User login
NETWORKS Pulmonary Physiology, Function, and Rehabilitation Disaster Response Pulmonary Vascular Disease Thoracic Oncology
Clinical utility of the acute bronchodilator response
Recently, numerous articles evaluating the acute bronchodilator (BD) response in various disease states have appeared in the literature (Chest. 2015;148[6]:1489; J Thorac Dis. 2016;8[1]:14; Int J Chron Obstruct Pulmon Dis. 2016;11:93; Respir Med. 2016;112:45). New algorithms have been proposed to improve quality control in BD (Eur Clin Respir J. 2015;30;2).
In our lab, requests for pre- and post-BD spirometry continue unabated. Undoubtedly, many labs comply with these requests without regard for pre-BD values. The number of these requests far exceeds the number needed to confirm asthma diagnosis, or to assure that post-BD FEV1/FVC ratio remains below 0.7 for COPD diagnosis, which are the only universally accepted indications for BD testing.
Acute BD testing technique, interpretation, and clinical application involve important issues that remain unresolved, even in COPD where this test has been studied more than any other disease state except asthma (Chest. 2011;140[4]:1055; Int J Chron Obstruct Pulmon Dis. 2015;10:407). There remains no clear consensus for a clinically relevant BD response. The ACCP definition proposed in 1974 (FEV1 improvement by greater than 15%) has not been updated, and the widely used ATS/ERS definition (FEV1 and/or FVC improvement by greater than 12% and 200 mL) is felt to be arbitrary and based more on expert opinion than scientific evidence (Respir Care. 2012;57[10]:1564). Literature review (excluding asthma) reveals no well-done, reproducible studies that demonstrate meaningful or widely applicable uses for the acute BD response.
Overcoming the many factors influencing acute bronchodilator testing, developing a unified definition for a positive test, and then showing a predictive significance to the acute-BD response is an extremely difficult task. Until this test is further studied in a rigorous manner, any meaning attached to a positive response outside of asthma is purely arbitrary.
Dr. Oleh Hnatiuk, FCCP
Steering Committee Member
Gun violence in the hospital
Thirty-one thousand fatal gunshot wounds (GSW) occur in the United States each year and are increasing; 55% are self-inflicted, mostly isolated incidents. However, mass shooting events (MSE = more than 3 victims) are rising with 355 events in 2015 (462 deaths and 1,314 injuries). The mortality of GSW has risen due to the use of high caliber automatic handguns. Health-care providers, facilities, and systems need to include preparation for primary prevention and secondary mitigation for violent acts of this nature.
MSE attacker demographics reveal a male predominance (90%) with ethnicity mirroring the US population (65% Caucasian, 16% black, and 9% Asian) and mainly occurring in urban settings. The psychosocial basis of these changes is complex and multifactorial. Two-thirds of mass shooters have a history of mental illness with paranoid schizophrenia predominating. Motives are shifting from self-destruction to grievance-related events. Targets and victims of GSW violence also seem to be changing, and health-care workers are potential targets for GSW violence.
A 12-year review of hospital shooting events (HSE) found 154 events with 235 victims. There is a rise in this type of violent act. Grievance motives are dominant in these events. Most HSE occur in the ED or at the entrance to the hospital or parking lot (77%). The case fatality rate in HSE averages 50%. The perpetrators are injured in 85% of cases. Nurses are the most common victims of HSE.
Prevention strategies such as metal detectors, camera surveillance, strengthened security staff, and emergency protocols are vital. However, in many hospitals, these strategies are inadequate or not considered. Secondary mitigation requires special education and training and some material preparation to be successful. Providers must consider themselves potential gun violence victims. We encourage all medical providers to engage in planning and preparation for HSE, as well as advocate for gun safety laws
Dr. Dennis Amundson, FCCP
NetWork Member
Critical violent injury in the United States: A review and call to action. Crit Care Med. 2015;43(11):2460-2466.
Hospital-based shooting in the United States: 2000-2011. Ann Emerg Med. 2012;60(6):790-798.
The epidemiology of trauma-related mortality in the United States From 2002-2012. J Trauma Acute Care Surg. 2014;76(4):913-920.
Balloon pulmonary angioplasty for CTEPH
The gold-standard treatment for chronic thromboembolic pulmonary hypertension (CTEPH) is pulmonary thromboendarterectomy (PTE). However, not every patient is a surgical candidate, including those who are deemed technically inoperable (after review by a multidisciplinary, experienced CTEPH team) or those whose goals of care are more palliative.
Such factors created an opportunity for an alternative procedure to manage CTEPH: catheter-based balloon pulmonary angioplasty (BPA). Despite the limited success with early BPA experience, with initial set-backs including high reperfusion edema rates and other procedure complications, BPA has become more refined over time. Initially led by the efforts of several groups based in Japan, modifications included greater precision in “right-sizing” balloons, staging the procedure (average two to five sessions/patient), and better vascular imaging techniques with advancing technical capabilities.
BPA has received attention due to the favorable hemodynamic and functional outcomes reported in select patients. Despite a lack of consensus regarding who might benefit most, these preliminary results have stimulated considerable interest for acquiring this technique worldwide.
Caution should be exercised when BPA is considered for CTEPH treatment. Critical to success is the selection of patients who might benefit, and adequate training and technical expertise is essential for BPA performance. For those with operable CTEPH who are otherwise surgical candidates, data do not yet exist to suggest BPA as a comparable alternative to PTE. Furthermore, the absence of head-to-head comparison between medical therapy and BPA for inoperable CTEPH further blurs the role BPA will have in this unique patient population. But, it holds promise, awaiting further trials data.
Dr. Wassim H. Fares, FCCP, NetWork Member
Dr. William R. Auger, FCCP, Steering Committee Member
Pulmonary nodules: Are you seeing spots?
Pulmonary nodules are increasingly being identified in clinical practice. A recent study estimated that 1.5 million nodules are identified annually in the United States (Gould et al. 2015; Am J Respir Crit Care Med. 192[10], 1208). This 10-fold increase in number over prior estimates reflects the steep escalation in utilization of CT scanning over the past several decades, and is likely to rise further as lung cancer screening is implemented. While the majority of nodules are benign, evaluation necessarily includes an assessment of the probability of malignancy, since this is a major driver of the decision as to whether no further intervention is required, or whether watchful surveillance or further noninvasive or invasive evaluation is appropriate (Gould et al., 2013). It is reassuring that experienced chest physicians perform well in the assessment of the probability of malignancy (Gould et al., 2013; Swensen et al., 1999), but also important to recognize that evidence-based guidelines for nodule evaluation as well as validated tools for assessing the likelihood of malignancy are readily available (Gould, Ananth, Barnett, & Veterans Affairs, 2007; Gould et al., 2013; McWilliams et al., 2013; Swensen, Silverstein, Ilstrup, Schleck, & Edell, 1997). It is important to engage our radiology colleagues in this discussion; guidelines from the Fleischner Society and the American College of Radiology for reporting on incidentally identified small solid nodules, incidentally identified subsolid nodules, and screening-detected nodules are individually distinct in definitions of abnormality as well as recommendations for follow up, and should be applied appropriately in the context of the individual patient as well as the situation for which the CT was performed (“Lung-RADS Version 1.0 Assessment Categories Release date: April 28, 2014,” 2014; MacMahon et al., 2005; Naidich et al., 2013). All of these potential sources of variation highlight the value of standardizing the approach to nodule evaluation, to ensure that appropriate evaluation will be done to maximize the likelihood of identifying nodules that are actually cancer, and minimize harm potentially incurred by unnecessary invasive and noninvasive testing of nodules that are actually benign.
Dr. Lynn Tanoue, FCCP
NetWork Chair
Gould MK, Ananth L, Barnett PG, and Veterans Affairs, S. C. S. G. A clinical model to estimate the pretest probability of lung cancer in patients with solitary pulmonary nodules. Chest. 2007;131(2):383-388.
Gould MK, Donington J, Lynch WR, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143(5 suppl):e93S.
Gould MK, Tang T, Liu IL, et al. Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med. 2015; 192(10):1208-1214.
Lung-RADS Version 1.0 Assessment Categories Release date: April 28,2014. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/LungRADS/AssessmentCategories.pdf. Accessed Oct 31, 2014.
MacMahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237(2):395-400.
McWilliams A, Tammemagi MC, Mayo JR, et al. Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369(10):910-919.
Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013;266(1):304-317.
Swensen SJ, Silverstein MD, Edell ES, et al. Solitary pulmonary nodules: clinical prediction model versus physicians. Mayo Clin Proc. 1999;74(4):319-329.
Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules: Application to small radiologically indeterminate nodules. Arch Intern Med. 1997;157(8): 849-855.
