User login
Regression, depression, and the facts of life
HISTORY: New school, old problems
Mr. E, age 13, was diagnosed with Down syndrome at birth and has mild mental retardation and bilateral sensorineural hearing loss. His pediatrician referred him to our child and adolescent psychiatry clinic for regressed behavior, depression, and apparent psychotic symptoms. He was also having problems sleeping and had begun puberty 8 months earlier.
Five months before referral, Mr. E had graduated from a small elementary school, where he was fully mainstreamed, to a large junior high school, where he spent most of the school day in a functional skills class. About that time, Mr. E began exhibiting nocturnal and daytime enuresis, loss of previously mastered skills, intolerance of novelty and change, and separation difficulty. Although toilet trained at age 7, he started having “accidents” at home, school, and elsewhere. He was reluctant to dress himself, and he resisted going to school.
The youth also talked to himself often and appeared to respond to internal stimuli. He “relived” conversations aloud, described imaginary friends to family and teachers, and spoke to a stuffed dog called Goofy. He would sit and stare into space for up to a half-hour, appearing preoccupied. Family members said he had exhibited these behaviors in grade school but until now appeared to have “outgrown” them.
Once sociable, Mr. E had become increasingly moody, negativistic, and isolative. He spent hours alone in his room. His mother, with whom he was close, reported that he was often angry with her for no apparent reason.
With puberty, his mother noted, Mr. E had begun kissing other developmentally disabled children. He also masturbated, but at his parents’ urging he restricted this activity to his room.
On evaluation, Mr. E was pleasant and outgoing. He had the facial dysmorphia and stature typical of Down syndrome. He smiled often and interacted well, and he attended and adapted to transitions in conversation and activities. His speech was dysarthric (with hyperglossia) and telegraphic; he could speak only four- to five-word sentences.
Was Mr. E exhibiting an adjustment reaction, depression, or a normal developmental response to puberty? Do his psychotic symptoms signal onset of schizophrenia?
Dr. Krassner’s and Kraus’ observations
Because Down syndrome is the most common genetic cause of mental retardation—seen in approximately 1 in 1,000 live births1—pediatricians and child psychiatrists see this disorder fairly frequently.
Regression, a form of coping exhibited by many children, is extremely common in youths with Down syndrome2 and often has a definite—though sometimes unclear—precipitant. We felt Mr. E’s move from a highly responsive, familiar school environment to a far less responsive one that accentuated his differences contributed to many of his symptoms.
Psychosis is less common in Down syndrome than in other developmental disabilities.2 Schizophrenia may occur, but diagnosis is complicated by cognition impairments, test-taking skills, and—in Mr. E’s case—inability to describe disordered thoughts or hallucinations due to poor language skills.3
Self-talk is common in Down syndrome and might be mistaken for psychosis. Note that despite his chronologic age, Mr. E is developmentally a 6-year-old, and self-talk and imaginary friends are considered normal behaviors for a child that age. What’s more, the stress of changing schools may have further compromised his developmental skills.
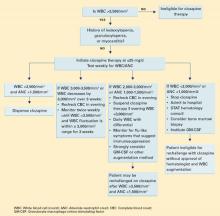
The FDA’s recent advisory about reports of increased suicidality in youths taking selective serotonin reuptake inhibitors (SSRIs) and other antidepressants for major depressive disorder during clinical trials has raised questions about using these agents in children and adolescents. Until more data become available, however, SSRIs remain the preferred drug therapy for pediatric depression.
- Based on our experience, we recommend citalopram, escitalopram, fluoxetine, and sertraline as first-line medications for pediatric depression because their side effects are relatively benign. The reported link between increased risk of suicidal ideation and behavior and use of paroxetine in pediatric patients has not been clearly established, so we cannot extrapolate that possible risk to other SSRIs.
- Newer antidepressants should be considered with caution in pediatric patients. Bupropion is contraindicated in patients with a history of seizures, bulimia, or anorexia. Mirtazapine is extremely sedating, with side effects such as weight gain and, in rare cases, agranulocytosis. Nefazodone comes with a “black box” warning for risk of liver toxicity. Trazodone is also sedating and carries a risk of priapism in boys.
- Older antidepressants, such as tricyclics, require extreme caution before prescribing to children and adolescents. Tricyclics, with their cardiac side effects, are not recommended for patients with Down syndrome, many of whom have cardiac pathology.
By contrast, depression is fairly common in Down syndrome, although it is much less prevalent in children than in adults with the developmental disorder.2
Finally, children with Down syndrome often enter puberty early, but without the cognitive or emotional maturity or knowledge to deal with the physiologic changes of adolescence.3 Parents often are reluctant to recognize their developmentally disabled child’s sexuality or are uncomfortable providing sexuality education.4 Mr. E’s parents clearly were unconvinced that his sexual behavior was normal for an adolescent.
TREATMENT Antidepressants lead to improvement
We felt Mr. E regressed secondary to emotional stress caused by switching schools. We viewed his psychotic symptoms as part of an adjustment disorder and attributed most of his other symptoms to depression. We anticipated Mr. E’s psychotic symptoms would remit spontaneously and focused on treating his mood and sleep disturbances.
We prescribed sertraline liquid suspension, 10 mg/d titrated across 3 weeks to 40 mg/d. We based our medication choice on clinical experience, mindful of a recent FDA advisory about the use of antidepressants in pediatric patients (Box 1). Also, the liquid suspension is easier to titrate than the tablet form, and we feared Mr. E might have trouble swallowing a tablet.
Mr. E’s mood and sociability improved after 3 to 4 weeks. Within 6 weeks, he regained some of his previously mastered daily activities. We added zolpidem, 10 mg nightly, to address his sleeping difficulties but discontinued the agent after 2 weeks, when his sleep patterns normalized.
At 2, 4, and 6 weeks, Mr. E was pleasant and cooperative, his thinking less concrete, and his speech more intelligible. His parents reported he was happier and more involved with family activities. At his mother’s request, sertraline was changed to 37.5 mg/d in tablet form. The patient remained stable for another month, during which his self-talk, though decreased, continued.
Two weeks later, Mr. E’s mother reported that, during a routine dermatologic examination for a chronic, presacral rash, the dermatologist noticed strategic shaving on the boy’s thighs, calves, and scrotum. Strategic shaving has been reported among sexually active youths as a means of purportedly increasing their sexual pleasure.
The dermatologist then told Mr. E’s mother that her son likely was sexually molested. Based on the boy’s differential rates of pubic hair growth, the doctor suspected that the molestation was chronic, dating back at least 3 months and probably continuing until the week before the examination. Upon hearing this, Mr. E’s parents were stunned and angry.
What behavioral signs might have suggested sexual abuse? How do the dermatologist’s findings alter diagnosis and treatment?
Dr. Krassner’s and Kraus’ observations
Given the dermatologist’s findings, Mr. E’s parents asked us whether their son’s presenting psychiatric symptoms were manifestations of posttraumatic stress disorder (PTSD).
Until now, explaining Mr. E’s symptoms as a reaction to changing schools seemed plausible. His symptoms were improving with treatment, and his sexual behaviors and interest in sexual topics were physiologically normal for his chronologic age. Despite his earlier pubertal experimentations, nothing in his psychosocial history indicated risk for sexual abuse or exploitation.
Still, children with Down syndrome are at higher risk for sexual exploitation than other children,4 so the possibility should have been explored with the parents. Psychiatrists should watch for physical signs of sexual abuse in these patients during the first examination (Box 2).4
But how is sexual abuse defined in this case? Deficient language skills prevented Mr. E from describing what happened to him, so determining whether he initiated sexual relations and with whom is nearly impossible. The act clearly could be considered abuse if Mr. E had been with an adult or older child—even if Mr. E consented. However, if Mr. E had initiated contact with another mentally retarded child, then cause, blame, and semantics become unclear. Either way, the incident could have caused PTSD.5
Diagnosing PTSD in non- or semi-verbal or retarded children is extremely difficult.6,7 Unlike adults with PTSD, pre-verbal children might not have recurrent, distressing recollections of the trauma, but symbolic displacement may characterize repetitive play, during which themes are expressed.8
Scheeringa et al have recommended PTSD criteria for preschool children, including:
- social withdrawal
- extreme temper tantrums
- loss of developmental skills
- new separation anxiety
- new onset of aggression
- new fears without obvious links to the trauma.5,6
Treating PTSD in children with developmental disabilities is also difficult. Modalities applicable to adults or mainstream children—such as psychodynamic psychotherapy, cognitive-behavioral therapy (CBT), exposure therapy, and medications—often do not help developmentally disabled children. For example, Mr. E lacks the cognitive apparatus to respond to CBT.
On the other hand, behavioral therapy, reducing risk factors, minimizing dissociative triggers, and educating patients, parents, friends, and teachers about PTSD can help patients such as Mr. E.5 Attempting to provide structure and maintain routines is a cornerstone of any intervention.
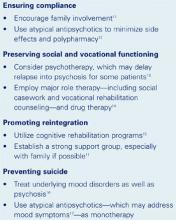
- Aggression
- Anxiety
- Behavior, learning problems at school
- Depression
- Heightened somatic concerns
- Sexualized behavior
- Sleep disturbance
- Withdrawal
FURTHER TREATMENT A family in turmoil
We addressed Mr. E’s symptoms as PTSD-related, though his poor language skills kept us from identifying a trauma. Based on data regarding pediatric PTSD treatment,9 we increased sertraline to 50 mg/d and then to 75 mg/d across 2 weeks.
However, an intense legal investigation brought on by the parents, combined with ensuing tumult within the family, worsened Mr. E’s symptoms. His self-talk became more pronounced and his isolative behavior reappeared, suggesting that the intrusive, repetitive questioning caused him to re-experience the trauma.
We again increased sertraline, to 100 mg/d, and offered supportive therapy to Mr. E. We tried to educate his parents about understanding his symptoms and managing his behavior and strongly recommended that they undergo crisis therapy to keep their reactions and emotions from hurting Mr. E. The parents declined, however, and alleged that we did not adequately support their pursuit of a diagnosis or legal action, which for them had become synonymous with treatment.
Mr. E’s mother brought her son to a psychologist, who engaged him in play therapy. She followed her son around, noting everything he said. All the while, she failed to resolve her guilt and anger. When we explained to her that these actions were hurting Mr. E’s progress, she terminated therapy.
How would you have tried to keep Mr. E’s family in therapy?
Dr. Krassner’s and Kraus’ observations
Treating psychopathology in children carries the risk of strained relations with the patient’s family. The risk increases exponentially for developmentally disabled children, as they have little or no input and their parents are exquisitely sensitive to their needs. Further, the revelation that the parents might have somehow failed to avert or anticipate danger to the child complicates their emotional response.
Although the child is the patient, the parent is the consumer. Failure to gain or keep the parents’ confidence will hinder or destroy therapy.
We might have protected our working relationship with Mr. E’s parents by recognizing how fragile they were and how intensely they would react to any constructive criticism. Paradoxically, for the short-term we could have tolerated their detrimental behaviors toward Mr. E (such as repeated questioning) in the hopes of protecting a long-term relationship. Spending more time exploring the guilt, anger, and confusion that tormented Mr. E’s parents—particularly his mother—also might have helped.
Related resources
- Ryan RM. Recognition of psychosis in persons who do not use spoken communication. In: Ancill RJ, Holliday S, Higenbottam J (eds). Schizophrenia: exploring the spectrum of psychosis. New York: John Wiley & Sons, 1994.
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
- Zolpidem • Ambien
1. Pueschel S. Children with Down syndrome. In: Levine M, Carey W, Crocker A, Gross R (eds). Developmental-behavioral pediatrics. Philadelphia: WB Saunders, 1983.
2. Hodapp RM. Down syndrome: developmental, psychiatric, and management issues. Child Adolesc Psychiatr Clin North Am 1996;5:881-94.
3. Feinstein C, Reiss AL. Psychiatric disorder in mentally retarded children and adolescents. Child Adolesc Psychiatr Clin North Am 1996;5:827-52.
4. Wilgosh L. Sexual abuse of children with disabilities: intervention and treatment issues for parents. Developmental Disabil Bull. Available at: http://www.ualberta.ca/~jpdasddc/bulletin/articles/wilgosh1993.html. Accessed Nov. 10, 2003.
5. Ryan RM. Posttraumatic stress disorder in persons with developmental disabilities. Community Health J 1994;30:45-54.
6. Scheeringa MS, Seanah CH, Myers L, Putnam FW. New findings on alternative criteria for PTSD in preschool children. J Am Acad Child Adolesc Psychiatry 2003;42:561-70.
7. Diagnostic and Statistical Manual of Mental Disorders (4th ed-text revision). Washington, DC: American Psychiatric Association, 2000.
8. Lonigan CJ, Phillips BM, Richey JA. Posttraumatic stress disorder in children: diagnosis, assessment, and associated features. Child Adolesc Psychiatr Clin North Am 2003;12:171-94.
9. Donnelly CL. Pharmacological treatment approaches for children and adolescents with posttraumatic stress disorder. Child Adolesc Psychiatr Clin North Am 2003;12:251-69.
HISTORY: New school, old problems
Mr. E, age 13, was diagnosed with Down syndrome at birth and has mild mental retardation and bilateral sensorineural hearing loss. His pediatrician referred him to our child and adolescent psychiatry clinic for regressed behavior, depression, and apparent psychotic symptoms. He was also having problems sleeping and had begun puberty 8 months earlier.
Five months before referral, Mr. E had graduated from a small elementary school, where he was fully mainstreamed, to a large junior high school, where he spent most of the school day in a functional skills class. About that time, Mr. E began exhibiting nocturnal and daytime enuresis, loss of previously mastered skills, intolerance of novelty and change, and separation difficulty. Although toilet trained at age 7, he started having “accidents” at home, school, and elsewhere. He was reluctant to dress himself, and he resisted going to school.
The youth also talked to himself often and appeared to respond to internal stimuli. He “relived” conversations aloud, described imaginary friends to family and teachers, and spoke to a stuffed dog called Goofy. He would sit and stare into space for up to a half-hour, appearing preoccupied. Family members said he had exhibited these behaviors in grade school but until now appeared to have “outgrown” them.
Once sociable, Mr. E had become increasingly moody, negativistic, and isolative. He spent hours alone in his room. His mother, with whom he was close, reported that he was often angry with her for no apparent reason.
With puberty, his mother noted, Mr. E had begun kissing other developmentally disabled children. He also masturbated, but at his parents’ urging he restricted this activity to his room.
On evaluation, Mr. E was pleasant and outgoing. He had the facial dysmorphia and stature typical of Down syndrome. He smiled often and interacted well, and he attended and adapted to transitions in conversation and activities. His speech was dysarthric (with hyperglossia) and telegraphic; he could speak only four- to five-word sentences.
Was Mr. E exhibiting an adjustment reaction, depression, or a normal developmental response to puberty? Do his psychotic symptoms signal onset of schizophrenia?
Dr. Krassner’s and Kraus’ observations
Because Down syndrome is the most common genetic cause of mental retardation—seen in approximately 1 in 1,000 live births1—pediatricians and child psychiatrists see this disorder fairly frequently.
Regression, a form of coping exhibited by many children, is extremely common in youths with Down syndrome2 and often has a definite—though sometimes unclear—precipitant. We felt Mr. E’s move from a highly responsive, familiar school environment to a far less responsive one that accentuated his differences contributed to many of his symptoms.
Psychosis is less common in Down syndrome than in other developmental disabilities.2 Schizophrenia may occur, but diagnosis is complicated by cognition impairments, test-taking skills, and—in Mr. E’s case—inability to describe disordered thoughts or hallucinations due to poor language skills.3
Self-talk is common in Down syndrome and might be mistaken for psychosis. Note that despite his chronologic age, Mr. E is developmentally a 6-year-old, and self-talk and imaginary friends are considered normal behaviors for a child that age. What’s more, the stress of changing schools may have further compromised his developmental skills.
The FDA’s recent advisory about reports of increased suicidality in youths taking selective serotonin reuptake inhibitors (SSRIs) and other antidepressants for major depressive disorder during clinical trials has raised questions about using these agents in children and adolescents. Until more data become available, however, SSRIs remain the preferred drug therapy for pediatric depression.
- Based on our experience, we recommend citalopram, escitalopram, fluoxetine, and sertraline as first-line medications for pediatric depression because their side effects are relatively benign. The reported link between increased risk of suicidal ideation and behavior and use of paroxetine in pediatric patients has not been clearly established, so we cannot extrapolate that possible risk to other SSRIs.
- Newer antidepressants should be considered with caution in pediatric patients. Bupropion is contraindicated in patients with a history of seizures, bulimia, or anorexia. Mirtazapine is extremely sedating, with side effects such as weight gain and, in rare cases, agranulocytosis. Nefazodone comes with a “black box” warning for risk of liver toxicity. Trazodone is also sedating and carries a risk of priapism in boys.
- Older antidepressants, such as tricyclics, require extreme caution before prescribing to children and adolescents. Tricyclics, with their cardiac side effects, are not recommended for patients with Down syndrome, many of whom have cardiac pathology.
By contrast, depression is fairly common in Down syndrome, although it is much less prevalent in children than in adults with the developmental disorder.2
Finally, children with Down syndrome often enter puberty early, but without the cognitive or emotional maturity or knowledge to deal with the physiologic changes of adolescence.3 Parents often are reluctant to recognize their developmentally disabled child’s sexuality or are uncomfortable providing sexuality education.4 Mr. E’s parents clearly were unconvinced that his sexual behavior was normal for an adolescent.
TREATMENT Antidepressants lead to improvement
We felt Mr. E regressed secondary to emotional stress caused by switching schools. We viewed his psychotic symptoms as part of an adjustment disorder and attributed most of his other symptoms to depression. We anticipated Mr. E’s psychotic symptoms would remit spontaneously and focused on treating his mood and sleep disturbances.
We prescribed sertraline liquid suspension, 10 mg/d titrated across 3 weeks to 40 mg/d. We based our medication choice on clinical experience, mindful of a recent FDA advisory about the use of antidepressants in pediatric patients (Box 1). Also, the liquid suspension is easier to titrate than the tablet form, and we feared Mr. E might have trouble swallowing a tablet.
Mr. E’s mood and sociability improved after 3 to 4 weeks. Within 6 weeks, he regained some of his previously mastered daily activities. We added zolpidem, 10 mg nightly, to address his sleeping difficulties but discontinued the agent after 2 weeks, when his sleep patterns normalized.
At 2, 4, and 6 weeks, Mr. E was pleasant and cooperative, his thinking less concrete, and his speech more intelligible. His parents reported he was happier and more involved with family activities. At his mother’s request, sertraline was changed to 37.5 mg/d in tablet form. The patient remained stable for another month, during which his self-talk, though decreased, continued.
Two weeks later, Mr. E’s mother reported that, during a routine dermatologic examination for a chronic, presacral rash, the dermatologist noticed strategic shaving on the boy’s thighs, calves, and scrotum. Strategic shaving has been reported among sexually active youths as a means of purportedly increasing their sexual pleasure.
The dermatologist then told Mr. E’s mother that her son likely was sexually molested. Based on the boy’s differential rates of pubic hair growth, the doctor suspected that the molestation was chronic, dating back at least 3 months and probably continuing until the week before the examination. Upon hearing this, Mr. E’s parents were stunned and angry.
What behavioral signs might have suggested sexual abuse? How do the dermatologist’s findings alter diagnosis and treatment?
Dr. Krassner’s and Kraus’ observations
Given the dermatologist’s findings, Mr. E’s parents asked us whether their son’s presenting psychiatric symptoms were manifestations of posttraumatic stress disorder (PTSD).
Until now, explaining Mr. E’s symptoms as a reaction to changing schools seemed plausible. His symptoms were improving with treatment, and his sexual behaviors and interest in sexual topics were physiologically normal for his chronologic age. Despite his earlier pubertal experimentations, nothing in his psychosocial history indicated risk for sexual abuse or exploitation.
Still, children with Down syndrome are at higher risk for sexual exploitation than other children,4 so the possibility should have been explored with the parents. Psychiatrists should watch for physical signs of sexual abuse in these patients during the first examination (Box 2).4
But how is sexual abuse defined in this case? Deficient language skills prevented Mr. E from describing what happened to him, so determining whether he initiated sexual relations and with whom is nearly impossible. The act clearly could be considered abuse if Mr. E had been with an adult or older child—even if Mr. E consented. However, if Mr. E had initiated contact with another mentally retarded child, then cause, blame, and semantics become unclear. Either way, the incident could have caused PTSD.5
Diagnosing PTSD in non- or semi-verbal or retarded children is extremely difficult.6,7 Unlike adults with PTSD, pre-verbal children might not have recurrent, distressing recollections of the trauma, but symbolic displacement may characterize repetitive play, during which themes are expressed.8
Scheeringa et al have recommended PTSD criteria for preschool children, including:
- social withdrawal
- extreme temper tantrums
- loss of developmental skills
- new separation anxiety
- new onset of aggression
- new fears without obvious links to the trauma.5,6
Treating PTSD in children with developmental disabilities is also difficult. Modalities applicable to adults or mainstream children—such as psychodynamic psychotherapy, cognitive-behavioral therapy (CBT), exposure therapy, and medications—often do not help developmentally disabled children. For example, Mr. E lacks the cognitive apparatus to respond to CBT.
On the other hand, behavioral therapy, reducing risk factors, minimizing dissociative triggers, and educating patients, parents, friends, and teachers about PTSD can help patients such as Mr. E.5 Attempting to provide structure and maintain routines is a cornerstone of any intervention.
- Aggression
- Anxiety
- Behavior, learning problems at school
- Depression
- Heightened somatic concerns
- Sexualized behavior
- Sleep disturbance
- Withdrawal
FURTHER TREATMENT A family in turmoil
We addressed Mr. E’s symptoms as PTSD-related, though his poor language skills kept us from identifying a trauma. Based on data regarding pediatric PTSD treatment,9 we increased sertraline to 50 mg/d and then to 75 mg/d across 2 weeks.
However, an intense legal investigation brought on by the parents, combined with ensuing tumult within the family, worsened Mr. E’s symptoms. His self-talk became more pronounced and his isolative behavior reappeared, suggesting that the intrusive, repetitive questioning caused him to re-experience the trauma.
We again increased sertraline, to 100 mg/d, and offered supportive therapy to Mr. E. We tried to educate his parents about understanding his symptoms and managing his behavior and strongly recommended that they undergo crisis therapy to keep their reactions and emotions from hurting Mr. E. The parents declined, however, and alleged that we did not adequately support their pursuit of a diagnosis or legal action, which for them had become synonymous with treatment.
Mr. E’s mother brought her son to a psychologist, who engaged him in play therapy. She followed her son around, noting everything he said. All the while, she failed to resolve her guilt and anger. When we explained to her that these actions were hurting Mr. E’s progress, she terminated therapy.
How would you have tried to keep Mr. E’s family in therapy?
Dr. Krassner’s and Kraus’ observations
Treating psychopathology in children carries the risk of strained relations with the patient’s family. The risk increases exponentially for developmentally disabled children, as they have little or no input and their parents are exquisitely sensitive to their needs. Further, the revelation that the parents might have somehow failed to avert or anticipate danger to the child complicates their emotional response.
Although the child is the patient, the parent is the consumer. Failure to gain or keep the parents’ confidence will hinder or destroy therapy.
We might have protected our working relationship with Mr. E’s parents by recognizing how fragile they were and how intensely they would react to any constructive criticism. Paradoxically, for the short-term we could have tolerated their detrimental behaviors toward Mr. E (such as repeated questioning) in the hopes of protecting a long-term relationship. Spending more time exploring the guilt, anger, and confusion that tormented Mr. E’s parents—particularly his mother—also might have helped.
Related resources
- Ryan RM. Recognition of psychosis in persons who do not use spoken communication. In: Ancill RJ, Holliday S, Higenbottam J (eds). Schizophrenia: exploring the spectrum of psychosis. New York: John Wiley & Sons, 1994.
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
- Zolpidem • Ambien
HISTORY: New school, old problems
Mr. E, age 13, was diagnosed with Down syndrome at birth and has mild mental retardation and bilateral sensorineural hearing loss. His pediatrician referred him to our child and adolescent psychiatry clinic for regressed behavior, depression, and apparent psychotic symptoms. He was also having problems sleeping and had begun puberty 8 months earlier.
Five months before referral, Mr. E had graduated from a small elementary school, where he was fully mainstreamed, to a large junior high school, where he spent most of the school day in a functional skills class. About that time, Mr. E began exhibiting nocturnal and daytime enuresis, loss of previously mastered skills, intolerance of novelty and change, and separation difficulty. Although toilet trained at age 7, he started having “accidents” at home, school, and elsewhere. He was reluctant to dress himself, and he resisted going to school.
The youth also talked to himself often and appeared to respond to internal stimuli. He “relived” conversations aloud, described imaginary friends to family and teachers, and spoke to a stuffed dog called Goofy. He would sit and stare into space for up to a half-hour, appearing preoccupied. Family members said he had exhibited these behaviors in grade school but until now appeared to have “outgrown” them.
Once sociable, Mr. E had become increasingly moody, negativistic, and isolative. He spent hours alone in his room. His mother, with whom he was close, reported that he was often angry with her for no apparent reason.
With puberty, his mother noted, Mr. E had begun kissing other developmentally disabled children. He also masturbated, but at his parents’ urging he restricted this activity to his room.
On evaluation, Mr. E was pleasant and outgoing. He had the facial dysmorphia and stature typical of Down syndrome. He smiled often and interacted well, and he attended and adapted to transitions in conversation and activities. His speech was dysarthric (with hyperglossia) and telegraphic; he could speak only four- to five-word sentences.
Was Mr. E exhibiting an adjustment reaction, depression, or a normal developmental response to puberty? Do his psychotic symptoms signal onset of schizophrenia?
Dr. Krassner’s and Kraus’ observations
Because Down syndrome is the most common genetic cause of mental retardation—seen in approximately 1 in 1,000 live births1—pediatricians and child psychiatrists see this disorder fairly frequently.
Regression, a form of coping exhibited by many children, is extremely common in youths with Down syndrome2 and often has a definite—though sometimes unclear—precipitant. We felt Mr. E’s move from a highly responsive, familiar school environment to a far less responsive one that accentuated his differences contributed to many of his symptoms.
Psychosis is less common in Down syndrome than in other developmental disabilities.2 Schizophrenia may occur, but diagnosis is complicated by cognition impairments, test-taking skills, and—in Mr. E’s case—inability to describe disordered thoughts or hallucinations due to poor language skills.3
Self-talk is common in Down syndrome and might be mistaken for psychosis. Note that despite his chronologic age, Mr. E is developmentally a 6-year-old, and self-talk and imaginary friends are considered normal behaviors for a child that age. What’s more, the stress of changing schools may have further compromised his developmental skills.
The FDA’s recent advisory about reports of increased suicidality in youths taking selective serotonin reuptake inhibitors (SSRIs) and other antidepressants for major depressive disorder during clinical trials has raised questions about using these agents in children and adolescents. Until more data become available, however, SSRIs remain the preferred drug therapy for pediatric depression.
- Based on our experience, we recommend citalopram, escitalopram, fluoxetine, and sertraline as first-line medications for pediatric depression because their side effects are relatively benign. The reported link between increased risk of suicidal ideation and behavior and use of paroxetine in pediatric patients has not been clearly established, so we cannot extrapolate that possible risk to other SSRIs.
- Newer antidepressants should be considered with caution in pediatric patients. Bupropion is contraindicated in patients with a history of seizures, bulimia, or anorexia. Mirtazapine is extremely sedating, with side effects such as weight gain and, in rare cases, agranulocytosis. Nefazodone comes with a “black box” warning for risk of liver toxicity. Trazodone is also sedating and carries a risk of priapism in boys.
- Older antidepressants, such as tricyclics, require extreme caution before prescribing to children and adolescents. Tricyclics, with their cardiac side effects, are not recommended for patients with Down syndrome, many of whom have cardiac pathology.
By contrast, depression is fairly common in Down syndrome, although it is much less prevalent in children than in adults with the developmental disorder.2
Finally, children with Down syndrome often enter puberty early, but without the cognitive or emotional maturity or knowledge to deal with the physiologic changes of adolescence.3 Parents often are reluctant to recognize their developmentally disabled child’s sexuality or are uncomfortable providing sexuality education.4 Mr. E’s parents clearly were unconvinced that his sexual behavior was normal for an adolescent.
TREATMENT Antidepressants lead to improvement
We felt Mr. E regressed secondary to emotional stress caused by switching schools. We viewed his psychotic symptoms as part of an adjustment disorder and attributed most of his other symptoms to depression. We anticipated Mr. E’s psychotic symptoms would remit spontaneously and focused on treating his mood and sleep disturbances.
We prescribed sertraline liquid suspension, 10 mg/d titrated across 3 weeks to 40 mg/d. We based our medication choice on clinical experience, mindful of a recent FDA advisory about the use of antidepressants in pediatric patients (Box 1). Also, the liquid suspension is easier to titrate than the tablet form, and we feared Mr. E might have trouble swallowing a tablet.
Mr. E’s mood and sociability improved after 3 to 4 weeks. Within 6 weeks, he regained some of his previously mastered daily activities. We added zolpidem, 10 mg nightly, to address his sleeping difficulties but discontinued the agent after 2 weeks, when his sleep patterns normalized.
At 2, 4, and 6 weeks, Mr. E was pleasant and cooperative, his thinking less concrete, and his speech more intelligible. His parents reported he was happier and more involved with family activities. At his mother’s request, sertraline was changed to 37.5 mg/d in tablet form. The patient remained stable for another month, during which his self-talk, though decreased, continued.
Two weeks later, Mr. E’s mother reported that, during a routine dermatologic examination for a chronic, presacral rash, the dermatologist noticed strategic shaving on the boy’s thighs, calves, and scrotum. Strategic shaving has been reported among sexually active youths as a means of purportedly increasing their sexual pleasure.
The dermatologist then told Mr. E’s mother that her son likely was sexually molested. Based on the boy’s differential rates of pubic hair growth, the doctor suspected that the molestation was chronic, dating back at least 3 months and probably continuing until the week before the examination. Upon hearing this, Mr. E’s parents were stunned and angry.
What behavioral signs might have suggested sexual abuse? How do the dermatologist’s findings alter diagnosis and treatment?
Dr. Krassner’s and Kraus’ observations
Given the dermatologist’s findings, Mr. E’s parents asked us whether their son’s presenting psychiatric symptoms were manifestations of posttraumatic stress disorder (PTSD).
Until now, explaining Mr. E’s symptoms as a reaction to changing schools seemed plausible. His symptoms were improving with treatment, and his sexual behaviors and interest in sexual topics were physiologically normal for his chronologic age. Despite his earlier pubertal experimentations, nothing in his psychosocial history indicated risk for sexual abuse or exploitation.
Still, children with Down syndrome are at higher risk for sexual exploitation than other children,4 so the possibility should have been explored with the parents. Psychiatrists should watch for physical signs of sexual abuse in these patients during the first examination (Box 2).4
But how is sexual abuse defined in this case? Deficient language skills prevented Mr. E from describing what happened to him, so determining whether he initiated sexual relations and with whom is nearly impossible. The act clearly could be considered abuse if Mr. E had been with an adult or older child—even if Mr. E consented. However, if Mr. E had initiated contact with another mentally retarded child, then cause, blame, and semantics become unclear. Either way, the incident could have caused PTSD.5
Diagnosing PTSD in non- or semi-verbal or retarded children is extremely difficult.6,7 Unlike adults with PTSD, pre-verbal children might not have recurrent, distressing recollections of the trauma, but symbolic displacement may characterize repetitive play, during which themes are expressed.8
Scheeringa et al have recommended PTSD criteria for preschool children, including:
- social withdrawal
- extreme temper tantrums
- loss of developmental skills
- new separation anxiety
- new onset of aggression
- new fears without obvious links to the trauma.5,6
Treating PTSD in children with developmental disabilities is also difficult. Modalities applicable to adults or mainstream children—such as psychodynamic psychotherapy, cognitive-behavioral therapy (CBT), exposure therapy, and medications—often do not help developmentally disabled children. For example, Mr. E lacks the cognitive apparatus to respond to CBT.
On the other hand, behavioral therapy, reducing risk factors, minimizing dissociative triggers, and educating patients, parents, friends, and teachers about PTSD can help patients such as Mr. E.5 Attempting to provide structure and maintain routines is a cornerstone of any intervention.
- Aggression
- Anxiety
- Behavior, learning problems at school
- Depression
- Heightened somatic concerns
- Sexualized behavior
- Sleep disturbance
- Withdrawal
FURTHER TREATMENT A family in turmoil
We addressed Mr. E’s symptoms as PTSD-related, though his poor language skills kept us from identifying a trauma. Based on data regarding pediatric PTSD treatment,9 we increased sertraline to 50 mg/d and then to 75 mg/d across 2 weeks.
However, an intense legal investigation brought on by the parents, combined with ensuing tumult within the family, worsened Mr. E’s symptoms. His self-talk became more pronounced and his isolative behavior reappeared, suggesting that the intrusive, repetitive questioning caused him to re-experience the trauma.
We again increased sertraline, to 100 mg/d, and offered supportive therapy to Mr. E. We tried to educate his parents about understanding his symptoms and managing his behavior and strongly recommended that they undergo crisis therapy to keep their reactions and emotions from hurting Mr. E. The parents declined, however, and alleged that we did not adequately support their pursuit of a diagnosis or legal action, which for them had become synonymous with treatment.
Mr. E’s mother brought her son to a psychologist, who engaged him in play therapy. She followed her son around, noting everything he said. All the while, she failed to resolve her guilt and anger. When we explained to her that these actions were hurting Mr. E’s progress, she terminated therapy.
How would you have tried to keep Mr. E’s family in therapy?
Dr. Krassner’s and Kraus’ observations
Treating psychopathology in children carries the risk of strained relations with the patient’s family. The risk increases exponentially for developmentally disabled children, as they have little or no input and their parents are exquisitely sensitive to their needs. Further, the revelation that the parents might have somehow failed to avert or anticipate danger to the child complicates their emotional response.
Although the child is the patient, the parent is the consumer. Failure to gain or keep the parents’ confidence will hinder or destroy therapy.
We might have protected our working relationship with Mr. E’s parents by recognizing how fragile they were and how intensely they would react to any constructive criticism. Paradoxically, for the short-term we could have tolerated their detrimental behaviors toward Mr. E (such as repeated questioning) in the hopes of protecting a long-term relationship. Spending more time exploring the guilt, anger, and confusion that tormented Mr. E’s parents—particularly his mother—also might have helped.
Related resources
- Ryan RM. Recognition of psychosis in persons who do not use spoken communication. In: Ancill RJ, Holliday S, Higenbottam J (eds). Schizophrenia: exploring the spectrum of psychosis. New York: John Wiley & Sons, 1994.
Drug brand names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
- Zolpidem • Ambien
1. Pueschel S. Children with Down syndrome. In: Levine M, Carey W, Crocker A, Gross R (eds). Developmental-behavioral pediatrics. Philadelphia: WB Saunders, 1983.
2. Hodapp RM. Down syndrome: developmental, psychiatric, and management issues. Child Adolesc Psychiatr Clin North Am 1996;5:881-94.
3. Feinstein C, Reiss AL. Psychiatric disorder in mentally retarded children and adolescents. Child Adolesc Psychiatr Clin North Am 1996;5:827-52.
4. Wilgosh L. Sexual abuse of children with disabilities: intervention and treatment issues for parents. Developmental Disabil Bull. Available at: http://www.ualberta.ca/~jpdasddc/bulletin/articles/wilgosh1993.html. Accessed Nov. 10, 2003.
5. Ryan RM. Posttraumatic stress disorder in persons with developmental disabilities. Community Health J 1994;30:45-54.
6. Scheeringa MS, Seanah CH, Myers L, Putnam FW. New findings on alternative criteria for PTSD in preschool children. J Am Acad Child Adolesc Psychiatry 2003;42:561-70.
7. Diagnostic and Statistical Manual of Mental Disorders (4th ed-text revision). Washington, DC: American Psychiatric Association, 2000.
8. Lonigan CJ, Phillips BM, Richey JA. Posttraumatic stress disorder in children: diagnosis, assessment, and associated features. Child Adolesc Psychiatr Clin North Am 2003;12:171-94.
9. Donnelly CL. Pharmacological treatment approaches for children and adolescents with posttraumatic stress disorder. Child Adolesc Psychiatr Clin North Am 2003;12:251-69.
1. Pueschel S. Children with Down syndrome. In: Levine M, Carey W, Crocker A, Gross R (eds). Developmental-behavioral pediatrics. Philadelphia: WB Saunders, 1983.
2. Hodapp RM. Down syndrome: developmental, psychiatric, and management issues. Child Adolesc Psychiatr Clin North Am 1996;5:881-94.
3. Feinstein C, Reiss AL. Psychiatric disorder in mentally retarded children and adolescents. Child Adolesc Psychiatr Clin North Am 1996;5:827-52.
4. Wilgosh L. Sexual abuse of children with disabilities: intervention and treatment issues for parents. Developmental Disabil Bull. Available at: http://www.ualberta.ca/~jpdasddc/bulletin/articles/wilgosh1993.html. Accessed Nov. 10, 2003.
5. Ryan RM. Posttraumatic stress disorder in persons with developmental disabilities. Community Health J 1994;30:45-54.
6. Scheeringa MS, Seanah CH, Myers L, Putnam FW. New findings on alternative criteria for PTSD in preschool children. J Am Acad Child Adolesc Psychiatry 2003;42:561-70.
7. Diagnostic and Statistical Manual of Mental Disorders (4th ed-text revision). Washington, DC: American Psychiatric Association, 2000.
8. Lonigan CJ, Phillips BM, Richey JA. Posttraumatic stress disorder in children: diagnosis, assessment, and associated features. Child Adolesc Psychiatr Clin North Am 2003;12:171-94.
9. Donnelly CL. Pharmacological treatment approaches for children and adolescents with posttraumatic stress disorder. Child Adolesc Psychiatr Clin North Am 2003;12:251-69.
Beware the men with toupees
HISTORY: Treatment-refractory depression
Mr. S, age 78, has a history of depression that has not responded to selective serotonin reuptake inhibitors and electroconvulsive therapy (ECT).
According to his niece, Mr. S had become withdrawn, suspicious, and forgetful. Several times over the past year, police found him wandering the streets and brought him to the community hospital’s emergency room.
During one emergency room visit, he complained of decreased appetite, poor sleep, and depressed mood. He was subsequently admitted to the psychiatric unit, where he was treated with ECT and discharged on citalopram, 20 mg/d. His symptoms did not improve and he became ataxic and incontinent of urine.
Mr. S’ family placed him in a nursing home, where he became increasingly paranoid. The attending physician prescribed risperidone, 3 mg/d, with no effect. He was then transferred to our psychiatric facility.
At admission, Mr. S told us that a group of men disguised in toupees and mustaches were out to kill him. He said these men had recently killed his niece—with whom he had just spoken on the phone and had seen at the hospital. He suspected that these men were after his money, hired a woman to impersonate his niece and spy on him, and planned to bury his body and his niece’s in a remote place.
On evaluation, Mr. S was suspicious, guarded, and uncooperative, and often ended conversations abruptly. He denied auditory and visual hallucinations, was not suicidal or homicidal, and denied abusing drugs or alcohol. He said constant fear of his imminent murder left him feeling depressed.
Physical and neurologic exams were unremarkable except for mild ataxia. Mr. S’ Folstein Mini-Mental State Examination score was 19/30, indicating moderate cognitive impairment.
Mr. S’ history and behavior suggest depression with psychotic features. Do we have enough information for a diagnosis?
Dr. Greenberg’s and Tampi’s observations
Mr. S is displaying mood symptoms consistent with his prior diagnosis of depression, but with new-onset psychosis as well.
Because of Mr. S’ neurobiologic symptoms, it is improper to diagnose depression with psychotic features without first performing a full medical and neurologic workup. The differential diagnosis needs to include medical and neurologic diagnoses, including:
- delirium secondary to urinary tract infection
- Alzheimer’s and/or vascular dementia
- normal-pressure hydrocephalus
- substance abuse.
A complete dementia and delirium workup and detailed medical history are imperative.
FURTHER HISTORY: Risky behavior
Further history reveals that Mr. S had been having sexual intercourse with prostitutes since his early teens and that this habit continued into his 70s. He had been diagnosed with syphilis in his teens and again in his 50s. Both times he refused to complete the recommended penicillin regimen because he was embarrassed by the diagnosis and had falsely believed that a single penicillin injection would cure him.
Lab tests showed a white blood cell count of 3.5 and a weakly reactive serum venereal disease research laboratory (VDRL) reading.
Reporting of syphilis cases in the United States began in 1941.1 At about that time, Yale University and the Mayo Clinic began conducting clinical trials of penicillin in syphilis treatment.2
Thanks to the advent of penicillin, syphilis incidence has declined dramatically since 1943, when 575,593 cases were reported.3 Only 5,979 cases were reported to the U.S. Centers for Disease Control and Prevention in 2000.4 A slight increase in cases, mainly among homosexual men, was reported in 2001.1,4
The AIDS epidemic and the emergence of crack/cocaine use5,6 were believed to have triggered a brief increase in cases that peaked in 1990. This was likely caused by the high-risk sexual behavior observed in individuals with sexually transmitted diseases and the practice of exchanging sex for drugs.6
Could Mr. S’ syphilis—inadequately treated in his youth—be causing his depression and paranoia decades later? If so, how would you confirm this finding?
Dr. Greenberg’s and Tampi’s observations
Mr. S has a longstanding history of syphilis secondary to high-risk sexual activity. This, combined with the lab findings and his worsening depression and paranoia, points to possible neurosyphilis.
Syphilis, caused by the spirochete Treponema pallidum., can traverse mucous membranes and abraded skin. Transmission is most common during sexual activity but also occurs through blood transfusions and nonsexual lesion contact and from mother to fetus.
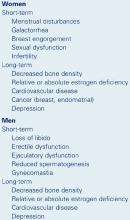
Prevalence
- 6,103 cases reported in 2001
- More prevalent among men than women (2.1:1), probably because of elevated prevalence among homosexual men
- African-Americans accounted for 62% of cases in 2001. Prevalence in African–Americans that year was 16 times greater than in whites
Risk factors
- Presence of HIV infection or other sexually transmitted disease
- Unprotected sex
- Residence in urban areas
- Substance abuse
- Homosexuality
Source: References 5 and 6
Because syphilis and its psychiatric effects are relatively uncommon (Box 1), many psychiatrists do not consider neurosyphilis in high-risk patients who present with depression, dementia, or psychosis (Box 2).
HOW SYPHILIS BECOMES NEUROSYPHILIS
Primary syphilis incubates for 10 to 90 days following infection. After this period, an infectious chancre appears along with regional adenopathy. If untreated, the chancre will disappear but the infection will progress.
Secondary syphilis is characterized by skin manifestations and occasionally affects the joints, eyes, bones, kidneys, liver, and CNS. Common effects include condylomata—highly infectious warty lesions—and a diffuse maculopapular rash on the palms and soles. These lesions disappear if left untreated, but most patients then either enter syphilis’ latent stage or experience a potentially fatal relapse of secondary syphilis.5
Latent syphilis usually remains latent or resolves, but about one-third of patients with latent syphilis slowly progress to tertiary syphilis. Neurosyphilis, one of the main forms of tertiary syphilis, can surface 5 to 35 years after an untreated primary infection.7
There are four categories of neurosyphilis:
- General paresis results in dementia, changes in personality, transient hemiparesis, depression, and psychosis.
- Tabes dorsalis degenerates the posterior columns and dorsal root ganglia of the spinal cord. This results in ataxia, parasthesias, decreased proprioception and vibratory sense, Argyll Robertson pupil (an optical disorder in which the pupil does not react normally to light), neurogenic bladder, and sharp shooting pains throughout the body.
- Meningovascular neurosyphilis can result in cranial nerve abnormalities, symptoms of meningitis, and cerebral infarctions.
- Asymptomatic but with CSF positive for syphilis.
Neurosyphilis is fatal if untreated, and treatment usually does not eliminate symptoms but prevents further progression. Approximately 8% of patients with untreated primary syphilis develop neurosyphilis.5,7
Standard nontreponemal tests, such as the VDRL or rapid plasmin reagin, can be used to screen for syphilis. Because these tests often produce false positives, confirm positive results with a syphilis-specific test, such as the fluorescent treponemal antibody absorption (FTA-ABS) test, microhemagglutination assay for antibodies to T pallidum., and the T pallidum. hemagglutination assay.
If neurosyphilis is suspected, CSF testing is strongly recommended. Diagnostic findings include elevated white blood cell and protein counts and a positive VDRL. If the CSF is negative, refer the patient for treatment anyway because false negatives are common. Patients with consistent neurologic symptoms, positive VDRL and/or FTA-ABS, and negative CSF are diagnosed with neurosyphilis and warrant treatment.7
How would you manage Mr. S’ psychiatric symptoms concomitant with medical treatment of late-stage syphilis?
