User login
Proper Inpatient Documentation, Coding Essential to Avoid a Medicare Audit
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
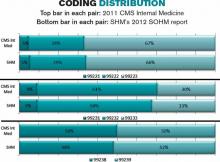
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Delay in ICD-10 Implementation to Impact Hospitalists, Physicians, Payers
On April 1, President Obama signed into law a bill that again delays a permanent fix of the sustainable growth rate formula, or SGR, the so-called “doc fix.” The bill also contained a surprise provision added by Congress to delay implementation of the switch from ICD-9 to ICD-10. The mandated conversion was supposed to take place by October 1 of this year; its delay will have a range of impacts on everyone from physicians to payers.
Hospitalists and others must weigh their options going forward, as many health systems and groups are already well on their way toward compliance with the 2014 deadline.
At this point, prevailing wisdom is that Congress added the delay as an appeasement to physician groups that would be unhappy about its failure to pass an SGR replacement, says Jeffrey Smith, senior director of federal affairs for CHIME, the College of Healthcare Information Management Executives.
“The appeasement, if in fact that was the motivation, was too little too late,” Smith says, adding Congress “caused a lot of unnecessary chaos.”
For instance, according to Modern Healthcare, executives at Catholic Health Initiatives had already invested millions of dollars updating software programs to handle the coding switch ahead of a new electronic health record system roll-out in 89 of its hospitals, which would not have been ready by the ICD-10 deadline.
“Anyone in the process has to circle the wagons again and reconsider their timelines,” Smith says. “The legislation has punished people trying to do the right thing.”
The transition to ICD-10 is a massive update to the 30-year-old ICD-9 codes, which no longer adequately reflect medical diagnoses, procedures, technology, and knowledge. There are five times more diagnosis codes and 21 times more procedural codes in ICD-10. It’s been on the table for at least a decade, and this was not the first delay.
In 2012, when fewer groups were on their way to compliance, CMS estimated that a one-year push-back of ICD-10 conversion could cost up to $306 million. With the latest delay, the American Health Information Management Association says CMS now estimates those costs between $1 billion and $6.6 billion.
However, according to the American Medical Association, which has actively lobbied to stop ICD-10 altogether, the costs of implementing ICD-10 range from $57,000 for small physician practices to as high as $8 million for large practices.
The increased number of codes, the increased number of characters per code, and the increased specificity require significant planning, training, software updates, and financial investments.
The Medical Group Management Association (MGMA) also pushed for ICD-10 delay, concerned that many groups would not be ready by Oct. 1. MGMA surveys showed as much, says Robert Tennant, senior policy advisor for MGMA.“We were concerned that if everyone has to flip the switch at the same time, there will be huge problems, as there were for healthcare.gov,” Tennant explains.
What MGMA would like to see is more thorough end-to-end testing and staggered roll-outs. Hospitals and health plans should be permitted to start using ICD-10 coding when they're ready, even if ahead of the next deadline, Tennant said. MGMA would also like to see a period of dual coding built in.
The ball is now in CMS' court.
“I think that CMS has within its power … the ability to embolden the industry to be more confident,” Smith says. “Even if it’s not going to require ICD-10 codes [by October 2014], hopefully they are still doing testing, still doing benchmarking, and by the time the deadline rolls around, it will touch every sector of the healthcare economy.”
Hospitalists, Smith says, should be more involved in the conversation going forward, to help maintain the momentum and preserve the investments made by their groups and institutions. Those not ready should push for compliance, rather than finding themselves in the same position a year from now.
Many of the hospital CIOs (chief information officers) he has talked to say that while they are stopping the car, they are keeping the engine running. Some will push for dual coding, even if only internally, because it’s proving to be a valuable tool in understanding their patient populations.
“It’s a frustrating time any time you have to kind of stop something with so much momentum, with hundreds of millions, if not billions, spent in advance of the conversion,” Smith says. “It does nothing to help care in this country to stay on ICD-9. Everybody understands those codes are completely exhausted, and the data we are getting out of it, while workable, is certainly not going to get us where we need to be in terms of transforming healthcare.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
On April 1, President Obama signed into law a bill that again delays a permanent fix of the sustainable growth rate formula, or SGR, the so-called “doc fix.” The bill also contained a surprise provision added by Congress to delay implementation of the switch from ICD-9 to ICD-10. The mandated conversion was supposed to take place by October 1 of this year; its delay will have a range of impacts on everyone from physicians to payers.
Hospitalists and others must weigh their options going forward, as many health systems and groups are already well on their way toward compliance with the 2014 deadline.
At this point, prevailing wisdom is that Congress added the delay as an appeasement to physician groups that would be unhappy about its failure to pass an SGR replacement, says Jeffrey Smith, senior director of federal affairs for CHIME, the College of Healthcare Information Management Executives.
“The appeasement, if in fact that was the motivation, was too little too late,” Smith says, adding Congress “caused a lot of unnecessary chaos.”
For instance, according to Modern Healthcare, executives at Catholic Health Initiatives had already invested millions of dollars updating software programs to handle the coding switch ahead of a new electronic health record system roll-out in 89 of its hospitals, which would not have been ready by the ICD-10 deadline.
“Anyone in the process has to circle the wagons again and reconsider their timelines,” Smith says. “The legislation has punished people trying to do the right thing.”
The transition to ICD-10 is a massive update to the 30-year-old ICD-9 codes, which no longer adequately reflect medical diagnoses, procedures, technology, and knowledge. There are five times more diagnosis codes and 21 times more procedural codes in ICD-10. It’s been on the table for at least a decade, and this was not the first delay.
In 2012, when fewer groups were on their way to compliance, CMS estimated that a one-year push-back of ICD-10 conversion could cost up to $306 million. With the latest delay, the American Health Information Management Association says CMS now estimates those costs between $1 billion and $6.6 billion.
However, according to the American Medical Association, which has actively lobbied to stop ICD-10 altogether, the costs of implementing ICD-10 range from $57,000 for small physician practices to as high as $8 million for large practices.
The increased number of codes, the increased number of characters per code, and the increased specificity require significant planning, training, software updates, and financial investments.
The Medical Group Management Association (MGMA) also pushed for ICD-10 delay, concerned that many groups would not be ready by Oct. 1. MGMA surveys showed as much, says Robert Tennant, senior policy advisor for MGMA.“We were concerned that if everyone has to flip the switch at the same time, there will be huge problems, as there were for healthcare.gov,” Tennant explains.
What MGMA would like to see is more thorough end-to-end testing and staggered roll-outs. Hospitals and health plans should be permitted to start using ICD-10 coding when they're ready, even if ahead of the next deadline, Tennant said. MGMA would also like to see a period of dual coding built in.
The ball is now in CMS' court.
“I think that CMS has within its power … the ability to embolden the industry to be more confident,” Smith says. “Even if it’s not going to require ICD-10 codes [by October 2014], hopefully they are still doing testing, still doing benchmarking, and by the time the deadline rolls around, it will touch every sector of the healthcare economy.”
Hospitalists, Smith says, should be more involved in the conversation going forward, to help maintain the momentum and preserve the investments made by their groups and institutions. Those not ready should push for compliance, rather than finding themselves in the same position a year from now.
Many of the hospital CIOs (chief information officers) he has talked to say that while they are stopping the car, they are keeping the engine running. Some will push for dual coding, even if only internally, because it’s proving to be a valuable tool in understanding their patient populations.
“It’s a frustrating time any time you have to kind of stop something with so much momentum, with hundreds of millions, if not billions, spent in advance of the conversion,” Smith says. “It does nothing to help care in this country to stay on ICD-9. Everybody understands those codes are completely exhausted, and the data we are getting out of it, while workable, is certainly not going to get us where we need to be in terms of transforming healthcare.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
On April 1, President Obama signed into law a bill that again delays a permanent fix of the sustainable growth rate formula, or SGR, the so-called “doc fix.” The bill also contained a surprise provision added by Congress to delay implementation of the switch from ICD-9 to ICD-10. The mandated conversion was supposed to take place by October 1 of this year; its delay will have a range of impacts on everyone from physicians to payers.
Hospitalists and others must weigh their options going forward, as many health systems and groups are already well on their way toward compliance with the 2014 deadline.
At this point, prevailing wisdom is that Congress added the delay as an appeasement to physician groups that would be unhappy about its failure to pass an SGR replacement, says Jeffrey Smith, senior director of federal affairs for CHIME, the College of Healthcare Information Management Executives.
“The appeasement, if in fact that was the motivation, was too little too late,” Smith says, adding Congress “caused a lot of unnecessary chaos.”
For instance, according to Modern Healthcare, executives at Catholic Health Initiatives had already invested millions of dollars updating software programs to handle the coding switch ahead of a new electronic health record system roll-out in 89 of its hospitals, which would not have been ready by the ICD-10 deadline.
“Anyone in the process has to circle the wagons again and reconsider their timelines,” Smith says. “The legislation has punished people trying to do the right thing.”
The transition to ICD-10 is a massive update to the 30-year-old ICD-9 codes, which no longer adequately reflect medical diagnoses, procedures, technology, and knowledge. There are five times more diagnosis codes and 21 times more procedural codes in ICD-10. It’s been on the table for at least a decade, and this was not the first delay.
In 2012, when fewer groups were on their way to compliance, CMS estimated that a one-year push-back of ICD-10 conversion could cost up to $306 million. With the latest delay, the American Health Information Management Association says CMS now estimates those costs between $1 billion and $6.6 billion.
However, according to the American Medical Association, which has actively lobbied to stop ICD-10 altogether, the costs of implementing ICD-10 range from $57,000 for small physician practices to as high as $8 million for large practices.
The increased number of codes, the increased number of characters per code, and the increased specificity require significant planning, training, software updates, and financial investments.
The Medical Group Management Association (MGMA) also pushed for ICD-10 delay, concerned that many groups would not be ready by Oct. 1. MGMA surveys showed as much, says Robert Tennant, senior policy advisor for MGMA.“We were concerned that if everyone has to flip the switch at the same time, there will be huge problems, as there were for healthcare.gov,” Tennant explains.
What MGMA would like to see is more thorough end-to-end testing and staggered roll-outs. Hospitals and health plans should be permitted to start using ICD-10 coding when they're ready, even if ahead of the next deadline, Tennant said. MGMA would also like to see a period of dual coding built in.
The ball is now in CMS' court.
“I think that CMS has within its power … the ability to embolden the industry to be more confident,” Smith says. “Even if it’s not going to require ICD-10 codes [by October 2014], hopefully they are still doing testing, still doing benchmarking, and by the time the deadline rolls around, it will touch every sector of the healthcare economy.”
Hospitalists, Smith says, should be more involved in the conversation going forward, to help maintain the momentum and preserve the investments made by their groups and institutions. Those not ready should push for compliance, rather than finding themselves in the same position a year from now.
Many of the hospital CIOs (chief information officers) he has talked to say that while they are stopping the car, they are keeping the engine running. Some will push for dual coding, even if only internally, because it’s proving to be a valuable tool in understanding their patient populations.
“It’s a frustrating time any time you have to kind of stop something with so much momentum, with hundreds of millions, if not billions, spent in advance of the conversion,” Smith says. “It does nothing to help care in this country to stay on ICD-9. Everybody understands those codes are completely exhausted, and the data we are getting out of it, while workable, is certainly not going to get us where we need to be in terms of transforming healthcare.”
Kelly April Tyrrell is a freelance writer in Madison, Wis.
Medicare Rule Change Raises Stakes for Hospital Discharge Planning
When she presents information to hospitalists about the little-known revision to Medicare’s condition of participation for discharge planning by hospitals, most hospitalists have no idea what Amy Boutwell, MD, MPP, is talking about. Even hospitalists who are active in their institutions’ efforts to improve transitions of care out of the hospital setting are unaware of the change, which was published in the Centers for Medicare & Medicaid Services’ Transmittal 87 and became effective July 19, 2013.
“I just don’t hear hospital professionals talking about it,” says Dr. Boutwell, a hospitalist at Newton-Wellesley Hospital and president of Collaborative Healthcare Strategies in Lexington, Mass. “When I say, ‘There are new rules of the road for discharge planning and evaluation,’ many are not aware of it.”
The revised condition states that the hospital must have a discharge planning process that applies to all patients—not just Medicare beneficiaries. Not every patient needs to have a written discharge plan—although this is recommended—but all patients should be screened and, if indicated, evaluated at an early stage of their hospitalization for risk of adverse post-discharge outcomes. Observation patients are not included in this requirement.
The discharge plan is different from a discharge summary document, which must be completed by the inpatient attending physician, not the hospital, and is not directly addressed in the regulation. The regulation does address the need for transfer of essential information to the next provider of care and says the hospital should have a written policy and procedure in place for discharge planning. The policy and procedure should be developed with input from medical staff and approved by the hospital’s governing body.
Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation.
—Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST
Transmittal 87 represents the first major update of the discharge planning regulation (Standard 482.43) and accompanying interpretive guidelines in more than a decade, Dr. Boutwell says. It consolidates and reorganizes 24 “tags” of regulatory language down to 13 and contains blue advisory boxes recommending best practices in discharge planning, drawn from the suggestions of a technical expert panel convened by CMS.
That panel included many of the country’s recognized thought leaders on improving care transitions, such as Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST; Eric Coleman, MD, MPH, head of the University of Colorado’s division of health care policy and research and creator of the widely-adopted Care Transitions Program (caretransitions.org), and Dr. Boutwell, co-founder of the STAAR initiative (www.ihi.org/engage/Initiatives/completed/STAAR).
The new condition raises baseline expectations for discharge planning and elevates care transitions efforts from a quality improvement issue to the realm of regulatory compliance, Dr. Boutwell says.
“This goes way beyond case review,” she adds. “It represents an evolution from discharge planning case by case to a system for improving transitions of care [for the hospital]. I’m impressed.”
The recommendations are consistent with best practices promoted by Project BOOST, STAAR, Project RED [Re-Engineered Discharge], and other national quality initiatives for improving care transitions.
“Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation,” Dr. Williams says.
In the Byzantine structure of federal regulations, Medicare’s conditions of participation are the regulations providers must meet in order to participate in the Medicare program and bill for their services. Condition-level citations, if not resolved, can cause hospitals to be decertified from Medicare. The accompanying interpretive guidelines, with survey protocols, are the playbook to help state auditors and providers know how to interpret and apply the language of the regulations. The suggestions and examples of best practices contained in the new condition are not required of hospitals but, if followed, could increase their likelihood of achieving better patient outcomes and staying in compliance with the regulations on surveys.
“If hospitals were to actually implement all of the CMS advisory practice recommendations contained in this 35-page document, they’d be in really good shape for effectively managing transitions of care,” says Teresa L. Hamblin, RN, MS, a CMS consultant with Joint Commission Resources. “The government has provided robust practice recommendations that are a model for what hospitals can do. I’d advise doing your best to implement these recommendations. Check your current processes using this detailed document for reference.”
Discharge planning starts at admission, Hamblin says. If the hospitalist assumes that responsibility, it becomes easier to leave a paper trail in the patient’s chart. Other important lessons for hospitalists include participation in a multidisciplinary approach to discharge planning (i.e., interdisciplinary rounding) and development of policies and procedures in this area.
“If the hospital has not elected to do a discharge plan on every patient, request this for your own patients and recommend it as a policy,” Hamblin says. “Go the extra mile, making follow-up appointments for your patients, filling prescriptions in house, and calling the patient 24 to 72 hours after discharge.”
Weekend coverage, when case managers typically are not present, is a particular challenge in care transitions.
“Encourage your hospital to provide reliable weekend coverage for discharge planning. Involve the nurses,” Hamblin says. “Anything the hospitalist can do to help the hospital close this gap is important.”
Larry Beresford is a freelance writer in Alameda, Calif.
When she presents information to hospitalists about the little-known revision to Medicare’s condition of participation for discharge planning by hospitals, most hospitalists have no idea what Amy Boutwell, MD, MPP, is talking about. Even hospitalists who are active in their institutions’ efforts to improve transitions of care out of the hospital setting are unaware of the change, which was published in the Centers for Medicare & Medicaid Services’ Transmittal 87 and became effective July 19, 2013.
“I just don’t hear hospital professionals talking about it,” says Dr. Boutwell, a hospitalist at Newton-Wellesley Hospital and president of Collaborative Healthcare Strategies in Lexington, Mass. “When I say, ‘There are new rules of the road for discharge planning and evaluation,’ many are not aware of it.”
The revised condition states that the hospital must have a discharge planning process that applies to all patients—not just Medicare beneficiaries. Not every patient needs to have a written discharge plan—although this is recommended—but all patients should be screened and, if indicated, evaluated at an early stage of their hospitalization for risk of adverse post-discharge outcomes. Observation patients are not included in this requirement.
The discharge plan is different from a discharge summary document, which must be completed by the inpatient attending physician, not the hospital, and is not directly addressed in the regulation. The regulation does address the need for transfer of essential information to the next provider of care and says the hospital should have a written policy and procedure in place for discharge planning. The policy and procedure should be developed with input from medical staff and approved by the hospital’s governing body.
Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation.
—Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST
Transmittal 87 represents the first major update of the discharge planning regulation (Standard 482.43) and accompanying interpretive guidelines in more than a decade, Dr. Boutwell says. It consolidates and reorganizes 24 “tags” of regulatory language down to 13 and contains blue advisory boxes recommending best practices in discharge planning, drawn from the suggestions of a technical expert panel convened by CMS.
That panel included many of the country’s recognized thought leaders on improving care transitions, such as Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST; Eric Coleman, MD, MPH, head of the University of Colorado’s division of health care policy and research and creator of the widely-adopted Care Transitions Program (caretransitions.org), and Dr. Boutwell, co-founder of the STAAR initiative (www.ihi.org/engage/Initiatives/completed/STAAR).
The new condition raises baseline expectations for discharge planning and elevates care transitions efforts from a quality improvement issue to the realm of regulatory compliance, Dr. Boutwell says.
“This goes way beyond case review,” she adds. “It represents an evolution from discharge planning case by case to a system for improving transitions of care [for the hospital]. I’m impressed.”
The recommendations are consistent with best practices promoted by Project BOOST, STAAR, Project RED [Re-Engineered Discharge], and other national quality initiatives for improving care transitions.
“Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation,” Dr. Williams says.
In the Byzantine structure of federal regulations, Medicare’s conditions of participation are the regulations providers must meet in order to participate in the Medicare program and bill for their services. Condition-level citations, if not resolved, can cause hospitals to be decertified from Medicare. The accompanying interpretive guidelines, with survey protocols, are the playbook to help state auditors and providers know how to interpret and apply the language of the regulations. The suggestions and examples of best practices contained in the new condition are not required of hospitals but, if followed, could increase their likelihood of achieving better patient outcomes and staying in compliance with the regulations on surveys.
“If hospitals were to actually implement all of the CMS advisory practice recommendations contained in this 35-page document, they’d be in really good shape for effectively managing transitions of care,” says Teresa L. Hamblin, RN, MS, a CMS consultant with Joint Commission Resources. “The government has provided robust practice recommendations that are a model for what hospitals can do. I’d advise doing your best to implement these recommendations. Check your current processes using this detailed document for reference.”
Discharge planning starts at admission, Hamblin says. If the hospitalist assumes that responsibility, it becomes easier to leave a paper trail in the patient’s chart. Other important lessons for hospitalists include participation in a multidisciplinary approach to discharge planning (i.e., interdisciplinary rounding) and development of policies and procedures in this area.
“If the hospital has not elected to do a discharge plan on every patient, request this for your own patients and recommend it as a policy,” Hamblin says. “Go the extra mile, making follow-up appointments for your patients, filling prescriptions in house, and calling the patient 24 to 72 hours after discharge.”
Weekend coverage, when case managers typically are not present, is a particular challenge in care transitions.
“Encourage your hospital to provide reliable weekend coverage for discharge planning. Involve the nurses,” Hamblin says. “Anything the hospitalist can do to help the hospital close this gap is important.”
Larry Beresford is a freelance writer in Alameda, Calif.
When she presents information to hospitalists about the little-known revision to Medicare’s condition of participation for discharge planning by hospitals, most hospitalists have no idea what Amy Boutwell, MD, MPP, is talking about. Even hospitalists who are active in their institutions’ efforts to improve transitions of care out of the hospital setting are unaware of the change, which was published in the Centers for Medicare & Medicaid Services’ Transmittal 87 and became effective July 19, 2013.
“I just don’t hear hospital professionals talking about it,” says Dr. Boutwell, a hospitalist at Newton-Wellesley Hospital and president of Collaborative Healthcare Strategies in Lexington, Mass. “When I say, ‘There are new rules of the road for discharge planning and evaluation,’ many are not aware of it.”
The revised condition states that the hospital must have a discharge planning process that applies to all patients—not just Medicare beneficiaries. Not every patient needs to have a written discharge plan—although this is recommended—but all patients should be screened and, if indicated, evaluated at an early stage of their hospitalization for risk of adverse post-discharge outcomes. Observation patients are not included in this requirement.
The discharge plan is different from a discharge summary document, which must be completed by the inpatient attending physician, not the hospital, and is not directly addressed in the regulation. The regulation does address the need for transfer of essential information to the next provider of care and says the hospital should have a written policy and procedure in place for discharge planning. The policy and procedure should be developed with input from medical staff and approved by the hospital’s governing body.
Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation.
—Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST
Transmittal 87 represents the first major update of the discharge planning regulation (Standard 482.43) and accompanying interpretive guidelines in more than a decade, Dr. Boutwell says. It consolidates and reorganizes 24 “tags” of regulatory language down to 13 and contains blue advisory boxes recommending best practices in discharge planning, drawn from the suggestions of a technical expert panel convened by CMS.
That panel included many of the country’s recognized thought leaders on improving care transitions, such as Mark Williams, MD, FACP, SFHM, principal investigator of SHM’s Project BOOST; Eric Coleman, MD, MPH, head of the University of Colorado’s division of health care policy and research and creator of the widely-adopted Care Transitions Program (caretransitions.org), and Dr. Boutwell, co-founder of the STAAR initiative (www.ihi.org/engage/Initiatives/completed/STAAR).
The new condition raises baseline expectations for discharge planning and elevates care transitions efforts from a quality improvement issue to the realm of regulatory compliance, Dr. Boutwell says.
“This goes way beyond case review,” she adds. “It represents an evolution from discharge planning case by case to a system for improving transitions of care [for the hospital]. I’m impressed.”
The recommendations are consistent with best practices promoted by Project BOOST, STAAR, Project RED [Re-Engineered Discharge], and other national quality initiatives for improving care transitions.
“Any hospitalist participating with a hospital QI team involved in Project BOOST is helping their hospital comply with this condition of participation,” Dr. Williams says.
In the Byzantine structure of federal regulations, Medicare’s conditions of participation are the regulations providers must meet in order to participate in the Medicare program and bill for their services. Condition-level citations, if not resolved, can cause hospitals to be decertified from Medicare. The accompanying interpretive guidelines, with survey protocols, are the playbook to help state auditors and providers know how to interpret and apply the language of the regulations. The suggestions and examples of best practices contained in the new condition are not required of hospitals but, if followed, could increase their likelihood of achieving better patient outcomes and staying in compliance with the regulations on surveys.
“If hospitals were to actually implement all of the CMS advisory practice recommendations contained in this 35-page document, they’d be in really good shape for effectively managing transitions of care,” says Teresa L. Hamblin, RN, MS, a CMS consultant with Joint Commission Resources. “The government has provided robust practice recommendations that are a model for what hospitals can do. I’d advise doing your best to implement these recommendations. Check your current processes using this detailed document for reference.”
Discharge planning starts at admission, Hamblin says. If the hospitalist assumes that responsibility, it becomes easier to leave a paper trail in the patient’s chart. Other important lessons for hospitalists include participation in a multidisciplinary approach to discharge planning (i.e., interdisciplinary rounding) and development of policies and procedures in this area.
“If the hospital has not elected to do a discharge plan on every patient, request this for your own patients and recommend it as a policy,” Hamblin says. “Go the extra mile, making follow-up appointments for your patients, filling prescriptions in house, and calling the patient 24 to 72 hours after discharge.”
Weekend coverage, when case managers typically are not present, is a particular challenge in care transitions.
“Encourage your hospital to provide reliable weekend coverage for discharge planning. Involve the nurses,” Hamblin says. “Anything the hospitalist can do to help the hospital close this gap is important.”
Larry Beresford is a freelance writer in Alameda, Calif.
SGR Reform, ICD-10 Implementation Delays Frustrate Hospitalists, Physicians
Congress has once again delayed implementation of draconian Medicare cuts tied to the sustainable growth rate (SGR) formula. It was the 17th temporary patch applied to the ailing physician reimbursement program, so the decision caused little surprise.
But with the same legislation—the Protecting Access to Medicare Act of 2014—being used to delay the long-awaited debut of ICD-10, many hospitalists and physicians couldn’t help but wonder whether billing and coding would now be as much of a political football as the SGR fix.1
The upshot: It doesn’t seem that way.
“I think it’s two separate issues,” says Phyllis “PJ” Floyd, RN, BSN, MBA, NE-BC, CCA, director of health information services and clinical documentation improvement at Medical University of South Carolina (MUSC) in Charleston, S.C. “The fact that it was all in one bill, I don’t know that it was well thought out as much as it was, ‘Let’s put the ICD-10 in here at the same time.’
“It was just a few sentences, and then it wasn’t even brought up in the discussion on the floor.”
Four policy wonks interviewed by The Hospitalist concurred that while tying the ICD-10 delay to the SGR issue was an unexpected and frustrating development, the coding system likely will be implemented in the relative short term. Meanwhile, a long-term resolution of the SGR dilemma remains much more elusive.
“For about 12 hours, I felt relief about the ICD-10 [being delayed], and then I just realized, it’s still coming, presumably,” says John Nelson, MD, MHM, a co-founder and past president of SHM and medical director of the hospitalist practice at Overlake Hospital Medical Center in Bellevue, Wash. “[It’s] like a patient who needs surgery and finds out it’s canceled for the day and he’ll have it tomorrow. Well, that’s good for right now, but [he] still has to face this eventually.”
“Doc-Pay” Fix Near?
Congress’ recent decision to delay both an SGR fix and the ICD-10 are troubling to some hospitalists and others for different reasons.
The SGR extension through this year’s end means that physicians do not face a 24% cut to physician payments under Medicare. SHM has long lobbied against temporary patches to the SGR, repeatedly backing legislation that would once and for all scrap the formula and replace it with something sustainable.
The SGR formula was first crafted in 1997, but the now often-delayed cuts were a byproduct of the federal sequester that was included in the Budget Control Act of 2011. At the time, the massive reduction to Medicare payments was tied to political brinksmanship over the country’s debt ceiling. The cuts were implemented as a doomsday scenario that was never likely to actually happen, but despite negotiations over the past three years, no long-term compromise can be found. Paying for the reform remains the main stumbling block.
“I think, this year, Congress was as close as it’s been in a long time to enacting a serious fix, aided by the agreement of major professional societies like the American College of Physicians and American College of Surgeons,” says David Howard, PhD, an associate professor in the department of health policy and management at the Rollins School of Public Health at Emory University in Atlanta. “They were all on board with this solution. ... Who knows, maybe if the economic situation continues to improve [and] tax revenues continue to go up...that will create a more favorable environment for compromise.”
Dr. Howard adds that while Congress might be close to a solution in theory, agreement on how to offset the roughly $100 billion in costs “is just very difficult.” That is why the healthcare professor is pessimistic that a long-term fix is truly at hand.
“The places where Congress might have looked for savings to offset the cost of the doc fix, such as hospital reimbursement rates or payment rates to Medicare Advantage plans—those are exactly the areas that the Affordable Care Act is targeting to pay for insurance expansion,” Dr. Howard adds. “So those areas of savings are not going to be available to offset the cost of the doc fix.”
