User login
CHEST Foundation Update
During this past year, the CHEST Foundation reached impressive new heights. Nearly a half a million dollars in research grants were awarded, with over $41,000 supporting community service programs ranging from critical care training in Tanzania to asthma education camps for the underserved children in San Antonio, Texas.
Our Disease Awareness Campaigns remain stronger than ever, reaching millions of sports fans at the Daytona 500, Brickyard 400, NASCAR Sprint Cup Race at Chicagoland, and the Indianapolis 500 with lung health public service announcements. In addition to the wide-reaching campaigns, our partnership with the American Lung Association will result in patient education information on 40 lung disease topics, some of which are already accessible on the ALA website, lung.org.
The CHEST Foundation is making a substantial impact on worldwide lung health. More than 95 cents of every dollar raised by the CHEST Foundation goes toward advancing our mission-based programming. Every cent and every donation matters: $100 can support the cost to print 250 “Healthy Lungs Passports” for children; $250 can supply a pulmonary reference textbook for physicians in Tanzania; $500 would help cover travel expenses for 20 home visits to teach children with asthma, and their parents, how to better control their condition; and $750 could fund a laptop computer and projector used to deliver chest medicine training for medical personnel in Africa.
With each contribution, our ability to make an impact on global lung health strengthens. We would like to thank all of our donors for being advocates for our mission—to champion lung health. Our list of achievements and successes is long because of the important role that our members play in ensuring the CHEST Foundation’s efforts to build healthier communities and save lives.
We hope that you will continue to embrace the foundation with enthusiasm, and include us in your end-of-year giving. To make a donation and learn more about the foundation, visit chestnet.org/foundation, or call us at 224/521-9527.
During this past year, the CHEST Foundation reached impressive new heights. Nearly a half a million dollars in research grants were awarded, with over $41,000 supporting community service programs ranging from critical care training in Tanzania to asthma education camps for the underserved children in San Antonio, Texas.
Our Disease Awareness Campaigns remain stronger than ever, reaching millions of sports fans at the Daytona 500, Brickyard 400, NASCAR Sprint Cup Race at Chicagoland, and the Indianapolis 500 with lung health public service announcements. In addition to the wide-reaching campaigns, our partnership with the American Lung Association will result in patient education information on 40 lung disease topics, some of which are already accessible on the ALA website, lung.org.
The CHEST Foundation is making a substantial impact on worldwide lung health. More than 95 cents of every dollar raised by the CHEST Foundation goes toward advancing our mission-based programming. Every cent and every donation matters: $100 can support the cost to print 250 “Healthy Lungs Passports” for children; $250 can supply a pulmonary reference textbook for physicians in Tanzania; $500 would help cover travel expenses for 20 home visits to teach children with asthma, and their parents, how to better control their condition; and $750 could fund a laptop computer and projector used to deliver chest medicine training for medical personnel in Africa.
With each contribution, our ability to make an impact on global lung health strengthens. We would like to thank all of our donors for being advocates for our mission—to champion lung health. Our list of achievements and successes is long because of the important role that our members play in ensuring the CHEST Foundation’s efforts to build healthier communities and save lives.
We hope that you will continue to embrace the foundation with enthusiasm, and include us in your end-of-year giving. To make a donation and learn more about the foundation, visit chestnet.org/foundation, or call us at 224/521-9527.
During this past year, the CHEST Foundation reached impressive new heights. Nearly a half a million dollars in research grants were awarded, with over $41,000 supporting community service programs ranging from critical care training in Tanzania to asthma education camps for the underserved children in San Antonio, Texas.
Our Disease Awareness Campaigns remain stronger than ever, reaching millions of sports fans at the Daytona 500, Brickyard 400, NASCAR Sprint Cup Race at Chicagoland, and the Indianapolis 500 with lung health public service announcements. In addition to the wide-reaching campaigns, our partnership with the American Lung Association will result in patient education information on 40 lung disease topics, some of which are already accessible on the ALA website, lung.org.
The CHEST Foundation is making a substantial impact on worldwide lung health. More than 95 cents of every dollar raised by the CHEST Foundation goes toward advancing our mission-based programming. Every cent and every donation matters: $100 can support the cost to print 250 “Healthy Lungs Passports” for children; $250 can supply a pulmonary reference textbook for physicians in Tanzania; $500 would help cover travel expenses for 20 home visits to teach children with asthma, and their parents, how to better control their condition; and $750 could fund a laptop computer and projector used to deliver chest medicine training for medical personnel in Africa.
With each contribution, our ability to make an impact on global lung health strengthens. We would like to thank all of our donors for being advocates for our mission—to champion lung health. Our list of achievements and successes is long because of the important role that our members play in ensuring the CHEST Foundation’s efforts to build healthier communities and save lives.
We hope that you will continue to embrace the foundation with enthusiasm, and include us in your end-of-year giving. To make a donation and learn more about the foundation, visit chestnet.org/foundation, or call us at 224/521-9527.
New Section Editor for PULMONARY PERSPECTIVES®
We welcome Dr. Nitin Puri, FCCP, as our new Section Editor for Pulmonary Perspectives.
He is an Assistant Professor of Medicine at Cooper Medical School of Rowan University, Camden, N.J.
He did his Internal Medicine training at Grady Hospital in Atlanta at Morehouse School of Medicine and his Pulmonary Medicine and Critical Care Medicine training was done at Cooper Hospital.
He is the Associate Program Director for Critical Care Medicine and was previously Director of the Cardiac Surgery ICU at Inova Fairfax, Falls Church, Virginia.
Dr. Puri’s special interests include quality improvement, bedside ultrasound, and mechanical circulatory support.
We welcome Dr. Nitin Puri, FCCP, as our new Section Editor for Pulmonary Perspectives.
He is an Assistant Professor of Medicine at Cooper Medical School of Rowan University, Camden, N.J.
He did his Internal Medicine training at Grady Hospital in Atlanta at Morehouse School of Medicine and his Pulmonary Medicine and Critical Care Medicine training was done at Cooper Hospital.
He is the Associate Program Director for Critical Care Medicine and was previously Director of the Cardiac Surgery ICU at Inova Fairfax, Falls Church, Virginia.
Dr. Puri’s special interests include quality improvement, bedside ultrasound, and mechanical circulatory support.
We welcome Dr. Nitin Puri, FCCP, as our new Section Editor for Pulmonary Perspectives.
He is an Assistant Professor of Medicine at Cooper Medical School of Rowan University, Camden, N.J.
He did his Internal Medicine training at Grady Hospital in Atlanta at Morehouse School of Medicine and his Pulmonary Medicine and Critical Care Medicine training was done at Cooper Hospital.
He is the Associate Program Director for Critical Care Medicine and was previously Director of the Cardiac Surgery ICU at Inova Fairfax, Falls Church, Virginia.
Dr. Puri’s special interests include quality improvement, bedside ultrasound, and mechanical circulatory support.
Changing the Publishing Paradigm of CHEST
Note: This article excerpts content from the January 2016 CHEST editorial (Irwin RS, Welch SJ, Rice J, French CT. Spread the word about CHEST in 2016: An ever-rising impact factor, content innovations, launching a new partnership with Elsevier, and protecting the name and legacy of the journal. Chest. 2016;149(1):1-6).
Since its inception in 1935, CHEST had been self-published by the American College of Chest Physicians. Starting this month, January 2016, CHEST has chosen to work in partnership with Elsevier as its publisher. While CHEST will maintain editorial control over the journal, this partnership will allow us to grow the reach and awareness of the journal, provide world class data reporting and trend analysis, increase our outreach for the best clinical research in the field, and provide a competitive business backbone to increase our support for the CHEST organization. We are confident that the global footprint of Elsevier, its Science Direct and Clinical Key content delivery platforms, and its commitment to attracting the best clinical science for the journal, will provide the resources for CHEST to continue to evolve, innovate, and bring our readers the most relevant, cutting-edge content to help them provide the best patient care every minute of every day. Please join us in celebrating a new relationship that we believe will benefit our readers, our parent CHEST organization and its membership, and our new business partner, Elsevier.
Elsevier Content Innovations and Benefits for Authors and Readers
Some exciting new content innovations will be available to CHEST authors and readers through Elsevier’s Science Direct platform.
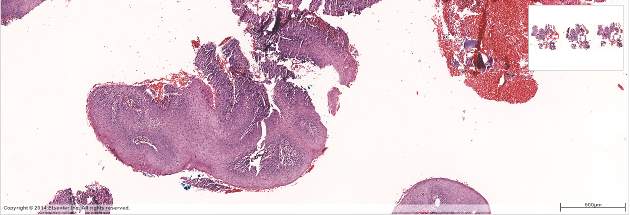
These will include (1) a virtual microscope that will allow authors to submit high-resolution figures that can be viewed and zoomed in to great detail not previously possible (Fig 1);
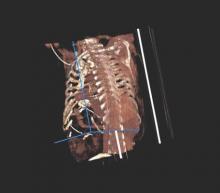
(2) interactive case reports that will allow us to modify case-based sections like Pearls and Chest Imaging so that the reader has to select the right answer from multiple choices; (3) multimedia audio slide summaries that will allow authors to record up to a 5-minute audio file, with slides, that summarizes their paper; and (4) interactive 3-D radiologic imaging that will allow conversion of images to an interactive 3-D model (Fig 2).
These innovations will be implemented throughout 2016, and instructions on how to use them have been added to our Instructions to Authors, which can be found at: http://journal.publications.chestnet.org/ss/forauthors.aspx
We are actively assessing other innovations that may be implemented at a later date. A list and description of the content innovations discussed above, as well as ones we are considering, can be found at:
https://www.elsevier.com/books-and-journals/content-innovation#list.
In addition, the partnership with Elsevier will allow for a number of benefits to authors and readers. First of all, we will no longer charge authors for submission of color figures. We believe this will enhance the visual appeal of articles and provide more clarity when looking at data plots and graphs, as color will be easier to discern than gray scale. In addition, Elsevier teams will redraw figures and use color in graphs and charts where appropriate to create consistency in the look and feel of the journal, improving readability and data interpretation by the reader. Second, Elsevier will provide an author dashboard, so that the author can see information about their article, such as citation statistics and bibliometrics, as well as usage and downloads. And, in order to facilitate wider dissemination of our correspondence, we are moving that section from an online-only status and putting it back into the print journal, as well as online. We are excited to offer all of these services to our authors and readers.
