User login
Technology-Supported Apprenticeship in the Management of Hypertension: A Randomized Controlled Trial
From the Massachusetts Institute of Technology (Dr. Moore, Dr. Moss and Mr. Gilroy) and the Massachusetts General Hospital (Ms. Marshall, Dr. Judge, Dr. Crocker, and Dr. Zusman), Boston, MA.
Abstract
- Objective: To compare technology-supported appren-ticeship in hypertension management with a successful coaching model at Massachusetts General Hospital.
- Methods: A randomized controlled trial was conducted. Adult patients with uncontrolled essential hypertension (average blood pressure (BP) 148/87 mm Hg) were recruited in a staggered fashion for a 12-week study period. Intervention subjects received apprenticeship support from a nurse health coach through the CollaboRhythm application on a tablet computer. Patients self-tracked medication adherence and blood pressure (via wireless device) and the coach helped them to continuously progress through lifestyle change and medication adjustment using integrated messaging. Control subjects received support from the same coach but through traditional channels of office visits, phone calls, and e-mail.
- Results: 42 of 44 subjects completed the study. Intervention subjects achieved a greater decrease in systolic BP at 12 weeks than control subjects (26.3 mm Hg vs. 16.0 mm Hg, P = 0.009). A greater percentage of intervention subjects achieved goal BP ≤ 130/80 mm Hg (75.0% vs. 31.8%, P = 0.003) and 100% of them achieved goal BP ≤ 140/90 mmHg. They also rated the experience higher, although this finding was not statistically significant (8.9 vs. 7.6, P = 0.12). There was a trend toward increased cost for intervention subjects ($67.50 vs. $53.41, P = 0.15), but the projected cost is much less than standard care ($248/patient/year).
- Conclusion: This study provides encouraging evidence that technology-supported apprenticeship can improve the outcomes, cost, and experience of care in managing hypertension.
Hypertension affects approximately 33% of the U.S. adult population [1]. Antihypertensive treatment has been shown to be effective at preventing complications [2,3]. Unfortunately, estimates suggest that the majority of those diagnosed with hypertension do not have their blood pressure controlled [1]. This failure is due to both clinician and patient factors. Mean adherence of clinicians to guidelines is estimated at 53.5% [4]. An electronic monitoring study showed that half of patients who are prescribed medications stop taking them within 1 year [5]. Of those who take their medications, about 10% have adherence issues on any given day and about 50% have significant adherence issues in the course of their treatment [5]. Adherence to diet and exercise self-management is even more dismal, with rates below 20% [6]. Hypertension is an expensive problem with direct medical costs (treatment and complications) greater than $100 billion a year and equally high indirect costs (lost productivity) [7–9].
In the management of chronic diseases, there is a significant trend toward empowering patients with more control and toward providing more longitudinal coaching from clinicians and from peers [10–15]. Technology-supported apprenticeship is a model of chronic disease management that builds on the success of self-management and coaching, but it is more ambitious in that its goal is for patients to lead their care with the support of health coaches and supervising clinicians. It is informed by the field of learning science, particularly in how technology can be used effectively to support learning [16–20]. Apprenticeship refers to the tutelage of a community of novices in a skill or trade by one or more masters through situated learning. Situated learning refers to the process in which novices learn through participation in legitimate tasks in the same physical and social context where they will need to perform them once independent [21,22]. It is opposed to learning through contrived exercises in an artificial environment like a classroom.
In technology-supported apprenticeship, patients are the novice apprentices of master coaches. Technology provides scaffolding and communication tools to allow coaches to support the patient in the management of disease within the context of daily life rather than in the clinician’s office. Patients are supported in gradually developing self-efficacy and independence until they are skilled enough to lead their care and even to help coach others to success. The hypothesis is that embracing the contribution of the patient to this extent will reap unparalleled rewards in the experience, outcomes, and cost of care.
We conducted a randomized controlled trial to assess whether a technology-supported apprenticeship in hyper-tension management would improve blood pressure control compared with a successful coaching model.
Methods
Setting
The health coaching model at the Ambulatory Practice of the Future (APF) at the Massachusetts General Hospital is designed to impact the whole health ofpatients. In the scope of hypertension management, a nurse health coach, under the supervision of a physician, is responsible for improving outcomes through longitudinal support via office visits, phone calls, and e-mails. Diet, exercise, stress management, and medication therapy are all emphasized through health coaching techniques, such as motivational interviewing and appreciative inquiry [23,24]. Patients are referred to dieticians, exercise coaches, mind-body specialists, and others as desired. Prior to the start of this study, the APF was outperforming the national average with ~70% of hypertensive patients in the practice below clinically recommended goal blood pressures.
Recruitment
The study was advertised to all clinical staff of the APF through word of mouth. Since the practice was relatively young, it also had a registry of patients with elevated blood pressure that had not been addressed. Adult patients (> 18 years old) from the registry or from routine visits with essential hypertension (average blood pressure ≥ 140/90 and ≤ 180/120) who were taking 0 or 1 medications and had internet connectivity were eligible for inclusion in the study. Patients with a history of hypotension, syncope, hypertensive urgency, hypertensive emergency, labile hypertension, and proven coronary artery disease were excluded, as were patients with significant visual, auditory, or cognitive impairment and patients who were not proficient in English. Clinical staff notified the nurse health coach for the study on identification of any eligible subjects. The same nurse health coach recruited and cared for all intervention and control subjects.
The nurse health coach contacted each eligible patient to assess interest. Interested patients were scheduled for an appointment to commence the study. A process of written informed consent was carried out with each study subject. Each subject was assigned the next sequential study number, which was pre-randomized to either the intervention or the control group.
The study period for each subject was 12 weeks +/– 2 weeks with staggered recruitment. Twelve weeks represents the minimal time required to progress through the standardized Medication Adjustment Plan that was used, assuming a minimum time of 2 weeks on each medication before a change is considered. A recruitment window from 1 March 2013 until 31 May 2013 was used. The goal was to recruit between 40 and 60 subjects, since statistical analysis revealed that a sample size of 36 was sufficient to detect a 5 mm Hg difference in the decrease in systolic blood pressure between groups given a 4 mm Hg standard deviation.
Intervention
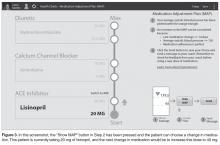
CollaboRhythm is a software platform that was developed at the MIT Media Lab and designed to support the principles of technology-supported apprenticeship. Patient tracking tools document progress, visualizations highlight associations between actions and outcomes, and personalized decision support encourages self-efficacy. Powerful virtual visits and instant messaging allow master clinicians to provide adaptive coaching within the context of daily life rather than in the artificial environment of the office. Applications can be deployed cross-platform to cell phones, tablets, computers, etc.
A simplified system was created for hypertension management. It is optimized for tablet deployment and focuses on instant messaging for communications. The patient uses a wireless blood pressure monitor (D40b model by ForaCare®) to take blood pressure measurements. The device is paired with a tablet application to automatically report measurements. The patient self-reports medication adherence using the tablet application. Patient data is visualized in a daily clock and weekly charts to promote proactive behavior and self-reflection. Decision support for medication adjustment is paired with the charts. The patient’s data are synchronized with the coach’s tablet application via a collaborative health record server implemented using the Indivo X personally controlled health record (Children’s Hospital Boston, indivohealth.org) code base. Instant messaging between the patient and coach is implemented using a real-time messaging server. The applications for the patient and the coach are identical, but the coach’s application is configured to allow switching between patient records in order to manage a number of patients.
The user experience was designed based on our years of exploration at the MIT Media Lab of the psychology of illness and the impact that technology could have on patient empowerment and patient-clinician collaboration. It is important to note that the CollaboRhythm application is different from typical electronic reminder applications. In fact, the application never alarms at patients, even if they forget to perform their health actions. Instead, the application focuses on providing awareness for proactive decision-making, self-reflection, and support from the coach.
Protocol Common to Control and Intervention Subjects
Following informed consent, a baseline blood pressure and heart rate were measured for each subject using the same automated sphygmomanometer. Weight was also measured and a hypertension knowledge assessment (a simple survey about normal blood pressures and the effects of diet, exercise, and medication that was created for the purpose of this study) was completed. The initial medication load was determined using the Medication Adjustment Plan as a reference and each dose step as a unit of 1. For example, if a subject was already on lisinopril 40 mg at the start of the study, the initial medication load was 2.
The nurse health coach conducted an introductory visit with each subject including motivational interviewing to assess their health values and to discuss
hypertension management goals. The subject and coach made shared decisions about diet, exercise, stress management, and medication. The same medication titration algorithm was used for both control and interventional
subjects.
At the conclusion of the study period, subjects in both groups returned for an exit visit. Blood pressure and heart rate were measured using the same automated sphygmomanometer that was used at the initial visit. Weight was measured using the same scale as the initial visit. A hypertension knowledge assessment was completed and an exit interview was conducted. The change in medication load was determined as well. For example, if a subject started the study on lisinopril 20 mg and ended the study on lisinopril 40 mg, the increase in medication load was 1.
