User login
Intercepting Wrong-Patient Orders in a Computerized Provider Order Entry System
Clinical question: Does implementing a patient verification dialog that appears at the beginning of each ordering session, accompanied by a 2.5-second delay, decrease wrong-patient orders?
Background: Computerized provider order entry (CPOE) is known to increase the rate of wrong-patient order entry and, although the rate in the ED has not been well characterized, CPOE wrong-patient order entry has been known to lead to fatalities in the emergency setting.
Study design: A parallel-controlled, experimental, before-after design.
Setting: Five teaching hospital EDs were included in New York City: two adult EDs, two pediatric EDs, and a combined ED, all totaling 250,000 annual visits.
Synopsis: The EDs in this study implemented a patient verification module into their Allscripts system. This verification included three identifiers: full name, birth date, and medical record number. A 2.5-second delay in ability to close the alert was implemented. All patients in the ED rooms were included in the analysis. The primary outcome was intercepted wrong-patient orders, as measured by number of retract and re-order events.
A baseline data set over four months was compared to immediate post-intervention data, as well as data two years post-intervention, with 30% and 25% reductions in the rate of wrong-patient orders, respectively. Of all retractions, 41% were for diagnostic procedures, 21% for medications, and 38% were nursing and miscellaneous orders. The majority of orders were placed by resident physicians (51%), followed by attending physicians (34%), physician assistants (12%), and others (3%).
This method of observation is limited to identified and corrected wrong-patient orders.
Bottom line: Implementing a patient verification alert can significantly decrease the number of order retractions and re-orders due to wrong-patient order entry in the ED setting.
Citation: Green RA, Hripcsak G, Salmasian H, et al. Intercepting wrong-patient orders in a computerized provider order entry system [published online ahead of print December 17, 2014]. Ann Emerg Med.
Clinical question: Does implementing a patient verification dialog that appears at the beginning of each ordering session, accompanied by a 2.5-second delay, decrease wrong-patient orders?
Background: Computerized provider order entry (CPOE) is known to increase the rate of wrong-patient order entry and, although the rate in the ED has not been well characterized, CPOE wrong-patient order entry has been known to lead to fatalities in the emergency setting.
Study design: A parallel-controlled, experimental, before-after design.
Setting: Five teaching hospital EDs were included in New York City: two adult EDs, two pediatric EDs, and a combined ED, all totaling 250,000 annual visits.
Synopsis: The EDs in this study implemented a patient verification module into their Allscripts system. This verification included three identifiers: full name, birth date, and medical record number. A 2.5-second delay in ability to close the alert was implemented. All patients in the ED rooms were included in the analysis. The primary outcome was intercepted wrong-patient orders, as measured by number of retract and re-order events.
A baseline data set over four months was compared to immediate post-intervention data, as well as data two years post-intervention, with 30% and 25% reductions in the rate of wrong-patient orders, respectively. Of all retractions, 41% were for diagnostic procedures, 21% for medications, and 38% were nursing and miscellaneous orders. The majority of orders were placed by resident physicians (51%), followed by attending physicians (34%), physician assistants (12%), and others (3%).
This method of observation is limited to identified and corrected wrong-patient orders.
Bottom line: Implementing a patient verification alert can significantly decrease the number of order retractions and re-orders due to wrong-patient order entry in the ED setting.
Citation: Green RA, Hripcsak G, Salmasian H, et al. Intercepting wrong-patient orders in a computerized provider order entry system [published online ahead of print December 17, 2014]. Ann Emerg Med.
Clinical question: Does implementing a patient verification dialog that appears at the beginning of each ordering session, accompanied by a 2.5-second delay, decrease wrong-patient orders?
Background: Computerized provider order entry (CPOE) is known to increase the rate of wrong-patient order entry and, although the rate in the ED has not been well characterized, CPOE wrong-patient order entry has been known to lead to fatalities in the emergency setting.
Study design: A parallel-controlled, experimental, before-after design.
Setting: Five teaching hospital EDs were included in New York City: two adult EDs, two pediatric EDs, and a combined ED, all totaling 250,000 annual visits.
Synopsis: The EDs in this study implemented a patient verification module into their Allscripts system. This verification included three identifiers: full name, birth date, and medical record number. A 2.5-second delay in ability to close the alert was implemented. All patients in the ED rooms were included in the analysis. The primary outcome was intercepted wrong-patient orders, as measured by number of retract and re-order events.
A baseline data set over four months was compared to immediate post-intervention data, as well as data two years post-intervention, with 30% and 25% reductions in the rate of wrong-patient orders, respectively. Of all retractions, 41% were for diagnostic procedures, 21% for medications, and 38% were nursing and miscellaneous orders. The majority of orders were placed by resident physicians (51%), followed by attending physicians (34%), physician assistants (12%), and others (3%).
This method of observation is limited to identified and corrected wrong-patient orders.
Bottom line: Implementing a patient verification alert can significantly decrease the number of order retractions and re-orders due to wrong-patient order entry in the ED setting.
Citation: Green RA, Hripcsak G, Salmasian H, et al. Intercepting wrong-patient orders in a computerized provider order entry system [published online ahead of print December 17, 2014]. Ann Emerg Med.
Epidemiology of Peri-Operative, Transfusion-Associated, Circulatory Overload
Clinical question: What is the incidence of transfusion-associated circulatory overload (TACO) as it relates to specific characteristics of patients and transfusion situations?
Background: TACO is the second-leading cause of transfusion-related fatalities; however, the epidemiology of TACO is centered mostly on patients in the ICU, and the epidemiology for noncardiac surgical patients is not well characterized. This might result in suboptimal care delivery and unfavorable outcomes in peri-operative patients.
Study design: Retrospective cohort study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Using an electronic algorithm, 2,162 and 1,908 patients in 2004 and 2011, respectively, were screened for TACO if they received intra-operative transfusions during noncardiac surgery with general anesthesia. Analyses evaluated associations between patient and transfusion characteristics with TACO rates. Patients with TACO were compared to complication-free transfused counterparts.
The incidence of TACO increased significantly with the volume of blood product transfused, advanced age, and total intra-operative fluid balance. Mixed blood products had highest incidence of TACO, followed by fresh frozen plasma. Vascular, transplant, and thoracic surgeries had the highest, and obstetric and gynecologic surgeries the lowest TACO rates. Patients with TACO, compared with their counterparts, had a longer ICU and hospital length of stay.
The study population is derived from a single tertiary care referral center and confounded by referral bias, and, therefore, not easily generalizable. Also, results cannot be generalized to nongeneral anesthesia patients.
Although associations were noted between certain characteristics and the development of TACO, more robust and definitive evaluations of TACO risk factors are needed, as many rates were not adjusted for confounding factors.
Bottom line: Understanding characteristics of at-risk patients may facilitate improved decision making regarding transfusion strategies for peri-operative noncardiac surgical patients.
Citation: Clifford L, Jia Q, Yadav H, et al. Characterizing the epidemiology of perioperative transfusion-associated circulatory overload. Anesthesiology. 2015;122(1):21-28.
Clinical question: What is the incidence of transfusion-associated circulatory overload (TACO) as it relates to specific characteristics of patients and transfusion situations?
Background: TACO is the second-leading cause of transfusion-related fatalities; however, the epidemiology of TACO is centered mostly on patients in the ICU, and the epidemiology for noncardiac surgical patients is not well characterized. This might result in suboptimal care delivery and unfavorable outcomes in peri-operative patients.
Study design: Retrospective cohort study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Using an electronic algorithm, 2,162 and 1,908 patients in 2004 and 2011, respectively, were screened for TACO if they received intra-operative transfusions during noncardiac surgery with general anesthesia. Analyses evaluated associations between patient and transfusion characteristics with TACO rates. Patients with TACO were compared to complication-free transfused counterparts.
The incidence of TACO increased significantly with the volume of blood product transfused, advanced age, and total intra-operative fluid balance. Mixed blood products had highest incidence of TACO, followed by fresh frozen plasma. Vascular, transplant, and thoracic surgeries had the highest, and obstetric and gynecologic surgeries the lowest TACO rates. Patients with TACO, compared with their counterparts, had a longer ICU and hospital length of stay.
The study population is derived from a single tertiary care referral center and confounded by referral bias, and, therefore, not easily generalizable. Also, results cannot be generalized to nongeneral anesthesia patients.
Although associations were noted between certain characteristics and the development of TACO, more robust and definitive evaluations of TACO risk factors are needed, as many rates were not adjusted for confounding factors.
Bottom line: Understanding characteristics of at-risk patients may facilitate improved decision making regarding transfusion strategies for peri-operative noncardiac surgical patients.
Citation: Clifford L, Jia Q, Yadav H, et al. Characterizing the epidemiology of perioperative transfusion-associated circulatory overload. Anesthesiology. 2015;122(1):21-28.
Clinical question: What is the incidence of transfusion-associated circulatory overload (TACO) as it relates to specific characteristics of patients and transfusion situations?
Background: TACO is the second-leading cause of transfusion-related fatalities; however, the epidemiology of TACO is centered mostly on patients in the ICU, and the epidemiology for noncardiac surgical patients is not well characterized. This might result in suboptimal care delivery and unfavorable outcomes in peri-operative patients.
Study design: Retrospective cohort study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Using an electronic algorithm, 2,162 and 1,908 patients in 2004 and 2011, respectively, were screened for TACO if they received intra-operative transfusions during noncardiac surgery with general anesthesia. Analyses evaluated associations between patient and transfusion characteristics with TACO rates. Patients with TACO were compared to complication-free transfused counterparts.
The incidence of TACO increased significantly with the volume of blood product transfused, advanced age, and total intra-operative fluid balance. Mixed blood products had highest incidence of TACO, followed by fresh frozen plasma. Vascular, transplant, and thoracic surgeries had the highest, and obstetric and gynecologic surgeries the lowest TACO rates. Patients with TACO, compared with their counterparts, had a longer ICU and hospital length of stay.
The study population is derived from a single tertiary care referral center and confounded by referral bias, and, therefore, not easily generalizable. Also, results cannot be generalized to nongeneral anesthesia patients.
Although associations were noted between certain characteristics and the development of TACO, more robust and definitive evaluations of TACO risk factors are needed, as many rates were not adjusted for confounding factors.
Bottom line: Understanding characteristics of at-risk patients may facilitate improved decision making regarding transfusion strategies for peri-operative noncardiac surgical patients.
Citation: Clifford L, Jia Q, Yadav H, et al. Characterizing the epidemiology of perioperative transfusion-associated circulatory overload. Anesthesiology. 2015;122(1):21-28.
The Spectrum of Acute Encephalitis
Clinical question: What characteristics in patients with acute encephalitis portend a worse prognosis?
Background: Acute encephalitis is a serious neurologic disease with high levels of associated morbidity, mortality, and cost of care. Yet, little is known about the factors that affect the outcome of patients with encephalitis.
Study design: Retrospective chart review of all consecutive patients diagnosed with acute encephalitis.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: A retrospective chart review revealed 198 patients with encephalitis, grouped into viral, autoimmune, or unknown/other encephalitis categories, with mortality rates of 8%, 12%, and 5%, respectively. Researchers calculated a modified Rankin Scale score (mRS) on factors associated with good (mRS=0-2) or poor (mRS=3-6) outcome after one year. Factors associated with poor outcome included age 65 or older, immunocompromised state, coma, mechanical ventilation, and acute thrombocytopenia. Unlike some previous studies, MRI findings and seizure activity did not portend a poor outcome. For viral encephalitis, cerebrospinal fluid polymorphonuclear cell count was also strongly associated with poor outcome.
This is one of the first studies to evaluate functional outcome or distant follow-up; however, it has inherent biases related to the retrospective design, and the results are not necessarily generalizable to all hospitals; there might be an underlying referral bias, given the fact that one third of the patients were referred to the center for further evaluation.
This study does suggest aggressive treatment should be pursued, even in patients with severe presentation, given the possibility of favorable recovery.
Bottom line: Advanced age, immunocompromised state, coma, mechanical ventilation, and acute thrombocytopenia portend a worse outcome for patients with acute encephalitis.
Citation: Singh TD, Fugate JE, Rabinstein AA. The spectrum of acute encephalitis: causes, management, and predictors of outcome. Neurology. 2015;84(4):359-366.
Clinical question: What characteristics in patients with acute encephalitis portend a worse prognosis?
