User login
Provider Recommendation Key in HPV Vaccine Initiation
DENVER – Provider recommendation is strongly associated with initiation of the human papillomavirus vaccine in teenage females, results from a national survey demonstrated.
"It’s important for providers to take the time to counsel and recommend the HPV vaccine and communicate the benefits and the risks of the vaccination, as well as the risk of getting HPV disease as teenagers," Dr. Christina G. Dorell said in an interview during a poster session at the annual meeting of the Pediatric Academic Societies.
Dr. Dorell of the immunization services division at the Centers for Disease Control and Prevention, Atlanta, presented findings from the 2008-2009 National Immunization Survey Teen (NIS-Teen), which was analyzed to determine human papillomavirus (HPV) vaccination coverage among females aged 13-17 years. The NIS-Teen is composed of two parts: a random-digit–dialed telephone survey of parents or guardians of adolescents aged 13-17 years, and a mailed survey to all vaccination providers identified by the parent and for which consent was granted.
The researchers evaluated associations of select socioeconomic characteristics, intention to vaccinate, and HPV status. They used multivariable logistic regression to examine associations while controlling for other factors, including state of residence.
Of the 18,288 females surveyed, 41% received at least one HPV dose. Of those, 53% completed the three-dose series.
The probability of HPV vaccination occurring is 2.6 times higher for adolescents who receive a provider recommendation than for adolescents who do not receive a provider recommendation. Other factors independently associated with HPV vaccine initiation were older age, having a preventive visit at age 11 or 12 years, being eligible for state Children’s Health Insurance Program (CHIP) or Vaccines for Children (VFC) program, having a mother younger than age 34 years, having a mother who never married, and not receiving all vaccines at public facilities.
More than half of white females (60%) completed the vaccination series, compared with 46% of blacks and 40% of Hispanics. Other factors independently associated with completing the vaccination series were having a mother aged 45 or older, being knowledgeable about HPV disease, and not receiving all vaccines at public facilities.
The main reported reasons parents do not intend for their daughters to receive the HPV vaccination in the next 12 months were lack of knowledge (19%), considering it not needed or not necessary (19%), the fact that their daughters were not sexually active (18%), and that they did not receive a provider recommendation (13%).
Dr. Dorell acknowledged certain limitations of the study, including the fact that the telephone portion of the survey was using land line phones only, thus contributing to a noncoverage bias of wireless-only households. It’s also possible that some of the provider data or vaccination histories may be incomplete, she said. However, she pointed out that one of the main strengths of the NIS-Teen "is that it is the only nationally representative survey that reports vaccination coverage estimates from provider-reported data, which is the gold standard for measuring vaccination coverage."
Dr. Dorell said that she had no relevant financial disclosures.
DENVER – Provider recommendation is strongly associated with initiation of the human papillomavirus vaccine in teenage females, results from a national survey demonstrated.
"It’s important for providers to take the time to counsel and recommend the HPV vaccine and communicate the benefits and the risks of the vaccination, as well as the risk of getting HPV disease as teenagers," Dr. Christina G. Dorell said in an interview during a poster session at the annual meeting of the Pediatric Academic Societies.
Dr. Dorell of the immunization services division at the Centers for Disease Control and Prevention, Atlanta, presented findings from the 2008-2009 National Immunization Survey Teen (NIS-Teen), which was analyzed to determine human papillomavirus (HPV) vaccination coverage among females aged 13-17 years. The NIS-Teen is composed of two parts: a random-digit–dialed telephone survey of parents or guardians of adolescents aged 13-17 years, and a mailed survey to all vaccination providers identified by the parent and for which consent was granted.
The researchers evaluated associations of select socioeconomic characteristics, intention to vaccinate, and HPV status. They used multivariable logistic regression to examine associations while controlling for other factors, including state of residence.
Of the 18,288 females surveyed, 41% received at least one HPV dose. Of those, 53% completed the three-dose series.
The probability of HPV vaccination occurring is 2.6 times higher for adolescents who receive a provider recommendation than for adolescents who do not receive a provider recommendation. Other factors independently associated with HPV vaccine initiation were older age, having a preventive visit at age 11 or 12 years, being eligible for state Children’s Health Insurance Program (CHIP) or Vaccines for Children (VFC) program, having a mother younger than age 34 years, having a mother who never married, and not receiving all vaccines at public facilities.
More than half of white females (60%) completed the vaccination series, compared with 46% of blacks and 40% of Hispanics. Other factors independently associated with completing the vaccination series were having a mother aged 45 or older, being knowledgeable about HPV disease, and not receiving all vaccines at public facilities.
The main reported reasons parents do not intend for their daughters to receive the HPV vaccination in the next 12 months were lack of knowledge (19%), considering it not needed or not necessary (19%), the fact that their daughters were not sexually active (18%), and that they did not receive a provider recommendation (13%).
Dr. Dorell acknowledged certain limitations of the study, including the fact that the telephone portion of the survey was using land line phones only, thus contributing to a noncoverage bias of wireless-only households. It’s also possible that some of the provider data or vaccination histories may be incomplete, she said. However, she pointed out that one of the main strengths of the NIS-Teen "is that it is the only nationally representative survey that reports vaccination coverage estimates from provider-reported data, which is the gold standard for measuring vaccination coverage."
Dr. Dorell said that she had no relevant financial disclosures.
DENVER – Provider recommendation is strongly associated with initiation of the human papillomavirus vaccine in teenage females, results from a national survey demonstrated.
"It’s important for providers to take the time to counsel and recommend the HPV vaccine and communicate the benefits and the risks of the vaccination, as well as the risk of getting HPV disease as teenagers," Dr. Christina G. Dorell said in an interview during a poster session at the annual meeting of the Pediatric Academic Societies.
Dr. Dorell of the immunization services division at the Centers for Disease Control and Prevention, Atlanta, presented findings from the 2008-2009 National Immunization Survey Teen (NIS-Teen), which was analyzed to determine human papillomavirus (HPV) vaccination coverage among females aged 13-17 years. The NIS-Teen is composed of two parts: a random-digit–dialed telephone survey of parents or guardians of adolescents aged 13-17 years, and a mailed survey to all vaccination providers identified by the parent and for which consent was granted.
The researchers evaluated associations of select socioeconomic characteristics, intention to vaccinate, and HPV status. They used multivariable logistic regression to examine associations while controlling for other factors, including state of residence.
Of the 18,288 females surveyed, 41% received at least one HPV dose. Of those, 53% completed the three-dose series.
The probability of HPV vaccination occurring is 2.6 times higher for adolescents who receive a provider recommendation than for adolescents who do not receive a provider recommendation. Other factors independently associated with HPV vaccine initiation were older age, having a preventive visit at age 11 or 12 years, being eligible for state Children’s Health Insurance Program (CHIP) or Vaccines for Children (VFC) program, having a mother younger than age 34 years, having a mother who never married, and not receiving all vaccines at public facilities.
More than half of white females (60%) completed the vaccination series, compared with 46% of blacks and 40% of Hispanics. Other factors independently associated with completing the vaccination series were having a mother aged 45 or older, being knowledgeable about HPV disease, and not receiving all vaccines at public facilities.
The main reported reasons parents do not intend for their daughters to receive the HPV vaccination in the next 12 months were lack of knowledge (19%), considering it not needed or not necessary (19%), the fact that their daughters were not sexually active (18%), and that they did not receive a provider recommendation (13%).
Dr. Dorell acknowledged certain limitations of the study, including the fact that the telephone portion of the survey was using land line phones only, thus contributing to a noncoverage bias of wireless-only households. It’s also possible that some of the provider data or vaccination histories may be incomplete, she said. However, she pointed out that one of the main strengths of the NIS-Teen "is that it is the only nationally representative survey that reports vaccination coverage estimates from provider-reported data, which is the gold standard for measuring vaccination coverage."
Dr. Dorell said that she had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: The probability of HPV vaccination occurring is 2.6 times higher for adolescents who receive a provider recommendation than it is for adolescents who do not receive a provider recommendation.
Data Source: Results from 18,228 females aged 13-17 years who participated in the National Immunization Survey–Teen 2008-2009.
Disclosures: Dr. Dorell said that she had no relevant financial disclosures.
Weekly E-Mails, Texts Help Keep Families on Weight-Loss Track
DENVER – When 45 families in Brooklyn, N.Y., got weekly reminders to keep to their diets – delivered by e-mail, text message, or voice mail – they stuck with their weight-loss programs longer, according to a study at Brooklyn’s Maimonides Infants and Children’s Hospital.
The messages came once a week on Thursday afternoon, when most parents did their grocery shopping. "They wanted the reminder [then] so that when they reached for [fattening] food, they saw the message and said ‘okay, let’s keep our family on track,’ " lead investigator Rachel Friedman, Ph.D., said at the annual meeting of the Pediatric Academic Societies.
The program, Kids Weight Down, focuses on children aged 2-18 years, but also helps their families. The messages went to parents, and supplemented weekly parenting and exercise classes during the program’s maintenance phase.
Of the 45 families who got them, 37 (83%) remained in the program after 3 months, and 31 (68%) remained in the program at 1 year. Among the 45 families in the program who did not get the messages, only half remained at 3 months, and fewer than 10 were left at 1 year.
The families were demographically similar and equally motivated; Dr. Friedman and her colleagues think the messages made the difference. Families want to be healthy and want to stay in the program, but "just need an extra push. That’s what the technology is doing," she said.
They wanted to get the messages, too. "Without hesitation, they provided cell phone numbers, e-mail addresses, home phone numbers. There wasn’t one who requested to not be part of this study." Plus, "it cost us nothing; it cost them nothing," Dr. Friedman said.
She and her colleagues came up with the idea after hearing how text messages from doctors help people quit smoking and take better care of their diabetes. Kids Weight Down had a problem with attrition during the maintenance phase, so they decided to give electronic messaging a try.
The program consists of 3 months of cognitive-behavioral obesity treatment, followed by the year-long maintenance phase with weekly classes plus individualized quarterly meetings with families.
Children and their families work with psychologists, nutritionists, exercise physiologists, and endocrinologists on nutritional education, awareness of binge triggers, increases in activity, self-esteem, and other issues.
Across both groups of 45 families, children had body mass indexes above the 95th percentile for age and sex; 65% were female, and 77% were of Hispanic ethnicity. They were 8 years old on average.
Messages were short and helpful. One said, "Remember your 543210 goal this week. Memorial Day is a great time for family fun. Turn off the TV, and plan a family activity outdoors."
The numbers 543210 stand for five daily servings of fruits and vegetables; no more than 4 hours without a healthy meal or snack; three meals every day; less than 2 hours of screen time every day; 1 hour or more of exercise; and zero sugary drinks.
Dr. Friedman and her colleagues are following the families to see if their persistence translates to better lipid profiles, weight management, and other outcomes. In the meantime, messaging has been extended to additional families.
Dr. Friedman said she had no relevant financial disclosures.
DENVER – When 45 families in Brooklyn, N.Y., got weekly reminders to keep to their diets – delivered by e-mail, text message, or voice mail – they stuck with their weight-loss programs longer, according to a study at Brooklyn’s Maimonides Infants and Children’s Hospital.
The messages came once a week on Thursday afternoon, when most parents did their grocery shopping. "They wanted the reminder [then] so that when they reached for [fattening] food, they saw the message and said ‘okay, let’s keep our family on track,’ " lead investigator Rachel Friedman, Ph.D., said at the annual meeting of the Pediatric Academic Societies.
The program, Kids Weight Down, focuses on children aged 2-18 years, but also helps their families. The messages went to parents, and supplemented weekly parenting and exercise classes during the program’s maintenance phase.
Of the 45 families who got them, 37 (83%) remained in the program after 3 months, and 31 (68%) remained in the program at 1 year. Among the 45 families in the program who did not get the messages, only half remained at 3 months, and fewer than 10 were left at 1 year.
The families were demographically similar and equally motivated; Dr. Friedman and her colleagues think the messages made the difference. Families want to be healthy and want to stay in the program, but "just need an extra push. That’s what the technology is doing," she said.
They wanted to get the messages, too. "Without hesitation, they provided cell phone numbers, e-mail addresses, home phone numbers. There wasn’t one who requested to not be part of this study." Plus, "it cost us nothing; it cost them nothing," Dr. Friedman said.
She and her colleagues came up with the idea after hearing how text messages from doctors help people quit smoking and take better care of their diabetes. Kids Weight Down had a problem with attrition during the maintenance phase, so they decided to give electronic messaging a try.
The program consists of 3 months of cognitive-behavioral obesity treatment, followed by the year-long maintenance phase with weekly classes plus individualized quarterly meetings with families.
Children and their families work with psychologists, nutritionists, exercise physiologists, and endocrinologists on nutritional education, awareness of binge triggers, increases in activity, self-esteem, and other issues.
Across both groups of 45 families, children had body mass indexes above the 95th percentile for age and sex; 65% were female, and 77% were of Hispanic ethnicity. They were 8 years old on average.
