User login
The cataclysmic COVID-19 pandemic: THIS CHANGES EVERYTHING!
It was unthinkable, but it has happened. A virulent and invisible virus, 10 microns in size, with no vaccine or cure yet, shut down our nation, the third largest country in the world with 330 million people. Overnight, our thriving cities became ghost towns. Schools were closed. Millions of businesses, restaurants, and stores were abruptly shuttered. Sporting events were instantly canceled. Air travel came to a halt.
The largest economy in the world started to tank. Millions of people lost their jobs and were forced to stay home. The vital structures of society were dismantled. Our vibrant culture came to a screeching halt. It’s a nightmare scenario that even the most imaginative science fiction writers could not have envisioned. By any measure, the coronavirus disease 2019 (COVID-19) pandemic unraveled everything, and became a human catastrophe and a social calamity reminiscent of the deadly 1918 influenza pandemic, or the devastating plagues that decimated Europe during the Middle Ages.
The human toll in death and suffering was the real disaster. Emergency departments and hospitals filled up with victims of the scourge, sickly and unable to breathe as the virus hijacked their red blood cells and lungs, and destroyed their alveoli. Compounding the disaster was a lack of medical supplies. The country was clearly caught off-guard, completely unprepared for the scale of the pandemic and the massive onslaught of desperately ill people requiring intensive care and special equipment. In addition, health care staff became stretched beyond the limit, and entire hospitals were transformed overnight into highly specialized ICUs. Medical care for millions with non-COVID-19 conditions was put on hold so that vital resources could be diverted to the desperately ill victims of these infections. Many physicians, nurses, and respiratory therapists—laudable heroes—succumbed to the perverse virus exhaled by their patients.
Insidious social effects
COVID-19 is not only a murderer, but also a thief. It stole our Spring; our religious holidays (Easter and Passover); classroom education in schools and colleges; the Prom; weddings; graduation ceremonies; proper funerals; concerts; football, basketball, hockey, and baseball games; Broadway shows; and even data from animal research. More important, it robbed us of our peace of mind, our liberty, and our pursuit of small pleasures such as family gatherings or schmoozing with friends at a nice restaurant. COVID-19 is a cruel, dastardly scoundrel.
I write this editorial as I sit at home, which I have not left for several weeks, like hundreds of millions in our country and around the world. We were all glued to TV news or the internet to learn about the latest updates, including the grim news of those who got infected, hospitalized, or passed away. Fear of dying permeated all age groups, especially those who were older and infirmed.
Making it worse was the relentless uncertainty. When will it end? Gradually or suddenly? When is it going to be safe to go to work again, or to visit our loved ones and our friends? When can we see our patients face-to-face instead of remotely by phone or video conferencing? When can we have live meetings instead of virtual video conferences? When will stores open so we can shop? When can we take our children or grandchildren to a baseball game or a show? Will the virus return next winter for another cycle of mayhem and social paralysis? When will the economy start to rebound, and how long will that take? Will our retirement accounts recoup their losses? So many questions with no clear answers. A malignant uncertainty, indeed.
And there are our patients who live with anxiety and depression, whose anguish is intensifying as they sit alone in their apartments or homes, struggling to cope with this sudden, overwhelming stress. How will they react to this pandemic? Obviously, a life-threatening event such as a deadly pandemic with no cure is likely to produce an acute stress reaction and, ultimately, posttraumatic stress disorder (PTSD). And if COVID-19 returns next year for another unwelcome visit, PTSD symptoms will get a booster shot and lead to severe anxiety, depression, or suicide. Psychiatrists and other mental health professionals, who were already stretched thin, must contend with another crisis that has destabilized millions of patients receiving psychiatric care, or new patients who seek help for themselves or their family members.
Continue to: One intervention that is emerging...
One intervention that is emerging on a large scale is online therapy. This includes reassurance and supportive therapy, cognitive-behavioral therapy, relaxation techniques, stress management, resilience training, mindfulness, and online group therapy. Those therapies can be effective for stress-induced anxiety and dysphoria when pharmacotherapy is not available, and can provide patients with tools and techniques that can be implemented by the patients themselves in the absence of a physician or nurse practitioner to prescribe a medication.
Lessons learned
This pandemic has taught us many lessons: that life as we know it should not be taken for granted, and can change drastically overnight; that human life is fragile and can be destroyed rapidly and ruthlessly on an unimaginable scale by an invisible enemy; that scientific drug development research by the often maligned pharmaceutical industry is indispensable to our well-being; that policymakers must always prepare for the worst and must have a well-designed disaster plan; that modifying human behavior and full compliance with public health measures are vital and can be the most effective way to prevent the spread of catastrophic pandemics, viral or otherwise; that we must all learn how to be resilient to cope with solitude and restricted mobility or socialization; that the human ingenuity and innovation that created technologies to enable virtual connectivity among us, even when we are isolated, has been a lifesaver during health crises such as the COVID-19 pandemic; that the clinicians and health care workers treating highly infectious and desperately ill patients are genuine heroes who deserve our respect and gratitude; and that magnificent altruism outstrips and outshines the selfish hoarding and profiteering that may emerge during life-threatening pandemics.
And that we shall overcome this horrid pandemic, a ghastly tribulation that changed everything.
It was unthinkable, but it has happened. A virulent and invisible virus, 10 microns in size, with no vaccine or cure yet, shut down our nation, the third largest country in the world with 330 million people. Overnight, our thriving cities became ghost towns. Schools were closed. Millions of businesses, restaurants, and stores were abruptly shuttered. Sporting events were instantly canceled. Air travel came to a halt.
The largest economy in the world started to tank. Millions of people lost their jobs and were forced to stay home. The vital structures of society were dismantled. Our vibrant culture came to a screeching halt. It’s a nightmare scenario that even the most imaginative science fiction writers could not have envisioned. By any measure, the coronavirus disease 2019 (COVID-19) pandemic unraveled everything, and became a human catastrophe and a social calamity reminiscent of the deadly 1918 influenza pandemic, or the devastating plagues that decimated Europe during the Middle Ages.
The human toll in death and suffering was the real disaster. Emergency departments and hospitals filled up with victims of the scourge, sickly and unable to breathe as the virus hijacked their red blood cells and lungs, and destroyed their alveoli. Compounding the disaster was a lack of medical supplies. The country was clearly caught off-guard, completely unprepared for the scale of the pandemic and the massive onslaught of desperately ill people requiring intensive care and special equipment. In addition, health care staff became stretched beyond the limit, and entire hospitals were transformed overnight into highly specialized ICUs. Medical care for millions with non-COVID-19 conditions was put on hold so that vital resources could be diverted to the desperately ill victims of these infections. Many physicians, nurses, and respiratory therapists—laudable heroes—succumbed to the perverse virus exhaled by their patients.
Insidious social effects
COVID-19 is not only a murderer, but also a thief. It stole our Spring; our religious holidays (Easter and Passover); classroom education in schools and colleges; the Prom; weddings; graduation ceremonies; proper funerals; concerts; football, basketball, hockey, and baseball games; Broadway shows; and even data from animal research. More important, it robbed us of our peace of mind, our liberty, and our pursuit of small pleasures such as family gatherings or schmoozing with friends at a nice restaurant. COVID-19 is a cruel, dastardly scoundrel.
I write this editorial as I sit at home, which I have not left for several weeks, like hundreds of millions in our country and around the world. We were all glued to TV news or the internet to learn about the latest updates, including the grim news of those who got infected, hospitalized, or passed away. Fear of dying permeated all age groups, especially those who were older and infirmed.
Making it worse was the relentless uncertainty. When will it end? Gradually or suddenly? When is it going to be safe to go to work again, or to visit our loved ones and our friends? When can we see our patients face-to-face instead of remotely by phone or video conferencing? When can we have live meetings instead of virtual video conferences? When will stores open so we can shop? When can we take our children or grandchildren to a baseball game or a show? Will the virus return next winter for another cycle of mayhem and social paralysis? When will the economy start to rebound, and how long will that take? Will our retirement accounts recoup their losses? So many questions with no clear answers. A malignant uncertainty, indeed.
And there are our patients who live with anxiety and depression, whose anguish is intensifying as they sit alone in their apartments or homes, struggling to cope with this sudden, overwhelming stress. How will they react to this pandemic? Obviously, a life-threatening event such as a deadly pandemic with no cure is likely to produce an acute stress reaction and, ultimately, posttraumatic stress disorder (PTSD). And if COVID-19 returns next year for another unwelcome visit, PTSD symptoms will get a booster shot and lead to severe anxiety, depression, or suicide. Psychiatrists and other mental health professionals, who were already stretched thin, must contend with another crisis that has destabilized millions of patients receiving psychiatric care, or new patients who seek help for themselves or their family members.
Continue to: One intervention that is emerging...
One intervention that is emerging on a large scale is online therapy. This includes reassurance and supportive therapy, cognitive-behavioral therapy, relaxation techniques, stress management, resilience training, mindfulness, and online group therapy. Those therapies can be effective for stress-induced anxiety and dysphoria when pharmacotherapy is not available, and can provide patients with tools and techniques that can be implemented by the patients themselves in the absence of a physician or nurse practitioner to prescribe a medication.
Lessons learned
This pandemic has taught us many lessons: that life as we know it should not be taken for granted, and can change drastically overnight; that human life is fragile and can be destroyed rapidly and ruthlessly on an unimaginable scale by an invisible enemy; that scientific drug development research by the often maligned pharmaceutical industry is indispensable to our well-being; that policymakers must always prepare for the worst and must have a well-designed disaster plan; that modifying human behavior and full compliance with public health measures are vital and can be the most effective way to prevent the spread of catastrophic pandemics, viral or otherwise; that we must all learn how to be resilient to cope with solitude and restricted mobility or socialization; that the human ingenuity and innovation that created technologies to enable virtual connectivity among us, even when we are isolated, has been a lifesaver during health crises such as the COVID-19 pandemic; that the clinicians and health care workers treating highly infectious and desperately ill patients are genuine heroes who deserve our respect and gratitude; and that magnificent altruism outstrips and outshines the selfish hoarding and profiteering that may emerge during life-threatening pandemics.
And that we shall overcome this horrid pandemic, a ghastly tribulation that changed everything.
It was unthinkable, but it has happened. A virulent and invisible virus, 10 microns in size, with no vaccine or cure yet, shut down our nation, the third largest country in the world with 330 million people. Overnight, our thriving cities became ghost towns. Schools were closed. Millions of businesses, restaurants, and stores were abruptly shuttered. Sporting events were instantly canceled. Air travel came to a halt.
The largest economy in the world started to tank. Millions of people lost their jobs and were forced to stay home. The vital structures of society were dismantled. Our vibrant culture came to a screeching halt. It’s a nightmare scenario that even the most imaginative science fiction writers could not have envisioned. By any measure, the coronavirus disease 2019 (COVID-19) pandemic unraveled everything, and became a human catastrophe and a social calamity reminiscent of the deadly 1918 influenza pandemic, or the devastating plagues that decimated Europe during the Middle Ages.
The human toll in death and suffering was the real disaster. Emergency departments and hospitals filled up with victims of the scourge, sickly and unable to breathe as the virus hijacked their red blood cells and lungs, and destroyed their alveoli. Compounding the disaster was a lack of medical supplies. The country was clearly caught off-guard, completely unprepared for the scale of the pandemic and the massive onslaught of desperately ill people requiring intensive care and special equipment. In addition, health care staff became stretched beyond the limit, and entire hospitals were transformed overnight into highly specialized ICUs. Medical care for millions with non-COVID-19 conditions was put on hold so that vital resources could be diverted to the desperately ill victims of these infections. Many physicians, nurses, and respiratory therapists—laudable heroes—succumbed to the perverse virus exhaled by their patients.
Insidious social effects
COVID-19 is not only a murderer, but also a thief. It stole our Spring; our religious holidays (Easter and Passover); classroom education in schools and colleges; the Prom; weddings; graduation ceremonies; proper funerals; concerts; football, basketball, hockey, and baseball games; Broadway shows; and even data from animal research. More important, it robbed us of our peace of mind, our liberty, and our pursuit of small pleasures such as family gatherings or schmoozing with friends at a nice restaurant. COVID-19 is a cruel, dastardly scoundrel.
I write this editorial as I sit at home, which I have not left for several weeks, like hundreds of millions in our country and around the world. We were all glued to TV news or the internet to learn about the latest updates, including the grim news of those who got infected, hospitalized, or passed away. Fear of dying permeated all age groups, especially those who were older and infirmed.
Making it worse was the relentless uncertainty. When will it end? Gradually or suddenly? When is it going to be safe to go to work again, or to visit our loved ones and our friends? When can we see our patients face-to-face instead of remotely by phone or video conferencing? When can we have live meetings instead of virtual video conferences? When will stores open so we can shop? When can we take our children or grandchildren to a baseball game or a show? Will the virus return next winter for another cycle of mayhem and social paralysis? When will the economy start to rebound, and how long will that take? Will our retirement accounts recoup their losses? So many questions with no clear answers. A malignant uncertainty, indeed.
And there are our patients who live with anxiety and depression, whose anguish is intensifying as they sit alone in their apartments or homes, struggling to cope with this sudden, overwhelming stress. How will they react to this pandemic? Obviously, a life-threatening event such as a deadly pandemic with no cure is likely to produce an acute stress reaction and, ultimately, posttraumatic stress disorder (PTSD). And if COVID-19 returns next year for another unwelcome visit, PTSD symptoms will get a booster shot and lead to severe anxiety, depression, or suicide. Psychiatrists and other mental health professionals, who were already stretched thin, must contend with another crisis that has destabilized millions of patients receiving psychiatric care, or new patients who seek help for themselves or their family members.
Continue to: One intervention that is emerging...
One intervention that is emerging on a large scale is online therapy. This includes reassurance and supportive therapy, cognitive-behavioral therapy, relaxation techniques, stress management, resilience training, mindfulness, and online group therapy. Those therapies can be effective for stress-induced anxiety and dysphoria when pharmacotherapy is not available, and can provide patients with tools and techniques that can be implemented by the patients themselves in the absence of a physician or nurse practitioner to prescribe a medication.
Lessons learned
This pandemic has taught us many lessons: that life as we know it should not be taken for granted, and can change drastically overnight; that human life is fragile and can be destroyed rapidly and ruthlessly on an unimaginable scale by an invisible enemy; that scientific drug development research by the often maligned pharmaceutical industry is indispensable to our well-being; that policymakers must always prepare for the worst and must have a well-designed disaster plan; that modifying human behavior and full compliance with public health measures are vital and can be the most effective way to prevent the spread of catastrophic pandemics, viral or otherwise; that we must all learn how to be resilient to cope with solitude and restricted mobility or socialization; that the human ingenuity and innovation that created technologies to enable virtual connectivity among us, even when we are isolated, has been a lifesaver during health crises such as the COVID-19 pandemic; that the clinicians and health care workers treating highly infectious and desperately ill patients are genuine heroes who deserve our respect and gratitude; and that magnificent altruism outstrips and outshines the selfish hoarding and profiteering that may emerge during life-threatening pandemics.
And that we shall overcome this horrid pandemic, a ghastly tribulation that changed everything.
Prescribing aspirin to improve pregnancy outcomes: Expand the indications? Increase the dose?
Authors of a recent Cochrane review concluded that low-dose aspirin treatment of 1,000 pregnant women at risk of developing preeclampsia resulted in 16 fewer cases of preeclampsia, 16 fewer preterm births, 7 fewer cases of small-for-gestational age newborns, and 5 fewer fetal or neonatal deaths.1
The American College of Obstetricians and Gynecologists (ACOG) and the US Preventive Services Task Force (USPSTF) recommend treatment with 81 mg of aspirin daily, initiated before 16 weeks of pregnancy to prevent preeclampsia in women with one major risk factor (personal history of preeclampsia, multifetal gestation, chronic hypertension, type 1 or 2 diabetes, renal or autoimmune disease) or at least two moderate risk factors (nulliparity; obesity; mother or sister with preeclampsia; a sociodemographic characteristic such as African American race or low socioeconomic status; age ≥35 years; personal history factors such as prior low birth weight infant, previous adverse pregnancy outcome, or >10-year interpregnancy interval).2,3 Healthy pregnant women with a previous uncomplicated full-term delivery do not need treatment with low-dose aspirin.2,3
However, evolving data and expert opinion suggest that expanding the indications for aspirin treatment and increasing the recommended dose of aspirin may be warranted.
Nulliparity
Nulliparity is the single clinical characteristic that is associated with the greatest number of cases of preeclampsia.4 Hence, from a public health perspective, reducing the rate of preeclampsia among nulliparous women is a top priority.
ACOG and USPSTF do not recommend aspirin treatment for all nulliparous women because risk factors help to identify those nulliparous women who benefit from aspirin treatment.
However, a recent cost-effectiveness analysis compared the health care costs and rates of preeclampsia for 4 prevention strategies among all pregnant women in the United States (nulliparous and parous)5:
- no aspirin use
- use of aspirin based on biomarker and ultrasound measurements
- use of aspirin based on USPSTF guidelines for identifying women at risk
- prescription of aspirin to all pregnant women.
Health care costs and rates of preeclampsia were lowest with the universal prescription of aspirin to all pregnant women in the United States. Compared with universal prescription of aspirin, the USPSTF approach, the biomarker-ultrasound approach, and the no aspirin approach were associated with 346, 308, and 762 additional cases of preeclampsia per 100,000 women. In sensitivity analyses, universal aspirin was the optimal strategy under most assumptions.
Another cost effectiveness analysis concluded that among nulliparous pregnant women, universal aspirin treatment was superior to aspirin treatment based on biomarker-ultrasound identification of women at high risk.6
In a recent clinical trial performed in India, Guatemala, Pakistan, Democratic Republic of Congo, Kenya, and Zambia, 14,361 nulliparous women were randomly assigned to placebo or 81 mg of aspirin daily between 6 and 14 weeks of gestation.7 Preterm birth (<37 weeks’ gestation) occurred in 13.1% and 11.6% of women treated with placebo or aspirin (relative risk [RR], 0.89; 95% confidence interval [CI], 0.81 to 0.98, P = .012). Most of the decrease in preterm birth appeared to be due to a decrease in the rate of preeclampsia in the aspirin-treated nulliparous women. The investigators also noted that aspirin treatment of nulliparous women resulted in a statistically significant decrease in perinatal mortality (RR, 0.86) and early preterm delivery, <34 weeks’ gestation (RR, 0.75).
