User login
The Hospitalist only
How’s your postacute network doing?
By now, nearly all hospitals are developing networks of postacute facilities for some or all of their patients, such as those in ACOs, bundled payments, or other value-based programs. Commonly referred to as preferred providers, performance networks, narrow networks, or similar, these networks of skilled nursing facilities (SNFs) and other entities that provide postacute care (like home health agencies) are usually chosen because they have demonstrated that they provide high quality, cost-effective care for patients after they leave the hospital.
While case managers are often the ones who counsel patients and caregivers on the details of the network, hospitalists should have at least a high-level grasp of which facilities are on the list and what the network selection criteria are. I would argue that hospitalists should lead the discussion with patients on postacute facility selection as it relates to which facilities are in the network and why going to a network facility is advantageous. Why? Because as hospitalist practices begin to share clinical and financial risk for patients, or at least become eligible to share in savings as MACRA encourages, they will have a vested interest in network facilities’ performance.
Postacute care network selection criteria
There is a range of criteria – usually incorporating measures of quality and efficiency – for including providers like SNFs in networks. In terms of quality, criteria can include physician/provider availability, star ratings on Nursing Home Compare, care transitions measures, Department of Public Health inspection survey scores, Joint Commission accreditation, etc.
A few caveats regarding specific selection criteria:
Star ratings on Nursing Home Compare
These are derived from nursing staffing ratios, health inspections, and 16 quality measures. More than half of the quality measures pertain to long-stay residents who typically are not in the ACO or bundled payment program for which the network was created (these are usually short-stay patients).
SNF length of stay
High readmission rates from a SNF can actually lower its length of stay, so including “balancing” measures such as readmissions should be considered.
What about patient choice?
Narrow postacute networks are not only becoming the norm, but there is also broad recognition from CMS, MedPAC, and industry leaders that value-based payment programs require such networks to succeed. That said, case managers and other discharge planners may still resist networks on the grounds that they might be perceived as restricting patient choice. One approach to balancing differing views on patient choice is to give patients the traditional longer list of available postacute providers, and also furnish the shorter network list accompanied by an explanation of why certain SNFs are in the network. Thankfully, as ACOs and bundles become widespread, resistance to narrow networks is dying down.
What role should hospitalists play in network referrals?
High functioning hospitalist practices should lead the discussion with patients and the health care team on referrals to network SNFs. Why? Patients are looking for their doctors to guide them on such decisions. Only if the physician opts not to have the discussion will patients look to the case manager for direction on which postacute facility to choose. A better option still would be for the hospitalists to partner with case managers to have the conversation with patients. In such a scenario, the hospitalist can begin the discussion and cover the major points, and the case manager can follow with more detailed information. For less mature hospitalist practices, the case manager can play a larger role in the discussion. In any case, as value-based models become ubiquitous, and shared savings become a driver of hospitalist revenue, hospitalists’ knowledge of and active participation in conversations around narrow networks and referrals will be necessary.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn. He is a cofounder and past president of SHM.
By now, nearly all hospitals are developing networks of postacute facilities for some or all of their patients, such as those in ACOs, bundled payments, or other value-based programs. Commonly referred to as preferred providers, performance networks, narrow networks, or similar, these networks of skilled nursing facilities (SNFs) and other entities that provide postacute care (like home health agencies) are usually chosen because they have demonstrated that they provide high quality, cost-effective care for patients after they leave the hospital.
While case managers are often the ones who counsel patients and caregivers on the details of the network, hospitalists should have at least a high-level grasp of which facilities are on the list and what the network selection criteria are. I would argue that hospitalists should lead the discussion with patients on postacute facility selection as it relates to which facilities are in the network and why going to a network facility is advantageous. Why? Because as hospitalist practices begin to share clinical and financial risk for patients, or at least become eligible to share in savings as MACRA encourages, they will have a vested interest in network facilities’ performance.
Postacute care network selection criteria
There is a range of criteria – usually incorporating measures of quality and efficiency – for including providers like SNFs in networks. In terms of quality, criteria can include physician/provider availability, star ratings on Nursing Home Compare, care transitions measures, Department of Public Health inspection survey scores, Joint Commission accreditation, etc.
A few caveats regarding specific selection criteria:
Star ratings on Nursing Home Compare
These are derived from nursing staffing ratios, health inspections, and 16 quality measures. More than half of the quality measures pertain to long-stay residents who typically are not in the ACO or bundled payment program for which the network was created (these are usually short-stay patients).
SNF length of stay
High readmission rates from a SNF can actually lower its length of stay, so including “balancing” measures such as readmissions should be considered.
What about patient choice?
Narrow postacute networks are not only becoming the norm, but there is also broad recognition from CMS, MedPAC, and industry leaders that value-based payment programs require such networks to succeed. That said, case managers and other discharge planners may still resist networks on the grounds that they might be perceived as restricting patient choice. One approach to balancing differing views on patient choice is to give patients the traditional longer list of available postacute providers, and also furnish the shorter network list accompanied by an explanation of why certain SNFs are in the network. Thankfully, as ACOs and bundles become widespread, resistance to narrow networks is dying down.
What role should hospitalists play in network referrals?
High functioning hospitalist practices should lead the discussion with patients and the health care team on referrals to network SNFs. Why? Patients are looking for their doctors to guide them on such decisions. Only if the physician opts not to have the discussion will patients look to the case manager for direction on which postacute facility to choose. A better option still would be for the hospitalists to partner with case managers to have the conversation with patients. In such a scenario, the hospitalist can begin the discussion and cover the major points, and the case manager can follow with more detailed information. For less mature hospitalist practices, the case manager can play a larger role in the discussion. In any case, as value-based models become ubiquitous, and shared savings become a driver of hospitalist revenue, hospitalists’ knowledge of and active participation in conversations around narrow networks and referrals will be necessary.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn. He is a cofounder and past president of SHM.
By now, nearly all hospitals are developing networks of postacute facilities for some or all of their patients, such as those in ACOs, bundled payments, or other value-based programs. Commonly referred to as preferred providers, performance networks, narrow networks, or similar, these networks of skilled nursing facilities (SNFs) and other entities that provide postacute care (like home health agencies) are usually chosen because they have demonstrated that they provide high quality, cost-effective care for patients after they leave the hospital.
While case managers are often the ones who counsel patients and caregivers on the details of the network, hospitalists should have at least a high-level grasp of which facilities are on the list and what the network selection criteria are. I would argue that hospitalists should lead the discussion with patients on postacute facility selection as it relates to which facilities are in the network and why going to a network facility is advantageous. Why? Because as hospitalist practices begin to share clinical and financial risk for patients, or at least become eligible to share in savings as MACRA encourages, they will have a vested interest in network facilities’ performance.
Postacute care network selection criteria
There is a range of criteria – usually incorporating measures of quality and efficiency – for including providers like SNFs in networks. In terms of quality, criteria can include physician/provider availability, star ratings on Nursing Home Compare, care transitions measures, Department of Public Health inspection survey scores, Joint Commission accreditation, etc.
A few caveats regarding specific selection criteria:
Star ratings on Nursing Home Compare
These are derived from nursing staffing ratios, health inspections, and 16 quality measures. More than half of the quality measures pertain to long-stay residents who typically are not in the ACO or bundled payment program for which the network was created (these are usually short-stay patients).
SNF length of stay
High readmission rates from a SNF can actually lower its length of stay, so including “balancing” measures such as readmissions should be considered.
What about patient choice?
Narrow postacute networks are not only becoming the norm, but there is also broad recognition from CMS, MedPAC, and industry leaders that value-based payment programs require such networks to succeed. That said, case managers and other discharge planners may still resist networks on the grounds that they might be perceived as restricting patient choice. One approach to balancing differing views on patient choice is to give patients the traditional longer list of available postacute providers, and also furnish the shorter network list accompanied by an explanation of why certain SNFs are in the network. Thankfully, as ACOs and bundles become widespread, resistance to narrow networks is dying down.
What role should hospitalists play in network referrals?
High functioning hospitalist practices should lead the discussion with patients and the health care team on referrals to network SNFs. Why? Patients are looking for their doctors to guide them on such decisions. Only if the physician opts not to have the discussion will patients look to the case manager for direction on which postacute facility to choose. A better option still would be for the hospitalists to partner with case managers to have the conversation with patients. In such a scenario, the hospitalist can begin the discussion and cover the major points, and the case manager can follow with more detailed information. For less mature hospitalist practices, the case manager can play a larger role in the discussion. In any case, as value-based models become ubiquitous, and shared savings become a driver of hospitalist revenue, hospitalists’ knowledge of and active participation in conversations around narrow networks and referrals will be necessary.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn. He is a cofounder and past president of SHM.
Transitioning from your current medical practice: an abbreviated step-by-step guide
You have decided it is time to move on from your current hospital or medical group position and transition into a new role. While this decision is exciting and well-earned after years of hard work, it is critical that you make a plan and take specific steps to ensure that the transition is seamless.
The steps below are recommendations to make this process smoother.
Step 1: Determine how you are leaving the practice and your proposed timeline
Before anything else, you should decide how you are leaving your practice. Are you leaving the practice of medicine altogether, or are you simply leaving your current position for a different position elsewhere? This distinction will dictate what steps are necessary. Timing is also critical when leaving a practice, as it will dictate what steps should be taken and when. Having specific but realistic goals is imperative. Select a goal date for leaving the practice, but be aware that this goal may need to be adjusted.
Step 2: Create your team of advisers
Whether you are leaving your current practice or transitioning to a different position, it is extremely important to have the right individuals on your team. You should consider enlisting an attorney, a financial adviser, and an accountant to help facilitate the process. Enlisting lawyers with certain areas of expertise, such as in the areas of employment restrictive covenants, health care, or tax, may also be extremely beneficial and helpful throughout the process.
Step 3: Review your current employment agreement
It is quite likely that at the onset of your current employment arrangement, you signed an employment agreement with your hospital or group. You will want to carefully review this agreement, as it may contain provisions that can affect the steps you should take before you leave your current practice and work elsewhere. These provisions include the following:
a) Noncompetition provisions
It is critical to determine whether or not there are any restrictive covenants in your employment agreement that limit where you can work after you transition from your current practice into a new role. Restrictive covenants include noncompetition and nonsolicitation provisions, and prohibit employees from working at certain places or in certain geographic areas after they leave their current place of employment. Rules surrounding restrictive covenants vary from state to state. If there are restrictive covenants in your agreement, be sure to understand the scope of the covenant, including the geographic and temporal scope, as well as the types of medicine you are prohibited from practicing. If the covenants seem too broad or unnecessarily restrictive, consult with an attorney, as overly broad or unduly burdensome covenants are often unenforceable. However, a state-by-state analysis is required.
b) Notice and termination provisions
It is important to review whether or not there are any notice requirements in your employment agreement, which may require you to notify your employer in advance of a departure. Make sure to comply with the time requirements in the notice provision to avoid a breach of the agreement. It is also critical to determine whether terminating an agreement early will result in any termination penalties. At times, employers will impose a penalty if an employee prematurely terminates a working relationship. Understanding the penalties associated with terminating your agreement will allow you to decide whether you want to cancel the agreement and pay the penalty or push back your timeline until the end of the agreement’s term to avoid termination fees.
Step 4: Licensure obligations
Further, if your practice bills Medicare, you will want to file certain forms with Medicare to show that you are either changing your practice location or leaving medicine. For example, if you are leaving the hospital or group to practice elsewhere, you will need to fill out forms in order for your old group to submit claims and receive payments for Medicare services you provided while you were still part of that group. Furthermore, you will need to file reassignment forms to allow your new practice to bill on your behalf. Understanding which forms to complete can be confusing, so enlisting the help of a healthcare attorney may be worthwhile.
Step 5: Discuss your transition with your insurance representative
Even after you leave your current practice, you may be exposed to litigation for services you provided while you were employed or otherwise retained by such practice. To ensure that you are protected, discuss your insurance policy with your insurance representative. Review whether your insurance policy is “occurrence” or “claims-made.” If you have an occurrence policy, you are protected from covered incidents that occur during the policy period, regardless if your policy is still in existence. Claims-made policies only provide coverage for claims where both the incident and the claim occur during the policy period. For example, if you cancel your policy on March 1, and are sued on April 1 for an incident that allegedly occurred on Feb. 1, your claims-made insurance policy will not protect you. Therefore, it is important to analyze your policies to determine if tail insurance is needed.
There are a number of other issues you will want to address before you leave your practice, including financial responsibilities and medical record and privacy obligations. To ensure that you leave your practice properly, you should contact an experienced lawyer who can help you navigate this process.
Steven M. Harris is a nationally recognized health care attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
You have decided it is time to move on from your current hospital or medical group position and transition into a new role. While this decision is exciting and well-earned after years of hard work, it is critical that you make a plan and take specific steps to ensure that the transition is seamless.
The steps below are recommendations to make this process smoother.
Step 1: Determine how you are leaving the practice and your proposed timeline
Before anything else, you should decide how you are leaving your practice. Are you leaving the practice of medicine altogether, or are you simply leaving your current position for a different position elsewhere? This distinction will dictate what steps are necessary. Timing is also critical when leaving a practice, as it will dictate what steps should be taken and when. Having specific but realistic goals is imperative. Select a goal date for leaving the practice, but be aware that this goal may need to be adjusted.
Step 2: Create your team of advisers
Whether you are leaving your current practice or transitioning to a different position, it is extremely important to have the right individuals on your team. You should consider enlisting an attorney, a financial adviser, and an accountant to help facilitate the process. Enlisting lawyers with certain areas of expertise, such as in the areas of employment restrictive covenants, health care, or tax, may also be extremely beneficial and helpful throughout the process.
Step 3: Review your current employment agreement
It is quite likely that at the onset of your current employment arrangement, you signed an employment agreement with your hospital or group. You will want to carefully review this agreement, as it may contain provisions that can affect the steps you should take before you leave your current practice and work elsewhere. These provisions include the following:
a) Noncompetition provisions
It is critical to determine whether or not there are any restrictive covenants in your employment agreement that limit where you can work after you transition from your current practice into a new role. Restrictive covenants include noncompetition and nonsolicitation provisions, and prohibit employees from working at certain places or in certain geographic areas after they leave their current place of employment. Rules surrounding restrictive covenants vary from state to state. If there are restrictive covenants in your agreement, be sure to understand the scope of the covenant, including the geographic and temporal scope, as well as the types of medicine you are prohibited from practicing. If the covenants seem too broad or unnecessarily restrictive, consult with an attorney, as overly broad or unduly burdensome covenants are often unenforceable. However, a state-by-state analysis is required.
b) Notice and termination provisions
It is important to review whether or not there are any notice requirements in your employment agreement, which may require you to notify your employer in advance of a departure. Make sure to comply with the time requirements in the notice provision to avoid a breach of the agreement. It is also critical to determine whether terminating an agreement early will result in any termination penalties. At times, employers will impose a penalty if an employee prematurely terminates a working relationship. Understanding the penalties associated with terminating your agreement will allow you to decide whether you want to cancel the agreement and pay the penalty or push back your timeline until the end of the agreement’s term to avoid termination fees.
Step 4: Licensure obligations
Further, if your practice bills Medicare, you will want to file certain forms with Medicare to show that you are either changing your practice location or leaving medicine. For example, if you are leaving the hospital or group to practice elsewhere, you will need to fill out forms in order for your old group to submit claims and receive payments for Medicare services you provided while you were still part of that group. Furthermore, you will need to file reassignment forms to allow your new practice to bill on your behalf. Understanding which forms to complete can be confusing, so enlisting the help of a healthcare attorney may be worthwhile.
Step 5: Discuss your transition with your insurance representative
Even after you leave your current practice, you may be exposed to litigation for services you provided while you were employed or otherwise retained by such practice. To ensure that you are protected, discuss your insurance policy with your insurance representative. Review whether your insurance policy is “occurrence” or “claims-made.” If you have an occurrence policy, you are protected from covered incidents that occur during the policy period, regardless if your policy is still in existence. Claims-made policies only provide coverage for claims where both the incident and the claim occur during the policy period. For example, if you cancel your policy on March 1, and are sued on April 1 for an incident that allegedly occurred on Feb. 1, your claims-made insurance policy will not protect you. Therefore, it is important to analyze your policies to determine if tail insurance is needed.
There are a number of other issues you will want to address before you leave your practice, including financial responsibilities and medical record and privacy obligations. To ensure that you leave your practice properly, you should contact an experienced lawyer who can help you navigate this process.
Steven M. Harris is a nationally recognized health care attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
You have decided it is time to move on from your current hospital or medical group position and transition into a new role. While this decision is exciting and well-earned after years of hard work, it is critical that you make a plan and take specific steps to ensure that the transition is seamless.
The steps below are recommendations to make this process smoother.
Step 1: Determine how you are leaving the practice and your proposed timeline
Before anything else, you should decide how you are leaving your practice. Are you leaving the practice of medicine altogether, or are you simply leaving your current position for a different position elsewhere? This distinction will dictate what steps are necessary. Timing is also critical when leaving a practice, as it will dictate what steps should be taken and when. Having specific but realistic goals is imperative. Select a goal date for leaving the practice, but be aware that this goal may need to be adjusted.
Step 2: Create your team of advisers
Whether you are leaving your current practice or transitioning to a different position, it is extremely important to have the right individuals on your team. You should consider enlisting an attorney, a financial adviser, and an accountant to help facilitate the process. Enlisting lawyers with certain areas of expertise, such as in the areas of employment restrictive covenants, health care, or tax, may also be extremely beneficial and helpful throughout the process.
Step 3: Review your current employment agreement
It is quite likely that at the onset of your current employment arrangement, you signed an employment agreement with your hospital or group. You will want to carefully review this agreement, as it may contain provisions that can affect the steps you should take before you leave your current practice and work elsewhere. These provisions include the following:
a) Noncompetition provisions
It is critical to determine whether or not there are any restrictive covenants in your employment agreement that limit where you can work after you transition from your current practice into a new role. Restrictive covenants include noncompetition and nonsolicitation provisions, and prohibit employees from working at certain places or in certain geographic areas after they leave their current place of employment. Rules surrounding restrictive covenants vary from state to state. If there are restrictive covenants in your agreement, be sure to understand the scope of the covenant, including the geographic and temporal scope, as well as the types of medicine you are prohibited from practicing. If the covenants seem too broad or unnecessarily restrictive, consult with an attorney, as overly broad or unduly burdensome covenants are often unenforceable. However, a state-by-state analysis is required.
b) Notice and termination provisions
It is important to review whether or not there are any notice requirements in your employment agreement, which may require you to notify your employer in advance of a departure. Make sure to comply with the time requirements in the notice provision to avoid a breach of the agreement. It is also critical to determine whether terminating an agreement early will result in any termination penalties. At times, employers will impose a penalty if an employee prematurely terminates a working relationship. Understanding the penalties associated with terminating your agreement will allow you to decide whether you want to cancel the agreement and pay the penalty or push back your timeline until the end of the agreement’s term to avoid termination fees.
