User login
Multiply Your Contacts
Networking is crucial to career advancement, no matter what your long-term goals are. Connecting with others in hospital medicine, general healthcare, and business can build your knowledge base, your support system, and your reputation. But how—and why—should hospitalists present themselves to the influential people they need to know?
The Need to Network
You may think it’s not necessary to expand your list of contacts within hospital medicine. Put another way, why bother to network? Vineet Arora, MD, MA, assistant professor of medicine at the Pritzker School of Medicine at University of Chicago, points to a paper, “Strength of Weak Ties,” published in the May 1973 American Journal of Sociology by sociologist Mark Granovetter. In the paper, he presents a social science theory that says “the people who are most helpful to you are those who you don’t know well,” Dr. Arora says. Granovetter’s theory suggests that in marketing or politics, the weak ties enable individuals to reach populations and audiences that are not accessible via strong ties.
“It’s not your friends or the people you know the best who are most likely to help you get a job,” Dr. Arora says. “Those people have already helped you as much as they can.” The main lesson here, she says, is to “think carefully about reaching outside your comfort zone. Introduce yourself to a stranger; it’s to your advantage to cultivate these weak ties.”
To increase your number of “weak ties” in hospital medicine, follow these simple steps:
Step 1: Establish Goals
Consider why you’re networking in order to focus your efforts and target your contacts. Are you looking for a new position? Do you want to transform yourself into the go-to hospitalist in a specific clinical area? Are you looking to learn leadership skills?
Once you’ve determined what you want to get out of networking—and it might be more than one goal—outline a brief elevator speech. It’s a one-minute explanation of who you are and what you’re interested in. It will prepare you to open a conversation with a stranger. “You should present yourself in a concise way,” Dr. Arora stresses. “State who you are and what your interests are.”
Step 2: Make a Plan
Once you know your goals and are able to state them clearly and eloquently, map out your networking strategy. You may simply keep this in the back of your mind for the short term, or you may specifically plan on attending events that will allow you to network with the appropriate people, such as hiring managers, experts in your area of interest, or HM movers and shakers.
“Figure out who the people are in your field of interest who are making waves, and go where they are,” Dr. Arora says. But “don’t just attend the meetings. Be proactive.”
Choose your conferences wisely. For example, if you’re interested in leadership skills or a leadership position, consider SHM’s biannual Leadership Academy. “Not only is this a terrific learning opportunity, it’s a very strong networking environment,” says Russell L. Holman, MD, chief operating officer for Cogent Healthcare in Nashville, Tenn., and past president of SHM. “You’re sharing a room with 120 or 130 leaders or leaders-in-training.”
Dozens of annual conferences and courses are available for networking, including clinical CME courses offered by universities. “The American College of Physician Executives [ACPE] has advanced training courses not only in management, but in quality improvement and a variety of other interests,” Dr. Holman explains.
Networking at industry events may not have an immediate payoff, Dr. Arora warns. “You’re probably not going to land a job or land an opportunity at a meeting,” she says, “but you float your name and get to know people.”
Step 3: Let the Networking Begin
With your short speech ready to go, attend a conference or meeting with key industry leaders and simply approach influential individuals you’d like to meet.
“The way it’s done is even more important than where and when you do it,” Dr. Holman says. “You don’t want to come across as pushy, aggressive, or needy.” Simply introduce yourself with a handshake, rely on your elevator speech for a brief explanation, then give that person a chance to talk. Ask questions about how their career advanced, then ask if they know of any opportunities for you, he says.
If your initial conversation is rushed—say, you’re approaching a speaker after a presentation—keep your conversation brief. “At an event like an SHM meeting, it may be difficult to catch certain people,” Dr. Holman says. “If you can, at least shake their hand and exchange business cards, then follow up with an e-mail and ask for 15 minutes of their time. This is very acceptable; it happens to me all the time.”
Another key piece of advice: “Don’t ask them to contact you—you be the one to send an e-mail,” Dr. Holman says.
Step 4: Follow Up
Soon after the in-person meeting, send a follow-up e-mail. Carefully consider your subject line to ensure your message is read. Reference your encounter in the message (e.g., “We met after your presentation at the conference in Miami”) to remind the person who you are. Depending on your goals, you may ask for information to be forwarded, contacts for additional networking, or request a brief telephone conversation.
“A lot of speakers post their e-mail in their presentation,” Dr. Arora points out. “If you don’t get a chance to talk to them in person, send them a message after you get home. People love to get feedback. Comment on their presentation and introduce yourself that way.”
Hospitalists can strengthen their connections with an offer to reciprocate: “You want to be as helpful as you are helped,” Dr. Holman says. “End the conversation with the offer: ‘If there is any way that I can help you, let me know.’ ”
Set goals, practice your elevator speech, venture out and introduce yourself, and follow up.
These simple steps will help you in your networking efforts, and likely will help advance your career. TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
Networking is crucial to career advancement, no matter what your long-term goals are. Connecting with others in hospital medicine, general healthcare, and business can build your knowledge base, your support system, and your reputation. But how—and why—should hospitalists present themselves to the influential people they need to know?
The Need to Network
You may think it’s not necessary to expand your list of contacts within hospital medicine. Put another way, why bother to network? Vineet Arora, MD, MA, assistant professor of medicine at the Pritzker School of Medicine at University of Chicago, points to a paper, “Strength of Weak Ties,” published in the May 1973 American Journal of Sociology by sociologist Mark Granovetter. In the paper, he presents a social science theory that says “the people who are most helpful to you are those who you don’t know well,” Dr. Arora says. Granovetter’s theory suggests that in marketing or politics, the weak ties enable individuals to reach populations and audiences that are not accessible via strong ties.
“It’s not your friends or the people you know the best who are most likely to help you get a job,” Dr. Arora says. “Those people have already helped you as much as they can.” The main lesson here, she says, is to “think carefully about reaching outside your comfort zone. Introduce yourself to a stranger; it’s to your advantage to cultivate these weak ties.”
To increase your number of “weak ties” in hospital medicine, follow these simple steps:
Step 1: Establish Goals
Consider why you’re networking in order to focus your efforts and target your contacts. Are you looking for a new position? Do you want to transform yourself into the go-to hospitalist in a specific clinical area? Are you looking to learn leadership skills?
Once you’ve determined what you want to get out of networking—and it might be more than one goal—outline a brief elevator speech. It’s a one-minute explanation of who you are and what you’re interested in. It will prepare you to open a conversation with a stranger. “You should present yourself in a concise way,” Dr. Arora stresses. “State who you are and what your interests are.”
Step 2: Make a Plan
Once you know your goals and are able to state them clearly and eloquently, map out your networking strategy. You may simply keep this in the back of your mind for the short term, or you may specifically plan on attending events that will allow you to network with the appropriate people, such as hiring managers, experts in your area of interest, or HM movers and shakers.
“Figure out who the people are in your field of interest who are making waves, and go where they are,” Dr. Arora says. But “don’t just attend the meetings. Be proactive.”
Choose your conferences wisely. For example, if you’re interested in leadership skills or a leadership position, consider SHM’s biannual Leadership Academy. “Not only is this a terrific learning opportunity, it’s a very strong networking environment,” says Russell L. Holman, MD, chief operating officer for Cogent Healthcare in Nashville, Tenn., and past president of SHM. “You’re sharing a room with 120 or 130 leaders or leaders-in-training.”
Dozens of annual conferences and courses are available for networking, including clinical CME courses offered by universities. “The American College of Physician Executives [ACPE] has advanced training courses not only in management, but in quality improvement and a variety of other interests,” Dr. Holman explains.
Networking at industry events may not have an immediate payoff, Dr. Arora warns. “You’re probably not going to land a job or land an opportunity at a meeting,” she says, “but you float your name and get to know people.”
Step 3: Let the Networking Begin
With your short speech ready to go, attend a conference or meeting with key industry leaders and simply approach influential individuals you’d like to meet.
“The way it’s done is even more important than where and when you do it,” Dr. Holman says. “You don’t want to come across as pushy, aggressive, or needy.” Simply introduce yourself with a handshake, rely on your elevator speech for a brief explanation, then give that person a chance to talk. Ask questions about how their career advanced, then ask if they know of any opportunities for you, he says.
If your initial conversation is rushed—say, you’re approaching a speaker after a presentation—keep your conversation brief. “At an event like an SHM meeting, it may be difficult to catch certain people,” Dr. Holman says. “If you can, at least shake their hand and exchange business cards, then follow up with an e-mail and ask for 15 minutes of their time. This is very acceptable; it happens to me all the time.”
Another key piece of advice: “Don’t ask them to contact you—you be the one to send an e-mail,” Dr. Holman says.
Step 4: Follow Up
Soon after the in-person meeting, send a follow-up e-mail. Carefully consider your subject line to ensure your message is read. Reference your encounter in the message (e.g., “We met after your presentation at the conference in Miami”) to remind the person who you are. Depending on your goals, you may ask for information to be forwarded, contacts for additional networking, or request a brief telephone conversation.
“A lot of speakers post their e-mail in their presentation,” Dr. Arora points out. “If you don’t get a chance to talk to them in person, send them a message after you get home. People love to get feedback. Comment on their presentation and introduce yourself that way.”
Hospitalists can strengthen their connections with an offer to reciprocate: “You want to be as helpful as you are helped,” Dr. Holman says. “End the conversation with the offer: ‘If there is any way that I can help you, let me know.’ ”
Set goals, practice your elevator speech, venture out and introduce yourself, and follow up.
These simple steps will help you in your networking efforts, and likely will help advance your career. TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
Networking is crucial to career advancement, no matter what your long-term goals are. Connecting with others in hospital medicine, general healthcare, and business can build your knowledge base, your support system, and your reputation. But how—and why—should hospitalists present themselves to the influential people they need to know?
The Need to Network
You may think it’s not necessary to expand your list of contacts within hospital medicine. Put another way, why bother to network? Vineet Arora, MD, MA, assistant professor of medicine at the Pritzker School of Medicine at University of Chicago, points to a paper, “Strength of Weak Ties,” published in the May 1973 American Journal of Sociology by sociologist Mark Granovetter. In the paper, he presents a social science theory that says “the people who are most helpful to you are those who you don’t know well,” Dr. Arora says. Granovetter’s theory suggests that in marketing or politics, the weak ties enable individuals to reach populations and audiences that are not accessible via strong ties.
“It’s not your friends or the people you know the best who are most likely to help you get a job,” Dr. Arora says. “Those people have already helped you as much as they can.” The main lesson here, she says, is to “think carefully about reaching outside your comfort zone. Introduce yourself to a stranger; it’s to your advantage to cultivate these weak ties.”
To increase your number of “weak ties” in hospital medicine, follow these simple steps:
Step 1: Establish Goals
Consider why you’re networking in order to focus your efforts and target your contacts. Are you looking for a new position? Do you want to transform yourself into the go-to hospitalist in a specific clinical area? Are you looking to learn leadership skills?
Once you’ve determined what you want to get out of networking—and it might be more than one goal—outline a brief elevator speech. It’s a one-minute explanation of who you are and what you’re interested in. It will prepare you to open a conversation with a stranger. “You should present yourself in a concise way,” Dr. Arora stresses. “State who you are and what your interests are.”
Step 2: Make a Plan
Once you know your goals and are able to state them clearly and eloquently, map out your networking strategy. You may simply keep this in the back of your mind for the short term, or you may specifically plan on attending events that will allow you to network with the appropriate people, such as hiring managers, experts in your area of interest, or HM movers and shakers.
“Figure out who the people are in your field of interest who are making waves, and go where they are,” Dr. Arora says. But “don’t just attend the meetings. Be proactive.”
Choose your conferences wisely. For example, if you’re interested in leadership skills or a leadership position, consider SHM’s biannual Leadership Academy. “Not only is this a terrific learning opportunity, it’s a very strong networking environment,” says Russell L. Holman, MD, chief operating officer for Cogent Healthcare in Nashville, Tenn., and past president of SHM. “You’re sharing a room with 120 or 130 leaders or leaders-in-training.”
Dozens of annual conferences and courses are available for networking, including clinical CME courses offered by universities. “The American College of Physician Executives [ACPE] has advanced training courses not only in management, but in quality improvement and a variety of other interests,” Dr. Holman explains.
Networking at industry events may not have an immediate payoff, Dr. Arora warns. “You’re probably not going to land a job or land an opportunity at a meeting,” she says, “but you float your name and get to know people.”
Step 3: Let the Networking Begin
With your short speech ready to go, attend a conference or meeting with key industry leaders and simply approach influential individuals you’d like to meet.
“The way it’s done is even more important than where and when you do it,” Dr. Holman says. “You don’t want to come across as pushy, aggressive, or needy.” Simply introduce yourself with a handshake, rely on your elevator speech for a brief explanation, then give that person a chance to talk. Ask questions about how their career advanced, then ask if they know of any opportunities for you, he says.
If your initial conversation is rushed—say, you’re approaching a speaker after a presentation—keep your conversation brief. “At an event like an SHM meeting, it may be difficult to catch certain people,” Dr. Holman says. “If you can, at least shake their hand and exchange business cards, then follow up with an e-mail and ask for 15 minutes of their time. This is very acceptable; it happens to me all the time.”
Another key piece of advice: “Don’t ask them to contact you—you be the one to send an e-mail,” Dr. Holman says.
Step 4: Follow Up
Soon after the in-person meeting, send a follow-up e-mail. Carefully consider your subject line to ensure your message is read. Reference your encounter in the message (e.g., “We met after your presentation at the conference in Miami”) to remind the person who you are. Depending on your goals, you may ask for information to be forwarded, contacts for additional networking, or request a brief telephone conversation.
“A lot of speakers post their e-mail in their presentation,” Dr. Arora points out. “If you don’t get a chance to talk to them in person, send them a message after you get home. People love to get feedback. Comment on their presentation and introduce yourself that way.”
Hospitalists can strengthen their connections with an offer to reciprocate: “You want to be as helpful as you are helped,” Dr. Holman says. “End the conversation with the offer: ‘If there is any way that I can help you, let me know.’ ”
Set goals, practice your elevator speech, venture out and introduce yourself, and follow up.
These simple steps will help you in your networking efforts, and likely will help advance your career. TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
To Crush or Not to Crush
There are multiple reasons for crushing tablets or capsule contents before administering medications, but there are numerous medications that should not be crushed. These medications should not be chewed, either, usually due to their specific formulations and their pharmacokinetic properties.1 Most of the no-crush medications are sustained-release, oral-dosage formulas. The majority of extended-release products should not be crushed or chewed, although there are some newer slow-release tablet formulations available that are scored and can be divided or halved (e.g., Toprol XL).
A common reason for crushing a tablet or capsule is for use by a hospitalized patient with an enteral feeding tube. A recent review in the American Journal of Health-System Pharmacy provides more details about administering medications in patients with enteral feeding tubes.2 Oral solutions can be used when commercially available and medically appropriate. If an oral solution or suspension is not available, the hospital pharmacy should be consulted to determine if a liquid formulation of the product can be extemporaneously prepared. In some cases, after careful consideration of compatibility, stability, and drug absorption changes, an injectable formulation of a product may be used. You should always consult your hospital pharmacist for information on this modality of drug administration.
Some patients have difficulty swallowing tablets or capsules; some dislike the taste. In these cases, crushing of medication for powdered delivery (to be mixed with food or beverages) should be considered. But beware of certain caveats, as not all medications are suitable for crushing. Generally, meds that should not be crushed fall into one of these categories:
- Sustained-release tablets, which can be composed of multiple layers for different drug release times, as can beads within capsules. Some of the more common prefixes or suffixes for sustained-release, controlled-release, or controlled-delivery products include: 12-hour, 24-hour, CC, CD, CR, ER, LA, Retard, SA, Slo-, SR, XL, XR, or XT.
- Enteric-coated tablets, which are formulated because certain drugs can be irritating to the stomach or are degraded by stomach acid. By enteric-coating tablets or capsule beads, the drug’s release can be delayed until it reaches the small intestine. Prefixes include EN- and EC-.
Other medications have objectionable tastes and are sugar-coated to improve tolerability. If this type of medication is crushed, the patient would be subject to its unpleasant taste, which could significantly impair medication adherence. Additionally, both sublingual and effervescent medications should not be crushed because it will decrease the medication’s effectiveness.
Hospital Pharmacy publishes a wall chart that includes many of these types of formulations, along with their do’s and don’ts. If there is ever any doubt about the best way to administer a particular product or whether it can be halved or crushed, ask your pharmacist.3 TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1. Mitchell J. Oral dosage forms that should not be crushed or chewed: facts and comparisons 4.0. Hospital Pharmacy Web site. Available at: online.factsandcomparisons.com/Viewer.aspx?book=atoz&monoID=fandc-atoz1040. Accessed March 5, 2009.
2. Williams NT. Medication administration through enteral feeding tubes. Am J Health Syst Pharm. 2008;65(24):2347-2357.
3. Mitchell JF. Oral dosage forms that should not be crushed: wall chart. Wolters Kluwer Health Web site. Available at: www.factsandcomparisons.com/Products/product.aspx?id=1111. Accessed Jan. 26, 2009.
4. Mylan's Matrix receives final FDA approval for the generic version of the antiretroviral Zerit capsules. Wolters Kluwer Health Web site. Available at: http://mylan.mediaroom.com/index.php?s=43&item=399. Accessed Jan. 23, 2009.
5. Product approval information. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/Cber/products/Cinryze.htm. Accessed Jan. 14, 2009.
6. FDA licenses for marketing new therapy for rare genetic disease. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/bbs/topics/NEWS/2008/NEW01903.html. Accessed Jan. 14, 2009.
7. Sancuso patch approved for nausea and vomiting. Monthly Prescribing Reference Web site. Available at: www.empr.com/Sancusopatchapprovedfornauseaandvomiting/article/122384/. Accessed Jan. 14, 2009.
8. TussiCaps now available for cough suppression. Monthly Prescribing Reference Web site. Available at: www.empr.com/TussiCapsnowavailableforcoughsuppression/article/122377/. Accessed Jan. 14, 2009.
9. UCB’s Vimpat approved by U.S. FDA as adjunctive therapy for partial onset seizures in adults. Medical News Today Web site. Available at: www.medicalnewstoday.com/articles/127354.php. Accessed Jan. 14, 2009.
10. Apriso granted FDA marketing approval for maintenance of remission of ulcerative colitis. Medical News Today Web site. Available at: http://www.medicalnewstoday.com/articles/127839.php. Accessed Jan. 14, 2009.
11. http://biz.yahoo.com/ap/081106/cv_therapeutics _ranexa.html?.v=1. Accessed February 2, 2009.
12. FDA approves Seroquel for bipolar maintenance. Monthly Prescribing Reference Web site. Available at: www.prescribingreference.com/news/showNews/which/SeroquelXRForBipolar10101. Accessed Jan. 14, 2009.
13. Seroquel XR Web site. Available at: www.pharmacistelink.com/news/2009/01/14_seroquel.pdf. Accessed Jan. 23, 2009.
14. Peck P. Smoking cessation drug linked to 1,001 new serious adverse events. Medpage Today Web site. Available at: www.medpagetoday.com/PrimaryCare/Smoking/11428. Accessed Jan. 14, 2009.
15. Public health advisory: important information on Chantix (varenicline). U.S. Food and Drug Administration Web site. Available at: www.fda.gov/CDER/Drug/advisory/varenicline.htm. Accessed Jan. 14, 2009.
There are multiple reasons for crushing tablets or capsule contents before administering medications, but there are numerous medications that should not be crushed. These medications should not be chewed, either, usually due to their specific formulations and their pharmacokinetic properties.1 Most of the no-crush medications are sustained-release, oral-dosage formulas. The majority of extended-release products should not be crushed or chewed, although there are some newer slow-release tablet formulations available that are scored and can be divided or halved (e.g., Toprol XL).
A common reason for crushing a tablet or capsule is for use by a hospitalized patient with an enteral feeding tube. A recent review in the American Journal of Health-System Pharmacy provides more details about administering medications in patients with enteral feeding tubes.2 Oral solutions can be used when commercially available and medically appropriate. If an oral solution or suspension is not available, the hospital pharmacy should be consulted to determine if a liquid formulation of the product can be extemporaneously prepared. In some cases, after careful consideration of compatibility, stability, and drug absorption changes, an injectable formulation of a product may be used. You should always consult your hospital pharmacist for information on this modality of drug administration.
Some patients have difficulty swallowing tablets or capsules; some dislike the taste. In these cases, crushing of medication for powdered delivery (to be mixed with food or beverages) should be considered. But beware of certain caveats, as not all medications are suitable for crushing. Generally, meds that should not be crushed fall into one of these categories:
- Sustained-release tablets, which can be composed of multiple layers for different drug release times, as can beads within capsules. Some of the more common prefixes or suffixes for sustained-release, controlled-release, or controlled-delivery products include: 12-hour, 24-hour, CC, CD, CR, ER, LA, Retard, SA, Slo-, SR, XL, XR, or XT.
- Enteric-coated tablets, which are formulated because certain drugs can be irritating to the stomach or are degraded by stomach acid. By enteric-coating tablets or capsule beads, the drug’s release can be delayed until it reaches the small intestine. Prefixes include EN- and EC-.
Other medications have objectionable tastes and are sugar-coated to improve tolerability. If this type of medication is crushed, the patient would be subject to its unpleasant taste, which could significantly impair medication adherence. Additionally, both sublingual and effervescent medications should not be crushed because it will decrease the medication’s effectiveness.
Hospital Pharmacy publishes a wall chart that includes many of these types of formulations, along with their do’s and don’ts. If there is ever any doubt about the best way to administer a particular product or whether it can be halved or crushed, ask your pharmacist.3 TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1. Mitchell J. Oral dosage forms that should not be crushed or chewed: facts and comparisons 4.0. Hospital Pharmacy Web site. Available at: online.factsandcomparisons.com/Viewer.aspx?book=atoz&monoID=fandc-atoz1040. Accessed March 5, 2009.
2. Williams NT. Medication administration through enteral feeding tubes. Am J Health Syst Pharm. 2008;65(24):2347-2357.
3. Mitchell JF. Oral dosage forms that should not be crushed: wall chart. Wolters Kluwer Health Web site. Available at: www.factsandcomparisons.com/Products/product.aspx?id=1111. Accessed Jan. 26, 2009.