Protocol Specifics for Intervention Subjects
The apprenticeship model of chronic disease management was discussed with the nurse health coach and with APF team prior to the study. It was also implicit in the design of the CollaboRhythm tablet application.
During the introduction visit, subjects in the inter-vention group received instructions from the nurse health coach on how to use the CollaboRhythm tablet application to self-track their medication adherence, to review progress using the charts, to propose or agree with changes in hypertension medications, and to communicate with messages.
Subjects in the intervention group received their hyper-tension care through the CollaboRhythm tablet application. All instant messages between the intervention subjects and the nurse health coach were automatically documented electronically. Other forms of communication were documented in a spreadsheet. During the exit visit, the tablet computer and the wireless blood pressure meter were returned.
Protocol Specifics for Control Subjects
Between the introduction and exit visits, subjects in the control group received standard hypertension care from the nurse health coach at the APF. The coach instructed subjects to check their blood pressures 3 to 5 times a week. They had the option of purchasing a cuff, using a monitor at work, or using a monitor at a facility such as a pharmacy or grocery store. Communication took place through
office visits, phone calls, and e-mails. All communications with control subjects were documented for the purposes of this study by the nurse health coach in a spread-
sheet.
Outcomes of Interest
The primary outcomes of interest were the absolute decrease in systolic and diastolic blood pressure and the number of subjects who reached the blood pressure goal of less than or equal to 130/80 mm Hg. This more aggressive blood pressure goal was chosen for a number of reasons: (1) it is not uncommon to set a lower blood pressure goal for home measurements to avoid patients hovering just at the 140/90 goal and not getting the true benefit of reduced blood pressure; and (2) subjects were supported in improving diet, exercise, and stress management in addition to pharmacologic therapy. The 140/90 cut-off (now 150/90 in patients over 60) is focused on pharmacologic therapy [2,3].
The secondary outcomes included the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg (for comparison to other published literature), the number of subjects who achieved greater than a 10 mm Hg decrease in systolic and greater than a 5 mm Hg decrease in diastolic blood pressure, the change in medication load, the absolute decrease in weight, the number of subjects who lost at least 5 lb, a hypertension knowledge score assessed by a pre- and post-study test, a rating of satisfaction in care, and the amount of clinician time required in the care.
Statistical Methods
The study results were analyzed by the intention-to-treat approach. All subjects who returned for the final study visit were included in the analysis regardless of their adherence to the protocol. Subjects who did not return for the study exit visit were not included in the analysis because it would be impossible to determine the change in blood pressure without a final measurement. A 2-tailed Student’s t test for independent samples was used for all comparisons of the mean of continuous variables between the control and intervention groups. A 2-tailed Student’s t test for dependent samples was used for all comparisons between pre- and post-study variables within the control and the intervention group. A chi-square test was used for all comparisons of categorical variables between the groups, except when the expected values in the 2x2 table were below 5. Fisher’s exact test was used in this scenario, which applied to the secondary outcome of the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg.
Oversight
This study was approved by the institutional review boards at the Massachusetts Institute of Technology and the Massachusetts General Hospital.
Results
There were a total of 44 subjects recruited for the study. One intervention subject and one control subject were lost to follow-up, leaving 42 subjects who completed the study exit visit.
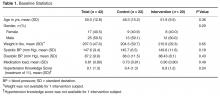
Baseline Statistics
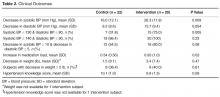
Clinical Outcomes
Cost
 Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Experience
Thirteen control subjects and 16 intervention subjects provided an experience rating during their exit interview from the study. There was a trend toward greater satisfaction by intervention subjects that was not statistically significant (8.9 vs. 7.6, P = 0.12). The majority of feedback from intervention subjects was obtained through the exit interview. The feedback was overwhelmingly positive. All of the subjects wanted to continue using the CollaboRhythm application after the end of the study. Some who had reached goal only wanted to use it sporadically as a “check-in,” but the majority wanted to use it daily as they had for the study for an indefinite period of time. They felt that the burden of reporting was easily balanced by the value of being able to track progress and get the efficient support of a health coach. They related that awareness of the associations between actions (diet, exercise, stress management, medication adherence) and blood pressure outcomes was integral to their success and their positive experience with the application. Subjects responded very favorably to the concept of leading their care. Some comments from patients include: “It felt good to take responsibility,” “No one has ever asked me to take responsibility for my health,” and “I developed confidence that I never would have had.” The nurse coach commented multiple times how delighted she was with the level of patient engagement and excitement. She also did not want to stop using the application at the end of the study.
The main complaints about the program from both subjects and the health coach were on performance. They wanted the application to load faster and to save data faster.
Discussion
This study provides encouraging evidence that technology-supported apprenticeship can dramatically improve the outcomes, cost, and experience of care in the management of hypertension.
A 26.3 mm Hg average decrease in systolic blood pressure for intervention subjects in 3 months is significantly better than the standard of care and the best of the best in published interventions. [1,11–14]. The same is true for a rate of 100% of patients achieving goal blood pressure < 140/90 mm Hg.
We believe several factors contribute to the success of our program: (1) supporting subjects in the mission of leading their care, (2) rich real-time feedback for self-reflection, (3) emphasis on short-term goals, (4) promise of medication reduction with goal achievement, and (5) social support and accountability that come with having a continuously available coach who had immediate data access.
Other studies have had web communication components, self-titration components, and coaching components. In a progressive study by McManus [11], subjects in the intervention group self-tracked their blood pressure and self-titrated their hypertension medications while control subjects received routine care. Self-managing patients achieved a decrease in systolic blood pressure of 17.6 mm Hg over 12 months while controls only achieved a decrease of 12.2 mm Hg. Self-managing patients were more aggressive in adding new medications and did not have increased incidence of side effects. A study by Green [12] showed that subjects with home blood pressure monitoring, a web training course, and web-based pharmacist coaching achieved a 14.2 mm Hg decrease in systolic blood pressure over 12 months and that 56% reached goal blood pressure (< 140/90 mm Hg). Subjects who received routine care only achieved a 5.3 mm Hg decrease in systolic blood pressure and only 31% reached goal blood pressure. Margolis [13] and Magid [14] conducted studies similar to Green's with pharmacist-led care. In Margolis’ study, 71.8% of inter-vention subjects study achieved goal at 6 months with a mean decrease in systolic blood pressure of 21.5 mm Hg. These results were impressively stable at 18 months [13]. In Magid’s study, 54.1% of intervention subjects achieved goal at 6 months with a mean decrease in systolic blood pressure of 20.7 mm Hg [14].
The technology-supported apprenticeship model was inspired by the exceptional results of these studies, but we believe that it represents a significant step forward in patient engagement. In these studies, the tools were typically more burdensome than empowering, the titration more prescriptive than motivational, and the coaching more timed and paternalistic than continuous and nurturing. Technology-supported apprenticeship relies on more powerful tools for collaboration and aspires for the patient to lead the care rather than the clinician. It has the potential to produce greater self-efficacy, which results in better outcomes at lower cost.
Cost Implications
The 100% rate of attainment of systolic blood pressure < 140 mm Hg in our intervention subjects has the poten-tial to contribute to substantial cost savings through reducing complications. The cost of complications per patient per year is approximately $1275, and attainment of goal blood pressure on average results in approximately 35% decrease in complications [2,7–9] Therefore, it is reasonable to expect at least $446 savings in downstream costs per patient per year with this intervention. This has notable public health implications given that there are approximately 32 million patients in the United States with diagnosed hypertension that is uncontrolled [1]. Cost saving at scale could be more than $14 billion.
Typically, interventions that produce downstream savings in health care require some upstream investment. An exciting aspect of this intervention is that it was significantly less costly, at $67.50 per patient, as compared with the standard of care, at $248 per patient per year [7–9]. Most of the responsibility was embraced by the patients, and the nurse coach needed only to provide occasional social and clinical support. Return office visits were almost completely eliminated and goals were achieved in a fraction of the time. The cost of the technology is effectively negligible given that patients will be able to use their own cell phones and tablets and their own blood pressure cuffs. Based on the prevalence of hypertension, a primary care practice with 2000 patients would be expected to have 600 with hypertension. At $180.50 in savings per patient per year, a profit of $108,300 could be retained if the same reimbursement was provided for this more effective care. At the same time, this more efficient and scalable model of care could allow a practice to care for a larger number of patients without compromising the experience for patients or clinicians.
Limitations and Future Directions
An important limitation of this study is its small sample size. The efficiency and cost analysis suggests that the intervention is highly suitable for scaling but, until this is studied, there is the risk that the small sample size may misrepresent the average effect on a larger population and overestimate the size of a population that a coach can manage. Future work will need to include much larger populations.