Step 4: Licensure obligations
Further, if your practice bills Medicare, you will want to file certain forms with Medicare to show that you are either changing your practice location or leaving medicine. For example, if you are leaving the hospital or group to practice elsewhere, you will need to fill out forms in order for your old group to submit claims and receive payments for Medicare services you provided while you were still part of that group. Furthermore, you will need to file reassignment forms to allow your new practice to bill on your behalf. Understanding which forms to complete can be confusing, so enlisting the help of a healthcare attorney may be worthwhile.
Step 5: Discuss your transition with your insurance representative
Even after you leave your current practice, you may be exposed to litigation for services you provided while you were employed or otherwise retained by such practice. To ensure that you are protected, discuss your insurance policy with your insurance representative. Review whether your insurance policy is “occurrence” or “claims-made.” If you have an occurrence policy, you are protected from covered incidents that occur during the policy period, regardless if your policy is still in existence. Claims-made policies only provide coverage for claims where both the incident and the claim occur during the policy period. For example, if you cancel your policy on March 1, and are sued on April 1 for an incident that allegedly occurred on Feb. 1, your claims-made insurance policy will not protect you. Therefore, it is important to analyze your policies to determine if tail insurance is needed.
There are a number of other issues you will want to address before you leave your practice, including financial responsibilities and medical record and privacy obligations. To ensure that you leave your practice properly, you should contact an experienced lawyer who can help you navigate this process.
Steven M. Harris is a nationally recognized health care attorney and a member of the law firm McDonald Hopkins LLC in Chicago. Write to him at [email protected].
Sneak Peak: The Hospital Leader Blog
FEATURED POST: “A Renewed Call to Overhaul Hospital Observation Care”
In response to concerns about Medicare beneficiary out-of-pocket financial risk, Congress unanimously passed the NOTICE Act, which President Obama signed into law August 5, 2015. This law states that all Medicare beneficiaries hospitalized for 24 hours or more as outpatients under observation must to be notified in writing that they are outpatients “not later than 36 hours after the time such individual begins receiving such services” as well as the associated “implications for cost-sharing.” Last month, the Centers for Medicare & Medicaid Services (CMS) released the final Medicare Outpatient Observation Notice (MOON) that hospitals will start delivering to patients no later than March 8, 2017 to comply with the law. Patients or their representatives must sign the form to acknowledge receipt.
First, Medicare beneficiaries are notified after they have been hospitalized, certainly after they could make an informed decision about accepting observation care. Second, patients or their representative must sign the form, yet it is unclear if this signature holds the patient financially liable, particularly if signed by a representative with no legal authority over the patient’s financial affairs. Third, the form does nothing for a patient’s right to appeal their status. And because observation is a billing distinction, the field at the top of the form requiring hospitals to specify why the patient is not an inpatient is circular reasoning, as patients are outpatients only when they fail to meet Medicare inpatient billing criteria.
Perhaps most importantly, the primary purpose of the NOTICE Act – to inform beneficiaries of the “implications for cost-sharing” when hospitalized under observation – cannot truly be accomplished.
On December 19, 2016, the Department of Health and Human Services Office of Inspector General (OIG) issued the best cost-sharing data available to date describing observation hospital care under the 2-midnight rule. In their report, the OIG used FY 2014 data to compare cost of short outpatient and inpatient stays with similar diagnoses. But because hospitalized outpatients under observation pay a copayment for each individual hospital service, financial risk is not directly correlated with a diagnosis but instead the result of the number, cost, and complexity of services rendered in the hospital, with no limit on the additive amount of per-service deductibles. In contrast, the inpatient deductible is finite per benefit period.
As the OIG report does not provide an accounting of services rendered nor comparison based on equivalent services, it isn’t clear how these cost estimates will help inform discussions when my observation patients receive their MOON.
Dr. Sheehy is a physician and associate professor at the University of Wisconsin School of Medicine and Public Health.
Read the full text of this blog post at http://blogs.hospitalmedicine.org/Blog/a-renewed-call-to-overhaul-hospital-observation-care/
Also on The Hospital Leader…
• New ABIM MOC Two-Year Plan for Internal Medicine Threatens the Focused Practice in Hospital Medicine By Burke Kealey, MD, SFHM
• The Nursing Home Get Out of Jail Card (“We Don’t Want Our Patient Back”). It’s Now Adios. By Brad Flansbaum, DO, MPH, MHM
• The Inmates Are Running the Asylum By Tracy Cardin, ACNP-BC, SFHM
• Do Clinicians Understand Quality Metric Data? By Danielle Scheurer, MD, MSCR, SFHM
• Fake News! Get Your Fake News Here! By Jordan Messler, MD, SFHM
FEATURED POST: “A Renewed Call to Overhaul Hospital Observation Care”
In response to concerns about Medicare beneficiary out-of-pocket financial risk, Congress unanimously passed the NOTICE Act, which President Obama signed into law August 5, 2015. This law states that all Medicare beneficiaries hospitalized for 24 hours or more as outpatients under observation must to be notified in writing that they are outpatients “not later than 36 hours after the time such individual begins receiving such services” as well as the associated “implications for cost-sharing.” Last month, the Centers for Medicare & Medicaid Services (CMS) released the final Medicare Outpatient Observation Notice (MOON) that hospitals will start delivering to patients no later than March 8, 2017 to comply with the law. Patients or their representatives must sign the form to acknowledge receipt.
First, Medicare beneficiaries are notified after they have been hospitalized, certainly after they could make an informed decision about accepting observation care. Second, patients or their representative must sign the form, yet it is unclear if this signature holds the patient financially liable, particularly if signed by a representative with no legal authority over the patient’s financial affairs. Third, the form does nothing for a patient’s right to appeal their status. And because observation is a billing distinction, the field at the top of the form requiring hospitals to specify why the patient is not an inpatient is circular reasoning, as patients are outpatients only when they fail to meet Medicare inpatient billing criteria.
Perhaps most importantly, the primary purpose of the NOTICE Act – to inform beneficiaries of the “implications for cost-sharing” when hospitalized under observation – cannot truly be accomplished.
On December 19, 2016, the Department of Health and Human Services Office of Inspector General (OIG) issued the best cost-sharing data available to date describing observation hospital care under the 2-midnight rule. In their report, the OIG used FY 2014 data to compare cost of short outpatient and inpatient stays with similar diagnoses. But because hospitalized outpatients under observation pay a copayment for each individual hospital service, financial risk is not directly correlated with a diagnosis but instead the result of the number, cost, and complexity of services rendered in the hospital, with no limit on the additive amount of per-service deductibles. In contrast, the inpatient deductible is finite per benefit period.
As the OIG report does not provide an accounting of services rendered nor comparison based on equivalent services, it isn’t clear how these cost estimates will help inform discussions when my observation patients receive their MOON.
Dr. Sheehy is a physician and associate professor at the University of Wisconsin School of Medicine and Public Health.
Read the full text of this blog post at http://blogs.hospitalmedicine.org/Blog/a-renewed-call-to-overhaul-hospital-observation-care/
Also on The Hospital Leader…
• New ABIM MOC Two-Year Plan for Internal Medicine Threatens the Focused Practice in Hospital Medicine By Burke Kealey, MD, SFHM
• The Nursing Home Get Out of Jail Card (“We Don’t Want Our Patient Back”). It’s Now Adios. By Brad Flansbaum, DO, MPH, MHM
• The Inmates Are Running the Asylum By Tracy Cardin, ACNP-BC, SFHM
• Do Clinicians Understand Quality Metric Data? By Danielle Scheurer, MD, MSCR, SFHM
• Fake News! Get Your Fake News Here! By Jordan Messler, MD, SFHM
FEATURED POST: “A Renewed Call to Overhaul Hospital Observation Care”
In response to concerns about Medicare beneficiary out-of-pocket financial risk, Congress unanimously passed the NOTICE Act, which President Obama signed into law August 5, 2015. This law states that all Medicare beneficiaries hospitalized for 24 hours or more as outpatients under observation must to be notified in writing that they are outpatients “not later than 36 hours after the time such individual begins receiving such services” as well as the associated “implications for cost-sharing.” Last month, the Centers for Medicare & Medicaid Services (CMS) released the final Medicare Outpatient Observation Notice (MOON) that hospitals will start delivering to patients no later than March 8, 2017 to comply with the law. Patients or their representatives must sign the form to acknowledge receipt.
First, Medicare beneficiaries are notified after they have been hospitalized, certainly after they could make an informed decision about accepting observation care. Second, patients or their representative must sign the form, yet it is unclear if this signature holds the patient financially liable, particularly if signed by a representative with no legal authority over the patient’s financial affairs. Third, the form does nothing for a patient’s right to appeal their status. And because observation is a billing distinction, the field at the top of the form requiring hospitals to specify why the patient is not an inpatient is circular reasoning, as patients are outpatients only when they fail to meet Medicare inpatient billing criteria.
Perhaps most importantly, the primary purpose of the NOTICE Act – to inform beneficiaries of the “implications for cost-sharing” when hospitalized under observation – cannot truly be accomplished.
On December 19, 2016, the Department of Health and Human Services Office of Inspector General (OIG) issued the best cost-sharing data available to date describing observation hospital care under the 2-midnight rule. In their report, the OIG used FY 2014 data to compare cost of short outpatient and inpatient stays with similar diagnoses. But because hospitalized outpatients under observation pay a copayment for each individual hospital service, financial risk is not directly correlated with a diagnosis but instead the result of the number, cost, and complexity of services rendered in the hospital, with no limit on the additive amount of per-service deductibles. In contrast, the inpatient deductible is finite per benefit period.
As the OIG report does not provide an accounting of services rendered nor comparison based on equivalent services, it isn’t clear how these cost estimates will help inform discussions when my observation patients receive their MOON.
Dr. Sheehy is a physician and associate professor at the University of Wisconsin School of Medicine and Public Health.
Read the full text of this blog post at http://blogs.hospitalmedicine.org/Blog/a-renewed-call-to-overhaul-hospital-observation-care/
Also on The Hospital Leader…
• New ABIM MOC Two-Year Plan for Internal Medicine Threatens the Focused Practice in Hospital Medicine By Burke Kealey, MD, SFHM
• The Nursing Home Get Out of Jail Card (“We Don’t Want Our Patient Back”). It’s Now Adios. By Brad Flansbaum, DO, MPH, MHM
• The Inmates Are Running the Asylum By Tracy Cardin, ACNP-BC, SFHM
• Do Clinicians Understand Quality Metric Data? By Danielle Scheurer, MD, MSCR, SFHM
• Fake News! Get Your Fake News Here! By Jordan Messler, MD, SFHM
What do you call a general medicine hospitalist who focuses on comanaging with a single medical subspecialty?
For more than 2 decades, U.S. health systems have drawn on hospitalists’ expertise to lower length of stay and enhance safety for general medical patients. Many hospital medicine groups have extended this successful practice model across a growing list of services, stretching the role of generalists as far as it can go. While a diverse scope of practice excites some hospitalists, others find career satisfaction with a specific patient population. Some even balk at rotating through all of the possible primary and comanagement services staffed by their group. A growing number of job opportunities have emerged for individuals who are drawn to a specialized patient population but either remain generalist at heart or don’t want to complete a fellowship.
The latest State of Hospital Medicine (SoHM) report provides new insight into this trend, which brings our unique talents to subspecialty populations.
To understand the prevalence of this practice style, the following topic was added to the 2016 SoHM survey: “Some hospital medicine groups include hospitalists who focus their practice exclusively or predominantly in a single medical subspecialty area (e.g., a general internist who exclusively cares for patients on an oncology service in collaboration with oncologists).” Groups were asked to report whether one or more members of their group practiced this way and with which specialty. Although less than a quarter of groups responded to this question, we learned that a substantial portion of respondent groups employ such individuals (see table below).
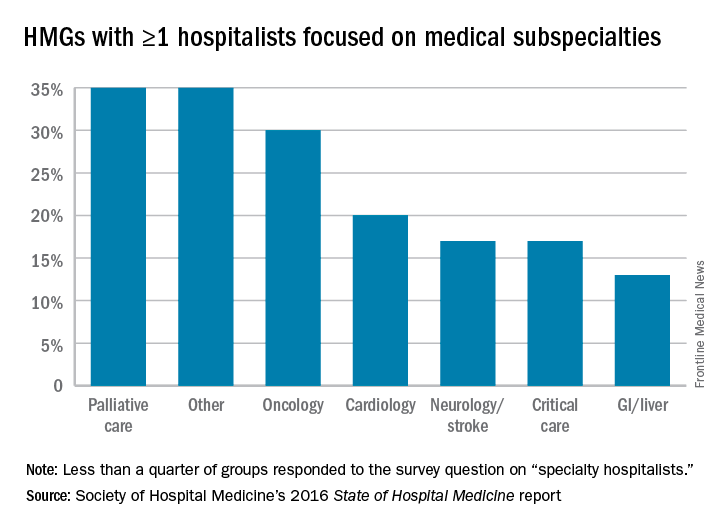
We look forward to tracking this area with subsequent surveys. Already, national meetings are developing for specialty hospitalists (for example, in oncology), and we see opportunities for specialty hospitalists to network through the Society of Hospital Medicine annual meeting and HMX online. My prediction is for growth in the number of groups reporting the employment of specialty hospitalists, but only time will tell. Hospital medicine group leaders should consider both participating in the next SOHM survey and digging into the details of the current report as ways to advance the best practices for developing specialty hospitalist positions.
Dr. White is associate professor of medicine at the University of Washington, Seattle, and a member of SHM’s Practice Analysis Committee.
For more than 2 decades, U.S. health systems have drawn on hospitalists’ expertise to lower length of stay and enhance safety for general medical patients. Many hospital medicine groups have extended this successful practice model across a growing list of services, stretching the role of generalists as far as it can go. While a diverse scope of practice excites some hospitalists, others find career satisfaction with a specific patient population. Some even balk at rotating through all of the possible primary and comanagement services staffed by their group. A growing number of job opportunities have emerged for individuals who are drawn to a specialized patient population but either remain generalist at heart or don’t want to complete a fellowship.
The latest State of Hospital Medicine (SoHM) report provides new insight into this trend, which brings our unique talents to subspecialty populations.
To understand the prevalence of this practice style, the following topic was added to the 2016 SoHM survey: “Some hospital medicine groups include hospitalists who focus their practice exclusively or predominantly in a single medical subspecialty area (e.g., a general internist who exclusively cares for patients on an oncology service in collaboration with oncologists).” Groups were asked to report whether one or more members of their group practiced this way and with which specialty. Although less than a quarter of groups responded to this question, we learned that a substantial portion of respondent groups employ such individuals (see table below).
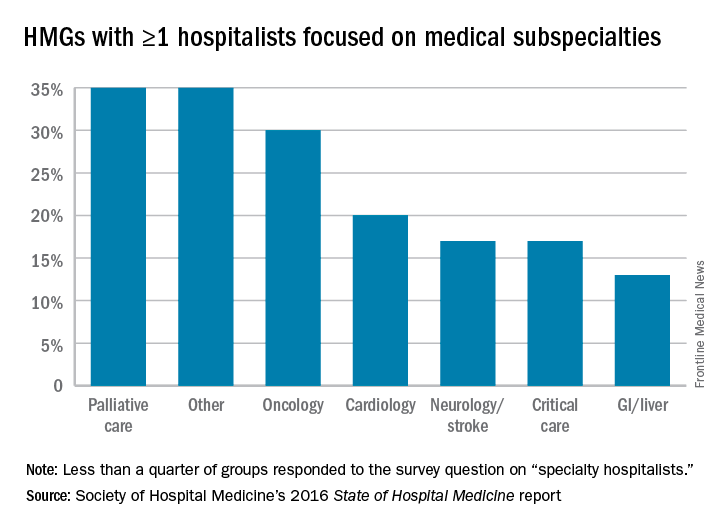
We look forward to tracking this area with subsequent surveys. Already, national meetings are developing for specialty hospitalists (for example, in oncology), and we see opportunities for specialty hospitalists to network through the Society of Hospital Medicine annual meeting and HMX online. My prediction is for growth in the number of groups reporting the employment of specialty hospitalists, but only time will tell. Hospital medicine group leaders should consider both participating in the next SOHM survey and digging into the details of the current report as ways to advance the best practices for developing specialty hospitalist positions.
Dr. White is associate professor of medicine at the University of Washington, Seattle, and a member of SHM’s Practice Analysis Committee.
For more than 2 decades, U.S. health systems have drawn on hospitalists’ expertise to lower length of stay and enhance safety for general medical patients. Many hospital medicine groups have extended this successful practice model across a growing list of services, stretching the role of generalists as far as it can go. While a diverse scope of practice excites some hospitalists, others find career satisfaction with a specific patient population. Some even balk at rotating through all of the possible primary and comanagement services staffed by their group. A growing number of job opportunities have emerged for individuals who are drawn to a specialized patient population but either remain generalist at heart or don’t want to complete a fellowship.
The latest State of Hospital Medicine (SoHM) report provides new insight into this trend, which brings our unique talents to subspecialty populations.
To understand the prevalence of this practice style, the following topic was added to the 2016 SoHM survey: “Some hospital medicine groups include hospitalists who focus their practice exclusively or predominantly in a single medical subspecialty area (e.g., a general internist who exclusively cares for patients on an oncology service in collaboration with oncologists).” Groups were asked to report whether one or more members of their group practiced this way and with which specialty. Although less than a quarter of groups responded to this question, we learned that a substantial portion of respondent groups employ such individuals (see table below).
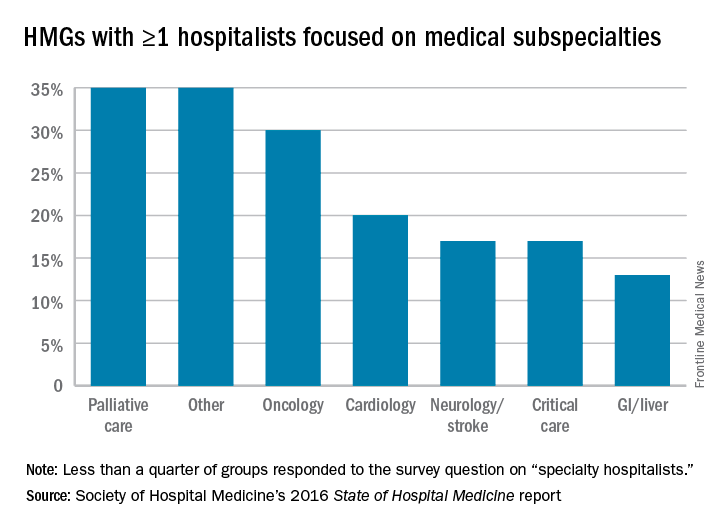
We look forward to tracking this area with subsequent surveys. Already, national meetings are developing for specialty hospitalists (for example, in oncology), and we see opportunities for specialty hospitalists to network through the Society of Hospital Medicine annual meeting and HMX online. My prediction is for growth in the number of groups reporting the employment of specialty hospitalists, but only time will tell. Hospital medicine group leaders should consider both participating in the next SOHM survey and digging into the details of the current report as ways to advance the best practices for developing specialty hospitalist positions.