Messages were short and helpful. One said, "Remember your 543210 goal this week. Memorial Day is a great time for family fun. Turn off the TV, and plan a family activity outdoors."
The numbers 543210 stand for five daily servings of fruits and vegetables; no more than 4 hours without a healthy meal or snack; three meals every day; less than 2 hours of screen time every day; 1 hour or more of exercise; and zero sugary drinks.
Dr. Friedman and her colleagues are following the families to see if their persistence translates to better lipid profiles, weight management, and other outcomes. In the meantime, messaging has been extended to additional families.
Dr. Friedman said she had no relevant financial disclosures.
DENVER – When 45 families in Brooklyn, N.Y., got weekly reminders to keep to their diets – delivered by e-mail, text message, or voice mail – they stuck with their weight-loss programs longer, according to a study at Brooklyn’s Maimonides Infants and Children’s Hospital.
The messages came once a week on Thursday afternoon, when most parents did their grocery shopping. "They wanted the reminder [then] so that when they reached for [fattening] food, they saw the message and said ‘okay, let’s keep our family on track,’ " lead investigator Rachel Friedman, Ph.D., said at the annual meeting of the Pediatric Academic Societies.
The program, Kids Weight Down, focuses on children aged 2-18 years, but also helps their families. The messages went to parents, and supplemented weekly parenting and exercise classes during the program’s maintenance phase.
Of the 45 families who got them, 37 (83%) remained in the program after 3 months, and 31 (68%) remained in the program at 1 year. Among the 45 families in the program who did not get the messages, only half remained at 3 months, and fewer than 10 were left at 1 year.
The families were demographically similar and equally motivated; Dr. Friedman and her colleagues think the messages made the difference. Families want to be healthy and want to stay in the program, but "just need an extra push. That’s what the technology is doing," she said.
They wanted to get the messages, too. "Without hesitation, they provided cell phone numbers, e-mail addresses, home phone numbers. There wasn’t one who requested to not be part of this study." Plus, "it cost us nothing; it cost them nothing," Dr. Friedman said.
She and her colleagues came up with the idea after hearing how text messages from doctors help people quit smoking and take better care of their diabetes. Kids Weight Down had a problem with attrition during the maintenance phase, so they decided to give electronic messaging a try.
The program consists of 3 months of cognitive-behavioral obesity treatment, followed by the year-long maintenance phase with weekly classes plus individualized quarterly meetings with families.
Children and their families work with psychologists, nutritionists, exercise physiologists, and endocrinologists on nutritional education, awareness of binge triggers, increases in activity, self-esteem, and other issues.
Across both groups of 45 families, children had body mass indexes above the 95th percentile for age and sex; 65% were female, and 77% were of Hispanic ethnicity. They were 8 years old on average.
Messages were short and helpful. One said, "Remember your 543210 goal this week. Memorial Day is a great time for family fun. Turn off the TV, and plan a family activity outdoors."
The numbers 543210 stand for five daily servings of fruits and vegetables; no more than 4 hours without a healthy meal or snack; three meals every day; less than 2 hours of screen time every day; 1 hour or more of exercise; and zero sugary drinks.
Dr. Friedman and her colleagues are following the families to see if their persistence translates to better lipid profiles, weight management, and other outcomes. In the meantime, messaging has been extended to additional families.
Dr. Friedman said she had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: Of 45 families who received weekly electronic reminders to stick to their diets, 37 (83%) remained in their weight-loss program at 3 months. Only about half of 45 families who didn’t get the reminders stayed at 3 months.
Data Source: Prospective study of 90 children aged 2-18 years who participated in the Kids Weight Down program.
Disclosures: Dr. Friedman said she had no relevant financial disclosures.
Simple Scoring System Assesses Pediatric Dehydration
DENVER – A scoring system based on five clinical parameters accurately assessed mild and moderate dehydration in children presenting to an emergency department with gastroenteritis and correlated with the need for intravenous fluids and hospital admission, according to a pilot study.
"Being able to objectively assess how dehydrated children are is really important – you don’t want to be giving children IV fluids if they don’t need them or admitting them if they don’t need it," said lead investigator Dr. Ming Chien, a pediatric emergency medicine fellow at Phoenix Children’s Hospital. "Conversely, you don’t want to be treating a child less than what they should be receiving."
But there are no robust, well-validated scoring systems for dehydration at the moment, he said said at the annual meeting of the Pediatric Academic Societies, so he and his colleagues decided to work on one themselves.
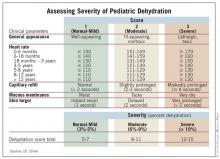
The system assigns a score of 1-3 to general appearance, heart rate, capillary refill, mucous membrane moisture, and skin turgor.
Those factors were picked because they have the strongest support in the medical literature, Dr. Chien noted, and they are objective. "You are not relying on [parents to tell you] the child has made wet diapers or is still making tears. You remove as much of the subjective [as possible] out of assessing children for gastroenteritis," he explained.
A capillary refill of less than 2 seconds, for example, earns a score of 1, 2-3 seconds a score of 2, and 4 or more seconds a score of 3. Similarly, skin that snaps back into place in 1 second receives a turgor score of 1, in 2 seconds a score of 2, and in more than 2 seconds a score of 3.
The scores are then added; 5-7 indicates no or mild dehydration, 8-11 indicates moderate dehydration, and 12-15 indicates severe dehydration.
To test the system’s validity, doctors and nurses weighed and scored 102 children 1 month to 15 years old who presented to the hospital’s emergency department with vomiting, diarrhea, and decreased oral intake, plus clinical concern for dehydration. Treating clinicians were blinded to the scores.
A total of 74 patients were able to return to the hospital a week later – after they had recovered – to be reweighed. The investigators assumed that those post-recovery results were the patients’ baseline weights. Comparing those assumed baseline weights to initial weights when patients first arrived at the ED, researchers were able to estimate children’s percent dehydrations when they first arrived at the ED. By percent dehydration, 64 of the 74 children had been mildly dehydrated, 9 were moderately dehydrated, and 1 was severely dehydrated.
The initial dehydration severity scores showed a statistically significant correlation with percent dehydration, though not a strong correlation. Higher scores correlated more strongly with increased likelihoods of receiving IV fluids and being admitted to the hospital, correlations that also were significant.
The scoring system is a work in progress, however. "We need bigger numbers," Dr. Chien said, as well as more severely dehydrated patients for further testing. Also, while capillary refill, skin turgor, and general appearance strongly and significantly correlated with percent dehydration, heart rate and mucous membrane moisture were less robust factors.
Even so, "the score does definitely seem to correlate with percent dehydration," he said.
Dr. Chien said he had no disclosures.
DENVER – A scoring system based on five clinical parameters accurately assessed mild and moderate dehydration in children presenting to an emergency department with gastroenteritis and correlated with the need for intravenous fluids and hospital admission, according to a pilot study.
"Being able to objectively assess how dehydrated children are is really important – you don’t want to be giving children IV fluids if they don’t need them or admitting them if they don’t need it," said lead investigator Dr. Ming Chien, a pediatric emergency medicine fellow at Phoenix Children’s Hospital. "Conversely, you don’t want to be treating a child less than what they should be receiving."
But there are no robust, well-validated scoring systems for dehydration at the moment, he said said at the annual meeting of the Pediatric Academic Societies, so he and his colleagues decided to work on one themselves.
The system assigns a score of 1-3 to general appearance, heart rate, capillary refill, mucous membrane moisture, and skin turgor.
Those factors were picked because they have the strongest support in the medical literature, Dr. Chien noted, and they are objective. "You are not relying on [parents to tell you] the child has made wet diapers or is still making tears. You remove as much of the subjective [as possible] out of assessing children for gastroenteritis," he explained.
A capillary refill of less than 2 seconds, for example, earns a score of 1, 2-3 seconds a score of 2, and 4 or more seconds a score of 3. Similarly, skin that snaps back into place in 1 second receives a turgor score of 1, in 2 seconds a score of 2, and in more than 2 seconds a score of 3.
The scores are then added; 5-7 indicates no or mild dehydration, 8-11 indicates moderate dehydration, and 12-15 indicates severe dehydration.
To test the system’s validity, doctors and nurses weighed and scored 102 children 1 month to 15 years old who presented to the hospital’s emergency department with vomiting, diarrhea, and decreased oral intake, plus clinical concern for dehydration. Treating clinicians were blinded to the scores.
A total of 74 patients were able to return to the hospital a week later – after they had recovered – to be reweighed. The investigators assumed that those post-recovery results were the patients’ baseline weights. Comparing those assumed baseline weights to initial weights when patients first arrived at the ED, researchers were able to estimate children’s percent dehydrations when they first arrived at the ED. By percent dehydration, 64 of the 74 children had been mildly dehydrated, 9 were moderately dehydrated, and 1 was severely dehydrated.
The initial dehydration severity scores showed a statistically significant correlation with percent dehydration, though not a strong correlation. Higher scores correlated more strongly with increased likelihoods of receiving IV fluids and being admitted to the hospital, correlations that also were significant.
The scoring system is a work in progress, however. "We need bigger numbers," Dr. Chien said, as well as more severely dehydrated patients for further testing. Also, while capillary refill, skin turgor, and general appearance strongly and significantly correlated with percent dehydration, heart rate and mucous membrane moisture were less robust factors.
Even so, "the score does definitely seem to correlate with percent dehydration," he said.
Dr. Chien said he had no disclosures.
DENVER – A scoring system based on five clinical parameters accurately assessed mild and moderate dehydration in children presenting to an emergency department with gastroenteritis and correlated with the need for intravenous fluids and hospital admission, according to a pilot study.
"Being able to objectively assess how dehydrated children are is really important – you don’t want to be giving children IV fluids if they don’t need them or admitting them if they don’t need it," said lead investigator Dr. Ming Chien, a pediatric emergency medicine fellow at Phoenix Children’s Hospital. "Conversely, you don’t want to be treating a child less than what they should be receiving."
But there are no robust, well-validated scoring systems for dehydration at the moment, he said said at the annual meeting of the Pediatric Academic Societies, so he and his colleagues decided to work on one themselves.
The system assigns a score of 1-3 to general appearance, heart rate, capillary refill, mucous membrane moisture, and skin turgor.
Those factors were picked because they have the strongest support in the medical literature, Dr. Chien noted, and they are objective. "You are not relying on [parents to tell you] the child has made wet diapers or is still making tears. You remove as much of the subjective [as possible] out of assessing children for gastroenteritis," he explained.
A capillary refill of less than 2 seconds, for example, earns a score of 1, 2-3 seconds a score of 2, and 4 or more seconds a score of 3. Similarly, skin that snaps back into place in 1 second receives a turgor score of 1, in 2 seconds a score of 2, and in more than 2 seconds a score of 3.
The scores are then added; 5-7 indicates no or mild dehydration, 8-11 indicates moderate dehydration, and 12-15 indicates severe dehydration.
To test the system’s validity, doctors and nurses weighed and scored 102 children 1 month to 15 years old who presented to the hospital’s emergency department with vomiting, diarrhea, and decreased oral intake, plus clinical concern for dehydration. Treating clinicians were blinded to the scores.
A total of 74 patients were able to return to the hospital a week later – after they had recovered – to be reweighed. The investigators assumed that those post-recovery results were the patients’ baseline weights. Comparing those assumed baseline weights to initial weights when patients first arrived at the ED, researchers were able to estimate children’s percent dehydrations when they first arrived at the ED. By percent dehydration, 64 of the 74 children had been mildly dehydrated, 9 were moderately dehydrated, and 1 was severely dehydrated.
The initial dehydration severity scores showed a statistically significant correlation with percent dehydration, though not a strong correlation. Higher scores correlated more strongly with increased likelihoods of receiving IV fluids and being admitted to the hospital, correlations that also were significant.
The scoring system is a work in progress, however. "We need bigger numbers," Dr. Chien said, as well as more severely dehydrated patients for further testing. Also, while capillary refill, skin turgor, and general appearance strongly and significantly correlated with percent dehydration, heart rate and mucous membrane moisture were less robust factors.
Even so, "the score does definitely seem to correlate with percent dehydration," he said.
Dr. Chien said he had no disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: A scoring system that measured general appearance, heart rate, capillary refill, mucous membrane moisture, and skin turgor correlated with percent dehydration in 74 children presenting with gastroenteritis to an emergency department.
Data Source: Blinded, prospective pilot study.
Disclosures: Dr. Ming said he had no disclosures.
Simple Scoring System Assesses Pediatric Dehydration
DENVER – A scoring system based on five clinical parameters accurately assessed mild and moderate dehydration in children presenting to an emergency department with gastroenteritis and correlated with the need for intravenous fluids and hospital admission, according to a pilot study.
"Being able to objectively assess how dehydrated children are is really important – you don’t want to be giving children IV fluids if they don’t need them or admitting them if they don’t need it," said lead investigator Dr. Ming Chien, a pediatric emergency medicine fellow at Phoenix Children’s Hospital. "Conversely, you don’t want to be treating a child less than what they should be receiving."
