User login
Standard Discharge Communication Process Improves Verbal Handoffs between Hospitalists, PCPs
Clinical question: Can a standardized discharge communication process, coupled with an electronic health record (EHR) system, improve the proportion of completed verbal handoffs from in-hospital physicians to PCPs within 24 hours of patient discharge?
Background: Discharge from the hospital setting is known to be a transition of care fraught with patient safety risks, with more than half of discharged patients experiencing at least one error.1 Previous studies identified core elements that pediatric hospitalists and PCPs consider essential in discharge communication, which included:
- Pending laboratory or test results;
- Follow-up appointments;
- Discharge medications;
- Admission and discharge diagnoses;
- Dates of admission and discharge; and
- Suggested management plan.2
Rates of transmission and receipt of information have been found to be suboptimal after hospital discharge, and PCPs have been found to be less satisfied than hospitalists with communication.2,3 Additionally, PCPs and hospitalists have been found to have incongruent views on who should be responsible for pending labs, adverse events, or status changes, differences which can have safety implications.3 PCPs who refer to general hospitals have been found to report superior completeness of discharge communication compared to freestanding children’s hospitals, where resident physicians are generally responsible for discharge summary completion.4 Standardizing and promoting a process of verbal handoff after hospital discharge may address some of these safety concerns, although a relationship has not been established between aspects of discharge communication and associated adverse clinical outcomes.5
Study design: Quality improvement study using improvement science methods and run charts.
Setting: An urban, 598-bed, freestanding children’s hospital.
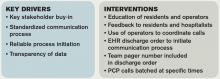
Synopsis: A 24/7 telephone operator service had been established at the investigators’ institution that was designed to facilitate communication between providers inside and outside the institution. At baseline, only 52% of hospital medicine (HM) provider discharges had a record of a discharge day call initiated to the PCP. A project team consisting of hospitalists, a chief resident, operator service administrators, and IT analysts identified system issues that led to unsuccessful communication, which facilitated identification of key drivers of improving communication and associated interventions (see Table 1).
Discharging physicians, who were usually residents, were instructed to call the operator at the time of discharge. Operators would page the PCP, and PCPs were expected to return the page within 20 minutes. Discharging physicians were expected to return the call to the operator within two to four minutes. The EHR generated a message to the operator whenever a discharge order was placed for an HM patient, leading the operator to page the discharging physician to initiate the call.
Adaptations after project initiation included:
- Reassigning primary responsibility for discharge phone calls to the daily on-call resident, if the discharging physician was not available.
- Establishing a non-changing pager number on the automated discharge notification that would always reach the appropriate team member.
- Batching discharge phone calls at times of increased resident availability to minimize hold times for PCPs and work interruptions for discharging physicians.
Weekly failure data was generated and reviewed by the improvement team, and a call record was linked to the patient’s medical record. Team-specific and overall results for HM teams were posted weekly on a run-chart. The primary outcome measure was the percentage of completed calls between PCP and HM physician within 24 hours of discharge.
Over the approximately 32-month study period, the percentage of calls initiated improved from 50% to 97% after four interventions. After one year, data was collected to assess percentage of calls completed, a number that rose from 80% in the first eight weeks to a median of 93%, which was sustained for 18 months.
Bottom line: Utilizing improvement methods and reliability science, a process of improving verbal handoffs between hospital-based physicians and PCPs within 24 hours after discharge led to a sustained improvement, to above 90%, in successful verbal handoffs.
Citation: Mussman GM, Vossmeyer MT, Brady PW, Warrick DM, Simmons JM, White CM. Improving the reliability of verbal communication between primary care physicians and pediatric hospitalists at hospital discharge [published online ahead of print May 29, 2015]. J Hosp Med. doi: 10.1002/jhm.2392.

Clinical Shorts
MAJORITY OF NONOBSTRUCTING ASYMPTOMATIC RENAL STONES REMAIN ASYMPTOMATIC OVER TIME
Retrospective trial of active surveillance of asymptomatic nonobstructing renal calculi demonstrated that 28% of stones became symptomatic, with 17% requiring surgical intervention and 2% causing asymptomatic hydronephrosis over three years.
Citation: Dropkin BM, Moses RA, Sharma D, Pais VM Jr. The natural history of nonobstructing asymptomatic renal stones managed with active surveillance. J Urol. 2015;193(4):1265-1269.
CPR USE IS HIGH, YET OUTCOMES ARE POOR IN HEMODIALYSIS PATIENTS
In a national cohort of hemodialysis patients, receipt of in-hospital CPR was significantly higher (6.3% vs. 0.3%) than the general population, but post-discharge survival was substantially shorter (33 vs. five months).
Citation: Wong SY, Kreuter W, Curtis JR, Hall YN, O’Hare AM. Trends in in-hospital cardiopulmonary resuscitation and survival in adults receiving maintenance dialysis. JAMA Intern Med. 2015;175(6):1028-1035. doi:10.1001/jamainternmed.2015.0406.
ULTRASOUND GUIDANCE INCREASES RATE OF SUCCESSFUL FIRST ATTEMPT RADIAL ARTERY CANNULATION
Randomized controlled trial of 749 anesthesia trainees showed that ultrasound guidance increased rate of first attempt radial artery cannulation by 14% when compared to Doppler and palpation (95% CI 5-22%).
Citation: Ueda K, Bayman EO, Johnson C, Odum NJ, Lee JJ. A randomised controlled trial of radial artery cannulation guided by Doppler vs palpation vs ultrasound [published online ahead of print April 8, 2015]. Anaesthesia. doi: 10.1111/anae.13062.
NO DIFFERENCE BETWEEN EPIDURAL STEROID INJECTIONS AND GABAPENTIN FOR TREATMENT OF LUMBOSACRAL RADICULAR PAIN
Multicenter, randomized study found no difference in lumbosacral radicular pain at one and three months in patients treated with epidural steroid injection versus gabapentin.
Citation: Cohen SP, Hanling S, Bicket MC, et al. Epidural steroid injections compared with gabapentin for lumbosacral radicular pain: multicenter randomized double blind comparative efficacy study. BMJ. 2015;350:h1748 doi: 10.1136/bmj.h1748.
References
- Smith K. Effective communication with primary care providers. Pediatr Clin North Am. 2014;61(4):671-679.
- Coghlin DT, Leyenaar JK, Shen M, et al. Pediatric discharge content: a multisite assessment of physician preferences and experiences. Hosp Pediatr. 2014;4(1):9-15.
- Ruth JL, Geskey JM, Shaffer ML, Bramley HP, Paul IM. Evaluating communication between pediatric primary care physicians and hospitalists. Clin Pediatr (Phila). 2011;50(10):923-928.
- Leyenaar JK, Bergert L, Mallory LA, et al. Pediatric primary care providers’ perspectives regarding hospital discharge communication: a mixed methods analysis. Acad Pediatr. 2015;15(1):61-68.
- Bell CM, Schnipper JL, Auerbach AD, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381-386.
Clinical question: Can a standardized discharge communication process, coupled with an electronic health record (EHR) system, improve the proportion of completed verbal handoffs from in-hospital physicians to PCPs within 24 hours of patient discharge?
Background: Discharge from the hospital setting is known to be a transition of care fraught with patient safety risks, with more than half of discharged patients experiencing at least one error.1 Previous studies identified core elements that pediatric hospitalists and PCPs consider essential in discharge communication, which included:
- Pending laboratory or test results;
- Follow-up appointments;
- Discharge medications;
- Admission and discharge diagnoses;
- Dates of admission and discharge; and
- Suggested management plan.2
Rates of transmission and receipt of information have been found to be suboptimal after hospital discharge, and PCPs have been found to be less satisfied than hospitalists with communication.2,3 Additionally, PCPs and hospitalists have been found to have incongruent views on who should be responsible for pending labs, adverse events, or status changes, differences which can have safety implications.3 PCPs who refer to general hospitals have been found to report superior completeness of discharge communication compared to freestanding children’s hospitals, where resident physicians are generally responsible for discharge summary completion.4 Standardizing and promoting a process of verbal handoff after hospital discharge may address some of these safety concerns, although a relationship has not been established between aspects of discharge communication and associated adverse clinical outcomes.5
Study design: Quality improvement study using improvement science methods and run charts.
Setting: An urban, 598-bed, freestanding children’s hospital.
Synopsis: A 24/7 telephone operator service had been established at the investigators’ institution that was designed to facilitate communication between providers inside and outside the institution. At baseline, only 52% of hospital medicine (HM) provider discharges had a record of a discharge day call initiated to the PCP. A project team consisting of hospitalists, a chief resident, operator service administrators, and IT analysts identified system issues that led to unsuccessful communication, which facilitated identification of key drivers of improving communication and associated interventions (see Table 1).
Discharging physicians, who were usually residents, were instructed to call the operator at the time of discharge. Operators would page the PCP, and PCPs were expected to return the page within 20 minutes. Discharging physicians were expected to return the call to the operator within two to four minutes. The EHR generated a message to the operator whenever a discharge order was placed for an HM patient, leading the operator to page the discharging physician to initiate the call.
Adaptations after project initiation included:
- Reassigning primary responsibility for discharge phone calls to the daily on-call resident, if the discharging physician was not available.
- Establishing a non-changing pager number on the automated discharge notification that would always reach the appropriate team member.
- Batching discharge phone calls at times of increased resident availability to minimize hold times for PCPs and work interruptions for discharging physicians.
Weekly failure data was generated and reviewed by the improvement team, and a call record was linked to the patient’s medical record. Team-specific and overall results for HM teams were posted weekly on a run-chart. The primary outcome measure was the percentage of completed calls between PCP and HM physician within 24 hours of discharge.
Over the approximately 32-month study period, the percentage of calls initiated improved from 50% to 97% after four interventions. After one year, data was collected to assess percentage of calls completed, a number that rose from 80% in the first eight weeks to a median of 93%, which was sustained for 18 months.
Bottom line: Utilizing improvement methods and reliability science, a process of improving verbal handoffs between hospital-based physicians and PCPs within 24 hours after discharge led to a sustained improvement, to above 90%, in successful verbal handoffs.
Citation: Mussman GM, Vossmeyer MT, Brady PW, Warrick DM, Simmons JM, White CM. Improving the reliability of verbal communication between primary care physicians and pediatric hospitalists at hospital discharge [published online ahead of print May 29, 2015]. J Hosp Med. doi: 10.1002/jhm.2392.

