User login
Special Interest Groups Target Healthcare Waste
As HM ramps up its efforts to eliminate wasteful and unnecessary medical treatments through its participation in the American Board of Internal Medicine (ABIM) Foundation’s Choosing Wisely Campaign (choosingwisely.org), two new policy reports help to delineate the problem of waste in healthcare.
The Health Affairs health policy brief “Reducing Waste in Health Care” concludes that a third or more of U.S. healthcare spending could be considered wasteful.4 Its categories of waste include unnecessary services, inefficiently delivered services, excessive prices and administrative costs, fraud, and abuse—along with a handful of categories familiar to hospitalists: failures of care coordination, avoidable hospital readmissions, and missed prevention opportunities.
The policy brief offers potential solutions, including increased provider use of digital data to improve care coordination and delivery, and heightened transparency of provider performance for consumers.
On Jan. 10, the Commonwealth Fund proposed a new set of strategies to slow health spending growth by $2 trillion dollars over the next 10 years.5 The report outlines a broad set of policies to change the way healthcare is paid for, accelerating a variety of delivery system innovations already under way; disseminate better quality and cost information to enhance consumers’ ability to choose high-value care; and address the market forces that drive up costs.
“We know that by innovating and coordinating care, our healthcare system can provide better care at lower cost,” Commonwealth Fund president David Blumenthal, MD, said in the report.
References
- Health Affairs. Health Policy Brief: Reducing Waste in Health Care. Health Affairs website. Available at: http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=82. Accessed Jan. 10, 2013.
- The Commonwealth Fund Commission on a High Performance Health System. Confronting Costs: Stabilizing U.S. Health Spending While Moving Toward a High Performance Health Care System. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/Publications/Fund-Reports/2013/Jan/Confronting-Costs.aspx?page=all. Accessed Feb. 2, 2013.
As HM ramps up its efforts to eliminate wasteful and unnecessary medical treatments through its participation in the American Board of Internal Medicine (ABIM) Foundation’s Choosing Wisely Campaign (choosingwisely.org), two new policy reports help to delineate the problem of waste in healthcare.
The Health Affairs health policy brief “Reducing Waste in Health Care” concludes that a third or more of U.S. healthcare spending could be considered wasteful.4 Its categories of waste include unnecessary services, inefficiently delivered services, excessive prices and administrative costs, fraud, and abuse—along with a handful of categories familiar to hospitalists: failures of care coordination, avoidable hospital readmissions, and missed prevention opportunities.
The policy brief offers potential solutions, including increased provider use of digital data to improve care coordination and delivery, and heightened transparency of provider performance for consumers.
On Jan. 10, the Commonwealth Fund proposed a new set of strategies to slow health spending growth by $2 trillion dollars over the next 10 years.5 The report outlines a broad set of policies to change the way healthcare is paid for, accelerating a variety of delivery system innovations already under way; disseminate better quality and cost information to enhance consumers’ ability to choose high-value care; and address the market forces that drive up costs.
“We know that by innovating and coordinating care, our healthcare system can provide better care at lower cost,” Commonwealth Fund president David Blumenthal, MD, said in the report.
References
- Health Affairs. Health Policy Brief: Reducing Waste in Health Care. Health Affairs website. Available at: http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=82. Accessed Jan. 10, 2013.
- The Commonwealth Fund Commission on a High Performance Health System. Confronting Costs: Stabilizing U.S. Health Spending While Moving Toward a High Performance Health Care System. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/Publications/Fund-Reports/2013/Jan/Confronting-Costs.aspx?page=all. Accessed Feb. 2, 2013.
As HM ramps up its efforts to eliminate wasteful and unnecessary medical treatments through its participation in the American Board of Internal Medicine (ABIM) Foundation’s Choosing Wisely Campaign (choosingwisely.org), two new policy reports help to delineate the problem of waste in healthcare.
The Health Affairs health policy brief “Reducing Waste in Health Care” concludes that a third or more of U.S. healthcare spending could be considered wasteful.4 Its categories of waste include unnecessary services, inefficiently delivered services, excessive prices and administrative costs, fraud, and abuse—along with a handful of categories familiar to hospitalists: failures of care coordination, avoidable hospital readmissions, and missed prevention opportunities.
The policy brief offers potential solutions, including increased provider use of digital data to improve care coordination and delivery, and heightened transparency of provider performance for consumers.
On Jan. 10, the Commonwealth Fund proposed a new set of strategies to slow health spending growth by $2 trillion dollars over the next 10 years.5 The report outlines a broad set of policies to change the way healthcare is paid for, accelerating a variety of delivery system innovations already under way; disseminate better quality and cost information to enhance consumers’ ability to choose high-value care; and address the market forces that drive up costs.
“We know that by innovating and coordinating care, our healthcare system can provide better care at lower cost,” Commonwealth Fund president David Blumenthal, MD, said in the report.
References
- Health Affairs. Health Policy Brief: Reducing Waste in Health Care. Health Affairs website. Available at: http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=82. Accessed Jan. 10, 2013.
- The Commonwealth Fund Commission on a High Performance Health System. Confronting Costs: Stabilizing U.S. Health Spending While Moving Toward a High Performance Health Care System. The Commonwealth Fund website. Available at: http://www.commonwealthfund.org/Publications/Fund-Reports/2013/Jan/Confronting-Costs.aspx?page=all. Accessed Feb. 2, 2013.
Medicare Funding May Become Enormous Burden for Generations of Future Taxpayers
February 2033
Dear sons:
Now that most of my baby boomer friends are 80 or 90 years old and are still hanging on, I wanted to apologize for leaving you in such a mess. Looking back, we all should have made some tough choices back in 2013, when some thoughtful belt-tightening would have created a fiscally sound ability for our country to provide healthcare and a safety net, not only to our senior citizens, but to all Americans. After today’s riots across the country, I felt I had to reach out to you and beg you to let rational minds prevail.
My fellow seniors, who paid into the Medicare and Social Security programs through our payroll taxes during the 30 to 40 years we worked in American industries, believe we are entitled to live forever with unlimited healthcare paid for by you. We are lined up almost every day at one doctor’s office or another to have our fourth joint replacement or our monthly MRI. Even though the actuaries tell us we all blew through our own contributions to Medicare sometime around our 75th birthdays, the general thinking of my friends on the golf course is that we paid for our parents’ healthcare and retirement, and you should just suck it up and stop whining.
Now I do admit that my friends tend to overlook the fact that when we were just in our 50s, like you are now, there were eight or nine workers (i.e. taxpayers) for every retiree. Now it seems it is one taxpayer working to support one retiree. The math just doesn’t work anymore. No wonder your tax burden is so suffocating that young workers can’t afford a home or a second car or even a vacation. I can see why there is talk by some of rationing care, but some of the rhetoric is kind of frightening.
Yes, there are more 90-year-olds with severe dementia on chronic dialysis than I would like to see. I don’t necessarily agree that everyone has a right to die with a normal BUN. Our generation did some great things with immunizations, cancer prevention, reducing the risks of coronary heart disease, and stroke prevention and treatment. The end result is that many of those who would have died earlier have lived beyond our country’s means to provide for them. For heaven’s sake, there are more than 1 million Americans over the age of 100 today. Once a woman gets past 65, it seems they are destined to live indefinitely.
Believe it or not, I was around in the 1960s when Medicare was first discussed and people were looking at life expectancies in the early 70s. No one saw the advent of so much expensive technology in diagnostic testing and surgical intervention. Despite more bipartisan national commissions and reports than I care to remember, no president or Congress has had the cojones to make the tough choices to provide the basic health needs for seniors in a fiscally sound system that doesn’t overwhelm the workforce.