Clinical utility of the acute bronchodilator response
Recently, numerous articles evaluating the acute bronchodilator (BD) response in various disease states have appeared in the literature (Chest. 2015;148[6]:1489; J Thorac Dis. 2016;8[1]:14; Int J Chron Obstruct Pulmon Dis. 2016;11:93; Respir Med. 2016;112:45). New algorithms have been proposed to improve quality control in BD (Eur Clin Respir J. 2015;30;2).
In our lab, requests for pre- and post-BD spirometry continue unabated. Undoubtedly, many labs comply with these requests without regard for pre-BD values. The number of these requests far exceeds the number needed to confirm asthma diagnosis, or to assure that post-BD FEV1/FVC ratio remains below 0.7 for COPD diagnosis, which are the only universally accepted indications for BD testing.
Acute BD testing technique, interpretation, and clinical application involve important issues that remain unresolved, even in COPD where this test has been studied more than any other disease state except asthma (Chest. 2011;140[4]:1055; Int J Chron Obstruct Pulmon Dis. 2015;10:407). There remains no clear consensus for a clinically relevant BD response. The ACCP definition proposed in 1974 (FEV1 improvement by greater than 15%) has not been updated, and the widely used ATS/ERS definition (FEV1 and/or FVC improvement by greater than 12% and 200 mL) is felt to be arbitrary and based more on expert opinion than scientific evidence (Respir Care. 2012;57[10]:1564). Literature review (excluding asthma) reveals no well-done, reproducible studies that demonstrate meaningful or widely applicable uses for the acute BD response.
Overcoming the many factors influencing acute bronchodilator testing, developing a unified definition for a positive test, and then showing a predictive significance to the acute-BD response is an extremely difficult task. Until this test is further studied in a rigorous manner, any meaning attached to a positive response outside of asthma is purely arbitrary.
Dr. Oleh Hnatiuk, FCCP
Steering Committee Member
Gun violence in the hospital
Thirty-one thousand fatal gunshot wounds (GSW) occur in the United States each year and are increasing; 55% are self-inflicted, mostly isolated incidents. However, mass shooting events (MSE = more than 3 victims) are rising with 355 events in 2015 (462 deaths and 1,314 injuries). The mortality of GSW has risen due to the use of high caliber automatic handguns. Health-care providers, facilities, and systems need to include preparation for primary prevention and secondary mitigation for violent acts of this nature.
MSE attacker demographics reveal a male predominance (90%) with ethnicity mirroring the US population (65% Caucasian, 16% black, and 9% Asian) and mainly occurring in urban settings. The psychosocial basis of these changes is complex and multifactorial. Two-thirds of mass shooters have a history of mental illness with paranoid schizophrenia predominating. Motives are shifting from self-destruction to grievance-related events. Targets and victims of GSW violence also seem to be changing, and health-care workers are potential targets for GSW violence.
A 12-year review of hospital shooting events (HSE) found 154 events with 235 victims. There is a rise in this type of violent act. Grievance motives are dominant in these events. Most HSE occur in the ED or at the entrance to the hospital or parking lot (77%). The case fatality rate in HSE averages 50%. The perpetrators are injured in 85% of cases. Nurses are the most common victims of HSE.
Prevention strategies such as metal detectors, camera surveillance, strengthened security staff, and emergency protocols are vital. However, in many hospitals, these strategies are inadequate or not considered. Secondary mitigation requires special education and training and some material preparation to be successful. Providers must consider themselves potential gun violence victims. We encourage all medical providers to engage in planning and preparation for HSE, as well as advocate for gun safety laws
Dr. Dennis Amundson, FCCP
NetWork Member
Critical violent injury in the United States: A review and call to action. Crit Care Med. 2015;43(11):2460-2466.
Hospital-based shooting in the United States: 2000-2011. Ann Emerg Med. 2012;60(6):790-798.
The epidemiology of trauma-related mortality in the United States From 2002-2012. J Trauma Acute Care Surg. 2014;76(4):913-920.
Balloon pulmonary angioplasty for CTEPH
The gold-standard treatment for chronic thromboembolic pulmonary hypertension (CTEPH) is pulmonary thromboendarterectomy (PTE). However, not every patient is a surgical candidate, including those who are deemed technically inoperable (after review by a multidisciplinary, experienced CTEPH team) or those whose goals of care are more palliative.
Such factors created an opportunity for an alternative procedure to manage CTEPH: catheter-based balloon pulmonary angioplasty (BPA). Despite the limited success with early BPA experience, with initial set-backs including high reperfusion edema rates and other procedure complications, BPA has become more refined over time. Initially led by the efforts of several groups based in Japan, modifications included greater precision in “right-sizing” balloons, staging the procedure (average two to five sessions/patient), and better vascular imaging techniques with advancing technical capabilities.
BPA has received attention due to the favorable hemodynamic and functional outcomes reported in select patients. Despite a lack of consensus regarding who might benefit most, these preliminary results have stimulated considerable interest for acquiring this technique worldwide.
Caution should be exercised when BPA is considered for CTEPH treatment. Critical to success is the selection of patients who might benefit, and adequate training and technical expertise is essential for BPA performance. For those with operable CTEPH who are otherwise surgical candidates, data do not yet exist to suggest BPA as a comparable alternative to PTE. Furthermore, the absence of head-to-head comparison between medical therapy and BPA for inoperable CTEPH further blurs the role BPA will have in this unique patient population. But, it holds promise, awaiting further trials data.
Dr. Wassim H. Fares, FCCP, NetWork Member
Dr. William R. Auger, FCCP, Steering Committee Member
Pulmonary nodules: Are you seeing spots?
Pulmonary nodules are increasingly being identified in clinical practice. A recent study estimated that 1.5 million nodules are identified annually in the United States (Gould et al. 2015; Am J Respir Crit Care Med. 192[10], 1208). This 10-fold increase in number over prior estimates reflects the steep escalation in utilization of CT scanning over the past several decades, and is likely to rise further as lung cancer screening is implemented. While the majority of nodules are benign, evaluation necessarily includes an assessment of the probability of malignancy, since this is a major driver of the decision as to whether no further intervention is required, or whether watchful surveillance or further noninvasive or invasive evaluation is appropriate (Gould et al., 2013). It is reassuring that experienced chest physicians perform well in the assessment of the probability of malignancy (Gould et al., 2013; Swensen et al., 1999), but also important to recognize that evidence-based guidelines for nodule evaluation as well as validated tools for assessing the likelihood of malignancy are readily available (Gould, Ananth, Barnett, & Veterans Affairs, 2007; Gould et al., 2013; McWilliams et al., 2013; Swensen, Silverstein, Ilstrup, Schleck, & Edell, 1997). It is important to engage our radiology colleagues in this discussion; guidelines from the Fleischner Society and the American College of Radiology for reporting on incidentally identified small solid nodules, incidentally identified subsolid nodules, and screening-detected nodules are individually distinct in definitions of abnormality as well as recommendations for follow up, and should be applied appropriately in the context of the individual patient as well as the situation for which the CT was performed (“Lung-RADS Version 1.0 Assessment Categories Release date: April 28, 2014,” 2014; MacMahon et al., 2005; Naidich et al., 2013). All of these potential sources of variation highlight the value of standardizing the approach to nodule evaluation, to ensure that appropriate evaluation will be done to maximize the likelihood of identifying nodules that are actually cancer, and minimize harm potentially incurred by unnecessary invasive and noninvasive testing of nodules that are actually benign.
Dr. Lynn Tanoue, FCCP
NetWork Chair
Gould MK, Ananth L, Barnett PG, and Veterans Affairs, S. C. S. G. A clinical model to estimate the pretest probability of lung cancer in patients with solitary pulmonary nodules. Chest. 2007;131(2):383-388.
Gould MK, Donington J, Lynch WR, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143(5 suppl):e93S.
Gould MK, Tang T, Liu IL, et al. Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med. 2015; 192(10):1208-1214.
Lung-RADS Version 1.0 Assessment Categories Release date: April 28,2014. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/LungRADS/AssessmentCategories.pdf. Accessed Oct 31, 2014.
MacMahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237(2):395-400.
McWilliams A, Tammemagi MC, Mayo JR, et al. Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369(10):910-919.
Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013;266(1):304-317.
Swensen SJ, Silverstein MD, Edell ES, et al. Solitary pulmonary nodules: clinical prediction model versus physicians. Mayo Clin Proc. 1999;74(4):319-329.
Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules: Application to small radiologically indeterminate nodules. Arch Intern Med. 1997;157(8): 849-855.
Clinical utility of the acute bronchodilator response
Recently, numerous articles evaluating the acute bronchodilator (BD) response in various disease states have appeared in the literature (Chest. 2015;148[6]:1489; J Thorac Dis. 2016;8[1]:14; Int J Chron Obstruct Pulmon Dis. 2016;11:93; Respir Med. 2016;112:45). New algorithms have been proposed to improve quality control in BD (Eur Clin Respir J. 2015;30;2).