Dr. White is associate professor of medicine at the University of Washington, Seattle, and a member of SHM’s Practice Analysis Committee.
Disappointment in article on NP, PA roles in HM groups
Editor’s note: The following “Letter to the Editor” was first emailed to the Society of Hospital Medicine, its board president, and John Nelson, MD, MHM, the author of the article, “Hospitalist Roles for NPs and PAs,” which published in the January 2017 issue. All parties agreed to publish the email exchange in The Hospitalist.
Sent: Sunday, February 12, 2017 9:59 AM
Subject: Offensive article on hospitalist roles for NPs, PAs
All,
I have been a hospitalist NP (nurse practitioner) for a decade and found the article in the January issue of The Hospitalist, Volume 21, Number 1, on the Hospitalist Roles for NPs and PAs, offensive and uninformed, with an intolerable amount of personal opinion not backed by research.
I am disappointed that The Hospitalist would publish such a low-class article. Your [magazine] promotes membership to all APPs (advanced practice providers), yet you publish articles that show a study with a positive finding yet allow and highlight an incredibly negative and offensive snippet. The highlighted box states that “Any group that thinks this study is evidence that adding more APPs and having them manage a high number of patients relatively independently will go well in any setting is MISTAKEN ... But it does offer a STORY of one place where, with careful planning and execution, it went OK.”
I can only say that the physicians, APPs, and hospital group who did this study would likely also be offended for taking their study and turning it into a “story.”
EDUCATE yourselves. There are numerous studies out there showing care by APP’s is cost effective, efficient, and with excellent care outcomes. There is a national group, APPex (Advanced Practice Provider Executives), that can give you all the studies you would want showing this information. Or contact the national NP or PA groups.
I am a working hospitalist NP and appreciate my physician colleagues and have their respect. This “John” person obviously doesn’t respect APPs and to publish him is just disheartening.
This publication could have and should have done better. You have one APP on your editorial advisory board – it appears you need more.
Marci Harris, MSN, FNP, ACNP
Acute Care Nurse Practitioner
Hospitalist/Internal Medicine
McKee Medical Center, Loveland, Colo.
Dr. Nelson responds:
Thanks for your message, Marci. It seems clear you’ve thought a lot about NPs and PAs in hospitalist practices and have arrived at conclusions that differ from what I wrote. Your voice and views are welcome.
I certainly didn’t intend to offend anyone, including those who might see all of this very differently from me.
As I mention in the first paragraph, I’m very supportive of NPs and PAs in hospitalist practices. And I wanted to write about this particular study precisely because it provides data that is very supportive of their contributions.
The point I was trying to make in the column is that there is value in careful planning around roles and who does what. A sports team could recruit the most talented players but still won’t perform well if they don’t develop and execute a good plan around who does what and how they work together. Simply having talented people on the team isn’t enough. I think the same is true of hospitalist teams.
The hospitalist group in the study has an impressively detailed plan for new provider (APC and MD alike) orientation and has a lot of operating processes that help ensure the PAs and MDs work effectively together. My experience is that many hospitalists groups have never developed such a plan.
John Nelson, MD, MHM
Partner, Nelson Flores Hospital Medicine Consultants, Bellevue, Wash.
Editor’s note: The following “Letter to the Editor” was first emailed to the Society of Hospital Medicine, its board president, and John Nelson, MD, MHM, the author of the article, “Hospitalist Roles for NPs and PAs,” which published in the January 2017 issue. All parties agreed to publish the email exchange in The Hospitalist.
Sent: Sunday, February 12, 2017 9:59 AM
Subject: Offensive article on hospitalist roles for NPs, PAs
All,
I have been a hospitalist NP (nurse practitioner) for a decade and found the article in the January issue of The Hospitalist, Volume 21, Number 1, on the Hospitalist Roles for NPs and PAs, offensive and uninformed, with an intolerable amount of personal opinion not backed by research.
I am disappointed that The Hospitalist would publish such a low-class article. Your [magazine] promotes membership to all APPs (advanced practice providers), yet you publish articles that show a study with a positive finding yet allow and highlight an incredibly negative and offensive snippet. The highlighted box states that “Any group that thinks this study is evidence that adding more APPs and having them manage a high number of patients relatively independently will go well in any setting is MISTAKEN ... But it does offer a STORY of one place where, with careful planning and execution, it went OK.”
I can only say that the physicians, APPs, and hospital group who did this study would likely also be offended for taking their study and turning it into a “story.”
EDUCATE yourselves. There are numerous studies out there showing care by APP’s is cost effective, efficient, and with excellent care outcomes. There is a national group, APPex (Advanced Practice Provider Executives), that can give you all the studies you would want showing this information. Or contact the national NP or PA groups.
I am a working hospitalist NP and appreciate my physician colleagues and have their respect. This “John” person obviously doesn’t respect APPs and to publish him is just disheartening.
This publication could have and should have done better. You have one APP on your editorial advisory board – it appears you need more.
Marci Harris, MSN, FNP, ACNP
Acute Care Nurse Practitioner
Hospitalist/Internal Medicine
McKee Medical Center, Loveland, Colo.
Dr. Nelson responds:
Thanks for your message, Marci. It seems clear you’ve thought a lot about NPs and PAs in hospitalist practices and have arrived at conclusions that differ from what I wrote. Your voice and views are welcome.
I certainly didn’t intend to offend anyone, including those who might see all of this very differently from me.
As I mention in the first paragraph, I’m very supportive of NPs and PAs in hospitalist practices. And I wanted to write about this particular study precisely because it provides data that is very supportive of their contributions.
The point I was trying to make in the column is that there is value in careful planning around roles and who does what. A sports team could recruit the most talented players but still won’t perform well if they don’t develop and execute a good plan around who does what and how they work together. Simply having talented people on the team isn’t enough. I think the same is true of hospitalist teams.
The hospitalist group in the study has an impressively detailed plan for new provider (APC and MD alike) orientation and has a lot of operating processes that help ensure the PAs and MDs work effectively together. My experience is that many hospitalists groups have never developed such a plan.
John Nelson, MD, MHM
Partner, Nelson Flores Hospital Medicine Consultants, Bellevue, Wash.
Editor’s note: The following “Letter to the Editor” was first emailed to the Society of Hospital Medicine, its board president, and John Nelson, MD, MHM, the author of the article, “Hospitalist Roles for NPs and PAs,” which published in the January 2017 issue. All parties agreed to publish the email exchange in The Hospitalist.
Sent: Sunday, February 12, 2017 9:59 AM
Subject: Offensive article on hospitalist roles for NPs, PAs
All,
I have been a hospitalist NP (nurse practitioner) for a decade and found the article in the January issue of The Hospitalist, Volume 21, Number 1, on the Hospitalist Roles for NPs and PAs, offensive and uninformed, with an intolerable amount of personal opinion not backed by research.
I am disappointed that The Hospitalist would publish such a low-class article. Your [magazine] promotes membership to all APPs (advanced practice providers), yet you publish articles that show a study with a positive finding yet allow and highlight an incredibly negative and offensive snippet. The highlighted box states that “Any group that thinks this study is evidence that adding more APPs and having them manage a high number of patients relatively independently will go well in any setting is MISTAKEN ... But it does offer a STORY of one place where, with careful planning and execution, it went OK.”
I can only say that the physicians, APPs, and hospital group who did this study would likely also be offended for taking their study and turning it into a “story.”
EDUCATE yourselves. There are numerous studies out there showing care by APP’s is cost effective, efficient, and with excellent care outcomes. There is a national group, APPex (Advanced Practice Provider Executives), that can give you all the studies you would want showing this information. Or contact the national NP or PA groups.
I am a working hospitalist NP and appreciate my physician colleagues and have their respect. This “John” person obviously doesn’t respect APPs and to publish him is just disheartening.
This publication could have and should have done better. You have one APP on your editorial advisory board – it appears you need more.
Marci Harris, MSN, FNP, ACNP
Acute Care Nurse Practitioner
Hospitalist/Internal Medicine
McKee Medical Center, Loveland, Colo.
Dr. Nelson responds:
Thanks for your message, Marci. It seems clear you’ve thought a lot about NPs and PAs in hospitalist practices and have arrived at conclusions that differ from what I wrote. Your voice and views are welcome.
I certainly didn’t intend to offend anyone, including those who might see all of this very differently from me.
As I mention in the first paragraph, I’m very supportive of NPs and PAs in hospitalist practices. And I wanted to write about this particular study precisely because it provides data that is very supportive of their contributions.
The point I was trying to make in the column is that there is value in careful planning around roles and who does what. A sports team could recruit the most talented players but still won’t perform well if they don’t develop and execute a good plan around who does what and how they work together. Simply having talented people on the team isn’t enough. I think the same is true of hospitalist teams.
The hospitalist group in the study has an impressively detailed plan for new provider (APC and MD alike) orientation and has a lot of operating processes that help ensure the PAs and MDs work effectively together. My experience is that many hospitalists groups have never developed such a plan.
John Nelson, MD, MHM
Partner, Nelson Flores Hospital Medicine Consultants, Bellevue, Wash.
Trending at the Society of Hospital Medicine
Calling all pediatric hospitalists
Register for Pediatric Hospital Medicine 2017 (PHM17), the premier educational conference for pediatric hospitalists and other clinicians who care for hospitalized children. Re-energize your practice with the latest research, best practices, innovations, and more.
Register before June 7 to receive the early-bird rates. Visit www.peds2017.org for more information.
SHM can prepare you for MACRA
Visit www.macraforhm.org for general information and details in the MACRA FAQ and MIPS Tips links.
Don’t miss five new tracks at HM17
- Learn how to avoid diagnostic and therapeutic overuse, and how to move towards the right care for every hospital medicine patient with the High Value Care Track.
- Don’t miss the Clinical Updates Track, which provides evidence-based updates from recent literature published in medicine subspecialty fields and specific topic areas that all hospitalists need to know.
- Accurate and timely diagnosis are the two cornerstones of high-quality patient care. Find out what topics are in the Diagnostic Reasoning Track.
- Learn from experts during the Health Policy Track who will discuss the most current health care policy issues as they impact hospitalists and what we can expect from a new Presidential administration and changes in Congress.
- The Mini Medical Education Track is for hospitalists who are interested in improving their teaching skills.
Learn more about the HM17 schedule and offerings at www.hospitalmedicine2017.org/schedule.
Prepare for the entire Focused Practice in Hospital Medicine (FPHM) exam with SPARK ONE
This self-paced study guide engages learners through an open-book format, allowing users to review detailed learning objectives and discussion points and define individual areas of strengths and weaknesses. SHM members Save $150! Learn more at www.hospitalmedicine.org/sparkone.
Improve your treatment of VTE during Blood Clot Awareness Month
March is Blood Clot Awareness Month, and SHM recently introduced a new toolkit and guide surrounding treatment of venous thromboembolism (VTE) in the hospital setting. SHM has a history of providing cutting-edge resources in this space, and Steven B. Deitelzweig, MD, MMM, SFHM, FACP, FACC, system chairman of hospital medicine at Oschner Health System in New Orleans, was integral in editing SHM’s VTE treatment mentored implementation guide and online toolkit.
“SHM has an established track record of implementing evidence-based and guideline-driven learnings successfully, and we continue to see improvement across multiple facilities based on this work with this disease,” Dr. Deitelzweig says. “Whenever possible, I would strongly recommend taking full advantage of SHM’s outstanding programs as they are intensely developed by experts for adoption at hospitals of different sizes, including community and academic centers.”
SHM can help you and your hospital improve treatment of VTE as well – learn how at www.hospitalmedicine.org/vtetreatment.
Share patient experience success stories
Our Patient Experience Committee wants to showcase stories of when care teams or their counterparts in the hospital made a notable shift in a patient’s experience: a special moment or interaction; a successful improvement project; an award for excellence in practice; a memo of commendation; a letter from a patient. Email examples of success to Claudia Stahl at [email protected] by May 11. Submissions can include photos, letters, or videos. SHM will share these moments that “made all the difference” with members on its website via other channels soon to be announced.
Brett Radler is SHM’s communications specialist.
Not a member? Know someone who should be? Visit www.joinshm.org to learn about the opportunities we can offer hospital medicine professionals.
Calling all pediatric hospitalists
Register for Pediatric Hospital Medicine 2017 (PHM17), the premier educational conference for pediatric hospitalists and other clinicians who care for hospitalized children. Re-energize your practice with the latest research, best practices, innovations, and more.
Register before June 7 to receive the early-bird rates. Visit www.peds2017.org for more information.
SHM can prepare you for MACRA
Visit www.macraforhm.org for general information and details in the MACRA FAQ and MIPS Tips links.
Don’t miss five new tracks at HM17
- Learn how to avoid diagnostic and therapeutic overuse, and how to move towards the right care for every hospital medicine patient with the High Value Care Track.
- Don’t miss the Clinical Updates Track, which provides evidence-based updates from recent literature published in medicine subspecialty fields and specific topic areas that all hospitalists need to know.
- Accurate and timely diagnosis are the two cornerstones of high-quality patient care. Find out what topics are in the Diagnostic Reasoning Track.
- Learn from experts during the Health Policy Track who will discuss the most current health care policy issues as they impact hospitalists and what we can expect from a new Presidential administration and changes in Congress.
- The Mini Medical Education Track is for hospitalists who are interested in improving their teaching skills.
Learn more about the HM17 schedule and offerings at www.hospitalmedicine2017.org/schedule.
Prepare for the entire Focused Practice in Hospital Medicine (FPHM) exam with SPARK ONE
This self-paced study guide engages learners through an open-book format, allowing users to review detailed learning objectives and discussion points and define individual areas of strengths and weaknesses. SHM members Save $150! Learn more at www.hospitalmedicine.org/sparkone.
Improve your treatment of VTE during Blood Clot Awareness Month
March is Blood Clot Awareness Month, and SHM recently introduced a new toolkit and guide surrounding treatment of venous thromboembolism (VTE) in the hospital setting. SHM has a history of providing cutting-edge resources in this space, and Steven B. Deitelzweig, MD, MMM, SFHM, FACP, FACC, system chairman of hospital medicine at Oschner Health System in New Orleans, was integral in editing SHM’s VTE treatment mentored implementation guide and online toolkit.
“SHM has an established track record of implementing evidence-based and guideline-driven learnings successfully, and we continue to see improvement across multiple facilities based on this work with this disease,” Dr. Deitelzweig says. “Whenever possible, I would strongly recommend taking full advantage of SHM’s outstanding programs as they are intensely developed by experts for adoption at hospitals of different sizes, including community and academic centers.”
SHM can help you and your hospital improve treatment of VTE as well – learn how at www.hospitalmedicine.org/vtetreatment.
Share patient experience success stories
Our Patient Experience Committee wants to showcase stories of when care teams or their counterparts in the hospital made a notable shift in a patient’s experience: a special moment or interaction; a successful improvement project; an award for excellence in practice; a memo of commendation; a letter from a patient. Email examples of success to Claudia Stahl at [email protected] by May 11. Submissions can include photos, letters, or videos. SHM will share these moments that “made all the difference” with members on its website via other channels soon to be announced.
Brett Radler is SHM’s communications specialist.
Not a member? Know someone who should be? Visit www.joinshm.org to learn about the opportunities we can offer hospital medicine professionals.
Calling all pediatric hospitalists
Register for Pediatric Hospital Medicine 2017 (PHM17), the premier educational conference for pediatric hospitalists and other clinicians who care for hospitalized children. Re-energize your practice with the latest research, best practices, innovations, and more.
Register before June 7 to receive the early-bird rates. Visit www.peds2017.org for more information.
SHM can prepare you for MACRA
Visit www.macraforhm.org for general information and details in the MACRA FAQ and MIPS Tips links.
Don’t miss five new tracks at HM17
- Learn how to avoid diagnostic and therapeutic overuse, and how to move towards the right care for every hospital medicine patient with the High Value Care Track.
- Don’t miss the Clinical Updates Track, which provides evidence-based updates from recent literature published in medicine subspecialty fields and specific topic areas that all hospitalists need to know.
- Accurate and timely diagnosis are the two cornerstones of high-quality patient care. Find out what topics are in the Diagnostic Reasoning Track.
- Learn from experts during the Health Policy Track who will discuss the most current health care policy issues as they impact hospitalists and what we can expect from a new Presidential administration and changes in Congress.
- The Mini Medical Education Track is for hospitalists who are interested in improving their teaching skills.
Learn more about the HM17 schedule and offerings at www.hospitalmedicine2017.org/schedule.
Prepare for the entire Focused Practice in Hospital Medicine (FPHM) exam with SPARK ONE
This self-paced study guide engages learners through an open-book format, allowing users to review detailed learning objectives and discussion points and define individual areas of strengths and weaknesses. SHM members Save $150! Learn more at www.hospitalmedicine.org/sparkone.
Improve your treatment of VTE during Blood Clot Awareness Month
March is Blood Clot Awareness Month, and SHM recently introduced a new toolkit and guide surrounding treatment of venous thromboembolism (VTE) in the hospital setting. SHM has a history of providing cutting-edge resources in this space, and Steven B. Deitelzweig, MD, MMM, SFHM, FACP, FACC, system chairman of hospital medicine at Oschner Health System in New Orleans, was integral in editing SHM’s VTE treatment mentored implementation guide and online toolkit.
“SHM has an established track record of implementing evidence-based and guideline-driven learnings successfully, and we continue to see improvement across multiple facilities based on this work with this disease,” Dr. Deitelzweig says. “Whenever possible, I would strongly recommend taking full advantage of SHM’s outstanding programs as they are intensely developed by experts for adoption at hospitals of different sizes, including community and academic centers.”
SHM can help you and your hospital improve treatment of VTE as well – learn how at www.hospitalmedicine.org/vtetreatment.
Share patient experience success stories
Our Patient Experience Committee wants to showcase stories of when care teams or their counterparts in the hospital made a notable shift in a patient’s experience: a special moment or interaction; a successful improvement project; an award for excellence in practice; a memo of commendation; a letter from a patient. Email examples of success to Claudia Stahl at [email protected] by May 11. Submissions can include photos, letters, or videos. SHM will share these moments that “made all the difference” with members on its website via other channels soon to be announced.
Brett Radler is SHM’s communications specialist.
