User login
The psychotic pot smoker
CASE: Scared and confused
Mr. C, age 28, presents to the emergency department (ED) in police custody with agitation and altered mental status. Earlier that evening, Mr. C’s girlfriend noticed he was talking to himself while watching television. A few hours later, Mr. C thought someone was breaking into his house. Mr. C ran out of the house screaming for help, broke his neighbor’s window, and eventually called the police. When the police arrived Mr. C was wearing only his underwear, shaking, and bleeding from his hands. He said he was afraid and refused to respond to police instructions. Police officers used an electronic stun gun to facilitate transport to the hospital.
Mr. C admits to smoking 3 to 4 marijuana joints daily for the past 16 years. His last drug use was 2 hours before his symptoms began. Mr. C suggests that someone may have adulterated his marijuana joint but he has no factual basis for this accusation. He denies using alcohol and other illicit drugs and has no personal or family psychiatric history. He denies recent fever, loss of consciousness, chest pain, weakness, myalgia, or headache. Medically stable, his only complaint is mild hand pain.
Mr. C is alert, awake, and oriented to his name, and he responds properly to questions. He is tachycardic (101 bpm), his blood pressure is 149/57 mm Hg with normal S1 and S2 sounds, and he has no meningismus or nystagmus. Glasgow Coma Scale score is 15. He has increased deep tendon reflexes on the right upper and lower limb with good hand-grip and multiple abrasions and lacerations on his hands.
The authors’ observations
New-onset psychosis can have a wide differential diagnosis, particularly when reliable history is not available. Mr. C’s allegation that someone tampered with his marijuana raises 2 possibilities: embalming fluid (form-aldehyde) toxicity or PCP intoxication.
Embalming fluid toxicity can cause:
- agitation and sudden unpredictable behavior
- confusion or toxic delirium
- coma or seizure
- cerebral and pulmonary edema or death in severe cases.
The terms “wet,” “sherm,” “fly,” “amp,” or “illy” are used to describe a marijuana cigarette that has been dipped into embalming fluid, dried, and then smoked.1 The effect is similar to that of PCP and causes extreme hallucinations. Reported highs last 30 minutes to 1 hour.2
Symptomatology of PCP intoxication may be indistinguishable from functional psychosis (Table 1).3 Visual, auditory, and tactile misperceptions are common and highly changeable disorientation often is accompanied by alternating periods of lethargy and fearful agitation. These patients typically show catatonic posturing and/or stereotyped movement. Somatic sensations appear to be disassociated; patients may misperceive pain, distance, and time. Patients taking PCP rarely admit to true hallucinations; however their thinking usually is grossly disoriented.4 Symptoms of delirium may last from 30 minutes to 6 hours in 80% of cases; 12% of patients may remain symptomatic for 12 hours. Violent behavior and agitation usually lasts only a few hours.5
Long-term marijuana abuse can lead to psychosis6 but acute onset is not typical, and recent prospective trials raised doubts that cannabis would be a sole factor.7 Instead, cannabis may be 1 of several factors that contribute to psychosis, particularly in patients who are predisposed.
Table 1
Phencyclidine (PCP) intoxication: What to look for
| Findings | Percentage of cases |
|---|---|
| Nystagmus | 57.4% |
| Hypertension | 57.0% |
| Delirium | 36.9% |
| Violent behavior | 35.4% |
| Agitation | 34.0% |
| Tachycardia | 30.0% |
| Bizarre behavior | 28.5% |
| Hallucinations/delusions | 18.5% |
| Unconsciousness | 10.6% |
| Lethargy/stupor | 6.6% |
| Hypothermia | 6.4% |
| Generalized rigidity | 5.2% |
| Profuse sweating | 3.9% |
| No behavior effect | 3.5% |
| Grand mal seizure | 3.1% |
| Source: Reference 3 | |
Possible neurologic causes
Complex partial seizures—also known as psychomotor epilepsy—are caused by a surge of electrical activity in the brain. Seizures often involve 1 of the brain’s temporal lobes but can affect any brain region. Symptoms include:
- impaired social interaction
- inability to control one’s movements
- alogia
- amnesia.
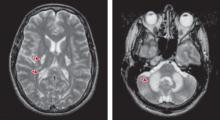
Episodes typically start with a blank stare followed by automatisms. The actions and movements often are unorganized or confused. Motor symptoms typically last for 1 to 2 minutes and confusion persists for another 1 to 2 minutes.8 In rare cases, a patient may become agitated or engage in behaviors such as undressing. Complex partial seizures may cause a person to run in apparent fear, cry out, or repeat a phrase.9 Electroencephalogram, CT, MRI, or positron-emission tomography scan could reveal any intracranial focus of complex partial seizures.
We suspect PCP or embalming fluid intoxication and initiate supportive therapy.
EVALUATION: Still confused
Initial baseline labs include a urine drug screen (UDS), chest radiography, ECG, and head CT. Mr. C’s UDS is positive for cannabis. A specific PCP assay is negative. White blood cell count (WBC) is 22,000/μL with high neutrophil count (88%), creatine kinase (CK) is 458 U/L, and urinalyis reveals protein 75 mg/dL and ketone 50 mg/dL. Head CT is negative for any acute process (click here for detailed description of Mr. C�s hospital course while in the ED).
During psychiatric evaluation 7 hours after presentation, Mr. C’s speech is loose and somewhat pressured, but intelligible. He cannot follow commands. Mr. C is delusional and appears to be hallucinating. He can repeat 3 words immediately but not after 3 minutes. We start Mr. C on divalproex, 1,500 mg/d, haloperidol, 6 mg/d, and IV lorazepam, 2 mg as needed for agitation. Although mildly disoriented, he gradually becomes less agitated.
The authors’ observations
At this point further evaluation is needed. Mr. C’s elevated WBC count could explain his fluctuating symptoms. He cannot provide further history and his family denies any past psychiatric episodes. Thyroid-stimulating hormone, B12, and folate levels are within normal limits. A negative LP rules out meningitic infection. We give Mr. C a diagnosis of psychosis NOS (Table 2).10
Table 2
DSM-IV-TR criteria for psychotic disorder, not otherwise specified
| This category includes psychotic symptomatology (ie, delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior) about which there is inadequate information to make a specific diagnosis or about which there is contradictory information, or disorders with psychotic symptoms that do not meet the criteria for any specific psychotic disorder. Examples include: |
|
| Source: Reference 10 |
TREATMENT: Medication choices
After 8 hours in the ED, Mr. C is transferred to the medical unit, where he becomes agitated and complains of auditory and visual hallucinations. He receives divalproex, 750 mg, haloperidol, 3 mg, and IM diphenhydramine, 50 mg, to calm him. He remains agitated but not violent until bedtime. At midnight he is agitated and violent and receives another dose of haloperidol and IM diphenhydramine with IV lorazepam, 2 mg. These medications calm him and he is able to sleep until morning.
Morning labs reveal CK is 674 U/L and WBC decreased to 13,200/μL. Mr. C denies any distress but after the fourth dose of haloperidol, he develops dystonia of his arms so we discontinue this medication. We start aripiprazole, 10 mg/d gradually increased to 30 mg/d, and Mr. C receives 1 injection of diphenhydramine. He responds well to the treatment.
The next few hours are uneventful but then Mr. C becomes verbally abusive to his relatives and sitter; physical restraints are ordered and he receives IM ziprasidone, 20 mg, and IV lorazepam, 2 mg. He remains awake and babbling. His perception continues to wax and wane and his words are jumbled. He remains calm until the next morning (click here for detailed description of Mr. C�s hospital course while on the medical unit).
After 4 days on the medical unit Mr. C is transferred to the psychiatry unit, where he is angry, belligerent, and hostile, but not placed in restraints. His symptoms resolve in 2 days without any further episodes of violent behavior.
OUTCOME: Solving the puzzle
When Mr. C becomes cooperative, he gives a detailed history. He repeats his suspicion of smoking adulterated marijuana, but during detailed questioning, he admits to using alprazolam, which he purchased illegally, to sleep for the past 6 to 7 months. He started with 1 or 2 “footballs” (1 to 2 mg) and gradually increased to 3 or 4 “bars” (6 to 8 mg) each day. Mr. C could no longer afford the drug and last took alprazolam 6 days before his symptoms began. He says that after stopping alprazolam he felt anxious and could not sleep. His girlfriend adds that he was irritable and “he had not been acting himself” several days before admission. She says he complained of hearing the voice of God, particularly when he was not taking alprazolam.
Mr. C’s hand wounds heal and his vitals are normal during his 1-week stay on the psychiatric unit. His interactions with staff and peers improve. Aripiprazole is tapered and discontinued; divalproex is reduced to 1,000 mg/d. Mr. C is discharged 11 days after presentation and prescribed divalproex, 1,000 mg/d, with instructions to taper the drug over several days to prevent withdrawal seizures before stopping it in 1 week.
Mr. C does not return for his follow-up appointment; however, in a telephone follow-up 6 months later, he denies experiencing withdrawal symptoms after discharge. Mr. C is now undergoing drug rehabilitation.
The authors’ observations
Benzodiazepine withdrawal symptoms occur 7 to 10 days after abrupt cessation (Table 3).10 Symptoms are similar to those of alcohol withdrawal and include tachycardia, hypertension, clouding of consciousness, and auditory and visual hallucinations.11 Serious reactions to benzodiazepine withdrawal include seizures and death.12
Because of the high prevalence of poly-substance misuse, obtain a detailed substance use history in patients undergoing benzodiazepine withdrawal to determine the likelihood of polysubstance withdrawal.13 A cross-tolerant sedative such as clonazepam could prevent withdrawal symptoms as the dose is gradually decreased. Long-acting benzodiazepines such as clonazepam or diazepam are recommended.14
In Mr. C’s case, minor withdrawal symptoms, such as disturbed sleep and irritability, began 3 to 4 days after discontinuing benzodiazepines15 and preceded development of psychosis. Withdrawal symptoms usually resolve after 2 weeks.16 Mr. C responded only partially to IV lorazepam because he did not receive the total replacement dose. Had we known he was experiencing benzodiazepine withdrawal, Mr. C could have been managed with detoxi"cation of the primary drug, alprazolam, with diazepam substitution and tapering over 3 weeks.17
Table 3
Criteria for sedative, hypnotic, or anxiolytic withdrawal
| A. Cessation of (or reduction in) sedative, hypnotic, or anxiolytic use that has been heavy and prolonged |
B. Two (or more) of the following, developing within several hours to a few days after Criterion A:
|
| C. The symptoms in Criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| D. The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder |
| Source: Reference 10 |
Related Resource
- Vikander B, Koechling UM, Borg S, et al. Benzodiazepine tapering: a prospective study. Nord J Psychiatry. 2010; 64(4):273-282.
Drug Brand Names
- Alprazolam • Xanax
- Aripiprazole • Abilify
- Chlordiazepoxide • Librium
- Diazepam • Valium
- Diphenhydramine • Diphenhydramine injection
- Divalproex • Depakote
- Haloperidol • Haldol
- Lorazepam • Ativan
- Ziprasidone • Geodon
Acknowledgements
The authors wish to thank Reena Kumar, MD, and Sonja Gennuso, fourth-year medical student at Louisiana State University Health Sciences Center, Shreveport, for their help in preparing this manuscript.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Table 1
Mr. C’s hospital course in the emergency department
| Time after presentation | Description |
|---|---|
| 2 hours | Mr. C is alert and oriented to his name and place. He rests comfortably but asks questions about his girlfriend and uncle, falsely believing they are in the emergency department |
| 4 hours | Hand lacerations are repaired, but Mr. C continues to dig in his wounds with the opposite hand and place it over his mouth despite constant redirection. He reports hearing his uncle’s voice behind the curtain. He then uses the pulse oximeter as a telephone and holds a conversation with his uncle on the other side of the curtain. On redirection, Mr. C replies that the pulse oximeter looks like a telephone and begins mumbling to himself |
| 5 hours | Mr. C continues to mumble but responds when directly questioned. He keeps insisting that the pulse oximeter is a telephone and that he can tell his uncle to come over from the other side of the curtain. He continues to act inappropriately despite the presence of family members but he is aware of their identities |
| 6 hours | Mr. C becomes disoriented and agitated and pulls out his IV line. Because of the high WBC count, we order blood cultures and a urine culture and give him IV antibiotics |
| WBC: white blood cell count | |
Table 2
Mr. C’s hospital course on the medical unit
| Time after presentation | Description |
|---|---|
| 54 hours | He is oriented to person and place. Staff notices he is talking to someone in the room but no one is present. Mr. C appears to be responding to visual hallucinations, but upon questioning he denies any symptoms. Restraints are discontinued. Divalproex is increased to 2,000 mg/d |
| 62 hours | Mr. C remains calm for several hours but later begins hallucinating and calls to his mother and others when no one is in the room. He receives IV lorazepam, 2 mg, without much response. Again he is placed in restraints and receives another dose of IV lorazepam, 3 mg, and IM ziprasidone, 20 mg. He becomes calmer. Restraints are continued as a precautionary measure. Mr. C calms down after several hours but cannot sleep |
| 78 hours | The next morning, Mr. C remains agitated and aggressive with loud speech. He denies any further hallucinations but talks to an invisible person. He remains in restraints and receives his routine medications. His blood pressure is 141/99 mm Hg and pulse is 110. Pulse rate normalizes during the day and he becomes calmer but seclusive |
1. Office of National Drug Control Policy. Street terms: drugs and the drug trade. Available at:http://www.whitehousedrugpolicy.gov/streetterms/ByType.asp?intTypeID=1. Accessed July 26, 2010.
2. Elwood WN. TCADA research brief: “Fry:” a study of adolescents’ use of embalming fluid with marijuana and tobacco. Texas Commission on Alcohol and Drug Abuse. 1998. Available at:http://www.dshs.state.tx.us/sa/research/populations/fry.pdf. Accessed August 9, 2010.
3. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: incidence of clinical findings in 1,000 cases. Ann Emerg Med. 1981;10(5):237-242.
4. Aniline O, Pitts FN, Jr. Phencyclidine (PCP): a review and perspectives. Crit Rev Toxicol. 1982;10(2):145-177.
5. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: clinical patterns, complications, and treatment. Ann Emerg Med. 1981;10(6):290-297.
6. Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187-194.
7. Degenhardt L, Hall W. Cannabis and psychosis. Curr Psychiatry Rep. 2002;4(3):191-196.
8. Carroll E, Benbadis SR. Complex partial seizures. eMedicine. April 21, 2010. Available at:http://emedicine.medscape.com/article/1183962-overview. Accessed July 20, 2010.
9. Epilepsy.com. Complex partial seizures. Available at: http://www.epilepsy.com/epilepsy/seizure_complexpartial. Accessed July 20, 2010.
10. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
11. Mellor CS, Jain VK. Diazepam withdrawal syndrome: its prolonged and changing nature. Can Med Assoc J. 1982;127(11):1093-1096.
12. Lann MA, Molina DK. A fatal case of benzodiazepine withdrawal. Am J Forensic Med Pathol. 2009;30(2):177-179.
13. Busto UE, Romach MK, Sellers EM. Multiple drug use and psychiatric comorbidity in patients admitted to the hospital with severe benzodiazepine dependence. J Clin Psychopharmacol. 1996;16(1):51-57.
14. Franklin JE, Jr., Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:400–401.
15. Preskorn SH, Denner LJ. Benzodiazepines and withdrawal psychosis. Report of three cases. JAMA. 1977;237(1):36-38.
16. Miller F, Nulsen J. Single case study. Diazepam (valium) detoxification. J Nerv Ment Dis. 1979;167:637-638.
17. Seivewright N, Dougal W. Withdrawal symptoms from high dose benzodiazepines in poly drug users. Drug Alcohol Depend. 1993;32(1):15-23.
CASE: Scared and confused
Mr. C, age 28, presents to the emergency department (ED) in police custody with agitation and altered mental status. Earlier that evening, Mr. C’s girlfriend noticed he was talking to himself while watching television. A few hours later, Mr. C thought someone was breaking into his house. Mr. C ran out of the house screaming for help, broke his neighbor’s window, and eventually called the police. When the police arrived Mr. C was wearing only his underwear, shaking, and bleeding from his hands. He said he was afraid and refused to respond to police instructions. Police officers used an electronic stun gun to facilitate transport to the hospital.
Mr. C admits to smoking 3 to 4 marijuana joints daily for the past 16 years. His last drug use was 2 hours before his symptoms began. Mr. C suggests that someone may have adulterated his marijuana joint but he has no factual basis for this accusation. He denies using alcohol and other illicit drugs and has no personal or family psychiatric history. He denies recent fever, loss of consciousness, chest pain, weakness, myalgia, or headache. Medically stable, his only complaint is mild hand pain.
Mr. C is alert, awake, and oriented to his name, and he responds properly to questions. He is tachycardic (101 bpm), his blood pressure is 149/57 mm Hg with normal S1 and S2 sounds, and he has no meningismus or nystagmus. Glasgow Coma Scale score is 15. He has increased deep tendon reflexes on the right upper and lower limb with good hand-grip and multiple abrasions and lacerations on his hands.
The authors’ observations
New-onset psychosis can have a wide differential diagnosis, particularly when reliable history is not available. Mr. C’s allegation that someone tampered with his marijuana raises 2 possibilities: embalming fluid (form-aldehyde) toxicity or PCP intoxication.
Embalming fluid toxicity can cause:
- agitation and sudden unpredictable behavior
- confusion or toxic delirium
- coma or seizure
- cerebral and pulmonary edema or death in severe cases.
The terms “wet,” “sherm,” “fly,” “amp,” or “illy” are used to describe a marijuana cigarette that has been dipped into embalming fluid, dried, and then smoked.1 The effect is similar to that of PCP and causes extreme hallucinations. Reported highs last 30 minutes to 1 hour.2
Symptomatology of PCP intoxication may be indistinguishable from functional psychosis (Table 1).3 Visual, auditory, and tactile misperceptions are common and highly changeable disorientation often is accompanied by alternating periods of lethargy and fearful agitation. These patients typically show catatonic posturing and/or stereotyped movement. Somatic sensations appear to be disassociated; patients may misperceive pain, distance, and time. Patients taking PCP rarely admit to true hallucinations; however their thinking usually is grossly disoriented.4 Symptoms of delirium may last from 30 minutes to 6 hours in 80% of cases; 12% of patients may remain symptomatic for 12 hours. Violent behavior and agitation usually lasts only a few hours.5
Long-term marijuana abuse can lead to psychosis6 but acute onset is not typical, and recent prospective trials raised doubts that cannabis would be a sole factor.7 Instead, cannabis may be 1 of several factors that contribute to psychosis, particularly in patients who are predisposed.
Table 1
Phencyclidine (PCP) intoxication: What to look for
| Findings | Percentage of cases |
|---|---|
| Nystagmus | 57.4% |
| Hypertension | 57.0% |
| Delirium | 36.9% |
| Violent behavior | 35.4% |
| Agitation | 34.0% |
| Tachycardia | 30.0% |
| Bizarre behavior | 28.5% |
| Hallucinations/delusions | 18.5% |
| Unconsciousness | 10.6% |
| Lethargy/stupor | 6.6% |
| Hypothermia | 6.4% |
| Generalized rigidity | 5.2% |
| Profuse sweating | 3.9% |
| No behavior effect | 3.5% |
| Grand mal seizure | 3.1% |
| Source: Reference 3 | |
Possible neurologic causes
Complex partial seizures—also known as psychomotor epilepsy—are caused by a surge of electrical activity in the brain. Seizures often involve 1 of the brain’s temporal lobes but can affect any brain region. Symptoms include:
- impaired social interaction
- inability to control one’s movements
- alogia
- amnesia.
Episodes typically start with a blank stare followed by automatisms. The actions and movements often are unorganized or confused. Motor symptoms typically last for 1 to 2 minutes and confusion persists for another 1 to 2 minutes.8 In rare cases, a patient may become agitated or engage in behaviors such as undressing. Complex partial seizures may cause a person to run in apparent fear, cry out, or repeat a phrase.9 Electroencephalogram, CT, MRI, or positron-emission tomography scan could reveal any intracranial focus of complex partial seizures.
We suspect PCP or embalming fluid intoxication and initiate supportive therapy.
EVALUATION: Still confused
Initial baseline labs include a urine drug screen (UDS), chest radiography, ECG, and head CT. Mr. C’s UDS is positive for cannabis. A specific PCP assay is negative. White blood cell count (WBC) is 22,000/μL with high neutrophil count (88%), creatine kinase (CK) is 458 U/L, and urinalyis reveals protein 75 mg/dL and ketone 50 mg/dL. Head CT is negative for any acute process (click here for detailed description of Mr. C�s hospital course while in the ED).
During psychiatric evaluation 7 hours after presentation, Mr. C’s speech is loose and somewhat pressured, but intelligible. He cannot follow commands. Mr. C is delusional and appears to be hallucinating. He can repeat 3 words immediately but not after 3 minutes. We start Mr. C on divalproex, 1,500 mg/d, haloperidol, 6 mg/d, and IV lorazepam, 2 mg as needed for agitation. Although mildly disoriented, he gradually becomes less agitated.
The authors’ observations
At this point further evaluation is needed. Mr. C’s elevated WBC count could explain his fluctuating symptoms. He cannot provide further history and his family denies any past psychiatric episodes. Thyroid-stimulating hormone, B12, and folate levels are within normal limits. A negative LP rules out meningitic infection. We give Mr. C a diagnosis of psychosis NOS (Table 2).10
Table 2
DSM-IV-TR criteria for psychotic disorder, not otherwise specified
| This category includes psychotic symptomatology (ie, delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior) about which there is inadequate information to make a specific diagnosis or about which there is contradictory information, or disorders with psychotic symptoms that do not meet the criteria for any specific psychotic disorder. Examples include: |
|
| Source: Reference 10 |
TREATMENT: Medication choices
After 8 hours in the ED, Mr. C is transferred to the medical unit, where he becomes agitated and complains of auditory and visual hallucinations. He receives divalproex, 750 mg, haloperidol, 3 mg, and IM diphenhydramine, 50 mg, to calm him. He remains agitated but not violent until bedtime. At midnight he is agitated and violent and receives another dose of haloperidol and IM diphenhydramine with IV lorazepam, 2 mg. These medications calm him and he is able to sleep until morning.
Morning labs reveal CK is 674 U/L and WBC decreased to 13,200/μL. Mr. C denies any distress but after the fourth dose of haloperidol, he develops dystonia of his arms so we discontinue this medication. We start aripiprazole, 10 mg/d gradually increased to 30 mg/d, and Mr. C receives 1 injection of diphenhydramine. He responds well to the treatment.
The next few hours are uneventful but then Mr. C becomes verbally abusive to his relatives and sitter; physical restraints are ordered and he receives IM ziprasidone, 20 mg, and IV lorazepam, 2 mg. He remains awake and babbling. His perception continues to wax and wane and his words are jumbled. He remains calm until the next morning (click here for detailed description of Mr. C�s hospital course while on the medical unit).
After 4 days on the medical unit Mr. C is transferred to the psychiatry unit, where he is angry, belligerent, and hostile, but not placed in restraints. His symptoms resolve in 2 days without any further episodes of violent behavior.
OUTCOME: Solving the puzzle
When Mr. C becomes cooperative, he gives a detailed history. He repeats his suspicion of smoking adulterated marijuana, but during detailed questioning, he admits to using alprazolam, which he purchased illegally, to sleep for the past 6 to 7 months. He started with 1 or 2 “footballs” (1 to 2 mg) and gradually increased to 3 or 4 “bars” (6 to 8 mg) each day. Mr. C could no longer afford the drug and last took alprazolam 6 days before his symptoms began. He says that after stopping alprazolam he felt anxious and could not sleep. His girlfriend adds that he was irritable and “he had not been acting himself” several days before admission. She says he complained of hearing the voice of God, particularly when he was not taking alprazolam.
Mr. C’s hand wounds heal and his vitals are normal during his 1-week stay on the psychiatric unit. His interactions with staff and peers improve. Aripiprazole is tapered and discontinued; divalproex is reduced to 1,000 mg/d. Mr. C is discharged 11 days after presentation and prescribed divalproex, 1,000 mg/d, with instructions to taper the drug over several days to prevent withdrawal seizures before stopping it in 1 week.
Mr. C does not return for his follow-up appointment; however, in a telephone follow-up 6 months later, he denies experiencing withdrawal symptoms after discharge. Mr. C is now undergoing drug rehabilitation.
The authors’ observations
Benzodiazepine withdrawal symptoms occur 7 to 10 days after abrupt cessation (Table 3).10 Symptoms are similar to those of alcohol withdrawal and include tachycardia, hypertension, clouding of consciousness, and auditory and visual hallucinations.11 Serious reactions to benzodiazepine withdrawal include seizures and death.12
Because of the high prevalence of poly-substance misuse, obtain a detailed substance use history in patients undergoing benzodiazepine withdrawal to determine the likelihood of polysubstance withdrawal.13 A cross-tolerant sedative such as clonazepam could prevent withdrawal symptoms as the dose is gradually decreased. Long-acting benzodiazepines such as clonazepam or diazepam are recommended.14
In Mr. C’s case, minor withdrawal symptoms, such as disturbed sleep and irritability, began 3 to 4 days after discontinuing benzodiazepines15 and preceded development of psychosis. Withdrawal symptoms usually resolve after 2 weeks.16 Mr. C responded only partially to IV lorazepam because he did not receive the total replacement dose. Had we known he was experiencing benzodiazepine withdrawal, Mr. C could have been managed with detoxi"cation of the primary drug, alprazolam, with diazepam substitution and tapering over 3 weeks.17
Table 3
Criteria for sedative, hypnotic, or anxiolytic withdrawal
| A. Cessation of (or reduction in) sedative, hypnotic, or anxiolytic use that has been heavy and prolonged |
B. Two (or more) of the following, developing within several hours to a few days after Criterion A:
|
| C. The symptoms in Criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| D. The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder |
| Source: Reference 10 |
Related Resource
- Vikander B, Koechling UM, Borg S, et al. Benzodiazepine tapering: a prospective study. Nord J Psychiatry. 2010; 64(4):273-282.
Drug Brand Names
- Alprazolam • Xanax
- Aripiprazole • Abilify
- Chlordiazepoxide • Librium
- Diazepam • Valium
- Diphenhydramine • Diphenhydramine injection
- Divalproex • Depakote
- Haloperidol • Haldol
- Lorazepam • Ativan
- Ziprasidone • Geodon
Acknowledgements
The authors wish to thank Reena Kumar, MD, and Sonja Gennuso, fourth-year medical student at Louisiana State University Health Sciences Center, Shreveport, for their help in preparing this manuscript.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Table 1
Mr. C’s hospital course in the emergency department
| Time after presentation | Description |
|---|---|
| 2 hours | Mr. C is alert and oriented to his name and place. He rests comfortably but asks questions about his girlfriend and uncle, falsely believing they are in the emergency department |
| 4 hours | Hand lacerations are repaired, but Mr. C continues to dig in his wounds with the opposite hand and place it over his mouth despite constant redirection. He reports hearing his uncle’s voice behind the curtain. He then uses the pulse oximeter as a telephone and holds a conversation with his uncle on the other side of the curtain. On redirection, Mr. C replies that the pulse oximeter looks like a telephone and begins mumbling to himself |
| 5 hours | Mr. C continues to mumble but responds when directly questioned. He keeps insisting that the pulse oximeter is a telephone and that he can tell his uncle to come over from the other side of the curtain. He continues to act inappropriately despite the presence of family members but he is aware of their identities |
| 6 hours | Mr. C becomes disoriented and agitated and pulls out his IV line. Because of the high WBC count, we order blood cultures and a urine culture and give him IV antibiotics |
| WBC: white blood cell count | |
Table 2
Mr. C’s hospital course on the medical unit
| Time after presentation | Description |
|---|---|
| 54 hours | He is oriented to person and place. Staff notices he is talking to someone in the room but no one is present. Mr. C appears to be responding to visual hallucinations, but upon questioning he denies any symptoms. Restraints are discontinued. Divalproex is increased to 2,000 mg/d |
| 62 hours | Mr. C remains calm for several hours but later begins hallucinating and calls to his mother and others when no one is in the room. He receives IV lorazepam, 2 mg, without much response. Again he is placed in restraints and receives another dose of IV lorazepam, 3 mg, and IM ziprasidone, 20 mg. He becomes calmer. Restraints are continued as a precautionary measure. Mr. C calms down after several hours but cannot sleep |
| 78 hours | The next morning, Mr. C remains agitated and aggressive with loud speech. He denies any further hallucinations but talks to an invisible person. He remains in restraints and receives his routine medications. His blood pressure is 141/99 mm Hg and pulse is 110. Pulse rate normalizes during the day and he becomes calmer but seclusive |
CASE: Scared and confused
Mr. C, age 28, presents to the emergency department (ED) in police custody with agitation and altered mental status. Earlier that evening, Mr. C’s girlfriend noticed he was talking to himself while watching television. A few hours later, Mr. C thought someone was breaking into his house. Mr. C ran out of the house screaming for help, broke his neighbor’s window, and eventually called the police. When the police arrived Mr. C was wearing only his underwear, shaking, and bleeding from his hands. He said he was afraid and refused to respond to police instructions. Police officers used an electronic stun gun to facilitate transport to the hospital.
Mr. C admits to smoking 3 to 4 marijuana joints daily for the past 16 years. His last drug use was 2 hours before his symptoms began. Mr. C suggests that someone may have adulterated his marijuana joint but he has no factual basis for this accusation. He denies using alcohol and other illicit drugs and has no personal or family psychiatric history. He denies recent fever, loss of consciousness, chest pain, weakness, myalgia, or headache. Medically stable, his only complaint is mild hand pain.
Mr. C is alert, awake, and oriented to his name, and he responds properly to questions. He is tachycardic (101 bpm), his blood pressure is 149/57 mm Hg with normal S1 and S2 sounds, and he has no meningismus or nystagmus. Glasgow Coma Scale score is 15. He has increased deep tendon reflexes on the right upper and lower limb with good hand-grip and multiple abrasions and lacerations on his hands.
The authors’ observations
New-onset psychosis can have a wide differential diagnosis, particularly when reliable history is not available. Mr. C’s allegation that someone tampered with his marijuana raises 2 possibilities: embalming fluid (form-aldehyde) toxicity or PCP intoxication.
Embalming fluid toxicity can cause:
- agitation and sudden unpredictable behavior
- confusion or toxic delirium
- coma or seizure
- cerebral and pulmonary edema or death in severe cases.
The terms “wet,” “sherm,” “fly,” “amp,” or “illy” are used to describe a marijuana cigarette that has been dipped into embalming fluid, dried, and then smoked.1 The effect is similar to that of PCP and causes extreme hallucinations. Reported highs last 30 minutes to 1 hour.2
Symptomatology of PCP intoxication may be indistinguishable from functional psychosis (Table 1).3 Visual, auditory, and tactile misperceptions are common and highly changeable disorientation often is accompanied by alternating periods of lethargy and fearful agitation. These patients typically show catatonic posturing and/or stereotyped movement. Somatic sensations appear to be disassociated; patients may misperceive pain, distance, and time. Patients taking PCP rarely admit to true hallucinations; however their thinking usually is grossly disoriented.4 Symptoms of delirium may last from 30 minutes to 6 hours in 80% of cases; 12% of patients may remain symptomatic for 12 hours. Violent behavior and agitation usually lasts only a few hours.5
Long-term marijuana abuse can lead to psychosis6 but acute onset is not typical, and recent prospective trials raised doubts that cannabis would be a sole factor.7 Instead, cannabis may be 1 of several factors that contribute to psychosis, particularly in patients who are predisposed.
Table 1
Phencyclidine (PCP) intoxication: What to look for
| Findings | Percentage of cases |
|---|---|
| Nystagmus | 57.4% |
| Hypertension | 57.0% |
| Delirium | 36.9% |
| Violent behavior | 35.4% |
| Agitation | 34.0% |
| Tachycardia | 30.0% |
| Bizarre behavior | 28.5% |
| Hallucinations/delusions | 18.5% |
| Unconsciousness | 10.6% |
| Lethargy/stupor | 6.6% |
| Hypothermia | 6.4% |
| Generalized rigidity | 5.2% |
| Profuse sweating | 3.9% |
| No behavior effect | 3.5% |
| Grand mal seizure | 3.1% |
| Source: Reference 3 | |
Possible neurologic causes
Complex partial seizures—also known as psychomotor epilepsy—are caused by a surge of electrical activity in the brain. Seizures often involve 1 of the brain’s temporal lobes but can affect any brain region. Symptoms include:
- impaired social interaction
- inability to control one’s movements
- alogia
- amnesia.
Episodes typically start with a blank stare followed by automatisms. The actions and movements often are unorganized or confused. Motor symptoms typically last for 1 to 2 minutes and confusion persists for another 1 to 2 minutes.8 In rare cases, a patient may become agitated or engage in behaviors such as undressing. Complex partial seizures may cause a person to run in apparent fear, cry out, or repeat a phrase.9 Electroencephalogram, CT, MRI, or positron-emission tomography scan could reveal any intracranial focus of complex partial seizures.
We suspect PCP or embalming fluid intoxication and initiate supportive therapy.
EVALUATION: Still confused
Initial baseline labs include a urine drug screen (UDS), chest radiography, ECG, and head CT. Mr. C’s UDS is positive for cannabis. A specific PCP assay is negative. White blood cell count (WBC) is 22,000/μL with high neutrophil count (88%), creatine kinase (CK) is 458 U/L, and urinalyis reveals protein 75 mg/dL and ketone 50 mg/dL. Head CT is negative for any acute process (click here for detailed description of Mr. C�s hospital course while in the ED).
During psychiatric evaluation 7 hours after presentation, Mr. C’s speech is loose and somewhat pressured, but intelligible. He cannot follow commands. Mr. C is delusional and appears to be hallucinating. He can repeat 3 words immediately but not after 3 minutes. We start Mr. C on divalproex, 1,500 mg/d, haloperidol, 6 mg/d, and IV lorazepam, 2 mg as needed for agitation. Although mildly disoriented, he gradually becomes less agitated.
The authors’ observations
At this point further evaluation is needed. Mr. C’s elevated WBC count could explain his fluctuating symptoms. He cannot provide further history and his family denies any past psychiatric episodes. Thyroid-stimulating hormone, B12, and folate levels are within normal limits. A negative LP rules out meningitic infection. We give Mr. C a diagnosis of psychosis NOS (Table 2).10
Table 2
DSM-IV-TR criteria for psychotic disorder, not otherwise specified
| This category includes psychotic symptomatology (ie, delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior) about which there is inadequate information to make a specific diagnosis or about which there is contradictory information, or disorders with psychotic symptoms that do not meet the criteria for any specific psychotic disorder. Examples include: |
|
| Source: Reference 10 |
TREATMENT: Medication choices
After 8 hours in the ED, Mr. C is transferred to the medical unit, where he becomes agitated and complains of auditory and visual hallucinations. He receives divalproex, 750 mg, haloperidol, 3 mg, and IM diphenhydramine, 50 mg, to calm him. He remains agitated but not violent until bedtime. At midnight he is agitated and violent and receives another dose of haloperidol and IM diphenhydramine with IV lorazepam, 2 mg. These medications calm him and he is able to sleep until morning.
Morning labs reveal CK is 674 U/L and WBC decreased to 13,200/μL. Mr. C denies any distress but after the fourth dose of haloperidol, he develops dystonia of his arms so we discontinue this medication. We start aripiprazole, 10 mg/d gradually increased to 30 mg/d, and Mr. C receives 1 injection of diphenhydramine. He responds well to the treatment.
The next few hours are uneventful but then Mr. C becomes verbally abusive to his relatives and sitter; physical restraints are ordered and he receives IM ziprasidone, 20 mg, and IV lorazepam, 2 mg. He remains awake and babbling. His perception continues to wax and wane and his words are jumbled. He remains calm until the next morning (click here for detailed description of Mr. C�s hospital course while on the medical unit).
After 4 days on the medical unit Mr. C is transferred to the psychiatry unit, where he is angry, belligerent, and hostile, but not placed in restraints. His symptoms resolve in 2 days without any further episodes of violent behavior.
OUTCOME: Solving the puzzle
When Mr. C becomes cooperative, he gives a detailed history. He repeats his suspicion of smoking adulterated marijuana, but during detailed questioning, he admits to using alprazolam, which he purchased illegally, to sleep for the past 6 to 7 months. He started with 1 or 2 “footballs” (1 to 2 mg) and gradually increased to 3 or 4 “bars” (6 to 8 mg) each day. Mr. C could no longer afford the drug and last took alprazolam 6 days before his symptoms began. He says that after stopping alprazolam he felt anxious and could not sleep. His girlfriend adds that he was irritable and “he had not been acting himself” several days before admission. She says he complained of hearing the voice of God, particularly when he was not taking alprazolam.
Mr. C’s hand wounds heal and his vitals are normal during his 1-week stay on the psychiatric unit. His interactions with staff and peers improve. Aripiprazole is tapered and discontinued; divalproex is reduced to 1,000 mg/d. Mr. C is discharged 11 days after presentation and prescribed divalproex, 1,000 mg/d, with instructions to taper the drug over several days to prevent withdrawal seizures before stopping it in 1 week.
Mr. C does not return for his follow-up appointment; however, in a telephone follow-up 6 months later, he denies experiencing withdrawal symptoms after discharge. Mr. C is now undergoing drug rehabilitation.
The authors’ observations
Benzodiazepine withdrawal symptoms occur 7 to 10 days after abrupt cessation (Table 3).10 Symptoms are similar to those of alcohol withdrawal and include tachycardia, hypertension, clouding of consciousness, and auditory and visual hallucinations.11 Serious reactions to benzodiazepine withdrawal include seizures and death.12
Because of the high prevalence of poly-substance misuse, obtain a detailed substance use history in patients undergoing benzodiazepine withdrawal to determine the likelihood of polysubstance withdrawal.13 A cross-tolerant sedative such as clonazepam could prevent withdrawal symptoms as the dose is gradually decreased. Long-acting benzodiazepines such as clonazepam or diazepam are recommended.14
In Mr. C’s case, minor withdrawal symptoms, such as disturbed sleep and irritability, began 3 to 4 days after discontinuing benzodiazepines15 and preceded development of psychosis. Withdrawal symptoms usually resolve after 2 weeks.16 Mr. C responded only partially to IV lorazepam because he did not receive the total replacement dose. Had we known he was experiencing benzodiazepine withdrawal, Mr. C could have been managed with detoxi"cation of the primary drug, alprazolam, with diazepam substitution and tapering over 3 weeks.17
Table 3
Criteria for sedative, hypnotic, or anxiolytic withdrawal
| A. Cessation of (or reduction in) sedative, hypnotic, or anxiolytic use that has been heavy and prolonged |
B. Two (or more) of the following, developing within several hours to a few days after Criterion A:
|
| C. The symptoms in Criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| D. The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder |
| Source: Reference 10 |
Related Resource
- Vikander B, Koechling UM, Borg S, et al. Benzodiazepine tapering: a prospective study. Nord J Psychiatry. 2010; 64(4):273-282.
Drug Brand Names
- Alprazolam • Xanax
- Aripiprazole • Abilify
- Chlordiazepoxide • Librium
- Diazepam • Valium
- Diphenhydramine • Diphenhydramine injection
- Divalproex • Depakote
- Haloperidol • Haldol
- Lorazepam • Ativan
- Ziprasidone • Geodon
Acknowledgements
The authors wish to thank Reena Kumar, MD, and Sonja Gennuso, fourth-year medical student at Louisiana State University Health Sciences Center, Shreveport, for their help in preparing this manuscript.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Table 1
Mr. C’s hospital course in the emergency department
| Time after presentation | Description |
|---|---|
| 2 hours | Mr. C is alert and oriented to his name and place. He rests comfortably but asks questions about his girlfriend and uncle, falsely believing they are in the emergency department |
| 4 hours | Hand lacerations are repaired, but Mr. C continues to dig in his wounds with the opposite hand and place it over his mouth despite constant redirection. He reports hearing his uncle’s voice behind the curtain. He then uses the pulse oximeter as a telephone and holds a conversation with his uncle on the other side of the curtain. On redirection, Mr. C replies that the pulse oximeter looks like a telephone and begins mumbling to himself |
| 5 hours | Mr. C continues to mumble but responds when directly questioned. He keeps insisting that the pulse oximeter is a telephone and that he can tell his uncle to come over from the other side of the curtain. He continues to act inappropriately despite the presence of family members but he is aware of their identities |
| 6 hours | Mr. C becomes disoriented and agitated and pulls out his IV line. Because of the high WBC count, we order blood cultures and a urine culture and give him IV antibiotics |
| WBC: white blood cell count | |
Table 2
Mr. C’s hospital course on the medical unit
| Time after presentation | Description |
|---|---|
| 54 hours | He is oriented to person and place. Staff notices he is talking to someone in the room but no one is present. Mr. C appears to be responding to visual hallucinations, but upon questioning he denies any symptoms. Restraints are discontinued. Divalproex is increased to 2,000 mg/d |
| 62 hours | Mr. C remains calm for several hours but later begins hallucinating and calls to his mother and others when no one is in the room. He receives IV lorazepam, 2 mg, without much response. Again he is placed in restraints and receives another dose of IV lorazepam, 3 mg, and IM ziprasidone, 20 mg. He becomes calmer. Restraints are continued as a precautionary measure. Mr. C calms down after several hours but cannot sleep |
| 78 hours | The next morning, Mr. C remains agitated and aggressive with loud speech. He denies any further hallucinations but talks to an invisible person. He remains in restraints and receives his routine medications. His blood pressure is 141/99 mm Hg and pulse is 110. Pulse rate normalizes during the day and he becomes calmer but seclusive |
1. Office of National Drug Control Policy. Street terms: drugs and the drug trade. Available at:http://www.whitehousedrugpolicy.gov/streetterms/ByType.asp?intTypeID=1. Accessed July 26, 2010.
2. Elwood WN. TCADA research brief: “Fry:” a study of adolescents’ use of embalming fluid with marijuana and tobacco. Texas Commission on Alcohol and Drug Abuse. 1998. Available at:http://www.dshs.state.tx.us/sa/research/populations/fry.pdf. Accessed August 9, 2010.
3. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: incidence of clinical findings in 1,000 cases. Ann Emerg Med. 1981;10(5):237-242.
4. Aniline O, Pitts FN, Jr. Phencyclidine (PCP): a review and perspectives. Crit Rev Toxicol. 1982;10(2):145-177.
5. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: clinical patterns, complications, and treatment. Ann Emerg Med. 1981;10(6):290-297.
6. Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187-194.
7. Degenhardt L, Hall W. Cannabis and psychosis. Curr Psychiatry Rep. 2002;4(3):191-196.
8. Carroll E, Benbadis SR. Complex partial seizures. eMedicine. April 21, 2010. Available at:http://emedicine.medscape.com/article/1183962-overview. Accessed July 20, 2010.
9. Epilepsy.com. Complex partial seizures. Available at: http://www.epilepsy.com/epilepsy/seizure_complexpartial. Accessed July 20, 2010.
10. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
11. Mellor CS, Jain VK. Diazepam withdrawal syndrome: its prolonged and changing nature. Can Med Assoc J. 1982;127(11):1093-1096.
12. Lann MA, Molina DK. A fatal case of benzodiazepine withdrawal. Am J Forensic Med Pathol. 2009;30(2):177-179.
13. Busto UE, Romach MK, Sellers EM. Multiple drug use and psychiatric comorbidity in patients admitted to the hospital with severe benzodiazepine dependence. J Clin Psychopharmacol. 1996;16(1):51-57.
14. Franklin JE, Jr., Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:400–401.
15. Preskorn SH, Denner LJ. Benzodiazepines and withdrawal psychosis. Report of three cases. JAMA. 1977;237(1):36-38.
16. Miller F, Nulsen J. Single case study. Diazepam (valium) detoxification. J Nerv Ment Dis. 1979;167:637-638.
17. Seivewright N, Dougal W. Withdrawal symptoms from high dose benzodiazepines in poly drug users. Drug Alcohol Depend. 1993;32(1):15-23.
1. Office of National Drug Control Policy. Street terms: drugs and the drug trade. Available at:http://www.whitehousedrugpolicy.gov/streetterms/ByType.asp?intTypeID=1. Accessed July 26, 2010.
2. Elwood WN. TCADA research brief: “Fry:” a study of adolescents’ use of embalming fluid with marijuana and tobacco. Texas Commission on Alcohol and Drug Abuse. 1998. Available at:http://www.dshs.state.tx.us/sa/research/populations/fry.pdf. Accessed August 9, 2010.
3. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: incidence of clinical findings in 1,000 cases. Ann Emerg Med. 1981;10(5):237-242.
4. Aniline O, Pitts FN, Jr. Phencyclidine (PCP): a review and perspectives. Crit Rev Toxicol. 1982;10(2):145-177.
5. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: clinical patterns, complications, and treatment. Ann Emerg Med. 1981;10(6):290-297.
6. Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187-194.
7. Degenhardt L, Hall W. Cannabis and psychosis. Curr Psychiatry Rep. 2002;4(3):191-196.
8. Carroll E, Benbadis SR. Complex partial seizures. eMedicine. April 21, 2010. Available at:http://emedicine.medscape.com/article/1183962-overview. Accessed July 20, 2010.
9. Epilepsy.com. Complex partial seizures. Available at: http://www.epilepsy.com/epilepsy/seizure_complexpartial. Accessed July 20, 2010.
10. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
11. Mellor CS, Jain VK. Diazepam withdrawal syndrome: its prolonged and changing nature. Can Med Assoc J. 1982;127(11):1093-1096.
12. Lann MA, Molina DK. A fatal case of benzodiazepine withdrawal. Am J Forensic Med Pathol. 2009;30(2):177-179.
13. Busto UE, Romach MK, Sellers EM. Multiple drug use and psychiatric comorbidity in patients admitted to the hospital with severe benzodiazepine dependence. J Clin Psychopharmacol. 1996;16(1):51-57.
14. Franklin JE, Jr., Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:400–401.
15. Preskorn SH, Denner LJ. Benzodiazepines and withdrawal psychosis. Report of three cases. JAMA. 1977;237(1):36-38.
16. Miller F, Nulsen J. Single case study. Diazepam (valium) detoxification. J Nerv Ment Dis. 1979;167:637-638.
17. Seivewright N, Dougal W. Withdrawal symptoms from high dose benzodiazepines in poly drug users. Drug Alcohol Depend. 1993;32(1):15-23.
Uncooperative and manic
CASE: New-onset mania
Ms. Z, age 69, is admitted to our hospital’s medical unit after developing manic symptoms. Her medical history includes hemodialysis-dependent chronic kidney disease, Parkinson’s disease stabilized by carbidopa/levodopa, 75/300 mg/d, for 4 years, diet-controlled type 2 diabetes mellitus, hypertension, hyperlipidemia, myelodysplasia, and acid reflux. She experiences mild anxiety, which has been stable for many years with escitalopram, 10 mg/d, but has no history of alcohol or drug abuse and no family history of psychiatric illness.
The staff at her assisted living facility reports that 8 days ago Ms. Z was mildly irritable and argumentative regarding her medications and 7 days ago began to refuse all medications. Six days ago she refused dialysis, reportedly because she was angry at the staff. One day later, the staff noticed Ms. Z had developed manic symptoms, including decreased need for sleep (only 2 hours a night), talkativeness, counting things and spelling words rapidly out loud, and making explicit drawings of men. Ms. Z refused her next 2 dialysis treatments and her manic symptoms worsened. She explained that all her medical problems had been “cured.” She inaccurately exclaimed that she can urinate, even though she is anuric, and that she can walk after not having done so for 5 years.
During our interview, Ms. Z is disheveled and exhibits pressured speech, often interrupting the interviewer. Her affect is euphoric and expansive. She perseverates on patenting her cures for diabetes and Parkinson’s disease, endorses hypersexuality, and denies hallucinations. Folstein Mini-Mental State Exam score is 18/28; however, Ms. Z refuses to participate in elements of cognitive testing, including writing a sentence, drawing pentagons, or drawing a clock, all of which would reveal her tremor. We note no disorientation or waxing and waning of attention or consciousness. She is fully oriented to person, place, time, and purpose and can perform serial 7s and spell a word backwards.
The authors’ observations
A number of factors suggest that Ms. Z’s manic symptoms likely are caused by a medical problem (Table 1).1 She has no family history and only minimal personal history of psychiatric illness, and new-onset bipolar disorder in a 69-year-old woman is unusual.2 Given Ms. Z’s acute change in mental status and numerous medical problems, we consider delirium. Because Ms. Z does not exhibit disorientation or waxing and waning of attention or consciousness, we feel delirium is unlikely to be the primary diagnosis.
Table 1
Criteria for mood disorder due to a general medical condition
A. A prominent and persistent disturbance in mood predominates in the clinical picture and is characterized by either (or both) of the following:
|
| B. There is evidence from the history, physical examination, or laboratory findings that the disturbance is the direct physiological consequence of a general medical condition |
| C. The disturbance is not better accounted for by another mental disorder |
| D. The disturbance does not occur exclusively during the course of a delirium |
| E. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| Source: Reference 1 |
EVALUATION: Clues to the cause
Physical exam reveals stable vital signs, and resting tremor and mild cogwheel rigidity in her right upper extremity consistent with Parkinson’s disease. Laboratory results show elevated blood urea nitrogen (65 mg/dL) and creatinine (8 mg/dL) and stably low white cell count (2.9/μL) and platelets (118x103/μL), which are consistent with her known myelodysplasia. Results for urinalysis, B12, folate, thyroid-stimulating hormone, electrolytes, glucose, liver function, antinuclear antibodies, and rapid plasma reagin are unremarkable. Ms. Z’s elevated blood urea nitrogen and creatinine are expected because she recently refused dialysis. We consider that uremia could be causing her manic symptoms; however, with only 2 case reports of uremia-induced mania in the literature over the past century, we want to rule out other potential causes.3,4
A CT of Ms. Z’s brain is normal. The neurology service performs an EEG and results show mild disorganization with a predominantly posterior rhythm of 8 to 9 Hz symmetrically, occasional periods of slowing, and no epileptiform activity or evidence of encephalopathy; these findings are consistent with end-stage renal disease.
The authors’ observations
Although mood disorder due to a general medical condition—in this case, mania secondary to uremia—was our primary consideration, at this point we could not rule out subclinical delirium. In delirium, we would expect EEG to show diffuse slowing of background rhythm, which we did not see with Ms. Z. However, occasional periods of slowing indicate that delirium was a possible factor.