In our lab, requests for pre- and post-BD spirometry continue unabated. Undoubtedly, many labs comply with these requests without regard for pre-BD values. The number of these requests far exceeds the number needed to confirm asthma diagnosis, or to assure that post-BD FEV1/FVC ratio remains below 0.7 for COPD diagnosis, which are the only universally accepted indications for BD testing.
Acute BD testing technique, interpretation, and clinical application involve important issues that remain unresolved, even in COPD where this test has been studied more than any other disease state except asthma (Chest. 2011;140[4]:1055; Int J Chron Obstruct Pulmon Dis. 2015;10:407). There remains no clear consensus for a clinically relevant BD response. The ACCP definition proposed in 1974 (FEV1 improvement by greater than 15%) has not been updated, and the widely used ATS/ERS definition (FEV1 and/or FVC improvement by greater than 12% and 200 mL) is felt to be arbitrary and based more on expert opinion than scientific evidence (Respir Care. 2012;57[10]:1564). Literature review (excluding asthma) reveals no well-done, reproducible studies that demonstrate meaningful or widely applicable uses for the acute BD response.
Overcoming the many factors influencing acute bronchodilator testing, developing a unified definition for a positive test, and then showing a predictive significance to the acute-BD response is an extremely difficult task. Until this test is further studied in a rigorous manner, any meaning attached to a positive response outside of asthma is purely arbitrary.
Dr. Oleh Hnatiuk, FCCP
Steering Committee Member
Gun violence in the hospital
Thirty-one thousand fatal gunshot wounds (GSW) occur in the United States each year and are increasing; 55% are self-inflicted, mostly isolated incidents. However, mass shooting events (MSE = more than 3 victims) are rising with 355 events in 2015 (462 deaths and 1,314 injuries). The mortality of GSW has risen due to the use of high caliber automatic handguns. Health-care providers, facilities, and systems need to include preparation for primary prevention and secondary mitigation for violent acts of this nature.
MSE attacker demographics reveal a male predominance (90%) with ethnicity mirroring the US population (65% Caucasian, 16% black, and 9% Asian) and mainly occurring in urban settings. The psychosocial basis of these changes is complex and multifactorial. Two-thirds of mass shooters have a history of mental illness with paranoid schizophrenia predominating. Motives are shifting from self-destruction to grievance-related events. Targets and victims of GSW violence also seem to be changing, and health-care workers are potential targets for GSW violence.
A 12-year review of hospital shooting events (HSE) found 154 events with 235 victims. There is a rise in this type of violent act. Grievance motives are dominant in these events. Most HSE occur in the ED or at the entrance to the hospital or parking lot (77%). The case fatality rate in HSE averages 50%. The perpetrators are injured in 85% of cases. Nurses are the most common victims of HSE.
Prevention strategies such as metal detectors, camera surveillance, strengthened security staff, and emergency protocols are vital. However, in many hospitals, these strategies are inadequate or not considered. Secondary mitigation requires special education and training and some material preparation to be successful. Providers must consider themselves potential gun violence victims. We encourage all medical providers to engage in planning and preparation for HSE, as well as advocate for gun safety laws
Dr. Dennis Amundson, FCCP
NetWork Member
Critical violent injury in the United States: A review and call to action. Crit Care Med. 2015;43(11):2460-2466.
Hospital-based shooting in the United States: 2000-2011. Ann Emerg Med. 2012;60(6):790-798.
The epidemiology of trauma-related mortality in the United States From 2002-2012. J Trauma Acute Care Surg. 2014;76(4):913-920.
Balloon pulmonary angioplasty for CTEPH
The gold-standard treatment for chronic thromboembolic pulmonary hypertension (CTEPH) is pulmonary thromboendarterectomy (PTE). However, not every patient is a surgical candidate, including those who are deemed technically inoperable (after review by a multidisciplinary, experienced CTEPH team) or those whose goals of care are more palliative.
Such factors created an opportunity for an alternative procedure to manage CTEPH: catheter-based balloon pulmonary angioplasty (BPA). Despite the limited success with early BPA experience, with initial set-backs including high reperfusion edema rates and other procedure complications, BPA has become more refined over time. Initially led by the efforts of several groups based in Japan, modifications included greater precision in “right-sizing” balloons, staging the procedure (average two to five sessions/patient), and better vascular imaging techniques with advancing technical capabilities.
BPA has received attention due to the favorable hemodynamic and functional outcomes reported in select patients. Despite a lack of consensus regarding who might benefit most, these preliminary results have stimulated considerable interest for acquiring this technique worldwide.
Caution should be exercised when BPA is considered for CTEPH treatment. Critical to success is the selection of patients who might benefit, and adequate training and technical expertise is essential for BPA performance. For those with operable CTEPH who are otherwise surgical candidates, data do not yet exist to suggest BPA as a comparable alternative to PTE. Furthermore, the absence of head-to-head comparison between medical therapy and BPA for inoperable CTEPH further blurs the role BPA will have in this unique patient population. But, it holds promise, awaiting further trials data.
Dr. Wassim H. Fares, FCCP, NetWork Member
Dr. William R. Auger, FCCP, Steering Committee Member
Pulmonary nodules: Are you seeing spots?
Pulmonary nodules are increasingly being identified in clinical practice. A recent study estimated that 1.5 million nodules are identified annually in the United States (Gould et al. 2015; Am J Respir Crit Care Med. 192[10], 1208). This 10-fold increase in number over prior estimates reflects the steep escalation in utilization of CT scanning over the past several decades, and is likely to rise further as lung cancer screening is implemented. While the majority of nodules are benign, evaluation necessarily includes an assessment of the probability of malignancy, since this is a major driver of the decision as to whether no further intervention is required, or whether watchful surveillance or further noninvasive or invasive evaluation is appropriate (Gould et al., 2013). It is reassuring that experienced chest physicians perform well in the assessment of the probability of malignancy (Gould et al., 2013; Swensen et al., 1999), but also important to recognize that evidence-based guidelines for nodule evaluation as well as validated tools for assessing the likelihood of malignancy are readily available (Gould, Ananth, Barnett, & Veterans Affairs, 2007; Gould et al., 2013; McWilliams et al., 2013; Swensen, Silverstein, Ilstrup, Schleck, & Edell, 1997). It is important to engage our radiology colleagues in this discussion; guidelines from the Fleischner Society and the American College of Radiology for reporting on incidentally identified small solid nodules, incidentally identified subsolid nodules, and screening-detected nodules are individually distinct in definitions of abnormality as well as recommendations for follow up, and should be applied appropriately in the context of the individual patient as well as the situation for which the CT was performed (“Lung-RADS Version 1.0 Assessment Categories Release date: April 28, 2014,” 2014; MacMahon et al., 2005; Naidich et al., 2013). All of these potential sources of variation highlight the value of standardizing the approach to nodule evaluation, to ensure that appropriate evaluation will be done to maximize the likelihood of identifying nodules that are actually cancer, and minimize harm potentially incurred by unnecessary invasive and noninvasive testing of nodules that are actually benign.
Dr. Lynn Tanoue, FCCP
NetWork Chair
Gould MK, Ananth L, Barnett PG, and Veterans Affairs, S. C. S. G. A clinical model to estimate the pretest probability of lung cancer in patients with solitary pulmonary nodules. Chest. 2007;131(2):383-388.
Gould MK, Donington J, Lynch WR, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143(5 suppl):e93S.
Gould MK, Tang T, Liu IL, et al. Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med. 2015; 192(10):1208-1214.
Lung-RADS Version 1.0 Assessment Categories Release date: April 28,2014. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/LungRADS/AssessmentCategories.pdf. Accessed Oct 31, 2014.
MacMahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237(2):395-400.
McWilliams A, Tammemagi MC, Mayo JR, et al. Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369(10):910-919.
Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013;266(1):304-317.
Swensen SJ, Silverstein MD, Edell ES, et al. Solitary pulmonary nodules: clinical prediction model versus physicians. Mayo Clin Proc. 1999;74(4):319-329.
Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules: Application to small radiologically indeterminate nodules. Arch Intern Med. 1997;157(8): 849-855.
This Month in CHEST: Editor’s Picks
Editorial
New Sepsis Criteria: A Change We Should Not Make.By Dr. S. Q. Simpson.
Giants in Chest Medicine
Arthur P. Wheeler, MD, FCCP. By Dr. G. R. Bernard.
Topics In Practice Management
Update on Exhaled Nitric Oxide in Clinical Practice.By Dr. S.R. Mummadi and Dr. P.Y. Hahn.
Original Research
Airway Surfactant Protein D Deficiency in Adults With Severe Asthma.By Dr. R.A. Mackay et al.
