User login
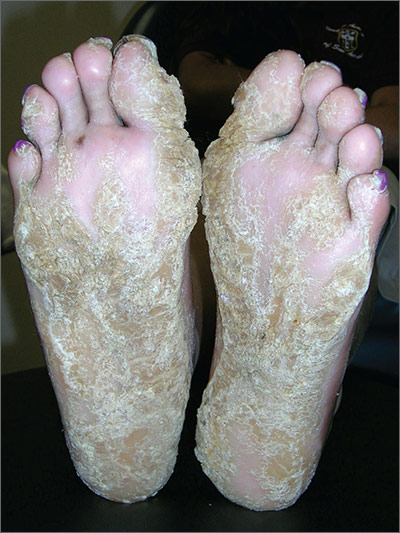
Thickening of skin on feet
The FP recognized this as diffuse palmoplantar keratoderma of the palms and soles. This is an inherited genodermatosis that may be autosomal dominant or sporadic. Palmoplantar keratoderma includes a rare heterogeneous group of disorders that are characterized by thickening of the palms and the soles that can also be an associated feature of some very rare syndromes. The patient in this case had diffuse hyperkeratosis, which can be distributed over most of the plantar surface.
This condition can be differentiated from plantar warts as it is present on more diffuse locations on the palmoplantar surfaces (including palms and soles) and it lacks the black dots of thrombosed capillaries that are seen in plantar warts.
There is no cure for this genetic condition and the goals of treatment are functional and cosmetic improvement. The FP prescribed 12% ammonium lactate as an emollient and keratolytic. The patient applied this twice daily with some symptomatic relief. The family hoped that there would be some genetic treatment for this in the future.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Plantar warts. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:766-770.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
The FP recognized this as diffuse palmoplantar keratoderma of the palms and soles. This is an inherited genodermatosis that may be autosomal dominant or sporadic. Palmoplantar keratoderma includes a rare heterogeneous group of disorders that are characterized by thickening of the palms and the soles that can also be an associated feature of some very rare syndromes. The patient in this case had diffuse hyperkeratosis, which can be distributed over most of the plantar surface.
This condition can be differentiated from plantar warts as it is present on more diffuse locations on the palmoplantar surfaces (including palms and soles) and it lacks the black dots of thrombosed capillaries that are seen in plantar warts.
There is no cure for this genetic condition and the goals of treatment are functional and cosmetic improvement. The FP prescribed 12% ammonium lactate as an emollient and keratolytic. The patient applied this twice daily with some symptomatic relief. The family hoped that there would be some genetic treatment for this in the future.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Plantar warts. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:766-770.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
The FP recognized this as diffuse palmoplantar keratoderma of the palms and soles. This is an inherited genodermatosis that may be autosomal dominant or sporadic. Palmoplantar keratoderma includes a rare heterogeneous group of disorders that are characterized by thickening of the palms and the soles that can also be an associated feature of some very rare syndromes. The patient in this case had diffuse hyperkeratosis, which can be distributed over most of the plantar surface.
This condition can be differentiated from plantar warts as it is present on more diffuse locations on the palmoplantar surfaces (including palms and soles) and it lacks the black dots of thrombosed capillaries that are seen in plantar warts.
There is no cure for this genetic condition and the goals of treatment are functional and cosmetic improvement. The FP prescribed 12% ammonium lactate as an emollient and keratolytic. The patient applied this twice daily with some symptomatic relief. The family hoped that there would be some genetic treatment for this in the future.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Plantar warts. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:766-770.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
Scaly palms and soles
The FP recognized this as focal palmoplantar keratoderma of the palms and soles, which is an inherited genodermatosis that is autosomal dominant. The lesions are located mainly on high pressure areas and spare the arches of the feet.
Palmoplantar keratoderma includes a rare heterogeneous group of disorders that are characterized by thickening of the palms and the soles that can also be an associated feature of some very rare syndromes. The patient in this case had focal hyperkeratosis, which is located mainly on pressure points and sites of recurrent friction.