4. Mylan's Matrix receives final FDA approval for the generic version of the antiretroviral Zerit capsules. Wolters Kluwer Health Web site. Available at: http://mylan.mediaroom.com/index.php?s=43&item=399. Accessed Jan. 23, 2009.
5. Product approval information. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/Cber/products/Cinryze.htm. Accessed Jan. 14, 2009.
6. FDA licenses for marketing new therapy for rare genetic disease. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/bbs/topics/NEWS/2008/NEW01903.html. Accessed Jan. 14, 2009.
7. Sancuso patch approved for nausea and vomiting. Monthly Prescribing Reference Web site. Available at: www.empr.com/Sancusopatchapprovedfornauseaandvomiting/article/122384/. Accessed Jan. 14, 2009.
8. TussiCaps now available for cough suppression. Monthly Prescribing Reference Web site. Available at: www.empr.com/TussiCapsnowavailableforcoughsuppression/article/122377/. Accessed Jan. 14, 2009.
9. UCB’s Vimpat approved by U.S. FDA as adjunctive therapy for partial onset seizures in adults. Medical News Today Web site. Available at: www.medicalnewstoday.com/articles/127354.php. Accessed Jan. 14, 2009.
10. Apriso granted FDA marketing approval for maintenance of remission of ulcerative colitis. Medical News Today Web site. Available at: http://www.medicalnewstoday.com/articles/127839.php. Accessed Jan. 14, 2009.
11. http://biz.yahoo.com/ap/081106/cv_therapeutics _ranexa.html?.v=1. Accessed February 2, 2009.
12. FDA approves Seroquel for bipolar maintenance. Monthly Prescribing Reference Web site. Available at: www.prescribingreference.com/news/showNews/which/SeroquelXRForBipolar10101. Accessed Jan. 14, 2009.
13. Seroquel XR Web site. Available at: www.pharmacistelink.com/news/2009/01/14_seroquel.pdf. Accessed Jan. 23, 2009.
14. Peck P. Smoking cessation drug linked to 1,001 new serious adverse events. Medpage Today Web site. Available at: www.medpagetoday.com/PrimaryCare/Smoking/11428. Accessed Jan. 14, 2009.
15. Public health advisory: important information on Chantix (varenicline). U.S. Food and Drug Administration Web site. Available at: www.fda.gov/CDER/Drug/advisory/varenicline.htm. Accessed Jan. 14, 2009.
There are multiple reasons for crushing tablets or capsule contents before administering medications, but there are numerous medications that should not be crushed. These medications should not be chewed, either, usually due to their specific formulations and their pharmacokinetic properties.1 Most of the no-crush medications are sustained-release, oral-dosage formulas. The majority of extended-release products should not be crushed or chewed, although there are some newer slow-release tablet formulations available that are scored and can be divided or halved (e.g., Toprol XL).
A common reason for crushing a tablet or capsule is for use by a hospitalized patient with an enteral feeding tube. A recent review in the American Journal of Health-System Pharmacy provides more details about administering medications in patients with enteral feeding tubes.2 Oral solutions can be used when commercially available and medically appropriate. If an oral solution or suspension is not available, the hospital pharmacy should be consulted to determine if a liquid formulation of the product can be extemporaneously prepared. In some cases, after careful consideration of compatibility, stability, and drug absorption changes, an injectable formulation of a product may be used. You should always consult your hospital pharmacist for information on this modality of drug administration.
Some patients have difficulty swallowing tablets or capsules; some dislike the taste. In these cases, crushing of medication for powdered delivery (to be mixed with food or beverages) should be considered. But beware of certain caveats, as not all medications are suitable for crushing. Generally, meds that should not be crushed fall into one of these categories:
- Sustained-release tablets, which can be composed of multiple layers for different drug release times, as can beads within capsules. Some of the more common prefixes or suffixes for sustained-release, controlled-release, or controlled-delivery products include: 12-hour, 24-hour, CC, CD, CR, ER, LA, Retard, SA, Slo-, SR, XL, XR, or XT.
- Enteric-coated tablets, which are formulated because certain drugs can be irritating to the stomach or are degraded by stomach acid. By enteric-coating tablets or capsule beads, the drug’s release can be delayed until it reaches the small intestine. Prefixes include EN- and EC-.
Other medications have objectionable tastes and are sugar-coated to improve tolerability. If this type of medication is crushed, the patient would be subject to its unpleasant taste, which could significantly impair medication adherence. Additionally, both sublingual and effervescent medications should not be crushed because it will decrease the medication’s effectiveness.
Hospital Pharmacy publishes a wall chart that includes many of these types of formulations, along with their do’s and don’ts. If there is ever any doubt about the best way to administer a particular product or whether it can be halved or crushed, ask your pharmacist.3 TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1. Mitchell J. Oral dosage forms that should not be crushed or chewed: facts and comparisons 4.0. Hospital Pharmacy Web site. Available at: online.factsandcomparisons.com/Viewer.aspx?book=atoz&monoID=fandc-atoz1040. Accessed March 5, 2009.
2. Williams NT. Medication administration through enteral feeding tubes. Am J Health Syst Pharm. 2008;65(24):2347-2357.
3. Mitchell JF. Oral dosage forms that should not be crushed: wall chart. Wolters Kluwer Health Web site. Available at: www.factsandcomparisons.com/Products/product.aspx?id=1111. Accessed Jan. 26, 2009.
4. Mylan's Matrix receives final FDA approval for the generic version of the antiretroviral Zerit capsules. Wolters Kluwer Health Web site. Available at: http://mylan.mediaroom.com/index.php?s=43&item=399. Accessed Jan. 23, 2009.
5. Product approval information. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/Cber/products/Cinryze.htm. Accessed Jan. 14, 2009.
6. FDA licenses for marketing new therapy for rare genetic disease. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/bbs/topics/NEWS/2008/NEW01903.html. Accessed Jan. 14, 2009.
7. Sancuso patch approved for nausea and vomiting. Monthly Prescribing Reference Web site. Available at: www.empr.com/Sancusopatchapprovedfornauseaandvomiting/article/122384/. Accessed Jan. 14, 2009.
8. TussiCaps now available for cough suppression. Monthly Prescribing Reference Web site. Available at: www.empr.com/TussiCapsnowavailableforcoughsuppression/article/122377/. Accessed Jan. 14, 2009.
9. UCB’s Vimpat approved by U.S. FDA as adjunctive therapy for partial onset seizures in adults. Medical News Today Web site. Available at: www.medicalnewstoday.com/articles/127354.php. Accessed Jan. 14, 2009.
10. Apriso granted FDA marketing approval for maintenance of remission of ulcerative colitis. Medical News Today Web site. Available at: http://www.medicalnewstoday.com/articles/127839.php. Accessed Jan. 14, 2009.
11. http://biz.yahoo.com/ap/081106/cv_therapeutics _ranexa.html?.v=1. Accessed February 2, 2009.
12. FDA approves Seroquel for bipolar maintenance. Monthly Prescribing Reference Web site. Available at: www.prescribingreference.com/news/showNews/which/SeroquelXRForBipolar10101. Accessed Jan. 14, 2009.
13. Seroquel XR Web site. Available at: www.pharmacistelink.com/news/2009/01/14_seroquel.pdf. Accessed Jan. 23, 2009.
14. Peck P. Smoking cessation drug linked to 1,001 new serious adverse events. Medpage Today Web site. Available at: www.medpagetoday.com/PrimaryCare/Smoking/11428. Accessed Jan. 14, 2009.
15. Public health advisory: important information on Chantix (varenicline). U.S. Food and Drug Administration Web site. Available at: www.fda.gov/CDER/Drug/advisory/varenicline.htm. Accessed Jan. 14, 2009.
Eliminate Inconsistency
Three years ago, Andrew Masica, MD, MSCI, joined the MedProvider Inpatient Care Unit hospitalist group at Baylor University Medical Center (BUMC) in Dallas just as the national debate on Medicare recidivism rates was focusing on high-risk populations.
Dr. Masica’s master’s degree in clinical investigation, combined with the roughly 35 hospitalists operating at the 900-bed BUMC, suggested it made sense to see what Baylor’s doctors could add to the conversation. And a study was born: “Reduction of 30-Day Post-Discharge Hospital Readmission or ED Visit Rates in High-Risk Elderly Medical Patients Through Delivery of a Targeted Care Bundle.” The single-center study will be published in this month’s Journal of Hospital Medicine.
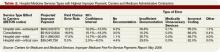
The study found readmission/ED visit rates were lower after 30 days for those given an individualized care bundle of educational information compared with those who received the center’s standard treatment (10% individualized care bundle compared with 38.1% for standard treatment, P=0.04). Analysis also showed that for those patients who had a readmission or post-discharge ED visit, the time interval to the second event was longer in the intervention group compared with the control group (36.2 days to 15.7 days, P=0.05). At 60 days, however, readmission/ED visit rates were not affected positively for the intervention group versus the control group (42.9% vs. 30%, P=0.52).
The study team emphasizes that its small sample size—20 in the intervention group, 21 in the control—make it nearly impossible to extrapolate the results to large population sets; however, the results fuel the debate. “We don’t want to overstate our conclusions,” says Dr. Masica, the principal study investigator. “Important questions need to be asked. Is it the specific characteristics of the care coordinators? Can you reproduce this at other facilities? Is it the care bundle or the personnel? …We view this as early-phase work that people can build upon.”
Expansion Opportunity
Still, Dr. Masica believes hospitalist-centric conclusions can be reached. Since the study used in-house personnel only, other HM groups could easily reproduce the bundle without added expense. Additionally, because the coordinated-care approach involves a checklist of patient interaction activities, not medical procedures, the barrier to replication is further reduced. However, hospitalists will need the cooperation of more than their own medical directors.
In BUMC’s case, that meant the assistance of patient-care support services and the pharmacy department. Liz Youngblood, RN, MBA, supervised the care coordination in her role as vice president of patient-care support services for the Baylor Health Care System. Brian Cohen, PharmD, MS, was the pharmacy lead. Dr. Masica notes the confluence between departments was one of the keys to the reduction in recidivism over the first 30 days post-discharge.
“If you pick the high-risk patients and deliver the care in a bundle, you would be able to improve outcomes,” Dr. Masica says. “When you deliver just pieces of the care—just the coordinated care or just the pharmacist—you get inconsistencies.”
The first struggle BUMC researchers encountered—once they secured funding from Baylor’s Institute for Health Care Research and Improvement—was enrolling enough patients who met the criteria set for the study. The high-risk patient thresholds were:
- At least 70 years old;
- Regular use of at least five medications;
- At least three chronic, comorbid conditions;
- Assistance with at least one activity of daily living; and
- Preadmission residence at home or at an assisted-living facility with a reasonable expectation of disposition back to that residence.
Researchers also wanted patients with common DRGs admitted, and set exclusion criteria as well: lack of fluency in English; admission primarily for a surgical procedure; terminal diagnosis with life expectancy of less than six months; and residency in a long-term care facility. Patients who could not be enrolled within 72 hours of admission were excluded.
Dr. Masica notes hospitalists interested in replicating the research should pay attention to the consent forms they used. When the Baylor team conducted its research from March to September 2007, they used a long-form consent waiver. Baylor’s consent form for similar studies has since been shortened, and Dr. Masica says a less complicated form would have helped encourage more patients to enroll. In the end, 60 patients declined to enroll in the Baylor study and 56 were unable to give their consent due to impairment.
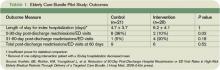
Once enrolled, the patients were delivered the care bundle in stages (see Table 1). Care coordinators (CCs) saw patients daily, instructing them on specific health conditions with an eye toward teaching home care, should post-discharge problems arise. Clinical pharmacists (CPs) visited patients to focus on medication reconciliation and education. CCs and CPs would follow up with post-discharge phone calls to confirm receipt of medical equipment and medications, use and affects of those medications, home-health arrangements, and to schedule follow-up appointments. If patients indicated any issues, the coordinators recommended action plans.
“It would be surprising to find out how little patients really understand about why they’re in the hospital and what they’re being treated for,” Youngblood says. “To have the reinforcement is really valuable.”
Care Continuum
One topic the study skirts is the ever-contentious realm of post-discharge care and who takes over responsibility for patient care. While the Baylor study examined readmission/ED visit rates through 60 days, Dr. Masica says a transitional-care program is the best way to manage that care continuum.
“We did see a difference at 30 days,” Dr. Masica says. “At 60 days, that effectively washed out. That makes sense. You can only control things so much from the hospital side. After 30 days, you need transitional care, good primary care.”
Baylor’s research team is working on a follow-up study that would apply the coordinated-care bundle to specific disease management. Youngblood notes that directing specific services at a targeted population—for example, congestive heart failure patients—should show an even more concentrated reduction of 30-day recidivism. “The key is to identify the high-risk groups,” he says. “You can’t apply this to every single patient. That would be low-yield. Your yield is going to come in on the very high-risk folks.” TH
Richard Quinn is a freelance writer based in New Jersey.
Three years ago, Andrew Masica, MD, MSCI, joined the MedProvider Inpatient Care Unit hospitalist group at Baylor University Medical Center (BUMC) in Dallas just as the national debate on Medicare recidivism rates was focusing on high-risk populations.
Dr. Masica’s master’s degree in clinical investigation, combined with the roughly 35 hospitalists operating at the 900-bed BUMC, suggested it made sense to see what Baylor’s doctors could add to the conversation. And a study was born: “Reduction of 30-Day Post-Discharge Hospital Readmission or ED Visit Rates in High-Risk Elderly Medical Patients Through Delivery of a Targeted Care Bundle.” The single-center study will be published in this month’s Journal of Hospital Medicine.
The study found readmission/ED visit rates were lower after 30 days for those given an individualized care bundle of educational information compared with those who received the center’s standard treatment (10% individualized care bundle compared with 38.1% for standard treatment, P=0.04). Analysis also showed that for those patients who had a readmission or post-discharge ED visit, the time interval to the second event was longer in the intervention group compared with the control group (36.2 days to 15.7 days, P=0.05). At 60 days, however, readmission/ED visit rates were not affected positively for the intervention group versus the control group (42.9% vs. 30%, P=0.52).
The study team emphasizes that its small sample size—20 in the intervention group, 21 in the control—make it nearly impossible to extrapolate the results to large population sets; however, the results fuel the debate. “We don’t want to overstate our conclusions,” says Dr. Masica, the principal study investigator. “Important questions need to be asked. Is it the specific characteristics of the care coordinators? Can you reproduce this at other facilities? Is it the care bundle or the personnel? …We view this as early-phase work that people can build upon.”
Expansion Opportunity
Still, Dr. Masica believes hospitalist-centric conclusions can be reached. Since the study used in-house personnel only, other HM groups could easily reproduce the bundle without added expense. Additionally, because the coordinated-care approach involves a checklist of patient interaction activities, not medical procedures, the barrier to replication is further reduced. However, hospitalists will need the cooperation of more than their own medical directors.
In BUMC’s case, that meant the assistance of patient-care support services and the pharmacy department. Liz Youngblood, RN, MBA, supervised the care coordination in her role as vice president of patient-care support services for the Baylor Health Care System. Brian Cohen, PharmD, MS, was the pharmacy lead. Dr. Masica notes the confluence between departments was one of the keys to the reduction in recidivism over the first 30 days post-discharge.
“If you pick the high-risk patients and deliver the care in a bundle, you would be able to improve outcomes,” Dr. Masica says. “When you deliver just pieces of the care—just the coordinated care or just the pharmacist—you get inconsistencies.”
The first struggle BUMC researchers encountered—once they secured funding from Baylor’s Institute for Health Care Research and Improvement—was enrolling enough patients who met the criteria set for the study. The high-risk patient thresholds were:
- At least 70 years old;
- Regular use of at least five medications;
- At least three chronic, comorbid conditions;
- Assistance with at least one activity of daily living; and
- Preadmission residence at home or at an assisted-living facility with a reasonable expectation of disposition back to that residence.
Researchers also wanted patients with common DRGs admitted, and set exclusion criteria as well: lack of fluency in English; admission primarily for a surgical procedure; terminal diagnosis with life expectancy of less than six months; and residency in a long-term care facility. Patients who could not be enrolled within 72 hours of admission were excluded.
Dr. Masica notes hospitalists interested in replicating the research should pay attention to the consent forms they used. When the Baylor team conducted its research from March to September 2007, they used a long-form consent waiver. Baylor’s consent form for similar studies has since been shortened, and Dr. Masica says a less complicated form would have helped encourage more patients to enroll. In the end, 60 patients declined to enroll in the Baylor study and 56 were unable to give their consent due to impairment.
Once enrolled, the patients were delivered the care bundle in stages (see Table 1). Care coordinators (CCs) saw patients daily, instructing them on specific health conditions with an eye toward teaching home care, should post-discharge problems arise. Clinical pharmacists (CPs) visited patients to focus on medication reconciliation and education. CCs and CPs would follow up with post-discharge phone calls to confirm receipt of medical equipment and medications, use and affects of those medications, home-health arrangements, and to schedule follow-up appointments. If patients indicated any issues, the coordinators recommended action plans.
“It would be surprising to find out how little patients really understand about why they’re in the hospital and what they’re being treated for,” Youngblood says. “To have the reinforcement is really valuable.”
Care Continuum
One topic the study skirts is the ever-contentious realm of post-discharge care and who takes over responsibility for patient care. While the Baylor study examined readmission/ED visit rates through 60 days, Dr. Masica says a transitional-care program is the best way to manage that care continuum.
“We did see a difference at 30 days,” Dr. Masica says. “At 60 days, that effectively washed out. That makes sense. You can only control things so much from the hospital side. After 30 days, you need transitional care, good primary care.”
Baylor’s research team is working on a follow-up study that would apply the coordinated-care bundle to specific disease management. Youngblood notes that directing specific services at a targeted population—for example, congestive heart failure patients—should show an even more concentrated reduction of 30-day recidivism. “The key is to identify the high-risk groups,” he says. “You can’t apply this to every single patient. That would be low-yield. Your yield is going to come in on the very high-risk folks.” TH
Richard Quinn is a freelance writer based in New Jersey.
Three years ago, Andrew Masica, MD, MSCI, joined the MedProvider Inpatient Care Unit hospitalist group at Baylor University Medical Center (BUMC) in Dallas just as the national debate on Medicare recidivism rates was focusing on high-risk populations.
Dr. Masica’s master’s degree in clinical investigation, combined with the roughly 35 hospitalists operating at the 900-bed BUMC, suggested it made sense to see what Baylor’s doctors could add to the conversation. And a study was born: “Reduction of 30-Day Post-Discharge Hospital Readmission or ED Visit Rates in High-Risk Elderly Medical Patients Through Delivery of a Targeted Care Bundle.” The single-center study will be published in this month’s Journal of Hospital Medicine.
The study found readmission/ED visit rates were lower after 30 days for those given an individualized care bundle of educational information compared with those who received the center’s standard treatment (10% individualized care bundle compared with 38.1% for standard treatment, P=0.04). Analysis also showed that for those patients who had a readmission or post-discharge ED visit, the time interval to the second event was longer in the intervention group compared with the control group (36.2 days to 15.7 days, P=0.05). At 60 days, however, readmission/ED visit rates were not affected positively for the intervention group versus the control group (42.9% vs. 30%, P=0.52).
The study team emphasizes that its small sample size—20 in the intervention group, 21 in the control—make it nearly impossible to extrapolate the results to large population sets; however, the results fuel the debate. “We don’t want to overstate our conclusions,” says Dr. Masica, the principal study investigator. “Important questions need to be asked. Is it the specific characteristics of the care coordinators? Can you reproduce this at other facilities? Is it the care bundle or the personnel? …We view this as early-phase work that people can build upon.”
Expansion Opportunity
Still, Dr. Masica believes hospitalist-centric conclusions can be reached. Since the study used in-house personnel only, other HM groups could easily reproduce the bundle without added expense. Additionally, because the coordinated-care approach involves a checklist of patient interaction activities, not medical procedures, the barrier to replication is further reduced. However, hospitalists will need the cooperation of more than their own medical directors.
In BUMC’s case, that meant the assistance of patient-care support services and the pharmacy department. Liz Youngblood, RN, MBA, supervised the care coordination in her role as vice president of patient-care support services for the Baylor Health Care System. Brian Cohen, PharmD, MS, was the pharmacy lead. Dr. Masica notes the confluence between departments was one of the keys to the reduction in recidivism over the first 30 days post-discharge.
“If you pick the high-risk patients and deliver the care in a bundle, you would be able to improve outcomes,” Dr. Masica says. “When you deliver just pieces of the care—just the coordinated care or just the pharmacist—you get inconsistencies.”
The first struggle BUMC researchers encountered—once they secured funding from Baylor’s Institute for Health Care Research and Improvement—was enrolling enough patients who met the criteria set for the study. The high-risk patient thresholds were:
- At least 70 years old;
- Regular use of at least five medications;
- At least three chronic, comorbid conditions;
- Assistance with at least one activity of daily living; and
- Preadmission residence at home or at an assisted-living facility with a reasonable expectation of disposition back to that residence.
Researchers also wanted patients with common DRGs admitted, and set exclusion criteria as well: lack of fluency in English; admission primarily for a surgical procedure; terminal diagnosis with life expectancy of less than six months; and residency in a long-term care facility. Patients who could not be enrolled within 72 hours of admission were excluded.
Dr. Masica notes hospitalists interested in replicating the research should pay attention to the consent forms they used. When the Baylor team conducted its research from March to September 2007, they used a long-form consent waiver. Baylor’s consent form for similar studies has since been shortened, and Dr. Masica says a less complicated form would have helped encourage more patients to enroll. In the end, 60 patients declined to enroll in the Baylor study and 56 were unable to give their consent due to impairment.
Once enrolled, the patients were delivered the care bundle in stages (see Table 1). Care coordinators (CCs) saw patients daily, instructing them on specific health conditions with an eye toward teaching home care, should post-discharge problems arise. Clinical pharmacists (CPs) visited patients to focus on medication reconciliation and education. CCs and CPs would follow up with post-discharge phone calls to confirm receipt of medical equipment and medications, use and affects of those medications, home-health arrangements, and to schedule follow-up appointments. If patients indicated any issues, the coordinators recommended action plans.
“It would be surprising to find out how little patients really understand about why they’re in the hospital and what they’re being treated for,” Youngblood says. “To have the reinforcement is really valuable.”