But there are no robust, well-validated scoring systems for dehydration at the moment, he said said at the annual meeting of the Pediatric Academic Societies, so he and his colleagues decided to work on one themselves.
The system assigns a score of 1-3 to general appearance, heart rate, capillary refill, mucous membrane moisture, and skin turgor.
Those factors were picked because they have the strongest support in the medical literature, Dr. Chien noted, and they are objective. "You are not relying on [parents to tell you] the child has made wet diapers or is still making tears. You remove as much of the subjective [as possible] out of assessing children for gastroenteritis," he explained.
A capillary refill of less than 2 seconds, for example, earns a score of 1, 2-3 seconds a score of 2, and 4 or more seconds a score of 3. Similarly, skin that snaps back into place in 1 second receives a turgor score of 1, in 2 seconds a score of 2, and in more than 2 seconds a score of 3.
The scores are then added; 5-7 indicates no or mild dehydration, 8-11 indicates moderate dehydration, and 12-15 indicates severe dehydration.
To test the system’s validity, doctors and nurses weighed and scored 102 children 1 month to 15 years old who presented to the hospital’s emergency department with vomiting, diarrhea, and decreased oral intake, plus clinical concern for dehydration. Treating clinicians were blinded to the scores.
A total of 74 patients were able to return to the hospital a week later – after they had recovered – to be reweighed. The investigators assumed that those post-recovery results were the patients’ baseline weights. Comparing those assumed baseline weights to initial weights when patients first arrived at the ED, researchers were able to estimate children’s percent dehydrations when they first arrived at the ED. By percent dehydration, 64 of the 74 children had been mildly dehydrated, 9 were moderately dehydrated, and 1 was severely dehydrated.
The initial dehydration severity scores showed a statistically significant correlation with percent dehydration, though not a strong correlation. Higher scores correlated more strongly with increased likelihoods of receiving IV fluids and being admitted to the hospital, correlations that also were significant.
The scoring system is a work in progress, however. "We need bigger numbers," Dr. Chien said, as well as more severely dehydrated patients for further testing. Also, while capillary refill, skin turgor, and general appearance strongly and significantly correlated with percent dehydration, heart rate and mucous membrane moisture were less robust factors.
Even so, "the score does definitely seem to correlate with percent dehydration," he said.
Dr. Chien said he had no disclosures.
DENVER – A scoring system based on five clinical parameters accurately assessed mild and moderate dehydration in children presenting to an emergency department with gastroenteritis and correlated with the need for intravenous fluids and hospital admission, according to a pilot study.
"Being able to objectively assess how dehydrated children are is really important – you don’t want to be giving children IV fluids if they don’t need them or admitting them if they don’t need it," said lead investigator Dr. Ming Chien, a pediatric emergency medicine fellow at Phoenix Children’s Hospital. "Conversely, you don’t want to be treating a child less than what they should be receiving."
But there are no robust, well-validated scoring systems for dehydration at the moment, he said said at the annual meeting of the Pediatric Academic Societies, so he and his colleagues decided to work on one themselves.
The system assigns a score of 1-3 to general appearance, heart rate, capillary refill, mucous membrane moisture, and skin turgor.
Those factors were picked because they have the strongest support in the medical literature, Dr. Chien noted, and they are objective. "You are not relying on [parents to tell you] the child has made wet diapers or is still making tears. You remove as much of the subjective [as possible] out of assessing children for gastroenteritis," he explained.
A capillary refill of less than 2 seconds, for example, earns a score of 1, 2-3 seconds a score of 2, and 4 or more seconds a score of 3. Similarly, skin that snaps back into place in 1 second receives a turgor score of 1, in 2 seconds a score of 2, and in more than 2 seconds a score of 3.
The scores are then added; 5-7 indicates no or mild dehydration, 8-11 indicates moderate dehydration, and 12-15 indicates severe dehydration.
To test the system’s validity, doctors and nurses weighed and scored 102 children 1 month to 15 years old who presented to the hospital’s emergency department with vomiting, diarrhea, and decreased oral intake, plus clinical concern for dehydration. Treating clinicians were blinded to the scores.
A total of 74 patients were able to return to the hospital a week later – after they had recovered – to be reweighed. The investigators assumed that those post-recovery results were the patients’ baseline weights. Comparing those assumed baseline weights to initial weights when patients first arrived at the ED, researchers were able to estimate children’s percent dehydrations when they first arrived at the ED. By percent dehydration, 64 of the 74 children had been mildly dehydrated, 9 were moderately dehydrated, and 1 was severely dehydrated.
The initial dehydration severity scores showed a statistically significant correlation with percent dehydration, though not a strong correlation. Higher scores correlated more strongly with increased likelihoods of receiving IV fluids and being admitted to the hospital, correlations that also were significant.
The scoring system is a work in progress, however. "We need bigger numbers," Dr. Chien said, as well as more severely dehydrated patients for further testing. Also, while capillary refill, skin turgor, and general appearance strongly and significantly correlated with percent dehydration, heart rate and mucous membrane moisture were less robust factors.
Even so, "the score does definitely seem to correlate with percent dehydration," he said.
Dr. Chien said he had no disclosures.
DENVER – A scoring system based on five clinical parameters accurately assessed mild and moderate dehydration in children presenting to an emergency department with gastroenteritis and correlated with the need for intravenous fluids and hospital admission, according to a pilot study.
"Being able to objectively assess how dehydrated children are is really important – you don’t want to be giving children IV fluids if they don’t need them or admitting them if they don’t need it," said lead investigator Dr. Ming Chien, a pediatric emergency medicine fellow at Phoenix Children’s Hospital. "Conversely, you don’t want to be treating a child less than what they should be receiving."
But there are no robust, well-validated scoring systems for dehydration at the moment, he said said at the annual meeting of the Pediatric Academic Societies, so he and his colleagues decided to work on one themselves.
The system assigns a score of 1-3 to general appearance, heart rate, capillary refill, mucous membrane moisture, and skin turgor.
Those factors were picked because they have the strongest support in the medical literature, Dr. Chien noted, and they are objective. "You are not relying on [parents to tell you] the child has made wet diapers or is still making tears. You remove as much of the subjective [as possible] out of assessing children for gastroenteritis," he explained.
A capillary refill of less than 2 seconds, for example, earns a score of 1, 2-3 seconds a score of 2, and 4 or more seconds a score of 3. Similarly, skin that snaps back into place in 1 second receives a turgor score of 1, in 2 seconds a score of 2, and in more than 2 seconds a score of 3.
The scores are then added; 5-7 indicates no or mild dehydration, 8-11 indicates moderate dehydration, and 12-15 indicates severe dehydration.
To test the system’s validity, doctors and nurses weighed and scored 102 children 1 month to 15 years old who presented to the hospital’s emergency department with vomiting, diarrhea, and decreased oral intake, plus clinical concern for dehydration. Treating clinicians were blinded to the scores.
A total of 74 patients were able to return to the hospital a week later – after they had recovered – to be reweighed. The investigators assumed that those post-recovery results were the patients’ baseline weights. Comparing those assumed baseline weights to initial weights when patients first arrived at the ED, researchers were able to estimate children’s percent dehydrations when they first arrived at the ED. By percent dehydration, 64 of the 74 children had been mildly dehydrated, 9 were moderately dehydrated, and 1 was severely dehydrated.
The initial dehydration severity scores showed a statistically significant correlation with percent dehydration, though not a strong correlation. Higher scores correlated more strongly with increased likelihoods of receiving IV fluids and being admitted to the hospital, correlations that also were significant.
The scoring system is a work in progress, however. "We need bigger numbers," Dr. Chien said, as well as more severely dehydrated patients for further testing. Also, while capillary refill, skin turgor, and general appearance strongly and significantly correlated with percent dehydration, heart rate and mucous membrane moisture were less robust factors.
Even so, "the score does definitely seem to correlate with percent dehydration," he said.
Dr. Chien said he had no disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Prehospital Methylprednisolone May Benefit Children With Asthma Exacerbations
DENVER – If emergency workers give children with acute asthma exacerbations intravenous methylprednisolone before they reach the hospital, those children end up spending less time in the emergency department, and perhaps have shorter hospital stays if they are admitted, according to a study from the Baylor College of Medicine.
"This is something that’s been shown in adult populations to work quite well in mitigating the negative outcomes associated with asthma exacerbations," and now for the first time it’s been shown to help children, too, said the study’s lead author, Dr. David N.R. Hooke, at the annual meeting of the Pediatric Academic Societies.
The Houston Fire Department – which handles medical emergency calls in Houston – added intravenous methylprednisolone (Solu-Medrol) to its asthma exacerbation protocol in the spring of 2008, said Dr. Hooke, a Baylor fellow in pediatric emergency medicine.
Giving IV methylprednisolone in the field for acute exacerbations isn’t something done everywhere, Dr. Hooke said, but it makes sense given the adult outcomes and also because steroids in the hospital and outpatient setting are known to shorten exacerbations.
In general, "the Houston Fire Department is very open to putting together pediatric protocols for prehospital care. The push right now is toward getting these children treated as quickly as possible," he said.
Dr. Hooke and his colleagues compared outcomes for 32 children brought to the Texas Children’s Hospital, Houston, with acute asthma exacerbations during May 2007–April 2008, before the addition of IV methylprednisolone, to outcomes for 32 children brought there for the same problem during May 2008–July 2010, with the patients matched by triage acuity.
The children in the later group received 2 mg/kg of the medication 23 minutes, on average, before they arrived at hospital. Children in the earlier group received IV methylprednisolone as well, but waited an average of 84 minutes in the emergency department before getting it. Both groups received continuous albuterol by nebulizer throughout transport.
Receiving IV methylprednisolone sooner seemed to make a difference. The mean emergency department length of stay for the later group was 237 minutes, compared with 338 minutes for children treated earlier, a significant difference.
Similarly, the mean hospital length of stay was 2.2 days in the children treated after April 2008, compared with 3 days in the group treated earlier. That finding was not significant (P = .056), but did demonstrate a trend toward shorter hospital stays, Dr. Hooke said.
The study had several limitations. Because the children were matched by acuity, there was wide variation in age and gender between two groups; 22 (69%) of children in the post–protocol change group were boys, and the mean age in that group was 9.8 years. In the earlier group, 12 (38%) were boys, and the group’s mean age was 6.6.
Also, the study did not meet its target sample size, perhaps because emergency workers were slow to adopt the new protocol. "Larger sample sizes are necessary to determine the effect with greater confidence," Dr. Hooke and his colleagues concluded.
Finally, when methylprednisolone was added to the protocol, ipratropium was dropped. "There have been several research papers that have questioned the utility of ipratropium in patients younger than 12," and it’s expensive, Dr. Hooke noted.
Removing it from the protocol is a possible confounder, "but from my personal experience, I do not believe that the addition or removal of ipratropium made much difference," he said.
Even with the limitations, "the prehospital setting provides the opportunity to initiate timely treatment for asthma exacerbations," the researchers concluded.
Asthma isn’t the only target for prehospital care. "Other things can be done as well, such as getting acutely dehydrated children rehydrated either by mouth or by vein," something not often done in the field, Dr. Hooke said.
For clinicians interested in such measures, "the main thing is to form bridges with their [emergency medical services] companies and get these sorts of protocols in place," he said.
That could be problematic in some places. "A lot of cities don’t have a unified provider of services like Houston does. They have many different companies sort of doing what they want to do," making it harder for protocol changes to be widely adopted, he said.
But "if we can help children and reduce costs, it’s important, especially in the environment we practice in now," he said.
The study received no external funding. Dr. Hooke said he has no disclosures.
DENVER – If emergency workers give children with acute asthma exacerbations intravenous methylprednisolone before they reach the hospital, those children end up spending less time in the emergency department, and perhaps have shorter hospital stays if they are admitted, according to a study from the Baylor College of Medicine.
"This is something that’s been shown in adult populations to work quite well in mitigating the negative outcomes associated with asthma exacerbations," and now for the first time it’s been shown to help children, too, said the study’s lead author, Dr. David N.R. Hooke, at the annual meeting of the Pediatric Academic Societies.
The Houston Fire Department – which handles medical emergency calls in Houston – added intravenous methylprednisolone (Solu-Medrol) to its asthma exacerbation protocol in the spring of 2008, said Dr. Hooke, a Baylor fellow in pediatric emergency medicine.
Giving IV methylprednisolone in the field for acute exacerbations isn’t something done everywhere, Dr. Hooke said, but it makes sense given the adult outcomes and also because steroids in the hospital and outpatient setting are known to shorten exacerbations.
In general, "the Houston Fire Department is very open to putting together pediatric protocols for prehospital care. The push right now is toward getting these children treated as quickly as possible," he said.
Dr. Hooke and his colleagues compared outcomes for 32 children brought to the Texas Children’s Hospital, Houston, with acute asthma exacerbations during May 2007–April 2008, before the addition of IV methylprednisolone, to outcomes for 32 children brought there for the same problem during May 2008–July 2010, with the patients matched by triage acuity.