ICD-10 Delays “Unfair”
The medical coding conundrum presents a different set of issues. The delay in transitioning healthcare providers from the ICD-9 medical coding classification system to the more complicated ICD-10 means the upgraded system is now against an Oct. 1, 2015, deadline. This comes after the Centers for Medicare & Medicaid Services (CMS) already pushed back the original implementation date for ICD-10 by one year.
SHM Public Policy Committee member Joshua Lenchus, DO, RPh, FACP, SFHM, says he thinks most doctors are content with the delay, particularly in light of some estimates that show that only about 20% of physicians “have actually initiated the ICD-10 transition.” But he also notes that it’s unfair to the health systems that have prepared for ICD-10.
“ICD-9 has a little more than 14,000 diagnostic codes and nearly 4,000 procedural codes. That is to be contrasted to ICD-10, which has more than 68,000 diagnostic codes ... and over 72,000 procedural codes,” Dr. Lenchus says. “So, it is not surprising that many take solace in the delay.”
–Dr. Lenchus
Dr. Nelson says the level of frustration for hospitalists is growing; however, the level of disruption for hospitals and health systems is reaching a boiling point.
“Of course, in some places, hospitalists may be the physician lead on ICD-10 efforts, so [they are] very much wrapped up in the problem of ‘What do we do now?’”
The answer, at least to the Coalition for ICD-10, a group of medical/technology trade groups, is to fight to ensure that the delays go no further. In an April letter to CMS Administrator Marilyn Tavenner, the coalition made that case, noting that in 2012, “CMS estimated the cost to the healthcare industry of a one-year delay to be as much as $6.6 billion, or approximately 30% of the $22 billion that CMS estimated had been invested or budgeted for ICD-10 implementation.”2
The letter went on to explain that the disruption and cost will grow each time the ICD-10 deadline is pushed.
“Furthermore, as CMS stated in 2012, implementation costs will continue to increase considerably with every year of a delay,” according to the letter. “The lost opportunity costs of failing to move to a more effective code set also continue to climb every year.”
Stay Engaged, Switch Gears
One of Floyd’s biggest concerns is that the ICD-10 implementation delays will affect physician engagement. The hospitalist groups at MUSC began training for ICD-10 in January 2013; however, the preparation and training were geared toward a 2014 implementation.
“You have to switch gears a little bit,” she says. “What we plan to do now is begin to do heavy auditing, and then from those audits we can give real-time feedback on what we’re doing well and what we’re not doing well. So I think that will be a method for engagement.”
She urges hospitalists, practice leaders, and informatics professionals to discuss ICD-10 not as a theoretical application, but as one tied to reimbursement that will have major impact in the years ahead. To that end, the American Health Information Management Association highlights the fact that the new coding system will result in higher-quality data that can improve performance measures, provide “increased sensitivity” to reimbursement methodologies, and help with stronger public health surveillance.3
“A lot of physicians see this as a hospital issue, and I think that’s why they shy away,” Floyd says. “Now there are some physicians who are interested in how well the hospital does, but the other piece is that it does affect things like [reduced] risk of mortality [and] comparison of data worldwide—those are things that we just have to continue to reiterate … and give them real examples.”
Richard Quinn is a freelance writer in New Jersey.
References
- Govtrack. H.R. 4302: Protecting Access to Medicare Act of 2014. https://www.govtrack.us/congress/bills/113/hr4302. Accessed June 5, 2014.
- Coalition for ICD. Letter to CMS Administrator Tavenner, April 11, 2014. http://coalitionforicd10.wordpress.com/2014/03/26/letter-from-the-coalition-for-icd-10. Accessed June 5, 2014.
- American Health Information Management Association. ICD-10-CM/PCS Transition: Planning and Preparation Checklist. http://journal.ahima.org/wp-content/uploads/ICD10-checklist.pdf. Accessed June 5, 2014.
Congress has once again delayed implementation of draconian Medicare cuts tied to the sustainable growth rate (SGR) formula. It was the 17th temporary patch applied to the ailing physician reimbursement program, so the decision caused little surprise.
But with the same legislation—the Protecting Access to Medicare Act of 2014—being used to delay the long-awaited debut of ICD-10, many hospitalists and physicians couldn’t help but wonder whether billing and coding would now be as much of a political football as the SGR fix.1
The upshot: It doesn’t seem that way.
“I think it’s two separate issues,” says Phyllis “PJ” Floyd, RN, BSN, MBA, NE-BC, CCA, director of health information services and clinical documentation improvement at Medical University of South Carolina (MUSC) in Charleston, S.C. “The fact that it was all in one bill, I don’t know that it was well thought out as much as it was, ‘Let’s put the ICD-10 in here at the same time.’
“It was just a few sentences, and then it wasn’t even brought up in the discussion on the floor.”
Four policy wonks interviewed by The Hospitalist concurred that while tying the ICD-10 delay to the SGR issue was an unexpected and frustrating development, the coding system likely will be implemented in the relative short term. Meanwhile, a long-term resolution of the SGR dilemma remains much more elusive.
“For about 12 hours, I felt relief about the ICD-10 [being delayed], and then I just realized, it’s still coming, presumably,” says John Nelson, MD, MHM, a co-founder and past president of SHM and medical director of the hospitalist practice at Overlake Hospital Medical Center in Bellevue, Wash. “[It’s] like a patient who needs surgery and finds out it’s canceled for the day and he’ll have it tomorrow. Well, that’s good for right now, but [he] still has to face this eventually.”
“Doc-Pay” Fix Near?
Congress’ recent decision to delay both an SGR fix and the ICD-10 are troubling to some hospitalists and others for different reasons.
The SGR extension through this year’s end means that physicians do not face a 24% cut to physician payments under Medicare. SHM has long lobbied against temporary patches to the SGR, repeatedly backing legislation that would once and for all scrap the formula and replace it with something sustainable.
The SGR formula was first crafted in 1997, but the now often-delayed cuts were a byproduct of the federal sequester that was included in the Budget Control Act of 2011. At the time, the massive reduction to Medicare payments was tied to political brinksmanship over the country’s debt ceiling. The cuts were implemented as a doomsday scenario that was never likely to actually happen, but despite negotiations over the past three years, no long-term compromise can be found. Paying for the reform remains the main stumbling block.
“I think, this year, Congress was as close as it’s been in a long time to enacting a serious fix, aided by the agreement of major professional societies like the American College of Physicians and American College of Surgeons,” says David Howard, PhD, an associate professor in the department of health policy and management at the Rollins School of Public Health at Emory University in Atlanta. “They were all on board with this solution. ... Who knows, maybe if the economic situation continues to improve [and] tax revenues continue to go up...that will create a more favorable environment for compromise.”
Dr. Howard adds that while Congress might be close to a solution in theory, agreement on how to offset the roughly $100 billion in costs “is just very difficult.” That is why the healthcare professor is pessimistic that a long-term fix is truly at hand.
“The places where Congress might have looked for savings to offset the cost of the doc fix, such as hospital reimbursement rates or payment rates to Medicare Advantage plans—those are exactly the areas that the Affordable Care Act is targeting to pay for insurance expansion,” Dr. Howard adds. “So those areas of savings are not going to be available to offset the cost of the doc fix.”
ICD-10 Delays “Unfair”
The medical coding conundrum presents a different set of issues. The delay in transitioning healthcare providers from the ICD-9 medical coding classification system to the more complicated ICD-10 means the upgraded system is now against an Oct. 1, 2015, deadline. This comes after the Centers for Medicare & Medicaid Services (CMS) already pushed back the original implementation date for ICD-10 by one year.
SHM Public Policy Committee member Joshua Lenchus, DO, RPh, FACP, SFHM, says he thinks most doctors are content with the delay, particularly in light of some estimates that show that only about 20% of physicians “have actually initiated the ICD-10 transition.” But he also notes that it’s unfair to the health systems that have prepared for ICD-10.
“ICD-9 has a little more than 14,000 diagnostic codes and nearly 4,000 procedural codes. That is to be contrasted to ICD-10, which has more than 68,000 diagnostic codes ... and over 72,000 procedural codes,” Dr. Lenchus says. “So, it is not surprising that many take solace in the delay.”
–Dr. Lenchus
Dr. Nelson says the level of frustration for hospitalists is growing; however, the level of disruption for hospitals and health systems is reaching a boiling point.
“Of course, in some places, hospitalists may be the physician lead on ICD-10 efforts, so [they are] very much wrapped up in the problem of ‘What do we do now?’”
The answer, at least to the Coalition for ICD-10, a group of medical/technology trade groups, is to fight to ensure that the delays go no further. In an April letter to CMS Administrator Marilyn Tavenner, the coalition made that case, noting that in 2012, “CMS estimated the cost to the healthcare industry of a one-year delay to be as much as $6.6 billion, or approximately 30% of the $22 billion that CMS estimated had been invested or budgeted for ICD-10 implementation.”2
The letter went on to explain that the disruption and cost will grow each time the ICD-10 deadline is pushed.
“Furthermore, as CMS stated in 2012, implementation costs will continue to increase considerably with every year of a delay,” according to the letter. “The lost opportunity costs of failing to move to a more effective code set also continue to climb every year.”
Stay Engaged, Switch Gears
One of Floyd’s biggest concerns is that the ICD-10 implementation delays will affect physician engagement. The hospitalist groups at MUSC began training for ICD-10 in January 2013; however, the preparation and training were geared toward a 2014 implementation.
“You have to switch gears a little bit,” she says. “What we plan to do now is begin to do heavy auditing, and then from those audits we can give real-time feedback on what we’re doing well and what we’re not doing well. So I think that will be a method for engagement.”
She urges hospitalists, practice leaders, and informatics professionals to discuss ICD-10 not as a theoretical application, but as one tied to reimbursement that will have major impact in the years ahead. To that end, the American Health Information Management Association highlights the fact that the new coding system will result in higher-quality data that can improve performance measures, provide “increased sensitivity” to reimbursement methodologies, and help with stronger public health surveillance.3
“A lot of physicians see this as a hospital issue, and I think that’s why they shy away,” Floyd says. “Now there are some physicians who are interested in how well the hospital does, but the other piece is that it does affect things like [reduced] risk of mortality [and] comparison of data worldwide—those are things that we just have to continue to reiterate … and give them real examples.”
Richard Quinn is a freelance writer in New Jersey.
References
- Govtrack. H.R. 4302: Protecting Access to Medicare Act of 2014. https://www.govtrack.us/congress/bills/113/hr4302. Accessed June 5, 2014.
- Coalition for ICD. Letter to CMS Administrator Tavenner, April 11, 2014. http://coalitionforicd10.wordpress.com/2014/03/26/letter-from-the-coalition-for-icd-10. Accessed June 5, 2014.
- American Health Information Management Association. ICD-10-CM/PCS Transition: Planning and Preparation Checklist. http://journal.ahima.org/wp-content/uploads/ICD10-checklist.pdf. Accessed June 5, 2014.
Congress has once again delayed implementation of draconian Medicare cuts tied to the sustainable growth rate (SGR) formula. It was the 17th temporary patch applied to the ailing physician reimbursement program, so the decision caused little surprise.
But with the same legislation—the Protecting Access to Medicare Act of 2014—being used to delay the long-awaited debut of ICD-10, many hospitalists and physicians couldn’t help but wonder whether billing and coding would now be as much of a political football as the SGR fix.1
The upshot: It doesn’t seem that way.
“I think it’s two separate issues,” says Phyllis “PJ” Floyd, RN, BSN, MBA, NE-BC, CCA, director of health information services and clinical documentation improvement at Medical University of South Carolina (MUSC) in Charleston, S.C. “The fact that it was all in one bill, I don’t know that it was well thought out as much as it was, ‘Let’s put the ICD-10 in here at the same time.’
“It was just a few sentences, and then it wasn’t even brought up in the discussion on the floor.”
Four policy wonks interviewed by The Hospitalist concurred that while tying the ICD-10 delay to the SGR issue was an unexpected and frustrating development, the coding system likely will be implemented in the relative short term. Meanwhile, a long-term resolution of the SGR dilemma remains much more elusive.
“For about 12 hours, I felt relief about the ICD-10 [being delayed], and then I just realized, it’s still coming, presumably,” says John Nelson, MD, MHM, a co-founder and past president of SHM and medical director of the hospitalist practice at Overlake Hospital Medical Center in Bellevue, Wash. “[It’s] like a patient who needs surgery and finds out it’s canceled for the day and he’ll have it tomorrow. Well, that’s good for right now, but [he] still has to face this eventually.”
“Doc-Pay” Fix Near?
Congress’ recent decision to delay both an SGR fix and the ICD-10 are troubling to some hospitalists and others for different reasons.
The SGR extension through this year’s end means that physicians do not face a 24% cut to physician payments under Medicare. SHM has long lobbied against temporary patches to the SGR, repeatedly backing legislation that would once and for all scrap the formula and replace it with something sustainable.
The SGR formula was first crafted in 1997, but the now often-delayed cuts were a byproduct of the federal sequester that was included in the Budget Control Act of 2011. At the time, the massive reduction to Medicare payments was tied to political brinksmanship over the country’s debt ceiling. The cuts were implemented as a doomsday scenario that was never likely to actually happen, but despite negotiations over the past three years, no long-term compromise can be found. Paying for the reform remains the main stumbling block.
“I think, this year, Congress was as close as it’s been in a long time to enacting a serious fix, aided by the agreement of major professional societies like the American College of Physicians and American College of Surgeons,” says David Howard, PhD, an associate professor in the department of health policy and management at the Rollins School of Public Health at Emory University in Atlanta. “They were all on board with this solution. ... Who knows, maybe if the economic situation continues to improve [and] tax revenues continue to go up...that will create a more favorable environment for compromise.”