Not a member? Know someone who should be? Visit www.joinshm.org to learn about the opportunities we can offer hospital medicine professionals.
Are you getting the most out of your EHR?
Sparrow Health System in Lansing, Mich., went live with its electronic health record (EHR) system at its main hospital on Dec. 1, 2012. For a year and a half, the system was untapped, innovation-wise. Very few features were turned on, and it sat relatively idle with regard to quality improvement. Hospitalists and others used the EHR, but not ambitiously. Everyone, essentially, used the post-launch period to catch their breath. Some even decided it would be the perfect time to retire, rather than confront the new reality of the EHR.
“It took a good 6 months, probably longer for some, for people to feel comfortable, to start smiling again and really feel like, ‘This isn’t so bad and actually might be working for us,’ ” said Carol Nwelue, MD, medical director of Sparrow’s adult hospitalist service.
Although Sparrow is now probably ahead of the curve when it comes to maximizing its EHR use, its story carries themes that are familiar to hospitalists and to the medical field: The beginning is scary and bumpy; there typically is a long getting-used-to period; and then some hospitalists get ansty and try to get more out of the system, but only gradually – and not without pain.
The bottom line is that most hospitals have a long way to go, said Venkataraman Palabindala, MD, a hospitalist and assistant professor of medicine at the University of Mississippi Medical Center in Jackson.
“We are nowhere close to using the technology to maximum benefit,” said Dr. Palabindala, also a member of the Society of Hospital Medicine’s information technology committee.
How well hospitalists are maximizing their use of EHRs varies from center to center and doctor to doctor. But, for those that are more advanced, Dr. Palabindala and other advocates of better EHR use mention these characteristics that drive the change:
- They have hospitalist leaders with a strong interest in IT who like to tinker and refine – and then share the tricks that work with others at their center.
- They belong to EHR-related committees or work at centers with hospitalists with a big presence in those committees.
- They keep their eyes on what other centers are doing with EHRs and use those projects as models for projects at their own centers.
- They are willing to make changes in their own processes, when feasible, so that they can better dovetail with the EHR.
- They keep their lines of communication open with their EHR vendors.
- They attend user meetings to get questions answered and share information and experiences.
At Sparrow, two committees – one nurse-led and one physician-led – guide EHR enhancement. The committees are a place where, yes, doctors can vent about the EHR (the phrase they use is “pain points”), but also a place where they can get constructive feedback. The committees also keep an eye out for EHR projects elsewhere that they might be able to do themselves.
EHR: a CAUTI example
In 2014, Sparrow doctors and nurses wanted to lower their number of catheter-associated urinary tract infections (CAUTI). With the EHR that had gone live 2 years before, they had the data that they needed. They just had to figure out how to turn the data into a workable plan. Ah, if only things were so simple with EHRs. As any health center that has gone through the great transition from paper to digital can attest, having the data only puts you at the foot of the mountain.
But using a program that Texas Health System had developed as a model, Sparrow got its CAUTI program up and running. The new system included not just a placement order, but the discontinuation order, too. Advisories on best practice were built into the work flow, including alerts on when catheters had been in for 48 hours, and metrics were created to track how well the whole thing worked.
“Once the data [were] obtained and validated, it was quickly shown that more needed to be done within this clinical program to impact our CAUTI numbers,” she said. “With collaboration from end users, the system was tweaked more and BPAs (best practice advisories) were added and removed in certain areas and shifted the focus from physician-facing to nursing-facing in most areas.”
It appears to be working: CAUTI incidence at 836-bed Sparrow Hospital has dropped from a total of 52 in 2014 to 11 over the first 3 quarters of 2016.
Sparrow has also built programs to better use its EHR for sepsis, medical reconciliation, and methicillin-resistant Staphylococcus aureus screening, and one is being developed for heart failure.
Vendor engagement = QI opportunity
Sparrow and many other health systems are motivated to use more of Epic’s features and to innovate through an Epic rewards program that gives rebates for advanced use that can total hundreds of thousands of dollars. That innovation helps Epic problem solve and it can then point to that innovation in its marketing.
Almost all hospitals, and their hospitalists, are using the EHR for such basics as reducing unnecessary testing, medical reconciliation, and to document more accurately, said Eric Helsher, vice president of client success at Epic, whose job is to foster the spread of new and better ways to use the EHR. Most hospitals use the EHR, to at least some degree, for targeted quality improvement (QI) and patient safety programs, he said.
Dr. Palabindala pointed to record-sharing features as a way clinicians can share records within minutes without having to bother with faxing or emailing. Integrating smart-paging into the EHR is another way for doctors to communicate – it may not be as good as a phone call, but it’s less disruptive during a workday, he notes.
Epic is just now rolling out a secure text-messaging system hospitalists and others can use to communicate with one another – the header of the text thread clearly shows the patient it is referencing, Mr. Helsher said. Other EHR uses, such as telemedicine, are being used around the country but are far less widespread. But users are generally becoming more ambitious, he said.
“For the last 5-10 years, we’ve been in such an implementation rush,” Mr. Helsher explained. “ Now, at much more of a macro scale, the mentality has changed to ‘OK, we have these systems, let’s go from the implementation era to the value era.’ ”
Corinne Boudreau, senior marketing manager of physician experience at Meditech, said their sepsis tool has been very popular, while messaging features and shortcut commands for simpler charting are gradually coming into wider use. Meditech also expects their Web-based EHR – designed to give patients access on their mobile devices – will give doctors the mobility they want.
Still, there’s a wide range in how much hospitalists and other doctors are using even the fundamental tools that are available to them.
“I think that between implementation and maximization there is a period of adoption, and I think that that’s where a lot of folks are these days,” she said.
As “physician engagement” has become a buzzword in the industry, Meditech has worked with physician leaders on how to get doctors to absorb the message that the EHR really can help them do their jobs better.
“If you get [doctors] at the right time, you show them how it can make things easier or take time off their workload,” Ms. Boudreau said. “For some physicians that time to get them might be first thing in the morning before they see patients. Another physician might want to do it in the evening. If you hit that evening physician in the morning, you’ve missed that window of opportunity.”
Given the demands on doctors’ time and either an inability or unwillingness to put the time in that’s needed to learn about all functions the EHR can offer, there’s a growing acknowledgment that doctors often can’t simply do this on their own.
“There’s more recognition that this is a project that needs to be resourced,” Ms. Boudreau said. “They’re already strapped for time; to put something additional on top of it needs to be accommodated for. It needs to be resourced in terms of time, it needs to be resourced in terms of compensation. There need to be governance and support of that.”
Early adopters vs. late bloomers
Many hospitalists and HM groups have advanced, but some places have lagged behind, said John Nelson, MD, MHM, a veteran hospitalist, practice management consultant, and longtime columnist with The Hospitalist.
“We find it’s reasonably common to go to a place where they’re still keeping their census in an Excel spreadsheet,” he said. “Last year, we found people who do billing on paper and index cards.”
He said that often, a failure to adopt new EHR functionality isn’t because hospitals and HM groups are avoiding it. He said he sees IT shortcomings as a major blocker.
“They want to use it,” he said. “Inertia might be part of the reason people are failing to fully capture the benefit the EHR could offer, [but] the bigger reason is local IT configurations and support.”
As an example, Dr. Nelson explained that at some of the centers he has worked with the name of the attending physician is not always reflected in the EHR. That’s a big no-no, he said. The problem, he’s sometimes found, isn’t really the EHR, but quirks in the hospital system: The EHR is locked down for that information and can be changed only by a person in the admitting department.
“It would require the hospitalist to call down [to admissions] and get someone else to make that change – and that’s tedious a big headache. They give up and don’t do it anymore,” he said. “Ideally, you’d want to make it so the hospitalists can make the change themselves.”
At his center, Overlake Hospital Medical Center in Bellevue, Wash., a go-to hospitalist is David Chu, MD, who has gone through Epic training and shares tips with colleagues. He is one of a relatively few physicians there who has taken the time to use the drop-down menu feature for putting information into a chart.
That might sound like a fairly basic use for a multimillion-dollar EHR system. But it still can take hours and hours to get it right.
“The way to do it is a little bit of a programmer’s way of looking at things,” Dr. Chu said, noting it involves programming-style language with double colons, commas, and quotations marks.
“For me, I think it took a good 10, 12, 15 hours on my part to get things going,” he said. “It was a good time investment up front to help me on that end, but it’s just hard getting people to want to commit that time, especially if they’re not that savvy with computers.”
His hospitalist colleague, Ryan Chew, MD, is more advanced – he has a taxonomy-like shorthand he uses to give him the right set of basic fields for a given type of case. For someone admitted with pneumonia, he’d want to know certain things all the time. Were they short of breath? Did they have chest pain? What were their vital signs? What about inflammatory markers?
Dr. Chew can get all of those fields to pop up by typing “.rchppneumonia.” The “.” means that a special code is to follow. The “rc” is for Ryan Chew, the “hp” is for history and physical, and “pneumonia,” is the type of case. For cases that require other information to be entered, he can add that as needed.
Hospitalists might try to write shortcut phrases, but unless they have a well-defined system, it won’t be helpful over the long run, he said.
“If you don’t have a good organization system … you’ll never remember it,” Dr. Chew said.
But even he hasn’t created the drop-down menus. He said he just hasn’t been willing to take the time, especially since he feels his own way of doing things seems to be working just fine.
Effort is essential
Expanding the functionalities of the EHR takes effort, no doubt. As a result, some physicians and hospitalist groups have not been open-minded to the idea – and opportunities – of the EHR as a database.
“I think for some people, even still, working with the EHR, it’s become more something they’ve learned to get used to rather than something that they sought to take advantage of, in terms of helping things,” Dr. Chew said. “They’re still working against the EHR a little bit.”
Dr. Palabindala agreed, and said that regardless of resistance or complaint, EHRs work.
“No matter how much we argue, it is proven in multiple studies that EHRs showed increased patient safety and better documentation and better transfer of the data,” he said.
He suggests hospitalists make more of an effort.
“I strongly encourage hospitalists to be part of the every EHR-related committee, including CPOE [computerized physician order entry], analytics, and utilization-review committees,” he said. “Learning about the upgrades and learning about all the possible options, exploring clinical informatics on a regular basis is important. I also encourage [hospitalists] to participate in online, EHR-related surveys to learn more about the EHR utility and what is missing in their home institution.”
He acknowledges that it’s “hard to develop a passion.” Then he put it in terms he thought might resonate: “Think of it like a new version of smart phone. Show the enthusiasm as if you are ready for next version of iPhone or Pixel.” TH
Is hospitalists’ EHR efficiency taken advantage of?
Even though their level of EHR use can be hit or miss, hospitalists tend to be ahead of the game, many agree. But that can come with some drawbacks. They’re often the go-to people everyone else in the hospital relies on to handle the system that some think is too unwieldy to bother with.
“One thing that really distinguishes hospitalists from many other providers, particularly on the inpatient side, is just the frequency with which they use the EHR,” said Eric Helsher of Epic. Many hospitalists are chosen by administrators to test pilot projects for that reason, he adds. “They want to get it out there with a group who they know will have a lot of exposure to the system and may be more willing to make those changes for long-term gain.”
Sometimes that expertise leads to situations that go beyond the hospitalist simply being leaders of change – they’re doing work they were never really intended to do.
John Nelson, MD, MHM, a hospitalist consultant based in Seattle, said hospitalists tell him that a subspecialist might handle a case but will not want to be the attending physician specifically so they don’t have to deal with the EHR. He said the specialist in such cases will say something along the lines of, “You can call me, I’ll help you, and I’ll come by and say hello to the patient and make the care decisions, but I need you to be the attending so you can document in the chart and you can do the med rec because ‘I can’t figure out how to do those buttons right.’ ”
Some will ask hospitalists “for a hand” with a case when really all they want is for the hospitalist to enter information into the system. It’s a tricky situation for the hospitalist, Dr. Nelson said.
“Some will be transparent and say I don’t really have a medical question – I just can’t figure out how to do the med rec and the discharge, so would you do it?” he said, adding the systems issues are largely because of new rounding patterns sparked by HM’s expanding role in-hospital. “I think it meaningfully contributes to what I perceive to be a decline in hospitalist morale in the last 2 or 3 years.”
Tom Collins is a freelance writer in South Florida.
Sparrow Health System in Lansing, Mich., went live with its electronic health record (EHR) system at its main hospital on Dec. 1, 2012. For a year and a half, the system was untapped, innovation-wise. Very few features were turned on, and it sat relatively idle with regard to quality improvement. Hospitalists and others used the EHR, but not ambitiously. Everyone, essentially, used the post-launch period to catch their breath. Some even decided it would be the perfect time to retire, rather than confront the new reality of the EHR.
“It took a good 6 months, probably longer for some, for people to feel comfortable, to start smiling again and really feel like, ‘This isn’t so bad and actually might be working for us,’ ” said Carol Nwelue, MD, medical director of Sparrow’s adult hospitalist service.
Although Sparrow is now probably ahead of the curve when it comes to maximizing its EHR use, its story carries themes that are familiar to hospitalists and to the medical field: The beginning is scary and bumpy; there typically is a long getting-used-to period; and then some hospitalists get ansty and try to get more out of the system, but only gradually – and not without pain.
The bottom line is that most hospitals have a long way to go, said Venkataraman Palabindala, MD, a hospitalist and assistant professor of medicine at the University of Mississippi Medical Center in Jackson.
“We are nowhere close to using the technology to maximum benefit,” said Dr. Palabindala, also a member of the Society of Hospital Medicine’s information technology committee.
How well hospitalists are maximizing their use of EHRs varies from center to center and doctor to doctor. But, for those that are more advanced, Dr. Palabindala and other advocates of better EHR use mention these characteristics that drive the change:
- They have hospitalist leaders with a strong interest in IT who like to tinker and refine – and then share the tricks that work with others at their center.
- They belong to EHR-related committees or work at centers with hospitalists with a big presence in those committees.
- They keep their eyes on what other centers are doing with EHRs and use those projects as models for projects at their own centers.
- They are willing to make changes in their own processes, when feasible, so that they can better dovetail with the EHR.
- They keep their lines of communication open with their EHR vendors.
- They attend user meetings to get questions answered and share information and experiences.
At Sparrow, two committees – one nurse-led and one physician-led – guide EHR enhancement. The committees are a place where, yes, doctors can vent about the EHR (the phrase they use is “pain points”), but also a place where they can get constructive feedback. The committees also keep an eye out for EHR projects elsewhere that they might be able to do themselves.
EHR: a CAUTI example
In 2014, Sparrow doctors and nurses wanted to lower their number of catheter-associated urinary tract infections (CAUTI). With the EHR that had gone live 2 years before, they had the data that they needed. They just had to figure out how to turn the data into a workable plan. Ah, if only things were so simple with EHRs. As any health center that has gone through the great transition from paper to digital can attest, having the data only puts you at the foot of the mountain.
But using a program that Texas Health System had developed as a model, Sparrow got its CAUTI program up and running. The new system included not just a placement order, but the discontinuation order, too. Advisories on best practice were built into the work flow, including alerts on when catheters had been in for 48 hours, and metrics were created to track how well the whole thing worked.
“Once the data [were] obtained and validated, it was quickly shown that more needed to be done within this clinical program to impact our CAUTI numbers,” she said. “With collaboration from end users, the system was tweaked more and BPAs (best practice advisories) were added and removed in certain areas and shifted the focus from physician-facing to nursing-facing in most areas.”
It appears to be working: CAUTI incidence at 836-bed Sparrow Hospital has dropped from a total of 52 in 2014 to 11 over the first 3 quarters of 2016.
Sparrow has also built programs to better use its EHR for sepsis, medical reconciliation, and methicillin-resistant Staphylococcus aureus screening, and one is being developed for heart failure.
Vendor engagement = QI opportunity
Sparrow and many other health systems are motivated to use more of Epic’s features and to innovate through an Epic rewards program that gives rebates for advanced use that can total hundreds of thousands of dollars. That innovation helps Epic problem solve and it can then point to that innovation in its marketing.
Almost all hospitals, and their hospitalists, are using the EHR for such basics as reducing unnecessary testing, medical reconciliation, and to document more accurately, said Eric Helsher, vice president of client success at Epic, whose job is to foster the spread of new and better ways to use the EHR. Most hospitals use the EHR, to at least some degree, for targeted quality improvement (QI) and patient safety programs, he said.
Dr. Palabindala pointed to record-sharing features as a way clinicians can share records within minutes without having to bother with faxing or emailing. Integrating smart-paging into the EHR is another way for doctors to communicate – it may not be as good as a phone call, but it’s less disruptive during a workday, he notes.
Epic is just now rolling out a secure text-messaging system hospitalists and others can use to communicate with one another – the header of the text thread clearly shows the patient it is referencing, Mr. Helsher said. Other EHR uses, such as telemedicine, are being used around the country but are far less widespread. But users are generally becoming more ambitious, he said.
“For the last 5-10 years, we’ve been in such an implementation rush,” Mr. Helsher explained. “ Now, at much more of a macro scale, the mentality has changed to ‘OK, we have these systems, let’s go from the implementation era to the value era.’ ”
Corinne Boudreau, senior marketing manager of physician experience at Meditech, said their sepsis tool has been very popular, while messaging features and shortcut commands for simpler charting are gradually coming into wider use. Meditech also expects their Web-based EHR – designed to give patients access on their mobile devices – will give doctors the mobility they want.
Still, there’s a wide range in how much hospitalists and other doctors are using even the fundamental tools that are available to them.
“I think that between implementation and maximization there is a period of adoption, and I think that that’s where a lot of folks are these days,” she said.
As “physician engagement” has become a buzzword in the industry, Meditech has worked with physician leaders on how to get doctors to absorb the message that the EHR really can help them do their jobs better.
“If you get [doctors] at the right time, you show them how it can make things easier or take time off their workload,” Ms. Boudreau said. “For some physicians that time to get them might be first thing in the morning before they see patients. Another physician might want to do it in the evening. If you hit that evening physician in the morning, you’ve missed that window of opportunity.”
Given the demands on doctors’ time and either an inability or unwillingness to put the time in that’s needed to learn about all functions the EHR can offer, there’s a growing acknowledgment that doctors often can’t simply do this on their own.
“There’s more recognition that this is a project that needs to be resourced,” Ms. Boudreau said. “They’re already strapped for time; to put something additional on top of it needs to be accommodated for. It needs to be resourced in terms of time, it needs to be resourced in terms of compensation. There need to be governance and support of that.”
Early adopters vs. late bloomers
Many hospitalists and HM groups have advanced, but some places have lagged behind, said John Nelson, MD, MHM, a veteran hospitalist, practice management consultant, and longtime columnist with The Hospitalist.
“We find it’s reasonably common to go to a place where they’re still keeping their census in an Excel spreadsheet,” he said. “Last year, we found people who do billing on paper and index cards.”
