User login
The Hospitalist only
NAM offers recommendations to fight clinician burnout
WASHINGTON – a condition now estimated to affect a third to a half of clinicians in the United States, according to a report from an influential federal panel.
The National Academy of Medicine (NAM) on Oct. 23 released a report, “Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being.” The report calls for a broad and unified approach to tackling the root causes of burnout.
There must be a concerted effort by leaders of many fields of health care to create less stressful workplaces for clinicians, Pascale Carayon, PhD, cochair of the NAM committee that produced the report, said during the NAM press event.
“This is not an easy process,” said Dr. Carayon, a researcher into patient safety issues at the University of Wisconsin–Madison. “There is no single solution.”
The NAM report assigns specific tasks to many different participants in health care through a six-goal approach, as described below.
–Create positive workplaces. Leaders of health care systems should consider how their business and management decisions will affect clinicians’ jobs, taking into account the potential to add to their levels of burnout. Executives need to continuously monitor and evaluate the extent of burnout in their organizations, and report on this at least annually.
–Address burnout in training and in clinicians’ early years. Medical, nursing, and pharmacy schools should consider steps such as monitoring workload, implementing pass-fail grading, improving access to scholarships and affordable loans, and creating new loan repayment systems.
–Reduce administrative burden. Federal and state bodies and organizations such as the National Quality Forum should reconsider how their regulations and recommendations contribute to burnout. Organizations should seek to eliminate tasks that do not improve the care of patients.
–Improve usability and relevance of health information technology (IT). Medical organizations should develop and buy systems that are as user-friendly and easy to operate as possible. They also should look to use IT to reduce documentation demands and automate nonessential tasks.
–Reduce stigma and improve burnout recovery services. State officials and legislative bodies should make it easier for clinicians to use employee assistance programs, peer support programs, and mental health providers without the information being admissible in malpractice litigation. The report notes the recommendations from the Federation of State Medical Boards, American Medical Association, and the American Psychiatric Association on limiting inquiries in licensing applications about a clinician’s mental health. Questions should focus on current impairment rather than reach well into a clinician’s past.
–Create a national research agenda on clinician well-being. By the end of 2020, federal agencies – including the Agency for Healthcare Research and Quality, the National Institute for Occupational Safety and Health, the Health Resources and Services Administration, and the U.S. Department of Veterans Affairs – should develop a coordinated research agenda on clinician burnout, the report said.
In casting a wide net and assigning specific tasks, the NAM report seeks to establish efforts to address clinician burnout as a broad and shared responsibility. It would be too easy for different medical organizations to depict addressing burnout as being outside of their responsibilities, Christine K. Cassel, MD, the cochair of the NAM committee that produced the report, said during the press event.
“Nothing could be farther from the truth. Everyone is necessary to solve this problem,” said Dr. Cassel, who is a former chief executive officer of the National Quality Forum.
Darrell G. Kirch, MD, chief executive of the Association of American Medical Colleges, described the report as a “call to action” at the press event.
Previously published research has found between 35% and 54% of nurses and physicians in the United States have substantial symptoms of burnout, with the prevalence of burnout ranging between 45% and 60% for medical students and residents, the NAM report said.
Leaders of health organizations must consider how the policies they set will add stress for clinicians and make them less effective in caring for patients, said Vindell Washington, MD, chief medical officer of Blue Cross Blue Shield of Louisiana and a member of the NAM committee that wrote the report.
“Those linkages should be incentives and motivations for boards and leaders more broadly to act on the problem,” Dr. Washington said at the NAM event.
Dr. Kirch said he experienced burnout as a first-year medical student. He said a “brilliant aspect” of the NAM report is its emphasis on burnout as a response to the conditions under which medicine is practiced. In the past, burnout has been viewed as being the fault of the physician or nurse experiencing it, with the response then being to try to “fix” this individual, Dr. Kirch said at the event.
The NAM report instead defines burnout as a “work-related phenomenon studied since at least the 1970s,” in which an individual may experience exhaustion and detachment. Depression and other mental health issues such as anxiety disorders and addiction can follow burnout, he said. “That involves a real human toll.”
Joe Rotella, MD, MBA, chief medical officer at American Academy of Hospice and Palliative Medicine, said in an interview that this NAM paper has the potential to spark the kind of transformation that its earlier research did for the quality of care. Then called the Institute of Medicine(IOM), NAM in 1999 issued a report, “To Err Is Human,” which is broadly seen as a key catalyst in efforts in the ensuing decades to improve the quality of care. IOM then followed up with a 2001 report, “Crossing the Quality Chasm.”
“Those papers over a period of time really did change the way we do health care,” said Dr. Rotella, who was not involved with the NAM report.
In Dr. Rotella’s view, the NAM report provides a solid framework for what remains a daunting task, addressing the many factors involved in burnout.
“The most exciting thing about this is that they don’t have 500 recommendations. They had six and that’s something people can organize around,” he said. “They are not small goals. I’m not saying they are simple.”
The NAM report delves into the factors that contribute to burnout. These include a maze of government and commercial insurance plans that create “a confusing and onerous environment for clinicians,” with many of them juggling “multiple payment systems with complex rules, processes, metrics, and incentives that may frequently change.”
Clinicians face a growing field of measurements intended to judge the quality of their performance. While some of these are useful, others are duplicative and some are not relevant to patient care, the NAM report said.
The report also noted that many clinicians describe electronic health records (EHRs) as taking a toll on their work and private lives. Previously published research has found that for every hour spent with a patient, physicians spend an additional 1-2 hours on the EHR at work, with additional time needed to complete this data entry at home after work hours, the report said.
In an interview, Cynda Rushton, RN, PhD, a Johns Hopkins University researcher and a member of the NAM committee that produced the report, said this new publication will support efforts to overhaul many aspects of current medical practice. She said she hopes it will be a “catalyst for bold and fundamental reform.
“It’s taking a deep dive into the evidence to see how we can begin to dismantle the system’s contributions to burnout,” she said. “No longer can we put Band-Aids on a gaping wound.”
WASHINGTON – a condition now estimated to affect a third to a half of clinicians in the United States, according to a report from an influential federal panel.
The National Academy of Medicine (NAM) on Oct. 23 released a report, “Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being.” The report calls for a broad and unified approach to tackling the root causes of burnout.
There must be a concerted effort by leaders of many fields of health care to create less stressful workplaces for clinicians, Pascale Carayon, PhD, cochair of the NAM committee that produced the report, said during the NAM press event.
“This is not an easy process,” said Dr. Carayon, a researcher into patient safety issues at the University of Wisconsin–Madison. “There is no single solution.”
The NAM report assigns specific tasks to many different participants in health care through a six-goal approach, as described below.
–Create positive workplaces. Leaders of health care systems should consider how their business and management decisions will affect clinicians’ jobs, taking into account the potential to add to their levels of burnout. Executives need to continuously monitor and evaluate the extent of burnout in their organizations, and report on this at least annually.
–Address burnout in training and in clinicians’ early years. Medical, nursing, and pharmacy schools should consider steps such as monitoring workload, implementing pass-fail grading, improving access to scholarships and affordable loans, and creating new loan repayment systems.
–Reduce administrative burden. Federal and state bodies and organizations such as the National Quality Forum should reconsider how their regulations and recommendations contribute to burnout. Organizations should seek to eliminate tasks that do not improve the care of patients.
–Improve usability and relevance of health information technology (IT). Medical organizations should develop and buy systems that are as user-friendly and easy to operate as possible. They also should look to use IT to reduce documentation demands and automate nonessential tasks.
–Reduce stigma and improve burnout recovery services. State officials and legislative bodies should make it easier for clinicians to use employee assistance programs, peer support programs, and mental health providers without the information being admissible in malpractice litigation. The report notes the recommendations from the Federation of State Medical Boards, American Medical Association, and the American Psychiatric Association on limiting inquiries in licensing applications about a clinician’s mental health. Questions should focus on current impairment rather than reach well into a clinician’s past.
–Create a national research agenda on clinician well-being. By the end of 2020, federal agencies – including the Agency for Healthcare Research and Quality, the National Institute for Occupational Safety and Health, the Health Resources and Services Administration, and the U.S. Department of Veterans Affairs – should develop a coordinated research agenda on clinician burnout, the report said.
In casting a wide net and assigning specific tasks, the NAM report seeks to establish efforts to address clinician burnout as a broad and shared responsibility. It would be too easy for different medical organizations to depict addressing burnout as being outside of their responsibilities, Christine K. Cassel, MD, the cochair of the NAM committee that produced the report, said during the press event.
“Nothing could be farther from the truth. Everyone is necessary to solve this problem,” said Dr. Cassel, who is a former chief executive officer of the National Quality Forum.
Darrell G. Kirch, MD, chief executive of the Association of American Medical Colleges, described the report as a “call to action” at the press event.
Previously published research has found between 35% and 54% of nurses and physicians in the United States have substantial symptoms of burnout, with the prevalence of burnout ranging between 45% and 60% for medical students and residents, the NAM report said.
Leaders of health organizations must consider how the policies they set will add stress for clinicians and make them less effective in caring for patients, said Vindell Washington, MD, chief medical officer of Blue Cross Blue Shield of Louisiana and a member of the NAM committee that wrote the report.
“Those linkages should be incentives and motivations for boards and leaders more broadly to act on the problem,” Dr. Washington said at the NAM event.
Dr. Kirch said he experienced burnout as a first-year medical student. He said a “brilliant aspect” of the NAM report is its emphasis on burnout as a response to the conditions under which medicine is practiced. In the past, burnout has been viewed as being the fault of the physician or nurse experiencing it, with the response then being to try to “fix” this individual, Dr. Kirch said at the event.
The NAM report instead defines burnout as a “work-related phenomenon studied since at least the 1970s,” in which an individual may experience exhaustion and detachment. Depression and other mental health issues such as anxiety disorders and addiction can follow burnout, he said. “That involves a real human toll.”
Joe Rotella, MD, MBA, chief medical officer at American Academy of Hospice and Palliative Medicine, said in an interview that this NAM paper has the potential to spark the kind of transformation that its earlier research did for the quality of care. Then called the Institute of Medicine(IOM), NAM in 1999 issued a report, “To Err Is Human,” which is broadly seen as a key catalyst in efforts in the ensuing decades to improve the quality of care. IOM then followed up with a 2001 report, “Crossing the Quality Chasm.”
“Those papers over a period of time really did change the way we do health care,” said Dr. Rotella, who was not involved with the NAM report.
In Dr. Rotella’s view, the NAM report provides a solid framework for what remains a daunting task, addressing the many factors involved in burnout.
“The most exciting thing about this is that they don’t have 500 recommendations. They had six and that’s something people can organize around,” he said. “They are not small goals. I’m not saying they are simple.”
The NAM report delves into the factors that contribute to burnout. These include a maze of government and commercial insurance plans that create “a confusing and onerous environment for clinicians,” with many of them juggling “multiple payment systems with complex rules, processes, metrics, and incentives that may frequently change.”
Clinicians face a growing field of measurements intended to judge the quality of their performance. While some of these are useful, others are duplicative and some are not relevant to patient care, the NAM report said.
The report also noted that many clinicians describe electronic health records (EHRs) as taking a toll on their work and private lives. Previously published research has found that for every hour spent with a patient, physicians spend an additional 1-2 hours on the EHR at work, with additional time needed to complete this data entry at home after work hours, the report said.
In an interview, Cynda Rushton, RN, PhD, a Johns Hopkins University researcher and a member of the NAM committee that produced the report, said this new publication will support efforts to overhaul many aspects of current medical practice. She said she hopes it will be a “catalyst for bold and fundamental reform.
“It’s taking a deep dive into the evidence to see how we can begin to dismantle the system’s contributions to burnout,” she said. “No longer can we put Band-Aids on a gaping wound.”
WASHINGTON – a condition now estimated to affect a third to a half of clinicians in the United States, according to a report from an influential federal panel.
The National Academy of Medicine (NAM) on Oct. 23 released a report, “Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being.” The report calls for a broad and unified approach to tackling the root causes of burnout.
There must be a concerted effort by leaders of many fields of health care to create less stressful workplaces for clinicians, Pascale Carayon, PhD, cochair of the NAM committee that produced the report, said during the NAM press event.
“This is not an easy process,” said Dr. Carayon, a researcher into patient safety issues at the University of Wisconsin–Madison. “There is no single solution.”
The NAM report assigns specific tasks to many different participants in health care through a six-goal approach, as described below.
–Create positive workplaces. Leaders of health care systems should consider how their business and management decisions will affect clinicians’ jobs, taking into account the potential to add to their levels of burnout. Executives need to continuously monitor and evaluate the extent of burnout in their organizations, and report on this at least annually.
–Address burnout in training and in clinicians’ early years. Medical, nursing, and pharmacy schools should consider steps such as monitoring workload, implementing pass-fail grading, improving access to scholarships and affordable loans, and creating new loan repayment systems.
–Reduce administrative burden. Federal and state bodies and organizations such as the National Quality Forum should reconsider how their regulations and recommendations contribute to burnout. Organizations should seek to eliminate tasks that do not improve the care of patients.
–Improve usability and relevance of health information technology (IT). Medical organizations should develop and buy systems that are as user-friendly and easy to operate as possible. They also should look to use IT to reduce documentation demands and automate nonessential tasks.
–Reduce stigma and improve burnout recovery services. State officials and legislative bodies should make it easier for clinicians to use employee assistance programs, peer support programs, and mental health providers without the information being admissible in malpractice litigation. The report notes the recommendations from the Federation of State Medical Boards, American Medical Association, and the American Psychiatric Association on limiting inquiries in licensing applications about a clinician’s mental health. Questions should focus on current impairment rather than reach well into a clinician’s past.
–Create a national research agenda on clinician well-being. By the end of 2020, federal agencies – including the Agency for Healthcare Research and Quality, the National Institute for Occupational Safety and Health, the Health Resources and Services Administration, and the U.S. Department of Veterans Affairs – should develop a coordinated research agenda on clinician burnout, the report said.
In casting a wide net and assigning specific tasks, the NAM report seeks to establish efforts to address clinician burnout as a broad and shared responsibility. It would be too easy for different medical organizations to depict addressing burnout as being outside of their responsibilities, Christine K. Cassel, MD, the cochair of the NAM committee that produced the report, said during the press event.
“Nothing could be farther from the truth. Everyone is necessary to solve this problem,” said Dr. Cassel, who is a former chief executive officer of the National Quality Forum.
Darrell G. Kirch, MD, chief executive of the Association of American Medical Colleges, described the report as a “call to action” at the press event.
Previously published research has found between 35% and 54% of nurses and physicians in the United States have substantial symptoms of burnout, with the prevalence of burnout ranging between 45% and 60% for medical students and residents, the NAM report said.
Leaders of health organizations must consider how the policies they set will add stress for clinicians and make them less effective in caring for patients, said Vindell Washington, MD, chief medical officer of Blue Cross Blue Shield of Louisiana and a member of the NAM committee that wrote the report.
“Those linkages should be incentives and motivations for boards and leaders more broadly to act on the problem,” Dr. Washington said at the NAM event.
Dr. Kirch said he experienced burnout as a first-year medical student. He said a “brilliant aspect” of the NAM report is its emphasis on burnout as a response to the conditions under which medicine is practiced. In the past, burnout has been viewed as being the fault of the physician or nurse experiencing it, with the response then being to try to “fix” this individual, Dr. Kirch said at the event.
The NAM report instead defines burnout as a “work-related phenomenon studied since at least the 1970s,” in which an individual may experience exhaustion and detachment. Depression and other mental health issues such as anxiety disorders and addiction can follow burnout, he said. “That involves a real human toll.”
Joe Rotella, MD, MBA, chief medical officer at American Academy of Hospice and Palliative Medicine, said in an interview that this NAM paper has the potential to spark the kind of transformation that its earlier research did for the quality of care. Then called the Institute of Medicine(IOM), NAM in 1999 issued a report, “To Err Is Human,” which is broadly seen as a key catalyst in efforts in the ensuing decades to improve the quality of care. IOM then followed up with a 2001 report, “Crossing the Quality Chasm.”
“Those papers over a period of time really did change the way we do health care,” said Dr. Rotella, who was not involved with the NAM report.
In Dr. Rotella’s view, the NAM report provides a solid framework for what remains a daunting task, addressing the many factors involved in burnout.
“The most exciting thing about this is that they don’t have 500 recommendations. They had six and that’s something people can organize around,” he said. “They are not small goals. I’m not saying they are simple.”
The NAM report delves into the factors that contribute to burnout. These include a maze of government and commercial insurance plans that create “a confusing and onerous environment for clinicians,” with many of them juggling “multiple payment systems with complex rules, processes, metrics, and incentives that may frequently change.”
Clinicians face a growing field of measurements intended to judge the quality of their performance. While some of these are useful, others are duplicative and some are not relevant to patient care, the NAM report said.
The report also noted that many clinicians describe electronic health records (EHRs) as taking a toll on their work and private lives. Previously published research has found that for every hour spent with a patient, physicians spend an additional 1-2 hours on the EHR at work, with additional time needed to complete this data entry at home after work hours, the report said.
In an interview, Cynda Rushton, RN, PhD, a Johns Hopkins University researcher and a member of the NAM committee that produced the report, said this new publication will support efforts to overhaul many aspects of current medical practice. She said she hopes it will be a “catalyst for bold and fundamental reform.
“It’s taking a deep dive into the evidence to see how we can begin to dismantle the system’s contributions to burnout,” she said. “No longer can we put Band-Aids on a gaping wound.”
The growing NP and PA workforce in hospital medicine
High rate of turnover among NPs, PAs
If you were a physician hospitalist in a group serving adults in 2017 you probably worked with nurse practitioners (NPs) and/or physician assistants (PAs). Seventy-seven percent of hospital medicine groups (HMGs) employed NPs and PAs that year.
In addition, the larger the group, the more likely the group was to have NPs and PAs as part of their practice model – 89% of hospital medicine groups with more than 30 physician had NPs and/or PAs as partners. In addition, the mean number of physicians for adult hospital medicine groups was 17.9. The same practices employed an average of 3.5 NPs, and 2.6 PAs.
Based on these numbers, there are just under three physicians per NP and PA in the typical HMG serving adults. This is all according to data from the 2018 State of Hospital Medicine (SoHM) report that was published in 2019 by the Society of Hospital Medicine.