Clinical Shorts
MAJORITY OF NONOBSTRUCTING ASYMPTOMATIC RENAL STONES REMAIN ASYMPTOMATIC OVER TIME
Retrospective trial of active surveillance of asymptomatic nonobstructing renal calculi demonstrated that 28% of stones became symptomatic, with 17% requiring surgical intervention and 2% causing asymptomatic hydronephrosis over three years.
Citation: Dropkin BM, Moses RA, Sharma D, Pais VM Jr. The natural history of nonobstructing asymptomatic renal stones managed with active surveillance. J Urol. 2015;193(4):1265-1269.
CPR USE IS HIGH, YET OUTCOMES ARE POOR IN HEMODIALYSIS PATIENTS
In a national cohort of hemodialysis patients, receipt of in-hospital CPR was significantly higher (6.3% vs. 0.3%) than the general population, but post-discharge survival was substantially shorter (33 vs. five months).
Citation: Wong SY, Kreuter W, Curtis JR, Hall YN, O’Hare AM. Trends in in-hospital cardiopulmonary resuscitation and survival in adults receiving maintenance dialysis. JAMA Intern Med. 2015;175(6):1028-1035. doi:10.1001/jamainternmed.2015.0406.
ULTRASOUND GUIDANCE INCREASES RATE OF SUCCESSFUL FIRST ATTEMPT RADIAL ARTERY CANNULATION
Randomized controlled trial of 749 anesthesia trainees showed that ultrasound guidance increased rate of first attempt radial artery cannulation by 14% when compared to Doppler and palpation (95% CI 5-22%).
Citation: Ueda K, Bayman EO, Johnson C, Odum NJ, Lee JJ. A randomised controlled trial of radial artery cannulation guided by Doppler vs palpation vs ultrasound [published online ahead of print April 8, 2015]. Anaesthesia. doi: 10.1111/anae.13062.
NO DIFFERENCE BETWEEN EPIDURAL STEROID INJECTIONS AND GABAPENTIN FOR TREATMENT OF LUMBOSACRAL RADICULAR PAIN
Multicenter, randomized study found no difference in lumbosacral radicular pain at one and three months in patients treated with epidural steroid injection versus gabapentin.
Citation: Cohen SP, Hanling S, Bicket MC, et al. Epidural steroid injections compared with gabapentin for lumbosacral radicular pain: multicenter randomized double blind comparative efficacy study. BMJ. 2015;350:h1748 doi: 10.1136/bmj.h1748.
References
- Smith K. Effective communication with primary care providers. Pediatr Clin North Am. 2014;61(4):671-679.
- Coghlin DT, Leyenaar JK, Shen M, et al. Pediatric discharge content: a multisite assessment of physician preferences and experiences. Hosp Pediatr. 2014;4(1):9-15.
- Ruth JL, Geskey JM, Shaffer ML, Bramley HP, Paul IM. Evaluating communication between pediatric primary care physicians and hospitalists. Clin Pediatr (Phila). 2011;50(10):923-928.
- Leyenaar JK, Bergert L, Mallory LA, et al. Pediatric primary care providers’ perspectives regarding hospital discharge communication: a mixed methods analysis. Acad Pediatr. 2015;15(1):61-68.
- Bell CM, Schnipper JL, Auerbach AD, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381-386.
Clinical question: Can a standardized discharge communication process, coupled with an electronic health record (EHR) system, improve the proportion of completed verbal handoffs from in-hospital physicians to PCPs within 24 hours of patient discharge?
Background: Discharge from the hospital setting is known to be a transition of care fraught with patient safety risks, with more than half of discharged patients experiencing at least one error.1 Previous studies identified core elements that pediatric hospitalists and PCPs consider essential in discharge communication, which included:
- Pending laboratory or test results;
- Follow-up appointments;
- Discharge medications;
- Admission and discharge diagnoses;
- Dates of admission and discharge; and
- Suggested management plan.2
Rates of transmission and receipt of information have been found to be suboptimal after hospital discharge, and PCPs have been found to be less satisfied than hospitalists with communication.2,3 Additionally, PCPs and hospitalists have been found to have incongruent views on who should be responsible for pending labs, adverse events, or status changes, differences which can have safety implications.3 PCPs who refer to general hospitals have been found to report superior completeness of discharge communication compared to freestanding children’s hospitals, where resident physicians are generally responsible for discharge summary completion.4 Standardizing and promoting a process of verbal handoff after hospital discharge may address some of these safety concerns, although a relationship has not been established between aspects of discharge communication and associated adverse clinical outcomes.5
Study design: Quality improvement study using improvement science methods and run charts.
Setting: An urban, 598-bed, freestanding children’s hospital.
Synopsis: A 24/7 telephone operator service had been established at the investigators’ institution that was designed to facilitate communication between providers inside and outside the institution. At baseline, only 52% of hospital medicine (HM) provider discharges had a record of a discharge day call initiated to the PCP. A project team consisting of hospitalists, a chief resident, operator service administrators, and IT analysts identified system issues that led to unsuccessful communication, which facilitated identification of key drivers of improving communication and associated interventions (see Table 1).
Discharging physicians, who were usually residents, were instructed to call the operator at the time of discharge. Operators would page the PCP, and PCPs were expected to return the page within 20 minutes. Discharging physicians were expected to return the call to the operator within two to four minutes. The EHR generated a message to the operator whenever a discharge order was placed for an HM patient, leading the operator to page the discharging physician to initiate the call.
Adaptations after project initiation included:
- Reassigning primary responsibility for discharge phone calls to the daily on-call resident, if the discharging physician was not available.
- Establishing a non-changing pager number on the automated discharge notification that would always reach the appropriate team member.
- Batching discharge phone calls at times of increased resident availability to minimize hold times for PCPs and work interruptions for discharging physicians.
Weekly failure data was generated and reviewed by the improvement team, and a call record was linked to the patient’s medical record. Team-specific and overall results for HM teams were posted weekly on a run-chart. The primary outcome measure was the percentage of completed calls between PCP and HM physician within 24 hours of discharge.
Over the approximately 32-month study period, the percentage of calls initiated improved from 50% to 97% after four interventions. After one year, data was collected to assess percentage of calls completed, a number that rose from 80% in the first eight weeks to a median of 93%, which was sustained for 18 months.
Bottom line: Utilizing improvement methods and reliability science, a process of improving verbal handoffs between hospital-based physicians and PCPs within 24 hours after discharge led to a sustained improvement, to above 90%, in successful verbal handoffs.
Citation: Mussman GM, Vossmeyer MT, Brady PW, Warrick DM, Simmons JM, White CM. Improving the reliability of verbal communication between primary care physicians and pediatric hospitalists at hospital discharge [published online ahead of print May 29, 2015]. J Hosp Med. doi: 10.1002/jhm.2392.

Clinical Shorts
MAJORITY OF NONOBSTRUCTING ASYMPTOMATIC RENAL STONES REMAIN ASYMPTOMATIC OVER TIME
Retrospective trial of active surveillance of asymptomatic nonobstructing renal calculi demonstrated that 28% of stones became symptomatic, with 17% requiring surgical intervention and 2% causing asymptomatic hydronephrosis over three years.
Citation: Dropkin BM, Moses RA, Sharma D, Pais VM Jr. The natural history of nonobstructing asymptomatic renal stones managed with active surveillance. J Urol. 2015;193(4):1265-1269.
CPR USE IS HIGH, YET OUTCOMES ARE POOR IN HEMODIALYSIS PATIENTS
In a national cohort of hemodialysis patients, receipt of in-hospital CPR was significantly higher (6.3% vs. 0.3%) than the general population, but post-discharge survival was substantially shorter (33 vs. five months).
Citation: Wong SY, Kreuter W, Curtis JR, Hall YN, O’Hare AM. Trends in in-hospital cardiopulmonary resuscitation and survival in adults receiving maintenance dialysis. JAMA Intern Med. 2015;175(6):1028-1035. doi:10.1001/jamainternmed.2015.0406.
ULTRASOUND GUIDANCE INCREASES RATE OF SUCCESSFUL FIRST ATTEMPT RADIAL ARTERY CANNULATION
Randomized controlled trial of 749 anesthesia trainees showed that ultrasound guidance increased rate of first attempt radial artery cannulation by 14% when compared to Doppler and palpation (95% CI 5-22%).
Citation: Ueda K, Bayman EO, Johnson C, Odum NJ, Lee JJ. A randomised controlled trial of radial artery cannulation guided by Doppler vs palpation vs ultrasound [published online ahead of print April 8, 2015]. Anaesthesia. doi: 10.1111/anae.13062.
NO DIFFERENCE BETWEEN EPIDURAL STEROID INJECTIONS AND GABAPENTIN FOR TREATMENT OF LUMBOSACRAL RADICULAR PAIN
Multicenter, randomized study found no difference in lumbosacral radicular pain at one and three months in patients treated with epidural steroid injection versus gabapentin.
Citation: Cohen SP, Hanling S, Bicket MC, et al. Epidural steroid injections compared with gabapentin for lumbosacral radicular pain: multicenter randomized double blind comparative efficacy study. BMJ. 2015;350:h1748 doi: 10.1136/bmj.h1748.
References
- Smith K. Effective communication with primary care providers. Pediatr Clin North Am. 2014;61(4):671-679.
- Coghlin DT, Leyenaar JK, Shen M, et al. Pediatric discharge content: a multisite assessment of physician preferences and experiences. Hosp Pediatr. 2014;4(1):9-15.
- Ruth JL, Geskey JM, Shaffer ML, Bramley HP, Paul IM. Evaluating communication between pediatric primary care physicians and hospitalists. Clin Pediatr (Phila). 2011;50(10):923-928.
- Leyenaar JK, Bergert L, Mallory LA, et al. Pediatric primary care providers’ perspectives regarding hospital discharge communication: a mixed methods analysis. Acad Pediatr. 2015;15(1):61-68.
- Bell CM, Schnipper JL, Auerbach AD, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381-386.
Nomogram Predicts Post-Operative Readmission
Clinical question: Can a nomogram accurately predict a patient’s risk of post-operative 30-day readmission?