He said that often, a failure to adopt new EHR functionality isn’t because hospitals and HM groups are avoiding it. He said he sees IT shortcomings as a major blocker.
“They want to use it,” he said. “Inertia might be part of the reason people are failing to fully capture the benefit the EHR could offer, [but] the bigger reason is local IT configurations and support.”
As an example, Dr. Nelson explained that at some of the centers he has worked with the name of the attending physician is not always reflected in the EHR. That’s a big no-no, he said. The problem, he’s sometimes found, isn’t really the EHR, but quirks in the hospital system: The EHR is locked down for that information and can be changed only by a person in the admitting department.
“It would require the hospitalist to call down [to admissions] and get someone else to make that change – and that’s tedious a big headache. They give up and don’t do it anymore,” he said. “Ideally, you’d want to make it so the hospitalists can make the change themselves.”
At his center, Overlake Hospital Medical Center in Bellevue, Wash., a go-to hospitalist is David Chu, MD, who has gone through Epic training and shares tips with colleagues. He is one of a relatively few physicians there who has taken the time to use the drop-down menu feature for putting information into a chart.
That might sound like a fairly basic use for a multimillion-dollar EHR system. But it still can take hours and hours to get it right.
“The way to do it is a little bit of a programmer’s way of looking at things,” Dr. Chu said, noting it involves programming-style language with double colons, commas, and quotations marks.
“For me, I think it took a good 10, 12, 15 hours on my part to get things going,” he said. “It was a good time investment up front to help me on that end, but it’s just hard getting people to want to commit that time, especially if they’re not that savvy with computers.”
His hospitalist colleague, Ryan Chew, MD, is more advanced – he has a taxonomy-like shorthand he uses to give him the right set of basic fields for a given type of case. For someone admitted with pneumonia, he’d want to know certain things all the time. Were they short of breath? Did they have chest pain? What were their vital signs? What about inflammatory markers?
Dr. Chew can get all of those fields to pop up by typing “.rchppneumonia.” The “.” means that a special code is to follow. The “rc” is for Ryan Chew, the “hp” is for history and physical, and “pneumonia,” is the type of case. For cases that require other information to be entered, he can add that as needed.
Hospitalists might try to write shortcut phrases, but unless they have a well-defined system, it won’t be helpful over the long run, he said.
“If you don’t have a good organization system … you’ll never remember it,” Dr. Chew said.
But even he hasn’t created the drop-down menus. He said he just hasn’t been willing to take the time, especially since he feels his own way of doing things seems to be working just fine.
Effort is essential
Expanding the functionalities of the EHR takes effort, no doubt. As a result, some physicians and hospitalist groups have not been open-minded to the idea – and opportunities – of the EHR as a database.
“I think for some people, even still, working with the EHR, it’s become more something they’ve learned to get used to rather than something that they sought to take advantage of, in terms of helping things,” Dr. Chew said. “They’re still working against the EHR a little bit.”
Dr. Palabindala agreed, and said that regardless of resistance or complaint, EHRs work.
“No matter how much we argue, it is proven in multiple studies that EHRs showed increased patient safety and better documentation and better transfer of the data,” he said.
He suggests hospitalists make more of an effort.
“I strongly encourage hospitalists to be part of the every EHR-related committee, including CPOE [computerized physician order entry], analytics, and utilization-review committees,” he said. “Learning about the upgrades and learning about all the possible options, exploring clinical informatics on a regular basis is important. I also encourage [hospitalists] to participate in online, EHR-related surveys to learn more about the EHR utility and what is missing in their home institution.”
He acknowledges that it’s “hard to develop a passion.” Then he put it in terms he thought might resonate: “Think of it like a new version of smart phone. Show the enthusiasm as if you are ready for next version of iPhone or Pixel.” TH
Is hospitalists’ EHR efficiency taken advantage of?
Even though their level of EHR use can be hit or miss, hospitalists tend to be ahead of the game, many agree. But that can come with some drawbacks. They’re often the go-to people everyone else in the hospital relies on to handle the system that some think is too unwieldy to bother with.
“One thing that really distinguishes hospitalists from many other providers, particularly on the inpatient side, is just the frequency with which they use the EHR,” said Eric Helsher of Epic. Many hospitalists are chosen by administrators to test pilot projects for that reason, he adds. “They want to get it out there with a group who they know will have a lot of exposure to the system and may be more willing to make those changes for long-term gain.”
Sometimes that expertise leads to situations that go beyond the hospitalist simply being leaders of change – they’re doing work they were never really intended to do.
John Nelson, MD, MHM, a hospitalist consultant based in Seattle, said hospitalists tell him that a subspecialist might handle a case but will not want to be the attending physician specifically so they don’t have to deal with the EHR. He said the specialist in such cases will say something along the lines of, “You can call me, I’ll help you, and I’ll come by and say hello to the patient and make the care decisions, but I need you to be the attending so you can document in the chart and you can do the med rec because ‘I can’t figure out how to do those buttons right.’ ”
Some will ask hospitalists “for a hand” with a case when really all they want is for the hospitalist to enter information into the system. It’s a tricky situation for the hospitalist, Dr. Nelson said.
“Some will be transparent and say I don’t really have a medical question – I just can’t figure out how to do the med rec and the discharge, so would you do it?” he said, adding the systems issues are largely because of new rounding patterns sparked by HM’s expanding role in-hospital. “I think it meaningfully contributes to what I perceive to be a decline in hospitalist morale in the last 2 or 3 years.”
Tom Collins is a freelance writer in South Florida.
Sparrow Health System in Lansing, Mich., went live with its electronic health record (EHR) system at its main hospital on Dec. 1, 2012. For a year and a half, the system was untapped, innovation-wise. Very few features were turned on, and it sat relatively idle with regard to quality improvement. Hospitalists and others used the EHR, but not ambitiously. Everyone, essentially, used the post-launch period to catch their breath. Some even decided it would be the perfect time to retire, rather than confront the new reality of the EHR.
“It took a good 6 months, probably longer for some, for people to feel comfortable, to start smiling again and really feel like, ‘This isn’t so bad and actually might be working for us,’ ” said Carol Nwelue, MD, medical director of Sparrow’s adult hospitalist service.
Although Sparrow is now probably ahead of the curve when it comes to maximizing its EHR use, its story carries themes that are familiar to hospitalists and to the medical field: The beginning is scary and bumpy; there typically is a long getting-used-to period; and then some hospitalists get ansty and try to get more out of the system, but only gradually – and not without pain.
The bottom line is that most hospitals have a long way to go, said Venkataraman Palabindala, MD, a hospitalist and assistant professor of medicine at the University of Mississippi Medical Center in Jackson.
“We are nowhere close to using the technology to maximum benefit,” said Dr. Palabindala, also a member of the Society of Hospital Medicine’s information technology committee.
How well hospitalists are maximizing their use of EHRs varies from center to center and doctor to doctor. But, for those that are more advanced, Dr. Palabindala and other advocates of better EHR use mention these characteristics that drive the change:
- They have hospitalist leaders with a strong interest in IT who like to tinker and refine – and then share the tricks that work with others at their center.
- They belong to EHR-related committees or work at centers with hospitalists with a big presence in those committees.
- They keep their eyes on what other centers are doing with EHRs and use those projects as models for projects at their own centers.
- They are willing to make changes in their own processes, when feasible, so that they can better dovetail with the EHR.
- They keep their lines of communication open with their EHR vendors.
- They attend user meetings to get questions answered and share information and experiences.
At Sparrow, two committees – one nurse-led and one physician-led – guide EHR enhancement. The committees are a place where, yes, doctors can vent about the EHR (the phrase they use is “pain points”), but also a place where they can get constructive feedback. The committees also keep an eye out for EHR projects elsewhere that they might be able to do themselves.
EHR: a CAUTI example
In 2014, Sparrow doctors and nurses wanted to lower their number of catheter-associated urinary tract infections (CAUTI). With the EHR that had gone live 2 years before, they had the data that they needed. They just had to figure out how to turn the data into a workable plan. Ah, if only things were so simple with EHRs. As any health center that has gone through the great transition from paper to digital can attest, having the data only puts you at the foot of the mountain.
But using a program that Texas Health System had developed as a model, Sparrow got its CAUTI program up and running. The new system included not just a placement order, but the discontinuation order, too. Advisories on best practice were built into the work flow, including alerts on when catheters had been in for 48 hours, and metrics were created to track how well the whole thing worked.
“Once the data [were] obtained and validated, it was quickly shown that more needed to be done within this clinical program to impact our CAUTI numbers,” she said. “With collaboration from end users, the system was tweaked more and BPAs (best practice advisories) were added and removed in certain areas and shifted the focus from physician-facing to nursing-facing in most areas.”
It appears to be working: CAUTI incidence at 836-bed Sparrow Hospital has dropped from a total of 52 in 2014 to 11 over the first 3 quarters of 2016.
Sparrow has also built programs to better use its EHR for sepsis, medical reconciliation, and methicillin-resistant Staphylococcus aureus screening, and one is being developed for heart failure.
Vendor engagement = QI opportunity
Sparrow and many other health systems are motivated to use more of Epic’s features and to innovate through an Epic rewards program that gives rebates for advanced use that can total hundreds of thousands of dollars. That innovation helps Epic problem solve and it can then point to that innovation in its marketing.
Almost all hospitals, and their hospitalists, are using the EHR for such basics as reducing unnecessary testing, medical reconciliation, and to document more accurately, said Eric Helsher, vice president of client success at Epic, whose job is to foster the spread of new and better ways to use the EHR. Most hospitals use the EHR, to at least some degree, for targeted quality improvement (QI) and patient safety programs, he said.
Dr. Palabindala pointed to record-sharing features as a way clinicians can share records within minutes without having to bother with faxing or emailing. Integrating smart-paging into the EHR is another way for doctors to communicate – it may not be as good as a phone call, but it’s less disruptive during a workday, he notes.
Epic is just now rolling out a secure text-messaging system hospitalists and others can use to communicate with one another – the header of the text thread clearly shows the patient it is referencing, Mr. Helsher said. Other EHR uses, such as telemedicine, are being used around the country but are far less widespread. But users are generally becoming more ambitious, he said.
“For the last 5-10 years, we’ve been in such an implementation rush,” Mr. Helsher explained. “ Now, at much more of a macro scale, the mentality has changed to ‘OK, we have these systems, let’s go from the implementation era to the value era.’ ”
Corinne Boudreau, senior marketing manager of physician experience at Meditech, said their sepsis tool has been very popular, while messaging features and shortcut commands for simpler charting are gradually coming into wider use. Meditech also expects their Web-based EHR – designed to give patients access on their mobile devices – will give doctors the mobility they want.
Still, there’s a wide range in how much hospitalists and other doctors are using even the fundamental tools that are available to them.
“I think that between implementation and maximization there is a period of adoption, and I think that that’s where a lot of folks are these days,” she said.
As “physician engagement” has become a buzzword in the industry, Meditech has worked with physician leaders on how to get doctors to absorb the message that the EHR really can help them do their jobs better.
“If you get [doctors] at the right time, you show them how it can make things easier or take time off their workload,” Ms. Boudreau said. “For some physicians that time to get them might be first thing in the morning before they see patients. Another physician might want to do it in the evening. If you hit that evening physician in the morning, you’ve missed that window of opportunity.”
Given the demands on doctors’ time and either an inability or unwillingness to put the time in that’s needed to learn about all functions the EHR can offer, there’s a growing acknowledgment that doctors often can’t simply do this on their own.
“There’s more recognition that this is a project that needs to be resourced,” Ms. Boudreau said. “They’re already strapped for time; to put something additional on top of it needs to be accommodated for. It needs to be resourced in terms of time, it needs to be resourced in terms of compensation. There need to be governance and support of that.”
Early adopters vs. late bloomers
Many hospitalists and HM groups have advanced, but some places have lagged behind, said John Nelson, MD, MHM, a veteran hospitalist, practice management consultant, and longtime columnist with The Hospitalist.
“We find it’s reasonably common to go to a place where they’re still keeping their census in an Excel spreadsheet,” he said. “Last year, we found people who do billing on paper and index cards.”
He said that often, a failure to adopt new EHR functionality isn’t because hospitals and HM groups are avoiding it. He said he sees IT shortcomings as a major blocker.
“They want to use it,” he said. “Inertia might be part of the reason people are failing to fully capture the benefit the EHR could offer, [but] the bigger reason is local IT configurations and support.”
As an example, Dr. Nelson explained that at some of the centers he has worked with the name of the attending physician is not always reflected in the EHR. That’s a big no-no, he said. The problem, he’s sometimes found, isn’t really the EHR, but quirks in the hospital system: The EHR is locked down for that information and can be changed only by a person in the admitting department.
“It would require the hospitalist to call down [to admissions] and get someone else to make that change – and that’s tedious a big headache. They give up and don’t do it anymore,” he said. “Ideally, you’d want to make it so the hospitalists can make the change themselves.”
At his center, Overlake Hospital Medical Center in Bellevue, Wash., a go-to hospitalist is David Chu, MD, who has gone through Epic training and shares tips with colleagues. He is one of a relatively few physicians there who has taken the time to use the drop-down menu feature for putting information into a chart.
That might sound like a fairly basic use for a multimillion-dollar EHR system. But it still can take hours and hours to get it right.
“The way to do it is a little bit of a programmer’s way of looking at things,” Dr. Chu said, noting it involves programming-style language with double colons, commas, and quotations marks.
“For me, I think it took a good 10, 12, 15 hours on my part to get things going,” he said. “It was a good time investment up front to help me on that end, but it’s just hard getting people to want to commit that time, especially if they’re not that savvy with computers.”
His hospitalist colleague, Ryan Chew, MD, is more advanced – he has a taxonomy-like shorthand he uses to give him the right set of basic fields for a given type of case. For someone admitted with pneumonia, he’d want to know certain things all the time. Were they short of breath? Did they have chest pain? What were their vital signs? What about inflammatory markers?
Dr. Chew can get all of those fields to pop up by typing “.rchppneumonia.” The “.” means that a special code is to follow. The “rc” is for Ryan Chew, the “hp” is for history and physical, and “pneumonia,” is the type of case. For cases that require other information to be entered, he can add that as needed.
Hospitalists might try to write shortcut phrases, but unless they have a well-defined system, it won’t be helpful over the long run, he said.
“If you don’t have a good organization system … you’ll never remember it,” Dr. Chew said.
But even he hasn’t created the drop-down menus. He said he just hasn’t been willing to take the time, especially since he feels his own way of doing things seems to be working just fine.
Effort is essential
Expanding the functionalities of the EHR takes effort, no doubt. As a result, some physicians and hospitalist groups have not been open-minded to the idea – and opportunities – of the EHR as a database.
“I think for some people, even still, working with the EHR, it’s become more something they’ve learned to get used to rather than something that they sought to take advantage of, in terms of helping things,” Dr. Chew said. “They’re still working against the EHR a little bit.”
Dr. Palabindala agreed, and said that regardless of resistance or complaint, EHRs work.
“No matter how much we argue, it is proven in multiple studies that EHRs showed increased patient safety and better documentation and better transfer of the data,” he said.
He suggests hospitalists make more of an effort.
“I strongly encourage hospitalists to be part of the every EHR-related committee, including CPOE [computerized physician order entry], analytics, and utilization-review committees,” he said. “Learning about the upgrades and learning about all the possible options, exploring clinical informatics on a regular basis is important. I also encourage [hospitalists] to participate in online, EHR-related surveys to learn more about the EHR utility and what is missing in their home institution.”
He acknowledges that it’s “hard to develop a passion.” Then he put it in terms he thought might resonate: “Think of it like a new version of smart phone. Show the enthusiasm as if you are ready for next version of iPhone or Pixel.” TH
Is hospitalists’ EHR efficiency taken advantage of?
Even though their level of EHR use can be hit or miss, hospitalists tend to be ahead of the game, many agree. But that can come with some drawbacks. They’re often the go-to people everyone else in the hospital relies on to handle the system that some think is too unwieldy to bother with.
“One thing that really distinguishes hospitalists from many other providers, particularly on the inpatient side, is just the frequency with which they use the EHR,” said Eric Helsher of Epic. Many hospitalists are chosen by administrators to test pilot projects for that reason, he adds. “They want to get it out there with a group who they know will have a lot of exposure to the system and may be more willing to make those changes for long-term gain.”
Sometimes that expertise leads to situations that go beyond the hospitalist simply being leaders of change – they’re doing work they were never really intended to do.
John Nelson, MD, MHM, a hospitalist consultant based in Seattle, said hospitalists tell him that a subspecialist might handle a case but will not want to be the attending physician specifically so they don’t have to deal with the EHR. He said the specialist in such cases will say something along the lines of, “You can call me, I’ll help you, and I’ll come by and say hello to the patient and make the care decisions, but I need you to be the attending so you can document in the chart and you can do the med rec because ‘I can’t figure out how to do those buttons right.’ ”
Some will ask hospitalists “for a hand” with a case when really all they want is for the hospitalist to enter information into the system. It’s a tricky situation for the hospitalist, Dr. Nelson said.
“Some will be transparent and say I don’t really have a medical question – I just can’t figure out how to do the med rec and the discharge, so would you do it?” he said, adding the systems issues are largely because of new rounding patterns sparked by HM’s expanding role in-hospital. “I think it meaningfully contributes to what I perceive to be a decline in hospitalist morale in the last 2 or 3 years.”
Tom Collins is a freelance writer in South Florida.
MACRA: What every hospitalist needs to know
In April 2015, President Obama signed the bipartisan Medicare Access and CHIP Reauthorization Act (MACRA) into law, effectively altering the future of the Medicare payment system for providers. MACRA not only removed the Sustainable Growth Rate, but also encouraged quality measure development, expanded the use of Medicare data, and locked provider payment rates to near zero growth.
For Medicare payments, MACRA created the Quality Payment Program, which breaks down clinical payments into two pathways: the Merit-Based Incentive Payment System (MIPS) combining current pay-for-performance programs into one consolidated payment system, and Alternative Payment Models (APMs), incentivizing payment models that move away from a fee-for-service system.
Both pathways incur risk, as well as rewards:
• MIPS. –4% penalty up to 12% positive adjustment in year 1 based on 2017 data reported and collected by the CMS, growing over time to include payment adjustments from –9% to +27% in future years.
• APMs. If the provider is eligible, a 5% payment increase from 2019 to 2024, with no reporting requirements, and exemption from MIPS.
Who is included in the program?
All clinicians who receive Medicare Physician Fee Schedule payments, including physicians, physician assistants, and nurse practitioners, will be affected by this program. The only providers who are exempt from the program are those who fall under low-volume thresholds (either less than $30,000 in Medicare Part B charges or less than 101 Medicare patients) or those in their first year with Medicare.
What is MIPS?