Dr. Greenberg’s and Tampi’s observations
Although no specific guidelines exist for treating psychosis secondary to neurosyphilis, atypical antipsychotics remain the first-line treatment. Atypicals do not interact significantly with penicillin and can be given safely with syphilis treatment. Atypicals also are better tolerated than typical antipsychotics and produce fewer extrapyramidal symptoms, which are common among older patients and those with neurologic diseases.
Screening for syphilis. Every patient with a history of high-risk sexual behavior who presents with new-onset dementia or psychosis should be screened for syphilis. Sexual history can be difficult to obtain from some patients and family members, so communication between providers becomes crucial. Obtain lab test results from other care team members to monitor compliance, and coordinate patient education with other doctors on safe sexual practices.
TREATMENT: Taking his medicine
Mr. S refused further testing and emergency conservatorship was sought. Citalopram was discontinued and risperidone was gradually increased to 6 mg at bedtime. He remained paranoid and delusional.
A brain MRI showed chronic ischemic small-vessel disease. HIV testing was negative, and serum FTA-ABS was reactive. CSF showed elevated protein and white blood cell count with a nonreactive VDRL and a reactive FTA-ABS. A diagnosis of neurosyphilis was made, and treatment was initiated with aqueous crystalline penicillin G, 4 million units every 4 hours for 2 weeks.
Mr. S was discharged back to the nursing home where his penicillin injections were continued. His paranoia diminished slightly but he remained ataxic, incontinent, and confused. He was discharged from the nursing home but needed confirmative HIV screening and repeated CSF testing to determine if syphilis treatment was effective.
Six months after treatment, Mr. S’ niece reports that his paranoia has decreased. He has not needed additional psychiatric hospitalizations.
Related resources
- Merck Manual. www.merck.com. Search: “syphilis”
- U.S. Centers for Disease Control and Prevention—Syphilis elimination: History in the making. www.cdc.gov. Click on “Health Topics A-Z,” then click on “S” and find “syphilis.”
- National Institute of Allergy and Infectious Disease. www.niaid.nih.gov. Search: “syphilis”
Drug brand names
- Citalopram • Celexa
- Risperidone • Risperdal
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. U.S. Centers for Disease Control and Prevention. Primary and secondary syphilis—United States, 2000-2001. MMWR Morb Mortal Wkly Rep. 2002;51:971-3.
2. Mandell GL, Petri WA. Antimicrobial agents: penicillins, cephalosporins, and other beta-lactam antibiotics. In:Hardman JG, Limbird LE, Molinoff PB, et al (eds) Goodman and Gilman’s the pharmacological basis of therapeutics. (9th ed). New York: McGraw-Hill, 1996;1073-4.
3. Lukehart SA, Holmes KK. Spirochetal diseases. In: Braunwald E, Fauci AS, Kasper DL, et al (eds). Harrison’s principles of internal medicine. (14th ed). New York: McGraw-Hill, 1998;1023.-
4. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2001 supplement, syphilis surveillance report. Available at: http://www.cdc.gov/std/stats/2001syphilis.htm. Accessed October 10, 2003.
5. Jacobs RA. Infectious diseases: spirochetal. In: Tierney LM, McPhee SJ, Papadakis MA (eds). Current medical diagnosis and treatment. (39th ed). New York: Lange Medical Books/McGraw-Hill, 2000;1376-86.
6. Hutto B. Syphilis in clinical psychiatry: a review. Psychosomatics. 2001;42:453-60.
7. Carpenter CJ, Lederman MM, Salata RA. Sexually transmitted diseases. In: Andreoli TE, Bennett JC, Carpenter CJ, Plum F (eds). Cecil essentials of medicine. (4th ed). Philadelphia: WB Saunders Co, 1997;742-5.
HISTORY: Treatment-refractory depression
Mr. S, age 78, has a history of depression that has not responded to selective serotonin reuptake inhibitors and electroconvulsive therapy (ECT).
According to his niece, Mr. S had become withdrawn, suspicious, and forgetful. Several times over the past year, police found him wandering the streets and brought him to the community hospital’s emergency room.
During one emergency room visit, he complained of decreased appetite, poor sleep, and depressed mood. He was subsequently admitted to the psychiatric unit, where he was treated with ECT and discharged on citalopram, 20 mg/d. His symptoms did not improve and he became ataxic and incontinent of urine.
Mr. S’ family placed him in a nursing home, where he became increasingly paranoid. The attending physician prescribed risperidone, 3 mg/d, with no effect. He was then transferred to our psychiatric facility.
At admission, Mr. S told us that a group of men disguised in toupees and mustaches were out to kill him. He said these men had recently killed his niece—with whom he had just spoken on the phone and had seen at the hospital. He suspected that these men were after his money, hired a woman to impersonate his niece and spy on him, and planned to bury his body and his niece’s in a remote place.
On evaluation, Mr. S was suspicious, guarded, and uncooperative, and often ended conversations abruptly. He denied auditory and visual hallucinations, was not suicidal or homicidal, and denied abusing drugs or alcohol. He said constant fear of his imminent murder left him feeling depressed.
Physical and neurologic exams were unremarkable except for mild ataxia. Mr. S’ Folstein Mini-Mental State Examination score was 19/30, indicating moderate cognitive impairment.
Mr. S’ history and behavior suggest depression with psychotic features. Do we have enough information for a diagnosis?
Dr. Greenberg’s and Tampi’s observations
Mr. S is displaying mood symptoms consistent with his prior diagnosis of depression, but with new-onset psychosis as well.
Because of Mr. S’ neurobiologic symptoms, it is improper to diagnose depression with psychotic features without first performing a full medical and neurologic workup. The differential diagnosis needs to include medical and neurologic diagnoses, including:
- delirium secondary to urinary tract infection
- Alzheimer’s and/or vascular dementia
- normal-pressure hydrocephalus
- substance abuse.
A complete dementia and delirium workup and detailed medical history are imperative.
FURTHER HISTORY: Risky behavior
Further history reveals that Mr. S had been having sexual intercourse with prostitutes since his early teens and that this habit continued into his 70s. He had been diagnosed with syphilis in his teens and again in his 50s. Both times he refused to complete the recommended penicillin regimen because he was embarrassed by the diagnosis and had falsely believed that a single penicillin injection would cure him.
Lab tests showed a white blood cell count of 3.5 and a weakly reactive serum venereal disease research laboratory (VDRL) reading.
Reporting of syphilis cases in the United States began in 1941.1 At about that time, Yale University and the Mayo Clinic began conducting clinical trials of penicillin in syphilis treatment.2
Thanks to the advent of penicillin, syphilis incidence has declined dramatically since 1943, when 575,593 cases were reported.3 Only 5,979 cases were reported to the U.S. Centers for Disease Control and Prevention in 2000.4 A slight increase in cases, mainly among homosexual men, was reported in 2001.1,4
The AIDS epidemic and the emergence of crack/cocaine use5,6 were believed to have triggered a brief increase in cases that peaked in 1990. This was likely caused by the high-risk sexual behavior observed in individuals with sexually transmitted diseases and the practice of exchanging sex for drugs.6
Could Mr. S’ syphilis—inadequately treated in his youth—be causing his depression and paranoia decades later? If so, how would you confirm this finding?
Dr. Greenberg’s and Tampi’s observations
Mr. S has a longstanding history of syphilis secondary to high-risk sexual activity. This, combined with the lab findings and his worsening depression and paranoia, points to possible neurosyphilis.
Syphilis, caused by the spirochete Treponema pallidum., can traverse mucous membranes and abraded skin. Transmission is most common during sexual activity but also occurs through blood transfusions and nonsexual lesion contact and from mother to fetus.
Prevalence
- 6,103 cases reported in 2001
- More prevalent among men than women (2.1:1), probably because of elevated prevalence among homosexual men
- African-Americans accounted for 62% of cases in 2001. Prevalence in African–Americans that year was 16 times greater than in whites
Risk factors
- Presence of HIV infection or other sexually transmitted disease
- Unprotected sex
- Residence in urban areas
- Substance abuse
- Homosexuality
Source: References 5 and 6
Because syphilis and its psychiatric effects are relatively uncommon (Box 1), many psychiatrists do not consider neurosyphilis in high-risk patients who present with depression, dementia, or psychosis (Box 2).
HOW SYPHILIS BECOMES NEUROSYPHILIS
Primary syphilis incubates for 10 to 90 days following infection. After this period, an infectious chancre appears along with regional adenopathy. If untreated, the chancre will disappear but the infection will progress.
Secondary syphilis is characterized by skin manifestations and occasionally affects the joints, eyes, bones, kidneys, liver, and CNS. Common effects include condylomata—highly infectious warty lesions—and a diffuse maculopapular rash on the palms and soles. These lesions disappear if left untreated, but most patients then either enter syphilis’ latent stage or experience a potentially fatal relapse of secondary syphilis.5
Latent syphilis usually remains latent or resolves, but about one-third of patients with latent syphilis slowly progress to tertiary syphilis. Neurosyphilis, one of the main forms of tertiary syphilis, can surface 5 to 35 years after an untreated primary infection.7
There are four categories of neurosyphilis:
- General paresis results in dementia, changes in personality, transient hemiparesis, depression, and psychosis.
- Tabes dorsalis degenerates the posterior columns and dorsal root ganglia of the spinal cord. This results in ataxia, parasthesias, decreased proprioception and vibratory sense, Argyll Robertson pupil (an optical disorder in which the pupil does not react normally to light), neurogenic bladder, and sharp shooting pains throughout the body.
- Meningovascular neurosyphilis can result in cranial nerve abnormalities, symptoms of meningitis, and cerebral infarctions.
- Asymptomatic but with CSF positive for syphilis.
Neurosyphilis is fatal if untreated, and treatment usually does not eliminate symptoms but prevents further progression. Approximately 8% of patients with untreated primary syphilis develop neurosyphilis.5,7
Standard nontreponemal tests, such as the VDRL or rapid plasmin reagin, can be used to screen for syphilis. Because these tests often produce false positives, confirm positive results with a syphilis-specific test, such as the fluorescent treponemal antibody absorption (FTA-ABS) test, microhemagglutination assay for antibodies to T pallidum., and the T pallidum. hemagglutination assay.
If neurosyphilis is suspected, CSF testing is strongly recommended. Diagnostic findings include elevated white blood cell and protein counts and a positive VDRL. If the CSF is negative, refer the patient for treatment anyway because false negatives are common. Patients with consistent neurologic symptoms, positive VDRL and/or FTA-ABS, and negative CSF are diagnosed with neurosyphilis and warrant treatment.7
How would you manage Mr. S’ psychiatric symptoms concomitant with medical treatment of late-stage syphilis?
Dr. Greenberg’s and Tampi’s observations
Although no specific guidelines exist for treating psychosis secondary to neurosyphilis, atypical antipsychotics remain the first-line treatment. Atypicals do not interact significantly with penicillin and can be given safely with syphilis treatment. Atypicals also are better tolerated than typical antipsychotics and produce fewer extrapyramidal symptoms, which are common among older patients and those with neurologic diseases.
Screening for syphilis. Every patient with a history of high-risk sexual behavior who presents with new-onset dementia or psychosis should be screened for syphilis. Sexual history can be difficult to obtain from some patients and family members, so communication between providers becomes crucial. Obtain lab test results from other care team members to monitor compliance, and coordinate patient education with other doctors on safe sexual practices.
TREATMENT: Taking his medicine
Mr. S refused further testing and emergency conservatorship was sought. Citalopram was discontinued and risperidone was gradually increased to 6 mg at bedtime. He remained paranoid and delusional.
A brain MRI showed chronic ischemic small-vessel disease. HIV testing was negative, and serum FTA-ABS was reactive. CSF showed elevated protein and white blood cell count with a nonreactive VDRL and a reactive FTA-ABS. A diagnosis of neurosyphilis was made, and treatment was initiated with aqueous crystalline penicillin G, 4 million units every 4 hours for 2 weeks.
Mr. S was discharged back to the nursing home where his penicillin injections were continued. His paranoia diminished slightly but he remained ataxic, incontinent, and confused. He was discharged from the nursing home but needed confirmative HIV screening and repeated CSF testing to determine if syphilis treatment was effective.
Six months after treatment, Mr. S’ niece reports that his paranoia has decreased. He has not needed additional psychiatric hospitalizations.
Related resources
- Merck Manual. www.merck.com. Search: “syphilis”
- U.S. Centers for Disease Control and Prevention—Syphilis elimination: History in the making. www.cdc.gov. Click on “Health Topics A-Z,” then click on “S” and find “syphilis.”
- National Institute of Allergy and Infectious Disease. www.niaid.nih.gov. Search: “syphilis”
Drug brand names
- Citalopram • Celexa
- Risperidone • Risperdal
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
HISTORY: Treatment-refractory depression
Mr. S, age 78, has a history of depression that has not responded to selective serotonin reuptake inhibitors and electroconvulsive therapy (ECT).
According to his niece, Mr. S had become withdrawn, suspicious, and forgetful. Several times over the past year, police found him wandering the streets and brought him to the community hospital’s emergency room.
During one emergency room visit, he complained of decreased appetite, poor sleep, and depressed mood. He was subsequently admitted to the psychiatric unit, where he was treated with ECT and discharged on citalopram, 20 mg/d. His symptoms did not improve and he became ataxic and incontinent of urine.
Mr. S’ family placed him in a nursing home, where he became increasingly paranoid. The attending physician prescribed risperidone, 3 mg/d, with no effect. He was then transferred to our psychiatric facility.
At admission, Mr. S told us that a group of men disguised in toupees and mustaches were out to kill him. He said these men had recently killed his niece—with whom he had just spoken on the phone and had seen at the hospital. He suspected that these men were after his money, hired a woman to impersonate his niece and spy on him, and planned to bury his body and his niece’s in a remote place.
On evaluation, Mr. S was suspicious, guarded, and uncooperative, and often ended conversations abruptly. He denied auditory and visual hallucinations, was not suicidal or homicidal, and denied abusing drugs or alcohol. He said constant fear of his imminent murder left him feeling depressed.
Physical and neurologic exams were unremarkable except for mild ataxia. Mr. S’ Folstein Mini-Mental State Examination score was 19/30, indicating moderate cognitive impairment.
Mr. S’ history and behavior suggest depression with psychotic features. Do we have enough information for a diagnosis?
Dr. Greenberg’s and Tampi’s observations
Mr. S is displaying mood symptoms consistent with his prior diagnosis of depression, but with new-onset psychosis as well.
Because of Mr. S’ neurobiologic symptoms, it is improper to diagnose depression with psychotic features without first performing a full medical and neurologic workup. The differential diagnosis needs to include medical and neurologic diagnoses, including:
- delirium secondary to urinary tract infection
- Alzheimer’s and/or vascular dementia
- normal-pressure hydrocephalus
- substance abuse.
A complete dementia and delirium workup and detailed medical history are imperative.
FURTHER HISTORY: Risky behavior
Further history reveals that Mr. S had been having sexual intercourse with prostitutes since his early teens and that this habit continued into his 70s. He had been diagnosed with syphilis in his teens and again in his 50s. Both times he refused to complete the recommended penicillin regimen because he was embarrassed by the diagnosis and had falsely believed that a single penicillin injection would cure him.
Lab tests showed a white blood cell count of 3.5 and a weakly reactive serum venereal disease research laboratory (VDRL) reading.
Reporting of syphilis cases in the United States began in 1941.1 At about that time, Yale University and the Mayo Clinic began conducting clinical trials of penicillin in syphilis treatment.2
Thanks to the advent of penicillin, syphilis incidence has declined dramatically since 1943, when 575,593 cases were reported.3 Only 5,979 cases were reported to the U.S. Centers for Disease Control and Prevention in 2000.4 A slight increase in cases, mainly among homosexual men, was reported in 2001.1,4
The AIDS epidemic and the emergence of crack/cocaine use5,6 were believed to have triggered a brief increase in cases that peaked in 1990. This was likely caused by the high-risk sexual behavior observed in individuals with sexually transmitted diseases and the practice of exchanging sex for drugs.6
Could Mr. S’ syphilis—inadequately treated in his youth—be causing his depression and paranoia decades later? If so, how would you confirm this finding?
Dr. Greenberg’s and Tampi’s observations
Mr. S has a longstanding history of syphilis secondary to high-risk sexual activity. This, combined with the lab findings and his worsening depression and paranoia, points to possible neurosyphilis.
Syphilis, caused by the spirochete Treponema pallidum., can traverse mucous membranes and abraded skin. Transmission is most common during sexual activity but also occurs through blood transfusions and nonsexual lesion contact and from mother to fetus.
Prevalence
- 6,103 cases reported in 2001
- More prevalent among men than women (2.1:1), probably because of elevated prevalence among homosexual men
- African-Americans accounted for 62% of cases in 2001. Prevalence in African–Americans that year was 16 times greater than in whites
Risk factors
- Presence of HIV infection or other sexually transmitted disease
- Unprotected sex
- Residence in urban areas
- Substance abuse
- Homosexuality
Source: References 5 and 6
Because syphilis and its psychiatric effects are relatively uncommon (Box 1), many psychiatrists do not consider neurosyphilis in high-risk patients who present with depression, dementia, or psychosis (Box 2).
HOW SYPHILIS BECOMES NEUROSYPHILIS
Primary syphilis incubates for 10 to 90 days following infection. After this period, an infectious chancre appears along with regional adenopathy. If untreated, the chancre will disappear but the infection will progress.
Secondary syphilis is characterized by skin manifestations and occasionally affects the joints, eyes, bones, kidneys, liver, and CNS. Common effects include condylomata—highly infectious warty lesions—and a diffuse maculopapular rash on the palms and soles. These lesions disappear if left untreated, but most patients then either enter syphilis’ latent stage or experience a potentially fatal relapse of secondary syphilis.5
Latent syphilis usually remains latent or resolves, but about one-third of patients with latent syphilis slowly progress to tertiary syphilis. Neurosyphilis, one of the main forms of tertiary syphilis, can surface 5 to 35 years after an untreated primary infection.7
There are four categories of neurosyphilis:
- General paresis results in dementia, changes in personality, transient hemiparesis, depression, and psychosis.
- Tabes dorsalis degenerates the posterior columns and dorsal root ganglia of the spinal cord. This results in ataxia, parasthesias, decreased proprioception and vibratory sense, Argyll Robertson pupil (an optical disorder in which the pupil does not react normally to light), neurogenic bladder, and sharp shooting pains throughout the body.
- Meningovascular neurosyphilis can result in cranial nerve abnormalities, symptoms of meningitis, and cerebral infarctions.
- Asymptomatic but with CSF positive for syphilis.
Neurosyphilis is fatal if untreated, and treatment usually does not eliminate symptoms but prevents further progression. Approximately 8% of patients with untreated primary syphilis develop neurosyphilis.5,7
Standard nontreponemal tests, such as the VDRL or rapid plasmin reagin, can be used to screen for syphilis. Because these tests often produce false positives, confirm positive results with a syphilis-specific test, such as the fluorescent treponemal antibody absorption (FTA-ABS) test, microhemagglutination assay for antibodies to T pallidum., and the T pallidum. hemagglutination assay.
If neurosyphilis is suspected, CSF testing is strongly recommended. Diagnostic findings include elevated white blood cell and protein counts and a positive VDRL. If the CSF is negative, refer the patient for treatment anyway because false negatives are common. Patients with consistent neurologic symptoms, positive VDRL and/or FTA-ABS, and negative CSF are diagnosed with neurosyphilis and warrant treatment.7
How would you manage Mr. S’ psychiatric symptoms concomitant with medical treatment of late-stage syphilis?
Dr. Greenberg’s and Tampi’s observations
Although no specific guidelines exist for treating psychosis secondary to neurosyphilis, atypical antipsychotics remain the first-line treatment. Atypicals do not interact significantly with penicillin and can be given safely with syphilis treatment. Atypicals also are better tolerated than typical antipsychotics and produce fewer extrapyramidal symptoms, which are common among older patients and those with neurologic diseases.
Screening for syphilis. Every patient with a history of high-risk sexual behavior who presents with new-onset dementia or psychosis should be screened for syphilis. Sexual history can be difficult to obtain from some patients and family members, so communication between providers becomes crucial. Obtain lab test results from other care team members to monitor compliance, and coordinate patient education with other doctors on safe sexual practices.
TREATMENT: Taking his medicine
Mr. S refused further testing and emergency conservatorship was sought. Citalopram was discontinued and risperidone was gradually increased to 6 mg at bedtime. He remained paranoid and delusional.
A brain MRI showed chronic ischemic small-vessel disease. HIV testing was negative, and serum FTA-ABS was reactive. CSF showed elevated protein and white blood cell count with a nonreactive VDRL and a reactive FTA-ABS. A diagnosis of neurosyphilis was made, and treatment was initiated with aqueous crystalline penicillin G, 4 million units every 4 hours for 2 weeks.
Mr. S was discharged back to the nursing home where his penicillin injections were continued. His paranoia diminished slightly but he remained ataxic, incontinent, and confused. He was discharged from the nursing home but needed confirmative HIV screening and repeated CSF testing to determine if syphilis treatment was effective.
Six months after treatment, Mr. S’ niece reports that his paranoia has decreased. He has not needed additional psychiatric hospitalizations.
Related resources
- Merck Manual. www.merck.com. Search: “syphilis”
- U.S. Centers for Disease Control and Prevention—Syphilis elimination: History in the making. www.cdc.gov. Click on “Health Topics A-Z,” then click on “S” and find “syphilis.”
- National Institute of Allergy and Infectious Disease. www.niaid.nih.gov. Search: “syphilis”
Drug brand names
- Citalopram • Celexa
- Risperidone • Risperdal
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. U.S. Centers for Disease Control and Prevention. Primary and secondary syphilis—United States, 2000-2001. MMWR Morb Mortal Wkly Rep. 2002;51:971-3.
2. Mandell GL, Petri WA. Antimicrobial agents: penicillins, cephalosporins, and other beta-lactam antibiotics. In:Hardman JG, Limbird LE, Molinoff PB, et al (eds) Goodman and Gilman’s the pharmacological basis of therapeutics. (9th ed). New York: McGraw-Hill, 1996;1073-4.
3. Lukehart SA, Holmes KK. Spirochetal diseases. In: Braunwald E, Fauci AS, Kasper DL, et al (eds). Harrison’s principles of internal medicine. (14th ed). New York: McGraw-Hill, 1998;1023.-
4. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2001 supplement, syphilis surveillance report. Available at: http://www.cdc.gov/std/stats/2001syphilis.htm. Accessed October 10, 2003.
5. Jacobs RA. Infectious diseases: spirochetal. In: Tierney LM, McPhee SJ, Papadakis MA (eds). Current medical diagnosis and treatment. (39th ed). New York: Lange Medical Books/McGraw-Hill, 2000;1376-86.
6. Hutto B. Syphilis in clinical psychiatry: a review. Psychosomatics. 2001;42:453-60.
7. Carpenter CJ, Lederman MM, Salata RA. Sexually transmitted diseases. In: Andreoli TE, Bennett JC, Carpenter CJ, Plum F (eds). Cecil essentials of medicine. (4th ed). Philadelphia: WB Saunders Co, 1997;742-5.
1. U.S. Centers for Disease Control and Prevention. Primary and secondary syphilis—United States, 2000-2001. MMWR Morb Mortal Wkly Rep. 2002;51:971-3.
2. Mandell GL, Petri WA. Antimicrobial agents: penicillins, cephalosporins, and other beta-lactam antibiotics. In:Hardman JG, Limbird LE, Molinoff PB, et al (eds) Goodman and Gilman’s the pharmacological basis of therapeutics. (9th ed). New York: McGraw-Hill, 1996;1073-4.
3. Lukehart SA, Holmes KK. Spirochetal diseases. In: Braunwald E, Fauci AS, Kasper DL, et al (eds). Harrison’s principles of internal medicine. (14th ed). New York: McGraw-Hill, 1998;1023.-
4. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2001 supplement, syphilis surveillance report. Available at: http://www.cdc.gov/std/stats/2001syphilis.htm. Accessed October 10, 2003.
5. Jacobs RA. Infectious diseases: spirochetal. In: Tierney LM, McPhee SJ, Papadakis MA (eds). Current medical diagnosis and treatment. (39th ed). New York: Lange Medical Books/McGraw-Hill, 2000;1376-86.
6. Hutto B. Syphilis in clinical psychiatry: a review. Psychosomatics. 2001;42:453-60.
7. Carpenter CJ, Lederman MM, Salata RA. Sexually transmitted diseases. In: Andreoli TE, Bennett JC, Carpenter CJ, Plum F (eds). Cecil essentials of medicine. (4th ed). Philadelphia: WB Saunders Co, 1997;742-5.
When a mother’s love hurts
INITIAL PRESENTATION: A sickly child
Ms. J, age 35, was referred to a psychiatrist after she was observed endangering her daughter. The child’s pediatrician provided the following history.
The 4-year-old has frequently required medical attention. As a baby, she wore a breathing monitor at home for almost 1 year after her mother expressed fear that she would die of apnea. Throughout her early years, the child was treated for asthma and abdominal pain and for bruises her parents said were caused when she fell out of her crib.
Recently, the child has suffered with recurring skin infections over her arm and shoulders. Her mother treated those with prescribed topical and oral antibiotics and dressings. The wounds would heal briefly, then become inflamed again.
The pediatrician consulted with a child psychiatrist, who suggested that the girl be hospitalized for a day so that doctors could examine the wound. Despite the mother’s protests, her daughter was hospitalized.
That day, Ms. J visited her daughter, unaware that the hospital room was equipped with a concealed video camera. As she was leaving late that evening, she lifted her daughter’s bandages as if to check them, then applied irritants to the wounds.
When the staff confronted her about this destructive behavior toward her daughter, Ms. J denied it had occurred. Upon seeing the videotape, however, she wept profusely, exclaiming, “I didn’t mean any harm.”
Ms. J does not fit the profile of a child abuser. Aside from part-time clerical work at home, she is a full-time mother who is intensely involved in every aspect of her daughter’s life. Before the videotaped incident, her pediatrician’s office staff had described her as caring and loving, and she had brought them thank-you gifts.
On psychiatric evaluation, Ms. J’s speech is coherent and logical, and she has no delusions or hallucinations. In describing her childhood, she recalls her parents arguing constantly. Her father, with whom she had little contact, traveled extensively on business. At home, her mother ruled with an iron fist. Any show of rebellion by Ms. J or her siblings led to a sharp slap on the shoulders.
Ms. J had few friends in grade school. In college, she earned good grades but often visited the infirmary with nonspecific complaints. She was hospitalized twice without a conclusive diagnosis. She twice saw a psychiatrist to address her medical symptoms and feelings of emptiness.
Table
Defining symptoms, features of Munchausen’s syndrome
Major symptoms
|
Secondary features
|
After college, Ms. J worked as a teacher’s aide. At age 30 she married a teacher, and their daughter was born 1 year later. The marriage ended in divorce after 3 years. After divorce the husband tried to visit the daughter but Ms. J interfered, insisting, “I’m enough.”
Ms. J told the psychiatrist that her ex-husband at times accused her of being “too clingy.” If he went to a sporting event, she would repeatedly ask what time he would come home. If she had to go shopping and he was home, she would ask him to drop everything and accompany her.
Does Ms. J’s behavior suggest a straightforward personality disorder, or would you consider a factitious disorder?
Dr. Messer’s observations
Ms. J recalled a childhood fraught with rejection and abuse. This finding, plus the deliberate injury to her daughter, points to a diagnosis of Munchausen’s syndrome by proxy.
Although not listed in DSM-IV-TR, Munchausen’s is the most severe form of factitious disorder (Table). First described in 1951, the disorder is named for Baron Karl von Munchausen, an 18th-century German nobleman known for telling tall tales about his life and exploits.1
In 1977, British pediatrician Roy Meadow described Munchausen’s syndrome by proxy, in which parents induce symptoms in their children—such as by injuring them with drugs or bacterial contaminants—then have doctors treat them.2 Because persons with Munchausen’s tend to frequently change their names and locales, the incidence of Munchausen’s and Munchausen’s by proxy has never been accurately gauged.
Munchausen’s occurs in both sexes, although men tend to exhibit more-dramatic symptoms such as self-induced fevers, bleeding, and seizures. Antisocial behavior is common among men with Munchausen’s, and many are jailed at some point. One man flying from New York to London feigned a heart attack so convincingly that he forced an emergency landing in Halifax, Nova Scotia, where he was hospitalized and released with a referral to his cardiologist.
By contrast, women with Munchausen’s or Munchausen’s by proxy—often nurses or hospital personnel—are more difficult to diagnose because they usually are agreeable and compliant with medical staff. Staff members tend to ask themselves, “Could such a caring person be putting us on?”
Some persons with Munchausen’s visit disease-specific support groups and draw attention or sympathy by faking illness. Having amassed significant medical knowledge through Web searches and frequent doctor visits, they present themselves as both patient and lofty advisor. Their antisocial tendencies can negatively alter group discussions, and the revelation that a fellow group member is an impostor can distress legitimate participants.3
Ms. J exhibited no evidence of a delusional disorder, which occurs rarely among parents with Munchausen’s by proxy. Her allegedly “clingy” (dependent) behavior toward her daughter and ex-husband, however, indicates borderline personality disorder or antisocial personality disorder, which are common in both forms of Munchausen’s. Like Ms. J, these patients
- have strong fears of rejection and abandonment
- are often impulsive
- exhibit damaging behavior to self or others
- have an unstable sense of self
- are unusually willing to comply with clinical tests or procedures
- and describe feelings of emptiness.
How would you confirm a diagnosis of Munchausen’s? What features in Ms J’s case distinguish Munchausen’s from other factitious disorders?Box
- Munchausen’s syndrome by proxy has been reported in women who were sexually abused in their youth. As adults, some of these women become hypervigilant against sexual abuse of their children.
- The disorder has been cited in several legal cases in which a suspect—usually a teacher or religious leader—was falsely accused of sexually molesting a child.4 Psychiatrists involved as expert witnesses or examiners in such cases should consider these allegations as a possible manifestation of Munchausen’s.
- If the accused denies the charges and no evidence is uncovered, the alleged victim’s mother should be interviewed. In some cases the mother was sexually abused and sought help, but the perpetrator was never apprehended. She may harbor resentment toward men and repeatedly ask her child whether he or she has been touched inappropriately. The child—besieged by frequent inquiries or unsure of what constitutes an inappropriate touch—may answer "yes," prompting the mother to press charges against the named individual.
Dr. Messer’s observations
When taking the patient history, look for:
- a pattern of rejection or abuse in youth. In women who have been sexually molested, Munchausen’s by proxy may manifest as allegations that their children have been touched inappropriately (Box).4
- history of multiple surgeries.5 Because Munchausen’s can coexist with genuine physical illness, the psychiatrist and other doctors need to carefully review the findings to determine the existence of medical symptoms or Munchausen’s. Doctors usually choose to operate if there is any suspicion that medical symptoms exist.
- memories of sympathetic and nurturing medical care early in life. A severe emotional crisis can awaken these memories. For example, emotional pain after a divorce or break-up can trigger a Munchausen’s episode in a subconscious attempt to repair this hurt.
Carefully reviewing the history will turn up glaring discrepancies in the patient’s account of his or her illness. Patients with Munchausen’s or Munchausen’s by proxy usually present to numerous clinicians and do not describe their “illness” the same way twice. Sharing information with other members of the care team—many of whom may feel anger after learning that a patient has been feigning illness—is crucial to confirming the diagnosis.
DIFFERENTIAL DIAGNOSIS
Munchausen’s should not be confused with symptoms of other lookalike disorders:
- Hypochondriasis applies to patients who are convinced they have a serious illness despite lack of a medical basis. The person may misinterpret normal bodily functions and suffer severe distress. The symptoms may express inner psychic conflict.
- Somatoform disorder is a physical complaint that cannot be explained as a known medical condition. This may include preoccupation with an imagined defect in appearance or loss of physical capacity. The deficit usually coincides with emotional conflict and—unlike Munchausen’s—there is no fabrication of illness.
- Malingerers purposely fake physical symptoms for specific gain, such as money, hospital care, disability, drugs, or avoiding military duty.
Persons with Munchausen’s have no external incentive for their behavior. Aside from the medical staff’s admiration, Ms. J had nothing to gain from injuring her daughter or portraying her as sickly.
TREATMENT: Coming home
Ms. J’s daughter responded well after being placed in the home of a relative who had a 3-year-old daughter of her own. Ms. J was allowed to see her daughter for 2 hours each day under strict supervision by a retired schoolteacher hired by the family. If Ms. J. violated the agreement, such as by leaving the house with her daughter, she was prohibited from seeing her child the next day.
Ms. J agreed to long-term therapy; in exchange, judicial proceedings were deferred. In most cases, the mother is referred to police and charged with child abuse/endangerment. However, the medical staff in this case felt treatment and supervision would provide ample rehabilitation.
The mother was referred to a psychiatrist trained in psychoanalysis. By making her aware of her unconscious responses, the doctor sought to improve Ms. J’s ability to cope with stress. Patients with a borderline personality disorder seldom respond in psychoanalysis, but Ms. J exhibited significant ego strengths and intelligence—and was motivated to regain custody of her daughter.
Ms. J’s transference response was predictable: She tried to please the doctor in everything she said or did. This reaction was analyzed and the insight helped Ms. J understand why she exaggerated or exacerbated normal childhood illnesses in her daughter. She discovered that she had hungered for approval since childhood and went as far as injuring her daughter to achieve this fulfillment. Early in treatment she developed a mantra: “I have behaved toward my daughter as my mother behaved toward me.”
After 8 months of therapy 3 times a week, Ms. J regained custody. She continued to receive once-weekly psychotherapy for 1 year.
Two years after regaining custody, Ms. J developed a stable, loving relationship with her daughter. She works full-time while her daughter is in high school and participates in many activities. The relative who assumed temporary custody stays in touch, as does her pediatrician.
The girl is seen by her father on alternate weekends. She tells friends she wants to become a nurse.
How can psychiatrists facilitate early diagnosis and treatment of Munchausen’s?
Dr. Messer’s observations
Although primary care physicians or general surgeons treat most patients with Munchausen’s, the disorder is psychiatric in nature.
For that reason, psychiatrists should participate when possible in the early medical workup of a patient who presents with an apparently severe illness. This way, the psychiatrist can:
- help detect Munchausen’s or another factitious disorder sooner
- establish a rapport with the patient early on. If Munchausen’s is subsequently diagnosed, the patient may be less likely to resist treatment or bolt when confronted.
When confronting someone suspected of fabricating or inducing symptoms, tell the patient that he or she might have Munchausen’s syndrome. Describe the disorder and cite cases, then challenge the patient to find a more appropriate way to cope with stress.
Related resources
- Adshead G, Brooke D (eds). Munchausen's syndrome by proxy. Current issues in assessment, treatment and research. Singapore: World Scientific Publishing, 2001.
- Munchausen’s syndrome by proxy. www.gktscientific.com
1. Asher R. Munchausen’s syndrome. Lancet 1951;1:580-5.
2. Meadow R. False allegations of abuse and Munchausen’s syndrome by proxy. Arch Dis Child 1993;68:444-7.
3. Feldman MD, Eisendrath SJ. The spectrum of factitious disorders. Washington, DC: American Psychiatric Publishing, 1998.
4. Schreier HA. Repeated false allegations of sexual abuse presenting to sheriffs: when is it Munchausen’s by proxy? Child Abuse Negl 1996;20:985-91.
5. Menninger KA. Polysurgery and polysurgical addiction. Psychoanal Q 1934;3:883-9.
INITIAL PRESENTATION: A sickly child
Ms. J, age 35, was referred to a psychiatrist after she was observed endangering her daughter. The child’s pediatrician provided the following history.
The 4-year-old has frequently required medical attention. As a baby, she wore a breathing monitor at home for almost 1 year after her mother expressed fear that she would die of apnea. Throughout her early years, the child was treated for asthma and abdominal pain and for bruises her parents said were caused when she fell out of her crib.
Recently, the child has suffered with recurring skin infections over her arm and shoulders. Her mother treated those with prescribed topical and oral antibiotics and dressings. The wounds would heal briefly, then become inflamed again.
The pediatrician consulted with a child psychiatrist, who suggested that the girl be hospitalized for a day so that doctors could examine the wound. Despite the mother’s protests, her daughter was hospitalized.
That day, Ms. J visited her daughter, unaware that the hospital room was equipped with a concealed video camera. As she was leaving late that evening, she lifted her daughter’s bandages as if to check them, then applied irritants to the wounds.
When the staff confronted her about this destructive behavior toward her daughter, Ms. J denied it had occurred. Upon seeing the videotape, however, she wept profusely, exclaiming, “I didn’t mean any harm.”
Ms. J does not fit the profile of a child abuser. Aside from part-time clerical work at home, she is a full-time mother who is intensely involved in every aspect of her daughter’s life. Before the videotaped incident, her pediatrician’s office staff had described her as caring and loving, and she had brought them thank-you gifts.
On psychiatric evaluation, Ms. J’s speech is coherent and logical, and she has no delusions or hallucinations. In describing her childhood, she recalls her parents arguing constantly. Her father, with whom she had little contact, traveled extensively on business. At home, her mother ruled with an iron fist. Any show of rebellion by Ms. J or her siblings led to a sharp slap on the shoulders.
Ms. J had few friends in grade school. In college, she earned good grades but often visited the infirmary with nonspecific complaints. She was hospitalized twice without a conclusive diagnosis. She twice saw a psychiatrist to address her medical symptoms and feelings of emptiness.
Table
Defining symptoms, features of Munchausen’s syndrome
Major symptoms
|
Secondary features
|
After college, Ms. J worked as a teacher’s aide. At age 30 she married a teacher, and their daughter was born 1 year later. The marriage ended in divorce after 3 years. After divorce the husband tried to visit the daughter but Ms. J interfered, insisting, “I’m enough.”
Ms. J told the psychiatrist that her ex-husband at times accused her of being “too clingy.” If he went to a sporting event, she would repeatedly ask what time he would come home. If she had to go shopping and he was home, she would ask him to drop everything and accompany her.
Does Ms. J’s behavior suggest a straightforward personality disorder, or would you consider a factitious disorder?
Dr. Messer’s observations
Ms. J recalled a childhood fraught with rejection and abuse. This finding, plus the deliberate injury to her daughter, points to a diagnosis of Munchausen’s syndrome by proxy.
Although not listed in DSM-IV-TR, Munchausen’s is the most severe form of factitious disorder (Table). First described in 1951, the disorder is named for Baron Karl von Munchausen, an 18th-century German nobleman known for telling tall tales about his life and exploits.1
In 1977, British pediatrician Roy Meadow described Munchausen’s syndrome by proxy, in which parents induce symptoms in their children—such as by injuring them with drugs or bacterial contaminants—then have doctors treat them.2 Because persons with Munchausen’s tend to frequently change their names and locales, the incidence of Munchausen’s and Munchausen’s by proxy has never been accurately gauged.
Munchausen’s occurs in both sexes, although men tend to exhibit more-dramatic symptoms such as self-induced fevers, bleeding, and seizures. Antisocial behavior is common among men with Munchausen’s, and many are jailed at some point. One man flying from New York to London feigned a heart attack so convincingly that he forced an emergency landing in Halifax, Nova Scotia, where he was hospitalized and released with a referral to his cardiologist.
By contrast, women with Munchausen’s or Munchausen’s by proxy—often nurses or hospital personnel—are more difficult to diagnose because they usually are agreeable and compliant with medical staff. Staff members tend to ask themselves, “Could such a caring person be putting us on?”
Some persons with Munchausen’s visit disease-specific support groups and draw attention or sympathy by faking illness. Having amassed significant medical knowledge through Web searches and frequent doctor visits, they present themselves as both patient and lofty advisor. Their antisocial tendencies can negatively alter group discussions, and the revelation that a fellow group member is an impostor can distress legitimate participants.3
Ms. J exhibited no evidence of a delusional disorder, which occurs rarely among parents with Munchausen’s by proxy. Her allegedly “clingy” (dependent) behavior toward her daughter and ex-husband, however, indicates borderline personality disorder or antisocial personality disorder, which are common in both forms of Munchausen’s. Like Ms. J, these patients
- have strong fears of rejection and abandonment
- are often impulsive
- exhibit damaging behavior to self or others
- have an unstable sense of self
- are unusually willing to comply with clinical tests or procedures
- and describe feelings of emptiness.
How would you confirm a diagnosis of Munchausen’s? What features in Ms J’s case distinguish Munchausen’s from other factitious disorders?Box
- Munchausen’s syndrome by proxy has been reported in women who were sexually abused in their youth. As adults, some of these women become hypervigilant against sexual abuse of their children.
- The disorder has been cited in several legal cases in which a suspect—usually a teacher or religious leader—was falsely accused of sexually molesting a child.4 Psychiatrists involved as expert witnesses or examiners in such cases should consider these allegations as a possible manifestation of Munchausen’s.
- If the accused denies the charges and no evidence is uncovered, the alleged victim’s mother should be interviewed. In some cases the mother was sexually abused and sought help, but the perpetrator was never apprehended. She may harbor resentment toward men and repeatedly ask her child whether he or she has been touched inappropriately. The child—besieged by frequent inquiries or unsure of what constitutes an inappropriate touch—may answer "yes," prompting the mother to press charges against the named individual.
Dr. Messer’s observations
When taking the patient history, look for:
- a pattern of rejection or abuse in youth. In women who have been sexually molested, Munchausen’s by proxy may manifest as allegations that their children have been touched inappropriately (Box).4
- history of multiple surgeries.5 Because Munchausen’s can coexist with genuine physical illness, the psychiatrist and other doctors need to carefully review the findings to determine the existence of medical symptoms or Munchausen’s. Doctors usually choose to operate if there is any suspicion that medical symptoms exist.
- memories of sympathetic and nurturing medical care early in life. A severe emotional crisis can awaken these memories. For example, emotional pain after a divorce or break-up can trigger a Munchausen’s episode in a subconscious attempt to repair this hurt.
Carefully reviewing the history will turn up glaring discrepancies in the patient’s account of his or her illness. Patients with Munchausen’s or Munchausen’s by proxy usually present to numerous clinicians and do not describe their “illness” the same way twice. Sharing information with other members of the care team—many of whom may feel anger after learning that a patient has been feigning illness—is crucial to confirming the diagnosis.
DIFFERENTIAL DIAGNOSIS
Munchausen’s should not be confused with symptoms of other lookalike disorders:
- Hypochondriasis applies to patients who are convinced they have a serious illness despite lack of a medical basis. The person may misinterpret normal bodily functions and suffer severe distress. The symptoms may express inner psychic conflict.
- Somatoform disorder is a physical complaint that cannot be explained as a known medical condition. This may include preoccupation with an imagined defect in appearance or loss of physical capacity. The deficit usually coincides with emotional conflict and—unlike Munchausen’s—there is no fabrication of illness.
- Malingerers purposely fake physical symptoms for specific gain, such as money, hospital care, disability, drugs, or avoiding military duty.
Persons with Munchausen’s have no external incentive for their behavior. Aside from the medical staff’s admiration, Ms. J had nothing to gain from injuring her daughter or portraying her as sickly.
TREATMENT: Coming home
Ms. J’s daughter responded well after being placed in the home of a relative who had a 3-year-old daughter of her own. Ms. J was allowed to see her daughter for 2 hours each day under strict supervision by a retired schoolteacher hired by the family. If Ms. J. violated the agreement, such as by leaving the house with her daughter, she was prohibited from seeing her child the next day.
Ms. J agreed to long-term therapy; in exchange, judicial proceedings were deferred. In most cases, the mother is referred to police and charged with child abuse/endangerment. However, the medical staff in this case felt treatment and supervision would provide ample rehabilitation.
The mother was referred to a psychiatrist trained in psychoanalysis. By making her aware of her unconscious responses, the doctor sought to improve Ms. J’s ability to cope with stress. Patients with a borderline personality disorder seldom respond in psychoanalysis, but Ms. J exhibited significant ego strengths and intelligence—and was motivated to regain custody of her daughter.
Ms. J’s transference response was predictable: She tried to please the doctor in everything she said or did. This reaction was analyzed and the insight helped Ms. J understand why she exaggerated or exacerbated normal childhood illnesses in her daughter. She discovered that she had hungered for approval since childhood and went as far as injuring her daughter to achieve this fulfillment. Early in treatment she developed a mantra: “I have behaved toward my daughter as my mother behaved toward me.”
After 8 months of therapy 3 times a week, Ms. J regained custody. She continued to receive once-weekly psychotherapy for 1 year.
Two years after regaining custody, Ms. J developed a stable, loving relationship with her daughter. She works full-time while her daughter is in high school and participates in many activities. The relative who assumed temporary custody stays in touch, as does her pediatrician.
The girl is seen by her father on alternate weekends. She tells friends she wants to become a nurse.
How can psychiatrists facilitate early diagnosis and treatment of Munchausen’s?
Dr. Messer’s observations
Although primary care physicians or general surgeons treat most patients with Munchausen’s, the disorder is psychiatric in nature.