Background: Medicare and Medicaid have implemented penalties for hospitals with high readmission rates. While this does not yet apply to post-operative readmissions, there is concern that it soon will. Algorithms for predicting readmission have been developed for medical patients; however, to date, no such tool has been developed for post-operative patients.
Study design: Retrospective review and prospective validation of a predictive nomogram.
Setting: Single academic hospital.
Synopsis: Using the American College of Surgeons’ National Surgical Quality Improvement Program (ACS NSQIP) and hospital billing data, a retrospective analysis of 2,799 patients who had elective surgery between 2006 and 2011 was performed in order to develop a predictive nomogram for post-operative readmissions. Pre-operative, operative, and post-operative variables associated with readmission were evaluated, and the following variables were found to be independently associated with readmission:
- Bleeding disorder;
- Prolonged procedure length;
- In-hospital complications;
- Dependent functional status; and/or
- Higher care at discharge.
Using a linear regression model, a nomogram was developed that was prospectively validated in 255 patients from a single center. The nomogram accurately predicted the risk of post-operative readmission (C statistic=0.756) in the prospective analysis.
The nomogram has limited generalizability given the fact that it included patients from a single institution; it would benefit from external validation before widespread use.
Bottom line: The use of this predictive nomogram could aid in identifying patients at high risk of readmission.
Citation: Tevis SE, Weber SM, Kent KC, Kennedy GD. Nomogram to predict postoperative readmission in patients who undergo general surgery. JAMA Surg. 2015;150(6):505-510. doi: 10.1001/jamasurg.2014.4043.
Clinical question: Can a nomogram accurately predict a patient’s risk of post-operative 30-day readmission?
Background: Medicare and Medicaid have implemented penalties for hospitals with high readmission rates. While this does not yet apply to post-operative readmissions, there is concern that it soon will. Algorithms for predicting readmission have been developed for medical patients; however, to date, no such tool has been developed for post-operative patients.
Study design: Retrospective review and prospective validation of a predictive nomogram.
Setting: Single academic hospital.
Synopsis: Using the American College of Surgeons’ National Surgical Quality Improvement Program (ACS NSQIP) and hospital billing data, a retrospective analysis of 2,799 patients who had elective surgery between 2006 and 2011 was performed in order to develop a predictive nomogram for post-operative readmissions. Pre-operative, operative, and post-operative variables associated with readmission were evaluated, and the following variables were found to be independently associated with readmission:
- Bleeding disorder;
- Prolonged procedure length;
- In-hospital complications;
- Dependent functional status; and/or
- Higher care at discharge.
Using a linear regression model, a nomogram was developed that was prospectively validated in 255 patients from a single center. The nomogram accurately predicted the risk of post-operative readmission (C statistic=0.756) in the prospective analysis.
The nomogram has limited generalizability given the fact that it included patients from a single institution; it would benefit from external validation before widespread use.
Bottom line: The use of this predictive nomogram could aid in identifying patients at high risk of readmission.
Citation: Tevis SE, Weber SM, Kent KC, Kennedy GD. Nomogram to predict postoperative readmission in patients who undergo general surgery. JAMA Surg. 2015;150(6):505-510. doi: 10.1001/jamasurg.2014.4043.
Clinical question: Can a nomogram accurately predict a patient’s risk of post-operative 30-day readmission?
Background: Medicare and Medicaid have implemented penalties for hospitals with high readmission rates. While this does not yet apply to post-operative readmissions, there is concern that it soon will. Algorithms for predicting readmission have been developed for medical patients; however, to date, no such tool has been developed for post-operative patients.
Study design: Retrospective review and prospective validation of a predictive nomogram.
Setting: Single academic hospital.
Synopsis: Using the American College of Surgeons’ National Surgical Quality Improvement Program (ACS NSQIP) and hospital billing data, a retrospective analysis of 2,799 patients who had elective surgery between 2006 and 2011 was performed in order to develop a predictive nomogram for post-operative readmissions. Pre-operative, operative, and post-operative variables associated with readmission were evaluated, and the following variables were found to be independently associated with readmission:
- Bleeding disorder;
- Prolonged procedure length;
- In-hospital complications;
- Dependent functional status; and/or
- Higher care at discharge.
Using a linear regression model, a nomogram was developed that was prospectively validated in 255 patients from a single center. The nomogram accurately predicted the risk of post-operative readmission (C statistic=0.756) in the prospective analysis.
The nomogram has limited generalizability given the fact that it included patients from a single institution; it would benefit from external validation before widespread use.
Bottom line: The use of this predictive nomogram could aid in identifying patients at high risk of readmission.
Citation: Tevis SE, Weber SM, Kent KC, Kennedy GD. Nomogram to predict postoperative readmission in patients who undergo general surgery. JAMA Surg. 2015;150(6):505-510. doi: 10.1001/jamasurg.2014.4043.
Antibiotic Stewardship and Hospitalists: How to Educate Patients on Antibiotics
Editor’s note: This article originally appeared on SHM’s official blog, “The Hospital Leader,” in June 2015.
“Tell me what you know about antibiotics.”
That’s the discussion I start with hospitalized patients all the time, right after they ask me to prescribe antibiotics for their simple cough or other viral-like illness.
And, from their perspective, asking for antibiotics makes sense. After all, antibiotics have been the physician’s knee-jerk reaction to a number of patient symptoms for decades, especially for a cough or upper respiratory infection. We have inadvertently trained our patients that there is an easy solution to almost any common medical problem.
But patients often answer my question with something like “not much,” coupled with a little surprise that I haven’t already started ordering the prescription.
That’s when I talk about the potential harms of antibiotics. And that’s also when their eyebrows go up. I start with the easy harms, like the fact that many antibiotics can cause diarrhea, a symptom nobody wants to deal with along with their runny nose. Then I move on to the big ones: Use of antibiotics today could make the patient resistant to antibiotics later in life, when they might really need them, and using antibiotics can lead to other painful and even fatal conditions, like Clostridium difficile.
After that, every patient agrees with my recommendations that we hold off on antibiotics for certain, particularly viral-like, ailments.
Change the Conversation. Change the Approach.
It’s a longer conversation, but it’s worth it. Overuse of antibiotics affects not only the patient in front of me, but also entire communities. By creating antibiotic-resistant bacteria, we make everyone more vulnerable to the very diseases the antibiotics were originally intended to treat, like tuberculosis, staph infections, and numerous others.
That’s why the hospitalists in my hospital at Johns Hopkins Bayview teamed up with the infectious diseases division to improve our approach to cellulitis and antibiotic use.
In short, cellulitis is a bacterial skin infection. The most feared bacterial skin infection is MRSA (methicillin-resistant Staphylococcus aureus), a “super bug” that requires highly selective antibiotics like vancomycin; however, other more common and less virulent bacteria also cause cellulitis, and they don’t need super bug fighter medications. Some types of skin ailments, like those caused by poor circulation in the legs, are not infectious at all but can look like cellulitis, even to experienced doctors.
Thanks to the collaboration between infectious disease doctors and hospitalists, the hospitalists are much less likely to prescribe inappropriate antibiotics. That’s a triple-win: It reduces the length of stay for the patient, the incidence of C. diff, and costs.
The Front Line
This concern isn’t limited to a single hospital. There are now more than 44,000 hospitalists nationwide, and every one of us plays an important role in antibiotic stewardship. The bedside is the front line of the fight against antibiotic resistance.
tuberculosis, staph infections, and numerous others.
—Eric Howell, MD, SFHM
There are more than 5,000 hospitals across the country, and hospitalists in every one of them must take responsibility for the appropriate use of antibiotics for their patients.
Announcing SHM’s National Commitment to Antibiotic Stewardship
SHM was proud to join more than 150 major organizations at the White House Forum on Antibiotic Stewardship to announce commitments to implement changes over the next five years that will slow the emergence of antibiotic-resistant bacteria, detect resistant strains, preserve the efficacy of our existing antibiotics, and prevent the spread of resistant infections.
Specifically, SHM has committed to three national initiatives that are aligned with our organizational goal of providing the best possible care for the hospitalized patient and the federal government’s dedication to this important issue:
- Enhance hospitalists’ awareness of key antimicrobial stewardship best practices and ask them to formally commit to at least two behavior changes to reduce inappropriate antimicrobial use and antimicrobial resistance;
- Support national initiatives that advocate for the appropriate use of antimicrobials and promote strategies to reduce antimicrobial resistance; and
- Identify partnerships and other opportunities to support the development of a comprehensive program to implement antimicrobial stewardship best practices in America’s hospitals.
These commitments, which I shared with White House Forum participants, play to the strengths of hospitalists in healthcare: advocacy on behalf of patients and quality improvement and collaboration with others.
What Hospitalists Can Do Now
I also know, however, that you aren’t the kind of people to wait for official pronouncements and campaigns to start a program that will improve the care of hospitalized patients. That’s why SHM and I are recommending that all hospitalists begin to take steps immediately to address this national healthcare crisis:
- Start the conversation with your patients. It’s easy to prescribe antibiotics, but it can also be harmful. Talk with your patients about when antibiotics are medically appropriate and the potential harms they may cause.
- Prescribe antibiotics for specific diagnoses. Prescribing “just in case” is a prescription for antibiotic resistance. Make sure you understand the signs and symptoms of the conditions for which you’re prescribing antibiotics. As we learned at our hospital, cellulitis and venous insufficiency can look similar, but only one responds to antibiotic treatment.
- Work with your infectious disease colleagues. They can help you create systems and diagnose patients to help improve your hospital’s antibiotic stewardship.
After all, we are on the front lines, protecting our current and future patients. And we can’t afford to wait.
Dr. Howell is a veteran hospitalist at Johns Hopkins Bayview Hospital in Baltimore and a past president of SHM.
Editor’s note: This article originally appeared on SHM’s official blog, “The Hospital Leader,” in June 2015.
“Tell me what you know about antibiotics.”
That’s the discussion I start with hospitalized patients all the time, right after they ask me to prescribe antibiotics for their simple cough or other viral-like illness.
And, from their perspective, asking for antibiotics makes sense. After all, antibiotics have been the physician’s knee-jerk reaction to a number of patient symptoms for decades, especially for a cough or upper respiratory infection. We have inadvertently trained our patients that there is an easy solution to almost any common medical problem.
But patients often answer my question with something like “not much,” coupled with a little surprise that I haven’t already started ordering the prescription.