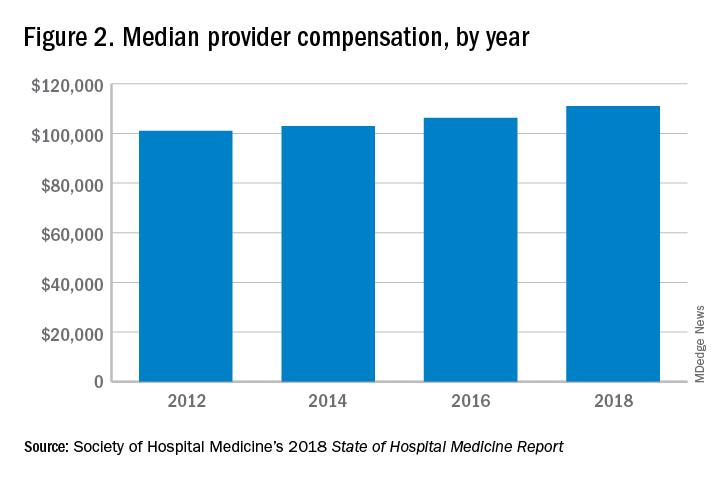
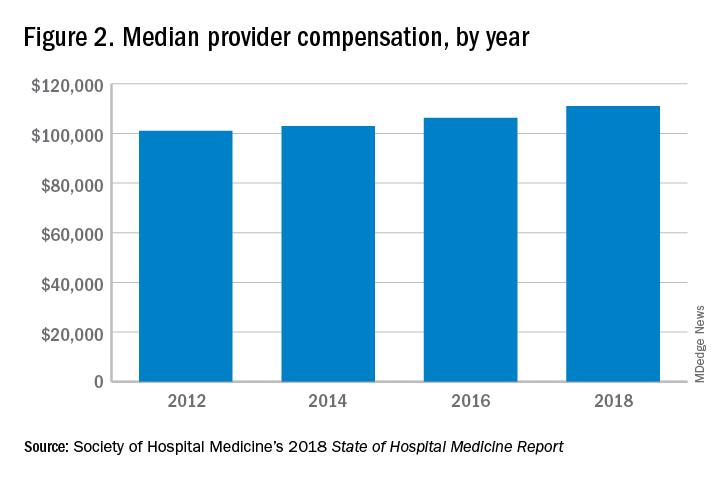
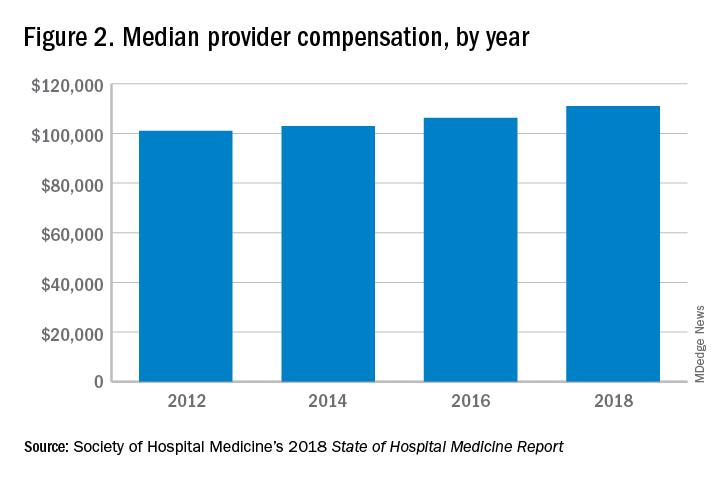
These observations lead to a number of questions. One thing that is not clear from the SoHM is why NPs and PAs are becoming a larger part of the hospital medicine workforce, but there are some insights and conjecture that can be drawn from the data. The first is economics. Over 6 years, the median incomes of NPs and PAs have risen a relatively modest 10%; over the same period physician hospitalists have seen a whopping 23.6% median pay increase.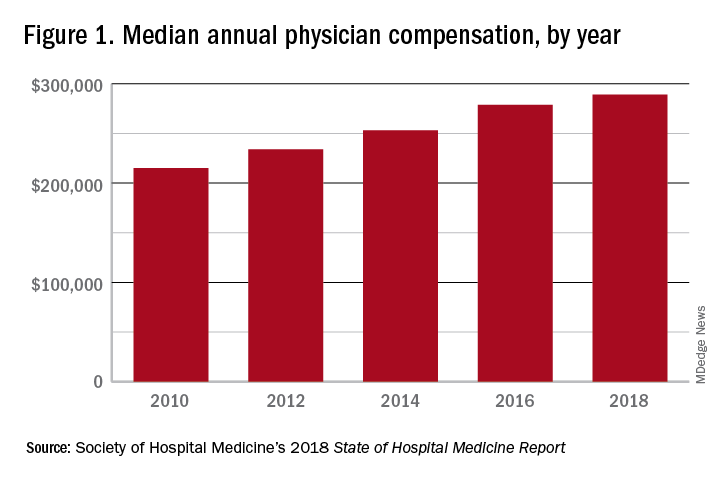
One argument against economics as a driving force behind greater use of NPs and PAs in the hospital medicine workforce is the billing patterns of HMGs that use NPs and PAs. Ten percent of HMGs do not have their NPs and PAs bill at all. The distribution of HMGs that predominantly bill NP and PA services as shared visits, versus having NPs and PAs bill independently, has also not changed much over the years, with 22% of HMGs having NPs and PAs bill independently as a predominant model. This would seem to suggest that some HMGs may not have learned how to deploy NPs and PAs effectively.
While inefficiency can be due to hospital bylaws, the culture of the hospital medicine group, or the skill set of the NPs and PAs working in HMGs – it would seem that if the driving force for the increase in the utilization of NPs and PAs in HMGs was financial, then that would also result in more of these providers billing independently, or alternatively, an increase in hospitalist physician productivity, which the data do not show. However, multistate HMGs may have this figured out better than some of the rest of us – 78% of these HMGs have NPs and PAs billing independently! All other categories of HMGs together are around 13%, with the next highest being hospital or health system integrated delivery systems, where NPs/PAs bill independently about 15% of the time.
In the last 2 years of the survey, there have been marked increases in the number of NPs and PAs at HMGs performing “nontraditional” services. For example, outpatient work has increased from 11% to 17%, and work in the postacute space has increased from 13% to 25%. Work in behavioral health and alcohol and drug rehab facilities has also increased, from 17% to 26%. As HMGs seek to rationalize their workforce while expanding, it is possible that decision makers have felt that it was either more economical to place NPs and PAs in positions where they are seeing these patients, or it was more aligned with the NP/PA skill set, or both. In any event, as the scope of hospital medicine broadens, the use of PAs and NPs has also increased – which is probably not coincidental.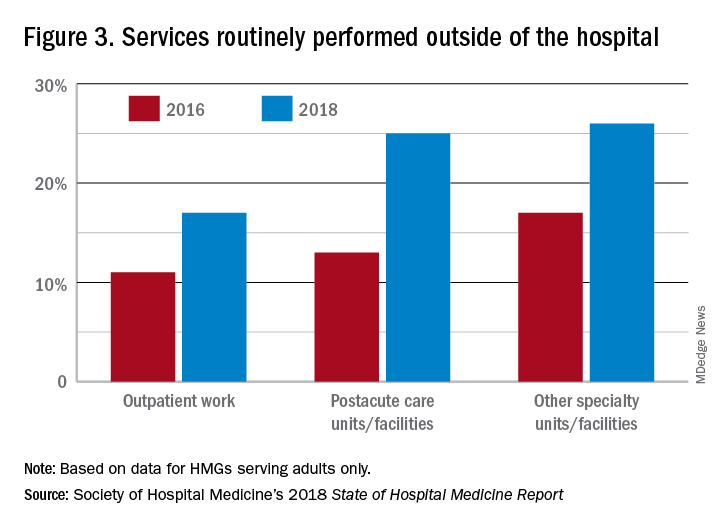
The average hospital medicine group continues to have staff openings. Workforce shortages may be leading to what in the past may have been considered physician openings being filled by NPs and PAs. Only 33% of HMGs reported having all their physician openings filled. Median physician shortage was 12% of total approved staffing. Given concerns in hospital medicine about provider burnout, the number of hospital medicine openings is no doubt a concern to HMG leaders and hospitalists. And necessity being the mother of invention, HMG leadership must be thinking differently than in the past about open positions and the skill mix needed to fill them. I believe this is leading to NPs and PAs being considered more often for a role that would have been open only to a physician in the past.
Just as open positions are a concern, so is turnover. One striking finding in the SoHM is the very high rate of turnover among NPs and PAs – a whopping 19.1% per year. For physicians, the same rate was 7.4% and has been declining every survey for many years. While NPs and PAs may be intended to stabilize the workforce, because of how this is being done in some groups, NPs and PAs may instead be a destabilizing factor. Rapid growth can lead to haphazard onboarding and less than clearly defined roles. NPs and PAs may often be placed into roles for which they are not yet prepared. In addition, the pay disparity between NPs and PAs and physicians has increased. As a new field, and with many HMGs still rapidly growing, increased thoughtfulness and maturity about how NPs and PAs are integrated into hospital medicine practices should lead to less turnover and better HMG stability in the future.
These observations could mark a future that includes higher pay for hospital medicine PAs and NPs (and potentially a slowdown in salary growth for physicians); HMGs taking steps to make the financial model more attractive by having NPs and PAs bill independently more often; and HMGs and their leaders engaging NPs and PAs by more clearly defining roles, shoring up onboarding and mentoring programs, and other measures that decrease turnover. This would help to make hospital medicine a career destination, rather than a stopping off point for NPs and PAs, much as it has become for internists over the past 20 years.
Dr. Frederickson is medical director, hospital medicine and palliative care, at CHI Health, Omaha, Neb., and assistant professor at Creighton University, Omaha.
High rate of turnover among NPs, PAs
High rate of turnover among NPs, PAs
If you were a physician hospitalist in a group serving adults in 2017 you probably worked with nurse practitioners (NPs) and/or physician assistants (PAs). Seventy-seven percent of hospital medicine groups (HMGs) employed NPs and PAs that year.
In addition, the larger the group, the more likely the group was to have NPs and PAs as part of their practice model – 89% of hospital medicine groups with more than 30 physician had NPs and/or PAs as partners. In addition, the mean number of physicians for adult hospital medicine groups was 17.9. The same practices employed an average of 3.5 NPs, and 2.6 PAs.
Based on these numbers, there are just under three physicians per NP and PA in the typical HMG serving adults. This is all according to data from the 2018 State of Hospital Medicine (SoHM) report that was published in 2019 by the Society of Hospital Medicine.
These observations lead to a number of questions. One thing that is not clear from the SoHM is why NPs and PAs are becoming a larger part of the hospital medicine workforce, but there are some insights and conjecture that can be drawn from the data. The first is economics. Over 6 years, the median incomes of NPs and PAs have risen a relatively modest 10%; over the same period physician hospitalists have seen a whopping 23.6% median pay increase.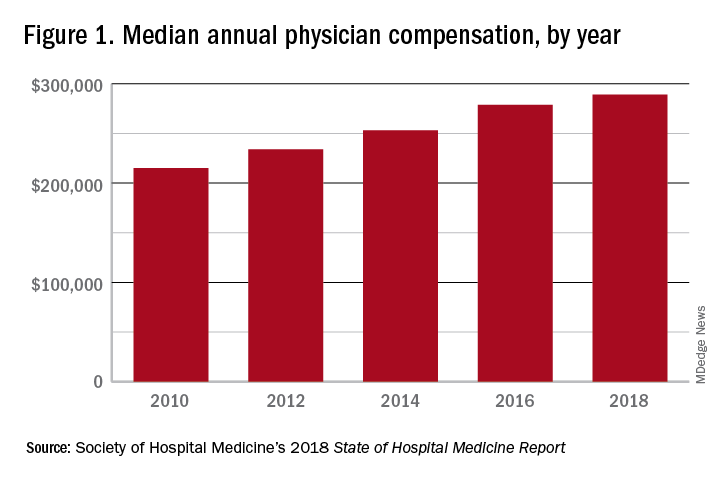
One argument against economics as a driving force behind greater use of NPs and PAs in the hospital medicine workforce is the billing patterns of HMGs that use NPs and PAs. Ten percent of HMGs do not have their NPs and PAs bill at all. The distribution of HMGs that predominantly bill NP and PA services as shared visits, versus having NPs and PAs bill independently, has also not changed much over the years, with 22% of HMGs having NPs and PAs bill independently as a predominant model. This would seem to suggest that some HMGs may not have learned how to deploy NPs and PAs effectively.
While inefficiency can be due to hospital bylaws, the culture of the hospital medicine group, or the skill set of the NPs and PAs working in HMGs – it would seem that if the driving force for the increase in the utilization of NPs and PAs in HMGs was financial, then that would also result in more of these providers billing independently, or alternatively, an increase in hospitalist physician productivity, which the data do not show. However, multistate HMGs may have this figured out better than some of the rest of us – 78% of these HMGs have NPs and PAs billing independently! All other categories of HMGs together are around 13%, with the next highest being hospital or health system integrated delivery systems, where NPs/PAs bill independently about 15% of the time.
In the last 2 years of the survey, there have been marked increases in the number of NPs and PAs at HMGs performing “nontraditional” services. For example, outpatient work has increased from 11% to 17%, and work in the postacute space has increased from 13% to 25%. Work in behavioral health and alcohol and drug rehab facilities has also increased, from 17% to 26%. As HMGs seek to rationalize their workforce while expanding, it is possible that decision makers have felt that it was either more economical to place NPs and PAs in positions where they are seeing these patients, or it was more aligned with the NP/PA skill set, or both. In any event, as the scope of hospital medicine broadens, the use of PAs and NPs has also increased – which is probably not coincidental.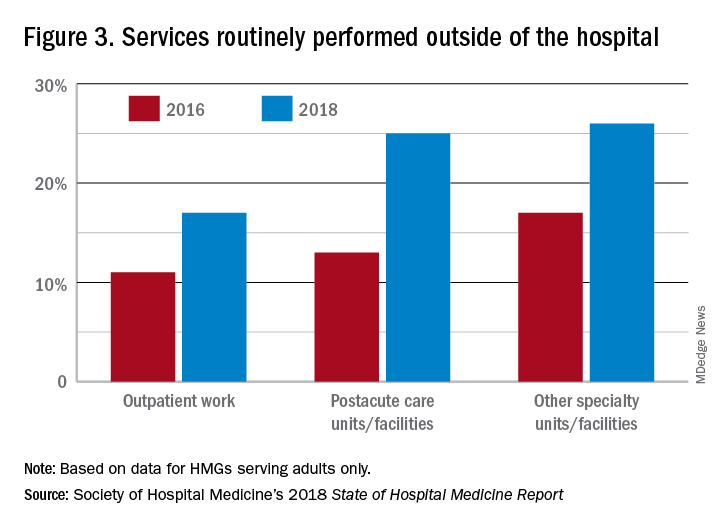
The average hospital medicine group continues to have staff openings. Workforce shortages may be leading to what in the past may have been considered physician openings being filled by NPs and PAs. Only 33% of HMGs reported having all their physician openings filled. Median physician shortage was 12% of total approved staffing. Given concerns in hospital medicine about provider burnout, the number of hospital medicine openings is no doubt a concern to HMG leaders and hospitalists. And necessity being the mother of invention, HMG leadership must be thinking differently than in the past about open positions and the skill mix needed to fill them. I believe this is leading to NPs and PAs being considered more often for a role that would have been open only to a physician in the past.
Just as open positions are a concern, so is turnover. One striking finding in the SoHM is the very high rate of turnover among NPs and PAs – a whopping 19.1% per year. For physicians, the same rate was 7.4% and has been declining every survey for many years. While NPs and PAs may be intended to stabilize the workforce, because of how this is being done in some groups, NPs and PAs may instead be a destabilizing factor. Rapid growth can lead to haphazard onboarding and less than clearly defined roles. NPs and PAs may often be placed into roles for which they are not yet prepared. In addition, the pay disparity between NPs and PAs and physicians has increased. As a new field, and with many HMGs still rapidly growing, increased thoughtfulness and maturity about how NPs and PAs are integrated into hospital medicine practices should lead to less turnover and better HMG stability in the future.
These observations could mark a future that includes higher pay for hospital medicine PAs and NPs (and potentially a slowdown in salary growth for physicians); HMGs taking steps to make the financial model more attractive by having NPs and PAs bill independently more often; and HMGs and their leaders engaging NPs and PAs by more clearly defining roles, shoring up onboarding and mentoring programs, and other measures that decrease turnover. This would help to make hospital medicine a career destination, rather than a stopping off point for NPs and PAs, much as it has become for internists over the past 20 years.
Dr. Frederickson is medical director, hospital medicine and palliative care, at CHI Health, Omaha, Neb., and assistant professor at Creighton University, Omaha.
If you were a physician hospitalist in a group serving adults in 2017 you probably worked with nurse practitioners (NPs) and/or physician assistants (PAs). Seventy-seven percent of hospital medicine groups (HMGs) employed NPs and PAs that year.
In addition, the larger the group, the more likely the group was to have NPs and PAs as part of their practice model – 89% of hospital medicine groups with more than 30 physician had NPs and/or PAs as partners. In addition, the mean number of physicians for adult hospital medicine groups was 17.9. The same practices employed an average of 3.5 NPs, and 2.6 PAs.
Based on these numbers, there are just under three physicians per NP and PA in the typical HMG serving adults. This is all according to data from the 2018 State of Hospital Medicine (SoHM) report that was published in 2019 by the Society of Hospital Medicine.
These observations lead to a number of questions. One thing that is not clear from the SoHM is why NPs and PAs are becoming a larger part of the hospital medicine workforce, but there are some insights and conjecture that can be drawn from the data. The first is economics. Over 6 years, the median incomes of NPs and PAs have risen a relatively modest 10%; over the same period physician hospitalists have seen a whopping 23.6% median pay increase.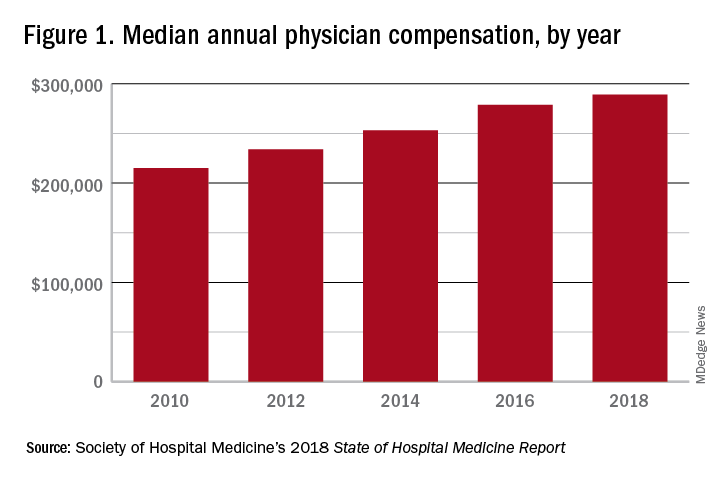
One argument against economics as a driving force behind greater use of NPs and PAs in the hospital medicine workforce is the billing patterns of HMGs that use NPs and PAs. Ten percent of HMGs do not have their NPs and PAs bill at all. The distribution of HMGs that predominantly bill NP and PA services as shared visits, versus having NPs and PAs bill independently, has also not changed much over the years, with 22% of HMGs having NPs and PAs bill independently as a predominant model. This would seem to suggest that some HMGs may not have learned how to deploy NPs and PAs effectively.
While inefficiency can be due to hospital bylaws, the culture of the hospital medicine group, or the skill set of the NPs and PAs working in HMGs – it would seem that if the driving force for the increase in the utilization of NPs and PAs in HMGs was financial, then that would also result in more of these providers billing independently, or alternatively, an increase in hospitalist physician productivity, which the data do not show. However, multistate HMGs may have this figured out better than some of the rest of us – 78% of these HMGs have NPs and PAs billing independently! All other categories of HMGs together are around 13%, with the next highest being hospital or health system integrated delivery systems, where NPs/PAs bill independently about 15% of the time.