Palmoplantar keratoderma can be differentiated from plantar warts as it is present on more diffuse locations on the palmoplantar surfaces (including palms and soles) and it lacks the black dots of thrombosed capillaries that are seen in plantar warts.
There is no cure for this genetic condition and the goals of treatment are functional and cosmetic improvement. The FP prescribed 12% ammonium lactate as an emollient and keratolytic. The patient applied this twice daily with some symptomatic relief.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Plantar warts. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:766-770.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
The FP recognized this as focal palmoplantar keratoderma of the palms and soles, which is an inherited genodermatosis that is autosomal dominant. The lesions are located mainly on high pressure areas and spare the arches of the feet.
Palmoplantar keratoderma includes a rare heterogeneous group of disorders that are characterized by thickening of the palms and the soles that can also be an associated feature of some very rare syndromes. The patient in this case had focal hyperkeratosis, which is located mainly on pressure points and sites of recurrent friction.
Palmoplantar keratoderma can be differentiated from plantar warts as it is present on more diffuse locations on the palmoplantar surfaces (including palms and soles) and it lacks the black dots of thrombosed capillaries that are seen in plantar warts.
There is no cure for this genetic condition and the goals of treatment are functional and cosmetic improvement. The FP prescribed 12% ammonium lactate as an emollient and keratolytic. The patient applied this twice daily with some symptomatic relief.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Plantar warts. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:766-770.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
The FP recognized this as focal palmoplantar keratoderma of the palms and soles, which is an inherited genodermatosis that is autosomal dominant. The lesions are located mainly on high pressure areas and spare the arches of the feet.
Palmoplantar keratoderma includes a rare heterogeneous group of disorders that are characterized by thickening of the palms and the soles that can also be an associated feature of some very rare syndromes. The patient in this case had focal hyperkeratosis, which is located mainly on pressure points and sites of recurrent friction.
Palmoplantar keratoderma can be differentiated from plantar warts as it is present on more diffuse locations on the palmoplantar surfaces (including palms and soles) and it lacks the black dots of thrombosed capillaries that are seen in plantar warts.
There is no cure for this genetic condition and the goals of treatment are functional and cosmetic improvement. The FP prescribed 12% ammonium lactate as an emollient and keratolytic. The patient applied this twice daily with some symptomatic relief.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Plantar warts. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:766-770.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
Growths on palms
The FP diagnosed this patient with palmar warts, which are similar in morphology to plantar warts. Plantar (or palmar) warts are lesions caused by human papillomavirus (HPV) that occur on the soles of the feet and palms of the hands. Plantar warts occur mostly in adolescents and young adults and affect up to 10% of people in these age groups.
Plantar warts usually occur at points of maximum pressure, such as on the heels or over the heads of the metatarsal bones, but may appear anywhere on the plantar surface, including the tips of the toes. A cluster of multiple warts that appear to fuse together is referred to as a mosaic wart. HIV is a risk factor for any type of HPV infection.
Distinguish warts from calluses by noting the skin lines; warts lack skin lines crossing their surface, whereas normal skin lines cross through a callus without any disturbance. Additionally, plantar/palmar warts may have a highly organized mosaic pattern on the surface when examined with a hand lens and have prominent black dots (thrombosed capillaries).
The most common treatments for warts include topical salicylic acid and cryotherapy. Topical salicylic acid preparations are nonscarring, minimally painful, and relatively effective, but require persistent application of medication once a day for weeks to months. Cryotherapy with liquid nitrogen therapy is commonly used, but plantar warts are more resistant than other HPV lesions. The liquid nitrogen is applied to form a freeze ball that covers the lesion and 2 mm of surrounding normal tissue for usually 10 to 20 seconds per treatment. This can be performed as a single long freeze or divided into 2 freezing episodes with thawing in between. This allows for more freeze time in a way that is less painful to the patient.