I know the slogans urge a move from Medicare to “MediCan’t.” I know some want to bar seniors from getting flu shots and want to have pneumonia be the old man’s friend again. I sense a feeling that the elderly are becoming the enemy of the working class. I hear the rants that most of our nation’s wealth is held by those over 65, yet my generation wants more and more, feeling we paid for this and we deserve everything we have coming to us.
Once again, sorry this all had to fall on you, but I have got to run. I am going to see your grandmother. I can’t believe how well she is recovering from arthroscopic surgery. Pretty amazing for someone who is 105 years old.
Love,
Dad
Dr. Wellikson is CEO of SHM.
February 2033
Dear sons:
Now that most of my baby boomer friends are 80 or 90 years old and are still hanging on, I wanted to apologize for leaving you in such a mess. Looking back, we all should have made some tough choices back in 2013, when some thoughtful belt-tightening would have created a fiscally sound ability for our country to provide healthcare and a safety net, not only to our senior citizens, but to all Americans. After today’s riots across the country, I felt I had to reach out to you and beg you to let rational minds prevail.
My fellow seniors, who paid into the Medicare and Social Security programs through our payroll taxes during the 30 to 40 years we worked in American industries, believe we are entitled to live forever with unlimited healthcare paid for by you. We are lined up almost every day at one doctor’s office or another to have our fourth joint replacement or our monthly MRI. Even though the actuaries tell us we all blew through our own contributions to Medicare sometime around our 75th birthdays, the general thinking of my friends on the golf course is that we paid for our parents’ healthcare and retirement, and you should just suck it up and stop whining.
Now I do admit that my friends tend to overlook the fact that when we were just in our 50s, like you are now, there were eight or nine workers (i.e. taxpayers) for every retiree. Now it seems it is one taxpayer working to support one retiree. The math just doesn’t work anymore. No wonder your tax burden is so suffocating that young workers can’t afford a home or a second car or even a vacation. I can see why there is talk by some of rationing care, but some of the rhetoric is kind of frightening.
Yes, there are more 90-year-olds with severe dementia on chronic dialysis than I would like to see. I don’t necessarily agree that everyone has a right to die with a normal BUN. Our generation did some great things with immunizations, cancer prevention, reducing the risks of coronary heart disease, and stroke prevention and treatment. The end result is that many of those who would have died earlier have lived beyond our country’s means to provide for them. For heaven’s sake, there are more than 1 million Americans over the age of 100 today. Once a woman gets past 65, it seems they are destined to live indefinitely.
Believe it or not, I was around in the 1960s when Medicare was first discussed and people were looking at life expectancies in the early 70s. No one saw the advent of so much expensive technology in diagnostic testing and surgical intervention. Despite more bipartisan national commissions and reports than I care to remember, no president or Congress has had the cojones to make the tough choices to provide the basic health needs for seniors in a fiscally sound system that doesn’t overwhelm the workforce.
I know the slogans urge a move from Medicare to “MediCan’t.” I know some want to bar seniors from getting flu shots and want to have pneumonia be the old man’s friend again. I sense a feeling that the elderly are becoming the enemy of the working class. I hear the rants that most of our nation’s wealth is held by those over 65, yet my generation wants more and more, feeling we paid for this and we deserve everything we have coming to us.
Once again, sorry this all had to fall on you, but I have got to run. I am going to see your grandmother. I can’t believe how well she is recovering from arthroscopic surgery. Pretty amazing for someone who is 105 years old.
Love,
Dad
Dr. Wellikson is CEO of SHM.
February 2033
Dear sons:
Now that most of my baby boomer friends are 80 or 90 years old and are still hanging on, I wanted to apologize for leaving you in such a mess. Looking back, we all should have made some tough choices back in 2013, when some thoughtful belt-tightening would have created a fiscally sound ability for our country to provide healthcare and a safety net, not only to our senior citizens, but to all Americans. After today’s riots across the country, I felt I had to reach out to you and beg you to let rational minds prevail.
My fellow seniors, who paid into the Medicare and Social Security programs through our payroll taxes during the 30 to 40 years we worked in American industries, believe we are entitled to live forever with unlimited healthcare paid for by you. We are lined up almost every day at one doctor’s office or another to have our fourth joint replacement or our monthly MRI. Even though the actuaries tell us we all blew through our own contributions to Medicare sometime around our 75th birthdays, the general thinking of my friends on the golf course is that we paid for our parents’ healthcare and retirement, and you should just suck it up and stop whining.
Now I do admit that my friends tend to overlook the fact that when we were just in our 50s, like you are now, there were eight or nine workers (i.e. taxpayers) for every retiree. Now it seems it is one taxpayer working to support one retiree. The math just doesn’t work anymore. No wonder your tax burden is so suffocating that young workers can’t afford a home or a second car or even a vacation. I can see why there is talk by some of rationing care, but some of the rhetoric is kind of frightening.
Yes, there are more 90-year-olds with severe dementia on chronic dialysis than I would like to see. I don’t necessarily agree that everyone has a right to die with a normal BUN. Our generation did some great things with immunizations, cancer prevention, reducing the risks of coronary heart disease, and stroke prevention and treatment. The end result is that many of those who would have died earlier have lived beyond our country’s means to provide for them. For heaven’s sake, there are more than 1 million Americans over the age of 100 today. Once a woman gets past 65, it seems they are destined to live indefinitely.
Believe it or not, I was around in the 1960s when Medicare was first discussed and people were looking at life expectancies in the early 70s. No one saw the advent of so much expensive technology in diagnostic testing and surgical intervention. Despite more bipartisan national commissions and reports than I care to remember, no president or Congress has had the cojones to make the tough choices to provide the basic health needs for seniors in a fiscally sound system that doesn’t overwhelm the workforce.
I know the slogans urge a move from Medicare to “MediCan’t.” I know some want to bar seniors from getting flu shots and want to have pneumonia be the old man’s friend again. I sense a feeling that the elderly are becoming the enemy of the working class. I hear the rants that most of our nation’s wealth is held by those over 65, yet my generation wants more and more, feeling we paid for this and we deserve everything we have coming to us.
Once again, sorry this all had to fall on you, but I have got to run. I am going to see your grandmother. I can’t believe how well she is recovering from arthroscopic surgery. Pretty amazing for someone who is 105 years old.
Love,
Dad
Dr. Wellikson is CEO of SHM.
Southern Hospital Medicine Conference Drives Home the Value of Hospitalists
More than 300 hospitalists and other clinicians recently attended the 13th annual Southern Hospital Medicine Conference in Atlanta. The conference is a joint collaboration between the Emory University School of Medicine in Atlanta and Ochsner Health System New Orleans. The meeting site has alternated between the two cities each year since 2005.
The prevailing conference theme in 2012 was “Value and Values in Hospital Medicine,” alluding to the value that hospitalists bring to the medical community and hospitals and the values shared by hospitalists. The conference offered five pre-courses and more than 50 sessions focused on educating hospitalists on current best practices within core topic areas, including clinical care, quality improvement, healthcare information technology, innovative care models, systems of care, and transitions of care. A judged poster competition featured research and clinical vignettes abstracts, with interesting clinical cases as well as new research in hospital medicine.