For that reason, psychiatrists should participate when possible in the early medical workup of a patient who presents with an apparently severe illness. This way, the psychiatrist can:
- help detect Munchausen’s or another factitious disorder sooner
- establish a rapport with the patient early on. If Munchausen’s is subsequently diagnosed, the patient may be less likely to resist treatment or bolt when confronted.
When confronting someone suspected of fabricating or inducing symptoms, tell the patient that he or she might have Munchausen’s syndrome. Describe the disorder and cite cases, then challenge the patient to find a more appropriate way to cope with stress.
Related resources
- Adshead G, Brooke D (eds). Munchausen's syndrome by proxy. Current issues in assessment, treatment and research. Singapore: World Scientific Publishing, 2001.
- Munchausen’s syndrome by proxy. www.gktscientific.com
INITIAL PRESENTATION: A sickly child
Ms. J, age 35, was referred to a psychiatrist after she was observed endangering her daughter. The child’s pediatrician provided the following history.
The 4-year-old has frequently required medical attention. As a baby, she wore a breathing monitor at home for almost 1 year after her mother expressed fear that she would die of apnea. Throughout her early years, the child was treated for asthma and abdominal pain and for bruises her parents said were caused when she fell out of her crib.
Recently, the child has suffered with recurring skin infections over her arm and shoulders. Her mother treated those with prescribed topical and oral antibiotics and dressings. The wounds would heal briefly, then become inflamed again.
The pediatrician consulted with a child psychiatrist, who suggested that the girl be hospitalized for a day so that doctors could examine the wound. Despite the mother’s protests, her daughter was hospitalized.
That day, Ms. J visited her daughter, unaware that the hospital room was equipped with a concealed video camera. As she was leaving late that evening, she lifted her daughter’s bandages as if to check them, then applied irritants to the wounds.
When the staff confronted her about this destructive behavior toward her daughter, Ms. J denied it had occurred. Upon seeing the videotape, however, she wept profusely, exclaiming, “I didn’t mean any harm.”
Ms. J does not fit the profile of a child abuser. Aside from part-time clerical work at home, she is a full-time mother who is intensely involved in every aspect of her daughter’s life. Before the videotaped incident, her pediatrician’s office staff had described her as caring and loving, and she had brought them thank-you gifts.
On psychiatric evaluation, Ms. J’s speech is coherent and logical, and she has no delusions or hallucinations. In describing her childhood, she recalls her parents arguing constantly. Her father, with whom she had little contact, traveled extensively on business. At home, her mother ruled with an iron fist. Any show of rebellion by Ms. J or her siblings led to a sharp slap on the shoulders.
Ms. J had few friends in grade school. In college, she earned good grades but often visited the infirmary with nonspecific complaints. She was hospitalized twice without a conclusive diagnosis. She twice saw a psychiatrist to address her medical symptoms and feelings of emptiness.
Table
Defining symptoms, features of Munchausen’s syndrome
Major symptoms
|
Secondary features
|
After college, Ms. J worked as a teacher’s aide. At age 30 she married a teacher, and their daughter was born 1 year later. The marriage ended in divorce after 3 years. After divorce the husband tried to visit the daughter but Ms. J interfered, insisting, “I’m enough.”
Ms. J told the psychiatrist that her ex-husband at times accused her of being “too clingy.” If he went to a sporting event, she would repeatedly ask what time he would come home. If she had to go shopping and he was home, she would ask him to drop everything and accompany her.
Does Ms. J’s behavior suggest a straightforward personality disorder, or would you consider a factitious disorder?
Dr. Messer’s observations
Ms. J recalled a childhood fraught with rejection and abuse. This finding, plus the deliberate injury to her daughter, points to a diagnosis of Munchausen’s syndrome by proxy.
Although not listed in DSM-IV-TR, Munchausen’s is the most severe form of factitious disorder (Table). First described in 1951, the disorder is named for Baron Karl von Munchausen, an 18th-century German nobleman known for telling tall tales about his life and exploits.1
In 1977, British pediatrician Roy Meadow described Munchausen’s syndrome by proxy, in which parents induce symptoms in their children—such as by injuring them with drugs or bacterial contaminants—then have doctors treat them.2 Because persons with Munchausen’s tend to frequently change their names and locales, the incidence of Munchausen’s and Munchausen’s by proxy has never been accurately gauged.
Munchausen’s occurs in both sexes, although men tend to exhibit more-dramatic symptoms such as self-induced fevers, bleeding, and seizures. Antisocial behavior is common among men with Munchausen’s, and many are jailed at some point. One man flying from New York to London feigned a heart attack so convincingly that he forced an emergency landing in Halifax, Nova Scotia, where he was hospitalized and released with a referral to his cardiologist.
By contrast, women with Munchausen’s or Munchausen’s by proxy—often nurses or hospital personnel—are more difficult to diagnose because they usually are agreeable and compliant with medical staff. Staff members tend to ask themselves, “Could such a caring person be putting us on?”
Some persons with Munchausen’s visit disease-specific support groups and draw attention or sympathy by faking illness. Having amassed significant medical knowledge through Web searches and frequent doctor visits, they present themselves as both patient and lofty advisor. Their antisocial tendencies can negatively alter group discussions, and the revelation that a fellow group member is an impostor can distress legitimate participants.3
Ms. J exhibited no evidence of a delusional disorder, which occurs rarely among parents with Munchausen’s by proxy. Her allegedly “clingy” (dependent) behavior toward her daughter and ex-husband, however, indicates borderline personality disorder or antisocial personality disorder, which are common in both forms of Munchausen’s. Like Ms. J, these patients
- have strong fears of rejection and abandonment
- are often impulsive
- exhibit damaging behavior to self or others
- have an unstable sense of self
- are unusually willing to comply with clinical tests or procedures
- and describe feelings of emptiness.
How would you confirm a diagnosis of Munchausen’s? What features in Ms J’s case distinguish Munchausen’s from other factitious disorders?Box
- Munchausen’s syndrome by proxy has been reported in women who were sexually abused in their youth. As adults, some of these women become hypervigilant against sexual abuse of their children.
- The disorder has been cited in several legal cases in which a suspect—usually a teacher or religious leader—was falsely accused of sexually molesting a child.4 Psychiatrists involved as expert witnesses or examiners in such cases should consider these allegations as a possible manifestation of Munchausen’s.
- If the accused denies the charges and no evidence is uncovered, the alleged victim’s mother should be interviewed. In some cases the mother was sexually abused and sought help, but the perpetrator was never apprehended. She may harbor resentment toward men and repeatedly ask her child whether he or she has been touched inappropriately. The child—besieged by frequent inquiries or unsure of what constitutes an inappropriate touch—may answer "yes," prompting the mother to press charges against the named individual.
Dr. Messer’s observations
When taking the patient history, look for:
- a pattern of rejection or abuse in youth. In women who have been sexually molested, Munchausen’s by proxy may manifest as allegations that their children have been touched inappropriately (Box).4
- history of multiple surgeries.5 Because Munchausen’s can coexist with genuine physical illness, the psychiatrist and other doctors need to carefully review the findings to determine the existence of medical symptoms or Munchausen’s. Doctors usually choose to operate if there is any suspicion that medical symptoms exist.
- memories of sympathetic and nurturing medical care early in life. A severe emotional crisis can awaken these memories. For example, emotional pain after a divorce or break-up can trigger a Munchausen’s episode in a subconscious attempt to repair this hurt.
Carefully reviewing the history will turn up glaring discrepancies in the patient’s account of his or her illness. Patients with Munchausen’s or Munchausen’s by proxy usually present to numerous clinicians and do not describe their “illness” the same way twice. Sharing information with other members of the care team—many of whom may feel anger after learning that a patient has been feigning illness—is crucial to confirming the diagnosis.
DIFFERENTIAL DIAGNOSIS
Munchausen’s should not be confused with symptoms of other lookalike disorders:
- Hypochondriasis applies to patients who are convinced they have a serious illness despite lack of a medical basis. The person may misinterpret normal bodily functions and suffer severe distress. The symptoms may express inner psychic conflict.
- Somatoform disorder is a physical complaint that cannot be explained as a known medical condition. This may include preoccupation with an imagined defect in appearance or loss of physical capacity. The deficit usually coincides with emotional conflict and—unlike Munchausen’s—there is no fabrication of illness.
- Malingerers purposely fake physical symptoms for specific gain, such as money, hospital care, disability, drugs, or avoiding military duty.
Persons with Munchausen’s have no external incentive for their behavior. Aside from the medical staff’s admiration, Ms. J had nothing to gain from injuring her daughter or portraying her as sickly.
TREATMENT: Coming home
Ms. J’s daughter responded well after being placed in the home of a relative who had a 3-year-old daughter of her own. Ms. J was allowed to see her daughter for 2 hours each day under strict supervision by a retired schoolteacher hired by the family. If Ms. J. violated the agreement, such as by leaving the house with her daughter, she was prohibited from seeing her child the next day.
Ms. J agreed to long-term therapy; in exchange, judicial proceedings were deferred. In most cases, the mother is referred to police and charged with child abuse/endangerment. However, the medical staff in this case felt treatment and supervision would provide ample rehabilitation.
The mother was referred to a psychiatrist trained in psychoanalysis. By making her aware of her unconscious responses, the doctor sought to improve Ms. J’s ability to cope with stress. Patients with a borderline personality disorder seldom respond in psychoanalysis, but Ms. J exhibited significant ego strengths and intelligence—and was motivated to regain custody of her daughter.
Ms. J’s transference response was predictable: She tried to please the doctor in everything she said or did. This reaction was analyzed and the insight helped Ms. J understand why she exaggerated or exacerbated normal childhood illnesses in her daughter. She discovered that she had hungered for approval since childhood and went as far as injuring her daughter to achieve this fulfillment. Early in treatment she developed a mantra: “I have behaved toward my daughter as my mother behaved toward me.”
After 8 months of therapy 3 times a week, Ms. J regained custody. She continued to receive once-weekly psychotherapy for 1 year.
Two years after regaining custody, Ms. J developed a stable, loving relationship with her daughter. She works full-time while her daughter is in high school and participates in many activities. The relative who assumed temporary custody stays in touch, as does her pediatrician.
The girl is seen by her father on alternate weekends. She tells friends she wants to become a nurse.
How can psychiatrists facilitate early diagnosis and treatment of Munchausen’s?
Dr. Messer’s observations
Although primary care physicians or general surgeons treat most patients with Munchausen’s, the disorder is psychiatric in nature.
For that reason, psychiatrists should participate when possible in the early medical workup of a patient who presents with an apparently severe illness. This way, the psychiatrist can:
- help detect Munchausen’s or another factitious disorder sooner
- establish a rapport with the patient early on. If Munchausen’s is subsequently diagnosed, the patient may be less likely to resist treatment or bolt when confronted.
When confronting someone suspected of fabricating or inducing symptoms, tell the patient that he or she might have Munchausen’s syndrome. Describe the disorder and cite cases, then challenge the patient to find a more appropriate way to cope with stress.
Related resources
- Adshead G, Brooke D (eds). Munchausen's syndrome by proxy. Current issues in assessment, treatment and research. Singapore: World Scientific Publishing, 2001.
- Munchausen’s syndrome by proxy. www.gktscientific.com
1. Asher R. Munchausen’s syndrome. Lancet 1951;1:580-5.
2. Meadow R. False allegations of abuse and Munchausen’s syndrome by proxy. Arch Dis Child 1993;68:444-7.
3. Feldman MD, Eisendrath SJ. The spectrum of factitious disorders. Washington, DC: American Psychiatric Publishing, 1998.
4. Schreier HA. Repeated false allegations of sexual abuse presenting to sheriffs: when is it Munchausen’s by proxy? Child Abuse Negl 1996;20:985-91.
5. Menninger KA. Polysurgery and polysurgical addiction. Psychoanal Q 1934;3:883-9.
1. Asher R. Munchausen’s syndrome. Lancet 1951;1:580-5.
2. Meadow R. False allegations of abuse and Munchausen’s syndrome by proxy. Arch Dis Child 1993;68:444-7.
3. Feldman MD, Eisendrath SJ. The spectrum of factitious disorders. Washington, DC: American Psychiatric Publishing, 1998.
4. Schreier HA. Repeated false allegations of sexual abuse presenting to sheriffs: when is it Munchausen’s by proxy? Child Abuse Negl 1996;20:985-91.
5. Menninger KA. Polysurgery and polysurgical addiction. Psychoanal Q 1934;3:883-9.
Psychosis or ‘cultural paranoia?’
Culture-related anxiety and paranoia can be difficult to treat because they are reinforced by socially normative practices and beliefs.1 As in the two cases described below, psychiatric patients with deep underlying mistrust may view a therapist from another culture—even though well-meaning—as a racist oppressor.
The clinician’s approach to therapy can help prevent cultural misunderstandings and—most important—misdiagnosis (Box).
MR. A’S CASE: ‘She’s out to get me’
Mr. A, age 38 and African-American, was admitted to the inpatient psychiatry service with neurovegetative depressive symptoms and apparent delusional thinking.
His wife of 20 years, also African-American, was concerned that he was becoming increasingly irrational. She said he accused her of conspiring with his predominantly white supervisors to “bring about my destruction.”
Mr. A consented to admission, acknowledging to the psychiatrist that he had felt depressed and at times considered suicide. He complained that he had recently experienced several unusual “happenings:”
- Pointing to recent weight loss, Mr. A feared someone was poisoning his food or that he had swallowed a “tracking” device.
- Mr. A feared that workers who were repairing flood damage in his home were sent to kill him. He remained home during the project, but the fear drove him to a panic attack.
- After more than 18 years working for the same employer with no notable interpersonal difficulties, Mr. A suddenly could not get along with his coworkers. He accused one colleague of following him to a restaurant.
Mr. A had no previous psychiatric disorder, but some distant relatives had schizophrenia. He was diagnosed as having major depressive disorder, severe with psychotic features; delusional disorder was ruled out. He was prescribed olanzapine, 10 mg at bedtime, and fluoxetine, 20 mg/d.
In the hospital, Mr. A spoke normally with no agitation, increased activity, or evidence of racing thoughts. In group therapy, he explained that he felt “confused.” He also disclosed that a recent extramarital affair left him feeling extremely guilty.
- Set treatment goals at the start. Make sure you and the patient agree on these goals.
- Make sure the patient understands he or she can cease treatment at any time. Stress that you are there simply to help achieve the patient’s stated goals.
- Avoid direct empathic statements during psychotherapy (eg, “You feel angry”); the patient may suspect you are imposing your beliefs. Indirect statements (eg, “It wouldn’t surprise me if you felt angry”) convey curiosity about the patient’s reactions and invite further discussion.
- Admit when you do not understand a culturally specific colloquialism or mannerism, and ask the patient to explain it at the next session. This usually encourages the patient to keep the follow-up appointment.
A few days later, Mr. A’s suicidal and paranoid ideations disappeared. He expressed anger only while discussing his diagnosis with the attending psychiatrist, who is white. The patient feared that being diagnosed with a psychotic illness would hurt his career. He admitted he felt depressed, but insisted that he now realized his paranoid thoughts were irrational.
Mr. A was discharged after 6 days. He remained on fluoxetine, 20 mg/d; olanzapine was discontinued due to excessive sedation.
The patient also entered insight-oriented psychotherapy to address his depression. Mr. A and the therapist, who is white, spent most of the initial sessions discussing their racial differences. At one point, Mr. A complained to the therapist that white physicians were trying to “railroad” him because of his race.
After nine sessions, Mr. A revealed that he felt isolated at an early age, thinking that others “will use what they know about me against me.” He described growing up in a predominantly black community where most of his neighbors felt oppressed by white people. As therapy progressed, Mr. A realized that this experience influenced his attitudes about race, and that his extramarital affair destroyed his sense of self-trust, which may have fueled his mistrust of others.
After 20 sessions, his marriage and work relationships were stable and his overall mood was much improved. His Outcome Questionnaire 45.2 score decreased across 12 months from 88 (moderate to severe distress) to 55 (level of distress similar to that of non-patients). Delusional behavior has not re-emerged, although his comments continue to reflect mistrust of his supervisors and of white people in general.
What would your diagnosis be? What clues would you gather from Mr. A’s pretreatment behavior and from his progress in therapy?
Dr. Benzick’s observations
Mr. A’s diagnosis upon admission reflected the psychiatrist’s belief that he suffered fixed delusions. By definition, however, a delusion is a false belief that is not “ordinarily accepted by other members of the person’s culture or subculture.”2
Growing up, Mr. A shared his neighbors’ suspicion of white people. Further, his overvalued conspiracy theory involving his wife might have projected his own guilt over his infidelity onto a pre-existing paranoid personality.
Based on his psychosocial history, rapid progress in psychotherapy, and marked improvement in Outcome Questionnaire 45.2 scores, Mr. A does not have a personality disorder. What’s more, paranoid ideation is not uncommon in African-Americans with depressive symptoms, as demonstrated by Bazargan et al. 3
Mr. A’s diagnosis was changed to major depressive disorder, moderate, in partial remission. He is still seen approximately every 6 weeks for medication maintenance; he continues taking fluoxetine, 20 mg/d.
MR. B’S CASE: ‘Singled’ out
Mr. B, age 42 and African-American, was referred from an alcohol rehabilitation program to the psychiatry unit after exhibiting depressive and paranoid symptoms.
After 17 years with his employer, he started clashing with his supervisors and coworkers—most of whom are white. He claimed his colleagues were talking behind his back, jealous that he is single and spends his evenings at nightclubs. He alleged that his bosses were singling him out after he was transferred to another department and reprimanded for arriving late to work. Resultant worry about job security brought on panic symptoms (shortness of breath, lightheadedness, dissociative feelings, and palpitations).
Upon further questioning, Mr. B said he felt depressed and isolated. He had been prescribed nortriptyline 2 years ago but discontinued it after a few weeks because of side effects.
Mr. B said that not having a steady companion contributed to his depression and alcohol use. He had been drinking heavily for about 3 years, consuming at least a six-pack daily. He acknowledged that his suspicion of his white coworkers long preceded his alcoholism. Still, he did not see this mistrust as a problem.
Mr. B was diagnosed with major depressive disorder, severe with psychotic features. Treatment consisted of:
- paroxetine, 20 mg/d
- attendance at Alcoholics Anonymous meetings (at least three meetings per week were recommended)
- and 12 sessions of interpersonal psychotherapy. During these sessions, the therapist began to uncover the roots of Mr. B’s symptoms.
School days. Mr. B described how, as a little boy, he once watched his mother being beaten by his drunken father. He told the therapist that the beatings occurred frequently.
When he was age 5, Mr. B’s parents divorced and he and his mother moved to a mostly white Midwest neighborhood so that he could attend a high school with an advanced music program (he was honored for exceptional talent on several instruments).
In his youth, Mr. B’s mother repeatedly told him that teachers and students would treat him “differently” because of his color, though she never explained what she meant. While in high school, he began to worry about his social functioning, appearance, work performance, and future accomplishments.
After four psychotherapy sessions, Mr. B revealed that while in grade school, he was sexually assaulted by an older white boy. For more than 30 years, he had told no one. He denied hyperautonomic and re-experiencing symptoms but realized that this incident may have kept him from starting a romantic relationship.
After psychotherapy, Mr. B reported reduced depression and increased social interaction. His Beck Depression Inventory score dropped from 23 (moderate depression) to 4 (normal mood), and his Beck Anxiety Inventory score improved from 33 (moderate anxiety) to 3 (very low anxiety). He has been sober for 6 months and handles stress more effectively, although his mistrust toward coworkers is still apparent.
How would you diagnose Mr. B? Do his symptoms characterize “psychotic features” or an anxiety or alcohol-related disorder?
Dr. Benzick’s observations
Mr. B’s case illustrates how deep-seated cultural perceptions and past trauma together can cause severe anxiety—and how that anxiety can be misperceived as psychosis.4 Anxiety also can manifest as paranoia in “psychotically vulnerable” individuals.5-7
Chronic anxiety seemed to cause Mr. B’s depressed mood and social withdrawal. Several anxiety disorder diagnoses were considered, including:
- panic disorder
- posttraumatic stress disorder
- social phobia
- alcohol-induced anxiety disorder
- and generalized anxiety disorder.
Mr. B, however, exhibited no evidence of repeated episodic anxiety, nor did he describe reexperiencing phenomena. His anxiety extended beyond social situations and preceded his heavy alcohol consumption. Paranoid personality disorder was also considered, but Mr. B sought relationships and lacked the angry, unforgiving qualities associated with this pathology. Finally, a battery of psychological tests did not reveal frank psychosis but suggested an avoidant personality style.
Mr. B’s diagnosis was changed to generalized anxiety disorder. He requested a trial off medications during the latter stages of therapy, but his severe anxiety returned. He was then prescribed venlafaxine, 37.5 mg/d titrated to 225 mg/d across 3 weeks. His anxiety symptoms again abated.
How could Mr A’s and Mr. B’s doctors have avoided their initial misdiagnoses?
Dr. Benzick’s observations
“Cultural paranoia” describes adaptive or healthy responses by African-Americans living in a society they perceive as racially prejudiced.8 Several researchers have studied this concept of protecting self-esteem by blaming an external source for negative events. Women who plausibly attribute unflattering feedback to prejudice exhibit higher self-esteem.9 A person who believes he or she is a target of discrimination identifies more strongly with his or her racial or ethnic group, leading to reduced depression, higher self-esteem, and improved psychological adjustment.9
Perceived discrimination, however, can also elicit feelings of hopelessness and resignation when it leads to widespread bias against the alleged oppressing racial or ethnic group. The resulting sense of social exclusion has been linked to lower self-esteem and higher rates of anxiety and depression.9 Thus, the individual’s environment and ability to develop relationships will determine whether “cultural paranoia” is “adaptive.”
Paranoia or prejudice? Distinguishing culturally sanctioned “paranoia” from “prejudice” can be difficult. “Prejudice” is defined as the negative evaluation of a group or individual based on group membership.10 “Paranoia” (using the DSM-IV definition of “paranoid ideation”) is a belief of less than delusional intensity “involving suspiciousness or the belief that one is being harassed, persecuted, or unfairly treated.”2
So while an individual may be prejudiced toward a group, cultural paranoia would exist only if other family members or acquaintances believe the other group is conspiring against them. Additionally, while prejudice tends to be ego-syntonic,11 paranoia is more distressing because it produces heightened vigilance and possibly fear.
Both cases describe how a lack of cultural understanding between African-American patients and physicians of other ethnicities or races can lead to misdiagnosis of psychosis.12 They also illustrate that while prejudice may be tightly focused (eg, hatred of anyone from a specific racial or ethnic group), paranoid ideation can be generalized. For example, Mr. A believed that his wife, an African-American, conspired with his white supervisors against him.
Mr. A’s and Mr. B’s depressive and anxiety symptoms unmasked longstanding, deeply rooted beliefs. Both patients’ neurovegetative symptoms responded to medication and brief psychotherapy, and both returned to prior levels of functioning. The underlying mistrust remained, however.
Related resources
- Lu FG. Annotated bibliography on cultural psychiatry and related topics-June 2003. Available at: http://www.admsep.org/culture.html. Accessed July 18, 2003.
- Forsell Y, Henderson S. Epidemiology of paranoid disorders in an elderly population. Br J Psychiatry 1998; 172:429-32.
Drug brand names
- Fluoxetine • Prozac
- Olanzapine • Zyprexa
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Venlafaxine • Effexor
Disclosure
Dr. Benzick reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Kirmayer LJ, Young A, Hayton BC. The cultural context of anxiety disorders. Psychiatr Clin North Am 1995;18:503-21.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed-text revision). Washington, DC. American Psychiatric Association, 2000.
3. Bazargan M, Bazargan S, King L. Paranoid ideation among elderly African American persons. Gerontologist 2001;41:366-73.
4. Newhill CE. The role of culture in the development of paranoid symptomatology. Am J Orthopsychiatry 1990;60:176-85.
5. Bermanzohn PC, Arlow PB, Pitch RJ, Siris SG. Panic and paranoia (letter). J Clin Psychiatry 1997;58:325.-
6. Bermanzohn PC, Arlow PB, Albert C, Siris SG. Relationship of panic attacks to paranoia. Am J Psychiatry 1999;156:1469.-
7. Galynker I, Ieronimo C, Perez-Acquino A, et al. Panic attacks with psychotic features. J Clin Psychiatry 1996;57:402-6.
8. Ridley CR. Clinical treatment of the nondisclosing black client. A therapeutic paradox. Am Psychol 1984;39:1233-43.
9. Branscombe NR, Schmitt MT, Harvey RD. Perceiving pervasive discrimination among African Americans: implications for group identification and well-being. J Pers Soc Psychol 1999;77:135-49.
10. Crandall CS, Eshleman A, O’Brien L. Social norms and suppression of prejudice: the struggle for internalization. J Pers Soc Psychol 2002;82:359-78.
11. Ryan MK, Buirski P. Prejudice as a function of self-organization. Psychoanalytic Psychol 2001;18:21-36.
12. Whaley AL. Psychometric analysis of the cultural mistrust inventory with a black psychiatric inpatient sample. J Clin Psychology 2002;58:383-96.
Culture-related anxiety and paranoia can be difficult to treat because they are reinforced by socially normative practices and beliefs.1 As in the two cases described below, psychiatric patients with deep underlying mistrust may view a therapist from another culture—even though well-meaning—as a racist oppressor.
The clinician’s approach to therapy can help prevent cultural misunderstandings and—most important—misdiagnosis (Box).
MR. A’S CASE: ‘She’s out to get me’
Mr. A, age 38 and African-American, was admitted to the inpatient psychiatry service with neurovegetative depressive symptoms and apparent delusional thinking.
His wife of 20 years, also African-American, was concerned that he was becoming increasingly irrational. She said he accused her of conspiring with his predominantly white supervisors to “bring about my destruction.”
Mr. A consented to admission, acknowledging to the psychiatrist that he had felt depressed and at times considered suicide. He complained that he had recently experienced several unusual “happenings:”
- Pointing to recent weight loss, Mr. A feared someone was poisoning his food or that he had swallowed a “tracking” device.
- Mr. A feared that workers who were repairing flood damage in his home were sent to kill him. He remained home during the project, but the fear drove him to a panic attack.
- After more than 18 years working for the same employer with no notable interpersonal difficulties, Mr. A suddenly could not get along with his coworkers. He accused one colleague of following him to a restaurant.
Mr. A had no previous psychiatric disorder, but some distant relatives had schizophrenia. He was diagnosed as having major depressive disorder, severe with psychotic features; delusional disorder was ruled out. He was prescribed olanzapine, 10 mg at bedtime, and fluoxetine, 20 mg/d.
In the hospital, Mr. A spoke normally with no agitation, increased activity, or evidence of racing thoughts. In group therapy, he explained that he felt “confused.” He also disclosed that a recent extramarital affair left him feeling extremely guilty.
- Set treatment goals at the start. Make sure you and the patient agree on these goals.
- Make sure the patient understands he or she can cease treatment at any time. Stress that you are there simply to help achieve the patient’s stated goals.
- Avoid direct empathic statements during psychotherapy (eg, “You feel angry”); the patient may suspect you are imposing your beliefs. Indirect statements (eg, “It wouldn’t surprise me if you felt angry”) convey curiosity about the patient’s reactions and invite further discussion.
- Admit when you do not understand a culturally specific colloquialism or mannerism, and ask the patient to explain it at the next session. This usually encourages the patient to keep the follow-up appointment.
A few days later, Mr. A’s suicidal and paranoid ideations disappeared. He expressed anger only while discussing his diagnosis with the attending psychiatrist, who is white. The patient feared that being diagnosed with a psychotic illness would hurt his career. He admitted he felt depressed, but insisted that he now realized his paranoid thoughts were irrational.
Mr. A was discharged after 6 days. He remained on fluoxetine, 20 mg/d; olanzapine was discontinued due to excessive sedation.
The patient also entered insight-oriented psychotherapy to address his depression. Mr. A and the therapist, who is white, spent most of the initial sessions discussing their racial differences. At one point, Mr. A complained to the therapist that white physicians were trying to “railroad” him because of his race.
After nine sessions, Mr. A revealed that he felt isolated at an early age, thinking that others “will use what they know about me against me.” He described growing up in a predominantly black community where most of his neighbors felt oppressed by white people. As therapy progressed, Mr. A realized that this experience influenced his attitudes about race, and that his extramarital affair destroyed his sense of self-trust, which may have fueled his mistrust of others.
After 20 sessions, his marriage and work relationships were stable and his overall mood was much improved. His Outcome Questionnaire 45.2 score decreased across 12 months from 88 (moderate to severe distress) to 55 (level of distress similar to that of non-patients). Delusional behavior has not re-emerged, although his comments continue to reflect mistrust of his supervisors and of white people in general.
What would your diagnosis be? What clues would you gather from Mr. A’s pretreatment behavior and from his progress in therapy?
Dr. Benzick’s observations
Mr. A’s diagnosis upon admission reflected the psychiatrist’s belief that he suffered fixed delusions. By definition, however, a delusion is a false belief that is not “ordinarily accepted by other members of the person’s culture or subculture.”2
Growing up, Mr. A shared his neighbors’ suspicion of white people. Further, his overvalued conspiracy theory involving his wife might have projected his own guilt over his infidelity onto a pre-existing paranoid personality.
Based on his psychosocial history, rapid progress in psychotherapy, and marked improvement in Outcome Questionnaire 45.2 scores, Mr. A does not have a personality disorder. What’s more, paranoid ideation is not uncommon in African-Americans with depressive symptoms, as demonstrated by Bazargan et al. 3
Mr. A’s diagnosis was changed to major depressive disorder, moderate, in partial remission. He is still seen approximately every 6 weeks for medication maintenance; he continues taking fluoxetine, 20 mg/d.
MR. B’S CASE: ‘Singled’ out
Mr. B, age 42 and African-American, was referred from an alcohol rehabilitation program to the psychiatry unit after exhibiting depressive and paranoid symptoms.
After 17 years with his employer, he started clashing with his supervisors and coworkers—most of whom are white. He claimed his colleagues were talking behind his back, jealous that he is single and spends his evenings at nightclubs. He alleged that his bosses were singling him out after he was transferred to another department and reprimanded for arriving late to work. Resultant worry about job security brought on panic symptoms (shortness of breath, lightheadedness, dissociative feelings, and palpitations).
Upon further questioning, Mr. B said he felt depressed and isolated. He had been prescribed nortriptyline 2 years ago but discontinued it after a few weeks because of side effects.
Mr. B said that not having a steady companion contributed to his depression and alcohol use. He had been drinking heavily for about 3 years, consuming at least a six-pack daily. He acknowledged that his suspicion of his white coworkers long preceded his alcoholism. Still, he did not see this mistrust as a problem.
Mr. B was diagnosed with major depressive disorder, severe with psychotic features. Treatment consisted of:
- paroxetine, 20 mg/d
- attendance at Alcoholics Anonymous meetings (at least three meetings per week were recommended)
- and 12 sessions of interpersonal psychotherapy. During these sessions, the therapist began to uncover the roots of Mr. B’s symptoms.
School days. Mr. B described how, as a little boy, he once watched his mother being beaten by his drunken father. He told the therapist that the beatings occurred frequently.
When he was age 5, Mr. B’s parents divorced and he and his mother moved to a mostly white Midwest neighborhood so that he could attend a high school with an advanced music program (he was honored for exceptional talent on several instruments).
In his youth, Mr. B’s mother repeatedly told him that teachers and students would treat him “differently” because of his color, though she never explained what she meant. While in high school, he began to worry about his social functioning, appearance, work performance, and future accomplishments.
After four psychotherapy sessions, Mr. B revealed that while in grade school, he was sexually assaulted by an older white boy. For more than 30 years, he had told no one. He denied hyperautonomic and re-experiencing symptoms but realized that this incident may have kept him from starting a romantic relationship.
After psychotherapy, Mr. B reported reduced depression and increased social interaction. His Beck Depression Inventory score dropped from 23 (moderate depression) to 4 (normal mood), and his Beck Anxiety Inventory score improved from 33 (moderate anxiety) to 3 (very low anxiety). He has been sober for 6 months and handles stress more effectively, although his mistrust toward coworkers is still apparent.
How would you diagnose Mr. B? Do his symptoms characterize “psychotic features” or an anxiety or alcohol-related disorder?
Dr. Benzick’s observations
Mr. B’s case illustrates how deep-seated cultural perceptions and past trauma together can cause severe anxiety—and how that anxiety can be misperceived as psychosis.4 Anxiety also can manifest as paranoia in “psychotically vulnerable” individuals.5-7
Chronic anxiety seemed to cause Mr. B’s depressed mood and social withdrawal. Several anxiety disorder diagnoses were considered, including:
- panic disorder
- posttraumatic stress disorder
- social phobia
- alcohol-induced anxiety disorder
- and generalized anxiety disorder.
Mr. B, however, exhibited no evidence of repeated episodic anxiety, nor did he describe reexperiencing phenomena. His anxiety extended beyond social situations and preceded his heavy alcohol consumption. Paranoid personality disorder was also considered, but Mr. B sought relationships and lacked the angry, unforgiving qualities associated with this pathology. Finally, a battery of psychological tests did not reveal frank psychosis but suggested an avoidant personality style.
Mr. B’s diagnosis was changed to generalized anxiety disorder. He requested a trial off medications during the latter stages of therapy, but his severe anxiety returned. He was then prescribed venlafaxine, 37.5 mg/d titrated to 225 mg/d across 3 weeks. His anxiety symptoms again abated.
How could Mr A’s and Mr. B’s doctors have avoided their initial misdiagnoses?
Dr. Benzick’s observations
“Cultural paranoia” describes adaptive or healthy responses by African-Americans living in a society they perceive as racially prejudiced.8 Several researchers have studied this concept of protecting self-esteem by blaming an external source for negative events. Women who plausibly attribute unflattering feedback to prejudice exhibit higher self-esteem.9 A person who believes he or she is a target of discrimination identifies more strongly with his or her racial or ethnic group, leading to reduced depression, higher self-esteem, and improved psychological adjustment.9
Perceived discrimination, however, can also elicit feelings of hopelessness and resignation when it leads to widespread bias against the alleged oppressing racial or ethnic group. The resulting sense of social exclusion has been linked to lower self-esteem and higher rates of anxiety and depression.9 Thus, the individual’s environment and ability to develop relationships will determine whether “cultural paranoia” is “adaptive.”
Paranoia or prejudice? Distinguishing culturally sanctioned “paranoia” from “prejudice” can be difficult. “Prejudice” is defined as the negative evaluation of a group or individual based on group membership.10 “Paranoia” (using the DSM-IV definition of “paranoid ideation”) is a belief of less than delusional intensity “involving suspiciousness or the belief that one is being harassed, persecuted, or unfairly treated.”2
So while an individual may be prejudiced toward a group, cultural paranoia would exist only if other family members or acquaintances believe the other group is conspiring against them. Additionally, while prejudice tends to be ego-syntonic,11 paranoia is more distressing because it produces heightened vigilance and possibly fear.
Both cases describe how a lack of cultural understanding between African-American patients and physicians of other ethnicities or races can lead to misdiagnosis of psychosis.12 They also illustrate that while prejudice may be tightly focused (eg, hatred of anyone from a specific racial or ethnic group), paranoid ideation can be generalized. For example, Mr. A believed that his wife, an African-American, conspired with his white supervisors against him.
Mr. A’s and Mr. B’s depressive and anxiety symptoms unmasked longstanding, deeply rooted beliefs. Both patients’ neurovegetative symptoms responded to medication and brief psychotherapy, and both returned to prior levels of functioning. The underlying mistrust remained, however.
Related resources
- Lu FG. Annotated bibliography on cultural psychiatry and related topics-June 2003. Available at: http://www.admsep.org/culture.html. Accessed July 18, 2003.
- Forsell Y, Henderson S. Epidemiology of paranoid disorders in an elderly population. Br J Psychiatry 1998; 172:429-32.
Drug brand names
- Fluoxetine • Prozac
- Olanzapine • Zyprexa
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Venlafaxine • Effexor
Disclosure
Dr. Benzick reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Culture-related anxiety and paranoia can be difficult to treat because they are reinforced by socially normative practices and beliefs.1 As in the two cases described below, psychiatric patients with deep underlying mistrust may view a therapist from another culture—even though well-meaning—as a racist oppressor.
The clinician’s approach to therapy can help prevent cultural misunderstandings and—most important—misdiagnosis (Box).
MR. A’S CASE: ‘She’s out to get me’
Mr. A, age 38 and African-American, was admitted to the inpatient psychiatry service with neurovegetative depressive symptoms and apparent delusional thinking.
His wife of 20 years, also African-American, was concerned that he was becoming increasingly irrational. She said he accused her of conspiring with his predominantly white supervisors to “bring about my destruction.”
Mr. A consented to admission, acknowledging to the psychiatrist that he had felt depressed and at times considered suicide. He complained that he had recently experienced several unusual “happenings:”
- Pointing to recent weight loss, Mr. A feared someone was poisoning his food or that he had swallowed a “tracking” device.
- Mr. A feared that workers who were repairing flood damage in his home were sent to kill him. He remained home during the project, but the fear drove him to a panic attack.
- After more than 18 years working for the same employer with no notable interpersonal difficulties, Mr. A suddenly could not get along with his coworkers. He accused one colleague of following him to a restaurant.
Mr. A had no previous psychiatric disorder, but some distant relatives had schizophrenia. He was diagnosed as having major depressive disorder, severe with psychotic features; delusional disorder was ruled out. He was prescribed olanzapine, 10 mg at bedtime, and fluoxetine, 20 mg/d.
In the hospital, Mr. A spoke normally with no agitation, increased activity, or evidence of racing thoughts. In group therapy, he explained that he felt “confused.” He also disclosed that a recent extramarital affair left him feeling extremely guilty.
- Set treatment goals at the start. Make sure you and the patient agree on these goals.
- Make sure the patient understands he or she can cease treatment at any time. Stress that you are there simply to help achieve the patient’s stated goals.
- Avoid direct empathic statements during psychotherapy (eg, “You feel angry”); the patient may suspect you are imposing your beliefs. Indirect statements (eg, “It wouldn’t surprise me if you felt angry”) convey curiosity about the patient’s reactions and invite further discussion.
- Admit when you do not understand a culturally specific colloquialism or mannerism, and ask the patient to explain it at the next session. This usually encourages the patient to keep the follow-up appointment.
A few days later, Mr. A’s suicidal and paranoid ideations disappeared. He expressed anger only while discussing his diagnosis with the attending psychiatrist, who is white. The patient feared that being diagnosed with a psychotic illness would hurt his career. He admitted he felt depressed, but insisted that he now realized his paranoid thoughts were irrational.
Mr. A was discharged after 6 days. He remained on fluoxetine, 20 mg/d; olanzapine was discontinued due to excessive sedation.
The patient also entered insight-oriented psychotherapy to address his depression. Mr. A and the therapist, who is white, spent most of the initial sessions discussing their racial differences. At one point, Mr. A complained to the therapist that white physicians were trying to “railroad” him because of his race.
After nine sessions, Mr. A revealed that he felt isolated at an early age, thinking that others “will use what they know about me against me.” He described growing up in a predominantly black community where most of his neighbors felt oppressed by white people. As therapy progressed, Mr. A realized that this experience influenced his attitudes about race, and that his extramarital affair destroyed his sense of self-trust, which may have fueled his mistrust of others.
After 20 sessions, his marriage and work relationships were stable and his overall mood was much improved. His Outcome Questionnaire 45.2 score decreased across 12 months from 88 (moderate to severe distress) to 55 (level of distress similar to that of non-patients). Delusional behavior has not re-emerged, although his comments continue to reflect mistrust of his supervisors and of white people in general.
What would your diagnosis be? What clues would you gather from Mr. A’s pretreatment behavior and from his progress in therapy?
Dr. Benzick’s observations
Mr. A’s diagnosis upon admission reflected the psychiatrist’s belief that he suffered fixed delusions. By definition, however, a delusion is a false belief that is not “ordinarily accepted by other members of the person’s culture or subculture.”2
Growing up, Mr. A shared his neighbors’ suspicion of white people. Further, his overvalued conspiracy theory involving his wife might have projected his own guilt over his infidelity onto a pre-existing paranoid personality.
Based on his psychosocial history, rapid progress in psychotherapy, and marked improvement in Outcome Questionnaire 45.2 scores, Mr. A does not have a personality disorder. What’s more, paranoid ideation is not uncommon in African-Americans with depressive symptoms, as demonstrated by Bazargan et al. 3
Mr. A’s diagnosis was changed to major depressive disorder, moderate, in partial remission. He is still seen approximately every 6 weeks for medication maintenance; he continues taking fluoxetine, 20 mg/d.
MR. B’S CASE: ‘Singled’ out
Mr. B, age 42 and African-American, was referred from an alcohol rehabilitation program to the psychiatry unit after exhibiting depressive and paranoid symptoms.
After 17 years with his employer, he started clashing with his supervisors and coworkers—most of whom are white. He claimed his colleagues were talking behind his back, jealous that he is single and spends his evenings at nightclubs. He alleged that his bosses were singling him out after he was transferred to another department and reprimanded for arriving late to work. Resultant worry about job security brought on panic symptoms (shortness of breath, lightheadedness, dissociative feelings, and palpitations).
Upon further questioning, Mr. B said he felt depressed and isolated. He had been prescribed nortriptyline 2 years ago but discontinued it after a few weeks because of side effects.
Mr. B said that not having a steady companion contributed to his depression and alcohol use. He had been drinking heavily for about 3 years, consuming at least a six-pack daily. He acknowledged that his suspicion of his white coworkers long preceded his alcoholism. Still, he did not see this mistrust as a problem.
Mr. B was diagnosed with major depressive disorder, severe with psychotic features. Treatment consisted of:
- paroxetine, 20 mg/d
- attendance at Alcoholics Anonymous meetings (at least three meetings per week were recommended)
- and 12 sessions of interpersonal psychotherapy. During these sessions, the therapist began to uncover the roots of Mr. B’s symptoms.
School days. Mr. B described how, as a little boy, he once watched his mother being beaten by his drunken father. He told the therapist that the beatings occurred frequently.
When he was age 5, Mr. B’s parents divorced and he and his mother moved to a mostly white Midwest neighborhood so that he could attend a high school with an advanced music program (he was honored for exceptional talent on several instruments).
In his youth, Mr. B’s mother repeatedly told him that teachers and students would treat him “differently” because of his color, though she never explained what she meant. While in high school, he began to worry about his social functioning, appearance, work performance, and future accomplishments.
After four psychotherapy sessions, Mr. B revealed that while in grade school, he was sexually assaulted by an older white boy. For more than 30 years, he had told no one. He denied hyperautonomic and re-experiencing symptoms but realized that this incident may have kept him from starting a romantic relationship.
After psychotherapy, Mr. B reported reduced depression and increased social interaction. His Beck Depression Inventory score dropped from 23 (moderate depression) to 4 (normal mood), and his Beck Anxiety Inventory score improved from 33 (moderate anxiety) to 3 (very low anxiety). He has been sober for 6 months and handles stress more effectively, although his mistrust toward coworkers is still apparent.
How would you diagnose Mr. B? Do his symptoms characterize “psychotic features” or an anxiety or alcohol-related disorder?
Dr. Benzick’s observations
Mr. B’s case illustrates how deep-seated cultural perceptions and past trauma together can cause severe anxiety—and how that anxiety can be misperceived as psychosis.4 Anxiety also can manifest as paranoia in “psychotically vulnerable” individuals.5-7
Chronic anxiety seemed to cause Mr. B’s depressed mood and social withdrawal. Several anxiety disorder diagnoses were considered, including:
- panic disorder
- posttraumatic stress disorder
- social phobia
- alcohol-induced anxiety disorder
- and generalized anxiety disorder.
Mr. B, however, exhibited no evidence of repeated episodic anxiety, nor did he describe reexperiencing phenomena. His anxiety extended beyond social situations and preceded his heavy alcohol consumption. Paranoid personality disorder was also considered, but Mr. B sought relationships and lacked the angry, unforgiving qualities associated with this pathology. Finally, a battery of psychological tests did not reveal frank psychosis but suggested an avoidant personality style.
Mr. B’s diagnosis was changed to generalized anxiety disorder. He requested a trial off medications during the latter stages of therapy, but his severe anxiety returned. He was then prescribed venlafaxine, 37.5 mg/d titrated to 225 mg/d across 3 weeks. His anxiety symptoms again abated.
How could Mr A’s and Mr. B’s doctors have avoided their initial misdiagnoses?
Dr. Benzick’s observations
“Cultural paranoia” describes adaptive or healthy responses by African-Americans living in a society they perceive as racially prejudiced.8 Several researchers have studied this concept of protecting self-esteem by blaming an external source for negative events. Women who plausibly attribute unflattering feedback to prejudice exhibit higher self-esteem.9 A person who believes he or she is a target of discrimination identifies more strongly with his or her racial or ethnic group, leading to reduced depression, higher self-esteem, and improved psychological adjustment.9
Perceived discrimination, however, can also elicit feelings of hopelessness and resignation when it leads to widespread bias against the alleged oppressing racial or ethnic group. The resulting sense of social exclusion has been linked to lower self-esteem and higher rates of anxiety and depression.9 Thus, the individual’s environment and ability to develop relationships will determine whether “cultural paranoia” is “adaptive.”
