User login
Weight Watchers for the Facebook Era—How Does It Compare to the Do-It-Yourself Approach?
Study Overview
Objective. To compare weight loss among patients using self-directed methods vs. those participating in a multi-component Weight Watchers (WW) program where participants could access content in person, online, or using mobile applications.
Study design. Randomized trial funded by Weight Watchers International.
Setting and participants. A market research firm was used to identify potentially eligible persons in a Northeastern U.S. metro area. Of those who responded to emails describing the project (n = 336), 292 were deemed eligible based on having a body mass index (BMI) between 27 and 40 kg/m2, not currently being on a diet or taking weight-loss medications, and not reporting any medical conditions that could interfere with their participation in a weight loss program (eg, thyroid disease, cardiac disease, pregnancy, cancer).
Eligible participants who consented were computer randomized to 1 of 2 arms. The intervention arm participants were provided with free access to the WW program, and those in the control group received only informational materials. The WW program consisted of putting participants on a food and physical activity plan and providing them with group support, as well as teaching them skills to help promote behavior change in a series of 24 weekly in-person meetings. In addition to in-person meetings, information and support could be accessed online and using mobile devices that allowed the formation of an online community with message board capabilities. Participants were followed for a 24-week period with weigh-ins at baseline and 3 and 6 months.
Main outcome measures. The primary outcomes in this study were the difference between the groups in BMI or weight at 3 and 6 months. BMI was measured at in-person study visits. Repeated-measures ANOVA was used to compare the groups, both on persons who completed the trial and also with an intention-to-treat sub-analysis where the last available measure was carried forward to the 6-month mark for those who were lost to follow-up.
Secondary outcomes included evaluation of the impact of mode (in person, online, or mobile device) and frequency of access of the WW program on BMI change. Participants were categorized as having high attendance if they came to more than 50% of the in-person sessions, or low attendance if they came to fewer. They were categorized as frequent or infrequent users of the web or mobile interfaces dichotomized around self-reported use of at least 2 times per week. One-way ANOVA was used to compare weight losses according to the type and frequency of access amongst WW participants. Logistic regression was used to evaluate the impact of the exposure of high vs. low attendance on dichotomized weight loss outcomes at the 5% and 10% level.
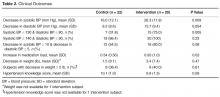
Results. There were no significant differences between the WW (n = 147) and self-help (n = 145) arms with respect to baseline characteristics. The sample was predominantly female (89.8%), middle aged (mean (SD) 46.5 (10.5) yr), and white (90.7%). The mean BMI at baseline was in the class I (BMI ≥ 30 but < 35) obesity category (mean (SD) 33.0 (3.6) kg/m2). Of the total sample of 292 initial participants, 257 (88%) completed the 6-month trial.
Both primary and intention-to-treat analyses revealed a greater degree of weight loss (or BMI reduction) among WW versus self-help participants. Specifically, the WW participants lost a mean of 4.6 kg at 6 months, and the self-help participants lost a mean of 0.6 kg. When the outcome was dichotomized around probability of achieving at least a 5% or 10% weight loss, WW participants were far more likely to achieve both outcomes (5% loss: odds ratio [OR] 8.0, 95% CI 3.9-16.2; 10% loss: OR 8.8, 95% CI 3.0-25.9). The most rapid weight loss period for WW participants was clearly in the first 3 months of the trial, after which weight loss slowed considerably.
Among the WW participants, when individuals were compared according to how many modes of access they used (0, 1, 2 or 3), participants using all 3 modes had significantly greater weight loss (P < 0.01) than all others. Mean weight loss was approximately equal between persons who used 1 or 2 modes of access. Overall weight loss at 6 months varied from a mean of 2 kg in the “0 components group” to approximately 4.5 kg in the 1 or 2 components group, to almost 10 kg in the 3 components group. Frequency of contact (in person or electronically) also corresponded to the amount of weight lost.
On average, the WW group attended fewer than 50% of the available 24 weekly sessions (mean (sd) 9.1 (7.3) sessions attended). However, those who came to at least 12 sessions were far more likely to achieve 5% and/or 10% weight losses than those who attended fewer sessions (5% loss: OR 11.2, 95% CI 4.6-26.9; 10% loss: OR 15.5, 95% CI 5.6-43.2). Frequent (vs. less frequent) use of the online website and mobile devices were also associated with statistically significant improvements in weight loss; however, the magnitude of effect for these modalities was much smaller than for the frequency of in person visits. Frequent website users, for example, had an OR of 3.1 (95% CI 1.5-6.5) for achieving a 5% weight loss compared with less frequent users, and frequent mobile app users had an OR of 2.0 (95% CI 1.0-4.1) for achieving that 5% loss compared with nonfrequent users. Stepwise regression models supported this pattern, indicating that the greatest predictor of weight loss was attendance at in-person meetings, accounting for 29.4% of the variance in 6-month weight losses.
Conclusion. Participants randomized to participate in a commercially available weight loss program with access to in-person, online, and mobile support lost significantly more weight than those who attempted to lose weight via self-help.
Commentary
With the prevalence of obesity in the United States now exceeding 30% [1], primary care physicians are routinely asked to counsel patients on the dangers of excess weight or to provide advice on how best to lose weight. In light of time demands, lack of expertise in weight loss management, and, historically, lack of reimbursement for obesity-specific care, primary care practices have not traditionally been ideal locations for provision of weight management services [2]. Behavioral approaches to weight loss require relatively high-frequency contact for a period of at least several months in order to provide the greatest chance of patients successfully losing weight [3]. In fact, many behavior change programs are modeled after the Diabetes Prevention Program, which relied on 24 weekly face-to-face visits (followed by every other week visits) in order for participants to achieve even modest weight losses (5%-10% of starting weight) [4]. To integrate such a program into most primary care practices has not been widely feasible, however. For physicians practicing in large academic centers, there may be specialized weight clinics where patients can be referred to receive such care, but for most community physicians and those practicing in smaller organizations, finding the right place to refer patients interested in weight loss via diet and exercise can be difficult. As a result of this and other factors, many patients elect to self-manage their own weight loss attempts with limited success.
One option for primary care physicians who do not feel comfortable or able to oversee the behavioral weight loss attempts of their patients is to consider referral to a commercial weight loss program, such as the one examined in this study. There are several such programs throughout the United States, and, as pointed out by these authors, the WW program itself has funded previous research studies, including one randomized trial that showed modestly superior weight loss outcomes amongst its participants, as compared to self-directed therapy [5]. A 2005 systematic review of commercially available weight loss programs concluded that there was limited evidence to support the use of such programs, particularly those that were internet-based [6]. The current study builds upon existing work by evaluating the impact of the newer, 3-modality (in-person, online, and mobile) WW intervention. Such an evaluation is important given the present-day near ubiquity of smartphone and internet access for most middle-aged US adults.
This randomized controlled trial tested this newer-modality WW program against self-directed behavioral weight loss therapy and found that participants achieved greater weight loss with the WW program. The randomized design was a strength of the study, as was the use of intention-to-treat analysis (although loss to follow-up was relatively minimal). The findings of improved weight loss amongst WW participants are not novel, however, they underscore that this program is a viable option for patients who are financially able (and motivated) to commit to such an endeavor. In terms of evaluating the added value of internet-based and mobile applications to the traditional in-person visit, although the authors note that participants who used all 3 modalities lost the most weight, it was in-person visit attendance that accounted for the greatest share of weight loss success. Thus, the internet and mobile app access methods ought not be considered as replacements for the in-person visits but rather as supplements, which does not support their use as an alternative for busy people who don’t have time to participate in person. Additionally, as noted by the authors in their discussion section, the number of components accessed by participants could merely be a marker for level of motivation—thus it was higher motivation levels perhaps driving the weight loss, rather than an additive effect of the 3 modalities. Because motivation to change was not assessed in this study, it is difficult to know what role this factor played in weight loss for the WW participants.
Unfortunately, the trial did not follow participants past the end of the intervention period to determine whether the weight changes were maintained once WW participation was complete. At least 1 prior study evaluating this program, however, showed that despite some weight regain, participants in this commercial program do maintain a larger degree of weight loss than their self-management counterparts at up to 2 years after randomization [6].
The generalizability of these study findings may be somewhat limited based on the demographics of trial participants. Nearly all of them were non-Hispanic white women, which is not too surprising given the nature of the intervention. It does raise an important question, however, about whether similar programs are available for (or of interest to) male and/or non-white patients. While it is possible that the geographic area they sampled from for the study was simply predominated by non-Hispanic white residents, no data were provided about the sampling pool, so one can only assume a somewhat biased response based on the nature of the intervention. Additionally, the patients in this study were, on average, class I obesity patients and lost only a moderate amount of weight. Furthermore, medically complex persons were excluded from participating. Providers caring for patients with more severe degrees of obesity and/or those who have multiple poorly controlled medical conditions should carefully consider whether such patients are appropriate for commercial programs before referring them, and should calibrate their patients’ expectations of the degree and durability of weight loss that will be obtained through such programs.
The participants in this trial received the WW intervention free of charge, which would obviously not be the case for real-world patients enrolling in commercial weight loss programs. Cost, therefore, might be an important barrier to assess prior to referring any patients to such programs. However, the idea of paying for the intervention might paradoxically improve outcomes—the concept of having “skin in the game,” or feeling more compelled to participate in something you have paid for, a popular concept in behavioral economics, could come into play in this context. Paying for WW might “frame” the service as desirable, making people more likely to attend, as opposed to essentially being paid to do it (as in this study), which might have framed it more as a chore, or something undesirable [7].
Finally, given the possible upcoming shift in provider reimbursement for obesity-related counseling heralded by 2012 Centers for Medicare and Medicaid coverage changes [8], providers may become increasingly comfortable managing their patients’ weight loss attempts in the primary care setting, decreasing the need for outsourcing to commercial programs in the near future.
Applications for Clinical Practice
Commercial weight loss programs with combined modalities of in-person, online, and mobile support can provide an alternative to self-directed weight loss, particularly for patients in the demographic groups targeted by such programs. Clinicians who do not feel able to provide such care in the clinical context, or who do not have referral access to clinical weight loss programs might consider referral to commercial programs for some patients. Appropriate selection of patients is important, however, and physicians should consider factors such as financial means, desired amount of weight loss, and medical complexity before recommending such a program. Furthermore, the evidence surrounding long-term maintenance of weight loss after participation in such programs is weak.
—Kristina Lewis, MD, MPH
1. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491–7.
2. Tsai AG, Wadden TA. Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med 2009;24:1073–9.
3. Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am 2011;34:841–59.
4. DPP Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403.
5. Heshka S, Anderson JW, Atkinson RL, et al. Weight loss with self-help compared with a structured commercial program: a randomized trial. JAMA 2003;289:1792–8.
6. Tsai AG, Wadden TA. Systematic review: an evaluation of major commercial weight loss programs in the United States. Ann Intern Med 2005;142:56–66.
7. Zimmerman FJ. Using behavioral economics to promote physical activity. Prev Med 2009;49:289–91.
8. Centers for Medicare and Medicaid Services. Decision memo for intensive behavioral therapy for obesity. 2012.
Study Overview
Objective. To compare weight loss among patients using self-directed methods vs. those participating in a multi-component Weight Watchers (WW) program where participants could access content in person, online, or using mobile applications.
Study design. Randomized trial funded by Weight Watchers International.
Setting and participants. A market research firm was used to identify potentially eligible persons in a Northeastern U.S. metro area. Of those who responded to emails describing the project (n = 336), 292 were deemed eligible based on having a body mass index (BMI) between 27 and 40 kg/m2, not currently being on a diet or taking weight-loss medications, and not reporting any medical conditions that could interfere with their participation in a weight loss program (eg, thyroid disease, cardiac disease, pregnancy, cancer).
Eligible participants who consented were computer randomized to 1 of 2 arms. The intervention arm participants were provided with free access to the WW program, and those in the control group received only informational materials. The WW program consisted of putting participants on a food and physical activity plan and providing them with group support, as well as teaching them skills to help promote behavior change in a series of 24 weekly in-person meetings. In addition to in-person meetings, information and support could be accessed online and using mobile devices that allowed the formation of an online community with message board capabilities. Participants were followed for a 24-week period with weigh-ins at baseline and 3 and 6 months.
Main outcome measures. The primary outcomes in this study were the difference between the groups in BMI or weight at 3 and 6 months. BMI was measured at in-person study visits. Repeated-measures ANOVA was used to compare the groups, both on persons who completed the trial and also with an intention-to-treat sub-analysis where the last available measure was carried forward to the 6-month mark for those who were lost to follow-up.
Secondary outcomes included evaluation of the impact of mode (in person, online, or mobile device) and frequency of access of the WW program on BMI change. Participants were categorized as having high attendance if they came to more than 50% of the in-person sessions, or low attendance if they came to fewer. They were categorized as frequent or infrequent users of the web or mobile interfaces dichotomized around self-reported use of at least 2 times per week. One-way ANOVA was used to compare weight losses according to the type and frequency of access amongst WW participants. Logistic regression was used to evaluate the impact of the exposure of high vs. low attendance on dichotomized weight loss outcomes at the 5% and 10% level.
Results. There were no significant differences between the WW (n = 147) and self-help (n = 145) arms with respect to baseline characteristics. The sample was predominantly female (89.8%), middle aged (mean (SD) 46.5 (10.5) yr), and white (90.7%). The mean BMI at baseline was in the class I (BMI ≥ 30 but < 35) obesity category (mean (SD) 33.0 (3.6) kg/m2). Of the total sample of 292 initial participants, 257 (88%) completed the 6-month trial.
Both primary and intention-to-treat analyses revealed a greater degree of weight loss (or BMI reduction) among WW versus self-help participants. Specifically, the WW participants lost a mean of 4.6 kg at 6 months, and the self-help participants lost a mean of 0.6 kg. When the outcome was dichotomized around probability of achieving at least a 5% or 10% weight loss, WW participants were far more likely to achieve both outcomes (5% loss: odds ratio [OR] 8.0, 95% CI 3.9-16.2; 10% loss: OR 8.8, 95% CI 3.0-25.9). The most rapid weight loss period for WW participants was clearly in the first 3 months of the trial, after which weight loss slowed considerably.
Among the WW participants, when individuals were compared according to how many modes of access they used (0, 1, 2 or 3), participants using all 3 modes had significantly greater weight loss (P < 0.01) than all others. Mean weight loss was approximately equal between persons who used 1 or 2 modes of access. Overall weight loss at 6 months varied from a mean of 2 kg in the “0 components group” to approximately 4.5 kg in the 1 or 2 components group, to almost 10 kg in the 3 components group. Frequency of contact (in person or electronically) also corresponded to the amount of weight lost.
On average, the WW group attended fewer than 50% of the available 24 weekly sessions (mean (sd) 9.1 (7.3) sessions attended). However, those who came to at least 12 sessions were far more likely to achieve 5% and/or 10% weight losses than those who attended fewer sessions (5% loss: OR 11.2, 95% CI 4.6-26.9; 10% loss: OR 15.5, 95% CI 5.6-43.2). Frequent (vs. less frequent) use of the online website and mobile devices were also associated with statistically significant improvements in weight loss; however, the magnitude of effect for these modalities was much smaller than for the frequency of in person visits. Frequent website users, for example, had an OR of 3.1 (95% CI 1.5-6.5) for achieving a 5% weight loss compared with less frequent users, and frequent mobile app users had an OR of 2.0 (95% CI 1.0-4.1) for achieving that 5% loss compared with nonfrequent users. Stepwise regression models supported this pattern, indicating that the greatest predictor of weight loss was attendance at in-person meetings, accounting for 29.4% of the variance in 6-month weight losses.
Conclusion. Participants randomized to participate in a commercially available weight loss program with access to in-person, online, and mobile support lost significantly more weight than those who attempted to lose weight via self-help.
Commentary
With the prevalence of obesity in the United States now exceeding 30% [1], primary care physicians are routinely asked to counsel patients on the dangers of excess weight or to provide advice on how best to lose weight. In light of time demands, lack of expertise in weight loss management, and, historically, lack of reimbursement for obesity-specific care, primary care practices have not traditionally been ideal locations for provision of weight management services [2]. Behavioral approaches to weight loss require relatively high-frequency contact for a period of at least several months in order to provide the greatest chance of patients successfully losing weight [3]. In fact, many behavior change programs are modeled after the Diabetes Prevention Program, which relied on 24 weekly face-to-face visits (followed by every other week visits) in order for participants to achieve even modest weight losses (5%-10% of starting weight) [4]. To integrate such a program into most primary care practices has not been widely feasible, however. For physicians practicing in large academic centers, there may be specialized weight clinics where patients can be referred to receive such care, but for most community physicians and those practicing in smaller organizations, finding the right place to refer patients interested in weight loss via diet and exercise can be difficult. As a result of this and other factors, many patients elect to self-manage their own weight loss attempts with limited success.
One option for primary care physicians who do not feel comfortable or able to oversee the behavioral weight loss attempts of their patients is to consider referral to a commercial weight loss program, such as the one examined in this study. There are several such programs throughout the United States, and, as pointed out by these authors, the WW program itself has funded previous research studies, including one randomized trial that showed modestly superior weight loss outcomes amongst its participants, as compared to self-directed therapy [5]. A 2005 systematic review of commercially available weight loss programs concluded that there was limited evidence to support the use of such programs, particularly those that were internet-based [6]. The current study builds upon existing work by evaluating the impact of the newer, 3-modality (in-person, online, and mobile) WW intervention. Such an evaluation is important given the present-day near ubiquity of smartphone and internet access for most middle-aged US adults.
This randomized controlled trial tested this newer-modality WW program against self-directed behavioral weight loss therapy and found that participants achieved greater weight loss with the WW program. The randomized design was a strength of the study, as was the use of intention-to-treat analysis (although loss to follow-up was relatively minimal). The findings of improved weight loss amongst WW participants are not novel, however, they underscore that this program is a viable option for patients who are financially able (and motivated) to commit to such an endeavor. In terms of evaluating the added value of internet-based and mobile applications to the traditional in-person visit, although the authors note that participants who used all 3 modalities lost the most weight, it was in-person visit attendance that accounted for the greatest share of weight loss success. Thus, the internet and mobile app access methods ought not be considered as replacements for the in-person visits but rather as supplements, which does not support their use as an alternative for busy people who don’t have time to participate in person. Additionally, as noted by the authors in their discussion section, the number of components accessed by participants could merely be a marker for level of motivation—thus it was higher motivation levels perhaps driving the weight loss, rather than an additive effect of the 3 modalities. Because motivation to change was not assessed in this study, it is difficult to know what role this factor played in weight loss for the WW participants.
Unfortunately, the trial did not follow participants past the end of the intervention period to determine whether the weight changes were maintained once WW participation was complete. At least 1 prior study evaluating this program, however, showed that despite some weight regain, participants in this commercial program do maintain a larger degree of weight loss than their self-management counterparts at up to 2 years after randomization [6].
The generalizability of these study findings may be somewhat limited based on the demographics of trial participants. Nearly all of them were non-Hispanic white women, which is not too surprising given the nature of the intervention. It does raise an important question, however, about whether similar programs are available for (or of interest to) male and/or non-white patients. While it is possible that the geographic area they sampled from for the study was simply predominated by non-Hispanic white residents, no data were provided about the sampling pool, so one can only assume a somewhat biased response based on the nature of the intervention. Additionally, the patients in this study were, on average, class I obesity patients and lost only a moderate amount of weight. Furthermore, medically complex persons were excluded from participating. Providers caring for patients with more severe degrees of obesity and/or those who have multiple poorly controlled medical conditions should carefully consider whether such patients are appropriate for commercial programs before referring them, and should calibrate their patients’ expectations of the degree and durability of weight loss that will be obtained through such programs.
The participants in this trial received the WW intervention free of charge, which would obviously not be the case for real-world patients enrolling in commercial weight loss programs. Cost, therefore, might be an important barrier to assess prior to referring any patients to such programs. However, the idea of paying for the intervention might paradoxically improve outcomes—the concept of having “skin in the game,” or feeling more compelled to participate in something you have paid for, a popular concept in behavioral economics, could come into play in this context. Paying for WW might “frame” the service as desirable, making people more likely to attend, as opposed to essentially being paid to do it (as in this study), which might have framed it more as a chore, or something undesirable [7].
Finally, given the possible upcoming shift in provider reimbursement for obesity-related counseling heralded by 2012 Centers for Medicare and Medicaid coverage changes [8], providers may become increasingly comfortable managing their patients’ weight loss attempts in the primary care setting, decreasing the need for outsourcing to commercial programs in the near future.
Applications for Clinical Practice
Commercial weight loss programs with combined modalities of in-person, online, and mobile support can provide an alternative to self-directed weight loss, particularly for patients in the demographic groups targeted by such programs. Clinicians who do not feel able to provide such care in the clinical context, or who do not have referral access to clinical weight loss programs might consider referral to commercial programs for some patients. Appropriate selection of patients is important, however, and physicians should consider factors such as financial means, desired amount of weight loss, and medical complexity before recommending such a program. Furthermore, the evidence surrounding long-term maintenance of weight loss after participation in such programs is weak.
—Kristina Lewis, MD, MPH
Study Overview
Objective. To compare weight loss among patients using self-directed methods vs. those participating in a multi-component Weight Watchers (WW) program where participants could access content in person, online, or using mobile applications.
Study design. Randomized trial funded by Weight Watchers International.
Setting and participants. A market research firm was used to identify potentially eligible persons in a Northeastern U.S. metro area. Of those who responded to emails describing the project (n = 336), 292 were deemed eligible based on having a body mass index (BMI) between 27 and 40 kg/m2, not currently being on a diet or taking weight-loss medications, and not reporting any medical conditions that could interfere with their participation in a weight loss program (eg, thyroid disease, cardiac disease, pregnancy, cancer).