Universal prescription of low-dose aspirin to nulliparous women in order to prevent preeclampsia and preterm birth may become recognized as an optimal public health strategy. As a step toward universal prescription of aspirin to nulliparous women, an opt-out rather than a screen-in strategy might be considered.8

Continue to: Booking systolic blood pressure, 120 to 134 mm Hg...
Booking systolic blood pressure, 120 to 134 mm Hg
All obstetricians recognize that women with chronic hypertension should be treated with low-dose aspirin because they are at high risk for preeclampsia. However, there is evidence that nulliparous women with a booking systolic pressure ≥120 mm Hg might also benefit from low-dose aspirin treatment. In one US trial, 3,135 nulliparous normotensive women (booking blood pressure [BP] <135/85 mm Hg) were randomly assigned to treatment with aspirin (60 mg daily) or placebo initiated between 13 and 26 weeks’ gestation. Preeclampsia occurred in 6.3% and 4.6% of the women treated with placebo or aspirin, respectively (RR, 0.7; 95% CI, 0.6–1.0; P = .05).9 A secondary analysis showed that, among 519 nulliparous women with a booking systolic BP from 120 to 134 mm Hg, compared with placebo, low-dose aspirin treatment reduced the rate of preeclampsia from 11.9% to 5.6%.9 Aspirin did not reduce the rate of preeclampsia among nulliparous women with a booking systolic BP <120 mm Hg.9 A systematic review of risk factors for developing preeclampsia reported that a booking diastolic BP of ≥80 mm Hg was associated with an increased risk of developing preeclampsia (RR, 1.38).10
The American Heart Association (AHA) and the American College of Cardiology (ACC) recently updated the definition of hypertension.11 Normal BP is now defined as a systolic pressure <120 mm Hg and diastolic pressure <80 mm Hg. Elevated BP is a systolic pressure of 120 to 129 mm Hg and diastolic pressure of <80 mm Hg. Stage I hypertension is a systolic BP from 130 to 139 mm Hg or diastolic blood pressure from 80 to 89 mm Hg. Stage II hypertension is a systolic BP of ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg.11
A recent study reported that 90% of women at 12 weeks’ gestation have a BP of ≤130 mm Hg systolic and ≤80 mm Hg diastolic, suggesting that the AHA-ACC criteria for stage I hypertension are reasonable.12 Obstetricians have not yet fully adopted the AHA-ACC criteria for defining stage I hypertension in pregnant women. Future research may demonstrate that a booking systolic BP
≥130 mm Hg or a diastolic BP ≥80 mm Hg are major risk factors for developing preeclampsia and warrant treatment with low-dose aspirin.

Continue to: Pregnancy resulting from fertility therapy...
Pregnancy resulting from fertility therapy
Current ACOG and USPSTF guidelines do not specifically identify pregnancies resulting from assisted reproductive technology as a major or moderate risk factor for preeclampsia.2,3 In a study comparing 83,582 births resulting from in vitro fertilization (IVF) and 1,382,311 births to fertile women, treatment with autologous cryopreserved embryos (adjusted odds ratio [aOR], 1.30), fresh donor embryos (aOR, 1.92), and cryopreserved donor embryos (aOR, 1.70) significantly increased the risk of preeclampsia.13 However, use of fresh autologous embryos did not increase the risk of preeclampsia (aOR, 1.04). These associations persisted after controlling for diabetes, hypertension, body mass index, and cause of infertility.13
Other studies also have reported that use of cryopreserved embryos is associated with a higher rate of preeclampsia than use of fresh autologous embryos. In a study of 825 infertile women undergoing IVF and randomly assigned to single embryo cryopreserved or fresh cycles, the rate of preeclampsia was 3.1% and 1.0% in the pregnancies that resulted from cryopreserved versus fresh cycles.14
What is the optimal dose of aspirin?
ACOG and the USPSTF recommend aspirin 81 mg daily for the prevention of preeclampsia.2,3 The International Federation of Gynecology and Obstetrics (FIGO) recommends aspirin 150 mg daily for the prevention of preeclampsia.15 The FIGO recommendation is based, in part, on the results of a large international clinical trial that randomly assigned 1,776 women at high risk for preeclampsia as determined by clinical factors plus biomarker and ultrasound screening to receive aspirin 150 mg daily or placebo daily initiated at 11 to 14 weeks’ gestation and continued until 36 weeks’ gestation.16 Preeclampsia before 37 weeks’ gestation occurred in 4.3% and 1.6% of women in the placebo and aspirin groups (OR, 0.38; 95% CI, 0.20–0.74; P = .004).16 FIGO recommends that women at risk for preeclampsia with a body mass <40 kg take aspirin 100 mg daily and women with a body mass ≥40 kg take aspirin at a dose of 150 mg daily. For women who live in a country where aspirin is not available in a pill containing 150 mg, FIGO recommends taking two 81 mg tablets.15 FIGO recommends initiating aspirin between 11 and 14 weeks and 6 days of gestation and continuing aspirin therapy until 36 weeks of gestation.15
Aspirin is an inexpensive intervention with many possible benefits
For many nulliparous women and some parous women aspirin treatment initiated early in pregnancy will improve maternal and newborn outcomes, including reducing the risk of preeclampsia, preterm birth, and intrauterine growth restriction.1 Obstetricians may want to begin to expand the indications for offering aspirin to prevent preeclampsia from those recommended by ACOG and the USPSTF to include nulliparous women with a booking systolic pressure of 120 to 134 mm Hg and women whose pregnancy was the result of an assisted reproduction treatment that used cryopreserved embryos. In addition, obstetricians who currently prescribe 81 mg of aspirin daily might want to consider increasing the prescribed dose to 162 mg of aspirin daily (two 81 mg tablets daily or one-half of a 325 mg tablet). Aspirin costs about less than 5 cents per 81 mg tablet (according to GoodRx website). It is an inexpensive intervention that could benefit many mothers and newborns. ●
- Duley L, Meher S, Hunter KE, et al. Antiplatelet agents for preventing pre-eclampsia and its complications. Cochrane Database Syst Rev. 2019;CD004659.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 743: low-dose aspirin use during pregnancy. Obstet Gynecol. 2018;132:e44-e52.
- LeFevre ML; U.S. Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: U.S. Preventive Services Task Force Recommendation Statement. Ann Int Med. 2014;161: 819-826.
- Bartsch E, Medcalf KE, Park AL, et al. Clinical risk factors for pre-eclampsia determined in early pregnancy: systematic review and meta-analysis of large cohort studies. BMJ. 2016;353:i1753.
- Mallampati D, Grobman W, Rouse DJ, et al. Strategies for prescribing aspirin to prevent preeclampsia: a cost-effectiveness analysis. Obstet Gynecol. 2019;134:537-544.
- Mone F, O’Mahony JF, Tyrrell E, et al. Preeclampsia prevention using routine versus screening test-indicated aspirin in low-risk women. Hypertension. 2018;72:1391-1396.
- Hoffman MK, Goudar SS, Kodkany BS, et al. Low-dose aspirin for the prevention of preterm delivery in nulliparous women with a singleton pregnancy (ASPIRIN): a randomised, double-blind, placebo-controlled trial. Lancet. 2020;395:285-293.
- Ayala NK, Rouse DJ. A nudge toward universal aspirin for preeclampsia prevention. Obstet Gynecol. 2019;133:725-728.
- Sibai BM, Caritis SN, Thom E, et al. Prevention of preeclampsia with low-dose aspirin in healthy, nulliparous pregnant women. The National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1993;329:1213-1218.
- Duckitt K, Harrington D. Risk factors for preeclampsia at antenatal booking: systematic review of controlled studies. BMJ. 2005;330:565.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199-2269.
- Green LJ, Mackillop LH, Salvi D, et al. Gestation-specific vital sign reference ranges in pregnancy. Obstet Gynecol. 2020;135:653-664.
- Luke B, Brown MB, Eisenberg ML, et al. In vitro fertilization and risk for hypertensive disorders of pregnancy: associations with treatment parameters. Am J Obstet Gynecol. October 17, 2019. doi:10.1016/j.ajog.2019.10.003.
- Wei D, Liu JY, Sun Y, et al. Frozen versus fresh single blastocyst transfer in ovulatory women: a multicentre, randomised controlled trial. Lancet. 2019;393:1310-1318.
- Poon LC, Shennan A, Hyett JA, et al. International Federation of Gynecology and Obstetrics (FIGO) initiative on preeclampsia: A pragmatic guide for first-trimester screening and prevention. Int J Gynaecol Obstet. 2019;145(suppl 1):1-33.
- Rolnik DL, Wright D, Poon LC, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377:613-622.
Authors of a recent Cochrane review concluded that low-dose aspirin treatment of 1,000 pregnant women at risk of developing preeclampsia resulted in 16 fewer cases of preeclampsia, 16 fewer preterm births, 7 fewer cases of small-for-gestational age newborns, and 5 fewer fetal or neonatal deaths.1
The American College of Obstetricians and Gynecologists (ACOG) and the US Preventive Services Task Force (USPSTF) recommend treatment with 81 mg of aspirin daily, initiated before 16 weeks of pregnancy to prevent preeclampsia in women with one major risk factor (personal history of preeclampsia, multifetal gestation, chronic hypertension, type 1 or 2 diabetes, renal or autoimmune disease) or at least two moderate risk factors (nulliparity; obesity; mother or sister with preeclampsia; a sociodemographic characteristic such as African American race or low socioeconomic status; age ≥35 years; personal history factors such as prior low birth weight infant, previous adverse pregnancy outcome, or >10-year interpregnancy interval).2,3 Healthy pregnant women with a previous uncomplicated full-term delivery do not need treatment with low-dose aspirin.2,3
However, evolving data and expert opinion suggest that expanding the indications for aspirin treatment and increasing the recommended dose of aspirin may be warranted.
Nulliparity
Nulliparity is the single clinical characteristic that is associated with the greatest number of cases of preeclampsia.4 Hence, from a public health perspective, reducing the rate of preeclampsia among nulliparous women is a top priority.
ACOG and USPSTF do not recommend aspirin treatment for all nulliparous women because risk factors help to identify those nulliparous women who benefit from aspirin treatment.
However, a recent cost-effectiveness analysis compared the health care costs and rates of preeclampsia for 4 prevention strategies among all pregnant women in the United States (nulliparous and parous)5:
- no aspirin use
- use of aspirin based on biomarker and ultrasound measurements
- use of aspirin based on USPSTF guidelines for identifying women at risk
- prescription of aspirin to all pregnant women.
Health care costs and rates of preeclampsia were lowest with the universal prescription of aspirin to all pregnant women in the United States. Compared with universal prescription of aspirin, the USPSTF approach, the biomarker-ultrasound approach, and the no aspirin approach were associated with 346, 308, and 762 additional cases of preeclampsia per 100,000 women. In sensitivity analyses, universal aspirin was the optimal strategy under most assumptions.
Another cost effectiveness analysis concluded that among nulliparous pregnant women, universal aspirin treatment was superior to aspirin treatment based on biomarker-ultrasound identification of women at high risk.6
In a recent clinical trial performed in India, Guatemala, Pakistan, Democratic Republic of Congo, Kenya, and Zambia, 14,361 nulliparous women were randomly assigned to placebo or 81 mg of aspirin daily between 6 and 14 weeks of gestation.7 Preterm birth (<37 weeks’ gestation) occurred in 13.1% and 11.6% of women treated with placebo or aspirin (relative risk [RR], 0.89; 95% confidence interval [CI], 0.81 to 0.98, P = .012). Most of the decrease in preterm birth appeared to be due to a decrease in the rate of preeclampsia in the aspirin-treated nulliparous women. The investigators also noted that aspirin treatment of nulliparous women resulted in a statistically significant decrease in perinatal mortality (RR, 0.86) and early preterm delivery, <34 weeks’ gestation (RR, 0.75).
Universal prescription of low-dose aspirin to nulliparous women in order to prevent preeclampsia and preterm birth may become recognized as an optimal public health strategy. As a step toward universal prescription of aspirin to nulliparous women, an opt-out rather than a screen-in strategy might be considered.8

Continue to: Booking systolic blood pressure, 120 to 134 mm Hg...
Booking systolic blood pressure, 120 to 134 mm Hg
All obstetricians recognize that women with chronic hypertension should be treated with low-dose aspirin because they are at high risk for preeclampsia. However, there is evidence that nulliparous women with a booking systolic pressure ≥120 mm Hg might also benefit from low-dose aspirin treatment. In one US trial, 3,135 nulliparous normotensive women (booking blood pressure [BP] <135/85 mm Hg) were randomly assigned to treatment with aspirin (60 mg daily) or placebo initiated between 13 and 26 weeks’ gestation. Preeclampsia occurred in 6.3% and 4.6% of the women treated with placebo or aspirin, respectively (RR, 0.7; 95% CI, 0.6–1.0; P = .05).9 A secondary analysis showed that, among 519 nulliparous women with a booking systolic BP from 120 to 134 mm Hg, compared with placebo, low-dose aspirin treatment reduced the rate of preeclampsia from 11.9% to 5.6%.9 Aspirin did not reduce the rate of preeclampsia among nulliparous women with a booking systolic BP <120 mm Hg.9 A systematic review of risk factors for developing preeclampsia reported that a booking diastolic BP of ≥80 mm Hg was associated with an increased risk of developing preeclampsia (RR, 1.38).10
The American Heart Association (AHA) and the American College of Cardiology (ACC) recently updated the definition of hypertension.11 Normal BP is now defined as a systolic pressure <120 mm Hg and diastolic pressure <80 mm Hg. Elevated BP is a systolic pressure of 120 to 129 mm Hg and diastolic pressure of <80 mm Hg. Stage I hypertension is a systolic BP from 130 to 139 mm Hg or diastolic blood pressure from 80 to 89 mm Hg. Stage II hypertension is a systolic BP of ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg.11
A recent study reported that 90% of women at 12 weeks’ gestation have a BP of ≤130 mm Hg systolic and ≤80 mm Hg diastolic, suggesting that the AHA-ACC criteria for stage I hypertension are reasonable.12 Obstetricians have not yet fully adopted the AHA-ACC criteria for defining stage I hypertension in pregnant women. Future research may demonstrate that a booking systolic BP
≥130 mm Hg or a diastolic BP ≥80 mm Hg are major risk factors for developing preeclampsia and warrant treatment with low-dose aspirin.

Continue to: Pregnancy resulting from fertility therapy...
Pregnancy resulting from fertility therapy
Current ACOG and USPSTF guidelines do not specifically identify pregnancies resulting from assisted reproductive technology as a major or moderate risk factor for preeclampsia.2,3 In a study comparing 83,582 births resulting from in vitro fertilization (IVF) and 1,382,311 births to fertile women, treatment with autologous cryopreserved embryos (adjusted odds ratio [aOR], 1.30), fresh donor embryos (aOR, 1.92), and cryopreserved donor embryos (aOR, 1.70) significantly increased the risk of preeclampsia.13 However, use of fresh autologous embryos did not increase the risk of preeclampsia (aOR, 1.04). These associations persisted after controlling for diabetes, hypertension, body mass index, and cause of infertility.13
Other studies also have reported that use of cryopreserved embryos is associated with a higher rate of preeclampsia than use of fresh autologous embryos. In a study of 825 infertile women undergoing IVF and randomly assigned to single embryo cryopreserved or fresh cycles, the rate of preeclampsia was 3.1% and 1.0% in the pregnancies that resulted from cryopreserved versus fresh cycles.14
What is the optimal dose of aspirin?
ACOG and the USPSTF recommend aspirin 81 mg daily for the prevention of preeclampsia.2,3 The International Federation of Gynecology and Obstetrics (FIGO) recommends aspirin 150 mg daily for the prevention of preeclampsia.15 The FIGO recommendation is based, in part, on the results of a large international clinical trial that randomly assigned 1,776 women at high risk for preeclampsia as determined by clinical factors plus biomarker and ultrasound screening to receive aspirin 150 mg daily or placebo daily initiated at 11 to 14 weeks’ gestation and continued until 36 weeks’ gestation.16 Preeclampsia before 37 weeks’ gestation occurred in 4.3% and 1.6% of women in the placebo and aspirin groups (OR, 0.38; 95% CI, 0.20–0.74; P = .004).16 FIGO recommends that women at risk for preeclampsia with a body mass <40 kg take aspirin 100 mg daily and women with a body mass ≥40 kg take aspirin at a dose of 150 mg daily. For women who live in a country where aspirin is not available in a pill containing 150 mg, FIGO recommends taking two 81 mg tablets.15 FIGO recommends initiating aspirin between 11 and 14 weeks and 6 days of gestation and continuing aspirin therapy until 36 weeks of gestation.15
Aspirin is an inexpensive intervention with many possible benefits
For many nulliparous women and some parous women aspirin treatment initiated early in pregnancy will improve maternal and newborn outcomes, including reducing the risk of preeclampsia, preterm birth, and intrauterine growth restriction.1 Obstetricians may want to begin to expand the indications for offering aspirin to prevent preeclampsia from those recommended by ACOG and the USPSTF to include nulliparous women with a booking systolic pressure of 120 to 134 mm Hg and women whose pregnancy was the result of an assisted reproduction treatment that used cryopreserved embryos. In addition, obstetricians who currently prescribe 81 mg of aspirin daily might want to consider increasing the prescribed dose to 162 mg of aspirin daily (two 81 mg tablets daily or one-half of a 325 mg tablet). Aspirin costs about less than 5 cents per 81 mg tablet (according to GoodRx website). It is an inexpensive intervention that could benefit many mothers and newborns. ●
Authors of a recent Cochrane review concluded that low-dose aspirin treatment of 1,000 pregnant women at risk of developing preeclampsia resulted in 16 fewer cases of preeclampsia, 16 fewer preterm births, 7 fewer cases of small-for-gestational age newborns, and 5 fewer fetal or neonatal deaths.1
The American College of Obstetricians and Gynecologists (ACOG) and the US Preventive Services Task Force (USPSTF) recommend treatment with 81 mg of aspirin daily, initiated before 16 weeks of pregnancy to prevent preeclampsia in women with one major risk factor (personal history of preeclampsia, multifetal gestation, chronic hypertension, type 1 or 2 diabetes, renal or autoimmune disease) or at least two moderate risk factors (nulliparity; obesity; mother or sister with preeclampsia; a sociodemographic characteristic such as African American race or low socioeconomic status; age ≥35 years; personal history factors such as prior low birth weight infant, previous adverse pregnancy outcome, or >10-year interpregnancy interval).2,3 Healthy pregnant women with a previous uncomplicated full-term delivery do not need treatment with low-dose aspirin.2,3
However, evolving data and expert opinion suggest that expanding the indications for aspirin treatment and increasing the recommended dose of aspirin may be warranted.