We want to assure our authors that all of these content innovations and benefits will be free of charge!
Innovation is not new for CHEST. A blog on The Scholarly Kitchen, written by Kent Anderson, noted “One frequent design challenge for both print and online is to make multimedia content more apparent to online users. The Chest redesign is notable in this regard, as the editorial explaining it carefully demonstrates how to access video, audio, and data options around articles. It reads like an instruction manual, which is not a criticism. Change has to be handled carefully, and most journals (and organizations in general) under-communicate changes and benefits to their customers. On the strategic front, the Chest redesign is geared to providing more online-only content, a strong trend among journals, especially as print advertising continues a slow and steady decline.” http://scholarlykitchen.sspnet.org/2014/07/07/the-journal-redesign-more-complicated-more-costly-and-more-strategic-than-ever/
We would be remiss if we didn’t thank you, our readers, members, authors, contributors, and peer reviewers, for the important roles you play in ensuring the success of our efforts to provide the best clinical content to the CHEST readership. Thank you for your ongoing support and contributions to CHEST.
Note: This article excerpts content from the January 2016 CHEST editorial (Irwin RS, Welch SJ, Rice J, French CT. Spread the word about CHEST in 2016: An ever-rising impact factor, content innovations, launching a new partnership with Elsevier, and protecting the name and legacy of the journal. Chest. 2016;149(1):1-6).
Since its inception in 1935, CHEST had been self-published by the American College of Chest Physicians. Starting this month, January 2016, CHEST has chosen to work in partnership with Elsevier as its publisher. While CHEST will maintain editorial control over the journal, this partnership will allow us to grow the reach and awareness of the journal, provide world class data reporting and trend analysis, increase our outreach for the best clinical research in the field, and provide a competitive business backbone to increase our support for the CHEST organization. We are confident that the global footprint of Elsevier, its Science Direct and Clinical Key content delivery platforms, and its commitment to attracting the best clinical science for the journal, will provide the resources for CHEST to continue to evolve, innovate, and bring our readers the most relevant, cutting-edge content to help them provide the best patient care every minute of every day. Please join us in celebrating a new relationship that we believe will benefit our readers, our parent CHEST organization and its membership, and our new business partner, Elsevier.
Elsevier Content Innovations and Benefits for Authors and Readers
Some exciting new content innovations will be available to CHEST authors and readers through Elsevier’s Science Direct platform.
These will include (1) a virtual microscope that will allow authors to submit high-resolution figures that can be viewed and zoomed in to great detail not previously possible (Fig 1);
(2) interactive case reports that will allow us to modify case-based sections like Pearls and Chest Imaging so that the reader has to select the right answer from multiple choices; (3) multimedia audio slide summaries that will allow authors to record up to a 5-minute audio file, with slides, that summarizes their paper; and (4) interactive 3-D radiologic imaging that will allow conversion of images to an interactive 3-D model (Fig 2).
These innovations will be implemented throughout 2016, and instructions on how to use them have been added to our Instructions to Authors, which can be found at: http://journal.publications.chestnet.org/ss/forauthors.aspx
We are actively assessing other innovations that may be implemented at a later date. A list and description of the content innovations discussed above, as well as ones we are considering, can be found at:
https://www.elsevier.com/books-and-journals/content-innovation#list.
In addition, the partnership with Elsevier will allow for a number of benefits to authors and readers. First of all, we will no longer charge authors for submission of color figures. We believe this will enhance the visual appeal of articles and provide more clarity when looking at data plots and graphs, as color will be easier to discern than gray scale. In addition, Elsevier teams will redraw figures and use color in graphs and charts where appropriate to create consistency in the look and feel of the journal, improving readability and data interpretation by the reader. Second, Elsevier will provide an author dashboard, so that the author can see information about their article, such as citation statistics and bibliometrics, as well as usage and downloads. And, in order to facilitate wider dissemination of our correspondence, we are moving that section from an online-only status and putting it back into the print journal, as well as online. We are excited to offer all of these services to our authors and readers.
We want to assure our authors that all of these content innovations and benefits will be free of charge!
Innovation is not new for CHEST. A blog on The Scholarly Kitchen, written by Kent Anderson, noted “One frequent design challenge for both print and online is to make multimedia content more apparent to online users. The Chest redesign is notable in this regard, as the editorial explaining it carefully demonstrates how to access video, audio, and data options around articles. It reads like an instruction manual, which is not a criticism. Change has to be handled carefully, and most journals (and organizations in general) under-communicate changes and benefits to their customers. On the strategic front, the Chest redesign is geared to providing more online-only content, a strong trend among journals, especially as print advertising continues a slow and steady decline.” http://scholarlykitchen.sspnet.org/2014/07/07/the-journal-redesign-more-complicated-more-costly-and-more-strategic-than-ever/
We would be remiss if we didn’t thank you, our readers, members, authors, contributors, and peer reviewers, for the important roles you play in ensuring the success of our efforts to provide the best clinical content to the CHEST readership. Thank you for your ongoing support and contributions to CHEST.
Note: This article excerpts content from the January 2016 CHEST editorial (Irwin RS, Welch SJ, Rice J, French CT. Spread the word about CHEST in 2016: An ever-rising impact factor, content innovations, launching a new partnership with Elsevier, and protecting the name and legacy of the journal. Chest. 2016;149(1):1-6).
Since its inception in 1935, CHEST had been self-published by the American College of Chest Physicians. Starting this month, January 2016, CHEST has chosen to work in partnership with Elsevier as its publisher. While CHEST will maintain editorial control over the journal, this partnership will allow us to grow the reach and awareness of the journal, provide world class data reporting and trend analysis, increase our outreach for the best clinical research in the field, and provide a competitive business backbone to increase our support for the CHEST organization. We are confident that the global footprint of Elsevier, its Science Direct and Clinical Key content delivery platforms, and its commitment to attracting the best clinical science for the journal, will provide the resources for CHEST to continue to evolve, innovate, and bring our readers the most relevant, cutting-edge content to help them provide the best patient care every minute of every day. Please join us in celebrating a new relationship that we believe will benefit our readers, our parent CHEST organization and its membership, and our new business partner, Elsevier.
Elsevier Content Innovations and Benefits for Authors and Readers
Some exciting new content innovations will be available to CHEST authors and readers through Elsevier’s Science Direct platform.
These will include (1) a virtual microscope that will allow authors to submit high-resolution figures that can be viewed and zoomed in to great detail not previously possible (Fig 1);
(2) interactive case reports that will allow us to modify case-based sections like Pearls and Chest Imaging so that the reader has to select the right answer from multiple choices; (3) multimedia audio slide summaries that will allow authors to record up to a 5-minute audio file, with slides, that summarizes their paper; and (4) interactive 3-D radiologic imaging that will allow conversion of images to an interactive 3-D model (Fig 2).
These innovations will be implemented throughout 2016, and instructions on how to use them have been added to our Instructions to Authors, which can be found at: http://journal.publications.chestnet.org/ss/forauthors.aspx
We are actively assessing other innovations that may be implemented at a later date. A list and description of the content innovations discussed above, as well as ones we are considering, can be found at:
https://www.elsevier.com/books-and-journals/content-innovation#list.
In addition, the partnership with Elsevier will allow for a number of benefits to authors and readers. First of all, we will no longer charge authors for submission of color figures. We believe this will enhance the visual appeal of articles and provide more clarity when looking at data plots and graphs, as color will be easier to discern than gray scale. In addition, Elsevier teams will redraw figures and use color in graphs and charts where appropriate to create consistency in the look and feel of the journal, improving readability and data interpretation by the reader. Second, Elsevier will provide an author dashboard, so that the author can see information about their article, such as citation statistics and bibliometrics, as well as usage and downloads. And, in order to facilitate wider dissemination of our correspondence, we are moving that section from an online-only status and putting it back into the print journal, as well as online. We are excited to offer all of these services to our authors and readers.
We want to assure our authors that all of these content innovations and benefits will be free of charge!
Innovation is not new for CHEST. A blog on The Scholarly Kitchen, written by Kent Anderson, noted “One frequent design challenge for both print and online is to make multimedia content more apparent to online users. The Chest redesign is notable in this regard, as the editorial explaining it carefully demonstrates how to access video, audio, and data options around articles. It reads like an instruction manual, which is not a criticism. Change has to be handled carefully, and most journals (and organizations in general) under-communicate changes and benefits to their customers. On the strategic front, the Chest redesign is geared to providing more online-only content, a strong trend among journals, especially as print advertising continues a slow and steady decline.” http://scholarlykitchen.sspnet.org/2014/07/07/the-journal-redesign-more-complicated-more-costly-and-more-strategic-than-ever/
We would be remiss if we didn’t thank you, our readers, members, authors, contributors, and peer reviewers, for the important roles you play in ensuring the success of our efforts to provide the best clinical content to the CHEST readership. Thank you for your ongoing support and contributions to CHEST.
NEW - Earn CME credit AND MOC points at CHEST live learning courses
Effective September 30, the American Board of Internal Medicine (ABIM) in collaboration with the Accreditation Council for Continuing Medical Education (ACCME) implemented a process for providers like CHEST to deliver educational activities that offer both MOC (Maintenance of Certification) points and CME (Continuing Medical Education) credits.
This will increase the number of MOC offerings available to CHEST members and minimize the time, effort, and resources needed for members to earn both MOC and CME.
As a result of this development, live learning courses offered at the CHEST Innovation, Simulation, and Training Center are now eligible for Maintenance of Certification (MOC).
CHEST will submit your MOC points directly to ABIM (minimum performance scores required). MOC points will correspond to the number of AMA PRA Category 1 Credits™ offered and claimed for the course.
More About MOC (http://www.chestnet.org/Education/Advanced-Clinical-Training/MOC-PIMs)
Live Learning Courses (chestnet.org/live-learning)
Effective September 30, the American Board of Internal Medicine (ABIM) in collaboration with the Accreditation Council for Continuing Medical Education (ACCME) implemented a process for providers like CHEST to deliver educational activities that offer both MOC (Maintenance of Certification) points and CME (Continuing Medical Education) credits.
This will increase the number of MOC offerings available to CHEST members and minimize the time, effort, and resources needed for members to earn both MOC and CME.