Paranoia or prejudice? Distinguishing culturally sanctioned “paranoia” from “prejudice” can be difficult. “Prejudice” is defined as the negative evaluation of a group or individual based on group membership.10 “Paranoia” (using the DSM-IV definition of “paranoid ideation”) is a belief of less than delusional intensity “involving suspiciousness or the belief that one is being harassed, persecuted, or unfairly treated.”2
So while an individual may be prejudiced toward a group, cultural paranoia would exist only if other family members or acquaintances believe the other group is conspiring against them. Additionally, while prejudice tends to be ego-syntonic,11 paranoia is more distressing because it produces heightened vigilance and possibly fear.
Both cases describe how a lack of cultural understanding between African-American patients and physicians of other ethnicities or races can lead to misdiagnosis of psychosis.12 They also illustrate that while prejudice may be tightly focused (eg, hatred of anyone from a specific racial or ethnic group), paranoid ideation can be generalized. For example, Mr. A believed that his wife, an African-American, conspired with his white supervisors against him.
Mr. A’s and Mr. B’s depressive and anxiety symptoms unmasked longstanding, deeply rooted beliefs. Both patients’ neurovegetative symptoms responded to medication and brief psychotherapy, and both returned to prior levels of functioning. The underlying mistrust remained, however.
Related resources
- Lu FG. Annotated bibliography on cultural psychiatry and related topics-June 2003. Available at: http://www.admsep.org/culture.html. Accessed July 18, 2003.
- Forsell Y, Henderson S. Epidemiology of paranoid disorders in an elderly population. Br J Psychiatry 1998; 172:429-32.
Drug brand names
- Fluoxetine • Prozac
- Olanzapine • Zyprexa
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Venlafaxine • Effexor
Disclosure
Dr. Benzick reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Kirmayer LJ, Young A, Hayton BC. The cultural context of anxiety disorders. Psychiatr Clin North Am 1995;18:503-21.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed-text revision). Washington, DC. American Psychiatric Association, 2000.
3. Bazargan M, Bazargan S, King L. Paranoid ideation among elderly African American persons. Gerontologist 2001;41:366-73.
4. Newhill CE. The role of culture in the development of paranoid symptomatology. Am J Orthopsychiatry 1990;60:176-85.
5. Bermanzohn PC, Arlow PB, Pitch RJ, Siris SG. Panic and paranoia (letter). J Clin Psychiatry 1997;58:325.-
6. Bermanzohn PC, Arlow PB, Albert C, Siris SG. Relationship of panic attacks to paranoia. Am J Psychiatry 1999;156:1469.-
7. Galynker I, Ieronimo C, Perez-Acquino A, et al. Panic attacks with psychotic features. J Clin Psychiatry 1996;57:402-6.
8. Ridley CR. Clinical treatment of the nondisclosing black client. A therapeutic paradox. Am Psychol 1984;39:1233-43.
9. Branscombe NR, Schmitt MT, Harvey RD. Perceiving pervasive discrimination among African Americans: implications for group identification and well-being. J Pers Soc Psychol 1999;77:135-49.
10. Crandall CS, Eshleman A, O’Brien L. Social norms and suppression of prejudice: the struggle for internalization. J Pers Soc Psychol 2002;82:359-78.
11. Ryan MK, Buirski P. Prejudice as a function of self-organization. Psychoanalytic Psychol 2001;18:21-36.
12. Whaley AL. Psychometric analysis of the cultural mistrust inventory with a black psychiatric inpatient sample. J Clin Psychology 2002;58:383-96.
1. Kirmayer LJ, Young A, Hayton BC. The cultural context of anxiety disorders. Psychiatr Clin North Am 1995;18:503-21.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed-text revision). Washington, DC. American Psychiatric Association, 2000.
3. Bazargan M, Bazargan S, King L. Paranoid ideation among elderly African American persons. Gerontologist 2001;41:366-73.
4. Newhill CE. The role of culture in the development of paranoid symptomatology. Am J Orthopsychiatry 1990;60:176-85.
5. Bermanzohn PC, Arlow PB, Pitch RJ, Siris SG. Panic and paranoia (letter). J Clin Psychiatry 1997;58:325.-
6. Bermanzohn PC, Arlow PB, Albert C, Siris SG. Relationship of panic attacks to paranoia. Am J Psychiatry 1999;156:1469.-
7. Galynker I, Ieronimo C, Perez-Acquino A, et al. Panic attacks with psychotic features. J Clin Psychiatry 1996;57:402-6.
8. Ridley CR. Clinical treatment of the nondisclosing black client. A therapeutic paradox. Am Psychol 1984;39:1233-43.
9. Branscombe NR, Schmitt MT, Harvey RD. Perceiving pervasive discrimination among African Americans: implications for group identification and well-being. J Pers Soc Psychol 1999;77:135-49.
10. Crandall CS, Eshleman A, O’Brien L. Social norms and suppression of prejudice: the struggle for internalization. J Pers Soc Psychol 2002;82:359-78.
11. Ryan MK, Buirski P. Prejudice as a function of self-organization. Psychoanalytic Psychol 2001;18:21-36.
12. Whaley AL. Psychometric analysis of the cultural mistrust inventory with a black psychiatric inpatient sample. J Clin Psychology 2002;58:383-96.
Clozapine therapy: Timing is everything
HISTORY: Six years of psychosis
Ms. G, age 37, has had paranoid schizophrenia f or 6 years, resulting in numerous hospitalizations and continuous outpatient follow-up. Her family is supportive and supervises her when she’s not hospitalized.
Though fluent in English, Ms. G—a Polish immigrant—speaks primarily in her native tongue during psychotic episodes and becomes increasingly paranoid toward neighbors. As her condition degenerates, she hears her late father’s voice criticizing her. Because of marked social withdrawal and isolation, she cannot maintain basic interpersonal skills or live independently. Her psychosis, apathy, avolition, withdrawal, and lack of focus have persisted despite trials of numerous antipsychotics, including olanzapine, 25 mg nightly for 1 month, and quetiapine, 300 mg bid for 3 weeks.
What are the drug therapy options for this patient?
The authors’ observations
“Treatment-refractory” schizophrenia has numerous definitions. One that is widely accepted but cumbersome—used in the multicenter clozapine trial1 —requires a 5-year absence of periods of good functioning in patients taking an antipsychotic at dosages equivalent to chlorpromazine, 1,000 mg/d. In that time, the patient must have received two or more antipsychotic classes for at least 6 weeks each without achieving significant relief. The Brief Psychiatric Rating Scale (BPRS) score must be at least 45, with item scores of moderate severity for two or more of the following:
- disorganization
- suspiciousness
- hallucinatory behavior
- unusual thought content.
The Clinical Global Impression (CGI) Scale score must be at least 4 (moderately ill). Also, a 6-week trial of haloperidol, with a mean dosage of 60 mg/d:
- must fail to decrease the BPRS score by 20% or to below 35
- or must fail to decrease the CGI severity score to 3 (mildly ill).1
In 1990, an international study group defined treatment-refractory schizophrenia as “the presence of ongoing psychotic symptoms with substantial functional disability and/or behavioral deviances that persist in well-diagnosed persons with schizophrenia despite reasonable and customary pharmacological and psychosocial treatment that has been provided for an adequate period.”2 This definition is far more useful to clinical practice and also considers psychosocial function. Seven levels of treatment response and resistance were suggested, based on presence of positive and negative symptoms, personal and social functioning, and CGI scores.2
Meltzer3 proposed that any person not returning to his or her highest premorbid level of functioning with a tolerable antipsychotic be considered refractory and thus a possible candidate for clozapine therapy.
Ms. G’s illness meets the definition of treatment-refractory schizophrenia. Her CGI score at baseline was 5—severely ill—and several medication trials at sufficient dosages failed to control her positive or negative symptoms. Upon psychotic decompensation, she required prolonged hospitalization and could no longer live independently or work. At this point, she is a possible candidate for clozapine therapy.
TREATMENT: Starting clozapine
Ms. G was started on clozapine, 25 mg at night, titrated to 300 mg at bedtime.
Two weeks later, her paranoia and auditory hallucinations diminished, her interpersonal relationships improved, she was less withdrawn, her thoughts became more organized, and her range of affect expanded. She functioned at her highest level since her initial presentation based on clinical observation and family reports. Her CGI Global Improvement score at this point was 2 (much improved).
Ms. G. continued to take clozapine, 300 mg/d, for 2 years while undergoing weekly blood tests for white blood cell counts (WBC) with differentials. She did not require hospitalization for schizophrenia during this time, and her WBC count averaged between 4,000 and 4,500/mm3, well within the normal range of 3,500 to 12,000/mm3.
Then one day—after maintaining a relatively stable WBC for several weeks—a blood test revealed a WBC of 2,700/mm3. Ms. G exhibited no objective signs of immunosuppression, such as fever or infection. Still, the psychiatrist immediately discontinued clozapine.
Was the treating psychiatrist justified in immediately stopping clozapine after one low WBC reading?
The authors’ observations
Leukopenia, defined as a WBC <3,000/mm3, and agranulocytosis, defined as an absolute neutrophil count <500/mm3, are well-documented adverse reactions to clozapine. Early data on clozapine-associated agranulocytosis cases prior to 1989 suggest that up to 32% were fatal,4 but relatively few cases have occurred since the Clozaril National Registry was instituted in 1977.4,5 Between 1977 and 1997, 585 clozapine-associated agranulocytosis cases were reported in the United States; 19 of these were fatal, suggesting a mortality rate of 3.2% and attesting to the effectiveness of FDA-mandated WBC testing. During this period, 150,409 patients received clozapine.4
The agranulocytosis risk does not appear to be dose-related but declines substantially after the 10th week. Three out of 1,000 patients who take clozapine for 1 year are likely to develop agranulocytosis at the 3- to 6-month mark.4 Although the incidence continues to drop after month 6, it never reaches zero.4-6
Table
Life-threatening effects of clozapine and their reported frequency of occurrence
| Adverse effect | Incidence rate among clozapine users |
|---|---|
| Agranulocytosis | 3/1000 person years* at 6 months |
| Hepatitis | Less than 1% |
| Hyperglycemia with ketoacidosis | Unknown, case reports |
| Myocarditis | 5.0-96.6 cases/100,000 patient years |
| Neuroleptic malignant syndrome | Unknown, several case reports |
| Orthostasis with cardiac collapse | 1/3,000 cases |
| Pulmonary embolism | 1/3,450 person years |
| Seizures | 5% after 1 year of therapy |
| * Person year = 1 person taking medication for 1 year | |
| Source: Clozaril prescribing information. In: Physicians’ Desk Reference (57th ed). Montvale, NJ: Thomson Healthcare, 2003. | |
Other severe adverse effects of clozapine include myocarditis associated with cardiac failure, orthostatic hypotension with circulatory collapse, and rhabdomyolysis (Table).4,7 Leukocytosis and eosinophilia are generally transient and self-limited but may predict agranulocytosis.8,9 The risk of seizure occurs most commonly at dosages greater than 500 mg/d.4
Given these potentially fatal effects, the authors’ treatment guidelines call for potential suspension of clozapine therapy when the WBC is consistently <3,000 mm3 (Algorithm).
CONTINUED TREATMENT: A difficult decision
Ms. G was switched to quetiapine, 100 mg nightly, titrated to 800 mg/d in divided doses.
Approximately 3 weeks later, Ms. G was hospitalized for renewed severe paranoia and command-type auditory hallucinations accompanied by prominent mood lability, avolition, and thought disorganization. During her 7-week hospitalization, she underwent sequential and sometimes overlapping trials of:
- ziprasidone, 160 mg bid
- risperidone, 3 mg bid
- trifluoperazine, 3 mg bid
- haloperidol, 10 mg bid
- divalproex sodium, 500 mg bid
- and carbamazepine, 400 mg bid.
None of these trials significantly improved her psychosis or mood.
At this point, the treating psychiatrists faced a difficult but clear decision: Ms. G was rechallenged on clozapine, 25 mg nightly, titrated again to 300 mg nightly. After she provided informed consent, her WBC was monitored twice daily—morning and evening—for agranulocytosis and to examine WBC patterns. Her average daily WBC counts were 4,200/mm3 in the morning and 5,500/mm3 at night. No physical signs of agranulocytosis emerged.
One week after restarting clozapine, Ms. G became less paranoid and socially more appropriate. Her thought process became increasingly organized, and after 4 weeks she reached her baseline status based upon family reports and the clinician’s CGI Global Improvement rating of 2 (much improved). Her auditory hallucinations resolved, and she was discharged to her family’s care.
Twice-daily blood testing was stopped at discharge. Ms. G continues to take clozapine and receives blood tests every 2 weeks, with no apparent signs of agranulocytosis.
Algorithm Suggested guidelines for managing WBC counts during clozapine therapy
Two treatments for clozapine-dependent agranulocytosis have been described.
- Granulocyte-macrophage colony-stimulating factor (GM-CSF) is a glycoprotein that has been shown to stimulate proliferation of precursor cells in bone marrow and their differentiation into granulocytes and macrophages. Researchers have reported that GM-CSF treatment allows patients to continue taking clozapine after an episode of severe neutropenia.10-12
- Lithium salts have been reported to exploit the natural leukocytosis observed with lithium to counter clozapine-related leukopenia.13 Use of lithium to displace white blood cells has been debated, and anecdotal evidence suggests that combining lithium with clozapine may increase the chance of seizure and neuroleptic malignant syndrome.4 Still, cases reported by Adityanjee and Blier suggest that lithium augmentation is cost-effective and efficacious.14,15
How could Ms. G’s doctors have avoided stopping her clozapine therapy and her subsequent decompensation?
The authors’ observations
Aggressive blood testing and cessation of clozapine therapy are indicated when onset of granulocytopenia and agranulocytosis are suspected. Even with early detection and discontinuation, the chance of infectious disease poses a danger for up to 4 weeks until WBC levels return to normal.4
Given Ms. G’s lack of response to other antipsychotics, however, we had to consider resuming clozapine therapy. Studies have described agranulocytosis management strategies that may allow patients to keep taking clozapine despite low WBC counts (Box).
We also considered the timing of Ms. G’s blood test that showed a WBC count <2,700/mm3. Ahokas16 suggests that evening WBC counts are significantly higher than those taken in the morning and that granulocytes fluctuate in a diurnal pattern. Ms. G’s evening WBC counts were on average 1,300/mm3 higher than morning levels. Allowing for this diurnal variation and comparing evening blood samples could have averted the interruption in Ms. G’s clozapine therapy and prevented relapse in a patient with highly treatment-refractory schizophrenia.
Related resources
- Chong SA, Remington G. Clozapine augmentation: safety and efficacy. Schizophr Bull 2000;26:421-40.
- Emsley R, Oosthuizen P. The new and evolving pharmacotherapy of schizophrenia. Psychiatr Clin North Am 2003;26:141-63.
- Barnas C, Zwierzina H, Hummer M, Sperner-Unterweger B, Stern A, Fleischhacker WW. Granulocyte-macrophage colony-stimulating factor (GM-CSF) treatment of clozapine-induced agranulocytosis: a case report. J Clin Psychiatry 1992;53:245-7.
Drug brand names
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- GM-CSF—Filgrastim • Neupogen
- Haloperidol • Haldol
- Lithium • Eskalith, Lithobid, others
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Trifluoperazine • Stelazine
- Ziprasidone • Geodon
Disclosure
Dr. Rao is a speaker for Pfizer Inc.
Drs. Goforth, Raval, and Sharma report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kane J, Honigfeld G, Singer J, Meltzer H. Clozapine for the treatment resistant schizophrenic: a double blind comparison with chlorpromazine. Arch Gen Psychiatry 1988;45:789-96.
2. Brenner HD, Dencker SJ, Goldstein MJ, et al. Defining treatment refractoriness in schizophrenia. Schizophr Bull 1990;16:551-61.
3. Meltzer HY. Clozapine: is another view valid? Am J Psychiatry 1995;152:821-5.
4. Clozaril prescribing information. In: Physicians’ Desk Reference. (57th ed). Montvale, NJ: Thomson Healthcare, 2003.
5. Alvir JM, Lieberman JA, Safferman AZ, et al. Clozapine-induced agranulocytosis. Incidence and risk factors in the United States. N Engl J Med. 1993;329:162-7.
6. Honigfeld G. Effects of the clozapine national registry system on incidence of deaths related to agranulocytosis. Psychiatr Serv 1996;47:52-6.
7. Scelsa SN, Simpson DM, McQuistion HL, et al. Clozapineinduced myotoxicity in patients with chronic psychotic disorders. Neurology 1996;47:1518-23.
8. Ames D, Wirshing WC, Baker RW, et al. Predictive value of eosinophilia for neutropenia during clozapine treatment. J Clin Psychiatry 1996;57:579-81.
9. Alvir JM, Lieberman JA, Safferman AZ. Do white-cell count spikes predict agranulocytosis in clozapine recipients? Psychopharmacol Bull 1995;31:311-14.
10. Sperner-Unterweger B, Czeipek I, Gaggl S, et al. Treatment of severe clozapine-induced neutropenia with granulocyte colonystimulating factor (G-CSF). Remission despite continuous treatment with clozapine. Br J Psychiatry 1998;172:82-4.
11. Chengappa KN, Gopalani A, Haught MK, et al. The treatment of clozapine-associated agranulocytosis with granulocyte colony-stimulating factor (G-CSF). Psychopharmacol Bull 1996;32:111-21.
12. Lamberti JS, Bellnier TJ, Schwarzkopf SB, Schneider E. Filgrastim treatment of three patients with clozapine-induced agranulocytosis. J Clin Psychiatry 1995;56:256-9.
13. Boshes RA, Manschreck TC, Desrosiers J, et al. Initiation of clozapine therapy in a patient with preexisting leukopenia: a discussion of the rationale of current treatment options. Ann Clin Psychiatry 2001;13:233-7.
14. Adityanjee. Modification of clozapine-induced leukopenia and neutropenia with lithium carbonate. Am J Psychiatry 1995;152:648-9.
15. Blier P, Slater S, Measham T, et al. Lithium and clozapine-induced neutropenia/agranulocytosis. Int Clin Psychopharmacol 1998;13:137-40.
16. Ahokas A, Elonen E. Circadian rhythm of white blood cells during clozapine treatment. Psychopharmacology 1999;144:301-2.
HISTORY: Six years of psychosis
Ms. G, age 37, has had paranoid schizophrenia f or 6 years, resulting in numerous hospitalizations and continuous outpatient follow-up. Her family is supportive and supervises her when she’s not hospitalized.
Though fluent in English, Ms. G—a Polish immigrant—speaks primarily in her native tongue during psychotic episodes and becomes increasingly paranoid toward neighbors. As her condition degenerates, she hears her late father’s voice criticizing her. Because of marked social withdrawal and isolation, she cannot maintain basic interpersonal skills or live independently. Her psychosis, apathy, avolition, withdrawal, and lack of focus have persisted despite trials of numerous antipsychotics, including olanzapine, 25 mg nightly for 1 month, and quetiapine, 300 mg bid for 3 weeks.
What are the drug therapy options for this patient?
The authors’ observations
“Treatment-refractory” schizophrenia has numerous definitions. One that is widely accepted but cumbersome—used in the multicenter clozapine trial1 —requires a 5-year absence of periods of good functioning in patients taking an antipsychotic at dosages equivalent to chlorpromazine, 1,000 mg/d. In that time, the patient must have received two or more antipsychotic classes for at least 6 weeks each without achieving significant relief. The Brief Psychiatric Rating Scale (BPRS) score must be at least 45, with item scores of moderate severity for two or more of the following:
- disorganization
- suspiciousness
- hallucinatory behavior
- unusual thought content.
The Clinical Global Impression (CGI) Scale score must be at least 4 (moderately ill). Also, a 6-week trial of haloperidol, with a mean dosage of 60 mg/d:
- must fail to decrease the BPRS score by 20% or to below 35
- or must fail to decrease the CGI severity score to 3 (mildly ill).1
In 1990, an international study group defined treatment-refractory schizophrenia as “the presence of ongoing psychotic symptoms with substantial functional disability and/or behavioral deviances that persist in well-diagnosed persons with schizophrenia despite reasonable and customary pharmacological and psychosocial treatment that has been provided for an adequate period.”2 This definition is far more useful to clinical practice and also considers psychosocial function. Seven levels of treatment response and resistance were suggested, based on presence of positive and negative symptoms, personal and social functioning, and CGI scores.2
Meltzer3 proposed that any person not returning to his or her highest premorbid level of functioning with a tolerable antipsychotic be considered refractory and thus a possible candidate for clozapine therapy.
Ms. G’s illness meets the definition of treatment-refractory schizophrenia. Her CGI score at baseline was 5—severely ill—and several medication trials at sufficient dosages failed to control her positive or negative symptoms. Upon psychotic decompensation, she required prolonged hospitalization and could no longer live independently or work. At this point, she is a possible candidate for clozapine therapy.
TREATMENT: Starting clozapine
Ms. G was started on clozapine, 25 mg at night, titrated to 300 mg at bedtime.
Two weeks later, her paranoia and auditory hallucinations diminished, her interpersonal relationships improved, she was less withdrawn, her thoughts became more organized, and her range of affect expanded. She functioned at her highest level since her initial presentation based on clinical observation and family reports. Her CGI Global Improvement score at this point was 2 (much improved).
Ms. G. continued to take clozapine, 300 mg/d, for 2 years while undergoing weekly blood tests for white blood cell counts (WBC) with differentials. She did not require hospitalization for schizophrenia during this time, and her WBC count averaged between 4,000 and 4,500/mm3, well within the normal range of 3,500 to 12,000/mm3.
Then one day—after maintaining a relatively stable WBC for several weeks—a blood test revealed a WBC of 2,700/mm3. Ms. G exhibited no objective signs of immunosuppression, such as fever or infection. Still, the psychiatrist immediately discontinued clozapine.
Was the treating psychiatrist justified in immediately stopping clozapine after one low WBC reading?
The authors’ observations
Leukopenia, defined as a WBC <3,000/mm3, and agranulocytosis, defined as an absolute neutrophil count <500/mm3, are well-documented adverse reactions to clozapine. Early data on clozapine-associated agranulocytosis cases prior to 1989 suggest that up to 32% were fatal,4 but relatively few cases have occurred since the Clozaril National Registry was instituted in 1977.4,5 Between 1977 and 1997, 585 clozapine-associated agranulocytosis cases were reported in the United States; 19 of these were fatal, suggesting a mortality rate of 3.2% and attesting to the effectiveness of FDA-mandated WBC testing. During this period, 150,409 patients received clozapine.4
The agranulocytosis risk does not appear to be dose-related but declines substantially after the 10th week. Three out of 1,000 patients who take clozapine for 1 year are likely to develop agranulocytosis at the 3- to 6-month mark.4 Although the incidence continues to drop after month 6, it never reaches zero.4-6
Table
Life-threatening effects of clozapine and their reported frequency of occurrence
| Adverse effect | Incidence rate among clozapine users |
|---|---|
| Agranulocytosis | 3/1000 person years* at 6 months |
| Hepatitis | Less than 1% |
| Hyperglycemia with ketoacidosis | Unknown, case reports |
| Myocarditis | 5.0-96.6 cases/100,000 patient years |
| Neuroleptic malignant syndrome | Unknown, several case reports |
| Orthostasis with cardiac collapse | 1/3,000 cases |
| Pulmonary embolism | 1/3,450 person years |
| Seizures | 5% after 1 year of therapy |
| * Person year = 1 person taking medication for 1 year | |
| Source: Clozaril prescribing information. In: Physicians’ Desk Reference (57th ed). Montvale, NJ: Thomson Healthcare, 2003. | |
Other severe adverse effects of clozapine include myocarditis associated with cardiac failure, orthostatic hypotension with circulatory collapse, and rhabdomyolysis (Table).4,7 Leukocytosis and eosinophilia are generally transient and self-limited but may predict agranulocytosis.8,9 The risk of seizure occurs most commonly at dosages greater than 500 mg/d.4
Given these potentially fatal effects, the authors’ treatment guidelines call for potential suspension of clozapine therapy when the WBC is consistently <3,000 mm3 (Algorithm).
CONTINUED TREATMENT: A difficult decision
Ms. G was switched to quetiapine, 100 mg nightly, titrated to 800 mg/d in divided doses.
Approximately 3 weeks later, Ms. G was hospitalized for renewed severe paranoia and command-type auditory hallucinations accompanied by prominent mood lability, avolition, and thought disorganization. During her 7-week hospitalization, she underwent sequential and sometimes overlapping trials of:
- ziprasidone, 160 mg bid
- risperidone, 3 mg bid
- trifluoperazine, 3 mg bid
- haloperidol, 10 mg bid
- divalproex sodium, 500 mg bid
- and carbamazepine, 400 mg bid.
None of these trials significantly improved her psychosis or mood.
At this point, the treating psychiatrists faced a difficult but clear decision: Ms. G was rechallenged on clozapine, 25 mg nightly, titrated again to 300 mg nightly. After she provided informed consent, her WBC was monitored twice daily—morning and evening—for agranulocytosis and to examine WBC patterns. Her average daily WBC counts were 4,200/mm3 in the morning and 5,500/mm3 at night. No physical signs of agranulocytosis emerged.
One week after restarting clozapine, Ms. G became less paranoid and socially more appropriate. Her thought process became increasingly organized, and after 4 weeks she reached her baseline status based upon family reports and the clinician’s CGI Global Improvement rating of 2 (much improved). Her auditory hallucinations resolved, and she was discharged to her family’s care.
Twice-daily blood testing was stopped at discharge. Ms. G continues to take clozapine and receives blood tests every 2 weeks, with no apparent signs of agranulocytosis.
Algorithm Suggested guidelines for managing WBC counts during clozapine therapy
Two treatments for clozapine-dependent agranulocytosis have been described.
- Granulocyte-macrophage colony-stimulating factor (GM-CSF) is a glycoprotein that has been shown to stimulate proliferation of precursor cells in bone marrow and their differentiation into granulocytes and macrophages. Researchers have reported that GM-CSF treatment allows patients to continue taking clozapine after an episode of severe neutropenia.10-12
- Lithium salts have been reported to exploit the natural leukocytosis observed with lithium to counter clozapine-related leukopenia.13 Use of lithium to displace white blood cells has been debated, and anecdotal evidence suggests that combining lithium with clozapine may increase the chance of seizure and neuroleptic malignant syndrome.4 Still, cases reported by Adityanjee and Blier suggest that lithium augmentation is cost-effective and efficacious.14,15
How could Ms. G’s doctors have avoided stopping her clozapine therapy and her subsequent decompensation?
The authors’ observations
Aggressive blood testing and cessation of clozapine therapy are indicated when onset of granulocytopenia and agranulocytosis are suspected. Even with early detection and discontinuation, the chance of infectious disease poses a danger for up to 4 weeks until WBC levels return to normal.4
Given Ms. G’s lack of response to other antipsychotics, however, we had to consider resuming clozapine therapy. Studies have described agranulocytosis management strategies that may allow patients to keep taking clozapine despite low WBC counts (Box).
We also considered the timing of Ms. G’s blood test that showed a WBC count <2,700/mm3. Ahokas16 suggests that evening WBC counts are significantly higher than those taken in the morning and that granulocytes fluctuate in a diurnal pattern. Ms. G’s evening WBC counts were on average 1,300/mm3 higher than morning levels. Allowing for this diurnal variation and comparing evening blood samples could have averted the interruption in Ms. G’s clozapine therapy and prevented relapse in a patient with highly treatment-refractory schizophrenia.
Related resources
- Chong SA, Remington G. Clozapine augmentation: safety and efficacy. Schizophr Bull 2000;26:421-40.
- Emsley R, Oosthuizen P. The new and evolving pharmacotherapy of schizophrenia. Psychiatr Clin North Am 2003;26:141-63.
- Barnas C, Zwierzina H, Hummer M, Sperner-Unterweger B, Stern A, Fleischhacker WW. Granulocyte-macrophage colony-stimulating factor (GM-CSF) treatment of clozapine-induced agranulocytosis: a case report. J Clin Psychiatry 1992;53:245-7.
Drug brand names
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- GM-CSF—Filgrastim • Neupogen
- Haloperidol • Haldol
- Lithium • Eskalith, Lithobid, others
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Trifluoperazine • Stelazine
- Ziprasidone • Geodon
Disclosure
Dr. Rao is a speaker for Pfizer Inc.
Drs. Goforth, Raval, and Sharma report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
HISTORY: Six years of psychosis
Ms. G, age 37, has had paranoid schizophrenia f or 6 years, resulting in numerous hospitalizations and continuous outpatient follow-up. Her family is supportive and supervises her when she’s not hospitalized.
Though fluent in English, Ms. G—a Polish immigrant—speaks primarily in her native tongue during psychotic episodes and becomes increasingly paranoid toward neighbors. As her condition degenerates, she hears her late father’s voice criticizing her. Because of marked social withdrawal and isolation, she cannot maintain basic interpersonal skills or live independently. Her psychosis, apathy, avolition, withdrawal, and lack of focus have persisted despite trials of numerous antipsychotics, including olanzapine, 25 mg nightly for 1 month, and quetiapine, 300 mg bid for 3 weeks.
What are the drug therapy options for this patient?
The authors’ observations
“Treatment-refractory” schizophrenia has numerous definitions. One that is widely accepted but cumbersome—used in the multicenter clozapine trial1 —requires a 5-year absence of periods of good functioning in patients taking an antipsychotic at dosages equivalent to chlorpromazine, 1,000 mg/d. In that time, the patient must have received two or more antipsychotic classes for at least 6 weeks each without achieving significant relief. The Brief Psychiatric Rating Scale (BPRS) score must be at least 45, with item scores of moderate severity for two or more of the following:
- disorganization
- suspiciousness
- hallucinatory behavior
- unusual thought content.
The Clinical Global Impression (CGI) Scale score must be at least 4 (moderately ill). Also, a 6-week trial of haloperidol, with a mean dosage of 60 mg/d:
- must fail to decrease the BPRS score by 20% or to below 35
- or must fail to decrease the CGI severity score to 3 (mildly ill).1
In 1990, an international study group defined treatment-refractory schizophrenia as “the presence of ongoing psychotic symptoms with substantial functional disability and/or behavioral deviances that persist in well-diagnosed persons with schizophrenia despite reasonable and customary pharmacological and psychosocial treatment that has been provided for an adequate period.”2 This definition is far more useful to clinical practice and also considers psychosocial function. Seven levels of treatment response and resistance were suggested, based on presence of positive and negative symptoms, personal and social functioning, and CGI scores.2
Meltzer3 proposed that any person not returning to his or her highest premorbid level of functioning with a tolerable antipsychotic be considered refractory and thus a possible candidate for clozapine therapy.
Ms. G’s illness meets the definition of treatment-refractory schizophrenia. Her CGI score at baseline was 5—severely ill—and several medication trials at sufficient dosages failed to control her positive or negative symptoms. Upon psychotic decompensation, she required prolonged hospitalization and could no longer live independently or work. At this point, she is a possible candidate for clozapine therapy.
TREATMENT: Starting clozapine
Ms. G was started on clozapine, 25 mg at night, titrated to 300 mg at bedtime.
Two weeks later, her paranoia and auditory hallucinations diminished, her interpersonal relationships improved, she was less withdrawn, her thoughts became more organized, and her range of affect expanded. She functioned at her highest level since her initial presentation based on clinical observation and family reports. Her CGI Global Improvement score at this point was 2 (much improved).
Ms. G. continued to take clozapine, 300 mg/d, for 2 years while undergoing weekly blood tests for white blood cell counts (WBC) with differentials. She did not require hospitalization for schizophrenia during this time, and her WBC count averaged between 4,000 and 4,500/mm3, well within the normal range of 3,500 to 12,000/mm3.
Then one day—after maintaining a relatively stable WBC for several weeks—a blood test revealed a WBC of 2,700/mm3. Ms. G exhibited no objective signs of immunosuppression, such as fever or infection. Still, the psychiatrist immediately discontinued clozapine.
Was the treating psychiatrist justified in immediately stopping clozapine after one low WBC reading?
The authors’ observations
Leukopenia, defined as a WBC <3,000/mm3, and agranulocytosis, defined as an absolute neutrophil count <500/mm3, are well-documented adverse reactions to clozapine. Early data on clozapine-associated agranulocytosis cases prior to 1989 suggest that up to 32% were fatal,4 but relatively few cases have occurred since the Clozaril National Registry was instituted in 1977.4,5 Between 1977 and 1997, 585 clozapine-associated agranulocytosis cases were reported in the United States; 19 of these were fatal, suggesting a mortality rate of 3.2% and attesting to the effectiveness of FDA-mandated WBC testing. During this period, 150,409 patients received clozapine.4
The agranulocytosis risk does not appear to be dose-related but declines substantially after the 10th week. Three out of 1,000 patients who take clozapine for 1 year are likely to develop agranulocytosis at the 3- to 6-month mark.4 Although the incidence continues to drop after month 6, it never reaches zero.4-6
Table
Life-threatening effects of clozapine and their reported frequency of occurrence
| Adverse effect | Incidence rate among clozapine users |
|---|---|
| Agranulocytosis | 3/1000 person years* at 6 months |
| Hepatitis | Less than 1% |
| Hyperglycemia with ketoacidosis | Unknown, case reports |
| Myocarditis | 5.0-96.6 cases/100,000 patient years |
| Neuroleptic malignant syndrome | Unknown, several case reports |
| Orthostasis with cardiac collapse | 1/3,000 cases |
| Pulmonary embolism | 1/3,450 person years |
| Seizures | 5% after 1 year of therapy |
| * Person year = 1 person taking medication for 1 year | |
| Source: Clozaril prescribing information. In: Physicians’ Desk Reference (57th ed). Montvale, NJ: Thomson Healthcare, 2003. | |
Other severe adverse effects of clozapine include myocarditis associated with cardiac failure, orthostatic hypotension with circulatory collapse, and rhabdomyolysis (Table).4,7 Leukocytosis and eosinophilia are generally transient and self-limited but may predict agranulocytosis.8,9 The risk of seizure occurs most commonly at dosages greater than 500 mg/d.4
Given these potentially fatal effects, the authors’ treatment guidelines call for potential suspension of clozapine therapy when the WBC is consistently <3,000 mm3 (Algorithm).
CONTINUED TREATMENT: A difficult decision
Ms. G was switched to quetiapine, 100 mg nightly, titrated to 800 mg/d in divided doses.
Approximately 3 weeks later, Ms. G was hospitalized for renewed severe paranoia and command-type auditory hallucinations accompanied by prominent mood lability, avolition, and thought disorganization. During her 7-week hospitalization, she underwent sequential and sometimes overlapping trials of:
- ziprasidone, 160 mg bid
- risperidone, 3 mg bid
- trifluoperazine, 3 mg bid
- haloperidol, 10 mg bid
- divalproex sodium, 500 mg bid
- and carbamazepine, 400 mg bid.
None of these trials significantly improved her psychosis or mood.
At this point, the treating psychiatrists faced a difficult but clear decision: Ms. G was rechallenged on clozapine, 25 mg nightly, titrated again to 300 mg nightly. After she provided informed consent, her WBC was monitored twice daily—morning and evening—for agranulocytosis and to examine WBC patterns. Her average daily WBC counts were 4,200/mm3 in the morning and 5,500/mm3 at night. No physical signs of agranulocytosis emerged.
One week after restarting clozapine, Ms. G became less paranoid and socially more appropriate. Her thought process became increasingly organized, and after 4 weeks she reached her baseline status based upon family reports and the clinician’s CGI Global Improvement rating of 2 (much improved). Her auditory hallucinations resolved, and she was discharged to her family’s care.
Twice-daily blood testing was stopped at discharge. Ms. G continues to take clozapine and receives blood tests every 2 weeks, with no apparent signs of agranulocytosis.
Algorithm Suggested guidelines for managing WBC counts during clozapine therapy
Two treatments for clozapine-dependent agranulocytosis have been described.
- Granulocyte-macrophage colony-stimulating factor (GM-CSF) is a glycoprotein that has been shown to stimulate proliferation of precursor cells in bone marrow and their differentiation into granulocytes and macrophages. Researchers have reported that GM-CSF treatment allows patients to continue taking clozapine after an episode of severe neutropenia.10-12
- Lithium salts have been reported to exploit the natural leukocytosis observed with lithium to counter clozapine-related leukopenia.13 Use of lithium to displace white blood cells has been debated, and anecdotal evidence suggests that combining lithium with clozapine may increase the chance of seizure and neuroleptic malignant syndrome.4 Still, cases reported by Adityanjee and Blier suggest that lithium augmentation is cost-effective and efficacious.14,15
How could Ms. G’s doctors have avoided stopping her clozapine therapy and her subsequent decompensation?
The authors’ observations
Aggressive blood testing and cessation of clozapine therapy are indicated when onset of granulocytopenia and agranulocytosis are suspected. Even with early detection and discontinuation, the chance of infectious disease poses a danger for up to 4 weeks until WBC levels return to normal.4
Given Ms. G’s lack of response to other antipsychotics, however, we had to consider resuming clozapine therapy. Studies have described agranulocytosis management strategies that may allow patients to keep taking clozapine despite low WBC counts (Box).
We also considered the timing of Ms. G’s blood test that showed a WBC count <2,700/mm3. Ahokas16 suggests that evening WBC counts are significantly higher than those taken in the morning and that granulocytes fluctuate in a diurnal pattern. Ms. G’s evening WBC counts were on average 1,300/mm3 higher than morning levels. Allowing for this diurnal variation and comparing evening blood samples could have averted the interruption in Ms. G’s clozapine therapy and prevented relapse in a patient with highly treatment-refractory schizophrenia.
Related resources
- Chong SA, Remington G. Clozapine augmentation: safety and efficacy. Schizophr Bull 2000;26:421-40.
- Emsley R, Oosthuizen P. The new and evolving pharmacotherapy of schizophrenia. Psychiatr Clin North Am 2003;26:141-63.
- Barnas C, Zwierzina H, Hummer M, Sperner-Unterweger B, Stern A, Fleischhacker WW. Granulocyte-macrophage colony-stimulating factor (GM-CSF) treatment of clozapine-induced agranulocytosis: a case report. J Clin Psychiatry 1992;53:245-7.
Drug brand names
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- GM-CSF—Filgrastim • Neupogen
- Haloperidol • Haldol
- Lithium • Eskalith, Lithobid, others
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Trifluoperazine • Stelazine
- Ziprasidone • Geodon
Disclosure
Dr. Rao is a speaker for Pfizer Inc.
Drs. Goforth, Raval, and Sharma report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kane J, Honigfeld G, Singer J, Meltzer H. Clozapine for the treatment resistant schizophrenic: a double blind comparison with chlorpromazine. Arch Gen Psychiatry 1988;45:789-96.
2. Brenner HD, Dencker SJ, Goldstein MJ, et al. Defining treatment refractoriness in schizophrenia. Schizophr Bull 1990;16:551-61.
3. Meltzer HY. Clozapine: is another view valid? Am J Psychiatry 1995;152:821-5.
4. Clozaril prescribing information. In: Physicians’ Desk Reference. (57th ed). Montvale, NJ: Thomson Healthcare, 2003.
5. Alvir JM, Lieberman JA, Safferman AZ, et al. Clozapine-induced agranulocytosis. Incidence and risk factors in the United States. N Engl J Med. 1993;329:162-7.
6. Honigfeld G. Effects of the clozapine national registry system on incidence of deaths related to agranulocytosis. Psychiatr Serv 1996;47:52-6.
7. Scelsa SN, Simpson DM, McQuistion HL, et al. Clozapineinduced myotoxicity in patients with chronic psychotic disorders. Neurology 1996;47:1518-23.
8. Ames D, Wirshing WC, Baker RW, et al. Predictive value of eosinophilia for neutropenia during clozapine treatment. J Clin Psychiatry 1996;57:579-81.
9. Alvir JM, Lieberman JA, Safferman AZ. Do white-cell count spikes predict agranulocytosis in clozapine recipients? Psychopharmacol Bull 1995;31:311-14.
10. Sperner-Unterweger B, Czeipek I, Gaggl S, et al. Treatment of severe clozapine-induced neutropenia with granulocyte colonystimulating factor (G-CSF). Remission despite continuous treatment with clozapine. Br J Psychiatry 1998;172:82-4.
11. Chengappa KN, Gopalani A, Haught MK, et al. The treatment of clozapine-associated agranulocytosis with granulocyte colony-stimulating factor (G-CSF). Psychopharmacol Bull 1996;32:111-21.
12. Lamberti JS, Bellnier TJ, Schwarzkopf SB, Schneider E. Filgrastim treatment of three patients with clozapine-induced agranulocytosis. J Clin Psychiatry 1995;56:256-9.
13. Boshes RA, Manschreck TC, Desrosiers J, et al. Initiation of clozapine therapy in a patient with preexisting leukopenia: a discussion of the rationale of current treatment options. Ann Clin Psychiatry 2001;13:233-7.
14. Adityanjee. Modification of clozapine-induced leukopenia and neutropenia with lithium carbonate. Am J Psychiatry 1995;152:648-9.
15. Blier P, Slater S, Measham T, et al. Lithium and clozapine-induced neutropenia/agranulocytosis. Int Clin Psychopharmacol 1998;13:137-40.
16. Ahokas A, Elonen E. Circadian rhythm of white blood cells during clozapine treatment. Psychopharmacology 1999;144:301-2.
1. Kane J, Honigfeld G, Singer J, Meltzer H. Clozapine for the treatment resistant schizophrenic: a double blind comparison with chlorpromazine. Arch Gen Psychiatry 1988;45:789-96.
2. Brenner HD, Dencker SJ, Goldstein MJ, et al. Defining treatment refractoriness in schizophrenia. Schizophr Bull 1990;16:551-61.
3. Meltzer HY. Clozapine: is another view valid? Am J Psychiatry 1995;152:821-5.
4. Clozaril prescribing information. In: Physicians’ Desk Reference. (57th ed). Montvale, NJ: Thomson Healthcare, 2003.
5. Alvir JM, Lieberman JA, Safferman AZ, et al. Clozapine-induced agranulocytosis. Incidence and risk factors in the United States. N Engl J Med. 1993;329:162-7.
6. Honigfeld G. Effects of the clozapine national registry system on incidence of deaths related to agranulocytosis. Psychiatr Serv 1996;47:52-6.
7. Scelsa SN, Simpson DM, McQuistion HL, et al. Clozapineinduced myotoxicity in patients with chronic psychotic disorders. Neurology 1996;47:1518-23.
8. Ames D, Wirshing WC, Baker RW, et al. Predictive value of eosinophilia for neutropenia during clozapine treatment. J Clin Psychiatry 1996;57:579-81.
9. Alvir JM, Lieberman JA, Safferman AZ. Do white-cell count spikes predict agranulocytosis in clozapine recipients? Psychopharmacol Bull 1995;31:311-14.
10. Sperner-Unterweger B, Czeipek I, Gaggl S, et al. Treatment of severe clozapine-induced neutropenia with granulocyte colonystimulating factor (G-CSF). Remission despite continuous treatment with clozapine. Br J Psychiatry 1998;172:82-4.
11. Chengappa KN, Gopalani A, Haught MK, et al. The treatment of clozapine-associated agranulocytosis with granulocyte colony-stimulating factor (G-CSF). Psychopharmacol Bull 1996;32:111-21.
12. Lamberti JS, Bellnier TJ, Schwarzkopf SB, Schneider E. Filgrastim treatment of three patients with clozapine-induced agranulocytosis. J Clin Psychiatry 1995;56:256-9.
13. Boshes RA, Manschreck TC, Desrosiers J, et al. Initiation of clozapine therapy in a patient with preexisting leukopenia: a discussion of the rationale of current treatment options. Ann Clin Psychiatry 2001;13:233-7.
14. Adityanjee. Modification of clozapine-induced leukopenia and neutropenia with lithium carbonate. Am J Psychiatry 1995;152:648-9.
15. Blier P, Slater S, Measham T, et al. Lithium and clozapine-induced neutropenia/agranulocytosis. Int Clin Psychopharmacol 1998;13:137-40.
16. Ahokas A, Elonen E. Circadian rhythm of white blood cells during clozapine treatment. Psychopharmacology 1999;144:301-2.
Getting patients to talk about priapism
CHIEF COMPLAINT: Anxiety and disordered sleep
Mr. Q, a college sophomore, reported symptoms of insomnia, anxiety, and sadness to the university health service. When in bed, he said, he would ruminate about whether he had studied adequately and would ultimately qualify for a graduate program. He exhibited no pervasive sadness, loss of interest or motivation, suicidal ideation, or loss of self-esteem. His medical history revealed no serious illness.