That’s when I talk about the potential harms of antibiotics. And that’s also when their eyebrows go up. I start with the easy harms, like the fact that many antibiotics can cause diarrhea, a symptom nobody wants to deal with along with their runny nose. Then I move on to the big ones: Use of antibiotics today could make the patient resistant to antibiotics later in life, when they might really need them, and using antibiotics can lead to other painful and even fatal conditions, like Clostridium difficile.
After that, every patient agrees with my recommendations that we hold off on antibiotics for certain, particularly viral-like, ailments.
Change the Conversation. Change the Approach.
It’s a longer conversation, but it’s worth it. Overuse of antibiotics affects not only the patient in front of me, but also entire communities. By creating antibiotic-resistant bacteria, we make everyone more vulnerable to the very diseases the antibiotics were originally intended to treat, like tuberculosis, staph infections, and numerous others.
That’s why the hospitalists in my hospital at Johns Hopkins Bayview teamed up with the infectious diseases division to improve our approach to cellulitis and antibiotic use.
In short, cellulitis is a bacterial skin infection. The most feared bacterial skin infection is MRSA (methicillin-resistant Staphylococcus aureus), a “super bug” that requires highly selective antibiotics like vancomycin; however, other more common and less virulent bacteria also cause cellulitis, and they don’t need super bug fighter medications. Some types of skin ailments, like those caused by poor circulation in the legs, are not infectious at all but can look like cellulitis, even to experienced doctors.
Thanks to the collaboration between infectious disease doctors and hospitalists, the hospitalists are much less likely to prescribe inappropriate antibiotics. That’s a triple-win: It reduces the length of stay for the patient, the incidence of C. diff, and costs.
The Front Line
This concern isn’t limited to a single hospital. There are now more than 44,000 hospitalists nationwide, and every one of us plays an important role in antibiotic stewardship. The bedside is the front line of the fight against antibiotic resistance.
tuberculosis, staph infections, and numerous others.
—Eric Howell, MD, SFHM
There are more than 5,000 hospitals across the country, and hospitalists in every one of them must take responsibility for the appropriate use of antibiotics for their patients.
Announcing SHM’s National Commitment to Antibiotic Stewardship
SHM was proud to join more than 150 major organizations at the White House Forum on Antibiotic Stewardship to announce commitments to implement changes over the next five years that will slow the emergence of antibiotic-resistant bacteria, detect resistant strains, preserve the efficacy of our existing antibiotics, and prevent the spread of resistant infections.
Specifically, SHM has committed to three national initiatives that are aligned with our organizational goal of providing the best possible care for the hospitalized patient and the federal government’s dedication to this important issue:
- Enhance hospitalists’ awareness of key antimicrobial stewardship best practices and ask them to formally commit to at least two behavior changes to reduce inappropriate antimicrobial use and antimicrobial resistance;
- Support national initiatives that advocate for the appropriate use of antimicrobials and promote strategies to reduce antimicrobial resistance; and
- Identify partnerships and other opportunities to support the development of a comprehensive program to implement antimicrobial stewardship best practices in America’s hospitals.
These commitments, which I shared with White House Forum participants, play to the strengths of hospitalists in healthcare: advocacy on behalf of patients and quality improvement and collaboration with others.
What Hospitalists Can Do Now
I also know, however, that you aren’t the kind of people to wait for official pronouncements and campaigns to start a program that will improve the care of hospitalized patients. That’s why SHM and I are recommending that all hospitalists begin to take steps immediately to address this national healthcare crisis:
- Start the conversation with your patients. It’s easy to prescribe antibiotics, but it can also be harmful. Talk with your patients about when antibiotics are medically appropriate and the potential harms they may cause.
- Prescribe antibiotics for specific diagnoses. Prescribing “just in case” is a prescription for antibiotic resistance. Make sure you understand the signs and symptoms of the conditions for which you’re prescribing antibiotics. As we learned at our hospital, cellulitis and venous insufficiency can look similar, but only one responds to antibiotic treatment.
- Work with your infectious disease colleagues. They can help you create systems and diagnose patients to help improve your hospital’s antibiotic stewardship.
After all, we are on the front lines, protecting our current and future patients. And we can’t afford to wait.
Dr. Howell is a veteran hospitalist at Johns Hopkins Bayview Hospital in Baltimore and a past president of SHM.
Editor’s note: This article originally appeared on SHM’s official blog, “The Hospital Leader,” in June 2015.
“Tell me what you know about antibiotics.”
That’s the discussion I start with hospitalized patients all the time, right after they ask me to prescribe antibiotics for their simple cough or other viral-like illness.
And, from their perspective, asking for antibiotics makes sense. After all, antibiotics have been the physician’s knee-jerk reaction to a number of patient symptoms for decades, especially for a cough or upper respiratory infection. We have inadvertently trained our patients that there is an easy solution to almost any common medical problem.
But patients often answer my question with something like “not much,” coupled with a little surprise that I haven’t already started ordering the prescription.
That’s when I talk about the potential harms of antibiotics. And that’s also when their eyebrows go up. I start with the easy harms, like the fact that many antibiotics can cause diarrhea, a symptom nobody wants to deal with along with their runny nose. Then I move on to the big ones: Use of antibiotics today could make the patient resistant to antibiotics later in life, when they might really need them, and using antibiotics can lead to other painful and even fatal conditions, like Clostridium difficile.
After that, every patient agrees with my recommendations that we hold off on antibiotics for certain, particularly viral-like, ailments.
Change the Conversation. Change the Approach.
It’s a longer conversation, but it’s worth it. Overuse of antibiotics affects not only the patient in front of me, but also entire communities. By creating antibiotic-resistant bacteria, we make everyone more vulnerable to the very diseases the antibiotics were originally intended to treat, like tuberculosis, staph infections, and numerous others.
That’s why the hospitalists in my hospital at Johns Hopkins Bayview teamed up with the infectious diseases division to improve our approach to cellulitis and antibiotic use.
In short, cellulitis is a bacterial skin infection. The most feared bacterial skin infection is MRSA (methicillin-resistant Staphylococcus aureus), a “super bug” that requires highly selective antibiotics like vancomycin; however, other more common and less virulent bacteria also cause cellulitis, and they don’t need super bug fighter medications. Some types of skin ailments, like those caused by poor circulation in the legs, are not infectious at all but can look like cellulitis, even to experienced doctors.
Thanks to the collaboration between infectious disease doctors and hospitalists, the hospitalists are much less likely to prescribe inappropriate antibiotics. That’s a triple-win: It reduces the length of stay for the patient, the incidence of C. diff, and costs.
The Front Line
This concern isn’t limited to a single hospital. There are now more than 44,000 hospitalists nationwide, and every one of us plays an important role in antibiotic stewardship. The bedside is the front line of the fight against antibiotic resistance.
tuberculosis, staph infections, and numerous others.
—Eric Howell, MD, SFHM
There are more than 5,000 hospitals across the country, and hospitalists in every one of them must take responsibility for the appropriate use of antibiotics for their patients.
Announcing SHM’s National Commitment to Antibiotic Stewardship
SHM was proud to join more than 150 major organizations at the White House Forum on Antibiotic Stewardship to announce commitments to implement changes over the next five years that will slow the emergence of antibiotic-resistant bacteria, detect resistant strains, preserve the efficacy of our existing antibiotics, and prevent the spread of resistant infections.
Specifically, SHM has committed to three national initiatives that are aligned with our organizational goal of providing the best possible care for the hospitalized patient and the federal government’s dedication to this important issue:
- Enhance hospitalists’ awareness of key antimicrobial stewardship best practices and ask them to formally commit to at least two behavior changes to reduce inappropriate antimicrobial use and antimicrobial resistance;
- Support national initiatives that advocate for the appropriate use of antimicrobials and promote strategies to reduce antimicrobial resistance; and
- Identify partnerships and other opportunities to support the development of a comprehensive program to implement antimicrobial stewardship best practices in America’s hospitals.
These commitments, which I shared with White House Forum participants, play to the strengths of hospitalists in healthcare: advocacy on behalf of patients and quality improvement and collaboration with others.
What Hospitalists Can Do Now
I also know, however, that you aren’t the kind of people to wait for official pronouncements and campaigns to start a program that will improve the care of hospitalized patients. That’s why SHM and I are recommending that all hospitalists begin to take steps immediately to address this national healthcare crisis:
- Start the conversation with your patients. It’s easy to prescribe antibiotics, but it can also be harmful. Talk with your patients about when antibiotics are medically appropriate and the potential harms they may cause.
- Prescribe antibiotics for specific diagnoses. Prescribing “just in case” is a prescription for antibiotic resistance. Make sure you understand the signs and symptoms of the conditions for which you’re prescribing antibiotics. As we learned at our hospital, cellulitis and venous insufficiency can look similar, but only one responds to antibiotic treatment.
- Work with your infectious disease colleagues. They can help you create systems and diagnose patients to help improve your hospital’s antibiotic stewardship.
After all, we are on the front lines, protecting our current and future patients. And we can’t afford to wait.
Dr. Howell is a veteran hospitalist at Johns Hopkins Bayview Hospital in Baltimore and a past president of SHM.
Antiepileptic Drugs Reduce Risk of Recurrent Unprovoked Seizures
Clinical question: What are the updated recommendations for treating first unprovoked seizure in adults?
Background: Approximately 150,000 adults present with an unprovoked first seizure in the U.S. annually, and these events are associated with physical and psychological trauma. Prior guidelines discussed evaluation of unprovoked first seizures in adults but did not address management. This publication aims to analyze existing evidence regarding prognosis and therapy with antiepileptic drugs (AEDs).
Study design: Evidence-based appraisal of a systematic review.
Setting: Literature published from 1966 to 2013 on MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials.
Synopsis: Ten prognostic studies describing risk of recurrence were found. Generalized tonic-clonic seizures were the major seizure type. Cumulative incidence of recurrent seizure increased over time, with the majority occurring within the first two years, regardless of treatment with AED; however, there were treatment differences among these studies and wide variation in recurrence rates.
Recurrence risk was lower with AED therapy, though patients were not randomized. Increased risk of recurrence was associated with prior brain lesion causing the seizure, EEG with epileptiform abnormalities, imaging abnormality, and nocturnal seizure.
