User login
CHEST membership is moving forward
We asked you, and you told us what you need to make your tomorrows greater than today. That’s why we’re upgrading our membership philosophy and structure starting this May, allowing you to:
• Collaborate more with integrated programming and CHEST membership available to all members of your clinical care team.
• Engage more by choosing the membership level that gives you the benefits you want.
• Achieve more with streamlined access to our online systems, making it easier than ever to tap into the wealth of resources CHEST offers you.
Learn more about the new membership model at chestnet.org/tomorrow. See videos of Dr. Curtis N. Sessler, FCCP, CHEST President, explaining why we’re changing the membership model, and Paul Markowski, CHEST EVP/ CEO, describing the benefits of the three levels of membership. Get answers to commonly asked questions, and, if your question isn’t answered there, submit a question of your own. Visit now to find out how your CHEST membership can help make your tomorrows greater than today.
We asked you, and you told us what you need to make your tomorrows greater than today. That’s why we’re upgrading our membership philosophy and structure starting this May, allowing you to:
• Collaborate more with integrated programming and CHEST membership available to all members of your clinical care team.
• Engage more by choosing the membership level that gives you the benefits you want.
• Achieve more with streamlined access to our online systems, making it easier than ever to tap into the wealth of resources CHEST offers you.
Learn more about the new membership model at chestnet.org/tomorrow. See videos of Dr. Curtis N. Sessler, FCCP, CHEST President, explaining why we’re changing the membership model, and Paul Markowski, CHEST EVP/ CEO, describing the benefits of the three levels of membership. Get answers to commonly asked questions, and, if your question isn’t answered there, submit a question of your own. Visit now to find out how your CHEST membership can help make your tomorrows greater than today.
We asked you, and you told us what you need to make your tomorrows greater than today. That’s why we’re upgrading our membership philosophy and structure starting this May, allowing you to:
• Collaborate more with integrated programming and CHEST membership available to all members of your clinical care team.
• Engage more by choosing the membership level that gives you the benefits you want.
• Achieve more with streamlined access to our online systems, making it easier than ever to tap into the wealth of resources CHEST offers you.
Learn more about the new membership model at chestnet.org/tomorrow. See videos of Dr. Curtis N. Sessler, FCCP, CHEST President, explaining why we’re changing the membership model, and Paul Markowski, CHEST EVP/ CEO, describing the benefits of the three levels of membership. Get answers to commonly asked questions, and, if your question isn’t answered there, submit a question of your own. Visit now to find out how your CHEST membership can help make your tomorrows greater than today.
New Publisher for CHEST
Elsevier, a world-leading provider of scientific, technical, and medical information products and services, and the American College of Chest Physicians (CHEST), a world-renowned publisher of evidence-based practice guidelines in chest medicine, have announced that Elsevier will publish the organization’s flagship journal CHEST as of January 1, 2016. This significant and exciting piece of news that will positively affect the future of the journal is a licensing agreement, wherein CHEST retains all ownership of the journal, copyright, trademark, and editorial decision-making. Elsevier’s role will be heavily focused on the business and operational aspects of publishing the journal and will provide significant resources to help us continue to take CHEST to a higher level.
“We are excited to begin this new relationship with Elsevier and we look forward to CHEST’s continued success under this collaboration,” said Paul Markowski, CEO and Executive Vice President of the American College of Chest Physicians. “CHEST will remain a leading publication designed to aid clinicians in providing the best patient care possible.”
Dr. Richard Irwin, Master FCCP, and Editor in Chief of the journal, said, “Our publishing agreement with Elsevier will allow CHEST to remain competitive, will help us to distribute research papers to a larger audience, and will allow us to better attract higher profile clinical research from around the world. We anticipate many enhancements to the journal, which will benefit our authors, members, and readers.
”The relationship with Elsevier will allow CHEST to leverage the global capabilities of Elsevier, its ScienceDirect platform, and its new ClinicalKey service to distribute the journal to an even larger audience than ever and attract higher profile research from around the world.
Elsevier, a world-leading provider of scientific, technical, and medical information products and services, and the American College of Chest Physicians (CHEST), a world-renowned publisher of evidence-based practice guidelines in chest medicine, have announced that Elsevier will publish the organization’s flagship journal CHEST as of January 1, 2016. This significant and exciting piece of news that will positively affect the future of the journal is a licensing agreement, wherein CHEST retains all ownership of the journal, copyright, trademark, and editorial decision-making. Elsevier’s role will be heavily focused on the business and operational aspects of publishing the journal and will provide significant resources to help us continue to take CHEST to a higher level.
“We are excited to begin this new relationship with Elsevier and we look forward to CHEST’s continued success under this collaboration,” said Paul Markowski, CEO and Executive Vice President of the American College of Chest Physicians. “CHEST will remain a leading publication designed to aid clinicians in providing the best patient care possible.”
Dr. Richard Irwin, Master FCCP, and Editor in Chief of the journal, said, “Our publishing agreement with Elsevier will allow CHEST to remain competitive, will help us to distribute research papers to a larger audience, and will allow us to better attract higher profile clinical research from around the world. We anticipate many enhancements to the journal, which will benefit our authors, members, and readers.
”The relationship with Elsevier will allow CHEST to leverage the global capabilities of Elsevier, its ScienceDirect platform, and its new ClinicalKey service to distribute the journal to an even larger audience than ever and attract higher profile research from around the world.
Elsevier, a world-leading provider of scientific, technical, and medical information products and services, and the American College of Chest Physicians (CHEST), a world-renowned publisher of evidence-based practice guidelines in chest medicine, have announced that Elsevier will publish the organization’s flagship journal CHEST as of January 1, 2016. This significant and exciting piece of news that will positively affect the future of the journal is a licensing agreement, wherein CHEST retains all ownership of the journal, copyright, trademark, and editorial decision-making. Elsevier’s role will be heavily focused on the business and operational aspects of publishing the journal and will provide significant resources to help us continue to take CHEST to a higher level.
“We are excited to begin this new relationship with Elsevier and we look forward to CHEST’s continued success under this collaboration,” said Paul Markowski, CEO and Executive Vice President of the American College of Chest Physicians. “CHEST will remain a leading publication designed to aid clinicians in providing the best patient care possible.”
Dr. Richard Irwin, Master FCCP, and Editor in Chief of the journal, said, “Our publishing agreement with Elsevier will allow CHEST to remain competitive, will help us to distribute research papers to a larger audience, and will allow us to better attract higher profile clinical research from around the world. We anticipate many enhancements to the journal, which will benefit our authors, members, and readers.
”The relationship with Elsevier will allow CHEST to leverage the global capabilities of Elsevier, its ScienceDirect platform, and its new ClinicalKey service to distribute the journal to an even larger audience than ever and attract higher profile research from around the world.
From the EVP/CEO: AMS: Offering Solutions to Make Your Tomorrows > Today
As a membership organization, CHEST is committed to supporting you and offering solutions that can make your tomorrows greater than today. It’s incumbent on us to ensure you continually derive value from our organization, and that’s the motive that led us to implement a robust, new association management software (AMS) system to improve and simplify the way you engage with us online. The AMS is scheduled to go live the first week of May, so I’d like to share what that will mean for you.
The main benefit you’ll notice with our AMS is single sign-on. Single sign-on is a feature that connects related, but independent, software systems, so a user can log in once and access all systems without needing to log in repeatedly for each individual system. Today, you’re required to log in to each of our systems separately. Single sign-on will connect the systems for our store, Learning Site, CME claiming, event registration, hotel reservations, session submission, and conflict of interest disclosure. When you log in to any of these systems, you’ll have access to all of them without needing to log in again. You’ll be able to efficiently and smoothly move from one system to the next without interruption for signing in.
For the most part, you won’t see many changes to chestnet.org after the AMS is live. The interface will remain very familiar—until you visit the store. Our online store has had a major facelift! You’ll immediately notice cleaner, more attractive page designs and more intuitive navigation. And, new to the store is an easy way to renew your CHEST membership. If you have trouble finding what you’re looking for, the upgraded search feature will allow you to filter results with further refinement. You’ll be able to limit your search to the store only or continue to search across chestnet.org, the journal CHEST, and our meeting sites. It will be an improved shopping experience, offering popular features similar to other retail sites.
The CHEST staff has been very committed to implementing the AMS, working hard for many months. They’ve developed, designed, trained, tested, and debugged to deliver a better experience for you come May. Despite this skilled and careful work, it’s realistic to expect there may be initial hiccoughs after the AMS goes live. If you experience any difficulty whatsoever, I encourage you to contact our Customer Support team at [email protected], 800/343-2227, or 224/521-9800. They’re top notch and will be ready to help you resolve your issues as quickly as possible.
I’m looking forward to going live with the AMS in May. But, I don’t think of that day as our finish line, marking the end of months of intense development work. Rather, it’s our starting line, marking the beginning of improved online solutions to enhance your engagement with us. And, since it’s only the beginning, you can expect that we’ll continue our work to help you achieve more through improved access to information and resources online. It’s our way of offering solutions to help make your tomorrow greater than today.Check out the new AMS features some time next month, and let me know what you think. And, as always, I invite you to follow me on Twitter (@PMarkowskiACCP), or look for me at upcoming CHEST events.