The student health psychiatrist diagnosed Mr. Q as having generalized anxiety disorder. She prescribed trazodone, up to 100 mg/d as needed, for the insomnia. For the next 3 weeks, he took one 25 mg dose each night. After that time, Mr. Q reported that the trazodone alleviated the insomnia and that he felt more rested and could study more effectively. He had stopped taking the medication.
Mr. Q, however, did not tell the health service psychiatrist that he had also experienced an uncomfortable erection that lasted about 4 hours and was not precipitated or accompanied by sexual activity. He finally experienced detumescence after several cold showers. He did not inform her of the episode because he felt embarrassed to discuss “such a thing” with a female physician.
After his anxiety and insomnia resurfaced, Mr. Q was referred to one of the authors.
Why did Mr. Q. develop priapism? How would you counsel him at this point?
Dr. Freed’s and Dr. Muskin’s observations
Priapism refers to a prolonged and painful erection that results from sustained blood flow into the corpora cavernosa. In contrast to a normal erection, both the corpus spongiosum and glans penis remain flaccid. Medical complications and reactions to drugs are well-documented causes.
Table 1
Drugs reported to cause priapism
| Antidepressants |
| Trazodone and, in rare cases, phenelzine and sertraline; bupropion has been associated with clitoral priapism3 |
| Antihypertensives that act via alpha blockade Labetalol, prazosin3-5 |
| Metoclopramide when taken with thioridazine3,4 |
| Sildenafil citrate6 (rare case reports) |
| Substances of abuse |
| Alcohol, marijuana, crack cocaine |
| Typical and atypical antipsychotics |
| Chlorpromazine, clozapine, fluphenazine, haloperidol, mesoridazine, molindone, levomepromazine, perphenazine, promazine, risperidone, thioridazine, thiothixene3-5 |
An erection in priapism may result from sexual stimulation/activity, although this is not typical. Sexually stimulated erections in priapism persist hours after the stimulation ceases.
High-flow priapism is rare, painless, and occurs when well-oxygenated blood stays in the corpora cavernosa. It may result from perineal trauma creating a fistula between an artery and the cavernosa. Because the blood is oxygenated, there is no tissue damage, intervention is not urgent, and the prognosis usually is good.
Low-flow priapism, the more prevalent type, is painful and occurs when venous blood remains in the corpora, resulting in hypoxia and ischemia. Approximately 50% of low-flow priapism cases can result in impotence.1
Because men often are embarrassed by priapism, they may not seek medical attention or mention a prior episode to their physicians. This neglect can be dangerous: Painful erections that persist for more than 4 hours can lead to impotence if left untreated.
The physician must surmount the patient’s reluctance to discuss the symptom. Inquiring about past priapism episodes as part of a complete patient history is essential. We suggest routinely asking patients taking priapism-causing psychotropics (Table 1) if they’ve had a recent erectile problem. Mentioning that a medication can cause uncomfortable and serious sexual side effects may prompt the patient to discuss such problems.
Above all, be direct. A straightforward inquiry about a sensitive medical condition usually draws an honest answer; the patient then realizes the subject is important and should not be embarrassed about it.
After the patient discloses a priapism episode, ask him:
- Was the erection related to sexual activity or desire?
- Were you using any other medications or illicit drugs when the erection occurred?
- Do you have a systemic blood disorder?
- Did you feel any pain during your erection? If so, how long did it persist?
Men who present during a priapism episode should immediately be sent to the ER for urologic treatment. Patients reporting a recent sustained erection should be referred to a urologist if they need to keep taking the priapism-causing drug. Urologic treatment is not necessary if the patient stops the medication and the priapism resolves.
Men who have had at least one past priapism episode and those taking alpha-adrenergic blockers should be instructed to visit the ER immediately if a painful, persistent erection develops. Patients also should be warned not to induce detumescence (such as by taking cold showers, drinking alcohol, or engaging in sexual activity) if the erection persists for more than 2 hours. Any delay in emergency care could lead to impotence.
HISTORY: A probable side effect
Because Mr. Q had no other past erectile problems, we strongly suspected his priapism was medication-induced. He reported he had neither been drinking nor taking illicit drugs or other medications when the erection occurred.
Mr. Q also was convinced that the trazodone had caused the sustained erection. He said, however, he was never informed that priapism was a potential side effect of that medication.
Would you resume trazodone, switch to another sleep-promoting or antianxiety medication, or consider other therapy?
Dr. Freed’s and Dr. Muskin’s observations
The prevalence of priapism is not known, although yearly estimates range from 1/1,000 to 1/10,000 patients who take trazodone.2
Trazodone, an alpha-adrenergic blocker, is most commonly implicated among psychotropics in causing priapism.2 Blockade of alpha-adrenergic receptors in the corpora cavernosa creates a parasympathetic imbalance favoring erection and prevents sympathetic-mediated detumescence. Histaminic, beta-adrenergic, and adrenergic/cholinergic components may also contribute to priapism.
Other medications associated with priapism include antipsychotics, antihypertensives, anticoagulants, some antidepressants, and antiimpotence medications injected into the penis.
Low-flow priapism can also be caused by systemic disorders (Table 2), including malignancies—particularly when a tumor has infiltrated the penis—and carcinoma of the bladder or prostate. Prostatitis has been implicated in some cases.
Table 2
Systemic illnesses and conditions that can cause priapism
|
Because Mr. Q has had at least one priapism episode, we would avoid prescribing any agent with alpha-adrenergic blocking properties.
Could Mr. Q’s response to trazodone have been dose-related? How would you ensure that the patient understands a medication’s risks?
Dr. Freed’s and Dr. Muskin’s observations
No findings indicate that trazodone-related priapism is dose-related. Several cases of men developing sustained priapism—resulting in permanent injury and impotence—have been reported after initial dosages of 25 and 50 mg/d.1,4,7 In a study using the FDA Spontaneous Reporting System, Warner et al found that priapism with trazodone was most likely to occur within the first month of treatment and at dosages 150 mg/d.7 Still other reports indicate that new-onset priapism may occur after years of treatment.3
Priapism refers to a painful, prolonged erection that occurs in the absence of sexual stimulation or does not remit after sexual activity.
Several psychotropic drugs, most often trazodone (Desyrel), can cause priapism. This can occur even if the medication is taken at a low dosage or taken only once.
Individuals who have had prior prolonged erections are more susceptible to priapism. Certain medical conditions, many medications, and substance abuse can also increase the risk of priapism. This effect may be additive.
If the erection lasts more than 2 hours, the patient must obtain emergency care. Impotence has been reported after erections lasting 4 hours or longer.
Mr. Z filed suit in Pennsylvania state court against his pharmacy and emergency room doctor. He alleged that he developed priapism after taking one dose of trazodone for disordered sleep. He subsequently became impotent.
Christopher T. Rhodes, PhD, a professor of pharmaceutics at the University of Rhode Island, was an expert witness in that 2000 trial. According to Dr. Rhodes, court testimony revealed that the ER physician had not informed the patient about the possibility of priapism or about the need to obtain emergency treatment for a sustained erection. Dr. Rhodes adds that the pharmacy handout for trazodone did not list priapism as a possible adverse effect.
The court ruled in favor of the patient, judging that the “quality of advice” was inadequate. The patient was awarded an unspecified sum.
Despite its association with priapism, trazodone is used frequently in men and is a popular medication for disordered sleep. Nierenberg et al demonstrated improved sleep in 67% of depressed patients with insomnia who received trazodone either for depression or disordered sleep.8
When prescribing a priapism-causing agent, make sure the patient understands that erectile effects—though rare—can occur. Consider giving patients an informed consent form explaining the association between psychotropics and priapism and the potential long-term health implications (Box 1). Include the form in the patient’s record for documentation in the event of a malpractice lawsuit (Box 2).
FURTHER TREATMENT: Learning how to cope
Self-hypnosis/relaxation therapy was initiated to address Mr. Q’s anxiety and insomnia. The patient quickly learned the hypnosis techniques and his anxiety/insomnia symptoms began to resolve almost immediately.
Mr. Q’s priapism resolved spontaneously with no apparent erectile dysfunction. He was referred back to the university health service and has been in apparent good health since.
Related resources
- Sleepnet.com. Information on sleep disorders and sleep hygiene. http://www.sleepnet.com/
- National Center on Sleep Disorders Research http://www.nhlbi.nih.gov/about/ncsdr/
Drug brand names
- Bupropion • Wellbutrin
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Labetalol • Trandate
- Levomepromazine • Nozinan
- Mesoridazine • Serentil
- Metoclopramide • Reglan
- Molindone • Lidone
- Perphenazine • Trilafon
- Phenelzine • Nardil
- Prazosin • Minipress
- Promazine • Sparine
- Risperidone • Risperdal
- Sertraline • Zoloft
- Sildenafil citrate • Viagra
- Thioridazine • Mellaril
- Thiothixene • Navane
- Trazodone • Desyrel
Disclosure
Dr. Freed reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Muskin receives research/grant support from Bristol-Myers Squibb Co., is a speaker for and consultant to Bristol-Myers Squibb Co., Forest Laboratories, GlaxoSmithKline, Janssen Pharmaceutica, and Pfizer Inc.; and is a speaker for Cephalon Inc. and Eli Lilly and Co.
1. Weiner DM, Lowe FC. Psychotropic drug-induced priapism. CNS Drugs 1998;9:371-9.
2. Rhodes CT. Trazodone and priapism—implications for responses to adverse events. Clin Res Regulatory Affairs 2001;18:47-52.
3. Compton MT, Miller AH. Priapism associated with conventional and atypical antipsychotic medications: a review. J Clin Psychiatry 2001;62:362-6.
4. Thompson JW, Ware MR, Blashfield RK. Psychotropic medication and priapism: a comprehensive review. J Clin Psychiatry 1990;51:430-3.
5. Reeves RR, Kimble R. Prolonged erections associated with ziprasidone treatment: a case report. J Clin Psychiatry 2003;64:97-8.
6. Sur RL, Kane CJ. Sildenafil citrate-associated priapism. Urology 2000;55:950.-
7. Warner MD, Peabody CA, Whiteford HA, Hollister LE. Trazodone and priapism. J Clin Psychiatry 1987;48:244-5.
8. Nierenberg AA, Adler LA, Peselow E, et al. Trazodone for antidepressant-associated insomnia. Am J Psychiatry 1994;151:1069-72.
CHIEF COMPLAINT: Anxiety and disordered sleep
Mr. Q, a college sophomore, reported symptoms of insomnia, anxiety, and sadness to the university health service. When in bed, he said, he would ruminate about whether he had studied adequately and would ultimately qualify for a graduate program. He exhibited no pervasive sadness, loss of interest or motivation, suicidal ideation, or loss of self-esteem. His medical history revealed no serious illness.
The student health psychiatrist diagnosed Mr. Q as having generalized anxiety disorder. She prescribed trazodone, up to 100 mg/d as needed, for the insomnia. For the next 3 weeks, he took one 25 mg dose each night. After that time, Mr. Q reported that the trazodone alleviated the insomnia and that he felt more rested and could study more effectively. He had stopped taking the medication.
Mr. Q, however, did not tell the health service psychiatrist that he had also experienced an uncomfortable erection that lasted about 4 hours and was not precipitated or accompanied by sexual activity. He finally experienced detumescence after several cold showers. He did not inform her of the episode because he felt embarrassed to discuss “such a thing” with a female physician.
After his anxiety and insomnia resurfaced, Mr. Q was referred to one of the authors.
Why did Mr. Q. develop priapism? How would you counsel him at this point?
Dr. Freed’s and Dr. Muskin’s observations
Priapism refers to a prolonged and painful erection that results from sustained blood flow into the corpora cavernosa. In contrast to a normal erection, both the corpus spongiosum and glans penis remain flaccid. Medical complications and reactions to drugs are well-documented causes.
Table 1
Drugs reported to cause priapism
| Antidepressants |
| Trazodone and, in rare cases, phenelzine and sertraline; bupropion has been associated with clitoral priapism3 |
| Antihypertensives that act via alpha blockade Labetalol, prazosin3-5 |
| Metoclopramide when taken with thioridazine3,4 |
| Sildenafil citrate6 (rare case reports) |
| Substances of abuse |
| Alcohol, marijuana, crack cocaine |
| Typical and atypical antipsychotics |
| Chlorpromazine, clozapine, fluphenazine, haloperidol, mesoridazine, molindone, levomepromazine, perphenazine, promazine, risperidone, thioridazine, thiothixene3-5 |
An erection in priapism may result from sexual stimulation/activity, although this is not typical. Sexually stimulated erections in priapism persist hours after the stimulation ceases.
High-flow priapism is rare, painless, and occurs when well-oxygenated blood stays in the corpora cavernosa. It may result from perineal trauma creating a fistula between an artery and the cavernosa. Because the blood is oxygenated, there is no tissue damage, intervention is not urgent, and the prognosis usually is good.
Low-flow priapism, the more prevalent type, is painful and occurs when venous blood remains in the corpora, resulting in hypoxia and ischemia. Approximately 50% of low-flow priapism cases can result in impotence.1
Because men often are embarrassed by priapism, they may not seek medical attention or mention a prior episode to their physicians. This neglect can be dangerous: Painful erections that persist for more than 4 hours can lead to impotence if left untreated.
The physician must surmount the patient’s reluctance to discuss the symptom. Inquiring about past priapism episodes as part of a complete patient history is essential. We suggest routinely asking patients taking priapism-causing psychotropics (Table 1) if they’ve had a recent erectile problem. Mentioning that a medication can cause uncomfortable and serious sexual side effects may prompt the patient to discuss such problems.
Above all, be direct. A straightforward inquiry about a sensitive medical condition usually draws an honest answer; the patient then realizes the subject is important and should not be embarrassed about it.
After the patient discloses a priapism episode, ask him:
- Was the erection related to sexual activity or desire?
- Were you using any other medications or illicit drugs when the erection occurred?
- Do you have a systemic blood disorder?
- Did you feel any pain during your erection? If so, how long did it persist?
Men who present during a priapism episode should immediately be sent to the ER for urologic treatment. Patients reporting a recent sustained erection should be referred to a urologist if they need to keep taking the priapism-causing drug. Urologic treatment is not necessary if the patient stops the medication and the priapism resolves.
Men who have had at least one past priapism episode and those taking alpha-adrenergic blockers should be instructed to visit the ER immediately if a painful, persistent erection develops. Patients also should be warned not to induce detumescence (such as by taking cold showers, drinking alcohol, or engaging in sexual activity) if the erection persists for more than 2 hours. Any delay in emergency care could lead to impotence.
HISTORY: A probable side effect
Because Mr. Q had no other past erectile problems, we strongly suspected his priapism was medication-induced. He reported he had neither been drinking nor taking illicit drugs or other medications when the erection occurred.
Mr. Q also was convinced that the trazodone had caused the sustained erection. He said, however, he was never informed that priapism was a potential side effect of that medication.
Would you resume trazodone, switch to another sleep-promoting or antianxiety medication, or consider other therapy?
Dr. Freed’s and Dr. Muskin’s observations
The prevalence of priapism is not known, although yearly estimates range from 1/1,000 to 1/10,000 patients who take trazodone.2
Trazodone, an alpha-adrenergic blocker, is most commonly implicated among psychotropics in causing priapism.2 Blockade of alpha-adrenergic receptors in the corpora cavernosa creates a parasympathetic imbalance favoring erection and prevents sympathetic-mediated detumescence. Histaminic, beta-adrenergic, and adrenergic/cholinergic components may also contribute to priapism.
Other medications associated with priapism include antipsychotics, antihypertensives, anticoagulants, some antidepressants, and antiimpotence medications injected into the penis.
Low-flow priapism can also be caused by systemic disorders (Table 2), including malignancies—particularly when a tumor has infiltrated the penis—and carcinoma of the bladder or prostate. Prostatitis has been implicated in some cases.
Table 2
Systemic illnesses and conditions that can cause priapism
|
Because Mr. Q has had at least one priapism episode, we would avoid prescribing any agent with alpha-adrenergic blocking properties.
Could Mr. Q’s response to trazodone have been dose-related? How would you ensure that the patient understands a medication’s risks?
Dr. Freed’s and Dr. Muskin’s observations
No findings indicate that trazodone-related priapism is dose-related. Several cases of men developing sustained priapism—resulting in permanent injury and impotence—have been reported after initial dosages of 25 and 50 mg/d.1,4,7 In a study using the FDA Spontaneous Reporting System, Warner et al found that priapism with trazodone was most likely to occur within the first month of treatment and at dosages 150 mg/d.7 Still other reports indicate that new-onset priapism may occur after years of treatment.3
Priapism refers to a painful, prolonged erection that occurs in the absence of sexual stimulation or does not remit after sexual activity.
Several psychotropic drugs, most often trazodone (Desyrel), can cause priapism. This can occur even if the medication is taken at a low dosage or taken only once.
Individuals who have had prior prolonged erections are more susceptible to priapism. Certain medical conditions, many medications, and substance abuse can also increase the risk of priapism. This effect may be additive.
If the erection lasts more than 2 hours, the patient must obtain emergency care. Impotence has been reported after erections lasting 4 hours or longer.
Mr. Z filed suit in Pennsylvania state court against his pharmacy and emergency room doctor. He alleged that he developed priapism after taking one dose of trazodone for disordered sleep. He subsequently became impotent.
Christopher T. Rhodes, PhD, a professor of pharmaceutics at the University of Rhode Island, was an expert witness in that 2000 trial. According to Dr. Rhodes, court testimony revealed that the ER physician had not informed the patient about the possibility of priapism or about the need to obtain emergency treatment for a sustained erection. Dr. Rhodes adds that the pharmacy handout for trazodone did not list priapism as a possible adverse effect.
The court ruled in favor of the patient, judging that the “quality of advice” was inadequate. The patient was awarded an unspecified sum.
Despite its association with priapism, trazodone is used frequently in men and is a popular medication for disordered sleep. Nierenberg et al demonstrated improved sleep in 67% of depressed patients with insomnia who received trazodone either for depression or disordered sleep.8
When prescribing a priapism-causing agent, make sure the patient understands that erectile effects—though rare—can occur. Consider giving patients an informed consent form explaining the association between psychotropics and priapism and the potential long-term health implications (Box 1). Include the form in the patient’s record for documentation in the event of a malpractice lawsuit (Box 2).
FURTHER TREATMENT: Learning how to cope
Self-hypnosis/relaxation therapy was initiated to address Mr. Q’s anxiety and insomnia. The patient quickly learned the hypnosis techniques and his anxiety/insomnia symptoms began to resolve almost immediately.
Mr. Q’s priapism resolved spontaneously with no apparent erectile dysfunction. He was referred back to the university health service and has been in apparent good health since.
Related resources
- Sleepnet.com. Information on sleep disorders and sleep hygiene. http://www.sleepnet.com/
- National Center on Sleep Disorders Research http://www.nhlbi.nih.gov/about/ncsdr/
Drug brand names
- Bupropion • Wellbutrin
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Labetalol • Trandate
- Levomepromazine • Nozinan
- Mesoridazine • Serentil
- Metoclopramide • Reglan
- Molindone • Lidone
- Perphenazine • Trilafon
- Phenelzine • Nardil
- Prazosin • Minipress
- Promazine • Sparine
- Risperidone • Risperdal
- Sertraline • Zoloft
- Sildenafil citrate • Viagra
- Thioridazine • Mellaril
- Thiothixene • Navane
- Trazodone • Desyrel
Disclosure
Dr. Freed reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Muskin receives research/grant support from Bristol-Myers Squibb Co., is a speaker for and consultant to Bristol-Myers Squibb Co., Forest Laboratories, GlaxoSmithKline, Janssen Pharmaceutica, and Pfizer Inc.; and is a speaker for Cephalon Inc. and Eli Lilly and Co.
CHIEF COMPLAINT: Anxiety and disordered sleep
Mr. Q, a college sophomore, reported symptoms of insomnia, anxiety, and sadness to the university health service. When in bed, he said, he would ruminate about whether he had studied adequately and would ultimately qualify for a graduate program. He exhibited no pervasive sadness, loss of interest or motivation, suicidal ideation, or loss of self-esteem. His medical history revealed no serious illness.
The student health psychiatrist diagnosed Mr. Q as having generalized anxiety disorder. She prescribed trazodone, up to 100 mg/d as needed, for the insomnia. For the next 3 weeks, he took one 25 mg dose each night. After that time, Mr. Q reported that the trazodone alleviated the insomnia and that he felt more rested and could study more effectively. He had stopped taking the medication.
Mr. Q, however, did not tell the health service psychiatrist that he had also experienced an uncomfortable erection that lasted about 4 hours and was not precipitated or accompanied by sexual activity. He finally experienced detumescence after several cold showers. He did not inform her of the episode because he felt embarrassed to discuss “such a thing” with a female physician.
After his anxiety and insomnia resurfaced, Mr. Q was referred to one of the authors.
Why did Mr. Q. develop priapism? How would you counsel him at this point?
Dr. Freed’s and Dr. Muskin’s observations
Priapism refers to a prolonged and painful erection that results from sustained blood flow into the corpora cavernosa. In contrast to a normal erection, both the corpus spongiosum and glans penis remain flaccid. Medical complications and reactions to drugs are well-documented causes.
Table 1
Drugs reported to cause priapism
| Antidepressants |
| Trazodone and, in rare cases, phenelzine and sertraline; bupropion has been associated with clitoral priapism3 |
| Antihypertensives that act via alpha blockade Labetalol, prazosin3-5 |
| Metoclopramide when taken with thioridazine3,4 |
| Sildenafil citrate6 (rare case reports) |
| Substances of abuse |
| Alcohol, marijuana, crack cocaine |
| Typical and atypical antipsychotics |
| Chlorpromazine, clozapine, fluphenazine, haloperidol, mesoridazine, molindone, levomepromazine, perphenazine, promazine, risperidone, thioridazine, thiothixene3-5 |
An erection in priapism may result from sexual stimulation/activity, although this is not typical. Sexually stimulated erections in priapism persist hours after the stimulation ceases.
High-flow priapism is rare, painless, and occurs when well-oxygenated blood stays in the corpora cavernosa. It may result from perineal trauma creating a fistula between an artery and the cavernosa. Because the blood is oxygenated, there is no tissue damage, intervention is not urgent, and the prognosis usually is good.
Low-flow priapism, the more prevalent type, is painful and occurs when venous blood remains in the corpora, resulting in hypoxia and ischemia. Approximately 50% of low-flow priapism cases can result in impotence.1
Because men often are embarrassed by priapism, they may not seek medical attention or mention a prior episode to their physicians. This neglect can be dangerous: Painful erections that persist for more than 4 hours can lead to impotence if left untreated.
The physician must surmount the patient’s reluctance to discuss the symptom. Inquiring about past priapism episodes as part of a complete patient history is essential. We suggest routinely asking patients taking priapism-causing psychotropics (Table 1) if they’ve had a recent erectile problem. Mentioning that a medication can cause uncomfortable and serious sexual side effects may prompt the patient to discuss such problems.
Above all, be direct. A straightforward inquiry about a sensitive medical condition usually draws an honest answer; the patient then realizes the subject is important and should not be embarrassed about it.
After the patient discloses a priapism episode, ask him:
- Was the erection related to sexual activity or desire?
- Were you using any other medications or illicit drugs when the erection occurred?
- Do you have a systemic blood disorder?
- Did you feel any pain during your erection? If so, how long did it persist?
Men who present during a priapism episode should immediately be sent to the ER for urologic treatment. Patients reporting a recent sustained erection should be referred to a urologist if they need to keep taking the priapism-causing drug. Urologic treatment is not necessary if the patient stops the medication and the priapism resolves.
Men who have had at least one past priapism episode and those taking alpha-adrenergic blockers should be instructed to visit the ER immediately if a painful, persistent erection develops. Patients also should be warned not to induce detumescence (such as by taking cold showers, drinking alcohol, or engaging in sexual activity) if the erection persists for more than 2 hours. Any delay in emergency care could lead to impotence.
HISTORY: A probable side effect
Because Mr. Q had no other past erectile problems, we strongly suspected his priapism was medication-induced. He reported he had neither been drinking nor taking illicit drugs or other medications when the erection occurred.
Mr. Q also was convinced that the trazodone had caused the sustained erection. He said, however, he was never informed that priapism was a potential side effect of that medication.
Would you resume trazodone, switch to another sleep-promoting or antianxiety medication, or consider other therapy?
Dr. Freed’s and Dr. Muskin’s observations
The prevalence of priapism is not known, although yearly estimates range from 1/1,000 to 1/10,000 patients who take trazodone.2
Trazodone, an alpha-adrenergic blocker, is most commonly implicated among psychotropics in causing priapism.2 Blockade of alpha-adrenergic receptors in the corpora cavernosa creates a parasympathetic imbalance favoring erection and prevents sympathetic-mediated detumescence. Histaminic, beta-adrenergic, and adrenergic/cholinergic components may also contribute to priapism.
Other medications associated with priapism include antipsychotics, antihypertensives, anticoagulants, some antidepressants, and antiimpotence medications injected into the penis.
Low-flow priapism can also be caused by systemic disorders (Table 2), including malignancies—particularly when a tumor has infiltrated the penis—and carcinoma of the bladder or prostate. Prostatitis has been implicated in some cases.
Table 2
Systemic illnesses and conditions that can cause priapism
|
Because Mr. Q has had at least one priapism episode, we would avoid prescribing any agent with alpha-adrenergic blocking properties.
Could Mr. Q’s response to trazodone have been dose-related? How would you ensure that the patient understands a medication’s risks?
Dr. Freed’s and Dr. Muskin’s observations
No findings indicate that trazodone-related priapism is dose-related. Several cases of men developing sustained priapism—resulting in permanent injury and impotence—have been reported after initial dosages of 25 and 50 mg/d.1,4,7 In a study using the FDA Spontaneous Reporting System, Warner et al found that priapism with trazodone was most likely to occur within the first month of treatment and at dosages 150 mg/d.7 Still other reports indicate that new-onset priapism may occur after years of treatment.3
Priapism refers to a painful, prolonged erection that occurs in the absence of sexual stimulation or does not remit after sexual activity.
Several psychotropic drugs, most often trazodone (Desyrel), can cause priapism. This can occur even if the medication is taken at a low dosage or taken only once.
Individuals who have had prior prolonged erections are more susceptible to priapism. Certain medical conditions, many medications, and substance abuse can also increase the risk of priapism. This effect may be additive.
If the erection lasts more than 2 hours, the patient must obtain emergency care. Impotence has been reported after erections lasting 4 hours or longer.
Mr. Z filed suit in Pennsylvania state court against his pharmacy and emergency room doctor. He alleged that he developed priapism after taking one dose of trazodone for disordered sleep. He subsequently became impotent.
Christopher T. Rhodes, PhD, a professor of pharmaceutics at the University of Rhode Island, was an expert witness in that 2000 trial. According to Dr. Rhodes, court testimony revealed that the ER physician had not informed the patient about the possibility of priapism or about the need to obtain emergency treatment for a sustained erection. Dr. Rhodes adds that the pharmacy handout for trazodone did not list priapism as a possible adverse effect.
The court ruled in favor of the patient, judging that the “quality of advice” was inadequate. The patient was awarded an unspecified sum.
Despite its association with priapism, trazodone is used frequently in men and is a popular medication for disordered sleep. Nierenberg et al demonstrated improved sleep in 67% of depressed patients with insomnia who received trazodone either for depression or disordered sleep.8
When prescribing a priapism-causing agent, make sure the patient understands that erectile effects—though rare—can occur. Consider giving patients an informed consent form explaining the association between psychotropics and priapism and the potential long-term health implications (Box 1). Include the form in the patient’s record for documentation in the event of a malpractice lawsuit (Box 2).
FURTHER TREATMENT: Learning how to cope
Self-hypnosis/relaxation therapy was initiated to address Mr. Q’s anxiety and insomnia. The patient quickly learned the hypnosis techniques and his anxiety/insomnia symptoms began to resolve almost immediately.
Mr. Q’s priapism resolved spontaneously with no apparent erectile dysfunction. He was referred back to the university health service and has been in apparent good health since.
Related resources
- Sleepnet.com. Information on sleep disorders and sleep hygiene. http://www.sleepnet.com/
- National Center on Sleep Disorders Research http://www.nhlbi.nih.gov/about/ncsdr/
Drug brand names
- Bupropion • Wellbutrin
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Labetalol • Trandate
- Levomepromazine • Nozinan
- Mesoridazine • Serentil
- Metoclopramide • Reglan
- Molindone • Lidone
- Perphenazine • Trilafon
- Phenelzine • Nardil
- Prazosin • Minipress
- Promazine • Sparine
- Risperidone • Risperdal
- Sertraline • Zoloft
- Sildenafil citrate • Viagra
- Thioridazine • Mellaril
- Thiothixene • Navane
- Trazodone • Desyrel
Disclosure
Dr. Freed reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Muskin receives research/grant support from Bristol-Myers Squibb Co., is a speaker for and consultant to Bristol-Myers Squibb Co., Forest Laboratories, GlaxoSmithKline, Janssen Pharmaceutica, and Pfizer Inc.; and is a speaker for Cephalon Inc. and Eli Lilly and Co.
1. Weiner DM, Lowe FC. Psychotropic drug-induced priapism. CNS Drugs 1998;9:371-9.
2. Rhodes CT. Trazodone and priapism—implications for responses to adverse events. Clin Res Regulatory Affairs 2001;18:47-52.
3. Compton MT, Miller AH. Priapism associated with conventional and atypical antipsychotic medications: a review. J Clin Psychiatry 2001;62:362-6.
4. Thompson JW, Ware MR, Blashfield RK. Psychotropic medication and priapism: a comprehensive review. J Clin Psychiatry 1990;51:430-3.
5. Reeves RR, Kimble R. Prolonged erections associated with ziprasidone treatment: a case report. J Clin Psychiatry 2003;64:97-8.
6. Sur RL, Kane CJ. Sildenafil citrate-associated priapism. Urology 2000;55:950.-
7. Warner MD, Peabody CA, Whiteford HA, Hollister LE. Trazodone and priapism. J Clin Psychiatry 1987;48:244-5.
8. Nierenberg AA, Adler LA, Peselow E, et al. Trazodone for antidepressant-associated insomnia. Am J Psychiatry 1994;151:1069-72.
1. Weiner DM, Lowe FC. Psychotropic drug-induced priapism. CNS Drugs 1998;9:371-9.
2. Rhodes CT. Trazodone and priapism—implications for responses to adverse events. Clin Res Regulatory Affairs 2001;18:47-52.
3. Compton MT, Miller AH. Priapism associated with conventional and atypical antipsychotic medications: a review. J Clin Psychiatry 2001;62:362-6.
4. Thompson JW, Ware MR, Blashfield RK. Psychotropic medication and priapism: a comprehensive review. J Clin Psychiatry 1990;51:430-3.
5. Reeves RR, Kimble R. Prolonged erections associated with ziprasidone treatment: a case report. J Clin Psychiatry 2003;64:97-8.
6. Sur RL, Kane CJ. Sildenafil citrate-associated priapism. Urology 2000;55:950.-
7. Warner MD, Peabody CA, Whiteford HA, Hollister LE. Trazodone and priapism. J Clin Psychiatry 1987;48:244-5.
8. Nierenberg AA, Adler LA, Peselow E, et al. Trazodone for antidepressant-associated insomnia. Am J Psychiatry 1994;151:1069-72.
Treating schizophrenia in the ‘real world’
HISTORY: Jesus’ ‘cousin’
Mr. F, age 60, was hospitalized in May 1995 after expressing fear he would hurt—or kill—himself or someone else. He cooperated with admission procedures but refused to participate in ward activities or meetings. His hygiene was poor, he made little eye contact, and reportedly heard voices. Two days after admission, he emphatically denied suicidal or homicidal ideation and was discharged against medical advice.
Two weeks later, Mr. F was readmitted after his symptoms worsened. He said voices told him that he was a cousin to Jesus Christ and that he had telepathic abilities. He also reported visual hallucinations.
Twice divorced, Mr. F has three uncles who have been diagnosed with schizophrenia. His late father had a history of alcohol abuse, and his late mother suffered from Alzheimer’s disease.
Mr. F lived a normal life until 1975, when he began drinking heavily. Three years later, he quit his job of 11 years at the local airport. At that time, he told a psychiatrist that “people are out to get me. I feel nervous a lot.” He was diagnosed as having generalized anxiety disorder and treated with diazepam, 20 mg/d.
Four months later he complained of severe insomnia, was diagnosed with depression, and was prescribed amitriptyline, 100 mg at bedtime. He was hospitalized 1 week later after he complained of chest pain and expressed paranoid thoughts. During the 3-week hospitalization, he experienced persecutory delusions and heard voices telling him he was “damned.” He was diagnosed with paranoid schizophrenia and alcohol dependence. The amitriptyline was stopped, and Mr. F was discharged on chlorpromazine, 300 mg/d.
From 1978 to 1995, Mr. F was hospitalized 35 times, often at his family’s urging after he made threats or became violent at home. He once kicked his elderly father and another time was jailed after a domestic violence incident. Religious delusions characterized his thought content. Thought blocking, flight of ideas, and somatic and sexual delusions were also apparent.
Was Mr. F’s diagnosis accurate, or do his frequent psychotic episodes meet criteria for a type of mania?
Dr. Canive’s observations
Diagnoses of mania or mood disorder with psychotic features were not considered because Mr. F never experienced a distinct period of persistently expansive or depressed mood.
Mr. F’s initial complaints of increased anxiety and depression were considered prodromal symptoms of schizophrenia and may have reflected his inability to discuss or cope with his delusions and hallucinations during the initial evaluation. What’s more, his occupational functioning gradually deteriorated months before his initial mental health assessment.
TREATMENT: Many medications, no progress
At different times from 1978 to 1995, Mr. F had taken chlorpromazine, 100 to 300 mg/d; thioridazine, 50 to 200 mg/d; loxapine, 25 mg/d; fluphenazine, 5 to 10 mg/d; haloperidol, 2 to 4 mg/d, and fluphenazine decanoate, 3.125 to 6.25 mg biweekly, as well as concomitant anticholinergics, benzodiazepines, or other hypnotics.
A closer look at Mr. F’s chart revealed that medication noncompliance often preceded hospitalization. He was extremely prone to antipsychotic-related extrapyramidal symptoms (EPS), even at low dosages. Whenever motor symptoms surfaced, he would stop taking his antipsychotics.
Buccolingual tardive dyskinesia (TD) was first noticed in 1987. Four years later, an Abnormal Involuntary Movement Scale (AIMS) exam revealed mild TD that was managed with vitamin E, 400 IU/d.
While hospitalized, Mr. F many times received injectable antipsychotics and benzodiazepines, mostly to control violence. Depot antipsychotics also were tried in an effort to promote compliance, but recurrent alcohol abuse often triggered a relapse.
How would you confront Mr. F’s history of noncompliance? Can his delusions be controlled without prompting severe motor effects?
Dr. Canive’s observations
For Mr. F, poor tolerability, incomplete efficacy, and variable compliance have repeatedly led to symptom exacerbation and hospitalization. Low dosing because of sensitivity to EPS may partially explain his insufficient response to antipsychotics.
In 1995, after numerous unsuccessful drug treatments, we considered entering Mr. F into a phase II clinical trial of the atypical antipsychotic aripiprazole.
Now FDA-approved for treatment of schizophrenia, aripiprazole decreases dopaminergic transmission in the nigrostriatal and tuberoinfundibular pathways, thus reducing the likelihood of EPS.1,2 Also, aripiprazole’s dopamine-serotonin stabilization effects have been reported in clinical trials to improve tolerability, compliance, and overall effectiveness in patients with schizophrenia.3
Common side effects of aripiprazole are mild nausea, insomnia, and restlessness, although data indicate that these effects have a low prevalence and disappear within 2 weeks. If insomnia and restlessness are prominent, a low-dose, short-acting benzodiazepine may be added, tapered after 1 week, and discontinued at week 2.
Table
Mr. F’s progress while taking aripiprazole, 1995-2003
| Visit | CGI-S | CGI-G | PANSS Positive | PANSS Negative | PANSS total | Clinical correlates |
|---|---|---|---|---|---|---|
| Baseline | 4 | 5 | 24 | 21 | 94 | —- |
| Week 2 | 3 | 2 | N/A | N/A | N/A | Positive, negative symptoms much improved |
| Week 12 | 3 | 2 | 11 | 16 | 56 | Mr. F’s understanding about his illness, life, socioeconomic issues much improved |
| Week 76 | 3 | 2 | 11 | 18 | 56 | Activity level increased; starts doing yard work to supplement disability income |
| Week 88 | 3 | 2 | 12 | 14 | 52 | Volunteers as courier at local hospital; continues to do yard work |
| Week 226 | 2 | 2 | 9 | 12 | 42 | Starts steady work as a janitor and security aid |
| Week 284 | 2 | 2 | 9 | 14 | 45 | Concerned about losing Social Security benefits, since he is working 40 hours a week. |
| Week 328 | 3 | 1 | 11 | 15 | 52 | Discharged from hospital after psychotic relapse. Looking for apartment. |
| Week 384 (Final visit) | 3 | 1 | 9 | 12 | 45 | Father died the previous week. Mr. F accepted his father’s passing well. Open-label study terminated. Patient continued on aripiprazole, 20 mg/d. |
What the scores mean
Clinical Global Impression-Severity of Illness (CGI-S)—Scores range from 1 to 7, with 1 meaning normal (normal, minimal, mild, moderate, moderately severe, severe, among the most extreme).
Clinical Global Impression-Global Improvement (CGI-G)—Scores range from 1 to 7, with 1 meaning very much improved (very much improved, much improved, improved, unchanged, little worse, much worse, very much worse).
Positive and Negative Syndrome Scale (PANSS) Positive—consists of 7 items (delusions, conceptual disorganization, hallucinatory behavior, excitement, grandiosity, suspiciousness/persecution, hostility); scores range from 7 to 49 and decrease as patients improve.
PANSS Negative—consists of 7 items (blunted affect, emotional withdrawal, poor rapport, passive pathetic withdrawal, difficulty in abstract thinking, lack of spontaneity and flow of conversation, stereotyped thinking); scores range from 7 to 49 and decrease as patients improve.
PANSS General—consists of 16 items (somatic concern, anxiety, guilt feelings, tension, mannerism and posturing, depression, motor retardation, uncooperativeness, unusual thought content, disorientation, poor attention, lack of judgment and insight, disturbance of volition, poor impulse control, preoccupation, active social avoidance). Scores range from 16 to 112 and decrease as patients improve.
CONTINUED TREATMENT: A new trial
Mr. F participated in a 4-week, double-blind, placebo-controlled trial of aripiprazole, 2, 10, or 30 mg/d, versus haloperidol, 10 mg/d.
One month later, he entered a second aripiprazole trial: a 4-day, open-label study starting at 5 mg/d with titration to 20 mg/d. In the interval between the two trials, Mr. F was prescribed thiothixene, 10 mg/d, and benztropine, 2 mg at bedtime.
During the 4-day trial, he complained of insomnia and was given chloral hydrate, 500 to 1,000 mg at bedtime. He also complained of anxiety and was started on lorazepam, 2 mg bid.
After completing the open-label aripiprazole trial, Mr. F exhibited no behavioral problems and complied with ward routine. He was discharged after 17 days, at which time he denied auditory or visual hallucinations. His thinking seemed clear and his insight improved. His Global Assessment of Functioning (GAF) score at discharge was 55, suggesting moderate symptoms and difficulty in social and occupational functioning.
For the next 5 1/2 years, Mr. F was maintained on aripiprazole, 20 mg/d, as part of the same ongoing open-label trial. During that period he also took lorazepam, 1 mg bid prn; oxazepam, 15 mg bid; or clonazepam, 0.5 mg bid, for anxiety.
Mr. F. exhibited significant sustained improvement as measured with the Positive and Negative Symptom Scale (PANSS), Clinical Global Impression scale (CGI), and GAF (Table). His TD remained mild throughout the trial, as determined through AIMS scores. He also reported no EPS, akathisia, or other adverse events.
About 18 months after starting aripiprazole, Mr. F resumed working part time. In September 2001, he stopped receiving disability benefits and started supporting himself again.
FOLLOW-UP: ‘The voices were ugly’
In December 2001, after 6 years without hospitalization, Mr. F was back in the psychiatric ward. One week before admission, he reported that he had been having panic attacks because “the voices were ugly.” He only slept 4 to 5 hours per night.
He then revealed that he had stopped taking aripiprazole for 2 weeks because he had no longer felt ill. He was still taking his lorazepam, however.
Mr. F appeared mildly anxious upon presentation and his affect was blunted. On examination, his thought processes were linear; he was once again hearing voices and experiencing delusions of telepathic control.
The patient was placed back on aripiprazole, 20 mg/d. His behavior on the ward improved dramatically, and the frequency and severity of his delusions and auditory hallucinations decreased gradually.
At discharge, Mr. F’s insight was good, his delusions had disappeared, and auditory hallucinations were rare. He was instructed to continue the aripiprazole and was prescribed clonazepam, 0.5 mg bid, for his anxiety and trazodone, 50 mg at bed-time, to help his sleep.
Since then, Mr. F has lived on his own, is working steadily, and has not required hospitalization. He stopped taking trazodone soon after discharge, but continues taking aripiprazole and clonazepam as prescribed. His hygiene is good, and he is making amends with family members. He attends church every Sunday—free of the messianic delusions that once tormented him. He also stopped abusing alcohol on his own in 1995 and has remained abstinent since.
How can we ensure that patients with schizophrenia keep taking their medications—regardless of whether symptoms are present?
Dr. Canive’s observations
Clinical trials measure a drug’s efficacy under highly controlled circumstances. In the “real world,” however, noncompliance due to intolerability can undermine a medication’s effectiveness.
Too often noncompliance—stemming from abatement of symptoms or the emergence of side effects—derails treatment of schizophrenia. Misdrahi et al found that medication noncompliance accounts for 40% of schizophrenia relapses occurring more than 1 year after patients’ first hospitalization.4
Given aripiprazole’s 75-hour half-life, one might not expect to see symptoms emerge so soon after discontinuation. It is possible that:
- Mr. F. abstained from aripiprazole longer than he realized—or admitted
- Unidentified stressful life events also exacerbated symptoms and precipitated hospitalization.
When Mr. F consistently followed his regimen, his positive symptoms abated and he could attempt to live a normal life.
Our patients must understand that schizophrenia is a lifelong illness and that continued adherence to medication—even when symptoms do not exist—is crucial. A strong therapeutic alliance,5 increased social support, adjunctive cognitive-behavioral therapy, psychosocial interventions,6 and medications with fewer and less-severe side effects may help patients embrace this message.
Related resources
- Tamminga CA. Partial dopamine agonists in the treatment of psychosis. J Neural Transm 2002;109:411-20.
Drug brand names
- Amitriptyline • Elavil
- Aripiprazole • Abilify
- Benztropine • Cogentin
- Chlorpromazine • Thorazine
- Clonazepam • Klonopin
- Diazepam • Valium
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Lorazepam • Ativan
- Loxapine • Loxitane
- Oxazepam • Serax
- Thiothixene • Navane
- Trazodone • Desyrel
Disclosure
The author receives research/grant support from and is a speaker for and consultant to Bristol-Myers Squibb Co. He also receives research/grant support from and/or is a speaker for AstraZeneca Pharmaceuticals, Janssen Pharmaceutica, and Eli Lilly and Co.
1. Aripiprazole prescribing information. Bristol-Myers Squibb Co. and Otsuka America Pharmaceutical, 2002.
2. Kane JM, Carson WH, Saha AR, et al. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry 2002;63:763-71.
3. Burris KD, Molski TF, Xu C, et al. Aripiprazole, a novel antipsychotic, is a high-affinity partial agonist at human dopamine D2 receptors. J Pharmacol Exp Ther 2002;302:381-9.
4. Misdrahi D, Llorca PM, Lancon C, Bayle FJ. Compliance in schizophrenia: Predictive factors, therapeutical considerations and research implications (French). Encephale 2002;3:266-72.
5. Weiss KA, Smith TE, Hull JW, et al. Predictors of risk of nonadherence in outpatients with schizophrenia and other psychotic disorders. Schizophr Bull 2002;28:341-9.
6. Perkins DO. Predictors of noncompliance in patients with schizophrenia. J Clin Psychiatry 2002;63:1121-8.
HISTORY: Jesus’ ‘cousin’
Mr. F, age 60, was hospitalized in May 1995 after expressing fear he would hurt—or kill—himself or someone else. He cooperated with admission procedures but refused to participate in ward activities or meetings. His hygiene was poor, he made little eye contact, and reportedly heard voices. Two days after admission, he emphatically denied suicidal or homicidal ideation and was discharged against medical advice.
Two weeks later, Mr. F was readmitted after his symptoms worsened. He said voices told him that he was a cousin to Jesus Christ and that he had telepathic abilities. He also reported visual hallucinations.
Twice divorced, Mr. F has three uncles who have been diagnosed with schizophrenia. His late father had a history of alcohol abuse, and his late mother suffered from Alzheimer’s disease.