Nulliparity
Nulliparity is the single clinical characteristic that is associated with the greatest number of cases of preeclampsia.4 Hence, from a public health perspective, reducing the rate of preeclampsia among nulliparous women is a top priority.
ACOG and USPSTF do not recommend aspirin treatment for all nulliparous women because risk factors help to identify those nulliparous women who benefit from aspirin treatment.
However, a recent cost-effectiveness analysis compared the health care costs and rates of preeclampsia for 4 prevention strategies among all pregnant women in the United States (nulliparous and parous)5:
- no aspirin use
- use of aspirin based on biomarker and ultrasound measurements
- use of aspirin based on USPSTF guidelines for identifying women at risk
- prescription of aspirin to all pregnant women.
Health care costs and rates of preeclampsia were lowest with the universal prescription of aspirin to all pregnant women in the United States. Compared with universal prescription of aspirin, the USPSTF approach, the biomarker-ultrasound approach, and the no aspirin approach were associated with 346, 308, and 762 additional cases of preeclampsia per 100,000 women. In sensitivity analyses, universal aspirin was the optimal strategy under most assumptions.
Another cost effectiveness analysis concluded that among nulliparous pregnant women, universal aspirin treatment was superior to aspirin treatment based on biomarker-ultrasound identification of women at high risk.6
In a recent clinical trial performed in India, Guatemala, Pakistan, Democratic Republic of Congo, Kenya, and Zambia, 14,361 nulliparous women were randomly assigned to placebo or 81 mg of aspirin daily between 6 and 14 weeks of gestation.7 Preterm birth (<37 weeks’ gestation) occurred in 13.1% and 11.6% of women treated with placebo or aspirin (relative risk [RR], 0.89; 95% confidence interval [CI], 0.81 to 0.98, P = .012). Most of the decrease in preterm birth appeared to be due to a decrease in the rate of preeclampsia in the aspirin-treated nulliparous women. The investigators also noted that aspirin treatment of nulliparous women resulted in a statistically significant decrease in perinatal mortality (RR, 0.86) and early preterm delivery, <34 weeks’ gestation (RR, 0.75).
Universal prescription of low-dose aspirin to nulliparous women in order to prevent preeclampsia and preterm birth may become recognized as an optimal public health strategy. As a step toward universal prescription of aspirin to nulliparous women, an opt-out rather than a screen-in strategy might be considered.8

Continue to: Booking systolic blood pressure, 120 to 134 mm Hg...
Booking systolic blood pressure, 120 to 134 mm Hg
All obstetricians recognize that women with chronic hypertension should be treated with low-dose aspirin because they are at high risk for preeclampsia. However, there is evidence that nulliparous women with a booking systolic pressure ≥120 mm Hg might also benefit from low-dose aspirin treatment. In one US trial, 3,135 nulliparous normotensive women (booking blood pressure [BP] <135/85 mm Hg) were randomly assigned to treatment with aspirin (60 mg daily) or placebo initiated between 13 and 26 weeks’ gestation. Preeclampsia occurred in 6.3% and 4.6% of the women treated with placebo or aspirin, respectively (RR, 0.7; 95% CI, 0.6–1.0; P = .05).9 A secondary analysis showed that, among 519 nulliparous women with a booking systolic BP from 120 to 134 mm Hg, compared with placebo, low-dose aspirin treatment reduced the rate of preeclampsia from 11.9% to 5.6%.9 Aspirin did not reduce the rate of preeclampsia among nulliparous women with a booking systolic BP <120 mm Hg.9 A systematic review of risk factors for developing preeclampsia reported that a booking diastolic BP of ≥80 mm Hg was associated with an increased risk of developing preeclampsia (RR, 1.38).10
The American Heart Association (AHA) and the American College of Cardiology (ACC) recently updated the definition of hypertension.11 Normal BP is now defined as a systolic pressure <120 mm Hg and diastolic pressure <80 mm Hg. Elevated BP is a systolic pressure of 120 to 129 mm Hg and diastolic pressure of <80 mm Hg. Stage I hypertension is a systolic BP from 130 to 139 mm Hg or diastolic blood pressure from 80 to 89 mm Hg. Stage II hypertension is a systolic BP of ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg.11
A recent study reported that 90% of women at 12 weeks’ gestation have a BP of ≤130 mm Hg systolic and ≤80 mm Hg diastolic, suggesting that the AHA-ACC criteria for stage I hypertension are reasonable.12 Obstetricians have not yet fully adopted the AHA-ACC criteria for defining stage I hypertension in pregnant women. Future research may demonstrate that a booking systolic BP
≥130 mm Hg or a diastolic BP ≥80 mm Hg are major risk factors for developing preeclampsia and warrant treatment with low-dose aspirin.

Continue to: Pregnancy resulting from fertility therapy...
Pregnancy resulting from fertility therapy
Current ACOG and USPSTF guidelines do not specifically identify pregnancies resulting from assisted reproductive technology as a major or moderate risk factor for preeclampsia.2,3 In a study comparing 83,582 births resulting from in vitro fertilization (IVF) and 1,382,311 births to fertile women, treatment with autologous cryopreserved embryos (adjusted odds ratio [aOR], 1.30), fresh donor embryos (aOR, 1.92), and cryopreserved donor embryos (aOR, 1.70) significantly increased the risk of preeclampsia.13 However, use of fresh autologous embryos did not increase the risk of preeclampsia (aOR, 1.04). These associations persisted after controlling for diabetes, hypertension, body mass index, and cause of infertility.13
Other studies also have reported that use of cryopreserved embryos is associated with a higher rate of preeclampsia than use of fresh autologous embryos. In a study of 825 infertile women undergoing IVF and randomly assigned to single embryo cryopreserved or fresh cycles, the rate of preeclampsia was 3.1% and 1.0% in the pregnancies that resulted from cryopreserved versus fresh cycles.14
What is the optimal dose of aspirin?
ACOG and the USPSTF recommend aspirin 81 mg daily for the prevention of preeclampsia.2,3 The International Federation of Gynecology and Obstetrics (FIGO) recommends aspirin 150 mg daily for the prevention of preeclampsia.15 The FIGO recommendation is based, in part, on the results of a large international clinical trial that randomly assigned 1,776 women at high risk for preeclampsia as determined by clinical factors plus biomarker and ultrasound screening to receive aspirin 150 mg daily or placebo daily initiated at 11 to 14 weeks’ gestation and continued until 36 weeks’ gestation.16 Preeclampsia before 37 weeks’ gestation occurred in 4.3% and 1.6% of women in the placebo and aspirin groups (OR, 0.38; 95% CI, 0.20–0.74; P = .004).16 FIGO recommends that women at risk for preeclampsia with a body mass <40 kg take aspirin 100 mg daily and women with a body mass ≥40 kg take aspirin at a dose of 150 mg daily. For women who live in a country where aspirin is not available in a pill containing 150 mg, FIGO recommends taking two 81 mg tablets.15 FIGO recommends initiating aspirin between 11 and 14 weeks and 6 days of gestation and continuing aspirin therapy until 36 weeks of gestation.15
Aspirin is an inexpensive intervention with many possible benefits
For many nulliparous women and some parous women aspirin treatment initiated early in pregnancy will improve maternal and newborn outcomes, including reducing the risk of preeclampsia, preterm birth, and intrauterine growth restriction.1 Obstetricians may want to begin to expand the indications for offering aspirin to prevent preeclampsia from those recommended by ACOG and the USPSTF to include nulliparous women with a booking systolic pressure of 120 to 134 mm Hg and women whose pregnancy was the result of an assisted reproduction treatment that used cryopreserved embryos. In addition, obstetricians who currently prescribe 81 mg of aspirin daily might want to consider increasing the prescribed dose to 162 mg of aspirin daily (two 81 mg tablets daily or one-half of a 325 mg tablet). Aspirin costs about less than 5 cents per 81 mg tablet (according to GoodRx website). It is an inexpensive intervention that could benefit many mothers and newborns. ●
- Duley L, Meher S, Hunter KE, et al. Antiplatelet agents for preventing pre-eclampsia and its complications. Cochrane Database Syst Rev. 2019;CD004659.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 743: low-dose aspirin use during pregnancy. Obstet Gynecol. 2018;132:e44-e52.
- LeFevre ML; U.S. Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: U.S. Preventive Services Task Force Recommendation Statement. Ann Int Med. 2014;161: 819-826.
- Bartsch E, Medcalf KE, Park AL, et al. Clinical risk factors for pre-eclampsia determined in early pregnancy: systematic review and meta-analysis of large cohort studies. BMJ. 2016;353:i1753.
- Mallampati D, Grobman W, Rouse DJ, et al. Strategies for prescribing aspirin to prevent preeclampsia: a cost-effectiveness analysis. Obstet Gynecol. 2019;134:537-544.
- Mone F, O’Mahony JF, Tyrrell E, et al. Preeclampsia prevention using routine versus screening test-indicated aspirin in low-risk women. Hypertension. 2018;72:1391-1396.
- Hoffman MK, Goudar SS, Kodkany BS, et al. Low-dose aspirin for the prevention of preterm delivery in nulliparous women with a singleton pregnancy (ASPIRIN): a randomised, double-blind, placebo-controlled trial. Lancet. 2020;395:285-293.
- Ayala NK, Rouse DJ. A nudge toward universal aspirin for preeclampsia prevention. Obstet Gynecol. 2019;133:725-728.
- Sibai BM, Caritis SN, Thom E, et al. Prevention of preeclampsia with low-dose aspirin in healthy, nulliparous pregnant women. The National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1993;329:1213-1218.
- Duckitt K, Harrington D. Risk factors for preeclampsia at antenatal booking: systematic review of controlled studies. BMJ. 2005;330:565.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199-2269.
- Green LJ, Mackillop LH, Salvi D, et al. Gestation-specific vital sign reference ranges in pregnancy. Obstet Gynecol. 2020;135:653-664.
- Luke B, Brown MB, Eisenberg ML, et al. In vitro fertilization and risk for hypertensive disorders of pregnancy: associations with treatment parameters. Am J Obstet Gynecol. October 17, 2019. doi:10.1016/j.ajog.2019.10.003.
- Wei D, Liu JY, Sun Y, et al. Frozen versus fresh single blastocyst transfer in ovulatory women: a multicentre, randomised controlled trial. Lancet. 2019;393:1310-1318.
- Poon LC, Shennan A, Hyett JA, et al. International Federation of Gynecology and Obstetrics (FIGO) initiative on preeclampsia: A pragmatic guide for first-trimester screening and prevention. Int J Gynaecol Obstet. 2019;145(suppl 1):1-33.
- Rolnik DL, Wright D, Poon LC, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377:613-622.
- Duley L, Meher S, Hunter KE, et al. Antiplatelet agents for preventing pre-eclampsia and its complications. Cochrane Database Syst Rev. 2019;CD004659.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 743: low-dose aspirin use during pregnancy. Obstet Gynecol. 2018;132:e44-e52.
- LeFevre ML; U.S. Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: U.S. Preventive Services Task Force Recommendation Statement. Ann Int Med. 2014;161: 819-826.
- Bartsch E, Medcalf KE, Park AL, et al. Clinical risk factors for pre-eclampsia determined in early pregnancy: systematic review and meta-analysis of large cohort studies. BMJ. 2016;353:i1753.
- Mallampati D, Grobman W, Rouse DJ, et al. Strategies for prescribing aspirin to prevent preeclampsia: a cost-effectiveness analysis. Obstet Gynecol. 2019;134:537-544.
- Mone F, O’Mahony JF, Tyrrell E, et al. Preeclampsia prevention using routine versus screening test-indicated aspirin in low-risk women. Hypertension. 2018;72:1391-1396.
- Hoffman MK, Goudar SS, Kodkany BS, et al. Low-dose aspirin for the prevention of preterm delivery in nulliparous women with a singleton pregnancy (ASPIRIN): a randomised, double-blind, placebo-controlled trial. Lancet. 2020;395:285-293.
- Ayala NK, Rouse DJ. A nudge toward universal aspirin for preeclampsia prevention. Obstet Gynecol. 2019;133:725-728.
- Sibai BM, Caritis SN, Thom E, et al. Prevention of preeclampsia with low-dose aspirin in healthy, nulliparous pregnant women. The National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1993;329:1213-1218.
- Duckitt K, Harrington D. Risk factors for preeclampsia at antenatal booking: systematic review of controlled studies. BMJ. 2005;330:565.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199-2269.
- Green LJ, Mackillop LH, Salvi D, et al. Gestation-specific vital sign reference ranges in pregnancy. Obstet Gynecol. 2020;135:653-664.
- Luke B, Brown MB, Eisenberg ML, et al. In vitro fertilization and risk for hypertensive disorders of pregnancy: associations with treatment parameters. Am J Obstet Gynecol. October 17, 2019. doi:10.1016/j.ajog.2019.10.003.
- Wei D, Liu JY, Sun Y, et al. Frozen versus fresh single blastocyst transfer in ovulatory women: a multicentre, randomised controlled trial. Lancet. 2019;393:1310-1318.
- Poon LC, Shennan A, Hyett JA, et al. International Federation of Gynecology and Obstetrics (FIGO) initiative on preeclampsia: A pragmatic guide for first-trimester screening and prevention. Int J Gynaecol Obstet. 2019;145(suppl 1):1-33.
- Rolnik DL, Wright D, Poon LC, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377:613-622.
Pre-authorization is illegal, unethical, and adversely disrupts patient care
Pre-authorization is a despicable scam. It’s a national racket by avaricious insurance companies, and it must be stopped. Since it first reared its ugly head 2 decades ago, it has inflicted great harm to countless patients, demoralized their physicians, and needlessly imposed higher costs in clinical practice while simultaneously depriving patients of the treatment their physicians prescribed for them.
Pre-authorization has become the nemesis of medical care. It recklessly and arbitrarily vetoes the clinical decision-making of competent physicians doing their best to address their patients’ medical needs. Yet, despite its outrageous disruption of the clinical practice of hundreds of thousands of practitioners, it continues unabated, without a forceful pushback. It has become the “new normal,” but in fact, it is the “new abnormal.” This harassment of clinicians must be outlawed.
Think about it: Pre-authorization is essentially practicing medicine without a license, which is a felony. When a remote and invisible insurance company staff member either prevents a patient from receiving a medication prescribed by that patient’s personal physician following a full diagnostic evaluation or pressures the physician to prescribe a different medication, he/she is basically deciding what the treatment should be for a patient who that insurance company employee has never seen, let alone examined. How did for-profit insurance companies empower themselves to tyrannize clinical practice so that the treatment administered isn’t customized to the patient’s need but instead to fatten the profits of the insurance company? That is patently unethical, in addition to being a felonious practice of medicine by an absentee person unqualified to decide what a patient needs without a direct examination.
Consider the multiple malignant consequences of such brazen and egregious restriction or distortion of medical care:
1. The physician’s clinical judgment is abrogated, even when it is clearly in the patient’s best interest.
2. Patients are deprived of receiving the medication that their personal physician deemed optimal.
3. The physician in private practice has to spend an inordinate amount of time going to web sites, such as CoverMyMeds.com, to fill out extensive forms containing numerous questions about the patient’s illness and diagnosis, and then selecting from a list of medications that the insurance company ironically labels as “smart choices.” These medications often are not necessarily what the physician considers a smart choice, but are the cheapest (regardless of whether their efficacy, safety, or tolerability are the best fit for the patient). After the physician completes the forms, there is a waiting period, followed by additional questions that consume more valuable time and take the physician away from seeing more patients. Some busy colleagues told me they often take the pre-authorization “homework” with them to do at home, consuming part of what should be their family time. For physicians who see patients in an institutional “clinic,” medical assistants or nurses must be hired at significant expense to work full-time on pre-authorizations, adding to the overhead of the clinic while increasing the profits of the third-party insurer.
4. Patients who have been stable on a medication for months, even years, are forced to switch to another medication if they change jobs and become covered by a different insurance company that does not have the patient’s current medication on their infamous list of “approved drugs,” an evil euphemism for “cheapest drugs.” Switching medications is known to be a possibly hazardous process with lower efficacy and/or tolerability, but that appears to be irrelevant to the insurance company. The welfare of the patient is not on the insurance company’s radar screen, perhaps because it is crowded out by dollar signs. We should all urge policymakers to pass legislation that goes beyond requiring insurance companies to cover “pre-existing conditions” and expands it to cover “pre-existing medications.”
Continue to: Often, frustrated physicians...
5. Often, frustrated physicians who do not want to see their patients receive a medication they do not believe is appropriate may spend valuable time writing letters of appeal, making phone calls, or printing and faxing scientific articles to the insurance company to convince them to authorize a medication that is not on the “approved list.” Based on my own clinical experience, that justification sometimes works and sometimes doesn’t.
6. Physicians are inevitably and understandably demoralized because their expertise and sound clinical judgment are arbitrarily dismissed and overruled by an invisible insurance employee whose knowledge about and compassion for the patient is miniscule at best.
7. New medication development has collided with the biased despotism of pre-authorization, which generally rejects any new medication (always costlier than generics) irrespective of whether the new medication was demonstrated in controlled clinical trials to have a measurably better profile than older generics. This has ominous implications for numerous medical disorders that do not have any approved medications (for psychiatry, a published study1 found that 82% of DSM disorders do not have a FDA-approved medication).
The lack of utilizing newly introduced medications has discouraged the pharmaceutical industry from investing to develop innovative new mechanisms of action for a variety of complex neuropsychiatric medical conditions. Some companies have already abandoned psychiatric drug development, which is dire for clinical care because pharmaceutical companies are the only entities that develop new treatments for our patients (some health care professionals wish the government had a pharmaceutical agency that develops medications for various illness, but no such agency has ever existed).
8. Hospitalization for a seriously ill patient is either denied, delayed, or eventually approved for an absurdly short period (a few days), which is woefully inadequate, culminating in discharging patients with unresolved symptoms. This can lead to disastrous consequences, including suicide, homicide, or incarceration.
Continue to: I have been personally infuriated...