As a membership organization, CHEST is committed to supporting you and offering solutions that can make your tomorrows greater than today. It’s incumbent on us to ensure you continually derive value from our organization, and that’s the motive that led us to implement a robust, new association management software (AMS) system to improve and simplify the way you engage with us online. The AMS is scheduled to go live the first week of May, so I’d like to share what that will mean for you.
The main benefit you’ll notice with our AMS is single sign-on. Single sign-on is a feature that connects related, but independent, software systems, so a user can log in once and access all systems without needing to log in repeatedly for each individual system. Today, you’re required to log in to each of our systems separately. Single sign-on will connect the systems for our store, Learning Site, CME claiming, event registration, hotel reservations, session submission, and conflict of interest disclosure. When you log in to any of these systems, you’ll have access to all of them without needing to log in again. You’ll be able to efficiently and smoothly move from one system to the next without interruption for signing in.
For the most part, you won’t see many changes to chestnet.org after the AMS is live. The interface will remain very familiar—until you visit the store. Our online store has had a major facelift! You’ll immediately notice cleaner, more attractive page designs and more intuitive navigation. And, new to the store is an easy way to renew your CHEST membership. If you have trouble finding what you’re looking for, the upgraded search feature will allow you to filter results with further refinement. You’ll be able to limit your search to the store only or continue to search across chestnet.org, the journal CHEST, and our meeting sites. It will be an improved shopping experience, offering popular features similar to other retail sites.
The CHEST staff has been very committed to implementing the AMS, working hard for many months. They’ve developed, designed, trained, tested, and debugged to deliver a better experience for you come May. Despite this skilled and careful work, it’s realistic to expect there may be initial hiccoughs after the AMS goes live. If you experience any difficulty whatsoever, I encourage you to contact our Customer Support team at [email protected], 800/343-2227, or 224/521-9800. They’re top notch and will be ready to help you resolve your issues as quickly as possible.
I’m looking forward to going live with the AMS in May. But, I don’t think of that day as our finish line, marking the end of months of intense development work. Rather, it’s our starting line, marking the beginning of improved online solutions to enhance your engagement with us. And, since it’s only the beginning, you can expect that we’ll continue our work to help you achieve more through improved access to information and resources online. It’s our way of offering solutions to help make your tomorrow greater than today.Check out the new AMS features some time next month, and let me know what you think. And, as always, I invite you to follow me on Twitter (@PMarkowskiACCP), or look for me at upcoming CHEST events.
As a membership organization, CHEST is committed to supporting you and offering solutions that can make your tomorrows greater than today. It’s incumbent on us to ensure you continually derive value from our organization, and that’s the motive that led us to implement a robust, new association management software (AMS) system to improve and simplify the way you engage with us online. The AMS is scheduled to go live the first week of May, so I’d like to share what that will mean for you.
The main benefit you’ll notice with our AMS is single sign-on. Single sign-on is a feature that connects related, but independent, software systems, so a user can log in once and access all systems without needing to log in repeatedly for each individual system. Today, you’re required to log in to each of our systems separately. Single sign-on will connect the systems for our store, Learning Site, CME claiming, event registration, hotel reservations, session submission, and conflict of interest disclosure. When you log in to any of these systems, you’ll have access to all of them without needing to log in again. You’ll be able to efficiently and smoothly move from one system to the next without interruption for signing in.
For the most part, you won’t see many changes to chestnet.org after the AMS is live. The interface will remain very familiar—until you visit the store. Our online store has had a major facelift! You’ll immediately notice cleaner, more attractive page designs and more intuitive navigation. And, new to the store is an easy way to renew your CHEST membership. If you have trouble finding what you’re looking for, the upgraded search feature will allow you to filter results with further refinement. You’ll be able to limit your search to the store only or continue to search across chestnet.org, the journal CHEST, and our meeting sites. It will be an improved shopping experience, offering popular features similar to other retail sites.
The CHEST staff has been very committed to implementing the AMS, working hard for many months. They’ve developed, designed, trained, tested, and debugged to deliver a better experience for you come May. Despite this skilled and careful work, it’s realistic to expect there may be initial hiccoughs after the AMS goes live. If you experience any difficulty whatsoever, I encourage you to contact our Customer Support team at [email protected], 800/343-2227, or 224/521-9800. They’re top notch and will be ready to help you resolve your issues as quickly as possible.
I’m looking forward to going live with the AMS in May. But, I don’t think of that day as our finish line, marking the end of months of intense development work. Rather, it’s our starting line, marking the beginning of improved online solutions to enhance your engagement with us. And, since it’s only the beginning, you can expect that we’ll continue our work to help you achieve more through improved access to information and resources online. It’s our way of offering solutions to help make your tomorrow greater than today.Check out the new AMS features some time next month, and let me know what you think. And, as always, I invite you to follow me on Twitter (@PMarkowskiACCP), or look for me at upcoming CHEST events.
Visit Montréal’s Past, Be Part of Chest Medicine’s Future
Montréal, Canada, will welcome the CHEST Annual Meeting 2015, October 24 – 28, and it couldn’t be more appropriate. Montréal will set a perfect backdrop of old world charm mixed with North American Energy. CHEST will fit right in with over 8 decades of clinically relevant annual meetings and its exciting schedule of innovative, state-of-the-art educational opportunities. You may come for the education, but you won’t want to leave without exploring this charming city.
Just minutes away from the Palais des congrès de Montréal, the convention center, Old Montréal offers a glimpse into Montréal’s history blended with hip, urban hotspots. Complete with cobblestone paths, chic art galleries, 19th century architecture, and trendy boutiques, this neighborhood will keep you busy during your spare time.
Start planning your itinerary today with these recommended spots in Old Montréal:
• Visit Notre-Dame Basilica. This Gothic Revival style church was built between 1672 and 1683. Admire the dramatic architecture and the beautiful, colorful interior as you take a guided tour to learn about the history, architecture, and much more.
• Go shopping and dine at Marche Bonsecours. This historic building is currently home to galleries, boutiques, and restaurants. You’ll recognize it’s imposing silver dome in this historic district.
• Explore the outdoors at The Quays of the Old Port, a park that runs alongside the St. Lawrence River. You’ll find festivals and cultural events year-round. Plus, there are walking paths, restaurants, and terraces with beautiful views of the city.
• Learn about local history at the Pointe-a-Calliere, Montréal Museum of Archaeology and History. This national historical and archaeological site leads visitors through centuries of history.
• Visit Chateau Ramezay, a private museum that details the history of Québec and Montréal.
• Dine at Olive & Gourmando. While there is regularly a line to get into this cafe, the cuisine is worth the wait. You’ll enjoy creative sandwiches, local beer and wine selections, and pastries galore!
After you visit the past in Old Montréal’s historic neighborhood, you’ll find yourself recharged and ready for the latest in pulmonary, critical care, and sleep medicine education. CHEST 2015 will give you a glimpse into the future of chest medicine with the latest guidelines, abstracts, and simulation education. Find everything you need to know to make the best clinical decisions and inspire your patient care. Learn more at chestmeeting.chestnet.org.
Montréal, Canada, will welcome the CHEST Annual Meeting 2015, October 24 – 28, and it couldn’t be more appropriate. Montréal will set a perfect backdrop of old world charm mixed with North American Energy. CHEST will fit right in with over 8 decades of clinically relevant annual meetings and its exciting schedule of innovative, state-of-the-art educational opportunities. You may come for the education, but you won’t want to leave without exploring this charming city.
Just minutes away from the Palais des congrès de Montréal, the convention center, Old Montréal offers a glimpse into Montréal’s history blended with hip, urban hotspots. Complete with cobblestone paths, chic art galleries, 19th century architecture, and trendy boutiques, this neighborhood will keep you busy during your spare time.
Start planning your itinerary today with these recommended spots in Old Montréal:
• Visit Notre-Dame Basilica. This Gothic Revival style church was built between 1672 and 1683. Admire the dramatic architecture and the beautiful, colorful interior as you take a guided tour to learn about the history, architecture, and much more.
• Go shopping and dine at Marche Bonsecours. This historic building is currently home to galleries, boutiques, and restaurants. You’ll recognize it’s imposing silver dome in this historic district.
• Explore the outdoors at The Quays of the Old Port, a park that runs alongside the St. Lawrence River. You’ll find festivals and cultural events year-round. Plus, there are walking paths, restaurants, and terraces with beautiful views of the city.
• Learn about local history at the Pointe-a-Calliere, Montréal Museum of Archaeology and History. This national historical and archaeological site leads visitors through centuries of history.
• Visit Chateau Ramezay, a private museum that details the history of Québec and Montréal.
• Dine at Olive & Gourmando. While there is regularly a line to get into this cafe, the cuisine is worth the wait. You’ll enjoy creative sandwiches, local beer and wine selections, and pastries galore!
After you visit the past in Old Montréal’s historic neighborhood, you’ll find yourself recharged and ready for the latest in pulmonary, critical care, and sleep medicine education. CHEST 2015 will give you a glimpse into the future of chest medicine with the latest guidelines, abstracts, and simulation education. Find everything you need to know to make the best clinical decisions and inspire your patient care. Learn more at chestmeeting.chestnet.org.