Mr. F lived a normal life until 1975, when he began drinking heavily. Three years later, he quit his job of 11 years at the local airport. At that time, he told a psychiatrist that “people are out to get me. I feel nervous a lot.” He was diagnosed as having generalized anxiety disorder and treated with diazepam, 20 mg/d.
Four months later he complained of severe insomnia, was diagnosed with depression, and was prescribed amitriptyline, 100 mg at bedtime. He was hospitalized 1 week later after he complained of chest pain and expressed paranoid thoughts. During the 3-week hospitalization, he experienced persecutory delusions and heard voices telling him he was “damned.” He was diagnosed with paranoid schizophrenia and alcohol dependence. The amitriptyline was stopped, and Mr. F was discharged on chlorpromazine, 300 mg/d.
From 1978 to 1995, Mr. F was hospitalized 35 times, often at his family’s urging after he made threats or became violent at home. He once kicked his elderly father and another time was jailed after a domestic violence incident. Religious delusions characterized his thought content. Thought blocking, flight of ideas, and somatic and sexual delusions were also apparent.
Was Mr. F’s diagnosis accurate, or do his frequent psychotic episodes meet criteria for a type of mania?
Dr. Canive’s observations
Diagnoses of mania or mood disorder with psychotic features were not considered because Mr. F never experienced a distinct period of persistently expansive or depressed mood.
Mr. F’s initial complaints of increased anxiety and depression were considered prodromal symptoms of schizophrenia and may have reflected his inability to discuss or cope with his delusions and hallucinations during the initial evaluation. What’s more, his occupational functioning gradually deteriorated months before his initial mental health assessment.
TREATMENT: Many medications, no progress
At different times from 1978 to 1995, Mr. F had taken chlorpromazine, 100 to 300 mg/d; thioridazine, 50 to 200 mg/d; loxapine, 25 mg/d; fluphenazine, 5 to 10 mg/d; haloperidol, 2 to 4 mg/d, and fluphenazine decanoate, 3.125 to 6.25 mg biweekly, as well as concomitant anticholinergics, benzodiazepines, or other hypnotics.
A closer look at Mr. F’s chart revealed that medication noncompliance often preceded hospitalization. He was extremely prone to antipsychotic-related extrapyramidal symptoms (EPS), even at low dosages. Whenever motor symptoms surfaced, he would stop taking his antipsychotics.
Buccolingual tardive dyskinesia (TD) was first noticed in 1987. Four years later, an Abnormal Involuntary Movement Scale (AIMS) exam revealed mild TD that was managed with vitamin E, 400 IU/d.
While hospitalized, Mr. F many times received injectable antipsychotics and benzodiazepines, mostly to control violence. Depot antipsychotics also were tried in an effort to promote compliance, but recurrent alcohol abuse often triggered a relapse.
How would you confront Mr. F’s history of noncompliance? Can his delusions be controlled without prompting severe motor effects?
Dr. Canive’s observations
For Mr. F, poor tolerability, incomplete efficacy, and variable compliance have repeatedly led to symptom exacerbation and hospitalization. Low dosing because of sensitivity to EPS may partially explain his insufficient response to antipsychotics.
In 1995, after numerous unsuccessful drug treatments, we considered entering Mr. F into a phase II clinical trial of the atypical antipsychotic aripiprazole.
Now FDA-approved for treatment of schizophrenia, aripiprazole decreases dopaminergic transmission in the nigrostriatal and tuberoinfundibular pathways, thus reducing the likelihood of EPS.1,2 Also, aripiprazole’s dopamine-serotonin stabilization effects have been reported in clinical trials to improve tolerability, compliance, and overall effectiveness in patients with schizophrenia.3
Common side effects of aripiprazole are mild nausea, insomnia, and restlessness, although data indicate that these effects have a low prevalence and disappear within 2 weeks. If insomnia and restlessness are prominent, a low-dose, short-acting benzodiazepine may be added, tapered after 1 week, and discontinued at week 2.
Table
Mr. F’s progress while taking aripiprazole, 1995-2003
| Visit | CGI-S | CGI-G | PANSS Positive | PANSS Negative | PANSS total | Clinical correlates |
|---|---|---|---|---|---|---|
| Baseline | 4 | 5 | 24 | 21 | 94 | —- |
| Week 2 | 3 | 2 | N/A | N/A | N/A | Positive, negative symptoms much improved |
| Week 12 | 3 | 2 | 11 | 16 | 56 | Mr. F’s understanding about his illness, life, socioeconomic issues much improved |
| Week 76 | 3 | 2 | 11 | 18 | 56 | Activity level increased; starts doing yard work to supplement disability income |
| Week 88 | 3 | 2 | 12 | 14 | 52 | Volunteers as courier at local hospital; continues to do yard work |
| Week 226 | 2 | 2 | 9 | 12 | 42 | Starts steady work as a janitor and security aid |
| Week 284 | 2 | 2 | 9 | 14 | 45 | Concerned about losing Social Security benefits, since he is working 40 hours a week. |
| Week 328 | 3 | 1 | 11 | 15 | 52 | Discharged from hospital after psychotic relapse. Looking for apartment. |
| Week 384 (Final visit) | 3 | 1 | 9 | 12 | 45 | Father died the previous week. Mr. F accepted his father’s passing well. Open-label study terminated. Patient continued on aripiprazole, 20 mg/d. |
What the scores mean
Clinical Global Impression-Severity of Illness (CGI-S)—Scores range from 1 to 7, with 1 meaning normal (normal, minimal, mild, moderate, moderately severe, severe, among the most extreme).
Clinical Global Impression-Global Improvement (CGI-G)—Scores range from 1 to 7, with 1 meaning very much improved (very much improved, much improved, improved, unchanged, little worse, much worse, very much worse).
Positive and Negative Syndrome Scale (PANSS) Positive—consists of 7 items (delusions, conceptual disorganization, hallucinatory behavior, excitement, grandiosity, suspiciousness/persecution, hostility); scores range from 7 to 49 and decrease as patients improve.
PANSS Negative—consists of 7 items (blunted affect, emotional withdrawal, poor rapport, passive pathetic withdrawal, difficulty in abstract thinking, lack of spontaneity and flow of conversation, stereotyped thinking); scores range from 7 to 49 and decrease as patients improve.
PANSS General—consists of 16 items (somatic concern, anxiety, guilt feelings, tension, mannerism and posturing, depression, motor retardation, uncooperativeness, unusual thought content, disorientation, poor attention, lack of judgment and insight, disturbance of volition, poor impulse control, preoccupation, active social avoidance). Scores range from 16 to 112 and decrease as patients improve.
CONTINUED TREATMENT: A new trial
Mr. F participated in a 4-week, double-blind, placebo-controlled trial of aripiprazole, 2, 10, or 30 mg/d, versus haloperidol, 10 mg/d.
One month later, he entered a second aripiprazole trial: a 4-day, open-label study starting at 5 mg/d with titration to 20 mg/d. In the interval between the two trials, Mr. F was prescribed thiothixene, 10 mg/d, and benztropine, 2 mg at bedtime.
During the 4-day trial, he complained of insomnia and was given chloral hydrate, 500 to 1,000 mg at bedtime. He also complained of anxiety and was started on lorazepam, 2 mg bid.
After completing the open-label aripiprazole trial, Mr. F exhibited no behavioral problems and complied with ward routine. He was discharged after 17 days, at which time he denied auditory or visual hallucinations. His thinking seemed clear and his insight improved. His Global Assessment of Functioning (GAF) score at discharge was 55, suggesting moderate symptoms and difficulty in social and occupational functioning.
For the next 5 1/2 years, Mr. F was maintained on aripiprazole, 20 mg/d, as part of the same ongoing open-label trial. During that period he also took lorazepam, 1 mg bid prn; oxazepam, 15 mg bid; or clonazepam, 0.5 mg bid, for anxiety.
Mr. F. exhibited significant sustained improvement as measured with the Positive and Negative Symptom Scale (PANSS), Clinical Global Impression scale (CGI), and GAF (Table). His TD remained mild throughout the trial, as determined through AIMS scores. He also reported no EPS, akathisia, or other adverse events.
About 18 months after starting aripiprazole, Mr. F resumed working part time. In September 2001, he stopped receiving disability benefits and started supporting himself again.
FOLLOW-UP: ‘The voices were ugly’
In December 2001, after 6 years without hospitalization, Mr. F was back in the psychiatric ward. One week before admission, he reported that he had been having panic attacks because “the voices were ugly.” He only slept 4 to 5 hours per night.
He then revealed that he had stopped taking aripiprazole for 2 weeks because he had no longer felt ill. He was still taking his lorazepam, however.
Mr. F appeared mildly anxious upon presentation and his affect was blunted. On examination, his thought processes were linear; he was once again hearing voices and experiencing delusions of telepathic control.
The patient was placed back on aripiprazole, 20 mg/d. His behavior on the ward improved dramatically, and the frequency and severity of his delusions and auditory hallucinations decreased gradually.
At discharge, Mr. F’s insight was good, his delusions had disappeared, and auditory hallucinations were rare. He was instructed to continue the aripiprazole and was prescribed clonazepam, 0.5 mg bid, for his anxiety and trazodone, 50 mg at bed-time, to help his sleep.
Since then, Mr. F has lived on his own, is working steadily, and has not required hospitalization. He stopped taking trazodone soon after discharge, but continues taking aripiprazole and clonazepam as prescribed. His hygiene is good, and he is making amends with family members. He attends church every Sunday—free of the messianic delusions that once tormented him. He also stopped abusing alcohol on his own in 1995 and has remained abstinent since.
How can we ensure that patients with schizophrenia keep taking their medications—regardless of whether symptoms are present?
Dr. Canive’s observations
Clinical trials measure a drug’s efficacy under highly controlled circumstances. In the “real world,” however, noncompliance due to intolerability can undermine a medication’s effectiveness.
Too often noncompliance—stemming from abatement of symptoms or the emergence of side effects—derails treatment of schizophrenia. Misdrahi et al found that medication noncompliance accounts for 40% of schizophrenia relapses occurring more than 1 year after patients’ first hospitalization.4
Given aripiprazole’s 75-hour half-life, one might not expect to see symptoms emerge so soon after discontinuation. It is possible that:
- Mr. F. abstained from aripiprazole longer than he realized—or admitted
- Unidentified stressful life events also exacerbated symptoms and precipitated hospitalization.
When Mr. F consistently followed his regimen, his positive symptoms abated and he could attempt to live a normal life.
Our patients must understand that schizophrenia is a lifelong illness and that continued adherence to medication—even when symptoms do not exist—is crucial. A strong therapeutic alliance,5 increased social support, adjunctive cognitive-behavioral therapy, psychosocial interventions,6 and medications with fewer and less-severe side effects may help patients embrace this message.
Related resources
- Tamminga CA. Partial dopamine agonists in the treatment of psychosis. J Neural Transm 2002;109:411-20.
Drug brand names
- Amitriptyline • Elavil
- Aripiprazole • Abilify
- Benztropine • Cogentin
- Chlorpromazine • Thorazine
- Clonazepam • Klonopin
- Diazepam • Valium
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Lorazepam • Ativan
- Loxapine • Loxitane
- Oxazepam • Serax
- Thiothixene • Navane
- Trazodone • Desyrel
Disclosure
The author receives research/grant support from and is a speaker for and consultant to Bristol-Myers Squibb Co. He also receives research/grant support from and/or is a speaker for AstraZeneca Pharmaceuticals, Janssen Pharmaceutica, and Eli Lilly and Co.
HISTORY: Jesus’ ‘cousin’
Mr. F, age 60, was hospitalized in May 1995 after expressing fear he would hurt—or kill—himself or someone else. He cooperated with admission procedures but refused to participate in ward activities or meetings. His hygiene was poor, he made little eye contact, and reportedly heard voices. Two days after admission, he emphatically denied suicidal or homicidal ideation and was discharged against medical advice.
Two weeks later, Mr. F was readmitted after his symptoms worsened. He said voices told him that he was a cousin to Jesus Christ and that he had telepathic abilities. He also reported visual hallucinations.
Twice divorced, Mr. F has three uncles who have been diagnosed with schizophrenia. His late father had a history of alcohol abuse, and his late mother suffered from Alzheimer’s disease.
Mr. F lived a normal life until 1975, when he began drinking heavily. Three years later, he quit his job of 11 years at the local airport. At that time, he told a psychiatrist that “people are out to get me. I feel nervous a lot.” He was diagnosed as having generalized anxiety disorder and treated with diazepam, 20 mg/d.
Four months later he complained of severe insomnia, was diagnosed with depression, and was prescribed amitriptyline, 100 mg at bedtime. He was hospitalized 1 week later after he complained of chest pain and expressed paranoid thoughts. During the 3-week hospitalization, he experienced persecutory delusions and heard voices telling him he was “damned.” He was diagnosed with paranoid schizophrenia and alcohol dependence. The amitriptyline was stopped, and Mr. F was discharged on chlorpromazine, 300 mg/d.
From 1978 to 1995, Mr. F was hospitalized 35 times, often at his family’s urging after he made threats or became violent at home. He once kicked his elderly father and another time was jailed after a domestic violence incident. Religious delusions characterized his thought content. Thought blocking, flight of ideas, and somatic and sexual delusions were also apparent.
Was Mr. F’s diagnosis accurate, or do his frequent psychotic episodes meet criteria for a type of mania?
Dr. Canive’s observations
Diagnoses of mania or mood disorder with psychotic features were not considered because Mr. F never experienced a distinct period of persistently expansive or depressed mood.
Mr. F’s initial complaints of increased anxiety and depression were considered prodromal symptoms of schizophrenia and may have reflected his inability to discuss or cope with his delusions and hallucinations during the initial evaluation. What’s more, his occupational functioning gradually deteriorated months before his initial mental health assessment.
TREATMENT: Many medications, no progress
At different times from 1978 to 1995, Mr. F had taken chlorpromazine, 100 to 300 mg/d; thioridazine, 50 to 200 mg/d; loxapine, 25 mg/d; fluphenazine, 5 to 10 mg/d; haloperidol, 2 to 4 mg/d, and fluphenazine decanoate, 3.125 to 6.25 mg biweekly, as well as concomitant anticholinergics, benzodiazepines, or other hypnotics.
A closer look at Mr. F’s chart revealed that medication noncompliance often preceded hospitalization. He was extremely prone to antipsychotic-related extrapyramidal symptoms (EPS), even at low dosages. Whenever motor symptoms surfaced, he would stop taking his antipsychotics.
Buccolingual tardive dyskinesia (TD) was first noticed in 1987. Four years later, an Abnormal Involuntary Movement Scale (AIMS) exam revealed mild TD that was managed with vitamin E, 400 IU/d.
While hospitalized, Mr. F many times received injectable antipsychotics and benzodiazepines, mostly to control violence. Depot antipsychotics also were tried in an effort to promote compliance, but recurrent alcohol abuse often triggered a relapse.
How would you confront Mr. F’s history of noncompliance? Can his delusions be controlled without prompting severe motor effects?
Dr. Canive’s observations
For Mr. F, poor tolerability, incomplete efficacy, and variable compliance have repeatedly led to symptom exacerbation and hospitalization. Low dosing because of sensitivity to EPS may partially explain his insufficient response to antipsychotics.
In 1995, after numerous unsuccessful drug treatments, we considered entering Mr. F into a phase II clinical trial of the atypical antipsychotic aripiprazole.
Now FDA-approved for treatment of schizophrenia, aripiprazole decreases dopaminergic transmission in the nigrostriatal and tuberoinfundibular pathways, thus reducing the likelihood of EPS.1,2 Also, aripiprazole’s dopamine-serotonin stabilization effects have been reported in clinical trials to improve tolerability, compliance, and overall effectiveness in patients with schizophrenia.3
Common side effects of aripiprazole are mild nausea, insomnia, and restlessness, although data indicate that these effects have a low prevalence and disappear within 2 weeks. If insomnia and restlessness are prominent, a low-dose, short-acting benzodiazepine may be added, tapered after 1 week, and discontinued at week 2.
Table
Mr. F’s progress while taking aripiprazole, 1995-2003
| Visit | CGI-S | CGI-G | PANSS Positive | PANSS Negative | PANSS total | Clinical correlates |
|---|---|---|---|---|---|---|
| Baseline | 4 | 5 | 24 | 21 | 94 | —- |
| Week 2 | 3 | 2 | N/A | N/A | N/A | Positive, negative symptoms much improved |
| Week 12 | 3 | 2 | 11 | 16 | 56 | Mr. F’s understanding about his illness, life, socioeconomic issues much improved |
| Week 76 | 3 | 2 | 11 | 18 | 56 | Activity level increased; starts doing yard work to supplement disability income |
| Week 88 | 3 | 2 | 12 | 14 | 52 | Volunteers as courier at local hospital; continues to do yard work |
| Week 226 | 2 | 2 | 9 | 12 | 42 | Starts steady work as a janitor and security aid |
| Week 284 | 2 | 2 | 9 | 14 | 45 | Concerned about losing Social Security benefits, since he is working 40 hours a week. |
| Week 328 | 3 | 1 | 11 | 15 | 52 | Discharged from hospital after psychotic relapse. Looking for apartment. |
| Week 384 (Final visit) | 3 | 1 | 9 | 12 | 45 | Father died the previous week. Mr. F accepted his father’s passing well. Open-label study terminated. Patient continued on aripiprazole, 20 mg/d. |
What the scores mean
Clinical Global Impression-Severity of Illness (CGI-S)—Scores range from 1 to 7, with 1 meaning normal (normal, minimal, mild, moderate, moderately severe, severe, among the most extreme).
Clinical Global Impression-Global Improvement (CGI-G)—Scores range from 1 to 7, with 1 meaning very much improved (very much improved, much improved, improved, unchanged, little worse, much worse, very much worse).
Positive and Negative Syndrome Scale (PANSS) Positive—consists of 7 items (delusions, conceptual disorganization, hallucinatory behavior, excitement, grandiosity, suspiciousness/persecution, hostility); scores range from 7 to 49 and decrease as patients improve.
PANSS Negative—consists of 7 items (blunted affect, emotional withdrawal, poor rapport, passive pathetic withdrawal, difficulty in abstract thinking, lack of spontaneity and flow of conversation, stereotyped thinking); scores range from 7 to 49 and decrease as patients improve.
PANSS General—consists of 16 items (somatic concern, anxiety, guilt feelings, tension, mannerism and posturing, depression, motor retardation, uncooperativeness, unusual thought content, disorientation, poor attention, lack of judgment and insight, disturbance of volition, poor impulse control, preoccupation, active social avoidance). Scores range from 16 to 112 and decrease as patients improve.
CONTINUED TREATMENT: A new trial
Mr. F participated in a 4-week, double-blind, placebo-controlled trial of aripiprazole, 2, 10, or 30 mg/d, versus haloperidol, 10 mg/d.
One month later, he entered a second aripiprazole trial: a 4-day, open-label study starting at 5 mg/d with titration to 20 mg/d. In the interval between the two trials, Mr. F was prescribed thiothixene, 10 mg/d, and benztropine, 2 mg at bedtime.
During the 4-day trial, he complained of insomnia and was given chloral hydrate, 500 to 1,000 mg at bedtime. He also complained of anxiety and was started on lorazepam, 2 mg bid.
After completing the open-label aripiprazole trial, Mr. F exhibited no behavioral problems and complied with ward routine. He was discharged after 17 days, at which time he denied auditory or visual hallucinations. His thinking seemed clear and his insight improved. His Global Assessment of Functioning (GAF) score at discharge was 55, suggesting moderate symptoms and difficulty in social and occupational functioning.
For the next 5 1/2 years, Mr. F was maintained on aripiprazole, 20 mg/d, as part of the same ongoing open-label trial. During that period he also took lorazepam, 1 mg bid prn; oxazepam, 15 mg bid; or clonazepam, 0.5 mg bid, for anxiety.
Mr. F. exhibited significant sustained improvement as measured with the Positive and Negative Symptom Scale (PANSS), Clinical Global Impression scale (CGI), and GAF (Table). His TD remained mild throughout the trial, as determined through AIMS scores. He also reported no EPS, akathisia, or other adverse events.
About 18 months after starting aripiprazole, Mr. F resumed working part time. In September 2001, he stopped receiving disability benefits and started supporting himself again.
FOLLOW-UP: ‘The voices were ugly’
In December 2001, after 6 years without hospitalization, Mr. F was back in the psychiatric ward. One week before admission, he reported that he had been having panic attacks because “the voices were ugly.” He only slept 4 to 5 hours per night.
He then revealed that he had stopped taking aripiprazole for 2 weeks because he had no longer felt ill. He was still taking his lorazepam, however.
Mr. F appeared mildly anxious upon presentation and his affect was blunted. On examination, his thought processes were linear; he was once again hearing voices and experiencing delusions of telepathic control.
The patient was placed back on aripiprazole, 20 mg/d. His behavior on the ward improved dramatically, and the frequency and severity of his delusions and auditory hallucinations decreased gradually.
At discharge, Mr. F’s insight was good, his delusions had disappeared, and auditory hallucinations were rare. He was instructed to continue the aripiprazole and was prescribed clonazepam, 0.5 mg bid, for his anxiety and trazodone, 50 mg at bed-time, to help his sleep.
Since then, Mr. F has lived on his own, is working steadily, and has not required hospitalization. He stopped taking trazodone soon after discharge, but continues taking aripiprazole and clonazepam as prescribed. His hygiene is good, and he is making amends with family members. He attends church every Sunday—free of the messianic delusions that once tormented him. He also stopped abusing alcohol on his own in 1995 and has remained abstinent since.
How can we ensure that patients with schizophrenia keep taking their medications—regardless of whether symptoms are present?
Dr. Canive’s observations
Clinical trials measure a drug’s efficacy under highly controlled circumstances. In the “real world,” however, noncompliance due to intolerability can undermine a medication’s effectiveness.
Too often noncompliance—stemming from abatement of symptoms or the emergence of side effects—derails treatment of schizophrenia. Misdrahi et al found that medication noncompliance accounts for 40% of schizophrenia relapses occurring more than 1 year after patients’ first hospitalization.4
Given aripiprazole’s 75-hour half-life, one might not expect to see symptoms emerge so soon after discontinuation. It is possible that:
- Mr. F. abstained from aripiprazole longer than he realized—or admitted
- Unidentified stressful life events also exacerbated symptoms and precipitated hospitalization.
When Mr. F consistently followed his regimen, his positive symptoms abated and he could attempt to live a normal life.
Our patients must understand that schizophrenia is a lifelong illness and that continued adherence to medication—even when symptoms do not exist—is crucial. A strong therapeutic alliance,5 increased social support, adjunctive cognitive-behavioral therapy, psychosocial interventions,6 and medications with fewer and less-severe side effects may help patients embrace this message.
Related resources
- Tamminga CA. Partial dopamine agonists in the treatment of psychosis. J Neural Transm 2002;109:411-20.
Drug brand names
- Amitriptyline • Elavil
- Aripiprazole • Abilify
- Benztropine • Cogentin
- Chlorpromazine • Thorazine
- Clonazepam • Klonopin
- Diazepam • Valium
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Lorazepam • Ativan
- Loxapine • Loxitane
- Oxazepam • Serax
- Thiothixene • Navane
- Trazodone • Desyrel
Disclosure
The author receives research/grant support from and is a speaker for and consultant to Bristol-Myers Squibb Co. He also receives research/grant support from and/or is a speaker for AstraZeneca Pharmaceuticals, Janssen Pharmaceutica, and Eli Lilly and Co.
1. Aripiprazole prescribing information. Bristol-Myers Squibb Co. and Otsuka America Pharmaceutical, 2002.
2. Kane JM, Carson WH, Saha AR, et al. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry 2002;63:763-71.
3. Burris KD, Molski TF, Xu C, et al. Aripiprazole, a novel antipsychotic, is a high-affinity partial agonist at human dopamine D2 receptors. J Pharmacol Exp Ther 2002;302:381-9.
4. Misdrahi D, Llorca PM, Lancon C, Bayle FJ. Compliance in schizophrenia: Predictive factors, therapeutical considerations and research implications (French). Encephale 2002;3:266-72.
5. Weiss KA, Smith TE, Hull JW, et al. Predictors of risk of nonadherence in outpatients with schizophrenia and other psychotic disorders. Schizophr Bull 2002;28:341-9.
6. Perkins DO. Predictors of noncompliance in patients with schizophrenia. J Clin Psychiatry 2002;63:1121-8.
1. Aripiprazole prescribing information. Bristol-Myers Squibb Co. and Otsuka America Pharmaceutical, 2002.
2. Kane JM, Carson WH, Saha AR, et al. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry 2002;63:763-71.
3. Burris KD, Molski TF, Xu C, et al. Aripiprazole, a novel antipsychotic, is a high-affinity partial agonist at human dopamine D2 receptors. J Pharmacol Exp Ther 2002;302:381-9.
4. Misdrahi D, Llorca PM, Lancon C, Bayle FJ. Compliance in schizophrenia: Predictive factors, therapeutical considerations and research implications (French). Encephale 2002;3:266-72.
5. Weiss KA, Smith TE, Hull JW, et al. Predictors of risk of nonadherence in outpatients with schizophrenia and other psychotic disorders. Schizophr Bull 2002;28:341-9.
6. Perkins DO. Predictors of noncompliance in patients with schizophrenia. J Clin Psychiatry 2002;63:1121-8.
Birds, butterflies and bullfrogs: When patients ‘see things’
HISTORY: A sudden vision
Ms. K, 73, was in reasonably good health when one day she suddenly noticed red, green, and yellow birds and butterflies covering her wall.
Ms. K, who lives alone, was frightened at first, but she did not immediately alert anyone because she thought she “was just seeing things, and they’ll go away.”
Instead, she saw more visions over the next 3 months. She once “watched” as two doctors and a nun carried a middle-aged burn victim into her apartment. She remembers seeing the doctors put a “patch” over the woman’s body. To Ms. K, this experience seemed so shockingly real that she called 911, reporting, “That woman should have been in the hospital!”
She reports that a pack of butterflies once “followed” her to the market. She vividly recalls how they crawled about her shoes and legs as she entered the store. When asked if anyone noticed her insect-covered extremities, she replied matter-of-factly, “Maybe it’s not for them to see, maybe it’s just for me,” as if her hallucinations were a divine gift.
Ms. K’s hallucinations usually occur at home, where she spends most of her time. She says that the images are fleeting, lasting from a few seconds to several minutes, and that the creatures fly silently around her room.
Ms. K’s daughter grew concerned that the hallucinations were increasingly diminishing her mother’s ability to care for herself. She brought Ms. K into our emergency department, from which the patient was admitted.
On admission, Ms. K said she had lost 20 lbs within 6 months, and that “concentrating on those things in the house” was impairing her sleep. She denied recent illness, trauma, loss of conscious ness, changes in medications, seizures, drug or alcohol use, suicidal or homicidal ideation, or specific stress in her life. She added that she often cooks for herself—only to lose her appetite after seeing bugs and other creatures crawl into her food.
Her medical history includes hypertension, type 2 diabetes mellitus, peripheral vascular disease, urinary incontinence, gastroesophageal reflux, glaucoma in her left eye, and bilateral cataracts. She denies any psychiatric history and adds that she had never experienced hallucinations until about 3 months before hospitalization. She also denies any history of auditory, tactile, or olfactory hallucinations.
Would you suspect a primary psychotic illness? What clinical tests might help us understand Ms. K’s progressively debilitating visual hallucinations?
The authors’ observations
Ms. K’s case places us at the crossroads of psychiatric disturbances and medical conditions that can present as or precipitate apparent psychiatric symptoms. Delirium, dementia, psychosis, endocrinopathies, encephalitis, electrolyte disturbances, drug abuse/withdrawal, and occipital or temporal lobe seizures are all possible differential diagnoses (Table 1).
A cognitive function screening and a battery of laboratory tests, imaging scans, and neurologic and vision exams are needed to uncover the cause of her hallucinations.
EVALUATION: Looking for clues
Ms. K’s left pupil was fixed at 6 mm and did not respond to light, while the right pupil was regular and reactive to light at 3 mm. Using a Snellen eye chart, her visual acuity was poor: 20/100 to 20/200 in her right eye and less than 20/200 in the left eye. She scored a 29 out of 30 on the Folstein Mini-Mental State Examination (MMSE), indicating her cognition was intact. The remainder of the neurologic exam was unremarkable.
At admission, Ms. K’s medications included metoprolol, 100 mg qd, for hypertension; lansoprazole, 30 mg qd, for gastroesophageal reflux; tolterodine, 2 mg bid, and oxybutynin, 10 mg qd, for urinary incontinence; repaglinide, 2 mg bid, for type 2 diabetes; and three ophthalmic agents: brimonidine, prednisolone, and dorzolamide/timolol. The patient had been maintained on these medications for more than 2 years with no recent changes in dosing.
Results of Ms. K’s lab studies were normal, including a basic metabolic panel, CBC, liver function tests, urinalysis, B12, thyroid panel, rapid plasma reagin test, and urine drug screen.
A head CT without contrast revealed chronic small-vessel ischemic white matter disease and a chronic infarct of the left cerebellar hemisphere. No acute intracranial hemorrhages, masses, or other abnormalities were noted. No seizures were seen on EEG.
Table 1
Common causes of visual hallucinations
| Schizophrenia |
| Delirium |
| Dementias |
| Substance-induced psychosis |
| Electrolyte disturbances |
| Occipital and temporal lobe epilepsy |
| Charles Bonnet syndrome |
What do the laboratory and imaging tests reveal about Ms. K’s hallucinations? Is her diagnosis delirium? Alzheimer’s or other type of dementia? Schizophrenia?
The authors’ observations
Visual hallucinations—often of deceased parents or siblings, unknown intruders, and animals—can occur in up to 25% of patients with Alzheimer’s-type dementia.1 Also, patients with Lewy body dementia often present with well-formed visual hallucinations, which are thought to result from temporal lobe involvement by the characteristic Lewy bodies.
To diagnose dementia, DSM-IV requires the presence of multiple cognitive deficits manifested by memory impairment and one or more of the following:
- aphasia
- apraxia
- agnosia
- disturbance of executive functioning.2
Ms. K exhibited none of these characteristics, and she retained full executive function—she could balance her checkbook, buy groceries, and cook for herself. Also, her MMSE score was high.
Ms. K showed no consciousness fluctuations or attention deficits, two features commonly seen in delirium. She was alert and oriented throughout the interview, and her flow of thought, speech, language, and attention were appropriate. Therefore, delirium can be reasonably excluded.
The hallucinations probably do not signal onset of schizophrenia because of Ms. K’s age at presentation, lack of family history of psychotic disorder, and paucity of negative symptoms. Auditory hallucinations are much more common in psychosis, and isolated visual hallucinations rarely occur in schizophrenia.
Finally, Ms. K’s electrophysiologic, laboratory, and imaging studies revealed isolated systolic hypertension, low visual acuity, and a mild gait disturbance. Severe left lens opacification accounted for the patient’s discordant pupillary light reflex. None of these findings explained her visual hallucinations, however.
Is a non-psychiatric disorder causing Ms. K’s hallucinations? What type of medication might alleviate her symptoms?
The authors’ observations
Given Ms. K’s strong cognitive function and poor visual acuity, we concluded that her hallucinations may fit the criteria for Charles Bonnet syndrome (CBS), a poorly understood medical phenomenon.
CBS is characterized by complex visual hallucinations in visually impaired elderly patients without cognitive deficits (Table 2).3,4 Swiss philosopher Charles Bonnet first described the disorder in 1760 to explain the vivid visual hallucinations of his 89-year-old grandfather, who had severe cataracts but no cognitive deficits.3 Bonnet’s grandfather claimed to have visions of men, women, birds, buildings, and tapestries.3
CBS is increasingly recognized and reported, but the medical community has never formed a universally accepted definition for this phenomenon. Persons with CBS react positively or negatively to their hallucinations, and the images may stimulate anxiety, anger, or mild paranoia. Research has focused on prevalence, risk indicators, and treatment.
Table 2
Charles Bonnet syndrome: fast facts
|
Teunisse et al determined that visual hallucinations plague up to 14% of sight-impaired persons.4,5 The hallucinations vary widely: people, animals, flowers, vehicles, buildings, and sometimes complete scenes.4,5 Significant risk factors for CBS include advanced age and low visual acuity.4,5 Loneliness, introversion, and shyness are additional risk indicators in older, visually handicapped persons.6 Therefore, social isolation may be a predisposing factor.
Drug treatment of visual hallucinations in CBS currently includes antipsychotics, such as quetiapine (25 to 100 mg/d) and risperidone (0.25 to 1.0 mg/d).7 However, mixed results have been reported after use of antipsychotics in CBS; one patient’s visual hallucinations were exacerbated after risperidone was initiated.8 Case reports have also described the use of valproate, carbamazepine, and ondansetron in CBS.9-11
Empathy and patient education are the cornerstones of CBS treatment.3 Patients need to be reassured that their visions are benign. For many, simply increasing the amount of ambient light in the home can reduce hallucinations.
TREATMENT A frog in the toilet
Ms. K was started on quetiapine, 25 mg bid, to try to promote restorative sleep and resolve her hallucinations. Up to 18% of persons treated with quetiapine report somnolence as an adverse effect, vs. 3 to 8% of those treated with risperidone.12
During her hospital stay, Ms. K experienced no visual hallucinations during the day but reported seeing a grayish-brown bullfrog in the toilet at night. This hallucination did not frighten her; she would simply close the bathroom door and wait until the bullfrog “disappeared.”
Her sleep improved, as did her appetite. She participated in daily group sessions and socialized with other patients.
After 12 days, Ms. K was discharged. To decrease her social isolation, we encouraged her to participate in a day program for seniors. We also continued her on quetiapine, 25 mg bid.
Five months later, her primary care physician reports that Ms. K remains symptom free while maintaining her quetiapine dosage.
Related resources
- Royal National Institute of the Blind: Fact sheet for Charles Bonnet syndrome. Available at: http://www.rnib.org.uk/info/cbsfin.htm
- Verstraten PFJ. The Charles Bonnet syndrome: Development of a protocol for clinical practice in a multidisciplinary approach from assessment to intervention. Available at: http://www.rehab-syn.enter.iris.se/kc-syn/cb.htm
- Adamczyk DT. Optometric educators. Am I seeing things? Optometry Today June 18, 1999:37-9. Available at: http://www.optometry.co.uk/articles/19990618/Adamczyk.pdf
Drug brand names
- Brimonidine Ophthalmic • Alphagan
- Carbamazepine • Tegretol
- Dorzolamide/Timolol • Cosopt
- Lansoprazole • Prevacid
- Metoprolol • Toprol XL
- Ondansetron • Zofran
- Oxybutynin • Ditropan XL
- Quetiapine • Seroquel
- Repaglinide • Prandin
- Risperidone • Risperdal
- Tolterodine • Detrol
- Valproate • Depakote
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with competing manufacturers.
1. Geldmacher DS, Whitehouse PJ. Current concepts: evaluation of dementia. JAMA 1996;335:330-6.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, rev). Washington, DC: American Psychiatric Press, 2000.
3. Fernandez A, Lichtshein G, Vieweg WV. The Charles Bonnet syndrome: a review. J Nerv Ment Dis 1997;185:195-200.
4. Teunisse RJ, Cruysberg , JR, Hoefnagels WH, et al. Risk indicators for the Charles Bonnet syndrome. J Nerv Ment Dis 1998;186:190-2.
5. Teunisse RJ, Cruysberg J, Verbeek A, Zitman FG. The Charles Bonnet syndrome: a large prospective study in the Netherlands. A study of the prevalence of the Charles Bonnet syndrome and associated factors in 500 patients attending the University Department of Ophthalmology at Nijme. Br J Psychiatry 1995;166(2):254-7.
6. Teunisse RJ, Cruysberg JR, Hoefnagels WH, et al. Social and psychological characteristics of elderly visually handicapped patients with the Charles Bonnet Syndrome. Compr Psychiatry 1999;40(4):315-19.
7. Rovner BW. The Charles Bonnet syndrome: Visual hallucinations caused by visual impairment. Geriatrics 2002;57:45-6.
8. Kornreich C, Dan B, Verbanck P, Pelc I. Treating Charles Bonnet syndrome: understanding inconsistency. J Clin Psychopharmacol 2000;20(3):396.-
9. Hori H, Terao T, Shiraishi Y, Nakamura J. Treatment of Charles Bonnet syndrome with valproate. Int Clin Psychopharmacol 2000;15:117-19.
10. Batra A, Bartels M, Wormstall H. Therapeutic options in Charles Bonnet syndrome. Acta Psychiatr Scand 1997;96:129-33.
11. Nevins M. Charles Bonnet syndrome. J Am Geriatr Soc 1997;45:894.-
12. Brown C, Markowitz J, Moore T, Parker N. Atypical antipsychotics, part II: adverse effects, drug interactions, and efficacy. Ann Pharmacother 1999;33:210-17.
HISTORY: A sudden vision
Ms. K, 73, was in reasonably good health when one day she suddenly noticed red, green, and yellow birds and butterflies covering her wall.
Ms. K, who lives alone, was frightened at first, but she did not immediately alert anyone because she thought she “was just seeing things, and they’ll go away.”
Instead, she saw more visions over the next 3 months. She once “watched” as two doctors and a nun carried a middle-aged burn victim into her apartment. She remembers seeing the doctors put a “patch” over the woman’s body. To Ms. K, this experience seemed so shockingly real that she called 911, reporting, “That woman should have been in the hospital!”
She reports that a pack of butterflies once “followed” her to the market. She vividly recalls how they crawled about her shoes and legs as she entered the store. When asked if anyone noticed her insect-covered extremities, she replied matter-of-factly, “Maybe it’s not for them to see, maybe it’s just for me,” as if her hallucinations were a divine gift.
Ms. K’s hallucinations usually occur at home, where she spends most of her time. She says that the images are fleeting, lasting from a few seconds to several minutes, and that the creatures fly silently around her room.
Ms. K’s daughter grew concerned that the hallucinations were increasingly diminishing her mother’s ability to care for herself. She brought Ms. K into our emergency department, from which the patient was admitted.
On admission, Ms. K said she had lost 20 lbs within 6 months, and that “concentrating on those things in the house” was impairing her sleep. She denied recent illness, trauma, loss of conscious ness, changes in medications, seizures, drug or alcohol use, suicidal or homicidal ideation, or specific stress in her life. She added that she often cooks for herself—only to lose her appetite after seeing bugs and other creatures crawl into her food.
Her medical history includes hypertension, type 2 diabetes mellitus, peripheral vascular disease, urinary incontinence, gastroesophageal reflux, glaucoma in her left eye, and bilateral cataracts. She denies any psychiatric history and adds that she had never experienced hallucinations until about 3 months before hospitalization. She also denies any history of auditory, tactile, or olfactory hallucinations.
Would you suspect a primary psychotic illness? What clinical tests might help us understand Ms. K’s progressively debilitating visual hallucinations?
The authors’ observations
Ms. K’s case places us at the crossroads of psychiatric disturbances and medical conditions that can present as or precipitate apparent psychiatric symptoms. Delirium, dementia, psychosis, endocrinopathies, encephalitis, electrolyte disturbances, drug abuse/withdrawal, and occipital or temporal lobe seizures are all possible differential diagnoses (Table 1).
A cognitive function screening and a battery of laboratory tests, imaging scans, and neurologic and vision exams are needed to uncover the cause of her hallucinations.
EVALUATION: Looking for clues
Ms. K’s left pupil was fixed at 6 mm and did not respond to light, while the right pupil was regular and reactive to light at 3 mm. Using a Snellen eye chart, her visual acuity was poor: 20/100 to 20/200 in her right eye and less than 20/200 in the left eye. She scored a 29 out of 30 on the Folstein Mini-Mental State Examination (MMSE), indicating her cognition was intact. The remainder of the neurologic exam was unremarkable.
At admission, Ms. K’s medications included metoprolol, 100 mg qd, for hypertension; lansoprazole, 30 mg qd, for gastroesophageal reflux; tolterodine, 2 mg bid, and oxybutynin, 10 mg qd, for urinary incontinence; repaglinide, 2 mg bid, for type 2 diabetes; and three ophthalmic agents: brimonidine, prednisolone, and dorzolamide/timolol. The patient had been maintained on these medications for more than 2 years with no recent changes in dosing.
Results of Ms. K’s lab studies were normal, including a basic metabolic panel, CBC, liver function tests, urinalysis, B12, thyroid panel, rapid plasma reagin test, and urine drug screen.
A head CT without contrast revealed chronic small-vessel ischemic white matter disease and a chronic infarct of the left cerebellar hemisphere. No acute intracranial hemorrhages, masses, or other abnormalities were noted. No seizures were seen on EEG.
Table 1
Common causes of visual hallucinations
| Schizophrenia |
| Delirium |
| Dementias |
| Substance-induced psychosis |
| Electrolyte disturbances |
| Occipital and temporal lobe epilepsy |
| Charles Bonnet syndrome |
What do the laboratory and imaging tests reveal about Ms. K’s hallucinations? Is her diagnosis delirium? Alzheimer’s or other type of dementia? Schizophrenia?
The authors’ observations
Visual hallucinations—often of deceased parents or siblings, unknown intruders, and animals—can occur in up to 25% of patients with Alzheimer’s-type dementia.1 Also, patients with Lewy body dementia often present with well-formed visual hallucinations, which are thought to result from temporal lobe involvement by the characteristic Lewy bodies.
To diagnose dementia, DSM-IV requires the presence of multiple cognitive deficits manifested by memory impairment and one or more of the following:
- aphasia
- apraxia
- agnosia
- disturbance of executive functioning.2
Ms. K exhibited none of these characteristics, and she retained full executive function—she could balance her checkbook, buy groceries, and cook for herself. Also, her MMSE score was high.
Ms. K showed no consciousness fluctuations or attention deficits, two features commonly seen in delirium. She was alert and oriented throughout the interview, and her flow of thought, speech, language, and attention were appropriate. Therefore, delirium can be reasonably excluded.
The hallucinations probably do not signal onset of schizophrenia because of Ms. K’s age at presentation, lack of family history of psychotic disorder, and paucity of negative symptoms. Auditory hallucinations are much more common in psychosis, and isolated visual hallucinations rarely occur in schizophrenia.
Finally, Ms. K’s electrophysiologic, laboratory, and imaging studies revealed isolated systolic hypertension, low visual acuity, and a mild gait disturbance. Severe left lens opacification accounted for the patient’s discordant pupillary light reflex. None of these findings explained her visual hallucinations, however.
Is a non-psychiatric disorder causing Ms. K’s hallucinations? What type of medication might alleviate her symptoms?
The authors’ observations
Given Ms. K’s strong cognitive function and poor visual acuity, we concluded that her hallucinations may fit the criteria for Charles Bonnet syndrome (CBS), a poorly understood medical phenomenon.
CBS is characterized by complex visual hallucinations in visually impaired elderly patients without cognitive deficits (Table 2).3,4 Swiss philosopher Charles Bonnet first described the disorder in 1760 to explain the vivid visual hallucinations of his 89-year-old grandfather, who had severe cataracts but no cognitive deficits.3 Bonnet’s grandfather claimed to have visions of men, women, birds, buildings, and tapestries.3
CBS is increasingly recognized and reported, but the medical community has never formed a universally accepted definition for this phenomenon. Persons with CBS react positively or negatively to their hallucinations, and the images may stimulate anxiety, anger, or mild paranoia. Research has focused on prevalence, risk indicators, and treatment.
Table 2
Charles Bonnet syndrome: fast facts
|
Teunisse et al determined that visual hallucinations plague up to 14% of sight-impaired persons.4,5 The hallucinations vary widely: people, animals, flowers, vehicles, buildings, and sometimes complete scenes.4,5 Significant risk factors for CBS include advanced age and low visual acuity.4,5 Loneliness, introversion, and shyness are additional risk indicators in older, visually handicapped persons.6 Therefore, social isolation may be a predisposing factor.
Drug treatment of visual hallucinations in CBS currently includes antipsychotics, such as quetiapine (25 to 100 mg/d) and risperidone (0.25 to 1.0 mg/d).7 However, mixed results have been reported after use of antipsychotics in CBS; one patient’s visual hallucinations were exacerbated after risperidone was initiated.8 Case reports have also described the use of valproate, carbamazepine, and ondansetron in CBS.9-11
Empathy and patient education are the cornerstones of CBS treatment.3 Patients need to be reassured that their visions are benign. For many, simply increasing the amount of ambient light in the home can reduce hallucinations.
TREATMENT A frog in the toilet
Ms. K was started on quetiapine, 25 mg bid, to try to promote restorative sleep and resolve her hallucinations. Up to 18% of persons treated with quetiapine report somnolence as an adverse effect, vs. 3 to 8% of those treated with risperidone.12
During her hospital stay, Ms. K experienced no visual hallucinations during the day but reported seeing a grayish-brown bullfrog in the toilet at night. This hallucination did not frighten her; she would simply close the bathroom door and wait until the bullfrog “disappeared.”
Her sleep improved, as did her appetite. She participated in daily group sessions and socialized with other patients.
After 12 days, Ms. K was discharged. To decrease her social isolation, we encouraged her to participate in a day program for seniors. We also continued her on quetiapine, 25 mg bid.