Dr. Howard adds that while Congress might be close to a solution in theory, agreement on how to offset the roughly $100 billion in costs “is just very difficult.” That is why the healthcare professor is pessimistic that a long-term fix is truly at hand.
“The places where Congress might have looked for savings to offset the cost of the doc fix, such as hospital reimbursement rates or payment rates to Medicare Advantage plans—those are exactly the areas that the Affordable Care Act is targeting to pay for insurance expansion,” Dr. Howard adds. “So those areas of savings are not going to be available to offset the cost of the doc fix.”
ICD-10 Delays “Unfair”
The medical coding conundrum presents a different set of issues. The delay in transitioning healthcare providers from the ICD-9 medical coding classification system to the more complicated ICD-10 means the upgraded system is now against an Oct. 1, 2015, deadline. This comes after the Centers for Medicare & Medicaid Services (CMS) already pushed back the original implementation date for ICD-10 by one year.
SHM Public Policy Committee member Joshua Lenchus, DO, RPh, FACP, SFHM, says he thinks most doctors are content with the delay, particularly in light of some estimates that show that only about 20% of physicians “have actually initiated the ICD-10 transition.” But he also notes that it’s unfair to the health systems that have prepared for ICD-10.
“ICD-9 has a little more than 14,000 diagnostic codes and nearly 4,000 procedural codes. That is to be contrasted to ICD-10, which has more than 68,000 diagnostic codes ... and over 72,000 procedural codes,” Dr. Lenchus says. “So, it is not surprising that many take solace in the delay.”
–Dr. Lenchus
Dr. Nelson says the level of frustration for hospitalists is growing; however, the level of disruption for hospitals and health systems is reaching a boiling point.
“Of course, in some places, hospitalists may be the physician lead on ICD-10 efforts, so [they are] very much wrapped up in the problem of ‘What do we do now?’”
The answer, at least to the Coalition for ICD-10, a group of medical/technology trade groups, is to fight to ensure that the delays go no further. In an April letter to CMS Administrator Marilyn Tavenner, the coalition made that case, noting that in 2012, “CMS estimated the cost to the healthcare industry of a one-year delay to be as much as $6.6 billion, or approximately 30% of the $22 billion that CMS estimated had been invested or budgeted for ICD-10 implementation.”2
The letter went on to explain that the disruption and cost will grow each time the ICD-10 deadline is pushed.
“Furthermore, as CMS stated in 2012, implementation costs will continue to increase considerably with every year of a delay,” according to the letter. “The lost opportunity costs of failing to move to a more effective code set also continue to climb every year.”
Stay Engaged, Switch Gears
One of Floyd’s biggest concerns is that the ICD-10 implementation delays will affect physician engagement. The hospitalist groups at MUSC began training for ICD-10 in January 2013; however, the preparation and training were geared toward a 2014 implementation.
“You have to switch gears a little bit,” she says. “What we plan to do now is begin to do heavy auditing, and then from those audits we can give real-time feedback on what we’re doing well and what we’re not doing well. So I think that will be a method for engagement.”
She urges hospitalists, practice leaders, and informatics professionals to discuss ICD-10 not as a theoretical application, but as one tied to reimbursement that will have major impact in the years ahead. To that end, the American Health Information Management Association highlights the fact that the new coding system will result in higher-quality data that can improve performance measures, provide “increased sensitivity” to reimbursement methodologies, and help with stronger public health surveillance.3
“A lot of physicians see this as a hospital issue, and I think that’s why they shy away,” Floyd says. “Now there are some physicians who are interested in how well the hospital does, but the other piece is that it does affect things like [reduced] risk of mortality [and] comparison of data worldwide—those are things that we just have to continue to reiterate … and give them real examples.”
Richard Quinn is a freelance writer in New Jersey.
References
- Govtrack. H.R. 4302: Protecting Access to Medicare Act of 2014. https://www.govtrack.us/congress/bills/113/hr4302. Accessed June 5, 2014.
- Coalition for ICD. Letter to CMS Administrator Tavenner, April 11, 2014. http://coalitionforicd10.wordpress.com/2014/03/26/letter-from-the-coalition-for-icd-10. Accessed June 5, 2014.
- American Health Information Management Association. ICD-10-CM/PCS Transition: Planning and Preparation Checklist. http://journal.ahima.org/wp-content/uploads/ICD10-checklist.pdf. Accessed June 5, 2014.
Bill to Clarify Three-Midnight Rule for Medicare Patients Gains Support from Congress, Hospitalists
In 2010, my office received a call from a Norwich, Conn., family whose 89-year-old father had fallen and broken his hip. After he was treated in the local hospital for four days, his doctor prescribed follow-on skilled nursing facility (SNF) care. Upon his arrival at the nursing home, his family was informed that they would have to pay more than $10,000 up front to cover the cost of his care: Because he had never been admitted to the hospital as an inpatient, Medicare would not cover the prescribed rehabilitative care that he needed to return home safely.
I know that hospitalists are already far too familiar with stories like this. Together, we can work to make sure it doesn’t happen again.
Support Is Growing
For me, that family’s story was a call for action. Shortly after speaking with the family, I introduced the Improving Access to Medicare Coverage Act (H.R. 1179). The bill is simple: It would restore the three-day hospital stay standard for SNF coverage, whether the stay is coded as inpatient under Part A or outpatient observation under Part B. Two Congresses later, support for the proposal is growing. In the 113th Congress, the bill has 137 bipartisan cosponsors, an indication of how widespread this problem is for Medicare beneficiaries.
The outdated Medicare law on skilled nursing care coverage is creating financial and healthcare dilemmas for families across the country. Under current law, beneficiaries must have a hospital inpatient stay of at least three days in order to qualify for Medicare coverage SNF benefits; however, more and more patients are being coded under observation status, and access to post-acute SNF care is diminishing. Patients are suffering, and healthcare providers are caught in the middle.
In fact, the Office of the Inspector General at the Department of Health and Human Services released a report last fall that showed that Medicare beneficiaries in 2012 had more than 600,000 hospital stays that lasted three nights, yet none were admitted as inpatients. Even though these beneficiaries likely received the same care inpatients received, their observation status designation disqualified them from Medicare coverage of the SNF benefit. For their families, prescribed follow-on SNF care would have an out-of-pocket cost averaging more than $10,000. For seniors on fixed incomes, that is a devastating financial penalty for a service that should be covered by their health plans.

—Rep. Joe Courtney
Administrative Oversight
There are many reasons for the growth in observation status treatments, but a primary driver is increasing scrutiny of admitting practices by recovery audit contractors (RACs). The consequences of RAC review processes have created difficult situations for hospitals, because admitting decisions are reviewable for three years, and hospitals can be hit with claw-back penalties for payments on behalf of patients RACs determine were incorrectly admitted. To prevent costly penalties and protracted appeals of individual cases, many hospitals feel an understandable amount of pressure to err on the side of treating patients under outpatient observation status covered under Part B.
The original intent of the three-day inpatient stay requirement was to serve as a tangible measure of medical necessity of SNF care. And, when the three-day inpatient stay prerequisite was written into law, long-term hospital observation stays were nonexistent. This intent has been lost in a changing system of hospital oversight under RACs and admitting practices.
The impact on patients and families is tragic.
Ann Sheehy, MD, MS, FHM, a hospitalist speaking on behalf of the Society of Hospital Medicine on a recent conference call I hosted, detailed the scenes she sees every day with her own patients. She described how doctors, knowing that a patient lacks the means to pay for rehabilitative care out of pocket and the support system to recover safely at home, sometimes keep the patient in the hospital longer, at a higher cost to Medicare. In other cases, Dr. Sheehy noted that patients end up back in the hospital soon after being discharged, having foregone expensive SNF care and subsequently suffered preventable injuries and illnesses. Both of these outcomes are bad for patients—and bad for Medicare expenditures.
Three-Day Fix
While the problem of observation status treatment is complex, the solution is simple.
As observation status becomes more ingrained in the healthcare lexicon, a legislative fix to restore the three-day hospital stay standard is needed now more than ever. Three days in the hospital—whether as an inpatient or under outpatient observation—should count for three days in the hospital when Medicare determines eligibility for SNF coverage.
My bill, H.R. 1179, is the most direct solution to rectify the flaw that leaves hundreds of thousands of beneficiaries wondering how their stay in the hospital does not “count” and scrambling to figure out how to pay for care—or foregoing it entirely. The strong support in the advocacy community for this legislation—especially from SHM—and the sway of outside groups cannot be overstated. In Washington’s current climate, the only thing that moves bipartisan issues forward is outside pressure.
Together, I hope hospitalists and members of Congress will reach the critical mass needed to pass this legislation and ensure that Medicare beneficiaries are covered for medically necessary care.
Joseph “Joe” Courtney is the U.S. Representative for Connecticut’s second congressional district, serving since 2007. The district includes most of the eastern third of the state, including Norwich and New London.
In 2010, my office received a call from a Norwich, Conn., family whose 89-year-old father had fallen and broken his hip. After he was treated in the local hospital for four days, his doctor prescribed follow-on skilled nursing facility (SNF) care. Upon his arrival at the nursing home, his family was informed that they would have to pay more than $10,000 up front to cover the cost of his care: Because he had never been admitted to the hospital as an inpatient, Medicare would not cover the prescribed rehabilitative care that he needed to return home safely.
I know that hospitalists are already far too familiar with stories like this. Together, we can work to make sure it doesn’t happen again.
Support Is Growing
For me, that family’s story was a call for action. Shortly after speaking with the family, I introduced the Improving Access to Medicare Coverage Act (H.R. 1179). The bill is simple: It would restore the three-day hospital stay standard for SNF coverage, whether the stay is coded as inpatient under Part A or outpatient observation under Part B. Two Congresses later, support for the proposal is growing. In the 113th Congress, the bill has 137 bipartisan cosponsors, an indication of how widespread this problem is for Medicare beneficiaries.
The outdated Medicare law on skilled nursing care coverage is creating financial and healthcare dilemmas for families across the country. Under current law, beneficiaries must have a hospital inpatient stay of at least three days in order to qualify for Medicare coverage SNF benefits; however, more and more patients are being coded under observation status, and access to post-acute SNF care is diminishing. Patients are suffering, and healthcare providers are caught in the middle.
In fact, the Office of the Inspector General at the Department of Health and Human Services released a report last fall that showed that Medicare beneficiaries in 2012 had more than 600,000 hospital stays that lasted three nights, yet none were admitted as inpatients. Even though these beneficiaries likely received the same care inpatients received, their observation status designation disqualified them from Medicare coverage of the SNF benefit. For their families, prescribed follow-on SNF care would have an out-of-pocket cost averaging more than $10,000. For seniors on fixed incomes, that is a devastating financial penalty for a service that should be covered by their health plans.

—Rep. Joe Courtney
Administrative Oversight
There are many reasons for the growth in observation status treatments, but a primary driver is increasing scrutiny of admitting practices by recovery audit contractors (RACs). The consequences of RAC review processes have created difficult situations for hospitals, because admitting decisions are reviewable for three years, and hospitals can be hit with claw-back penalties for payments on behalf of patients RACs determine were incorrectly admitted. To prevent costly penalties and protracted appeals of individual cases, many hospitals feel an understandable amount of pressure to err on the side of treating patients under outpatient observation status covered under Part B.
The original intent of the three-day inpatient stay requirement was to serve as a tangible measure of medical necessity of SNF care. And, when the three-day inpatient stay prerequisite was written into law, long-term hospital observation stays were nonexistent. This intent has been lost in a changing system of hospital oversight under RACs and admitting practices.
The impact on patients and families is tragic.
Ann Sheehy, MD, MS, FHM, a hospitalist speaking on behalf of the Society of Hospital Medicine on a recent conference call I hosted, detailed the scenes she sees every day with her own patients. She described how doctors, knowing that a patient lacks the means to pay for rehabilitative care out of pocket and the support system to recover safely at home, sometimes keep the patient in the hospital longer, at a higher cost to Medicare. In other cases, Dr. Sheehy noted that patients end up back in the hospital soon after being discharged, having foregone expensive SNF care and subsequently suffered preventable injuries and illnesses. Both of these outcomes are bad for patients—and bad for Medicare expenditures.
Three-Day Fix
While the problem of observation status treatment is complex, the solution is simple.
As observation status becomes more ingrained in the healthcare lexicon, a legislative fix to restore the three-day hospital stay standard is needed now more than ever. Three days in the hospital—whether as an inpatient or under outpatient observation—should count for three days in the hospital when Medicare determines eligibility for SNF coverage.
My bill, H.R. 1179, is the most direct solution to rectify the flaw that leaves hundreds of thousands of beneficiaries wondering how their stay in the hospital does not “count” and scrambling to figure out how to pay for care—or foregoing it entirely. The strong support in the advocacy community for this legislation—especially from SHM—and the sway of outside groups cannot be overstated. In Washington’s current climate, the only thing that moves bipartisan issues forward is outside pressure.
Together, I hope hospitalists and members of Congress will reach the critical mass needed to pass this legislation and ensure that Medicare beneficiaries are covered for medically necessary care.
Joseph “Joe” Courtney is the U.S. Representative for Connecticut’s second congressional district, serving since 2007. The district includes most of the eastern third of the state, including Norwich and New London.
In 2010, my office received a call from a Norwich, Conn., family whose 89-year-old father had fallen and broken his hip. After he was treated in the local hospital for four days, his doctor prescribed follow-on skilled nursing facility (SNF) care. Upon his arrival at the nursing home, his family was informed that they would have to pay more than $10,000 up front to cover the cost of his care: Because he had never been admitted to the hospital as an inpatient, Medicare would not cover the prescribed rehabilitative care that he needed to return home safely.
I know that hospitalists are already far too familiar with stories like this. Together, we can work to make sure it doesn’t happen again.
Support Is Growing
For me, that family’s story was a call for action. Shortly after speaking with the family, I introduced the Improving Access to Medicare Coverage Act (H.R. 1179). The bill is simple: It would restore the three-day hospital stay standard for SNF coverage, whether the stay is coded as inpatient under Part A or outpatient observation under Part B. Two Congresses later, support for the proposal is growing. In the 113th Congress, the bill has 137 bipartisan cosponsors, an indication of how widespread this problem is for Medicare beneficiaries.
