User login
Planning for future college expenses with 529 accounts
Financial planning for families can involve multiple investment goals. The big ones usually are investing for retirement and for your children’s college expenses. With any investment strategy, once you have identified an investment goal, you will want to utilize the right investment account to achieve that goal. If investing for future college expenses is your goal, then one of the investment accounts you will want to utilize is called a 529 plan.
What is a 529 plan?
A 529 plan is a tax-favored account authorized by Section 529 of the Internal Revenue Code and sponsored by a state or educational institution. These plans have specific tax-saving features to them, compared with other taxable accounts, which are listed below. To begin with, there are two types of 529 plans: prepaid tuition plans and education savings plans. Every state has at least one type of 529 plan. Additionally, some private colleges sponsor a prepaid tuition plan.
Prepaid tuition plan
The first type of 529 account is a prepaid tuition plan. These let an account owner purchase college credits (or units) for participating colleges or universities at today’s prices to be used for the student’s future tuition charges. The states that sponsor prepaid plans do so primarily for the benefit of their in-state public colleges and universities. Things to know about the prepaid plans: States may or may not guarantee that the prepaid units keep up with increases in tuition charges. The plan also may have a state residency requirement. If the student decides not to attend one of the eligible schools, the equivalent payout may be less than had the student attended one of the participating institutions. There are no federal guarantees on the state prepaid plans and they are not available for private elementary and high school programs.
Education savings plan
The second type of 529 account is an education savings plan, an investment account into which you can invest your after-tax dollars. The intent with these accounts is to grow the balance for use at a future date. These are tax-deferred accounts, which means each year the interest, dividends, and capital gains created within the account do not show up on your tax return. If the funds are used for a “qualified” higher-education expense, then gains on the account are not taxed upon withdrawal.
As with most investments, the longer your money is invested, the more time it has to grow via accumulated interest, dividends, and appreciation. The larger the growth, the larger the tax benefits. This offers a tremendous advantage for a high-income and high-tax bracket household to invest for future goals (such as private school tuition or college expenses). By contrast, if you had invested in a fully taxable account, you would be subject to taxes each year on the interest, dividends, and capital gain distributions. Also, with taxable accounts, your investments would be subject to capital gains tax on the growth when they are sold to pay for those future expenses.
An account owner may choose among a range of investment options that the 529 plan provides. These are typically individual mutual funds or preformed mutual fund portfolios. The portfolios may have a fixed allocation percentage that stays the same over time or come “age-weighted,” meaning the investment allocation becomes more conservative the closer the student gets to college age when withdrawals would occur. This is a similar approach to the “target retirement date” offerings one sees in retirement accounts.
If one is using the 529 account for the student’s elementary or high school years, the investment time frame may be shorter and necessitate a more conservative approach, as the time for withdrawals would be nearer than the college years. As with most investments, the account can lose value based on investment performance.
Owner versus beneficiary
There are two parties to any 529 plan account: The account owner, who has control over the account and can name the beneficiary to the account, and the beneficiary (the student). The account owner can change beneficiaries on the account and can even name themselves as the beneficiary. One can name anyone as the beneficiary (e.g., child, friend, relative, yourself). You can be proactive by creating an account and naming yourself the beneficiary now, before switching to your child in the future. The account owner can live in one state with the beneficiary in another and invest in the 529 from a third state, and the student may eventually go to an educational institution in a fourth state. The 529 education savings account is not limited to any specific college, as a prepaid plan may be.
Withdrawals from 529s
If a 529 account withdrawal is for qualified higher education expenses or tuition for elementary or secondary schools, earnings are not subject to federal income tax or, in many cases, state income tax. Qualified withdrawals need to take place in the same tax year as the qualified expense.
Withdrawals not used for qualified higher education expenses in that year are considered “nonqualified” and would be subject to tax and 10% penalty on the earnings. State and local taxes may apply as well.
You can use the proceeds from the account free of taxes for the following qualified higher-education expenses:
- Tuition and school fees for both full and part time students at an eligible college, university, trade, or vocational institution.
- Room and board if the student is enrolled at more than half-time status. The amount up to the school’s room and board charges are eligible if paid directly to the school or to a landlord if living in nonschool housing. If actual charges to the landlord exceed the schools’ charges, then the amount above the school’s charges would be considered an excess withdrawal.
- Required books, supplies, and equipment for the academic program. Computer and technology equipment, printers, and required software, and such related services as Internet access also are qualified expenses.
- Private elementary or secondary school tuition up to $10,000 annually also is a qualified expense for 529 withdrawals.
Health insurance for the student and transportation-related costs to and from the school are not qualified expenses.
Contributions and fees
Like all investments, the fees associated with a 529 account need to be considered, as excess fees lower the investment returns. Prepaid tuition plans may charge initial application, transaction, and ongoing administrative fees. Investment 529 accounts may also have administrative costs such as program management fees, per-transaction fees, and the underlying investment expense ratios. Some states have broker-sold plans as well as direct-sold plans. Broker-sold plans can be purchased only through a broker and have the additional expenses associated with that either in the form of a load (sales charge) or higher expense ratio.
Contributions to a 529 plan can only be made in cash. If you currently have other investments, they need to be liquidated first (with the associated tax consequence) and then the proceeds invested into the 529 plan. Establishing the account and ongoing contributions are subject to gift tax limits ($15,000 for 2019). A married couple may make a “joint gift” to the account to double the limit. The 529 plans also allow the owner to front-load the account in 1 year with up to 5 years’ worth of gift limit contributions all at once. This lump sum is treated for tax reasons as a pro-rata 5 consecutive years of contributions all at once. Any additional gifts to that beneficiary during that year and the remaining four would be subject to gift tax issues if it means the annual gift limits were exceeded. Contributions are considered a “completed gift” for gift- and estate-tax purposes even though the account owner retains an element of control. The up-front 5-year gift election is available only on 529 accounts and is a great way for parents and grandparents (hint-hint) to reduce their estates and get a significant initial balance into the account. This can come in handy for those who may have procrastinated working toward this investment goal and need to catch up.
If the beneficiary does not need all or some of the funds for qualified higher education expenses, the account owner has options: One can change beneficiary to another relative who may need the funds or keep the account going and eventually add a grandchild as a beneficiary. Graduate school expenses also are eligible. A student can have multiple 529 accounts set up in their name.
Additional tax considerations
Education Tax Credits like the American Opportunity Tax Credit and the Lifetime Learning Credit have income phase-outs that you may or may not be eligible for based on your income. Education expenses used to qualify for the tax-free withdrawal from a 529 plan cannot be used to claim these tax credits. Several states offer state income tax deductions for contributions to a 529 plan but may have eligibility limited to the in-state plan only. It is wise to look to your own state’s plan first to see if that is the case and consider that as a factor when you choose a plan right for you. Refer to your tax professional for your eligibility.
In conclusion, 529 savings plans represent a tax-free way to grow your investments for future education expenses down the road, even if you don’t have a child yet. Speak to your financial adviser to learn about plans and contribution schedules that work with your current and future investing goals.
Good sources for further information include:
- www.savingforcollege.com.
- www.irs.gov/forms-pubs/about-publication-970.
- www.finra.org/investors/saving-college.
Mr. Clancy is director of financial planning, Drexel University College of Medicine.
Financial planning for families can involve multiple investment goals. The big ones usually are investing for retirement and for your children’s college expenses. With any investment strategy, once you have identified an investment goal, you will want to utilize the right investment account to achieve that goal. If investing for future college expenses is your goal, then one of the investment accounts you will want to utilize is called a 529 plan.
What is a 529 plan?
A 529 plan is a tax-favored account authorized by Section 529 of the Internal Revenue Code and sponsored by a state or educational institution. These plans have specific tax-saving features to them, compared with other taxable accounts, which are listed below. To begin with, there are two types of 529 plans: prepaid tuition plans and education savings plans. Every state has at least one type of 529 plan. Additionally, some private colleges sponsor a prepaid tuition plan.
Prepaid tuition plan
The first type of 529 account is a prepaid tuition plan. These let an account owner purchase college credits (or units) for participating colleges or universities at today’s prices to be used for the student’s future tuition charges. The states that sponsor prepaid plans do so primarily for the benefit of their in-state public colleges and universities. Things to know about the prepaid plans: States may or may not guarantee that the prepaid units keep up with increases in tuition charges. The plan also may have a state residency requirement. If the student decides not to attend one of the eligible schools, the equivalent payout may be less than had the student attended one of the participating institutions. There are no federal guarantees on the state prepaid plans and they are not available for private elementary and high school programs.
Education savings plan
The second type of 529 account is an education savings plan, an investment account into which you can invest your after-tax dollars. The intent with these accounts is to grow the balance for use at a future date. These are tax-deferred accounts, which means each year the interest, dividends, and capital gains created within the account do not show up on your tax return. If the funds are used for a “qualified” higher-education expense, then gains on the account are not taxed upon withdrawal.
As with most investments, the longer your money is invested, the more time it has to grow via accumulated interest, dividends, and appreciation. The larger the growth, the larger the tax benefits. This offers a tremendous advantage for a high-income and high-tax bracket household to invest for future goals (such as private school tuition or college expenses). By contrast, if you had invested in a fully taxable account, you would be subject to taxes each year on the interest, dividends, and capital gain distributions. Also, with taxable accounts, your investments would be subject to capital gains tax on the growth when they are sold to pay for those future expenses.
An account owner may choose among a range of investment options that the 529 plan provides. These are typically individual mutual funds or preformed mutual fund portfolios. The portfolios may have a fixed allocation percentage that stays the same over time or come “age-weighted,” meaning the investment allocation becomes more conservative the closer the student gets to college age when withdrawals would occur. This is a similar approach to the “target retirement date” offerings one sees in retirement accounts.
If one is using the 529 account for the student’s elementary or high school years, the investment time frame may be shorter and necessitate a more conservative approach, as the time for withdrawals would be nearer than the college years. As with most investments, the account can lose value based on investment performance.
Owner versus beneficiary
There are two parties to any 529 plan account: The account owner, who has control over the account and can name the beneficiary to the account, and the beneficiary (the student). The account owner can change beneficiaries on the account and can even name themselves as the beneficiary. One can name anyone as the beneficiary (e.g., child, friend, relative, yourself). You can be proactive by creating an account and naming yourself the beneficiary now, before switching to your child in the future. The account owner can live in one state with the beneficiary in another and invest in the 529 from a third state, and the student may eventually go to an educational institution in a fourth state. The 529 education savings account is not limited to any specific college, as a prepaid plan may be.
Withdrawals from 529s
If a 529 account withdrawal is for qualified higher education expenses or tuition for elementary or secondary schools, earnings are not subject to federal income tax or, in many cases, state income tax. Qualified withdrawals need to take place in the same tax year as the qualified expense.
Withdrawals not used for qualified higher education expenses in that year are considered “nonqualified” and would be subject to tax and 10% penalty on the earnings. State and local taxes may apply as well.
You can use the proceeds from the account free of taxes for the following qualified higher-education expenses:
- Tuition and school fees for both full and part time students at an eligible college, university, trade, or vocational institution.
- Room and board if the student is enrolled at more than half-time status. The amount up to the school’s room and board charges are eligible if paid directly to the school or to a landlord if living in nonschool housing. If actual charges to the landlord exceed the schools’ charges, then the amount above the school’s charges would be considered an excess withdrawal.
- Required books, supplies, and equipment for the academic program. Computer and technology equipment, printers, and required software, and such related services as Internet access also are qualified expenses.
- Private elementary or secondary school tuition up to $10,000 annually also is a qualified expense for 529 withdrawals.
Health insurance for the student and transportation-related costs to and from the school are not qualified expenses.
Contributions and fees
Like all investments, the fees associated with a 529 account need to be considered, as excess fees lower the investment returns. Prepaid tuition plans may charge initial application, transaction, and ongoing administrative fees. Investment 529 accounts may also have administrative costs such as program management fees, per-transaction fees, and the underlying investment expense ratios. Some states have broker-sold plans as well as direct-sold plans. Broker-sold plans can be purchased only through a broker and have the additional expenses associated with that either in the form of a load (sales charge) or higher expense ratio.
Contributions to a 529 plan can only be made in cash. If you currently have other investments, they need to be liquidated first (with the associated tax consequence) and then the proceeds invested into the 529 plan. Establishing the account and ongoing contributions are subject to gift tax limits ($15,000 for 2019). A married couple may make a “joint gift” to the account to double the limit. The 529 plans also allow the owner to front-load the account in 1 year with up to 5 years’ worth of gift limit contributions all at once. This lump sum is treated for tax reasons as a pro-rata 5 consecutive years of contributions all at once. Any additional gifts to that beneficiary during that year and the remaining four would be subject to gift tax issues if it means the annual gift limits were exceeded. Contributions are considered a “completed gift” for gift- and estate-tax purposes even though the account owner retains an element of control. The up-front 5-year gift election is available only on 529 accounts and is a great way for parents and grandparents (hint-hint) to reduce their estates and get a significant initial balance into the account. This can come in handy for those who may have procrastinated working toward this investment goal and need to catch up.
If the beneficiary does not need all or some of the funds for qualified higher education expenses, the account owner has options: One can change beneficiary to another relative who may need the funds or keep the account going and eventually add a grandchild as a beneficiary. Graduate school expenses also are eligible. A student can have multiple 529 accounts set up in their name.
Additional tax considerations
Education Tax Credits like the American Opportunity Tax Credit and the Lifetime Learning Credit have income phase-outs that you may or may not be eligible for based on your income. Education expenses used to qualify for the tax-free withdrawal from a 529 plan cannot be used to claim these tax credits. Several states offer state income tax deductions for contributions to a 529 plan but may have eligibility limited to the in-state plan only. It is wise to look to your own state’s plan first to see if that is the case and consider that as a factor when you choose a plan right for you. Refer to your tax professional for your eligibility.
In conclusion, 529 savings plans represent a tax-free way to grow your investments for future education expenses down the road, even if you don’t have a child yet. Speak to your financial adviser to learn about plans and contribution schedules that work with your current and future investing goals.
Good sources for further information include:
- www.savingforcollege.com.
- www.irs.gov/forms-pubs/about-publication-970.
- www.finra.org/investors/saving-college.
Mr. Clancy is director of financial planning, Drexel University College of Medicine.
Financial planning for families can involve multiple investment goals. The big ones usually are investing for retirement and for your children’s college expenses. With any investment strategy, once you have identified an investment goal, you will want to utilize the right investment account to achieve that goal. If investing for future college expenses is your goal, then one of the investment accounts you will want to utilize is called a 529 plan.
What is a 529 plan?
A 529 plan is a tax-favored account authorized by Section 529 of the Internal Revenue Code and sponsored by a state or educational institution. These plans have specific tax-saving features to them, compared with other taxable accounts, which are listed below. To begin with, there are two types of 529 plans: prepaid tuition plans and education savings plans. Every state has at least one type of 529 plan. Additionally, some private colleges sponsor a prepaid tuition plan.
Prepaid tuition plan
The first type of 529 account is a prepaid tuition plan. These let an account owner purchase college credits (or units) for participating colleges or universities at today’s prices to be used for the student’s future tuition charges. The states that sponsor prepaid plans do so primarily for the benefit of their in-state public colleges and universities. Things to know about the prepaid plans: States may or may not guarantee that the prepaid units keep up with increases in tuition charges. The plan also may have a state residency requirement. If the student decides not to attend one of the eligible schools, the equivalent payout may be less than had the student attended one of the participating institutions. There are no federal guarantees on the state prepaid plans and they are not available for private elementary and high school programs.
Education savings plan
The second type of 529 account is an education savings plan, an investment account into which you can invest your after-tax dollars. The intent with these accounts is to grow the balance for use at a future date. These are tax-deferred accounts, which means each year the interest, dividends, and capital gains created within the account do not show up on your tax return. If the funds are used for a “qualified” higher-education expense, then gains on the account are not taxed upon withdrawal.
As with most investments, the longer your money is invested, the more time it has to grow via accumulated interest, dividends, and appreciation. The larger the growth, the larger the tax benefits. This offers a tremendous advantage for a high-income and high-tax bracket household to invest for future goals (such as private school tuition or college expenses). By contrast, if you had invested in a fully taxable account, you would be subject to taxes each year on the interest, dividends, and capital gain distributions. Also, with taxable accounts, your investments would be subject to capital gains tax on the growth when they are sold to pay for those future expenses.
An account owner may choose among a range of investment options that the 529 plan provides. These are typically individual mutual funds or preformed mutual fund portfolios. The portfolios may have a fixed allocation percentage that stays the same over time or come “age-weighted,” meaning the investment allocation becomes more conservative the closer the student gets to college age when withdrawals would occur. This is a similar approach to the “target retirement date” offerings one sees in retirement accounts.
If one is using the 529 account for the student’s elementary or high school years, the investment time frame may be shorter and necessitate a more conservative approach, as the time for withdrawals would be nearer than the college years. As with most investments, the account can lose value based on investment performance.
Owner versus beneficiary
There are two parties to any 529 plan account: The account owner, who has control over the account and can name the beneficiary to the account, and the beneficiary (the student). The account owner can change beneficiaries on the account and can even name themselves as the beneficiary. One can name anyone as the beneficiary (e.g., child, friend, relative, yourself). You can be proactive by creating an account and naming yourself the beneficiary now, before switching to your child in the future. The account owner can live in one state with the beneficiary in another and invest in the 529 from a third state, and the student may eventually go to an educational institution in a fourth state. The 529 education savings account is not limited to any specific college, as a prepaid plan may be.
Withdrawals from 529s
If a 529 account withdrawal is for qualified higher education expenses or tuition for elementary or secondary schools, earnings are not subject to federal income tax or, in many cases, state income tax. Qualified withdrawals need to take place in the same tax year as the qualified expense.
Withdrawals not used for qualified higher education expenses in that year are considered “nonqualified” and would be subject to tax and 10% penalty on the earnings. State and local taxes may apply as well.
You can use the proceeds from the account free of taxes for the following qualified higher-education expenses:
- Tuition and school fees for both full and part time students at an eligible college, university, trade, or vocational institution.
- Room and board if the student is enrolled at more than half-time status. The amount up to the school’s room and board charges are eligible if paid directly to the school or to a landlord if living in nonschool housing. If actual charges to the landlord exceed the schools’ charges, then the amount above the school’s charges would be considered an excess withdrawal.
- Required books, supplies, and equipment for the academic program. Computer and technology equipment, printers, and required software, and such related services as Internet access also are qualified expenses.
- Private elementary or secondary school tuition up to $10,000 annually also is a qualified expense for 529 withdrawals.
Health insurance for the student and transportation-related costs to and from the school are not qualified expenses.
Contributions and fees
Like all investments, the fees associated with a 529 account need to be considered, as excess fees lower the investment returns. Prepaid tuition plans may charge initial application, transaction, and ongoing administrative fees. Investment 529 accounts may also have administrative costs such as program management fees, per-transaction fees, and the underlying investment expense ratios. Some states have broker-sold plans as well as direct-sold plans. Broker-sold plans can be purchased only through a broker and have the additional expenses associated with that either in the form of a load (sales charge) or higher expense ratio.
Contributions to a 529 plan can only be made in cash. If you currently have other investments, they need to be liquidated first (with the associated tax consequence) and then the proceeds invested into the 529 plan. Establishing the account and ongoing contributions are subject to gift tax limits ($15,000 for 2019). A married couple may make a “joint gift” to the account to double the limit. The 529 plans also allow the owner to front-load the account in 1 year with up to 5 years’ worth of gift limit contributions all at once. This lump sum is treated for tax reasons as a pro-rata 5 consecutive years of contributions all at once. Any additional gifts to that beneficiary during that year and the remaining four would be subject to gift tax issues if it means the annual gift limits were exceeded. Contributions are considered a “completed gift” for gift- and estate-tax purposes even though the account owner retains an element of control. The up-front 5-year gift election is available only on 529 accounts and is a great way for parents and grandparents (hint-hint) to reduce their estates and get a significant initial balance into the account. This can come in handy for those who may have procrastinated working toward this investment goal and need to catch up.
If the beneficiary does not need all or some of the funds for qualified higher education expenses, the account owner has options: One can change beneficiary to another relative who may need the funds or keep the account going and eventually add a grandchild as a beneficiary. Graduate school expenses also are eligible. A student can have multiple 529 accounts set up in their name.
Additional tax considerations
Education Tax Credits like the American Opportunity Tax Credit and the Lifetime Learning Credit have income phase-outs that you may or may not be eligible for based on your income. Education expenses used to qualify for the tax-free withdrawal from a 529 plan cannot be used to claim these tax credits. Several states offer state income tax deductions for contributions to a 529 plan but may have eligibility limited to the in-state plan only. It is wise to look to your own state’s plan first to see if that is the case and consider that as a factor when you choose a plan right for you. Refer to your tax professional for your eligibility.
In conclusion, 529 savings plans represent a tax-free way to grow your investments for future education expenses down the road, even if you don’t have a child yet. Speak to your financial adviser to learn about plans and contribution schedules that work with your current and future investing goals.
Good sources for further information include:
- www.savingforcollege.com.
- www.irs.gov/forms-pubs/about-publication-970.
- www.finra.org/investors/saving-college.
Mr. Clancy is director of financial planning, Drexel University College of Medicine.
New feature debuts, how to address reviewer criticism, and more!
Dear Colleagues,
The November issue of The New Gastroenterologist is packed with some great articles! First, this issue’s In Focus article addresses the increasingly important topic of endoscopic management of obesity. In the article, the authors, Pichamol Jirapinyo and Christopher Thompson (Brigham and Women’s Hospital), provide an outstanding overview of the approved and up-and-coming endoscopic therapies that can be used to help treat the obesity epidemic. This is an area that we will inevitably see more of in our practices.
A new feature in this issue of The New Gastroenterologist is a column focused on early career gastroenterologists who are going into private practice, which was curated in conjunction with the Digestive Health Physicians Association. This month’s article by Fred Rosenberg (North Shore Endoscopy Center) provides an overview of private practice gastroenterology models. I look forward to making this column a recurring feature of future issues.
Additionally, using their wealth of experience, former CGH editor in chief Hashem El-Serag and current CGH editor in chief Fasiha Kanwal (Baylor) provide an enlightening piece on how to address reviewer criticism, which will no doubt be very helpful for those of us looking to publish. There is also a helpful article about grant writing tips authored by two successfully funded early career basic scientists, Arthur Beyder (Mayo) and Christina Twyman-Saint Victor (University of Pennsylvania).
For those considering pursuing extra training in IBD either during or after GI fellowship, Siddharth Singh (UCSD) goes through the different advanced training options that are now available in IBD. And finally, as many are laying down roots in new places, buying a house will almost inevitably be on the horizon. To help guide you through the mortgage preapproval process, Rob Wishnick (Guaranteed Rate) provides some useful insights from his many years of experience in the home loan industry.
Please check out “In Case You Missed It” to see other articles from the last quarter in AGA publications that may be of interest to you. And, if you have any ideas or want to contribute to The New Gastroenterologist, please contact me at [email protected] or the managing editor, Ryan Farrell, at [email protected].
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an assistant professor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
Dear Colleagues,
The November issue of The New Gastroenterologist is packed with some great articles! First, this issue’s In Focus article addresses the increasingly important topic of endoscopic management of obesity. In the article, the authors, Pichamol Jirapinyo and Christopher Thompson (Brigham and Women’s Hospital), provide an outstanding overview of the approved and up-and-coming endoscopic therapies that can be used to help treat the obesity epidemic. This is an area that we will inevitably see more of in our practices.
A new feature in this issue of The New Gastroenterologist is a column focused on early career gastroenterologists who are going into private practice, which was curated in conjunction with the Digestive Health Physicians Association. This month’s article by Fred Rosenberg (North Shore Endoscopy Center) provides an overview of private practice gastroenterology models. I look forward to making this column a recurring feature of future issues.
Additionally, using their wealth of experience, former CGH editor in chief Hashem El-Serag and current CGH editor in chief Fasiha Kanwal (Baylor) provide an enlightening piece on how to address reviewer criticism, which will no doubt be very helpful for those of us looking to publish. There is also a helpful article about grant writing tips authored by two successfully funded early career basic scientists, Arthur Beyder (Mayo) and Christina Twyman-Saint Victor (University of Pennsylvania).
For those considering pursuing extra training in IBD either during or after GI fellowship, Siddharth Singh (UCSD) goes through the different advanced training options that are now available in IBD. And finally, as many are laying down roots in new places, buying a house will almost inevitably be on the horizon. To help guide you through the mortgage preapproval process, Rob Wishnick (Guaranteed Rate) provides some useful insights from his many years of experience in the home loan industry.
Please check out “In Case You Missed It” to see other articles from the last quarter in AGA publications that may be of interest to you. And, if you have any ideas or want to contribute to The New Gastroenterologist, please contact me at [email protected] or the managing editor, Ryan Farrell, at [email protected].