One of the highlights of this year’s conference was the keynote address delivered by Dr. William A. Bornstein, chief quality and medical officer of Emory Healthcare. Dr. Bornstein discussed the various aspects of quality and cost in hospital care. He described the challenges in defining quality and measuring cost when trying to calculate the “value” equation in medicine (value=quality/cost). He outlined the Institute of Medicine’s previously described STEEEP (safe, timely, effective, efficient, equitable, patient-centered) aims of quality in 2001.
Dr. Bornstein’s own definition for quality is “partnering with patients and families to reliably, 100% of the time, deliver when, where, and how they want it—and with minimal waste—care based on the best available evidence and consistent with patient and family values and preferences.” To measure outcome, he said, we need to address system structure (what’s in place before the patient arrives), process (what we do for the patient), and culture (how we can get the buy-in from all stakeholders). The sum of these factors achieves outcome, which requires risk adjustment and, ideally, long-term follow-up data, he said.
Dr. Bornstein also discussed the need to develop standard processes whereby equivalent clinicians can follow similar processes to achieve the same results. When physicians “do it the same” (i.e. standardized protocols), error rates and cost decrease, he explained.
Dr. Bornstein also focused on transformative solutions to address problems in healthcare as a whole, rather than attempting to fix problems piecemeal.
Jason Stein, MD, SFHM, offered another conference highlight: a pre-conference program and plenary session on an innovative approach to improve hospital outcomes through implementation of the accountable-care unit (ACU). Dr. Stein, director of the clinical research program at Emory School of Medicine, described the current state of hospital care as asynchronous, with various providers caring for the patient without much coordination. For example, the physician sees the patient at 9 a.m., followed by the nurse at 10 a.m., and then finally the visiting family at 11 a.m. The ACU model of care would involve all the providers rounding with the patient and family at a scheduled time daily to provide synchronous care.
Dr. Stein described an ACU as a geographic inpatient area consistently responsible for the clinical, service, and cost outcomes it produces. Features of this unit include:
- Assignment of physicians by units to enhance predictability;
- Cohesiveness and communication;
- Structured interdisciplinary bedside rounds to consistently deliver evidence-based, patient-centered care;
- Evaluation of performance data by unit instead of facility or service line; and
- A dyad partnership involving a nurse unit director and a physician unit medical director.
ACU implementation at Emory has led to decreased mortality, reduced length of stay, and improved patient satisfaction compared to traditional units, according to Dr. Stein. While the ACU might not be suited for all, he said, all hospitals can learn from various components of this innovative approach to deliver better patient care.
The ever-changing state of HM in the U.S. remains a challenge, but it continues to generate innovation and excitement. The high number of engaged participants from 30 different states attending the 13th annual Southern Hospital Medicine Conference demonstrates that hospitalists are eager to learn and ready to improve their practice in order to provide high-value healthcare in U.S. hospitals today.
Dr. Lee is vice chairman in the department of hospital medicine at Ochsner Health System. Dr. Smith is an assistant director for education in the division of hospital medicine at Emory University. Dr. Deitelzweig is system chairman in the department of hospital medicine and medical director for regional business development at Ochsner Health System. Dr. Wang is the division director of hospital medicine at Emory University. Dr. Dressler is director for education in the division of hospital medicine and an associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory University.
More than 300 hospitalists and other clinicians recently attended the 13th annual Southern Hospital Medicine Conference in Atlanta. The conference is a joint collaboration between the Emory University School of Medicine in Atlanta and Ochsner Health System New Orleans. The meeting site has alternated between the two cities each year since 2005.
The prevailing conference theme in 2012 was “Value and Values in Hospital Medicine,” alluding to the value that hospitalists bring to the medical community and hospitals and the values shared by hospitalists. The conference offered five pre-courses and more than 50 sessions focused on educating hospitalists on current best practices within core topic areas, including clinical care, quality improvement, healthcare information technology, innovative care models, systems of care, and transitions of care. A judged poster competition featured research and clinical vignettes abstracts, with interesting clinical cases as well as new research in hospital medicine.
One of the highlights of this year’s conference was the keynote address delivered by Dr. William A. Bornstein, chief quality and medical officer of Emory Healthcare. Dr. Bornstein discussed the various aspects of quality and cost in hospital care. He described the challenges in defining quality and measuring cost when trying to calculate the “value” equation in medicine (value=quality/cost). He outlined the Institute of Medicine’s previously described STEEEP (safe, timely, effective, efficient, equitable, patient-centered) aims of quality in 2001.
Dr. Bornstein’s own definition for quality is “partnering with patients and families to reliably, 100% of the time, deliver when, where, and how they want it—and with minimal waste—care based on the best available evidence and consistent with patient and family values and preferences.” To measure outcome, he said, we need to address system structure (what’s in place before the patient arrives), process (what we do for the patient), and culture (how we can get the buy-in from all stakeholders). The sum of these factors achieves outcome, which requires risk adjustment and, ideally, long-term follow-up data, he said.
Dr. Bornstein also discussed the need to develop standard processes whereby equivalent clinicians can follow similar processes to achieve the same results. When physicians “do it the same” (i.e. standardized protocols), error rates and cost decrease, he explained.
Dr. Bornstein also focused on transformative solutions to address problems in healthcare as a whole, rather than attempting to fix problems piecemeal.
Jason Stein, MD, SFHM, offered another conference highlight: a pre-conference program and plenary session on an innovative approach to improve hospital outcomes through implementation of the accountable-care unit (ACU). Dr. Stein, director of the clinical research program at Emory School of Medicine, described the current state of hospital care as asynchronous, with various providers caring for the patient without much coordination. For example, the physician sees the patient at 9 a.m., followed by the nurse at 10 a.m., and then finally the visiting family at 11 a.m. The ACU model of care would involve all the providers rounding with the patient and family at a scheduled time daily to provide synchronous care.
Dr. Stein described an ACU as a geographic inpatient area consistently responsible for the clinical, service, and cost outcomes it produces. Features of this unit include:
- Assignment of physicians by units to enhance predictability;
- Cohesiveness and communication;
- Structured interdisciplinary bedside rounds to consistently deliver evidence-based, patient-centered care;
- Evaluation of performance data by unit instead of facility or service line; and
- A dyad partnership involving a nurse unit director and a physician unit medical director.
ACU implementation at Emory has led to decreased mortality, reduced length of stay, and improved patient satisfaction compared to traditional units, according to Dr. Stein. While the ACU might not be suited for all, he said, all hospitals can learn from various components of this innovative approach to deliver better patient care.
The ever-changing state of HM in the U.S. remains a challenge, but it continues to generate innovation and excitement. The high number of engaged participants from 30 different states attending the 13th annual Southern Hospital Medicine Conference demonstrates that hospitalists are eager to learn and ready to improve their practice in order to provide high-value healthcare in U.S. hospitals today.
Dr. Lee is vice chairman in the department of hospital medicine at Ochsner Health System. Dr. Smith is an assistant director for education in the division of hospital medicine at Emory University. Dr. Deitelzweig is system chairman in the department of hospital medicine and medical director for regional business development at Ochsner Health System. Dr. Wang is the division director of hospital medicine at Emory University. Dr. Dressler is director for education in the division of hospital medicine and an associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory University.
More than 300 hospitalists and other clinicians recently attended the 13th annual Southern Hospital Medicine Conference in Atlanta. The conference is a joint collaboration between the Emory University School of Medicine in Atlanta and Ochsner Health System New Orleans. The meeting site has alternated between the two cities each year since 2005.