Background: Acute encephalitis is a serious neurologic disease with high levels of associated morbidity, mortality, and cost of care. Yet, little is known about the factors that affect the outcome of patients with encephalitis.
Study design: Retrospective chart review of all consecutive patients diagnosed with acute encephalitis.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: A retrospective chart review revealed 198 patients with encephalitis, grouped into viral, autoimmune, or unknown/other encephalitis categories, with mortality rates of 8%, 12%, and 5%, respectively. Researchers calculated a modified Rankin Scale score (mRS) on factors associated with good (mRS=0-2) or poor (mRS=3-6) outcome after one year. Factors associated with poor outcome included age 65 or older, immunocompromised state, coma, mechanical ventilation, and acute thrombocytopenia. Unlike some previous studies, MRI findings and seizure activity did not portend a poor outcome. For viral encephalitis, cerebrospinal fluid polymorphonuclear cell count was also strongly associated with poor outcome.
This is one of the first studies to evaluate functional outcome or distant follow-up; however, it has inherent biases related to the retrospective design, and the results are not necessarily generalizable to all hospitals; there might be an underlying referral bias, given the fact that one third of the patients were referred to the center for further evaluation.
This study does suggest aggressive treatment should be pursued, even in patients with severe presentation, given the possibility of favorable recovery.
Bottom line: Advanced age, immunocompromised state, coma, mechanical ventilation, and acute thrombocytopenia portend a worse outcome for patients with acute encephalitis.
Citation: Singh TD, Fugate JE, Rabinstein AA. The spectrum of acute encephalitis: causes, management, and predictors of outcome. Neurology. 2015;84(4):359-366.
Clinical question: What characteristics in patients with acute encephalitis portend a worse prognosis?
Background: Acute encephalitis is a serious neurologic disease with high levels of associated morbidity, mortality, and cost of care. Yet, little is known about the factors that affect the outcome of patients with encephalitis.
Study design: Retrospective chart review of all consecutive patients diagnosed with acute encephalitis.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: A retrospective chart review revealed 198 patients with encephalitis, grouped into viral, autoimmune, or unknown/other encephalitis categories, with mortality rates of 8%, 12%, and 5%, respectively. Researchers calculated a modified Rankin Scale score (mRS) on factors associated with good (mRS=0-2) or poor (mRS=3-6) outcome after one year. Factors associated with poor outcome included age 65 or older, immunocompromised state, coma, mechanical ventilation, and acute thrombocytopenia. Unlike some previous studies, MRI findings and seizure activity did not portend a poor outcome. For viral encephalitis, cerebrospinal fluid polymorphonuclear cell count was also strongly associated with poor outcome.
This is one of the first studies to evaluate functional outcome or distant follow-up; however, it has inherent biases related to the retrospective design, and the results are not necessarily generalizable to all hospitals; there might be an underlying referral bias, given the fact that one third of the patients were referred to the center for further evaluation.
This study does suggest aggressive treatment should be pursued, even in patients with severe presentation, given the possibility of favorable recovery.
Bottom line: Advanced age, immunocompromised state, coma, mechanical ventilation, and acute thrombocytopenia portend a worse outcome for patients with acute encephalitis.
Citation: Singh TD, Fugate JE, Rabinstein AA. The spectrum of acute encephalitis: causes, management, and predictors of outcome. Neurology. 2015;84(4):359-366.
Peri-Operative Hyperglycemia and Risk of Adverse Events in Diabetic Patients
Clinical question: How does peri-operative hyperglycemia affect the risk of adverse events in diabetic patients compared to nondiabetic patients?
Background: Peri-operative hyperglycemia is associated with increased rates of infection, myocardial infarction, stroke, and death. Recent studies suggest that nondiabetics are more prone to hyperglycemia-related complications than diabetics. This study sought to analyze the effect and mechanism by which nondiabetics may be at increased risk for such complications.
Study Design: Retrospective cohort study.
Setting: Fifty-three hospitals in Washington.
Synopsis: Among 40,836 patients who underwent surgery, diabetics had a higher rate of peri-operative adverse events overall compared to nondiabetics (12% vs. 9%, P<0.001). Peri-operative hyperglycemia, defined as blood glucose 180 or greater, was also associated with an increased rate of adverse events. Ironically, this association was more significant in nondiabetic patients [OR 1.6; 95% CI, 1.3-2.1] than in diabetic patients (OR, 0.8; 95% CI, 0.6-1.0). Although the exact reason for this is unknown, existing theories include the following:
- Diabetics are more apt to receive insulin for peri-operative hyperglycemia than nondiabetics (P<0.001);
- Hyperglycemia in diabetics may be a less reliable marker of surgical stress than in nondiabetics; and
- Diabetics may be better adapted to hyperglycemia than nondiabetics.
Bottom Line: Peri-operative hyperglycemia leads to an increased risk of adverse events; this relationship is more pronounced in nondiabetic patients than in diabetic patients.
Citation: Kotagal M, Symons RG, Hirsch IB, et al. Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg. 2015;261(1):97-103.
Clinical question: How does peri-operative hyperglycemia affect the risk of adverse events in diabetic patients compared to nondiabetic patients?
Background: Peri-operative hyperglycemia is associated with increased rates of infection, myocardial infarction, stroke, and death. Recent studies suggest that nondiabetics are more prone to hyperglycemia-related complications than diabetics. This study sought to analyze the effect and mechanism by which nondiabetics may be at increased risk for such complications.
Study Design: Retrospective cohort study.
Setting: Fifty-three hospitals in Washington.
Synopsis: Among 40,836 patients who underwent surgery, diabetics had a higher rate of peri-operative adverse events overall compared to nondiabetics (12% vs. 9%, P<0.001). Peri-operative hyperglycemia, defined as blood glucose 180 or greater, was also associated with an increased rate of adverse events. Ironically, this association was more significant in nondiabetic patients [OR 1.6; 95% CI, 1.3-2.1] than in diabetic patients (OR, 0.8; 95% CI, 0.6-1.0). Although the exact reason for this is unknown, existing theories include the following:
- Diabetics are more apt to receive insulin for peri-operative hyperglycemia than nondiabetics (P<0.001);
- Hyperglycemia in diabetics may be a less reliable marker of surgical stress than in nondiabetics; and
- Diabetics may be better adapted to hyperglycemia than nondiabetics.
Bottom Line: Peri-operative hyperglycemia leads to an increased risk of adverse events; this relationship is more pronounced in nondiabetic patients than in diabetic patients.
Citation: Kotagal M, Symons RG, Hirsch IB, et al. Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg. 2015;261(1):97-103.
Clinical question: How does peri-operative hyperglycemia affect the risk of adverse events in diabetic patients compared to nondiabetic patients?
Background: Peri-operative hyperglycemia is associated with increased rates of infection, myocardial infarction, stroke, and death. Recent studies suggest that nondiabetics are more prone to hyperglycemia-related complications than diabetics. This study sought to analyze the effect and mechanism by which nondiabetics may be at increased risk for such complications.
Study Design: Retrospective cohort study.
Setting: Fifty-three hospitals in Washington.
Synopsis: Among 40,836 patients who underwent surgery, diabetics had a higher rate of peri-operative adverse events overall compared to nondiabetics (12% vs. 9%, P<0.001). Peri-operative hyperglycemia, defined as blood glucose 180 or greater, was also associated with an increased rate of adverse events. Ironically, this association was more significant in nondiabetic patients [OR 1.6; 95% CI, 1.3-2.1] than in diabetic patients (OR, 0.8; 95% CI, 0.6-1.0). Although the exact reason for this is unknown, existing theories include the following:
- Diabetics are more apt to receive insulin for peri-operative hyperglycemia than nondiabetics (P<0.001);
- Hyperglycemia in diabetics may be a less reliable marker of surgical stress than in nondiabetics; and
- Diabetics may be better adapted to hyperglycemia than nondiabetics.
Bottom Line: Peri-operative hyperglycemia leads to an increased risk of adverse events; this relationship is more pronounced in nondiabetic patients than in diabetic patients.
Citation: Kotagal M, Symons RG, Hirsch IB, et al. Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg. 2015;261(1):97-103.
Complaints Against Doctors Linked to Depression, Defensive Medicine
Clinical question: What is the impact of complaints on doctors’ psychological welfare and health?
Background: Studies have shown that malpractice litigation is associated with physician depression and suicide. Though complaints and investigations are part of appropriate physician oversight, unintentional consequences, such as defensive medicine and physician burnout, often occur.
Study design: Cross-sectional, anonymous survey study.
Setting: Surveys sent to members of the British Medical Association.
Synopsis: Only 8.3% of 95,636 invited physicians completed the survey. This study demonstrated that 16.9% of doctors with recent or ongoing complaints reported clinically significant symptoms of moderate to severe depression, compared to 9.5% of doctors with no complaints; 15% of doctors in the recent complaints group reported clinically significant levels of anxiety, compared to 7.3% of doctors with no complaints. Overall, 84.7% of doctors with a recent complaint and 79.9% with a past complaint reported changing the way they practiced medicine as a result of the complaint.
Since this study is a cross-sectional survey, it does not prove causation; it is possible that doctors with depression and anxiety are more likely to have complaints filed against them.
Bottom line: Doctors involved with complaints have a high prevalence of depression, anxiety, and suicidal ideation.
Citation: Bourne T, Wynants L, Peters M, et al. The impact of complaints procedures on the welfare, health and clinical practise of 7926 doctors in the UK: a cross-sectional survey. BMJ Open. 2015;5(1):e006687.
Clinical question: What is the impact of complaints on doctors’ psychological welfare and health?
Background: Studies have shown that malpractice litigation is associated with physician depression and suicide. Though complaints and investigations are part of appropriate physician oversight, unintentional consequences, such as defensive medicine and physician burnout, often occur.
Study design: Cross-sectional, anonymous survey study.
Setting: Surveys sent to members of the British Medical Association.
Synopsis: Only 8.3% of 95,636 invited physicians completed the survey. This study demonstrated that 16.9% of doctors with recent or ongoing complaints reported clinically significant symptoms of moderate to severe depression, compared to 9.5% of doctors with no complaints; 15% of doctors in the recent complaints group reported clinically significant levels of anxiety, compared to 7.3% of doctors with no complaints. Overall, 84.7% of doctors with a recent complaint and 79.9% with a past complaint reported changing the way they practiced medicine as a result of the complaint.
Since this study is a cross-sectional survey, it does not prove causation; it is possible that doctors with depression and anxiety are more likely to have complaints filed against them.
Bottom line: Doctors involved with complaints have a high prevalence of depression, anxiety, and suicidal ideation.
Citation: Bourne T, Wynants L, Peters M, et al. The impact of complaints procedures on the welfare, health and clinical practise of 7926 doctors in the UK: a cross-sectional survey. BMJ Open. 2015;5(1):e006687.
Clinical question: What is the impact of complaints on doctors’ psychological welfare and health?
Background: Studies have shown that malpractice litigation is associated with physician depression and suicide. Though complaints and investigations are part of appropriate physician oversight, unintentional consequences, such as defensive medicine and physician burnout, often occur.
Study design: Cross-sectional, anonymous survey study.
Setting: Surveys sent to members of the British Medical Association.
Synopsis: Only 8.3% of 95,636 invited physicians completed the survey. This study demonstrated that 16.9% of doctors with recent or ongoing complaints reported clinically significant symptoms of moderate to severe depression, compared to 9.5% of doctors with no complaints; 15% of doctors in the recent complaints group reported clinically significant levels of anxiety, compared to 7.3% of doctors with no complaints. Overall, 84.7% of doctors with a recent complaint and 79.9% with a past complaint reported changing the way they practiced medicine as a result of the complaint.
Since this study is a cross-sectional survey, it does not prove causation; it is possible that doctors with depression and anxiety are more likely to have complaints filed against them.
Bottom line: Doctors involved with complaints have a high prevalence of depression, anxiety, and suicidal ideation.
Citation: Bourne T, Wynants L, Peters M, et al. The impact of complaints procedures on the welfare, health and clinical practise of 7926 doctors in the UK: a cross-sectional survey. BMJ Open. 2015;5(1):e006687.
ICU Delirium: Little Attributable Mortality after Adjustment
Clinical question: Does delirium contribute to chance of death?
Background: Delirium is a well-recognized predictor of mortality. Prior observational studies have estimated a risk of death two to four times higher in ICU patients with delirium compared with those who do not experience delirium. The degree to which this association reflects a causal relationship is debated.