In the last 2 years of the survey, there have been marked increases in the number of NPs and PAs at HMGs performing “nontraditional” services. For example, outpatient work has increased from 11% to 17%, and work in the postacute space has increased from 13% to 25%. Work in behavioral health and alcohol and drug rehab facilities has also increased, from 17% to 26%. As HMGs seek to rationalize their workforce while expanding, it is possible that decision makers have felt that it was either more economical to place NPs and PAs in positions where they are seeing these patients, or it was more aligned with the NP/PA skill set, or both. In any event, as the scope of hospital medicine broadens, the use of PAs and NPs has also increased – which is probably not coincidental.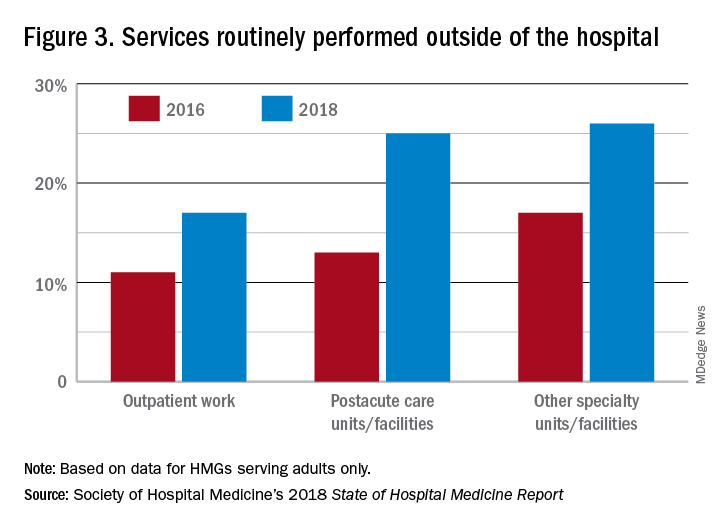
The average hospital medicine group continues to have staff openings. Workforce shortages may be leading to what in the past may have been considered physician openings being filled by NPs and PAs. Only 33% of HMGs reported having all their physician openings filled. Median physician shortage was 12% of total approved staffing. Given concerns in hospital medicine about provider burnout, the number of hospital medicine openings is no doubt a concern to HMG leaders and hospitalists. And necessity being the mother of invention, HMG leadership must be thinking differently than in the past about open positions and the skill mix needed to fill them. I believe this is leading to NPs and PAs being considered more often for a role that would have been open only to a physician in the past.
Just as open positions are a concern, so is turnover. One striking finding in the SoHM is the very high rate of turnover among NPs and PAs – a whopping 19.1% per year. For physicians, the same rate was 7.4% and has been declining every survey for many years. While NPs and PAs may be intended to stabilize the workforce, because of how this is being done in some groups, NPs and PAs may instead be a destabilizing factor. Rapid growth can lead to haphazard onboarding and less than clearly defined roles. NPs and PAs may often be placed into roles for which they are not yet prepared. In addition, the pay disparity between NPs and PAs and physicians has increased. As a new field, and with many HMGs still rapidly growing, increased thoughtfulness and maturity about how NPs and PAs are integrated into hospital medicine practices should lead to less turnover and better HMG stability in the future.
These observations could mark a future that includes higher pay for hospital medicine PAs and NPs (and potentially a slowdown in salary growth for physicians); HMGs taking steps to make the financial model more attractive by having NPs and PAs bill independently more often; and HMGs and their leaders engaging NPs and PAs by more clearly defining roles, shoring up onboarding and mentoring programs, and other measures that decrease turnover. This would help to make hospital medicine a career destination, rather than a stopping off point for NPs and PAs, much as it has become for internists over the past 20 years.
Dr. Frederickson is medical director, hospital medicine and palliative care, at CHI Health, Omaha, Neb., and assistant professor at Creighton University, Omaha.
Gender bias and pediatric hospital medicine
Where do we go from here?
Autumn is a busy time for pediatric hospitalists, with this autumn being particularly eventful as the first American Board of Pediatrics (ABP) certifying exam for Pediatric Hospital Medicine (PHM) will be offered on Nov. 12, 2019.
More than 1,600 med/peds and pediatric hospitalists applied to be eligible for the 2019 exam, 71% of whom were women. At least 3.9% of those applicants were denied eligibility for the 2019 exam.1 These denials resulted in discussions on the American Academy of Pediatrics Section on Hospital Medicine (AAP SOHM) email listserv related to unintentional gender bias.
PHM was first recognized as a subspecialty by the American Board of Medical Specialties in December 2015.2 Since that time, the ABP’s PHM sub-board developed eligibility criteria for practicing pediatric and med/peds hospitalists to apply for the exam. The sub-board identified three paths: a training pathway for applicants who had completed a 2-year PHM fellowship, a practice pathway for those satisfying ABP criteria for clinical activity in PHM, and a combined pathway for applicants who had completed PHM fellowships lasting less than 2 years.
Based on these pathways, 1,627 applicants applied for eligibility for the first PHM board certification exam.1 However, many concerns arose with the practice pathway eligibility criteria.
The PHM practice pathway initially included the following eligibility criteria:
• General pediatrics board certification.
• PHM practice “look back” period ends on or before June 30 of the exam year and starts 4 years earlier.
• More than 0.5 FTE professional PHM-related activities (patient-care, research, administration), defined as more than 900 hours/year every year for the preceding 4 years.
• More than 0.25 FTE direct patient care of hospitalized children, defined as more than 450 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice interruptions cannot exceed 3 months in the preceding 4 years, or 6 months in the preceding 5 years.
• Practice experience and hours were acquired in the United States and Canada.1,3
The start date and practice interruptions criteria in the practice pathway posed hurdles for many female applicants. Many women voiced concerns about feeling disadvantaged when applying for the PHM certifying exam and some of these women shared their concerns on the AAP SOHM email listserv. In response to these concerns, the PHM community called for increased transparency from the ABP related to denials, specifically related to unintentional gender bias against women applying for the exam.
David Skey, MD, and Jamee Walters, MD, pediatric hospitalists at Arnold Palmer Medical Center in Orlando, heard these concerns and decided to draft a petition with the help of legal counsel. The petition “demand[ed] immediate action,” and “request[ed] a formal response from the ABP regarding the practice pathway criteria.” The petition also stated that there was insufficient data to determine if the practice pathway “disadvantages women.” The petition asked the ABP to “facilitate a timely analysis to determine if gender bias” was present, or to perform an internal analysis and “release the findings publicly.”4
The petition was shared with the PHM community via the AAP SOHM listserv on July 29, 2019. Dr. Walters stated she was pleased by the response she and Dr. Skey received from the PHM community, on and off the AAP SOHM listserv. The petition was submitted to the ABP on Aug. 6, 2019, with 1,479 signatures.
On Aug. 29, 2019, the ABP’s response was shared on the AAP SOHM email listserv1 and was later published in the Journal of Hospital Medicine as a Special Announcement.5 In its response, the ABP stated that the gender bias allegation was “not supported by the facts” as there was “no significant difference between the percentage of women and men who were denied” eligibility.”5 In addressing the gender bias allegations and clarifying the practice pathway eligibility, the ABP removed the practice interruption criteria and modified the practice pathway criteria as follows:
• General pediatrics board certification.
• PHM practice started on or before July 2015 (for board eligibility in 2019).
• Professional PHM-related activities (patient-care, research, administration), defined as more than 900-1000 hours/year every year for the preceding 4 years.
• Direct patient care of hospitalized children, defined as more than 450-500 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice experience and hours were acquired in the United States and Canada.1
Following the release of the ABP’s response, many members of the PHM community remain concerned about the ABP’s revised criteria. Arti Desai, MD, pediatric hospitalist at Seattle Children’s and senior author on a “Perspectives in Hospital Medicine” in the Journal of Hospital Medicine,6 was appreciative that the ABP chose to remove the practice interruptions criterion. However, she and her colleagues remain concerned about lingering gender bias in the ABP’s practice pathway eligibility criteria surrounding the “start date” criterion. The authors state that this criterion differentially affects women, as women may take time off during or after residency for maternity or family leave. Dr. Desai states that this criterion alone can affect a woman’s chance for being eligible for the practice pathway.
Other members of the PHM community also expressed concerns about the ABP’s response to the PHM petition. Beth C. Natt, MD, pediatric hospitalist and director of pediatric hospital medicine regional programs at Connecticut Children’s in Hartford, felt that the population may have been self-selected, as the ABP’s data were limited to individuals who applied for exam eligibility. She was concerned that the data excluded pediatric hospitalists who chose not to apply because of uncertainty about meeting eligibility criteria. Klint Schwenk, MD, pediatric hospitalist at Norton Children’s Hospital in Louisville, Ky., stated that he wished the ABP had addressed the number of pediatric hospitalists who elected not to apply based on fear of ineligibility before concluding that there was no bias. He likened the ABP’s response to that of study authors omitting selection bias when discussing the limitations of their study.
Courtney Edgar-Zarate, MD, med/peds hospitalist and associate program director of the internal medicine/pediatrics residency at the University of Arkansas, expressed concerns that the ABP’s stringent clinical patient care hours criterion may unintentionally result in ineligibility for many mid-career or senior med/peds hospitalists. Dr. Edgar-Zarate also voiced concerns that graduating med/peds residents were electing not to pursue careers in hospital medicine because they would be required to complete a PHM fellowship to become a pediatric hospitalist, when a similar fellowship is not required to practice adult hospital medicine.
The Society of Hospital Medicine shared its position in regard to the ABP’s response in a Special Announcement in the Journal of Hospital Medicine.7 In it, SHM’s pediatric leaders recognized physicians for the excellent care they provide to hospitalized children. They stated that SHM would continue to support all hospitalists, independent of board eligibility status, and would continue to offer these hospitalists the merit-based Fellow designation. SHM’s pediatric leaders also proposed future directions for the ABP, including a Focused Practice Pathway in Hospital Medicine (FPHM), such as what the American Board of Internal Medicine and the American Board of Family Medicine have adopted for board recertification in internal medicine and family medicine. This maintenance of certification program that allows physicians primarily practicing in inpatient settings to focus their continuing education on inpatient practice, and is not a subspecialty.7
Dr. Edgar-Zarate fully supports the future directions for pediatric hospitalists outlined in SHM’s Special Announcement. She hopes that the ABP will support the FPHM. She feels the FPHM will encourage more med/peds physicians to practice med/peds hospital medicine. L. Nell Hodo, MD, a family medicine–trained pediatric hospitalist at Icahn School of Medicine at Mount Sinai in New York, joins Dr. Edgar-Zarate in supporting an FPHM for PHM, and feels that it will open the door for hospitalists who are ineligible for the practice pathway to be able to focus their recertification on the inpatient setting.
Dr. Hodo and Dr. Desai hope that rather than excluding those who are not PHM board eligible/certified, institutions and professional organizations will consider all qualifications when hiring, mentoring, and promoting physicians who care for hospitalized children. Dr. Natt, Dr. Schwenk, Dr. Edgar-Zarate, and Dr. Hodo appreciate that SHM is leading the way, and will continue to allow all hospitalists who care for children to receive Fellow designation.
Dr. Kumar is clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University and a pediatric hospitalist at Cleveland Clinic Children’s. She is the pediatric editor of The Hospitalist.
References
1. The American Board of Pediatrics. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. https://www.abp.org/sites/abp/files/phm-petition-response.pdf. Published 2019.
2. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). doi: 10.1542/peds.2016-1823.
3. The American Board of Pediatrics. Pediatric Hospital Medicine Certification. https://www.abp.org/content/pediatric-hospital-medicine-certification. Published 2019.
4. Skey D. Pediatric Hospitalists, It’s time to take a stand on the PHM Boards Application Process! Five Dog Development, LLC.
5. Nichols DG, Woods SZ. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):586-8. doi: 10.12788/jhm.3322.
6. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019 Oct;14(10):630-2. doi: 10.12788/jhm.3331.
7. Chang WW et al. Society of Hospital Medicine position on the American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):589-90. doi: 10.12788/jhm.3326.
Where do we go from here?
Where do we go from here?
Autumn is a busy time for pediatric hospitalists, with this autumn being particularly eventful as the first American Board of Pediatrics (ABP) certifying exam for Pediatric Hospital Medicine (PHM) will be offered on Nov. 12, 2019.
More than 1,600 med/peds and pediatric hospitalists applied to be eligible for the 2019 exam, 71% of whom were women. At least 3.9% of those applicants were denied eligibility for the 2019 exam.1 These denials resulted in discussions on the American Academy of Pediatrics Section on Hospital Medicine (AAP SOHM) email listserv related to unintentional gender bias.
PHM was first recognized as a subspecialty by the American Board of Medical Specialties in December 2015.2 Since that time, the ABP’s PHM sub-board developed eligibility criteria for practicing pediatric and med/peds hospitalists to apply for the exam. The sub-board identified three paths: a training pathway for applicants who had completed a 2-year PHM fellowship, a practice pathway for those satisfying ABP criteria for clinical activity in PHM, and a combined pathway for applicants who had completed PHM fellowships lasting less than 2 years.
Based on these pathways, 1,627 applicants applied for eligibility for the first PHM board certification exam.1 However, many concerns arose with the practice pathway eligibility criteria.
The PHM practice pathway initially included the following eligibility criteria:
• General pediatrics board certification.
• PHM practice “look back” period ends on or before June 30 of the exam year and starts 4 years earlier.
• More than 0.5 FTE professional PHM-related activities (patient-care, research, administration), defined as more than 900 hours/year every year for the preceding 4 years.
• More than 0.25 FTE direct patient care of hospitalized children, defined as more than 450 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice interruptions cannot exceed 3 months in the preceding 4 years, or 6 months in the preceding 5 years.
• Practice experience and hours were acquired in the United States and Canada.1,3
The start date and practice interruptions criteria in the practice pathway posed hurdles for many female applicants. Many women voiced concerns about feeling disadvantaged when applying for the PHM certifying exam and some of these women shared their concerns on the AAP SOHM email listserv. In response to these concerns, the PHM community called for increased transparency from the ABP related to denials, specifically related to unintentional gender bias against women applying for the exam.
David Skey, MD, and Jamee Walters, MD, pediatric hospitalists at Arnold Palmer Medical Center in Orlando, heard these concerns and decided to draft a petition with the help of legal counsel. The petition “demand[ed] immediate action,” and “request[ed] a formal response from the ABP regarding the practice pathway criteria.” The petition also stated that there was insufficient data to determine if the practice pathway “disadvantages women.” The petition asked the ABP to “facilitate a timely analysis to determine if gender bias” was present, or to perform an internal analysis and “release the findings publicly.”4
The petition was shared with the PHM community via the AAP SOHM listserv on July 29, 2019. Dr. Walters stated she was pleased by the response she and Dr. Skey received from the PHM community, on and off the AAP SOHM listserv. The petition was submitted to the ABP on Aug. 6, 2019, with 1,479 signatures.
On Aug. 29, 2019, the ABP’s response was shared on the AAP SOHM email listserv1 and was later published in the Journal of Hospital Medicine as a Special Announcement.5 In its response, the ABP stated that the gender bias allegation was “not supported by the facts” as there was “no significant difference between the percentage of women and men who were denied” eligibility.”5 In addressing the gender bias allegations and clarifying the practice pathway eligibility, the ABP removed the practice interruption criteria and modified the practice pathway criteria as follows:
• General pediatrics board certification.
• PHM practice started on or before July 2015 (for board eligibility in 2019).
• Professional PHM-related activities (patient-care, research, administration), defined as more than 900-1000 hours/year every year for the preceding 4 years.
• Direct patient care of hospitalized children, defined as more than 450-500 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice experience and hours were acquired in the United States and Canada.1
Following the release of the ABP’s response, many members of the PHM community remain concerned about the ABP’s revised criteria. Arti Desai, MD, pediatric hospitalist at Seattle Children’s and senior author on a “Perspectives in Hospital Medicine” in the Journal of Hospital Medicine,6 was appreciative that the ABP chose to remove the practice interruptions criterion. However, she and her colleagues remain concerned about lingering gender bias in the ABP’s practice pathway eligibility criteria surrounding the “start date” criterion. The authors state that this criterion differentially affects women, as women may take time off during or after residency for maternity or family leave. Dr. Desai states that this criterion alone can affect a woman’s chance for being eligible for the practice pathway.
Other members of the PHM community also expressed concerns about the ABP’s response to the PHM petition. Beth C. Natt, MD, pediatric hospitalist and director of pediatric hospital medicine regional programs at Connecticut Children’s in Hartford, felt that the population may have been self-selected, as the ABP’s data were limited to individuals who applied for exam eligibility. She was concerned that the data excluded pediatric hospitalists who chose not to apply because of uncertainty about meeting eligibility criteria. Klint Schwenk, MD, pediatric hospitalist at Norton Children’s Hospital in Louisville, Ky., stated that he wished the ABP had addressed the number of pediatric hospitalists who elected not to apply based on fear of ineligibility before concluding that there was no bias. He likened the ABP’s response to that of study authors omitting selection bias when discussing the limitations of their study.
Courtney Edgar-Zarate, MD, med/peds hospitalist and associate program director of the internal medicine/pediatrics residency at the University of Arkansas, expressed concerns that the ABP’s stringent clinical patient care hours criterion may unintentionally result in ineligibility for many mid-career or senior med/peds hospitalists. Dr. Edgar-Zarate also voiced concerns that graduating med/peds residents were electing not to pursue careers in hospital medicine because they would be required to complete a PHM fellowship to become a pediatric hospitalist, when a similar fellowship is not required to practice adult hospital medicine.
The Society of Hospital Medicine shared its position in regard to the ABP’s response in a Special Announcement in the Journal of Hospital Medicine.7 In it, SHM’s pediatric leaders recognized physicians for the excellent care they provide to hospitalized children. They stated that SHM would continue to support all hospitalists, independent of board eligibility status, and would continue to offer these hospitalists the merit-based Fellow designation. SHM’s pediatric leaders also proposed future directions for the ABP, including a Focused Practice Pathway in Hospital Medicine (FPHM), such as what the American Board of Internal Medicine and the American Board of Family Medicine have adopted for board recertification in internal medicine and family medicine. This maintenance of certification program that allows physicians primarily practicing in inpatient settings to focus their continuing education on inpatient practice, and is not a subspecialty.7
Dr. Edgar-Zarate fully supports the future directions for pediatric hospitalists outlined in SHM’s Special Announcement. She hopes that the ABP will support the FPHM. She feels the FPHM will encourage more med/peds physicians to practice med/peds hospital medicine. L. Nell Hodo, MD, a family medicine–trained pediatric hospitalist at Icahn School of Medicine at Mount Sinai in New York, joins Dr. Edgar-Zarate in supporting an FPHM for PHM, and feels that it will open the door for hospitalists who are ineligible for the practice pathway to be able to focus their recertification on the inpatient setting.
Dr. Hodo and Dr. Desai hope that rather than excluding those who are not PHM board eligible/certified, institutions and professional organizations will consider all qualifications when hiring, mentoring, and promoting physicians who care for hospitalized children. Dr. Natt, Dr. Schwenk, Dr. Edgar-Zarate, and Dr. Hodo appreciate that SHM is leading the way, and will continue to allow all hospitalists who care for children to receive Fellow designation.