Parkinson’s disease is known to be a rare predisposing factor for mania—possibly related to potential manicogenic properties of dopaminergic medications5—but this would not explain new-onset mania in the context of uremia in a patient whose carbidopa/levodopa dose had been stable for several years. It is possible that Ms. Z’s refusal of dialysis could have led to build-up of carbidopa/levodopa in her blood, thereby contributing to mania; however, when she began feeling irritable, she refused several of her medications, including carbidopa/levodopa. Therefore, it is unlikely that carbidopa/levodopa accumulated to toxic levels.
We carefully evaluated Ms. Z’s complete medication list to determine if other drugs could be contributing factors. She has been taking escitalopram for anxiety for several years. Although Ms. Z had no personal or family history of bipolar disorder and no past hypomania or agitation associated with this medication, we discontinue escitalopram in case it was contributing to her manic symptoms. Ms. Z also receives amlodipine, 5 mg/d for hypertension; atorvastatin, 20 mg/d, for hyperlipidemia; pantoprazole, 40 mg/d, for acid reflux; metoprolol, 100 mg/d, for hypertension; aspirin, 81 mg/d, for cardioprotection; and fish oil, 2000 mg/d, for cardioprotection. We do not feel that any of these medications significantly contribute to her current state.
TREATMENT: Restarting dialysis
We start Ms. Z on olanzapine, 5 mg/d, for manic symptoms 1 day after admission, and resume dialysis treatments 1 day later. Because of concerns that olanzapine could worsen her myelodysplasia, we switch to aripiprazole, titrating up to 30 mg/d, 4 days later. After 2 dialysis treatments, her manic symptoms begin to resolve.
The authors’ observations
A number of factors suggest that uremia likely is causing Ms. Z’s manic symptoms. Her symptoms suddenly developed shortly after her first missed dialysis treatment, but gradually resolved after re-initiating dialysis. It is possible that antipsychotics relieved her manic symptoms, but this does not detract from the factors that make a causal relationship between uremia and mania likely.
Manic symptoms have been reported to be precipitated by a variety of medical problems, including metabolic disturbances, infections such as human immunodeficiency virus brain infection, neurologic disorders, brain neoplasms, or traumatic brain injuries (Table 2).6,7 End-stage renal disease frequently is associated with psychiatric manifestations—including depression, psychosis, delirium, and dementia—but mania is not a typical presentation. It is possible that this condition occurs more often but is not recognized.
Table 2
Common causes of secondary mania
| Metabolic/endocrine disturbances (hyperthyroidism, hyperadrenalism) |
| Infections (HIV) |
| Neurologic disorders (cerebrovascular accident, multiple sclerosis, Parkinson’s disease, epilepsy, Huntington’s disease) |
| Brain neoplasms |
| Traumatic brain injuries |
| Medications (anabolic steroids, antidepressants, corticosteroids, dextromethorphan, dopamine agonists, hypericum, isoniazid, stimulants, ephedrine, zidovudine) |
| Substance abuse (cocaine, amphetamines) |
| HIV: human immunodeficiency virus |
| Source: References 6,7 |
Kidney disease and psychotropics
We considered the effect of dialysis on psychotropics when selecting pharmacotherapy for Ms. Z’s manic symptoms. Haloperidol is not renally cleared so no dosage adjustment is necessary;8 however, this potent dopamine D2-blocker could have worsened Ms. Z’s parkinsonism. Lithium is contraindicated in acute renal failure. Valproic acid clearance is reduced in renal failure, but because it is cleared by hemodialysis, dosage adjustment is not recommended for dialysis patients.8 However, Ms. Z’s myelodysplasia is a contraindication for valproic acid as well as carbamazepine. With atypical antipsychotics as our primary options, we noted that olanzapine, quetiapine, or aripiprazole do not require dosage adjustments for dialysis patients.8,9 Of these, we eventually chose aripiprazole because we felt that it was least likely to exacerbate Ms. Z’s myelodysplasia.10
How uremia might cause mania
The pathophysiology of uremia-induced mania remains speculative. Possible factors include:
- Chronic renal failure can cause an elevation in plasma free tryptophan, a serotonin (5-HT) precursor.11 Postmortem examination of brains of patients who died in uremic coma show elevated 5-HT.12 Moreover, cerebrospinal fluid of patients with chronic renal failure has shown increased 5-hydroxyindoleacetic acid, the major 5-HT metabolite.13 Increased 5-HT could cause mania in some uremic patients, similar to how serotonergic medications can precipitate mania in some patients.
- Circulating ß-endorphin levels are increased in renal failure.14 ß-endorphins increase animal locomotor activity, which is the basis of an animal model of mania.15,16 Therefore, uremia-induced mania could be partly related to elevated ß-endorphin levels.
This case demonstrates that mania could be a psychiatric manifestation of end-stage renal disease. Clinicians should be aware of this possibility, and further study should examine underlying pathophysiologic changes in uremia and other secondary causes of mania that might lead to such a mood state.
OUTCOME: Lasting improvement
At discharge 17 days after admission, Ms. Z is back to her baseline mental state. Her aripiprazole dose is tapered to 20 mg/d with no return of manic symptoms. After 10 weeks, aripiprazole is discontinued, with no recurrence of mania.
Related Resource
- Arora M, Daughton J. Mania in the medically ill. Curr Psychiatry Rep. 2007;9(3):232-235.
Drug Brand Names
- Amlodipine • Norvasc
- Aripiprazole • Abilify
- Atorvastatin • Lipitor
- Carbamazepine • Tegretol
- Carbidopa/levodopa • Sinemet
- Escitalopram • Lexapro
- Haloperidol • Haldol
- Isoniazid • Nydrazid
- Lithium • Eskalith, Lithobid
- Metoprolol • Lopressor
- Olanzapine • Zyprexa
- Pantoprazole • Protonix
- Quetiapine • Seroquel
- Valproic acid • Depakote
- Zidovudine • Retrovir
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
2. Depp CA, Jeste DV. Bipolar disorder in older adults: a critical review. Bipolar Disord. 2004;6:343-367.
3. El-Mallakh RS, Shrader SA, Widger E. Mania as a manifestation of end-stage renal disease. J Nerv Ment Dis. 1987;175:243-245.
4. Thomas CS, Neale TJ. Organic manic syndrome associated with advanced uraemia due to polycystic kidney disease. Br J Psychiatry. 1991;158:119-121.
5. Kim E, Zwil AS, McAllister TW, et al. Treatment of organic bipolar mood disorders in Parkinson’s disease. J Neuropsychiatry Clin Neurosci. 1994;6:181-184.
6. Levenson JL. Psychosis in the medically ill. Primary Psychiatry. 2005;12(8):16-18.
7. Arora M, Daughton J. Mania in the medically ill. Curr Psychiatry Rep. 2007;9(3):232-235.
8. McLaren KD, Marangell LB. Special considerations in the treatment of patients with bipolar disorder and medical comorbidities. Ann Gen Hosp Psychiatry. 2004;3(1):7.-
9. Mallikaarjun S, Shoaf SE, Boulton DW, et al. Effects of hepatic or renal impairment on the pharmacokinetics of aripiprazole. Clin Pharmacokinet. 2008;47(8):533-542.
10. Stip E, Langlois R, Thuot C, et al. Fatal agranulocytosis: the use of olanzapine in a patient with schizophrenia and myelodysplasia. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(1):297-300.
11. de Torrente A, Glazer GB, Gulyassy P. Reduced in vitro binding of tryptophan by plasma in uremia. Kidney Int. 1974;6:222-229.
12. Jellinger E, Irsigler K, Kothbauer P, et al. Brain monoamines in metabolic coma. Excerpta Medica. 1977;427:169.-
13. Sullivan PA, Murnaghan D, Callaghan N, et al. Cerebral transmitter precursors and metabolites in advanced renal disease. J Neurol Neurosurg Psychiatry. 1978;41:581-588.
14. Aronin N, Krieger DT. Plasma immunoreactive beta-endorphin is elevated in uraemia. Clin Endocrinol (Oxf). 1983;18:459-464.
15. Holtzman SG. Behavioral effects of separate and combined administration of naloxone and D-amphetamine. J Pharmacol Exp Ther. 1974;189:51-60.
16. Segal DS, Browne RG, Derrington DC. Characteristics of beta-endorphin induced behavioral activation and immobilization. In: Usdin E, Bunney WE, Kline NS, eds. Endorphins in mental health research. New York, NY: Oxford University Press; 1979.
CASE: New-onset mania
Ms. Z, age 69, is admitted to our hospital’s medical unit after developing manic symptoms. Her medical history includes hemodialysis-dependent chronic kidney disease, Parkinson’s disease stabilized by carbidopa/levodopa, 75/300 mg/d, for 4 years, diet-controlled type 2 diabetes mellitus, hypertension, hyperlipidemia, myelodysplasia, and acid reflux. She experiences mild anxiety, which has been stable for many years with escitalopram, 10 mg/d, but has no history of alcohol or drug abuse and no family history of psychiatric illness.
The staff at her assisted living facility reports that 8 days ago Ms. Z was mildly irritable and argumentative regarding her medications and 7 days ago began to refuse all medications. Six days ago she refused dialysis, reportedly because she was angry at the staff. One day later, the staff noticed Ms. Z had developed manic symptoms, including decreased need for sleep (only 2 hours a night), talkativeness, counting things and spelling words rapidly out loud, and making explicit drawings of men. Ms. Z refused her next 2 dialysis treatments and her manic symptoms worsened. She explained that all her medical problems had been “cured.” She inaccurately exclaimed that she can urinate, even though she is anuric, and that she can walk after not having done so for 5 years.
During our interview, Ms. Z is disheveled and exhibits pressured speech, often interrupting the interviewer. Her affect is euphoric and expansive. She perseverates on patenting her cures for diabetes and Parkinson’s disease, endorses hypersexuality, and denies hallucinations. Folstein Mini-Mental State Exam score is 18/28; however, Ms. Z refuses to participate in elements of cognitive testing, including writing a sentence, drawing pentagons, or drawing a clock, all of which would reveal her tremor. We note no disorientation or waxing and waning of attention or consciousness. She is fully oriented to person, place, time, and purpose and can perform serial 7s and spell a word backwards.
The authors’ observations
A number of factors suggest that Ms. Z’s manic symptoms likely are caused by a medical problem (Table 1).1 She has no family history and only minimal personal history of psychiatric illness, and new-onset bipolar disorder in a 69-year-old woman is unusual.2 Given Ms. Z’s acute change in mental status and numerous medical problems, we consider delirium. Because Ms. Z does not exhibit disorientation or waxing and waning of attention or consciousness, we feel delirium is unlikely to be the primary diagnosis.
Table 1
Criteria for mood disorder due to a general medical condition
A. A prominent and persistent disturbance in mood predominates in the clinical picture and is characterized by either (or both) of the following:
|
| B. There is evidence from the history, physical examination, or laboratory findings that the disturbance is the direct physiological consequence of a general medical condition |
| C. The disturbance is not better accounted for by another mental disorder |
| D. The disturbance does not occur exclusively during the course of a delirium |
| E. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| Source: Reference 1 |
EVALUATION: Clues to the cause
Physical exam reveals stable vital signs, and resting tremor and mild cogwheel rigidity in her right upper extremity consistent with Parkinson’s disease. Laboratory results show elevated blood urea nitrogen (65 mg/dL) and creatinine (8 mg/dL) and stably low white cell count (2.9/μL) and platelets (118x103/μL), which are consistent with her known myelodysplasia. Results for urinalysis, B12, folate, thyroid-stimulating hormone, electrolytes, glucose, liver function, antinuclear antibodies, and rapid plasma reagin are unremarkable. Ms. Z’s elevated blood urea nitrogen and creatinine are expected because she recently refused dialysis. We consider that uremia could be causing her manic symptoms; however, with only 2 case reports of uremia-induced mania in the literature over the past century, we want to rule out other potential causes.3,4
A CT of Ms. Z’s brain is normal. The neurology service performs an EEG and results show mild disorganization with a predominantly posterior rhythm of 8 to 9 Hz symmetrically, occasional periods of slowing, and no epileptiform activity or evidence of encephalopathy; these findings are consistent with end-stage renal disease.
The authors’ observations
Although mood disorder due to a general medical condition—in this case, mania secondary to uremia—was our primary consideration, at this point we could not rule out subclinical delirium. In delirium, we would expect EEG to show diffuse slowing of background rhythm, which we did not see with Ms. Z. However, occasional periods of slowing indicate that delirium was a possible factor.
Parkinson’s disease is known to be a rare predisposing factor for mania—possibly related to potential manicogenic properties of dopaminergic medications5—but this would not explain new-onset mania in the context of uremia in a patient whose carbidopa/levodopa dose had been stable for several years. It is possible that Ms. Z’s refusal of dialysis could have led to build-up of carbidopa/levodopa in her blood, thereby contributing to mania; however, when she began feeling irritable, she refused several of her medications, including carbidopa/levodopa. Therefore, it is unlikely that carbidopa/levodopa accumulated to toxic levels.
We carefully evaluated Ms. Z’s complete medication list to determine if other drugs could be contributing factors. She has been taking escitalopram for anxiety for several years. Although Ms. Z had no personal or family history of bipolar disorder and no past hypomania or agitation associated with this medication, we discontinue escitalopram in case it was contributing to her manic symptoms. Ms. Z also receives amlodipine, 5 mg/d for hypertension; atorvastatin, 20 mg/d, for hyperlipidemia; pantoprazole, 40 mg/d, for acid reflux; metoprolol, 100 mg/d, for hypertension; aspirin, 81 mg/d, for cardioprotection; and fish oil, 2000 mg/d, for cardioprotection. We do not feel that any of these medications significantly contribute to her current state.
TREATMENT: Restarting dialysis
We start Ms. Z on olanzapine, 5 mg/d, for manic symptoms 1 day after admission, and resume dialysis treatments 1 day later. Because of concerns that olanzapine could worsen her myelodysplasia, we switch to aripiprazole, titrating up to 30 mg/d, 4 days later. After 2 dialysis treatments, her manic symptoms begin to resolve.
The authors’ observations
A number of factors suggest that uremia likely is causing Ms. Z’s manic symptoms. Her symptoms suddenly developed shortly after her first missed dialysis treatment, but gradually resolved after re-initiating dialysis. It is possible that antipsychotics relieved her manic symptoms, but this does not detract from the factors that make a causal relationship between uremia and mania likely.
Manic symptoms have been reported to be precipitated by a variety of medical problems, including metabolic disturbances, infections such as human immunodeficiency virus brain infection, neurologic disorders, brain neoplasms, or traumatic brain injuries (Table 2).6,7 End-stage renal disease frequently is associated with psychiatric manifestations—including depression, psychosis, delirium, and dementia—but mania is not a typical presentation. It is possible that this condition occurs more often but is not recognized.
Table 2
Common causes of secondary mania
| Metabolic/endocrine disturbances (hyperthyroidism, hyperadrenalism) |
| Infections (HIV) |
| Neurologic disorders (cerebrovascular accident, multiple sclerosis, Parkinson’s disease, epilepsy, Huntington’s disease) |
| Brain neoplasms |
| Traumatic brain injuries |
| Medications (anabolic steroids, antidepressants, corticosteroids, dextromethorphan, dopamine agonists, hypericum, isoniazid, stimulants, ephedrine, zidovudine) |
| Substance abuse (cocaine, amphetamines) |
| HIV: human immunodeficiency virus |
| Source: References 6,7 |
Kidney disease and psychotropics
We considered the effect of dialysis on psychotropics when selecting pharmacotherapy for Ms. Z’s manic symptoms. Haloperidol is not renally cleared so no dosage adjustment is necessary;8 however, this potent dopamine D2-blocker could have worsened Ms. Z’s parkinsonism. Lithium is contraindicated in acute renal failure. Valproic acid clearance is reduced in renal failure, but because it is cleared by hemodialysis, dosage adjustment is not recommended for dialysis patients.8 However, Ms. Z’s myelodysplasia is a contraindication for valproic acid as well as carbamazepine. With atypical antipsychotics as our primary options, we noted that olanzapine, quetiapine, or aripiprazole do not require dosage adjustments for dialysis patients.8,9 Of these, we eventually chose aripiprazole because we felt that it was least likely to exacerbate Ms. Z’s myelodysplasia.10
How uremia might cause mania
The pathophysiology of uremia-induced mania remains speculative. Possible factors include:
- Chronic renal failure can cause an elevation in plasma free tryptophan, a serotonin (5-HT) precursor.11 Postmortem examination of brains of patients who died in uremic coma show elevated 5-HT.12 Moreover, cerebrospinal fluid of patients with chronic renal failure has shown increased 5-hydroxyindoleacetic acid, the major 5-HT metabolite.13 Increased 5-HT could cause mania in some uremic patients, similar to how serotonergic medications can precipitate mania in some patients.
- Circulating ß-endorphin levels are increased in renal failure.14 ß-endorphins increase animal locomotor activity, which is the basis of an animal model of mania.15,16 Therefore, uremia-induced mania could be partly related to elevated ß-endorphin levels.
This case demonstrates that mania could be a psychiatric manifestation of end-stage renal disease. Clinicians should be aware of this possibility, and further study should examine underlying pathophysiologic changes in uremia and other secondary causes of mania that might lead to such a mood state.
OUTCOME: Lasting improvement
At discharge 17 days after admission, Ms. Z is back to her baseline mental state. Her aripiprazole dose is tapered to 20 mg/d with no return of manic symptoms. After 10 weeks, aripiprazole is discontinued, with no recurrence of mania.
Related Resource
- Arora M, Daughton J. Mania in the medically ill. Curr Psychiatry Rep. 2007;9(3):232-235.
Drug Brand Names
- Amlodipine • Norvasc
- Aripiprazole • Abilify
- Atorvastatin • Lipitor
- Carbamazepine • Tegretol
- Carbidopa/levodopa • Sinemet
- Escitalopram • Lexapro
- Haloperidol • Haldol
- Isoniazid • Nydrazid
- Lithium • Eskalith, Lithobid
- Metoprolol • Lopressor
- Olanzapine • Zyprexa
- Pantoprazole • Protonix
- Quetiapine • Seroquel
- Valproic acid • Depakote
- Zidovudine • Retrovir
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: New-onset mania
Ms. Z, age 69, is admitted to our hospital’s medical unit after developing manic symptoms. Her medical history includes hemodialysis-dependent chronic kidney disease, Parkinson’s disease stabilized by carbidopa/levodopa, 75/300 mg/d, for 4 years, diet-controlled type 2 diabetes mellitus, hypertension, hyperlipidemia, myelodysplasia, and acid reflux. She experiences mild anxiety, which has been stable for many years with escitalopram, 10 mg/d, but has no history of alcohol or drug abuse and no family history of psychiatric illness.
The staff at her assisted living facility reports that 8 days ago Ms. Z was mildly irritable and argumentative regarding her medications and 7 days ago began to refuse all medications. Six days ago she refused dialysis, reportedly because she was angry at the staff. One day later, the staff noticed Ms. Z had developed manic symptoms, including decreased need for sleep (only 2 hours a night), talkativeness, counting things and spelling words rapidly out loud, and making explicit drawings of men. Ms. Z refused her next 2 dialysis treatments and her manic symptoms worsened. She explained that all her medical problems had been “cured.” She inaccurately exclaimed that she can urinate, even though she is anuric, and that she can walk after not having done so for 5 years.
During our interview, Ms. Z is disheveled and exhibits pressured speech, often interrupting the interviewer. Her affect is euphoric and expansive. She perseverates on patenting her cures for diabetes and Parkinson’s disease, endorses hypersexuality, and denies hallucinations. Folstein Mini-Mental State Exam score is 18/28; however, Ms. Z refuses to participate in elements of cognitive testing, including writing a sentence, drawing pentagons, or drawing a clock, all of which would reveal her tremor. We note no disorientation or waxing and waning of attention or consciousness. She is fully oriented to person, place, time, and purpose and can perform serial 7s and spell a word backwards.
The authors’ observations
A number of factors suggest that Ms. Z’s manic symptoms likely are caused by a medical problem (Table 1).1 She has no family history and only minimal personal history of psychiatric illness, and new-onset bipolar disorder in a 69-year-old woman is unusual.2 Given Ms. Z’s acute change in mental status and numerous medical problems, we consider delirium. Because Ms. Z does not exhibit disorientation or waxing and waning of attention or consciousness, we feel delirium is unlikely to be the primary diagnosis.
Table 1
Criteria for mood disorder due to a general medical condition
A. A prominent and persistent disturbance in mood predominates in the clinical picture and is characterized by either (or both) of the following:
|
| B. There is evidence from the history, physical examination, or laboratory findings that the disturbance is the direct physiological consequence of a general medical condition |
| C. The disturbance is not better accounted for by another mental disorder |
| D. The disturbance does not occur exclusively during the course of a delirium |
| E. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| Source: Reference 1 |
EVALUATION: Clues to the cause
Physical exam reveals stable vital signs, and resting tremor and mild cogwheel rigidity in her right upper extremity consistent with Parkinson’s disease. Laboratory results show elevated blood urea nitrogen (65 mg/dL) and creatinine (8 mg/dL) and stably low white cell count (2.9/μL) and platelets (118x103/μL), which are consistent with her known myelodysplasia. Results for urinalysis, B12, folate, thyroid-stimulating hormone, electrolytes, glucose, liver function, antinuclear antibodies, and rapid plasma reagin are unremarkable. Ms. Z’s elevated blood urea nitrogen and creatinine are expected because she recently refused dialysis. We consider that uremia could be causing her manic symptoms; however, with only 2 case reports of uremia-induced mania in the literature over the past century, we want to rule out other potential causes.3,4
A CT of Ms. Z’s brain is normal. The neurology service performs an EEG and results show mild disorganization with a predominantly posterior rhythm of 8 to 9 Hz symmetrically, occasional periods of slowing, and no epileptiform activity or evidence of encephalopathy; these findings are consistent with end-stage renal disease.
The authors’ observations
Although mood disorder due to a general medical condition—in this case, mania secondary to uremia—was our primary consideration, at this point we could not rule out subclinical delirium. In delirium, we would expect EEG to show diffuse slowing of background rhythm, which we did not see with Ms. Z. However, occasional periods of slowing indicate that delirium was a possible factor.
Parkinson’s disease is known to be a rare predisposing factor for mania—possibly related to potential manicogenic properties of dopaminergic medications5—but this would not explain new-onset mania in the context of uremia in a patient whose carbidopa/levodopa dose had been stable for several years. It is possible that Ms. Z’s refusal of dialysis could have led to build-up of carbidopa/levodopa in her blood, thereby contributing to mania; however, when she began feeling irritable, she refused several of her medications, including carbidopa/levodopa. Therefore, it is unlikely that carbidopa/levodopa accumulated to toxic levels.
We carefully evaluated Ms. Z’s complete medication list to determine if other drugs could be contributing factors. She has been taking escitalopram for anxiety for several years. Although Ms. Z had no personal or family history of bipolar disorder and no past hypomania or agitation associated with this medication, we discontinue escitalopram in case it was contributing to her manic symptoms. Ms. Z also receives amlodipine, 5 mg/d for hypertension; atorvastatin, 20 mg/d, for hyperlipidemia; pantoprazole, 40 mg/d, for acid reflux; metoprolol, 100 mg/d, for hypertension; aspirin, 81 mg/d, for cardioprotection; and fish oil, 2000 mg/d, for cardioprotection. We do not feel that any of these medications significantly contribute to her current state.
TREATMENT: Restarting dialysis
We start Ms. Z on olanzapine, 5 mg/d, for manic symptoms 1 day after admission, and resume dialysis treatments 1 day later. Because of concerns that olanzapine could worsen her myelodysplasia, we switch to aripiprazole, titrating up to 30 mg/d, 4 days later. After 2 dialysis treatments, her manic symptoms begin to resolve.
The authors’ observations
A number of factors suggest that uremia likely is causing Ms. Z’s manic symptoms. Her symptoms suddenly developed shortly after her first missed dialysis treatment, but gradually resolved after re-initiating dialysis. It is possible that antipsychotics relieved her manic symptoms, but this does not detract from the factors that make a causal relationship between uremia and mania likely.
Manic symptoms have been reported to be precipitated by a variety of medical problems, including metabolic disturbances, infections such as human immunodeficiency virus brain infection, neurologic disorders, brain neoplasms, or traumatic brain injuries (Table 2).6,7 End-stage renal disease frequently is associated with psychiatric manifestations—including depression, psychosis, delirium, and dementia—but mania is not a typical presentation. It is possible that this condition occurs more often but is not recognized.
Table 2
Common causes of secondary mania
| Metabolic/endocrine disturbances (hyperthyroidism, hyperadrenalism) |
| Infections (HIV) |
| Neurologic disorders (cerebrovascular accident, multiple sclerosis, Parkinson’s disease, epilepsy, Huntington’s disease) |
| Brain neoplasms |
| Traumatic brain injuries |
| Medications (anabolic steroids, antidepressants, corticosteroids, dextromethorphan, dopamine agonists, hypericum, isoniazid, stimulants, ephedrine, zidovudine) |
| Substance abuse (cocaine, amphetamines) |
| HIV: human immunodeficiency virus |
| Source: References 6,7 |
Kidney disease and psychotropics
We considered the effect of dialysis on psychotropics when selecting pharmacotherapy for Ms. Z’s manic symptoms. Haloperidol is not renally cleared so no dosage adjustment is necessary;8 however, this potent dopamine D2-blocker could have worsened Ms. Z’s parkinsonism. Lithium is contraindicated in acute renal failure. Valproic acid clearance is reduced in renal failure, but because it is cleared by hemodialysis, dosage adjustment is not recommended for dialysis patients.8 However, Ms. Z’s myelodysplasia is a contraindication for valproic acid as well as carbamazepine. With atypical antipsychotics as our primary options, we noted that olanzapine, quetiapine, or aripiprazole do not require dosage adjustments for dialysis patients.8,9 Of these, we eventually chose aripiprazole because we felt that it was least likely to exacerbate Ms. Z’s myelodysplasia.10
How uremia might cause mania
The pathophysiology of uremia-induced mania remains speculative. Possible factors include:
- Chronic renal failure can cause an elevation in plasma free tryptophan, a serotonin (5-HT) precursor.11 Postmortem examination of brains of patients who died in uremic coma show elevated 5-HT.12 Moreover, cerebrospinal fluid of patients with chronic renal failure has shown increased 5-hydroxyindoleacetic acid, the major 5-HT metabolite.13 Increased 5-HT could cause mania in some uremic patients, similar to how serotonergic medications can precipitate mania in some patients.
- Circulating ß-endorphin levels are increased in renal failure.14 ß-endorphins increase animal locomotor activity, which is the basis of an animal model of mania.15,16 Therefore, uremia-induced mania could be partly related to elevated ß-endorphin levels.
This case demonstrates that mania could be a psychiatric manifestation of end-stage renal disease. Clinicians should be aware of this possibility, and further study should examine underlying pathophysiologic changes in uremia and other secondary causes of mania that might lead to such a mood state.
OUTCOME: Lasting improvement
At discharge 17 days after admission, Ms. Z is back to her baseline mental state. Her aripiprazole dose is tapered to 20 mg/d with no return of manic symptoms. After 10 weeks, aripiprazole is discontinued, with no recurrence of mania.
Related Resource
- Arora M, Daughton J. Mania in the medically ill. Curr Psychiatry Rep. 2007;9(3):232-235.
Drug Brand Names
- Amlodipine • Norvasc
- Aripiprazole • Abilify
- Atorvastatin • Lipitor
- Carbamazepine • Tegretol
- Carbidopa/levodopa • Sinemet
- Escitalopram • Lexapro
- Haloperidol • Haldol
- Isoniazid • Nydrazid
- Lithium • Eskalith, Lithobid
- Metoprolol • Lopressor
- Olanzapine • Zyprexa
- Pantoprazole • Protonix
- Quetiapine • Seroquel
- Valproic acid • Depakote
- Zidovudine • Retrovir
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
2. Depp CA, Jeste DV. Bipolar disorder in older adults: a critical review. Bipolar Disord. 2004;6:343-367.
3. El-Mallakh RS, Shrader SA, Widger E. Mania as a manifestation of end-stage renal disease. J Nerv Ment Dis. 1987;175:243-245.
4. Thomas CS, Neale TJ. Organic manic syndrome associated with advanced uraemia due to polycystic kidney disease. Br J Psychiatry. 1991;158:119-121.
5. Kim E, Zwil AS, McAllister TW, et al. Treatment of organic bipolar mood disorders in Parkinson’s disease. J Neuropsychiatry Clin Neurosci. 1994;6:181-184.
6. Levenson JL. Psychosis in the medically ill. Primary Psychiatry. 2005;12(8):16-18.
7. Arora M, Daughton J. Mania in the medically ill. Curr Psychiatry Rep. 2007;9(3):232-235.
8. McLaren KD, Marangell LB. Special considerations in the treatment of patients with bipolar disorder and medical comorbidities. Ann Gen Hosp Psychiatry. 2004;3(1):7.-
9. Mallikaarjun S, Shoaf SE, Boulton DW, et al. Effects of hepatic or renal impairment on the pharmacokinetics of aripiprazole. Clin Pharmacokinet. 2008;47(8):533-542.
10. Stip E, Langlois R, Thuot C, et al. Fatal agranulocytosis: the use of olanzapine in a patient with schizophrenia and myelodysplasia. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(1):297-300.
11. de Torrente A, Glazer GB, Gulyassy P. Reduced in vitro binding of tryptophan by plasma in uremia. Kidney Int. 1974;6:222-229.
12. Jellinger E, Irsigler K, Kothbauer P, et al. Brain monoamines in metabolic coma. Excerpta Medica. 1977;427:169.-
13. Sullivan PA, Murnaghan D, Callaghan N, et al. Cerebral transmitter precursors and metabolites in advanced renal disease. J Neurol Neurosurg Psychiatry. 1978;41:581-588.
14. Aronin N, Krieger DT. Plasma immunoreactive beta-endorphin is elevated in uraemia. Clin Endocrinol (Oxf). 1983;18:459-464.
15. Holtzman SG. Behavioral effects of separate and combined administration of naloxone and D-amphetamine. J Pharmacol Exp Ther. 1974;189:51-60.
16. Segal DS, Browne RG, Derrington DC. Characteristics of beta-endorphin induced behavioral activation and immobilization. In: Usdin E, Bunney WE, Kline NS, eds. Endorphins in mental health research. New York, NY: Oxford University Press; 1979.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
2. Depp CA, Jeste DV. Bipolar disorder in older adults: a critical review. Bipolar Disord. 2004;6:343-367.
3. El-Mallakh RS, Shrader SA, Widger E. Mania as a manifestation of end-stage renal disease. J Nerv Ment Dis. 1987;175:243-245.
4. Thomas CS, Neale TJ. Organic manic syndrome associated with advanced uraemia due to polycystic kidney disease. Br J Psychiatry. 1991;158:119-121.
5. Kim E, Zwil AS, McAllister TW, et al. Treatment of organic bipolar mood disorders in Parkinson’s disease. J Neuropsychiatry Clin Neurosci. 1994;6:181-184.
6. Levenson JL. Psychosis in the medically ill. Primary Psychiatry. 2005;12(8):16-18.
7. Arora M, Daughton J. Mania in the medically ill. Curr Psychiatry Rep. 2007;9(3):232-235.
8. McLaren KD, Marangell LB. Special considerations in the treatment of patients with bipolar disorder and medical comorbidities. Ann Gen Hosp Psychiatry. 2004;3(1):7.-
9. Mallikaarjun S, Shoaf SE, Boulton DW, et al. Effects of hepatic or renal impairment on the pharmacokinetics of aripiprazole. Clin Pharmacokinet. 2008;47(8):533-542.
10. Stip E, Langlois R, Thuot C, et al. Fatal agranulocytosis: the use of olanzapine in a patient with schizophrenia and myelodysplasia. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(1):297-300.
11. de Torrente A, Glazer GB, Gulyassy P. Reduced in vitro binding of tryptophan by plasma in uremia. Kidney Int. 1974;6:222-229.
12. Jellinger E, Irsigler K, Kothbauer P, et al. Brain monoamines in metabolic coma. Excerpta Medica. 1977;427:169.-
13. Sullivan PA, Murnaghan D, Callaghan N, et al. Cerebral transmitter precursors and metabolites in advanced renal disease. J Neurol Neurosurg Psychiatry. 1978;41:581-588.
14. Aronin N, Krieger DT. Plasma immunoreactive beta-endorphin is elevated in uraemia. Clin Endocrinol (Oxf). 1983;18:459-464.
15. Holtzman SG. Behavioral effects of separate and combined administration of naloxone and D-amphetamine. J Pharmacol Exp Ther. 1974;189:51-60.
16. Segal DS, Browne RG, Derrington DC. Characteristics of beta-endorphin induced behavioral activation and immobilization. In: Usdin E, Bunney WE, Kline NS, eds. Endorphins in mental health research. New York, NY: Oxford University Press; 1979.
The woman who saw the light
HISTORY: Visual disturbances
Ms. G, age 30, has schizoaffective disorder and presents with worsening auditory hallucinations, paranoid delusions, and thought broadcasting and insertion, which is suspected to be related to a change from olanzapine to aripiprazole. She complains of visual disturbances—a hallucination of flashing lights—that she describes as occurring “all the time, like salt-and-pepper dancing, and sometimes splotches.” Her visual symptoms are worse when she closes her eyes and in dimly lit environments, but occur in daylight as well. Her vision is otherwise unimpaired.
The visual disturbances started with Ms. G’s first psychotic break at age 23 and have persisted continuously. She reports that at first, the spots were more intense, like an incessant strobe light. These symptoms are aggravated by sleep deprivation and anger and improve only with topiramate, 100 mg/d, which was prescribed a year earlier after a neurologic consultation but discontinued because of cognitive side effects.
Ms. G also complains of dull, aching, continuous headaches in the center of her forehead, which do not wake her, are not worse in the morning, and do not vary with the intensity of her visual symptoms. The headaches are incorporated into her system of delusions; she believes they “drain the electricity from her head” and make her feel better. She denies a history of migraines. Ms. G has a history of experiencing well-formed visual hallucinations, such as the devil, but has not had them for several years.
She had 5 to 10 episodes over the last 2 years that she describes as seizures—“an earthquake, a huge whooshing noise,” accompanied by heart palpitations that occur with stress, in public, in bright lights, or whenever she feels vulnerable. These episodes are not associated with loss of consciousness, incontinence, amnesia, or post-ictal confusion and she can stop them with relaxation techniques such as deep breathing and reminding herself to calm down. The last episode was 2 months ago and seemed unrelated to her visual phenomena. She also complains of occasional paresthesias in her extremities but denies dizziness, presyncope, or blurry or double vision.
Ms. G is obese and has no history of head injury or birth defects. Her family history is negative for epilepsy; however, her mother has bipolar disorder and father has schizophrenia. Her medications are phentermine, 37.5 mg/d for short-term management of obesity, oxcarbazepine, 600 mg/d for supposed partial seizures, sertraline, 100 mg/d for depression, aripiprazole, 10 mg/d, and nizatidine, 150 mg/d, for gastroesophageal reflux disease. She does not use alcohol, cigarettes, or illicit drugs. Ms. G obtained a master’s degree in health communications and works as a research assistant at a local medical school.
The authors’ observations
Visual hallucinations are not distortions of reality but original false perceptions that co-occur with real perceptions.1 They vary from simple, elemental hallucinations involving flashes of light or geometric figures to more complex elaborations such as seeing crawling insects or a flock of angels.2 Hallucinations can originate anywhere in the visual system from the lens to the visual cortex and can be vascular, toxic, electrophysiologic, structural, or neurochemical manifestations of neurologic, psychiatric, or ophthalmologic disorders. Depending on the hallucination’s etiology, treatment varies from emergent ophthalmologic examination and retinal surgery to antipsychotic therapy to simple observation. Photopsia is a perception of flashing lights, and its etiology varies; causes can be categorized as emergent or nonemergent.
Emergent causes of photopsia typically have a sudden onset, often can be diagnosed from associated symptoms or medical history, and must be recognized quickly to prevent permanent vision loss. Posterior vitreous detachment and retinal tearing can manifest as flashes of light, floaters, or blurred vision in the peripheral visual field that are worse in dim illumination and localizable by the patient. Retinal detachment can cause photopsia, floaters, or a “curtain” or “shadow” moving over the visual field, which may be accompanied by central or peripheral vision loss.3 Severe myopia is a risk factor for retinal detachment.
New-onset photopsia can suggest cytomegaloviral retinitis in an immune-compromised patient, and ocular-vascular crisis in a patient with sickle cell disease. New-onset or recurrent photopsia with bilateral blurred vision, ataxia, vertigo, dysarthria, or drop attacks may be caused by vertebrobasilar artery insufficiency (VBAI). Photopsia has been reported as the presenting symptom in carotid artery dissection.4 Photopsia correlated with eye movement implicates the retina or optic nerve. All of these etiologies except for VBAI should be referred to an ophthalmologist for indirect ophthalmoscopy and evaluation.
Nonemergent causes of photopsia include:
- drug toxicity
- migraine headache
- thyroid ophthalmopathy
- arteriovenous malformations
- seizures
- psychiatric disorders.
Digoxin, cocaine, paclitaxel, and clomiphene may have ocular side effects, including photopsia. The first symptoms of digitalis toxicity often are visual and include photopsia, yellow or green discoloration of the visual field, halos, and the appearance of frost over objects.5 Signs of cocaine intoxication can include visual hallucinations such as photopsia, shadows, moving objects, and insects crawling and co-occurring euphoria, hypervigilance, impaired judgment, and autonomic changes such as tachycardia, pupillary dilation, hypertension, and nausea.6 High-dose paclitaxel infusion has been reported to cause photopsia.7 Clomiphene can cause flickering lights and shimmering that persists after discontinuing the medication.8
Migraine with aura, which includes photopsia 39% of the time,9 often involves an expanding central visual disturbance or scotoma, and usually is confined to 1 visual field but may involve both. The aura typically lasts 10 to 20 minutes and often is followed by headache. Patients often report a history of episodic stereotyped auras and headache. Ocular examination is normal.
Ophthalmic migraine, also known as ocular or retinal migraine, is thought to be caused by transient vasospasm of the choroidal or retinal arteries and can be precipitated by postural changes, exercise, and oral contraceptives. It manifests as a gradual visual disturbance in a mosaic scotomata pattern that enlarges, producing total unilateral visual loss lasting from minutes to an hour, and—misleadingly—can be associated with minimal or no headache. Ocular examination is normal, and a personal or family history of migraine confirms the diagnosis.
Seizure activity in the occipital cortex and adjacent association areas can produce static light and stars. In a prospective study of 18 patients with occipital epilepsy, visual seizures lasted from a few seconds to 3 minutes—although rarely 20 to 150 minutes—and occurred in multiple clusters a day or week.10 All but 2 patients had secondary generalized tonic-clonic convulsions. Occipital seizures often are misdiagnosed as the visual aura of migraine, particularly when elementary visual hallucinations are followed by post-ictal headache and vomiting.11 Lights with a color or a spherical shape suggest occipital epilepsy. Consider ordering an electroencephalogram (EEG) if the clinical diagnosis is unclear.
EXAMINATION: No obvious cause
During a mental status exam, Ms. G is pleasant, cooperative, alert, and oriented to person, place, and time. Her speech is fluent, her affect is full, and she describes her mood as a “sensitive, overwhelmed state.” Her thoughts occasionally are tangential, and she perseverates on guilty, embarrassed, and paranoid thoughts. She has auditory hallucinations and experiences photopsia during the interview, but denies other visual hallucinations. She shows no deficits in attention, concentration, memory, language, calculations, visuospatial abilities, or general fund of knowledge.
Her physical exam shows pupils that are equal, round, and reactive to light with normal extraocular movements, intact visual fields, 20/20 visual acuity in both eyes with glasses, and sharp optic disc margins with no retinal abnormalities apparent on funduscopic exam. The rest of her physical and neurologic exam is normal. Her complete blood count, electrolytes, kidney, liver function tests, urinalysis, and serum toxicology screens are normal. She has no history of immunodeficiency.
An MRI performed a year earlier showed mild diffuse congestion of a left maxillary sinus but no other intracranial abnormalities, and a waking EEG with sphenoidal electrodes was normal.
The authors’ observations
Evaluation of patients with photopsia includes taking a history and performing an eye examination including visual acuity testing, visual field testing, and funduscopic examination. The appearance, location, and duration of photopsia may help narrow the differential diagnosis and identify emergent cases (Table 1 and Table 2). Seizure activity associated with flashing lights suggests occipital epilepsy. A history of hypertension, diabetes, or polymyalgia rheumatica points to vascular causes, and hyperthyroidism suggests that flashing lights may be phosphenes of Graves’ disease. Myopia or eye trauma could indicate vitreous traction. Prescription medications and illicit drug use may point to a toxic etiology.12
Table 1
Diagnoses suggested by photopsia phenomena
| Feature | Suggested diagnosis |
|---|---|
| Appearance | |
| Twinkling lights with grey spots | Emboli |
| Zigzag lines | Occipital epilepsy |
| White flashes | Vitreous traction on the retina |
| Flickering lights and shimmering | Clomiphene use |
| Temporally located flashes of light, floaters, or blurred vision that is worse in dim illumination | Posterior vitreous detachment and retinal tearing |
| Location | |
| Temporal | Migraine or retinal pathology |
| Central | Occipital lesion or embolus |
| Monocular | Retinal pathology |
| Binocular | Cerebral cause |
| Duration | |
| Lightning quick | Vitreous detachment |
| Lasts up to 30 minutes | Migraine or occipital epilepsy |
Table 2
Photopsia differential diagnosis: Look for co-occurring symptoms
| Co-occurring symptoms | Suggests |
|---|---|
| Seizure activity associated with flashing lights | Occipital epilepsy |
| Yellow or green discoloration to the visual field, halos, and appearance of frost over objects | Digitalis toxicity |
| Shadows, moving objects, and insects crawling with co-occurring euphoria, hypervigilance, impaired judgment, and autonomic changes such as tachycardia, pupillary dilation, hypertension, and nausea | Cocaine intoxication |
| Floaters, or a ‘curtain’ or ‘shadow’ moving over the visual field, which may be accompanied by central or peripheral vision loss | Retinal detachment |
| Bilateral blurred vision, ataxia, vertigo, dysarthria, or drop attacks | Vertebrobasilar artery insufficiency |
OUTCOME: Diagnosis of exclusion
Ms. G’s visual disturbance resembles vitreous detachment or classic migraine; however, the onset is not sudden, her funduscopic exam is normal, and she has no discrete episodes with concomitant headache. Ms. G’s improvement with topiramate is inconsistent with an ophthalmic origin because such photopsia should not improve with medication. It is consistent with recurrent seizures or status epilepticus of the occipital cortex; however, she did not experience multiple discrete episodes a day or generalized seizures experienced by most occipital seizure patients, and her EEG and clinical history are not consistent with seizures. Because we cannot rule out occipital lobe epilepsy, we refer Ms. G for repeat EEG and routine ophthalmologic exam, both of which are normal.
Perceptual disturbances are common in schizoaffective disorder and schizophrenia,13-15 which we consider the most likely etiology of Ms. G’s photopsia, given her normal neurologic and ophthalmologic examinations. We switch her from aripiprazole to ziprasidone, 40 mg/d, discontinue phentermine, and taper and discontinue oxcarbazepine.
Related resources
- Ophthalmology Web. www.ophthalmologyweb.com.
- Aleman A, Larøi F. Hallucinations: the science of idiosyncratic perception. Washington, DC: American Psychological Association; 2008.
Drug Brand Names
- Aripiprazole • Abilify
- Clomiphene • Clomid, Serophene
- Digoxin • Lanoxin
- Nizatidine • Axid
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Paclitaxel • Onxol, Taxol
- Phentermine • Adipex-P, Inoamin
- Sertraline • Zoloft
- Topiramate • Topamax
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Jaspers K. General psychopathology. Manchester, United Kingdom: Manchester University Press; 1962.
2. Manford M, Andermann F. Complex visual hallucinations. Clinical and neurobiological insights. Brain. 1998;121:1819-1840.
3. Amos JF. Differential diagnosis of common etiologies of photopsia. J Am Optom Assoc. 1999;70(8):485-504.
4. Biousse V, Touboul PJ, D’Anglejan-Chatillon J, et al. Ophthalmologic manifestations of internal carotid artery dissection. Am J Ophthalmol. 1998;126(4):565-577.
5. Butler VP, Jr, Odel JG, Rath E, et al. Digitalis-induced visual disturbances with therapeutic serum digitalis concentrations. Ann Intern Med. 1995;123(9):676-680.
6. Mitchell J, Vierkant AD. Delusions and hallucinations of cocaine abusers and paranoid schizophrenics: a comparative study. J Psychol. 1991;125(3):301-310.
7. Seidman AD, Barrett S, Canezo S. Photopsia during 3-hour paclitaxel administration at doses > or = 250 mg/m2. J Clin Oncol. 1994;12(8):1741-1742.
8. Purvin VA. Visual disturbance secondary to clomiphene citrate. Arch Ophthalmol. 1995;113(4):482-484.
9. Queiroz LP, Rapoport AM, Weeks RE, et al. Characteristics of migraine visual aura. Headache. 1997;37(3):137-141.
10. Panayiotopoulos CP. Visual phenomena and headache in occipital epilepsy: a review, a systematic study and differentiation from migraine. Epileptic Disord. 1999;1(4):205-216.
11. Walker MC, Smith SJ, Sisodiya SM, et al. Case of simple partial status epilepticus in occipital lobe epilepsy misdiagnosed as migraine: clinical, electrophysiological, and magnetic resonance imaging characteristics. Epilepsia. 1995;36(12):1233-1236.
12. Lichter M. Flashing lights—a warning. The Canadian Journal of Diagnosis. 2002;19:31-35.
13. Parnas J, Handest P, Saebye D, et al. Anomalies of subjective experience in schizophrenia and psychotic bipolar illness. Acta Psychiatr Scand. 2003;108(2):126-133.
14. Phillipson OT, Harris JP. Perceptual changes in schizophrenia: a questionnaire survey. Psychol Med. 1985;15(4):859-866.
15. Cutting J, Dunne F. Subjective experience of schizophrenia. Schizophr Bull. 1989;15(2):217-231.
HISTORY: Visual disturbances
Ms. G, age 30, has schizoaffective disorder and presents with worsening auditory hallucinations, paranoid delusions, and thought broadcasting and insertion, which is suspected to be related to a change from olanzapine to aripiprazole. She complains of visual disturbances—a hallucination of flashing lights—that she describes as occurring “all the time, like salt-and-pepper dancing, and sometimes splotches.” Her visual symptoms are worse when she closes her eyes and in dimly lit environments, but occur in daylight as well. Her vision is otherwise unimpaired.
The visual disturbances started with Ms. G’s first psychotic break at age 23 and have persisted continuously. She reports that at first, the spots were more intense, like an incessant strobe light. These symptoms are aggravated by sleep deprivation and anger and improve only with topiramate, 100 mg/d, which was prescribed a year earlier after a neurologic consultation but discontinued because of cognitive side effects.
Ms. G also complains of dull, aching, continuous headaches in the center of her forehead, which do not wake her, are not worse in the morning, and do not vary with the intensity of her visual symptoms. The headaches are incorporated into her system of delusions; she believes they “drain the electricity from her head” and make her feel better. She denies a history of migraines. Ms. G has a history of experiencing well-formed visual hallucinations, such as the devil, but has not had them for several years.
She had 5 to 10 episodes over the last 2 years that she describes as seizures—“an earthquake, a huge whooshing noise,” accompanied by heart palpitations that occur with stress, in public, in bright lights, or whenever she feels vulnerable. These episodes are not associated with loss of consciousness, incontinence, amnesia, or post-ictal confusion and she can stop them with relaxation techniques such as deep breathing and reminding herself to calm down. The last episode was 2 months ago and seemed unrelated to her visual phenomena. She also complains of occasional paresthesias in her extremities but denies dizziness, presyncope, or blurry or double vision.
Ms. G is obese and has no history of head injury or birth defects. Her family history is negative for epilepsy; however, her mother has bipolar disorder and father has schizophrenia. Her medications are phentermine, 37.5 mg/d for short-term management of obesity, oxcarbazepine, 600 mg/d for supposed partial seizures, sertraline, 100 mg/d for depression, aripiprazole, 10 mg/d, and nizatidine, 150 mg/d, for gastroesophageal reflux disease. She does not use alcohol, cigarettes, or illicit drugs. Ms. G obtained a master’s degree in health communications and works as a research assistant at a local medical school.
The authors’ observations
Visual hallucinations are not distortions of reality but original false perceptions that co-occur with real perceptions.1 They vary from simple, elemental hallucinations involving flashes of light or geometric figures to more complex elaborations such as seeing crawling insects or a flock of angels.2 Hallucinations can originate anywhere in the visual system from the lens to the visual cortex and can be vascular, toxic, electrophysiologic, structural, or neurochemical manifestations of neurologic, psychiatric, or ophthalmologic disorders. Depending on the hallucination’s etiology, treatment varies from emergent ophthalmologic examination and retinal surgery to antipsychotic therapy to simple observation. Photopsia is a perception of flashing lights, and its etiology varies; causes can be categorized as emergent or nonemergent.
Emergent causes of photopsia typically have a sudden onset, often can be diagnosed from associated symptoms or medical history, and must be recognized quickly to prevent permanent vision loss. Posterior vitreous detachment and retinal tearing can manifest as flashes of light, floaters, or blurred vision in the peripheral visual field that are worse in dim illumination and localizable by the patient. Retinal detachment can cause photopsia, floaters, or a “curtain” or “shadow” moving over the visual field, which may be accompanied by central or peripheral vision loss.3 Severe myopia is a risk factor for retinal detachment.
New-onset photopsia can suggest cytomegaloviral retinitis in an immune-compromised patient, and ocular-vascular crisis in a patient with sickle cell disease. New-onset or recurrent photopsia with bilateral blurred vision, ataxia, vertigo, dysarthria, or drop attacks may be caused by vertebrobasilar artery insufficiency (VBAI). Photopsia has been reported as the presenting symptom in carotid artery dissection.4 Photopsia correlated with eye movement implicates the retina or optic nerve. All of these etiologies except for VBAI should be referred to an ophthalmologist for indirect ophthalmoscopy and evaluation.
Nonemergent causes of photopsia include:
- drug toxicity
- migraine headache
- thyroid ophthalmopathy
- arteriovenous malformations
- seizures
- psychiatric disorders.