Study design: Prospective cohort study; used logistic regression and competing risks survival analyses along with a marginal structural model analysis to adjust for both baseline characteristics and severity of illness developing during ICU stay.
Setting: Single ICU in the Netherlands.
Synopsis: Regression analysis of 1,112 ICU patients confirmed the strong association between delirium and mortality; however, additional analysis, adjusting for the severity of illness as it progressed during the ICU stay, attenuated the relationship to nonsignificance. This suggests that both delirium and mortality were being driven by the common underlying illness.
In post hoc analysis, only persistent delirium was associated with a small increase in mortality. Although this observational study can neither prove nor disprove causation, the adjustment for changing severity of illness during the ICU stay was more sophisticated than prior studies. This study suggests that delirium and mortality are likely companions on the road of critical illness but that one may not directly cause the other.
Bottom line: Delirium in the ICU likely does not cause death, but its presence portends increased risk of mortality.
Citations: Klouwenberg PM, Zaal IJ, Spitoni C, et al. The attributable mortality of delirium in critically ill patients: prospective cohort study. BMJ. 2014;349:g6652. Inouye SK, Westendorp RGJ, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-922.
Clinical question: Does delirium contribute to chance of death?
Background: Delirium is a well-recognized predictor of mortality. Prior observational studies have estimated a risk of death two to four times higher in ICU patients with delirium compared with those who do not experience delirium. The degree to which this association reflects a causal relationship is debated.
Study design: Prospective cohort study; used logistic regression and competing risks survival analyses along with a marginal structural model analysis to adjust for both baseline characteristics and severity of illness developing during ICU stay.
Setting: Single ICU in the Netherlands.
Synopsis: Regression analysis of 1,112 ICU patients confirmed the strong association between delirium and mortality; however, additional analysis, adjusting for the severity of illness as it progressed during the ICU stay, attenuated the relationship to nonsignificance. This suggests that both delirium and mortality were being driven by the common underlying illness.
In post hoc analysis, only persistent delirium was associated with a small increase in mortality. Although this observational study can neither prove nor disprove causation, the adjustment for changing severity of illness during the ICU stay was more sophisticated than prior studies. This study suggests that delirium and mortality are likely companions on the road of critical illness but that one may not directly cause the other.
Bottom line: Delirium in the ICU likely does not cause death, but its presence portends increased risk of mortality.
Citations: Klouwenberg PM, Zaal IJ, Spitoni C, et al. The attributable mortality of delirium in critically ill patients: prospective cohort study. BMJ. 2014;349:g6652. Inouye SK, Westendorp RGJ, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-922.
Clinical question: Does delirium contribute to chance of death?
Background: Delirium is a well-recognized predictor of mortality. Prior observational studies have estimated a risk of death two to four times higher in ICU patients with delirium compared with those who do not experience delirium. The degree to which this association reflects a causal relationship is debated.
Study design: Prospective cohort study; used logistic regression and competing risks survival analyses along with a marginal structural model analysis to adjust for both baseline characteristics and severity of illness developing during ICU stay.
Setting: Single ICU in the Netherlands.
Synopsis: Regression analysis of 1,112 ICU patients confirmed the strong association between delirium and mortality; however, additional analysis, adjusting for the severity of illness as it progressed during the ICU stay, attenuated the relationship to nonsignificance. This suggests that both delirium and mortality were being driven by the common underlying illness.
In post hoc analysis, only persistent delirium was associated with a small increase in mortality. Although this observational study can neither prove nor disprove causation, the adjustment for changing severity of illness during the ICU stay was more sophisticated than prior studies. This study suggests that delirium and mortality are likely companions on the road of critical illness but that one may not directly cause the other.
Bottom line: Delirium in the ICU likely does not cause death, but its presence portends increased risk of mortality.
Citations: Klouwenberg PM, Zaal IJ, Spitoni C, et al. The attributable mortality of delirium in critically ill patients: prospective cohort study. BMJ. 2014;349:g6652. Inouye SK, Westendorp RGJ, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-922.
What Is the Appropriate Medical and Interventional Treatment for Hyperacute Ischemic Stroke?
Case
A 70-year-old woman was brought to the ED by ambulance with slurred speech after a fall. She arrived in the ED three hours and 29 minutes after the last time she was known to be normal. On initial examination, she had a National Institutes of Health Stroke Scale (NIHSS) score of 13, with a left facial droop, left hemiplegia, and right gaze deviation. Her acute noncontrast head computed tomography (CT), CT angiogram, and CT perfusion scans are shown in Figure 1.
How should this patient’s acute stroke be managed at this time?
Overview
Pathophysiology/Epidemiology: Stroke is the fourth most common cause of death in the United States and the main cause of disability, resulting in substantial healthcare expenditures.1 Ischemic stroke accounts for about 85% of all stroke cases and has several subtypes. The most common causes of ischemic stroke are small vessel thrombosis, large vessel thromboembolism, and cardioembolism. Both small vessel thrombosis and large vessel thromboembolism often are related to typical atherosclerotic risk factors, and cardioembolism is most often related to atrial fibrillation/flutter.
Minimizing death and disability from stroke is dependent on prevention measures, as well as early response to the onset of symptoms. The typical patient loses 1.9 million neurons for every minute a stroke is untreated—hence the popular adage “Time is Brain.”2 Although the appropriate management and time window of stroke treatment have been somewhat controversial, the acuity of treatment is now undisputed. Intravenous thrombolysis with tPA, also known as alteplase, has been an FDA-approved treatment for stroke since 1996, yet, as of 2006, only 2.4% of patients hospitalized for ischemic stroke were treated with IV tPA.3
The etiology of stroke, in most cases, does not change management in the hyperacute period, when thrombolysis is appropriate regardless of etiology.
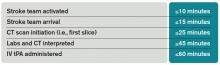
Timely evaluation: Although recognition of stroke symptoms by the public and pre-hospital management is a barrier in the treatment of acute stroke, this article will focus on appropriate ED and in-hospital treatment of stroke. Given the urgent need for management of acute ischemic stroke, it is critical that hospitals have an efficient process for identifying possible strokes and beginning treatment early. In order to accomplish these objectives, the National Institute of Neurological Disorders and Stroke (NINDS) has established goals for time frames of evaluation and management of patients with stroke in the ED (see Table 1).4
The role of the hospitalist: Hospitalists can play critical roles both as part of a primary stroke team and in identifying missed strokes. Some acute stroke teams have included hospitalists due to their ability to help with medical management, identify mimics, and assess medical contraindications to thrombolytic therapy. In addition, hospitalists may be the first to recognize a stroke in the ED when evaluating a patient with symptoms confused with a medical condition, or when a stroke occurs in an inpatient. In both of these situations, as first responders, hospitalists have knowledge of stroke evaluation and treatment that is crucial in beginning the evaluation and triggering a stroke alert.
Diagnostic tools: The initial evaluation of a patient with a possible stroke includes a brief but thorough history of current symptoms, as well as past medical and medication histories. The most critical piece of information to obtain from patients, family members, or bystanders is the time of symptom onset, or the time the patient was last known normal, so that the options for treatment can be evaluated early.
After basic stabilization of ABCs—airway maintenance, breathing and ventilation, and circulation— a brief but thorough neurologic examination is critical to define severity of neurologic injury and to help localize injury. Some standardized tools help with rapid assessment, including the NIHSS. The NIHSS is a standardized and reproducible evaluation that can be performed by many different specialties and levels of healthcare providers and provides information about stroke severity, localization, and prognosis.5 NIHSS offers free online certification.
Imaging: Early brain imaging and interpretation is another important piece of the acute evaluation of stroke. The most commonly used first-line imaging is noncontrast head CT, which is widely available and quickly performed. This type of imaging is sensitive for intracranial hemorrhage and can help distinguish nonvascular causes of symptoms such as tumor. CT is not sensitive for early signs of infarct, and, most often, initial CT findings are normal in early ischemic stroke. In patients who are candidates for intravenous fibrinolysis, ruling out hemorrhage is the main priority. Noncontrast head CT is the only imaging necessary to make decisions regarding IV thrombolytic treatment.
For further treatment decisions beyond IV tPA, intracranial and extracranial vascular imaging can help with decision making. All patients with stroke should have extracranial vascular imaging to help determine the etiology of stroke and evaluate the need for carotid endarterectomy or stenting for symptomatic stenosis in the days to weeks after stroke. More acutely, vascular imaging can be used to identify large vessel occlusions, in consideration of endovascular intervention (discussed in further detail below). CT angiography, magnetic resonance (MR) angiography, and conventional angiography are all options for evaluating the vasculature, though the first two are generally used as a noninvasive first step. Carotid ultrasound is often considered but only evaluates the extracranial anterior circulation; posterior circulation vessel abnormalities (like dissection) and intracranial abnormalities (like stenosis) may be missed. Although tPA decisions are not based upon these imaging modalities, secondary stroke prevention decisions may be altered by the findings.4
Perfusion imaging is the newest addition to acute stroke imaging, but its utility in guiding decision making remains unclear. Perfusion imaging provides hemodynamic information, ideally to identify areas of infarct versus ischemic penumbra, an area at risk of becoming ischemic. The use of perfusion imaging to identify good candidates for reperfusion (with IV tPA or with interventional techniques) is controversial.9 It is clear that perfusion imaging should not delay the time to treatment for IV tPA within the 4.5-hour window.
Windows: Current guidelines for administration of IV tPA for acute stroke are based in large part on two pivotal studies—the NINDS tPA Stroke Trial and the European Cooperative Acute Stroke Study III (ECASS III).6,7 IV alteplase for the treatment of acute stroke was approved by the FDA in 1996 following publication of the NINDS tPA Stroke Trial. This placebo-controlled randomized trial of 624 patients within three hours of ischemic stroke onset found that treatment with IV alteplase improved the odds of minimal or no disability at three months by approximately 30%. The rate of symptomatic intracranial hemorrhage was higher in the tPA group (6.4%) compared to the placebo group (0.6%), but mortality was not significantly different at three months. Though the benefit of IV tPA was clear in the three-hour window, subgroup analyses and further studies have clarified that treatment earlier in the window provides further benefit.
Given the difficulty of achieving treatment in short time windows, further studies have aimed to evaluate the utility of IV thrombolysis beyond the three-hour time window. While early studies found no clear benefit in extending the window, pooled analyses suggested a benefit in the three to 4.5-hour window, and ECASS III was designed to evaluate this window. This randomized placebo-controlled study used similar inclusion criteria to the NINDS study, with the exception of the time window, and excluded patients more than 80 years old, with large stroke (NIHSS score greater than 25), on anticoagulation (regardless of INR [international normalized ratio]), and with a history of prior stroke and diabetes. Again, in line with prior findings of time-dependent response to tPA, the study found that the IV tPA group were more likely than the placebo group to have good functional outcomes at three months, but the magnitude of this effect was lower than the one seen in the studies of the zero- to three-hour window. The rate of symptomatic intracranial hemorrhage in the 4.5-hour window was 7.9% using the NINDS tPA Stroke Trial criteria.
The American Heart Association/American Stroke Association (AHA/ASA) guidelines now recommend the use of IV tPA for patients within three hours of onset of ischemic stroke, with treatment initiated as quickly as possible (Class I; Level A). Although it has not been FDA approved, IV tPA treatment of eligible patients within the three to 4.5-hour window is recommended as Class I-Level B evidence with exclusions as in the ECASS study.4 Inclusion and exclusion criteria for tPA according to AHA/ASA guidelines can be found in Table 2.
IA thrombolysis/thrombectomy: Over the last two decades, there has been great interest in endovascular treatment of acute ischemic stroke and large advances in the numbers and types of treatments available. The FDA has approved multiple devices developed for mechanical thrombectomy based on their ability to recanalize vessels; however, to date, there is no clear evidence that thrombectomy improves patient outcomes. Several studies of endovascular therapy were recently published, including the Interventional Management of Stroke III (IMS 3) study, the Mechanical Retrieval and Recanalization of Stroke Clots using Embolectomy (MR RESCUE) study, and the SYNTHESIS Expansion study.8,9,10 None of these studies showed a benefit to endovascular treatment; however, critics have pointed out many flaws in these studies, including protracted time to treatment and patient selection. Furthermore, the most recent devices, like Solitaire and Trevo, were not used in most patients.