Dr. Kumar is clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University and a pediatric hospitalist at Cleveland Clinic Children’s. She is the pediatric editor of The Hospitalist.
References
1. The American Board of Pediatrics. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. https://www.abp.org/sites/abp/files/phm-petition-response.pdf. Published 2019.
2. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). doi: 10.1542/peds.2016-1823.
3. The American Board of Pediatrics. Pediatric Hospital Medicine Certification. https://www.abp.org/content/pediatric-hospital-medicine-certification. Published 2019.
4. Skey D. Pediatric Hospitalists, It’s time to take a stand on the PHM Boards Application Process! Five Dog Development, LLC.
5. Nichols DG, Woods SZ. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):586-8. doi: 10.12788/jhm.3322.
6. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019 Oct;14(10):630-2. doi: 10.12788/jhm.3331.
7. Chang WW et al. Society of Hospital Medicine position on the American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):589-90. doi: 10.12788/jhm.3326.
Autumn is a busy time for pediatric hospitalists, with this autumn being particularly eventful as the first American Board of Pediatrics (ABP) certifying exam for Pediatric Hospital Medicine (PHM) will be offered on Nov. 12, 2019.
More than 1,600 med/peds and pediatric hospitalists applied to be eligible for the 2019 exam, 71% of whom were women. At least 3.9% of those applicants were denied eligibility for the 2019 exam.1 These denials resulted in discussions on the American Academy of Pediatrics Section on Hospital Medicine (AAP SOHM) email listserv related to unintentional gender bias.
PHM was first recognized as a subspecialty by the American Board of Medical Specialties in December 2015.2 Since that time, the ABP’s PHM sub-board developed eligibility criteria for practicing pediatric and med/peds hospitalists to apply for the exam. The sub-board identified three paths: a training pathway for applicants who had completed a 2-year PHM fellowship, a practice pathway for those satisfying ABP criteria for clinical activity in PHM, and a combined pathway for applicants who had completed PHM fellowships lasting less than 2 years.
Based on these pathways, 1,627 applicants applied for eligibility for the first PHM board certification exam.1 However, many concerns arose with the practice pathway eligibility criteria.
The PHM practice pathway initially included the following eligibility criteria:
• General pediatrics board certification.
• PHM practice “look back” period ends on or before June 30 of the exam year and starts 4 years earlier.
• More than 0.5 FTE professional PHM-related activities (patient-care, research, administration), defined as more than 900 hours/year every year for the preceding 4 years.
• More than 0.25 FTE direct patient care of hospitalized children, defined as more than 450 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice interruptions cannot exceed 3 months in the preceding 4 years, or 6 months in the preceding 5 years.
• Practice experience and hours were acquired in the United States and Canada.1,3
The start date and practice interruptions criteria in the practice pathway posed hurdles for many female applicants. Many women voiced concerns about feeling disadvantaged when applying for the PHM certifying exam and some of these women shared their concerns on the AAP SOHM email listserv. In response to these concerns, the PHM community called for increased transparency from the ABP related to denials, specifically related to unintentional gender bias against women applying for the exam.
David Skey, MD, and Jamee Walters, MD, pediatric hospitalists at Arnold Palmer Medical Center in Orlando, heard these concerns and decided to draft a petition with the help of legal counsel. The petition “demand[ed] immediate action,” and “request[ed] a formal response from the ABP regarding the practice pathway criteria.” The petition also stated that there was insufficient data to determine if the practice pathway “disadvantages women.” The petition asked the ABP to “facilitate a timely analysis to determine if gender bias” was present, or to perform an internal analysis and “release the findings publicly.”4
The petition was shared with the PHM community via the AAP SOHM listserv on July 29, 2019. Dr. Walters stated she was pleased by the response she and Dr. Skey received from the PHM community, on and off the AAP SOHM listserv. The petition was submitted to the ABP on Aug. 6, 2019, with 1,479 signatures.
On Aug. 29, 2019, the ABP’s response was shared on the AAP SOHM email listserv1 and was later published in the Journal of Hospital Medicine as a Special Announcement.5 In its response, the ABP stated that the gender bias allegation was “not supported by the facts” as there was “no significant difference between the percentage of women and men who were denied” eligibility.”5 In addressing the gender bias allegations and clarifying the practice pathway eligibility, the ABP removed the practice interruption criteria and modified the practice pathway criteria as follows:
• General pediatrics board certification.
• PHM practice started on or before July 2015 (for board eligibility in 2019).
• Professional PHM-related activities (patient-care, research, administration), defined as more than 900-1000 hours/year every year for the preceding 4 years.
• Direct patient care of hospitalized children, defined as more than 450-500 hours/year every year for the preceding 4 years.
• Practice covers the full range of hospitalized children with regard to age, diagnoses, and complexity.
• Practice experience and hours were acquired in the United States and Canada.1
Following the release of the ABP’s response, many members of the PHM community remain concerned about the ABP’s revised criteria. Arti Desai, MD, pediatric hospitalist at Seattle Children’s and senior author on a “Perspectives in Hospital Medicine” in the Journal of Hospital Medicine,6 was appreciative that the ABP chose to remove the practice interruptions criterion. However, she and her colleagues remain concerned about lingering gender bias in the ABP’s practice pathway eligibility criteria surrounding the “start date” criterion. The authors state that this criterion differentially affects women, as women may take time off during or after residency for maternity or family leave. Dr. Desai states that this criterion alone can affect a woman’s chance for being eligible for the practice pathway.
Other members of the PHM community also expressed concerns about the ABP’s response to the PHM petition. Beth C. Natt, MD, pediatric hospitalist and director of pediatric hospital medicine regional programs at Connecticut Children’s in Hartford, felt that the population may have been self-selected, as the ABP’s data were limited to individuals who applied for exam eligibility. She was concerned that the data excluded pediatric hospitalists who chose not to apply because of uncertainty about meeting eligibility criteria. Klint Schwenk, MD, pediatric hospitalist at Norton Children’s Hospital in Louisville, Ky., stated that he wished the ABP had addressed the number of pediatric hospitalists who elected not to apply based on fear of ineligibility before concluding that there was no bias. He likened the ABP’s response to that of study authors omitting selection bias when discussing the limitations of their study.
Courtney Edgar-Zarate, MD, med/peds hospitalist and associate program director of the internal medicine/pediatrics residency at the University of Arkansas, expressed concerns that the ABP’s stringent clinical patient care hours criterion may unintentionally result in ineligibility for many mid-career or senior med/peds hospitalists. Dr. Edgar-Zarate also voiced concerns that graduating med/peds residents were electing not to pursue careers in hospital medicine because they would be required to complete a PHM fellowship to become a pediatric hospitalist, when a similar fellowship is not required to practice adult hospital medicine.
The Society of Hospital Medicine shared its position in regard to the ABP’s response in a Special Announcement in the Journal of Hospital Medicine.7 In it, SHM’s pediatric leaders recognized physicians for the excellent care they provide to hospitalized children. They stated that SHM would continue to support all hospitalists, independent of board eligibility status, and would continue to offer these hospitalists the merit-based Fellow designation. SHM’s pediatric leaders also proposed future directions for the ABP, including a Focused Practice Pathway in Hospital Medicine (FPHM), such as what the American Board of Internal Medicine and the American Board of Family Medicine have adopted for board recertification in internal medicine and family medicine. This maintenance of certification program that allows physicians primarily practicing in inpatient settings to focus their continuing education on inpatient practice, and is not a subspecialty.7
Dr. Edgar-Zarate fully supports the future directions for pediatric hospitalists outlined in SHM’s Special Announcement. She hopes that the ABP will support the FPHM. She feels the FPHM will encourage more med/peds physicians to practice med/peds hospital medicine. L. Nell Hodo, MD, a family medicine–trained pediatric hospitalist at Icahn School of Medicine at Mount Sinai in New York, joins Dr. Edgar-Zarate in supporting an FPHM for PHM, and feels that it will open the door for hospitalists who are ineligible for the practice pathway to be able to focus their recertification on the inpatient setting.
Dr. Hodo and Dr. Desai hope that rather than excluding those who are not PHM board eligible/certified, institutions and professional organizations will consider all qualifications when hiring, mentoring, and promoting physicians who care for hospitalized children. Dr. Natt, Dr. Schwenk, Dr. Edgar-Zarate, and Dr. Hodo appreciate that SHM is leading the way, and will continue to allow all hospitalists who care for children to receive Fellow designation.
Dr. Kumar is clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University and a pediatric hospitalist at Cleveland Clinic Children’s. She is the pediatric editor of The Hospitalist.
References
1. The American Board of Pediatrics. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. https://www.abp.org/sites/abp/files/phm-petition-response.pdf. Published 2019.
2. Barrett DJ, McGuinness GA, Cunha CA, et al. Pediatric hospital medicine: A proposed new subspecialty. Pediatrics. 2017;139(3). doi: 10.1542/peds.2016-1823.
3. The American Board of Pediatrics. Pediatric Hospital Medicine Certification. https://www.abp.org/content/pediatric-hospital-medicine-certification. Published 2019.
4. Skey D. Pediatric Hospitalists, It’s time to take a stand on the PHM Boards Application Process! Five Dog Development, LLC.
5. Nichols DG, Woods SZ. The American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):586-8. doi: 10.12788/jhm.3322.
6. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019 Oct;14(10):630-2. doi: 10.12788/jhm.3331.
7. Chang WW et al. Society of Hospital Medicine position on the American Board of Pediatrics response to the Pediatric Hospital Medicine petition. J Hosp Med. 2019 Oct;14(10):589-90. doi: 10.12788/jhm.3326.
Who makes the rules? CMS and IPPS
Major MS-DRG changes postponed
The introduction of the Medicare Inpatient Prospective Payment System (IPPS) through amendment of the Social Security Act in 1983 transformed hospital reimbursement in the United States. Under the IPPS, a new form of Medicare prospective payment that paid hospitals a fixed amount per discharge for inpatient services was created: the diagnosis-related group (DRG). This eliminated the preceding retrospective cost reimbursement system in an attempt to stop health care price inflation.
Each DRG represents a grouping of similar conditions and procedures for services provided during an inpatient hospitalization reimbursed under Medicare Part A. The Centers for Medicare & Medicaid Services uses the Medicare Severity DRG (MS-DRG) system to account for severity of illness and resource consumption. There are three levels of severity based upon secondary diagnosis: major complication/comorbidity (MCC), complication/comorbidity (CC), and noncomplication/comorbidity (non-CC).
Payment rates are defined by base rates for operating costs and capital-related costs which are adjusted for relative weight (the average cost within a DRG, compared with the average Medicare case cost) and market condition adjustments. As the largest single health care payer in the United States, CMS’ annual changes to the IPPS have a major impact on hospital reimbursement.
In May 2019, CMS released its annual proposed rule for the Hospital IPPS suggesting extensive changes to MS-DRG reimbursements. Notably, CMS proposed changing the severity level of nearly 1,500 diagnosis codes by adjusting their categorization between MCC, CC, or non-CC. The majority of these changes included downgrading MCCs to CCs or non-CCs. In fact, 87% of the changes involved a downgrade from one of the higher severity levels to a non-CC level, while only 13% involved an upgrade from a lower severity level to MCC level.
The CMS derived these changes from an algorithmic review and input from their clinical advisors to determine each diagnoses impact on resource utilization. Multiple major groups of codes were included in the downgraded groups, including secondary cancer diagnoses, organ transplant status, and hip fracture.
Evaluating codes based on coded resource use alone could have had a major negative impact on the clinical practice of hospitalists as it undervalues cognitive and clinical work associated with these secondary diagnoses. As an example, malignant neoplasm of head of pancreas (ICD-10, C25.0) was proposed to move to a non-CC. Under CMS’ proposed rule, if a patient was admitted with complications of pancreatic cancer such as cholangitis caused by biliary obstruction, the pancreatic cancer diagnosis would not serve as a CC since the primary condition for which the patient was hospitalized would be cholangitis. The anticipated increase in such a patient’s length of stay, severity of illness, and expected resource utilization would be grossly misrepresented in this case by CMS’ proposed rule changes. CMS also proposed to move major organ-transplant status (including heart, lung, kidney, and pancreas) from CC to non-CC status. Again, the cognitive work and resource utilization required to manage these patients would be underrepresented with this change, given the increased complexity of managing immunosuppressant medications or conducting an infectious diagnostic work-up in immunosuppressed patients.
The Society of Hospital Medicine Public Policy Committee provides comments annually to CMS on the IPPS, advocating for hospitalists and patients. After advocacy efforts from SHM and other groups, expressing concern about making such significant changes to the DRG system without further study, the IPPS final rule was released on August 2, 2019. SHM’s efforts paid off. The final rule excluded the proposed broad changes to the MS-DRG system that were in the proposed rule.
In deciding not to finalize the proposed severity level changes, CMS wrote that the adoption of these broad changes will be postponed in order “to fully consider the technical feedback provided” regarding the proposal. The final rule also describes making a “test GROUPER [software program] publicly available to allow for impact testing,” and allows for the possibility of phasing in changes and eliciting feedback. SHM is fully supportive of the decision to postpone major changes to the MS-DRG system in the IPPS until further review is obtained, and will continue to monitor this issue and provide appropriate input to CMS for our hospitalist members.
As hospitalists, it is important to understand the foundational role that public policy and CMS rule creation have on our work. Influencing change to the MS-DRG system is yet another example of how SHM’s work has impacted the policy domain, limiting negative effects on our members and advancing the practice of hospital medicine.
Dr. Biebelhausen is head of the section of hospital medicine at Virginia Mason Medical Center, Seattle. Dr. Cowart is a hospitalist at the Mayo Clinic in Jacksonville, Fla. Dr. Hamilton is a hospitalist and associate chief quality officer at the Cleveland Clinic.
Major MS-DRG changes postponed
Major MS-DRG changes postponed
The introduction of the Medicare Inpatient Prospective Payment System (IPPS) through amendment of the Social Security Act in 1983 transformed hospital reimbursement in the United States. Under the IPPS, a new form of Medicare prospective payment that paid hospitals a fixed amount per discharge for inpatient services was created: the diagnosis-related group (DRG). This eliminated the preceding retrospective cost reimbursement system in an attempt to stop health care price inflation.
Each DRG represents a grouping of similar conditions and procedures for services provided during an inpatient hospitalization reimbursed under Medicare Part A. The Centers for Medicare & Medicaid Services uses the Medicare Severity DRG (MS-DRG) system to account for severity of illness and resource consumption. There are three levels of severity based upon secondary diagnosis: major complication/comorbidity (MCC), complication/comorbidity (CC), and noncomplication/comorbidity (non-CC).
Payment rates are defined by base rates for operating costs and capital-related costs which are adjusted for relative weight (the average cost within a DRG, compared with the average Medicare case cost) and market condition adjustments. As the largest single health care payer in the United States, CMS’ annual changes to the IPPS have a major impact on hospital reimbursement.
In May 2019, CMS released its annual proposed rule for the Hospital IPPS suggesting extensive changes to MS-DRG reimbursements. Notably, CMS proposed changing the severity level of nearly 1,500 diagnosis codes by adjusting their categorization between MCC, CC, or non-CC. The majority of these changes included downgrading MCCs to CCs or non-CCs. In fact, 87% of the changes involved a downgrade from one of the higher severity levels to a non-CC level, while only 13% involved an upgrade from a lower severity level to MCC level.
The CMS derived these changes from an algorithmic review and input from their clinical advisors to determine each diagnoses impact on resource utilization. Multiple major groups of codes were included in the downgraded groups, including secondary cancer diagnoses, organ transplant status, and hip fracture.
Evaluating codes based on coded resource use alone could have had a major negative impact on the clinical practice of hospitalists as it undervalues cognitive and clinical work associated with these secondary diagnoses. As an example, malignant neoplasm of head of pancreas (ICD-10, C25.0) was proposed to move to a non-CC. Under CMS’ proposed rule, if a patient was admitted with complications of pancreatic cancer such as cholangitis caused by biliary obstruction, the pancreatic cancer diagnosis would not serve as a CC since the primary condition for which the patient was hospitalized would be cholangitis. The anticipated increase in such a patient’s length of stay, severity of illness, and expected resource utilization would be grossly misrepresented in this case by CMS’ proposed rule changes. CMS also proposed to move major organ-transplant status (including heart, lung, kidney, and pancreas) from CC to non-CC status. Again, the cognitive work and resource utilization required to manage these patients would be underrepresented with this change, given the increased complexity of managing immunosuppressant medications or conducting an infectious diagnostic work-up in immunosuppressed patients.
The Society of Hospital Medicine Public Policy Committee provides comments annually to CMS on the IPPS, advocating for hospitalists and patients. After advocacy efforts from SHM and other groups, expressing concern about making such significant changes to the DRG system without further study, the IPPS final rule was released on August 2, 2019. SHM’s efforts paid off. The final rule excluded the proposed broad changes to the MS-DRG system that were in the proposed rule.
In deciding not to finalize the proposed severity level changes, CMS wrote that the adoption of these broad changes will be postponed in order “to fully consider the technical feedback provided” regarding the proposal. The final rule also describes making a “test GROUPER [software program] publicly available to allow for impact testing,” and allows for the possibility of phasing in changes and eliciting feedback. SHM is fully supportive of the decision to postpone major changes to the MS-DRG system in the IPPS until further review is obtained, and will continue to monitor this issue and provide appropriate input to CMS for our hospitalist members.
As hospitalists, it is important to understand the foundational role that public policy and CMS rule creation have on our work. Influencing change to the MS-DRG system is yet another example of how SHM’s work has impacted the policy domain, limiting negative effects on our members and advancing the practice of hospital medicine.
Dr. Biebelhausen is head of the section of hospital medicine at Virginia Mason Medical Center, Seattle. Dr. Cowart is a hospitalist at the Mayo Clinic in Jacksonville, Fla. Dr. Hamilton is a hospitalist and associate chief quality officer at the Cleveland Clinic.
The introduction of the Medicare Inpatient Prospective Payment System (IPPS) through amendment of the Social Security Act in 1983 transformed hospital reimbursement in the United States. Under the IPPS, a new form of Medicare prospective payment that paid hospitals a fixed amount per discharge for inpatient services was created: the diagnosis-related group (DRG). This eliminated the preceding retrospective cost reimbursement system in an attempt to stop health care price inflation.
Each DRG represents a grouping of similar conditions and procedures for services provided during an inpatient hospitalization reimbursed under Medicare Part A. The Centers for Medicare & Medicaid Services uses the Medicare Severity DRG (MS-DRG) system to account for severity of illness and resource consumption. There are three levels of severity based upon secondary diagnosis: major complication/comorbidity (MCC), complication/comorbidity (CC), and noncomplication/comorbidity (non-CC).
Payment rates are defined by base rates for operating costs and capital-related costs which are adjusted for relative weight (the average cost within a DRG, compared with the average Medicare case cost) and market condition adjustments. As the largest single health care payer in the United States, CMS’ annual changes to the IPPS have a major impact on hospital reimbursement.
In May 2019, CMS released its annual proposed rule for the Hospital IPPS suggesting extensive changes to MS-DRG reimbursements. Notably, CMS proposed changing the severity level of nearly 1,500 diagnosis codes by adjusting their categorization between MCC, CC, or non-CC. The majority of these changes included downgrading MCCs to CCs or non-CCs. In fact, 87% of the changes involved a downgrade from one of the higher severity levels to a non-CC level, while only 13% involved an upgrade from a lower severity level to MCC level.