As a result of this development, live learning courses offered at the CHEST Innovation, Simulation, and Training Center are now eligible for Maintenance of Certification (MOC).
CHEST will submit your MOC points directly to ABIM (minimum performance scores required). MOC points will correspond to the number of AMA PRA Category 1 Credits™ offered and claimed for the course.
More About MOC (http://www.chestnet.org/Education/Advanced-Clinical-Training/MOC-PIMs)
Live Learning Courses (chestnet.org/live-learning)
Effective September 30, the American Board of Internal Medicine (ABIM) in collaboration with the Accreditation Council for Continuing Medical Education (ACCME) implemented a process for providers like CHEST to deliver educational activities that offer both MOC (Maintenance of Certification) points and CME (Continuing Medical Education) credits.
This will increase the number of MOC offerings available to CHEST members and minimize the time, effort, and resources needed for members to earn both MOC and CME.
As a result of this development, live learning courses offered at the CHEST Innovation, Simulation, and Training Center are now eligible for Maintenance of Certification (MOC).
CHEST will submit your MOC points directly to ABIM (minimum performance scores required). MOC points will correspond to the number of AMA PRA Category 1 Credits™ offered and claimed for the course.
More About MOC (http://www.chestnet.org/Education/Advanced-Clinical-Training/MOC-PIMs)
Live Learning Courses (chestnet.org/live-learning)
A Time to Look Back…and Forward
It’s December—the end of the calendar year and a time of reflection. When I look back on the goals we set for CHEST in 2015, I’m enthusiastic by what I see. We concentrated our efforts around the five main goals from our strategic plan to focus our work. There are many noteworthy accomplishments in each, but I’ll highlight just a few.
Goal 1: CHEST provides the total education solution with content customized to fit individual learner needs and schedules.
We held a very successful annual meeting in Montréal with more than 7,000 total attendees. Throughout the year, we hosted 19 live learning simulation courses in our Innovation, Simulation, and Training Center, reaching over 900 learners. With a full line of courses scheduled for 2016, we’re on track to continue providing quality education next year. People have already begun registering. Check out the calendar at chestnet.org/live-learning.
Goal 2: CHEST has a wide array of new, relevant, and useful guidelines, standards, and complementary programs that guide the profession.
We released eight guidelines and consensus statements in 2015. (Visit journal.publications.chestnet.org/ss/guidelines.aspx for the complete list.) And, following our model to publish updates to topics as new evidence is evaluated, we released seven chapter updates to Diagnosis and Management of Cough: Evidence-Based Clinical Practice Guidelines.
Beginning January 2016, Elsevier, a world-leading provider of scientific products and services, will publish the journal CHEST, allowing us to deliver research to a larger audience and attract higher profile clinical research from around the world. I’m looking forward to seeing the impact of this new partnership.
Goal 3: CHEST has a meaningful impact on global lung health and patient care.
We continue to host international education events around the world. In 2015, we offered “Best of CHEST” courses in Argentina and Beijing, a board review course in Turkey, simulation training at ERS in Amsterdam, four GAIN Europe courses, and sent CHEST faculty to international education events around the globe. Through disease awareness campaigns, the CHEST Foundation is reaching both patients and clinicians. This past year, the foundation promoted the importance of understanding COPD with both English and Spanish resources. In addition, the foundation teamed up with the Foundation for Sarcoidosis Research to launch “Sarcoidosis: Seek Answers. Inspire Results” and built awareness of lung health and lung cancer at major sporting events.
Goal 4: CHEST optimizes its assets to achieve its mission and ensure execution of its strategic plan.
Our greatest asset is our membership. In May 2015, we updated our membership model to reflect emerging, team-based health-care models and opened membership to the entire chest medicine team. Team-based care is consistent with how health care is practiced, and it’s the way to keep advancing patient care. Under our new model, we’ve gained 90% of US chest medicine fellows-in-training as members and have maintained a 90% membership retention rate.
Another asset, our journal CHEST, continues to be respected around the world. The CHEST Impact Factor rose again to 7.483. CHEST now ranks fifth of 54 journals in the Respiratory Medicine category and second of 27 in the Critical Care category. We continue using our social media outlets to serve as thought leaders in chest medicine. Over the past year, our Twitter followers grew to more than 10,000, and our Facebook fans topped 90,000. These numbers indicate those with interest in chest medicine are taking note and engaging with us.
Goal 5: CHEST has a strong and diverse financial base.
I’m happy to report we had positive financial performances for CHEST, the CHEST Foundation, and CHEST Enterprises. We controlled key expenses throughout the year while achieving the highest-ever revenue on the CHEST Annual Meeting, attracting higher royalties and advertising revenue, and more to improve margins. Moving into 2016, we’re financially stable because of our many valued assets.
CHEST accomplished much more during 2015, and I invite you to read the details in our Advancement and Impact Report, available on chestnet.org under the “About” tab. The report recaps our accomplishments during the presidential term of Dr. Curt Sessler, FCCP, and it represents a culmination of the work of our leaders and members. CHEST has a proud history of dedicated members committed to advancing chest medicine and patient care. Your contributions continue to make our organization a success, and I look forward to beginning another outstanding year in 2016.
As always, feel free to connect with me if you have anything on your mind. I invite you to follow me on Twitter (@PMarkowskiACCP), or look for me at upcoming CHEST events.
It’s December—the end of the calendar year and a time of reflection. When I look back on the goals we set for CHEST in 2015, I’m enthusiastic by what I see. We concentrated our efforts around the five main goals from our strategic plan to focus our work. There are many noteworthy accomplishments in each, but I’ll highlight just a few.
Goal 1: CHEST provides the total education solution with content customized to fit individual learner needs and schedules.
We held a very successful annual meeting in Montréal with more than 7,000 total attendees. Throughout the year, we hosted 19 live learning simulation courses in our Innovation, Simulation, and Training Center, reaching over 900 learners. With a full line of courses scheduled for 2016, we’re on track to continue providing quality education next year. People have already begun registering. Check out the calendar at chestnet.org/live-learning.
Goal 2: CHEST has a wide array of new, relevant, and useful guidelines, standards, and complementary programs that guide the profession.
We released eight guidelines and consensus statements in 2015. (Visit journal.publications.chestnet.org/ss/guidelines.aspx for the complete list.) And, following our model to publish updates to topics as new evidence is evaluated, we released seven chapter updates to Diagnosis and Management of Cough: Evidence-Based Clinical Practice Guidelines.
Beginning January 2016, Elsevier, a world-leading provider of scientific products and services, will publish the journal CHEST, allowing us to deliver research to a larger audience and attract higher profile clinical research from around the world. I’m looking forward to seeing the impact of this new partnership.
Goal 3: CHEST has a meaningful impact on global lung health and patient care.
We continue to host international education events around the world. In 2015, we offered “Best of CHEST” courses in Argentina and Beijing, a board review course in Turkey, simulation training at ERS in Amsterdam, four GAIN Europe courses, and sent CHEST faculty to international education events around the globe. Through disease awareness campaigns, the CHEST Foundation is reaching both patients and clinicians. This past year, the foundation promoted the importance of understanding COPD with both English and Spanish resources. In addition, the foundation teamed up with the Foundation for Sarcoidosis Research to launch “Sarcoidosis: Seek Answers. Inspire Results” and built awareness of lung health and lung cancer at major sporting events.
Goal 4: CHEST optimizes its assets to achieve its mission and ensure execution of its strategic plan.
Our greatest asset is our membership. In May 2015, we updated our membership model to reflect emerging, team-based health-care models and opened membership to the entire chest medicine team. Team-based care is consistent with how health care is practiced, and it’s the way to keep advancing patient care. Under our new model, we’ve gained 90% of US chest medicine fellows-in-training as members and have maintained a 90% membership retention rate.
Another asset, our journal CHEST, continues to be respected around the world. The CHEST Impact Factor rose again to 7.483. CHEST now ranks fifth of 54 journals in the Respiratory Medicine category and second of 27 in the Critical Care category. We continue using our social media outlets to serve as thought leaders in chest medicine. Over the past year, our Twitter followers grew to more than 10,000, and our Facebook fans topped 90,000. These numbers indicate those with interest in chest medicine are taking note and engaging with us.
Goal 5: CHEST has a strong and diverse financial base.
I’m happy to report we had positive financial performances for CHEST, the CHEST Foundation, and CHEST Enterprises. We controlled key expenses throughout the year while achieving the highest-ever revenue on the CHEST Annual Meeting, attracting higher royalties and advertising revenue, and more to improve margins. Moving into 2016, we’re financially stable because of our many valued assets.
CHEST accomplished much more during 2015, and I invite you to read the details in our Advancement and Impact Report, available on chestnet.org under the “About” tab. The report recaps our accomplishments during the presidential term of Dr. Curt Sessler, FCCP, and it represents a culmination of the work of our leaders and members. CHEST has a proud history of dedicated members committed to advancing chest medicine and patient care. Your contributions continue to make our organization a success, and I look forward to beginning another outstanding year in 2016.
As always, feel free to connect with me if you have anything on your mind. I invite you to follow me on Twitter (@PMarkowskiACCP), or look for me at upcoming CHEST events.
It’s December—the end of the calendar year and a time of reflection. When I look back on the goals we set for CHEST in 2015, I’m enthusiastic by what I see. We concentrated our efforts around the five main goals from our strategic plan to focus our work. There are many noteworthy accomplishments in each, but I’ll highlight just a few.
Goal 1: CHEST provides the total education solution with content customized to fit individual learner needs and schedules.
We held a very successful annual meeting in Montréal with more than 7,000 total attendees. Throughout the year, we hosted 19 live learning simulation courses in our Innovation, Simulation, and Training Center, reaching over 900 learners. With a full line of courses scheduled for 2016, we’re on track to continue providing quality education next year. People have already begun registering. Check out the calendar at chestnet.org/live-learning.
Goal 2: CHEST has a wide array of new, relevant, and useful guidelines, standards, and complementary programs that guide the profession.
We released eight guidelines and consensus statements in 2015. (Visit journal.publications.chestnet.org/ss/guidelines.aspx for the complete list.) And, following our model to publish updates to topics as new evidence is evaluated, we released seven chapter updates to Diagnosis and Management of Cough: Evidence-Based Clinical Practice Guidelines.