Five studies were reviewed for prognosis following immediate AED therapy. Immediate AED treatment reduced risk of recurrence by 35% over the first two years. Among studies, “immediate” ranged from within one week to up to three months. Two studies described long-term prognosis, concluding that immediate AED treatment was unlikely to improve the chance of sustained seizure remission.
Five studies were used to describe adverse events in patients treated with AED. Adverse event incidence varied from 7% to 31%, and the incidents that occurred were largely mild and were reversible.
Bottom line: In adults presenting with unprovoked first seizure, the risk of recurrence is highest in the first two years and can be reduced with immediate AED therapy, though AED therapy was not shown to improve long-term prognosis.
Citation: Krumholz A, Wiebe S, Gronseth GS, et al. Evidence-based guideline: management of an unprovoked first seizure in adults. Report of the Guideline Development Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2015;84(16):1705-1713.
Clinical question: What are the updated recommendations for treating first unprovoked seizure in adults?
Background: Approximately 150,000 adults present with an unprovoked first seizure in the U.S. annually, and these events are associated with physical and psychological trauma. Prior guidelines discussed evaluation of unprovoked first seizures in adults but did not address management. This publication aims to analyze existing evidence regarding prognosis and therapy with antiepileptic drugs (AEDs).
Study design: Evidence-based appraisal of a systematic review.
Setting: Literature published from 1966 to 2013 on MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials.
Synopsis: Ten prognostic studies describing risk of recurrence were found. Generalized tonic-clonic seizures were the major seizure type. Cumulative incidence of recurrent seizure increased over time, with the majority occurring within the first two years, regardless of treatment with AED; however, there were treatment differences among these studies and wide variation in recurrence rates.
Recurrence risk was lower with AED therapy, though patients were not randomized. Increased risk of recurrence was associated with prior brain lesion causing the seizure, EEG with epileptiform abnormalities, imaging abnormality, and nocturnal seizure.
Five studies were reviewed for prognosis following immediate AED therapy. Immediate AED treatment reduced risk of recurrence by 35% over the first two years. Among studies, “immediate” ranged from within one week to up to three months. Two studies described long-term prognosis, concluding that immediate AED treatment was unlikely to improve the chance of sustained seizure remission.
Five studies were used to describe adverse events in patients treated with AED. Adverse event incidence varied from 7% to 31%, and the incidents that occurred were largely mild and were reversible.
Bottom line: In adults presenting with unprovoked first seizure, the risk of recurrence is highest in the first two years and can be reduced with immediate AED therapy, though AED therapy was not shown to improve long-term prognosis.
Citation: Krumholz A, Wiebe S, Gronseth GS, et al. Evidence-based guideline: management of an unprovoked first seizure in adults. Report of the Guideline Development Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2015;84(16):1705-1713.
Clinical question: What are the updated recommendations for treating first unprovoked seizure in adults?
Background: Approximately 150,000 adults present with an unprovoked first seizure in the U.S. annually, and these events are associated with physical and psychological trauma. Prior guidelines discussed evaluation of unprovoked first seizures in adults but did not address management. This publication aims to analyze existing evidence regarding prognosis and therapy with antiepileptic drugs (AEDs).
Study design: Evidence-based appraisal of a systematic review.
Setting: Literature published from 1966 to 2013 on MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials.
Synopsis: Ten prognostic studies describing risk of recurrence were found. Generalized tonic-clonic seizures were the major seizure type. Cumulative incidence of recurrent seizure increased over time, with the majority occurring within the first two years, regardless of treatment with AED; however, there were treatment differences among these studies and wide variation in recurrence rates.
Recurrence risk was lower with AED therapy, though patients were not randomized. Increased risk of recurrence was associated with prior brain lesion causing the seizure, EEG with epileptiform abnormalities, imaging abnormality, and nocturnal seizure.
Five studies were reviewed for prognosis following immediate AED therapy. Immediate AED treatment reduced risk of recurrence by 35% over the first two years. Among studies, “immediate” ranged from within one week to up to three months. Two studies described long-term prognosis, concluding that immediate AED treatment was unlikely to improve the chance of sustained seizure remission.
Five studies were used to describe adverse events in patients treated with AED. Adverse event incidence varied from 7% to 31%, and the incidents that occurred were largely mild and were reversible.
Bottom line: In adults presenting with unprovoked first seizure, the risk of recurrence is highest in the first two years and can be reduced with immediate AED therapy, though AED therapy was not shown to improve long-term prognosis.
Citation: Krumholz A, Wiebe S, Gronseth GS, et al. Evidence-based guideline: management of an unprovoked first seizure in adults. Report of the Guideline Development Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2015;84(16):1705-1713.
PPI Usage with SBP Prophylaxis Predicts Recurrent Infections in Cirrhosis
Clinical question: What are the risk factors for development of a recurrent infection in cirrhotic patients hospitalized with an initial infection?
Background: Infections are a major cause of morbidity and mortality in patients with cirrhosis. Prior retrospective data suggest that proton pump inhibitors (PPIs) increase the risk of infections in cirrhotic patients, while beta blockers do not. This study sought to prospectively evaluate risk factors for recurrent infections in hospitalized patients with cirrhosis.
Study design: Prospective, multicenter study.
Setting: Twelve North American hospitalists enrolled in the North American Consortium for the Study of End-Stage Liver Disease.
Synopsis: Researchers enrolled 188 hospitalized cirrhotic patients who had or developed an infection during their hospitalization. Patients were followed for six months to determine risk of development of subsequent infection and to identify independent risk factors associated with recurrent infections.
Forty-five percent of patients developed a subsequent infection, 74% of which occurred in a different location than the primary infection. This risk was independent of liver disease severity.
Age (OR 1.06; CI 1.02-1.11), PPI use (OR 2.72; CI 1.30-5.71), and spontaneous bacterial peritonitis (SBP) prophylaxis (OR 3.66; CI 1.60-8.37) were found to be independent predictors of recurrent infections. Beta blocker use did not differ between those who developed an infection and those who did not. An initial infection of SBP (compared to other infection sites) was protective (OR 0.37; CI 0.15-0.91) against subsequent infection.
Notably, study size was small, and 18% of patients were lost to follow-up. Further studies are needed to determine effective strategies to prevent recurrent infections in cirrhotics.
Bottom line: Cirrhotic patients hospitalized with an infection are at high risk of recurrent infections, and the long-term use of SBP prophylaxis and PPIs independently increase this risk.
Citation: O’Leary JG, Reddy KR, Wong F, et al. Long-term use of antibiotics and proton pump inhibitors predict development of infections in patients with cirrhosis. Clinical Gastro Hepatol. 2015;13(4):753-759.
Clinical question: What are the risk factors for development of a recurrent infection in cirrhotic patients hospitalized with an initial infection?
Background: Infections are a major cause of morbidity and mortality in patients with cirrhosis. Prior retrospective data suggest that proton pump inhibitors (PPIs) increase the risk of infections in cirrhotic patients, while beta blockers do not. This study sought to prospectively evaluate risk factors for recurrent infections in hospitalized patients with cirrhosis.
Study design: Prospective, multicenter study.
Setting: Twelve North American hospitalists enrolled in the North American Consortium for the Study of End-Stage Liver Disease.
Synopsis: Researchers enrolled 188 hospitalized cirrhotic patients who had or developed an infection during their hospitalization. Patients were followed for six months to determine risk of development of subsequent infection and to identify independent risk factors associated with recurrent infections.
Forty-five percent of patients developed a subsequent infection, 74% of which occurred in a different location than the primary infection. This risk was independent of liver disease severity.
Age (OR 1.06; CI 1.02-1.11), PPI use (OR 2.72; CI 1.30-5.71), and spontaneous bacterial peritonitis (SBP) prophylaxis (OR 3.66; CI 1.60-8.37) were found to be independent predictors of recurrent infections. Beta blocker use did not differ between those who developed an infection and those who did not. An initial infection of SBP (compared to other infection sites) was protective (OR 0.37; CI 0.15-0.91) against subsequent infection.
Notably, study size was small, and 18% of patients were lost to follow-up. Further studies are needed to determine effective strategies to prevent recurrent infections in cirrhotics.
Bottom line: Cirrhotic patients hospitalized with an infection are at high risk of recurrent infections, and the long-term use of SBP prophylaxis and PPIs independently increase this risk.
Citation: O’Leary JG, Reddy KR, Wong F, et al. Long-term use of antibiotics and proton pump inhibitors predict development of infections in patients with cirrhosis. Clinical Gastro Hepatol. 2015;13(4):753-759.
Clinical question: What are the risk factors for development of a recurrent infection in cirrhotic patients hospitalized with an initial infection?
Background: Infections are a major cause of morbidity and mortality in patients with cirrhosis. Prior retrospective data suggest that proton pump inhibitors (PPIs) increase the risk of infections in cirrhotic patients, while beta blockers do not. This study sought to prospectively evaluate risk factors for recurrent infections in hospitalized patients with cirrhosis.
Study design: Prospective, multicenter study.
Setting: Twelve North American hospitalists enrolled in the North American Consortium for the Study of End-Stage Liver Disease.
Synopsis: Researchers enrolled 188 hospitalized cirrhotic patients who had or developed an infection during their hospitalization. Patients were followed for six months to determine risk of development of subsequent infection and to identify independent risk factors associated with recurrent infections.
Forty-five percent of patients developed a subsequent infection, 74% of which occurred in a different location than the primary infection. This risk was independent of liver disease severity.
Age (OR 1.06; CI 1.02-1.11), PPI use (OR 2.72; CI 1.30-5.71), and spontaneous bacterial peritonitis (SBP) prophylaxis (OR 3.66; CI 1.60-8.37) were found to be independent predictors of recurrent infections. Beta blocker use did not differ between those who developed an infection and those who did not. An initial infection of SBP (compared to other infection sites) was protective (OR 0.37; CI 0.15-0.91) against subsequent infection.
Notably, study size was small, and 18% of patients were lost to follow-up. Further studies are needed to determine effective strategies to prevent recurrent infections in cirrhotics.
Bottom line: Cirrhotic patients hospitalized with an infection are at high risk of recurrent infections, and the long-term use of SBP prophylaxis and PPIs independently increase this risk.
Citation: O’Leary JG, Reddy KR, Wong F, et al. Long-term use of antibiotics and proton pump inhibitors predict development of infections in patients with cirrhosis. Clinical Gastro Hepatol. 2015;13(4):753-759.