The children in the later group received 2 mg/kg of the medication 23 minutes, on average, before they arrived at hospital. Children in the earlier group received IV methylprednisolone as well, but waited an average of 84 minutes in the emergency department before getting it. Both groups received continuous albuterol by nebulizer throughout transport.
Receiving IV methylprednisolone sooner seemed to make a difference. The mean emergency department length of stay for the later group was 237 minutes, compared with 338 minutes for children treated earlier, a significant difference.
Similarly, the mean hospital length of stay was 2.2 days in the children treated after April 2008, compared with 3 days in the group treated earlier. That finding was not significant (P = .056), but did demonstrate a trend toward shorter hospital stays, Dr. Hooke said.
The study had several limitations. Because the children were matched by acuity, there was wide variation in age and gender between two groups; 22 (69%) of children in the post–protocol change group were boys, and the mean age in that group was 9.8 years. In the earlier group, 12 (38%) were boys, and the group’s mean age was 6.6.
Also, the study did not meet its target sample size, perhaps because emergency workers were slow to adopt the new protocol. "Larger sample sizes are necessary to determine the effect with greater confidence," Dr. Hooke and his colleagues concluded.
Finally, when methylprednisolone was added to the protocol, ipratropium was dropped. "There have been several research papers that have questioned the utility of ipratropium in patients younger than 12," and it’s expensive, Dr. Hooke noted.
Removing it from the protocol is a possible confounder, "but from my personal experience, I do not believe that the addition or removal of ipratropium made much difference," he said.
Even with the limitations, "the prehospital setting provides the opportunity to initiate timely treatment for asthma exacerbations," the researchers concluded.
Asthma isn’t the only target for prehospital care. "Other things can be done as well, such as getting acutely dehydrated children rehydrated either by mouth or by vein," something not often done in the field, Dr. Hooke said.
For clinicians interested in such measures, "the main thing is to form bridges with their [emergency medical services] companies and get these sorts of protocols in place," he said.
That could be problematic in some places. "A lot of cities don’t have a unified provider of services like Houston does. They have many different companies sort of doing what they want to do," making it harder for protocol changes to be widely adopted, he said.
But "if we can help children and reduce costs, it’s important, especially in the environment we practice in now," he said.
The study received no external funding. Dr. Hooke said he has no disclosures.
DENVER – If emergency workers give children with acute asthma exacerbations intravenous methylprednisolone before they reach the hospital, those children end up spending less time in the emergency department, and perhaps have shorter hospital stays if they are admitted, according to a study from the Baylor College of Medicine.
"This is something that’s been shown in adult populations to work quite well in mitigating the negative outcomes associated with asthma exacerbations," and now for the first time it’s been shown to help children, too, said the study’s lead author, Dr. David N.R. Hooke, at the annual meeting of the Pediatric Academic Societies.
The Houston Fire Department – which handles medical emergency calls in Houston – added intravenous methylprednisolone (Solu-Medrol) to its asthma exacerbation protocol in the spring of 2008, said Dr. Hooke, a Baylor fellow in pediatric emergency medicine.
Giving IV methylprednisolone in the field for acute exacerbations isn’t something done everywhere, Dr. Hooke said, but it makes sense given the adult outcomes and also because steroids in the hospital and outpatient setting are known to shorten exacerbations.
In general, "the Houston Fire Department is very open to putting together pediatric protocols for prehospital care. The push right now is toward getting these children treated as quickly as possible," he said.
Dr. Hooke and his colleagues compared outcomes for 32 children brought to the Texas Children’s Hospital, Houston, with acute asthma exacerbations during May 2007–April 2008, before the addition of IV methylprednisolone, to outcomes for 32 children brought there for the same problem during May 2008–July 2010, with the patients matched by triage acuity.
The children in the later group received 2 mg/kg of the medication 23 minutes, on average, before they arrived at hospital. Children in the earlier group received IV methylprednisolone as well, but waited an average of 84 minutes in the emergency department before getting it. Both groups received continuous albuterol by nebulizer throughout transport.
Receiving IV methylprednisolone sooner seemed to make a difference. The mean emergency department length of stay for the later group was 237 minutes, compared with 338 minutes for children treated earlier, a significant difference.
Similarly, the mean hospital length of stay was 2.2 days in the children treated after April 2008, compared with 3 days in the group treated earlier. That finding was not significant (P = .056), but did demonstrate a trend toward shorter hospital stays, Dr. Hooke said.
The study had several limitations. Because the children were matched by acuity, there was wide variation in age and gender between two groups; 22 (69%) of children in the post–protocol change group were boys, and the mean age in that group was 9.8 years. In the earlier group, 12 (38%) were boys, and the group’s mean age was 6.6.
Also, the study did not meet its target sample size, perhaps because emergency workers were slow to adopt the new protocol. "Larger sample sizes are necessary to determine the effect with greater confidence," Dr. Hooke and his colleagues concluded.
Finally, when methylprednisolone was added to the protocol, ipratropium was dropped. "There have been several research papers that have questioned the utility of ipratropium in patients younger than 12," and it’s expensive, Dr. Hooke noted.
Removing it from the protocol is a possible confounder, "but from my personal experience, I do not believe that the addition or removal of ipratropium made much difference," he said.
Even with the limitations, "the prehospital setting provides the opportunity to initiate timely treatment for asthma exacerbations," the researchers concluded.
Asthma isn’t the only target for prehospital care. "Other things can be done as well, such as getting acutely dehydrated children rehydrated either by mouth or by vein," something not often done in the field, Dr. Hooke said.
For clinicians interested in such measures, "the main thing is to form bridges with their [emergency medical services] companies and get these sorts of protocols in place," he said.
That could be problematic in some places. "A lot of cities don’t have a unified provider of services like Houston does. They have many different companies sort of doing what they want to do," making it harder for protocol changes to be widely adopted, he said.
But "if we can help children and reduce costs, it’s important, especially in the environment we practice in now," he said.
The study received no external funding. Dr. Hooke said he has no disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: Children with acute asthma exacerbations who received IV methylprednisolone before reaching the hospital spent an average of 237 minutes in the ED; those who did not spent 338 minutes, a significant difference.
Data Source: Retrospective case-control study of children with acute asthma brought to one hospital: 32 received IV methylprednisolone en route and 32 did not.
Disclosures: The study received no external funding. Dr. Hooke said he has no disclosures.
Vaccine Recommendations Don't Boost Teen Preventive Visits
DENVER – Although new adolescent vaccine recommendations disseminated between 2005 and early 2007 for meningococcal, tetanus-diphtheria-pertussis, and human papillomavirus vaccines were anticipated to increase the proportion of adolescents with an annual preventive visit, no such impact has occurred, results from a large national survey demonstrated.
However, the rates of vaccination-only visits did increase, researchers led by Christina S. Albertin, M.P.H., reported during a poster session at the annual meeting of the Pediatric Academic Societies. The findings suggest that patterns of primary care delivery did not appear to change as a result of the new recommendations for this population.
"Additional methods, such as reminder recall interventions for annual well care visits, may be needed to bring additional adolescents in for recommended preventive care," the researchers wrote in their poster.
Ms. Albertin and her associates from the division of general pediatrics at the University of Rochester, N.Y., analyzed Medical Expenditure Panel Survey data for any medical visits, well-care visits, and vaccine-only visits made by adolescents, aged 11-21 years, during two time periods: 2004-2005 (before the vaccine recommendations) and 2007-2008 (after the recommendations). They compared visit rates overall and by age group (11-13 years, 14-17 years, and 18-21 years), sex, race/ethnic group, insurance status, and household income. They used chi square analysis to compare rates between the two time periods, controlling for the complex sample design.
Ms. Albertin presented findings from 2,693 adolescents studied in 2004-2005 and 1,988 adolescents studied in 2007-2008.
Between the two time periods, no significant changes in the percentage of adolescents with any medical visit overall were observed (73% vs. 72%, respectively), nor were any changes seen among any of the subgroups following the recommendations. In addition, the percentage of well child visits did not change significantly overall (they remained at 41% for both time periods), or among any of the subgroups.
The average number of visits with a vaccination overall increased significantly from 0.08% in 2004-2005 to 0.14% in 2007-2008. Likewise, the percentage of adolescents who reported a visit with a vaccination increased from 8% to 11%. The subgroups with significant increases included adolescents aged 14-17 years, females, whites, privately insured, and those from families with the highest income level.
"The data seem to show that in the initial 21 months or so following the recommendations, pediatricians focused on fitting vaccinations into existing visits, not expanding the number of [patient] visits," Ms. Albertin said in an interview. "I’m surprised by the results given that there are Tdap vaccine requirements in many states."
She went on to explain that through 2008, only 16 states had school requirements for the Tdap vaccine. "Now, projected through 2011 it looks like that’s going to more than double," she said. "As a result, I think that we will slowly see an increase in both immunization-only and preventive visits."
Ms. Albertin said that she had no relevant financial conflicts to disclose.
DENVER – Although new adolescent vaccine recommendations disseminated between 2005 and early 2007 for meningococcal, tetanus-diphtheria-pertussis, and human papillomavirus vaccines were anticipated to increase the proportion of adolescents with an annual preventive visit, no such impact has occurred, results from a large national survey demonstrated.
However, the rates of vaccination-only visits did increase, researchers led by Christina S. Albertin, M.P.H., reported during a poster session at the annual meeting of the Pediatric Academic Societies. The findings suggest that patterns of primary care delivery did not appear to change as a result of the new recommendations for this population.
"Additional methods, such as reminder recall interventions for annual well care visits, may be needed to bring additional adolescents in for recommended preventive care," the researchers wrote in their poster.
Ms. Albertin and her associates from the division of general pediatrics at the University of Rochester, N.Y., analyzed Medical Expenditure Panel Survey data for any medical visits, well-care visits, and vaccine-only visits made by adolescents, aged 11-21 years, during two time periods: 2004-2005 (before the vaccine recommendations) and 2007-2008 (after the recommendations). They compared visit rates overall and by age group (11-13 years, 14-17 years, and 18-21 years), sex, race/ethnic group, insurance status, and household income. They used chi square analysis to compare rates between the two time periods, controlling for the complex sample design.
Ms. Albertin presented findings from 2,693 adolescents studied in 2004-2005 and 1,988 adolescents studied in 2007-2008.
Between the two time periods, no significant changes in the percentage of adolescents with any medical visit overall were observed (73% vs. 72%, respectively), nor were any changes seen among any of the subgroups following the recommendations. In addition, the percentage of well child visits did not change significantly overall (they remained at 41% for both time periods), or among any of the subgroups.
The average number of visits with a vaccination overall increased significantly from 0.08% in 2004-2005 to 0.14% in 2007-2008. Likewise, the percentage of adolescents who reported a visit with a vaccination increased from 8% to 11%. The subgroups with significant increases included adolescents aged 14-17 years, females, whites, privately insured, and those from families with the highest income level.
"The data seem to show that in the initial 21 months or so following the recommendations, pediatricians focused on fitting vaccinations into existing visits, not expanding the number of [patient] visits," Ms. Albertin said in an interview. "I’m surprised by the results given that there are Tdap vaccine requirements in many states."
She went on to explain that through 2008, only 16 states had school requirements for the Tdap vaccine. "Now, projected through 2011 it looks like that’s going to more than double," she said. "As a result, I think that we will slowly see an increase in both immunization-only and preventive visits."
Ms. Albertin said that she had no relevant financial conflicts to disclose.
DENVER – Although new adolescent vaccine recommendations disseminated between 2005 and early 2007 for meningococcal, tetanus-diphtheria-pertussis, and human papillomavirus vaccines were anticipated to increase the proportion of adolescents with an annual preventive visit, no such impact has occurred, results from a large national survey demonstrated.
However, the rates of vaccination-only visits did increase, researchers led by Christina S. Albertin, M.P.H., reported during a poster session at the annual meeting of the Pediatric Academic Societies. The findings suggest that patterns of primary care delivery did not appear to change as a result of the new recommendations for this population.
"Additional methods, such as reminder recall interventions for annual well care visits, may be needed to bring additional adolescents in for recommended preventive care," the researchers wrote in their poster.
Ms. Albertin and her associates from the division of general pediatrics at the University of Rochester, N.Y., analyzed Medical Expenditure Panel Survey data for any medical visits, well-care visits, and vaccine-only visits made by adolescents, aged 11-21 years, during two time periods: 2004-2005 (before the vaccine recommendations) and 2007-2008 (after the recommendations). They compared visit rates overall and by age group (11-13 years, 14-17 years, and 18-21 years), sex, race/ethnic group, insurance status, and household income. They used chi square analysis to compare rates between the two time periods, controlling for the complex sample design.
Ms. Albertin presented findings from 2,693 adolescents studied in 2004-2005 and 1,988 adolescents studied in 2007-2008.