Digoxin, cocaine, paclitaxel, and clomiphene may have ocular side effects, including photopsia. The first symptoms of digitalis toxicity often are visual and include photopsia, yellow or green discoloration of the visual field, halos, and the appearance of frost over objects.5 Signs of cocaine intoxication can include visual hallucinations such as photopsia, shadows, moving objects, and insects crawling and co-occurring euphoria, hypervigilance, impaired judgment, and autonomic changes such as tachycardia, pupillary dilation, hypertension, and nausea.6 High-dose paclitaxel infusion has been reported to cause photopsia.7 Clomiphene can cause flickering lights and shimmering that persists after discontinuing the medication.8
Migraine with aura, which includes photopsia 39% of the time,9 often involves an expanding central visual disturbance or scotoma, and usually is confined to 1 visual field but may involve both. The aura typically lasts 10 to 20 minutes and often is followed by headache. Patients often report a history of episodic stereotyped auras and headache. Ocular examination is normal.
Ophthalmic migraine, also known as ocular or retinal migraine, is thought to be caused by transient vasospasm of the choroidal or retinal arteries and can be precipitated by postural changes, exercise, and oral contraceptives. It manifests as a gradual visual disturbance in a mosaic scotomata pattern that enlarges, producing total unilateral visual loss lasting from minutes to an hour, and—misleadingly—can be associated with minimal or no headache. Ocular examination is normal, and a personal or family history of migraine confirms the diagnosis.
Seizure activity in the occipital cortex and adjacent association areas can produce static light and stars. In a prospective study of 18 patients with occipital epilepsy, visual seizures lasted from a few seconds to 3 minutes—although rarely 20 to 150 minutes—and occurred in multiple clusters a day or week.10 All but 2 patients had secondary generalized tonic-clonic convulsions. Occipital seizures often are misdiagnosed as the visual aura of migraine, particularly when elementary visual hallucinations are followed by post-ictal headache and vomiting.11 Lights with a color or a spherical shape suggest occipital epilepsy. Consider ordering an electroencephalogram (EEG) if the clinical diagnosis is unclear.
EXAMINATION: No obvious cause
During a mental status exam, Ms. G is pleasant, cooperative, alert, and oriented to person, place, and time. Her speech is fluent, her affect is full, and she describes her mood as a “sensitive, overwhelmed state.” Her thoughts occasionally are tangential, and she perseverates on guilty, embarrassed, and paranoid thoughts. She has auditory hallucinations and experiences photopsia during the interview, but denies other visual hallucinations. She shows no deficits in attention, concentration, memory, language, calculations, visuospatial abilities, or general fund of knowledge.
Her physical exam shows pupils that are equal, round, and reactive to light with normal extraocular movements, intact visual fields, 20/20 visual acuity in both eyes with glasses, and sharp optic disc margins with no retinal abnormalities apparent on funduscopic exam. The rest of her physical and neurologic exam is normal. Her complete blood count, electrolytes, kidney, liver function tests, urinalysis, and serum toxicology screens are normal. She has no history of immunodeficiency.
An MRI performed a year earlier showed mild diffuse congestion of a left maxillary sinus but no other intracranial abnormalities, and a waking EEG with sphenoidal electrodes was normal.
The authors’ observations
Evaluation of patients with photopsia includes taking a history and performing an eye examination including visual acuity testing, visual field testing, and funduscopic examination. The appearance, location, and duration of photopsia may help narrow the differential diagnosis and identify emergent cases (Table 1 and Table 2). Seizure activity associated with flashing lights suggests occipital epilepsy. A history of hypertension, diabetes, or polymyalgia rheumatica points to vascular causes, and hyperthyroidism suggests that flashing lights may be phosphenes of Graves’ disease. Myopia or eye trauma could indicate vitreous traction. Prescription medications and illicit drug use may point to a toxic etiology.12
Table 1
Diagnoses suggested by photopsia phenomena
| Feature | Suggested diagnosis |
|---|---|
| Appearance | |
| Twinkling lights with grey spots | Emboli |
| Zigzag lines | Occipital epilepsy |
| White flashes | Vitreous traction on the retina |
| Flickering lights and shimmering | Clomiphene use |
| Temporally located flashes of light, floaters, or blurred vision that is worse in dim illumination | Posterior vitreous detachment and retinal tearing |
| Location | |
| Temporal | Migraine or retinal pathology |
| Central | Occipital lesion or embolus |
| Monocular | Retinal pathology |
| Binocular | Cerebral cause |
| Duration | |
| Lightning quick | Vitreous detachment |
| Lasts up to 30 minutes | Migraine or occipital epilepsy |
Table 2
Photopsia differential diagnosis: Look for co-occurring symptoms
| Co-occurring symptoms | Suggests |
|---|---|
| Seizure activity associated with flashing lights | Occipital epilepsy |
| Yellow or green discoloration to the visual field, halos, and appearance of frost over objects | Digitalis toxicity |
| Shadows, moving objects, and insects crawling with co-occurring euphoria, hypervigilance, impaired judgment, and autonomic changes such as tachycardia, pupillary dilation, hypertension, and nausea | Cocaine intoxication |
| Floaters, or a ‘curtain’ or ‘shadow’ moving over the visual field, which may be accompanied by central or peripheral vision loss | Retinal detachment |
| Bilateral blurred vision, ataxia, vertigo, dysarthria, or drop attacks | Vertebrobasilar artery insufficiency |
OUTCOME: Diagnosis of exclusion
Ms. G’s visual disturbance resembles vitreous detachment or classic migraine; however, the onset is not sudden, her funduscopic exam is normal, and she has no discrete episodes with concomitant headache. Ms. G’s improvement with topiramate is inconsistent with an ophthalmic origin because such photopsia should not improve with medication. It is consistent with recurrent seizures or status epilepticus of the occipital cortex; however, she did not experience multiple discrete episodes a day or generalized seizures experienced by most occipital seizure patients, and her EEG and clinical history are not consistent with seizures. Because we cannot rule out occipital lobe epilepsy, we refer Ms. G for repeat EEG and routine ophthalmologic exam, both of which are normal.
Perceptual disturbances are common in schizoaffective disorder and schizophrenia,13-15 which we consider the most likely etiology of Ms. G’s photopsia, given her normal neurologic and ophthalmologic examinations. We switch her from aripiprazole to ziprasidone, 40 mg/d, discontinue phentermine, and taper and discontinue oxcarbazepine.
Related resources
- Ophthalmology Web. www.ophthalmologyweb.com.
- Aleman A, Larøi F. Hallucinations: the science of idiosyncratic perception. Washington, DC: American Psychological Association; 2008.
Drug Brand Names
- Aripiprazole • Abilify
- Clomiphene • Clomid, Serophene
- Digoxin • Lanoxin
- Nizatidine • Axid
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Paclitaxel • Onxol, Taxol
- Phentermine • Adipex-P, Inoamin
- Sertraline • Zoloft
- Topiramate • Topamax
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
HISTORY: Visual disturbances
Ms. G, age 30, has schizoaffective disorder and presents with worsening auditory hallucinations, paranoid delusions, and thought broadcasting and insertion, which is suspected to be related to a change from olanzapine to aripiprazole. She complains of visual disturbances—a hallucination of flashing lights—that she describes as occurring “all the time, like salt-and-pepper dancing, and sometimes splotches.” Her visual symptoms are worse when she closes her eyes and in dimly lit environments, but occur in daylight as well. Her vision is otherwise unimpaired.
The visual disturbances started with Ms. G’s first psychotic break at age 23 and have persisted continuously. She reports that at first, the spots were more intense, like an incessant strobe light. These symptoms are aggravated by sleep deprivation and anger and improve only with topiramate, 100 mg/d, which was prescribed a year earlier after a neurologic consultation but discontinued because of cognitive side effects.
Ms. G also complains of dull, aching, continuous headaches in the center of her forehead, which do not wake her, are not worse in the morning, and do not vary with the intensity of her visual symptoms. The headaches are incorporated into her system of delusions; she believes they “drain the electricity from her head” and make her feel better. She denies a history of migraines. Ms. G has a history of experiencing well-formed visual hallucinations, such as the devil, but has not had them for several years.
She had 5 to 10 episodes over the last 2 years that she describes as seizures—“an earthquake, a huge whooshing noise,” accompanied by heart palpitations that occur with stress, in public, in bright lights, or whenever she feels vulnerable. These episodes are not associated with loss of consciousness, incontinence, amnesia, or post-ictal confusion and she can stop them with relaxation techniques such as deep breathing and reminding herself to calm down. The last episode was 2 months ago and seemed unrelated to her visual phenomena. She also complains of occasional paresthesias in her extremities but denies dizziness, presyncope, or blurry or double vision.
Ms. G is obese and has no history of head injury or birth defects. Her family history is negative for epilepsy; however, her mother has bipolar disorder and father has schizophrenia. Her medications are phentermine, 37.5 mg/d for short-term management of obesity, oxcarbazepine, 600 mg/d for supposed partial seizures, sertraline, 100 mg/d for depression, aripiprazole, 10 mg/d, and nizatidine, 150 mg/d, for gastroesophageal reflux disease. She does not use alcohol, cigarettes, or illicit drugs. Ms. G obtained a master’s degree in health communications and works as a research assistant at a local medical school.
The authors’ observations
Visual hallucinations are not distortions of reality but original false perceptions that co-occur with real perceptions.1 They vary from simple, elemental hallucinations involving flashes of light or geometric figures to more complex elaborations such as seeing crawling insects or a flock of angels.2 Hallucinations can originate anywhere in the visual system from the lens to the visual cortex and can be vascular, toxic, electrophysiologic, structural, or neurochemical manifestations of neurologic, psychiatric, or ophthalmologic disorders. Depending on the hallucination’s etiology, treatment varies from emergent ophthalmologic examination and retinal surgery to antipsychotic therapy to simple observation. Photopsia is a perception of flashing lights, and its etiology varies; causes can be categorized as emergent or nonemergent.
Emergent causes of photopsia typically have a sudden onset, often can be diagnosed from associated symptoms or medical history, and must be recognized quickly to prevent permanent vision loss. Posterior vitreous detachment and retinal tearing can manifest as flashes of light, floaters, or blurred vision in the peripheral visual field that are worse in dim illumination and localizable by the patient. Retinal detachment can cause photopsia, floaters, or a “curtain” or “shadow” moving over the visual field, which may be accompanied by central or peripheral vision loss.3 Severe myopia is a risk factor for retinal detachment.
New-onset photopsia can suggest cytomegaloviral retinitis in an immune-compromised patient, and ocular-vascular crisis in a patient with sickle cell disease. New-onset or recurrent photopsia with bilateral blurred vision, ataxia, vertigo, dysarthria, or drop attacks may be caused by vertebrobasilar artery insufficiency (VBAI). Photopsia has been reported as the presenting symptom in carotid artery dissection.4 Photopsia correlated with eye movement implicates the retina or optic nerve. All of these etiologies except for VBAI should be referred to an ophthalmologist for indirect ophthalmoscopy and evaluation.
Nonemergent causes of photopsia include:
- drug toxicity
- migraine headache
- thyroid ophthalmopathy
- arteriovenous malformations
- seizures
- psychiatric disorders.
Digoxin, cocaine, paclitaxel, and clomiphene may have ocular side effects, including photopsia. The first symptoms of digitalis toxicity often are visual and include photopsia, yellow or green discoloration of the visual field, halos, and the appearance of frost over objects.5 Signs of cocaine intoxication can include visual hallucinations such as photopsia, shadows, moving objects, and insects crawling and co-occurring euphoria, hypervigilance, impaired judgment, and autonomic changes such as tachycardia, pupillary dilation, hypertension, and nausea.6 High-dose paclitaxel infusion has been reported to cause photopsia.7 Clomiphene can cause flickering lights and shimmering that persists after discontinuing the medication.8
Migraine with aura, which includes photopsia 39% of the time,9 often involves an expanding central visual disturbance or scotoma, and usually is confined to 1 visual field but may involve both. The aura typically lasts 10 to 20 minutes and often is followed by headache. Patients often report a history of episodic stereotyped auras and headache. Ocular examination is normal.
Ophthalmic migraine, also known as ocular or retinal migraine, is thought to be caused by transient vasospasm of the choroidal or retinal arteries and can be precipitated by postural changes, exercise, and oral contraceptives. It manifests as a gradual visual disturbance in a mosaic scotomata pattern that enlarges, producing total unilateral visual loss lasting from minutes to an hour, and—misleadingly—can be associated with minimal or no headache. Ocular examination is normal, and a personal or family history of migraine confirms the diagnosis.
Seizure activity in the occipital cortex and adjacent association areas can produce static light and stars. In a prospective study of 18 patients with occipital epilepsy, visual seizures lasted from a few seconds to 3 minutes—although rarely 20 to 150 minutes—and occurred in multiple clusters a day or week.10 All but 2 patients had secondary generalized tonic-clonic convulsions. Occipital seizures often are misdiagnosed as the visual aura of migraine, particularly when elementary visual hallucinations are followed by post-ictal headache and vomiting.11 Lights with a color or a spherical shape suggest occipital epilepsy. Consider ordering an electroencephalogram (EEG) if the clinical diagnosis is unclear.
EXAMINATION: No obvious cause
During a mental status exam, Ms. G is pleasant, cooperative, alert, and oriented to person, place, and time. Her speech is fluent, her affect is full, and she describes her mood as a “sensitive, overwhelmed state.” Her thoughts occasionally are tangential, and she perseverates on guilty, embarrassed, and paranoid thoughts. She has auditory hallucinations and experiences photopsia during the interview, but denies other visual hallucinations. She shows no deficits in attention, concentration, memory, language, calculations, visuospatial abilities, or general fund of knowledge.
Her physical exam shows pupils that are equal, round, and reactive to light with normal extraocular movements, intact visual fields, 20/20 visual acuity in both eyes with glasses, and sharp optic disc margins with no retinal abnormalities apparent on funduscopic exam. The rest of her physical and neurologic exam is normal. Her complete blood count, electrolytes, kidney, liver function tests, urinalysis, and serum toxicology screens are normal. She has no history of immunodeficiency.
An MRI performed a year earlier showed mild diffuse congestion of a left maxillary sinus but no other intracranial abnormalities, and a waking EEG with sphenoidal electrodes was normal.
The authors’ observations
Evaluation of patients with photopsia includes taking a history and performing an eye examination including visual acuity testing, visual field testing, and funduscopic examination. The appearance, location, and duration of photopsia may help narrow the differential diagnosis and identify emergent cases (Table 1 and Table 2). Seizure activity associated with flashing lights suggests occipital epilepsy. A history of hypertension, diabetes, or polymyalgia rheumatica points to vascular causes, and hyperthyroidism suggests that flashing lights may be phosphenes of Graves’ disease. Myopia or eye trauma could indicate vitreous traction. Prescription medications and illicit drug use may point to a toxic etiology.12
Table 1
Diagnoses suggested by photopsia phenomena
| Feature | Suggested diagnosis |
|---|---|
| Appearance | |
| Twinkling lights with grey spots | Emboli |
| Zigzag lines | Occipital epilepsy |
| White flashes | Vitreous traction on the retina |
| Flickering lights and shimmering | Clomiphene use |
| Temporally located flashes of light, floaters, or blurred vision that is worse in dim illumination | Posterior vitreous detachment and retinal tearing |
| Location | |
| Temporal | Migraine or retinal pathology |
| Central | Occipital lesion or embolus |
| Monocular | Retinal pathology |
| Binocular | Cerebral cause |
| Duration | |
| Lightning quick | Vitreous detachment |
| Lasts up to 30 minutes | Migraine or occipital epilepsy |
Table 2
Photopsia differential diagnosis: Look for co-occurring symptoms
| Co-occurring symptoms | Suggests |
|---|---|
| Seizure activity associated with flashing lights | Occipital epilepsy |
| Yellow or green discoloration to the visual field, halos, and appearance of frost over objects | Digitalis toxicity |
| Shadows, moving objects, and insects crawling with co-occurring euphoria, hypervigilance, impaired judgment, and autonomic changes such as tachycardia, pupillary dilation, hypertension, and nausea | Cocaine intoxication |
| Floaters, or a ‘curtain’ or ‘shadow’ moving over the visual field, which may be accompanied by central or peripheral vision loss | Retinal detachment |
| Bilateral blurred vision, ataxia, vertigo, dysarthria, or drop attacks | Vertebrobasilar artery insufficiency |
OUTCOME: Diagnosis of exclusion
Ms. G’s visual disturbance resembles vitreous detachment or classic migraine; however, the onset is not sudden, her funduscopic exam is normal, and she has no discrete episodes with concomitant headache. Ms. G’s improvement with topiramate is inconsistent with an ophthalmic origin because such photopsia should not improve with medication. It is consistent with recurrent seizures or status epilepticus of the occipital cortex; however, she did not experience multiple discrete episodes a day or generalized seizures experienced by most occipital seizure patients, and her EEG and clinical history are not consistent with seizures. Because we cannot rule out occipital lobe epilepsy, we refer Ms. G for repeat EEG and routine ophthalmologic exam, both of which are normal.
Perceptual disturbances are common in schizoaffective disorder and schizophrenia,13-15 which we consider the most likely etiology of Ms. G’s photopsia, given her normal neurologic and ophthalmologic examinations. We switch her from aripiprazole to ziprasidone, 40 mg/d, discontinue phentermine, and taper and discontinue oxcarbazepine.
Related resources
- Ophthalmology Web. www.ophthalmologyweb.com.
- Aleman A, Larøi F. Hallucinations: the science of idiosyncratic perception. Washington, DC: American Psychological Association; 2008.
Drug Brand Names
- Aripiprazole • Abilify
- Clomiphene • Clomid, Serophene
- Digoxin • Lanoxin
- Nizatidine • Axid
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Paclitaxel • Onxol, Taxol
- Phentermine • Adipex-P, Inoamin
- Sertraline • Zoloft
- Topiramate • Topamax
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Jaspers K. General psychopathology. Manchester, United Kingdom: Manchester University Press; 1962.
2. Manford M, Andermann F. Complex visual hallucinations. Clinical and neurobiological insights. Brain. 1998;121:1819-1840.
3. Amos JF. Differential diagnosis of common etiologies of photopsia. J Am Optom Assoc. 1999;70(8):485-504.
4. Biousse V, Touboul PJ, D’Anglejan-Chatillon J, et al. Ophthalmologic manifestations of internal carotid artery dissection. Am J Ophthalmol. 1998;126(4):565-577.
5. Butler VP, Jr, Odel JG, Rath E, et al. Digitalis-induced visual disturbances with therapeutic serum digitalis concentrations. Ann Intern Med. 1995;123(9):676-680.
6. Mitchell J, Vierkant AD. Delusions and hallucinations of cocaine abusers and paranoid schizophrenics: a comparative study. J Psychol. 1991;125(3):301-310.
7. Seidman AD, Barrett S, Canezo S. Photopsia during 3-hour paclitaxel administration at doses > or = 250 mg/m2. J Clin Oncol. 1994;12(8):1741-1742.
8. Purvin VA. Visual disturbance secondary to clomiphene citrate. Arch Ophthalmol. 1995;113(4):482-484.
9. Queiroz LP, Rapoport AM, Weeks RE, et al. Characteristics of migraine visual aura. Headache. 1997;37(3):137-141.
10. Panayiotopoulos CP. Visual phenomena and headache in occipital epilepsy: a review, a systematic study and differentiation from migraine. Epileptic Disord. 1999;1(4):205-216.
11. Walker MC, Smith SJ, Sisodiya SM, et al. Case of simple partial status epilepticus in occipital lobe epilepsy misdiagnosed as migraine: clinical, electrophysiological, and magnetic resonance imaging characteristics. Epilepsia. 1995;36(12):1233-1236.
12. Lichter M. Flashing lights—a warning. The Canadian Journal of Diagnosis. 2002;19:31-35.
13. Parnas J, Handest P, Saebye D, et al. Anomalies of subjective experience in schizophrenia and psychotic bipolar illness. Acta Psychiatr Scand. 2003;108(2):126-133.
14. Phillipson OT, Harris JP. Perceptual changes in schizophrenia: a questionnaire survey. Psychol Med. 1985;15(4):859-866.
15. Cutting J, Dunne F. Subjective experience of schizophrenia. Schizophr Bull. 1989;15(2):217-231.
1. Jaspers K. General psychopathology. Manchester, United Kingdom: Manchester University Press; 1962.
2. Manford M, Andermann F. Complex visual hallucinations. Clinical and neurobiological insights. Brain. 1998;121:1819-1840.
3. Amos JF. Differential diagnosis of common etiologies of photopsia. J Am Optom Assoc. 1999;70(8):485-504.
4. Biousse V, Touboul PJ, D’Anglejan-Chatillon J, et al. Ophthalmologic manifestations of internal carotid artery dissection. Am J Ophthalmol. 1998;126(4):565-577.
5. Butler VP, Jr, Odel JG, Rath E, et al. Digitalis-induced visual disturbances with therapeutic serum digitalis concentrations. Ann Intern Med. 1995;123(9):676-680.
6. Mitchell J, Vierkant AD. Delusions and hallucinations of cocaine abusers and paranoid schizophrenics: a comparative study. J Psychol. 1991;125(3):301-310.
7. Seidman AD, Barrett S, Canezo S. Photopsia during 3-hour paclitaxel administration at doses > or = 250 mg/m2. J Clin Oncol. 1994;12(8):1741-1742.
8. Purvin VA. Visual disturbance secondary to clomiphene citrate. Arch Ophthalmol. 1995;113(4):482-484.
9. Queiroz LP, Rapoport AM, Weeks RE, et al. Characteristics of migraine visual aura. Headache. 1997;37(3):137-141.
10. Panayiotopoulos CP. Visual phenomena and headache in occipital epilepsy: a review, a systematic study and differentiation from migraine. Epileptic Disord. 1999;1(4):205-216.
11. Walker MC, Smith SJ, Sisodiya SM, et al. Case of simple partial status epilepticus in occipital lobe epilepsy misdiagnosed as migraine: clinical, electrophysiological, and magnetic resonance imaging characteristics. Epilepsia. 1995;36(12):1233-1236.
12. Lichter M. Flashing lights—a warning. The Canadian Journal of Diagnosis. 2002;19:31-35.
13. Parnas J, Handest P, Saebye D, et al. Anomalies of subjective experience in schizophrenia and psychotic bipolar illness. Acta Psychiatr Scand. 2003;108(2):126-133.
14. Phillipson OT, Harris JP. Perceptual changes in schizophrenia: a questionnaire survey. Psychol Med. 1985;15(4):859-866.
15. Cutting J, Dunne F. Subjective experience of schizophrenia. Schizophr Bull. 1989;15(2):217-231.
The manipulative self-harmer
CASE: Self-destructive behaviors
After being acquitted of 4 counts of second-degree forgery for writing checks from her mother’s bank account, Ms. L, age 52, is sent to the state hospital for a forensic examination to determine competency. Two years later she is granted conditional release from the hospital, transferred to our not-for-profit community mental health center, and enrolled in an intensive inpatient treatment program to monitor forensic patients. She is legally required to comply with treatment recommendations.
At admission, Ms. L is diagnosed with major depression, recurrent, and borderline personality disorder (BPD). She has no history of antisocial behavior or criminal acts other than forging checks and has never spent time in prison, which makes it unlikely she has co morbid antisocial personality disorder (Table 1).1
Over the next 5 years Ms. L tests limits with the treatment team and acts out by engaging in self-harming behaviors. In 1 instance, she cuts her forearm deeply, stuffs the wound with mayonnaise and paper towels, and wraps her arm with a bandage. She wears a long-sleeved shirt to hide her wound, which is not discovered until a severe infection develops.
Ms. L has difficulty with coping skills and interpersonal relationships. She approaches others with ambivalence and mistrust and consistently expects them to demean or take advantage of her. Ms. L is manipulative, at times injuring herself after perceived wrongdoings by staff. For example, after her therapist reschedules a meeting because of an emergency, Ms. L pours scalding water on her foot.
Table 1
Cluster B personality disorders: Differential diagnosis
| Diagnosis | Features |
|---|---|
| Borderline personality disorder | Self-destructiveness, angry disruptions in close relationships, and chronic feelings of deep emptiness and loneliness |
| Histrionic personality disorder | Attention seeking, manipulative behavior, and rapidly shifting emotions |
| Antisocial personality disorder | Manipulative to gain profit, power, or other material gratification |
| Source: Reference 1 | |
The authors’ observations
Ms. L consistently displays 3 common constructs of BPD:
- primitive defense mechanisms
- identity diffusion
- generally intact reality testing.2
Defense mechanisms are psychological attempts to deal with intrapsychic stress. Splitting—vacillating between extremes of idealization and devaluation—is a fundamental primitive defense mechanism that is the root of BPD.2 Identity diffusion causes confusion about life goals and values and feelings of boredom and emptiness. This internal world leads a patient to have the same perception of the external world, which explains many symptoms of BPD, such as rapidly shifting moods, intense anger, lack of clear sense of self, fear of abandonment, and unstable and intense interpersonal relationships.2
Early in treatment, Ms. L had difficulty breaking a cycle of self-defeating behavior, such as destroying personal items, trying to hang herself, and gluing an ear plug in her ear. During an argument with a staff member, Ms. L punched a wall and fractured her left hand. BPD patients sometimes will “up the ante” when acting out. For example, one of our patients claimed to have planted a bomb in an elementary school and another swallowed inedible objects, including spoons, forks, and butter knives. In Ms. L’s case, we addressed her self-harm behavior by helping her:
- develop less destructive coping skills such as drawing or painting
- identify irrational thoughts that contribute to self harm.
HISTORY: Troubled past
Raised by her biologic parents, Ms. L met all developmental milestones. She denies a history of childhood abuse but reports experiencing “depression and memory loss” and relationship problems with her parents during adolescence. As a child she often missed school because she “did not want anyone to know what a disgusting person I was” and “I should have my head cut open and cut into little pieces for thinking such mean thoughts.” Ms. L dropped out of school in the twelfth grade but obtained her general educational development certificate.
Notes and letters Ms. L wrote while in treatment consistently refer to her negative self-image. Ms. L writes that she feels she does not deserve to “be a part of this world,” is “never good enough for anyone,” and “should be thrown away with the garbage.”
Ms. L vacillates between desiring a closer relationship with her parents, especially her mother, and wanting to “cut them out of my life for good.” She has minimal contact with her older sister. Ms. L is divorced and has 2 adult sons. She was involved sporadically in her sons’ lives when they were children, but now has no contact with them.
BPD and crime
Ms. L is enrolled in the “911 program,” which monitors individuals who have been found not guilty by reason of mental defect. Individuals with BPD often are convicted of serious and violent crimes, which may be because of BPD features such as interpersonal hostility and self-harm. Impulsivity, substance abuse, and parental neglect—all of which are associated with BPD—can increase risk of criminality.3 There is no evidence to suggest a direct link between BPD and criminality; however, over-representation of BPD in prison populations suggest that in severe cases it may increase criminogenic risk.1,3
TREATMENT: Worsened depression
When Ms. L arrives at our facility, her medication regimen includes fluoxetine, 80 mg/d, risperidone, 2 mg/d, and buspirone, 20 mg/d. Risperidone and buspirone are discontinued because of perceived lack of efficacy. Venlafaxine XR is added and titrated to 300 mg/d, and Ms. L receives lorazepam, 1 and 2 mg as needed. However, lorazepam carries risks because impulsivity and impaired judgment—which are common in BPD—can lead to dependence and abuse. We feel that in a supervised setting the risks can be managed.
Recently, staff witnessed Ms. L experiencing an episode that appeared to be a grand mal seizure. After Ms. L is evaluated at the local emergency room, her EEG is normal, but a neurologic consult recommends discontinuing fluoxetine or venlafaxine XR because they may have contributed to the seizure. We taper and discontinue venlafaxine XR but Ms. L complains bitterly that she is getting increasingly depressed. On several occasions she attempts to pit team members against each other.
Ms. L falls, injures her back, and begins to abuse opiates. After her prescription runs out, she obtains more from an intellectually limited patient in her treatment program. Ms. L says she is getting more depressed, threatens suicide, and is placed in a more restrictive in-patient setting. We consider adding pregabalin to address her pain and help with anxiety and impulse control but the consulting neurologist prescribes carbamazepine, 400 mg/d, and her pain improves.5,6
The authors’ observations
BPD treatment primarily is psychotherapeutic and emphasizes skill building (Table 2) with focused, symptom-targeted pharmacotherapy as indicated.4 Pharmacotherapy typically targets 3 domains:
- affective dysregulation
- impulsive-behavioral dyscontrol symptoms
- cognitive-perceptual symptoms.
Patients with prominent anxiety may benefit from benzodiazepines, although research on these agents for BPD is limited. Recent studies show efficacy with fluoxetine, olanzapine, or a combination of both,7 and divalproex.8 Preliminary data supports the use of topiramate, quetiapine, risperidone, ziprasidone, lamotrigine, and clonidine (Table 3).9-14 A recent review and meta-analysis showed efficacy with topira-mate, lamotrigine, valproate, aripiprazole, and olanzapine.15
For Ms. L, we restart venlafaxine at a lower dose of 50 mg/d and titrate it to 150 mg/d, which is still lower than her previous dose of 300 mg/d. She has no recurrence of seizures and her depression improves.
Table 2
Features of psychotherapeutic modalities for BPD
| Description | Mode of treatment | Skills taught | |
|---|---|---|---|
| Dialectical behavior therapy | Manualized, time-limited, cognitive-behavioral approach based on the biosocial theory of BPD | Individual therapy, group skills training, telephone contact, and therapist consultation | Core mindfulness skills, interpersonal effectiveness skills, emotion modulation skills, and distress tolerance skills |
| Systems Training for Emotional Predictability and Problem Solving | Manual-based, group treatment that includes a systems component to train family members, friends, and significant others | 20-week basic skills group and a 1-year, twice-monthly advanced group program; utilizes a classroom ‘seminar’ format | Awareness of illness, emotion management skills, and behavior management skills |
| BPD: borderline personality disorder | |||
Table 3
Pharmacotherapy for BPD: What the evidence says
| Study | Design | Results |
|---|---|---|
| Hollander et al, 20039 | 96 patients with Cluster B personality disorders randomized to divalproex or placebo for 12 weeks | Divalproex was superior to placebo in treating impulsive aggression, irritability, and global severity |
| Hilger et al, 200310 | Case report of 2 women with BPD and severe self-mutilation receiving quetiapine monotherapy | Quetiapine resulted in a marked improvement of impulsive behavior and overall level of function |
| Rizvi, 200211 | Case report of a 14-year-old female with borderline personality traits admitted to an inpatient facility for suicide attempt, impulsive behavior, and mood lability. Lamotrigine was started at 25 mg/d and titrated to 200 mg/d. At admission, she was receiving clonazepam, valproic acid, quetiapine, and fluoxetine, which were tapered and discontinued | Over 6 months of inpatient treatment, suicidal behavior and ideation diminished and impulse control and mood lability improved; continued improvement at 1-year follow up |
| Rocca et al, 200212 | 15 BPD outpatients with aggressive behavior given risperidone (mean dose 3.27 mg/d) in an 8-week open-label study | Risperidone produced a significant reduction in aggression based on AQ scores, reduction in depressive symptoms, and an increase in energy and global functioning |
| Philipsen et al, 200413 | 14 women with BPD given oral clonidine, 75 and 150 µg, while experiencing strong aversive inner tension and urge to commit self-injury | Clonidine significantly decreased aversive inner tension, dissociative symptoms, and urge to commit self-injury as measured by self rated scales |
| Pascual et al, 200414 | A 2-week open-label study of 10 females and 2 males presenting to psychiatric emergency service for self-injurious behavior, aggression/hostility, loss of impulse control, and severe anxiety/depressive symptoms received IM ziprasidone, 20 mg, followed by flexible oral dosing between 40 mg/d and 160 mg/d | 9 patients who completed the study showed statistically significant improvements on CGI-S, HAM-D-17, HAM-A, BPRS, and BIS |
| AQ: Aggression Questionnaire; BIS: Barratt Impulsiveness Scale; BPD: borderline personality disorder; BPRS: Brief Psychiatric Rating Scale; CGI-S: Clinical Global Impressions-Severity of Illness; HAM-A: Hamilton Anxiety Rating scale; HAM-D-17: 17-item Hamilton Depression Rating scale | ||
OUTCOME: Some improvement
Ms. L has no dramatic suicidal gestures for 3 years. Although she continues to engage in self-injurious behaviors, the intensity and frequency are reduced and she does not inflict any serious injury for 18 months. Her mood and behavior continue to oscillate; she is relatively calm and satisfied 1 week, angry and assaultive the next. This stormy course is expected given her BPD diagnosis.
Initially, Ms. L resided in a locked residential unit and was minimally compliant with treatment recommendations and unit policies. As treatment progressed she moved to a different locked unit and eventually to an apartment. Recently, she was placed in a more restrictive setting because her hostile and self-destructive behavior escalated.
The authors’ observations
Ms. L is no different from most Axis II Cluster B disordered patients. During treatment she shows improvement by refraining from self-destructive behaviors for up to 18 months, but she then briefly reverts back to maladaptive behaviors. Ms. L resides in a very structured treatment setting. It is not clear if the gains she made in treatment would have been possible if she was living on her own in the community.
One year after finishing the court-mandated “911 program,” Ms. L lives in the community, draws and paints quite well, attends weekly individual and group therapy, and refrains from self-mutilation. She still experiences volatile moods, but can handle them without inflicting self injury.
Related resources
- Oldham JM. Guideline watch: practice guideline for the treatment of patients with borderline personality disorder. Arlington, VA: American Psychiatric Association; 2005. www.psychiatryonline.com/content.aspx?aID=148722.
- Koenigsberg HW, Kernberg OF, Stone MH, et al. Borderline patients: extending the limits of treatability. New York, NY: Basic Books; 2000.
Drug brand names
- Aripiprazole • Abilify
- Buspirone • Buspar
- Carbamazepine • Tegretol
- Clonidine • Catapres
- Divalproex • Depakote
- Fluoxetine • Prozac
- Fluoxetine-olanzapine • Symbyax
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Pregabalin • Lyrica
- Risperidone • Risperdal
- Topiramate • Topamax
- Valproic acid • Depakene
- Venlafaxine XR • Effexor XR
- Ziprasidone • Geodon
Disclosures
Dr. Hashmi is on the speakers bureau for AstraZeneca, Eli Lilly and Company, and Janssen.
Dr. Vowell reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
2. Koenigsberg HW, Kernberg OF, Stone MH, et al. Borderline patients: extending the limits of treatability. New York, NY: Basic Books; 2000.
3. Nee C, Farman S. Female prisoners with borderline personality disorder: some promising treatment developments. Crim Behav Ment Health. 2005;15:2-16.
4. Oldham JM, Bender DS, Skodol AE, et al. Testing an APA practice guideline: symptom-targeted medication utilization for patients with borderline personality disorder. J Psychiatr Pract. 2004;10:156-161.
5. American Psychiatric Association Practice Guidelines. Practice guideline for the treatment of patients with borderline personality disorder. Am J Psychiatry. 2001;158(suppl 10):1-52.
6. Yatham LN. Newer anticonvulsants in the treatment of bipolar disorder. J Clin Psychiatry. 2004;65(suppl 10):28-35.
7. Rinne T, van den Brink W, Wouters L, et al. SSRI treatment of borderline personality disorder: a randomized, placebo-controlled clinical trial for female patients with borderline personality disorder. Am J Psychiatry. 2002;159(12):2048-2054.
8. Zanarini MC, Frankenburg FR, Parachini EA. A preliminary, randomized trial of fluoxetine, olanzapine, and the olanzapine-fluoxetine combination in women with borderline personality disorder. J Clin Psychiatry. 2004;65(7):903-907.
9. Hollander E, Tracy KA, Swann AC, et al. Divalproex in the treatment of impulsive aggression: efficacy in cluster B personality disorders. Neuropsychopharmacology. 2003;28(6):1186-1197.
10. Hilger E, Barnas C, Kasper S. Quetiapine in the treatment of borderline personality disorder. World J Biol Psychiatry. 2003;4(1):42-44.
11. Rizvi ST. Lamotrigine and borderline personality disorder. J Child Adolesc Psychopharmacol. 2002;12(4):365-366.
12. Rocca P, Marchiaro L, Cocuzza E, et al. Treatment of borderline personality disorder with risperidone. J Clin Psychiatry. 2002;63(3):241-244.
13. Philipsen A, Richter H, Schmahl C, et al. Clonidine in acute aversive inner tension and self-injurious behavior in female patients with borderline personality disorder. J Clin Psychiatry. 2004;65(10):1414-1419.
14. Pascual JC, Oller S, Soler J, et al. Ziprasidone in the acute treatment of borderline personality disorder in psychiatric emergency services. J Clin Psychiatry. 2004;65(9):1281-1282.
15. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196(1):4-12.
CASE: Self-destructive behaviors
After being acquitted of 4 counts of second-degree forgery for writing checks from her mother’s bank account, Ms. L, age 52, is sent to the state hospital for a forensic examination to determine competency. Two years later she is granted conditional release from the hospital, transferred to our not-for-profit community mental health center, and enrolled in an intensive inpatient treatment program to monitor forensic patients. She is legally required to comply with treatment recommendations.
At admission, Ms. L is diagnosed with major depression, recurrent, and borderline personality disorder (BPD). She has no history of antisocial behavior or criminal acts other than forging checks and has never spent time in prison, which makes it unlikely she has co morbid antisocial personality disorder (Table 1).1
Over the next 5 years Ms. L tests limits with the treatment team and acts out by engaging in self-harming behaviors. In 1 instance, she cuts her forearm deeply, stuffs the wound with mayonnaise and paper towels, and wraps her arm with a bandage. She wears a long-sleeved shirt to hide her wound, which is not discovered until a severe infection develops.
Ms. L has difficulty with coping skills and interpersonal relationships. She approaches others with ambivalence and mistrust and consistently expects them to demean or take advantage of her. Ms. L is manipulative, at times injuring herself after perceived wrongdoings by staff. For example, after her therapist reschedules a meeting because of an emergency, Ms. L pours scalding water on her foot.
Table 1
Cluster B personality disorders: Differential diagnosis
| Diagnosis | Features |
|---|---|
| Borderline personality disorder | Self-destructiveness, angry disruptions in close relationships, and chronic feelings of deep emptiness and loneliness |
| Histrionic personality disorder | Attention seeking, manipulative behavior, and rapidly shifting emotions |
| Antisocial personality disorder | Manipulative to gain profit, power, or other material gratification |
| Source: Reference 1 | |
The authors’ observations
Ms. L consistently displays 3 common constructs of BPD:
- primitive defense mechanisms
- identity diffusion
- generally intact reality testing.2
Defense mechanisms are psychological attempts to deal with intrapsychic stress. Splitting—vacillating between extremes of idealization and devaluation—is a fundamental primitive defense mechanism that is the root of BPD.2 Identity diffusion causes confusion about life goals and values and feelings of boredom and emptiness. This internal world leads a patient to have the same perception of the external world, which explains many symptoms of BPD, such as rapidly shifting moods, intense anger, lack of clear sense of self, fear of abandonment, and unstable and intense interpersonal relationships.2
Early in treatment, Ms. L had difficulty breaking a cycle of self-defeating behavior, such as destroying personal items, trying to hang herself, and gluing an ear plug in her ear. During an argument with a staff member, Ms. L punched a wall and fractured her left hand. BPD patients sometimes will “up the ante” when acting out. For example, one of our patients claimed to have planted a bomb in an elementary school and another swallowed inedible objects, including spoons, forks, and butter knives. In Ms. L’s case, we addressed her self-harm behavior by helping her:
- develop less destructive coping skills such as drawing or painting
- identify irrational thoughts that contribute to self harm.
HISTORY: Troubled past
Raised by her biologic parents, Ms. L met all developmental milestones. She denies a history of childhood abuse but reports experiencing “depression and memory loss” and relationship problems with her parents during adolescence. As a child she often missed school because she “did not want anyone to know what a disgusting person I was” and “I should have my head cut open and cut into little pieces for thinking such mean thoughts.” Ms. L dropped out of school in the twelfth grade but obtained her general educational development certificate.
Notes and letters Ms. L wrote while in treatment consistently refer to her negative self-image. Ms. L writes that she feels she does not deserve to “be a part of this world,” is “never good enough for anyone,” and “should be thrown away with the garbage.”
Ms. L vacillates between desiring a closer relationship with her parents, especially her mother, and wanting to “cut them out of my life for good.” She has minimal contact with her older sister. Ms. L is divorced and has 2 adult sons. She was involved sporadically in her sons’ lives when they were children, but now has no contact with them.
BPD and crime
Ms. L is enrolled in the “911 program,” which monitors individuals who have been found not guilty by reason of mental defect. Individuals with BPD often are convicted of serious and violent crimes, which may be because of BPD features such as interpersonal hostility and self-harm. Impulsivity, substance abuse, and parental neglect—all of which are associated with BPD—can increase risk of criminality.3 There is no evidence to suggest a direct link between BPD and criminality; however, over-representation of BPD in prison populations suggest that in severe cases it may increase criminogenic risk.1,3
TREATMENT: Worsened depression
When Ms. L arrives at our facility, her medication regimen includes fluoxetine, 80 mg/d, risperidone, 2 mg/d, and buspirone, 20 mg/d. Risperidone and buspirone are discontinued because of perceived lack of efficacy. Venlafaxine XR is added and titrated to 300 mg/d, and Ms. L receives lorazepam, 1 and 2 mg as needed. However, lorazepam carries risks because impulsivity and impaired judgment—which are common in BPD—can lead to dependence and abuse. We feel that in a supervised setting the risks can be managed.
Recently, staff witnessed Ms. L experiencing an episode that appeared to be a grand mal seizure. After Ms. L is evaluated at the local emergency room, her EEG is normal, but a neurologic consult recommends discontinuing fluoxetine or venlafaxine XR because they may have contributed to the seizure. We taper and discontinue venlafaxine XR but Ms. L complains bitterly that she is getting increasingly depressed. On several occasions she attempts to pit team members against each other.
Ms. L falls, injures her back, and begins to abuse opiates. After her prescription runs out, she obtains more from an intellectually limited patient in her treatment program. Ms. L says she is getting more depressed, threatens suicide, and is placed in a more restrictive in-patient setting. We consider adding pregabalin to address her pain and help with anxiety and impulse control but the consulting neurologist prescribes carbamazepine, 400 mg/d, and her pain improves.5,6
The authors’ observations
BPD treatment primarily is psychotherapeutic and emphasizes skill building (Table 2) with focused, symptom-targeted pharmacotherapy as indicated.4 Pharmacotherapy typically targets 3 domains:
- affective dysregulation
- impulsive-behavioral dyscontrol symptoms
- cognitive-perceptual symptoms.
Patients with prominent anxiety may benefit from benzodiazepines, although research on these agents for BPD is limited. Recent studies show efficacy with fluoxetine, olanzapine, or a combination of both,7 and divalproex.8 Preliminary data supports the use of topiramate, quetiapine, risperidone, ziprasidone, lamotrigine, and clonidine (Table 3).9-14 A recent review and meta-analysis showed efficacy with topira-mate, lamotrigine, valproate, aripiprazole, and olanzapine.15
For Ms. L, we restart venlafaxine at a lower dose of 50 mg/d and titrate it to 150 mg/d, which is still lower than her previous dose of 300 mg/d. She has no recurrence of seizures and her depression improves.
Table 2
Features of psychotherapeutic modalities for BPD
| Description | Mode of treatment | Skills taught | |
|---|---|---|---|
| Dialectical behavior therapy | Manualized, time-limited, cognitive-behavioral approach based on the biosocial theory of BPD | Individual therapy, group skills training, telephone contact, and therapist consultation | Core mindfulness skills, interpersonal effectiveness skills, emotion modulation skills, and distress tolerance skills |
| Systems Training for Emotional Predictability and Problem Solving | Manual-based, group treatment that includes a systems component to train family members, friends, and significant others | 20-week basic skills group and a 1-year, twice-monthly advanced group program; utilizes a classroom ‘seminar’ format | Awareness of illness, emotion management skills, and behavior management skills |
| BPD: borderline personality disorder | |||
Table 3
Pharmacotherapy for BPD: What the evidence says
| Study | Design | Results |
|---|---|---|
| Hollander et al, 20039 | 96 patients with Cluster B personality disorders randomized to divalproex or placebo for 12 weeks | Divalproex was superior to placebo in treating impulsive aggression, irritability, and global severity |
| Hilger et al, 200310 | Case report of 2 women with BPD and severe self-mutilation receiving quetiapine monotherapy | Quetiapine resulted in a marked improvement of impulsive behavior and overall level of function |
| Rizvi, 200211 | Case report of a 14-year-old female with borderline personality traits admitted to an inpatient facility for suicide attempt, impulsive behavior, and mood lability. Lamotrigine was started at 25 mg/d and titrated to 200 mg/d. At admission, she was receiving clonazepam, valproic acid, quetiapine, and fluoxetine, which were tapered and discontinued | Over 6 months of inpatient treatment, suicidal behavior and ideation diminished and impulse control and mood lability improved; continued improvement at 1-year follow up |
| Rocca et al, 200212 | 15 BPD outpatients with aggressive behavior given risperidone (mean dose 3.27 mg/d) in an 8-week open-label study | Risperidone produced a significant reduction in aggression based on AQ scores, reduction in depressive symptoms, and an increase in energy and global functioning |
| Philipsen et al, 200413 | 14 women with BPD given oral clonidine, 75 and 150 µg, while experiencing strong aversive inner tension and urge to commit self-injury | Clonidine significantly decreased aversive inner tension, dissociative symptoms, and urge to commit self-injury as measured by self rated scales |
| Pascual et al, 200414 | A 2-week open-label study of 10 females and 2 males presenting to psychiatric emergency service for self-injurious behavior, aggression/hostility, loss of impulse control, and severe anxiety/depressive symptoms received IM ziprasidone, 20 mg, followed by flexible oral dosing between 40 mg/d and 160 mg/d | 9 patients who completed the study showed statistically significant improvements on CGI-S, HAM-D-17, HAM-A, BPRS, and BIS |
| AQ: Aggression Questionnaire; BIS: Barratt Impulsiveness Scale; BPD: borderline personality disorder; BPRS: Brief Psychiatric Rating Scale; CGI-S: Clinical Global Impressions-Severity of Illness; HAM-A: Hamilton Anxiety Rating scale; HAM-D-17: 17-item Hamilton Depression Rating scale | ||
OUTCOME: Some improvement
Ms. L has no dramatic suicidal gestures for 3 years. Although she continues to engage in self-injurious behaviors, the intensity and frequency are reduced and she does not inflict any serious injury for 18 months. Her mood and behavior continue to oscillate; she is relatively calm and satisfied 1 week, angry and assaultive the next. This stormy course is expected given her BPD diagnosis.
Initially, Ms. L resided in a locked residential unit and was minimally compliant with treatment recommendations and unit policies. As treatment progressed she moved to a different locked unit and eventually to an apartment. Recently, she was placed in a more restrictive setting because her hostile and self-destructive behavior escalated.
The authors’ observations
Ms. L is no different from most Axis II Cluster B disordered patients. During treatment she shows improvement by refraining from self-destructive behaviors for up to 18 months, but she then briefly reverts back to maladaptive behaviors. Ms. L resides in a very structured treatment setting. It is not clear if the gains she made in treatment would have been possible if she was living on her own in the community.
One year after finishing the court-mandated “911 program,” Ms. L lives in the community, draws and paints quite well, attends weekly individual and group therapy, and refrains from self-mutilation. She still experiences volatile moods, but can handle them without inflicting self injury.
Related resources
- Oldham JM. Guideline watch: practice guideline for the treatment of patients with borderline personality disorder. Arlington, VA: American Psychiatric Association; 2005. www.psychiatryonline.com/content.aspx?aID=148722.
- Koenigsberg HW, Kernberg OF, Stone MH, et al. Borderline patients: extending the limits of treatability. New York, NY: Basic Books; 2000.
Drug brand names
- Aripiprazole • Abilify
- Buspirone • Buspar
- Carbamazepine • Tegretol
- Clonidine • Catapres
- Divalproex • Depakote
- Fluoxetine • Prozac
- Fluoxetine-olanzapine • Symbyax
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Pregabalin • Lyrica
- Risperidone • Risperdal
- Topiramate • Topamax
- Valproic acid • Depakene
- Venlafaxine XR • Effexor XR
- Ziprasidone • Geodon
Disclosures
Dr. Hashmi is on the speakers bureau for AstraZeneca, Eli Lilly and Company, and Janssen.
Dr. Vowell reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Self-destructive behaviors
After being acquitted of 4 counts of second-degree forgery for writing checks from her mother’s bank account, Ms. L, age 52, is sent to the state hospital for a forensic examination to determine competency. Two years later she is granted conditional release from the hospital, transferred to our not-for-profit community mental health center, and enrolled in an intensive inpatient treatment program to monitor forensic patients. She is legally required to comply with treatment recommendations.
At admission, Ms. L is diagnosed with major depression, recurrent, and borderline personality disorder (BPD). She has no history of antisocial behavior or criminal acts other than forging checks and has never spent time in prison, which makes it unlikely she has co morbid antisocial personality disorder (Table 1).1
Over the next 5 years Ms. L tests limits with the treatment team and acts out by engaging in self-harming behaviors. In 1 instance, she cuts her forearm deeply, stuffs the wound with mayonnaise and paper towels, and wraps her arm with a bandage. She wears a long-sleeved shirt to hide her wound, which is not discovered until a severe infection develops.
Ms. L has difficulty with coping skills and interpersonal relationships. She approaches others with ambivalence and mistrust and consistently expects them to demean or take advantage of her. Ms. L is manipulative, at times injuring herself after perceived wrongdoings by staff. For example, after her therapist reschedules a meeting because of an emergency, Ms. L pours scalding water on her foot.
Table 1
Cluster B personality disorders: Differential diagnosis
| Diagnosis | Features |
|---|---|
| Borderline personality disorder | Self-destructiveness, angry disruptions in close relationships, and chronic feelings of deep emptiness and loneliness |
| Histrionic personality disorder | Attention seeking, manipulative behavior, and rapidly shifting emotions |
| Antisocial personality disorder | Manipulative to gain profit, power, or other material gratification |
| Source: Reference 1 | |
The authors’ observations
Ms. L consistently displays 3 common constructs of BPD:
- primitive defense mechanisms
- identity diffusion
- generally intact reality testing.2
Defense mechanisms are psychological attempts to deal with intrapsychic stress. Splitting—vacillating between extremes of idealization and devaluation—is a fundamental primitive defense mechanism that is the root of BPD.2 Identity diffusion causes confusion about life goals and values and feelings of boredom and emptiness. This internal world leads a patient to have the same perception of the external world, which explains many symptoms of BPD, such as rapidly shifting moods, intense anger, lack of clear sense of self, fear of abandonment, and unstable and intense interpersonal relationships.2
Early in treatment, Ms. L had difficulty breaking a cycle of self-defeating behavior, such as destroying personal items, trying to hang herself, and gluing an ear plug in her ear. During an argument with a staff member, Ms. L punched a wall and fractured her left hand. BPD patients sometimes will “up the ante” when acting out. For example, one of our patients claimed to have planted a bomb in an elementary school and another swallowed inedible objects, including spoons, forks, and butter knives. In Ms. L’s case, we addressed her self-harm behavior by helping her:
- develop less destructive coping skills such as drawing or painting
- identify irrational thoughts that contribute to self harm.