Another limitation was the short follow-up period. A key benefit of apprenticeship is that it theoretically results in greater and more sustainable self-efficacy than other models of patient engagement that are not as grounded in learning science and that do not engage the patient as deeply. Follow-up visits for both control and intervention subjects will be conducted at 1 year to assess the sustainability of the blood pressure improvements.
The fact that the population was from a single practice also presents the possibility that the subjects being studied were more interested and/or capable than a larger, more general population. This is likely to be true, since many of the patients at the APF sought it out in the hope of receiving a new health care experience. Future work will need to address patient populations from diverse socioeconomic situations and diverse cultures. Based on pilot studies that we have done with diverse populations with HIV, hypertension, and diabetes, we believe that patients who are more disempowered and disenfranchised at baseline attain greater benefit from becoming apprentices in their care.
Another potential limitation is that hypertension was treated in isolation in this study. In fact, many of the subjects had comorbid conditions and were being treated for them simultaneously at the APF. Future work will need to address how the apprenticeship approach and accompanying technology can support the management of multiple comorbid conditions. At the same time, we believe that setting aggressive goals for one condition at a time and achieving these goals over a short period, such as 3 months, will be an important strategy in effectively engaging patients as active participants in their care and helping them to develop self-efficacy. As they develop competency for one condition, they become more capable of managing the others. If they were to attempt to tackle all of the problems simultaneously, it could be overwhelming and ineffective.
Conclusions
This study provides encouraging evidence that, in the management of hypertension, technology-supported apprenticeship can improve the outcomes, cost, and experience of care. By embracing the potential of patients while at the same time optimizing support from clinicians and leveraging information technology for cost-effective scaling, it has the potential to have a tremendous impact across the spectrum of chronic disease.
Three core tenants of technology-supported apprenticeship have surfaced as the product of this work, and they may serve as a useful guide to other efforts improving care delivery: First, patients are the most underutilized resource in health care. Technology-supported apprenticeship harnesses the contribution of the patient and values the development of self-efficacy to the extent that apprentices can become masters. It supports patients in achieving a pinnacle of patient empowerment.
Second, health takes place in the everyday lives of patients, not in a doctor’s office or hospital. Technology-supported apprenticeship appreciates that situated learning is the key to mastery of chronic disease management and strives to support patients continuously in the context of their lives.
Third, collaboration and information transparency, not just information access, are critical. Technology-supported apprenticeship embraces information technology to maximize collaboration among novices and masters and to provide common ground through complete transparency.
Acknowledgments: This study was completed as part of John O. Moore’s PhD thesis at the MIT Media Lab. Mitchel Resnick, PhD, and Pattie Maes, PhD, were members of the thesis committee along with authors Franklin H. Moss, PhD, and David C. Judge, MD, and their advice was critical in the development of the technology-supported apprenticeship approach.
Corresponding author: John O. Moore, MD, PhD, [email protected]
Funding/support: This work was supported, in part, by the CIMIT Prize for Primary Healthcare from the Center for Integration of Medicine & Innovative Technology, Boston, MA.
Financial disclosures: John O. Moore, Frank Moss, and Scott Gilroy have a health information technology company focused on building software solutions for improving chronic disease management. This company does not yet have a product for sale.
1. Recent trends in the prevalence of high blood pressure and its treatment and control. National Center for Health Statistics. Hyattsville, MD; 2010.
2. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–72. Erratum in: JAMA 2003;290:197.
3. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20.
4. Ardery G, Carter BL, Milchak JL, et al. Explicit and implicit evaluation of physician adherence to hypertension guidelines. J Clin Hypertens (Greenwich) 2007;9:113–9.
5. Vrijens B, Vincze G, Kristanto P, et al. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008;336:1114–7.
6. Mellen PB, Gao SK, Vitolins MZ, Goff DC Jr. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med 2008;168:308–14.
7. Davis K. Expenditures for hypertension among adults age 18 and older, 2009: estimates for the U.S. civilian noninstitutionalized population. Rockville, MD: Agency for Healthcare Research and Quality; June 2012. Available at http://meps.ahrq.gov/mepsweb/data_files/publications/st371/stat371.shtml.
8. Hodgson TA, Liming C. Medical care expenditures for hypertension, its complications, and its comorbidities. Med Care 2001;39:599–615.
9. Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011;123:933–44.
10. Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20:64–78.
11. McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomized controlled trial. Lancet 2010;376:163–72.
12. Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA 2008;299:2857–67.
13. Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA 2013;310:46–56.
14. Magid DJ, Olson KL, Billups SJ, et al. A pharmacist-led, American Heart Association Heart360 Web-enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes 2013;6:157–63.
15. Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ 2009;35:641–51.
16. Collins A, Brown J, Newman SE. Cognitive apprenticeship: Teaching the crafts of reading, writing, and mathematics. In: Knowing, learning, and instruction: Essays in honor of Robert Glaser. Lawrence Erlbaum Associates; 1989:453–94.
17. Resnick M. Rethinking learning in the digital age. In: Kirkman G, editor. The global information technology report: readiness for a networked world. Oxford University Press; 2002.
18. Koschmann T. Paradigm shifts and instructional technology. In: Koschmann T, editor. CSCL: Theory and practice of an emerging paradigm. Lawrence Erlbaum Associates; 1996:83–124.
19. Brown JS, Adler RP. Minds on fire: open education, the long tail, and learning 2.0. Educause Rev 2008;43:16–32.
20. Collins A, Halverson R. The second educational revolution: rethinking education in the age of technology. J Comp Assist Learn 2010;26:18–27.
21. Dewey J. Experience and education. New York: Collier Books; 1938.
22. Lave J. Situated learning: legitimate peripheral participation (Learning in Doing: Social, Cognitive, and Computational Perspectives). Cambridge University Press; 1991.
23. Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol 2009;64:527–37.
24. Moore SM, Charvat J. Promoting health behavior change using appreciative inquiry: moving from deficit models to affirmation models of care. Fam Community Health 2007;30 Supp 1:S64–74.
From the Massachusetts Institute of Technology (Dr. Moore, Dr. Moss and Mr. Gilroy) and the Massachusetts General Hospital (Ms. Marshall, Dr. Judge, Dr. Crocker, and Dr. Zusman), Boston, MA.
Abstract
- Objective: To compare technology-supported appren-ticeship in hypertension management with a successful coaching model at Massachusetts General Hospital.
- Methods: A randomized controlled trial was conducted. Adult patients with uncontrolled essential hypertension (average blood pressure (BP) 148/87 mm Hg) were recruited in a staggered fashion for a 12-week study period. Intervention subjects received apprenticeship support from a nurse health coach through the CollaboRhythm application on a tablet computer. Patients self-tracked medication adherence and blood pressure (via wireless device) and the coach helped them to continuously progress through lifestyle change and medication adjustment using integrated messaging. Control subjects received support from the same coach but through traditional channels of office visits, phone calls, and e-mail.
- Results: 42 of 44 subjects completed the study. Intervention subjects achieved a greater decrease in systolic BP at 12 weeks than control subjects (26.3 mm Hg vs. 16.0 mm Hg, P = 0.009). A greater percentage of intervention subjects achieved goal BP ≤ 130/80 mm Hg (75.0% vs. 31.8%, P = 0.003) and 100% of them achieved goal BP ≤ 140/90 mmHg. They also rated the experience higher, although this finding was not statistically significant (8.9 vs. 7.6, P = 0.12). There was a trend toward increased cost for intervention subjects ($67.50 vs. $53.41, P = 0.15), but the projected cost is much less than standard care ($248/patient/year).
- Conclusion: This study provides encouraging evidence that technology-supported apprenticeship can improve the outcomes, cost, and experience of care in managing hypertension.
Hypertension affects approximately 33% of the U.S. adult population [1]. Antihypertensive treatment has been shown to be effective at preventing complications [2,3]. Unfortunately, estimates suggest that the majority of those diagnosed with hypertension do not have their blood pressure controlled [1]. This failure is due to both clinician and patient factors. Mean adherence of clinicians to guidelines is estimated at 53.5% [4]. An electronic monitoring study showed that half of patients who are prescribed medications stop taking them within 1 year [5]. Of those who take their medications, about 10% have adherence issues on any given day and about 50% have significant adherence issues in the course of their treatment [5]. Adherence to diet and exercise self-management is even more dismal, with rates below 20% [6]. Hypertension is an expensive problem with direct medical costs (treatment and complications) greater than $100 billion a year and equally high indirect costs (lost productivity) [7–9].
In the management of chronic diseases, there is a significant trend toward empowering patients with more control and toward providing more longitudinal coaching from clinicians and from peers [10–15]. Technology-supported apprenticeship is a model of chronic disease management that builds on the success of self-management and coaching, but it is more ambitious in that its goal is for patients to lead their care with the support of health coaches and supervising clinicians. It is informed by the field of learning science, particularly in how technology can be used effectively to support learning [16–20]. Apprenticeship refers to the tutelage of a community of novices in a skill or trade by one or more masters through situated learning. Situated learning refers to the process in which novices learn through participation in legitimate tasks in the same physical and social context where they will need to perform them once independent [21,22]. It is opposed to learning through contrived exercises in an artificial environment like a classroom.