Three more recent trials found promising results for interventional treatment.11-13 The trials ranged from 70 to 500 patients with anterior circulation strokes with a large vessel occlusion; each study found a statistically significant improvement in functional independence at three months in the intervention group.12,13 Intravenous tPA was given in 72.7% to 100% of patients.11,12 Intervention to reperfusion was very quick in each study.
Some possible reasons for the more successful outcomes include the high proportion of newer devices for thrombectomy used and rapid treatment of symptoms, with symptom onset to groin puncture medians ranging from 185 minutes to 260 minutes.11,13 It remains clear that careful patient selection should occur, and those who are not candidates for intravenous therapy who present inside an appropriate time window could be considered. Time from symptom onset continues to be an important piece of making decisions about candidates for interventional treatment, but some advocate for the use of advanced imaging modalities, such as DWI imaging on MRI, or MR, or CT perfusion imaging, to help decide who could be a candidate.
Back to the Case
IV tPA was given to the patient 30 minutes after presentation. She met all inclusion and exclusion criteria for treatment and received the best-proven therapy for acute ischemic stroke. Due to her severe symptoms, the neurointerventional team was consulted for possible thrombectomy. This decision is controversial, as there is no proven benefit to intraarterial therapy. She was a possible candidate because of her time to presentation, large vessel occlusion, and substantial penumbra with CT imaging (see Figure 1).
About 20 minutes after treatment, she began to improve, now lifting her left arm and leg against gravity and showing less dysarthria. The decision was made to perform a conventional angiogram to reevaluate her blood vessels and to consider thrombectomy based upon the result. The majority of her middle cerebral artery had recanalized, so no further interventions were needed.
Bottom Line
Intravenous tPA (alteplase) is indicated for patients presenting within 4.5 hours of last known normal. Careful patient selection should occur if additional therapies are considered.
Drs. Poisson and Simpson are a neurohospitalists in the department of neurology at the University of Colorado Denver in Aurora.
References
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28-e292.
- Saver JL. Time is brain–quantified. Stroke. 2006;37(1):263-266.
- Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med. 2010;5(7):406-409.
- Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947. Lyden P, Raman R, Liu L, Emr M, Warren M, Marler
- J. National Institutes of Health Stroke Scale certification is reliable across multiple venues. Stroke. 2009;40(7):2507-2511.
- Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333(24):1581-1587.
- Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317-1329. Broderick JP, Palesch YY, Demchuk AM, et al Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368(10):893-903.
- Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368(10):914-923.
- Ciccone A, Valvassori L, Nichelatti M, et al. SYNTHESIS Expansion Investigators. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013;368(10):904-913.
- Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030.
- Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-1018.
- Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20.
Case
A 70-year-old woman was brought to the ED by ambulance with slurred speech after a fall. She arrived in the ED three hours and 29 minutes after the last time she was known to be normal. On initial examination, she had a National Institutes of Health Stroke Scale (NIHSS) score of 13, with a left facial droop, left hemiplegia, and right gaze deviation. Her acute noncontrast head computed tomography (CT), CT angiogram, and CT perfusion scans are shown in Figure 1.
How should this patient’s acute stroke be managed at this time?
Overview
Pathophysiology/Epidemiology: Stroke is the fourth most common cause of death in the United States and the main cause of disability, resulting in substantial healthcare expenditures.1 Ischemic stroke accounts for about 85% of all stroke cases and has several subtypes. The most common causes of ischemic stroke are small vessel thrombosis, large vessel thromboembolism, and cardioembolism. Both small vessel thrombosis and large vessel thromboembolism often are related to typical atherosclerotic risk factors, and cardioembolism is most often related to atrial fibrillation/flutter.
Minimizing death and disability from stroke is dependent on prevention measures, as well as early response to the onset of symptoms. The typical patient loses 1.9 million neurons for every minute a stroke is untreated—hence the popular adage “Time is Brain.”2 Although the appropriate management and time window of stroke treatment have been somewhat controversial, the acuity of treatment is now undisputed. Intravenous thrombolysis with tPA, also known as alteplase, has been an FDA-approved treatment for stroke since 1996, yet, as of 2006, only 2.4% of patients hospitalized for ischemic stroke were treated with IV tPA.3
The etiology of stroke, in most cases, does not change management in the hyperacute period, when thrombolysis is appropriate regardless of etiology.
Timely evaluation: Although recognition of stroke symptoms by the public and pre-hospital management is a barrier in the treatment of acute stroke, this article will focus on appropriate ED and in-hospital treatment of stroke. Given the urgent need for management of acute ischemic stroke, it is critical that hospitals have an efficient process for identifying possible strokes and beginning treatment early. In order to accomplish these objectives, the National Institute of Neurological Disorders and Stroke (NINDS) has established goals for time frames of evaluation and management of patients with stroke in the ED (see Table 1).4
The role of the hospitalist: Hospitalists can play critical roles both as part of a primary stroke team and in identifying missed strokes. Some acute stroke teams have included hospitalists due to their ability to help with medical management, identify mimics, and assess medical contraindications to thrombolytic therapy. In addition, hospitalists may be the first to recognize a stroke in the ED when evaluating a patient with symptoms confused with a medical condition, or when a stroke occurs in an inpatient. In both of these situations, as first responders, hospitalists have knowledge of stroke evaluation and treatment that is crucial in beginning the evaluation and triggering a stroke alert.
Diagnostic tools: The initial evaluation of a patient with a possible stroke includes a brief but thorough history of current symptoms, as well as past medical and medication histories. The most critical piece of information to obtain from patients, family members, or bystanders is the time of symptom onset, or the time the patient was last known normal, so that the options for treatment can be evaluated early.
After basic stabilization of ABCs—airway maintenance, breathing and ventilation, and circulation— a brief but thorough neurologic examination is critical to define severity of neurologic injury and to help localize injury. Some standardized tools help with rapid assessment, including the NIHSS. The NIHSS is a standardized and reproducible evaluation that can be performed by many different specialties and levels of healthcare providers and provides information about stroke severity, localization, and prognosis.5 NIHSS offers free online certification.
Imaging: Early brain imaging and interpretation is another important piece of the acute evaluation of stroke. The most commonly used first-line imaging is noncontrast head CT, which is widely available and quickly performed. This type of imaging is sensitive for intracranial hemorrhage and can help distinguish nonvascular causes of symptoms such as tumor. CT is not sensitive for early signs of infarct, and, most often, initial CT findings are normal in early ischemic stroke. In patients who are candidates for intravenous fibrinolysis, ruling out hemorrhage is the main priority. Noncontrast head CT is the only imaging necessary to make decisions regarding IV thrombolytic treatment.
For further treatment decisions beyond IV tPA, intracranial and extracranial vascular imaging can help with decision making. All patients with stroke should have extracranial vascular imaging to help determine the etiology of stroke and evaluate the need for carotid endarterectomy or stenting for symptomatic stenosis in the days to weeks after stroke. More acutely, vascular imaging can be used to identify large vessel occlusions, in consideration of endovascular intervention (discussed in further detail below). CT angiography, magnetic resonance (MR) angiography, and conventional angiography are all options for evaluating the vasculature, though the first two are generally used as a noninvasive first step. Carotid ultrasound is often considered but only evaluates the extracranial anterior circulation; posterior circulation vessel abnormalities (like dissection) and intracranial abnormalities (like stenosis) may be missed. Although tPA decisions are not based upon these imaging modalities, secondary stroke prevention decisions may be altered by the findings.4
Perfusion imaging is the newest addition to acute stroke imaging, but its utility in guiding decision making remains unclear. Perfusion imaging provides hemodynamic information, ideally to identify areas of infarct versus ischemic penumbra, an area at risk of becoming ischemic. The use of perfusion imaging to identify good candidates for reperfusion (with IV tPA or with interventional techniques) is controversial.9 It is clear that perfusion imaging should not delay the time to treatment for IV tPA within the 4.5-hour window.
Windows: Current guidelines for administration of IV tPA for acute stroke are based in large part on two pivotal studies—the NINDS tPA Stroke Trial and the European Cooperative Acute Stroke Study III (ECASS III).6,7 IV alteplase for the treatment of acute stroke was approved by the FDA in 1996 following publication of the NINDS tPA Stroke Trial. This placebo-controlled randomized trial of 624 patients within three hours of ischemic stroke onset found that treatment with IV alteplase improved the odds of minimal or no disability at three months by approximately 30%. The rate of symptomatic intracranial hemorrhage was higher in the tPA group (6.4%) compared to the placebo group (0.6%), but mortality was not significantly different at three months. Though the benefit of IV tPA was clear in the three-hour window, subgroup analyses and further studies have clarified that treatment earlier in the window provides further benefit.
Given the difficulty of achieving treatment in short time windows, further studies have aimed to evaluate the utility of IV thrombolysis beyond the three-hour time window. While early studies found no clear benefit in extending the window, pooled analyses suggested a benefit in the three to 4.5-hour window, and ECASS III was designed to evaluate this window. This randomized placebo-controlled study used similar inclusion criteria to the NINDS study, with the exception of the time window, and excluded patients more than 80 years old, with large stroke (NIHSS score greater than 25), on anticoagulation (regardless of INR [international normalized ratio]), and with a history of prior stroke and diabetes. Again, in line with prior findings of time-dependent response to tPA, the study found that the IV tPA group were more likely than the placebo group to have good functional outcomes at three months, but the magnitude of this effect was lower than the one seen in the studies of the zero- to three-hour window. The rate of symptomatic intracranial hemorrhage in the 4.5-hour window was 7.9% using the NINDS tPA Stroke Trial criteria.
The American Heart Association/American Stroke Association (AHA/ASA) guidelines now recommend the use of IV tPA for patients within three hours of onset of ischemic stroke, with treatment initiated as quickly as possible (Class I; Level A). Although it has not been FDA approved, IV tPA treatment of eligible patients within the three to 4.5-hour window is recommended as Class I-Level B evidence with exclusions as in the ECASS study.4 Inclusion and exclusion criteria for tPA according to AHA/ASA guidelines can be found in Table 2.
IA thrombolysis/thrombectomy: Over the last two decades, there has been great interest in endovascular treatment of acute ischemic stroke and large advances in the numbers and types of treatments available. The FDA has approved multiple devices developed for mechanical thrombectomy based on their ability to recanalize vessels; however, to date, there is no clear evidence that thrombectomy improves patient outcomes. Several studies of endovascular therapy were recently published, including the Interventional Management of Stroke III (IMS 3) study, the Mechanical Retrieval and Recanalization of Stroke Clots using Embolectomy (MR RESCUE) study, and the SYNTHESIS Expansion study.8,9,10 None of these studies showed a benefit to endovascular treatment; however, critics have pointed out many flaws in these studies, including protracted time to treatment and patient selection. Furthermore, the most recent devices, like Solitaire and Trevo, were not used in most patients.
Three more recent trials found promising results for interventional treatment.11-13 The trials ranged from 70 to 500 patients with anterior circulation strokes with a large vessel occlusion; each study found a statistically significant improvement in functional independence at three months in the intervention group.12,13 Intravenous tPA was given in 72.7% to 100% of patients.11,12 Intervention to reperfusion was very quick in each study.
Some possible reasons for the more successful outcomes include the high proportion of newer devices for thrombectomy used and rapid treatment of symptoms, with symptom onset to groin puncture medians ranging from 185 minutes to 260 minutes.11,13 It remains clear that careful patient selection should occur, and those who are not candidates for intravenous therapy who present inside an appropriate time window could be considered. Time from symptom onset continues to be an important piece of making decisions about candidates for interventional treatment, but some advocate for the use of advanced imaging modalities, such as DWI imaging on MRI, or MR, or CT perfusion imaging, to help decide who could be a candidate.
Back to the Case
IV tPA was given to the patient 30 minutes after presentation. She met all inclusion and exclusion criteria for treatment and received the best-proven therapy for acute ischemic stroke. Due to her severe symptoms, the neurointerventional team was consulted for possible thrombectomy. This decision is controversial, as there is no proven benefit to intraarterial therapy. She was a possible candidate because of her time to presentation, large vessel occlusion, and substantial penumbra with CT imaging (see Figure 1).
About 20 minutes after treatment, she began to improve, now lifting her left arm and leg against gravity and showing less dysarthria. The decision was made to perform a conventional angiogram to reevaluate her blood vessels and to consider thrombectomy based upon the result. The majority of her middle cerebral artery had recanalized, so no further interventions were needed.