Between the two time periods, no significant changes in the percentage of adolescents with any medical visit overall were observed (73% vs. 72%, respectively), nor were any changes seen among any of the subgroups following the recommendations. In addition, the percentage of well child visits did not change significantly overall (they remained at 41% for both time periods), or among any of the subgroups.
The average number of visits with a vaccination overall increased significantly from 0.08% in 2004-2005 to 0.14% in 2007-2008. Likewise, the percentage of adolescents who reported a visit with a vaccination increased from 8% to 11%. The subgroups with significant increases included adolescents aged 14-17 years, females, whites, privately insured, and those from families with the highest income level.
"The data seem to show that in the initial 21 months or so following the recommendations, pediatricians focused on fitting vaccinations into existing visits, not expanding the number of [patient] visits," Ms. Albertin said in an interview. "I’m surprised by the results given that there are Tdap vaccine requirements in many states."
She went on to explain that through 2008, only 16 states had school requirements for the Tdap vaccine. "Now, projected through 2011 it looks like that’s going to more than double," she said. "As a result, I think that we will slowly see an increase in both immunization-only and preventive visits."
Ms. Albertin said that she had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: Between 2004-2005 and 2007-2008, no significant changes in the percentage of adolescents with any medical visit overall were observed (73% vs. 72%, respectively). The percentage of well child visits remained unchanged between the two time periods at 41%, but the average number of visits with a vaccination overall increased significantly from 0.08% in 2004-2005 to 0.14% in 2007-2008.
Data Source: An analysis of Medical Expenditure Survey data from 2,693 adolescents studied in 2004-2005 (before the vaccine recommendations), compared with 1,988 adolescents studied in 2007-2008 (after the recommendations).
Disclosures: Ms. Albertin said that she had no relevant financial disclosures.
Vaccine Recommendations Don't Boost Teen Preventive Visits
DENVER – Although new adolescent vaccine recommendations disseminated between 2005 and early 2007 for meningococcal, tetanus-diphtheria-pertussis, and human papillomavirus vaccines were anticipated to increase the proportion of adolescents with an annual preventive visit, no such impact has occurred, results from a large national survey demonstrated.
However, the rates of vaccination-only visits did increase, researchers led by Christina S. Albertin, M.P.H., reported during a poster session at the annual meeting of the Pediatric Academic Societies. The findings suggest that patterns of primary care delivery did not appear to change as a result of the new recommendations for this population.
"Additional methods, such as reminder recall interventions for annual well care visits, may be needed to bring additional adolescents in for recommended preventive care," the researchers wrote in their poster.
Ms. Albertin and her associates from the division of general pediatrics at the University of Rochester, N.Y., analyzed Medical Expenditure Panel Survey data for any medical visits, well-care visits, and vaccine-only visits made by adolescents, aged 11-21 years, during two time periods: 2004-2005 (before the vaccine recommendations) and 2007-2008 (after the recommendations). They compared visit rates overall and by age group (11-13 years, 14-17 years, and 18-21 years), sex, race/ethnic group, insurance status, and household income. They used chi square analysis to compare rates between the two time periods, controlling for the complex sample design.
Ms. Albertin presented findings from 2,693 adolescents studied in 2004-2005 and 1,988 adolescents studied in 2007-2008.
Between the two time periods, no significant changes in the percentage of adolescents with any medical visit overall were observed (73% vs. 72%, respectively), nor were any changes seen among any of the subgroups following the recommendations. In addition, the percentage of well child visits did not change significantly overall (they remained at 41% for both time periods), or among any of the subgroups.
The average number of visits with a vaccination overall increased significantly from 0.08% in 2004-2005 to 0.14% in 2007-2008. Likewise, the percentage of adolescents who reported a visit with a vaccination increased from 8% to 11%. The subgroups with significant increases included adolescents aged 14-17 years, females, whites, privately insured, and those from families with the highest income level.
"The data seem to show that in the initial 21 months or so following the recommendations, pediatricians focused on fitting vaccinations into existing visits, not expanding the number of [patient] visits," Ms. Albertin said in an interview. "I’m surprised by the results given that there are Tdap vaccine requirements in many states."
She went on to explain that through 2008, only 16 states had school requirements for the Tdap vaccine. "Now, projected through 2011 it looks like that’s going to more than double," she said. "As a result, I think that we will slowly see an increase in both immunization-only and preventive visits."
Ms. Albertin said that she had no relevant financial conflicts to disclose.
DENVER – Although new adolescent vaccine recommendations disseminated between 2005 and early 2007 for meningococcal, tetanus-diphtheria-pertussis, and human papillomavirus vaccines were anticipated to increase the proportion of adolescents with an annual preventive visit, no such impact has occurred, results from a large national survey demonstrated.
However, the rates of vaccination-only visits did increase, researchers led by Christina S. Albertin, M.P.H., reported during a poster session at the annual meeting of the Pediatric Academic Societies. The findings suggest that patterns of primary care delivery did not appear to change as a result of the new recommendations for this population.
"Additional methods, such as reminder recall interventions for annual well care visits, may be needed to bring additional adolescents in for recommended preventive care," the researchers wrote in their poster.
Ms. Albertin and her associates from the division of general pediatrics at the University of Rochester, N.Y., analyzed Medical Expenditure Panel Survey data for any medical visits, well-care visits, and vaccine-only visits made by adolescents, aged 11-21 years, during two time periods: 2004-2005 (before the vaccine recommendations) and 2007-2008 (after the recommendations). They compared visit rates overall and by age group (11-13 years, 14-17 years, and 18-21 years), sex, race/ethnic group, insurance status, and household income. They used chi square analysis to compare rates between the two time periods, controlling for the complex sample design.
Ms. Albertin presented findings from 2,693 adolescents studied in 2004-2005 and 1,988 adolescents studied in 2007-2008.
Between the two time periods, no significant changes in the percentage of adolescents with any medical visit overall were observed (73% vs. 72%, respectively), nor were any changes seen among any of the subgroups following the recommendations. In addition, the percentage of well child visits did not change significantly overall (they remained at 41% for both time periods), or among any of the subgroups.
The average number of visits with a vaccination overall increased significantly from 0.08% in 2004-2005 to 0.14% in 2007-2008. Likewise, the percentage of adolescents who reported a visit with a vaccination increased from 8% to 11%. The subgroups with significant increases included adolescents aged 14-17 years, females, whites, privately insured, and those from families with the highest income level.
"The data seem to show that in the initial 21 months or so following the recommendations, pediatricians focused on fitting vaccinations into existing visits, not expanding the number of [patient] visits," Ms. Albertin said in an interview. "I’m surprised by the results given that there are Tdap vaccine requirements in many states."
She went on to explain that through 2008, only 16 states had school requirements for the Tdap vaccine. "Now, projected through 2011 it looks like that’s going to more than double," she said. "As a result, I think that we will slowly see an increase in both immunization-only and preventive visits."
Ms. Albertin said that she had no relevant financial conflicts to disclose.
DENVER – Although new adolescent vaccine recommendations disseminated between 2005 and early 2007 for meningococcal, tetanus-diphtheria-pertussis, and human papillomavirus vaccines were anticipated to increase the proportion of adolescents with an annual preventive visit, no such impact has occurred, results from a large national survey demonstrated.
However, the rates of vaccination-only visits did increase, researchers led by Christina S. Albertin, M.P.H., reported during a poster session at the annual meeting of the Pediatric Academic Societies. The findings suggest that patterns of primary care delivery did not appear to change as a result of the new recommendations for this population.
"Additional methods, such as reminder recall interventions for annual well care visits, may be needed to bring additional adolescents in for recommended preventive care," the researchers wrote in their poster.
Ms. Albertin and her associates from the division of general pediatrics at the University of Rochester, N.Y., analyzed Medical Expenditure Panel Survey data for any medical visits, well-care visits, and vaccine-only visits made by adolescents, aged 11-21 years, during two time periods: 2004-2005 (before the vaccine recommendations) and 2007-2008 (after the recommendations). They compared visit rates overall and by age group (11-13 years, 14-17 years, and 18-21 years), sex, race/ethnic group, insurance status, and household income. They used chi square analysis to compare rates between the two time periods, controlling for the complex sample design.
Ms. Albertin presented findings from 2,693 adolescents studied in 2004-2005 and 1,988 adolescents studied in 2007-2008.
Between the two time periods, no significant changes in the percentage of adolescents with any medical visit overall were observed (73% vs. 72%, respectively), nor were any changes seen among any of the subgroups following the recommendations. In addition, the percentage of well child visits did not change significantly overall (they remained at 41% for both time periods), or among any of the subgroups.
The average number of visits with a vaccination overall increased significantly from 0.08% in 2004-2005 to 0.14% in 2007-2008. Likewise, the percentage of adolescents who reported a visit with a vaccination increased from 8% to 11%. The subgroups with significant increases included adolescents aged 14-17 years, females, whites, privately insured, and those from families with the highest income level.
"The data seem to show that in the initial 21 months or so following the recommendations, pediatricians focused on fitting vaccinations into existing visits, not expanding the number of [patient] visits," Ms. Albertin said in an interview. "I’m surprised by the results given that there are Tdap vaccine requirements in many states."
She went on to explain that through 2008, only 16 states had school requirements for the Tdap vaccine. "Now, projected through 2011 it looks like that’s going to more than double," she said. "As a result, I think that we will slowly see an increase in both immunization-only and preventive visits."
Ms. Albertin said that she had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: Between 2004-2005 and 2007-2008, no significant changes in the percentage of adolescents with any medical visit overall were observed (73% vs. 72%, respectively). The percentage of well child visits remained unchanged between the two time periods at 41%, but the average number of visits with a vaccination overall increased significantly from 0.08% in 2004-2005 to 0.14% in 2007-2008.
Data Source: An analysis of Medical Expenditure Survey data from 2,693 adolescents studied in 2004-2005 (before the vaccine recommendations), compared with 1,988 adolescents studied in 2007-2008 (after the recommendations).
Disclosures: Ms. Albertin said that she had no relevant financial disclosures.
Having a Favorite Alcohol Brand Ups Risk for Binge Drinking
DENVER – Underage, adolescent alcohol drinkers who endorse a favorite brand are significantly more likely to report recent binge drinking than are those who have no favorite brand.
In addition, the amount of money a company spent on television advertising to promote its brand was directly associated with choice of brand and increased risk for problematic alcohol use, according to a nationally-representative survey of 2,699 individuals aged 16-20 years.
"Underage drinkers preferentially choose highly advertised brands as ‘favorites.’ This suggests that marketing is indeed influencing their choice of beverage," Dr. Susanne E. Tanski said at the annual meeting of the Pediatric Academic Societies.
Based on the findings, physicians could screen patients for problem drinking if they endorse a favorite brand. Doctors also could advocate for an increase in the voluntary advertising restrictions for "hard alcohol" television advertising to protect underage drinkers, Dr. Tanski said. Currently, such advertisements are placed only in media where at least 70% of audience is reasonably expected to be 21 years or older.
"If you turn on [ESPN] SportsCenter any night, you see a tremendous number of alcohol ads," said Dr. Tanski, who is on the pediatric faculty at Dartmouth Medical School in Lebanon, N.H.
Nearly two-thirds of respondents reported they had ever tried alcohol (1,734 adolescents, 64%), and almost 21% had binged in the previous 30 days. Binge drinking was defined as consuming five or more alcoholic drinks at a time.
Of those who had ever had a full drink (not a sip or taste), 68% said they had a favorite brand. "We took anything they told us. It was a long list [158 brands], but some we were not able to verify (e.g, ‘X-Ray’)."
Favorite drinks included a distilled spirit brand by 53%, beer brand by almost 43%, and wine/cider by nearly 3%. The remaining drinks were unknown brand names. Results suggest that the distilled spirits industry is making inroads into the adolescent market, the authors stated.
"The winner for this was Smirnoff, and a close second was Budweiser," Dr. Tanski said. As a caveat, she added, she and her colleagues did not distinguish between hard liquor brands and their malt beverage drinks (for example, Smirnoff vodka was not distinguished from Smirnoff Ice or Bacardi rum from Bacardi Breezers).
In addition, favorites varied by sex, with girls more likely to endorse Smirnoff and boys more likely to say Budweiser was their favorite. A meeting attendee asked if Dr. Tanski differentiated between advertising geared toward men or women. "Most of Budweiser ads are advertised to men, but there are some geared to women also. That is something we can certainly look at."
Girls also chose, in order, Budweiser, Corona, Grey Goose, Bacardi, Captain Morgan, Coors, Skyy, Miller, and Absolut as their top favorites. Male adolescents, after Budweiser, chose Smirnoff, Coors, Corona, Miller, Captain Morgan, Heineken, Grey Goose, Jack Daniels, and Bacardi.
Binge drinking within the past 30 days did not differ significantly between those who endorsed a favorite distilled spirit vs. a beer brand. Another significant difference was binge drinking prevalence among those teenagers who reported a favorite alcohol brand, which ranged from 28% to 71% depending on brand, vs. 11% among those with no favorite.