Nontoxigenic C. diff Spores May Decrease Rates of Recurrent CDI
Clinical question: Is treatment with nontoxigenic C. diff strain M-3 (NTCD-M3) safe and effective in preventing recurrent Clostridium difficile infection (CDI)?
Background: C. diff is the most commonly identified healthcare pathogen, and CDI has a 25%-30% recurrence rate. Not all C. diff strains produce toxins, and gastrointestinal (GI) tract colonization with NTCD has been shown to prevent CDI when the patient is subsequently exposed to a toxigenic strain.
Study design: Multicenter, phase 2, randomized, double-blind, placebo-controlled, dose-ranging trial.
Setting: Forty-four centers in the U.S., Canada, and Europe.
Synopsis: Patients who had clinically recovered from CDI were randomized to placebo or NTCD-M3 at a dose of 104 spores/day for seven days, 107 spores/day for seven days, or 107 spores per day for 14 days. Patients were excluded who had multiple recurrences or other significant GI illnesses, were treated with antimicrobials other than metronidazole or PO [by mouth] vancomycin, had planned antibiotics, were unable to take PO, or had immunosuppression. Patients were monitored for side effects, rates of colonization, and incidence of CDI recurrence within six weeks.
Both overall and serious treatment-emergent adverse events were similar in patients receiving NTCD-M3 and those receiving placebo, but no statistical analysis was performed. Headache was more common in treatment groups.
CDI recurrence occurred in 31% of placebo patients and 11% of patients who received NTCD-M3 (OR 0.28). Fecal colonization was achieved in 69% of NTCD-M3 patients; this subset of patients had a 2% recurrence. Patients who received NTDC but did not achieve GI colonization had rates of recurrent CDI similar to placebo.
Bottom line: Use of NTCD-M3 spores appears safe and well tolerated and led to decreased recurrent CDI, primarily in patients who achieved fecal colonization.
Citation: Gerding DN, Meyer T, Lee C, et al. Administration of spores of nontoxigenic Clostridium difficile strain M3 for prevention of recurrent C. difficile infection: a randomized clinical trial. JAMA. 2015;313(17):1719-1727.
Clinical question: Is treatment with nontoxigenic C. diff strain M-3 (NTCD-M3) safe and effective in preventing recurrent Clostridium difficile infection (CDI)?
Background: C. diff is the most commonly identified healthcare pathogen, and CDI has a 25%-30% recurrence rate. Not all C. diff strains produce toxins, and gastrointestinal (GI) tract colonization with NTCD has been shown to prevent CDI when the patient is subsequently exposed to a toxigenic strain.
Study design: Multicenter, phase 2, randomized, double-blind, placebo-controlled, dose-ranging trial.
Setting: Forty-four centers in the U.S., Canada, and Europe.
Synopsis: Patients who had clinically recovered from CDI were randomized to placebo or NTCD-M3 at a dose of 104 spores/day for seven days, 107 spores/day for seven days, or 107 spores per day for 14 days. Patients were excluded who had multiple recurrences or other significant GI illnesses, were treated with antimicrobials other than metronidazole or PO [by mouth] vancomycin, had planned antibiotics, were unable to take PO, or had immunosuppression. Patients were monitored for side effects, rates of colonization, and incidence of CDI recurrence within six weeks.
Both overall and serious treatment-emergent adverse events were similar in patients receiving NTCD-M3 and those receiving placebo, but no statistical analysis was performed. Headache was more common in treatment groups.
CDI recurrence occurred in 31% of placebo patients and 11% of patients who received NTCD-M3 (OR 0.28). Fecal colonization was achieved in 69% of NTCD-M3 patients; this subset of patients had a 2% recurrence. Patients who received NTDC but did not achieve GI colonization had rates of recurrent CDI similar to placebo.
Bottom line: Use of NTCD-M3 spores appears safe and well tolerated and led to decreased recurrent CDI, primarily in patients who achieved fecal colonization.
Citation: Gerding DN, Meyer T, Lee C, et al. Administration of spores of nontoxigenic Clostridium difficile strain M3 for prevention of recurrent C. difficile infection: a randomized clinical trial. JAMA. 2015;313(17):1719-1727.
Clinical question: Is treatment with nontoxigenic C. diff strain M-3 (NTCD-M3) safe and effective in preventing recurrent Clostridium difficile infection (CDI)?
Background: C. diff is the most commonly identified healthcare pathogen, and CDI has a 25%-30% recurrence rate. Not all C. diff strains produce toxins, and gastrointestinal (GI) tract colonization with NTCD has been shown to prevent CDI when the patient is subsequently exposed to a toxigenic strain.
Study design: Multicenter, phase 2, randomized, double-blind, placebo-controlled, dose-ranging trial.
Setting: Forty-four centers in the U.S., Canada, and Europe.
Synopsis: Patients who had clinically recovered from CDI were randomized to placebo or NTCD-M3 at a dose of 104 spores/day for seven days, 107 spores/day for seven days, or 107 spores per day for 14 days. Patients were excluded who had multiple recurrences or other significant GI illnesses, were treated with antimicrobials other than metronidazole or PO [by mouth] vancomycin, had planned antibiotics, were unable to take PO, or had immunosuppression. Patients were monitored for side effects, rates of colonization, and incidence of CDI recurrence within six weeks.
Both overall and serious treatment-emergent adverse events were similar in patients receiving NTCD-M3 and those receiving placebo, but no statistical analysis was performed. Headache was more common in treatment groups.
CDI recurrence occurred in 31% of placebo patients and 11% of patients who received NTCD-M3 (OR 0.28). Fecal colonization was achieved in 69% of NTCD-M3 patients; this subset of patients had a 2% recurrence. Patients who received NTDC but did not achieve GI colonization had rates of recurrent CDI similar to placebo.
Bottom line: Use of NTCD-M3 spores appears safe and well tolerated and led to decreased recurrent CDI, primarily in patients who achieved fecal colonization.
Citation: Gerding DN, Meyer T, Lee C, et al. Administration of spores of nontoxigenic Clostridium difficile strain M3 for prevention of recurrent C. difficile infection: a randomized clinical trial. JAMA. 2015;313(17):1719-1727.
Retrievable IVC Plus Anticoagulation Does Not Reduce Risk of Recurrent Pulmonary Embolism
Clinical question: Does a retrievable inferior vena cava (IVC) filter in addition to anticoagulation in patients with an acute pulmonary embolism (PE) decrease the risk of recurrent PE?
Background: Inferior vena cava placement has increased dramatically over the last three decades. Although IVC filter placement benefits patients with a contraindication to anticoagulation, the benefit of a temporary IVC filter in addition to anticoagulation to prevent PE in patients at high risk of recurrence is unknown.
Study design: Randomized, open-label.
Setting: Seventeen French hospitals.
Synopsis: Nearly 400 patients with an acute PE associated with lower extremity thrombosis and at least one additional risk factor for severity were randomized to anticoagulation in combination with a retrievable IVC filter versus anticoagulation alone. Risk factors included age, active cancer, chronic cardiac or respiratory disease, recent ischemic stroke with leg paralysis, bilateral deep vein thrombosis, or right ventricular failure or myocardial injury. Both groups received anticoagulation for six months.
Overall, there was no difference in fatal or symptomatic nonfatal PE in each group at three and six months.
The open-label design is subject to interpretative bias. A blinded outcome assessment committee and a central randomization process were implemented in order to minimize bias. In addition, the study could have been underpowered given the limited number of patients and low PE recurrence rate.
Bottom line: In patients with an acute PE at high risk of recurrent PE, retrievable IVC filter in addition to standard anticoagulation therapy does not decrease the risk of recurrence.
Citation: Mismetti, P, Laporte, S, Pellerin O, et al. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism. JAMA. 2015;313(16):1627-1635.
Clinical question: Does a retrievable inferior vena cava (IVC) filter in addition to anticoagulation in patients with an acute pulmonary embolism (PE) decrease the risk of recurrent PE?
Background: Inferior vena cava placement has increased dramatically over the last three decades. Although IVC filter placement benefits patients with a contraindication to anticoagulation, the benefit of a temporary IVC filter in addition to anticoagulation to prevent PE in patients at high risk of recurrence is unknown.
Study design: Randomized, open-label.
Setting: Seventeen French hospitals.
Synopsis: Nearly 400 patients with an acute PE associated with lower extremity thrombosis and at least one additional risk factor for severity were randomized to anticoagulation in combination with a retrievable IVC filter versus anticoagulation alone. Risk factors included age, active cancer, chronic cardiac or respiratory disease, recent ischemic stroke with leg paralysis, bilateral deep vein thrombosis, or right ventricular failure or myocardial injury. Both groups received anticoagulation for six months.
Overall, there was no difference in fatal or symptomatic nonfatal PE in each group at three and six months.
The open-label design is subject to interpretative bias. A blinded outcome assessment committee and a central randomization process were implemented in order to minimize bias. In addition, the study could have been underpowered given the limited number of patients and low PE recurrence rate.
Bottom line: In patients with an acute PE at high risk of recurrent PE, retrievable IVC filter in addition to standard anticoagulation therapy does not decrease the risk of recurrence.
Citation: Mismetti, P, Laporte, S, Pellerin O, et al. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism. JAMA. 2015;313(16):1627-1635.
Clinical question: Does a retrievable inferior vena cava (IVC) filter in addition to anticoagulation in patients with an acute pulmonary embolism (PE) decrease the risk of recurrent PE?
Background: Inferior vena cava placement has increased dramatically over the last three decades. Although IVC filter placement benefits patients with a contraindication to anticoagulation, the benefit of a temporary IVC filter in addition to anticoagulation to prevent PE in patients at high risk of recurrence is unknown.
Study design: Randomized, open-label.
Setting: Seventeen French hospitals.
Synopsis: Nearly 400 patients with an acute PE associated with lower extremity thrombosis and at least one additional risk factor for severity were randomized to anticoagulation in combination with a retrievable IVC filter versus anticoagulation alone. Risk factors included age, active cancer, chronic cardiac or respiratory disease, recent ischemic stroke with leg paralysis, bilateral deep vein thrombosis, or right ventricular failure or myocardial injury. Both groups received anticoagulation for six months.
Overall, there was no difference in fatal or symptomatic nonfatal PE in each group at three and six months.