Bottom Line
Intravenous tPA (alteplase) is indicated for patients presenting within 4.5 hours of last known normal. Careful patient selection should occur if additional therapies are considered.
Drs. Poisson and Simpson are a neurohospitalists in the department of neurology at the University of Colorado Denver in Aurora.
References
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28-e292.
- Saver JL. Time is brain–quantified. Stroke. 2006;37(1):263-266.
- Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med. 2010;5(7):406-409.
- Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947. Lyden P, Raman R, Liu L, Emr M, Warren M, Marler
- J. National Institutes of Health Stroke Scale certification is reliable across multiple venues. Stroke. 2009;40(7):2507-2511.
- Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333(24):1581-1587.
- Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317-1329. Broderick JP, Palesch YY, Demchuk AM, et al Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368(10):893-903.
- Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368(10):914-923.
- Ciccone A, Valvassori L, Nichelatti M, et al. SYNTHESIS Expansion Investigators. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013;368(10):904-913.
- Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030.
- Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-1018.
- Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20.
Case
A 70-year-old woman was brought to the ED by ambulance with slurred speech after a fall. She arrived in the ED three hours and 29 minutes after the last time she was known to be normal. On initial examination, she had a National Institutes of Health Stroke Scale (NIHSS) score of 13, with a left facial droop, left hemiplegia, and right gaze deviation. Her acute noncontrast head computed tomography (CT), CT angiogram, and CT perfusion scans are shown in Figure 1.
How should this patient’s acute stroke be managed at this time?
Overview
Pathophysiology/Epidemiology: Stroke is the fourth most common cause of death in the United States and the main cause of disability, resulting in substantial healthcare expenditures.1 Ischemic stroke accounts for about 85% of all stroke cases and has several subtypes. The most common causes of ischemic stroke are small vessel thrombosis, large vessel thromboembolism, and cardioembolism. Both small vessel thrombosis and large vessel thromboembolism often are related to typical atherosclerotic risk factors, and cardioembolism is most often related to atrial fibrillation/flutter.
Minimizing death and disability from stroke is dependent on prevention measures, as well as early response to the onset of symptoms. The typical patient loses 1.9 million neurons for every minute a stroke is untreated—hence the popular adage “Time is Brain.”2 Although the appropriate management and time window of stroke treatment have been somewhat controversial, the acuity of treatment is now undisputed. Intravenous thrombolysis with tPA, also known as alteplase, has been an FDA-approved treatment for stroke since 1996, yet, as of 2006, only 2.4% of patients hospitalized for ischemic stroke were treated with IV tPA.3
The etiology of stroke, in most cases, does not change management in the hyperacute period, when thrombolysis is appropriate regardless of etiology.
Timely evaluation: Although recognition of stroke symptoms by the public and pre-hospital management is a barrier in the treatment of acute stroke, this article will focus on appropriate ED and in-hospital treatment of stroke. Given the urgent need for management of acute ischemic stroke, it is critical that hospitals have an efficient process for identifying possible strokes and beginning treatment early. In order to accomplish these objectives, the National Institute of Neurological Disorders and Stroke (NINDS) has established goals for time frames of evaluation and management of patients with stroke in the ED (see Table 1).4
The role of the hospitalist: Hospitalists can play critical roles both as part of a primary stroke team and in identifying missed strokes. Some acute stroke teams have included hospitalists due to their ability to help with medical management, identify mimics, and assess medical contraindications to thrombolytic therapy. In addition, hospitalists may be the first to recognize a stroke in the ED when evaluating a patient with symptoms confused with a medical condition, or when a stroke occurs in an inpatient. In both of these situations, as first responders, hospitalists have knowledge of stroke evaluation and treatment that is crucial in beginning the evaluation and triggering a stroke alert.
Diagnostic tools: The initial evaluation of a patient with a possible stroke includes a brief but thorough history of current symptoms, as well as past medical and medication histories. The most critical piece of information to obtain from patients, family members, or bystanders is the time of symptom onset, or the time the patient was last known normal, so that the options for treatment can be evaluated early.
After basic stabilization of ABCs—airway maintenance, breathing and ventilation, and circulation— a brief but thorough neurologic examination is critical to define severity of neurologic injury and to help localize injury. Some standardized tools help with rapid assessment, including the NIHSS. The NIHSS is a standardized and reproducible evaluation that can be performed by many different specialties and levels of healthcare providers and provides information about stroke severity, localization, and prognosis.5 NIHSS offers free online certification.
Imaging: Early brain imaging and interpretation is another important piece of the acute evaluation of stroke. The most commonly used first-line imaging is noncontrast head CT, which is widely available and quickly performed. This type of imaging is sensitive for intracranial hemorrhage and can help distinguish nonvascular causes of symptoms such as tumor. CT is not sensitive for early signs of infarct, and, most often, initial CT findings are normal in early ischemic stroke. In patients who are candidates for intravenous fibrinolysis, ruling out hemorrhage is the main priority. Noncontrast head CT is the only imaging necessary to make decisions regarding IV thrombolytic treatment.
For further treatment decisions beyond IV tPA, intracranial and extracranial vascular imaging can help with decision making. All patients with stroke should have extracranial vascular imaging to help determine the etiology of stroke and evaluate the need for carotid endarterectomy or stenting for symptomatic stenosis in the days to weeks after stroke. More acutely, vascular imaging can be used to identify large vessel occlusions, in consideration of endovascular intervention (discussed in further detail below). CT angiography, magnetic resonance (MR) angiography, and conventional angiography are all options for evaluating the vasculature, though the first two are generally used as a noninvasive first step. Carotid ultrasound is often considered but only evaluates the extracranial anterior circulation; posterior circulation vessel abnormalities (like dissection) and intracranial abnormalities (like stenosis) may be missed. Although tPA decisions are not based upon these imaging modalities, secondary stroke prevention decisions may be altered by the findings.4
Perfusion imaging is the newest addition to acute stroke imaging, but its utility in guiding decision making remains unclear. Perfusion imaging provides hemodynamic information, ideally to identify areas of infarct versus ischemic penumbra, an area at risk of becoming ischemic. The use of perfusion imaging to identify good candidates for reperfusion (with IV tPA or with interventional techniques) is controversial.9 It is clear that perfusion imaging should not delay the time to treatment for IV tPA within the 4.5-hour window.
Windows: Current guidelines for administration of IV tPA for acute stroke are based in large part on two pivotal studies—the NINDS tPA Stroke Trial and the European Cooperative Acute Stroke Study III (ECASS III).6,7 IV alteplase for the treatment of acute stroke was approved by the FDA in 1996 following publication of the NINDS tPA Stroke Trial. This placebo-controlled randomized trial of 624 patients within three hours of ischemic stroke onset found that treatment with IV alteplase improved the odds of minimal or no disability at three months by approximately 30%. The rate of symptomatic intracranial hemorrhage was higher in the tPA group (6.4%) compared to the placebo group (0.6%), but mortality was not significantly different at three months. Though the benefit of IV tPA was clear in the three-hour window, subgroup analyses and further studies have clarified that treatment earlier in the window provides further benefit.
Given the difficulty of achieving treatment in short time windows, further studies have aimed to evaluate the utility of IV thrombolysis beyond the three-hour time window. While early studies found no clear benefit in extending the window, pooled analyses suggested a benefit in the three to 4.5-hour window, and ECASS III was designed to evaluate this window. This randomized placebo-controlled study used similar inclusion criteria to the NINDS study, with the exception of the time window, and excluded patients more than 80 years old, with large stroke (NIHSS score greater than 25), on anticoagulation (regardless of INR [international normalized ratio]), and with a history of prior stroke and diabetes. Again, in line with prior findings of time-dependent response to tPA, the study found that the IV tPA group were more likely than the placebo group to have good functional outcomes at three months, but the magnitude of this effect was lower than the one seen in the studies of the zero- to three-hour window. The rate of symptomatic intracranial hemorrhage in the 4.5-hour window was 7.9% using the NINDS tPA Stroke Trial criteria.
The American Heart Association/American Stroke Association (AHA/ASA) guidelines now recommend the use of IV tPA for patients within three hours of onset of ischemic stroke, with treatment initiated as quickly as possible (Class I; Level A). Although it has not been FDA approved, IV tPA treatment of eligible patients within the three to 4.5-hour window is recommended as Class I-Level B evidence with exclusions as in the ECASS study.4 Inclusion and exclusion criteria for tPA according to AHA/ASA guidelines can be found in Table 2.
IA thrombolysis/thrombectomy: Over the last two decades, there has been great interest in endovascular treatment of acute ischemic stroke and large advances in the numbers and types of treatments available. The FDA has approved multiple devices developed for mechanical thrombectomy based on their ability to recanalize vessels; however, to date, there is no clear evidence that thrombectomy improves patient outcomes. Several studies of endovascular therapy were recently published, including the Interventional Management of Stroke III (IMS 3) study, the Mechanical Retrieval and Recanalization of Stroke Clots using Embolectomy (MR RESCUE) study, and the SYNTHESIS Expansion study.8,9,10 None of these studies showed a benefit to endovascular treatment; however, critics have pointed out many flaws in these studies, including protracted time to treatment and patient selection. Furthermore, the most recent devices, like Solitaire and Trevo, were not used in most patients.
Three more recent trials found promising results for interventional treatment.11-13 The trials ranged from 70 to 500 patients with anterior circulation strokes with a large vessel occlusion; each study found a statistically significant improvement in functional independence at three months in the intervention group.12,13 Intravenous tPA was given in 72.7% to 100% of patients.11,12 Intervention to reperfusion was very quick in each study.
Some possible reasons for the more successful outcomes include the high proportion of newer devices for thrombectomy used and rapid treatment of symptoms, with symptom onset to groin puncture medians ranging from 185 minutes to 260 minutes.11,13 It remains clear that careful patient selection should occur, and those who are not candidates for intravenous therapy who present inside an appropriate time window could be considered. Time from symptom onset continues to be an important piece of making decisions about candidates for interventional treatment, but some advocate for the use of advanced imaging modalities, such as DWI imaging on MRI, or MR, or CT perfusion imaging, to help decide who could be a candidate.
Back to the Case
IV tPA was given to the patient 30 minutes after presentation. She met all inclusion and exclusion criteria for treatment and received the best-proven therapy for acute ischemic stroke. Due to her severe symptoms, the neurointerventional team was consulted for possible thrombectomy. This decision is controversial, as there is no proven benefit to intraarterial therapy. She was a possible candidate because of her time to presentation, large vessel occlusion, and substantial penumbra with CT imaging (see Figure 1).
About 20 minutes after treatment, she began to improve, now lifting her left arm and leg against gravity and showing less dysarthria. The decision was made to perform a conventional angiogram to reevaluate her blood vessels and to consider thrombectomy based upon the result. The majority of her middle cerebral artery had recanalized, so no further interventions were needed.
Bottom Line
Intravenous tPA (alteplase) is indicated for patients presenting within 4.5 hours of last known normal. Careful patient selection should occur if additional therapies are considered.
Drs. Poisson and Simpson are a neurohospitalists in the department of neurology at the University of Colorado Denver in Aurora.
References
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28-e292.
- Saver JL. Time is brain–quantified. Stroke. 2006;37(1):263-266.
- Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med. 2010;5(7):406-409.
- Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947. Lyden P, Raman R, Liu L, Emr M, Warren M, Marler
- J. National Institutes of Health Stroke Scale certification is reliable across multiple venues. Stroke. 2009;40(7):2507-2511.
- Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333(24):1581-1587.
- Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317-1329. Broderick JP, Palesch YY, Demchuk AM, et al Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368(10):893-903.
- Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368(10):914-923.
- Ciccone A, Valvassori L, Nichelatti M, et al. SYNTHESIS Expansion Investigators. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013;368(10):904-913.
- Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030.
- Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-1018.
- Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20.
HM15 Session Analysis: End-of-Life Discussions
Presenter: Julia Ragland, MD, FHM
Summation: Discussion of Prognosis in Advance Illness is a key component of informed decision-making and should be undertaken during a “Sentinel Hospitalization” and at times of other “triggers”. End-of-Life discussions are critical for providing the best care for patients with advanced diseases.
A Sentinel Hospitalization is a hospitalization in the patient’s disease course that heralds a need to reassess prognosis, patient understanding, treatment options and intensities, and goals of care.