In this case, the patient chose cryotherapy and arranged for a follow-up appointment in 3 to 4 weeks for a second round.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Plantar warts. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:766-770.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
The FP diagnosed this patient with palmar warts, which are similar in morphology to plantar warts. Plantar (or palmar) warts are lesions caused by human papillomavirus (HPV) that occur on the soles of the feet and palms of the hands. Plantar warts occur mostly in adolescents and young adults and affect up to 10% of people in these age groups.
Plantar warts usually occur at points of maximum pressure, such as on the heels or over the heads of the metatarsal bones, but may appear anywhere on the plantar surface, including the tips of the toes. A cluster of multiple warts that appear to fuse together is referred to as a mosaic wart. HIV is a risk factor for any type of HPV infection.
Distinguish warts from calluses by noting the skin lines; warts lack skin lines crossing their surface, whereas normal skin lines cross through a callus without any disturbance. Additionally, plantar/palmar warts may have a highly organized mosaic pattern on the surface when examined with a hand lens and have prominent black dots (thrombosed capillaries).
The most common treatments for warts include topical salicylic acid and cryotherapy. Topical salicylic acid preparations are nonscarring, minimally painful, and relatively effective, but require persistent application of medication once a day for weeks to months. Cryotherapy with liquid nitrogen therapy is commonly used, but plantar warts are more resistant than other HPV lesions. The liquid nitrogen is applied to form a freeze ball that covers the lesion and 2 mm of surrounding normal tissue for usually 10 to 20 seconds per treatment. This can be performed as a single long freeze or divided into 2 freezing episodes with thawing in between. This allows for more freeze time in a way that is less painful to the patient.
In this case, the patient chose cryotherapy and arranged for a follow-up appointment in 3 to 4 weeks for a second round.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Plantar warts. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:766-770.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
The FP diagnosed this patient with palmar warts, which are similar in morphology to plantar warts. Plantar (or palmar) warts are lesions caused by human papillomavirus (HPV) that occur on the soles of the feet and palms of the hands. Plantar warts occur mostly in adolescents and young adults and affect up to 10% of people in these age groups.
Plantar warts usually occur at points of maximum pressure, such as on the heels or over the heads of the metatarsal bones, but may appear anywhere on the plantar surface, including the tips of the toes. A cluster of multiple warts that appear to fuse together is referred to as a mosaic wart. HIV is a risk factor for any type of HPV infection.
Distinguish warts from calluses by noting the skin lines; warts lack skin lines crossing their surface, whereas normal skin lines cross through a callus without any disturbance. Additionally, plantar/palmar warts may have a highly organized mosaic pattern on the surface when examined with a hand lens and have prominent black dots (thrombosed capillaries).
The most common treatments for warts include topical salicylic acid and cryotherapy. Topical salicylic acid preparations are nonscarring, minimally painful, and relatively effective, but require persistent application of medication once a day for weeks to months. Cryotherapy with liquid nitrogen therapy is commonly used, but plantar warts are more resistant than other HPV lesions. The liquid nitrogen is applied to form a freeze ball that covers the lesion and 2 mm of surrounding normal tissue for usually 10 to 20 seconds per treatment. This can be performed as a single long freeze or divided into 2 freezing episodes with thawing in between. This allows for more freeze time in a way that is less painful to the patient.
In this case, the patient chose cryotherapy and arranged for a follow-up appointment in 3 to 4 weeks for a second round.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Plantar warts. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:766-770.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
Pruritic hyperpigmented patch on back
A 60-year-old woman visited our clinic complaining of an area on the right side of her middle back that was itchy, and had been bothering her for the past 10 years. She said her symptoms began without a trigger, and that a darkened area had appeared in the location of the itch. She had already been prescribed topical corticosteroids and antifungals and had tried over-the counter aids, but nothing relieved the itch. The patient had a history of cervical radiculopathy and was morbidly obese at the time of the visit.