The prevailing conference theme in 2012 was “Value and Values in Hospital Medicine,” alluding to the value that hospitalists bring to the medical community and hospitals and the values shared by hospitalists. The conference offered five pre-courses and more than 50 sessions focused on educating hospitalists on current best practices within core topic areas, including clinical care, quality improvement, healthcare information technology, innovative care models, systems of care, and transitions of care. A judged poster competition featured research and clinical vignettes abstracts, with interesting clinical cases as well as new research in hospital medicine.
One of the highlights of this year’s conference was the keynote address delivered by Dr. William A. Bornstein, chief quality and medical officer of Emory Healthcare. Dr. Bornstein discussed the various aspects of quality and cost in hospital care. He described the challenges in defining quality and measuring cost when trying to calculate the “value” equation in medicine (value=quality/cost). He outlined the Institute of Medicine’s previously described STEEEP (safe, timely, effective, efficient, equitable, patient-centered) aims of quality in 2001.
Dr. Bornstein’s own definition for quality is “partnering with patients and families to reliably, 100% of the time, deliver when, where, and how they want it—and with minimal waste—care based on the best available evidence and consistent with patient and family values and preferences.” To measure outcome, he said, we need to address system structure (what’s in place before the patient arrives), process (what we do for the patient), and culture (how we can get the buy-in from all stakeholders). The sum of these factors achieves outcome, which requires risk adjustment and, ideally, long-term follow-up data, he said.
Dr. Bornstein also discussed the need to develop standard processes whereby equivalent clinicians can follow similar processes to achieve the same results. When physicians “do it the same” (i.e. standardized protocols), error rates and cost decrease, he explained.
Dr. Bornstein also focused on transformative solutions to address problems in healthcare as a whole, rather than attempting to fix problems piecemeal.
Jason Stein, MD, SFHM, offered another conference highlight: a pre-conference program and plenary session on an innovative approach to improve hospital outcomes through implementation of the accountable-care unit (ACU). Dr. Stein, director of the clinical research program at Emory School of Medicine, described the current state of hospital care as asynchronous, with various providers caring for the patient without much coordination. For example, the physician sees the patient at 9 a.m., followed by the nurse at 10 a.m., and then finally the visiting family at 11 a.m. The ACU model of care would involve all the providers rounding with the patient and family at a scheduled time daily to provide synchronous care.
Dr. Stein described an ACU as a geographic inpatient area consistently responsible for the clinical, service, and cost outcomes it produces. Features of this unit include:
- Assignment of physicians by units to enhance predictability;
- Cohesiveness and communication;
- Structured interdisciplinary bedside rounds to consistently deliver evidence-based, patient-centered care;
- Evaluation of performance data by unit instead of facility or service line; and
- A dyad partnership involving a nurse unit director and a physician unit medical director.
ACU implementation at Emory has led to decreased mortality, reduced length of stay, and improved patient satisfaction compared to traditional units, according to Dr. Stein. While the ACU might not be suited for all, he said, all hospitals can learn from various components of this innovative approach to deliver better patient care.
The ever-changing state of HM in the U.S. remains a challenge, but it continues to generate innovation and excitement. The high number of engaged participants from 30 different states attending the 13th annual Southern Hospital Medicine Conference demonstrates that hospitalists are eager to learn and ready to improve their practice in order to provide high-value healthcare in U.S. hospitals today.
Dr. Lee is vice chairman in the department of hospital medicine at Ochsner Health System. Dr. Smith is an assistant director for education in the division of hospital medicine at Emory University. Dr. Deitelzweig is system chairman in the department of hospital medicine and medical director for regional business development at Ochsner Health System. Dr. Wang is the division director of hospital medicine at Emory University. Dr. Dressler is director for education in the division of hospital medicine and an associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory University.
Effect of Nonpayment on Nosocomial Infection Rates in U.S. Hospitals
Clinical question: Did the 2008 Center for Medicare & Medicaid Services (CMS) policy denying additional payment for hospital-acquired conditions result in decreased rates of nosocomial infections?
Background: In an effort to curtail preventable complications, CMS implemented a policy of nonpayment for certain healthcare-acquired conditions beginning in October 2008. The effect of this policy on rates of nosocomial infections, including central venous catheter-associated bloodstream infections and catheter-associated urinary tract infections, is unknown.
Study design: Quasi-experimental.
Setting: Data collected from 398 hospitals participating in the National Healthcare Safety Network of the Centers for Disease Control and Prevention.
Synopsis: Investigators analyzed rates of nosocomial infections in participating hospitals before and after implementation of the 2008 nonpayment policy. The rates of decline in central venous catheter infections were not significantly different in the pre-implementation and post-implementation periods (4.8% per quarter and 4.7% per quarter, respectively; incidence-rate ratio 1.0; P=0.97). Similar results were found with regard to catheter-associated UTIs before and after policy initiation (3.9% per quarter and 0.9% per quarter, incidence-rate ratio 1.03; P=0.08). Results did not vary between states with and without mandatory reporting of nosocomial infections.
While this study’s broad scope limits the ability to draw firm conclusions, it does highlight the need for careful evaluation and quantification of the outcomes resulting from CMS’ expansion of policies for financial incentives and disincentives.
Bottom line: National rates of decline in nosocomial infections were unchanged before and after implementation of CMS’ nonpayment policy in 2008.
Citation: Lee GM, Kleinman K, Soumerai SB, et al. Effect of nonpayment for preventable infections in U.S. hospitals. N Engl J Med. 2012;367:1428-1437
Clinical question: Did the 2008 Center for Medicare & Medicaid Services (CMS) policy denying additional payment for hospital-acquired conditions result in decreased rates of nosocomial infections?
Background: In an effort to curtail preventable complications, CMS implemented a policy of nonpayment for certain healthcare-acquired conditions beginning in October 2008. The effect of this policy on rates of nosocomial infections, including central venous catheter-associated bloodstream infections and catheter-associated urinary tract infections, is unknown.
Study design: Quasi-experimental.
Setting: Data collected from 398 hospitals participating in the National Healthcare Safety Network of the Centers for Disease Control and Prevention.
Synopsis: Investigators analyzed rates of nosocomial infections in participating hospitals before and after implementation of the 2008 nonpayment policy. The rates of decline in central venous catheter infections were not significantly different in the pre-implementation and post-implementation periods (4.8% per quarter and 4.7% per quarter, respectively; incidence-rate ratio 1.0; P=0.97). Similar results were found with regard to catheter-associated UTIs before and after policy initiation (3.9% per quarter and 0.9% per quarter, incidence-rate ratio 1.03; P=0.08). Results did not vary between states with and without mandatory reporting of nosocomial infections.
While this study’s broad scope limits the ability to draw firm conclusions, it does highlight the need for careful evaluation and quantification of the outcomes resulting from CMS’ expansion of policies for financial incentives and disincentives.
Bottom line: National rates of decline in nosocomial infections were unchanged before and after implementation of CMS’ nonpayment policy in 2008.
Citation: Lee GM, Kleinman K, Soumerai SB, et al. Effect of nonpayment for preventable infections in U.S. hospitals. N Engl J Med. 2012;367:1428-1437
Clinical question: Did the 2008 Center for Medicare & Medicaid Services (CMS) policy denying additional payment for hospital-acquired conditions result in decreased rates of nosocomial infections?
Background: In an effort to curtail preventable complications, CMS implemented a policy of nonpayment for certain healthcare-acquired conditions beginning in October 2008. The effect of this policy on rates of nosocomial infections, including central venous catheter-associated bloodstream infections and catheter-associated urinary tract infections, is unknown.
Study design: Quasi-experimental.
Setting: Data collected from 398 hospitals participating in the National Healthcare Safety Network of the Centers for Disease Control and Prevention.