Other triggers for discussing prognosis: new diagnosis of serious illness, major medical decision with uncertain outcome, frequent hospitalizations for advanced disease, patient/family query prognosis, patient/family request treatment inconsistent with good clinical judgment (futile care), patient actively dying, “No” answer to “Surprise Question” (“would you be surprised if this patient died in the next year?”)
How can we prognosticate? Data from studies, Clinical intuition and experience, Prognostic indices, Key indicators of worsening prognosis (declining functional status, weight loss/malnutrition, co-morbidities, frequent hospitalizations)
Resources for Prognostication: ePrognosis, Seattle Heart Failure Model, MELD, Charlson Comorbidity Index, MJHSpalliativeinstitute.org/e-learning, Palliative Care Fast Facts mobile app
Ask-Tell-Ask method for communicating prognosis
- ASK: if they want to talk about prognosis and what they already know
- TELL: give information in small amounts, build on what they already know, use simple straight-forward language
- ASK: repeat understanding of what has been said, if they would like to hear more
Key Points/HM Takeaways:
- Estimating and discussing prognosis are core competencies for hospitalists and should be utilized during a “sentinel hospitalization”
- Prognostic awareness in advanced illness is key for:
- Informed decision making (CPR, procedures, chemo, et al)
- Determining realistic goals of care
- Providing patient centered care
- Most patients and families want prognostic information, but not always- must ask to know. Give the patient the option not to discuss prognosis.
- Ask-Tell-Ask approach for discussing prognosis is effective
Presenter: Julia Ragland, MD, FHM
Summation: Discussion of Prognosis in Advance Illness is a key component of informed decision-making and should be undertaken during a “Sentinel Hospitalization” and at times of other “triggers”. End-of-Life discussions are critical for providing the best care for patients with advanced diseases.
A Sentinel Hospitalization is a hospitalization in the patient’s disease course that heralds a need to reassess prognosis, patient understanding, treatment options and intensities, and goals of care.
Other triggers for discussing prognosis: new diagnosis of serious illness, major medical decision with uncertain outcome, frequent hospitalizations for advanced disease, patient/family query prognosis, patient/family request treatment inconsistent with good clinical judgment (futile care), patient actively dying, “No” answer to “Surprise Question” (“would you be surprised if this patient died in the next year?”)
How can we prognosticate? Data from studies, Clinical intuition and experience, Prognostic indices, Key indicators of worsening prognosis (declining functional status, weight loss/malnutrition, co-morbidities, frequent hospitalizations)
Resources for Prognostication: ePrognosis, Seattle Heart Failure Model, MELD, Charlson Comorbidity Index, MJHSpalliativeinstitute.org/e-learning, Palliative Care Fast Facts mobile app
Ask-Tell-Ask method for communicating prognosis
- ASK: if they want to talk about prognosis and what they already know
- TELL: give information in small amounts, build on what they already know, use simple straight-forward language
- ASK: repeat understanding of what has been said, if they would like to hear more
Key Points/HM Takeaways:
- Estimating and discussing prognosis are core competencies for hospitalists and should be utilized during a “sentinel hospitalization”
- Prognostic awareness in advanced illness is key for:
- Informed decision making (CPR, procedures, chemo, et al)
- Determining realistic goals of care
- Providing patient centered care
- Most patients and families want prognostic information, but not always- must ask to know. Give the patient the option not to discuss prognosis.
- Ask-Tell-Ask approach for discussing prognosis is effective
Presenter: Julia Ragland, MD, FHM
Summation: Discussion of Prognosis in Advance Illness is a key component of informed decision-making and should be undertaken during a “Sentinel Hospitalization” and at times of other “triggers”. End-of-Life discussions are critical for providing the best care for patients with advanced diseases.
A Sentinel Hospitalization is a hospitalization in the patient’s disease course that heralds a need to reassess prognosis, patient understanding, treatment options and intensities, and goals of care.
Other triggers for discussing prognosis: new diagnosis of serious illness, major medical decision with uncertain outcome, frequent hospitalizations for advanced disease, patient/family query prognosis, patient/family request treatment inconsistent with good clinical judgment (futile care), patient actively dying, “No” answer to “Surprise Question” (“would you be surprised if this patient died in the next year?”)
How can we prognosticate? Data from studies, Clinical intuition and experience, Prognostic indices, Key indicators of worsening prognosis (declining functional status, weight loss/malnutrition, co-morbidities, frequent hospitalizations)
Resources for Prognostication: ePrognosis, Seattle Heart Failure Model, MELD, Charlson Comorbidity Index, MJHSpalliativeinstitute.org/e-learning, Palliative Care Fast Facts mobile app
Ask-Tell-Ask method for communicating prognosis
- ASK: if they want to talk about prognosis and what they already know
- TELL: give information in small amounts, build on what they already know, use simple straight-forward language
- ASK: repeat understanding of what has been said, if they would like to hear more
Key Points/HM Takeaways:
- Estimating and discussing prognosis are core competencies for hospitalists and should be utilized during a “sentinel hospitalization”
- Prognostic awareness in advanced illness is key for:
- Informed decision making (CPR, procedures, chemo, et al)
- Determining realistic goals of care
- Providing patient centered care
- Most patients and families want prognostic information, but not always- must ask to know. Give the patient the option not to discuss prognosis.
- Ask-Tell-Ask approach for discussing prognosis is effective
Nine Things Hospitalists Need to Know about Treating Patients with Endocrine Disorders
Diabetes is as prevalent in hospitals today as lab coats and heart monitors. More than 8% of the population—almost 26 million people—and nearly 27% (11 million) of Americans 65 or older have diabetes, according to American Diabetes Association (ADA) statistics. That makes diabetes one of the most common conditions hospitalists face day in and day out.
Other endocrine disorders also pose a challenge to hospitalists because they may be relatively uncommon, endocrinologists say.
The Hospitalist spoke to several endocrinologists and veteran hospitalists, mining their backgrounds and observations for tips on caring for hospitalized patients with endocrine disorders. Here are nine things they think hospitalists need to know:
1. Realize the far-reaching impact of good care for diabetic patients.
Part of the reason this is important is the numbers of patients with the disease who will be hospitalized and come under the care of a hospitalist.
“They’re coming in for a host of medical conditions, not the least of which is that diabetes is a comorbid factor that goes along with it,” says John Anderson, MD, the ADA’s immediate past president of medicine and science and an internist and diabetician at The Frist Clinic in Nashville, Tenn. “For those who are critically ill—those having bypass, those having stroke—diabetes is overrepresented even more once they get inside the hospital and in the intensive care unit.”
Job No. 1, controlling blood sugar, can have broad implications, he says.
“We know that control of their glucose through the hospital stay actually makes a difference in long-term outcomes, particularly things like surgery, coronary bypass grafting, that type of thing,” he says, noting that the standard of care is to try to keep glucose under 200. “A lot of studies have been done that demonstrate that really poor control of glucose in the hospital, regardless of the disease entity they’re in with, can lead to worsening long-term outcomes. It’s really imperative that you control the blood sugar.1,2

—John Anderson, MD, past president, American Diabetes Association, internist and diabetician, The Frist Clinic, Nashville, Tenn.
“However, the other part of this is…that if you control it so tightly that these patients are dropping their blood sugar and having significant hypoglycemia problems in the hospital, that’s not good either.”
2. You probably shouldn’t be testing for thyroid-stimulating hormone (TSH) level by itself in an acutely ill inpatient.
Simply put, the results probably won’t be useful, says Tamara Wexler, MD, PhD, an endocrinologist attending at Massachusetts General Hospital in Boston.
“TSH alone, for some reason, seems to be often measured,” she says, but “it’s extremely rarely indicated during acute hospitalization.”
TSH is “notoriously spurious” in inpatients, she adds, because the stress of an illness can make the test difficult to interpret.
“Many endocrine hormone levels are affected by stress, for example, and thus are better measured in an outpatient setting than in an acute hospitalized illness because of the impact of the illness on interpreting the test results,” she says.
Euthyroid sick syndrome—or “sick euthyroid”—is a term used for abnormalities in thyroid tests in patients with systemic illnesses that are nonthyroidal.
In cases in which thyroid dysfunction is strongly suspected, TSH should be measured in conjunction with other levels, such as a free thyroxine (free T4) level, Dr. Wexler says.
3. Don’t forget to watch potassium in patients with diabetic ketoacidosis (DKA).
A patient with a normal level of potassium, or even a high one, at baseline can encounter a problem with plummeting levels, says Bruce Mitchell, MD, director of hospital medicine services at Emory Hospital Midtown and assistant professor of hospital medicine at Emory University in Atlanta.
“Once you start insulin and correcting the hyperosmolality, the potassium shifts,” says Dr. Mitchell, who has a particular interest in endocrinology, “so it can become abnormally low fairly quickly.
“You start the insulin and fluids; then all of a sudden that person’s potassium is drastically abnormal and they’re coding,” he says. “It’s important to make sure your hospital’s diabetic ketoacidosis protocol includes frequent potassium checks.”
4. Be sure to wait long enough before rechecking TSH after a medication change.
It takes several weeks before thyroid medication dose changes start to show their effects, says Jeffrey Greenwald, MD, a hospitalist at Massachusetts General with expertise in endocrinology. Guidelines published in 2012 by the American Association of Clinical Endocrinologists and the American Thyroid Association recommend rechecking TSH within four to eight weeks.3

“It bears reminding that [for] patients who have recently changed their thyroid medication dose, you need to wait several weeks before you recheck their TSH,” he says. “That’s another reason why the TSH can be somewhat difficult to interpret.
“There’s a tendency that I have seen, too, if the TSH is high and they’re on thyroid replacement, to want to adjust the dose while they’re in the hospital, which is probably not the time to do it.”
5. When administering insulin, factor in soon-to-arrive meals and give prandial insulin as needed.
If patients with diabetes are receiving insulin in the hospital, even if their glucose is in the normal range, they will need insulin if they’re about to have a carb-loaded breakfast, says Jose Florez, MD, PhD, an endocrinologist at Massachusetts General and associate professor of medicine at Harvard Medical School in Boston.
“A person with a glucose of 98 who is about to eat pancakes needs standing short-acting insulin regardless of the fingerstick,” Dr. Florez says. “A person with a glucose of 250 who is about to eat needs both the correction insulin and the amount needed to handle the impending carbohydrate load.”
“The person not only needs to correct what the glucose is at the moment, but they also need to account for the impending carbohydrate intake,” he says.
Dr. Anderson says he always cautions those caring for hospitalized diabetic patients against using the “sliding-scale philosophy”—marked by set amounts of long-acting insulin and set amounts of carbohydrate intake—because it’s overly formulaic for that setting.
“It leads to really variable glucoses,” he says, “and usually not good control.”
6. Giving isotonic fluids to someone who has fixed water retention or hypertonic urine can worsen the problem.
This can stem from an incomplete or incorrect evaluation of hyponatremia, which is a common problem in hospitalized patients. When hyponatremia is present, the first order of business should be to exclude pseudohyponatremia and confirm that it’s hypotonic hyponatremia.
After confirmation, the volume status should be assessed. One useful way to do this is to measure urine creatinine, urine sodium, and urine osmolality (osm), Dr. Florez says. If a patient has water retention or hypertonic urine from syndrome of inappropriate diuretic hormone secretion (SIADH), hypothyroidism, or glucocorticoid deficiency, the hospitalist needs to act accordingly.
“If the urine osm is high, higher than the serum osm, and is fixed at that level for some reason…giving that person isotonic fluids will lead to additional water retention and make the situation worse,” he says. “It’s very important to assess the volume status and establish the cause. And then, if you’re going to give fluids, be mindful of what the urine might look like. Do not give fluids that are hypotonic with respect to what the urine is making, unless you are completely convinced that the person is dry and therefore needs volume.”

7. Encourage patients to check their own glucose and administer their own insulin while still in the hospital.
“We often deal with patients who start insulin treatment for diabetes during an admission or who seem not to be doing very well giving insulin at home,” Dr. Wexler says. “Many patients can benefit from supervised insulin injections and glucose testing.”
Going through the process while in the hospital with supervision can be a good refresher, she says.
“You don’t have to necessarily order specific diabetic teaching,” she adds, noting that not all hospitals have diabetic educators available at all times.
A patient might be waiting for diabetic teaching before discharge, but this might be one way to speed the process, Dr. Wexler says. She suggests teaching by example.