The CMS derived these changes from an algorithmic review and input from their clinical advisors to determine each diagnoses impact on resource utilization. Multiple major groups of codes were included in the downgraded groups, including secondary cancer diagnoses, organ transplant status, and hip fracture.
Evaluating codes based on coded resource use alone could have had a major negative impact on the clinical practice of hospitalists as it undervalues cognitive and clinical work associated with these secondary diagnoses. As an example, malignant neoplasm of head of pancreas (ICD-10, C25.0) was proposed to move to a non-CC. Under CMS’ proposed rule, if a patient was admitted with complications of pancreatic cancer such as cholangitis caused by biliary obstruction, the pancreatic cancer diagnosis would not serve as a CC since the primary condition for which the patient was hospitalized would be cholangitis. The anticipated increase in such a patient’s length of stay, severity of illness, and expected resource utilization would be grossly misrepresented in this case by CMS’ proposed rule changes. CMS also proposed to move major organ-transplant status (including heart, lung, kidney, and pancreas) from CC to non-CC status. Again, the cognitive work and resource utilization required to manage these patients would be underrepresented with this change, given the increased complexity of managing immunosuppressant medications or conducting an infectious diagnostic work-up in immunosuppressed patients.
The Society of Hospital Medicine Public Policy Committee provides comments annually to CMS on the IPPS, advocating for hospitalists and patients. After advocacy efforts from SHM and other groups, expressing concern about making such significant changes to the DRG system without further study, the IPPS final rule was released on August 2, 2019. SHM’s efforts paid off. The final rule excluded the proposed broad changes to the MS-DRG system that were in the proposed rule.
In deciding not to finalize the proposed severity level changes, CMS wrote that the adoption of these broad changes will be postponed in order “to fully consider the technical feedback provided” regarding the proposal. The final rule also describes making a “test GROUPER [software program] publicly available to allow for impact testing,” and allows for the possibility of phasing in changes and eliciting feedback. SHM is fully supportive of the decision to postpone major changes to the MS-DRG system in the IPPS until further review is obtained, and will continue to monitor this issue and provide appropriate input to CMS for our hospitalist members.
As hospitalists, it is important to understand the foundational role that public policy and CMS rule creation have on our work. Influencing change to the MS-DRG system is yet another example of how SHM’s work has impacted the policy domain, limiting negative effects on our members and advancing the practice of hospital medicine.
Dr. Biebelhausen is head of the section of hospital medicine at Virginia Mason Medical Center, Seattle. Dr. Cowart is a hospitalist at the Mayo Clinic in Jacksonville, Fla. Dr. Hamilton is a hospitalist and associate chief quality officer at the Cleveland Clinic.
Considering the value of productivity bonuses
Connect high-value care with reimbursement
Physician payment models that include productivity bonuses are widespread, says Reshma Gupta, MD, MSHPM.
“These payment models are thought to affect clinician behavior, with productivity bonuses incentivizing clinicians to do more. While new policies aim to reduce total costs of care, little is known about the association between physician payment models and the culture of delivering high-value care,” said Dr. Gupta, the medical director for quality improvement at UCLA Health in Los Angeles.
To find out if hospitalist reimbursement models are associated with high-value culture in university, community, and safety-net hospitals, internal medicine hospitalists from 12 hospitals across California completed a cross-sectional survey assessing their perceptions of high-value care culture within their institutions. Dr. Gupta and colleagues summarized the results.
The study found that nearly 30% of hospitalists who were sampled reported payment with productivity bonuses, while only 5% of hospitalists sampled reported quality or value-based bonuses, Dr. Gupta said. “Hospitalists who reported payment with productivity bonuses were more likely to report lower high-value care culture within their programs.”
Hospitalist leaders interested in improving high-value care culture can use the High Value Care Culture Survey (http://www.highvaluecareculturesurvey.com) to quickly assess the culture within their programs, diagnose areas of opportunity and target improvement efforts.
“They can test new physician payment models within their programs and evaluate their high-value care culture to identify areas of opportunity for improvement,” Dr. Gupta said.
Reference
1. Gupta R et al. Association between hospitalist productivity payments and high-value care culture. J Hosp Med. 2019;1;16-21.
Connect high-value care with reimbursement
Connect high-value care with reimbursement
Physician payment models that include productivity bonuses are widespread, says Reshma Gupta, MD, MSHPM.
“These payment models are thought to affect clinician behavior, with productivity bonuses incentivizing clinicians to do more. While new policies aim to reduce total costs of care, little is known about the association between physician payment models and the culture of delivering high-value care,” said Dr. Gupta, the medical director for quality improvement at UCLA Health in Los Angeles.
To find out if hospitalist reimbursement models are associated with high-value culture in university, community, and safety-net hospitals, internal medicine hospitalists from 12 hospitals across California completed a cross-sectional survey assessing their perceptions of high-value care culture within their institutions. Dr. Gupta and colleagues summarized the results.
The study found that nearly 30% of hospitalists who were sampled reported payment with productivity bonuses, while only 5% of hospitalists sampled reported quality or value-based bonuses, Dr. Gupta said. “Hospitalists who reported payment with productivity bonuses were more likely to report lower high-value care culture within their programs.”
Hospitalist leaders interested in improving high-value care culture can use the High Value Care Culture Survey (http://www.highvaluecareculturesurvey.com) to quickly assess the culture within their programs, diagnose areas of opportunity and target improvement efforts.
“They can test new physician payment models within their programs and evaluate their high-value care culture to identify areas of opportunity for improvement,” Dr. Gupta said.
Reference
1. Gupta R et al. Association between hospitalist productivity payments and high-value care culture. J Hosp Med. 2019;1;16-21.
Physician payment models that include productivity bonuses are widespread, says Reshma Gupta, MD, MSHPM.
“These payment models are thought to affect clinician behavior, with productivity bonuses incentivizing clinicians to do more. While new policies aim to reduce total costs of care, little is known about the association between physician payment models and the culture of delivering high-value care,” said Dr. Gupta, the medical director for quality improvement at UCLA Health in Los Angeles.
To find out if hospitalist reimbursement models are associated with high-value culture in university, community, and safety-net hospitals, internal medicine hospitalists from 12 hospitals across California completed a cross-sectional survey assessing their perceptions of high-value care culture within their institutions. Dr. Gupta and colleagues summarized the results.
The study found that nearly 30% of hospitalists who were sampled reported payment with productivity bonuses, while only 5% of hospitalists sampled reported quality or value-based bonuses, Dr. Gupta said. “Hospitalists who reported payment with productivity bonuses were more likely to report lower high-value care culture within their programs.”
Hospitalist leaders interested in improving high-value care culture can use the High Value Care Culture Survey (http://www.highvaluecareculturesurvey.com) to quickly assess the culture within their programs, diagnose areas of opportunity and target improvement efforts.
“They can test new physician payment models within their programs and evaluate their high-value care culture to identify areas of opportunity for improvement,” Dr. Gupta said.
Reference
1. Gupta R et al. Association between hospitalist productivity payments and high-value care culture. J Hosp Med. 2019;1;16-21.
Labeling of medication warnings
Question: Which one of the following statements regarding medication warnings is incorrect?
A. The drug package “insert” or “label” contains, among other things, a drug’s pharmacology, indications, contraindications, risks and warnings.
B. The Physicians’ Desk Reference (PDR) is an annually updated drug compendium, which can be admitted into evidence as a learned treatise.
C. Drug labeling is a dual responsibility of the manufacturer and the Food and Drug Administration.
D. The FDA is solely responsible for a drug’s warnings and sets the absolute standard of care regarding side effects and complications.
E. State law can impose liability for negligent failure to warn even if the FDA has not included the warning in the drug’s label.
Answer: D. In medical products liability, injured plaintiffs frequently claim a failure to warn of known risks. An example is the cardiovascular deaths caused by Vioxx, a nonsteroidal, anti-inflammatory drug that was withdrawn in 2004. Other examples alleging failure to warn are Actos-associated bladder cancer and Baycol-related rhabdomyolysis. At the time of product approval, the FDA sets out the labeling that goes with each drug, and then makes periodic changes to reflect new indications, warnings and risks. The manufacturer has the prime responsibility for submitting all updated information, especially of augmented risks that come with field experience. In 2012, for example, the FDA mandated the revision of the labeling of Lipitor and other statins to warn of the increased risk of diabetes.
The drug manufacturer stands in the unique position as having the most detailed and up-to-date data and bears a serious responsibility to submit its full findings to the FDA, including its request for label change. Litigation over failure to warn of risks frequently turns on whether the drug manufacturer knew or should have known, had failed to inform the FDA, or whether the FDA itself had declined to make the changes, e.g., because of incomplete or premature data. Notwithstanding the FDA’s overarching federal status, a plaintiff may still attempt to use state tort law to hold a manufacturer liable should the federally approved labeling be silent on the matter.
Two U.S. Supreme Court cases sought to clarify the rules under which a drug manufacturer, when sued for failure to warn, may seek protection under its FDA-approved labeling. The first case involved Diana Levine, a Vermont musician and migraine sufferer, who lost her arm after the drug Phenergan, given by intravenous push, accidentally entered an artery and caused gangrene. Although the intravenous use of Phenergan is approved by the FDA and the risk of such use is clearly stated in the drug’s package insert, the lawsuit alleged that under state law, such a warning was inadequate and should have been strengthened to prohibit this mode of administration. A Vermont jury awarded damages of $6.7 million. On appeal, Wyeth, the defendant pharmaceutical company, maintained that its warning was appropriate, as it had been approved by the federal government through the FDA. It further argued that the drug’s package insert could not be unilaterally altered or modified without running afoul of federal regulations.
In a 6-3 decision,1 the U.S. Supreme Court ruled that the manufacturer was in fact at liberty to issue a more stringent warning, and FDA approval does not bar lawsuits. The Court opined that “Federal law does not pre-empt Levine’s claim that Phenergan’s label did not contain an adequate warning about the IV-push method of administration.” Wyeth had argued that it was impossible for the company to provide additional warnings, since it was the FDA that made the sole determination of the nature and scope of a drug’s label. However, the court held that Wyeth never attempted to change the label to warn of the risk and failed to provide “clear” evidence that the FDA would have prevented it from changing its label. Without defining what constituted “clear” evidence, it rejected Wyeth’s broad assertion that unilaterally changing the Phenergan label would have violated federal law, which was based on the fundamental misunderstanding that the FDA, rather than the manufacturer, bears primary responsibility for drug labeling.
In 2019, the landmark case of Merck Sharp & Dohme Corp v. Albrecht et al.2 reached the U.S. Supreme Court. This class-action suit involved more than 500 individuals who took Fosamax, an effective anti-resorptive drug for treating osteoporosis, and suffered atypical femoral fractures between 1999 and 2010. When the FDA first approved of the manufacture and sale of Fosamax in 1995, the Fosamax label did not warn of the then-speculative risk of atypical femoral fractures. But stronger evidence connecting Fosamax to atypical fractures developed after 1995, prompting the FDA to add a warning in 2011. Merck argued that plaintiffs’ state-law failure-to-warn claims should be dismissed as preempted by federal law. It conceded that the FDA regulations would have permitted Merck to try to change the label to add a warning before 2010 but believed the FDA would have rejected that attempt. In particular, it claimed that the FDA’s rejection of Merck’s 2008 attempt to warn of a risk of “stress fractures” showed that the FDA would also have rejected any attempt by Merck to warn of the risk of atypical femoral fractures. In short, Merck was relying on the legal doctrine of “impossibility preemption,” i.e., it was impossible to comply with both state law (adequate label warning of atypical fractures) and federal law (FDA control of warning labels). The plaintiffs’ position was that Merck’s proposed warning to the FDA had minimized the seriousness of the femoral fracture risk, characterizing them only as “stress fractures.”3
The Court’s earlier Levine decision had held that a state-law failure-to-warn claim is preempted where there is “clear” evidence the FDA would not have approved a label change. In the Albrecht decision, which also sided with the plaintiffs, the court indicated that “Clear evidence is evidence that shows the court that the drug manufacturer fully informed the FDA of the justifications for the warning required by state law and that the FDA, in turn, informed the drug manufacturer that the FDA would not approve a change to the drug’s label to include that warning.” The court also held that issues relating to presumption of impossibility are law-based, and thus it remains for the judge, not the jury, to make that determination.
Issuing timely warnings regarding medical products promotes patient safety, and the law appears to place the major onus on the manufacturer. Still, striking the proper balance is important. During oral arguments in Albrecht, Associate Justice Neil Gorsuch is said to have cautioned against “ ... incentives for companies to submit weakly supported label changes to the agency, knowing that when those label changes are rejected the companies will be free of further liability.” And as pointed out in the earlier cited Johnston article: “ ... a system that creates incentives for manufacturers to over-warn physicians and patients could harm patients by listing the important warnings of adverse effects among numerous less important warnings, which may discourage physicians and patients from choosing potentially useful drugs. On the other hand, a shift of responsibility for labeling to the FDA raises questions about whether the agency, which has resources that are dwarfed by the combined resources of industry, is necessarily capable to serve in this role ...”
Finally, this issue is more complex for devices because of the Medical Device Amendments Act of 1976 (MDA), which may preempt state-based lawsuits. In a claim brought after a Medtronic catheter ruptured in a patient’s coronary artery during heart surgery, the plaintiff alleged that the device was designed, labeled, and manufactured in a manner that violated New York common law. The case was appealed to the U.S. Supreme Court. The court held that the MDA preempted petitioner’s common-law claims challenging the safety or effectiveness of a medical device marketed in a form that received premarket approval from the FDA.4 The court ruled that MDA created a scheme of federal safety oversight for medical devices while sweeping back state oversight schemes.
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Wyeth v. Levine, 555 U.S. 2 (2009).
2. Merck, Sharp & Dohme Corp. v. Albrecht et al., 587 U. S. ____ (2019).
3. Johnston MC et al., A new Supreme Court ruling on drug liability. JAMA 2019;322(7):607-8.
4. Riegel v. Medtronic, 128 S. Ct. 999 (2008).
Question: Which one of the following statements regarding medication warnings is incorrect?
A. The drug package “insert” or “label” contains, among other things, a drug’s pharmacology, indications, contraindications, risks and warnings.
B. The Physicians’ Desk Reference (PDR) is an annually updated drug compendium, which can be admitted into evidence as a learned treatise.
C. Drug labeling is a dual responsibility of the manufacturer and the Food and Drug Administration.
D. The FDA is solely responsible for a drug’s warnings and sets the absolute standard of care regarding side effects and complications.
E. State law can impose liability for negligent failure to warn even if the FDA has not included the warning in the drug’s label.
Answer: D. In medical products liability, injured plaintiffs frequently claim a failure to warn of known risks. An example is the cardiovascular deaths caused by Vioxx, a nonsteroidal, anti-inflammatory drug that was withdrawn in 2004. Other examples alleging failure to warn are Actos-associated bladder cancer and Baycol-related rhabdomyolysis. At the time of product approval, the FDA sets out the labeling that goes with each drug, and then makes periodic changes to reflect new indications, warnings and risks. The manufacturer has the prime responsibility for submitting all updated information, especially of augmented risks that come with field experience. In 2012, for example, the FDA mandated the revision of the labeling of Lipitor and other statins to warn of the increased risk of diabetes.
The drug manufacturer stands in the unique position as having the most detailed and up-to-date data and bears a serious responsibility to submit its full findings to the FDA, including its request for label change. Litigation over failure to warn of risks frequently turns on whether the drug manufacturer knew or should have known, had failed to inform the FDA, or whether the FDA itself had declined to make the changes, e.g., because of incomplete or premature data. Notwithstanding the FDA’s overarching federal status, a plaintiff may still attempt to use state tort law to hold a manufacturer liable should the federally approved labeling be silent on the matter.
Two U.S. Supreme Court cases sought to clarify the rules under which a drug manufacturer, when sued for failure to warn, may seek protection under its FDA-approved labeling. The first case involved Diana Levine, a Vermont musician and migraine sufferer, who lost her arm after the drug Phenergan, given by intravenous push, accidentally entered an artery and caused gangrene. Although the intravenous use of Phenergan is approved by the FDA and the risk of such use is clearly stated in the drug’s package insert, the lawsuit alleged that under state law, such a warning was inadequate and should have been strengthened to prohibit this mode of administration. A Vermont jury awarded damages of $6.7 million. On appeal, Wyeth, the defendant pharmaceutical company, maintained that its warning was appropriate, as it had been approved by the federal government through the FDA. It further argued that the drug’s package insert could not be unilaterally altered or modified without running afoul of federal regulations.
In a 6-3 decision,1 the U.S. Supreme Court ruled that the manufacturer was in fact at liberty to issue a more stringent warning, and FDA approval does not bar lawsuits. The Court opined that “Federal law does not pre-empt Levine’s claim that Phenergan’s label did not contain an adequate warning about the IV-push method of administration.” Wyeth had argued that it was impossible for the company to provide additional warnings, since it was the FDA that made the sole determination of the nature and scope of a drug’s label. However, the court held that Wyeth never attempted to change the label to warn of the risk and failed to provide “clear” evidence that the FDA would have prevented it from changing its label. Without defining what constituted “clear” evidence, it rejected Wyeth’s broad assertion that unilaterally changing the Phenergan label would have violated federal law, which was based on the fundamental misunderstanding that the FDA, rather than the manufacturer, bears primary responsibility for drug labeling.
In 2019, the landmark case of Merck Sharp & Dohme Corp v. Albrecht et al.2 reached the U.S. Supreme Court. This class-action suit involved more than 500 individuals who took Fosamax, an effective anti-resorptive drug for treating osteoporosis, and suffered atypical femoral fractures between 1999 and 2010. When the FDA first approved of the manufacture and sale of Fosamax in 1995, the Fosamax label did not warn of the then-speculative risk of atypical femoral fractures. But stronger evidence connecting Fosamax to atypical fractures developed after 1995, prompting the FDA to add a warning in 2011. Merck argued that plaintiffs’ state-law failure-to-warn claims should be dismissed as preempted by federal law. It conceded that the FDA regulations would have permitted Merck to try to change the label to add a warning before 2010 but believed the FDA would have rejected that attempt. In particular, it claimed that the FDA’s rejection of Merck’s 2008 attempt to warn of a risk of “stress fractures” showed that the FDA would also have rejected any attempt by Merck to warn of the risk of atypical femoral fractures. In short, Merck was relying on the legal doctrine of “impossibility preemption,” i.e., it was impossible to comply with both state law (adequate label warning of atypical fractures) and federal law (FDA control of warning labels). The plaintiffs’ position was that Merck’s proposed warning to the FDA had minimized the seriousness of the femoral fracture risk, characterizing them only as “stress fractures.”3
The Court’s earlier Levine decision had held that a state-law failure-to-warn claim is preempted where there is “clear” evidence the FDA would not have approved a label change. In the Albrecht decision, which also sided with the plaintiffs, the court indicated that “Clear evidence is evidence that shows the court that the drug manufacturer fully informed the FDA of the justifications for the warning required by state law and that the FDA, in turn, informed the drug manufacturer that the FDA would not approve a change to the drug’s label to include that warning.” The court also held that issues relating to presumption of impossibility are law-based, and thus it remains for the judge, not the jury, to make that determination.