Eligible participants who consented were computer randomized to 1 of 2 arms. The intervention arm participants were provided with free access to the WW program, and those in the control group received only informational materials. The WW program consisted of putting participants on a food and physical activity plan and providing them with group support, as well as teaching them skills to help promote behavior change in a series of 24 weekly in-person meetings. In addition to in-person meetings, information and support could be accessed online and using mobile devices that allowed the formation of an online community with message board capabilities. Participants were followed for a 24-week period with weigh-ins at baseline and 3 and 6 months.
Main outcome measures. The primary outcomes in this study were the difference between the groups in BMI or weight at 3 and 6 months. BMI was measured at in-person study visits. Repeated-measures ANOVA was used to compare the groups, both on persons who completed the trial and also with an intention-to-treat sub-analysis where the last available measure was carried forward to the 6-month mark for those who were lost to follow-up.
Secondary outcomes included evaluation of the impact of mode (in person, online, or mobile device) and frequency of access of the WW program on BMI change. Participants were categorized as having high attendance if they came to more than 50% of the in-person sessions, or low attendance if they came to fewer. They were categorized as frequent or infrequent users of the web or mobile interfaces dichotomized around self-reported use of at least 2 times per week. One-way ANOVA was used to compare weight losses according to the type and frequency of access amongst WW participants. Logistic regression was used to evaluate the impact of the exposure of high vs. low attendance on dichotomized weight loss outcomes at the 5% and 10% level.
Results. There were no significant differences between the WW (n = 147) and self-help (n = 145) arms with respect to baseline characteristics. The sample was predominantly female (89.8%), middle aged (mean (SD) 46.5 (10.5) yr), and white (90.7%). The mean BMI at baseline was in the class I (BMI ≥ 30 but < 35) obesity category (mean (SD) 33.0 (3.6) kg/m2). Of the total sample of 292 initial participants, 257 (88%) completed the 6-month trial.
Both primary and intention-to-treat analyses revealed a greater degree of weight loss (or BMI reduction) among WW versus self-help participants. Specifically, the WW participants lost a mean of 4.6 kg at 6 months, and the self-help participants lost a mean of 0.6 kg. When the outcome was dichotomized around probability of achieving at least a 5% or 10% weight loss, WW participants were far more likely to achieve both outcomes (5% loss: odds ratio [OR] 8.0, 95% CI 3.9-16.2; 10% loss: OR 8.8, 95% CI 3.0-25.9). The most rapid weight loss period for WW participants was clearly in the first 3 months of the trial, after which weight loss slowed considerably.
Among the WW participants, when individuals were compared according to how many modes of access they used (0, 1, 2 or 3), participants using all 3 modes had significantly greater weight loss (P < 0.01) than all others. Mean weight loss was approximately equal between persons who used 1 or 2 modes of access. Overall weight loss at 6 months varied from a mean of 2 kg in the “0 components group” to approximately 4.5 kg in the 1 or 2 components group, to almost 10 kg in the 3 components group. Frequency of contact (in person or electronically) also corresponded to the amount of weight lost.
On average, the WW group attended fewer than 50% of the available 24 weekly sessions (mean (sd) 9.1 (7.3) sessions attended). However, those who came to at least 12 sessions were far more likely to achieve 5% and/or 10% weight losses than those who attended fewer sessions (5% loss: OR 11.2, 95% CI 4.6-26.9; 10% loss: OR 15.5, 95% CI 5.6-43.2). Frequent (vs. less frequent) use of the online website and mobile devices were also associated with statistically significant improvements in weight loss; however, the magnitude of effect for these modalities was much smaller than for the frequency of in person visits. Frequent website users, for example, had an OR of 3.1 (95% CI 1.5-6.5) for achieving a 5% weight loss compared with less frequent users, and frequent mobile app users had an OR of 2.0 (95% CI 1.0-4.1) for achieving that 5% loss compared with nonfrequent users. Stepwise regression models supported this pattern, indicating that the greatest predictor of weight loss was attendance at in-person meetings, accounting for 29.4% of the variance in 6-month weight losses.
Conclusion. Participants randomized to participate in a commercially available weight loss program with access to in-person, online, and mobile support lost significantly more weight than those who attempted to lose weight via self-help.
Commentary
With the prevalence of obesity in the United States now exceeding 30% [1], primary care physicians are routinely asked to counsel patients on the dangers of excess weight or to provide advice on how best to lose weight. In light of time demands, lack of expertise in weight loss management, and, historically, lack of reimbursement for obesity-specific care, primary care practices have not traditionally been ideal locations for provision of weight management services [2]. Behavioral approaches to weight loss require relatively high-frequency contact for a period of at least several months in order to provide the greatest chance of patients successfully losing weight [3]. In fact, many behavior change programs are modeled after the Diabetes Prevention Program, which relied on 24 weekly face-to-face visits (followed by every other week visits) in order for participants to achieve even modest weight losses (5%-10% of starting weight) [4]. To integrate such a program into most primary care practices has not been widely feasible, however. For physicians practicing in large academic centers, there may be specialized weight clinics where patients can be referred to receive such care, but for most community physicians and those practicing in smaller organizations, finding the right place to refer patients interested in weight loss via diet and exercise can be difficult. As a result of this and other factors, many patients elect to self-manage their own weight loss attempts with limited success.
One option for primary care physicians who do not feel comfortable or able to oversee the behavioral weight loss attempts of their patients is to consider referral to a commercial weight loss program, such as the one examined in this study. There are several such programs throughout the United States, and, as pointed out by these authors, the WW program itself has funded previous research studies, including one randomized trial that showed modestly superior weight loss outcomes amongst its participants, as compared to self-directed therapy [5]. A 2005 systematic review of commercially available weight loss programs concluded that there was limited evidence to support the use of such programs, particularly those that were internet-based [6]. The current study builds upon existing work by evaluating the impact of the newer, 3-modality (in-person, online, and mobile) WW intervention. Such an evaluation is important given the present-day near ubiquity of smartphone and internet access for most middle-aged US adults.
This randomized controlled trial tested this newer-modality WW program against self-directed behavioral weight loss therapy and found that participants achieved greater weight loss with the WW program. The randomized design was a strength of the study, as was the use of intention-to-treat analysis (although loss to follow-up was relatively minimal). The findings of improved weight loss amongst WW participants are not novel, however, they underscore that this program is a viable option for patients who are financially able (and motivated) to commit to such an endeavor. In terms of evaluating the added value of internet-based and mobile applications to the traditional in-person visit, although the authors note that participants who used all 3 modalities lost the most weight, it was in-person visit attendance that accounted for the greatest share of weight loss success. Thus, the internet and mobile app access methods ought not be considered as replacements for the in-person visits but rather as supplements, which does not support their use as an alternative for busy people who don’t have time to participate in person. Additionally, as noted by the authors in their discussion section, the number of components accessed by participants could merely be a marker for level of motivation—thus it was higher motivation levels perhaps driving the weight loss, rather than an additive effect of the 3 modalities. Because motivation to change was not assessed in this study, it is difficult to know what role this factor played in weight loss for the WW participants.
Unfortunately, the trial did not follow participants past the end of the intervention period to determine whether the weight changes were maintained once WW participation was complete. At least 1 prior study evaluating this program, however, showed that despite some weight regain, participants in this commercial program do maintain a larger degree of weight loss than their self-management counterparts at up to 2 years after randomization [6].
The generalizability of these study findings may be somewhat limited based on the demographics of trial participants. Nearly all of them were non-Hispanic white women, which is not too surprising given the nature of the intervention. It does raise an important question, however, about whether similar programs are available for (or of interest to) male and/or non-white patients. While it is possible that the geographic area they sampled from for the study was simply predominated by non-Hispanic white residents, no data were provided about the sampling pool, so one can only assume a somewhat biased response based on the nature of the intervention. Additionally, the patients in this study were, on average, class I obesity patients and lost only a moderate amount of weight. Furthermore, medically complex persons were excluded from participating. Providers caring for patients with more severe degrees of obesity and/or those who have multiple poorly controlled medical conditions should carefully consider whether such patients are appropriate for commercial programs before referring them, and should calibrate their patients’ expectations of the degree and durability of weight loss that will be obtained through such programs.
The participants in this trial received the WW intervention free of charge, which would obviously not be the case for real-world patients enrolling in commercial weight loss programs. Cost, therefore, might be an important barrier to assess prior to referring any patients to such programs. However, the idea of paying for the intervention might paradoxically improve outcomes—the concept of having “skin in the game,” or feeling more compelled to participate in something you have paid for, a popular concept in behavioral economics, could come into play in this context. Paying for WW might “frame” the service as desirable, making people more likely to attend, as opposed to essentially being paid to do it (as in this study), which might have framed it more as a chore, or something undesirable [7].
Finally, given the possible upcoming shift in provider reimbursement for obesity-related counseling heralded by 2012 Centers for Medicare and Medicaid coverage changes [8], providers may become increasingly comfortable managing their patients’ weight loss attempts in the primary care setting, decreasing the need for outsourcing to commercial programs in the near future.
Applications for Clinical Practice
Commercial weight loss programs with combined modalities of in-person, online, and mobile support can provide an alternative to self-directed weight loss, particularly for patients in the demographic groups targeted by such programs. Clinicians who do not feel able to provide such care in the clinical context, or who do not have referral access to clinical weight loss programs might consider referral to commercial programs for some patients. Appropriate selection of patients is important, however, and physicians should consider factors such as financial means, desired amount of weight loss, and medical complexity before recommending such a program. Furthermore, the evidence surrounding long-term maintenance of weight loss after participation in such programs is weak.
—Kristina Lewis, MD, MPH
1. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491–7.
2. Tsai AG, Wadden TA. Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med 2009;24:1073–9.
3. Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am 2011;34:841–59.
4. DPP Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403.
5. Heshka S, Anderson JW, Atkinson RL, et al. Weight loss with self-help compared with a structured commercial program: a randomized trial. JAMA 2003;289:1792–8.
6. Tsai AG, Wadden TA. Systematic review: an evaluation of major commercial weight loss programs in the United States. Ann Intern Med 2005;142:56–66.
7. Zimmerman FJ. Using behavioral economics to promote physical activity. Prev Med 2009;49:289–91.
8. Centers for Medicare and Medicaid Services. Decision memo for intensive behavioral therapy for obesity. 2012.
1. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491–7.
2. Tsai AG, Wadden TA. Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med 2009;24:1073–9.
3. Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am 2011;34:841–59.
4. DPP Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403.
5. Heshka S, Anderson JW, Atkinson RL, et al. Weight loss with self-help compared with a structured commercial program: a randomized trial. JAMA 2003;289:1792–8.
6. Tsai AG, Wadden TA. Systematic review: an evaluation of major commercial weight loss programs in the United States. Ann Intern Med 2005;142:56–66.
7. Zimmerman FJ. Using behavioral economics to promote physical activity. Prev Med 2009;49:289–91.
8. Centers for Medicare and Medicaid Services. Decision memo for intensive behavioral therapy for obesity. 2012.
Good Midlife Dietary Habits May Increase Likelihood of Healthy Aging
Study Overview
Objective. To evaluate the contribution of dietary habits in midlife on healthy aging.
Study design. Observational investigation of an ongoing cohort study.
Setting and participants. Participants were gathered from the Nurses’ Health Study, a cohort of 121,700 married female nurses who have completed health-related questionnaires every 2 years since 1976. Data on race was not originally collected, but a subsample analysis revealed that the cohort of nurses was > 98% white [1]. A subset of this cohort (n = 19,415) older than age 70 years from 1995 and 2002 and who received additional cognitive testing was chosen as the population of interest for this study. The investigators excluded participants with missing data (n = 5878) on important covariates and participants who had any of 11 chronic diseases in midlife (n = 2585), obtained from questionnaires in the 1980s. 10,670 participants were included in the final analysis.
Main outcome measures. Participants were dichotomized as “healthy agers” or “usual agers” on the basis of 4 health domains measured in 2000. Persons free of 11 chronic diseases, without cognitive impairment, without physical limitations, and with intact mental health were designated “healthy agers,” with the remainder designated “usual agers.” For each domain, specific criteria were employed to indicate impairment. Cognitive impairment was defined as a score of 31 or greater on the Telephone Interview for Cognitive Status. Investigators used the Medical Outcomes Short-Form 36 health survey (SF-36) to measure physical impairment and mental health. Participants who reported being limited at least “a little” on moderate activities or limited “a lot” on strenuous activities were classified as physically impaired. Intact mental health was defined as a score above the cohort’s median on the mental health subscale of the SF-36.
Dietary habits were ascertained at midlife by an average of the 1984 and 1986 food frequency questionnaire (FFQ) data. Using these data, the authors calculated the Alternative Healthy Eating-2010 (AHEI-2010) and the Alternate Mediterranean Diet (A-MeDi) scores. AHEH-2010 incorporates the latest knowledge on the benefits and harms of foods and nutrients on the risk of chronic disease. It has 11 domains (including whole grain intake, vegetable intake, and lower intake of trans fats, among others) which are each scored 0 (worst) to 10 (best). The A-MeDi score assesses adherence to the traditional Mediterranean diet, which includes intake of vegetables, fruits, nuts, legumes, and moderate alcohol intake, among others. Each of 9 categories is rated 0 or 1, with 1 representing healthy intake.
Covariates included sociodemographic, lifestyle, and health-related measures obtained either in 1984 or 1986. These included age; educational level; household income and home value estimated from census tract data; marital status; family history of diabetes, cancer, and myocardial infarction; physical activity; smoking; multivitamin and aspirin use; BMI; history of high blood pressure; and hypercholesterolemia. BMI was obtained via self-report and averaged from among values obtained in 1984 and 1986; these have previously been shown to have excellent correlation (r = 0.97) to standardized examinations [2].
The authors standardized baseline characteristics for each study participant based upon the age at which they entered the study. They used logistic regression to estimate the odds of being a “healthy ager” in the year 2000 by quintile of AHEI-2010 and A-MeDi scores.
Main results. Of the 10,670 participants, 1171 (11%) were labeled “healthy agers” and 9499 (89%) were labeled “usual agers.” Prevalence in each of the 4 health domains varied widely: 9599 (90%) of the 10670 participants had no cognitive impairment, 7234 (67.8%) had no chronic diseases, 4606 (43.2%) had no mental health limitations, and 2905 (27.2%) had no impairment of physical functioning.
Investigators presented data comparing healthy agers and usual agers at baseline without tests for significance. The mean age of healthy agers and usual agers was comparable (58.6 [SD = 2.5] vs. 59.1 [SD = 2.5]). Healthy agers had lower prevalence of obesity (3% vs. 13%), ever smoking (54% vs. 47%), higher mean physical activity (19.4 MET h/wk [SD = 21.7] vs. 14.1 MET h/wk [SD = 19.8]), lower energy intake (1692 kcal/d [SD = 472] vs. 1743 kcal/d [SD = 477]) and lower prevalence of hypertension (20% vs. 32%) and hypercholesterolemia (12% vs. 17%). Healthy agers also had higher baseline AHEI-2010 (53.2 [SD = 10.3] vs. 50.6 [SD = 10.1]) and A-MeDi scores in midlife (4.5 [SD = 1.6] vs. 4.3 [SD = 1.7]).
Greater scores on the AHEI-2010 and A-MeDi measures in midlife were associated with greater odds of healthy aging in multivariate analysis. After adjusting for all covariates, women in the highest quintile of AHEI-2010 scores at baseline had 34% greater odds (95% CI, 9% to 66%) of being healthy agers compared to women in the lowest quintile. Likewise, adjusted analyses reported women in the highest quintile of A-MeDi scores had 46% greater odds (95% CI, 17% to 83%) of being healthy agers.
Secondary analyses tested each component of healthy aging for associations with AHEI-2010 and A-MeDi scores in midlife. Associations were overall weaker, but no impairment of physical function and no limitation of mental health were both found to be significant after adjustment for covariates. Women in the highest quintile of AHEI-2010 scores at baseline had 23% (95% CI, 11% to 36%) and 13% (95% CI, 5% to 22%) greater odds, respectively, of not having any physical limitations or mental health impairments in late life compared to women in the lowest quintile. Likewise, women in the highest quintile of A-MeDi scores at baseline had 14% (95% CI, 3% to 26%) and 12% (95% CI, 4% to 20%) greater odds, respectively, of not having any physical limitations or mental health impairments in late life compared to women in the lowest quintile.
The authors also tested the effect of individual components of dietary patterns on healthy aging, comparing those in the highest quintile versus those in the lowest quintile for each measure. Persons with the greatest intake of fruits had 46% (95% CI, 15% to 85%) greater odds of being healthy agers compared to those with the lowest intake of fruits. Persons with the highest intake of alcohol had 28% greater odds (95% CI, 4% to 56%) of being healthy agers compared to those with the lowest intake of alcohol. Conversely, those with lower intake of sugar-sweetened beverages (OR, 1.28 [95% CI, 1.03 to 1.58]) and non-omega 3 polyunsaturated fatty acids (OR, 1.38 [CI, 1.10 to 1.73]) had better odds of being healthy agers compared to those with higher intakes.
Conclusion. Women with healthy dietary patterns at midlife had significantly greater odds of being healthy agers in later life after adjusting for potential con-founders. Results were consistent in direction and effect size when using either the AHEI-2010 score or the A-MeDi score. The effects of healthy diet at midlife seemed to have the strongest association with physical impairment scores and mental health scores. Higher intake of fruits and alcohol along with lower intake of sugar-sweetened beverages and polyunsaturated fatty acids seemed to have the most power for predicting healthy aging.
Commentary
These results are consistent with current knowledge, which indicates the health benefits of a balanced, healthy diet high in fruits, vegetables, whole grains, nuts, and legumes and low in red or other processed meats. There is high quality evidence linking each dietary measure to health outcomes. Adherence to the Alternative Healthy Eating Index has been related to lower mortality rates [3], decreased risk of cardiovascular disease [4], and decreased risk of type 2 diabetes and the metabolic syndrome [5]. Likewise, adherence to the Mediterranean diet is associated with reductions in overall mortality, cardiovascular incidence and mortality, cancer incidence and mortality, and neurodegenerative diseases [6]. Both diets endorse moderate alcohol intake, which was associated with lower rates of all-cause and cardiovascular mortality in a meta-analysis [7]. Alcohol is theorized to produce decreased platelet aggregation, increase HDL cholesterol, and increase endothelial vasorelaxation [8]. Polyphenols, most prominent in red wines, may have additional effects which include vaso-relaxation of aortic rings, reduced thrombosis and inflammation, and increased fibrinolysis [9]. Nevertheless, heavy alcohol use may increase cardiovascular mortality, hypertension, and hyperlipidemia [8]. This study concluded that higher alcohol intake was related to being a healthy ager; this may be because there are few heavy alcohol users in this cohort, though this hypothesis was not tested in the study.
Any observational study is subject to debate about the confounders chosen for analysis and potential biases. The authors report that the most powerful confounders in this analysis were BMI, physical activity, and smoking, all of which have been well established as predictors for health in later life [10]. Nonetheless, important potential confounders not used in analysis included the baseline prevalence of mental health problems, cognitive limitations, and physical limitations, all of which were not available.
The greatest concern about of this study is a potential lack of generalizability given the population surveyed. The Nurses’ Health Study consists of a cohort of female, married, predominantly white registered nurses [1]. For instance, African Americans have a greater burden of hypertension than non-Hispanic whites after accounting for dietary differences [11], a higher degree of late-life cognitive dysfunction [12], and greater risk of developing late-life physical disability [13]. Also, race and ethnicity may impact eating patterns, food preferences, and food availability in ways that are difficult to predict. In addition, nurses in the cohort were probably of similar socioeconomic status given their shared occupation, though the authors did not report the variation in median household incomes obtained from census tract analysis in this study [14]. Results might change if the sample was less homogeneous. Nonetheless, the results are consistent with current knowledge, biologically plausible, and clinically meaningful.
Applications for Clinical Practice
Integrating dietary changes in middle-aged women may be an important means of decreasing morbidity in older age and improving physical and mental health functioning later in life. Health care providers should discuss the future benefits of healthy eating on quality of life in order to encourage patients in midlife to alter their diet in meaningful ways. While it may be difficult to generalize these findings to patients of different genders, races, or ethnicities, the biological underpinnings of the data make it hard dispute the conclusions presented in the study.
—Hector Perez, MD, and Melanie Jay, MD, MS
1. Hemenway D, Colditz GA, Willett WC, et al. Fractures and lifestyle: effect of cigarette smoking, alcohol intake, and relative weight on the risk of hip and forearm fractures in middle-aged women. Am J Public Health 1988;78:1554–8.
2. Rimm EB, Stampfer MJ, Colditz GA, et al. Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1990;1:466–73.
3. Akbaraly TN, Ferrie JE, Berr C, et al. Alternative Healthy Eating Index and mortality over 18 y of follow-up: results from the Whitehall II cohort. Am J Clin Nutr 2011;94:247–53.
4. McCullough ML, Feskanich D, Stampfer MJ, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr 2002;76:1261–71.
5. Akbaraly TN, Singh-Manoux A, Tabak AG, et al. Overall diet history and reversibility of the metabolic syndrome over 5 years: the Whitehall II prospective cohort study. Diabetes Care 2010;33:2339–41.
6. Sofi F, Abbate R, Gensini GF, et al. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr 2010;92:1189–96.
7. Di Castelnuovo A, Costanzo S, Bagnardi V, et al. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med 2006;166:2437–45.
8. Costanzo S, Di Castelnuovo A, Donati MB, et al. Cardiovascular and overall mortality risk in relation to alcohol consumption in patients with cardiovascular disease. Circulation 2010;121:1951–9.
9. Booyse FM, Pan W, Grenett HE, et al. Mechanism by which alcohol and wine polyphenols affect coronary heart disease risk. Ann Epidemiol 2007;17:S24–S31.
10. Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med 2012;55:163–70.
11. Diaz VA, Mainous AG, Koopman RJ, et al. Race and diet in the overweight: association with cardiovascular risk in a nationally representative sample. Nutrition 2005;21:718–25.
12. Sloan FA, Wang J. Disparities among older adults in measures of cognitive function by race or ethnicity. J Gerontol B Psychol Sci Soc Sci 2005;60:P242–50.