8. Patients on steroids every day are at risk for adrenal insufficiency.
Even if they aren’t on corticosteroids when they present, hospitalists should think of these patients as “at risk for adrenal insufficiency and potentially immunocompromised,” Dr. Greenwald says. “The bigger issue in most cases is the adrenal insufficiency.”
That means their bodies can’t mount an appropriate response to stress.
“And without that appropriate response of additional stress hormone the body would normally make, they may not be able, for example, to maintain their blood pressure,” he says. “This can be extremely dangerous.”
Inhaled steroids, and topical steroids if they are applied to broken skin, can have a kind of stealth effect.
“That’s something to keep in mind,” Dr. Wexler says, noting the connection between blood pressure management and endocrine conditions.
9. Thyroid hormone might not be as well absorbed under certain conditions.
With calcium or iron supplementation, thyroid hormones might present a problem, Dr. Wexler says. For patients at home taking thyroid hormone appropriately (an hour or two separated from calcium or iron supplementation), there “should be no issue,” she says. “But if they are administered at the same time at the hospital, patients may not absorb the full dose.”
Tom Collins is a freelance writer in South Florida.
References
- Omar AS, Salama A, Allam M, et al. Association of time in blood glucose range with outcomes following cardiac surgery. BMC Anesthesiol. 2015;15(1):14.
- Han HS, Kang SB. Relations between long-term glycemic control and postoperative wound and infectious complications after total knee arthroplasty in type 2 diabetics. Clin Orthop Surg. 2013;5(2):118–123.
- Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract. 2012;18(6):988-1028.
- Supit EJ, Peiris AN. Interpretation of laboratory thyroid function tests for the primary care physician. South Med J. 2002;95(5):481-485.
Diabetes is as prevalent in hospitals today as lab coats and heart monitors. More than 8% of the population—almost 26 million people—and nearly 27% (11 million) of Americans 65 or older have diabetes, according to American Diabetes Association (ADA) statistics. That makes diabetes one of the most common conditions hospitalists face day in and day out.
Other endocrine disorders also pose a challenge to hospitalists because they may be relatively uncommon, endocrinologists say.
The Hospitalist spoke to several endocrinologists and veteran hospitalists, mining their backgrounds and observations for tips on caring for hospitalized patients with endocrine disorders. Here are nine things they think hospitalists need to know:
1. Realize the far-reaching impact of good care for diabetic patients.
Part of the reason this is important is the numbers of patients with the disease who will be hospitalized and come under the care of a hospitalist.
“They’re coming in for a host of medical conditions, not the least of which is that diabetes is a comorbid factor that goes along with it,” says John Anderson, MD, the ADA’s immediate past president of medicine and science and an internist and diabetician at The Frist Clinic in Nashville, Tenn. “For those who are critically ill—those having bypass, those having stroke—diabetes is overrepresented even more once they get inside the hospital and in the intensive care unit.”
Job No. 1, controlling blood sugar, can have broad implications, he says.
“We know that control of their glucose through the hospital stay actually makes a difference in long-term outcomes, particularly things like surgery, coronary bypass grafting, that type of thing,” he says, noting that the standard of care is to try to keep glucose under 200. “A lot of studies have been done that demonstrate that really poor control of glucose in the hospital, regardless of the disease entity they’re in with, can lead to worsening long-term outcomes. It’s really imperative that you control the blood sugar.1,2

—John Anderson, MD, past president, American Diabetes Association, internist and diabetician, The Frist Clinic, Nashville, Tenn.
“However, the other part of this is…that if you control it so tightly that these patients are dropping their blood sugar and having significant hypoglycemia problems in the hospital, that’s not good either.”
2. You probably shouldn’t be testing for thyroid-stimulating hormone (TSH) level by itself in an acutely ill inpatient.
Simply put, the results probably won’t be useful, says Tamara Wexler, MD, PhD, an endocrinologist attending at Massachusetts General Hospital in Boston.
“TSH alone, for some reason, seems to be often measured,” she says, but “it’s extremely rarely indicated during acute hospitalization.”
TSH is “notoriously spurious” in inpatients, she adds, because the stress of an illness can make the test difficult to interpret.
“Many endocrine hormone levels are affected by stress, for example, and thus are better measured in an outpatient setting than in an acute hospitalized illness because of the impact of the illness on interpreting the test results,” she says.
Euthyroid sick syndrome—or “sick euthyroid”—is a term used for abnormalities in thyroid tests in patients with systemic illnesses that are nonthyroidal.
In cases in which thyroid dysfunction is strongly suspected, TSH should be measured in conjunction with other levels, such as a free thyroxine (free T4) level, Dr. Wexler says.
3. Don’t forget to watch potassium in patients with diabetic ketoacidosis (DKA).
A patient with a normal level of potassium, or even a high one, at baseline can encounter a problem with plummeting levels, says Bruce Mitchell, MD, director of hospital medicine services at Emory Hospital Midtown and assistant professor of hospital medicine at Emory University in Atlanta.
“Once you start insulin and correcting the hyperosmolality, the potassium shifts,” says Dr. Mitchell, who has a particular interest in endocrinology, “so it can become abnormally low fairly quickly.
“You start the insulin and fluids; then all of a sudden that person’s potassium is drastically abnormal and they’re coding,” he says. “It’s important to make sure your hospital’s diabetic ketoacidosis protocol includes frequent potassium checks.”
4. Be sure to wait long enough before rechecking TSH after a medication change.
It takes several weeks before thyroid medication dose changes start to show their effects, says Jeffrey Greenwald, MD, a hospitalist at Massachusetts General with expertise in endocrinology. Guidelines published in 2012 by the American Association of Clinical Endocrinologists and the American Thyroid Association recommend rechecking TSH within four to eight weeks.3

“It bears reminding that [for] patients who have recently changed their thyroid medication dose, you need to wait several weeks before you recheck their TSH,” he says. “That’s another reason why the TSH can be somewhat difficult to interpret.
“There’s a tendency that I have seen, too, if the TSH is high and they’re on thyroid replacement, to want to adjust the dose while they’re in the hospital, which is probably not the time to do it.”
5. When administering insulin, factor in soon-to-arrive meals and give prandial insulin as needed.
If patients with diabetes are receiving insulin in the hospital, even if their glucose is in the normal range, they will need insulin if they’re about to have a carb-loaded breakfast, says Jose Florez, MD, PhD, an endocrinologist at Massachusetts General and associate professor of medicine at Harvard Medical School in Boston.
“A person with a glucose of 98 who is about to eat pancakes needs standing short-acting insulin regardless of the fingerstick,” Dr. Florez says. “A person with a glucose of 250 who is about to eat needs both the correction insulin and the amount needed to handle the impending carbohydrate load.”
“The person not only needs to correct what the glucose is at the moment, but they also need to account for the impending carbohydrate intake,” he says.
Dr. Anderson says he always cautions those caring for hospitalized diabetic patients against using the “sliding-scale philosophy”—marked by set amounts of long-acting insulin and set amounts of carbohydrate intake—because it’s overly formulaic for that setting.
“It leads to really variable glucoses,” he says, “and usually not good control.”
6. Giving isotonic fluids to someone who has fixed water retention or hypertonic urine can worsen the problem.
This can stem from an incomplete or incorrect evaluation of hyponatremia, which is a common problem in hospitalized patients. When hyponatremia is present, the first order of business should be to exclude pseudohyponatremia and confirm that it’s hypotonic hyponatremia.
After confirmation, the volume status should be assessed. One useful way to do this is to measure urine creatinine, urine sodium, and urine osmolality (osm), Dr. Florez says. If a patient has water retention or hypertonic urine from syndrome of inappropriate diuretic hormone secretion (SIADH), hypothyroidism, or glucocorticoid deficiency, the hospitalist needs to act accordingly.
“If the urine osm is high, higher than the serum osm, and is fixed at that level for some reason…giving that person isotonic fluids will lead to additional water retention and make the situation worse,” he says. “It’s very important to assess the volume status and establish the cause. And then, if you’re going to give fluids, be mindful of what the urine might look like. Do not give fluids that are hypotonic with respect to what the urine is making, unless you are completely convinced that the person is dry and therefore needs volume.”

7. Encourage patients to check their own glucose and administer their own insulin while still in the hospital.
“We often deal with patients who start insulin treatment for diabetes during an admission or who seem not to be doing very well giving insulin at home,” Dr. Wexler says. “Many patients can benefit from supervised insulin injections and glucose testing.”
Going through the process while in the hospital with supervision can be a good refresher, she says.
“You don’t have to necessarily order specific diabetic teaching,” she adds, noting that not all hospitals have diabetic educators available at all times.
A patient might be waiting for diabetic teaching before discharge, but this might be one way to speed the process, Dr. Wexler says. She suggests teaching by example.
8. Patients on steroids every day are at risk for adrenal insufficiency.
Even if they aren’t on corticosteroids when they present, hospitalists should think of these patients as “at risk for adrenal insufficiency and potentially immunocompromised,” Dr. Greenwald says. “The bigger issue in most cases is the adrenal insufficiency.”
That means their bodies can’t mount an appropriate response to stress.
“And without that appropriate response of additional stress hormone the body would normally make, they may not be able, for example, to maintain their blood pressure,” he says. “This can be extremely dangerous.”
Inhaled steroids, and topical steroids if they are applied to broken skin, can have a kind of stealth effect.
“That’s something to keep in mind,” Dr. Wexler says, noting the connection between blood pressure management and endocrine conditions.
9. Thyroid hormone might not be as well absorbed under certain conditions.
With calcium or iron supplementation, thyroid hormones might present a problem, Dr. Wexler says. For patients at home taking thyroid hormone appropriately (an hour or two separated from calcium or iron supplementation), there “should be no issue,” she says. “But if they are administered at the same time at the hospital, patients may not absorb the full dose.”
Tom Collins is a freelance writer in South Florida.
References
- Omar AS, Salama A, Allam M, et al. Association of time in blood glucose range with outcomes following cardiac surgery. BMC Anesthesiol. 2015;15(1):14.
- Han HS, Kang SB. Relations between long-term glycemic control and postoperative wound and infectious complications after total knee arthroplasty in type 2 diabetics. Clin Orthop Surg. 2013;5(2):118–123.
- Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract. 2012;18(6):988-1028.
- Supit EJ, Peiris AN. Interpretation of laboratory thyroid function tests for the primary care physician. South Med J. 2002;95(5):481-485.
Diabetes is as prevalent in hospitals today as lab coats and heart monitors. More than 8% of the population—almost 26 million people—and nearly 27% (11 million) of Americans 65 or older have diabetes, according to American Diabetes Association (ADA) statistics. That makes diabetes one of the most common conditions hospitalists face day in and day out.
Other endocrine disorders also pose a challenge to hospitalists because they may be relatively uncommon, endocrinologists say.
The Hospitalist spoke to several endocrinologists and veteran hospitalists, mining their backgrounds and observations for tips on caring for hospitalized patients with endocrine disorders. Here are nine things they think hospitalists need to know:
1. Realize the far-reaching impact of good care for diabetic patients.
Part of the reason this is important is the numbers of patients with the disease who will be hospitalized and come under the care of a hospitalist.
“They’re coming in for a host of medical conditions, not the least of which is that diabetes is a comorbid factor that goes along with it,” says John Anderson, MD, the ADA’s immediate past president of medicine and science and an internist and diabetician at The Frist Clinic in Nashville, Tenn. “For those who are critically ill—those having bypass, those having stroke—diabetes is overrepresented even more once they get inside the hospital and in the intensive care unit.”
Job No. 1, controlling blood sugar, can have broad implications, he says.
“We know that control of their glucose through the hospital stay actually makes a difference in long-term outcomes, particularly things like surgery, coronary bypass grafting, that type of thing,” he says, noting that the standard of care is to try to keep glucose under 200. “A lot of studies have been done that demonstrate that really poor control of glucose in the hospital, regardless of the disease entity they’re in with, can lead to worsening long-term outcomes. It’s really imperative that you control the blood sugar.1,2

—John Anderson, MD, past president, American Diabetes Association, internist and diabetician, The Frist Clinic, Nashville, Tenn.
“However, the other part of this is…that if you control it so tightly that these patients are dropping their blood sugar and having significant hypoglycemia problems in the hospital, that’s not good either.”