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an assistant professor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
Dear Colleagues,
The November issue of The New Gastroenterologist is packed with some great articles! First, this issue’s In Focus article addresses the increasingly important topic of endoscopic management of obesity. In the article, the authors, Pichamol Jirapinyo and Christopher Thompson (Brigham and Women’s Hospital), provide an outstanding overview of the approved and up-and-coming endoscopic therapies that can be used to help treat the obesity epidemic. This is an area that we will inevitably see more of in our practices.
A new feature in this issue of The New Gastroenterologist is a column focused on early career gastroenterologists who are going into private practice, which was curated in conjunction with the Digestive Health Physicians Association. This month’s article by Fred Rosenberg (North Shore Endoscopy Center) provides an overview of private practice gastroenterology models. I look forward to making this column a recurring feature of future issues.
Additionally, using their wealth of experience, former CGH editor in chief Hashem El-Serag and current CGH editor in chief Fasiha Kanwal (Baylor) provide an enlightening piece on how to address reviewer criticism, which will no doubt be very helpful for those of us looking to publish. There is also a helpful article about grant writing tips authored by two successfully funded early career basic scientists, Arthur Beyder (Mayo) and Christina Twyman-Saint Victor (University of Pennsylvania).
For those considering pursuing extra training in IBD either during or after GI fellowship, Siddharth Singh (UCSD) goes through the different advanced training options that are now available in IBD. And finally, as many are laying down roots in new places, buying a house will almost inevitably be on the horizon. To help guide you through the mortgage preapproval process, Rob Wishnick (Guaranteed Rate) provides some useful insights from his many years of experience in the home loan industry.
Please check out “In Case You Missed It” to see other articles from the last quarter in AGA publications that may be of interest to you. And, if you have any ideas or want to contribute to The New Gastroenterologist, please contact me at [email protected] or the managing editor, Ryan Farrell, at [email protected].
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an assistant professor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
Endoscopic management of obesity
Editor's Note
Gastroenterologists are becoming increasingly involved in the management of obesity. While prior therapy for obesity was mainly based on lifestyle changes, medication, or surgery, the new and exciting field of endoscopic bariatric and metabolic therapies has recently garnered incredible attention and momentum.
In this quarter’s In Focus article, brought to you by The New Gastroenterologist, Pichamol Jirapinyo and Christopher Thompson (Brigham and Women’s Hospital) provide an outstanding overview of the gastric and small bowel endoscopic interventions that are either already approved for use in obesity or currently being studied. This field is moving incredibly fast, and knowledge and understanding of these endoscopic therapies for obesity will undoubtedly be important for our field.
Bryson W. Katona, MD, PhD
Editor in Chief, The New Gastroenterologist
Introduction
Obesity is a rising pandemic. As of 2016, 93.3 million U.S. adults had obesity, representing 39.8% of our adult population.1 It is estimated that approximately $147 billion is spent annually on caring for patients with obesity. Traditionally, the management of obesity includes lifestyle therapy (diet and exercise), pharmacotherapy (six Food and Drug Administration–approved medications for obesity), and bariatric surgery (sleeve gastrectomy [SG] and Roux-en-Y gastric bypass [RYGB]). Nevertheless, intensive lifestyle intervention and pharmacotherapy are associated with approximately 3.1%-6.6% total weight loss (TWL),2-7 and bariatric surgery is associated with 20%-33.3% TWL.8 However, less than 2% of patients who are eligible for bariatric surgery elect to undergo surgery, leaving a large proportion of patients with obesity untreated or undertreated.9
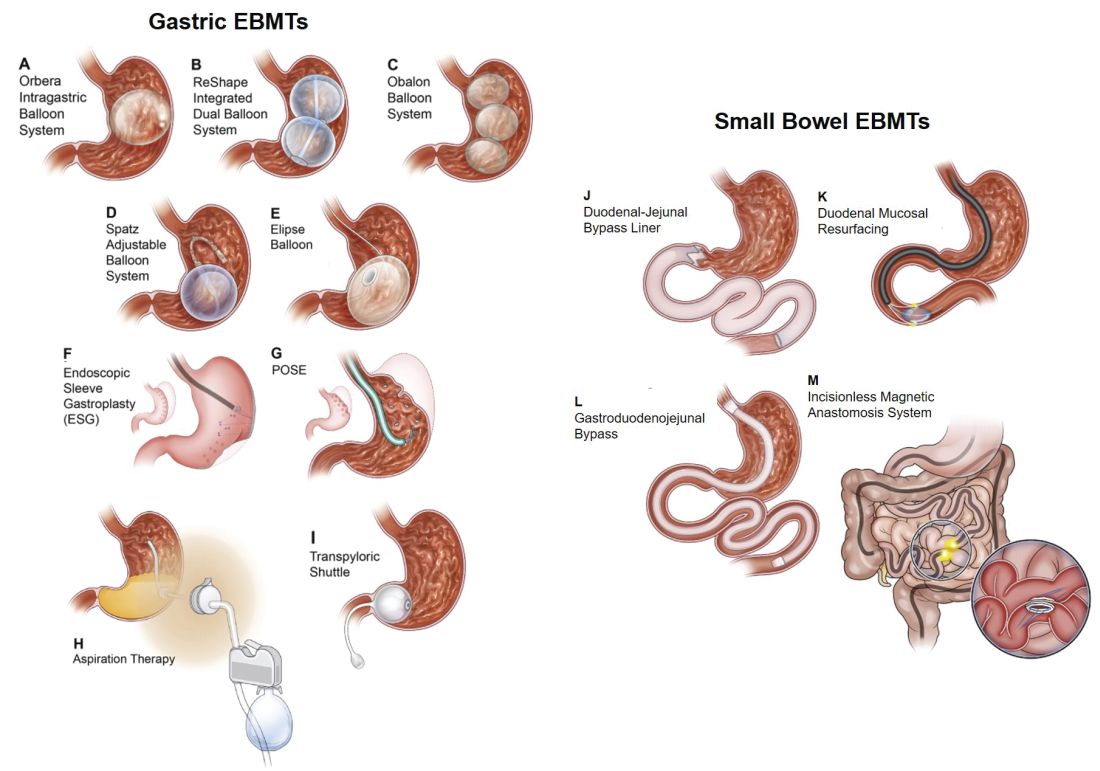
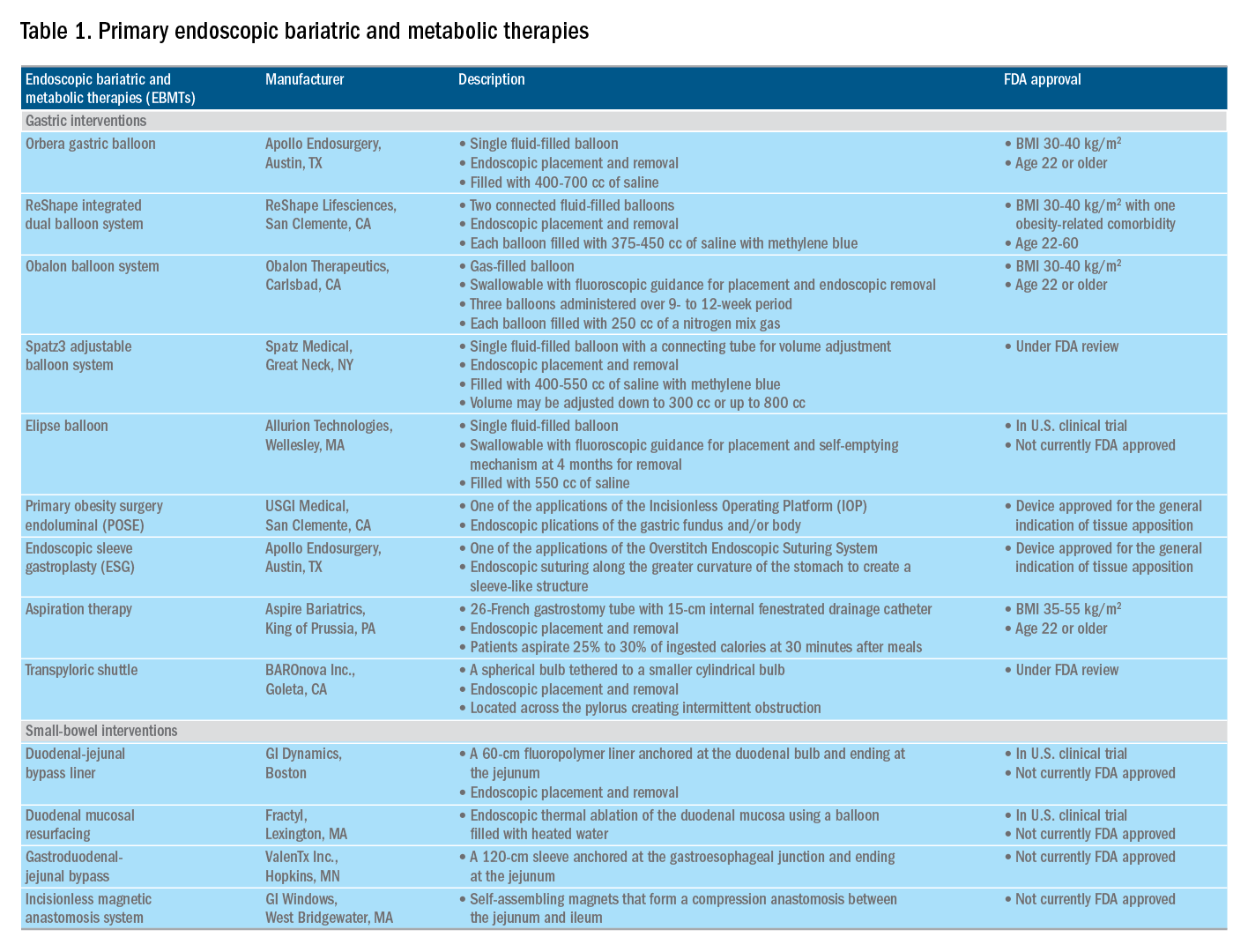
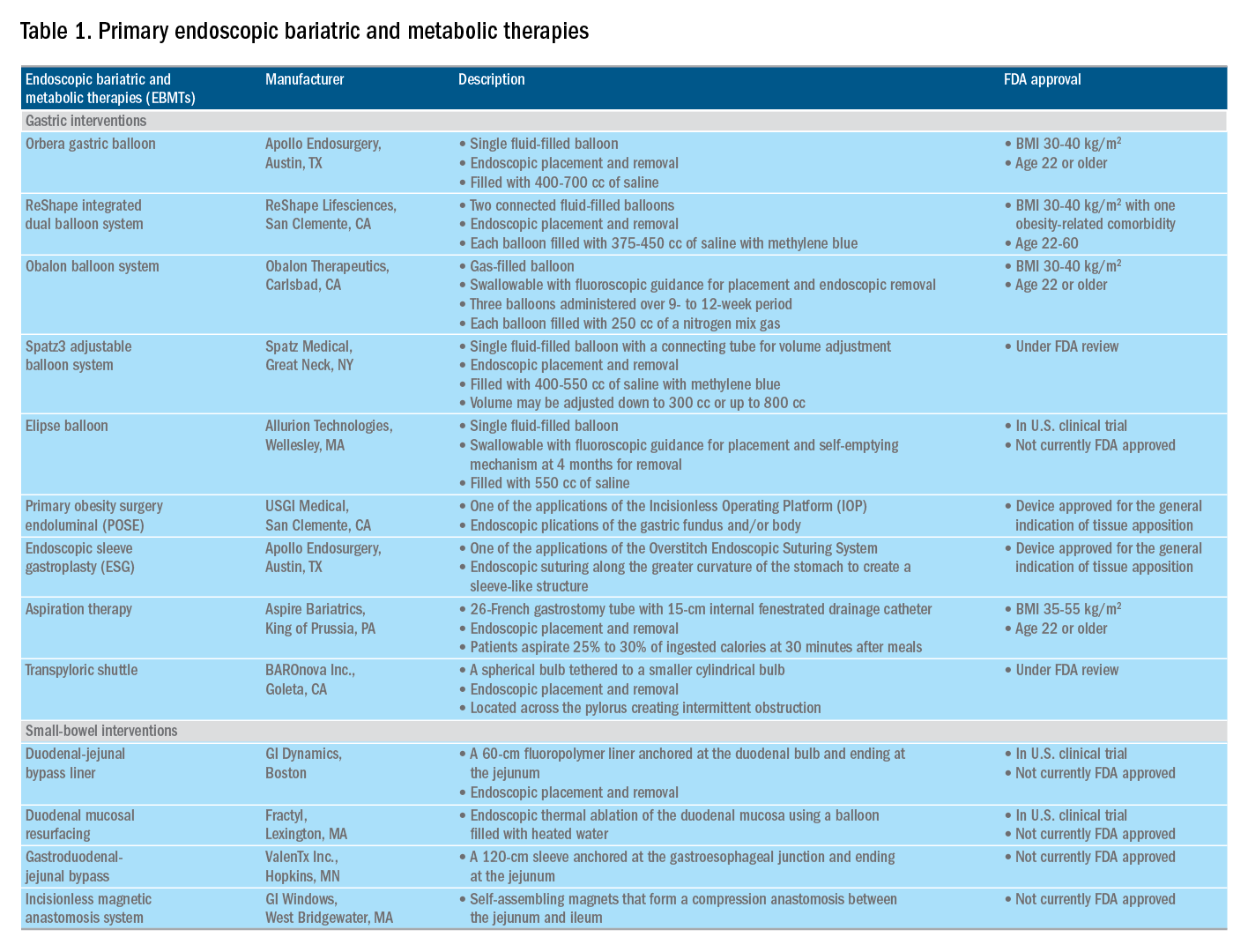
Endoscopic bariatric and metabolic therapies (EBMTs) encompass an emerging field for the treatment of obesity. In general, EBMTs are associated with greater weight loss than are lifestyle intervention and pharmacotherapy, but with a less- invasive risk profile than bariatric surgery. EBMTs may be divided into two general categories – gastric and small bowel interventions (Figure 1 and Table 1). Gastric EBMTs are effective at treating obesity, while small bowel EBMTs are effective at treating metabolic diseases with a variable weight loss profile depending on the device.10,11
Of note, a variety of study designs (including retrospective series, prospective series, and randomized trials with and without shams) have been employed, which can affect outcomes. Therefore, weight loss comparisons among studies are challenging and should be considered in this context.
Gastric interventions
Currently, there are three types of EBMTs that are FDA approved and used for the treatment of obesity. These include intragastric balloons (IGBs), plications and suturing, and aspiration therapy (AT). Other technologies that are under investigation also will be briefly covered.
Intragastric balloons
An intragastric balloon is a space-occupying device that is placed in the stomach. The mechanism of action of IGBs involves delaying gastric emptying, which leads to increased satiety.12 There are several types of IGBs available worldwide differing in techniques of placement and removal (endoscopic versus fluoroscopic versus swallowable), materials used to fill the balloon (fluid-filled versus air-filled), and the number of balloons placed (single versus duo versus three-balloon). At the time of this writing, three IGBs are approved by the FDA (Orbera, ReShape, and Obalon), all for patients with body mass indexes of 30-40 kg/m2, and two others are in the process of obtaining FDA approval (Spatz and Elipse).
Orbera gastric balloon (Apollo Endosurgery, Austin, Tex.) is a single fluid-filled IGB that is endoscopically placed and removed at 6 months. The balloon is filled with 400-700 cc of saline with or without methylene blue (to identify leakage or rupture). Recently, Orbera365, which allows the balloon to stay for 12 months instead of 6 months, has become available in Europe; however, it is yet to be approved in the United States. The U.S. pivotal trial (Orbera trial) including 255 subjects (125 Orbera arm versus 130 non-sham control arm) demonstrated 10.2% TWL in the Orbera group compared with 3.3% TWL in the control group at 6 months based on intention-to-treat (ITT) analysis. This difference persisted at 12 months (6 months after explantation) with 7.6% TWL for the Orbera group versus 3.1% TWL for the control group.13,14
ReShape integrated dual balloon system (ReShape Lifesciences, San Clemente, Calif.) consists of two connected fluid-filled balloons that are endoscopically placed and removed at 6 months. Each balloon is filled with 375-450 cc of saline mixed with methylene blue. The U.S. pivotal trial (REDUCE trial) including 326 subjects (187 ReShape arm versus 139 sham arm) demonstrated 6.8% TWL in the ReShape group compared with 3.3% TWL in the sham group at 6 months based on ITT analysis.15,16
Obalon balloon system (Obalon Therapeutics, Carlsbad, Calif.) is a swallowable, gas-filled balloon system that requires endoscopy only for removal. During placement, a capsule is swallowed under fluoroscopic guidance. The balloon is then inflated with 250 cc of nitrogen mix gas prior to tube detachment. Up to three balloons may be swallowed sequentially at 1-month intervals. At 6 months from the first balloon placement, all balloons are removed endoscopically. The U.S. pivotal trial (SMART trial) including 366 subjects (185 Obalon arm versus 181 sham capsule arm) demonstrated 6.6% TWL in the Obalon group compared with 3.4% TWL in the sham group at 6 months based on ITT analysis.17,18
Two other balloons that are currently under investigation in the United States are the Spatz3 adjustable balloon system (Spatz Medical, Great Neck, N.Y.) and Elipse balloon (Allurion Technologies, Wellesley, Mass.). The Spatz3 is a fluid-filled balloon that is placed and removed endoscopically. It consists of a single balloon and a connecting tube that allows volume adjustment for control of symptoms and possible augmentation of weight loss. The U.S. pivotal trial was recently completed and the data are being reviewed by the FDA. The Elipse is a swallowable fluid-filled balloon that does not require endoscopy for placement or removal. At 4 months, the balloon releases fluid allowing it to empty and pass naturally. The U.S. pivotal trial (ENLIGHTEN trial) is currently underway.
A meta-analysis of randomized controlled trials revealed improvement in most metabolic parameters (diastolic blood pressure, fasting glucose, hemoglobin A1c, and waist circumference) following IGB compared with controls.19 Nausea and vomiting are seen in approximately 30% and should be addressed appropriately. Pooled serious adverse event (SAE) rate was 1.5%, which included migration, perforation, and death. Since 2016, 14 deaths have been reported according to the FDA MAUDE database. Corporate response was that over 295,000 balloons had been distributed worldwide with a mortality rate of less than 0.01%.20
Plication and suturing
Currently, there are two endoscopic devices that are approved for the general indication of tissue apposition. These include the Incisionless Operating Platform (IOP) (USGI Medical, San Clemente, Calif.) and the Overstitch endoscopic suturing system (Apollo Endosurgery, Austin, Tex.). These devices are used to remodel the stomach to create a sleeve-like structure to induce weight loss.
The IOP system consists of a transport, which is a 54-Fr flexible endoscope. It consists of four working channels that accommodate a G-Prox (for tissue approximation), a G-Lix (for tissue grasping), and an ultrathin endoscope (for visualization). In April 2008, Horgan performed the first-in-human primary obesity surgery endoluminal (POSE) procedure in Argentina. The procedure involves the use of the IOP system to place plications primarily in the fundus to modify gastric accommodation.21 The U.S. pivotal trial (ESSENTIAL trial) including 332 subjects (221 POSE arm versus 111 sham arm) demonstrated 5.0% TWL in the POSE group compared with 1.4% in the sham group at 12 months based on ITT analysis.22 A European multicenter randomized controlled trial (MILEPOST trial) including 44 subjects (34 POSE arm versus 10 non-sham control arm) demonstrated 13.0% TWL in the POSE group compared with 5.3% TWL in the control group at 12 months.23 A recent meta-analysis including five studies with 586 subjects showed pooled weight loss of 13.2% at 12-15 months following POSE with a pooled serious adverse event rate of 3.2%.24 These included extraluminal bleeding, minor bleeding at the suture site, hepatic abscess, chest pain, nausea, vomiting, and abdominal pain. A distal POSE procedure with a new plication pattern focusing on the gastric body to augment the effect on gastric emptying has also been described.25
The Overstitch is an endoscopic suturing device that is mounted on a double-channel endoscope. At the tip of the scope, there is a curved suture arm and an anchor exchange that allow the needle to pass back and forth to perform full-thickness bites. The tissue helix may also be placed through the second channel to grasp tissue. In April 2012, Thompson performed the first-in-human endoscopic sutured/sleeve gastroplasty (ESG) procedure in India, which was published together with cases performed in Panama and the Dominican Republic.26-28 This procedure involves the use of the Overstitch device to place several sets of running sutures along the greater curvature of the stomach to create a sleeve-like structure. It is thought to delay gastric emptying and therefore increase satiety.29 The largest multicenter retrospective study including 248 patients demonstrated 18.6% TWL at 2 years with 2% SAE rate including perigastric fluid collections, extraluminal hemorrhage, pulmonary embolism, pneumoperitoneum, and pneumothorax.30
Aspiration therapy
Aspiration therapy (AT; Aspire Bariatrics, King of Prussia, Pa.) allows patients to remove 25%-30% of ingested calories at approximately 30 minutes after meals. AT consists of an A-tube, which is a 26-Fr gastrostomy tube with a 15-cm fenestrated drainage catheter placed endoscopically via a standard pull technique. At 1-2 weeks after A-tube placement, the tube is cut down to the skin and connected to the port prior to aspiration. AT is approved for patients with a BMI of 35-55 kg/m2.31 The U.S. pivotal trial (PATHWAY trial) including 207 subjects (137 AT arm versus 70 non-sham control arm) demonstrated 12.1% TWL in the AT group compared to 3.5% in the control group at 12 months based on ITT analysis. The SAE rate was 3.6% including severe abdominal pain, peritonitis, prepyloric ulcer, and A-tube replacement due to skin-port malfunction.32
Transpyloric shuttle
The transpyloric shuttle (TPS; BAROnova, Goleta, Calif.) consists of a spherical bulb that is attached to a smaller cylindrical bulb by a flexible tether. It is placed and removed endoscopically at 6 months. TPS resides across the pylorus creating intermittent obstruction that may result in delayed gastric emptying. A pilot study including 20 patients demonstrated 14.5% TWL at 6 months.33 The U.S. pivotal trial (ENDObesity II trial) was recently completed and the data are being reviewed by the FDA.
Revision for weight regain following bariatric surgery

Weight regain is common following RYGB34,35 and can be associated with dilation of the gastrojejunal anastomosis (GJA).36 Several procedures have been developed to treat this condition by focusing on reduction of GJA size and are available in the United States (Figure 2). These procedures have level I evidence supporting their use and include transoral outlet reduction (TORe) and restorative obesity surgery endoluminal (ROSE).37 TORe involves the use of the Overstitch to place sutures at the GJA. At 1 year, patients had 8.4% TWL with improvement in comorbidities.38 Weight loss remained significant up to 3-5 years.39,40 The modern ROSE procedure utilizes the IOP system to place plications at the GJA and distal gastric pouch following argon plasma coagulation (APC). A small series showed 12.4% TWL at 6 months.41 APC is also currently being investigated as a standalone therapy for weight regain in this population.
Small bowel interventions
There are several small bowel interventions, with different mechanisms of action, available internationally. Many of these are under investigation in the United States; however, none are currently FDA approved.
Duodenal-jejunal bypass liner
Duodenal-jejunal bypass liner (DJBL; GI Dynamics, Boston, Mass.) is a 60-cm fluoropolymer liner that is endoscopically placed and removed at 12 months. It is anchored at the duodenal bulb and ends at the jejunum. By excluding direct contact between chyme and the proximal small bowel, DJBL is thought to work via foregut mechanism where there is less inhibition of the incretin effect (greater increase in insulin secretion following oral glucose administration compared to intravenous glucose administration due to gut-derived factors that enhance insulin secretion) leading to improved insulin resistance. In addition, the enteral transit of chyme and bile is altered suggesting the possible role of the hindgut mechanism. The previous U.S. pivotal trial (ENDO trial) met efficacy endpoints. However, the study was stopped early by the company because of a hepatic abscess rate of 3.5%, all of which were treated conservatively.42 A new U.S. pivotal study is currently planned. A meta-analysis of 17 published studies, all of which were from outside the United States, demonstrated a significant decrease in hemoglobin A1c of 1.3% and 18.9% TWL at 1 year following implantation in patients with obesity with concomitant diabetes.43
Duodenal mucosal resurfacing
Duodenal mucosal resurfacing (Fractyl, Lexington, Mass.) involves saline lifting of the duodenal mucosa circumferentially prior to thermal ablation using an inflated balloon filled with heated water. It is hypothesized that this may reset the diseased duodenal enteroendocrine cells leading to restoration of the incretin effect. A pilot study including 39 patients with poorly controlled diabetes demonstrated a decrease in hemoglobin A1c of 1.2%. The SAE rate was 7.7% including duodenal stenosis, all of which were treated with balloon dilation.44 The U.S. pivotal trial is currently planned.