Outcomes of Nurse Practitioner–Delivered Critical Care: A Prospective Cohort Study.By Dr. J.S. Landsperger et al.
Editorial
New Sepsis Criteria: A Change We Should Not Make.By Dr. S. Q. Simpson.
Giants in Chest Medicine
Arthur P. Wheeler, MD, FCCP. By Dr. G. R. Bernard.
Topics In Practice Management
Update on Exhaled Nitric Oxide in Clinical Practice.By Dr. S.R. Mummadi and Dr. P.Y. Hahn.
Original Research
Airway Surfactant Protein D Deficiency in Adults With Severe Asthma.By Dr. R.A. Mackay et al.
Outcomes of Nurse Practitioner–Delivered Critical Care: A Prospective Cohort Study.By Dr. J.S. Landsperger et al.
Editorial
New Sepsis Criteria: A Change We Should Not Make.By Dr. S. Q. Simpson.
Giants in Chest Medicine
Arthur P. Wheeler, MD, FCCP. By Dr. G. R. Bernard.
Topics In Practice Management
Update on Exhaled Nitric Oxide in Clinical Practice.By Dr. S.R. Mummadi and Dr. P.Y. Hahn.
Original Research
Airway Surfactant Protein D Deficiency in Adults With Severe Asthma.By Dr. R.A. Mackay et al.
Outcomes of Nurse Practitioner–Delivered Critical Care: A Prospective Cohort Study.By Dr. J.S. Landsperger et al.
2016 NetWorks Challenge
In March, the foundation kicked off the 2016 NetWorks Challenge, and we’re delighted to see a very enthusiastic response from our NetWorks Steering Committee members. In fact, we are thrilled to announce that the first NetWorks Steering Committee to achieve 100% participation is the Women’s Health NetWork. Every member on the steering committee made a donation to the CHEST Foundation last month.
“Physicians are competitive by nature and always welcome a challenge; the CHEST Foundation challenge is no exception,” stated Ghada Bourjeily, MD, FCCP, and Chair of the Women’s Health NetWork. “The Women’s Health NetWork Steering Committee members jumped on the opportunity to donate as soon as they heard about this great opportunity and donated to the CHEST Foundation.”
This year, the prizes for winning the NetWorks Challenge are more enticing than ever before. In the first round, the highest percentage of participation by a NetWork Steering Committee will receive additional time for the NetWorks Featured Lecture at CHEST 2016. And, for the very first time, the CHEST Foundation is offering up to two travel grants to CHEST 2016. In the second round, the top two NetWorks Steering Committees that are able to contribute the highest total amount will receive a seat on the CHEST Foundation’s Awards Committee and a potential clinical research grant. Up to two travel grants to CHEST 2017 will also be awarded in the final round to the NetWork that has the highest percentage of participation among their membership.
David Schulman, MD, MPH, FCCP, Chair of the Council of NetWorks, recently commented on why it is critical to take part in the NetWorks Challenge. “Participating in the NetWorks Challenge will serve many great purposes. First, it’s an opportunity to give to a great organization that does fantastic work. Second, if you’re a member of a NetWork and you participate, it allows your NetWork to achieve greatness. How? Because you get extra time at the annual meeting to show off your wares to your members by letting your national leaders speak to your members. Third, you can get travel grants for your colleagues, which allow them to attend the annual Meeting at no cost. Fourth, you can participate in awarding grants to next year’s foundation awardees as a public member of the CHEST Foundation Awards Committee. In short, there is no reason not to give to the foundation as part of the NetWorks Challenge.”
In March, the foundation kicked off the 2016 NetWorks Challenge, and we’re delighted to see a very enthusiastic response from our NetWorks Steering Committee members. In fact, we are thrilled to announce that the first NetWorks Steering Committee to achieve 100% participation is the Women’s Health NetWork. Every member on the steering committee made a donation to the CHEST Foundation last month.
“Physicians are competitive by nature and always welcome a challenge; the CHEST Foundation challenge is no exception,” stated Ghada Bourjeily, MD, FCCP, and Chair of the Women’s Health NetWork. “The Women’s Health NetWork Steering Committee members jumped on the opportunity to donate as soon as they heard about this great opportunity and donated to the CHEST Foundation.”
This year, the prizes for winning the NetWorks Challenge are more enticing than ever before. In the first round, the highest percentage of participation by a NetWork Steering Committee will receive additional time for the NetWorks Featured Lecture at CHEST 2016. And, for the very first time, the CHEST Foundation is offering up to two travel grants to CHEST 2016. In the second round, the top two NetWorks Steering Committees that are able to contribute the highest total amount will receive a seat on the CHEST Foundation’s Awards Committee and a potential clinical research grant. Up to two travel grants to CHEST 2017 will also be awarded in the final round to the NetWork that has the highest percentage of participation among their membership.
David Schulman, MD, MPH, FCCP, Chair of the Council of NetWorks, recently commented on why it is critical to take part in the NetWorks Challenge. “Participating in the NetWorks Challenge will serve many great purposes. First, it’s an opportunity to give to a great organization that does fantastic work. Second, if you’re a member of a NetWork and you participate, it allows your NetWork to achieve greatness. How? Because you get extra time at the annual meeting to show off your wares to your members by letting your national leaders speak to your members. Third, you can get travel grants for your colleagues, which allow them to attend the annual Meeting at no cost. Fourth, you can participate in awarding grants to next year’s foundation awardees as a public member of the CHEST Foundation Awards Committee. In short, there is no reason not to give to the foundation as part of the NetWorks Challenge.”
In March, the foundation kicked off the 2016 NetWorks Challenge, and we’re delighted to see a very enthusiastic response from our NetWorks Steering Committee members. In fact, we are thrilled to announce that the first NetWorks Steering Committee to achieve 100% participation is the Women’s Health NetWork. Every member on the steering committee made a donation to the CHEST Foundation last month.
“Physicians are competitive by nature and always welcome a challenge; the CHEST Foundation challenge is no exception,” stated Ghada Bourjeily, MD, FCCP, and Chair of the Women’s Health NetWork. “The Women’s Health NetWork Steering Committee members jumped on the opportunity to donate as soon as they heard about this great opportunity and donated to the CHEST Foundation.”
This year, the prizes for winning the NetWorks Challenge are more enticing than ever before. In the first round, the highest percentage of participation by a NetWork Steering Committee will receive additional time for the NetWorks Featured Lecture at CHEST 2016. And, for the very first time, the CHEST Foundation is offering up to two travel grants to CHEST 2016. In the second round, the top two NetWorks Steering Committees that are able to contribute the highest total amount will receive a seat on the CHEST Foundation’s Awards Committee and a potential clinical research grant. Up to two travel grants to CHEST 2017 will also be awarded in the final round to the NetWork that has the highest percentage of participation among their membership.
David Schulman, MD, MPH, FCCP, Chair of the Council of NetWorks, recently commented on why it is critical to take part in the NetWorks Challenge. “Participating in the NetWorks Challenge will serve many great purposes. First, it’s an opportunity to give to a great organization that does fantastic work. Second, if you’re a member of a NetWork and you participate, it allows your NetWork to achieve greatness. How? Because you get extra time at the annual meeting to show off your wares to your members by letting your national leaders speak to your members. Third, you can get travel grants for your colleagues, which allow them to attend the annual Meeting at no cost. Fourth, you can participate in awarding grants to next year’s foundation awardees as a public member of the CHEST Foundation Awards Committee. In short, there is no reason not to give to the foundation as part of the NetWorks Challenge.”
The Changing Face of MOC More information
On April 8, 2106, CHEST joined 29 other medical specialty societies at the American Board of Internal Medicine’s (ABIM’s) biannual Liaison Committee on Certification and Recertification (LCCR) meeting in Philadelphia. The meeting focused on the changing face of Maintenance of Certification (MOC) and the vision ABIM has for the future of MOC.
President Richard J. Baron, MD, responded to a letter signed by several medical specialty societies, asking for clarification on ABIM’s vision and philosophy for MOC and the future changes ABIM is considering for the MOC program. Dr. Baron articulated the desire for MOC to be relevant to physicians’ practices in collaboration with the ABIM and the medical specialty societies, to produce, “a credential that speaks to whether physicians are staying current in knowledge and practice over the course of their career in their specialty.”