Care Continuum
One topic the study skirts is the ever-contentious realm of post-discharge care and who takes over responsibility for patient care. While the Baylor study examined readmission/ED visit rates through 60 days, Dr. Masica says a transitional-care program is the best way to manage that care continuum.
“We did see a difference at 30 days,” Dr. Masica says. “At 60 days, that effectively washed out. That makes sense. You can only control things so much from the hospital side. After 30 days, you need transitional care, good primary care.”
Baylor’s research team is working on a follow-up study that would apply the coordinated-care bundle to specific disease management. Youngblood notes that directing specific services at a targeted population—for example, congestive heart failure patients—should show an even more concentrated reduction of 30-day recidivism. “The key is to identify the high-risk groups,” he says. “You can’t apply this to every single patient. That would be low-yield. Your yield is going to come in on the very high-risk folks.” TH
Richard Quinn is a freelance writer based in New Jersey.
The latest research you need to know
In This Edition
- Generic vs. brand-name drugs.
- Rapid-response teams and mortality.
- A new prediction rule for mortality in acute pancreatitis.
- Viral causes of community-acquired pneumonia.
- Intensive insulin therapy in the ICU.
- New preoperative and intraoperative risk factors.
- Timing of ICU feedings and mortality.
- Aspirin as primary prevention in diabetics.
Generic, Brand-Name Drugs Used for Cardiovascular Disease Are Clinically Equivalent
Clinical question: Is there a clinical risk when substituting generic drugs for brand-name drugs in the treatment of cardiovascular disease?
Background: Spending on healthcare in the U.S. has reached critical levels. Increasing prescription drug costs make up a large portion of healthcare expenditures. The high cost of medicines directly affect adherence to treatment regimens and contribute to poor health outcomes. Cardiovascular drugs make up the largest portion of outpatient prescription drug spending.
Study design: Systematic review of relevant articles with a meta-analysis performed to determine an aggregate effect size.
Setting: Multiple locations and varied patient populations.
Synopsis: A total of 47 articles were included in the review, of which 38 were randomized controlled trials (RCTs). The studies measured both clinical efficacy and safety end points. More than half the articles were published prior to 2000. Clinical equivalence was noted in all seven beta-blocker RCTs; 10 of 11 diuretic RCTs; five of seven calcium-channel-blocker RCTs; all three antiplatelet-agent RCTs (clopidogrel, enteric-coated aspirin); two statin RCTs; one ACE-inhibitor RCT; and one alpha-blocker RCT. For drugs with a narrow therapeutic index, clinical equivalence was noted in all five warfarin RCTs and a single Class 1 anti-arrhythmic-agent RCT.
The aggregate effect size was -0.03 (95% CI, -0.15 to 0.08), which indicates nearly complete overlap of the generic and brand-name distributions. The data show no evidence of superiority of brand-name to generic drugs in clinical outcomes measured in the various studies.
In a separate review of editorials addressing generic substitution for cardiovascular drugs, 53% expressed a negative view of generic-drug substitution.
Bottom line: There is clinical equivalency between generic and brand-name drugs used in the treatment of cardiovascular disease. Despite this conclusion, a substantial number of editorials advise against generic substitution, which affects both patient and physician drug preferences.
Citation: Kesselheim A, Misono A, Lee J, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008; 300(21):2514-2526.
RRT Implement-ation Doesn’t Affect Hospitalwide Code Rates or Mortality
Clinical question: Does the use of a rapid-response team (RRT) affect hospitalwide code rates and mortality?
Background: In the 100,000 Lives campaign, the Institute for Healthcare Improvement recommended that hospitals implement RRTs to help reduce preventable, in-hospital deaths. Studies have demonstrated that rates of non-ICU codes decrease after RRT implementation. It is unclear if this translates to changes in mortality rates.
Study design: Prospective cohort study of adult inpatients.
Setting: Saint Luke’s Hospital, a 404-bed tertiary-care academic hospital in Kansas City, Mo.
Synopsis: The hospital documented a total of 376 RRT activations. After RRT implementation, mean hospitalwide code rates decreased to 7.5 per 1,000 admissions from 11.2 per 1,000 admissions. This was not associated with a statistically significant reduction in hospitalwide code rates (adjusted odds ratio 0.76; 95% CI; 0.57-1.01; P=0.06). Secondary analyses noted lower rates of non-ICU codes (0.59; 95% CI, 0.40-0.89) compared with ICU codes (0.95; 95% CI; 0.64-1.43; P=0.03 for interaction). Finally, the RRT implementation was not associated with lower hospital-wide mortality (0.95; 95% CI; 0.81-1.11; P=0.52).
Secondary analyses also revealed few instances of RRT undertreatment or underutilization that may have affected the mortality numbers.
A limitation of this study is that it was slightly underpowered (78%) to detect a significant mortality difference. The findings also represent a single institution experience, and may not be generalized to other adult hospital settings or RRT programs.
Bottom line: Implementation of an RRT does not confer lower rates of hospital-wide code arrests or mortality.
Citation: Chan P, Khalid A, Longmore L, et al. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA. 2008;300(21):2506-2513.
Simple Scoring System Provides Timely Prediction of Mortality in Acute Pancreatitis
Clinical question: How can physicians predict mortality in acute pancreatitis?
Background: Historical predictors of mortality in acute pancreatitis require up to 48 hours of data, such as with the Ranson Criteria, or extensive amounts of data, such as with the APACHE II score. An easier tool is needed to predict which patients are at higher risk of mortality.
Study design: Retrospective cohort.
Setting: Patients in the Cardinal Health clinical outcomes research database, which supports public reporting of hospital performance.
Synopsis: The authors identified patients with the principal diagnosis of pancreatitis from 2000-2001 and explored numerous diagnostic findings available within the first 24 hours. Ultimately, BUN >25, impaired mental status, presence of SIRS (systemic inflammatory response syndrome), age >60, and presence of a pleural effusion were found to be predictive of mortality. These diagnostic findings correspond to the mnemonic BISAP. The BISAP score was then validated in a second cohort that included patients from 2004-2005.
Each finding in the BISAP score was given one point. A score of less than 2 was present in approximately 60% of patients admitted with acute pancreatitis, and corresponded to a mortality of less than 1%. A score of 2 corresponded to a mortality of 2%. Higher scores were associated with steeply increasing mortality, with a score of 5 corresponding with greater than 20% mortality.
The BISAP score performed similarly to the APACHE II score, but the former is easier to calculate on the day of admission and has fewer parameters. A more challenging research step will be to demonstrate that using the BISAP score to determine treatment strategies can affect patient outcomes.
Bottom line: The easy-to-calculate BISAP score is a new method for predicting mortality in patients with acute pancreatitis. This tool should help hospitalists determine, on the day of admission, to what extent patients with acute pancreatitis need aggressive management, such as ICU admission and early involvement of specialists.
Citation: Wu B, Johannes R, Sun X, Tabak Y, Conwell D, Banks P. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57(12): 1698-1703.
Nasal Swabs Identify Viral Causes in CAP Patients
Clinical question: How often is viral infection associated with community-acquired pneumonia (CAP) in adults?
Background: CAP is a clinically important disease that is associated with significant hospitalization and mortality. CAP treatment guidelines acknowledge respiratory viruses as an etiology for pneumonia, but few recommendations are made regarding management of these viral infections.
Study design: Prospective study.
Setting: Five hospitals in Edmonton, Alberta, from 2004-2006.
Synopsis: The authors enrolled 193 hospitalized adults, median age 71. Nucleic amplification tests (NATs) from nasopharyngeal swab specimens were tested for human metapneumovirus, respiratory syncytial virus, rhinovirus, parainfluenza virus 1-4, coronaviruses, and adenovirus.
Fifteen percent of these patients had a nasal swab positive for a viral infection. Interestingly, 4% of patients had both a positive viral nasal swab and positive bacterial cultures. Compared with bacterial infection, patients with viral infection tended to be older (76 vs. 64 years, P=0.01), have limited ambulation (66% vs. 32%, P=0.006), and have a history of cardiac disease (66% vs. 32%, P=0.02). Patients with bacterial pneumonia showed a statistically significant trend toward having chest pain, an abnormal white blood count, and a lobar infiltrate on chest X-ray.
Further investigations might look at how nasal swab data could be used to improve infection control within the hospital for patients found to have easily transmissible viruses. Further research could explore the feasibility of avoiding antibiotic use in patients found to have viral pneumonia, assuming bacterial co-infection is reliably excluded.
Bottom line: Nasal swabs using NAT technology could play a significant role in identifying pathogens in CAP patients. How this technology should affect clinical decision-making and how it might improve outcomes remains unknown.
Citation: Johnstone J, Majumdar S, Fox J, Marrie T. Viral infection in adults hospitalized with community-acquired pneumonia: prevalence, pathogens, and presentation. Chest. 2008;134(6):1141-1148.
Intensive Insulin Therapy Doesn’t Reduce ICU Mortality
Clinical question: Does the use of intensive insulin therapy decrease mortality in the intensive-care unit (ICU)?
Background: In 2001, Van den Berghe et al (N Engl J Med. 2001;345(19):1359-67) reported a reduction in morbidity and mortality with intensive insulin therapy (IIT) in surgical ICU patients. This study led to the adoption of IIT protocols in many hospitals. Since 2001, further studies have failed to reproduce the same dramatic benefit of IIT.
Study design: Randomized, controlled trial.
Setting: National Guard King Abdulaziz Medical City, a tertiary-care teaching hospital in Saudi Arabia.
Synopsis: Patients were included in this study if they were 18 years or older with serum glucose levels greater than 110 mg/dL during the first 24 hours of ICU admission. There were multiple exclusion criteria, including patients with Type I diabetes, documented hypoglycemia on ICU admission (glucose <40), or diabetic ketoacidosis.
Enrolled patients were randomized to IIT or conventional insulin therapy (CIT). A multidisciplinary team designed the protocols to maintain glucose levels of 80 to 110 mg/dL and 180 to 200 mg/dL in the IIT and the CIT groups, respectively. The primary endpoint measured was ICU mortality.
The study did not produce a statistically significant difference in ICU mortality (13.5% for IIT vs. 17.1% for CIT; P=0.30). The adjusted hypoglycemia rate was 6.8 per 100 treatment days with IIT and 0.4 per 100 treatment days with CIT (P<0.0001). Patients with hypoglycemia had higher ICU mortality (23.8% vs. 13.7%, P=0.02).
In the measurement of secondary endpoints, there was a trend toward lower episodes of severe sepsis and septic shock in the IIT group (20.7% in IIT vs. 27.2% in CIT, P=0.08). However, this result was not statistically significant.
Bottom line: This well-designed study failed to show a survival benefit with IIT use in the critical-care setting. Given the findings of this and several other recent studies, one should question whether IIT should be prescribed as the standard of care in all critically-ill patients.
Citation: Arabi Y, Dabbagh O, Tamim H, et al. Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Crit Care Med. 2008;36(12):3190-3197.
Preoperative and Intraoperative Predictors of Cardiac Adverse Events
Clinical question: What are the incidence and risk factors for perioperative cardiac adverse events after noncardiac surgery?
Background: In the past few decades, the incidence of cardiac adverse events (CAEs) for a general surgery population has remained largely unchanged (approximately 1%). This is in spite of multiple studies evaluating predictive models and attempts at preventive treatment, including preoperative coronary revascularization and perioperative beta blockers.
Study design: Prospective observational study.
Setting: Single, large, tertiary-care university hospital.
Synopsis: A total of 7,740 cases were reviewed in this study, which consisted of general surgery (4,937), vascular surgery (1,846), and urological surgery (957). A trained nurse followed up for perioperative CAEs as many as 30 days after the operation via medical chart review, phone calls, and letters. CAEs were defined as: Q-wave myocardial infarction (MI), non-ST elevation MI, cardiac arrest, or new cardiac dysrhythmia. A total of 83 CAEs (1.1% of patients) had cardiac arrest, with cardiac dysrhythmia being most common.
A total of seven preoperative risk factors were identified as independent predictors for CAEs: age 68, BMI 30, emergent surgery, prior coronary intervention or cardiac surgery, active congestive heart failure, cerebrovascular disease, and hypertension. In addition, two intraoperative risk factors were identified: intraoperative transfusion of packed red blood cells and operative duration of 3.8 hours. (The P value was 0.05 for all independent predictors.)
A further evaluation of intraoperative parameters of high-risk patients experiencing a CAE showed that these patients were more likely to have an episode of mean arterial pressure (MAP) <50 mmHg, an episode of 40% decrease in MAP, and an episode of tachycardia (heart rate >100).
Bottom line: A combination of preoperative predictors and intraoperative elements can help improve risk assessment for perioperative CAEs after noncardiac surgery.
Citation: Kheterpal S, O’Reilly M, Englesbe M, et al. Preoperative and intraoperative predictors of cardiac adverse events after general, vascular, and urological surgery. Anesthesiology. 2009;110(1):58-66.
Early Feeding in the ICU Does Not Affect Hospital Mortality
Clinical question: Will implementing evidence-based feeding guidelines improve feeding practices and reduce mortality in ICU patients?
Background: There is evidence suggesting that providing nutritional support to ICU patients within 24 hours of admission may decrease mortality. It is widely understood that patient care varies between ICUs, and there exist no uniform, evidence-based guidelines for nutritional support. Many patients remain unfed after 48 hours.
Study design: Cluster, randomized-controlled trial.
Setting: ICUs in 27 community and tertiary-care hospitals in Australia and New Zealand.
Synopsis: Hospitals were randomized to intervention or control groups. Dietitian and intensivist co-investigators from intervention ICUs developed guidelines using the Clinical Practice Guideline Development Cycle. Control ICUs were requested to make no new ICU nutritional management changes. The study enrolled 1,118 eligible patients and included adults expected to stay longer than two days. Excluded were patients taking oral diets, patients receiving palliative care or with suspected brain death, and patients sent from other facilities.
Guidelines were implemented using several methods—educational outreach visits, one-on-one conversations, active reminders, passive reminders, and educational in-services. The guidelines were successful in evoking significant practice changes in all of the intervention ICUs. Significantly more patients received nutritional support during their ICU stays in guideline ICUs, and patients in these ICUs were fed significantly earlier. There were, however, no significant differences between guideline and control ICUs with regard to hospital discharge mortality (28.9% vs. 27.4%; 95% CI; -6.3% to 12.0%; P=0.75). The groups also showed no statistical difference in hospital or ICU length of stay.
Bottom line: Significantly more patients in the guideline ICUs were fed within 24 hours, but this did not translate into improvements in mortality or other clinical outcomes.
Citation: Doig G, Simpson F, Finfer S, et al. Effect of evidence-based feeding guidelines on mortality of critically ill adults: a cluster randomized controlled trial. JAMA. 2008;300(23):2731-2741.
Low-Dose Aspirin Doesn’t Reduce Cardiovascular Events in Type 2 Diabetes Patients
Clinical question: Is low-dose aspirin effective for the primary prevention of atherosclerotic events in patients with Type 2 diabetes?
Background: Diabetes is a significant risk factor for cardiovascular events. Several prior studies have shown that aspirin therapy is effective as a secondary prevention strategy for cardiovascular events. The American Diabetes Association also recommends use of aspirin as a primary prevention strategy. Clinical trial data is currently insufficient in this area.
Study design: Prospective, randomized, open-label, controlled trial with blinded endpoint assessment.
Setting: 163 institutions in Japan.
Synopsis: The study enrolled 2,539 diabetic patients between 30 and 85 years old—mean age was 65—and included patients without EKG changes or a significant history or ongoing treatment of atherosclerotic disease. Patients were randomly assigned into an aspirin group (81 mg or 100 mg once daily) or a nonaspirin group. Patients had a median follow up of 4.37 years.
The primary endpoint was any atherosclerotic event, ranging from sudden death to ischemic heart disease or stroke. The incidence of atherosclerotic events was not statistically different in the aspirin group (68 events, 5.4%) than in the nonaspirin group (86 events, 6.7%) (HR, 0.80; 95% CI; 0.58-1.10; log-rank test, P=0.16). However, there was a suggested benefit of primary prevention in the subgroup aged 65 years or older. In addition, the combined endpoint of fatal coronary and cerebrovascular events occurred in one patient in the aspirin group and 10 patients in the nonaspirin group (HR, 0.10; 95 % CI, 0.01-0.79; P=.0037). This study is limited by the low incidence of atherosclerotic disease in Japan.
Bottom line: Low-dose aspirin used in patients with Type 2 diabetes does not significantly demonstrate primary prevention of cardiovascular events.
Citation: Ogawa H, Nakayama M, Morimoto T, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2008;300(18):2134-2141. TH
In This Edition
- Generic vs. brand-name drugs.
- Rapid-response teams and mortality.
- A new prediction rule for mortality in acute pancreatitis.
- Viral causes of community-acquired pneumonia.
- Intensive insulin therapy in the ICU.
- New preoperative and intraoperative risk factors.
- Timing of ICU feedings and mortality.
- Aspirin as primary prevention in diabetics.
Generic, Brand-Name Drugs Used for Cardiovascular Disease Are Clinically Equivalent
Clinical question: Is there a clinical risk when substituting generic drugs for brand-name drugs in the treatment of cardiovascular disease?
Background: Spending on healthcare in the U.S. has reached critical levels. Increasing prescription drug costs make up a large portion of healthcare expenditures. The high cost of medicines directly affect adherence to treatment regimens and contribute to poor health outcomes. Cardiovascular drugs make up the largest portion of outpatient prescription drug spending.
Study design: Systematic review of relevant articles with a meta-analysis performed to determine an aggregate effect size.
Setting: Multiple locations and varied patient populations.
Synopsis: A total of 47 articles were included in the review, of which 38 were randomized controlled trials (RCTs). The studies measured both clinical efficacy and safety end points. More than half the articles were published prior to 2000. Clinical equivalence was noted in all seven beta-blocker RCTs; 10 of 11 diuretic RCTs; five of seven calcium-channel-blocker RCTs; all three antiplatelet-agent RCTs (clopidogrel, enteric-coated aspirin); two statin RCTs; one ACE-inhibitor RCT; and one alpha-blocker RCT. For drugs with a narrow therapeutic index, clinical equivalence was noted in all five warfarin RCTs and a single Class 1 anti-arrhythmic-agent RCT.
The aggregate effect size was -0.03 (95% CI, -0.15 to 0.08), which indicates nearly complete overlap of the generic and brand-name distributions. The data show no evidence of superiority of brand-name to generic drugs in clinical outcomes measured in the various studies.
In a separate review of editorials addressing generic substitution for cardiovascular drugs, 53% expressed a negative view of generic-drug substitution.
Bottom line: There is clinical equivalency between generic and brand-name drugs used in the treatment of cardiovascular disease. Despite this conclusion, a substantial number of editorials advise against generic substitution, which affects both patient and physician drug preferences.
Citation: Kesselheim A, Misono A, Lee J, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008; 300(21):2514-2526.
RRT Implement-ation Doesn’t Affect Hospitalwide Code Rates or Mortality
Clinical question: Does the use of a rapid-response team (RRT) affect hospitalwide code rates and mortality?
Background: In the 100,000 Lives campaign, the Institute for Healthcare Improvement recommended that hospitals implement RRTs to help reduce preventable, in-hospital deaths. Studies have demonstrated that rates of non-ICU codes decrease after RRT implementation. It is unclear if this translates to changes in mortality rates.
Study design: Prospective cohort study of adult inpatients.
Setting: Saint Luke’s Hospital, a 404-bed tertiary-care academic hospital in Kansas City, Mo.
Synopsis: The hospital documented a total of 376 RRT activations. After RRT implementation, mean hospitalwide code rates decreased to 7.5 per 1,000 admissions from 11.2 per 1,000 admissions. This was not associated with a statistically significant reduction in hospitalwide code rates (adjusted odds ratio 0.76; 95% CI; 0.57-1.01; P=0.06). Secondary analyses noted lower rates of non-ICU codes (0.59; 95% CI, 0.40-0.89) compared with ICU codes (0.95; 95% CI; 0.64-1.43; P=0.03 for interaction). Finally, the RRT implementation was not associated with lower hospital-wide mortality (0.95; 95% CI; 0.81-1.11; P=0.52).
Secondary analyses also revealed few instances of RRT undertreatment or underutilization that may have affected the mortality numbers.
A limitation of this study is that it was slightly underpowered (78%) to detect a significant mortality difference. The findings also represent a single institution experience, and may not be generalized to other adult hospital settings or RRT programs.
Bottom line: Implementation of an RRT does not confer lower rates of hospital-wide code arrests or mortality.
Citation: Chan P, Khalid A, Longmore L, et al. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA. 2008;300(21):2506-2513.
Simple Scoring System Provides Timely Prediction of Mortality in Acute Pancreatitis
Clinical question: How can physicians predict mortality in acute pancreatitis?
Background: Historical predictors of mortality in acute pancreatitis require up to 48 hours of data, such as with the Ranson Criteria, or extensive amounts of data, such as with the APACHE II score. An easier tool is needed to predict which patients are at higher risk of mortality.
Study design: Retrospective cohort.
Setting: Patients in the Cardinal Health clinical outcomes research database, which supports public reporting of hospital performance.
Synopsis: The authors identified patients with the principal diagnosis of pancreatitis from 2000-2001 and explored numerous diagnostic findings available within the first 24 hours. Ultimately, BUN >25, impaired mental status, presence of SIRS (systemic inflammatory response syndrome), age >60, and presence of a pleural effusion were found to be predictive of mortality. These diagnostic findings correspond to the mnemonic BISAP. The BISAP score was then validated in a second cohort that included patients from 2004-2005.
Each finding in the BISAP score was given one point. A score of less than 2 was present in approximately 60% of patients admitted with acute pancreatitis, and corresponded to a mortality of less than 1%. A score of 2 corresponded to a mortality of 2%. Higher scores were associated with steeply increasing mortality, with a score of 5 corresponding with greater than 20% mortality.
The BISAP score performed similarly to the APACHE II score, but the former is easier to calculate on the day of admission and has fewer parameters. A more challenging research step will be to demonstrate that using the BISAP score to determine treatment strategies can affect patient outcomes.
Bottom line: The easy-to-calculate BISAP score is a new method for predicting mortality in patients with acute pancreatitis. This tool should help hospitalists determine, on the day of admission, to what extent patients with acute pancreatitis need aggressive management, such as ICU admission and early involvement of specialists.