Overall prevalence of binge drinking was 25% among girls and 39% among boys. Both girls and boys who chose Coors beer as their favorite were at particularly high risk for binge drinking. For example, 70% of the boys who said they were likely to binge drink chose Coors as their favorite brand. Miller beer and Grey Goose vodka also scored high for binge drinking among girls, as did Jack Daniels and Captain Morgan among boys.
A significant correlation between brand preference among these adolescents and marketing expenditures suggest marketing plays a role in choice of a favorite brand. Using the most recent data available from Nielsen, Budweiser spent $1.1 billion on television advertising in 2009. Smirnoff advertising expenditure was $63 million during the same year, Dr. Tanski said, "So they got a lot of bang for their buck."
In 1996, the Distilled Spirits Council of the United States lifted its voluntary ban on "hard alcohol" advertising on television, starting with cable TV. The major television networks began allowing such advertisements in 2001, when NBC aired a Smirnoff ad during Saturday Night Live. More recently, in 2009, CBS aired an Absolut advertisement during the Grammy Awards. "As you all well know, there is lot more hard alcohol or distilled spirits advertising on major networks now," Dr. Tanski said. ABC, which is owned by Disney, has not aired "hard alcohol" advertising.
Self-reported drinking behavior is a potential limitation of the study. This was a sample from a longitudinal survey of media exposure and adolescent behavior. In addition, this sample, while national, might not be representative of groups with higher attrition in the survey over time, such as poorer or minority adolescents. Also, because the study was cross-sectional, no causality can be implied, Dr. Tanski said.
Dr. Tanski said that she had no relevant disclosures.
DENVER – Underage, adolescent alcohol drinkers who endorse a favorite brand are significantly more likely to report recent binge drinking than are those who have no favorite brand.
In addition, the amount of money a company spent on television advertising to promote its brand was directly associated with choice of brand and increased risk for problematic alcohol use, according to a nationally-representative survey of 2,699 individuals aged 16-20 years.
"Underage drinkers preferentially choose highly advertised brands as ‘favorites.’ This suggests that marketing is indeed influencing their choice of beverage," Dr. Susanne E. Tanski said at the annual meeting of the Pediatric Academic Societies.
Based on the findings, physicians could screen patients for problem drinking if they endorse a favorite brand. Doctors also could advocate for an increase in the voluntary advertising restrictions for "hard alcohol" television advertising to protect underage drinkers, Dr. Tanski said. Currently, such advertisements are placed only in media where at least 70% of audience is reasonably expected to be 21 years or older.
"If you turn on [ESPN] SportsCenter any night, you see a tremendous number of alcohol ads," said Dr. Tanski, who is on the pediatric faculty at Dartmouth Medical School in Lebanon, N.H.
Nearly two-thirds of respondents reported they had ever tried alcohol (1,734 adolescents, 64%), and almost 21% had binged in the previous 30 days. Binge drinking was defined as consuming five or more alcoholic drinks at a time.
Of those who had ever had a full drink (not a sip or taste), 68% said they had a favorite brand. "We took anything they told us. It was a long list [158 brands], but some we were not able to verify (e.g, ‘X-Ray’)."
Favorite drinks included a distilled spirit brand by 53%, beer brand by almost 43%, and wine/cider by nearly 3%. The remaining drinks were unknown brand names. Results suggest that the distilled spirits industry is making inroads into the adolescent market, the authors stated.
"The winner for this was Smirnoff, and a close second was Budweiser," Dr. Tanski said. As a caveat, she added, she and her colleagues did not distinguish between hard liquor brands and their malt beverage drinks (for example, Smirnoff vodka was not distinguished from Smirnoff Ice or Bacardi rum from Bacardi Breezers).
In addition, favorites varied by sex, with girls more likely to endorse Smirnoff and boys more likely to say Budweiser was their favorite. A meeting attendee asked if Dr. Tanski differentiated between advertising geared toward men or women. "Most of Budweiser ads are advertised to men, but there are some geared to women also. That is something we can certainly look at."
Girls also chose, in order, Budweiser, Corona, Grey Goose, Bacardi, Captain Morgan, Coors, Skyy, Miller, and Absolut as their top favorites. Male adolescents, after Budweiser, chose Smirnoff, Coors, Corona, Miller, Captain Morgan, Heineken, Grey Goose, Jack Daniels, and Bacardi.
Binge drinking within the past 30 days did not differ significantly between those who endorsed a favorite distilled spirit vs. a beer brand. Another significant difference was binge drinking prevalence among those teenagers who reported a favorite alcohol brand, which ranged from 28% to 71% depending on brand, vs. 11% among those with no favorite.
Overall prevalence of binge drinking was 25% among girls and 39% among boys. Both girls and boys who chose Coors beer as their favorite were at particularly high risk for binge drinking. For example, 70% of the boys who said they were likely to binge drink chose Coors as their favorite brand. Miller beer and Grey Goose vodka also scored high for binge drinking among girls, as did Jack Daniels and Captain Morgan among boys.
A significant correlation between brand preference among these adolescents and marketing expenditures suggest marketing plays a role in choice of a favorite brand. Using the most recent data available from Nielsen, Budweiser spent $1.1 billion on television advertising in 2009. Smirnoff advertising expenditure was $63 million during the same year, Dr. Tanski said, "So they got a lot of bang for their buck."
In 1996, the Distilled Spirits Council of the United States lifted its voluntary ban on "hard alcohol" advertising on television, starting with cable TV. The major television networks began allowing such advertisements in 2001, when NBC aired a Smirnoff ad during Saturday Night Live. More recently, in 2009, CBS aired an Absolut advertisement during the Grammy Awards. "As you all well know, there is lot more hard alcohol or distilled spirits advertising on major networks now," Dr. Tanski said. ABC, which is owned by Disney, has not aired "hard alcohol" advertising.
Self-reported drinking behavior is a potential limitation of the study. This was a sample from a longitudinal survey of media exposure and adolescent behavior. In addition, this sample, while national, might not be representative of groups with higher attrition in the survey over time, such as poorer or minority adolescents. Also, because the study was cross-sectional, no causality can be implied, Dr. Tanski said.
Dr. Tanski said that she had no relevant disclosures.
DENVER – Underage, adolescent alcohol drinkers who endorse a favorite brand are significantly more likely to report recent binge drinking than are those who have no favorite brand.
In addition, the amount of money a company spent on television advertising to promote its brand was directly associated with choice of brand and increased risk for problematic alcohol use, according to a nationally-representative survey of 2,699 individuals aged 16-20 years.
"Underage drinkers preferentially choose highly advertised brands as ‘favorites.’ This suggests that marketing is indeed influencing their choice of beverage," Dr. Susanne E. Tanski said at the annual meeting of the Pediatric Academic Societies.
Based on the findings, physicians could screen patients for problem drinking if they endorse a favorite brand. Doctors also could advocate for an increase in the voluntary advertising restrictions for "hard alcohol" television advertising to protect underage drinkers, Dr. Tanski said. Currently, such advertisements are placed only in media where at least 70% of audience is reasonably expected to be 21 years or older.
"If you turn on [ESPN] SportsCenter any night, you see a tremendous number of alcohol ads," said Dr. Tanski, who is on the pediatric faculty at Dartmouth Medical School in Lebanon, N.H.
Nearly two-thirds of respondents reported they had ever tried alcohol (1,734 adolescents, 64%), and almost 21% had binged in the previous 30 days. Binge drinking was defined as consuming five or more alcoholic drinks at a time.
Of those who had ever had a full drink (not a sip or taste), 68% said they had a favorite brand. "We took anything they told us. It was a long list [158 brands], but some we were not able to verify (e.g, ‘X-Ray’)."
Favorite drinks included a distilled spirit brand by 53%, beer brand by almost 43%, and wine/cider by nearly 3%. The remaining drinks were unknown brand names. Results suggest that the distilled spirits industry is making inroads into the adolescent market, the authors stated.
"The winner for this was Smirnoff, and a close second was Budweiser," Dr. Tanski said. As a caveat, she added, she and her colleagues did not distinguish between hard liquor brands and their malt beverage drinks (for example, Smirnoff vodka was not distinguished from Smirnoff Ice or Bacardi rum from Bacardi Breezers).
In addition, favorites varied by sex, with girls more likely to endorse Smirnoff and boys more likely to say Budweiser was their favorite. A meeting attendee asked if Dr. Tanski differentiated between advertising geared toward men or women. "Most of Budweiser ads are advertised to men, but there are some geared to women also. That is something we can certainly look at."
Girls also chose, in order, Budweiser, Corona, Grey Goose, Bacardi, Captain Morgan, Coors, Skyy, Miller, and Absolut as their top favorites. Male adolescents, after Budweiser, chose Smirnoff, Coors, Corona, Miller, Captain Morgan, Heineken, Grey Goose, Jack Daniels, and Bacardi.
Binge drinking within the past 30 days did not differ significantly between those who endorsed a favorite distilled spirit vs. a beer brand. Another significant difference was binge drinking prevalence among those teenagers who reported a favorite alcohol brand, which ranged from 28% to 71% depending on brand, vs. 11% among those with no favorite.
Overall prevalence of binge drinking was 25% among girls and 39% among boys. Both girls and boys who chose Coors beer as their favorite were at particularly high risk for binge drinking. For example, 70% of the boys who said they were likely to binge drink chose Coors as their favorite brand. Miller beer and Grey Goose vodka also scored high for binge drinking among girls, as did Jack Daniels and Captain Morgan among boys.
A significant correlation between brand preference among these adolescents and marketing expenditures suggest marketing plays a role in choice of a favorite brand. Using the most recent data available from Nielsen, Budweiser spent $1.1 billion on television advertising in 2009. Smirnoff advertising expenditure was $63 million during the same year, Dr. Tanski said, "So they got a lot of bang for their buck."
In 1996, the Distilled Spirits Council of the United States lifted its voluntary ban on "hard alcohol" advertising on television, starting with cable TV. The major television networks began allowing such advertisements in 2001, when NBC aired a Smirnoff ad during Saturday Night Live. More recently, in 2009, CBS aired an Absolut advertisement during the Grammy Awards. "As you all well know, there is lot more hard alcohol or distilled spirits advertising on major networks now," Dr. Tanski said. ABC, which is owned by Disney, has not aired "hard alcohol" advertising.
Self-reported drinking behavior is a potential limitation of the study. This was a sample from a longitudinal survey of media exposure and adolescent behavior. In addition, this sample, while national, might not be representative of groups with higher attrition in the survey over time, such as poorer or minority adolescents. Also, because the study was cross-sectional, no causality can be implied, Dr. Tanski said.
Dr. Tanski said that she had no relevant disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: Almost 21% of 2,699 individuals aged 16-20 years reported binge drinking in the previous 30 days, and those who had a favorite brand were at higher risk for this problematic drinking.
Data Source: Cross-sectional sample of a longitudinal survey of media exposure and adolescent behavior.
Disclosures: Dr. Tanski said she had no relevant disclosures.
Having a Favorite Alcohol Brand Ups the Risk for Binge Drinking
DENVER – Underage, adolescent alcohol drinkers who endorse a favorite brand are significantly more likely to report recent binge drinking than are those who have no favorite brand.
In addition, the amount of money a company spent on television advertising to promote its brand was directly associated with choice of brand and increased risk for problematic alcohol use, according to a nationally-representative survey of 2,699 individuals aged 16-20 years.
"Underage drinkers preferentially choose highly advertised brands as ‘favorites.’ This suggests that marketing is indeed influencing their choice of beverage," Dr. Susanne E. Tanski said at the annual meeting of the Pediatric Academic Societies.
Based on the findings, physicians could screen patients for problem drinking if they endorse a favorite brand. Doctors also could advocate for an increase in the voluntary advertising restrictions for "hard alcohol" television advertising to protect underage drinkers, Dr. Tanski said. Currently, such advertisements are placed only in media where at least 70% of audience is reasonably expected to be 21 years or older.
"If you turn on [ESPN] SportsCenter any night, you see a tremendous number of alcohol ads," said Dr. Tanski, who is on the pediatric faculty at Dartmouth Medical School in Lebanon, N.H.
Nearly two-thirds of respondents reported they had ever tried alcohol (1,734 adolescents, 64%), and almost 21% had binged in the previous 30 days. Binge drinking was defined as consuming five or more alcoholic drinks at a time.
Of those who had ever had a full drink (not a sip or taste), 68% said they had a favorite brand. "We took anything they told us. It was a long list [158 brands], but some we were not able to verify (e.g, ‘X-Ray’)."
Favorite drinks included a distilled spirit brand by 53%, beer brand by almost 43%, and wine/cider by nearly 3%. The remaining drinks were unknown brand names. Results suggest that the distilled spirits industry is making inroads into the adolescent market, the authors stated.
"The winner for this was Smirnoff, and a close second was Budweiser," Dr. Tanski said. As a caveat, she added, she and her colleagues did not distinguish between hard liquor brands and their malt beverage drinks (for example, Smirnoff vodka was not distinguished from Smirnoff Ice or Bacardi rum from Bacardi Breezers).