Synopsis: Investigators analyzed rates of nosocomial infections in participating hospitals before and after implementation of the 2008 nonpayment policy. The rates of decline in central venous catheter infections were not significantly different in the pre-implementation and post-implementation periods (4.8% per quarter and 4.7% per quarter, respectively; incidence-rate ratio 1.0; P=0.97). Similar results were found with regard to catheter-associated UTIs before and after policy initiation (3.9% per quarter and 0.9% per quarter, incidence-rate ratio 1.03; P=0.08). Results did not vary between states with and without mandatory reporting of nosocomial infections.
While this study’s broad scope limits the ability to draw firm conclusions, it does highlight the need for careful evaluation and quantification of the outcomes resulting from CMS’ expansion of policies for financial incentives and disincentives.
Bottom line: National rates of decline in nosocomial infections were unchanged before and after implementation of CMS’ nonpayment policy in 2008.
Citation: Lee GM, Kleinman K, Soumerai SB, et al. Effect of nonpayment for preventable infections in U.S. hospitals. N Engl J Med. 2012;367:1428-1437
Win Whitcomb: Mortality Rates Become a Measuring Stick for Hospital Performance
—Blue Oyster Cult
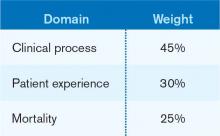
The designers of the hospital value-based purchasing (HVBP) program sought to include outcomes measures in 2014, and when they did, mortality was their choice. Specifically, HVBP for fiscal-year 2014 (starting October 2013) will include 30-day mortality rates for myocardial infarction, heart failure, and pneumonia. The weighting for the mortality domain will be 25% (see Table 1).
To review the requirements for the HVBP program in FY2014: All hospitals will have 1.25% of their Medicare inpatient payments withheld. They can earn back none, some, all, or an amount in excess of the 1.25%, depending on performance in the performance domains. To put it in perspective, 1.25% of Medicare inpatient payments for a 320-bed hospital are about $1 million. Such a hospital will have about $250,000 at risk in the mortality domain in FY2014.
Given the role hospitalists play in quality and safety initiatives, and the importance of medical record documentation in defining the risk of mortality and severity of illness, we can be crucial players in how our hospitals perform with regard to mortality.
Focus Areas for Mortality Reduction
Although many hospitalists might think that reducing mortality is like “boiling the ocean,” there are some areas where we can clearly focus our attention. There are four priority areas we should target in the coming years (also see Figure 1):
Reduce harm. This may take the form of reducing hospital-acquired infections, such as catheter-related UTIs, Clostridium difficile, and central-line-associated bloodstream infections, or reducing hospital-acquired VTE, falls, and delirium. Many hospital-acquired conditions have a collection, or bundle, of preventive practices. Hospitalists can work both in an institutional leadership capacity and in the course of daily clinical practice to implement bundles and best practices to reduce patient harm.
Improve teamwork. With hospitalists, “you started to have teams caring for inpatients in a coordinated way. So I regard this as [hospitalists] coming into their own, their vision of the future starting to really take hold,” said Brent James, coauthor of the recent Institute of Medicine report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Partly, we’ve accomplished this through simply “showing up” and partly we’ve done it through becoming students of the art and science of teamwork. An example of teamwork training, developed by the Defense Department and the Agency for Healthcare Quality and Research (AHRQ), is TeamSTEPPS, which offers a systematic approach to cooperation, coordination, and communication among team members. Optimal patient resuscitation, in-hospital handoffs, rapid-response teams, and early-warning systems are essential pieces of teamwork that may reduce mortality.
Improve evidence-based care. This domain covers process measures aimed at optimizing care, including reducing mortality. For HVBP in particular, myocardial infarction, heart failure, and pneumonia are the focus.
Improve transitions of care. Best practices for care transitions and reducing readmissions, including advance-care planning, involvement of palliative care and hospice, and coordination with post-acute care, can be a key part of reducing 30-day mortality.
Documentation Integrity
Accurately capturing a patient’s condition in the medical record is crucial to assigning severity of illness and risk of mortality. Because mortality rates are severity-adjusted, accurate documentation is another important dimension to potentially improving a hospital’s performance with regard to the mortality domain. This is one more reason to work closely with your hospital’s documentation specialists.
Don’t Be Afraid...
Proponents of mortality as a quality measure point to it as the ultimate reflection of the care provided. While moving the needle might seem like a task too big to undertake, a disciplined approach to the elements of the driver diagram combined with a robust documentation program can provide your institution with a tangible focus on this definitive measure.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
—Blue Oyster Cult
The designers of the hospital value-based purchasing (HVBP) program sought to include outcomes measures in 2014, and when they did, mortality was their choice. Specifically, HVBP for fiscal-year 2014 (starting October 2013) will include 30-day mortality rates for myocardial infarction, heart failure, and pneumonia. The weighting for the mortality domain will be 25% (see Table 1).
To review the requirements for the HVBP program in FY2014: All hospitals will have 1.25% of their Medicare inpatient payments withheld. They can earn back none, some, all, or an amount in excess of the 1.25%, depending on performance in the performance domains. To put it in perspective, 1.25% of Medicare inpatient payments for a 320-bed hospital are about $1 million. Such a hospital will have about $250,000 at risk in the mortality domain in FY2014.
Given the role hospitalists play in quality and safety initiatives, and the importance of medical record documentation in defining the risk of mortality and severity of illness, we can be crucial players in how our hospitals perform with regard to mortality.
Focus Areas for Mortality Reduction
Although many hospitalists might think that reducing mortality is like “boiling the ocean,” there are some areas where we can clearly focus our attention. There are four priority areas we should target in the coming years (also see Figure 1):
Reduce harm. This may take the form of reducing hospital-acquired infections, such as catheter-related UTIs, Clostridium difficile, and central-line-associated bloodstream infections, or reducing hospital-acquired VTE, falls, and delirium. Many hospital-acquired conditions have a collection, or bundle, of preventive practices. Hospitalists can work both in an institutional leadership capacity and in the course of daily clinical practice to implement bundles and best practices to reduce patient harm.
Improve teamwork. With hospitalists, “you started to have teams caring for inpatients in a coordinated way. So I regard this as [hospitalists] coming into their own, their vision of the future starting to really take hold,” said Brent James, coauthor of the recent Institute of Medicine report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Partly, we’ve accomplished this through simply “showing up” and partly we’ve done it through becoming students of the art and science of teamwork. An example of teamwork training, developed by the Defense Department and the Agency for Healthcare Quality and Research (AHRQ), is TeamSTEPPS, which offers a systematic approach to cooperation, coordination, and communication among team members. Optimal patient resuscitation, in-hospital handoffs, rapid-response teams, and early-warning systems are essential pieces of teamwork that may reduce mortality.
Improve evidence-based care. This domain covers process measures aimed at optimizing care, including reducing mortality. For HVBP in particular, myocardial infarction, heart failure, and pneumonia are the focus.
Improve transitions of care. Best practices for care transitions and reducing readmissions, including advance-care planning, involvement of palliative care and hospice, and coordination with post-acute care, can be a key part of reducing 30-day mortality.
Documentation Integrity
Accurately capturing a patient’s condition in the medical record is crucial to assigning severity of illness and risk of mortality. Because mortality rates are severity-adjusted, accurate documentation is another important dimension to potentially improving a hospital’s performance with regard to the mortality domain. This is one more reason to work closely with your hospital’s documentation specialists.
Don’t Be Afraid...