I have been personally infuriated many times because of the adverse impact pre-authorization had on my patients. One example that still haunts me is a 23-year-old college graduate with severe treatment-resistant depression who failed multiple antidepressant trials, including IV ketamine. She harbored daily thoughts of suicide (throwing herself in front of a train, which she saw daily as she drove to work). She admitted to frequently contemplating which dress she should wear in her coffin. Based on several published double-blind studies showing that modafinil improved bipolar depression,2 I prescribed modafinil, 200 mg/d, as adjunctive treatment to venlafaxine, 300 mg/d, and she improved significantly for 10 months. Suddenly, the insurance company refused to renew her refill of modafinil, and it took 4 weeks of incessant communication (phone calls, faxes, letters, sending published articles) before it was finally approved. In the meantime, the patient deteriorated and began to have active suicidal urges. When she was restarted on modafinil, she never achieved the same level of improvement she had prior to discontinuing modafinil. The insurance company damaged this patient’s recovery with its refusal to authorize a medication that was “not approved” for depression despite the clear benefit it had provided this treatment-resistant patient for almost 1 year. Their motive was clearly to avoid covering the high cost of modafinil, regardless of this patient’s high risk of suicide.
Every physician can recite a litany of complaints about the evil of pre-authorizations. We must therefore unite and vigorously lobby legislators to pass laws that protect patients and uphold physicians’ authority to determine the right treatment for their patients. We must terminate the plague of pre-authorization that takes our patients hostage to the greed of insurance companies, who have no regard to the agony of patients who are prevented from receiving the medication that their personal physician prescribes. Physicians’ well-being would be greatly enhanced if they were not enslaved to the avarice of insurance companies.
The travesty of pre-authorization and its pervasive and deleterious effects on medical care, society, and citizens must be stopped. It’s a plague that sacrifices the practice of medicine on the altar of financial greed. Just because it has gone on for many years does not mean it should be accepted as the “new normal.” It must be condemned as the “new abnormal,” a cancerous lesion on health care delivery that must be excised and discarded.
1. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
2. Nunez NA, Singh B, Romo-Nava F, et al. Efficacy and tolerability of adjunctive modafinil/armodafinil in bipolar depression: a meta-analysis of randomized controlled trials. Bipolar Dipsord. 2019;10.1111/bdi.12859. doi: 10.1111/bdi.12859
Pre-authorization is a despicable scam. It’s a national racket by avaricious insurance companies, and it must be stopped. Since it first reared its ugly head 2 decades ago, it has inflicted great harm to countless patients, demoralized their physicians, and needlessly imposed higher costs in clinical practice while simultaneously depriving patients of the treatment their physicians prescribed for them.
Pre-authorization has become the nemesis of medical care. It recklessly and arbitrarily vetoes the clinical decision-making of competent physicians doing their best to address their patients’ medical needs. Yet, despite its outrageous disruption of the clinical practice of hundreds of thousands of practitioners, it continues unabated, without a forceful pushback. It has become the “new normal,” but in fact, it is the “new abnormal.” This harassment of clinicians must be outlawed.
Think about it: Pre-authorization is essentially practicing medicine without a license, which is a felony. When a remote and invisible insurance company staff member either prevents a patient from receiving a medication prescribed by that patient’s personal physician following a full diagnostic evaluation or pressures the physician to prescribe a different medication, he/she is basically deciding what the treatment should be for a patient who that insurance company employee has never seen, let alone examined. How did for-profit insurance companies empower themselves to tyrannize clinical practice so that the treatment administered isn’t customized to the patient’s need but instead to fatten the profits of the insurance company? That is patently unethical, in addition to being a felonious practice of medicine by an absentee person unqualified to decide what a patient needs without a direct examination.
Consider the multiple malignant consequences of such brazen and egregious restriction or distortion of medical care:
1. The physician’s clinical judgment is abrogated, even when it is clearly in the patient’s best interest.
2. Patients are deprived of receiving the medication that their personal physician deemed optimal.
3. The physician in private practice has to spend an inordinate amount of time going to web sites, such as CoverMyMeds.com, to fill out extensive forms containing numerous questions about the patient’s illness and diagnosis, and then selecting from a list of medications that the insurance company ironically labels as “smart choices.” These medications often are not necessarily what the physician considers a smart choice, but are the cheapest (regardless of whether their efficacy, safety, or tolerability are the best fit for the patient). After the physician completes the forms, there is a waiting period, followed by additional questions that consume more valuable time and take the physician away from seeing more patients. Some busy colleagues told me they often take the pre-authorization “homework” with them to do at home, consuming part of what should be their family time. For physicians who see patients in an institutional “clinic,” medical assistants or nurses must be hired at significant expense to work full-time on pre-authorizations, adding to the overhead of the clinic while increasing the profits of the third-party insurer.
4. Patients who have been stable on a medication for months, even years, are forced to switch to another medication if they change jobs and become covered by a different insurance company that does not have the patient’s current medication on their infamous list of “approved drugs,” an evil euphemism for “cheapest drugs.” Switching medications is known to be a possibly hazardous process with lower efficacy and/or tolerability, but that appears to be irrelevant to the insurance company. The welfare of the patient is not on the insurance company’s radar screen, perhaps because it is crowded out by dollar signs. We should all urge policymakers to pass legislation that goes beyond requiring insurance companies to cover “pre-existing conditions” and expands it to cover “pre-existing medications.”
Continue to: Often, frustrated physicians...
5. Often, frustrated physicians who do not want to see their patients receive a medication they do not believe is appropriate may spend valuable time writing letters of appeal, making phone calls, or printing and faxing scientific articles to the insurance company to convince them to authorize a medication that is not on the “approved list.” Based on my own clinical experience, that justification sometimes works and sometimes doesn’t.
6. Physicians are inevitably and understandably demoralized because their expertise and sound clinical judgment are arbitrarily dismissed and overruled by an invisible insurance employee whose knowledge about and compassion for the patient is miniscule at best.
7. New medication development has collided with the biased despotism of pre-authorization, which generally rejects any new medication (always costlier than generics) irrespective of whether the new medication was demonstrated in controlled clinical trials to have a measurably better profile than older generics. This has ominous implications for numerous medical disorders that do not have any approved medications (for psychiatry, a published study1 found that 82% of DSM disorders do not have a FDA-approved medication).
The lack of utilizing newly introduced medications has discouraged the pharmaceutical industry from investing to develop innovative new mechanisms of action for a variety of complex neuropsychiatric medical conditions. Some companies have already abandoned psychiatric drug development, which is dire for clinical care because pharmaceutical companies are the only entities that develop new treatments for our patients (some health care professionals wish the government had a pharmaceutical agency that develops medications for various illness, but no such agency has ever existed).
8. Hospitalization for a seriously ill patient is either denied, delayed, or eventually approved for an absurdly short period (a few days), which is woefully inadequate, culminating in discharging patients with unresolved symptoms. This can lead to disastrous consequences, including suicide, homicide, or incarceration.
Continue to: I have been personally infuriated...
I have been personally infuriated many times because of the adverse impact pre-authorization had on my patients. One example that still haunts me is a 23-year-old college graduate with severe treatment-resistant depression who failed multiple antidepressant trials, including IV ketamine. She harbored daily thoughts of suicide (throwing herself in front of a train, which she saw daily as she drove to work). She admitted to frequently contemplating which dress she should wear in her coffin. Based on several published double-blind studies showing that modafinil improved bipolar depression,2 I prescribed modafinil, 200 mg/d, as adjunctive treatment to venlafaxine, 300 mg/d, and she improved significantly for 10 months. Suddenly, the insurance company refused to renew her refill of modafinil, and it took 4 weeks of incessant communication (phone calls, faxes, letters, sending published articles) before it was finally approved. In the meantime, the patient deteriorated and began to have active suicidal urges. When she was restarted on modafinil, she never achieved the same level of improvement she had prior to discontinuing modafinil. The insurance company damaged this patient’s recovery with its refusal to authorize a medication that was “not approved” for depression despite the clear benefit it had provided this treatment-resistant patient for almost 1 year. Their motive was clearly to avoid covering the high cost of modafinil, regardless of this patient’s high risk of suicide.
Every physician can recite a litany of complaints about the evil of pre-authorizations. We must therefore unite and vigorously lobby legislators to pass laws that protect patients and uphold physicians’ authority to determine the right treatment for their patients. We must terminate the plague of pre-authorization that takes our patients hostage to the greed of insurance companies, who have no regard to the agony of patients who are prevented from receiving the medication that their personal physician prescribes. Physicians’ well-being would be greatly enhanced if they were not enslaved to the avarice of insurance companies.
The travesty of pre-authorization and its pervasive and deleterious effects on medical care, society, and citizens must be stopped. It’s a plague that sacrifices the practice of medicine on the altar of financial greed. Just because it has gone on for many years does not mean it should be accepted as the “new normal.” It must be condemned as the “new abnormal,” a cancerous lesion on health care delivery that must be excised and discarded.
Pre-authorization is a despicable scam. It’s a national racket by avaricious insurance companies, and it must be stopped. Since it first reared its ugly head 2 decades ago, it has inflicted great harm to countless patients, demoralized their physicians, and needlessly imposed higher costs in clinical practice while simultaneously depriving patients of the treatment their physicians prescribed for them.
Pre-authorization has become the nemesis of medical care. It recklessly and arbitrarily vetoes the clinical decision-making of competent physicians doing their best to address their patients’ medical needs. Yet, despite its outrageous disruption of the clinical practice of hundreds of thousands of practitioners, it continues unabated, without a forceful pushback. It has become the “new normal,” but in fact, it is the “new abnormal.” This harassment of clinicians must be outlawed.
Think about it: Pre-authorization is essentially practicing medicine without a license, which is a felony. When a remote and invisible insurance company staff member either prevents a patient from receiving a medication prescribed by that patient’s personal physician following a full diagnostic evaluation or pressures the physician to prescribe a different medication, he/she is basically deciding what the treatment should be for a patient who that insurance company employee has never seen, let alone examined. How did for-profit insurance companies empower themselves to tyrannize clinical practice so that the treatment administered isn’t customized to the patient’s need but instead to fatten the profits of the insurance company? That is patently unethical, in addition to being a felonious practice of medicine by an absentee person unqualified to decide what a patient needs without a direct examination.
Consider the multiple malignant consequences of such brazen and egregious restriction or distortion of medical care:
1. The physician’s clinical judgment is abrogated, even when it is clearly in the patient’s best interest.
2. Patients are deprived of receiving the medication that their personal physician deemed optimal.
3. The physician in private practice has to spend an inordinate amount of time going to web sites, such as CoverMyMeds.com, to fill out extensive forms containing numerous questions about the patient’s illness and diagnosis, and then selecting from a list of medications that the insurance company ironically labels as “smart choices.” These medications often are not necessarily what the physician considers a smart choice, but are the cheapest (regardless of whether their efficacy, safety, or tolerability are the best fit for the patient). After the physician completes the forms, there is a waiting period, followed by additional questions that consume more valuable time and take the physician away from seeing more patients. Some busy colleagues told me they often take the pre-authorization “homework” with them to do at home, consuming part of what should be their family time. For physicians who see patients in an institutional “clinic,” medical assistants or nurses must be hired at significant expense to work full-time on pre-authorizations, adding to the overhead of the clinic while increasing the profits of the third-party insurer.
4. Patients who have been stable on a medication for months, even years, are forced to switch to another medication if they change jobs and become covered by a different insurance company that does not have the patient’s current medication on their infamous list of “approved drugs,” an evil euphemism for “cheapest drugs.” Switching medications is known to be a possibly hazardous process with lower efficacy and/or tolerability, but that appears to be irrelevant to the insurance company. The welfare of the patient is not on the insurance company’s radar screen, perhaps because it is crowded out by dollar signs. We should all urge policymakers to pass legislation that goes beyond requiring insurance companies to cover “pre-existing conditions” and expands it to cover “pre-existing medications.”
Continue to: Often, frustrated physicians...
5. Often, frustrated physicians who do not want to see their patients receive a medication they do not believe is appropriate may spend valuable time writing letters of appeal, making phone calls, or printing and faxing scientific articles to the insurance company to convince them to authorize a medication that is not on the “approved list.” Based on my own clinical experience, that justification sometimes works and sometimes doesn’t.
6. Physicians are inevitably and understandably demoralized because their expertise and sound clinical judgment are arbitrarily dismissed and overruled by an invisible insurance employee whose knowledge about and compassion for the patient is miniscule at best.
7. New medication development has collided with the biased despotism of pre-authorization, which generally rejects any new medication (always costlier than generics) irrespective of whether the new medication was demonstrated in controlled clinical trials to have a measurably better profile than older generics. This has ominous implications for numerous medical disorders that do not have any approved medications (for psychiatry, a published study1 found that 82% of DSM disorders do not have a FDA-approved medication).
The lack of utilizing newly introduced medications has discouraged the pharmaceutical industry from investing to develop innovative new mechanisms of action for a variety of complex neuropsychiatric medical conditions. Some companies have already abandoned psychiatric drug development, which is dire for clinical care because pharmaceutical companies are the only entities that develop new treatments for our patients (some health care professionals wish the government had a pharmaceutical agency that develops medications for various illness, but no such agency has ever existed).
8. Hospitalization for a seriously ill patient is either denied, delayed, or eventually approved for an absurdly short period (a few days), which is woefully inadequate, culminating in discharging patients with unresolved symptoms. This can lead to disastrous consequences, including suicide, homicide, or incarceration.
Continue to: I have been personally infuriated...
I have been personally infuriated many times because of the adverse impact pre-authorization had on my patients. One example that still haunts me is a 23-year-old college graduate with severe treatment-resistant depression who failed multiple antidepressant trials, including IV ketamine. She harbored daily thoughts of suicide (throwing herself in front of a train, which she saw daily as she drove to work). She admitted to frequently contemplating which dress she should wear in her coffin. Based on several published double-blind studies showing that modafinil improved bipolar depression,2 I prescribed modafinil, 200 mg/d, as adjunctive treatment to venlafaxine, 300 mg/d, and she improved significantly for 10 months. Suddenly, the insurance company refused to renew her refill of modafinil, and it took 4 weeks of incessant communication (phone calls, faxes, letters, sending published articles) before it was finally approved. In the meantime, the patient deteriorated and began to have active suicidal urges. When she was restarted on modafinil, she never achieved the same level of improvement she had prior to discontinuing modafinil. The insurance company damaged this patient’s recovery with its refusal to authorize a medication that was “not approved” for depression despite the clear benefit it had provided this treatment-resistant patient for almost 1 year. Their motive was clearly to avoid covering the high cost of modafinil, regardless of this patient’s high risk of suicide.
Every physician can recite a litany of complaints about the evil of pre-authorizations. We must therefore unite and vigorously lobby legislators to pass laws that protect patients and uphold physicians’ authority to determine the right treatment for their patients. We must terminate the plague of pre-authorization that takes our patients hostage to the greed of insurance companies, who have no regard to the agony of patients who are prevented from receiving the medication that their personal physician prescribes. Physicians’ well-being would be greatly enhanced if they were not enslaved to the avarice of insurance companies.
The travesty of pre-authorization and its pervasive and deleterious effects on medical care, society, and citizens must be stopped. It’s a plague that sacrifices the practice of medicine on the altar of financial greed. Just because it has gone on for many years does not mean it should be accepted as the “new normal.” It must be condemned as the “new abnormal,” a cancerous lesion on health care delivery that must be excised and discarded.
1. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
2. Nunez NA, Singh B, Romo-Nava F, et al. Efficacy and tolerability of adjunctive modafinil/armodafinil in bipolar depression: a meta-analysis of randomized controlled trials. Bipolar Dipsord. 2019;10.1111/bdi.12859. doi: 10.1111/bdi.12859
1. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
2. Nunez NA, Singh B, Romo-Nava F, et al. Efficacy and tolerability of adjunctive modafinil/armodafinil in bipolar depression: a meta-analysis of randomized controlled trials. Bipolar Dipsord. 2019;10.1111/bdi.12859. doi: 10.1111/bdi.12859
During a viral pandemic, anxiety is endemic: The psychiatric aspects of COVID-19
Fear of dying is considered “normal.” However, the ongoing threat of a potentially fatal viral infection can cause panic, anxiety, and an exaggerated fear of illness and death. The relentless spread of the coronavirus infectious disease that began in late 2019 (COVID-19) is spawning widespread anxiety, panic, and worry about one’s health and the health of loved ones. The viral pandemic has triggered a parallel anxiety epidemic.
Making things worse is that no vaccine has yet been developed, and for individuals who do get infected, there are no specific treatments other than supportive care, such as ventilators. Members of the public have been urged to practice sensible preventative measures, including handwashing, sanitizing certain items and surfaces, and—particularly challenging—self-isolation and social distancing. The public has channeled its fear into frantic buying and hoarding of food and non-food items, especially masks, sanitizers, soap, disinfectant wipes, and toilet paper (perhaps preparing for gastrointestinal hyperactivity during anxiety); canceling flights; avoiding group activities; and self-isolation or, for those exposed to the virus, quarantine. Anxiety is palpable. The facial masks that people wear are ironically unmasking their inner agitation and disquietude.
Our role as psychiatrists
As psychiatrists, we have an important role to play in such times, especially for our patients who already have anxiety disorders or depression. The additional emotional burden of this escalating health crisis is exacerbating the mental anguish of our patients (in addition to those who may soon become new patients). The anxiety and panic attacks due to “imagined” doom and gloom are now intensified by anxiety due to a “real” fatal threat. The effect on some vulnerable patients can be devastating, and may culminate in an acute stress reaction and future posttraumatic stress disorder. There are also reports of “psychogenic COVID-19” conversion reaction, with symptoms of sore throat, dyspnea, and even psychogenic fever. Paradoxically, self-isolation and social distancing, which are recommended to prevent the human-to-human spread of the virus, may further worsen anxiety and depression by reducing the comfort of intimacy and social contacts.
Individuals with depression will also experience an increased risk of symptom breakthrough despite receiving treatment. Stress is well known to trigger or exacerbate depression. Thus, the sense of helplessness and hopelessness during depression may intensify among our patients with pre-existing mood disorders, and suicidal ideation may resurface. Making things worse is the unfortunate timing of the COVID-19 pandemic. Spring is the peak season for the re-emergence of depression and suicide attempts. The ongoing stress of the health crisis, coupled with the onset of spring, may coalesce into a dreadful synergy for relapse among vulnerable individuals with unipolar or bipolar depression.