Montréal, Canada, will welcome the CHEST Annual Meeting 2015, October 24 – 28, and it couldn’t be more appropriate. Montréal will set a perfect backdrop of old world charm mixed with North American Energy. CHEST will fit right in with over 8 decades of clinically relevant annual meetings and its exciting schedule of innovative, state-of-the-art educational opportunities. You may come for the education, but you won’t want to leave without exploring this charming city.
Just minutes away from the Palais des congrès de Montréal, the convention center, Old Montréal offers a glimpse into Montréal’s history blended with hip, urban hotspots. Complete with cobblestone paths, chic art galleries, 19th century architecture, and trendy boutiques, this neighborhood will keep you busy during your spare time.
Start planning your itinerary today with these recommended spots in Old Montréal:
• Visit Notre-Dame Basilica. This Gothic Revival style church was built between 1672 and 1683. Admire the dramatic architecture and the beautiful, colorful interior as you take a guided tour to learn about the history, architecture, and much more.
• Go shopping and dine at Marche Bonsecours. This historic building is currently home to galleries, boutiques, and restaurants. You’ll recognize it’s imposing silver dome in this historic district.
• Explore the outdoors at The Quays of the Old Port, a park that runs alongside the St. Lawrence River. You’ll find festivals and cultural events year-round. Plus, there are walking paths, restaurants, and terraces with beautiful views of the city.
• Learn about local history at the Pointe-a-Calliere, Montréal Museum of Archaeology and History. This national historical and archaeological site leads visitors through centuries of history.
• Visit Chateau Ramezay, a private museum that details the history of Québec and Montréal.
• Dine at Olive & Gourmando. While there is regularly a line to get into this cafe, the cuisine is worth the wait. You’ll enjoy creative sandwiches, local beer and wine selections, and pastries galore!
After you visit the past in Old Montréal’s historic neighborhood, you’ll find yourself recharged and ready for the latest in pulmonary, critical care, and sleep medicine education. CHEST 2015 will give you a glimpse into the future of chest medicine with the latest guidelines, abstracts, and simulation education. Find everything you need to know to make the best clinical decisions and inspire your patient care. Learn more at chestmeeting.chestnet.org.
Sarcoidosis Patient Education Campaign
In honor of National Sarcoidosis Awareness month, the CHEST Foundation and Foundation for Sarcoidosis Research (FSR) have launched Sarcoidosis: Seek Answers. Inspire Results., a nationwide campaign encouraging patients with sarcoidosis to take a proactive role in their treatment plan (www.stopsarcoidosis.org/patient-resources/what-is-sarcoidosis).
This rare, autoimmune disease, which affects the lungs in 90% of cases, can often mimic other conditions as well, further adding to the complexity of the disorder. For instance, sarcoidosis can mimic fungal or mycobacterial infections, chronic beryllium disease, hypersensitivity pneumonitis, rheumatologic syndromes, lymphoma, tumor-associated granulomas, pulmonary fibrosis, and more. Lung symptoms often include a cough that does not go away, shortness of breath, and chest pain. About one-third of patients will also experience nonspecific symptoms, such as fever, fatigue, weight loss, night sweats, and an overall feeling of ill health. Key diagnostic tools include chest radiographs, laboratory blood tests, breathing tests, and a biopsy.
Anyone can develop sarcoidosis; however, for reasons not yet understood by medical science, the condition is more prevalent among African-Americans and people of Northern European – particularly Scandinavian – descent. Sarcoidosis most commonly occurs among people between the ages of 20 and 40.
If diagnosed and under good medical care, most cases of sarcoidosis have a positive prognosis and do not cause lasting damage to the body. However, 30% to 40% of people living with sarcoidosis have a persistent condition that may require personalized treatment – including co-consultation with other organ specialists, as indicated – to control symptoms.
To this end, the Seek Answers. Inspire Results. campaign encourages physician/patient dialogue, as well as treatment compliance. For educational tools to share with patients, including the “Sarcoid Five” – five questions designed to jumpstart physician/patient conversations – visit chestnet.org/sarcoid.
Patient education resources supported in part by a grant from Mallinckrodt Pharmaceuticals Autoimmune and Rare Diseases.
For further reading:
www.stopsarcoidosis.org/patient-resources/what-is-sarcoidosis/
In honor of National Sarcoidosis Awareness month, the CHEST Foundation and Foundation for Sarcoidosis Research (FSR) have launched Sarcoidosis: Seek Answers. Inspire Results., a nationwide campaign encouraging patients with sarcoidosis to take a proactive role in their treatment plan (www.stopsarcoidosis.org/patient-resources/what-is-sarcoidosis).
This rare, autoimmune disease, which affects the lungs in 90% of cases, can often mimic other conditions as well, further adding to the complexity of the disorder. For instance, sarcoidosis can mimic fungal or mycobacterial infections, chronic beryllium disease, hypersensitivity pneumonitis, rheumatologic syndromes, lymphoma, tumor-associated granulomas, pulmonary fibrosis, and more. Lung symptoms often include a cough that does not go away, shortness of breath, and chest pain. About one-third of patients will also experience nonspecific symptoms, such as fever, fatigue, weight loss, night sweats, and an overall feeling of ill health. Key diagnostic tools include chest radiographs, laboratory blood tests, breathing tests, and a biopsy.
Anyone can develop sarcoidosis; however, for reasons not yet understood by medical science, the condition is more prevalent among African-Americans and people of Northern European – particularly Scandinavian – descent. Sarcoidosis most commonly occurs among people between the ages of 20 and 40.
If diagnosed and under good medical care, most cases of sarcoidosis have a positive prognosis and do not cause lasting damage to the body. However, 30% to 40% of people living with sarcoidosis have a persistent condition that may require personalized treatment – including co-consultation with other organ specialists, as indicated – to control symptoms.
To this end, the Seek Answers. Inspire Results. campaign encourages physician/patient dialogue, as well as treatment compliance. For educational tools to share with patients, including the “Sarcoid Five” – five questions designed to jumpstart physician/patient conversations – visit chestnet.org/sarcoid.
Patient education resources supported in part by a grant from Mallinckrodt Pharmaceuticals Autoimmune and Rare Diseases.
For further reading:
www.stopsarcoidosis.org/patient-resources/what-is-sarcoidosis/
In honor of National Sarcoidosis Awareness month, the CHEST Foundation and Foundation for Sarcoidosis Research (FSR) have launched Sarcoidosis: Seek Answers. Inspire Results., a nationwide campaign encouraging patients with sarcoidosis to take a proactive role in their treatment plan (www.stopsarcoidosis.org/patient-resources/what-is-sarcoidosis).
This rare, autoimmune disease, which affects the lungs in 90% of cases, can often mimic other conditions as well, further adding to the complexity of the disorder. For instance, sarcoidosis can mimic fungal or mycobacterial infections, chronic beryllium disease, hypersensitivity pneumonitis, rheumatologic syndromes, lymphoma, tumor-associated granulomas, pulmonary fibrosis, and more. Lung symptoms often include a cough that does not go away, shortness of breath, and chest pain. About one-third of patients will also experience nonspecific symptoms, such as fever, fatigue, weight loss, night sweats, and an overall feeling of ill health. Key diagnostic tools include chest radiographs, laboratory blood tests, breathing tests, and a biopsy.
Anyone can develop sarcoidosis; however, for reasons not yet understood by medical science, the condition is more prevalent among African-Americans and people of Northern European – particularly Scandinavian – descent. Sarcoidosis most commonly occurs among people between the ages of 20 and 40.
If diagnosed and under good medical care, most cases of sarcoidosis have a positive prognosis and do not cause lasting damage to the body. However, 30% to 40% of people living with sarcoidosis have a persistent condition that may require personalized treatment – including co-consultation with other organ specialists, as indicated – to control symptoms.
To this end, the Seek Answers. Inspire Results. campaign encourages physician/patient dialogue, as well as treatment compliance. For educational tools to share with patients, including the “Sarcoid Five” – five questions designed to jumpstart physician/patient conversations – visit chestnet.org/sarcoid.
Patient education resources supported in part by a grant from Mallinckrodt Pharmaceuticals Autoimmune and Rare Diseases.
For further reading:
www.stopsarcoidosis.org/patient-resources/what-is-sarcoidosis/
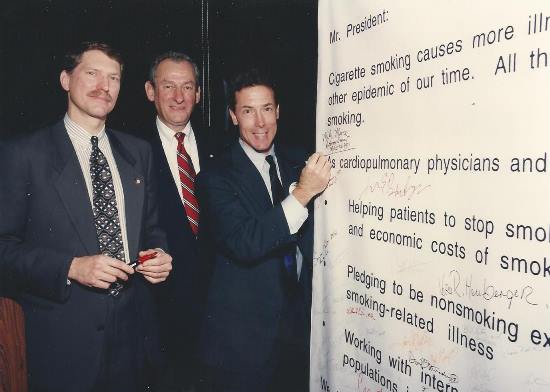
Catching Up With Our Past Presidents
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new in their lives.