Proponents of mortality as a quality measure point to it as the ultimate reflection of the care provided. While moving the needle might seem like a task too big to undertake, a disciplined approach to the elements of the driver diagram combined with a robust documentation program can provide your institution with a tangible focus on this definitive measure.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
—Blue Oyster Cult
The designers of the hospital value-based purchasing (HVBP) program sought to include outcomes measures in 2014, and when they did, mortality was their choice. Specifically, HVBP for fiscal-year 2014 (starting October 2013) will include 30-day mortality rates for myocardial infarction, heart failure, and pneumonia. The weighting for the mortality domain will be 25% (see Table 1).
To review the requirements for the HVBP program in FY2014: All hospitals will have 1.25% of their Medicare inpatient payments withheld. They can earn back none, some, all, or an amount in excess of the 1.25%, depending on performance in the performance domains. To put it in perspective, 1.25% of Medicare inpatient payments for a 320-bed hospital are about $1 million. Such a hospital will have about $250,000 at risk in the mortality domain in FY2014.
Given the role hospitalists play in quality and safety initiatives, and the importance of medical record documentation in defining the risk of mortality and severity of illness, we can be crucial players in how our hospitals perform with regard to mortality.
Focus Areas for Mortality Reduction
Although many hospitalists might think that reducing mortality is like “boiling the ocean,” there are some areas where we can clearly focus our attention. There are four priority areas we should target in the coming years (also see Figure 1):
Reduce harm. This may take the form of reducing hospital-acquired infections, such as catheter-related UTIs, Clostridium difficile, and central-line-associated bloodstream infections, or reducing hospital-acquired VTE, falls, and delirium. Many hospital-acquired conditions have a collection, or bundle, of preventive practices. Hospitalists can work both in an institutional leadership capacity and in the course of daily clinical practice to implement bundles and best practices to reduce patient harm.
Improve teamwork. With hospitalists, “you started to have teams caring for inpatients in a coordinated way. So I regard this as [hospitalists] coming into their own, their vision of the future starting to really take hold,” said Brent James, coauthor of the recent Institute of Medicine report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Partly, we’ve accomplished this through simply “showing up” and partly we’ve done it through becoming students of the art and science of teamwork. An example of teamwork training, developed by the Defense Department and the Agency for Healthcare Quality and Research (AHRQ), is TeamSTEPPS, which offers a systematic approach to cooperation, coordination, and communication among team members. Optimal patient resuscitation, in-hospital handoffs, rapid-response teams, and early-warning systems are essential pieces of teamwork that may reduce mortality.
Improve evidence-based care. This domain covers process measures aimed at optimizing care, including reducing mortality. For HVBP in particular, myocardial infarction, heart failure, and pneumonia are the focus.
Improve transitions of care. Best practices for care transitions and reducing readmissions, including advance-care planning, involvement of palliative care and hospice, and coordination with post-acute care, can be a key part of reducing 30-day mortality.
Documentation Integrity
Accurately capturing a patient’s condition in the medical record is crucial to assigning severity of illness and risk of mortality. Because mortality rates are severity-adjusted, accurate documentation is another important dimension to potentially improving a hospital’s performance with regard to the mortality domain. This is one more reason to work closely with your hospital’s documentation specialists.
Don’t Be Afraid...
Proponents of mortality as a quality measure point to it as the ultimate reflection of the care provided. While moving the needle might seem like a task too big to undertake, a disciplined approach to the elements of the driver diagram combined with a robust documentation program can provide your institution with a tangible focus on this definitive measure.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Multidisciplinary Palliative-Care Consults Help Reduce Hospital Readmissions
Research on seriously ill, hospitalized, Medicare-age patients finds that those who received inpatient consultations from a multidisciplinary, palliative-care team (including a physician, nurse, and social worker) had lower 30-day hospital readmission rates.1 Ten percent of discharged patients who received the palliative-care consult were readmitted within 30 days at an urban HMO medical center in Los Angeles County during the same period, even though they were sicker than the overall discharged population.
Receipt of hospice care or home-based palliative-care services following discharge was also associated with significantly lower rates of readmissions, suggesting opportunities for systemic cost savings from earlier access to longitudinal, or ongoing, palliative-care services, says Susan Enguidanos, MPH, PhD, assistant professor of gerontology at the University of Southern California in Los Angeles. Patients discharged from the hospital without any follow-up care in the home had higher odds of readmission.
“Hospitals and medical centers should seriously consider an inpatient palliative care consultation team for many reasons, mostly arising from findings from other studies that have demonstrated improved quality of life, pain and symptom management, satisfaction with medical care, and other promising outcomes,” Dr. Enguidanos says. “Our study suggests that longitudinal palliative care is also associated with the lower readmission rate.”
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
Research on seriously ill, hospitalized, Medicare-age patients finds that those who received inpatient consultations from a multidisciplinary, palliative-care team (including a physician, nurse, and social worker) had lower 30-day hospital readmission rates.1 Ten percent of discharged patients who received the palliative-care consult were readmitted within 30 days at an urban HMO medical center in Los Angeles County during the same period, even though they were sicker than the overall discharged population.
Receipt of hospice care or home-based palliative-care services following discharge was also associated with significantly lower rates of readmissions, suggesting opportunities for systemic cost savings from earlier access to longitudinal, or ongoing, palliative-care services, says Susan Enguidanos, MPH, PhD, assistant professor of gerontology at the University of Southern California in Los Angeles. Patients discharged from the hospital without any follow-up care in the home had higher odds of readmission.
“Hospitals and medical centers should seriously consider an inpatient palliative care consultation team for many reasons, mostly arising from findings from other studies that have demonstrated improved quality of life, pain and symptom management, satisfaction with medical care, and other promising outcomes,” Dr. Enguidanos says. “Our study suggests that longitudinal palliative care is also associated with the lower readmission rate.”
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
Research on seriously ill, hospitalized, Medicare-age patients finds that those who received inpatient consultations from a multidisciplinary, palliative-care team (including a physician, nurse, and social worker) had lower 30-day hospital readmission rates.1 Ten percent of discharged patients who received the palliative-care consult were readmitted within 30 days at an urban HMO medical center in Los Angeles County during the same period, even though they were sicker than the overall discharged population.
Receipt of hospice care or home-based palliative-care services following discharge was also associated with significantly lower rates of readmissions, suggesting opportunities for systemic cost savings from earlier access to longitudinal, or ongoing, palliative-care services, says Susan Enguidanos, MPH, PhD, assistant professor of gerontology at the University of Southern California in Los Angeles. Patients discharged from the hospital without any follow-up care in the home had higher odds of readmission.
“Hospitals and medical centers should seriously consider an inpatient palliative care consultation team for many reasons, mostly arising from findings from other studies that have demonstrated improved quality of life, pain and symptom management, satisfaction with medical care, and other promising outcomes,” Dr. Enguidanos says. “Our study suggests that longitudinal palliative care is also associated with the lower readmission rate.”
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
VTE Pathway Improves Outcomes for Uninsured Patients
A poster presented at HM12 in San Diego last April describes a standardized, systematic, multidisciplinary clinical pathway for treating acute VTE (venous thromboembolism) in an urban hospital serving a high proportion of the uninsured.3 Implementing the pathway in February 2011 “dramatically reduced hospital utilization and cost, particularly among uninsured patients,” who were previously shown to have increased length of stay, cost, and emergency department recidivism, says lead author Gregory Misky, MD, a hospitalist at the University of Colorado Denver.