Dr. Richard G. Battaglia, ABIM Chief Medical Officer, and Eric McKeeby, ABIM Director of Community Engagement, reported the results of a membership survey and focus group discussions regarding ABIM’s Assessment 2020 Report, published in September 2015. They highlighted the challenges, opportunities, and future plans for the MOC program, in light of diplomates’ input through these mechanisms. In the feedback received, the majority of diplomates favored a move away from the secure 10-year MOC recertification examination. Several options were presented, including smaller, more frequent exams, secure exams taken from home or office, and the ability to “test out” of the 10-year exam by successfully completing smaller assessments along the way. Ultimately, participants favored a move away from assessment and toward learning and improvement through a mechanism that is relevant to their real-world practices. Dr. Baron noted the ABIM survey results in which 76.3% of diplomates said they wanted the MOC credential to mean “I am staying current in the knowledge I need to practice,” and he reiterated the Board’s commitment to developing assessment approaches that would result in a meaningful credential based on performance. The ABIM Board of Directors met in April, with the exam format being a priority for them.
Regarding the future of MOC, while the practice assessment requirement is on hold through 2018, ABIM recognizes the work in this area many physicians are currently doing. By early 2017, ABIM is planning on extending the partnership with ACCME to recognize practice assessment activities, along with current medical knowledge activities, for both CME and MOC. This expansion would include blended activities that meet both medical knowledge and practice assessment requirements.
In addition to ABIM staff’s perspectives, three medical societies, including CHEST, reported on their MOC efforts. Heather Dethloff, CHEST Education and Accreditation Specialist, participated in a panel discussion, along with the Endocrine Society and the American Academy of Hospice and Palliative Medicine regarding the ongoing efforts to incorporate MOC into educational activities within their organizations. Successes and challenges encountered through the ABIM MOC certification process were the topics for discussion. During this presentation, CHEST announced its plan to incorporate ABIM MOC into the entire CHEST Annual Meeting 2016; details will be communicated to CHEST members and meeting registrants in coming months.
Throughout these changes to the MOC program, CHEST has been, and will continue to be, in communication with ABIM, advocating for our members. Any questions or concerns about this process can be directed to Heather Dethloff, Education and Accreditation Specialist, at [email protected].
More information
New ABIM Survey Indicates Physician Interest in Potential Changes to MOC Assessment: www.abim.org/news/new-abim-survey-indicates-physician-interest-in-potential-changes-to-moc-assessment.aspx
On April 8, 2106, CHEST joined 29 other medical specialty societies at the American Board of Internal Medicine’s (ABIM’s) biannual Liaison Committee on Certification and Recertification (LCCR) meeting in Philadelphia. The meeting focused on the changing face of Maintenance of Certification (MOC) and the vision ABIM has for the future of MOC.
President Richard J. Baron, MD, responded to a letter signed by several medical specialty societies, asking for clarification on ABIM’s vision and philosophy for MOC and the future changes ABIM is considering for the MOC program. Dr. Baron articulated the desire for MOC to be relevant to physicians’ practices in collaboration with the ABIM and the medical specialty societies, to produce, “a credential that speaks to whether physicians are staying current in knowledge and practice over the course of their career in their specialty.”
Dr. Richard G. Battaglia, ABIM Chief Medical Officer, and Eric McKeeby, ABIM Director of Community Engagement, reported the results of a membership survey and focus group discussions regarding ABIM’s Assessment 2020 Report, published in September 2015. They highlighted the challenges, opportunities, and future plans for the MOC program, in light of diplomates’ input through these mechanisms. In the feedback received, the majority of diplomates favored a move away from the secure 10-year MOC recertification examination. Several options were presented, including smaller, more frequent exams, secure exams taken from home or office, and the ability to “test out” of the 10-year exam by successfully completing smaller assessments along the way. Ultimately, participants favored a move away from assessment and toward learning and improvement through a mechanism that is relevant to their real-world practices. Dr. Baron noted the ABIM survey results in which 76.3% of diplomates said they wanted the MOC credential to mean “I am staying current in the knowledge I need to practice,” and he reiterated the Board’s commitment to developing assessment approaches that would result in a meaningful credential based on performance. The ABIM Board of Directors met in April, with the exam format being a priority for them.
Regarding the future of MOC, while the practice assessment requirement is on hold through 2018, ABIM recognizes the work in this area many physicians are currently doing. By early 2017, ABIM is planning on extending the partnership with ACCME to recognize practice assessment activities, along with current medical knowledge activities, for both CME and MOC. This expansion would include blended activities that meet both medical knowledge and practice assessment requirements.
In addition to ABIM staff’s perspectives, three medical societies, including CHEST, reported on their MOC efforts. Heather Dethloff, CHEST Education and Accreditation Specialist, participated in a panel discussion, along with the Endocrine Society and the American Academy of Hospice and Palliative Medicine regarding the ongoing efforts to incorporate MOC into educational activities within their organizations. Successes and challenges encountered through the ABIM MOC certification process were the topics for discussion. During this presentation, CHEST announced its plan to incorporate ABIM MOC into the entire CHEST Annual Meeting 2016; details will be communicated to CHEST members and meeting registrants in coming months.
Throughout these changes to the MOC program, CHEST has been, and will continue to be, in communication with ABIM, advocating for our members. Any questions or concerns about this process can be directed to Heather Dethloff, Education and Accreditation Specialist, at [email protected].
More information
New ABIM Survey Indicates Physician Interest in Potential Changes to MOC Assessment: www.abim.org/news/new-abim-survey-indicates-physician-interest-in-potential-changes-to-moc-assessment.aspx
On April 8, 2106, CHEST joined 29 other medical specialty societies at the American Board of Internal Medicine’s (ABIM’s) biannual Liaison Committee on Certification and Recertification (LCCR) meeting in Philadelphia. The meeting focused on the changing face of Maintenance of Certification (MOC) and the vision ABIM has for the future of MOC.
President Richard J. Baron, MD, responded to a letter signed by several medical specialty societies, asking for clarification on ABIM’s vision and philosophy for MOC and the future changes ABIM is considering for the MOC program. Dr. Baron articulated the desire for MOC to be relevant to physicians’ practices in collaboration with the ABIM and the medical specialty societies, to produce, “a credential that speaks to whether physicians are staying current in knowledge and practice over the course of their career in their specialty.”
Dr. Richard G. Battaglia, ABIM Chief Medical Officer, and Eric McKeeby, ABIM Director of Community Engagement, reported the results of a membership survey and focus group discussions regarding ABIM’s Assessment 2020 Report, published in September 2015. They highlighted the challenges, opportunities, and future plans for the MOC program, in light of diplomates’ input through these mechanisms. In the feedback received, the majority of diplomates favored a move away from the secure 10-year MOC recertification examination. Several options were presented, including smaller, more frequent exams, secure exams taken from home or office, and the ability to “test out” of the 10-year exam by successfully completing smaller assessments along the way. Ultimately, participants favored a move away from assessment and toward learning and improvement through a mechanism that is relevant to their real-world practices. Dr. Baron noted the ABIM survey results in which 76.3% of diplomates said they wanted the MOC credential to mean “I am staying current in the knowledge I need to practice,” and he reiterated the Board’s commitment to developing assessment approaches that would result in a meaningful credential based on performance. The ABIM Board of Directors met in April, with the exam format being a priority for them.
Regarding the future of MOC, while the practice assessment requirement is on hold through 2018, ABIM recognizes the work in this area many physicians are currently doing. By early 2017, ABIM is planning on extending the partnership with ACCME to recognize practice assessment activities, along with current medical knowledge activities, for both CME and MOC. This expansion would include blended activities that meet both medical knowledge and practice assessment requirements.
In addition to ABIM staff’s perspectives, three medical societies, including CHEST, reported on their MOC efforts. Heather Dethloff, CHEST Education and Accreditation Specialist, participated in a panel discussion, along with the Endocrine Society and the American Academy of Hospice and Palliative Medicine regarding the ongoing efforts to incorporate MOC into educational activities within their organizations. Successes and challenges encountered through the ABIM MOC certification process were the topics for discussion. During this presentation, CHEST announced its plan to incorporate ABIM MOC into the entire CHEST Annual Meeting 2016; details will be communicated to CHEST members and meeting registrants in coming months.
Throughout these changes to the MOC program, CHEST has been, and will continue to be, in communication with ABIM, advocating for our members. Any questions or concerns about this process can be directed to Heather Dethloff, Education and Accreditation Specialist, at [email protected].
More information
New ABIM Survey Indicates Physician Interest in Potential Changes to MOC Assessment: www.abim.org/news/new-abim-survey-indicates-physician-interest-in-potential-changes-to-moc-assessment.aspx
Catching up with our past presidents
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new in their lives.
Kalpalatha K. Guntupalli, MD, Master FCCP, MACP, FCCM
Frances K. Friedman and Oscar Friedman, MD ’36 Endowed Professor for Pulmonary Disorders; and Chief, Section of Pulmonary, Critical Care, and Sleep Medicine, Department of Medicine, Baylor College of Medicine.
President 2009-2010
November 1, 2009, is clearly etched into my memory. I was sworn in as the 73rd President, and 3rd woman President, of the American College of Chest Physicians during CHEST Annual Meeting 2009 in San Diego.