13. Dunlop DD, Song J, Manheim LM, et al. Racial/ethnic differences in the development of disability among older adults. Am J Public Health 2007;97:2209–15.
14. Puett RC, Schwartz J, Hart JE, et al. Chronic particulate exposure, mortality, and coronary heart disease in the nurses’ health study. Am J Epidemiol 2008;168:1161–8.
Study Overview
Objective. To evaluate the contribution of dietary habits in midlife on healthy aging.
Study design. Observational investigation of an ongoing cohort study.
Setting and participants. Participants were gathered from the Nurses’ Health Study, a cohort of 121,700 married female nurses who have completed health-related questionnaires every 2 years since 1976. Data on race was not originally collected, but a subsample analysis revealed that the cohort of nurses was > 98% white [1]. A subset of this cohort (n = 19,415) older than age 70 years from 1995 and 2002 and who received additional cognitive testing was chosen as the population of interest for this study. The investigators excluded participants with missing data (n = 5878) on important covariates and participants who had any of 11 chronic diseases in midlife (n = 2585), obtained from questionnaires in the 1980s. 10,670 participants were included in the final analysis.
Main outcome measures. Participants were dichotomized as “healthy agers” or “usual agers” on the basis of 4 health domains measured in 2000. Persons free of 11 chronic diseases, without cognitive impairment, without physical limitations, and with intact mental health were designated “healthy agers,” with the remainder designated “usual agers.” For each domain, specific criteria were employed to indicate impairment. Cognitive impairment was defined as a score of 31 or greater on the Telephone Interview for Cognitive Status. Investigators used the Medical Outcomes Short-Form 36 health survey (SF-36) to measure physical impairment and mental health. Participants who reported being limited at least “a little” on moderate activities or limited “a lot” on strenuous activities were classified as physically impaired. Intact mental health was defined as a score above the cohort’s median on the mental health subscale of the SF-36.
Dietary habits were ascertained at midlife by an average of the 1984 and 1986 food frequency questionnaire (FFQ) data. Using these data, the authors calculated the Alternative Healthy Eating-2010 (AHEI-2010) and the Alternate Mediterranean Diet (A-MeDi) scores. AHEH-2010 incorporates the latest knowledge on the benefits and harms of foods and nutrients on the risk of chronic disease. It has 11 domains (including whole grain intake, vegetable intake, and lower intake of trans fats, among others) which are each scored 0 (worst) to 10 (best). The A-MeDi score assesses adherence to the traditional Mediterranean diet, which includes intake of vegetables, fruits, nuts, legumes, and moderate alcohol intake, among others. Each of 9 categories is rated 0 or 1, with 1 representing healthy intake.
Covariates included sociodemographic, lifestyle, and health-related measures obtained either in 1984 or 1986. These included age; educational level; household income and home value estimated from census tract data; marital status; family history of diabetes, cancer, and myocardial infarction; physical activity; smoking; multivitamin and aspirin use; BMI; history of high blood pressure; and hypercholesterolemia. BMI was obtained via self-report and averaged from among values obtained in 1984 and 1986; these have previously been shown to have excellent correlation (r = 0.97) to standardized examinations [2].
The authors standardized baseline characteristics for each study participant based upon the age at which they entered the study. They used logistic regression to estimate the odds of being a “healthy ager” in the year 2000 by quintile of AHEI-2010 and A-MeDi scores.
Main results. Of the 10,670 participants, 1171 (11%) were labeled “healthy agers” and 9499 (89%) were labeled “usual agers.” Prevalence in each of the 4 health domains varied widely: 9599 (90%) of the 10670 participants had no cognitive impairment, 7234 (67.8%) had no chronic diseases, 4606 (43.2%) had no mental health limitations, and 2905 (27.2%) had no impairment of physical functioning.
Investigators presented data comparing healthy agers and usual agers at baseline without tests for significance. The mean age of healthy agers and usual agers was comparable (58.6 [SD = 2.5] vs. 59.1 [SD = 2.5]). Healthy agers had lower prevalence of obesity (3% vs. 13%), ever smoking (54% vs. 47%), higher mean physical activity (19.4 MET h/wk [SD = 21.7] vs. 14.1 MET h/wk [SD = 19.8]), lower energy intake (1692 kcal/d [SD = 472] vs. 1743 kcal/d [SD = 477]) and lower prevalence of hypertension (20% vs. 32%) and hypercholesterolemia (12% vs. 17%). Healthy agers also had higher baseline AHEI-2010 (53.2 [SD = 10.3] vs. 50.6 [SD = 10.1]) and A-MeDi scores in midlife (4.5 [SD = 1.6] vs. 4.3 [SD = 1.7]).
Greater scores on the AHEI-2010 and A-MeDi measures in midlife were associated with greater odds of healthy aging in multivariate analysis. After adjusting for all covariates, women in the highest quintile of AHEI-2010 scores at baseline had 34% greater odds (95% CI, 9% to 66%) of being healthy agers compared to women in the lowest quintile. Likewise, adjusted analyses reported women in the highest quintile of A-MeDi scores had 46% greater odds (95% CI, 17% to 83%) of being healthy agers.
Secondary analyses tested each component of healthy aging for associations with AHEI-2010 and A-MeDi scores in midlife. Associations were overall weaker, but no impairment of physical function and no limitation of mental health were both found to be significant after adjustment for covariates. Women in the highest quintile of AHEI-2010 scores at baseline had 23% (95% CI, 11% to 36%) and 13% (95% CI, 5% to 22%) greater odds, respectively, of not having any physical limitations or mental health impairments in late life compared to women in the lowest quintile. Likewise, women in the highest quintile of A-MeDi scores at baseline had 14% (95% CI, 3% to 26%) and 12% (95% CI, 4% to 20%) greater odds, respectively, of not having any physical limitations or mental health impairments in late life compared to women in the lowest quintile.
The authors also tested the effect of individual components of dietary patterns on healthy aging, comparing those in the highest quintile versus those in the lowest quintile for each measure. Persons with the greatest intake of fruits had 46% (95% CI, 15% to 85%) greater odds of being healthy agers compared to those with the lowest intake of fruits. Persons with the highest intake of alcohol had 28% greater odds (95% CI, 4% to 56%) of being healthy agers compared to those with the lowest intake of alcohol. Conversely, those with lower intake of sugar-sweetened beverages (OR, 1.28 [95% CI, 1.03 to 1.58]) and non-omega 3 polyunsaturated fatty acids (OR, 1.38 [CI, 1.10 to 1.73]) had better odds of being healthy agers compared to those with higher intakes.
Conclusion. Women with healthy dietary patterns at midlife had significantly greater odds of being healthy agers in later life after adjusting for potential con-founders. Results were consistent in direction and effect size when using either the AHEI-2010 score or the A-MeDi score. The effects of healthy diet at midlife seemed to have the strongest association with physical impairment scores and mental health scores. Higher intake of fruits and alcohol along with lower intake of sugar-sweetened beverages and polyunsaturated fatty acids seemed to have the most power for predicting healthy aging.
Commentary
These results are consistent with current knowledge, which indicates the health benefits of a balanced, healthy diet high in fruits, vegetables, whole grains, nuts, and legumes and low in red or other processed meats. There is high quality evidence linking each dietary measure to health outcomes. Adherence to the Alternative Healthy Eating Index has been related to lower mortality rates [3], decreased risk of cardiovascular disease [4], and decreased risk of type 2 diabetes and the metabolic syndrome [5]. Likewise, adherence to the Mediterranean diet is associated with reductions in overall mortality, cardiovascular incidence and mortality, cancer incidence and mortality, and neurodegenerative diseases [6]. Both diets endorse moderate alcohol intake, which was associated with lower rates of all-cause and cardiovascular mortality in a meta-analysis [7]. Alcohol is theorized to produce decreased platelet aggregation, increase HDL cholesterol, and increase endothelial vasorelaxation [8]. Polyphenols, most prominent in red wines, may have additional effects which include vaso-relaxation of aortic rings, reduced thrombosis and inflammation, and increased fibrinolysis [9]. Nevertheless, heavy alcohol use may increase cardiovascular mortality, hypertension, and hyperlipidemia [8]. This study concluded that higher alcohol intake was related to being a healthy ager; this may be because there are few heavy alcohol users in this cohort, though this hypothesis was not tested in the study.
Any observational study is subject to debate about the confounders chosen for analysis and potential biases. The authors report that the most powerful confounders in this analysis were BMI, physical activity, and smoking, all of which have been well established as predictors for health in later life [10]. Nonetheless, important potential confounders not used in analysis included the baseline prevalence of mental health problems, cognitive limitations, and physical limitations, all of which were not available.
The greatest concern about of this study is a potential lack of generalizability given the population surveyed. The Nurses’ Health Study consists of a cohort of female, married, predominantly white registered nurses [1]. For instance, African Americans have a greater burden of hypertension than non-Hispanic whites after accounting for dietary differences [11], a higher degree of late-life cognitive dysfunction [12], and greater risk of developing late-life physical disability [13]. Also, race and ethnicity may impact eating patterns, food preferences, and food availability in ways that are difficult to predict. In addition, nurses in the cohort were probably of similar socioeconomic status given their shared occupation, though the authors did not report the variation in median household incomes obtained from census tract analysis in this study [14]. Results might change if the sample was less homogeneous. Nonetheless, the results are consistent with current knowledge, biologically plausible, and clinically meaningful.
Applications for Clinical Practice
Integrating dietary changes in middle-aged women may be an important means of decreasing morbidity in older age and improving physical and mental health functioning later in life. Health care providers should discuss the future benefits of healthy eating on quality of life in order to encourage patients in midlife to alter their diet in meaningful ways. While it may be difficult to generalize these findings to patients of different genders, races, or ethnicities, the biological underpinnings of the data make it hard dispute the conclusions presented in the study.
—Hector Perez, MD, and Melanie Jay, MD, MS
Study Overview
Objective. To evaluate the contribution of dietary habits in midlife on healthy aging.
Study design. Observational investigation of an ongoing cohort study.
Setting and participants. Participants were gathered from the Nurses’ Health Study, a cohort of 121,700 married female nurses who have completed health-related questionnaires every 2 years since 1976. Data on race was not originally collected, but a subsample analysis revealed that the cohort of nurses was > 98% white [1]. A subset of this cohort (n = 19,415) older than age 70 years from 1995 and 2002 and who received additional cognitive testing was chosen as the population of interest for this study. The investigators excluded participants with missing data (n = 5878) on important covariates and participants who had any of 11 chronic diseases in midlife (n = 2585), obtained from questionnaires in the 1980s. 10,670 participants were included in the final analysis.
Main outcome measures. Participants were dichotomized as “healthy agers” or “usual agers” on the basis of 4 health domains measured in 2000. Persons free of 11 chronic diseases, without cognitive impairment, without physical limitations, and with intact mental health were designated “healthy agers,” with the remainder designated “usual agers.” For each domain, specific criteria were employed to indicate impairment. Cognitive impairment was defined as a score of 31 or greater on the Telephone Interview for Cognitive Status. Investigators used the Medical Outcomes Short-Form 36 health survey (SF-36) to measure physical impairment and mental health. Participants who reported being limited at least “a little” on moderate activities or limited “a lot” on strenuous activities were classified as physically impaired. Intact mental health was defined as a score above the cohort’s median on the mental health subscale of the SF-36.
Dietary habits were ascertained at midlife by an average of the 1984 and 1986 food frequency questionnaire (FFQ) data. Using these data, the authors calculated the Alternative Healthy Eating-2010 (AHEI-2010) and the Alternate Mediterranean Diet (A-MeDi) scores. AHEH-2010 incorporates the latest knowledge on the benefits and harms of foods and nutrients on the risk of chronic disease. It has 11 domains (including whole grain intake, vegetable intake, and lower intake of trans fats, among others) which are each scored 0 (worst) to 10 (best). The A-MeDi score assesses adherence to the traditional Mediterranean diet, which includes intake of vegetables, fruits, nuts, legumes, and moderate alcohol intake, among others. Each of 9 categories is rated 0 or 1, with 1 representing healthy intake.
Covariates included sociodemographic, lifestyle, and health-related measures obtained either in 1984 or 1986. These included age; educational level; household income and home value estimated from census tract data; marital status; family history of diabetes, cancer, and myocardial infarction; physical activity; smoking; multivitamin and aspirin use; BMI; history of high blood pressure; and hypercholesterolemia. BMI was obtained via self-report and averaged from among values obtained in 1984 and 1986; these have previously been shown to have excellent correlation (r = 0.97) to standardized examinations [2].
The authors standardized baseline characteristics for each study participant based upon the age at which they entered the study. They used logistic regression to estimate the odds of being a “healthy ager” in the year 2000 by quintile of AHEI-2010 and A-MeDi scores.
Main results. Of the 10,670 participants, 1171 (11%) were labeled “healthy agers” and 9499 (89%) were labeled “usual agers.” Prevalence in each of the 4 health domains varied widely: 9599 (90%) of the 10670 participants had no cognitive impairment, 7234 (67.8%) had no chronic diseases, 4606 (43.2%) had no mental health limitations, and 2905 (27.2%) had no impairment of physical functioning.
Investigators presented data comparing healthy agers and usual agers at baseline without tests for significance. The mean age of healthy agers and usual agers was comparable (58.6 [SD = 2.5] vs. 59.1 [SD = 2.5]). Healthy agers had lower prevalence of obesity (3% vs. 13%), ever smoking (54% vs. 47%), higher mean physical activity (19.4 MET h/wk [SD = 21.7] vs. 14.1 MET h/wk [SD = 19.8]), lower energy intake (1692 kcal/d [SD = 472] vs. 1743 kcal/d [SD = 477]) and lower prevalence of hypertension (20% vs. 32%) and hypercholesterolemia (12% vs. 17%). Healthy agers also had higher baseline AHEI-2010 (53.2 [SD = 10.3] vs. 50.6 [SD = 10.1]) and A-MeDi scores in midlife (4.5 [SD = 1.6] vs. 4.3 [SD = 1.7]).
Greater scores on the AHEI-2010 and A-MeDi measures in midlife were associated with greater odds of healthy aging in multivariate analysis. After adjusting for all covariates, women in the highest quintile of AHEI-2010 scores at baseline had 34% greater odds (95% CI, 9% to 66%) of being healthy agers compared to women in the lowest quintile. Likewise, adjusted analyses reported women in the highest quintile of A-MeDi scores had 46% greater odds (95% CI, 17% to 83%) of being healthy agers.
Secondary analyses tested each component of healthy aging for associations with AHEI-2010 and A-MeDi scores in midlife. Associations were overall weaker, but no impairment of physical function and no limitation of mental health were both found to be significant after adjustment for covariates. Women in the highest quintile of AHEI-2010 scores at baseline had 23% (95% CI, 11% to 36%) and 13% (95% CI, 5% to 22%) greater odds, respectively, of not having any physical limitations or mental health impairments in late life compared to women in the lowest quintile. Likewise, women in the highest quintile of A-MeDi scores at baseline had 14% (95% CI, 3% to 26%) and 12% (95% CI, 4% to 20%) greater odds, respectively, of not having any physical limitations or mental health impairments in late life compared to women in the lowest quintile.
The authors also tested the effect of individual components of dietary patterns on healthy aging, comparing those in the highest quintile versus those in the lowest quintile for each measure. Persons with the greatest intake of fruits had 46% (95% CI, 15% to 85%) greater odds of being healthy agers compared to those with the lowest intake of fruits. Persons with the highest intake of alcohol had 28% greater odds (95% CI, 4% to 56%) of being healthy agers compared to those with the lowest intake of alcohol. Conversely, those with lower intake of sugar-sweetened beverages (OR, 1.28 [95% CI, 1.03 to 1.58]) and non-omega 3 polyunsaturated fatty acids (OR, 1.38 [CI, 1.10 to 1.73]) had better odds of being healthy agers compared to those with higher intakes.
Conclusion. Women with healthy dietary patterns at midlife had significantly greater odds of being healthy agers in later life after adjusting for potential con-founders. Results were consistent in direction and effect size when using either the AHEI-2010 score or the A-MeDi score. The effects of healthy diet at midlife seemed to have the strongest association with physical impairment scores and mental health scores. Higher intake of fruits and alcohol along with lower intake of sugar-sweetened beverages and polyunsaturated fatty acids seemed to have the most power for predicting healthy aging.
Commentary
These results are consistent with current knowledge, which indicates the health benefits of a balanced, healthy diet high in fruits, vegetables, whole grains, nuts, and legumes and low in red or other processed meats. There is high quality evidence linking each dietary measure to health outcomes. Adherence to the Alternative Healthy Eating Index has been related to lower mortality rates [3], decreased risk of cardiovascular disease [4], and decreased risk of type 2 diabetes and the metabolic syndrome [5]. Likewise, adherence to the Mediterranean diet is associated with reductions in overall mortality, cardiovascular incidence and mortality, cancer incidence and mortality, and neurodegenerative diseases [6]. Both diets endorse moderate alcohol intake, which was associated with lower rates of all-cause and cardiovascular mortality in a meta-analysis [7]. Alcohol is theorized to produce decreased platelet aggregation, increase HDL cholesterol, and increase endothelial vasorelaxation [8]. Polyphenols, most prominent in red wines, may have additional effects which include vaso-relaxation of aortic rings, reduced thrombosis and inflammation, and increased fibrinolysis [9]. Nevertheless, heavy alcohol use may increase cardiovascular mortality, hypertension, and hyperlipidemia [8]. This study concluded that higher alcohol intake was related to being a healthy ager; this may be because there are few heavy alcohol users in this cohort, though this hypothesis was not tested in the study.
Any observational study is subject to debate about the confounders chosen for analysis and potential biases. The authors report that the most powerful confounders in this analysis were BMI, physical activity, and smoking, all of which have been well established as predictors for health in later life [10]. Nonetheless, important potential confounders not used in analysis included the baseline prevalence of mental health problems, cognitive limitations, and physical limitations, all of which were not available.
The greatest concern about of this study is a potential lack of generalizability given the population surveyed. The Nurses’ Health Study consists of a cohort of female, married, predominantly white registered nurses [1]. For instance, African Americans have a greater burden of hypertension than non-Hispanic whites after accounting for dietary differences [11], a higher degree of late-life cognitive dysfunction [12], and greater risk of developing late-life physical disability [13]. Also, race and ethnicity may impact eating patterns, food preferences, and food availability in ways that are difficult to predict. In addition, nurses in the cohort were probably of similar socioeconomic status given their shared occupation, though the authors did not report the variation in median household incomes obtained from census tract analysis in this study [14]. Results might change if the sample was less homogeneous. Nonetheless, the results are consistent with current knowledge, biologically plausible, and clinically meaningful.
Applications for Clinical Practice
Integrating dietary changes in middle-aged women may be an important means of decreasing morbidity in older age and improving physical and mental health functioning later in life. Health care providers should discuss the future benefits of healthy eating on quality of life in order to encourage patients in midlife to alter their diet in meaningful ways. While it may be difficult to generalize these findings to patients of different genders, races, or ethnicities, the biological underpinnings of the data make it hard dispute the conclusions presented in the study.
—Hector Perez, MD, and Melanie Jay, MD, MS
1. Hemenway D, Colditz GA, Willett WC, et al. Fractures and lifestyle: effect of cigarette smoking, alcohol intake, and relative weight on the risk of hip and forearm fractures in middle-aged women. Am J Public Health 1988;78:1554–8.
2. Rimm EB, Stampfer MJ, Colditz GA, et al. Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1990;1:466–73.
3. Akbaraly TN, Ferrie JE, Berr C, et al. Alternative Healthy Eating Index and mortality over 18 y of follow-up: results from the Whitehall II cohort. Am J Clin Nutr 2011;94:247–53.
4. McCullough ML, Feskanich D, Stampfer MJ, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr 2002;76:1261–71.
5. Akbaraly TN, Singh-Manoux A, Tabak AG, et al. Overall diet history and reversibility of the metabolic syndrome over 5 years: the Whitehall II prospective cohort study. Diabetes Care 2010;33:2339–41.
6. Sofi F, Abbate R, Gensini GF, et al. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr 2010;92:1189–96.
7. Di Castelnuovo A, Costanzo S, Bagnardi V, et al. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med 2006;166:2437–45.
8. Costanzo S, Di Castelnuovo A, Donati MB, et al. Cardiovascular and overall mortality risk in relation to alcohol consumption in patients with cardiovascular disease. Circulation 2010;121:1951–9.
9. Booyse FM, Pan W, Grenett HE, et al. Mechanism by which alcohol and wine polyphenols affect coronary heart disease risk. Ann Epidemiol 2007;17:S24–S31.
10. Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med 2012;55:163–70.
11. Diaz VA, Mainous AG, Koopman RJ, et al. Race and diet in the overweight: association with cardiovascular risk in a nationally representative sample. Nutrition 2005;21:718–25.
12. Sloan FA, Wang J. Disparities among older adults in measures of cognitive function by race or ethnicity. J Gerontol B Psychol Sci Soc Sci 2005;60:P242–50.
13. Dunlop DD, Song J, Manheim LM, et al. Racial/ethnic differences in the development of disability among older adults. Am J Public Health 2007;97:2209–15.
14. Puett RC, Schwartz J, Hart JE, et al. Chronic particulate exposure, mortality, and coronary heart disease in the nurses’ health study. Am J Epidemiol 2008;168:1161–8.
1. Hemenway D, Colditz GA, Willett WC, et al. Fractures and lifestyle: effect of cigarette smoking, alcohol intake, and relative weight on the risk of hip and forearm fractures in middle-aged women. Am J Public Health 1988;78:1554–8.
2. Rimm EB, Stampfer MJ, Colditz GA, et al. Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1990;1:466–73.
3. Akbaraly TN, Ferrie JE, Berr C, et al. Alternative Healthy Eating Index and mortality over 18 y of follow-up: results from the Whitehall II cohort. Am J Clin Nutr 2011;94:247–53.