Citation: Wu B, Johannes R, Sun X, Tabak Y, Conwell D, Banks P. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57(12): 1698-1703.
Nasal Swabs Identify Viral Causes in CAP Patients
Clinical question: How often is viral infection associated with community-acquired pneumonia (CAP) in adults?
Background: CAP is a clinically important disease that is associated with significant hospitalization and mortality. CAP treatment guidelines acknowledge respiratory viruses as an etiology for pneumonia, but few recommendations are made regarding management of these viral infections.
Study design: Prospective study.
Setting: Five hospitals in Edmonton, Alberta, from 2004-2006.
Synopsis: The authors enrolled 193 hospitalized adults, median age 71. Nucleic amplification tests (NATs) from nasopharyngeal swab specimens were tested for human metapneumovirus, respiratory syncytial virus, rhinovirus, parainfluenza virus 1-4, coronaviruses, and adenovirus.
Fifteen percent of these patients had a nasal swab positive for a viral infection. Interestingly, 4% of patients had both a positive viral nasal swab and positive bacterial cultures. Compared with bacterial infection, patients with viral infection tended to be older (76 vs. 64 years, P=0.01), have limited ambulation (66% vs. 32%, P=0.006), and have a history of cardiac disease (66% vs. 32%, P=0.02). Patients with bacterial pneumonia showed a statistically significant trend toward having chest pain, an abnormal white blood count, and a lobar infiltrate on chest X-ray.
Further investigations might look at how nasal swab data could be used to improve infection control within the hospital for patients found to have easily transmissible viruses. Further research could explore the feasibility of avoiding antibiotic use in patients found to have viral pneumonia, assuming bacterial co-infection is reliably excluded.
Bottom line: Nasal swabs using NAT technology could play a significant role in identifying pathogens in CAP patients. How this technology should affect clinical decision-making and how it might improve outcomes remains unknown.
Citation: Johnstone J, Majumdar S, Fox J, Marrie T. Viral infection in adults hospitalized with community-acquired pneumonia: prevalence, pathogens, and presentation. Chest. 2008;134(6):1141-1148.
Intensive Insulin Therapy Doesn’t Reduce ICU Mortality
Clinical question: Does the use of intensive insulin therapy decrease mortality in the intensive-care unit (ICU)?
Background: In 2001, Van den Berghe et al (N Engl J Med. 2001;345(19):1359-67) reported a reduction in morbidity and mortality with intensive insulin therapy (IIT) in surgical ICU patients. This study led to the adoption of IIT protocols in many hospitals. Since 2001, further studies have failed to reproduce the same dramatic benefit of IIT.
Study design: Randomized, controlled trial.
Setting: National Guard King Abdulaziz Medical City, a tertiary-care teaching hospital in Saudi Arabia.
Synopsis: Patients were included in this study if they were 18 years or older with serum glucose levels greater than 110 mg/dL during the first 24 hours of ICU admission. There were multiple exclusion criteria, including patients with Type I diabetes, documented hypoglycemia on ICU admission (glucose <40), or diabetic ketoacidosis.
Enrolled patients were randomized to IIT or conventional insulin therapy (CIT). A multidisciplinary team designed the protocols to maintain glucose levels of 80 to 110 mg/dL and 180 to 200 mg/dL in the IIT and the CIT groups, respectively. The primary endpoint measured was ICU mortality.
The study did not produce a statistically significant difference in ICU mortality (13.5% for IIT vs. 17.1% for CIT; P=0.30). The adjusted hypoglycemia rate was 6.8 per 100 treatment days with IIT and 0.4 per 100 treatment days with CIT (P<0.0001). Patients with hypoglycemia had higher ICU mortality (23.8% vs. 13.7%, P=0.02).
In the measurement of secondary endpoints, there was a trend toward lower episodes of severe sepsis and septic shock in the IIT group (20.7% in IIT vs. 27.2% in CIT, P=0.08). However, this result was not statistically significant.
Bottom line: This well-designed study failed to show a survival benefit with IIT use in the critical-care setting. Given the findings of this and several other recent studies, one should question whether IIT should be prescribed as the standard of care in all critically-ill patients.
Citation: Arabi Y, Dabbagh O, Tamim H, et al. Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Crit Care Med. 2008;36(12):3190-3197.
Preoperative and Intraoperative Predictors of Cardiac Adverse Events
Clinical question: What are the incidence and risk factors for perioperative cardiac adverse events after noncardiac surgery?
Background: In the past few decades, the incidence of cardiac adverse events (CAEs) for a general surgery population has remained largely unchanged (approximately 1%). This is in spite of multiple studies evaluating predictive models and attempts at preventive treatment, including preoperative coronary revascularization and perioperative beta blockers.
Study design: Prospective observational study.
Setting: Single, large, tertiary-care university hospital.
Synopsis: A total of 7,740 cases were reviewed in this study, which consisted of general surgery (4,937), vascular surgery (1,846), and urological surgery (957). A trained nurse followed up for perioperative CAEs as many as 30 days after the operation via medical chart review, phone calls, and letters. CAEs were defined as: Q-wave myocardial infarction (MI), non-ST elevation MI, cardiac arrest, or new cardiac dysrhythmia. A total of 83 CAEs (1.1% of patients) had cardiac arrest, with cardiac dysrhythmia being most common.
A total of seven preoperative risk factors were identified as independent predictors for CAEs: age 68, BMI 30, emergent surgery, prior coronary intervention or cardiac surgery, active congestive heart failure, cerebrovascular disease, and hypertension. In addition, two intraoperative risk factors were identified: intraoperative transfusion of packed red blood cells and operative duration of 3.8 hours. (The P value was 0.05 for all independent predictors.)
A further evaluation of intraoperative parameters of high-risk patients experiencing a CAE showed that these patients were more likely to have an episode of mean arterial pressure (MAP) <50 mmHg, an episode of 40% decrease in MAP, and an episode of tachycardia (heart rate >100).
Bottom line: A combination of preoperative predictors and intraoperative elements can help improve risk assessment for perioperative CAEs after noncardiac surgery.
Citation: Kheterpal S, O’Reilly M, Englesbe M, et al. Preoperative and intraoperative predictors of cardiac adverse events after general, vascular, and urological surgery. Anesthesiology. 2009;110(1):58-66.
Early Feeding in the ICU Does Not Affect Hospital Mortality
Clinical question: Will implementing evidence-based feeding guidelines improve feeding practices and reduce mortality in ICU patients?
Background: There is evidence suggesting that providing nutritional support to ICU patients within 24 hours of admission may decrease mortality. It is widely understood that patient care varies between ICUs, and there exist no uniform, evidence-based guidelines for nutritional support. Many patients remain unfed after 48 hours.
Study design: Cluster, randomized-controlled trial.
Setting: ICUs in 27 community and tertiary-care hospitals in Australia and New Zealand.
Synopsis: Hospitals were randomized to intervention or control groups. Dietitian and intensivist co-investigators from intervention ICUs developed guidelines using the Clinical Practice Guideline Development Cycle. Control ICUs were requested to make no new ICU nutritional management changes. The study enrolled 1,118 eligible patients and included adults expected to stay longer than two days. Excluded were patients taking oral diets, patients receiving palliative care or with suspected brain death, and patients sent from other facilities.
Guidelines were implemented using several methods—educational outreach visits, one-on-one conversations, active reminders, passive reminders, and educational in-services. The guidelines were successful in evoking significant practice changes in all of the intervention ICUs. Significantly more patients received nutritional support during their ICU stays in guideline ICUs, and patients in these ICUs were fed significantly earlier. There were, however, no significant differences between guideline and control ICUs with regard to hospital discharge mortality (28.9% vs. 27.4%; 95% CI; -6.3% to 12.0%; P=0.75). The groups also showed no statistical difference in hospital or ICU length of stay.
Bottom line: Significantly more patients in the guideline ICUs were fed within 24 hours, but this did not translate into improvements in mortality or other clinical outcomes.
Citation: Doig G, Simpson F, Finfer S, et al. Effect of evidence-based feeding guidelines on mortality of critically ill adults: a cluster randomized controlled trial. JAMA. 2008;300(23):2731-2741.
Low-Dose Aspirin Doesn’t Reduce Cardiovascular Events in Type 2 Diabetes Patients
Clinical question: Is low-dose aspirin effective for the primary prevention of atherosclerotic events in patients with Type 2 diabetes?
Background: Diabetes is a significant risk factor for cardiovascular events. Several prior studies have shown that aspirin therapy is effective as a secondary prevention strategy for cardiovascular events. The American Diabetes Association also recommends use of aspirin as a primary prevention strategy. Clinical trial data is currently insufficient in this area.
Study design: Prospective, randomized, open-label, controlled trial with blinded endpoint assessment.
Setting: 163 institutions in Japan.
Synopsis: The study enrolled 2,539 diabetic patients between 30 and 85 years old—mean age was 65—and included patients without EKG changes or a significant history or ongoing treatment of atherosclerotic disease. Patients were randomly assigned into an aspirin group (81 mg or 100 mg once daily) or a nonaspirin group. Patients had a median follow up of 4.37 years.
The primary endpoint was any atherosclerotic event, ranging from sudden death to ischemic heart disease or stroke. The incidence of atherosclerotic events was not statistically different in the aspirin group (68 events, 5.4%) than in the nonaspirin group (86 events, 6.7%) (HR, 0.80; 95% CI; 0.58-1.10; log-rank test, P=0.16). However, there was a suggested benefit of primary prevention in the subgroup aged 65 years or older. In addition, the combined endpoint of fatal coronary and cerebrovascular events occurred in one patient in the aspirin group and 10 patients in the nonaspirin group (HR, 0.10; 95 % CI, 0.01-0.79; P=.0037). This study is limited by the low incidence of atherosclerotic disease in Japan.
Bottom line: Low-dose aspirin used in patients with Type 2 diabetes does not significantly demonstrate primary prevention of cardiovascular events.
Citation: Ogawa H, Nakayama M, Morimoto T, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2008;300(18):2134-2141. TH
In This Edition
- Generic vs. brand-name drugs.
- Rapid-response teams and mortality.
- A new prediction rule for mortality in acute pancreatitis.
- Viral causes of community-acquired pneumonia.
- Intensive insulin therapy in the ICU.
- New preoperative and intraoperative risk factors.
- Timing of ICU feedings and mortality.
- Aspirin as primary prevention in diabetics.
Generic, Brand-Name Drugs Used for Cardiovascular Disease Are Clinically Equivalent
Clinical question: Is there a clinical risk when substituting generic drugs for brand-name drugs in the treatment of cardiovascular disease?
Background: Spending on healthcare in the U.S. has reached critical levels. Increasing prescription drug costs make up a large portion of healthcare expenditures. The high cost of medicines directly affect adherence to treatment regimens and contribute to poor health outcomes. Cardiovascular drugs make up the largest portion of outpatient prescription drug spending.
Study design: Systematic review of relevant articles with a meta-analysis performed to determine an aggregate effect size.
Setting: Multiple locations and varied patient populations.
Synopsis: A total of 47 articles were included in the review, of which 38 were randomized controlled trials (RCTs). The studies measured both clinical efficacy and safety end points. More than half the articles were published prior to 2000. Clinical equivalence was noted in all seven beta-blocker RCTs; 10 of 11 diuretic RCTs; five of seven calcium-channel-blocker RCTs; all three antiplatelet-agent RCTs (clopidogrel, enteric-coated aspirin); two statin RCTs; one ACE-inhibitor RCT; and one alpha-blocker RCT. For drugs with a narrow therapeutic index, clinical equivalence was noted in all five warfarin RCTs and a single Class 1 anti-arrhythmic-agent RCT.
The aggregate effect size was -0.03 (95% CI, -0.15 to 0.08), which indicates nearly complete overlap of the generic and brand-name distributions. The data show no evidence of superiority of brand-name to generic drugs in clinical outcomes measured in the various studies.
In a separate review of editorials addressing generic substitution for cardiovascular drugs, 53% expressed a negative view of generic-drug substitution.
Bottom line: There is clinical equivalency between generic and brand-name drugs used in the treatment of cardiovascular disease. Despite this conclusion, a substantial number of editorials advise against generic substitution, which affects both patient and physician drug preferences.
Citation: Kesselheim A, Misono A, Lee J, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008; 300(21):2514-2526.
RRT Implement-ation Doesn’t Affect Hospitalwide Code Rates or Mortality
Clinical question: Does the use of a rapid-response team (RRT) affect hospitalwide code rates and mortality?
Background: In the 100,000 Lives campaign, the Institute for Healthcare Improvement recommended that hospitals implement RRTs to help reduce preventable, in-hospital deaths. Studies have demonstrated that rates of non-ICU codes decrease after RRT implementation. It is unclear if this translates to changes in mortality rates.
Study design: Prospective cohort study of adult inpatients.
Setting: Saint Luke’s Hospital, a 404-bed tertiary-care academic hospital in Kansas City, Mo.
Synopsis: The hospital documented a total of 376 RRT activations. After RRT implementation, mean hospitalwide code rates decreased to 7.5 per 1,000 admissions from 11.2 per 1,000 admissions. This was not associated with a statistically significant reduction in hospitalwide code rates (adjusted odds ratio 0.76; 95% CI; 0.57-1.01; P=0.06). Secondary analyses noted lower rates of non-ICU codes (0.59; 95% CI, 0.40-0.89) compared with ICU codes (0.95; 95% CI; 0.64-1.43; P=0.03 for interaction). Finally, the RRT implementation was not associated with lower hospital-wide mortality (0.95; 95% CI; 0.81-1.11; P=0.52).
Secondary analyses also revealed few instances of RRT undertreatment or underutilization that may have affected the mortality numbers.
A limitation of this study is that it was slightly underpowered (78%) to detect a significant mortality difference. The findings also represent a single institution experience, and may not be generalized to other adult hospital settings or RRT programs.
Bottom line: Implementation of an RRT does not confer lower rates of hospital-wide code arrests or mortality.
Citation: Chan P, Khalid A, Longmore L, et al. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA. 2008;300(21):2506-2513.
Simple Scoring System Provides Timely Prediction of Mortality in Acute Pancreatitis
Clinical question: How can physicians predict mortality in acute pancreatitis?
Background: Historical predictors of mortality in acute pancreatitis require up to 48 hours of data, such as with the Ranson Criteria, or extensive amounts of data, such as with the APACHE II score. An easier tool is needed to predict which patients are at higher risk of mortality.
Study design: Retrospective cohort.
Setting: Patients in the Cardinal Health clinical outcomes research database, which supports public reporting of hospital performance.
Synopsis: The authors identified patients with the principal diagnosis of pancreatitis from 2000-2001 and explored numerous diagnostic findings available within the first 24 hours. Ultimately, BUN >25, impaired mental status, presence of SIRS (systemic inflammatory response syndrome), age >60, and presence of a pleural effusion were found to be predictive of mortality. These diagnostic findings correspond to the mnemonic BISAP. The BISAP score was then validated in a second cohort that included patients from 2004-2005.
Each finding in the BISAP score was given one point. A score of less than 2 was present in approximately 60% of patients admitted with acute pancreatitis, and corresponded to a mortality of less than 1%. A score of 2 corresponded to a mortality of 2%. Higher scores were associated with steeply increasing mortality, with a score of 5 corresponding with greater than 20% mortality.
The BISAP score performed similarly to the APACHE II score, but the former is easier to calculate on the day of admission and has fewer parameters. A more challenging research step will be to demonstrate that using the BISAP score to determine treatment strategies can affect patient outcomes.
Bottom line: The easy-to-calculate BISAP score is a new method for predicting mortality in patients with acute pancreatitis. This tool should help hospitalists determine, on the day of admission, to what extent patients with acute pancreatitis need aggressive management, such as ICU admission and early involvement of specialists.
Citation: Wu B, Johannes R, Sun X, Tabak Y, Conwell D, Banks P. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57(12): 1698-1703.
Nasal Swabs Identify Viral Causes in CAP Patients
Clinical question: How often is viral infection associated with community-acquired pneumonia (CAP) in adults?
Background: CAP is a clinically important disease that is associated with significant hospitalization and mortality. CAP treatment guidelines acknowledge respiratory viruses as an etiology for pneumonia, but few recommendations are made regarding management of these viral infections.
Study design: Prospective study.
Setting: Five hospitals in Edmonton, Alberta, from 2004-2006.
Synopsis: The authors enrolled 193 hospitalized adults, median age 71. Nucleic amplification tests (NATs) from nasopharyngeal swab specimens were tested for human metapneumovirus, respiratory syncytial virus, rhinovirus, parainfluenza virus 1-4, coronaviruses, and adenovirus.
Fifteen percent of these patients had a nasal swab positive for a viral infection. Interestingly, 4% of patients had both a positive viral nasal swab and positive bacterial cultures. Compared with bacterial infection, patients with viral infection tended to be older (76 vs. 64 years, P=0.01), have limited ambulation (66% vs. 32%, P=0.006), and have a history of cardiac disease (66% vs. 32%, P=0.02). Patients with bacterial pneumonia showed a statistically significant trend toward having chest pain, an abnormal white blood count, and a lobar infiltrate on chest X-ray.
Further investigations might look at how nasal swab data could be used to improve infection control within the hospital for patients found to have easily transmissible viruses. Further research could explore the feasibility of avoiding antibiotic use in patients found to have viral pneumonia, assuming bacterial co-infection is reliably excluded.
Bottom line: Nasal swabs using NAT technology could play a significant role in identifying pathogens in CAP patients. How this technology should affect clinical decision-making and how it might improve outcomes remains unknown.
Citation: Johnstone J, Majumdar S, Fox J, Marrie T. Viral infection in adults hospitalized with community-acquired pneumonia: prevalence, pathogens, and presentation. Chest. 2008;134(6):1141-1148.
Intensive Insulin Therapy Doesn’t Reduce ICU Mortality
Clinical question: Does the use of intensive insulin therapy decrease mortality in the intensive-care unit (ICU)?
Background: In 2001, Van den Berghe et al (N Engl J Med. 2001;345(19):1359-67) reported a reduction in morbidity and mortality with intensive insulin therapy (IIT) in surgical ICU patients. This study led to the adoption of IIT protocols in many hospitals. Since 2001, further studies have failed to reproduce the same dramatic benefit of IIT.
Study design: Randomized, controlled trial.
Setting: National Guard King Abdulaziz Medical City, a tertiary-care teaching hospital in Saudi Arabia.
Synopsis: Patients were included in this study if they were 18 years or older with serum glucose levels greater than 110 mg/dL during the first 24 hours of ICU admission. There were multiple exclusion criteria, including patients with Type I diabetes, documented hypoglycemia on ICU admission (glucose <40), or diabetic ketoacidosis.
Enrolled patients were randomized to IIT or conventional insulin therapy (CIT). A multidisciplinary team designed the protocols to maintain glucose levels of 80 to 110 mg/dL and 180 to 200 mg/dL in the IIT and the CIT groups, respectively. The primary endpoint measured was ICU mortality.
The study did not produce a statistically significant difference in ICU mortality (13.5% for IIT vs. 17.1% for CIT; P=0.30). The adjusted hypoglycemia rate was 6.8 per 100 treatment days with IIT and 0.4 per 100 treatment days with CIT (P<0.0001). Patients with hypoglycemia had higher ICU mortality (23.8% vs. 13.7%, P=0.02).
In the measurement of secondary endpoints, there was a trend toward lower episodes of severe sepsis and septic shock in the IIT group (20.7% in IIT vs. 27.2% in CIT, P=0.08). However, this result was not statistically significant.
Bottom line: This well-designed study failed to show a survival benefit with IIT use in the critical-care setting. Given the findings of this and several other recent studies, one should question whether IIT should be prescribed as the standard of care in all critically-ill patients.
Citation: Arabi Y, Dabbagh O, Tamim H, et al. Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Crit Care Med. 2008;36(12):3190-3197.
Preoperative and Intraoperative Predictors of Cardiac Adverse Events
Clinical question: What are the incidence and risk factors for perioperative cardiac adverse events after noncardiac surgery?
Background: In the past few decades, the incidence of cardiac adverse events (CAEs) for a general surgery population has remained largely unchanged (approximately 1%). This is in spite of multiple studies evaluating predictive models and attempts at preventive treatment, including preoperative coronary revascularization and perioperative beta blockers.
Study design: Prospective observational study.
Setting: Single, large, tertiary-care university hospital.
Synopsis: A total of 7,740 cases were reviewed in this study, which consisted of general surgery (4,937), vascular surgery (1,846), and urological surgery (957). A trained nurse followed up for perioperative CAEs as many as 30 days after the operation via medical chart review, phone calls, and letters. CAEs were defined as: Q-wave myocardial infarction (MI), non-ST elevation MI, cardiac arrest, or new cardiac dysrhythmia. A total of 83 CAEs (1.1% of patients) had cardiac arrest, with cardiac dysrhythmia being most common.
A total of seven preoperative risk factors were identified as independent predictors for CAEs: age 68, BMI 30, emergent surgery, prior coronary intervention or cardiac surgery, active congestive heart failure, cerebrovascular disease, and hypertension. In addition, two intraoperative risk factors were identified: intraoperative transfusion of packed red blood cells and operative duration of 3.8 hours. (The P value was 0.05 for all independent predictors.)
A further evaluation of intraoperative parameters of high-risk patients experiencing a CAE showed that these patients were more likely to have an episode of mean arterial pressure (MAP) <50 mmHg, an episode of 40% decrease in MAP, and an episode of tachycardia (heart rate >100).
Bottom line: A combination of preoperative predictors and intraoperative elements can help improve risk assessment for perioperative CAEs after noncardiac surgery.
Citation: Kheterpal S, O’Reilly M, Englesbe M, et al. Preoperative and intraoperative predictors of cardiac adverse events after general, vascular, and urological surgery. Anesthesiology. 2009;110(1):58-66.
Early Feeding in the ICU Does Not Affect Hospital Mortality
Clinical question: Will implementing evidence-based feeding guidelines improve feeding practices and reduce mortality in ICU patients?
Background: There is evidence suggesting that providing nutritional support to ICU patients within 24 hours of admission may decrease mortality. It is widely understood that patient care varies between ICUs, and there exist no uniform, evidence-based guidelines for nutritional support. Many patients remain unfed after 48 hours.
Study design: Cluster, randomized-controlled trial.
Setting: ICUs in 27 community and tertiary-care hospitals in Australia and New Zealand.