Five months later, her primary care physician reports that Ms. K remains symptom free while maintaining her quetiapine dosage.
Related resources
- Royal National Institute of the Blind: Fact sheet for Charles Bonnet syndrome. Available at: http://www.rnib.org.uk/info/cbsfin.htm
- Verstraten PFJ. The Charles Bonnet syndrome: Development of a protocol for clinical practice in a multidisciplinary approach from assessment to intervention. Available at: http://www.rehab-syn.enter.iris.se/kc-syn/cb.htm
- Adamczyk DT. Optometric educators. Am I seeing things? Optometry Today June 18, 1999:37-9. Available at: http://www.optometry.co.uk/articles/19990618/Adamczyk.pdf
Drug brand names
- Brimonidine Ophthalmic • Alphagan
- Carbamazepine • Tegretol
- Dorzolamide/Timolol • Cosopt
- Lansoprazole • Prevacid
- Metoprolol • Toprol XL
- Ondansetron • Zofran
- Oxybutynin • Ditropan XL
- Quetiapine • Seroquel
- Repaglinide • Prandin
- Risperidone • Risperdal
- Tolterodine • Detrol
- Valproate • Depakote
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with competing manufacturers.
HISTORY: A sudden vision
Ms. K, 73, was in reasonably good health when one day she suddenly noticed red, green, and yellow birds and butterflies covering her wall.
Ms. K, who lives alone, was frightened at first, but she did not immediately alert anyone because she thought she “was just seeing things, and they’ll go away.”
Instead, she saw more visions over the next 3 months. She once “watched” as two doctors and a nun carried a middle-aged burn victim into her apartment. She remembers seeing the doctors put a “patch” over the woman’s body. To Ms. K, this experience seemed so shockingly real that she called 911, reporting, “That woman should have been in the hospital!”
She reports that a pack of butterflies once “followed” her to the market. She vividly recalls how they crawled about her shoes and legs as she entered the store. When asked if anyone noticed her insect-covered extremities, she replied matter-of-factly, “Maybe it’s not for them to see, maybe it’s just for me,” as if her hallucinations were a divine gift.
Ms. K’s hallucinations usually occur at home, where she spends most of her time. She says that the images are fleeting, lasting from a few seconds to several minutes, and that the creatures fly silently around her room.
Ms. K’s daughter grew concerned that the hallucinations were increasingly diminishing her mother’s ability to care for herself. She brought Ms. K into our emergency department, from which the patient was admitted.
On admission, Ms. K said she had lost 20 lbs within 6 months, and that “concentrating on those things in the house” was impairing her sleep. She denied recent illness, trauma, loss of conscious ness, changes in medications, seizures, drug or alcohol use, suicidal or homicidal ideation, or specific stress in her life. She added that she often cooks for herself—only to lose her appetite after seeing bugs and other creatures crawl into her food.
Her medical history includes hypertension, type 2 diabetes mellitus, peripheral vascular disease, urinary incontinence, gastroesophageal reflux, glaucoma in her left eye, and bilateral cataracts. She denies any psychiatric history and adds that she had never experienced hallucinations until about 3 months before hospitalization. She also denies any history of auditory, tactile, or olfactory hallucinations.
Would you suspect a primary psychotic illness? What clinical tests might help us understand Ms. K’s progressively debilitating visual hallucinations?
The authors’ observations
Ms. K’s case places us at the crossroads of psychiatric disturbances and medical conditions that can present as or precipitate apparent psychiatric symptoms. Delirium, dementia, psychosis, endocrinopathies, encephalitis, electrolyte disturbances, drug abuse/withdrawal, and occipital or temporal lobe seizures are all possible differential diagnoses (Table 1).
A cognitive function screening and a battery of laboratory tests, imaging scans, and neurologic and vision exams are needed to uncover the cause of her hallucinations.
EVALUATION: Looking for clues
Ms. K’s left pupil was fixed at 6 mm and did not respond to light, while the right pupil was regular and reactive to light at 3 mm. Using a Snellen eye chart, her visual acuity was poor: 20/100 to 20/200 in her right eye and less than 20/200 in the left eye. She scored a 29 out of 30 on the Folstein Mini-Mental State Examination (MMSE), indicating her cognition was intact. The remainder of the neurologic exam was unremarkable.
At admission, Ms. K’s medications included metoprolol, 100 mg qd, for hypertension; lansoprazole, 30 mg qd, for gastroesophageal reflux; tolterodine, 2 mg bid, and oxybutynin, 10 mg qd, for urinary incontinence; repaglinide, 2 mg bid, for type 2 diabetes; and three ophthalmic agents: brimonidine, prednisolone, and dorzolamide/timolol. The patient had been maintained on these medications for more than 2 years with no recent changes in dosing.
Results of Ms. K’s lab studies were normal, including a basic metabolic panel, CBC, liver function tests, urinalysis, B12, thyroid panel, rapid plasma reagin test, and urine drug screen.
A head CT without contrast revealed chronic small-vessel ischemic white matter disease and a chronic infarct of the left cerebellar hemisphere. No acute intracranial hemorrhages, masses, or other abnormalities were noted. No seizures were seen on EEG.
Table 1
Common causes of visual hallucinations
| Schizophrenia |
| Delirium |
| Dementias |
| Substance-induced psychosis |
| Electrolyte disturbances |
| Occipital and temporal lobe epilepsy |
| Charles Bonnet syndrome |
What do the laboratory and imaging tests reveal about Ms. K’s hallucinations? Is her diagnosis delirium? Alzheimer’s or other type of dementia? Schizophrenia?
The authors’ observations
Visual hallucinations—often of deceased parents or siblings, unknown intruders, and animals—can occur in up to 25% of patients with Alzheimer’s-type dementia.1 Also, patients with Lewy body dementia often present with well-formed visual hallucinations, which are thought to result from temporal lobe involvement by the characteristic Lewy bodies.
To diagnose dementia, DSM-IV requires the presence of multiple cognitive deficits manifested by memory impairment and one or more of the following:
- aphasia
- apraxia
- agnosia
- disturbance of executive functioning.2
Ms. K exhibited none of these characteristics, and she retained full executive function—she could balance her checkbook, buy groceries, and cook for herself. Also, her MMSE score was high.
Ms. K showed no consciousness fluctuations or attention deficits, two features commonly seen in delirium. She was alert and oriented throughout the interview, and her flow of thought, speech, language, and attention were appropriate. Therefore, delirium can be reasonably excluded.
The hallucinations probably do not signal onset of schizophrenia because of Ms. K’s age at presentation, lack of family history of psychotic disorder, and paucity of negative symptoms. Auditory hallucinations are much more common in psychosis, and isolated visual hallucinations rarely occur in schizophrenia.
Finally, Ms. K’s electrophysiologic, laboratory, and imaging studies revealed isolated systolic hypertension, low visual acuity, and a mild gait disturbance. Severe left lens opacification accounted for the patient’s discordant pupillary light reflex. None of these findings explained her visual hallucinations, however.
Is a non-psychiatric disorder causing Ms. K’s hallucinations? What type of medication might alleviate her symptoms?
The authors’ observations
Given Ms. K’s strong cognitive function and poor visual acuity, we concluded that her hallucinations may fit the criteria for Charles Bonnet syndrome (CBS), a poorly understood medical phenomenon.
CBS is characterized by complex visual hallucinations in visually impaired elderly patients without cognitive deficits (Table 2).3,4 Swiss philosopher Charles Bonnet first described the disorder in 1760 to explain the vivid visual hallucinations of his 89-year-old grandfather, who had severe cataracts but no cognitive deficits.3 Bonnet’s grandfather claimed to have visions of men, women, birds, buildings, and tapestries.3
CBS is increasingly recognized and reported, but the medical community has never formed a universally accepted definition for this phenomenon. Persons with CBS react positively or negatively to their hallucinations, and the images may stimulate anxiety, anger, or mild paranoia. Research has focused on prevalence, risk indicators, and treatment.
Table 2
Charles Bonnet syndrome: fast facts
|
Teunisse et al determined that visual hallucinations plague up to 14% of sight-impaired persons.4,5 The hallucinations vary widely: people, animals, flowers, vehicles, buildings, and sometimes complete scenes.4,5 Significant risk factors for CBS include advanced age and low visual acuity.4,5 Loneliness, introversion, and shyness are additional risk indicators in older, visually handicapped persons.6 Therefore, social isolation may be a predisposing factor.
Drug treatment of visual hallucinations in CBS currently includes antipsychotics, such as quetiapine (25 to 100 mg/d) and risperidone (0.25 to 1.0 mg/d).7 However, mixed results have been reported after use of antipsychotics in CBS; one patient’s visual hallucinations were exacerbated after risperidone was initiated.8 Case reports have also described the use of valproate, carbamazepine, and ondansetron in CBS.9-11
Empathy and patient education are the cornerstones of CBS treatment.3 Patients need to be reassured that their visions are benign. For many, simply increasing the amount of ambient light in the home can reduce hallucinations.
TREATMENT A frog in the toilet
Ms. K was started on quetiapine, 25 mg bid, to try to promote restorative sleep and resolve her hallucinations. Up to 18% of persons treated with quetiapine report somnolence as an adverse effect, vs. 3 to 8% of those treated with risperidone.12
During her hospital stay, Ms. K experienced no visual hallucinations during the day but reported seeing a grayish-brown bullfrog in the toilet at night. This hallucination did not frighten her; she would simply close the bathroom door and wait until the bullfrog “disappeared.”
Her sleep improved, as did her appetite. She participated in daily group sessions and socialized with other patients.
After 12 days, Ms. K was discharged. To decrease her social isolation, we encouraged her to participate in a day program for seniors. We also continued her on quetiapine, 25 mg bid.
Five months later, her primary care physician reports that Ms. K remains symptom free while maintaining her quetiapine dosage.
Related resources
- Royal National Institute of the Blind: Fact sheet for Charles Bonnet syndrome. Available at: http://www.rnib.org.uk/info/cbsfin.htm
- Verstraten PFJ. The Charles Bonnet syndrome: Development of a protocol for clinical practice in a multidisciplinary approach from assessment to intervention. Available at: http://www.rehab-syn.enter.iris.se/kc-syn/cb.htm
- Adamczyk DT. Optometric educators. Am I seeing things? Optometry Today June 18, 1999:37-9. Available at: http://www.optometry.co.uk/articles/19990618/Adamczyk.pdf
Drug brand names
- Brimonidine Ophthalmic • Alphagan
- Carbamazepine • Tegretol
- Dorzolamide/Timolol • Cosopt
- Lansoprazole • Prevacid
- Metoprolol • Toprol XL
- Ondansetron • Zofran
- Oxybutynin • Ditropan XL
- Quetiapine • Seroquel
- Repaglinide • Prandin
- Risperidone • Risperdal
- Tolterodine • Detrol
- Valproate • Depakote
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with competing manufacturers.
1. Geldmacher DS, Whitehouse PJ. Current concepts: evaluation of dementia. JAMA 1996;335:330-6.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, rev). Washington, DC: American Psychiatric Press, 2000.
3. Fernandez A, Lichtshein G, Vieweg WV. The Charles Bonnet syndrome: a review. J Nerv Ment Dis 1997;185:195-200.
4. Teunisse RJ, Cruysberg , JR, Hoefnagels WH, et al. Risk indicators for the Charles Bonnet syndrome. J Nerv Ment Dis 1998;186:190-2.
5. Teunisse RJ, Cruysberg J, Verbeek A, Zitman FG. The Charles Bonnet syndrome: a large prospective study in the Netherlands. A study of the prevalence of the Charles Bonnet syndrome and associated factors in 500 patients attending the University Department of Ophthalmology at Nijme. Br J Psychiatry 1995;166(2):254-7.
6. Teunisse RJ, Cruysberg JR, Hoefnagels WH, et al. Social and psychological characteristics of elderly visually handicapped patients with the Charles Bonnet Syndrome. Compr Psychiatry 1999;40(4):315-19.
7. Rovner BW. The Charles Bonnet syndrome: Visual hallucinations caused by visual impairment. Geriatrics 2002;57:45-6.
8. Kornreich C, Dan B, Verbanck P, Pelc I. Treating Charles Bonnet syndrome: understanding inconsistency. J Clin Psychopharmacol 2000;20(3):396.-
9. Hori H, Terao T, Shiraishi Y, Nakamura J. Treatment of Charles Bonnet syndrome with valproate. Int Clin Psychopharmacol 2000;15:117-19.
10. Batra A, Bartels M, Wormstall H. Therapeutic options in Charles Bonnet syndrome. Acta Psychiatr Scand 1997;96:129-33.
11. Nevins M. Charles Bonnet syndrome. J Am Geriatr Soc 1997;45:894.-
12. Brown C, Markowitz J, Moore T, Parker N. Atypical antipsychotics, part II: adverse effects, drug interactions, and efficacy. Ann Pharmacother 1999;33:210-17.
1. Geldmacher DS, Whitehouse PJ. Current concepts: evaluation of dementia. JAMA 1996;335:330-6.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, rev). Washington, DC: American Psychiatric Press, 2000.
3. Fernandez A, Lichtshein G, Vieweg WV. The Charles Bonnet syndrome: a review. J Nerv Ment Dis 1997;185:195-200.
4. Teunisse RJ, Cruysberg , JR, Hoefnagels WH, et al. Risk indicators for the Charles Bonnet syndrome. J Nerv Ment Dis 1998;186:190-2.
5. Teunisse RJ, Cruysberg J, Verbeek A, Zitman FG. The Charles Bonnet syndrome: a large prospective study in the Netherlands. A study of the prevalence of the Charles Bonnet syndrome and associated factors in 500 patients attending the University Department of Ophthalmology at Nijme. Br J Psychiatry 1995;166(2):254-7.
6. Teunisse RJ, Cruysberg JR, Hoefnagels WH, et al. Social and psychological characteristics of elderly visually handicapped patients with the Charles Bonnet Syndrome. Compr Psychiatry 1999;40(4):315-19.
7. Rovner BW. The Charles Bonnet syndrome: Visual hallucinations caused by visual impairment. Geriatrics 2002;57:45-6.
8. Kornreich C, Dan B, Verbanck P, Pelc I. Treating Charles Bonnet syndrome: understanding inconsistency. J Clin Psychopharmacol 2000;20(3):396.-
9. Hori H, Terao T, Shiraishi Y, Nakamura J. Treatment of Charles Bonnet syndrome with valproate. Int Clin Psychopharmacol 2000;15:117-19.
10. Batra A, Bartels M, Wormstall H. Therapeutic options in Charles Bonnet syndrome. Acta Psychiatr Scand 1997;96:129-33.
11. Nevins M. Charles Bonnet syndrome. J Am Geriatr Soc 1997;45:894.-
12. Brown C, Markowitz J, Moore T, Parker N. Atypical antipsychotics, part II: adverse effects, drug interactions, and efficacy. Ann Pharmacother 1999;33:210-17.
The search for the hidden depressant
History: Initial symptoms
Ms. G, 17, has battled attention-deficit/hyperactivity disorder (ADHD) since age 6, and within the past 2 years was also diagnosed as having schizoaffective disorder, bipolar type. An outpatient child psychiatrist and a therapist have helped keep her symptoms in control through much of her life.
During one recent visit to her psychiatrist, however, she complained of decreased energy, increased crying spells, broken sleep, and a depressed mood. She reported that these symptoms began approximately 2 months before the visit, and neither she nor her parents could identify a clear-cut cause.
Throughout her life she has complied with her drug regimens. For 2 years she has been taking divalproex sodium, 500 mg twice daily to manage her manic and depressive episodes, dextroamphetamine sulfate, 30 mg in the morning for her ADHD; risperidone, 2 mg at bedtime for her psychotic symptoms; and mestranol, 60 mcg/d, plus norethindrone, 1 mg/d, for contraception. A recent valproic acid reading of 62 μg/ml is consistent with levels over the last 2 years.
During previous psychotic episodes, Ms. G often became delusional and paranoid with command-type hallucinations. She destroyed her room during her most recent episode.
Ms. G’s adoptive mother accompanied her during this visit. She is concerned for her daughter, especially with the start of school about 1 month away.
Which would you address first: the depression or the psychosis? Would you change Ms. G’s medication and if so, how?
Figure 1 DEPRESSION IN SCHIZOPHRENIA: IMPROVING OUTCOMES
Drs. Yu’s and Maguire’s observations
Complaints of depression in a patient with schizoaffective disorder are especially concerning because multiple domains could be affected (Figure 1). For patients with schizophrenia, the 60% lifetime incidence of major depressive disorder substantially exceeds the 8 to 26% risk in the general population. Ms. G’s comorbid depression also may predispose her to an increased rate of relapse into schizoaffective psychosis, poor treatment response, and a longer duration of psychotic illness that could require hospitalization.1
Although Ms. G’s divalproex level was therapeutic (between 50 and 100 μg/ml), some data indicate that valproic acid may be less effective in schizoaffective disorder than in bipolar I disorder. Still, treatment of schizoaffective disorder often follows antimanic and antidepressant protocols.2
Treatment: An agent is added
The outpatient psychiatrist adds fluoxetine, 20 mg each morning, to address Ms. G’s depressive symptoms. She reports no improvement after 1 month, and her fluoxetine is increased to 30 mg/d.
Three weeks later, Ms. G’s parents bring her to the psychiatrist for an emergency visit. She reports suicidal ideation over the previous month. Rolling up both sleeves, she reveals several superficial cuts on her forearms and wrists that she inflicted after breaking up with her boyfriend.
Her mother, appearing anxious and overwhelmed, reports that her daughter pushed her because she had refused to give Ms. G her calling card. She had told her mother that she wanted to call a boy in Utah that she had met over the Internet.
Ms. G’s speech is noticeably pressured and she is extremely distractible. Her mother notes that her daughter is sleeping only 2 to 3 hours a night, yet exhibits no decrease in energy. Still depressed, her affect is markedly labile, crying at one moment when discussing her suicidality, then railing at her mother when she tries to explain Ms. G’s aggressiveness. When the psychiatrist recommends hospitalization to stabilize her symptoms, she vehemently demands to be let out so that she can run in front of a moving car. The police are called, and she is restrained and brought into the hospital.
What caused Ms. G’s sudden decline? How would you address it?
Drs. Yu’s and Maguire’s observations
Although antidepressants can effectively treat depression in schizoaffective disorder, many of these medications can trigger a manic episode,3 which can include mania, mixed mania with depression, or rapid cycling every few days or hours. In Ms. G’s case, an increase in serotonin due to the fluoxetine may have caused her mania.
We would stop the fluoxetine and see if her manic symptoms resolve. Fluoxetine’s long half-life (4 to 16 days) cuts down the odds of a serotonin-discontinuation syndrome, making immediate discontinuation feasible.
Still, the cause of Ms. G’s depressive symptoms remains unknown. At this stage, observation in the adolescent inpatient ward holds our best hope of reaching a definitive diagnosis.
Treatment: A diagnostic clue surfaces
Blood tests on admission (including a negative drug screen for narcotics or other depressogenic substances) are normal, and her valproic acid level is 61 μg/ml. Her divalproex is increased to 500 mg in the morning and 750 mg at bedtime, and she is tapered off fluoxetine. Her symptoms gradually improve with the change in the medications and her attendance in milieu and group therapy on the ward. A second valproic acid reading on day three of hospitalization is 67 μg/ml.
That day, a nurse informs the inpatient child/adolescent psychiatrist that Ms. G has requested extra hospital gowns. Ms. G later reveals that for about 4 months she has been producing a milky discharge from both breasts, and that the flow has been increasing in frequency and quantity. She adds that she has not menstruated for almost 5 months and complains of breast tenderness.
What do Ms. G’s latest symptoms suggest? How will your response to these symptoms affect treatment?
Drs. Yu’s and Maguire’s observations
Complaints of menstrual irregularities, breast tenderness, and galactorrhea should arouse suspicions of hyperprolactinemia. Because tumors that raise prolactin levels are rare, medications are the most likely culprit in Ms. G’s case. Dopamine blockade within the tuberoinfundibular tract is the mechanism of action behind prolactin elevation.4
Prolactin levels in patients with schizophrenia are generally normal (1 to 25 mg/L) prior to treatment,5 but have been known to increase with use of typical antipsychotics. The atypical antipsychotic risperidone has been associated with dose-related increases in plasma prolactin concentration, although Kleinberg et al found no correlation between risperidone-induced plasma prolactin concentrations and adverse events.6
Figure 2 POSSIBLE ADVERSE EFFECTS OF HYPERPROLACTINEMIA8
Prolactin-sparing atypical antipsychotics such as olanzapine, quetiapine, ziprasidone, and aripiprazole may cause a transient prolactin increase in the first few weeks of use. These levels tend to remain within the normal range before decreasing to baseline levels or lower.7,8
Prolactin elevation in women may lead to an estrogen deficiency, causing changes in mood and cognition and psychopathology9 that can manifest as increased depression, anxiety, and hostility.10 Hyperprolactinemia can also cause depression in men, though the mechanism of action is unknown.
Prolactin elevation can lead to numerous other health disturbances (Figure 2). When screening women who are taking antipsychotics, ask about menstrual irregularities, sexual dysfunction, breast tenderness, and galactorrhea. Ask male patients about a loss of libido, erectile dysfunction, ejaculatory dysfunction, and gynecomastia.
When hyperprolactinemia becomes apparent, we suggest discontinuing the offending drug and, if necessary:
- switching to a prolactin-sparing atypical antipsychotic
- or trying another agent, such as bromocriptine or pergolide, if switching to another antipsychotic is infeasible.10,11
Baseline prolactin levels should be measured before starting any prolactin-elevating antipsychotic. Because prolactin levels may not correlate with severity of clinical symptoms, the net change in these levels may be a better indicator.4 If prolactin levels exceed 100 mg/L, consider an MRI with fine cuts though the sellae to check for a primary adenoma.4
Conclusion: A cause is found
An MRI of Ms. G’s head is normal, but her serum prolactin level is 125 μg/L. Her risperidone is tapered off, and olanzapine, 10 mg at bedtime, is started with her mother’s consent. Two days later, her prolactin level drops to 85 μg/L. Notable improvement is reported on day seven of hospitalization; she is sleeping and eating well with no suicidal or homicidal ideations and notes no psychotic symptoms. She is discharged that day.
Two weeks later, Ms. G’s improvement continues. Lab tests reveal normal prolactin levels. Over the next few months, she remains stable, attends school, and takes her medications with no adverse effects.
Related resources
- Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002; 63(suppl 4):56-62. Available at: www.psychiatrist.com/supplenet/v63s04/v63s0408.pdf. Accessed March 11, 2003.
Drug brand names
- Aripiprazole • Abilify
- Dextroamphetamine sulfate • Dexadrine
- Divalproex sodium • Depakote
- Fluoxetine • Prozac
- Mestranol • Necon 1/50
- Norethindrone • Activella
- Pergolide • Permax
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
Dr. Yu receives research/grant support from, is a consultant to, and/or is a speaker for Cephalon Inc., Eli Lilly and Co., Novartis Pharmaceuticals Corp., and Pfizer Inc.
Dr. Maguire receives research/grant support from, is a consultant to, and/or is a speaker for Eli Lilly and Co., Pfizer Inc., Forest Laboratories, and GlaxoSmithKline.
1. Bartels SJ, Drake RE. Depressive symptoms in schizophrenia: comprehensive differential diagnosis. Compr Psychiatry 1988;29(5):467-83.
2. Sadock BJ, Sadock VA. Kaplan and Sadock’s comprehensive textbook of psychiatry (7th ed). Philadelphia Lippincott Williams & Wilkins, 2000.
3. Stahl SM. Essential psychopharmacology: neuroscientific basis and practical application (2nd ed). Cambridge, UK: Cambridge University Press, 2000:chap 5.
4. Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002;63(suppl 4):56-62.
5. Kuruvilla A, Srikrishna G, Peedicayil J, et al. A study on serum prolactin levels in schizophrenia: correlation with positive and negative symptoms. Int Clin Psychopharmacol 1993;8:177-9.
6. Kleinberg DL, Davis JM, De Coster R, et al. Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol 1999;19:57-61.
7. Petty RG. Prolactin and antipsychotic medications: mechanisms of actions. Schizophr Res 1999;35(suppl):S67-S73.
8. Tran PV, Hamilton SH, Kuntz AJ, et al. Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacology 1997;17:407-18.
9. Panay N, Studd JW. The psychotherapeutic effects of estrogens. Gynecol Endocrinol 1998;12:353-65.
10. Kellner R, Buckman MT, Fava M, et al. Prolactin, aggression and hostility: a discussion of recent studies. Psychiatry Dev 1984;2:131-8.
11. Pharoah FM, Mari JJ, Streiner D. Family intervention for schizophrenia. Cochrane Database Syst Rev 2000;(2):CD000088.-
12. Weiden PJ, Aquila R, Emanuel M, Zygmunt A. Long-term considerations after switching antipsychotics. J Clin Psychiatry 1998;59(suppl 19):36-49.
13. Goldberg SC, Schooler NR, Hogarty GE, et al. Prediction of relapse in schizophrenic outpatients treated by drug and sociotherapy. Arch Gen Psychiatry 1977;34:171-84.
14. Hogarty GE, Ulrich RF. The limitations of antipsychotic medication on schizophrenia relapse and adjustment and the contributions of psychosocial treatment. J Psychiatr Res 1998;32:243-50.
15. Bellack AS, Gold JM, Buchanan RW. Cognitive rehabilitation for schizophrenia: problems, prospects, and strategies. Schizophr Bull 1999;25:257-75.
16. Siris SG. Assessment and treatment of secondary depression in schizophrenia. Psychiatr Ann 1994;24:463-7.
17. Keck PE, Jr, Strakowski SM, McElroy SL. The efficacy of atypical antipsychotics in the treatment of depressive symptoms, hostility and suicidality in patients with schizophrenia. J Clin Psychiatry 2000;61(suppl 3):4-9.
18. Mattox JH, Buckman MT, Bernstein J, et al. Dopamine agonists for reducing depression associated with hyperprolactinemia. J Reprod Med 1986;31:694-8.
History: Initial symptoms
Ms. G, 17, has battled attention-deficit/hyperactivity disorder (ADHD) since age 6, and within the past 2 years was also diagnosed as having schizoaffective disorder, bipolar type. An outpatient child psychiatrist and a therapist have helped keep her symptoms in control through much of her life.
During one recent visit to her psychiatrist, however, she complained of decreased energy, increased crying spells, broken sleep, and a depressed mood. She reported that these symptoms began approximately 2 months before the visit, and neither she nor her parents could identify a clear-cut cause.
Throughout her life she has complied with her drug regimens. For 2 years she has been taking divalproex sodium, 500 mg twice daily to manage her manic and depressive episodes, dextroamphetamine sulfate, 30 mg in the morning for her ADHD; risperidone, 2 mg at bedtime for her psychotic symptoms; and mestranol, 60 mcg/d, plus norethindrone, 1 mg/d, for contraception. A recent valproic acid reading of 62 μg/ml is consistent with levels over the last 2 years.
During previous psychotic episodes, Ms. G often became delusional and paranoid with command-type hallucinations. She destroyed her room during her most recent episode.
Ms. G’s adoptive mother accompanied her during this visit. She is concerned for her daughter, especially with the start of school about 1 month away.
Which would you address first: the depression or the psychosis? Would you change Ms. G’s medication and if so, how?
Figure 1 DEPRESSION IN SCHIZOPHRENIA: IMPROVING OUTCOMES
Drs. Yu’s and Maguire’s observations
Complaints of depression in a patient with schizoaffective disorder are especially concerning because multiple domains could be affected (Figure 1). For patients with schizophrenia, the 60% lifetime incidence of major depressive disorder substantially exceeds the 8 to 26% risk in the general population. Ms. G’s comorbid depression also may predispose her to an increased rate of relapse into schizoaffective psychosis, poor treatment response, and a longer duration of psychotic illness that could require hospitalization.1
Although Ms. G’s divalproex level was therapeutic (between 50 and 100 μg/ml), some data indicate that valproic acid may be less effective in schizoaffective disorder than in bipolar I disorder. Still, treatment of schizoaffective disorder often follows antimanic and antidepressant protocols.2
Treatment: An agent is added
The outpatient psychiatrist adds fluoxetine, 20 mg each morning, to address Ms. G’s depressive symptoms. She reports no improvement after 1 month, and her fluoxetine is increased to 30 mg/d.
Three weeks later, Ms. G’s parents bring her to the psychiatrist for an emergency visit. She reports suicidal ideation over the previous month. Rolling up both sleeves, she reveals several superficial cuts on her forearms and wrists that she inflicted after breaking up with her boyfriend.
Her mother, appearing anxious and overwhelmed, reports that her daughter pushed her because she had refused to give Ms. G her calling card. She had told her mother that she wanted to call a boy in Utah that she had met over the Internet.
Ms. G’s speech is noticeably pressured and she is extremely distractible. Her mother notes that her daughter is sleeping only 2 to 3 hours a night, yet exhibits no decrease in energy. Still depressed, her affect is markedly labile, crying at one moment when discussing her suicidality, then railing at her mother when she tries to explain Ms. G’s aggressiveness. When the psychiatrist recommends hospitalization to stabilize her symptoms, she vehemently demands to be let out so that she can run in front of a moving car. The police are called, and she is restrained and brought into the hospital.
What caused Ms. G’s sudden decline? How would you address it?
Drs. Yu’s and Maguire’s observations
Although antidepressants can effectively treat depression in schizoaffective disorder, many of these medications can trigger a manic episode,3 which can include mania, mixed mania with depression, or rapid cycling every few days or hours. In Ms. G’s case, an increase in serotonin due to the fluoxetine may have caused her mania.
We would stop the fluoxetine and see if her manic symptoms resolve. Fluoxetine’s long half-life (4 to 16 days) cuts down the odds of a serotonin-discontinuation syndrome, making immediate discontinuation feasible.
Still, the cause of Ms. G’s depressive symptoms remains unknown. At this stage, observation in the adolescent inpatient ward holds our best hope of reaching a definitive diagnosis.
Treatment: A diagnostic clue surfaces
Blood tests on admission (including a negative drug screen for narcotics or other depressogenic substances) are normal, and her valproic acid level is 61 μg/ml. Her divalproex is increased to 500 mg in the morning and 750 mg at bedtime, and she is tapered off fluoxetine. Her symptoms gradually improve with the change in the medications and her attendance in milieu and group therapy on the ward. A second valproic acid reading on day three of hospitalization is 67 μg/ml.
That day, a nurse informs the inpatient child/adolescent psychiatrist that Ms. G has requested extra hospital gowns. Ms. G later reveals that for about 4 months she has been producing a milky discharge from both breasts, and that the flow has been increasing in frequency and quantity. She adds that she has not menstruated for almost 5 months and complains of breast tenderness.
What do Ms. G’s latest symptoms suggest? How will your response to these symptoms affect treatment?
Drs. Yu’s and Maguire’s observations
Complaints of menstrual irregularities, breast tenderness, and galactorrhea should arouse suspicions of hyperprolactinemia. Because tumors that raise prolactin levels are rare, medications are the most likely culprit in Ms. G’s case. Dopamine blockade within the tuberoinfundibular tract is the mechanism of action behind prolactin elevation.4
Prolactin levels in patients with schizophrenia are generally normal (1 to 25 mg/L) prior to treatment,5 but have been known to increase with use of typical antipsychotics. The atypical antipsychotic risperidone has been associated with dose-related increases in plasma prolactin concentration, although Kleinberg et al found no correlation between risperidone-induced plasma prolactin concentrations and adverse events.6
Figure 2 POSSIBLE ADVERSE EFFECTS OF HYPERPROLACTINEMIA8
Prolactin-sparing atypical antipsychotics such as olanzapine, quetiapine, ziprasidone, and aripiprazole may cause a transient prolactin increase in the first few weeks of use. These levels tend to remain within the normal range before decreasing to baseline levels or lower.7,8
Prolactin elevation in women may lead to an estrogen deficiency, causing changes in mood and cognition and psychopathology9 that can manifest as increased depression, anxiety, and hostility.10 Hyperprolactinemia can also cause depression in men, though the mechanism of action is unknown.
Prolactin elevation can lead to numerous other health disturbances (Figure 2). When screening women who are taking antipsychotics, ask about menstrual irregularities, sexual dysfunction, breast tenderness, and galactorrhea. Ask male patients about a loss of libido, erectile dysfunction, ejaculatory dysfunction, and gynecomastia.
When hyperprolactinemia becomes apparent, we suggest discontinuing the offending drug and, if necessary:
- switching to a prolactin-sparing atypical antipsychotic
- or trying another agent, such as bromocriptine or pergolide, if switching to another antipsychotic is infeasible.10,11
Baseline prolactin levels should be measured before starting any prolactin-elevating antipsychotic. Because prolactin levels may not correlate with severity of clinical symptoms, the net change in these levels may be a better indicator.4 If prolactin levels exceed 100 mg/L, consider an MRI with fine cuts though the sellae to check for a primary adenoma.4
Conclusion: A cause is found
An MRI of Ms. G’s head is normal, but her serum prolactin level is 125 μg/L. Her risperidone is tapered off, and olanzapine, 10 mg at bedtime, is started with her mother’s consent. Two days later, her prolactin level drops to 85 μg/L. Notable improvement is reported on day seven of hospitalization; she is sleeping and eating well with no suicidal or homicidal ideations and notes no psychotic symptoms. She is discharged that day.
Two weeks later, Ms. G’s improvement continues. Lab tests reveal normal prolactin levels. Over the next few months, she remains stable, attends school, and takes her medications with no adverse effects.
Related resources
- Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002; 63(suppl 4):56-62. Available at: www.psychiatrist.com/supplenet/v63s04/v63s0408.pdf. Accessed March 11, 2003.
Drug brand names
- Aripiprazole • Abilify
- Dextroamphetamine sulfate • Dexadrine
- Divalproex sodium • Depakote
- Fluoxetine • Prozac
- Mestranol • Necon 1/50
- Norethindrone • Activella
- Pergolide • Permax
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
Dr. Yu receives research/grant support from, is a consultant to, and/or is a speaker for Cephalon Inc., Eli Lilly and Co., Novartis Pharmaceuticals Corp., and Pfizer Inc.
Dr. Maguire receives research/grant support from, is a consultant to, and/or is a speaker for Eli Lilly and Co., Pfizer Inc., Forest Laboratories, and GlaxoSmithKline.
History: Initial symptoms
Ms. G, 17, has battled attention-deficit/hyperactivity disorder (ADHD) since age 6, and within the past 2 years was also diagnosed as having schizoaffective disorder, bipolar type. An outpatient child psychiatrist and a therapist have helped keep her symptoms in control through much of her life.
During one recent visit to her psychiatrist, however, she complained of decreased energy, increased crying spells, broken sleep, and a depressed mood. She reported that these symptoms began approximately 2 months before the visit, and neither she nor her parents could identify a clear-cut cause.
Throughout her life she has complied with her drug regimens. For 2 years she has been taking divalproex sodium, 500 mg twice daily to manage her manic and depressive episodes, dextroamphetamine sulfate, 30 mg in the morning for her ADHD; risperidone, 2 mg at bedtime for her psychotic symptoms; and mestranol, 60 mcg/d, plus norethindrone, 1 mg/d, for contraception. A recent valproic acid reading of 62 μg/ml is consistent with levels over the last 2 years.
During previous psychotic episodes, Ms. G often became delusional and paranoid with command-type hallucinations. She destroyed her room during her most recent episode.
Ms. G’s adoptive mother accompanied her during this visit. She is concerned for her daughter, especially with the start of school about 1 month away.
Which would you address first: the depression or the psychosis? Would you change Ms. G’s medication and if so, how?
Figure 1 DEPRESSION IN SCHIZOPHRENIA: IMPROVING OUTCOMES
Drs. Yu’s and Maguire’s observations
Complaints of depression in a patient with schizoaffective disorder are especially concerning because multiple domains could be affected (Figure 1). For patients with schizophrenia, the 60% lifetime incidence of major depressive disorder substantially exceeds the 8 to 26% risk in the general population. Ms. G’s comorbid depression also may predispose her to an increased rate of relapse into schizoaffective psychosis, poor treatment response, and a longer duration of psychotic illness that could require hospitalization.1
Although Ms. G’s divalproex level was therapeutic (between 50 and 100 μg/ml), some data indicate that valproic acid may be less effective in schizoaffective disorder than in bipolar I disorder. Still, treatment of schizoaffective disorder often follows antimanic and antidepressant protocols.2
Treatment: An agent is added
The outpatient psychiatrist adds fluoxetine, 20 mg each morning, to address Ms. G’s depressive symptoms. She reports no improvement after 1 month, and her fluoxetine is increased to 30 mg/d.
Three weeks later, Ms. G’s parents bring her to the psychiatrist for an emergency visit. She reports suicidal ideation over the previous month. Rolling up both sleeves, she reveals several superficial cuts on her forearms and wrists that she inflicted after breaking up with her boyfriend.
Her mother, appearing anxious and overwhelmed, reports that her daughter pushed her because she had refused to give Ms. G her calling card. She had told her mother that she wanted to call a boy in Utah that she had met over the Internet.
Ms. G’s speech is noticeably pressured and she is extremely distractible. Her mother notes that her daughter is sleeping only 2 to 3 hours a night, yet exhibits no decrease in energy. Still depressed, her affect is markedly labile, crying at one moment when discussing her suicidality, then railing at her mother when she tries to explain Ms. G’s aggressiveness. When the psychiatrist recommends hospitalization to stabilize her symptoms, she vehemently demands to be let out so that she can run in front of a moving car. The police are called, and she is restrained and brought into the hospital.
What caused Ms. G’s sudden decline? How would you address it?
Drs. Yu’s and Maguire’s observations
Although antidepressants can effectively treat depression in schizoaffective disorder, many of these medications can trigger a manic episode,3 which can include mania, mixed mania with depression, or rapid cycling every few days or hours. In Ms. G’s case, an increase in serotonin due to the fluoxetine may have caused her mania.
We would stop the fluoxetine and see if her manic symptoms resolve. Fluoxetine’s long half-life (4 to 16 days) cuts down the odds of a serotonin-discontinuation syndrome, making immediate discontinuation feasible.
Still, the cause of Ms. G’s depressive symptoms remains unknown. At this stage, observation in the adolescent inpatient ward holds our best hope of reaching a definitive diagnosis.
Treatment: A diagnostic clue surfaces
Blood tests on admission (including a negative drug screen for narcotics or other depressogenic substances) are normal, and her valproic acid level is 61 μg/ml. Her divalproex is increased to 500 mg in the morning and 750 mg at bedtime, and she is tapered off fluoxetine. Her symptoms gradually improve with the change in the medications and her attendance in milieu and group therapy on the ward. A second valproic acid reading on day three of hospitalization is 67 μg/ml.
That day, a nurse informs the inpatient child/adolescent psychiatrist that Ms. G has requested extra hospital gowns. Ms. G later reveals that for about 4 months she has been producing a milky discharge from both breasts, and that the flow has been increasing in frequency and quantity. She adds that she has not menstruated for almost 5 months and complains of breast tenderness.
What do Ms. G’s latest symptoms suggest? How will your response to these symptoms affect treatment?
Drs. Yu’s and Maguire’s observations
Complaints of menstrual irregularities, breast tenderness, and galactorrhea should arouse suspicions of hyperprolactinemia. Because tumors that raise prolactin levels are rare, medications are the most likely culprit in Ms. G’s case. Dopamine blockade within the tuberoinfundibular tract is the mechanism of action behind prolactin elevation.4
Prolactin levels in patients with schizophrenia are generally normal (1 to 25 mg/L) prior to treatment,5 but have been known to increase with use of typical antipsychotics. The atypical antipsychotic risperidone has been associated with dose-related increases in plasma prolactin concentration, although Kleinberg et al found no correlation between risperidone-induced plasma prolactin concentrations and adverse events.6
Figure 2 POSSIBLE ADVERSE EFFECTS OF HYPERPROLACTINEMIA8
Prolactin-sparing atypical antipsychotics such as olanzapine, quetiapine, ziprasidone, and aripiprazole may cause a transient prolactin increase in the first few weeks of use. These levels tend to remain within the normal range before decreasing to baseline levels or lower.7,8
Prolactin elevation in women may lead to an estrogen deficiency, causing changes in mood and cognition and psychopathology9 that can manifest as increased depression, anxiety, and hostility.10 Hyperprolactinemia can also cause depression in men, though the mechanism of action is unknown.
Prolactin elevation can lead to numerous other health disturbances (Figure 2). When screening women who are taking antipsychotics, ask about menstrual irregularities, sexual dysfunction, breast tenderness, and galactorrhea. Ask male patients about a loss of libido, erectile dysfunction, ejaculatory dysfunction, and gynecomastia.
When hyperprolactinemia becomes apparent, we suggest discontinuing the offending drug and, if necessary:
- switching to a prolactin-sparing atypical antipsychotic
- or trying another agent, such as bromocriptine or pergolide, if switching to another antipsychotic is infeasible.10,11
Baseline prolactin levels should be measured before starting any prolactin-elevating antipsychotic. Because prolactin levels may not correlate with severity of clinical symptoms, the net change in these levels may be a better indicator.4 If prolactin levels exceed 100 mg/L, consider an MRI with fine cuts though the sellae to check for a primary adenoma.4
Conclusion: A cause is found
An MRI of Ms. G’s head is normal, but her serum prolactin level is 125 μg/L. Her risperidone is tapered off, and olanzapine, 10 mg at bedtime, is started with her mother’s consent. Two days later, her prolactin level drops to 85 μg/L. Notable improvement is reported on day seven of hospitalization; she is sleeping and eating well with no suicidal or homicidal ideations and notes no psychotic symptoms. She is discharged that day.
Two weeks later, Ms. G’s improvement continues. Lab tests reveal normal prolactin levels. Over the next few months, she remains stable, attends school, and takes her medications with no adverse effects.
Related resources
- Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002; 63(suppl 4):56-62. Available at: www.psychiatrist.com/supplenet/v63s04/v63s0408.pdf. Accessed March 11, 2003.
Drug brand names
- Aripiprazole • Abilify
- Dextroamphetamine sulfate • Dexadrine
- Divalproex sodium • Depakote
- Fluoxetine • Prozac
- Mestranol • Necon 1/50
- Norethindrone • Activella
- Pergolide • Permax
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
Dr. Yu receives research/grant support from, is a consultant to, and/or is a speaker for Cephalon Inc., Eli Lilly and Co., Novartis Pharmaceuticals Corp., and Pfizer Inc.
Dr. Maguire receives research/grant support from, is a consultant to, and/or is a speaker for Eli Lilly and Co., Pfizer Inc., Forest Laboratories, and GlaxoSmithKline.
1. Bartels SJ, Drake RE. Depressive symptoms in schizophrenia: comprehensive differential diagnosis. Compr Psychiatry 1988;29(5):467-83.
2. Sadock BJ, Sadock VA. Kaplan and Sadock’s comprehensive textbook of psychiatry (7th ed). Philadelphia Lippincott Williams & Wilkins, 2000.
3. Stahl SM. Essential psychopharmacology: neuroscientific basis and practical application (2nd ed). Cambridge, UK: Cambridge University Press, 2000:chap 5.
4. Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002;63(suppl 4):56-62.
5. Kuruvilla A, Srikrishna G, Peedicayil J, et al. A study on serum prolactin levels in schizophrenia: correlation with positive and negative symptoms. Int Clin Psychopharmacol 1993;8:177-9.
6. Kleinberg DL, Davis JM, De Coster R, et al. Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol 1999;19:57-61.
7. Petty RG. Prolactin and antipsychotic medications: mechanisms of actions. Schizophr Res 1999;35(suppl):S67-S73.
8. Tran PV, Hamilton SH, Kuntz AJ, et al. Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacology 1997;17:407-18.
9. Panay N, Studd JW. The psychotherapeutic effects of estrogens. Gynecol Endocrinol 1998;12:353-65.
10. Kellner R, Buckman MT, Fava M, et al. Prolactin, aggression and hostility: a discussion of recent studies. Psychiatry Dev 1984;2:131-8.
11. Pharoah FM, Mari JJ, Streiner D. Family intervention for schizophrenia. Cochrane Database Syst Rev 2000;(2):CD000088.-
12. Weiden PJ, Aquila R, Emanuel M, Zygmunt A. Long-term considerations after switching antipsychotics. J Clin Psychiatry 1998;59(suppl 19):36-49.
13. Goldberg SC, Schooler NR, Hogarty GE, et al. Prediction of relapse in schizophrenic outpatients treated by drug and sociotherapy. Arch Gen Psychiatry 1977;34:171-84.
14. Hogarty GE, Ulrich RF. The limitations of antipsychotic medication on schizophrenia relapse and adjustment and the contributions of psychosocial treatment. J Psychiatr Res 1998;32:243-50.
15. Bellack AS, Gold JM, Buchanan RW. Cognitive rehabilitation for schizophrenia: problems, prospects, and strategies. Schizophr Bull 1999;25:257-75.