4. McCullough ML, Feskanich D, Stampfer MJ, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr 2002;76:1261–71.
5. Akbaraly TN, Singh-Manoux A, Tabak AG, et al. Overall diet history and reversibility of the metabolic syndrome over 5 years: the Whitehall II prospective cohort study. Diabetes Care 2010;33:2339–41.
6. Sofi F, Abbate R, Gensini GF, et al. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr 2010;92:1189–96.
7. Di Castelnuovo A, Costanzo S, Bagnardi V, et al. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med 2006;166:2437–45.
8. Costanzo S, Di Castelnuovo A, Donati MB, et al. Cardiovascular and overall mortality risk in relation to alcohol consumption in patients with cardiovascular disease. Circulation 2010;121:1951–9.
9. Booyse FM, Pan W, Grenett HE, et al. Mechanism by which alcohol and wine polyphenols affect coronary heart disease risk. Ann Epidemiol 2007;17:S24–S31.
10. Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med 2012;55:163–70.
11. Diaz VA, Mainous AG, Koopman RJ, et al. Race and diet in the overweight: association with cardiovascular risk in a nationally representative sample. Nutrition 2005;21:718–25.
12. Sloan FA, Wang J. Disparities among older adults in measures of cognitive function by race or ethnicity. J Gerontol B Psychol Sci Soc Sci 2005;60:P242–50.
13. Dunlop DD, Song J, Manheim LM, et al. Racial/ethnic differences in the development of disability among older adults. Am J Public Health 2007;97:2209–15.
14. Puett RC, Schwartz J, Hart JE, et al. Chronic particulate exposure, mortality, and coronary heart disease in the nurses’ health study. Am J Epidemiol 2008;168:1161–8.
Technology-Supported Apprenticeship in the Management of Hypertension: A Randomized Controlled Trial
From the Massachusetts Institute of Technology (Dr. Moore, Dr. Moss and Mr. Gilroy) and the Massachusetts General Hospital (Ms. Marshall, Dr. Judge, Dr. Crocker, and Dr. Zusman), Boston, MA.
Abstract
- Objective: To compare technology-supported appren-ticeship in hypertension management with a successful coaching model at Massachusetts General Hospital.
- Methods: A randomized controlled trial was conducted. Adult patients with uncontrolled essential hypertension (average blood pressure (BP) 148/87 mm Hg) were recruited in a staggered fashion for a 12-week study period. Intervention subjects received apprenticeship support from a nurse health coach through the CollaboRhythm application on a tablet computer. Patients self-tracked medication adherence and blood pressure (via wireless device) and the coach helped them to continuously progress through lifestyle change and medication adjustment using integrated messaging. Control subjects received support from the same coach but through traditional channels of office visits, phone calls, and e-mail.
- Results: 42 of 44 subjects completed the study. Intervention subjects achieved a greater decrease in systolic BP at 12 weeks than control subjects (26.3 mm Hg vs. 16.0 mm Hg, P = 0.009). A greater percentage of intervention subjects achieved goal BP ≤ 130/80 mm Hg (75.0% vs. 31.8%, P = 0.003) and 100% of them achieved goal BP ≤ 140/90 mmHg. They also rated the experience higher, although this finding was not statistically significant (8.9 vs. 7.6, P = 0.12). There was a trend toward increased cost for intervention subjects ($67.50 vs. $53.41, P = 0.15), but the projected cost is much less than standard care ($248/patient/year).
- Conclusion: This study provides encouraging evidence that technology-supported apprenticeship can improve the outcomes, cost, and experience of care in managing hypertension.
Hypertension affects approximately 33% of the U.S. adult population [1]. Antihypertensive treatment has been shown to be effective at preventing complications [2,3]. Unfortunately, estimates suggest that the majority of those diagnosed with hypertension do not have their blood pressure controlled [1]. This failure is due to both clinician and patient factors. Mean adherence of clinicians to guidelines is estimated at 53.5% [4]. An electronic monitoring study showed that half of patients who are prescribed medications stop taking them within 1 year [5]. Of those who take their medications, about 10% have adherence issues on any given day and about 50% have significant adherence issues in the course of their treatment [5]. Adherence to diet and exercise self-management is even more dismal, with rates below 20% [6]. Hypertension is an expensive problem with direct medical costs (treatment and complications) greater than $100 billion a year and equally high indirect costs (lost productivity) [7–9].
In the management of chronic diseases, there is a significant trend toward empowering patients with more control and toward providing more longitudinal coaching from clinicians and from peers [10–15]. Technology-supported apprenticeship is a model of chronic disease management that builds on the success of self-management and coaching, but it is more ambitious in that its goal is for patients to lead their care with the support of health coaches and supervising clinicians. It is informed by the field of learning science, particularly in how technology can be used effectively to support learning [16–20]. Apprenticeship refers to the tutelage of a community of novices in a skill or trade by one or more masters through situated learning. Situated learning refers to the process in which novices learn through participation in legitimate tasks in the same physical and social context where they will need to perform them once independent [21,22]. It is opposed to learning through contrived exercises in an artificial environment like a classroom.
In technology-supported apprenticeship, patients are the novice apprentices of master coaches. Technology provides scaffolding and communication tools to allow coaches to support the patient in the management of disease within the context of daily life rather than in the clinician’s office. Patients are supported in gradually developing self-efficacy and independence until they are skilled enough to lead their care and even to help coach others to success. The hypothesis is that embracing the contribution of the patient to this extent will reap unparalleled rewards in the experience, outcomes, and cost of care.
We conducted a randomized controlled trial to assess whether a technology-supported apprenticeship in hyper-tension management would improve blood pressure control compared with a successful coaching model.
Methods
Setting
The health coaching model at the Ambulatory Practice of the Future (APF) at the Massachusetts General Hospital is designed to impact the whole health ofpatients. In the scope of hypertension management, a nurse health coach, under the supervision of a physician, is responsible for improving outcomes through longitudinal support via office visits, phone calls, and e-mails. Diet, exercise, stress management, and medication therapy are all emphasized through health coaching techniques, such as motivational interviewing and appreciative inquiry [23,24]. Patients are referred to dieticians, exercise coaches, mind-body specialists, and others as desired. Prior to the start of this study, the APF was outperforming the national average with ~70% of hypertensive patients in the practice below clinically recommended goal blood pressures.
Recruitment
The study was advertised to all clinical staff of the APF through word of mouth. Since the practice was relatively young, it also had a registry of patients with elevated blood pressure that had not been addressed. Adult patients (> 18 years old) from the registry or from routine visits with essential hypertension (average blood pressure ≥ 140/90 and ≤ 180/120) who were taking 0 or 1 medications and had internet connectivity were eligible for inclusion in the study. Patients with a history of hypotension, syncope, hypertensive urgency, hypertensive emergency, labile hypertension, and proven coronary artery disease were excluded, as were patients with significant visual, auditory, or cognitive impairment and patients who were not proficient in English. Clinical staff notified the nurse health coach for the study on identification of any eligible subjects. The same nurse health coach recruited and cared for all intervention and control subjects.
The nurse health coach contacted each eligible patient to assess interest. Interested patients were scheduled for an appointment to commence the study. A process of written informed consent was carried out with each study subject. Each subject was assigned the next sequential study number, which was pre-randomized to either the intervention or the control group.
The study period for each subject was 12 weeks +/– 2 weeks with staggered recruitment. Twelve weeks represents the minimal time required to progress through the standardized Medication Adjustment Plan that was used, assuming a minimum time of 2 weeks on each medication before a change is considered. A recruitment window from 1 March 2013 until 31 May 2013 was used. The goal was to recruit between 40 and 60 subjects, since statistical analysis revealed that a sample size of 36 was sufficient to detect a 5 mm Hg difference in the decrease in systolic blood pressure between groups given a 4 mm Hg standard deviation.
Intervention
CollaboRhythm is a software platform that was developed at the MIT Media Lab and designed to support the principles of technology-supported apprenticeship. Patient tracking tools document progress, visualizations highlight associations between actions and outcomes, and personalized decision support encourages self-efficacy. Powerful virtual visits and instant messaging allow master clinicians to provide adaptive coaching within the context of daily life rather than in the artificial environment of the office. Applications can be deployed cross-platform to cell phones, tablets, computers, etc.
A simplified system was created for hypertension management. It is optimized for tablet deployment and focuses on instant messaging for communications. The patient uses a wireless blood pressure monitor (D40b model by ForaCare®) to take blood pressure measurements. The device is paired with a tablet application to automatically report measurements. The patient self-reports medication adherence using the tablet application. Patient data is visualized in a daily clock and weekly charts to promote proactive behavior and self-reflection. Decision support for medication adjustment is paired with the charts. The patient’s data are synchronized with the coach’s tablet application via a collaborative health record server implemented using the Indivo X personally controlled health record (Children’s Hospital Boston, indivohealth.org) code base. Instant messaging between the patient and coach is implemented using a real-time messaging server. The applications for the patient and the coach are identical, but the coach’s application is configured to allow switching between patient records in order to manage a number of patients.
The user experience was designed based on our years of exploration at the MIT Media Lab of the psychology of illness and the impact that technology could have on patient empowerment and patient-clinician collaboration. It is important to note that the CollaboRhythm application is different from typical electronic reminder applications. In fact, the application never alarms at patients, even if they forget to perform their health actions. Instead, the application focuses on providing awareness for proactive decision-making, self-reflection, and support from the coach.
Protocol Common to Control and Intervention Subjects
Following informed consent, a baseline blood pressure and heart rate were measured for each subject using the same automated sphygmomanometer. Weight was also measured and a hypertension knowledge assessment (a simple survey about normal blood pressures and the effects of diet, exercise, and medication that was created for the purpose of this study) was completed. The initial medication load was determined using the Medication Adjustment Plan as a reference and each dose step as a unit of 1. For example, if a subject was already on lisinopril 40 mg at the start of the study, the initial medication load was 2.
The nurse health coach conducted an introductory visit with each subject including motivational interviewing to assess their health values and to discuss
hypertension management goals. The subject and coach made shared decisions about diet, exercise, stress management, and medication. The same medication titration algorithm was used for both control and interventional
subjects.
At the conclusion of the study period, subjects in both groups returned for an exit visit. Blood pressure and heart rate were measured using the same automated sphygmomanometer that was used at the initial visit. Weight was measured using the same scale as the initial visit. A hypertension knowledge assessment was completed and an exit interview was conducted. The change in medication load was determined as well. For example, if a subject started the study on lisinopril 20 mg and ended the study on lisinopril 40 mg, the increase in medication load was 1.
Protocol Specifics for Intervention Subjects
The apprenticeship model of chronic disease management was discussed with the nurse health coach and with APF team prior to the study. It was also implicit in the design of the CollaboRhythm tablet application.
During the introduction visit, subjects in the inter-vention group received instructions from the nurse health coach on how to use the CollaboRhythm tablet application to self-track their medication adherence, to review progress using the charts, to propose or agree with changes in hypertension medications, and to communicate with messages.
Subjects in the intervention group received their hyper-tension care through the CollaboRhythm tablet application. All instant messages between the intervention subjects and the nurse health coach were automatically documented electronically. Other forms of communication were documented in a spreadsheet. During the exit visit, the tablet computer and the wireless blood pressure meter were returned.
Protocol Specifics for Control Subjects
Between the introduction and exit visits, subjects in the control group received standard hypertension care from the nurse health coach at the APF. The coach instructed subjects to check their blood pressures 3 to 5 times a week. They had the option of purchasing a cuff, using a monitor at work, or using a monitor at a facility such as a pharmacy or grocery store. Communication took place through
office visits, phone calls, and e-mails. All communications with control subjects were documented for the purposes of this study by the nurse health coach in a spread-
sheet.
Outcomes of Interest
The primary outcomes of interest were the absolute decrease in systolic and diastolic blood pressure and the number of subjects who reached the blood pressure goal of less than or equal to 130/80 mm Hg. This more aggressive blood pressure goal was chosen for a number of reasons: (1) it is not uncommon to set a lower blood pressure goal for home measurements to avoid patients hovering just at the 140/90 goal and not getting the true benefit of reduced blood pressure; and (2) subjects were supported in improving diet, exercise, and stress management in addition to pharmacologic therapy. The 140/90 cut-off (now 150/90 in patients over 60) is focused on pharmacologic therapy [2,3].
The secondary outcomes included the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg (for comparison to other published literature), the number of subjects who achieved greater than a 10 mm Hg decrease in systolic and greater than a 5 mm Hg decrease in diastolic blood pressure, the change in medication load, the absolute decrease in weight, the number of subjects who lost at least 5 lb, a hypertension knowledge score assessed by a pre- and post-study test, a rating of satisfaction in care, and the amount of clinician time required in the care.
Statistical Methods
The study results were analyzed by the intention-to-treat approach. All subjects who returned for the final study visit were included in the analysis regardless of their adherence to the protocol. Subjects who did not return for the study exit visit were not included in the analysis because it would be impossible to determine the change in blood pressure without a final measurement. A 2-tailed Student’s t test for independent samples was used for all comparisons of the mean of continuous variables between the control and intervention groups. A 2-tailed Student’s t test for dependent samples was used for all comparisons between pre- and post-study variables within the control and the intervention group. A chi-square test was used for all comparisons of categorical variables between the groups, except when the expected values in the 2x2 table were below 5. Fisher’s exact test was used in this scenario, which applied to the secondary outcome of the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg.
Oversight
This study was approved by the institutional review boards at the Massachusetts Institute of Technology and the Massachusetts General Hospital.
Results
There were a total of 44 subjects recruited for the study. One intervention subject and one control subject were lost to follow-up, leaving 42 subjects who completed the study exit visit.
Baseline Statistics
Clinical Outcomes
Cost
 Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Experience
Thirteen control subjects and 16 intervention subjects provided an experience rating during their exit interview from the study. There was a trend toward greater satisfaction by intervention subjects that was not statistically significant (8.9 vs. 7.6, P = 0.12). The majority of feedback from intervention subjects was obtained through the exit interview. The feedback was overwhelmingly positive. All of the subjects wanted to continue using the CollaboRhythm application after the end of the study. Some who had reached goal only wanted to use it sporadically as a “check-in,” but the majority wanted to use it daily as they had for the study for an indefinite period of time. They felt that the burden of reporting was easily balanced by the value of being able to track progress and get the efficient support of a health coach. They related that awareness of the associations between actions (diet, exercise, stress management, medication adherence) and blood pressure outcomes was integral to their success and their positive experience with the application. Subjects responded very favorably to the concept of leading their care. Some comments from patients include: “It felt good to take responsibility,” “No one has ever asked me to take responsibility for my health,” and “I developed confidence that I never would have had.” The nurse coach commented multiple times how delighted she was with the level of patient engagement and excitement. She also did not want to stop using the application at the end of the study.
The main complaints about the program from both subjects and the health coach were on performance. They wanted the application to load faster and to save data faster.
Discussion
This study provides encouraging evidence that technology-supported apprenticeship can dramatically improve the outcomes, cost, and experience of care in the management of hypertension.
A 26.3 mm Hg average decrease in systolic blood pressure for intervention subjects in 3 months is significantly better than the standard of care and the best of the best in published interventions. [1,11–14]. The same is true for a rate of 100% of patients achieving goal blood pressure < 140/90 mm Hg.
We believe several factors contribute to the success of our program: (1) supporting subjects in the mission of leading their care, (2) rich real-time feedback for self-reflection, (3) emphasis on short-term goals, (4) promise of medication reduction with goal achievement, and (5) social support and accountability that come with having a continuously available coach who had immediate data access.
Other studies have had web communication components, self-titration components, and coaching components. In a progressive study by McManus [11], subjects in the intervention group self-tracked their blood pressure and self-titrated their hypertension medications while control subjects received routine care. Self-managing patients achieved a decrease in systolic blood pressure of 17.6 mm Hg over 12 months while controls only achieved a decrease of 12.2 mm Hg. Self-managing patients were more aggressive in adding new medications and did not have increased incidence of side effects. A study by Green [12] showed that subjects with home blood pressure monitoring, a web training course, and web-based pharmacist coaching achieved a 14.2 mm Hg decrease in systolic blood pressure over 12 months and that 56% reached goal blood pressure (< 140/90 mm Hg). Subjects who received routine care only achieved a 5.3 mm Hg decrease in systolic blood pressure and only 31% reached goal blood pressure. Margolis [13] and Magid [14] conducted studies similar to Green's with pharmacist-led care. In Margolis’ study, 71.8% of inter-vention subjects study achieved goal at 6 months with a mean decrease in systolic blood pressure of 21.5 mm Hg. These results were impressively stable at 18 months [13]. In Magid’s study, 54.1% of intervention subjects achieved goal at 6 months with a mean decrease in systolic blood pressure of 20.7 mm Hg [14].
The technology-supported apprenticeship model was inspired by the exceptional results of these studies, but we believe that it represents a significant step forward in patient engagement. In these studies, the tools were typically more burdensome than empowering, the titration more prescriptive than motivational, and the coaching more timed and paternalistic than continuous and nurturing. Technology-supported apprenticeship relies on more powerful tools for collaboration and aspires for the patient to lead the care rather than the clinician. It has the potential to produce greater self-efficacy, which results in better outcomes at lower cost.
Cost Implications
The 100% rate of attainment of systolic blood pressure < 140 mm Hg in our intervention subjects has the poten-tial to contribute to substantial cost savings through reducing complications. The cost of complications per patient per year is approximately $1275, and attainment of goal blood pressure on average results in approximately 35% decrease in complications [2,7–9] Therefore, it is reasonable to expect at least $446 savings in downstream costs per patient per year with this intervention. This has notable public health implications given that there are approximately 32 million patients in the United States with diagnosed hypertension that is uncontrolled [1]. Cost saving at scale could be more than $14 billion.
Typically, interventions that produce downstream savings in health care require some upstream investment. An exciting aspect of this intervention is that it was significantly less costly, at $67.50 per patient, as compared with the standard of care, at $248 per patient per year [7–9]. Most of the responsibility was embraced by the patients, and the nurse coach needed only to provide occasional social and clinical support. Return office visits were almost completely eliminated and goals were achieved in a fraction of the time. The cost of the technology is effectively negligible given that patients will be able to use their own cell phones and tablets and their own blood pressure cuffs. Based on the prevalence of hypertension, a primary care practice with 2000 patients would be expected to have 600 with hypertension. At $180.50 in savings per patient per year, a profit of $108,300 could be retained if the same reimbursement was provided for this more effective care. At the same time, this more efficient and scalable model of care could allow a practice to care for a larger number of patients without compromising the experience for patients or clinicians.
Limitations and Future Directions
An important limitation of this study is its small sample size. The efficiency and cost analysis suggests that the intervention is highly suitable for scaling but, until this is studied, there is the risk that the small sample size may misrepresent the average effect on a larger population and overestimate the size of a population that a coach can manage. Future work will need to include much larger populations.
Another limitation was the short follow-up period. A key benefit of apprenticeship is that it theoretically results in greater and more sustainable self-efficacy than other models of patient engagement that are not as grounded in learning science and that do not engage the patient as deeply. Follow-up visits for both control and intervention subjects will be conducted at 1 year to assess the sustainability of the blood pressure improvements.
The fact that the population was from a single practice also presents the possibility that the subjects being studied were more interested and/or capable than a larger, more general population. This is likely to be true, since many of the patients at the APF sought it out in the hope of receiving a new health care experience. Future work will need to address patient populations from diverse socioeconomic situations and diverse cultures. Based on pilot studies that we have done with diverse populations with HIV, hypertension, and diabetes, we believe that patients who are more disempowered and disenfranchised at baseline attain greater benefit from becoming apprentices in their care.
Another potential limitation is that hypertension was treated in isolation in this study. In fact, many of the subjects had comorbid conditions and were being treated for them simultaneously at the APF. Future work will need to address how the apprenticeship approach and accompanying technology can support the management of multiple comorbid conditions. At the same time, we believe that setting aggressive goals for one condition at a time and achieving these goals over a short period, such as 3 months, will be an important strategy in effectively engaging patients as active participants in their care and helping them to develop self-efficacy. As they develop competency for one condition, they become more capable of managing the others. If they were to attempt to tackle all of the problems simultaneously, it could be overwhelming and ineffective.
Conclusions
This study provides encouraging evidence that, in the management of hypertension, technology-supported apprenticeship can improve the outcomes, cost, and experience of care. By embracing the potential of patients while at the same time optimizing support from clinicians and leveraging information technology for cost-effective scaling, it has the potential to have a tremendous impact across the spectrum of chronic disease.
Three core tenants of technology-supported apprenticeship have surfaced as the product of this work, and they may serve as a useful guide to other efforts improving care delivery: First, patients are the most underutilized resource in health care. Technology-supported apprenticeship harnesses the contribution of the patient and values the development of self-efficacy to the extent that apprentices can become masters. It supports patients in achieving a pinnacle of patient empowerment.
Second, health takes place in the everyday lives of patients, not in a doctor’s office or hospital. Technology-supported apprenticeship appreciates that situated learning is the key to mastery of chronic disease management and strives to support patients continuously in the context of their lives.
Third, collaboration and information transparency, not just information access, are critical. Technology-supported apprenticeship embraces information technology to maximize collaboration among novices and masters and to provide common ground through complete transparency.
Acknowledgments: This study was completed as part of John O. Moore’s PhD thesis at the MIT Media Lab. Mitchel Resnick, PhD, and Pattie Maes, PhD, were members of the thesis committee along with authors Franklin H. Moss, PhD, and David C. Judge, MD, and their advice was critical in the development of the technology-supported apprenticeship approach.
Corresponding author: John O. Moore, MD, PhD, [email protected]
Funding/support: This work was supported, in part, by the CIMIT Prize for Primary Healthcare from the Center for Integration of Medicine & Innovative Technology, Boston, MA.
Financial disclosures: John O. Moore, Frank Moss, and Scott Gilroy have a health information technology company focused on building software solutions for improving chronic disease management. This company does not yet have a product for sale.
1. Recent trends in the prevalence of high blood pressure and its treatment and control. National Center for Health Statistics. Hyattsville, MD; 2010.
2. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–72. Erratum in: JAMA 2003;290:197.
3. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20.
4. Ardery G, Carter BL, Milchak JL, et al. Explicit and implicit evaluation of physician adherence to hypertension guidelines. J Clin Hypertens (Greenwich) 2007;9:113–9.
5. Vrijens B, Vincze G, Kristanto P, et al. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008;336:1114–7.
6. Mellen PB, Gao SK, Vitolins MZ, Goff DC Jr. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med 2008;168:308–14.
7. Davis K. Expenditures for hypertension among adults age 18 and older, 2009: estimates for the U.S. civilian noninstitutionalized population. Rockville, MD: Agency for Healthcare Research and Quality; June 2012. Available at http://meps.ahrq.gov/mepsweb/data_files/publications/st371/stat371.shtml.
8. Hodgson TA, Liming C. Medical care expenditures for hypertension, its complications, and its comorbidities. Med Care 2001;39:599–615.
9. Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011;123:933–44.
10. Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20:64–78.
11. McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomized controlled trial. Lancet 2010;376:163–72.
12. Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA 2008;299:2857–67.
13. Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA 2013;310:46–56.
14. Magid DJ, Olson KL, Billups SJ, et al. A pharmacist-led, American Heart Association Heart360 Web-enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes 2013;6:157–63.
15. Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ 2009;35:641–51.
16. Collins A, Brown J, Newman SE. Cognitive apprenticeship: Teaching the crafts of reading, writing, and mathematics. In: Knowing, learning, and instruction: Essays in honor of Robert Glaser. Lawrence Erlbaum Associates; 1989:453–94.
17. Resnick M. Rethinking learning in the digital age. In: Kirkman G, editor. The global information technology report: readiness for a networked world. Oxford University Press; 2002.
18. Koschmann T. Paradigm shifts and instructional technology. In: Koschmann T, editor. CSCL: Theory and practice of an emerging paradigm. Lawrence Erlbaum Associates; 1996:83–124.
19. Brown JS, Adler RP. Minds on fire: open education, the long tail, and learning 2.0. Educause Rev 2008;43:16–32.
20. Collins A, Halverson R. The second educational revolution: rethinking education in the age of technology. J Comp Assist Learn 2010;26:18–27.
21. Dewey J. Experience and education. New York: Collier Books; 1938.
22. Lave J. Situated learning: legitimate peripheral participation (Learning in Doing: Social, Cognitive, and Computational Perspectives). Cambridge University Press; 1991.
23. Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol 2009;64:527–37.
24. Moore SM, Charvat J. Promoting health behavior change using appreciative inquiry: moving from deficit models to affirmation models of care. Fam Community Health 2007;30 Supp 1:S64–74.
From the Massachusetts Institute of Technology (Dr. Moore, Dr. Moss and Mr. Gilroy) and the Massachusetts General Hospital (Ms. Marshall, Dr. Judge, Dr. Crocker, and Dr. Zusman), Boston, MA.
Abstract
- Objective: To compare technology-supported appren-ticeship in hypertension management with a successful coaching model at Massachusetts General Hospital.
- Methods: A randomized controlled trial was conducted. Adult patients with uncontrolled essential hypertension (average blood pressure (BP) 148/87 mm Hg) were recruited in a staggered fashion for a 12-week study period. Intervention subjects received apprenticeship support from a nurse health coach through the CollaboRhythm application on a tablet computer. Patients self-tracked medication adherence and blood pressure (via wireless device) and the coach helped them to continuously progress through lifestyle change and medication adjustment using integrated messaging. Control subjects received support from the same coach but through traditional channels of office visits, phone calls, and e-mail.
- Results: 42 of 44 subjects completed the study. Intervention subjects achieved a greater decrease in systolic BP at 12 weeks than control subjects (26.3 mm Hg vs. 16.0 mm Hg, P = 0.009). A greater percentage of intervention subjects achieved goal BP ≤ 130/80 mm Hg (75.0% vs. 31.8%, P = 0.003) and 100% of them achieved goal BP ≤ 140/90 mmHg. They also rated the experience higher, although this finding was not statistically significant (8.9 vs. 7.6, P = 0.12). There was a trend toward increased cost for intervention subjects ($67.50 vs. $53.41, P = 0.15), but the projected cost is much less than standard care ($248/patient/year).
- Conclusion: This study provides encouraging evidence that technology-supported apprenticeship can improve the outcomes, cost, and experience of care in managing hypertension.
Hypertension affects approximately 33% of the U.S. adult population [1]. Antihypertensive treatment has been shown to be effective at preventing complications [2,3]. Unfortunately, estimates suggest that the majority of those diagnosed with hypertension do not have their blood pressure controlled [1]. This failure is due to both clinician and patient factors. Mean adherence of clinicians to guidelines is estimated at 53.5% [4]. An electronic monitoring study showed that half of patients who are prescribed medications stop taking them within 1 year [5]. Of those who take their medications, about 10% have adherence issues on any given day and about 50% have significant adherence issues in the course of their treatment [5]. Adherence to diet and exercise self-management is even more dismal, with rates below 20% [6]. Hypertension is an expensive problem with direct medical costs (treatment and complications) greater than $100 billion a year and equally high indirect costs (lost productivity) [7–9].
In the management of chronic diseases, there is a significant trend toward empowering patients with more control and toward providing more longitudinal coaching from clinicians and from peers [10–15]. Technology-supported apprenticeship is a model of chronic disease management that builds on the success of self-management and coaching, but it is more ambitious in that its goal is for patients to lead their care with the support of health coaches and supervising clinicians. It is informed by the field of learning science, particularly in how technology can be used effectively to support learning [16–20]. Apprenticeship refers to the tutelage of a community of novices in a skill or trade by one or more masters through situated learning. Situated learning refers to the process in which novices learn through participation in legitimate tasks in the same physical and social context where they will need to perform them once independent [21,22]. It is opposed to learning through contrived exercises in an artificial environment like a classroom.
In technology-supported apprenticeship, patients are the novice apprentices of master coaches. Technology provides scaffolding and communication tools to allow coaches to support the patient in the management of disease within the context of daily life rather than in the clinician’s office. Patients are supported in gradually developing self-efficacy and independence until they are skilled enough to lead their care and even to help coach others to success. The hypothesis is that embracing the contribution of the patient to this extent will reap unparalleled rewards in the experience, outcomes, and cost of care.
We conducted a randomized controlled trial to assess whether a technology-supported apprenticeship in hyper-tension management would improve blood pressure control compared with a successful coaching model.
Methods
Setting
The health coaching model at the Ambulatory Practice of the Future (APF) at the Massachusetts General Hospital is designed to impact the whole health ofpatients. In the scope of hypertension management, a nurse health coach, under the supervision of a physician, is responsible for improving outcomes through longitudinal support via office visits, phone calls, and e-mails. Diet, exercise, stress management, and medication therapy are all emphasized through health coaching techniques, such as motivational interviewing and appreciative inquiry [23,24]. Patients are referred to dieticians, exercise coaches, mind-body specialists, and others as desired. Prior to the start of this study, the APF was outperforming the national average with ~70% of hypertensive patients in the practice below clinically recommended goal blood pressures.
Recruitment
The study was advertised to all clinical staff of the APF through word of mouth. Since the practice was relatively young, it also had a registry of patients with elevated blood pressure that had not been addressed. Adult patients (> 18 years old) from the registry or from routine visits with essential hypertension (average blood pressure ≥ 140/90 and ≤ 180/120) who were taking 0 or 1 medications and had internet connectivity were eligible for inclusion in the study. Patients with a history of hypotension, syncope, hypertensive urgency, hypertensive emergency, labile hypertension, and proven coronary artery disease were excluded, as were patients with significant visual, auditory, or cognitive impairment and patients who were not proficient in English. Clinical staff notified the nurse health coach for the study on identification of any eligible subjects. The same nurse health coach recruited and cared for all intervention and control subjects.
The nurse health coach contacted each eligible patient to assess interest. Interested patients were scheduled for an appointment to commence the study. A process of written informed consent was carried out with each study subject. Each subject was assigned the next sequential study number, which was pre-randomized to either the intervention or the control group.
The study period for each subject was 12 weeks +/– 2 weeks with staggered recruitment. Twelve weeks represents the minimal time required to progress through the standardized Medication Adjustment Plan that was used, assuming a minimum time of 2 weeks on each medication before a change is considered. A recruitment window from 1 March 2013 until 31 May 2013 was used. The goal was to recruit between 40 and 60 subjects, since statistical analysis revealed that a sample size of 36 was sufficient to detect a 5 mm Hg difference in the decrease in systolic blood pressure between groups given a 4 mm Hg standard deviation.
Intervention
CollaboRhythm is a software platform that was developed at the MIT Media Lab and designed to support the principles of technology-supported apprenticeship. Patient tracking tools document progress, visualizations highlight associations between actions and outcomes, and personalized decision support encourages self-efficacy. Powerful virtual visits and instant messaging allow master clinicians to provide adaptive coaching within the context of daily life rather than in the artificial environment of the office. Applications can be deployed cross-platform to cell phones, tablets, computers, etc.
A simplified system was created for hypertension management. It is optimized for tablet deployment and focuses on instant messaging for communications. The patient uses a wireless blood pressure monitor (D40b model by ForaCare®) to take blood pressure measurements. The device is paired with a tablet application to automatically report measurements. The patient self-reports medication adherence using the tablet application. Patient data is visualized in a daily clock and weekly charts to promote proactive behavior and self-reflection. Decision support for medication adjustment is paired with the charts. The patient’s data are synchronized with the coach’s tablet application via a collaborative health record server implemented using the Indivo X personally controlled health record (Children’s Hospital Boston, indivohealth.org) code base. Instant messaging between the patient and coach is implemented using a real-time messaging server. The applications for the patient and the coach are identical, but the coach’s application is configured to allow switching between patient records in order to manage a number of patients.
The user experience was designed based on our years of exploration at the MIT Media Lab of the psychology of illness and the impact that technology could have on patient empowerment and patient-clinician collaboration. It is important to note that the CollaboRhythm application is different from typical electronic reminder applications. In fact, the application never alarms at patients, even if they forget to perform their health actions. Instead, the application focuses on providing awareness for proactive decision-making, self-reflection, and support from the coach.
Protocol Common to Control and Intervention Subjects
Following informed consent, a baseline blood pressure and heart rate were measured for each subject using the same automated sphygmomanometer. Weight was also measured and a hypertension knowledge assessment (a simple survey about normal blood pressures and the effects of diet, exercise, and medication that was created for the purpose of this study) was completed. The initial medication load was determined using the Medication Adjustment Plan as a reference and each dose step as a unit of 1. For example, if a subject was already on lisinopril 40 mg at the start of the study, the initial medication load was 2.
The nurse health coach conducted an introductory visit with each subject including motivational interviewing to assess their health values and to discuss
hypertension management goals. The subject and coach made shared decisions about diet, exercise, stress management, and medication. The same medication titration algorithm was used for both control and interventional
subjects.
At the conclusion of the study period, subjects in both groups returned for an exit visit. Blood pressure and heart rate were measured using the same automated sphygmomanometer that was used at the initial visit. Weight was measured using the same scale as the initial visit. A hypertension knowledge assessment was completed and an exit interview was conducted. The change in medication load was determined as well. For example, if a subject started the study on lisinopril 20 mg and ended the study on lisinopril 40 mg, the increase in medication load was 1.
Protocol Specifics for Intervention Subjects
The apprenticeship model of chronic disease management was discussed with the nurse health coach and with APF team prior to the study. It was also implicit in the design of the CollaboRhythm tablet application.
During the introduction visit, subjects in the inter-vention group received instructions from the nurse health coach on how to use the CollaboRhythm tablet application to self-track their medication adherence, to review progress using the charts, to propose or agree with changes in hypertension medications, and to communicate with messages.
Subjects in the intervention group received their hyper-tension care through the CollaboRhythm tablet application. All instant messages between the intervention subjects and the nurse health coach were automatically documented electronically. Other forms of communication were documented in a spreadsheet. During the exit visit, the tablet computer and the wireless blood pressure meter were returned.
Protocol Specifics for Control Subjects
Between the introduction and exit visits, subjects in the control group received standard hypertension care from the nurse health coach at the APF. The coach instructed subjects to check their blood pressures 3 to 5 times a week. They had the option of purchasing a cuff, using a monitor at work, or using a monitor at a facility such as a pharmacy or grocery store. Communication took place through
office visits, phone calls, and e-mails. All communications with control subjects were documented for the purposes of this study by the nurse health coach in a spread-
sheet.
Outcomes of Interest
The primary outcomes of interest were the absolute decrease in systolic and diastolic blood pressure and the number of subjects who reached the blood pressure goal of less than or equal to 130/80 mm Hg. This more aggressive blood pressure goal was chosen for a number of reasons: (1) it is not uncommon to set a lower blood pressure goal for home measurements to avoid patients hovering just at the 140/90 goal and not getting the true benefit of reduced blood pressure; and (2) subjects were supported in improving diet, exercise, and stress management in addition to pharmacologic therapy. The 140/90 cut-off (now 150/90 in patients over 60) is focused on pharmacologic therapy [2,3].
The secondary outcomes included the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg (for comparison to other published literature), the number of subjects who achieved greater than a 10 mm Hg decrease in systolic and greater than a 5 mm Hg decrease in diastolic blood pressure, the change in medication load, the absolute decrease in weight, the number of subjects who lost at least 5 lb, a hypertension knowledge score assessed by a pre- and post-study test, a rating of satisfaction in care, and the amount of clinician time required in the care.
Statistical Methods
The study results were analyzed by the intention-to-treat approach. All subjects who returned for the final study visit were included in the analysis regardless of their adherence to the protocol. Subjects who did not return for the study exit visit were not included in the analysis because it would be impossible to determine the change in blood pressure without a final measurement. A 2-tailed Student’s t test for independent samples was used for all comparisons of the mean of continuous variables between the control and intervention groups. A 2-tailed Student’s t test for dependent samples was used for all comparisons between pre- and post-study variables within the control and the intervention group. A chi-square test was used for all comparisons of categorical variables between the groups, except when the expected values in the 2x2 table were below 5. Fisher’s exact test was used in this scenario, which applied to the secondary outcome of the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg.
Oversight
This study was approved by the institutional review boards at the Massachusetts Institute of Technology and the Massachusetts General Hospital.
Results
There were a total of 44 subjects recruited for the study. One intervention subject and one control subject were lost to follow-up, leaving 42 subjects who completed the study exit visit.
Baseline Statistics
Clinical Outcomes
Cost
 Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Experience
Thirteen control subjects and 16 intervention subjects provided an experience rating during their exit interview from the study. There was a trend toward greater satisfaction by intervention subjects that was not statistically significant (8.9 vs. 7.6, P = 0.12). The majority of feedback from intervention subjects was obtained through the exit interview. The feedback was overwhelmingly positive. All of the subjects wanted to continue using the CollaboRhythm application after the end of the study. Some who had reached goal only wanted to use it sporadically as a “check-in,” but the majority wanted to use it daily as they had for the study for an indefinite period of time. They felt that the burden of reporting was easily balanced by the value of being able to track progress and get the efficient support of a health coach. They related that awareness of the associations between actions (diet, exercise, stress management, medication adherence) and blood pressure outcomes was integral to their success and their positive experience with the application. Subjects responded very favorably to the concept of leading their care. Some comments from patients include: “It felt good to take responsibility,” “No one has ever asked me to take responsibility for my health,” and “I developed confidence that I never would have had.” The nurse coach commented multiple times how delighted she was with the level of patient engagement and excitement. She also did not want to stop using the application at the end of the study.
The main complaints about the program from both subjects and the health coach were on performance. They wanted the application to load faster and to save data faster.
Discussion
This study provides encouraging evidence that technology-supported apprenticeship can dramatically improve the outcomes, cost, and experience of care in the management of hypertension.
A 26.3 mm Hg average decrease in systolic blood pressure for intervention subjects in 3 months is significantly better than the standard of care and the best of the best in published interventions. [1,11–14]. The same is true for a rate of 100% of patients achieving goal blood pressure < 140/90 mm Hg.
We believe several factors contribute to the success of our program: (1) supporting subjects in the mission of leading their care, (2) rich real-time feedback for self-reflection, (3) emphasis on short-term goals, (4) promise of medication reduction with goal achievement, and (5) social support and accountability that come with having a continuously available coach who had immediate data access.
Other studies have had web communication components, self-titration components, and coaching components. In a progressive study by McManus [11], subjects in the intervention group self-tracked their blood pressure and self-titrated their hypertension medications while control subjects received routine care. Self-managing patients achieved a decrease in systolic blood pressure of 17.6 mm Hg over 12 months while controls only achieved a decrease of 12.2 mm Hg. Self-managing patients were more aggressive in adding new medications and did not have increased incidence of side effects. A study by Green [12] showed that subjects with home blood pressure monitoring, a web training course, and web-based pharmacist coaching achieved a 14.2 mm Hg decrease in systolic blood pressure over 12 months and that 56% reached goal blood pressure (< 140/90 mm Hg). Subjects who received routine care only achieved a 5.3 mm Hg decrease in systolic blood pressure and only 31% reached goal blood pressure. Margolis [13] and Magid [14] conducted studies similar to Green's with pharmacist-led care. In Margolis’ study, 71.8% of inter-vention subjects study achieved goal at 6 months with a mean decrease in systolic blood pressure of 21.5 mm Hg. These results were impressively stable at 18 months [13]. In Magid’s study, 54.1% of intervention subjects achieved goal at 6 months with a mean decrease in systolic blood pressure of 20.7 mm Hg [14].
The technology-supported apprenticeship model was inspired by the exceptional results of these studies, but we believe that it represents a significant step forward in patient engagement. In these studies, the tools were typically more burdensome than empowering, the titration more prescriptive than motivational, and the coaching more timed and paternalistic than continuous and nurturing. Technology-supported apprenticeship relies on more powerful tools for collaboration and aspires for the patient to lead the care rather than the clinician. It has the potential to produce greater self-efficacy, which results in better outcomes at lower cost.
Cost Implications
The 100% rate of attainment of systolic blood pressure < 140 mm Hg in our intervention subjects has the poten-tial to contribute to substantial cost savings through reducing complications. The cost of complications per patient per year is approximately $1275, and attainment of goal blood pressure on average results in approximately 35% decrease in complications [2,7–9] Therefore, it is reasonable to expect at least $446 savings in downstream costs per patient per year with this intervention. This has notable public health implications given that there are approximately 32 million patients in the United States with diagnosed hypertension that is uncontrolled [1]. Cost saving at scale could be more than $14 billion.
Typically, interventions that produce downstream savings in health care require some upstream investment. An exciting aspect of this intervention is that it was significantly less costly, at $67.50 per patient, as compared with the standard of care, at $248 per patient per year [7–9]. Most of the responsibility was embraced by the patients, and the nurse coach needed only to provide occasional social and clinical support. Return office visits were almost completely eliminated and goals were achieved in a fraction of the time. The cost of the technology is effectively negligible given that patients will be able to use their own cell phones and tablets and their own blood pressure cuffs. Based on the prevalence of hypertension, a primary care practice with 2000 patients would be expected to have 600 with hypertension. At $180.50 in savings per patient per year, a profit of $108,300 could be retained if the same reimbursement was provided for this more effective care. At the same time, this more efficient and scalable model of care could allow a practice to care for a larger number of patients without compromising the experience for patients or clinicians.
Limitations and Future Directions
An important limitation of this study is its small sample size. The efficiency and cost analysis suggests that the intervention is highly suitable for scaling but, until this is studied, there is the risk that the small sample size may misrepresent the average effect on a larger population and overestimate the size of a population that a coach can manage. Future work will need to include much larger populations.
Another limitation was the short follow-up period. A key benefit of apprenticeship is that it theoretically results in greater and more sustainable self-efficacy than other models of patient engagement that are not as grounded in learning science and that do not engage the patient as deeply. Follow-up visits for both control and intervention subjects will be conducted at 1 year to assess the sustainability of the blood pressure improvements.
The fact that the population was from a single practice also presents the possibility that the subjects being studied were more interested and/or capable than a larger, more general population. This is likely to be true, since many of the patients at the APF sought it out in the hope of receiving a new health care experience. Future work will need to address patient populations from diverse socioeconomic situations and diverse cultures. Based on pilot studies that we have done with diverse populations with HIV, hypertension, and diabetes, we believe that patients who are more disempowered and disenfranchised at baseline attain greater benefit from becoming apprentices in their care.
Another potential limitation is that hypertension was treated in isolation in this study. In fact, many of the subjects had comorbid conditions and were being treated for them simultaneously at the APF. Future work will need to address how the apprenticeship approach and accompanying technology can support the management of multiple comorbid conditions. At the same time, we believe that setting aggressive goals for one condition at a time and achieving these goals over a short period, such as 3 months, will be an important strategy in effectively engaging patients as active participants in their care and helping them to develop self-efficacy. As they develop competency for one condition, they become more capable of managing the others. If they were to attempt to tackle all of the problems simultaneously, it could be overwhelming and ineffective.
Conclusions
This study provides encouraging evidence that, in the management of hypertension, technology-supported apprenticeship can improve the outcomes, cost, and experience of care. By embracing the potential of patients while at the same time optimizing support from clinicians and leveraging information technology for cost-effective scaling, it has the potential to have a tremendous impact across the spectrum of chronic disease.
Three core tenants of technology-supported apprenticeship have surfaced as the product of this work, and they may serve as a useful guide to other efforts improving care delivery: First, patients are the most underutilized resource in health care. Technology-supported apprenticeship harnesses the contribution of the patient and values the development of self-efficacy to the extent that apprentices can become masters. It supports patients in achieving a pinnacle of patient empowerment.
Second, health takes place in the everyday lives of patients, not in a doctor’s office or hospital. Technology-supported apprenticeship appreciates that situated learning is the key to mastery of chronic disease management and strives to support patients continuously in the context of their lives.