In technology-supported apprenticeship, patients are the novice apprentices of master coaches. Technology provides scaffolding and communication tools to allow coaches to support the patient in the management of disease within the context of daily life rather than in the clinician’s office. Patients are supported in gradually developing self-efficacy and independence until they are skilled enough to lead their care and even to help coach others to success. The hypothesis is that embracing the contribution of the patient to this extent will reap unparalleled rewards in the experience, outcomes, and cost of care.
We conducted a randomized controlled trial to assess whether a technology-supported apprenticeship in hyper-tension management would improve blood pressure control compared with a successful coaching model.
Methods
Setting
The health coaching model at the Ambulatory Practice of the Future (APF) at the Massachusetts General Hospital is designed to impact the whole health ofpatients. In the scope of hypertension management, a nurse health coach, under the supervision of a physician, is responsible for improving outcomes through longitudinal support via office visits, phone calls, and e-mails. Diet, exercise, stress management, and medication therapy are all emphasized through health coaching techniques, such as motivational interviewing and appreciative inquiry [23,24]. Patients are referred to dieticians, exercise coaches, mind-body specialists, and others as desired. Prior to the start of this study, the APF was outperforming the national average with ~70% of hypertensive patients in the practice below clinically recommended goal blood pressures.
Recruitment
The study was advertised to all clinical staff of the APF through word of mouth. Since the practice was relatively young, it also had a registry of patients with elevated blood pressure that had not been addressed. Adult patients (> 18 years old) from the registry or from routine visits with essential hypertension (average blood pressure ≥ 140/90 and ≤ 180/120) who were taking 0 or 1 medications and had internet connectivity were eligible for inclusion in the study. Patients with a history of hypotension, syncope, hypertensive urgency, hypertensive emergency, labile hypertension, and proven coronary artery disease were excluded, as were patients with significant visual, auditory, or cognitive impairment and patients who were not proficient in English. Clinical staff notified the nurse health coach for the study on identification of any eligible subjects. The same nurse health coach recruited and cared for all intervention and control subjects.
The nurse health coach contacted each eligible patient to assess interest. Interested patients were scheduled for an appointment to commence the study. A process of written informed consent was carried out with each study subject. Each subject was assigned the next sequential study number, which was pre-randomized to either the intervention or the control group.
The study period for each subject was 12 weeks +/– 2 weeks with staggered recruitment. Twelve weeks represents the minimal time required to progress through the standardized Medication Adjustment Plan that was used, assuming a minimum time of 2 weeks on each medication before a change is considered. A recruitment window from 1 March 2013 until 31 May 2013 was used. The goal was to recruit between 40 and 60 subjects, since statistical analysis revealed that a sample size of 36 was sufficient to detect a 5 mm Hg difference in the decrease in systolic blood pressure between groups given a 4 mm Hg standard deviation.
Intervention
CollaboRhythm is a software platform that was developed at the MIT Media Lab and designed to support the principles of technology-supported apprenticeship. Patient tracking tools document progress, visualizations highlight associations between actions and outcomes, and personalized decision support encourages self-efficacy. Powerful virtual visits and instant messaging allow master clinicians to provide adaptive coaching within the context of daily life rather than in the artificial environment of the office. Applications can be deployed cross-platform to cell phones, tablets, computers, etc.
A simplified system was created for hypertension management. It is optimized for tablet deployment and focuses on instant messaging for communications. The patient uses a wireless blood pressure monitor (D40b model by ForaCare®) to take blood pressure measurements. The device is paired with a tablet application to automatically report measurements. The patient self-reports medication adherence using the tablet application. Patient data is visualized in a daily clock and weekly charts to promote proactive behavior and self-reflection. Decision support for medication adjustment is paired with the charts. The patient’s data are synchronized with the coach’s tablet application via a collaborative health record server implemented using the Indivo X personally controlled health record (Children’s Hospital Boston, indivohealth.org) code base. Instant messaging between the patient and coach is implemented using a real-time messaging server. The applications for the patient and the coach are identical, but the coach’s application is configured to allow switching between patient records in order to manage a number of patients.
The user experience was designed based on our years of exploration at the MIT Media Lab of the psychology of illness and the impact that technology could have on patient empowerment and patient-clinician collaboration. It is important to note that the CollaboRhythm application is different from typical electronic reminder applications. In fact, the application never alarms at patients, even if they forget to perform their health actions. Instead, the application focuses on providing awareness for proactive decision-making, self-reflection, and support from the coach.
Protocol Common to Control and Intervention Subjects
Following informed consent, a baseline blood pressure and heart rate were measured for each subject using the same automated sphygmomanometer. Weight was also measured and a hypertension knowledge assessment (a simple survey about normal blood pressures and the effects of diet, exercise, and medication that was created for the purpose of this study) was completed. The initial medication load was determined using the Medication Adjustment Plan as a reference and each dose step as a unit of 1. For example, if a subject was already on lisinopril 40 mg at the start of the study, the initial medication load was 2.
The nurse health coach conducted an introductory visit with each subject including motivational interviewing to assess their health values and to discuss
hypertension management goals. The subject and coach made shared decisions about diet, exercise, stress management, and medication. The same medication titration algorithm was used for both control and interventional
subjects.
At the conclusion of the study period, subjects in both groups returned for an exit visit. Blood pressure and heart rate were measured using the same automated sphygmomanometer that was used at the initial visit. Weight was measured using the same scale as the initial visit. A hypertension knowledge assessment was completed and an exit interview was conducted. The change in medication load was determined as well. For example, if a subject started the study on lisinopril 20 mg and ended the study on lisinopril 40 mg, the increase in medication load was 1.
Protocol Specifics for Intervention Subjects
The apprenticeship model of chronic disease management was discussed with the nurse health coach and with APF team prior to the study. It was also implicit in the design of the CollaboRhythm tablet application.
During the introduction visit, subjects in the inter-vention group received instructions from the nurse health coach on how to use the CollaboRhythm tablet application to self-track their medication adherence, to review progress using the charts, to propose or agree with changes in hypertension medications, and to communicate with messages.
Subjects in the intervention group received their hyper-tension care through the CollaboRhythm tablet application. All instant messages between the intervention subjects and the nurse health coach were automatically documented electronically. Other forms of communication were documented in a spreadsheet. During the exit visit, the tablet computer and the wireless blood pressure meter were returned.
Protocol Specifics for Control Subjects
Between the introduction and exit visits, subjects in the control group received standard hypertension care from the nurse health coach at the APF. The coach instructed subjects to check their blood pressures 3 to 5 times a week. They had the option of purchasing a cuff, using a monitor at work, or using a monitor at a facility such as a pharmacy or grocery store. Communication took place through
office visits, phone calls, and e-mails. All communications with control subjects were documented for the purposes of this study by the nurse health coach in a spread-
sheet.
Outcomes of Interest
The primary outcomes of interest were the absolute decrease in systolic and diastolic blood pressure and the number of subjects who reached the blood pressure goal of less than or equal to 130/80 mm Hg. This more aggressive blood pressure goal was chosen for a number of reasons: (1) it is not uncommon to set a lower blood pressure goal for home measurements to avoid patients hovering just at the 140/90 goal and not getting the true benefit of reduced blood pressure; and (2) subjects were supported in improving diet, exercise, and stress management in addition to pharmacologic therapy. The 140/90 cut-off (now 150/90 in patients over 60) is focused on pharmacologic therapy [2,3].
The secondary outcomes included the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg (for comparison to other published literature), the number of subjects who achieved greater than a 10 mm Hg decrease in systolic and greater than a 5 mm Hg decrease in diastolic blood pressure, the change in medication load, the absolute decrease in weight, the number of subjects who lost at least 5 lb, a hypertension knowledge score assessed by a pre- and post-study test, a rating of satisfaction in care, and the amount of clinician time required in the care.
Statistical Methods
The study results were analyzed by the intention-to-treat approach. All subjects who returned for the final study visit were included in the analysis regardless of their adherence to the protocol. Subjects who did not return for the study exit visit were not included in the analysis because it would be impossible to determine the change in blood pressure without a final measurement. A 2-tailed Student’s t test for independent samples was used for all comparisons of the mean of continuous variables between the control and intervention groups. A 2-tailed Student’s t test for dependent samples was used for all comparisons between pre- and post-study variables within the control and the intervention group. A chi-square test was used for all comparisons of categorical variables between the groups, except when the expected values in the 2x2 table were below 5. Fisher’s exact test was used in this scenario, which applied to the secondary outcome of the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg.
Oversight
This study was approved by the institutional review boards at the Massachusetts Institute of Technology and the Massachusetts General Hospital.
Results
There were a total of 44 subjects recruited for the study. One intervention subject and one control subject were lost to follow-up, leaving 42 subjects who completed the study exit visit.