James B. D. Mark, MD, FCCP
President 1994-1995
My presidential year began in New Orleans at CHEST 1994. The welcoming reception, which was Halloween-themed, started the year off with a bang. Attendees were encouraged to wear costumes and many did so. Two robbers, complete with trick-or-treat bags and masks. crashed the party and helped themselves to unattended purses and more. They were caught in the act by one of the guests and turned over to the New Orleans police. ... and the year just got better!
Two highlights were travel to the Asia-Pacific Congress on Diseases of the Chest in Hong Kong and to the meeting of the European Respiratory Society in Barcelona. The delegation from the ACCP was well received at both meetings. Memorable, also, was a leadership luncheon meeting with the American Thoracic Society in Seattle. Dr. Claude Lenfant, Director of the NHLBI, attended the luncheon. He said at the time that he had given many talks to lay and professional groups over the years and that during the question-and-answer periods, he had never had a question asked about lung disease, only heart disease, the clear implication being that we “Lungies” better get our message out to the public. Interacting with the staff of the ACCP and many members of leadership during the year was a stimulating and memorable experience.
I am currently Professor of Cardiothoracic Surgery, Emeritus at Stanford University School of Medicine. I achieved Emeritus status at Stanford in 1996, but continued to operate for another year and be active clinically for several more years. I no longer see patients but do attend conferences each week. I go to few professional meetings, national or international, but do travel with my wife and family. A highlight was a trip to Rwanda, Kenya, and Tanzania recently. My exercise regimen includes walking, going to the gym for light workouts, and playing golf. Where but the Stanford Golf Course can a previous Heisman Trophy winner, Jim Plunkett, be in the foursome ahead of you and an ex-Secretary of State, Condoleezza Rice, be in the one behind you?
James B. D. Mark, MD, FCCP
Professor of Cardiothoracic Surgery, Emeritus
Stanford University School of Medicine
President, American College of Chest Physicians, 1994-1995
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new in their lives.
James B. D. Mark, MD, FCCP
President 1994-1995
My presidential year began in New Orleans at CHEST 1994. The welcoming reception, which was Halloween-themed, started the year off with a bang. Attendees were encouraged to wear costumes and many did so. Two robbers, complete with trick-or-treat bags and masks. crashed the party and helped themselves to unattended purses and more. They were caught in the act by one of the guests and turned over to the New Orleans police. ... and the year just got better!
Two highlights were travel to the Asia-Pacific Congress on Diseases of the Chest in Hong Kong and to the meeting of the European Respiratory Society in Barcelona. The delegation from the ACCP was well received at both meetings. Memorable, also, was a leadership luncheon meeting with the American Thoracic Society in Seattle. Dr. Claude Lenfant, Director of the NHLBI, attended the luncheon. He said at the time that he had given many talks to lay and professional groups over the years and that during the question-and-answer periods, he had never had a question asked about lung disease, only heart disease, the clear implication being that we “Lungies” better get our message out to the public. Interacting with the staff of the ACCP and many members of leadership during the year was a stimulating and memorable experience.
I am currently Professor of Cardiothoracic Surgery, Emeritus at Stanford University School of Medicine. I achieved Emeritus status at Stanford in 1996, but continued to operate for another year and be active clinically for several more years. I no longer see patients but do attend conferences each week. I go to few professional meetings, national or international, but do travel with my wife and family. A highlight was a trip to Rwanda, Kenya, and Tanzania recently. My exercise regimen includes walking, going to the gym for light workouts, and playing golf. Where but the Stanford Golf Course can a previous Heisman Trophy winner, Jim Plunkett, be in the foursome ahead of you and an ex-Secretary of State, Condoleezza Rice, be in the one behind you?
James B. D. Mark, MD, FCCP
Professor of Cardiothoracic Surgery, Emeritus
Stanford University School of Medicine
President, American College of Chest Physicians, 1994-1995
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new in their lives.
James B. D. Mark, MD, FCCP
President 1994-1995
My presidential year began in New Orleans at CHEST 1994. The welcoming reception, which was Halloween-themed, started the year off with a bang. Attendees were encouraged to wear costumes and many did so. Two robbers, complete with trick-or-treat bags and masks. crashed the party and helped themselves to unattended purses and more. They were caught in the act by one of the guests and turned over to the New Orleans police. ... and the year just got better!
Two highlights were travel to the Asia-Pacific Congress on Diseases of the Chest in Hong Kong and to the meeting of the European Respiratory Society in Barcelona. The delegation from the ACCP was well received at both meetings. Memorable, also, was a leadership luncheon meeting with the American Thoracic Society in Seattle. Dr. Claude Lenfant, Director of the NHLBI, attended the luncheon. He said at the time that he had given many talks to lay and professional groups over the years and that during the question-and-answer periods, he had never had a question asked about lung disease, only heart disease, the clear implication being that we “Lungies” better get our message out to the public. Interacting with the staff of the ACCP and many members of leadership during the year was a stimulating and memorable experience.
I am currently Professor of Cardiothoracic Surgery, Emeritus at Stanford University School of Medicine. I achieved Emeritus status at Stanford in 1996, but continued to operate for another year and be active clinically for several more years. I no longer see patients but do attend conferences each week. I go to few professional meetings, national or international, but do travel with my wife and family. A highlight was a trip to Rwanda, Kenya, and Tanzania recently. My exercise regimen includes walking, going to the gym for light workouts, and playing golf. Where but the Stanford Golf Course can a previous Heisman Trophy winner, Jim Plunkett, be in the foursome ahead of you and an ex-Secretary of State, Condoleezza Rice, be in the one behind you?
James B. D. Mark, MD, FCCP
Professor of Cardiothoracic Surgery, Emeritus
Stanford University School of Medicine
President, American College of Chest Physicians, 1994-1995
Make Plans Now to Attend CHEST 2015
October 24-28
Montréal, Canada
Montréal is a lively city with multicultural influences that make the city tick. What better place for CHEST 2015, where we’ll connect a global community in clinical chest medicine? As always, our program will deliver current pulmonary, critical care, and sleep medicine topics, presented by world-renowned faculty using innovative instruction formats—like hands-on simulation and interactive case discussions—to offer popular options for learning. Take advantage of these opportunities now:
Call for Abstracts
Submission Deadline: April 1
Submit an abstract of your original investigative work for presentation at the meeting. Accepted abstracts will be published in an online supplement to CHEST. Three types of abstracts will be considered:
• Slide presentations
• Poster presentations
• Poster discussions
Learn more and submit at chestmeeting.chestnet.org.
Call for Case Reports
Submission Deadline: April 1
Submit case reports for presentation during special sessions. Accepted case reports (excluding clinical case puzzlers) will be published in an online supplement to CHEST. Four types of case reports will be considered:
• Affiliate case reports
• Medical student/resident case reports
• Global case reports
• Clinical case puzzlers
Learn more and submit at chestmeeting.chestnet.org.
Call for Moderators
Moderators are needed on-site during the meeting. Responsibilities include reviewing the abstracts and case reports prior to the meeting, then facilitating discussion, questions, and answers within your assigned session(s). All slide sessions and most poster sessions will have two moderators. Moderators will be recognized in the CHEST 2015 program and will receive a reduced registration rate to the meeting. Travel reimbursement will not be offered. Learn more at chestmeeting.chestnet.org.
The CHEST Foundation 2015 Grants Program
Application Deadline: April 30
The CHEST Foundation tradition of recognizing and rewarding health-care professionals for scholarly projects and research continues. Grants for both leaders in chest medicine and young investigators are available, including:
• CHEST Foundation and the Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency - $25,000 1-year grant
• CHEST Foundation Research Grant in Women’s Lung Health - $10,000 1-year grant
• CHEST Foundation Research Grant in Pulmonary Fibrosis - $30,000 1-year grant
• CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease - $50,000 1-year grant
• CHEST Diversity Committee Minority Investigator Research Grant - $25,000 1-year grant
• Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP - up to $15,000 1-year grant
• CHEST Foundation Research Grant in Pulmonary Arterial Hypertension - $50,000 1-year grant
• Eli Lilly and Company Distinguished Scholar in Critical Care Medicine - $150,000 for 3 years
See which grants you are eligible for, and apply today at chestnet.org/grants.
Play CHEST Challenge
Game Ends: May 30
CHEST affiliate members, play CHEST Challenge to test your knowledge of pulmonary, critical care, and sleep medicine while competing for prizes.
The three top-scoring programs will compete in the CHEST Challenge Championship at CHEST Annual Meeting 2015. All championship players will receive:
• Airfare and registration to CHEST Annual Meeting 2015 in Montréal, Canada
• Complimentary hotel
• Cash prizes
Game on! Learn more at chestchallenge.org.
October 24-28
Montréal, Canada
Montréal is a lively city with multicultural influences that make the city tick. What better place for CHEST 2015, where we’ll connect a global community in clinical chest medicine? As always, our program will deliver current pulmonary, critical care, and sleep medicine topics, presented by world-renowned faculty using innovative instruction formats—like hands-on simulation and interactive case discussions—to offer popular options for learning. Take advantage of these opportunities now:
Call for Abstracts
Submission Deadline: April 1
Submit an abstract of your original investigative work for presentation at the meeting. Accepted abstracts will be published in an online supplement to CHEST. Three types of abstracts will be considered:
• Slide presentations
• Poster presentations
• Poster discussions
Learn more and submit at chestmeeting.chestnet.org.