Third, collaboration and information transparency, not just information access, are critical. Technology-supported apprenticeship embraces information technology to maximize collaboration among novices and masters and to provide common ground through complete transparency.
Acknowledgments: This study was completed as part of John O. Moore’s PhD thesis at the MIT Media Lab. Mitchel Resnick, PhD, and Pattie Maes, PhD, were members of the thesis committee along with authors Franklin H. Moss, PhD, and David C. Judge, MD, and their advice was critical in the development of the technology-supported apprenticeship approach.
Corresponding author: John O. Moore, MD, PhD, [email protected]
Funding/support: This work was supported, in part, by the CIMIT Prize for Primary Healthcare from the Center for Integration of Medicine & Innovative Technology, Boston, MA.
Financial disclosures: John O. Moore, Frank Moss, and Scott Gilroy have a health information technology company focused on building software solutions for improving chronic disease management. This company does not yet have a product for sale.
From the Massachusetts Institute of Technology (Dr. Moore, Dr. Moss and Mr. Gilroy) and the Massachusetts General Hospital (Ms. Marshall, Dr. Judge, Dr. Crocker, and Dr. Zusman), Boston, MA.
Abstract
- Objective: To compare technology-supported appren-ticeship in hypertension management with a successful coaching model at Massachusetts General Hospital.
- Methods: A randomized controlled trial was conducted. Adult patients with uncontrolled essential hypertension (average blood pressure (BP) 148/87 mm Hg) were recruited in a staggered fashion for a 12-week study period. Intervention subjects received apprenticeship support from a nurse health coach through the CollaboRhythm application on a tablet computer. Patients self-tracked medication adherence and blood pressure (via wireless device) and the coach helped them to continuously progress through lifestyle change and medication adjustment using integrated messaging. Control subjects received support from the same coach but through traditional channels of office visits, phone calls, and e-mail.
- Results: 42 of 44 subjects completed the study. Intervention subjects achieved a greater decrease in systolic BP at 12 weeks than control subjects (26.3 mm Hg vs. 16.0 mm Hg, P = 0.009). A greater percentage of intervention subjects achieved goal BP ≤ 130/80 mm Hg (75.0% vs. 31.8%, P = 0.003) and 100% of them achieved goal BP ≤ 140/90 mmHg. They also rated the experience higher, although this finding was not statistically significant (8.9 vs. 7.6, P = 0.12). There was a trend toward increased cost for intervention subjects ($67.50 vs. $53.41, P = 0.15), but the projected cost is much less than standard care ($248/patient/year).
- Conclusion: This study provides encouraging evidence that technology-supported apprenticeship can improve the outcomes, cost, and experience of care in managing hypertension.
Hypertension affects approximately 33% of the U.S. adult population [1]. Antihypertensive treatment has been shown to be effective at preventing complications [2,3]. Unfortunately, estimates suggest that the majority of those diagnosed with hypertension do not have their blood pressure controlled [1]. This failure is due to both clinician and patient factors. Mean adherence of clinicians to guidelines is estimated at 53.5% [4]. An electronic monitoring study showed that half of patients who are prescribed medications stop taking them within 1 year [5]. Of those who take their medications, about 10% have adherence issues on any given day and about 50% have significant adherence issues in the course of their treatment [5]. Adherence to diet and exercise self-management is even more dismal, with rates below 20% [6]. Hypertension is an expensive problem with direct medical costs (treatment and complications) greater than $100 billion a year and equally high indirect costs (lost productivity) [7–9].
In the management of chronic diseases, there is a significant trend toward empowering patients with more control and toward providing more longitudinal coaching from clinicians and from peers [10–15]. Technology-supported apprenticeship is a model of chronic disease management that builds on the success of self-management and coaching, but it is more ambitious in that its goal is for patients to lead their care with the support of health coaches and supervising clinicians. It is informed by the field of learning science, particularly in how technology can be used effectively to support learning [16–20]. Apprenticeship refers to the tutelage of a community of novices in a skill or trade by one or more masters through situated learning. Situated learning refers to the process in which novices learn through participation in legitimate tasks in the same physical and social context where they will need to perform them once independent [21,22]. It is opposed to learning through contrived exercises in an artificial environment like a classroom.
In technology-supported apprenticeship, patients are the novice apprentices of master coaches. Technology provides scaffolding and communication tools to allow coaches to support the patient in the management of disease within the context of daily life rather than in the clinician’s office. Patients are supported in gradually developing self-efficacy and independence until they are skilled enough to lead their care and even to help coach others to success. The hypothesis is that embracing the contribution of the patient to this extent will reap unparalleled rewards in the experience, outcomes, and cost of care.
We conducted a randomized controlled trial to assess whether a technology-supported apprenticeship in hyper-tension management would improve blood pressure control compared with a successful coaching model.
Methods
Setting
The health coaching model at the Ambulatory Practice of the Future (APF) at the Massachusetts General Hospital is designed to impact the whole health ofpatients. In the scope of hypertension management, a nurse health coach, under the supervision of a physician, is responsible for improving outcomes through longitudinal support via office visits, phone calls, and e-mails. Diet, exercise, stress management, and medication therapy are all emphasized through health coaching techniques, such as motivational interviewing and appreciative inquiry [23,24]. Patients are referred to dieticians, exercise coaches, mind-body specialists, and others as desired. Prior to the start of this study, the APF was outperforming the national average with ~70% of hypertensive patients in the practice below clinically recommended goal blood pressures.
Recruitment
The study was advertised to all clinical staff of the APF through word of mouth. Since the practice was relatively young, it also had a registry of patients with elevated blood pressure that had not been addressed. Adult patients (> 18 years old) from the registry or from routine visits with essential hypertension (average blood pressure ≥ 140/90 and ≤ 180/120) who were taking 0 or 1 medications and had internet connectivity were eligible for inclusion in the study. Patients with a history of hypotension, syncope, hypertensive urgency, hypertensive emergency, labile hypertension, and proven coronary artery disease were excluded, as were patients with significant visual, auditory, or cognitive impairment and patients who were not proficient in English. Clinical staff notified the nurse health coach for the study on identification of any eligible subjects. The same nurse health coach recruited and cared for all intervention and control subjects.
The nurse health coach contacted each eligible patient to assess interest. Interested patients were scheduled for an appointment to commence the study. A process of written informed consent was carried out with each study subject. Each subject was assigned the next sequential study number, which was pre-randomized to either the intervention or the control group.
The study period for each subject was 12 weeks +/– 2 weeks with staggered recruitment. Twelve weeks represents the minimal time required to progress through the standardized Medication Adjustment Plan that was used, assuming a minimum time of 2 weeks on each medication before a change is considered. A recruitment window from 1 March 2013 until 31 May 2013 was used. The goal was to recruit between 40 and 60 subjects, since statistical analysis revealed that a sample size of 36 was sufficient to detect a 5 mm Hg difference in the decrease in systolic blood pressure between groups given a 4 mm Hg standard deviation.
Intervention
CollaboRhythm is a software platform that was developed at the MIT Media Lab and designed to support the principles of technology-supported apprenticeship. Patient tracking tools document progress, visualizations highlight associations between actions and outcomes, and personalized decision support encourages self-efficacy. Powerful virtual visits and instant messaging allow master clinicians to provide adaptive coaching within the context of daily life rather than in the artificial environment of the office. Applications can be deployed cross-platform to cell phones, tablets, computers, etc.
A simplified system was created for hypertension management. It is optimized for tablet deployment and focuses on instant messaging for communications. The patient uses a wireless blood pressure monitor (D40b model by ForaCare®) to take blood pressure measurements. The device is paired with a tablet application to automatically report measurements. The patient self-reports medication adherence using the tablet application. Patient data is visualized in a daily clock and weekly charts to promote proactive behavior and self-reflection. Decision support for medication adjustment is paired with the charts. The patient’s data are synchronized with the coach’s tablet application via a collaborative health record server implemented using the Indivo X personally controlled health record (Children’s Hospital Boston, indivohealth.org) code base. Instant messaging between the patient and coach is implemented using a real-time messaging server. The applications for the patient and the coach are identical, but the coach’s application is configured to allow switching between patient records in order to manage a number of patients.
The user experience was designed based on our years of exploration at the MIT Media Lab of the psychology of illness and the impact that technology could have on patient empowerment and patient-clinician collaboration. It is important to note that the CollaboRhythm application is different from typical electronic reminder applications. In fact, the application never alarms at patients, even if they forget to perform their health actions. Instead, the application focuses on providing awareness for proactive decision-making, self-reflection, and support from the coach.
Protocol Common to Control and Intervention Subjects
Following informed consent, a baseline blood pressure and heart rate were measured for each subject using the same automated sphygmomanometer. Weight was also measured and a hypertension knowledge assessment (a simple survey about normal blood pressures and the effects of diet, exercise, and medication that was created for the purpose of this study) was completed. The initial medication load was determined using the Medication Adjustment Plan as a reference and each dose step as a unit of 1. For example, if a subject was already on lisinopril 40 mg at the start of the study, the initial medication load was 2.
The nurse health coach conducted an introductory visit with each subject including motivational interviewing to assess their health values and to discuss
hypertension management goals. The subject and coach made shared decisions about diet, exercise, stress management, and medication. The same medication titration algorithm was used for both control and interventional
subjects.
At the conclusion of the study period, subjects in both groups returned for an exit visit. Blood pressure and heart rate were measured using the same automated sphygmomanometer that was used at the initial visit. Weight was measured using the same scale as the initial visit. A hypertension knowledge assessment was completed and an exit interview was conducted. The change in medication load was determined as well. For example, if a subject started the study on lisinopril 20 mg and ended the study on lisinopril 40 mg, the increase in medication load was 1.
Protocol Specifics for Intervention Subjects
The apprenticeship model of chronic disease management was discussed with the nurse health coach and with APF team prior to the study. It was also implicit in the design of the CollaboRhythm tablet application.
During the introduction visit, subjects in the inter-vention group received instructions from the nurse health coach on how to use the CollaboRhythm tablet application to self-track their medication adherence, to review progress using the charts, to propose or agree with changes in hypertension medications, and to communicate with messages.
Subjects in the intervention group received their hyper-tension care through the CollaboRhythm tablet application. All instant messages between the intervention subjects and the nurse health coach were automatically documented electronically. Other forms of communication were documented in a spreadsheet. During the exit visit, the tablet computer and the wireless blood pressure meter were returned.
Protocol Specifics for Control Subjects
Between the introduction and exit visits, subjects in the control group received standard hypertension care from the nurse health coach at the APF. The coach instructed subjects to check their blood pressures 3 to 5 times a week. They had the option of purchasing a cuff, using a monitor at work, or using a monitor at a facility such as a pharmacy or grocery store. Communication took place through
office visits, phone calls, and e-mails. All communications with control subjects were documented for the purposes of this study by the nurse health coach in a spread-
sheet.
Outcomes of Interest
The primary outcomes of interest were the absolute decrease in systolic and diastolic blood pressure and the number of subjects who reached the blood pressure goal of less than or equal to 130/80 mm Hg. This more aggressive blood pressure goal was chosen for a number of reasons: (1) it is not uncommon to set a lower blood pressure goal for home measurements to avoid patients hovering just at the 140/90 goal and not getting the true benefit of reduced blood pressure; and (2) subjects were supported in improving diet, exercise, and stress management in addition to pharmacologic therapy. The 140/90 cut-off (now 150/90 in patients over 60) is focused on pharmacologic therapy [2,3].
The secondary outcomes included the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg (for comparison to other published literature), the number of subjects who achieved greater than a 10 mm Hg decrease in systolic and greater than a 5 mm Hg decrease in diastolic blood pressure, the change in medication load, the absolute decrease in weight, the number of subjects who lost at least 5 lb, a hypertension knowledge score assessed by a pre- and post-study test, a rating of satisfaction in care, and the amount of clinician time required in the care.
Statistical Methods
The study results were analyzed by the intention-to-treat approach. All subjects who returned for the final study visit were included in the analysis regardless of their adherence to the protocol. Subjects who did not return for the study exit visit were not included in the analysis because it would be impossible to determine the change in blood pressure without a final measurement. A 2-tailed Student’s t test for independent samples was used for all comparisons of the mean of continuous variables between the control and intervention groups. A 2-tailed Student’s t test for dependent samples was used for all comparisons between pre- and post-study variables within the control and the intervention group. A chi-square test was used for all comparisons of categorical variables between the groups, except when the expected values in the 2x2 table were below 5. Fisher’s exact test was used in this scenario, which applied to the secondary outcome of the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg.
Oversight
This study was approved by the institutional review boards at the Massachusetts Institute of Technology and the Massachusetts General Hospital.
Results
There were a total of 44 subjects recruited for the study. One intervention subject and one control subject were lost to follow-up, leaving 42 subjects who completed the study exit visit.
Baseline Statistics
Clinical Outcomes
Cost
 Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Experience
Thirteen control subjects and 16 intervention subjects provided an experience rating during their exit interview from the study. There was a trend toward greater satisfaction by intervention subjects that was not statistically significant (8.9 vs. 7.6, P = 0.12). The majority of feedback from intervention subjects was obtained through the exit interview. The feedback was overwhelmingly positive. All of the subjects wanted to continue using the CollaboRhythm application after the end of the study. Some who had reached goal only wanted to use it sporadically as a “check-in,” but the majority wanted to use it daily as they had for the study for an indefinite period of time. They felt that the burden of reporting was easily balanced by the value of being able to track progress and get the efficient support of a health coach. They related that awareness of the associations between actions (diet, exercise, stress management, medication adherence) and blood pressure outcomes was integral to their success and their positive experience with the application. Subjects responded very favorably to the concept of leading their care. Some comments from patients include: “It felt good to take responsibility,” “No one has ever asked me to take responsibility for my health,” and “I developed confidence that I never would have had.” The nurse coach commented multiple times how delighted she was with the level of patient engagement and excitement. She also did not want to stop using the application at the end of the study.
The main complaints about the program from both subjects and the health coach were on performance. They wanted the application to load faster and to save data faster.
Discussion
This study provides encouraging evidence that technology-supported apprenticeship can dramatically improve the outcomes, cost, and experience of care in the management of hypertension.
A 26.3 mm Hg average decrease in systolic blood pressure for intervention subjects in 3 months is significantly better than the standard of care and the best of the best in published interventions. [1,11–14]. The same is true for a rate of 100% of patients achieving goal blood pressure < 140/90 mm Hg.
We believe several factors contribute to the success of our program: (1) supporting subjects in the mission of leading their care, (2) rich real-time feedback for self-reflection, (3) emphasis on short-term goals, (4) promise of medication reduction with goal achievement, and (5) social support and accountability that come with having a continuously available coach who had immediate data access.
Other studies have had web communication components, self-titration components, and coaching components. In a progressive study by McManus [11], subjects in the intervention group self-tracked their blood pressure and self-titrated their hypertension medications while control subjects received routine care. Self-managing patients achieved a decrease in systolic blood pressure of 17.6 mm Hg over 12 months while controls only achieved a decrease of 12.2 mm Hg. Self-managing patients were more aggressive in adding new medications and did not have increased incidence of side effects. A study by Green [12] showed that subjects with home blood pressure monitoring, a web training course, and web-based pharmacist coaching achieved a 14.2 mm Hg decrease in systolic blood pressure over 12 months and that 56% reached goal blood pressure (< 140/90 mm Hg). Subjects who received routine care only achieved a 5.3 mm Hg decrease in systolic blood pressure and only 31% reached goal blood pressure. Margolis [13] and Magid [14] conducted studies similar to Green's with pharmacist-led care. In Margolis’ study, 71.8% of inter-vention subjects study achieved goal at 6 months with a mean decrease in systolic blood pressure of 21.5 mm Hg. These results were impressively stable at 18 months [13]. In Magid’s study, 54.1% of intervention subjects achieved goal at 6 months with a mean decrease in systolic blood pressure of 20.7 mm Hg [14].
The technology-supported apprenticeship model was inspired by the exceptional results of these studies, but we believe that it represents a significant step forward in patient engagement. In these studies, the tools were typically more burdensome than empowering, the titration more prescriptive than motivational, and the coaching more timed and paternalistic than continuous and nurturing. Technology-supported apprenticeship relies on more powerful tools for collaboration and aspires for the patient to lead the care rather than the clinician. It has the potential to produce greater self-efficacy, which results in better outcomes at lower cost.
Cost Implications
The 100% rate of attainment of systolic blood pressure < 140 mm Hg in our intervention subjects has the poten-tial to contribute to substantial cost savings through reducing complications. The cost of complications per patient per year is approximately $1275, and attainment of goal blood pressure on average results in approximately 35% decrease in complications [2,7–9] Therefore, it is reasonable to expect at least $446 savings in downstream costs per patient per year with this intervention. This has notable public health implications given that there are approximately 32 million patients in the United States with diagnosed hypertension that is uncontrolled [1]. Cost saving at scale could be more than $14 billion.
Typically, interventions that produce downstream savings in health care require some upstream investment. An exciting aspect of this intervention is that it was significantly less costly, at $67.50 per patient, as compared with the standard of care, at $248 per patient per year [7–9]. Most of the responsibility was embraced by the patients, and the nurse coach needed only to provide occasional social and clinical support. Return office visits were almost completely eliminated and goals were achieved in a fraction of the time. The cost of the technology is effectively negligible given that patients will be able to use their own cell phones and tablets and their own blood pressure cuffs. Based on the prevalence of hypertension, a primary care practice with 2000 patients would be expected to have 600 with hypertension. At $180.50 in savings per patient per year, a profit of $108,300 could be retained if the same reimbursement was provided for this more effective care. At the same time, this more efficient and scalable model of care could allow a practice to care for a larger number of patients without compromising the experience for patients or clinicians.
Limitations and Future Directions
An important limitation of this study is its small sample size. The efficiency and cost analysis suggests that the intervention is highly suitable for scaling but, until this is studied, there is the risk that the small sample size may misrepresent the average effect on a larger population and overestimate the size of a population that a coach can manage. Future work will need to include much larger populations.
Another limitation was the short follow-up period. A key benefit of apprenticeship is that it theoretically results in greater and more sustainable self-efficacy than other models of patient engagement that are not as grounded in learning science and that do not engage the patient as deeply. Follow-up visits for both control and intervention subjects will be conducted at 1 year to assess the sustainability of the blood pressure improvements.
The fact that the population was from a single practice also presents the possibility that the subjects being studied were more interested and/or capable than a larger, more general population. This is likely to be true, since many of the patients at the APF sought it out in the hope of receiving a new health care experience. Future work will need to address patient populations from diverse socioeconomic situations and diverse cultures. Based on pilot studies that we have done with diverse populations with HIV, hypertension, and diabetes, we believe that patients who are more disempowered and disenfranchised at baseline attain greater benefit from becoming apprentices in their care.
Another potential limitation is that hypertension was treated in isolation in this study. In fact, many of the subjects had comorbid conditions and were being treated for them simultaneously at the APF. Future work will need to address how the apprenticeship approach and accompanying technology can support the management of multiple comorbid conditions. At the same time, we believe that setting aggressive goals for one condition at a time and achieving these goals over a short period, such as 3 months, will be an important strategy in effectively engaging patients as active participants in their care and helping them to develop self-efficacy. As they develop competency for one condition, they become more capable of managing the others. If they were to attempt to tackle all of the problems simultaneously, it could be overwhelming and ineffective.
Conclusions
This study provides encouraging evidence that, in the management of hypertension, technology-supported apprenticeship can improve the outcomes, cost, and experience of care. By embracing the potential of patients while at the same time optimizing support from clinicians and leveraging information technology for cost-effective scaling, it has the potential to have a tremendous impact across the spectrum of chronic disease.
Three core tenants of technology-supported apprenticeship have surfaced as the product of this work, and they may serve as a useful guide to other efforts improving care delivery: First, patients are the most underutilized resource in health care. Technology-supported apprenticeship harnesses the contribution of the patient and values the development of self-efficacy to the extent that apprentices can become masters. It supports patients in achieving a pinnacle of patient empowerment.
Second, health takes place in the everyday lives of patients, not in a doctor’s office or hospital. Technology-supported apprenticeship appreciates that situated learning is the key to mastery of chronic disease management and strives to support patients continuously in the context of their lives.
Third, collaboration and information transparency, not just information access, are critical. Technology-supported apprenticeship embraces information technology to maximize collaboration among novices and masters and to provide common ground through complete transparency.
Acknowledgments: This study was completed as part of John O. Moore’s PhD thesis at the MIT Media Lab. Mitchel Resnick, PhD, and Pattie Maes, PhD, were members of the thesis committee along with authors Franklin H. Moss, PhD, and David C. Judge, MD, and their advice was critical in the development of the technology-supported apprenticeship approach.
Corresponding author: John O. Moore, MD, PhD, [email protected]
Funding/support: This work was supported, in part, by the CIMIT Prize for Primary Healthcare from the Center for Integration of Medicine & Innovative Technology, Boston, MA.
Financial disclosures: John O. Moore, Frank Moss, and Scott Gilroy have a health information technology company focused on building software solutions for improving chronic disease management. This company does not yet have a product for sale.
1. Recent trends in the prevalence of high blood pressure and its treatment and control. National Center for Health Statistics. Hyattsville, MD; 2010.
2. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–72. Erratum in: JAMA 2003;290:197.
3. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20.
4. Ardery G, Carter BL, Milchak JL, et al. Explicit and implicit evaluation of physician adherence to hypertension guidelines. J Clin Hypertens (Greenwich) 2007;9:113–9.
5. Vrijens B, Vincze G, Kristanto P, et al. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008;336:1114–7.
6. Mellen PB, Gao SK, Vitolins MZ, Goff DC Jr. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med 2008;168:308–14.
7. Davis K. Expenditures for hypertension among adults age 18 and older, 2009: estimates for the U.S. civilian noninstitutionalized population. Rockville, MD: Agency for Healthcare Research and Quality; June 2012. Available at http://meps.ahrq.gov/mepsweb/data_files/publications/st371/stat371.shtml.