The open-label design is subject to interpretative bias. A blinded outcome assessment committee and a central randomization process were implemented in order to minimize bias. In addition, the study could have been underpowered given the limited number of patients and low PE recurrence rate.
Bottom line: In patients with an acute PE at high risk of recurrent PE, retrievable IVC filter in addition to standard anticoagulation therapy does not decrease the risk of recurrence.
Citation: Mismetti, P, Laporte, S, Pellerin O, et al. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism. JAMA. 2015;313(16):1627-1635.
PHM15: Evidence-Based Diagnostic Evaluation of Infants Presenting with an Apparent Life Threatening Event
Summary:
Presenters of the PHM15 session "Evidence Based Diagnostic Evaluation of Infants Presenting with an Apparent Life Threatening Event" discussed four main diagnostic categories for ALTEs: cardiac, infectious, non-accidental trauma/neurologic, and gastrointestinal. They reviewed the incidence of each of these diagnoses in infants presenting with ALTE, discussed the utility of various diagnostic modalities, and suggested elements of the history and physical that might make those etiologies higher on the differential.
The evidence shows a 0%-2% rate of cardiac disease in infants presenting with ALTE. Given low sensitivity and low specificity for echocardiograms in these patients, the presenters did not recommend routine echocardiograms in all patients. Given high sensitivity and low specificity for EKGs, they suggested EKGs could be considered to help exclude cardiac etiologies, but cautioned that the high false positive rate could lead to additional unnecessary testing. They did not find a high association between most historical facts and an increased likelihood of cardiac etiologies in patients presenting with an ALTE.
Infectious etiologies discussed included bacteremia (0%-2.5%), UTI (0%-7.7%), meningitis (0%-1.2%) and pertussis (0.6%-9.2%), with rates in ALTE as noted.
Again, the literature does not support the use of routine testing for these diagnoses unless there are suggestive clinical findings. Findings that might warrant further infectious investigations:
- Multiple events,
- Prematurity,
- Fever/hypothermia,
- Toxic appearance,
- Altered mental status, or
- Clinical signs of pertussis.
From their literature review, the speakers found a 1.4%-3.7% rate of non-accidental trauma in infants presenting with an ALTE. They did not feel there was sufficient evidence to support skeletal surveys or dilated ophthalmologic exams as part of a standard ALTE workup. Historical clues that might lead the provider to consider NAT include recurrent events, a history of SIDS or ALTE in siblings, delay in seeking care or a confusing history. Suggestive physical exam findings included blood in the nose/mouth, abnormal neurological exam, ear bruising, oral injuries, or bruising in a non-mobile child.
Regarding GE reflux, the presenters discussed the difficulty in identifying the incidence since temporal association does not necessarily equate with causation. They did not recommend routine testing for GER or acid suppression in low risk patients, but said patients could be counseled on various behavioral interventions such as avoiding tobacco and overfeeding, providing frequent burping and upright positioning and exclusive breastfeeding.
Finally, the speakers discussed the upcoming practice guideline for the management of patients with ALTE. They reviewed the proposed change in nomenclature, with the transition to "BRUE" (brief resolved unexplained event), as well as a new algorithm for the evaluation of low-risk patients. The new guidelines currently are being reviewed, with plans to be published and available for general dissemination within the next 12 months. TH
Amanda Rogers, MD, is a hospitalist and assistant professor in the Department of Pediatrics, Section of Hospital Medicine, at the Medical College of Wisconsin in Milwaukee.
Summary:
Presenters of the PHM15 session "Evidence Based Diagnostic Evaluation of Infants Presenting with an Apparent Life Threatening Event" discussed four main diagnostic categories for ALTEs: cardiac, infectious, non-accidental trauma/neurologic, and gastrointestinal. They reviewed the incidence of each of these diagnoses in infants presenting with ALTE, discussed the utility of various diagnostic modalities, and suggested elements of the history and physical that might make those etiologies higher on the differential.
The evidence shows a 0%-2% rate of cardiac disease in infants presenting with ALTE. Given low sensitivity and low specificity for echocardiograms in these patients, the presenters did not recommend routine echocardiograms in all patients. Given high sensitivity and low specificity for EKGs, they suggested EKGs could be considered to help exclude cardiac etiologies, but cautioned that the high false positive rate could lead to additional unnecessary testing. They did not find a high association between most historical facts and an increased likelihood of cardiac etiologies in patients presenting with an ALTE.
Infectious etiologies discussed included bacteremia (0%-2.5%), UTI (0%-7.7%), meningitis (0%-1.2%) and pertussis (0.6%-9.2%), with rates in ALTE as noted.
Again, the literature does not support the use of routine testing for these diagnoses unless there are suggestive clinical findings. Findings that might warrant further infectious investigations:
- Multiple events,
- Prematurity,
- Fever/hypothermia,
- Toxic appearance,
- Altered mental status, or
- Clinical signs of pertussis.
From their literature review, the speakers found a 1.4%-3.7% rate of non-accidental trauma in infants presenting with an ALTE. They did not feel there was sufficient evidence to support skeletal surveys or dilated ophthalmologic exams as part of a standard ALTE workup. Historical clues that might lead the provider to consider NAT include recurrent events, a history of SIDS or ALTE in siblings, delay in seeking care or a confusing history. Suggestive physical exam findings included blood in the nose/mouth, abnormal neurological exam, ear bruising, oral injuries, or bruising in a non-mobile child.
Regarding GE reflux, the presenters discussed the difficulty in identifying the incidence since temporal association does not necessarily equate with causation. They did not recommend routine testing for GER or acid suppression in low risk patients, but said patients could be counseled on various behavioral interventions such as avoiding tobacco and overfeeding, providing frequent burping and upright positioning and exclusive breastfeeding.
Finally, the speakers discussed the upcoming practice guideline for the management of patients with ALTE. They reviewed the proposed change in nomenclature, with the transition to "BRUE" (brief resolved unexplained event), as well as a new algorithm for the evaluation of low-risk patients. The new guidelines currently are being reviewed, with plans to be published and available for general dissemination within the next 12 months. TH
Amanda Rogers, MD, is a hospitalist and assistant professor in the Department of Pediatrics, Section of Hospital Medicine, at the Medical College of Wisconsin in Milwaukee.
Summary:
Presenters of the PHM15 session "Evidence Based Diagnostic Evaluation of Infants Presenting with an Apparent Life Threatening Event" discussed four main diagnostic categories for ALTEs: cardiac, infectious, non-accidental trauma/neurologic, and gastrointestinal. They reviewed the incidence of each of these diagnoses in infants presenting with ALTE, discussed the utility of various diagnostic modalities, and suggested elements of the history and physical that might make those etiologies higher on the differential.
The evidence shows a 0%-2% rate of cardiac disease in infants presenting with ALTE. Given low sensitivity and low specificity for echocardiograms in these patients, the presenters did not recommend routine echocardiograms in all patients. Given high sensitivity and low specificity for EKGs, they suggested EKGs could be considered to help exclude cardiac etiologies, but cautioned that the high false positive rate could lead to additional unnecessary testing. They did not find a high association between most historical facts and an increased likelihood of cardiac etiologies in patients presenting with an ALTE.
Infectious etiologies discussed included bacteremia (0%-2.5%), UTI (0%-7.7%), meningitis (0%-1.2%) and pertussis (0.6%-9.2%), with rates in ALTE as noted.
Again, the literature does not support the use of routine testing for these diagnoses unless there are suggestive clinical findings. Findings that might warrant further infectious investigations:
- Multiple events,
- Prematurity,
- Fever/hypothermia,
- Toxic appearance,
- Altered mental status, or
- Clinical signs of pertussis.
From their literature review, the speakers found a 1.4%-3.7% rate of non-accidental trauma in infants presenting with an ALTE. They did not feel there was sufficient evidence to support skeletal surveys or dilated ophthalmologic exams as part of a standard ALTE workup. Historical clues that might lead the provider to consider NAT include recurrent events, a history of SIDS or ALTE in siblings, delay in seeking care or a confusing history. Suggestive physical exam findings included blood in the nose/mouth, abnormal neurological exam, ear bruising, oral injuries, or bruising in a non-mobile child.
Regarding GE reflux, the presenters discussed the difficulty in identifying the incidence since temporal association does not necessarily equate with causation. They did not recommend routine testing for GER or acid suppression in low risk patients, but said patients could be counseled on various behavioral interventions such as avoiding tobacco and overfeeding, providing frequent burping and upright positioning and exclusive breastfeeding.
Finally, the speakers discussed the upcoming practice guideline for the management of patients with ALTE. They reviewed the proposed change in nomenclature, with the transition to "BRUE" (brief resolved unexplained event), as well as a new algorithm for the evaluation of low-risk patients. The new guidelines currently are being reviewed, with plans to be published and available for general dissemination within the next 12 months. TH
Amanda Rogers, MD, is a hospitalist and assistant professor in the Department of Pediatrics, Section of Hospital Medicine, at the Medical College of Wisconsin in Milwaukee.
Small Bowel Block in Elderly Merits Full Hospitalization
NEW YORK (Reuters Health) - The "vast majority" of elderly patients admitted with small bowel obstruction (SBO) are hospitalized for more than two days, and the diagnosis alone should allow appropriate Medicare coverage, according to a new study.
In a paper online July 1 in Annals of Surgery, Dr. Zara Cooper, of Brigham and Women's Hospital, Boston, and colleagues noted that their study was prompted by the Two-Midnight Rule established by the Centers for Medicare & Medicaid Services (CMS) in 2013.
The authors explained that if a physician expects a patient to need a hospital stay that crosses two midnights and thus admits the patient, related costs may be covered. However, shorter stays are deemed as observational and can raise the possibility of non-reimbursement for hospitals.
For example, if someone is admitted as an inpatient, but discharged in less than two days, payment will be made only if it can be documented that a longer stay was reasonably expected and unforeseen circumstances led to the shorter stay. Hospital stays that are incorrectly classified or have improperly documented changes in admission status will not be paid.
However, Dr. Cooper told Reuters Health by email, "Older patients with SBO, a very common diagnosis, should be presumed to be admitted for more than two midnights and hospitals should not get penalized."
She and her colleagues pointed out that SBO accounts for about 15% of surgical admissions to U.S. hospitals and more than $1 billion in annual hospital charges. However, diagnosis requires surgeons to observe patients to determine if surgery is warranted.