HISTORY: Troubled past
Raised by her biologic parents, Ms. L met all developmental milestones. She denies a history of childhood abuse but reports experiencing “depression and memory loss” and relationship problems with her parents during adolescence. As a child she often missed school because she “did not want anyone to know what a disgusting person I was” and “I should have my head cut open and cut into little pieces for thinking such mean thoughts.” Ms. L dropped out of school in the twelfth grade but obtained her general educational development certificate.
Notes and letters Ms. L wrote while in treatment consistently refer to her negative self-image. Ms. L writes that she feels she does not deserve to “be a part of this world,” is “never good enough for anyone,” and “should be thrown away with the garbage.”
Ms. L vacillates between desiring a closer relationship with her parents, especially her mother, and wanting to “cut them out of my life for good.” She has minimal contact with her older sister. Ms. L is divorced and has 2 adult sons. She was involved sporadically in her sons’ lives when they were children, but now has no contact with them.
BPD and crime
Ms. L is enrolled in the “911 program,” which monitors individuals who have been found not guilty by reason of mental defect. Individuals with BPD often are convicted of serious and violent crimes, which may be because of BPD features such as interpersonal hostility and self-harm. Impulsivity, substance abuse, and parental neglect—all of which are associated with BPD—can increase risk of criminality.3 There is no evidence to suggest a direct link between BPD and criminality; however, over-representation of BPD in prison populations suggest that in severe cases it may increase criminogenic risk.1,3
TREATMENT: Worsened depression
When Ms. L arrives at our facility, her medication regimen includes fluoxetine, 80 mg/d, risperidone, 2 mg/d, and buspirone, 20 mg/d. Risperidone and buspirone are discontinued because of perceived lack of efficacy. Venlafaxine XR is added and titrated to 300 mg/d, and Ms. L receives lorazepam, 1 and 2 mg as needed. However, lorazepam carries risks because impulsivity and impaired judgment—which are common in BPD—can lead to dependence and abuse. We feel that in a supervised setting the risks can be managed.
Recently, staff witnessed Ms. L experiencing an episode that appeared to be a grand mal seizure. After Ms. L is evaluated at the local emergency room, her EEG is normal, but a neurologic consult recommends discontinuing fluoxetine or venlafaxine XR because they may have contributed to the seizure. We taper and discontinue venlafaxine XR but Ms. L complains bitterly that she is getting increasingly depressed. On several occasions she attempts to pit team members against each other.
Ms. L falls, injures her back, and begins to abuse opiates. After her prescription runs out, she obtains more from an intellectually limited patient in her treatment program. Ms. L says she is getting more depressed, threatens suicide, and is placed in a more restrictive in-patient setting. We consider adding pregabalin to address her pain and help with anxiety and impulse control but the consulting neurologist prescribes carbamazepine, 400 mg/d, and her pain improves.5,6
The authors’ observations
BPD treatment primarily is psychotherapeutic and emphasizes skill building (Table 2) with focused, symptom-targeted pharmacotherapy as indicated.4 Pharmacotherapy typically targets 3 domains:
- affective dysregulation
- impulsive-behavioral dyscontrol symptoms
- cognitive-perceptual symptoms.
Patients with prominent anxiety may benefit from benzodiazepines, although research on these agents for BPD is limited. Recent studies show efficacy with fluoxetine, olanzapine, or a combination of both,7 and divalproex.8 Preliminary data supports the use of topiramate, quetiapine, risperidone, ziprasidone, lamotrigine, and clonidine (Table 3).9-14 A recent review and meta-analysis showed efficacy with topira-mate, lamotrigine, valproate, aripiprazole, and olanzapine.15
For Ms. L, we restart venlafaxine at a lower dose of 50 mg/d and titrate it to 150 mg/d, which is still lower than her previous dose of 300 mg/d. She has no recurrence of seizures and her depression improves.
Table 2
Features of psychotherapeutic modalities for BPD
| Description | Mode of treatment | Skills taught | |
|---|---|---|---|
| Dialectical behavior therapy | Manualized, time-limited, cognitive-behavioral approach based on the biosocial theory of BPD | Individual therapy, group skills training, telephone contact, and therapist consultation | Core mindfulness skills, interpersonal effectiveness skills, emotion modulation skills, and distress tolerance skills |
| Systems Training for Emotional Predictability and Problem Solving | Manual-based, group treatment that includes a systems component to train family members, friends, and significant others | 20-week basic skills group and a 1-year, twice-monthly advanced group program; utilizes a classroom ‘seminar’ format | Awareness of illness, emotion management skills, and behavior management skills |
| BPD: borderline personality disorder | |||
Table 3
Pharmacotherapy for BPD: What the evidence says
| Study | Design | Results |
|---|---|---|
| Hollander et al, 20039 | 96 patients with Cluster B personality disorders randomized to divalproex or placebo for 12 weeks | Divalproex was superior to placebo in treating impulsive aggression, irritability, and global severity |
| Hilger et al, 200310 | Case report of 2 women with BPD and severe self-mutilation receiving quetiapine monotherapy | Quetiapine resulted in a marked improvement of impulsive behavior and overall level of function |
| Rizvi, 200211 | Case report of a 14-year-old female with borderline personality traits admitted to an inpatient facility for suicide attempt, impulsive behavior, and mood lability. Lamotrigine was started at 25 mg/d and titrated to 200 mg/d. At admission, she was receiving clonazepam, valproic acid, quetiapine, and fluoxetine, which were tapered and discontinued | Over 6 months of inpatient treatment, suicidal behavior and ideation diminished and impulse control and mood lability improved; continued improvement at 1-year follow up |
| Rocca et al, 200212 | 15 BPD outpatients with aggressive behavior given risperidone (mean dose 3.27 mg/d) in an 8-week open-label study | Risperidone produced a significant reduction in aggression based on AQ scores, reduction in depressive symptoms, and an increase in energy and global functioning |
| Philipsen et al, 200413 | 14 women with BPD given oral clonidine, 75 and 150 µg, while experiencing strong aversive inner tension and urge to commit self-injury | Clonidine significantly decreased aversive inner tension, dissociative symptoms, and urge to commit self-injury as measured by self rated scales |
| Pascual et al, 200414 | A 2-week open-label study of 10 females and 2 males presenting to psychiatric emergency service for self-injurious behavior, aggression/hostility, loss of impulse control, and severe anxiety/depressive symptoms received IM ziprasidone, 20 mg, followed by flexible oral dosing between 40 mg/d and 160 mg/d | 9 patients who completed the study showed statistically significant improvements on CGI-S, HAM-D-17, HAM-A, BPRS, and BIS |
| AQ: Aggression Questionnaire; BIS: Barratt Impulsiveness Scale; BPD: borderline personality disorder; BPRS: Brief Psychiatric Rating Scale; CGI-S: Clinical Global Impressions-Severity of Illness; HAM-A: Hamilton Anxiety Rating scale; HAM-D-17: 17-item Hamilton Depression Rating scale | ||
OUTCOME: Some improvement
Ms. L has no dramatic suicidal gestures for 3 years. Although she continues to engage in self-injurious behaviors, the intensity and frequency are reduced and she does not inflict any serious injury for 18 months. Her mood and behavior continue to oscillate; she is relatively calm and satisfied 1 week, angry and assaultive the next. This stormy course is expected given her BPD diagnosis.
Initially, Ms. L resided in a locked residential unit and was minimally compliant with treatment recommendations and unit policies. As treatment progressed she moved to a different locked unit and eventually to an apartment. Recently, she was placed in a more restrictive setting because her hostile and self-destructive behavior escalated.
The authors’ observations
Ms. L is no different from most Axis II Cluster B disordered patients. During treatment she shows improvement by refraining from self-destructive behaviors for up to 18 months, but she then briefly reverts back to maladaptive behaviors. Ms. L resides in a very structured treatment setting. It is not clear if the gains she made in treatment would have been possible if she was living on her own in the community.
One year after finishing the court-mandated “911 program,” Ms. L lives in the community, draws and paints quite well, attends weekly individual and group therapy, and refrains from self-mutilation. She still experiences volatile moods, but can handle them without inflicting self injury.
Related resources
- Oldham JM. Guideline watch: practice guideline for the treatment of patients with borderline personality disorder. Arlington, VA: American Psychiatric Association; 2005. www.psychiatryonline.com/content.aspx?aID=148722.
- Koenigsberg HW, Kernberg OF, Stone MH, et al. Borderline patients: extending the limits of treatability. New York, NY: Basic Books; 2000.
Drug brand names
- Aripiprazole • Abilify
- Buspirone • Buspar
- Carbamazepine • Tegretol
- Clonidine • Catapres
- Divalproex • Depakote
- Fluoxetine • Prozac
- Fluoxetine-olanzapine • Symbyax
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Pregabalin • Lyrica
- Risperidone • Risperdal
- Topiramate • Topamax
- Valproic acid • Depakene
- Venlafaxine XR • Effexor XR
- Ziprasidone • Geodon
Disclosures
Dr. Hashmi is on the speakers bureau for AstraZeneca, Eli Lilly and Company, and Janssen.
Dr. Vowell reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
2. Koenigsberg HW, Kernberg OF, Stone MH, et al. Borderline patients: extending the limits of treatability. New York, NY: Basic Books; 2000.
3. Nee C, Farman S. Female prisoners with borderline personality disorder: some promising treatment developments. Crim Behav Ment Health. 2005;15:2-16.
4. Oldham JM, Bender DS, Skodol AE, et al. Testing an APA practice guideline: symptom-targeted medication utilization for patients with borderline personality disorder. J Psychiatr Pract. 2004;10:156-161.
5. American Psychiatric Association Practice Guidelines. Practice guideline for the treatment of patients with borderline personality disorder. Am J Psychiatry. 2001;158(suppl 10):1-52.
6. Yatham LN. Newer anticonvulsants in the treatment of bipolar disorder. J Clin Psychiatry. 2004;65(suppl 10):28-35.
7. Rinne T, van den Brink W, Wouters L, et al. SSRI treatment of borderline personality disorder: a randomized, placebo-controlled clinical trial for female patients with borderline personality disorder. Am J Psychiatry. 2002;159(12):2048-2054.
8. Zanarini MC, Frankenburg FR, Parachini EA. A preliminary, randomized trial of fluoxetine, olanzapine, and the olanzapine-fluoxetine combination in women with borderline personality disorder. J Clin Psychiatry. 2004;65(7):903-907.
9. Hollander E, Tracy KA, Swann AC, et al. Divalproex in the treatment of impulsive aggression: efficacy in cluster B personality disorders. Neuropsychopharmacology. 2003;28(6):1186-1197.
10. Hilger E, Barnas C, Kasper S. Quetiapine in the treatment of borderline personality disorder. World J Biol Psychiatry. 2003;4(1):42-44.
11. Rizvi ST. Lamotrigine and borderline personality disorder. J Child Adolesc Psychopharmacol. 2002;12(4):365-366.
12. Rocca P, Marchiaro L, Cocuzza E, et al. Treatment of borderline personality disorder with risperidone. J Clin Psychiatry. 2002;63(3):241-244.
13. Philipsen A, Richter H, Schmahl C, et al. Clonidine in acute aversive inner tension and self-injurious behavior in female patients with borderline personality disorder. J Clin Psychiatry. 2004;65(10):1414-1419.
14. Pascual JC, Oller S, Soler J, et al. Ziprasidone in the acute treatment of borderline personality disorder in psychiatric emergency services. J Clin Psychiatry. 2004;65(9):1281-1282.
15. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196(1):4-12.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
2. Koenigsberg HW, Kernberg OF, Stone MH, et al. Borderline patients: extending the limits of treatability. New York, NY: Basic Books; 2000.
3. Nee C, Farman S. Female prisoners with borderline personality disorder: some promising treatment developments. Crim Behav Ment Health. 2005;15:2-16.
4. Oldham JM, Bender DS, Skodol AE, et al. Testing an APA practice guideline: symptom-targeted medication utilization for patients with borderline personality disorder. J Psychiatr Pract. 2004;10:156-161.
5. American Psychiatric Association Practice Guidelines. Practice guideline for the treatment of patients with borderline personality disorder. Am J Psychiatry. 2001;158(suppl 10):1-52.
6. Yatham LN. Newer anticonvulsants in the treatment of bipolar disorder. J Clin Psychiatry. 2004;65(suppl 10):28-35.
7. Rinne T, van den Brink W, Wouters L, et al. SSRI treatment of borderline personality disorder: a randomized, placebo-controlled clinical trial for female patients with borderline personality disorder. Am J Psychiatry. 2002;159(12):2048-2054.
8. Zanarini MC, Frankenburg FR, Parachini EA. A preliminary, randomized trial of fluoxetine, olanzapine, and the olanzapine-fluoxetine combination in women with borderline personality disorder. J Clin Psychiatry. 2004;65(7):903-907.
9. Hollander E, Tracy KA, Swann AC, et al. Divalproex in the treatment of impulsive aggression: efficacy in cluster B personality disorders. Neuropsychopharmacology. 2003;28(6):1186-1197.
10. Hilger E, Barnas C, Kasper S. Quetiapine in the treatment of borderline personality disorder. World J Biol Psychiatry. 2003;4(1):42-44.
11. Rizvi ST. Lamotrigine and borderline personality disorder. J Child Adolesc Psychopharmacol. 2002;12(4):365-366.
12. Rocca P, Marchiaro L, Cocuzza E, et al. Treatment of borderline personality disorder with risperidone. J Clin Psychiatry. 2002;63(3):241-244.
13. Philipsen A, Richter H, Schmahl C, et al. Clonidine in acute aversive inner tension and self-injurious behavior in female patients with borderline personality disorder. J Clin Psychiatry. 2004;65(10):1414-1419.
14. Pascual JC, Oller S, Soler J, et al. Ziprasidone in the acute treatment of borderline personality disorder in psychiatric emergency services. J Clin Psychiatry. 2004;65(9):1281-1282.
15. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196(1):4-12.
Nighttime anxieties
CASE: Stress and chest pain
A primary care physician refers Mr. J, age 40, to our mental health clinic for evaluation of anxiety symptoms. Almost a decade ago Mr. J presented to his primary care physician with anxiety and panic attacks that included chest pain and shortness of breath. Various pharmacologic treatments, including paroxetine, were only moderately successful until 4 years ago, when Mr. J began nighttime continuous positive airway pressure (CPAP) therapy and pramipexole, 0.25 to 0.5 mg/d, for obstructive sleep apnea (OSA), at which point his anxiety completely resolved.
Mr. J reported no anxiety for many years, but when shortness of breath, palpitations, and chest pain re-emerge, he consults his primary care physician. After a negative workup for myocardial infarction, Mr. J is started on short-term beta-blocker therapy and restarted on paroxetine, 20 mg/d. A sleep medicine specialist repeats polysomnography and makes slight adjustments to Mr. J’s CPAP therapy. Mr. J relocates to our city and his new primary care physician refers Mr. J to our mental health clinic.
In addition to OSA, Mr. J has mild anemia, hyperlipidemia, and vitamin D deficiency. Mr. J was adopted and has no knowledge of his family psychiatric or medical history. His mental status is normal. Mr. J is not obese, exercises regularly, and has slight micrognathia. His current medications include paroxetine, 20 mg/d, modafinil, 200 mg/d, and ergocalciferol, 50,000 units/week for vitamin D deficiency.
Mr. J says he experienced a single panic attack 7 months ago, but none since then. However, he complains of chronic chest pressure and mild intermittent anxiety associated with the stress of his new job and recent relocation.
The authors’ observations
Mr. J’s anxiety resolved fully only after receiving treatment for OSA, which is characterized by episodes of blocked breathing during sleep (Table 1).1 Multiple studies show a significant association between OSA and panic attacks.2-5 In a survey of 301 sleep apnea patients, Edlund et al6 demonstrated that OSA may cause nocturnal panic attacks. Untreated OSA can worsen anxiety symptoms. In a study of 242 OSA patients, those who were not compliant with CPAP therapy had significantly higher anxiety scores as measured on the Hospital Anxiety and Depression Scale.7
OSA treatment options include CPAP, oral appliance, and surgery; weight loss and positional therapy may help. Thyroid function, B12, folate, ferritin, and iron studies, and complete blood count can rule out secondary causes of OSA.
Table 1
Obstructive sleep apnea risk factors, symptoms, and features
| Established risk factors | Obesity, craniofacial abnormalities, upper airway soft tissue abnormalities, male sex |
| Potential risk factors | Heredity, smoking, nasal congestion, diabetes |
| Symptoms | Daytime sleepiness; nonrestorative sleep; witnessed apneas by bed partner; awakening with choking; nocturnal restlessness; insomnia with frequent awakenings; impaired concentration; cognitive deficits; mood changes; morning headaches; vivid, strange, or threatening dreams; gastroesophageal reflux |
| Common features in patients with obstructive sleep apnea | Obesity, large neck circumference, systemic hypertension, hypercapnia, cardiovascular or cerebrovascular disease, cardiac dysrhythmias, narrow or ‘crowded’ airway, pulmonary hypertension, cor pulmonale, polycythemia |
| Source: Reference 1 | |
HISTORY: A succession of diagnoses
Approximately 9 years ago, Mr. J experienced several episodes of waking in the middle of the night from a bad dream with severe shortness of breath and chest pain. He also reported increasing fatigue, anxiety, and stress regarding work, graduate school, and his wife’s recent miscarriage. After negative cardiac workups, his primary care physician diagnosed panic attacks. He referred Mr. J to stress management classes and prescribed clonazepam, 1.5 mg/d, which was discontinued after 2 months.
One week after discontinuing clonazepam, Mr. J experienced chest pain, shortness of breath, and anxiety while awake. A cardiologist ruled out cardiac pathology. Mr. J’s primary care physician prescribed sertraline, 25 mg/d, and propranolol, 60 mg/d and 10 mg as needed, for anxiety.
Shortly after, Mr. J moved to a different city. His new primary care physician discontinued sertraline and propranolol and started paroxetine, titrated to 20 mg/d. A psychiatrist diagnosed Mr. J with panic disorder without agoraphobia, continued paroxetine, and added alprazolam, 1 mg/d as needed. Mr. J’s anxiety symptoms were moderately controlled for several years.
After his son was diagnosed with attention-deficit/hyperactivity disorder (ADHD), Mr. J also was evaluated and found to have ADHD and major depressive disorder, single episode. Mr. J received methylphenidate, 54 mg/d, and paroxetine was titrated to 40 mg/d, with moderate results.
Approximately 6 years before presenting to our clinic, Mr. J reported worsening daytime fatigue, which was treated with modafinil, 200 mg/d. He experienced significant improvement. The next year methylphenidate was switched to amphetamine/dextroamphetamine, then discontinued because of side effects. His physician started Mr. J on atomoxetine, which also was discontinued because of side effects.
Two years later, Mr. J complained of gradual worsening daytime sleepiness. Polysomnography revealed that Mr. J had severe OSA and periodic limb movement disorder. After he began nighttime CPAP and pramipexole, 0.25 to 0.5 mg/d, and continued modafinil, 200 mg/d, his anxiety symptoms completely resolved. Several months later Mr. J’s physician discontinued paroxetine because Mr. J reported it caused mildly decreased concentration.
The authors’ observations
The etiology of Mr. J’s anxiety is unclear; however, he does not meet criteria for:
- panic disorder, because he denies persistent concern about having more attacks or the implications or consequences of panic attacks, or significant change in behavior related to panic attacks (Table 2)8
- generalized anxiety disorder, because between panic attacks Mr. J’s baseline anxiety related to “real-world” stressors is mild, intermittent, and easily controllable8
- substance-induced anxiety disorder, because Mr. J denies using caffeine, tobacco, alcohol, or illicit drugs. Also, for many years he worked for a company that performed random drug screening.
Table 2
Diagnostic criteria for panic disorder without agoraphobia
| A. Both 1 and 2: 1. Recurrent unexpected panic attacks 2. At least one of the attacks has been followed by 1 month (or more) of 1 (or more) of the following: a. Persistent concern about having additional attacks b. Worry about the implications of the attack or its consequences (eg, losing control, having a heart attack, ‘going crazy’) c. A significant change in behavior related to the attacks |
| B. Absence of agoraphobia |
| C. The panic attacks are not due to the direct physiologic effects of a substance (eg, a drug of abuse, a medication) or a general medical condition (eg, hyperthyroidism). |
| D. The panic attacks are not better accounted for by another mental disorder, such as social phobia (eg, occurring on exposure to feared social situations), specific phobia (eg, on exposure to a specific phobic situation), obsessive-compulsive disorder (eg, on exposure to dirt in someone with an obsession about contamination), posttraumatic stress disorder (eg, in response to stimuli associated with a severe stressor), or separation anxiety disorder (eg, in response to being away from home or close relatives). |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 |
Although it is difficult to draw a conclusion from a single case, Mr. J’s dramatic improvement with CPAP warrants speculation about possible etiologic relationships among daytime panic attacks, nighttime panic attacks, and OSA.
According to DSM-IV-TR, a panic attack has a distinct period of intense fear or discomfort (Table 3).8 Recurrent panic attacks can lead to anticipatory anxiety, which is an intense fear and/or dread of having another panic attack.9 According to Steven Reiss’ expectancy theory, anxiety sensitivity—ie, the fear of anxiety or fear of fear—may be a risk factor for panic disorder.10 Therefore, past panic attacks may increase the likelihood of future panic attacks.
Table 3
Diagnostic criteria for panic attack*
A discrete period of intense fear or discomfort, in which 4 (or more) of the following symptoms developed abruptly and reached a peak within 10 minutes:
|
| *Panic attacks occur in the context of several anxiety disorders and cannot be diagnosed as a separate entity |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 |
Mr. J’s panic symptoms may be caused by multiple OSA-induced nocturnal panic attacks. These nighttime panic attacks may predispose him to daytime attacks. It is possible that Mr. J had subclinical panic disorder before developing OSA. In this scenario, his OSA-induced nocturnal panic attacks may have worsened his panic disorder. Unfortunately, we do not know precisely how long Mr. J has had OSA—only that he was diagnosed with the condition 4 years before presenting to our clinic.
Mr. J responded moderately to paroxetine monotherapy but experienced rapid resolution of his panic attacks with a combination of paroxetine and CPAP. CPAP monotherapy sufficiently prevented panic attacks for 4 years. Finally, when Mr. J experienced a single panic attack several months before presenting to our clinic—at the end of a very stressful year—reintroducing paroxetine prevented subsequent attacks. This supports our hypothesis that OSA may predispose or indirectly cause patients to develop daytime panic attacks. Alternately, this case suggests that OSA may cause subclinical panic disorder to present as an acute condition.
We rule out anxiety disorder secondary to a general medical condition (OSA) and diagnose Mr. J with anxiety disorder not otherwise specified.
The authors’ observations
We continue paroxetine at 20 mg/d because it was working fairly well with minimal side effects. The sleep medicine specialist maintained modafinil, 200 mg/d. Laboratory studies—including a comprehensive metabolic panel, complete blood count with differential, and thyroid stimulating hormone—were within normal limits except a fasting blood glucose of 123 mg/dL, for which we referred Mr. J to his primary care physician.
OUTCOME: Discontinue paroxetine?
One month later, Mr. J denies panic attacks, other anxiety symptoms, or other psychiatric symptoms and is sleeping well. However, he reports that his mildly decreased concentration persists and he wants to stop paroxetine.
After discussing the risks and benefits, Mr. J and the treatment team decide to continue paroxetine at 20 mg/d. We cite peer-reviewed literature that recommends continuing antidepressants for at least 1 year and possibly indefinitely after symptom resolution to control panic disorder symptoms.9 In addition, we discuss the lack of studies comparing different lengths of treatment with SSRIs for apparent OSA-induced panic attacks that respond to SSRI/CPAP therapy. Because Mr. J was doing well and experiencing minimal side effects, he feels he would be better served with a longer period of psychopharmacologic treatment.
Six months later, Mr. J says his anxiety symptoms are well controlled and generally unchanged except for an occasional “little flutter” of anxiety every 3 or 4 days that lasts several seconds. For 1 year, he reports no recurrence of panic attacks, compliance with CPAP, and stable OSA.
Related resource
- Saunamäki T, Jehkonen M. Depression and anxiety in obstructive sleep apnea syndrome: a review. Acta Neurol Scand. 2007;116(5):277-288.
Drug brand names
- Alprazolam • Xanax
- Amphetamine/dextroamphetamine • Adderall
- Atomoxetine • Strattera
- Clonazepam • Klonopin
- Ergocalciferol • Calciferol
- Modafinil • Provigil
- Methylphenidate extended release • Concerta
- Paroxetine • Paxil
- Pramipexole • Mirapex
- Propranolol • Inderal
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Strohl K, Basner R, Sanders M, et al. Overview of obstructive sleep apnea in adults. UpToDate Online. May 2009. Available at: http://uptodateonline.com/online/content/topic.do?topicKey=sleepdis/12387&selectedTitle=1~150&source=search_result. Accessed September 1, 2009.
2. Chung SA, Jairam S, Hussain MR, et al. How, what, and why of sleep apnea. Perspectives for primary care physicians. Can Fam Physician. 2002;48:1073-1080.
3. Sharafkhaneh A, Giray N, Richardson P, et al. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep. 2005;28(11):1405-1411.
4. Victor LD. Obstructive sleep apnea. Am Fam Physician. 1999;60(8):2279-2286.
5. Lopes FL, Nardi AE, Nascimento I, et al. Nocturnal panic attacks. Arq Neuropsiquiatr. 2002;60:717-720.
6. Edlund MJ, McNamara ME, Millman RP. Sleep apnea and panic attacks. Compr Psychiatry. 1991;32(2):130-132.
7. Kjelsberg FN, Ruud EA, Stavem K. Predictors of symptoms of anxiety and depression in obstructive sleep apnea. Sleep Med. 2005;6(4):341-346.
8. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000:432,440,476.
9. Strahl N. Clinical study guide for the oral boards in psychiatry. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc; 2005:244-246.
10. Reiss S. Expectancy model of fear, anxiety, and panic. Clin Psychol Rev. 1991;11:141-153.
CASE: Stress and chest pain
A primary care physician refers Mr. J, age 40, to our mental health clinic for evaluation of anxiety symptoms. Almost a decade ago Mr. J presented to his primary care physician with anxiety and panic attacks that included chest pain and shortness of breath. Various pharmacologic treatments, including paroxetine, were only moderately successful until 4 years ago, when Mr. J began nighttime continuous positive airway pressure (CPAP) therapy and pramipexole, 0.25 to 0.5 mg/d, for obstructive sleep apnea (OSA), at which point his anxiety completely resolved.
Mr. J reported no anxiety for many years, but when shortness of breath, palpitations, and chest pain re-emerge, he consults his primary care physician. After a negative workup for myocardial infarction, Mr. J is started on short-term beta-blocker therapy and restarted on paroxetine, 20 mg/d. A sleep medicine specialist repeats polysomnography and makes slight adjustments to Mr. J’s CPAP therapy. Mr. J relocates to our city and his new primary care physician refers Mr. J to our mental health clinic.
In addition to OSA, Mr. J has mild anemia, hyperlipidemia, and vitamin D deficiency. Mr. J was adopted and has no knowledge of his family psychiatric or medical history. His mental status is normal. Mr. J is not obese, exercises regularly, and has slight micrognathia. His current medications include paroxetine, 20 mg/d, modafinil, 200 mg/d, and ergocalciferol, 50,000 units/week for vitamin D deficiency.
Mr. J says he experienced a single panic attack 7 months ago, but none since then. However, he complains of chronic chest pressure and mild intermittent anxiety associated with the stress of his new job and recent relocation.
The authors’ observations
Mr. J’s anxiety resolved fully only after receiving treatment for OSA, which is characterized by episodes of blocked breathing during sleep (Table 1).1 Multiple studies show a significant association between OSA and panic attacks.2-5 In a survey of 301 sleep apnea patients, Edlund et al6 demonstrated that OSA may cause nocturnal panic attacks. Untreated OSA can worsen anxiety symptoms. In a study of 242 OSA patients, those who were not compliant with CPAP therapy had significantly higher anxiety scores as measured on the Hospital Anxiety and Depression Scale.7
OSA treatment options include CPAP, oral appliance, and surgery; weight loss and positional therapy may help. Thyroid function, B12, folate, ferritin, and iron studies, and complete blood count can rule out secondary causes of OSA.
Table 1
Obstructive sleep apnea risk factors, symptoms, and features
| Established risk factors | Obesity, craniofacial abnormalities, upper airway soft tissue abnormalities, male sex |
| Potential risk factors | Heredity, smoking, nasal congestion, diabetes |
| Symptoms | Daytime sleepiness; nonrestorative sleep; witnessed apneas by bed partner; awakening with choking; nocturnal restlessness; insomnia with frequent awakenings; impaired concentration; cognitive deficits; mood changes; morning headaches; vivid, strange, or threatening dreams; gastroesophageal reflux |
| Common features in patients with obstructive sleep apnea | Obesity, large neck circumference, systemic hypertension, hypercapnia, cardiovascular or cerebrovascular disease, cardiac dysrhythmias, narrow or ‘crowded’ airway, pulmonary hypertension, cor pulmonale, polycythemia |
| Source: Reference 1 | |
HISTORY: A succession of diagnoses
Approximately 9 years ago, Mr. J experienced several episodes of waking in the middle of the night from a bad dream with severe shortness of breath and chest pain. He also reported increasing fatigue, anxiety, and stress regarding work, graduate school, and his wife’s recent miscarriage. After negative cardiac workups, his primary care physician diagnosed panic attacks. He referred Mr. J to stress management classes and prescribed clonazepam, 1.5 mg/d, which was discontinued after 2 months.
One week after discontinuing clonazepam, Mr. J experienced chest pain, shortness of breath, and anxiety while awake. A cardiologist ruled out cardiac pathology. Mr. J’s primary care physician prescribed sertraline, 25 mg/d, and propranolol, 60 mg/d and 10 mg as needed, for anxiety.
Shortly after, Mr. J moved to a different city. His new primary care physician discontinued sertraline and propranolol and started paroxetine, titrated to 20 mg/d. A psychiatrist diagnosed Mr. J with panic disorder without agoraphobia, continued paroxetine, and added alprazolam, 1 mg/d as needed. Mr. J’s anxiety symptoms were moderately controlled for several years.
After his son was diagnosed with attention-deficit/hyperactivity disorder (ADHD), Mr. J also was evaluated and found to have ADHD and major depressive disorder, single episode. Mr. J received methylphenidate, 54 mg/d, and paroxetine was titrated to 40 mg/d, with moderate results.
Approximately 6 years before presenting to our clinic, Mr. J reported worsening daytime fatigue, which was treated with modafinil, 200 mg/d. He experienced significant improvement. The next year methylphenidate was switched to amphetamine/dextroamphetamine, then discontinued because of side effects. His physician started Mr. J on atomoxetine, which also was discontinued because of side effects.
Two years later, Mr. J complained of gradual worsening daytime sleepiness. Polysomnography revealed that Mr. J had severe OSA and periodic limb movement disorder. After he began nighttime CPAP and pramipexole, 0.25 to 0.5 mg/d, and continued modafinil, 200 mg/d, his anxiety symptoms completely resolved. Several months later Mr. J’s physician discontinued paroxetine because Mr. J reported it caused mildly decreased concentration.
The authors’ observations
The etiology of Mr. J’s anxiety is unclear; however, he does not meet criteria for:
- panic disorder, because he denies persistent concern about having more attacks or the implications or consequences of panic attacks, or significant change in behavior related to panic attacks (Table 2)8
- generalized anxiety disorder, because between panic attacks Mr. J’s baseline anxiety related to “real-world” stressors is mild, intermittent, and easily controllable8
- substance-induced anxiety disorder, because Mr. J denies using caffeine, tobacco, alcohol, or illicit drugs. Also, for many years he worked for a company that performed random drug screening.
Table 2
Diagnostic criteria for panic disorder without agoraphobia
| A. Both 1 and 2: 1. Recurrent unexpected panic attacks 2. At least one of the attacks has been followed by 1 month (or more) of 1 (or more) of the following: a. Persistent concern about having additional attacks b. Worry about the implications of the attack or its consequences (eg, losing control, having a heart attack, ‘going crazy’) c. A significant change in behavior related to the attacks |
| B. Absence of agoraphobia |
| C. The panic attacks are not due to the direct physiologic effects of a substance (eg, a drug of abuse, a medication) or a general medical condition (eg, hyperthyroidism). |
| D. The panic attacks are not better accounted for by another mental disorder, such as social phobia (eg, occurring on exposure to feared social situations), specific phobia (eg, on exposure to a specific phobic situation), obsessive-compulsive disorder (eg, on exposure to dirt in someone with an obsession about contamination), posttraumatic stress disorder (eg, in response to stimuli associated with a severe stressor), or separation anxiety disorder (eg, in response to being away from home or close relatives). |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 |
Although it is difficult to draw a conclusion from a single case, Mr. J’s dramatic improvement with CPAP warrants speculation about possible etiologic relationships among daytime panic attacks, nighttime panic attacks, and OSA.
According to DSM-IV-TR, a panic attack has a distinct period of intense fear or discomfort (Table 3).8 Recurrent panic attacks can lead to anticipatory anxiety, which is an intense fear and/or dread of having another panic attack.9 According to Steven Reiss’ expectancy theory, anxiety sensitivity—ie, the fear of anxiety or fear of fear—may be a risk factor for panic disorder.10 Therefore, past panic attacks may increase the likelihood of future panic attacks.
Table 3
Diagnostic criteria for panic attack*
A discrete period of intense fear or discomfort, in which 4 (or more) of the following symptoms developed abruptly and reached a peak within 10 minutes:
|
| *Panic attacks occur in the context of several anxiety disorders and cannot be diagnosed as a separate entity |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 |
Mr. J’s panic symptoms may be caused by multiple OSA-induced nocturnal panic attacks. These nighttime panic attacks may predispose him to daytime attacks. It is possible that Mr. J had subclinical panic disorder before developing OSA. In this scenario, his OSA-induced nocturnal panic attacks may have worsened his panic disorder. Unfortunately, we do not know precisely how long Mr. J has had OSA—only that he was diagnosed with the condition 4 years before presenting to our clinic.
Mr. J responded moderately to paroxetine monotherapy but experienced rapid resolution of his panic attacks with a combination of paroxetine and CPAP. CPAP monotherapy sufficiently prevented panic attacks for 4 years. Finally, when Mr. J experienced a single panic attack several months before presenting to our clinic—at the end of a very stressful year—reintroducing paroxetine prevented subsequent attacks. This supports our hypothesis that OSA may predispose or indirectly cause patients to develop daytime panic attacks. Alternately, this case suggests that OSA may cause subclinical panic disorder to present as an acute condition.
We rule out anxiety disorder secondary to a general medical condition (OSA) and diagnose Mr. J with anxiety disorder not otherwise specified.
The authors’ observations
We continue paroxetine at 20 mg/d because it was working fairly well with minimal side effects. The sleep medicine specialist maintained modafinil, 200 mg/d. Laboratory studies—including a comprehensive metabolic panel, complete blood count with differential, and thyroid stimulating hormone—were within normal limits except a fasting blood glucose of 123 mg/dL, for which we referred Mr. J to his primary care physician.
OUTCOME: Discontinue paroxetine?
One month later, Mr. J denies panic attacks, other anxiety symptoms, or other psychiatric symptoms and is sleeping well. However, he reports that his mildly decreased concentration persists and he wants to stop paroxetine.
After discussing the risks and benefits, Mr. J and the treatment team decide to continue paroxetine at 20 mg/d. We cite peer-reviewed literature that recommends continuing antidepressants for at least 1 year and possibly indefinitely after symptom resolution to control panic disorder symptoms.9 In addition, we discuss the lack of studies comparing different lengths of treatment with SSRIs for apparent OSA-induced panic attacks that respond to SSRI/CPAP therapy. Because Mr. J was doing well and experiencing minimal side effects, he feels he would be better served with a longer period of psychopharmacologic treatment.
Six months later, Mr. J says his anxiety symptoms are well controlled and generally unchanged except for an occasional “little flutter” of anxiety every 3 or 4 days that lasts several seconds. For 1 year, he reports no recurrence of panic attacks, compliance with CPAP, and stable OSA.
Related resource
- Saunamäki T, Jehkonen M. Depression and anxiety in obstructive sleep apnea syndrome: a review. Acta Neurol Scand. 2007;116(5):277-288.
Drug brand names
- Alprazolam • Xanax
- Amphetamine/dextroamphetamine • Adderall
- Atomoxetine • Strattera
- Clonazepam • Klonopin
- Ergocalciferol • Calciferol
- Modafinil • Provigil
- Methylphenidate extended release • Concerta
- Paroxetine • Paxil
- Pramipexole • Mirapex
- Propranolol • Inderal
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Stress and chest pain
A primary care physician refers Mr. J, age 40, to our mental health clinic for evaluation of anxiety symptoms. Almost a decade ago Mr. J presented to his primary care physician with anxiety and panic attacks that included chest pain and shortness of breath. Various pharmacologic treatments, including paroxetine, were only moderately successful until 4 years ago, when Mr. J began nighttime continuous positive airway pressure (CPAP) therapy and pramipexole, 0.25 to 0.5 mg/d, for obstructive sleep apnea (OSA), at which point his anxiety completely resolved.
Mr. J reported no anxiety for many years, but when shortness of breath, palpitations, and chest pain re-emerge, he consults his primary care physician. After a negative workup for myocardial infarction, Mr. J is started on short-term beta-blocker therapy and restarted on paroxetine, 20 mg/d. A sleep medicine specialist repeats polysomnography and makes slight adjustments to Mr. J’s CPAP therapy. Mr. J relocates to our city and his new primary care physician refers Mr. J to our mental health clinic.
In addition to OSA, Mr. J has mild anemia, hyperlipidemia, and vitamin D deficiency. Mr. J was adopted and has no knowledge of his family psychiatric or medical history. His mental status is normal. Mr. J is not obese, exercises regularly, and has slight micrognathia. His current medications include paroxetine, 20 mg/d, modafinil, 200 mg/d, and ergocalciferol, 50,000 units/week for vitamin D deficiency.
Mr. J says he experienced a single panic attack 7 months ago, but none since then. However, he complains of chronic chest pressure and mild intermittent anxiety associated with the stress of his new job and recent relocation.
The authors’ observations
Mr. J’s anxiety resolved fully only after receiving treatment for OSA, which is characterized by episodes of blocked breathing during sleep (Table 1).1 Multiple studies show a significant association between OSA and panic attacks.2-5 In a survey of 301 sleep apnea patients, Edlund et al6 demonstrated that OSA may cause nocturnal panic attacks. Untreated OSA can worsen anxiety symptoms. In a study of 242 OSA patients, those who were not compliant with CPAP therapy had significantly higher anxiety scores as measured on the Hospital Anxiety and Depression Scale.7
OSA treatment options include CPAP, oral appliance, and surgery; weight loss and positional therapy may help. Thyroid function, B12, folate, ferritin, and iron studies, and complete blood count can rule out secondary causes of OSA.
Table 1
Obstructive sleep apnea risk factors, symptoms, and features
| Established risk factors | Obesity, craniofacial abnormalities, upper airway soft tissue abnormalities, male sex |
| Potential risk factors | Heredity, smoking, nasal congestion, diabetes |
| Symptoms | Daytime sleepiness; nonrestorative sleep; witnessed apneas by bed partner; awakening with choking; nocturnal restlessness; insomnia with frequent awakenings; impaired concentration; cognitive deficits; mood changes; morning headaches; vivid, strange, or threatening dreams; gastroesophageal reflux |
| Common features in patients with obstructive sleep apnea | Obesity, large neck circumference, systemic hypertension, hypercapnia, cardiovascular or cerebrovascular disease, cardiac dysrhythmias, narrow or ‘crowded’ airway, pulmonary hypertension, cor pulmonale, polycythemia |
| Source: Reference 1 | |
HISTORY: A succession of diagnoses
Approximately 9 years ago, Mr. J experienced several episodes of waking in the middle of the night from a bad dream with severe shortness of breath and chest pain. He also reported increasing fatigue, anxiety, and stress regarding work, graduate school, and his wife’s recent miscarriage. After negative cardiac workups, his primary care physician diagnosed panic attacks. He referred Mr. J to stress management classes and prescribed clonazepam, 1.5 mg/d, which was discontinued after 2 months.
One week after discontinuing clonazepam, Mr. J experienced chest pain, shortness of breath, and anxiety while awake. A cardiologist ruled out cardiac pathology. Mr. J’s primary care physician prescribed sertraline, 25 mg/d, and propranolol, 60 mg/d and 10 mg as needed, for anxiety.
Shortly after, Mr. J moved to a different city. His new primary care physician discontinued sertraline and propranolol and started paroxetine, titrated to 20 mg/d. A psychiatrist diagnosed Mr. J with panic disorder without agoraphobia, continued paroxetine, and added alprazolam, 1 mg/d as needed. Mr. J’s anxiety symptoms were moderately controlled for several years.
After his son was diagnosed with attention-deficit/hyperactivity disorder (ADHD), Mr. J also was evaluated and found to have ADHD and major depressive disorder, single episode. Mr. J received methylphenidate, 54 mg/d, and paroxetine was titrated to 40 mg/d, with moderate results.
Approximately 6 years before presenting to our clinic, Mr. J reported worsening daytime fatigue, which was treated with modafinil, 200 mg/d. He experienced significant improvement. The next year methylphenidate was switched to amphetamine/dextroamphetamine, then discontinued because of side effects. His physician started Mr. J on atomoxetine, which also was discontinued because of side effects.
Two years later, Mr. J complained of gradual worsening daytime sleepiness. Polysomnography revealed that Mr. J had severe OSA and periodic limb movement disorder. After he began nighttime CPAP and pramipexole, 0.25 to 0.5 mg/d, and continued modafinil, 200 mg/d, his anxiety symptoms completely resolved. Several months later Mr. J’s physician discontinued paroxetine because Mr. J reported it caused mildly decreased concentration.
The authors’ observations
The etiology of Mr. J’s anxiety is unclear; however, he does not meet criteria for:
- panic disorder, because he denies persistent concern about having more attacks or the implications or consequences of panic attacks, or significant change in behavior related to panic attacks (Table 2)8
- generalized anxiety disorder, because between panic attacks Mr. J’s baseline anxiety related to “real-world” stressors is mild, intermittent, and easily controllable8
- substance-induced anxiety disorder, because Mr. J denies using caffeine, tobacco, alcohol, or illicit drugs. Also, for many years he worked for a company that performed random drug screening.
Table 2
Diagnostic criteria for panic disorder without agoraphobia
| A. Both 1 and 2: 1. Recurrent unexpected panic attacks 2. At least one of the attacks has been followed by 1 month (or more) of 1 (or more) of the following: a. Persistent concern about having additional attacks b. Worry about the implications of the attack or its consequences (eg, losing control, having a heart attack, ‘going crazy’) c. A significant change in behavior related to the attacks |
| B. Absence of agoraphobia |
| C. The panic attacks are not due to the direct physiologic effects of a substance (eg, a drug of abuse, a medication) or a general medical condition (eg, hyperthyroidism). |
| D. The panic attacks are not better accounted for by another mental disorder, such as social phobia (eg, occurring on exposure to feared social situations), specific phobia (eg, on exposure to a specific phobic situation), obsessive-compulsive disorder (eg, on exposure to dirt in someone with an obsession about contamination), posttraumatic stress disorder (eg, in response to stimuli associated with a severe stressor), or separation anxiety disorder (eg, in response to being away from home or close relatives). |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 |
Although it is difficult to draw a conclusion from a single case, Mr. J’s dramatic improvement with CPAP warrants speculation about possible etiologic relationships among daytime panic attacks, nighttime panic attacks, and OSA.
According to DSM-IV-TR, a panic attack has a distinct period of intense fear or discomfort (Table 3).8 Recurrent panic attacks can lead to anticipatory anxiety, which is an intense fear and/or dread of having another panic attack.9 According to Steven Reiss’ expectancy theory, anxiety sensitivity—ie, the fear of anxiety or fear of fear—may be a risk factor for panic disorder.10 Therefore, past panic attacks may increase the likelihood of future panic attacks.
Table 3
Diagnostic criteria for panic attack*
A discrete period of intense fear or discomfort, in which 4 (or more) of the following symptoms developed abruptly and reached a peak within 10 minutes:
|
| *Panic attacks occur in the context of several anxiety disorders and cannot be diagnosed as a separate entity |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 |
Mr. J’s panic symptoms may be caused by multiple OSA-induced nocturnal panic attacks. These nighttime panic attacks may predispose him to daytime attacks. It is possible that Mr. J had subclinical panic disorder before developing OSA. In this scenario, his OSA-induced nocturnal panic attacks may have worsened his panic disorder. Unfortunately, we do not know precisely how long Mr. J has had OSA—only that he was diagnosed with the condition 4 years before presenting to our clinic.
Mr. J responded moderately to paroxetine monotherapy but experienced rapid resolution of his panic attacks with a combination of paroxetine and CPAP. CPAP monotherapy sufficiently prevented panic attacks for 4 years. Finally, when Mr. J experienced a single panic attack several months before presenting to our clinic—at the end of a very stressful year—reintroducing paroxetine prevented subsequent attacks. This supports our hypothesis that OSA may predispose or indirectly cause patients to develop daytime panic attacks. Alternately, this case suggests that OSA may cause subclinical panic disorder to present as an acute condition.
We rule out anxiety disorder secondary to a general medical condition (OSA) and diagnose Mr. J with anxiety disorder not otherwise specified.
The authors’ observations
We continue paroxetine at 20 mg/d because it was working fairly well with minimal side effects. The sleep medicine specialist maintained modafinil, 200 mg/d. Laboratory studies—including a comprehensive metabolic panel, complete blood count with differential, and thyroid stimulating hormone—were within normal limits except a fasting blood glucose of 123 mg/dL, for which we referred Mr. J to his primary care physician.
OUTCOME: Discontinue paroxetine?
One month later, Mr. J denies panic attacks, other anxiety symptoms, or other psychiatric symptoms and is sleeping well. However, he reports that his mildly decreased concentration persists and he wants to stop paroxetine.
After discussing the risks and benefits, Mr. J and the treatment team decide to continue paroxetine at 20 mg/d. We cite peer-reviewed literature that recommends continuing antidepressants for at least 1 year and possibly indefinitely after symptom resolution to control panic disorder symptoms.9 In addition, we discuss the lack of studies comparing different lengths of treatment with SSRIs for apparent OSA-induced panic attacks that respond to SSRI/CPAP therapy. Because Mr. J was doing well and experiencing minimal side effects, he feels he would be better served with a longer period of psychopharmacologic treatment.
Six months later, Mr. J says his anxiety symptoms are well controlled and generally unchanged except for an occasional “little flutter” of anxiety every 3 or 4 days that lasts several seconds. For 1 year, he reports no recurrence of panic attacks, compliance with CPAP, and stable OSA.
Related resource
- Saunamäki T, Jehkonen M. Depression and anxiety in obstructive sleep apnea syndrome: a review. Acta Neurol Scand. 2007;116(5):277-288.
Drug brand names
- Alprazolam • Xanax
- Amphetamine/dextroamphetamine • Adderall
- Atomoxetine • Strattera
- Clonazepam • Klonopin
- Ergocalciferol • Calciferol
- Modafinil • Provigil
- Methylphenidate extended release • Concerta
- Paroxetine • Paxil
- Pramipexole • Mirapex
- Propranolol • Inderal
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Strohl K, Basner R, Sanders M, et al. Overview of obstructive sleep apnea in adults. UpToDate Online. May 2009. Available at: http://uptodateonline.com/online/content/topic.do?topicKey=sleepdis/12387&selectedTitle=1~150&source=search_result. Accessed September 1, 2009.
2. Chung SA, Jairam S, Hussain MR, et al. How, what, and why of sleep apnea. Perspectives for primary care physicians. Can Fam Physician. 2002;48:1073-1080.
3. Sharafkhaneh A, Giray N, Richardson P, et al. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep. 2005;28(11):1405-1411.
4. Victor LD. Obstructive sleep apnea. Am Fam Physician. 1999;60(8):2279-2286.
5. Lopes FL, Nardi AE, Nascimento I, et al. Nocturnal panic attacks. Arq Neuropsiquiatr. 2002;60:717-720.
6. Edlund MJ, McNamara ME, Millman RP. Sleep apnea and panic attacks. Compr Psychiatry. 1991;32(2):130-132.
7. Kjelsberg FN, Ruud EA, Stavem K. Predictors of symptoms of anxiety and depression in obstructive sleep apnea. Sleep Med. 2005;6(4):341-346.
8. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000:432,440,476.
9. Strahl N. Clinical study guide for the oral boards in psychiatry. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc; 2005:244-246.
10. Reiss S. Expectancy model of fear, anxiety, and panic. Clin Psychol Rev. 1991;11:141-153.
1. Strohl K, Basner R, Sanders M, et al. Overview of obstructive sleep apnea in adults. UpToDate Online. May 2009. Available at: http://uptodateonline.com/online/content/topic.do?topicKey=sleepdis/12387&selectedTitle=1~150&source=search_result. Accessed September 1, 2009.
2. Chung SA, Jairam S, Hussain MR, et al. How, what, and why of sleep apnea. Perspectives for primary care physicians. Can Fam Physician. 2002;48:1073-1080.
3. Sharafkhaneh A, Giray N, Richardson P, et al. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep. 2005;28(11):1405-1411.
4. Victor LD. Obstructive sleep apnea. Am Fam Physician. 1999;60(8):2279-2286.
5. Lopes FL, Nardi AE, Nascimento I, et al. Nocturnal panic attacks. Arq Neuropsiquiatr. 2002;60:717-720.
6. Edlund MJ, McNamara ME, Millman RP. Sleep apnea and panic attacks. Compr Psychiatry. 1991;32(2):130-132.
7. Kjelsberg FN, Ruud EA, Stavem K. Predictors of symptoms of anxiety and depression in obstructive sleep apnea. Sleep Med. 2005;6(4):341-346.
8. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000:432,440,476.
9. Strahl N. Clinical study guide for the oral boards in psychiatry. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc; 2005:244-246.