8. Hodgson TA, Liming C. Medical care expenditures for hypertension, its complications, and its comorbidities. Med Care 2001;39:599–615.
9. Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011;123:933–44.
10. Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20:64–78.
11. McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomized controlled trial. Lancet 2010;376:163–72.
12. Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA 2008;299:2857–67.
13. Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA 2013;310:46–56.
14. Magid DJ, Olson KL, Billups SJ, et al. A pharmacist-led, American Heart Association Heart360 Web-enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes 2013;6:157–63.
15. Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ 2009;35:641–51.
16. Collins A, Brown J, Newman SE. Cognitive apprenticeship: Teaching the crafts of reading, writing, and mathematics. In: Knowing, learning, and instruction: Essays in honor of Robert Glaser. Lawrence Erlbaum Associates; 1989:453–94.
17. Resnick M. Rethinking learning in the digital age. In: Kirkman G, editor. The global information technology report: readiness for a networked world. Oxford University Press; 2002.
18. Koschmann T. Paradigm shifts and instructional technology. In: Koschmann T, editor. CSCL: Theory and practice of an emerging paradigm. Lawrence Erlbaum Associates; 1996:83–124.
19. Brown JS, Adler RP. Minds on fire: open education, the long tail, and learning 2.0. Educause Rev 2008;43:16–32.
20. Collins A, Halverson R. The second educational revolution: rethinking education in the age of technology. J Comp Assist Learn 2010;26:18–27.
21. Dewey J. Experience and education. New York: Collier Books; 1938.
22. Lave J. Situated learning: legitimate peripheral participation (Learning in Doing: Social, Cognitive, and Computational Perspectives). Cambridge University Press; 1991.
23. Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol 2009;64:527–37.
24. Moore SM, Charvat J. Promoting health behavior change using appreciative inquiry: moving from deficit models to affirmation models of care. Fam Community Health 2007;30 Supp 1:S64–74.
1. Recent trends in the prevalence of high blood pressure and its treatment and control. National Center for Health Statistics. Hyattsville, MD; 2010.
2. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–72. Erratum in: JAMA 2003;290:197.
3. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20.
4. Ardery G, Carter BL, Milchak JL, et al. Explicit and implicit evaluation of physician adherence to hypertension guidelines. J Clin Hypertens (Greenwich) 2007;9:113–9.
5. Vrijens B, Vincze G, Kristanto P, et al. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008;336:1114–7.
6. Mellen PB, Gao SK, Vitolins MZ, Goff DC Jr. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med 2008;168:308–14.
7. Davis K. Expenditures for hypertension among adults age 18 and older, 2009: estimates for the U.S. civilian noninstitutionalized population. Rockville, MD: Agency for Healthcare Research and Quality; June 2012. Available at http://meps.ahrq.gov/mepsweb/data_files/publications/st371/stat371.shtml.
8. Hodgson TA, Liming C. Medical care expenditures for hypertension, its complications, and its comorbidities. Med Care 2001;39:599–615.
9. Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011;123:933–44.
10. Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20:64–78.
11. McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomized controlled trial. Lancet 2010;376:163–72.
12. Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA 2008;299:2857–67.
13. Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA 2013;310:46–56.
14. Magid DJ, Olson KL, Billups SJ, et al. A pharmacist-led, American Heart Association Heart360 Web-enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes 2013;6:157–63.
15. Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ 2009;35:641–51.
16. Collins A, Brown J, Newman SE. Cognitive apprenticeship: Teaching the crafts of reading, writing, and mathematics. In: Knowing, learning, and instruction: Essays in honor of Robert Glaser. Lawrence Erlbaum Associates; 1989:453–94.
17. Resnick M. Rethinking learning in the digital age. In: Kirkman G, editor. The global information technology report: readiness for a networked world. Oxford University Press; 2002.
18. Koschmann T. Paradigm shifts and instructional technology. In: Koschmann T, editor. CSCL: Theory and practice of an emerging paradigm. Lawrence Erlbaum Associates; 1996:83–124.
19. Brown JS, Adler RP. Minds on fire: open education, the long tail, and learning 2.0. Educause Rev 2008;43:16–32.
20. Collins A, Halverson R. The second educational revolution: rethinking education in the age of technology. J Comp Assist Learn 2010;26:18–27.
21. Dewey J. Experience and education. New York: Collier Books; 1938.
22. Lave J. Situated learning: legitimate peripheral participation (Learning in Doing: Social, Cognitive, and Computational Perspectives). Cambridge University Press; 1991.
23. Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol 2009;64:527–37.
24. Moore SM, Charvat J. Promoting health behavior change using appreciative inquiry: moving from deficit models to affirmation models of care. Fam Community Health 2007;30 Supp 1:S64–74.
What Is the Global Burden of Unsafe Medical Care?
Study Overview
Objective. To examine the global burden of unsafe medical care and its comparative frequency in low/middle-income vs. high-income countries.
Design. Analytical modeling of aggregated data from observational studies.
Data. Two primary sources of data were used. First, the team conducted a search of over 16,000 articles written in English after 1976 that aimed for a comprehensive exam-ination of both peer-reviewed and non–peer-reviewed studies that focused on 7 inpatient adverse events (see below), and the clinical features of the patients who were injured from them. Two separate literature reviews were conducted in 2007 through early 2008 and then repeated in 2011. Discussions with international experts in each topic area informed the selection process. The second source of data was epidemiological studies commissioned by the World Health Organization (WHO). These aimed to identify inpatient adverse events using a 2-stage medical record review in 26 hospitals across 8 low- and middle-income countries (LMICs) in the Eastern Mediterranean and North Africanregions, and 35 hospitals across 5 countries in Latin America.
Main outcome measures. 7 types of adverse events were evaluated in the analysis: (1) adverse drug events, (2) catheter-related urinary tract infection, (3) catheter-related blood stream infections, (4) nosocomial pneumonia, (5) venous thromboembolism, (6) falls, and (7) pressure ulcers (decubiti). The global burden of disease (GBD) is a standard metric that uses disability-adjusted life years (DALYs) as a proxy measure of morbidity and mortality related to a specific condition. The GBD DALYs model requires several key inputs: the number of people affected, the age at which they are affected, and the clinical consequence of the adverse events. In this study, a single average age per event was used instead of the standard GBD calculations by age and sex. Each input of GBD and DALYs was calculated separately for high-income countries (HICs) versus LMICs. The World Bank sets the income categorization for countries and adjusts the information on an annual basis. Countries in each category share common characteristics of socioeconomic development and epidemiological profiles.
Main results. The rate of hospitalization in HICs was higher than in LMICs: 10.8 vs. 3.7 per 100 citizens per year. There were large variations in the reported incidence of adverse events in both HICs and LMICs. Of the 7 adverse events assessed, adverse drug events were the most common type in HICs, with an incidence rate of 5.0%. In LMICs, venous thromboembolism was most common, with an incidence rate of 3.0%. Catheter-related blood stream infection, venous thromboembolism, and pressure ulcers had comparable rates between HICs and LMIC . The authors estimated that for every 100 hospitalizations, approximately 14.2 adverse events in HICs and 12.7 in LMICs. This is roughly 16.8 million injuries annually among hospitalized patients in HICs. LMICs and experienced approximately 50% more adverse events than HICs. Of note, LMICs had 5 times the population of HICs but the authors did not calculate proportional incidence rates.
The authors estimated 22.6 million DALYs lost due to these adverse events in 2009 globally. Unsurprisingly, the number of DALYs lost were more than twice as high as in LMICs as they were in HICs. This is likely due to the combination of weaker health systems and human resources for health shortages in those countries. In LMICs, venous thromboembolism was the main source of lost DALYs. Although incidences of hospital-acquired infections--such as nosocomial pneumonia, catheter-related blood stream and urinary tract infections--were smaller, they caused a comparable number of DALYs lost. Premature death from adverse events was the primary source of DALYs lost for all countries.
Conclusion. Adverse events from unsafe care is a significant problem across all countries.
Commentary
Globally, the efforts to improve health care delivery for diseases that cause substantial morbidity and mortality have been largely successful. For example, antimalarial drugs and antiretroviral therapies have become more accessible to patients in need [1,2]. However, in order to create more sustainable model, the health care systems of developing countries need sustainable investments to care for their growing populations and increasing medical needs [3,4]. Allengranzi et al [5] concluded from a systemic review that health care–associated infections are ubiquitous and occur at much higher rates in LMICs than in HICs. Findings from this study support those from Allengranzi’s review.
This study helped further our understanding of and explored the impact of unsafe medical care on GBD and DALYs. Several other adverse events related to unsafe care, such as unsafe surgery, harms due to counterfeit drugs, unsafe childbirth and unsafe blood use, were not included in this study due to data limitations. The estimated lost DALYs would be much higher if these events were counted.
This study has several strengths. First, the authors sought out the best available data from a large number of sources. Evidence selected for the analysis came from studies with good quality ratings. The 7 outcome measures used in this study are now standard minimum reporting data internationally. Nonetheless, several limitations are present. As the authors noted, the lack of availability high-quality data is common in international analyses. There can be reporting delays, data collection errors due to a lack of technical capacity, and corruption problems that may influence data quality. Poor reporting practices may exclude or underreport adverse events. Also, the paucity of data for some variables limited the calculation of estimates Second, few studies used standardized approaches in their data collection and analysis, contributing to data inconsistencies that may affect the reliability of the results. Third, the same life expectancy value (the WHO standard) was used for all individuals regardless of their countries’ life expectancy. The authors acknowledged that this approach was controversial and may have resulted in a different number of DALYs lost. Finally, only English-language publications were used, which may have influenced the findings. Latin America, the former Soviet Union states, and many Asian countries have growing bodies of research published in their native languages.
Despite the limitations, the study is one of the first systematic analyses of GBD, the outcomes of unsafe medical care, and associated lost DALYs. The analysis identified that a majority of the harms from adverse events occur in LMICs. Policies addressing, supporting, and enforcing patient safety measures during the health care experience will help ensure reductions in mortality and morbidity in LMICs. Improving the safety of the healthcare system should be a major policy and research emphasis across the globe.
Applications for Clinical Practice
Even though patient safety initiatives have been at the forefront of many organizational policies and health care provider education since the 1999 Institute of Medicine report “Crossing the Quality Chasm,” this study reminds practitioners that safe clinical practice is essential for reducing domestic disease burden. The cost of adverse events from unsafe practice in the United States was estimated to be around $16.6 billion in 2004 alone [6]. With the World Health Organization calling for strengthened research infrastructure across the globe and LMICs now seeing the value of data for health systems policymaking and management, future research will help to further refine the methods developed in this study.
—Jin Jun, MSN, APRN-BC, CCRN, and Allison Squires, PhD, RN
1. Kaplan J, Hanson D, Dworkin M, et al. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretroviral therapy, Clin Infect Dis 2000;30 Suppl 1:S5–14.
2. Eaton J, et al. Health benefits, costs, and cost-effectiveness of earlier eligibility for adult antiretroviral therapy and expanded treatment coverage: a cmbined analysis of 12 mathematical models, Lancet Global Health 2014;2:e23–34.
3. Mills A, Brugha R, Hanson K, et al. What can be done about the private health sector in low-income countries? Bull World Health Org 2002;80:325–30.
4. Schlein K, De La Cruz A, Gopalakrishnan T, Montagu D. Private sector delivery of health services in developing countries: a mixed-methods study on quality assurance in social franchises, BMC Health Serv Res 2013;13:4.
5. Allegranzi B, Bagheri N, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis, Lancet 2011;377;
228–41.
6. Jha A, Chan D, Ridgway A, et al. Improving safety and eliminating redundant tests: cutting costs in US hospitals. Health Affairs 2009;28:1475–84.
Study Overview
Objective. To examine the global burden of unsafe medical care and its comparative frequency in low/middle-income vs. high-income countries.
Design. Analytical modeling of aggregated data from observational studies.
Data. Two primary sources of data were used. First, the team conducted a search of over 16,000 articles written in English after 1976 that aimed for a comprehensive exam-ination of both peer-reviewed and non–peer-reviewed studies that focused on 7 inpatient adverse events (see below), and the clinical features of the patients who were injured from them. Two separate literature reviews were conducted in 2007 through early 2008 and then repeated in 2011. Discussions with international experts in each topic area informed the selection process. The second source of data was epidemiological studies commissioned by the World Health Organization (WHO). These aimed to identify inpatient adverse events using a 2-stage medical record review in 26 hospitals across 8 low- and middle-income countries (LMICs) in the Eastern Mediterranean and North Africanregions, and 35 hospitals across 5 countries in Latin America.
Main outcome measures. 7 types of adverse events were evaluated in the analysis: (1) adverse drug events, (2) catheter-related urinary tract infection, (3) catheter-related blood stream infections, (4) nosocomial pneumonia, (5) venous thromboembolism, (6) falls, and (7) pressure ulcers (decubiti). The global burden of disease (GBD) is a standard metric that uses disability-adjusted life years (DALYs) as a proxy measure of morbidity and mortality related to a specific condition. The GBD DALYs model requires several key inputs: the number of people affected, the age at which they are affected, and the clinical consequence of the adverse events. In this study, a single average age per event was used instead of the standard GBD calculations by age and sex. Each input of GBD and DALYs was calculated separately for high-income countries (HICs) versus LMICs. The World Bank sets the income categorization for countries and adjusts the information on an annual basis. Countries in each category share common characteristics of socioeconomic development and epidemiological profiles.
Main results. The rate of hospitalization in HICs was higher than in LMICs: 10.8 vs. 3.7 per 100 citizens per year. There were large variations in the reported incidence of adverse events in both HICs and LMICs. Of the 7 adverse events assessed, adverse drug events were the most common type in HICs, with an incidence rate of 5.0%. In LMICs, venous thromboembolism was most common, with an incidence rate of 3.0%. Catheter-related blood stream infection, venous thromboembolism, and pressure ulcers had comparable rates between HICs and LMIC . The authors estimated that for every 100 hospitalizations, approximately 14.2 adverse events in HICs and 12.7 in LMICs. This is roughly 16.8 million injuries annually among hospitalized patients in HICs. LMICs and experienced approximately 50% more adverse events than HICs. Of note, LMICs had 5 times the population of HICs but the authors did not calculate proportional incidence rates.
The authors estimated 22.6 million DALYs lost due to these adverse events in 2009 globally. Unsurprisingly, the number of DALYs lost were more than twice as high as in LMICs as they were in HICs. This is likely due to the combination of weaker health systems and human resources for health shortages in those countries. In LMICs, venous thromboembolism was the main source of lost DALYs. Although incidences of hospital-acquired infections--such as nosocomial pneumonia, catheter-related blood stream and urinary tract infections--were smaller, they caused a comparable number of DALYs lost. Premature death from adverse events was the primary source of DALYs lost for all countries.
Conclusion. Adverse events from unsafe care is a significant problem across all countries.
Commentary
Globally, the efforts to improve health care delivery for diseases that cause substantial morbidity and mortality have been largely successful. For example, antimalarial drugs and antiretroviral therapies have become more accessible to patients in need [1,2]. However, in order to create more sustainable model, the health care systems of developing countries need sustainable investments to care for their growing populations and increasing medical needs [3,4]. Allengranzi et al [5] concluded from a systemic review that health care–associated infections are ubiquitous and occur at much higher rates in LMICs than in HICs. Findings from this study support those from Allengranzi’s review.
This study helped further our understanding of and explored the impact of unsafe medical care on GBD and DALYs. Several other adverse events related to unsafe care, such as unsafe surgery, harms due to counterfeit drugs, unsafe childbirth and unsafe blood use, were not included in this study due to data limitations. The estimated lost DALYs would be much higher if these events were counted.
This study has several strengths. First, the authors sought out the best available data from a large number of sources. Evidence selected for the analysis came from studies with good quality ratings. The 7 outcome measures used in this study are now standard minimum reporting data internationally. Nonetheless, several limitations are present. As the authors noted, the lack of availability high-quality data is common in international analyses. There can be reporting delays, data collection errors due to a lack of technical capacity, and corruption problems that may influence data quality. Poor reporting practices may exclude or underreport adverse events. Also, the paucity of data for some variables limited the calculation of estimates Second, few studies used standardized approaches in their data collection and analysis, contributing to data inconsistencies that may affect the reliability of the results. Third, the same life expectancy value (the WHO standard) was used for all individuals regardless of their countries’ life expectancy. The authors acknowledged that this approach was controversial and may have resulted in a different number of DALYs lost. Finally, only English-language publications were used, which may have influenced the findings. Latin America, the former Soviet Union states, and many Asian countries have growing bodies of research published in their native languages.
Despite the limitations, the study is one of the first systematic analyses of GBD, the outcomes of unsafe medical care, and associated lost DALYs. The analysis identified that a majority of the harms from adverse events occur in LMICs. Policies addressing, supporting, and enforcing patient safety measures during the health care experience will help ensure reductions in mortality and morbidity in LMICs. Improving the safety of the healthcare system should be a major policy and research emphasis across the globe.
Applications for Clinical Practice
Even though patient safety initiatives have been at the forefront of many organizational policies and health care provider education since the 1999 Institute of Medicine report “Crossing the Quality Chasm,” this study reminds practitioners that safe clinical practice is essential for reducing domestic disease burden. The cost of adverse events from unsafe practice in the United States was estimated to be around $16.6 billion in 2004 alone [6]. With the World Health Organization calling for strengthened research infrastructure across the globe and LMICs now seeing the value of data for health systems policymaking and management, future research will help to further refine the methods developed in this study.
—Jin Jun, MSN, APRN-BC, CCRN, and Allison Squires, PhD, RN
Study Overview
Objective. To examine the global burden of unsafe medical care and its comparative frequency in low/middle-income vs. high-income countries.
Design. Analytical modeling of aggregated data from observational studies.
Data. Two primary sources of data were used. First, the team conducted a search of over 16,000 articles written in English after 1976 that aimed for a comprehensive exam-ination of both peer-reviewed and non–peer-reviewed studies that focused on 7 inpatient adverse events (see below), and the clinical features of the patients who were injured from them. Two separate literature reviews were conducted in 2007 through early 2008 and then repeated in 2011. Discussions with international experts in each topic area informed the selection process. The second source of data was epidemiological studies commissioned by the World Health Organization (WHO). These aimed to identify inpatient adverse events using a 2-stage medical record review in 26 hospitals across 8 low- and middle-income countries (LMICs) in the Eastern Mediterranean and North Africanregions, and 35 hospitals across 5 countries in Latin America.
Main outcome measures. 7 types of adverse events were evaluated in the analysis: (1) adverse drug events, (2) catheter-related urinary tract infection, (3) catheter-related blood stream infections, (4) nosocomial pneumonia, (5) venous thromboembolism, (6) falls, and (7) pressure ulcers (decubiti). The global burden of disease (GBD) is a standard metric that uses disability-adjusted life years (DALYs) as a proxy measure of morbidity and mortality related to a specific condition. The GBD DALYs model requires several key inputs: the number of people affected, the age at which they are affected, and the clinical consequence of the adverse events. In this study, a single average age per event was used instead of the standard GBD calculations by age and sex. Each input of GBD and DALYs was calculated separately for high-income countries (HICs) versus LMICs. The World Bank sets the income categorization for countries and adjusts the information on an annual basis. Countries in each category share common characteristics of socioeconomic development and epidemiological profiles.
Main results. The rate of hospitalization in HICs was higher than in LMICs: 10.8 vs. 3.7 per 100 citizens per year. There were large variations in the reported incidence of adverse events in both HICs and LMICs. Of the 7 adverse events assessed, adverse drug events were the most common type in HICs, with an incidence rate of 5.0%. In LMICs, venous thromboembolism was most common, with an incidence rate of 3.0%. Catheter-related blood stream infection, venous thromboembolism, and pressure ulcers had comparable rates between HICs and LMIC . The authors estimated that for every 100 hospitalizations, approximately 14.2 adverse events in HICs and 12.7 in LMICs. This is roughly 16.8 million injuries annually among hospitalized patients in HICs. LMICs and experienced approximately 50% more adverse events than HICs. Of note, LMICs had 5 times the population of HICs but the authors did not calculate proportional incidence rates.
The authors estimated 22.6 million DALYs lost due to these adverse events in 2009 globally. Unsurprisingly, the number of DALYs lost were more than twice as high as in LMICs as they were in HICs. This is likely due to the combination of weaker health systems and human resources for health shortages in those countries. In LMICs, venous thromboembolism was the main source of lost DALYs. Although incidences of hospital-acquired infections--such as nosocomial pneumonia, catheter-related blood stream and urinary tract infections--were smaller, they caused a comparable number of DALYs lost. Premature death from adverse events was the primary source of DALYs lost for all countries.
Conclusion. Adverse events from unsafe care is a significant problem across all countries.
Commentary
Globally, the efforts to improve health care delivery for diseases that cause substantial morbidity and mortality have been largely successful. For example, antimalarial drugs and antiretroviral therapies have become more accessible to patients in need [1,2]. However, in order to create more sustainable model, the health care systems of developing countries need sustainable investments to care for their growing populations and increasing medical needs [3,4]. Allengranzi et al [5] concluded from a systemic review that health care–associated infections are ubiquitous and occur at much higher rates in LMICs than in HICs. Findings from this study support those from Allengranzi’s review.
This study helped further our understanding of and explored the impact of unsafe medical care on GBD and DALYs. Several other adverse events related to unsafe care, such as unsafe surgery, harms due to counterfeit drugs, unsafe childbirth and unsafe blood use, were not included in this study due to data limitations. The estimated lost DALYs would be much higher if these events were counted.