Synopsis: Hospitals were randomized to intervention or control groups. Dietitian and intensivist co-investigators from intervention ICUs developed guidelines using the Clinical Practice Guideline Development Cycle. Control ICUs were requested to make no new ICU nutritional management changes. The study enrolled 1,118 eligible patients and included adults expected to stay longer than two days. Excluded were patients taking oral diets, patients receiving palliative care or with suspected brain death, and patients sent from other facilities.
Guidelines were implemented using several methods—educational outreach visits, one-on-one conversations, active reminders, passive reminders, and educational in-services. The guidelines were successful in evoking significant practice changes in all of the intervention ICUs. Significantly more patients received nutritional support during their ICU stays in guideline ICUs, and patients in these ICUs were fed significantly earlier. There were, however, no significant differences between guideline and control ICUs with regard to hospital discharge mortality (28.9% vs. 27.4%; 95% CI; -6.3% to 12.0%; P=0.75). The groups also showed no statistical difference in hospital or ICU length of stay.
Bottom line: Significantly more patients in the guideline ICUs were fed within 24 hours, but this did not translate into improvements in mortality or other clinical outcomes.
Citation: Doig G, Simpson F, Finfer S, et al. Effect of evidence-based feeding guidelines on mortality of critically ill adults: a cluster randomized controlled trial. JAMA. 2008;300(23):2731-2741.
Low-Dose Aspirin Doesn’t Reduce Cardiovascular Events in Type 2 Diabetes Patients
Clinical question: Is low-dose aspirin effective for the primary prevention of atherosclerotic events in patients with Type 2 diabetes?
Background: Diabetes is a significant risk factor for cardiovascular events. Several prior studies have shown that aspirin therapy is effective as a secondary prevention strategy for cardiovascular events. The American Diabetes Association also recommends use of aspirin as a primary prevention strategy. Clinical trial data is currently insufficient in this area.
Study design: Prospective, randomized, open-label, controlled trial with blinded endpoint assessment.
Setting: 163 institutions in Japan.
Synopsis: The study enrolled 2,539 diabetic patients between 30 and 85 years old—mean age was 65—and included patients without EKG changes or a significant history or ongoing treatment of atherosclerotic disease. Patients were randomly assigned into an aspirin group (81 mg or 100 mg once daily) or a nonaspirin group. Patients had a median follow up of 4.37 years.
The primary endpoint was any atherosclerotic event, ranging from sudden death to ischemic heart disease or stroke. The incidence of atherosclerotic events was not statistically different in the aspirin group (68 events, 5.4%) than in the nonaspirin group (86 events, 6.7%) (HR, 0.80; 95% CI; 0.58-1.10; log-rank test, P=0.16). However, there was a suggested benefit of primary prevention in the subgroup aged 65 years or older. In addition, the combined endpoint of fatal coronary and cerebrovascular events occurred in one patient in the aspirin group and 10 patients in the nonaspirin group (HR, 0.10; 95 % CI, 0.01-0.79; P=.0037). This study is limited by the low incidence of atherosclerotic disease in Japan.
Bottom line: Low-dose aspirin used in patients with Type 2 diabetes does not significantly demonstrate primary prevention of cardiovascular events.
Citation: Ogawa H, Nakayama M, Morimoto T, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2008;300(18):2134-2141. TH
Telemedicine Can Help Solve Intensivist Shortage
Having spent my medical career in the ICU and the hospital, I have followed the recent articles on the struggle to care for ICU patients with interest. Gretchen Henkel’s article on hospitalists filling ICU manpower gaps (“The New Intensivists,” October 2008, p. 1) poses a very real question for community hospitals, which face the greatest challenges in this area. Two issues are common: 1) difficulty in providing 24/7 ICU coverage and 2) the competing priorities that ICU medical leaders face. For these challenges, telemedicine offers a possible solution.
This unique, high-intensity, multidisciplinary approach to the patient population—an integral part of intensivist training—is a proven process shown to have meaningful results in the ICU. However, the team approach to managing ICU patients can be hard to come by. As suggested in Henkel’s article, there are several ways to approach this, but simply having a hospitalist consult on an ICU patient is not, I believe, a solution. Not only can this add to the strain on a hospitalist team, but a proactive approach to the ICU patient also can be hampered by the need for hospitalists to be present in the medical-surgical areas. Ideally, an intensivist should lead a multiprofessional team; however, there is a tremendous intensivist shortage, with less than 20% of ICUs staffed with them. Telemedicine offers a way to bridge the gap of expertise and manpower in many settings, bringing intensivists to the forefront of the ICU multidisciplinary team.
For the multidisciplinary approach to be effective, a physician must be committed to creating the team and identifying the measures that it will impact. In many community hospitals, this is the ICU medical director. However, competing priorities can make this directive difficult to achieve. Teleintensivists, intensivists that practice medicine via telemedicine, proactively establish best practices and a multidisciplinary approach, thus dramatically affecting the quality and financial metrics of the ICU.
Lack of 24/7 ICU coverage is another big challenge for community hospitals. Trying to meet this challenge by simply adding intensivists is likely to be met with defeat, given the shortage of hospitalists. And adding more hospitalists in the ICU continues to drive the hospitalist shortage. There is a variety of solutions for bedside procedures; however, the constant need to respond to phone calls and unpredictable patient interventions remains. While utilizing midlevel providers can help, this approach is not likely to support the demand of the aging population.
Hospitals increasingly are considering telemedicine to meet the 24/7 need. Teleintensivists have risen to add manpower and immediate response to ICU patients. Without the distraction of constant interruptions and with a process to manage the deluge of data, community hospitals with teleintensivist programs are seeing a drop in ventilator-associated pneumonia, better blood glucose management, and compliance with sepsis and other bundles.
This proactive approach to ICU patient care has led to significant decreases in mortality and lengths of stay.
A recent article in The New York Times focused on “disruptive innovation” in healthcare.1 Given the pressing issues facing the industry, disruptive innovation―at the bedside as well as with telemedicine technology―will be a key factor in meeting our ICU needs successfully.
Mary Jo Gorman, MD, MBA
Editor’s note: Dr. Gorman, a former SHM president, is the CEO of St. Louis-based Advanced ICU Care, which provides intensivists to community hospitals using telemedicine. TH
Reference
1. Rae-Dupree J. Disruptive innovation, applied to health care. The New York Times Web site. Available at: www.nytimes.com/2009/02/01/business/01unbox.html?scp=1&sq=disruptive%20innovation&st=cse. Accessed March 3, 2009.
Having spent my medical career in the ICU and the hospital, I have followed the recent articles on the struggle to care for ICU patients with interest. Gretchen Henkel’s article on hospitalists filling ICU manpower gaps (“The New Intensivists,” October 2008, p. 1) poses a very real question for community hospitals, which face the greatest challenges in this area. Two issues are common: 1) difficulty in providing 24/7 ICU coverage and 2) the competing priorities that ICU medical leaders face. For these challenges, telemedicine offers a possible solution.
This unique, high-intensity, multidisciplinary approach to the patient population—an integral part of intensivist training—is a proven process shown to have meaningful results in the ICU. However, the team approach to managing ICU patients can be hard to come by. As suggested in Henkel’s article, there are several ways to approach this, but simply having a hospitalist consult on an ICU patient is not, I believe, a solution. Not only can this add to the strain on a hospitalist team, but a proactive approach to the ICU patient also can be hampered by the need for hospitalists to be present in the medical-surgical areas. Ideally, an intensivist should lead a multiprofessional team; however, there is a tremendous intensivist shortage, with less than 20% of ICUs staffed with them. Telemedicine offers a way to bridge the gap of expertise and manpower in many settings, bringing intensivists to the forefront of the ICU multidisciplinary team.
For the multidisciplinary approach to be effective, a physician must be committed to creating the team and identifying the measures that it will impact. In many community hospitals, this is the ICU medical director. However, competing priorities can make this directive difficult to achieve. Teleintensivists, intensivists that practice medicine via telemedicine, proactively establish best practices and a multidisciplinary approach, thus dramatically affecting the quality and financial metrics of the ICU.
Lack of 24/7 ICU coverage is another big challenge for community hospitals. Trying to meet this challenge by simply adding intensivists is likely to be met with defeat, given the shortage of hospitalists. And adding more hospitalists in the ICU continues to drive the hospitalist shortage. There is a variety of solutions for bedside procedures; however, the constant need to respond to phone calls and unpredictable patient interventions remains. While utilizing midlevel providers can help, this approach is not likely to support the demand of the aging population.
Hospitals increasingly are considering telemedicine to meet the 24/7 need. Teleintensivists have risen to add manpower and immediate response to ICU patients. Without the distraction of constant interruptions and with a process to manage the deluge of data, community hospitals with teleintensivist programs are seeing a drop in ventilator-associated pneumonia, better blood glucose management, and compliance with sepsis and other bundles.
This proactive approach to ICU patient care has led to significant decreases in mortality and lengths of stay.
A recent article in The New York Times focused on “disruptive innovation” in healthcare.1 Given the pressing issues facing the industry, disruptive innovation―at the bedside as well as with telemedicine technology―will be a key factor in meeting our ICU needs successfully.
Mary Jo Gorman, MD, MBA
Editor’s note: Dr. Gorman, a former SHM president, is the CEO of St. Louis-based Advanced ICU Care, which provides intensivists to community hospitals using telemedicine. TH
Reference
1. Rae-Dupree J. Disruptive innovation, applied to health care. The New York Times Web site. Available at: www.nytimes.com/2009/02/01/business/01unbox.html?scp=1&sq=disruptive%20innovation&st=cse. Accessed March 3, 2009.
Having spent my medical career in the ICU and the hospital, I have followed the recent articles on the struggle to care for ICU patients with interest. Gretchen Henkel’s article on hospitalists filling ICU manpower gaps (“The New Intensivists,” October 2008, p. 1) poses a very real question for community hospitals, which face the greatest challenges in this area. Two issues are common: 1) difficulty in providing 24/7 ICU coverage and 2) the competing priorities that ICU medical leaders face. For these challenges, telemedicine offers a possible solution.
This unique, high-intensity, multidisciplinary approach to the patient population—an integral part of intensivist training—is a proven process shown to have meaningful results in the ICU. However, the team approach to managing ICU patients can be hard to come by. As suggested in Henkel’s article, there are several ways to approach this, but simply having a hospitalist consult on an ICU patient is not, I believe, a solution. Not only can this add to the strain on a hospitalist team, but a proactive approach to the ICU patient also can be hampered by the need for hospitalists to be present in the medical-surgical areas. Ideally, an intensivist should lead a multiprofessional team; however, there is a tremendous intensivist shortage, with less than 20% of ICUs staffed with them. Telemedicine offers a way to bridge the gap of expertise and manpower in many settings, bringing intensivists to the forefront of the ICU multidisciplinary team.
For the multidisciplinary approach to be effective, a physician must be committed to creating the team and identifying the measures that it will impact. In many community hospitals, this is the ICU medical director. However, competing priorities can make this directive difficult to achieve. Teleintensivists, intensivists that practice medicine via telemedicine, proactively establish best practices and a multidisciplinary approach, thus dramatically affecting the quality and financial metrics of the ICU.
Lack of 24/7 ICU coverage is another big challenge for community hospitals. Trying to meet this challenge by simply adding intensivists is likely to be met with defeat, given the shortage of hospitalists. And adding more hospitalists in the ICU continues to drive the hospitalist shortage. There is a variety of solutions for bedside procedures; however, the constant need to respond to phone calls and unpredictable patient interventions remains. While utilizing midlevel providers can help, this approach is not likely to support the demand of the aging population.
Hospitals increasingly are considering telemedicine to meet the 24/7 need. Teleintensivists have risen to add manpower and immediate response to ICU patients. Without the distraction of constant interruptions and with a process to manage the deluge of data, community hospitals with teleintensivist programs are seeing a drop in ventilator-associated pneumonia, better blood glucose management, and compliance with sepsis and other bundles.
This proactive approach to ICU patient care has led to significant decreases in mortality and lengths of stay.
A recent article in The New York Times focused on “disruptive innovation” in healthcare.1 Given the pressing issues facing the industry, disruptive innovation―at the bedside as well as with telemedicine technology―will be a key factor in meeting our ICU needs successfully.
Mary Jo Gorman, MD, MBA
Editor’s note: Dr. Gorman, a former SHM president, is the CEO of St. Louis-based Advanced ICU Care, which provides intensivists to community hospitals using telemedicine. TH
Reference
1. Rae-Dupree J. Disruptive innovation, applied to health care. The New York Times Web site. Available at: www.nytimes.com/2009/02/01/business/01unbox.html?scp=1&sq=disruptive%20innovation&st=cse. Accessed March 3, 2009.
Non-Physician Providers: Vital HM Resources
Enter text here
Enter text here
Enter text here
Project BOOST Expands
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) is an initiative to improve practices in transition care and reduce readmission rates for hospitals across the country. The project’s toolkit, mentoring program, and national advocacy efforts have proven so successful that the program is expanding this year.
In 2008, SHM began the first round of the Project BOOST mentoring program in six pilot hospitals. The first full cycle of Project BOOST mentoring sites began in March at 24 sites. The Hospitalist will feature updates on the full cycle of Project BOOST later this year. For more information about Project BOOST, visit www.hospitalmedicine.org/BOOST or e-mail [email protected].
As a pilot site, Southwestern Vermont Medical Center in Bennington has worked with mentors for the past six months. We caught up with project leader Jennifer Fells, RN, MS, to discuss the institution’s participation.
—Jennifer Fells, RN, MS, Southwestern Vermont Medical Center, Bennington
Question: Why did your group choose to participate in the mentoring program?
Answer: We wanted to reduce our readmission rate, and we knew we weren’t doing a service to patients. This was also a goal of our organization overall; it’s not only a benefit to the hospital, but a larger value when the patient goes back to the community.
Q: How has the BOOST mentoring program benefited your program?
A: It helped us get organized by beginning the process and affirmed our belief that there were ways to address readmissions. The toolkit has proved to be invaluable. The mentors helped us keep on track and offered us guidance. They share the experiences of the other Project BOOST teams, and we benefit from that information.
The changes in the approach to the discharge process were a surprise to us. After we developed our team, we discovered how fragmented the discharge process was throughout the entire organization. Discharges were handled over multiple disciplines, and it was fragmented by design.
For example, our documentation, discharge plans, discharge recommendations, and patient-education materials are in different parts of our documentation system.
Q: What did you learn about your program through the initial Project BOOST step: analyze care delivery?
A: We realized that disciplines were not coordinated with one another and there was not enough time for the physician to complete the discharge plan. The process was cumbersome, awkward, and very time-consuming. We were looking to create efficiency in the information that needs to be coordinated to do those discharge orders.
Q: What additional changes do you hope to see in the remaining time with BOOST mentors?
A: We definitely hope to improve our process. We want to have implemented the tools and have a coordinated discharge process, and a centralized way to communicate the discharge plan. We found a lack of communication creates a barrier among disciplines, and we hope to correct that and become more customer-friendly to patients.
Q: How did your site’s BOOST mentor assist in the implementation process? What was the outcome?
A: Our site mentor helped with the clarification of data to be collected for measurement, keeping us on track with the toolkit, and served as another set of eyes. When you are in an organization, and even when you have the appropriate team, you always need somebody to say, “What do you think about this?” or “Did you think about this item?”
It’s another perspective, sharing gained knowledge from other organizations. That’s very critical.
SHM marketing coordinator Nadia Clenending contributed to this report.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) is an initiative to improve practices in transition care and reduce readmission rates for hospitals across the country. The project’s toolkit, mentoring program, and national advocacy efforts have proven so successful that the program is expanding this year.
In 2008, SHM began the first round of the Project BOOST mentoring program in six pilot hospitals. The first full cycle of Project BOOST mentoring sites began in March at 24 sites. The Hospitalist will feature updates on the full cycle of Project BOOST later this year. For more information about Project BOOST, visit www.hospitalmedicine.org/BOOST or e-mail [email protected].
As a pilot site, Southwestern Vermont Medical Center in Bennington has worked with mentors for the past six months. We caught up with project leader Jennifer Fells, RN, MS, to discuss the institution’s participation.
—Jennifer Fells, RN, MS, Southwestern Vermont Medical Center, Bennington
Question: Why did your group choose to participate in the mentoring program?
Answer: We wanted to reduce our readmission rate, and we knew we weren’t doing a service to patients. This was also a goal of our organization overall; it’s not only a benefit to the hospital, but a larger value when the patient goes back to the community.
Q: How has the BOOST mentoring program benefited your program?
A: It helped us get organized by beginning the process and affirmed our belief that there were ways to address readmissions. The toolkit has proved to be invaluable. The mentors helped us keep on track and offered us guidance. They share the experiences of the other Project BOOST teams, and we benefit from that information.
The changes in the approach to the discharge process were a surprise to us. After we developed our team, we discovered how fragmented the discharge process was throughout the entire organization. Discharges were handled over multiple disciplines, and it was fragmented by design.
For example, our documentation, discharge plans, discharge recommendations, and patient-education materials are in different parts of our documentation system.
Q: What did you learn about your program through the initial Project BOOST step: analyze care delivery?
A: We realized that disciplines were not coordinated with one another and there was not enough time for the physician to complete the discharge plan. The process was cumbersome, awkward, and very time-consuming. We were looking to create efficiency in the information that needs to be coordinated to do those discharge orders.
Q: What additional changes do you hope to see in the remaining time with BOOST mentors?
A: We definitely hope to improve our process. We want to have implemented the tools and have a coordinated discharge process, and a centralized way to communicate the discharge plan. We found a lack of communication creates a barrier among disciplines, and we hope to correct that and become more customer-friendly to patients.
Q: How did your site’s BOOST mentor assist in the implementation process? What was the outcome?
A: Our site mentor helped with the clarification of data to be collected for measurement, keeping us on track with the toolkit, and served as another set of eyes. When you are in an organization, and even when you have the appropriate team, you always need somebody to say, “What do you think about this?” or “Did you think about this item?”
It’s another perspective, sharing gained knowledge from other organizations. That’s very critical.
SHM marketing coordinator Nadia Clenending contributed to this report.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions) is an initiative to improve practices in transition care and reduce readmission rates for hospitals across the country. The project’s toolkit, mentoring program, and national advocacy efforts have proven so successful that the program is expanding this year.
In 2008, SHM began the first round of the Project BOOST mentoring program in six pilot hospitals. The first full cycle of Project BOOST mentoring sites began in March at 24 sites. The Hospitalist will feature updates on the full cycle of Project BOOST later this year. For more information about Project BOOST, visit www.hospitalmedicine.org/BOOST or e-mail [email protected].
As a pilot site, Southwestern Vermont Medical Center in Bennington has worked with mentors for the past six months. We caught up with project leader Jennifer Fells, RN, MS, to discuss the institution’s participation.
—Jennifer Fells, RN, MS, Southwestern Vermont Medical Center, Bennington
Question: Why did your group choose to participate in the mentoring program?
Answer: We wanted to reduce our readmission rate, and we knew we weren’t doing a service to patients. This was also a goal of our organization overall; it’s not only a benefit to the hospital, but a larger value when the patient goes back to the community.
Q: How has the BOOST mentoring program benefited your program?
A: It helped us get organized by beginning the process and affirmed our belief that there were ways to address readmissions. The toolkit has proved to be invaluable. The mentors helped us keep on track and offered us guidance. They share the experiences of the other Project BOOST teams, and we benefit from that information.
The changes in the approach to the discharge process were a surprise to us. After we developed our team, we discovered how fragmented the discharge process was throughout the entire organization. Discharges were handled over multiple disciplines, and it was fragmented by design.
For example, our documentation, discharge plans, discharge recommendations, and patient-education materials are in different parts of our documentation system.
Q: What did you learn about your program through the initial Project BOOST step: analyze care delivery?
A: We realized that disciplines were not coordinated with one another and there was not enough time for the physician to complete the discharge plan. The process was cumbersome, awkward, and very time-consuming. We were looking to create efficiency in the information that needs to be coordinated to do those discharge orders.
Q: What additional changes do you hope to see in the remaining time with BOOST mentors?
A: We definitely hope to improve our process. We want to have implemented the tools and have a coordinated discharge process, and a centralized way to communicate the discharge plan. We found a lack of communication creates a barrier among disciplines, and we hope to correct that and become more customer-friendly to patients.
Q: How did your site’s BOOST mentor assist in the implementation process? What was the outcome?
A: Our site mentor helped with the clarification of data to be collected for measurement, keeping us on track with the toolkit, and served as another set of eyes. When you are in an organization, and even when you have the appropriate team, you always need somebody to say, “What do you think about this?” or “Did you think about this item?”
It’s another perspective, sharing gained knowledge from other organizations. That’s very critical.
SHM marketing coordinator Nadia Clenending contributed to this report.
Malpractice Chronicle
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Sedation Masks Neurologic Damage
While making pizza deliveries, an 18-year-old man was involved in a motor vehicle collision. The delivery vehicle was T-boned by two cars whose drivers were racing with their headlights off. The patient was taken to a hospital, where he was diagnosed with a fractured femur, facial fractures, cuts, and abrasions. He was given a Glasgow Coma Scale score of 15 out of 15. CT was read with normal results.
The man began to develop respiratory problems, and other patients were arriving, so the decision was made to transfer him to another facility. The plaintiff was intubated for flight, which required sedation and pharmacologic paralysis.
At the receiving hospital, the patient was assessed by an emergency department (ED) physician and a trauma surgeon. Both doctors suspected an acute closed head injury. Sedation and pharmacologic paralysis were continued in the ED and after the man’s transfer to the ICU; this made it impossible to conduct an accurate neurologic assessment. The patient’s health care providers relied on the fact that he had previously been pronounced neurologically stable and had had normal CT results.
After transfer to the lCU, the man’s facial injuries were repaired. In the early morning hours he was transferred to the operating room for repair of the femur. During this surgery, the patient sustained a 20- to 30-minute period of hypotension, which persisted after his return to the ICU. Medications were administered for the hypotension, and sedation was continued for several more hours. When the patient did not wake up, sedation was discontinued.
CT was ordered, and it revealed mild to moderate brain swelling. Mannitol and other agents were administered. A neurology consult was obtained, and an intracranial pressure monitor was placed.