Patients with obsessive-compulsive disorder (OCD) are known to be averse to imagined germs and may wash their hands multiple times a day. An epidemic in which all health officials strongly urge washing one’s hands is very likely to exacerbate the compulsive handwashing of persons with OCD and significantly increase their anxiety. Because their other obsessions and compulsions may also increase in frequency and intensity, they will need our attention as their psychiatrists.
The viral pandemic is eerily similar to a natural disaster such as a hurricane of tornado, both of which physically destroy towns and flatten homes. The COVID-19 pandemic is damaging social structures and obliterating the fabric of global human relations. Consider the previously unimaginable disruption of what makes a vibrant society: schools, colleges, sporting events, concerts, Broadway shows, houses of worship, festivals, conferences, conventions, busy airports/train stations/bus stations, and spontaneous community gatherings. The sudden shock of upheaval in our daily lives may not only cause a hollow sense of emptiness and grief, but also have residual economic and emotional consequences. Nothing can be taken for granted anymore, and nothing is permanent. Cynicism may rise about maintaining life as we know it.
Rising to the challenge
Physicians and clinicians across all specialties are rising to the challenge of the pandemic, whether to manage the immediate physical or emotional impacts of the health crisis or its anticipated consequences (including the economic sequelae). The often-demonized pharmaceutical industry is urgently summoning all its resources to develop both a vaccine as well as biologic treatments for this potentially fatal viral infection. The government is removing regulatory barriers to expedite solutions to the crisis. A welcome public-private partnership is expediting the availability of and access to testing for the virus. The toxic political partisanship has temporarily given way to collaboration in crafting laws that can mitigate the corrosive effects of the health crisis on businesses and individuals. All these salubrious repercussions of the pandemic are heartening and indicative of how a crisis can often bring out the best among us humans.
Continue to: Let's acknowledge the benefits...
Let’s acknowledge the benefits of the internet and the often-maligned social media. At a time of social isolation and cancellation of popular recreational activities (March Madness, NBA games, spring training baseball, movie theaters, concerts, religious congregations, partying with friends), the internet can offset the pain of mandated isolation by connecting all of us virtually, thus alleviating the emptiness that comes with isolation and boredom laced with anxiety. The damaging effects of a viral pandemic on human well-being would have been much worse if the internet did not exist.
Before the internet, television was a major escape, and for many it still is. But there is a downside: the wall-to-wall coverage of the local, national, and international effects of the pandemic can be alarming, and could increase distress even among persons who don’t have an anxiety disorder. Paradoxically, fear of going outdoors (agoraphobia) has suddenly become a necessary coping mechanism during a viral pandemic, instead of its traditional status as a “disabling symptom.”
Thank heavens for advances in technology. School children and college students can continue their education remotely without the risks of spreading infection by going to crowded classrooms. Scientific interactions and collaboration as well as business communications can remain active via videoconferencing technology, such as Zoom, Skype, or WebEx, without having to walk in crowded airports and fly to other cities on planes with recirculated air. Also, individuals who live far from family or friends can use their smartphones to see and chat with their loved ones. And cellphones remain a convenient method of staying in touch with the latest developments or making a “call to action” locally, national, and internationally.
During these oppressive and exceptional times, special attention and support must be provided to vulnerable populations, especially individuals with psychiatric illnesses, older adults who are physically infirm, and young children. Providing medical care, including psychiatric care, is essential to prevent the escalation of anxiety and panic among children and adults alike, and to prevent physical deterioration or death. This health crisis must be tackled with biopsychosocial approaches. And we, psychiatrists, must support and educate our patients and the public about stress management, and remind all about the transiency of epidemics as exemplified by the 1918 Spanish flu, the 1957 Asian flu, the 1968 Hong Kong flu, the 1982 human immunodeficiency virus, the 2002 severe acute respiratory syndrome virus, the 2009 Swine flu, the 2013 Ebola virus, and the 2016 Zika virus, all of which are now distant memories. The current COVID-19 pandemic should inoculate us to be more prepared and resilient for the inevitable future pandemics.
Fear of dying is considered “normal.” However, the ongoing threat of a potentially fatal viral infection can cause panic, anxiety, and an exaggerated fear of illness and death. The relentless spread of the coronavirus infectious disease that began in late 2019 (COVID-19) is spawning widespread anxiety, panic, and worry about one’s health and the health of loved ones. The viral pandemic has triggered a parallel anxiety epidemic.
Making things worse is that no vaccine has yet been developed, and for individuals who do get infected, there are no specific treatments other than supportive care, such as ventilators. Members of the public have been urged to practice sensible preventative measures, including handwashing, sanitizing certain items and surfaces, and—particularly challenging—self-isolation and social distancing. The public has channeled its fear into frantic buying and hoarding of food and non-food items, especially masks, sanitizers, soap, disinfectant wipes, and toilet paper (perhaps preparing for gastrointestinal hyperactivity during anxiety); canceling flights; avoiding group activities; and self-isolation or, for those exposed to the virus, quarantine. Anxiety is palpable. The facial masks that people wear are ironically unmasking their inner agitation and disquietude.
Our role as psychiatrists
As psychiatrists, we have an important role to play in such times, especially for our patients who already have anxiety disorders or depression. The additional emotional burden of this escalating health crisis is exacerbating the mental anguish of our patients (in addition to those who may soon become new patients). The anxiety and panic attacks due to “imagined” doom and gloom are now intensified by anxiety due to a “real” fatal threat. The effect on some vulnerable patients can be devastating, and may culminate in an acute stress reaction and future posttraumatic stress disorder. There are also reports of “psychogenic COVID-19” conversion reaction, with symptoms of sore throat, dyspnea, and even psychogenic fever. Paradoxically, self-isolation and social distancing, which are recommended to prevent the human-to-human spread of the virus, may further worsen anxiety and depression by reducing the comfort of intimacy and social contacts.
Individuals with depression will also experience an increased risk of symptom breakthrough despite receiving treatment. Stress is well known to trigger or exacerbate depression. Thus, the sense of helplessness and hopelessness during depression may intensify among our patients with pre-existing mood disorders, and suicidal ideation may resurface. Making things worse is the unfortunate timing of the COVID-19 pandemic. Spring is the peak season for the re-emergence of depression and suicide attempts. The ongoing stress of the health crisis, coupled with the onset of spring, may coalesce into a dreadful synergy for relapse among vulnerable individuals with unipolar or bipolar depression.
Patients with obsessive-compulsive disorder (OCD) are known to be averse to imagined germs and may wash their hands multiple times a day. An epidemic in which all health officials strongly urge washing one’s hands is very likely to exacerbate the compulsive handwashing of persons with OCD and significantly increase their anxiety. Because their other obsessions and compulsions may also increase in frequency and intensity, they will need our attention as their psychiatrists.
The viral pandemic is eerily similar to a natural disaster such as a hurricane of tornado, both of which physically destroy towns and flatten homes. The COVID-19 pandemic is damaging social structures and obliterating the fabric of global human relations. Consider the previously unimaginable disruption of what makes a vibrant society: schools, colleges, sporting events, concerts, Broadway shows, houses of worship, festivals, conferences, conventions, busy airports/train stations/bus stations, and spontaneous community gatherings. The sudden shock of upheaval in our daily lives may not only cause a hollow sense of emptiness and grief, but also have residual economic and emotional consequences. Nothing can be taken for granted anymore, and nothing is permanent. Cynicism may rise about maintaining life as we know it.
Rising to the challenge
Physicians and clinicians across all specialties are rising to the challenge of the pandemic, whether to manage the immediate physical or emotional impacts of the health crisis or its anticipated consequences (including the economic sequelae). The often-demonized pharmaceutical industry is urgently summoning all its resources to develop both a vaccine as well as biologic treatments for this potentially fatal viral infection. The government is removing regulatory barriers to expedite solutions to the crisis. A welcome public-private partnership is expediting the availability of and access to testing for the virus. The toxic political partisanship has temporarily given way to collaboration in crafting laws that can mitigate the corrosive effects of the health crisis on businesses and individuals. All these salubrious repercussions of the pandemic are heartening and indicative of how a crisis can often bring out the best among us humans.
Continue to: Let's acknowledge the benefits...
Let’s acknowledge the benefits of the internet and the often-maligned social media. At a time of social isolation and cancellation of popular recreational activities (March Madness, NBA games, spring training baseball, movie theaters, concerts, religious congregations, partying with friends), the internet can offset the pain of mandated isolation by connecting all of us virtually, thus alleviating the emptiness that comes with isolation and boredom laced with anxiety. The damaging effects of a viral pandemic on human well-being would have been much worse if the internet did not exist.
Before the internet, television was a major escape, and for many it still is. But there is a downside: the wall-to-wall coverage of the local, national, and international effects of the pandemic can be alarming, and could increase distress even among persons who don’t have an anxiety disorder. Paradoxically, fear of going outdoors (agoraphobia) has suddenly become a necessary coping mechanism during a viral pandemic, instead of its traditional status as a “disabling symptom.”
Thank heavens for advances in technology. School children and college students can continue their education remotely without the risks of spreading infection by going to crowded classrooms. Scientific interactions and collaboration as well as business communications can remain active via videoconferencing technology, such as Zoom, Skype, or WebEx, without having to walk in crowded airports and fly to other cities on planes with recirculated air. Also, individuals who live far from family or friends can use their smartphones to see and chat with their loved ones. And cellphones remain a convenient method of staying in touch with the latest developments or making a “call to action” locally, national, and internationally.
During these oppressive and exceptional times, special attention and support must be provided to vulnerable populations, especially individuals with psychiatric illnesses, older adults who are physically infirm, and young children. Providing medical care, including psychiatric care, is essential to prevent the escalation of anxiety and panic among children and adults alike, and to prevent physical deterioration or death. This health crisis must be tackled with biopsychosocial approaches. And we, psychiatrists, must support and educate our patients and the public about stress management, and remind all about the transiency of epidemics as exemplified by the 1918 Spanish flu, the 1957 Asian flu, the 1968 Hong Kong flu, the 1982 human immunodeficiency virus, the 2002 severe acute respiratory syndrome virus, the 2009 Swine flu, the 2013 Ebola virus, and the 2016 Zika virus, all of which are now distant memories. The current COVID-19 pandemic should inoculate us to be more prepared and resilient for the inevitable future pandemics.
Fear of dying is considered “normal.” However, the ongoing threat of a potentially fatal viral infection can cause panic, anxiety, and an exaggerated fear of illness and death. The relentless spread of the coronavirus infectious disease that began in late 2019 (COVID-19) is spawning widespread anxiety, panic, and worry about one’s health and the health of loved ones. The viral pandemic has triggered a parallel anxiety epidemic.
Making things worse is that no vaccine has yet been developed, and for individuals who do get infected, there are no specific treatments other than supportive care, such as ventilators. Members of the public have been urged to practice sensible preventative measures, including handwashing, sanitizing certain items and surfaces, and—particularly challenging—self-isolation and social distancing. The public has channeled its fear into frantic buying and hoarding of food and non-food items, especially masks, sanitizers, soap, disinfectant wipes, and toilet paper (perhaps preparing for gastrointestinal hyperactivity during anxiety); canceling flights; avoiding group activities; and self-isolation or, for those exposed to the virus, quarantine. Anxiety is palpable. The facial masks that people wear are ironically unmasking their inner agitation and disquietude.
Our role as psychiatrists
As psychiatrists, we have an important role to play in such times, especially for our patients who already have anxiety disorders or depression. The additional emotional burden of this escalating health crisis is exacerbating the mental anguish of our patients (in addition to those who may soon become new patients). The anxiety and panic attacks due to “imagined” doom and gloom are now intensified by anxiety due to a “real” fatal threat. The effect on some vulnerable patients can be devastating, and may culminate in an acute stress reaction and future posttraumatic stress disorder. There are also reports of “psychogenic COVID-19” conversion reaction, with symptoms of sore throat, dyspnea, and even psychogenic fever. Paradoxically, self-isolation and social distancing, which are recommended to prevent the human-to-human spread of the virus, may further worsen anxiety and depression by reducing the comfort of intimacy and social contacts.
Individuals with depression will also experience an increased risk of symptom breakthrough despite receiving treatment. Stress is well known to trigger or exacerbate depression. Thus, the sense of helplessness and hopelessness during depression may intensify among our patients with pre-existing mood disorders, and suicidal ideation may resurface. Making things worse is the unfortunate timing of the COVID-19 pandemic. Spring is the peak season for the re-emergence of depression and suicide attempts. The ongoing stress of the health crisis, coupled with the onset of spring, may coalesce into a dreadful synergy for relapse among vulnerable individuals with unipolar or bipolar depression.
Patients with obsessive-compulsive disorder (OCD) are known to be averse to imagined germs and may wash their hands multiple times a day. An epidemic in which all health officials strongly urge washing one’s hands is very likely to exacerbate the compulsive handwashing of persons with OCD and significantly increase their anxiety. Because their other obsessions and compulsions may also increase in frequency and intensity, they will need our attention as their psychiatrists.
The viral pandemic is eerily similar to a natural disaster such as a hurricane of tornado, both of which physically destroy towns and flatten homes. The COVID-19 pandemic is damaging social structures and obliterating the fabric of global human relations. Consider the previously unimaginable disruption of what makes a vibrant society: schools, colleges, sporting events, concerts, Broadway shows, houses of worship, festivals, conferences, conventions, busy airports/train stations/bus stations, and spontaneous community gatherings. The sudden shock of upheaval in our daily lives may not only cause a hollow sense of emptiness and grief, but also have residual economic and emotional consequences. Nothing can be taken for granted anymore, and nothing is permanent. Cynicism may rise about maintaining life as we know it.
Rising to the challenge
Physicians and clinicians across all specialties are rising to the challenge of the pandemic, whether to manage the immediate physical or emotional impacts of the health crisis or its anticipated consequences (including the economic sequelae). The often-demonized pharmaceutical industry is urgently summoning all its resources to develop both a vaccine as well as biologic treatments for this potentially fatal viral infection. The government is removing regulatory barriers to expedite solutions to the crisis. A welcome public-private partnership is expediting the availability of and access to testing for the virus. The toxic political partisanship has temporarily given way to collaboration in crafting laws that can mitigate the corrosive effects of the health crisis on businesses and individuals. All these salubrious repercussions of the pandemic are heartening and indicative of how a crisis can often bring out the best among us humans.
Continue to: Let's acknowledge the benefits...
Let’s acknowledge the benefits of the internet and the often-maligned social media. At a time of social isolation and cancellation of popular recreational activities (March Madness, NBA games, spring training baseball, movie theaters, concerts, religious congregations, partying with friends), the internet can offset the pain of mandated isolation by connecting all of us virtually, thus alleviating the emptiness that comes with isolation and boredom laced with anxiety. The damaging effects of a viral pandemic on human well-being would have been much worse if the internet did not exist.
Before the internet, television was a major escape, and for many it still is. But there is a downside: the wall-to-wall coverage of the local, national, and international effects of the pandemic can be alarming, and could increase distress even among persons who don’t have an anxiety disorder. Paradoxically, fear of going outdoors (agoraphobia) has suddenly become a necessary coping mechanism during a viral pandemic, instead of its traditional status as a “disabling symptom.”
Thank heavens for advances in technology. School children and college students can continue their education remotely without the risks of spreading infection by going to crowded classrooms. Scientific interactions and collaboration as well as business communications can remain active via videoconferencing technology, such as Zoom, Skype, or WebEx, without having to walk in crowded airports and fly to other cities on planes with recirculated air. Also, individuals who live far from family or friends can use their smartphones to see and chat with their loved ones. And cellphones remain a convenient method of staying in touch with the latest developments or making a “call to action” locally, national, and internationally.
During these oppressive and exceptional times, special attention and support must be provided to vulnerable populations, especially individuals with psychiatric illnesses, older adults who are physically infirm, and young children. Providing medical care, including psychiatric care, is essential to prevent the escalation of anxiety and panic among children and adults alike, and to prevent physical deterioration or death. This health crisis must be tackled with biopsychosocial approaches. And we, psychiatrists, must support and educate our patients and the public about stress management, and remind all about the transiency of epidemics as exemplified by the 1918 Spanish flu, the 1957 Asian flu, the 1968 Hong Kong flu, the 1982 human immunodeficiency virus, the 2002 severe acute respiratory syndrome virus, the 2009 Swine flu, the 2013 Ebola virus, and the 2016 Zika virus, all of which are now distant memories. The current COVID-19 pandemic should inoculate us to be more prepared and resilient for the inevitable future pandemics.
What is the role of the ObGyn in preventing and treating obesity?
Obesity is a disease causing a public health crisis. In the United States, tobacco use and obesity are the two most important causes of preventable premature death. They result in an estimated 480,0001 and 300,0002 premature deaths per year, respectively. Obesity is a major contributor to diabetes mellitus, hypertension, dyslipidemia, and coronary heart disease. Obesity is also associated with increased rates of colon, breast, and endometrial cancer. Experts predict that in 2030, 50% of adults in the United States will have a body mass index (BMI) ≥ 30 kg/m2, and 25% will have a BMI ≥ 35 kg/m2.3 More women than men are predicted to be severely obese (FIGURE).3
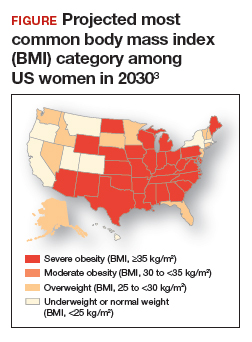
As clinicians we need to increase our efforts to reduce the epidemic of obesity. ObGyns can play an important role in preventing and managing obesity, by recommending primary-care weight management practices, prescribing medications that influence central metabolism, and referring appropriate patients to bariatric surgery centers of excellence.
Primary-care weight management
Measuring BMI and recommending interventions to prevent and treat obesity are important components of a health maintenance encounter. For women who are overweight or obese, dietary changes and exercise are important recommendations. The American Heart Association recommends the following lifestyle interventions4:
- Eat a high-quality diet that includes vegetables, fruit, whole grains, beans, legumes, nuts, plant-based protein, lean animal protein, and fish.
- Limit intake of sugary drinks and foods, fatty or processed meats, full-fat dairy products, eggs, highly processed foods, and tropical oils.
- Exercise at least 150 minutes weekly at a moderate activity level, including muscle-strengthening activity.
- Reduce prolonged intervals of sitting.
- Consider using an activity tracker to monitor activity level.