Baseline Statistics
Clinical Outcomes
Cost
 Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Experience
Thirteen control subjects and 16 intervention subjects provided an experience rating during their exit interview from the study. There was a trend toward greater satisfaction by intervention subjects that was not statistically significant (8.9 vs. 7.6, P = 0.12). The majority of feedback from intervention subjects was obtained through the exit interview. The feedback was overwhelmingly positive. All of the subjects wanted to continue using the CollaboRhythm application after the end of the study. Some who had reached goal only wanted to use it sporadically as a “check-in,” but the majority wanted to use it daily as they had for the study for an indefinite period of time. They felt that the burden of reporting was easily balanced by the value of being able to track progress and get the efficient support of a health coach. They related that awareness of the associations between actions (diet, exercise, stress management, medication adherence) and blood pressure outcomes was integral to their success and their positive experience with the application. Subjects responded very favorably to the concept of leading their care. Some comments from patients include: “It felt good to take responsibility,” “No one has ever asked me to take responsibility for my health,” and “I developed confidence that I never would have had.” The nurse coach commented multiple times how delighted she was with the level of patient engagement and excitement. She also did not want to stop using the application at the end of the study.
The main complaints about the program from both subjects and the health coach were on performance. They wanted the application to load faster and to save data faster.
Discussion
This study provides encouraging evidence that technology-supported apprenticeship can dramatically improve the outcomes, cost, and experience of care in the management of hypertension.
A 26.3 mm Hg average decrease in systolic blood pressure for intervention subjects in 3 months is significantly better than the standard of care and the best of the best in published interventions. [1,11–14]. The same is true for a rate of 100% of patients achieving goal blood pressure < 140/90 mm Hg.
We believe several factors contribute to the success of our program: (1) supporting subjects in the mission of leading their care, (2) rich real-time feedback for self-reflection, (3) emphasis on short-term goals, (4) promise of medication reduction with goal achievement, and (5) social support and accountability that come with having a continuously available coach who had immediate data access.
Other studies have had web communication components, self-titration components, and coaching components. In a progressive study by McManus [11], subjects in the intervention group self-tracked their blood pressure and self-titrated their hypertension medications while control subjects received routine care. Self-managing patients achieved a decrease in systolic blood pressure of 17.6 mm Hg over 12 months while controls only achieved a decrease of 12.2 mm Hg. Self-managing patients were more aggressive in adding new medications and did not have increased incidence of side effects. A study by Green [12] showed that subjects with home blood pressure monitoring, a web training course, and web-based pharmacist coaching achieved a 14.2 mm Hg decrease in systolic blood pressure over 12 months and that 56% reached goal blood pressure (< 140/90 mm Hg). Subjects who received routine care only achieved a 5.3 mm Hg decrease in systolic blood pressure and only 31% reached goal blood pressure. Margolis [13] and Magid [14] conducted studies similar to Green's with pharmacist-led care. In Margolis’ study, 71.8% of inter-vention subjects study achieved goal at 6 months with a mean decrease in systolic blood pressure of 21.5 mm Hg. These results were impressively stable at 18 months [13]. In Magid’s study, 54.1% of intervention subjects achieved goal at 6 months with a mean decrease in systolic blood pressure of 20.7 mm Hg [14].
The technology-supported apprenticeship model was inspired by the exceptional results of these studies, but we believe that it represents a significant step forward in patient engagement. In these studies, the tools were typically more burdensome than empowering, the titration more prescriptive than motivational, and the coaching more timed and paternalistic than continuous and nurturing. Technology-supported apprenticeship relies on more powerful tools for collaboration and aspires for the patient to lead the care rather than the clinician. It has the potential to produce greater self-efficacy, which results in better outcomes at lower cost.
Cost Implications
The 100% rate of attainment of systolic blood pressure < 140 mm Hg in our intervention subjects has the poten-tial to contribute to substantial cost savings through reducing complications. The cost of complications per patient per year is approximately $1275, and attainment of goal blood pressure on average results in approximately 35% decrease in complications [2,7–9] Therefore, it is reasonable to expect at least $446 savings in downstream costs per patient per year with this intervention. This has notable public health implications given that there are approximately 32 million patients in the United States with diagnosed hypertension that is uncontrolled [1]. Cost saving at scale could be more than $14 billion.
Typically, interventions that produce downstream savings in health care require some upstream investment. An exciting aspect of this intervention is that it was significantly less costly, at $67.50 per patient, as compared with the standard of care, at $248 per patient per year [7–9]. Most of the responsibility was embraced by the patients, and the nurse coach needed only to provide occasional social and clinical support. Return office visits were almost completely eliminated and goals were achieved in a fraction of the time. The cost of the technology is effectively negligible given that patients will be able to use their own cell phones and tablets and their own blood pressure cuffs. Based on the prevalence of hypertension, a primary care practice with 2000 patients would be expected to have 600 with hypertension. At $180.50 in savings per patient per year, a profit of $108,300 could be retained if the same reimbursement was provided for this more effective care. At the same time, this more efficient and scalable model of care could allow a practice to care for a larger number of patients without compromising the experience for patients or clinicians.
Limitations and Future Directions
An important limitation of this study is its small sample size. The efficiency and cost analysis suggests that the intervention is highly suitable for scaling but, until this is studied, there is the risk that the small sample size may misrepresent the average effect on a larger population and overestimate the size of a population that a coach can manage. Future work will need to include much larger populations.
Another limitation was the short follow-up period. A key benefit of apprenticeship is that it theoretically results in greater and more sustainable self-efficacy than other models of patient engagement that are not as grounded in learning science and that do not engage the patient as deeply. Follow-up visits for both control and intervention subjects will be conducted at 1 year to assess the sustainability of the blood pressure improvements.
The fact that the population was from a single practice also presents the possibility that the subjects being studied were more interested and/or capable than a larger, more general population. This is likely to be true, since many of the patients at the APF sought it out in the hope of receiving a new health care experience. Future work will need to address patient populations from diverse socioeconomic situations and diverse cultures. Based on pilot studies that we have done with diverse populations with HIV, hypertension, and diabetes, we believe that patients who are more disempowered and disenfranchised at baseline attain greater benefit from becoming apprentices in their care.
Another potential limitation is that hypertension was treated in isolation in this study. In fact, many of the subjects had comorbid conditions and were being treated for them simultaneously at the APF. Future work will need to address how the apprenticeship approach and accompanying technology can support the management of multiple comorbid conditions. At the same time, we believe that setting aggressive goals for one condition at a time and achieving these goals over a short period, such as 3 months, will be an important strategy in effectively engaging patients as active participants in their care and helping them to develop self-efficacy. As they develop competency for one condition, they become more capable of managing the others. If they were to attempt to tackle all of the problems simultaneously, it could be overwhelming and ineffective.
Conclusions
This study provides encouraging evidence that, in the management of hypertension, technology-supported apprenticeship can improve the outcomes, cost, and experience of care. By embracing the potential of patients while at the same time optimizing support from clinicians and leveraging information technology for cost-effective scaling, it has the potential to have a tremendous impact across the spectrum of chronic disease.
Three core tenants of technology-supported apprenticeship have surfaced as the product of this work, and they may serve as a useful guide to other efforts improving care delivery: First, patients are the most underutilized resource in health care. Technology-supported apprenticeship harnesses the contribution of the patient and values the development of self-efficacy to the extent that apprentices can become masters. It supports patients in achieving a pinnacle of patient empowerment.
Second, health takes place in the everyday lives of patients, not in a doctor’s office or hospital. Technology-supported apprenticeship appreciates that situated learning is the key to mastery of chronic disease management and strives to support patients continuously in the context of their lives.
Third, collaboration and information transparency, not just information access, are critical. Technology-supported apprenticeship embraces information technology to maximize collaboration among novices and masters and to provide common ground through complete transparency.
Acknowledgments: This study was completed as part of John O. Moore’s PhD thesis at the MIT Media Lab. Mitchel Resnick, PhD, and Pattie Maes, PhD, were members of the thesis committee along with authors Franklin H. Moss, PhD, and David C. Judge, MD, and their advice was critical in the development of the technology-supported apprenticeship approach.
Corresponding author: John O. Moore, MD, PhD, [email protected]
Funding/support: This work was supported, in part, by the CIMIT Prize for Primary Healthcare from the Center for Integration of Medicine & Innovative Technology, Boston, MA.
Financial disclosures: John O. Moore, Frank Moss, and Scott Gilroy have a health information technology company focused on building software solutions for improving chronic disease management. This company does not yet have a product for sale.
From the Massachusetts Institute of Technology (Dr. Moore, Dr. Moss and Mr. Gilroy) and the Massachusetts General Hospital (Ms. Marshall, Dr. Judge, Dr. Crocker, and Dr. Zusman), Boston, MA.
Abstract
- Objective: To compare technology-supported appren-ticeship in hypertension management with a successful coaching model at Massachusetts General Hospital.