Eventually, the plaintiff was diagnosed with a severe brain injury. He has undergone considerable rehabilitation and treatment, but his prospects for further recovery are not promising.
The plaintiff claimed that the receiving physicians should have been on the alert for deterioration of the plaintiff’s neurologic status and that the sedation should have been discontinued so that an accurate neurologic assessment could be performed. The plaintiff also claimed that surgery to repair the femur was not appropriate without a current accurate assessment of his neurologic status.
The defendant claimed that the plaintiff’s brain injury was caused by the collision and was not related to his subsequent medical care. According to the defendant, the plaintiff’s brain scans revealed diffuse axial injury, which is not amenable to treatment. The defendant also claimed that it was reasonable to have relied on the negative CT results and the normal neurologic examination from the transferring hospital.
After the underlying motor vehicle accident claim was resolved, the malpractice action and the plaintiff’s workers compensation claim proceeded. The medical malpractice claims were resolved with a $2,375,000 mediated settlement.
Bedsore Requires Debridement, Leads to Sepsis
At age 58, a man underwent coronary artery bypass surgery in July 1999. Shortly after the procedure, the patient experienced a stroke. He remained hospitalized in the defendant facility under the care of Dr. W., the defendant physician.
Several weeks later, the patient developed a sacral bedsore. He underwent three surgical debridements but developed sepsis. The bedsore allegedly worsened until the man’s death in January 2000.
The plaintiff claimed that the defendants failed to properly reposition the decedent and failed to treat the bedsore appropriately as soon as it developed. The plaintiff reached a confidential settlement with the nurses involved, and the matter proceeded against Dr. W. He claimed that the decedent’s diabetes made it impossible for the wound to heal and that nothing would have changed the outcome.
According to a published account, a $300,000 verdict was returned. A posttrial motion was pending.
Hernia Repaired, Recurrence Overlooked
A woman with a diagnosis of paraesophageal hernia was referred to the defendant surgeon, who recommended and performed laparoscopic surgery. The procedure involved reduction and repair of the patient’s large paraesophageal hernia, followed by Nissen fundoplication. A chest x-ray performed two days later revealed a large hiatal hernia, small to moderate-sized bilateral pleural effusions, and atelectasis in the left lung base. The woman was discharged from the hospital the next day.
Three days later, she presented to the emergency department, complaining of abdominal pain and shortness of breath. Chest x-rays again revealed the hiatal hernia, and no improvement was seen on repeat chest x-rays the next day. An upper gastrointestinal (GI) study was ordered. During the test, the patient’s condition declined, and she was transferred to the ICU.
After exploratory surgery revealed a constriction of the stomach and tissue necroses, the patient underwent cholecystectomy, resection of the proximal two-thirds of the stomach, and esophagogastrostomy with insertion of a feeding jejunostomy tube. Despite additional surgery, the woman died a few days later as a result of acute respiratory distress syndrome.
The plaintiff claimed that the defendant surgeon should have followed up on the chest x-ray following the initial surgery. On the patient’s return to the hospital, it was additionally charged, he should have inserted a nasogastric tube and ordered CT or an upper GI series immediately.
The defendant claimed that paraesophageal hernia repairs tend to fail and that it was not alarming that the hernia had recurred. The defendant maintained that the decedent’s symptoms were consistent with gas bloat syndrome, a common side effect of Nissen fundoplication. The defendant also claimed that even if the recommended diagnostic workup had been initiated earlier, she would have died in any event.
A defense verdict was returned.
House MD Forgoes Cardiology Consult
A 60-year-old woman was brought to the defendant hospital’s emergency department (ED) complaining of chest pain, nausea, and diaphoresis. She reported a family history of heart disease and a personal history of hypertension and high cholesterol.
In the ED, the patient was treated with aspirin and nitroglycerin. ECG revealed an old inferior infarct and was consistent with acute anterior ischemia. A diagnosis of unstable angina was made. The patient was admitted to a cardiac telemetry unit, and the on-call cardiologist was asked to consult. The plan for care included serial ECG and enzyme studies.
Shortly after midnight, the house officer was contacted by a unit nurse and informed about a report of an elevated troponin level. The house officer saw the patient, but his examination failed to elicit complaints of chest pain or shortness of breath and he pronounced it unremarkable.
Six hours later, the woman was found in cardiac arrest. Her heartbeat was restored, but she had experienced brain damage. She was transferred to another hospital for cardiac catheterization and stenting. Cardiac catheterization revealed single-vessel disease, with 99% to 100% occlusion of the left anterior descending artery. The decedent did not regain consciousness and was placed on a ventilator. A week later, she was removed from the ventilator and died.
The plaintiff claimed that the house officer should have ordered a stat cardiology consultation, which would have led to appropriate treatment and prevented the decedent’s massive myocardial infarction and death.
According to a published account, a $600,000 settlement was reached.
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Sedation Masks Neurologic Damage
While making pizza deliveries, an 18-year-old man was involved in a motor vehicle collision. The delivery vehicle was T-boned by two cars whose drivers were racing with their headlights off. The patient was taken to a hospital, where he was diagnosed with a fractured femur, facial fractures, cuts, and abrasions. He was given a Glasgow Coma Scale score of 15 out of 15. CT was read with normal results.
The man began to develop respiratory problems, and other patients were arriving, so the decision was made to transfer him to another facility. The plaintiff was intubated for flight, which required sedation and pharmacologic paralysis.
At the receiving hospital, the patient was assessed by an emergency department (ED) physician and a trauma surgeon. Both doctors suspected an acute closed head injury. Sedation and pharmacologic paralysis were continued in the ED and after the man’s transfer to the ICU; this made it impossible to conduct an accurate neurologic assessment. The patient’s health care providers relied on the fact that he had previously been pronounced neurologically stable and had had normal CT results.
After transfer to the lCU, the man’s facial injuries were repaired. In the early morning hours he was transferred to the operating room for repair of the femur. During this surgery, the patient sustained a 20- to 30-minute period of hypotension, which persisted after his return to the ICU. Medications were administered for the hypotension, and sedation was continued for several more hours. When the patient did not wake up, sedation was discontinued.
CT was ordered, and it revealed mild to moderate brain swelling. Mannitol and other agents were administered. A neurology consult was obtained, and an intracranial pressure monitor was placed.
Eventually, the plaintiff was diagnosed with a severe brain injury. He has undergone considerable rehabilitation and treatment, but his prospects for further recovery are not promising.
The plaintiff claimed that the receiving physicians should have been on the alert for deterioration of the plaintiff’s neurologic status and that the sedation should have been discontinued so that an accurate neurologic assessment could be performed. The plaintiff also claimed that surgery to repair the femur was not appropriate without a current accurate assessment of his neurologic status.
The defendant claimed that the plaintiff’s brain injury was caused by the collision and was not related to his subsequent medical care. According to the defendant, the plaintiff’s brain scans revealed diffuse axial injury, which is not amenable to treatment. The defendant also claimed that it was reasonable to have relied on the negative CT results and the normal neurologic examination from the transferring hospital.
After the underlying motor vehicle accident claim was resolved, the malpractice action and the plaintiff’s workers compensation claim proceeded. The medical malpractice claims were resolved with a $2,375,000 mediated settlement.
Bedsore Requires Debridement, Leads to Sepsis
At age 58, a man underwent coronary artery bypass surgery in July 1999. Shortly after the procedure, the patient experienced a stroke. He remained hospitalized in the defendant facility under the care of Dr. W., the defendant physician.
Several weeks later, the patient developed a sacral bedsore. He underwent three surgical debridements but developed sepsis. The bedsore allegedly worsened until the man’s death in January 2000.
The plaintiff claimed that the defendants failed to properly reposition the decedent and failed to treat the bedsore appropriately as soon as it developed. The plaintiff reached a confidential settlement with the nurses involved, and the matter proceeded against Dr. W. He claimed that the decedent’s diabetes made it impossible for the wound to heal and that nothing would have changed the outcome.
According to a published account, a $300,000 verdict was returned. A posttrial motion was pending.
Hernia Repaired, Recurrence Overlooked
A woman with a diagnosis of paraesophageal hernia was referred to the defendant surgeon, who recommended and performed laparoscopic surgery. The procedure involved reduction and repair of the patient’s large paraesophageal hernia, followed by Nissen fundoplication. A chest x-ray performed two days later revealed a large hiatal hernia, small to moderate-sized bilateral pleural effusions, and atelectasis in the left lung base. The woman was discharged from the hospital the next day.
Three days later, she presented to the emergency department, complaining of abdominal pain and shortness of breath. Chest x-rays again revealed the hiatal hernia, and no improvement was seen on repeat chest x-rays the next day. An upper gastrointestinal (GI) study was ordered. During the test, the patient’s condition declined, and she was transferred to the ICU.
After exploratory surgery revealed a constriction of the stomach and tissue necroses, the patient underwent cholecystectomy, resection of the proximal two-thirds of the stomach, and esophagogastrostomy with insertion of a feeding jejunostomy tube. Despite additional surgery, the woman died a few days later as a result of acute respiratory distress syndrome.
The plaintiff claimed that the defendant surgeon should have followed up on the chest x-ray following the initial surgery. On the patient’s return to the hospital, it was additionally charged, he should have inserted a nasogastric tube and ordered CT or an upper GI series immediately.
The defendant claimed that paraesophageal hernia repairs tend to fail and that it was not alarming that the hernia had recurred. The defendant maintained that the decedent’s symptoms were consistent with gas bloat syndrome, a common side effect of Nissen fundoplication. The defendant also claimed that even if the recommended diagnostic workup had been initiated earlier, she would have died in any event.
A defense verdict was returned.
House MD Forgoes Cardiology Consult
A 60-year-old woman was brought to the defendant hospital’s emergency department (ED) complaining of chest pain, nausea, and diaphoresis. She reported a family history of heart disease and a personal history of hypertension and high cholesterol.
In the ED, the patient was treated with aspirin and nitroglycerin. ECG revealed an old inferior infarct and was consistent with acute anterior ischemia. A diagnosis of unstable angina was made. The patient was admitted to a cardiac telemetry unit, and the on-call cardiologist was asked to consult. The plan for care included serial ECG and enzyme studies.
Shortly after midnight, the house officer was contacted by a unit nurse and informed about a report of an elevated troponin level. The house officer saw the patient, but his examination failed to elicit complaints of chest pain or shortness of breath and he pronounced it unremarkable.
Six hours later, the woman was found in cardiac arrest. Her heartbeat was restored, but she had experienced brain damage. She was transferred to another hospital for cardiac catheterization and stenting. Cardiac catheterization revealed single-vessel disease, with 99% to 100% occlusion of the left anterior descending artery. The decedent did not regain consciousness and was placed on a ventilator. A week later, she was removed from the ventilator and died.
The plaintiff claimed that the house officer should have ordered a stat cardiology consultation, which would have led to appropriate treatment and prevented the decedent’s massive myocardial infarction and death.
According to a published account, a $600,000 settlement was reached.
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Sedation Masks Neurologic Damage
While making pizza deliveries, an 18-year-old man was involved in a motor vehicle collision. The delivery vehicle was T-boned by two cars whose drivers were racing with their headlights off. The patient was taken to a hospital, where he was diagnosed with a fractured femur, facial fractures, cuts, and abrasions. He was given a Glasgow Coma Scale score of 15 out of 15. CT was read with normal results.
The man began to develop respiratory problems, and other patients were arriving, so the decision was made to transfer him to another facility. The plaintiff was intubated for flight, which required sedation and pharmacologic paralysis.
At the receiving hospital, the patient was assessed by an emergency department (ED) physician and a trauma surgeon. Both doctors suspected an acute closed head injury. Sedation and pharmacologic paralysis were continued in the ED and after the man’s transfer to the ICU; this made it impossible to conduct an accurate neurologic assessment. The patient’s health care providers relied on the fact that he had previously been pronounced neurologically stable and had had normal CT results.
After transfer to the lCU, the man’s facial injuries were repaired. In the early morning hours he was transferred to the operating room for repair of the femur. During this surgery, the patient sustained a 20- to 30-minute period of hypotension, which persisted after his return to the ICU. Medications were administered for the hypotension, and sedation was continued for several more hours. When the patient did not wake up, sedation was discontinued.
CT was ordered, and it revealed mild to moderate brain swelling. Mannitol and other agents were administered. A neurology consult was obtained, and an intracranial pressure monitor was placed.
Eventually, the plaintiff was diagnosed with a severe brain injury. He has undergone considerable rehabilitation and treatment, but his prospects for further recovery are not promising.
The plaintiff claimed that the receiving physicians should have been on the alert for deterioration of the plaintiff’s neurologic status and that the sedation should have been discontinued so that an accurate neurologic assessment could be performed. The plaintiff also claimed that surgery to repair the femur was not appropriate without a current accurate assessment of his neurologic status.
The defendant claimed that the plaintiff’s brain injury was caused by the collision and was not related to his subsequent medical care. According to the defendant, the plaintiff’s brain scans revealed diffuse axial injury, which is not amenable to treatment. The defendant also claimed that it was reasonable to have relied on the negative CT results and the normal neurologic examination from the transferring hospital.
After the underlying motor vehicle accident claim was resolved, the malpractice action and the plaintiff’s workers compensation claim proceeded. The medical malpractice claims were resolved with a $2,375,000 mediated settlement.
Bedsore Requires Debridement, Leads to Sepsis
At age 58, a man underwent coronary artery bypass surgery in July 1999. Shortly after the procedure, the patient experienced a stroke. He remained hospitalized in the defendant facility under the care of Dr. W., the defendant physician.
Several weeks later, the patient developed a sacral bedsore. He underwent three surgical debridements but developed sepsis. The bedsore allegedly worsened until the man’s death in January 2000.
The plaintiff claimed that the defendants failed to properly reposition the decedent and failed to treat the bedsore appropriately as soon as it developed. The plaintiff reached a confidential settlement with the nurses involved, and the matter proceeded against Dr. W. He claimed that the decedent’s diabetes made it impossible for the wound to heal and that nothing would have changed the outcome.
According to a published account, a $300,000 verdict was returned. A posttrial motion was pending.
Hernia Repaired, Recurrence Overlooked
A woman with a diagnosis of paraesophageal hernia was referred to the defendant surgeon, who recommended and performed laparoscopic surgery. The procedure involved reduction and repair of the patient’s large paraesophageal hernia, followed by Nissen fundoplication. A chest x-ray performed two days later revealed a large hiatal hernia, small to moderate-sized bilateral pleural effusions, and atelectasis in the left lung base. The woman was discharged from the hospital the next day.
Three days later, she presented to the emergency department, complaining of abdominal pain and shortness of breath. Chest x-rays again revealed the hiatal hernia, and no improvement was seen on repeat chest x-rays the next day. An upper gastrointestinal (GI) study was ordered. During the test, the patient’s condition declined, and she was transferred to the ICU.
After exploratory surgery revealed a constriction of the stomach and tissue necroses, the patient underwent cholecystectomy, resection of the proximal two-thirds of the stomach, and esophagogastrostomy with insertion of a feeding jejunostomy tube. Despite additional surgery, the woman died a few days later as a result of acute respiratory distress syndrome.
The plaintiff claimed that the defendant surgeon should have followed up on the chest x-ray following the initial surgery. On the patient’s return to the hospital, it was additionally charged, he should have inserted a nasogastric tube and ordered CT or an upper GI series immediately.
The defendant claimed that paraesophageal hernia repairs tend to fail and that it was not alarming that the hernia had recurred. The defendant maintained that the decedent’s symptoms were consistent with gas bloat syndrome, a common side effect of Nissen fundoplication. The defendant also claimed that even if the recommended diagnostic workup had been initiated earlier, she would have died in any event.
A defense verdict was returned.
House MD Forgoes Cardiology Consult
A 60-year-old woman was brought to the defendant hospital’s emergency department (ED) complaining of chest pain, nausea, and diaphoresis. She reported a family history of heart disease and a personal history of hypertension and high cholesterol.
In the ED, the patient was treated with aspirin and nitroglycerin. ECG revealed an old inferior infarct and was consistent with acute anterior ischemia. A diagnosis of unstable angina was made. The patient was admitted to a cardiac telemetry unit, and the on-call cardiologist was asked to consult. The plan for care included serial ECG and enzyme studies.
Shortly after midnight, the house officer was contacted by a unit nurse and informed about a report of an elevated troponin level. The house officer saw the patient, but his examination failed to elicit complaints of chest pain or shortness of breath and he pronounced it unremarkable.
Six hours later, the woman was found in cardiac arrest. Her heartbeat was restored, but she had experienced brain damage. She was transferred to another hospital for cardiac catheterization and stenting. Cardiac catheterization revealed single-vessel disease, with 99% to 100% occlusion of the left anterior descending artery. The decedent did not regain consciousness and was placed on a ventilator. A week later, she was removed from the ventilator and died.
The plaintiff claimed that the house officer should have ordered a stat cardiology consultation, which would have led to appropriate treatment and prevented the decedent’s massive myocardial infarction and death.
According to a published account, a $600,000 settlement was reached.
The latest research you need to know
Literature at a Glance
A guide to this month’s studies.
- Score predicts risk of intracerebral hemorrhage after thrombolysis.
- Trigylcerides and stroke-risk predictors.
- PPI use and risk of community-acquired pneumonia.
- Clopidogrel before coronary intervention might improve outcomes.
- High-dose clopidogrel after coronary intervention is beneficial.
- B-type natriuretic peptide level and sepsis.
- Thrombolytic use in pulmonary embolism.
- Hospitalists and ED patient flow.
Simple Clinical Score Predicts Intracerebral Hemorrhage after Thrombolysis
Clinical question: Is there a simple scoring tool that will predict the risk of intracerebral hemorrhage (ICH) following IV tissue-plasminogen activator (t-PA) in ischemic strokes?
Background: The use of t-PA in acute ischemic stroke (AIS) is about 2% to 4%, due in part to fear of conversion of an ischemic event to an ICH. Several studies using t-PA after AIS have identified risk factors for ICH; however, none has looked at the cumulative risk and prognosis for an individual candidate based on these factors.
Study design: Retrospective, observational cohort study.
Setting: The National Institute of Neurological Disorders and Stroke Trials 1 and 2, and consecutive patients treated at Beth Israel Deaconess Medical Center, Boston.
Synopsis: After an extensive literature review, a five-point scale to determine the risk of hemorrhage after t-PA (HAT) was developed using the top four predictive factors based on odds ratios. These included the National Institutes of Health Stroke Scale (NIHSS), presence and extent of hypodensity on initial CT scan, history of diabetes, and high baseline serum glucose. The predictive value of this scale was tested against two independent cohorts of patients with AIS treated with IV t-PA. The HAT scale was able to reasonably predict both the risk of ICH following t-PA and the functional outcome at 90 days. Higher scores on the scale tended to do worse, especially scores of three or more. Its retrospective nature and small number of patients experiencing ICH limit this study.
Bottom line: The HAT score is a quick bedside tool that can help in the counseling of patients and families in conjunction with the risks and benefits of t-PA after ischemic stroke.
Citation: Lou M, Safdar A, Mehdiratta M, et al. The HAT Score: a simple grading scale for predicting hemorrhage after thrombolysis. Neurology. 2008;71:1417-1423.
Nonfasting Triglycerides Predict Stroke Risk
Clinical question: Is there a correlation between nonfasting triglyceride levels and ischemic stroke?
Background: Most individuals are in a nonfasting state, with the exception of several hours prior to breakfast. Fasting cholesterol levels exclude most remnant lipoproteins, which might play a role in early atherosclerotic disease. Increased levels of triglycerides in a nonfasting state indicate the presence of these remnants.
Study design: Prospective, population-based cohort study.
Setting: The Copenhagen City Heart Study.
Synopsis: The study included 13,956 individuals between the ages of 20 and 93 with a follow-up period of up to 31 years. Cholesterol levels were checked during four evaluation periods: 1976-1978, 1981-1983, 1991-1994, and 2001-2003. Eighty-two percent of the participants had eaten a meal within three hours of the blood draw; the other 18% had eaten more than three hours prior to the draw. The study showed an association between increasing nonfasting triglyceride levels and a step-wise increase in the risk of ischemic stroke. The highest risk came in individuals with nonfasting triglyceride levels > 443mg/dl, which was associated with a three- to fourfold greater risk of ischemic stroke. The study was limited in that it evaluated a homogenous group of individuals, which may not reflect other racial or ethnic populations.
Bottom line: Increasing levels of nonfasting triglycerides are associated with an increased risk of ischemic stroke.
Citation: Freiberg J, Tybjaerg-Hansen A, Jensen JS, Nordestgaard BG. Nonfasting triglycerides and risk of ischemic stroke in the general population. JAMA. 2008;300(18):2142-2152.
Proton-Pump Inhibitor (PPI) Use Increases the Risk of Community-Acquired Pneumonia (CAP)
Clinical question: Is there an association between PPI use and CAP?
Background: CAP is associated with significant morbidity, annually accounting for billions of healthcare dollars. Proton-pump inhibitors (PPI) are a mainstay treatment for gastric acid suppression. Previous studies have suggested using PPIs may increase the risk of developing CAP.
Study design: Nested case control study.
Setting: Outpatient general practices, United Kingdom.
Synopsis: The association between PPI use and CAP was evaluated in a cohort of more than 7 million patients using the UK’s general-practice research database. Eligible participants were divided into two groups: case patients and control patients. Initial results indicated an increased risk of CAP with PPI use. After adjusting for confounding variables, the use of a PPI was strongly associated with CAP development when used within 30 days prior of the diagnosis, and most notably within 48 hours of diagnosis. It also was noted that the risk of developing CAP with longer-term PPI use was much lower. This inverse temporal relationship was noted in two previous studies. The limitations of this study were related to presumed adherence and compliance with PPI therapy. There also was no radiographic data to support the diagnosis of pneumonia in these cases, both of which could bias the results.
Bottom line: There appears to be an increased risk of CAP with PPI use. This risk is most notable within 48 hours. However, long-term, chronic PPI use was not associated with an increased risk of CAP.
Citation: Sarkar M, Hennessy S, Yang YX. Proton-pump inhibitor use and the risk for community-acquired pneumonia. Ann Intern Med. 2008;149:391-398.
Clopidogrel Prior to Percutaneous Intervention (PCI) Might Improve Outcomes in Patients with Acute ST-Elevation Myocardial Infarction (STEMI)
Clinical question: Does pretreatment with clopidogrel prior to PCI in acute STEMI improve outcomes?