In addition, favorites varied by sex, with girls more likely to endorse Smirnoff and boys more likely to say Budweiser was their favorite. A meeting attendee asked if Dr. Tanski differentiated between advertising geared toward men or women. "Most of Budweiser ads are advertised to men, but there are some geared to women also. That is something we can certainly look at."
Girls also chose, in order, Budweiser, Corona, Grey Goose, Bacardi, Captain Morgan, Coors, Skyy, Miller, and Absolut as their top favorites. Male adolescents, after Budweiser, chose Smirnoff, Coors, Corona, Miller, Captain Morgan, Heineken, Grey Goose, Jack Daniels, and Bacardi.
Binge drinking within the past 30 days did not differ significantly between those who endorsed a favorite distilled spirit vs. a beer brand. Another significant difference was binge drinking prevalence among those teenagers who reported a favorite alcohol brand, which ranged from 28% to 71% depending on brand, vs. 11% among those with no favorite.
Overall prevalence of binge drinking was 25% among girls and 39% among boys. Both girls and boys who chose Coors beer as their favorite were at particularly high risk for binge drinking. For example, 70% of the boys who said they were likely to binge drink chose Coors as their favorite brand. Miller beer and Grey Goose vodka also scored high for binge drinking among girls, as did Jack Daniels and Captain Morgan among boys.
A significant correlation between brand preference among these adolescents and marketing expenditures suggest marketing plays a role in choice of a favorite brand. Using the most recent data available from Nielsen, Budweiser spent $1.1 billion on television advertising in 2009. Smirnoff advertising expenditure was $63 million during the same year, Dr. Tanski said, "So they got a lot of bang for their buck."
In 1996, the Distilled Spirits Council of the United States lifted its voluntary ban on "hard alcohol" advertising on television, starting with cable TV. The major television networks began allowing such advertisements in 2001, when NBC aired a Smirnoff ad during Saturday Night Live. More recently, in 2009, CBS aired an Absolut advertisement during the Grammy Awards. "As you all well know, there is lot more hard alcohol or distilled spirits advertising on major networks now," Dr. Tanski said. ABC, which is owned by Disney, has not aired "hard alcohol" advertising.
Self-reported drinking behavior is a potential limitation of the study. This was a sample from a longitudinal survey of media exposure and adolescent behavior. In addition, this sample, while national, might not be representative of groups with higher attrition in the survey over time, such as poorer or minority adolescents. Also, because the study was cross-sectional, no causality can be implied, Dr. Tanski said.
Dr. Tanski said that she had no relevant disclosures.
DENVER – Underage, adolescent alcohol drinkers who endorse a favorite brand are significantly more likely to report recent binge drinking than are those who have no favorite brand.
In addition, the amount of money a company spent on television advertising to promote its brand was directly associated with choice of brand and increased risk for problematic alcohol use, according to a nationally-representative survey of 2,699 individuals aged 16-20 years.
"Underage drinkers preferentially choose highly advertised brands as ‘favorites.’ This suggests that marketing is indeed influencing their choice of beverage," Dr. Susanne E. Tanski said at the annual meeting of the Pediatric Academic Societies.
Based on the findings, physicians could screen patients for problem drinking if they endorse a favorite brand. Doctors also could advocate for an increase in the voluntary advertising restrictions for "hard alcohol" television advertising to protect underage drinkers, Dr. Tanski said. Currently, such advertisements are placed only in media where at least 70% of audience is reasonably expected to be 21 years or older.
"If you turn on [ESPN] SportsCenter any night, you see a tremendous number of alcohol ads," said Dr. Tanski, who is on the pediatric faculty at Dartmouth Medical School in Lebanon, N.H.
Nearly two-thirds of respondents reported they had ever tried alcohol (1,734 adolescents, 64%), and almost 21% had binged in the previous 30 days. Binge drinking was defined as consuming five or more alcoholic drinks at a time.
Of those who had ever had a full drink (not a sip or taste), 68% said they had a favorite brand. "We took anything they told us. It was a long list [158 brands], but some we were not able to verify (e.g, ‘X-Ray’)."
Favorite drinks included a distilled spirit brand by 53%, beer brand by almost 43%, and wine/cider by nearly 3%. The remaining drinks were unknown brand names. Results suggest that the distilled spirits industry is making inroads into the adolescent market, the authors stated.
"The winner for this was Smirnoff, and a close second was Budweiser," Dr. Tanski said. As a caveat, she added, she and her colleagues did not distinguish between hard liquor brands and their malt beverage drinks (for example, Smirnoff vodka was not distinguished from Smirnoff Ice or Bacardi rum from Bacardi Breezers).
In addition, favorites varied by sex, with girls more likely to endorse Smirnoff and boys more likely to say Budweiser was their favorite. A meeting attendee asked if Dr. Tanski differentiated between advertising geared toward men or women. "Most of Budweiser ads are advertised to men, but there are some geared to women also. That is something we can certainly look at."
Girls also chose, in order, Budweiser, Corona, Grey Goose, Bacardi, Captain Morgan, Coors, Skyy, Miller, and Absolut as their top favorites. Male adolescents, after Budweiser, chose Smirnoff, Coors, Corona, Miller, Captain Morgan, Heineken, Grey Goose, Jack Daniels, and Bacardi.
Binge drinking within the past 30 days did not differ significantly between those who endorsed a favorite distilled spirit vs. a beer brand. Another significant difference was binge drinking prevalence among those teenagers who reported a favorite alcohol brand, which ranged from 28% to 71% depending on brand, vs. 11% among those with no favorite.
Overall prevalence of binge drinking was 25% among girls and 39% among boys. Both girls and boys who chose Coors beer as their favorite were at particularly high risk for binge drinking. For example, 70% of the boys who said they were likely to binge drink chose Coors as their favorite brand. Miller beer and Grey Goose vodka also scored high for binge drinking among girls, as did Jack Daniels and Captain Morgan among boys.
A significant correlation between brand preference among these adolescents and marketing expenditures suggest marketing plays a role in choice of a favorite brand. Using the most recent data available from Nielsen, Budweiser spent $1.1 billion on television advertising in 2009. Smirnoff advertising expenditure was $63 million during the same year, Dr. Tanski said, "So they got a lot of bang for their buck."
In 1996, the Distilled Spirits Council of the United States lifted its voluntary ban on "hard alcohol" advertising on television, starting with cable TV. The major television networks began allowing such advertisements in 2001, when NBC aired a Smirnoff ad during Saturday Night Live. More recently, in 2009, CBS aired an Absolut advertisement during the Grammy Awards. "As you all well know, there is lot more hard alcohol or distilled spirits advertising on major networks now," Dr. Tanski said. ABC, which is owned by Disney, has not aired "hard alcohol" advertising.
Self-reported drinking behavior is a potential limitation of the study. This was a sample from a longitudinal survey of media exposure and adolescent behavior. In addition, this sample, while national, might not be representative of groups with higher attrition in the survey over time, such as poorer or minority adolescents. Also, because the study was cross-sectional, no causality can be implied, Dr. Tanski said.
Dr. Tanski said that she had no relevant disclosures.
DENVER – Underage, adolescent alcohol drinkers who endorse a favorite brand are significantly more likely to report recent binge drinking than are those who have no favorite brand.
In addition, the amount of money a company spent on television advertising to promote its brand was directly associated with choice of brand and increased risk for problematic alcohol use, according to a nationally-representative survey of 2,699 individuals aged 16-20 years.
"Underage drinkers preferentially choose highly advertised brands as ‘favorites.’ This suggests that marketing is indeed influencing their choice of beverage," Dr. Susanne E. Tanski said at the annual meeting of the Pediatric Academic Societies.
Based on the findings, physicians could screen patients for problem drinking if they endorse a favorite brand. Doctors also could advocate for an increase in the voluntary advertising restrictions for "hard alcohol" television advertising to protect underage drinkers, Dr. Tanski said. Currently, such advertisements are placed only in media where at least 70% of audience is reasonably expected to be 21 years or older.
"If you turn on [ESPN] SportsCenter any night, you see a tremendous number of alcohol ads," said Dr. Tanski, who is on the pediatric faculty at Dartmouth Medical School in Lebanon, N.H.
Nearly two-thirds of respondents reported they had ever tried alcohol (1,734 adolescents, 64%), and almost 21% had binged in the previous 30 days. Binge drinking was defined as consuming five or more alcoholic drinks at a time.
Of those who had ever had a full drink (not a sip or taste), 68% said they had a favorite brand. "We took anything they told us. It was a long list [158 brands], but some we were not able to verify (e.g, ‘X-Ray’)."
Favorite drinks included a distilled spirit brand by 53%, beer brand by almost 43%, and wine/cider by nearly 3%. The remaining drinks were unknown brand names. Results suggest that the distilled spirits industry is making inroads into the adolescent market, the authors stated.
"The winner for this was Smirnoff, and a close second was Budweiser," Dr. Tanski said. As a caveat, she added, she and her colleagues did not distinguish between hard liquor brands and their malt beverage drinks (for example, Smirnoff vodka was not distinguished from Smirnoff Ice or Bacardi rum from Bacardi Breezers).
In addition, favorites varied by sex, with girls more likely to endorse Smirnoff and boys more likely to say Budweiser was their favorite. A meeting attendee asked if Dr. Tanski differentiated between advertising geared toward men or women. "Most of Budweiser ads are advertised to men, but there are some geared to women also. That is something we can certainly look at."
Girls also chose, in order, Budweiser, Corona, Grey Goose, Bacardi, Captain Morgan, Coors, Skyy, Miller, and Absolut as their top favorites. Male adolescents, after Budweiser, chose Smirnoff, Coors, Corona, Miller, Captain Morgan, Heineken, Grey Goose, Jack Daniels, and Bacardi.
Binge drinking within the past 30 days did not differ significantly between those who endorsed a favorite distilled spirit vs. a beer brand. Another significant difference was binge drinking prevalence among those teenagers who reported a favorite alcohol brand, which ranged from 28% to 71% depending on brand, vs. 11% among those with no favorite.
Overall prevalence of binge drinking was 25% among girls and 39% among boys. Both girls and boys who chose Coors beer as their favorite were at particularly high risk for binge drinking. For example, 70% of the boys who said they were likely to binge drink chose Coors as their favorite brand. Miller beer and Grey Goose vodka also scored high for binge drinking among girls, as did Jack Daniels and Captain Morgan among boys.
A significant correlation between brand preference among these adolescents and marketing expenditures suggest marketing plays a role in choice of a favorite brand. Using the most recent data available from Nielsen, Budweiser spent $1.1 billion on television advertising in 2009. Smirnoff advertising expenditure was $63 million during the same year, Dr. Tanski said, "So they got a lot of bang for their buck."
In 1996, the Distilled Spirits Council of the United States lifted its voluntary ban on "hard alcohol" advertising on television, starting with cable TV. The major television networks began allowing such advertisements in 2001, when NBC aired a Smirnoff ad during Saturday Night Live. More recently, in 2009, CBS aired an Absolut advertisement during the Grammy Awards. "As you all well know, there is lot more hard alcohol or distilled spirits advertising on major networks now," Dr. Tanski said. ABC, which is owned by Disney, has not aired "hard alcohol" advertising.
Self-reported drinking behavior is a potential limitation of the study. This was a sample from a longitudinal survey of media exposure and adolescent behavior. In addition, this sample, while national, might not be representative of groups with higher attrition in the survey over time, such as poorer or minority adolescents. Also, because the study was cross-sectional, no causality can be implied, Dr. Tanski said.
Dr. Tanski said that she had no relevant disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: Almost 21% of 2,699 individuals aged 16-20 years reported binge drinking in the previous 30 days, and those who had a favorite brand were at higher risk for this problematic drinking.
Data Source: Cross-sectional sample of a longitudinal survey of media exposure and adolescent behavior.
Disclosures: Dr. Tanski said she had no relevant disclosures.
Having a Favorite Alcohol Brand Ups Risk For Binge Drinking
DENVER – Underage, adolescent alcohol drinkers who endorse a favorite brand are significantly more likely to report recent binge drinking than are those who have no favorite brand.
In addition, the amount of money a company spent on television advertising to promote its brand was directly associated with choice of brand and increased risk for problematic alcohol use, according to a nationally-representative survey of 2,699 individuals aged 16-20 years.
"Underage drinkers preferentially choose highly advertised brands as ‘favorites.’ This suggests that marketing is indeed influencing their choice of beverage," Dr. Susanne E. Tanski said at the annual meeting of the Pediatric Academic Societies.
Based on the findings, physicians could screen patients for problem drinking if they endorse a favorite brand. Doctors also could advocate for an increase in the voluntary advertising restrictions for "hard alcohol" television advertising to protect underage drinkers, Dr. Tanski said. Currently, such advertisements are placed only in media where at least 70% of audience is reasonably expected to be 21 years or older.