I consider the 2 years leading up to the presidency and the year following my term as the best years of my professional career. They were action packed, full of excitement that gave immense satisfaction. During my year, the longtime EVP/CEO, Al Lever, retired, and we welcomed the new EVP/CEO Mr. Paul Markowski.
To make the transition easier, I started the “4 Ps” call of the 4 Presidents (President-Designate, President-Elect, President, and the Past President), a weekly call to catch up and keep everyone in the loop. This has since become a tradition in the organization.
My theme for the year was “Act local, Think global.” We started many international initiatives, in the Middle East, India, China, and South America, that have since evolved into successful programs. In 2010, as members of the Federation of International Respiratory Societies (FIRS), we celebrated the “Year of the Lung.” We participated in the “world spirometry day” (102,487 spirometries were done globally) and did many other programs to increase awareness of lung disease. We held a long-term strategic retreat developing goals for the College. We implemented many other process-driven initiatives under the new CEO’s leadership.
Land was acquired where the new beautiful headquarters building now stands.
What is life like after CHEST Presidency?
I was very honored in 2012 to receive the “Pravasi Bharatiya Samman,” the highest award bestowed on a nonresident Indian by the President of India or distinguished members of the Indian Diaspora to “honor exceptional and meritorious contributions in their chosen field/profession and enhancing the image of India.” In 2013, I spent 4 months as a Fulbright Scholar forming an ARDS network in India, and in 2015, I was honored as a Master FCCP by our own organization.
As the Section Chief, I have been busy building a “Lung Institute” and ICU services along with many new initiatives in our very active Pulmonary/CC/Sleep section at Baylor College of Medicine.
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new in their lives.
Kalpalatha K. Guntupalli, MD, Master FCCP, MACP, FCCM
Frances K. Friedman and Oscar Friedman, MD ’36 Endowed Professor for Pulmonary Disorders; and Chief, Section of Pulmonary, Critical Care, and Sleep Medicine, Department of Medicine, Baylor College of Medicine.
President 2009-2010
November 1, 2009, is clearly etched into my memory. I was sworn in as the 73rd President, and 3rd woman President, of the American College of Chest Physicians during CHEST Annual Meeting 2009 in San Diego.
I consider the 2 years leading up to the presidency and the year following my term as the best years of my professional career. They were action packed, full of excitement that gave immense satisfaction. During my year, the longtime EVP/CEO, Al Lever, retired, and we welcomed the new EVP/CEO Mr. Paul Markowski.
To make the transition easier, I started the “4 Ps” call of the 4 Presidents (President-Designate, President-Elect, President, and the Past President), a weekly call to catch up and keep everyone in the loop. This has since become a tradition in the organization.
My theme for the year was “Act local, Think global.” We started many international initiatives, in the Middle East, India, China, and South America, that have since evolved into successful programs. In 2010, as members of the Federation of International Respiratory Societies (FIRS), we celebrated the “Year of the Lung.” We participated in the “world spirometry day” (102,487 spirometries were done globally) and did many other programs to increase awareness of lung disease. We held a long-term strategic retreat developing goals for the College. We implemented many other process-driven initiatives under the new CEO’s leadership.
Land was acquired where the new beautiful headquarters building now stands.
What is life like after CHEST Presidency?
I was very honored in 2012 to receive the “Pravasi Bharatiya Samman,” the highest award bestowed on a nonresident Indian by the President of India or distinguished members of the Indian Diaspora to “honor exceptional and meritorious contributions in their chosen field/profession and enhancing the image of India.” In 2013, I spent 4 months as a Fulbright Scholar forming an ARDS network in India, and in 2015, I was honored as a Master FCCP by our own organization.
As the Section Chief, I have been busy building a “Lung Institute” and ICU services along with many new initiatives in our very active Pulmonary/CC/Sleep section at Baylor College of Medicine.
Where are they now? What have they been up to? CHEST’s Past Presidents each forged the way for the many successes of the American College of Chest Physicians (CHEST), leading to enhanced patient care around the globe. Their outstanding leadership and vision are evidenced today in many of CHEST’s current initiatives, and now it is time to check in with these past leaders to give us a look at what’s new in their lives.
Kalpalatha K. Guntupalli, MD, Master FCCP, MACP, FCCM
Frances K. Friedman and Oscar Friedman, MD ’36 Endowed Professor for Pulmonary Disorders; and Chief, Section of Pulmonary, Critical Care, and Sleep Medicine, Department of Medicine, Baylor College of Medicine.
President 2009-2010
November 1, 2009, is clearly etched into my memory. I was sworn in as the 73rd President, and 3rd woman President, of the American College of Chest Physicians during CHEST Annual Meeting 2009 in San Diego.
I consider the 2 years leading up to the presidency and the year following my term as the best years of my professional career. They were action packed, full of excitement that gave immense satisfaction. During my year, the longtime EVP/CEO, Al Lever, retired, and we welcomed the new EVP/CEO Mr. Paul Markowski.
To make the transition easier, I started the “4 Ps” call of the 4 Presidents (President-Designate, President-Elect, President, and the Past President), a weekly call to catch up and keep everyone in the loop. This has since become a tradition in the organization.
My theme for the year was “Act local, Think global.” We started many international initiatives, in the Middle East, India, China, and South America, that have since evolved into successful programs. In 2010, as members of the Federation of International Respiratory Societies (FIRS), we celebrated the “Year of the Lung.” We participated in the “world spirometry day” (102,487 spirometries were done globally) and did many other programs to increase awareness of lung disease. We held a long-term strategic retreat developing goals for the College. We implemented many other process-driven initiatives under the new CEO’s leadership.
Land was acquired where the new beautiful headquarters building now stands.
What is life like after CHEST Presidency?
I was very honored in 2012 to receive the “Pravasi Bharatiya Samman,” the highest award bestowed on a nonresident Indian by the President of India or distinguished members of the Indian Diaspora to “honor exceptional and meritorious contributions in their chosen field/profession and enhancing the image of India.” In 2013, I spent 4 months as a Fulbright Scholar forming an ARDS network in India, and in 2015, I was honored as a Master FCCP by our own organization.
As the Section Chief, I have been busy building a “Lung Institute” and ICU services along with many new initiatives in our very active Pulmonary/CC/Sleep section at Baylor College of Medicine.
National Sarcoidosis Awareness Month
In conjunction with National Sarcoidosis Awareness Month in April, and in partnership with the Foundation for Sarcoidosis Research (FSR), the CHEST Foundation has launched the second annual Seek Answers. Inspire Results. campaign. This national awareness effort encourages people living with sarcoidosis to take a proactive role in their care.
Throughout the campaign, CHEST Foundation and FSR are providing people living with sarcoidosis and their caregivers the tools necessary to understand and manage their unique condition through individual provider and patient toolkits. One of the materials included within these toolkits is the “Sarcoid Five.” Due to the variability of disease presentation, the “Sarcoid Five” provides a list of five questions designed to start proactive patient-doctor conversations and help people living with sarcoidosis to understand treatment options and create a personalized plan to control their individual condition.
Additional campaign materials include a radio media tour, social media sharable images, infographics, as well as compelling digital assets, including a video and interactive, Web-based element.
Further information can be found at chestnet.org/sarcoid.
In conjunction with National Sarcoidosis Awareness Month in April, and in partnership with the Foundation for Sarcoidosis Research (FSR), the CHEST Foundation has launched the second annual Seek Answers. Inspire Results. campaign. This national awareness effort encourages people living with sarcoidosis to take a proactive role in their care.
Throughout the campaign, CHEST Foundation and FSR are providing people living with sarcoidosis and their caregivers the tools necessary to understand and manage their unique condition through individual provider and patient toolkits. One of the materials included within these toolkits is the “Sarcoid Five.” Due to the variability of disease presentation, the “Sarcoid Five” provides a list of five questions designed to start proactive patient-doctor conversations and help people living with sarcoidosis to understand treatment options and create a personalized plan to control their individual condition.
Additional campaign materials include a radio media tour, social media sharable images, infographics, as well as compelling digital assets, including a video and interactive, Web-based element.
Further information can be found at chestnet.org/sarcoid.
In conjunction with National Sarcoidosis Awareness Month in April, and in partnership with the Foundation for Sarcoidosis Research (FSR), the CHEST Foundation has launched the second annual Seek Answers. Inspire Results. campaign. This national awareness effort encourages people living with sarcoidosis to take a proactive role in their care.
Throughout the campaign, CHEST Foundation and FSR are providing people living with sarcoidosis and their caregivers the tools necessary to understand and manage their unique condition through individual provider and patient toolkits. One of the materials included within these toolkits is the “Sarcoid Five.” Due to the variability of disease presentation, the “Sarcoid Five” provides a list of five questions designed to start proactive patient-doctor conversations and help people living with sarcoidosis to understand treatment options and create a personalized plan to control their individual condition.