Beginning January 2016, Elsevier, a world-leading provider of scientific products and services, will publish the journal CHEST, allowing us to deliver research to a larger audience and attract higher profile clinical research from around the world. I’m looking forward to seeing the impact of this new partnership.
Goal 3: CHEST has a meaningful impact on global lung health and patient care.
We continue to host international education events around the world. In 2015, we offered “Best of CHEST” courses in Argentina and Beijing, a board review course in Turkey, simulation training at ERS in Amsterdam, four GAIN Europe courses, and sent CHEST faculty to international education events around the globe. Through disease awareness campaigns, the CHEST Foundation is reaching both patients and clinicians. This past year, the foundation promoted the importance of understanding COPD with both English and Spanish resources. In addition, the foundation teamed up with the Foundation for Sarcoidosis Research to launch “Sarcoidosis: Seek Answers. Inspire Results” and built awareness of lung health and lung cancer at major sporting events.
Goal 4: CHEST optimizes its assets to achieve its mission and ensure execution of its strategic plan.
Our greatest asset is our membership. In May 2015, we updated our membership model to reflect emerging, team-based health-care models and opened membership to the entire chest medicine team. Team-based care is consistent with how health care is practiced, and it’s the way to keep advancing patient care. Under our new model, we’ve gained 90% of US chest medicine fellows-in-training as members and have maintained a 90% membership retention rate.
Another asset, our journal CHEST, continues to be respected around the world. The CHEST Impact Factor rose again to 7.483. CHEST now ranks fifth of 54 journals in the Respiratory Medicine category and second of 27 in the Critical Care category. We continue using our social media outlets to serve as thought leaders in chest medicine. Over the past year, our Twitter followers grew to more than 10,000, and our Facebook fans topped 90,000. These numbers indicate those with interest in chest medicine are taking note and engaging with us.
Goal 5: CHEST has a strong and diverse financial base.
I’m happy to report we had positive financial performances for CHEST, the CHEST Foundation, and CHEST Enterprises. We controlled key expenses throughout the year while achieving the highest-ever revenue on the CHEST Annual Meeting, attracting higher royalties and advertising revenue, and more to improve margins. Moving into 2016, we’re financially stable because of our many valued assets.
CHEST accomplished much more during 2015, and I invite you to read the details in our Advancement and Impact Report, available on chestnet.org under the “About” tab. The report recaps our accomplishments during the presidential term of Dr. Curt Sessler, FCCP, and it represents a culmination of the work of our leaders and members. CHEST has a proud history of dedicated members committed to advancing chest medicine and patient care. Your contributions continue to make our organization a success, and I look forward to beginning another outstanding year in 2016.
As always, feel free to connect with me if you have anything on your mind. I invite you to follow me on Twitter (@PMarkowskiACCP), or look for me at upcoming CHEST events.
CHEST announces Dr. Barbara Phillips as its 78th President
The American College of Chest Physicians (CHEST) has announced Dr. Barbara Phillips as its new President, effective November 1. At CHEST 2015 in Montréal, the appointments of Dr. Gerard Silvestri as President-Elect and Dr. John Studdard as President-Designate were confirmed, and Dr. Curtis Sessler, who completed his term as President and became Immediate Past President of CHEST was honored.
Barbara Phillips, MD, MSPH, FCCP, is a Professor of Pulmonary, Critical Care, and Sleep Medicine in the Department of Internal Medicine, and Medical Director of the Sleep Laboratory at the University of Kentucky College of Medicine. She is board-certified in internal medicine, pulmonary medicine, and sleep medicine. After joining CHEST as an affiliate member in 1982, Dr. Phillips advanced to Fellow in 1983. She became a member of the Sleep Medicine NetWork and CHEST Governor of Kentucky. She has chaired the Sleep Institute and is Editor of CHEST SEEK Sleep Medicine (Second, Third, and Fourth Editions). Dr. Phillips also served for 8 years as a Regent-at-Large for the American College of Chest Physicians. Besides her work with CHEST, Dr. Phillips chaired the National Sleep Foundation and has served on the boards of the American Lung Association, the American Academy of Sleep Medicine, and the American Board of Sleep Medicine. Dr. Phillips received a Sleep Academic Award from the National Institutes of Health and was presented with the College Medalist Award at CHEST 2013. Dr. Phillips’ research interests include the effects of sleep apnea on performance and outcomes, genetic risk factors for sleep apnea, nonpharmacologic treatment of sleep apnea, and sleep in aging.
Gerard Silvestri, MD, FCCP, is the Hillenbrand Professor of Thoracic Oncology and Vice-Chair of Medicine for Faculty Development at the Medical University of South Carolina. He completed his fellowship training in pulmonary and critical care at Dartmouth. He has an advanced degree in the evaluative clinical sciences, also from Dartmouth. He is a lung cancer and interventional pulmonologist with an interest in health services research, lung cancer screening, nodule evaluation and management, and staging of lung cancer. After becoming a Fellow of the American College of Chest Physicians in 1998, Dr. Silvestri became active with the NetWorks, serving on the Steering Committees of the Thoracic Oncology and the Interventional Chest/Diagnostic Procedures NetWorks, eventually chairing the Thoracic Oncology NetWork. Dr. Silvestri has also served on the Nominating Committee, the CHEST Scientific Program Committee, the CHEST Foundation Development Committee, as Treasurer and Trustee on the foundation’s Board of Trustees, and as a Regent-at-Large for the American College of Chest Physicians for 3 years. At CHEST 2012, Dr. Silvestri was awarded the Pasquale Ciaglia Memorial Lecture in Interventional Medicine, and at CHEST 2014, he received the Edward C. Rosenow III, MD, Master FCCP/Master Teacher Honor Lecture. Dr. Silvestri has authored more than 200 scientific articles, book chapters, and editorials, and he currently serves on the editorial board of the journal CHEST.
John Studdard, MD, FCCP, is a pulmonary and critical care physician in private practice with Jackson Pulmonary Associates in Jackson, Mississippi. Dr. Studdard completed his fellowship training at the Mayo Graduate School of Medicine. He has served in numerous CHEST leadership roles, including President and Chair of the CHEST Foundation, the philanthropic arm of CHEST; chair of the Government Relations Committee; member of the Marketing Committee; and Ex Officio member of the Diversity Committee, Scientific Program Committee, and Financial Oversight Committee. Dr. Studdard’s dedication to reducing the number of patients he treats for tobacco-related diseases, and his leadership qualities led him to serve as representative for CHEST in the negotiations with the tobacco industry leading to the Attorneys General Master Settlement Agreement of 1998. More recently, in his roles with the CHEST Foundation, Dr. Studdard served as a vice chair of the Beyond Our Walls capital campaign, the CHEST Foundation Nominating Committee, and several foundation work groups.
Curtis N. Sessler MD, FCCP, is the Orhan Muren Distinguished Professor of Medicine at Virginia Commonwealth University (VCU) Health System in the Division of Pulmonary and Critical Care Medicine, where he is Director of the Center for Adult Critical Care and Medical Director of Critical Care and the Medical Respiratory ICU. Dr. Sessler is an enthusiastic clinician and educator who has received teaching awards at VCU, including the School of Medicine Educational Innovation Award. His research interests include ICU sedation, mechanical ventilation, and infection prevention, authoring more than 300 articles, book chapters, books, and abstracts. He has served on a variety of multisociety task forces addressing research, training competency, workforce shortage, and ICU burnout. He is Past President of the Virginia Thoracic Society and has served as Chair of the Pulmonary and Allergy Drug Advisory Committee of the US FDA. An active member of CHEST, he has served on the Board of Regents and as Chair of the Critical Care Section, Chair of the Council of Sections, Chair of the Critical Care Institute, Program Chair for the 2003 CHEST annual meeting, and an Ex Officio member of the CHEST Foundation Board of Trustees. He received the Roger C. Bone Memorial Lecture award in 2010. He is a member of the editorial board of CHEST, Editor in Chief of CHEST SEEK Critical Care Medicine, and is co-section editor for Contemporary Reviews in Critical Care Medicine (in CHEST).
The American College of Chest Physicians (CHEST) has announced Dr. Barbara Phillips as its new President, effective November 1. At CHEST 2015 in Montréal, the appointments of Dr. Gerard Silvestri as President-Elect and Dr. John Studdard as President-Designate were confirmed, and Dr. Curtis Sessler, who completed his term as President and became Immediate Past President of CHEST was honored.
Barbara Phillips, MD, MSPH, FCCP, is a Professor of Pulmonary, Critical Care, and Sleep Medicine in the Department of Internal Medicine, and Medical Director of the Sleep Laboratory at the University of Kentucky College of Medicine. She is board-certified in internal medicine, pulmonary medicine, and sleep medicine. After joining CHEST as an affiliate member in 1982, Dr. Phillips advanced to Fellow in 1983. She became a member of the Sleep Medicine NetWork and CHEST Governor of Kentucky. She has chaired the Sleep Institute and is Editor of CHEST SEEK Sleep Medicine (Second, Third, and Fourth Editions). Dr. Phillips also served for 8 years as a Regent-at-Large for the American College of Chest Physicians. Besides her work with CHEST, Dr. Phillips chaired the National Sleep Foundation and has served on the boards of the American Lung Association, the American Academy of Sleep Medicine, and the American Board of Sleep Medicine. Dr. Phillips received a Sleep Academic Award from the National Institutes of Health and was presented with the College Medalist Award at CHEST 2013. Dr. Phillips’ research interests include the effects of sleep apnea on performance and outcomes, genetic risk factors for sleep apnea, nonpharmacologic treatment of sleep apnea, and sleep in aging.