Call for Case Reports
Submission Deadline: April 1
Submit case reports for presentation during special sessions. Accepted case reports (excluding clinical case puzzlers) will be published in an online supplement to CHEST. Four types of case reports will be considered:
• Affiliate case reports
• Medical student/resident case reports
• Global case reports
• Clinical case puzzlers
Learn more and submit at chestmeeting.chestnet.org.
Call for Moderators
Moderators are needed on-site during the meeting. Responsibilities include reviewing the abstracts and case reports prior to the meeting, then facilitating discussion, questions, and answers within your assigned session(s). All slide sessions and most poster sessions will have two moderators. Moderators will be recognized in the CHEST 2015 program and will receive a reduced registration rate to the meeting. Travel reimbursement will not be offered. Learn more at chestmeeting.chestnet.org.
The CHEST Foundation 2015 Grants Program
Application Deadline: April 30
The CHEST Foundation tradition of recognizing and rewarding health-care professionals for scholarly projects and research continues. Grants for both leaders in chest medicine and young investigators are available, including:
• CHEST Foundation and the Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency - $25,000 1-year grant
• CHEST Foundation Research Grant in Women’s Lung Health - $10,000 1-year grant
• CHEST Foundation Research Grant in Pulmonary Fibrosis - $30,000 1-year grant
• CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease - $50,000 1-year grant
• CHEST Diversity Committee Minority Investigator Research Grant - $25,000 1-year grant
• Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP - up to $15,000 1-year grant
• CHEST Foundation Research Grant in Pulmonary Arterial Hypertension - $50,000 1-year grant
• Eli Lilly and Company Distinguished Scholar in Critical Care Medicine - $150,000 for 3 years
See which grants you are eligible for, and apply today at chestnet.org/grants.
Play CHEST Challenge
Game Ends: May 30
CHEST affiliate members, play CHEST Challenge to test your knowledge of pulmonary, critical care, and sleep medicine while competing for prizes.
The three top-scoring programs will compete in the CHEST Challenge Championship at CHEST Annual Meeting 2015. All championship players will receive:
• Airfare and registration to CHEST Annual Meeting 2015 in Montréal, Canada
• Complimentary hotel
• Cash prizes
Game on! Learn more at chestchallenge.org.
October 24-28
Montréal, Canada
Montréal is a lively city with multicultural influences that make the city tick. What better place for CHEST 2015, where we’ll connect a global community in clinical chest medicine? As always, our program will deliver current pulmonary, critical care, and sleep medicine topics, presented by world-renowned faculty using innovative instruction formats—like hands-on simulation and interactive case discussions—to offer popular options for learning. Take advantage of these opportunities now:
Call for Abstracts
Submission Deadline: April 1
Submit an abstract of your original investigative work for presentation at the meeting. Accepted abstracts will be published in an online supplement to CHEST. Three types of abstracts will be considered:
• Slide presentations
• Poster presentations
• Poster discussions
Learn more and submit at chestmeeting.chestnet.org.
Call for Case Reports
Submission Deadline: April 1
Submit case reports for presentation during special sessions. Accepted case reports (excluding clinical case puzzlers) will be published in an online supplement to CHEST. Four types of case reports will be considered:
• Affiliate case reports
• Medical student/resident case reports
• Global case reports
• Clinical case puzzlers
Learn more and submit at chestmeeting.chestnet.org.
Call for Moderators
Moderators are needed on-site during the meeting. Responsibilities include reviewing the abstracts and case reports prior to the meeting, then facilitating discussion, questions, and answers within your assigned session(s). All slide sessions and most poster sessions will have two moderators. Moderators will be recognized in the CHEST 2015 program and will receive a reduced registration rate to the meeting. Travel reimbursement will not be offered. Learn more at chestmeeting.chestnet.org.
The CHEST Foundation 2015 Grants Program
Application Deadline: April 30
The CHEST Foundation tradition of recognizing and rewarding health-care professionals for scholarly projects and research continues. Grants for both leaders in chest medicine and young investigators are available, including:
• CHEST Foundation and the Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency - $25,000 1-year grant
• CHEST Foundation Research Grant in Women’s Lung Health - $10,000 1-year grant
• CHEST Foundation Research Grant in Pulmonary Fibrosis - $30,000 1-year grant
• CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease - $50,000 1-year grant
• CHEST Diversity Committee Minority Investigator Research Grant - $25,000 1-year grant
• Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP - up to $15,000 1-year grant
• CHEST Foundation Research Grant in Pulmonary Arterial Hypertension - $50,000 1-year grant
• Eli Lilly and Company Distinguished Scholar in Critical Care Medicine - $150,000 for 3 years
See which grants you are eligible for, and apply today at chestnet.org/grants.
Play CHEST Challenge
Game Ends: May 30
CHEST affiliate members, play CHEST Challenge to test your knowledge of pulmonary, critical care, and sleep medicine while competing for prizes.
The three top-scoring programs will compete in the CHEST Challenge Championship at CHEST Annual Meeting 2015. All championship players will receive:
• Airfare and registration to CHEST Annual Meeting 2015 in Montréal, Canada
• Complimentary hotel
• Cash prizes
Game on! Learn more at chestchallenge.org.
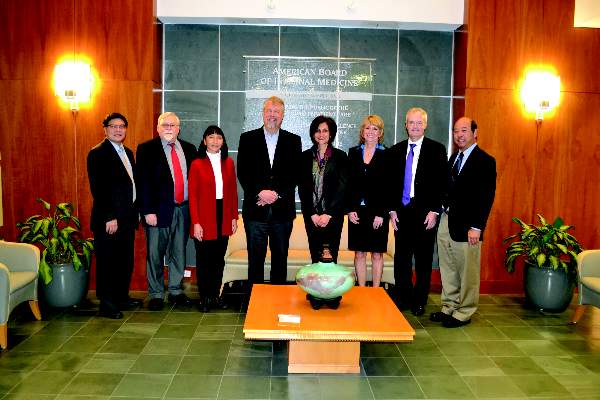
Meet ABIM’s Pulmonary Disease Board
As you have likely heard, the American Board of Internal Medicine (ABIM) has recently introduced a number of changes to its Maintenance of Certification (MOC) program, but what you may not know is that its governance structure has also undergone some important changes, including the formation of new specialty boards. In the past, the specialty boards or test writing committees were charged with developing new exam questions, and due to the amount of time and effort involved in this process, they had little time to weigh in on specialty-specific issues related to certification and MOC.
One of the major criticisms of the MOC program is that certain requirements do not have options relevant to specific specialties or that on-the-ground physicians were not engaged in the process. In direct response to that criticism, ABIM established these specialty boards so they could:
• Define, refine, and set standards for certification and MOC in the discipline;
• Perform oversight/review of performance assessments in the discipline; and to
• Build partnerships with societies and other organizational stakeholders.
The secure examination will continue to be developed by a separate, dedicated group of physicians but will now be referred to as exam committees, ie, Pulmonary Disease Board Exam Committee.
As the Chair of the ABIM’s Pulmonary Disease Board, I am excited to take this opportunity to introduce the role of this newly formed specialty board, as well as introduce its members.
The ABIM Pulmonary Disease Board, along with nine other specialty boards, held their inaugural meetings this fall. Each of the specialty boards consist of practicing ABIM Board-Certified physicians, an intraprofessional team member, and a patient representative. Members of the ABIM Pulmonary Disease Board include:
Dr. Serpil C. Erzurum, Chair, Cleveland, OH
I am board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, practice Pulmonary Medicine at the Cleveland Clinic and serve as the Alfred Lerner Chair of the Department of Pathobiology in the Lerner Research Institute.
Dr. Kevin M. Chan, FCCP, Ann Arbor, MI
Dr. Chan, who is board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, is Fellowship Program Director for the Division of Pulmonary and Critical Care Medicine, and Medical Director of Lung Transplantation at the University of Michigan.
Dr. John Allen Cooper, Birmingham, AL
Dr. Cooper, who is board certified in Internal Medicine and Pulmonary Disease, is Professor of Medicine at the University of Alabama Medical School, and Chief of the Pulmonary Section at the Birmingham Veterans Administration Medical Center.
Dean R. Hess, PhD, RRT, FCCP, Boston, MA
Dr. Hess, our intra-professional member, is Assistant Director of Respiratory Care, Massachusetts General Hospital, and Associate Professor of Anesthesia, Harvard Medical School.
Tommye Lambert, MBA, MDIV, Hoover, AL
Mrs. Lambert, our patient representative, is a leader in the caregiver community who focuses on patient-doctor communication and collaboration and was primary caregiver for 28 years to her daughter who suffered with cystic fibrosis. Mrs. Lambert earned her MDIV at Beeson Divinity School, Samford University, and her Executive MBA from the University of Alabama.
Dr. Michael E. Nelson, FCCP, Shawnee Mission, KS
Dr. Nelson, who is board-certified in Internal Medicine, Sleep Medicine, Pulmonary Disease, and Critical Care Medicine, is a practicing physician in Shawnee Mission, Kansas, and Medical Director of the Sleep Laboratory of the Shawnee Mission Medical Center.