On examination, the pruritic area consisted of a hyperpigmented, non-infiltrated 7-cm patch that was lateral to the vertebral column and within the dermatomes T4 to T6 (FIGURE). The patient also had hyperesthesia to light touch in this region and scratch abrasions.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Notalgia paresthetica
The location of the pruritic area and the patient’s clinical presentation led us to diagnose notalgia paresthetica. NP is a common dermatologic complaint characterized by unilateral pruritus that is medial or inferior to the scapula with dermatomal distribution.
The etiology of NP remains unknown, although it is thought to be a neuropathic itch caused by afferent nerve entrapment. The dorsal rami of the thoracic spinal nerves T2 to T6 are considered to be responsible for these symptoms. NP is not only a skin disease, but a cutaneous sign of an underlying spinal condition, including degenerative cervical spine disease.1-3
NP is a clinical diagnosis. There is typically a history of localized pruritus on the unilateral infrascapula area and there are few or no visible signs of disease. Patients frequently report a spider-bite sensation, prickly feelings, and/or an indescribable itch sensation. In addition, they may experience dysesthesia with diffuse mild burning, some surface numbness, and “under the skin” discomfort.
On physical examination, the patient may have a unilateral and ill-defined tan, pink, or hyperpigmented nonindurated patch on the infrascapular back that is a result of long-time scratching. Secondary skin changes such as lichenification, excoriations, eczema, xerosis, and infection often occur. Mild sensory alterations to light touch, vibration, and pin pricks may round out the clinical picture.1-3 Atypical forms of NP include localized pruritus on the upper back, neck, scalp, or shoulder.
Pruritus without other skin lesions can help pinpoint the Dx
The differential diagnosis for NP includes atopic dermatitis, contact dermatitis, drug eruptions, herpes zoster, idiopathic pruritus and systemic disease (such as renal, cholestatic, or hematologic pruritus, or pruritus associated with malignancy), tinea corporis, tinea versicolor, and xerosis.
Clues in the history. The chronic evolution of pruritus without other skin lesions, like vesicles or squamous areas, and the location of a hyperpigmented patch near the scapula region in a midlife patient, should prompt you to consider NP. A biopsy may show signs of post-inflammatory infiltrate of the papillary dermis with dermal melanophages.4,5
Although imaging tests are not required for a diagnosis of NP, basic cervical and possibly thoracic radiographs or magnetic resonance imaging (MRI) may be helpful in patients with symptoms of spine pain, tenderness, spasms, decreased range of motion, or any history of spinal trauma or injury. The images may reveal spinal disorders, including osteoarthritic lesions such as kyphosis, kyphoscoliosis, and vertebral hyperostosis.4
The exact cause of NP is unclear, but the evidence suggests that it results from damage to the cutaneous branches of the posterior divisions of the spinal nerves. This can occur by either impingement from degenerative changes in the spine or by spasms in the paraspinal musculature.2
The itch is neuropathic; antihistamines, steroids won’t help
It is difficult to treat NP without treating the underlying disease, which is usually spinal damage.4 Little has been published on the treatment of NP, and most of the literature on the subject involves case reports. Because the pruritus in NP is neuropathic, antihistamines and topical steroids are ineffective.4
The most commonly used treatment for NP among dermatologists is capsaicin as a 0.025% cream or 8% patch. One study with 20 patients reported improvement of pruritus in 70% of patients at 2 weeks, with some relapsing in about a month.6
Another treatment that has been used is cutaneous botulinum toxin type A injections, but its use is controversial. This strategy was proposed by Weinfeld7 after successful treatment of 2 patients. However, other studies have had variable outcomes with no resolution of pruritus.8
Other treatments include gabapentin,9 transcutaneous electrical nerve stimulation,10 and narrow-band ultraviolet-B.11 It is appropriate to consider surgical decompression or neurolysis of the nerve when other forms of treatment fail.12
Our patient was treated with topical capsaicin cream 0.25 mg/g, which lessened the intensity of her itching. After 2 months, the patient reported improvement of her symptoms.
CORRESPONDENCE
Joana Sequeira, MD, Estrada da Mata nº56, Leiria, Portugal; [email protected].