"If you turn on [ESPN] SportsCenter any night, you see a tremendous number of alcohol ads," said Dr. Tanski, who is on the pediatric faculty at Dartmouth Medical School in Lebanon, N.H.
Nearly two-thirds of respondents reported they had ever tried alcohol (1,734 adolescents, 64%), and almost 21% had binged in the previous 30 days. Binge drinking was defined as consuming five or more alcoholic drinks at a time.
Of those who had ever had a full drink (not a sip or taste), 68% said they had a favorite brand. "We took anything they told us. It was a long list [158 brands], but some we were not able to verify (e.g, ‘X-Ray’)."
Favorite drinks included a distilled spirit brand by 53%, beer brand by almost 43%, and wine/cider by nearly 3%. The remaining drinks were unknown brand names. Results suggest that the distilled spirits industry is making inroads into the adolescent market, the authors stated.
"The winner for this was Smirnoff, and a close second was Budweiser," Dr. Tanski said. As a caveat, she added, she and her colleagues did not distinguish between hard liquor brands and their malt beverage drinks (for example, Smirnoff vodka was not distinguished from Smirnoff Ice or Bacardi rum from Bacardi Breezers).
In addition, favorites varied by sex, with girls more likely to endorse Smirnoff and boys more likely to say Budweiser was their favorite. A meeting attendee asked if Dr. Tanski differentiated between advertising geared toward men or women. "Most of Budweiser ads are advertised to men, but there are some geared to women also. That is something we can certainly look at."
Girls also chose, in order, Budweiser, Corona, Grey Goose, Bacardi, Captain Morgan, Coors, Skyy, Miller, and Absolut as their top favorites. Male adolescents, after Budweiser, chose Smirnoff, Coors, Corona, Miller, Captain Morgan, Heineken, Grey Goose, Jack Daniels, and Bacardi.
Binge drinking within the past 30 days did not differ significantly between those who endorsed a favorite distilled spirit vs. a beer brand. Another significant difference was binge drinking prevalence among those teenagers who reported a favorite alcohol brand, which ranged from 28% to 71% depending on brand, vs. 11% among those with no favorite.
Overall prevalence of binge drinking was 25% among girls and 39% among boys. Both girls and boys who chose Coors beer as their favorite were at particularly high risk for binge drinking. For example, 70% of the boys who said they were likely to binge drink chose Coors as their favorite brand. Miller beer and Grey Goose vodka also scored high for binge drinking among girls, as did Jack Daniels and Captain Morgan among boys.
A significant correlation between brand preference among these adolescents and marketing expenditures suggest marketing plays a role in choice of a favorite brand. Using the most recent data available from Nielsen, Budweiser spent $1.1 billion on television advertising in 2009. Smirnoff advertising expenditure was $63 million during the same year, Dr. Tanski said, "So they got a lot of bang for their buck."
In 1996, the Distilled Spirits Council of the United States lifted its voluntary ban on "hard alcohol" advertising on television, starting with cable TV. The major television networks began allowing such advertisements in 2001, when NBC aired a Smirnoff ad during Saturday Night Live. More recently, in 2009, CBS aired an Absolut advertisement during the Grammy Awards. "As you all well know, there is lot more hard alcohol or distilled spirits advertising on major networks now," Dr. Tanski said. ABC, which is owned by Disney, has not aired "hard alcohol" advertising.
Self-reported drinking behavior is a potential limitation of the study. This was a sample from a longitudinal survey of media exposure and adolescent behavior. In addition, this sample, while national, might not be representative of groups with higher attrition in the survey over time, such as poorer or minority adolescents. Also, because the study was cross-sectional, no causality can be implied, Dr. Tanski said.
Dr. Tanski said that she had no relevant disclosures.
DENVER – Underage, adolescent alcohol drinkers who endorse a favorite brand are significantly more likely to report recent binge drinking than are those who have no favorite brand.
In addition, the amount of money a company spent on television advertising to promote its brand was directly associated with choice of brand and increased risk for problematic alcohol use, according to a nationally-representative survey of 2,699 individuals aged 16-20 years.
"Underage drinkers preferentially choose highly advertised brands as ‘favorites.’ This suggests that marketing is indeed influencing their choice of beverage," Dr. Susanne E. Tanski said at the annual meeting of the Pediatric Academic Societies.
Based on the findings, physicians could screen patients for problem drinking if they endorse a favorite brand. Doctors also could advocate for an increase in the voluntary advertising restrictions for "hard alcohol" television advertising to protect underage drinkers, Dr. Tanski said. Currently, such advertisements are placed only in media where at least 70% of audience is reasonably expected to be 21 years or older.
"If you turn on [ESPN] SportsCenter any night, you see a tremendous number of alcohol ads," said Dr. Tanski, who is on the pediatric faculty at Dartmouth Medical School in Lebanon, N.H.
Nearly two-thirds of respondents reported they had ever tried alcohol (1,734 adolescents, 64%), and almost 21% had binged in the previous 30 days. Binge drinking was defined as consuming five or more alcoholic drinks at a time.
Of those who had ever had a full drink (not a sip or taste), 68% said they had a favorite brand. "We took anything they told us. It was a long list [158 brands], but some we were not able to verify (e.g, ‘X-Ray’)."
Favorite drinks included a distilled spirit brand by 53%, beer brand by almost 43%, and wine/cider by nearly 3%. The remaining drinks were unknown brand names. Results suggest that the distilled spirits industry is making inroads into the adolescent market, the authors stated.
"The winner for this was Smirnoff, and a close second was Budweiser," Dr. Tanski said. As a caveat, she added, she and her colleagues did not distinguish between hard liquor brands and their malt beverage drinks (for example, Smirnoff vodka was not distinguished from Smirnoff Ice or Bacardi rum from Bacardi Breezers).
In addition, favorites varied by sex, with girls more likely to endorse Smirnoff and boys more likely to say Budweiser was their favorite. A meeting attendee asked if Dr. Tanski differentiated between advertising geared toward men or women. "Most of Budweiser ads are advertised to men, but there are some geared to women also. That is something we can certainly look at."
Girls also chose, in order, Budweiser, Corona, Grey Goose, Bacardi, Captain Morgan, Coors, Skyy, Miller, and Absolut as their top favorites. Male adolescents, after Budweiser, chose Smirnoff, Coors, Corona, Miller, Captain Morgan, Heineken, Grey Goose, Jack Daniels, and Bacardi.
Binge drinking within the past 30 days did not differ significantly between those who endorsed a favorite distilled spirit vs. a beer brand. Another significant difference was binge drinking prevalence among those teenagers who reported a favorite alcohol brand, which ranged from 28% to 71% depending on brand, vs. 11% among those with no favorite.
Overall prevalence of binge drinking was 25% among girls and 39% among boys. Both girls and boys who chose Coors beer as their favorite were at particularly high risk for binge drinking. For example, 70% of the boys who said they were likely to binge drink chose Coors as their favorite brand. Miller beer and Grey Goose vodka also scored high for binge drinking among girls, as did Jack Daniels and Captain Morgan among boys.
A significant correlation between brand preference among these adolescents and marketing expenditures suggest marketing plays a role in choice of a favorite brand. Using the most recent data available from Nielsen, Budweiser spent $1.1 billion on television advertising in 2009. Smirnoff advertising expenditure was $63 million during the same year, Dr. Tanski said, "So they got a lot of bang for their buck."
In 1996, the Distilled Spirits Council of the United States lifted its voluntary ban on "hard alcohol" advertising on television, starting with cable TV. The major television networks began allowing such advertisements in 2001, when NBC aired a Smirnoff ad during Saturday Night Live. More recently, in 2009, CBS aired an Absolut advertisement during the Grammy Awards. "As you all well know, there is lot more hard alcohol or distilled spirits advertising on major networks now," Dr. Tanski said. ABC, which is owned by Disney, has not aired "hard alcohol" advertising.
Self-reported drinking behavior is a potential limitation of the study. This was a sample from a longitudinal survey of media exposure and adolescent behavior. In addition, this sample, while national, might not be representative of groups with higher attrition in the survey over time, such as poorer or minority adolescents. Also, because the study was cross-sectional, no causality can be implied, Dr. Tanski said.
Dr. Tanski said that she had no relevant disclosures.
DENVER – Underage, adolescent alcohol drinkers who endorse a favorite brand are significantly more likely to report recent binge drinking than are those who have no favorite brand.
In addition, the amount of money a company spent on television advertising to promote its brand was directly associated with choice of brand and increased risk for problematic alcohol use, according to a nationally-representative survey of 2,699 individuals aged 16-20 years.
"Underage drinkers preferentially choose highly advertised brands as ‘favorites.’ This suggests that marketing is indeed influencing their choice of beverage," Dr. Susanne E. Tanski said at the annual meeting of the Pediatric Academic Societies.
Based on the findings, physicians could screen patients for problem drinking if they endorse a favorite brand. Doctors also could advocate for an increase in the voluntary advertising restrictions for "hard alcohol" television advertising to protect underage drinkers, Dr. Tanski said. Currently, such advertisements are placed only in media where at least 70% of audience is reasonably expected to be 21 years or older.
"If you turn on [ESPN] SportsCenter any night, you see a tremendous number of alcohol ads," said Dr. Tanski, who is on the pediatric faculty at Dartmouth Medical School in Lebanon, N.H.
Nearly two-thirds of respondents reported they had ever tried alcohol (1,734 adolescents, 64%), and almost 21% had binged in the previous 30 days. Binge drinking was defined as consuming five or more alcoholic drinks at a time.
Of those who had ever had a full drink (not a sip or taste), 68% said they had a favorite brand. "We took anything they told us. It was a long list [158 brands], but some we were not able to verify (e.g, ‘X-Ray’)."
Favorite drinks included a distilled spirit brand by 53%, beer brand by almost 43%, and wine/cider by nearly 3%. The remaining drinks were unknown brand names. Results suggest that the distilled spirits industry is making inroads into the adolescent market, the authors stated.
"The winner for this was Smirnoff, and a close second was Budweiser," Dr. Tanski said. As a caveat, she added, she and her colleagues did not distinguish between hard liquor brands and their malt beverage drinks (for example, Smirnoff vodka was not distinguished from Smirnoff Ice or Bacardi rum from Bacardi Breezers).
In addition, favorites varied by sex, with girls more likely to endorse Smirnoff and boys more likely to say Budweiser was their favorite. A meeting attendee asked if Dr. Tanski differentiated between advertising geared toward men or women. "Most of Budweiser ads are advertised to men, but there are some geared to women also. That is something we can certainly look at."
Girls also chose, in order, Budweiser, Corona, Grey Goose, Bacardi, Captain Morgan, Coors, Skyy, Miller, and Absolut as their top favorites. Male adolescents, after Budweiser, chose Smirnoff, Coors, Corona, Miller, Captain Morgan, Heineken, Grey Goose, Jack Daniels, and Bacardi.
Binge drinking within the past 30 days did not differ significantly between those who endorsed a favorite distilled spirit vs. a beer brand. Another significant difference was binge drinking prevalence among those teenagers who reported a favorite alcohol brand, which ranged from 28% to 71% depending on brand, vs. 11% among those with no favorite.
Overall prevalence of binge drinking was 25% among girls and 39% among boys. Both girls and boys who chose Coors beer as their favorite were at particularly high risk for binge drinking. For example, 70% of the boys who said they were likely to binge drink chose Coors as their favorite brand. Miller beer and Grey Goose vodka also scored high for binge drinking among girls, as did Jack Daniels and Captain Morgan among boys.
A significant correlation between brand preference among these adolescents and marketing expenditures suggest marketing plays a role in choice of a favorite brand. Using the most recent data available from Nielsen, Budweiser spent $1.1 billion on television advertising in 2009. Smirnoff advertising expenditure was $63 million during the same year, Dr. Tanski said, "So they got a lot of bang for their buck."
In 1996, the Distilled Spirits Council of the United States lifted its voluntary ban on "hard alcohol" advertising on television, starting with cable TV. The major television networks began allowing such advertisements in 2001, when NBC aired a Smirnoff ad during Saturday Night Live. More recently, in 2009, CBS aired an Absolut advertisement during the Grammy Awards. "As you all well know, there is lot more hard alcohol or distilled spirits advertising on major networks now," Dr. Tanski said. ABC, which is owned by Disney, has not aired "hard alcohol" advertising.
Self-reported drinking behavior is a potential limitation of the study. This was a sample from a longitudinal survey of media exposure and adolescent behavior. In addition, this sample, while national, might not be representative of groups with higher attrition in the survey over time, such as poorer or minority adolescents. Also, because the study was cross-sectional, no causality can be implied, Dr. Tanski said.
Dr. Tanski said that she had no relevant disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: Almost 21% of 2,699 individuals aged 16-20 years reported binge drinking in the previous 30 days, and those who had a favorite brand were at higher risk for this problematic drinking.
Data Source: Cross-sectional sample of a longitudinal survey of media exposure and adolescent behavior.
Disclosures: Dr. Tanski said she had no relevant disclosures.