Dr. Stanton T. Siu, Oakland, CA
Dr. Siu, who is board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, is Chief of Pulmonary Medicine and Director of Graduate and Undergraduate Medical Education for Kaiser Permanente East Bay in Northern California, and Full Clinical Professor at the University of California San Francisco.
Dr. Lynn T. Tanoue, FCCP, New Haven, CT
Dr. Tanoue, who is board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, is Professor of Medicine and Clinical Chief of the Section of Pulmonary, Critical Care, and Sleep Medicine, and Vice-Chair for Clinical Affairs in the Department of Internal Medicine at Yale School of Medicine. As a longtime member and current Chair of ABIM’s Pulmonary Disease Board Exam Committee, Dr. Tanoue works closely with me in planning and carrying out the work of the Pulmonary Disease Board.
I am honored to lead such a diverse group of professionals from across the spectrum of pulmonary disease and look forward to sharing updates with you as we embark on our work of ensuring the relevancy of MOC to pulmonary disease physicians across the country.
Further information about ABIM’s new governance structure may be found via the ABIM website: www.abim.org/about/governance
As you have likely heard, the American Board of Internal Medicine (ABIM) has recently introduced a number of changes to its Maintenance of Certification (MOC) program, but what you may not know is that its governance structure has also undergone some important changes, including the formation of new specialty boards. In the past, the specialty boards or test writing committees were charged with developing new exam questions, and due to the amount of time and effort involved in this process, they had little time to weigh in on specialty-specific issues related to certification and MOC.
One of the major criticisms of the MOC program is that certain requirements do not have options relevant to specific specialties or that on-the-ground physicians were not engaged in the process. In direct response to that criticism, ABIM established these specialty boards so they could:
• Define, refine, and set standards for certification and MOC in the discipline;
• Perform oversight/review of performance assessments in the discipline; and to
• Build partnerships with societies and other organizational stakeholders.
The secure examination will continue to be developed by a separate, dedicated group of physicians but will now be referred to as exam committees, ie, Pulmonary Disease Board Exam Committee.
As the Chair of the ABIM’s Pulmonary Disease Board, I am excited to take this opportunity to introduce the role of this newly formed specialty board, as well as introduce its members.
The ABIM Pulmonary Disease Board, along with nine other specialty boards, held their inaugural meetings this fall. Each of the specialty boards consist of practicing ABIM Board-Certified physicians, an intraprofessional team member, and a patient representative. Members of the ABIM Pulmonary Disease Board include:
Dr. Serpil C. Erzurum, Chair, Cleveland, OH
I am board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, practice Pulmonary Medicine at the Cleveland Clinic and serve as the Alfred Lerner Chair of the Department of Pathobiology in the Lerner Research Institute.
Dr. Kevin M. Chan, FCCP, Ann Arbor, MI
Dr. Chan, who is board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, is Fellowship Program Director for the Division of Pulmonary and Critical Care Medicine, and Medical Director of Lung Transplantation at the University of Michigan.
Dr. John Allen Cooper, Birmingham, AL
Dr. Cooper, who is board certified in Internal Medicine and Pulmonary Disease, is Professor of Medicine at the University of Alabama Medical School, and Chief of the Pulmonary Section at the Birmingham Veterans Administration Medical Center.
Dean R. Hess, PhD, RRT, FCCP, Boston, MA
Dr. Hess, our intra-professional member, is Assistant Director of Respiratory Care, Massachusetts General Hospital, and Associate Professor of Anesthesia, Harvard Medical School.
Tommye Lambert, MBA, MDIV, Hoover, AL
Mrs. Lambert, our patient representative, is a leader in the caregiver community who focuses on patient-doctor communication and collaboration and was primary caregiver for 28 years to her daughter who suffered with cystic fibrosis. Mrs. Lambert earned her MDIV at Beeson Divinity School, Samford University, and her Executive MBA from the University of Alabama.
Dr. Michael E. Nelson, FCCP, Shawnee Mission, KS
Dr. Nelson, who is board-certified in Internal Medicine, Sleep Medicine, Pulmonary Disease, and Critical Care Medicine, is a practicing physician in Shawnee Mission, Kansas, and Medical Director of the Sleep Laboratory of the Shawnee Mission Medical Center.
Dr. Stanton T. Siu, Oakland, CA
Dr. Siu, who is board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, is Chief of Pulmonary Medicine and Director of Graduate and Undergraduate Medical Education for Kaiser Permanente East Bay in Northern California, and Full Clinical Professor at the University of California San Francisco.
Dr. Lynn T. Tanoue, FCCP, New Haven, CT
Dr. Tanoue, who is board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, is Professor of Medicine and Clinical Chief of the Section of Pulmonary, Critical Care, and Sleep Medicine, and Vice-Chair for Clinical Affairs in the Department of Internal Medicine at Yale School of Medicine. As a longtime member and current Chair of ABIM’s Pulmonary Disease Board Exam Committee, Dr. Tanoue works closely with me in planning and carrying out the work of the Pulmonary Disease Board.
I am honored to lead such a diverse group of professionals from across the spectrum of pulmonary disease and look forward to sharing updates with you as we embark on our work of ensuring the relevancy of MOC to pulmonary disease physicians across the country.
Further information about ABIM’s new governance structure may be found via the ABIM website: www.abim.org/about/governance
As you have likely heard, the American Board of Internal Medicine (ABIM) has recently introduced a number of changes to its Maintenance of Certification (MOC) program, but what you may not know is that its governance structure has also undergone some important changes, including the formation of new specialty boards. In the past, the specialty boards or test writing committees were charged with developing new exam questions, and due to the amount of time and effort involved in this process, they had little time to weigh in on specialty-specific issues related to certification and MOC.
One of the major criticisms of the MOC program is that certain requirements do not have options relevant to specific specialties or that on-the-ground physicians were not engaged in the process. In direct response to that criticism, ABIM established these specialty boards so they could:
• Define, refine, and set standards for certification and MOC in the discipline;
• Perform oversight/review of performance assessments in the discipline; and to
• Build partnerships with societies and other organizational stakeholders.
The secure examination will continue to be developed by a separate, dedicated group of physicians but will now be referred to as exam committees, ie, Pulmonary Disease Board Exam Committee.
As the Chair of the ABIM’s Pulmonary Disease Board, I am excited to take this opportunity to introduce the role of this newly formed specialty board, as well as introduce its members.
The ABIM Pulmonary Disease Board, along with nine other specialty boards, held their inaugural meetings this fall. Each of the specialty boards consist of practicing ABIM Board-Certified physicians, an intraprofessional team member, and a patient representative. Members of the ABIM Pulmonary Disease Board include:
Dr. Serpil C. Erzurum, Chair, Cleveland, OH
I am board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, practice Pulmonary Medicine at the Cleveland Clinic and serve as the Alfred Lerner Chair of the Department of Pathobiology in the Lerner Research Institute.
Dr. Kevin M. Chan, FCCP, Ann Arbor, MI
Dr. Chan, who is board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, is Fellowship Program Director for the Division of Pulmonary and Critical Care Medicine, and Medical Director of Lung Transplantation at the University of Michigan.
Dr. John Allen Cooper, Birmingham, AL
Dr. Cooper, who is board certified in Internal Medicine and Pulmonary Disease, is Professor of Medicine at the University of Alabama Medical School, and Chief of the Pulmonary Section at the Birmingham Veterans Administration Medical Center.
Dean R. Hess, PhD, RRT, FCCP, Boston, MA
Dr. Hess, our intra-professional member, is Assistant Director of Respiratory Care, Massachusetts General Hospital, and Associate Professor of Anesthesia, Harvard Medical School.
Tommye Lambert, MBA, MDIV, Hoover, AL
Mrs. Lambert, our patient representative, is a leader in the caregiver community who focuses on patient-doctor communication and collaboration and was primary caregiver for 28 years to her daughter who suffered with cystic fibrosis. Mrs. Lambert earned her MDIV at Beeson Divinity School, Samford University, and her Executive MBA from the University of Alabama.
Dr. Michael E. Nelson, FCCP, Shawnee Mission, KS
Dr. Nelson, who is board-certified in Internal Medicine, Sleep Medicine, Pulmonary Disease, and Critical Care Medicine, is a practicing physician in Shawnee Mission, Kansas, and Medical Director of the Sleep Laboratory of the Shawnee Mission Medical Center.
Dr. Stanton T. Siu, Oakland, CA
Dr. Siu, who is board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, is Chief of Pulmonary Medicine and Director of Graduate and Undergraduate Medical Education for Kaiser Permanente East Bay in Northern California, and Full Clinical Professor at the University of California San Francisco.
Dr. Lynn T. Tanoue, FCCP, New Haven, CT
Dr. Tanoue, who is board-certified in Internal Medicine, Pulmonary Disease, and Critical Care Medicine, is Professor of Medicine and Clinical Chief of the Section of Pulmonary, Critical Care, and Sleep Medicine, and Vice-Chair for Clinical Affairs in the Department of Internal Medicine at Yale School of Medicine. As a longtime member and current Chair of ABIM’s Pulmonary Disease Board Exam Committee, Dr. Tanoue works closely with me in planning and carrying out the work of the Pulmonary Disease Board.
I am honored to lead such a diverse group of professionals from across the spectrum of pulmonary disease and look forward to sharing updates with you as we embark on our work of ensuring the relevancy of MOC to pulmonary disease physicians across the country.