16. Siris SG. Assessment and treatment of secondary depression in schizophrenia. Psychiatr Ann 1994;24:463-7.
17. Keck PE, Jr, Strakowski SM, McElroy SL. The efficacy of atypical antipsychotics in the treatment of depressive symptoms, hostility and suicidality in patients with schizophrenia. J Clin Psychiatry 2000;61(suppl 3):4-9.
18. Mattox JH, Buckman MT, Bernstein J, et al. Dopamine agonists for reducing depression associated with hyperprolactinemia. J Reprod Med 1986;31:694-8.
1. Bartels SJ, Drake RE. Depressive symptoms in schizophrenia: comprehensive differential diagnosis. Compr Psychiatry 1988;29(5):467-83.
2. Sadock BJ, Sadock VA. Kaplan and Sadock’s comprehensive textbook of psychiatry (7th ed). Philadelphia Lippincott Williams & Wilkins, 2000.
3. Stahl SM. Essential psychopharmacology: neuroscientific basis and practical application (2nd ed). Cambridge, UK: Cambridge University Press, 2000:chap 5.
4. Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002;63(suppl 4):56-62.
5. Kuruvilla A, Srikrishna G, Peedicayil J, et al. A study on serum prolactin levels in schizophrenia: correlation with positive and negative symptoms. Int Clin Psychopharmacol 1993;8:177-9.
6. Kleinberg DL, Davis JM, De Coster R, et al. Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol 1999;19:57-61.
7. Petty RG. Prolactin and antipsychotic medications: mechanisms of actions. Schizophr Res 1999;35(suppl):S67-S73.
8. Tran PV, Hamilton SH, Kuntz AJ, et al. Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacology 1997;17:407-18.
9. Panay N, Studd JW. The psychotherapeutic effects of estrogens. Gynecol Endocrinol 1998;12:353-65.
10. Kellner R, Buckman MT, Fava M, et al. Prolactin, aggression and hostility: a discussion of recent studies. Psychiatry Dev 1984;2:131-8.
11. Pharoah FM, Mari JJ, Streiner D. Family intervention for schizophrenia. Cochrane Database Syst Rev 2000;(2):CD000088.-
12. Weiden PJ, Aquila R, Emanuel M, Zygmunt A. Long-term considerations after switching antipsychotics. J Clin Psychiatry 1998;59(suppl 19):36-49.
13. Goldberg SC, Schooler NR, Hogarty GE, et al. Prediction of relapse in schizophrenic outpatients treated by drug and sociotherapy. Arch Gen Psychiatry 1977;34:171-84.
14. Hogarty GE, Ulrich RF. The limitations of antipsychotic medication on schizophrenia relapse and adjustment and the contributions of psychosocial treatment. J Psychiatr Res 1998;32:243-50.
15. Bellack AS, Gold JM, Buchanan RW. Cognitive rehabilitation for schizophrenia: problems, prospects, and strategies. Schizophr Bull 1999;25:257-75.
16. Siris SG. Assessment and treatment of secondary depression in schizophrenia. Psychiatr Ann 1994;24:463-7.
17. Keck PE, Jr, Strakowski SM, McElroy SL. The efficacy of atypical antipsychotics in the treatment of depressive symptoms, hostility and suicidality in patients with schizophrenia. J Clin Psychiatry 2000;61(suppl 3):4-9.
18. Mattox JH, Buckman MT, Bernstein J, et al. Dopamine agonists for reducing depression associated with hyperprolactinemia. J Reprod Med 1986;31:694-8.
Treating persistent psychosis with cognitive-behavioral therapy
History: A secluded life
Mr. K, 31, immigrated to Brooklyn as a child with his family. At age 19, he was working as an auto mechanic in a relative’s garage when he had his first psychotic episode. He was hospitalized and diagnosed with paranoid schizophrenia, which was confirmed by his subsequent course of illness and a recent structured diagnostic interview.
Since becoming ill, Mr. K almost never leaves his house and socializes only with his mother and sister. Unable to work, he helps around the house and often cares for his nieces and nephews. He has no history of substance abuse and has been faithfully taking his medication since his last hospitalization 8 years ago.
Mr. K’s outpatient clinic chart reflects concern about persistent negative symptoms. He hardly speaks in session. Even when “stable,” his social and vocational functioning has been poor. Therapeutic dosages of oral haloperidol, haloperidol decanoate, and fluphenazine have not worked, and trials of risperidone and olanzapine—administered in therapeutic dosages for at least 3 months—were only slightly more effective. Attempts to treat his social withdrawal as a depressive symptom equivalent, with use of adjunctive selective serotonin reuptake inhibitors, also have been disappointing.
We eventually discovered that his so-called negative symptoms were in fact the manifestation of persistent positive symptoms (Table 1). His social withdrawal stemmed not from lack of motivation but from ideas of reference and constant paranoid fears. He believed that if he left the house, a street gang would kill him or his family. When he did venture outdoors, he thought that strangers were ridiculing or insulting him or intended to brutally attack him.
Mr. K spent much of his time at home reading, occasionally visiting the public library just long enough to check out a few books. Family members convinced him to attend church services, but he could not interact with other parishioners because he feared they would find out something was “wrong” with him.
How would you address Mr. K’s positive symptoms? Would you try another antipsychotic after lack of response to five other agents?
Drug treatment: A clinical trial
After a thorough evaluation, Mr. K entered a clinical trial during which he began taking another antipsy-chotic. But after 4 months at high therapeutic dosages, his positive symptoms showed no change from baseline.
We then recommended that Mr. K try clozapine. His persistent paranoid delusions and lack of response to other antipsychotics made him an ideal candidate for this agent. Because he was compliant, motivated, and had available family support, we were confident that he could surmount the vicissitudes of a clozapine trial.
Mr. K refused to try clozapine, however. After so many unsuccessful medication trials over the years, he said he felt some (albeit minor) benefits from his current study medication and wanted to stick with it.
What treatment options remain for Mr. K?
Dr. Weiden’s and Burkholder’s observations
Although the newer antipsychotics have greatly improved outcomes in schizophrenia over the past decade, many patients still battle persistent psychotic (positive) symptoms despite compliance with these medications.1 While clozapine remains the treatment of choice for positive symptoms, some patients cannot—or will not—take it because of its burdensome side-effect profile.
It is well accepted that supportive psychotherapy can help a person with schizophrenia confront the secondary issues of loss, disability, and stigma. But psychotherapy is rarely considered as an adjunct therapy for treatment-resistant positive symptoms. Skepticism about the role of psychotherapy is understandable, because older studies that demonstrated psychoanalytic psychotherapy’s lack of effect on schizophrenia’s positive symptoms2 have driven psychiatric medical education and practice for the past half-century. Other non-psychoanalytic therapeutic approaches had not been studied until recently, so most of us generalized from the disappointing results of the psychoanalytic psychotherapy research.
Still, there is a resurgence of interest in using cognitive-behavioral principles to treat core schizophrenia symptoms. Several randomized, controlled studies—almost all performed in the United Kingdom—have demonstrated that a cognitive-behavioral therapy (CBT) approach, modified for schizophrenia, is superior to more traditional supportive therapies in treating persistent positive and negative symptoms.3-5 Until recently, CBT for schizophrenia has generated little interest or research on this side of the Atlantic.
Continued treatment: A new approach
At this point, we decided to address Mr. K’s paranoid symptoms with CBT-based psychotherapy. The patient, whom we’d been seeing twice monthly for medication management, agreed to weekly 45-minute CBT sessions across 3 months. A third-year resident who had treated Mr. K during the antipsychotic clinical trial administered the therapy as described in the literature.4-6
During the first sessions, we found that some of Mr. K's fears of leaving the house stemmed from living in a poor inner-city neighborhood with a high rate of violent crime. A few sessions later, Mr. K was able to question some of his beliefs that assassins had targeted his family.
By the fourth week, the therapist discovered that Mr. K liked to read and viewed the local library as a reasonably safe place. Mr. K agreed to visit the library once a week and to record his experiences commuting to and from there.
After roughly 8 weeks of treatment, Mr. K was visiting the library twice a week, usually for 90 minutes at a time. He reported that he “had a good time,” but still suspected other library patrons were talking about him. Upon exploring these suspicions, we learned that Mr. K feared other library goers viewed him as “stupid” and that this fear was exacerbating some of his paranoid delusions.
Table 1
POSITIVE SYMPTOMS THATMAYAPPEARASNEGATIVE SYMPTOMS
| Apparent negative symptom | Underlying psychotic symptom |
|---|---|
| Apathy |
|
| Social withdrawal |
|
| Poor hygiene |
|
Once Mr. K acknowledged that his mental illness was not outwardly recognizable, we could convince him that his fear of appearing “stupid” should not keep him housebound. He began to visit the library more frequently. Although he was still anxious, it no longer took him all day to summon the courage to leave home.
After about 10 weeks of treatment, Mr. K began going on bike rides twice a week. We were concerned that he was making too many changes at once, but he insisted he felt more “comfortable” and enjoyed the exercise.
Did cognitive-behavioral therapy contribute to Mr. K’s improvement? How did the therapist’s treatment differ from accepted protocols?
Dr. Weiden’s and Burkholder’s observations
You might be thinking, “This sounds no different from what I do in practice!” The patient was reassured and encouraged to go out and live his life despite having symptoms.
In practice, however, some techniques used in the CBT approach to psychosis are quite different; some techniques are not intuitive, and some contradict most standard teachings of supportive psychotherapy in this country.
The CBT approach used for Mr. K differed greatly from traditional “medical model” supportive psychotherapy. The therapist:
- rejected a “brain disorder” approach to describing his illness7
- used the stress-vulnerability model to explain positive symptoms
- viewed psychotic symptoms as normal reactions rather than pathologic response
- considered psychological factors behind specific psychotic symptoms (Table 2).8
The “brain disorder” explanation. The Kraepelinian model, which characterizes schizophrenia as a degenerative brain disorder, drives patient education. For example, one brochure for patients and their families refers to schizophrenia as “a brain disorder like Alzheimer’s disease.”
Such a comparison could devastate a young adult who is overwhelmed by symptoms and after being told he had a “brain disorder” that “interfered with his cognition.” While this corresponded with our knowledge of schizophrenia, he took this to mean he is “retarded” and “stupid.”
Table 2
UNDERSTANDING PSYCHOSIS WITHIN THE COGNITIVE-BEHAVIORAL MODEL
| Theory | Implications |
|---|---|
| Psychosis lies on one end of a continuum | Psychosis may be the extreme end of normal cognitive, perceptual experiences |
| Delusions can be modified by others under some circumstances | Consider reducing delusional belief or distress by verbal interventions* |
| The stress-vulnerability model represents a more appropriate explanation of symptoms | Emphasizes stress as a possible cause of symptoms; specifying a diagnosis of schizophrenia can be contraindicated |
| Psychotic symptoms may be a normal response | Normalize symptoms, behavior as much as possible |
| Nature of psychotic symptoms is based on specific circumstances | Explore life events that have a specific psychological context for the individual |
| Psychotic symptoms may be secondary to congnitiive dysfunction | Trace the origins of hallucinations or delusions to specific cognitive overload or stress |
| * This is not meant to endorse a confrontational approach. | |
Telling the patient that he or she has schizophrenia– known in some clinical circles as “the S word”–is not necessary and may even be harmful in some cases. We’re not saying that giving a diagnosis of schizophrenia or using a medical model approach is wrong. However, patient education based on symptoms instead of diagnosis may be more conducive in some cases.
The stress-vulnerability model explains psychosis without having to use a diagnostic label. Mr. K’s previous understanding of schizophrenia dovetailed with his low self-esteem. His self-perceived stupidity also had discouraged him from confronting his paranoid anxieties.
Once he realized that unrelenting psychotic symptoms—not his IQ—held him back, we could form a treatment plan. We explained Mr. K’s paranoid symptoms with the stress-vulnerability model: His fears and suspicions worsened whenever he was under stress. This allowed us to sidestep the “brain disorder” model that demoralized him.
By no means, however, did we reject the notion that schizophrenia has a biologic basis. Even if “schizophrenia” is never mentioned, this diagnosis still guides treatment.
Viewing psychotic symptoms as normal reactions. The therapist extensively examined Mr. K’s safety concerns for himself and his family. The therapist acknowledged that these concerns were legitimate, as the patient lives in an inner-city neighborhood plagued by violent crime. Mr. K was then praised for his devotion to his family.
By applying normalization techniques,9 the therapist found fact-based aspects of the delusional beliefs. Normalizing Mr. K’s safety concerns made him feel validated. From there, we could map out a plan for him to periodically leave his home. We devised a routine that addressed his safety concerns: He went to the library only in daylight. He chose a subway route that was less convenient but made him feel more comfortable. Once at the library, he called home to make sure his family was safe, then sat at an open table so he could watch other library patrons come and go.
Once this routine was established, we could address the more idiosyncratic delusions that caused Mr. K considerable stress and anxiety. We asked him to explain the evidence behind his belief that trained assassins were targeting his family. He could not do so and eventually admitted that this thinking was misguided. His fears gradually shifted from specific threats targeted at him and his family to nonspecific fears of the randomness and unfairness of life.
Placing psychosis in psychological context. We tried to understand the psychology of his paranoid thoughts while viewing his symptoms as part of a neurobiologic disorder.
What initially looked like “garden variety” paranoid delusions had a psychological meaning to Mr. K. His dread of public humiliation was intertwined with his fear of assassination. Once understood, these two fears could be isolated and became easier to treat.10 We traced Mr. K’s fear for his family’s safety to his being the oldest male in a matriarchal household. Because his illness prevented him from assuming the role of breadwinner, all that was left was for him to guard his family from the imagined threat of assassination.
Caveats The CBT techniques outlined in the literature for schizophrenia vary greatly from those used in depression or anxiety disorders. In order for CBT to be effective in schizophrenia, the therapist must have considerable experience working with patients with schizophrenia and must receive specialized training and supervision in CBT techniques modified for persons with schizophrenia.
Further, Mr. K continued to take his antipsychotic medication during the 3-month CBT course. We are not suggesting that CBT be administered in lieu of drug therapy, nor can we claim that CBT will be consistently effective against positive symptoms. What’s more, this case does not take into consideration patients who are persistently psychotic because of suboptimal dosing, poor compliance, or substance abuse.
Follow-up: Continued progress
Mr. K continued to improve after the CBT sessions ended. He completed a summer art class despite recurrent paranoia and lingering fears of social interaction. As of this writing, he was considering taking another course.
Three months after his last session, Mr. K was still regularly visiting the library. He also began walking his niece to and from school each day. His paranoid ideation and ideas of reference appeared to be lessening in intensity. Last fall, he joined a gym. He also reported comfortably conversing with people other than immediate family members or mental health clinicians.
Related resources
- Grech E. A review of the current evidence for the use of psychological interventions in psychosis. Int J Psychosoc Rehab 2002;6:79-88.
- Jones C, Cormac I, et al. Cognitive behaviour therapy for schizophrenia. Cochrane Library Issue 4, 2001. Available at: http://www.mediscope.ch/cochrane-abstracts/ab000524.htm. Accessed Feb. 10, 2003.
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Risperidone • Risperdal
Disclosure
Dr. Weiden reports that he receives research/grant support from, is a consultant to, and/or is a speaker for AstraZeneca Pharmaceuticals, Bristol-Myers Squibb Co., Pfizer Inc., and Janssen Pharmaceutica.
Dr. Burkholder reports that she is a consultant and speaker for Pfizer Inc. and Eli Lilly and Co.
Acknowledgments
The authors wish to thank Catie Camille for her assistance in preparing this article, and Drs. Motaz El Rafae and Najma Khanani for the care they provided to Mr. K.
1. Drake RE, Sederer LI. The adverse effects of intensive treatment of chronic schizophrenia. Compr Psychiatry 1986;27(4):313-26.
2. May PRA. Treatment of schizophrenia. New York: Science House, 1968:352.
3. Tarrier N, Beckett R, Harwood S, et al. A trial of two cognitive-behavioural methods of treating drug-resistant psychotic symptoms in schizophrenic patients, I: outcome. Br J Psychiatry 1993;162:524-32.
4. Sensky T, Turkington D, Kingdon D, et al. A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms of schizophrenia resistant to medication. Arch Gen Psychiatry 2000;57(2):165-72.
5. Turkington D, Kingdon D, Turner T. Effectiveness of a brief cognitive-behavioural therapy intervention in the treatment of schizophrenia. Br J Psychiatry 2002;180:523-7.
6. Kingdon DG, Turkington D. Cognitive-behavioral therapy of schizophrenia. New York: Guilford Publications, 1994.
7. Kemp R, Kirov G, Everitt B, et al. Randomised controlled trial of compliance therapy: 18-month follow-up. Br J Psychiatry 1998;172:413-9.
8. Turkington D, Siddle R. Improving understanding and coping in people with schizophrenia by changing attitudes. Psychiatr Rehabil Skills 2000;4(2):300-20.
9. Weiden PJ, Havens LL. Psychotherapeutic management techniques in the treatment of outpatients with schizophrenia. Hosp Community Psychiatry 1994;45:549-55.
10. Link B, Mirotznik J, Cullen FT. The effectiveness of stigma coping orientations: Can negative consequences of mental illness labeling be avoided? J Health Soc Behav 1991;32(3):302-20.
11. Weiden PJ, Aquila R, Emanuel R, Zygmunt A. Long-term considerations after switching antipsychotics. J Clin Psychiatry 1998;59(suppl 19):36-49.
History: A secluded life
Mr. K, 31, immigrated to Brooklyn as a child with his family. At age 19, he was working as an auto mechanic in a relative’s garage when he had his first psychotic episode. He was hospitalized and diagnosed with paranoid schizophrenia, which was confirmed by his subsequent course of illness and a recent structured diagnostic interview.
Since becoming ill, Mr. K almost never leaves his house and socializes only with his mother and sister. Unable to work, he helps around the house and often cares for his nieces and nephews. He has no history of substance abuse and has been faithfully taking his medication since his last hospitalization 8 years ago.
Mr. K’s outpatient clinic chart reflects concern about persistent negative symptoms. He hardly speaks in session. Even when “stable,” his social and vocational functioning has been poor. Therapeutic dosages of oral haloperidol, haloperidol decanoate, and fluphenazine have not worked, and trials of risperidone and olanzapine—administered in therapeutic dosages for at least 3 months—were only slightly more effective. Attempts to treat his social withdrawal as a depressive symptom equivalent, with use of adjunctive selective serotonin reuptake inhibitors, also have been disappointing.
We eventually discovered that his so-called negative symptoms were in fact the manifestation of persistent positive symptoms (Table 1). His social withdrawal stemmed not from lack of motivation but from ideas of reference and constant paranoid fears. He believed that if he left the house, a street gang would kill him or his family. When he did venture outdoors, he thought that strangers were ridiculing or insulting him or intended to brutally attack him.
Mr. K spent much of his time at home reading, occasionally visiting the public library just long enough to check out a few books. Family members convinced him to attend church services, but he could not interact with other parishioners because he feared they would find out something was “wrong” with him.
How would you address Mr. K’s positive symptoms? Would you try another antipsychotic after lack of response to five other agents?
Drug treatment: A clinical trial
After a thorough evaluation, Mr. K entered a clinical trial during which he began taking another antipsy-chotic. But after 4 months at high therapeutic dosages, his positive symptoms showed no change from baseline.
We then recommended that Mr. K try clozapine. His persistent paranoid delusions and lack of response to other antipsychotics made him an ideal candidate for this agent. Because he was compliant, motivated, and had available family support, we were confident that he could surmount the vicissitudes of a clozapine trial.
Mr. K refused to try clozapine, however. After so many unsuccessful medication trials over the years, he said he felt some (albeit minor) benefits from his current study medication and wanted to stick with it.
What treatment options remain for Mr. K?
Dr. Weiden’s and Burkholder’s observations
Although the newer antipsychotics have greatly improved outcomes in schizophrenia over the past decade, many patients still battle persistent psychotic (positive) symptoms despite compliance with these medications.1 While clozapine remains the treatment of choice for positive symptoms, some patients cannot—or will not—take it because of its burdensome side-effect profile.
It is well accepted that supportive psychotherapy can help a person with schizophrenia confront the secondary issues of loss, disability, and stigma. But psychotherapy is rarely considered as an adjunct therapy for treatment-resistant positive symptoms. Skepticism about the role of psychotherapy is understandable, because older studies that demonstrated psychoanalytic psychotherapy’s lack of effect on schizophrenia’s positive symptoms2 have driven psychiatric medical education and practice for the past half-century. Other non-psychoanalytic therapeutic approaches had not been studied until recently, so most of us generalized from the disappointing results of the psychoanalytic psychotherapy research.
Still, there is a resurgence of interest in using cognitive-behavioral principles to treat core schizophrenia symptoms. Several randomized, controlled studies—almost all performed in the United Kingdom—have demonstrated that a cognitive-behavioral therapy (CBT) approach, modified for schizophrenia, is superior to more traditional supportive therapies in treating persistent positive and negative symptoms.3-5 Until recently, CBT for schizophrenia has generated little interest or research on this side of the Atlantic.
Continued treatment: A new approach
At this point, we decided to address Mr. K’s paranoid symptoms with CBT-based psychotherapy. The patient, whom we’d been seeing twice monthly for medication management, agreed to weekly 45-minute CBT sessions across 3 months. A third-year resident who had treated Mr. K during the antipsychotic clinical trial administered the therapy as described in the literature.4-6
During the first sessions, we found that some of Mr. K's fears of leaving the house stemmed from living in a poor inner-city neighborhood with a high rate of violent crime. A few sessions later, Mr. K was able to question some of his beliefs that assassins had targeted his family.
By the fourth week, the therapist discovered that Mr. K liked to read and viewed the local library as a reasonably safe place. Mr. K agreed to visit the library once a week and to record his experiences commuting to and from there.
After roughly 8 weeks of treatment, Mr. K was visiting the library twice a week, usually for 90 minutes at a time. He reported that he “had a good time,” but still suspected other library patrons were talking about him. Upon exploring these suspicions, we learned that Mr. K feared other library goers viewed him as “stupid” and that this fear was exacerbating some of his paranoid delusions.
Table 1
POSITIVE SYMPTOMS THATMAYAPPEARASNEGATIVE SYMPTOMS
| Apparent negative symptom | Underlying psychotic symptom |
|---|---|
| Apathy |
|
| Social withdrawal |
|
| Poor hygiene |
|
Once Mr. K acknowledged that his mental illness was not outwardly recognizable, we could convince him that his fear of appearing “stupid” should not keep him housebound. He began to visit the library more frequently. Although he was still anxious, it no longer took him all day to summon the courage to leave home.
After about 10 weeks of treatment, Mr. K began going on bike rides twice a week. We were concerned that he was making too many changes at once, but he insisted he felt more “comfortable” and enjoyed the exercise.
Did cognitive-behavioral therapy contribute to Mr. K’s improvement? How did the therapist’s treatment differ from accepted protocols?
Dr. Weiden’s and Burkholder’s observations
You might be thinking, “This sounds no different from what I do in practice!” The patient was reassured and encouraged to go out and live his life despite having symptoms.
In practice, however, some techniques used in the CBT approach to psychosis are quite different; some techniques are not intuitive, and some contradict most standard teachings of supportive psychotherapy in this country.
The CBT approach used for Mr. K differed greatly from traditional “medical model” supportive psychotherapy. The therapist:
- rejected a “brain disorder” approach to describing his illness7
- used the stress-vulnerability model to explain positive symptoms
- viewed psychotic symptoms as normal reactions rather than pathologic response
- considered psychological factors behind specific psychotic symptoms (Table 2).8
The “brain disorder” explanation. The Kraepelinian model, which characterizes schizophrenia as a degenerative brain disorder, drives patient education. For example, one brochure for patients and their families refers to schizophrenia as “a brain disorder like Alzheimer’s disease.”
Such a comparison could devastate a young adult who is overwhelmed by symptoms and after being told he had a “brain disorder” that “interfered with his cognition.” While this corresponded with our knowledge of schizophrenia, he took this to mean he is “retarded” and “stupid.”
Table 2
UNDERSTANDING PSYCHOSIS WITHIN THE COGNITIVE-BEHAVIORAL MODEL
| Theory | Implications |
|---|---|
| Psychosis lies on one end of a continuum | Psychosis may be the extreme end of normal cognitive, perceptual experiences |
| Delusions can be modified by others under some circumstances | Consider reducing delusional belief or distress by verbal interventions* |
| The stress-vulnerability model represents a more appropriate explanation of symptoms | Emphasizes stress as a possible cause of symptoms; specifying a diagnosis of schizophrenia can be contraindicated |
| Psychotic symptoms may be a normal response | Normalize symptoms, behavior as much as possible |
| Nature of psychotic symptoms is based on specific circumstances | Explore life events that have a specific psychological context for the individual |
| Psychotic symptoms may be secondary to congnitiive dysfunction | Trace the origins of hallucinations or delusions to specific cognitive overload or stress |
| * This is not meant to endorse a confrontational approach. | |
Telling the patient that he or she has schizophrenia– known in some clinical circles as “the S word”–is not necessary and may even be harmful in some cases. We’re not saying that giving a diagnosis of schizophrenia or using a medical model approach is wrong. However, patient education based on symptoms instead of diagnosis may be more conducive in some cases.
The stress-vulnerability model explains psychosis without having to use a diagnostic label. Mr. K’s previous understanding of schizophrenia dovetailed with his low self-esteem. His self-perceived stupidity also had discouraged him from confronting his paranoid anxieties.
Once he realized that unrelenting psychotic symptoms—not his IQ—held him back, we could form a treatment plan. We explained Mr. K’s paranoid symptoms with the stress-vulnerability model: His fears and suspicions worsened whenever he was under stress. This allowed us to sidestep the “brain disorder” model that demoralized him.
By no means, however, did we reject the notion that schizophrenia has a biologic basis. Even if “schizophrenia” is never mentioned, this diagnosis still guides treatment.
Viewing psychotic symptoms as normal reactions. The therapist extensively examined Mr. K’s safety concerns for himself and his family. The therapist acknowledged that these concerns were legitimate, as the patient lives in an inner-city neighborhood plagued by violent crime. Mr. K was then praised for his devotion to his family.
By applying normalization techniques,9 the therapist found fact-based aspects of the delusional beliefs. Normalizing Mr. K’s safety concerns made him feel validated. From there, we could map out a plan for him to periodically leave his home. We devised a routine that addressed his safety concerns: He went to the library only in daylight. He chose a subway route that was less convenient but made him feel more comfortable. Once at the library, he called home to make sure his family was safe, then sat at an open table so he could watch other library patrons come and go.
Once this routine was established, we could address the more idiosyncratic delusions that caused Mr. K considerable stress and anxiety. We asked him to explain the evidence behind his belief that trained assassins were targeting his family. He could not do so and eventually admitted that this thinking was misguided. His fears gradually shifted from specific threats targeted at him and his family to nonspecific fears of the randomness and unfairness of life.
Placing psychosis in psychological context. We tried to understand the psychology of his paranoid thoughts while viewing his symptoms as part of a neurobiologic disorder.
What initially looked like “garden variety” paranoid delusions had a psychological meaning to Mr. K. His dread of public humiliation was intertwined with his fear of assassination. Once understood, these two fears could be isolated and became easier to treat.10 We traced Mr. K’s fear for his family’s safety to his being the oldest male in a matriarchal household. Because his illness prevented him from assuming the role of breadwinner, all that was left was for him to guard his family from the imagined threat of assassination.
Caveats The CBT techniques outlined in the literature for schizophrenia vary greatly from those used in depression or anxiety disorders. In order for CBT to be effective in schizophrenia, the therapist must have considerable experience working with patients with schizophrenia and must receive specialized training and supervision in CBT techniques modified for persons with schizophrenia.
Further, Mr. K continued to take his antipsychotic medication during the 3-month CBT course. We are not suggesting that CBT be administered in lieu of drug therapy, nor can we claim that CBT will be consistently effective against positive symptoms. What’s more, this case does not take into consideration patients who are persistently psychotic because of suboptimal dosing, poor compliance, or substance abuse.
Follow-up: Continued progress
Mr. K continued to improve after the CBT sessions ended. He completed a summer art class despite recurrent paranoia and lingering fears of social interaction. As of this writing, he was considering taking another course.
Three months after his last session, Mr. K was still regularly visiting the library. He also began walking his niece to and from school each day. His paranoid ideation and ideas of reference appeared to be lessening in intensity. Last fall, he joined a gym. He also reported comfortably conversing with people other than immediate family members or mental health clinicians.
Related resources
- Grech E. A review of the current evidence for the use of psychological interventions in psychosis. Int J Psychosoc Rehab 2002;6:79-88.
- Jones C, Cormac I, et al. Cognitive behaviour therapy for schizophrenia. Cochrane Library Issue 4, 2001. Available at: http://www.mediscope.ch/cochrane-abstracts/ab000524.htm. Accessed Feb. 10, 2003.
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Risperidone • Risperdal
Disclosure
Dr. Weiden reports that he receives research/grant support from, is a consultant to, and/or is a speaker for AstraZeneca Pharmaceuticals, Bristol-Myers Squibb Co., Pfizer Inc., and Janssen Pharmaceutica.
Dr. Burkholder reports that she is a consultant and speaker for Pfizer Inc. and Eli Lilly and Co.
Acknowledgments
The authors wish to thank Catie Camille for her assistance in preparing this article, and Drs. Motaz El Rafae and Najma Khanani for the care they provided to Mr. K.
History: A secluded life
Mr. K, 31, immigrated to Brooklyn as a child with his family. At age 19, he was working as an auto mechanic in a relative’s garage when he had his first psychotic episode. He was hospitalized and diagnosed with paranoid schizophrenia, which was confirmed by his subsequent course of illness and a recent structured diagnostic interview.
Since becoming ill, Mr. K almost never leaves his house and socializes only with his mother and sister. Unable to work, he helps around the house and often cares for his nieces and nephews. He has no history of substance abuse and has been faithfully taking his medication since his last hospitalization 8 years ago.
Mr. K’s outpatient clinic chart reflects concern about persistent negative symptoms. He hardly speaks in session. Even when “stable,” his social and vocational functioning has been poor. Therapeutic dosages of oral haloperidol, haloperidol decanoate, and fluphenazine have not worked, and trials of risperidone and olanzapine—administered in therapeutic dosages for at least 3 months—were only slightly more effective. Attempts to treat his social withdrawal as a depressive symptom equivalent, with use of adjunctive selective serotonin reuptake inhibitors, also have been disappointing.
We eventually discovered that his so-called negative symptoms were in fact the manifestation of persistent positive symptoms (Table 1). His social withdrawal stemmed not from lack of motivation but from ideas of reference and constant paranoid fears. He believed that if he left the house, a street gang would kill him or his family. When he did venture outdoors, he thought that strangers were ridiculing or insulting him or intended to brutally attack him.
Mr. K spent much of his time at home reading, occasionally visiting the public library just long enough to check out a few books. Family members convinced him to attend church services, but he could not interact with other parishioners because he feared they would find out something was “wrong” with him.
How would you address Mr. K’s positive symptoms? Would you try another antipsychotic after lack of response to five other agents?
Drug treatment: A clinical trial
After a thorough evaluation, Mr. K entered a clinical trial during which he began taking another antipsy-chotic. But after 4 months at high therapeutic dosages, his positive symptoms showed no change from baseline.
We then recommended that Mr. K try clozapine. His persistent paranoid delusions and lack of response to other antipsychotics made him an ideal candidate for this agent. Because he was compliant, motivated, and had available family support, we were confident that he could surmount the vicissitudes of a clozapine trial.
Mr. K refused to try clozapine, however. After so many unsuccessful medication trials over the years, he said he felt some (albeit minor) benefits from his current study medication and wanted to stick with it.
What treatment options remain for Mr. K?
Dr. Weiden’s and Burkholder’s observations
Although the newer antipsychotics have greatly improved outcomes in schizophrenia over the past decade, many patients still battle persistent psychotic (positive) symptoms despite compliance with these medications.1 While clozapine remains the treatment of choice for positive symptoms, some patients cannot—or will not—take it because of its burdensome side-effect profile.
It is well accepted that supportive psychotherapy can help a person with schizophrenia confront the secondary issues of loss, disability, and stigma. But psychotherapy is rarely considered as an adjunct therapy for treatment-resistant positive symptoms. Skepticism about the role of psychotherapy is understandable, because older studies that demonstrated psychoanalytic psychotherapy’s lack of effect on schizophrenia’s positive symptoms2 have driven psychiatric medical education and practice for the past half-century. Other non-psychoanalytic therapeutic approaches had not been studied until recently, so most of us generalized from the disappointing results of the psychoanalytic psychotherapy research.
Still, there is a resurgence of interest in using cognitive-behavioral principles to treat core schizophrenia symptoms. Several randomized, controlled studies—almost all performed in the United Kingdom—have demonstrated that a cognitive-behavioral therapy (CBT) approach, modified for schizophrenia, is superior to more traditional supportive therapies in treating persistent positive and negative symptoms.3-5 Until recently, CBT for schizophrenia has generated little interest or research on this side of the Atlantic.
Continued treatment: A new approach
At this point, we decided to address Mr. K’s paranoid symptoms with CBT-based psychotherapy. The patient, whom we’d been seeing twice monthly for medication management, agreed to weekly 45-minute CBT sessions across 3 months. A third-year resident who had treated Mr. K during the antipsychotic clinical trial administered the therapy as described in the literature.4-6
During the first sessions, we found that some of Mr. K's fears of leaving the house stemmed from living in a poor inner-city neighborhood with a high rate of violent crime. A few sessions later, Mr. K was able to question some of his beliefs that assassins had targeted his family.
By the fourth week, the therapist discovered that Mr. K liked to read and viewed the local library as a reasonably safe place. Mr. K agreed to visit the library once a week and to record his experiences commuting to and from there.
After roughly 8 weeks of treatment, Mr. K was visiting the library twice a week, usually for 90 minutes at a time. He reported that he “had a good time,” but still suspected other library patrons were talking about him. Upon exploring these suspicions, we learned that Mr. K feared other library goers viewed him as “stupid” and that this fear was exacerbating some of his paranoid delusions.
Table 1
POSITIVE SYMPTOMS THATMAYAPPEARASNEGATIVE SYMPTOMS
| Apparent negative symptom | Underlying psychotic symptom |
|---|---|
| Apathy |
|
| Social withdrawal |
|
| Poor hygiene |
|
Once Mr. K acknowledged that his mental illness was not outwardly recognizable, we could convince him that his fear of appearing “stupid” should not keep him housebound. He began to visit the library more frequently. Although he was still anxious, it no longer took him all day to summon the courage to leave home.
After about 10 weeks of treatment, Mr. K began going on bike rides twice a week. We were concerned that he was making too many changes at once, but he insisted he felt more “comfortable” and enjoyed the exercise.
Did cognitive-behavioral therapy contribute to Mr. K’s improvement? How did the therapist’s treatment differ from accepted protocols?
Dr. Weiden’s and Burkholder’s observations
You might be thinking, “This sounds no different from what I do in practice!” The patient was reassured and encouraged to go out and live his life despite having symptoms.
In practice, however, some techniques used in the CBT approach to psychosis are quite different; some techniques are not intuitive, and some contradict most standard teachings of supportive psychotherapy in this country.
The CBT approach used for Mr. K differed greatly from traditional “medical model” supportive psychotherapy. The therapist:
- rejected a “brain disorder” approach to describing his illness7
- used the stress-vulnerability model to explain positive symptoms
- viewed psychotic symptoms as normal reactions rather than pathologic response
- considered psychological factors behind specific psychotic symptoms (Table 2).8
The “brain disorder” explanation. The Kraepelinian model, which characterizes schizophrenia as a degenerative brain disorder, drives patient education. For example, one brochure for patients and their families refers to schizophrenia as “a brain disorder like Alzheimer’s disease.”
Such a comparison could devastate a young adult who is overwhelmed by symptoms and after being told he had a “brain disorder” that “interfered with his cognition.” While this corresponded with our knowledge of schizophrenia, he took this to mean he is “retarded” and “stupid.”
Table 2
UNDERSTANDING PSYCHOSIS WITHIN THE COGNITIVE-BEHAVIORAL MODEL
| Theory | Implications |
|---|---|
| Psychosis lies on one end of a continuum | Psychosis may be the extreme end of normal cognitive, perceptual experiences |
| Delusions can be modified by others under some circumstances | Consider reducing delusional belief or distress by verbal interventions* |
| The stress-vulnerability model represents a more appropriate explanation of symptoms | Emphasizes stress as a possible cause of symptoms; specifying a diagnosis of schizophrenia can be contraindicated |
| Psychotic symptoms may be a normal response | Normalize symptoms, behavior as much as possible |
| Nature of psychotic symptoms is based on specific circumstances | Explore life events that have a specific psychological context for the individual |
| Psychotic symptoms may be secondary to congnitiive dysfunction | Trace the origins of hallucinations or delusions to specific cognitive overload or stress |
| * This is not meant to endorse a confrontational approach. | |
Telling the patient that he or she has schizophrenia– known in some clinical circles as “the S word”–is not necessary and may even be harmful in some cases. We’re not saying that giving a diagnosis of schizophrenia or using a medical model approach is wrong. However, patient education based on symptoms instead of diagnosis may be more conducive in some cases.
The stress-vulnerability model explains psychosis without having to use a diagnostic label. Mr. K’s previous understanding of schizophrenia dovetailed with his low self-esteem. His self-perceived stupidity also had discouraged him from confronting his paranoid anxieties.
Once he realized that unrelenting psychotic symptoms—not his IQ—held him back, we could form a treatment plan. We explained Mr. K’s paranoid symptoms with the stress-vulnerability model: His fears and suspicions worsened whenever he was under stress. This allowed us to sidestep the “brain disorder” model that demoralized him.
By no means, however, did we reject the notion that schizophrenia has a biologic basis. Even if “schizophrenia” is never mentioned, this diagnosis still guides treatment.
Viewing psychotic symptoms as normal reactions. The therapist extensively examined Mr. K’s safety concerns for himself and his family. The therapist acknowledged that these concerns were legitimate, as the patient lives in an inner-city neighborhood plagued by violent crime. Mr. K was then praised for his devotion to his family.
By applying normalization techniques,9 the therapist found fact-based aspects of the delusional beliefs. Normalizing Mr. K’s safety concerns made him feel validated. From there, we could map out a plan for him to periodically leave his home. We devised a routine that addressed his safety concerns: He went to the library only in daylight. He chose a subway route that was less convenient but made him feel more comfortable. Once at the library, he called home to make sure his family was safe, then sat at an open table so he could watch other library patrons come and go.
Once this routine was established, we could address the more idiosyncratic delusions that caused Mr. K considerable stress and anxiety. We asked him to explain the evidence behind his belief that trained assassins were targeting his family. He could not do so and eventually admitted that this thinking was misguided. His fears gradually shifted from specific threats targeted at him and his family to nonspecific fears of the randomness and unfairness of life.
Placing psychosis in psychological context. We tried to understand the psychology of his paranoid thoughts while viewing his symptoms as part of a neurobiologic disorder.
What initially looked like “garden variety” paranoid delusions had a psychological meaning to Mr. K. His dread of public humiliation was intertwined with his fear of assassination. Once understood, these two fears could be isolated and became easier to treat.10 We traced Mr. K’s fear for his family’s safety to his being the oldest male in a matriarchal household. Because his illness prevented him from assuming the role of breadwinner, all that was left was for him to guard his family from the imagined threat of assassination.
Caveats The CBT techniques outlined in the literature for schizophrenia vary greatly from those used in depression or anxiety disorders. In order for CBT to be effective in schizophrenia, the therapist must have considerable experience working with patients with schizophrenia and must receive specialized training and supervision in CBT techniques modified for persons with schizophrenia.
Further, Mr. K continued to take his antipsychotic medication during the 3-month CBT course. We are not suggesting that CBT be administered in lieu of drug therapy, nor can we claim that CBT will be consistently effective against positive symptoms. What’s more, this case does not take into consideration patients who are persistently psychotic because of suboptimal dosing, poor compliance, or substance abuse.
Follow-up: Continued progress
Mr. K continued to improve after the CBT sessions ended. He completed a summer art class despite recurrent paranoia and lingering fears of social interaction. As of this writing, he was considering taking another course.
Three months after his last session, Mr. K was still regularly visiting the library. He also began walking his niece to and from school each day. His paranoid ideation and ideas of reference appeared to be lessening in intensity. Last fall, he joined a gym. He also reported comfortably conversing with people other than immediate family members or mental health clinicians.
Related resources
- Grech E. A review of the current evidence for the use of psychological interventions in psychosis. Int J Psychosoc Rehab 2002;6:79-88.
- Jones C, Cormac I, et al. Cognitive behaviour therapy for schizophrenia. Cochrane Library Issue 4, 2001. Available at: http://www.mediscope.ch/cochrane-abstracts/ab000524.htm. Accessed Feb. 10, 2003.
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Risperidone • Risperdal
Disclosure
Dr. Weiden reports that he receives research/grant support from, is a consultant to, and/or is a speaker for AstraZeneca Pharmaceuticals, Bristol-Myers Squibb Co., Pfizer Inc., and Janssen Pharmaceutica.
Dr. Burkholder reports that she is a consultant and speaker for Pfizer Inc. and Eli Lilly and Co.
Acknowledgments
The authors wish to thank Catie Camille for her assistance in preparing this article, and Drs. Motaz El Rafae and Najma Khanani for the care they provided to Mr. K.
1. Drake RE, Sederer LI. The adverse effects of intensive treatment of chronic schizophrenia. Compr Psychiatry 1986;27(4):313-26.
2. May PRA. Treatment of schizophrenia. New York: Science House, 1968:352.
3. Tarrier N, Beckett R, Harwood S, et al. A trial of two cognitive-behavioural methods of treating drug-resistant psychotic symptoms in schizophrenic patients, I: outcome. Br J Psychiatry 1993;162:524-32.
4. Sensky T, Turkington D, Kingdon D, et al. A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms of schizophrenia resistant to medication. Arch Gen Psychiatry 2000;57(2):165-72.
5. Turkington D, Kingdon D, Turner T. Effectiveness of a brief cognitive-behavioural therapy intervention in the treatment of schizophrenia. Br J Psychiatry 2002;180:523-7.
6. Kingdon DG, Turkington D. Cognitive-behavioral therapy of schizophrenia. New York: Guilford Publications, 1994.
7. Kemp R, Kirov G, Everitt B, et al. Randomised controlled trial of compliance therapy: 18-month follow-up. Br J Psychiatry 1998;172:413-9.
8. Turkington D, Siddle R. Improving understanding and coping in people with schizophrenia by changing attitudes. Psychiatr Rehabil Skills 2000;4(2):300-20.
9. Weiden PJ, Havens LL. Psychotherapeutic management techniques in the treatment of outpatients with schizophrenia. Hosp Community Psychiatry 1994;45:549-55.
10. Link B, Mirotznik J, Cullen FT. The effectiveness of stigma coping orientations: Can negative consequences of mental illness labeling be avoided? J Health Soc Behav 1991;32(3):302-20.
11. Weiden PJ, Aquila R, Emanuel R, Zygmunt A. Long-term considerations after switching antipsychotics. J Clin Psychiatry 1998;59(suppl 19):36-49.
1. Drake RE, Sederer LI. The adverse effects of intensive treatment of chronic schizophrenia. Compr Psychiatry 1986;27(4):313-26.
2. May PRA. Treatment of schizophrenia. New York: Science House, 1968:352.
3. Tarrier N, Beckett R, Harwood S, et al. A trial of two cognitive-behavioural methods of treating drug-resistant psychotic symptoms in schizophrenic patients, I: outcome. Br J Psychiatry 1993;162:524-32.
4. Sensky T, Turkington D, Kingdon D, et al. A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms of schizophrenia resistant to medication. Arch Gen Psychiatry 2000;57(2):165-72.
5. Turkington D, Kingdon D, Turner T. Effectiveness of a brief cognitive-behavioural therapy intervention in the treatment of schizophrenia. Br J Psychiatry 2002;180:523-7.
6. Kingdon DG, Turkington D. Cognitive-behavioral therapy of schizophrenia. New York: Guilford Publications, 1994.
7. Kemp R, Kirov G, Everitt B, et al. Randomised controlled trial of compliance therapy: 18-month follow-up. Br J Psychiatry 1998;172:413-9.
8. Turkington D, Siddle R. Improving understanding and coping in people with schizophrenia by changing attitudes. Psychiatr Rehabil Skills 2000;4(2):300-20.
9. Weiden PJ, Havens LL. Psychotherapeutic management techniques in the treatment of outpatients with schizophrenia. Hosp Community Psychiatry 1994;45:549-55.
10. Link B, Mirotznik J, Cullen FT. The effectiveness of stigma coping orientations: Can negative consequences of mental illness labeling be avoided? J Health Soc Behav 1991;32(3):302-20.
11. Weiden PJ, Aquila R, Emanuel R, Zygmunt A. Long-term considerations after switching antipsychotics. J Clin Psychiatry 1998;59(suppl 19):36-49.