The outdated Medicare law on skilled nursing care coverage is creating financial and healthcare dilemmas for families across the country. Under current law, beneficiaries must have a hospital inpatient stay of at least three days in order to qualify for Medicare coverage SNF benefits; however, more and more patients are being coded under observation status, and access to post-acute SNF care is diminishing. Patients are suffering, and healthcare providers are caught in the middle.
In fact, the Office of the Inspector General at the Department of Health and Human Services released a report last fall that showed that Medicare beneficiaries in 2012 had more than 600,000 hospital stays that lasted three nights, yet none were admitted as inpatients. Even though these beneficiaries likely received the same care inpatients received, their observation status designation disqualified them from Medicare coverage of the SNF benefit. For their families, prescribed follow-on SNF care would have an out-of-pocket cost averaging more than $10,000. For seniors on fixed incomes, that is a devastating financial penalty for a service that should be covered by their health plans.

—Rep. Joe Courtney
Administrative Oversight
There are many reasons for the growth in observation status treatments, but a primary driver is increasing scrutiny of admitting practices by recovery audit contractors (RACs). The consequences of RAC review processes have created difficult situations for hospitals, because admitting decisions are reviewable for three years, and hospitals can be hit with claw-back penalties for payments on behalf of patients RACs determine were incorrectly admitted. To prevent costly penalties and protracted appeals of individual cases, many hospitals feel an understandable amount of pressure to err on the side of treating patients under outpatient observation status covered under Part B.
The original intent of the three-day inpatient stay requirement was to serve as a tangible measure of medical necessity of SNF care. And, when the three-day inpatient stay prerequisite was written into law, long-term hospital observation stays were nonexistent. This intent has been lost in a changing system of hospital oversight under RACs and admitting practices.
The impact on patients and families is tragic.
Ann Sheehy, MD, MS, FHM, a hospitalist speaking on behalf of the Society of Hospital Medicine on a recent conference call I hosted, detailed the scenes she sees every day with her own patients. She described how doctors, knowing that a patient lacks the means to pay for rehabilitative care out of pocket and the support system to recover safely at home, sometimes keep the patient in the hospital longer, at a higher cost to Medicare. In other cases, Dr. Sheehy noted that patients end up back in the hospital soon after being discharged, having foregone expensive SNF care and subsequently suffered preventable injuries and illnesses. Both of these outcomes are bad for patients—and bad for Medicare expenditures.
Three-Day Fix
While the problem of observation status treatment is complex, the solution is simple.
As observation status becomes more ingrained in the healthcare lexicon, a legislative fix to restore the three-day hospital stay standard is needed now more than ever. Three days in the hospital—whether as an inpatient or under outpatient observation—should count for three days in the hospital when Medicare determines eligibility for SNF coverage.
My bill, H.R. 1179, is the most direct solution to rectify the flaw that leaves hundreds of thousands of beneficiaries wondering how their stay in the hospital does not “count” and scrambling to figure out how to pay for care—or foregoing it entirely. The strong support in the advocacy community for this legislation—especially from SHM—and the sway of outside groups cannot be overstated. In Washington’s current climate, the only thing that moves bipartisan issues forward is outside pressure.
Together, I hope hospitalists and members of Congress will reach the critical mass needed to pass this legislation and ensure that Medicare beneficiaries are covered for medically necessary care.
Joseph “Joe” Courtney is the U.S. Representative for Connecticut’s second congressional district, serving since 2007. The district includes most of the eastern third of the state, including Norwich and New London.
Society of Hospital Medicine Ranks Observation Status a Priority Advocacy Issue
The use of observation status within hospitals has risen over the last several years, creating the potential for negative financial impacts on patients and mounting headaches for hospitalists. Historically, the intent of observation status was to provide care in designated hospital units for short-stay patients with well-defined diagnoses, according to Medicare; however, as a result of complex federal policy and the realities of hospital care, patients under observation often receive care in general hospital beds, with stays that can extend past the 48-hour benchmark set by the Centers for Medicare & Medicaid Services (CMS).
Almost all hospitalists are familiar with the implications of observation status for their patients, and SHM has taken a leadership role in advocating for positive changes that benefit both the patient and hospitalist workflow.
Today, patients under observation often receive identical care to that received by inpatients but are billed as outpatients under Medicare Part B. This results in high deductibles, additional cost sharing, and out-of-pocket costs for medications. Complicating the issue more, hospitals in most states are not required to notify patients that they are coded as outpatients, leaving them with the impression that they have been admitted, until they receive their hospital bill.
In an attempt to curb the overuse of hospital observation status and clarify guidelines pertaining to inpatient admission decisions, CMS changed the rules for admitting patients in August 2013. Under what is now known as the “Two-Midnight Rule,” if a patient is expected to stay longer than two midnights and their stay is documented as medically necessary, they are an inpatient; fewer than two midnights constitutes outpatient services.
Even though the two-midnight rule is intended to simplify admission decisions, hospitalists have expressed a general apprehension regarding the impact of observation status. If a patient classified as an inpatient is discharged before two midnights, Medicare recovery auditors may deem the inpatient classification unnecessary, potentially resulting in loss of payment for medical services rendered.
For patients, the new rule does not remedy the fact that days spent under observation do not count toward the three-day inpatient stay requirement needed for skill nursing facility (SNF) post-acute care under Medicare. Consequently, thousands of patients classified under outpatient status have no choice but to pay for SNF care themselves, or forego the treatment altogether, creating possible complications in their care and delays in recovery.
Hospitalist concern over this issue has prompted SHM to rank observation status as a priority advocacy issue. Hospitalists are ideally situated to be part of a meaningful solution, and SHM’s Public Policy Committee has set out to do just that.
The first step will be to fully understand the experiences and perspectives regarding observation policy among hospitalists. SHM’s Public Policy Committee and government relations team have developed a survey for a group of randomized members. While individual anecdotal accounts are available, this is the first time the issue will be addressed on an aggregate level. Responses from survey participants will be used to frame the hospitalist perspective, help to bolster advocacy and educational efforts within SHM, and, ultimately, bring about possible policy revisions.
Hospitalists not receiving the survey can help by joining SHM’s Grassroots Network and lending their voice to the effort. To get involved, visit www.hospitalmedicine.org/advocacy.
NaDea Jeter is a member of SHM’s government relations team.
The use of observation status within hospitals has risen over the last several years, creating the potential for negative financial impacts on patients and mounting headaches for hospitalists. Historically, the intent of observation status was to provide care in designated hospital units for short-stay patients with well-defined diagnoses, according to Medicare; however, as a result of complex federal policy and the realities of hospital care, patients under observation often receive care in general hospital beds, with stays that can extend past the 48-hour benchmark set by the Centers for Medicare & Medicaid Services (CMS).
Almost all hospitalists are familiar with the implications of observation status for their patients, and SHM has taken a leadership role in advocating for positive changes that benefit both the patient and hospitalist workflow.
Today, patients under observation often receive identical care to that received by inpatients but are billed as outpatients under Medicare Part B. This results in high deductibles, additional cost sharing, and out-of-pocket costs for medications. Complicating the issue more, hospitals in most states are not required to notify patients that they are coded as outpatients, leaving them with the impression that they have been admitted, until they receive their hospital bill.
In an attempt to curb the overuse of hospital observation status and clarify guidelines pertaining to inpatient admission decisions, CMS changed the rules for admitting patients in August 2013. Under what is now known as the “Two-Midnight Rule,” if a patient is expected to stay longer than two midnights and their stay is documented as medically necessary, they are an inpatient; fewer than two midnights constitutes outpatient services.
Even though the two-midnight rule is intended to simplify admission decisions, hospitalists have expressed a general apprehension regarding the impact of observation status. If a patient classified as an inpatient is discharged before two midnights, Medicare recovery auditors may deem the inpatient classification unnecessary, potentially resulting in loss of payment for medical services rendered.
For patients, the new rule does not remedy the fact that days spent under observation do not count toward the three-day inpatient stay requirement needed for skill nursing facility (SNF) post-acute care under Medicare. Consequently, thousands of patients classified under outpatient status have no choice but to pay for SNF care themselves, or forego the treatment altogether, creating possible complications in their care and delays in recovery.
Hospitalist concern over this issue has prompted SHM to rank observation status as a priority advocacy issue. Hospitalists are ideally situated to be part of a meaningful solution, and SHM’s Public Policy Committee has set out to do just that.
The first step will be to fully understand the experiences and perspectives regarding observation policy among hospitalists. SHM’s Public Policy Committee and government relations team have developed a survey for a group of randomized members. While individual anecdotal accounts are available, this is the first time the issue will be addressed on an aggregate level. Responses from survey participants will be used to frame the hospitalist perspective, help to bolster advocacy and educational efforts within SHM, and, ultimately, bring about possible policy revisions.
Hospitalists not receiving the survey can help by joining SHM’s Grassroots Network and lending their voice to the effort. To get involved, visit www.hospitalmedicine.org/advocacy.
NaDea Jeter is a member of SHM’s government relations team.
The use of observation status within hospitals has risen over the last several years, creating the potential for negative financial impacts on patients and mounting headaches for hospitalists. Historically, the intent of observation status was to provide care in designated hospital units for short-stay patients with well-defined diagnoses, according to Medicare; however, as a result of complex federal policy and the realities of hospital care, patients under observation often receive care in general hospital beds, with stays that can extend past the 48-hour benchmark set by the Centers for Medicare & Medicaid Services (CMS).
Almost all hospitalists are familiar with the implications of observation status for their patients, and SHM has taken a leadership role in advocating for positive changes that benefit both the patient and hospitalist workflow.
Today, patients under observation often receive identical care to that received by inpatients but are billed as outpatients under Medicare Part B. This results in high deductibles, additional cost sharing, and out-of-pocket costs for medications. Complicating the issue more, hospitals in most states are not required to notify patients that they are coded as outpatients, leaving them with the impression that they have been admitted, until they receive their hospital bill.
In an attempt to curb the overuse of hospital observation status and clarify guidelines pertaining to inpatient admission decisions, CMS changed the rules for admitting patients in August 2013. Under what is now known as the “Two-Midnight Rule,” if a patient is expected to stay longer than two midnights and their stay is documented as medically necessary, they are an inpatient; fewer than two midnights constitutes outpatient services.
Even though the two-midnight rule is intended to simplify admission decisions, hospitalists have expressed a general apprehension regarding the impact of observation status. If a patient classified as an inpatient is discharged before two midnights, Medicare recovery auditors may deem the inpatient classification unnecessary, potentially resulting in loss of payment for medical services rendered.
For patients, the new rule does not remedy the fact that days spent under observation do not count toward the three-day inpatient stay requirement needed for skill nursing facility (SNF) post-acute care under Medicare. Consequently, thousands of patients classified under outpatient status have no choice but to pay for SNF care themselves, or forego the treatment altogether, creating possible complications in their care and delays in recovery.
Hospitalist concern over this issue has prompted SHM to rank observation status as a priority advocacy issue. Hospitalists are ideally situated to be part of a meaningful solution, and SHM’s Public Policy Committee has set out to do just that.
The first step will be to fully understand the experiences and perspectives regarding observation policy among hospitalists. SHM’s Public Policy Committee and government relations team have developed a survey for a group of randomized members. While individual anecdotal accounts are available, this is the first time the issue will be addressed on an aggregate level. Responses from survey participants will be used to frame the hospitalist perspective, help to bolster advocacy and educational efforts within SHM, and, ultimately, bring about possible policy revisions.
Hospitalists not receiving the survey can help by joining SHM’s Grassroots Network and lending their voice to the effort. To get involved, visit www.hospitalmedicine.org/advocacy.
NaDea Jeter is a member of SHM’s government relations team.
Delays, Controversy Muddle CMS’ Two-Midnight Rule for Hospital Patient Admissions
A new rule issued by the Centers for Medicare & Medicaid Services (CMS) is at the center of controversy fueled by competing interests and lack of clarity. And, for the fourth time since the two-midnight rule was introduced in the 2014 Hospital Inpatient Prospective Payment System, its implementation has been delayed. Hospitals and providers have until March 31, 2015, before auditors begin scrutinizing patient admission statuses for reimbursement determination.
The rule requires Medicare and Medicaid patients spending fewer than two midnights receiving hospital care to be classified as outpatient or under observation. Patients spending more than two midnights will be considered inpatient. Only physicians can make the determination, and the clock begins ticking the moment care begins.
The rule also cuts hospital inpatient reimbursement by 0.2%, because CMS believes the number of inpatient admissions will increase.

–Joanna Hiatt Kim, vice president of payment policy for the American Hospital Association
The rule pits private Medicare auditors (Medicare Administrative Contractors, MACs, and Recovery Audit Contractors, RACs), who have a financial stake in denying inpatient claims, against hospitals and physicians. It does little to clear confusion for patients when it comes time for them to pay their bills.
Patients generally are unaware whether they’ve been admitted or are under observation. But observation status leaves them on the hook for any skilled nursing care they receive following discharge and for the costs of routine maintenance drugs hospitals give them for chronic conditions.
Beneficiaries also are not eligible for Medicare Part A skilled nursing care coverage if they were an inpatient for fewer than 72 hours, and observation days do not count toward the three-day requirement. The two-midnight rule adds another “layer” to the equation, says Bradley Flansbaum, DO, MPH, FACP, a hospitalist and clinical assistant professor of medicine at NYU School of Medicine in New York City.
At the same time, hospitals now face penalties for patients readmitted within 30 days of discharge for a similar episode of care. Observation status offers a measure of protection in the event patients return.
The number of observation patients increased 69% between 2006 and 2011, according to federal data cited by Kaiser Health News, and the number of observation patients staying more than 48 hours increased from 3% to 8% during this same period.