Further information about ABIM’s new governance structure may be found via the ABIM website: www.abim.org/about/governance
NAMDRC Hosts a 2-Day Roundtable on “Respiratory Compromise”
NAMDRC is bringing together representatives of key medical societies, including CHEST, ATS, AARC, SCCM, AACN, SHM (hospitalists), PPAHS (patient safety), and ACEP (emergency physicians) to address respiratory compromise, that cascade of events that moves from respiratory insufficiency to respiratory failure to respiratory arrest. Recognizing that respiratory compromise occurs in various settings, the conference, Feb 26-27 in Orlando, Florida, will focus on the hospital setting.
In addition to society representatives, the NAMDRC leadership, in consultation with recognized experts, has also invited several key opinion leaders to participate, including physicians, respiratory therapists, and nurses.
There are several challenges facing the participants, perhaps paramount is to define the concept of “respiratory compromise.” Some of have signaled, “I know it when I see it,” but the expectation is to formulate a specific clinical definition of the respiratory deterioration, and devise a recognition pathway that can easily be used in the hospital setting to identify patients earlier in the course of this cascade.
How to identify high risk patients is critical to the discussion, because it is generally believed that this is where resources need to be focused, both from a personnel and monitoring perspective. Can consensus be drawn to determine which patient characteristics can reliably classify that patient into a high risk for respiratory compromise, and, if so, those characteristics should be delineated. The corollary challenge is to identify the low risk patients so that inappropriate resources are not focused where such efforts might not be necessary.
Individual hospital policies are integral to this issue, as the relative value of rapid response teams appears to vary greatly. Add to the equation a recent Wall Street Journal article (http://online.wsj.com/search/term.html?KEYWORDS=Heart%20attack) that highlighted the success of managing heart attacks outside the hospital but the notable challenges of managing those events when they occur within the inpatient population.
Another key challenge facing roundtable participants will be to focus their discussions on what clinical parameters should be monitored and which, if any, should be put on the back burner. There is a relatively wide variation of views regarding what should be monitored, what thresholds are problematic and indicative of a declining patient, and what actions need to be taken, and how swiftly, to abate the downward cascade of respiratory compromise. A related challenge facing participants is, “should the industry be moving toward refinement of their monitoring technologies to give physicians and the health-care team more valuable and more timely information? Are we monitoring the right parameters, or are we monitoring what the technology allows us to monitor? Are there gaps that can be addressed?”
While no one is confident of the specific direction these discussions will take, it is likely that not only will the proceedings be documented for submission for publication, but it may very well lead to other conferences that focus on respiratory compromise in other settings. Both the skilled nursing facility and long-term acute care hospital settings provide care for a spectrum of pulmonary/ventilator patients, and the characteristics of their potential cascade of deterioration may or may not be the same as in an acute care hospital. The challenges are similar, but solutions may be different—a subject for further discussion.
This conference is just one example of NAMDRC’s approach to a range of pulmonary-related clinical issues. While NAMDRC’s broad mission is to “improve access to quality care for patients with respiratory disease by removing regulatory and legislative barriers to appropriate treatment,” the roundtable does fit into the mission because of growing concerns that we are facing challenges that are solvable if we take the initiative to address solutions to these challenges.
Another very broad challenge facing NAMDRC is its belief that the growing area of home mechanical ventilation is being shaped by archaic and outdated legislation and regulation. In fact, in a discussion with Marilyn Tavenner, CMS Administrator (and critical care nurse by training) last August, she conceded that the laws and regulations have not kept pace with innovations as basic as noninvasive mechanical ventilation. The idea that mechanical ventilation involves intubation or tracheostomy is universally recognized as archaic. As archaic is the concept that, by definition, ending mechanical ventilation leads to imminent death. While that may have reflected technologies of the 1980s and early 1990s, it is not reflective of today’s standards of care. Amending the existing laws and regulations in this area may become a high priority for NAMDRC over the next few years.
For membership information, visit the NAMDRC website at www.namdrc.org or call 703/752-4359.
NAMDRC is bringing together representatives of key medical societies, including CHEST, ATS, AARC, SCCM, AACN, SHM (hospitalists), PPAHS (patient safety), and ACEP (emergency physicians) to address respiratory compromise, that cascade of events that moves from respiratory insufficiency to respiratory failure to respiratory arrest. Recognizing that respiratory compromise occurs in various settings, the conference, Feb 26-27 in Orlando, Florida, will focus on the hospital setting.
In addition to society representatives, the NAMDRC leadership, in consultation with recognized experts, has also invited several key opinion leaders to participate, including physicians, respiratory therapists, and nurses.
There are several challenges facing the participants, perhaps paramount is to define the concept of “respiratory compromise.” Some of have signaled, “I know it when I see it,” but the expectation is to formulate a specific clinical definition of the respiratory deterioration, and devise a recognition pathway that can easily be used in the hospital setting to identify patients earlier in the course of this cascade.
How to identify high risk patients is critical to the discussion, because it is generally believed that this is where resources need to be focused, both from a personnel and monitoring perspective. Can consensus be drawn to determine which patient characteristics can reliably classify that patient into a high risk for respiratory compromise, and, if so, those characteristics should be delineated. The corollary challenge is to identify the low risk patients so that inappropriate resources are not focused where such efforts might not be necessary.
Individual hospital policies are integral to this issue, as the relative value of rapid response teams appears to vary greatly. Add to the equation a recent Wall Street Journal article (http://online.wsj.com/search/term.html?KEYWORDS=Heart%20attack) that highlighted the success of managing heart attacks outside the hospital but the notable challenges of managing those events when they occur within the inpatient population.
Another key challenge facing roundtable participants will be to focus their discussions on what clinical parameters should be monitored and which, if any, should be put on the back burner. There is a relatively wide variation of views regarding what should be monitored, what thresholds are problematic and indicative of a declining patient, and what actions need to be taken, and how swiftly, to abate the downward cascade of respiratory compromise. A related challenge facing participants is, “should the industry be moving toward refinement of their monitoring technologies to give physicians and the health-care team more valuable and more timely information? Are we monitoring the right parameters, or are we monitoring what the technology allows us to monitor? Are there gaps that can be addressed?”
While no one is confident of the specific direction these discussions will take, it is likely that not only will the proceedings be documented for submission for publication, but it may very well lead to other conferences that focus on respiratory compromise in other settings. Both the skilled nursing facility and long-term acute care hospital settings provide care for a spectrum of pulmonary/ventilator patients, and the characteristics of their potential cascade of deterioration may or may not be the same as in an acute care hospital. The challenges are similar, but solutions may be different—a subject for further discussion.
This conference is just one example of NAMDRC’s approach to a range of pulmonary-related clinical issues. While NAMDRC’s broad mission is to “improve access to quality care for patients with respiratory disease by removing regulatory and legislative barriers to appropriate treatment,” the roundtable does fit into the mission because of growing concerns that we are facing challenges that are solvable if we take the initiative to address solutions to these challenges.
Another very broad challenge facing NAMDRC is its belief that the growing area of home mechanical ventilation is being shaped by archaic and outdated legislation and regulation. In fact, in a discussion with Marilyn Tavenner, CMS Administrator (and critical care nurse by training) last August, she conceded that the laws and regulations have not kept pace with innovations as basic as noninvasive mechanical ventilation. The idea that mechanical ventilation involves intubation or tracheostomy is universally recognized as archaic. As archaic is the concept that, by definition, ending mechanical ventilation leads to imminent death. While that may have reflected technologies of the 1980s and early 1990s, it is not reflective of today’s standards of care. Amending the existing laws and regulations in this area may become a high priority for NAMDRC over the next few years.
For membership information, visit the NAMDRC website at www.namdrc.org or call 703/752-4359.
NAMDRC is bringing together representatives of key medical societies, including CHEST, ATS, AARC, SCCM, AACN, SHM (hospitalists), PPAHS (patient safety), and ACEP (emergency physicians) to address respiratory compromise, that cascade of events that moves from respiratory insufficiency to respiratory failure to respiratory arrest. Recognizing that respiratory compromise occurs in various settings, the conference, Feb 26-27 in Orlando, Florida, will focus on the hospital setting.
In addition to society representatives, the NAMDRC leadership, in consultation with recognized experts, has also invited several key opinion leaders to participate, including physicians, respiratory therapists, and nurses.
There are several challenges facing the participants, perhaps paramount is to define the concept of “respiratory compromise.” Some of have signaled, “I know it when I see it,” but the expectation is to formulate a specific clinical definition of the respiratory deterioration, and devise a recognition pathway that can easily be used in the hospital setting to identify patients earlier in the course of this cascade.
How to identify high risk patients is critical to the discussion, because it is generally believed that this is where resources need to be focused, both from a personnel and monitoring perspective. Can consensus be drawn to determine which patient characteristics can reliably classify that patient into a high risk for respiratory compromise, and, if so, those characteristics should be delineated. The corollary challenge is to identify the low risk patients so that inappropriate resources are not focused where such efforts might not be necessary.