Issuing timely warnings regarding medical products promotes patient safety, and the law appears to place the major onus on the manufacturer. Still, striking the proper balance is important. During oral arguments in Albrecht, Associate Justice Neil Gorsuch is said to have cautioned against “ ... incentives for companies to submit weakly supported label changes to the agency, knowing that when those label changes are rejected the companies will be free of further liability.” And as pointed out in the earlier cited Johnston article: “ ... a system that creates incentives for manufacturers to over-warn physicians and patients could harm patients by listing the important warnings of adverse effects among numerous less important warnings, which may discourage physicians and patients from choosing potentially useful drugs. On the other hand, a shift of responsibility for labeling to the FDA raises questions about whether the agency, which has resources that are dwarfed by the combined resources of industry, is necessarily capable to serve in this role ...”
Finally, this issue is more complex for devices because of the Medical Device Amendments Act of 1976 (MDA), which may preempt state-based lawsuits. In a claim brought after a Medtronic catheter ruptured in a patient’s coronary artery during heart surgery, the plaintiff alleged that the device was designed, labeled, and manufactured in a manner that violated New York common law. The case was appealed to the U.S. Supreme Court. The court held that the MDA preempted petitioner’s common-law claims challenging the safety or effectiveness of a medical device marketed in a form that received premarket approval from the FDA.4 The court ruled that MDA created a scheme of federal safety oversight for medical devices while sweeping back state oversight schemes.
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Wyeth v. Levine, 555 U.S. 2 (2009).
2. Merck, Sharp & Dohme Corp. v. Albrecht et al., 587 U. S. ____ (2019).
3. Johnston MC et al., A new Supreme Court ruling on drug liability. JAMA 2019;322(7):607-8.
4. Riegel v. Medtronic, 128 S. Ct. 999 (2008).
Question: Which one of the following statements regarding medication warnings is incorrect?
A. The drug package “insert” or “label” contains, among other things, a drug’s pharmacology, indications, contraindications, risks and warnings.
B. The Physicians’ Desk Reference (PDR) is an annually updated drug compendium, which can be admitted into evidence as a learned treatise.
C. Drug labeling is a dual responsibility of the manufacturer and the Food and Drug Administration.
D. The FDA is solely responsible for a drug’s warnings and sets the absolute standard of care regarding side effects and complications.
E. State law can impose liability for negligent failure to warn even if the FDA has not included the warning in the drug’s label.
Answer: D. In medical products liability, injured plaintiffs frequently claim a failure to warn of known risks. An example is the cardiovascular deaths caused by Vioxx, a nonsteroidal, anti-inflammatory drug that was withdrawn in 2004. Other examples alleging failure to warn are Actos-associated bladder cancer and Baycol-related rhabdomyolysis. At the time of product approval, the FDA sets out the labeling that goes with each drug, and then makes periodic changes to reflect new indications, warnings and risks. The manufacturer has the prime responsibility for submitting all updated information, especially of augmented risks that come with field experience. In 2012, for example, the FDA mandated the revision of the labeling of Lipitor and other statins to warn of the increased risk of diabetes.
The drug manufacturer stands in the unique position as having the most detailed and up-to-date data and bears a serious responsibility to submit its full findings to the FDA, including its request for label change. Litigation over failure to warn of risks frequently turns on whether the drug manufacturer knew or should have known, had failed to inform the FDA, or whether the FDA itself had declined to make the changes, e.g., because of incomplete or premature data. Notwithstanding the FDA’s overarching federal status, a plaintiff may still attempt to use state tort law to hold a manufacturer liable should the federally approved labeling be silent on the matter.
Two U.S. Supreme Court cases sought to clarify the rules under which a drug manufacturer, when sued for failure to warn, may seek protection under its FDA-approved labeling. The first case involved Diana Levine, a Vermont musician and migraine sufferer, who lost her arm after the drug Phenergan, given by intravenous push, accidentally entered an artery and caused gangrene. Although the intravenous use of Phenergan is approved by the FDA and the risk of such use is clearly stated in the drug’s package insert, the lawsuit alleged that under state law, such a warning was inadequate and should have been strengthened to prohibit this mode of administration. A Vermont jury awarded damages of $6.7 million. On appeal, Wyeth, the defendant pharmaceutical company, maintained that its warning was appropriate, as it had been approved by the federal government through the FDA. It further argued that the drug’s package insert could not be unilaterally altered or modified without running afoul of federal regulations.
In a 6-3 decision,1 the U.S. Supreme Court ruled that the manufacturer was in fact at liberty to issue a more stringent warning, and FDA approval does not bar lawsuits. The Court opined that “Federal law does not pre-empt Levine’s claim that Phenergan’s label did not contain an adequate warning about the IV-push method of administration.” Wyeth had argued that it was impossible for the company to provide additional warnings, since it was the FDA that made the sole determination of the nature and scope of a drug’s label. However, the court held that Wyeth never attempted to change the label to warn of the risk and failed to provide “clear” evidence that the FDA would have prevented it from changing its label. Without defining what constituted “clear” evidence, it rejected Wyeth’s broad assertion that unilaterally changing the Phenergan label would have violated federal law, which was based on the fundamental misunderstanding that the FDA, rather than the manufacturer, bears primary responsibility for drug labeling.
In 2019, the landmark case of Merck Sharp & Dohme Corp v. Albrecht et al.2 reached the U.S. Supreme Court. This class-action suit involved more than 500 individuals who took Fosamax, an effective anti-resorptive drug for treating osteoporosis, and suffered atypical femoral fractures between 1999 and 2010. When the FDA first approved of the manufacture and sale of Fosamax in 1995, the Fosamax label did not warn of the then-speculative risk of atypical femoral fractures. But stronger evidence connecting Fosamax to atypical fractures developed after 1995, prompting the FDA to add a warning in 2011. Merck argued that plaintiffs’ state-law failure-to-warn claims should be dismissed as preempted by federal law. It conceded that the FDA regulations would have permitted Merck to try to change the label to add a warning before 2010 but believed the FDA would have rejected that attempt. In particular, it claimed that the FDA’s rejection of Merck’s 2008 attempt to warn of a risk of “stress fractures” showed that the FDA would also have rejected any attempt by Merck to warn of the risk of atypical femoral fractures. In short, Merck was relying on the legal doctrine of “impossibility preemption,” i.e., it was impossible to comply with both state law (adequate label warning of atypical fractures) and federal law (FDA control of warning labels). The plaintiffs’ position was that Merck’s proposed warning to the FDA had minimized the seriousness of the femoral fracture risk, characterizing them only as “stress fractures.”3
The Court’s earlier Levine decision had held that a state-law failure-to-warn claim is preempted where there is “clear” evidence the FDA would not have approved a label change. In the Albrecht decision, which also sided with the plaintiffs, the court indicated that “Clear evidence is evidence that shows the court that the drug manufacturer fully informed the FDA of the justifications for the warning required by state law and that the FDA, in turn, informed the drug manufacturer that the FDA would not approve a change to the drug’s label to include that warning.” The court also held that issues relating to presumption of impossibility are law-based, and thus it remains for the judge, not the jury, to make that determination.
Issuing timely warnings regarding medical products promotes patient safety, and the law appears to place the major onus on the manufacturer. Still, striking the proper balance is important. During oral arguments in Albrecht, Associate Justice Neil Gorsuch is said to have cautioned against “ ... incentives for companies to submit weakly supported label changes to the agency, knowing that when those label changes are rejected the companies will be free of further liability.” And as pointed out in the earlier cited Johnston article: “ ... a system that creates incentives for manufacturers to over-warn physicians and patients could harm patients by listing the important warnings of adverse effects among numerous less important warnings, which may discourage physicians and patients from choosing potentially useful drugs. On the other hand, a shift of responsibility for labeling to the FDA raises questions about whether the agency, which has resources that are dwarfed by the combined resources of industry, is necessarily capable to serve in this role ...”
Finally, this issue is more complex for devices because of the Medical Device Amendments Act of 1976 (MDA), which may preempt state-based lawsuits. In a claim brought after a Medtronic catheter ruptured in a patient’s coronary artery during heart surgery, the plaintiff alleged that the device was designed, labeled, and manufactured in a manner that violated New York common law. The case was appealed to the U.S. Supreme Court. The court held that the MDA preempted petitioner’s common-law claims challenging the safety or effectiveness of a medical device marketed in a form that received premarket approval from the FDA.4 The court ruled that MDA created a scheme of federal safety oversight for medical devices while sweeping back state oversight schemes.
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Wyeth v. Levine, 555 U.S. 2 (2009).
2. Merck, Sharp & Dohme Corp. v. Albrecht et al., 587 U. S. ____ (2019).
3. Johnston MC et al., A new Supreme Court ruling on drug liability. JAMA 2019;322(7):607-8.
4. Riegel v. Medtronic, 128 S. Ct. 999 (2008).
Palliative care programs continue growth in U.S. hospitals
Growth continues among palliative care programs in the United States, although access often depends “more upon accidents of geography than it does upon the needs of patients,” according to the Center to Advance Palliative Care and the National Palliative Care Research Center.
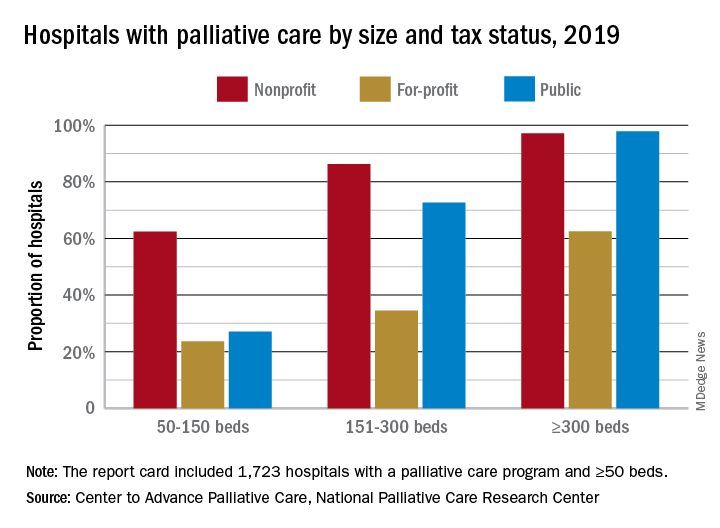
“As is true for many aspects of health care, geography is destiny. Where you live determines your access to the best quality of life and highest quality of care during a serious illness,” said Diane E. Meier, MD, director of the Center to Advance Palliative Care, in a written statement.
the two organizations said in their 2019 report card on palliative care access. What hasn’t changed since 2015, however, is the country’s overall grade, which remains a B.
Delaware, New Hampshire, Rhode Island, and Vermont have a palliative care program in all of their hospitals with 50 or more beds and each earned a grade of A (palliative care rate of greater than 80%), along with 17 other states. The lowest-performing states – Alabama, Mississippi, New Mexico, Oklahoma, and Wyoming – all received Ds for having a rate below 40%, the CAPC said.
The urban/rural divide also is prominent in palliative care: “90% of hospitals with palliative care are in urban areas. Only 17% of rural hospitals with fifty or more beds report palliative care programs,” the report said.
Hospital type is another source of disparity. Small, nonprofit hospitals are much more likely to offer access to palliative care than either for-profit or public facilities of the same size, but the gap closes as size increases, at least between nonprofit and public hospitals. For the largest institutions, the public hospitals pull into the lead, 98% versus 97%, over the nonprofits, with the for-profit facilities well behind at 63%.
“High quality palliative care has been shown to improve patient and family quality of life, improve patients’ and families’ health care experiences, and in certain diseases, prolong life. Palliative care has also been shown to improve hospital efficiency and reduce unnecessary spending,” said R. Sean Morrison, MD, director of the National Palliative Care Research Center.
The report card is based on data from the American Hospital Association’s Annual Survey Database, with additional data from the National Palliative Care Registry and Center to Advance Palliative Care’s Mapping Community Palliative Care initiative. The final sample included 2,409 hospitals with 50 or more beds.
Growth continues among palliative care programs in the United States, although access often depends “more upon accidents of geography than it does upon the needs of patients,” according to the Center to Advance Palliative Care and the National Palliative Care Research Center.
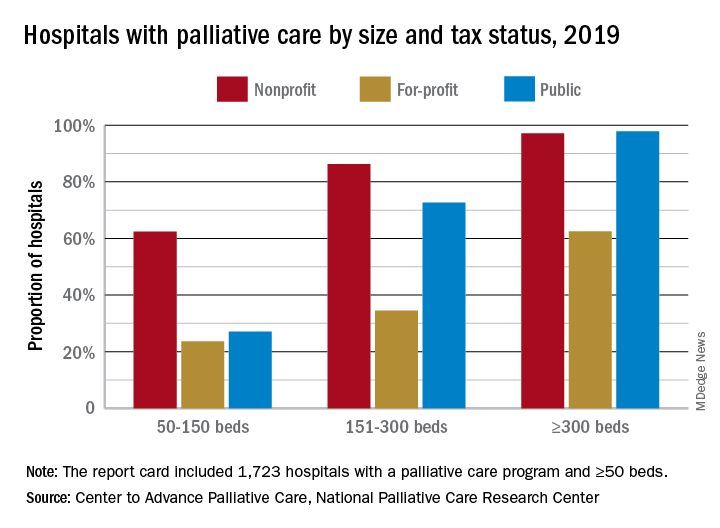
“As is true for many aspects of health care, geography is destiny. Where you live determines your access to the best quality of life and highest quality of care during a serious illness,” said Diane E. Meier, MD, director of the Center to Advance Palliative Care, in a written statement.
the two organizations said in their 2019 report card on palliative care access. What hasn’t changed since 2015, however, is the country’s overall grade, which remains a B.
Delaware, New Hampshire, Rhode Island, and Vermont have a palliative care program in all of their hospitals with 50 or more beds and each earned a grade of A (palliative care rate of greater than 80%), along with 17 other states. The lowest-performing states – Alabama, Mississippi, New Mexico, Oklahoma, and Wyoming – all received Ds for having a rate below 40%, the CAPC said.
The urban/rural divide also is prominent in palliative care: “90% of hospitals with palliative care are in urban areas. Only 17% of rural hospitals with fifty or more beds report palliative care programs,” the report said.
Hospital type is another source of disparity. Small, nonprofit hospitals are much more likely to offer access to palliative care than either for-profit or public facilities of the same size, but the gap closes as size increases, at least between nonprofit and public hospitals. For the largest institutions, the public hospitals pull into the lead, 98% versus 97%, over the nonprofits, with the for-profit facilities well behind at 63%.
“High quality palliative care has been shown to improve patient and family quality of life, improve patients’ and families’ health care experiences, and in certain diseases, prolong life. Palliative care has also been shown to improve hospital efficiency and reduce unnecessary spending,” said R. Sean Morrison, MD, director of the National Palliative Care Research Center.
The report card is based on data from the American Hospital Association’s Annual Survey Database, with additional data from the National Palliative Care Registry and Center to Advance Palliative Care’s Mapping Community Palliative Care initiative. The final sample included 2,409 hospitals with 50 or more beds.
Growth continues among palliative care programs in the United States, although access often depends “more upon accidents of geography than it does upon the needs of patients,” according to the Center to Advance Palliative Care and the National Palliative Care Research Center.
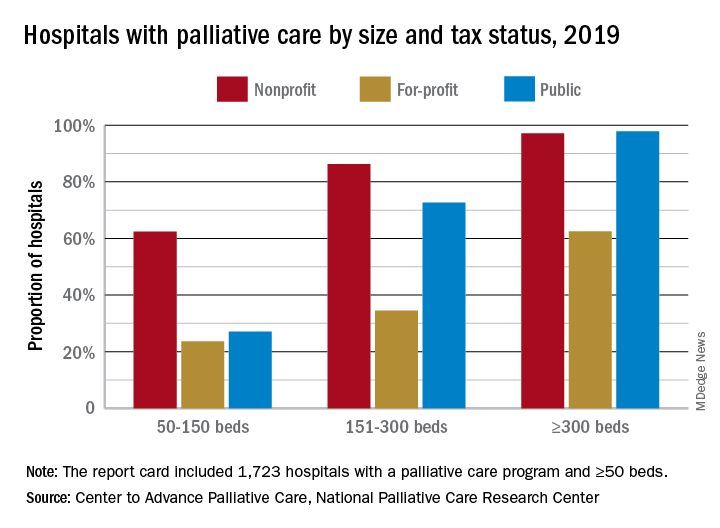
“As is true for many aspects of health care, geography is destiny. Where you live determines your access to the best quality of life and highest quality of care during a serious illness,” said Diane E. Meier, MD, director of the Center to Advance Palliative Care, in a written statement.
the two organizations said in their 2019 report card on palliative care access. What hasn’t changed since 2015, however, is the country’s overall grade, which remains a B.
Delaware, New Hampshire, Rhode Island, and Vermont have a palliative care program in all of their hospitals with 50 or more beds and each earned a grade of A (palliative care rate of greater than 80%), along with 17 other states. The lowest-performing states – Alabama, Mississippi, New Mexico, Oklahoma, and Wyoming – all received Ds for having a rate below 40%, the CAPC said.
The urban/rural divide also is prominent in palliative care: “90% of hospitals with palliative care are in urban areas. Only 17% of rural hospitals with fifty or more beds report palliative care programs,” the report said.
Hospital type is another source of disparity. Small, nonprofit hospitals are much more likely to offer access to palliative care than either for-profit or public facilities of the same size, but the gap closes as size increases, at least between nonprofit and public hospitals. For the largest institutions, the public hospitals pull into the lead, 98% versus 97%, over the nonprofits, with the for-profit facilities well behind at 63%.
“High quality palliative care has been shown to improve patient and family quality of life, improve patients’ and families’ health care experiences, and in certain diseases, prolong life. Palliative care has also been shown to improve hospital efficiency and reduce unnecessary spending,” said R. Sean Morrison, MD, director of the National Palliative Care Research Center.
The report card is based on data from the American Hospital Association’s Annual Survey Database, with additional data from the National Palliative Care Registry and Center to Advance Palliative Care’s Mapping Community Palliative Care initiative. The final sample included 2,409 hospitals with 50 or more beds.
Observation versus inpatient status
A dilemma for hospitalists and patients
A federal effort to reduce health care expenditures has left many older Medicare recipients experiencing the sticker shock of “observation status.” Patients who are not sick enough to meet inpatient admission criteria, however, still require hospitalization, and may be placed under Medicare observation care.
Seniors can get frustrated, confused, and anxious as their status can be changed while they are in the hospital, and they may receive large medical bills after they are discharged. The Centers for Medicare & Medicaid Services’ “3-day rule” mandates that Medicare will not pay for skilled nursing facility care unless the patient is admitted as an “inpatient” for at least 3 days. Observation days do not count towards this 3-day hospital stay.
There has been an increase in outpatient services over the years since 2006. The 2018 State of Hospital Medicine Report (SoHM) highlights the percentage of discharges based on hospitalists’ billed Current Procedural Terminology codes. Codes 99217 (observation discharge) and 99238-99239 (inpatient discharge) were used to calculate the percentages. 80.7% of adult medicine hospitalist discharges were coded using inpatient discharge codes, while 19.3% of patients were discharged with observation discharge codes.