- Methods: A randomized controlled trial was conducted. Adult patients with uncontrolled essential hypertension (average blood pressure (BP) 148/87 mm Hg) were recruited in a staggered fashion for a 12-week study period. Intervention subjects received apprenticeship support from a nurse health coach through the CollaboRhythm application on a tablet computer. Patients self-tracked medication adherence and blood pressure (via wireless device) and the coach helped them to continuously progress through lifestyle change and medication adjustment using integrated messaging. Control subjects received support from the same coach but through traditional channels of office visits, phone calls, and e-mail.
- Results: 42 of 44 subjects completed the study. Intervention subjects achieved a greater decrease in systolic BP at 12 weeks than control subjects (26.3 mm Hg vs. 16.0 mm Hg, P = 0.009). A greater percentage of intervention subjects achieved goal BP ≤ 130/80 mm Hg (75.0% vs. 31.8%, P = 0.003) and 100% of them achieved goal BP ≤ 140/90 mmHg. They also rated the experience higher, although this finding was not statistically significant (8.9 vs. 7.6, P = 0.12). There was a trend toward increased cost for intervention subjects ($67.50 vs. $53.41, P = 0.15), but the projected cost is much less than standard care ($248/patient/year).
- Conclusion: This study provides encouraging evidence that technology-supported apprenticeship can improve the outcomes, cost, and experience of care in managing hypertension.
Hypertension affects approximately 33% of the U.S. adult population [1]. Antihypertensive treatment has been shown to be effective at preventing complications [2,3]. Unfortunately, estimates suggest that the majority of those diagnosed with hypertension do not have their blood pressure controlled [1]. This failure is due to both clinician and patient factors. Mean adherence of clinicians to guidelines is estimated at 53.5% [4]. An electronic monitoring study showed that half of patients who are prescribed medications stop taking them within 1 year [5]. Of those who take their medications, about 10% have adherence issues on any given day and about 50% have significant adherence issues in the course of their treatment [5]. Adherence to diet and exercise self-management is even more dismal, with rates below 20% [6]. Hypertension is an expensive problem with direct medical costs (treatment and complications) greater than $100 billion a year and equally high indirect costs (lost productivity) [7–9].
In the management of chronic diseases, there is a significant trend toward empowering patients with more control and toward providing more longitudinal coaching from clinicians and from peers [10–15]. Technology-supported apprenticeship is a model of chronic disease management that builds on the success of self-management and coaching, but it is more ambitious in that its goal is for patients to lead their care with the support of health coaches and supervising clinicians. It is informed by the field of learning science, particularly in how technology can be used effectively to support learning [16–20]. Apprenticeship refers to the tutelage of a community of novices in a skill or trade by one or more masters through situated learning. Situated learning refers to the process in which novices learn through participation in legitimate tasks in the same physical and social context where they will need to perform them once independent [21,22]. It is opposed to learning through contrived exercises in an artificial environment like a classroom.
In technology-supported apprenticeship, patients are the novice apprentices of master coaches. Technology provides scaffolding and communication tools to allow coaches to support the patient in the management of disease within the context of daily life rather than in the clinician’s office. Patients are supported in gradually developing self-efficacy and independence until they are skilled enough to lead their care and even to help coach others to success. The hypothesis is that embracing the contribution of the patient to this extent will reap unparalleled rewards in the experience, outcomes, and cost of care.
We conducted a randomized controlled trial to assess whether a technology-supported apprenticeship in hyper-tension management would improve blood pressure control compared with a successful coaching model.
Methods
Setting
The health coaching model at the Ambulatory Practice of the Future (APF) at the Massachusetts General Hospital is designed to impact the whole health ofpatients. In the scope of hypertension management, a nurse health coach, under the supervision of a physician, is responsible for improving outcomes through longitudinal support via office visits, phone calls, and e-mails. Diet, exercise, stress management, and medication therapy are all emphasized through health coaching techniques, such as motivational interviewing and appreciative inquiry [23,24]. Patients are referred to dieticians, exercise coaches, mind-body specialists, and others as desired. Prior to the start of this study, the APF was outperforming the national average with ~70% of hypertensive patients in the practice below clinically recommended goal blood pressures.
Recruitment
The study was advertised to all clinical staff of the APF through word of mouth. Since the practice was relatively young, it also had a registry of patients with elevated blood pressure that had not been addressed. Adult patients (> 18 years old) from the registry or from routine visits with essential hypertension (average blood pressure ≥ 140/90 and ≤ 180/120) who were taking 0 or 1 medications and had internet connectivity were eligible for inclusion in the study. Patients with a history of hypotension, syncope, hypertensive urgency, hypertensive emergency, labile hypertension, and proven coronary artery disease were excluded, as were patients with significant visual, auditory, or cognitive impairment and patients who were not proficient in English. Clinical staff notified the nurse health coach for the study on identification of any eligible subjects. The same nurse health coach recruited and cared for all intervention and control subjects.
The nurse health coach contacted each eligible patient to assess interest. Interested patients were scheduled for an appointment to commence the study. A process of written informed consent was carried out with each study subject. Each subject was assigned the next sequential study number, which was pre-randomized to either the intervention or the control group.
The study period for each subject was 12 weeks +/– 2 weeks with staggered recruitment. Twelve weeks represents the minimal time required to progress through the standardized Medication Adjustment Plan that was used, assuming a minimum time of 2 weeks on each medication before a change is considered. A recruitment window from 1 March 2013 until 31 May 2013 was used. The goal was to recruit between 40 and 60 subjects, since statistical analysis revealed that a sample size of 36 was sufficient to detect a 5 mm Hg difference in the decrease in systolic blood pressure between groups given a 4 mm Hg standard deviation.
Intervention
CollaboRhythm is a software platform that was developed at the MIT Media Lab and designed to support the principles of technology-supported apprenticeship. Patient tracking tools document progress, visualizations highlight associations between actions and outcomes, and personalized decision support encourages self-efficacy. Powerful virtual visits and instant messaging allow master clinicians to provide adaptive coaching within the context of daily life rather than in the artificial environment of the office. Applications can be deployed cross-platform to cell phones, tablets, computers, etc.
A simplified system was created for hypertension management. It is optimized for tablet deployment and focuses on instant messaging for communications. The patient uses a wireless blood pressure monitor (D40b model by ForaCare®) to take blood pressure measurements. The device is paired with a tablet application to automatically report measurements. The patient self-reports medication adherence using the tablet application. Patient data is visualized in a daily clock and weekly charts to promote proactive behavior and self-reflection. Decision support for medication adjustment is paired with the charts. The patient’s data are synchronized with the coach’s tablet application via a collaborative health record server implemented using the Indivo X personally controlled health record (Children’s Hospital Boston, indivohealth.org) code base. Instant messaging between the patient and coach is implemented using a real-time messaging server. The applications for the patient and the coach are identical, but the coach’s application is configured to allow switching between patient records in order to manage a number of patients.
The user experience was designed based on our years of exploration at the MIT Media Lab of the psychology of illness and the impact that technology could have on patient empowerment and patient-clinician collaboration. It is important to note that the CollaboRhythm application is different from typical electronic reminder applications. In fact, the application never alarms at patients, even if they forget to perform their health actions. Instead, the application focuses on providing awareness for proactive decision-making, self-reflection, and support from the coach.
Protocol Common to Control and Intervention Subjects
Following informed consent, a baseline blood pressure and heart rate were measured for each subject using the same automated sphygmomanometer. Weight was also measured and a hypertension knowledge assessment (a simple survey about normal blood pressures and the effects of diet, exercise, and medication that was created for the purpose of this study) was completed. The initial medication load was determined using the Medication Adjustment Plan as a reference and each dose step as a unit of 1. For example, if a subject was already on lisinopril 40 mg at the start of the study, the initial medication load was 2.
The nurse health coach conducted an introductory visit with each subject including motivational interviewing to assess their health values and to discuss
hypertension management goals. The subject and coach made shared decisions about diet, exercise, stress management, and medication. The same medication titration algorithm was used for both control and interventional
subjects.
At the conclusion of the study period, subjects in both groups returned for an exit visit. Blood pressure and heart rate were measured using the same automated sphygmomanometer that was used at the initial visit. Weight was measured using the same scale as the initial visit. A hypertension knowledge assessment was completed and an exit interview was conducted. The change in medication load was determined as well. For example, if a subject started the study on lisinopril 20 mg and ended the study on lisinopril 40 mg, the increase in medication load was 1.
Protocol Specifics for Intervention Subjects
The apprenticeship model of chronic disease management was discussed with the nurse health coach and with APF team prior to the study. It was also implicit in the design of the CollaboRhythm tablet application.
During the introduction visit, subjects in the inter-vention group received instructions from the nurse health coach on how to use the CollaboRhythm tablet application to self-track their medication adherence, to review progress using the charts, to propose or agree with changes in hypertension medications, and to communicate with messages.