10. Reiss S. Expectancy model of fear, anxiety, and panic. Clin Psychol Rev. 1991;11:141-153.
The woman who wasn’t there
CASE: Feeling detached
Ms. A, age 23, presents to our clinic complaining of feeling detached for the past 4 years. She says she feels “fuzzy all the time, like I lost touch with reality 4 years ago and really miss it.” She complains of “confused thinking,” excessive tiredness and weakness, depression, and anxiety. She says, “It feels like I’m watching my life on television; I don’t feel any emotions.” These symptoms began immediately after a college party, which the police stopped because of underage drinking. She says, “I don’t know why, but that party set it off, and it feels like I am in a dream all the time.”
For the last 4 years, Ms. A has been working as a waitress and is now engaged. She presents to our clinic because the treatments she has been receiving are ineffective and she wants to feel her emotions again, especially before her wedding.
Ms. A has no history of mania, depression, or psychosis. She says she was an anxious child and suffered from anorexia nervosa between age 13 and 14. She experienced occasional panic attacks beginning in high school that were triggered by feeling overwhelmed or frustrated with not feeling normal. During these panic attacks, Ms. A experienced tightness in her chest and dizziness. She denies suicidal or homicidal ideation or attempts.
At age 18, she was sexually assaulted. Ongoing stressors include living in a dangerous neighborhood, having her car broken into, her father’s disapproval of her fiancé, and wanting to get married. She drank heavily in college, but has used alcohol infrequently since then.
Ms. A’s father has a history of anxiety. She describes him as domineering and her mother as very emotional and always wanting to be her friend. Ms. A says she struggles with relationships, employment, and plans for advancement, all of which are moderately to severely affected by her depersonalization symptoms. During the initial appointment, we diagnose Ms. A with generalized anxiety disorder, panic disorder, and major depressive disorder (MDD).
Which diagnoses would you include among the differential diagnosis?
- posttraumatic stress disorder (PTSD)
- MDD with psychotic features
- depersonalization disorder
- schizophrenia, undifferentiated type
- psychosis not otherwise specified
The authors’ observations
Depersonalization symptoms can occur in a variety of situations, including:
- mentally healthy persons suffering from acute stressors, fatigue, or drug use
- neuropsychiatric conditions such as epilepsy
- migraine
- anxiety disorders
- depressive disorders
- schizophrenia.1
Transient depersonalization symptoms are common and have been found in 2.4% of the general population.2 Community surveys using standardized diagnostic interviews reveal 1-month prevalence rates of 1.6% to 1.9% in 2 UK samples.3,4 Depersonalization symptoms are brief and less debilitating than depersonalization disorder.
Depersonalization rarely presents as a primary disorder, when symptoms persist chronically. Rating scales (Table 1)5-7 and DSM-IV-TR criteria (Table 2) can help assess symptom severity and differentiate transient symptoms from a disorder. Psychiatric conditions that commonly are comorbid with depersonalization disorder appear in Table 3.8 Triggers for a first episode of depersonalization disorder include:
Table 1
Assessing for depersonalization: 3 rating scales
| Scale | Description |
|---|---|
| Cambridge Depersonalization Scale5 | 29-item, self-report questionnaire meant to capture frequency and duration of depersonalization symptoms over the previous 6 months |
| Depersonalization Severity Scale6 | Covers a range of axis I and II psychopathology |
| Dissociative Experiences Scale7 | 28-item, self-report instrument to measure dissociation |
- psychological stressors (31%)
- substance abuse (25%)
- physical stressor (12%)
- situational stressor (17%)
- social and/or relationship problems (10%)
- trauma (6%)
- panic/anxiety (2%).8
Although Ms. A experiences depersonalization—constant numbness and emptiness—when she thinks about the sexual assault, she does not meet criteria for PTSD because she denies re-experiencing the assault, hyperarousal, and avoidance behaviors.
Ms. A meets all 4 DSM-IV-TR criteria for depersonalization disorder (Table 2). She experiences persistent feelings of detachment, which cause her considerable distress. Her reality testing is intact and these experiences are not due to a general medical condition, another mental disorder, or direct physiological effects of a substance.
Table 2
DSM-IV-TR criteria for depersonalization disorder
| A. Persistent and recurrent experiences of feeling detached from oneself and as if one is an outside observer of one’s mental processes or body. B. During the depersonalization experience, reality testing remains intact. C. The depersonalization causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. D. The depersonalization experience does not occur exclusively during the course of another mental disorder, such as schizophrenia, panic disorder, acute stress disorder, or another dissociative disorder, and is not due to the direct physiological effects of a substance (eg, a drug of abuse or a medication) or a general medical condition (eg, temporal lobe epilepsy). |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text revision. Washington, DC: American Psychiatric Association; 2004 |
Which medications would you consider for Ms. A?
- benzodiazepine plus a tricyclic antidepressant (TCA)
- selective serotonin reuptake inhibitor (SSRI) plus a benzodiazepine
- trazodone plus bupropion
- atypical antipsychotic plus a benzodiazepine and a TCA
TREATMENT: Insufficient response
Ms. A’s previous psychiatrist prescribed various SSRIs and selective serotonin-norepinephrine reuptake inhibitors, including sertraline, escitalopram, citalopram, paroxetine, and venlafaxine, for depression and anxiety with little or no benefit. When she presented at our clinic, Ms. A was taking clonazepam, 0.25 mg as needed, and fluvoxamine, 50 mg/d, which she said helped her anxiety a little, but not depersonalization symptoms. She received supportive psychotherapy provided during biweekly 30-minute medication management visits.
We add aripiprazole, 2.5 mg/d, to augment fluvoxamine’s antidepressant effect and reduce her anxiety and dissociative symptoms. At the next visit 5 weeks later, she reports her depersonalization symptoms gradually lessened from 10 to 6 on a 10-point self-report scale.
We discontinue fluvoxamine after 5 weeks because it no longer significantly contributes to her recovery. We add amantadine, 100 mg/d, based on the belief that dopamine augmentation might help reduce her symptoms. Ms. A reports improved depersonalization symptoms over the next 4 weeks (5/10). However, a week later she says she feels her anxiety is worsening the depersonalization symptoms. We start buspirone, 7.5 mg/d titrated to 15 mg/d over 4 weeks, Ms. A reports feeling worse so we discontinue the drug.
Next Ms. A complains of excessive sleepiness, which seems to be related to amantadine, so we discontinue it. We start bupropion, 150 mg/d and titrate it to 450 mg/d, which we hope will reduce her fatigue, anxiety, depersonalization, and depression. Bupropion’s effect on norepinephrine and dopamine reuptake and a study of autonomic blunting in depersonalization9 justify our selection.
After 3 months, Ms. A stops taking aripiprazole because it is too costly. The following month she presents with severe anxiety and low-to-moderate depression. Clonazepam and bupropion are discontinued and replaced with diazepam, 20 mg/d, and clomipramine, 25 mg/d at bedtime titrated to 75 mg/d. Our decision is guided by a study on the efficacy of clomipramine in treating depersonalization10 and our desire to aggressively treat her anxiety and depression. After 2 weeks, Ms. A says her anxiety and depression have resolved completely but the depersonalization symptoms persist. We restart amantadine, 100 mg as needed, for anorgasmia.
Because of her persistent complaints of depersonalization, after discussion with Ms. A, we decide to return to what had helped her at the beginning of treatment and restart aripiprazole, 2.5 mg/d. Four months later, she reports her depersonalization symptoms have resolved completely. At this time, her regimen consists of clomipramine, 50 mg at bedtime, diazepam, 10 mg at bedtime, and aripiprazole, 2.5 mg/d.
Which neurotransmitter systems have been implicated in depersonalization disorder?
- HPA axis
- serotonin system
- norepinephrine-dopamine system
- dopamine-serotonin system
- all of the above
The authors’ observations
The neurobiology of emotion processing is still unclear but some evidence indicates that the amygdala, anterior cingulate cortex, and medial prefrontal cortex might be involved in emotion regulation and integration.
Depersonalization disorder is associated with HPA axis dysregulation and patients with depersonalization disorder have a lower basal cortisol level compared with patients with MDD.11,12 Simeon et al9 found a marked basal norepinephrine decline with increasing depersonalization severity.
Various SSRIs,13,14 TCAs,10,15,16 citalopram-olanzapine combination, naltrexone, citalopram-clonazepam combination,17 and fluoxetine-buspirone combination18 have been studied as treatment for depersonalization disorder. We present the first case report of aripiprazole to treat depersonalization disorder. A previous study19 of quetiapine—a low potency blocker of dopamine D2 receptors, which also has a high affinity for serotonin 5-HT2A receptors—suggested a potential role in improving emotional numbing symptoms in depersonalization/derealization disorder. The authors hypothesized that quetiapine may facilitate dopamine and serotonin neurotransmissions in the anterior limbic cortex and prefrontal cortex, which are involved in emotional experiences.
Other treatment options
The kappa opioid system also is implicated in depersonalization. Enadoline, a selective k-opioid agonist, has been shown to cause depersonalization symptoms in healthy subjects.20 High doses of opioid antagonists, such as naltrexone, have been used successfully to treat depersonalization symptoms in patients with borderline personality disorder,21 PTSD,22 and depersonalization disorder.23
Ketamine—which can produce depersonalization—increases glutamate transmission, which suggests that drugs that affect the glutamate system might be targets for future investigation. Similarly, smoking marijuana can induce depersonalization, which indicates that cannabinoid receptors might be another area for research. Hallucinogens, such as lysergic acid diethylamide, psilocybin, and dimethyltryptamine, can produce temporary depersonalization. These drugs are 5-HT2 agonists (HT2A, HT2C), which gives weight to using 5-HT2 antagonists to treat depersonalization.
Psychodynamic approaches based on self-constancy—cohesiveness and stability of self-representation—may be helpful, especially in patients with acute symptoms.24 Cognitive-behavioral therapy may be effective and could be divided into 2 phases:
Table 3
Depersonalization comorbidity: Common disorders
| Disorder | Percentage of depersonalization patients reporting comorbidity |
|---|---|
| Anxiety | 45% |
| Major depressive disorder | 41% |
| Panic disorder | 22% |
| Agoraphobia | 11% |
| Source: Reference 8 | |
- nonspecific interventions such as activity scheduling, graded exposure to avoidance behaviors, and negative automatic thought charts
- techniques to facilitate controlled re-experiencing of emotions and refocusing of attention away from the self and the depersonalization experience.25
Measures such as relaxation techniques, breathing exercises, yoga, tai chi, and meditation also might help decrease anxiety.
OUTCOME: Why did it work?
Ms. A responded partially to the diazepam-clomipramine combination but experienced a full response only after we added aripiprazole. We are not certain whether her response was caused by aripiprazole, a delayed action of clomipramine, or a spontaneous remission. Aripiprazole, 2.5 mg/d, was the first medication we added when Ms. A presented to our clinic and she had reported a partial response to the drug. Aripiprazole was also the last medication added before she experienced response, which lasted for at least 5 months, after which Ms. A was lost to follow-up.
The authors’ observations
We believe that aripiprazole might rebalance serotonin/dopamine neurotransmission for some patients with depersonalization disorder. We theorize that aripiprazole’s blockade of serotonin 2A receptors may enhance dopamine release in certain areas of the brain, possibly improving cognitive and affective symptoms. Depersonalization may be a symptom of worsening psychiatric illness and justifies the use of intensive pharmacologic and psychological therapy.
Related resource
- Simeon D. Feeling unreal: Depersonalization disorder and loss of self. New York, NY: Oxford University Press; 2006.
Drug brand names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bupropion • Wellbutrin
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clonazepam • Klonopin
- Diazepam • Valium
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Ketamine • Ketalar
- Naltrexone • ReVia
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Simeon D. Depersonalisation disorder: a contemporary overview. CNS Drugs. 2004;18(6):343-354.
2. Ross CA, Joshi S, Currie R. Dissociative experiences in the general population: a factor analysis. Hosp Community Psychiatry. 1991;42:297-301.
3. Bebbington PE, Hurry J, Tennant C, et al. Epidemiology of mental disorders in Camberwell. Psychol Med. 1981;11(3):561-579.
4. Bebbington PE, Marsden L, Brewin CR. The need for psychiatric treatment in the general population: the Camberwell needs for care survey. Psychol Med. 1997;27(4):821-834.
5. Sierra M, Berrios GE. The Cambridge Depersonalization Scale: a new instrument for the measurement of depersonalization. Psychiatry Res. 2000;93(2):153-164.
6. Simeon D, Guralnik O, Schmeidler J. Development of a depersonalization severity scale. J Trauma Stress. 2001;14(2):341-349.
7. Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis. 1986;174(12):727-735.
8. Baker D, Earle M, Medford N, et al. Illness perceptions in depersonalization disorder: testing an illness attribution model. Clin Psychol Psychother. 2007;14(2):105-116.
9. Simeon D, Guralnik O, Knutelska M, et al. Basal norepinephrine in depersonalization disorder. Psychiatry Res. 2003;121(1):93-97.
10. Simeon D, Stein DJ, Hollander E. Treatment of depersonalization disorder with clomipramine. Biol Psychiatry. 1998;44(4):302-303.
11. Simeon D, Guralnik O, Knutelska M, et al. Hypothalamic-pituitary-adrenal axis dysregulation in depersonalization disorder. Neuropsychopharmacology. 2001;25(45):793-795.
12. Stanton BR, David AS, Cleare AJ, et al. Basal activity of the hypothalamic-pituitary-adrenal axis in patients with depersonalization disorder. Psychiatry Res. 2001;104(1):85-89.
13. Fichtner CG, Horevitz RP, Braun BG. Fluoxetine in depersonalization disorder. Am J Psychiatry. 1992;149(12):1750-1751.
14. Hollander E, Liebowitz MR, DeCaria C, et al. Treatment of depersonalization with serotonin reuptake blockers. J Clin Psychopharmacol. 1990;10(3):200-203.
15. Noyes R, Jr, Kuperman S, Olson SB. Desipramine: a possible treatment for depersonalization disorder. Can J Psychiatry. 1987;32(9):782-784.
16. Simeon D, Stein DJ, Hollander E. Treatment of depersonalization disorder with clomipramine. Biol Psychiatry. 1998;44(4):302-303.
17. Sachdev P. Citalopram-clonazepam combination for primary depersonalization disorder: a case report. Aust N Z J Psychiatry. 2002;36(3):424-425.
18. Abbas S, Chandra PS, Srivastava M. The use of fluoxetine and buspirone for treatment-refractory depersonalization disorder. J Clin Psychiatry. 1995;56(10):484.-
19. Mancini-Marie A, Fahim C, Potvin S, et al. Quetiapine: focus on emotional numbing in depersonalization disorder: an fMRI case report. Eur Psychiatry. 2006;21(8):574-577.
20. Walsh SL, Geter-Douglas B, Strain EC, et al. Enadoline and butorphanol: evaluation of kappa-agonists on cocaine pharmacodynamics and cocaine self-administration in humans. J Pharmacol Exp Ther. 2001;299(1):147-158.
21. Bohus MJ, Landwehrmeyer B, Stiglmayr CE, et al. Naltrexone in the treatment of dissociative symptoms in patients with borderline personality disorder: a open label trial. J Clin Psychiatry. 1999;60(9):598-603.
22. Glover H. A preliminary trial of nalmefene for the treatment of emotional numbing in combat veterans with posttraumatic stress disorder. Isr J Psychiatry Relat Sci. 1993;30(4):255-263.
23. Nuller YL, Morozova MG, Kushnir ON, et al. Effect of naloxone therapy on depersonalization: a pilot study. J Psychopharmacol. 2001;15(2):93-95.
24. Frances A, Sacks M, Aronoff S. Depersonalization: a self-relations perspective. Int J Psychanal. 1977;58:325-331.
25. Hunter ECM, Phillips ML, Chalder T, et al. Depersonalization disorder: a cognitive-behavioural conceptualization. Behav Res Ther. 2003;41(12):1451-1467.
CASE: Feeling detached
Ms. A, age 23, presents to our clinic complaining of feeling detached for the past 4 years. She says she feels “fuzzy all the time, like I lost touch with reality 4 years ago and really miss it.” She complains of “confused thinking,” excessive tiredness and weakness, depression, and anxiety. She says, “It feels like I’m watching my life on television; I don’t feel any emotions.” These symptoms began immediately after a college party, which the police stopped because of underage drinking. She says, “I don’t know why, but that party set it off, and it feels like I am in a dream all the time.”
For the last 4 years, Ms. A has been working as a waitress and is now engaged. She presents to our clinic because the treatments she has been receiving are ineffective and she wants to feel her emotions again, especially before her wedding.
Ms. A has no history of mania, depression, or psychosis. She says she was an anxious child and suffered from anorexia nervosa between age 13 and 14. She experienced occasional panic attacks beginning in high school that were triggered by feeling overwhelmed or frustrated with not feeling normal. During these panic attacks, Ms. A experienced tightness in her chest and dizziness. She denies suicidal or homicidal ideation or attempts.
At age 18, she was sexually assaulted. Ongoing stressors include living in a dangerous neighborhood, having her car broken into, her father’s disapproval of her fiancé, and wanting to get married. She drank heavily in college, but has used alcohol infrequently since then.
Ms. A’s father has a history of anxiety. She describes him as domineering and her mother as very emotional and always wanting to be her friend. Ms. A says she struggles with relationships, employment, and plans for advancement, all of which are moderately to severely affected by her depersonalization symptoms. During the initial appointment, we diagnose Ms. A with generalized anxiety disorder, panic disorder, and major depressive disorder (MDD).
Which diagnoses would you include among the differential diagnosis?
- posttraumatic stress disorder (PTSD)
- MDD with psychotic features
- depersonalization disorder
- schizophrenia, undifferentiated type
- psychosis not otherwise specified
The authors’ observations
Depersonalization symptoms can occur in a variety of situations, including:
- mentally healthy persons suffering from acute stressors, fatigue, or drug use
- neuropsychiatric conditions such as epilepsy
- migraine
- anxiety disorders
- depressive disorders
- schizophrenia.1
Transient depersonalization symptoms are common and have been found in 2.4% of the general population.2 Community surveys using standardized diagnostic interviews reveal 1-month prevalence rates of 1.6% to 1.9% in 2 UK samples.3,4 Depersonalization symptoms are brief and less debilitating than depersonalization disorder.
Depersonalization rarely presents as a primary disorder, when symptoms persist chronically. Rating scales (Table 1)5-7 and DSM-IV-TR criteria (Table 2) can help assess symptom severity and differentiate transient symptoms from a disorder. Psychiatric conditions that commonly are comorbid with depersonalization disorder appear in Table 3.8 Triggers for a first episode of depersonalization disorder include:
Table 1
Assessing for depersonalization: 3 rating scales
| Scale | Description |
|---|---|
| Cambridge Depersonalization Scale5 | 29-item, self-report questionnaire meant to capture frequency and duration of depersonalization symptoms over the previous 6 months |
| Depersonalization Severity Scale6 | Covers a range of axis I and II psychopathology |
| Dissociative Experiences Scale7 | 28-item, self-report instrument to measure dissociation |
- psychological stressors (31%)
- substance abuse (25%)
- physical stressor (12%)
- situational stressor (17%)
- social and/or relationship problems (10%)
- trauma (6%)
- panic/anxiety (2%).8
Although Ms. A experiences depersonalization—constant numbness and emptiness—when she thinks about the sexual assault, she does not meet criteria for PTSD because she denies re-experiencing the assault, hyperarousal, and avoidance behaviors.
Ms. A meets all 4 DSM-IV-TR criteria for depersonalization disorder (Table 2). She experiences persistent feelings of detachment, which cause her considerable distress. Her reality testing is intact and these experiences are not due to a general medical condition, another mental disorder, or direct physiological effects of a substance.
Table 2
DSM-IV-TR criteria for depersonalization disorder
| A. Persistent and recurrent experiences of feeling detached from oneself and as if one is an outside observer of one’s mental processes or body. B. During the depersonalization experience, reality testing remains intact. C. The depersonalization causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. D. The depersonalization experience does not occur exclusively during the course of another mental disorder, such as schizophrenia, panic disorder, acute stress disorder, or another dissociative disorder, and is not due to the direct physiological effects of a substance (eg, a drug of abuse or a medication) or a general medical condition (eg, temporal lobe epilepsy). |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text revision. Washington, DC: American Psychiatric Association; 2004 |
Which medications would you consider for Ms. A?
- benzodiazepine plus a tricyclic antidepressant (TCA)
- selective serotonin reuptake inhibitor (SSRI) plus a benzodiazepine
- trazodone plus bupropion
- atypical antipsychotic plus a benzodiazepine and a TCA
TREATMENT: Insufficient response
Ms. A’s previous psychiatrist prescribed various SSRIs and selective serotonin-norepinephrine reuptake inhibitors, including sertraline, escitalopram, citalopram, paroxetine, and venlafaxine, for depression and anxiety with little or no benefit. When she presented at our clinic, Ms. A was taking clonazepam, 0.25 mg as needed, and fluvoxamine, 50 mg/d, which she said helped her anxiety a little, but not depersonalization symptoms. She received supportive psychotherapy provided during biweekly 30-minute medication management visits.
We add aripiprazole, 2.5 mg/d, to augment fluvoxamine’s antidepressant effect and reduce her anxiety and dissociative symptoms. At the next visit 5 weeks later, she reports her depersonalization symptoms gradually lessened from 10 to 6 on a 10-point self-report scale.
We discontinue fluvoxamine after 5 weeks because it no longer significantly contributes to her recovery. We add amantadine, 100 mg/d, based on the belief that dopamine augmentation might help reduce her symptoms. Ms. A reports improved depersonalization symptoms over the next 4 weeks (5/10). However, a week later she says she feels her anxiety is worsening the depersonalization symptoms. We start buspirone, 7.5 mg/d titrated to 15 mg/d over 4 weeks, Ms. A reports feeling worse so we discontinue the drug.
Next Ms. A complains of excessive sleepiness, which seems to be related to amantadine, so we discontinue it. We start bupropion, 150 mg/d and titrate it to 450 mg/d, which we hope will reduce her fatigue, anxiety, depersonalization, and depression. Bupropion’s effect on norepinephrine and dopamine reuptake and a study of autonomic blunting in depersonalization9 justify our selection.
After 3 months, Ms. A stops taking aripiprazole because it is too costly. The following month she presents with severe anxiety and low-to-moderate depression. Clonazepam and bupropion are discontinued and replaced with diazepam, 20 mg/d, and clomipramine, 25 mg/d at bedtime titrated to 75 mg/d. Our decision is guided by a study on the efficacy of clomipramine in treating depersonalization10 and our desire to aggressively treat her anxiety and depression. After 2 weeks, Ms. A says her anxiety and depression have resolved completely but the depersonalization symptoms persist. We restart amantadine, 100 mg as needed, for anorgasmia.
Because of her persistent complaints of depersonalization, after discussion with Ms. A, we decide to return to what had helped her at the beginning of treatment and restart aripiprazole, 2.5 mg/d. Four months later, she reports her depersonalization symptoms have resolved completely. At this time, her regimen consists of clomipramine, 50 mg at bedtime, diazepam, 10 mg at bedtime, and aripiprazole, 2.5 mg/d.
Which neurotransmitter systems have been implicated in depersonalization disorder?
- HPA axis
- serotonin system
- norepinephrine-dopamine system
- dopamine-serotonin system
- all of the above
The authors’ observations
The neurobiology of emotion processing is still unclear but some evidence indicates that the amygdala, anterior cingulate cortex, and medial prefrontal cortex might be involved in emotion regulation and integration.
Depersonalization disorder is associated with HPA axis dysregulation and patients with depersonalization disorder have a lower basal cortisol level compared with patients with MDD.11,12 Simeon et al9 found a marked basal norepinephrine decline with increasing depersonalization severity.
Various SSRIs,13,14 TCAs,10,15,16 citalopram-olanzapine combination, naltrexone, citalopram-clonazepam combination,17 and fluoxetine-buspirone combination18 have been studied as treatment for depersonalization disorder. We present the first case report of aripiprazole to treat depersonalization disorder. A previous study19 of quetiapine—a low potency blocker of dopamine D2 receptors, which also has a high affinity for serotonin 5-HT2A receptors—suggested a potential role in improving emotional numbing symptoms in depersonalization/derealization disorder. The authors hypothesized that quetiapine may facilitate dopamine and serotonin neurotransmissions in the anterior limbic cortex and prefrontal cortex, which are involved in emotional experiences.
Other treatment options
The kappa opioid system also is implicated in depersonalization. Enadoline, a selective k-opioid agonist, has been shown to cause depersonalization symptoms in healthy subjects.20 High doses of opioid antagonists, such as naltrexone, have been used successfully to treat depersonalization symptoms in patients with borderline personality disorder,21 PTSD,22 and depersonalization disorder.23
Ketamine—which can produce depersonalization—increases glutamate transmission, which suggests that drugs that affect the glutamate system might be targets for future investigation. Similarly, smoking marijuana can induce depersonalization, which indicates that cannabinoid receptors might be another area for research. Hallucinogens, such as lysergic acid diethylamide, psilocybin, and dimethyltryptamine, can produce temporary depersonalization. These drugs are 5-HT2 agonists (HT2A, HT2C), which gives weight to using 5-HT2 antagonists to treat depersonalization.
Psychodynamic approaches based on self-constancy—cohesiveness and stability of self-representation—may be helpful, especially in patients with acute symptoms.24 Cognitive-behavioral therapy may be effective and could be divided into 2 phases:
Table 3
Depersonalization comorbidity: Common disorders
| Disorder | Percentage of depersonalization patients reporting comorbidity |
|---|---|
| Anxiety | 45% |
| Major depressive disorder | 41% |
| Panic disorder | 22% |
| Agoraphobia | 11% |
| Source: Reference 8 | |
- nonspecific interventions such as activity scheduling, graded exposure to avoidance behaviors, and negative automatic thought charts
- techniques to facilitate controlled re-experiencing of emotions and refocusing of attention away from the self and the depersonalization experience.25
Measures such as relaxation techniques, breathing exercises, yoga, tai chi, and meditation also might help decrease anxiety.
OUTCOME: Why did it work?
Ms. A responded partially to the diazepam-clomipramine combination but experienced a full response only after we added aripiprazole. We are not certain whether her response was caused by aripiprazole, a delayed action of clomipramine, or a spontaneous remission. Aripiprazole, 2.5 mg/d, was the first medication we added when Ms. A presented to our clinic and she had reported a partial response to the drug. Aripiprazole was also the last medication added before she experienced response, which lasted for at least 5 months, after which Ms. A was lost to follow-up.
The authors’ observations
We believe that aripiprazole might rebalance serotonin/dopamine neurotransmission for some patients with depersonalization disorder. We theorize that aripiprazole’s blockade of serotonin 2A receptors may enhance dopamine release in certain areas of the brain, possibly improving cognitive and affective symptoms. Depersonalization may be a symptom of worsening psychiatric illness and justifies the use of intensive pharmacologic and psychological therapy.
Related resource
- Simeon D. Feeling unreal: Depersonalization disorder and loss of self. New York, NY: Oxford University Press; 2006.
Drug brand names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bupropion • Wellbutrin
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clonazepam • Klonopin
- Diazepam • Valium
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Ketamine • Ketalar
- Naltrexone • ReVia
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Feeling detached
Ms. A, age 23, presents to our clinic complaining of feeling detached for the past 4 years. She says she feels “fuzzy all the time, like I lost touch with reality 4 years ago and really miss it.” She complains of “confused thinking,” excessive tiredness and weakness, depression, and anxiety. She says, “It feels like I’m watching my life on television; I don’t feel any emotions.” These symptoms began immediately after a college party, which the police stopped because of underage drinking. She says, “I don’t know why, but that party set it off, and it feels like I am in a dream all the time.”
For the last 4 years, Ms. A has been working as a waitress and is now engaged. She presents to our clinic because the treatments she has been receiving are ineffective and she wants to feel her emotions again, especially before her wedding.
Ms. A has no history of mania, depression, or psychosis. She says she was an anxious child and suffered from anorexia nervosa between age 13 and 14. She experienced occasional panic attacks beginning in high school that were triggered by feeling overwhelmed or frustrated with not feeling normal. During these panic attacks, Ms. A experienced tightness in her chest and dizziness. She denies suicidal or homicidal ideation or attempts.
At age 18, she was sexually assaulted. Ongoing stressors include living in a dangerous neighborhood, having her car broken into, her father’s disapproval of her fiancé, and wanting to get married. She drank heavily in college, but has used alcohol infrequently since then.
Ms. A’s father has a history of anxiety. She describes him as domineering and her mother as very emotional and always wanting to be her friend. Ms. A says she struggles with relationships, employment, and plans for advancement, all of which are moderately to severely affected by her depersonalization symptoms. During the initial appointment, we diagnose Ms. A with generalized anxiety disorder, panic disorder, and major depressive disorder (MDD).
Which diagnoses would you include among the differential diagnosis?
- posttraumatic stress disorder (PTSD)
- MDD with psychotic features
- depersonalization disorder
- schizophrenia, undifferentiated type
- psychosis not otherwise specified
The authors’ observations
Depersonalization symptoms can occur in a variety of situations, including:
- mentally healthy persons suffering from acute stressors, fatigue, or drug use
- neuropsychiatric conditions such as epilepsy
- migraine
- anxiety disorders
- depressive disorders
- schizophrenia.1
Transient depersonalization symptoms are common and have been found in 2.4% of the general population.2 Community surveys using standardized diagnostic interviews reveal 1-month prevalence rates of 1.6% to 1.9% in 2 UK samples.3,4 Depersonalization symptoms are brief and less debilitating than depersonalization disorder.
Depersonalization rarely presents as a primary disorder, when symptoms persist chronically. Rating scales (Table 1)5-7 and DSM-IV-TR criteria (Table 2) can help assess symptom severity and differentiate transient symptoms from a disorder. Psychiatric conditions that commonly are comorbid with depersonalization disorder appear in Table 3.8 Triggers for a first episode of depersonalization disorder include:
Table 1
Assessing for depersonalization: 3 rating scales
| Scale | Description |
|---|---|
| Cambridge Depersonalization Scale5 | 29-item, self-report questionnaire meant to capture frequency and duration of depersonalization symptoms over the previous 6 months |
| Depersonalization Severity Scale6 | Covers a range of axis I and II psychopathology |
| Dissociative Experiences Scale7 | 28-item, self-report instrument to measure dissociation |
- psychological stressors (31%)
- substance abuse (25%)
- physical stressor (12%)
- situational stressor (17%)
- social and/or relationship problems (10%)
- trauma (6%)
- panic/anxiety (2%).8
Although Ms. A experiences depersonalization—constant numbness and emptiness—when she thinks about the sexual assault, she does not meet criteria for PTSD because she denies re-experiencing the assault, hyperarousal, and avoidance behaviors.
Ms. A meets all 4 DSM-IV-TR criteria for depersonalization disorder (Table 2). She experiences persistent feelings of detachment, which cause her considerable distress. Her reality testing is intact and these experiences are not due to a general medical condition, another mental disorder, or direct physiological effects of a substance.
Table 2
DSM-IV-TR criteria for depersonalization disorder
| A. Persistent and recurrent experiences of feeling detached from oneself and as if one is an outside observer of one’s mental processes or body. B. During the depersonalization experience, reality testing remains intact. C. The depersonalization causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. D. The depersonalization experience does not occur exclusively during the course of another mental disorder, such as schizophrenia, panic disorder, acute stress disorder, or another dissociative disorder, and is not due to the direct physiological effects of a substance (eg, a drug of abuse or a medication) or a general medical condition (eg, temporal lobe epilepsy). |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text revision. Washington, DC: American Psychiatric Association; 2004 |
Which medications would you consider for Ms. A?
- benzodiazepine plus a tricyclic antidepressant (TCA)
- selective serotonin reuptake inhibitor (SSRI) plus a benzodiazepine
- trazodone plus bupropion
- atypical antipsychotic plus a benzodiazepine and a TCA
TREATMENT: Insufficient response
Ms. A’s previous psychiatrist prescribed various SSRIs and selective serotonin-norepinephrine reuptake inhibitors, including sertraline, escitalopram, citalopram, paroxetine, and venlafaxine, for depression and anxiety with little or no benefit. When she presented at our clinic, Ms. A was taking clonazepam, 0.25 mg as needed, and fluvoxamine, 50 mg/d, which she said helped her anxiety a little, but not depersonalization symptoms. She received supportive psychotherapy provided during biweekly 30-minute medication management visits.
We add aripiprazole, 2.5 mg/d, to augment fluvoxamine’s antidepressant effect and reduce her anxiety and dissociative symptoms. At the next visit 5 weeks later, she reports her depersonalization symptoms gradually lessened from 10 to 6 on a 10-point self-report scale.
We discontinue fluvoxamine after 5 weeks because it no longer significantly contributes to her recovery. We add amantadine, 100 mg/d, based on the belief that dopamine augmentation might help reduce her symptoms. Ms. A reports improved depersonalization symptoms over the next 4 weeks (5/10). However, a week later she says she feels her anxiety is worsening the depersonalization symptoms. We start buspirone, 7.5 mg/d titrated to 15 mg/d over 4 weeks, Ms. A reports feeling worse so we discontinue the drug.
Next Ms. A complains of excessive sleepiness, which seems to be related to amantadine, so we discontinue it. We start bupropion, 150 mg/d and titrate it to 450 mg/d, which we hope will reduce her fatigue, anxiety, depersonalization, and depression. Bupropion’s effect on norepinephrine and dopamine reuptake and a study of autonomic blunting in depersonalization9 justify our selection.
After 3 months, Ms. A stops taking aripiprazole because it is too costly. The following month she presents with severe anxiety and low-to-moderate depression. Clonazepam and bupropion are discontinued and replaced with diazepam, 20 mg/d, and clomipramine, 25 mg/d at bedtime titrated to 75 mg/d. Our decision is guided by a study on the efficacy of clomipramine in treating depersonalization10 and our desire to aggressively treat her anxiety and depression. After 2 weeks, Ms. A says her anxiety and depression have resolved completely but the depersonalization symptoms persist. We restart amantadine, 100 mg as needed, for anorgasmia.
Because of her persistent complaints of depersonalization, after discussion with Ms. A, we decide to return to what had helped her at the beginning of treatment and restart aripiprazole, 2.5 mg/d. Four months later, she reports her depersonalization symptoms have resolved completely. At this time, her regimen consists of clomipramine, 50 mg at bedtime, diazepam, 10 mg at bedtime, and aripiprazole, 2.5 mg/d.
Which neurotransmitter systems have been implicated in depersonalization disorder?
- HPA axis
- serotonin system
- norepinephrine-dopamine system
- dopamine-serotonin system
- all of the above
The authors’ observations
The neurobiology of emotion processing is still unclear but some evidence indicates that the amygdala, anterior cingulate cortex, and medial prefrontal cortex might be involved in emotion regulation and integration.
Depersonalization disorder is associated with HPA axis dysregulation and patients with depersonalization disorder have a lower basal cortisol level compared with patients with MDD.11,12 Simeon et al9 found a marked basal norepinephrine decline with increasing depersonalization severity.
Various SSRIs,13,14 TCAs,10,15,16 citalopram-olanzapine combination, naltrexone, citalopram-clonazepam combination,17 and fluoxetine-buspirone combination18 have been studied as treatment for depersonalization disorder. We present the first case report of aripiprazole to treat depersonalization disorder. A previous study19 of quetiapine—a low potency blocker of dopamine D2 receptors, which also has a high affinity for serotonin 5-HT2A receptors—suggested a potential role in improving emotional numbing symptoms in depersonalization/derealization disorder. The authors hypothesized that quetiapine may facilitate dopamine and serotonin neurotransmissions in the anterior limbic cortex and prefrontal cortex, which are involved in emotional experiences.
Other treatment options
The kappa opioid system also is implicated in depersonalization. Enadoline, a selective k-opioid agonist, has been shown to cause depersonalization symptoms in healthy subjects.20 High doses of opioid antagonists, such as naltrexone, have been used successfully to treat depersonalization symptoms in patients with borderline personality disorder,21 PTSD,22 and depersonalization disorder.23
Ketamine—which can produce depersonalization—increases glutamate transmission, which suggests that drugs that affect the glutamate system might be targets for future investigation. Similarly, smoking marijuana can induce depersonalization, which indicates that cannabinoid receptors might be another area for research. Hallucinogens, such as lysergic acid diethylamide, psilocybin, and dimethyltryptamine, can produce temporary depersonalization. These drugs are 5-HT2 agonists (HT2A, HT2C), which gives weight to using 5-HT2 antagonists to treat depersonalization.
Psychodynamic approaches based on self-constancy—cohesiveness and stability of self-representation—may be helpful, especially in patients with acute symptoms.24 Cognitive-behavioral therapy may be effective and could be divided into 2 phases:
Table 3
Depersonalization comorbidity: Common disorders
| Disorder | Percentage of depersonalization patients reporting comorbidity |
|---|---|
| Anxiety | 45% |
| Major depressive disorder | 41% |
| Panic disorder | 22% |
| Agoraphobia | 11% |
| Source: Reference 8 | |
- nonspecific interventions such as activity scheduling, graded exposure to avoidance behaviors, and negative automatic thought charts
- techniques to facilitate controlled re-experiencing of emotions and refocusing of attention away from the self and the depersonalization experience.25
Measures such as relaxation techniques, breathing exercises, yoga, tai chi, and meditation also might help decrease anxiety.
OUTCOME: Why did it work?
Ms. A responded partially to the diazepam-clomipramine combination but experienced a full response only after we added aripiprazole. We are not certain whether her response was caused by aripiprazole, a delayed action of clomipramine, or a spontaneous remission. Aripiprazole, 2.5 mg/d, was the first medication we added when Ms. A presented to our clinic and she had reported a partial response to the drug. Aripiprazole was also the last medication added before she experienced response, which lasted for at least 5 months, after which Ms. A was lost to follow-up.
The authors’ observations
We believe that aripiprazole might rebalance serotonin/dopamine neurotransmission for some patients with depersonalization disorder. We theorize that aripiprazole’s blockade of serotonin 2A receptors may enhance dopamine release in certain areas of the brain, possibly improving cognitive and affective symptoms. Depersonalization may be a symptom of worsening psychiatric illness and justifies the use of intensive pharmacologic and psychological therapy.
Related resource
- Simeon D. Feeling unreal: Depersonalization disorder and loss of self. New York, NY: Oxford University Press; 2006.
Drug brand names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bupropion • Wellbutrin
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clonazepam • Klonopin
- Diazepam • Valium
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Ketamine • Ketalar
- Naltrexone • ReVia
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Trazodone • Desyrel
- Venlafaxine • Effexor
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Simeon D. Depersonalisation disorder: a contemporary overview. CNS Drugs. 2004;18(6):343-354.
2. Ross CA, Joshi S, Currie R. Dissociative experiences in the general population: a factor analysis. Hosp Community Psychiatry. 1991;42:297-301.
3. Bebbington PE, Hurry J, Tennant C, et al. Epidemiology of mental disorders in Camberwell. Psychol Med. 1981;11(3):561-579.
4. Bebbington PE, Marsden L, Brewin CR. The need for psychiatric treatment in the general population: the Camberwell needs for care survey. Psychol Med. 1997;27(4):821-834.
5. Sierra M, Berrios GE. The Cambridge Depersonalization Scale: a new instrument for the measurement of depersonalization. Psychiatry Res. 2000;93(2):153-164.
6. Simeon D, Guralnik O, Schmeidler J. Development of a depersonalization severity scale. J Trauma Stress. 2001;14(2):341-349.
7. Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis. 1986;174(12):727-735.
8. Baker D, Earle M, Medford N, et al. Illness perceptions in depersonalization disorder: testing an illness attribution model. Clin Psychol Psychother. 2007;14(2):105-116.
9. Simeon D, Guralnik O, Knutelska M, et al. Basal norepinephrine in depersonalization disorder. Psychiatry Res. 2003;121(1):93-97.
10. Simeon D, Stein DJ, Hollander E. Treatment of depersonalization disorder with clomipramine. Biol Psychiatry. 1998;44(4):302-303.
11. Simeon D, Guralnik O, Knutelska M, et al. Hypothalamic-pituitary-adrenal axis dysregulation in depersonalization disorder. Neuropsychopharmacology. 2001;25(45):793-795.
12. Stanton BR, David AS, Cleare AJ, et al. Basal activity of the hypothalamic-pituitary-adrenal axis in patients with depersonalization disorder. Psychiatry Res. 2001;104(1):85-89.
13. Fichtner CG, Horevitz RP, Braun BG. Fluoxetine in depersonalization disorder. Am J Psychiatry. 1992;149(12):1750-1751.
14. Hollander E, Liebowitz MR, DeCaria C, et al. Treatment of depersonalization with serotonin reuptake blockers. J Clin Psychopharmacol. 1990;10(3):200-203.
15. Noyes R, Jr, Kuperman S, Olson SB. Desipramine: a possible treatment for depersonalization disorder. Can J Psychiatry. 1987;32(9):782-784.
16. Simeon D, Stein DJ, Hollander E. Treatment of depersonalization disorder with clomipramine. Biol Psychiatry. 1998;44(4):302-303.
17. Sachdev P. Citalopram-clonazepam combination for primary depersonalization disorder: a case report. Aust N Z J Psychiatry. 2002;36(3):424-425.
18. Abbas S, Chandra PS, Srivastava M. The use of fluoxetine and buspirone for treatment-refractory depersonalization disorder. J Clin Psychiatry. 1995;56(10):484.-
19. Mancini-Marie A, Fahim C, Potvin S, et al. Quetiapine: focus on emotional numbing in depersonalization disorder: an fMRI case report. Eur Psychiatry. 2006;21(8):574-577.
20. Walsh SL, Geter-Douglas B, Strain EC, et al. Enadoline and butorphanol: evaluation of kappa-agonists on cocaine pharmacodynamics and cocaine self-administration in humans. J Pharmacol Exp Ther. 2001;299(1):147-158.
21. Bohus MJ, Landwehrmeyer B, Stiglmayr CE, et al. Naltrexone in the treatment of dissociative symptoms in patients with borderline personality disorder: a open label trial. J Clin Psychiatry. 1999;60(9):598-603.
22. Glover H. A preliminary trial of nalmefene for the treatment of emotional numbing in combat veterans with posttraumatic stress disorder. Isr J Psychiatry Relat Sci. 1993;30(4):255-263.
23. Nuller YL, Morozova MG, Kushnir ON, et al. Effect of naloxone therapy on depersonalization: a pilot study. J Psychopharmacol. 2001;15(2):93-95.
24. Frances A, Sacks M, Aronoff S. Depersonalization: a self-relations perspective. Int J Psychanal. 1977;58:325-331.
25. Hunter ECM, Phillips ML, Chalder T, et al. Depersonalization disorder: a cognitive-behavioural conceptualization. Behav Res Ther. 2003;41(12):1451-1467.
1. Simeon D. Depersonalisation disorder: a contemporary overview. CNS Drugs. 2004;18(6):343-354.
2. Ross CA, Joshi S, Currie R. Dissociative experiences in the general population: a factor analysis. Hosp Community Psychiatry. 1991;42:297-301.
3. Bebbington PE, Hurry J, Tennant C, et al. Epidemiology of mental disorders in Camberwell. Psychol Med. 1981;11(3):561-579.
4. Bebbington PE, Marsden L, Brewin CR. The need for psychiatric treatment in the general population: the Camberwell needs for care survey. Psychol Med. 1997;27(4):821-834.
5. Sierra M, Berrios GE. The Cambridge Depersonalization Scale: a new instrument for the measurement of depersonalization. Psychiatry Res. 2000;93(2):153-164.
6. Simeon D, Guralnik O, Schmeidler J. Development of a depersonalization severity scale. J Trauma Stress. 2001;14(2):341-349.
7. Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis. 1986;174(12):727-735.
8. Baker D, Earle M, Medford N, et al. Illness perceptions in depersonalization disorder: testing an illness attribution model. Clin Psychol Psychother. 2007;14(2):105-116.
9. Simeon D, Guralnik O, Knutelska M, et al. Basal norepinephrine in depersonalization disorder. Psychiatry Res. 2003;121(1):93-97.
10. Simeon D, Stein DJ, Hollander E. Treatment of depersonalization disorder with clomipramine. Biol Psychiatry. 1998;44(4):302-303.
11. Simeon D, Guralnik O, Knutelska M, et al. Hypothalamic-pituitary-adrenal axis dysregulation in depersonalization disorder. Neuropsychopharmacology. 2001;25(45):793-795.
12. Stanton BR, David AS, Cleare AJ, et al. Basal activity of the hypothalamic-pituitary-adrenal axis in patients with depersonalization disorder. Psychiatry Res. 2001;104(1):85-89.
13. Fichtner CG, Horevitz RP, Braun BG. Fluoxetine in depersonalization disorder. Am J Psychiatry. 1992;149(12):1750-1751.
14. Hollander E, Liebowitz MR, DeCaria C, et al. Treatment of depersonalization with serotonin reuptake blockers. J Clin Psychopharmacol. 1990;10(3):200-203.
15. Noyes R, Jr, Kuperman S, Olson SB. Desipramine: a possible treatment for depersonalization disorder. Can J Psychiatry. 1987;32(9):782-784.
16. Simeon D, Stein DJ, Hollander E. Treatment of depersonalization disorder with clomipramine. Biol Psychiatry. 1998;44(4):302-303.
17. Sachdev P. Citalopram-clonazepam combination for primary depersonalization disorder: a case report. Aust N Z J Psychiatry. 2002;36(3):424-425.
18. Abbas S, Chandra PS, Srivastava M. The use of fluoxetine and buspirone for treatment-refractory depersonalization disorder. J Clin Psychiatry. 1995;56(10):484.-
19. Mancini-Marie A, Fahim C, Potvin S, et al. Quetiapine: focus on emotional numbing in depersonalization disorder: an fMRI case report. Eur Psychiatry. 2006;21(8):574-577.
20. Walsh SL, Geter-Douglas B, Strain EC, et al. Enadoline and butorphanol: evaluation of kappa-agonists on cocaine pharmacodynamics and cocaine self-administration in humans. J Pharmacol Exp Ther. 2001;299(1):147-158.
21. Bohus MJ, Landwehrmeyer B, Stiglmayr CE, et al. Naltrexone in the treatment of dissociative symptoms in patients with borderline personality disorder: a open label trial. J Clin Psychiatry. 1999;60(9):598-603.
22. Glover H. A preliminary trial of nalmefene for the treatment of emotional numbing in combat veterans with posttraumatic stress disorder. Isr J Psychiatry Relat Sci. 1993;30(4):255-263.
23. Nuller YL, Morozova MG, Kushnir ON, et al. Effect of naloxone therapy on depersonalization: a pilot study. J Psychopharmacol. 2001;15(2):93-95.
24. Frances A, Sacks M, Aronoff S. Depersonalization: a self-relations perspective. Int J Psychanal. 1977;58:325-331.
25. Hunter ECM, Phillips ML, Chalder T, et al. Depersonalization disorder: a cognitive-behavioural conceptualization. Behav Res Ther. 2003;41(12):1451-1467.
Did brain trauma lead to crime?
CASE: Self-reported TBI
When charged with raping a 19-year-old woman, Mr. P, age 32, pleads not guilty by reason of insanity (NGRI). He has a self-reported history of traumatic brain injury (TBI) and claims that since suffering a blow to the head 8 years before the rape, he has experienced episodes of personality changes, psychosis, and violent behavior. Mr. P is adamant that any wrongdoing on his part was beyond his control, and he argues that consequences of the brain injury, such as hallucinations and aggressive behavior, had recently emerged. The court asks that a forensic psychiatrist evaluate Mr. P.
An only child, Mr. P was raised by his mother in an inner city area. His father was dependent on alcohol and cocaine and abandoned the family shortly after Mr. P’s birth. Mr. P abuses alcohol, as evidenced by previous driving under the influence charges, but denies illicit drug use. He graduated from high school with average grades and denies a history of disciplinary action at school or home. Although Mr. P was charged with misdemeanors in his late teens, the sexual assault is his first felony charge. Mr. P describes himself as a “charmer.”
After high school, Mr. P worked full-time in construction, where he claims he suffered a traumatic blow to the head. Despite this injury, he continued to work and socialize and never sought treatment at a mental health clinic.
The authors’ observations
Although defendants may legitimately suffer from TBI and resultant complications, many individuals capitalize on a history of minor head injury to support their NGRI defense.1 Forensic psychiatrists must retain a healthy degree of clinical suspicion for malingering in defendants who claim NGRI as a result of complications from brain injury, especially when the injury and complications are not documented and simply patient-reported.
TBI is a CNS injury that occurs when an outside force traumatically injures the brain and can cause a variety of physical, cognitive, emotional, and behavioral effects ( Table 1 ).2 Cognitive deficits include:
- impaired attention
- disrupted insight
- poor judgment
- thought disorders.
Reduced processing speed, distractibility, and deficits in executive functions such as abstract reasoning, planning, problem solving, and multitasking have been documented. Memory loss—the most common cognitive impairment among head-injured people—occurs in 20% to 79% of people with closed head trauma, depending on injury severity.3 People who have suffered TBI may have difficulty understanding or producing spoken or written language, or with more subtle aspects of communication, such as body language.
TBI may cause emotional or behavioral problems and personality changes. Mood and affect changes are common. TBI predisposes patients to obsessive-compulsive disorder, substance abuse, dysthymia, clinical depression, bipolar disorder, phobias, panic disorder, and schizophrenia.4 Frontal lobe injuries have been correlated with disinhibition and inappropriate or childish behavior, and temporal lobe injuries with irritability and aggression.5
Table 1
TBI symptoms correspond to area of injury
| Area of injury | Motor/sensory | Psychiatric/behavioral | Cognitive |
|---|---|---|---|
| Brain stem | Decreased vital capacity in breathing, dysphagia | Sleep difficulties | Inability to categorize objects, difficulty with organization |
| Frontal lobe | Aphasia, praxis | Disinhibition, personality changes | Impaired executive function |
| Cerebellum | Nystagmus, tremor | Labile emotions | Inability to process information |
| Parietal lobe | Apraxia | Personality changes | Neglect |
| Occipital lobe | Visual field cuts; diminished proprioception | Visual hallucinations | Color agnosia; inability to recognize words; difficulty reading, writing, and recognizing drawn objects |
| Temporal lobe | Seizure | Libido changes, humorless verbosity, aggression, olfactory perceptual changes | Prosopagnosia, aphasia, agnosia, memory loss, inattention |
| TBI: traumatic brain injury | |||
| Source: Reference 2 | |||
TBI and the insanity defense
The M’Naghten Rule of 1843 requires that for an insanity defense, the defendant must have a mental disease or defect that causes him not to know the nature and quality or the wrongfulness of his act.6 TBI is an abnormal condition of the mind leading to a mental disease that can substantially affect control of emotions and behaviors.