1. Stumpf A, Ständer S. Neuropathic itch: diagnosis and management. Dermatol Ther. 2013;26:104-109.
2. Ellis C. Notalgia paresthetica: the unreachable itch. Dermatol Pract Concept. 2013;3:3-6.
3. Bolognia JL, Jorizzo JL, Schaffer JV, eds. Pruritus and dysesthesia. In: Dermatology. 3rd ed. Philadelphia, PA: Elsevier Saunders;2012:121.
4. Raison-Peyron N, Meunier L, Acevedo M, et al. Notalgia paresthetica: clinical, physiopathological and therapeutic aspects. A study of 12 cases. J Eur Acad Dermatol Venereol. 1999;12:215-221.
5. Savk O, Savk E. Investigation of spinal pathology in notalgia paresthetica. J Am Acad Dermatol. 2005;52:1085-1087.
6. Wallengren J, Klinker M. Successful treatment of notalgia paresthetica with topical capsaicin: vehicle-controlled, double-blind, crossover study. J Am Acad Dermatol. 1995;32:287-289.
7. Weinfeld PK. Successful treatment of notalgia paresthetica with botulinum toxin type A. Arch Dermatol. 2007;143:980-982.
8. Pérez-Pérez L, García-Gavín J, Allegue F, et al. Notalgia paresthetica: treatment using intradermal botulinum toxin A. Actas Dermosifiliogr. 2014;105:74-77.
9. Maciel AA, Cunha PR, Laraia IO, et al. Efficacy of gabapentin in the improvement of pruritus and quality of life of patients with nostalgia paresthetica. An Bras Dermatol. 2014;89:570-575.
10. Savk E, Savk O, Sendur F. Transcutaneous electrical nerve stimulation offers partial relief in notalgia paresthetica patients with a relevant spinal pathology. J Dermatol. 2007;34:315-319.
11. Pérez-Pérez L, Allegue F, Fabeiro JM, et al. Notalgia paresthesica successfully treated with narrow-band UVB: report of five cases. J Eur Acad Dermatol Venereol. 2010;24:730-732.
12. Williams EH, Rosson GD, Elsamanoudi I, et al. Surgical decompression for notalgia paresthetica: a case report. Microsurgery. 2010;30:70-72.
A 60-year-old woman visited our clinic complaining of an area on the right side of her middle back that was itchy, and had been bothering her for the past 10 years. She said her symptoms began without a trigger, and that a darkened area had appeared in the location of the itch. She had already been prescribed topical corticosteroids and antifungals and had tried over-the counter aids, but nothing relieved the itch. The patient had a history of cervical radiculopathy and was morbidly obese at the time of the visit.
On examination, the pruritic area consisted of a hyperpigmented, non-infiltrated 7-cm patch that was lateral to the vertebral column and within the dermatomes T4 to T6 (FIGURE). The patient also had hyperesthesia to light touch in this region and scratch abrasions.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Notalgia paresthetica
The location of the pruritic area and the patient’s clinical presentation led us to diagnose notalgia paresthetica. NP is a common dermatologic complaint characterized by unilateral pruritus that is medial or inferior to the scapula with dermatomal distribution.
The etiology of NP remains unknown, although it is thought to be a neuropathic itch caused by afferent nerve entrapment. The dorsal rami of the thoracic spinal nerves T2 to T6 are considered to be responsible for these symptoms. NP is not only a skin disease, but a cutaneous sign of an underlying spinal condition, including degenerative cervical spine disease.1-3
NP is a clinical diagnosis. There is typically a history of localized pruritus on the unilateral infrascapula area and there are few or no visible signs of disease. Patients frequently report a spider-bite sensation, prickly feelings, and/or an indescribable itch sensation. In addition, they may experience dysesthesia with diffuse mild burning, some surface numbness, and “under the skin” discomfort.