MIPS requires reporting in four categories that determine a physician’s payment adjustment:
• Quality, which replaces the Physician Quality Reporting System (PQRS).
• Cost, which replaces the value-based modifier.
• Advancing Care Information (ACI), which replaces the meaningful use program.
• Improvement activities, a new category, but one in which hospitalists should excel, as they are already participating in many of the activities.
Each category is given relative weight, which the CMS will adjust in the first few years of the program.
Note that in the first year (2017), cost will be calculated, but not used to determine payment amount, hence this category gets a 0% weighting. Also, there are significant differences between how most providers’ MIPS score will be calculated with respect to category weights, and how this will be done for hospitalists.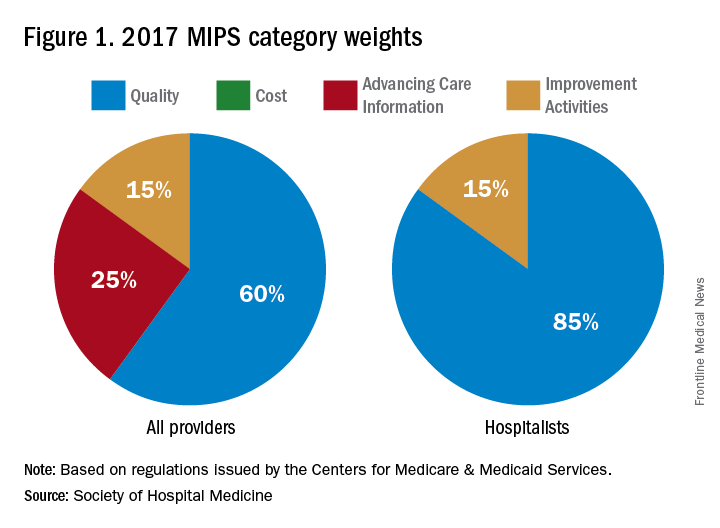
In addition to cost, the ACI will not play a role in the 2019 performance scores for hospitalists. However, hospitalists who practice in noninpatient settings, such as skilled nursing facilities or ambulatory clinics, will be subject to the ACI unless they apply for exceptions.
The quality category requires physicians to report on 6 of the 271 measures available. Hospitalists can report from the hospitalist-specific specialty set for which the Society of Hospital Medicine (SHM) was successful in advocating. Although continued cooperation between the CMS and SHM is necessary to fine-tune the measures, below are those that the SHM believes are reportable by, and most relevant to, hospitalists.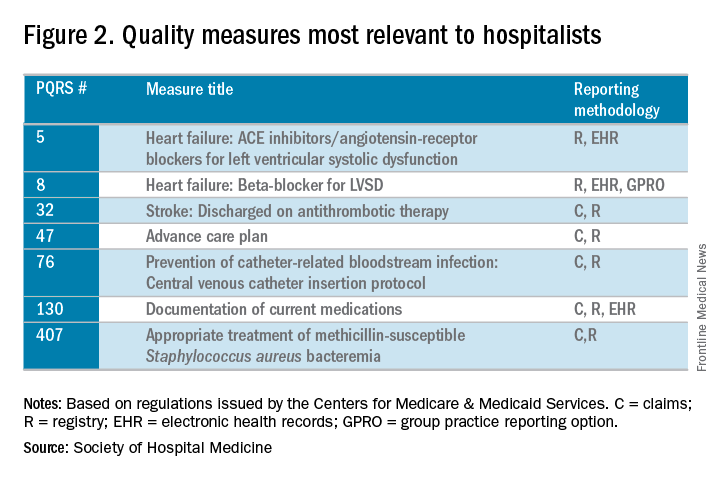
The improvement activities category will determine 15% of hospitalists’ performance in the MIPS. To receive full credit for this category, hospitalists must report on activities totaling 40 points. There are 92 available activities across eight different categories – 20 points for those that have a “high” weight determination and 10 points for those with medium weight.
In 2017, the CMS will calculate the cost category for providers, but it will not be counted toward the overall score. The data will still be collected based on Medicare Part A and Part B costs and will be reported to groups. Over time, this category will increase in scoring weight.
The Advancing Care Information category replaces the meaningful use program. This category will still promote EHR use, but hospitalists should be exempt from this category because of their “hospital-based” practice setting. This exemption is the reason why the quality category counts for 85% of the hospitalists’ score.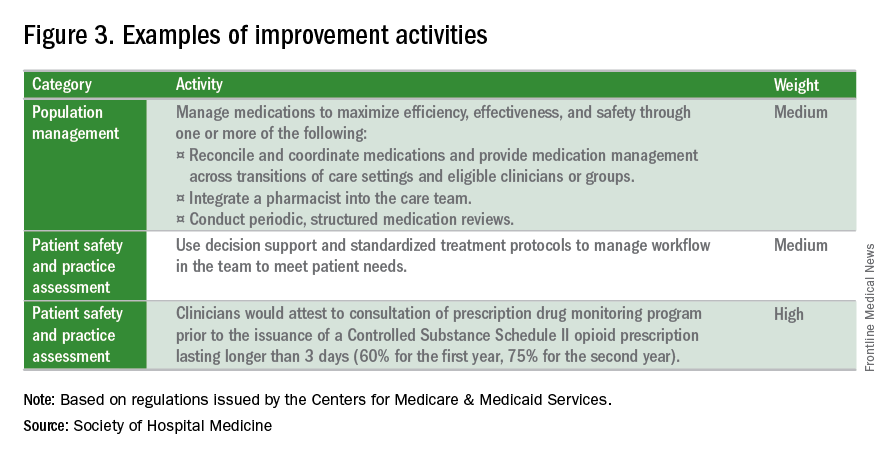
What is the APM Track?
The Alternative Payment Model pathway will be difficult for hospitalists to participate in, given its current criteria. Only advanced APMs will qualify, and for an APM to qualify as advanced, its clinicians/groups must use certified EHR technology, tie clinician payments to quality measures, and bear greater than nominal financial risk for outcomes and expenses, or qualify as a medical home. A provider must also meet rather high patient or payment thresholds coming from the model (greater than 25% of Medicare payments or greater than 20% of patients as part of an APM) in order to qualify.
Nominal financial risk is defined as either meeting revenue standards (at risk of losing 7% of its own revenues when Medicare expenditures are higher than expected) or benchmark-based standards (at risk of repaying the CMS up to a maximum of 3% of total Medicare expenditures).
Many hospitalists are participating in the Bundled Payments for Care Improvement (BPCI) model, but in its current form, it does not qualify as an APM for 2017 reporting.
The CMS has indicated that new voluntary bundled payment models that meet advanced APM criteria will be developed, but as of 2017, the list of APMs is slim, including only the Comprehensive ESRD Care, Comprehensive Primary Care Plus, Next Generation ACO, Shared Savings Program Tracks 2 and 3, and Oncology Care models.
Interested in learning more?
The SHM is working relentlessly in advocating on the behalf of hospitalists, and is constantly developing resources that will better prepare hospitalists for success within this program. If you are interested in learning more, check out the following resources:
• The SHM’s MACRA for Hospitalists website. Learn more about MACRA and its impact on hospitalists at www.macraforhm.org.
• The SHM’s annual meeting. A health policy track has been approved for HM17, including two sessions May 4 from 7:45 a.m.–8:35 a.m., “Hot Topics in Health Policy for Hospitalists,” and from 8:45 a.m.–9:40 a.m., “The Impact of the New Administration on Health Care Reform.” A MACRA-specific session will be held May 4 from 9:50 a.m.–10:45 a.m., “Tips for MIPS and Beyond,” as well as an Advocacy and Public Policy Special Interest Forum on May 2 from 4:30 p.m.–5:25 p.m.
• HMX. Join the advocacy and public policy community on HMX to learn more about dynamic changes in public policy and be a part of the conversation.
• Connect with SHM staff. Email Josh Boswell, SHM’s director of government relations, at [email protected].
• The CMS website. An easy to navigate site, the CMS’s MACRA-specific site, qpp.cms.gov, has additional resources and educational tools.
Dr. Lenchus is associate professor of clinical medicine, anesthesiology, and radiology, University of Miami Miller School of Medicine, and associate director, University of Miami/Jackson Memorial Hospital Center for Patient Safety, Miami.
Dr. Dutta is interim division chief, division of hospital medicine; medical director, attending/APP directed services; and assistant professor, department of internal medicine, Rush Medical College in Chicago.
Dr. Afsar-Manesh is chief quality officer, department of medicine, UCLA Health in Los Angeles, and treasurer of SHM’s board of directors.
All three are members of SHM’s Public Policy Committee.
In April 2015, President Obama signed the bipartisan Medicare Access and CHIP Reauthorization Act (MACRA) into law, effectively altering the future of the Medicare payment system for providers. MACRA not only removed the Sustainable Growth Rate, but also encouraged quality measure development, expanded the use of Medicare data, and locked provider payment rates to near zero growth.
For Medicare payments, MACRA created the Quality Payment Program, which breaks down clinical payments into two pathways: the Merit-Based Incentive Payment System (MIPS) combining current pay-for-performance programs into one consolidated payment system, and Alternative Payment Models (APMs), incentivizing payment models that move away from a fee-for-service system.
Both pathways incur risk, as well as rewards:
• MIPS. –4% penalty up to 12% positive adjustment in year 1 based on 2017 data reported and collected by the CMS, growing over time to include payment adjustments from –9% to +27% in future years.
• APMs. If the provider is eligible, a 5% payment increase from 2019 to 2024, with no reporting requirements, and exemption from MIPS.
Who is included in the program?
All clinicians who receive Medicare Physician Fee Schedule payments, including physicians, physician assistants, and nurse practitioners, will be affected by this program. The only providers who are exempt from the program are those who fall under low-volume thresholds (either less than $30,000 in Medicare Part B charges or less than 101 Medicare patients) or those in their first year with Medicare.
What is MIPS?
MIPS requires reporting in four categories that determine a physician’s payment adjustment:
• Quality, which replaces the Physician Quality Reporting System (PQRS).
• Cost, which replaces the value-based modifier.
• Advancing Care Information (ACI), which replaces the meaningful use program.
• Improvement activities, a new category, but one in which hospitalists should excel, as they are already participating in many of the activities.
Each category is given relative weight, which the CMS will adjust in the first few years of the program.
Note that in the first year (2017), cost will be calculated, but not used to determine payment amount, hence this category gets a 0% weighting. Also, there are significant differences between how most providers’ MIPS score will be calculated with respect to category weights, and how this will be done for hospitalists.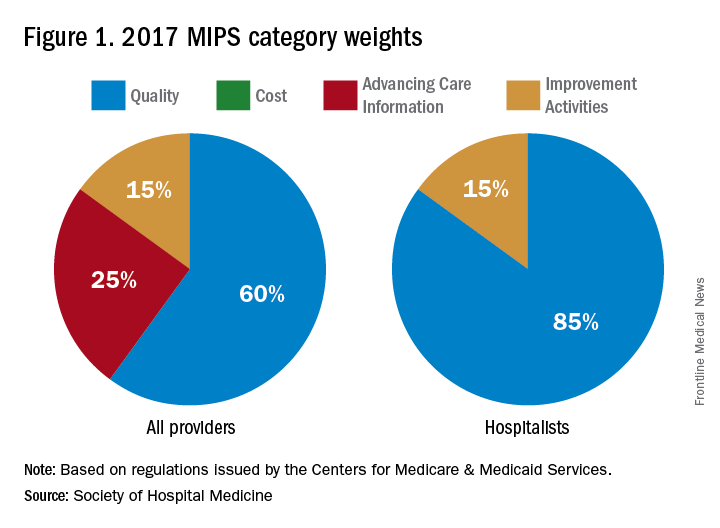
In addition to cost, the ACI will not play a role in the 2019 performance scores for hospitalists. However, hospitalists who practice in noninpatient settings, such as skilled nursing facilities or ambulatory clinics, will be subject to the ACI unless they apply for exceptions.
The quality category requires physicians to report on 6 of the 271 measures available. Hospitalists can report from the hospitalist-specific specialty set for which the Society of Hospital Medicine (SHM) was successful in advocating. Although continued cooperation between the CMS and SHM is necessary to fine-tune the measures, below are those that the SHM believes are reportable by, and most relevant to, hospitalists.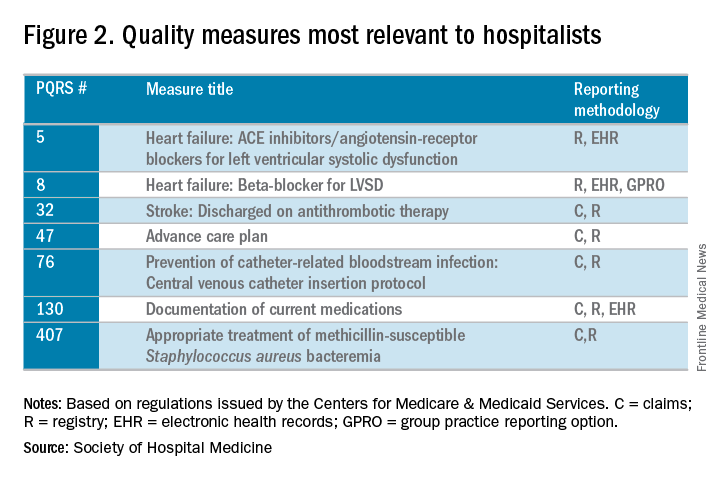
The improvement activities category will determine 15% of hospitalists’ performance in the MIPS. To receive full credit for this category, hospitalists must report on activities totaling 40 points. There are 92 available activities across eight different categories – 20 points for those that have a “high” weight determination and 10 points for those with medium weight.
In 2017, the CMS will calculate the cost category for providers, but it will not be counted toward the overall score. The data will still be collected based on Medicare Part A and Part B costs and will be reported to groups. Over time, this category will increase in scoring weight.
The Advancing Care Information category replaces the meaningful use program. This category will still promote EHR use, but hospitalists should be exempt from this category because of their “hospital-based” practice setting. This exemption is the reason why the quality category counts for 85% of the hospitalists’ score.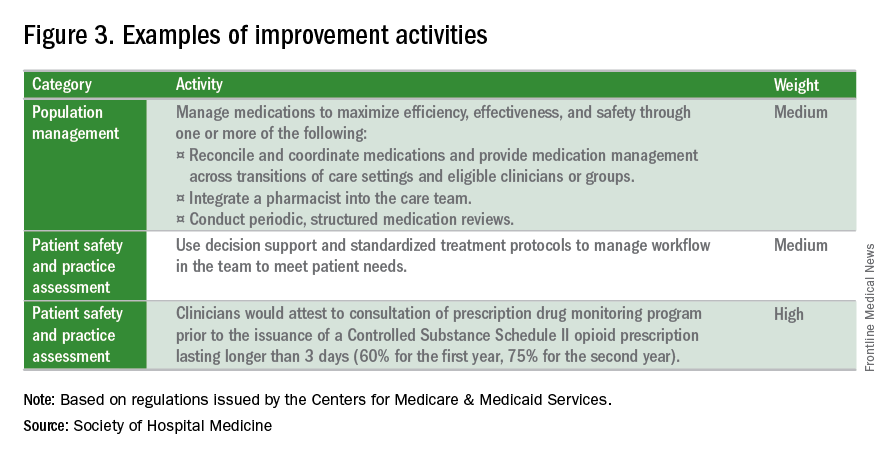
What is the APM Track?
The Alternative Payment Model pathway will be difficult for hospitalists to participate in, given its current criteria. Only advanced APMs will qualify, and for an APM to qualify as advanced, its clinicians/groups must use certified EHR technology, tie clinician payments to quality measures, and bear greater than nominal financial risk for outcomes and expenses, or qualify as a medical home. A provider must also meet rather high patient or payment thresholds coming from the model (greater than 25% of Medicare payments or greater than 20% of patients as part of an APM) in order to qualify.
Nominal financial risk is defined as either meeting revenue standards (at risk of losing 7% of its own revenues when Medicare expenditures are higher than expected) or benchmark-based standards (at risk of repaying the CMS up to a maximum of 3% of total Medicare expenditures).
Many hospitalists are participating in the Bundled Payments for Care Improvement (BPCI) model, but in its current form, it does not qualify as an APM for 2017 reporting.
The CMS has indicated that new voluntary bundled payment models that meet advanced APM criteria will be developed, but as of 2017, the list of APMs is slim, including only the Comprehensive ESRD Care, Comprehensive Primary Care Plus, Next Generation ACO, Shared Savings Program Tracks 2 and 3, and Oncology Care models.
Interested in learning more?
The SHM is working relentlessly in advocating on the behalf of hospitalists, and is constantly developing resources that will better prepare hospitalists for success within this program. If you are interested in learning more, check out the following resources:
• The SHM’s MACRA for Hospitalists website. Learn more about MACRA and its impact on hospitalists at www.macraforhm.org.
• The SHM’s annual meeting. A health policy track has been approved for HM17, including two sessions May 4 from 7:45 a.m.–8:35 a.m., “Hot Topics in Health Policy for Hospitalists,” and from 8:45 a.m.–9:40 a.m., “The Impact of the New Administration on Health Care Reform.” A MACRA-specific session will be held May 4 from 9:50 a.m.–10:45 a.m., “Tips for MIPS and Beyond,” as well as an Advocacy and Public Policy Special Interest Forum on May 2 from 4:30 p.m.–5:25 p.m.
• HMX. Join the advocacy and public policy community on HMX to learn more about dynamic changes in public policy and be a part of the conversation.
• Connect with SHM staff. Email Josh Boswell, SHM’s director of government relations, at [email protected].
• The CMS website. An easy to navigate site, the CMS’s MACRA-specific site, qpp.cms.gov, has additional resources and educational tools.
Dr. Lenchus is associate professor of clinical medicine, anesthesiology, and radiology, University of Miami Miller School of Medicine, and associate director, University of Miami/Jackson Memorial Hospital Center for Patient Safety, Miami.
Dr. Dutta is interim division chief, division of hospital medicine; medical director, attending/APP directed services; and assistant professor, department of internal medicine, Rush Medical College in Chicago.
Dr. Afsar-Manesh is chief quality officer, department of medicine, UCLA Health in Los Angeles, and treasurer of SHM’s board of directors.
All three are members of SHM’s Public Policy Committee.
In April 2015, President Obama signed the bipartisan Medicare Access and CHIP Reauthorization Act (MACRA) into law, effectively altering the future of the Medicare payment system for providers. MACRA not only removed the Sustainable Growth Rate, but also encouraged quality measure development, expanded the use of Medicare data, and locked provider payment rates to near zero growth.
For Medicare payments, MACRA created the Quality Payment Program, which breaks down clinical payments into two pathways: the Merit-Based Incentive Payment System (MIPS) combining current pay-for-performance programs into one consolidated payment system, and Alternative Payment Models (APMs), incentivizing payment models that move away from a fee-for-service system.