Additional campaign materials include a radio media tour, social media sharable images, infographics, as well as compelling digital assets, including a video and interactive, Web-based element.
Further information can be found at chestnet.org/sarcoid.
In Memoriam
Dr. Robert O. Crapo, FCCP, died on December 26, 2015. He was a Professor of Medicine at the University of Utah and the Director of the Pulmonary Function Laboratory at LDS Hospital, a laboratory that was internationally regarded for many contributions to understanding pulmonary function and pulmonary function testing.
At this teaching laboratory where countless fellows, residents, and students learned the principles of pulmonary function testing, basic respiratory physiology, and how lung function tests could help them diagnose and treat lung disease, Dr. Crapo was a master teacher. Dr. Crapo received the 2006 Distinguished Scientist Honor Lecture award from the American College of Chest Physicians. We extend our condolences to the Crapo family.
Dr. Robert O. Crapo, FCCP, died on December 26, 2015. He was a Professor of Medicine at the University of Utah and the Director of the Pulmonary Function Laboratory at LDS Hospital, a laboratory that was internationally regarded for many contributions to understanding pulmonary function and pulmonary function testing.
At this teaching laboratory where countless fellows, residents, and students learned the principles of pulmonary function testing, basic respiratory physiology, and how lung function tests could help them diagnose and treat lung disease, Dr. Crapo was a master teacher. Dr. Crapo received the 2006 Distinguished Scientist Honor Lecture award from the American College of Chest Physicians. We extend our condolences to the Crapo family.
Dr. Robert O. Crapo, FCCP, died on December 26, 2015. He was a Professor of Medicine at the University of Utah and the Director of the Pulmonary Function Laboratory at LDS Hospital, a laboratory that was internationally regarded for many contributions to understanding pulmonary function and pulmonary function testing.
At this teaching laboratory where countless fellows, residents, and students learned the principles of pulmonary function testing, basic respiratory physiology, and how lung function tests could help them diagnose and treat lung disease, Dr. Crapo was a master teacher. Dr. Crapo received the 2006 Distinguished Scientist Honor Lecture award from the American College of Chest Physicians. We extend our condolences to the Crapo family.
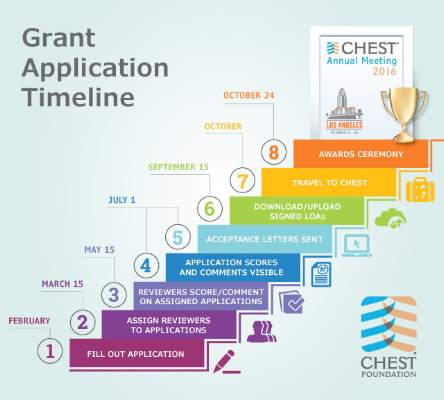
CHEST Foundation Grants: How will you help champion lung health?
The CHEST Foundation expanded its grant offerings in 2016 with the addition of two new research grants that will broaden the program’s reach and scope. As of February 1, the foundation began accepting applications for research grants, community service projects, and distinguished scholar research projects. These grants have a powerful impact on our grantees’ ability to champion lung health, and they also assist young investigators like Dr. Kerri Johannson in gaining research and project management skills, while assisting in advancing their careers.
“Being awarded a grant is validation that somebody else believes in your idea and that your project could be fruitful and contribute meaningfully to the field,” stated Johannson. “It actually begets more opportunities. I am forever grateful to the CHEST Foundation for providing me with this opportunity.” The CHEST Foundation’s Clinical Research Grant in Pulmonary Fibrosis, along with Genentech, funded her 2013 project, Ambient Air Pollution Exposure and Clinical Outcomes in Idiopathic Pulmonary Fibrosis. Dr. Johannson’s research focuses on analyzing air pollution exposures and short-term variability in lung function for patients with idiopathic pulmonary fibrosis (IPF).
Her patients were given home breathing machines, so they could do breathing tests at home to show how their lung function fluctuated over shorter periods of time. “I was interested in looking at whether or not and how that correlated with their air quality in the regional area.” She said about her project, “No one has ever looked at it before. It’s usually a long-term study, such as every 3 months or changes over a year in clinical trials, but it turns out there is actually a large portion of patients with a lot of short-term variability that has an impact for clinical trial outcomes and measures.”
The deadline for applications is quickly approaching. CHEST Foundation grants help make your research and community service projects possible. Please take advantage of our substantive grant program, and remember that the submissions will be accepted until April 30. How will you help champion lung health? Apply for a CHEST Foundation grant today by going to chestnet.org/grants.
The CHEST Foundation expanded its grant offerings in 2016 with the addition of two new research grants that will broaden the program’s reach and scope. As of February 1, the foundation began accepting applications for research grants, community service projects, and distinguished scholar research projects. These grants have a powerful impact on our grantees’ ability to champion lung health, and they also assist young investigators like Dr. Kerri Johannson in gaining research and project management skills, while assisting in advancing their careers.
“Being awarded a grant is validation that somebody else believes in your idea and that your project could be fruitful and contribute meaningfully to the field,” stated Johannson. “It actually begets more opportunities. I am forever grateful to the CHEST Foundation for providing me with this opportunity.” The CHEST Foundation’s Clinical Research Grant in Pulmonary Fibrosis, along with Genentech, funded her 2013 project, Ambient Air Pollution Exposure and Clinical Outcomes in Idiopathic Pulmonary Fibrosis. Dr. Johannson’s research focuses on analyzing air pollution exposures and short-term variability in lung function for patients with idiopathic pulmonary fibrosis (IPF).
Her patients were given home breathing machines, so they could do breathing tests at home to show how their lung function fluctuated over shorter periods of time. “I was interested in looking at whether or not and how that correlated with their air quality in the regional area.” She said about her project, “No one has ever looked at it before. It’s usually a long-term study, such as every 3 months or changes over a year in clinical trials, but it turns out there is actually a large portion of patients with a lot of short-term variability that has an impact for clinical trial outcomes and measures.”
The deadline for applications is quickly approaching. CHEST Foundation grants help make your research and community service projects possible. Please take advantage of our substantive grant program, and remember that the submissions will be accepted until April 30. How will you help champion lung health? Apply for a CHEST Foundation grant today by going to chestnet.org/grants.
The CHEST Foundation expanded its grant offerings in 2016 with the addition of two new research grants that will broaden the program’s reach and scope. As of February 1, the foundation began accepting applications for research grants, community service projects, and distinguished scholar research projects. These grants have a powerful impact on our grantees’ ability to champion lung health, and they also assist young investigators like Dr. Kerri Johannson in gaining research and project management skills, while assisting in advancing their careers.
“Being awarded a grant is validation that somebody else believes in your idea and that your project could be fruitful and contribute meaningfully to the field,” stated Johannson. “It actually begets more opportunities. I am forever grateful to the CHEST Foundation for providing me with this opportunity.” The CHEST Foundation’s Clinical Research Grant in Pulmonary Fibrosis, along with Genentech, funded her 2013 project, Ambient Air Pollution Exposure and Clinical Outcomes in Idiopathic Pulmonary Fibrosis. Dr. Johannson’s research focuses on analyzing air pollution exposures and short-term variability in lung function for patients with idiopathic pulmonary fibrosis (IPF).
Her patients were given home breathing machines, so they could do breathing tests at home to show how their lung function fluctuated over shorter periods of time. “I was interested in looking at whether or not and how that correlated with their air quality in the regional area.” She said about her project, “No one has ever looked at it before. It’s usually a long-term study, such as every 3 months or changes over a year in clinical trials, but it turns out there is actually a large portion of patients with a lot of short-term variability that has an impact for clinical trial outcomes and measures.”
The deadline for applications is quickly approaching. CHEST Foundation grants help make your research and community service projects possible. Please take advantage of our substantive grant program, and remember that the submissions will be accepted until April 30. How will you help champion lung health? Apply for a CHEST Foundation grant today by going to chestnet.org/grants.
Lights, camera, action! CHEST 2016 visits Los Angeles
We’re gearing up to visit the entertainment capital of the world on October 22 - 26 for CHEST 2016. We will dazzle Los Angeles and the chest medicine community with current pulmonary, critical care, and sleep medicine topics presented by world-renowned faculty in a variety of innovative instruction formats. You won’t want to miss our cutting-edge education; and, in your free time, we want to make sure you take in all that Los Angeles has to offer. Follow our suggestions below, and we’ll make sure you’ve seen the most famous hot spots in LA.