“The concern is that [the two-midnight rule] sets an arbitrary time threshold that dictates where a patient should be placed,” says Joanna Hiatt Kim, vice president of payment policy for the American Hospital Association. The AHA opposes aspects of the rule and was involved in legislation to delay implementation.
“We feel time should not be the only factor taken into account,” Hiatt Kim adds. “It should be a decision a physician reaches based on a patient’s condition.”
Good Intentions
The rule states that hospital stays fewer than two midnights are generally medically inappropriate for inpatient designation. The services provided are not at issue, but CMS believes those administered during a short stay could be provided on a less expensive outpatient basis.
Dr. Flansbaum, a member of SHM’s Public Policy Committee, says the language of medical necessity that designates status is unclear, though CMS has given physicians the benefit of the doubt.
“We are looking for clear signals from providers for how we determine when someone is appropriately inpatient and when they’re observation,” he explains.
Although medical needs can be quantified, there are often other, nonmedical factors that put patients at risk and influence when and whether a patient is admitted. Physicians routinely weigh these factors on behalf of their patients.
“Risk isn’t necessarily implied by just a dangerous blood value,” Dr. Flansbaum says. “If something is not right in the transition zone or in the community, I think those [factors] need to be taken into account.”
Physicians are being given “a lot of latitude” in CMS’ new rule, he notes.
Clarification
In recent clarification, CMS highlighted exceptions to the rule. If “unforeseen circumstances” shorten the anticipated stay of someone initially deemed inpatient—transfer to another hospital, death, or clinical improvement in fewer than two midnights, for example—CMS can advise auditors to approve the inpatient claim.
Additionally, CMS will maintain a list of services considered “inpatient only,” regardless of stay duration.
But creating a list of every medically necessary service is an “administrative black hole,” says Dr. Flansbaum, though he believes that with enough time and clarity, compliance with the two-midnight rule is possible.
Kelly April Tyrrell is a freelance writer in Wilmington, Del.
A new rule issued by the Centers for Medicare & Medicaid Services (CMS) is at the center of controversy fueled by competing interests and lack of clarity. And, for the fourth time since the two-midnight rule was introduced in the 2014 Hospital Inpatient Prospective Payment System, its implementation has been delayed. Hospitals and providers have until March 31, 2015, before auditors begin scrutinizing patient admission statuses for reimbursement determination.
The rule requires Medicare and Medicaid patients spending fewer than two midnights receiving hospital care to be classified as outpatient or under observation. Patients spending more than two midnights will be considered inpatient. Only physicians can make the determination, and the clock begins ticking the moment care begins.
The rule also cuts hospital inpatient reimbursement by 0.2%, because CMS believes the number of inpatient admissions will increase.

–Joanna Hiatt Kim, vice president of payment policy for the American Hospital Association
The rule pits private Medicare auditors (Medicare Administrative Contractors, MACs, and Recovery Audit Contractors, RACs), who have a financial stake in denying inpatient claims, against hospitals and physicians. It does little to clear confusion for patients when it comes time for them to pay their bills.
Patients generally are unaware whether they’ve been admitted or are under observation. But observation status leaves them on the hook for any skilled nursing care they receive following discharge and for the costs of routine maintenance drugs hospitals give them for chronic conditions.
Beneficiaries also are not eligible for Medicare Part A skilled nursing care coverage if they were an inpatient for fewer than 72 hours, and observation days do not count toward the three-day requirement. The two-midnight rule adds another “layer” to the equation, says Bradley Flansbaum, DO, MPH, FACP, a hospitalist and clinical assistant professor of medicine at NYU School of Medicine in New York City.
At the same time, hospitals now face penalties for patients readmitted within 30 days of discharge for a similar episode of care. Observation status offers a measure of protection in the event patients return.
The number of observation patients increased 69% between 2006 and 2011, according to federal data cited by Kaiser Health News, and the number of observation patients staying more than 48 hours increased from 3% to 8% during this same period.
“The concern is that [the two-midnight rule] sets an arbitrary time threshold that dictates where a patient should be placed,” says Joanna Hiatt Kim, vice president of payment policy for the American Hospital Association. The AHA opposes aspects of the rule and was involved in legislation to delay implementation.
“We feel time should not be the only factor taken into account,” Hiatt Kim adds. “It should be a decision a physician reaches based on a patient’s condition.”
Good Intentions
The rule states that hospital stays fewer than two midnights are generally medically inappropriate for inpatient designation. The services provided are not at issue, but CMS believes those administered during a short stay could be provided on a less expensive outpatient basis.
Dr. Flansbaum, a member of SHM’s Public Policy Committee, says the language of medical necessity that designates status is unclear, though CMS has given physicians the benefit of the doubt.
“We are looking for clear signals from providers for how we determine when someone is appropriately inpatient and when they’re observation,” he explains.
Although medical needs can be quantified, there are often other, nonmedical factors that put patients at risk and influence when and whether a patient is admitted. Physicians routinely weigh these factors on behalf of their patients.
“Risk isn’t necessarily implied by just a dangerous blood value,” Dr. Flansbaum says. “If something is not right in the transition zone or in the community, I think those [factors] need to be taken into account.”
Physicians are being given “a lot of latitude” in CMS’ new rule, he notes.
Clarification
In recent clarification, CMS highlighted exceptions to the rule. If “unforeseen circumstances” shorten the anticipated stay of someone initially deemed inpatient—transfer to another hospital, death, or clinical improvement in fewer than two midnights, for example—CMS can advise auditors to approve the inpatient claim.
Additionally, CMS will maintain a list of services considered “inpatient only,” regardless of stay duration.
But creating a list of every medically necessary service is an “administrative black hole,” says Dr. Flansbaum, though he believes that with enough time and clarity, compliance with the two-midnight rule is possible.
Kelly April Tyrrell is a freelance writer in Wilmington, Del.
A new rule issued by the Centers for Medicare & Medicaid Services (CMS) is at the center of controversy fueled by competing interests and lack of clarity. And, for the fourth time since the two-midnight rule was introduced in the 2014 Hospital Inpatient Prospective Payment System, its implementation has been delayed. Hospitals and providers have until March 31, 2015, before auditors begin scrutinizing patient admission statuses for reimbursement determination.
The rule requires Medicare and Medicaid patients spending fewer than two midnights receiving hospital care to be classified as outpatient or under observation. Patients spending more than two midnights will be considered inpatient. Only physicians can make the determination, and the clock begins ticking the moment care begins.
The rule also cuts hospital inpatient reimbursement by 0.2%, because CMS believes the number of inpatient admissions will increase.

–Joanna Hiatt Kim, vice president of payment policy for the American Hospital Association
The rule pits private Medicare auditors (Medicare Administrative Contractors, MACs, and Recovery Audit Contractors, RACs), who have a financial stake in denying inpatient claims, against hospitals and physicians. It does little to clear confusion for patients when it comes time for them to pay their bills.
Patients generally are unaware whether they’ve been admitted or are under observation. But observation status leaves them on the hook for any skilled nursing care they receive following discharge and for the costs of routine maintenance drugs hospitals give them for chronic conditions.
Beneficiaries also are not eligible for Medicare Part A skilled nursing care coverage if they were an inpatient for fewer than 72 hours, and observation days do not count toward the three-day requirement. The two-midnight rule adds another “layer” to the equation, says Bradley Flansbaum, DO, MPH, FACP, a hospitalist and clinical assistant professor of medicine at NYU School of Medicine in New York City.
At the same time, hospitals now face penalties for patients readmitted within 30 days of discharge for a similar episode of care. Observation status offers a measure of protection in the event patients return.
The number of observation patients increased 69% between 2006 and 2011, according to federal data cited by Kaiser Health News, and the number of observation patients staying more than 48 hours increased from 3% to 8% during this same period.
“The concern is that [the two-midnight rule] sets an arbitrary time threshold that dictates where a patient should be placed,” says Joanna Hiatt Kim, vice president of payment policy for the American Hospital Association. The AHA opposes aspects of the rule and was involved in legislation to delay implementation.
“We feel time should not be the only factor taken into account,” Hiatt Kim adds. “It should be a decision a physician reaches based on a patient’s condition.”
Good Intentions
The rule states that hospital stays fewer than two midnights are generally medically inappropriate for inpatient designation. The services provided are not at issue, but CMS believes those administered during a short stay could be provided on a less expensive outpatient basis.
Dr. Flansbaum, a member of SHM’s Public Policy Committee, says the language of medical necessity that designates status is unclear, though CMS has given physicians the benefit of the doubt.
“We are looking for clear signals from providers for how we determine when someone is appropriately inpatient and when they’re observation,” he explains.
Although medical needs can be quantified, there are often other, nonmedical factors that put patients at risk and influence when and whether a patient is admitted. Physicians routinely weigh these factors on behalf of their patients.
“Risk isn’t necessarily implied by just a dangerous blood value,” Dr. Flansbaum says. “If something is not right in the transition zone or in the community, I think those [factors] need to be taken into account.”
Physicians are being given “a lot of latitude” in CMS’ new rule, he notes.
Clarification
In recent clarification, CMS highlighted exceptions to the rule. If “unforeseen circumstances” shorten the anticipated stay of someone initially deemed inpatient—transfer to another hospital, death, or clinical improvement in fewer than two midnights, for example—CMS can advise auditors to approve the inpatient claim.
Additionally, CMS will maintain a list of services considered “inpatient only,” regardless of stay duration.
But creating a list of every medically necessary service is an “administrative black hole,” says Dr. Flansbaum, though he believes that with enough time and clarity, compliance with the two-midnight rule is possible.
Kelly April Tyrrell is a freelance writer in Wilmington, Del.
Federal Grant Extends Anti-Infection Initiative
The American Hospital Association’s Health Research and Educational Trust (HRET) recently obtained a grant from the federal Agency for Healthcare Research and Quality to expand CUSP, the Comprehensive Unit-based Safety Program for reducing catheter-associated urinary tract infections (CAUTI) and other healthcare-associated infections, to nursing homes and skilled nursing facilities nationwide.
CUSP has posted a 40% reduction in central line-associated bloodstream infections (CLABSI) in 1,000 participating hospitals by providing education and support and an evidence-based protocol. The grant will be administered by HRET in partnership with others, including the University of Michigan Health System, the Association for Professionals in Infection Control and Epidemiology, and SHM.
Meanwhile, a study published in the American Journal of Infection Control found that rates of catheter-associated urinary tract infections in adult patients given urinary catheter placements dropped nationwide to 5.3% in 2010 from 9.4% in 2001.3 The retrospective analysis of data from the National Hospital Discharge Survey found that CAUTI-related mortality and associated length of hospital stay also declined during the same period.
Larry Beresford is a freelance writer in Alameda, Calif.
The American Hospital Association’s Health Research and Educational Trust (HRET) recently obtained a grant from the federal Agency for Healthcare Research and Quality to expand CUSP, the Comprehensive Unit-based Safety Program for reducing catheter-associated urinary tract infections (CAUTI) and other healthcare-associated infections, to nursing homes and skilled nursing facilities nationwide.
CUSP has posted a 40% reduction in central line-associated bloodstream infections (CLABSI) in 1,000 participating hospitals by providing education and support and an evidence-based protocol. The grant will be administered by HRET in partnership with others, including the University of Michigan Health System, the Association for Professionals in Infection Control and Epidemiology, and SHM.
Meanwhile, a study published in the American Journal of Infection Control found that rates of catheter-associated urinary tract infections in adult patients given urinary catheter placements dropped nationwide to 5.3% in 2010 from 9.4% in 2001.3 The retrospective analysis of data from the National Hospital Discharge Survey found that CAUTI-related mortality and associated length of hospital stay also declined during the same period.
Larry Beresford is a freelance writer in Alameda, Calif.
The American Hospital Association’s Health Research and Educational Trust (HRET) recently obtained a grant from the federal Agency for Healthcare Research and Quality to expand CUSP, the Comprehensive Unit-based Safety Program for reducing catheter-associated urinary tract infections (CAUTI) and other healthcare-associated infections, to nursing homes and skilled nursing facilities nationwide.
CUSP has posted a 40% reduction in central line-associated bloodstream infections (CLABSI) in 1,000 participating hospitals by providing education and support and an evidence-based protocol. The grant will be administered by HRET in partnership with others, including the University of Michigan Health System, the Association for Professionals in Infection Control and Epidemiology, and SHM.
Meanwhile, a study published in the American Journal of Infection Control found that rates of catheter-associated urinary tract infections in adult patients given urinary catheter placements dropped nationwide to 5.3% in 2010 from 9.4% in 2001.3 The retrospective analysis of data from the National Hospital Discharge Survey found that CAUTI-related mortality and associated length of hospital stay also declined during the same period.
Larry Beresford is a freelance writer in Alameda, Calif.
How Will New Physician Value-Based Payment Modifier Affect Medicare Reimbursements?
We talk a lot about value in healthcare—about how to enhance quality and reduce cost—because we all know both need an incredible amount of work. One tactic Medicare is using to improve the value equation on a large scale is aggregating and displaying physician-specific “value” metrics. These metrics, which will be used to deduct or enhance reimbursement for physicians, are known as the Physician Value-Based Payment Modifier (PVBM).
This program has been enacted fairly rapidly since the passage of the Affordable Care Act; it is being rolled out first to large physician practices, then to all groups by 2017. Those with superior performance in both quality and cost will experience as much as a 2% higher reimbursement, while groups with average performance will remain financially neutral and those who show lower performance or choose not to report will be penalized up to 1% of Medicare reimbursement. This first round, for larger groups of 100-plus physicians, will affect about 30% of all U.S. physicians. The second round, for groups of 10 or more physicians, will affect about another third of physicians. The last round, for groups with fewer than 10 physicians, will be applicable to the remaining physicians practicing in the U.S.