Nevertheless, TBI-induced criminality remains controversial.7 Theories on the etiology of impulse dyscontrol resulting from TBI have suggested structural damage to the brain and altered neurotransmitters. In TBI, the amygdala—which is located within the anterior temporal lobe and adjoins emotions to thoughts—often is injured. Damage to this structure leads to poor impulse control and violent behavior. Damage to specific neurotransmitter systems that causes elevated norepinephrine and dopamine levels and reduced serotonin levels have also been implicated as a cause of impulse dyscontrol in TBI patients.8
In theory, TBI patients potentially could have enough cognitive impairment to have a substantial lack of appreciation of the criminality or wrongfulness of an act. TBI-related impulsivity and cognitive impairment can lead to recklessness and negligence.9 The U.S. Supreme Court has acknowledged that CNS dysfunction affects judgment, reality testing, and self-control.10
EVALUATION: Vague answers
To determine whether Mr. P’s defense is plausible, the forensic psychiatrist must pay attention to the details of the patient’s presentation and history. During the interview, Mr. P quickly shifts from cooperative to obstinate and restricted. He ruminates on the head injury causing him to suffer auditory hallucinations, which he claims he always obeys. Mr. P refuses to provide details of the hallucinations, however, and answers most questions about the head injury or his defense with vague answers, including “I don’t know.”
Because of Mr. P’s reluctance to share information, his lack of psychiatric symptoms other than those he self-reports, and the presence of potential secondary gain from an NGRI defense, the psychiatrist begins to suspect malingering.
The authors’ observations
Malingering is a condition—not a diagnosis—characterized by intentional production of false or grossly exaggerated physical or psychological symptoms motivated by external incentives.11 The presence of external incentives distinguishes malingering from psychiatric illnesses such as factitious and somatoform disorders, in which there is no apparent external incentive. Malingering of psychiatric symptoms occurs in up to 20% of forensic patients, 5% of military recruits, and 1% of mental health patients.5 Stimuli for malingering range from seeking food and shelter to avoiding criminal responsibility ( Table 2 ). Malingering is more common in individuals being evaluated for criminal responsibility than for competence to stand trial. The 3 categories of malingering are:
Table 2
Common external incentives for malingering
| Evading criminal responsibility |
| Disability claims/financial gain |
| Avoiding military duty |
| Evading work |
| Obtaining drugs |
| Seeking food/shelter |
- pure malingering—feigning a nonexistent disorder
- partial malingering—consciously exaggerating real symptoms
- false imputation—ascribing real symptoms to a cause the individual knows is unrelated to the symptoms.12
Determining if a defendant with a history of TBI is malingering requires a multi-step approach that encompasses the clinical interview, a thorough review of collateral data, and focused psychological testing. In interviews, psychiatrists detect approximately 50% of lies, which is no better than would be discovered by chance.13 If you suspect a patient is malingering, combine a structured clinical interview with collateral sources such as old hospital records, treatment history, insurance records, police reports, and interviews with close family and friends.
TBI patients’ poor cognition, memory deficits, and inattention will prove challenging. Malingering patients who attempt to capitalize on a pre-existing TBI to evade responsibility for a current criminal charge may grossly exaggerate or even fake intellectual deficits. Be patient with such defendants and remain aware that such people will give vague or hedging answers to straightforward questions, often accompanied by “I don’t know.” Prolonging the interview may be helpful because it may fatigue a defendant who is faking.12
Some patients who malinger after sustaining a TBI will attempt to feign psychotic symptoms. Table 3 14 illustrates criteria for assessing a patient suspected of malingering psychosis and Table 4 14 highlights atypical psychotic symptoms that suggest feigning illness. Malingering of psychosis can be both assessed in the interview and through testing.
Table 3
Criteria for malingered psychosis
| A. Understandable motive to malinger |
| B. Marked variability of presentation as evidenced by ≥1 of the following: 1. Marked discrepancies in interview and non-interview behaviors 2. Gross inconsistencies in reported psychotic symptoms 3. Blatant contradictions between reported prior episodes and documented psychiatric history |
| C. Improbable psychiatric symptoms as evidenced by ≥1 of the following: 1. Reporting elaborate psychotic symptoms that lack common paranoid, grandiose, or religious themes 2. Sudden emergence of purported symptoms to explain antisocial behavior 3. Atypical hallucinations and delusions |
| D. Confirmation of malingering by either: 1. Admission of malingering following confrontation, or 2. Presence of strong corroborative information, such as psychometric data or history of malingering |
| Source: Reference 14 |
Table 4
Atypical psychotic symptoms that suggest malingering
| Hallucinations |
| Continuous rather than intermittent |
| Vague or inaudible auditory hallucinations |
| Stilted language reported in hallucinations |
| Inability to state strategies to diminish voices |
| Self-report that all command hallucinations were obeyed |
| Visual hallucinations in black and white |
| Delusions |
| Abrupt onset or termination |
| Eagerness to call attention to delusions |
| Conduct markedly inconsistent with delusions |
| Bizarre content without disordered thinking |
| Source: Reference 14 |
Psychological testing
Several standardized diagnostic instruments can be used to help determine whether a patient is feigning or exaggerating psychotic symptoms or cognitive impairments ( Table 5 ). Testing for a patient such as Mr. P—who attributes any criminal wrongdoing to psychosis and also cites limited cognition as a reason for trouble in the interview—would include personality tests, tests to assess exaggerations of psychosis, and cognitive tests.
In the forensic setting, the preferred personality test is the MMPI-2.15 It consists of 567 items, with 10 clinical scales and several validity scales. The F scale, “faking good” or “faking bad,” detects people who are answering questions with the goal of appearing better or worse than they actually are. The Personal Assessment Inventory (PAI)16 is a 344-item test with a 4-point response format. The 22 scales cover a range of important axis I and II psychopathology.
SIRS17 is the gold standard in detecting malingered psychiatric illness; it includes questions about rare symptoms and uncommon symptom pairing. M-FAST18 was developed to provide a brief, reliable screen for malingered mental illness. It has shown good validity and high correlation with the SIRS and MMPI-2.
Tests of exaggerated cognitive impairment are extremely important in evaluating patients who claim to suffer from complications following TBI. TOMM19 —a 50-item recognition test designed to discriminate between true memory-impaired patients and malingerers—is the most studied and valid of such tests. Defendants’ scores that meet the recommended criteria for detecting malingering—≥5 errors on the retention trial—were found to also report a history of head injury.1
Although not as well validated, the Portland Digit Recognition Test (PDRT)20 is an alternative to the TOMM. This test is a forced-choice measure of recognition designed for assessing the possibility of malingering in individuals claiming mental illness because of head injury. The Victoria Symptoms Validity Test (VSVT)21 is used in outpatient and inpatient settings and also uses a forced-choice model to assess possible exaggeration or feigning of cognitive impairments. Finally, the Word Memory Test (WMT)22 is a neuropsychological assessment that evaluates the effort participants put forth.
Table 5
Standardized diagnostic instruments for detecting malingering
| Test | Clinical use |
|---|---|
| Personality | |
| MMPI-2 | F scale detects lying. Several validity scales |
| PAI | Covers a range of axis I and II psychopathology |
| Psychotic symptoms | |
| SIRS | Gold standard in detecting exaggerated psychotic symptoms |
| M-FAST | Screening tool to assess exaggerated psychosis; brief and reliable |
| Cognitive impairment | |
| TOMM | Highest validity of all tools to test memory malingering |
| PDRT | Assesses the possibility of malingering. Not widely studied and validity/reliability are suspect |
| VSVT | Useful for inpatient and outpatient settings |
| WMT | Evaluates effort put forth by the participant |
| M-FAST: Miller Forensic Assessment of Symptoms Test; MMPI-2: Minnesota Multiphasic Personality Inventory; PAI: Personal Assessment Inventory; PDRT: Portland Digit Recognition Test; SIRS: Structured Interview of Reported Symptoms; TOMM: Test of Memory Malingering; VSVT: Victoria Symptoms Validity Test; WMT: Word Memory Test | |
OUTCOME: Unsupported claims
Mr. P’s hospital records reveal a very minor head trauma that resulted in no structural brain abnormalities on imaging tests. Collateral interviews with Mr. P’s family and close friends fail to support the defendant’s claim that after the accident he began to experience behavioral changes and periods of psychosis. Mr. P’s SIRS and TOMM scores indicate malingering, and the psychiatrist did not support his NGRI defense.
Related resource
- Williamson DJ. Neurocognitive impairment: feigned, exaggerated, or real? Current Psychiatry. 2007;6(8):19-37.
Disclosure
Dr. Nasrallah receives research grant/research support from Forest Pharmaceuticals, GlaxoSmithKline, Janssen, Otsuka America Pharmaceuticals, Pfizer Inc., Roche, sanofi-aventis, and Shire, is on the advisory board of Abbott Laboratories, AstraZeneca, Janssen, Novartis, Pfizer Inc., and Merck, and is on the speakers’ bureau for Abbott Laboratories, AstraZeneca, Janssen, Novartis, Pfizer Inc., and Merck.
Dr. Farrell reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Delain SL, Stafford KP, Yosef SB. Use of the TOMM in a criminal court forensic assessment setting. Assessment. 2003;10(4):370-381.
2. Rao V, Lyketsos C. Neuropsychiatric sequelae of traumatic brain injury Psychosomatics. 2000;41:95-103.
3. Hall RC, Hall RC, Chapman MJ. Definition, diagnosis, and forensic implications of postconcussional syndrome. Psychosomatics. 2005;46(3):195-202.
4. Arlinghaus KA, Shoaib AM, Price TRP. Neuropsychiatric assessment. In: Silver JM, McAllister TW, Yudofsky SC. Textbook of traumatic brain injury. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:63-65.
5. West S, Noffsinger S. Is this patient not guilty by reason of insanity? Current Psychiatry. 2005;5(8):54-62.
6. Barzman D, Kennedy J, Fozdar M. Does traumatic brain injury cause violence? Current Psychiatry. 2002;1(4):49-55.
7. Silver JM, Yudofsky SC, Hales RE. Neuropsychiatry of traumatic brain injury. Washington, DC: American Psychiatric Press, Inc.; 1994.
8. Melton GB, Petrila J, Poythress NG, et al. Psychological evaluations for the courts. New York, NY: The Guilford Press; 1997.
9. Lewis DO, Pincus JH, Feldman M, et al. Psychiatric, neurological, and psychoeducational characteristics of 15 death row inmates in the United States. Am J Psychiatry. 1986;143:838-845.
10. Diagnostic and statistical manual of mental disorders, 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
11. Sadock VA. Kaplan and Sadock’s synopsis of psychiatry. Philadelphia, PA: Lippincott, Williams, and Wilkins; 2007:887.
12. Resnick PJ. Faking it: how to determine malingered psychosis. Current Psychiatry. 2005;4(11):12-25.
13. Samuel RZ, Mittenberg W. Determination of malingering in disability claims. Primary Psychiatry. 2005;12(12):60-68.
14. Resnick PJ. Malingered psychosis. In: Rogers R, ed. Clinical assessment of malingering. 2nd ed. New York, NY: The Guilford Press; 1997:47-67.
15. Hathaway SR, McKinley JC. The Minnesota Multiphasic Personality Inventory-2. Minneapolis, MN: University of Minnesota Press; 1989.
16. Rogers R, Sewell KW, Morey LC, et al. Detection of feigned mental disorder on the personality assessment inventory: a discriminate analysis. J Pers Assess. 1996;67:629-640.
17. Rogers R, Bagby RM, Dickens SE. Structured Interview of Reported Symptoms (SIRS). Lutz, FL: Psychological Assessment Resources; 1992.
18. Miller H. Miller Forensic Assessment of Symptoms Test (M-FAST). Professional Manual. Lutz, FL: Psychological Assessment Resources; 2001.
19. Tombaugh TN. The Test of Memory Malingering. Toronto, ON, Canada: Multi-Health Systems; 1996.
20. Binder LM. Malingering following minor head trauma. Clin Neuropsychol. 1990;4:25-36.
21. Slick D, Hopp G, Strauss E, et al. Victoria Symptom Validity Test professional manual. Lutz, FL: Psychological Assessment Resources; 1997.
22. Green P. Word Memory Test. Edmonton, Alberta, Canada: Green’s Publishing; 2003.
CASE: Self-reported TBI
When charged with raping a 19-year-old woman, Mr. P, age 32, pleads not guilty by reason of insanity (NGRI). He has a self-reported history of traumatic brain injury (TBI) and claims that since suffering a blow to the head 8 years before the rape, he has experienced episodes of personality changes, psychosis, and violent behavior. Mr. P is adamant that any wrongdoing on his part was beyond his control, and he argues that consequences of the brain injury, such as hallucinations and aggressive behavior, had recently emerged. The court asks that a forensic psychiatrist evaluate Mr. P.
An only child, Mr. P was raised by his mother in an inner city area. His father was dependent on alcohol and cocaine and abandoned the family shortly after Mr. P’s birth. Mr. P abuses alcohol, as evidenced by previous driving under the influence charges, but denies illicit drug use. He graduated from high school with average grades and denies a history of disciplinary action at school or home. Although Mr. P was charged with misdemeanors in his late teens, the sexual assault is his first felony charge. Mr. P describes himself as a “charmer.”
After high school, Mr. P worked full-time in construction, where he claims he suffered a traumatic blow to the head. Despite this injury, he continued to work and socialize and never sought treatment at a mental health clinic.
The authors’ observations
Although defendants may legitimately suffer from TBI and resultant complications, many individuals capitalize on a history of minor head injury to support their NGRI defense.1 Forensic psychiatrists must retain a healthy degree of clinical suspicion for malingering in defendants who claim NGRI as a result of complications from brain injury, especially when the injury and complications are not documented and simply patient-reported.
TBI is a CNS injury that occurs when an outside force traumatically injures the brain and can cause a variety of physical, cognitive, emotional, and behavioral effects ( Table 1 ).2 Cognitive deficits include:
- impaired attention
- disrupted insight
- poor judgment
- thought disorders.
Reduced processing speed, distractibility, and deficits in executive functions such as abstract reasoning, planning, problem solving, and multitasking have been documented. Memory loss—the most common cognitive impairment among head-injured people—occurs in 20% to 79% of people with closed head trauma, depending on injury severity.3 People who have suffered TBI may have difficulty understanding or producing spoken or written language, or with more subtle aspects of communication, such as body language.
TBI may cause emotional or behavioral problems and personality changes. Mood and affect changes are common. TBI predisposes patients to obsessive-compulsive disorder, substance abuse, dysthymia, clinical depression, bipolar disorder, phobias, panic disorder, and schizophrenia.4 Frontal lobe injuries have been correlated with disinhibition and inappropriate or childish behavior, and temporal lobe injuries with irritability and aggression.5
Table 1
TBI symptoms correspond to area of injury
| Area of injury | Motor/sensory | Psychiatric/behavioral | Cognitive |
|---|---|---|---|
| Brain stem | Decreased vital capacity in breathing, dysphagia | Sleep difficulties | Inability to categorize objects, difficulty with organization |
| Frontal lobe | Aphasia, praxis | Disinhibition, personality changes | Impaired executive function |
| Cerebellum | Nystagmus, tremor | Labile emotions | Inability to process information |
| Parietal lobe | Apraxia | Personality changes | Neglect |
| Occipital lobe | Visual field cuts; diminished proprioception | Visual hallucinations | Color agnosia; inability to recognize words; difficulty reading, writing, and recognizing drawn objects |
| Temporal lobe | Seizure | Libido changes, humorless verbosity, aggression, olfactory perceptual changes | Prosopagnosia, aphasia, agnosia, memory loss, inattention |
| TBI: traumatic brain injury | |||
| Source: Reference 2 | |||
TBI and the insanity defense
The M’Naghten Rule of 1843 requires that for an insanity defense, the defendant must have a mental disease or defect that causes him not to know the nature and quality or the wrongfulness of his act.6 TBI is an abnormal condition of the mind leading to a mental disease that can substantially affect control of emotions and behaviors.
Nevertheless, TBI-induced criminality remains controversial.7 Theories on the etiology of impulse dyscontrol resulting from TBI have suggested structural damage to the brain and altered neurotransmitters. In TBI, the amygdala—which is located within the anterior temporal lobe and adjoins emotions to thoughts—often is injured. Damage to this structure leads to poor impulse control and violent behavior. Damage to specific neurotransmitter systems that causes elevated norepinephrine and dopamine levels and reduced serotonin levels have also been implicated as a cause of impulse dyscontrol in TBI patients.8
In theory, TBI patients potentially could have enough cognitive impairment to have a substantial lack of appreciation of the criminality or wrongfulness of an act. TBI-related impulsivity and cognitive impairment can lead to recklessness and negligence.9 The U.S. Supreme Court has acknowledged that CNS dysfunction affects judgment, reality testing, and self-control.10
EVALUATION: Vague answers
To determine whether Mr. P’s defense is plausible, the forensic psychiatrist must pay attention to the details of the patient’s presentation and history. During the interview, Mr. P quickly shifts from cooperative to obstinate and restricted. He ruminates on the head injury causing him to suffer auditory hallucinations, which he claims he always obeys. Mr. P refuses to provide details of the hallucinations, however, and answers most questions about the head injury or his defense with vague answers, including “I don’t know.”
Because of Mr. P’s reluctance to share information, his lack of psychiatric symptoms other than those he self-reports, and the presence of potential secondary gain from an NGRI defense, the psychiatrist begins to suspect malingering.
The authors’ observations
Malingering is a condition—not a diagnosis—characterized by intentional production of false or grossly exaggerated physical or psychological symptoms motivated by external incentives.11 The presence of external incentives distinguishes malingering from psychiatric illnesses such as factitious and somatoform disorders, in which there is no apparent external incentive. Malingering of psychiatric symptoms occurs in up to 20% of forensic patients, 5% of military recruits, and 1% of mental health patients.5 Stimuli for malingering range from seeking food and shelter to avoiding criminal responsibility ( Table 2 ). Malingering is more common in individuals being evaluated for criminal responsibility than for competence to stand trial. The 3 categories of malingering are:
Table 2
Common external incentives for malingering
| Evading criminal responsibility |
| Disability claims/financial gain |
| Avoiding military duty |
| Evading work |
| Obtaining drugs |
| Seeking food/shelter |
- pure malingering—feigning a nonexistent disorder
- partial malingering—consciously exaggerating real symptoms
- false imputation—ascribing real symptoms to a cause the individual knows is unrelated to the symptoms.12
Determining if a defendant with a history of TBI is malingering requires a multi-step approach that encompasses the clinical interview, a thorough review of collateral data, and focused psychological testing. In interviews, psychiatrists detect approximately 50% of lies, which is no better than would be discovered by chance.13 If you suspect a patient is malingering, combine a structured clinical interview with collateral sources such as old hospital records, treatment history, insurance records, police reports, and interviews with close family and friends.
TBI patients’ poor cognition, memory deficits, and inattention will prove challenging. Malingering patients who attempt to capitalize on a pre-existing TBI to evade responsibility for a current criminal charge may grossly exaggerate or even fake intellectual deficits. Be patient with such defendants and remain aware that such people will give vague or hedging answers to straightforward questions, often accompanied by “I don’t know.” Prolonging the interview may be helpful because it may fatigue a defendant who is faking.12
Some patients who malinger after sustaining a TBI will attempt to feign psychotic symptoms. Table 3 14 illustrates criteria for assessing a patient suspected of malingering psychosis and Table 4 14 highlights atypical psychotic symptoms that suggest feigning illness. Malingering of psychosis can be both assessed in the interview and through testing.
Table 3
Criteria for malingered psychosis
| A. Understandable motive to malinger |
| B. Marked variability of presentation as evidenced by ≥1 of the following: 1. Marked discrepancies in interview and non-interview behaviors 2. Gross inconsistencies in reported psychotic symptoms 3. Blatant contradictions between reported prior episodes and documented psychiatric history |
| C. Improbable psychiatric symptoms as evidenced by ≥1 of the following: 1. Reporting elaborate psychotic symptoms that lack common paranoid, grandiose, or religious themes 2. Sudden emergence of purported symptoms to explain antisocial behavior 3. Atypical hallucinations and delusions |
| D. Confirmation of malingering by either: 1. Admission of malingering following confrontation, or 2. Presence of strong corroborative information, such as psychometric data or history of malingering |
| Source: Reference 14 |
Table 4
Atypical psychotic symptoms that suggest malingering
| Hallucinations |
| Continuous rather than intermittent |
| Vague or inaudible auditory hallucinations |
| Stilted language reported in hallucinations |
| Inability to state strategies to diminish voices |
| Self-report that all command hallucinations were obeyed |
| Visual hallucinations in black and white |
| Delusions |
| Abrupt onset or termination |
| Eagerness to call attention to delusions |
| Conduct markedly inconsistent with delusions |
| Bizarre content without disordered thinking |
| Source: Reference 14 |
Psychological testing
Several standardized diagnostic instruments can be used to help determine whether a patient is feigning or exaggerating psychotic symptoms or cognitive impairments ( Table 5 ). Testing for a patient such as Mr. P—who attributes any criminal wrongdoing to psychosis and also cites limited cognition as a reason for trouble in the interview—would include personality tests, tests to assess exaggerations of psychosis, and cognitive tests.
In the forensic setting, the preferred personality test is the MMPI-2.15 It consists of 567 items, with 10 clinical scales and several validity scales. The F scale, “faking good” or “faking bad,” detects people who are answering questions with the goal of appearing better or worse than they actually are. The Personal Assessment Inventory (PAI)16 is a 344-item test with a 4-point response format. The 22 scales cover a range of important axis I and II psychopathology.
SIRS17 is the gold standard in detecting malingered psychiatric illness; it includes questions about rare symptoms and uncommon symptom pairing. M-FAST18 was developed to provide a brief, reliable screen for malingered mental illness. It has shown good validity and high correlation with the SIRS and MMPI-2.
Tests of exaggerated cognitive impairment are extremely important in evaluating patients who claim to suffer from complications following TBI. TOMM19 —a 50-item recognition test designed to discriminate between true memory-impaired patients and malingerers—is the most studied and valid of such tests. Defendants’ scores that meet the recommended criteria for detecting malingering—≥5 errors on the retention trial—were found to also report a history of head injury.1
Although not as well validated, the Portland Digit Recognition Test (PDRT)20 is an alternative to the TOMM. This test is a forced-choice measure of recognition designed for assessing the possibility of malingering in individuals claiming mental illness because of head injury. The Victoria Symptoms Validity Test (VSVT)21 is used in outpatient and inpatient settings and also uses a forced-choice model to assess possible exaggeration or feigning of cognitive impairments. Finally, the Word Memory Test (WMT)22 is a neuropsychological assessment that evaluates the effort participants put forth.
Table 5
Standardized diagnostic instruments for detecting malingering
| Test | Clinical use |
|---|---|
| Personality | |
| MMPI-2 | F scale detects lying. Several validity scales |
| PAI | Covers a range of axis I and II psychopathology |
| Psychotic symptoms | |
| SIRS | Gold standard in detecting exaggerated psychotic symptoms |
| M-FAST | Screening tool to assess exaggerated psychosis; brief and reliable |
| Cognitive impairment | |
| TOMM | Highest validity of all tools to test memory malingering |
| PDRT | Assesses the possibility of malingering. Not widely studied and validity/reliability are suspect |
| VSVT | Useful for inpatient and outpatient settings |
| WMT | Evaluates effort put forth by the participant |
| M-FAST: Miller Forensic Assessment of Symptoms Test; MMPI-2: Minnesota Multiphasic Personality Inventory; PAI: Personal Assessment Inventory; PDRT: Portland Digit Recognition Test; SIRS: Structured Interview of Reported Symptoms; TOMM: Test of Memory Malingering; VSVT: Victoria Symptoms Validity Test; WMT: Word Memory Test | |
OUTCOME: Unsupported claims
Mr. P’s hospital records reveal a very minor head trauma that resulted in no structural brain abnormalities on imaging tests. Collateral interviews with Mr. P’s family and close friends fail to support the defendant’s claim that after the accident he began to experience behavioral changes and periods of psychosis. Mr. P’s SIRS and TOMM scores indicate malingering, and the psychiatrist did not support his NGRI defense.
Related resource
- Williamson DJ. Neurocognitive impairment: feigned, exaggerated, or real? Current Psychiatry. 2007;6(8):19-37.
Disclosure
Dr. Nasrallah receives research grant/research support from Forest Pharmaceuticals, GlaxoSmithKline, Janssen, Otsuka America Pharmaceuticals, Pfizer Inc., Roche, sanofi-aventis, and Shire, is on the advisory board of Abbott Laboratories, AstraZeneca, Janssen, Novartis, Pfizer Inc., and Merck, and is on the speakers’ bureau for Abbott Laboratories, AstraZeneca, Janssen, Novartis, Pfizer Inc., and Merck.
Dr. Farrell reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Self-reported TBI
When charged with raping a 19-year-old woman, Mr. P, age 32, pleads not guilty by reason of insanity (NGRI). He has a self-reported history of traumatic brain injury (TBI) and claims that since suffering a blow to the head 8 years before the rape, he has experienced episodes of personality changes, psychosis, and violent behavior. Mr. P is adamant that any wrongdoing on his part was beyond his control, and he argues that consequences of the brain injury, such as hallucinations and aggressive behavior, had recently emerged. The court asks that a forensic psychiatrist evaluate Mr. P.
An only child, Mr. P was raised by his mother in an inner city area. His father was dependent on alcohol and cocaine and abandoned the family shortly after Mr. P’s birth. Mr. P abuses alcohol, as evidenced by previous driving under the influence charges, but denies illicit drug use. He graduated from high school with average grades and denies a history of disciplinary action at school or home. Although Mr. P was charged with misdemeanors in his late teens, the sexual assault is his first felony charge. Mr. P describes himself as a “charmer.”
After high school, Mr. P worked full-time in construction, where he claims he suffered a traumatic blow to the head. Despite this injury, he continued to work and socialize and never sought treatment at a mental health clinic.
The authors’ observations
Although defendants may legitimately suffer from TBI and resultant complications, many individuals capitalize on a history of minor head injury to support their NGRI defense.1 Forensic psychiatrists must retain a healthy degree of clinical suspicion for malingering in defendants who claim NGRI as a result of complications from brain injury, especially when the injury and complications are not documented and simply patient-reported.
TBI is a CNS injury that occurs when an outside force traumatically injures the brain and can cause a variety of physical, cognitive, emotional, and behavioral effects ( Table 1 ).2 Cognitive deficits include:
- impaired attention
- disrupted insight
- poor judgment
- thought disorders.
Reduced processing speed, distractibility, and deficits in executive functions such as abstract reasoning, planning, problem solving, and multitasking have been documented. Memory loss—the most common cognitive impairment among head-injured people—occurs in 20% to 79% of people with closed head trauma, depending on injury severity.3 People who have suffered TBI may have difficulty understanding or producing spoken or written language, or with more subtle aspects of communication, such as body language.
TBI may cause emotional or behavioral problems and personality changes. Mood and affect changes are common. TBI predisposes patients to obsessive-compulsive disorder, substance abuse, dysthymia, clinical depression, bipolar disorder, phobias, panic disorder, and schizophrenia.4 Frontal lobe injuries have been correlated with disinhibition and inappropriate or childish behavior, and temporal lobe injuries with irritability and aggression.5
Table 1
TBI symptoms correspond to area of injury
| Area of injury | Motor/sensory | Psychiatric/behavioral | Cognitive |
|---|---|---|---|
| Brain stem | Decreased vital capacity in breathing, dysphagia | Sleep difficulties | Inability to categorize objects, difficulty with organization |
| Frontal lobe | Aphasia, praxis | Disinhibition, personality changes | Impaired executive function |
| Cerebellum | Nystagmus, tremor | Labile emotions | Inability to process information |
| Parietal lobe | Apraxia | Personality changes | Neglect |
| Occipital lobe | Visual field cuts; diminished proprioception | Visual hallucinations | Color agnosia; inability to recognize words; difficulty reading, writing, and recognizing drawn objects |
| Temporal lobe | Seizure | Libido changes, humorless verbosity, aggression, olfactory perceptual changes | Prosopagnosia, aphasia, agnosia, memory loss, inattention |
| TBI: traumatic brain injury | |||
| Source: Reference 2 | |||
TBI and the insanity defense
The M’Naghten Rule of 1843 requires that for an insanity defense, the defendant must have a mental disease or defect that causes him not to know the nature and quality or the wrongfulness of his act.6 TBI is an abnormal condition of the mind leading to a mental disease that can substantially affect control of emotions and behaviors.
Nevertheless, TBI-induced criminality remains controversial.7 Theories on the etiology of impulse dyscontrol resulting from TBI have suggested structural damage to the brain and altered neurotransmitters. In TBI, the amygdala—which is located within the anterior temporal lobe and adjoins emotions to thoughts—often is injured. Damage to this structure leads to poor impulse control and violent behavior. Damage to specific neurotransmitter systems that causes elevated norepinephrine and dopamine levels and reduced serotonin levels have also been implicated as a cause of impulse dyscontrol in TBI patients.8
In theory, TBI patients potentially could have enough cognitive impairment to have a substantial lack of appreciation of the criminality or wrongfulness of an act. TBI-related impulsivity and cognitive impairment can lead to recklessness and negligence.9 The U.S. Supreme Court has acknowledged that CNS dysfunction affects judgment, reality testing, and self-control.10
EVALUATION: Vague answers
To determine whether Mr. P’s defense is plausible, the forensic psychiatrist must pay attention to the details of the patient’s presentation and history. During the interview, Mr. P quickly shifts from cooperative to obstinate and restricted. He ruminates on the head injury causing him to suffer auditory hallucinations, which he claims he always obeys. Mr. P refuses to provide details of the hallucinations, however, and answers most questions about the head injury or his defense with vague answers, including “I don’t know.”
Because of Mr. P’s reluctance to share information, his lack of psychiatric symptoms other than those he self-reports, and the presence of potential secondary gain from an NGRI defense, the psychiatrist begins to suspect malingering.
The authors’ observations
Malingering is a condition—not a diagnosis—characterized by intentional production of false or grossly exaggerated physical or psychological symptoms motivated by external incentives.11 The presence of external incentives distinguishes malingering from psychiatric illnesses such as factitious and somatoform disorders, in which there is no apparent external incentive. Malingering of psychiatric symptoms occurs in up to 20% of forensic patients, 5% of military recruits, and 1% of mental health patients.5 Stimuli for malingering range from seeking food and shelter to avoiding criminal responsibility ( Table 2 ). Malingering is more common in individuals being evaluated for criminal responsibility than for competence to stand trial. The 3 categories of malingering are:
Table 2
Common external incentives for malingering
| Evading criminal responsibility |
| Disability claims/financial gain |
| Avoiding military duty |
| Evading work |
| Obtaining drugs |
| Seeking food/shelter |
- pure malingering—feigning a nonexistent disorder
- partial malingering—consciously exaggerating real symptoms
- false imputation—ascribing real symptoms to a cause the individual knows is unrelated to the symptoms.12
Determining if a defendant with a history of TBI is malingering requires a multi-step approach that encompasses the clinical interview, a thorough review of collateral data, and focused psychological testing. In interviews, psychiatrists detect approximately 50% of lies, which is no better than would be discovered by chance.13 If you suspect a patient is malingering, combine a structured clinical interview with collateral sources such as old hospital records, treatment history, insurance records, police reports, and interviews with close family and friends.
TBI patients’ poor cognition, memory deficits, and inattention will prove challenging. Malingering patients who attempt to capitalize on a pre-existing TBI to evade responsibility for a current criminal charge may grossly exaggerate or even fake intellectual deficits. Be patient with such defendants and remain aware that such people will give vague or hedging answers to straightforward questions, often accompanied by “I don’t know.” Prolonging the interview may be helpful because it may fatigue a defendant who is faking.12
Some patients who malinger after sustaining a TBI will attempt to feign psychotic symptoms. Table 3 14 illustrates criteria for assessing a patient suspected of malingering psychosis and Table 4 14 highlights atypical psychotic symptoms that suggest feigning illness. Malingering of psychosis can be both assessed in the interview and through testing.
Table 3
Criteria for malingered psychosis
| A. Understandable motive to malinger |
| B. Marked variability of presentation as evidenced by ≥1 of the following: 1. Marked discrepancies in interview and non-interview behaviors 2. Gross inconsistencies in reported psychotic symptoms 3. Blatant contradictions between reported prior episodes and documented psychiatric history |
| C. Improbable psychiatric symptoms as evidenced by ≥1 of the following: 1. Reporting elaborate psychotic symptoms that lack common paranoid, grandiose, or religious themes 2. Sudden emergence of purported symptoms to explain antisocial behavior 3. Atypical hallucinations and delusions |
| D. Confirmation of malingering by either: 1. Admission of malingering following confrontation, or 2. Presence of strong corroborative information, such as psychometric data or history of malingering |
| Source: Reference 14 |
Table 4
Atypical psychotic symptoms that suggest malingering
| Hallucinations |
| Continuous rather than intermittent |
| Vague or inaudible auditory hallucinations |
| Stilted language reported in hallucinations |
| Inability to state strategies to diminish voices |
| Self-report that all command hallucinations were obeyed |
| Visual hallucinations in black and white |
| Delusions |
| Abrupt onset or termination |
| Eagerness to call attention to delusions |
| Conduct markedly inconsistent with delusions |
| Bizarre content without disordered thinking |
| Source: Reference 14 |
Psychological testing
Several standardized diagnostic instruments can be used to help determine whether a patient is feigning or exaggerating psychotic symptoms or cognitive impairments ( Table 5 ). Testing for a patient such as Mr. P—who attributes any criminal wrongdoing to psychosis and also cites limited cognition as a reason for trouble in the interview—would include personality tests, tests to assess exaggerations of psychosis, and cognitive tests.
In the forensic setting, the preferred personality test is the MMPI-2.15 It consists of 567 items, with 10 clinical scales and several validity scales. The F scale, “faking good” or “faking bad,” detects people who are answering questions with the goal of appearing better or worse than they actually are. The Personal Assessment Inventory (PAI)16 is a 344-item test with a 4-point response format. The 22 scales cover a range of important axis I and II psychopathology.
SIRS17 is the gold standard in detecting malingered psychiatric illness; it includes questions about rare symptoms and uncommon symptom pairing. M-FAST18 was developed to provide a brief, reliable screen for malingered mental illness. It has shown good validity and high correlation with the SIRS and MMPI-2.
Tests of exaggerated cognitive impairment are extremely important in evaluating patients who claim to suffer from complications following TBI. TOMM19 —a 50-item recognition test designed to discriminate between true memory-impaired patients and malingerers—is the most studied and valid of such tests. Defendants’ scores that meet the recommended criteria for detecting malingering—≥5 errors on the retention trial—were found to also report a history of head injury.1
Although not as well validated, the Portland Digit Recognition Test (PDRT)20 is an alternative to the TOMM. This test is a forced-choice measure of recognition designed for assessing the possibility of malingering in individuals claiming mental illness because of head injury. The Victoria Symptoms Validity Test (VSVT)21 is used in outpatient and inpatient settings and also uses a forced-choice model to assess possible exaggeration or feigning of cognitive impairments. Finally, the Word Memory Test (WMT)22 is a neuropsychological assessment that evaluates the effort participants put forth.
Table 5
Standardized diagnostic instruments for detecting malingering
| Test | Clinical use |
|---|---|
| Personality | |
| MMPI-2 | F scale detects lying. Several validity scales |
| PAI | Covers a range of axis I and II psychopathology |
| Psychotic symptoms | |
| SIRS | Gold standard in detecting exaggerated psychotic symptoms |
| M-FAST | Screening tool to assess exaggerated psychosis; brief and reliable |
| Cognitive impairment | |
| TOMM | Highest validity of all tools to test memory malingering |
| PDRT | Assesses the possibility of malingering. Not widely studied and validity/reliability are suspect |
| VSVT | Useful for inpatient and outpatient settings |
| WMT | Evaluates effort put forth by the participant |
| M-FAST: Miller Forensic Assessment of Symptoms Test; MMPI-2: Minnesota Multiphasic Personality Inventory; PAI: Personal Assessment Inventory; PDRT: Portland Digit Recognition Test; SIRS: Structured Interview of Reported Symptoms; TOMM: Test of Memory Malingering; VSVT: Victoria Symptoms Validity Test; WMT: Word Memory Test | |
OUTCOME: Unsupported claims
Mr. P’s hospital records reveal a very minor head trauma that resulted in no structural brain abnormalities on imaging tests. Collateral interviews with Mr. P’s family and close friends fail to support the defendant’s claim that after the accident he began to experience behavioral changes and periods of psychosis. Mr. P’s SIRS and TOMM scores indicate malingering, and the psychiatrist did not support his NGRI defense.
Related resource
- Williamson DJ. Neurocognitive impairment: feigned, exaggerated, or real? Current Psychiatry. 2007;6(8):19-37.
Disclosure
Dr. Nasrallah receives research grant/research support from Forest Pharmaceuticals, GlaxoSmithKline, Janssen, Otsuka America Pharmaceuticals, Pfizer Inc., Roche, sanofi-aventis, and Shire, is on the advisory board of Abbott Laboratories, AstraZeneca, Janssen, Novartis, Pfizer Inc., and Merck, and is on the speakers’ bureau for Abbott Laboratories, AstraZeneca, Janssen, Novartis, Pfizer Inc., and Merck.
Dr. Farrell reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Delain SL, Stafford KP, Yosef SB. Use of the TOMM in a criminal court forensic assessment setting. Assessment. 2003;10(4):370-381.
2. Rao V, Lyketsos C. Neuropsychiatric sequelae of traumatic brain injury Psychosomatics. 2000;41:95-103.
3. Hall RC, Hall RC, Chapman MJ. Definition, diagnosis, and forensic implications of postconcussional syndrome. Psychosomatics. 2005;46(3):195-202.
4. Arlinghaus KA, Shoaib AM, Price TRP. Neuropsychiatric assessment. In: Silver JM, McAllister TW, Yudofsky SC. Textbook of traumatic brain injury. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:63-65.
5. West S, Noffsinger S. Is this patient not guilty by reason of insanity? Current Psychiatry. 2005;5(8):54-62.
6. Barzman D, Kennedy J, Fozdar M. Does traumatic brain injury cause violence? Current Psychiatry. 2002;1(4):49-55.
7. Silver JM, Yudofsky SC, Hales RE. Neuropsychiatry of traumatic brain injury. Washington, DC: American Psychiatric Press, Inc.; 1994.
8. Melton GB, Petrila J, Poythress NG, et al. Psychological evaluations for the courts. New York, NY: The Guilford Press; 1997.
9. Lewis DO, Pincus JH, Feldman M, et al. Psychiatric, neurological, and psychoeducational characteristics of 15 death row inmates in the United States. Am J Psychiatry. 1986;143:838-845.
10. Diagnostic and statistical manual of mental disorders, 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
11. Sadock VA. Kaplan and Sadock’s synopsis of psychiatry. Philadelphia, PA: Lippincott, Williams, and Wilkins; 2007:887.
12. Resnick PJ. Faking it: how to determine malingered psychosis. Current Psychiatry. 2005;4(11):12-25.
13. Samuel RZ, Mittenberg W. Determination of malingering in disability claims. Primary Psychiatry. 2005;12(12):60-68.
14. Resnick PJ. Malingered psychosis. In: Rogers R, ed. Clinical assessment of malingering. 2nd ed. New York, NY: The Guilford Press; 1997:47-67.
15. Hathaway SR, McKinley JC. The Minnesota Multiphasic Personality Inventory-2. Minneapolis, MN: University of Minnesota Press; 1989.
16. Rogers R, Sewell KW, Morey LC, et al. Detection of feigned mental disorder on the personality assessment inventory: a discriminate analysis. J Pers Assess. 1996;67:629-640.
17. Rogers R, Bagby RM, Dickens SE. Structured Interview of Reported Symptoms (SIRS). Lutz, FL: Psychological Assessment Resources; 1992.
18. Miller H. Miller Forensic Assessment of Symptoms Test (M-FAST). Professional Manual. Lutz, FL: Psychological Assessment Resources; 2001.
19. Tombaugh TN. The Test of Memory Malingering. Toronto, ON, Canada: Multi-Health Systems; 1996.
20. Binder LM. Malingering following minor head trauma. Clin Neuropsychol. 1990;4:25-36.
21. Slick D, Hopp G, Strauss E, et al. Victoria Symptom Validity Test professional manual. Lutz, FL: Psychological Assessment Resources; 1997.
22. Green P. Word Memory Test. Edmonton, Alberta, Canada: Green’s Publishing; 2003.
1. Delain SL, Stafford KP, Yosef SB. Use of the TOMM in a criminal court forensic assessment setting. Assessment. 2003;10(4):370-381.
2. Rao V, Lyketsos C. Neuropsychiatric sequelae of traumatic brain injury Psychosomatics. 2000;41:95-103.
3. Hall RC, Hall RC, Chapman MJ. Definition, diagnosis, and forensic implications of postconcussional syndrome. Psychosomatics. 2005;46(3):195-202.
4. Arlinghaus KA, Shoaib AM, Price TRP. Neuropsychiatric assessment. In: Silver JM, McAllister TW, Yudofsky SC. Textbook of traumatic brain injury. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:63-65.
5. West S, Noffsinger S. Is this patient not guilty by reason of insanity? Current Psychiatry. 2005;5(8):54-62.
6. Barzman D, Kennedy J, Fozdar M. Does traumatic brain injury cause violence? Current Psychiatry. 2002;1(4):49-55.
7. Silver JM, Yudofsky SC, Hales RE. Neuropsychiatry of traumatic brain injury. Washington, DC: American Psychiatric Press, Inc.; 1994.
8. Melton GB, Petrila J, Poythress NG, et al. Psychological evaluations for the courts. New York, NY: The Guilford Press; 1997.
9. Lewis DO, Pincus JH, Feldman M, et al. Psychiatric, neurological, and psychoeducational characteristics of 15 death row inmates in the United States. Am J Psychiatry. 1986;143:838-845.
10. Diagnostic and statistical manual of mental disorders, 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
11. Sadock VA. Kaplan and Sadock’s synopsis of psychiatry. Philadelphia, PA: Lippincott, Williams, and Wilkins; 2007:887.
12. Resnick PJ. Faking it: how to determine malingered psychosis. Current Psychiatry. 2005;4(11):12-25.
13. Samuel RZ, Mittenberg W. Determination of malingering in disability claims. Primary Psychiatry. 2005;12(12):60-68.
14. Resnick PJ. Malingered psychosis. In: Rogers R, ed. Clinical assessment of malingering. 2nd ed. New York, NY: The Guilford Press; 1997:47-67.
15. Hathaway SR, McKinley JC. The Minnesota Multiphasic Personality Inventory-2. Minneapolis, MN: University of Minnesota Press; 1989.
16. Rogers R, Sewell KW, Morey LC, et al. Detection of feigned mental disorder on the personality assessment inventory: a discriminate analysis. J Pers Assess. 1996;67:629-640.
17. Rogers R, Bagby RM, Dickens SE. Structured Interview of Reported Symptoms (SIRS). Lutz, FL: Psychological Assessment Resources; 1992.
18. Miller H. Miller Forensic Assessment of Symptoms Test (M-FAST). Professional Manual. Lutz, FL: Psychological Assessment Resources; 2001.
19. Tombaugh TN. The Test of Memory Malingering. Toronto, ON, Canada: Multi-Health Systems; 1996.
20. Binder LM. Malingering following minor head trauma. Clin Neuropsychol. 1990;4:25-36.
21. Slick D, Hopp G, Strauss E, et al. Victoria Symptom Validity Test professional manual. Lutz, FL: Psychological Assessment Resources; 1997.
22. Green P. Word Memory Test. Edmonton, Alberta, Canada: Green’s Publishing; 2003.
Chasing the dragon
CASE: Confusion after discharge
Mr. G, age 37, is transferred to our medical center from a local hospital for treatment of altered mental status. His wife reports that 1 month ago he had been admitted to a different hospital for a heroin overdose. His urine toxicology screen then was positive for benzodiazepines, cocaine, and opioids. Mr. G’s 2-week stay was complicated by respiratory arrest, intubation, and mechanical ventilation. He also developed hypotension, acute renal failure, and aspiration pneumonia, but recovered.
His wife says 2 weeks after Mr. G was discharged home, she noticed he was becoming increasingly confused and forgetful. Initially she observed dificulty with short-term memory. He was involved in a motor vehicle accident far from home while reporting to a job he no longer held. She found him confused and watering the lawn in the rain. After she discovered him talking on the phone with no one on the line, she brought him to the emergency room (ER).
His urine toxicology screen was negative. Routine examination of cerebrospinal fluid and tests for glucose, protein, lactate, lactate dehydrogenase, red blood cell count, white blood cell count with differential, syphilis serology, Gram’s stain, and bacterial culture were negative.
Brain MRI showed diffuse new white matter signal abnormality superior to the tentorium of the cerebellum, suggestive of low-grade white matter ischemia or inflammation. Mr. G’s mental status did not improve in the ER, and he was transferred to our facility.
The authors’ observations
Based on abnormal brain imaging findings, we initially suspect a type of white matter disorder ( Table 1 ).1 We attempt to conduct a thorough history.
Table 1
Differential diagnoses: Types of white matter disorders
| Category | Example |
|---|---|
| Genetic | Metachromatic leukodystrophy |
| Demyelinative | Multiple sclerosis |
| Infectious | AIDS dementia complex |
| Inflammatory | Systemic lupus erythematosus |
| Toxic | Toluene leukoencephalopathy |
| Metabolic | Vitamin B12 deficiency |
| Vascular | Binswanger’s disease* |
| Traumatic | Traumatic brain injury |
| Neoplastic | Gliomatosis cerebri |
| Hydrocephalic | Normal pressure hydrocephalus |
| *Degenerative dementia caused by thinning of subcortical white matter of the brain | |
| AIDS: acquired immune deficiency syndrome | |
| Source: Reference 1 | |
HISTORY: Missing information
Attempts to obtain collateral information are largely unsuccessful. Mr. G denies having a history of medical or psychiatric illness. He is vague about substance use but may have a history of opioid and cocaine dependence and alcohol abuse. He says he takes no prescribed or over-the-counter medications and has no known drug allergies.
Mr. G’s wife provides limited additional information. She married Mr. G 6 months ago; before that, he was in jail for 3.5 years for unclear reasons. He is unemployed, and the couple has no children.
Mr. G’s wife reports that Mr. G’s father had a history of diabetes mellitus and dialysis and died in his 40s from “Staph infection of the brain.” Mr. G is estranged from his mother. He has no family history of neurologic or psychiatric illness.
Mr. G’s wife denies that her husband has had recent fever, chills, weight loss, nausea, vomiting, diarrhea, or skin rash. He has no history of alcohol withdrawal symptoms, seizures, headache, diplopia, vertigo, hearing loss, swallowing difficulty, focal weakness, or sensory or speech changes. She did not notice personality or behavior changes in her husband before his recent confusion.
The authors’ observations
During our interview, Mr. G maintains minimal eye contact. His speech is minimal with impaired fluency; he responds to questions with 1- or 2-word answers. He describes his mood as “fine” but exhibits an incongruent and constricted affect, alternately laughing and crying. We are unable to assess his thought process and content because Mr. G is emotionally labile and unable to respond rationally to many of our questions. Mr. G’s insight and judgment are poor. His hygiene, grooming, and teeth also are poor, and he is wearing diapers for bowel/bladder incontinence.
Mr. G scores 9/30 on the Mini-Mental State Exam (MMSE), indicating severe cognitive impairment. He is not oriented to place or time, and cannot:
- spell “world” backwards
- subtract serial 7s from 100
- repeat the phrase “no ifs, ands, or buts”
- name 5 U.S. cities
- write any words
- copy a figure of intersecting pentagons.
Neurologic exam reveals apathy, inattention, impaired executive function, and generalized hyperreflexia with bilateral unsustained ankle clonus and Babinski’s sign. In addition, Mr. G has a snout reflex, bilateral hand and foot grasping, and bilateral palmomental reflexes but no mydriasis or nasal septum perforation. Repeat MRI shows the same white matter changes.
Based on Mr. G’s history and brain imaging findings, we suspect that he is suffering from toxic leukoencephalopathy. He meets these diagnostic criteria:
- documented exposure to a toxin
- neurobehavioral deficits
- neuroradiologic abnormalities.2
Toxic leukoencephalopathy can be caused by environmental exposure, radiation, chemotherapy, or substance abuse.3 Because Mr. G has a history of substance abuse, we believe his symptoms developed as a result of heroin vapor inhalation.
‘Chasing the dragon’
Inhaling heroin vapor is known by drug users as “chasing the dragon.” Users place a small amount of heroin powder on aluminum foil, which they heat from below with a flame. The heroin liquidizes and emits a white vapor, which users inhale.3
This method of heroin use can result in a form of toxic spongiform leukoencephalopathy. Brain imaging shows widespread white matter hyperintensities involving both supra and infratentorial compartments that are considered highly specific for this type of leukoencephalopathy ( Figure ). These hyperintensities are most commonly found in the:
- posterior cerebral and cerebellar white matter
- cerebellar peduncles
- splenium of the corpus callosum
- posterior limb of the internal capsule.4
Involvement of the cerebellum and posterior limb of the internal capsule while sparing the anterior limb helps to distinguish heroin vapor inhalation from other causes of toxic leukoencephalopathy.3 Extensive damage to the white matter is believed to be caused by a contaminant that is activated when heroin is heated.4,5
Toxic leukoencephalopathy has not been observed in heroin users who snort or inject the drug. Despite the prevalence of heroin abuse, fewer than 100 cases of leukoencephalopathy associated with heroin vapor inhalation have been reported as of 2000, the most recent year for which data are available.6 Patients with this form of leukoencephalopathy typically progress through 3 clinical stages: initial, intermediate, and terminal ( Table 2 ).4
Figure: White matter changes in a patient who inhaled heroin vapor
Photos: © Frank Gaillard/Radiopaedia.org
Seen on brain MRI as ultra-white patches, white matter hyperintensities (WMHs) are areas of increased signal intensity that indicate injury to the axons. In this typical patient (not Mr. G) who developed toxic leukoencephalopathy from heroin vapor inhalation, WMHs are evident in supra and infratentorial compartments, with characteristic involvement of the posterior limb of the internal capsule and cerebellum. Table 2
Stages of heroin vapor inhalation leukoencephalopathy
| Stage | Features |
|---|---|
| Initial | Soft (pseudobulbar) speech, cerebellar ataxia, motor restlessness, apathy/bradyphrenia |
| Intermediate | Pyramidal tract lesions, pseudobulbar reflexes, spastic paresis, tremor/myoclonic jerks, choreoathetoid movements |
| Terminal | Stretching spasms, hypotonic paresis, akinetic mutism, central pyrexia, death |
| Source: Reference 4 | |
TREATMENT Stimulant medication
We prescribe methylphenidate, 2.5 mg bid, to which Mr. G responds well. His cognition and mood improve, he is more goal-directed in his responses, and his MMSE score increases to 13/30. Mr. G eventually is able to converse minimally, and he confirms that he had heated heroin on a piece of foil and inhaled the vapors through his mouth.