Gastroduodenal-jejunal bypass
Gastroduodenal-jejunal bypass (ValenTx., Hopkins, Minn.) is a 120-cm sleeve that is anchored at the gastroesophageal junction to create the anatomic changes of RYGB. It is placed and removed endoscopically with laparoscopic assistance. A pilot study including 12 patients demonstrated 35.9% excess weight loss at 12 months. Two out of 12 patients had early device removal due to intolerance and they were not included in the weight loss analysis.45
Incisionless magnetic anastomosis system
The incisionless magnetic anastomosis system (GI Windows, West Bridgewater, Mass.) consists of self-assembling magnets that are deployed under fluoroscopic guidance through the working channel of colonoscopes to form magnetic octagons in the jejunum and ileum. After a week, a compression anastomosis is formed and the coupled magnets pass spontaneously. A pilot study including 10 patients showed 14.6% TWL and a decrease in hemoglobin A1c of 1.9% (for patients with diabetes) at 1 year.46 A randomized study outside the United States is currently underway.
Summary
Endoscopic bariatric and metabolic therapies are emerging as first-line treatments for obesity in many populations. They can serve as a gap therapy for patients who do not qualify for surgery, but also may have a specific role in the treatment of metabolic comorbidities. This field will continue to develop and improve with the introduction of personalized medicine leading to better patient selection, and newer combination therapies. It is time for gastroenterologists to become more involved in the management of this challenging condition.
Dr. Jirapinyo is an advanced and bariatric endoscopy fellow, Brigham and Women’s Hospital, Harvard Medical School, Boston; Dr. Thompson is director of therapeutic endoscopy, Brigham and Women’s Hospital, and associate professor of medicine, Harvard Medical School. Dr. Jirapinyo has served as a consultant for GI Dynamics and holds royalties for Endosim. Dr. Thompson has contracted research for Aspire Bariatrics, USGI Medical, Spatz, and Apollo Endosurgery; has served as a consultant for Boston Scientific, Covidien, USGI Medical, Olympus, and Fractyl; holds stocks and royalties for GI Windows and Endosim, and has served as an expert reviewer for GI Dynamics.
References
1. CDC. From https://www.cdc.gov/obesity/data/adult.html. Accessed on 11 September 2018.
2. Aronne LJ et al. Obesity. 2013;21:2163-71.
3. Torgerson JS et al. Diabetes Care. 2004;27:155-61.
4. Allison DB et al. Obesity. 2012;20:330-42.
5. Smith SR et al. N Engl J Med. 2010;363:245-56.
6. Apovian CM et al. Obesity. 2013;21:935-43.
7. Pi-Sunyer X et al. N Engl J Med. 2015;373:11-22.
8. Colguitt JL et al. Cochrane Database Syst Rev. 2014;8(8):CD003641.
9. Ponce J et al. Surg Obes Relat Dis. 2015;11(6):1199-200.
10. Jirapinyo P, Thompson CC et al. Clin Gastroenterol Hepatol. 2017;15(5):619-30.
11. Sullivan S et al.Gastroenterology. 2017;152(7):1791-801.
12. Gomez V et al. Obesity. 2016;24(9):1849-53.
13. Food and Drug Administration. Summary of safety and effectiveness data (SSED) ORBERA Intragastric Balloon System. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf14/P140008b.pdf. 2015:1-32.
14. Abu Dayyeh BK et al. Gastrointest Endosc. 2015;81:AB147.
15. Food and Drug Administration. Summary of safety and effectiveness data (SSED) ReShape Integrated Dual Balloon System. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf14/P140012b.pdf. 2015:1-43.
16. Ponce J et al. Surg Obes Relat Dis. 2015;11:874-81.
17. Food and Drug Administration. Summary and effectiveness data (SSED): Obalon Balloon System. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf16/P160001b.pdf. 2016:1-46.
18. Sullivan S et al. Gastroenterology. 2016;150:S1267.
19. Popov VB et al. Am J Gastroenterol. 2017;112:429-39.
20. Abu Dayyeh BK et al. Gastrointest Endosc. 2015;82(3):425-38.
21. Espinos JC et al. Obes Surg. 2013;23(9):1375-83.
22. Sullivan S et al. Obesity. 2017;25:294-301.
23. Miller K et al. Obesity Surg. 2017;27(2):310-22.
24. Jirapinyo P et al. Gastrointest Endosc. 2018;87(6):AB604-AB605.
25. Jirapinyo P, Thompson CC. Video GIE. 2018;3(10):296-300.
26. Campos J et al. SAGES 2013 Presentation. Baltimore, MD. 19 April 2013.
27. Kumar N et al. Gastroenterology. 2014;146(5):S571-2.
28. Kumar N et al. Surg Endosc. 2018;32(4):2159-64.
29. Abu Dayyeh BK et al. Clin Gastroenterol Hepatol. 2017;15:37-43.
30. Lopez-Nava G et al. Obes Surg. 2017;27(10):2649-55.
31. Food and Drug Administration. Summary of safety and effectiveness (SSED): AspireAssist. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf15/p150024b.pdf. FDA,ed,2016:1-36.
32. Thompson CC et al. Am J Gastroenterol. 2017;112:447-57.
33. SAGES abstract archives. SAGES. Available from: http://www.sages.org/meetings/annual-meeting/abstracts-archive/first-clinical-experience-with-the-transpyloric-shuttle-tpsr-device-a-non-surgical-endoscopic treatment-for-obesity-results-from-a-3-month-and-6-month-study. Accessed Sept. 12, 2018.
34. Sjostrom L et al. N Engl J Med. 2007;357:741-52.
35. Adams TD et al. N Engl J Med. 2017;377:1143-55.
36. Abu Dayyeh BK et al. Clin Gastroenterol Hepatol. 2011;9:228-33.
37. Thompson CC et al. Gastroenterology. 2013;145(1):129-37.
38. Jirapinyo P et al. Endoscopy. 2018;50(4):371-7.
39. Kumar N, Thompson CC. Gastrointest Endosc. 2016;83(4):776-9.
40. Jirapinyo P et al. Gastrointest Endosc. 2017;85(5):AB93-94.
41. Jirapinyo P, Thompson CC et al. Comparison of a novel plication technique to suturing for endoscopic outlet reduction for the treatment of weight regain after Roux-en-Y gastric bypass. Obesity Week 2018. Poster presentation.
42. Kaplan LM et al. EndoBarrier therapy is associated with glycemic improvement, weight loss and safety issues in patients with obesity and type 2 diabetes on oral anti-hyperglycemic agents (The ENDO Trial). In: Oral Presentation at the 76th American Diabetes Association (ADA) Annual Meeting: 2016 June 10-14: New Orleans. Abstract number 362-LB.
43. Jirapinyo P et al. Diabetes Care. 2018;41(5):1106-15.
44. Rajagopalan H et al. Diabetes Care. 2016;39(12):2254-61.
45. Sandler BJ et al. Surgical Endosc. 2015;29:3298-303.
46. Machytka E et al. Gastrointest Endosc. 2017;86(5):904-12.
Editor's Note
Gastroenterologists are becoming increasingly involved in the management of obesity. While prior therapy for obesity was mainly based on lifestyle changes, medication, or surgery, the new and exciting field of endoscopic bariatric and metabolic therapies has recently garnered incredible attention and momentum.
In this quarter’s In Focus article, brought to you by The New Gastroenterologist, Pichamol Jirapinyo and Christopher Thompson (Brigham and Women’s Hospital) provide an outstanding overview of the gastric and small bowel endoscopic interventions that are either already approved for use in obesity or currently being studied. This field is moving incredibly fast, and knowledge and understanding of these endoscopic therapies for obesity will undoubtedly be important for our field.
Bryson W. Katona, MD, PhD
Editor in Chief, The New Gastroenterologist
Introduction
Obesity is a rising pandemic. As of 2016, 93.3 million U.S. adults had obesity, representing 39.8% of our adult population.1 It is estimated that approximately $147 billion is spent annually on caring for patients with obesity. Traditionally, the management of obesity includes lifestyle therapy (diet and exercise), pharmacotherapy (six Food and Drug Administration–approved medications for obesity), and bariatric surgery (sleeve gastrectomy [SG] and Roux-en-Y gastric bypass [RYGB]). Nevertheless, intensive lifestyle intervention and pharmacotherapy are associated with approximately 3.1%-6.6% total weight loss (TWL),2-7 and bariatric surgery is associated with 20%-33.3% TWL.8 However, less than 2% of patients who are eligible for bariatric surgery elect to undergo surgery, leaving a large proportion of patients with obesity untreated or undertreated.9
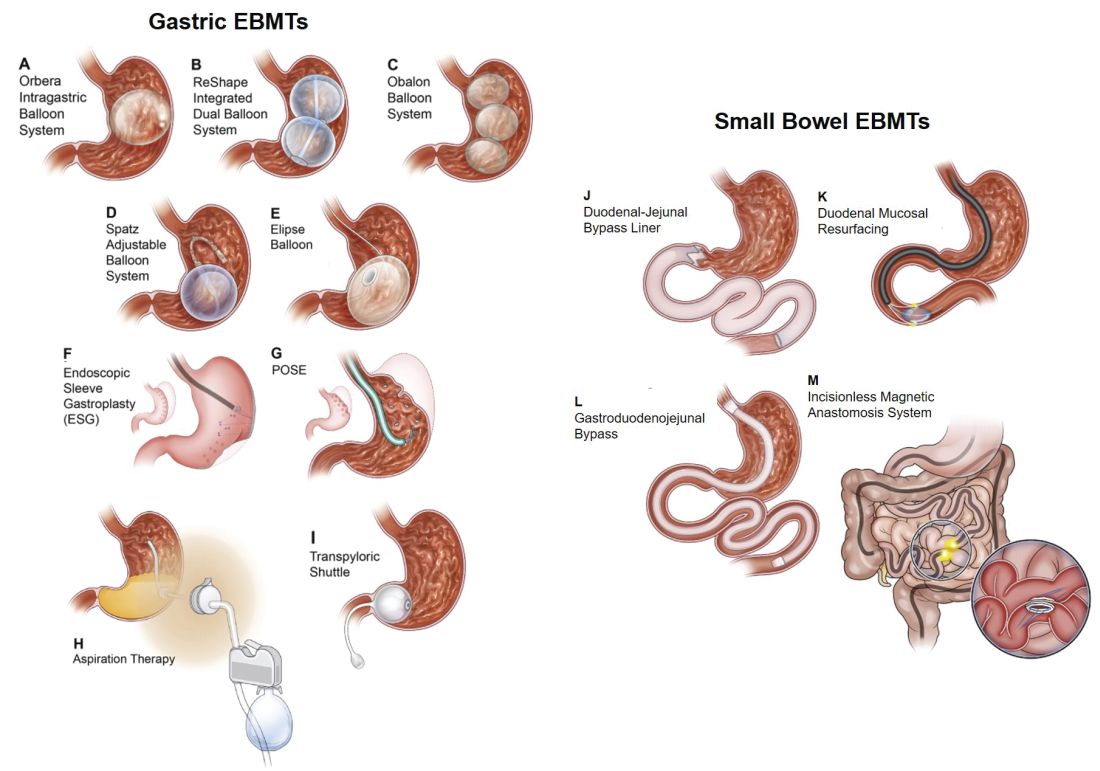
Endoscopic bariatric and metabolic therapies (EBMTs) encompass an emerging field for the treatment of obesity. In general, EBMTs are associated with greater weight loss than are lifestyle intervention and pharmacotherapy, but with a less- invasive risk profile than bariatric surgery. EBMTs may be divided into two general categories – gastric and small bowel interventions (Figure 1 and Table 1). Gastric EBMTs are effective at treating obesity, while small bowel EBMTs are effective at treating metabolic diseases with a variable weight loss profile depending on the device.10,11
Of note, a variety of study designs (including retrospective series, prospective series, and randomized trials with and without shams) have been employed, which can affect outcomes. Therefore, weight loss comparisons among studies are challenging and should be considered in this context.
Gastric interventions
Currently, there are three types of EBMTs that are FDA approved and used for the treatment of obesity. These include intragastric balloons (IGBs), plications and suturing, and aspiration therapy (AT). Other technologies that are under investigation also will be briefly covered.
Intragastric balloons
An intragastric balloon is a space-occupying device that is placed in the stomach. The mechanism of action of IGBs involves delaying gastric emptying, which leads to increased satiety.12 There are several types of IGBs available worldwide differing in techniques of placement and removal (endoscopic versus fluoroscopic versus swallowable), materials used to fill the balloon (fluid-filled versus air-filled), and the number of balloons placed (single versus duo versus three-balloon). At the time of this writing, three IGBs are approved by the FDA (Orbera, ReShape, and Obalon), all for patients with body mass indexes of 30-40 kg/m2, and two others are in the process of obtaining FDA approval (Spatz and Elipse).
Orbera gastric balloon (Apollo Endosurgery, Austin, Tex.) is a single fluid-filled IGB that is endoscopically placed and removed at 6 months. The balloon is filled with 400-700 cc of saline with or without methylene blue (to identify leakage or rupture). Recently, Orbera365, which allows the balloon to stay for 12 months instead of 6 months, has become available in Europe; however, it is yet to be approved in the United States. The U.S. pivotal trial (Orbera trial) including 255 subjects (125 Orbera arm versus 130 non-sham control arm) demonstrated 10.2% TWL in the Orbera group compared with 3.3% TWL in the control group at 6 months based on intention-to-treat (ITT) analysis. This difference persisted at 12 months (6 months after explantation) with 7.6% TWL for the Orbera group versus 3.1% TWL for the control group.13,14
ReShape integrated dual balloon system (ReShape Lifesciences, San Clemente, Calif.) consists of two connected fluid-filled balloons that are endoscopically placed and removed at 6 months. Each balloon is filled with 375-450 cc of saline mixed with methylene blue. The U.S. pivotal trial (REDUCE trial) including 326 subjects (187 ReShape arm versus 139 sham arm) demonstrated 6.8% TWL in the ReShape group compared with 3.3% TWL in the sham group at 6 months based on ITT analysis.15,16
Obalon balloon system (Obalon Therapeutics, Carlsbad, Calif.) is a swallowable, gas-filled balloon system that requires endoscopy only for removal. During placement, a capsule is swallowed under fluoroscopic guidance. The balloon is then inflated with 250 cc of nitrogen mix gas prior to tube detachment. Up to three balloons may be swallowed sequentially at 1-month intervals. At 6 months from the first balloon placement, all balloons are removed endoscopically. The U.S. pivotal trial (SMART trial) including 366 subjects (185 Obalon arm versus 181 sham capsule arm) demonstrated 6.6% TWL in the Obalon group compared with 3.4% TWL in the sham group at 6 months based on ITT analysis.17,18
Two other balloons that are currently under investigation in the United States are the Spatz3 adjustable balloon system (Spatz Medical, Great Neck, N.Y.) and Elipse balloon (Allurion Technologies, Wellesley, Mass.). The Spatz3 is a fluid-filled balloon that is placed and removed endoscopically. It consists of a single balloon and a connecting tube that allows volume adjustment for control of symptoms and possible augmentation of weight loss. The U.S. pivotal trial was recently completed and the data are being reviewed by the FDA. The Elipse is a swallowable fluid-filled balloon that does not require endoscopy for placement or removal. At 4 months, the balloon releases fluid allowing it to empty and pass naturally. The U.S. pivotal trial (ENLIGHTEN trial) is currently underway.
A meta-analysis of randomized controlled trials revealed improvement in most metabolic parameters (diastolic blood pressure, fasting glucose, hemoglobin A1c, and waist circumference) following IGB compared with controls.19 Nausea and vomiting are seen in approximately 30% and should be addressed appropriately. Pooled serious adverse event (SAE) rate was 1.5%, which included migration, perforation, and death. Since 2016, 14 deaths have been reported according to the FDA MAUDE database. Corporate response was that over 295,000 balloons had been distributed worldwide with a mortality rate of less than 0.01%.20
Plication and suturing
Currently, there are two endoscopic devices that are approved for the general indication of tissue apposition. These include the Incisionless Operating Platform (IOP) (USGI Medical, San Clemente, Calif.) and the Overstitch endoscopic suturing system (Apollo Endosurgery, Austin, Tex.). These devices are used to remodel the stomach to create a sleeve-like structure to induce weight loss.
The IOP system consists of a transport, which is a 54-Fr flexible endoscope. It consists of four working channels that accommodate a G-Prox (for tissue approximation), a G-Lix (for tissue grasping), and an ultrathin endoscope (for visualization). In April 2008, Horgan performed the first-in-human primary obesity surgery endoluminal (POSE) procedure in Argentina. The procedure involves the use of the IOP system to place plications primarily in the fundus to modify gastric accommodation.21 The U.S. pivotal trial (ESSENTIAL trial) including 332 subjects (221 POSE arm versus 111 sham arm) demonstrated 5.0% TWL in the POSE group compared with 1.4% in the sham group at 12 months based on ITT analysis.22 A European multicenter randomized controlled trial (MILEPOST trial) including 44 subjects (34 POSE arm versus 10 non-sham control arm) demonstrated 13.0% TWL in the POSE group compared with 5.3% TWL in the control group at 12 months.23 A recent meta-analysis including five studies with 586 subjects showed pooled weight loss of 13.2% at 12-15 months following POSE with a pooled serious adverse event rate of 3.2%.24 These included extraluminal bleeding, minor bleeding at the suture site, hepatic abscess, chest pain, nausea, vomiting, and abdominal pain. A distal POSE procedure with a new plication pattern focusing on the gastric body to augment the effect on gastric emptying has also been described.25
The Overstitch is an endoscopic suturing device that is mounted on a double-channel endoscope. At the tip of the scope, there is a curved suture arm and an anchor exchange that allow the needle to pass back and forth to perform full-thickness bites. The tissue helix may also be placed through the second channel to grasp tissue. In April 2012, Thompson performed the first-in-human endoscopic sutured/sleeve gastroplasty (ESG) procedure in India, which was published together with cases performed in Panama and the Dominican Republic.26-28 This procedure involves the use of the Overstitch device to place several sets of running sutures along the greater curvature of the stomach to create a sleeve-like structure. It is thought to delay gastric emptying and therefore increase satiety.29 The largest multicenter retrospective study including 248 patients demonstrated 18.6% TWL at 2 years with 2% SAE rate including perigastric fluid collections, extraluminal hemorrhage, pulmonary embolism, pneumoperitoneum, and pneumothorax.30
Aspiration therapy
Aspiration therapy (AT; Aspire Bariatrics, King of Prussia, Pa.) allows patients to remove 25%-30% of ingested calories at approximately 30 minutes after meals. AT consists of an A-tube, which is a 26-Fr gastrostomy tube with a 15-cm fenestrated drainage catheter placed endoscopically via a standard pull technique. At 1-2 weeks after A-tube placement, the tube is cut down to the skin and connected to the port prior to aspiration. AT is approved for patients with a BMI of 35-55 kg/m2.31 The U.S. pivotal trial (PATHWAY trial) including 207 subjects (137 AT arm versus 70 non-sham control arm) demonstrated 12.1% TWL in the AT group compared to 3.5% in the control group at 12 months based on ITT analysis. The SAE rate was 3.6% including severe abdominal pain, peritonitis, prepyloric ulcer, and A-tube replacement due to skin-port malfunction.32
Transpyloric shuttle
The transpyloric shuttle (TPS; BAROnova, Goleta, Calif.) consists of a spherical bulb that is attached to a smaller cylindrical bulb by a flexible tether. It is placed and removed endoscopically at 6 months. TPS resides across the pylorus creating intermittent obstruction that may result in delayed gastric emptying. A pilot study including 20 patients demonstrated 14.5% TWL at 6 months.33 The U.S. pivotal trial (ENDObesity II trial) was recently completed and the data are being reviewed by the FDA.
Revision for weight regain following bariatric surgery

Weight regain is common following RYGB34,35 and can be associated with dilation of the gastrojejunal anastomosis (GJA).36 Several procedures have been developed to treat this condition by focusing on reduction of GJA size and are available in the United States (Figure 2). These procedures have level I evidence supporting their use and include transoral outlet reduction (TORe) and restorative obesity surgery endoluminal (ROSE).37 TORe involves the use of the Overstitch to place sutures at the GJA. At 1 year, patients had 8.4% TWL with improvement in comorbidities.38 Weight loss remained significant up to 3-5 years.39,40 The modern ROSE procedure utilizes the IOP system to place plications at the GJA and distal gastric pouch following argon plasma coagulation (APC). A small series showed 12.4% TWL at 6 months.41 APC is also currently being investigated as a standalone therapy for weight regain in this population.
Small bowel interventions
There are several small bowel interventions, with different mechanisms of action, available internationally. Many of these are under investigation in the United States; however, none are currently FDA approved.
Duodenal-jejunal bypass liner
Duodenal-jejunal bypass liner (DJBL; GI Dynamics, Boston, Mass.) is a 60-cm fluoropolymer liner that is endoscopically placed and removed at 12 months. It is anchored at the duodenal bulb and ends at the jejunum. By excluding direct contact between chyme and the proximal small bowel, DJBL is thought to work via foregut mechanism where there is less inhibition of the incretin effect (greater increase in insulin secretion following oral glucose administration compared to intravenous glucose administration due to gut-derived factors that enhance insulin secretion) leading to improved insulin resistance. In addition, the enteral transit of chyme and bile is altered suggesting the possible role of the hindgut mechanism. The previous U.S. pivotal trial (ENDO trial) met efficacy endpoints. However, the study was stopped early by the company because of a hepatic abscess rate of 3.5%, all of which were treated conservatively.42 A new U.S. pivotal study is currently planned. A meta-analysis of 17 published studies, all of which were from outside the United States, demonstrated a significant decrease in hemoglobin A1c of 1.3% and 18.9% TWL at 1 year following implantation in patients with obesity with concomitant diabetes.43
Duodenal mucosal resurfacing
Duodenal mucosal resurfacing (Fractyl, Lexington, Mass.) involves saline lifting of the duodenal mucosa circumferentially prior to thermal ablation using an inflated balloon filled with heated water. It is hypothesized that this may reset the diseased duodenal enteroendocrine cells leading to restoration of the incretin effect. A pilot study including 39 patients with poorly controlled diabetes demonstrated a decrease in hemoglobin A1c of 1.2%. The SAE rate was 7.7% including duodenal stenosis, all of which were treated with balloon dilation.44 The U.S. pivotal trial is currently planned.
Gastroduodenal-jejunal bypass
Gastroduodenal-jejunal bypass (ValenTx., Hopkins, Minn.) is a 120-cm sleeve that is anchored at the gastroesophageal junction to create the anatomic changes of RYGB. It is placed and removed endoscopically with laparoscopic assistance. A pilot study including 12 patients demonstrated 35.9% excess weight loss at 12 months. Two out of 12 patients had early device removal due to intolerance and they were not included in the weight loss analysis.45
Incisionless magnetic anastomosis system
The incisionless magnetic anastomosis system (GI Windows, West Bridgewater, Mass.) consists of self-assembling magnets that are deployed under fluoroscopic guidance through the working channel of colonoscopes to form magnetic octagons in the jejunum and ileum. After a week, a compression anastomosis is formed and the coupled magnets pass spontaneously. A pilot study including 10 patients showed 14.6% TWL and a decrease in hemoglobin A1c of 1.9% (for patients with diabetes) at 1 year.46 A randomized study outside the United States is currently underway.
Summary
Endoscopic bariatric and metabolic therapies are emerging as first-line treatments for obesity in many populations. They can serve as a gap therapy for patients who do not qualify for surgery, but also may have a specific role in the treatment of metabolic comorbidities. This field will continue to develop and improve with the introduction of personalized medicine leading to better patient selection, and newer combination therapies. It is time for gastroenterologists to become more involved in the management of this challenging condition.
Dr. Jirapinyo is an advanced and bariatric endoscopy fellow, Brigham and Women’s Hospital, Harvard Medical School, Boston; Dr. Thompson is director of therapeutic endoscopy, Brigham and Women’s Hospital, and associate professor of medicine, Harvard Medical School. Dr. Jirapinyo has served as a consultant for GI Dynamics and holds royalties for Endosim. Dr. Thompson has contracted research for Aspire Bariatrics, USGI Medical, Spatz, and Apollo Endosurgery; has served as a consultant for Boston Scientific, Covidien, USGI Medical, Olympus, and Fractyl; holds stocks and royalties for GI Windows and Endosim, and has served as an expert reviewer for GI Dynamics.
References
1. CDC. From https://www.cdc.gov/obesity/data/adult.html. Accessed on 11 September 2018.
2. Aronne LJ et al. Obesity. 2013;21:2163-71.
3. Torgerson JS et al. Diabetes Care. 2004;27:155-61.
4. Allison DB et al. Obesity. 2012;20:330-42.
5. Smith SR et al. N Engl J Med. 2010;363:245-56.
6. Apovian CM et al. Obesity. 2013;21:935-43.
7. Pi-Sunyer X et al. N Engl J Med. 2015;373:11-22.
8. Colguitt JL et al. Cochrane Database Syst Rev. 2014;8(8):CD003641.
9. Ponce J et al. Surg Obes Relat Dis. 2015;11(6):1199-200.
10. Jirapinyo P, Thompson CC et al. Clin Gastroenterol Hepatol. 2017;15(5):619-30.
11. Sullivan S et al.Gastroenterology. 2017;152(7):1791-801.
12. Gomez V et al. Obesity. 2016;24(9):1849-53.
13. Food and Drug Administration. Summary of safety and effectiveness data (SSED) ORBERA Intragastric Balloon System. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf14/P140008b.pdf. 2015:1-32.