Background: Extant guidelines for early utilization of clopidogrel in STEMI patients are based on results of studies of patients with non-ST-elevation acute coronary syndromes or treatment with thrombolytics.
Study design: Systematic review.
Setting: MEDLINE and Cochrane Controlled Trials Register of randomized controlled trials.
Synopsis: The authors selected 38 treatment groups, including 8,429 patients with STEMI who underwent primary PCI. They found a statistically significant difference in initial patency, and further found clopidogrel pretreatment was an independent predictor of early reperfusion and improved clinical outcome. This study suggests a benefit to pretreatment with clopidogrel but likely is not sufficient to establish such pretreatment as the standard of care. The limitations of this study were a retrospective review/meta-analysis, as the ability to limit the influence of confounding variables is reduced.
Bottom line: Pretreatment with clopidogrel in patients with acute STEMI undergoing primary PCI appears beneficial based on the results of this review of available evidence.
Citation: Vlaar PJ, Svilaas T, Damman K, et al. Impact of pretreatment with clopidogrel on initial patency and outcomes in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review. Circulation. 2008;118:1828-1836.
High-Dose Clopidogrel after PCI Is Beneficial
Clinical question: Does high-dose clopidogrel improve patient outcome following PCI?
Background: Studies have shown antiplatelet resistance after PCI is associated with an increased risk of cardiovascular events, including in-stent thrombosis and death. Other studies have shown the benefit of high-dose clopidogrel by the inhibition of platelet aggregation. Limited information is available regarding the applicability to patients after PCI.
Study design: Retrospective study of 2,954 consecutive patients divided into two groups, low-dose and high-dose clopidogrel use.
Setting: Single hospital in France.
Synopsis: The low-dose study group undergoing PCI was pretreated with 300 mg clopidogrel, followed by ASA 75 mg and clopidogrel 75 mg daily for two months. The second group undergoing PCI was pretreated with 600 mg clopidogrel followed by ASA 75 mg and clopidogrel 150 mg for 15 days, then maintained on ASA 75 mg and clopidogrel 75 mg. Patients received follow-up at two months and were evaluated for in-stent thrombosis, myocardial infarction (MI), death, and hemorrhagic complications. The two groups were matched one-to-one using propensity scoring and the nearest-pair-matching method blinded to patient outcome.
The high-dose clopidogrel group showed a decreased incidence of MI, in-stent thrombosis, and death. This benefit confirms the importance of achieving early and adequate antiplatelet therapy. However, the study authors noted a higher percentage of major bleeding and minor bleeding, although the increase was not statistically significant (2.8% vs. 3.5%, P=0.379, and 7.4% vs. 8.2%, P=0.699, respectively).
Bottom line: High-dose clopidogrel before and within the first 15 days after PCI decreases the risk of MI, in-stent thrombosis, and death, with no statistical increase in bleeding complications. Long-range studies beyond the two-month interval might be beneficial.
Citation: Lemesle G, Delhaye C, Sudre A, et al. Impact of high loading and maintenance dose of clopidogrel within the first 15 days after percutaneous coronary intervention on patient outcome. Am Heart J. 2008;10:1-8.
B-Type Natriuretic Peptide (BNP) Identifies Patients Developing Sepsis-Induced Myocardial Depression
Clinical question: Can plasma BNP be used as a marker to identify patients at risk for sepsis-induced depression of myocardial function?
Background: Previous studies have established BNP levels are increased in patients with septic shock but have not examined the relationship between plasma BNP concentration and left ventricular (LV) systolic dysfunction.
Study design: Prospective cohort.
Setting: Academic medical center.
Synopsis: The authors divided 93 prospectively selected ICU patients with severe sepsis into two groups: one with normal left ventricular (LV) function and a group with LV systolic dysfunction. Comparison of the plasma BNP concentrations between these two groups demonstrated a significant positive correlation between the BNP level and the degree of LV systolic dysfunction, suggesting BNP is a reasonable marker for identification of septic patients with sepsis-induced myocardial depression.
Further, the study’s results suggest BNP measurements early in the course of septic shock might be useful prognostic indicators. However, it is unclear to what extent the knowledge gained from such measurements would alter care management, or how BNP compares to echocardiography in terms of diagnostic and prognostic utility. Thus, these results might not be adequate to justify the routine measurement of BNP in patients with severe sepsis.
Bottom line: Elevated BNP in septic patients is associated with the presence or risk of sepsis-induced myocardial depression, and might be a negative prognostic indicator.
Citation: Post F, Weilemann LS, Messow CM, Sinning C, Munzel T. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36:3030–3037.
High Risk of Death with Thrombolytic Use in Low-Risk Pulmonary Embolism (PE)
Clinical question: Is there an advantage to thrombolytic therapy in the treatment of acute PE versus treatment with unfractionated or low-molecular-weight (LMW) heparin?
Background: Given the high mortality linked to PE, consistent indications for thrombolytic therapy in acute PE are needed. An assessment of the prevalence of thrombolytic therapy and mortality, as compared with standard anticoagulation, has been described inconsistently.
Study design: Retrospective cohort study.
Setting: 186 acute-care hospitals in Pennsylvania.
Synopsis: Using a database of ICD-9 codes, 15,116 patients were reviewed. Logistic regression was used to evaluate the association between thrombolytic therapy and 30-day mortality. Poisson regression was used to evaluate the association between thrombolytic therapy and in-hospital mortality. For those receiving thrombolysis and considered unlikely candidates for the therapy based on documentation at presentation (low predicted probability), the in-hospital mortality and overall 30-day mortality rate were higher when compared with those who did not receive thrombolysis. An exception to this was a group of patients with high predicted probability of receiving thrombolysis. In this group, thrombolysis was not associated with increased risk. Limitations to the study include lack of assessment of right ventricular function, changes in condition after presentation, lack of long-term outcomes, and lack of exact cause of death.
Bottom line: Thrombolytic therapy is associated with higher mortality in patients with hemodynamically uncomplicated PE, and therefore not indicated. Thrombolytic therapy in a subgroup of patients with hemodynamic instability or right ventricular dysfunction improves the clinical course and outcome.
Citation: Ibrahim SA, Stone RA, Obrosky S, Geng M, Fine MJ, Aujesky D. Thrombolytic therapy and mortality in patients with acute pulmonary embolism. Arch Intern Med. 2008;168(20):2183-2190.
Hospitalists Improve Patient Flow in the ED
Clinical question: Can active-bed management by hospitalists reduce ED throughput times and diversionary status?
Background: ED overcrowding leads to ambulance diversion, which has been associated with increased mortality. A primary cause of ED crowding is inpatient boarding, which can reduce patient satisfaction and quality of care. Previous studies targeting the ED have had little impact on throughput and ambulance diversion.
Study design: Pre-post case study in a single institution.
Setting: Academic teaching hospital in Baltimore.
Synopsis: ED throughput times and ambulance diversion hours were measured for all adult patients registered in the department from November 2005 to February 2006 (control period) and November 2006 to February 2007 (intervention period). Active-bed management was defined as appointing a hospitalist to assess bed availability in real time and assigning department of medicine admissions to the appropriate clinical setting, as well as the creation of a bed director. Although the ED census was 8.8% higher during the intervention period, throughput time for admitted patients decreased by 98 minutes per patient, to 458 from 360. The time spent under diversionary status for overcrowding or lack of ICU beds decreased by 6% and 27%, respectively. Limitations of this study include the pre-post design and the implementation at a single institution. Additionally, active-bed management is expensive, and in this case required the hiring of three full-time-equivalent faculty. However, this study successfully demonstrates that a quality improvement partnership between hospitalists and the ED can substantially reduce overcrowding.
Bottom line: Active-bed management by hospitalists improves ED throughput by decreasing the length of time admitted patients spend in the ED and reducing ambulance diversion hours.
Citation: Howell E, Bessman E, Kravet S, Kolodner K, Marshall R, Wright S. Active bed management by hospitalists and emergency department throughput. Ann Int Med. 2008;149(11):804-810.
Literature at a Glance
A guide to this month’s studies.
- Score predicts risk of intracerebral hemorrhage after thrombolysis.
- Trigylcerides and stroke-risk predictors.
- PPI use and risk of community-acquired pneumonia.
- Clopidogrel before coronary intervention might improve outcomes.
- High-dose clopidogrel after coronary intervention is beneficial.
- B-type natriuretic peptide level and sepsis.
- Thrombolytic use in pulmonary embolism.
- Hospitalists and ED patient flow.
Simple Clinical Score Predicts Intracerebral Hemorrhage after Thrombolysis
Clinical question: Is there a simple scoring tool that will predict the risk of intracerebral hemorrhage (ICH) following IV tissue-plasminogen activator (t-PA) in ischemic strokes?
Background: The use of t-PA in acute ischemic stroke (AIS) is about 2% to 4%, due in part to fear of conversion of an ischemic event to an ICH. Several studies using t-PA after AIS have identified risk factors for ICH; however, none has looked at the cumulative risk and prognosis for an individual candidate based on these factors.
Study design: Retrospective, observational cohort study.
Setting: The National Institute of Neurological Disorders and Stroke Trials 1 and 2, and consecutive patients treated at Beth Israel Deaconess Medical Center, Boston.
Synopsis: After an extensive literature review, a five-point scale to determine the risk of hemorrhage after t-PA (HAT) was developed using the top four predictive factors based on odds ratios. These included the National Institutes of Health Stroke Scale (NIHSS), presence and extent of hypodensity on initial CT scan, history of diabetes, and high baseline serum glucose. The predictive value of this scale was tested against two independent cohorts of patients with AIS treated with IV t-PA. The HAT scale was able to reasonably predict both the risk of ICH following t-PA and the functional outcome at 90 days. Higher scores on the scale tended to do worse, especially scores of three or more. Its retrospective nature and small number of patients experiencing ICH limit this study.
Bottom line: The HAT score is a quick bedside tool that can help in the counseling of patients and families in conjunction with the risks and benefits of t-PA after ischemic stroke.
Citation: Lou M, Safdar A, Mehdiratta M, et al. The HAT Score: a simple grading scale for predicting hemorrhage after thrombolysis. Neurology. 2008;71:1417-1423.
Nonfasting Triglycerides Predict Stroke Risk
Clinical question: Is there a correlation between nonfasting triglyceride levels and ischemic stroke?
Background: Most individuals are in a nonfasting state, with the exception of several hours prior to breakfast. Fasting cholesterol levels exclude most remnant lipoproteins, which might play a role in early atherosclerotic disease. Increased levels of triglycerides in a nonfasting state indicate the presence of these remnants.
Study design: Prospective, population-based cohort study.
Setting: The Copenhagen City Heart Study.
Synopsis: The study included 13,956 individuals between the ages of 20 and 93 with a follow-up period of up to 31 years. Cholesterol levels were checked during four evaluation periods: 1976-1978, 1981-1983, 1991-1994, and 2001-2003. Eighty-two percent of the participants had eaten a meal within three hours of the blood draw; the other 18% had eaten more than three hours prior to the draw. The study showed an association between increasing nonfasting triglyceride levels and a step-wise increase in the risk of ischemic stroke. The highest risk came in individuals with nonfasting triglyceride levels > 443mg/dl, which was associated with a three- to fourfold greater risk of ischemic stroke. The study was limited in that it evaluated a homogenous group of individuals, which may not reflect other racial or ethnic populations.
Bottom line: Increasing levels of nonfasting triglycerides are associated with an increased risk of ischemic stroke.
Citation: Freiberg J, Tybjaerg-Hansen A, Jensen JS, Nordestgaard BG. Nonfasting triglycerides and risk of ischemic stroke in the general population. JAMA. 2008;300(18):2142-2152.
Proton-Pump Inhibitor (PPI) Use Increases the Risk of Community-Acquired Pneumonia (CAP)
Clinical question: Is there an association between PPI use and CAP?
Background: CAP is associated with significant morbidity, annually accounting for billions of healthcare dollars. Proton-pump inhibitors (PPI) are a mainstay treatment for gastric acid suppression. Previous studies have suggested using PPIs may increase the risk of developing CAP.
Study design: Nested case control study.
Setting: Outpatient general practices, United Kingdom.
Synopsis: The association between PPI use and CAP was evaluated in a cohort of more than 7 million patients using the UK’s general-practice research database. Eligible participants were divided into two groups: case patients and control patients. Initial results indicated an increased risk of CAP with PPI use. After adjusting for confounding variables, the use of a PPI was strongly associated with CAP development when used within 30 days prior of the diagnosis, and most notably within 48 hours of diagnosis. It also was noted that the risk of developing CAP with longer-term PPI use was much lower. This inverse temporal relationship was noted in two previous studies. The limitations of this study were related to presumed adherence and compliance with PPI therapy. There also was no radiographic data to support the diagnosis of pneumonia in these cases, both of which could bias the results.
Bottom line: There appears to be an increased risk of CAP with PPI use. This risk is most notable within 48 hours. However, long-term, chronic PPI use was not associated with an increased risk of CAP.
Citation: Sarkar M, Hennessy S, Yang YX. Proton-pump inhibitor use and the risk for community-acquired pneumonia. Ann Intern Med. 2008;149:391-398.
Clopidogrel Prior to Percutaneous Intervention (PCI) Might Improve Outcomes in Patients with Acute ST-Elevation Myocardial Infarction (STEMI)
Clinical question: Does pretreatment with clopidogrel prior to PCI in acute STEMI improve outcomes?
Background: Extant guidelines for early utilization of clopidogrel in STEMI patients are based on results of studies of patients with non-ST-elevation acute coronary syndromes or treatment with thrombolytics.
Study design: Systematic review.
Setting: MEDLINE and Cochrane Controlled Trials Register of randomized controlled trials.
Synopsis: The authors selected 38 treatment groups, including 8,429 patients with STEMI who underwent primary PCI. They found a statistically significant difference in initial patency, and further found clopidogrel pretreatment was an independent predictor of early reperfusion and improved clinical outcome. This study suggests a benefit to pretreatment with clopidogrel but likely is not sufficient to establish such pretreatment as the standard of care. The limitations of this study were a retrospective review/meta-analysis, as the ability to limit the influence of confounding variables is reduced.
Bottom line: Pretreatment with clopidogrel in patients with acute STEMI undergoing primary PCI appears beneficial based on the results of this review of available evidence.
Citation: Vlaar PJ, Svilaas T, Damman K, et al. Impact of pretreatment with clopidogrel on initial patency and outcomes in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review. Circulation. 2008;118:1828-1836.
High-Dose Clopidogrel after PCI Is Beneficial
Clinical question: Does high-dose clopidogrel improve patient outcome following PCI?
Background: Studies have shown antiplatelet resistance after PCI is associated with an increased risk of cardiovascular events, including in-stent thrombosis and death. Other studies have shown the benefit of high-dose clopidogrel by the inhibition of platelet aggregation. Limited information is available regarding the applicability to patients after PCI.
Study design: Retrospective study of 2,954 consecutive patients divided into two groups, low-dose and high-dose clopidogrel use.
Setting: Single hospital in France.
Synopsis: The low-dose study group undergoing PCI was pretreated with 300 mg clopidogrel, followed by ASA 75 mg and clopidogrel 75 mg daily for two months. The second group undergoing PCI was pretreated with 600 mg clopidogrel followed by ASA 75 mg and clopidogrel 150 mg for 15 days, then maintained on ASA 75 mg and clopidogrel 75 mg. Patients received follow-up at two months and were evaluated for in-stent thrombosis, myocardial infarction (MI), death, and hemorrhagic complications. The two groups were matched one-to-one using propensity scoring and the nearest-pair-matching method blinded to patient outcome.
The high-dose clopidogrel group showed a decreased incidence of MI, in-stent thrombosis, and death. This benefit confirms the importance of achieving early and adequate antiplatelet therapy. However, the study authors noted a higher percentage of major bleeding and minor bleeding, although the increase was not statistically significant (2.8% vs. 3.5%, P=0.379, and 7.4% vs. 8.2%, P=0.699, respectively).
Bottom line: High-dose clopidogrel before and within the first 15 days after PCI decreases the risk of MI, in-stent thrombosis, and death, with no statistical increase in bleeding complications. Long-range studies beyond the two-month interval might be beneficial.
Citation: Lemesle G, Delhaye C, Sudre A, et al. Impact of high loading and maintenance dose of clopidogrel within the first 15 days after percutaneous coronary intervention on patient outcome. Am Heart J. 2008;10:1-8.
B-Type Natriuretic Peptide (BNP) Identifies Patients Developing Sepsis-Induced Myocardial Depression
Clinical question: Can plasma BNP be used as a marker to identify patients at risk for sepsis-induced depression of myocardial function?
Background: Previous studies have established BNP levels are increased in patients with septic shock but have not examined the relationship between plasma BNP concentration and left ventricular (LV) systolic dysfunction.
Study design: Prospective cohort.
Setting: Academic medical center.
Synopsis: The authors divided 93 prospectively selected ICU patients with severe sepsis into two groups: one with normal left ventricular (LV) function and a group with LV systolic dysfunction. Comparison of the plasma BNP concentrations between these two groups demonstrated a significant positive correlation between the BNP level and the degree of LV systolic dysfunction, suggesting BNP is a reasonable marker for identification of septic patients with sepsis-induced myocardial depression.
Further, the study’s results suggest BNP measurements early in the course of septic shock might be useful prognostic indicators. However, it is unclear to what extent the knowledge gained from such measurements would alter care management, or how BNP compares to echocardiography in terms of diagnostic and prognostic utility. Thus, these results might not be adequate to justify the routine measurement of BNP in patients with severe sepsis.
Bottom line: Elevated BNP in septic patients is associated with the presence or risk of sepsis-induced myocardial depression, and might be a negative prognostic indicator.
Citation: Post F, Weilemann LS, Messow CM, Sinning C, Munzel T. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36:3030–3037.
High Risk of Death with Thrombolytic Use in Low-Risk Pulmonary Embolism (PE)
Clinical question: Is there an advantage to thrombolytic therapy in the treatment of acute PE versus treatment with unfractionated or low-molecular-weight (LMW) heparin?
Background: Given the high mortality linked to PE, consistent indications for thrombolytic therapy in acute PE are needed. An assessment of the prevalence of thrombolytic therapy and mortality, as compared with standard anticoagulation, has been described inconsistently.
Study design: Retrospective cohort study.
Setting: 186 acute-care hospitals in Pennsylvania.
Synopsis: Using a database of ICD-9 codes, 15,116 patients were reviewed. Logistic regression was used to evaluate the association between thrombolytic therapy and 30-day mortality. Poisson regression was used to evaluate the association between thrombolytic therapy and in-hospital mortality. For those receiving thrombolysis and considered unlikely candidates for the therapy based on documentation at presentation (low predicted probability), the in-hospital mortality and overall 30-day mortality rate were higher when compared with those who did not receive thrombolysis. An exception to this was a group of patients with high predicted probability of receiving thrombolysis. In this group, thrombolysis was not associated with increased risk. Limitations to the study include lack of assessment of right ventricular function, changes in condition after presentation, lack of long-term outcomes, and lack of exact cause of death.
Bottom line: Thrombolytic therapy is associated with higher mortality in patients with hemodynamically uncomplicated PE, and therefore not indicated. Thrombolytic therapy in a subgroup of patients with hemodynamic instability or right ventricular dysfunction improves the clinical course and outcome.
Citation: Ibrahim SA, Stone RA, Obrosky S, Geng M, Fine MJ, Aujesky D. Thrombolytic therapy and mortality in patients with acute pulmonary embolism. Arch Intern Med. 2008;168(20):2183-2190.
Hospitalists Improve Patient Flow in the ED
Clinical question: Can active-bed management by hospitalists reduce ED throughput times and diversionary status?
Background: ED overcrowding leads to ambulance diversion, which has been associated with increased mortality. A primary cause of ED crowding is inpatient boarding, which can reduce patient satisfaction and quality of care. Previous studies targeting the ED have had little impact on throughput and ambulance diversion.
Study design: Pre-post case study in a single institution.
Setting: Academic teaching hospital in Baltimore.
Synopsis: ED throughput times and ambulance diversion hours were measured for all adult patients registered in the department from November 2005 to February 2006 (control period) and November 2006 to February 2007 (intervention period). Active-bed management was defined as appointing a hospitalist to assess bed availability in real time and assigning department of medicine admissions to the appropriate clinical setting, as well as the creation of a bed director. Although the ED census was 8.8% higher during the intervention period, throughput time for admitted patients decreased by 98 minutes per patient, to 458 from 360. The time spent under diversionary status for overcrowding or lack of ICU beds decreased by 6% and 27%, respectively. Limitations of this study include the pre-post design and the implementation at a single institution. Additionally, active-bed management is expensive, and in this case required the hiring of three full-time-equivalent faculty. However, this study successfully demonstrates that a quality improvement partnership between hospitalists and the ED can substantially reduce overcrowding.
Bottom line: Active-bed management by hospitalists improves ED throughput by decreasing the length of time admitted patients spend in the ED and reducing ambulance diversion hours.
Citation: Howell E, Bessman E, Kravet S, Kolodner K, Marshall R, Wright S. Active bed management by hospitalists and emergency department throughput. Ann Int Med. 2008;149(11):804-810.
Literature at a Glance
A guide to this month’s studies.
- Score predicts risk of intracerebral hemorrhage after thrombolysis.
- Trigylcerides and stroke-risk predictors.
- PPI use and risk of community-acquired pneumonia.
- Clopidogrel before coronary intervention might improve outcomes.
- High-dose clopidogrel after coronary intervention is beneficial.
- B-type natriuretic peptide level and sepsis.
- Thrombolytic use in pulmonary embolism.
- Hospitalists and ED patient flow.
Simple Clinical Score Predicts Intracerebral Hemorrhage after Thrombolysis
Clinical question: Is there a simple scoring tool that will predict the risk of intracerebral hemorrhage (ICH) following IV tissue-plasminogen activator (t-PA) in ischemic strokes?
Background: The use of t-PA in acute ischemic stroke (AIS) is about 2% to 4%, due in part to fear of conversion of an ischemic event to an ICH. Several studies using t-PA after AIS have identified risk factors for ICH; however, none has looked at the cumulative risk and prognosis for an individual candidate based on these factors.
Study design: Retrospective, observational cohort study.
Setting: The National Institute of Neurological Disorders and Stroke Trials 1 and 2, and consecutive patients treated at Beth Israel Deaconess Medical Center, Boston.