Mr. G reports on the day of discharge that he still has cravings for illicit drugs and plans to continue using them. He is not interested in chemical dependency treatment.
The authors’ observations
Little published data exist on treating toxic leukoencephalopathy. Treatment mainly is supportive, although some researchers have suggested a role for coenzyme Q and vitamin supplements.3
Some studies have found methylphenidate beneficial in treating cognitive slowing in cancer patients.1,7 The extent of Mr. G’s cognitive impairment—which was severe—and evidence supporting stimulant medication prompted us to prescribe a low-dose methylphenidate trial, even though we were well aware of its abuse potential. Mr. G improved after starting methylphenidate, but unfortunately he was lost to follow-up.
Related resource
- Filley CM, Kleinschmidt-Demasters BK. Toxic leukoencephalopathy. N Engl J Med. 2001;345(6):425-432.
Drug brand name
- Methylphenidate • Ritalin
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Filley CM. Neurobehavioral aspects of cerebral white matter disorders. Psychiatr Clin North Am. 2005;28(3):685-700.
2. Jordan JD, Lloyd T, Pardo-Villamizar C. Case 16: Chasing the dragon. Medscape General Medicine. 2007;9(2):14.-Available at: http://www.medscape.com/viewarticle/554308. Accessed December 7, 2009.
3. Keogh CF, Andrews GT, Spacey SD, et al. Neuroimaging features of heroin inhalation toxicity: “chasing the dragon.” Am J Roentgen. 2003;180:847-850.
4. Hagel J, Andrews G, Vertinsky T, et al. “Chasing the dragon”—imaging of heroin inhalation leukoencephalopathy. Can Assoc Radiol J. 2005;56(4):199-203.
5. Wolters EC, van Wijngaarden GK, Stam FC, et al. Leucoencephalopathy after inhaling “heroin” pyrolysate. Lancet. 1982;2:1233-1237.
6. Hill MD, Cooper PW, Perry JR. Chasing the dragon—neurological toxicity associated with inhalation of heroin vapor: case report. CMAJ. 2000;162:236-238.
7. Weitzner MA, Meyers CA, Valentine AD. Methylphenidate in the treatment of neurobehavioral slowing associated with cancer and cancer treatment. J Neuropsychiatry Clin Neurosci. 1995;7:347-350.
CASE: Confusion after discharge
Mr. G, age 37, is transferred to our medical center from a local hospital for treatment of altered mental status. His wife reports that 1 month ago he had been admitted to a different hospital for a heroin overdose. His urine toxicology screen then was positive for benzodiazepines, cocaine, and opioids. Mr. G’s 2-week stay was complicated by respiratory arrest, intubation, and mechanical ventilation. He also developed hypotension, acute renal failure, and aspiration pneumonia, but recovered.
His wife says 2 weeks after Mr. G was discharged home, she noticed he was becoming increasingly confused and forgetful. Initially she observed dificulty with short-term memory. He was involved in a motor vehicle accident far from home while reporting to a job he no longer held. She found him confused and watering the lawn in the rain. After she discovered him talking on the phone with no one on the line, she brought him to the emergency room (ER).
His urine toxicology screen was negative. Routine examination of cerebrospinal fluid and tests for glucose, protein, lactate, lactate dehydrogenase, red blood cell count, white blood cell count with differential, syphilis serology, Gram’s stain, and bacterial culture were negative.
Brain MRI showed diffuse new white matter signal abnormality superior to the tentorium of the cerebellum, suggestive of low-grade white matter ischemia or inflammation. Mr. G’s mental status did not improve in the ER, and he was transferred to our facility.
The authors’ observations
Based on abnormal brain imaging findings, we initially suspect a type of white matter disorder ( Table 1 ).1 We attempt to conduct a thorough history.
Table 1
Differential diagnoses: Types of white matter disorders
| Category | Example |
|---|---|
| Genetic | Metachromatic leukodystrophy |
| Demyelinative | Multiple sclerosis |
| Infectious | AIDS dementia complex |
| Inflammatory | Systemic lupus erythematosus |
| Toxic | Toluene leukoencephalopathy |
| Metabolic | Vitamin B12 deficiency |
| Vascular | Binswanger’s disease* |
| Traumatic | Traumatic brain injury |
| Neoplastic | Gliomatosis cerebri |
| Hydrocephalic | Normal pressure hydrocephalus |
| *Degenerative dementia caused by thinning of subcortical white matter of the brain | |
| AIDS: acquired immune deficiency syndrome | |
| Source: Reference 1 | |
HISTORY: Missing information
Attempts to obtain collateral information are largely unsuccessful. Mr. G denies having a history of medical or psychiatric illness. He is vague about substance use but may have a history of opioid and cocaine dependence and alcohol abuse. He says he takes no prescribed or over-the-counter medications and has no known drug allergies.
Mr. G’s wife provides limited additional information. She married Mr. G 6 months ago; before that, he was in jail for 3.5 years for unclear reasons. He is unemployed, and the couple has no children.
Mr. G’s wife reports that Mr. G’s father had a history of diabetes mellitus and dialysis and died in his 40s from “Staph infection of the brain.” Mr. G is estranged from his mother. He has no family history of neurologic or psychiatric illness.
Mr. G’s wife denies that her husband has had recent fever, chills, weight loss, nausea, vomiting, diarrhea, or skin rash. He has no history of alcohol withdrawal symptoms, seizures, headache, diplopia, vertigo, hearing loss, swallowing difficulty, focal weakness, or sensory or speech changes. She did not notice personality or behavior changes in her husband before his recent confusion.
The authors’ observations
During our interview, Mr. G maintains minimal eye contact. His speech is minimal with impaired fluency; he responds to questions with 1- or 2-word answers. He describes his mood as “fine” but exhibits an incongruent and constricted affect, alternately laughing and crying. We are unable to assess his thought process and content because Mr. G is emotionally labile and unable to respond rationally to many of our questions. Mr. G’s insight and judgment are poor. His hygiene, grooming, and teeth also are poor, and he is wearing diapers for bowel/bladder incontinence.
Mr. G scores 9/30 on the Mini-Mental State Exam (MMSE), indicating severe cognitive impairment. He is not oriented to place or time, and cannot:
- spell “world” backwards
- subtract serial 7s from 100
- repeat the phrase “no ifs, ands, or buts”
- name 5 U.S. cities
- write any words
- copy a figure of intersecting pentagons.
Neurologic exam reveals apathy, inattention, impaired executive function, and generalized hyperreflexia with bilateral unsustained ankle clonus and Babinski’s sign. In addition, Mr. G has a snout reflex, bilateral hand and foot grasping, and bilateral palmomental reflexes but no mydriasis or nasal septum perforation. Repeat MRI shows the same white matter changes.
Based on Mr. G’s history and brain imaging findings, we suspect that he is suffering from toxic leukoencephalopathy. He meets these diagnostic criteria:
- documented exposure to a toxin
- neurobehavioral deficits
- neuroradiologic abnormalities.2
Toxic leukoencephalopathy can be caused by environmental exposure, radiation, chemotherapy, or substance abuse.3 Because Mr. G has a history of substance abuse, we believe his symptoms developed as a result of heroin vapor inhalation.
‘Chasing the dragon’
Inhaling heroin vapor is known by drug users as “chasing the dragon.” Users place a small amount of heroin powder on aluminum foil, which they heat from below with a flame. The heroin liquidizes and emits a white vapor, which users inhale.3
This method of heroin use can result in a form of toxic spongiform leukoencephalopathy. Brain imaging shows widespread white matter hyperintensities involving both supra and infratentorial compartments that are considered highly specific for this type of leukoencephalopathy ( Figure ). These hyperintensities are most commonly found in the:
- posterior cerebral and cerebellar white matter
- cerebellar peduncles
- splenium of the corpus callosum
- posterior limb of the internal capsule.4
Involvement of the cerebellum and posterior limb of the internal capsule while sparing the anterior limb helps to distinguish heroin vapor inhalation from other causes of toxic leukoencephalopathy.3 Extensive damage to the white matter is believed to be caused by a contaminant that is activated when heroin is heated.4,5
Toxic leukoencephalopathy has not been observed in heroin users who snort or inject the drug. Despite the prevalence of heroin abuse, fewer than 100 cases of leukoencephalopathy associated with heroin vapor inhalation have been reported as of 2000, the most recent year for which data are available.6 Patients with this form of leukoencephalopathy typically progress through 3 clinical stages: initial, intermediate, and terminal ( Table 2 ).4
Figure: White matter changes in a patient who inhaled heroin vapor
Photos: © Frank Gaillard/Radiopaedia.org
Seen on brain MRI as ultra-white patches, white matter hyperintensities (WMHs) are areas of increased signal intensity that indicate injury to the axons. In this typical patient (not Mr. G) who developed toxic leukoencephalopathy from heroin vapor inhalation, WMHs are evident in supra and infratentorial compartments, with characteristic involvement of the posterior limb of the internal capsule and cerebellum. Table 2
Stages of heroin vapor inhalation leukoencephalopathy
| Stage | Features |
|---|---|
| Initial | Soft (pseudobulbar) speech, cerebellar ataxia, motor restlessness, apathy/bradyphrenia |
| Intermediate | Pyramidal tract lesions, pseudobulbar reflexes, spastic paresis, tremor/myoclonic jerks, choreoathetoid movements |
| Terminal | Stretching spasms, hypotonic paresis, akinetic mutism, central pyrexia, death |
| Source: Reference 4 | |
TREATMENT Stimulant medication
We prescribe methylphenidate, 2.5 mg bid, to which Mr. G responds well. His cognition and mood improve, he is more goal-directed in his responses, and his MMSE score increases to 13/30. Mr. G eventually is able to converse minimally, and he confirms that he had heated heroin on a piece of foil and inhaled the vapors through his mouth.
Mr. G reports on the day of discharge that he still has cravings for illicit drugs and plans to continue using them. He is not interested in chemical dependency treatment.
The authors’ observations
Little published data exist on treating toxic leukoencephalopathy. Treatment mainly is supportive, although some researchers have suggested a role for coenzyme Q and vitamin supplements.3
Some studies have found methylphenidate beneficial in treating cognitive slowing in cancer patients.1,7 The extent of Mr. G’s cognitive impairment—which was severe—and evidence supporting stimulant medication prompted us to prescribe a low-dose methylphenidate trial, even though we were well aware of its abuse potential. Mr. G improved after starting methylphenidate, but unfortunately he was lost to follow-up.
Related resource
- Filley CM, Kleinschmidt-Demasters BK. Toxic leukoencephalopathy. N Engl J Med. 2001;345(6):425-432.
Drug brand name
- Methylphenidate • Ritalin
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Confusion after discharge
Mr. G, age 37, is transferred to our medical center from a local hospital for treatment of altered mental status. His wife reports that 1 month ago he had been admitted to a different hospital for a heroin overdose. His urine toxicology screen then was positive for benzodiazepines, cocaine, and opioids. Mr. G’s 2-week stay was complicated by respiratory arrest, intubation, and mechanical ventilation. He also developed hypotension, acute renal failure, and aspiration pneumonia, but recovered.
His wife says 2 weeks after Mr. G was discharged home, she noticed he was becoming increasingly confused and forgetful. Initially she observed dificulty with short-term memory. He was involved in a motor vehicle accident far from home while reporting to a job he no longer held. She found him confused and watering the lawn in the rain. After she discovered him talking on the phone with no one on the line, she brought him to the emergency room (ER).
His urine toxicology screen was negative. Routine examination of cerebrospinal fluid and tests for glucose, protein, lactate, lactate dehydrogenase, red blood cell count, white blood cell count with differential, syphilis serology, Gram’s stain, and bacterial culture were negative.
Brain MRI showed diffuse new white matter signal abnormality superior to the tentorium of the cerebellum, suggestive of low-grade white matter ischemia or inflammation. Mr. G’s mental status did not improve in the ER, and he was transferred to our facility.
The authors’ observations
Based on abnormal brain imaging findings, we initially suspect a type of white matter disorder ( Table 1 ).1 We attempt to conduct a thorough history.
Table 1
Differential diagnoses: Types of white matter disorders
| Category | Example |
|---|---|
| Genetic | Metachromatic leukodystrophy |
| Demyelinative | Multiple sclerosis |
| Infectious | AIDS dementia complex |
| Inflammatory | Systemic lupus erythematosus |
| Toxic | Toluene leukoencephalopathy |
| Metabolic | Vitamin B12 deficiency |
| Vascular | Binswanger’s disease* |
| Traumatic | Traumatic brain injury |
| Neoplastic | Gliomatosis cerebri |
| Hydrocephalic | Normal pressure hydrocephalus |
| *Degenerative dementia caused by thinning of subcortical white matter of the brain | |
| AIDS: acquired immune deficiency syndrome | |
| Source: Reference 1 | |
HISTORY: Missing information
Attempts to obtain collateral information are largely unsuccessful. Mr. G denies having a history of medical or psychiatric illness. He is vague about substance use but may have a history of opioid and cocaine dependence and alcohol abuse. He says he takes no prescribed or over-the-counter medications and has no known drug allergies.
Mr. G’s wife provides limited additional information. She married Mr. G 6 months ago; before that, he was in jail for 3.5 years for unclear reasons. He is unemployed, and the couple has no children.
Mr. G’s wife reports that Mr. G’s father had a history of diabetes mellitus and dialysis and died in his 40s from “Staph infection of the brain.” Mr. G is estranged from his mother. He has no family history of neurologic or psychiatric illness.
Mr. G’s wife denies that her husband has had recent fever, chills, weight loss, nausea, vomiting, diarrhea, or skin rash. He has no history of alcohol withdrawal symptoms, seizures, headache, diplopia, vertigo, hearing loss, swallowing difficulty, focal weakness, or sensory or speech changes. She did not notice personality or behavior changes in her husband before his recent confusion.
The authors’ observations
During our interview, Mr. G maintains minimal eye contact. His speech is minimal with impaired fluency; he responds to questions with 1- or 2-word answers. He describes his mood as “fine” but exhibits an incongruent and constricted affect, alternately laughing and crying. We are unable to assess his thought process and content because Mr. G is emotionally labile and unable to respond rationally to many of our questions. Mr. G’s insight and judgment are poor. His hygiene, grooming, and teeth also are poor, and he is wearing diapers for bowel/bladder incontinence.
Mr. G scores 9/30 on the Mini-Mental State Exam (MMSE), indicating severe cognitive impairment. He is not oriented to place or time, and cannot:
- spell “world” backwards
- subtract serial 7s from 100
- repeat the phrase “no ifs, ands, or buts”
- name 5 U.S. cities
- write any words
- copy a figure of intersecting pentagons.
Neurologic exam reveals apathy, inattention, impaired executive function, and generalized hyperreflexia with bilateral unsustained ankle clonus and Babinski’s sign. In addition, Mr. G has a snout reflex, bilateral hand and foot grasping, and bilateral palmomental reflexes but no mydriasis or nasal septum perforation. Repeat MRI shows the same white matter changes.
Based on Mr. G’s history and brain imaging findings, we suspect that he is suffering from toxic leukoencephalopathy. He meets these diagnostic criteria:
- documented exposure to a toxin
- neurobehavioral deficits
- neuroradiologic abnormalities.2
Toxic leukoencephalopathy can be caused by environmental exposure, radiation, chemotherapy, or substance abuse.3 Because Mr. G has a history of substance abuse, we believe his symptoms developed as a result of heroin vapor inhalation.
‘Chasing the dragon’
Inhaling heroin vapor is known by drug users as “chasing the dragon.” Users place a small amount of heroin powder on aluminum foil, which they heat from below with a flame. The heroin liquidizes and emits a white vapor, which users inhale.3
This method of heroin use can result in a form of toxic spongiform leukoencephalopathy. Brain imaging shows widespread white matter hyperintensities involving both supra and infratentorial compartments that are considered highly specific for this type of leukoencephalopathy ( Figure ). These hyperintensities are most commonly found in the:
- posterior cerebral and cerebellar white matter
- cerebellar peduncles
- splenium of the corpus callosum
- posterior limb of the internal capsule.4
Involvement of the cerebellum and posterior limb of the internal capsule while sparing the anterior limb helps to distinguish heroin vapor inhalation from other causes of toxic leukoencephalopathy.3 Extensive damage to the white matter is believed to be caused by a contaminant that is activated when heroin is heated.4,5
Toxic leukoencephalopathy has not been observed in heroin users who snort or inject the drug. Despite the prevalence of heroin abuse, fewer than 100 cases of leukoencephalopathy associated with heroin vapor inhalation have been reported as of 2000, the most recent year for which data are available.6 Patients with this form of leukoencephalopathy typically progress through 3 clinical stages: initial, intermediate, and terminal ( Table 2 ).4
Figure: White matter changes in a patient who inhaled heroin vapor
Photos: © Frank Gaillard/Radiopaedia.org
Seen on brain MRI as ultra-white patches, white matter hyperintensities (WMHs) are areas of increased signal intensity that indicate injury to the axons. In this typical patient (not Mr. G) who developed toxic leukoencephalopathy from heroin vapor inhalation, WMHs are evident in supra and infratentorial compartments, with characteristic involvement of the posterior limb of the internal capsule and cerebellum. Table 2
Stages of heroin vapor inhalation leukoencephalopathy
| Stage | Features |
|---|---|
| Initial | Soft (pseudobulbar) speech, cerebellar ataxia, motor restlessness, apathy/bradyphrenia |
| Intermediate | Pyramidal tract lesions, pseudobulbar reflexes, spastic paresis, tremor/myoclonic jerks, choreoathetoid movements |
| Terminal | Stretching spasms, hypotonic paresis, akinetic mutism, central pyrexia, death |
| Source: Reference 4 | |
TREATMENT Stimulant medication
We prescribe methylphenidate, 2.5 mg bid, to which Mr. G responds well. His cognition and mood improve, he is more goal-directed in his responses, and his MMSE score increases to 13/30. Mr. G eventually is able to converse minimally, and he confirms that he had heated heroin on a piece of foil and inhaled the vapors through his mouth.
Mr. G reports on the day of discharge that he still has cravings for illicit drugs and plans to continue using them. He is not interested in chemical dependency treatment.
The authors’ observations
Little published data exist on treating toxic leukoencephalopathy. Treatment mainly is supportive, although some researchers have suggested a role for coenzyme Q and vitamin supplements.3
Some studies have found methylphenidate beneficial in treating cognitive slowing in cancer patients.1,7 The extent of Mr. G’s cognitive impairment—which was severe—and evidence supporting stimulant medication prompted us to prescribe a low-dose methylphenidate trial, even though we were well aware of its abuse potential. Mr. G improved after starting methylphenidate, but unfortunately he was lost to follow-up.
Related resource
- Filley CM, Kleinschmidt-Demasters BK. Toxic leukoencephalopathy. N Engl J Med. 2001;345(6):425-432.
Drug brand name
- Methylphenidate • Ritalin
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Filley CM. Neurobehavioral aspects of cerebral white matter disorders. Psychiatr Clin North Am. 2005;28(3):685-700.
2. Jordan JD, Lloyd T, Pardo-Villamizar C. Case 16: Chasing the dragon. Medscape General Medicine. 2007;9(2):14.-Available at: http://www.medscape.com/viewarticle/554308. Accessed December 7, 2009.
3. Keogh CF, Andrews GT, Spacey SD, et al. Neuroimaging features of heroin inhalation toxicity: “chasing the dragon.” Am J Roentgen. 2003;180:847-850.
4. Hagel J, Andrews G, Vertinsky T, et al. “Chasing the dragon”—imaging of heroin inhalation leukoencephalopathy. Can Assoc Radiol J. 2005;56(4):199-203.
5. Wolters EC, van Wijngaarden GK, Stam FC, et al. Leucoencephalopathy after inhaling “heroin” pyrolysate. Lancet. 1982;2:1233-1237.
6. Hill MD, Cooper PW, Perry JR. Chasing the dragon—neurological toxicity associated with inhalation of heroin vapor: case report. CMAJ. 2000;162:236-238.
7. Weitzner MA, Meyers CA, Valentine AD. Methylphenidate in the treatment of neurobehavioral slowing associated with cancer and cancer treatment. J Neuropsychiatry Clin Neurosci. 1995;7:347-350.
1. Filley CM. Neurobehavioral aspects of cerebral white matter disorders. Psychiatr Clin North Am. 2005;28(3):685-700.
2. Jordan JD, Lloyd T, Pardo-Villamizar C. Case 16: Chasing the dragon. Medscape General Medicine. 2007;9(2):14.-Available at: http://www.medscape.com/viewarticle/554308. Accessed December 7, 2009.
3. Keogh CF, Andrews GT, Spacey SD, et al. Neuroimaging features of heroin inhalation toxicity: “chasing the dragon.” Am J Roentgen. 2003;180:847-850.
4. Hagel J, Andrews G, Vertinsky T, et al. “Chasing the dragon”—imaging of heroin inhalation leukoencephalopathy. Can Assoc Radiol J. 2005;56(4):199-203.
5. Wolters EC, van Wijngaarden GK, Stam FC, et al. Leucoencephalopathy after inhaling “heroin” pyrolysate. Lancet. 1982;2:1233-1237.
6. Hill MD, Cooper PW, Perry JR. Chasing the dragon—neurological toxicity associated with inhalation of heroin vapor: case report. CMAJ. 2000;162:236-238.
7. Weitzner MA, Meyers CA, Valentine AD. Methylphenidate in the treatment of neurobehavioral slowing associated with cancer and cancer treatment. J Neuropsychiatry Clin Neurosci. 1995;7:347-350.
Terrifying visions
CASE: Seeing things
Family members bring Mrs. L, age 82, to the emergency room (ER) because she is agitated, nervous, and carries a knife “for protection.” In the past few months, she has been seeing things her family could not, such as bugs in her food and people trying to break into her house. Mrs. L becomes increasingly frightened and angry because her family denies seeing these things. Her family is concerned she might hurt herself or others.
Despite some hearing loss, Mrs. L had been relatively healthy and independent until a few years ago, when her vision decreased secondary to age-related macular degeneration and diabetic retinopathy. In addition to sensory impairment and diabetes mellitus, her medical history includes mild hypothyroidism and intervertebral disc herniation. She has no history of liver disease or alcohol or substance abuse. A few weeks ago Mrs. L’s primary care physician began treating her with donepezil, 5 mg/d, because he suspected dementia was causing her hallucinations. Otherwise, she has no psychiatric history.
On exam, Mrs. L is easily directable and cooperative. She seems angry because no one believes her; she reports seeing a cat that nobody else could see in the ER immediately before being evaluated. She is frightened because she believes her hallucinations are real, although she is unable to explain them. Mrs. L reports feeling anxious most of the time and having difficulty sleeping because of her fears. She also feels sad and occasionally worthless because she cannot see or hear as well as when she was younger.
A mental status examination shows partial impairment of concentration and short-term memory, but Mrs. L is alert and oriented. No theme of delusions is detected. She has no physical complaints, and physical examination is unremarkable.
The authors’ observations
Mrs. L presented with new-onset agitation, visual hallucinations, and mildly decreased concentration and short-term memory. Our next step after history and examination was to perform laboratory testing to narrow the diagnosis ( Table 1 ).
A basic electrolyte panel including kidney function can point toward electrolyte imbalance or uremia as a cause of delirium. Mrs. L’s basic metabolic panel and liver function were normal. Urinalysis ruled out urinary tract infection.
Mrs. L’s thyroid-stimulating hormone (TSH) level was mildly elevated at 5.6 mU/L (in our laboratory, the upper normal limit is 5.2 mU/L). Hypothyroidism and hyperthyroidism are not associated with hallucinations, but hyperthyroidism is an important medical cause of anxiety and hypothyroidism can cause a dementia-like presentation. CT of the head to rule out a space-occupying lesion or acute process—such as cerebrovascular accident—shows only chronic vascular changes.
Based on Mrs. L’s history, physical examination, and lab results, we provisionally diagnose dementia, Alzheimer’s type with psychotic features, and prescribe quetiapine, 25 mg at bedtime. We offer to admit Mrs. L, but she and her family prefer close outpatient follow-up. After discussing safety concerns and pharmacotherapy with the patient and her family, we discharge Mrs. L home and advise her to follow up with the psychiatric clinic.
Table 1
Suggested workup for elderly patients with hallucinations
| History and physical exam |
| History of dementia, mood disorder, Parkinson’s disease, or drug abuse |
| Presence of delusions or mood/anxiety symptoms |
| Detailed medication history |
| Level of consciousness, alertness, and cognitive function assessment (eg, MMSE) |
| Vital signs (instability may reflect delirium, meningitis/encephalitis, or intoxication) |
| Physical exam (may confirm acute medical illness causing delirium) |
| Neurologic exam (may show focal neurologic signs reflecting space-occupying lesion, signs of Parkinson’s disease, vitamin B12 deficiency) |
| Ophthalmologic history/exam |
| Investigations |
| Electrolyte imbalance, especially calcium |
| Glucose level |
| Uremia, impaired liver function, and increased ammonia |
| CBC |
| Urine drug screen |
| Urinalysis, culture, and sensitivity |
| Additional tests |
| VDRL |
| Arterial blood gas |
| ECG and cardiac enzymes |
| Chest radiography |
| Vitamin B12/folate |
| TSH |
| EEG |
| Serum drug levels |
| CT/MRI of the head |
| Lumbar puncture and cerebrospinal fluid analysis |
| Heavy metal screen |
| HIV screen |
| CBC: complete blood count; CT: computed tomography; ECG: electrocardiography; EEG: electroencephalography; HIV: human immunodeficiency virus; MMSE: Mini-Mental State Exam; MRI: magnetic resonance imaging; TSH: thyroid-stimulating hormone; VDRL: venereal disease research laboratory |
EVALUATION: Lasting hallucinations
Quetiapine improves Mrs. L’s sleep and agitation but does not reduce her hallucinations. She sees a helicopter planting wires on a tree next to her house, a snake in the house, children in her room (some are “beautiful”), fire, and creatures with scary faces. These hallucinations occur mostly when she is alone. She denies hearing or touching the things she sees but continues to feel fear and anxiety when she sees them, although this diminishes with education and reassurance.
The authors’ observations
In Mrs. L’s subsequent psychiatry clinic visits, we gather additional information that helped us rule out several differential diagnoses ( Table 2 ).
The most common causes of new-onset psychosis in later life are:
- dementia-related syndromes with psychosis, delirium, or drug-induced psychosis
- primary psychiatric disorders, most commonly depression.1
Alzheimer’s disease has been associated with up to a 60% incidence of psychotic symptoms at some point in the disease course.2 Although Mrs. L’s short-term memory had declined in recent years, she does not have aphasia, apraxia, agnosia, or decrease in mental executive functioning to meet Alzheimer’s dementia criteria.
Perceptual disturbance is a feature of delirium that can cause agitation and hallucinations in elderly patients. However, Mrs. L did not have a decreased level of consciousness or an acute medical illness that would explain delirium.
Despite Mrs. L’s symptoms and progressive hearing and vision loss with resultant disability, she generally was organized in terms of basic self-care, hygiene, and activities of daily living. She was able to have a conversation when she could hear the physician. Surprisingly, her Mini-Mental State Examination (MMSE) score was within normal limits or only mildly impaired at office visits. This was not compatible with the initial diagnosis of dementia, although it may suggest mild cognitive impairment.
Mrs. L took donepezil as prescribed by her primary care physician for only a few weeks before we stopped it. We attributed Mrs. L’s slightly impaired concentration and short-term memory in the ER to the anxiety and stress of oscillating visual hallucinations.
Schizophrenia is another cause of psychosis, but Mrs. L had no history of negative symptoms, delusions, disorganized speech/behavior, or family history of psychotic disorders. In addition, schizophrenia is most likely to appear in a patient’s third decade. Although more common in women than men, late-onset schizophrenia—defined as onset after age 40—has a 1-year prevalence rate of 0.6%3 and therefore is an unlikely cause of Mrs. L’s symptoms.
Mrs. L had no history of neurologic deficit to suggest cerebrovascular disease or space-occupying brain lesion. Her TSH, which was slightly increased when she presented in the ER, was normal on subsequent testing. Folic acid and vitamin B12 were normal. We ordered brain MRI to rule out organic causes not seen with CT, but Mrs. L felt claustrophobic in the machine and could not finish the test.
EEG was ordered to rule out epilepsy. Hallucinations can be a prominent component of seizures and are more common when the seizure focus is in the left temporal lobe.4 However, the development of psychotic symptoms often follows the onset of seizures by approximately 14 to 17 years.5 Although Mrs. L never obtained the ordered EEG, the absence of a history of clinical seizures or focal neurologic signs makes it unlikely that epilepsy accounted for her hallucinations. The normal workup ruled out most possible medical/organic causes of Mrs. L’s visual hallucinations.
We considered depression with psychotic features because Mrs. L had occasional depressed mood, feelings of worthlessness, and low self-esteem. These symptoms started only after she began losing her vision and hearing and she did not experience them most of the time. Furthermore, her predominant negative feeling was anxiety related to the hallucinations. Mrs. L had no other depressive symptoms such as guilt or loss of appetite.
Table 2
Differential diagnosis of hallucinations in elderly patients
| Diagnosis | Comments |
|---|---|
| Delirium | Secondary to a generalized medical condition, substance-induced, or substance withdrawal |
| Dementia | Alzheimer’s, vascular, Lewy body, or less common types |
| Parkinson’s disease | Medications can induce visual hallucinations |
| Brain tumor/mass/CVA | Usually accompanied by other neurologic symptoms and signs |
| Schizophrenia | Usually starts in early adulthood |
| Mood disorder with psychotic features | Depression can present as pseudodementia in elderly patients |
| Drug abuse/withdrawal or side effect | Numerous medications are known to worsen delirium in elderly patients |
| Other causes | HIV, tertiary syphilis, Charles Bonnet syndrome |
| CVA: cerebrovascular accident; HIV: human immunodeficiency virus | |
A diagnosis of exclusion
We began to suspect that Mrs. L had Charles Bonnet syndrome (CBS), a condition in which visually impaired persons experience visual hallucinations without other known mental illnesses. These hallucinations tend to be complex, vivid, and elaborate, lasting from a few seconds to most of the day.6,7 CBS occurs in 10% to 15% of patients with visual impairment, including up to 3.5% of elderly patients referred to psychiatrists for visual hallucinations.7,8 CBS is most common among the elderly because of the high prevalence of visual impairment in this population.
Many patients with CBS are aware that their hallucinations are not real.7 Mrs. L’s presentation was atypical because she believed what she was seeing was real and because most images were terrifying, which also is not usually the case in CBS.
CBS frequently goes unrecognized in clinical practice.9 Patients who admit to experiencing hallucinations often are labeled demented or psychotic.10 The course of CBS is categorized in 3 patterns:
- episodic (in this least common pattern, hallucinations occur over days to months and then resolve)
- periodic (hallucinatory activity alternates with phases of remission)
- continuous (patients experience no hallucination-free intervals).7,11
The pathophysiology of CBS is not fully understood. The deafferentation hypothesis suggests that reduced or absent visual system stimulation leads to increased excitability of areas of the cerebral cortex associated with vision, resulting in phantom vision.6,7,12
CBS has no universally accepted diagnostic criteria; it is a diagnosis of exclusion. Because we ruled out medical and organic causes, dementia, delirium, schizophrenia, and depression with psychotic features—and because Mrs. L had advanced macular degeneration and retinopathy—we believed CBS was a likely diagnosis. We referred her to an ophthalmologist, who confirmed the CBS diagnosis.
TREATMENT: Temporary improvement
We prescribe low-dose lorazepam, 0.5 to 1 mg every 8 hours as needed for agitation, and increase quetiapine to 50 mg up to twice a day as needed. These approaches fail because of excessive sedation and delayed onset of action in relation to the fast onset of Mrs. L’s hallucinations.
Based on a published report, we prescribe gabapentin, 100 mg bid, which seems to help Mrs. L. For several months, her hallucinations are reduced, and she occasionally experiences a hallucination-free day. After several months, however, the frequency of her hallucinations increases. Mrs. L refuses to take a higher dosage of gabapentin because she doesn’t like “a lot of medicine.”
Her cognitive function remains mostly stable over the next few months, with an MMSE score of 23+/-1, which is equal to 25.6 +/- 1 when corrected for unperformed tasks secondary to severe visual impairment. She develops no aphasia, apraxia, or agnosia.
Educating Mrs. L about her illness—reassuring her that she is not “crazy”—helped to decrease her anxiety, as did teaching her family to acknowledge the hallucinations and react appropriately. Mrs. L’s hallucinations are less frequent when she interacts with other people and more frequent when she is alone with less sensory stimulation. Although Mrs. L has not yet recovered, a low dose of gabapentin temporarily decreased hallucinations and anxiety.
The authors’ observations
CBS treatment is based mostly on case reports. No pharmacologic treatment is universally effective, but anticonvulsants may help reduce hallucinations.7 Low-dose gabapentin is reported to have produced permanent remission.13
Patients may benefit from using magnifiers and other low-vision devices to maximize residual sight. Increased social interaction and brighter lighting also may help.7 Reassuring the patient that the hallucinations are not real and do not indicate mental illness can be strongly therapeutic.7 Hallucinations may resolve spontaneously, with improved vision, or with increased social interaction.7
Related Resource
- Menon GJ, Rahman I, Menon SJ, et al. Complex visual hallucinations in the visually impaired: the Charles Bonnet syndrome. Surv Ophthalmol. 2003;48:58-72.
Drug Brand Names
- Donepezil • Aricept
- Gabapentin • Neurontin
- Lorazepam • Ativan
- Quetiapine • Seroquel
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Brown FW. Late-life psychosis: making the diagnosis and controlling symptoms. Geriatrics. 1998;53:26-42.
2. Lautenschlager NT, Forstl H. Organic psychosis. Curr Psychiatry Rep. 2001;3:319-325.
3. Mortensen PB, Pedersen CB, Westergaard T, et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med. 1999;340:603-608.
4. Roberts GW, Done DJ, Bruton C, et al. A “mock up” of schizophrenia: temporal lobe epilepsy and schizophrenia-like psychosis. Biol Psychiatry. 1990;28:127-143.
5. Bruton CJ, Stevens JR, Frith CD. Epilepsy, psychosis, and schizophrenia: clinical and neuropathologic correlations. Neurology. 1994;44:34-42.
6. Jacob A, Prasad S, Boggild M, et al. Charles Bonnet syndrome—elderly people and visual hallucinations. BMJ. 2004;328(7455):1552-1554.
7. Menon GJ, Rahman I, Menon SJ, et al. Complex visual hallucinations in the visually impaired: the Charles Bonnet syndrome. Surv Ophthalmol. 2003;48:58-72.
8. O’Reilly R, Chamberlaine C. Charles Bonnet syndrome: incidence and demographic and clinical features. Can J Psychiatry. 1996;41(4):259-260.
9. Brown GC, Murphy RP. Visual symptoms associated with choroidal neovascularization. Photopsias and the Charles Bonnet syndrome. Arch Ophthalmol. 1992;110(9):1251-1256.
10. Hart J. Phantom visions: real enough to touch. Elder Care. 1997;9(1):30-32.
11. de Morsier G. Le Syndrome de Charles Bonnet: hallucinations visuelles des viellards sans deficience mentale. Ann Med Psychol. 1967;125:677-702.
12. Manford M, Andermann F. Complex visual hallucinations. Clinical and neurobiological insights. Brain. 1998;121:1819-1840.
13. Paulig M, Mentrup H. Charles Bonnet’s syndrome: complete remission of complex visual hallucinations treated by gabapentin. J Neurol Neurosurg Psychiatry. 2001;70(6):813-814.
CASE: Seeing things
Family members bring Mrs. L, age 82, to the emergency room (ER) because she is agitated, nervous, and carries a knife “for protection.” In the past few months, she has been seeing things her family could not, such as bugs in her food and people trying to break into her house. Mrs. L becomes increasingly frightened and angry because her family denies seeing these things. Her family is concerned she might hurt herself or others.
Despite some hearing loss, Mrs. L had been relatively healthy and independent until a few years ago, when her vision decreased secondary to age-related macular degeneration and diabetic retinopathy. In addition to sensory impairment and diabetes mellitus, her medical history includes mild hypothyroidism and intervertebral disc herniation. She has no history of liver disease or alcohol or substance abuse. A few weeks ago Mrs. L’s primary care physician began treating her with donepezil, 5 mg/d, because he suspected dementia was causing her hallucinations. Otherwise, she has no psychiatric history.
On exam, Mrs. L is easily directable and cooperative. She seems angry because no one believes her; she reports seeing a cat that nobody else could see in the ER immediately before being evaluated. She is frightened because she believes her hallucinations are real, although she is unable to explain them. Mrs. L reports feeling anxious most of the time and having difficulty sleeping because of her fears. She also feels sad and occasionally worthless because she cannot see or hear as well as when she was younger.
A mental status examination shows partial impairment of concentration and short-term memory, but Mrs. L is alert and oriented. No theme of delusions is detected. She has no physical complaints, and physical examination is unremarkable.
The authors’ observations
Mrs. L presented with new-onset agitation, visual hallucinations, and mildly decreased concentration and short-term memory. Our next step after history and examination was to perform laboratory testing to narrow the diagnosis ( Table 1 ).
A basic electrolyte panel including kidney function can point toward electrolyte imbalance or uremia as a cause of delirium. Mrs. L’s basic metabolic panel and liver function were normal. Urinalysis ruled out urinary tract infection.
Mrs. L’s thyroid-stimulating hormone (TSH) level was mildly elevated at 5.6 mU/L (in our laboratory, the upper normal limit is 5.2 mU/L). Hypothyroidism and hyperthyroidism are not associated with hallucinations, but hyperthyroidism is an important medical cause of anxiety and hypothyroidism can cause a dementia-like presentation. CT of the head to rule out a space-occupying lesion or acute process—such as cerebrovascular accident—shows only chronic vascular changes.
Based on Mrs. L’s history, physical examination, and lab results, we provisionally diagnose dementia, Alzheimer’s type with psychotic features, and prescribe quetiapine, 25 mg at bedtime. We offer to admit Mrs. L, but she and her family prefer close outpatient follow-up. After discussing safety concerns and pharmacotherapy with the patient and her family, we discharge Mrs. L home and advise her to follow up with the psychiatric clinic.
Table 1
Suggested workup for elderly patients with hallucinations
| History and physical exam |
| History of dementia, mood disorder, Parkinson’s disease, or drug abuse |
| Presence of delusions or mood/anxiety symptoms |
| Detailed medication history |
| Level of consciousness, alertness, and cognitive function assessment (eg, MMSE) |
| Vital signs (instability may reflect delirium, meningitis/encephalitis, or intoxication) |
| Physical exam (may confirm acute medical illness causing delirium) |
| Neurologic exam (may show focal neurologic signs reflecting space-occupying lesion, signs of Parkinson’s disease, vitamin B12 deficiency) |
| Ophthalmologic history/exam |
| Investigations |
| Electrolyte imbalance, especially calcium |
| Glucose level |
| Uremia, impaired liver function, and increased ammonia |
| CBC |
| Urine drug screen |
| Urinalysis, culture, and sensitivity |
| Additional tests |
| VDRL |
| Arterial blood gas |
| ECG and cardiac enzymes |
| Chest radiography |
| Vitamin B12/folate |
| TSH |
| EEG |
| Serum drug levels |
| CT/MRI of the head |
| Lumbar puncture and cerebrospinal fluid analysis |
| Heavy metal screen |
| HIV screen |
| CBC: complete blood count; CT: computed tomography; ECG: electrocardiography; EEG: electroencephalography; HIV: human immunodeficiency virus; MMSE: Mini-Mental State Exam; MRI: magnetic resonance imaging; TSH: thyroid-stimulating hormone; VDRL: venereal disease research laboratory |
EVALUATION: Lasting hallucinations
Quetiapine improves Mrs. L’s sleep and agitation but does not reduce her hallucinations. She sees a helicopter planting wires on a tree next to her house, a snake in the house, children in her room (some are “beautiful”), fire, and creatures with scary faces. These hallucinations occur mostly when she is alone. She denies hearing or touching the things she sees but continues to feel fear and anxiety when she sees them, although this diminishes with education and reassurance.
The authors’ observations
In Mrs. L’s subsequent psychiatry clinic visits, we gather additional information that helped us rule out several differential diagnoses ( Table 2 ).
The most common causes of new-onset psychosis in later life are:
- dementia-related syndromes with psychosis, delirium, or drug-induced psychosis
- primary psychiatric disorders, most commonly depression.1
Alzheimer’s disease has been associated with up to a 60% incidence of psychotic symptoms at some point in the disease course.2 Although Mrs. L’s short-term memory had declined in recent years, she does not have aphasia, apraxia, agnosia, or decrease in mental executive functioning to meet Alzheimer’s dementia criteria.
Perceptual disturbance is a feature of delirium that can cause agitation and hallucinations in elderly patients. However, Mrs. L did not have a decreased level of consciousness or an acute medical illness that would explain delirium.
Despite Mrs. L’s symptoms and progressive hearing and vision loss with resultant disability, she generally was organized in terms of basic self-care, hygiene, and activities of daily living. She was able to have a conversation when she could hear the physician. Surprisingly, her Mini-Mental State Examination (MMSE) score was within normal limits or only mildly impaired at office visits. This was not compatible with the initial diagnosis of dementia, although it may suggest mild cognitive impairment.
Mrs. L took donepezil as prescribed by her primary care physician for only a few weeks before we stopped it. We attributed Mrs. L’s slightly impaired concentration and short-term memory in the ER to the anxiety and stress of oscillating visual hallucinations.
Schizophrenia is another cause of psychosis, but Mrs. L had no history of negative symptoms, delusions, disorganized speech/behavior, or family history of psychotic disorders. In addition, schizophrenia is most likely to appear in a patient’s third decade. Although more common in women than men, late-onset schizophrenia—defined as onset after age 40—has a 1-year prevalence rate of 0.6%3 and therefore is an unlikely cause of Mrs. L’s symptoms.
Mrs. L had no history of neurologic deficit to suggest cerebrovascular disease or space-occupying brain lesion. Her TSH, which was slightly increased when she presented in the ER, was normal on subsequent testing. Folic acid and vitamin B12 were normal. We ordered brain MRI to rule out organic causes not seen with CT, but Mrs. L felt claustrophobic in the machine and could not finish the test.
EEG was ordered to rule out epilepsy. Hallucinations can be a prominent component of seizures and are more common when the seizure focus is in the left temporal lobe.4 However, the development of psychotic symptoms often follows the onset of seizures by approximately 14 to 17 years.5 Although Mrs. L never obtained the ordered EEG, the absence of a history of clinical seizures or focal neurologic signs makes it unlikely that epilepsy accounted for her hallucinations. The normal workup ruled out most possible medical/organic causes of Mrs. L’s visual hallucinations.
We considered depression with psychotic features because Mrs. L had occasional depressed mood, feelings of worthlessness, and low self-esteem. These symptoms started only after she began losing her vision and hearing and she did not experience them most of the time. Furthermore, her predominant negative feeling was anxiety related to the hallucinations. Mrs. L had no other depressive symptoms such as guilt or loss of appetite.
Table 2
Differential diagnosis of hallucinations in elderly patients
| Diagnosis | Comments |
|---|---|
| Delirium | Secondary to a generalized medical condition, substance-induced, or substance withdrawal |
| Dementia | Alzheimer’s, vascular, Lewy body, or less common types |
| Parkinson’s disease | Medications can induce visual hallucinations |
| Brain tumor/mass/CVA | Usually accompanied by other neurologic symptoms and signs |
| Schizophrenia | Usually starts in early adulthood |
| Mood disorder with psychotic features | Depression can present as pseudodementia in elderly patients |
| Drug abuse/withdrawal or side effect | Numerous medications are known to worsen delirium in elderly patients |
| Other causes | HIV, tertiary syphilis, Charles Bonnet syndrome |
| CVA: cerebrovascular accident; HIV: human immunodeficiency virus | |
A diagnosis of exclusion
We began to suspect that Mrs. L had Charles Bonnet syndrome (CBS), a condition in which visually impaired persons experience visual hallucinations without other known mental illnesses. These hallucinations tend to be complex, vivid, and elaborate, lasting from a few seconds to most of the day.6,7 CBS occurs in 10% to 15% of patients with visual impairment, including up to 3.5% of elderly patients referred to psychiatrists for visual hallucinations.7,8 CBS is most common among the elderly because of the high prevalence of visual impairment in this population.
Many patients with CBS are aware that their hallucinations are not real.7 Mrs. L’s presentation was atypical because she believed what she was seeing was real and because most images were terrifying, which also is not usually the case in CBS.
CBS frequently goes unrecognized in clinical practice.9 Patients who admit to experiencing hallucinations often are labeled demented or psychotic.10 The course of CBS is categorized in 3 patterns:
- episodic (in this least common pattern, hallucinations occur over days to months and then resolve)
- periodic (hallucinatory activity alternates with phases of remission)
- continuous (patients experience no hallucination-free intervals).7,11
The pathophysiology of CBS is not fully understood. The deafferentation hypothesis suggests that reduced or absent visual system stimulation leads to increased excitability of areas of the cerebral cortex associated with vision, resulting in phantom vision.6,7,12
CBS has no universally accepted diagnostic criteria; it is a diagnosis of exclusion. Because we ruled out medical and organic causes, dementia, delirium, schizophrenia, and depression with psychotic features—and because Mrs. L had advanced macular degeneration and retinopathy—we believed CBS was a likely diagnosis. We referred her to an ophthalmologist, who confirmed the CBS diagnosis.
TREATMENT: Temporary improvement
We prescribe low-dose lorazepam, 0.5 to 1 mg every 8 hours as needed for agitation, and increase quetiapine to 50 mg up to twice a day as needed. These approaches fail because of excessive sedation and delayed onset of action in relation to the fast onset of Mrs. L’s hallucinations.
Based on a published report, we prescribe gabapentin, 100 mg bid, which seems to help Mrs. L. For several months, her hallucinations are reduced, and she occasionally experiences a hallucination-free day. After several months, however, the frequency of her hallucinations increases. Mrs. L refuses to take a higher dosage of gabapentin because she doesn’t like “a lot of medicine.”
Her cognitive function remains mostly stable over the next few months, with an MMSE score of 23+/-1, which is equal to 25.6 +/- 1 when corrected for unperformed tasks secondary to severe visual impairment. She develops no aphasia, apraxia, or agnosia.
Educating Mrs. L about her illness—reassuring her that she is not “crazy”—helped to decrease her anxiety, as did teaching her family to acknowledge the hallucinations and react appropriately. Mrs. L’s hallucinations are less frequent when she interacts with other people and more frequent when she is alone with less sensory stimulation. Although Mrs. L has not yet recovered, a low dose of gabapentin temporarily decreased hallucinations and anxiety.
The authors’ observations
CBS treatment is based mostly on case reports. No pharmacologic treatment is universally effective, but anticonvulsants may help reduce hallucinations.7 Low-dose gabapentin is reported to have produced permanent remission.13
Patients may benefit from using magnifiers and other low-vision devices to maximize residual sight. Increased social interaction and brighter lighting also may help.7 Reassuring the patient that the hallucinations are not real and do not indicate mental illness can be strongly therapeutic.7 Hallucinations may resolve spontaneously, with improved vision, or with increased social interaction.7
Related Resource
- Menon GJ, Rahman I, Menon SJ, et al. Complex visual hallucinations in the visually impaired: the Charles Bonnet syndrome. Surv Ophthalmol. 2003;48:58-72.
Drug Brand Names
- Donepezil • Aricept
- Gabapentin • Neurontin
- Lorazepam • Ativan
- Quetiapine • Seroquel
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Seeing things
Family members bring Mrs. L, age 82, to the emergency room (ER) because she is agitated, nervous, and carries a knife “for protection.” In the past few months, she has been seeing things her family could not, such as bugs in her food and people trying to break into her house. Mrs. L becomes increasingly frightened and angry because her family denies seeing these things. Her family is concerned she might hurt herself or others.
Despite some hearing loss, Mrs. L had been relatively healthy and independent until a few years ago, when her vision decreased secondary to age-related macular degeneration and diabetic retinopathy. In addition to sensory impairment and diabetes mellitus, her medical history includes mild hypothyroidism and intervertebral disc herniation. She has no history of liver disease or alcohol or substance abuse. A few weeks ago Mrs. L’s primary care physician began treating her with donepezil, 5 mg/d, because he suspected dementia was causing her hallucinations. Otherwise, she has no psychiatric history.
On exam, Mrs. L is easily directable and cooperative. She seems angry because no one believes her; she reports seeing a cat that nobody else could see in the ER immediately before being evaluated. She is frightened because she believes her hallucinations are real, although she is unable to explain them. Mrs. L reports feeling anxious most of the time and having difficulty sleeping because of her fears. She also feels sad and occasionally worthless because she cannot see or hear as well as when she was younger.
A mental status examination shows partial impairment of concentration and short-term memory, but Mrs. L is alert and oriented. No theme of delusions is detected. She has no physical complaints, and physical examination is unremarkable.
The authors’ observations
Mrs. L presented with new-onset agitation, visual hallucinations, and mildly decreased concentration and short-term memory. Our next step after history and examination was to perform laboratory testing to narrow the diagnosis ( Table 1 ).
A basic electrolyte panel including kidney function can point toward electrolyte imbalance or uremia as a cause of delirium. Mrs. L’s basic metabolic panel and liver function were normal. Urinalysis ruled out urinary tract infection.
Mrs. L’s thyroid-stimulating hormone (TSH) level was mildly elevated at 5.6 mU/L (in our laboratory, the upper normal limit is 5.2 mU/L). Hypothyroidism and hyperthyroidism are not associated with hallucinations, but hyperthyroidism is an important medical cause of anxiety and hypothyroidism can cause a dementia-like presentation. CT of the head to rule out a space-occupying lesion or acute process—such as cerebrovascular accident—shows only chronic vascular changes.
Based on Mrs. L’s history, physical examination, and lab results, we provisionally diagnose dementia, Alzheimer’s type with psychotic features, and prescribe quetiapine, 25 mg at bedtime. We offer to admit Mrs. L, but she and her family prefer close outpatient follow-up. After discussing safety concerns and pharmacotherapy with the patient and her family, we discharge Mrs. L home and advise her to follow up with the psychiatric clinic.