Gerard Silvestri, MD, FCCP, is the Hillenbrand Professor of Thoracic Oncology and Vice-Chair of Medicine for Faculty Development at the Medical University of South Carolina. He completed his fellowship training in pulmonary and critical care at Dartmouth. He has an advanced degree in the evaluative clinical sciences, also from Dartmouth. He is a lung cancer and interventional pulmonologist with an interest in health services research, lung cancer screening, nodule evaluation and management, and staging of lung cancer. After becoming a Fellow of the American College of Chest Physicians in 1998, Dr. Silvestri became active with the NetWorks, serving on the Steering Committees of the Thoracic Oncology and the Interventional Chest/Diagnostic Procedures NetWorks, eventually chairing the Thoracic Oncology NetWork. Dr. Silvestri has also served on the Nominating Committee, the CHEST Scientific Program Committee, the CHEST Foundation Development Committee, as Treasurer and Trustee on the foundation’s Board of Trustees, and as a Regent-at-Large for the American College of Chest Physicians for 3 years. At CHEST 2012, Dr. Silvestri was awarded the Pasquale Ciaglia Memorial Lecture in Interventional Medicine, and at CHEST 2014, he received the Edward C. Rosenow III, MD, Master FCCP/Master Teacher Honor Lecture. Dr. Silvestri has authored more than 200 scientific articles, book chapters, and editorials, and he currently serves on the editorial board of the journal CHEST.
John Studdard, MD, FCCP, is a pulmonary and critical care physician in private practice with Jackson Pulmonary Associates in Jackson, Mississippi. Dr. Studdard completed his fellowship training at the Mayo Graduate School of Medicine. He has served in numerous CHEST leadership roles, including President and Chair of the CHEST Foundation, the philanthropic arm of CHEST; chair of the Government Relations Committee; member of the Marketing Committee; and Ex Officio member of the Diversity Committee, Scientific Program Committee, and Financial Oversight Committee. Dr. Studdard’s dedication to reducing the number of patients he treats for tobacco-related diseases, and his leadership qualities led him to serve as representative for CHEST in the negotiations with the tobacco industry leading to the Attorneys General Master Settlement Agreement of 1998. More recently, in his roles with the CHEST Foundation, Dr. Studdard served as a vice chair of the Beyond Our Walls capital campaign, the CHEST Foundation Nominating Committee, and several foundation work groups.
Curtis N. Sessler MD, FCCP, is the Orhan Muren Distinguished Professor of Medicine at Virginia Commonwealth University (VCU) Health System in the Division of Pulmonary and Critical Care Medicine, where he is Director of the Center for Adult Critical Care and Medical Director of Critical Care and the Medical Respiratory ICU. Dr. Sessler is an enthusiastic clinician and educator who has received teaching awards at VCU, including the School of Medicine Educational Innovation Award. His research interests include ICU sedation, mechanical ventilation, and infection prevention, authoring more than 300 articles, book chapters, books, and abstracts. He has served on a variety of multisociety task forces addressing research, training competency, workforce shortage, and ICU burnout. He is Past President of the Virginia Thoracic Society and has served as Chair of the Pulmonary and Allergy Drug Advisory Committee of the US FDA. An active member of CHEST, he has served on the Board of Regents and as Chair of the Critical Care Section, Chair of the Council of Sections, Chair of the Critical Care Institute, Program Chair for the 2003 CHEST annual meeting, and an Ex Officio member of the CHEST Foundation Board of Trustees. He received the Roger C. Bone Memorial Lecture award in 2010. He is a member of the editorial board of CHEST, Editor in Chief of CHEST SEEK Critical Care Medicine, and is co-section editor for Contemporary Reviews in Critical Care Medicine (in CHEST).
The American College of Chest Physicians (CHEST) has announced Dr. Barbara Phillips as its new President, effective November 1. At CHEST 2015 in Montréal, the appointments of Dr. Gerard Silvestri as President-Elect and Dr. John Studdard as President-Designate were confirmed, and Dr. Curtis Sessler, who completed his term as President and became Immediate Past President of CHEST was honored.
Barbara Phillips, MD, MSPH, FCCP, is a Professor of Pulmonary, Critical Care, and Sleep Medicine in the Department of Internal Medicine, and Medical Director of the Sleep Laboratory at the University of Kentucky College of Medicine. She is board-certified in internal medicine, pulmonary medicine, and sleep medicine. After joining CHEST as an affiliate member in 1982, Dr. Phillips advanced to Fellow in 1983. She became a member of the Sleep Medicine NetWork and CHEST Governor of Kentucky. She has chaired the Sleep Institute and is Editor of CHEST SEEK Sleep Medicine (Second, Third, and Fourth Editions). Dr. Phillips also served for 8 years as a Regent-at-Large for the American College of Chest Physicians. Besides her work with CHEST, Dr. Phillips chaired the National Sleep Foundation and has served on the boards of the American Lung Association, the American Academy of Sleep Medicine, and the American Board of Sleep Medicine. Dr. Phillips received a Sleep Academic Award from the National Institutes of Health and was presented with the College Medalist Award at CHEST 2013. Dr. Phillips’ research interests include the effects of sleep apnea on performance and outcomes, genetic risk factors for sleep apnea, nonpharmacologic treatment of sleep apnea, and sleep in aging.
Gerard Silvestri, MD, FCCP, is the Hillenbrand Professor of Thoracic Oncology and Vice-Chair of Medicine for Faculty Development at the Medical University of South Carolina. He completed his fellowship training in pulmonary and critical care at Dartmouth. He has an advanced degree in the evaluative clinical sciences, also from Dartmouth. He is a lung cancer and interventional pulmonologist with an interest in health services research, lung cancer screening, nodule evaluation and management, and staging of lung cancer. After becoming a Fellow of the American College of Chest Physicians in 1998, Dr. Silvestri became active with the NetWorks, serving on the Steering Committees of the Thoracic Oncology and the Interventional Chest/Diagnostic Procedures NetWorks, eventually chairing the Thoracic Oncology NetWork. Dr. Silvestri has also served on the Nominating Committee, the CHEST Scientific Program Committee, the CHEST Foundation Development Committee, as Treasurer and Trustee on the foundation’s Board of Trustees, and as a Regent-at-Large for the American College of Chest Physicians for 3 years. At CHEST 2012, Dr. Silvestri was awarded the Pasquale Ciaglia Memorial Lecture in Interventional Medicine, and at CHEST 2014, he received the Edward C. Rosenow III, MD, Master FCCP/Master Teacher Honor Lecture. Dr. Silvestri has authored more than 200 scientific articles, book chapters, and editorials, and he currently serves on the editorial board of the journal CHEST.
John Studdard, MD, FCCP, is a pulmonary and critical care physician in private practice with Jackson Pulmonary Associates in Jackson, Mississippi. Dr. Studdard completed his fellowship training at the Mayo Graduate School of Medicine. He has served in numerous CHEST leadership roles, including President and Chair of the CHEST Foundation, the philanthropic arm of CHEST; chair of the Government Relations Committee; member of the Marketing Committee; and Ex Officio member of the Diversity Committee, Scientific Program Committee, and Financial Oversight Committee. Dr. Studdard’s dedication to reducing the number of patients he treats for tobacco-related diseases, and his leadership qualities led him to serve as representative for CHEST in the negotiations with the tobacco industry leading to the Attorneys General Master Settlement Agreement of 1998. More recently, in his roles with the CHEST Foundation, Dr. Studdard served as a vice chair of the Beyond Our Walls capital campaign, the CHEST Foundation Nominating Committee, and several foundation work groups.
Curtis N. Sessler MD, FCCP, is the Orhan Muren Distinguished Professor of Medicine at Virginia Commonwealth University (VCU) Health System in the Division of Pulmonary and Critical Care Medicine, where he is Director of the Center for Adult Critical Care and Medical Director of Critical Care and the Medical Respiratory ICU. Dr. Sessler is an enthusiastic clinician and educator who has received teaching awards at VCU, including the School of Medicine Educational Innovation Award. His research interests include ICU sedation, mechanical ventilation, and infection prevention, authoring more than 300 articles, book chapters, books, and abstracts. He has served on a variety of multisociety task forces addressing research, training competency, workforce shortage, and ICU burnout. He is Past President of the Virginia Thoracic Society and has served as Chair of the Pulmonary and Allergy Drug Advisory Committee of the US FDA. An active member of CHEST, he has served on the Board of Regents and as Chair of the Critical Care Section, Chair of the Council of Sections, Chair of the Critical Care Institute, Program Chair for the 2003 CHEST annual meeting, and an Ex Officio member of the CHEST Foundation Board of Trustees. He received the Roger C. Bone Memorial Lecture award in 2010. He is a member of the editorial board of CHEST, Editor in Chief of CHEST SEEK Critical Care Medicine, and is co-section editor for Contemporary Reviews in Critical Care Medicine (in CHEST).
Societies Join NAMDRC and CHEST on Regulatory Push; Respiratory Compromise Institute Announces Two Research Projects
NAMDRC and CHEST, along with the ATS and AARC, have submitted a series of recommendations to CMS to address an archaic, outdated Decision Memo from 2001 that stipulates that patients who receive home mechanical ventilation must have an artificial airway AND must succumb to death if the ventilator is removed. Even though the Decision Memo clearly signals that contractors have discretion in applying the rule, all the DME MACs have pushed forward with it in an attempt to control the growing use of noninvasive home mechanical ventilation, usually billed under HCPCS code E0464.
There are several moving pieces to this issue, and finding consensus was a challenge. While everyone agreed with the problems that have apparently triggered a review by the Office of the Inspector General, finding specific solutions to guide CMS took several months of collaborative work. Because CMS rejects all textbook definitions of mechanical ventilators, as well as FDA classifications, our approach was to explain that the presence of respiratory failure, by well accepted standards of care, includes use of a mechanical ventilator. Therefore, by defining “respiratory failure” and accepting the principle of mechanical ventilation as integral to treatment, a revised policy can now be created by CMS that reflects 2015 standards of care. Importantly, the societies also emphasized that chronic respiratory failure is not always a 24/7 medical phenomena; rather, it can occur nocturnally, intermittently, or progress into a 24/7 reality. In all of these examples, mechanical ventilation is warranted as long as respiratory failure is documented.
Tangential but integral to this issue is the barrier to bilevel devices, called respiratory-assist devices (RADs) by CMS. Because the rules for access to these devices are currently so problematic, physicians understandably make the shift to ordering NIV because that is the only option available for treatment for the patient. Therefore, integral to the recommendations related to home mechanical ventilation, the societies made a series of recommendations for improvement in RAD policies, as well. These recommendations are available on the NAMDRC website at www.namdrc.org.