Both pathways incur risk, as well as rewards:
• MIPS. –4% penalty up to 12% positive adjustment in year 1 based on 2017 data reported and collected by the CMS, growing over time to include payment adjustments from –9% to +27% in future years.
• APMs. If the provider is eligible, a 5% payment increase from 2019 to 2024, with no reporting requirements, and exemption from MIPS.
Who is included in the program?
All clinicians who receive Medicare Physician Fee Schedule payments, including physicians, physician assistants, and nurse practitioners, will be affected by this program. The only providers who are exempt from the program are those who fall under low-volume thresholds (either less than $30,000 in Medicare Part B charges or less than 101 Medicare patients) or those in their first year with Medicare.
What is MIPS?
MIPS requires reporting in four categories that determine a physician’s payment adjustment:
• Quality, which replaces the Physician Quality Reporting System (PQRS).
• Cost, which replaces the value-based modifier.
• Advancing Care Information (ACI), which replaces the meaningful use program.
• Improvement activities, a new category, but one in which hospitalists should excel, as they are already participating in many of the activities.
Each category is given relative weight, which the CMS will adjust in the first few years of the program.
Note that in the first year (2017), cost will be calculated, but not used to determine payment amount, hence this category gets a 0% weighting. Also, there are significant differences between how most providers’ MIPS score will be calculated with respect to category weights, and how this will be done for hospitalists.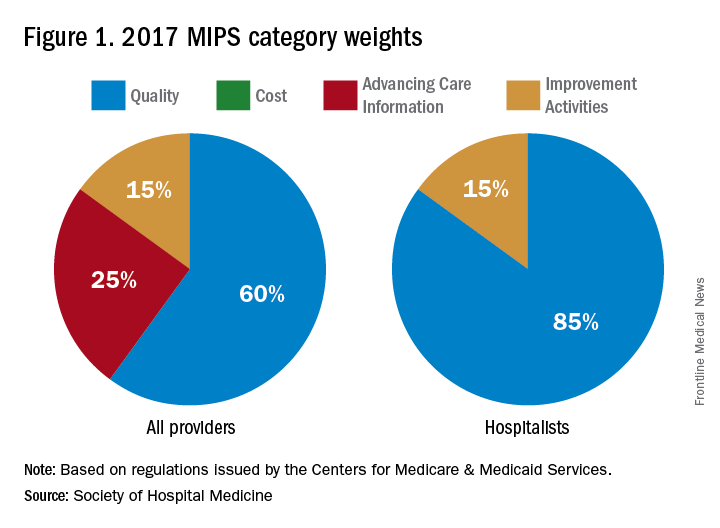
In addition to cost, the ACI will not play a role in the 2019 performance scores for hospitalists. However, hospitalists who practice in noninpatient settings, such as skilled nursing facilities or ambulatory clinics, will be subject to the ACI unless they apply for exceptions.
The quality category requires physicians to report on 6 of the 271 measures available. Hospitalists can report from the hospitalist-specific specialty set for which the Society of Hospital Medicine (SHM) was successful in advocating. Although continued cooperation between the CMS and SHM is necessary to fine-tune the measures, below are those that the SHM believes are reportable by, and most relevant to, hospitalists.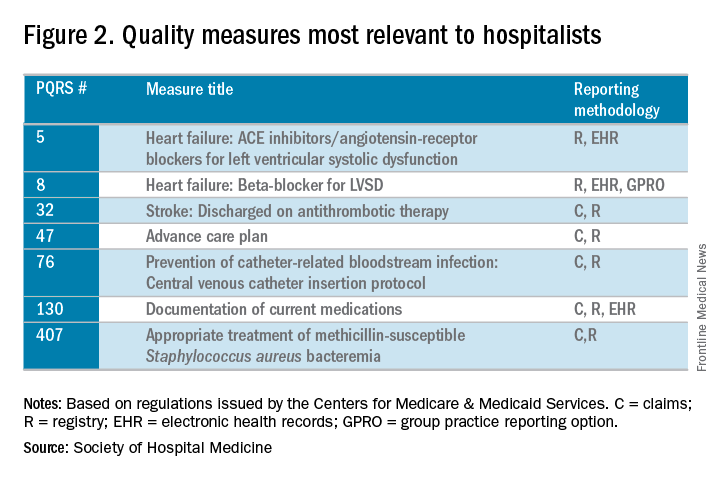
The improvement activities category will determine 15% of hospitalists’ performance in the MIPS. To receive full credit for this category, hospitalists must report on activities totaling 40 points. There are 92 available activities across eight different categories – 20 points for those that have a “high” weight determination and 10 points for those with medium weight.
In 2017, the CMS will calculate the cost category for providers, but it will not be counted toward the overall score. The data will still be collected based on Medicare Part A and Part B costs and will be reported to groups. Over time, this category will increase in scoring weight.
The Advancing Care Information category replaces the meaningful use program. This category will still promote EHR use, but hospitalists should be exempt from this category because of their “hospital-based” practice setting. This exemption is the reason why the quality category counts for 85% of the hospitalists’ score.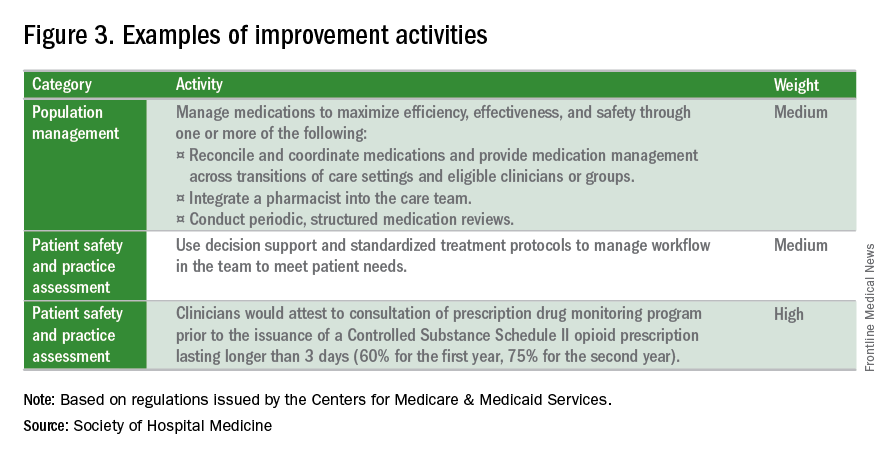
What is the APM Track?
The Alternative Payment Model pathway will be difficult for hospitalists to participate in, given its current criteria. Only advanced APMs will qualify, and for an APM to qualify as advanced, its clinicians/groups must use certified EHR technology, tie clinician payments to quality measures, and bear greater than nominal financial risk for outcomes and expenses, or qualify as a medical home. A provider must also meet rather high patient or payment thresholds coming from the model (greater than 25% of Medicare payments or greater than 20% of patients as part of an APM) in order to qualify.
Nominal financial risk is defined as either meeting revenue standards (at risk of losing 7% of its own revenues when Medicare expenditures are higher than expected) or benchmark-based standards (at risk of repaying the CMS up to a maximum of 3% of total Medicare expenditures).
Many hospitalists are participating in the Bundled Payments for Care Improvement (BPCI) model, but in its current form, it does not qualify as an APM for 2017 reporting.
The CMS has indicated that new voluntary bundled payment models that meet advanced APM criteria will be developed, but as of 2017, the list of APMs is slim, including only the Comprehensive ESRD Care, Comprehensive Primary Care Plus, Next Generation ACO, Shared Savings Program Tracks 2 and 3, and Oncology Care models.
Interested in learning more?
The SHM is working relentlessly in advocating on the behalf of hospitalists, and is constantly developing resources that will better prepare hospitalists for success within this program. If you are interested in learning more, check out the following resources:
• The SHM’s MACRA for Hospitalists website. Learn more about MACRA and its impact on hospitalists at www.macraforhm.org.
• The SHM’s annual meeting. A health policy track has been approved for HM17, including two sessions May 4 from 7:45 a.m.–8:35 a.m., “Hot Topics in Health Policy for Hospitalists,” and from 8:45 a.m.–9:40 a.m., “The Impact of the New Administration on Health Care Reform.” A MACRA-specific session will be held May 4 from 9:50 a.m.–10:45 a.m., “Tips for MIPS and Beyond,” as well as an Advocacy and Public Policy Special Interest Forum on May 2 from 4:30 p.m.–5:25 p.m.
• HMX. Join the advocacy and public policy community on HMX to learn more about dynamic changes in public policy and be a part of the conversation.
• Connect with SHM staff. Email Josh Boswell, SHM’s director of government relations, at [email protected].
• The CMS website. An easy to navigate site, the CMS’s MACRA-specific site, qpp.cms.gov, has additional resources and educational tools.
Dr. Lenchus is associate professor of clinical medicine, anesthesiology, and radiology, University of Miami Miller School of Medicine, and associate director, University of Miami/Jackson Memorial Hospital Center for Patient Safety, Miami.
Dr. Dutta is interim division chief, division of hospital medicine; medical director, attending/APP directed services; and assistant professor, department of internal medicine, Rush Medical College in Chicago.
Dr. Afsar-Manesh is chief quality officer, department of medicine, UCLA Health in Los Angeles, and treasurer of SHM’s board of directors.
All three are members of SHM’s Public Policy Committee.
The beginning of the end
No matter on which side of the aisle you sit, and even if you’d prefer to just sit in your car and check Instagram, the results of the November election were likely a surprise. Speculation abounds by pundits and so-called experts as to what a Trump presidency means for health care in this country. The shape and scope of health care initiatives that a Trump administration will attempt to advance in place of the Affordable Care Act (ACA), which has likely met its demise, is unknown at the time of this writing. How Trump’s new initiatives fare in Congress and then get translated into practical changes in health care delivery and financing is even more muddled.
The U.S. medical community has remained largely silent, which is wise given the lack of evidence that would support any rational prediction, but perhaps it’s easier to pronounce judgment from across the pond. The Lancet recently reported the comment of Sophie Harman, PhD, a political scientist at Queen Mary University in London, who told an audience at the London School of Hygiene & Tropical Medicine to “ignore the dead cat in the room.”1 I spent 6 months of my residency in the United Kingdom, and this phrase never came up in my travels across the wards, streets, and pubs of the mother country. Apparently, the “dead cat strategy” is a legislative maneuver to distract attention from a party’s political shortcomings by raising a ruckus about a salacious or social hot-button topic. In this case, the dead cat may just be the carcass of Obamacare, exuding the fetor of millions of people losing their health insurance.
The BMJ, another respected U.K. journal, offered the pronouncement by Don Berwick, MD, former administrator of the Centers for Medicare & Medicaid Services, that Trump’s election would be “disastrous” for U.S. health care, but not much else.2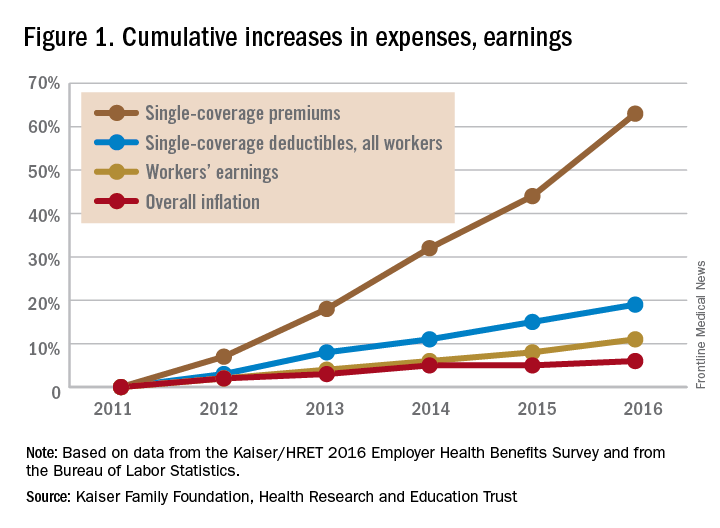
Out-of-pocket health care expenses for patients and families insured under Medicaid and its ACA-mandated expansion decreased to, on average, less than $500 per year; however, 19 states, all with Republican governors, blocked the Medicaid expansion.5 This denied more than 2.5 million people Medicaid coverage in these states; the overwhelming majority of these people remained uninsured. Uninsured people incur significant out-of-pocket costs when they do require health care, and have worse outcomes.6,7 The end of ACA throws Medicaid expansion in any state, with its protections to limit out-of-pocket expenses, into doubt.
Before the ACA expanded Medicaid coverage, patients faced significant wait times and travel costs associated with the low numbers of providers accepting Medicaid’s low reimbursement rate.8 These numbers had begun to improve after the ACA increased primary care physicians’ Medicaid reimbursements to Medicare rates in 2013 and 2014, but only a limited number of states will continue the increases after the end of federal subsidies.
For people who purchased plans on the ACA’s marketplace, out-of-pocket exposure is capped in 2017 at no more than $7,150 for an individual plan and $14,300 for a family plan before marketplace subsidies. Even those who qualified for cost-sharing deductions, with incomes between 100% and 250% of the federal poverty level, had out-of-pocket caps that varied widely depending on plan and state. For example, in 2016 at the $17,000 annual income level, out-of-pocket caps could range from $500 to $2,250.9
Clinician concern
On a provider level, incentives to reduce readmissions and limit health care–associated harm events mandated by the ACA may soon evaporate, throwing into question many quality metrics pursued by health systems. In response, will health system administrators abandon efforts to reduce readmissions and hospital-acquired conditions (HACs)? Or will health systems, despite the lack of a Medicare penalty “stick,” move forward with efforts to reduce readmissions and HACs? There’s no question of what would benefit the pocketbooks of our patients the most – every hospitalization results in significant direct out-of-pocket costs, not to mention lost productivity and income.10
It seems unlikely that a Republican-led government will pursue efforts to decrease out-of-pocket expenses. More likely, new proposals will aim to provide tax benefits to encourage use of health savings accounts (HSAs), continuing the shift of health care to employees.11 HSAs benefit employers, who pay less for the health care costs of employees, but are associated with worsened adherence to recommended treatments for patients.8,12
A 2016 study analyzed health care policies considered by Trump, including the following:
- Full repeal of the ACA.
- Repeal of the ACA plus tax deductions of health insurance premiums.
- Repeal of the ACA plus block grants to states for Medicaid and Children’s Health Insurance Program (CHIP).
- Repeal plus promotion of selling health insurance across state lines.
Not surprisingly, all four scenarios resulted in significant increases in out-of-pocket expenses for those in individual insurance plans.13
Although at the time of writing, the “replace” segment of “repeal-and-replace” is not known, Mr. Trump’s nominee for Secretary of Health and Human Services (HHS), Rep. Tom Price (R-Ga.), has given a hint of what he would champion based on his prior legislative proposals. Along with his support of increasing accessibility of armor-piercing bullets, reduced regulations on cigars, and opposition to expanding the State Children’s Health Insurance Program, he proposed H.R. 2300, “Empower Patients First Act.” This would eliminate the ACA’s Medicaid expansion and replace it with flat tax credits based on age, not income, which turns out to offer greater subsidies relative to income for those with higher incomes. A 30-year-old would, on average, face a premium bill of $2,532, along with a potential out-of-pocket liability of $7,000, with only a $1,200 credit to cover this from Mr. Price’s plan.14
In sum
So what’s a conscientious advocate for the physical and financial health of patients to do? Beyond political action, hospitalists need to keep abreast of the effect of changes in health care policy on their patients, as unpleasant as it may be. Do you know what the copays and out-of-pocket costs are for your patient’s (or your own) health care? Knowing how your recommendations for treatment and follow-up affect your patient’s pocketbook will not only help protect their finances, but will also protect their health, as people are less likely to be compliant with treatment if it involves out-of-pocket costs.
And easy as it would be to simply tune out the partisan rancor, stay engaged as a citizen, if for nothing else, the benefit of your patients.
Dr. Chang is pediatric editor of The Hospitalist. He is associate clinical professor of pediatrics at the University of Massachusetts, Worcester, and chief of pediatric hospital medicine at Baystate Children's Hospital, Springfield, Mass. Send comments and questions to [email protected].
References
1. Horton R. Offline: Looking forward to Donald Trump. The Lancet. 2016;388[10061]:2726.
2. Page L. What Donald Trump would do with the US healthcare system. BMJ. 2016;353:i2996.
3. Uberoi N, Finegold, K. and Gee, E. Health Insurance Coverage and the Affordable Care Act, 2010-2016. Department of Health and Human Services, ASPE Issue Brief, 2016 March 3.
4. Claxton G, Rae M, Long M, Damico A, Whitmore H, Foster G. Health Benefits In 2016: Family Premiums Rose Modestly, And Offer Rates Remained Stable. Health Aff (Millwood). 2016 Sep. doi: 10.1377/hlthaff.2016.0951.
5. Ku L, Broaddus M. Public and private health insurance: stacking up the costs. Health Aff (Millwood). 2008;27:w318-327.
6. Waters H, Steinhardt L, Oliver TR, Burton A, Milner S. The costs of non-insurance in Maryland. J Health Care Poor Underserved. 2007 Feb;18[1]:139-51.
7. Cheung MR. Lack of health insurance increases all cause and all cancer mortality in adults: an analysis of National Health and Nutrition Examination Survey (NHANES III) data. Asian Pac J Cancer Prev. 2013;14[4]:2259-63.
8. Gillis JZ, Yazdany J, Trupin L, et al. Medicaid and access to care among persons with systemic lupus erythematosus. Arthritis Rheum. 2007;57[4]:601-7.
9. Collins SR, Gunja M, Beutel S. How Will the Affordable Care Act’s Cost-Sharing Reductions Affect Consumers’ Out-of-Pocket Costs in 2016? Issue Brief (Commonw Fund) 2016;6:1-17.
10. Leader S, Yang H, DeVincenzo J, Jacobson P, Marcin JP, Murray DL. Time and out-of-pocket costs associated with respiratory syncytial virus hospitalization of infants. Value Health. 2003;6[2]:100-6.
11. Antos J CJ. The House Republicans’ Health Plan. Bethesda, MD: Health Affairs Blog, Project HOPE; 2016 June 22.
12. Fronstin P, Roebuck MC. Health care spending after adopting a full-replacement, high-deductible health plan with a health savings account: a five-year study. EBRI Issue Brief 2013 July:3-15.
13. Saltzman E EC. Donald Trump’s Health Care Reform Proposals: Anticipated Effects on Insurance Coverage, Out-of-Pocket Costs, and the Federal Deficit. The Commonwealth Fund September 2016.
14. Glied SA, Frank RG. Care for the Vulnerable vs. Cash for the Powerful – Trump’s Pick for HHS. N Engl J Med. 2017;376:103-5.