14. Abu Dayyeh BK et al. Gastrointest Endosc. 2015;81:AB147.
15. Food and Drug Administration. Summary of safety and effectiveness data (SSED) ReShape Integrated Dual Balloon System. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf14/P140012b.pdf. 2015:1-43.
16. Ponce J et al. Surg Obes Relat Dis. 2015;11:874-81.
17. Food and Drug Administration. Summary and effectiveness data (SSED): Obalon Balloon System. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf16/P160001b.pdf. 2016:1-46.
18. Sullivan S et al. Gastroenterology. 2016;150:S1267.
19. Popov VB et al. Am J Gastroenterol. 2017;112:429-39.
20. Abu Dayyeh BK et al. Gastrointest Endosc. 2015;82(3):425-38.
21. Espinos JC et al. Obes Surg. 2013;23(9):1375-83.
22. Sullivan S et al. Obesity. 2017;25:294-301.
23. Miller K et al. Obesity Surg. 2017;27(2):310-22.
24. Jirapinyo P et al. Gastrointest Endosc. 2018;87(6):AB604-AB605.
25. Jirapinyo P, Thompson CC. Video GIE. 2018;3(10):296-300.
26. Campos J et al. SAGES 2013 Presentation. Baltimore, MD. 19 April 2013.
27. Kumar N et al. Gastroenterology. 2014;146(5):S571-2.
28. Kumar N et al. Surg Endosc. 2018;32(4):2159-64.
29. Abu Dayyeh BK et al. Clin Gastroenterol Hepatol. 2017;15:37-43.
30. Lopez-Nava G et al. Obes Surg. 2017;27(10):2649-55.
31. Food and Drug Administration. Summary of safety and effectiveness (SSED): AspireAssist. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf15/p150024b.pdf. FDA,ed,2016:1-36.
32. Thompson CC et al. Am J Gastroenterol. 2017;112:447-57.
33. SAGES abstract archives. SAGES. Available from: http://www.sages.org/meetings/annual-meeting/abstracts-archive/first-clinical-experience-with-the-transpyloric-shuttle-tpsr-device-a-non-surgical-endoscopic treatment-for-obesity-results-from-a-3-month-and-6-month-study. Accessed Sept. 12, 2018.
34. Sjostrom L et al. N Engl J Med. 2007;357:741-52.
35. Adams TD et al. N Engl J Med. 2017;377:1143-55.
36. Abu Dayyeh BK et al. Clin Gastroenterol Hepatol. 2011;9:228-33.
37. Thompson CC et al. Gastroenterology. 2013;145(1):129-37.
38. Jirapinyo P et al. Endoscopy. 2018;50(4):371-7.
39. Kumar N, Thompson CC. Gastrointest Endosc. 2016;83(4):776-9.
40. Jirapinyo P et al. Gastrointest Endosc. 2017;85(5):AB93-94.
41. Jirapinyo P, Thompson CC et al. Comparison of a novel plication technique to suturing for endoscopic outlet reduction for the treatment of weight regain after Roux-en-Y gastric bypass. Obesity Week 2018. Poster presentation.
42. Kaplan LM et al. EndoBarrier therapy is associated with glycemic improvement, weight loss and safety issues in patients with obesity and type 2 diabetes on oral anti-hyperglycemic agents (The ENDO Trial). In: Oral Presentation at the 76th American Diabetes Association (ADA) Annual Meeting: 2016 June 10-14: New Orleans. Abstract number 362-LB.
43. Jirapinyo P et al. Diabetes Care. 2018;41(5):1106-15.
44. Rajagopalan H et al. Diabetes Care. 2016;39(12):2254-61.
45. Sandler BJ et al. Surgical Endosc. 2015;29:3298-303.
46. Machytka E et al. Gastrointest Endosc. 2017;86(5):904-12.
Editor's Note
Gastroenterologists are becoming increasingly involved in the management of obesity. While prior therapy for obesity was mainly based on lifestyle changes, medication, or surgery, the new and exciting field of endoscopic bariatric and metabolic therapies has recently garnered incredible attention and momentum.
In this quarter’s In Focus article, brought to you by The New Gastroenterologist, Pichamol Jirapinyo and Christopher Thompson (Brigham and Women’s Hospital) provide an outstanding overview of the gastric and small bowel endoscopic interventions that are either already approved for use in obesity or currently being studied. This field is moving incredibly fast, and knowledge and understanding of these endoscopic therapies for obesity will undoubtedly be important for our field.
Bryson W. Katona, MD, PhD
Editor in Chief, The New Gastroenterologist
Introduction
Obesity is a rising pandemic. As of 2016, 93.3 million U.S. adults had obesity, representing 39.8% of our adult population.1 It is estimated that approximately $147 billion is spent annually on caring for patients with obesity. Traditionally, the management of obesity includes lifestyle therapy (diet and exercise), pharmacotherapy (six Food and Drug Administration–approved medications for obesity), and bariatric surgery (sleeve gastrectomy [SG] and Roux-en-Y gastric bypass [RYGB]). Nevertheless, intensive lifestyle intervention and pharmacotherapy are associated with approximately 3.1%-6.6% total weight loss (TWL),2-7 and bariatric surgery is associated with 20%-33.3% TWL.8 However, less than 2% of patients who are eligible for bariatric surgery elect to undergo surgery, leaving a large proportion of patients with obesity untreated or undertreated.9
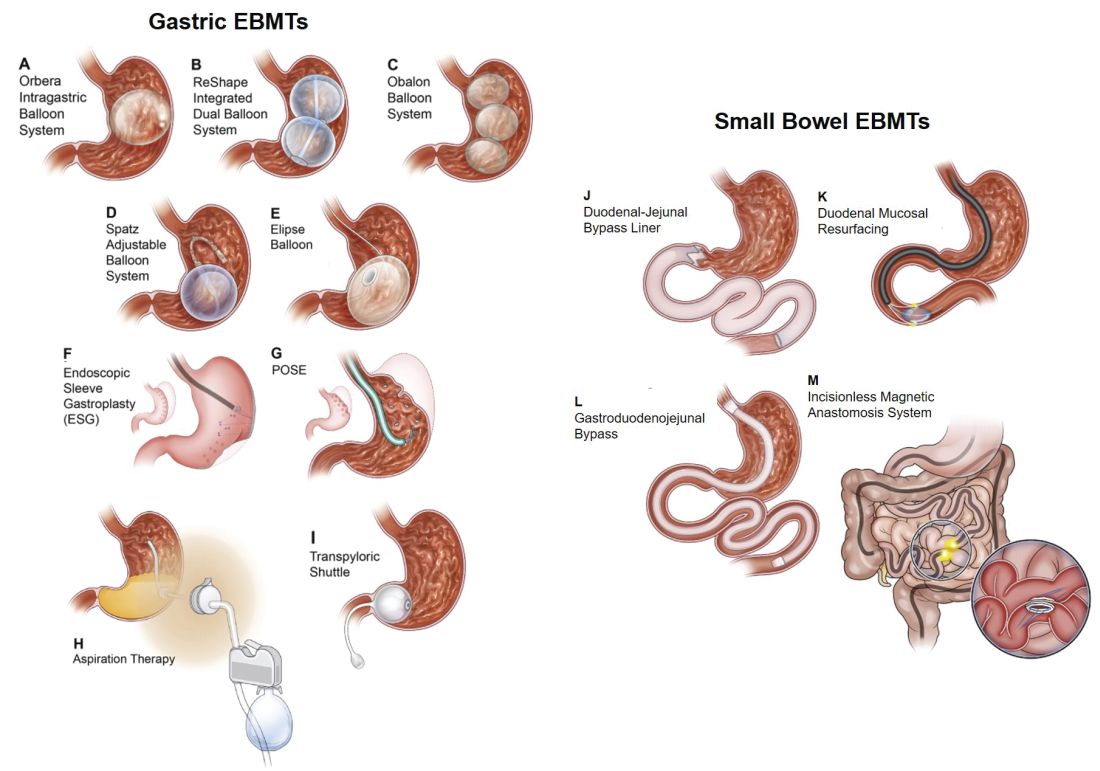
Endoscopic bariatric and metabolic therapies (EBMTs) encompass an emerging field for the treatment of obesity. In general, EBMTs are associated with greater weight loss than are lifestyle intervention and pharmacotherapy, but with a less- invasive risk profile than bariatric surgery. EBMTs may be divided into two general categories – gastric and small bowel interventions (Figure 1 and Table 1). Gastric EBMTs are effective at treating obesity, while small bowel EBMTs are effective at treating metabolic diseases with a variable weight loss profile depending on the device.10,11
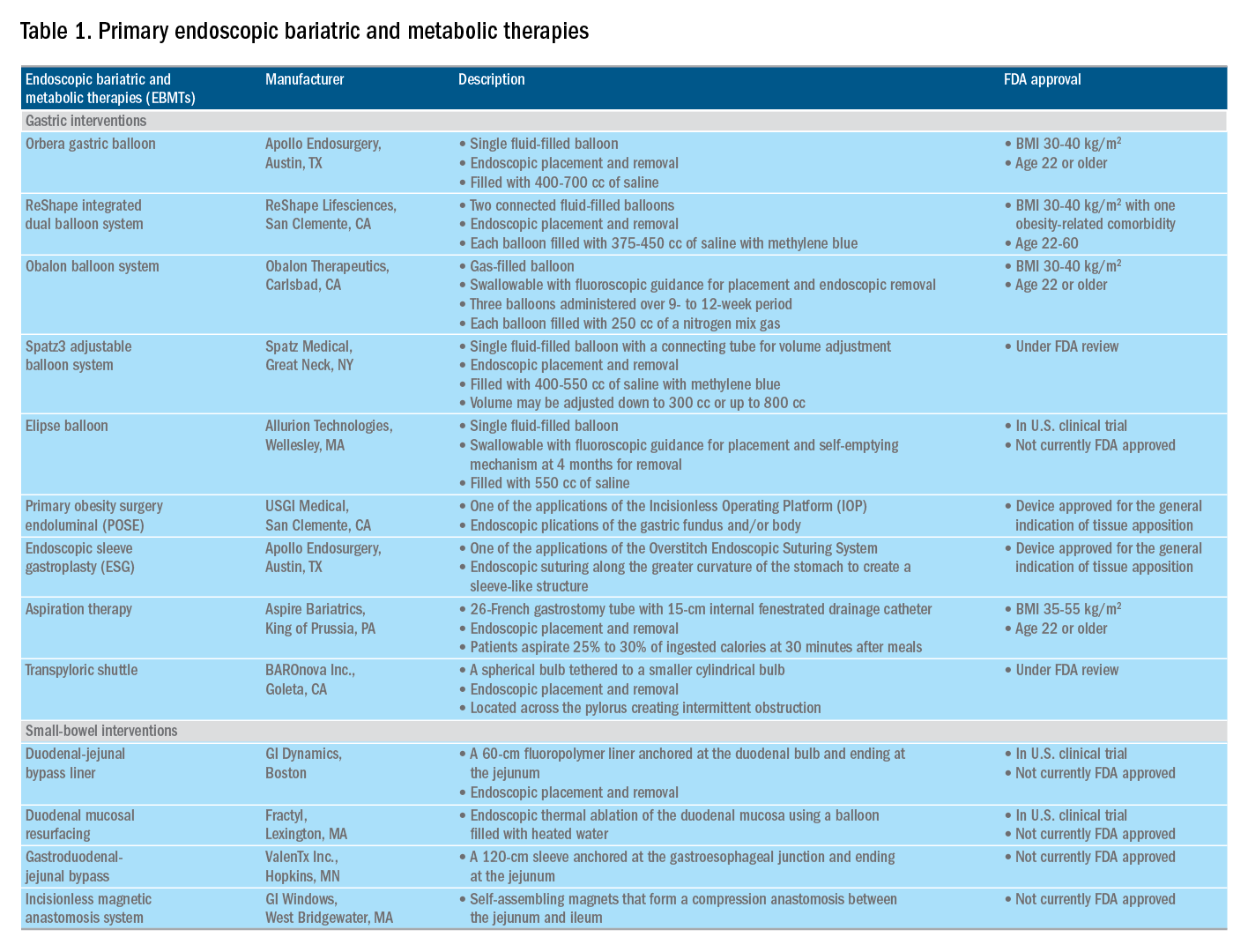
Of note, a variety of study designs (including retrospective series, prospective series, and randomized trials with and without shams) have been employed, which can affect outcomes. Therefore, weight loss comparisons among studies are challenging and should be considered in this context.
Gastric interventions
Currently, there are three types of EBMTs that are FDA approved and used for the treatment of obesity. These include intragastric balloons (IGBs), plications and suturing, and aspiration therapy (AT). Other technologies that are under investigation also will be briefly covered.
Intragastric balloons
An intragastric balloon is a space-occupying device that is placed in the stomach. The mechanism of action of IGBs involves delaying gastric emptying, which leads to increased satiety.12 There are several types of IGBs available worldwide differing in techniques of placement and removal (endoscopic versus fluoroscopic versus swallowable), materials used to fill the balloon (fluid-filled versus air-filled), and the number of balloons placed (single versus duo versus three-balloon). At the time of this writing, three IGBs are approved by the FDA (Orbera, ReShape, and Obalon), all for patients with body mass indexes of 30-40 kg/m2, and two others are in the process of obtaining FDA approval (Spatz and Elipse).
Orbera gastric balloon (Apollo Endosurgery, Austin, Tex.) is a single fluid-filled IGB that is endoscopically placed and removed at 6 months. The balloon is filled with 400-700 cc of saline with or without methylene blue (to identify leakage or rupture). Recently, Orbera365, which allows the balloon to stay for 12 months instead of 6 months, has become available in Europe; however, it is yet to be approved in the United States. The U.S. pivotal trial (Orbera trial) including 255 subjects (125 Orbera arm versus 130 non-sham control arm) demonstrated 10.2% TWL in the Orbera group compared with 3.3% TWL in the control group at 6 months based on intention-to-treat (ITT) analysis. This difference persisted at 12 months (6 months after explantation) with 7.6% TWL for the Orbera group versus 3.1% TWL for the control group.13,14
ReShape integrated dual balloon system (ReShape Lifesciences, San Clemente, Calif.) consists of two connected fluid-filled balloons that are endoscopically placed and removed at 6 months. Each balloon is filled with 375-450 cc of saline mixed with methylene blue. The U.S. pivotal trial (REDUCE trial) including 326 subjects (187 ReShape arm versus 139 sham arm) demonstrated 6.8% TWL in the ReShape group compared with 3.3% TWL in the sham group at 6 months based on ITT analysis.15,16
Obalon balloon system (Obalon Therapeutics, Carlsbad, Calif.) is a swallowable, gas-filled balloon system that requires endoscopy only for removal. During placement, a capsule is swallowed under fluoroscopic guidance. The balloon is then inflated with 250 cc of nitrogen mix gas prior to tube detachment. Up to three balloons may be swallowed sequentially at 1-month intervals. At 6 months from the first balloon placement, all balloons are removed endoscopically. The U.S. pivotal trial (SMART trial) including 366 subjects (185 Obalon arm versus 181 sham capsule arm) demonstrated 6.6% TWL in the Obalon group compared with 3.4% TWL in the sham group at 6 months based on ITT analysis.17,18
Two other balloons that are currently under investigation in the United States are the Spatz3 adjustable balloon system (Spatz Medical, Great Neck, N.Y.) and Elipse balloon (Allurion Technologies, Wellesley, Mass.). The Spatz3 is a fluid-filled balloon that is placed and removed endoscopically. It consists of a single balloon and a connecting tube that allows volume adjustment for control of symptoms and possible augmentation of weight loss. The U.S. pivotal trial was recently completed and the data are being reviewed by the FDA. The Elipse is a swallowable fluid-filled balloon that does not require endoscopy for placement or removal. At 4 months, the balloon releases fluid allowing it to empty and pass naturally. The U.S. pivotal trial (ENLIGHTEN trial) is currently underway.
A meta-analysis of randomized controlled trials revealed improvement in most metabolic parameters (diastolic blood pressure, fasting glucose, hemoglobin A1c, and waist circumference) following IGB compared with controls.19 Nausea and vomiting are seen in approximately 30% and should be addressed appropriately. Pooled serious adverse event (SAE) rate was 1.5%, which included migration, perforation, and death. Since 2016, 14 deaths have been reported according to the FDA MAUDE database. Corporate response was that over 295,000 balloons had been distributed worldwide with a mortality rate of less than 0.01%.20
Plication and suturing
Currently, there are two endoscopic devices that are approved for the general indication of tissue apposition. These include the Incisionless Operating Platform (IOP) (USGI Medical, San Clemente, Calif.) and the Overstitch endoscopic suturing system (Apollo Endosurgery, Austin, Tex.). These devices are used to remodel the stomach to create a sleeve-like structure to induce weight loss.
The IOP system consists of a transport, which is a 54-Fr flexible endoscope. It consists of four working channels that accommodate a G-Prox (for tissue approximation), a G-Lix (for tissue grasping), and an ultrathin endoscope (for visualization). In April 2008, Horgan performed the first-in-human primary obesity surgery endoluminal (POSE) procedure in Argentina. The procedure involves the use of the IOP system to place plications primarily in the fundus to modify gastric accommodation.21 The U.S. pivotal trial (ESSENTIAL trial) including 332 subjects (221 POSE arm versus 111 sham arm) demonstrated 5.0% TWL in the POSE group compared with 1.4% in the sham group at 12 months based on ITT analysis.22 A European multicenter randomized controlled trial (MILEPOST trial) including 44 subjects (34 POSE arm versus 10 non-sham control arm) demonstrated 13.0% TWL in the POSE group compared with 5.3% TWL in the control group at 12 months.23 A recent meta-analysis including five studies with 586 subjects showed pooled weight loss of 13.2% at 12-15 months following POSE with a pooled serious adverse event rate of 3.2%.24 These included extraluminal bleeding, minor bleeding at the suture site, hepatic abscess, chest pain, nausea, vomiting, and abdominal pain. A distal POSE procedure with a new plication pattern focusing on the gastric body to augment the effect on gastric emptying has also been described.25
The Overstitch is an endoscopic suturing device that is mounted on a double-channel endoscope. At the tip of the scope, there is a curved suture arm and an anchor exchange that allow the needle to pass back and forth to perform full-thickness bites. The tissue helix may also be placed through the second channel to grasp tissue. In April 2012, Thompson performed the first-in-human endoscopic sutured/sleeve gastroplasty (ESG) procedure in India, which was published together with cases performed in Panama and the Dominican Republic.26-28 This procedure involves the use of the Overstitch device to place several sets of running sutures along the greater curvature of the stomach to create a sleeve-like structure. It is thought to delay gastric emptying and therefore increase satiety.29 The largest multicenter retrospective study including 248 patients demonstrated 18.6% TWL at 2 years with 2% SAE rate including perigastric fluid collections, extraluminal hemorrhage, pulmonary embolism, pneumoperitoneum, and pneumothorax.30
Aspiration therapy
Aspiration therapy (AT; Aspire Bariatrics, King of Prussia, Pa.) allows patients to remove 25%-30% of ingested calories at approximately 30 minutes after meals. AT consists of an A-tube, which is a 26-Fr gastrostomy tube with a 15-cm fenestrated drainage catheter placed endoscopically via a standard pull technique. At 1-2 weeks after A-tube placement, the tube is cut down to the skin and connected to the port prior to aspiration. AT is approved for patients with a BMI of 35-55 kg/m2.31 The U.S. pivotal trial (PATHWAY trial) including 207 subjects (137 AT arm versus 70 non-sham control arm) demonstrated 12.1% TWL in the AT group compared to 3.5% in the control group at 12 months based on ITT analysis. The SAE rate was 3.6% including severe abdominal pain, peritonitis, prepyloric ulcer, and A-tube replacement due to skin-port malfunction.32
Transpyloric shuttle
The transpyloric shuttle (TPS; BAROnova, Goleta, Calif.) consists of a spherical bulb that is attached to a smaller cylindrical bulb by a flexible tether. It is placed and removed endoscopically at 6 months. TPS resides across the pylorus creating intermittent obstruction that may result in delayed gastric emptying. A pilot study including 20 patients demonstrated 14.5% TWL at 6 months.33 The U.S. pivotal trial (ENDObesity II trial) was recently completed and the data are being reviewed by the FDA.
Revision for weight regain following bariatric surgery

Weight regain is common following RYGB34,35 and can be associated with dilation of the gastrojejunal anastomosis (GJA).36 Several procedures have been developed to treat this condition by focusing on reduction of GJA size and are available in the United States (Figure 2). These procedures have level I evidence supporting their use and include transoral outlet reduction (TORe) and restorative obesity surgery endoluminal (ROSE).37 TORe involves the use of the Overstitch to place sutures at the GJA. At 1 year, patients had 8.4% TWL with improvement in comorbidities.38 Weight loss remained significant up to 3-5 years.39,40 The modern ROSE procedure utilizes the IOP system to place plications at the GJA and distal gastric pouch following argon plasma coagulation (APC). A small series showed 12.4% TWL at 6 months.41 APC is also currently being investigated as a standalone therapy for weight regain in this population.
Small bowel interventions
There are several small bowel interventions, with different mechanisms of action, available internationally. Many of these are under investigation in the United States; however, none are currently FDA approved.
Duodenal-jejunal bypass liner
Duodenal-jejunal bypass liner (DJBL; GI Dynamics, Boston, Mass.) is a 60-cm fluoropolymer liner that is endoscopically placed and removed at 12 months. It is anchored at the duodenal bulb and ends at the jejunum. By excluding direct contact between chyme and the proximal small bowel, DJBL is thought to work via foregut mechanism where there is less inhibition of the incretin effect (greater increase in insulin secretion following oral glucose administration compared to intravenous glucose administration due to gut-derived factors that enhance insulin secretion) leading to improved insulin resistance. In addition, the enteral transit of chyme and bile is altered suggesting the possible role of the hindgut mechanism. The previous U.S. pivotal trial (ENDO trial) met efficacy endpoints. However, the study was stopped early by the company because of a hepatic abscess rate of 3.5%, all of which were treated conservatively.42 A new U.S. pivotal study is currently planned. A meta-analysis of 17 published studies, all of which were from outside the United States, demonstrated a significant decrease in hemoglobin A1c of 1.3% and 18.9% TWL at 1 year following implantation in patients with obesity with concomitant diabetes.43
Duodenal mucosal resurfacing
Duodenal mucosal resurfacing (Fractyl, Lexington, Mass.) involves saline lifting of the duodenal mucosa circumferentially prior to thermal ablation using an inflated balloon filled with heated water. It is hypothesized that this may reset the diseased duodenal enteroendocrine cells leading to restoration of the incretin effect. A pilot study including 39 patients with poorly controlled diabetes demonstrated a decrease in hemoglobin A1c of 1.2%. The SAE rate was 7.7% including duodenal stenosis, all of which were treated with balloon dilation.44 The U.S. pivotal trial is currently planned.
Gastroduodenal-jejunal bypass
Gastroduodenal-jejunal bypass (ValenTx., Hopkins, Minn.) is a 120-cm sleeve that is anchored at the gastroesophageal junction to create the anatomic changes of RYGB. It is placed and removed endoscopically with laparoscopic assistance. A pilot study including 12 patients demonstrated 35.9% excess weight loss at 12 months. Two out of 12 patients had early device removal due to intolerance and they were not included in the weight loss analysis.45
Incisionless magnetic anastomosis system
The incisionless magnetic anastomosis system (GI Windows, West Bridgewater, Mass.) consists of self-assembling magnets that are deployed under fluoroscopic guidance through the working channel of colonoscopes to form magnetic octagons in the jejunum and ileum. After a week, a compression anastomosis is formed and the coupled magnets pass spontaneously. A pilot study including 10 patients showed 14.6% TWL and a decrease in hemoglobin A1c of 1.9% (for patients with diabetes) at 1 year.46 A randomized study outside the United States is currently underway.
Summary
Endoscopic bariatric and metabolic therapies are emerging as first-line treatments for obesity in many populations. They can serve as a gap therapy for patients who do not qualify for surgery, but also may have a specific role in the treatment of metabolic comorbidities. This field will continue to develop and improve with the introduction of personalized medicine leading to better patient selection, and newer combination therapies. It is time for gastroenterologists to become more involved in the management of this challenging condition.
Dr. Jirapinyo is an advanced and bariatric endoscopy fellow, Brigham and Women’s Hospital, Harvard Medical School, Boston; Dr. Thompson is director of therapeutic endoscopy, Brigham and Women’s Hospital, and associate professor of medicine, Harvard Medical School. Dr. Jirapinyo has served as a consultant for GI Dynamics and holds royalties for Endosim. Dr. Thompson has contracted research for Aspire Bariatrics, USGI Medical, Spatz, and Apollo Endosurgery; has served as a consultant for Boston Scientific, Covidien, USGI Medical, Olympus, and Fractyl; holds stocks and royalties for GI Windows and Endosim, and has served as an expert reviewer for GI Dynamics.