Individual hospital policies are integral to this issue, as the relative value of rapid response teams appears to vary greatly. Add to the equation a recent Wall Street Journal article (http://online.wsj.com/search/term.html?KEYWORDS=Heart%20attack) that highlighted the success of managing heart attacks outside the hospital but the notable challenges of managing those events when they occur within the inpatient population.
Another key challenge facing roundtable participants will be to focus their discussions on what clinical parameters should be monitored and which, if any, should be put on the back burner. There is a relatively wide variation of views regarding what should be monitored, what thresholds are problematic and indicative of a declining patient, and what actions need to be taken, and how swiftly, to abate the downward cascade of respiratory compromise. A related challenge facing participants is, “should the industry be moving toward refinement of their monitoring technologies to give physicians and the health-care team more valuable and more timely information? Are we monitoring the right parameters, or are we monitoring what the technology allows us to monitor? Are there gaps that can be addressed?”
While no one is confident of the specific direction these discussions will take, it is likely that not only will the proceedings be documented for submission for publication, but it may very well lead to other conferences that focus on respiratory compromise in other settings. Both the skilled nursing facility and long-term acute care hospital settings provide care for a spectrum of pulmonary/ventilator patients, and the characteristics of their potential cascade of deterioration may or may not be the same as in an acute care hospital. The challenges are similar, but solutions may be different—a subject for further discussion.
This conference is just one example of NAMDRC’s approach to a range of pulmonary-related clinical issues. While NAMDRC’s broad mission is to “improve access to quality care for patients with respiratory disease by removing regulatory and legislative barriers to appropriate treatment,” the roundtable does fit into the mission because of growing concerns that we are facing challenges that are solvable if we take the initiative to address solutions to these challenges.
Another very broad challenge facing NAMDRC is its belief that the growing area of home mechanical ventilation is being shaped by archaic and outdated legislation and regulation. In fact, in a discussion with Marilyn Tavenner, CMS Administrator (and critical care nurse by training) last August, she conceded that the laws and regulations have not kept pace with innovations as basic as noninvasive mechanical ventilation. The idea that mechanical ventilation involves intubation or tracheostomy is universally recognized as archaic. As archaic is the concept that, by definition, ending mechanical ventilation leads to imminent death. While that may have reflected technologies of the 1980s and early 1990s, it is not reflective of today’s standards of care. Amending the existing laws and regulations in this area may become a high priority for NAMDRC over the next few years.
For membership information, visit the NAMDRC website at www.namdrc.org or call 703/752-4359.
CHEST PREP – Industry-Focused, Disease-State Education
Did you know the American College of Chest Physicians (CHEST) has provided disease-state-specific education for pharmaceutical and medical device representatives for more than 12 years?
The CHEST Professional Representative Education Program, or PREP, is an unbranded disease-state clinical immersion program. The PREP Team works with pharmaceutical and medical device companies to understand their learning objectives and the educational needs of their representatives. We then develop a customized program to address those specific needs. Each program uses different learning methods—problem-based case studies, patient testimony, simulation, and faculty-led workshops—to create a dynamic learning environment that increases interaction and develops deeper comprehension. The PREP curriculum is based on evidence-based clinical practice guidelines and consensus statements. Each program is created by clinical thought leaders and delivered by expert faculty, typically drawn from our CHEST membership. PREP courses are held at leading hospitals and academic medical centers throughout the country, as well as the CHEST Innovation, Simulation, and Training Center in Glenview, Illinois.
Participants, who successfully complete the course objectives, including the post-course knowledge assessment, are awarded a Certificate of Completion valid for a 3-year period.
More importantly, they gain the most current, in-depth clinical information needed to engage with health-care professionals—knowledgeably, confidently, and meaningfully. This translates to better-educated representatives who interact with you as you make clinical decisions that enhance patient outcomes.
CHEST has trained over 4,000 sales representatives over the past 2 years. Not only has CHEST conducted PREP programs for disease states such as atrial fibrillation, venous thromboembolism (VTE), and COPD, PREP programs are also available for women’s health, oncology, and interventional radiology through strategic agreements with the American Congress of Obstetricians and Gynecologists (ACOG), the American Society of Clinical Oncology (ASCO), and the Society of Interventional Radiology (SIR).
The PREP Team recently conducted a very successful Prostate Cancer PREP course at Huntsman Cancer Institute in Salt Lake City, Utah. This course is the first of four to be conducted over the next few months at academic medical centers around the country. Over 100 pharmaceutical sales representatives will participate in this PREP, which was developed and is being conducted through CHEST’s agreement with ASCO.
There are several exciting opportunities coming up in the next few months, as the PREP Team continues to expand the PREP offerings to meet the needs of the industry.
If you would like to develop curriculum content or participate as faculty for a PREP course or to receive more information about how your hospital or medical center can become a course site, please contact me at [email protected] or 224/521-9518.
Did you know the American College of Chest Physicians (CHEST) has provided disease-state-specific education for pharmaceutical and medical device representatives for more than 12 years?
The CHEST Professional Representative Education Program, or PREP, is an unbranded disease-state clinical immersion program. The PREP Team works with pharmaceutical and medical device companies to understand their learning objectives and the educational needs of their representatives. We then develop a customized program to address those specific needs. Each program uses different learning methods—problem-based case studies, patient testimony, simulation, and faculty-led workshops—to create a dynamic learning environment that increases interaction and develops deeper comprehension. The PREP curriculum is based on evidence-based clinical practice guidelines and consensus statements. Each program is created by clinical thought leaders and delivered by expert faculty, typically drawn from our CHEST membership. PREP courses are held at leading hospitals and academic medical centers throughout the country, as well as the CHEST Innovation, Simulation, and Training Center in Glenview, Illinois.
Participants, who successfully complete the course objectives, including the post-course knowledge assessment, are awarded a Certificate of Completion valid for a 3-year period.
More importantly, they gain the most current, in-depth clinical information needed to engage with health-care professionals—knowledgeably, confidently, and meaningfully. This translates to better-educated representatives who interact with you as you make clinical decisions that enhance patient outcomes.
CHEST has trained over 4,000 sales representatives over the past 2 years. Not only has CHEST conducted PREP programs for disease states such as atrial fibrillation, venous thromboembolism (VTE), and COPD, PREP programs are also available for women’s health, oncology, and interventional radiology through strategic agreements with the American Congress of Obstetricians and Gynecologists (ACOG), the American Society of Clinical Oncology (ASCO), and the Society of Interventional Radiology (SIR).
The PREP Team recently conducted a very successful Prostate Cancer PREP course at Huntsman Cancer Institute in Salt Lake City, Utah. This course is the first of four to be conducted over the next few months at academic medical centers around the country. Over 100 pharmaceutical sales representatives will participate in this PREP, which was developed and is being conducted through CHEST’s agreement with ASCO.
There are several exciting opportunities coming up in the next few months, as the PREP Team continues to expand the PREP offerings to meet the needs of the industry.
If you would like to develop curriculum content or participate as faculty for a PREP course or to receive more information about how your hospital or medical center can become a course site, please contact me at [email protected] or 224/521-9518.
Did you know the American College of Chest Physicians (CHEST) has provided disease-state-specific education for pharmaceutical and medical device representatives for more than 12 years?
The CHEST Professional Representative Education Program, or PREP, is an unbranded disease-state clinical immersion program. The PREP Team works with pharmaceutical and medical device companies to understand their learning objectives and the educational needs of their representatives. We then develop a customized program to address those specific needs. Each program uses different learning methods—problem-based case studies, patient testimony, simulation, and faculty-led workshops—to create a dynamic learning environment that increases interaction and develops deeper comprehension. The PREP curriculum is based on evidence-based clinical practice guidelines and consensus statements. Each program is created by clinical thought leaders and delivered by expert faculty, typically drawn from our CHEST membership. PREP courses are held at leading hospitals and academic medical centers throughout the country, as well as the CHEST Innovation, Simulation, and Training Center in Glenview, Illinois.
Participants, who successfully complete the course objectives, including the post-course knowledge assessment, are awarded a Certificate of Completion valid for a 3-year period.
More importantly, they gain the most current, in-depth clinical information needed to engage with health-care professionals—knowledgeably, confidently, and meaningfully. This translates to better-educated representatives who interact with you as you make clinical decisions that enhance patient outcomes.
CHEST has trained over 4,000 sales representatives over the past 2 years. Not only has CHEST conducted PREP programs for disease states such as atrial fibrillation, venous thromboembolism (VTE), and COPD, PREP programs are also available for women’s health, oncology, and interventional radiology through strategic agreements with the American Congress of Obstetricians and Gynecologists (ACOG), the American Society of Clinical Oncology (ASCO), and the Society of Interventional Radiology (SIR).
The PREP Team recently conducted a very successful Prostate Cancer PREP course at Huntsman Cancer Institute in Salt Lake City, Utah. This course is the first of four to be conducted over the next few months at academic medical centers around the country. Over 100 pharmaceutical sales representatives will participate in this PREP, which was developed and is being conducted through CHEST’s agreement with ASCO.
There are several exciting opportunities coming up in the next few months, as the PREP Team continues to expand the PREP offerings to meet the needs of the industry.
If you would like to develop curriculum content or participate as faculty for a PREP course or to receive more information about how your hospital or medical center can become a course site, please contact me at [email protected] or 224/521-9518.