On physical examination, the patient may have a unilateral and ill-defined tan, pink, or hyperpigmented nonindurated patch on the infrascapular back that is a result of long-time scratching. Secondary skin changes such as lichenification, excoriations, eczema, xerosis, and infection often occur. Mild sensory alterations to light touch, vibration, and pin pricks may round out the clinical picture.1-3 Atypical forms of NP include localized pruritus on the upper back, neck, scalp, or shoulder.
Pruritus without other skin lesions can help pinpoint the Dx
The differential diagnosis for NP includes atopic dermatitis, contact dermatitis, drug eruptions, herpes zoster, idiopathic pruritus and systemic disease (such as renal, cholestatic, or hematologic pruritus, or pruritus associated with malignancy), tinea corporis, tinea versicolor, and xerosis.
Clues in the history. The chronic evolution of pruritus without other skin lesions, like vesicles or squamous areas, and the location of a hyperpigmented patch near the scapula region in a midlife patient, should prompt you to consider NP. A biopsy may show signs of post-inflammatory infiltrate of the papillary dermis with dermal melanophages.4,5
Although imaging tests are not required for a diagnosis of NP, basic cervical and possibly thoracic radiographs or magnetic resonance imaging (MRI) may be helpful in patients with symptoms of spine pain, tenderness, spasms, decreased range of motion, or any history of spinal trauma or injury. The images may reveal spinal disorders, including osteoarthritic lesions such as kyphosis, kyphoscoliosis, and vertebral hyperostosis.4
The exact cause of NP is unclear, but the evidence suggests that it results from damage to the cutaneous branches of the posterior divisions of the spinal nerves. This can occur by either impingement from degenerative changes in the spine or by spasms in the paraspinal musculature.2
The itch is neuropathic; antihistamines, steroids won’t help
It is difficult to treat NP without treating the underlying disease, which is usually spinal damage.4 Little has been published on the treatment of NP, and most of the literature on the subject involves case reports. Because the pruritus in NP is neuropathic, antihistamines and topical steroids are ineffective.4
The most commonly used treatment for NP among dermatologists is capsaicin as a 0.025% cream or 8% patch. One study with 20 patients reported improvement of pruritus in 70% of patients at 2 weeks, with some relapsing in about a month.6
Another treatment that has been used is cutaneous botulinum toxin type A injections, but its use is controversial. This strategy was proposed by Weinfeld7 after successful treatment of 2 patients. However, other studies have had variable outcomes with no resolution of pruritus.8
Other treatments include gabapentin,9 transcutaneous electrical nerve stimulation,10 and narrow-band ultraviolet-B.11 It is appropriate to consider surgical decompression or neurolysis of the nerve when other forms of treatment fail.12
Our patient was treated with topical capsaicin cream 0.25 mg/g, which lessened the intensity of her itching. After 2 months, the patient reported improvement of her symptoms.
CORRESPONDENCE
Joana Sequeira, MD, Estrada da Mata nº56, Leiria, Portugal; [email protected].
A 60-year-old woman visited our clinic complaining of an area on the right side of her middle back that was itchy, and had been bothering her for the past 10 years. She said her symptoms began without a trigger, and that a darkened area had appeared in the location of the itch. She had already been prescribed topical corticosteroids and antifungals and had tried over-the counter aids, but nothing relieved the itch. The patient had a history of cervical radiculopathy and was morbidly obese at the time of the visit.
On examination, the pruritic area consisted of a hyperpigmented, non-infiltrated 7-cm patch that was lateral to the vertebral column and within the dermatomes T4 to T6 (FIGURE). The patient also had hyperesthesia to light touch in this region and scratch abrasions.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Notalgia paresthetica
The location of the pruritic area and the patient’s clinical presentation led us to diagnose notalgia paresthetica. NP is a common dermatologic complaint characterized by unilateral pruritus that is medial or inferior to the scapula with dermatomal distribution.