Hollywood
When you think of Los Angeles, Hollywood is sure to be top of mind. Hollywood is about a 25-minute drive from the Convention Center, so make sure you have time for a longer excursion. You’ll enjoy the recognizable Hollywood sign, built in 1923, and the Hollywood Walk of Fame. You can also check out the Dolby Theater, home to the Academy Awards until at least 2033, or Runyon Canyon, a famous park known for great views of the city and celebrity sightings.
Beaches
If Hollywood doesn’t allure you, maybe you’d rather take it easy at one of Los Angeles’s famous beaches. If you like to people watch, Venice Beach will keep you interested with body builders, jugglers, palm readers, folk artists, and many other personalities. If you’re interested in surfing, Malibu Surfrider Beach is known for amateurs and experienced surfers alike to find great waves. Santa Monica Beach is one of the most popular beaches for its volleyball, bike riding, and sunbathing. Or check out Long Beach, home to the Queen Mary, a floating hotel aboard an iconic 1936 ocean liner. With 75 miles of coast, you’re sure to find the beach that you’re looking for.
Shopping
Make sure to explore the LA Fashion District in downtown LA, where you’ll find many top shopping centers to choose from. If you’re looking for luxury, Rodeo Drive in Beverly Hills offers extravagant shopping and dining experiences. Or, if you’re intrigued by bargain hunting, there are also plenty of opportunities for outlet shopping in Camarillo, the Citadel, Desert Hills, and Ontario Mills.
Television Show Taping
Maybe you’ve always dreamed of being part of a live studio audience. Choose from a wide array of shows filmed in Los Angeles, and lucky you, October is in the heart of peak production season. If you want to attend a show taping, order tickets in advance. Check out a vendor, such as Audiences Unlimited or Hollywood Tickets, both of which feature sitcoms and talk shows. You can also look at a specific show’s website to find tickets. Attending a TV show taping can be an exciting and unique LA experience, and, best of all, it’s free!
Los Angeles will keep you entertained with its glamour and glitz. Learn more about tourism opportunities at discoverlosangeles.com, and find out more about CHEST 2016 at chestmeeting.chestnet.org.
We’re gearing up to visit the entertainment capital of the world on October 22 - 26 for CHEST 2016. We will dazzle Los Angeles and the chest medicine community with current pulmonary, critical care, and sleep medicine topics presented by world-renowned faculty in a variety of innovative instruction formats. You won’t want to miss our cutting-edge education; and, in your free time, we want to make sure you take in all that Los Angeles has to offer. Follow our suggestions below, and we’ll make sure you’ve seen the most famous hot spots in LA.
Hollywood
When you think of Los Angeles, Hollywood is sure to be top of mind. Hollywood is about a 25-minute drive from the Convention Center, so make sure you have time for a longer excursion. You’ll enjoy the recognizable Hollywood sign, built in 1923, and the Hollywood Walk of Fame. You can also check out the Dolby Theater, home to the Academy Awards until at least 2033, or Runyon Canyon, a famous park known for great views of the city and celebrity sightings.
Beaches
If Hollywood doesn’t allure you, maybe you’d rather take it easy at one of Los Angeles’s famous beaches. If you like to people watch, Venice Beach will keep you interested with body builders, jugglers, palm readers, folk artists, and many other personalities. If you’re interested in surfing, Malibu Surfrider Beach is known for amateurs and experienced surfers alike to find great waves. Santa Monica Beach is one of the most popular beaches for its volleyball, bike riding, and sunbathing. Or check out Long Beach, home to the Queen Mary, a floating hotel aboard an iconic 1936 ocean liner. With 75 miles of coast, you’re sure to find the beach that you’re looking for.
Shopping
Make sure to explore the LA Fashion District in downtown LA, where you’ll find many top shopping centers to choose from. If you’re looking for luxury, Rodeo Drive in Beverly Hills offers extravagant shopping and dining experiences. Or, if you’re intrigued by bargain hunting, there are also plenty of opportunities for outlet shopping in Camarillo, the Citadel, Desert Hills, and Ontario Mills.
Television Show Taping
Maybe you’ve always dreamed of being part of a live studio audience. Choose from a wide array of shows filmed in Los Angeles, and lucky you, October is in the heart of peak production season. If you want to attend a show taping, order tickets in advance. Check out a vendor, such as Audiences Unlimited or Hollywood Tickets, both of which feature sitcoms and talk shows. You can also look at a specific show’s website to find tickets. Attending a TV show taping can be an exciting and unique LA experience, and, best of all, it’s free!
Los Angeles will keep you entertained with its glamour and glitz. Learn more about tourism opportunities at discoverlosangeles.com, and find out more about CHEST 2016 at chestmeeting.chestnet.org.
We’re gearing up to visit the entertainment capital of the world on October 22 - 26 for CHEST 2016. We will dazzle Los Angeles and the chest medicine community with current pulmonary, critical care, and sleep medicine topics presented by world-renowned faculty in a variety of innovative instruction formats. You won’t want to miss our cutting-edge education; and, in your free time, we want to make sure you take in all that Los Angeles has to offer. Follow our suggestions below, and we’ll make sure you’ve seen the most famous hot spots in LA.
Hollywood
When you think of Los Angeles, Hollywood is sure to be top of mind. Hollywood is about a 25-minute drive from the Convention Center, so make sure you have time for a longer excursion. You’ll enjoy the recognizable Hollywood sign, built in 1923, and the Hollywood Walk of Fame. You can also check out the Dolby Theater, home to the Academy Awards until at least 2033, or Runyon Canyon, a famous park known for great views of the city and celebrity sightings.
Beaches
If Hollywood doesn’t allure you, maybe you’d rather take it easy at one of Los Angeles’s famous beaches. If you like to people watch, Venice Beach will keep you interested with body builders, jugglers, palm readers, folk artists, and many other personalities. If you’re interested in surfing, Malibu Surfrider Beach is known for amateurs and experienced surfers alike to find great waves. Santa Monica Beach is one of the most popular beaches for its volleyball, bike riding, and sunbathing. Or check out Long Beach, home to the Queen Mary, a floating hotel aboard an iconic 1936 ocean liner. With 75 miles of coast, you’re sure to find the beach that you’re looking for.
Shopping
Make sure to explore the LA Fashion District in downtown LA, where you’ll find many top shopping centers to choose from. If you’re looking for luxury, Rodeo Drive in Beverly Hills offers extravagant shopping and dining experiences. Or, if you’re intrigued by bargain hunting, there are also plenty of opportunities for outlet shopping in Camarillo, the Citadel, Desert Hills, and Ontario Mills.
Television Show Taping
Maybe you’ve always dreamed of being part of a live studio audience. Choose from a wide array of shows filmed in Los Angeles, and lucky you, October is in the heart of peak production season. If you want to attend a show taping, order tickets in advance. Check out a vendor, such as Audiences Unlimited or Hollywood Tickets, both of which feature sitcoms and talk shows. You can also look at a specific show’s website to find tickets. Attending a TV show taping can be an exciting and unique LA experience, and, best of all, it’s free!
Los Angeles will keep you entertained with its glamour and glitz. Learn more about tourism opportunities at discoverlosangeles.com, and find out more about CHEST 2016 at chestmeeting.chestnet.org.
Sepsis guidelines ... opening a conversation
The March issue of CHEST Physician featured an article entitled “Sepsis, Septic Shock Redefined by Critical Care Groups.” Dr. Steven Q. Simpson, FCCP, has commented in an editorial entitled, “New Sepsis Criteria: A Change We Should Not Make,” that can currently be found at CHEST Online First at http://journal.publications.chestnet.org/article.aspx?articleid=2499560. This editorial will appear in print in the May issue of the journal CHEST. Also, in the May issue, watch for a podcast discussion between Dr. Simpson and Dr. C. S. Deutschman, one of the authors of the sepsis consensus document.
The March issue of CHEST Physician featured an article entitled “Sepsis, Septic Shock Redefined by Critical Care Groups.” Dr. Steven Q. Simpson, FCCP, has commented in an editorial entitled, “New Sepsis Criteria: A Change We Should Not Make,” that can currently be found at CHEST Online First at http://journal.publications.chestnet.org/article.aspx?articleid=2499560. This editorial will appear in print in the May issue of the journal CHEST. Also, in the May issue, watch for a podcast discussion between Dr. Simpson and Dr. C. S. Deutschman, one of the authors of the sepsis consensus document.
The March issue of CHEST Physician featured an article entitled “Sepsis, Septic Shock Redefined by Critical Care Groups.” Dr. Steven Q. Simpson, FCCP, has commented in an editorial entitled, “New Sepsis Criteria: A Change We Should Not Make,” that can currently be found at CHEST Online First at http://journal.publications.chestnet.org/article.aspx?articleid=2499560. This editorial will appear in print in the May issue of the journal CHEST. Also, in the May issue, watch for a podcast discussion between Dr. Simpson and Dr. C. S. Deutschman, one of the authors of the sepsis consensus document.