis, Missouri, provided inspiration and encouragement in the development of the manuscript.
Disclosure
Dr. Afanasevich reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. The Nielsen Company. How people watch: a global Nielsen consumer report. http://www.nielsen.com/content/dam/ corporate/mx/reports/2011/Lo-que-la-gente-ve.pdf. Published August 2010. Accessed March 17, 2015.
2. Almond S. Connection error. Spirit Magazine. April 2014:76-86.
3. Waelder R. Basic theory of psychoanalysis. New York, NY: International Universities Press; 1960.
4. Tronick E, Als H, Adamson L, et al. The infant’s response to entrapment between contradictory messages in face-to-face interaction. J Am Acad Child Psychiatry. 1978;17(1):1-13.
5. Winnicott DW. The child, the family, and the outside world. London, United Kingdom: Penguin Books; 1964.
1. The Nielsen Company. How people watch: a global Nielsen consumer report. http://www.nielsen.com/content/dam/ corporate/mx/reports/2011/Lo-que-la-gente-ve.pdf. Published August 2010. Accessed March 17, 2015.
2. Almond S. Connection error. Spirit Magazine. April 2014:76-86.
3. Waelder R. Basic theory of psychoanalysis. New York, NY: International Universities Press; 1960.
4. Tronick E, Als H, Adamson L, et al. The infant’s response to entrapment between contradictory messages in face-to-face interaction. J Am Acad Child Psychiatry. 1978;17(1):1-13.
5. Winnicott DW. The child, the family, and the outside world. London, United Kingdom: Penguin Books; 1964.