In the 2016 SoHM report, the ratio was 76.0% inpatient and 21.1% observation codes and in the 2014 report we saw 80.3% inpatient and 16.1% observation discharges (see table 1). But in both of those surveys, same-day admission/discharge codes were also separately reported, which did not occur in 2018. That makes year-over-year comparison of the data challenging.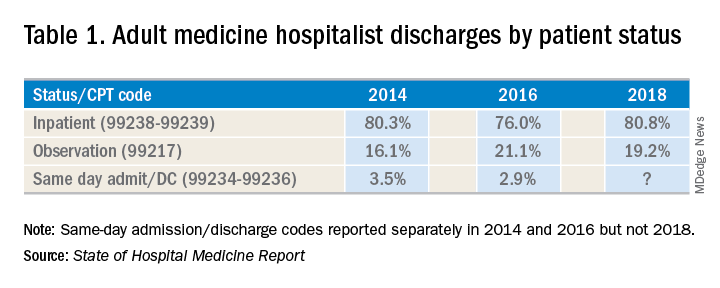
Interestingly, the 2017 CMS data on Evaluation and Management Codes by Specialty for the first time included separate data for hospitalists, based on hospitalists who credentialed with Medicare using the new C6 specialty code. Based on that data, when looking only at inpatient (99238-99239) and observation (99217) codes, 83% of the discharges were inpatient and 17% were observation.
Physicians feel the pressure of strained patient-physician relationships as a consequence of patients feeling the brunt of the financing gap related to observation status. Patients often feel they were not warned adequately about the financial ramifications of observation status. Even if Medicare beneficiaries have received the Medicare Outpatient Observation Notice, outlined by the Notice of Observation Treatment and Implication for Care Eligibility Act, they have no rights to appeal.
Currently Medicare beneficiaries admitted as inpatients only incur a Part A deductible; they are not liable for tests, procedures, and nursing care. On the other hand, in observation status all services are billed separately. For Medicare Part B services (which covers observation care) patients must pay 20% of services after the Part B deductible, which could result in a huge financial burden. Costs for skilled nursing facilities, when they are not covered by Medicare Part A, because of the 3-day rule, can easily go up to $20,000 or more. Medicare beneficiaries have no cap on costs for an observation stay. In some cases, hospitals have to apply a condition code 44 and retroactively change the stay to observation status.
I attended the 2019 Society of Hospital Medicine Annual Conference in Washington. Hospitalists from all parts of the country advocated on Capitol Hill against the “observation bill,” and “meet and greets” with congressional representatives increased their opposition to the bill. These efforts may work in favor of protecting patients from surprise medical bills. Hospital medicine physicians are on the front lines for providing health care in the hospital setting; they have demanded a fix to this legislative loophole which brings high out of pocket costs to our nation’s most vulnerable seniors. The observation status “2-midnight rule” utilized by CMS has increased financial barriers and decreased access to postacute care, affecting the provision of high-quality care for patients.
My hospital has a utilization review committee which reviews all cases to determine the appropriateness of an inpatient versus an observation designation. (An interesting question is whether the financial resources used to support this additional staff could be better assigned to provide high-quality care.) Distribution of these patients is determined on very specific criteria as outlined by Medicare. Observation is basically considered a billing method implemented by payers to decrease dollars paid to acute care hospitals for inpatient care. It pertains to admission status, not to the level of care provided in the hospital. Unfortunately, it is felt that no two payers define observation the same way. A few examples of common observation diagnoses are chest pain, abdominal pain, syncope, and migraine headache; in other words, patients with diagnoses where it is suspected that a less than 24-hour stay in the hospital could be sufficient.
Observation care is increasing and can sometimes contribute to work flow impediments and frustrations in hospitalists; thus, hospitalists are demanding reform. It has been proposed that observation could be eliminated altogether by creating a payment blend of inpatient/outpatient rates. Another option could be to assign lower Diagnosis Related Group coding to lower acuity disease processes, instead of separate observation reimbursement.
Patients and doctors lament that “Once you are in the hospital, you are admitted!” I don’t know the right answer that would solve the observation versus inpatient dilemma, but it is intriguing to consider changes in policy that might focus on the complete elimination of observation status.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
A dilemma for hospitalists and patients
A dilemma for hospitalists and patients
A federal effort to reduce health care expenditures has left many older Medicare recipients experiencing the sticker shock of “observation status.” Patients who are not sick enough to meet inpatient admission criteria, however, still require hospitalization, and may be placed under Medicare observation care.
Seniors can get frustrated, confused, and anxious as their status can be changed while they are in the hospital, and they may receive large medical bills after they are discharged. The Centers for Medicare & Medicaid Services’ “3-day rule” mandates that Medicare will not pay for skilled nursing facility care unless the patient is admitted as an “inpatient” for at least 3 days. Observation days do not count towards this 3-day hospital stay.
There has been an increase in outpatient services over the years since 2006. The 2018 State of Hospital Medicine Report (SoHM) highlights the percentage of discharges based on hospitalists’ billed Current Procedural Terminology codes. Codes 99217 (observation discharge) and 99238-99239 (inpatient discharge) were used to calculate the percentages. 80.7% of adult medicine hospitalist discharges were coded using inpatient discharge codes, while 19.3% of patients were discharged with observation discharge codes.
In the 2016 SoHM report, the ratio was 76.0% inpatient and 21.1% observation codes and in the 2014 report we saw 80.3% inpatient and 16.1% observation discharges (see table 1). But in both of those surveys, same-day admission/discharge codes were also separately reported, which did not occur in 2018. That makes year-over-year comparison of the data challenging.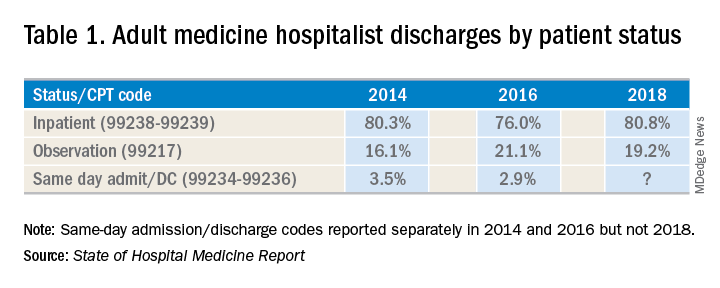
Interestingly, the 2017 CMS data on Evaluation and Management Codes by Specialty for the first time included separate data for hospitalists, based on hospitalists who credentialed with Medicare using the new C6 specialty code. Based on that data, when looking only at inpatient (99238-99239) and observation (99217) codes, 83% of the discharges were inpatient and 17% were observation.
Physicians feel the pressure of strained patient-physician relationships as a consequence of patients feeling the brunt of the financing gap related to observation status. Patients often feel they were not warned adequately about the financial ramifications of observation status. Even if Medicare beneficiaries have received the Medicare Outpatient Observation Notice, outlined by the Notice of Observation Treatment and Implication for Care Eligibility Act, they have no rights to appeal.
Currently Medicare beneficiaries admitted as inpatients only incur a Part A deductible; they are not liable for tests, procedures, and nursing care. On the other hand, in observation status all services are billed separately. For Medicare Part B services (which covers observation care) patients must pay 20% of services after the Part B deductible, which could result in a huge financial burden. Costs for skilled nursing facilities, when they are not covered by Medicare Part A, because of the 3-day rule, can easily go up to $20,000 or more. Medicare beneficiaries have no cap on costs for an observation stay. In some cases, hospitals have to apply a condition code 44 and retroactively change the stay to observation status.
I attended the 2019 Society of Hospital Medicine Annual Conference in Washington. Hospitalists from all parts of the country advocated on Capitol Hill against the “observation bill,” and “meet and greets” with congressional representatives increased their opposition to the bill. These efforts may work in favor of protecting patients from surprise medical bills. Hospital medicine physicians are on the front lines for providing health care in the hospital setting; they have demanded a fix to this legislative loophole which brings high out of pocket costs to our nation’s most vulnerable seniors. The observation status “2-midnight rule” utilized by CMS has increased financial barriers and decreased access to postacute care, affecting the provision of high-quality care for patients.
My hospital has a utilization review committee which reviews all cases to determine the appropriateness of an inpatient versus an observation designation. (An interesting question is whether the financial resources used to support this additional staff could be better assigned to provide high-quality care.) Distribution of these patients is determined on very specific criteria as outlined by Medicare. Observation is basically considered a billing method implemented by payers to decrease dollars paid to acute care hospitals for inpatient care. It pertains to admission status, not to the level of care provided in the hospital. Unfortunately, it is felt that no two payers define observation the same way. A few examples of common observation diagnoses are chest pain, abdominal pain, syncope, and migraine headache; in other words, patients with diagnoses where it is suspected that a less than 24-hour stay in the hospital could be sufficient.
Observation care is increasing and can sometimes contribute to work flow impediments and frustrations in hospitalists; thus, hospitalists are demanding reform. It has been proposed that observation could be eliminated altogether by creating a payment blend of inpatient/outpatient rates. Another option could be to assign lower Diagnosis Related Group coding to lower acuity disease processes, instead of separate observation reimbursement.
Patients and doctors lament that “Once you are in the hospital, you are admitted!” I don’t know the right answer that would solve the observation versus inpatient dilemma, but it is intriguing to consider changes in policy that might focus on the complete elimination of observation status.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
A federal effort to reduce health care expenditures has left many older Medicare recipients experiencing the sticker shock of “observation status.” Patients who are not sick enough to meet inpatient admission criteria, however, still require hospitalization, and may be placed under Medicare observation care.
Seniors can get frustrated, confused, and anxious as their status can be changed while they are in the hospital, and they may receive large medical bills after they are discharged. The Centers for Medicare & Medicaid Services’ “3-day rule” mandates that Medicare will not pay for skilled nursing facility care unless the patient is admitted as an “inpatient” for at least 3 days. Observation days do not count towards this 3-day hospital stay.
There has been an increase in outpatient services over the years since 2006. The 2018 State of Hospital Medicine Report (SoHM) highlights the percentage of discharges based on hospitalists’ billed Current Procedural Terminology codes. Codes 99217 (observation discharge) and 99238-99239 (inpatient discharge) were used to calculate the percentages. 80.7% of adult medicine hospitalist discharges were coded using inpatient discharge codes, while 19.3% of patients were discharged with observation discharge codes.
In the 2016 SoHM report, the ratio was 76.0% inpatient and 21.1% observation codes and in the 2014 report we saw 80.3% inpatient and 16.1% observation discharges (see table 1). But in both of those surveys, same-day admission/discharge codes were also separately reported, which did not occur in 2018. That makes year-over-year comparison of the data challenging.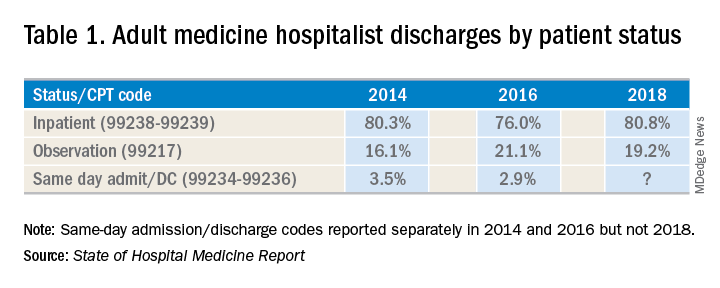
Interestingly, the 2017 CMS data on Evaluation and Management Codes by Specialty for the first time included separate data for hospitalists, based on hospitalists who credentialed with Medicare using the new C6 specialty code. Based on that data, when looking only at inpatient (99238-99239) and observation (99217) codes, 83% of the discharges were inpatient and 17% were observation.
Physicians feel the pressure of strained patient-physician relationships as a consequence of patients feeling the brunt of the financing gap related to observation status. Patients often feel they were not warned adequately about the financial ramifications of observation status. Even if Medicare beneficiaries have received the Medicare Outpatient Observation Notice, outlined by the Notice of Observation Treatment and Implication for Care Eligibility Act, they have no rights to appeal.
Currently Medicare beneficiaries admitted as inpatients only incur a Part A deductible; they are not liable for tests, procedures, and nursing care. On the other hand, in observation status all services are billed separately. For Medicare Part B services (which covers observation care) patients must pay 20% of services after the Part B deductible, which could result in a huge financial burden. Costs for skilled nursing facilities, when they are not covered by Medicare Part A, because of the 3-day rule, can easily go up to $20,000 or more. Medicare beneficiaries have no cap on costs for an observation stay. In some cases, hospitals have to apply a condition code 44 and retroactively change the stay to observation status.
I attended the 2019 Society of Hospital Medicine Annual Conference in Washington. Hospitalists from all parts of the country advocated on Capitol Hill against the “observation bill,” and “meet and greets” with congressional representatives increased their opposition to the bill. These efforts may work in favor of protecting patients from surprise medical bills. Hospital medicine physicians are on the front lines for providing health care in the hospital setting; they have demanded a fix to this legislative loophole which brings high out of pocket costs to our nation’s most vulnerable seniors. The observation status “2-midnight rule” utilized by CMS has increased financial barriers and decreased access to postacute care, affecting the provision of high-quality care for patients.
My hospital has a utilization review committee which reviews all cases to determine the appropriateness of an inpatient versus an observation designation. (An interesting question is whether the financial resources used to support this additional staff could be better assigned to provide high-quality care.) Distribution of these patients is determined on very specific criteria as outlined by Medicare. Observation is basically considered a billing method implemented by payers to decrease dollars paid to acute care hospitals for inpatient care. It pertains to admission status, not to the level of care provided in the hospital. Unfortunately, it is felt that no two payers define observation the same way. A few examples of common observation diagnoses are chest pain, abdominal pain, syncope, and migraine headache; in other words, patients with diagnoses where it is suspected that a less than 24-hour stay in the hospital could be sufficient.
Observation care is increasing and can sometimes contribute to work flow impediments and frustrations in hospitalists; thus, hospitalists are demanding reform. It has been proposed that observation could be eliminated altogether by creating a payment blend of inpatient/outpatient rates. Another option could be to assign lower Diagnosis Related Group coding to lower acuity disease processes, instead of separate observation reimbursement.
Patients and doctors lament that “Once you are in the hospital, you are admitted!” I don’t know the right answer that would solve the observation versus inpatient dilemma, but it is intriguing to consider changes in policy that might focus on the complete elimination of observation status.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
Battling hospitalist burnout
Higher salaries are not sufficient
Hospitalist Rahul C. Borsadia, MD, had been working with Orlando Health Inpatient Medicine Group since the year of its founding in 2011.
The salaries of the practice’s physicians back then were based on relative value units (RVU) – the more patients that physicians saw, the higher their salaries. But a problem arose, Dr. Borsadia said. Physicians were trying to squeeze in two dozen or more patients a day “in a practice that is modeled for quality.”
“By the time the end of the day comes, it’s 9 or 10 p.m. and you are leaving but coming back at 6:30 the next morning. So, lack of sleep, more patients, striving to earn that higher salary,” he said. “The desire to perform quality work with that kind of patient load was not fulfilled and that lead to dissatisfaction and stress, which lead to irritation and exodus from the group.”
Three years ago, the practice transitioned to a throughput process with a census limit of 18 patients or less, without an RVU system, but with salary incentives based on patient satisfaction, billing, and documentation.
“We’ve not had anybody leave the hospital because of burnout or dissatisfaction” since the new system was put into place, Dr. Borsadia said. “Less burnout means more people are happy.”
Although symptoms of burnout still seem to be rampant across hospital medicine, hospitalists are putting potential solutions into place. And – sometimes – they are making progress, through tweaks in schedules and responsibilities, incentives suited to different goals, and better communication.
Scheduling problems
The need for continuing efforts to improve the work experience for hospitalists is apparent, said Henry Michtalik, MD, MPH, MHS, assistant professor of general internal medicine at Johns Hopkins, Baltimore, who led a workshop on the topic at the 2019 Annual Conference of the Society of Hospital Medicine (HM19).
A 2016 survey of academic general internal medicine clinicians – including about 600 hospitalists and outpatient physicians – found that 67% reported high stress, 38% said they were “burned out,” 50% said they felt they had “low control” over their work, and 60% said they felt high documentation pressures. Still, 68% said they were satisfied with the values of their departments.
Hospitalists surveyed were actually less likely to say they were burned out, compared with outpatient internists – 52%, compared with 55% – but they were more likely to score low on a scale measuring personal accomplishments, compared with the outpatient clinicians – 20% to 10%. The survey found no significant difference between the two groups in depression or suicidality. But with 40% reporting depression and 10% reporting thoughts of suicide, the numbers virtually cry out for solutions.
Hospitalists in the HM19 workshop, as in other sessions at the Annual Conference, questioned whether the standard 7-days-on, 7-days-off work schedule – seven 12-hour shifts followed by 7 days off – allows hospitalists to pair their works lives with their personal lives in a sustainable way. They described the way that the stress and fatigue of such an intense work period bleeds into the days off that follow after it.
“By the end of seven 12’s, they’re bleary eyed, they’re upset, they go home (for) 2 days of washout before they even start to enjoy whatever life they have left,” said Jonathan Martin, MD, director of medicine at Cumberland Medical Center in Crossville, Tenn. “It’s hard to get hospitalists to buy in, which increases their dissatisfaction.”
Dr. Michtalik had a similar perspective.
“You just shut the rest of your life down completely for those 7 days and then, on your 7 days off, you’ve scheduled your life,” he said. “But that last off day – day number 7 – you feel that pit in your stomach, that the streak is coming.” He joked that the feeling was similar to the dread inspired by the phrase “winter is coming” in the popular HBO series “Game of Thrones.”
Systematic reviews of the literature have found that it’s mostly changes at the organization level – rather than changes that an individual physician makes on his or her own – that tend to make significant differences. Changes to structure, communication, and scheduling tend to work better than working on mindfulness, education, or trying to improve resilience, Dr. Michtalik said.
In one study discussed at the HM19 workshop, researchers compared a schedule in which an intensivist works in-house for 7 days, with home call at night, to a schedule in which the intensivist is completely off at night, with an in-house intensivist covering the night shift. The schedule in which the intensivist was truly off for the night significantly reduced reports of burnout, while not affecting length of stay or patient-experience outcomes.
Dr. Michtalik said that another study compared 4-week rotations to 2-week rotations for attending physicians. Researchers found that the 2-week version resulted in lower reports of burnout, with readmissions and patient experience unaffected, although they noted that residents tended to prefer 4-week schedules because they felt it resulted in better relationships with the attending physician.
Perhaps the dominant factor in job satisfaction that’s been identified in surveys is how physicians, patients, and administrators relate to one another, Dr. Michtalik said.
“The important concept here is that relationships were really important in driving job satisfaction, whether that be with our colleagues, our patients, or with the staff that you’re working with,” he said. “It’s always easier to decline a consultation or have a bad interaction with someone over the phone than it is if you actually know them or you are communicating face to face. That’s why it’s important to develop these kinds of relationships, which also put a face to what’s going on.”
Beyond salary adjustments
Hospitalists attending the HM19 workshop said they thought that participating in administration committees at their own institutions helps keep hospitalists involved in hospital matters, limiting the effects of burnout and improving workplace satisfaction.