On the face of it, the program does seem to be a potentially effective tactic for improving value on a large scale, holding individual physicians accountable for their own individual patient-care performance. A few fatal flaws in the program as it currently stands make it extraordinarily unlikely to be universally adopted by all physicians, however. Here are a few of those flaws:1,2
1 Uncertain yield: Because it is essentially a “zero-sum game” for Medicare, the incentive or penalty for a physician (or the physician’s group) depends on the performance of all the other physicians’ or groups’ performance. As a result, there is incredible uncertainty as to how strong a physician’s performance actually needs to be, year to year, to result in a bonus payment. Given that many of the metrics will require some type of investment to perform well, such as information technology infrastructure or a quality coordinator, there is an equal amount of uncertainty about how much investment will be needed to get a certain budgetary yield. For smaller physician practices, taking a 1% to 2% reduction in Medicare reimbursements may be easier to weather financially than investing in the infrastructure needed to reliably hit the quality metrics for every relevant patient.
2 Uncertain benchmarks: Unlike many hospital quality metrics, which have been publicly displayed for years, physician-level value metrics are just now being reported publicly. This leaves uncertainty about how strong a physician’s performance needs to be in order to be better than average. In the hospital value-based purchasing program, “average” performance is extremely good, in the 98% to 99% compliance range for most metrics. It is less clear what compliance range will be “average” in the physician-based program.
3 Physician variability: More than a half million physicians in the U.S. bill Medicare, and their practice types range from primary care solo practice to multi-group specialty practice. Motivating all brands to understand, measure, report, and improve quality metrics is a yeoman’s task, unlikely to be successful in the short term. Most physicians have not received any formal education or training in quality improvement, so they may not even have the skill set required to improve their metrics into a highly reliable range, worthy of bonus designation.
4 Metric identity and attribution: Because the repertoire of physician types is broad, the ability of each physician type to have a set of metrics that they understand and can identify with is extremely unlikely. In addition, attribution of patients and their associated metrics to any single physician is complicated, especially for patients who are cared for by many different physicians across a number of settings. For hospitalists, the attribution issue is a fatal flaw, as many groups routinely “hand off” patients among other hospitalists in their group, at least once if not several times during a typical hospital stay. The same is true of many other hospital-based specialty physicians.
5 Playing to the test: As with other pay-for-performance programs, there is a legitimate concern that physicians will be overwhelmingly motivated to play to the test, so that their efforts to perform exceedingly well at a few metrics will crowd out and hinder their performance on unmeasured metrics. This tendency can result in lower-value care in the sum total, even if the metrics show stellar performance.
6 Reducing the risk: As seen in other pay-for-performance programs, there is a legitimate concern that physicians will be overwhelmingly motivated to avoid caring for patients who are likely to be unpredictable, including those with multiple co-morbid conditions or with complex social situations; these patients are likely to perform less well on any metric, despite risk adjusting (which is inherently imperfect). This is a well-known and documented risk of publicly reported programs, and there is no reason to believe the PVBM program will be immune to this risk.
In Sum
Because these flaws seem so daunting at first glance, many physicians and physician groups will be tempted to reject the program outright and take the financial hit induced by nonparticipation. An alternative approach is to embrace all of the value programs outright, investing time and energy in improving the metrics that are truly valuable to both patients and providers.
Regardless of which regulatory agency is demanding performance, we need to be active participants in foraging out what metrics and attribution logic are most appropriate. For hospitalists, these could include risk-adjusted device days, appropriate prescribing and unprescribing of antibiotics, judicious utilization of diagnostic testing, and measurements of patient functional status and/or mobility.
Value metrics are here to stay, including those attributable to individual physicians; our job now is to advocate for meaningful metrics and meaningful attribution, which can and should motivate hospitalists to enhance their patients’ quality of life at a lower cost.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
We talk a lot about value in healthcare—about how to enhance quality and reduce cost—because we all know both need an incredible amount of work. One tactic Medicare is using to improve the value equation on a large scale is aggregating and displaying physician-specific “value” metrics. These metrics, which will be used to deduct or enhance reimbursement for physicians, are known as the Physician Value-Based Payment Modifier (PVBM).
This program has been enacted fairly rapidly since the passage of the Affordable Care Act; it is being rolled out first to large physician practices, then to all groups by 2017. Those with superior performance in both quality and cost will experience as much as a 2% higher reimbursement, while groups with average performance will remain financially neutral and those who show lower performance or choose not to report will be penalized up to 1% of Medicare reimbursement. This first round, for larger groups of 100-plus physicians, will affect about 30% of all U.S. physicians. The second round, for groups of 10 or more physicians, will affect about another third of physicians. The last round, for groups with fewer than 10 physicians, will be applicable to the remaining physicians practicing in the U.S.
On the face of it, the program does seem to be a potentially effective tactic for improving value on a large scale, holding individual physicians accountable for their own individual patient-care performance. A few fatal flaws in the program as it currently stands make it extraordinarily unlikely to be universally adopted by all physicians, however. Here are a few of those flaws:1,2
1 Uncertain yield: Because it is essentially a “zero-sum game” for Medicare, the incentive or penalty for a physician (or the physician’s group) depends on the performance of all the other physicians’ or groups’ performance. As a result, there is incredible uncertainty as to how strong a physician’s performance actually needs to be, year to year, to result in a bonus payment. Given that many of the metrics will require some type of investment to perform well, such as information technology infrastructure or a quality coordinator, there is an equal amount of uncertainty about how much investment will be needed to get a certain budgetary yield. For smaller physician practices, taking a 1% to 2% reduction in Medicare reimbursements may be easier to weather financially than investing in the infrastructure needed to reliably hit the quality metrics for every relevant patient.
2 Uncertain benchmarks: Unlike many hospital quality metrics, which have been publicly displayed for years, physician-level value metrics are just now being reported publicly. This leaves uncertainty about how strong a physician’s performance needs to be in order to be better than average. In the hospital value-based purchasing program, “average” performance is extremely good, in the 98% to 99% compliance range for most metrics. It is less clear what compliance range will be “average” in the physician-based program.
3 Physician variability: More than a half million physicians in the U.S. bill Medicare, and their practice types range from primary care solo practice to multi-group specialty practice. Motivating all brands to understand, measure, report, and improve quality metrics is a yeoman’s task, unlikely to be successful in the short term. Most physicians have not received any formal education or training in quality improvement, so they may not even have the skill set required to improve their metrics into a highly reliable range, worthy of bonus designation.
4 Metric identity and attribution: Because the repertoire of physician types is broad, the ability of each physician type to have a set of metrics that they understand and can identify with is extremely unlikely. In addition, attribution of patients and their associated metrics to any single physician is complicated, especially for patients who are cared for by many different physicians across a number of settings. For hospitalists, the attribution issue is a fatal flaw, as many groups routinely “hand off” patients among other hospitalists in their group, at least once if not several times during a typical hospital stay. The same is true of many other hospital-based specialty physicians.
5 Playing to the test: As with other pay-for-performance programs, there is a legitimate concern that physicians will be overwhelmingly motivated to play to the test, so that their efforts to perform exceedingly well at a few metrics will crowd out and hinder their performance on unmeasured metrics. This tendency can result in lower-value care in the sum total, even if the metrics show stellar performance.
6 Reducing the risk: As seen in other pay-for-performance programs, there is a legitimate concern that physicians will be overwhelmingly motivated to avoid caring for patients who are likely to be unpredictable, including those with multiple co-morbid conditions or with complex social situations; these patients are likely to perform less well on any metric, despite risk adjusting (which is inherently imperfect). This is a well-known and documented risk of publicly reported programs, and there is no reason to believe the PVBM program will be immune to this risk.
In Sum
Because these flaws seem so daunting at first glance, many physicians and physician groups will be tempted to reject the program outright and take the financial hit induced by nonparticipation. An alternative approach is to embrace all of the value programs outright, investing time and energy in improving the metrics that are truly valuable to both patients and providers.
Regardless of which regulatory agency is demanding performance, we need to be active participants in foraging out what metrics and attribution logic are most appropriate. For hospitalists, these could include risk-adjusted device days, appropriate prescribing and unprescribing of antibiotics, judicious utilization of diagnostic testing, and measurements of patient functional status and/or mobility.
Value metrics are here to stay, including those attributable to individual physicians; our job now is to advocate for meaningful metrics and meaningful attribution, which can and should motivate hospitalists to enhance their patients’ quality of life at a lower cost.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
We talk a lot about value in healthcare—about how to enhance quality and reduce cost—because we all know both need an incredible amount of work. One tactic Medicare is using to improve the value equation on a large scale is aggregating and displaying physician-specific “value” metrics. These metrics, which will be used to deduct or enhance reimbursement for physicians, are known as the Physician Value-Based Payment Modifier (PVBM).
This program has been enacted fairly rapidly since the passage of the Affordable Care Act; it is being rolled out first to large physician practices, then to all groups by 2017. Those with superior performance in both quality and cost will experience as much as a 2% higher reimbursement, while groups with average performance will remain financially neutral and those who show lower performance or choose not to report will be penalized up to 1% of Medicare reimbursement. This first round, for larger groups of 100-plus physicians, will affect about 30% of all U.S. physicians. The second round, for groups of 10 or more physicians, will affect about another third of physicians. The last round, for groups with fewer than 10 physicians, will be applicable to the remaining physicians practicing in the U.S.
On the face of it, the program does seem to be a potentially effective tactic for improving value on a large scale, holding individual physicians accountable for their own individual patient-care performance. A few fatal flaws in the program as it currently stands make it extraordinarily unlikely to be universally adopted by all physicians, however. Here are a few of those flaws:1,2
1 Uncertain yield: Because it is essentially a “zero-sum game” for Medicare, the incentive or penalty for a physician (or the physician’s group) depends on the performance of all the other physicians’ or groups’ performance. As a result, there is incredible uncertainty as to how strong a physician’s performance actually needs to be, year to year, to result in a bonus payment. Given that many of the metrics will require some type of investment to perform well, such as information technology infrastructure or a quality coordinator, there is an equal amount of uncertainty about how much investment will be needed to get a certain budgetary yield. For smaller physician practices, taking a 1% to 2% reduction in Medicare reimbursements may be easier to weather financially than investing in the infrastructure needed to reliably hit the quality metrics for every relevant patient.
2 Uncertain benchmarks: Unlike many hospital quality metrics, which have been publicly displayed for years, physician-level value metrics are just now being reported publicly. This leaves uncertainty about how strong a physician’s performance needs to be in order to be better than average. In the hospital value-based purchasing program, “average” performance is extremely good, in the 98% to 99% compliance range for most metrics. It is less clear what compliance range will be “average” in the physician-based program.
3 Physician variability: More than a half million physicians in the U.S. bill Medicare, and their practice types range from primary care solo practice to multi-group specialty practice. Motivating all brands to understand, measure, report, and improve quality metrics is a yeoman’s task, unlikely to be successful in the short term. Most physicians have not received any formal education or training in quality improvement, so they may not even have the skill set required to improve their metrics into a highly reliable range, worthy of bonus designation.
4 Metric identity and attribution: Because the repertoire of physician types is broad, the ability of each physician type to have a set of metrics that they understand and can identify with is extremely unlikely. In addition, attribution of patients and their associated metrics to any single physician is complicated, especially for patients who are cared for by many different physicians across a number of settings. For hospitalists, the attribution issue is a fatal flaw, as many groups routinely “hand off” patients among other hospitalists in their group, at least once if not several times during a typical hospital stay. The same is true of many other hospital-based specialty physicians.
5 Playing to the test: As with other pay-for-performance programs, there is a legitimate concern that physicians will be overwhelmingly motivated to play to the test, so that their efforts to perform exceedingly well at a few metrics will crowd out and hinder their performance on unmeasured metrics. This tendency can result in lower-value care in the sum total, even if the metrics show stellar performance.
6 Reducing the risk: As seen in other pay-for-performance programs, there is a legitimate concern that physicians will be overwhelmingly motivated to avoid caring for patients who are likely to be unpredictable, including those with multiple co-morbid conditions or with complex social situations; these patients are likely to perform less well on any metric, despite risk adjusting (which is inherently imperfect). This is a well-known and documented risk of publicly reported programs, and there is no reason to believe the PVBM program will be immune to this risk.
In Sum
Because these flaws seem so daunting at first glance, many physicians and physician groups will be tempted to reject the program outright and take the financial hit induced by nonparticipation. An alternative approach is to embrace all of the value programs outright, investing time and energy in improving the metrics that are truly valuable to both patients and providers.
Regardless of which regulatory agency is demanding performance, we need to be active participants in foraging out what metrics and attribution logic are most appropriate. For hospitalists, these could include risk-adjusted device days, appropriate prescribing and unprescribing of antibiotics, judicious utilization of diagnostic testing, and measurements of patient functional status and/or mobility.
Value metrics are here to stay, including those attributable to individual physicians; our job now is to advocate for meaningful metrics and meaningful attribution, which can and should motivate hospitalists to enhance their patients’ quality of life at a lower cost.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
Centers for Medicare & Medicaid Services Modify Physician Quality Reporting System
Only 27% of eligible providers participated in the Physician Quality Reporting System (PQRS) in 2011—roughly 26,500 medical practices and 266,500 medical professionals, according to the Centers for Medicare & Medicaid Services (CMS).
“A lot of physicians have walked away [from PQRS] feeling like there are not sufficient measures for them to be measured against,” says Cheryl Damberg, senior principal researcher at RAND corporation and professor at the Pardee RAND Graduate School in Santa Monica, Calif.
Encouraging more participation from hospitalists has been the goal of the Society of Hospital Medicine (SHM) for the last several years, says Gregory Seymann, MD, SFHM, clinical professor and chief in the division of hospital medicine at University of California San Diego Health Sciences and chair of SHM’s Performance Measurement and Reporting Committee (PMRC).
“The committee has tried to champion it the best we can, making sure the measures that are there and in development meet the needs of the specialty,” Dr. Seymann says.
In just one year, the SHM committee managed to increase hospitalist reportable measures in PQRS from a paltry 11—half of which were only for stroke patients—to 21, which now includes things like diabetes exams, osteoporosis management, documentation of current medications, and community-acquired pneumonia treatment.