This study has several strengths. First, the authors sought out the best available data from a large number of sources. Evidence selected for the analysis came from studies with good quality ratings. The 7 outcome measures used in this study are now standard minimum reporting data internationally. Nonetheless, several limitations are present. As the authors noted, the lack of availability high-quality data is common in international analyses. There can be reporting delays, data collection errors due to a lack of technical capacity, and corruption problems that may influence data quality. Poor reporting practices may exclude or underreport adverse events. Also, the paucity of data for some variables limited the calculation of estimates Second, few studies used standardized approaches in their data collection and analysis, contributing to data inconsistencies that may affect the reliability of the results. Third, the same life expectancy value (the WHO standard) was used for all individuals regardless of their countries’ life expectancy. The authors acknowledged that this approach was controversial and may have resulted in a different number of DALYs lost. Finally, only English-language publications were used, which may have influenced the findings. Latin America, the former Soviet Union states, and many Asian countries have growing bodies of research published in their native languages.
Despite the limitations, the study is one of the first systematic analyses of GBD, the outcomes of unsafe medical care, and associated lost DALYs. The analysis identified that a majority of the harms from adverse events occur in LMICs. Policies addressing, supporting, and enforcing patient safety measures during the health care experience will help ensure reductions in mortality and morbidity in LMICs. Improving the safety of the healthcare system should be a major policy and research emphasis across the globe.
Applications for Clinical Practice
Even though patient safety initiatives have been at the forefront of many organizational policies and health care provider education since the 1999 Institute of Medicine report “Crossing the Quality Chasm,” this study reminds practitioners that safe clinical practice is essential for reducing domestic disease burden. The cost of adverse events from unsafe practice in the United States was estimated to be around $16.6 billion in 2004 alone [6]. With the World Health Organization calling for strengthened research infrastructure across the globe and LMICs now seeing the value of data for health systems policymaking and management, future research will help to further refine the methods developed in this study.
—Jin Jun, MSN, APRN-BC, CCRN, and Allison Squires, PhD, RN
1. Kaplan J, Hanson D, Dworkin M, et al. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretroviral therapy, Clin Infect Dis 2000;30 Suppl 1:S5–14.
2. Eaton J, et al. Health benefits, costs, and cost-effectiveness of earlier eligibility for adult antiretroviral therapy and expanded treatment coverage: a cmbined analysis of 12 mathematical models, Lancet Global Health 2014;2:e23–34.
3. Mills A, Brugha R, Hanson K, et al. What can be done about the private health sector in low-income countries? Bull World Health Org 2002;80:325–30.
4. Schlein K, De La Cruz A, Gopalakrishnan T, Montagu D. Private sector delivery of health services in developing countries: a mixed-methods study on quality assurance in social franchises, BMC Health Serv Res 2013;13:4.
5. Allegranzi B, Bagheri N, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis, Lancet 2011;377;
228–41.
6. Jha A, Chan D, Ridgway A, et al. Improving safety and eliminating redundant tests: cutting costs in US hospitals. Health Affairs 2009;28:1475–84.
1. Kaplan J, Hanson D, Dworkin M, et al. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretroviral therapy, Clin Infect Dis 2000;30 Suppl 1:S5–14.
2. Eaton J, et al. Health benefits, costs, and cost-effectiveness of earlier eligibility for adult antiretroviral therapy and expanded treatment coverage: a cmbined analysis of 12 mathematical models, Lancet Global Health 2014;2:e23–34.
3. Mills A, Brugha R, Hanson K, et al. What can be done about the private health sector in low-income countries? Bull World Health Org 2002;80:325–30.
4. Schlein K, De La Cruz A, Gopalakrishnan T, Montagu D. Private sector delivery of health services in developing countries: a mixed-methods study on quality assurance in social franchises, BMC Health Serv Res 2013;13:4.
5. Allegranzi B, Bagheri N, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis, Lancet 2011;377;
228–41.
6. Jha A, Chan D, Ridgway A, et al. Improving safety and eliminating redundant tests: cutting costs in US hospitals. Health Affairs 2009;28:1475–84.
Does Bioelectrical Impedance Analysis Provide a Reliable Diagnosis of Secondary Lymphedema in Breast Cancer Patients?
Study Overview
Objective. To evaluate the reliability, sensitivity, and specificity of bioelectrical impedance analysis (BIA) in the diagnosis of secondary lymphedema.
Design. Cross-sectional study utilizing test-retest method
Setting and participants. The researchers used a purposeful sampling technique to recruit women between 2010 and 2011 from a metropolitan cancer center and communities in the New York City metropolitan area. Participants included women who were 18 years of age or older and able to read and write in English. Exclusion criteria included patients with bilateral breast disease, recurrent cancer, artificial limb, knee, or hip, and kidney or heart failure. Study participants were divided into 3 groups: breast cancer survivors with lymphedema, those at risk for lymphedema, and healthy adult women (no history of breast cancer or lymphedema). Women in the at risk category had to have completed surgical treatment, chemotherapy and/or radiation within the 5 years prior to the study enrollment.
Measurements. Patient’s arms were measured by the same 2 researchers using sequential circumferential measurements. BIA was measured in all patients with the ImpXCA (Impedimed Inc, Pittsford, NY), an FDA-approved device that measures impedance and resistance of the extracellular fluid. The ImpXCA utilizes a scale to correlate BIA to an L-Dex (lymphedema index) ratio; –10 to +10 defines the normal range of L-Dex values for a patient without lymphedema. Measurements were taken at 5-minute increments for a total of 3 times at the same visit to test for stability of BIA.
Main results. 250 patients were in the sample: 42 with known lymphedema, 148 at risk for lymphedema, and 60 healthy female adults. L-Dex ratios ranged from –9.7 to 7.7 in the healthy population, –9.6 to 36.9 in the at risk group, and 0.9 to 115 in the group with lymphedema. Mean L-Dex ratios were significantly different between the healthy and lymphedema groups (P < 0.001) and the at risk and lymphedema groups (P < 0.001). There was no difference between the at risk and healthy groups (P = 0.85). Utilizing an L-Dex ratio cutoff of 7.1 provided 80% sensitivity and 90% specificity in the diagnosis of secondary lymphedema.
Reliability and reproducibility of BIA by ImpXCA using the L-Dex ratio was assessed using a test-retest method. Intra-class correlation coefficients (ICC) provided strong stability for the repeated measurements in the healthy group, with ICC = 0.99 (95% CI, 0.99–0.99), and in the at risk group, with ICC = 0.99 (95% CI, 0.99–0.99). There was also fair agreement in the repeated measurements in the lymphedema group, with ICC = 0.69 (95% CI, 0.58-0.82). All of these findings were statistically significant (P < 0.001).
Conclusion. The L-Dex ratio is reliable and reproducible and may be helpful in distinguishing women with lymphedema from those without lymphedema. BIA in conjunction with other tools, such as self-report of symptoms, circumferential measurements, and clinical observation, may have a role in diagnosing lymphedema.
Commentary
The first year and a half following surgical treatment for breast cancer is when providers tend to diagnose the initial onset of lymphedema [1]. Many women, however, go undiagnosed until the illness has progressed. Earlier treatment has the potential to improve patient outcomes [2]. Although awareness of secondary lymphedema among breast cancer survivors has increased over the past 10 years, the diagnosis remains difficult and the development of effective diagnostic tools continues to challenge health care providers.
The current gold standard for diagnosis is the water displacement method where the affected and unaffected extremities are each placed into a tank of water, and the displaced water is measured [3]. Greater than a 200 mL discrepancy between arms is used to make a diagnosis of lymphedema. While useful, this measurement is messy and difficult to set up, and thus underutilized. Many providers have turned to circumferential measurements as their primary method to diagnose and monitor lymphedema [4]. However, this method may miss patients in the earlier stages of lymphedema, since it measures the size of limbs rather than changes in the tissue. Without a definitive test to diagnose lymphedema, researchers and health care providers continue to search for the most accurate, reliable, and feasible means to assist in the diagnosis.
This cross-sectional study suggests that L-Dex can be helpful in detecting lymphedema. A weakness of the study is that the investigators did not compare the results of BIA to the current gold standard of water displacement, but rather to circumferential measurement. In addition, while all results were reproducible, the difference between groups was notable in terms of age and body mass index, making it difficult to generalize to all patients at risk for lymphedema or differentiate results by those same variables. Although having the same 2 investigators obtain circumferential tape measurements is preferable to having multiple investigators do so, such measurements are still at risk for human error.
BIA shows promise as a diagnostic tool. Future studies should include healthy patients with characteristics similar to those of at risk patients and lymphedema patients. Efforts also could be directed towards determining whether combining BIA with other methods, such as self-report, circumferential measurements, and close observation, may offer greater sensitivity and specificity than one method alone.
Applications for Clinical Practice
Secondary lymphedema is a common complication caused by surgical treatment of breast cancer. Early treatment is linked to a decrease in debilitating factors such as immobility of affected joints, skin changes, and risk for infection. Measurement of extracellular fluid utilizing L-Dex ratios produces reliable and repeatable results in the assessment for lymphedema. Paired with additional tools and resources it may be helpful in making a diagnosis, which is normally difficult in its earliest stages. The early diagnosis of secondary lymphedema may allow for improved quality of life for survivors of breast cancer.
—Jennifer L. Nahum, MSN, CPNP-AC, PPCNP-BC, and Allison Squires, PhD, RN
1. Czerniec SA, Ward LC, Lee MJ, et al. Segmental measurement of breast cancer-related arm lymphoedema using perometry and bioimpedance spectroscopy. Support Care Cancer. 2011;19:703–10.
2. Damstra RJ, Voesten HG, van Schelven WD, van der Lei B. Lymphatic venous anastomosis (LVA) for treatment of secondary arm lymphedema. A prospective study of 11 LVA procedures in 10 patients with breast cancer related lymphedema and a critical review of the literature. Breast Cancer Res Treat 2009;113:199–206.
3. Brorson H, Höijer P. Standardised measurements used to order compression garments can be used to calculate arm volumes to evaluate lymphoedema treatment. Plast Surg Hand Surg 2012;46:410–5.
4. Langbecker D, Hayes SC, Newman B, Janda M. Treatment for upper-limb and lower-limb lymphedema by professionals specializing in lymphedema care. Eur J Cancer Care (Engl). 2008;17:557–64.
Study Overview
Objective. To evaluate the reliability, sensitivity, and specificity of bioelectrical impedance analysis (BIA) in the diagnosis of secondary lymphedema.
Design. Cross-sectional study utilizing test-retest method
Setting and participants. The researchers used a purposeful sampling technique to recruit women between 2010 and 2011 from a metropolitan cancer center and communities in the New York City metropolitan area. Participants included women who were 18 years of age or older and able to read and write in English. Exclusion criteria included patients with bilateral breast disease, recurrent cancer, artificial limb, knee, or hip, and kidney or heart failure. Study participants were divided into 3 groups: breast cancer survivors with lymphedema, those at risk for lymphedema, and healthy adult women (no history of breast cancer or lymphedema). Women in the at risk category had to have completed surgical treatment, chemotherapy and/or radiation within the 5 years prior to the study enrollment.
Measurements. Patient’s arms were measured by the same 2 researchers using sequential circumferential measurements. BIA was measured in all patients with the ImpXCA (Impedimed Inc, Pittsford, NY), an FDA-approved device that measures impedance and resistance of the extracellular fluid. The ImpXCA utilizes a scale to correlate BIA to an L-Dex (lymphedema index) ratio; –10 to +10 defines the normal range of L-Dex values for a patient without lymphedema. Measurements were taken at 5-minute increments for a total of 3 times at the same visit to test for stability of BIA.
Main results. 250 patients were in the sample: 42 with known lymphedema, 148 at risk for lymphedema, and 60 healthy female adults. L-Dex ratios ranged from –9.7 to 7.7 in the healthy population, –9.6 to 36.9 in the at risk group, and 0.9 to 115 in the group with lymphedema. Mean L-Dex ratios were significantly different between the healthy and lymphedema groups (P < 0.001) and the at risk and lymphedema groups (P < 0.001). There was no difference between the at risk and healthy groups (P = 0.85). Utilizing an L-Dex ratio cutoff of 7.1 provided 80% sensitivity and 90% specificity in the diagnosis of secondary lymphedema.
Reliability and reproducibility of BIA by ImpXCA using the L-Dex ratio was assessed using a test-retest method. Intra-class correlation coefficients (ICC) provided strong stability for the repeated measurements in the healthy group, with ICC = 0.99 (95% CI, 0.99–0.99), and in the at risk group, with ICC = 0.99 (95% CI, 0.99–0.99). There was also fair agreement in the repeated measurements in the lymphedema group, with ICC = 0.69 (95% CI, 0.58-0.82). All of these findings were statistically significant (P < 0.001).
Conclusion. The L-Dex ratio is reliable and reproducible and may be helpful in distinguishing women with lymphedema from those without lymphedema. BIA in conjunction with other tools, such as self-report of symptoms, circumferential measurements, and clinical observation, may have a role in diagnosing lymphedema.
Commentary
The first year and a half following surgical treatment for breast cancer is when providers tend to diagnose the initial onset of lymphedema [1]. Many women, however, go undiagnosed until the illness has progressed. Earlier treatment has the potential to improve patient outcomes [2]. Although awareness of secondary lymphedema among breast cancer survivors has increased over the past 10 years, the diagnosis remains difficult and the development of effective diagnostic tools continues to challenge health care providers.
The current gold standard for diagnosis is the water displacement method where the affected and unaffected extremities are each placed into a tank of water, and the displaced water is measured [3]. Greater than a 200 mL discrepancy between arms is used to make a diagnosis of lymphedema. While useful, this measurement is messy and difficult to set up, and thus underutilized. Many providers have turned to circumferential measurements as their primary method to diagnose and monitor lymphedema [4]. However, this method may miss patients in the earlier stages of lymphedema, since it measures the size of limbs rather than changes in the tissue. Without a definitive test to diagnose lymphedema, researchers and health care providers continue to search for the most accurate, reliable, and feasible means to assist in the diagnosis.
This cross-sectional study suggests that L-Dex can be helpful in detecting lymphedema. A weakness of the study is that the investigators did not compare the results of BIA to the current gold standard of water displacement, but rather to circumferential measurement. In addition, while all results were reproducible, the difference between groups was notable in terms of age and body mass index, making it difficult to generalize to all patients at risk for lymphedema or differentiate results by those same variables. Although having the same 2 investigators obtain circumferential tape measurements is preferable to having multiple investigators do so, such measurements are still at risk for human error.
BIA shows promise as a diagnostic tool. Future studies should include healthy patients with characteristics similar to those of at risk patients and lymphedema patients. Efforts also could be directed towards determining whether combining BIA with other methods, such as self-report, circumferential measurements, and close observation, may offer greater sensitivity and specificity than one method alone.
Applications for Clinical Practice
Secondary lymphedema is a common complication caused by surgical treatment of breast cancer. Early treatment is linked to a decrease in debilitating factors such as immobility of affected joints, skin changes, and risk for infection. Measurement of extracellular fluid utilizing L-Dex ratios produces reliable and repeatable results in the assessment for lymphedema. Paired with additional tools and resources it may be helpful in making a diagnosis, which is normally difficult in its earliest stages. The early diagnosis of secondary lymphedema may allow for improved quality of life for survivors of breast cancer.
—Jennifer L. Nahum, MSN, CPNP-AC, PPCNP-BC, and Allison Squires, PhD, RN
Study Overview
Objective. To evaluate the reliability, sensitivity, and specificity of bioelectrical impedance analysis (BIA) in the diagnosis of secondary lymphedema.
Design. Cross-sectional study utilizing test-retest method
Setting and participants. The researchers used a purposeful sampling technique to recruit women between 2010 and 2011 from a metropolitan cancer center and communities in the New York City metropolitan area. Participants included women who were 18 years of age or older and able to read and write in English. Exclusion criteria included patients with bilateral breast disease, recurrent cancer, artificial limb, knee, or hip, and kidney or heart failure. Study participants were divided into 3 groups: breast cancer survivors with lymphedema, those at risk for lymphedema, and healthy adult women (no history of breast cancer or lymphedema). Women in the at risk category had to have completed surgical treatment, chemotherapy and/or radiation within the 5 years prior to the study enrollment.
Measurements. Patient’s arms were measured by the same 2 researchers using sequential circumferential measurements. BIA was measured in all patients with the ImpXCA (Impedimed Inc, Pittsford, NY), an FDA-approved device that measures impedance and resistance of the extracellular fluid. The ImpXCA utilizes a scale to correlate BIA to an L-Dex (lymphedema index) ratio; –10 to +10 defines the normal range of L-Dex values for a patient without lymphedema. Measurements were taken at 5-minute increments for a total of 3 times at the same visit to test for stability of BIA.
Main results. 250 patients were in the sample: 42 with known lymphedema, 148 at risk for lymphedema, and 60 healthy female adults. L-Dex ratios ranged from –9.7 to 7.7 in the healthy population, –9.6 to 36.9 in the at risk group, and 0.9 to 115 in the group with lymphedema. Mean L-Dex ratios were significantly different between the healthy and lymphedema groups (P < 0.001) and the at risk and lymphedema groups (P < 0.001). There was no difference between the at risk and healthy groups (P = 0.85). Utilizing an L-Dex ratio cutoff of 7.1 provided 80% sensitivity and 90% specificity in the diagnosis of secondary lymphedema.
Reliability and reproducibility of BIA by ImpXCA using the L-Dex ratio was assessed using a test-retest method. Intra-class correlation coefficients (ICC) provided strong stability for the repeated measurements in the healthy group, with ICC = 0.99 (95% CI, 0.99–0.99), and in the at risk group, with ICC = 0.99 (95% CI, 0.99–0.99). There was also fair agreement in the repeated measurements in the lymphedema group, with ICC = 0.69 (95% CI, 0.58-0.82). All of these findings were statistically significant (P < 0.001).
Conclusion. The L-Dex ratio is reliable and reproducible and may be helpful in distinguishing women with lymphedema from those without lymphedema. BIA in conjunction with other tools, such as self-report of symptoms, circumferential measurements, and clinical observation, may have a role in diagnosing lymphedema.
Commentary
The first year and a half following surgical treatment for breast cancer is when providers tend to diagnose the initial onset of lymphedema [1]. Many women, however, go undiagnosed until the illness has progressed. Earlier treatment has the potential to improve patient outcomes [2]. Although awareness of secondary lymphedema among breast cancer survivors has increased over the past 10 years, the diagnosis remains difficult and the development of effective diagnostic tools continues to challenge health care providers.
The current gold standard for diagnosis is the water displacement method where the affected and unaffected extremities are each placed into a tank of water, and the displaced water is measured [3]. Greater than a 200 mL discrepancy between arms is used to make a diagnosis of lymphedema. While useful, this measurement is messy and difficult to set up, and thus underutilized. Many providers have turned to circumferential measurements as their primary method to diagnose and monitor lymphedema [4]. However, this method may miss patients in the earlier stages of lymphedema, since it measures the size of limbs rather than changes in the tissue. Without a definitive test to diagnose lymphedema, researchers and health care providers continue to search for the most accurate, reliable, and feasible means to assist in the diagnosis.
This cross-sectional study suggests that L-Dex can be helpful in detecting lymphedema. A weakness of the study is that the investigators did not compare the results of BIA to the current gold standard of water displacement, but rather to circumferential measurement. In addition, while all results were reproducible, the difference between groups was notable in terms of age and body mass index, making it difficult to generalize to all patients at risk for lymphedema or differentiate results by those same variables. Although having the same 2 investigators obtain circumferential tape measurements is preferable to having multiple investigators do so, such measurements are still at risk for human error.
BIA shows promise as a diagnostic tool. Future studies should include healthy patients with characteristics similar to those of at risk patients and lymphedema patients. Efforts also could be directed towards determining whether combining BIA with other methods, such as self-report, circumferential measurements, and close observation, may offer greater sensitivity and specificity than one method alone.
Applications for Clinical Practice
Secondary lymphedema is a common complication caused by surgical treatment of breast cancer. Early treatment is linked to a decrease in debilitating factors such as immobility of affected joints, skin changes, and risk for infection. Measurement of extracellular fluid utilizing L-Dex ratios produces reliable and repeatable results in the assessment for lymphedema. Paired with additional tools and resources it may be helpful in making a diagnosis, which is normally difficult in its earliest stages. The early diagnosis of secondary lymphedema may allow for improved quality of life for survivors of breast cancer.
—Jennifer L. Nahum, MSN, CPNP-AC, PPCNP-BC, and Allison Squires, PhD, RN
1. Czerniec SA, Ward LC, Lee MJ, et al. Segmental measurement of breast cancer-related arm lymphoedema using perometry and bioimpedance spectroscopy. Support Care Cancer. 2011;19:703–10.
2. Damstra RJ, Voesten HG, van Schelven WD, van der Lei B. Lymphatic venous anastomosis (LVA) for treatment of secondary arm lymphedema. A prospective study of 11 LVA procedures in 10 patients with breast cancer related lymphedema and a critical review of the literature. Breast Cancer Res Treat 2009;113:199–206.
3. Brorson H, Höijer P. Standardised measurements used to order compression garments can be used to calculate arm volumes to evaluate lymphoedema treatment. Plast Surg Hand Surg 2012;46:410–5.
4. Langbecker D, Hayes SC, Newman B, Janda M. Treatment for upper-limb and lower-limb lymphedema by professionals specializing in lymphedema care. Eur J Cancer Care (Engl). 2008;17:557–64.
1. Czerniec SA, Ward LC, Lee MJ, et al. Segmental measurement of breast cancer-related arm lymphoedema using perometry and bioimpedance spectroscopy. Support Care Cancer. 2011;19:703–10.
2. Damstra RJ, Voesten HG, van Schelven WD, van der Lei B. Lymphatic venous anastomosis (LVA) for treatment of secondary arm lymphedema. A prospective study of 11 LVA procedures in 10 patients with breast cancer related lymphedema and a critical review of the literature. Breast Cancer Res Treat 2009;113:199–206.
3. Brorson H, Höijer P. Standardised measurements used to order compression garments can be used to calculate arm volumes to evaluate lymphoedema treatment. Plast Surg Hand Surg 2012;46:410–5.
4. Langbecker D, Hayes SC, Newman B, Janda M. Treatment for upper-limb and lower-limb lymphedema by professionals specializing in lymphedema care. Eur J Cancer Care (Engl). 2008;17:557–64.