Respiratory Compromise Institute: The Institute is currently pursuing two specific research endeavors, and the RFP for the large, meta-analysis is open for review at both the NAMDRC website www.namdrc.org and the Institute website, www.respiratorycompromise.org. The meta-analysis is a challenge because any literature search will reveal virtually nothing with the specific term “respiratory compromise” because of its newness. The challenge, therefore, is to conduct a broad search that encompasses all the key variables in the downward cascade from respiratory insufficiency to respiratory failure to respiratory arrest. That includes literature focusing on appropriate monitoring, treatment, therapies, outcomes, length of stay, etc. The Institute hopes to award the contract at the next meeting of its Clinical Advisory Committee, scheduled for March 1.
The second project focuses on Medicare data mining of hospital inpatient records. Beginning with a focus on records where respiratory failure is not present upon admission or within the first 24 hours following admission but present in the medical record, the data mining then expands outward to focus on the services provided, the length of stay, monitoring and therapies instituted, etc. A team of physician researchers are working with the data mining company to focus the research on specific ICD-9 codes (ICD-10 records will not appear in available data until late 2016/early 2017), CPT codes, and HCPCS codes. Hopefully, we will be able to begin with an initial 1 year snapshot, expanding to a multiyear longitudinal review to determine what trends, if any, exist. The data will then be sent to the physician researchers for analysis, and several papers will be generated as a result of those analyses.
NAMDRC Annual Meeting: The NAMDRC Annual Educational Conference is scheduled for March 3-5, 2016, in Palm Springs, California, at the Omni Rancho Las Palmas Resort. The entire program and registration information are available on the NAMDRC website. Registration for the conference is complimentary for new members who join NAMDRC after May 1, 2015, a value of $400. Physicians who want to take advantage of this special offer must contact the NAMDRC Executive Office at 703/752-4359.
NAMDRC and CHEST, along with the ATS and AARC, have submitted a series of recommendations to CMS to address an archaic, outdated Decision Memo from 2001 that stipulates that patients who receive home mechanical ventilation must have an artificial airway AND must succumb to death if the ventilator is removed. Even though the Decision Memo clearly signals that contractors have discretion in applying the rule, all the DME MACs have pushed forward with it in an attempt to control the growing use of noninvasive home mechanical ventilation, usually billed under HCPCS code E0464.
There are several moving pieces to this issue, and finding consensus was a challenge. While everyone agreed with the problems that have apparently triggered a review by the Office of the Inspector General, finding specific solutions to guide CMS took several months of collaborative work. Because CMS rejects all textbook definitions of mechanical ventilators, as well as FDA classifications, our approach was to explain that the presence of respiratory failure, by well accepted standards of care, includes use of a mechanical ventilator. Therefore, by defining “respiratory failure” and accepting the principle of mechanical ventilation as integral to treatment, a revised policy can now be created by CMS that reflects 2015 standards of care. Importantly, the societies also emphasized that chronic respiratory failure is not always a 24/7 medical phenomena; rather, it can occur nocturnally, intermittently, or progress into a 24/7 reality. In all of these examples, mechanical ventilation is warranted as long as respiratory failure is documented.
Tangential but integral to this issue is the barrier to bilevel devices, called respiratory-assist devices (RADs) by CMS. Because the rules for access to these devices are currently so problematic, physicians understandably make the shift to ordering NIV because that is the only option available for treatment for the patient. Therefore, integral to the recommendations related to home mechanical ventilation, the societies made a series of recommendations for improvement in RAD policies, as well. These recommendations are available on the NAMDRC website at www.namdrc.org.
Respiratory Compromise Institute: The Institute is currently pursuing two specific research endeavors, and the RFP for the large, meta-analysis is open for review at both the NAMDRC website www.namdrc.org and the Institute website, www.respiratorycompromise.org. The meta-analysis is a challenge because any literature search will reveal virtually nothing with the specific term “respiratory compromise” because of its newness. The challenge, therefore, is to conduct a broad search that encompasses all the key variables in the downward cascade from respiratory insufficiency to respiratory failure to respiratory arrest. That includes literature focusing on appropriate monitoring, treatment, therapies, outcomes, length of stay, etc. The Institute hopes to award the contract at the next meeting of its Clinical Advisory Committee, scheduled for March 1.
The second project focuses on Medicare data mining of hospital inpatient records. Beginning with a focus on records where respiratory failure is not present upon admission or within the first 24 hours following admission but present in the medical record, the data mining then expands outward to focus on the services provided, the length of stay, monitoring and therapies instituted, etc. A team of physician researchers are working with the data mining company to focus the research on specific ICD-9 codes (ICD-10 records will not appear in available data until late 2016/early 2017), CPT codes, and HCPCS codes. Hopefully, we will be able to begin with an initial 1 year snapshot, expanding to a multiyear longitudinal review to determine what trends, if any, exist. The data will then be sent to the physician researchers for analysis, and several papers will be generated as a result of those analyses.
NAMDRC Annual Meeting: The NAMDRC Annual Educational Conference is scheduled for March 3-5, 2016, in Palm Springs, California, at the Omni Rancho Las Palmas Resort. The entire program and registration information are available on the NAMDRC website. Registration for the conference is complimentary for new members who join NAMDRC after May 1, 2015, a value of $400. Physicians who want to take advantage of this special offer must contact the NAMDRC Executive Office at 703/752-4359.
NAMDRC and CHEST, along with the ATS and AARC, have submitted a series of recommendations to CMS to address an archaic, outdated Decision Memo from 2001 that stipulates that patients who receive home mechanical ventilation must have an artificial airway AND must succumb to death if the ventilator is removed. Even though the Decision Memo clearly signals that contractors have discretion in applying the rule, all the DME MACs have pushed forward with it in an attempt to control the growing use of noninvasive home mechanical ventilation, usually billed under HCPCS code E0464.
There are several moving pieces to this issue, and finding consensus was a challenge. While everyone agreed with the problems that have apparently triggered a review by the Office of the Inspector General, finding specific solutions to guide CMS took several months of collaborative work. Because CMS rejects all textbook definitions of mechanical ventilators, as well as FDA classifications, our approach was to explain that the presence of respiratory failure, by well accepted standards of care, includes use of a mechanical ventilator. Therefore, by defining “respiratory failure” and accepting the principle of mechanical ventilation as integral to treatment, a revised policy can now be created by CMS that reflects 2015 standards of care. Importantly, the societies also emphasized that chronic respiratory failure is not always a 24/7 medical phenomena; rather, it can occur nocturnally, intermittently, or progress into a 24/7 reality. In all of these examples, mechanical ventilation is warranted as long as respiratory failure is documented.
Tangential but integral to this issue is the barrier to bilevel devices, called respiratory-assist devices (RADs) by CMS. Because the rules for access to these devices are currently so problematic, physicians understandably make the shift to ordering NIV because that is the only option available for treatment for the patient. Therefore, integral to the recommendations related to home mechanical ventilation, the societies made a series of recommendations for improvement in RAD policies, as well. These recommendations are available on the NAMDRC website at www.namdrc.org.
Respiratory Compromise Institute: The Institute is currently pursuing two specific research endeavors, and the RFP for the large, meta-analysis is open for review at both the NAMDRC website www.namdrc.org and the Institute website, www.respiratorycompromise.org. The meta-analysis is a challenge because any literature search will reveal virtually nothing with the specific term “respiratory compromise” because of its newness. The challenge, therefore, is to conduct a broad search that encompasses all the key variables in the downward cascade from respiratory insufficiency to respiratory failure to respiratory arrest. That includes literature focusing on appropriate monitoring, treatment, therapies, outcomes, length of stay, etc. The Institute hopes to award the contract at the next meeting of its Clinical Advisory Committee, scheduled for March 1.
The second project focuses on Medicare data mining of hospital inpatient records. Beginning with a focus on records where respiratory failure is not present upon admission or within the first 24 hours following admission but present in the medical record, the data mining then expands outward to focus on the services provided, the length of stay, monitoring and therapies instituted, etc. A team of physician researchers are working with the data mining company to focus the research on specific ICD-9 codes (ICD-10 records will not appear in available data until late 2016/early 2017), CPT codes, and HCPCS codes. Hopefully, we will be able to begin with an initial 1 year snapshot, expanding to a multiyear longitudinal review to determine what trends, if any, exist. The data will then be sent to the physician researchers for analysis, and several papers will be generated as a result of those analyses.
NAMDRC Annual Meeting: The NAMDRC Annual Educational Conference is scheduled for March 3-5, 2016, in Palm Springs, California, at the Omni Rancho Las Palmas Resort. The entire program and registration information are available on the NAMDRC website. Registration for the conference is complimentary for new members who join NAMDRC after May 1, 2015, a value of $400. Physicians who want to take advantage of this special offer must contact the NAMDRC Executive Office at 703/752-4359.
PQRS Reporting
Do you understand your PQRS financial risk?
Successful reporting doesn’t just satisfy 2015 reporting requirements but will also help you to avoid fast approaching PQRS and Value-Based Modifier penalties.
Value Modifier Penalty for 2015 PQRS Nonreporters
• Groups with 2-9 Eligible Professionals (EPs) and solo practitioners: automatic -2.0% of Medicare Physician Fee Schedule (MPFS) downward adjustment
• Groups with 10+ EPs: Automatic -4.0% of MPFS downward adjustment
Quality-Tiering for Successful 2015 PQRS Reporters
• Groups with 2-9 EPs and solo practitioners: Upward or neutral value modifier adjustment only based on quality-tiering (+0.0% to +2.0x of MPFS)
• Groups with 10+ EPs: Upward, neutral, or downward value modifier adjustment based on quality-tiering (up to -4.0% to or +4.0x of MPFS)
Eligible professionals have several options to participate in annual PQRS reporting to avoid PQRS and VBM automatic penalties, including Measures Groups, Individual Measures, and Group Practice Reporting Option (GPRO) reporting for practices reporting through the GPRO.
Don’t know where to begin? The PQRSwizard, a CHEST-affiliated product, can help. The PQRSwizard is a fast, convenient, and cost-effective online tool to help collect and report quality measure data for the CMS PQRS incentive payment program. Similar to online tax preparation software, the PQRSwizard helps guide you through a few easy steps to help rapidly collect, validate, report, and submit the results to CMS for payment.
Learn more about PQRSwizard during a live demo on December 7 at 2:00 PM ET or on January 19 at 12:00 PM ET. CECity’s PQRS experts will provide a guided tour of reporting using the PQRSwizard. Register for the webinar by going to aquire.pqrswizard.com and clicking on “View webcasts.”