Clinicians should consider referring overweight and obese patients to a nutritionist for a consultation to plan how to consume a high-quality, low-calorie diet. A nutritionist can spend time with patients explaining options for implementing a calorie-restricted diet. In addition, some health insurers will require patients to participate in a supervised calorie-restricted diet plan for at least 6 months before authorizing coverage of expensive weight loss medications or bariatric surgery. In addition to recommending diet and exercise, ObGyns may consider prescribing metformin for their obese patients.
Continue to: Metformin...
Metformin
Metformin is approved for the treatment of type 2 diabetes mellitus. Unlike insulin therapy, which is associated with weight gain, metformin is associated with modest weight loss. The Diabetes Prevention Program (DPP) randomly assigned 3,234 nondiabetic participants with a fasting glucose level between 95 and 125 mg/dL and impaired glucose tolerance (140 to 199 mg/dL) after a 75-g oral glucose load to intensive lifestyle changes (calorie-restricted diet to achieve 7% weight loss plus 150 minutes of exercise weekly), metformin (850 mg twice daily), or placebo.5,6 The mean age of the participants was 51 years, with a mean BMI of 34 kg/m2. Most (68%) of the participants were women.
After 12 months of follow-up, mean weight loss in the intensive lifestyle change, metformin, and placebo groups was 6.5%, 2.7%, and 0.4%, respectively. After 2 years of treatment, weight loss among those who reliably took their metformin pills was approximately 4%, while participants in the placebo group had a 1% weight gain. Among those who continued to reliably take their metformin pills, the weight loss persisted through 9 years of follow up.
The mechanisms by which metformin causes weight loss are not clear. Metformin stimulates phosphorylation of adenosine monophosphate (AMP)-activated protein kinase, which regulates mitochondrial function, hepatic and muscle fatty acid oxidation, glucose transport, insulin secretion, and lipogenesis.7
Many ObGyns have experience in using metformin for the treatment of polycystic ovary syndrome or gestational diabetes. Hence, the dosing and adverse effects of metformin are familiar to many obstetricians-gynecologists. Metformin is contraindicated in individuals with creatinine clearance less than 30 mL/min. Rarely, metformin can cause lactic acidosis. According to Lexicomp,8 the most common adverse effects of metformin extended release (metformin ER) are diarrhea (17%), nausea and vomiting (7%), and decreased vitamin B12 concentration (7%) due to malabsorption in the terminal ileum. Of note, in the DPP study, hemoglobin concentration was slightly lower over time in the metformin compared with the placebo group (13.6 mg/dL vs 13.8 mg/dL, respectively; P<.001).6 Some experts recommend annual vitamin B12 measurement in individuals taking metformin.
In my practice, I only prescribe metformin ER. I usually start metformin treatment with one 750 mg ER tablet with dinner. If the patient tolerates that dose, I increase the dose to two 750 mg ER tablets with dinner. Metformin-induced adverse effects include diarrhea (17%) and nausea and vomiting (7%). Metformin ER is inexpensive. A one-month supply of metformin (sixty 750 mg tablets) costs between $4 and $21 at major pharmacies.9 Health insurance companies generally do not require preauthorization to cover metformin prescriptions.
Weight loss medications
US Food and Drug Administration (FDA)-approved weight loss medications include: liraglutide (Victoza), orlistat (Xenical, Alli), combination phentermine-extended release topiramate (Qsymia), and combination extended release naltrexone-bupropion (Contrave). All FDA-approved weight loss medications result in mean weight loss in the range of 6% to 10%. Many of these medications are very expensive (more than $200 per month).10 Insurance preauthorization is commonly required for these medications. For ObGyns, it may be best to refer patients who would like to use a weight loss medication to a specialist or specialty center with expertise in using these medications.
Sustainable weight loss is very difficult to achieve through dieting alone. A multitude of dietary interventions have been presented as “revolutionary approaches” to the challenging problem of sustainable weight loss, including the Paleo diet, the Vegan diet, the low-carb diet, the Dukan diet, the ultra-lowfat diet, the Atkins diet, the HCG diet, the Zone diet, the South Beach diet, the plant-based diet, the Mediterranean diet, the Asian diet, and intermittent fasting. Recently, intermittent fasting has been presented as the latest and greatest approach to dieting, with the dual goals of achieving weight loss and improved health.1 In some animal models, intermittent dieting has been shown to increase life-span, a finding that has attracted great interest. A major goal of intermittent fasting is to promote “metabolic switching” with increased reliance on ketones to fuel cellular energy needs.
Two approaches to “prescribing” an intermittent fasting diet are to limit food intake to a period of 6 to 10 hours each day or to markedly reduce caloric intake one or two days per week, for example to 750 calories in a 24-hour period. There are no long-term studies of the health outcomes associated with intermittent fasting. In head-to-head clinical trials of intermittent fasting and daily calorie restriction (classic dieting), both diets result in similar weight loss. For example, in one clinical trial 100 obese participants, with a mean body mass index (BMI) of 34 kg/m2 , including 86 women, were randomly assigned to2:
1. intermittent fasting (25% of energy needs every other day)
2. daily calorie restriction (75% of energy needs every day), or
3. no intervention.
After 12 months of follow up, the participants in the no intervention group had gained 0.5% of their starting weight. The intermittent fasting and the daily calorie restriction groups had similar amounts of weight loss, approximately 5% of their starting weight. More individuals dropped out of the study from the intermittent fasting group than the daily calorie restriction group (38% vs 29%, respectively).
In another clinical trial, 107 overweight or obese premenopausal women, average age 40 years and mean BMI 31 kg/m2 , were randomly assigned to intermittent fasting (25% of energy needs 2 days per week) or daily calorie restriction (75% of energy needs daily) for 6 months. The mean weight of the participants at baseline was 83 kg. Weight loss was similar in the intermittent fasting and daily calorie restriction groups, 6.4 kg (-7.7%) and 5.6 kg (-6.7%), respectively (P=.4).3
The investigators concluded that intermittent fasting and daily calorie restriction could both be offered as effective approaches to weight loss. My conclusion is that intermittent fasting is not a miracle dietary intervention, but it is another important option in the armamentarium of weight loss interventions.
References
1. de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging and disease. N Engl J Med. 2019;381:2541-2551.
2. Trepanowski JF, Kroeger CM, Barnosky A, et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: a randomized clinical trial. JAMA Intern Med. 2017;177:930-938.
3. Harvie MN, Pegington M, Mattson MP, et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disc disease risk markers: a randomized trial in young overweight women. Int J Obes (Lond). 2011;35:714-727.
Sleeve gastrectomy
Two children are playing in a school yard. One child proudly states, “My mother is an endocrinologist. She treats diabetes.” Not to be outdone, the other child replies, “My mother is a bariatric surgeon. She cures diabetes.”
The dialogue reflects the reality that bariatric surgery results in more reliable and significant weight loss than diet, exercise, or weight loss medications. Diet, exercise, and weight loss medications often result in a 5% to 10% decrease in weight, but bariatric surgery typically results in a 25% decrease in weight. Until recently, 3 bariatric surgical procedures were commonly performed: Roux-en-Y gastric bypass (RYGB), sleeve gastrectomy (SG), and adjustable gastric banding (AGB). AGB is now seldom performed because it is less effective than RYGB and SG. Two recently published randomized trials compared the long-term outcomes associated with RYGB and SG. The studies found that SG and RYGB result in a similar degree of weight loss. RYGB resulted in slightly more weight loss than SG, but SG was associated with a lower rate of major complications, such as internal hernias. SG takes much less time to perform than RYGB. SG has become the most commonly performed bariatric surgery in premenopausal women considering pregnancy because of the low risk of internal hernias.
In the Swiss Multicenter Bypass or Sleeve Study (SM-BOSS), 217 participants with a mean BMI of 44 kg/m2 and mean age of 45.5 years were randomly assigned to RYGB or SG and followed for 5 years.11 The majority (72%) of the participants were women. At 5 years of follow-up, in the RYGB and SG groups, mean weight loss was 37 kg and 33 kg, respectively (P=.19). In both groups, weight loss nadir was reached 12 to 24 months after surgery. Expressed as a percentage of original weight, weight loss in the RYGB and SG groups was -29% and -25%, respectively (P=.02). Gastric reflux worsened in both the RYGB and SG groups (6% vs 32%, respectively). The number of reoperations in the RYGB and SG groups was 22% and 16%. Of note, among individuals with prevalent diabetes, RYGB and SG resulted in remission of the diabetes in 68% and 62% of participants, respectively.
In the Sleeve vs Bypass study (SLEEVEPASS), 240 participants, with mean BMI of 46 kg/m2 and mean age of 48 years, were randomly assigned to RYGB or SG and followed for 5 years.12 Most (70%) of the participants were women. Following bariatric surgery, BMI decreased significantly in both groups. In the RYGB group, BMI decreased from 48 kg/m2 preoperatively to 35.4 kg/m2 at 5 years of follow up. In the SG group, BMI decreased from 47 kg/m2 preoperatively to 36.5 kg/m2 at 5 years of follow up. Late major complications (defined as complications occurring from 30 days to 5 years postoperatively) occurred more frequently in the RYGB group (15%) versus the SG group (8%). All the late major complications required reoperation. In the SG group, 7 of 10 reoperations were for severe gastric reflux disease. In the RYGB group 17 of 18 reoperations were for suspected internal hernia, requiring closure of a mesenteric defect at reoperation. There was no treatment-related mortality during the 5-year follow up.
Guidelines for bariatric surgery are BMI ≥ 40 kg/m2 without a comorbid illness or BMI ≥ 35 kg/m2 with at least one serious comorbid disease, such as diabetes.13 ObGyns can build a synergistic relationship with bariatric surgeons by referring eligible patients for surgical consultation and, in return, accepting referrals. A paradox and challenge is that many health insurers require patients to complete a supervised medical weight loss management program prior to being approved for bariatric surgery. However, the medical weight loss program might result in the patient no longer being eligible for insurance coverage of their surgery. For example, a patient who had a BMI of 42 kg/m2 prior to a medical weight loss management program who then lost enough weight to achieve a BMI of 38 kg/m2 might no longer be eligible for insurance coverage of a bariatric operation.14
Continue to: ObGyns need to prioritize treatment for obesity...
ObGyns need to prioritize treatment for obesity
Between 1959 and 2014, US life expectancy increased from 69.9 years to 79.1 years. However, in 2015 and 2016 life expectancy in the United States decreased slightly to 78.9 years, while continuing to improve in other countries.15 What could cause such an unexpected trend? Some experts believe that excess overweight and obesity in the US population, resulting in increased rates of diabetes, hypertension, and heart disease, accounts for a significant proportion of the life expectancy gap between US citizens and those who reside in Australia, Finland, Japan, and Sweden.16,17 All frontline clinicians play an important role in reversing the decades-long trend of increasing rates of overweight and obesity. Interventions that ObGyns could prioritize in their practices for treating overweight and obese patients include: a calorie-restricted diet, exercise, metformin, and SG.
- U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress. A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
- Allison DB, Fontaine KR, Manson JE, et al. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530-1538.
- Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381:2440-2450.
- American Heart Association. My life check | Life’s simple 7. https://www.heart.org/en/healthyliving/healthy-lifestyle/my-life-check--lifessimple-7. Reviewed May 2, 2018. Accessed February 10, 2020.
- Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
- Diabetes Prevention Program Research Group. Long-term safety, tolerability and weight loss associated with metformin in the Diabetes Prevention Program Outcomes Study. Diabetes Care. 2012;35:731-737.
- Winder WW, Hardie DG. Inactivation of acetylCoA carboxylase and activation of AMP-activated protein kinase in muscle during exercise. Am J Physiol. 1996;270(2 pt 1):E299-E304.
- Lexicomp. https://online.lexi.com/lco/action/ home. Accessed February 13, 2020.
- Metformin ER (Glucophage XR). GoodRX website. https://www.goodrx.com/metformin-erglucophage-xr?dosage=750mg&form=tablet&la bel_override=metformin+ER+%28Glucophage+X R%29&quantity=60. Accessed February 13, 2020.
- GoodRX website. www.goodrx.com. Accessed February 10, 2020.
- Peterli R, Wolnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018;319:255-265.
- Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: The SLEEVEPASS randomized clinical trial. JAMA. 2018;319:241-254.
- Rubino F, Nathan DM, Eckel RH, et al; Delegates of the 2nd Diabetes Surgery Summit. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Obes Surg. 2017;27:2-21.
- Gebran SG, Knighton B, Ngaage LM, et al. Insurance coverage criteria for bariatric surgery: a survey of policies. Obes Surg. 2020;30:707-713.
- Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959-2017. JAMA. 2019;322:1996-2016.
- Preston SH, Vierboom YC, Stokes A. The role of obesity in exceptionally slow US mortality improvement. Proc Natl Acad Sci U S A. 2019;115:957-961.
- Xu H, Cupples LA, Stokes A, et al. Association of obesity with mortality over 24 years of weight history: findings from the Framingham Heart Study. JAMA Network Open. 2018;1:e184587.
Obesity is a disease causing a public health crisis. In the United States, tobacco use and obesity are the two most important causes of preventable premature death. They result in an estimated 480,0001 and 300,0002 premature deaths per year, respectively. Obesity is a major contributor to diabetes mellitus, hypertension, dyslipidemia, and coronary heart disease. Obesity is also associated with increased rates of colon, breast, and endometrial cancer. Experts predict that in 2030, 50% of adults in the United States will have a body mass index (BMI) ≥ 30 kg/m2, and 25% will have a BMI ≥ 35 kg/m2.3 More women than men are predicted to be severely obese (FIGURE).3
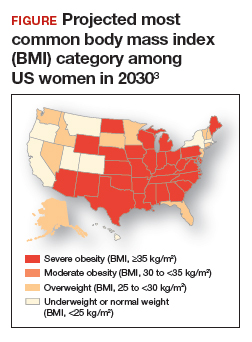
As clinicians we need to increase our efforts to reduce the epidemic of obesity. ObGyns can play an important role in preventing and managing obesity, by recommending primary-care weight management practices, prescribing medications that influence central metabolism, and referring appropriate patients to bariatric surgery centers of excellence.
Primary-care weight management
Measuring BMI and recommending interventions to prevent and treat obesity are important components of a health maintenance encounter. For women who are overweight or obese, dietary changes and exercise are important recommendations. The American Heart Association recommends the following lifestyle interventions4:
- Eat a high-quality diet that includes vegetables, fruit, whole grains, beans, legumes, nuts, plant-based protein, lean animal protein, and fish.
- Limit intake of sugary drinks and foods, fatty or processed meats, full-fat dairy products, eggs, highly processed foods, and tropical oils.
- Exercise at least 150 minutes weekly at a moderate activity level, including muscle-strengthening activity.
- Reduce prolonged intervals of sitting.
- Consider using an activity tracker to monitor activity level.
Clinicians should consider referring overweight and obese patients to a nutritionist for a consultation to plan how to consume a high-quality, low-calorie diet. A nutritionist can spend time with patients explaining options for implementing a calorie-restricted diet. In addition, some health insurers will require patients to participate in a supervised calorie-restricted diet plan for at least 6 months before authorizing coverage of expensive weight loss medications or bariatric surgery. In addition to recommending diet and exercise, ObGyns may consider prescribing metformin for their obese patients.
Continue to: Metformin...
Metformin
Metformin is approved for the treatment of type 2 diabetes mellitus. Unlike insulin therapy, which is associated with weight gain, metformin is associated with modest weight loss. The Diabetes Prevention Program (DPP) randomly assigned 3,234 nondiabetic participants with a fasting glucose level between 95 and 125 mg/dL and impaired glucose tolerance (140 to 199 mg/dL) after a 75-g oral glucose load to intensive lifestyle changes (calorie-restricted diet to achieve 7% weight loss plus 150 minutes of exercise weekly), metformin (850 mg twice daily), or placebo.5,6 The mean age of the participants was 51 years, with a mean BMI of 34 kg/m2. Most (68%) of the participants were women.
After 12 months of follow-up, mean weight loss in the intensive lifestyle change, metformin, and placebo groups was 6.5%, 2.7%, and 0.4%, respectively. After 2 years of treatment, weight loss among those who reliably took their metformin pills was approximately 4%, while participants in the placebo group had a 1% weight gain. Among those who continued to reliably take their metformin pills, the weight loss persisted through 9 years of follow up.
The mechanisms by which metformin causes weight loss are not clear. Metformin stimulates phosphorylation of adenosine monophosphate (AMP)-activated protein kinase, which regulates mitochondrial function, hepatic and muscle fatty acid oxidation, glucose transport, insulin secretion, and lipogenesis.7
Many ObGyns have experience in using metformin for the treatment of polycystic ovary syndrome or gestational diabetes. Hence, the dosing and adverse effects of metformin are familiar to many obstetricians-gynecologists. Metformin is contraindicated in individuals with creatinine clearance less than 30 mL/min. Rarely, metformin can cause lactic acidosis. According to Lexicomp,8 the most common adverse effects of metformin extended release (metformin ER) are diarrhea (17%), nausea and vomiting (7%), and decreased vitamin B12 concentration (7%) due to malabsorption in the terminal ileum. Of note, in the DPP study, hemoglobin concentration was slightly lower over time in the metformin compared with the placebo group (13.6 mg/dL vs 13.8 mg/dL, respectively; P<.001).6 Some experts recommend annual vitamin B12 measurement in individuals taking metformin.
In my practice, I only prescribe metformin ER. I usually start metformin treatment with one 750 mg ER tablet with dinner. If the patient tolerates that dose, I increase the dose to two 750 mg ER tablets with dinner. Metformin-induced adverse effects include diarrhea (17%) and nausea and vomiting (7%). Metformin ER is inexpensive. A one-month supply of metformin (sixty 750 mg tablets) costs between $4 and $21 at major pharmacies.9 Health insurance companies generally do not require preauthorization to cover metformin prescriptions.
Weight loss medications
US Food and Drug Administration (FDA)-approved weight loss medications include: liraglutide (Victoza), orlistat (Xenical, Alli), combination phentermine-extended release topiramate (Qsymia), and combination extended release naltrexone-bupropion (Contrave). All FDA-approved weight loss medications result in mean weight loss in the range of 6% to 10%. Many of these medications are very expensive (more than $200 per month).10 Insurance preauthorization is commonly required for these medications. For ObGyns, it may be best to refer patients who would like to use a weight loss medication to a specialist or specialty center with expertise in using these medications.