Subjects in the intervention group received their hyper-tension care through the CollaboRhythm tablet application. All instant messages between the intervention subjects and the nurse health coach were automatically documented electronically. Other forms of communication were documented in a spreadsheet. During the exit visit, the tablet computer and the wireless blood pressure meter were returned.
Protocol Specifics for Control Subjects
Between the introduction and exit visits, subjects in the control group received standard hypertension care from the nurse health coach at the APF. The coach instructed subjects to check their blood pressures 3 to 5 times a week. They had the option of purchasing a cuff, using a monitor at work, or using a monitor at a facility such as a pharmacy or grocery store. Communication took place through
office visits, phone calls, and e-mails. All communications with control subjects were documented for the purposes of this study by the nurse health coach in a spread-
sheet.
Outcomes of Interest
The primary outcomes of interest were the absolute decrease in systolic and diastolic blood pressure and the number of subjects who reached the blood pressure goal of less than or equal to 130/80 mm Hg. This more aggressive blood pressure goal was chosen for a number of reasons: (1) it is not uncommon to set a lower blood pressure goal for home measurements to avoid patients hovering just at the 140/90 goal and not getting the true benefit of reduced blood pressure; and (2) subjects were supported in improving diet, exercise, and stress management in addition to pharmacologic therapy. The 140/90 cut-off (now 150/90 in patients over 60) is focused on pharmacologic therapy [2,3].
The secondary outcomes included the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg (for comparison to other published literature), the number of subjects who achieved greater than a 10 mm Hg decrease in systolic and greater than a 5 mm Hg decrease in diastolic blood pressure, the change in medication load, the absolute decrease in weight, the number of subjects who lost at least 5 lb, a hypertension knowledge score assessed by a pre- and post-study test, a rating of satisfaction in care, and the amount of clinician time required in the care.
Statistical Methods
The study results were analyzed by the intention-to-treat approach. All subjects who returned for the final study visit were included in the analysis regardless of their adherence to the protocol. Subjects who did not return for the study exit visit were not included in the analysis because it would be impossible to determine the change in blood pressure without a final measurement. A 2-tailed Student’s t test for independent samples was used for all comparisons of the mean of continuous variables between the control and intervention groups. A 2-tailed Student’s t test for dependent samples was used for all comparisons between pre- and post-study variables within the control and the intervention group. A chi-square test was used for all comparisons of categorical variables between the groups, except when the expected values in the 2x2 table were below 5. Fisher’s exact test was used in this scenario, which applied to the secondary outcome of the number of subjects who reached the blood pressure goal of less than or equal to 140/90 mm Hg.
Oversight
This study was approved by the institutional review boards at the Massachusetts Institute of Technology and the Massachusetts General Hospital.
Results
There were a total of 44 subjects recruited for the study. One intervention subject and one control subject were lost to follow-up, leaving 42 subjects who completed the study exit visit.
Baseline Statistics
Clinical Outcomes
Cost
 Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Table 3 presents a summary of nurse coach communications with subjects and the corresponding cost. The coach communicated with intervention subjects primarily through instant messages using the CollaboRhythm tablet application. There were trends toward more e-mails, phone calls, and office visits in control subjects that were not statistically significant. The total nurse coach time spent per patient was calculated using the following assumptions: instant message = 5 minutes, e-mail = 10 minutes, phone call = 15 minutes, office visit = 30 minutes. It is of note that, although virtual visits (video conferences with the ability to co-navigate patient data) were available as a feature, none were conducted during the course of the study. There was a trend toward intervention subjects receiving more support from the nurse coach that was not statistically significant. The cost associated with nurse coach time was calculated for both control and intervention subjects using the assumption of $50/hour (based on $100,000/year average salary plus benefits for nurse with health coaching certification). On average, intervention subjects received 0.28 hours or 16.8 minutes more time at an additional cost of $14.09.
Experience
Thirteen control subjects and 16 intervention subjects provided an experience rating during their exit interview from the study. There was a trend toward greater satisfaction by intervention subjects that was not statistically significant (8.9 vs. 7.6, P = 0.12). The majority of feedback from intervention subjects was obtained through the exit interview. The feedback was overwhelmingly positive. All of the subjects wanted to continue using the CollaboRhythm application after the end of the study. Some who had reached goal only wanted to use it sporadically as a “check-in,” but the majority wanted to use it daily as they had for the study for an indefinite period of time. They felt that the burden of reporting was easily balanced by the value of being able to track progress and get the efficient support of a health coach. They related that awareness of the associations between actions (diet, exercise, stress management, medication adherence) and blood pressure outcomes was integral to their success and their positive experience with the application. Subjects responded very favorably to the concept of leading their care. Some comments from patients include: “It felt good to take responsibility,” “No one has ever asked me to take responsibility for my health,” and “I developed confidence that I never would have had.” The nurse coach commented multiple times how delighted she was with the level of patient engagement and excitement. She also did not want to stop using the application at the end of the study.
The main complaints about the program from both subjects and the health coach were on performance. They wanted the application to load faster and to save data faster.
Discussion
This study provides encouraging evidence that technology-supported apprenticeship can dramatically improve the outcomes, cost, and experience of care in the management of hypertension.
A 26.3 mm Hg average decrease in systolic blood pressure for intervention subjects in 3 months is significantly better than the standard of care and the best of the best in published interventions. [1,11–14]. The same is true for a rate of 100% of patients achieving goal blood pressure < 140/90 mm Hg.
We believe several factors contribute to the success of our program: (1) supporting subjects in the mission of leading their care, (2) rich real-time feedback for self-reflection, (3) emphasis on short-term goals, (4) promise of medication reduction with goal achievement, and (5) social support and accountability that come with having a continuously available coach who had immediate data access.
Other studies have had web communication components, self-titration components, and coaching components. In a progressive study by McManus [11], subjects in the intervention group self-tracked their blood pressure and self-titrated their hypertension medications while control subjects received routine care. Self-managing patients achieved a decrease in systolic blood pressure of 17.6 mm Hg over 12 months while controls only achieved a decrease of 12.2 mm Hg. Self-managing patients were more aggressive in adding new medications and did not have increased incidence of side effects. A study by Green [12] showed that subjects with home blood pressure monitoring, a web training course, and web-based pharmacist coaching achieved a 14.2 mm Hg decrease in systolic blood pressure over 12 months and that 56% reached goal blood pressure (< 140/90 mm Hg). Subjects who received routine care only achieved a 5.3 mm Hg decrease in systolic blood pressure and only 31% reached goal blood pressure. Margolis [13] and Magid [14] conducted studies similar to Green's with pharmacist-led care. In Margolis’ study, 71.8% of inter-vention subjects study achieved goal at 6 months with a mean decrease in systolic blood pressure of 21.5 mm Hg. These results were impressively stable at 18 months [13]. In Magid’s study, 54.1% of intervention subjects achieved goal at 6 months with a mean decrease in systolic blood pressure of 20.7 mm Hg [14].
The technology-supported apprenticeship model was inspired by the exceptional results of these studies, but we believe that it represents a significant step forward in patient engagement. In these studies, the tools were typically more burdensome than empowering, the titration more prescriptive than motivational, and the coaching more timed and paternalistic than continuous and nurturing. Technology-supported apprenticeship relies on more powerful tools for collaboration and aspires for the patient to lead the care rather than the clinician. It has the potential to produce greater self-efficacy, which results in better outcomes at lower cost.
Cost Implications
The 100% rate of attainment of systolic blood pressure < 140 mm Hg in our intervention subjects has the poten-tial to contribute to substantial cost savings through reducing complications. The cost of complications per patient per year is approximately $1275, and attainment of goal blood pressure on average results in approximately 35% decrease in complications [2,7–9] Therefore, it is reasonable to expect at least $446 savings in downstream costs per patient per year with this intervention. This has notable public health implications given that there are approximately 32 million patients in the United States with diagnosed hypertension that is uncontrolled [1]. Cost saving at scale could be more than $14 billion.
Typically, interventions that produce downstream savings in health care require some upstream investment. An exciting aspect of this intervention is that it was significantly less costly, at $67.50 per patient, as compared with the standard of care, at $248 per patient per year [7–9]. Most of the responsibility was embraced by the patients, and the nurse coach needed only to provide occasional social and clinical support. Return office visits were almost completely eliminated and goals were achieved in a fraction of the time. The cost of the technology is effectively negligible given that patients will be able to use their own cell phones and tablets and their own blood pressure cuffs. Based on the prevalence of hypertension, a primary care practice with 2000 patients would be expected to have 600 with hypertension. At $180.50 in savings per patient per year, a profit of $108,300 could be retained if the same reimbursement was provided for this more effective care. At the same time, this more efficient and scalable model of care could allow a practice to care for a larger number of patients without compromising the experience for patients or clinicians.