Synopsis: After an extensive literature review, a five-point scale to determine the risk of hemorrhage after t-PA (HAT) was developed using the top four predictive factors based on odds ratios. These included the National Institutes of Health Stroke Scale (NIHSS), presence and extent of hypodensity on initial CT scan, history of diabetes, and high baseline serum glucose. The predictive value of this scale was tested against two independent cohorts of patients with AIS treated with IV t-PA. The HAT scale was able to reasonably predict both the risk of ICH following t-PA and the functional outcome at 90 days. Higher scores on the scale tended to do worse, especially scores of three or more. Its retrospective nature and small number of patients experiencing ICH limit this study.
Bottom line: The HAT score is a quick bedside tool that can help in the counseling of patients and families in conjunction with the risks and benefits of t-PA after ischemic stroke.
Citation: Lou M, Safdar A, Mehdiratta M, et al. The HAT Score: a simple grading scale for predicting hemorrhage after thrombolysis. Neurology. 2008;71:1417-1423.
Nonfasting Triglycerides Predict Stroke Risk
Clinical question: Is there a correlation between nonfasting triglyceride levels and ischemic stroke?
Background: Most individuals are in a nonfasting state, with the exception of several hours prior to breakfast. Fasting cholesterol levels exclude most remnant lipoproteins, which might play a role in early atherosclerotic disease. Increased levels of triglycerides in a nonfasting state indicate the presence of these remnants.
Study design: Prospective, population-based cohort study.
Setting: The Copenhagen City Heart Study.
Synopsis: The study included 13,956 individuals between the ages of 20 and 93 with a follow-up period of up to 31 years. Cholesterol levels were checked during four evaluation periods: 1976-1978, 1981-1983, 1991-1994, and 2001-2003. Eighty-two percent of the participants had eaten a meal within three hours of the blood draw; the other 18% had eaten more than three hours prior to the draw. The study showed an association between increasing nonfasting triglyceride levels and a step-wise increase in the risk of ischemic stroke. The highest risk came in individuals with nonfasting triglyceride levels > 443mg/dl, which was associated with a three- to fourfold greater risk of ischemic stroke. The study was limited in that it evaluated a homogenous group of individuals, which may not reflect other racial or ethnic populations.
Bottom line: Increasing levels of nonfasting triglycerides are associated with an increased risk of ischemic stroke.
Citation: Freiberg J, Tybjaerg-Hansen A, Jensen JS, Nordestgaard BG. Nonfasting triglycerides and risk of ischemic stroke in the general population. JAMA. 2008;300(18):2142-2152.
Proton-Pump Inhibitor (PPI) Use Increases the Risk of Community-Acquired Pneumonia (CAP)
Clinical question: Is there an association between PPI use and CAP?
Background: CAP is associated with significant morbidity, annually accounting for billions of healthcare dollars. Proton-pump inhibitors (PPI) are a mainstay treatment for gastric acid suppression. Previous studies have suggested using PPIs may increase the risk of developing CAP.
Study design: Nested case control study.
Setting: Outpatient general practices, United Kingdom.
Synopsis: The association between PPI use and CAP was evaluated in a cohort of more than 7 million patients using the UK’s general-practice research database. Eligible participants were divided into two groups: case patients and control patients. Initial results indicated an increased risk of CAP with PPI use. After adjusting for confounding variables, the use of a PPI was strongly associated with CAP development when used within 30 days prior of the diagnosis, and most notably within 48 hours of diagnosis. It also was noted that the risk of developing CAP with longer-term PPI use was much lower. This inverse temporal relationship was noted in two previous studies. The limitations of this study were related to presumed adherence and compliance with PPI therapy. There also was no radiographic data to support the diagnosis of pneumonia in these cases, both of which could bias the results.
Bottom line: There appears to be an increased risk of CAP with PPI use. This risk is most notable within 48 hours. However, long-term, chronic PPI use was not associated with an increased risk of CAP.
Citation: Sarkar M, Hennessy S, Yang YX. Proton-pump inhibitor use and the risk for community-acquired pneumonia. Ann Intern Med. 2008;149:391-398.
Clopidogrel Prior to Percutaneous Intervention (PCI) Might Improve Outcomes in Patients with Acute ST-Elevation Myocardial Infarction (STEMI)
Clinical question: Does pretreatment with clopidogrel prior to PCI in acute STEMI improve outcomes?
Background: Extant guidelines for early utilization of clopidogrel in STEMI patients are based on results of studies of patients with non-ST-elevation acute coronary syndromes or treatment with thrombolytics.
Study design: Systematic review.
Setting: MEDLINE and Cochrane Controlled Trials Register of randomized controlled trials.
Synopsis: The authors selected 38 treatment groups, including 8,429 patients with STEMI who underwent primary PCI. They found a statistically significant difference in initial patency, and further found clopidogrel pretreatment was an independent predictor of early reperfusion and improved clinical outcome. This study suggests a benefit to pretreatment with clopidogrel but likely is not sufficient to establish such pretreatment as the standard of care. The limitations of this study were a retrospective review/meta-analysis, as the ability to limit the influence of confounding variables is reduced.
Bottom line: Pretreatment with clopidogrel in patients with acute STEMI undergoing primary PCI appears beneficial based on the results of this review of available evidence.
Citation: Vlaar PJ, Svilaas T, Damman K, et al. Impact of pretreatment with clopidogrel on initial patency and outcomes in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review. Circulation. 2008;118:1828-1836.
High-Dose Clopidogrel after PCI Is Beneficial
Clinical question: Does high-dose clopidogrel improve patient outcome following PCI?
Background: Studies have shown antiplatelet resistance after PCI is associated with an increased risk of cardiovascular events, including in-stent thrombosis and death. Other studies have shown the benefit of high-dose clopidogrel by the inhibition of platelet aggregation. Limited information is available regarding the applicability to patients after PCI.
Study design: Retrospective study of 2,954 consecutive patients divided into two groups, low-dose and high-dose clopidogrel use.
Setting: Single hospital in France.
Synopsis: The low-dose study group undergoing PCI was pretreated with 300 mg clopidogrel, followed by ASA 75 mg and clopidogrel 75 mg daily for two months. The second group undergoing PCI was pretreated with 600 mg clopidogrel followed by ASA 75 mg and clopidogrel 150 mg for 15 days, then maintained on ASA 75 mg and clopidogrel 75 mg. Patients received follow-up at two months and were evaluated for in-stent thrombosis, myocardial infarction (MI), death, and hemorrhagic complications. The two groups were matched one-to-one using propensity scoring and the nearest-pair-matching method blinded to patient outcome.
The high-dose clopidogrel group showed a decreased incidence of MI, in-stent thrombosis, and death. This benefit confirms the importance of achieving early and adequate antiplatelet therapy. However, the study authors noted a higher percentage of major bleeding and minor bleeding, although the increase was not statistically significant (2.8% vs. 3.5%, P=0.379, and 7.4% vs. 8.2%, P=0.699, respectively).
Bottom line: High-dose clopidogrel before and within the first 15 days after PCI decreases the risk of MI, in-stent thrombosis, and death, with no statistical increase in bleeding complications. Long-range studies beyond the two-month interval might be beneficial.
Citation: Lemesle G, Delhaye C, Sudre A, et al. Impact of high loading and maintenance dose of clopidogrel within the first 15 days after percutaneous coronary intervention on patient outcome. Am Heart J. 2008;10:1-8.
B-Type Natriuretic Peptide (BNP) Identifies Patients Developing Sepsis-Induced Myocardial Depression
Clinical question: Can plasma BNP be used as a marker to identify patients at risk for sepsis-induced depression of myocardial function?
Background: Previous studies have established BNP levels are increased in patients with septic shock but have not examined the relationship between plasma BNP concentration and left ventricular (LV) systolic dysfunction.
Study design: Prospective cohort.
Setting: Academic medical center.
Synopsis: The authors divided 93 prospectively selected ICU patients with severe sepsis into two groups: one with normal left ventricular (LV) function and a group with LV systolic dysfunction. Comparison of the plasma BNP concentrations between these two groups demonstrated a significant positive correlation between the BNP level and the degree of LV systolic dysfunction, suggesting BNP is a reasonable marker for identification of septic patients with sepsis-induced myocardial depression.
Further, the study’s results suggest BNP measurements early in the course of septic shock might be useful prognostic indicators. However, it is unclear to what extent the knowledge gained from such measurements would alter care management, or how BNP compares to echocardiography in terms of diagnostic and prognostic utility. Thus, these results might not be adequate to justify the routine measurement of BNP in patients with severe sepsis.
Bottom line: Elevated BNP in septic patients is associated with the presence or risk of sepsis-induced myocardial depression, and might be a negative prognostic indicator.
Citation: Post F, Weilemann LS, Messow CM, Sinning C, Munzel T. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36:3030–3037.
High Risk of Death with Thrombolytic Use in Low-Risk Pulmonary Embolism (PE)
Clinical question: Is there an advantage to thrombolytic therapy in the treatment of acute PE versus treatment with unfractionated or low-molecular-weight (LMW) heparin?
Background: Given the high mortality linked to PE, consistent indications for thrombolytic therapy in acute PE are needed. An assessment of the prevalence of thrombolytic therapy and mortality, as compared with standard anticoagulation, has been described inconsistently.
Study design: Retrospective cohort study.
Setting: 186 acute-care hospitals in Pennsylvania.
Synopsis: Using a database of ICD-9 codes, 15,116 patients were reviewed. Logistic regression was used to evaluate the association between thrombolytic therapy and 30-day mortality. Poisson regression was used to evaluate the association between thrombolytic therapy and in-hospital mortality. For those receiving thrombolysis and considered unlikely candidates for the therapy based on documentation at presentation (low predicted probability), the in-hospital mortality and overall 30-day mortality rate were higher when compared with those who did not receive thrombolysis. An exception to this was a group of patients with high predicted probability of receiving thrombolysis. In this group, thrombolysis was not associated with increased risk. Limitations to the study include lack of assessment of right ventricular function, changes in condition after presentation, lack of long-term outcomes, and lack of exact cause of death.
Bottom line: Thrombolytic therapy is associated with higher mortality in patients with hemodynamically uncomplicated PE, and therefore not indicated. Thrombolytic therapy in a subgroup of patients with hemodynamic instability or right ventricular dysfunction improves the clinical course and outcome.
Citation: Ibrahim SA, Stone RA, Obrosky S, Geng M, Fine MJ, Aujesky D. Thrombolytic therapy and mortality in patients with acute pulmonary embolism. Arch Intern Med. 2008;168(20):2183-2190.
Hospitalists Improve Patient Flow in the ED
Clinical question: Can active-bed management by hospitalists reduce ED throughput times and diversionary status?
Background: ED overcrowding leads to ambulance diversion, which has been associated with increased mortality. A primary cause of ED crowding is inpatient boarding, which can reduce patient satisfaction and quality of care. Previous studies targeting the ED have had little impact on throughput and ambulance diversion.
Study design: Pre-post case study in a single institution.
Setting: Academic teaching hospital in Baltimore.
Synopsis: ED throughput times and ambulance diversion hours were measured for all adult patients registered in the department from November 2005 to February 2006 (control period) and November 2006 to February 2007 (intervention period). Active-bed management was defined as appointing a hospitalist to assess bed availability in real time and assigning department of medicine admissions to the appropriate clinical setting, as well as the creation of a bed director. Although the ED census was 8.8% higher during the intervention period, throughput time for admitted patients decreased by 98 minutes per patient, to 458 from 360. The time spent under diversionary status for overcrowding or lack of ICU beds decreased by 6% and 27%, respectively. Limitations of this study include the pre-post design and the implementation at a single institution. Additionally, active-bed management is expensive, and in this case required the hiring of three full-time-equivalent faculty. However, this study successfully demonstrates that a quality improvement partnership between hospitalists and the ED can substantially reduce overcrowding.
Bottom line: Active-bed management by hospitalists improves ED throughput by decreasing the length of time admitted patients spend in the ED and reducing ambulance diversion hours.
Citation: Howell E, Bessman E, Kravet S, Kolodner K, Marshall R, Wright S. Active bed management by hospitalists and emergency department throughput. Ann Int Med. 2008;149(11):804-810.
Eagle-Eye Your Payors
Protection of the Medicare program has reached new heights in recent years. One of the most important ways hospitalist groups can protect their Medicare funding is the discovery and recovery of improper contractor payments of Medicare claims.
The Centers for Medicare and Medicaid Services (CMS) reviews various types of contractors—Medicare administrative contractors (MACs), carriers, durable medical equipment regional carriers (DMERCs), fiscal intermediaries (FIs), and quality improvement organizations (QIOs)—through its protection efforts as part of the Comprehensive Error Rate Testing (CERT) program and Hospital Payment Monitoring Program (HPMP). The CERT program’s contractors review physician (i.e., professional) claims processed by MACs and carriers.
The primary goal of a contractor is to “pay it right”—that is, pay the correct amount to the right provider for covered and correctly coded services.1 During the 12-month reporting period ending Sept. 30, 2007, the CERT program sampled 129,875 claims from carriers, DMERCs, FIs, and MACs.
The CERT contractor randomly and electronically selects about 172 claims each month from each type of claims-processing contractor. Since some of these contractors were transitioning to MACs, the target Part B (i.e., professional) sample size for the May 2008 report was approximately 2,000 reviewable claims per MAC cluster. However, this might have varied if a MAC was not processing claims during the entire sampling period.
Document Requests
Physicians need to be mindful of CERT requests for documentation. When possible, every attempt is made to benefit the physician. Initial CERT requests are attempted by way of a letter. If the physician does not respond within 30 days, the CERT contractor attempts one to three more contacts with correspondence and phone calls. If documentation is received after 75 days, it is considered “late.” It then will be reviewed, unless the reporting period has expired.
However, this should not be considered a prudent approach, and timely responses are ideal. If the physician offers no response, and documentation is not received, it is counted as a “no documentation” error.
Physicians often worry about accusations of fraud. The purpose of the CERT program is not to assume or accuse physicians of fraud, although it may serve as a deterrent. It does not, and cannot, label a claim fraudulent.
One scenario of potential fraud the CERT program is able to identify occurs when a CERT documentation contractor is unable to locate a provider or supplier when requesting medical record documentation.2
Outcomes
Individual contractors are notified of improper payments. These include overpayments and underpayments. Unfortunately, contractors do not have to resolve CERT issues involving underpayments, although they are encouraged to do so by CMS.
The CERT program identified overpayments totaling $875,005 during the 12-month reporting period, but collected only $650,418 in overpayments after consideration of appeals that overturned a CERT decision or the provider discontinued business operations. (See Table 1, p. 18, for error rates and Table 2, p. 18, for highest rates of improper payment)
To improve billing compliance and prevent repetitive errors, contractors must implement provider education regarding erroneously paid claims. A contractor may determine the best education method to distribute information about Medicare rules and effectively answer coverage and coding questions.
Some contractors have designed Web-based training modules, Web pages with frequently-asked-questions sections, or local coverage analyses to address contractor-specific errors. Detailed CERT contractor information can be found at www.cms.hhs.gov/ mcd/indexes.asp?from2=indexes.asp&
Due to its successful outcomes, future CMS goals include the continuation of the CERT program. MACs will look more closely at service types based on identified error rates.
Apart from CERT requests, prepayment contractor reviews already exist for most of the services included in Table 2 (p. 18). Timely response is crucial to justify and receive appropriate reimbursement. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Improper Medicare fee-for-service payments report: May 2008. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report.asp?from=public&which=long&reportID=9. Accessed Dec. 20, 2008.
2. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association; 2008.
Protection of the Medicare program has reached new heights in recent years. One of the most important ways hospitalist groups can protect their Medicare funding is the discovery and recovery of improper contractor payments of Medicare claims.
The Centers for Medicare and Medicaid Services (CMS) reviews various types of contractors—Medicare administrative contractors (MACs), carriers, durable medical equipment regional carriers (DMERCs), fiscal intermediaries (FIs), and quality improvement organizations (QIOs)—through its protection efforts as part of the Comprehensive Error Rate Testing (CERT) program and Hospital Payment Monitoring Program (HPMP). The CERT program’s contractors review physician (i.e., professional) claims processed by MACs and carriers.
The primary goal of a contractor is to “pay it right”—that is, pay the correct amount to the right provider for covered and correctly coded services.1 During the 12-month reporting period ending Sept. 30, 2007, the CERT program sampled 129,875 claims from carriers, DMERCs, FIs, and MACs.
The CERT contractor randomly and electronically selects about 172 claims each month from each type of claims-processing contractor. Since some of these contractors were transitioning to MACs, the target Part B (i.e., professional) sample size for the May 2008 report was approximately 2,000 reviewable claims per MAC cluster. However, this might have varied if a MAC was not processing claims during the entire sampling period.
Document Requests
Physicians need to be mindful of CERT requests for documentation. When possible, every attempt is made to benefit the physician. Initial CERT requests are attempted by way of a letter. If the physician does not respond within 30 days, the CERT contractor attempts one to three more contacts with correspondence and phone calls. If documentation is received after 75 days, it is considered “late.” It then will be reviewed, unless the reporting period has expired.
However, this should not be considered a prudent approach, and timely responses are ideal. If the physician offers no response, and documentation is not received, it is counted as a “no documentation” error.
Physicians often worry about accusations of fraud. The purpose of the CERT program is not to assume or accuse physicians of fraud, although it may serve as a deterrent. It does not, and cannot, label a claim fraudulent.
One scenario of potential fraud the CERT program is able to identify occurs when a CERT documentation contractor is unable to locate a provider or supplier when requesting medical record documentation.2
Outcomes
Individual contractors are notified of improper payments. These include overpayments and underpayments. Unfortunately, contractors do not have to resolve CERT issues involving underpayments, although they are encouraged to do so by CMS.
The CERT program identified overpayments totaling $875,005 during the 12-month reporting period, but collected only $650,418 in overpayments after consideration of appeals that overturned a CERT decision or the provider discontinued business operations. (See Table 1, p. 18, for error rates and Table 2, p. 18, for highest rates of improper payment)
To improve billing compliance and prevent repetitive errors, contractors must implement provider education regarding erroneously paid claims. A contractor may determine the best education method to distribute information about Medicare rules and effectively answer coverage and coding questions.
Some contractors have designed Web-based training modules, Web pages with frequently-asked-questions sections, or local coverage analyses to address contractor-specific errors. Detailed CERT contractor information can be found at www.cms.hhs.gov/ mcd/indexes.asp?from2=indexes.asp&
Due to its successful outcomes, future CMS goals include the continuation of the CERT program. MACs will look more closely at service types based on identified error rates.
Apart from CERT requests, prepayment contractor reviews already exist for most of the services included in Table 2 (p. 18). Timely response is crucial to justify and receive appropriate reimbursement. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Improper Medicare fee-for-service payments report: May 2008. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report.asp?from=public&which=long&reportID=9. Accessed Dec. 20, 2008.
2. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association; 2008.
Protection of the Medicare program has reached new heights in recent years. One of the most important ways hospitalist groups can protect their Medicare funding is the discovery and recovery of improper contractor payments of Medicare claims.
The Centers for Medicare and Medicaid Services (CMS) reviews various types of contractors—Medicare administrative contractors (MACs), carriers, durable medical equipment regional carriers (DMERCs), fiscal intermediaries (FIs), and quality improvement organizations (QIOs)—through its protection efforts as part of the Comprehensive Error Rate Testing (CERT) program and Hospital Payment Monitoring Program (HPMP). The CERT program’s contractors review physician (i.e., professional) claims processed by MACs and carriers.
The primary goal of a contractor is to “pay it right”—that is, pay the correct amount to the right provider for covered and correctly coded services.1 During the 12-month reporting period ending Sept. 30, 2007, the CERT program sampled 129,875 claims from carriers, DMERCs, FIs, and MACs.
The CERT contractor randomly and electronically selects about 172 claims each month from each type of claims-processing contractor. Since some of these contractors were transitioning to MACs, the target Part B (i.e., professional) sample size for the May 2008 report was approximately 2,000 reviewable claims per MAC cluster. However, this might have varied if a MAC was not processing claims during the entire sampling period.
Document Requests
Physicians need to be mindful of CERT requests for documentation. When possible, every attempt is made to benefit the physician. Initial CERT requests are attempted by way of a letter. If the physician does not respond within 30 days, the CERT contractor attempts one to three more contacts with correspondence and phone calls. If documentation is received after 75 days, it is considered “late.” It then will be reviewed, unless the reporting period has expired.
However, this should not be considered a prudent approach, and timely responses are ideal. If the physician offers no response, and documentation is not received, it is counted as a “no documentation” error.
Physicians often worry about accusations of fraud. The purpose of the CERT program is not to assume or accuse physicians of fraud, although it may serve as a deterrent. It does not, and cannot, label a claim fraudulent.
One scenario of potential fraud the CERT program is able to identify occurs when a CERT documentation contractor is unable to locate a provider or supplier when requesting medical record documentation.2
Outcomes
Individual contractors are notified of improper payments. These include overpayments and underpayments. Unfortunately, contractors do not have to resolve CERT issues involving underpayments, although they are encouraged to do so by CMS.
The CERT program identified overpayments totaling $875,005 during the 12-month reporting period, but collected only $650,418 in overpayments after consideration of appeals that overturned a CERT decision or the provider discontinued business operations. (See Table 1, p. 18, for error rates and Table 2, p. 18, for highest rates of improper payment)
To improve billing compliance and prevent repetitive errors, contractors must implement provider education regarding erroneously paid claims. A contractor may determine the best education method to distribute information about Medicare rules and effectively answer coverage and coding questions.
Some contractors have designed Web-based training modules, Web pages with frequently-asked-questions sections, or local coverage analyses to address contractor-specific errors. Detailed CERT contractor information can be found at www.cms.hhs.gov/ mcd/indexes.asp?from2=indexes.asp&
Due to its successful outcomes, future CMS goals include the continuation of the CERT program. MACs will look more closely at service types based on identified error rates.
Apart from CERT requests, prepayment contractor reviews already exist for most of the services included in Table 2 (p. 18). Timely response is crucial to justify and receive appropriate reimbursement. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Improper Medicare fee-for-service payments report: May 2008. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report.asp?from=public&which=long&reportID=9. Accessed Dec. 20, 2008.
2. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association; 2008.