The pathway—which aimed to standardize all VTE care from hospital presentation to post-discharge follow-up—contained multiple components, including education for staff, enhanced communication processes, written order sets, and a series of formal and informal meetings held with community providers, such as the clinics where these patients get their follow-up primary care. Dr. Misky collaborated with his university’s anticoagulation clinic to help identify primary-care physicians and clinics and arrange follow-up outpatient appointments much sooner than the patients could have obtained by themselves.
The prospective study compared 135 VTE patients presenting to the emergency department or admitted to a medicine service and receiving care under the pathway, compared with 234 VTE patients prior to its introduction. Length of stay dropped to 2.5 days from 4.2, and for uninsured patients it dropped even more, to 2.2 days from 5.5.
Dr. Misky says the data gathered since the San Diego conference “continue to show good results in resource utilization, particularly for the uninsured, with emergency department visits and readmissions slashed.” Readmissions have dropped to 5.2% from 9.8%—and to 3.5% from 11.6% for uninsured VTE patients. He suggests that the clinical pathway approach likely has implications for other diseases as well.
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
A poster presented at HM12 in San Diego last April describes a standardized, systematic, multidisciplinary clinical pathway for treating acute VTE (venous thromboembolism) in an urban hospital serving a high proportion of the uninsured.3 Implementing the pathway in February 2011 “dramatically reduced hospital utilization and cost, particularly among uninsured patients,” who were previously shown to have increased length of stay, cost, and emergency department recidivism, says lead author Gregory Misky, MD, a hospitalist at the University of Colorado Denver.
The pathway—which aimed to standardize all VTE care from hospital presentation to post-discharge follow-up—contained multiple components, including education for staff, enhanced communication processes, written order sets, and a series of formal and informal meetings held with community providers, such as the clinics where these patients get their follow-up primary care. Dr. Misky collaborated with his university’s anticoagulation clinic to help identify primary-care physicians and clinics and arrange follow-up outpatient appointments much sooner than the patients could have obtained by themselves.
The prospective study compared 135 VTE patients presenting to the emergency department or admitted to a medicine service and receiving care under the pathway, compared with 234 VTE patients prior to its introduction. Length of stay dropped to 2.5 days from 4.2, and for uninsured patients it dropped even more, to 2.2 days from 5.5.
Dr. Misky says the data gathered since the San Diego conference “continue to show good results in resource utilization, particularly for the uninsured, with emergency department visits and readmissions slashed.” Readmissions have dropped to 5.2% from 9.8%—and to 3.5% from 11.6% for uninsured VTE patients. He suggests that the clinical pathway approach likely has implications for other diseases as well.
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
A poster presented at HM12 in San Diego last April describes a standardized, systematic, multidisciplinary clinical pathway for treating acute VTE (venous thromboembolism) in an urban hospital serving a high proportion of the uninsured.3 Implementing the pathway in February 2011 “dramatically reduced hospital utilization and cost, particularly among uninsured patients,” who were previously shown to have increased length of stay, cost, and emergency department recidivism, says lead author Gregory Misky, MD, a hospitalist at the University of Colorado Denver.
The pathway—which aimed to standardize all VTE care from hospital presentation to post-discharge follow-up—contained multiple components, including education for staff, enhanced communication processes, written order sets, and a series of formal and informal meetings held with community providers, such as the clinics where these patients get their follow-up primary care. Dr. Misky collaborated with his university’s anticoagulation clinic to help identify primary-care physicians and clinics and arrange follow-up outpatient appointments much sooner than the patients could have obtained by themselves.
The prospective study compared 135 VTE patients presenting to the emergency department or admitted to a medicine service and receiving care under the pathway, compared with 234 VTE patients prior to its introduction. Length of stay dropped to 2.5 days from 4.2, and for uninsured patients it dropped even more, to 2.2 days from 5.5.
Dr. Misky says the data gathered since the San Diego conference “continue to show good results in resource utilization, particularly for the uninsured, with emergency department visits and readmissions slashed.” Readmissions have dropped to 5.2% from 9.8%—and to 3.5% from 11.6% for uninsured VTE patients. He suggests that the clinical pathway approach likely has implications for other diseases as well.
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
Well-Designed IT Systems Essential to Healthcare Integration
David Lawrence, MD, retired head of the Kaiser Foundation health plan, says in a recent Information Week article that it will be “nearly impossible” to achieve the goals of healthcare integration without the connectivity of a well-designed health IT system.4 Dr. Lawrence was a member of a committee that authored the recent report Order from Chaos: Accelerating Care Integration for the Lucian Leape Institute at the National Patient Care Safety Foundation. Failures of coordination most often happen during the crucial information transfers that happen during care transitions, but there has not been enough attention to how important information technology could be to these transfers, Dr. Lawrence told the magazine. “It’s the really complex stuff where this becomes particularly critical,” he said.
The federal Office of Inspector General (OIG) took the Centers for Medicare & Medicaid Services (CMS) to task in a November report for not having adequate oversight or safeguards for its EHR meaningful-use program.5 As a result, OIG described Medicare as “vulnerable” to fraud and abuse of incentive payments made to hospitals and health professionals, according to OIG. OIG recommends that CMS request and review supporting documentation for selected providers and issue guidance with specific examples of appropriate documentation. As of September 2012, CMS had paid out $4 billion in meaningful-use incentives to 1,400 hospitals and 82,000 professionals.
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
David Lawrence, MD, retired head of the Kaiser Foundation health plan, says in a recent Information Week article that it will be “nearly impossible” to achieve the goals of healthcare integration without the connectivity of a well-designed health IT system.4 Dr. Lawrence was a member of a committee that authored the recent report Order from Chaos: Accelerating Care Integration for the Lucian Leape Institute at the National Patient Care Safety Foundation. Failures of coordination most often happen during the crucial information transfers that happen during care transitions, but there has not been enough attention to how important information technology could be to these transfers, Dr. Lawrence told the magazine. “It’s the really complex stuff where this becomes particularly critical,” he said.
The federal Office of Inspector General (OIG) took the Centers for Medicare & Medicaid Services (CMS) to task in a November report for not having adequate oversight or safeguards for its EHR meaningful-use program.5 As a result, OIG described Medicare as “vulnerable” to fraud and abuse of incentive payments made to hospitals and health professionals, according to OIG. OIG recommends that CMS request and review supporting documentation for selected providers and issue guidance with specific examples of appropriate documentation. As of September 2012, CMS had paid out $4 billion in meaningful-use incentives to 1,400 hospitals and 82,000 professionals.
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
David Lawrence, MD, retired head of the Kaiser Foundation health plan, says in a recent Information Week article that it will be “nearly impossible” to achieve the goals of healthcare integration without the connectivity of a well-designed health IT system.4 Dr. Lawrence was a member of a committee that authored the recent report Order from Chaos: Accelerating Care Integration for the Lucian Leape Institute at the National Patient Care Safety Foundation. Failures of coordination most often happen during the crucial information transfers that happen during care transitions, but there has not been enough attention to how important information technology could be to these transfers, Dr. Lawrence told the magazine. “It’s the really complex stuff where this becomes particularly critical,” he said.
The federal Office of Inspector General (OIG) took the Centers for Medicare & Medicaid Services (CMS) to task in a November report for not having adequate oversight or safeguards for its EHR meaningful-use program.5 As a result, OIG described Medicare as “vulnerable” to fraud and abuse of incentive payments made to hospitals and health professionals, according to OIG. OIG recommends that CMS request and review supporting documentation for selected providers and issue guidance with specific examples of appropriate documentation. As of September 2012, CMS had paid out $4 billion in meaningful-use incentives to 1,400 hospitals and 82,000 professionals.