Sustainable weight loss is very difficult to achieve through dieting alone. A multitude of dietary interventions have been presented as “revolutionary approaches” to the challenging problem of sustainable weight loss, including the Paleo diet, the Vegan diet, the low-carb diet, the Dukan diet, the ultra-lowfat diet, the Atkins diet, the HCG diet, the Zone diet, the South Beach diet, the plant-based diet, the Mediterranean diet, the Asian diet, and intermittent fasting. Recently, intermittent fasting has been presented as the latest and greatest approach to dieting, with the dual goals of achieving weight loss and improved health.1 In some animal models, intermittent dieting has been shown to increase life-span, a finding that has attracted great interest. A major goal of intermittent fasting is to promote “metabolic switching” with increased reliance on ketones to fuel cellular energy needs.
Two approaches to “prescribing” an intermittent fasting diet are to limit food intake to a period of 6 to 10 hours each day or to markedly reduce caloric intake one or two days per week, for example to 750 calories in a 24-hour period. There are no long-term studies of the health outcomes associated with intermittent fasting. In head-to-head clinical trials of intermittent fasting and daily calorie restriction (classic dieting), both diets result in similar weight loss. For example, in one clinical trial 100 obese participants, with a mean body mass index (BMI) of 34 kg/m2 , including 86 women, were randomly assigned to2:
1. intermittent fasting (25% of energy needs every other day)
2. daily calorie restriction (75% of energy needs every day), or
3. no intervention.
After 12 months of follow up, the participants in the no intervention group had gained 0.5% of their starting weight. The intermittent fasting and the daily calorie restriction groups had similar amounts of weight loss, approximately 5% of their starting weight. More individuals dropped out of the study from the intermittent fasting group than the daily calorie restriction group (38% vs 29%, respectively).
In another clinical trial, 107 overweight or obese premenopausal women, average age 40 years and mean BMI 31 kg/m2 , were randomly assigned to intermittent fasting (25% of energy needs 2 days per week) or daily calorie restriction (75% of energy needs daily) for 6 months. The mean weight of the participants at baseline was 83 kg. Weight loss was similar in the intermittent fasting and daily calorie restriction groups, 6.4 kg (-7.7%) and 5.6 kg (-6.7%), respectively (P=.4).3
The investigators concluded that intermittent fasting and daily calorie restriction could both be offered as effective approaches to weight loss. My conclusion is that intermittent fasting is not a miracle dietary intervention, but it is another important option in the armamentarium of weight loss interventions.
References
1. de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging and disease. N Engl J Med. 2019;381:2541-2551.
2. Trepanowski JF, Kroeger CM, Barnosky A, et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: a randomized clinical trial. JAMA Intern Med. 2017;177:930-938.
3. Harvie MN, Pegington M, Mattson MP, et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disc disease risk markers: a randomized trial in young overweight women. Int J Obes (Lond). 2011;35:714-727.
Sleeve gastrectomy
Two children are playing in a school yard. One child proudly states, “My mother is an endocrinologist. She treats diabetes.” Not to be outdone, the other child replies, “My mother is a bariatric surgeon. She cures diabetes.”
The dialogue reflects the reality that bariatric surgery results in more reliable and significant weight loss than diet, exercise, or weight loss medications. Diet, exercise, and weight loss medications often result in a 5% to 10% decrease in weight, but bariatric surgery typically results in a 25% decrease in weight. Until recently, 3 bariatric surgical procedures were commonly performed: Roux-en-Y gastric bypass (RYGB), sleeve gastrectomy (SG), and adjustable gastric banding (AGB). AGB is now seldom performed because it is less effective than RYGB and SG. Two recently published randomized trials compared the long-term outcomes associated with RYGB and SG. The studies found that SG and RYGB result in a similar degree of weight loss. RYGB resulted in slightly more weight loss than SG, but SG was associated with a lower rate of major complications, such as internal hernias. SG takes much less time to perform than RYGB. SG has become the most commonly performed bariatric surgery in premenopausal women considering pregnancy because of the low risk of internal hernias.
In the Swiss Multicenter Bypass or Sleeve Study (SM-BOSS), 217 participants with a mean BMI of 44 kg/m2 and mean age of 45.5 years were randomly assigned to RYGB or SG and followed for 5 years.11 The majority (72%) of the participants were women. At 5 years of follow-up, in the RYGB and SG groups, mean weight loss was 37 kg and 33 kg, respectively (P=.19). In both groups, weight loss nadir was reached 12 to 24 months after surgery. Expressed as a percentage of original weight, weight loss in the RYGB and SG groups was -29% and -25%, respectively (P=.02). Gastric reflux worsened in both the RYGB and SG groups (6% vs 32%, respectively). The number of reoperations in the RYGB and SG groups was 22% and 16%. Of note, among individuals with prevalent diabetes, RYGB and SG resulted in remission of the diabetes in 68% and 62% of participants, respectively.
In the Sleeve vs Bypass study (SLEEVEPASS), 240 participants, with mean BMI of 46 kg/m2 and mean age of 48 years, were randomly assigned to RYGB or SG and followed for 5 years.12 Most (70%) of the participants were women. Following bariatric surgery, BMI decreased significantly in both groups. In the RYGB group, BMI decreased from 48 kg/m2 preoperatively to 35.4 kg/m2 at 5 years of follow up. In the SG group, BMI decreased from 47 kg/m2 preoperatively to 36.5 kg/m2 at 5 years of follow up. Late major complications (defined as complications occurring from 30 days to 5 years postoperatively) occurred more frequently in the RYGB group (15%) versus the SG group (8%). All the late major complications required reoperation. In the SG group, 7 of 10 reoperations were for severe gastric reflux disease. In the RYGB group 17 of 18 reoperations were for suspected internal hernia, requiring closure of a mesenteric defect at reoperation. There was no treatment-related mortality during the 5-year follow up.
Guidelines for bariatric surgery are BMI ≥ 40 kg/m2 without a comorbid illness or BMI ≥ 35 kg/m2 with at least one serious comorbid disease, such as diabetes.13 ObGyns can build a synergistic relationship with bariatric surgeons by referring eligible patients for surgical consultation and, in return, accepting referrals. A paradox and challenge is that many health insurers require patients to complete a supervised medical weight loss management program prior to being approved for bariatric surgery. However, the medical weight loss program might result in the patient no longer being eligible for insurance coverage of their surgery. For example, a patient who had a BMI of 42 kg/m2 prior to a medical weight loss management program who then lost enough weight to achieve a BMI of 38 kg/m2 might no longer be eligible for insurance coverage of a bariatric operation.14
Continue to: ObGyns need to prioritize treatment for obesity...
ObGyns need to prioritize treatment for obesity
Between 1959 and 2014, US life expectancy increased from 69.9 years to 79.1 years. However, in 2015 and 2016 life expectancy in the United States decreased slightly to 78.9 years, while continuing to improve in other countries.15 What could cause such an unexpected trend? Some experts believe that excess overweight and obesity in the US population, resulting in increased rates of diabetes, hypertension, and heart disease, accounts for a significant proportion of the life expectancy gap between US citizens and those who reside in Australia, Finland, Japan, and Sweden.16,17 All frontline clinicians play an important role in reversing the decades-long trend of increasing rates of overweight and obesity. Interventions that ObGyns could prioritize in their practices for treating overweight and obese patients include: a calorie-restricted diet, exercise, metformin, and SG.
Obesity is a disease causing a public health crisis. In the United States, tobacco use and obesity are the two most important causes of preventable premature death. They result in an estimated 480,0001 and 300,0002 premature deaths per year, respectively. Obesity is a major contributor to diabetes mellitus, hypertension, dyslipidemia, and coronary heart disease. Obesity is also associated with increased rates of colon, breast, and endometrial cancer. Experts predict that in 2030, 50% of adults in the United States will have a body mass index (BMI) ≥ 30 kg/m2, and 25% will have a BMI ≥ 35 kg/m2.3 More women than men are predicted to be severely obese (FIGURE).3
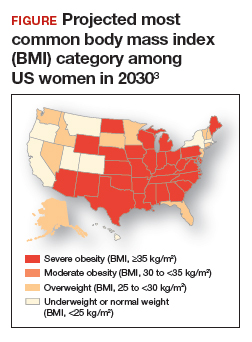
As clinicians we need to increase our efforts to reduce the epidemic of obesity. ObGyns can play an important role in preventing and managing obesity, by recommending primary-care weight management practices, prescribing medications that influence central metabolism, and referring appropriate patients to bariatric surgery centers of excellence.
Primary-care weight management
Measuring BMI and recommending interventions to prevent and treat obesity are important components of a health maintenance encounter. For women who are overweight or obese, dietary changes and exercise are important recommendations. The American Heart Association recommends the following lifestyle interventions4:
- Eat a high-quality diet that includes vegetables, fruit, whole grains, beans, legumes, nuts, plant-based protein, lean animal protein, and fish.
- Limit intake of sugary drinks and foods, fatty or processed meats, full-fat dairy products, eggs, highly processed foods, and tropical oils.
- Exercise at least 150 minutes weekly at a moderate activity level, including muscle-strengthening activity.
- Reduce prolonged intervals of sitting.
- Consider using an activity tracker to monitor activity level.
Clinicians should consider referring overweight and obese patients to a nutritionist for a consultation to plan how to consume a high-quality, low-calorie diet. A nutritionist can spend time with patients explaining options for implementing a calorie-restricted diet. In addition, some health insurers will require patients to participate in a supervised calorie-restricted diet plan for at least 6 months before authorizing coverage of expensive weight loss medications or bariatric surgery. In addition to recommending diet and exercise, ObGyns may consider prescribing metformin for their obese patients.
Continue to: Metformin...
Metformin
Metformin is approved for the treatment of type 2 diabetes mellitus. Unlike insulin therapy, which is associated with weight gain, metformin is associated with modest weight loss. The Diabetes Prevention Program (DPP) randomly assigned 3,234 nondiabetic participants with a fasting glucose level between 95 and 125 mg/dL and impaired glucose tolerance (140 to 199 mg/dL) after a 75-g oral glucose load to intensive lifestyle changes (calorie-restricted diet to achieve 7% weight loss plus 150 minutes of exercise weekly), metformin (850 mg twice daily), or placebo.5,6 The mean age of the participants was 51 years, with a mean BMI of 34 kg/m2. Most (68%) of the participants were women.
After 12 months of follow-up, mean weight loss in the intensive lifestyle change, metformin, and placebo groups was 6.5%, 2.7%, and 0.4%, respectively. After 2 years of treatment, weight loss among those who reliably took their metformin pills was approximately 4%, while participants in the placebo group had a 1% weight gain. Among those who continued to reliably take their metformin pills, the weight loss persisted through 9 years of follow up.
The mechanisms by which metformin causes weight loss are not clear. Metformin stimulates phosphorylation of adenosine monophosphate (AMP)-activated protein kinase, which regulates mitochondrial function, hepatic and muscle fatty acid oxidation, glucose transport, insulin secretion, and lipogenesis.7
Many ObGyns have experience in using metformin for the treatment of polycystic ovary syndrome or gestational diabetes. Hence, the dosing and adverse effects of metformin are familiar to many obstetricians-gynecologists. Metformin is contraindicated in individuals with creatinine clearance less than 30 mL/min. Rarely, metformin can cause lactic acidosis. According to Lexicomp,8 the most common adverse effects of metformin extended release (metformin ER) are diarrhea (17%), nausea and vomiting (7%), and decreased vitamin B12 concentration (7%) due to malabsorption in the terminal ileum. Of note, in the DPP study, hemoglobin concentration was slightly lower over time in the metformin compared with the placebo group (13.6 mg/dL vs 13.8 mg/dL, respectively; P<.001).6 Some experts recommend annual vitamin B12 measurement in individuals taking metformin.
In my practice, I only prescribe metformin ER. I usually start metformin treatment with one 750 mg ER tablet with dinner. If the patient tolerates that dose, I increase the dose to two 750 mg ER tablets with dinner. Metformin-induced adverse effects include diarrhea (17%) and nausea and vomiting (7%). Metformin ER is inexpensive. A one-month supply of metformin (sixty 750 mg tablets) costs between $4 and $21 at major pharmacies.9 Health insurance companies generally do not require preauthorization to cover metformin prescriptions.
Weight loss medications
US Food and Drug Administration (FDA)-approved weight loss medications include: liraglutide (Victoza), orlistat (Xenical, Alli), combination phentermine-extended release topiramate (Qsymia), and combination extended release naltrexone-bupropion (Contrave). All FDA-approved weight loss medications result in mean weight loss in the range of 6% to 10%. Many of these medications are very expensive (more than $200 per month).10 Insurance preauthorization is commonly required for these medications. For ObGyns, it may be best to refer patients who would like to use a weight loss medication to a specialist or specialty center with expertise in using these medications.
Sustainable weight loss is very difficult to achieve through dieting alone. A multitude of dietary interventions have been presented as “revolutionary approaches” to the challenging problem of sustainable weight loss, including the Paleo diet, the Vegan diet, the low-carb diet, the Dukan diet, the ultra-lowfat diet, the Atkins diet, the HCG diet, the Zone diet, the South Beach diet, the plant-based diet, the Mediterranean diet, the Asian diet, and intermittent fasting. Recently, intermittent fasting has been presented as the latest and greatest approach to dieting, with the dual goals of achieving weight loss and improved health.1 In some animal models, intermittent dieting has been shown to increase life-span, a finding that has attracted great interest. A major goal of intermittent fasting is to promote “metabolic switching” with increased reliance on ketones to fuel cellular energy needs.
Two approaches to “prescribing” an intermittent fasting diet are to limit food intake to a period of 6 to 10 hours each day or to markedly reduce caloric intake one or two days per week, for example to 750 calories in a 24-hour period. There are no long-term studies of the health outcomes associated with intermittent fasting. In head-to-head clinical trials of intermittent fasting and daily calorie restriction (classic dieting), both diets result in similar weight loss. For example, in one clinical trial 100 obese participants, with a mean body mass index (BMI) of 34 kg/m2 , including 86 women, were randomly assigned to2:
1. intermittent fasting (25% of energy needs every other day)
2. daily calorie restriction (75% of energy needs every day), or
3. no intervention.
After 12 months of follow up, the participants in the no intervention group had gained 0.5% of their starting weight. The intermittent fasting and the daily calorie restriction groups had similar amounts of weight loss, approximately 5% of their starting weight. More individuals dropped out of the study from the intermittent fasting group than the daily calorie restriction group (38% vs 29%, respectively).
In another clinical trial, 107 overweight or obese premenopausal women, average age 40 years and mean BMI 31 kg/m2 , were randomly assigned to intermittent fasting (25% of energy needs 2 days per week) or daily calorie restriction (75% of energy needs daily) for 6 months. The mean weight of the participants at baseline was 83 kg. Weight loss was similar in the intermittent fasting and daily calorie restriction groups, 6.4 kg (-7.7%) and 5.6 kg (-6.7%), respectively (P=.4).3
The investigators concluded that intermittent fasting and daily calorie restriction could both be offered as effective approaches to weight loss. My conclusion is that intermittent fasting is not a miracle dietary intervention, but it is another important option in the armamentarium of weight loss interventions.
References
1. de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging and disease. N Engl J Med. 2019;381:2541-2551.
2. Trepanowski JF, Kroeger CM, Barnosky A, et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: a randomized clinical trial. JAMA Intern Med. 2017;177:930-938.
3. Harvie MN, Pegington M, Mattson MP, et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disc disease risk markers: a randomized trial in young overweight women. Int J Obes (Lond). 2011;35:714-727.
Sleeve gastrectomy
Two children are playing in a school yard. One child proudly states, “My mother is an endocrinologist. She treats diabetes.” Not to be outdone, the other child replies, “My mother is a bariatric surgeon. She cures diabetes.”
The dialogue reflects the reality that bariatric surgery results in more reliable and significant weight loss than diet, exercise, or weight loss medications. Diet, exercise, and weight loss medications often result in a 5% to 10% decrease in weight, but bariatric surgery typically results in a 25% decrease in weight. Until recently, 3 bariatric surgical procedures were commonly performed: Roux-en-Y gastric bypass (RYGB), sleeve gastrectomy (SG), and adjustable gastric banding (AGB). AGB is now seldom performed because it is less effective than RYGB and SG. Two recently published randomized trials compared the long-term outcomes associated with RYGB and SG. The studies found that SG and RYGB result in a similar degree of weight loss. RYGB resulted in slightly more weight loss than SG, but SG was associated with a lower rate of major complications, such as internal hernias. SG takes much less time to perform than RYGB. SG has become the most commonly performed bariatric surgery in premenopausal women considering pregnancy because of the low risk of internal hernias.
In the Swiss Multicenter Bypass or Sleeve Study (SM-BOSS), 217 participants with a mean BMI of 44 kg/m2 and mean age of 45.5 years were randomly assigned to RYGB or SG and followed for 5 years.11 The majority (72%) of the participants were women. At 5 years of follow-up, in the RYGB and SG groups, mean weight loss was 37 kg and 33 kg, respectively (P=.19). In both groups, weight loss nadir was reached 12 to 24 months after surgery. Expressed as a percentage of original weight, weight loss in the RYGB and SG groups was -29% and -25%, respectively (P=.02). Gastric reflux worsened in both the RYGB and SG groups (6% vs 32%, respectively). The number of reoperations in the RYGB and SG groups was 22% and 16%. Of note, among individuals with prevalent diabetes, RYGB and SG resulted in remission of the diabetes in 68% and 62% of participants, respectively.
In the Sleeve vs Bypass study (SLEEVEPASS), 240 participants, with mean BMI of 46 kg/m2 and mean age of 48 years, were randomly assigned to RYGB or SG and followed for 5 years.12 Most (70%) of the participants were women. Following bariatric surgery, BMI decreased significantly in both groups. In the RYGB group, BMI decreased from 48 kg/m2 preoperatively to 35.4 kg/m2 at 5 years of follow up. In the SG group, BMI decreased from 47 kg/m2 preoperatively to 36.5 kg/m2 at 5 years of follow up. Late major complications (defined as complications occurring from 30 days to 5 years postoperatively) occurred more frequently in the RYGB group (15%) versus the SG group (8%). All the late major complications required reoperation. In the SG group, 7 of 10 reoperations were for severe gastric reflux disease. In the RYGB group 17 of 18 reoperations were for suspected internal hernia, requiring closure of a mesenteric defect at reoperation. There was no treatment-related mortality during the 5-year follow up.