Table 1
Suggested workup for elderly patients with hallucinations
| History and physical exam |
| History of dementia, mood disorder, Parkinson’s disease, or drug abuse |
| Presence of delusions or mood/anxiety symptoms |
| Detailed medication history |
| Level of consciousness, alertness, and cognitive function assessment (eg, MMSE) |
| Vital signs (instability may reflect delirium, meningitis/encephalitis, or intoxication) |
| Physical exam (may confirm acute medical illness causing delirium) |
| Neurologic exam (may show focal neurologic signs reflecting space-occupying lesion, signs of Parkinson’s disease, vitamin B12 deficiency) |
| Ophthalmologic history/exam |
| Investigations |
| Electrolyte imbalance, especially calcium |
| Glucose level |
| Uremia, impaired liver function, and increased ammonia |
| CBC |
| Urine drug screen |
| Urinalysis, culture, and sensitivity |
| Additional tests |
| VDRL |
| Arterial blood gas |
| ECG and cardiac enzymes |
| Chest radiography |
| Vitamin B12/folate |
| TSH |
| EEG |
| Serum drug levels |
| CT/MRI of the head |
| Lumbar puncture and cerebrospinal fluid analysis |
| Heavy metal screen |
| HIV screen |
| CBC: complete blood count; CT: computed tomography; ECG: electrocardiography; EEG: electroencephalography; HIV: human immunodeficiency virus; MMSE: Mini-Mental State Exam; MRI: magnetic resonance imaging; TSH: thyroid-stimulating hormone; VDRL: venereal disease research laboratory |
EVALUATION: Lasting hallucinations
Quetiapine improves Mrs. L’s sleep and agitation but does not reduce her hallucinations. She sees a helicopter planting wires on a tree next to her house, a snake in the house, children in her room (some are “beautiful”), fire, and creatures with scary faces. These hallucinations occur mostly when she is alone. She denies hearing or touching the things she sees but continues to feel fear and anxiety when she sees them, although this diminishes with education and reassurance.
The authors’ observations
In Mrs. L’s subsequent psychiatry clinic visits, we gather additional information that helped us rule out several differential diagnoses ( Table 2 ).
The most common causes of new-onset psychosis in later life are:
- dementia-related syndromes with psychosis, delirium, or drug-induced psychosis
- primary psychiatric disorders, most commonly depression.1
Alzheimer’s disease has been associated with up to a 60% incidence of psychotic symptoms at some point in the disease course.2 Although Mrs. L’s short-term memory had declined in recent years, she does not have aphasia, apraxia, agnosia, or decrease in mental executive functioning to meet Alzheimer’s dementia criteria.
Perceptual disturbance is a feature of delirium that can cause agitation and hallucinations in elderly patients. However, Mrs. L did not have a decreased level of consciousness or an acute medical illness that would explain delirium.
Despite Mrs. L’s symptoms and progressive hearing and vision loss with resultant disability, she generally was organized in terms of basic self-care, hygiene, and activities of daily living. She was able to have a conversation when she could hear the physician. Surprisingly, her Mini-Mental State Examination (MMSE) score was within normal limits or only mildly impaired at office visits. This was not compatible with the initial diagnosis of dementia, although it may suggest mild cognitive impairment.
Mrs. L took donepezil as prescribed by her primary care physician for only a few weeks before we stopped it. We attributed Mrs. L’s slightly impaired concentration and short-term memory in the ER to the anxiety and stress of oscillating visual hallucinations.
Schizophrenia is another cause of psychosis, but Mrs. L had no history of negative symptoms, delusions, disorganized speech/behavior, or family history of psychotic disorders. In addition, schizophrenia is most likely to appear in a patient’s third decade. Although more common in women than men, late-onset schizophrenia—defined as onset after age 40—has a 1-year prevalence rate of 0.6%3 and therefore is an unlikely cause of Mrs. L’s symptoms.
Mrs. L had no history of neurologic deficit to suggest cerebrovascular disease or space-occupying brain lesion. Her TSH, which was slightly increased when she presented in the ER, was normal on subsequent testing. Folic acid and vitamin B12 were normal. We ordered brain MRI to rule out organic causes not seen with CT, but Mrs. L felt claustrophobic in the machine and could not finish the test.
EEG was ordered to rule out epilepsy. Hallucinations can be a prominent component of seizures and are more common when the seizure focus is in the left temporal lobe.4 However, the development of psychotic symptoms often follows the onset of seizures by approximately 14 to 17 years.5 Although Mrs. L never obtained the ordered EEG, the absence of a history of clinical seizures or focal neurologic signs makes it unlikely that epilepsy accounted for her hallucinations. The normal workup ruled out most possible medical/organic causes of Mrs. L’s visual hallucinations.
We considered depression with psychotic features because Mrs. L had occasional depressed mood, feelings of worthlessness, and low self-esteem. These symptoms started only after she began losing her vision and hearing and she did not experience them most of the time. Furthermore, her predominant negative feeling was anxiety related to the hallucinations. Mrs. L had no other depressive symptoms such as guilt or loss of appetite.
Table 2
Differential diagnosis of hallucinations in elderly patients
| Diagnosis | Comments |
|---|---|
| Delirium | Secondary to a generalized medical condition, substance-induced, or substance withdrawal |
| Dementia | Alzheimer’s, vascular, Lewy body, or less common types |
| Parkinson’s disease | Medications can induce visual hallucinations |
| Brain tumor/mass/CVA | Usually accompanied by other neurologic symptoms and signs |
| Schizophrenia | Usually starts in early adulthood |
| Mood disorder with psychotic features | Depression can present as pseudodementia in elderly patients |
| Drug abuse/withdrawal or side effect | Numerous medications are known to worsen delirium in elderly patients |
| Other causes | HIV, tertiary syphilis, Charles Bonnet syndrome |
| CVA: cerebrovascular accident; HIV: human immunodeficiency virus | |
A diagnosis of exclusion
We began to suspect that Mrs. L had Charles Bonnet syndrome (CBS), a condition in which visually impaired persons experience visual hallucinations without other known mental illnesses. These hallucinations tend to be complex, vivid, and elaborate, lasting from a few seconds to most of the day.6,7 CBS occurs in 10% to 15% of patients with visual impairment, including up to 3.5% of elderly patients referred to psychiatrists for visual hallucinations.7,8 CBS is most common among the elderly because of the high prevalence of visual impairment in this population.
Many patients with CBS are aware that their hallucinations are not real.7 Mrs. L’s presentation was atypical because she believed what she was seeing was real and because most images were terrifying, which also is not usually the case in CBS.
CBS frequently goes unrecognized in clinical practice.9 Patients who admit to experiencing hallucinations often are labeled demented or psychotic.10 The course of CBS is categorized in 3 patterns:
- episodic (in this least common pattern, hallucinations occur over days to months and then resolve)
- periodic (hallucinatory activity alternates with phases of remission)
- continuous (patients experience no hallucination-free intervals).7,11
The pathophysiology of CBS is not fully understood. The deafferentation hypothesis suggests that reduced or absent visual system stimulation leads to increased excitability of areas of the cerebral cortex associated with vision, resulting in phantom vision.6,7,12
CBS has no universally accepted diagnostic criteria; it is a diagnosis of exclusion. Because we ruled out medical and organic causes, dementia, delirium, schizophrenia, and depression with psychotic features—and because Mrs. L had advanced macular degeneration and retinopathy—we believed CBS was a likely diagnosis. We referred her to an ophthalmologist, who confirmed the CBS diagnosis.
TREATMENT: Temporary improvement
We prescribe low-dose lorazepam, 0.5 to 1 mg every 8 hours as needed for agitation, and increase quetiapine to 50 mg up to twice a day as needed. These approaches fail because of excessive sedation and delayed onset of action in relation to the fast onset of Mrs. L’s hallucinations.
Based on a published report, we prescribe gabapentin, 100 mg bid, which seems to help Mrs. L. For several months, her hallucinations are reduced, and she occasionally experiences a hallucination-free day. After several months, however, the frequency of her hallucinations increases. Mrs. L refuses to take a higher dosage of gabapentin because she doesn’t like “a lot of medicine.”
Her cognitive function remains mostly stable over the next few months, with an MMSE score of 23+/-1, which is equal to 25.6 +/- 1 when corrected for unperformed tasks secondary to severe visual impairment. She develops no aphasia, apraxia, or agnosia.
Educating Mrs. L about her illness—reassuring her that she is not “crazy”—helped to decrease her anxiety, as did teaching her family to acknowledge the hallucinations and react appropriately. Mrs. L’s hallucinations are less frequent when she interacts with other people and more frequent when she is alone with less sensory stimulation. Although Mrs. L has not yet recovered, a low dose of gabapentin temporarily decreased hallucinations and anxiety.
The authors’ observations
CBS treatment is based mostly on case reports. No pharmacologic treatment is universally effective, but anticonvulsants may help reduce hallucinations.7 Low-dose gabapentin is reported to have produced permanent remission.13
Patients may benefit from using magnifiers and other low-vision devices to maximize residual sight. Increased social interaction and brighter lighting also may help.7 Reassuring the patient that the hallucinations are not real and do not indicate mental illness can be strongly therapeutic.7 Hallucinations may resolve spontaneously, with improved vision, or with increased social interaction.7
Related Resource
- Menon GJ, Rahman I, Menon SJ, et al. Complex visual hallucinations in the visually impaired: the Charles Bonnet syndrome. Surv Ophthalmol. 2003;48:58-72.
Drug Brand Names
- Donepezil • Aricept
- Gabapentin • Neurontin
- Lorazepam • Ativan
- Quetiapine • Seroquel
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Brown FW. Late-life psychosis: making the diagnosis and controlling symptoms. Geriatrics. 1998;53:26-42.
2. Lautenschlager NT, Forstl H. Organic psychosis. Curr Psychiatry Rep. 2001;3:319-325.
3. Mortensen PB, Pedersen CB, Westergaard T, et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med. 1999;340:603-608.
4. Roberts GW, Done DJ, Bruton C, et al. A “mock up” of schizophrenia: temporal lobe epilepsy and schizophrenia-like psychosis. Biol Psychiatry. 1990;28:127-143.
5. Bruton CJ, Stevens JR, Frith CD. Epilepsy, psychosis, and schizophrenia: clinical and neuropathologic correlations. Neurology. 1994;44:34-42.
6. Jacob A, Prasad S, Boggild M, et al. Charles Bonnet syndrome—elderly people and visual hallucinations. BMJ. 2004;328(7455):1552-1554.
7. Menon GJ, Rahman I, Menon SJ, et al. Complex visual hallucinations in the visually impaired: the Charles Bonnet syndrome. Surv Ophthalmol. 2003;48:58-72.
8. O’Reilly R, Chamberlaine C. Charles Bonnet syndrome: incidence and demographic and clinical features. Can J Psychiatry. 1996;41(4):259-260.
9. Brown GC, Murphy RP. Visual symptoms associated with choroidal neovascularization. Photopsias and the Charles Bonnet syndrome. Arch Ophthalmol. 1992;110(9):1251-1256.
10. Hart J. Phantom visions: real enough to touch. Elder Care. 1997;9(1):30-32.
11. de Morsier G. Le Syndrome de Charles Bonnet: hallucinations visuelles des viellards sans deficience mentale. Ann Med Psychol. 1967;125:677-702.
12. Manford M, Andermann F. Complex visual hallucinations. Clinical and neurobiological insights. Brain. 1998;121:1819-1840.
13. Paulig M, Mentrup H. Charles Bonnet’s syndrome: complete remission of complex visual hallucinations treated by gabapentin. J Neurol Neurosurg Psychiatry. 2001;70(6):813-814.
1. Brown FW. Late-life psychosis: making the diagnosis and controlling symptoms. Geriatrics. 1998;53:26-42.
2. Lautenschlager NT, Forstl H. Organic psychosis. Curr Psychiatry Rep. 2001;3:319-325.
3. Mortensen PB, Pedersen CB, Westergaard T, et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med. 1999;340:603-608.
4. Roberts GW, Done DJ, Bruton C, et al. A “mock up” of schizophrenia: temporal lobe epilepsy and schizophrenia-like psychosis. Biol Psychiatry. 1990;28:127-143.
5. Bruton CJ, Stevens JR, Frith CD. Epilepsy, psychosis, and schizophrenia: clinical and neuropathologic correlations. Neurology. 1994;44:34-42.
6. Jacob A, Prasad S, Boggild M, et al. Charles Bonnet syndrome—elderly people and visual hallucinations. BMJ. 2004;328(7455):1552-1554.
7. Menon GJ, Rahman I, Menon SJ, et al. Complex visual hallucinations in the visually impaired: the Charles Bonnet syndrome. Surv Ophthalmol. 2003;48:58-72.
8. O’Reilly R, Chamberlaine C. Charles Bonnet syndrome: incidence and demographic and clinical features. Can J Psychiatry. 1996;41(4):259-260.
9. Brown GC, Murphy RP. Visual symptoms associated with choroidal neovascularization. Photopsias and the Charles Bonnet syndrome. Arch Ophthalmol. 1992;110(9):1251-1256.
10. Hart J. Phantom visions: real enough to touch. Elder Care. 1997;9(1):30-32.
11. de Morsier G. Le Syndrome de Charles Bonnet: hallucinations visuelles des viellards sans deficience mentale. Ann Med Psychol. 1967;125:677-702.
12. Manford M, Andermann F. Complex visual hallucinations. Clinical and neurobiological insights. Brain. 1998;121:1819-1840.
13. Paulig M, Mentrup H. Charles Bonnet’s syndrome: complete remission of complex visual hallucinations treated by gabapentin. J Neurol Neurosurg Psychiatry. 2001;70(6):813-814.
The bedtime solution
CASE: Refractory depression
Ms. W, age 38, is brought to the emergency department after her son finds her unresponsive and calls 911. Suffering from worsening depression, she wrote a note telling her children goodbye, and overdosed on zolpidem from an old prescription and her daughter’s opioids. After being evaluated and medically cleared in the emergency department, Ms. W was admitted to the psychiatric unit.
Ms. W has a history of recurrent major depressive disorder that developed after she was sexually abused by a relative as a teen. She also has bulimia nervosa, alcohol dependence, and posttraumatic stress disorder. She was hospitalized twice for depression and suicidality but had not previously attempted suicide. In the mid-to-late 1990s, she had trials of paroxetine, clomipramine, lithium, and bupropion.
She was seen regularly in our outpatient psychiatry clinic for medication management and supportive psychotherapy. Since being followed in our clinic starting in early 2005, she has had the following medication trials:
- fluoxetine, citalopram, venlafaxine XR, and duloxetine for depression
- atomoxetine, buspirone, liothyronine, risperidone, and aripiprazole for antidepressant augmentation
- lorazepam, clonazepam, and gabapentin for anxiety
- zolpidem and trazodone for insomnia
- nortriptyline for migraine headache prophylaxis.
Some medications were not tolerated, primarily because of increased anxiety. Those that were tolerated were adequate trials in terms of dose titration and length. High-dose fluoxetine (80 mg/d) augmented by risperidone (0.375 to 0.5 mg/d) produced the most reliable and significant improvement.
Ms. W had 2 courses of electroconvulsive therapy (ECT) totaling 30 treatments—most recently in 2007—that resulted in significant memory loss with limited benefit. Premenstrual worsening of depression and suicidality were noted. In collaboration with her gynecologist, Ms. W was treated with a 3-month trial of leuprolide to suppress her ovarian axis, which was helpful. In 2008 she underwent bilateral oophorectomy. She has not had symptoms of mood elevation or psychosis. Family history includes schizophrenia, depression, anxiety, and alcoholism.
In the months before hospitalization, Ms. W had been increasingly depressed and intermittently suicidal, although she did not endorse a specific plan or intention to harm herself because she was concerned about the impact suicide would have on her children. Weight gain with risperidone had reactivated body image issues, so Ms. W stopped taking this medication 2 weeks before hospitalization. Her depression became worse, and she began using her husband’s hydrocodone/acetaminophen prescription.
The authors’ observations
Approximately 40% of patients with major depression fail to respond to an initial antidepressant trial.1 An additional 50% of these patients will be treatment-resistant to a subsequent antidepressant.1 Patients may be progressively less likely to respond to additional medication trials.2
One of the most rapid-acting and effective treatments for unipolar and bipolar depression is sleep deprivation. Wirz-Justice et al3 found total or partial sleep deprivation during the second half of the night induced rapid depression remission. Response rates range from 40% to 60% over hours to days.4 Sleep deprivation also can reduce suicidality in patients with seasonal depression.5 This treatment has not been widely employed, however, because up to 80% of patients who undergo sleep deprivation experience rapid and significant depressive relapse.4
Sleep deprivation usually is well tolerated. Potential side effects include:
- headache
- gastrointestinal upset
- fatigue
- cognitive impairment.
Less often, patients report worsening of depressive symptoms and, rarely, suicidal ideation or psychosis.4 Mania or hypomania are potential complications of sleep loss for patients with bipolar or unipolar depression. In a review, Oliwenstein6 suggested that rates of total sleep deprivation-induced mania are likely to be similar to or less than those reported for antidepressants. Because sleep deprivation can induce seizures, this therapy is contraindicated for patients with epilepsy or those at risk for seizures.4
Researchers have successfully explored strategies to reduce the rate of depressive relapse after sleep deprivation, including coadministering light therapy, antidepressants, lithium (particularly for bipolar depression), and sleep-phase advance.4 Sleep-phase advance involves shifting the sleep-wake schedule to a very early sleep time and wake-up time (such as 5 PM to midnight) for 1 day, and then pushing back this schedule by 1 or 2 hours each day until the patient is returned to a “normal” sleep schedule (such as 10 PM to 5 AM). Researchers have demonstrated that sleep-phase advance can have antidepressant effects.7
TREATMENT: Sleep manipulation
Ms. W is continued on fluoxetine, 80 mg/d. We opt for a trial of partial sleep deprivation and sleep-phase advance for Ms. W because of the severity of her depression, her multiple ineffective or poorly tolerated medication trials, and limited benefit from ECT. This treatment involves instituting partial sleep deprivation the first night and subsequently advancing her sleep phase over the next several days (Table 1).
Although she is sleepy the morning after partial sleep deprivation, Ms. W reports a marked improvement in her mood, decline in hopelessness, and absence of suicidal ideation. She continues the sleep-phase advance protocol for the next 3 nights and participates in cognitive-behavioral therapy groups and ward activities. Psychiatric unit staff support her continued wakefulness during sleep manipulation. Because Ms. W had previously responded to antidepressant augmentation with an atypical antipsychotic we add aripiprazole and titrate the dosage to 7.5 mg/d. We also continue fluoxetine, 80 mg/d, and add trazodone, 100 mg at bedtime, and hydroxyzine, 25 mg as needed.
Table 1
Ms. W’s chronotherapy protocol: Hours permitted for sleep*
| Day number | |||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Sleep deprivation | 9 PM to2 AM | ||||
| Sleep-phase advance | 5 PM to midnight | 7 PM to 2 AM | 9 PM to 4 AM | 10 PM to 5 AM | |
| *Treatment was implemented while Ms. W was hospitalized | |||||
The authors’ observations
Chronotherapy incorporates manipulations of the sleep/wake cycle such as sleep deprivation and dark or light therapy. It may use combinations of interventions to generate and sustain a response in patients with depression. In a 4-week pilot study, Moscovici et al8 employed a regimen of late partial sleep deprivation, light, and sleep-phase advance to generate and maintain an anti depressant response in 12 patients. Benedetti et al9 used a similar regimen plus lithium to successfully treat bipolar depression and sleep-phase advance to continue that response in 50% of patients for 3 months.
Circadian rhythms affect the function of serotonin (5-HT), norepinephrine, and dopamine.9,10 In a manner similar to antidepressant medications, sleep deprivation may up-regulate or otherwise alter these neurotransmitters’ function. In animals, sleep deprivation increases serotonin function.11 Several hypothetical mechanisms of action for sleep deprivation and other types of chronotherapies have been suggested (Table 2).11-14
Chronotherapies may affect function in brain pathways, as demonstrated by neuroimaging with positron emission tomography (PET) and functional magnetic resonance imaging (fMRI). Depression has been associated with increased or decreased brain activity measured by PET or fMRI in regions of the limbic cortex (cingulate and anterior cingulate) and frontal cortex.12
Wu et al13 examined patients treated for depression with medication and total sleep deprivation therapy. Response to treatment was associated with increased function in the cingulate, anterior cingulate, and medial prefrontal cortex as measured by PET. In contrast, mood improvement was associated with reduced baseline activity in the left medial prefrontal cortex, left frontal pole, and right lateral prefrontal cortex.
Researchers have noted the convergence of sleep-wake rhythms and abnormalities seen in depression and the subsequent link with improved sleep-wake cycles related to depression remission. Bunney and Potkin14 note the powerful effect of zeitgebers—environmental agents that reset the body’s internal clock. They suggested that sleep deprivation may affect the function of “master clock” genes involved in controlling the biological clock. These effects on the suprachiasmatic nucleus hypothalamic pacemaker may improve mood by altering control of genetic expression through chromatin remodeling of this master clock circuit.
Certain factors may increase the likelihood that a patient may respond to chronotherapy (Table 3).9,15-17
Table 2
Sleep deprivation for depression: Possible mechanisms
| Mechanism | Components |
|---|---|
| Alterations to neurotransmitter function | Serotonin, norepinephrine, dopamine11 |
| Alterations to endogenous circadian pacemaker function | Increased gene expression14 |
| Changes in perfusion/activity of brain regions | Anterior cingulate, frontal cortex regions12,13 |
Table 3
Factors that suggest a patient might respond to chronotherapy
| Diurnal mood variation15 |
| Endogenous depression including insomnia and anorexia16 |
| Abnormal dexamethasone suppression17 |
| High motivation for treatment |
| Bipolar depression (possibly)9 |
OUTCOME: Lasting improvement
Ms. W’s mood improvement is sustained during her week-long hospitalization. At discharge she is hopeful about the future and does not have thoughts of suicide.
At subsequent outpatient visits up to 4 months after discharge, her depressive symptoms remain improved. Patient Health Questionnaire scores indicate mild depression, but Ms. W is not suicidal. She maintains a sleep schedule of 10 PM to 6:30 AM and undergoes 10,000 lux bright light therapy, which she began shortly after discharge, for 30 minutes every morning. She works more productively in psychotherapy, focusing on her eating disorder and anxiety.
Related resource
- Wu JC, Kelsoe JR, Schachat C, et al. Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry. 2009; 66(3): 298-301.
Drug brand names
- Aripiprazole • Abilify
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clonazepam • Klonopin
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Gabapentin • Neurontin
- Hydrocodone/APAP • Vicodin
- Hydroxyzine • Atarax, Vistaril
- Leuprolide • Lupron
- Liothyronine • Cytomel
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Nortriptyline • Aventyl
- Paroxetine • Paxil
- Risperidone • Risperdal, Risperdal Consta
- Trazodone • Desyrel
- Venlafaxine XR • Effexor XR
- Zolpidem • Ambien
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. AHCPR Depression Guideline Panel. Clinical practice guideline number 5. Depression in primary care. Volume 2: Treatment of major depression. Rockville, MD: Agency for Health Care Policy and Research, Public Health Services, U.S. Department of Health and Human Services; 1993. AHCPR publication 93-0550.
2. Fava M, Rush JA, Wisniewski SR, et al. A comparison of mirtazapine and nortriptyline following two consecutive failed medication treatments for depressed outpatients: a STAR*D report. Am J Psychiatry. 2006;163(7):1161-1172.
3. Wirz-Justice A, Benedetti F, Berger M. Chronotherapeutics (light and wake therapy) in affective disorders. Psychol Med. 2005;35(7):939-944.
4. Giedke H, Schwärzler F. Therapeutic use of sleep deprivation in depression. Sleep Med Rev. 2002;6(5):361-377.
5. Lam RW, Tam EM, Shiah IS, et al. Effects of light therapy on suicidal ideation in patients with winter depression. J Clin Psychiatry. 2000;61(1):30-32.
6. Oliwenstein L. Lifting moods by losing sleep: an adjunct therapy for treating depression. Alternative and Complementary Therapies. 2006;12(2):66-70.
7. Wehr TA, Wirz-Justice A, Goodwin FK, et al. Phase advance of the circadian sleep-wake cycle as an antidepressant. Science. 1979;206(4419):710-713.
8. Moscovici L, Kotler M. A multistage chronobiologic intervention for the treatment of depression: a pilot study. J Affect Disord. 2009;116(3):201-217.
9. Benedetti F, Colombo C, Barbini B, et al. Morning sunlight reduces length of hospitalization in bipolar depression. J Affect Disord. 2001;62(3):221-223.
10. Benedetti F, Barbini B, Colombo C, et al. Chronotherapeutics in a psychiatric ward. Sleep Med Rev. 2007;11(6):509-522.
11. Lopez-Rodriguez F, Wilson CL, Maidment NT, et al. Total sleep deprivation increases extracellular serotonin in the rat hippocampus. Neuroscience. 2003;121(2):523-530.
12. Mayberg HS. Defining the neural circuitry of depression: toward a new nosology with therapeutic implications. Biol Psychiatry. 2007;61(6):729-730.
13. Wu JC, Gillin JC, Buchsbaum MS, et al. Sleep deprivation PET correlations of Hamilton symptom improvement ratings with changes in relative glucose metabolism in patients with depression. J Affect Disord. 2008;107(1-3):181-186.
14. Bunney JN, Potkin SG. Circadian abnormalities, molecular clock genes and chronobiological treatments in depression. Br Med Bull. 2008;86:23-32.
15. Benedetti F, Barbini B, Lucca A, et al. Sleep deprivation hastens the antidepressant action of fluoxetine. Eur Arch Psychiatry Clin Neurosci. 1997;247(2):100-103.
16. Vogel GW, Thurmond A, Gibbons P, et al. REM sleep reduction effects on depression syndromes. Arch Gen Psychiatry. 1975;32(6):765-777.
17. King D, Dowdy S, Jack R, et al. The dexamethasone suppression test as a predictor of sleep deprivation antidepressant effect. Psychiatry Res. 1982;7(1):93-99.
CASE: Refractory depression
Ms. W, age 38, is brought to the emergency department after her son finds her unresponsive and calls 911. Suffering from worsening depression, she wrote a note telling her children goodbye, and overdosed on zolpidem from an old prescription and her daughter’s opioids. After being evaluated and medically cleared in the emergency department, Ms. W was admitted to the psychiatric unit.
Ms. W has a history of recurrent major depressive disorder that developed after she was sexually abused by a relative as a teen. She also has bulimia nervosa, alcohol dependence, and posttraumatic stress disorder. She was hospitalized twice for depression and suicidality but had not previously attempted suicide. In the mid-to-late 1990s, she had trials of paroxetine, clomipramine, lithium, and bupropion.
She was seen regularly in our outpatient psychiatry clinic for medication management and supportive psychotherapy. Since being followed in our clinic starting in early 2005, she has had the following medication trials:
- fluoxetine, citalopram, venlafaxine XR, and duloxetine for depression
- atomoxetine, buspirone, liothyronine, risperidone, and aripiprazole for antidepressant augmentation
- lorazepam, clonazepam, and gabapentin for anxiety
- zolpidem and trazodone for insomnia
- nortriptyline for migraine headache prophylaxis.
Some medications were not tolerated, primarily because of increased anxiety. Those that were tolerated were adequate trials in terms of dose titration and length. High-dose fluoxetine (80 mg/d) augmented by risperidone (0.375 to 0.5 mg/d) produced the most reliable and significant improvement.
Ms. W had 2 courses of electroconvulsive therapy (ECT) totaling 30 treatments—most recently in 2007—that resulted in significant memory loss with limited benefit. Premenstrual worsening of depression and suicidality were noted. In collaboration with her gynecologist, Ms. W was treated with a 3-month trial of leuprolide to suppress her ovarian axis, which was helpful. In 2008 she underwent bilateral oophorectomy. She has not had symptoms of mood elevation or psychosis. Family history includes schizophrenia, depression, anxiety, and alcoholism.
In the months before hospitalization, Ms. W had been increasingly depressed and intermittently suicidal, although she did not endorse a specific plan or intention to harm herself because she was concerned about the impact suicide would have on her children. Weight gain with risperidone had reactivated body image issues, so Ms. W stopped taking this medication 2 weeks before hospitalization. Her depression became worse, and she began using her husband’s hydrocodone/acetaminophen prescription.
The authors’ observations
Approximately 40% of patients with major depression fail to respond to an initial antidepressant trial.1 An additional 50% of these patients will be treatment-resistant to a subsequent antidepressant.1 Patients may be progressively less likely to respond to additional medication trials.2
One of the most rapid-acting and effective treatments for unipolar and bipolar depression is sleep deprivation. Wirz-Justice et al3 found total or partial sleep deprivation during the second half of the night induced rapid depression remission. Response rates range from 40% to 60% over hours to days.4 Sleep deprivation also can reduce suicidality in patients with seasonal depression.5 This treatment has not been widely employed, however, because up to 80% of patients who undergo sleep deprivation experience rapid and significant depressive relapse.4
Sleep deprivation usually is well tolerated. Potential side effects include:
- headache
- gastrointestinal upset
- fatigue
- cognitive impairment.
Less often, patients report worsening of depressive symptoms and, rarely, suicidal ideation or psychosis.4 Mania or hypomania are potential complications of sleep loss for patients with bipolar or unipolar depression. In a review, Oliwenstein6 suggested that rates of total sleep deprivation-induced mania are likely to be similar to or less than those reported for antidepressants. Because sleep deprivation can induce seizures, this therapy is contraindicated for patients with epilepsy or those at risk for seizures.4
Researchers have successfully explored strategies to reduce the rate of depressive relapse after sleep deprivation, including coadministering light therapy, antidepressants, lithium (particularly for bipolar depression), and sleep-phase advance.4 Sleep-phase advance involves shifting the sleep-wake schedule to a very early sleep time and wake-up time (such as 5 PM to midnight) for 1 day, and then pushing back this schedule by 1 or 2 hours each day until the patient is returned to a “normal” sleep schedule (such as 10 PM to 5 AM). Researchers have demonstrated that sleep-phase advance can have antidepressant effects.7
TREATMENT: Sleep manipulation
Ms. W is continued on fluoxetine, 80 mg/d. We opt for a trial of partial sleep deprivation and sleep-phase advance for Ms. W because of the severity of her depression, her multiple ineffective or poorly tolerated medication trials, and limited benefit from ECT. This treatment involves instituting partial sleep deprivation the first night and subsequently advancing her sleep phase over the next several days (Table 1).
Although she is sleepy the morning after partial sleep deprivation, Ms. W reports a marked improvement in her mood, decline in hopelessness, and absence of suicidal ideation. She continues the sleep-phase advance protocol for the next 3 nights and participates in cognitive-behavioral therapy groups and ward activities. Psychiatric unit staff support her continued wakefulness during sleep manipulation. Because Ms. W had previously responded to antidepressant augmentation with an atypical antipsychotic we add aripiprazole and titrate the dosage to 7.5 mg/d. We also continue fluoxetine, 80 mg/d, and add trazodone, 100 mg at bedtime, and hydroxyzine, 25 mg as needed.
Table 1
Ms. W’s chronotherapy protocol: Hours permitted for sleep*
| Day number | |||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Sleep deprivation | 9 PM to2 AM | ||||
| Sleep-phase advance | 5 PM to midnight | 7 PM to 2 AM | 9 PM to 4 AM | 10 PM to 5 AM | |
| *Treatment was implemented while Ms. W was hospitalized | |||||
The authors’ observations
Chronotherapy incorporates manipulations of the sleep/wake cycle such as sleep deprivation and dark or light therapy. It may use combinations of interventions to generate and sustain a response in patients with depression. In a 4-week pilot study, Moscovici et al8 employed a regimen of late partial sleep deprivation, light, and sleep-phase advance to generate and maintain an anti depressant response in 12 patients. Benedetti et al9 used a similar regimen plus lithium to successfully treat bipolar depression and sleep-phase advance to continue that response in 50% of patients for 3 months.
Circadian rhythms affect the function of serotonin (5-HT), norepinephrine, and dopamine.9,10 In a manner similar to antidepressant medications, sleep deprivation may up-regulate or otherwise alter these neurotransmitters’ function. In animals, sleep deprivation increases serotonin function.11 Several hypothetical mechanisms of action for sleep deprivation and other types of chronotherapies have been suggested (Table 2).11-14
Chronotherapies may affect function in brain pathways, as demonstrated by neuroimaging with positron emission tomography (PET) and functional magnetic resonance imaging (fMRI). Depression has been associated with increased or decreased brain activity measured by PET or fMRI in regions of the limbic cortex (cingulate and anterior cingulate) and frontal cortex.12
Wu et al13 examined patients treated for depression with medication and total sleep deprivation therapy. Response to treatment was associated with increased function in the cingulate, anterior cingulate, and medial prefrontal cortex as measured by PET. In contrast, mood improvement was associated with reduced baseline activity in the left medial prefrontal cortex, left frontal pole, and right lateral prefrontal cortex.
Researchers have noted the convergence of sleep-wake rhythms and abnormalities seen in depression and the subsequent link with improved sleep-wake cycles related to depression remission. Bunney and Potkin14 note the powerful effect of zeitgebers—environmental agents that reset the body’s internal clock. They suggested that sleep deprivation may affect the function of “master clock” genes involved in controlling the biological clock. These effects on the suprachiasmatic nucleus hypothalamic pacemaker may improve mood by altering control of genetic expression through chromatin remodeling of this master clock circuit.
Certain factors may increase the likelihood that a patient may respond to chronotherapy (Table 3).9,15-17
Table 2
Sleep deprivation for depression: Possible mechanisms
| Mechanism | Components |
|---|---|
| Alterations to neurotransmitter function | Serotonin, norepinephrine, dopamine11 |
| Alterations to endogenous circadian pacemaker function | Increased gene expression14 |
| Changes in perfusion/activity of brain regions | Anterior cingulate, frontal cortex regions12,13 |
Table 3
Factors that suggest a patient might respond to chronotherapy
| Diurnal mood variation15 |
| Endogenous depression including insomnia and anorexia16 |
| Abnormal dexamethasone suppression17 |
| High motivation for treatment |
| Bipolar depression (possibly)9 |
OUTCOME: Lasting improvement
Ms. W’s mood improvement is sustained during her week-long hospitalization. At discharge she is hopeful about the future and does not have thoughts of suicide.
At subsequent outpatient visits up to 4 months after discharge, her depressive symptoms remain improved. Patient Health Questionnaire scores indicate mild depression, but Ms. W is not suicidal. She maintains a sleep schedule of 10 PM to 6:30 AM and undergoes 10,000 lux bright light therapy, which she began shortly after discharge, for 30 minutes every morning. She works more productively in psychotherapy, focusing on her eating disorder and anxiety.
Related resource
- Wu JC, Kelsoe JR, Schachat C, et al. Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry. 2009; 66(3): 298-301.
Drug brand names
- Aripiprazole • Abilify
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clonazepam • Klonopin
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Gabapentin • Neurontin
- Hydrocodone/APAP • Vicodin
- Hydroxyzine • Atarax, Vistaril
- Leuprolide • Lupron
- Liothyronine • Cytomel
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Nortriptyline • Aventyl
- Paroxetine • Paxil
- Risperidone • Risperdal, Risperdal Consta
- Trazodone • Desyrel
- Venlafaxine XR • Effexor XR
- Zolpidem • Ambien
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Refractory depression
Ms. W, age 38, is brought to the emergency department after her son finds her unresponsive and calls 911. Suffering from worsening depression, she wrote a note telling her children goodbye, and overdosed on zolpidem from an old prescription and her daughter’s opioids. After being evaluated and medically cleared in the emergency department, Ms. W was admitted to the psychiatric unit.
Ms. W has a history of recurrent major depressive disorder that developed after she was sexually abused by a relative as a teen. She also has bulimia nervosa, alcohol dependence, and posttraumatic stress disorder. She was hospitalized twice for depression and suicidality but had not previously attempted suicide. In the mid-to-late 1990s, she had trials of paroxetine, clomipramine, lithium, and bupropion.
She was seen regularly in our outpatient psychiatry clinic for medication management and supportive psychotherapy. Since being followed in our clinic starting in early 2005, she has had the following medication trials:
- fluoxetine, citalopram, venlafaxine XR, and duloxetine for depression
- atomoxetine, buspirone, liothyronine, risperidone, and aripiprazole for antidepressant augmentation
- lorazepam, clonazepam, and gabapentin for anxiety
- zolpidem and trazodone for insomnia
- nortriptyline for migraine headache prophylaxis.
Some medications were not tolerated, primarily because of increased anxiety. Those that were tolerated were adequate trials in terms of dose titration and length. High-dose fluoxetine (80 mg/d) augmented by risperidone (0.375 to 0.5 mg/d) produced the most reliable and significant improvement.
Ms. W had 2 courses of electroconvulsive therapy (ECT) totaling 30 treatments—most recently in 2007—that resulted in significant memory loss with limited benefit. Premenstrual worsening of depression and suicidality were noted. In collaboration with her gynecologist, Ms. W was treated with a 3-month trial of leuprolide to suppress her ovarian axis, which was helpful. In 2008 she underwent bilateral oophorectomy. She has not had symptoms of mood elevation or psychosis. Family history includes schizophrenia, depression, anxiety, and alcoholism.
In the months before hospitalization, Ms. W had been increasingly depressed and intermittently suicidal, although she did not endorse a specific plan or intention to harm herself because she was concerned about the impact suicide would have on her children. Weight gain with risperidone had reactivated body image issues, so Ms. W stopped taking this medication 2 weeks before hospitalization. Her depression became worse, and she began using her husband’s hydrocodone/acetaminophen prescription.
The authors’ observations
Approximately 40% of patients with major depression fail to respond to an initial antidepressant trial.1 An additional 50% of these patients will be treatment-resistant to a subsequent antidepressant.1 Patients may be progressively less likely to respond to additional medication trials.2
One of the most rapid-acting and effective treatments for unipolar and bipolar depression is sleep deprivation. Wirz-Justice et al3 found total or partial sleep deprivation during the second half of the night induced rapid depression remission. Response rates range from 40% to 60% over hours to days.4 Sleep deprivation also can reduce suicidality in patients with seasonal depression.5 This treatment has not been widely employed, however, because up to 80% of patients who undergo sleep deprivation experience rapid and significant depressive relapse.4
Sleep deprivation usually is well tolerated. Potential side effects include:
- headache
- gastrointestinal upset
- fatigue
- cognitive impairment.
Less often, patients report worsening of depressive symptoms and, rarely, suicidal ideation or psychosis.4 Mania or hypomania are potential complications of sleep loss for patients with bipolar or unipolar depression. In a review, Oliwenstein6 suggested that rates of total sleep deprivation-induced mania are likely to be similar to or less than those reported for antidepressants. Because sleep deprivation can induce seizures, this therapy is contraindicated for patients with epilepsy or those at risk for seizures.4
Researchers have successfully explored strategies to reduce the rate of depressive relapse after sleep deprivation, including coadministering light therapy, antidepressants, lithium (particularly for bipolar depression), and sleep-phase advance.4 Sleep-phase advance involves shifting the sleep-wake schedule to a very early sleep time and wake-up time (such as 5 PM to midnight) for 1 day, and then pushing back this schedule by 1 or 2 hours each day until the patient is returned to a “normal” sleep schedule (such as 10 PM to 5 AM). Researchers have demonstrated that sleep-phase advance can have antidepressant effects.7
TREATMENT: Sleep manipulation
Ms. W is continued on fluoxetine, 80 mg/d. We opt for a trial of partial sleep deprivation and sleep-phase advance for Ms. W because of the severity of her depression, her multiple ineffective or poorly tolerated medication trials, and limited benefit from ECT. This treatment involves instituting partial sleep deprivation the first night and subsequently advancing her sleep phase over the next several days (Table 1).
Although she is sleepy the morning after partial sleep deprivation, Ms. W reports a marked improvement in her mood, decline in hopelessness, and absence of suicidal ideation. She continues the sleep-phase advance protocol for the next 3 nights and participates in cognitive-behavioral therapy groups and ward activities. Psychiatric unit staff support her continued wakefulness during sleep manipulation. Because Ms. W had previously responded to antidepressant augmentation with an atypical antipsychotic we add aripiprazole and titrate the dosage to 7.5 mg/d. We also continue fluoxetine, 80 mg/d, and add trazodone, 100 mg at bedtime, and hydroxyzine, 25 mg as needed.
Table 1
Ms. W’s chronotherapy protocol: Hours permitted for sleep*
| Day number | |||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Sleep deprivation | 9 PM to2 AM | ||||
| Sleep-phase advance | 5 PM to midnight | 7 PM to 2 AM | 9 PM to 4 AM | 10 PM to 5 AM | |
| *Treatment was implemented while Ms. W was hospitalized | |||||
The authors’ observations
Chronotherapy incorporates manipulations of the sleep/wake cycle such as sleep deprivation and dark or light therapy. It may use combinations of interventions to generate and sustain a response in patients with depression. In a 4-week pilot study, Moscovici et al8 employed a regimen of late partial sleep deprivation, light, and sleep-phase advance to generate and maintain an anti depressant response in 12 patients. Benedetti et al9 used a similar regimen plus lithium to successfully treat bipolar depression and sleep-phase advance to continue that response in 50% of patients for 3 months.
Circadian rhythms affect the function of serotonin (5-HT), norepinephrine, and dopamine.9,10 In a manner similar to antidepressant medications, sleep deprivation may up-regulate or otherwise alter these neurotransmitters’ function. In animals, sleep deprivation increases serotonin function.11 Several hypothetical mechanisms of action for sleep deprivation and other types of chronotherapies have been suggested (Table 2).11-14
Chronotherapies may affect function in brain pathways, as demonstrated by neuroimaging with positron emission tomography (PET) and functional magnetic resonance imaging (fMRI). Depression has been associated with increased or decreased brain activity measured by PET or fMRI in regions of the limbic cortex (cingulate and anterior cingulate) and frontal cortex.12
Wu et al13 examined patients treated for depression with medication and total sleep deprivation therapy. Response to treatment was associated with increased function in the cingulate, anterior cingulate, and medial prefrontal cortex as measured by PET. In contrast, mood improvement was associated with reduced baseline activity in the left medial prefrontal cortex, left frontal pole, and right lateral prefrontal cortex.
Researchers have noted the convergence of sleep-wake rhythms and abnormalities seen in depression and the subsequent link with improved sleep-wake cycles related to depression remission. Bunney and Potkin14 note the powerful effect of zeitgebers—environmental agents that reset the body’s internal clock. They suggested that sleep deprivation may affect the function of “master clock” genes involved in controlling the biological clock. These effects on the suprachiasmatic nucleus hypothalamic pacemaker may improve mood by altering control of genetic expression through chromatin remodeling of this master clock circuit.
Certain factors may increase the likelihood that a patient may respond to chronotherapy (Table 3).9,15-17
Table 2
Sleep deprivation for depression: Possible mechanisms
| Mechanism | Components |
|---|---|
| Alterations to neurotransmitter function | Serotonin, norepinephrine, dopamine11 |
| Alterations to endogenous circadian pacemaker function | Increased gene expression14 |
| Changes in perfusion/activity of brain regions | Anterior cingulate, frontal cortex regions12,13 |
Table 3
Factors that suggest a patient might respond to chronotherapy
| Diurnal mood variation15 |
| Endogenous depression including insomnia and anorexia16 |
| Abnormal dexamethasone suppression17 |
| High motivation for treatment |
| Bipolar depression (possibly)9 |
OUTCOME: Lasting improvement
Ms. W’s mood improvement is sustained during her week-long hospitalization. At discharge she is hopeful about the future and does not have thoughts of suicide.
At subsequent outpatient visits up to 4 months after discharge, her depressive symptoms remain improved. Patient Health Questionnaire scores indicate mild depression, but Ms. W is not suicidal. She maintains a sleep schedule of 10 PM to 6:30 AM and undergoes 10,000 lux bright light therapy, which she began shortly after discharge, for 30 minutes every morning. She works more productively in psychotherapy, focusing on her eating disorder and anxiety.
Related resource
- Wu JC, Kelsoe JR, Schachat C, et al. Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry. 2009; 66(3): 298-301.
Drug brand names
- Aripiprazole • Abilify
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Buspirone • BuSpar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clonazepam • Klonopin
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Gabapentin • Neurontin
- Hydrocodone/APAP • Vicodin
- Hydroxyzine • Atarax, Vistaril
- Leuprolide • Lupron
- Liothyronine • Cytomel
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Nortriptyline • Aventyl
- Paroxetine • Paxil
- Risperidone • Risperdal, Risperdal Consta
- Trazodone • Desyrel
- Venlafaxine XR • Effexor XR
- Zolpidem • Ambien
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. AHCPR Depression Guideline Panel. Clinical practice guideline number 5. Depression in primary care. Volume 2: Treatment of major depression. Rockville, MD: Agency for Health Care Policy and Research, Public Health Services, U.S. Department of Health and Human Services; 1993. AHCPR publication 93-0550.
2. Fava M, Rush JA, Wisniewski SR, et al. A comparison of mirtazapine and nortriptyline following two consecutive failed medication treatments for depressed outpatients: a STAR*D report. Am J Psychiatry. 2006;163(7):1161-1172.
3. Wirz-Justice A, Benedetti F, Berger M. Chronotherapeutics (light and wake therapy) in affective disorders. Psychol Med. 2005;35(7):939-944.
4. Giedke H, Schwärzler F. Therapeutic use of sleep deprivation in depression. Sleep Med Rev. 2002;6(5):361-377.
5. Lam RW, Tam EM, Shiah IS, et al. Effects of light therapy on suicidal ideation in patients with winter depression. J Clin Psychiatry. 2000;61(1):30-32.
6. Oliwenstein L. Lifting moods by losing sleep: an adjunct therapy for treating depression. Alternative and Complementary Therapies. 2006;12(2):66-70.
7. Wehr TA, Wirz-Justice A, Goodwin FK, et al. Phase advance of the circadian sleep-wake cycle as an antidepressant. Science. 1979;206(4419):710-713.
8. Moscovici L, Kotler M. A multistage chronobiologic intervention for the treatment of depression: a pilot study. J Affect Disord. 2009;116(3):201-217.
9. Benedetti F, Colombo C, Barbini B, et al. Morning sunlight reduces length of hospitalization in bipolar depression. J Affect Disord. 2001;62(3):221-223.
10. Benedetti F, Barbini B, Colombo C, et al. Chronotherapeutics in a psychiatric ward. Sleep Med Rev. 2007;11(6):509-522.
11. Lopez-Rodriguez F, Wilson CL, Maidment NT, et al. Total sleep deprivation increases extracellular serotonin in the rat hippocampus. Neuroscience. 2003;121(2):523-530.
12. Mayberg HS. Defining the neural circuitry of depression: toward a new nosology with therapeutic implications. Biol Psychiatry. 2007;61(6):729-730.
13. Wu JC, Gillin JC, Buchsbaum MS, et al. Sleep deprivation PET correlations of Hamilton symptom improvement ratings with changes in relative glucose metabolism in patients with depression. J Affect Disord. 2008;107(1-3):181-186.
14. Bunney JN, Potkin SG. Circadian abnormalities, molecular clock genes and chronobiological treatments in depression. Br Med Bull. 2008;86:23-32.
15. Benedetti F, Barbini B, Lucca A, et al. Sleep deprivation hastens the antidepressant action of fluoxetine. Eur Arch Psychiatry Clin Neurosci. 1997;247(2):100-103.
16. Vogel GW, Thurmond A, Gibbons P, et al. REM sleep reduction effects on depression syndromes. Arch Gen Psychiatry. 1975;32(6):765-777.
17. King D, Dowdy S, Jack R, et al. The dexamethasone suppression test as a predictor of sleep deprivation antidepressant effect. Psychiatry Res. 1982;7(1):93-99.
1. AHCPR Depression Guideline Panel. Clinical practice guideline number 5. Depression in primary care. Volume 2: Treatment of major depression. Rockville, MD: Agency for Health Care Policy and Research, Public Health Services, U.S. Department of Health and Human Services; 1993. AHCPR publication 93-0550.
2. Fava M, Rush JA, Wisniewski SR, et al. A comparison of mirtazapine and nortriptyline following two consecutive failed medication treatments for depressed outpatients: a STAR*D report. Am J Psychiatry. 2006;163(7):1161-1172.
3. Wirz-Justice A, Benedetti F, Berger M. Chronotherapeutics (light and wake therapy) in affective disorders. Psychol Med. 2005;35(7):939-944.
4. Giedke H, Schwärzler F. Therapeutic use of sleep deprivation in depression. Sleep Med Rev. 2002;6(5):361-377.
5. Lam RW, Tam EM, Shiah IS, et al. Effects of light therapy on suicidal ideation in patients with winter depression. J Clin Psychiatry. 2000;61(1):30-32.
6. Oliwenstein L. Lifting moods by losing sleep: an adjunct therapy for treating depression. Alternative and Complementary Therapies. 2006;12(2):66-70.
7. Wehr TA, Wirz-Justice A, Goodwin FK, et al. Phase advance of the circadian sleep-wake cycle as an antidepressant. Science. 1979;206(4419):710-713.
8. Moscovici L, Kotler M. A multistage chronobiologic intervention for the treatment of depression: a pilot study. J Affect Disord. 2009;116(3):201-217.
9. Benedetti F, Colombo C, Barbini B, et al. Morning sunlight reduces length of hospitalization in bipolar depression. J Affect Disord. 2001;62(3):221-223.
10. Benedetti F, Barbini B, Colombo C, et al. Chronotherapeutics in a psychiatric ward. Sleep Med Rev. 2007;11(6):509-522.
11. Lopez-Rodriguez F, Wilson CL, Maidment NT, et al. Total sleep deprivation increases extracellular serotonin in the rat hippocampus. Neuroscience. 2003;121(2):523-530.
12. Mayberg HS. Defining the neural circuitry of depression: toward a new nosology with therapeutic implications. Biol Psychiatry. 2007;61(6):729-730.
13. Wu JC, Gillin JC, Buchsbaum MS, et al. Sleep deprivation PET correlations of Hamilton symptom improvement ratings with changes in relative glucose metabolism in patients with depression. J Affect Disord. 2008;107(1-3):181-186.
14. Bunney JN, Potkin SG. Circadian abnormalities, molecular clock genes and chronobiological treatments in depression. Br Med Bull. 2008;86:23-32.
15. Benedetti F, Barbini B, Lucca A, et al. Sleep deprivation hastens the antidepressant action of fluoxetine. Eur Arch Psychiatry Clin Neurosci. 1997;247(2):100-103.
16. Vogel GW, Thurmond A, Gibbons P, et al. REM sleep reduction effects on depression syndromes. Arch Gen Psychiatry. 1975;32(6):765-777.
17. King D, Dowdy S, Jack R, et al. The dexamethasone suppression test as a predictor of sleep deprivation antidepressant effect. Psychiatry Res. 1982;7(1):93-99.