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
Hospitalists Get Answers to Tough Healthcare Questions
When it comes to Medicare, the Affordable Care Act, and a host of other healthcare-reform-related topics, hospitalists have lots of good questions, such as:
- When does the Physician Value-Based Payment Modifier (VBPM) take effect? And will I be included?
- Which primary-care services are covered by the increased Medicaid payments?
- Are hospitalists eligible to bill for Medicare’s new CPT Transitional Care Management (TCM) codes? (see “New Codes Bridge Billing Gap,”).
Now, SHM’s Public Policy Committee has answered all of the above—and many more—in a set of three “Frequently Asked Questions” documents available at www.hospitalmedicine.org/advocacy. Each document goes in-depth on the most cutting-edge policy issues that are top of mind for hospitalists and the hospitals they serve on these issues:
The Physician Value-Based Payment Modifier (VBPM): The VBPM seeks to connect cost and quality of services in order to begin reimbursement for the value, rather than the quantity, of care. It combines the quality measuring in the Physician Quality Reporting System (PQRS), cost measures, and a payment adjustment for physicians. Measurement begins this year, and many hospitalists will be included.
Medicaid/Medicare parity regulation: On Nov. 1, 2012, the Centers for Medicare & Medicaid Services (CMS) released the final regulations implementing Section 1202 of the Affordable Care Act, which increases Medicaid payments for specified primary-care services to 100% of Medicare levels in 2013 and 2014.
New CPT Transitional Care Management (TCM) codes 99495-99496: CMS has created two new CPT Transitional Care Management (TCM) codes designed to improve care coordination and provide better incentives to ensure patients are seen in a physician’s office, rather than be at risk for readmission.
New Action: Getting Involved Just Got Easier
SHM’s Legislative Action Center also makes getting involved easier with a new grassroots outreach tool called Voter Voice. SHM’s first action alert on Voter Voice was sent to members in December. Hospitalists’ willingness to take a few minutes and contact their congressional leaders using Voter Voice increased SHM’s visibility to Congress by nearly five times compared with prior similar alerts.
Getting involved is easy and only takes a few seconds. You can use either your ZIP code to look up your members of Congress or search active legislation by keyword. SHM members can sign up for SHM Legislative Action Center alerts by entering their email address.
To download the new SHM advocacy FAQs or use the improved Legislative Action Center, visit www.hospitalmedicine.org/advocacy.
When it comes to Medicare, the Affordable Care Act, and a host of other healthcare-reform-related topics, hospitalists have lots of good questions, such as:
- When does the Physician Value-Based Payment Modifier (VBPM) take effect? And will I be included?
- Which primary-care services are covered by the increased Medicaid payments?
- Are hospitalists eligible to bill for Medicare’s new CPT Transitional Care Management (TCM) codes? (see “New Codes Bridge Billing Gap,”).
Now, SHM’s Public Policy Committee has answered all of the above—and many more—in a set of three “Frequently Asked Questions” documents available at www.hospitalmedicine.org/advocacy. Each document goes in-depth on the most cutting-edge policy issues that are top of mind for hospitalists and the hospitals they serve on these issues:
The Physician Value-Based Payment Modifier (VBPM): The VBPM seeks to connect cost and quality of services in order to begin reimbursement for the value, rather than the quantity, of care. It combines the quality measuring in the Physician Quality Reporting System (PQRS), cost measures, and a payment adjustment for physicians. Measurement begins this year, and many hospitalists will be included.
Medicaid/Medicare parity regulation: On Nov. 1, 2012, the Centers for Medicare & Medicaid Services (CMS) released the final regulations implementing Section 1202 of the Affordable Care Act, which increases Medicaid payments for specified primary-care services to 100% of Medicare levels in 2013 and 2014.
New CPT Transitional Care Management (TCM) codes 99495-99496: CMS has created two new CPT Transitional Care Management (TCM) codes designed to improve care coordination and provide better incentives to ensure patients are seen in a physician’s office, rather than be at risk for readmission.
New Action: Getting Involved Just Got Easier
SHM’s Legislative Action Center also makes getting involved easier with a new grassroots outreach tool called Voter Voice. SHM’s first action alert on Voter Voice was sent to members in December. Hospitalists’ willingness to take a few minutes and contact their congressional leaders using Voter Voice increased SHM’s visibility to Congress by nearly five times compared with prior similar alerts.
Getting involved is easy and only takes a few seconds. You can use either your ZIP code to look up your members of Congress or search active legislation by keyword. SHM members can sign up for SHM Legislative Action Center alerts by entering their email address.
To download the new SHM advocacy FAQs or use the improved Legislative Action Center, visit www.hospitalmedicine.org/advocacy.
When it comes to Medicare, the Affordable Care Act, and a host of other healthcare-reform-related topics, hospitalists have lots of good questions, such as:
- When does the Physician Value-Based Payment Modifier (VBPM) take effect? And will I be included?
- Which primary-care services are covered by the increased Medicaid payments?
- Are hospitalists eligible to bill for Medicare’s new CPT Transitional Care Management (TCM) codes? (see “New Codes Bridge Billing Gap,”).
Now, SHM’s Public Policy Committee has answered all of the above—and many more—in a set of three “Frequently Asked Questions” documents available at www.hospitalmedicine.org/advocacy. Each document goes in-depth on the most cutting-edge policy issues that are top of mind for hospitalists and the hospitals they serve on these issues:
The Physician Value-Based Payment Modifier (VBPM): The VBPM seeks to connect cost and quality of services in order to begin reimbursement for the value, rather than the quantity, of care. It combines the quality measuring in the Physician Quality Reporting System (PQRS), cost measures, and a payment adjustment for physicians. Measurement begins this year, and many hospitalists will be included.
Medicaid/Medicare parity regulation: On Nov. 1, 2012, the Centers for Medicare & Medicaid Services (CMS) released the final regulations implementing Section 1202 of the Affordable Care Act, which increases Medicaid payments for specified primary-care services to 100% of Medicare levels in 2013 and 2014.
New CPT Transitional Care Management (TCM) codes 99495-99496: CMS has created two new CPT Transitional Care Management (TCM) codes designed to improve care coordination and provide better incentives to ensure patients are seen in a physician’s office, rather than be at risk for readmission.
New Action: Getting Involved Just Got Easier
SHM’s Legislative Action Center also makes getting involved easier with a new grassroots outreach tool called Voter Voice. SHM’s first action alert on Voter Voice was sent to members in December. Hospitalists’ willingness to take a few minutes and contact their congressional leaders using Voter Voice increased SHM’s visibility to Congress by nearly five times compared with prior similar alerts.
Getting involved is easy and only takes a few seconds. You can use either your ZIP code to look up your members of Congress or search active legislation by keyword. SHM members can sign up for SHM Legislative Action Center alerts by entering their email address.
To download the new SHM advocacy FAQs or use the improved Legislative Action Center, visit www.hospitalmedicine.org/advocacy.
HMX Term of the Month: CMS 1500
Medical claim form established by CMS to submit paper claims to Medicare and Medicaid. Most commercial insurance carriers also require paper claims be submitted on CMS 1500s. The form is distinguished by its red ink.
Medical claim form established by CMS to submit paper claims to Medicare and Medicaid. Most commercial insurance carriers also require paper claims be submitted on CMS 1500s. The form is distinguished by its red ink.
Medical claim form established by CMS to submit paper claims to Medicare and Medicaid. Most commercial insurance carriers also require paper claims be submitted on CMS 1500s. The form is distinguished by its red ink.