Do you understand your PQRS financial risk?
Successful reporting doesn’t just satisfy 2015 reporting requirements but will also help you to avoid fast approaching PQRS and Value-Based Modifier penalties.
Value Modifier Penalty for 2015 PQRS Nonreporters
• Groups with 2-9 Eligible Professionals (EPs) and solo practitioners: automatic -2.0% of Medicare Physician Fee Schedule (MPFS) downward adjustment
• Groups with 10+ EPs: Automatic -4.0% of MPFS downward adjustment
Quality-Tiering for Successful 2015 PQRS Reporters
• Groups with 2-9 EPs and solo practitioners: Upward or neutral value modifier adjustment only based on quality-tiering (+0.0% to +2.0x of MPFS)
• Groups with 10+ EPs: Upward, neutral, or downward value modifier adjustment based on quality-tiering (up to -4.0% to or +4.0x of MPFS)
Eligible professionals have several options to participate in annual PQRS reporting to avoid PQRS and VBM automatic penalties, including Measures Groups, Individual Measures, and Group Practice Reporting Option (GPRO) reporting for practices reporting through the GPRO.
Don’t know where to begin? The PQRSwizard, a CHEST-affiliated product, can help. The PQRSwizard is a fast, convenient, and cost-effective online tool to help collect and report quality measure data for the CMS PQRS incentive payment program. Similar to online tax preparation software, the PQRSwizard helps guide you through a few easy steps to help rapidly collect, validate, report, and submit the results to CMS for payment.
Learn more about PQRSwizard during a live demo on December 7 at 2:00 PM ET or on January 19 at 12:00 PM ET. CECity’s PQRS experts will provide a guided tour of reporting using the PQRSwizard. Register for the webinar by going to aquire.pqrswizard.com and clicking on “View webcasts.”
Do you understand your PQRS financial risk?
Successful reporting doesn’t just satisfy 2015 reporting requirements but will also help you to avoid fast approaching PQRS and Value-Based Modifier penalties.
Value Modifier Penalty for 2015 PQRS Nonreporters
• Groups with 2-9 Eligible Professionals (EPs) and solo practitioners: automatic -2.0% of Medicare Physician Fee Schedule (MPFS) downward adjustment
• Groups with 10+ EPs: Automatic -4.0% of MPFS downward adjustment
Quality-Tiering for Successful 2015 PQRS Reporters
• Groups with 2-9 EPs and solo practitioners: Upward or neutral value modifier adjustment only based on quality-tiering (+0.0% to +2.0x of MPFS)
• Groups with 10+ EPs: Upward, neutral, or downward value modifier adjustment based on quality-tiering (up to -4.0% to or +4.0x of MPFS)
Eligible professionals have several options to participate in annual PQRS reporting to avoid PQRS and VBM automatic penalties, including Measures Groups, Individual Measures, and Group Practice Reporting Option (GPRO) reporting for practices reporting through the GPRO.
Don’t know where to begin? The PQRSwizard, a CHEST-affiliated product, can help. The PQRSwizard is a fast, convenient, and cost-effective online tool to help collect and report quality measure data for the CMS PQRS incentive payment program. Similar to online tax preparation software, the PQRSwizard helps guide you through a few easy steps to help rapidly collect, validate, report, and submit the results to CMS for payment.
Learn more about PQRSwizard during a live demo on December 7 at 2:00 PM ET or on January 19 at 12:00 PM ET. CECity’s PQRS experts will provide a guided tour of reporting using the PQRSwizard. Register for the webinar by going to aquire.pqrswizard.com and clicking on “View webcasts.”
ABIM Continues to Offer MOC Benefits for Newly Certified Internal Medicine Physicians and Fellows
If you are an American Board of Internal Medicine (ABIM) Board-Certified physician newly certified in Internal Medicine, or a fellow who has completed an accredited fellowship year, ABIM recognizes the work that goes into those efforts with fee waivers, credits, and MOC points.
When ABIM updated its MOC program in January 2014, the program was designed to provide continuous learning opportunities for doctors and to help physicians, their colleagues, and their patients know that they were staying current in knowledge and practice throughout their careers. Recognizing that those who have just completed training and those engaged in fellowship are just beginning their careers or are embedded in learning environments, ABIM wants to recognize this work as part of MOC and, thus, not burden these individuals with additional MOC costs or activities.
For those newly certified in Internal Medicine:
• Passing the Internal Medicine exam earns a waiver that covers the MOC program fee for the first calendar year after earning the certification.
• A diplomate will need to enroll in MOC but will not owe any fees through the subsequent calendar year ending December 31.
For those in ACGME-accredited fellowship training:
• For each year of successful ACGME-accredited fellowship training*, fellows earn:
• a full year’s MOC fee credit and
• 20 MOC points (10 in medical knowledge and 10 in practice assessment)
• The MOC fee credit, earned at the end of the academic year, will be applied to the following calendar year as long as the fee credit is claimed by logging into the Physician Login, clicking on “Enroll in MOC,” and applying the credit on the payment screen.
The fee credit is earned when the fellowship program director submits an evaluation via ABIM’s online clinical competence evaluation system (FasTrack®) following a year of successfully completed accredited fellowship training. It’s important to note that the fee credit is not automatically applied to a diplomate’s account; rather, every year a credit is earned, it must be claimed when enrolling in MOC via the Physician Login. Fellows and recent graduates are encouraged to make sure and confirm with their program director that evaluations have been submitted (via (ABIM’s online clinical competence evaluation system) by September after the training year was completed (most often training years end in June, but this may vary for some academic years at some institutions).
Please note - fellows and recent graduates (within 5 years of completing an initial certification examination in Internal Medicine or a subspecialty) will remain certified whether or not they choose to enroll in MOC; however, if they participate in an unaccredited training year either before or after accredited training years, they may need to pay an MOC program fee for that year in order to be reported as participating in MOC, since fee credits are granted for the calendar year after successful completion of accredited training years (most academic years end in June). Unaccredited years may include:
• year(s) spent working as a hospitalist between residency and fellowship,
• research years that are unaccredited, and
• a year as a chief resident, usually occurring immediately following residency before starting fellowship.
However, as noted above, if the fellow does not enroll in MOC and pay the MOC program fee for the calendar year after the unaccredited training year, they will remain certified as long as they are meeting all other programmatic requirements, but will be reported as not participating in MOC. The fellow will be reported as participating in MOC as soon as they enroll in the MOC program by either paying the MOC program fee or claiming the fee credit earned through fellowship training. Going forward, as they successfully complete accredited training years, they will receive the fee credit that can be applied to MOC program fee due each subsequent calendar year.
*Fellowship years in ABIM subspecialties completed in 2014 and after are eligible if accredited by the Accreditation Council for Graduate Medical Education (ACGME), the Royal College of Physicians and Surgeons of Canada, or the Professional Corporation of Physicians of Quebec. Currently, only accredited years are tracked by ABIM in its online clinical competence evaluation system, and, therefore, only the accredited years can be verified reliably across all programs for satisfactory completion. If in doubt, fellows should contact their program director to verify whether their training is accredited.
We encourage you to visit and subscribe to the Transforming ABIM blog (http://transforming.abim.blog) to learn more about ABIM’s ongoing discussions regarding certification and MOC and upcoming opportunities to provide input.
To learn more about your specific requirements and deadlines, or to check your certification status, log into www.abim.org to view your MOC Status Report.
We look forward to sharing more updates with you as we continue our work of ensuring the relevancy of MOC to pulmonary disease physicians across the country.
If you are an American Board of Internal Medicine (ABIM) Board-Certified physician newly certified in Internal Medicine, or a fellow who has completed an accredited fellowship year, ABIM recognizes the work that goes into those efforts with fee waivers, credits, and MOC points.
When ABIM updated its MOC program in January 2014, the program was designed to provide continuous learning opportunities for doctors and to help physicians, their colleagues, and their patients know that they were staying current in knowledge and practice throughout their careers. Recognizing that those who have just completed training and those engaged in fellowship are just beginning their careers or are embedded in learning environments, ABIM wants to recognize this work as part of MOC and, thus, not burden these individuals with additional MOC costs or activities.
For those newly certified in Internal Medicine:
• Passing the Internal Medicine exam earns a waiver that covers the MOC program fee for the first calendar year after earning the certification.
• A diplomate will need to enroll in MOC but will not owe any fees through the subsequent calendar year ending December 31.
For those in ACGME-accredited fellowship training:
• For each year of successful ACGME-accredited fellowship training*, fellows earn:
• a full year’s MOC fee credit and
• 20 MOC points (10 in medical knowledge and 10 in practice assessment)
• The MOC fee credit, earned at the end of the academic year, will be applied to the following calendar year as long as the fee credit is claimed by logging into the Physician Login, clicking on “Enroll in MOC,” and applying the credit on the payment screen.
The fee credit is earned when the fellowship program director submits an evaluation via ABIM’s online clinical competence evaluation system (FasTrack®) following a year of successfully completed accredited fellowship training. It’s important to note that the fee credit is not automatically applied to a diplomate’s account; rather, every year a credit is earned, it must be claimed when enrolling in MOC via the Physician Login. Fellows and recent graduates are encouraged to make sure and confirm with their program director that evaluations have been submitted (via (ABIM’s online clinical competence evaluation system) by September after the training year was completed (most often training years end in June, but this may vary for some academic years at some institutions).
Please note - fellows and recent graduates (within 5 years of completing an initial certification examination in Internal Medicine or a subspecialty) will remain certified whether or not they choose to enroll in MOC; however, if they participate in an unaccredited training year either before or after accredited training years, they may need to pay an MOC program fee for that year in order to be reported as participating in MOC, since fee credits are granted for the calendar year after successful completion of accredited training years (most academic years end in June). Unaccredited years may include:
• year(s) spent working as a hospitalist between residency and fellowship,
• research years that are unaccredited, and
• a year as a chief resident, usually occurring immediately following residency before starting fellowship.
However, as noted above, if the fellow does not enroll in MOC and pay the MOC program fee for the calendar year after the unaccredited training year, they will remain certified as long as they are meeting all other programmatic requirements, but will be reported as not participating in MOC. The fellow will be reported as participating in MOC as soon as they enroll in the MOC program by either paying the MOC program fee or claiming the fee credit earned through fellowship training. Going forward, as they successfully complete accredited training years, they will receive the fee credit that can be applied to MOC program fee due each subsequent calendar year.