No matter on which side of the aisle you sit, and even if you’d prefer to just sit in your car and check Instagram, the results of the November election were likely a surprise. Speculation abounds by pundits and so-called experts as to what a Trump presidency means for health care in this country. The shape and scope of health care initiatives that a Trump administration will attempt to advance in place of the Affordable Care Act (ACA), which has likely met its demise, is unknown at the time of this writing. How Trump’s new initiatives fare in Congress and then get translated into practical changes in health care delivery and financing is even more muddled.
The U.S. medical community has remained largely silent, which is wise given the lack of evidence that would support any rational prediction, but perhaps it’s easier to pronounce judgment from across the pond. The Lancet recently reported the comment of Sophie Harman, PhD, a political scientist at Queen Mary University in London, who told an audience at the London School of Hygiene & Tropical Medicine to “ignore the dead cat in the room.”1 I spent 6 months of my residency in the United Kingdom, and this phrase never came up in my travels across the wards, streets, and pubs of the mother country. Apparently, the “dead cat strategy” is a legislative maneuver to distract attention from a party’s political shortcomings by raising a ruckus about a salacious or social hot-button topic. In this case, the dead cat may just be the carcass of Obamacare, exuding the fetor of millions of people losing their health insurance.
The BMJ, another respected U.K. journal, offered the pronouncement by Don Berwick, MD, former administrator of the Centers for Medicare & Medicaid Services, that Trump’s election would be “disastrous” for U.S. health care, but not much else.2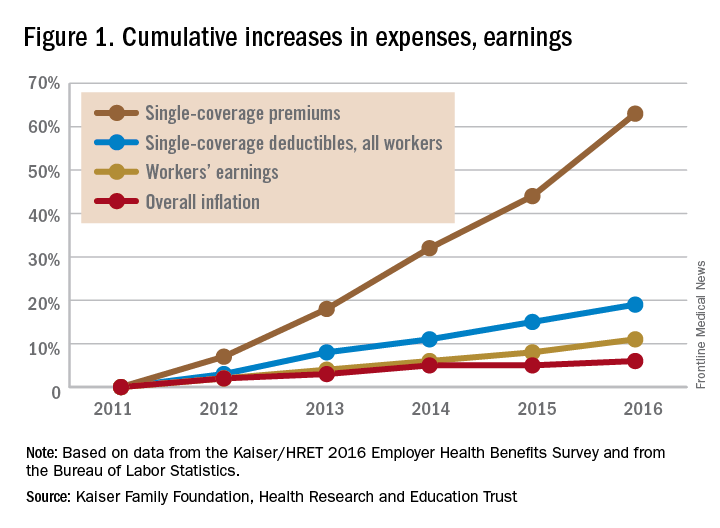
Out-of-pocket health care expenses for patients and families insured under Medicaid and its ACA-mandated expansion decreased to, on average, less than $500 per year; however, 19 states, all with Republican governors, blocked the Medicaid expansion.5 This denied more than 2.5 million people Medicaid coverage in these states; the overwhelming majority of these people remained uninsured. Uninsured people incur significant out-of-pocket costs when they do require health care, and have worse outcomes.6,7 The end of ACA throws Medicaid expansion in any state, with its protections to limit out-of-pocket expenses, into doubt.
Before the ACA expanded Medicaid coverage, patients faced significant wait times and travel costs associated with the low numbers of providers accepting Medicaid’s low reimbursement rate.8 These numbers had begun to improve after the ACA increased primary care physicians’ Medicaid reimbursements to Medicare rates in 2013 and 2014, but only a limited number of states will continue the increases after the end of federal subsidies.
For people who purchased plans on the ACA’s marketplace, out-of-pocket exposure is capped in 2017 at no more than $7,150 for an individual plan and $14,300 for a family plan before marketplace subsidies. Even those who qualified for cost-sharing deductions, with incomes between 100% and 250% of the federal poverty level, had out-of-pocket caps that varied widely depending on plan and state. For example, in 2016 at the $17,000 annual income level, out-of-pocket caps could range from $500 to $2,250.9
Clinician concern
On a provider level, incentives to reduce readmissions and limit health care–associated harm events mandated by the ACA may soon evaporate, throwing into question many quality metrics pursued by health systems. In response, will health system administrators abandon efforts to reduce readmissions and hospital-acquired conditions (HACs)? Or will health systems, despite the lack of a Medicare penalty “stick,” move forward with efforts to reduce readmissions and HACs? There’s no question of what would benefit the pocketbooks of our patients the most – every hospitalization results in significant direct out-of-pocket costs, not to mention lost productivity and income.10
It seems unlikely that a Republican-led government will pursue efforts to decrease out-of-pocket expenses. More likely, new proposals will aim to provide tax benefits to encourage use of health savings accounts (HSAs), continuing the shift of health care to employees.11 HSAs benefit employers, who pay less for the health care costs of employees, but are associated with worsened adherence to recommended treatments for patients.8,12
A 2016 study analyzed health care policies considered by Trump, including the following:
- Full repeal of the ACA.
- Repeal of the ACA plus tax deductions of health insurance premiums.
- Repeal of the ACA plus block grants to states for Medicaid and Children’s Health Insurance Program (CHIP).
- Repeal plus promotion of selling health insurance across state lines.
Not surprisingly, all four scenarios resulted in significant increases in out-of-pocket expenses for those in individual insurance plans.13
Although at the time of writing, the “replace” segment of “repeal-and-replace” is not known, Mr. Trump’s nominee for Secretary of Health and Human Services (HHS), Rep. Tom Price (R-Ga.), has given a hint of what he would champion based on his prior legislative proposals. Along with his support of increasing accessibility of armor-piercing bullets, reduced regulations on cigars, and opposition to expanding the State Children’s Health Insurance Program, he proposed H.R. 2300, “Empower Patients First Act.” This would eliminate the ACA’s Medicaid expansion and replace it with flat tax credits based on age, not income, which turns out to offer greater subsidies relative to income for those with higher incomes. A 30-year-old would, on average, face a premium bill of $2,532, along with a potential out-of-pocket liability of $7,000, with only a $1,200 credit to cover this from Mr. Price’s plan.14
In sum
So what’s a conscientious advocate for the physical and financial health of patients to do? Beyond political action, hospitalists need to keep abreast of the effect of changes in health care policy on their patients, as unpleasant as it may be. Do you know what the copays and out-of-pocket costs are for your patient’s (or your own) health care? Knowing how your recommendations for treatment and follow-up affect your patient’s pocketbook will not only help protect their finances, but will also protect their health, as people are less likely to be compliant with treatment if it involves out-of-pocket costs.
And easy as it would be to simply tune out the partisan rancor, stay engaged as a citizen, if for nothing else, the benefit of your patients.
Dr. Chang is pediatric editor of The Hospitalist. He is associate clinical professor of pediatrics at the University of Massachusetts, Worcester, and chief of pediatric hospital medicine at Baystate Children's Hospital, Springfield, Mass. Send comments and questions to [email protected].
References
1. Horton R. Offline: Looking forward to Donald Trump. The Lancet. 2016;388[10061]:2726.
2. Page L. What Donald Trump would do with the US healthcare system. BMJ. 2016;353:i2996.
3. Uberoi N, Finegold, K. and Gee, E. Health Insurance Coverage and the Affordable Care Act, 2010-2016. Department of Health and Human Services, ASPE Issue Brief, 2016 March 3.
4. Claxton G, Rae M, Long M, Damico A, Whitmore H, Foster G. Health Benefits In 2016: Family Premiums Rose Modestly, And Offer Rates Remained Stable. Health Aff (Millwood). 2016 Sep. doi: 10.1377/hlthaff.2016.0951.
5. Ku L, Broaddus M. Public and private health insurance: stacking up the costs. Health Aff (Millwood). 2008;27:w318-327.
6. Waters H, Steinhardt L, Oliver TR, Burton A, Milner S. The costs of non-insurance in Maryland. J Health Care Poor Underserved. 2007 Feb;18[1]:139-51.
7. Cheung MR. Lack of health insurance increases all cause and all cancer mortality in adults: an analysis of National Health and Nutrition Examination Survey (NHANES III) data. Asian Pac J Cancer Prev. 2013;14[4]:2259-63.
8. Gillis JZ, Yazdany J, Trupin L, et al. Medicaid and access to care among persons with systemic lupus erythematosus. Arthritis Rheum. 2007;57[4]:601-7.
9. Collins SR, Gunja M, Beutel S. How Will the Affordable Care Act’s Cost-Sharing Reductions Affect Consumers’ Out-of-Pocket Costs in 2016? Issue Brief (Commonw Fund) 2016;6:1-17.
10. Leader S, Yang H, DeVincenzo J, Jacobson P, Marcin JP, Murray DL. Time and out-of-pocket costs associated with respiratory syncytial virus hospitalization of infants. Value Health. 2003;6[2]:100-6.
11. Antos J CJ. The House Republicans’ Health Plan. Bethesda, MD: Health Affairs Blog, Project HOPE; 2016 June 22.
12. Fronstin P, Roebuck MC. Health care spending after adopting a full-replacement, high-deductible health plan with a health savings account: a five-year study. EBRI Issue Brief 2013 July:3-15.
13. Saltzman E EC. Donald Trump’s Health Care Reform Proposals: Anticipated Effects on Insurance Coverage, Out-of-Pocket Costs, and the Federal Deficit. The Commonwealth Fund September 2016.
14. Glied SA, Frank RG. Care for the Vulnerable vs. Cash for the Powerful – Trump’s Pick for HHS. N Engl J Med. 2017;376:103-5.
No matter on which side of the aisle you sit, and even if you’d prefer to just sit in your car and check Instagram, the results of the November election were likely a surprise. Speculation abounds by pundits and so-called experts as to what a Trump presidency means for health care in this country. The shape and scope of health care initiatives that a Trump administration will attempt to advance in place of the Affordable Care Act (ACA), which has likely met its demise, is unknown at the time of this writing. How Trump’s new initiatives fare in Congress and then get translated into practical changes in health care delivery and financing is even more muddled.
The U.S. medical community has remained largely silent, which is wise given the lack of evidence that would support any rational prediction, but perhaps it’s easier to pronounce judgment from across the pond. The Lancet recently reported the comment of Sophie Harman, PhD, a political scientist at Queen Mary University in London, who told an audience at the London School of Hygiene & Tropical Medicine to “ignore the dead cat in the room.”1 I spent 6 months of my residency in the United Kingdom, and this phrase never came up in my travels across the wards, streets, and pubs of the mother country. Apparently, the “dead cat strategy” is a legislative maneuver to distract attention from a party’s political shortcomings by raising a ruckus about a salacious or social hot-button topic. In this case, the dead cat may just be the carcass of Obamacare, exuding the fetor of millions of people losing their health insurance.
The BMJ, another respected U.K. journal, offered the pronouncement by Don Berwick, MD, former administrator of the Centers for Medicare & Medicaid Services, that Trump’s election would be “disastrous” for U.S. health care, but not much else.2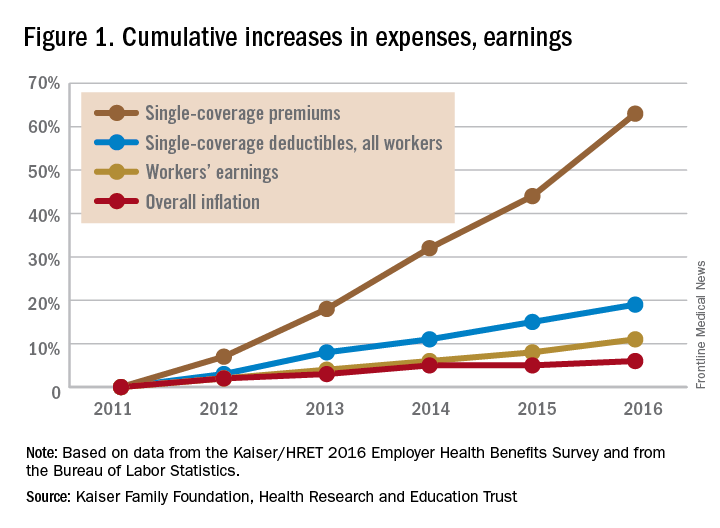
Out-of-pocket health care expenses for patients and families insured under Medicaid and its ACA-mandated expansion decreased to, on average, less than $500 per year; however, 19 states, all with Republican governors, blocked the Medicaid expansion.5 This denied more than 2.5 million people Medicaid coverage in these states; the overwhelming majority of these people remained uninsured. Uninsured people incur significant out-of-pocket costs when they do require health care, and have worse outcomes.6,7 The end of ACA throws Medicaid expansion in any state, with its protections to limit out-of-pocket expenses, into doubt.
Before the ACA expanded Medicaid coverage, patients faced significant wait times and travel costs associated with the low numbers of providers accepting Medicaid’s low reimbursement rate.8 These numbers had begun to improve after the ACA increased primary care physicians’ Medicaid reimbursements to Medicare rates in 2013 and 2014, but only a limited number of states will continue the increases after the end of federal subsidies.
For people who purchased plans on the ACA’s marketplace, out-of-pocket exposure is capped in 2017 at no more than $7,150 for an individual plan and $14,300 for a family plan before marketplace subsidies. Even those who qualified for cost-sharing deductions, with incomes between 100% and 250% of the federal poverty level, had out-of-pocket caps that varied widely depending on plan and state. For example, in 2016 at the $17,000 annual income level, out-of-pocket caps could range from $500 to $2,250.9
Clinician concern
On a provider level, incentives to reduce readmissions and limit health care–associated harm events mandated by the ACA may soon evaporate, throwing into question many quality metrics pursued by health systems. In response, will health system administrators abandon efforts to reduce readmissions and hospital-acquired conditions (HACs)? Or will health systems, despite the lack of a Medicare penalty “stick,” move forward with efforts to reduce readmissions and HACs? There’s no question of what would benefit the pocketbooks of our patients the most – every hospitalization results in significant direct out-of-pocket costs, not to mention lost productivity and income.10
It seems unlikely that a Republican-led government will pursue efforts to decrease out-of-pocket expenses. More likely, new proposals will aim to provide tax benefits to encourage use of health savings accounts (HSAs), continuing the shift of health care to employees.11 HSAs benefit employers, who pay less for the health care costs of employees, but are associated with worsened adherence to recommended treatments for patients.8,12
A 2016 study analyzed health care policies considered by Trump, including the following:
- Full repeal of the ACA.
- Repeal of the ACA plus tax deductions of health insurance premiums.
- Repeal of the ACA plus block grants to states for Medicaid and Children’s Health Insurance Program (CHIP).
- Repeal plus promotion of selling health insurance across state lines.
Not surprisingly, all four scenarios resulted in significant increases in out-of-pocket expenses for those in individual insurance plans.13
Although at the time of writing, the “replace” segment of “repeal-and-replace” is not known, Mr. Trump’s nominee for Secretary of Health and Human Services (HHS), Rep. Tom Price (R-Ga.), has given a hint of what he would champion based on his prior legislative proposals. Along with his support of increasing accessibility of armor-piercing bullets, reduced regulations on cigars, and opposition to expanding the State Children’s Health Insurance Program, he proposed H.R. 2300, “Empower Patients First Act.” This would eliminate the ACA’s Medicaid expansion and replace it with flat tax credits based on age, not income, which turns out to offer greater subsidies relative to income for those with higher incomes. A 30-year-old would, on average, face a premium bill of $2,532, along with a potential out-of-pocket liability of $7,000, with only a $1,200 credit to cover this from Mr. Price’s plan.14
In sum
So what’s a conscientious advocate for the physical and financial health of patients to do? Beyond political action, hospitalists need to keep abreast of the effect of changes in health care policy on their patients, as unpleasant as it may be. Do you know what the copays and out-of-pocket costs are for your patient’s (or your own) health care? Knowing how your recommendations for treatment and follow-up affect your patient’s pocketbook will not only help protect their finances, but will also protect their health, as people are less likely to be compliant with treatment if it involves out-of-pocket costs.
And easy as it would be to simply tune out the partisan rancor, stay engaged as a citizen, if for nothing else, the benefit of your patients.
Dr. Chang is pediatric editor of The Hospitalist. He is associate clinical professor of pediatrics at the University of Massachusetts, Worcester, and chief of pediatric hospital medicine at Baystate Children's Hospital, Springfield, Mass. Send comments and questions to [email protected].
References
1. Horton R. Offline: Looking forward to Donald Trump. The Lancet. 2016;388[10061]:2726.
2. Page L. What Donald Trump would do with the US healthcare system. BMJ. 2016;353:i2996.
3. Uberoi N, Finegold, K. and Gee, E. Health Insurance Coverage and the Affordable Care Act, 2010-2016. Department of Health and Human Services, ASPE Issue Brief, 2016 March 3.
4. Claxton G, Rae M, Long M, Damico A, Whitmore H, Foster G. Health Benefits In 2016: Family Premiums Rose Modestly, And Offer Rates Remained Stable. Health Aff (Millwood). 2016 Sep. doi: 10.1377/hlthaff.2016.0951.
5. Ku L, Broaddus M. Public and private health insurance: stacking up the costs. Health Aff (Millwood). 2008;27:w318-327.
6. Waters H, Steinhardt L, Oliver TR, Burton A, Milner S. The costs of non-insurance in Maryland. J Health Care Poor Underserved. 2007 Feb;18[1]:139-51.
7. Cheung MR. Lack of health insurance increases all cause and all cancer mortality in adults: an analysis of National Health and Nutrition Examination Survey (NHANES III) data. Asian Pac J Cancer Prev. 2013;14[4]:2259-63.
8. Gillis JZ, Yazdany J, Trupin L, et al. Medicaid and access to care among persons with systemic lupus erythematosus. Arthritis Rheum. 2007;57[4]:601-7.
9. Collins SR, Gunja M, Beutel S. How Will the Affordable Care Act’s Cost-Sharing Reductions Affect Consumers’ Out-of-Pocket Costs in 2016? Issue Brief (Commonw Fund) 2016;6:1-17.
10. Leader S, Yang H, DeVincenzo J, Jacobson P, Marcin JP, Murray DL. Time and out-of-pocket costs associated with respiratory syncytial virus hospitalization of infants. Value Health. 2003;6[2]:100-6.
11. Antos J CJ. The House Republicans’ Health Plan. Bethesda, MD: Health Affairs Blog, Project HOPE; 2016 June 22.
12. Fronstin P, Roebuck MC. Health care spending after adopting a full-replacement, high-deductible health plan with a health savings account: a five-year study. EBRI Issue Brief 2013 July:3-15.
13. Saltzman E EC. Donald Trump’s Health Care Reform Proposals: Anticipated Effects on Insurance Coverage, Out-of-Pocket Costs, and the Federal Deficit. The Commonwealth Fund September 2016.
14. Glied SA, Frank RG. Care for the Vulnerable vs. Cash for the Powerful – Trump’s Pick for HHS. N Engl J Med. 2017;376:103-5.