References
1. CDC. From https://www.cdc.gov/obesity/data/adult.html. Accessed on 11 September 2018.
2. Aronne LJ et al. Obesity. 2013;21:2163-71.
3. Torgerson JS et al. Diabetes Care. 2004;27:155-61.
4. Allison DB et al. Obesity. 2012;20:330-42.
5. Smith SR et al. N Engl J Med. 2010;363:245-56.
6. Apovian CM et al. Obesity. 2013;21:935-43.
7. Pi-Sunyer X et al. N Engl J Med. 2015;373:11-22.
8. Colguitt JL et al. Cochrane Database Syst Rev. 2014;8(8):CD003641.
9. Ponce J et al. Surg Obes Relat Dis. 2015;11(6):1199-200.
10. Jirapinyo P, Thompson CC et al. Clin Gastroenterol Hepatol. 2017;15(5):619-30.
11. Sullivan S et al.Gastroenterology. 2017;152(7):1791-801.
12. Gomez V et al. Obesity. 2016;24(9):1849-53.
13. Food and Drug Administration. Summary of safety and effectiveness data (SSED) ORBERA Intragastric Balloon System. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf14/P140008b.pdf. 2015:1-32.
14. Abu Dayyeh BK et al. Gastrointest Endosc. 2015;81:AB147.
15. Food and Drug Administration. Summary of safety and effectiveness data (SSED) ReShape Integrated Dual Balloon System. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf14/P140012b.pdf. 2015:1-43.
16. Ponce J et al. Surg Obes Relat Dis. 2015;11:874-81.
17. Food and Drug Administration. Summary and effectiveness data (SSED): Obalon Balloon System. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf16/P160001b.pdf. 2016:1-46.
18. Sullivan S et al. Gastroenterology. 2016;150:S1267.
19. Popov VB et al. Am J Gastroenterol. 2017;112:429-39.
20. Abu Dayyeh BK et al. Gastrointest Endosc. 2015;82(3):425-38.
21. Espinos JC et al. Obes Surg. 2013;23(9):1375-83.
22. Sullivan S et al. Obesity. 2017;25:294-301.
23. Miller K et al. Obesity Surg. 2017;27(2):310-22.
24. Jirapinyo P et al. Gastrointest Endosc. 2018;87(6):AB604-AB605.
25. Jirapinyo P, Thompson CC. Video GIE. 2018;3(10):296-300.
26. Campos J et al. SAGES 2013 Presentation. Baltimore, MD. 19 April 2013.
27. Kumar N et al. Gastroenterology. 2014;146(5):S571-2.
28. Kumar N et al. Surg Endosc. 2018;32(4):2159-64.
29. Abu Dayyeh BK et al. Clin Gastroenterol Hepatol. 2017;15:37-43.
30. Lopez-Nava G et al. Obes Surg. 2017;27(10):2649-55.
31. Food and Drug Administration. Summary of safety and effectiveness (SSED): AspireAssist. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf15/p150024b.pdf. FDA,ed,2016:1-36.
32. Thompson CC et al. Am J Gastroenterol. 2017;112:447-57.
33. SAGES abstract archives. SAGES. Available from: http://www.sages.org/meetings/annual-meeting/abstracts-archive/first-clinical-experience-with-the-transpyloric-shuttle-tpsr-device-a-non-surgical-endoscopic treatment-for-obesity-results-from-a-3-month-and-6-month-study. Accessed Sept. 12, 2018.
34. Sjostrom L et al. N Engl J Med. 2007;357:741-52.
35. Adams TD et al. N Engl J Med. 2017;377:1143-55.
36. Abu Dayyeh BK et al. Clin Gastroenterol Hepatol. 2011;9:228-33.
37. Thompson CC et al. Gastroenterology. 2013;145(1):129-37.
38. Jirapinyo P et al. Endoscopy. 2018;50(4):371-7.
39. Kumar N, Thompson CC. Gastrointest Endosc. 2016;83(4):776-9.
40. Jirapinyo P et al. Gastrointest Endosc. 2017;85(5):AB93-94.
41. Jirapinyo P, Thompson CC et al. Comparison of a novel plication technique to suturing for endoscopic outlet reduction for the treatment of weight regain after Roux-en-Y gastric bypass. Obesity Week 2018. Poster presentation.
42. Kaplan LM et al. EndoBarrier therapy is associated with glycemic improvement, weight loss and safety issues in patients with obesity and type 2 diabetes on oral anti-hyperglycemic agents (The ENDO Trial). In: Oral Presentation at the 76th American Diabetes Association (ADA) Annual Meeting: 2016 June 10-14: New Orleans. Abstract number 362-LB.
43. Jirapinyo P et al. Diabetes Care. 2018;41(5):1106-15.
44. Rajagopalan H et al. Diabetes Care. 2016;39(12):2254-61.
45. Sandler BJ et al. Surgical Endosc. 2015;29:3298-303.
46. Machytka E et al. Gastrointest Endosc. 2017;86(5):904-12.
AGA report from Capitol Hill
On Sept. 14, AGA held Advocacy Day. This was a day in which several AGA members met with staff of Congressional representatives on Capitol Hill to advocate for important issues within the field of gastroenterology. The three primary issues involved:
- Support of increased NIH funding.
- Requesting increased transparency in insurance-driven step-therapy protocols.
- Removal of the coinsurance or copayment for screening colonoscopies that become therapeutic, once polyps are identified and removed.
These issues support growth and autonomy of our field, while supporting the interests of our patients.
Advocacy is not difficult. Many of my fellow GIs are unnecessarily intimidated by this word; however, each individual has the ability and, arguably, the responsibility to shape the environment in which we practice. Opportunities to engage your representatives may be as simple as clicking a link, leaving a voicemail, or signing a petition, to testifying at hearings or hosting a representative at your own institution. AGA staff made participating in Advocacy Day very easy. Staff at AGA coordinate meetings between each advocate, and the offices of his or her local Congress members. AGA also provides brief training prior to these meetings; thus, no prior experience is required. I felt well prepared for the meetings with my local Congress staff members.
I chose to participate in Advocacy Day because I want to bring the experiences of my colleagues and patients to the doorsteps of those who make decisions about how we practice. I feel that it is important to stand up for our field and our patients, lest others make decisions for us. We do not have to feel powerless in a changing field. Let your voice be heard.
Dr. Anjou is a gastroenterologist at the University of Connecticut Health Center, Farmington, and member of the AGA Trainee and Early Career Committee and Quality Measures Committee.
On Sept. 14, AGA held Advocacy Day. This was a day in which several AGA members met with staff of Congressional representatives on Capitol Hill to advocate for important issues within the field of gastroenterology. The three primary issues involved:
- Support of increased NIH funding.
- Requesting increased transparency in insurance-driven step-therapy protocols.
- Removal of the coinsurance or copayment for screening colonoscopies that become therapeutic, once polyps are identified and removed.
These issues support growth and autonomy of our field, while supporting the interests of our patients.
Advocacy is not difficult. Many of my fellow GIs are unnecessarily intimidated by this word; however, each individual has the ability and, arguably, the responsibility to shape the environment in which we practice. Opportunities to engage your representatives may be as simple as clicking a link, leaving a voicemail, or signing a petition, to testifying at hearings or hosting a representative at your own institution. AGA staff made participating in Advocacy Day very easy. Staff at AGA coordinate meetings between each advocate, and the offices of his or her local Congress members. AGA also provides brief training prior to these meetings; thus, no prior experience is required. I felt well prepared for the meetings with my local Congress staff members.
I chose to participate in Advocacy Day because I want to bring the experiences of my colleagues and patients to the doorsteps of those who make decisions about how we practice. I feel that it is important to stand up for our field and our patients, lest others make decisions for us. We do not have to feel powerless in a changing field. Let your voice be heard.
Dr. Anjou is a gastroenterologist at the University of Connecticut Health Center, Farmington, and member of the AGA Trainee and Early Career Committee and Quality Measures Committee.
On Sept. 14, AGA held Advocacy Day. This was a day in which several AGA members met with staff of Congressional representatives on Capitol Hill to advocate for important issues within the field of gastroenterology. The three primary issues involved:
- Support of increased NIH funding.
- Requesting increased transparency in insurance-driven step-therapy protocols.
- Removal of the coinsurance or copayment for screening colonoscopies that become therapeutic, once polyps are identified and removed.
These issues support growth and autonomy of our field, while supporting the interests of our patients.
Advocacy is not difficult. Many of my fellow GIs are unnecessarily intimidated by this word; however, each individual has the ability and, arguably, the responsibility to shape the environment in which we practice. Opportunities to engage your representatives may be as simple as clicking a link, leaving a voicemail, or signing a petition, to testifying at hearings or hosting a representative at your own institution. AGA staff made participating in Advocacy Day very easy. Staff at AGA coordinate meetings between each advocate, and the offices of his or her local Congress members. AGA also provides brief training prior to these meetings; thus, no prior experience is required. I felt well prepared for the meetings with my local Congress staff members.
I chose to participate in Advocacy Day because I want to bring the experiences of my colleagues and patients to the doorsteps of those who make decisions about how we practice. I feel that it is important to stand up for our field and our patients, lest others make decisions for us. We do not have to feel powerless in a changing field. Let your voice be heard.
Dr. Anjou is a gastroenterologist at the University of Connecticut Health Center, Farmington, and member of the AGA Trainee and Early Career Committee and Quality Measures Committee.
Rising microbiome investigator: Ting-Chin David Shen, MD, PhD
We spoke with Dr. Shen, instructor of medicine at the University of Pennsylvania and the recipient of the AGA Research Foundation’s 2016 Microbiome Junior Investigator Award, to learn about his passion for gut microbiome research.
How would you sum up your research in one sentence?
My research examines the metabolic interactions between the gut microbiota and the mammalian host, with a particular emphasis on amino acid metabolism and nitrogen flux via the bacterial enzyme urease.
What impact do you hope your research will have on patients?
My hope is that by better understanding the biological mechanisms by which the gut microbiota impacts host metabolism, we can modulate its effects to treat a variety of conditions and diseases including hepatic encephalopathy, inborn errors of metabolism, obesity, malnutrition, etc.
What inspired you to focus your research career on the gut microbiome?
My clinical experience as a gastroenterologist inspired my interest in metabolic and nutritional research. When I learned of the impact that the gut microbiota has on host metabolism, it created an entirely different perspective for me in terms of thinking about how to treat metabolic and nutritional disorders. There are tremendous opportunities in modifying our gut microbiota in concert with dietary interventions in order to modulate our metabolism.
What recent publication from your lab best represents your work, if anyone wants to learn more?
The following work examined how the use of a defined bacterial consortium without urease activity can reduce colonic ammonia level upon inoculation into the gut and ameliorate morbidity and mortality in a murine model of liver disease.
Shen, T.D., Albenberg, L.A., Bittinger, K., et al, Engineering the Gut Microbiota to Treat Hyperammonemia. Journal of Clinical Investigation. 2015 Jul 1;125(7):2841-50.
We spoke with Dr. Shen, instructor of medicine at the University of Pennsylvania and the recipient of the AGA Research Foundation’s 2016 Microbiome Junior Investigator Award, to learn about his passion for gut microbiome research.
How would you sum up your research in one sentence?
My research examines the metabolic interactions between the gut microbiota and the mammalian host, with a particular emphasis on amino acid metabolism and nitrogen flux via the bacterial enzyme urease.
What impact do you hope your research will have on patients?
My hope is that by better understanding the biological mechanisms by which the gut microbiota impacts host metabolism, we can modulate its effects to treat a variety of conditions and diseases including hepatic encephalopathy, inborn errors of metabolism, obesity, malnutrition, etc.
What inspired you to focus your research career on the gut microbiome?
My clinical experience as a gastroenterologist inspired my interest in metabolic and nutritional research. When I learned of the impact that the gut microbiota has on host metabolism, it created an entirely different perspective for me in terms of thinking about how to treat metabolic and nutritional disorders. There are tremendous opportunities in modifying our gut microbiota in concert with dietary interventions in order to modulate our metabolism.
What recent publication from your lab best represents your work, if anyone wants to learn more?
The following work examined how the use of a defined bacterial consortium without urease activity can reduce colonic ammonia level upon inoculation into the gut and ameliorate morbidity and mortality in a murine model of liver disease.
Shen, T.D., Albenberg, L.A., Bittinger, K., et al, Engineering the Gut Microbiota to Treat Hyperammonemia. Journal of Clinical Investigation. 2015 Jul 1;125(7):2841-50.
We spoke with Dr. Shen, instructor of medicine at the University of Pennsylvania and the recipient of the AGA Research Foundation’s 2016 Microbiome Junior Investigator Award, to learn about his passion for gut microbiome research.
How would you sum up your research in one sentence?
My research examines the metabolic interactions between the gut microbiota and the mammalian host, with a particular emphasis on amino acid metabolism and nitrogen flux via the bacterial enzyme urease.
What impact do you hope your research will have on patients?
My hope is that by better understanding the biological mechanisms by which the gut microbiota impacts host metabolism, we can modulate its effects to treat a variety of conditions and diseases including hepatic encephalopathy, inborn errors of metabolism, obesity, malnutrition, etc.
What inspired you to focus your research career on the gut microbiome?
My clinical experience as a gastroenterologist inspired my interest in metabolic and nutritional research. When I learned of the impact that the gut microbiota has on host metabolism, it created an entirely different perspective for me in terms of thinking about how to treat metabolic and nutritional disorders. There are tremendous opportunities in modifying our gut microbiota in concert with dietary interventions in order to modulate our metabolism.
What recent publication from your lab best represents your work, if anyone wants to learn more?
The following work examined how the use of a defined bacterial consortium without urease activity can reduce colonic ammonia level upon inoculation into the gut and ameliorate morbidity and mortality in a murine model of liver disease.
Shen, T.D., Albenberg, L.A., Bittinger, K., et al, Engineering the Gut Microbiota to Treat Hyperammonemia. Journal of Clinical Investigation. 2015 Jul 1;125(7):2841-50.
AGA’s flagship research grant now accepting applications
The call for applications for 2019 Research Scholar Awards (RSA) is now open. An RSA enables young investigators to develop independent and productive research careers by ensuring protected time for research. And our commitment includes supporting the career development of all GI researchers, whether they focus on clinical or basic research. The deadline to apply is Dec. 14, 2018.
The call for applications for 2019 Research Scholar Awards (RSA) is now open. An RSA enables young investigators to develop independent and productive research careers by ensuring protected time for research. And our commitment includes supporting the career development of all GI researchers, whether they focus on clinical or basic research. The deadline to apply is Dec. 14, 2018.
The call for applications for 2019 Research Scholar Awards (RSA) is now open. An RSA enables young investigators to develop independent and productive research careers by ensuring protected time for research. And our commitment includes supporting the career development of all GI researchers, whether they focus on clinical or basic research. The deadline to apply is Dec. 14, 2018.
Private practice gastroenterology models: Weighing the options
Editor’s note: It is my pleasure to introduce this new quarterly column in The New Gastroenterologist that will be dedicated to addressing important topics for early-career GIs who are either considering a career or starting a career as an independent GI physician in practice. This column is a collaboration between the AGA’s The New Gastroenterologist and the Digestive Health Physicians Association (DHPA), a national advocacy organization of more than 1,800 gastroenterologists in 79 member practices, which is focused exclusively on policies that promote and protect the high-quality, cost-efficient care provided to patients in the independent GI-practice setting.
Bryson W. Katona, MD, PhD
Editor in Chief, The New Gastroenterologist
Educating and training for your life’s work has likely occupied much of the past 10 years including medical school, residency, and fellowship. When it comes to deciding the next steps, the options can seem daunting.
As a long-standing private practice gastroenterologist, I think it is important for early-career GIs to understand the different private practice options and the new challenges and opportunities that private practitioners are experiencing.
According to recent data, there are approximately 12,500 clinical gastroenterologists divided among private gastroenterology practice models, hospital-based employees, and large multispecialty groups. There are nearly 6,000 private practice gastroenterologists.
There has been ongoing dialogue among all health care system stakeholders and the public regarding health care delivery, access, and financing. For the past several years, private practice advocacy groups, including DHPA, have been urging the elimination of the Medicare “site of service” differential between hospital and nonhospital settings, which typically results in substantially higher costs for hospital-based services.
In the 2015 Balanced Budget Act, Congress mandated that patient services provided in off-campus locations acquired by hospitals after Nov.1, 2015, be paid at the nonhospital rate. The 2019 Medicare Outpatient Prospective Payment System/Ambulatory Surgical Center proposed rule takes additional steps in achieving site neutrality and will likely have the effect of tamping down hospitals’ incentives to acquire independent physician practices.
This is a positive step forward in preserving the cost-efficient, high-quality care provided in the independent GI medical setting. And, with the growing health needs of an aging population and an aging GI physician workforce (nearly half of gastroenterologists are older than 55 years old), there is sure to be an ongoing high demand for providers in our specialty.
Selecting the career path that best fits your goals, ambitions, and lifestyle can be challenging. But, our professional training has taught us that the best method for arriving at the correct course of action is to first understand the questions and then seek the answers – let’s get to it.
Private practice models: What are the options?
A lot has changed since I completed my fellowship training in 1978. But the most dramatic changes have happened in the past decade, including the trend of smaller practices consolidating into larger groups.
Traditionally, physicians and patients have favored individual and very-small-group practices. Patients view small-group practices as highly personalized. They come to appreciate knowing all the physicians and staff in a practice. These long-standing “family type” relationships among patients and providers that often develop in this clinical care setting engenders in both the patient and provider a high level of satisfaction with the type and experience of care provided.
New physicians who are part of a small group practice often have the opportunity to take an earlier and more active role within the leadership of the practice. Small groups typically look to new physicians to function as “innovators” who can introduce into the practice those cutting-edge treatments and procedures learned during fellowship.
In the past decade, however, the trend toward the disappearance of solo and very-small-group practices has accelerated. Today, very small groups face several challenges. Providing all the “necessities” that are now part of today’s medical practice can be daunting. Small-sized practices are less likely to integrate ancillary services (e.g., lab and pathology services, in-office infusions, dietary and weight loss management) that are more typically seen in larger practices. Patients may find this fragmentation of care burdensome when they have to go to several providers for treatment.
The difficulties of implementing and maintaining information technology, EHRs, and patient-engagement tools are often inversely related to group size. In addition, the ability and effectiveness of a group to negotiate with hospital systems and insurance companies can be easier for larger practices, although other local factors will also come into play.
Beyond the administrative aspects of running a small group practice, your views about work-life balance should also be an important consideration when choosing a career path. Understandably, issues of call coverage and time off can be more restrictive in small groups.
Is bigger better?
The consolidation seen in hospital systems and multispecialty groups has found its way into single specialty practices. Many urban areas now have GI group practices of 10 or more physicians. There are now approximately 15 groups with 40 or more gastroenterologists, including a few GI practices with 100 or more physicians.
Increasing the size of a practice has obvious potential advantages, including less burdensome on-call requirements and a lower per-physician cost of maintaining and operating the practice. Larger groups often have dedicated software development and IT support staff. Patients are engaged and can connect with their providers through all manner of social media.
Large practice size also can make it possible to enable physicians who may choose to focus on single areas of gastroenterology. This means that a physician who wants to subspecialize in areas such as inflammatory bowel disease, hepatology, woman’s health, and advanced therapeutic endoscopy, would have the requisite large patient base, through internal practice referral, to support subspecialization. Larger groups can also integrate ancillary services into their practice such as pathology, infusion therapy, and nonhospital-based endoscopy services.
However, there can be disadvantages to choosing a larger practice. As in other larger institutions, physicians practicing in larger-sized groups may feel somewhat removed from practice management decisions. It may take several years to become a partner in a large practice – if you are more interested in the opportunity to be involved in practice decisions, a smaller group may be right for you.
New trends in practice groups
Physicians are continuously looking for ways to practice effectively and efficiently while expanding the range of services offered (think obesity management). Independent practice physicians are finding it increasingly difficult to grow and manage successful organizations while they care for their patients. Larger practices now typically include areas such as nursing, information technology, human resources, billing, and practice administration. I trained to treat patients, not run a business – there was much I’ve learned along the way. Many schools now offer joint MD/MBA programs. This may help blend the clinical, operational, and business components of practice.
In a newly developing trend, practice groups are exploring strategic partnerships with private equity/venture capital, practice management companies, national ambulatory surgery center companies, and even managed care insurance companies. This creates the opportunity to forge partnerships with these various health care–focused groups, and results in investment in GI practices seeking experienced business leadership and management while remaining independent of a health system. Already well established in dermatology, ophthalmology, and anesthesia, this phenomenon is now beginning in gastroenterology.
There are many things to consider when choosing a career path. Independent practice in gastroenterology continues as a vitally important component of care delivery, and it’s my hope that the new generation of gastroenterologists finds their journey as rewarding and personally satisfying as mine has been.
Fred B. Rosenberg, MD, is a board-certified gastroenterologist and the medical director of the North Shore Endoscopy Center in Lake Bluff, Ill., the founding president of Illinois Gastroenterology Group, and immediate past president of DHPA.
Editor’s note: It is my pleasure to introduce this new quarterly column in The New Gastroenterologist that will be dedicated to addressing important topics for early-career GIs who are either considering a career or starting a career as an independent GI physician in practice. This column is a collaboration between the AGA’s The New Gastroenterologist and the Digestive Health Physicians Association (DHPA), a national advocacy organization of more than 1,800 gastroenterologists in 79 member practices, which is focused exclusively on policies that promote and protect the high-quality, cost-efficient care provided to patients in the independent GI-practice setting.
Bryson W. Katona, MD, PhD
Editor in Chief, The New Gastroenterologist
Educating and training for your life’s work has likely occupied much of the past 10 years including medical school, residency, and fellowship. When it comes to deciding the next steps, the options can seem daunting.
As a long-standing private practice gastroenterologist, I think it is important for early-career GIs to understand the different private practice options and the new challenges and opportunities that private practitioners are experiencing.
According to recent data, there are approximately 12,500 clinical gastroenterologists divided among private gastroenterology practice models, hospital-based employees, and large multispecialty groups. There are nearly 6,000 private practice gastroenterologists.
There has been ongoing dialogue among all health care system stakeholders and the public regarding health care delivery, access, and financing. For the past several years, private practice advocacy groups, including DHPA, have been urging the elimination of the Medicare “site of service” differential between hospital and nonhospital settings, which typically results in substantially higher costs for hospital-based services.
In the 2015 Balanced Budget Act, Congress mandated that patient services provided in off-campus locations acquired by hospitals after Nov.1, 2015, be paid at the nonhospital rate. The 2019 Medicare Outpatient Prospective Payment System/Ambulatory Surgical Center proposed rule takes additional steps in achieving site neutrality and will likely have the effect of tamping down hospitals’ incentives to acquire independent physician practices.
This is a positive step forward in preserving the cost-efficient, high-quality care provided in the independent GI medical setting. And, with the growing health needs of an aging population and an aging GI physician workforce (nearly half of gastroenterologists are older than 55 years old), there is sure to be an ongoing high demand for providers in our specialty.
Selecting the career path that best fits your goals, ambitions, and lifestyle can be challenging. But, our professional training has taught us that the best method for arriving at the correct course of action is to first understand the questions and then seek the answers – let’s get to it.
Private practice models: What are the options?
A lot has changed since I completed my fellowship training in 1978. But the most dramatic changes have happened in the past decade, including the trend of smaller practices consolidating into larger groups.
Traditionally, physicians and patients have favored individual and very-small-group practices. Patients view small-group practices as highly personalized. They come to appreciate knowing all the physicians and staff in a practice. These long-standing “family type” relationships among patients and providers that often develop in this clinical care setting engenders in both the patient and provider a high level of satisfaction with the type and experience of care provided.
New physicians who are part of a small group practice often have the opportunity to take an earlier and more active role within the leadership of the practice. Small groups typically look to new physicians to function as “innovators” who can introduce into the practice those cutting-edge treatments and procedures learned during fellowship.
In the past decade, however, the trend toward the disappearance of solo and very-small-group practices has accelerated. Today, very small groups face several challenges. Providing all the “necessities” that are now part of today’s medical practice can be daunting. Small-sized practices are less likely to integrate ancillary services (e.g., lab and pathology services, in-office infusions, dietary and weight loss management) that are more typically seen in larger practices. Patients may find this fragmentation of care burdensome when they have to go to several providers for treatment.
The difficulties of implementing and maintaining information technology, EHRs, and patient-engagement tools are often inversely related to group size. In addition, the ability and effectiveness of a group to negotiate with hospital systems and insurance companies can be easier for larger practices, although other local factors will also come into play.
Beyond the administrative aspects of running a small group practice, your views about work-life balance should also be an important consideration when choosing a career path. Understandably, issues of call coverage and time off can be more restrictive in small groups.
Is bigger better?
The consolidation seen in hospital systems and multispecialty groups has found its way into single specialty practices. Many urban areas now have GI group practices of 10 or more physicians. There are now approximately 15 groups with 40 or more gastroenterologists, including a few GI practices with 100 or more physicians.