Thus, the authors wrote, "It is critically important for surgeons to correctly assign admission status for patients with SBO to ensure that hospitals are reimbursed appropriately, and patients are not unduly burdened."
The investigators examined data on 855 older patients admitted with SBO from 2006 and 2013. Of these, 816 (95%) stayed for two midnights or longer. This was true of all patients aged 85 years or older (n=108, approximately 13%).
The only significant difference in clinical characteristics was the presence of inflammatory bowel disease. Of five such patients, only one stayed for less than two midnights.
"Based on our study and others," the investigators wrote, "we propose that hospital admission for SBO in elderly patients is sufficient justification for the reasonable expectation" of the required length of stay for reimbursement.
This also may be true of other conditions. Dr. Cooper concluded, "More studies like this are needed in surgical patients to better understand the impact of CMS admission guidelines. The rule may not make sense in certain populations, leading to heavy and unfair penalties for hospitals."
The authors reported no disclosures.
NEW YORK (Reuters Health) - The "vast majority" of elderly patients admitted with small bowel obstruction (SBO) are hospitalized for more than two days, and the diagnosis alone should allow appropriate Medicare coverage, according to a new study.
In a paper online July 1 in Annals of Surgery, Dr. Zara Cooper, of Brigham and Women's Hospital, Boston, and colleagues noted that their study was prompted by the Two-Midnight Rule established by the Centers for Medicare & Medicaid Services (CMS) in 2013.
The authors explained that if a physician expects a patient to need a hospital stay that crosses two midnights and thus admits the patient, related costs may be covered. However, shorter stays are deemed as observational and can raise the possibility of non-reimbursement for hospitals.
For example, if someone is admitted as an inpatient, but discharged in less than two days, payment will be made only if it can be documented that a longer stay was reasonably expected and unforeseen circumstances led to the shorter stay. Hospital stays that are incorrectly classified or have improperly documented changes in admission status will not be paid.
However, Dr. Cooper told Reuters Health by email, "Older patients with SBO, a very common diagnosis, should be presumed to be admitted for more than two midnights and hospitals should not get penalized."
She and her colleagues pointed out that SBO accounts for about 15% of surgical admissions to U.S. hospitals and more than $1 billion in annual hospital charges. However, diagnosis requires surgeons to observe patients to determine if surgery is warranted.
Thus, the authors wrote, "It is critically important for surgeons to correctly assign admission status for patients with SBO to ensure that hospitals are reimbursed appropriately, and patients are not unduly burdened."
The investigators examined data on 855 older patients admitted with SBO from 2006 and 2013. Of these, 816 (95%) stayed for two midnights or longer. This was true of all patients aged 85 years or older (n=108, approximately 13%).
The only significant difference in clinical characteristics was the presence of inflammatory bowel disease. Of five such patients, only one stayed for less than two midnights.
"Based on our study and others," the investigators wrote, "we propose that hospital admission for SBO in elderly patients is sufficient justification for the reasonable expectation" of the required length of stay for reimbursement.
This also may be true of other conditions. Dr. Cooper concluded, "More studies like this are needed in surgical patients to better understand the impact of CMS admission guidelines. The rule may not make sense in certain populations, leading to heavy and unfair penalties for hospitals."
The authors reported no disclosures.
NEW YORK (Reuters Health) - The "vast majority" of elderly patients admitted with small bowel obstruction (SBO) are hospitalized for more than two days, and the diagnosis alone should allow appropriate Medicare coverage, according to a new study.
In a paper online July 1 in Annals of Surgery, Dr. Zara Cooper, of Brigham and Women's Hospital, Boston, and colleagues noted that their study was prompted by the Two-Midnight Rule established by the Centers for Medicare & Medicaid Services (CMS) in 2013.
The authors explained that if a physician expects a patient to need a hospital stay that crosses two midnights and thus admits the patient, related costs may be covered. However, shorter stays are deemed as observational and can raise the possibility of non-reimbursement for hospitals.
For example, if someone is admitted as an inpatient, but discharged in less than two days, payment will be made only if it can be documented that a longer stay was reasonably expected and unforeseen circumstances led to the shorter stay. Hospital stays that are incorrectly classified or have improperly documented changes in admission status will not be paid.
However, Dr. Cooper told Reuters Health by email, "Older patients with SBO, a very common diagnosis, should be presumed to be admitted for more than two midnights and hospitals should not get penalized."
She and her colleagues pointed out that SBO accounts for about 15% of surgical admissions to U.S. hospitals and more than $1 billion in annual hospital charges. However, diagnosis requires surgeons to observe patients to determine if surgery is warranted.
Thus, the authors wrote, "It is critically important for surgeons to correctly assign admission status for patients with SBO to ensure that hospitals are reimbursed appropriately, and patients are not unduly burdened."
The investigators examined data on 855 older patients admitted with SBO from 2006 and 2013. Of these, 816 (95%) stayed for two midnights or longer. This was true of all patients aged 85 years or older (n=108, approximately 13%).
The only significant difference in clinical characteristics was the presence of inflammatory bowel disease. Of five such patients, only one stayed for less than two midnights.
"Based on our study and others," the investigators wrote, "we propose that hospital admission for SBO in elderly patients is sufficient justification for the reasonable expectation" of the required length of stay for reimbursement.
This also may be true of other conditions. Dr. Cooper concluded, "More studies like this are needed in surgical patients to better understand the impact of CMS admission guidelines. The rule may not make sense in certain populations, leading to heavy and unfair penalties for hospitals."
The authors reported no disclosures.
PHM15: How to Make Difficult Conversations Manageable
Summary:
One of PHM15's first sessions was a workshop led by Dr. Rachna May focusing on the role of pediatric hospitalists in end-of-life conversations.
Medically complex pediatric patients are more likely to have end-of-life care in the hospital, placing the pediatric hospitalist in a unique position to address end-of-life issues. Medically complex patients may have waxing and waning courses, with frequent admissions for acute illness. Following these admissions, they may not fully return to their pre-illness baseline, leading to an overall gradual decline in health. An opportunity for discussing quality of life is available with each acute illness and hospitalization.
These conversations, however, can be difficult to initiate and present several barriers to overcome. These barriers include:
- Unknown parental expectations regarding outcome,
- Lack of an established relationship with the patient and family, and
- Lack of readiness of the patient and family to discuss end-of-life decisions.
To overcome these barriers, providers must develop tools for delivery. They must find the right setting for the conversation, limit distractions, and avoid medical jargon. Begin with asking the patient and family's perceptions of the clinical prognosis and be honest when discussing the predicted medical outcomes for the patient. Open discussion of the prognosis allows autonomy in decision making, helps families feel supported, and can help them manage distress surrounding end-of-life care.
Such terminology as "do not resuscitate" can be interpreted as “doing nothing,” and result in feelings of guilt for a family desiring care for their child. Using a phrase such as "allowing a natural death" can alleviate feelings of guilt over end-of-life decisions and help the family actively provide care while optimizing quality of life. TH
Dr. Player is a hospitalist and assistant professor in the Department of Pediatrics at Medical College of Wisconsin, Children’s Hospital of Wisconsin in Milwaukee.
Summary:
One of PHM15's first sessions was a workshop led by Dr. Rachna May focusing on the role of pediatric hospitalists in end-of-life conversations.
Medically complex pediatric patients are more likely to have end-of-life care in the hospital, placing the pediatric hospitalist in a unique position to address end-of-life issues. Medically complex patients may have waxing and waning courses, with frequent admissions for acute illness. Following these admissions, they may not fully return to their pre-illness baseline, leading to an overall gradual decline in health. An opportunity for discussing quality of life is available with each acute illness and hospitalization.
These conversations, however, can be difficult to initiate and present several barriers to overcome. These barriers include:
- Unknown parental expectations regarding outcome,
- Lack of an established relationship with the patient and family, and
- Lack of readiness of the patient and family to discuss end-of-life decisions.
To overcome these barriers, providers must develop tools for delivery. They must find the right setting for the conversation, limit distractions, and avoid medical jargon. Begin with asking the patient and family's perceptions of the clinical prognosis and be honest when discussing the predicted medical outcomes for the patient. Open discussion of the prognosis allows autonomy in decision making, helps families feel supported, and can help them manage distress surrounding end-of-life care.
Such terminology as "do not resuscitate" can be interpreted as “doing nothing,” and result in feelings of guilt for a family desiring care for their child. Using a phrase such as "allowing a natural death" can alleviate feelings of guilt over end-of-life decisions and help the family actively provide care while optimizing quality of life. TH
Dr. Player is a hospitalist and assistant professor in the Department of Pediatrics at Medical College of Wisconsin, Children’s Hospital of Wisconsin in Milwaukee.
Summary:
One of PHM15's first sessions was a workshop led by Dr. Rachna May focusing on the role of pediatric hospitalists in end-of-life conversations.
Medically complex pediatric patients are more likely to have end-of-life care in the hospital, placing the pediatric hospitalist in a unique position to address end-of-life issues. Medically complex patients may have waxing and waning courses, with frequent admissions for acute illness. Following these admissions, they may not fully return to their pre-illness baseline, leading to an overall gradual decline in health. An opportunity for discussing quality of life is available with each acute illness and hospitalization.
These conversations, however, can be difficult to initiate and present several barriers to overcome. These barriers include:
- Unknown parental expectations regarding outcome,
- Lack of an established relationship with the patient and family, and
- Lack of readiness of the patient and family to discuss end-of-life decisions.
To overcome these barriers, providers must develop tools for delivery. They must find the right setting for the conversation, limit distractions, and avoid medical jargon. Begin with asking the patient and family's perceptions of the clinical prognosis and be honest when discussing the predicted medical outcomes for the patient. Open discussion of the prognosis allows autonomy in decision making, helps families feel supported, and can help them manage distress surrounding end-of-life care.
Such terminology as "do not resuscitate" can be interpreted as “doing nothing,” and result in feelings of guilt for a family desiring care for their child. Using a phrase such as "allowing a natural death" can alleviate feelings of guilt over end-of-life decisions and help the family actively provide care while optimizing quality of life. TH
Dr. Player is a hospitalist and assistant professor in the Department of Pediatrics at Medical College of Wisconsin, Children’s Hospital of Wisconsin in Milwaukee.