*Fellowship years in ABIM subspecialties completed in 2014 and after are eligible if accredited by the Accreditation Council for Graduate Medical Education (ACGME), the Royal College of Physicians and Surgeons of Canada, or the Professional Corporation of Physicians of Quebec. Currently, only accredited years are tracked by ABIM in its online clinical competence evaluation system, and, therefore, only the accredited years can be verified reliably across all programs for satisfactory completion. If in doubt, fellows should contact their program director to verify whether their training is accredited.
We encourage you to visit and subscribe to the Transforming ABIM blog (http://transforming.abim.blog) to learn more about ABIM’s ongoing discussions regarding certification and MOC and upcoming opportunities to provide input.
To learn more about your specific requirements and deadlines, or to check your certification status, log into www.abim.org to view your MOC Status Report.
We look forward to sharing more updates with you as we continue our work of ensuring the relevancy of MOC to pulmonary disease physicians across the country.
If you are an American Board of Internal Medicine (ABIM) Board-Certified physician newly certified in Internal Medicine, or a fellow who has completed an accredited fellowship year, ABIM recognizes the work that goes into those efforts with fee waivers, credits, and MOC points.
When ABIM updated its MOC program in January 2014, the program was designed to provide continuous learning opportunities for doctors and to help physicians, their colleagues, and their patients know that they were staying current in knowledge and practice throughout their careers. Recognizing that those who have just completed training and those engaged in fellowship are just beginning their careers or are embedded in learning environments, ABIM wants to recognize this work as part of MOC and, thus, not burden these individuals with additional MOC costs or activities.
For those newly certified in Internal Medicine:
• Passing the Internal Medicine exam earns a waiver that covers the MOC program fee for the first calendar year after earning the certification.
• A diplomate will need to enroll in MOC but will not owe any fees through the subsequent calendar year ending December 31.
For those in ACGME-accredited fellowship training:
• For each year of successful ACGME-accredited fellowship training*, fellows earn:
• a full year’s MOC fee credit and
• 20 MOC points (10 in medical knowledge and 10 in practice assessment)
• The MOC fee credit, earned at the end of the academic year, will be applied to the following calendar year as long as the fee credit is claimed by logging into the Physician Login, clicking on “Enroll in MOC,” and applying the credit on the payment screen.
The fee credit is earned when the fellowship program director submits an evaluation via ABIM’s online clinical competence evaluation system (FasTrack®) following a year of successfully completed accredited fellowship training. It’s important to note that the fee credit is not automatically applied to a diplomate’s account; rather, every year a credit is earned, it must be claimed when enrolling in MOC via the Physician Login. Fellows and recent graduates are encouraged to make sure and confirm with their program director that evaluations have been submitted (via (ABIM’s online clinical competence evaluation system) by September after the training year was completed (most often training years end in June, but this may vary for some academic years at some institutions).
Please note - fellows and recent graduates (within 5 years of completing an initial certification examination in Internal Medicine or a subspecialty) will remain certified whether or not they choose to enroll in MOC; however, if they participate in an unaccredited training year either before or after accredited training years, they may need to pay an MOC program fee for that year in order to be reported as participating in MOC, since fee credits are granted for the calendar year after successful completion of accredited training years (most academic years end in June). Unaccredited years may include:
• year(s) spent working as a hospitalist between residency and fellowship,
• research years that are unaccredited, and
• a year as a chief resident, usually occurring immediately following residency before starting fellowship.
However, as noted above, if the fellow does not enroll in MOC and pay the MOC program fee for the calendar year after the unaccredited training year, they will remain certified as long as they are meeting all other programmatic requirements, but will be reported as not participating in MOC. The fellow will be reported as participating in MOC as soon as they enroll in the MOC program by either paying the MOC program fee or claiming the fee credit earned through fellowship training. Going forward, as they successfully complete accredited training years, they will receive the fee credit that can be applied to MOC program fee due each subsequent calendar year.
*Fellowship years in ABIM subspecialties completed in 2014 and after are eligible if accredited by the Accreditation Council for Graduate Medical Education (ACGME), the Royal College of Physicians and Surgeons of Canada, or the Professional Corporation of Physicians of Quebec. Currently, only accredited years are tracked by ABIM in its online clinical competence evaluation system, and, therefore, only the accredited years can be verified reliably across all programs for satisfactory completion. If in doubt, fellows should contact their program director to verify whether their training is accredited.
We encourage you to visit and subscribe to the Transforming ABIM blog (http://transforming.abim.blog) to learn more about ABIM’s ongoing discussions regarding certification and MOC and upcoming opportunities to provide input.
To learn more about your specific requirements and deadlines, or to check your certification status, log into www.abim.org to view your MOC Status Report.
We look forward to sharing more updates with you as we continue our work of ensuring the relevancy of MOC to pulmonary disease physicians across the country.
Join Us at CHEST World Congress 2016
April 15 – 17, 2016
Shanghai, China, will set a perfect backdrop for CHEST World Congress 2016. This unique, modern city will keep you moving and thinking, as we make sure you’re informed on the latest updates and innovations in chest medicine.
CHEST, in collaboration with the Chinese Thoracic Society, will host this clinical event, featuring simulation-based education, case- and problem-based sessions, and evidence-based medicine for clinical respirologists, intensive care physicians, and specialists in sleep medicine.
On Friday, April 15, we’ll offer postgraduate courses for an intensive learning experience. With additional registration, you can choose from the following topics:
• Advanced Mechanical Ventilation
• Clinical Pulmonary Medicine: A Case-Based Review
• Lung Cancer Education Program: A Multidisciplinary Team-Bbased Approach
• Thoracic Ultrasonography for the Pulmonary and Critical Care Consultant
We’ll also enhance your skills in a hands-on clinical environment within our CHEST Simulation Center. Work with expert faculty to sharpen your skills and apply your knowledge using real equipment and simulators. With additional registration, you’ll choose from the following topics:
• Ultrasonography for the Assessment of Cardiopulmonary Failure
• Bronchoscopy Procedures: EBUS-TBNA, Radial EBUS, and Endobronchial Blockers
• Mechanical Ventilation: Techniques to Optimize Care of the Critically Ill Patient
• Home-Based Sleep Apnea Testing
• Advanced Positive Airway Pressure Devices and Downloads
• Pulmonary Function Testing: A Case-Based, Hands-On, Guidelines-Driven Practicum
When you have some free time, be sure to visit explore Shanghai. You will be immersed in a wonderful Chinese culture, complete with flavorful, authentic food; exquisite, local architecture and gardens; and a native language with beautifully written characters.
Learn more and register today at chestworldcongress2016.org/.
April 15 – 17, 2016
Shanghai, China, will set a perfect backdrop for CHEST World Congress 2016. This unique, modern city will keep you moving and thinking, as we make sure you’re informed on the latest updates and innovations in chest medicine.
CHEST, in collaboration with the Chinese Thoracic Society, will host this clinical event, featuring simulation-based education, case- and problem-based sessions, and evidence-based medicine for clinical respirologists, intensive care physicians, and specialists in sleep medicine.
On Friday, April 15, we’ll offer postgraduate courses for an intensive learning experience. With additional registration, you can choose from the following topics:
• Advanced Mechanical Ventilation
• Clinical Pulmonary Medicine: A Case-Based Review
• Lung Cancer Education Program: A Multidisciplinary Team-Bbased Approach
• Thoracic Ultrasonography for the Pulmonary and Critical Care Consultant
We’ll also enhance your skills in a hands-on clinical environment within our CHEST Simulation Center. Work with expert faculty to sharpen your skills and apply your knowledge using real equipment and simulators. With additional registration, you’ll choose from the following topics:
• Ultrasonography for the Assessment of Cardiopulmonary Failure
• Bronchoscopy Procedures: EBUS-TBNA, Radial EBUS, and Endobronchial Blockers
• Mechanical Ventilation: Techniques to Optimize Care of the Critically Ill Patient
• Home-Based Sleep Apnea Testing
• Advanced Positive Airway Pressure Devices and Downloads
• Pulmonary Function Testing: A Case-Based, Hands-On, Guidelines-Driven Practicum
When you have some free time, be sure to visit explore Shanghai. You will be immersed in a wonderful Chinese culture, complete with flavorful, authentic food; exquisite, local architecture and gardens; and a native language with beautifully written characters.
Learn more and register today at chestworldcongress2016.org/.
April 15 – 17, 2016
Shanghai, China, will set a perfect backdrop for CHEST World Congress 2016. This unique, modern city will keep you moving and thinking, as we make sure you’re informed on the latest updates and innovations in chest medicine.
CHEST, in collaboration with the Chinese Thoracic Society, will host this clinical event, featuring simulation-based education, case- and problem-based sessions, and evidence-based medicine for clinical respirologists, intensive care physicians, and specialists in sleep medicine.
On Friday, April 15, we’ll offer postgraduate courses for an intensive learning experience. With additional registration, you can choose from the following topics:
• Advanced Mechanical Ventilation
• Clinical Pulmonary Medicine: A Case-Based Review
• Lung Cancer Education Program: A Multidisciplinary Team-Bbased Approach
• Thoracic Ultrasonography for the Pulmonary and Critical Care Consultant
We’ll also enhance your skills in a hands-on clinical environment within our CHEST Simulation Center. Work with expert faculty to sharpen your skills and apply your knowledge using real equipment and simulators. With additional registration, you’ll choose from the following topics:
• Ultrasonography for the Assessment of Cardiopulmonary Failure
• Bronchoscopy Procedures: EBUS-TBNA, Radial EBUS, and Endobronchial Blockers
• Mechanical Ventilation: Techniques to Optimize Care of the Critically Ill Patient
• Home-Based Sleep Apnea Testing
• Advanced Positive Airway Pressure Devices and Downloads
• Pulmonary Function Testing: A Case-Based, Hands-On, Guidelines-Driven Practicum
When you have some free time, be sure to visit explore Shanghai. You will be immersed in a wonderful Chinese culture, complete with flavorful, authentic food; exquisite, local architecture and gardens; and a native language with beautifully written characters.
Learn more and register today at chestworldcongress2016.org/.