Increasing the size of a practice has obvious potential advantages, including less burdensome on-call requirements and a lower per-physician cost of maintaining and operating the practice. Larger groups often have dedicated software development and IT support staff. Patients are engaged and can connect with their providers through all manner of social media.
Large practice size also can make it possible to enable physicians who may choose to focus on single areas of gastroenterology. This means that a physician who wants to subspecialize in areas such as inflammatory bowel disease, hepatology, woman’s health, and advanced therapeutic endoscopy, would have the requisite large patient base, through internal practice referral, to support subspecialization. Larger groups can also integrate ancillary services into their practice such as pathology, infusion therapy, and nonhospital-based endoscopy services.
However, there can be disadvantages to choosing a larger practice. As in other larger institutions, physicians practicing in larger-sized groups may feel somewhat removed from practice management decisions. It may take several years to become a partner in a large practice – if you are more interested in the opportunity to be involved in practice decisions, a smaller group may be right for you.
New trends in practice groups
Physicians are continuously looking for ways to practice effectively and efficiently while expanding the range of services offered (think obesity management). Independent practice physicians are finding it increasingly difficult to grow and manage successful organizations while they care for their patients. Larger practices now typically include areas such as nursing, information technology, human resources, billing, and practice administration. I trained to treat patients, not run a business – there was much I’ve learned along the way. Many schools now offer joint MD/MBA programs. This may help blend the clinical, operational, and business components of practice.
In a newly developing trend, practice groups are exploring strategic partnerships with private equity/venture capital, practice management companies, national ambulatory surgery center companies, and even managed care insurance companies. This creates the opportunity to forge partnerships with these various health care–focused groups, and results in investment in GI practices seeking experienced business leadership and management while remaining independent of a health system. Already well established in dermatology, ophthalmology, and anesthesia, this phenomenon is now beginning in gastroenterology.
There are many things to consider when choosing a career path. Independent practice in gastroenterology continues as a vitally important component of care delivery, and it’s my hope that the new generation of gastroenterologists finds their journey as rewarding and personally satisfying as mine has been.
Fred B. Rosenberg, MD, is a board-certified gastroenterologist and the medical director of the North Shore Endoscopy Center in Lake Bluff, Ill., the founding president of Illinois Gastroenterology Group, and immediate past president of DHPA.
Editor’s note: It is my pleasure to introduce this new quarterly column in The New Gastroenterologist that will be dedicated to addressing important topics for early-career GIs who are either considering a career or starting a career as an independent GI physician in practice. This column is a collaboration between the AGA’s The New Gastroenterologist and the Digestive Health Physicians Association (DHPA), a national advocacy organization of more than 1,800 gastroenterologists in 79 member practices, which is focused exclusively on policies that promote and protect the high-quality, cost-efficient care provided to patients in the independent GI-practice setting.
Bryson W. Katona, MD, PhD
Editor in Chief, The New Gastroenterologist
Educating and training for your life’s work has likely occupied much of the past 10 years including medical school, residency, and fellowship. When it comes to deciding the next steps, the options can seem daunting.
As a long-standing private practice gastroenterologist, I think it is important for early-career GIs to understand the different private practice options and the new challenges and opportunities that private practitioners are experiencing.
According to recent data, there are approximately 12,500 clinical gastroenterologists divided among private gastroenterology practice models, hospital-based employees, and large multispecialty groups. There are nearly 6,000 private practice gastroenterologists.
There has been ongoing dialogue among all health care system stakeholders and the public regarding health care delivery, access, and financing. For the past several years, private practice advocacy groups, including DHPA, have been urging the elimination of the Medicare “site of service” differential between hospital and nonhospital settings, which typically results in substantially higher costs for hospital-based services.
In the 2015 Balanced Budget Act, Congress mandated that patient services provided in off-campus locations acquired by hospitals after Nov.1, 2015, be paid at the nonhospital rate. The 2019 Medicare Outpatient Prospective Payment System/Ambulatory Surgical Center proposed rule takes additional steps in achieving site neutrality and will likely have the effect of tamping down hospitals’ incentives to acquire independent physician practices.
This is a positive step forward in preserving the cost-efficient, high-quality care provided in the independent GI medical setting. And, with the growing health needs of an aging population and an aging GI physician workforce (nearly half of gastroenterologists are older than 55 years old), there is sure to be an ongoing high demand for providers in our specialty.
Selecting the career path that best fits your goals, ambitions, and lifestyle can be challenging. But, our professional training has taught us that the best method for arriving at the correct course of action is to first understand the questions and then seek the answers – let’s get to it.
Private practice models: What are the options?
A lot has changed since I completed my fellowship training in 1978. But the most dramatic changes have happened in the past decade, including the trend of smaller practices consolidating into larger groups.
Traditionally, physicians and patients have favored individual and very-small-group practices. Patients view small-group practices as highly personalized. They come to appreciate knowing all the physicians and staff in a practice. These long-standing “family type” relationships among patients and providers that often develop in this clinical care setting engenders in both the patient and provider a high level of satisfaction with the type and experience of care provided.
New physicians who are part of a small group practice often have the opportunity to take an earlier and more active role within the leadership of the practice. Small groups typically look to new physicians to function as “innovators” who can introduce into the practice those cutting-edge treatments and procedures learned during fellowship.
In the past decade, however, the trend toward the disappearance of solo and very-small-group practices has accelerated. Today, very small groups face several challenges. Providing all the “necessities” that are now part of today’s medical practice can be daunting. Small-sized practices are less likely to integrate ancillary services (e.g., lab and pathology services, in-office infusions, dietary and weight loss management) that are more typically seen in larger practices. Patients may find this fragmentation of care burdensome when they have to go to several providers for treatment.
The difficulties of implementing and maintaining information technology, EHRs, and patient-engagement tools are often inversely related to group size. In addition, the ability and effectiveness of a group to negotiate with hospital systems and insurance companies can be easier for larger practices, although other local factors will also come into play.
Beyond the administrative aspects of running a small group practice, your views about work-life balance should also be an important consideration when choosing a career path. Understandably, issues of call coverage and time off can be more restrictive in small groups.
Is bigger better?
The consolidation seen in hospital systems and multispecialty groups has found its way into single specialty practices. Many urban areas now have GI group practices of 10 or more physicians. There are now approximately 15 groups with 40 or more gastroenterologists, including a few GI practices with 100 or more physicians.
Increasing the size of a practice has obvious potential advantages, including less burdensome on-call requirements and a lower per-physician cost of maintaining and operating the practice. Larger groups often have dedicated software development and IT support staff. Patients are engaged and can connect with their providers through all manner of social media.
Large practice size also can make it possible to enable physicians who may choose to focus on single areas of gastroenterology. This means that a physician who wants to subspecialize in areas such as inflammatory bowel disease, hepatology, woman’s health, and advanced therapeutic endoscopy, would have the requisite large patient base, through internal practice referral, to support subspecialization. Larger groups can also integrate ancillary services into their practice such as pathology, infusion therapy, and nonhospital-based endoscopy services.
However, there can be disadvantages to choosing a larger practice. As in other larger institutions, physicians practicing in larger-sized groups may feel somewhat removed from practice management decisions. It may take several years to become a partner in a large practice – if you are more interested in the opportunity to be involved in practice decisions, a smaller group may be right for you.
New trends in practice groups
Physicians are continuously looking for ways to practice effectively and efficiently while expanding the range of services offered (think obesity management). Independent practice physicians are finding it increasingly difficult to grow and manage successful organizations while they care for their patients. Larger practices now typically include areas such as nursing, information technology, human resources, billing, and practice administration. I trained to treat patients, not run a business – there was much I’ve learned along the way. Many schools now offer joint MD/MBA programs. This may help blend the clinical, operational, and business components of practice.
In a newly developing trend, practice groups are exploring strategic partnerships with private equity/venture capital, practice management companies, national ambulatory surgery center companies, and even managed care insurance companies. This creates the opportunity to forge partnerships with these various health care–focused groups, and results in investment in GI practices seeking experienced business leadership and management while remaining independent of a health system. Already well established in dermatology, ophthalmology, and anesthesia, this phenomenon is now beginning in gastroenterology.
There are many things to consider when choosing a career path. Independent practice in gastroenterology continues as a vitally important component of care delivery, and it’s my hope that the new generation of gastroenterologists finds their journey as rewarding and personally satisfying as mine has been.
Fred B. Rosenberg, MD, is a board-certified gastroenterologist and the medical director of the North Shore Endoscopy Center in Lake Bluff, Ill., the founding president of Illinois Gastroenterology Group, and immediate past president of DHPA.
Calendar
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Dec. 10-11, 12-13, 2018; Jan. 16-17, 22-23, 23-24, 2019; Feb. 20-21, 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc
.Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Tampa, FL (12/10-11), Dallas, TX (12/12-13), Houston, TX (1/16-17), New Orleans, LA (1/22-23), Pittsburgh, PA (1/23-24), 2/20 (Hartford, CT)
Jan. 17-19, 2019
2019 GI Cancers Symposium
Join colleagues from across the globe in San Francisco to discover and share groundbreaking research in treating gastrointestinal cancers.
San Francisco, CA
Feb. 7–9, 2019
Crohn’s & Colitis Congress™ (A Partnership of the Crohn’s & Colitis Foundation and American Gastroenterological Association)
Expand your knowledge, network with IBD leaders, spark innovative research and get inspired to improve patient care.
Las Vegas, NV
March 8-9, 2019
2019 Women’s Leadership Conference
The conference is specifically designed for women looking to advance their careers, further professional goals, enhance personal growth and effectively network.
Bethesda, MD
March 8-10, 2019
FORWARD Program
AGA’s Fostering Opportunities Resulting in Workforce and Research Diversity (FORWARD) Program is a new initiative funded by NIH, supporting the career entry and development for underrepresented minority physician scientists in gastroenterology. The program provides concrete leadership and skill development that includes scientific manuscript and grant writing, research development, executive coaching and more.
Bethesda, MD
March 8-10, 2019
Future Leaders Program
The Future Leaders Program provides a pathway within the organization to network, connect with mentors, develop leadership skills and learn about AGA’s governance and operations while advancing your career and supporting the profession.
Bethesda, MD
March 23–24, 2019
2019 Gut Microbiota for Health World Summit
The 2019 program will present the latest evidence on the interaction between diet, nutrition and the gut microbiome. Learn how diet and nutrition are being used in concert with traditional therapies to manage GI disorders.
Miami, FL
May 18-21, 2019
Digestive Disease Week (DDW)®
DDW® is the world’s leading educational forum for academicians, clinicians, researchers, students and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery and related fields. Whether you work in patient care, research, education or administration, the DDW program offers something for you. DDW is co-sponsored by AGA, AASLD, ASGE and SSAT.
San Diego, CA
AWARDS APPLICATION DEADLINES
AGA-Rady Children’s Institute for Genomic Medicine Research Scholar Award in Pediatric Genomics
This award provides $90,000 per year for three years (totaling $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in gastroenterology, hepatology or related areas. The proposed research may be basic, translational or clinical and must use genomics as an approach to enhance understanding of pediatric digestive diseases toward prevention, treatment and/or cure of such diseases. The funded research must be conducted full-time at the Rady Children’s Institute for Genomic Medicine in San Diego, California, or at Rady Children’s Hospital – San Diego.
Application Deadline: Dec. 14, 2018
AGA-Bern Schwartz Family Fund Research Scholar Award in Pancreatic Cancer
This award provides $100,000 per year for three years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in pancreatic cancer research.
Application Deadline: Dec. 14, 2018
AGA Research Scholar Award (RSA)
This award provides $90,000 per year for three years (total $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in gastroenterology, hepatology or related areas.
Application Deadline: Dec. 14, 2018
AGA-Shire Research Scholar Award in Functional GI and Motility Disorders
This award provides $90,000 per year for three years (total $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in functional GI and motility disorders research.
Application Deadline: Dec. 14, 2018
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $90,000 per year for three years (total $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Dec. 14, 2018
AGA Fellow Abstract Award
This travel award provides nine $500 and one $1,000 prize to recipients who are MD, PhD or equivalent fellows presenting posters/oral sessions at Digestive Disease Week® (DDW).
Application Deadline: Feb. 15, 2019
AGA Moti L. & Kamla Rustgi International Travel Awards
This travel award provides two $750 prizes to recipients who are young basic, translational or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 15, 2019
AGA Student Abstract Award
This travel award provides nine $500 and one $1,000 prize to recipients who are high school, undergraduate, graduate, or medical students or residents (residents up to year three postgraduate) presenting posters/oral sessions at Digestive Disease Week® (DDW).
Application Deadline: Feb. 15, 2019
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Dec. 10-11, 12-13, 2018; Jan. 16-17, 22-23, 23-24, 2019; Feb. 20-21, 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc
.Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Tampa, FL (12/10-11), Dallas, TX (12/12-13), Houston, TX (1/16-17), New Orleans, LA (1/22-23), Pittsburgh, PA (1/23-24), 2/20 (Hartford, CT)
Jan. 17-19, 2019
2019 GI Cancers Symposium
Join colleagues from across the globe in San Francisco to discover and share groundbreaking research in treating gastrointestinal cancers.
San Francisco, CA
Feb. 7–9, 2019
Crohn’s & Colitis Congress™ (A Partnership of the Crohn’s & Colitis Foundation and American Gastroenterological Association)
Expand your knowledge, network with IBD leaders, spark innovative research and get inspired to improve patient care.
Las Vegas, NV
March 8-9, 2019
2019 Women’s Leadership Conference
The conference is specifically designed for women looking to advance their careers, further professional goals, enhance personal growth and effectively network.
Bethesda, MD
March 8-10, 2019
FORWARD Program
AGA’s Fostering Opportunities Resulting in Workforce and Research Diversity (FORWARD) Program is a new initiative funded by NIH, supporting the career entry and development for underrepresented minority physician scientists in gastroenterology. The program provides concrete leadership and skill development that includes scientific manuscript and grant writing, research development, executive coaching and more.
Bethesda, MD
March 8-10, 2019
Future Leaders Program
The Future Leaders Program provides a pathway within the organization to network, connect with mentors, develop leadership skills and learn about AGA’s governance and operations while advancing your career and supporting the profession.
Bethesda, MD
March 23–24, 2019
2019 Gut Microbiota for Health World Summit
The 2019 program will present the latest evidence on the interaction between diet, nutrition and the gut microbiome. Learn how diet and nutrition are being used in concert with traditional therapies to manage GI disorders.
Miami, FL
May 18-21, 2019
Digestive Disease Week (DDW)®
DDW® is the world’s leading educational forum for academicians, clinicians, researchers, students and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery and related fields. Whether you work in patient care, research, education or administration, the DDW program offers something for you. DDW is co-sponsored by AGA, AASLD, ASGE and SSAT.
San Diego, CA
AWARDS APPLICATION DEADLINES
AGA-Rady Children’s Institute for Genomic Medicine Research Scholar Award in Pediatric Genomics
This award provides $90,000 per year for three years (totaling $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in gastroenterology, hepatology or related areas. The proposed research may be basic, translational or clinical and must use genomics as an approach to enhance understanding of pediatric digestive diseases toward prevention, treatment and/or cure of such diseases. The funded research must be conducted full-time at the Rady Children’s Institute for Genomic Medicine in San Diego, California, or at Rady Children’s Hospital – San Diego.
Application Deadline: Dec. 14, 2018
AGA-Bern Schwartz Family Fund Research Scholar Award in Pancreatic Cancer
This award provides $100,000 per year for three years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in pancreatic cancer research.
Application Deadline: Dec. 14, 2018
AGA Research Scholar Award (RSA)
This award provides $90,000 per year for three years (total $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in gastroenterology, hepatology or related areas.
Application Deadline: Dec. 14, 2018
AGA-Shire Research Scholar Award in Functional GI and Motility Disorders
This award provides $90,000 per year for three years (total $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in functional GI and motility disorders research.
Application Deadline: Dec. 14, 2018
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $90,000 per year for three years (total $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Dec. 14, 2018
AGA Fellow Abstract Award
This travel award provides nine $500 and one $1,000 prize to recipients who are MD, PhD or equivalent fellows presenting posters/oral sessions at Digestive Disease Week® (DDW).
Application Deadline: Feb. 15, 2019
AGA Moti L. & Kamla Rustgi International Travel Awards
This travel award provides two $750 prizes to recipients who are young basic, translational or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 15, 2019
AGA Student Abstract Award
This travel award provides nine $500 and one $1,000 prize to recipients who are high school, undergraduate, graduate, or medical students or residents (residents up to year three postgraduate) presenting posters/oral sessions at Digestive Disease Week® (DDW).
Application Deadline: Feb. 15, 2019
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Dec. 10-11, 12-13, 2018; Jan. 16-17, 22-23, 23-24, 2019; Feb. 20-21, 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc
.Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Tampa, FL (12/10-11), Dallas, TX (12/12-13), Houston, TX (1/16-17), New Orleans, LA (1/22-23), Pittsburgh, PA (1/23-24), 2/20 (Hartford, CT)
Jan. 17-19, 2019
2019 GI Cancers Symposium
Join colleagues from across the globe in San Francisco to discover and share groundbreaking research in treating gastrointestinal cancers.
San Francisco, CA
Feb. 7–9, 2019
Crohn’s & Colitis Congress™ (A Partnership of the Crohn’s & Colitis Foundation and American Gastroenterological Association)
Expand your knowledge, network with IBD leaders, spark innovative research and get inspired to improve patient care.
Las Vegas, NV
March 8-9, 2019
2019 Women’s Leadership Conference
The conference is specifically designed for women looking to advance their careers, further professional goals, enhance personal growth and effectively network.
Bethesda, MD
March 8-10, 2019
FORWARD Program
AGA’s Fostering Opportunities Resulting in Workforce and Research Diversity (FORWARD) Program is a new initiative funded by NIH, supporting the career entry and development for underrepresented minority physician scientists in gastroenterology. The program provides concrete leadership and skill development that includes scientific manuscript and grant writing, research development, executive coaching and more.
Bethesda, MD
March 8-10, 2019
Future Leaders Program
The Future Leaders Program provides a pathway within the organization to network, connect with mentors, develop leadership skills and learn about AGA’s governance and operations while advancing your career and supporting the profession.
Bethesda, MD
March 23–24, 2019
2019 Gut Microbiota for Health World Summit
The 2019 program will present the latest evidence on the interaction between diet, nutrition and the gut microbiome. Learn how diet and nutrition are being used in concert with traditional therapies to manage GI disorders.
Miami, FL
May 18-21, 2019
Digestive Disease Week (DDW)®
DDW® is the world’s leading educational forum for academicians, clinicians, researchers, students and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery and related fields. Whether you work in patient care, research, education or administration, the DDW program offers something for you. DDW is co-sponsored by AGA, AASLD, ASGE and SSAT.
San Diego, CA
AWARDS APPLICATION DEADLINES
AGA-Rady Children’s Institute for Genomic Medicine Research Scholar Award in Pediatric Genomics
This award provides $90,000 per year for three years (totaling $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in gastroenterology, hepatology or related areas. The proposed research may be basic, translational or clinical and must use genomics as an approach to enhance understanding of pediatric digestive diseases toward prevention, treatment and/or cure of such diseases. The funded research must be conducted full-time at the Rady Children’s Institute for Genomic Medicine in San Diego, California, or at Rady Children’s Hospital – San Diego.
Application Deadline: Dec. 14, 2018
AGA-Bern Schwartz Family Fund Research Scholar Award in Pancreatic Cancer
This award provides $100,000 per year for three years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in pancreatic cancer research.
Application Deadline: Dec. 14, 2018
AGA Research Scholar Award (RSA)
This award provides $90,000 per year for three years (total $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in gastroenterology, hepatology or related areas.
Application Deadline: Dec. 14, 2018
AGA-Shire Research Scholar Award in Functional GI and Motility Disorders
This award provides $90,000 per year for three years (total $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in functional GI and motility disorders research.
Application Deadline: Dec. 14, 2018
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $90,000 per year for three years (total $270,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Dec. 14, 2018
AGA Fellow Abstract Award
This travel award provides nine $500 and one $1,000 prize to recipients who are MD, PhD or equivalent fellows presenting posters/oral sessions at Digestive Disease Week® (DDW).
Application Deadline: Feb. 15, 2019
AGA Moti L. & Kamla Rustgi International Travel Awards
This travel award provides two $750 prizes to recipients who are young basic, translational or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 15, 2019
AGA Student Abstract Award
This travel award provides nine $500 and one $1,000 prize to recipients who are high school, undergraduate, graduate, or medical students or residents (residents up to year three postgraduate) presenting posters/oral sessions at Digestive Disease Week® (DDW).
Application Deadline: Feb. 15, 2019
Don’t let the mortgage preapproval process give you a stomachache
You are trying to buy your first home. Maybe you have heard stories from family, friends, and colleagues about nightmare scenarios when purchasing a home. There are many facets to the home-financing process, and a little bit of planning can reduce a significant amount of time and stress. Where do you begin? What do lenders look for when preapproving a borrower? What steps do I take to get preapproved for a mortgage loan? This article will help guide you through these initial stages to ultimately guide you to settlement on your new home.
Where to begin?
- Start by drafting a budget. How much of a monthly housing payment can you afford? Planning a budget is an extremely valuable exercise at any point in life, not just when buying a home. Often, borrowers will ask the question “How much can I afford?” The better question to ask is “Can I qualify for a home that meets the maximum monthly payment I have budgeted for?”
- What funds would I use for purchasing a home? Down payments and closing costs can add up quickly. Do you have funds readily available in an account you hold? Will you be obtaining a gift from a family member? Generally, funds for down payment are not allowed to be borrowed, unless the money is coming from an account secured by your own assets (for instance, borrowing from your own retirement account). Don’t think you necessarily need to put 20% down. Some loan programs offer little or no down payment options, while other programs may offer down payment assistance options.
- If you are not aware of your credit standing, run a free credit report to verify accurate information. Federal law allows consumers to access one free credit report annually with each of the three credit bureaus (Equifax, Experian, TransUnion). Knowing your credit history and data on your credit report is very important. If there are known or unknown issues on your credit report, it’s always best to at least be informed. You can access your free report at www.annualcreditreport.com.
- Start planning ahead with some of the documentation you will need for a loan approval. Lenders will request items such as tax returns and W-2s from the past 2 years, your recent pay stubs covering a 30-day period, most recent 2 months asset account statements (bank accounts, investment accounts, retirement accounts, etc.), as well as other documentation, depending on your specific scenario.
What are lenders looking at when preapproving an applicant?
Many people will often start to search for homes without having prepared for the preapproval process. This is not necessarily an issue and it doesn’t mean you will not be preapproved. Planning ahead could help you avoid any unforeseen problems and avoid rushing into the mortgage application process when trying to place an offer on a home.
In addition to supplying information on residence and employment/student history for the past 2 years, there are three primary components to a borrower’s credit portfolio:
1) Debt-to-income ratio: What monthly expenses will show on your credit report (car loans/leases, student loans, credit card payments, personal loans/lines of credit, and mortgages for other properties owned)? Do you own any other real estate? Do you have other required obligations, such as alimony or child support payments? To calculate, first combine these liabilities on a monthly expense basis along with the new proposed monthly housing payment. Take these monthly liabilities and divide by monthly income. Gross income (pretax) for employees of a company they do not own is typically utilized (bonus or commission income can have some alternate rules to be allowed as qualifying income); for self-employed borrowers, tax returns will be required to be reviewed; tax write offs could reduce qualifying income. Self-employed individuals will typically need to show a 2-year income history via personal tax returns (as well as business tax returns if applicable). See Figure 1 for an example of a debt-to-income ratio calculation. Many loan programs will require a debt-to-income ratio of 45% or less. There are various loan programs that will be more or less restrictive than this percentage. A lender will be able to guide you to the proper program for your scenario.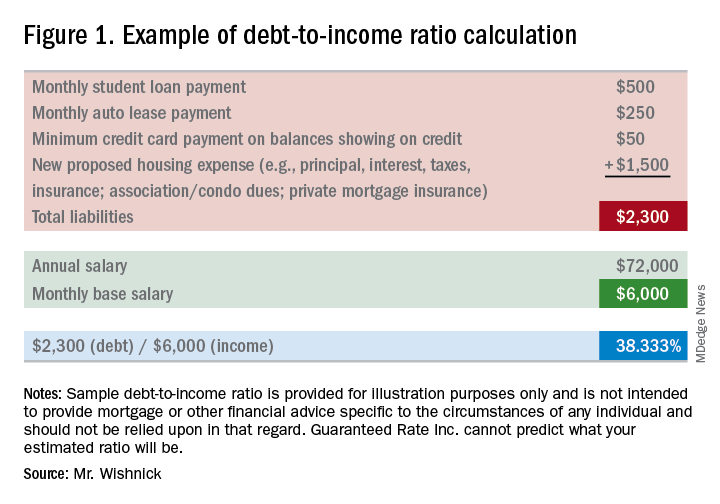
2) Liquid assets: Lenders will review the amount of liquid funds you have available for down payment, closing costs, and any necessary reserves. These may include, but are not limited to, checking/savings/money market accounts, investment accounts (stocks, bonds, mutual funds), and retirement funds. Are there enough allowable funds available for the down payment and closing costs, as well as any required reserves needed for qualification? Large non–payroll deposits can be required to be sourced to make sure the funds are from an allowable source.