Limitations and Future Directions
An important limitation of this study is its small sample size. The efficiency and cost analysis suggests that the intervention is highly suitable for scaling but, until this is studied, there is the risk that the small sample size may misrepresent the average effect on a larger population and overestimate the size of a population that a coach can manage. Future work will need to include much larger populations.
Another limitation was the short follow-up period. A key benefit of apprenticeship is that it theoretically results in greater and more sustainable self-efficacy than other models of patient engagement that are not as grounded in learning science and that do not engage the patient as deeply. Follow-up visits for both control and intervention subjects will be conducted at 1 year to assess the sustainability of the blood pressure improvements.
The fact that the population was from a single practice also presents the possibility that the subjects being studied were more interested and/or capable than a larger, more general population. This is likely to be true, since many of the patients at the APF sought it out in the hope of receiving a new health care experience. Future work will need to address patient populations from diverse socioeconomic situations and diverse cultures. Based on pilot studies that we have done with diverse populations with HIV, hypertension, and diabetes, we believe that patients who are more disempowered and disenfranchised at baseline attain greater benefit from becoming apprentices in their care.
Another potential limitation is that hypertension was treated in isolation in this study. In fact, many of the subjects had comorbid conditions and were being treated for them simultaneously at the APF. Future work will need to address how the apprenticeship approach and accompanying technology can support the management of multiple comorbid conditions. At the same time, we believe that setting aggressive goals for one condition at a time and achieving these goals over a short period, such as 3 months, will be an important strategy in effectively engaging patients as active participants in their care and helping them to develop self-efficacy. As they develop competency for one condition, they become more capable of managing the others. If they were to attempt to tackle all of the problems simultaneously, it could be overwhelming and ineffective.
Conclusions
This study provides encouraging evidence that, in the management of hypertension, technology-supported apprenticeship can improve the outcomes, cost, and experience of care. By embracing the potential of patients while at the same time optimizing support from clinicians and leveraging information technology for cost-effective scaling, it has the potential to have a tremendous impact across the spectrum of chronic disease.
Three core tenants of technology-supported apprenticeship have surfaced as the product of this work, and they may serve as a useful guide to other efforts improving care delivery: First, patients are the most underutilized resource in health care. Technology-supported apprenticeship harnesses the contribution of the patient and values the development of self-efficacy to the extent that apprentices can become masters. It supports patients in achieving a pinnacle of patient empowerment.
Second, health takes place in the everyday lives of patients, not in a doctor’s office or hospital. Technology-supported apprenticeship appreciates that situated learning is the key to mastery of chronic disease management and strives to support patients continuously in the context of their lives.
Third, collaboration and information transparency, not just information access, are critical. Technology-supported apprenticeship embraces information technology to maximize collaboration among novices and masters and to provide common ground through complete transparency.
Acknowledgments: This study was completed as part of John O. Moore’s PhD thesis at the MIT Media Lab. Mitchel Resnick, PhD, and Pattie Maes, PhD, were members of the thesis committee along with authors Franklin H. Moss, PhD, and David C. Judge, MD, and their advice was critical in the development of the technology-supported apprenticeship approach.
Corresponding author: John O. Moore, MD, PhD, [email protected]
Funding/support: This work was supported, in part, by the CIMIT Prize for Primary Healthcare from the Center for Integration of Medicine & Innovative Technology, Boston, MA.
Financial disclosures: John O. Moore, Frank Moss, and Scott Gilroy have a health information technology company focused on building software solutions for improving chronic disease management. This company does not yet have a product for sale.
1. Recent trends in the prevalence of high blood pressure and its treatment and control. National Center for Health Statistics. Hyattsville, MD; 2010.
2. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–72. Erratum in: JAMA 2003;290:197.
3. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20.
4. Ardery G, Carter BL, Milchak JL, et al. Explicit and implicit evaluation of physician adherence to hypertension guidelines. J Clin Hypertens (Greenwich) 2007;9:113–9.
5. Vrijens B, Vincze G, Kristanto P, et al. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008;336:1114–7.
6. Mellen PB, Gao SK, Vitolins MZ, Goff DC Jr. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med 2008;168:308–14.
7. Davis K. Expenditures for hypertension among adults age 18 and older, 2009: estimates for the U.S. civilian noninstitutionalized population. Rockville, MD: Agency for Healthcare Research and Quality; June 2012. Available at http://meps.ahrq.gov/mepsweb/data_files/publications/st371/stat371.shtml.
8. Hodgson TA, Liming C. Medical care expenditures for hypertension, its complications, and its comorbidities. Med Care 2001;39:599–615.
9. Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011;123:933–44.
10. Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20:64–78.
11. McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomized controlled trial. Lancet 2010;376:163–72.
12. Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA 2008;299:2857–67.
13. Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA 2013;310:46–56.
14. Magid DJ, Olson KL, Billups SJ, et al. A pharmacist-led, American Heart Association Heart360 Web-enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes 2013;6:157–63.
15. Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ 2009;35:641–51.
16. Collins A, Brown J, Newman SE. Cognitive apprenticeship: Teaching the crafts of reading, writing, and mathematics. In: Knowing, learning, and instruction: Essays in honor of Robert Glaser. Lawrence Erlbaum Associates; 1989:453–94.
17. Resnick M. Rethinking learning in the digital age. In: Kirkman G, editor. The global information technology report: readiness for a networked world. Oxford University Press; 2002.
18. Koschmann T. Paradigm shifts and instructional technology. In: Koschmann T, editor. CSCL: Theory and practice of an emerging paradigm. Lawrence Erlbaum Associates; 1996:83–124.
19. Brown JS, Adler RP. Minds on fire: open education, the long tail, and learning 2.0. Educause Rev 2008;43:16–32.
20. Collins A, Halverson R. The second educational revolution: rethinking education in the age of technology. J Comp Assist Learn 2010;26:18–27.
21. Dewey J. Experience and education. New York: Collier Books; 1938.
22. Lave J. Situated learning: legitimate peripheral participation (Learning in Doing: Social, Cognitive, and Computational Perspectives). Cambridge University Press; 1991.
23. Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol 2009;64:527–37.
24. Moore SM, Charvat J. Promoting health behavior change using appreciative inquiry: moving from deficit models to affirmation models of care. Fam Community Health 2007;30 Supp 1:S64–74.
1. Recent trends in the prevalence of high blood pressure and its treatment and control. National Center for Health Statistics. Hyattsville, MD; 2010.
2. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–72. Erratum in: JAMA 2003;290:197.
3. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20.
4. Ardery G, Carter BL, Milchak JL, et al. Explicit and implicit evaluation of physician adherence to hypertension guidelines. J Clin Hypertens (Greenwich) 2007;9:113–9.
5. Vrijens B, Vincze G, Kristanto P, et al. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008;336:1114–7.
6. Mellen PB, Gao SK, Vitolins MZ, Goff DC Jr. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med 2008;168:308–14.
7. Davis K. Expenditures for hypertension among adults age 18 and older, 2009: estimates for the U.S. civilian noninstitutionalized population. Rockville, MD: Agency for Healthcare Research and Quality; June 2012. Available at http://meps.ahrq.gov/mepsweb/data_files/publications/st371/stat371.shtml.
8. Hodgson TA, Liming C. Medical care expenditures for hypertension, its complications, and its comorbidities. Med Care 2001;39:599–615.
9. Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011;123:933–44.
10. Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20:64–78.
11. McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomized controlled trial. Lancet 2010;376:163–72.
12. Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA 2008;299:2857–67.
13. Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA 2013;310:46–56.
14. Magid DJ, Olson KL, Billups SJ, et al. A pharmacist-led, American Heart Association Heart360 Web-enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes 2013;6:157–63.
15. Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ 2009;35:641–51.
16. Collins A, Brown J, Newman SE. Cognitive apprenticeship: Teaching the crafts of reading, writing, and mathematics. In: Knowing, learning, and instruction: Essays in honor of Robert Glaser. Lawrence Erlbaum Associates; 1989:453–94.
17. Resnick M. Rethinking learning in the digital age. In: Kirkman G, editor. The global information technology report: readiness for a networked world. Oxford University Press; 2002.
18. Koschmann T. Paradigm shifts and instructional technology. In: Koschmann T, editor. CSCL: Theory and practice of an emerging paradigm. Lawrence Erlbaum Associates; 1996:83–124.
19. Brown JS, Adler RP. Minds on fire: open education, the long tail, and learning 2.0. Educause Rev 2008;43:16–32.
20. Collins A, Halverson R. The second educational revolution: rethinking education in the age of technology. J Comp Assist Learn 2010;26:18–27.
21. Dewey J. Experience and education. New York: Collier Books; 1938.
22. Lave J. Situated learning: legitimate peripheral participation (Learning in Doing: Social, Cognitive, and Computational Perspectives). Cambridge University Press; 1991.
23. Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol 2009;64:527–37.
24. Moore SM, Charvat J. Promoting health behavior change using appreciative inquiry: moving from deficit models to affirmation models of care. Fam Community Health 2007;30 Supp 1:S64–74.