Guidelines for bariatric surgery are BMI ≥ 40 kg/m2 without a comorbid illness or BMI ≥ 35 kg/m2 with at least one serious comorbid disease, such as diabetes.13 ObGyns can build a synergistic relationship with bariatric surgeons by referring eligible patients for surgical consultation and, in return, accepting referrals. A paradox and challenge is that many health insurers require patients to complete a supervised medical weight loss management program prior to being approved for bariatric surgery. However, the medical weight loss program might result in the patient no longer being eligible for insurance coverage of their surgery. For example, a patient who had a BMI of 42 kg/m2 prior to a medical weight loss management program who then lost enough weight to achieve a BMI of 38 kg/m2 might no longer be eligible for insurance coverage of a bariatric operation.14
Continue to: ObGyns need to prioritize treatment for obesity...
ObGyns need to prioritize treatment for obesity
Between 1959 and 2014, US life expectancy increased from 69.9 years to 79.1 years. However, in 2015 and 2016 life expectancy in the United States decreased slightly to 78.9 years, while continuing to improve in other countries.15 What could cause such an unexpected trend? Some experts believe that excess overweight and obesity in the US population, resulting in increased rates of diabetes, hypertension, and heart disease, accounts for a significant proportion of the life expectancy gap between US citizens and those who reside in Australia, Finland, Japan, and Sweden.16,17 All frontline clinicians play an important role in reversing the decades-long trend of increasing rates of overweight and obesity. Interventions that ObGyns could prioritize in their practices for treating overweight and obese patients include: a calorie-restricted diet, exercise, metformin, and SG.
- U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress. A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
- Allison DB, Fontaine KR, Manson JE, et al. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530-1538.
- Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381:2440-2450.
- American Heart Association. My life check | Life’s simple 7. https://www.heart.org/en/healthyliving/healthy-lifestyle/my-life-check--lifessimple-7. Reviewed May 2, 2018. Accessed February 10, 2020.
- Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
- Diabetes Prevention Program Research Group. Long-term safety, tolerability and weight loss associated with metformin in the Diabetes Prevention Program Outcomes Study. Diabetes Care. 2012;35:731-737.
- Winder WW, Hardie DG. Inactivation of acetylCoA carboxylase and activation of AMP-activated protein kinase in muscle during exercise. Am J Physiol. 1996;270(2 pt 1):E299-E304.
- Lexicomp. https://online.lexi.com/lco/action/ home. Accessed February 13, 2020.
- Metformin ER (Glucophage XR). GoodRX website. https://www.goodrx.com/metformin-erglucophage-xr?dosage=750mg&form=tablet&la bel_override=metformin+ER+%28Glucophage+X R%29&quantity=60. Accessed February 13, 2020.
- GoodRX website. www.goodrx.com. Accessed February 10, 2020.
- Peterli R, Wolnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018;319:255-265.
- Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: The SLEEVEPASS randomized clinical trial. JAMA. 2018;319:241-254.
- Rubino F, Nathan DM, Eckel RH, et al; Delegates of the 2nd Diabetes Surgery Summit. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Obes Surg. 2017;27:2-21.
- Gebran SG, Knighton B, Ngaage LM, et al. Insurance coverage criteria for bariatric surgery: a survey of policies. Obes Surg. 2020;30:707-713.
- Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959-2017. JAMA. 2019;322:1996-2016.
- Preston SH, Vierboom YC, Stokes A. The role of obesity in exceptionally slow US mortality improvement. Proc Natl Acad Sci U S A. 2019;115:957-961.
- Xu H, Cupples LA, Stokes A, et al. Association of obesity with mortality over 24 years of weight history: findings from the Framingham Heart Study. JAMA Network Open. 2018;1:e184587.
- U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress. A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
- Allison DB, Fontaine KR, Manson JE, et al. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530-1538.
- Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381:2440-2450.
- American Heart Association. My life check | Life’s simple 7. https://www.heart.org/en/healthyliving/healthy-lifestyle/my-life-check--lifessimple-7. Reviewed May 2, 2018. Accessed February 10, 2020.
- Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
- Diabetes Prevention Program Research Group. Long-term safety, tolerability and weight loss associated with metformin in the Diabetes Prevention Program Outcomes Study. Diabetes Care. 2012;35:731-737.
- Winder WW, Hardie DG. Inactivation of acetylCoA carboxylase and activation of AMP-activated protein kinase in muscle during exercise. Am J Physiol. 1996;270(2 pt 1):E299-E304.
- Lexicomp. https://online.lexi.com/lco/action/ home. Accessed February 13, 2020.
- Metformin ER (Glucophage XR). GoodRX website. https://www.goodrx.com/metformin-erglucophage-xr?dosage=750mg&form=tablet&la bel_override=metformin+ER+%28Glucophage+X R%29&quantity=60. Accessed February 13, 2020.
- GoodRX website. www.goodrx.com. Accessed February 10, 2020.
- Peterli R, Wolnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018;319:255-265.
- Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: The SLEEVEPASS randomized clinical trial. JAMA. 2018;319:241-254.
- Rubino F, Nathan DM, Eckel RH, et al; Delegates of the 2nd Diabetes Surgery Summit. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Obes Surg. 2017;27:2-21.
- Gebran SG, Knighton B, Ngaage LM, et al. Insurance coverage criteria for bariatric surgery: a survey of policies. Obes Surg. 2020;30:707-713.
- Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959-2017. JAMA. 2019;322:1996-2016.
- Preston SH, Vierboom YC, Stokes A. The role of obesity in exceptionally slow US mortality improvement. Proc Natl Acad Sci U S A. 2019;115:957-961.
- Xu H, Cupples LA, Stokes A, et al. Association of obesity with mortality over 24 years of weight history: findings from the Framingham Heart Study. JAMA Network Open. 2018;1:e184587.
Paradise lost: Life, liberty, and the pursuit of happiness among psychiatric patients
The United States Declaration of Independence is widely known for the words that begin its second paragraph:
We hold these truths to be self-evident, that all men are created equal, that they are endowed by their Creator with certain unalienable Rights, that among these are Life, Liberty and the pursuit of Happiness.
Those basic rights are accessible and exercised by all healthy US citizens, but for many individuals with psychiatric disorders, those inalienable rights may be elusive. Consider how they are compromised by untreated psychiatric illness.
Life. This is the most basic right. In the United States, healthy individuals cherish being alive, and many take it for granted, unlike the residents of nondemocratic countries, where persons may be killed by dictators for political or other reasons (Stalin and Hitler murdered millions of innocent people). In the past, persons with mental illness were considered possessed by demons and were killed or burned at the stake (as in the Middle Ages). But unfortunately, the current major risk for the loss of life among psychiatric patients is the patients themselves. Suicidal urges, attempts, and completions are of epidemic proportions and continue to rise every year. Our patients end their own lives because their illness prompts them to relinquish their life and to embrace untimely death. And once life is lost, all other rights are abdicated. Suicide attempts are common among patients who are diagnosed with bipolar disorder, major depressive disorder, schizophrenia, anxiety, obsessive-compulsive disorder (OCD), posttraumatic stress disorder, and borderline personality disorder. Sometimes, suicide is unintentional, such as when a patient with a substance use disorder inadvertently overdoses (as in the contemporary opioid epidemic) or ingests drugs laced with a deadly substance. For many untreated patients, life can be so fragile, tenuous, and tragically brief.
Liberty. Healthy citizens in the United States (and other democratic countries) have many liberties: where to live, what to do, where to move, what to say, what to believe, who to assemble with, what to eat or drink, whom to befriend, whom to marry, whether or not to procreate, and what to wear. They can choose to be an activist for any cause, no matter how quaint, or to disfigure their bodies with tattoos or piercings.
In contrast, the liberties of individuals with a psychiatric disorder can be compromised. In fact, patients’ liberties can be seriously shackled by their illness. A person with untreated schizophrenia can be enslaved by fixed irrational beliefs that may constrain their choices or determine how they live or relate to others. Command hallucinations can dictate what a patient should or mustn’t do. Poor reality testing detrimentally limits the options of a person with psychosis. A lack of insight deprives a patient with schizophrenia from rational decision-making. Self-neglect leads to physical, mental, and social deterioration.
For persons with depression, the range of liberties is shattered by social withdrawal, overwhelming guilt, sense of worthlessness, dismal hopelessness, doleful ruminations, and loss of appetite or sleep. The only rights that people with depression may exercise is to injure their body or end their life.
Think also of patients with OCD, who are subjugated by their ongoing obsessions or compulsive rituals; think of those with panic disorder who are unable to leave their home due to agoraphobia or
Continue to: Happiness
Happiness. I often wonder if most Americans these days are pursuing pleasure rather than happiness, seeking the momentary thrill and gratification instead of long-lasting happiness and joy. But persons with psychiatric brain disorders have great difficulty pursuing either pleasure or happiness. Anhedonia is a common symptom in schizophrenia and depression, depriving patients from experiencing enjoyable activities (ie, having fun) as they used to do before they got sick. Persons with anxiety have such emotional turmoil, it is hard for them to experience pleasure or happiness when feelings of impending doom permeates their souls. Persons with an addictive disorder are coerced to seek their substance for a momentary reward, only to spend a much longer time craving and seeking their substance of choice again and again. On the other end of the spectrum, for persons with mania, the excessive pursuit of high-risk pleasures can have grave consequences or embarrassment after they recover.
Happiness for patients with mental illness is possible only when they emerge from their illness and are “liberated” from the symptoms that disrupt their lives. As psychiatrists, we don’t just evaluate and treat patients with psychiatric illness—we restore their liberties and ability to pursue happiness and enjoy small pleasures.
The motto on the seal of the American University of Beirut, which I attended in my youth, is “That they may have life, and to have it abundantly.” As I have grown older and wiser, I have come to realize the true meaning of that motto. Life is a right we take for granted, but without it, we cannot exercise the various liberties, or be able to pursue happiness. I exercised my right to become a psychiatrist, and that provided me with lifelong happiness and satisfaction, especially when I prevent the loss of life of my patients, restore their liberty by ridding them of illness, and resurrect their ability to experience pleasure and pursue happiness.
The United States Declaration of Independence is widely known for the words that begin its second paragraph:
We hold these truths to be self-evident, that all men are created equal, that they are endowed by their Creator with certain unalienable Rights, that among these are Life, Liberty and the pursuit of Happiness.
Those basic rights are accessible and exercised by all healthy US citizens, but for many individuals with psychiatric disorders, those inalienable rights may be elusive. Consider how they are compromised by untreated psychiatric illness.
Life. This is the most basic right. In the United States, healthy individuals cherish being alive, and many take it for granted, unlike the residents of nondemocratic countries, where persons may be killed by dictators for political or other reasons (Stalin and Hitler murdered millions of innocent people). In the past, persons with mental illness were considered possessed by demons and were killed or burned at the stake (as in the Middle Ages). But unfortunately, the current major risk for the loss of life among psychiatric patients is the patients themselves. Suicidal urges, attempts, and completions are of epidemic proportions and continue to rise every year. Our patients end their own lives because their illness prompts them to relinquish their life and to embrace untimely death. And once life is lost, all other rights are abdicated. Suicide attempts are common among patients who are diagnosed with bipolar disorder, major depressive disorder, schizophrenia, anxiety, obsessive-compulsive disorder (OCD), posttraumatic stress disorder, and borderline personality disorder. Sometimes, suicide is unintentional, such as when a patient with a substance use disorder inadvertently overdoses (as in the contemporary opioid epidemic) or ingests drugs laced with a deadly substance. For many untreated patients, life can be so fragile, tenuous, and tragically brief.
Liberty. Healthy citizens in the United States (and other democratic countries) have many liberties: where to live, what to do, where to move, what to say, what to believe, who to assemble with, what to eat or drink, whom to befriend, whom to marry, whether or not to procreate, and what to wear. They can choose to be an activist for any cause, no matter how quaint, or to disfigure their bodies with tattoos or piercings.
In contrast, the liberties of individuals with a psychiatric disorder can be compromised. In fact, patients’ liberties can be seriously shackled by their illness. A person with untreated schizophrenia can be enslaved by fixed irrational beliefs that may constrain their choices or determine how they live or relate to others. Command hallucinations can dictate what a patient should or mustn’t do. Poor reality testing detrimentally limits the options of a person with psychosis. A lack of insight deprives a patient with schizophrenia from rational decision-making. Self-neglect leads to physical, mental, and social deterioration.
For persons with depression, the range of liberties is shattered by social withdrawal, overwhelming guilt, sense of worthlessness, dismal hopelessness, doleful ruminations, and loss of appetite or sleep. The only rights that people with depression may exercise is to injure their body or end their life.
Think also of patients with OCD, who are subjugated by their ongoing obsessions or compulsive rituals; think of those with panic disorder who are unable to leave their home due to agoraphobia or
Continue to: Happiness
Happiness. I often wonder if most Americans these days are pursuing pleasure rather than happiness, seeking the momentary thrill and gratification instead of long-lasting happiness and joy. But persons with psychiatric brain disorders have great difficulty pursuing either pleasure or happiness. Anhedonia is a common symptom in schizophrenia and depression, depriving patients from experiencing enjoyable activities (ie, having fun) as they used to do before they got sick. Persons with anxiety have such emotional turmoil, it is hard for them to experience pleasure or happiness when feelings of impending doom permeates their souls. Persons with an addictive disorder are coerced to seek their substance for a momentary reward, only to spend a much longer time craving and seeking their substance of choice again and again. On the other end of the spectrum, for persons with mania, the excessive pursuit of high-risk pleasures can have grave consequences or embarrassment after they recover.
Happiness for patients with mental illness is possible only when they emerge from their illness and are “liberated” from the symptoms that disrupt their lives. As psychiatrists, we don’t just evaluate and treat patients with psychiatric illness—we restore their liberties and ability to pursue happiness and enjoy small pleasures.
The motto on the seal of the American University of Beirut, which I attended in my youth, is “That they may have life, and to have it abundantly.” As I have grown older and wiser, I have come to realize the true meaning of that motto. Life is a right we take for granted, but without it, we cannot exercise the various liberties, or be able to pursue happiness. I exercised my right to become a psychiatrist, and that provided me with lifelong happiness and satisfaction, especially when I prevent the loss of life of my patients, restore their liberty by ridding them of illness, and resurrect their ability to experience pleasure and pursue happiness.
The United States Declaration of Independence is widely known for the words that begin its second paragraph:
We hold these truths to be self-evident, that all men are created equal, that they are endowed by their Creator with certain unalienable Rights, that among these are Life, Liberty and the pursuit of Happiness.
Those basic rights are accessible and exercised by all healthy US citizens, but for many individuals with psychiatric disorders, those inalienable rights may be elusive. Consider how they are compromised by untreated psychiatric illness.
Life. This is the most basic right. In the United States, healthy individuals cherish being alive, and many take it for granted, unlike the residents of nondemocratic countries, where persons may be killed by dictators for political or other reasons (Stalin and Hitler murdered millions of innocent people). In the past, persons with mental illness were considered possessed by demons and were killed or burned at the stake (as in the Middle Ages). But unfortunately, the current major risk for the loss of life among psychiatric patients is the patients themselves. Suicidal urges, attempts, and completions are of epidemic proportions and continue to rise every year. Our patients end their own lives because their illness prompts them to relinquish their life and to embrace untimely death. And once life is lost, all other rights are abdicated. Suicide attempts are common among patients who are diagnosed with bipolar disorder, major depressive disorder, schizophrenia, anxiety, obsessive-compulsive disorder (OCD), posttraumatic stress disorder, and borderline personality disorder. Sometimes, suicide is unintentional, such as when a patient with a substance use disorder inadvertently overdoses (as in the contemporary opioid epidemic) or ingests drugs laced with a deadly substance. For many untreated patients, life can be so fragile, tenuous, and tragically brief.
Liberty. Healthy citizens in the United States (and other democratic countries) have many liberties: where to live, what to do, where to move, what to say, what to believe, who to assemble with, what to eat or drink, whom to befriend, whom to marry, whether or not to procreate, and what to wear. They can choose to be an activist for any cause, no matter how quaint, or to disfigure their bodies with tattoos or piercings.
In contrast, the liberties of individuals with a psychiatric disorder can be compromised. In fact, patients’ liberties can be seriously shackled by their illness. A person with untreated schizophrenia can be enslaved by fixed irrational beliefs that may constrain their choices or determine how they live or relate to others. Command hallucinations can dictate what a patient should or mustn’t do. Poor reality testing detrimentally limits the options of a person with psychosis. A lack of insight deprives a patient with schizophrenia from rational decision-making. Self-neglect leads to physical, mental, and social deterioration.
For persons with depression, the range of liberties is shattered by social withdrawal, overwhelming guilt, sense of worthlessness, dismal hopelessness, doleful ruminations, and loss of appetite or sleep. The only rights that people with depression may exercise is to injure their body or end their life.
Think also of patients with OCD, who are subjugated by their ongoing obsessions or compulsive rituals; think of those with panic disorder who are unable to leave their home due to agoraphobia or
Continue to: Happiness
Happiness. I often wonder if most Americans these days are pursuing pleasure rather than happiness, seeking the momentary thrill and gratification instead of long-lasting happiness and joy. But persons with psychiatric brain disorders have great difficulty pursuing either pleasure or happiness. Anhedonia is a common symptom in schizophrenia and depression, depriving patients from experiencing enjoyable activities (ie, having fun) as they used to do before they got sick. Persons with anxiety have such emotional turmoil, it is hard for them to experience pleasure or happiness when feelings of impending doom permeates their souls. Persons with an addictive disorder are coerced to seek their substance for a momentary reward, only to spend a much longer time craving and seeking their substance of choice again and again. On the other end of the spectrum, for persons with mania, the excessive pursuit of high-risk pleasures can have grave consequences or embarrassment after they recover.
Happiness for patients with mental illness is possible only when they emerge from their illness and are “liberated” from the symptoms that disrupt their lives. As psychiatrists, we don’t just evaluate and treat patients with psychiatric illness—we restore their liberties and ability to pursue happiness and enjoy small pleasures.
The motto on the seal of the American University of Beirut, which I attended in my youth, is “That they may have life, and to have it abundantly.” As I have grown older and wiser, I have come to realize the true meaning of that motto. Life is a right we take for granted, but without it, we cannot exercise the various liberties, or be able to pursue happiness. I exercised my right to become a psychiatrist, and that provided me with lifelong happiness and satisfaction, especially when I prevent the loss of life of my patients, restore their liberty by ridding them of illness, and resurrect their ability to experience pleasure and pursue happiness.