3) Credit history/scores: Buying a home will be one of the largest purchases you will make in a lifetime. Credit scores have a major impact on the cost of credit (the interest rate you will obtain). Having higher scores could result in a lower interest rate, as well as open up certain loan programs that may be more advantageous for you. Oftentimes, lenders will take the middle of the three scores as your mortgage score (one score from each of the three credit bureaus). In most cases, if applying jointly, the lowest of the middle scores for all borrowers is the score that is used as the score for the applicants. In general, a 740 middle credit score is considered to be excellent for mortgage financing but is not a requirement for all programs.
**You may have heard about specific mortgage programs for physicians. These programs are intended for use for lesser down payments, and/or not calculating student loan payments when qualifying for home financing. As future income potential is typically not considered when determining debt-to-income ratios, not counting these liabilities potentially increases borrowing power.
You are now ready to be preapproved for mortgage financing. What should you do next?
- Talk to a trusted lender. Ask your real estate agent, family, friends, or colleagues for local lender recommendations. Real estate agents will want to make sure you have spoken with a lender and completed a preapproval application to ensure that you can be preapproved for financing before showing you homes. If you need a loan to purchase a home, a preapproval letter will be required to submit with an offer letter. The application contains questions such as your address and employment history for the past 2 years, income and asset information, as well as a series of other financial information. A hard credit inquiry will need to be performed in order for the lender to issue a preapproval. What should you expect from a lender in addition to competitive rates and an array of programs? Some people prefer more of a hands-on approach. Working with a lender who provides regular status updates and makes him/herself easily accessible for all of your questions can certainly be an attractive feature. Working with a local lender also may be reassuring, as he or she should have plenty of experience with the market in which you are purchasing.
- Search for homes. Upon being given the green light for your preapproval and a price range within your comfort zone, connect with your local real estate professional to search for homes. Plan to spend time with your agent discussing all your needs for your new home.
- Submit an offer. Your lender will be able to provide an estimate of closing costs and monthly payments for homes that you are considering buying before you make an offer. You will want to be sure you are comfortable with the financial obligation prior to making your offer. With your offer, an initial good faith deposit (earnest money deposit) will be required. Your real estate agent will guide you on the proper amount of the deposit.
Conclusion
Once you and the seller have come to terms, you will look to discuss with your lender the rate and program options to secure (locking in an interest rate and program), as well as to complete the formal mortgage application. The lender will request additional documentation, if you have not already provided documents, in order for you to obtain a conditional mortgage commitment. The lender also will order an appraisal to ensure the property value supports the price you have agreed to pay for it. Your real estate agent will guide you through the various deadlines and requirements in the contract for items like home inspections, ordering a title search to obtain title insurance, and other nonfinancing contingencies. Some areas may require attorneys for contract review and closing, which your agent will discuss with you. As you can see, buying a home is not an instant process. Taking the appropriate steps to prepare for your mortgage preapproval could save you a lot of time and stress.
Mr. Wishnick is a 15-year mortgage industry veteran, vice president of mortgage lending with Guaranteed Rate (NMLS #2611) and was ranked as a Top 1% mortgage originator by Mortgage Executive Magazine. He can be reached at [email protected].
All information provided in this publication is for informational and educational purposes only, and in no way is any of the content contained herein to be construed as financial, investment, or legal advice or instruction. Guaranteed Rate does not guarantee the quality, accuracy, completeness or timelines of the information in this publication.
You are trying to buy your first home. Maybe you have heard stories from family, friends, and colleagues about nightmare scenarios when purchasing a home. There are many facets to the home-financing process, and a little bit of planning can reduce a significant amount of time and stress. Where do you begin? What do lenders look for when preapproving a borrower? What steps do I take to get preapproved for a mortgage loan? This article will help guide you through these initial stages to ultimately guide you to settlement on your new home.
Where to begin?
- Start by drafting a budget. How much of a monthly housing payment can you afford? Planning a budget is an extremely valuable exercise at any point in life, not just when buying a home. Often, borrowers will ask the question “How much can I afford?” The better question to ask is “Can I qualify for a home that meets the maximum monthly payment I have budgeted for?”
- What funds would I use for purchasing a home? Down payments and closing costs can add up quickly. Do you have funds readily available in an account you hold? Will you be obtaining a gift from a family member? Generally, funds for down payment are not allowed to be borrowed, unless the money is coming from an account secured by your own assets (for instance, borrowing from your own retirement account). Don’t think you necessarily need to put 20% down. Some loan programs offer little or no down payment options, while other programs may offer down payment assistance options.
- If you are not aware of your credit standing, run a free credit report to verify accurate information. Federal law allows consumers to access one free credit report annually with each of the three credit bureaus (Equifax, Experian, TransUnion). Knowing your credit history and data on your credit report is very important. If there are known or unknown issues on your credit report, it’s always best to at least be informed. You can access your free report at www.annualcreditreport.com.
- Start planning ahead with some of the documentation you will need for a loan approval. Lenders will request items such as tax returns and W-2s from the past 2 years, your recent pay stubs covering a 30-day period, most recent 2 months asset account statements (bank accounts, investment accounts, retirement accounts, etc.), as well as other documentation, depending on your specific scenario.
What are lenders looking at when preapproving an applicant?
Many people will often start to search for homes without having prepared for the preapproval process. This is not necessarily an issue and it doesn’t mean you will not be preapproved. Planning ahead could help you avoid any unforeseen problems and avoid rushing into the mortgage application process when trying to place an offer on a home.
In addition to supplying information on residence and employment/student history for the past 2 years, there are three primary components to a borrower’s credit portfolio:
1) Debt-to-income ratio: What monthly expenses will show on your credit report (car loans/leases, student loans, credit card payments, personal loans/lines of credit, and mortgages for other properties owned)? Do you own any other real estate? Do you have other required obligations, such as alimony or child support payments? To calculate, first combine these liabilities on a monthly expense basis along with the new proposed monthly housing payment. Take these monthly liabilities and divide by monthly income. Gross income (pretax) for employees of a company they do not own is typically utilized (bonus or commission income can have some alternate rules to be allowed as qualifying income); for self-employed borrowers, tax returns will be required to be reviewed; tax write offs could reduce qualifying income. Self-employed individuals will typically need to show a 2-year income history via personal tax returns (as well as business tax returns if applicable). See Figure 1 for an example of a debt-to-income ratio calculation. Many loan programs will require a debt-to-income ratio of 45% or less. There are various loan programs that will be more or less restrictive than this percentage. A lender will be able to guide you to the proper program for your scenario.
2) Liquid assets: Lenders will review the amount of liquid funds you have available for down payment, closing costs, and any necessary reserves. These may include, but are not limited to, checking/savings/money market accounts, investment accounts (stocks, bonds, mutual funds), and retirement funds. Are there enough allowable funds available for the down payment and closing costs, as well as any required reserves needed for qualification? Large non–payroll deposits can be required to be sourced to make sure the funds are from an allowable source.
3) Credit history/scores: Buying a home will be one of the largest purchases you will make in a lifetime. Credit scores have a major impact on the cost of credit (the interest rate you will obtain). Having higher scores could result in a lower interest rate, as well as open up certain loan programs that may be more advantageous for you. Oftentimes, lenders will take the middle of the three scores as your mortgage score (one score from each of the three credit bureaus). In most cases, if applying jointly, the lowest of the middle scores for all borrowers is the score that is used as the score for the applicants. In general, a 740 middle credit score is considered to be excellent for mortgage financing but is not a requirement for all programs.
**You may have heard about specific mortgage programs for physicians. These programs are intended for use for lesser down payments, and/or not calculating student loan payments when qualifying for home financing. As future income potential is typically not considered when determining debt-to-income ratios, not counting these liabilities potentially increases borrowing power.
You are now ready to be preapproved for mortgage financing. What should you do next?
- Talk to a trusted lender. Ask your real estate agent, family, friends, or colleagues for local lender recommendations. Real estate agents will want to make sure you have spoken with a lender and completed a preapproval application to ensure that you can be preapproved for financing before showing you homes. If you need a loan to purchase a home, a preapproval letter will be required to submit with an offer letter. The application contains questions such as your address and employment history for the past 2 years, income and asset information, as well as a series of other financial information. A hard credit inquiry will need to be performed in order for the lender to issue a preapproval. What should you expect from a lender in addition to competitive rates and an array of programs? Some people prefer more of a hands-on approach. Working with a lender who provides regular status updates and makes him/herself easily accessible for all of your questions can certainly be an attractive feature. Working with a local lender also may be reassuring, as he or she should have plenty of experience with the market in which you are purchasing.
- Search for homes. Upon being given the green light for your preapproval and a price range within your comfort zone, connect with your local real estate professional to search for homes. Plan to spend time with your agent discussing all your needs for your new home.
- Submit an offer. Your lender will be able to provide an estimate of closing costs and monthly payments for homes that you are considering buying before you make an offer. You will want to be sure you are comfortable with the financial obligation prior to making your offer. With your offer, an initial good faith deposit (earnest money deposit) will be required. Your real estate agent will guide you on the proper amount of the deposit.
Conclusion
Once you and the seller have come to terms, you will look to discuss with your lender the rate and program options to secure (locking in an interest rate and program), as well as to complete the formal mortgage application. The lender will request additional documentation, if you have not already provided documents, in order for you to obtain a conditional mortgage commitment. The lender also will order an appraisal to ensure the property value supports the price you have agreed to pay for it. Your real estate agent will guide you through the various deadlines and requirements in the contract for items like home inspections, ordering a title search to obtain title insurance, and other nonfinancing contingencies. Some areas may require attorneys for contract review and closing, which your agent will discuss with you. As you can see, buying a home is not an instant process. Taking the appropriate steps to prepare for your mortgage preapproval could save you a lot of time and stress.
Mr. Wishnick is a 15-year mortgage industry veteran, vice president of mortgage lending with Guaranteed Rate (NMLS #2611) and was ranked as a Top 1% mortgage originator by Mortgage Executive Magazine. He can be reached at [email protected].
All information provided in this publication is for informational and educational purposes only, and in no way is any of the content contained herein to be construed as financial, investment, or legal advice or instruction. Guaranteed Rate does not guarantee the quality, accuracy, completeness or timelines of the information in this publication.
You are trying to buy your first home. Maybe you have heard stories from family, friends, and colleagues about nightmare scenarios when purchasing a home. There are many facets to the home-financing process, and a little bit of planning can reduce a significant amount of time and stress. Where do you begin? What do lenders look for when preapproving a borrower? What steps do I take to get preapproved for a mortgage loan? This article will help guide you through these initial stages to ultimately guide you to settlement on your new home.
Where to begin?
- Start by drafting a budget. How much of a monthly housing payment can you afford? Planning a budget is an extremely valuable exercise at any point in life, not just when buying a home. Often, borrowers will ask the question “How much can I afford?” The better question to ask is “Can I qualify for a home that meets the maximum monthly payment I have budgeted for?”
- What funds would I use for purchasing a home? Down payments and closing costs can add up quickly. Do you have funds readily available in an account you hold? Will you be obtaining a gift from a family member? Generally, funds for down payment are not allowed to be borrowed, unless the money is coming from an account secured by your own assets (for instance, borrowing from your own retirement account). Don’t think you necessarily need to put 20% down. Some loan programs offer little or no down payment options, while other programs may offer down payment assistance options.
- If you are not aware of your credit standing, run a free credit report to verify accurate information. Federal law allows consumers to access one free credit report annually with each of the three credit bureaus (Equifax, Experian, TransUnion). Knowing your credit history and data on your credit report is very important. If there are known or unknown issues on your credit report, it’s always best to at least be informed. You can access your free report at www.annualcreditreport.com.
- Start planning ahead with some of the documentation you will need for a loan approval. Lenders will request items such as tax returns and W-2s from the past 2 years, your recent pay stubs covering a 30-day period, most recent 2 months asset account statements (bank accounts, investment accounts, retirement accounts, etc.), as well as other documentation, depending on your specific scenario.
What are lenders looking at when preapproving an applicant?
Many people will often start to search for homes without having prepared for the preapproval process. This is not necessarily an issue and it doesn’t mean you will not be preapproved. Planning ahead could help you avoid any unforeseen problems and avoid rushing into the mortgage application process when trying to place an offer on a home.
In addition to supplying information on residence and employment/student history for the past 2 years, there are three primary components to a borrower’s credit portfolio:
1) Debt-to-income ratio: What monthly expenses will show on your credit report (car loans/leases, student loans, credit card payments, personal loans/lines of credit, and mortgages for other properties owned)? Do you own any other real estate? Do you have other required obligations, such as alimony or child support payments? To calculate, first combine these liabilities on a monthly expense basis along with the new proposed monthly housing payment. Take these monthly liabilities and divide by monthly income. Gross income (pretax) for employees of a company they do not own is typically utilized (bonus or commission income can have some alternate rules to be allowed as qualifying income); for self-employed borrowers, tax returns will be required to be reviewed; tax write offs could reduce qualifying income. Self-employed individuals will typically need to show a 2-year income history via personal tax returns (as well as business tax returns if applicable). See Figure 1 for an example of a debt-to-income ratio calculation. Many loan programs will require a debt-to-income ratio of 45% or less. There are various loan programs that will be more or less restrictive than this percentage. A lender will be able to guide you to the proper program for your scenario.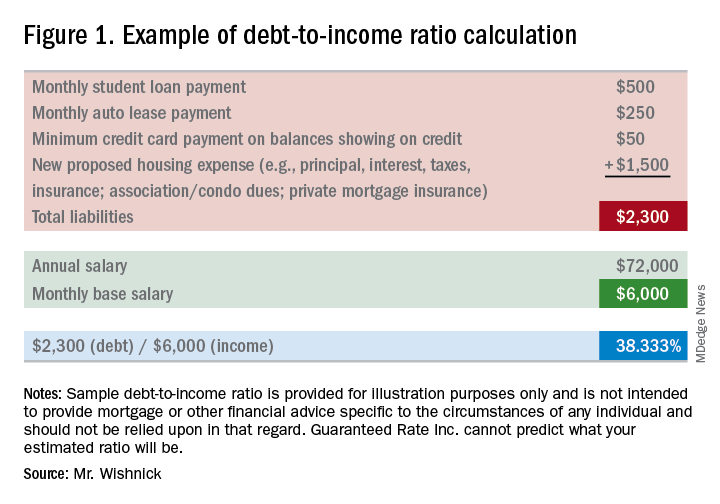
2) Liquid assets: Lenders will review the amount of liquid funds you have available for down payment, closing costs, and any necessary reserves. These may include, but are not limited to, checking/savings/money market accounts, investment accounts (stocks, bonds, mutual funds), and retirement funds. Are there enough allowable funds available for the down payment and closing costs, as well as any required reserves needed for qualification? Large non–payroll deposits can be required to be sourced to make sure the funds are from an allowable source.
3) Credit history/scores: Buying a home will be one of the largest purchases you will make in a lifetime. Credit scores have a major impact on the cost of credit (the interest rate you will obtain). Having higher scores could result in a lower interest rate, as well as open up certain loan programs that may be more advantageous for you. Oftentimes, lenders will take the middle of the three scores as your mortgage score (one score from each of the three credit bureaus). In most cases, if applying jointly, the lowest of the middle scores for all borrowers is the score that is used as the score for the applicants. In general, a 740 middle credit score is considered to be excellent for mortgage financing but is not a requirement for all programs.
**You may have heard about specific mortgage programs for physicians. These programs are intended for use for lesser down payments, and/or not calculating student loan payments when qualifying for home financing. As future income potential is typically not considered when determining debt-to-income ratios, not counting these liabilities potentially increases borrowing power.
You are now ready to be preapproved for mortgage financing. What should you do next?
- Talk to a trusted lender. Ask your real estate agent, family, friends, or colleagues for local lender recommendations. Real estate agents will want to make sure you have spoken with a lender and completed a preapproval application to ensure that you can be preapproved for financing before showing you homes. If you need a loan to purchase a home, a preapproval letter will be required to submit with an offer letter. The application contains questions such as your address and employment history for the past 2 years, income and asset information, as well as a series of other financial information. A hard credit inquiry will need to be performed in order for the lender to issue a preapproval. What should you expect from a lender in addition to competitive rates and an array of programs? Some people prefer more of a hands-on approach. Working with a lender who provides regular status updates and makes him/herself easily accessible for all of your questions can certainly be an attractive feature. Working with a local lender also may be reassuring, as he or she should have plenty of experience with the market in which you are purchasing.
- Search for homes. Upon being given the green light for your preapproval and a price range within your comfort zone, connect with your local real estate professional to search for homes. Plan to spend time with your agent discussing all your needs for your new home.
- Submit an offer. Your lender will be able to provide an estimate of closing costs and monthly payments for homes that you are considering buying before you make an offer. You will want to be sure you are comfortable with the financial obligation prior to making your offer. With your offer, an initial good faith deposit (earnest money deposit) will be required. Your real estate agent will guide you on the proper amount of the deposit.
Conclusion
Once you and the seller have come to terms, you will look to discuss with your lender the rate and program options to secure (locking in an interest rate and program), as well as to complete the formal mortgage application. The lender will request additional documentation, if you have not already provided documents, in order for you to obtain a conditional mortgage commitment. The lender also will order an appraisal to ensure the property value supports the price you have agreed to pay for it. Your real estate agent will guide you through the various deadlines and requirements in the contract for items like home inspections, ordering a title search to obtain title insurance, and other nonfinancing contingencies. Some areas may require attorneys for contract review and closing, which your agent will discuss with you. As you can see, buying a home is not an instant process. Taking the appropriate steps to prepare for your mortgage preapproval could save you a lot of time and stress.
Mr. Wishnick is a 15-year mortgage industry veteran, vice president of mortgage lending with Guaranteed Rate (NMLS #2611) and was ranked as a Top 1% mortgage originator by Mortgage Executive Magazine. He can be reached at [email protected].
All information provided in this publication is for informational and educational purposes only, and in no way is any of the content contained herein to be construed as financial, investment, or legal advice or instruction. Guaranteed Rate does not guarantee the quality, accuracy, completeness or timelines of the information in this publication.
Advanced training options in inflammatory bowel disease
The global incidence and prevalence of inflammatory bowel disease (IBD) is rising, and it is estimated that by 2025, approximately 2.2 million Americans will be living with this disease. At the same time, there have been several paradigm-changing scientific and medical advances in the understanding and management of IBD. As the diagnostic, therapeutic, and monitoring armamentarium in the management of IBD increases, so is the complexity of the decision making. Advanced concepts and training are often not covered adequately during a general gastroenterology fellowship. In a survey of 160 trainees, more than one-third of fellows did not feel “confident” or “mostly comfortable” with their level of IBD training. Yet, efficient dissemination, effective translation and integration of these advances into clinical practice is paramount to improving quality of care. To facilitate multiple goals as listed in Table 1, advanced training in the field of IBD is increasingly important. In this article, I review different training options available for young gastroenterologists.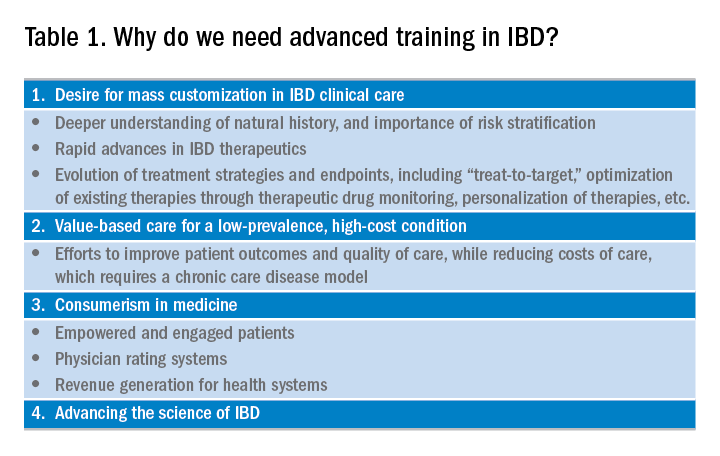
Readers are also directed to an excellent article by David Rubin, MD, published in Gastroenterology in 2015.
Advanced fellowship training in IBD
The most rigorous training in IBD is offered through dedicated advanced fellowships. Currently, there are more than 20 such fellowships in North America, most of them offered at large academic centers with nationally and internationally renowned faculty. These training positions are generally 1 year long, offered after completion of gastroenterology fellowship. The Accreditation Council of the Graduate Medical Education (ACGME) does not accredit these advanced training programs, and there is not a separate American Board of Internal Medicine (ABIM) certification for IBD. Funding of such programs comes from different sources including endowments, private foundations, institutional funds, pharmaceutical company grants, and even limited faculty appointments of the trainees. Though there is currently no official regulatory oversight and requirements, most programs have well-defined curricula covering diverse aspects of IBD care. This core curriculum has been nicely summarized in a recent article by Uma Mahadevan, MD, in Gastroenterology.
Clinical training in these programs is offered through a mix of outpatient IBD clinics (generally three to five clinics/week, with one or more senior IBD-focused faculty member), supervising general gastroenterology fellows for inpatient IBD care, dedicated IBD-focused endoscopy sessions (generally one or two sessions/week) including chromoendoscopy and stricture dilation, as well as formal and informal mentorship by one or more senior faculty members, time and mentorship for scholarly activities, and appropriate evaluation and feedback systems. In addition, most programs offer multidisciplinary training through dedicated clinics with colorectal surgeons (such as pouch clinics, etc.), opportunities for observing and interacting with radiologists, pathologists, psychologists, and dietitians.
There is no centralized application process and prospective applicants should reach out to their program directors and mentors regarding guidance, as well as program directors of specific training programs to learn more about these programs, generally in the second half of their gastroenterology training. The Crohn’s and Colitis Foundation maintains a list of fellowship training programs and appropriate contacts. In choosing a specific program, prospective fellows should consider the rigor and diversity of training, balance between service and scholarship, mentorship opportunities as well as the experience and outcomes of previous fellows in the program. Besides formal interviews at prospective program, fellows should utilize the networking opportunities afforded through the American Gastroenterological Association (both with senior faculty as well as through the Trainee and Early-Career Committee), the Crohn’s and Colitis Foundation as well as other organizations in learning more about programs.
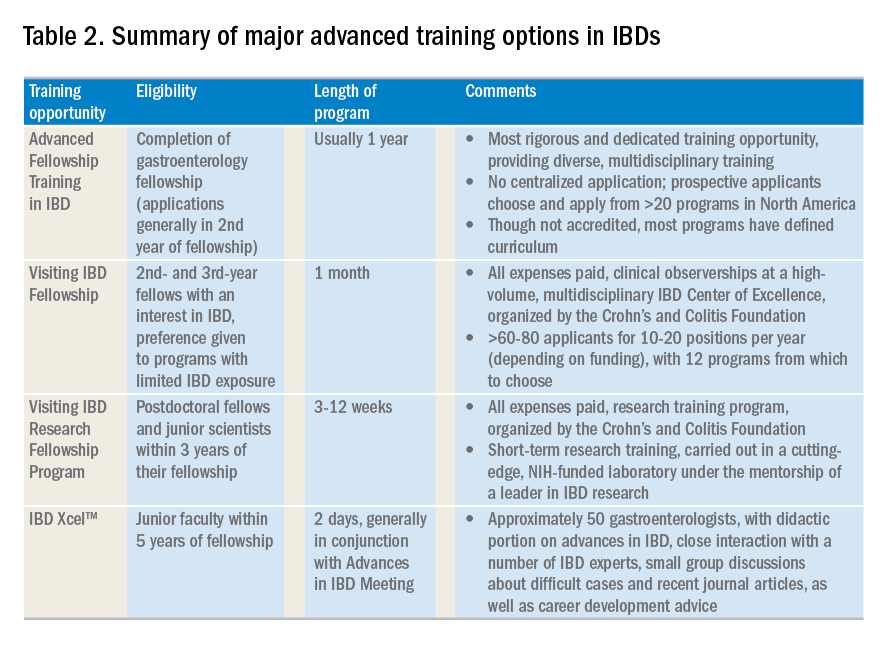
Visiting IBD Fellow Program: Clinical observership, through the Crohn’s and Colitis Foundation
The Visiting IBD Fellow Program – with the support of the Crohn’s and Colitis Foundation – which launched in 2006, arose from the need for immersive training in IBD, especially for fellows for whom IBD exposure may be limited. In this 1-month “observership,” interested 2nd and 3rd year fellows get the opportunity to observe faculty at a high-volume, multidisciplinary IBD Center of Excellence. Besides providing additional knowledge and expertise in the field, this also allows fellows the chance to understand how IBD Centers are set up, so they may seek to replicate similar models as local or regional IBD experts. Currently, 12 centers participate in this program. There is no cost to the fellows who are selected to participate, and all travel expenses and lodging are covered. The program significantly improved the fellows’ knowledge, skills, and attitudes toward IBD and has steadily gained in popularity, with more than 60-80 applicants for 10-20 positions per year (depending on funding). In addition to the clinical exposure, this experience also facilitates networking with faculty and other fellows at participating institutions. Full details of this program can be accessed from the Crohn’s and Colitis Foundation website.