The etiology of NP remains unknown, although it is thought to be a neuropathic itch caused by afferent nerve entrapment. The dorsal rami of the thoracic spinal nerves T2 to T6 are considered to be responsible for these symptoms. NP is not only a skin disease, but a cutaneous sign of an underlying spinal condition, including degenerative cervical spine disease.1-3
NP is a clinical diagnosis. There is typically a history of localized pruritus on the unilateral infrascapula area and there are few or no visible signs of disease. Patients frequently report a spider-bite sensation, prickly feelings, and/or an indescribable itch sensation. In addition, they may experience dysesthesia with diffuse mild burning, some surface numbness, and “under the skin” discomfort.
On physical examination, the patient may have a unilateral and ill-defined tan, pink, or hyperpigmented nonindurated patch on the infrascapular back that is a result of long-time scratching. Secondary skin changes such as lichenification, excoriations, eczema, xerosis, and infection often occur. Mild sensory alterations to light touch, vibration, and pin pricks may round out the clinical picture.1-3 Atypical forms of NP include localized pruritus on the upper back, neck, scalp, or shoulder.
Pruritus without other skin lesions can help pinpoint the Dx
The differential diagnosis for NP includes atopic dermatitis, contact dermatitis, drug eruptions, herpes zoster, idiopathic pruritus and systemic disease (such as renal, cholestatic, or hematologic pruritus, or pruritus associated with malignancy), tinea corporis, tinea versicolor, and xerosis.
Clues in the history. The chronic evolution of pruritus without other skin lesions, like vesicles or squamous areas, and the location of a hyperpigmented patch near the scapula region in a midlife patient, should prompt you to consider NP. A biopsy may show signs of post-inflammatory infiltrate of the papillary dermis with dermal melanophages.4,5
Although imaging tests are not required for a diagnosis of NP, basic cervical and possibly thoracic radiographs or magnetic resonance imaging (MRI) may be helpful in patients with symptoms of spine pain, tenderness, spasms, decreased range of motion, or any history of spinal trauma or injury. The images may reveal spinal disorders, including osteoarthritic lesions such as kyphosis, kyphoscoliosis, and vertebral hyperostosis.4
The exact cause of NP is unclear, but the evidence suggests that it results from damage to the cutaneous branches of the posterior divisions of the spinal nerves. This can occur by either impingement from degenerative changes in the spine or by spasms in the paraspinal musculature.2
The itch is neuropathic; antihistamines, steroids won’t help
It is difficult to treat NP without treating the underlying disease, which is usually spinal damage.4 Little has been published on the treatment of NP, and most of the literature on the subject involves case reports. Because the pruritus in NP is neuropathic, antihistamines and topical steroids are ineffective.4
The most commonly used treatment for NP among dermatologists is capsaicin as a 0.025% cream or 8% patch. One study with 20 patients reported improvement of pruritus in 70% of patients at 2 weeks, with some relapsing in about a month.6
Another treatment that has been used is cutaneous botulinum toxin type A injections, but its use is controversial. This strategy was proposed by Weinfeld7 after successful treatment of 2 patients. However, other studies have had variable outcomes with no resolution of pruritus.8
Other treatments include gabapentin,9 transcutaneous electrical nerve stimulation,10 and narrow-band ultraviolet-B.11 It is appropriate to consider surgical decompression or neurolysis of the nerve when other forms of treatment fail.12
Our patient was treated with topical capsaicin cream 0.25 mg/g, which lessened the intensity of her itching. After 2 months, the patient reported improvement of her symptoms.
CORRESPONDENCE
Joana Sequeira, MD, Estrada da Mata nº56, Leiria, Portugal; [email protected].
1. Stumpf A, Ständer S. Neuropathic itch: diagnosis and management. Dermatol Ther. 2013;26:104-109.
2. Ellis C. Notalgia paresthetica: the unreachable itch. Dermatol Pract Concept. 2013;3:3-6.
3. Bolognia JL, Jorizzo JL, Schaffer JV, eds. Pruritus and dysesthesia. In: Dermatology. 3rd ed. Philadelphia, PA: Elsevier Saunders;2012:121.