Kevin McAninch, DO, a hospitalist with Central Ohio Primary Care in Westerville, said a shift in work responsibilities has made an improvement at his hospital. There is now an “inpatient support center” – which has a physician and a nurse in an office taking calls from 6 p.m. to 7 a.m., so that rounders can stop taking floor calls during that time.
The system “takes the pressure off our admitters at night and our nurses because they’re not getting floor calls anymore, so they’re just taking care of the admissions from the ER,” he said.
A recurring theme of the discussion was that salary alone seems universally incapable of eradicating feelings of burnout. One hospitalist said that in surveys, higher-paid physicians insist that monetary compensation is their main driver, but still often complain of burnout because they must work extra shifts to earn that higher level of pay.
Instead, burnout and satisfaction indicators tend to have more do to with time, control, and support, Dr. Michtalik noted.
Mangla Gulati, MD, SFHM, chief quality officer at the University of Maryland Medical Center in Baltimore, said that there’s no big secret about what hospitalists want from their places of employment. They want things like getting patients to service faster so they can make diagnoses, making sure patients get the care they need, fixing the problems associated with electronic medical records, and having a work-life “integration.”
“The questions is – how do we get there?” Dr. Gulati wondered. She suggested that hospitalists have to be more assertive and explanatory in their interactions with members of the hospital C-suite.
“I think it’s really important for you to understand or ask your C-suite, ‘Where are you in this whole journey? What is your perception of wellness? Tell me some of the measures of staff wellness,’ ” she said.
If the C-suite says “we have no money” to make improvements, hospitalists must be willing to say, ‘Well, you’re going to have to invest a little bit.’ ” Dr. Gulati said. “What is the ROI (return on investment) on the turnover of a physician? Because when you turn a physician over, you have to recruit and hire new staff.”
Dr. Gulati said that hospitalists should provide C-suite leaders with a detailed walk-through of their actual workflows – what their workdays look like – because “it’s not something they’re familiar with.”
Aside from improving relations with hospital administration, Dr. Gulati suggested creating CME programs for wellness, offering time and funding for physician support meetings, supporting flexibility in work hours, and creating programs specifically to help clinicians with burnout symptoms.
She also touted the benefits of “Schwartz Rounds,” in which several medical disciplines gather to talk about a case that was particularly challenging, clinically complex, and emotionally draining for everyone involved.
At Cumberland Medical Center, Dr. Martin said he has two meetings a month with executives in the hospital’s C-suite. One is with his hospitalist group, TeamHealth, and one is more direct, between himself and hospital administrators. It’s just 2 hours a month, but these conversations have undoubtedly helped, he said, although he cautioned that “the meetings themselves don’t have as much meaning if you aren’t communicating effectively,” meaning hospitalists must understand how the C-suite thinks and learn to speak in terms they understand.
“When I go to the administration now and I say ‘Hey, this is a problem that we’re having. I need your help in solving it,’ the executives are much more likely to respond to me than if they’d never seen me, or only see me rarely,” Dr. Martin said.
As a result, a collaborative approach to such conversations tends to be more effective.
“If you go to the C-suite and say, ‘Here’s our issue, how can you help us?’ – as opposed to telling the administration, ‘This is what I need’ – they are more likely to work with you to generate a solution.”
Higher salaries are not sufficient
Higher salaries are not sufficient
Hospitalist Rahul C. Borsadia, MD, had been working with Orlando Health Inpatient Medicine Group since the year of its founding in 2011.
The salaries of the practice’s physicians back then were based on relative value units (RVU) – the more patients that physicians saw, the higher their salaries. But a problem arose, Dr. Borsadia said. Physicians were trying to squeeze in two dozen or more patients a day “in a practice that is modeled for quality.”
“By the time the end of the day comes, it’s 9 or 10 p.m. and you are leaving but coming back at 6:30 the next morning. So, lack of sleep, more patients, striving to earn that higher salary,” he said. “The desire to perform quality work with that kind of patient load was not fulfilled and that lead to dissatisfaction and stress, which lead to irritation and exodus from the group.”
Three years ago, the practice transitioned to a throughput process with a census limit of 18 patients or less, without an RVU system, but with salary incentives based on patient satisfaction, billing, and documentation.
“We’ve not had anybody leave the hospital because of burnout or dissatisfaction” since the new system was put into place, Dr. Borsadia said. “Less burnout means more people are happy.”
Although symptoms of burnout still seem to be rampant across hospital medicine, hospitalists are putting potential solutions into place. And – sometimes – they are making progress, through tweaks in schedules and responsibilities, incentives suited to different goals, and better communication.
Scheduling problems
The need for continuing efforts to improve the work experience for hospitalists is apparent, said Henry Michtalik, MD, MPH, MHS, assistant professor of general internal medicine at Johns Hopkins, Baltimore, who led a workshop on the topic at the 2019 Annual Conference of the Society of Hospital Medicine (HM19).
A 2016 survey of academic general internal medicine clinicians – including about 600 hospitalists and outpatient physicians – found that 67% reported high stress, 38% said they were “burned out,” 50% said they felt they had “low control” over their work, and 60% said they felt high documentation pressures. Still, 68% said they were satisfied with the values of their departments.
Hospitalists surveyed were actually less likely to say they were burned out, compared with outpatient internists – 52%, compared with 55% – but they were more likely to score low on a scale measuring personal accomplishments, compared with the outpatient clinicians – 20% to 10%. The survey found no significant difference between the two groups in depression or suicidality. But with 40% reporting depression and 10% reporting thoughts of suicide, the numbers virtually cry out for solutions.
Hospitalists in the HM19 workshop, as in other sessions at the Annual Conference, questioned whether the standard 7-days-on, 7-days-off work schedule – seven 12-hour shifts followed by 7 days off – allows hospitalists to pair their works lives with their personal lives in a sustainable way. They described the way that the stress and fatigue of such an intense work period bleeds into the days off that follow after it.
“By the end of seven 12’s, they’re bleary eyed, they’re upset, they go home (for) 2 days of washout before they even start to enjoy whatever life they have left,” said Jonathan Martin, MD, director of medicine at Cumberland Medical Center in Crossville, Tenn. “It’s hard to get hospitalists to buy in, which increases their dissatisfaction.”
Dr. Michtalik had a similar perspective.
“You just shut the rest of your life down completely for those 7 days and then, on your 7 days off, you’ve scheduled your life,” he said. “But that last off day – day number 7 – you feel that pit in your stomach, that the streak is coming.” He joked that the feeling was similar to the dread inspired by the phrase “winter is coming” in the popular HBO series “Game of Thrones.”
Systematic reviews of the literature have found that it’s mostly changes at the organization level – rather than changes that an individual physician makes on his or her own – that tend to make significant differences. Changes to structure, communication, and scheduling tend to work better than working on mindfulness, education, or trying to improve resilience, Dr. Michtalik said.
In one study discussed at the HM19 workshop, researchers compared a schedule in which an intensivist works in-house for 7 days, with home call at night, to a schedule in which the intensivist is completely off at night, with an in-house intensivist covering the night shift. The schedule in which the intensivist was truly off for the night significantly reduced reports of burnout, while not affecting length of stay or patient-experience outcomes.
Dr. Michtalik said that another study compared 4-week rotations to 2-week rotations for attending physicians. Researchers found that the 2-week version resulted in lower reports of burnout, with readmissions and patient experience unaffected, although they noted that residents tended to prefer 4-week schedules because they felt it resulted in better relationships with the attending physician.
Perhaps the dominant factor in job satisfaction that’s been identified in surveys is how physicians, patients, and administrators relate to one another, Dr. Michtalik said.
“The important concept here is that relationships were really important in driving job satisfaction, whether that be with our colleagues, our patients, or with the staff that you’re working with,” he said. “It’s always easier to decline a consultation or have a bad interaction with someone over the phone than it is if you actually know them or you are communicating face to face. That’s why it’s important to develop these kinds of relationships, which also put a face to what’s going on.”
Beyond salary adjustments
Hospitalists attending the HM19 workshop said they thought that participating in administration committees at their own institutions helps keep hospitalists involved in hospital matters, limiting the effects of burnout and improving workplace satisfaction.
Kevin McAninch, DO, a hospitalist with Central Ohio Primary Care in Westerville, said a shift in work responsibilities has made an improvement at his hospital. There is now an “inpatient support center” – which has a physician and a nurse in an office taking calls from 6 p.m. to 7 a.m., so that rounders can stop taking floor calls during that time.
The system “takes the pressure off our admitters at night and our nurses because they’re not getting floor calls anymore, so they’re just taking care of the admissions from the ER,” he said.
A recurring theme of the discussion was that salary alone seems universally incapable of eradicating feelings of burnout. One hospitalist said that in surveys, higher-paid physicians insist that monetary compensation is their main driver, but still often complain of burnout because they must work extra shifts to earn that higher level of pay.
Instead, burnout and satisfaction indicators tend to have more do to with time, control, and support, Dr. Michtalik noted.
Mangla Gulati, MD, SFHM, chief quality officer at the University of Maryland Medical Center in Baltimore, said that there’s no big secret about what hospitalists want from their places of employment. They want things like getting patients to service faster so they can make diagnoses, making sure patients get the care they need, fixing the problems associated with electronic medical records, and having a work-life “integration.”
“The questions is – how do we get there?” Dr. Gulati wondered. She suggested that hospitalists have to be more assertive and explanatory in their interactions with members of the hospital C-suite.
“I think it’s really important for you to understand or ask your C-suite, ‘Where are you in this whole journey? What is your perception of wellness? Tell me some of the measures of staff wellness,’ ” she said.
If the C-suite says “we have no money” to make improvements, hospitalists must be willing to say, ‘Well, you’re going to have to invest a little bit.’ ” Dr. Gulati said. “What is the ROI (return on investment) on the turnover of a physician? Because when you turn a physician over, you have to recruit and hire new staff.”
Dr. Gulati said that hospitalists should provide C-suite leaders with a detailed walk-through of their actual workflows – what their workdays look like – because “it’s not something they’re familiar with.”
Aside from improving relations with hospital administration, Dr. Gulati suggested creating CME programs for wellness, offering time and funding for physician support meetings, supporting flexibility in work hours, and creating programs specifically to help clinicians with burnout symptoms.
She also touted the benefits of “Schwartz Rounds,” in which several medical disciplines gather to talk about a case that was particularly challenging, clinically complex, and emotionally draining for everyone involved.
At Cumberland Medical Center, Dr. Martin said he has two meetings a month with executives in the hospital’s C-suite. One is with his hospitalist group, TeamHealth, and one is more direct, between himself and hospital administrators. It’s just 2 hours a month, but these conversations have undoubtedly helped, he said, although he cautioned that “the meetings themselves don’t have as much meaning if you aren’t communicating effectively,” meaning hospitalists must understand how the C-suite thinks and learn to speak in terms they understand.
“When I go to the administration now and I say ‘Hey, this is a problem that we’re having. I need your help in solving it,’ the executives are much more likely to respond to me than if they’d never seen me, or only see me rarely,” Dr. Martin said.
As a result, a collaborative approach to such conversations tends to be more effective.
“If you go to the C-suite and say, ‘Here’s our issue, how can you help us?’ – as opposed to telling the administration, ‘This is what I need’ – they are more likely to work with you to generate a solution.”
Hospitalist Rahul C. Borsadia, MD, had been working with Orlando Health Inpatient Medicine Group since the year of its founding in 2011.
The salaries of the practice’s physicians back then were based on relative value units (RVU) – the more patients that physicians saw, the higher their salaries. But a problem arose, Dr. Borsadia said. Physicians were trying to squeeze in two dozen or more patients a day “in a practice that is modeled for quality.”
“By the time the end of the day comes, it’s 9 or 10 p.m. and you are leaving but coming back at 6:30 the next morning. So, lack of sleep, more patients, striving to earn that higher salary,” he said. “The desire to perform quality work with that kind of patient load was not fulfilled and that lead to dissatisfaction and stress, which lead to irritation and exodus from the group.”
Three years ago, the practice transitioned to a throughput process with a census limit of 18 patients or less, without an RVU system, but with salary incentives based on patient satisfaction, billing, and documentation.
“We’ve not had anybody leave the hospital because of burnout or dissatisfaction” since the new system was put into place, Dr. Borsadia said. “Less burnout means more people are happy.”
Although symptoms of burnout still seem to be rampant across hospital medicine, hospitalists are putting potential solutions into place. And – sometimes – they are making progress, through tweaks in schedules and responsibilities, incentives suited to different goals, and better communication.
Scheduling problems
The need for continuing efforts to improve the work experience for hospitalists is apparent, said Henry Michtalik, MD, MPH, MHS, assistant professor of general internal medicine at Johns Hopkins, Baltimore, who led a workshop on the topic at the 2019 Annual Conference of the Society of Hospital Medicine (HM19).
A 2016 survey of academic general internal medicine clinicians – including about 600 hospitalists and outpatient physicians – found that 67% reported high stress, 38% said they were “burned out,” 50% said they felt they had “low control” over their work, and 60% said they felt high documentation pressures. Still, 68% said they were satisfied with the values of their departments.
Hospitalists surveyed were actually less likely to say they were burned out, compared with outpatient internists – 52%, compared with 55% – but they were more likely to score low on a scale measuring personal accomplishments, compared with the outpatient clinicians – 20% to 10%. The survey found no significant difference between the two groups in depression or suicidality. But with 40% reporting depression and 10% reporting thoughts of suicide, the numbers virtually cry out for solutions.
Hospitalists in the HM19 workshop, as in other sessions at the Annual Conference, questioned whether the standard 7-days-on, 7-days-off work schedule – seven 12-hour shifts followed by 7 days off – allows hospitalists to pair their works lives with their personal lives in a sustainable way. They described the way that the stress and fatigue of such an intense work period bleeds into the days off that follow after it.
“By the end of seven 12’s, they’re bleary eyed, they’re upset, they go home (for) 2 days of washout before they even start to enjoy whatever life they have left,” said Jonathan Martin, MD, director of medicine at Cumberland Medical Center in Crossville, Tenn. “It’s hard to get hospitalists to buy in, which increases their dissatisfaction.”
Dr. Michtalik had a similar perspective.
“You just shut the rest of your life down completely for those 7 days and then, on your 7 days off, you’ve scheduled your life,” he said. “But that last off day – day number 7 – you feel that pit in your stomach, that the streak is coming.” He joked that the feeling was similar to the dread inspired by the phrase “winter is coming” in the popular HBO series “Game of Thrones.”
Systematic reviews of the literature have found that it’s mostly changes at the organization level – rather than changes that an individual physician makes on his or her own – that tend to make significant differences. Changes to structure, communication, and scheduling tend to work better than working on mindfulness, education, or trying to improve resilience, Dr. Michtalik said.
In one study discussed at the HM19 workshop, researchers compared a schedule in which an intensivist works in-house for 7 days, with home call at night, to a schedule in which the intensivist is completely off at night, with an in-house intensivist covering the night shift. The schedule in which the intensivist was truly off for the night significantly reduced reports of burnout, while not affecting length of stay or patient-experience outcomes.
Dr. Michtalik said that another study compared 4-week rotations to 2-week rotations for attending physicians. Researchers found that the 2-week version resulted in lower reports of burnout, with readmissions and patient experience unaffected, although they noted that residents tended to prefer 4-week schedules because they felt it resulted in better relationships with the attending physician.
Perhaps the dominant factor in job satisfaction that’s been identified in surveys is how physicians, patients, and administrators relate to one another, Dr. Michtalik said.
“The important concept here is that relationships were really important in driving job satisfaction, whether that be with our colleagues, our patients, or with the staff that you’re working with,” he said. “It’s always easier to decline a consultation or have a bad interaction with someone over the phone than it is if you actually know them or you are communicating face to face. That’s why it’s important to develop these kinds of relationships, which also put a face to what’s going on.”
Beyond salary adjustments
Hospitalists attending the HM19 workshop said they thought that participating in administration committees at their own institutions helps keep hospitalists involved in hospital matters, limiting the effects of burnout and improving workplace satisfaction.
Kevin McAninch, DO, a hospitalist with Central Ohio Primary Care in Westerville, said a shift in work responsibilities has made an improvement at his hospital. There is now an “inpatient support center” – which has a physician and a nurse in an office taking calls from 6 p.m. to 7 a.m., so that rounders can stop taking floor calls during that time.
The system “takes the pressure off our admitters at night and our nurses because they’re not getting floor calls anymore, so they’re just taking care of the admissions from the ER,” he said.
A recurring theme of the discussion was that salary alone seems universally incapable of eradicating feelings of burnout. One hospitalist said that in surveys, higher-paid physicians insist that monetary compensation is their main driver, but still often complain of burnout because they must work extra shifts to earn that higher level of pay.
Instead, burnout and satisfaction indicators tend to have more do to with time, control, and support, Dr. Michtalik noted.
Mangla Gulati, MD, SFHM, chief quality officer at the University of Maryland Medical Center in Baltimore, said that there’s no big secret about what hospitalists want from their places of employment. They want things like getting patients to service faster so they can make diagnoses, making sure patients get the care they need, fixing the problems associated with electronic medical records, and having a work-life “integration.”
“The questions is – how do we get there?” Dr. Gulati wondered. She suggested that hospitalists have to be more assertive and explanatory in their interactions with members of the hospital C-suite.
“I think it’s really important for you to understand or ask your C-suite, ‘Where are you in this whole journey? What is your perception of wellness? Tell me some of the measures of staff wellness,’ ” she said.
If the C-suite says “we have no money” to make improvements, hospitalists must be willing to say, ‘Well, you’re going to have to invest a little bit.’ ” Dr. Gulati said. “What is the ROI (return on investment) on the turnover of a physician? Because when you turn a physician over, you have to recruit and hire new staff.”
Dr. Gulati said that hospitalists should provide C-suite leaders with a detailed walk-through of their actual workflows – what their workdays look like – because “it’s not something they’re familiar with.”
Aside from improving relations with hospital administration, Dr. Gulati suggested creating CME programs for wellness, offering time and funding for physician support meetings, supporting flexibility in work hours, and creating programs specifically to help clinicians with burnout symptoms.
She also touted the benefits of “Schwartz Rounds,” in which several medical disciplines gather to talk about a case that was particularly challenging, clinically complex, and emotionally draining for everyone involved.
At Cumberland Medical Center, Dr. Martin said he has two meetings a month with executives in the hospital’s C-suite. One is with his hospitalist group, TeamHealth, and one is more direct, between himself and hospital administrators. It’s just 2 hours a month, but these conversations have undoubtedly helped, he said, although he cautioned that “the meetings themselves don’t have as much meaning if you aren’t communicating effectively,” meaning hospitalists must understand how the C-suite thinks and learn to speak in terms they understand.
“When I go to the administration now and I say ‘Hey, this is a problem that we’re having. I need your help in solving it,’ the executives are much more likely to respond to me than if they’d never seen me, or only see me rarely,” Dr. Martin said.
As a result, a collaborative approach to such conversations tends to be more effective.
“If you go to the C-suite and say, ‘Here’s our issue, how can you help us?’ – as opposed to telling the administration, ‘This is what I need’ – they are more likely to work with you to generate a solution.”
