A similar, expenses-paid, abbreviated 3-day program of IBD preceptorship has been launched for advanced practice providers (qualified advanced-practice nurses, nurse practitioners, and physician assistants). This program provides preceptee exposure to medical, surgical, outpatient, and inpatient experiences with patients at a leading academic IBD center.
Visiting IBD Research Fellowship Program, through the Crohn’s and Colitis Foundation
The Crohn’s and Colitis Foundation recently launched a new, short-term, mentored research initiative designed to promote career advancement for talented junior investigators dedicated to IBD research, and to enable knowledge-sharing among leaders in the IBD field. The Foundation encourages outstanding young scientists (postdoctoral studies in the first 3 years of their fellowship), who would like to expand their expertise in IBD research to participate in this short-term research training, carried out in a cutting-edge, NIH-funded laboratory under the mentorship of a leader in IBD research. This all-expense covered 3-12 week rotation provides mentorship and technical training in a state-of-the-art research lab relevant to IBD, with an emphasis on preclinical research most closely relevant to human disease. Details of the program can be found on the Crohn’s and Colitis Foundation website.
IBD Xcel
In 2013, Cornerstones Health, a nonprofit medical education organization, launched a 2-day program dedicated to advances in the field of IBD for junior gastroenterologists within 5 years of completion of their fellowship training. The program includes a didactic component as well as close interaction with a number of IBD experts, small-group discussions about difficult cases, and recent journal articles, as well as career-development advice. The education component is free of cost to selected participants, though travel and housing expenses are not covered.
Besides these dedicated advanced training opportunities, there are major conferences that cover IBD extensively and exclusively. These include the annual Crohn’s and Colitis Congress® conducted jointly by the Crohn’s and Colitis Foundation and the American Gastroenterological Association, the annual Advances in Inflammatory Bowel Diseases through Imedex, the annual European Crohn’s and Colitis Congress, the American College of Gastroenterology’s IBD School, as well as several regional courses conducted throughout the country. In terms of networking opportunities for gastroenterology fellows interested in IBD and junior faculty, REACH-IBD (Rising Educators, Academicians and Clinicians Helping Inflammatory Bowel Disease), founded under the auspices of the Crohn’s and Colitis Foundation in 2013, provides a unique resource. This group is open to all clinical fellows, postdoctoral scientists, and junior faculty (pediatric and adult; medical and surgical specialties, as well as PhDs) less than 7 years out of training with a rank not higher than assistant professor. The mission is to facilitate networking and career development for clinical fellows, postdoctoral scientists, and junior faculty with an interest in IBD; increase active participation of our members in the clinical, educational, scientific, and research programs within the Crohn’s and Colitis Foundation; and foster collaborative research among our members within the Foundation. The group organizes specific breakout events at the Digestive Disease Week® and the annual Crohn’s and Colitis Congress, covering diverse topics such as setting up an IBD practice, funding opportunities, paper and grant writing, career advancement guidance. More information on this can be found on the Crohn’s and Colitis Foundation website.
To summarize, there are numerous opportunities of varying lengths to receive training in inflammatory bowel diseases. This exciting field is expanding at a rapid pace, and instead of limiting management to dedicated IBD Centers of Excellence, there is clear need for effective dissemination of new management approaches and incorporation of quality measures will likely raise the bar for all patients and physicians who care for them.
AGA offers IBD education
Check out AGA’s on-demand IBD education available in AGA University.
Dr. Singh is assistant professor of medicine, division of gastroenterology, University of California, San Diego. He is supported by the American College of Gastroenterology and Crohn’s and Colitis Foundation, has received research grants from Pfizer and AbbVie, and consulting fees from AbbVie, Takeda, and AMAG Pharmaceuticals.
The global incidence and prevalence of inflammatory bowel disease (IBD) is rising, and it is estimated that by 2025, approximately 2.2 million Americans will be living with this disease. At the same time, there have been several paradigm-changing scientific and medical advances in the understanding and management of IBD. As the diagnostic, therapeutic, and monitoring armamentarium in the management of IBD increases, so is the complexity of the decision making. Advanced concepts and training are often not covered adequately during a general gastroenterology fellowship. In a survey of 160 trainees, more than one-third of fellows did not feel “confident” or “mostly comfortable” with their level of IBD training. Yet, efficient dissemination, effective translation and integration of these advances into clinical practice is paramount to improving quality of care. To facilitate multiple goals as listed in Table 1, advanced training in the field of IBD is increasingly important. In this article, I review different training options available for young gastroenterologists.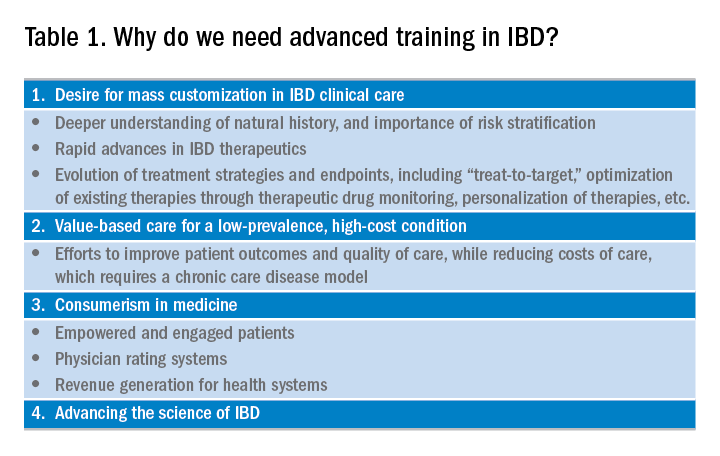
Readers are also directed to an excellent article by David Rubin, MD, published in Gastroenterology in 2015.
Advanced fellowship training in IBD
The most rigorous training in IBD is offered through dedicated advanced fellowships. Currently, there are more than 20 such fellowships in North America, most of them offered at large academic centers with nationally and internationally renowned faculty. These training positions are generally 1 year long, offered after completion of gastroenterology fellowship. The Accreditation Council of the Graduate Medical Education (ACGME) does not accredit these advanced training programs, and there is not a separate American Board of Internal Medicine (ABIM) certification for IBD. Funding of such programs comes from different sources including endowments, private foundations, institutional funds, pharmaceutical company grants, and even limited faculty appointments of the trainees. Though there is currently no official regulatory oversight and requirements, most programs have well-defined curricula covering diverse aspects of IBD care. This core curriculum has been nicely summarized in a recent article by Uma Mahadevan, MD, in Gastroenterology.
Clinical training in these programs is offered through a mix of outpatient IBD clinics (generally three to five clinics/week, with one or more senior IBD-focused faculty member), supervising general gastroenterology fellows for inpatient IBD care, dedicated IBD-focused endoscopy sessions (generally one or two sessions/week) including chromoendoscopy and stricture dilation, as well as formal and informal mentorship by one or more senior faculty members, time and mentorship for scholarly activities, and appropriate evaluation and feedback systems. In addition, most programs offer multidisciplinary training through dedicated clinics with colorectal surgeons (such as pouch clinics, etc.), opportunities for observing and interacting with radiologists, pathologists, psychologists, and dietitians.
There is no centralized application process and prospective applicants should reach out to their program directors and mentors regarding guidance, as well as program directors of specific training programs to learn more about these programs, generally in the second half of their gastroenterology training. The Crohn’s and Colitis Foundation maintains a list of fellowship training programs and appropriate contacts. In choosing a specific program, prospective fellows should consider the rigor and diversity of training, balance between service and scholarship, mentorship opportunities as well as the experience and outcomes of previous fellows in the program. Besides formal interviews at prospective program, fellows should utilize the networking opportunities afforded through the American Gastroenterological Association (both with senior faculty as well as through the Trainee and Early-Career Committee), the Crohn’s and Colitis Foundation as well as other organizations in learning more about programs.
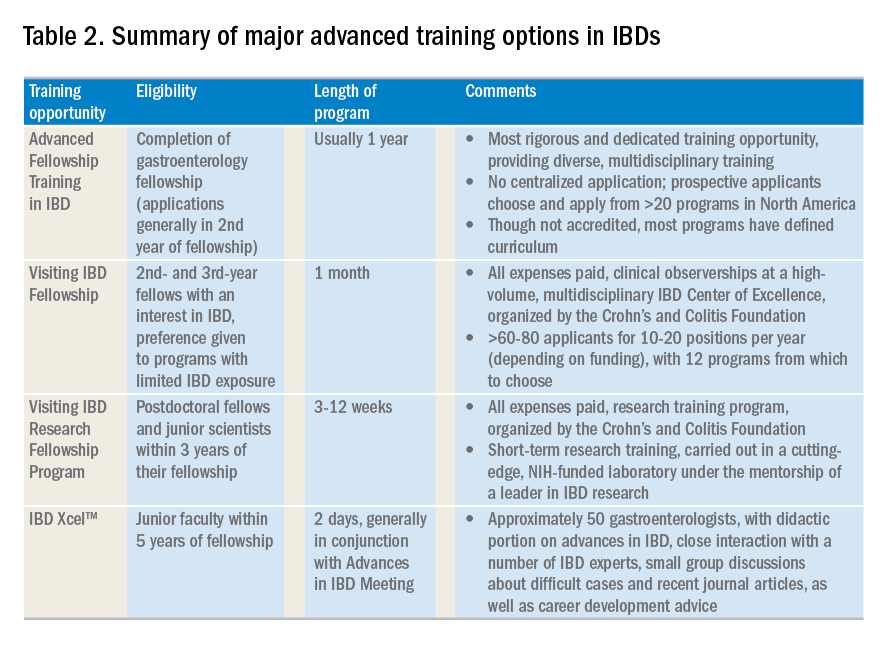
Visiting IBD Fellow Program: Clinical observership, through the Crohn’s and Colitis Foundation
The Visiting IBD Fellow Program – with the support of the Crohn’s and Colitis Foundation – which launched in 2006, arose from the need for immersive training in IBD, especially for fellows for whom IBD exposure may be limited. In this 1-month “observership,” interested 2nd and 3rd year fellows get the opportunity to observe faculty at a high-volume, multidisciplinary IBD Center of Excellence. Besides providing additional knowledge and expertise in the field, this also allows fellows the chance to understand how IBD Centers are set up, so they may seek to replicate similar models as local or regional IBD experts. Currently, 12 centers participate in this program. There is no cost to the fellows who are selected to participate, and all travel expenses and lodging are covered. The program significantly improved the fellows’ knowledge, skills, and attitudes toward IBD and has steadily gained in popularity, with more than 60-80 applicants for 10-20 positions per year (depending on funding). In addition to the clinical exposure, this experience also facilitates networking with faculty and other fellows at participating institutions. Full details of this program can be accessed from the Crohn’s and Colitis Foundation website.
A similar, expenses-paid, abbreviated 3-day program of IBD preceptorship has been launched for advanced practice providers (qualified advanced-practice nurses, nurse practitioners, and physician assistants). This program provides preceptee exposure to medical, surgical, outpatient, and inpatient experiences with patients at a leading academic IBD center.
Visiting IBD Research Fellowship Program, through the Crohn’s and Colitis Foundation
The Crohn’s and Colitis Foundation recently launched a new, short-term, mentored research initiative designed to promote career advancement for talented junior investigators dedicated to IBD research, and to enable knowledge-sharing among leaders in the IBD field. The Foundation encourages outstanding young scientists (postdoctoral studies in the first 3 years of their fellowship), who would like to expand their expertise in IBD research to participate in this short-term research training, carried out in a cutting-edge, NIH-funded laboratory under the mentorship of a leader in IBD research. This all-expense covered 3-12 week rotation provides mentorship and technical training in a state-of-the-art research lab relevant to IBD, with an emphasis on preclinical research most closely relevant to human disease. Details of the program can be found on the Crohn’s and Colitis Foundation website.
IBD Xcel
In 2013, Cornerstones Health, a nonprofit medical education organization, launched a 2-day program dedicated to advances in the field of IBD for junior gastroenterologists within 5 years of completion of their fellowship training. The program includes a didactic component as well as close interaction with a number of IBD experts, small-group discussions about difficult cases, and recent journal articles, as well as career-development advice. The education component is free of cost to selected participants, though travel and housing expenses are not covered.
Besides these dedicated advanced training opportunities, there are major conferences that cover IBD extensively and exclusively. These include the annual Crohn’s and Colitis Congress® conducted jointly by the Crohn’s and Colitis Foundation and the American Gastroenterological Association, the annual Advances in Inflammatory Bowel Diseases through Imedex, the annual European Crohn’s and Colitis Congress, the American College of Gastroenterology’s IBD School, as well as several regional courses conducted throughout the country. In terms of networking opportunities for gastroenterology fellows interested in IBD and junior faculty, REACH-IBD (Rising Educators, Academicians and Clinicians Helping Inflammatory Bowel Disease), founded under the auspices of the Crohn’s and Colitis Foundation in 2013, provides a unique resource. This group is open to all clinical fellows, postdoctoral scientists, and junior faculty (pediatric and adult; medical and surgical specialties, as well as PhDs) less than 7 years out of training with a rank not higher than assistant professor. The mission is to facilitate networking and career development for clinical fellows, postdoctoral scientists, and junior faculty with an interest in IBD; increase active participation of our members in the clinical, educational, scientific, and research programs within the Crohn’s and Colitis Foundation; and foster collaborative research among our members within the Foundation. The group organizes specific breakout events at the Digestive Disease Week® and the annual Crohn’s and Colitis Congress, covering diverse topics such as setting up an IBD practice, funding opportunities, paper and grant writing, career advancement guidance. More information on this can be found on the Crohn’s and Colitis Foundation website.
To summarize, there are numerous opportunities of varying lengths to receive training in inflammatory bowel diseases. This exciting field is expanding at a rapid pace, and instead of limiting management to dedicated IBD Centers of Excellence, there is clear need for effective dissemination of new management approaches and incorporation of quality measures will likely raise the bar for all patients and physicians who care for them.
AGA offers IBD education
Check out AGA’s on-demand IBD education available in AGA University.
Dr. Singh is assistant professor of medicine, division of gastroenterology, University of California, San Diego. He is supported by the American College of Gastroenterology and Crohn’s and Colitis Foundation, has received research grants from Pfizer and AbbVie, and consulting fees from AbbVie, Takeda, and AMAG Pharmaceuticals.
The global incidence and prevalence of inflammatory bowel disease (IBD) is rising, and it is estimated that by 2025, approximately 2.2 million Americans will be living with this disease. At the same time, there have been several paradigm-changing scientific and medical advances in the understanding and management of IBD. As the diagnostic, therapeutic, and monitoring armamentarium in the management of IBD increases, so is the complexity of the decision making. Advanced concepts and training are often not covered adequately during a general gastroenterology fellowship. In a survey of 160 trainees, more than one-third of fellows did not feel “confident” or “mostly comfortable” with their level of IBD training. Yet, efficient dissemination, effective translation and integration of these advances into clinical practice is paramount to improving quality of care. To facilitate multiple goals as listed in Table 1, advanced training in the field of IBD is increasingly important. In this article, I review different training options available for young gastroenterologists.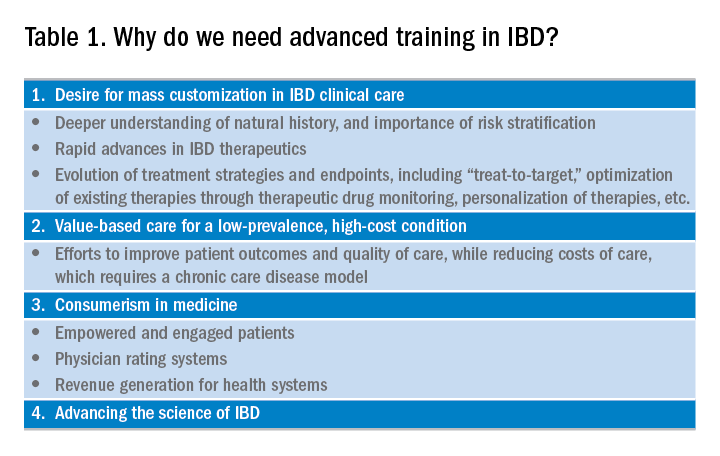
Readers are also directed to an excellent article by David Rubin, MD, published in Gastroenterology in 2015.
Advanced fellowship training in IBD
The most rigorous training in IBD is offered through dedicated advanced fellowships. Currently, there are more than 20 such fellowships in North America, most of them offered at large academic centers with nationally and internationally renowned faculty. These training positions are generally 1 year long, offered after completion of gastroenterology fellowship. The Accreditation Council of the Graduate Medical Education (ACGME) does not accredit these advanced training programs, and there is not a separate American Board of Internal Medicine (ABIM) certification for IBD. Funding of such programs comes from different sources including endowments, private foundations, institutional funds, pharmaceutical company grants, and even limited faculty appointments of the trainees. Though there is currently no official regulatory oversight and requirements, most programs have well-defined curricula covering diverse aspects of IBD care. This core curriculum has been nicely summarized in a recent article by Uma Mahadevan, MD, in Gastroenterology.
Clinical training in these programs is offered through a mix of outpatient IBD clinics (generally three to five clinics/week, with one or more senior IBD-focused faculty member), supervising general gastroenterology fellows for inpatient IBD care, dedicated IBD-focused endoscopy sessions (generally one or two sessions/week) including chromoendoscopy and stricture dilation, as well as formal and informal mentorship by one or more senior faculty members, time and mentorship for scholarly activities, and appropriate evaluation and feedback systems. In addition, most programs offer multidisciplinary training through dedicated clinics with colorectal surgeons (such as pouch clinics, etc.), opportunities for observing and interacting with radiologists, pathologists, psychologists, and dietitians.
There is no centralized application process and prospective applicants should reach out to their program directors and mentors regarding guidance, as well as program directors of specific training programs to learn more about these programs, generally in the second half of their gastroenterology training. The Crohn’s and Colitis Foundation maintains a list of fellowship training programs and appropriate contacts. In choosing a specific program, prospective fellows should consider the rigor and diversity of training, balance between service and scholarship, mentorship opportunities as well as the experience and outcomes of previous fellows in the program. Besides formal interviews at prospective program, fellows should utilize the networking opportunities afforded through the American Gastroenterological Association (both with senior faculty as well as through the Trainee and Early-Career Committee), the Crohn’s and Colitis Foundation as well as other organizations in learning more about programs.
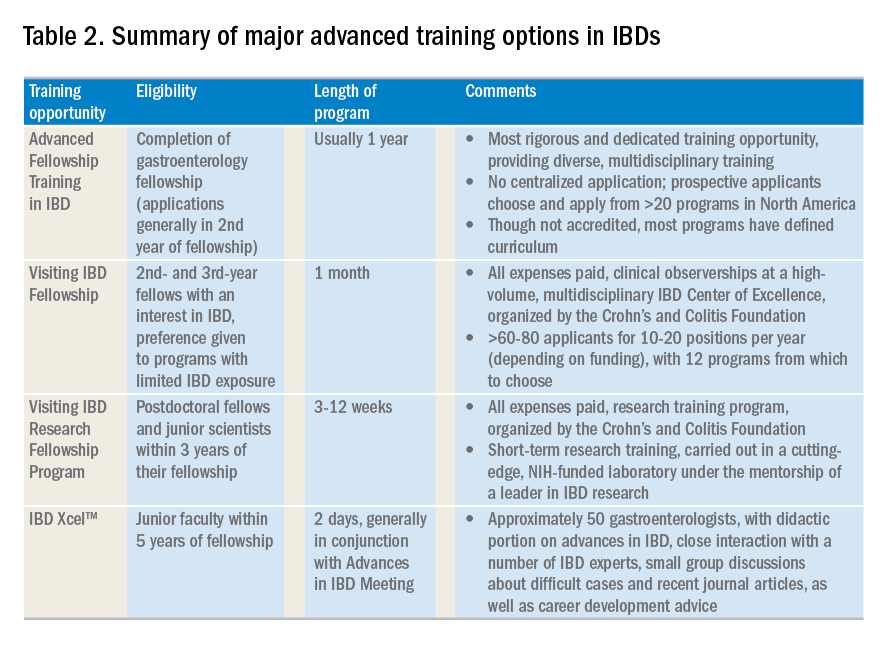
Visiting IBD Fellow Program: Clinical observership, through the Crohn’s and Colitis Foundation
The Visiting IBD Fellow Program – with the support of the Crohn’s and Colitis Foundation – which launched in 2006, arose from the need for immersive training in IBD, especially for fellows for whom IBD exposure may be limited. In this 1-month “observership,” interested 2nd and 3rd year fellows get the opportunity to observe faculty at a high-volume, multidisciplinary IBD Center of Excellence. Besides providing additional knowledge and expertise in the field, this also allows fellows the chance to understand how IBD Centers are set up, so they may seek to replicate similar models as local or regional IBD experts. Currently, 12 centers participate in this program. There is no cost to the fellows who are selected to participate, and all travel expenses and lodging are covered. The program significantly improved the fellows’ knowledge, skills, and attitudes toward IBD and has steadily gained in popularity, with more than 60-80 applicants for 10-20 positions per year (depending on funding). In addition to the clinical exposure, this experience also facilitates networking with faculty and other fellows at participating institutions. Full details of this program can be accessed from the Crohn’s and Colitis Foundation website.
A similar, expenses-paid, abbreviated 3-day program of IBD preceptorship has been launched for advanced practice providers (qualified advanced-practice nurses, nurse practitioners, and physician assistants). This program provides preceptee exposure to medical, surgical, outpatient, and inpatient experiences with patients at a leading academic IBD center.
Visiting IBD Research Fellowship Program, through the Crohn’s and Colitis Foundation
The Crohn’s and Colitis Foundation recently launched a new, short-term, mentored research initiative designed to promote career advancement for talented junior investigators dedicated to IBD research, and to enable knowledge-sharing among leaders in the IBD field. The Foundation encourages outstanding young scientists (postdoctoral studies in the first 3 years of their fellowship), who would like to expand their expertise in IBD research to participate in this short-term research training, carried out in a cutting-edge, NIH-funded laboratory under the mentorship of a leader in IBD research. This all-expense covered 3-12 week rotation provides mentorship and technical training in a state-of-the-art research lab relevant to IBD, with an emphasis on preclinical research most closely relevant to human disease. Details of the program can be found on the Crohn’s and Colitis Foundation website.
IBD Xcel
In 2013, Cornerstones Health, a nonprofit medical education organization, launched a 2-day program dedicated to advances in the field of IBD for junior gastroenterologists within 5 years of completion of their fellowship training. The program includes a didactic component as well as close interaction with a number of IBD experts, small-group discussions about difficult cases, and recent journal articles, as well as career-development advice. The education component is free of cost to selected participants, though travel and housing expenses are not covered.
Besides these dedicated advanced training opportunities, there are major conferences that cover IBD extensively and exclusively. These include the annual Crohn’s and Colitis Congress® conducted jointly by the Crohn’s and Colitis Foundation and the American Gastroenterological Association, the annual Advances in Inflammatory Bowel Diseases through Imedex, the annual European Crohn’s and Colitis Congress, the American College of Gastroenterology’s IBD School, as well as several regional courses conducted throughout the country. In terms of networking opportunities for gastroenterology fellows interested in IBD and junior faculty, REACH-IBD (Rising Educators, Academicians and Clinicians Helping Inflammatory Bowel Disease), founded under the auspices of the Crohn’s and Colitis Foundation in 2013, provides a unique resource. This group is open to all clinical fellows, postdoctoral scientists, and junior faculty (pediatric and adult; medical and surgical specialties, as well as PhDs) less than 7 years out of training with a rank not higher than assistant professor. The mission is to facilitate networking and career development for clinical fellows, postdoctoral scientists, and junior faculty with an interest in IBD; increase active participation of our members in the clinical, educational, scientific, and research programs within the Crohn’s and Colitis Foundation; and foster collaborative research among our members within the Foundation. The group organizes specific breakout events at the Digestive Disease Week® and the annual Crohn’s and Colitis Congress, covering diverse topics such as setting up an IBD practice, funding opportunities, paper and grant writing, career advancement guidance. More information on this can be found on the Crohn’s and Colitis Foundation website.
To summarize, there are numerous opportunities of varying lengths to receive training in inflammatory bowel diseases. This exciting field is expanding at a rapid pace, and instead of limiting management to dedicated IBD Centers of Excellence, there is clear need for effective dissemination of new management approaches and incorporation of quality measures will likely raise the bar for all patients and physicians who care for them.
AGA offers IBD education
Check out AGA’s on-demand IBD education available in AGA University.
Dr. Singh is assistant professor of medicine, division of gastroenterology, University of California, San Diego. He is supported by the American College of Gastroenterology and Crohn’s and Colitis Foundation, has received research grants from Pfizer and AbbVie, and consulting fees from AbbVie, Takeda, and AMAG Pharmaceuticals.