2. You probably shouldn’t be testing for thyroid-stimulating hormone (TSH) level by itself in an acutely ill inpatient.
Simply put, the results probably won’t be useful, says Tamara Wexler, MD, PhD, an endocrinologist attending at Massachusetts General Hospital in Boston.
“TSH alone, for some reason, seems to be often measured,” she says, but “it’s extremely rarely indicated during acute hospitalization.”
TSH is “notoriously spurious” in inpatients, she adds, because the stress of an illness can make the test difficult to interpret.
“Many endocrine hormone levels are affected by stress, for example, and thus are better measured in an outpatient setting than in an acute hospitalized illness because of the impact of the illness on interpreting the test results,” she says.
Euthyroid sick syndrome—or “sick euthyroid”—is a term used for abnormalities in thyroid tests in patients with systemic illnesses that are nonthyroidal.
In cases in which thyroid dysfunction is strongly suspected, TSH should be measured in conjunction with other levels, such as a free thyroxine (free T4) level, Dr. Wexler says.
3. Don’t forget to watch potassium in patients with diabetic ketoacidosis (DKA).
A patient with a normal level of potassium, or even a high one, at baseline can encounter a problem with plummeting levels, says Bruce Mitchell, MD, director of hospital medicine services at Emory Hospital Midtown and assistant professor of hospital medicine at Emory University in Atlanta.
“Once you start insulin and correcting the hyperosmolality, the potassium shifts,” says Dr. Mitchell, who has a particular interest in endocrinology, “so it can become abnormally low fairly quickly.
“You start the insulin and fluids; then all of a sudden that person’s potassium is drastically abnormal and they’re coding,” he says. “It’s important to make sure your hospital’s diabetic ketoacidosis protocol includes frequent potassium checks.”
4. Be sure to wait long enough before rechecking TSH after a medication change.
It takes several weeks before thyroid medication dose changes start to show their effects, says Jeffrey Greenwald, MD, a hospitalist at Massachusetts General with expertise in endocrinology. Guidelines published in 2012 by the American Association of Clinical Endocrinologists and the American Thyroid Association recommend rechecking TSH within four to eight weeks.3

“It bears reminding that [for] patients who have recently changed their thyroid medication dose, you need to wait several weeks before you recheck their TSH,” he says. “That’s another reason why the TSH can be somewhat difficult to interpret.
“There’s a tendency that I have seen, too, if the TSH is high and they’re on thyroid replacement, to want to adjust the dose while they’re in the hospital, which is probably not the time to do it.”
5. When administering insulin, factor in soon-to-arrive meals and give prandial insulin as needed.
If patients with diabetes are receiving insulin in the hospital, even if their glucose is in the normal range, they will need insulin if they’re about to have a carb-loaded breakfast, says Jose Florez, MD, PhD, an endocrinologist at Massachusetts General and associate professor of medicine at Harvard Medical School in Boston.
“A person with a glucose of 98 who is about to eat pancakes needs standing short-acting insulin regardless of the fingerstick,” Dr. Florez says. “A person with a glucose of 250 who is about to eat needs both the correction insulin and the amount needed to handle the impending carbohydrate load.”
“The person not only needs to correct what the glucose is at the moment, but they also need to account for the impending carbohydrate intake,” he says.
Dr. Anderson says he always cautions those caring for hospitalized diabetic patients against using the “sliding-scale philosophy”—marked by set amounts of long-acting insulin and set amounts of carbohydrate intake—because it’s overly formulaic for that setting.
“It leads to really variable glucoses,” he says, “and usually not good control.”
6. Giving isotonic fluids to someone who has fixed water retention or hypertonic urine can worsen the problem.
This can stem from an incomplete or incorrect evaluation of hyponatremia, which is a common problem in hospitalized patients. When hyponatremia is present, the first order of business should be to exclude pseudohyponatremia and confirm that it’s hypotonic hyponatremia.
After confirmation, the volume status should be assessed. One useful way to do this is to measure urine creatinine, urine sodium, and urine osmolality (osm), Dr. Florez says. If a patient has water retention or hypertonic urine from syndrome of inappropriate diuretic hormone secretion (SIADH), hypothyroidism, or glucocorticoid deficiency, the hospitalist needs to act accordingly.
“If the urine osm is high, higher than the serum osm, and is fixed at that level for some reason…giving that person isotonic fluids will lead to additional water retention and make the situation worse,” he says. “It’s very important to assess the volume status and establish the cause. And then, if you’re going to give fluids, be mindful of what the urine might look like. Do not give fluids that are hypotonic with respect to what the urine is making, unless you are completely convinced that the person is dry and therefore needs volume.”

7. Encourage patients to check their own glucose and administer their own insulin while still in the hospital.
“We often deal with patients who start insulin treatment for diabetes during an admission or who seem not to be doing very well giving insulin at home,” Dr. Wexler says. “Many patients can benefit from supervised insulin injections and glucose testing.”
Going through the process while in the hospital with supervision can be a good refresher, she says.
“You don’t have to necessarily order specific diabetic teaching,” she adds, noting that not all hospitals have diabetic educators available at all times.
A patient might be waiting for diabetic teaching before discharge, but this might be one way to speed the process, Dr. Wexler says. She suggests teaching by example.
8. Patients on steroids every day are at risk for adrenal insufficiency.
Even if they aren’t on corticosteroids when they present, hospitalists should think of these patients as “at risk for adrenal insufficiency and potentially immunocompromised,” Dr. Greenwald says. “The bigger issue in most cases is the adrenal insufficiency.”
That means their bodies can’t mount an appropriate response to stress.
“And without that appropriate response of additional stress hormone the body would normally make, they may not be able, for example, to maintain their blood pressure,” he says. “This can be extremely dangerous.”
Inhaled steroids, and topical steroids if they are applied to broken skin, can have a kind of stealth effect.
“That’s something to keep in mind,” Dr. Wexler says, noting the connection between blood pressure management and endocrine conditions.
9. Thyroid hormone might not be as well absorbed under certain conditions.
With calcium or iron supplementation, thyroid hormones might present a problem, Dr. Wexler says. For patients at home taking thyroid hormone appropriately (an hour or two separated from calcium or iron supplementation), there “should be no issue,” she says. “But if they are administered at the same time at the hospital, patients may not absorb the full dose.”
Tom Collins is a freelance writer in South Florida.
References
- Omar AS, Salama A, Allam M, et al. Association of time in blood glucose range with outcomes following cardiac surgery. BMC Anesthesiol. 2015;15(1):14.
- Han HS, Kang SB. Relations between long-term glycemic control and postoperative wound and infectious complications after total knee arthroplasty in type 2 diabetics. Clin Orthop Surg. 2013;5(2):118–123.
- Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract. 2012;18(6):988-1028.
- Supit EJ, Peiris AN. Interpretation of laboratory thyroid function tests for the primary care physician. South Med J. 2002;95(5):481-485.
Assessing, Managing Delirium in Hospitalized Patients
Summary: Delirium is a common problem in hospitalized patients, and all too often delirium is iatrogenic. Delirium is associated with poor outcomes such as prolonged hospitalization and functional decline, and it increases the risk of nursing home admission. The most common tool to assess the presence of delirium is the Confusion Assessment Method (CAM). Dr. Cumbler educated the audience on a more refined tool, the 3D CAM [PDF], and provided the algorithm for diagnosis and evaluation of hospital-onset delirium.
Where delirium is concerned (as with most conditions), “an ounce of prevention is worth a pound of cure.” Namely, avoid prescribing problem medications such as anticholinergics, sedative/hypnotics (except benzodiazepines for treatment of alcohol withdrawal), and antihistamines; and minimize narcotics, but don’t undertreat pain as uncontrolled pain is a more potent delirium trigger than narcotics.
Avoid sleep deprivation. Do we really require vital signs and phlebotomy between midnight and 6 a.m.? Make sure patients have their glasses and hearing aids, and keep them up and moving during daylight hours. Sleep and sensory deprivation are effective forms of human torture and are known to be rather disorienting.
Finally, antipsychotics are associated with increased mortality in dementia. Patients with agitated delirium may benefit from a low dose of haloperidol. When prescribing haloperidol, remember IV administration requires EKG monitoring (FDA black box warning), and a reasonable starting dose is 0.5 mg, NOT 5 mg.
HM takeaways:
- Use CAM, 3D CAM to diagnose delirium;
- Avoid anticholinergic medications (promethazine, cyclobenzaprine, oxybutynin, amitriptyline, prednisolone, theophylline, dixogin, furosemide);
- Minimize, but do not avoid, narcotics in patients with both pain and delirium;
- Use low-dose antipsychotics, not benzodiazepines, for agitated delirium; and
- STOP antipsychotics ASAP, ideally prior to discharge; if not prior to discharge, then include discontinuation date on discharge medication list. TH
Summary: Delirium is a common problem in hospitalized patients, and all too often delirium is iatrogenic. Delirium is associated with poor outcomes such as prolonged hospitalization and functional decline, and it increases the risk of nursing home admission. The most common tool to assess the presence of delirium is the Confusion Assessment Method (CAM). Dr. Cumbler educated the audience on a more refined tool, the 3D CAM [PDF], and provided the algorithm for diagnosis and evaluation of hospital-onset delirium.
Where delirium is concerned (as with most conditions), “an ounce of prevention is worth a pound of cure.” Namely, avoid prescribing problem medications such as anticholinergics, sedative/hypnotics (except benzodiazepines for treatment of alcohol withdrawal), and antihistamines; and minimize narcotics, but don’t undertreat pain as uncontrolled pain is a more potent delirium trigger than narcotics.
Avoid sleep deprivation. Do we really require vital signs and phlebotomy between midnight and 6 a.m.? Make sure patients have their glasses and hearing aids, and keep them up and moving during daylight hours. Sleep and sensory deprivation are effective forms of human torture and are known to be rather disorienting.
Finally, antipsychotics are associated with increased mortality in dementia. Patients with agitated delirium may benefit from a low dose of haloperidol. When prescribing haloperidol, remember IV administration requires EKG monitoring (FDA black box warning), and a reasonable starting dose is 0.5 mg, NOT 5 mg.
HM takeaways:
- Use CAM, 3D CAM to diagnose delirium;
- Avoid anticholinergic medications (promethazine, cyclobenzaprine, oxybutynin, amitriptyline, prednisolone, theophylline, dixogin, furosemide);
- Minimize, but do not avoid, narcotics in patients with both pain and delirium;
- Use low-dose antipsychotics, not benzodiazepines, for agitated delirium; and
- STOP antipsychotics ASAP, ideally prior to discharge; if not prior to discharge, then include discontinuation date on discharge medication list. TH
Summary: Delirium is a common problem in hospitalized patients, and all too often delirium is iatrogenic. Delirium is associated with poor outcomes such as prolonged hospitalization and functional decline, and it increases the risk of nursing home admission. The most common tool to assess the presence of delirium is the Confusion Assessment Method (CAM). Dr. Cumbler educated the audience on a more refined tool, the 3D CAM [PDF], and provided the algorithm for diagnosis and evaluation of hospital-onset delirium.
Where delirium is concerned (as with most conditions), “an ounce of prevention is worth a pound of cure.” Namely, avoid prescribing problem medications such as anticholinergics, sedative/hypnotics (except benzodiazepines for treatment of alcohol withdrawal), and antihistamines; and minimize narcotics, but don’t undertreat pain as uncontrolled pain is a more potent delirium trigger than narcotics.
Avoid sleep deprivation. Do we really require vital signs and phlebotomy between midnight and 6 a.m.? Make sure patients have their glasses and hearing aids, and keep them up and moving during daylight hours. Sleep and sensory deprivation are effective forms of human torture and are known to be rather disorienting.
Finally, antipsychotics are associated with increased mortality in dementia. Patients with agitated delirium may benefit from a low dose of haloperidol. When prescribing haloperidol, remember IV administration requires EKG monitoring (FDA black box warning), and a reasonable starting dose is 0.5 mg, NOT 5 mg.
HM takeaways:
- Use CAM, 3D CAM to diagnose delirium;
- Avoid anticholinergic medications (promethazine, cyclobenzaprine, oxybutynin, amitriptyline, prednisolone, theophylline, dixogin, furosemide);
- Minimize, but do not avoid, narcotics in patients with both pain and delirium;
- Use low-dose antipsychotics, not benzodiazepines, for agitated delirium; and
- STOP antipsychotics ASAP, ideally prior to discharge; if not prior to discharge, then include discontinuation date on discharge medication list. TH