For Comparison’s Sake
For the first couple of phases of PQRS reporting, very few measures were relevant to hospitalists, Dr. Seymann says. The committee worked to ensure that more measures were added and billing codes modified to include those used by the specialty. Hospital medicine is relatively new, not officially recognized by the American Board of Medical Specialties (ABMS), and hospitalists serve a unique role. Most hospitalists are in internal medicine, family medicine, or pediatrics, but they aren’t doing what the average primary care doctor does, like referral for breast cancer or colon cancer screening, Dr. Seymann adds. Additionally, they aren’t always the provider performing specific cardiac or neurological care.
Hospitalists’ patients usually are in the hospital because they are sick. They may have chronic disease or more complex medical needs (e.g. osteoporosis-related hip fracture) than the average population seen by a non-hospitalist PCP.
If hospitalists are compared to other PCPs, as is the plan in the Physician Value-Based Payment Modifier, it “looks like our patients are dying a lot more frequently, we’re spending a lot of money, and we’re not doing primary care,” Dr. Seymann explains.
New Brand, New Push
PQRS is not new; it is the rebranding of CMS’ Physician Quality Reporting Initiative (PQRI), launched in 2006. But changes to the program are part of a national push to improve healthcare quality and patient care while reimbursing for performance on outcome- and process-based measures instead of simply for the volume of services provided. Each year, CMS updates PQRS rules.
This year is the last one in which providers will receive a bonus for reporting through PQRS. Beginning next year, practitioners that don’t meet the reporting requirements for 2013 will incur a 1.5% penalty—with additional penalties for physicians in groups of 100 or more from the value-based payment modifier. This year also serves as the performance year for 2016, when a 2% penalty for insufficient reporting will be assessed.
In early December 2013, the Centers for Medicare & Medicaid Services (CMS) published the 2014 Physician Fee Schedule and, with it, the final rules for the PQRS. Although many physicians and specialist groups believed the measures included in PQRS in previous years were too limited, CMS has added the additional reporting methodology of qualified clinical data registries (QCDR), which can include measures outside of the PQRS—a marked shift from previous policies.
The rule change, Damberg says, should take some energy out of the discussion surrounding the program and allow more physicians to participate.
“From CMS’ perspective, they want doctors delivering the recommended care and they want doctors to be able to report it out easily,” Damberg says.
Moving Forward
In 2014, providers can submit measures through the new QCDR option, or submit PQRS-identified measures through a Medicare qualified registry, through electronic health records, through the group practice reporting option (GPRO), and through claims-based reporting (though this last option is expected to be phased out over time).
Registries themselves are not new, but they can cost millions of dollars to establish and as much as a million a year to maintain. They typically contain more clinical depth and specificity than claims data, and numerous studies show the use of registries leads to improved patient outcomes.
“We don’t know how many [existing] registries are going to qualify to become these qualified clinical data registries,” says Tom Granatir, senior vice president for health policy and external relations at ABMS. “It’s going to take some time for these registries to evolve.”
Qualified clinical data registries must be in operation for at least one year to be eligible for certification by Medicare. They must include performance data from other payers beyond Medicare. Not only must QCDRs be capable of capturing and sending data, they must also provide national benchmarks to those who submit and must report back at least four times per year.
Granatir believes the QCDR rule, which allows QCDR’s to report measures beyond those included in the PQRS program, will help increase participation and will lead to more practice-based measures, but he fears it may exclude some important nuances of day-to-day patient care.
“The whole point [of quality measure reporting] is to create more public transparency…but if you have measures that are not relevant to what is actually done in practices, then it’s not a useful dataset,” he says.
Ideally, Damberg says, PQRS and other performance measures should enable physicians to do what they do better.
“I think this is really going to raise the stakes for [hospitalists] if they want to control their destiny,” Damberg says. “I think they have to get really engaged in this game and take a pro-active role in looking at where the quality gaps are and how can they better benefit patients. That’s the ultimate goal.”
Kelly April Tyrrell is a freelance writer in Wilmington, Del.
Only 27% of eligible providers participated in the Physician Quality Reporting System (PQRS) in 2011—roughly 26,500 medical practices and 266,500 medical professionals, according to the Centers for Medicare & Medicaid Services (CMS).
“A lot of physicians have walked away [from PQRS] feeling like there are not sufficient measures for them to be measured against,” says Cheryl Damberg, senior principal researcher at RAND corporation and professor at the Pardee RAND Graduate School in Santa Monica, Calif.
Encouraging more participation from hospitalists has been the goal of the Society of Hospital Medicine (SHM) for the last several years, says Gregory Seymann, MD, SFHM, clinical professor and chief in the division of hospital medicine at University of California San Diego Health Sciences and chair of SHM’s Performance Measurement and Reporting Committee (PMRC).
“The committee has tried to champion it the best we can, making sure the measures that are there and in development meet the needs of the specialty,” Dr. Seymann says.
In just one year, the SHM committee managed to increase hospitalist reportable measures in PQRS from a paltry 11—half of which were only for stroke patients—to 21, which now includes things like diabetes exams, osteoporosis management, documentation of current medications, and community-acquired pneumonia treatment.
For Comparison’s Sake
For the first couple of phases of PQRS reporting, very few measures were relevant to hospitalists, Dr. Seymann says. The committee worked to ensure that more measures were added and billing codes modified to include those used by the specialty. Hospital medicine is relatively new, not officially recognized by the American Board of Medical Specialties (ABMS), and hospitalists serve a unique role. Most hospitalists are in internal medicine, family medicine, or pediatrics, but they aren’t doing what the average primary care doctor does, like referral for breast cancer or colon cancer screening, Dr. Seymann adds. Additionally, they aren’t always the provider performing specific cardiac or neurological care.
Hospitalists’ patients usually are in the hospital because they are sick. They may have chronic disease or more complex medical needs (e.g. osteoporosis-related hip fracture) than the average population seen by a non-hospitalist PCP.
If hospitalists are compared to other PCPs, as is the plan in the Physician Value-Based Payment Modifier, it “looks like our patients are dying a lot more frequently, we’re spending a lot of money, and we’re not doing primary care,” Dr. Seymann explains.
New Brand, New Push
PQRS is not new; it is the rebranding of CMS’ Physician Quality Reporting Initiative (PQRI), launched in 2006. But changes to the program are part of a national push to improve healthcare quality and patient care while reimbursing for performance on outcome- and process-based measures instead of simply for the volume of services provided. Each year, CMS updates PQRS rules.
This year is the last one in which providers will receive a bonus for reporting through PQRS. Beginning next year, practitioners that don’t meet the reporting requirements for 2013 will incur a 1.5% penalty—with additional penalties for physicians in groups of 100 or more from the value-based payment modifier. This year also serves as the performance year for 2016, when a 2% penalty for insufficient reporting will be assessed.
In early December 2013, the Centers for Medicare & Medicaid Services (CMS) published the 2014 Physician Fee Schedule and, with it, the final rules for the PQRS. Although many physicians and specialist groups believed the measures included in PQRS in previous years were too limited, CMS has added the additional reporting methodology of qualified clinical data registries (QCDR), which can include measures outside of the PQRS—a marked shift from previous policies.
The rule change, Damberg says, should take some energy out of the discussion surrounding the program and allow more physicians to participate.
“From CMS’ perspective, they want doctors delivering the recommended care and they want doctors to be able to report it out easily,” Damberg says.
Moving Forward
In 2014, providers can submit measures through the new QCDR option, or submit PQRS-identified measures through a Medicare qualified registry, through electronic health records, through the group practice reporting option (GPRO), and through claims-based reporting (though this last option is expected to be phased out over time).
Registries themselves are not new, but they can cost millions of dollars to establish and as much as a million a year to maintain. They typically contain more clinical depth and specificity than claims data, and numerous studies show the use of registries leads to improved patient outcomes.
“We don’t know how many [existing] registries are going to qualify to become these qualified clinical data registries,” says Tom Granatir, senior vice president for health policy and external relations at ABMS. “It’s going to take some time for these registries to evolve.”
Qualified clinical data registries must be in operation for at least one year to be eligible for certification by Medicare. They must include performance data from other payers beyond Medicare. Not only must QCDRs be capable of capturing and sending data, they must also provide national benchmarks to those who submit and must report back at least four times per year.
Granatir believes the QCDR rule, which allows QCDR’s to report measures beyond those included in the PQRS program, will help increase participation and will lead to more practice-based measures, but he fears it may exclude some important nuances of day-to-day patient care.
“The whole point [of quality measure reporting] is to create more public transparency…but if you have measures that are not relevant to what is actually done in practices, then it’s not a useful dataset,” he says.
Ideally, Damberg says, PQRS and other performance measures should enable physicians to do what they do better.
“I think this is really going to raise the stakes for [hospitalists] if they want to control their destiny,” Damberg says. “I think they have to get really engaged in this game and take a pro-active role in looking at where the quality gaps are and how can they better benefit patients. That’s the ultimate goal.”
Kelly April Tyrrell is a freelance writer in Wilmington, Del.
Only 27% of eligible providers participated in the Physician Quality Reporting System (PQRS) in 2011—roughly 26,500 medical practices and 266,500 medical professionals, according to the Centers for Medicare & Medicaid Services (CMS).
“A lot of physicians have walked away [from PQRS] feeling like there are not sufficient measures for them to be measured against,” says Cheryl Damberg, senior principal researcher at RAND corporation and professor at the Pardee RAND Graduate School in Santa Monica, Calif.
Encouraging more participation from hospitalists has been the goal of the Society of Hospital Medicine (SHM) for the last several years, says Gregory Seymann, MD, SFHM, clinical professor and chief in the division of hospital medicine at University of California San Diego Health Sciences and chair of SHM’s Performance Measurement and Reporting Committee (PMRC).
“The committee has tried to champion it the best we can, making sure the measures that are there and in development meet the needs of the specialty,” Dr. Seymann says.
In just one year, the SHM committee managed to increase hospitalist reportable measures in PQRS from a paltry 11—half of which were only for stroke patients—to 21, which now includes things like diabetes exams, osteoporosis management, documentation of current medications, and community-acquired pneumonia treatment.
For Comparison’s Sake
For the first couple of phases of PQRS reporting, very few measures were relevant to hospitalists, Dr. Seymann says. The committee worked to ensure that more measures were added and billing codes modified to include those used by the specialty. Hospital medicine is relatively new, not officially recognized by the American Board of Medical Specialties (ABMS), and hospitalists serve a unique role. Most hospitalists are in internal medicine, family medicine, or pediatrics, but they aren’t doing what the average primary care doctor does, like referral for breast cancer or colon cancer screening, Dr. Seymann adds. Additionally, they aren’t always the provider performing specific cardiac or neurological care.
Hospitalists’ patients usually are in the hospital because they are sick. They may have chronic disease or more complex medical needs (e.g. osteoporosis-related hip fracture) than the average population seen by a non-hospitalist PCP.
If hospitalists are compared to other PCPs, as is the plan in the Physician Value-Based Payment Modifier, it “looks like our patients are dying a lot more frequently, we’re spending a lot of money, and we’re not doing primary care,” Dr. Seymann explains.
New Brand, New Push
PQRS is not new; it is the rebranding of CMS’ Physician Quality Reporting Initiative (PQRI), launched in 2006. But changes to the program are part of a national push to improve healthcare quality and patient care while reimbursing for performance on outcome- and process-based measures instead of simply for the volume of services provided. Each year, CMS updates PQRS rules.
This year is the last one in which providers will receive a bonus for reporting through PQRS. Beginning next year, practitioners that don’t meet the reporting requirements for 2013 will incur a 1.5% penalty—with additional penalties for physicians in groups of 100 or more from the value-based payment modifier. This year also serves as the performance year for 2016, when a 2% penalty for insufficient reporting will be assessed.
In early December 2013, the Centers for Medicare & Medicaid Services (CMS) published the 2014 Physician Fee Schedule and, with it, the final rules for the PQRS. Although many physicians and specialist groups believed the measures included in PQRS in previous years were too limited, CMS has added the additional reporting methodology of qualified clinical data registries (QCDR), which can include measures outside of the PQRS—a marked shift from previous policies.
The rule change, Damberg says, should take some energy out of the discussion surrounding the program and allow more physicians to participate.
“From CMS’ perspective, they want doctors delivering the recommended care and they want doctors to be able to report it out easily,” Damberg says.
Moving Forward
In 2014, providers can submit measures through the new QCDR option, or submit PQRS-identified measures through a Medicare qualified registry, through electronic health records, through the group practice reporting option (GPRO), and through claims-based reporting (though this last option is expected to be phased out over time).
Registries themselves are not new, but they can cost millions of dollars to establish and as much as a million a year to maintain. They typically contain more clinical depth and specificity than claims data, and numerous studies show the use of registries leads to improved patient outcomes.
“We don’t know how many [existing] registries are going to qualify to become these qualified clinical data registries,” says Tom Granatir, senior vice president for health policy and external relations at ABMS. “It’s going to take some time for these registries to evolve.”
Qualified clinical data registries must be in operation for at least one year to be eligible for certification by Medicare. They must include performance data from other payers beyond Medicare. Not only must QCDRs be capable of capturing and sending data, they must also provide national benchmarks to those who submit and must report back at least four times per year.
Granatir believes the QCDR rule, which allows QCDR’s to report measures beyond those included in the PQRS program, will help increase participation and will lead to more practice-based measures, but he fears it may exclude some important nuances of day-to-day patient care.
“The whole point [of quality measure reporting] is to create more public transparency…but if you have measures that are not relevant to what is actually done in practices, then it’s not a useful dataset,” he says.
Ideally, Damberg says, PQRS and other performance measures should enable physicians to do what they do better.
“I think this is really going to raise the stakes for [hospitalists] if they want to control their destiny,” Damberg says. “I think they have to get really engaged in this game and take a pro-active role in looking at where the quality gaps are and how can they better benefit patients. That’s the ultimate goal.”
Kelly April Tyrrell is a freelance writer in Wilmington, Del.