4. Raison-Peyron N, Meunier L, Acevedo M, et al. Notalgia paresthetica: clinical, physiopathological and therapeutic aspects. A study of 12 cases. J Eur Acad Dermatol Venereol. 1999;12:215-221.
5. Savk O, Savk E. Investigation of spinal pathology in notalgia paresthetica. J Am Acad Dermatol. 2005;52:1085-1087.
6. Wallengren J, Klinker M. Successful treatment of notalgia paresthetica with topical capsaicin: vehicle-controlled, double-blind, crossover study. J Am Acad Dermatol. 1995;32:287-289.
7. Weinfeld PK. Successful treatment of notalgia paresthetica with botulinum toxin type A. Arch Dermatol. 2007;143:980-982.
8. Pérez-Pérez L, García-Gavín J, Allegue F, et al. Notalgia paresthetica: treatment using intradermal botulinum toxin A. Actas Dermosifiliogr. 2014;105:74-77.
9. Maciel AA, Cunha PR, Laraia IO, et al. Efficacy of gabapentin in the improvement of pruritus and quality of life of patients with nostalgia paresthetica. An Bras Dermatol. 2014;89:570-575.
10. Savk E, Savk O, Sendur F. Transcutaneous electrical nerve stimulation offers partial relief in notalgia paresthetica patients with a relevant spinal pathology. J Dermatol. 2007;34:315-319.
11. Pérez-Pérez L, Allegue F, Fabeiro JM, et al. Notalgia paresthesica successfully treated with narrow-band UVB: report of five cases. J Eur Acad Dermatol Venereol. 2010;24:730-732.
12. Williams EH, Rosson GD, Elsamanoudi I, et al. Surgical decompression for notalgia paresthetica: a case report. Microsurgery. 2010;30:70-72.
1. Stumpf A, Ständer S. Neuropathic itch: diagnosis and management. Dermatol Ther. 2013;26:104-109.
2. Ellis C. Notalgia paresthetica: the unreachable itch. Dermatol Pract Concept. 2013;3:3-6.
3. Bolognia JL, Jorizzo JL, Schaffer JV, eds. Pruritus and dysesthesia. In: Dermatology. 3rd ed. Philadelphia, PA: Elsevier Saunders;2012:121.
4. Raison-Peyron N, Meunier L, Acevedo M, et al. Notalgia paresthetica: clinical, physiopathological and therapeutic aspects. A study of 12 cases. J Eur Acad Dermatol Venereol. 1999;12:215-221.
5. Savk O, Savk E. Investigation of spinal pathology in notalgia paresthetica. J Am Acad Dermatol. 2005;52:1085-1087.
6. Wallengren J, Klinker M. Successful treatment of notalgia paresthetica with topical capsaicin: vehicle-controlled, double-blind, crossover study. J Am Acad Dermatol. 1995;32:287-289.
7. Weinfeld PK. Successful treatment of notalgia paresthetica with botulinum toxin type A. Arch Dermatol. 2007;143:980-982.
8. Pérez-Pérez L, García-Gavín J, Allegue F, et al. Notalgia paresthetica: treatment using intradermal botulinum toxin A. Actas Dermosifiliogr. 2014;105:74-77.
9. Maciel AA, Cunha PR, Laraia IO, et al. Efficacy of gabapentin in the improvement of pruritus and quality of life of patients with nostalgia paresthetica. An Bras Dermatol. 2014;89:570-575.
10. Savk E, Savk O, Sendur F. Transcutaneous electrical nerve stimulation offers partial relief in notalgia paresthetica patients with a relevant spinal pathology. J Dermatol. 2007;34:315-319.
11. Pérez-Pérez L, Allegue F, Fabeiro JM, et al. Notalgia paresthesica successfully treated with narrow-band UVB: report of five cases. J Eur Acad Dermatol Venereol. 2010;24:730-732.
12. Williams EH, Rosson GD, Elsamanoudi I, et al. Surgical decompression for notalgia paresthetica: a case report. Microsurgery. 2010;30:70-72.